User login
Is Vaginal Estrogen Safe in Breast Cancer Survivors?
TOPLINE:
Vaginal estrogen therapy does not increase the risk for recurrence in women with hormone receptor (HR)–negative breast cancer or in those with HR–positive tumors concurrently treated with tamoxifen but should be avoided in aromatase inhibitor users, a French study suggested.
METHODOLOGY:
- Survivors of breast cancer often experience genitourinary symptoms due to declining estrogen levels. Vaginal estrogen therapies, including estriol and promestriene (3-propyl ethyl, 17B-methyl estradiol), can prevent these symptoms, but the effect on breast cancer outcomes remains uncertain.
- Researchers used French insurance claims data to emulate a target trial assessing the effect of initiating vaginal estrogen therapy — any molecule, promestriene, or estriol — on disease-free survival in survivors of breast cancer.
- Patients included in the study had a median age of 54 years; 85% were HR-positive, and 15% were HR–negative. The researchers conducted subgroup analyses based on HR status and endocrine therapy regimen.
TAKEAWAY:
- Among 134,942 unique patients, 1739 started vaginal estrogen therapy — 56%, promestriene; 34%, estriol; and 10%, both.
- Initiation of vaginal estrogen therapy led to a modest decrease in disease-free survival in patients with HR–positive tumors (−2.1 percentage point at 5 years), particularly in those concurrently treated with an aromatase inhibitor (−3.0 percentage points).
- No decrease in disease-free survival was observed in patients with HR–negative tumors or in those treated with tamoxifen.
- In aromatase inhibitor users, starting estriol led to a “more severe and premature” decrease in disease-free survival (−4.2 percentage point after 3 years) compared with initiating promestriene (1.0 percentage point difference at 3 years).
IN PRACTICE:
“This study addresses a very important survivorship issue — sexual dysfunction in cancer patients — which is associated with anxiety and depression and should be considered a crucial component of survivorship care,” said study discussant Matteo Lambertini, MD, PhD, with University of Genova, Genova, Italy.
Our results suggest that using vaginal estrogen therapy “is safe in individuals with HR-negative tumors and in those concurrently treated with tamoxifen,” said study presenter Elise Dumas, PhD, with Institut Curie, Paris, France. For breast cancer survivors treated with aromatase inhibitors, vaginal estrogen therapy should be avoided as much as possible, but promestriene is preferred over estriol in this subgroup of patients.
SOURCE:
The research (Abstract 268MO) was presented at the European Society for Medical Oncology Breast Cancer 2024 Annual Congress on May 17, 2024.
LIMITATIONS:
No limitations were discussed in the presentation.
DISCLOSURES:
Funding was provided by Monoprix and the French National Cancer Institute. Dumas declared no conflicts of interest. Lambertini has financial relationships with various pharmaceutical companies including Roche, Novartis, AstraZeneca, Lilly, Exact Sciences, Pfizer, and others.
A version of this article first appeared on Medscape.com.
TOPLINE:
Vaginal estrogen therapy does not increase the risk for recurrence in women with hormone receptor (HR)–negative breast cancer or in those with HR–positive tumors concurrently treated with tamoxifen but should be avoided in aromatase inhibitor users, a French study suggested.
METHODOLOGY:
- Survivors of breast cancer often experience genitourinary symptoms due to declining estrogen levels. Vaginal estrogen therapies, including estriol and promestriene (3-propyl ethyl, 17B-methyl estradiol), can prevent these symptoms, but the effect on breast cancer outcomes remains uncertain.
- Researchers used French insurance claims data to emulate a target trial assessing the effect of initiating vaginal estrogen therapy — any molecule, promestriene, or estriol — on disease-free survival in survivors of breast cancer.
- Patients included in the study had a median age of 54 years; 85% were HR-positive, and 15% were HR–negative. The researchers conducted subgroup analyses based on HR status and endocrine therapy regimen.
TAKEAWAY:
- Among 134,942 unique patients, 1739 started vaginal estrogen therapy — 56%, promestriene; 34%, estriol; and 10%, both.
- Initiation of vaginal estrogen therapy led to a modest decrease in disease-free survival in patients with HR–positive tumors (−2.1 percentage point at 5 years), particularly in those concurrently treated with an aromatase inhibitor (−3.0 percentage points).
- No decrease in disease-free survival was observed in patients with HR–negative tumors or in those treated with tamoxifen.
- In aromatase inhibitor users, starting estriol led to a “more severe and premature” decrease in disease-free survival (−4.2 percentage point after 3 years) compared with initiating promestriene (1.0 percentage point difference at 3 years).
IN PRACTICE:
“This study addresses a very important survivorship issue — sexual dysfunction in cancer patients — which is associated with anxiety and depression and should be considered a crucial component of survivorship care,” said study discussant Matteo Lambertini, MD, PhD, with University of Genova, Genova, Italy.
Our results suggest that using vaginal estrogen therapy “is safe in individuals with HR-negative tumors and in those concurrently treated with tamoxifen,” said study presenter Elise Dumas, PhD, with Institut Curie, Paris, France. For breast cancer survivors treated with aromatase inhibitors, vaginal estrogen therapy should be avoided as much as possible, but promestriene is preferred over estriol in this subgroup of patients.
SOURCE:
The research (Abstract 268MO) was presented at the European Society for Medical Oncology Breast Cancer 2024 Annual Congress on May 17, 2024.
LIMITATIONS:
No limitations were discussed in the presentation.
DISCLOSURES:
Funding was provided by Monoprix and the French National Cancer Institute. Dumas declared no conflicts of interest. Lambertini has financial relationships with various pharmaceutical companies including Roche, Novartis, AstraZeneca, Lilly, Exact Sciences, Pfizer, and others.
A version of this article first appeared on Medscape.com.
TOPLINE:
Vaginal estrogen therapy does not increase the risk for recurrence in women with hormone receptor (HR)–negative breast cancer or in those with HR–positive tumors concurrently treated with tamoxifen but should be avoided in aromatase inhibitor users, a French study suggested.
METHODOLOGY:
- Survivors of breast cancer often experience genitourinary symptoms due to declining estrogen levels. Vaginal estrogen therapies, including estriol and promestriene (3-propyl ethyl, 17B-methyl estradiol), can prevent these symptoms, but the effect on breast cancer outcomes remains uncertain.
- Researchers used French insurance claims data to emulate a target trial assessing the effect of initiating vaginal estrogen therapy — any molecule, promestriene, or estriol — on disease-free survival in survivors of breast cancer.
- Patients included in the study had a median age of 54 years; 85% were HR-positive, and 15% were HR–negative. The researchers conducted subgroup analyses based on HR status and endocrine therapy regimen.
TAKEAWAY:
- Among 134,942 unique patients, 1739 started vaginal estrogen therapy — 56%, promestriene; 34%, estriol; and 10%, both.
- Initiation of vaginal estrogen therapy led to a modest decrease in disease-free survival in patients with HR–positive tumors (−2.1 percentage point at 5 years), particularly in those concurrently treated with an aromatase inhibitor (−3.0 percentage points).
- No decrease in disease-free survival was observed in patients with HR–negative tumors or in those treated with tamoxifen.
- In aromatase inhibitor users, starting estriol led to a “more severe and premature” decrease in disease-free survival (−4.2 percentage point after 3 years) compared with initiating promestriene (1.0 percentage point difference at 3 years).
IN PRACTICE:
“This study addresses a very important survivorship issue — sexual dysfunction in cancer patients — which is associated with anxiety and depression and should be considered a crucial component of survivorship care,” said study discussant Matteo Lambertini, MD, PhD, with University of Genova, Genova, Italy.
Our results suggest that using vaginal estrogen therapy “is safe in individuals with HR-negative tumors and in those concurrently treated with tamoxifen,” said study presenter Elise Dumas, PhD, with Institut Curie, Paris, France. For breast cancer survivors treated with aromatase inhibitors, vaginal estrogen therapy should be avoided as much as possible, but promestriene is preferred over estriol in this subgroup of patients.
SOURCE:
The research (Abstract 268MO) was presented at the European Society for Medical Oncology Breast Cancer 2024 Annual Congress on May 17, 2024.
LIMITATIONS:
No limitations were discussed in the presentation.
DISCLOSURES:
Funding was provided by Monoprix and the French National Cancer Institute. Dumas declared no conflicts of interest. Lambertini has financial relationships with various pharmaceutical companies including Roche, Novartis, AstraZeneca, Lilly, Exact Sciences, Pfizer, and others.
A version of this article first appeared on Medscape.com.
Helping Patients With Intellectual Disabilities Make Informed Decisions
BOSTON — Primary care clinicians caring for patients with intellectual and developmental disabilities often recommend guardianship, a responsibility with life-altering implications.
But only approximately 30% of primary care residency programs in the United States provide training on how to assess the ability of patients with disabilities to make decisions for themselves, and much of this training is optional, according to a recent study cited during a workshop at the 2024 annual meeting of the Society of General Internal Medicine.
Assessing the capacity of patients with disabilities involves navigating a maze of legal, ethical, and clinical considerations, according to Mary Thomas, MD, MPH, a clinical fellow in geriatrics at Yale University School of Medicine in New Haven, Connecticut, who co-moderated the workshop.
Guardianship, while sometimes necessary, can be overly restrictive and diminish patient autonomy, she said. The legal process — ultimately decided through the courts — gives a guardian permission to manage medical care and make decisions for someone who cannot make or communicate those decisions themselves.
Clinicians can assess patients through an evaluation of functional capacity, which allows them to observe a patient’s demeanor and administer a cognition test. Alternatives such as supported decision-making may be less restrictive and can better serve patients, she said. Supported decision-making allows for a person with disabilities to receive assistance from a supporter who can help a patient process medical conditions and treatment needs. The supporter helps empower capable patients to decide on their own.
Some states have introduced legislation that would legally recognize supported decision-making as a less restrictive alternative to guardianship or conservatorship, in which a court-appointed individual manages all aspects of a person’s life.
Sara Mixter, MD, MPH, an assistant professor of medicine and pediatrics at the Johns Hopkins University School of Medicine in Baltimore and a co-moderator of the workshop, called the use of inclusive language in patient communication the “first step toward fostering an environment where patients feel respected and understood.”
Inclusive conversations can include person-first language and using words such as “caregiver” rather than “caretaker.”
Dr. Thomas and Dr. Mixter also called for the directors of residency programs to provide more training on disabilities. They cited a 2023 survey of directors, many of whom said that educational boards do not require training in disability-specific care and that experts in the care of people with disabilities are few and far between.
“Education and awareness are key to overcoming the challenges we face,” Dr. Thomas said. “Improving our training programs means we can ensure that all patients receive the care and respect they deserve.”
Dr. Thomas and Dr. Mixter report no relevant disclosures.
A version of this article first appeared on Medscape.com.
BOSTON — Primary care clinicians caring for patients with intellectual and developmental disabilities often recommend guardianship, a responsibility with life-altering implications.
But only approximately 30% of primary care residency programs in the United States provide training on how to assess the ability of patients with disabilities to make decisions for themselves, and much of this training is optional, according to a recent study cited during a workshop at the 2024 annual meeting of the Society of General Internal Medicine.
Assessing the capacity of patients with disabilities involves navigating a maze of legal, ethical, and clinical considerations, according to Mary Thomas, MD, MPH, a clinical fellow in geriatrics at Yale University School of Medicine in New Haven, Connecticut, who co-moderated the workshop.
Guardianship, while sometimes necessary, can be overly restrictive and diminish patient autonomy, she said. The legal process — ultimately decided through the courts — gives a guardian permission to manage medical care and make decisions for someone who cannot make or communicate those decisions themselves.
Clinicians can assess patients through an evaluation of functional capacity, which allows them to observe a patient’s demeanor and administer a cognition test. Alternatives such as supported decision-making may be less restrictive and can better serve patients, she said. Supported decision-making allows for a person with disabilities to receive assistance from a supporter who can help a patient process medical conditions and treatment needs. The supporter helps empower capable patients to decide on their own.
Some states have introduced legislation that would legally recognize supported decision-making as a less restrictive alternative to guardianship or conservatorship, in which a court-appointed individual manages all aspects of a person’s life.
Sara Mixter, MD, MPH, an assistant professor of medicine and pediatrics at the Johns Hopkins University School of Medicine in Baltimore and a co-moderator of the workshop, called the use of inclusive language in patient communication the “first step toward fostering an environment where patients feel respected and understood.”
Inclusive conversations can include person-first language and using words such as “caregiver” rather than “caretaker.”
Dr. Thomas and Dr. Mixter also called for the directors of residency programs to provide more training on disabilities. They cited a 2023 survey of directors, many of whom said that educational boards do not require training in disability-specific care and that experts in the care of people with disabilities are few and far between.
“Education and awareness are key to overcoming the challenges we face,” Dr. Thomas said. “Improving our training programs means we can ensure that all patients receive the care and respect they deserve.”
Dr. Thomas and Dr. Mixter report no relevant disclosures.
A version of this article first appeared on Medscape.com.
BOSTON — Primary care clinicians caring for patients with intellectual and developmental disabilities often recommend guardianship, a responsibility with life-altering implications.
But only approximately 30% of primary care residency programs in the United States provide training on how to assess the ability of patients with disabilities to make decisions for themselves, and much of this training is optional, according to a recent study cited during a workshop at the 2024 annual meeting of the Society of General Internal Medicine.
Assessing the capacity of patients with disabilities involves navigating a maze of legal, ethical, and clinical considerations, according to Mary Thomas, MD, MPH, a clinical fellow in geriatrics at Yale University School of Medicine in New Haven, Connecticut, who co-moderated the workshop.
Guardianship, while sometimes necessary, can be overly restrictive and diminish patient autonomy, she said. The legal process — ultimately decided through the courts — gives a guardian permission to manage medical care and make decisions for someone who cannot make or communicate those decisions themselves.
Clinicians can assess patients through an evaluation of functional capacity, which allows them to observe a patient’s demeanor and administer a cognition test. Alternatives such as supported decision-making may be less restrictive and can better serve patients, she said. Supported decision-making allows for a person with disabilities to receive assistance from a supporter who can help a patient process medical conditions and treatment needs. The supporter helps empower capable patients to decide on their own.
Some states have introduced legislation that would legally recognize supported decision-making as a less restrictive alternative to guardianship or conservatorship, in which a court-appointed individual manages all aspects of a person’s life.
Sara Mixter, MD, MPH, an assistant professor of medicine and pediatrics at the Johns Hopkins University School of Medicine in Baltimore and a co-moderator of the workshop, called the use of inclusive language in patient communication the “first step toward fostering an environment where patients feel respected and understood.”
Inclusive conversations can include person-first language and using words such as “caregiver” rather than “caretaker.”
Dr. Thomas and Dr. Mixter also called for the directors of residency programs to provide more training on disabilities. They cited a 2023 survey of directors, many of whom said that educational boards do not require training in disability-specific care and that experts in the care of people with disabilities are few and far between.
“Education and awareness are key to overcoming the challenges we face,” Dr. Thomas said. “Improving our training programs means we can ensure that all patients receive the care and respect they deserve.”
Dr. Thomas and Dr. Mixter report no relevant disclosures.
A version of this article first appeared on Medscape.com.
