User login
Implicit bias in medicine and beyond
Recently, I reported to the Washtenaw County Circuit Courthouse in Ann Arbor, Mich., to fulfill my civic responsibility of jury duty. After check-in, a pool of 250 potential jurors were shown a video about implicit bias and shuttled off to different courtrooms for the jury selection process (voir dire, or “to speak the truth” in French). While not personally called up to the juror box on this day, I did have the opportunity to observe the attorneys and judge as they questioned potential jurors to uncover any indication that they might not be fair or impartial in judging the facts of this criminal case. After over 3 hours of questioning and several peremptory challenges, a jury was empaneled, and the rest of us were dismissed for the day.
In the legal system, implicit bias can adversely affect legal outcomes by impacting the beliefs and attitudes of multiple stakeholders, including attorneys and judges, litigants, witnesses, and of course jurors, threatening one of our society’s most fundamental principles of equal justice under the law. In the health care arena, implicit bias has been shown to impact patient-clinician communication and contribute to racial and ethnic disparities in patient outcomes. As a medical community, acknowledging and accepting the existence of implicit bias, its manifestations, and its impact is a critical first step to ensuring that every patient that walks into our exam rooms receives equitable care, and we can begin to move the needle in addressing persistent health disparities in patients with gastrointestinal diseases and beyond. While this is regrettably a politically charged topic in our current environment, I urge you to join me in reflecting on whether and how unconscious attitudes or stereotypes may unintentionally color the way in which you interact with patients in the clinic and serve to create or perpetuate inequities in treatment. (I also urge you to show up for jury duty!)
Turning to our April issue, we highlight two recent studies from AGA’s flagship journals, one showing an unexpected rise in pancreatic cancer incidence among women under the age of 55, and another evaluating survival outcomes by fibrosis stage in biopsy-proven nonalcoholic fatty liver disease. In this month’s Member Spotlight column, we introduce you to gastroenterologist Daniel Leffler, MD, who shares his experiences transitioning from a traditional academic career to a job in industry to further scientific advancements in celiac disease treatment. We hope you enjoy these articles and all the content included in our April issue!
Megan A. Adams, MD, JD, MSc
Recently, I reported to the Washtenaw County Circuit Courthouse in Ann Arbor, Mich., to fulfill my civic responsibility of jury duty. After check-in, a pool of 250 potential jurors were shown a video about implicit bias and shuttled off to different courtrooms for the jury selection process (voir dire, or “to speak the truth” in French). While not personally called up to the juror box on this day, I did have the opportunity to observe the attorneys and judge as they questioned potential jurors to uncover any indication that they might not be fair or impartial in judging the facts of this criminal case. After over 3 hours of questioning and several peremptory challenges, a jury was empaneled, and the rest of us were dismissed for the day.
In the legal system, implicit bias can adversely affect legal outcomes by impacting the beliefs and attitudes of multiple stakeholders, including attorneys and judges, litigants, witnesses, and of course jurors, threatening one of our society’s most fundamental principles of equal justice under the law. In the health care arena, implicit bias has been shown to impact patient-clinician communication and contribute to racial and ethnic disparities in patient outcomes. As a medical community, acknowledging and accepting the existence of implicit bias, its manifestations, and its impact is a critical first step to ensuring that every patient that walks into our exam rooms receives equitable care, and we can begin to move the needle in addressing persistent health disparities in patients with gastrointestinal diseases and beyond. While this is regrettably a politically charged topic in our current environment, I urge you to join me in reflecting on whether and how unconscious attitudes or stereotypes may unintentionally color the way in which you interact with patients in the clinic and serve to create or perpetuate inequities in treatment. (I also urge you to show up for jury duty!)
Turning to our April issue, we highlight two recent studies from AGA’s flagship journals, one showing an unexpected rise in pancreatic cancer incidence among women under the age of 55, and another evaluating survival outcomes by fibrosis stage in biopsy-proven nonalcoholic fatty liver disease. In this month’s Member Spotlight column, we introduce you to gastroenterologist Daniel Leffler, MD, who shares his experiences transitioning from a traditional academic career to a job in industry to further scientific advancements in celiac disease treatment. We hope you enjoy these articles and all the content included in our April issue!
Megan A. Adams, MD, JD, MSc
Recently, I reported to the Washtenaw County Circuit Courthouse in Ann Arbor, Mich., to fulfill my civic responsibility of jury duty. After check-in, a pool of 250 potential jurors were shown a video about implicit bias and shuttled off to different courtrooms for the jury selection process (voir dire, or “to speak the truth” in French). While not personally called up to the juror box on this day, I did have the opportunity to observe the attorneys and judge as they questioned potential jurors to uncover any indication that they might not be fair or impartial in judging the facts of this criminal case. After over 3 hours of questioning and several peremptory challenges, a jury was empaneled, and the rest of us were dismissed for the day.
In the legal system, implicit bias can adversely affect legal outcomes by impacting the beliefs and attitudes of multiple stakeholders, including attorneys and judges, litigants, witnesses, and of course jurors, threatening one of our society’s most fundamental principles of equal justice under the law. In the health care arena, implicit bias has been shown to impact patient-clinician communication and contribute to racial and ethnic disparities in patient outcomes. As a medical community, acknowledging and accepting the existence of implicit bias, its manifestations, and its impact is a critical first step to ensuring that every patient that walks into our exam rooms receives equitable care, and we can begin to move the needle in addressing persistent health disparities in patients with gastrointestinal diseases and beyond. While this is regrettably a politically charged topic in our current environment, I urge you to join me in reflecting on whether and how unconscious attitudes or stereotypes may unintentionally color the way in which you interact with patients in the clinic and serve to create or perpetuate inequities in treatment. (I also urge you to show up for jury duty!)
Turning to our April issue, we highlight two recent studies from AGA’s flagship journals, one showing an unexpected rise in pancreatic cancer incidence among women under the age of 55, and another evaluating survival outcomes by fibrosis stage in biopsy-proven nonalcoholic fatty liver disease. In this month’s Member Spotlight column, we introduce you to gastroenterologist Daniel Leffler, MD, who shares his experiences transitioning from a traditional academic career to a job in industry to further scientific advancements in celiac disease treatment. We hope you enjoy these articles and all the content included in our April issue!
Megan A. Adams, MD, JD, MSc
Are parents infecting their children with contagious negativity?
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
New antiobesity drugs will benefit many. Is that bad?
where some economists opined that their coverage would be disastrous for Medicare.
Among their concerns? The drugs need to be taken long term (just like drugs for any other chronic condition). The new drugs are more expensive than the old drugs (just like new drugs for any other chronic condition). Lots of people will want to take them (just like highly effective drugs for any other chronic condition that has a significant quality-of-life or clinical impact). The U.K. recommended that they be covered only for 2 years (unlike drugs for any other chronic condition). And the Institute for Clinical and Economic Review (ICER) on which they lean heavily decided that $13,618 annually was too expensive for a medication that leads to sustained 15%-20% weight losses and those losses’ consequential benefits.
As a clinician working with patients who sustain those levels of weight loss, I find that conclusion confusing. Whether by way of lifestyle alone, or more often by way of lifestyle efforts plus medication or lifestyle efforts plus surgery, the benefits reported and seen with 15%-20% weight losses are almost uniformly huge. Patients are regularly seen discontinuing or reducing the dosage of multiple medications as a result of improvements to multiple weight-responsive comorbidities, and they also report objective benefits to mood, sleep, mobility, pain, and energy. Losing that much weight changes lives. Not to mention the impact that that degree of loss has on the primary prevention of so many diseases, including plausible reductions in many common cancers – reductions that have been shown to occur after surgery-related weight losses and for which there’s no plausible reason to imagine that they wouldn’t occur with pharmaceutical-related losses.
Are those discussions found in the NEJM op-ed or in the ICER report? Well, yes, sort of. However, in the NEJM op-ed, the word “prevention” isn’t used once, and unlike with oral hypoglycemics or antihypertensives, the authors state that with antiobesity medications, additional research is needed to determine whether medication-induced changes to A1c, blood pressure, and waist circumference would have clinical benefits: “Antiobesity medications have been shown to improve the surrogate end points of weight, glycated hemoglobin levels, systolic blood pressure, and waist circumference. Long-term studies are needed, however, to clarify how medication-induced changes in these surrogate markers translate to health outcomes.”
Primary prevention is mentioned in the ICER review, but in the “limitations” section where the authors explain that they didn’t include it in their modeling: “The long-term benefits of preventing other comorbidities including cancer, chronic kidney disease, osteoarthritis, and sleep apnea were not explicitly modeled in the base case.”
And they pretended that the impact on existing weight-responsive comorbidities mostly didn’t exist, too: “To limit the complexity of the cost-effectiveness model and to prevent double-counting of treatment benefits, we limited the long-term effects of treatments for weight management to cardiovascular risk and delays in the onset and/or diagnosis of diabetes mellitus.”
As far as cardiovascular disease (CVD) benefits go, you might have thought that it would be a slam dunk on that basis alone, at least according to a recent simple back-of-the-envelope math exercise presented at a recent American College of Cardiology conference, which applied the semaglutide treatment group weight changes in the STEP 1 trial to estimate the population impact on weight and obesity in 30- to 74-year-olds without prior CVD, and estimated 10-year CVD risks utilizing the BMI-based Framingham CVD risk scores. By their accounting, semaglutide treatment in eligible American patients has the potential to prevent over 1.6 million CVD events over 10 years.
Finally, even putting aside ICER’s admittedly and exceedingly narrow base case, what lifestyle-alone studies could ICER possibly be comparing with drug efficacy? And what does “alone” mean? Does “alone” mean with a months- or years long interprofessional behavioral program? Does “alone” mean by way of diet books? Does “alone” mean by way of simply “moving more and eating less”? I’m not aware of robust studies demonstrating any long-term meaningful, predictable, reproducible, durable weight loss outcomes for any lifestyle-only approach, intensive or otherwise.
It’s difficult for me to imagine a situation in which a drug other than an antiobesity drug would be found to have too many benefits to include in your cost-effectiveness analysis but where you’d be comfortable to run that analysis anyhow, and then come out against the drug’s recommendation and fearmonger about its use.
But then again, systemic weight bias is a hell of a drug.
Dr. Freedhoff is associate professor, department of family medicine, University of Ottawa, and medical director, Bariatric Medical Institute, Ottawa. He disclosed ties with Constant Health and Novo Nordisk, and has shared opinions via Weighty Matters and social media.
A version of this article originally appeared on Medscape.com.
where some economists opined that their coverage would be disastrous for Medicare.
Among their concerns? The drugs need to be taken long term (just like drugs for any other chronic condition). The new drugs are more expensive than the old drugs (just like new drugs for any other chronic condition). Lots of people will want to take them (just like highly effective drugs for any other chronic condition that has a significant quality-of-life or clinical impact). The U.K. recommended that they be covered only for 2 years (unlike drugs for any other chronic condition). And the Institute for Clinical and Economic Review (ICER) on which they lean heavily decided that $13,618 annually was too expensive for a medication that leads to sustained 15%-20% weight losses and those losses’ consequential benefits.
As a clinician working with patients who sustain those levels of weight loss, I find that conclusion confusing. Whether by way of lifestyle alone, or more often by way of lifestyle efforts plus medication or lifestyle efforts plus surgery, the benefits reported and seen with 15%-20% weight losses are almost uniformly huge. Patients are regularly seen discontinuing or reducing the dosage of multiple medications as a result of improvements to multiple weight-responsive comorbidities, and they also report objective benefits to mood, sleep, mobility, pain, and energy. Losing that much weight changes lives. Not to mention the impact that that degree of loss has on the primary prevention of so many diseases, including plausible reductions in many common cancers – reductions that have been shown to occur after surgery-related weight losses and for which there’s no plausible reason to imagine that they wouldn’t occur with pharmaceutical-related losses.
Are those discussions found in the NEJM op-ed or in the ICER report? Well, yes, sort of. However, in the NEJM op-ed, the word “prevention” isn’t used once, and unlike with oral hypoglycemics or antihypertensives, the authors state that with antiobesity medications, additional research is needed to determine whether medication-induced changes to A1c, blood pressure, and waist circumference would have clinical benefits: “Antiobesity medications have been shown to improve the surrogate end points of weight, glycated hemoglobin levels, systolic blood pressure, and waist circumference. Long-term studies are needed, however, to clarify how medication-induced changes in these surrogate markers translate to health outcomes.”
Primary prevention is mentioned in the ICER review, but in the “limitations” section where the authors explain that they didn’t include it in their modeling: “The long-term benefits of preventing other comorbidities including cancer, chronic kidney disease, osteoarthritis, and sleep apnea were not explicitly modeled in the base case.”
And they pretended that the impact on existing weight-responsive comorbidities mostly didn’t exist, too: “To limit the complexity of the cost-effectiveness model and to prevent double-counting of treatment benefits, we limited the long-term effects of treatments for weight management to cardiovascular risk and delays in the onset and/or diagnosis of diabetes mellitus.”
As far as cardiovascular disease (CVD) benefits go, you might have thought that it would be a slam dunk on that basis alone, at least according to a recent simple back-of-the-envelope math exercise presented at a recent American College of Cardiology conference, which applied the semaglutide treatment group weight changes in the STEP 1 trial to estimate the population impact on weight and obesity in 30- to 74-year-olds without prior CVD, and estimated 10-year CVD risks utilizing the BMI-based Framingham CVD risk scores. By their accounting, semaglutide treatment in eligible American patients has the potential to prevent over 1.6 million CVD events over 10 years.
Finally, even putting aside ICER’s admittedly and exceedingly narrow base case, what lifestyle-alone studies could ICER possibly be comparing with drug efficacy? And what does “alone” mean? Does “alone” mean with a months- or years long interprofessional behavioral program? Does “alone” mean by way of diet books? Does “alone” mean by way of simply “moving more and eating less”? I’m not aware of robust studies demonstrating any long-term meaningful, predictable, reproducible, durable weight loss outcomes for any lifestyle-only approach, intensive or otherwise.
It’s difficult for me to imagine a situation in which a drug other than an antiobesity drug would be found to have too many benefits to include in your cost-effectiveness analysis but where you’d be comfortable to run that analysis anyhow, and then come out against the drug’s recommendation and fearmonger about its use.
But then again, systemic weight bias is a hell of a drug.
Dr. Freedhoff is associate professor, department of family medicine, University of Ottawa, and medical director, Bariatric Medical Institute, Ottawa. He disclosed ties with Constant Health and Novo Nordisk, and has shared opinions via Weighty Matters and social media.
A version of this article originally appeared on Medscape.com.
where some economists opined that their coverage would be disastrous for Medicare.
Among their concerns? The drugs need to be taken long term (just like drugs for any other chronic condition). The new drugs are more expensive than the old drugs (just like new drugs for any other chronic condition). Lots of people will want to take them (just like highly effective drugs for any other chronic condition that has a significant quality-of-life or clinical impact). The U.K. recommended that they be covered only for 2 years (unlike drugs for any other chronic condition). And the Institute for Clinical and Economic Review (ICER) on which they lean heavily decided that $13,618 annually was too expensive for a medication that leads to sustained 15%-20% weight losses and those losses’ consequential benefits.
As a clinician working with patients who sustain those levels of weight loss, I find that conclusion confusing. Whether by way of lifestyle alone, or more often by way of lifestyle efforts plus medication or lifestyle efforts plus surgery, the benefits reported and seen with 15%-20% weight losses are almost uniformly huge. Patients are regularly seen discontinuing or reducing the dosage of multiple medications as a result of improvements to multiple weight-responsive comorbidities, and they also report objective benefits to mood, sleep, mobility, pain, and energy. Losing that much weight changes lives. Not to mention the impact that that degree of loss has on the primary prevention of so many diseases, including plausible reductions in many common cancers – reductions that have been shown to occur after surgery-related weight losses and for which there’s no plausible reason to imagine that they wouldn’t occur with pharmaceutical-related losses.
Are those discussions found in the NEJM op-ed or in the ICER report? Well, yes, sort of. However, in the NEJM op-ed, the word “prevention” isn’t used once, and unlike with oral hypoglycemics or antihypertensives, the authors state that with antiobesity medications, additional research is needed to determine whether medication-induced changes to A1c, blood pressure, and waist circumference would have clinical benefits: “Antiobesity medications have been shown to improve the surrogate end points of weight, glycated hemoglobin levels, systolic blood pressure, and waist circumference. Long-term studies are needed, however, to clarify how medication-induced changes in these surrogate markers translate to health outcomes.”
