User login
ACOG, SMFM urge all pregnant women to get COVID-19 vaccine
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
Persistent Panniculitis in Dermatomyositis
To the Editor:
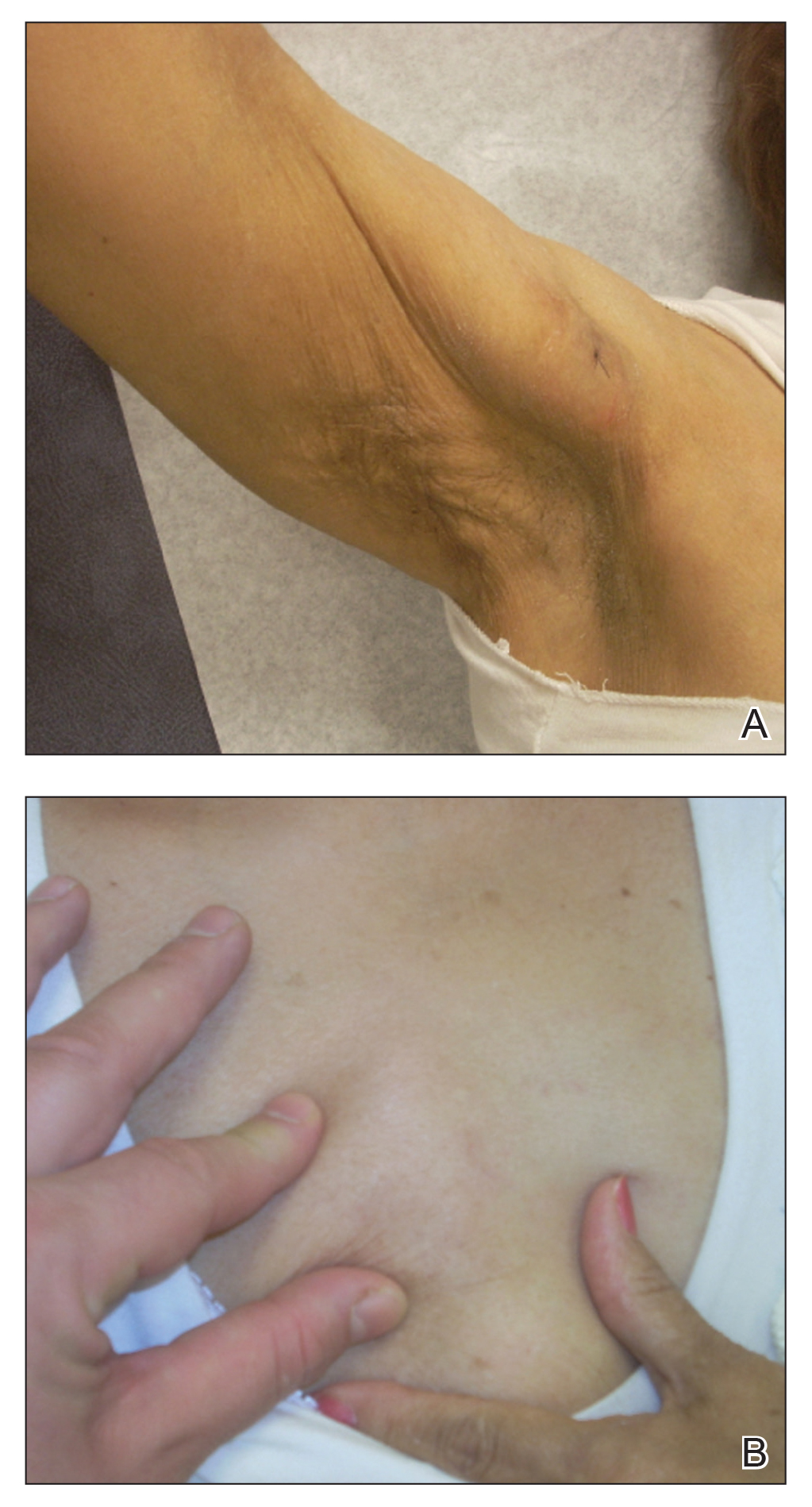
A 62-year-old woman with a history of dermatomyositis (DM) presented to dermatology clinic for evaluation of multiple subcutaneous nodules. Two years prior to the current presentation, the patient was diagnosed by her primary care physician with DM based on clinical presentation. She initially developed body aches, muscle pain, and weakness of the upper extremities, specifically around the shoulders, and later the lower extremities, specifically around the thighs. The initial physical examination revealed pain with movement, tenderness to palpation, and proximal extremity weakness. The patient also noted a 50-lb weight loss. Over the next year, she noted dysphagia and developed multiple subcutaneous nodules on the right arm, chest, and left axilla. Subsequently, she developed a violaceous, hyperpigmented, periorbital rash and erythema of the anterior chest. She did not experience hair loss, oral ulcers, photosensitivity, or joint pain.
Laboratory testing in the months following the initial presentation revealed a creatine phosphokinase level of 436 U/L (reference range, 20–200 U/L), an erythrocyte sedimentation rate of 60 mm/h (reference range, <31 mm/h), and an aldolase level of 10.4 U/L (reference range, 1.0–8.0 U/L). Lactate dehydrogenase and thyroid function tests were within normal limits. Antinuclear antibodies, anti–double-stranded DNA, anti-Smith antibodies, anti-ribonucleoprotein, anti–Jo-1 antibodies, and anti–smooth muscle antibodies all were negative. Total blood complement levels were elevated, but complement C3 and C4 were within normal limits. Imaging demonstrated normal chest radiographs, and a modified barium swallow confirmed swallowing dysfunction. A right quadricep muscle biopsy confirmed the diagnosis of DM. A malignancy work-up including mammography, colonoscopy, and computed tomography of the chest, abdomen, and pelvis was negative aside from nodular opacities in the chest. She was treated with prednisone (60 mg, 0.9 mg/kg) daily and methotrexate (15–20 mg) weekly for several months. While the treatment attenuated the rash and improved weakness, the nodules persisted, prompting a referral to dermatology.
Physical examination at the dermatology clinic demonstrated the persistent subcutaneous nodules were indurated and bilaterally located on the arms, axillae, chest, abdomen, buttocks, and thighs with no pain or erythema (Figure). Laboratory tests demonstrated a normal creatine phosphokinase level, elevated erythrocyte sedimentation rate (70 mm/h), and elevated aldolase level (9.3 U/L). Complement levels were elevated, though complement C3 and C4 remained within normal limits. Histopathology of nodules from the medial right upper arm and left thigh showed lobular panniculitis with fat necrosis, calcification, and interface changes. The patient was treated for several months with daily mycophenolate mofetil (1 g increased to 3 g) and daily hydroxychloroquine (200 mg) without any effect on the nodules.
The histologic features of panniculitis in lupus and DM are similar and include multifocal hyalinization of the subcuticular fat and diffuse lobular infiltrates of mature lymphocytes without nuclear atypia.1 Though clinical panniculitis is a rare finding in DM, histologic panniculitis is a relatively common finding.2 Despite the similar histopathology of lupus and DM, the presence of typical DM clinical and laboratory features in our patient (body aches, muscle pain, proximal weakness, cutaneous manifestations, elevated creatine phosphokinase, normal complement C3 and C4) made a diagnosis of DM more likely.
Clinical panniculitis is a rare subcutaneous manifestation of DM with around 50 cases reported in the literature (Table). A PubMed search of articles indexed for MEDLINE was conducted using the terms dermatomyositis and panniculitis through July 2019. Additionally, a full-text review and search of references within these articles was used to identify all cases of patients presenting with panniculitis in the setting of DM. Exclusion criteria were cases in which another etiology was considered likely (infectious panniculitis and lupus panniculitis) as well as those without an English translation. We identified 43 cases; the average age of the patients was 39.6 years, and 36 (83.7%) of the cases were women. Patients typically presented with persistent, indurated, painful, erythematous, nodular lesions localized to the arms, abdomen, buttocks, and thighs.
While panniculitis has been reported preceding and concurrent with a diagnosis of DM, a number of cases described presentation as late as 5 years following onset of classic DM symptoms.12,13,31 In some cases (3/43 [7.0%]), panniculitis was the only cutaneous manifestation of DM.15,33,36 However, it occurred more commonly with other characteristic skin findings, such as heliotrope rash or Gottron sign.Some investigators have recommended that panniculitis be included as a diagnostic feature of DM and that DM be considered in the differential diagnosis in isolated cases of panniculitis.25,33
Though it seems panniculitis in DM may correlate with a better prognosis, we identified underlying malignancies in 3 cases. Malignancies associated with panniculitis in DM included ovarian adenocarcinoma, nasopharyngeal carcinoma, and parotid carcinoma, indicating that appropriate cancer screening still is critical in the diagnostic workup.2,11,22
A majority of the reported panniculitis cases in DM have responded to treatment with prednisone; however, treatment with prednisone has been more recalcitrant in other cases. Reports of successful additional therapies include methotrexate, cyclosporine, azathioprine, hydroxychloroquine, intravenous immunoglobulin, mepacrine, or a combination of these entities.19,22 In most cases, improvement of the panniculitis and other DM symptoms occurred simultaneously.25 It is noteworthy that the muscular symptoms often resolved more rapidly than cutaneous manifestations.33 Few reported cases (6 including the current case) found a persistent panniculitis despite improvement and remission of the myositis.3,5,10,11,30
Our patient was treated with both prednisone and methotrexate for several months, leading to remission of muscular symptoms (along with return to baseline of creatine phosphokinase), yet the panniculitis did not improve. The subcutaneous nodules also did not respond to treatment with mycophenolate mofetil and hydroxychloroquine.
Recent immunohistochemical studies have suggested that panniculitic lesions show better outcomes with immunosuppressive therapy when compared with other DM-related skin lesions.40 However, this was not the case for our patient, who after months of immunosuppressive therapy showed complete resolution of the periorbital and chest rashes with persistence of multiple indurated subcutaneous nodules.
Our case adds to a number of reports of DM presenting with panniculitis. Our patient fit the classic demographic of previously reported cases, as she was an adult woman without evidence of underlying malignancy; however, our case remains an example of the therapeutic challenge that exists when encountering a persistent, treatment-resistant panniculitis despite resolution of all other features of DM.
- Wick MR. Panniculitis: a summary. Semin Diagn Pathol. 2017;34:261-272.
- Girouard SD, Velez NF, Penson RT, et al. Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol. 2012;148:740-744.
- van Dongen HM, van Vugt RM, Stoof TJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol. 2020;26:E187-E188.
- Choi YJ, Yoo WH. Panniculitis, a rare presentation of onset and exacerbation of juvenile dermatomyositis: a case report and literature review. Arch Rheumatol. 2018;33:367-371.
- Azevedo PO, Castellen NR, Salai AF, et al. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 2018;93:119-121.
- Agulló A, Hinds B, Larrea M, et al. Livedo racemosa, reticulated ulcerations, panniculitis and violaceous plaques in a 46-year-old woman. Indian Dermatol Online J. 2018;9:47-49.
- Hattori Y, Matsuyama K, Takahashi T, et al. Anti-MDA5 antibody-positive dermatomyositis presenting with cellulitis-like erythema on the mandible as an initial symptom. Case Rep Dermatol. 2018;10:110-114.
- Hasegawa A, Shimomura Y, Kibune N, et al. Panniculitis as the initial manifestation of dermatomyositis with anti-MDA5 antibody. Clin Exp Dermatol. 2017;42:551-553.
- Salman A, Kasapcopur O, Ergun T, et al. Panniculitis in juvenile dermatomyositis: report of a case and review of the published work. J Dermatol. 2016;43:951-953.
- Carroll M, Mellick N, Wagner G. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 2015;56:224‐226.
- Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201.
- Otero Rivas MM, Vicente Villa A, González Lara L, et al. Panniculitis in juvenile dermatomyositis. Clin Exp Dermatol. 2015;40:574-575.
- Yanaba K, Tanito K, Hamaguchi Y, et al. Anti‐transcription intermediary factor‐1γ/α/β antibody‐positive dermatomyositis associated with multiple panniculitis lesions. Int J Rheum Dis. 2015;20:1831-1834.