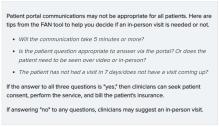
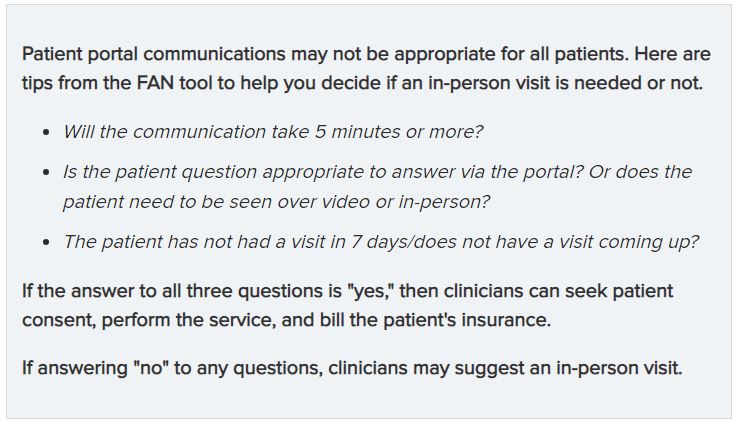
Asynchronous Primary Care Offers Challenges, Opportunities
BOSTON — Online patient portals have shifted patient expectations of how quickly clinicians respond and provide timely care, which can lead to burnout. But asynchronous care can, in some cases, be compensated and increase physician productivity and enhance patient care, according to experts who led a workshop at the Society of General Internal Medicine (SGIM) 2024 Annual Meeting.
Patient portal visits have increased in popularity and use since the COVID-19 pandemic. For primary care clinicians especially, the amount of time spent and the span of requests, from messages with new health concerns to requests for prescription refills, can be daunting.
“Understanding the nuances of these relationships is pivotal in navigating the evolution toward asynchronous care,” said Jennifer Schmidt, MD, an assistant professor of medicine at the Washington University School of Medicine in St. Louis, who co-moderated the workshop.
But patient portals can give clinicians another tool to deliver care beyond conventional office visits or telemedicine appointments, Dr. Schmidt said.
Clinicians can bill insurance if their response to a patient question takes longer than 5 minutes to compose. Responses to messages related to scheduling appointments, refilling prescriptions, or visit follow-ups are not billable.
Some participants at the session said their employers do not have policies that allow compensation for their work in patient portals. Others said their health systems have reported that patients who use portals more frequently have higher satisfaction scores.
Asynchronous care holds promise for extending care beyond traditional constraints, according to Stephen Fuest, MD, an assistant professor of internal medicine at the University of Colorado Anschutz Medical Campus in Aurora, Colorado, and a co-moderator of the workshop.
“By capitalizing on our experiences in designing and implementing systems for portal communication, we can find ways to optimize productivity and alleviate burnout,” Dr. Fuest said.
Dr. Fuest noted that while compensation rates for virtual care are lower than those for in-person, the lack of geographical barriers and time constraints allow clinicians to care for more patients. Asynchronous care also can limit losing patients to follow-up.
One participant noted that the use of the patient portal may increase disparities in care among non-English speaking patients who are unable to interpret communications or clinician notes.
Still, Dr. Schmidt said that asynchronous care is only as successful as the trust and rapport built between the clinician and the patient.
“Asynchronous care isn’t just a technological advancement, it’s a testament to the commitment to patient-centric care,” she said. “By embracing innovation responsibly, we’re ushering healthcare delivery characterized by efficiency, empathy, and empowerment.”
The moderators reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
BOSTON — Online patient portals have shifted patient expectations of how quickly clinicians respond and provide timely care, which can lead to burnout. But asynchronous care can, in some cases, be compensated and increase physician productivity and enhance patient care, according to experts who led a workshop at the Society of General Internal Medicine (SGIM) 2024 Annual Meeting.
Patient portal visits have increased in popularity and use since the COVID-19 pandemic. For primary care clinicians especially, the amount of time spent and the span of requests, from messages with new health concerns to requests for prescription refills, can be daunting.
“Understanding the nuances of these relationships is pivotal in navigating the evolution toward asynchronous care,” said Jennifer Schmidt, MD, an assistant professor of medicine at the Washington University School of Medicine in St. Louis, who co-moderated the workshop.
But patient portals can give clinicians another tool to deliver care beyond conventional office visits or telemedicine appointments, Dr. Schmidt said.
Clinicians can bill insurance if their response to a patient question takes longer than 5 minutes to compose. Responses to messages related to scheduling appointments, refilling prescriptions, or visit follow-ups are not billable.
Some participants at the session said their employers do not have policies that allow compensation for their work in patient portals. Others said their health systems have reported that patients who use portals more frequently have higher satisfaction scores.
Asynchronous care holds promise for extending care beyond traditional constraints, according to Stephen Fuest, MD, an assistant professor of internal medicine at the University of Colorado Anschutz Medical Campus in Aurora, Colorado, and a co-moderator of the workshop.
“By capitalizing on our experiences in designing and implementing systems for portal communication, we can find ways to optimize productivity and alleviate burnout,” Dr. Fuest said.
Dr. Fuest noted that while compensation rates for virtual care are lower than those for in-person, the lack of geographical barriers and time constraints allow clinicians to care for more patients. Asynchronous care also can limit losing patients to follow-up.
One participant noted that the use of the patient portal may increase disparities in care among non-English speaking patients who are unable to interpret communications or clinician notes.
Still, Dr. Schmidt said that asynchronous care is only as successful as the trust and rapport built between the clinician and the patient.
“Asynchronous care isn’t just a technological advancement, it’s a testament to the commitment to patient-centric care,” she said. “By embracing innovation responsibly, we’re ushering healthcare delivery characterized by efficiency, empathy, and empowerment.”
The moderators reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
BOSTON — Online patient portals have shifted patient expectations of how quickly clinicians respond and provide timely care, which can lead to burnout. But asynchronous care can, in some cases, be compensated and increase physician productivity and enhance patient care, according to experts who led a workshop at the Society of General Internal Medicine (SGIM) 2024 Annual Meeting.
Patient portal visits have increased in popularity and use since the COVID-19 pandemic. For primary care clinicians especially, the amount of time spent and the span of requests, from messages with new health concerns to requests for prescription refills, can be daunting.
“Understanding the nuances of these relationships is pivotal in navigating the evolution toward asynchronous care,” said Jennifer Schmidt, MD, an assistant professor of medicine at the Washington University School of Medicine in St. Louis, who co-moderated the workshop.
But patient portals can give clinicians another tool to deliver care beyond conventional office visits or telemedicine appointments, Dr. Schmidt said.
Clinicians can bill insurance if their response to a patient question takes longer than 5 minutes to compose. Responses to messages related to scheduling appointments, refilling prescriptions, or visit follow-ups are not billable.
Some participants at the session said their employers do not have policies that allow compensation for their work in patient portals. Others said their health systems have reported that patients who use portals more frequently have higher satisfaction scores.
Asynchronous care holds promise for extending care beyond traditional constraints, according to Stephen Fuest, MD, an assistant professor of internal medicine at the University of Colorado Anschutz Medical Campus in Aurora, Colorado, and a co-moderator of the workshop.
“By capitalizing on our experiences in designing and implementing systems for portal communication, we can find ways to optimize productivity and alleviate burnout,” Dr. Fuest said.
Dr. Fuest noted that while compensation rates for virtual care are lower than those for in-person, the lack of geographical barriers and time constraints allow clinicians to care for more patients. Asynchronous care also can limit losing patients to follow-up.
One participant noted that the use of the patient portal may increase disparities in care among non-English speaking patients who are unable to interpret communications or clinician notes.
Still, Dr. Schmidt said that asynchronous care is only as successful as the trust and rapport built between the clinician and the patient.
“Asynchronous care isn’t just a technological advancement, it’s a testament to the commitment to patient-centric care,” she said. “By embracing innovation responsibly, we’re ushering healthcare delivery characterized by efficiency, empathy, and empowerment.”
The moderators reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Study of AI for Retina Disease Finds Many Unusable Images
Artificial intelligence (AI) has drawn interest in ophthalmology for its potential to track disease trends in huge populations, such as the 38.4 million people in the United States with diabetes who are at risk for diabetic eye disease. However, a recent study using AI to detect diabetic retinopathy from retinal photo screenings has found wide disparities in the quality of data being fed into the algorithm.
And screening photos captured in nine primary care settings were three times more likely to be unusable than those obtained in two ophthalmology clinics, a study at Temple University in Philadelphia found. The results of the new research were reported at the Association for Research in Vision and Ophthalmology (ARVO) 2024 annual meeting.
“AI-assisted diabetic retinopathy screenings were more successful when completed in the ophthalmology clinic setting compared to the primary care setting,” study leader Madelyn Class, a medical student at Temple, told this news organization. One key difference, Ms. Class said, was that the specialty clinics used a photographer training in capturing ophthalmic images, while the primary care sites had medical assistants taking the photos.
Challenges of Screening in Primary Care
The American Diabetes Association acknowledged in a 2017 position statement that retinal photography has the potential to bring screening into settings where optometrists or ophthalmologists are unavailable. This study showed the potential may not yet be realized.
In the primary care setting, 42.5% of retinal photos were ungradable compared with 14.5% in the specialty settings.
The number of patients diagnosed with more-than-mild diabetic retinopathy also varied significantly between the two settings — 13% in primary care and 24% in ophthalmology — as did the rates of follow-up appointments: 58% and 80%, respectively.
“It seems user error played a role in the quality of photographs that were taken,” Ms. Class said. “Some of the images we received from the primary care settings were actually of the eyelid, or even the curtains on the wall, rather than the fundus.
“All the camera operators in the study received training on the imaging device,” Ms. Class added. “This suggests that some of the photographers were rushed, out of practice, or simply no longer interested in taking photos,” she said. “Apparently, we will have to continuously monitor the performance of each photographer to ensure that quality photos are being taken.”
The findings may also point to the need for using different equipment for screening in primary care, Ms. Class added. “Robotic as opposed to manual cameras may help eliminate some of the user error that was experienced with primary care screenings,” she said.
Need for Training ‘Fixable’
These findings demonstrate the challenges of capturing usable retinal images outside of an eye care professional’s office, according to Jennifer Lim, MD, director of the retina service at the University of Illinois Chicago.
“This study illustrates that implementation is the rub of AI,” Dr. Lim told this news organization. “Getting primary care doctors and clinics to want to adopt and figure out how to implement AI screening [for diabetic retinopathy] in a healthcare system is difficult, so I applaud the Temple University system for trying to integrate retinal photography-based AI screening into the primary care outpatient centers and comparing outcomes to the ophthalmology clinics.”
The study showed that photographers need not only initial training but also monitoring to avoid ungradable images, Dr. Lim added, a problem that is “fixable.”
“It’s going to take a lot of work to get the message out to the primary care practices that these autonomous, cloud-based systems are available and effective for detecting retinopathy,” she said.
But the effort is worth it, she added: “It doesn’t take much time to take these photos for diabetic retinopathy screening, and the potential benefits are huge because the earlier you diagnose diabetic retinopathy that’s more than mild, the more likely the patient can be sent for eye care in a timely fashion and thus prevent visual loss from diabetic retinopathy.”
Ms. Class had no relevant disclosures. Dr. Lim disclosed a past relationship with Eyenuk, the maker of retinal screening cameras.
A version of this article appeared on Medscape.com .
Artificial intelligence (AI) has drawn interest in ophthalmology for its potential to track disease trends in huge populations, such as the 38.4 million people in the United States with diabetes who are at risk for diabetic eye disease. However, a recent study using AI to detect diabetic retinopathy from retinal photo screenings has found wide disparities in the quality of data being fed into the algorithm.
And screening photos captured in nine primary care settings were three times more likely to be unusable than those obtained in two ophthalmology clinics, a study at Temple University in Philadelphia found. The results of the new research were reported at the Association for Research in Vision and Ophthalmology (ARVO) 2024 annual meeting.
“AI-assisted diabetic retinopathy screenings were more successful when completed in the ophthalmology clinic setting compared to the primary care setting,” study leader Madelyn Class, a medical student at Temple, told this news organization. One key difference, Ms. Class said, was that the specialty clinics used a photographer training in capturing ophthalmic images, while the primary care sites had medical assistants taking the photos.
Challenges of Screening in Primary Care
The American Diabetes Association acknowledged in a 2017 position statement that retinal photography has the potential to bring screening into settings where optometrists or ophthalmologists are unavailable. This study showed the potential may not yet be realized.
In the primary care setting, 42.5% of retinal photos were ungradable compared with 14.5% in the specialty settings.
The number of patients diagnosed with more-than-mild diabetic retinopathy also varied significantly between the two settings — 13% in primary care and 24% in ophthalmology — as did the rates of follow-up appointments: 58% and 80%, respectively.
“It seems user error played a role in the quality of photographs that were taken,” Ms. Class said. “Some of the images we received from the primary care settings were actually of the eyelid, or even the curtains on the wall, rather than the fundus.
“All the camera operators in the study received training on the imaging device,” Ms. Class added. “This suggests that some of the photographers were rushed, out of practice, or simply no longer interested in taking photos,” she said. “Apparently, we will have to continuously monitor the performance of each photographer to ensure that quality photos are being taken.”
The findings may also point to the need for using different equipment for screening in primary care, Ms. Class added. “Robotic as opposed to manual cameras may help eliminate some of the user error that was experienced with primary care screenings,” she said.
Need for Training ‘Fixable’
These findings demonstrate the challenges of capturing usable retinal images outside of an eye care professional’s office, according to Jennifer Lim, MD, director of the retina service at the University of Illinois Chicago.
“This study illustrates that implementation is the rub of AI,” Dr. Lim told this news organization. “Getting primary care doctors and clinics to want to adopt and figure out how to implement AI screening [for diabetic retinopathy] in a healthcare system is difficult, so I applaud the Temple University system for trying to integrate retinal photography-based AI screening into the primary care outpatient centers and comparing outcomes to the ophthalmology clinics.”
The study showed that photographers need not only initial training but also monitoring to avoid ungradable images, Dr. Lim added, a problem that is “fixable.”
“It’s going to take a lot of work to get the message out to the primary care practices that these autonomous, cloud-based systems are available and effective for detecting retinopathy,” she said.
But the effort is worth it, she added: “It doesn’t take much time to take these photos for diabetic retinopathy screening, and the potential benefits are huge because the earlier you diagnose diabetic retinopathy that’s more than mild, the more likely the patient can be sent for eye care in a timely fashion and thus prevent visual loss from diabetic retinopathy.”
Ms. Class had no relevant disclosures. Dr. Lim disclosed a past relationship with Eyenuk, the maker of retinal screening cameras.
A version of this article appeared on Medscape.com .
Artificial intelligence (AI) has drawn interest in ophthalmology for its potential to track disease trends in huge populations, such as the 38.4 million people in the United States with diabetes who are at risk for diabetic eye disease. However, a recent study using AI to detect diabetic retinopathy from retinal photo screenings has found wide disparities in the quality of data being fed into the algorithm.
And screening photos captured in nine primary care settings were three times more likely to be unusable than those obtained in two ophthalmology clinics, a study at Temple University in Philadelphia found. The results of the new research were reported at the Association for Research in Vision and Ophthalmology (ARVO) 2024 annual meeting.
“AI-assisted diabetic retinopathy screenings were more successful when completed in the ophthalmology clinic setting compared to the primary care setting,” study leader Madelyn Class, a medical student at Temple, told this news organization. One key difference, Ms. Class said, was that the specialty clinics used a photographer training in capturing ophthalmic images, while the primary care sites had medical assistants taking the photos.
Challenges of Screening in Primary Care
The American Diabetes Association acknowledged in a 2017 position statement that retinal photography has the potential to bring screening into settings where optometrists or ophthalmologists are unavailable. This study showed the potential may not yet be realized.
In the primary care setting, 42.5% of retinal photos were ungradable compared with 14.5% in the specialty settings.
The number of patients diagnosed with more-than-mild diabetic retinopathy also varied significantly between the two settings — 13% in primary care and 24% in ophthalmology — as did the rates of follow-up appointments: 58% and 80%, respectively.
“It seems user error played a role in the quality of photographs that were taken,” Ms. Class said. “Some of the images we received from the primary care settings were actually of the eyelid, or even the curtains on the wall, rather than the fundus.
“All the camera operators in the study received training on the imaging device,” Ms. Class added. “This suggests that some of the photographers were rushed, out of practice, or simply no longer interested in taking photos,” she said. “Apparently, we will have to continuously monitor the performance of each photographer to ensure that quality photos are being taken.”
