User login
Barriers to System Quality Improvement in Health Care
Corresponding author: Ebrahim Barkoudah, MD, MPH, Department of Medicine, Brigham and Women’s Hospital, Boston, MA; [email protected]
Process improvement in any industry sector aims to increase the efficiency of resource utilization and delivery methods (cost) and the quality of the product (outcomes), with the goal of ultimately achieving continuous development.1 In the health care industry, variation in processes and outcomes along with inefficiency in resource use that result in changes in value (the product of outcomes/costs) are the general targets of quality improvement (QI) efforts employing various implementation methodologies.2 When the ultimate aim is to serve the patient (customer), best clinical practice includes both maintaining high quality (individual care delivery) and controlling costs (efficient care system delivery), leading to optimal delivery (value-based care). High-quality individual care and efficient care delivery are not competing concepts, but when working to improve both health care outcomes and cost, traditional and nontraditional barriers to system QI often arise.3
The possible scenarios after a QI intervention include backsliding (regression to the mean over time), steady-state (minimal fixed improvement that could sustain), and continuous improvement (tangible enhancement after completing the intervention with legacy effect).4 The scalability of results can be considered during the process measurement and the intervention design phases of all QI projects; however, the complex nature of barriers in the health care environment during each level of implementation should be accounted for to prevent failure in the scalability phase.5
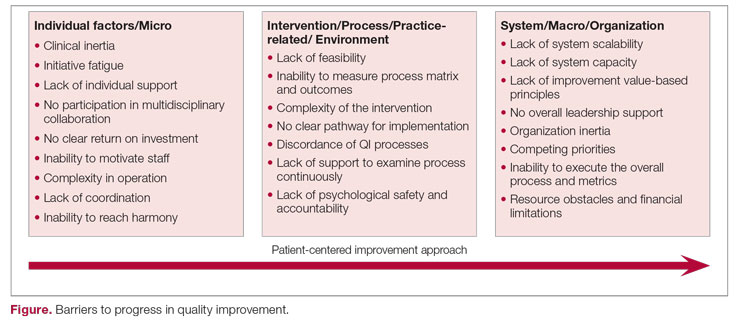
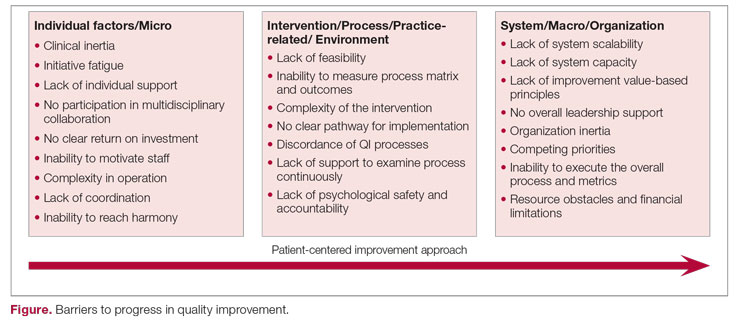
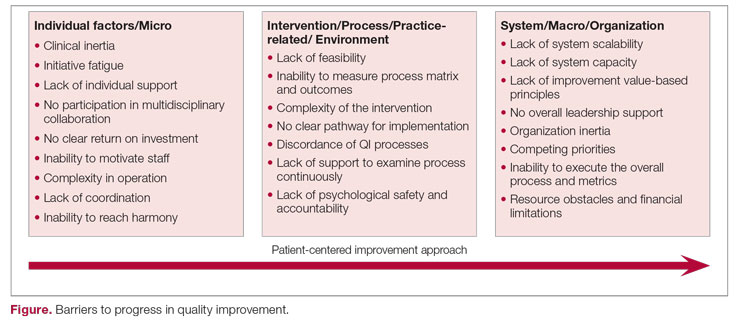
The barriers to optimal QI outcomes leading to continuous improvement are multifactorial and are related to intrinsic and extrinsic factors.6 These factors include 3 fundamental levels: (1) individual level inertia/beliefs, prior personal knowledge, and team-related factors7,8; (2) intervention-related and process-specific barriers and clinical practice obstacles; and (3) organizational level challenges and macro-level and population-level barriers (Figure). The obstacles faced during the implementation phase will likely include 2 of these levels simultaneously, which could add complexity and hinder or prevent the implementation of a tangible successful QI process and eventually lead to backsliding or minimal fixed improvement rather than continuous improvement. Furthermore, a patient-centered approach to QI would contribute to further complexity in design and execution, given the importance of reaching sustainable, meaningful improvement by adding elements of patient’s preferences, caregiver engagement, and the shared decision-making processes.9
Overcoming these multidomain barriers and reaching resilience and sustainability requires thoughtful planning and execution through a multifaceted approach.10 A meaningful start could include addressing the clinical inertia for the individual and the team by promoting open innovation and allowing outside institutional collaborations and ideas through networks.11 On the individual level, encouraging participation and motivating health care workers in QI to reach a multidisciplinary operation approach will lead to harmony in collaboration. Concurrently, the organization should support the QI capability and scalability by removing competing priorities and establishing effective leadership that ensures resource allocation, communicates clear value-based principles, and engenders a psychological safety environment.
A continuous improvement state is the optimal QI target, a target that can be attained by removing obstacles and paving a clear pathway to implementation. Focusing on the 3 levels of barriers will position the organization for meaningful and successful QI phases to achieve continuous improvement.
1. Adesola S, Baines T. Developing and evaluating a methodology for business process improvement. Business Process Manage J. 2005;11(1):37-46. doi:10.1108/14637150510578719
2. Gershon M. Choosing which process improvement methodology to implement. J Appl Business & Economics. 2010;10(5):61-69.
3. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business Press; 2006.
4. Holweg M, Davies J, De Meyer A, Lawson B, Schmenner RW. Process Theory: The Principles of Operations Management. Oxford University Press; 2018.
5. Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: what it will take to accelerate progress. Milbank Q. 1998;76(4):593-624. doi:10.1111/1468-0009.00107
6. Solomons NM, Spross JA. Evidence‐based practice barriers and facilitators from a continuous quality improvement perspective: an integrative review. J Nurs Manage. 2011;19(1):109-120. doi:10.1111/j.1365-2834.2010.01144.x
7. Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825-34. doi:10.7326/0003-4819-135-9-200111060-00012
8. Stevenson K, Baker R, Farooqi A, Sorrie R, Khunti K. Features of primary health care teams associated with successful quality improvement of diabetes care: a qualitative study. Fam Pract. 2001;18(1):21-26. doi:10.1093/fampra/18.1.21
9. What is patient-centered care? NEJM Catalyst. January 1, 2017. Accessed August 31, 2022. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0559
10. Kilbourne AM, Beck K, Spaeth‐Rublee B, et al. Measuring and improving the quality of mental health care: a global perspective. World Psychiatry. 2018;17(1):30-8. doi:10.1002/wps.20482
11. Huang HC, Lai MC, Lin LH, Chen CT. Overcoming organizational inertia to strengthen business model innovation: An open innovation perspective. J Organizational Change Manage. 2013;26(6):977-1002. doi:10.1108/JOCM-04-2012-0047
Corresponding author: Ebrahim Barkoudah, MD, MPH, Department of Medicine, Brigham and Women’s Hospital, Boston, MA; [email protected]
Process improvement in any industry sector aims to increase the efficiency of resource utilization and delivery methods (cost) and the quality of the product (outcomes), with the goal of ultimately achieving continuous development.1 In the health care industry, variation in processes and outcomes along with inefficiency in resource use that result in changes in value (the product of outcomes/costs) are the general targets of quality improvement (QI) efforts employing various implementation methodologies.2 When the ultimate aim is to serve the patient (customer), best clinical practice includes both maintaining high quality (individual care delivery) and controlling costs (efficient care system delivery), leading to optimal delivery (value-based care). High-quality individual care and efficient care delivery are not competing concepts, but when working to improve both health care outcomes and cost, traditional and nontraditional barriers to system QI often arise.3
The possible scenarios after a QI intervention include backsliding (regression to the mean over time), steady-state (minimal fixed improvement that could sustain), and continuous improvement (tangible enhancement after completing the intervention with legacy effect).4 The scalability of results can be considered during the process measurement and the intervention design phases of all QI projects; however, the complex nature of barriers in the health care environment during each level of implementation should be accounted for to prevent failure in the scalability phase.5
The barriers to optimal QI outcomes leading to continuous improvement are multifactorial and are related to intrinsic and extrinsic factors.6 These factors include 3 fundamental levels: (1) individual level inertia/beliefs, prior personal knowledge, and team-related factors7,8; (2) intervention-related and process-specific barriers and clinical practice obstacles; and (3) organizational level challenges and macro-level and population-level barriers (Figure). The obstacles faced during the implementation phase will likely include 2 of these levels simultaneously, which could add complexity and hinder or prevent the implementation of a tangible successful QI process and eventually lead to backsliding or minimal fixed improvement rather than continuous improvement. Furthermore, a patient-centered approach to QI would contribute to further complexity in design and execution, given the importance of reaching sustainable, meaningful improvement by adding elements of patient’s preferences, caregiver engagement, and the shared decision-making processes.9
Overcoming these multidomain barriers and reaching resilience and sustainability requires thoughtful planning and execution through a multifaceted approach.10 A meaningful start could include addressing the clinical inertia for the individual and the team by promoting open innovation and allowing outside institutional collaborations and ideas through networks.11 On the individual level, encouraging participation and motivating health care workers in QI to reach a multidisciplinary operation approach will lead to harmony in collaboration. Concurrently, the organization should support the QI capability and scalability by removing competing priorities and establishing effective leadership that ensures resource allocation, communicates clear value-based principles, and engenders a psychological safety environment.