- Pau-Charles I, Moreno PJ, Ortiz-Ibanez K, et al. Anti-MDA5 positive clinically amyopathic dermatomyositis presenting with severe cardiomyopathy. J Eur Acad Dermatol Venereol. 2014;28:1097-1102.
- Lamb R, Digby S, Stewart W, et al. Cutaneous ulceration: more than skin deep? Clin Exp Dermatol. 2013;38:443-445.
- Arias M, Hernández MI, Cunha LG, et al. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146-148.
- Hemmi S, Kushida R, Nishimura H, et al. Magnetic resonance imaging diagnosis of panniculitis in dermatomyositis. Muscle Nerve. 2010;41:151-153.
- Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41:547-549.
- Abdul‐Wahab A, Holden CA, Harland C, et al Calcific panniculitis in adult‐onset dermatomyositis. Clin Exp Dermatol. 2009;34:E854-E856.
- Carneiro S, Alvim G, Resende P, et al. Dermatomyositis with panniculitis. Skinmed. 2007;6:46-47.
- Carrera E, Lobrinus JA, Spertini O, et al. Dermatomyositis, lobarpanniculitis and inflammatory myopathy with abundant macrophages. Neuromuscul Disord. 2006;16:468-471.
- Lin JH, Chu CY, Lin RY. Panniculitis in adult onset dermatomyositis: report of two cases and review of the literature. Dermatol Sinica. 2006;24:194-200.
- Chen GY, Liu MF, Lee JY, et al. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005;15:396-400.
- Nakamori A, Yamaguchi Y, Kurimoto I, et al. Vesiculobullous dermatomyositis with panniculitis without muscle disease. J Am Acad Dermatol. 2003;49:1136-1139.
- Solans R, Cortés J, Selva A, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002;46:S148-S150.
- Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141-144.
- Lee MW, Lim YS, Choi JH, et al. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 1999;26:608‐610.
- Ghali FE, Reed AM, Groben PA, et al. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999;16:270-272.
- Molnar K, Kemeny L, Korom I, et al. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998;139:161‐163.
- Ishikawa O, Tamura A, Ryuzaki K, et al. Membranocystic changes in the panniculitis of dermatomyositis. Br J Dermatol. 1996;134:773-776.
- Sabroe RA, Wallington TB, Kennedy CT. Dermatomyositis treated with high-dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 1995;20:164-167.
- Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995;33:305-307.
- Fusade T, Belanyi P, Joly P, et al. Subcutaneous changes in dermatomyositis. Br J Dermatol. 1993;128:451-453.
- Winkelmann WJ, Billick RC, Srolovitz H. Dermatomyositis presenting as panniculitis. J Am Acad Dermatol. 1990;23:127-128.
- Commens C, O’Neill P, Walker G. Dermatomyositis associated with multifocal lipoatrophy. J Am Acad Dermatol. 1990;22:966-969.
- Raimer SS, Solomon AR, Daniels JC. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 1985;13(2 pt 2):366‐369.
- Feldman D, Hochberg MC, Zizic TM, et al. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 1983;10:85-89.
- Kimura S, Fukuyama Y. Tubular cytoplasmic inclusions in a case of childhood dermatomyositis with migratory subcutaneous nodules. Eur J Pediatr. 1977;125:275-283.
- Weber FP, Gray AMH. Chronic relapsing polydermatomyositis with predominant involvement of the subcutaneous fat. Br J Dermatol. 1924;36:544-560.
- Santos‐Briz A, Calle A, Linos K, et al. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-1359.
To the Editor:
A 62-year-old woman with a history of dermatomyositis (DM) presented to dermatology clinic for evaluation of multiple subcutaneous nodules. Two years prior to the current presentation, the patient was diagnosed by her primary care physician with DM based on clinical presentation. She initially developed body aches, muscle pain, and weakness of the upper extremities, specifically around the shoulders, and later the lower extremities, specifically around the thighs. The initial physical examination revealed pain with movement, tenderness to palpation, and proximal extremity weakness. The patient also noted a 50-lb weight loss. Over the next year, she noted dysphagia and developed multiple subcutaneous nodules on the right arm, chest, and left axilla. Subsequently, she developed a violaceous, hyperpigmented, periorbital rash and erythema of the anterior chest. She did not experience hair loss, oral ulcers, photosensitivity, or joint pain.
Laboratory testing in the months following the initial presentation revealed a creatine phosphokinase level of 436 U/L (reference range, 20–200 U/L), an erythrocyte sedimentation rate of 60 mm/h (reference range, <31 mm/h), and an aldolase level of 10.4 U/L (reference range, 1.0–8.0 U/L). Lactate dehydrogenase and thyroid function tests were within normal limits. Antinuclear antibodies, anti–double-stranded DNA, anti-Smith antibodies, anti-ribonucleoprotein, anti–Jo-1 antibodies, and anti–smooth muscle antibodies all were negative. Total blood complement levels were elevated, but complement C3 and C4 were within normal limits. Imaging demonstrated normal chest radiographs, and a modified barium swallow confirmed swallowing dysfunction. A right quadricep muscle biopsy confirmed the diagnosis of DM. A malignancy work-up including mammography, colonoscopy, and computed tomography of the chest, abdomen, and pelvis was negative aside from nodular opacities in the chest. She was treated with prednisone (60 mg, 0.9 mg/kg) daily and methotrexate (15–20 mg) weekly for several months. While the treatment attenuated the rash and improved weakness, the nodules persisted, prompting a referral to dermatology.
Physical examination at the dermatology clinic demonstrated the persistent subcutaneous nodules were indurated and bilaterally located on the arms, axillae, chest, abdomen, buttocks, and thighs with no pain or erythema (Figure). Laboratory tests demonstrated a normal creatine phosphokinase level, elevated erythrocyte sedimentation rate (70 mm/h), and elevated aldolase level (9.3 U/L). Complement levels were elevated, though complement C3 and C4 remained within normal limits. Histopathology of nodules from the medial right upper arm and left thigh showed lobular panniculitis with fat necrosis, calcification, and interface changes. The patient was treated for several months with daily mycophenolate mofetil (1 g increased to 3 g) and daily hydroxychloroquine (200 mg) without any effect on the nodules.
The histologic features of panniculitis in lupus and DM are similar and include multifocal hyalinization of the subcuticular fat and diffuse lobular infiltrates of mature lymphocytes without nuclear atypia.1 Though clinical panniculitis is a rare finding in DM, histologic panniculitis is a relatively common finding.2 Despite the similar histopathology of lupus and DM, the presence of typical DM clinical and laboratory features in our patient (body aches, muscle pain, proximal weakness, cutaneous manifestations, elevated creatine phosphokinase, normal complement C3 and C4) made a diagnosis of DM more likely.
Clinical panniculitis is a rare subcutaneous manifestation of DM with around 50 cases reported in the literature (Table). A PubMed search of articles indexed for MEDLINE was conducted using the terms dermatomyositis and panniculitis through July 2019. Additionally, a full-text review and search of references within these articles was used to identify all cases of patients presenting with panniculitis in the setting of DM. Exclusion criteria were cases in which another etiology was considered likely (infectious panniculitis and lupus panniculitis) as well as those without an English translation. We identified 43 cases; the average age of the patients was 39.6 years, and 36 (83.7%) of the cases were women. Patients typically presented with persistent, indurated, painful, erythematous, nodular lesions localized to the arms, abdomen, buttocks, and thighs.
While panniculitis has been reported preceding and concurrent with a diagnosis of DM, a number of cases described presentation as late as 5 years following onset of classic DM symptoms.12,13,31 In some cases (3/43 [7.0%]), panniculitis was the only cutaneous manifestation of DM.15,33,36 However, it occurred more commonly with other characteristic skin findings, such as heliotrope rash or Gottron sign.Some investigators have recommended that panniculitis be included as a diagnostic feature of DM and that DM be considered in the differential diagnosis in isolated cases of panniculitis.25,33
Though it seems panniculitis in DM may correlate with a better prognosis, we identified underlying malignancies in 3 cases. Malignancies associated with panniculitis in DM included ovarian adenocarcinoma, nasopharyngeal carcinoma, and parotid carcinoma, indicating that appropriate cancer screening still is critical in the diagnostic workup.2,11,22
A majority of the reported panniculitis cases in DM have responded to treatment with prednisone; however, treatment with prednisone has been more recalcitrant in other cases. Reports of successful additional therapies include methotrexate, cyclosporine, azathioprine, hydroxychloroquine, intravenous immunoglobulin, mepacrine, or a combination of these entities.19,22 In most cases, improvement of the panniculitis and other DM symptoms occurred simultaneously.25 It is noteworthy that the muscular symptoms often resolved more rapidly than cutaneous manifestations.33 Few reported cases (6 including the current case) found a persistent panniculitis despite improvement and remission of the myositis.3,5,10,11,30
Our patient was treated with both prednisone and methotrexate for several months, leading to remission of muscular symptoms (along with return to baseline of creatine phosphokinase), yet the panniculitis did not improve. The subcutaneous nodules also did not respond to treatment with mycophenolate mofetil and hydroxychloroquine.
Recent immunohistochemical studies have suggested that panniculitic lesions show better outcomes with immunosuppressive therapy when compared with other DM-related skin lesions.40 However, this was not the case for our patient, who after months of immunosuppressive therapy showed complete resolution of the periorbital and chest rashes with persistence of multiple indurated subcutaneous nodules.
Our case adds to a number of reports of DM presenting with panniculitis. Our patient fit the classic demographic of previously reported cases, as she was an adult woman without evidence of underlying malignancy; however, our case remains an example of the therapeutic challenge that exists when encountering a persistent, treatment-resistant panniculitis despite resolution of all other features of DM.
To the Editor:
A 62-year-old woman with a history of dermatomyositis (DM) presented to dermatology clinic for evaluation of multiple subcutaneous nodules. Two years prior to the current presentation, the patient was diagnosed by her primary care physician with DM based on clinical presentation. She initially developed body aches, muscle pain, and weakness of the upper extremities, specifically around the shoulders, and later the lower extremities, specifically around the thighs. The initial physical examination revealed pain with movement, tenderness to palpation, and proximal extremity weakness. The patient also noted a 50-lb weight loss. Over the next year, she noted dysphagia and developed multiple subcutaneous nodules on the right arm, chest, and left axilla. Subsequently, she developed a violaceous, hyperpigmented, periorbital rash and erythema of the anterior chest. She did not experience hair loss, oral ulcers, photosensitivity, or joint pain.
Laboratory testing in the months following the initial presentation revealed a creatine phosphokinase level of 436 U/L (reference range, 20–200 U/L), an erythrocyte sedimentation rate of 60 mm/h (reference range, <31 mm/h), and an aldolase level of 10.4 U/L (reference range, 1.0–8.0 U/L). Lactate dehydrogenase and thyroid function tests were within normal limits. Antinuclear antibodies, anti–double-stranded DNA, anti-Smith antibodies, anti-ribonucleoprotein, anti–Jo-1 antibodies, and anti–smooth muscle antibodies all were negative. Total blood complement levels were elevated, but complement C3 and C4 were within normal limits. Imaging demonstrated normal chest radiographs, and a modified barium swallow confirmed swallowing dysfunction. A right quadricep muscle biopsy confirmed the diagnosis of DM. A malignancy work-up including mammography, colonoscopy, and computed tomography of the chest, abdomen, and pelvis was negative aside from nodular opacities in the chest. She was treated with prednisone (60 mg, 0.9 mg/kg) daily and methotrexate (15–20 mg) weekly for several months. While the treatment attenuated the rash and improved weakness, the nodules persisted, prompting a referral to dermatology.
Physical examination at the dermatology clinic demonstrated the persistent subcutaneous nodules were indurated and bilaterally located on the arms, axillae, chest, abdomen, buttocks, and thighs with no pain or erythema (Figure). Laboratory tests demonstrated a normal creatine phosphokinase level, elevated erythrocyte sedimentation rate (70 mm/h), and elevated aldolase level (9.3 U/L). Complement levels were elevated, though complement C3 and C4 remained within normal limits. Histopathology of nodules from the medial right upper arm and left thigh showed lobular panniculitis with fat necrosis, calcification, and interface changes. The patient was treated for several months with daily mycophenolate mofetil (1 g increased to 3 g) and daily hydroxychloroquine (200 mg) without any effect on the nodules.