The findings may also point to the need for using different equipment for screening in primary care, Ms. Class added. “Robotic as opposed to manual cameras may help eliminate some of the user error that was experienced with primary care screenings,” she said.
Need for Training ‘Fixable’
These findings demonstrate the challenges of capturing usable retinal images outside of an eye care professional’s office, according to Jennifer Lim, MD, director of the retina service at the University of Illinois Chicago.
“This study illustrates that implementation is the rub of AI,” Dr. Lim told this news organization. “Getting primary care doctors and clinics to want to adopt and figure out how to implement AI screening [for diabetic retinopathy] in a healthcare system is difficult, so I applaud the Temple University system for trying to integrate retinal photography-based AI screening into the primary care outpatient centers and comparing outcomes to the ophthalmology clinics.”
The study showed that photographers need not only initial training but also monitoring to avoid ungradable images, Dr. Lim added, a problem that is “fixable.”
“It’s going to take a lot of work to get the message out to the primary care practices that these autonomous, cloud-based systems are available and effective for detecting retinopathy,” she said.
But the effort is worth it, she added: “It doesn’t take much time to take these photos for diabetic retinopathy screening, and the potential benefits are huge because the earlier you diagnose diabetic retinopathy that’s more than mild, the more likely the patient can be sent for eye care in a timely fashion and thus prevent visual loss from diabetic retinopathy.”
Ms. Class had no relevant disclosures. Dr. Lim disclosed a past relationship with Eyenuk, the maker of retinal screening cameras.
A version of this article appeared on Medscape.com .
GI Complications With GLP-1s for Weight Loss: Reexamining the Risks
WASHINGTON — In contrast with a previous study that found glucagon-like peptide 1 (GLP-1) receptor agonists associated with an increased risk for acute pancreatitis and bowel obstruction, a new retrospective study found no significant link to these complications.
One of the big differences from the previous study, published in JAMA in October 2023 by Sodhi and colleagues , is that the current research was able to account for initial body mass index (BMI), said Benjamin Liu, MD, a resident in internal medicine at Case Western Reserve University School of Medicine, Cleveland, Ohio.
This is important, he explained in his presentation (abstract 1074) at the annual Digestive Disease Week® 2024, because obesity on its own is associated with an increased risk for some of these gastrointestinal (GI) outcomes.
“They did an excellent study,” Dr. Liu said. “But their platform did not allow them to match participants for BMI.”
Another distinction between the two studies is that the JAMA study excluded people who had diabetes 90 days before or 30 days following the start of GLP-1 therapy.
Instead, Dr. Liu said, he and colleague Gengqing Song, MD, “just made it simple” and excluded anyone with diabetes or an A1c ≥ 6.5.
We didn’t want participants with diabetes because “we were looking at GLP-1s for weight loss,” Dr. Liu explained.
Although some clinical trials have already assessed adverse events of these medications, “clinical trials are not always a perfect representation of the real world,” Dr. Liu said in an interview. “So, it’s important to do real-world studies to see just what actually goes on.”
Reassessing GI Complications
In the current study, the researchers identified 105,793 patients from the TriNetX healthcare database taking a GLP-1, either semaglutide or liraglutide, for weight loss and 8794 patients taking 8 mg naltrexone/90 mg bupropion. After propensity matching, including for BMI, there were 8792 patients in each group.
They were identified in the database between 2011 and 2023. Researchers noted their first-ever occurrence of acute pancreatitis, bowel obstruction, gastroparesis, or biliary disease during the study period.
Participants had a BMI ≥ 30 kg/m2. In addition to BMI, propensity score matching included demographics, alcohol use, smoking, hyperlipidemia, and abdominal surgery. A second analysis specifically did not match participants for BMI.
The researchers found no significant association between GLP-1s and acute pancreatitis (adjusted hazard ratio [HR], 1.19; 95% CI, 0.66-2.14).
The labeling for semaglutide and liraglutide warns about an increased risk for acute pancreatitis, “but real-world studies and clinical trials are increasingly suggesting there is no increased risk,” Dr. Liu said.
They also did not find a significant association between GLP-1s and bowel obstruction (HR, 1.30; 95% CI, 0.69-2.18).
Despite the current findings, more research — especially prospective data — is needed to confirm pancreatitis as well as other GI risks like bowel obstruction potentially associated with GLP-1s, he added.
The study did, however, find an elevated risk for biliary disease (HR, 1.27; 95% CI, 1.02-1.59) in the BMI-matched cohorts.
This could be due to the rapidity of weight loss, Dr. Liu suggested. “We found that semaglutide caused more weight loss at 6 and 12 months than naltrexone/bupropion, and it did so at a faster rate. That falls in line with other data that suggest if you lose weight too fast, you actually have an increased risk of gallstones,” he said.
Rapid weight loss can release cholesterol into the body, which then collects in the bile ducts and causes gallstones. This risk for gallstone formation with rapid weight loss is also seen after bariatric surgery, Dr. Liu said.
Without BMI matching, he noted, the increased risk for biliary disease was no longer significant (HR, 1.21; 95% CI, 0.96-1.52).
The researchers also reported a significant association between GLP-1s and gastroparesis (HR, 2.30; 95% CI, 1.19-4.46), confirming the results of the JAMA study “but at a much lower incidence rate once we excluded all patients with diabetes,” said Dr. Liu. The JAMA study had a HR of 3.67 for gastroparesis (95% CI, 1.15-11.90).
Weighing in on the Results
“Overall, their study design looks sound,” said Mahyar Etminan, PharmD, associate professor of medicine at the University of British Columbia in Vancouver and an author of the JAMA study. He agreed that Dr. Liu’s research confirmed their findings about gastroparesis and biliary disease.
However, “I interpret the results with intestinal obstruction and pancreatitis as more inconclusive than no risk,” he added.
Session co-moderator and gastroenterologist and motility specialist with Stanford Health Care in California, Linda Anh Bui Nguyen, MD, AGAF, said that she thinks “it’s a promising study.
“But with any retrospective study where you’re looking at ICD-10 [International Classification of Diseases, Tenth Revision] codes, it really depends on the coders. The code could be subjective and could be wrong,” said Dr. Nguyen, clinical professor of medicine at Stanford Medical School, California.
For example, the diagnosis of gastroparesis requires a normal endoscopy and a gastric emptying test. “But we find that, frequently, patients are being given a diagnosis of gastroparesis without the test,” she said.
An unanswered question also remains regarding how pancreatitis or biliary disease is being diagnosed: “Was it imaging, lab testing, or symptoms?” she said in an interview. “For example, if patients had pain on the right side, did they call it biliary?”
Dr. Nguyen added that it is difficult to get this kind of detail in retrospective studies. She also agreed with Dr. Liu that prospective studies are warranted.
The study was independently supported. Dr. Liu, Dr. Etminan, and Dr. Nguyen had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
WASHINGTON — In contrast with a previous study that found glucagon-like peptide 1 (GLP-1) receptor agonists associated with an increased risk for acute pancreatitis and bowel obstruction, a new retrospective study found no significant link to these complications.
One of the big differences from the previous study, published in JAMA in October 2023 by Sodhi and colleagues , is that the current research was able to account for initial body mass index (BMI), said Benjamin Liu, MD, a resident in internal medicine at Case Western Reserve University School of Medicine, Cleveland, Ohio.
This is important, he explained in his presentation (abstract 1074) at the annual Digestive Disease Week® 2024, because obesity on its own is associated with an increased risk for some of these gastrointestinal (GI) outcomes.
“They did an excellent study,” Dr. Liu said. “But their platform did not allow them to match participants for BMI.”
Another distinction between the two studies is that the JAMA study excluded people who had diabetes 90 days before or 30 days following the start of GLP-1 therapy.
Instead, Dr. Liu said, he and colleague Gengqing Song, MD, “just made it simple” and excluded anyone with diabetes or an A1c ≥ 6.5.
We didn’t want participants with diabetes because “we were looking at GLP-1s for weight loss,” Dr. Liu explained.
Although some clinical trials have already assessed adverse events of these medications, “clinical trials are not always a perfect representation of the real world,” Dr. Liu said in an interview. “So, it’s important to do real-world studies to see just what actually goes on.”
Reassessing GI Complications
In the current study, the researchers identified 105,793 patients from the TriNetX healthcare database taking a GLP-1, either semaglutide or liraglutide, for weight loss and 8794 patients taking 8 mg naltrexone/90 mg bupropion. After propensity matching, including for BMI, there were 8792 patients in each group.
They were identified in the database between 2011 and 2023. Researchers noted their first-ever occurrence of acute pancreatitis, bowel obstruction, gastroparesis, or biliary disease during the study period.
Participants had a BMI ≥ 30 kg/m2. In addition to BMI, propensity score matching included demographics, alcohol use, smoking, hyperlipidemia, and abdominal surgery. A second analysis specifically did not match participants for BMI.
The researchers found no significant association between GLP-1s and acute pancreatitis (adjusted hazard ratio [HR], 1.19; 95% CI, 0.66-2.14).
The labeling for semaglutide and liraglutide warns about an increased risk for acute pancreatitis, “but real-world studies and clinical trials are increasingly suggesting there is no increased risk,” Dr. Liu said.
They also did not find a significant association between GLP-1s and bowel obstruction (HR, 1.30; 95% CI, 0.69-2.18).
Despite the current findings, more research — especially prospective data — is needed to confirm pancreatitis as well as other GI risks like bowel obstruction potentially associated with GLP-1s, he added.
The study did, however, find an elevated risk for biliary disease (HR, 1.27; 95% CI, 1.02-1.59) in the BMI-matched cohorts.
This could be due to the rapidity of weight loss, Dr. Liu suggested. “We found that semaglutide caused more weight loss at 6 and 12 months than naltrexone/bupropion, and it did so at a faster rate. That falls in line with other data that suggest if you lose weight too fast, you actually have an increased risk of gallstones,” he said.
Rapid weight loss can release cholesterol into the body, which then collects in the bile ducts and causes gallstones. This risk for gallstone formation with rapid weight loss is also seen after bariatric surgery, Dr. Liu said.
Without BMI matching, he noted, the increased risk for biliary disease was no longer significant (HR, 1.21; 95% CI, 0.96-1.52).
The researchers also reported a significant association between GLP-1s and gastroparesis (HR, 2.30; 95% CI, 1.19-4.46), confirming the results of the JAMA study “but at a much lower incidence rate once we excluded all patients with diabetes,” said Dr. Liu. The JAMA study had a HR of 3.67 for gastroparesis (95% CI, 1.15-11.90).
Weighing in on the Results
“Overall, their study design looks sound,” said Mahyar Etminan, PharmD, associate professor of medicine at the University of British Columbia in Vancouver and an author of the JAMA study. He agreed that Dr. Liu’s research confirmed their findings about gastroparesis and biliary disease.
However, “I interpret the results with intestinal obstruction and pancreatitis as more inconclusive than no risk,” he added.
Session co-moderator and gastroenterologist and motility specialist with Stanford Health Care in California, Linda Anh Bui Nguyen, MD, AGAF, said that she thinks “it’s a promising study.
“But with any retrospective study where you’re looking at ICD-10 [International Classification of Diseases, Tenth Revision] codes, it really depends on the coders. The code could be subjective and could be wrong,” said Dr. Nguyen, clinical professor of medicine at Stanford Medical School, California.
For example, the diagnosis of gastroparesis requires a normal endoscopy and a gastric emptying test. “But we find that, frequently, patients are being given a diagnosis of gastroparesis without the test,” she said.
An unanswered question also remains regarding how pancreatitis or biliary disease is being diagnosed: “Was it imaging, lab testing, or symptoms?” she said in an interview. “For example, if patients had pain on the right side, did they call it biliary?”
Dr. Nguyen added that it is difficult to get this kind of detail in retrospective studies. She also agreed with Dr. Liu that prospective studies are warranted.
The study was independently supported. Dr. Liu, Dr. Etminan, and Dr. Nguyen had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
WASHINGTON — In contrast with a previous study that found glucagon-like peptide 1 (GLP-1) receptor agonists associated with an increased risk for acute pancreatitis and bowel obstruction, a new retrospective study found no significant link to these complications.
One of the big differences from the previous study, published in JAMA in October 2023 by Sodhi and colleagues , is that the current research was able to account for initial body mass index (BMI), said Benjamin Liu, MD, a resident in internal medicine at Case Western Reserve University School of Medicine, Cleveland, Ohio.
This is important, he explained in his presentation (abstract 1074) at the annual Digestive Disease Week® 2024, because obesity on its own is associated with an increased risk for some of these gastrointestinal (GI) outcomes.
“They did an excellent study,” Dr. Liu said. “But their platform did not allow them to match participants for BMI.”
Another distinction between the two studies is that the JAMA study excluded people who had diabetes 90 days before or 30 days following the start of GLP-1 therapy.
Instead, Dr. Liu said, he and colleague Gengqing Song, MD, “just made it simple” and excluded anyone with diabetes or an A1c ≥ 6.5.
We didn’t want participants with diabetes because “we were looking at GLP-1s for weight loss,” Dr. Liu explained.
Although some clinical trials have already assessed adverse events of these medications, “clinical trials are not always a perfect representation of the real world,” Dr. Liu said in an interview. “So, it’s important to do real-world studies to see just what actually goes on.”
Reassessing GI Complications
In the current study, the researchers identified 105,793 patients from the TriNetX healthcare database taking a GLP-1, either semaglutide or liraglutide, for weight loss and 8794 patients taking 8 mg naltrexone/90 mg bupropion. After propensity matching, including for BMI, there were 8792 patients in each group.
They were identified in the database between 2011 and 2023. Researchers noted their first-ever occurrence of acute pancreatitis, bowel obstruction, gastroparesis, or biliary disease during the study period.
Participants had a BMI ≥ 30 kg/m2. In addition to BMI, propensity score matching included demographics, alcohol use, smoking, hyperlipidemia, and abdominal surgery. A second analysis specifically did not match participants for BMI.
The researchers found no significant association between GLP-1s and acute pancreatitis (adjusted hazard ratio [HR], 1.19; 95% CI, 0.66-2.14).
The labeling for semaglutide and liraglutide warns about an increased risk for acute pancreatitis, “but real-world studies and clinical trials are increasingly suggesting there is no increased risk,” Dr. Liu said.
They also did not find a significant association between GLP-1s and bowel obstruction (HR, 1.30; 95% CI, 0.69-2.18).
Despite the current findings, more research — especially prospective data — is needed to confirm pancreatitis as well as other GI risks like bowel obstruction potentially associated with GLP-1s, he added.
The study did, however, find an elevated risk for biliary disease (HR, 1.27; 95% CI, 1.02-1.59) in the BMI-matched cohorts.
This could be due to the rapidity of weight loss, Dr. Liu suggested. “We found that semaglutide caused more weight loss at 6 and 12 months than naltrexone/bupropion, and it did so at a faster rate. That falls in line with other data that suggest if you lose weight too fast, you actually have an increased risk of gallstones,” he said.
Rapid weight loss can release cholesterol into the body, which then collects in the bile ducts and causes gallstones. This risk for gallstone formation with rapid weight loss is also seen after bariatric surgery, Dr. Liu said.
Without BMI matching, he noted, the increased risk for biliary disease was no longer significant (HR, 1.21; 95% CI, 0.96-1.52).
The researchers also reported a significant association between GLP-1s and gastroparesis (HR, 2.30; 95% CI, 1.19-4.46), confirming the results of the JAMA study “but at a much lower incidence rate once we excluded all patients with diabetes,” said Dr. Liu. The JAMA study had a HR of 3.67 for gastroparesis (95% CI, 1.15-11.90).
Weighing in on the Results
“Overall, their study design looks sound,” said Mahyar Etminan, PharmD, associate professor of medicine at the University of British Columbia in Vancouver and an author of the JAMA study. He agreed that Dr. Liu’s research confirmed their findings about gastroparesis and biliary disease.
However, “I interpret the results with intestinal obstruction and pancreatitis as more inconclusive than no risk,” he added.