A continuous improvement state is the optimal QI target, a target that can be attained by removing obstacles and paving a clear pathway to implementation. Focusing on the 3 levels of barriers will position the organization for meaningful and successful QI phases to achieve continuous improvement.
Corresponding author: Ebrahim Barkoudah, MD, MPH, Department of Medicine, Brigham and Women’s Hospital, Boston, MA; [email protected]
Process improvement in any industry sector aims to increase the efficiency of resource utilization and delivery methods (cost) and the quality of the product (outcomes), with the goal of ultimately achieving continuous development.1 In the health care industry, variation in processes and outcomes along with inefficiency in resource use that result in changes in value (the product of outcomes/costs) are the general targets of quality improvement (QI) efforts employing various implementation methodologies.2 When the ultimate aim is to serve the patient (customer), best clinical practice includes both maintaining high quality (individual care delivery) and controlling costs (efficient care system delivery), leading to optimal delivery (value-based care). High-quality individual care and efficient care delivery are not competing concepts, but when working to improve both health care outcomes and cost, traditional and nontraditional barriers to system QI often arise.3
The possible scenarios after a QI intervention include backsliding (regression to the mean over time), steady-state (minimal fixed improvement that could sustain), and continuous improvement (tangible enhancement after completing the intervention with legacy effect).4 The scalability of results can be considered during the process measurement and the intervention design phases of all QI projects; however, the complex nature of barriers in the health care environment during each level of implementation should be accounted for to prevent failure in the scalability phase.5
The barriers to optimal QI outcomes leading to continuous improvement are multifactorial and are related to intrinsic and extrinsic factors.6 These factors include 3 fundamental levels: (1) individual level inertia/beliefs, prior personal knowledge, and team-related factors7,8; (2) intervention-related and process-specific barriers and clinical practice obstacles; and (3) organizational level challenges and macro-level and population-level barriers (Figure). The obstacles faced during the implementation phase will likely include 2 of these levels simultaneously, which could add complexity and hinder or prevent the implementation of a tangible successful QI process and eventually lead to backsliding or minimal fixed improvement rather than continuous improvement. Furthermore, a patient-centered approach to QI would contribute to further complexity in design and execution, given the importance of reaching sustainable, meaningful improvement by adding elements of patient’s preferences, caregiver engagement, and the shared decision-making processes.9
Overcoming these multidomain barriers and reaching resilience and sustainability requires thoughtful planning and execution through a multifaceted approach.10 A meaningful start could include addressing the clinical inertia for the individual and the team by promoting open innovation and allowing outside institutional collaborations and ideas through networks.11 On the individual level, encouraging participation and motivating health care workers in QI to reach a multidisciplinary operation approach will lead to harmony in collaboration. Concurrently, the organization should support the QI capability and scalability by removing competing priorities and establishing effective leadership that ensures resource allocation, communicates clear value-based principles, and engenders a psychological safety environment.
A continuous improvement state is the optimal QI target, a target that can be attained by removing obstacles and paving a clear pathway to implementation. Focusing on the 3 levels of barriers will position the organization for meaningful and successful QI phases to achieve continuous improvement.
1. Adesola S, Baines T. Developing and evaluating a methodology for business process improvement. Business Process Manage J. 2005;11(1):37-46. doi:10.1108/14637150510578719
2. Gershon M. Choosing which process improvement methodology to implement. J Appl Business & Economics. 2010;10(5):61-69.
3. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business Press; 2006.
4. Holweg M, Davies J, De Meyer A, Lawson B, Schmenner RW. Process Theory: The Principles of Operations Management. Oxford University Press; 2018.
5. Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: what it will take to accelerate progress. Milbank Q. 1998;76(4):593-624. doi:10.1111/1468-0009.00107
6. Solomons NM, Spross JA. Evidence‐based practice barriers and facilitators from a continuous quality improvement perspective: an integrative review. J Nurs Manage. 2011;19(1):109-120. doi:10.1111/j.1365-2834.2010.01144.x
7. Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825-34. doi:10.7326/0003-4819-135-9-200111060-00012
8. Stevenson K, Baker R, Farooqi A, Sorrie R, Khunti K. Features of primary health care teams associated with successful quality improvement of diabetes care: a qualitative study. Fam Pract. 2001;18(1):21-26. doi:10.1093/fampra/18.1.21
9. What is patient-centered care? NEJM Catalyst. January 1, 2017. Accessed August 31, 2022. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0559
10. Kilbourne AM, Beck K, Spaeth‐Rublee B, et al. Measuring and improving the quality of mental health care: a global perspective. World Psychiatry. 2018;17(1):30-8. doi:10.1002/wps.20482
11. Huang HC, Lai MC, Lin LH, Chen CT. Overcoming organizational inertia to strengthen business model innovation: An open innovation perspective. J Organizational Change Manage. 2013;26(6):977-1002. doi:10.1108/JOCM-04-2012-0047
1. Adesola S, Baines T. Developing and evaluating a methodology for business process improvement. Business Process Manage J. 2005;11(1):37-46. doi:10.1108/14637150510578719
2. Gershon M. Choosing which process improvement methodology to implement. J Appl Business & Economics. 2010;10(5):61-69.
3. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business Press; 2006.
4. Holweg M, Davies J, De Meyer A, Lawson B, Schmenner RW. Process Theory: The Principles of Operations Management. Oxford University Press; 2018.
5. Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: what it will take to accelerate progress. Milbank Q. 1998;76(4):593-624. doi:10.1111/1468-0009.00107
6. Solomons NM, Spross JA. Evidence‐based practice barriers and facilitators from a continuous quality improvement perspective: an integrative review. J Nurs Manage. 2011;19(1):109-120. doi:10.1111/j.1365-2834.2010.01144.x
7. Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825-34. doi:10.7326/0003-4819-135-9-200111060-00012
8. Stevenson K, Baker R, Farooqi A, Sorrie R, Khunti K. Features of primary health care teams associated with successful quality improvement of diabetes care: a qualitative study. Fam Pract. 2001;18(1):21-26. doi:10.1093/fampra/18.1.21
9. What is patient-centered care? NEJM Catalyst. January 1, 2017. Accessed August 31, 2022. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0559
10. Kilbourne AM, Beck K, Spaeth‐Rublee B, et al. Measuring and improving the quality of mental health care: a global perspective. World Psychiatry. 2018;17(1):30-8. doi:10.1002/wps.20482
11. Huang HC, Lai MC, Lin LH, Chen CT. Overcoming organizational inertia to strengthen business model innovation: An open innovation perspective. J Organizational Change Manage. 2013;26(6):977-1002. doi:10.1108/JOCM-04-2012-0047
Flashy, blingy doc sabotages his own malpractice trial in rural farm town
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
During a medical malpractice trial in New Jersey, jurors waited nearly 4 hours for the physician defendant to show up. When he did arrive, the body-building surgeon was sporting two thick gold chains and a diamond pinky ring, and had the top buttons of his shirt open enough to reveal his chest hair.
“This trial was in a very rural, farming community,” recalls medical liability defense attorney Catherine Flynn, of Flynn Watts LLC, based in Parsippany, N.J. “Many of the jurors were wearing flannel shirts and jeans. The doctor’s wife walked in wearing a five-carat diamond ring and other jewelry.”
Ms. Flynn took the couple aside and asked them to remove the jewelry. She explained that the opulent accessories could damage the jury’s view of the physician. The surgeon and his wife, however, refused to remove their jewelry, she said. They didn’t think it was a big deal.
The case against the surgeon involved intraoperative damage to a patient when the physician inadvertently removed a portion of nerve in the area of the procedure. After repair of the nerve, the patient had a positive result. However, the patient alleged the surgeon’s negligence resulted in permanent damage despite the successful repair.
Jurors ultimately found the physician negligent in the case and awarded the plaintiff $1.2 million. Ms. Flynn believes that physician’s flamboyant attire and arrogant nature tainted the jury’s decision.
“In certain counties in New Jersey, his attire would not have been a problem,” she said. “In this rural, farming county, it was a huge problem. You have to know your audience. There are a lot of other things that come into play in a medical malpractice case, but when it comes to damages in a case, you don’t want to be sending the message that supports what somebody’s bias may already be telling them about a doctor.”
The surgeon appealed the verdict, and the case ultimately settled for a lesser amount, according to Ms. Flynn.
An over-the-top wardrobe is just one way that physicians can negatively influence jurors during legal trials. From subtle facial expressions to sudden outbursts to downright rudeness, attorneys have witnessed countless examples of physicians sabotaging their own trials.
“The minute you enter the courthouse, jurors or potential jurors are sizing you up,” says health law attorney Michael Clark, of Womble Bond Dickinson (US) LLP, based in Houston. “The same phenomenon occurs in a deposition. Awareness of how you are being assessed at all times, and the image that is needed, is important since a negative impression by jurors can have a detrimental effect on a physician’s case.”
Juror: We didn’t like the doctor’s shoes
In another case, attorneys warned a physician defendant against dressing in his signature wardrobe during his trial. Against their advice, the doctor showed up daily to his trial in bright pastel, monochromatic suits with matching Gucci-brand shoes, said medical liability defense attorney Meredith C. Lander, of Kaufman Borgeest & Ryan LLP, based in Connecticut. On the witness stand, the doctor was long-winded and wasn’t “terribly likable,” Ms. Lander said.
However, the evidence weighed in the physician’s favor, and there was strong testimony by defense experts. The physician won the case, Ms. Lander said, but after the verdict, the jury foreperson approached the trial attorney and made some disparaging remarks about the defendant.