The histologic features of panniculitis in lupus and DM are similar and include multifocal hyalinization of the subcuticular fat and diffuse lobular infiltrates of mature lymphocytes without nuclear atypia.1 Though clinical panniculitis is a rare finding in DM, histologic panniculitis is a relatively common finding.2 Despite the similar histopathology of lupus and DM, the presence of typical DM clinical and laboratory features in our patient (body aches, muscle pain, proximal weakness, cutaneous manifestations, elevated creatine phosphokinase, normal complement C3 and C4) made a diagnosis of DM more likely.
Clinical panniculitis is a rare subcutaneous manifestation of DM with around 50 cases reported in the literature (Table). A PubMed search of articles indexed for MEDLINE was conducted using the terms dermatomyositis and panniculitis through July 2019. Additionally, a full-text review and search of references within these articles was used to identify all cases of patients presenting with panniculitis in the setting of DM. Exclusion criteria were cases in which another etiology was considered likely (infectious panniculitis and lupus panniculitis) as well as those without an English translation. We identified 43 cases; the average age of the patients was 39.6 years, and 36 (83.7%) of the cases were women. Patients typically presented with persistent, indurated, painful, erythematous, nodular lesions localized to the arms, abdomen, buttocks, and thighs.
While panniculitis has been reported preceding and concurrent with a diagnosis of DM, a number of cases described presentation as late as 5 years following onset of classic DM symptoms.12,13,31 In some cases (3/43 [7.0%]), panniculitis was the only cutaneous manifestation of DM.15,33,36 However, it occurred more commonly with other characteristic skin findings, such as heliotrope rash or Gottron sign.Some investigators have recommended that panniculitis be included as a diagnostic feature of DM and that DM be considered in the differential diagnosis in isolated cases of panniculitis.25,33
Though it seems panniculitis in DM may correlate with a better prognosis, we identified underlying malignancies in 3 cases. Malignancies associated with panniculitis in DM included ovarian adenocarcinoma, nasopharyngeal carcinoma, and parotid carcinoma, indicating that appropriate cancer screening still is critical in the diagnostic workup.2,11,22
A majority of the reported panniculitis cases in DM have responded to treatment with prednisone; however, treatment with prednisone has been more recalcitrant in other cases. Reports of successful additional therapies include methotrexate, cyclosporine, azathioprine, hydroxychloroquine, intravenous immunoglobulin, mepacrine, or a combination of these entities.19,22 In most cases, improvement of the panniculitis and other DM symptoms occurred simultaneously.25 It is noteworthy that the muscular symptoms often resolved more rapidly than cutaneous manifestations.33 Few reported cases (6 including the current case) found a persistent panniculitis despite improvement and remission of the myositis.3,5,10,11,30
Our patient was treated with both prednisone and methotrexate for several months, leading to remission of muscular symptoms (along with return to baseline of creatine phosphokinase), yet the panniculitis did not improve. The subcutaneous nodules also did not respond to treatment with mycophenolate mofetil and hydroxychloroquine.
Recent immunohistochemical studies have suggested that panniculitic lesions show better outcomes with immunosuppressive therapy when compared with other DM-related skin lesions.40 However, this was not the case for our patient, who after months of immunosuppressive therapy showed complete resolution of the periorbital and chest rashes with persistence of multiple indurated subcutaneous nodules.
Our case adds to a number of reports of DM presenting with panniculitis. Our patient fit the classic demographic of previously reported cases, as she was an adult woman without evidence of underlying malignancy; however, our case remains an example of the therapeutic challenge that exists when encountering a persistent, treatment-resistant panniculitis despite resolution of all other features of DM.
- Wick MR. Panniculitis: a summary. Semin Diagn Pathol. 2017;34:261-272.
- Girouard SD, Velez NF, Penson RT, et al. Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol. 2012;148:740-744.
- van Dongen HM, van Vugt RM, Stoof TJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol. 2020;26:E187-E188.
- Choi YJ, Yoo WH. Panniculitis, a rare presentation of onset and exacerbation of juvenile dermatomyositis: a case report and literature review. Arch Rheumatol. 2018;33:367-371.
- Azevedo PO, Castellen NR, Salai AF, et al. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 2018;93:119-121.
- Agulló A, Hinds B, Larrea M, et al. Livedo racemosa, reticulated ulcerations, panniculitis and violaceous plaques in a 46-year-old woman. Indian Dermatol Online J. 2018;9:47-49.
- Hattori Y, Matsuyama K, Takahashi T, et al. Anti-MDA5 antibody-positive dermatomyositis presenting with cellulitis-like erythema on the mandible as an initial symptom. Case Rep Dermatol. 2018;10:110-114.
- Hasegawa A, Shimomura Y, Kibune N, et al. Panniculitis as the initial manifestation of dermatomyositis with anti-MDA5 antibody. Clin Exp Dermatol. 2017;42:551-553.
- Salman A, Kasapcopur O, Ergun T, et al. Panniculitis in juvenile dermatomyositis: report of a case and review of the published work. J Dermatol. 2016;43:951-953.
- Carroll M, Mellick N, Wagner G. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 2015;56:224‐226.
- Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201.
- Otero Rivas MM, Vicente Villa A, González Lara L, et al. Panniculitis in juvenile dermatomyositis. Clin Exp Dermatol. 2015;40:574-575.
- Yanaba K, Tanito K, Hamaguchi Y, et al. Anti‐transcription intermediary factor‐1γ/α/β antibody‐positive dermatomyositis associated with multiple panniculitis lesions. Int J Rheum Dis. 2015;20:1831-1834.
- Pau-Charles I, Moreno PJ, Ortiz-Ibanez K, et al. Anti-MDA5 positive clinically amyopathic dermatomyositis presenting with severe cardiomyopathy. J Eur Acad Dermatol Venereol. 2014;28:1097-1102.
- Lamb R, Digby S, Stewart W, et al. Cutaneous ulceration: more than skin deep? Clin Exp Dermatol. 2013;38:443-445.
- Arias M, Hernández MI, Cunha LG, et al. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146-148.
- Hemmi S, Kushida R, Nishimura H, et al. Magnetic resonance imaging diagnosis of panniculitis in dermatomyositis. Muscle Nerve. 2010;41:151-153.
- Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41:547-549.
- Abdul‐Wahab A, Holden CA, Harland C, et al Calcific panniculitis in adult‐onset dermatomyositis. Clin Exp Dermatol. 2009;34:E854-E856.
- Carneiro S, Alvim G, Resende P, et al. Dermatomyositis with panniculitis. Skinmed. 2007;6:46-47.
- Carrera E, Lobrinus JA, Spertini O, et al. Dermatomyositis, lobarpanniculitis and inflammatory myopathy with abundant macrophages. Neuromuscul Disord. 2006;16:468-471.
- Lin JH, Chu CY, Lin RY. Panniculitis in adult onset dermatomyositis: report of two cases and review of the literature. Dermatol Sinica. 2006;24:194-200.
- Chen GY, Liu MF, Lee JY, et al. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005;15:396-400.
- Nakamori A, Yamaguchi Y, Kurimoto I, et al. Vesiculobullous dermatomyositis with panniculitis without muscle disease. J Am Acad Dermatol. 2003;49:1136-1139.
- Solans R, Cortés J, Selva A, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002;46:S148-S150.
- Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141-144.
- Lee MW, Lim YS, Choi JH, et al. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 1999;26:608‐610.
- Ghali FE, Reed AM, Groben PA, et al. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999;16:270-272.
- Molnar K, Kemeny L, Korom I, et al. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998;139:161‐163.
- Ishikawa O, Tamura A, Ryuzaki K, et al. Membranocystic changes in the panniculitis of dermatomyositis. Br J Dermatol. 1996;134:773-776.
- Sabroe RA, Wallington TB, Kennedy CT. Dermatomyositis treated with high-dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 1995;20:164-167.
- Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995;33:305-307.
- Fusade T, Belanyi P, Joly P, et al. Subcutaneous changes in dermatomyositis. Br J Dermatol. 1993;128:451-453.
- Winkelmann WJ, Billick RC, Srolovitz H. Dermatomyositis presenting as panniculitis. J Am Acad Dermatol. 1990;23:127-128.
- Commens C, O’Neill P, Walker G. Dermatomyositis associated with multifocal lipoatrophy. J Am Acad Dermatol. 1990;22:966-969.
- Raimer SS, Solomon AR, Daniels JC. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 1985;13(2 pt 2):366‐369.
- Feldman D, Hochberg MC, Zizic TM, et al. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 1983;10:85-89.
- Kimura S, Fukuyama Y. Tubular cytoplasmic inclusions in a case of childhood dermatomyositis with migratory subcutaneous nodules. Eur J Pediatr. 1977;125:275-283.
- Weber FP, Gray AMH. Chronic relapsing polydermatomyositis with predominant involvement of the subcutaneous fat. Br J Dermatol. 1924;36:544-560.
- Santos‐Briz A, Calle A, Linos K, et al. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-1359.
- Wick MR. Panniculitis: a summary. Semin Diagn Pathol. 2017;34:261-272.
- Girouard SD, Velez NF, Penson RT, et al. Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol. 2012;148:740-744.
- van Dongen HM, van Vugt RM, Stoof TJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol. 2020;26:E187-E188.
- Choi YJ, Yoo WH. Panniculitis, a rare presentation of onset and exacerbation of juvenile dermatomyositis: a case report and literature review. Arch Rheumatol. 2018;33:367-371.
- Azevedo PO, Castellen NR, Salai AF, et al. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 2018;93:119-121.
- Agulló A, Hinds B, Larrea M, et al. Livedo racemosa, reticulated ulcerations, panniculitis and violaceous plaques in a 46-year-old woman. Indian Dermatol Online J. 2018;9:47-49.
- Hattori Y, Matsuyama K, Takahashi T, et al. Anti-MDA5 antibody-positive dermatomyositis presenting with cellulitis-like erythema on the mandible as an initial symptom. Case Rep Dermatol. 2018;10:110-114.
- Hasegawa A, Shimomura Y, Kibune N, et al. Panniculitis as the initial manifestation of dermatomyositis with anti-MDA5 antibody. Clin Exp Dermatol. 2017;42:551-553.
- Salman A, Kasapcopur O, Ergun T, et al. Panniculitis in juvenile dermatomyositis: report of a case and review of the published work. J Dermatol. 2016;43:951-953.
- Carroll M, Mellick N, Wagner G. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 2015;56:224‐226.
- Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201.
- Otero Rivas MM, Vicente Villa A, González Lara L, et al. Panniculitis in juvenile dermatomyositis. Clin Exp Dermatol. 2015;40:574-575.
- Yanaba K, Tanito K, Hamaguchi Y, et al. Anti‐transcription intermediary factor‐1γ/α/β antibody‐positive dermatomyositis associated with multiple panniculitis lesions. Int J Rheum Dis. 2015;20:1831-1834.
- Pau-Charles I, Moreno PJ, Ortiz-Ibanez K, et al. Anti-MDA5 positive clinically amyopathic dermatomyositis presenting with severe cardiomyopathy. J Eur Acad Dermatol Venereol. 2014;28:1097-1102.
- Lamb R, Digby S, Stewart W, et al. Cutaneous ulceration: more than skin deep? Clin Exp Dermatol. 2013;38:443-445.
- Arias M, Hernández MI, Cunha LG, et al. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146-148.
- Hemmi S, Kushida R, Nishimura H, et al. Magnetic resonance imaging diagnosis of panniculitis in dermatomyositis. Muscle Nerve. 2010;41:151-153.
- Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41:547-549.
- Abdul‐Wahab A, Holden CA, Harland C, et al Calcific panniculitis in adult‐onset dermatomyositis. Clin Exp Dermatol. 2009;34:E854-E856.
- Carneiro S, Alvim G, Resende P, et al. Dermatomyositis with panniculitis. Skinmed. 2007;6:46-47.
- Carrera E, Lobrinus JA, Spertini O, et al. Dermatomyositis, lobarpanniculitis and inflammatory myopathy with abundant macrophages. Neuromuscul Disord. 2006;16:468-471.