Session co-moderator and gastroenterologist and motility specialist with Stanford Health Care in California, Linda Anh Bui Nguyen, MD, AGAF, said that she thinks “it’s a promising study.
“But with any retrospective study where you’re looking at ICD-10 [International Classification of Diseases, Tenth Revision] codes, it really depends on the coders. The code could be subjective and could be wrong,” said Dr. Nguyen, clinical professor of medicine at Stanford Medical School, California.
For example, the diagnosis of gastroparesis requires a normal endoscopy and a gastric emptying test. “But we find that, frequently, patients are being given a diagnosis of gastroparesis without the test,” she said.
An unanswered question also remains regarding how pancreatitis or biliary disease is being diagnosed: “Was it imaging, lab testing, or symptoms?” she said in an interview. “For example, if patients had pain on the right side, did they call it biliary?”
Dr. Nguyen added that it is difficult to get this kind of detail in retrospective studies. She also agreed with Dr. Liu that prospective studies are warranted.
The study was independently supported. Dr. Liu, Dr. Etminan, and Dr. Nguyen had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
FROM DDW 2024
Surgical Pearls and Wellness Tips From the American Academy of Dermatology Annual Meeting
Attendees of the 2024 American Academy of Dermatology annual meeting in San Diego, California, were eager to delve into the latest trends and advancements in dermatology and dermatologic surgery. This article provides a few key takeaways for residents from a range of engaging sessions, with an emphasis on procedural dermatology and physician health and well-being.
Practical Applications of Surgical Enhancements
In an informative session dedicated to dermatologic surgeons and their patients, “Simple Tricks and Practical Tips to Optimize the Surgical Experience for You and Your Patients,” attendees learned practical tips for enhancing the surgical experience. The discussion spanned various aspects of surgery, from managing preoperative anxiety with anxiolytics such as midazolam to the strategic use of skin hooks for delicate tissue manipulation. Midazolam is fast acting and its use is tailored to patient factors such as weight, hepatic function, and prior use. An innovative anxiety management algorithm combining “talkesethesia” with other methods such as anodynes and benzodiazepines underscored the importance of a calm patient in successful surgical outcomes. Talkesthesia involves engaging patients in soothing and distracting conversation throughout the procedure. This technique can include discussing nonmedical topics of interest with the patient—such as their hobbies, family, or favorite movies—to divert their attention from the surgical process and reduce anxiety. By creating a friendly and reassuring atmosphere, talkesthesia helps to establish trust between the patient and the medical team, ultimately contributing to a more relaxed and cooperative patient.1
The utility of skin hooks also was discussed, with an emphasis on their role in ensuring gentle tissue handling. The modified buried vertical mattress technique was discussed for its added benefits in wound approximation and strength. Emphasis was placed on the importance of maintaining a clear surgical field by electrocautery to ensure optimal visibility.
Focusing on the treatment of skin cancer, curettage alone was touted as a viable alternative to electrodesiccation and curettage, especially in reducing postoperative hypopigmentation while maintaining high cure rates. This method was shown to be effective in treating basal cell carcinoma and well-differentiated squamous cell carcinoma.2,3
Suturing techniques such as pulley, purse-string, and buried sutures offer efficiencies in time, cost, and improved healing in high-tension areas. These methods can contribute to postsurgical aesthetic and functional outcomes. Additionally, Dr. Desiree Ratner shared her tips for painless local anesthesia techniques, emphasizing the importance of patient comfort through methods such as slow injection and buffering of lidocaine. The next time you give a local anesthetic, try this technique to minimize pain: using a 30-gauge needle, hold the syringe with the bevel up, insert only the bevel into the skin (needle tip goes into the papillary dermis), and numb superficially around the periphery using as little volume as possible. Keep pressure slow and steady without moving the needle, then insert the needle only in previously anesthetized areas, numbing deeply only after the entire periphery has been anesthetized.
The session concluded with the recommendation to provide patients with a goody bag containing postoperative supplies. This thoughtful gesture not only enhances patient satisfaction but also addresses the practical aspect of postsurgery care, offering an inexpensive yet impactful way to ensure patients have the necessary supplies for their recovery.
Take-Home Point—This session distilled essential surgical enhancements into practical applications, emphasizing the importance of anxiety management, delicate tissue handling, innovative suturing techniques, and thoughtful patient care postsurgery. The overarching message highlighted the synergy between technical skill and patient-centric approaches in optimizing surgical outcomes, underscoring the significance of attention to detail in every aspect of patient care, from preoperative preparation to postoperative recovery.
Optimizing Safety and Ergonomics in Surgical Practices
Understanding the dynamics of surgical plume is crucial to safety in the operating room. The carcinogenic risk associated with surgical smoke is not trivial: exposure to the plume generated by monopolar electrocautery in a single day can be equivalent to smoking approximately 30 cigarettes, and a surgeon’s lifetime cancer risk from polycyclic aromatic hydrocarbons exposure is alarmingly high.4 To mitigate these risks, several strategies were recommended, including using lower-energy settings, choosing indirect or bipolar cautery, and ensuring efficient room ventilation with HEPA (high-efficiency particulate absorbing) filters to turn over air frequently. Additionally, employing the use of smoke evacuators and suction devices with proper filters can reduce particulate matter in the operating room.
The importance of the surgeon’s posture during procedures also was emphasized for ergonomic benefits and to minimize fatigue. Maintaining a neutral stance with the core and glutes engaged, standing on the balls of the feet, and aligning the table height to keep the hands at the lower chest level were recommended; this not only helps in reducing strain but also in maintaining precision during surgical tasks.
The surgeons on the panel also highlighted the novel use of hydrocolloid dressings with tattoo lasers, electrodesiccation and curettage for treating rhinophyma, and purse-string closure for chest defects as evolving practices to enhance outcomes and safety.
The session offered valuable insights into suturing techniques, advocating for the use of deep sutures—ideally Monocryl (Ethicon US, LLC)—for superficial closures and fast-absorbing gut sutures for patients who are not expected to return for suture removal. Keith LeBlanc Jr, MD, shared one of his favorite tricks for suturing fragile, sun-damaged skin on the forearm in elderly patients: apply adhesive skin closures aligned parallel to the suture line, then suture through them for extra support. This can help ensure a more secure closure.
In situations when no deep sutures are required, such as on the hair-bearing scalp, large bites through the galea using monofilament nonabsorbable sutures for up to 14 days or staples can offer favorable closures and enhanced hemostasis. Tranexamic acid has emerged as a versatile hemostatic agent—available in multiple forms ranging from direct injection to topical applications—and is cost-effective, enhancing its accessibility in various surgical settings.
A high proportion of patients are taken aback by the length of the scar following removal of what they perceive as a small skin cancer. Leslie Storey, MD, cleverly recommended using the back of a glove to mark surgical planning, giving the patient a visual guide for anticipating the size of the excision. This is a simple yet effective approach to enhance patient understanding and informed consent.
Lastly, the notion that “patients remember you if you don’t cause them pain” resonated deeply, underlining the importance of gentle techniques such as pinching the suture rather than pushing the wound edges together and asking assistants to maintain tension without obstructing the field. In the words of Seth Matarasso, MD: “If you pain ‘em, you won’t retain ‘em!”
Take-Home Point—The take-home message from the session was a comprehensive approach to surgical excellence that aligns technical proficiency with a strong emphasis on safety, patient comfort, and operative efficiency. Surgeons were advised to adopt practices that reduce the risks associated with surgical plume, maintain ergonomic discipline, and apply innovative suturing techniques to enhance patient outcomes. Compassionate patient care, innovative use of materials and methods, and a commitment to continual learning and adaptation of new evidence-based practices are paramount for the modern surgeon.
Approaches for Facial Reconstruction
The intricacies of multisubunit facial reconstruction were explored in a session that blended the pursuit of aesthetic harmony with functional restoration, “Simplifying the Complex: Reconstructing Multisubunit Defects.” The session began with an introduction to flap design principles, emphasizing the importance of thorough defect analysis and the strategic design of flaps. A key objective within this framework is the integration of the flap within existing cosmetic subunits to avoid unwanted effects such as unintended eyebrow elevation.
The concept of tissue reservoirs was discussed,focusing on regions such as the glabella as potential sources for skin recruitment. This then transitioned into a nuanced discussion on incision planning, underscoring the significance of aligning incision lines with relaxed skin tension lines to enhance healing and minimize scarring.
The topic of delayed reconstruction also was introduced as a deliberate tactic for high-risk tumor management. This approach allows for an in-depth pathologic examination and provides patients with more time for psychological adjustment, which may be particularly important for those with complex medical histories or those who require staged surgical interventions.
In a thorough examination of flap design techniques, the session highlighted the bilobed transposition flap as a versatile choice for nasal reconstruction, particularly apt for the distal third of the nose due to its design that harnesses skin from nonadjacent areas. Accompanying this was an exploration of Zitelli modifications, which enhance the bilobed flap by reducing issues such as pincushioning through a moderated rotation angle and the strategic incorporation of a Burow triangle.
Finally, the interpolated paranasal flap was discussed. This technique is designed to reduce the risk for cheek asymmetry and is suitable for patients with generous donor sites; however, this method requires diligent evaluation to avoid complications such as external nasal valve collapse.
Take-Home Point—This session highlighted approaches in facial reconstruction, emphasizing the necessity of strategic flap design and meticulous incision planning to maintain aesthetic harmony and functional integrity.
Strategies for Improving Physician Well-Being
Evidence-based recommendations to support physicians’ well-being are crucial as the health care system becomes increasingly demanding. Instead of focusing on aspects of the health care system that frequently are outside of physicians’ control, the session “A Realistic and Evidence-Based Roadmap for Thriving in Life and Career” discussed many practical, self-empowering tools and strategies to lead a happier and healthier life—both personally and professionally.
The speakers cautioned against the concept of an “unlimited ceiling” for achieving a certain goal, where an unlimited amount of time and energy is allowed to be dedicated to a given task over a period of time. They highlighted the potential consequences of this approach, such as stress, dissatisfaction, and ultimately burnout. The speakers explored the concept of well-being as a continuous journey rather than a destination, emphasizing that it is not the opposite of burnout. To promote well-being, the speakers advocated for utilizing concepts rooted in positive psychology to empower the individual rather than longing for a different environment. They hypothesized that changing one’s life can be accomplished by changing one’s mind, independent of the environment.
The roadmap for physician well-being, as presented by clinical psychologist Amy MacDonald, PsyD, commenced with urging the audience to introspect on situations and experiences, categorizing them into “feel good” and “feel bad” buckets. For every feel-good event, Dr. MacDonald proposed 5 mental exercises for optimized well-being: (1) control/increase: evaluate whether one can control or increase the frequency of the event; (2) consider: reflect on why this event feels good and explore other aspects to gain any additional joy from the event; (3) share: recognize that some feel goods are more joyous when shared; (4) value: connect the feel-good experiences with personal core values, as research shows value affirmations can buffer neuroendocrine and psychological stress responses; and (5) savor: deliberately relish each small or notable feel-good moment.
Similarly, after labeling an event as a feel-bad experience, Dr. MacDonald encouraged the audience to go through mental exercises to strengthen their well-being journey; however, before proceeding, she highlighted the importance of arming ourselves with self-compassion. The 5 mental exercises to address feel bads include (1) solve: assess whether we have control over the situation and attempt to make changes if possible; (2) reframe: explore new perspectives and assess assumptions without minimizing the situation; (3) connect: embrace the positive impact of safe human connections on our stress response; (4) reflect: search curiously using a compassionate lens for any existing patterns of reactions; and (5) accept and pivot: allow thoughts and feelings to exist and pivot to values-based engagement without waiting for the environment to change. Consistently seeking and appreciating feel goods while addressing rather than suppressing the feel bads can lead to joyful satisfaction and overall well-being.
Additional pearls for optimizing physician well-being included accurately labeling emotions rather than lumping them into an overarching theme (eg, stressed), avoiding comparisons with others, choosing courage over comfort, celebrating vulnerability, and embracing the ability to say no to prioritize engagements aligned with one’s purpose and values. Additional resources were shared for further reading, including Emotional Agility by Susan David, Daring Greatly and Rising Strong by Brené Brown, and Self-Compassion by Kristin Neff.
Take-Home Point—This lecture highlighted key strategies for physicians to improve their well-being, emphasizing self-empowerment and practical tools over external circumstances. It distinguished between productive and destructive influences on satisfaction, and emphasized decision-making aligned with personal values. The concept of well-being as a journey, not a destination, was central, encouraging positive psychology and self-reflection to enhance fulfillment. By focusing on amplifying feel-good experiences and addressing feel-bad experiences with resilience, the lecture advocated for internal over external change, offering a pathway to a balanced and satisfying professional and personal life for physicians.
Final Thoughts
The recent American Academy of Dermatology meeting offered valuable insights and practical pearls to enhance surgical practices and promote physician well-being, in addition to a wide range of topics beyond what is mentioned in this article. From optimizing surgical techniques to prioritizing patient care and safety, the sessions underscored the importance of continuous learning and adaptation in the ever-evolving field of dermatology. As we reflect on the lessons learned and the camaraderie shared during this gathering, let us carry forward these teachings to improve patient outcomes, foster innovation, and cultivate resilience in our pursuit of excellence. Together, we can continue to push the boundaries of dermatologic care while nurturing our own well-being and that of our colleagues, ensuring a brighter future for both patients and practitioners alike.
Acknowledgments—Sultan H. Qiblawi, MD, MBA; Eva Shelton, MD; and Christy T. Behnam, MD (all from Madison, Wisconsin), shared their insights and key takeaways from American Academy of Dermatology lecturers, which enriched the content of this article.
- Hills LS. Putting patients at ease with conversation. J Med Pract Manage. 2006;22:168-170.
- Barlow JO, Zalla MJ, Kyle A, et al. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54:1039-1045.
- Yakish K, Graham J, Hossler EW. Efficacy of curettage alone for invasive cutaneous squamous cell carcinoma: a retrospective cohort study. J Am Acad Dermatol. 2017;77:582-584.
- Shah NR. Commentary on: “surgical smoke—a health hazard in the operating theatre: a study to quantify exposure and a survey of the use of smoke extractor systems in UK plastic surgery units.”Ann Med Surg (Lond). 2012;1:23-24.
Attendees of the 2024 American Academy of Dermatology annual meeting in San Diego, California, were eager to delve into the latest trends and advancements in dermatology and dermatologic surgery. This article provides a few key takeaways for residents from a range of engaging sessions, with an emphasis on procedural dermatology and physician health and well-being.
Practical Applications of Surgical Enhancements
In an informative session dedicated to dermatologic surgeons and their patients, “Simple Tricks and Practical Tips to Optimize the Surgical Experience for You and Your Patients,” attendees learned practical tips for enhancing the surgical experience. The discussion spanned various aspects of surgery, from managing preoperative anxiety with anxiolytics such as midazolam to the strategic use of skin hooks for delicate tissue manipulation. Midazolam is fast acting and its use is tailored to patient factors such as weight, hepatic function, and prior use. An innovative anxiety management algorithm combining “talkesethesia” with other methods such as anodynes and benzodiazepines underscored the importance of a calm patient in successful surgical outcomes. Talkesthesia involves engaging patients in soothing and distracting conversation throughout the procedure. This technique can include discussing nonmedical topics of interest with the patient—such as their hobbies, family, or favorite movies—to divert their attention from the surgical process and reduce anxiety. By creating a friendly and reassuring atmosphere, talkesthesia helps to establish trust between the patient and the medical team, ultimately contributing to a more relaxed and cooperative patient.1
The utility of skin hooks also was discussed, with an emphasis on their role in ensuring gentle tissue handling. The modified buried vertical mattress technique was discussed for its added benefits in wound approximation and strength. Emphasis was placed on the importance of maintaining a clear surgical field by electrocautery to ensure optimal visibility.