“The foreperson said the jury didn’t like the doctor or his ‘Gucci suits and shoes,’ but they believed the experts,” Ms. Lander said.
Disruptive behavior can also harm jurors’ perception of physicians, Ms. Flynn adds. During one instance, a surgeon insisted on sitting next to Ms. Flynn, although she generally requests clients sit in the first row so that jurors are not so focused on their reactions during testimony. The surgeon loudly peppered Ms. Flynn with questions as witnesses testified, prompting a reprimand from the judge.
“The judge admonished the doctor several times and said, ‘Doctor, you’re raising your voice. You’ll get a chance to speak with your attorney during the break,’ ” Ms. Flynn recalled. “The doctor refused to stop talking, and the judge told him in front of the jury to go sit in the back of the courtroom. His reaction was, ‘Why do I have to move?! I need to sit here!’ ”
The surgeon eventually moved to the back of the courtroom and a sheriff’s deputy stood next to him. Testimony continued until a note in the form of a paper airplane landed on the table in front of Ms. Flynn. She carefully crumpled the note and tossed it in the wastebasket. Luckily, this drew a laugh from jurors, she said.
But things got worse when the surgeon testified. Rather than answer the questions, he interrupted and started telling jurors his own version of events.
“The judge finally said, ‘Doctor, if you don’t listen to your attorney and answer her questions, I’m going to make you get off the stand,’ ” Ms. Flynn said. “That was the most unbelievable, egregious self-sabotage trial moment I’ve ever experienced.”
Fortunately, the physician’s legal case was strong, and the experts who testified drove the defense’s side home, Ms. Flynn said. The surgeon won the case.
Attorney: Watch what you say in the elevator
Other, more subtle behaviors – while often unintentional – can also be damaging.
Physicians often let their guard down while outside the courtroom and can unknowingly wind up next to a juror in an elevator or standing in a hallway, said Laura Postilion, a partner at Quintairos, Prieto, Wood & Boyer, P.A., based in Chicago.
“For instance, a doctor is in an elevator and feels that some witness on the stand was lying,” Ms. Postilion said. “They might be very upset about it and start ranting about a witness lying, not realizing there is a juror is in the elevator with you.”
Physicians should also be cautious when speaking on the phone to their family or friends during a trial break.
“At the Daley Center in downtown Chicago, there are these long corridors and long line of windows; a lot of people will stand there during breaks. A doctor may be talking to his or her spouse and saying, ‘Yeah, this juror is sleeping!’ Jurors are [often] looking for drama. They’re looking for somebody letting their guard down. Hearing a doctor speak badly about them would certainly give them a reason to dislike the physician.”
Ms. Postilion warns against talking about jurors in or outside of the courtroom. This includes parking structures, she said.
Physicians can take additional steps to save themselves from negative judgment from jurors, attorneys say. Even before the trial starts, Ms. Postilion advises clients to make their social media accounts private. Some curious jurors may look up a physician’s social media accounts to learn more about their personal life, political leanings, or social beliefs, which could prejudice them against the doctor, she said.
Once on the stand, the words and tone used are key. The last thing a physician defendant wants is to come across as arrogant or condescending to jurors, said medical liability defense attorney Michael Moroney, of Flynn Watts LLC.
“For instance, a defendant might say, ‘Well, let me make this simple for you,’ as if they’re talking to a bunch of schoolchildren,” he said. “You don’t know who’s on the jury. That type of language can be offensive.”
Ms. Lander counsels her clients to refrain from using the common phrase, “honestly,” before answering questions on the stand.
“Everything you’re saying on the stand is presumed to be honest,” she said. “When you start an answer with, ‘Honestly…’ out of habit, it really does undercut everything that follows and everything else that’s already been said. It suggests that you were not being honest in your other answers.”
Attitude, body language speak volumes
Keep in mind that plaintiffs’ attorneys will try their best to rattle physicians on the stand and get them to appear unlikeable, says Mr. Clark, the Houston-based health law attorney. Physicians who lose their cool and begin arguing with attorneys play into their strategy.
“Plaintiffs’ attorneys have been trained in ways to get under their skin,” he said. “Righteous indignation and annoyance are best left for a rare occasion. Think about how you feel in a social setting when people are bickering in front of you. It’s uncomfortable at best. That’s how a jury feels too.”
Body language is also important, Mr. Clark notes. Physicians should avoid crossed arms, leaning back and rocking, or putting a hand on their mouth while testifying, he said. Many attorneys have practice sessions with their clients and record the interaction so that doctors can watch it and see how they look.
“Know your strengths and weaknesses,” he said. “Get help from your lawyer and perhaps consultants about how to improve these skills. Practice and preparation are important.”
Ms. Postilion goes over courtroom clothing with physician clients before trial. Anything “too flashy, too high-end, or too dumpy” should be avoided, she said. Getting accustomed to the courtroom and practicing in an empty courtroom are good ways to ensure that a physician’s voice is loud enough and projecting far enough in the courtroom, she adds.
“The doctor should try to be the best version of him- or herself to jurors,” she said. “A jury can pick up someone who’s trying to be something they’re not. A good attorney can help the doctor find the best version of themselves and capitalize on it. What is it that you want the jury to know about your care of the patient? Take that overall feeling and make sure it’s clearly expressed to the jury.”
A version of this article first appeared on Medscape.com.
When the public misplaces their trust
Not long ago, the grandmother of my son’s friend died of COVID-19 infection. She was elderly and unvaccinated. Her grandson had no regrets over her unvaccinated status. “Why would she inject poison into her body?” he said, and then expressed a strong opinion that she had died because the hospital physicians refused to give her ivermectin and hydroxychloroquine. My son, wisely, did not push the issue.
Soon thereafter, my personal family physician emailed a newsletter to his patients (me included) with 3 important messages: (1) COVID vaccines were available in the office; (2) He was not going to prescribe hydroxychloroquine, no matter how adamantly it was requested; and (3) He warned against threatening him or his staff with lawsuits or violence over refusal to prescribe any unproven medication.
How, as a country, have we come to this? A sizeable portion of the public trusts the advice of quacks, hacks, and political opportunists over that of the nation’s most expert scientists and physicians. The National Institutes of Health maintains a website with up-to-date recommendations on the use of treatments for COVID-19. They assess the existing evidence and make recommendations for or against a wide array of interventions. (They recommend against the use of both ivermectin and hydroxychloroquine.) The Centers for Disease Control and Prevention publishes extensively about the current knowledge on the safety and efficacy of vaccines. Neither agency is part of a “deep state” or conspiracy. They are comprised of some of the nation’s leading scientists, including physicians, trying to protect the public from disease and foster good health.
Sadly, some physicians have been a source of inaccurate vaccine information; some even prescribe ineffective treatments despite the evidence. These physicians are either letting their politics override their good sense or are improperly assessing the scientific literature, or both. Medical licensing agencies, and specialty certification boards, need to find ways to prevent this—ways that can survive judicial scrutiny and allow for legitimate scientific debate.
I have been tempted to just accept the current situation as the inevitable outcome of social media–fueled tribalism. But when we know that the COVID death rate among the unvaccinated is 9 times that of people who have received a booster dose,1 I can’t sit idly and watch the Internet pundits prevail. Instead, I continue to advise and teach my students to have confidence in trustworthy authorities and websites. Mistakes will be made; corrections will be issued. However, this is not evidence of malintent or incompetence, but rather, the scientific process in action.
I tell my students that one of the biggest challenges facing them and society is to figure out how to stop, or at least minimize the effects of, incorrect information, misleading statements, and outright lies in a society that values free speech. Physicians—young and old alike—must remain committed to communicating factual information to a not-always-receptive audience. And I wish my young colleagues luck; I hope that their passion for family medicine and their insights into social media may be just the combination that’s needed to redirect the public’s trust back to where it belongs during a health care crisis.
1. Fleming-Dutra KE. COVID-19 Epidemiology and Vaccination Rates in the United States. Presented to the Authorization Committee on Immunization Practices, July 19, 2022. Accessed August 9, 2022. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2022-07-19/02-COVID-Fleming-Dutra-508.pdf
Not long ago, the grandmother of my son’s friend died of COVID-19 infection. She was elderly and unvaccinated. Her grandson had no regrets over her unvaccinated status. “Why would she inject poison into her body?” he said, and then expressed a strong opinion that she had died because the hospital physicians refused to give her ivermectin and hydroxychloroquine. My son, wisely, did not push the issue.
Soon thereafter, my personal family physician emailed a newsletter to his patients (me included) with 3 important messages: (1) COVID vaccines were available in the office; (2) He was not going to prescribe hydroxychloroquine, no matter how adamantly it was requested; and (3) He warned against threatening him or his staff with lawsuits or violence over refusal to prescribe any unproven medication.
How, as a country, have we come to this? A sizeable portion of the public trusts the advice of quacks, hacks, and political opportunists over that of the nation’s most expert scientists and physicians. The National Institutes of Health maintains a website with up-to-date recommendations on the use of treatments for COVID-19. They assess the existing evidence and make recommendations for or against a wide array of interventions. (They recommend against the use of both ivermectin and hydroxychloroquine.) The Centers for Disease Control and Prevention publishes extensively about the current knowledge on the safety and efficacy of vaccines. Neither agency is part of a “deep state” or conspiracy. They are comprised of some of the nation’s leading scientists, including physicians, trying to protect the public from disease and foster good health.