Primary prevention is mentioned in the ICER review, but in the “limitations” section where the authors explain that they didn’t include it in their modeling: “The long-term benefits of preventing other comorbidities including cancer, chronic kidney disease, osteoarthritis, and sleep apnea were not explicitly modeled in the base case.”
And they pretended that the impact on existing weight-responsive comorbidities mostly didn’t exist, too: “To limit the complexity of the cost-effectiveness model and to prevent double-counting of treatment benefits, we limited the long-term effects of treatments for weight management to cardiovascular risk and delays in the onset and/or diagnosis of diabetes mellitus.”
As far as cardiovascular disease (CVD) benefits go, you might have thought that it would be a slam dunk on that basis alone, at least according to a recent simple back-of-the-envelope math exercise presented at a recent American College of Cardiology conference, which applied the semaglutide treatment group weight changes in the STEP 1 trial to estimate the population impact on weight and obesity in 30- to 74-year-olds without prior CVD, and estimated 10-year CVD risks utilizing the BMI-based Framingham CVD risk scores. By their accounting, semaglutide treatment in eligible American patients has the potential to prevent over 1.6 million CVD events over 10 years.
Finally, even putting aside ICER’s admittedly and exceedingly narrow base case, what lifestyle-alone studies could ICER possibly be comparing with drug efficacy? And what does “alone” mean? Does “alone” mean with a months- or years long interprofessional behavioral program? Does “alone” mean by way of diet books? Does “alone” mean by way of simply “moving more and eating less”? I’m not aware of robust studies demonstrating any long-term meaningful, predictable, reproducible, durable weight loss outcomes for any lifestyle-only approach, intensive or otherwise.
It’s difficult for me to imagine a situation in which a drug other than an antiobesity drug would be found to have too many benefits to include in your cost-effectiveness analysis but where you’d be comfortable to run that analysis anyhow, and then come out against the drug’s recommendation and fearmonger about its use.
But then again, systemic weight bias is a hell of a drug.
Dr. Freedhoff is associate professor, department of family medicine, University of Ottawa, and medical director, Bariatric Medical Institute, Ottawa. He disclosed ties with Constant Health and Novo Nordisk, and has shared opinions via Weighty Matters and social media.
A version of this article originally appeared on Medscape.com.
Don’t fear testing for, and delabeling, penicillin allergy
You are seeing a 28-year-old man for a same-day appointment. He has a history of opioid use disorder and chronic hepatitis C virus infection. He has been using injections of heroin and fentanyl for more than 6 years, and you can see in his medical record that he has had four outpatient appointments for cutaneous infections along with three emergency department visits for same in the past 2 years. His chief complaint today is pain over his left forearm for the past 3 days. He does not report fever or other constitutional symptoms.
Examination of the left forearm reveals 8 cm of erythema with induration and calor but no fluctuance. The area is moderately tender to palpation. He has no other abnormal findings on exam.
What’s your course of action?
Dr. Vega’s take
You want to treat this patient with antibiotics and close follow-up, and you note that he has a history of penicillin allergy. A note in his record states that he had a rash after receiving amoxicillin as a child.
Sometimes, we have to take the most expedient action in health care. But most of the time, we should do the right thing, even if it’s harder. I would gather more history of this reaction to penicillin and consider an oral challenge, hoping that the work that we put in to testing him for penicillin allergy pays dividends for him now and for years to come.
Penicillin allergy is very commonly listed in patient health records. In a retrospective analysis of the charts of 11,761 patients seen at a single U.S. urban outpatient system in 2012, 11.5% had documentation of penicillin allergy. Rash was the most common manifestation listed for allergy (37% of cases), followed by unknown symptoms (20%), hives (19%), swelling/angioedema (12%), and anaphylaxis (7%). Women were nearly twice as likely as men were to report a history of penicillin allergy, and patients of Asian descent had half the reported prevalence of penicillin allergy, compared with White patients.
Only 6% of the patients reporting penicillin allergy in this study had been referred to an allergy specialist. Given the consequences of true penicillin allergy, this rate is far too low. Patients with a history of penicillin allergy have higher risks for mortality from coexisting hematologic malignancies and penicillin-sensitive infections such as Staphylococcus species. They more frequently develop resistance to multiple antimicrobials and have longer average lengths of stay in the hospital.
Getting a good history for penicillin allergy can be challenging. Approximately three-quarters of penicillin allergies are diagnosed prior to age 3 years. Some children with a family history of penicillin allergy are mislabeled as having an active allergy, even though family history is not a significant contributor to penicillin allergy. Most rashes blamed on penicillin among children are actually not immunoglobulin (Ig) E–mediated and instead represent viral exanthems.
In response to these challenges, at the end of 2022, the American Academy of Allergy, Asthma & Immunology along with the American College of Allergy, Asthma and Immunology published new recommendations for the management of drug allergy. These recommendations provide an algorithm for the active reassessment of penicillin allergy. Like other recommendations in recent years, they call for a proactive approach in questioning the potential clinical consequences of the penicillin allergy listed in the health record.
First, the guidelines recommend against needing any testing for previous adverse reactions to penicillin, such as headache, nausea/vomiting, or diarrhea, that are not IgE-mediated. However, patients who have experienced these adverse reactions may still be reticent to take penicillin. For them and for adults with a history of mild to moderate reactions to penicillin more than 5 years ago, a single oral challenge test with amoxicillin is practical and can be used to exclude penicillin allergy.
The oral amoxicillin challenge
After patients take a treatment dose of oral amoxicillin, they should be observed for 1 hour for any objective reaction. The clinical setting should be able to support patients in the rare case of a more severe reaction to penicillin. Subjective symptoms such as pruritus without objective findings such as rash may be considered a successful challenge, and penicillin may be taken off the list of allergies. The treating team can bill CPT codes for drug challenge testing.
Some research has supported multidose testing with amoxicillin to assess for late reactions to a penicillin oral challenge, but the current guidelines recommend against this approach based on the very limited yield in finding additional cases of true allergy with extra doses of antibiotics. One method to address this issue is to have patients advise the practice if symptoms develop within 10 days of the oral challenge, with photos or prompt clinical evaluation to assess for an IgE-mediated reaction.
Many patients, and certainly some clinicians, will have significant trepidation regarding an oral challenge, despite the low risk for complications. For these patients, as well as children with a history of penicillin allergy and patients with a history of anaphylaxis to penicillin or probable IgE-mediated reaction to penicillin in the past several years, skin testing is recommended. Lower-risk patients might feel reassured to complete an oral challenge test after a negative skin test.
Penicillin skin testing is more reliable than a radioallergosorbent test or an enzyme-linked immunoassay and carries a high specificity. However, skin testing requires the specialized care of an allergy clinic, and this resource is limited in many communities.
Many patients will have negative oral challenge or skin testing for penicillin allergy, but there are still some critical responsibilities for the clinician after testing is complete. First, the label of penicillin allergy should be expunged from all available health records. Second, the clinician should communicate clearly and with empathy to the patient that they can take penicillin-based antibiotics safely and with confidence. Repeat testing is unnecessary unless new symptoms develop.
But the application of this policy to clinical practice is challenging on several levels, from patient and clinician fear to practical constraints on time.
Dr. Vega is health sciences clinical professor, family medicine, University of California, Irvine. He has disclosed ties with McNeil Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
You are seeing a 28-year-old man for a same-day appointment. He has a history of opioid use disorder and chronic hepatitis C virus infection. He has been using injections of heroin and fentanyl for more than 6 years, and you can see in his medical record that he has had four outpatient appointments for cutaneous infections along with three emergency department visits for same in the past 2 years. His chief complaint today is pain over his left forearm for the past 3 days. He does not report fever or other constitutional symptoms.
Examination of the left forearm reveals 8 cm of erythema with induration and calor but no fluctuance. The area is moderately tender to palpation. He has no other abnormal findings on exam.
What’s your course of action?
Dr. Vega’s take
You want to treat this patient with antibiotics and close follow-up, and you note that he has a history of penicillin allergy. A note in his record states that he had a rash after receiving amoxicillin as a child.
Sometimes, we have to take the most expedient action in health care. But most of the time, we should do the right thing, even if it’s harder. I would gather more history of this reaction to penicillin and consider an oral challenge, hoping that the work that we put in to testing him for penicillin allergy pays dividends for him now and for years to come.
Penicillin allergy is very commonly listed in patient health records. In a retrospective analysis of the charts of 11,761 patients seen at a single U.S. urban outpatient system in 2012, 11.5% had documentation of penicillin allergy. Rash was the most common manifestation listed for allergy (37% of cases), followed by unknown symptoms (20%), hives (19%), swelling/angioedema (12%), and anaphylaxis (7%). Women were nearly twice as likely as men were to report a history of penicillin allergy, and patients of Asian descent had half the reported prevalence of penicillin allergy, compared with White patients.
Only 6% of the patients reporting penicillin allergy in this study had been referred to an allergy specialist. Given the consequences of true penicillin allergy, this rate is far too low. Patients with a history of penicillin allergy have higher risks for mortality from coexisting hematologic malignancies and penicillin-sensitive infections such as Staphylococcus species. They more frequently develop resistance to multiple antimicrobials and have longer average lengths of stay in the hospital.
Getting a good history for penicillin allergy can be challenging. Approximately three-quarters of penicillin allergies are diagnosed prior to age 3 years. Some children with a family history of penicillin allergy are mislabeled as having an active allergy, even though family history is not a significant contributor to penicillin allergy. Most rashes blamed on penicillin among children are actually not immunoglobulin (Ig) E–mediated and instead represent viral exanthems.
In response to these challenges, at the end of 2022, the American Academy of Allergy, Asthma & Immunology along with the American College of Allergy, Asthma and Immunology published new recommendations for the management of drug allergy. These recommendations provide an algorithm for the active reassessment of penicillin allergy. Like other recommendations in recent years, they call for a proactive approach in questioning the potential clinical consequences of the penicillin allergy listed in the health record.
First, the guidelines recommend against needing any testing for previous adverse reactions to penicillin, such as headache, nausea/vomiting, or diarrhea, that are not IgE-mediated. However, patients who have experienced these adverse reactions may still be reticent to take penicillin. For them and for adults with a history of mild to moderate reactions to penicillin more than 5 years ago, a single oral challenge test with amoxicillin is practical and can be used to exclude penicillin allergy.
The oral amoxicillin challenge
After patients take a treatment dose of oral amoxicillin, they should be observed for 1 hour for any objective reaction. The clinical setting should be able to support patients in the rare case of a more severe reaction to penicillin. Subjective symptoms such as pruritus without objective findings such as rash may be considered a successful challenge, and penicillin may be taken off the list of allergies. The treating team can bill CPT codes for drug challenge testing.
Some research has supported multidose testing with amoxicillin to assess for late reactions to a penicillin oral challenge, but the current guidelines recommend against this approach based on the very limited yield in finding additional cases of true allergy with extra doses of antibiotics. One method to address this issue is to have patients advise the practice if symptoms develop within 10 days of the oral challenge, with photos or prompt clinical evaluation to assess for an IgE-mediated reaction.
Many patients, and certainly some clinicians, will have significant trepidation regarding an oral challenge, despite the low risk for complications. For these patients, as well as children with a history of penicillin allergy and patients with a history of anaphylaxis to penicillin or probable IgE-mediated reaction to penicillin in the past several years, skin testing is recommended. Lower-risk patients might feel reassured to complete an oral challenge test after a negative skin test.
Penicillin skin testing is more reliable than a radioallergosorbent test or an enzyme-linked immunoassay and carries a high specificity. However, skin testing requires the specialized care of an allergy clinic, and this resource is limited in many communities.
Many patients will have negative oral challenge or skin testing for penicillin allergy, but there are still some critical responsibilities for the clinician after testing is complete. First, the label of penicillin allergy should be expunged from all available health records. Second, the clinician should communicate clearly and with empathy to the patient that they can take penicillin-based antibiotics safely and with confidence. Repeat testing is unnecessary unless new symptoms develop.
But the application of this policy to clinical practice is challenging on several levels, from patient and clinician fear to practical constraints on time.
Dr. Vega is health sciences clinical professor, family medicine, University of California, Irvine. He has disclosed ties with McNeil Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
You are seeing a 28-year-old man for a same-day appointment. He has a history of opioid use disorder and chronic hepatitis C virus infection. He has been using injections of heroin and fentanyl for more than 6 years, and you can see in his medical record that he has had four outpatient appointments for cutaneous infections along with three emergency department visits for same in the past 2 years. His chief complaint today is pain over his left forearm for the past 3 days. He does not report fever or other constitutional symptoms.
Examination of the left forearm reveals 8 cm of erythema with induration and calor but no fluctuance. The area is moderately tender to palpation. He has no other abnormal findings on exam.
What’s your course of action?
Dr. Vega’s take
You want to treat this patient with antibiotics and close follow-up, and you note that he has a history of penicillin allergy. A note in his record states that he had a rash after receiving amoxicillin as a child.
Sometimes, we have to take the most expedient action in health care. But most of the time, we should do the right thing, even if it’s harder. I would gather more history of this reaction to penicillin and consider an oral challenge, hoping that the work that we put in to testing him for penicillin allergy pays dividends for him now and for years to come.
Penicillin allergy is very commonly listed in patient health records. In a retrospective analysis of the charts of 11,761 patients seen at a single U.S. urban outpatient system in 2012, 11.5% had documentation of penicillin allergy. Rash was the most common manifestation listed for allergy (37% of cases), followed by unknown symptoms (20%), hives (19%), swelling/angioedema (12%), and anaphylaxis (7%). Women were nearly twice as likely as men were to report a history of penicillin allergy, and patients of Asian descent had half the reported prevalence of penicillin allergy, compared with White patients.
Only 6% of the patients reporting penicillin allergy in this study had been referred to an allergy specialist. Given the consequences of true penicillin allergy, this rate is far too low. Patients with a history of penicillin allergy have higher risks for mortality from coexisting hematologic malignancies and penicillin-sensitive infections such as Staphylococcus species. They more frequently develop resistance to multiple antimicrobials and have longer average lengths of stay in the hospital.
Getting a good history for penicillin allergy can be challenging. Approximately three-quarters of penicillin allergies are diagnosed prior to age 3 years. Some children with a family history of penicillin allergy are mislabeled as having an active allergy, even though family history is not a significant contributor to penicillin allergy. Most rashes blamed on penicillin among children are actually not immunoglobulin (Ig) E–mediated and instead represent viral exanthems.
In response to these challenges, at the end of 2022, the American Academy of Allergy, Asthma & Immunology along with the American College of Allergy, Asthma and Immunology published new recommendations for the management of drug allergy. These recommendations provide an algorithm for the active reassessment of penicillin allergy. Like other recommendations in recent years, they call for a proactive approach in questioning the potential clinical consequences of the penicillin allergy listed in the health record.
First, the guidelines recommend against needing any testing for previous adverse reactions to penicillin, such as headache, nausea/vomiting, or diarrhea, that are not IgE-mediated. However, patients who have experienced these adverse reactions may still be reticent to take penicillin. For them and for adults with a history of mild to moderate reactions to penicillin more than 5 years ago, a single oral challenge test with amoxicillin is practical and can be used to exclude penicillin allergy.
The oral amoxicillin challenge
After patients take a treatment dose of oral amoxicillin, they should be observed for 1 hour for any objective reaction. The clinical setting should be able to support patients in the rare case of a more severe reaction to penicillin. Subjective symptoms such as pruritus without objective findings such as rash may be considered a successful challenge, and penicillin may be taken off the list of allergies. The treating team can bill CPT codes for drug challenge testing.
Some research has supported multidose testing with amoxicillin to assess for late reactions to a penicillin oral challenge, but the current guidelines recommend against this approach based on the very limited yield in finding additional cases of true allergy with extra doses of antibiotics. One method to address this issue is to have patients advise the practice if symptoms develop within 10 days of the oral challenge, with photos or prompt clinical evaluation to assess for an IgE-mediated reaction.
Many patients, and certainly some clinicians, will have significant trepidation regarding an oral challenge, despite the low risk for complications. For these patients, as well as children with a history of penicillin allergy and patients with a history of anaphylaxis to penicillin or probable IgE-mediated reaction to penicillin in the past several years, skin testing is recommended. Lower-risk patients might feel reassured to complete an oral challenge test after a negative skin test.