- Lin JH, Chu CY, Lin RY. Panniculitis in adult onset dermatomyositis: report of two cases and review of the literature. Dermatol Sinica. 2006;24:194-200.
- Chen GY, Liu MF, Lee JY, et al. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005;15:396-400.
- Nakamori A, Yamaguchi Y, Kurimoto I, et al. Vesiculobullous dermatomyositis with panniculitis without muscle disease. J Am Acad Dermatol. 2003;49:1136-1139.
- Solans R, Cortés J, Selva A, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002;46:S148-S150.
- Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141-144.
- Lee MW, Lim YS, Choi JH, et al. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 1999;26:608‐610.
- Ghali FE, Reed AM, Groben PA, et al. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999;16:270-272.
- Molnar K, Kemeny L, Korom I, et al. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998;139:161‐163.
- Ishikawa O, Tamura A, Ryuzaki K, et al. Membranocystic changes in the panniculitis of dermatomyositis. Br J Dermatol. 1996;134:773-776.
- Sabroe RA, Wallington TB, Kennedy CT. Dermatomyositis treated with high-dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 1995;20:164-167.
- Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995;33:305-307.
- Fusade T, Belanyi P, Joly P, et al. Subcutaneous changes in dermatomyositis. Br J Dermatol. 1993;128:451-453.
- Winkelmann WJ, Billick RC, Srolovitz H. Dermatomyositis presenting as panniculitis. J Am Acad Dermatol. 1990;23:127-128.
- Commens C, O’Neill P, Walker G. Dermatomyositis associated with multifocal lipoatrophy. J Am Acad Dermatol. 1990;22:966-969.
- Raimer SS, Solomon AR, Daniels JC. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 1985;13(2 pt 2):366‐369.
- Feldman D, Hochberg MC, Zizic TM, et al. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 1983;10:85-89.
- Kimura S, Fukuyama Y. Tubular cytoplasmic inclusions in a case of childhood dermatomyositis with migratory subcutaneous nodules. Eur J Pediatr. 1977;125:275-283.
- Weber FP, Gray AMH. Chronic relapsing polydermatomyositis with predominant involvement of the subcutaneous fat. Br J Dermatol. 1924;36:544-560.
- Santos‐Briz A, Calle A, Linos K, et al. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-1359.
Practice Points
- Clinical panniculitis is a rare subcutaneous manifestation of dermatomyositis (DM) that dermatologists must consider when evaluating patients with this condition.
- Panniculitis can precede, occur simultaneously with, or develop up to 5 years after onset of DM.
- Many patients suffer from treatment-resistant panniculitis in DM, suggesting that therapeutic management of this condition may require long-term and more aggressive treatment modalities.
COVID-19: Delta variant is raising the stakes
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Empathetic conversations with unvaccinated people desperately needed
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Diabetes drug’s new weight-loss indication fuels cost-benefit debate
The long list of side effects that follow ads for newer expensive drugs to treat type 2 diabetes sometimes include an unusual warning: They might cause weight loss. That side effect is one that many people – especially those with type 2 diabetes, which is associated with obesity – may desperately want.
So it’s no surprise that some of the same drugs are being reformulated and renamed by manufacturers as a new obesity treatment. No longer limited to the crowded field of treatments for type 2 diabetes, which affects about 10% of Americans, they join the far smaller number of drugs for obesity, which affects 42% of Americans and is ready to be mined for profit.
One that recently hit the market – winning Food and Drug Administration approval in June – is Novo Nordisk’s Wegovy (semaglutide), a higher-dose version of the company’s injectable diabetes drug, Ozempic.
Ozempic’s peppy ads suggest that people who use it might lose weight, but also include a disclaimer: that it “is not a weight-loss drug.” Now – with a new name – it is. And clinical trials showed using it leads to significant weight loss for many patients.
“People who go on this medication lose more weight than with any drug we’ve seen, ever,” said Fatima Cody Stanford, MD, MPH, an obesity medicine specialist at Massachusetts General Hospital and Harvard Medical School, both in Boston, who was not involved with any of the clinical trials.
But that leaves employers and insurers in the uncomfortable position of deciding if it’s worth it.
Wegovy’s monthly wholesale price tag – set at $1,349 – is about 58% more than Ozempic’s, although, the company pointed out, the drug’s injector pens contain more than twice as much of the active ingredient. Studies so far show that patients may need to take it indefinitely to maintain weight loss, translating to a tab that could top $323,000 over 20 years at the current price. Weight-loss treatments are not universally covered by insurance policies.
The arrival of this new class of weight-loss drugs – one from Lilly may soon follow – has created a thicket of issues for those who will pay for them. The decision is complicated by many unknowables concerning their long-term use and whether competition might eventually lower the price.
“The metric we try to use is value,” said James Gelfand, senior vice president for health policy at the ERISA Industry Committee, which represents large, self-insured employers. “If we pay for this drug, how much is this going to cost and how much value will it provide to the beneficiaries?”
Weight-loss treatments have had a lackluster past in this regard, with only modest results. Many employers and insurers likely remember Fen-Phen, a combination of fenfluramine and dexfenfluramine that was pulled from the market in the late 1990s for causing heart valve problems.
New drugs like Wegovy, more effective but also pricier than previous weight-loss treatments, will add more fuel to that debate.
Past treatments were shown to prompt weight loss in the range of 5%-10% of body weight. But many had relatively serious or unpleasant side effects.
Wegovy, however, helped patients lose an average of 15% of their body weight over 68 weeks in the main clinical trial that led to its approval. A comparison group that got a placebo injection lost an average of 2.5% over the same period. On the high end, nearly a third of patients in the treatment group lost 20% or more. Both groups had counseling on diet and exercise.
Side effects, generally considered mild, included nausea, diarrhea, vomiting, and constipation. A few patients developed pancreatitis, a serious inflammation of the pancreas. Like the diabetes medication, the drug carries a warning about a potential risk of a type of thyroid cancer.
Weight loss in those taking Wegovy puts it close to the 20%-25% losses seen with bariatric surgery, said Stanford, and well above the 3%-4% seen with diet and other lifestyle changes alone.
Participants also saw reductions in their waistlines and improvements in their blood pressure and blood sugar levels, which may mean they won’t develop diabetes, said Sean Wharton, MD, an internal medicine specialist and adjunct professor at York University in Toronto who was among the coauthors of the report outlining the results of the first clinical trial on Wegovy.
Since weight loss is known to reduce the risk of heart attack, high blood pressure and diabetes, might the new drug type be worth it?
Covering such treatment would be a sea change for Medicare, which specifically bars coverage for obesity medications or drugs for “anorexia, weight loss, or weight gain,” although it does pay for bariatric surgery. Pharmaceutical companies, patient advocates, and some medical professionals are backing proposed federal legislation to allow coverage. But the legislation, the Treat and Reduce Obesity Act, has not made progress despite being reintroduced every year since 2012, and sponsors are now asking federal officials instead to rewrite existing rules.
Private insurers will have to consider a cost-benefit analysis of adding Wegovy to their list of covered treatments, either broadly or with limits. Obesity was first recognized as a disease by the American Medical Association, easing the path for insurance coverage, in 2013.
“Employers are going to have a bit of a challenge” deciding whether to add the benefit to insurance offerings, said Steve Pearson, founder and president of the Institute for Clinical and Economic Review, which provides cost-benefit analyses of medical treatments but has not yet looked at Wegovy.
The trade-offs are embodied in patients like Phylander Pannell, a 49-year-old Largo, Md., woman who said she lost 65 pounds in a clinical trial of Wegovy. That study gave the drug to all participants for the first 20 weeks, then randomly assigned patients to get either the drug or a placebo for the next 48 weeks to determine what happens when the medication is stopped. Only after the trial ended did she find out she was in the treatment group the entire time.
Her weight fell slowly at first, then ramped up, eventually bringing her 190-pound frame down to about 125. Pains in her joints eased; she felt better all around.
“I definitely feel the drug was it for me,” said Ms. Pannell, who also followed the trial’s guidance on diet and exercise.
The study found that both groups lost weight in the initial 20 weeks, but those who continued to get the drug lost an additional average of 7.9% of their body weight. Those who got a placebo gained back nearly 7%.
After the trial ended, and the COVID-19 pandemic hit, Ms. Pannell regained some weight and is now at 155. She is eager to get back on the medication and hopes her job-based insurance will cover it.
Many employers do cover obesity drugs. For example, about 40% of private employer plans include Novo Nordisk’s once-daily injection called Saxenda on their health plans, said Michael Bachner, Novo Nordisk’s director of media relations.
He said the $1,349-a-month wholesale acquisition price of Wegovy was determined by making it equivalent to that of Saxenda, which is less effective.
Still, that is more than the $851 monthly wholesale price of Ozempic. But, he pointed out, the recommended dosage of Wegovy is more than twice that of Ozempic. Four milligrams come in the Ozempic injector pens for the month, while Wegovy has 9.6.
“There’s more drug in the pen,” Mr. Bachner said. “That drives the price up.”
He added: “This is not a 20-year-old drug that we now have a new indication for and are pricing it higher. It’s a whole different clinical program,” which required new trials.
Now scientists, employers, physicians, and patients will have to decide whether the new drugs are worth it.
Earlier estimates – some commissioned by Novo Nordisk – of the potential cost of adding an obesity drug benefit to Medicare showed an overall reduction in spending when better health from the resulting weight loss was factored in.
Still, those earlier estimates considered much less expensive drugs, including a range of generic and branded drugs costing as little as $7 a month to more than $300, a small fraction of Wegovy’s cost.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The long list of side effects that follow ads for newer expensive drugs to treat type 2 diabetes sometimes include an unusual warning: They might cause weight loss. That side effect is one that many people – especially those with type 2 diabetes, which is associated with obesity – may desperately want.
So it’s no surprise that some of the same drugs are being reformulated and renamed by manufacturers as a new obesity treatment. No longer limited to the crowded field of treatments for type 2 diabetes, which affects about 10% of Americans, they join the far smaller number of drugs for obesity, which affects 42% of Americans and is ready to be mined for profit.
One that recently hit the market – winning Food and Drug Administration approval in June – is Novo Nordisk’s Wegovy (semaglutide), a higher-dose version of the company’s injectable diabetes drug, Ozempic.
Ozempic’s peppy ads suggest that people who use it might lose weight, but also include a disclaimer: that it “is not a weight-loss drug.” Now – with a new name – it is. And clinical trials showed using it leads to significant weight loss for many patients.
“People who go on this medication lose more weight than with any drug we’ve seen, ever,” said Fatima Cody Stanford, MD, MPH, an obesity medicine specialist at Massachusetts General Hospital and Harvard Medical School, both in Boston, who was not involved with any of the clinical trials.
But that leaves employers and insurers in the uncomfortable position of deciding if it’s worth it.
Wegovy’s monthly wholesale price tag – set at $1,349 – is about 58% more than Ozempic’s, although, the company pointed out, the drug’s injector pens contain more than twice as much of the active ingredient. Studies so far show that patients may need to take it indefinitely to maintain weight loss, translating to a tab that could top $323,000 over 20 years at the current price. Weight-loss treatments are not universally covered by insurance policies.
The arrival of this new class of weight-loss drugs – one from Lilly may soon follow – has created a thicket of issues for those who will pay for them. The decision is complicated by many unknowables concerning their long-term use and whether competition might eventually lower the price.
“The metric we try to use is value,” said James Gelfand, senior vice president for health policy at the ERISA Industry Committee, which represents large, self-insured employers. “If we pay for this drug, how much is this going to cost and how much value will it provide to the beneficiaries?”
Weight-loss treatments have had a lackluster past in this regard, with only modest results. Many employers and insurers likely remember Fen-Phen, a combination of fenfluramine and dexfenfluramine that was pulled from the market in the late 1990s for causing heart valve problems.
New drugs like Wegovy, more effective but also pricier than previous weight-loss treatments, will add more fuel to that debate.
Past treatments were shown to prompt weight loss in the range of 5%-10% of body weight. But many had relatively serious or unpleasant side effects.
Wegovy, however, helped patients lose an average of 15% of their body weight over 68 weeks in the main clinical trial that led to its approval. A comparison group that got a placebo injection lost an average of 2.5% over the same period. On the high end, nearly a third of patients in the treatment group lost 20% or more. Both groups had counseling on diet and exercise.