Sadly, some physicians have been a source of inaccurate vaccine information; some even prescribe ineffective treatments despite the evidence. These physicians are either letting their politics override their good sense or are improperly assessing the scientific literature, or both. Medical licensing agencies, and specialty certification boards, need to find ways to prevent this—ways that can survive judicial scrutiny and allow for legitimate scientific debate.
I have been tempted to just accept the current situation as the inevitable outcome of social media–fueled tribalism. But when we know that the COVID death rate among the unvaccinated is 9 times that of people who have received a booster dose,1 I can’t sit idly and watch the Internet pundits prevail. Instead, I continue to advise and teach my students to have confidence in trustworthy authorities and websites. Mistakes will be made; corrections will be issued. However, this is not evidence of malintent or incompetence, but rather, the scientific process in action.
I tell my students that one of the biggest challenges facing them and society is to figure out how to stop, or at least minimize the effects of, incorrect information, misleading statements, and outright lies in a society that values free speech. Physicians—young and old alike—must remain committed to communicating factual information to a not-always-receptive audience. And I wish my young colleagues luck; I hope that their passion for family medicine and their insights into social media may be just the combination that’s needed to redirect the public’s trust back to where it belongs during a health care crisis.
Not long ago, the grandmother of my son’s friend died of COVID-19 infection. She was elderly and unvaccinated. Her grandson had no regrets over her unvaccinated status. “Why would she inject poison into her body?” he said, and then expressed a strong opinion that she had died because the hospital physicians refused to give her ivermectin and hydroxychloroquine. My son, wisely, did not push the issue.
Soon thereafter, my personal family physician emailed a newsletter to his patients (me included) with 3 important messages: (1) COVID vaccines were available in the office; (2) He was not going to prescribe hydroxychloroquine, no matter how adamantly it was requested; and (3) He warned against threatening him or his staff with lawsuits or violence over refusal to prescribe any unproven medication.
How, as a country, have we come to this? A sizeable portion of the public trusts the advice of quacks, hacks, and political opportunists over that of the nation’s most expert scientists and physicians. The National Institutes of Health maintains a website with up-to-date recommendations on the use of treatments for COVID-19. They assess the existing evidence and make recommendations for or against a wide array of interventions. (They recommend against the use of both ivermectin and hydroxychloroquine.) The Centers for Disease Control and Prevention publishes extensively about the current knowledge on the safety and efficacy of vaccines. Neither agency is part of a “deep state” or conspiracy. They are comprised of some of the nation’s leading scientists, including physicians, trying to protect the public from disease and foster good health.
Sadly, some physicians have been a source of inaccurate vaccine information; some even prescribe ineffective treatments despite the evidence. These physicians are either letting their politics override their good sense or are improperly assessing the scientific literature, or both. Medical licensing agencies, and specialty certification boards, need to find ways to prevent this—ways that can survive judicial scrutiny and allow for legitimate scientific debate.
I have been tempted to just accept the current situation as the inevitable outcome of social media–fueled tribalism. But when we know that the COVID death rate among the unvaccinated is 9 times that of people who have received a booster dose,1 I can’t sit idly and watch the Internet pundits prevail. Instead, I continue to advise and teach my students to have confidence in trustworthy authorities and websites. Mistakes will be made; corrections will be issued. However, this is not evidence of malintent or incompetence, but rather, the scientific process in action.
I tell my students that one of the biggest challenges facing them and society is to figure out how to stop, or at least minimize the effects of, incorrect information, misleading statements, and outright lies in a society that values free speech. Physicians—young and old alike—must remain committed to communicating factual information to a not-always-receptive audience. And I wish my young colleagues luck; I hope that their passion for family medicine and their insights into social media may be just the combination that’s needed to redirect the public’s trust back to where it belongs during a health care crisis.
1. Fleming-Dutra KE. COVID-19 Epidemiology and Vaccination Rates in the United States. Presented to the Authorization Committee on Immunization Practices, July 19, 2022. Accessed August 9, 2022. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2022-07-19/02-COVID-Fleming-Dutra-508.pdf
1. Fleming-Dutra KE. COVID-19 Epidemiology and Vaccination Rates in the United States. Presented to the Authorization Committee on Immunization Practices, July 19, 2022. Accessed August 9, 2022. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2022-07-19/02-COVID-Fleming-Dutra-508.pdf
Five contract red flags every physician should know
Recruiting health care workers is a challenge these days for both private practice and hospital employers, and competition can be fierce. In order to be competitive, employers need to review the package they are offering potential candidates and understand that it’s more than just compensation and benefits that matter.
As someone who reviews physician contracts extensively, there are some common examples of language that may cause a candidate to choose a different position.
Probationary period
Although every employer wants to find out if they like the physician or midlevel employee that they have just hired before fully committing, the inclusion of a probationary period (usually 90 days) is offensive to a candidate, especially one with a choice of contracts.
Essentially, the employer is asking the employee to (potentially) relocate, go through the credentialing process, and turn down other potential offers, all for the possibility that they could easily be terminated. Probationary periods typically allow an employee to be immediately terminated without notice or cause, which can then leave them stranded without a paycheck (and with a new home and/or other recent commitments).
Moreover, contracts with probationary periods tend to terminate the employee without covering any tail costs or clarifying that the employer will not enforce restrictive provisions (even if unlikely to be legally enforceable based on the short relationship).
It is important to understand that the process of a person finding a new position, which includes interviewing, contract negotiation, and credentialing, can take up to 6 months. For this reason, probationary provisions create real job insecurity for a candidate.
Entering into a new affiliation is a leap of faith both for the employer and the employee. If the circumstances do not work out, the employer should fairly compensate the employee for the notice period and ask them not to return to work or otherwise allow them to keep working the notice period while they search for a new position.
Acceleration of notice
Another objectionable provision that employers like to include in their contracts is one which allows the employer to accelerate and immediately terminate an employee who has given proper notice.
The contract will contain a standard notice provision, but when the health care professional submits notice, their last date is suddenly accelerated, and they are released without further compensation, notice, or benefits. This type of provision is particularly offensive to health care employees who take the step of giving proper contractual notice and, similar to the probationary language, can create real job insecurity for an employee who suddenly loses their paycheck and has no new job to start.
Medical workers should be paid for the entire notice period whether or not they are allowed to work. Unfortunately, this type of provision is sometimes hidden in contracts and not noticed by employees, who tend to focus on the notice provision itself. I consider this provision to be a red flag about the employer when I review clients’ contracts.
Malpractice tail
Although many employers will claim it is not unusual for an employee to pay for their own malpractice tail, in the current marketplace, the payment of tail can be a deciding factor in whether a candidate accepts a contract.
At a minimum, employers should consider paying for the tail under circumstances where they non-renew a contract, terminate without cause, or the contract is terminated for the employer’s breach. Similarly, I like to seek out payment of the tail by the employer where the contract is terminated owing to a change in the law, use of a force majeure provision, loss of the employer’s hospital contract, or similar provisions where termination is outside the control of the employee.
Employers should also consider a provision where they share the cost of a tail or cover the entire cost on the basis of years of service in order to stand out to a potential candidate.
Noncompete provisions
I do not find noncompete provisions to be generally unacceptable when properly written; however, employers should reevaluate the reasonableness of their noncompete language frequently, because such language can make the difference in whether a candidate accepts a contract.
A reasonable noncompete that only protects the employer as necessary and does not restrict the reasonable practice of medicine is always preferable and can be the deciding factor for a candidate. Tying enforcement of a noncompete to reasons for termination (similar to the tail) can also make a positive difference in a candidate’s review of a contract.
Egregious noncompetes, where the candidate is simply informed that the language is “not negotiable,” are unlikely to be compelling to a candidate with other options.
Specifics on location, call, schedule
One item potential employees find extremely frustrating about contracts is when it fails to include promises made regarding location, call, and schedule.
These particular items affect a physician’s expectations about a job, including commute time, family life, and lifestyle. An employer or recruiter that makes a lot of promises on these points but won’t commit to the details in writing (or at least offer mutual agreement on these issues) can cause an uncertain candidate to choose the job that offers greater certainty.
There are many provisions of a contract that can make a difference to a particular job applicant. A savvy employer seeking to capture a particular health care professional should find out what the specific goals and needs of the candidate might be and consider adjusting the contract to best satisfy the candidate.
At the end of the day, however, at least for those physicians and others reviewing contracts that are fairly equivalent, it may be the fairness of the contract provisions that end up being the deciding factor.
Ms. Adler is Health Law Group Practice Leader for the law firm Roetzel in Chicago. She reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Recruiting health care workers is a challenge these days for both private practice and hospital employers, and competition can be fierce. In order to be competitive, employers need to review the package they are offering potential candidates and understand that it’s more than just compensation and benefits that matter.
As someone who reviews physician contracts extensively, there are some common examples of language that may cause a candidate to choose a different position.
Probationary period
Although every employer wants to find out if they like the physician or midlevel employee that they have just hired before fully committing, the inclusion of a probationary period (usually 90 days) is offensive to a candidate, especially one with a choice of contracts.
Essentially, the employer is asking the employee to (potentially) relocate, go through the credentialing process, and turn down other potential offers, all for the possibility that they could easily be terminated. Probationary periods typically allow an employee to be immediately terminated without notice or cause, which can then leave them stranded without a paycheck (and with a new home and/or other recent commitments).
Moreover, contracts with probationary periods tend to terminate the employee without covering any tail costs or clarifying that the employer will not enforce restrictive provisions (even if unlikely to be legally enforceable based on the short relationship).
It is important to understand that the process of a person finding a new position, which includes interviewing, contract negotiation, and credentialing, can take up to 6 months. For this reason, probationary provisions create real job insecurity for a candidate.