Focusing on the treatment of skin cancer, curettage alone was touted as a viable alternative to electrodesiccation and curettage, especially in reducing postoperative hypopigmentation while maintaining high cure rates. This method was shown to be effective in treating basal cell carcinoma and well-differentiated squamous cell carcinoma.2,3
Suturing techniques such as pulley, purse-string, and buried sutures offer efficiencies in time, cost, and improved healing in high-tension areas. These methods can contribute to postsurgical aesthetic and functional outcomes. Additionally, Dr. Desiree Ratner shared her tips for painless local anesthesia techniques, emphasizing the importance of patient comfort through methods such as slow injection and buffering of lidocaine. The next time you give a local anesthetic, try this technique to minimize pain: using a 30-gauge needle, hold the syringe with the bevel up, insert only the bevel into the skin (needle tip goes into the papillary dermis), and numb superficially around the periphery using as little volume as possible. Keep pressure slow and steady without moving the needle, then insert the needle only in previously anesthetized areas, numbing deeply only after the entire periphery has been anesthetized.
The session concluded with the recommendation to provide patients with a goody bag containing postoperative supplies. This thoughtful gesture not only enhances patient satisfaction but also addresses the practical aspect of postsurgery care, offering an inexpensive yet impactful way to ensure patients have the necessary supplies for their recovery.
Take-Home Point—This session distilled essential surgical enhancements into practical applications, emphasizing the importance of anxiety management, delicate tissue handling, innovative suturing techniques, and thoughtful patient care postsurgery. The overarching message highlighted the synergy between technical skill and patient-centric approaches in optimizing surgical outcomes, underscoring the significance of attention to detail in every aspect of patient care, from preoperative preparation to postoperative recovery.
Optimizing Safety and Ergonomics in Surgical Practices
Understanding the dynamics of surgical plume is crucial to safety in the operating room. The carcinogenic risk associated with surgical smoke is not trivial: exposure to the plume generated by monopolar electrocautery in a single day can be equivalent to smoking approximately 30 cigarettes, and a surgeon’s lifetime cancer risk from polycyclic aromatic hydrocarbons exposure is alarmingly high.4 To mitigate these risks, several strategies were recommended, including using lower-energy settings, choosing indirect or bipolar cautery, and ensuring efficient room ventilation with HEPA (high-efficiency particulate absorbing) filters to turn over air frequently. Additionally, employing the use of smoke evacuators and suction devices with proper filters can reduce particulate matter in the operating room.
The importance of the surgeon’s posture during procedures also was emphasized for ergonomic benefits and to minimize fatigue. Maintaining a neutral stance with the core and glutes engaged, standing on the balls of the feet, and aligning the table height to keep the hands at the lower chest level were recommended; this not only helps in reducing strain but also in maintaining precision during surgical tasks.
The surgeons on the panel also highlighted the novel use of hydrocolloid dressings with tattoo lasers, electrodesiccation and curettage for treating rhinophyma, and purse-string closure for chest defects as evolving practices to enhance outcomes and safety.
The session offered valuable insights into suturing techniques, advocating for the use of deep sutures—ideally Monocryl (Ethicon US, LLC)—for superficial closures and fast-absorbing gut sutures for patients who are not expected to return for suture removal. Keith LeBlanc Jr, MD, shared one of his favorite tricks for suturing fragile, sun-damaged skin on the forearm in elderly patients: apply adhesive skin closures aligned parallel to the suture line, then suture through them for extra support. This can help ensure a more secure closure.
In situations when no deep sutures are required, such as on the hair-bearing scalp, large bites through the galea using monofilament nonabsorbable sutures for up to 14 days or staples can offer favorable closures and enhanced hemostasis. Tranexamic acid has emerged as a versatile hemostatic agent—available in multiple forms ranging from direct injection to topical applications—and is cost-effective, enhancing its accessibility in various surgical settings.
A high proportion of patients are taken aback by the length of the scar following removal of what they perceive as a small skin cancer. Leslie Storey, MD, cleverly recommended using the back of a glove to mark surgical planning, giving the patient a visual guide for anticipating the size of the excision. This is a simple yet effective approach to enhance patient understanding and informed consent.
Lastly, the notion that “patients remember you if you don’t cause them pain” resonated deeply, underlining the importance of gentle techniques such as pinching the suture rather than pushing the wound edges together and asking assistants to maintain tension without obstructing the field. In the words of Seth Matarasso, MD: “If you pain ‘em, you won’t retain ‘em!”
Take-Home Point—The take-home message from the session was a comprehensive approach to surgical excellence that aligns technical proficiency with a strong emphasis on safety, patient comfort, and operative efficiency. Surgeons were advised to adopt practices that reduce the risks associated with surgical plume, maintain ergonomic discipline, and apply innovative suturing techniques to enhance patient outcomes. Compassionate patient care, innovative use of materials and methods, and a commitment to continual learning and adaptation of new evidence-based practices are paramount for the modern surgeon.
Approaches for Facial Reconstruction
The intricacies of multisubunit facial reconstruction were explored in a session that blended the pursuit of aesthetic harmony with functional restoration, “Simplifying the Complex: Reconstructing Multisubunit Defects.” The session began with an introduction to flap design principles, emphasizing the importance of thorough defect analysis and the strategic design of flaps. A key objective within this framework is the integration of the flap within existing cosmetic subunits to avoid unwanted effects such as unintended eyebrow elevation.
The concept of tissue reservoirs was discussed,focusing on regions such as the glabella as potential sources for skin recruitment. This then transitioned into a nuanced discussion on incision planning, underscoring the significance of aligning incision lines with relaxed skin tension lines to enhance healing and minimize scarring.
The topic of delayed reconstruction also was introduced as a deliberate tactic for high-risk tumor management. This approach allows for an in-depth pathologic examination and provides patients with more time for psychological adjustment, which may be particularly important for those with complex medical histories or those who require staged surgical interventions.
In a thorough examination of flap design techniques, the session highlighted the bilobed transposition flap as a versatile choice for nasal reconstruction, particularly apt for the distal third of the nose due to its design that harnesses skin from nonadjacent areas. Accompanying this was an exploration of Zitelli modifications, which enhance the bilobed flap by reducing issues such as pincushioning through a moderated rotation angle and the strategic incorporation of a Burow triangle.
Finally, the interpolated paranasal flap was discussed. This technique is designed to reduce the risk for cheek asymmetry and is suitable for patients with generous donor sites; however, this method requires diligent evaluation to avoid complications such as external nasal valve collapse.
Take-Home Point—This session highlighted approaches in facial reconstruction, emphasizing the necessity of strategic flap design and meticulous incision planning to maintain aesthetic harmony and functional integrity.
Strategies for Improving Physician Well-Being
Evidence-based recommendations to support physicians’ well-being are crucial as the health care system becomes increasingly demanding. Instead of focusing on aspects of the health care system that frequently are outside of physicians’ control, the session “A Realistic and Evidence-Based Roadmap for Thriving in Life and Career” discussed many practical, self-empowering tools and strategies to lead a happier and healthier life—both personally and professionally.
The speakers cautioned against the concept of an “unlimited ceiling” for achieving a certain goal, where an unlimited amount of time and energy is allowed to be dedicated to a given task over a period of time. They highlighted the potential consequences of this approach, such as stress, dissatisfaction, and ultimately burnout. The speakers explored the concept of well-being as a continuous journey rather than a destination, emphasizing that it is not the opposite of burnout. To promote well-being, the speakers advocated for utilizing concepts rooted in positive psychology to empower the individual rather than longing for a different environment. They hypothesized that changing one’s life can be accomplished by changing one’s mind, independent of the environment.
The roadmap for physician well-being, as presented by clinical psychologist Amy MacDonald, PsyD, commenced with urging the audience to introspect on situations and experiences, categorizing them into “feel good” and “feel bad” buckets. For every feel-good event, Dr. MacDonald proposed 5 mental exercises for optimized well-being: (1) control/increase: evaluate whether one can control or increase the frequency of the event; (2) consider: reflect on why this event feels good and explore other aspects to gain any additional joy from the event; (3) share: recognize that some feel goods are more joyous when shared; (4) value: connect the feel-good experiences with personal core values, as research shows value affirmations can buffer neuroendocrine and psychological stress responses; and (5) savor: deliberately relish each small or notable feel-good moment.
Similarly, after labeling an event as a feel-bad experience, Dr. MacDonald encouraged the audience to go through mental exercises to strengthen their well-being journey; however, before proceeding, she highlighted the importance of arming ourselves with self-compassion. The 5 mental exercises to address feel bads include (1) solve: assess whether we have control over the situation and attempt to make changes if possible; (2) reframe: explore new perspectives and assess assumptions without minimizing the situation; (3) connect: embrace the positive impact of safe human connections on our stress response; (4) reflect: search curiously using a compassionate lens for any existing patterns of reactions; and (5) accept and pivot: allow thoughts and feelings to exist and pivot to values-based engagement without waiting for the environment to change. Consistently seeking and appreciating feel goods while addressing rather than suppressing the feel bads can lead to joyful satisfaction and overall well-being.
Additional pearls for optimizing physician well-being included accurately labeling emotions rather than lumping them into an overarching theme (eg, stressed), avoiding comparisons with others, choosing courage over comfort, celebrating vulnerability, and embracing the ability to say no to prioritize engagements aligned with one’s purpose and values. Additional resources were shared for further reading, including Emotional Agility by Susan David, Daring Greatly and Rising Strong by Brené Brown, and Self-Compassion by Kristin Neff.
Take-Home Point—This lecture highlighted key strategies for physicians to improve their well-being, emphasizing self-empowerment and practical tools over external circumstances. It distinguished between productive and destructive influences on satisfaction, and emphasized decision-making aligned with personal values. The concept of well-being as a journey, not a destination, was central, encouraging positive psychology and self-reflection to enhance fulfillment. By focusing on amplifying feel-good experiences and addressing feel-bad experiences with resilience, the lecture advocated for internal over external change, offering a pathway to a balanced and satisfying professional and personal life for physicians.
Final Thoughts
The recent American Academy of Dermatology meeting offered valuable insights and practical pearls to enhance surgical practices and promote physician well-being, in addition to a wide range of topics beyond what is mentioned in this article. From optimizing surgical techniques to prioritizing patient care and safety, the sessions underscored the importance of continuous learning and adaptation in the ever-evolving field of dermatology. As we reflect on the lessons learned and the camaraderie shared during this gathering, let us carry forward these teachings to improve patient outcomes, foster innovation, and cultivate resilience in our pursuit of excellence. Together, we can continue to push the boundaries of dermatologic care while nurturing our own well-being and that of our colleagues, ensuring a brighter future for both patients and practitioners alike.
Acknowledgments—Sultan H. Qiblawi, MD, MBA; Eva Shelton, MD; and Christy T. Behnam, MD (all from Madison, Wisconsin), shared their insights and key takeaways from American Academy of Dermatology lecturers, which enriched the content of this article.
Attendees of the 2024 American Academy of Dermatology annual meeting in San Diego, California, were eager to delve into the latest trends and advancements in dermatology and dermatologic surgery. This article provides a few key takeaways for residents from a range of engaging sessions, with an emphasis on procedural dermatology and physician health and well-being.
Practical Applications of Surgical Enhancements
In an informative session dedicated to dermatologic surgeons and their patients, “Simple Tricks and Practical Tips to Optimize the Surgical Experience for You and Your Patients,” attendees learned practical tips for enhancing the surgical experience. The discussion spanned various aspects of surgery, from managing preoperative anxiety with anxiolytics such as midazolam to the strategic use of skin hooks for delicate tissue manipulation. Midazolam is fast acting and its use is tailored to patient factors such as weight, hepatic function, and prior use. An innovative anxiety management algorithm combining “talkesethesia” with other methods such as anodynes and benzodiazepines underscored the importance of a calm patient in successful surgical outcomes. Talkesthesia involves engaging patients in soothing and distracting conversation throughout the procedure. This technique can include discussing nonmedical topics of interest with the patient—such as their hobbies, family, or favorite movies—to divert their attention from the surgical process and reduce anxiety. By creating a friendly and reassuring atmosphere, talkesthesia helps to establish trust between the patient and the medical team, ultimately contributing to a more relaxed and cooperative patient.1
The utility of skin hooks also was discussed, with an emphasis on their role in ensuring gentle tissue handling. The modified buried vertical mattress technique was discussed for its added benefits in wound approximation and strength. Emphasis was placed on the importance of maintaining a clear surgical field by electrocautery to ensure optimal visibility.
Focusing on the treatment of skin cancer, curettage alone was touted as a viable alternative to electrodesiccation and curettage, especially in reducing postoperative hypopigmentation while maintaining high cure rates. This method was shown to be effective in treating basal cell carcinoma and well-differentiated squamous cell carcinoma.2,3
Suturing techniques such as pulley, purse-string, and buried sutures offer efficiencies in time, cost, and improved healing in high-tension areas. These methods can contribute to postsurgical aesthetic and functional outcomes. Additionally, Dr. Desiree Ratner shared her tips for painless local anesthesia techniques, emphasizing the importance of patient comfort through methods such as slow injection and buffering of lidocaine. The next time you give a local anesthetic, try this technique to minimize pain: using a 30-gauge needle, hold the syringe with the bevel up, insert only the bevel into the skin (needle tip goes into the papillary dermis), and numb superficially around the periphery using as little volume as possible. Keep pressure slow and steady without moving the needle, then insert the needle only in previously anesthetized areas, numbing deeply only after the entire periphery has been anesthetized.
The session concluded with the recommendation to provide patients with a goody bag containing postoperative supplies. This thoughtful gesture not only enhances patient satisfaction but also addresses the practical aspect of postsurgery care, offering an inexpensive yet impactful way to ensure patients have the necessary supplies for their recovery.
Take-Home Point—This session distilled essential surgical enhancements into practical applications, emphasizing the importance of anxiety management, delicate tissue handling, innovative suturing techniques, and thoughtful patient care postsurgery. The overarching message highlighted the synergy between technical skill and patient-centric approaches in optimizing surgical outcomes, underscoring the significance of attention to detail in every aspect of patient care, from preoperative preparation to postoperative recovery.
Optimizing Safety and Ergonomics in Surgical Practices
Understanding the dynamics of surgical plume is crucial to safety in the operating room. The carcinogenic risk associated with surgical smoke is not trivial: exposure to the plume generated by monopolar electrocautery in a single day can be equivalent to smoking approximately 30 cigarettes, and a surgeon’s lifetime cancer risk from polycyclic aromatic hydrocarbons exposure is alarmingly high.4 To mitigate these risks, several strategies were recommended, including using lower-energy settings, choosing indirect or bipolar cautery, and ensuring efficient room ventilation with HEPA (high-efficiency particulate absorbing) filters to turn over air frequently. Additionally, employing the use of smoke evacuators and suction devices with proper filters can reduce particulate matter in the operating room.
The importance of the surgeon’s posture during procedures also was emphasized for ergonomic benefits and to minimize fatigue. Maintaining a neutral stance with the core and glutes engaged, standing on the balls of the feet, and aligning the table height to keep the hands at the lower chest level were recommended; this not only helps in reducing strain but also in maintaining precision during surgical tasks.
The surgeons on the panel also highlighted the novel use of hydrocolloid dressings with tattoo lasers, electrodesiccation and curettage for treating rhinophyma, and purse-string closure for chest defects as evolving practices to enhance outcomes and safety.
The session offered valuable insights into suturing techniques, advocating for the use of deep sutures—ideally Monocryl (Ethicon US, LLC)—for superficial closures and fast-absorbing gut sutures for patients who are not expected to return for suture removal. Keith LeBlanc Jr, MD, shared one of his favorite tricks for suturing fragile, sun-damaged skin on the forearm in elderly patients: apply adhesive skin closures aligned parallel to the suture line, then suture through them for extra support. This can help ensure a more secure closure.
In situations when no deep sutures are required, such as on the hair-bearing scalp, large bites through the galea using monofilament nonabsorbable sutures for up to 14 days or staples can offer favorable closures and enhanced hemostasis. Tranexamic acid has emerged as a versatile hemostatic agent—available in multiple forms ranging from direct injection to topical applications—and is cost-effective, enhancing its accessibility in various surgical settings.