Side effects, generally considered mild, included nausea, diarrhea, vomiting, and constipation. A few patients developed pancreatitis, a serious inflammation of the pancreas. Like the diabetes medication, the drug carries a warning about a potential risk of a type of thyroid cancer.
Weight loss in those taking Wegovy puts it close to the 20%-25% losses seen with bariatric surgery, said Stanford, and well above the 3%-4% seen with diet and other lifestyle changes alone.
Participants also saw reductions in their waistlines and improvements in their blood pressure and blood sugar levels, which may mean they won’t develop diabetes, said Sean Wharton, MD, an internal medicine specialist and adjunct professor at York University in Toronto who was among the coauthors of the report outlining the results of the first clinical trial on Wegovy.
Since weight loss is known to reduce the risk of heart attack, high blood pressure and diabetes, might the new drug type be worth it?
Covering such treatment would be a sea change for Medicare, which specifically bars coverage for obesity medications or drugs for “anorexia, weight loss, or weight gain,” although it does pay for bariatric surgery. Pharmaceutical companies, patient advocates, and some medical professionals are backing proposed federal legislation to allow coverage. But the legislation, the Treat and Reduce Obesity Act, has not made progress despite being reintroduced every year since 2012, and sponsors are now asking federal officials instead to rewrite existing rules.
Private insurers will have to consider a cost-benefit analysis of adding Wegovy to their list of covered treatments, either broadly or with limits. Obesity was first recognized as a disease by the American Medical Association, easing the path for insurance coverage, in 2013.
“Employers are going to have a bit of a challenge” deciding whether to add the benefit to insurance offerings, said Steve Pearson, founder and president of the Institute for Clinical and Economic Review, which provides cost-benefit analyses of medical treatments but has not yet looked at Wegovy.
The trade-offs are embodied in patients like Phylander Pannell, a 49-year-old Largo, Md., woman who said she lost 65 pounds in a clinical trial of Wegovy. That study gave the drug to all participants for the first 20 weeks, then randomly assigned patients to get either the drug or a placebo for the next 48 weeks to determine what happens when the medication is stopped. Only after the trial ended did she find out she was in the treatment group the entire time.
Her weight fell slowly at first, then ramped up, eventually bringing her 190-pound frame down to about 125. Pains in her joints eased; she felt better all around.
“I definitely feel the drug was it for me,” said Ms. Pannell, who also followed the trial’s guidance on diet and exercise.
The study found that both groups lost weight in the initial 20 weeks, but those who continued to get the drug lost an additional average of 7.9% of their body weight. Those who got a placebo gained back nearly 7%.
After the trial ended, and the COVID-19 pandemic hit, Ms. Pannell regained some weight and is now at 155. She is eager to get back on the medication and hopes her job-based insurance will cover it.
Many employers do cover obesity drugs. For example, about 40% of private employer plans include Novo Nordisk’s once-daily injection called Saxenda on their health plans, said Michael Bachner, Novo Nordisk’s director of media relations.
He said the $1,349-a-month wholesale acquisition price of Wegovy was determined by making it equivalent to that of Saxenda, which is less effective.
Still, that is more than the $851 monthly wholesale price of Ozempic. But, he pointed out, the recommended dosage of Wegovy is more than twice that of Ozempic. Four milligrams come in the Ozempic injector pens for the month, while Wegovy has 9.6.
“There’s more drug in the pen,” Mr. Bachner said. “That drives the price up.”
He added: “This is not a 20-year-old drug that we now have a new indication for and are pricing it higher. It’s a whole different clinical program,” which required new trials.
Now scientists, employers, physicians, and patients will have to decide whether the new drugs are worth it.
Earlier estimates – some commissioned by Novo Nordisk – of the potential cost of adding an obesity drug benefit to Medicare showed an overall reduction in spending when better health from the resulting weight loss was factored in.
Still, those earlier estimates considered much less expensive drugs, including a range of generic and branded drugs costing as little as $7 a month to more than $300, a small fraction of Wegovy’s cost.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The long list of side effects that follow ads for newer expensive drugs to treat type 2 diabetes sometimes include an unusual warning: They might cause weight loss. That side effect is one that many people – especially those with type 2 diabetes, which is associated with obesity – may desperately want.
So it’s no surprise that some of the same drugs are being reformulated and renamed by manufacturers as a new obesity treatment. No longer limited to the crowded field of treatments for type 2 diabetes, which affects about 10% of Americans, they join the far smaller number of drugs for obesity, which affects 42% of Americans and is ready to be mined for profit.
One that recently hit the market – winning Food and Drug Administration approval in June – is Novo Nordisk’s Wegovy (semaglutide), a higher-dose version of the company’s injectable diabetes drug, Ozempic.
Ozempic’s peppy ads suggest that people who use it might lose weight, but also include a disclaimer: that it “is not a weight-loss drug.” Now – with a new name – it is. And clinical trials showed using it leads to significant weight loss for many patients.
“People who go on this medication lose more weight than with any drug we’ve seen, ever,” said Fatima Cody Stanford, MD, MPH, an obesity medicine specialist at Massachusetts General Hospital and Harvard Medical School, both in Boston, who was not involved with any of the clinical trials.
But that leaves employers and insurers in the uncomfortable position of deciding if it’s worth it.
Wegovy’s monthly wholesale price tag – set at $1,349 – is about 58% more than Ozempic’s, although, the company pointed out, the drug’s injector pens contain more than twice as much of the active ingredient. Studies so far show that patients may need to take it indefinitely to maintain weight loss, translating to a tab that could top $323,000 over 20 years at the current price. Weight-loss treatments are not universally covered by insurance policies.
The arrival of this new class of weight-loss drugs – one from Lilly may soon follow – has created a thicket of issues for those who will pay for them. The decision is complicated by many unknowables concerning their long-term use and whether competition might eventually lower the price.
“The metric we try to use is value,” said James Gelfand, senior vice president for health policy at the ERISA Industry Committee, which represents large, self-insured employers. “If we pay for this drug, how much is this going to cost and how much value will it provide to the beneficiaries?”
Weight-loss treatments have had a lackluster past in this regard, with only modest results. Many employers and insurers likely remember Fen-Phen, a combination of fenfluramine and dexfenfluramine that was pulled from the market in the late 1990s for causing heart valve problems.
New drugs like Wegovy, more effective but also pricier than previous weight-loss treatments, will add more fuel to that debate.
Past treatments were shown to prompt weight loss in the range of 5%-10% of body weight. But many had relatively serious or unpleasant side effects.
Wegovy, however, helped patients lose an average of 15% of their body weight over 68 weeks in the main clinical trial that led to its approval. A comparison group that got a placebo injection lost an average of 2.5% over the same period. On the high end, nearly a third of patients in the treatment group lost 20% or more. Both groups had counseling on diet and exercise.
Side effects, generally considered mild, included nausea, diarrhea, vomiting, and constipation. A few patients developed pancreatitis, a serious inflammation of the pancreas. Like the diabetes medication, the drug carries a warning about a potential risk of a type of thyroid cancer.
Weight loss in those taking Wegovy puts it close to the 20%-25% losses seen with bariatric surgery, said Stanford, and well above the 3%-4% seen with diet and other lifestyle changes alone.
Participants also saw reductions in their waistlines and improvements in their blood pressure and blood sugar levels, which may mean they won’t develop diabetes, said Sean Wharton, MD, an internal medicine specialist and adjunct professor at York University in Toronto who was among the coauthors of the report outlining the results of the first clinical trial on Wegovy.
Since weight loss is known to reduce the risk of heart attack, high blood pressure and diabetes, might the new drug type be worth it?
Covering such treatment would be a sea change for Medicare, which specifically bars coverage for obesity medications or drugs for “anorexia, weight loss, or weight gain,” although it does pay for bariatric surgery. Pharmaceutical companies, patient advocates, and some medical professionals are backing proposed federal legislation to allow coverage. But the legislation, the Treat and Reduce Obesity Act, has not made progress despite being reintroduced every year since 2012, and sponsors are now asking federal officials instead to rewrite existing rules.
Private insurers will have to consider a cost-benefit analysis of adding Wegovy to their list of covered treatments, either broadly or with limits. Obesity was first recognized as a disease by the American Medical Association, easing the path for insurance coverage, in 2013.
“Employers are going to have a bit of a challenge” deciding whether to add the benefit to insurance offerings, said Steve Pearson, founder and president of the Institute for Clinical and Economic Review, which provides cost-benefit analyses of medical treatments but has not yet looked at Wegovy.
The trade-offs are embodied in patients like Phylander Pannell, a 49-year-old Largo, Md., woman who said she lost 65 pounds in a clinical trial of Wegovy. That study gave the drug to all participants for the first 20 weeks, then randomly assigned patients to get either the drug or a placebo for the next 48 weeks to determine what happens when the medication is stopped. Only after the trial ended did she find out she was in the treatment group the entire time.
Her weight fell slowly at first, then ramped up, eventually bringing her 190-pound frame down to about 125. Pains in her joints eased; she felt better all around.
“I definitely feel the drug was it for me,” said Ms. Pannell, who also followed the trial’s guidance on diet and exercise.
The study found that both groups lost weight in the initial 20 weeks, but those who continued to get the drug lost an additional average of 7.9% of their body weight. Those who got a placebo gained back nearly 7%.
After the trial ended, and the COVID-19 pandemic hit, Ms. Pannell regained some weight and is now at 155. She is eager to get back on the medication and hopes her job-based insurance will cover it.
Many employers do cover obesity drugs. For example, about 40% of private employer plans include Novo Nordisk’s once-daily injection called Saxenda on their health plans, said Michael Bachner, Novo Nordisk’s director of media relations.
He said the $1,349-a-month wholesale acquisition price of Wegovy was determined by making it equivalent to that of Saxenda, which is less effective.
Still, that is more than the $851 monthly wholesale price of Ozempic. But, he pointed out, the recommended dosage of Wegovy is more than twice that of Ozempic. Four milligrams come in the Ozempic injector pens for the month, while Wegovy has 9.6.
“There’s more drug in the pen,” Mr. Bachner said. “That drives the price up.”
He added: “This is not a 20-year-old drug that we now have a new indication for and are pricing it higher. It’s a whole different clinical program,” which required new trials.
Now scientists, employers, physicians, and patients will have to decide whether the new drugs are worth it.
Earlier estimates – some commissioned by Novo Nordisk – of the potential cost of adding an obesity drug benefit to Medicare showed an overall reduction in spending when better health from the resulting weight loss was factored in.
Still, those earlier estimates considered much less expensive drugs, including a range of generic and branded drugs costing as little as $7 a month to more than $300, a small fraction of Wegovy’s cost.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Vaccination alone won’t counter rise of resistant variants: Study
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
C. diff eradication not necessary for clinical cure of recurrent infections with fecal transplant
It’s not necessary to completely eradicate all Clostridioides difficile to successfully treat recurrent C. difficile infections with fecal microbiota transplant (FMT), according to a study presented online July 12 at the European Congress of Clinical Microbiology & Infectious Diseases.
C. difficile colonization persisted for 3 weeks after FMT in about one-quarter of patients, but it’s not clear whether this is a persistent infection, a newly acquired infection, or partial persistence of a mixed infection, said Elisabeth Terveer, MD, a medical microbiologist at Leiden (the Netherlands) University Medical Center. In addition, “82% of patients with detectable C. diff do not relapse, so it’s absolutely not necessary for a cure,” she said.
Several mechanisms explain why FMT is a highly effective therapy for recurrent C. difficile infections, including restoration of bacterial metabolism in the gut, immune modulation, and direct competition between bacteria, Dr. Terveer said, but it’s less clear whether eradication of C. difficile spores is among these mechanisms.
Between May 2016 and April 2020, the researchers analyzed fecal samples from 84 patients who took vancomycin for at least 4 days before undergoing FMT. The researchers took fecal samples from patients before FMT and 3 weeks after FMT to culture them and the donor samples for presence of C. difficile, and they assessed clinical outcomes at 3 weeks and 6 months after FMT.