Entering into a new affiliation is a leap of faith both for the employer and the employee. If the circumstances do not work out, the employer should fairly compensate the employee for the notice period and ask them not to return to work or otherwise allow them to keep working the notice period while they search for a new position.
Acceleration of notice
Another objectionable provision that employers like to include in their contracts is one which allows the employer to accelerate and immediately terminate an employee who has given proper notice.
The contract will contain a standard notice provision, but when the health care professional submits notice, their last date is suddenly accelerated, and they are released without further compensation, notice, or benefits. This type of provision is particularly offensive to health care employees who take the step of giving proper contractual notice and, similar to the probationary language, can create real job insecurity for an employee who suddenly loses their paycheck and has no new job to start.
Medical workers should be paid for the entire notice period whether or not they are allowed to work. Unfortunately, this type of provision is sometimes hidden in contracts and not noticed by employees, who tend to focus on the notice provision itself. I consider this provision to be a red flag about the employer when I review clients’ contracts.
Malpractice tail
Although many employers will claim it is not unusual for an employee to pay for their own malpractice tail, in the current marketplace, the payment of tail can be a deciding factor in whether a candidate accepts a contract.
At a minimum, employers should consider paying for the tail under circumstances where they non-renew a contract, terminate without cause, or the contract is terminated for the employer’s breach. Similarly, I like to seek out payment of the tail by the employer where the contract is terminated owing to a change in the law, use of a force majeure provision, loss of the employer’s hospital contract, or similar provisions where termination is outside the control of the employee.
Employers should also consider a provision where they share the cost of a tail or cover the entire cost on the basis of years of service in order to stand out to a potential candidate.
Noncompete provisions
I do not find noncompete provisions to be generally unacceptable when properly written; however, employers should reevaluate the reasonableness of their noncompete language frequently, because such language can make the difference in whether a candidate accepts a contract.
A reasonable noncompete that only protects the employer as necessary and does not restrict the reasonable practice of medicine is always preferable and can be the deciding factor for a candidate. Tying enforcement of a noncompete to reasons for termination (similar to the tail) can also make a positive difference in a candidate’s review of a contract.
Egregious noncompetes, where the candidate is simply informed that the language is “not negotiable,” are unlikely to be compelling to a candidate with other options.
Specifics on location, call, schedule
One item potential employees find extremely frustrating about contracts is when it fails to include promises made regarding location, call, and schedule.
These particular items affect a physician’s expectations about a job, including commute time, family life, and lifestyle. An employer or recruiter that makes a lot of promises on these points but won’t commit to the details in writing (or at least offer mutual agreement on these issues) can cause an uncertain candidate to choose the job that offers greater certainty.
There are many provisions of a contract that can make a difference to a particular job applicant. A savvy employer seeking to capture a particular health care professional should find out what the specific goals and needs of the candidate might be and consider adjusting the contract to best satisfy the candidate.
At the end of the day, however, at least for those physicians and others reviewing contracts that are fairly equivalent, it may be the fairness of the contract provisions that end up being the deciding factor.
Ms. Adler is Health Law Group Practice Leader for the law firm Roetzel in Chicago. She reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Recruiting health care workers is a challenge these days for both private practice and hospital employers, and competition can be fierce. In order to be competitive, employers need to review the package they are offering potential candidates and understand that it’s more than just compensation and benefits that matter.
As someone who reviews physician contracts extensively, there are some common examples of language that may cause a candidate to choose a different position.
Probationary period
Although every employer wants to find out if they like the physician or midlevel employee that they have just hired before fully committing, the inclusion of a probationary period (usually 90 days) is offensive to a candidate, especially one with a choice of contracts.
Essentially, the employer is asking the employee to (potentially) relocate, go through the credentialing process, and turn down other potential offers, all for the possibility that they could easily be terminated. Probationary periods typically allow an employee to be immediately terminated without notice or cause, which can then leave them stranded without a paycheck (and with a new home and/or other recent commitments).
Moreover, contracts with probationary periods tend to terminate the employee without covering any tail costs or clarifying that the employer will not enforce restrictive provisions (even if unlikely to be legally enforceable based on the short relationship).
It is important to understand that the process of a person finding a new position, which includes interviewing, contract negotiation, and credentialing, can take up to 6 months. For this reason, probationary provisions create real job insecurity for a candidate.
Entering into a new affiliation is a leap of faith both for the employer and the employee. If the circumstances do not work out, the employer should fairly compensate the employee for the notice period and ask them not to return to work or otherwise allow them to keep working the notice period while they search for a new position.
Acceleration of notice
Another objectionable provision that employers like to include in their contracts is one which allows the employer to accelerate and immediately terminate an employee who has given proper notice.
The contract will contain a standard notice provision, but when the health care professional submits notice, their last date is suddenly accelerated, and they are released without further compensation, notice, or benefits. This type of provision is particularly offensive to health care employees who take the step of giving proper contractual notice and, similar to the probationary language, can create real job insecurity for an employee who suddenly loses their paycheck and has no new job to start.
Medical workers should be paid for the entire notice period whether or not they are allowed to work. Unfortunately, this type of provision is sometimes hidden in contracts and not noticed by employees, who tend to focus on the notice provision itself. I consider this provision to be a red flag about the employer when I review clients’ contracts.
Malpractice tail
Although many employers will claim it is not unusual for an employee to pay for their own malpractice tail, in the current marketplace, the payment of tail can be a deciding factor in whether a candidate accepts a contract.
At a minimum, employers should consider paying for the tail under circumstances where they non-renew a contract, terminate without cause, or the contract is terminated for the employer’s breach. Similarly, I like to seek out payment of the tail by the employer where the contract is terminated owing to a change in the law, use of a force majeure provision, loss of the employer’s hospital contract, or similar provisions where termination is outside the control of the employee.
Employers should also consider a provision where they share the cost of a tail or cover the entire cost on the basis of years of service in order to stand out to a potential candidate.
Noncompete provisions
I do not find noncompete provisions to be generally unacceptable when properly written; however, employers should reevaluate the reasonableness of their noncompete language frequently, because such language can make the difference in whether a candidate accepts a contract.
A reasonable noncompete that only protects the employer as necessary and does not restrict the reasonable practice of medicine is always preferable and can be the deciding factor for a candidate. Tying enforcement of a noncompete to reasons for termination (similar to the tail) can also make a positive difference in a candidate’s review of a contract.
Egregious noncompetes, where the candidate is simply informed that the language is “not negotiable,” are unlikely to be compelling to a candidate with other options.
Specifics on location, call, schedule
One item potential employees find extremely frustrating about contracts is when it fails to include promises made regarding location, call, and schedule.
These particular items affect a physician’s expectations about a job, including commute time, family life, and lifestyle. An employer or recruiter that makes a lot of promises on these points but won’t commit to the details in writing (or at least offer mutual agreement on these issues) can cause an uncertain candidate to choose the job that offers greater certainty.
There are many provisions of a contract that can make a difference to a particular job applicant. A savvy employer seeking to capture a particular health care professional should find out what the specific goals and needs of the candidate might be and consider adjusting the contract to best satisfy the candidate.
At the end of the day, however, at least for those physicians and others reviewing contracts that are fairly equivalent, it may be the fairness of the contract provisions that end up being the deciding factor.
Ms. Adler is Health Law Group Practice Leader for the law firm Roetzel in Chicago. She reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A case for when, how, and why to evaluate capacity
Case
Ms. F. is a 68-year-old woman who presented to the hospital with sepsis, developed delirium, and stopped eating. Her clinicians recommended a PEG tube. Although she was inconsistently oriented to self, time, and place, she reiterated the same decision across multiple discussions: She did not want the PEG tube. Her replies to what would happen if she didn’t have the procedure and continued not to eat were consistent, too: “I’ll wither away.”
Ms. F. had impaired cognition. Do these impairments mean her clinicians should over-rule her choice? What evidence indicates whether she lacks decision-making capacity? This case of a patient refusing a potentially life-saving procedure amplifies the importance of asking these questions and integrating capacity assessments into clinical care. In this article, we will describe what capacity is, when and how to assess it, and the alternatives when a patient does not have capacity.
The ethical background
Before starting a medical treatment or procedure, a physician must obtain the patient’s informed consent. This is a core ethic of medicine. Informed consent describes the voluntary decision made by a competent patient following the disclosure of necessary information. Informed consent is key to achieving a balance between promoting patient self-determination and protecting vulnerable patients from harm. In most clinical encounters, informed consent unfolds effortlessly. However, in the care of patients who are acutely ill, particularly those in hospitals, fulfilling the ethic can be challenging.
It is important to have skills to recognize and address these challenges. One of the most common challenges to practicing the ethic of informed consent is the impact of illness on a person’s decision-making capacity. A patient who retains capacity ought to make his or her decisions and does not need someone else (a friend or a family member) to help with the decision.
Incapacity is unfortunately common among the acutely ill medical inpatient population, which typically skews older with more comorbidities.1 Impairments frequently are overlooked for a variety of reasons,2-6 including that many hospitalized patients do not challenge their doctors’ decisions. Doctors may be reluctant to assess capacity because the assessment may medically, legally, or ethically complicate the patient’s care.
Two common terms describe the outcome of an assessment of a patient’s decision-making abilities: competency and capacity. Competency describes a legal principle. It is granted or withdrawn by judicial review. The consequences of a judge rescinding competency are severe: A patient would need a guardian to make choices on his or her behalf.
Capacity, on the other hand, is a clinical concept. A physician assesses whether the patient can make a specific decision in a specific context. The difference between the two terms – competency and capacity – delineates what are the consequences of the assessment and which authority, a judge or a physician, has the right to withdraw a person’s decision-making authority.