Penicillin skin testing is more reliable than a radioallergosorbent test or an enzyme-linked immunoassay and carries a high specificity. However, skin testing requires the specialized care of an allergy clinic, and this resource is limited in many communities.
Many patients will have negative oral challenge or skin testing for penicillin allergy, but there are still some critical responsibilities for the clinician after testing is complete. First, the label of penicillin allergy should be expunged from all available health records. Second, the clinician should communicate clearly and with empathy to the patient that they can take penicillin-based antibiotics safely and with confidence. Repeat testing is unnecessary unless new symptoms develop.
But the application of this policy to clinical practice is challenging on several levels, from patient and clinician fear to practical constraints on time.
Dr. Vega is health sciences clinical professor, family medicine, University of California, Irvine. He has disclosed ties with McNeil Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
The physician as leader
Physicians are placed in positions of leadership by the medical team, by the community, and by society, particularly during times of crisis such as the COVID pandemic. They are looked to by the media at times of health care news such as the overturning of Roe v. Wade.1 In a 2015 survey of resident physicians, two-thirds agreed that a formalized leadership curriculum would help them become better supervisors and clinicians.2 While all physicians are viewed as leaders, the concept of leadership is rarely, if ever, described or developed as a part of medical training. This month’s column will provide insights into defining leadership as a physician in the medical and administrative settings.
Benefits of effective leadership
Physicians, whether they are clinicians, researchers, administrators, or teachers, are expected to oversee and engage their teams. A report by the Institute of Medicine recommended that academic health centers “develop leaders at all levels who can manage the organizational and system changes necessary to improve health through innovation in health professions education, patient care, and research.”3 Hospitals with higher-rated management practices and more highly rated boards of directors have been shown to deliver higher-quality care and better clinical outcomes, including lower mortality.
To illustrate, the clinicians at the Mayo Clinic annually rate their supervisors on a Leader Index, a simple 12-question survey of five leadership domains: truthfulness, transparency, character, capability, and partnership. All supervisors were physicians and scientists. Their findings revealed that for each one-point increase in composite leadership score, there was a 3.3% decrease in the likelihood of burnout and a 9.0% increase in the likelihood of satisfaction in the physicians supervised.4
Interprofessional teamwork and engagement are vital skills for a leader to create a successful team. Enhanced management practices have also been associated with higher patient approval ratings and better financial performance. Effective leadership additionally affects physician well-being, with stronger leadership associated with less physician burnout and higher satisfaction.5
Leadership styles enhance quality measures in health care.6 The most effective leadership styles are ones in which the staff feels they are part of a team, are engaged, and are mentored.7 While leadership styles can vary, the common theme is staff engagement. An authoritative style leader is one who mobilizes the team toward a vision, that is, “Come with me.” An affiliative style leader creates harmony and builds emotional bonds where “people come first.” Democratic leaders forge a consensus through staff participation by asking, “What do you think?” Finally, a leader who uses a coaching style helps staff to identify their strengths and weaknesses and work toward improvement. These leadership behaviors are in contradistinction to the unsuccessful coercive leader who demands immediate compliance, that is, “Do what I tell you.”
Five fundamental leadership principles are shown in Table 1.8
Effective leaders have an open (growth) mindset, unwavering attention to diversity, equity, and inclusion, and to building relationships and trust; they practice effective communication and listening, focus on results, and cocreate support structures.
A growth mindset is the belief that one’s abilities are not innate but can improve through effort and learning.9
Emotional intelligence
A survey of business senior managers rated the qualities found in the most outstanding leaders. Using objective criteria like profitability the study psychologists interviewed the highest-rated leaders to compare their capabilities. While intellects and cognitive skills were important, the results showed that emotional intelligence (EI) was twice as important as technical skills and IQ.10 As an example, in a 1996 study, when senior managers had an optimal level of EI, their division’s yearly earnings were 20% higher than estimated.11
EI is a leadership competency that deals with the ability to understand and manage your own emotions and your interactions with others.10 At the Cleveland Clinic, EI is exemplified by the acronym HEART, whereby the team strives to improve the patient experience, mainly when an error occurs. The health care team is using EI by showing its the ability to Hear, Empathize, Apologize, Reply, and Thank. When an untoward event occurs, the physician, as the leader of the team, must lead by example when communicating with staff and patients. EI consists of five components (Table 2).13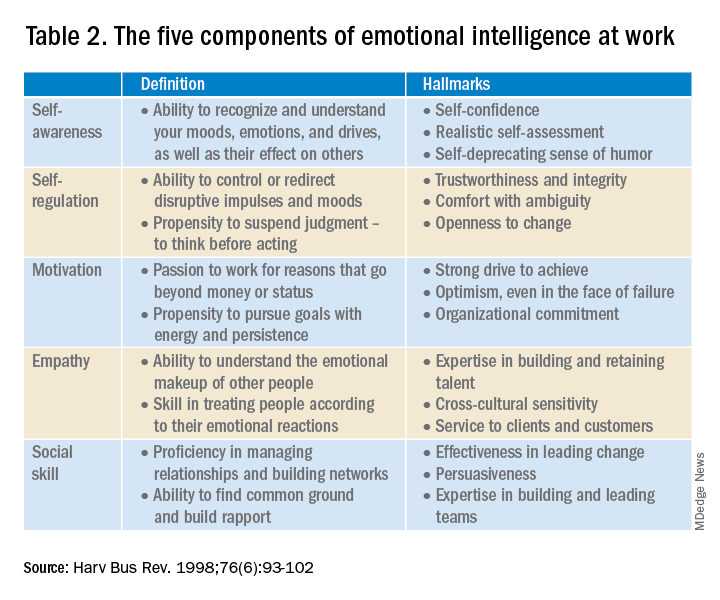
- Self-awareness is insight by which you can improve. Maintaining a journal of your daily thoughts may assist with this as well as simply pausing to pay attention during times of heightened emotions.
- Self-regulation shows control, that is, behaving according to your values, and being accountable and calm when challenged.
- Purpose, knowing your “why,” produces motivation and helps maintain optimism.
- Empathy shows the ability to understand the emotions of other people.
- Social skill is the ability to establish mutually rewarding relationships.
Given all the above benefits, it is no surprise that companies are actively trying use artificial intelligence to improve EI.12
Learning to be a leader
In medical school, students are expected to develop skills to handle and resolve conflicts, learn to share leadership, take mutual responsibility, and monitor their own performance.13 Although training of young physicians in leadership is not unprecedented, a systemic review revealed a lack of analytic studies to evaluate the effectiveness of the teaching methods.14 During undergraduate medical education, standard curricula and methods of instruction on leadership are not established, resulting in variable outcomes.
The Association of American Medical Colleges offers a curriculum, “Preparing Medical Students to Be Physician Leaders: A Leadership Training Program for Students Designed and Led by Students.”15 The objectives of this training are to help students identify their “personal style of leadership, recognize strengths and weaknesses, utilize effective communication strategies, appropriately delegate team member responsibilities, and provide constructive feedback to help improve team function.”
Take-home points
Following the completion of formal medical education, physicians are thrust into leadership roles. The key to being an effective leader is using EI to mentor the team and make staff feel connected to the team’s meaning and purpose, so they feel valued.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Carsen S and Xia C. McGill J Med. 2006 Jan;9(1):1-2.
2. Jardine D et al. J Grad Med Educ. 2015;7(2):307-9.
3. Institute of Medicine. Acad Emerg Med. July 2004;11(7):802-6.
4. Shanafelt TD et al. Mayo Clin Proc. April 2015;90(4):432-40.
5. Rotenstein LS et al. Harv Bus Rev. Oct. 17, 2018.
6. Sfantou SF. Healthcare 2017;5(4):73.
7. Goleman D. Harv Bus Rev. March-April 2000.
8. Collins-Nakai R. McGill J Med [Internet]. 2020 Dec. 1 [cited 2023 Mar. 28];9(1).
9. Dweck C. Harv Bus Rev. Jan. 13, 2016.
10. Goleman D. Harv Bus Rev. 1998 Nov-Dec;76(6):93-102..
11. Goleman D et al. Primal leadership: Realizing the power of emotional intelligence. Boston: Harvard Business School Publishing, 2002.12. Limon D and Plaster B. Harv Bus Rev. Jan. 25, 2022.
13. Chen T-Y. Tzu Chi Med J. Apr–Jun 2018;30(2):66-70.
14. Kumar B et al. BMC Med Educ. 2020;20:175.
15. Richards K et al. Med Ed Portal. Dec. 13 2019.
Physicians are placed in positions of leadership by the medical team, by the community, and by society, particularly during times of crisis such as the COVID pandemic. They are looked to by the media at times of health care news such as the overturning of Roe v. Wade.1 In a 2015 survey of resident physicians, two-thirds agreed that a formalized leadership curriculum would help them become better supervisors and clinicians.2 While all physicians are viewed as leaders, the concept of leadership is rarely, if ever, described or developed as a part of medical training. This month’s column will provide insights into defining leadership as a physician in the medical and administrative settings.
Benefits of effective leadership
Physicians, whether they are clinicians, researchers, administrators, or teachers, are expected to oversee and engage their teams. A report by the Institute of Medicine recommended that academic health centers “develop leaders at all levels who can manage the organizational and system changes necessary to improve health through innovation in health professions education, patient care, and research.”3 Hospitals with higher-rated management practices and more highly rated boards of directors have been shown to deliver higher-quality care and better clinical outcomes, including lower mortality.
To illustrate, the clinicians at the Mayo Clinic annually rate their supervisors on a Leader Index, a simple 12-question survey of five leadership domains: truthfulness, transparency, character, capability, and partnership. All supervisors were physicians and scientists. Their findings revealed that for each one-point increase in composite leadership score, there was a 3.3% decrease in the likelihood of burnout and a 9.0% increase in the likelihood of satisfaction in the physicians supervised.4
Interprofessional teamwork and engagement are vital skills for a leader to create a successful team. Enhanced management practices have also been associated with higher patient approval ratings and better financial performance. Effective leadership additionally affects physician well-being, with stronger leadership associated with less physician burnout and higher satisfaction.5
Leadership styles enhance quality measures in health care.6 The most effective leadership styles are ones in which the staff feels they are part of a team, are engaged, and are mentored.7 While leadership styles can vary, the common theme is staff engagement. An authoritative style leader is one who mobilizes the team toward a vision, that is, “Come with me.” An affiliative style leader creates harmony and builds emotional bonds where “people come first.” Democratic leaders forge a consensus through staff participation by asking, “What do you think?” Finally, a leader who uses a coaching style helps staff to identify their strengths and weaknesses and work toward improvement. These leadership behaviors are in contradistinction to the unsuccessful coercive leader who demands immediate compliance, that is, “Do what I tell you.”
Five fundamental leadership principles are shown in Table 1.8
Effective leaders have an open (growth) mindset, unwavering attention to diversity, equity, and inclusion, and to building relationships and trust; they practice effective communication and listening, focus on results, and cocreate support structures.
A growth mindset is the belief that one’s abilities are not innate but can improve through effort and learning.9
Emotional intelligence
A survey of business senior managers rated the qualities found in the most outstanding leaders. Using objective criteria like profitability the study psychologists interviewed the highest-rated leaders to compare their capabilities. While intellects and cognitive skills were important, the results showed that emotional intelligence (EI) was twice as important as technical skills and IQ.10 As an example, in a 1996 study, when senior managers had an optimal level of EI, their division’s yearly earnings were 20% higher than estimated.11
EI is a leadership competency that deals with the ability to understand and manage your own emotions and your interactions with others.10 At the Cleveland Clinic, EI is exemplified by the acronym HEART, whereby the team strives to improve the patient experience, mainly when an error occurs. The health care team is using EI by showing its the ability to Hear, Empathize, Apologize, Reply, and Thank. When an untoward event occurs, the physician, as the leader of the team, must lead by example when communicating with staff and patients. EI consists of five components (Table 2).13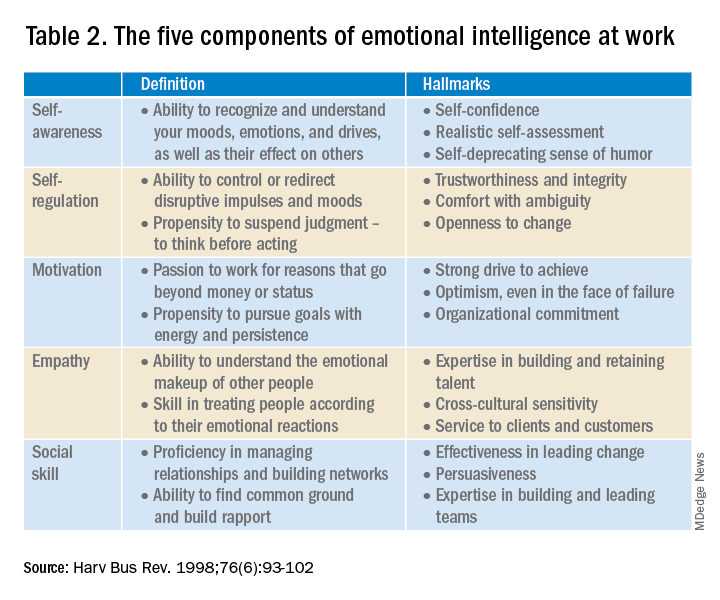
- Self-awareness is insight by which you can improve. Maintaining a journal of your daily thoughts may assist with this as well as simply pausing to pay attention during times of heightened emotions.
- Self-regulation shows control, that is, behaving according to your values, and being accountable and calm when challenged.
- Purpose, knowing your “why,” produces motivation and helps maintain optimism.
- Empathy shows the ability to understand the emotions of other people.
- Social skill is the ability to establish mutually rewarding relationships.
Given all the above benefits, it is no surprise that companies are actively trying use artificial intelligence to improve EI.12
Learning to be a leader
In medical school, students are expected to develop skills to handle and resolve conflicts, learn to share leadership, take mutual responsibility, and monitor their own performance.13 Although training of young physicians in leadership is not unprecedented, a systemic review revealed a lack of analytic studies to evaluate the effectiveness of the teaching methods.14 During undergraduate medical education, standard curricula and methods of instruction on leadership are not established, resulting in variable outcomes.
The Association of American Medical Colleges offers a curriculum, “Preparing Medical Students to Be Physician Leaders: A Leadership Training Program for Students Designed and Led by Students.”15 The objectives of this training are to help students identify their “personal style of leadership, recognize strengths and weaknesses, utilize effective communication strategies, appropriately delegate team member responsibilities, and provide constructive feedback to help improve team function.”
Take-home points
Following the completion of formal medical education, physicians are thrust into leadership roles. The key to being an effective leader is using EI to mentor the team and make staff feel connected to the team’s meaning and purpose, so they feel valued.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Carsen S and Xia C. McGill J Med. 2006 Jan;9(1):1-2.
2. Jardine D et al. J Grad Med Educ. 2015;7(2):307-9.
3. Institute of Medicine. Acad Emerg Med. July 2004;11(7):802-6.
4. Shanafelt TD et al. Mayo Clin Proc. April 2015;90(4):432-40.
5. Rotenstein LS et al. Harv Bus Rev. Oct. 17, 2018.
6. Sfantou SF. Healthcare 2017;5(4):73.
7. Goleman D. Harv Bus Rev. March-April 2000.
8. Collins-Nakai R. McGill J Med [Internet]. 2020 Dec. 1 [cited 2023 Mar. 28];9(1).
9. Dweck C. Harv Bus Rev. Jan. 13, 2016.
10. Goleman D. Harv Bus Rev. 1998 Nov-Dec;76(6):93-102..
11. Goleman D et al. Primal leadership: Realizing the power of emotional intelligence. Boston: Harvard Business School Publishing, 2002.12. Limon D and Plaster B. Harv Bus Rev. Jan. 25, 2022.
13. Chen T-Y. Tzu Chi Med J. Apr–Jun 2018;30(2):66-70.
14. Kumar B et al. BMC Med Educ. 2020;20:175.
15. Richards K et al. Med Ed Portal. Dec. 13 2019.
Physicians are placed in positions of leadership by the medical team, by the community, and by society, particularly during times of crisis such as the COVID pandemic. They are looked to by the media at times of health care news such as the overturning of Roe v. Wade.1 In a 2015 survey of resident physicians, two-thirds agreed that a formalized leadership curriculum would help them become better supervisors and clinicians.2 While all physicians are viewed as leaders, the concept of leadership is rarely, if ever, described or developed as a part of medical training. This month’s column will provide insights into defining leadership as a physician in the medical and administrative settings.