After antibiotic treatment but prior to FMT, 19% of patients (n = 16) still had a toxigenic C. difficile culture while the other 81% had a negative culture. None of the donor samples had a positive C. difficile culture. After FMT treatment, five patients who had a positive pre-FMT culture remained positive, and the other 11 were negative. Among the 81% of patients (n = 68) who had a negative culture just before FMT, 22 had a positive culture and 46 had a negative culture after FMT. Overall, 26% of patients post FMT had a positive C. difficile culture, a finding that was 10-fold higher than another study that assessed C. difficile with PCR testing, Dr. Terveer said.
The clinical cure rate after FMT was 94%, and five patients had relapses within 2 months of their FMT. These relapses were more prevalent in patients with a positive C. difficile culture prior to FMT (odds ratio [OR], 7.6; P = .045) and a positive C. difficile culture after FMT (OR, 13.6; P = .016). Still, 82% of patients who had a positive C. difficile culture post FMT remained clinically cured 2 months later.
It’s unclear why 19% of patients had a positive culture after their antibiotic pretreatment prior to FMT, Dr. Terveer said, but it may be because the pretreatment was of such a short duration.
“I think the advice should be: Give a full anti–C. diff antibiotic course to treat the C. diff infection, and then give FMT afterward to restore the microbiota and prevent further relapses,” Dr. Terveer told attendees.
Dimitri Drekonja, MD, chief of the Minneapolis VA Infectious Disease Section, said the findings were not necessarily surprising, but it would have been interesting for the researchers to have conducted DNA sequencing of the patients’ fecal samples post FMT to see what the biological diversity looked like.
“One school of thought has been that you have to repopulate the normal diverse microbiota of the colon” with FMT, and the other “is that you need to get rid of the C. diff that›s there,” Dr. Drekonja, who was not involved in the study, said in an interview. “I think more people think it’s the diverse microbiota because if it’s just getting rid of C. diff, we can get do that with antibiotics – but that gets rid of the other organisms.”
As long as you have a diverse microbiota post FMT, Dr. Drekonja said, then “having a few residual organisms, even if they get magnified in the culture process, is probably not that big a deal.”
But there’s a third school of thought that Dr. Drekonja said he himself falls into: “I don’t really care how it works, just that in well-done trials, it does work.” As long as large, robust, well-blinded trials show that FMT works, “I’m open to all sorts of ideas of what the mechanism is,” he said. “The main thing is that it does or doesn’t work.”
These findings basically reinforce current guidance not to test patients’ stools if they are asymptomatic, Dr. Drekonja said. In the past, clinicians sometimes tested patients’ stool after therapy to ensure the C. difficile was eradicated, regardless of whether the patient had symptoms of infection, he said.
“We’ve since become much more attuned that there are lots of people who have detectable C. diff in their stool without any symptoms,” whether detectable by culture or PCR, Dr. Drekonja said. “Generally, if you’re doing well and you’re not having diarrhea, don’t test, and if someone does test and finds it, pretend you didn’t see the test,” he advised. “This is a big part of diagnostic stewardship, which is: You don’t go testing people who are doing well.”
The Netherlands Donor Feces Bank used in the research is funded by a grant from Vedanta Biosciences. Dr. Drekonja had no disclosures.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center: www.gastro.org/Cdiff.
A version of this article first appeared on Medscape.com.
It’s not necessary to completely eradicate all Clostridioides difficile to successfully treat recurrent C. difficile infections with fecal microbiota transplant (FMT), according to a study presented online July 12 at the European Congress of Clinical Microbiology & Infectious Diseases.
C. difficile colonization persisted for 3 weeks after FMT in about one-quarter of patients, but it’s not clear whether this is a persistent infection, a newly acquired infection, or partial persistence of a mixed infection, said Elisabeth Terveer, MD, a medical microbiologist at Leiden (the Netherlands) University Medical Center. In addition, “82% of patients with detectable C. diff do not relapse, so it’s absolutely not necessary for a cure,” she said.
Several mechanisms explain why FMT is a highly effective therapy for recurrent C. difficile infections, including restoration of bacterial metabolism in the gut, immune modulation, and direct competition between bacteria, Dr. Terveer said, but it’s less clear whether eradication of C. difficile spores is among these mechanisms.
Between May 2016 and April 2020, the researchers analyzed fecal samples from 84 patients who took vancomycin for at least 4 days before undergoing FMT. The researchers took fecal samples from patients before FMT and 3 weeks after FMT to culture them and the donor samples for presence of C. difficile, and they assessed clinical outcomes at 3 weeks and 6 months after FMT.
After antibiotic treatment but prior to FMT, 19% of patients (n = 16) still had a toxigenic C. difficile culture while the other 81% had a negative culture. None of the donor samples had a positive C. difficile culture. After FMT treatment, five patients who had a positive pre-FMT culture remained positive, and the other 11 were negative. Among the 81% of patients (n = 68) who had a negative culture just before FMT, 22 had a positive culture and 46 had a negative culture after FMT. Overall, 26% of patients post FMT had a positive C. difficile culture, a finding that was 10-fold higher than another study that assessed C. difficile with PCR testing, Dr. Terveer said.
The clinical cure rate after FMT was 94%, and five patients had relapses within 2 months of their FMT. These relapses were more prevalent in patients with a positive C. difficile culture prior to FMT (odds ratio [OR], 7.6; P = .045) and a positive C. difficile culture after FMT (OR, 13.6; P = .016). Still, 82% of patients who had a positive C. difficile culture post FMT remained clinically cured 2 months later.
It’s unclear why 19% of patients had a positive culture after their antibiotic pretreatment prior to FMT, Dr. Terveer said, but it may be because the pretreatment was of such a short duration.
“I think the advice should be: Give a full anti–C. diff antibiotic course to treat the C. diff infection, and then give FMT afterward to restore the microbiota and prevent further relapses,” Dr. Terveer told attendees.
Dimitri Drekonja, MD, chief of the Minneapolis VA Infectious Disease Section, said the findings were not necessarily surprising, but it would have been interesting for the researchers to have conducted DNA sequencing of the patients’ fecal samples post FMT to see what the biological diversity looked like.
“One school of thought has been that you have to repopulate the normal diverse microbiota of the colon” with FMT, and the other “is that you need to get rid of the C. diff that›s there,” Dr. Drekonja, who was not involved in the study, said in an interview. “I think more people think it’s the diverse microbiota because if it’s just getting rid of C. diff, we can get do that with antibiotics – but that gets rid of the other organisms.”
As long as you have a diverse microbiota post FMT, Dr. Drekonja said, then “having a few residual organisms, even if they get magnified in the culture process, is probably not that big a deal.”
But there’s a third school of thought that Dr. Drekonja said he himself falls into: “I don’t really care how it works, just that in well-done trials, it does work.” As long as large, robust, well-blinded trials show that FMT works, “I’m open to all sorts of ideas of what the mechanism is,” he said. “The main thing is that it does or doesn’t work.”
These findings basically reinforce current guidance not to test patients’ stools if they are asymptomatic, Dr. Drekonja said. In the past, clinicians sometimes tested patients’ stool after therapy to ensure the C. difficile was eradicated, regardless of whether the patient had symptoms of infection, he said.
“We’ve since become much more attuned that there are lots of people who have detectable C. diff in their stool without any symptoms,” whether detectable by culture or PCR, Dr. Drekonja said. “Generally, if you’re doing well and you’re not having diarrhea, don’t test, and if someone does test and finds it, pretend you didn’t see the test,” he advised. “This is a big part of diagnostic stewardship, which is: You don’t go testing people who are doing well.”
The Netherlands Donor Feces Bank used in the research is funded by a grant from Vedanta Biosciences. Dr. Drekonja had no disclosures.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center: www.gastro.org/Cdiff.
A version of this article first appeared on Medscape.com.
It’s not necessary to completely eradicate all Clostridioides difficile to successfully treat recurrent C. difficile infections with fecal microbiota transplant (FMT), according to a study presented online July 12 at the European Congress of Clinical Microbiology & Infectious Diseases.
C. difficile colonization persisted for 3 weeks after FMT in about one-quarter of patients, but it’s not clear whether this is a persistent infection, a newly acquired infection, or partial persistence of a mixed infection, said Elisabeth Terveer, MD, a medical microbiologist at Leiden (the Netherlands) University Medical Center. In addition, “82% of patients with detectable C. diff do not relapse, so it’s absolutely not necessary for a cure,” she said.
Several mechanisms explain why FMT is a highly effective therapy for recurrent C. difficile infections, including restoration of bacterial metabolism in the gut, immune modulation, and direct competition between bacteria, Dr. Terveer said, but it’s less clear whether eradication of C. difficile spores is among these mechanisms.
Between May 2016 and April 2020, the researchers analyzed fecal samples from 84 patients who took vancomycin for at least 4 days before undergoing FMT. The researchers took fecal samples from patients before FMT and 3 weeks after FMT to culture them and the donor samples for presence of C. difficile, and they assessed clinical outcomes at 3 weeks and 6 months after FMT.
After antibiotic treatment but prior to FMT, 19% of patients (n = 16) still had a toxigenic C. difficile culture while the other 81% had a negative culture. None of the donor samples had a positive C. difficile culture. After FMT treatment, five patients who had a positive pre-FMT culture remained positive, and the other 11 were negative. Among the 81% of patients (n = 68) who had a negative culture just before FMT, 22 had a positive culture and 46 had a negative culture after FMT. Overall, 26% of patients post FMT had a positive C. difficile culture, a finding that was 10-fold higher than another study that assessed C. difficile with PCR testing, Dr. Terveer said.
The clinical cure rate after FMT was 94%, and five patients had relapses within 2 months of their FMT. These relapses were more prevalent in patients with a positive C. difficile culture prior to FMT (odds ratio [OR], 7.6; P = .045) and a positive C. difficile culture after FMT (OR, 13.6; P = .016). Still, 82% of patients who had a positive C. difficile culture post FMT remained clinically cured 2 months later.
It’s unclear why 19% of patients had a positive culture after their antibiotic pretreatment prior to FMT, Dr. Terveer said, but it may be because the pretreatment was of such a short duration.
“I think the advice should be: Give a full anti–C. diff antibiotic course to treat the C. diff infection, and then give FMT afterward to restore the microbiota and prevent further relapses,” Dr. Terveer told attendees.
Dimitri Drekonja, MD, chief of the Minneapolis VA Infectious Disease Section, said the findings were not necessarily surprising, but it would have been interesting for the researchers to have conducted DNA sequencing of the patients’ fecal samples post FMT to see what the biological diversity looked like.
“One school of thought has been that you have to repopulate the normal diverse microbiota of the colon” with FMT, and the other “is that you need to get rid of the C. diff that›s there,” Dr. Drekonja, who was not involved in the study, said in an interview. “I think more people think it’s the diverse microbiota because if it’s just getting rid of C. diff, we can get do that with antibiotics – but that gets rid of the other organisms.”
As long as you have a diverse microbiota post FMT, Dr. Drekonja said, then “having a few residual organisms, even if they get magnified in the culture process, is probably not that big a deal.”
But there’s a third school of thought that Dr. Drekonja said he himself falls into: “I don’t really care how it works, just that in well-done trials, it does work.” As long as large, robust, well-blinded trials show that FMT works, “I’m open to all sorts of ideas of what the mechanism is,” he said. “The main thing is that it does or doesn’t work.”
These findings basically reinforce current guidance not to test patients’ stools if they are asymptomatic, Dr. Drekonja said. In the past, clinicians sometimes tested patients’ stool after therapy to ensure the C. difficile was eradicated, regardless of whether the patient had symptoms of infection, he said.
“We’ve since become much more attuned that there are lots of people who have detectable C. diff in their stool without any symptoms,” whether detectable by culture or PCR, Dr. Drekonja said. “Generally, if you’re doing well and you’re not having diarrhea, don’t test, and if someone does test and finds it, pretend you didn’t see the test,” he advised. “This is a big part of diagnostic stewardship, which is: You don’t go testing people who are doing well.”
The Netherlands Donor Feces Bank used in the research is funded by a grant from Vedanta Biosciences. Dr. Drekonja had no disclosures.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center: www.gastro.org/Cdiff.
A version of this article first appeared on Medscape.com.