The judge offers a global assessment that can lead to a guardianship. The physician’s decision is temporal and situational. Patients can lack capacity when they are ill and recover it when they are healed. Capacity is specific to each medical decision that the patient makes and so a person can lack capacity to make some decisions but not others.
Ethical framework to make assessment
Capacity is described by four decisional abilities: 1) communicate a choice, 2) understand relevant information, 3) appreciation, and 4) reasoning.7
Communication of a choice may be verbal or nonverbal, but the patient must be able to indicate the treatment choice clearly and consistently. Understanding describes knowing essential information a physician has conveyed. This is assessed by having the patients say back what they were told, such as: “Can you tell me in your own words what is a PEG tube?”
The components of appreciation are: the diagnosis or disorder and the benefits and risks of the proposed intervention as it relates to the diagnosis or disorder. Patients who appreciate their disorder have insight into their condition: “I’m not eating because I have an infection.” This can be assessed with a question such as: “Can you tell me in your own words what are the risks or downsides to you?” This prompt assesses the patient’s appreciation of risk. Reframing the question to ask, “Can you tell me about the upsides of this intervention?” will assess the patient’s appreciation of benefit.
Reasoning assesses the thought process and rationale for a person’s decision. It has two components – comparative and consequential reasoning. The first compares the different choices presented about the proposed intervention: “How does having a PEG tube compare to not having it?” The second asks about the consequences of each choice: “What might happen to a person who has the PEG tube?”
The capacity assessment evaluates a patient's performance on these decision-making abilities. This informs the clinician’s judgment of whether the patient has the capacity to make a decision. A patient who has capacity makes the choice, regardless of the physician’s preference or recommendation.
The physician’s duty is to decide which decision-making abilities to assess. Choice and understanding are essential. In riskier or more consequential decisions, a physician may raise the rigor of the assessment to include appreciation and reasoning.8 It is common practice for physicians to raise the standard for when to evaluate and how extensive their evaluation is when the decision is life-altering, as with a PEG tube versus a more routine, non–life-altering decision such as drawing blood for a routine wellness visit.
A simple scoring rubric determines the patient’s ability to answer each question along a range from adequate = 2, marginal = 1, to inadequate = 0. The extremes or adequate or inadequate are straightforward. Judgment is needed when performance is marginal. In the case of repeated marginal answers, a physician must strongly consider whether the patient lacks capacity to make the decision in question.9
Who receives a capacity assessment and when?
A good doctor is a good teacher. A doctor should therefore check that patients understand what is happening with their health. Assessing understanding is simply good medicine; for example, a good teacher ought to be asking an unimpaired patient without impaired cognition, “Can you say back to me the key points of what I explained?” With this approach, every patient is effectively “screened” for a capacity impairment.
Certain patients ought to trigger a more thorough examination of decisional abilities. Across multiple articles, the strongest factors associated with incapacity are older age and diminished cognitive function (often detected by MMSE scores below the low 20s).1,7,10 Other factors that may amplify these deficits and thus should raise clinician concern would be patients with brain diseases such as Alzheimer’s or Parkinson’s, persons with lower education levels, or those who already have someone who helps them make decisions. To be sure, many older adults, even those with cognitive impairments, retain capacity, but extra protection should be in place to ensure their well-being.
Consequences of incapacity
If a careful assessment shows a patient has sound decision-making abilities, the patient is free to make the choice. On the other hand, a person does not have the capacity to make the decision at hand if he or she cannot communicate a choice or understand relevant information. Whether appreciation or reasoning ought to be assessed depends on the complexity and the significance of the decision. An assessment of decisional ability is not the end of the decision-making process. The goal is to maximize the patient’s autonomy.
Capacity can change over time. Factors that may inhibit capacity, such as medications, time of day, and even illness acuity, need to be accounted for and, if possible, addressed. The decision ought to be delayed, if possible, to a time when the patient has better chances of having capacity. If it is unlikely that patients’ status will change in the time frame needed to make the choice and they are found to not have capacity, then the decision making can be aided by advance directives or substitute decision makers such as family members or legal guardians.
Revisiting the case
Ms. F., who was delirious, retained notable decisional abilities. She understood the procedure of receiving the PEG tube and how the risk of continuing to not eat and not receive the PEG would result in dying by starvation. She appreciated her own diagnosis and how the proposed intervention could alter her condition. She appreciated how not having a PEG would lead to her death. Her choice to refuse the procedure was consistent. Ms. F. showed she retained capacity to make this decision. It was the physician’s duty to respect her autonomy and so to respect her refusal of the PEG.
Dr. Ney is a physician resident, department of psychiatry and human behavior, Thomas Jefferson University Hospital, Philadelphia. He has no conflicts to disclose. Dr. Karlawish is a professor in the departments of medicine, medical ethics and health policy, and neurology, University of Pennsylvania, Philadelphia. He is a site investigator for clinical trials sponsored by Biogen, Eisai, and Lilly.
References
1. Raymont V et al. Prevalence of mental incapacity in medical inpatients and associated risk factors: Cross-sectional study. Lancet. 2004;364(9443):1421-7. doi: 10.1016/S0140-6736(04)17224-3.
2. Hanson M and Pitt D. Informed consent for surgery: risk discussion and documentation. Can J Surg. 2017;60(1):69-70. doi: 10.1503/cjs.004816.
3. Dahlberg J et al. Lack of informed consent for surgical procedures by elderly patients with inability to consent: A retrospective chart review from an academic medical center in Norway. Patient Saf Surg. 2019;13:24. doi: 10.1186/s13037-019-0205-5.
4. Sessums LL et al. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-7. doi: 10.1001/jama.2011.1023.
5. Terranova C et al. Ethical and medicolegal implications of capacity of patients in geriatric surgery. Med Sci Law. 2013;53(3):166-71. doi: 10.1177/0025802412473963.
6. John S et al. Assessing patients decision-making capacity in the hospital setting: A literature review. Aust J Rural Health. 2020;28(2):141-8. doi: 10.1111/ajr.12592.
7. Kim SYH et al. Do clinicians follow a risk-sensitive model of capacity-determination? An experimental video survey. Psychosomatics. 2006;47(4):325-9. doi: 10.1176/appi.psy.47.4.325.
8. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-40. doi: 10.1056/NEJMcp074045.
9. Karlawish J. Measuring decision-making capacity in cognitively impaired individuals. Neurosignals. 2008;16(1):91-8. doi: 10.1159/000109763.
10. Christensen K et al. Decision-making capacity for informed consent in the older population. Bull Am Acad Psychiatry Law. 1995;23(3):353-65.
Case
Ms. F. is a 68-year-old woman who presented to the hospital with sepsis, developed delirium, and stopped eating. Her clinicians recommended a PEG tube. Although she was inconsistently oriented to self, time, and place, she reiterated the same decision across multiple discussions: She did not want the PEG tube. Her replies to what would happen if she didn’t have the procedure and continued not to eat were consistent, too: “I’ll wither away.”
Ms. F. had impaired cognition. Do these impairments mean her clinicians should over-rule her choice? What evidence indicates whether she lacks decision-making capacity? This case of a patient refusing a potentially life-saving procedure amplifies the importance of asking these questions and integrating capacity assessments into clinical care. In this article, we will describe what capacity is, when and how to assess it, and the alternatives when a patient does not have capacity.
The ethical background
Before starting a medical treatment or procedure, a physician must obtain the patient’s informed consent. This is a core ethic of medicine. Informed consent describes the voluntary decision made by a competent patient following the disclosure of necessary information. Informed consent is key to achieving a balance between promoting patient self-determination and protecting vulnerable patients from harm. In most clinical encounters, informed consent unfolds effortlessly. However, in the care of patients who are acutely ill, particularly those in hospitals, fulfilling the ethic can be challenging.
It is important to have skills to recognize and address these challenges. One of the most common challenges to practicing the ethic of informed consent is the impact of illness on a person’s decision-making capacity. A patient who retains capacity ought to make his or her decisions and does not need someone else (a friend or a family member) to help with the decision.
Incapacity is unfortunately common among the acutely ill medical inpatient population, which typically skews older with more comorbidities.1 Impairments frequently are overlooked for a variety of reasons,2-6 including that many hospitalized patients do not challenge their doctors’ decisions. Doctors may be reluctant to assess capacity because the assessment may medically, legally, or ethically complicate the patient’s care.
Two common terms describe the outcome of an assessment of a patient’s decision-making abilities: competency and capacity. Competency describes a legal principle. It is granted or withdrawn by judicial review. The consequences of a judge rescinding competency are severe: A patient would need a guardian to make choices on his or her behalf.
Capacity, on the other hand, is a clinical concept. A physician assesses whether the patient can make a specific decision in a specific context. The difference between the two terms – competency and capacity – delineates what are the consequences of the assessment and which authority, a judge or a physician, has the right to withdraw a person’s decision-making authority.
The judge offers a global assessment that can lead to a guardianship. The physician’s decision is temporal and situational. Patients can lack capacity when they are ill and recover it when they are healed. Capacity is specific to each medical decision that the patient makes and so a person can lack capacity to make some decisions but not others.
Ethical framework to make assessment
Capacity is described by four decisional abilities: 1) communicate a choice, 2) understand relevant information, 3) appreciation, and 4) reasoning.7
Communication of a choice may be verbal or nonverbal, but the patient must be able to indicate the treatment choice clearly and consistently. Understanding describes knowing essential information a physician has conveyed. This is assessed by having the patients say back what they were told, such as: “Can you tell me in your own words what is a PEG tube?”