Benefits of effective leadership
Physicians, whether they are clinicians, researchers, administrators, or teachers, are expected to oversee and engage their teams. A report by the Institute of Medicine recommended that academic health centers “develop leaders at all levels who can manage the organizational and system changes necessary to improve health through innovation in health professions education, patient care, and research.”3 Hospitals with higher-rated management practices and more highly rated boards of directors have been shown to deliver higher-quality care and better clinical outcomes, including lower mortality.
To illustrate, the clinicians at the Mayo Clinic annually rate their supervisors on a Leader Index, a simple 12-question survey of five leadership domains: truthfulness, transparency, character, capability, and partnership. All supervisors were physicians and scientists. Their findings revealed that for each one-point increase in composite leadership score, there was a 3.3% decrease in the likelihood of burnout and a 9.0% increase in the likelihood of satisfaction in the physicians supervised.4
Interprofessional teamwork and engagement are vital skills for a leader to create a successful team. Enhanced management practices have also been associated with higher patient approval ratings and better financial performance. Effective leadership additionally affects physician well-being, with stronger leadership associated with less physician burnout and higher satisfaction.5
Leadership styles enhance quality measures in health care.6 The most effective leadership styles are ones in which the staff feels they are part of a team, are engaged, and are mentored.7 While leadership styles can vary, the common theme is staff engagement. An authoritative style leader is one who mobilizes the team toward a vision, that is, “Come with me.” An affiliative style leader creates harmony and builds emotional bonds where “people come first.” Democratic leaders forge a consensus through staff participation by asking, “What do you think?” Finally, a leader who uses a coaching style helps staff to identify their strengths and weaknesses and work toward improvement. These leadership behaviors are in contradistinction to the unsuccessful coercive leader who demands immediate compliance, that is, “Do what I tell you.”
Five fundamental leadership principles are shown in Table 1.8
Effective leaders have an open (growth) mindset, unwavering attention to diversity, equity, and inclusion, and to building relationships and trust; they practice effective communication and listening, focus on results, and cocreate support structures.
A growth mindset is the belief that one’s abilities are not innate but can improve through effort and learning.9
Emotional intelligence
A survey of business senior managers rated the qualities found in the most outstanding leaders. Using objective criteria like profitability the study psychologists interviewed the highest-rated leaders to compare their capabilities. While intellects and cognitive skills were important, the results showed that emotional intelligence (EI) was twice as important as technical skills and IQ.10 As an example, in a 1996 study, when senior managers had an optimal level of EI, their division’s yearly earnings were 20% higher than estimated.11
EI is a leadership competency that deals with the ability to understand and manage your own emotions and your interactions with others.10 At the Cleveland Clinic, EI is exemplified by the acronym HEART, whereby the team strives to improve the patient experience, mainly when an error occurs. The health care team is using EI by showing its the ability to Hear, Empathize, Apologize, Reply, and Thank. When an untoward event occurs, the physician, as the leader of the team, must lead by example when communicating with staff and patients. EI consists of five components (Table 2).13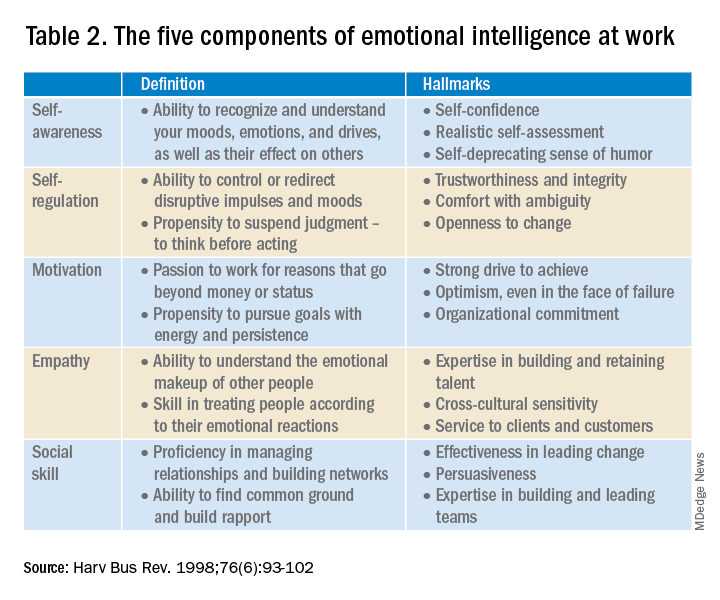
- Self-awareness is insight by which you can improve. Maintaining a journal of your daily thoughts may assist with this as well as simply pausing to pay attention during times of heightened emotions.
- Self-regulation shows control, that is, behaving according to your values, and being accountable and calm when challenged.
- Purpose, knowing your “why,” produces motivation and helps maintain optimism.
- Empathy shows the ability to understand the emotions of other people.
- Social skill is the ability to establish mutually rewarding relationships.
Given all the above benefits, it is no surprise that companies are actively trying use artificial intelligence to improve EI.12
Learning to be a leader
In medical school, students are expected to develop skills to handle and resolve conflicts, learn to share leadership, take mutual responsibility, and monitor their own performance.13 Although training of young physicians in leadership is not unprecedented, a systemic review revealed a lack of analytic studies to evaluate the effectiveness of the teaching methods.14 During undergraduate medical education, standard curricula and methods of instruction on leadership are not established, resulting in variable outcomes.
The Association of American Medical Colleges offers a curriculum, “Preparing Medical Students to Be Physician Leaders: A Leadership Training Program for Students Designed and Led by Students.”15 The objectives of this training are to help students identify their “personal style of leadership, recognize strengths and weaknesses, utilize effective communication strategies, appropriately delegate team member responsibilities, and provide constructive feedback to help improve team function.”
Take-home points
Following the completion of formal medical education, physicians are thrust into leadership roles. The key to being an effective leader is using EI to mentor the team and make staff feel connected to the team’s meaning and purpose, so they feel valued.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Carsen S and Xia C. McGill J Med. 2006 Jan;9(1):1-2.
2. Jardine D et al. J Grad Med Educ. 2015;7(2):307-9.
3. Institute of Medicine. Acad Emerg Med. July 2004;11(7):802-6.
4. Shanafelt TD et al. Mayo Clin Proc. April 2015;90(4):432-40.
5. Rotenstein LS et al. Harv Bus Rev. Oct. 17, 2018.
6. Sfantou SF. Healthcare 2017;5(4):73.
7. Goleman D. Harv Bus Rev. March-April 2000.
8. Collins-Nakai R. McGill J Med [Internet]. 2020 Dec. 1 [cited 2023 Mar. 28];9(1).
9. Dweck C. Harv Bus Rev. Jan. 13, 2016.
10. Goleman D. Harv Bus Rev. 1998 Nov-Dec;76(6):93-102..
11. Goleman D et al. Primal leadership: Realizing the power of emotional intelligence. Boston: Harvard Business School Publishing, 2002.12. Limon D and Plaster B. Harv Bus Rev. Jan. 25, 2022.
13. Chen T-Y. Tzu Chi Med J. Apr–Jun 2018;30(2):66-70.
14. Kumar B et al. BMC Med Educ. 2020;20:175.
15. Richards K et al. Med Ed Portal. Dec. 13 2019.
‘Excess’ deaths surging, but why?
This transcript has been edited for clarity.
“Excess deaths.” You’ve heard the phrase countless times by now. It is one of the myriad of previously esoteric epidemiology terms that the pandemic brought squarely into the zeitgeist.
As a sort of standard candle of the performance of a state or a region or a country in terms of health care, it has a lot of utility – if for nothing more than Monday-morning quarterbacking. But this week, I want to dig in on the concept a bit because, according to a new study, the excess death gap between the United States and Western Europe has never been higher.
You might imagine that the best way to figure this out is for some group of intelligent people to review each death and decide, somehow, whether it was expected or not. But aside from being impractical, this would end up being somewhat subjective. That older person who died from pneumonia – was that an expected death? Could it have been avoided?
Rather, the calculation of excess mortality relies on large numbers and statistical inference to compare an expected number of deaths with those that are observed.
The difference is excess mortality, even if you can never be sure whether any particular death was expected or not.
As always, however, the devil is in the details. What data do you use to define the expected number of deaths?
There are options here. Probably the most straightforward analysis uses past data from the country of interest. You look at annual deaths over some historical period of time and compare those numbers with the rates today. Two issues need to be accounted for here: population growth – a larger population will have more deaths, so you need to adjust the historical population with current levels, and demographic shifts – an older or more male population will have more deaths, so you need to adjust for that as well.
But provided you take care of those factors, you can estimate fairly well how many deaths you can expect to see in any given period of time.
Still, you should see right away that excess mortality is a relative concept. If you think that, just perhaps, the United States has some systematic failure to deliver care that has been stable and persistent over time, you wouldn’t capture that failing in an excess mortality calculation that uses U.S. historical data as the baseline.
The best way to get around that is to use data from other countries, and that’s just what this article – a rare single-author piece by Patrick Heuveline – does, calculating excess deaths in the United States by standardizing our mortality rates to the five largest Western European countries: the United Kingdom, France, Germany, Italy, and Spain.
Controlling for the differences in the demographics of that European population, here is the expected number of deaths in the United States over the past 5 years.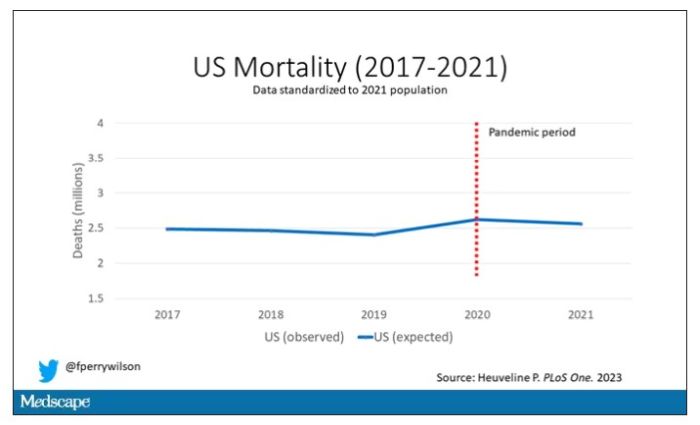
Note that there is a small uptick in expected deaths in 2020, reflecting the pandemic, which returns to baseline levels by 2021. This is because that’s what happened in Europe; by 2021, the excess mortality due to COVID-19 was quite low.
Here are the actual deaths in the US during that time.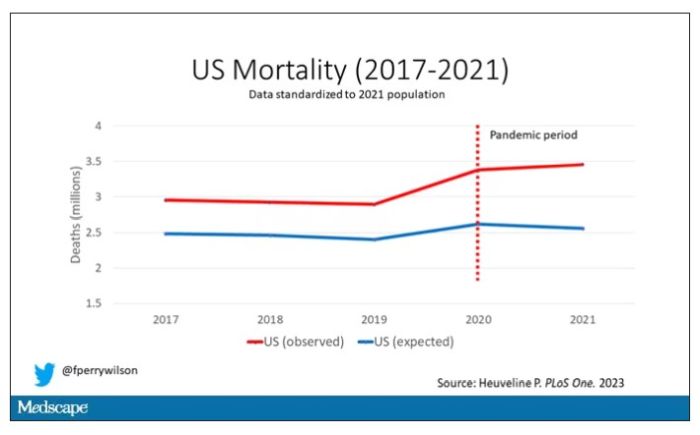
Highlighted here in green, then, is the excess mortality over time in the United States.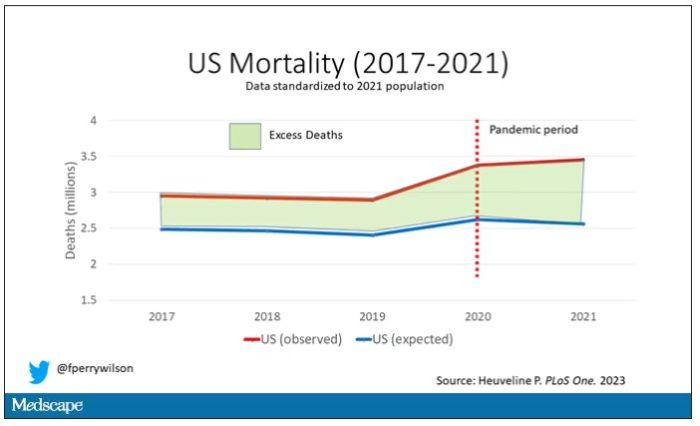
There are some fascinating and concerning findings here.
First of all, you can see that even before the pandemic, the United States has an excess mortality problem. This is not entirely a surprise; we’ve known that so-called “deaths of despair,” those due to alcohol abuse, drug overdoses, and suicide, are at an all-time high and tend to affect a “prime of life” population that would not otherwise be expected to die. In fact, fully 50% of the excess deaths in the United States occur in those between ages 15 and 64.
Excess deaths are also a concerning percentage of total deaths. In 2017, 17% of total deaths in the United States could be considered “excess.” In 2021, that number had doubled to 35%. Nearly 900,000 individuals in the United States died in 2021 who perhaps didn’t need to.
The obvious culprit to blame here is COVID, but COVID-associated excess deaths only explain about 50% of the excess we see in 2021. The rest reflect something even more concerning: a worsening of the failures of the past, perhaps exacerbated by the pandemic but not due to the virus itself.
Of course, we started this discussion acknowledging that the calculation of excess mortality is exquisitely dependent on how you model the expected number of deaths, and I’m sure some will take issue with the use of European numbers when applied to Americans. After all, Europe has, by and large, a robust public health service, socialized medicine, and healthcare that does not run the risk of bankrupting its citizens. How can we compare our outcomes to a place like that?
How indeed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven,Conn. He reported no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
“Excess deaths.” You’ve heard the phrase countless times by now. It is one of the myriad of previously esoteric epidemiology terms that the pandemic brought squarely into the zeitgeist.
As a sort of standard candle of the performance of a state or a region or a country in terms of health care, it has a lot of utility – if for nothing more than Monday-morning quarterbacking. But this week, I want to dig in on the concept a bit because, according to a new study, the excess death gap between the United States and Western Europe has never been higher.
You might imagine that the best way to figure this out is for some group of intelligent people to review each death and decide, somehow, whether it was expected or not. But aside from being impractical, this would end up being somewhat subjective. That older person who died from pneumonia – was that an expected death? Could it have been avoided?
Rather, the calculation of excess mortality relies on large numbers and statistical inference to compare an expected number of deaths with those that are observed.
The difference is excess mortality, even if you can never be sure whether any particular death was expected or not.
As always, however, the devil is in the details. What data do you use to define the expected number of deaths?
There are options here. Probably the most straightforward analysis uses past data from the country of interest. You look at annual deaths over some historical period of time and compare those numbers with the rates today. Two issues need to be accounted for here: population growth – a larger population will have more deaths, so you need to adjust the historical population with current levels, and demographic shifts – an older or more male population will have more deaths, so you need to adjust for that as well.
But provided you take care of those factors, you can estimate fairly well how many deaths you can expect to see in any given period of time.
Still, you should see right away that excess mortality is a relative concept. If you think that, just perhaps, the United States has some systematic failure to deliver care that has been stable and persistent over time, you wouldn’t capture that failing in an excess mortality calculation that uses U.S. historical data as the baseline.
The best way to get around that is to use data from other countries, and that’s just what this article – a rare single-author piece by Patrick Heuveline – does, calculating excess deaths in the United States by standardizing our mortality rates to the five largest Western European countries: the United Kingdom, France, Germany, Italy, and Spain.