Indoor masking needed in almost 70% of U.S. counties: CDC data
In announcing new guidance on July 27, the CDC said vaccinated people should wear face masks in indoor public places with “high” or “substantial” community transmission rates of COVID-19.
Data from the CDC shows that designation covers 69.3% of all counties in the United States – 52.2% (1,680 counties) with high community transmission rates and 17.1% (551 counties) with substantial rates.
A county has “high transmission” if it reports 100 or more weekly cases per 100,000 residents or a 10% or higher test positivity rate in the last 7 days, the CDC said. “Substantial transmission” means a county reports 50-99 weekly cases per 100,000 residents or has a positivity rate between 8% and 9.9% in the last 7 days.
About 23% of U.S. counties had moderate rates of community transmission, and 7.67% had low rates.
To find out the transmission rate in your county, go to the CDC COVID data tracker.
Smithsonian requiring masks again
The Smithsonian now requires all visitors over age 2, regardless of vaccination status, to wear face masks indoors and in all museum spaces.
The Smithsonian said in a news release that fully vaccinated visitors won’t have to wear masks at the National Zoo or outdoor gardens for museums.
The new rule goes into effect Aug. 6. It reverses a rule that said fully vaccinated visitors didn’t have to wear masks indoors beginning June 28.
Indoor face masks will be required throughout the District of Columbia beginning July 31., D.C. Mayor Muriel Bowser.
House Republicans protest face mask policy
About 40 maskless Republican members of the U.S. House of Representatives filed onto the Senate floor on July 29 to protest a new rule requiring House members to wear face masks, the Hill reported.
Congress’s attending doctor said in a memo that the 435 members of the House, plus workers, must wear masks indoors, but not the 100 members of the Senate. The Senate is a smaller body and has had better mask compliance than the House.
Rep. Ronny Jackson (R-Tex.), told the Hill that Republicans wanted to show “what it was like on the floor of the Senate versus the floor of the House. Obviously, it’s vastly different.”
Among the group of Republicans who filed onto the Senate floor were Rep. Lauren Boebert of Colorado, Rep. Matt Gaetz and Rep. Byron Donalds of Florida, Rep. Marjorie Taylor Greene of Georgia, Rep. Chip Roy and Rep. Louie Gohmert of Texas, Rep. Madison Cawthorn of North Carolina, Rep. Warren Davidson of Ohio, and Rep. Andy Biggs of Arizona.
A version of this article first appeared on WebMD.com.
In announcing new guidance on July 27, the CDC said vaccinated people should wear face masks in indoor public places with “high” or “substantial” community transmission rates of COVID-19.
Data from the CDC shows that designation covers 69.3% of all counties in the United States – 52.2% (1,680 counties) with high community transmission rates and 17.1% (551 counties) with substantial rates.
A county has “high transmission” if it reports 100 or more weekly cases per 100,000 residents or a 10% or higher test positivity rate in the last 7 days, the CDC said. “Substantial transmission” means a county reports 50-99 weekly cases per 100,000 residents or has a positivity rate between 8% and 9.9% in the last 7 days.
About 23% of U.S. counties had moderate rates of community transmission, and 7.67% had low rates.
To find out the transmission rate in your county, go to the CDC COVID data tracker.
Smithsonian requiring masks again
The Smithsonian now requires all visitors over age 2, regardless of vaccination status, to wear face masks indoors and in all museum spaces.
The Smithsonian said in a news release that fully vaccinated visitors won’t have to wear masks at the National Zoo or outdoor gardens for museums.
The new rule goes into effect Aug. 6. It reverses a rule that said fully vaccinated visitors didn’t have to wear masks indoors beginning June 28.
Indoor face masks will be required throughout the District of Columbia beginning July 31., D.C. Mayor Muriel Bowser.
House Republicans protest face mask policy
About 40 maskless Republican members of the U.S. House of Representatives filed onto the Senate floor on July 29 to protest a new rule requiring House members to wear face masks, the Hill reported.
Congress’s attending doctor said in a memo that the 435 members of the House, plus workers, must wear masks indoors, but not the 100 members of the Senate. The Senate is a smaller body and has had better mask compliance than the House.
Rep. Ronny Jackson (R-Tex.), told the Hill that Republicans wanted to show “what it was like on the floor of the Senate versus the floor of the House. Obviously, it’s vastly different.”
Among the group of Republicans who filed onto the Senate floor were Rep. Lauren Boebert of Colorado, Rep. Matt Gaetz and Rep. Byron Donalds of Florida, Rep. Marjorie Taylor Greene of Georgia, Rep. Chip Roy and Rep. Louie Gohmert of Texas, Rep. Madison Cawthorn of North Carolina, Rep. Warren Davidson of Ohio, and Rep. Andy Biggs of Arizona.
A version of this article first appeared on WebMD.com.
In announcing new guidance on July 27, the CDC said vaccinated people should wear face masks in indoor public places with “high” or “substantial” community transmission rates of COVID-19.
Data from the CDC shows that designation covers 69.3% of all counties in the United States – 52.2% (1,680 counties) with high community transmission rates and 17.1% (551 counties) with substantial rates.
A county has “high transmission” if it reports 100 or more weekly cases per 100,000 residents or a 10% or higher test positivity rate in the last 7 days, the CDC said. “Substantial transmission” means a county reports 50-99 weekly cases per 100,000 residents or has a positivity rate between 8% and 9.9% in the last 7 days.
About 23% of U.S. counties had moderate rates of community transmission, and 7.67% had low rates.
To find out the transmission rate in your county, go to the CDC COVID data tracker.
Smithsonian requiring masks again
The Smithsonian now requires all visitors over age 2, regardless of vaccination status, to wear face masks indoors and in all museum spaces.
The Smithsonian said in a news release that fully vaccinated visitors won’t have to wear masks at the National Zoo or outdoor gardens for museums.
The new rule goes into effect Aug. 6. It reverses a rule that said fully vaccinated visitors didn’t have to wear masks indoors beginning June 28.
Indoor face masks will be required throughout the District of Columbia beginning July 31., D.C. Mayor Muriel Bowser.
House Republicans protest face mask policy
About 40 maskless Republican members of the U.S. House of Representatives filed onto the Senate floor on July 29 to protest a new rule requiring House members to wear face masks, the Hill reported.
Congress’s attending doctor said in a memo that the 435 members of the House, plus workers, must wear masks indoors, but not the 100 members of the Senate. The Senate is a smaller body and has had better mask compliance than the House.
Rep. Ronny Jackson (R-Tex.), told the Hill that Republicans wanted to show “what it was like on the floor of the Senate versus the floor of the House. Obviously, it’s vastly different.”
Among the group of Republicans who filed onto the Senate floor were Rep. Lauren Boebert of Colorado, Rep. Matt Gaetz and Rep. Byron Donalds of Florida, Rep. Marjorie Taylor Greene of Georgia, Rep. Chip Roy and Rep. Louie Gohmert of Texas, Rep. Madison Cawthorn of North Carolina, Rep. Warren Davidson of Ohio, and Rep. Andy Biggs of Arizona.
A version of this article first appeared on WebMD.com.
‘War has changed’: CDC says Delta as contagious as chicken pox
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
COVID brings evolutionary virologists out of the shadows, into the fight
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
Needed: More studies of CSF molecular biomarkers in psychiatric disorders
Psychiatry and neurology are the brain’s twin medical disciplines. Unlike neurologic brain disorders, where localizing the “lesion” is a primary objective, psychiatric brain disorders are much more subtle, with no “gross” lesions but numerous cellular and molecular pathologies within neural circuits.
Measuring the molecular components of the cerebrospinal fluid (CSF), the glorious “sewage system” of the brain, may help reveal granular clues to the neurobiology of psychiatric disorders.
Mental illnesses involve the disruption of brain structures and functions in a diffuse manner across the cortex. Abnormal neuroplasticity has been implicated in several major psychiatric disorders. Examples include hypoplasia of the hippocampus in major depressive disorder and cortical thinning/dysplasia in schizophrenia. Reductions of neurotropic factors such as nerve growth factor or brain-derived neurotropic factor have been reported in mood and psychotic disorders, and appear to correlate with neuroplasticity changes.
Recent advances in psychiatric neuroscience have provided many clues to the pathophysiology of psychopathological conditions, including neuroinflammation, oxidative stress, apoptosis, impaired energy metabolism, abnormal metabolomics and lipidomics, and hypo- and hyperfunction of various neurotransmitters systems (especially glutamate N-methyl-
Thus, psychiatric research should focus on exploring and detecting molecular signatures (ie, biomarkers) of psychiatric disorders, including biomarkers of axonal and synaptic damage, glial activation, and oxidative stress. This is especially critical given the extensive heterogeneity of schizophrenia and mood and anxiety disorders. The CSF is a vastly unexploited substrate for discovering molecular biomarkers that will pave the way to precision psychiatry, and possibly open the door for completely new therapeutic strategies to tackle the most challenging neuropsychiatric disorders.
A role for CSF analysis
It’s quite puzzling why acute psychiatric episodes of schizophrenia, bipolar disorder, major depressive disorder, or panic attacks are not routinely assessed with a spinal tap, in conjunction with other brain measures such as neuroimaging (morphology, spectroscopy, cerebral blood flow, and diffusion tensor imaging) as well as a comprehensive neurocognitive examination and neurophysiological tests such as pre-pulse inhibition, mismatch negativity, and P-50, N-10, and P-300 evoked potentials. Combining CSF analysis with all those measures may help us stratify the spectra of psychosis, depression, and anxiety, as well as posttraumatic stress disorder and obsessive-compulsive disorder, into unique biotypes with overlapping clinical phenotypes and specific treatment approaches.
There are relatively few published CSF studies in psychiatric patients (mostly schizophrenia and bipolar and depressive disorders). The Table1-9 shows some of those findings. More than 365 biomarkers have been reported in schizophrenia, most of them in serum and tissue.10 However, none of them can be used for diagnostic purposes because schizophrenia is a syndrome comprised of several hundred different diseases (biotypes) that have similar clinical symptoms. Many of the serum and tissue biomarkers have not been studied in CSF, and they must if advances in the neurobiology and treatment of the psychotic and mood spectra are to be achieved. And adapting the CSF biomarkers described in neurologic disorders such as multiple sclerosis11 to schizophrenia and bipolar disorder (which also have well-established myelin pathologies) may yield a trove of neurobiologic findings.
If CSF studies eventually prove to be very useful for identifying subtypes for diagnosis and treatment, psychiatrists do not have to do the lumbar puncture themselves, but may refer patients to a “spinal tap” laboratory, just as they refer patients to a phlebotomy laboratory for routine blood tests. The adoption of CSF assessment in psychiatry will solidify its status as a clinical neuroscience, like its sister, neurology.
1. Vasic N, Connemann BJ, Wolf RC, et al. Cerebrospinal fluid biomarker candidates of schizophrenia: where do we stand? Eur Arch Psychiatry Clin Neurosci. 2012;262(5):375-391.
2. Pollak TA, Drndarski S, Stone JM, et al. The blood-brain barrier in psychosis. Lancet Psychiatry. 2018;5(1):79-92.
3. Katisko K, Cajanus A, Jääskeläinen O, et al. Serum neurofilament light chain is a discriminative biomarker between frontotemporal lobar degeneration and primary psychiatric disorders. J Neurol. 2020;267(1):162-167.
4. Bechter K, Reiber H, Herzog S, et al. Cerebrospinal fluid analysis in affective and schizophrenic spectrum disorders: identification of subgroups with immune responses and blood-CSF barrier dysfunction. J Psychiatr Res. 2010;44(5):321-330.
5. Hidese S, Hattori K, Sasayama D, et al. Cerebrospinal fluid neural cell adhesion molecule levels and their correlation with clinical variables in patients with schizophrenia, bipolar disorder, and major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2017;76:12-18.
6. Tunca Z, Kıvırcık Akdede B, Özerdem A, et al. Diverse glial cell line-derived neurotrophic factor (GDNF) support between mania and schizophrenia: a comparative study in four major psychiatric disorders. Eur Psychiatry. 2015;30(2):198-204.
7. Al Shweiki MR, Oeckl P, Steinacker P, et al. Major depressive disorder: insight into candidate cerebrospinal fluid protein biomarkers from proteomics studies. Expert Rev Proteomics. 2017;14(6):499-514.