The components of appreciation are: the diagnosis or disorder and the benefits and risks of the proposed intervention as it relates to the diagnosis or disorder. Patients who appreciate their disorder have insight into their condition: “I’m not eating because I have an infection.” This can be assessed with a question such as: “Can you tell me in your own words what are the risks or downsides to you?” This prompt assesses the patient’s appreciation of risk. Reframing the question to ask, “Can you tell me about the upsides of this intervention?” will assess the patient’s appreciation of benefit.
Reasoning assesses the thought process and rationale for a person’s decision. It has two components – comparative and consequential reasoning. The first compares the different choices presented about the proposed intervention: “How does having a PEG tube compare to not having it?” The second asks about the consequences of each choice: “What might happen to a person who has the PEG tube?”
The capacity assessment evaluates a patient's performance on these decision-making abilities. This informs the clinician’s judgment of whether the patient has the capacity to make a decision. A patient who has capacity makes the choice, regardless of the physician’s preference or recommendation.
The physician’s duty is to decide which decision-making abilities to assess. Choice and understanding are essential. In riskier or more consequential decisions, a physician may raise the rigor of the assessment to include appreciation and reasoning.8 It is common practice for physicians to raise the standard for when to evaluate and how extensive their evaluation is when the decision is life-altering, as with a PEG tube versus a more routine, non–life-altering decision such as drawing blood for a routine wellness visit.
A simple scoring rubric determines the patient’s ability to answer each question along a range from adequate = 2, marginal = 1, to inadequate = 0. The extremes or adequate or inadequate are straightforward. Judgment is needed when performance is marginal. In the case of repeated marginal answers, a physician must strongly consider whether the patient lacks capacity to make the decision in question.9
Who receives a capacity assessment and when?
A good doctor is a good teacher. A doctor should therefore check that patients understand what is happening with their health. Assessing understanding is simply good medicine; for example, a good teacher ought to be asking an unimpaired patient without impaired cognition, “Can you say back to me the key points of what I explained?” With this approach, every patient is effectively “screened” for a capacity impairment.
Certain patients ought to trigger a more thorough examination of decisional abilities. Across multiple articles, the strongest factors associated with incapacity are older age and diminished cognitive function (often detected by MMSE scores below the low 20s).1,7,10 Other factors that may amplify these deficits and thus should raise clinician concern would be patients with brain diseases such as Alzheimer’s or Parkinson’s, persons with lower education levels, or those who already have someone who helps them make decisions. To be sure, many older adults, even those with cognitive impairments, retain capacity, but extra protection should be in place to ensure their well-being.
Consequences of incapacity
If a careful assessment shows a patient has sound decision-making abilities, the patient is free to make the choice. On the other hand, a person does not have the capacity to make the decision at hand if he or she cannot communicate a choice or understand relevant information. Whether appreciation or reasoning ought to be assessed depends on the complexity and the significance of the decision. An assessment of decisional ability is not the end of the decision-making process. The goal is to maximize the patient’s autonomy.
Capacity can change over time. Factors that may inhibit capacity, such as medications, time of day, and even illness acuity, need to be accounted for and, if possible, addressed. The decision ought to be delayed, if possible, to a time when the patient has better chances of having capacity. If it is unlikely that patients’ status will change in the time frame needed to make the choice and they are found to not have capacity, then the decision making can be aided by advance directives or substitute decision makers such as family members or legal guardians.
Revisiting the case
Ms. F., who was delirious, retained notable decisional abilities. She understood the procedure of receiving the PEG tube and how the risk of continuing to not eat and not receive the PEG would result in dying by starvation. She appreciated her own diagnosis and how the proposed intervention could alter her condition. She appreciated how not having a PEG would lead to her death. Her choice to refuse the procedure was consistent. Ms. F. showed she retained capacity to make this decision. It was the physician’s duty to respect her autonomy and so to respect her refusal of the PEG.
Dr. Ney is a physician resident, department of psychiatry and human behavior, Thomas Jefferson University Hospital, Philadelphia. He has no conflicts to disclose. Dr. Karlawish is a professor in the departments of medicine, medical ethics and health policy, and neurology, University of Pennsylvania, Philadelphia. He is a site investigator for clinical trials sponsored by Biogen, Eisai, and Lilly.
References
1. Raymont V et al. Prevalence of mental incapacity in medical inpatients and associated risk factors: Cross-sectional study. Lancet. 2004;364(9443):1421-7. doi: 10.1016/S0140-6736(04)17224-3.
2. Hanson M and Pitt D. Informed consent for surgery: risk discussion and documentation. Can J Surg. 2017;60(1):69-70. doi: 10.1503/cjs.004816.
3. Dahlberg J et al. Lack of informed consent for surgical procedures by elderly patients with inability to consent: A retrospective chart review from an academic medical center in Norway. Patient Saf Surg. 2019;13:24. doi: 10.1186/s13037-019-0205-5.
4. Sessums LL et al. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-7. doi: 10.1001/jama.2011.1023.
5. Terranova C et al. Ethical and medicolegal implications of capacity of patients in geriatric surgery. Med Sci Law. 2013;53(3):166-71. doi: 10.1177/0025802412473963.
6. John S et al. Assessing patients decision-making capacity in the hospital setting: A literature review. Aust J Rural Health. 2020;28(2):141-8. doi: 10.1111/ajr.12592.
7. Kim SYH et al. Do clinicians follow a risk-sensitive model of capacity-determination? An experimental video survey. Psychosomatics. 2006;47(4):325-9. doi: 10.1176/appi.psy.47.4.325.
8. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-40. doi: 10.1056/NEJMcp074045.
9. Karlawish J. Measuring decision-making capacity in cognitively impaired individuals. Neurosignals. 2008;16(1):91-8. doi: 10.1159/000109763.
10. Christensen K et al. Decision-making capacity for informed consent in the older population. Bull Am Acad Psychiatry Law. 1995;23(3):353-65.
Case
Ms. F. is a 68-year-old woman who presented to the hospital with sepsis, developed delirium, and stopped eating. Her clinicians recommended a PEG tube. Although she was inconsistently oriented to self, time, and place, she reiterated the same decision across multiple discussions: She did not want the PEG tube. Her replies to what would happen if she didn’t have the procedure and continued not to eat were consistent, too: “I’ll wither away.”
Ms. F. had impaired cognition. Do these impairments mean her clinicians should over-rule her choice? What evidence indicates whether she lacks decision-making capacity? This case of a patient refusing a potentially life-saving procedure amplifies the importance of asking these questions and integrating capacity assessments into clinical care. In this article, we will describe what capacity is, when and how to assess it, and the alternatives when a patient does not have capacity.
The ethical background
Before starting a medical treatment or procedure, a physician must obtain the patient’s informed consent. This is a core ethic of medicine. Informed consent describes the voluntary decision made by a competent patient following the disclosure of necessary information. Informed consent is key to achieving a balance between promoting patient self-determination and protecting vulnerable patients from harm. In most clinical encounters, informed consent unfolds effortlessly. However, in the care of patients who are acutely ill, particularly those in hospitals, fulfilling the ethic can be challenging.
It is important to have skills to recognize and address these challenges. One of the most common challenges to practicing the ethic of informed consent is the impact of illness on a person’s decision-making capacity. A patient who retains capacity ought to make his or her decisions and does not need someone else (a friend or a family member) to help with the decision.
Incapacity is unfortunately common among the acutely ill medical inpatient population, which typically skews older with more comorbidities.1 Impairments frequently are overlooked for a variety of reasons,2-6 including that many hospitalized patients do not challenge their doctors’ decisions. Doctors may be reluctant to assess capacity because the assessment may medically, legally, or ethically complicate the patient’s care.
Two common terms describe the outcome of an assessment of a patient’s decision-making abilities: competency and capacity. Competency describes a legal principle. It is granted or withdrawn by judicial review. The consequences of a judge rescinding competency are severe: A patient would need a guardian to make choices on his or her behalf.
Capacity, on the other hand, is a clinical concept. A physician assesses whether the patient can make a specific decision in a specific context. The difference between the two terms – competency and capacity – delineates what are the consequences of the assessment and which authority, a judge or a physician, has the right to withdraw a person’s decision-making authority.
The judge offers a global assessment that can lead to a guardianship. The physician’s decision is temporal and situational. Patients can lack capacity when they are ill and recover it when they are healed. Capacity is specific to each medical decision that the patient makes and so a person can lack capacity to make some decisions but not others.
Ethical framework to make assessment
Capacity is described by four decisional abilities: 1) communicate a choice, 2) understand relevant information, 3) appreciation, and 4) reasoning.7
Communication of a choice may be verbal or nonverbal, but the patient must be able to indicate the treatment choice clearly and consistently. Understanding describes knowing essential information a physician has conveyed. This is assessed by having the patients say back what they were told, such as: “Can you tell me in your own words what is a PEG tube?”
The components of appreciation are: the diagnosis or disorder and the benefits and risks of the proposed intervention as it relates to the diagnosis or disorder. Patients who appreciate their disorder have insight into their condition: “I’m not eating because I have an infection.” This can be assessed with a question such as: “Can you tell me in your own words what are the risks or downsides to you?” This prompt assesses the patient’s appreciation of risk. Reframing the question to ask, “Can you tell me about the upsides of this intervention?” will assess the patient’s appreciation of benefit.
Reasoning assesses the thought process and rationale for a person’s decision. It has two components – comparative and consequential reasoning. The first compares the different choices presented about the proposed intervention: “How does having a PEG tube compare to not having it?” The second asks about the consequences of each choice: “What might happen to a person who has the PEG tube?”