A high proportion of patients are taken aback by the length of the scar following removal of what they perceive as a small skin cancer. Leslie Storey, MD, cleverly recommended using the back of a glove to mark surgical planning, giving the patient a visual guide for anticipating the size of the excision. This is a simple yet effective approach to enhance patient understanding and informed consent.
Lastly, the notion that “patients remember you if you don’t cause them pain” resonated deeply, underlining the importance of gentle techniques such as pinching the suture rather than pushing the wound edges together and asking assistants to maintain tension without obstructing the field. In the words of Seth Matarasso, MD: “If you pain ‘em, you won’t retain ‘em!”
Take-Home Point—The take-home message from the session was a comprehensive approach to surgical excellence that aligns technical proficiency with a strong emphasis on safety, patient comfort, and operative efficiency. Surgeons were advised to adopt practices that reduce the risks associated with surgical plume, maintain ergonomic discipline, and apply innovative suturing techniques to enhance patient outcomes. Compassionate patient care, innovative use of materials and methods, and a commitment to continual learning and adaptation of new evidence-based practices are paramount for the modern surgeon.
Approaches for Facial Reconstruction
The intricacies of multisubunit facial reconstruction were explored in a session that blended the pursuit of aesthetic harmony with functional restoration, “Simplifying the Complex: Reconstructing Multisubunit Defects.” The session began with an introduction to flap design principles, emphasizing the importance of thorough defect analysis and the strategic design of flaps. A key objective within this framework is the integration of the flap within existing cosmetic subunits to avoid unwanted effects such as unintended eyebrow elevation.
The concept of tissue reservoirs was discussed,focusing on regions such as the glabella as potential sources for skin recruitment. This then transitioned into a nuanced discussion on incision planning, underscoring the significance of aligning incision lines with relaxed skin tension lines to enhance healing and minimize scarring.
The topic of delayed reconstruction also was introduced as a deliberate tactic for high-risk tumor management. This approach allows for an in-depth pathologic examination and provides patients with more time for psychological adjustment, which may be particularly important for those with complex medical histories or those who require staged surgical interventions.
In a thorough examination of flap design techniques, the session highlighted the bilobed transposition flap as a versatile choice for nasal reconstruction, particularly apt for the distal third of the nose due to its design that harnesses skin from nonadjacent areas. Accompanying this was an exploration of Zitelli modifications, which enhance the bilobed flap by reducing issues such as pincushioning through a moderated rotation angle and the strategic incorporation of a Burow triangle.
Finally, the interpolated paranasal flap was discussed. This technique is designed to reduce the risk for cheek asymmetry and is suitable for patients with generous donor sites; however, this method requires diligent evaluation to avoid complications such as external nasal valve collapse.
Take-Home Point—This session highlighted approaches in facial reconstruction, emphasizing the necessity of strategic flap design and meticulous incision planning to maintain aesthetic harmony and functional integrity.
Strategies for Improving Physician Well-Being
Evidence-based recommendations to support physicians’ well-being are crucial as the health care system becomes increasingly demanding. Instead of focusing on aspects of the health care system that frequently are outside of physicians’ control, the session “A Realistic and Evidence-Based Roadmap for Thriving in Life and Career” discussed many practical, self-empowering tools and strategies to lead a happier and healthier life—both personally and professionally.
The speakers cautioned against the concept of an “unlimited ceiling” for achieving a certain goal, where an unlimited amount of time and energy is allowed to be dedicated to a given task over a period of time. They highlighted the potential consequences of this approach, such as stress, dissatisfaction, and ultimately burnout. The speakers explored the concept of well-being as a continuous journey rather than a destination, emphasizing that it is not the opposite of burnout. To promote well-being, the speakers advocated for utilizing concepts rooted in positive psychology to empower the individual rather than longing for a different environment. They hypothesized that changing one’s life can be accomplished by changing one’s mind, independent of the environment.
The roadmap for physician well-being, as presented by clinical psychologist Amy MacDonald, PsyD, commenced with urging the audience to introspect on situations and experiences, categorizing them into “feel good” and “feel bad” buckets. For every feel-good event, Dr. MacDonald proposed 5 mental exercises for optimized well-being: (1) control/increase: evaluate whether one can control or increase the frequency of the event; (2) consider: reflect on why this event feels good and explore other aspects to gain any additional joy from the event; (3) share: recognize that some feel goods are more joyous when shared; (4) value: connect the feel-good experiences with personal core values, as research shows value affirmations can buffer neuroendocrine and psychological stress responses; and (5) savor: deliberately relish each small or notable feel-good moment.
Similarly, after labeling an event as a feel-bad experience, Dr. MacDonald encouraged the audience to go through mental exercises to strengthen their well-being journey; however, before proceeding, she highlighted the importance of arming ourselves with self-compassion. The 5 mental exercises to address feel bads include (1) solve: assess whether we have control over the situation and attempt to make changes if possible; (2) reframe: explore new perspectives and assess assumptions without minimizing the situation; (3) connect: embrace the positive impact of safe human connections on our stress response; (4) reflect: search curiously using a compassionate lens for any existing patterns of reactions; and (5) accept and pivot: allow thoughts and feelings to exist and pivot to values-based engagement without waiting for the environment to change. Consistently seeking and appreciating feel goods while addressing rather than suppressing the feel bads can lead to joyful satisfaction and overall well-being.
Additional pearls for optimizing physician well-being included accurately labeling emotions rather than lumping them into an overarching theme (eg, stressed), avoiding comparisons with others, choosing courage over comfort, celebrating vulnerability, and embracing the ability to say no to prioritize engagements aligned with one’s purpose and values. Additional resources were shared for further reading, including Emotional Agility by Susan David, Daring Greatly and Rising Strong by Brené Brown, and Self-Compassion by Kristin Neff.
Take-Home Point—This lecture highlighted key strategies for physicians to improve their well-being, emphasizing self-empowerment and practical tools over external circumstances. It distinguished between productive and destructive influences on satisfaction, and emphasized decision-making aligned with personal values. The concept of well-being as a journey, not a destination, was central, encouraging positive psychology and self-reflection to enhance fulfillment. By focusing on amplifying feel-good experiences and addressing feel-bad experiences with resilience, the lecture advocated for internal over external change, offering a pathway to a balanced and satisfying professional and personal life for physicians.
Final Thoughts
The recent American Academy of Dermatology meeting offered valuable insights and practical pearls to enhance surgical practices and promote physician well-being, in addition to a wide range of topics beyond what is mentioned in this article. From optimizing surgical techniques to prioritizing patient care and safety, the sessions underscored the importance of continuous learning and adaptation in the ever-evolving field of dermatology. As we reflect on the lessons learned and the camaraderie shared during this gathering, let us carry forward these teachings to improve patient outcomes, foster innovation, and cultivate resilience in our pursuit of excellence. Together, we can continue to push the boundaries of dermatologic care while nurturing our own well-being and that of our colleagues, ensuring a brighter future for both patients and practitioners alike.
Acknowledgments—Sultan H. Qiblawi, MD, MBA; Eva Shelton, MD; and Christy T. Behnam, MD (all from Madison, Wisconsin), shared their insights and key takeaways from American Academy of Dermatology lecturers, which enriched the content of this article.
- Hills LS. Putting patients at ease with conversation. J Med Pract Manage. 2006;22:168-170.
- Barlow JO, Zalla MJ, Kyle A, et al. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54:1039-1045.
- Yakish K, Graham J, Hossler EW. Efficacy of curettage alone for invasive cutaneous squamous cell carcinoma: a retrospective cohort study. J Am Acad Dermatol. 2017;77:582-584.
- Shah NR. Commentary on: “surgical smoke—a health hazard in the operating theatre: a study to quantify exposure and a survey of the use of smoke extractor systems in UK plastic surgery units.”Ann Med Surg (Lond). 2012;1:23-24.
- Hills LS. Putting patients at ease with conversation. J Med Pract Manage. 2006;22:168-170.
- Barlow JO, Zalla MJ, Kyle A, et al. Treatment of basal cell carcinoma with curettage alone. J Am Acad Dermatol. 2006;54:1039-1045.
- Yakish K, Graham J, Hossler EW. Efficacy of curettage alone for invasive cutaneous squamous cell carcinoma: a retrospective cohort study. J Am Acad Dermatol. 2017;77:582-584.
- Shah NR. Commentary on: “surgical smoke—a health hazard in the operating theatre: a study to quantify exposure and a survey of the use of smoke extractor systems in UK plastic surgery units.”Ann Med Surg (Lond). 2012;1:23-24.
RESIDENT PEARLS
- By protecting yourself and ensuring your own longevity as a practicing physician, you will be better able to care for your patients over the long term. Focus on self-empowerment and positive psychology for a balanced life.
- Protect yourself from surgical plume by using smoke evacuators and ensuring proper room ventilation with HEPA (high-efficiency particulate absorbing) filters whenever possible. Stick to low-energy settings for electrocautery.
- During surgical procedures, maintain a neutral posture, keep your core and glutes engaged, and adjust the table height to reduce strain and improve precision.
In IBD Patients, Statin Use Associated with Lower Risk of Developing PSC
WASHINGTON — , according to a study presented at Digestive Disease Week® (DDW) 2024.
Statin use was associated with an 86% risk reduction, and only .09% of IBD patients who took statins developed PSC.
“We all take care of patients with liver disease, and we know what a significant burden PSC is. These patients have a significantly elevated risk of enhanced fibrosis and cirrhosis, multiple cancers, and cholangitis and sepsis,” said lead author Chiraag Kulkarni, MD, a gastroenterology fellow at Stanford (California) University Medical School.
“Despite this, we have to date no proven effective medical care for PSC,” he said. “However, over the last decade, there is growing evidence that statins may be beneficial in liver disease, and we see this evidence base stretching from basic science to clinical data.”
Dr. Kulkarni pointed to numerous studies that indicate statins may slow disease progression in steatotic liver disease, viral hepatitis, and cirrhosis. But could statins prevent the onset of PSC?
Because PSC incidence is low, Dr. Kulkarni and colleagues focused on a patient population with higher prevalence — those with IBD, who have an overall lifetime risk of 2% to 7%. The research team followed patients from the date of IBD diagnosis.
Among 33,813 patients with IBD in a national dataset from 2018 onward, 8813 used statins. Statin users tended to be older than non–statin users.
Overall, 181 patients developed new onset PSC during a median follow-up of about 45 months after initial IBD diagnosis. Only eight statin users (.09%) developed PSC, compared with 173 patients (.69%) in the control group.
In a propensity score-matched analysis, statin therapy was associated with a significantly lower risk of developing PSC (HR .14, P < .001). The associated E-value was 5.5, which suggested a robust finding and unlikely to be due to non-visible confounding.
The findings were consistent across secondary and sensitivity analyses, including by age, duration of statin use, and type of statin. For instance, for patients under age 50 where PSC is more likely to occur, statins were associated with a 90% reduction in PSC risk.
“We take away two things from this. First, it’s suggested that a protective effect occurs at ages where PSC is most likely to occur,” Dr. Kulkarni said. “Second, in combination with our propensity score-matched analysis, the results we are observing are not due to a survival bias, where the patients who survive to an age where statins are prescribed simply have a biologically different predilection for developing PSC.”
Statins also protected against PSC in both ulcerative colitis (HR .21) and Crohn’s disease (HR .15), as well as both women (HR .16) and men (HR .22).
Given the uncertainty about the optimal duration of statin therapy for a protective effect, Dr. Kulkarni and colleagues looked at a lag time of 12 months. They found statins were associated with an 84% risk reduction (HR .16), which was similar to the primary analysis.
The study was limited by the inability to capture dosage data or medication adherence. The findings raised several questions, Dr. Kulkarni said, such as the underlying mechanisms and clinical implications. For instance, the underlying mechanisms appear to be related to the pleiotropic effect of statins, modulation of gut inflammation, and alterations in bile acid profiles.
“This is really fascinating and interesting. I wonder about this as a primary prevention strategy in those who have normal cholesterol. Could this work or not?” said Gyongyi Szabo, MD, AGAF, chief academic officer at Beth Israel Deaconess Medical Center, Boston, who was a moderator for the Liver & Biliary Section Distinguished Abstract Plenary Session.
Dr. Kulkarni noted that these findings wouldn’t change clinical practice alone, but based on existing literature around statin hesitancy among patients with cardiovascular disease, the risk reduction for PSC could provide another reason to encourage patients to take them.
“To move this to a place where you can actually think about primary prevention, I think the biological mechanisms need to be teased out a little bit more,” Dr. Kulkarni said. “Then I think you probably still need to identify a higher-risk group than IBD alone.”
Dr. Kulkarni declared no disclosures.
WASHINGTON — , according to a study presented at Digestive Disease Week® (DDW) 2024.
Statin use was associated with an 86% risk reduction, and only .09% of IBD patients who took statins developed PSC.
“We all take care of patients with liver disease, and we know what a significant burden PSC is. These patients have a significantly elevated risk of enhanced fibrosis and cirrhosis, multiple cancers, and cholangitis and sepsis,” said lead author Chiraag Kulkarni, MD, a gastroenterology fellow at Stanford (California) University Medical School.
“Despite this, we have to date no proven effective medical care for PSC,” he said. “However, over the last decade, there is growing evidence that statins may be beneficial in liver disease, and we see this evidence base stretching from basic science to clinical data.”
Dr. Kulkarni pointed to numerous studies that indicate statins may slow disease progression in steatotic liver disease, viral hepatitis, and cirrhosis. But could statins prevent the onset of PSC?
Because PSC incidence is low, Dr. Kulkarni and colleagues focused on a patient population with higher prevalence — those with IBD, who have an overall lifetime risk of 2% to 7%. The research team followed patients from the date of IBD diagnosis.
Among 33,813 patients with IBD in a national dataset from 2018 onward, 8813 used statins. Statin users tended to be older than non–statin users.
Overall, 181 patients developed new onset PSC during a median follow-up of about 45 months after initial IBD diagnosis. Only eight statin users (.09%) developed PSC, compared with 173 patients (.69%) in the control group.
In a propensity score-matched analysis, statin therapy was associated with a significantly lower risk of developing PSC (HR .14, P < .001). The associated E-value was 5.5, which suggested a robust finding and unlikely to be due to non-visible confounding.
The findings were consistent across secondary and sensitivity analyses, including by age, duration of statin use, and type of statin. For instance, for patients under age 50 where PSC is more likely to occur, statins were associated with a 90% reduction in PSC risk.
“We take away two things from this. First, it’s suggested that a protective effect occurs at ages where PSC is most likely to occur,” Dr. Kulkarni said. “Second, in combination with our propensity score-matched analysis, the results we are observing are not due to a survival bias, where the patients who survive to an age where statins are prescribed simply have a biologically different predilection for developing PSC.”
Statins also protected against PSC in both ulcerative colitis (HR .21) and Crohn’s disease (HR .15), as well as both women (HR .16) and men (HR .22).
Given the uncertainty about the optimal duration of statin therapy for a protective effect, Dr. Kulkarni and colleagues looked at a lag time of 12 months. They found statins were associated with an 84% risk reduction (HR .16), which was similar to the primary analysis.
The study was limited by the inability to capture dosage data or medication adherence. The findings raised several questions, Dr. Kulkarni said, such as the underlying mechanisms and clinical implications. For instance, the underlying mechanisms appear to be related to the pleiotropic effect of statins, modulation of gut inflammation, and alterations in bile acid profiles.
“This is really fascinating and interesting. I wonder about this as a primary prevention strategy in those who have normal cholesterol. Could this work or not?” said Gyongyi Szabo, MD, AGAF, chief academic officer at Beth Israel Deaconess Medical Center, Boston, who was a moderator for the Liver & Biliary Section Distinguished Abstract Plenary Session.