8. Kroksmark H, Vinberg M. Does S100B have a potential role in affective disorders? A literature review. Nord J Psychiatry. 2018;72(7):462-470.
9. Orlovska-Waast S, Köhler-Forsberg O, Brix SW, et al. Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol Psychiatry. 2019;24(6):869-887.
10. Nasrallah HA. Lab tests for psychiatric disorders: few clinicians are aware of them. Current Psychiatry. 2013;12(2):5-7.
11. Porter L, Shoushtarizadeh A, Jelinek GA, et al. Metabolomic biomarkers of multiple sclerosis: a systematic review. Front Mol Biosci. 2020;7:574133. doi: 10.3389/fmolb.2020.574133
Psychiatry and neurology are the brain’s twin medical disciplines. Unlike neurologic brain disorders, where localizing the “lesion” is a primary objective, psychiatric brain disorders are much more subtle, with no “gross” lesions but numerous cellular and molecular pathologies within neural circuits.
Measuring the molecular components of the cerebrospinal fluid (CSF), the glorious “sewage system” of the brain, may help reveal granular clues to the neurobiology of psychiatric disorders.
Mental illnesses involve the disruption of brain structures and functions in a diffuse manner across the cortex. Abnormal neuroplasticity has been implicated in several major psychiatric disorders. Examples include hypoplasia of the hippocampus in major depressive disorder and cortical thinning/dysplasia in schizophrenia. Reductions of neurotropic factors such as nerve growth factor or brain-derived neurotropic factor have been reported in mood and psychotic disorders, and appear to correlate with neuroplasticity changes.
Recent advances in psychiatric neuroscience have provided many clues to the pathophysiology of psychopathological conditions, including neuroinflammation, oxidative stress, apoptosis, impaired energy metabolism, abnormal metabolomics and lipidomics, and hypo- and hyperfunction of various neurotransmitters systems (especially glutamate N-methyl-
Thus, psychiatric research should focus on exploring and detecting molecular signatures (ie, biomarkers) of psychiatric disorders, including biomarkers of axonal and synaptic damage, glial activation, and oxidative stress. This is especially critical given the extensive heterogeneity of schizophrenia and mood and anxiety disorders. The CSF is a vastly unexploited substrate for discovering molecular biomarkers that will pave the way to precision psychiatry, and possibly open the door for completely new therapeutic strategies to tackle the most challenging neuropsychiatric disorders.
A role for CSF analysis
It’s quite puzzling why acute psychiatric episodes of schizophrenia, bipolar disorder, major depressive disorder, or panic attacks are not routinely assessed with a spinal tap, in conjunction with other brain measures such as neuroimaging (morphology, spectroscopy, cerebral blood flow, and diffusion tensor imaging) as well as a comprehensive neurocognitive examination and neurophysiological tests such as pre-pulse inhibition, mismatch negativity, and P-50, N-10, and P-300 evoked potentials. Combining CSF analysis with all those measures may help us stratify the spectra of psychosis, depression, and anxiety, as well as posttraumatic stress disorder and obsessive-compulsive disorder, into unique biotypes with overlapping clinical phenotypes and specific treatment approaches.
There are relatively few published CSF studies in psychiatric patients (mostly schizophrenia and bipolar and depressive disorders). The Table1-9 shows some of those findings. More than 365 biomarkers have been reported in schizophrenia, most of them in serum and tissue.10 However, none of them can be used for diagnostic purposes because schizophrenia is a syndrome comprised of several hundred different diseases (biotypes) that have similar clinical symptoms. Many of the serum and tissue biomarkers have not been studied in CSF, and they must if advances in the neurobiology and treatment of the psychotic and mood spectra are to be achieved. And adapting the CSF biomarkers described in neurologic disorders such as multiple sclerosis11 to schizophrenia and bipolar disorder (which also have well-established myelin pathologies) may yield a trove of neurobiologic findings.
If CSF studies eventually prove to be very useful for identifying subtypes for diagnosis and treatment, psychiatrists do not have to do the lumbar puncture themselves, but may refer patients to a “spinal tap” laboratory, just as they refer patients to a phlebotomy laboratory for routine blood tests. The adoption of CSF assessment in psychiatry will solidify its status as a clinical neuroscience, like its sister, neurology.
Psychiatry and neurology are the brain’s twin medical disciplines. Unlike neurologic brain disorders, where localizing the “lesion” is a primary objective, psychiatric brain disorders are much more subtle, with no “gross” lesions but numerous cellular and molecular pathologies within neural circuits.
Measuring the molecular components of the cerebrospinal fluid (CSF), the glorious “sewage system” of the brain, may help reveal granular clues to the neurobiology of psychiatric disorders.
Mental illnesses involve the disruption of brain structures and functions in a diffuse manner across the cortex. Abnormal neuroplasticity has been implicated in several major psychiatric disorders. Examples include hypoplasia of the hippocampus in major depressive disorder and cortical thinning/dysplasia in schizophrenia. Reductions of neurotropic factors such as nerve growth factor or brain-derived neurotropic factor have been reported in mood and psychotic disorders, and appear to correlate with neuroplasticity changes.
Recent advances in psychiatric neuroscience have provided many clues to the pathophysiology of psychopathological conditions, including neuroinflammation, oxidative stress, apoptosis, impaired energy metabolism, abnormal metabolomics and lipidomics, and hypo- and hyperfunction of various neurotransmitters systems (especially glutamate N-methyl-
Thus, psychiatric research should focus on exploring and detecting molecular signatures (ie, biomarkers) of psychiatric disorders, including biomarkers of axonal and synaptic damage, glial activation, and oxidative stress. This is especially critical given the extensive heterogeneity of schizophrenia and mood and anxiety disorders. The CSF is a vastly unexploited substrate for discovering molecular biomarkers that will pave the way to precision psychiatry, and possibly open the door for completely new therapeutic strategies to tackle the most challenging neuropsychiatric disorders.
A role for CSF analysis
It’s quite puzzling why acute psychiatric episodes of schizophrenia, bipolar disorder, major depressive disorder, or panic attacks are not routinely assessed with a spinal tap, in conjunction with other brain measures such as neuroimaging (morphology, spectroscopy, cerebral blood flow, and diffusion tensor imaging) as well as a comprehensive neurocognitive examination and neurophysiological tests such as pre-pulse inhibition, mismatch negativity, and P-50, N-10, and P-300 evoked potentials. Combining CSF analysis with all those measures may help us stratify the spectra of psychosis, depression, and anxiety, as well as posttraumatic stress disorder and obsessive-compulsive disorder, into unique biotypes with overlapping clinical phenotypes and specific treatment approaches.
There are relatively few published CSF studies in psychiatric patients (mostly schizophrenia and bipolar and depressive disorders). The Table1-9 shows some of those findings. More than 365 biomarkers have been reported in schizophrenia, most of them in serum and tissue.10 However, none of them can be used for diagnostic purposes because schizophrenia is a syndrome comprised of several hundred different diseases (biotypes) that have similar clinical symptoms. Many of the serum and tissue biomarkers have not been studied in CSF, and they must if advances in the neurobiology and treatment of the psychotic and mood spectra are to be achieved. And adapting the CSF biomarkers described in neurologic disorders such as multiple sclerosis11 to schizophrenia and bipolar disorder (which also have well-established myelin pathologies) may yield a trove of neurobiologic findings.
If CSF studies eventually prove to be very useful for identifying subtypes for diagnosis and treatment, psychiatrists do not have to do the lumbar puncture themselves, but may refer patients to a “spinal tap” laboratory, just as they refer patients to a phlebotomy laboratory for routine blood tests. The adoption of CSF assessment in psychiatry will solidify its status as a clinical neuroscience, like its sister, neurology.
1. Vasic N, Connemann BJ, Wolf RC, et al. Cerebrospinal fluid biomarker candidates of schizophrenia: where do we stand? Eur Arch Psychiatry Clin Neurosci. 2012;262(5):375-391.
2. Pollak TA, Drndarski S, Stone JM, et al. The blood-brain barrier in psychosis. Lancet Psychiatry. 2018;5(1):79-92.
3. Katisko K, Cajanus A, Jääskeläinen O, et al. Serum neurofilament light chain is a discriminative biomarker between frontotemporal lobar degeneration and primary psychiatric disorders. J Neurol. 2020;267(1):162-167.
4. Bechter K, Reiber H, Herzog S, et al. Cerebrospinal fluid analysis in affective and schizophrenic spectrum disorders: identification of subgroups with immune responses and blood-CSF barrier dysfunction. J Psychiatr Res. 2010;44(5):321-330.
5. Hidese S, Hattori K, Sasayama D, et al. Cerebrospinal fluid neural cell adhesion molecule levels and their correlation with clinical variables in patients with schizophrenia, bipolar disorder, and major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2017;76:12-18.
6. Tunca Z, Kıvırcık Akdede B, Özerdem A, et al. Diverse glial cell line-derived neurotrophic factor (GDNF) support between mania and schizophrenia: a comparative study in four major psychiatric disorders. Eur Psychiatry. 2015;30(2):198-204.
7. Al Shweiki MR, Oeckl P, Steinacker P, et al. Major depressive disorder: insight into candidate cerebrospinal fluid protein biomarkers from proteomics studies. Expert Rev Proteomics. 2017;14(6):499-514.
8. Kroksmark H, Vinberg M. Does S100B have a potential role in affective disorders? A literature review. Nord J Psychiatry. 2018;72(7):462-470.
9. Orlovska-Waast S, Köhler-Forsberg O, Brix SW, et al. Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol Psychiatry. 2019;24(6):869-887.
10. Nasrallah HA. Lab tests for psychiatric disorders: few clinicians are aware of them. Current Psychiatry. 2013;12(2):5-7.
11. Porter L, Shoushtarizadeh A, Jelinek GA, et al. Metabolomic biomarkers of multiple sclerosis: a systematic review. Front Mol Biosci. 2020;7:574133. doi: 10.3389/fmolb.2020.574133
1. Vasic N, Connemann BJ, Wolf RC, et al. Cerebrospinal fluid biomarker candidates of schizophrenia: where do we stand? Eur Arch Psychiatry Clin Neurosci. 2012;262(5):375-391.
2. Pollak TA, Drndarski S, Stone JM, et al. The blood-brain barrier in psychosis. Lancet Psychiatry. 2018;5(1):79-92.
3. Katisko K, Cajanus A, Jääskeläinen O, et al. Serum neurofilament light chain is a discriminative biomarker between frontotemporal lobar degeneration and primary psychiatric disorders. J Neurol. 2020;267(1):162-167.
4. Bechter K, Reiber H, Herzog S, et al. Cerebrospinal fluid analysis in affective and schizophrenic spectrum disorders: identification of subgroups with immune responses and blood-CSF barrier dysfunction. J Psychiatr Res. 2010;44(5):321-330.
5. Hidese S, Hattori K, Sasayama D, et al. Cerebrospinal fluid neural cell adhesion molecule levels and their correlation with clinical variables in patients with schizophrenia, bipolar disorder, and major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2017;76:12-18.
6. Tunca Z, Kıvırcık Akdede B, Özerdem A, et al. Diverse glial cell line-derived neurotrophic factor (GDNF) support between mania and schizophrenia: a comparative study in four major psychiatric disorders. Eur Psychiatry. 2015;30(2):198-204.
7. Al Shweiki MR, Oeckl P, Steinacker P, et al. Major depressive disorder: insight into candidate cerebrospinal fluid protein biomarkers from proteomics studies. Expert Rev Proteomics. 2017;14(6):499-514.
8. Kroksmark H, Vinberg M. Does S100B have a potential role in affective disorders? A literature review. Nord J Psychiatry. 2018;72(7):462-470.
9. Orlovska-Waast S, Köhler-Forsberg O, Brix SW, et al. Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol Psychiatry. 2019;24(6):869-887.
10. Nasrallah HA. Lab tests for psychiatric disorders: few clinicians are aware of them. Current Psychiatry. 2013;12(2):5-7.
11. Porter L, Shoushtarizadeh A, Jelinek GA, et al. Metabolomic biomarkers of multiple sclerosis: a systematic review. Front Mol Biosci. 2020;7:574133. doi: 10.3389/fmolb.2020.574133