Controlling for the differences in the demographics of that European population, here is the expected number of deaths in the United States over the past 5 years.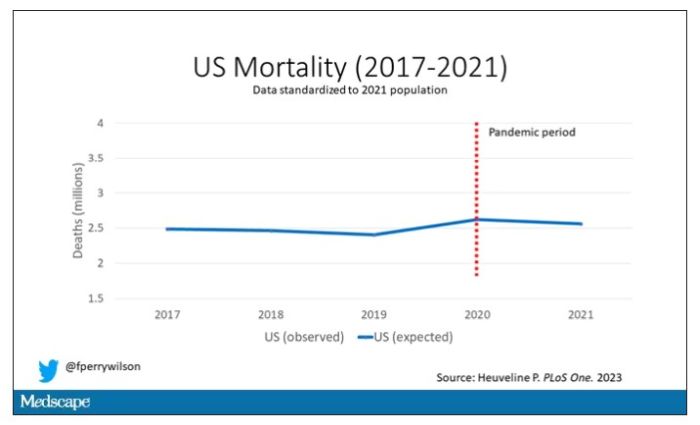
Note that there is a small uptick in expected deaths in 2020, reflecting the pandemic, which returns to baseline levels by 2021. This is because that’s what happened in Europe; by 2021, the excess mortality due to COVID-19 was quite low.
Here are the actual deaths in the US during that time.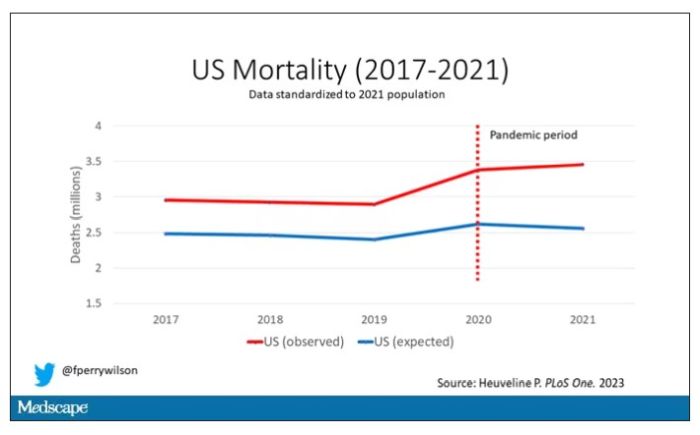
Highlighted here in green, then, is the excess mortality over time in the United States.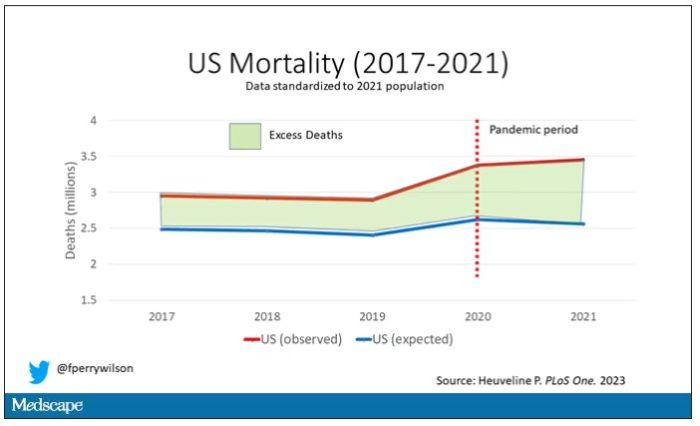
There are some fascinating and concerning findings here.
First of all, you can see that even before the pandemic, the United States has an excess mortality problem. This is not entirely a surprise; we’ve known that so-called “deaths of despair,” those due to alcohol abuse, drug overdoses, and suicide, are at an all-time high and tend to affect a “prime of life” population that would not otherwise be expected to die. In fact, fully 50% of the excess deaths in the United States occur in those between ages 15 and 64.
Excess deaths are also a concerning percentage of total deaths. In 2017, 17% of total deaths in the United States could be considered “excess.” In 2021, that number had doubled to 35%. Nearly 900,000 individuals in the United States died in 2021 who perhaps didn’t need to.
The obvious culprit to blame here is COVID, but COVID-associated excess deaths only explain about 50% of the excess we see in 2021. The rest reflect something even more concerning: a worsening of the failures of the past, perhaps exacerbated by the pandemic but not due to the virus itself.
Of course, we started this discussion acknowledging that the calculation of excess mortality is exquisitely dependent on how you model the expected number of deaths, and I’m sure some will take issue with the use of European numbers when applied to Americans. After all, Europe has, by and large, a robust public health service, socialized medicine, and healthcare that does not run the risk of bankrupting its citizens. How can we compare our outcomes to a place like that?
How indeed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven,Conn. He reported no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
“Excess deaths.” You’ve heard the phrase countless times by now. It is one of the myriad of previously esoteric epidemiology terms that the pandemic brought squarely into the zeitgeist.
As a sort of standard candle of the performance of a state or a region or a country in terms of health care, it has a lot of utility – if for nothing more than Monday-morning quarterbacking. But this week, I want to dig in on the concept a bit because, according to a new study, the excess death gap between the United States and Western Europe has never been higher.
You might imagine that the best way to figure this out is for some group of intelligent people to review each death and decide, somehow, whether it was expected or not. But aside from being impractical, this would end up being somewhat subjective. That older person who died from pneumonia – was that an expected death? Could it have been avoided?
Rather, the calculation of excess mortality relies on large numbers and statistical inference to compare an expected number of deaths with those that are observed.
The difference is excess mortality, even if you can never be sure whether any particular death was expected or not.
As always, however, the devil is in the details. What data do you use to define the expected number of deaths?
There are options here. Probably the most straightforward analysis uses past data from the country of interest. You look at annual deaths over some historical period of time and compare those numbers with the rates today. Two issues need to be accounted for here: population growth – a larger population will have more deaths, so you need to adjust the historical population with current levels, and demographic shifts – an older or more male population will have more deaths, so you need to adjust for that as well.
But provided you take care of those factors, you can estimate fairly well how many deaths you can expect to see in any given period of time.
Still, you should see right away that excess mortality is a relative concept. If you think that, just perhaps, the United States has some systematic failure to deliver care that has been stable and persistent over time, you wouldn’t capture that failing in an excess mortality calculation that uses U.S. historical data as the baseline.
The best way to get around that is to use data from other countries, and that’s just what this article – a rare single-author piece by Patrick Heuveline – does, calculating excess deaths in the United States by standardizing our mortality rates to the five largest Western European countries: the United Kingdom, France, Germany, Italy, and Spain.
Controlling for the differences in the demographics of that European population, here is the expected number of deaths in the United States over the past 5 years.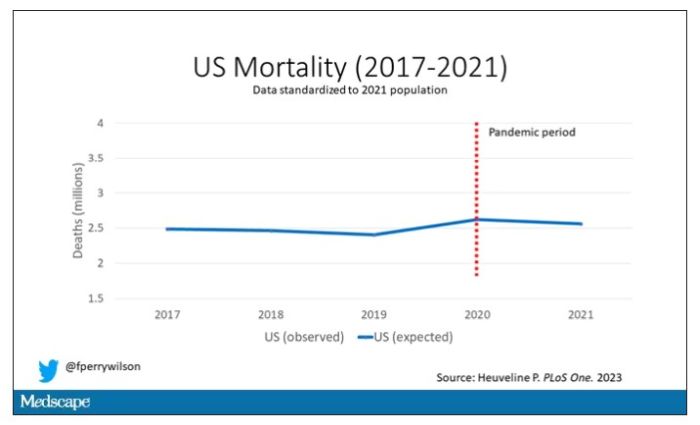
Note that there is a small uptick in expected deaths in 2020, reflecting the pandemic, which returns to baseline levels by 2021. This is because that’s what happened in Europe; by 2021, the excess mortality due to COVID-19 was quite low.
Here are the actual deaths in the US during that time.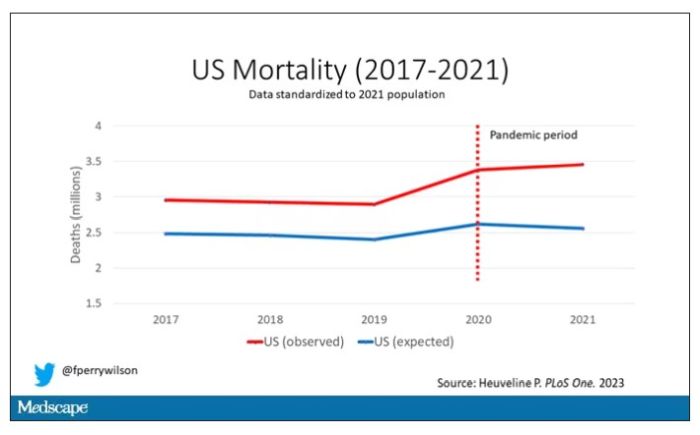
Highlighted here in green, then, is the excess mortality over time in the United States.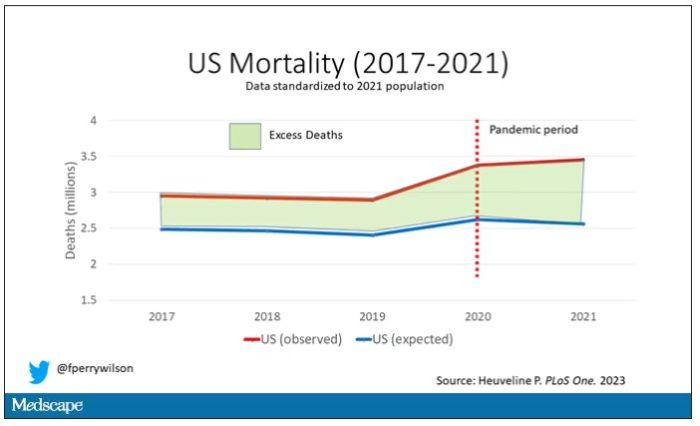
There are some fascinating and concerning findings here.
First of all, you can see that even before the pandemic, the United States has an excess mortality problem. This is not entirely a surprise; we’ve known that so-called “deaths of despair,” those due to alcohol abuse, drug overdoses, and suicide, are at an all-time high and tend to affect a “prime of life” population that would not otherwise be expected to die. In fact, fully 50% of the excess deaths in the United States occur in those between ages 15 and 64.
Excess deaths are also a concerning percentage of total deaths. In 2017, 17% of total deaths in the United States could be considered “excess.” In 2021, that number had doubled to 35%. Nearly 900,000 individuals in the United States died in 2021 who perhaps didn’t need to.
The obvious culprit to blame here is COVID, but COVID-associated excess deaths only explain about 50% of the excess we see in 2021. The rest reflect something even more concerning: a worsening of the failures of the past, perhaps exacerbated by the pandemic but not due to the virus itself.
Of course, we started this discussion acknowledging that the calculation of excess mortality is exquisitely dependent on how you model the expected number of deaths, and I’m sure some will take issue with the use of European numbers when applied to Americans. After all, Europe has, by and large, a robust public health service, socialized medicine, and healthcare that does not run the risk of bankrupting its citizens. How can we compare our outcomes to a place like that?
How indeed.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven,Conn. He reported no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
Is it time to stop treating high triglycerides?
The publication of the PROMINENT trial, where pemafibrate successfully lowered high levels but was not associated with a lower risk for cardiovascular events, reinforced the point. Is it time to stop measuring and treating high triglycerides?
There may be noncardiovascular reasons to treat hypertriglyceridemia. Pancreatitis is the most cited one, given that the risk for pancreatitis increases with increasing triglyceride levels, especially in patients with a prior episode.
There may also be practical reasons to lower trigs. Because most cholesterol panels use the Friedewald equation to calculate low-density lipoprotein cholesterol (LDL-C) rather than measuring it directly, very high triglyceride levels can invalidate the calculation and return error messages on lab reports.
But we now have alternatives to measuring LDL-C, including non–high-density lipoprotein cholesterol (HDL-C) and apolipoprotein B (apoB), that better predict risk and are usable even in the setting of nonfasting samples when triglycerides are elevated.
Independent cardiovascular risk factor?
If we are going to measure and treat high triglycerides for cardiovascular reasons, the relevant question is, are high triglycerides an independent risk factor for cardiovascular disease?
Proponents have a broad swath of supportive literature to point at. Multiple studies have shown an association between triglyceride levels and cardiovascular risk. The evidence even extends beyond traditional epidemiologic analyses, to genetic studies that should be free from some of the problems seen in observational cohorts.
But it is difficult to be certain whether these associations are causal or merely confounding. An unhealthy diet will increase triglycerides, as will alcohol. Patients with diabetes or metabolic syndrome have high triglycerides. So do patients with nephrotic syndrome or hypothyroidism, or hypertensive patients taking thiazide diuretics. Adjusting for these baseline factors is possible but imperfect, and residual confounding is always an issue. An analysis of the Reykjavik and the EPIC-Norfolk studies found an association between triglyceride levels and cardiovascular risk. That risk was attenuated, but not eliminated, when adjusted for traditional risk factors such as age, smoking, blood pressure, diabetes, and cholesterol.
Randomized trials of triglyceride-lowering therapies would help resolve the question of whether hypertriglyceridemia contributes to coronary disease or simply identifies high-risk patients. Early trials seemed to support the idea of a causal link. The Helsinki Heart Study randomized patients to gemfibrozil or placebo and found a 34% relative risk reduction in coronary artery disease with the fibrate. But gemfibrozil didn’t only reduce triglycerides. It also increased HDL-C and lowered LDL-C relative to placebo, which may explain the observed benefit.
Gemfibrozil is rarely used today because we can achieve much greater LDL-C reductions with statins, as well as ezetimibe and PCSK9 inhibitors. The success of these drugs may not leave any room for triglyceride-lowering medications.
The pre- vs. post-statin era
In the 2005 FIELD study, participants were randomized to receive fenofibrate or placebo. Although patients weren’t taking statin at study entry, 17% of the placebo group started taking one during the trial. Fenofibrate wasn’t associated with a reduction in the primary endpoint, a combination of coronary heart disease death or nonfatal myocardial infarction (MI). Among the many secondary endpoints, nonfatal MI was lower but cardiovascular mortality was not in the fibrate-treated patients. In the same vein, the 2010 ACCORD study randomized patients to receive simvastatin plus fenofibrate or simvastatin alone. The composite primary outcome of MI, stroke, and cardiovascular mortality was not lowered nor were any secondary outcomes with the combination therapy. In the statin era, triglyceride-lowering therapies have not shown much benefit.
The final nail in the coffin may very well be the aforementioned PROMINENT trial. The new agent, pemafibrate, fared no better than its predecessor fenofibrate. Pemafibrate had no impact on the study’s primary composite outcome of nonfatal MI, stroke, coronary revascularization, or cardiovascular death despite being very effective at lowering triglycerides (by more than 25%). Patients treated with pemafibrate had increased LDL-C and apoB compared with the placebo group. When you realize that, the results of the study are not very surprising.
Some point to the results of REDUCE-IT as proof that triglycerides are still a valid target for pharmacotherapy. The debate on whether REDUCE-IT tested a good drug or a bad placebo is one for another day. The salient point for today is that the benefits of eicosapentaenoic acid (EPA) were seen regardless of either baseline or final triglyceride level. EPA may lower cardiac risk, but there is no widespread consensus that it does so by lowering triglycerides. There may be other mechanisms at work.
You could still argue that high triglycerides have value as a risk prediction tool even if their role as a target for drug therapy is questionable. There was a time when medications to lower triglycerides had a benefit. But this is the post-statin era, and that time has passed.
If you see patients with high triglycerides, treating them with triglyceride-lowering medication probably isn’t going to reduce their cardiovascular risk. Dietary interventions, encouraging exercise, and reducing alcohol consumption are better options. Not only will they lead to lower cholesterol levels, but they’ll lower cardiovascular risk, too.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, with a degree in epidemiology. He has disclosed no relevant financial relationships. He spends most of his time doing things that he doesn’t get paid for, like research, teaching, and podcasting. Occasionally he finds time to practice cardiology to pay the rent. He realizes that half of his research findings will be disproved in 5 years; he just doesn’t know which half. He is a regular contributor to the Montreal Gazette, CJAD radio, and CTV television in Montreal and is host of the award-winning podcast The Body of Evidence. The Body of Evidence.
A version of this article originally appeared on Medscape.com.
The publication of the PROMINENT trial, where pemafibrate successfully lowered high levels but was not associated with a lower risk for cardiovascular events, reinforced the point. Is it time to stop measuring and treating high triglycerides?
There may be noncardiovascular reasons to treat hypertriglyceridemia. Pancreatitis is the most cited one, given that the risk for pancreatitis increases with increasing triglyceride levels, especially in patients with a prior episode.
There may also be practical reasons to lower trigs. Because most cholesterol panels use the Friedewald equation to calculate low-density lipoprotein cholesterol (LDL-C) rather than measuring it directly, very high triglyceride levels can invalidate the calculation and return error messages on lab reports.