Dr. Kulkarni noted that these findings wouldn’t change clinical practice alone, but based on existing literature around statin hesitancy among patients with cardiovascular disease, the risk reduction for PSC could provide another reason to encourage patients to take them.
“To move this to a place where you can actually think about primary prevention, I think the biological mechanisms need to be teased out a little bit more,” Dr. Kulkarni said. “Then I think you probably still need to identify a higher-risk group than IBD alone.”
Dr. Kulkarni declared no disclosures.
WASHINGTON — , according to a study presented at Digestive Disease Week® (DDW) 2024.
Statin use was associated with an 86% risk reduction, and only .09% of IBD patients who took statins developed PSC.
“We all take care of patients with liver disease, and we know what a significant burden PSC is. These patients have a significantly elevated risk of enhanced fibrosis and cirrhosis, multiple cancers, and cholangitis and sepsis,” said lead author Chiraag Kulkarni, MD, a gastroenterology fellow at Stanford (California) University Medical School.
“Despite this, we have to date no proven effective medical care for PSC,” he said. “However, over the last decade, there is growing evidence that statins may be beneficial in liver disease, and we see this evidence base stretching from basic science to clinical data.”
Dr. Kulkarni pointed to numerous studies that indicate statins may slow disease progression in steatotic liver disease, viral hepatitis, and cirrhosis. But could statins prevent the onset of PSC?
Because PSC incidence is low, Dr. Kulkarni and colleagues focused on a patient population with higher prevalence — those with IBD, who have an overall lifetime risk of 2% to 7%. The research team followed patients from the date of IBD diagnosis.
Among 33,813 patients with IBD in a national dataset from 2018 onward, 8813 used statins. Statin users tended to be older than non–statin users.
Overall, 181 patients developed new onset PSC during a median follow-up of about 45 months after initial IBD diagnosis. Only eight statin users (.09%) developed PSC, compared with 173 patients (.69%) in the control group.
In a propensity score-matched analysis, statin therapy was associated with a significantly lower risk of developing PSC (HR .14, P < .001). The associated E-value was 5.5, which suggested a robust finding and unlikely to be due to non-visible confounding.
The findings were consistent across secondary and sensitivity analyses, including by age, duration of statin use, and type of statin. For instance, for patients under age 50 where PSC is more likely to occur, statins were associated with a 90% reduction in PSC risk.
“We take away two things from this. First, it’s suggested that a protective effect occurs at ages where PSC is most likely to occur,” Dr. Kulkarni said. “Second, in combination with our propensity score-matched analysis, the results we are observing are not due to a survival bias, where the patients who survive to an age where statins are prescribed simply have a biologically different predilection for developing PSC.”
Statins also protected against PSC in both ulcerative colitis (HR .21) and Crohn’s disease (HR .15), as well as both women (HR .16) and men (HR .22).
Given the uncertainty about the optimal duration of statin therapy for a protective effect, Dr. Kulkarni and colleagues looked at a lag time of 12 months. They found statins were associated with an 84% risk reduction (HR .16), which was similar to the primary analysis.
The study was limited by the inability to capture dosage data or medication adherence. The findings raised several questions, Dr. Kulkarni said, such as the underlying mechanisms and clinical implications. For instance, the underlying mechanisms appear to be related to the pleiotropic effect of statins, modulation of gut inflammation, and alterations in bile acid profiles.
“This is really fascinating and interesting. I wonder about this as a primary prevention strategy in those who have normal cholesterol. Could this work or not?” said Gyongyi Szabo, MD, AGAF, chief academic officer at Beth Israel Deaconess Medical Center, Boston, who was a moderator for the Liver & Biliary Section Distinguished Abstract Plenary Session.
Dr. Kulkarni noted that these findings wouldn’t change clinical practice alone, but based on existing literature around statin hesitancy among patients with cardiovascular disease, the risk reduction for PSC could provide another reason to encourage patients to take them.
“To move this to a place where you can actually think about primary prevention, I think the biological mechanisms need to be teased out a little bit more,” Dr. Kulkarni said. “Then I think you probably still need to identify a higher-risk group than IBD alone.”
Dr. Kulkarni declared no disclosures.
FROM DDW 2024
Study Finds Immunosuppression Affects Risk for Poor Outcomes in Patients with cSCC
PHOENIX — Immunosuppression is an independent risk factor for poorer outcomes in patients with cutaneous squamous cell carcinoma (cSCC), according to new research that was presented at the American College of Mohs Surgery (ACMS) 2024 annual meeting.
Even though immunosuppression is strongly associated with an increased risk for cSCC, studies to date have generally not shown it to be an independent risk factor for metastasis and disease-specific death (DSD), after accounting for primary tumor stage.
“Solid organ transplant puts patients at risk for developing cutaneous squamous cell carcinoma, and it’s more likely to have aggressive features,” said study author Jason Klein, MD, PhD, a dermatology resident at University of Texas Southwestern Medical Center, Dallas. “But it’s still not known if immunosuppression is an independent risk factor.”
Other groups “have tried to tackle this, but they have all primarily been single-institution data,” he noted, adding that “results so far have been tipping the scale towards immunosuppression not being an independent risk factor” for worse outcomes.
Immunosuppressed individuals face a greater risk for cSCC than the general population and often present with more aggressive, multifocal disease. However, Dr. Klein explained that a previous retrospective study comprising a cohort of approximately 7600 tumors from two centers reported that immunosuppression was not an independent risk factor for both tumor metastasis and cancer-specific death after adjusting for tumor characteristics.
Tipped the Scale
Therefore, the goal of the current study was to repeat this analysis but in a much larger retrospective cohort. Dr. Klein and his colleagues pooled cSCC data from 12 dermatology centers (11 academic and one private) that were located in the United States, Spain, and Brazil. The cohort included 4392 patients (3769 immunocompetent patients and 623 immunosuppressed patients) with 19,237 tumors (15,191 immunocompetent and 4046 immunosuppressed). Study endpoints included local recurrence, metastasis (nodal, satellite/in-transit, and distant), DSD, and “major poor outcomes” (defined as metastasis and DSD combined).
About 30% of the immunosuppressed patients were organ transplant recipients (OTR) and 10% had chronic lymphocytic leukemia (CLL). Half of the immunocompetent patients (50.3%) underwent Mohs surgery as the primary treatment, as did 58.2% of the immunosuppressed patients.
On multivariable analysis, significant predictors of “major poor outcomes” included immunosuppression (subdistribution hazard ratio [SHR], 1.3; P = .04), Brigham and Women’s Hospital tumor stage (SHR 6.7 for T2a, 18.1 for T2b, and 37.2 for T3; P < .001 for all), location on the head/neck (SHR, 2.1; P < .001), and adjuvant radiation (SHR, 1.6; P < .001).
But when metastasis and DSD were evaluated separately, immunosuppression was only predictive of DSD (SHR, 1.7; P = .008) but not metastasis (SHR, 1.2; P = .21). Dr. Klein explained that they also conducted a separate subanalysis limited to OTR and patients with CLL, which demonstrated that immunosuppression was no longer a significant predictor of “major poor outcomes” (SHR, 0.9; P = .66 for OTR; SHR, 1.4; P = .25 for CLL).
“Organ transplant status and CLL were not independent risk factors for major poor outcomes,” he said. “But in summary, we may be tipping the scale to immunosuppression being a risk factor.”
Asked to comment on the findings, Naissan O. Wesley, MD, director of Mohs surgery, Skin Care and Laser Physicians of Beverly Hills, Los Angeles, California, stated that “this larger scale study presented at this meeting was important to further confirm what we see in everyday practice, that immunosuppression may lead to poorer outcomes in patients with cutaneous squamous cell carcinoma.”
Also weighing in on the data, Jesse M. Lewin, MD, chief of Mohs micrographic and dermatologic surgery, at the Icahn School of Medicine at Mount Sinai, New York City, noted that the treatment of cSCC in high-risk patients has been challenging because of the historical lack of data and large studies to guide management.
“The authors provide a large cohort to help stratify which patients are most at risk for poor outcomes, which can inform our decision to refer for neoadjuvant or adjuvant treatment and multi-disciplinary management,” he said. “This is the first step in being able to optimize cure in these patients.”
The study was independently supported. Dr. Klein, Dr. Lewin, and Dr. Wesley reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
PHOENIX — Immunosuppression is an independent risk factor for poorer outcomes in patients with cutaneous squamous cell carcinoma (cSCC), according to new research that was presented at the American College of Mohs Surgery (ACMS) 2024 annual meeting.
Even though immunosuppression is strongly associated with an increased risk for cSCC, studies to date have generally not shown it to be an independent risk factor for metastasis and disease-specific death (DSD), after accounting for primary tumor stage.
“Solid organ transplant puts patients at risk for developing cutaneous squamous cell carcinoma, and it’s more likely to have aggressive features,” said study author Jason Klein, MD, PhD, a dermatology resident at University of Texas Southwestern Medical Center, Dallas. “But it’s still not known if immunosuppression is an independent risk factor.”
Other groups “have tried to tackle this, but they have all primarily been single-institution data,” he noted, adding that “results so far have been tipping the scale towards immunosuppression not being an independent risk factor” for worse outcomes.
Immunosuppressed individuals face a greater risk for cSCC than the general population and often present with more aggressive, multifocal disease. However, Dr. Klein explained that a previous retrospective study comprising a cohort of approximately 7600 tumors from two centers reported that immunosuppression was not an independent risk factor for both tumor metastasis and cancer-specific death after adjusting for tumor characteristics.
Tipped the Scale
Therefore, the goal of the current study was to repeat this analysis but in a much larger retrospective cohort. Dr. Klein and his colleagues pooled cSCC data from 12 dermatology centers (11 academic and one private) that were located in the United States, Spain, and Brazil. The cohort included 4392 patients (3769 immunocompetent patients and 623 immunosuppressed patients) with 19,237 tumors (15,191 immunocompetent and 4046 immunosuppressed). Study endpoints included local recurrence, metastasis (nodal, satellite/in-transit, and distant), DSD, and “major poor outcomes” (defined as metastasis and DSD combined).
About 30% of the immunosuppressed patients were organ transplant recipients (OTR) and 10% had chronic lymphocytic leukemia (CLL). Half of the immunocompetent patients (50.3%) underwent Mohs surgery as the primary treatment, as did 58.2% of the immunosuppressed patients.
On multivariable analysis, significant predictors of “major poor outcomes” included immunosuppression (subdistribution hazard ratio [SHR], 1.3; P = .04), Brigham and Women’s Hospital tumor stage (SHR 6.7 for T2a, 18.1 for T2b, and 37.2 for T3; P < .001 for all), location on the head/neck (SHR, 2.1; P < .001), and adjuvant radiation (SHR, 1.6; P < .001).
But when metastasis and DSD were evaluated separately, immunosuppression was only predictive of DSD (SHR, 1.7; P = .008) but not metastasis (SHR, 1.2; P = .21). Dr. Klein explained that they also conducted a separate subanalysis limited to OTR and patients with CLL, which demonstrated that immunosuppression was no longer a significant predictor of “major poor outcomes” (SHR, 0.9; P = .66 for OTR; SHR, 1.4; P = .25 for CLL).
“Organ transplant status and CLL were not independent risk factors for major poor outcomes,” he said. “But in summary, we may be tipping the scale to immunosuppression being a risk factor.”
Asked to comment on the findings, Naissan O. Wesley, MD, director of Mohs surgery, Skin Care and Laser Physicians of Beverly Hills, Los Angeles, California, stated that “this larger scale study presented at this meeting was important to further confirm what we see in everyday practice, that immunosuppression may lead to poorer outcomes in patients with cutaneous squamous cell carcinoma.”
Also weighing in on the data, Jesse M. Lewin, MD, chief of Mohs micrographic and dermatologic surgery, at the Icahn School of Medicine at Mount Sinai, New York City, noted that the treatment of cSCC in high-risk patients has been challenging because of the historical lack of data and large studies to guide management.
“The authors provide a large cohort to help stratify which patients are most at risk for poor outcomes, which can inform our decision to refer for neoadjuvant or adjuvant treatment and multi-disciplinary management,” he said. “This is the first step in being able to optimize cure in these patients.”
The study was independently supported. Dr. Klein, Dr. Lewin, and Dr. Wesley reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
PHOENIX — Immunosuppression is an independent risk factor for poorer outcomes in patients with cutaneous squamous cell carcinoma (cSCC), according to new research that was presented at the American College of Mohs Surgery (ACMS) 2024 annual meeting.
Even though immunosuppression is strongly associated with an increased risk for cSCC, studies to date have generally not shown it to be an independent risk factor for metastasis and disease-specific death (DSD), after accounting for primary tumor stage.
“Solid organ transplant puts patients at risk for developing cutaneous squamous cell carcinoma, and it’s more likely to have aggressive features,” said study author Jason Klein, MD, PhD, a dermatology resident at University of Texas Southwestern Medical Center, Dallas. “But it’s still not known if immunosuppression is an independent risk factor.”
Other groups “have tried to tackle this, but they have all primarily been single-institution data,” he noted, adding that “results so far have been tipping the scale towards immunosuppression not being an independent risk factor” for worse outcomes.
Immunosuppressed individuals face a greater risk for cSCC than the general population and often present with more aggressive, multifocal disease. However, Dr. Klein explained that a previous retrospective study comprising a cohort of approximately 7600 tumors from two centers reported that immunosuppression was not an independent risk factor for both tumor metastasis and cancer-specific death after adjusting for tumor characteristics.
Tipped the Scale
Therefore, the goal of the current study was to repeat this analysis but in a much larger retrospective cohort. Dr. Klein and his colleagues pooled cSCC data from 12 dermatology centers (11 academic and one private) that were located in the United States, Spain, and Brazil. The cohort included 4392 patients (3769 immunocompetent patients and 623 immunosuppressed patients) with 19,237 tumors (15,191 immunocompetent and 4046 immunosuppressed). Study endpoints included local recurrence, metastasis (nodal, satellite/in-transit, and distant), DSD, and “major poor outcomes” (defined as metastasis and DSD combined).
About 30% of the immunosuppressed patients were organ transplant recipients (OTR) and 10% had chronic lymphocytic leukemia (CLL). Half of the immunocompetent patients (50.3%) underwent Mohs surgery as the primary treatment, as did 58.2% of the immunosuppressed patients.
On multivariable analysis, significant predictors of “major poor outcomes” included immunosuppression (subdistribution hazard ratio [SHR], 1.3; P = .04), Brigham and Women’s Hospital tumor stage (SHR 6.7 for T2a, 18.1 for T2b, and 37.2 for T3; P < .001 for all), location on the head/neck (SHR, 2.1; P < .001), and adjuvant radiation (SHR, 1.6; P < .001).
But when metastasis and DSD were evaluated separately, immunosuppression was only predictive of DSD (SHR, 1.7; P = .008) but not metastasis (SHR, 1.2; P = .21). Dr. Klein explained that they also conducted a separate subanalysis limited to OTR and patients with CLL, which demonstrated that immunosuppression was no longer a significant predictor of “major poor outcomes” (SHR, 0.9; P = .66 for OTR; SHR, 1.4; P = .25 for CLL).
“Organ transplant status and CLL were not independent risk factors for major poor outcomes,” he said. “But in summary, we may be tipping the scale to immunosuppression being a risk factor.”
Asked to comment on the findings, Naissan O. Wesley, MD, director of Mohs surgery, Skin Care and Laser Physicians of Beverly Hills, Los Angeles, California, stated that “this larger scale study presented at this meeting was important to further confirm what we see in everyday practice, that immunosuppression may lead to poorer outcomes in patients with cutaneous squamous cell carcinoma.”
Also weighing in on the data, Jesse M. Lewin, MD, chief of Mohs micrographic and dermatologic surgery, at the Icahn School of Medicine at Mount Sinai, New York City, noted that the treatment of cSCC in high-risk patients has been challenging because of the historical lack of data and large studies to guide management.
“The authors provide a large cohort to help stratify which patients are most at risk for poor outcomes, which can inform our decision to refer for neoadjuvant or adjuvant treatment and multi-disciplinary management,” he said. “This is the first step in being able to optimize cure in these patients.”
The study was independently supported. Dr. Klein, Dr. Lewin, and Dr. Wesley reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM ACMS 2024
Staving Off Obsolescence
I don’t write many checks anymore.
When I started my practice in 2000 I wrote a lot. Paychecks for my staff, my rent, insurance, IRA contributions, federal & state withholding, payments on my EMG machine, pretty much everything.
Checks are old. We’ve been using them in some form for roughly 2000 years.
But the online world has changed a lot of that. Now I write maybe 2-3 a month. I could probably do fewer, but haven’t bothered to set those accounts up that way.
I recently was down to my last few checks, so ordered replacements. The minimum order was 600. As I unpacked the box I realized they’re probably the last ones I’ll need, both because checks are gradually passing by and because there are more days behind in my neurology career than ahead.
The checks are a minor thing, but they do make you think. Certainly we’re in the last generation of people who will ever need to use paper checks. Some phrases like “blank check” will likely be with us long after they’re gone (like “dialing a phone”), but the real deal is heading the same way as 8-Track and VHS tapes.
As my 600 checks dwindle down, realistically, so will my career. There is no rewind button on life. I have no desire to leave medicine right now, but the passage of time changes things.
Does that mean I, like my checks, am also getting obsolete?
I hope not. I’d like to think I still have something to offer. I have 30 years of neurology experience behind me, and try to keep up to date on my field. My patients and staff depend on me to bring my best to the office every day.
I hope to stay that way to the end. I’d rather leave voluntarily, still at the top of my game. Even if I end up leaving a few unused checks behind.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
I don’t write many checks anymore.
When I started my practice in 2000 I wrote a lot. Paychecks for my staff, my rent, insurance, IRA contributions, federal & state withholding, payments on my EMG machine, pretty much everything.
Checks are old. We’ve been using them in some form for roughly 2000 years.
But the online world has changed a lot of that. Now I write maybe 2-3 a month. I could probably do fewer, but haven’t bothered to set those accounts up that way.
I recently was down to my last few checks, so ordered replacements. The minimum order was 600. As I unpacked the box I realized they’re probably the last ones I’ll need, both because checks are gradually passing by and because there are more days behind in my neurology career than ahead.
The checks are a minor thing, but they do make you think. Certainly we’re in the last generation of people who will ever need to use paper checks. Some phrases like “blank check” will likely be with us long after they’re gone (like “dialing a phone”), but the real deal is heading the same way as 8-Track and VHS tapes.
As my 600 checks dwindle down, realistically, so will my career. There is no rewind button on life. I have no desire to leave medicine right now, but the passage of time changes things.
Does that mean I, like my checks, am also getting obsolete?
I hope not. I’d like to think I still have something to offer. I have 30 years of neurology experience behind me, and try to keep up to date on my field. My patients and staff depend on me to bring my best to the office every day.
I hope to stay that way to the end. I’d rather leave voluntarily, still at the top of my game. Even if I end up leaving a few unused checks behind.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
I don’t write many checks anymore.
When I started my practice in 2000 I wrote a lot. Paychecks for my staff, my rent, insurance, IRA contributions, federal & state withholding, payments on my EMG machine, pretty much everything.
Checks are old. We’ve been using them in some form for roughly 2000 years.
But the online world has changed a lot of that. Now I write maybe 2-3 a month. I could probably do fewer, but haven’t bothered to set those accounts up that way.
I recently was down to my last few checks, so ordered replacements. The minimum order was 600. As I unpacked the box I realized they’re probably the last ones I’ll need, both because checks are gradually passing by and because there are more days behind in my neurology career than ahead.
The checks are a minor thing, but they do make you think. Certainly we’re in the last generation of people who will ever need to use paper checks. Some phrases like “blank check” will likely be with us long after they’re gone (like “dialing a phone”), but the real deal is heading the same way as 8-Track and VHS tapes.
As my 600 checks dwindle down, realistically, so will my career. There is no rewind button on life. I have no desire to leave medicine right now, but the passage of time changes things.
Does that mean I, like my checks, am also getting obsolete?
I hope not. I’d like to think I still have something to offer. I have 30 years of neurology experience behind me, and try to keep up to date on my field. My patients and staff depend on me to bring my best to the office every day.
I hope to stay that way to the end. I’d rather leave voluntarily, still at the top of my game. Even if I end up leaving a few unused checks behind.
Dr. Block has a solo neurology practice in Scottsdale, Arizona.
New TAVI Platform Adds More Valve Sizes to Choose From
PARIS — Intermediate valve sizes are at least as safe and effective as the standard sizes now available for transcatheter aortic valve implantation (TAVI), according to an international randomized trial.
In a head-to-head comparison, the LANDMARK trial looked at valves from the new balloon-expandable Myval® by Merril Life Sciences and compared them with the balloon-expandable Sapien® from Edwards Lifesciences and the self-expanding Evolut® valve from Medtronic.
The new Myval platform offers multiple valves sized at 1.5 mm intervals, while the other two have valves that are generally sized at intervals of 3.0 mm.
at the Congress of the European Association of Percutaneous Coronary Interventions 2024.
The LANDMARK Trial
The trial enrolled 768 patients at 31 sites in 16 countries. They were randomized in a 1:1 fashion to the new platform or to one of the standards to compare the concept of intermediate valves with contemporary standards.
Seven sizes of Myval valves were used in the study, ranging from 20 mm to 29 mm at 1.5 mm increments. Two more sizes, 30.5 mm and 32.0 mm, were not included in this analysis but are being following in a registry.
The study also used Sapien valves sized 20 mm, 23 mm, 26 mm, and 29 mm and Evolut valves sized 26 mm, 29 mm, and 34 mm. There is also a 23 mm Evolut valve available, but it was not selected by any of the participating investigators.
Of the 336 patients given Myval valves, 48% were an intermediate size not available on one of the other platforms.
For the primary composite efficacy and safety endpoint of all-cause mortality, fatal or nonfatal strokes, VARC 3 or 4 bleeding, acute kidney injury, major vascular injury, moderate or greater valve regurgitation, or conduction disturbances requiring a new permanent pacemaker, the difference in absolute risk was slightly lower in the Myval arm, at 24.7% vs 27.0%, but not statistically significant. With that numerical difference favoring the Myval platform, noninferiority was demonstrated at 30 days with a high level of statistical significance, Dr. Serruys reported.
When each endpoint, with the composite primary endpoint, was evaluated separately in a secondary analysis, all-cause mortality and stroke incidence were identical in the two arms.
Major bleeding and acute kidney injury were nonsignificantly more common in the Myval group, while the incidence of moderate or greater valve regurgitation, placement of a new permanent pacemaker, and major vascular complications were nonsignificantly less common.
Precise Matching
The effective orifice area was consistently higher in the group receiving an intermediate valve relative to a Sapien valve. This was not significant for the 20 mm valve size, but it did reach statistical significance for the rest of the sizes. In contrast, there was no significant difference with the Evolut series.
The data suggest that intermediate sizes “enable precise and appropriate matching of devices to an individual anatomy,” at least relative to Sapien, said Dr. Serruys.
Martin Leon, MD, of Columbia University in New York, called LANDMARK an important step for considering how comparative trials should be conducted in the future.
However, he challenged the idea that this study compared devices for both safety and efficacy. Despite the evidence it provides on device and procedural safety over the short-term, he said few conclusions can be drawn about comparative efficacy after just 30 days. Rather, the true comparative value of the trial will be derived from “rigorous late follow-up,” he said.
Longer Follow-Up to Come
Dr. Serruys acknowledged that the differences seen after 30 days have uncertain relevance to longer-term outcomes. He is planning to conduct a 10-year follow-up that “will unravel whether the documented effective orifice area of the Myval platform will have a beneficial impact on long-term patient prognosis and valve durability,” he said.
Leon agreed that, so far, these data do suggest superior hemodynamic performance with the intermediate sizing relative to valves in the Sapien platform, but the same cannot be said for the Evolut platform, and he pointed out that pooling data from the two platforms for the primary endpoint “makes comparisons difficult.”
And with about half of patients still fitted with the sizes already available, he said a deeper understanding was needed of how “adjustment strategies,” such as oversizing, affect long-term outcomes relative to platforms, such as Myval, with more valve sizes.
A version of this article appeared on Medscape.com.
PARIS — Intermediate valve sizes are at least as safe and effective as the standard sizes now available for transcatheter aortic valve implantation (TAVI), according to an international randomized trial.
In a head-to-head comparison, the LANDMARK trial looked at valves from the new balloon-expandable Myval® by Merril Life Sciences and compared them with the balloon-expandable Sapien® from Edwards Lifesciences and the self-expanding Evolut® valve from Medtronic.
The new Myval platform offers multiple valves sized at 1.5 mm intervals, while the other two have valves that are generally sized at intervals of 3.0 mm.
at the Congress of the European Association of Percutaneous Coronary Interventions 2024.
The LANDMARK Trial
The trial enrolled 768 patients at 31 sites in 16 countries. They were randomized in a 1:1 fashion to the new platform or to one of the standards to compare the concept of intermediate valves with contemporary standards.
Seven sizes of Myval valves were used in the study, ranging from 20 mm to 29 mm at 1.5 mm increments. Two more sizes, 30.5 mm and 32.0 mm, were not included in this analysis but are being following in a registry.
The study also used Sapien valves sized 20 mm, 23 mm, 26 mm, and 29 mm and Evolut valves sized 26 mm, 29 mm, and 34 mm. There is also a 23 mm Evolut valve available, but it was not selected by any of the participating investigators.
Of the 336 patients given Myval valves, 48% were an intermediate size not available on one of the other platforms.
For the primary composite efficacy and safety endpoint of all-cause mortality, fatal or nonfatal strokes, VARC 3 or 4 bleeding, acute kidney injury, major vascular injury, moderate or greater valve regurgitation, or conduction disturbances requiring a new permanent pacemaker, the difference in absolute risk was slightly lower in the Myval arm, at 24.7% vs 27.0%, but not statistically significant. With that numerical difference favoring the Myval platform, noninferiority was demonstrated at 30 days with a high level of statistical significance, Dr. Serruys reported.
When each endpoint, with the composite primary endpoint, was evaluated separately in a secondary analysis, all-cause mortality and stroke incidence were identical in the two arms.
Major bleeding and acute kidney injury were nonsignificantly more common in the Myval group, while the incidence of moderate or greater valve regurgitation, placement of a new permanent pacemaker, and major vascular complications were nonsignificantly less common.
Precise Matching
The effective orifice area was consistently higher in the group receiving an intermediate valve relative to a Sapien valve. This was not significant for the 20 mm valve size, but it did reach statistical significance for the rest of the sizes. In contrast, there was no significant difference with the Evolut series.
The data suggest that intermediate sizes “enable precise and appropriate matching of devices to an individual anatomy,” at least relative to Sapien, said Dr. Serruys.
Martin Leon, MD, of Columbia University in New York, called LANDMARK an important step for considering how comparative trials should be conducted in the future.
However, he challenged the idea that this study compared devices for both safety and efficacy. Despite the evidence it provides on device and procedural safety over the short-term, he said few conclusions can be drawn about comparative efficacy after just 30 days. Rather, the true comparative value of the trial will be derived from “rigorous late follow-up,” he said.
Longer Follow-Up to Come
Dr. Serruys acknowledged that the differences seen after 30 days have uncertain relevance to longer-term outcomes. He is planning to conduct a 10-year follow-up that “will unravel whether the documented effective orifice area of the Myval platform will have a beneficial impact on long-term patient prognosis and valve durability,” he said.
Leon agreed that, so far, these data do suggest superior hemodynamic performance with the intermediate sizing relative to valves in the Sapien platform, but the same cannot be said for the Evolut platform, and he pointed out that pooling data from the two platforms for the primary endpoint “makes comparisons difficult.”
And with about half of patients still fitted with the sizes already available, he said a deeper understanding was needed of how “adjustment strategies,” such as oversizing, affect long-term outcomes relative to platforms, such as Myval, with more valve sizes.
A version of this article appeared on Medscape.com.
PARIS — Intermediate valve sizes are at least as safe and effective as the standard sizes now available for transcatheter aortic valve implantation (TAVI), according to an international randomized trial.
In a head-to-head comparison, the LANDMARK trial looked at valves from the new balloon-expandable Myval® by Merril Life Sciences and compared them with the balloon-expandable Sapien® from Edwards Lifesciences and the self-expanding Evolut® valve from Medtronic.
The new Myval platform offers multiple valves sized at 1.5 mm intervals, while the other two have valves that are generally sized at intervals of 3.0 mm.
at the Congress of the European Association of Percutaneous Coronary Interventions 2024.
The LANDMARK Trial
The trial enrolled 768 patients at 31 sites in 16 countries. They were randomized in a 1:1 fashion to the new platform or to one of the standards to compare the concept of intermediate valves with contemporary standards.
Seven sizes of Myval valves were used in the study, ranging from 20 mm to 29 mm at 1.5 mm increments. Two more sizes, 30.5 mm and 32.0 mm, were not included in this analysis but are being following in a registry.
The study also used Sapien valves sized 20 mm, 23 mm, 26 mm, and 29 mm and Evolut valves sized 26 mm, 29 mm, and 34 mm. There is also a 23 mm Evolut valve available, but it was not selected by any of the participating investigators.
Of the 336 patients given Myval valves, 48% were an intermediate size not available on one of the other platforms.
For the primary composite efficacy and safety endpoint of all-cause mortality, fatal or nonfatal strokes, VARC 3 or 4 bleeding, acute kidney injury, major vascular injury, moderate or greater valve regurgitation, or conduction disturbances requiring a new permanent pacemaker, the difference in absolute risk was slightly lower in the Myval arm, at 24.7% vs 27.0%, but not statistically significant. With that numerical difference favoring the Myval platform, noninferiority was demonstrated at 30 days with a high level of statistical significance, Dr. Serruys reported.
When each endpoint, with the composite primary endpoint, was evaluated separately in a secondary analysis, all-cause mortality and stroke incidence were identical in the two arms.
Major bleeding and acute kidney injury were nonsignificantly more common in the Myval group, while the incidence of moderate or greater valve regurgitation, placement of a new permanent pacemaker, and major vascular complications were nonsignificantly less common.
Precise Matching
The effective orifice area was consistently higher in the group receiving an intermediate valve relative to a Sapien valve. This was not significant for the 20 mm valve size, but it did reach statistical significance for the rest of the sizes. In contrast, there was no significant difference with the Evolut series.
The data suggest that intermediate sizes “enable precise and appropriate matching of devices to an individual anatomy,” at least relative to Sapien, said Dr. Serruys.
Martin Leon, MD, of Columbia University in New York, called LANDMARK an important step for considering how comparative trials should be conducted in the future.
However, he challenged the idea that this study compared devices for both safety and efficacy. Despite the evidence it provides on device and procedural safety over the short-term, he said few conclusions can be drawn about comparative efficacy after just 30 days. Rather, the true comparative value of the trial will be derived from “rigorous late follow-up,” he said.
Longer Follow-Up to Come
Dr. Serruys acknowledged that the differences seen after 30 days have uncertain relevance to longer-term outcomes. He is planning to conduct a 10-year follow-up that “will unravel whether the documented effective orifice area of the Myval platform will have a beneficial impact on long-term patient prognosis and valve durability,” he said.
Leon agreed that, so far, these data do suggest superior hemodynamic performance with the intermediate sizing relative to valves in the Sapien platform, but the same cannot be said for the Evolut platform, and he pointed out that pooling data from the two platforms for the primary endpoint “makes comparisons difficult.”
And with about half of patients still fitted with the sizes already available, he said a deeper understanding was needed of how “adjustment strategies,” such as oversizing, affect long-term outcomes relative to platforms, such as Myval, with more valve sizes.
A version of this article appeared on Medscape.com.
FROM EUROPCR 2024