But we now have alternatives to measuring LDL-C, including non–high-density lipoprotein cholesterol (HDL-C) and apolipoprotein B (apoB), that better predict risk and are usable even in the setting of nonfasting samples when triglycerides are elevated.
Independent cardiovascular risk factor?
If we are going to measure and treat high triglycerides for cardiovascular reasons, the relevant question is, are high triglycerides an independent risk factor for cardiovascular disease?
Proponents have a broad swath of supportive literature to point at. Multiple studies have shown an association between triglyceride levels and cardiovascular risk. The evidence even extends beyond traditional epidemiologic analyses, to genetic studies that should be free from some of the problems seen in observational cohorts.
But it is difficult to be certain whether these associations are causal or merely confounding. An unhealthy diet will increase triglycerides, as will alcohol. Patients with diabetes or metabolic syndrome have high triglycerides. So do patients with nephrotic syndrome or hypothyroidism, or hypertensive patients taking thiazide diuretics. Adjusting for these baseline factors is possible but imperfect, and residual confounding is always an issue. An analysis of the Reykjavik and the EPIC-Norfolk studies found an association between triglyceride levels and cardiovascular risk. That risk was attenuated, but not eliminated, when adjusted for traditional risk factors such as age, smoking, blood pressure, diabetes, and cholesterol.
Randomized trials of triglyceride-lowering therapies would help resolve the question of whether hypertriglyceridemia contributes to coronary disease or simply identifies high-risk patients. Early trials seemed to support the idea of a causal link. The Helsinki Heart Study randomized patients to gemfibrozil or placebo and found a 34% relative risk reduction in coronary artery disease with the fibrate. But gemfibrozil didn’t only reduce triglycerides. It also increased HDL-C and lowered LDL-C relative to placebo, which may explain the observed benefit.
Gemfibrozil is rarely used today because we can achieve much greater LDL-C reductions with statins, as well as ezetimibe and PCSK9 inhibitors. The success of these drugs may not leave any room for triglyceride-lowering medications.
The pre- vs. post-statin era
In the 2005 FIELD study, participants were randomized to receive fenofibrate or placebo. Although patients weren’t taking statin at study entry, 17% of the placebo group started taking one during the trial. Fenofibrate wasn’t associated with a reduction in the primary endpoint, a combination of coronary heart disease death or nonfatal myocardial infarction (MI). Among the many secondary endpoints, nonfatal MI was lower but cardiovascular mortality was not in the fibrate-treated patients. In the same vein, the 2010 ACCORD study randomized patients to receive simvastatin plus fenofibrate or simvastatin alone. The composite primary outcome of MI, stroke, and cardiovascular mortality was not lowered nor were any secondary outcomes with the combination therapy. In the statin era, triglyceride-lowering therapies have not shown much benefit.
The final nail in the coffin may very well be the aforementioned PROMINENT trial. The new agent, pemafibrate, fared no better than its predecessor fenofibrate. Pemafibrate had no impact on the study’s primary composite outcome of nonfatal MI, stroke, coronary revascularization, or cardiovascular death despite being very effective at lowering triglycerides (by more than 25%). Patients treated with pemafibrate had increased LDL-C and apoB compared with the placebo group. When you realize that, the results of the study are not very surprising.
Some point to the results of REDUCE-IT as proof that triglycerides are still a valid target for pharmacotherapy. The debate on whether REDUCE-IT tested a good drug or a bad placebo is one for another day. The salient point for today is that the benefits of eicosapentaenoic acid (EPA) were seen regardless of either baseline or final triglyceride level. EPA may lower cardiac risk, but there is no widespread consensus that it does so by lowering triglycerides. There may be other mechanisms at work.
You could still argue that high triglycerides have value as a risk prediction tool even if their role as a target for drug therapy is questionable. There was a time when medications to lower triglycerides had a benefit. But this is the post-statin era, and that time has passed.
If you see patients with high triglycerides, treating them with triglyceride-lowering medication probably isn’t going to reduce their cardiovascular risk. Dietary interventions, encouraging exercise, and reducing alcohol consumption are better options. Not only will they lead to lower cholesterol levels, but they’ll lower cardiovascular risk, too.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, with a degree in epidemiology. He has disclosed no relevant financial relationships. He spends most of his time doing things that he doesn’t get paid for, like research, teaching, and podcasting. Occasionally he finds time to practice cardiology to pay the rent. He realizes that half of his research findings will be disproved in 5 years; he just doesn’t know which half. He is a regular contributor to the Montreal Gazette, CJAD radio, and CTV television in Montreal and is host of the award-winning podcast The Body of Evidence. The Body of Evidence.
A version of this article originally appeared on Medscape.com.
The publication of the PROMINENT trial, where pemafibrate successfully lowered high levels but was not associated with a lower risk for cardiovascular events, reinforced the point. Is it time to stop measuring and treating high triglycerides?
There may be noncardiovascular reasons to treat hypertriglyceridemia. Pancreatitis is the most cited one, given that the risk for pancreatitis increases with increasing triglyceride levels, especially in patients with a prior episode.
There may also be practical reasons to lower trigs. Because most cholesterol panels use the Friedewald equation to calculate low-density lipoprotein cholesterol (LDL-C) rather than measuring it directly, very high triglyceride levels can invalidate the calculation and return error messages on lab reports.
But we now have alternatives to measuring LDL-C, including non–high-density lipoprotein cholesterol (HDL-C) and apolipoprotein B (apoB), that better predict risk and are usable even in the setting of nonfasting samples when triglycerides are elevated.
Independent cardiovascular risk factor?
If we are going to measure and treat high triglycerides for cardiovascular reasons, the relevant question is, are high triglycerides an independent risk factor for cardiovascular disease?
Proponents have a broad swath of supportive literature to point at. Multiple studies have shown an association between triglyceride levels and cardiovascular risk. The evidence even extends beyond traditional epidemiologic analyses, to genetic studies that should be free from some of the problems seen in observational cohorts.
But it is difficult to be certain whether these associations are causal or merely confounding. An unhealthy diet will increase triglycerides, as will alcohol. Patients with diabetes or metabolic syndrome have high triglycerides. So do patients with nephrotic syndrome or hypothyroidism, or hypertensive patients taking thiazide diuretics. Adjusting for these baseline factors is possible but imperfect, and residual confounding is always an issue. An analysis of the Reykjavik and the EPIC-Norfolk studies found an association between triglyceride levels and cardiovascular risk. That risk was attenuated, but not eliminated, when adjusted for traditional risk factors such as age, smoking, blood pressure, diabetes, and cholesterol.
Randomized trials of triglyceride-lowering therapies would help resolve the question of whether hypertriglyceridemia contributes to coronary disease or simply identifies high-risk patients. Early trials seemed to support the idea of a causal link. The Helsinki Heart Study randomized patients to gemfibrozil or placebo and found a 34% relative risk reduction in coronary artery disease with the fibrate. But gemfibrozil didn’t only reduce triglycerides. It also increased HDL-C and lowered LDL-C relative to placebo, which may explain the observed benefit.
Gemfibrozil is rarely used today because we can achieve much greater LDL-C reductions with statins, as well as ezetimibe and PCSK9 inhibitors. The success of these drugs may not leave any room for triglyceride-lowering medications.
The pre- vs. post-statin era
In the 2005 FIELD study, participants were randomized to receive fenofibrate or placebo. Although patients weren’t taking statin at study entry, 17% of the placebo group started taking one during the trial. Fenofibrate wasn’t associated with a reduction in the primary endpoint, a combination of coronary heart disease death or nonfatal myocardial infarction (MI). Among the many secondary endpoints, nonfatal MI was lower but cardiovascular mortality was not in the fibrate-treated patients. In the same vein, the 2010 ACCORD study randomized patients to receive simvastatin plus fenofibrate or simvastatin alone. The composite primary outcome of MI, stroke, and cardiovascular mortality was not lowered nor were any secondary outcomes with the combination therapy. In the statin era, triglyceride-lowering therapies have not shown much benefit.
The final nail in the coffin may very well be the aforementioned PROMINENT trial. The new agent, pemafibrate, fared no better than its predecessor fenofibrate. Pemafibrate had no impact on the study’s primary composite outcome of nonfatal MI, stroke, coronary revascularization, or cardiovascular death despite being very effective at lowering triglycerides (by more than 25%). Patients treated with pemafibrate had increased LDL-C and apoB compared with the placebo group. When you realize that, the results of the study are not very surprising.
Some point to the results of REDUCE-IT as proof that triglycerides are still a valid target for pharmacotherapy. The debate on whether REDUCE-IT tested a good drug or a bad placebo is one for another day. The salient point for today is that the benefits of eicosapentaenoic acid (EPA) were seen regardless of either baseline or final triglyceride level. EPA may lower cardiac risk, but there is no widespread consensus that it does so by lowering triglycerides. There may be other mechanisms at work.
You could still argue that high triglycerides have value as a risk prediction tool even if their role as a target for drug therapy is questionable. There was a time when medications to lower triglycerides had a benefit. But this is the post-statin era, and that time has passed.
If you see patients with high triglycerides, treating them with triglyceride-lowering medication probably isn’t going to reduce their cardiovascular risk. Dietary interventions, encouraging exercise, and reducing alcohol consumption are better options. Not only will they lead to lower cholesterol levels, but they’ll lower cardiovascular risk, too.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, with a degree in epidemiology. He has disclosed no relevant financial relationships. He spends most of his time doing things that he doesn’t get paid for, like research, teaching, and podcasting. Occasionally he finds time to practice cardiology to pay the rent. He realizes that half of his research findings will be disproved in 5 years; he just doesn’t know which half. He is a regular contributor to the Montreal Gazette, CJAD radio, and CTV television in Montreal and is host of the award-winning podcast The Body of Evidence. The Body of Evidence.
A version of this article originally appeared on Medscape.com.
Stutz: The psychiatrist as movie star
For as long as I can remember, psychiatrists have talked about what the appropriate boundaries are for self-disclosure about personal issues with patients. There is obviously no exact answer as to what is acceptable to disclose; this depends on the doctor, the patient, the “brand” of psychotherapy, the patient’s issues, the nature of what is being disclosed, and maybe the alignment of the stars on that particular day. “Stutz,” the Netflix documentary that Oscar-nominated actor/director Jonah Hill has made about his psychiatrist, Phil Stutz, MD, adds a whole new chapter to the discussion.
“Okay, entertain me,” Dr. Stutz says as his patient takes a seat. The therapeutic relationship and the paradigm Dr. Stutz has created to help his patients has been healing for Jonah Hill. The very serious and intimate dialogue that follows unfolds with moments of humor, warmth, and open affection. Hill candidly tells us why he is making this documentary – to share what he has learned and to honor his therapist – but we don’t know why Dr. Stutz has agreed to the endeavor and we’re left to our own inferences.
Dr. Stutz is the coauthor, with Barry Michels, of a best-selling self-help book, “The Tools: 5 Tools to Help You Find Courage, Creativity, and Willpower – and Inspire You to Live Life in Forward Motion.” He talks about his restlessness with the psychodynamic method during his training as a resident in New York – he wanted to offer his patients more immediate relief and a supervisor told him, “Don’t you dare!”
In the film, he talks about giving patients hope and direction. And Hill makes the comment, “In traditional therapy, you’re paying this person and you save all your problems for them, and they just listen, and your friends – who are idiots – give you advice, unsolicited, and you want your friends just to listen, and you want your therapist to give you advice!” Dr. Stutz gives advice and he is like no other therapist Jonah has ever had.
The premise of the film is that we are watching a single therapy session and Dr. Stutz will discuss the use of his tools and techniques that Hill has found helpful. Jonah is the interviewer, and when the doctor suggests it would be helpful if Jonah talked about his life, the patient/director rebuffs him; this documentary is about the psychiatrist.
Early in the film an alarm goes off, Dr. Stutz does not hear it, and Jonah has to remind him that it’s time for him to take his pills. The psychiatrist has Parkinson’s disease and how it has affected him becomes one focal point for the film. We later learn that he lost a younger brother as a child (something Hill did not know before they started filming) and grew up in the shadow of that loss. His extroverted father made it clear that medicine was the only acceptable career path for his son, and his introverted and depressed mother spent her days proclaiming that all men were as awful as her own abusive father.
About a third of the way through the film, the focus shifts. Jonah suddenly confesses that he is feeling stuck with regard to the movie, that he is troubled by the fact that he has not been able to share his distress with Dr. Stutz during their real-life, unfilmed therapy sessions, and the viewers learn that the single-session concept was disingenuous – they have been filming this documentary for two years, against a green screen and not in an office, always wearing the same clothes, and Jonah pulls off a wig that he wears to disguise the fact that he changed his hairstyle months earlier.
It’s a bit unnerving as they throw the wig around, and Jonah agrees to be more open about the issues he has struggled with. He acknowledges that this has been difficult, and he says, “I just keep asking myself, like, was this a f***ing horrible idea for a patient to make a movie about his therapist?” From my perspective as a psychiatrist-viewer, it’s a good question to ask!
Dr. Stutz reassures Jonah that it is okay to be vulnerable. “Failure, weakness, vulnerability – it’s like a connector, it connects you to the rest of the world.” A super-sized cardboard cutout of an obese 14-year-old Jonah now joins the room, and we learn that he continues to struggle with his self-image. Things get more real.
Peppered throughout the film, there are lessons from Dr. Stutz about his “tools,” constructs he uses to help people restructure their worlds and take action to move forward. One such construct he calls “the maze,” which occurs when one person in an interpersonal relationship is waiting for fairness and becomes preoccupied with feeling injured.
Jonah inquires about Dr. Stutz’s romantic life and the therapist replies with a transparency that overrides our usual professional boundaries. We all learn that Dr. Stutz is not in a relationship, he’s never been married, but there is a woman he has had some involvement with on and off for 40 years. Jonah’s line of questioning rivals that of any therapist. “How do you think it affects you, having your mom hate men and you being a man?” Dr. Stutz admits that he can never feel safe with women. “Did you ever override that wall you built with your mom and get close to a woman?” When Jonah professes, “I don’t feel anything but love for you and I just want you to be happy,” my own feeling was that the tables had turned too far, that the therapist’s failed romantic life risked being a burden to the patient.
Still, there is something about the relationship between the two men that is touching and beautiful. Dr. Stutz as a therapist is charismatic, caring, self-assured, and optimistic, and he radiates hope and certainty. He mixes an intense intimacy with humor in a way that is both authentic and entertaining. The interspersed jokes break the intensity, but they don’t diminish his wisdom and the healing he imparts.
Dr. Stutz is a psychiatrist, and his strength is clearly as a psychotherapist, yet there is not a single mention of psychotropic medications – there is a banter about recreational drugs and medications for Parkinson’s disease. If Hill is taking medication for depression or anxiety, and if prescribing is part of Dr. Stutz’s arsenal, the viewer is not made aware of this.
Dr. Stutz eschews the slow, detached, and “neutral” pace of psychodynamic therapy and the whole concept of the therapist as a blank wall for the transference to play out on, but here the transference screams: Jonah loves him, he respect and honors him, he wants him to be happy, and he is afraid of losing him.
“Stutz” is a movie about a larger-than-life psychiatrist, one whose warmth and inspiration are healing. I imagine his tools are helpful, but his personality is what carries the load. If a viewer has not had experience with psychiatry, and this film inspires him to begin therapy, there may be a good deal of disappointment. In this case, the patient is a successful actor, and one might wonder if that, together with the entire years-long project of filming, has altered the relationship well beyond the usual therapeutic hour.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
For as long as I can remember, psychiatrists have talked about what the appropriate boundaries are for self-disclosure about personal issues with patients. There is obviously no exact answer as to what is acceptable to disclose; this depends on the doctor, the patient, the “brand” of psychotherapy, the patient’s issues, the nature of what is being disclosed, and maybe the alignment of the stars on that particular day. “Stutz,” the Netflix documentary that Oscar-nominated actor/director Jonah Hill has made about his psychiatrist, Phil Stutz, MD, adds a whole new chapter to the discussion.
“Okay, entertain me,” Dr. Stutz says as his patient takes a seat. The therapeutic relationship and the paradigm Dr. Stutz has created to help his patients has been healing for Jonah Hill. The very serious and intimate dialogue that follows unfolds with moments of humor, warmth, and open affection. Hill candidly tells us why he is making this documentary – to share what he has learned and to honor his therapist – but we don’t know why Dr. Stutz has agreed to the endeavor and we’re left to our own inferences.
Dr. Stutz is the coauthor, with Barry Michels, of a best-selling self-help book, “The Tools: 5 Tools to Help You Find Courage, Creativity, and Willpower – and Inspire You to Live Life in Forward Motion.” He talks about his restlessness with the psychodynamic method during his training as a resident in New York – he wanted to offer his patients more immediate relief and a supervisor told him, “Don’t you dare!”
In the film, he talks about giving patients hope and direction. And Hill makes the comment, “In traditional therapy, you’re paying this person and you save all your problems for them, and they just listen, and your friends – who are idiots – give you advice, unsolicited, and you want your friends just to listen, and you want your therapist to give you advice!” Dr. Stutz gives advice and he is like no other therapist Jonah has ever had.
The premise of the film is that we are watching a single therapy session and Dr. Stutz will discuss the use of his tools and techniques that Hill has found helpful. Jonah is the interviewer, and when the doctor suggests it would be helpful if Jonah talked about his life, the patient/director rebuffs him; this documentary is about the psychiatrist.
Early in the film an alarm goes off, Dr. Stutz does not hear it, and Jonah has to remind him that it’s time for him to take his pills. The psychiatrist has Parkinson’s disease and how it has affected him becomes one focal point for the film. We later learn that he lost a younger brother as a child (something Hill did not know before they started filming) and grew up in the shadow of that loss. His extroverted father made it clear that medicine was the only acceptable career path for his son, and his introverted and depressed mother spent her days proclaiming that all men were as awful as her own abusive father.
About a third of the way through the film, the focus shifts. Jonah suddenly confesses that he is feeling stuck with regard to the movie, that he is troubled by the fact that he has not been able to share his distress with Dr. Stutz during their real-life, unfilmed therapy sessions, and the viewers learn that the single-session concept was disingenuous – they have been filming this documentary for two years, against a green screen and not in an office, always wearing the same clothes, and Jonah pulls off a wig that he wears to disguise the fact that he changed his hairstyle months earlier.
It’s a bit unnerving as they throw the wig around, and Jonah agrees to be more open about the issues he has struggled with. He acknowledges that this has been difficult, and he says, “I just keep asking myself, like, was this a f***ing horrible idea for a patient to make a movie about his therapist?” From my perspective as a psychiatrist-viewer, it’s a good question to ask!
Dr. Stutz reassures Jonah that it is okay to be vulnerable. “Failure, weakness, vulnerability – it’s like a connector, it connects you to the rest of the world.” A super-sized cardboard cutout of an obese 14-year-old Jonah now joins the room, and we learn that he continues to struggle with his self-image. Things get more real.
Peppered throughout the film, there are lessons from Dr. Stutz about his “tools,” constructs he uses to help people restructure their worlds and take action to move forward. One such construct he calls “the maze,” which occurs when one person in an interpersonal relationship is waiting for fairness and becomes preoccupied with feeling injured.
Jonah inquires about Dr. Stutz’s romantic life and the therapist replies with a transparency that overrides our usual professional boundaries. We all learn that Dr. Stutz is not in a relationship, he’s never been married, but there is a woman he has had some involvement with on and off for 40 years. Jonah’s line of questioning rivals that of any therapist. “How do you think it affects you, having your mom hate men and you being a man?” Dr. Stutz admits that he can never feel safe with women. “Did you ever override that wall you built with your mom and get close to a woman?” When Jonah professes, “I don’t feel anything but love for you and I just want you to be happy,” my own feeling was that the tables had turned too far, that the therapist’s failed romantic life risked being a burden to the patient.
Still, there is something about the relationship between the two men that is touching and beautiful. Dr. Stutz as a therapist is charismatic, caring, self-assured, and optimistic, and he radiates hope and certainty. He mixes an intense intimacy with humor in a way that is both authentic and entertaining. The interspersed jokes break the intensity, but they don’t diminish his wisdom and the healing he imparts.
Dr. Stutz is a psychiatrist, and his strength is clearly as a psychotherapist, yet there is not a single mention of psychotropic medications – there is a banter about recreational drugs and medications for Parkinson’s disease. If Hill is taking medication for depression or anxiety, and if prescribing is part of Dr. Stutz’s arsenal, the viewer is not made aware of this.
Dr. Stutz eschews the slow, detached, and “neutral” pace of psychodynamic therapy and the whole concept of the therapist as a blank wall for the transference to play out on, but here the transference screams: Jonah loves him, he respect and honors him, he wants him to be happy, and he is afraid of losing him.
“Stutz” is a movie about a larger-than-life psychiatrist, one whose warmth and inspiration are healing. I imagine his tools are helpful, but his personality is what carries the load. If a viewer has not had experience with psychiatry, and this film inspires him to begin therapy, there may be a good deal of disappointment. In this case, the patient is a successful actor, and one might wonder if that, together with the entire years-long project of filming, has altered the relationship well beyond the usual therapeutic hour.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
For as long as I can remember, psychiatrists have talked about what the appropriate boundaries are for self-disclosure about personal issues with patients. There is obviously no exact answer as to what is acceptable to disclose; this depends on the doctor, the patient, the “brand” of psychotherapy, the patient’s issues, the nature of what is being disclosed, and maybe the alignment of the stars on that particular day. “Stutz,” the Netflix documentary that Oscar-nominated actor/director Jonah Hill has made about his psychiatrist, Phil Stutz, MD, adds a whole new chapter to the discussion.
“Okay, entertain me,” Dr. Stutz says as his patient takes a seat. The therapeutic relationship and the paradigm Dr. Stutz has created to help his patients has been healing for Jonah Hill. The very serious and intimate dialogue that follows unfolds with moments of humor, warmth, and open affection. Hill candidly tells us why he is making this documentary – to share what he has learned and to honor his therapist – but we don’t know why Dr. Stutz has agreed to the endeavor and we’re left to our own inferences.
Dr. Stutz is the coauthor, with Barry Michels, of a best-selling self-help book, “The Tools: 5 Tools to Help You Find Courage, Creativity, and Willpower – and Inspire You to Live Life in Forward Motion.” He talks about his restlessness with the psychodynamic method during his training as a resident in New York – he wanted to offer his patients more immediate relief and a supervisor told him, “Don’t you dare!”
In the film, he talks about giving patients hope and direction. And Hill makes the comment, “In traditional therapy, you’re paying this person and you save all your problems for them, and they just listen, and your friends – who are idiots – give you advice, unsolicited, and you want your friends just to listen, and you want your therapist to give you advice!” Dr. Stutz gives advice and he is like no other therapist Jonah has ever had.
The premise of the film is that we are watching a single therapy session and Dr. Stutz will discuss the use of his tools and techniques that Hill has found helpful. Jonah is the interviewer, and when the doctor suggests it would be helpful if Jonah talked about his life, the patient/director rebuffs him; this documentary is about the psychiatrist.
Early in the film an alarm goes off, Dr. Stutz does not hear it, and Jonah has to remind him that it’s time for him to take his pills. The psychiatrist has Parkinson’s disease and how it has affected him becomes one focal point for the film. We later learn that he lost a younger brother as a child (something Hill did not know before they started filming) and grew up in the shadow of that loss. His extroverted father made it clear that medicine was the only acceptable career path for his son, and his introverted and depressed mother spent her days proclaiming that all men were as awful as her own abusive father.
About a third of the way through the film, the focus shifts. Jonah suddenly confesses that he is feeling stuck with regard to the movie, that he is troubled by the fact that he has not been able to share his distress with Dr. Stutz during their real-life, unfilmed therapy sessions, and the viewers learn that the single-session concept was disingenuous – they have been filming this documentary for two years, against a green screen and not in an office, always wearing the same clothes, and Jonah pulls off a wig that he wears to disguise the fact that he changed his hairstyle months earlier.
It’s a bit unnerving as they throw the wig around, and Jonah agrees to be more open about the issues he has struggled with. He acknowledges that this has been difficult, and he says, “I just keep asking myself, like, was this a f***ing horrible idea for a patient to make a movie about his therapist?” From my perspective as a psychiatrist-viewer, it’s a good question to ask!
Dr. Stutz reassures Jonah that it is okay to be vulnerable. “Failure, weakness, vulnerability – it’s like a connector, it connects you to the rest of the world.” A super-sized cardboard cutout of an obese 14-year-old Jonah now joins the room, and we learn that he continues to struggle with his self-image. Things get more real.
Peppered throughout the film, there are lessons from Dr. Stutz about his “tools,” constructs he uses to help people restructure their worlds and take action to move forward. One such construct he calls “the maze,” which occurs when one person in an interpersonal relationship is waiting for fairness and becomes preoccupied with feeling injured.
Jonah inquires about Dr. Stutz’s romantic life and the therapist replies with a transparency that overrides our usual professional boundaries. We all learn that Dr. Stutz is not in a relationship, he’s never been married, but there is a woman he has had some involvement with on and off for 40 years. Jonah’s line of questioning rivals that of any therapist. “How do you think it affects you, having your mom hate men and you being a man?” Dr. Stutz admits that he can never feel safe with women. “Did you ever override that wall you built with your mom and get close to a woman?” When Jonah professes, “I don’t feel anything but love for you and I just want you to be happy,” my own feeling was that the tables had turned too far, that the therapist’s failed romantic life risked being a burden to the patient.
Still, there is something about the relationship between the two men that is touching and beautiful. Dr. Stutz as a therapist is charismatic, caring, self-assured, and optimistic, and he radiates hope and certainty. He mixes an intense intimacy with humor in a way that is both authentic and entertaining. The interspersed jokes break the intensity, but they don’t diminish his wisdom and the healing he imparts.
Dr. Stutz is a psychiatrist, and his strength is clearly as a psychotherapist, yet there is not a single mention of psychotropic medications – there is a banter about recreational drugs and medications for Parkinson’s disease. If Hill is taking medication for depression or anxiety, and if prescribing is part of Dr. Stutz’s arsenal, the viewer is not made aware of this.
Dr. Stutz eschews the slow, detached, and “neutral” pace of psychodynamic therapy and the whole concept of the therapist as a blank wall for the transference to play out on, but here the transference screams: Jonah loves him, he respect and honors him, he wants him to be happy, and he is afraid of losing him.
“Stutz” is a movie about a larger-than-life psychiatrist, one whose warmth and inspiration are healing. I imagine his tools are helpful, but his personality is what carries the load. If a viewer has not had experience with psychiatry, and this film inspires him to begin therapy, there may be a good deal of disappointment. In this case, the patient is a successful actor, and one might wonder if that, together with the entire years-long project of filming, has altered the relationship well beyond the usual therapeutic hour.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University in Baltimore.
Surgical management of borderline ovarian tumors, part 1
Borderline ovarian tumors (BOTs) are estimated to comprise 10%-15% of all epithelial tumors of the ovary. They are characterized by their behavior, which falls somewhere between benign ovarian masses and frank carcinomas. They have cytologic characteristics suggesting malignancy, such as higher cellular proliferation and more variable nuclear atypia, but, unlike carcinomas, they lack destructive stromal invasion. For decades after their recognition by the International Federation of Gynecology and Obstetrics in 1971, these tumors were classified as being of low malignant potential (and subsequently referred to as LMP tumors of the ovary). Beginning with the 2014 World Health Organization classification, the recommended terminology is now borderline tumor of the ovary.
The primary treatment for BOTs is surgery. With a mean age at diagnosis in the fifth decade, many patients with BOTs desire ovarian preservation to maintain fertility and/or prevent surgical menopause. This raises multiple questions regarding the use of fertility-sparing surgery for BOTs: What types of procedures are safe and should be offered? For those patients who undergo fertility-sparing surgery initially, is additional surgery indicated after completion of childbearing or at an age closer to natural menopause? What should this completion surgery include?
Ovarian-sparing surgery
The diagnosis of a BOT is frequently only confirmed after the decision for ovarian conservation has been made. What should be considered before electing to proceed with ovarian cystectomy instead of unilateral salpingo-oophorectomy (USO)?
Is the risk of recurrence higher with cystectomy versus oophorectomy?
Yes. The risk of recurrence of BOT appears to be higher after cystectomy than it is after oophorectomy. There is a large range reported in the literature, with the risk of recurrence after cystectomy described as between 12% and 58%. Most studies report recurrences between 25% and 35% of patients who undergo cystectomy. In contrast, the risk of recurrence after USO is often reported to be approximately 10%. Higher risk of recurrence after cystectomy is speculated to be due to leaving some BOT at the time of initial surgery.
Multiple meta-analyses have found an increased risk of recurrence after cystectomy. The risk of recurrence after unilateral cystectomy was 19.4%, compared with 9.1% after USO, in 2,145 patients included in a 2017 meta-analysis.1 Similarly, a 2021 meta-analysis found a significantly higher rate of BOT recurrence in patients who underwent unilateral or bilateral cystectomy compared with USO (odds ratio, 2.02; 95% confidence interval, 1.59-2.57).2
Does the higher recurrence risk translate into a difference in long-term outcomes?
No. Despite an increased risk of recurrence after cystectomy, ovarian-sparing surgery does not appear to alter patients’ survival. The pooled mortality estimate was 1.6% for those undergoing fertility-sparing surgery (95% CI, 0.011-0.023), compared with 2.0% for those undergoing radical surgery (95% CI, 0.014-0.029), in a 2015 meta-analysis of over 5,100 patients. The analysis included studies in which patients underwent unilateral cystectomy, bilateral cystectomy, USO, or USO plus contralateral cystectomy. The low mortality rate did not allow for comparison between the different types of fertility-sparing surgeries.3
Do we accept a higher risk of recurrence with ovarian sparing surgery to improve fertility?
Data are mixed. When we examine studies describing fertility rates after conservative surgery, there are significant limitations to interpreting the data available. Some studies do not differentiate among patients who underwent fertility-sparing surgery, or between those who had cystectomy versus USO. Other studies do not report the number of patients who tried to achieve pregnancy after surgery. Conception rates are reported to be as high as 88.2%, which was in 116 patients who were able to be reached after fertility-sparing surgery (retained at least one ovary). Of the 51 patients who tried to conceive, 45 were successful.4
Multiple studies and meta-analyses have shown no difference in postoperative pregnancy rates when comparing oophorectomy to cystectomy. For instance, in a 2021 meta-analysis, there was no significant difference noted in pregnancy rates between patients who underwent USO versus cystectomy (OR, 0.92; 95% CI, 0.60-1.42).
There are some data that support improved postoperative pregnancy rates in more conservative surgery, especially in the setting of bilateral BOT. In a small study of 32 patients who had laparoscopic staging for bilateral BOTs, patients were randomized to unilateral oophorectomy plus contralateral cystectomy or to bilateral cystectomy, which was referred to as ultraconservative surgery. The time to first recurrence was shorter in the ultraconservative group (although this lost significance when regression analysis was performed), but the time to first live birth was shorter and the relative chance of having a baby was higher in the bilateral cystectomy group.5
Ovarian-sparing procedures should be offered to patients in the setting of BOT. With ovarian-sparing surgery, it is important to counsel patients about the increased risk of recurrence and need for long-term follow-up. Pregnancy rates are generally good after fertility-sparing surgery. Surgery to conserve both ovaries does not seem to improve pregnancy rates in the setting of unilateral BOTs.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Jiao X et al. Int J Gynecol Cancer. 2017 Nov;27(9):1833-41.
2. Wang P and Fang L. World J Surg Oncol. 2021 Apr 21;19(1):132.
3. Vasconcelos I and de Sousa Mendes M. Eur J Cancer. 2015 Mar;51(5):620-31.
4. Song T et al. Int J Gynecol Cancer. 2011 May;21(4):640-6.
5. Palomba S et al. Hum Reprod. 2010 Aug;25(8):1966-72.
Borderline ovarian tumors (BOTs) are estimated to comprise 10%-15% of all epithelial tumors of the ovary. They are characterized by their behavior, which falls somewhere between benign ovarian masses and frank carcinomas. They have cytologic characteristics suggesting malignancy, such as higher cellular proliferation and more variable nuclear atypia, but, unlike carcinomas, they lack destructive stromal invasion. For decades after their recognition by the International Federation of Gynecology and Obstetrics in 1971, these tumors were classified as being of low malignant potential (and subsequently referred to as LMP tumors of the ovary). Beginning with the 2014 World Health Organization classification, the recommended terminology is now borderline tumor of the ovary.
The primary treatment for BOTs is surgery. With a mean age at diagnosis in the fifth decade, many patients with BOTs desire ovarian preservation to maintain fertility and/or prevent surgical menopause. This raises multiple questions regarding the use of fertility-sparing surgery for BOTs: What types of procedures are safe and should be offered? For those patients who undergo fertility-sparing surgery initially, is additional surgery indicated after completion of childbearing or at an age closer to natural menopause? What should this completion surgery include?
Ovarian-sparing surgery
The diagnosis of a BOT is frequently only confirmed after the decision for ovarian conservation has been made. What should be considered before electing to proceed with ovarian cystectomy instead of unilateral salpingo-oophorectomy (USO)?
Is the risk of recurrence higher with cystectomy versus oophorectomy?
Yes. The risk of recurrence of BOT appears to be higher after cystectomy than it is after oophorectomy. There is a large range reported in the literature, with the risk of recurrence after cystectomy described as between 12% and 58%. Most studies report recurrences between 25% and 35% of patients who undergo cystectomy. In contrast, the risk of recurrence after USO is often reported to be approximately 10%. Higher risk of recurrence after cystectomy is speculated to be due to leaving some BOT at the time of initial surgery.
Multiple meta-analyses have found an increased risk of recurrence after cystectomy. The risk of recurrence after unilateral cystectomy was 19.4%, compared with 9.1% after USO, in 2,145 patients included in a 2017 meta-analysis.1 Similarly, a 2021 meta-analysis found a significantly higher rate of BOT recurrence in patients who underwent unilateral or bilateral cystectomy compared with USO (odds ratio, 2.02; 95% confidence interval, 1.59-2.57).2
Does the higher recurrence risk translate into a difference in long-term outcomes?
No. Despite an increased risk of recurrence after cystectomy, ovarian-sparing surgery does not appear to alter patients’ survival. The pooled mortality estimate was 1.6% for those undergoing fertility-sparing surgery (95% CI, 0.011-0.023), compared with 2.0% for those undergoing radical surgery (95% CI, 0.014-0.029), in a 2015 meta-analysis of over 5,100 patients. The analysis included studies in which patients underwent unilateral cystectomy, bilateral cystectomy, USO, or USO plus contralateral cystectomy. The low mortality rate did not allow for comparison between the different types of fertility-sparing surgeries.3
Do we accept a higher risk of recurrence with ovarian sparing surgery to improve fertility?
Data are mixed. When we examine studies describing fertility rates after conservative surgery, there are significant limitations to interpreting the data available. Some studies do not differentiate among patients who underwent fertility-sparing surgery, or between those who had cystectomy versus USO. Other studies do not report the number of patients who tried to achieve pregnancy after surgery. Conception rates are reported to be as high as 88.2%, which was in 116 patients who were able to be reached after fertility-sparing surgery (retained at least one ovary). Of the 51 patients who tried to conceive, 45 were successful.4
Multiple studies and meta-analyses have shown no difference in postoperative pregnancy rates when comparing oophorectomy to cystectomy. For instance, in a 2021 meta-analysis, there was no significant difference noted in pregnancy rates between patients who underwent USO versus cystectomy (OR, 0.92; 95% CI, 0.60-1.42).
There are some data that support improved postoperative pregnancy rates in more conservative surgery, especially in the setting of bilateral BOT. In a small study of 32 patients who had laparoscopic staging for bilateral BOTs, patients were randomized to unilateral oophorectomy plus contralateral cystectomy or to bilateral cystectomy, which was referred to as ultraconservative surgery. The time to first recurrence was shorter in the ultraconservative group (although this lost significance when regression analysis was performed), but the time to first live birth was shorter and the relative chance of having a baby was higher in the bilateral cystectomy group.5
Ovarian-sparing procedures should be offered to patients in the setting of BOT. With ovarian-sparing surgery, it is important to counsel patients about the increased risk of recurrence and need for long-term follow-up. Pregnancy rates are generally good after fertility-sparing surgery. Surgery to conserve both ovaries does not seem to improve pregnancy rates in the setting of unilateral BOTs.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Jiao X et al. Int J Gynecol Cancer. 2017 Nov;27(9):1833-41.
2. Wang P and Fang L. World J Surg Oncol. 2021 Apr 21;19(1):132.
3. Vasconcelos I and de Sousa Mendes M. Eur J Cancer. 2015 Mar;51(5):620-31.
4. Song T et al. Int J Gynecol Cancer. 2011 May;21(4):640-6.
5. Palomba S et al. Hum Reprod. 2010 Aug;25(8):1966-72.
Borderline ovarian tumors (BOTs) are estimated to comprise 10%-15% of all epithelial tumors of the ovary. They are characterized by their behavior, which falls somewhere between benign ovarian masses and frank carcinomas. They have cytologic characteristics suggesting malignancy, such as higher cellular proliferation and more variable nuclear atypia, but, unlike carcinomas, they lack destructive stromal invasion. For decades after their recognition by the International Federation of Gynecology and Obstetrics in 1971, these tumors were classified as being of low malignant potential (and subsequently referred to as LMP tumors of the ovary). Beginning with the 2014 World Health Organization classification, the recommended terminology is now borderline tumor of the ovary.
The primary treatment for BOTs is surgery. With a mean age at diagnosis in the fifth decade, many patients with BOTs desire ovarian preservation to maintain fertility and/or prevent surgical menopause. This raises multiple questions regarding the use of fertility-sparing surgery for BOTs: What types of procedures are safe and should be offered? For those patients who undergo fertility-sparing surgery initially, is additional surgery indicated after completion of childbearing or at an age closer to natural menopause? What should this completion surgery include?
Ovarian-sparing surgery
The diagnosis of a BOT is frequently only confirmed after the decision for ovarian conservation has been made. What should be considered before electing to proceed with ovarian cystectomy instead of unilateral salpingo-oophorectomy (USO)?
Is the risk of recurrence higher with cystectomy versus oophorectomy?
Yes. The risk of recurrence of BOT appears to be higher after cystectomy than it is after oophorectomy. There is a large range reported in the literature, with the risk of recurrence after cystectomy described as between 12% and 58%. Most studies report recurrences between 25% and 35% of patients who undergo cystectomy. In contrast, the risk of recurrence after USO is often reported to be approximately 10%. Higher risk of recurrence after cystectomy is speculated to be due to leaving some BOT at the time of initial surgery.
Multiple meta-analyses have found an increased risk of recurrence after cystectomy. The risk of recurrence after unilateral cystectomy was 19.4%, compared with 9.1% after USO, in 2,145 patients included in a 2017 meta-analysis.1 Similarly, a 2021 meta-analysis found a significantly higher rate of BOT recurrence in patients who underwent unilateral or bilateral cystectomy compared with USO (odds ratio, 2.02; 95% confidence interval, 1.59-2.57).2
Does the higher recurrence risk translate into a difference in long-term outcomes?
No. Despite an increased risk of recurrence after cystectomy, ovarian-sparing surgery does not appear to alter patients’ survival. The pooled mortality estimate was 1.6% for those undergoing fertility-sparing surgery (95% CI, 0.011-0.023), compared with 2.0% for those undergoing radical surgery (95% CI, 0.014-0.029), in a 2015 meta-analysis of over 5,100 patients. The analysis included studies in which patients underwent unilateral cystectomy, bilateral cystectomy, USO, or USO plus contralateral cystectomy. The low mortality rate did not allow for comparison between the different types of fertility-sparing surgeries.3
Do we accept a higher risk of recurrence with ovarian sparing surgery to improve fertility?
Data are mixed. When we examine studies describing fertility rates after conservative surgery, there are significant limitations to interpreting the data available. Some studies do not differentiate among patients who underwent fertility-sparing surgery, or between those who had cystectomy versus USO. Other studies do not report the number of patients who tried to achieve pregnancy after surgery. Conception rates are reported to be as high as 88.2%, which was in 116 patients who were able to be reached after fertility-sparing surgery (retained at least one ovary). Of the 51 patients who tried to conceive, 45 were successful.4
Multiple studies and meta-analyses have shown no difference in postoperative pregnancy rates when comparing oophorectomy to cystectomy. For instance, in a 2021 meta-analysis, there was no significant difference noted in pregnancy rates between patients who underwent USO versus cystectomy (OR, 0.92; 95% CI, 0.60-1.42).
There are some data that support improved postoperative pregnancy rates in more conservative surgery, especially in the setting of bilateral BOT. In a small study of 32 patients who had laparoscopic staging for bilateral BOTs, patients were randomized to unilateral oophorectomy plus contralateral cystectomy or to bilateral cystectomy, which was referred to as ultraconservative surgery. The time to first recurrence was shorter in the ultraconservative group (although this lost significance when regression analysis was performed), but the time to first live birth was shorter and the relative chance of having a baby was higher in the bilateral cystectomy group.5
Ovarian-sparing procedures should be offered to patients in the setting of BOT. With ovarian-sparing surgery, it is important to counsel patients about the increased risk of recurrence and need for long-term follow-up. Pregnancy rates are generally good after fertility-sparing surgery. Surgery to conserve both ovaries does not seem to improve pregnancy rates in the setting of unilateral BOTs.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Jiao X et al. Int J Gynecol Cancer. 2017 Nov;27(9):1833-41.
2. Wang P and Fang L. World J Surg Oncol. 2021 Apr 21;19(1):132.
3. Vasconcelos I and de Sousa Mendes M. Eur J Cancer. 2015 Mar;51(5):620-31.
4. Song T et al. Int J Gynecol Cancer. 2011 May;21(4):640-6.
5. Palomba S et al. Hum Reprod. 2010 Aug;25(8):1966-72.
Life’s Essential 8: Higher scores extend health span
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. I’d like to talk with you about a recent report on
This study leveraged the UK Biobank and included more than 135,000 U.K. adults with a mean age of 55. The AHA metric was defined as including the following lifestyle behavioral factors:
- Not smoking.
- Regular physical activity.
- Healthy weight.
- Healthy diet.
- Healthy sleep (defined as an average of 7-9 hours nightly).
- Blood pressure in a healthy range.
- Blood glucose in a healthy range.
- Non-HDL cholesterol in a healthy range.
This study was just published in JAMA Internal Medicine. I’d like to acknowledge that I’m a coauthor of this study, along with my colleagues at Tulane.
We divided the study population into three groups: those with low, moderate, and high scores on the Life’s Essential 8 metric – low, moderate, and high cardiovascular health. Overall, the average life expectancy free of chronic disease was estimated to be age 50, with 25 additional years in men and 30 additional years in women.
We saw large differences across the Life’s Essential 8 metric group. Men with high cardiovascular health scores tended to have an additional 7 years of life expectancy free of chronic disease, compared with those who had poorer scores. In women, the difference was about 9.5 years between high scores and lower scores. Also, the number of years lived with chronic disease was compressed in those with high cardiovascular health scores. They tended to have fewer years living with those chronic diseases but more years living free of chronic diseases.
We were interested in how these results might differ by socioeconomic status, educational level, and income level, as well as the Townsend deprivation index. We were intrigued by the finding that the gain in life expectancy free of chronic disease was very similar across all socioeconomic strata – those with lower education and lower income gained as much in terms of chronic disease–free life expectancy as those who were in the higher socioeconomic strata.
Overall, the findings make a compelling case for the importance of lifestyle factors in extending health span and years free of chronic disease. It can be motivating to tell our patients that a healthy lifestyle not only extends life expectancy but also extends years of health free of chronic disease.
Nonetheless, we do have many disparities in life expectancy and health span. So it will be very important to population health to narrow those health disparities through education about the importance of lifestyle factors, more research on implementation of lifestyle factors and behaviors, and public policy to make a healthy lifestyle both affordable and accessible to all people across all of these socioeconomic groups.
Thank you so much for your attention.
JoAnn E. Manson, MD, DrPH, is professor of medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School, Boston.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. I’d like to talk with you about a recent report on
This study leveraged the UK Biobank and included more than 135,000 U.K. adults with a mean age of 55. The AHA metric was defined as including the following lifestyle behavioral factors:
- Not smoking.
- Regular physical activity.
- Healthy weight.
- Healthy diet.
- Healthy sleep (defined as an average of 7-9 hours nightly).
- Blood pressure in a healthy range.
- Blood glucose in a healthy range.
- Non-HDL cholesterol in a healthy range.
This study was just published in JAMA Internal Medicine. I’d like to acknowledge that I’m a coauthor of this study, along with my colleagues at Tulane.
We divided the study population into three groups: those with low, moderate, and high scores on the Life’s Essential 8 metric – low, moderate, and high cardiovascular health. Overall, the average life expectancy free of chronic disease was estimated to be age 50, with 25 additional years in men and 30 additional years in women.
We saw large differences across the Life’s Essential 8 metric group. Men with high cardiovascular health scores tended to have an additional 7 years of life expectancy free of chronic disease, compared with those who had poorer scores. In women, the difference was about 9.5 years between high scores and lower scores. Also, the number of years lived with chronic disease was compressed in those with high cardiovascular health scores. They tended to have fewer years living with those chronic diseases but more years living free of chronic diseases.
We were interested in how these results might differ by socioeconomic status, educational level, and income level, as well as the Townsend deprivation index. We were intrigued by the finding that the gain in life expectancy free of chronic disease was very similar across all socioeconomic strata – those with lower education and lower income gained as much in terms of chronic disease–free life expectancy as those who were in the higher socioeconomic strata.
Overall, the findings make a compelling case for the importance of lifestyle factors in extending health span and years free of chronic disease. It can be motivating to tell our patients that a healthy lifestyle not only extends life expectancy but also extends years of health free of chronic disease.
Nonetheless, we do have many disparities in life expectancy and health span. So it will be very important to population health to narrow those health disparities through education about the importance of lifestyle factors, more research on implementation of lifestyle factors and behaviors, and public policy to make a healthy lifestyle both affordable and accessible to all people across all of these socioeconomic groups.
Thank you so much for your attention.
JoAnn E. Manson, MD, DrPH, is professor of medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School, Boston.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital. I’d like to talk with you about a recent report on
This study leveraged the UK Biobank and included more than 135,000 U.K. adults with a mean age of 55. The AHA metric was defined as including the following lifestyle behavioral factors:
- Not smoking.
- Regular physical activity.
- Healthy weight.
- Healthy diet.
- Healthy sleep (defined as an average of 7-9 hours nightly).
- Blood pressure in a healthy range.
- Blood glucose in a healthy range.
- Non-HDL cholesterol in a healthy range.
This study was just published in JAMA Internal Medicine. I’d like to acknowledge that I’m a coauthor of this study, along with my colleagues at Tulane.
We divided the study population into three groups: those with low, moderate, and high scores on the Life’s Essential 8 metric – low, moderate, and high cardiovascular health. Overall, the average life expectancy free of chronic disease was estimated to be age 50, with 25 additional years in men and 30 additional years in women.
We saw large differences across the Life’s Essential 8 metric group. Men with high cardiovascular health scores tended to have an additional 7 years of life expectancy free of chronic disease, compared with those who had poorer scores. In women, the difference was about 9.5 years between high scores and lower scores. Also, the number of years lived with chronic disease was compressed in those with high cardiovascular health scores. They tended to have fewer years living with those chronic diseases but more years living free of chronic diseases.
We were interested in how these results might differ by socioeconomic status, educational level, and income level, as well as the Townsend deprivation index. We were intrigued by the finding that the gain in life expectancy free of chronic disease was very similar across all socioeconomic strata – those with lower education and lower income gained as much in terms of chronic disease–free life expectancy as those who were in the higher socioeconomic strata.
Overall, the findings make a compelling case for the importance of lifestyle factors in extending health span and years free of chronic disease. It can be motivating to tell our patients that a healthy lifestyle not only extends life expectancy but also extends years of health free of chronic disease.
Nonetheless, we do have many disparities in life expectancy and health span. So it will be very important to population health to narrow those health disparities through education about the importance of lifestyle factors, more research on implementation of lifestyle factors and behaviors, and public policy to make a healthy lifestyle both affordable and accessible to all people across all of these socioeconomic groups.
Thank you so much for your attention.
JoAnn E. Manson, MD, DrPH, is professor of medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School, Boston.
A version of this article first appeared on Medscape.com.