The capacity assessment evaluates a patient's performance on these decision-making abilities. This informs the clinician’s judgment of whether the patient has the capacity to make a decision. A patient who has capacity makes the choice, regardless of the physician’s preference or recommendation.
The physician’s duty is to decide which decision-making abilities to assess. Choice and understanding are essential. In riskier or more consequential decisions, a physician may raise the rigor of the assessment to include appreciation and reasoning.8 It is common practice for physicians to raise the standard for when to evaluate and how extensive their evaluation is when the decision is life-altering, as with a PEG tube versus a more routine, non–life-altering decision such as drawing blood for a routine wellness visit.
A simple scoring rubric determines the patient’s ability to answer each question along a range from adequate = 2, marginal = 1, to inadequate = 0. The extremes or adequate or inadequate are straightforward. Judgment is needed when performance is marginal. In the case of repeated marginal answers, a physician must strongly consider whether the patient lacks capacity to make the decision in question.9
Who receives a capacity assessment and when?
A good doctor is a good teacher. A doctor should therefore check that patients understand what is happening with their health. Assessing understanding is simply good medicine; for example, a good teacher ought to be asking an unimpaired patient without impaired cognition, “Can you say back to me the key points of what I explained?” With this approach, every patient is effectively “screened” for a capacity impairment.
Certain patients ought to trigger a more thorough examination of decisional abilities. Across multiple articles, the strongest factors associated with incapacity are older age and diminished cognitive function (often detected by MMSE scores below the low 20s).1,7,10 Other factors that may amplify these deficits and thus should raise clinician concern would be patients with brain diseases such as Alzheimer’s or Parkinson’s, persons with lower education levels, or those who already have someone who helps them make decisions. To be sure, many older adults, even those with cognitive impairments, retain capacity, but extra protection should be in place to ensure their well-being.
Consequences of incapacity
If a careful assessment shows a patient has sound decision-making abilities, the patient is free to make the choice. On the other hand, a person does not have the capacity to make the decision at hand if he or she cannot communicate a choice or understand relevant information. Whether appreciation or reasoning ought to be assessed depends on the complexity and the significance of the decision. An assessment of decisional ability is not the end of the decision-making process. The goal is to maximize the patient’s autonomy.
Capacity can change over time. Factors that may inhibit capacity, such as medications, time of day, and even illness acuity, need to be accounted for and, if possible, addressed. The decision ought to be delayed, if possible, to a time when the patient has better chances of having capacity. If it is unlikely that patients’ status will change in the time frame needed to make the choice and they are found to not have capacity, then the decision making can be aided by advance directives or substitute decision makers such as family members or legal guardians.
Revisiting the case
Ms. F., who was delirious, retained notable decisional abilities. She understood the procedure of receiving the PEG tube and how the risk of continuing to not eat and not receive the PEG would result in dying by starvation. She appreciated her own diagnosis and how the proposed intervention could alter her condition. She appreciated how not having a PEG would lead to her death. Her choice to refuse the procedure was consistent. Ms. F. showed she retained capacity to make this decision. It was the physician’s duty to respect her autonomy and so to respect her refusal of the PEG.
Dr. Ney is a physician resident, department of psychiatry and human behavior, Thomas Jefferson University Hospital, Philadelphia. He has no conflicts to disclose. Dr. Karlawish is a professor in the departments of medicine, medical ethics and health policy, and neurology, University of Pennsylvania, Philadelphia. He is a site investigator for clinical trials sponsored by Biogen, Eisai, and Lilly.
References
1. Raymont V et al. Prevalence of mental incapacity in medical inpatients and associated risk factors: Cross-sectional study. Lancet. 2004;364(9443):1421-7. doi: 10.1016/S0140-6736(04)17224-3.
2. Hanson M and Pitt D. Informed consent for surgery: risk discussion and documentation. Can J Surg. 2017;60(1):69-70. doi: 10.1503/cjs.004816.
3. Dahlberg J et al. Lack of informed consent for surgical procedures by elderly patients with inability to consent: A retrospective chart review from an academic medical center in Norway. Patient Saf Surg. 2019;13:24. doi: 10.1186/s13037-019-0205-5.
4. Sessums LL et al. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-7. doi: 10.1001/jama.2011.1023.
5. Terranova C et al. Ethical and medicolegal implications of capacity of patients in geriatric surgery. Med Sci Law. 2013;53(3):166-71. doi: 10.1177/0025802412473963.
6. John S et al. Assessing patients decision-making capacity in the hospital setting: A literature review. Aust J Rural Health. 2020;28(2):141-8. doi: 10.1111/ajr.12592.
7. Kim SYH et al. Do clinicians follow a risk-sensitive model of capacity-determination? An experimental video survey. Psychosomatics. 2006;47(4):325-9. doi: 10.1176/appi.psy.47.4.325.
8. Appelbaum PS. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-40. doi: 10.1056/NEJMcp074045.
9. Karlawish J. Measuring decision-making capacity in cognitively impaired individuals. Neurosignals. 2008;16(1):91-8. doi: 10.1159/000109763.
10. Christensen K et al. Decision-making capacity for informed consent in the older population. Bull Am Acad Psychiatry Law. 1995;23(3):353-65.
What role does social media have in GI?
Dear colleagues,
Most of us engage with social media, whether actively tweeting, following friends on Facebook, or discussing TikTok videos with family. Many gastroenterologists leverage social media to build their professional brand and to reach a wider audience. Others remain wary of committing a social media faux paux or worry about patient confidentiality. In this Perspectives column, Dr. Stephen Chris Pappas and Dr. Mohammad Bilal discuss the risks and benefits of social media for the practicing gastroenterologist. Dr. Pappas has a unique perspective as a gastroenterologist who is also trained as a lawyer, and Dr. Bilal speaks from a wealth of experience leading educational activities on social media. We look forward to hearing your thoughts on Twitter @AGA_GIHN and by email at [email protected].
Gyanprakash A. Ketwaroo, MD, MSc, an associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Carefully consider the plentiful risks, concerns
BY STEPHEN CHRIS PAPPAS, MD, JD, FAASLD, FACLM
Social media for gastroenterologists comes with benefits accompanied by pesky risks. The risks are pesky like a mosquito bite: An itching bite is annoying, but getting malaria is serious. Managing your unprofessional tweet to salvage your reputation is going to be annoying. Disclosing a patient's identity on social media is going to be serious; you could find yourself fired, fined, reprimanded, and without hospital privileges, as happened recently to a Rhode Island physician. I divide the risks of social media into legal risks (for example, disclosing patient identity or inadvertently creating a doctor-patient relationship), risks of compromising ethical standards (for example, impairing the doctor-patient relationship), and mixed legal/ethics risks (for example, inappropriate Twitter banter disparaging individuals, promotion of “fake news”). Fortunately, these risks are intuitive and can be mitigated by attention to some simple principles.
Disclosing a patient’s identity on social media is clearly in violation of privacy laws and other regulations. Since privacy compliance is drummed into us ad nauseum via annual compliance training, we could ask “how on earth could an inadvertent disclosure of identity occur?” We must remember that sites that are nominally termed “secure” may not be. As a general suggestion, I would regard social media of all types as open public forums with permanent postings. Even limited descriptions of a patient on social media may allow identification of the actual patient. The risk may be highest in smaller communities; in the past I assisted a small-town practitioner manage the fallout from inadvertently identifying a patient on his professional Facebook page by simply saying “I recently managed a 38-year-old pregnant woman with Crohn’s disease ...” That small amount of information allowed some members of his community to identify the specific patient. My suggestion would be to never talk about individual patients on social media. Phrase comments or questions generically; for example, “Crohn’s disease in pregnancy is managed with attention to ...”.
Another legal risk of social media engagement is to unknowingly create a patient-doctor relationship with a duty to treat, opening the door for exposure to malpractice litigation if something goes awry. A patient may interpret a social media interaction as establishing a patient-doctor relationship. While we think we know what defines a doctor-patient relationship, it’s not always clear and varies between jurisdictions. Indeed, a physician-patient relationship may not even be a necessary element of a claim for professional negligence (an issue shared with “curbside” consults). A recent court case in Minnesota ruled that a duty to care is established if “... it is reasonably foreseeable that the third party will rely on the physician’s acts and be harmed by a breach of the standard of care.” That case involved a telephone call, but you could see the standard easily morphing to apply to social media posts. Gastroenterologists should always talk about disease and treatment on social media in generic terms, preferably with appropriate caveats (for example, “Patients with cholestasis and intense itching may be treated with naloxone in selected cases after detailed assessment by a hepatologist”).
Impairing an established doctor-patient relationship by “friending” a patient on your personal Facebook risks a potential compromise of professional ethics, breaking the boundaries between profession and person for the gastroenterologist. The approach by most professional societies is that a “friend” on social media is equal to a friend in the real world; the same legal and ethical standards apply. Doctor-patient friendships may compromise objectivity, lead to preferential but not optimal therapy, and increase the risk of skirting around informed consent among other issues. Being friends on social media is discouraged, but not prohibited, by most professional societies and licensing bodies. In my opinion, that is sound advice. Over a career of more than 40 years, I have had patients who became friends, but only after I had transferred their care to another hepatologist.
More recently with escalating, aggressive, tones for social media communications, GI/hepatology practitioners must be aware of the serious risk of blurring their personal and professional online lives, particularly where Twitter is involved. The rapidity which people seem to want to reply to a tweet, the public and durable natures of a tweet, and the ability to significantly retweet and repost all spell potential disasters for the physician tweeting an inappropriate communication. Separation of personal and professional social media accounts is strongly encouraged but alone is not enough; you are never totally anonymous online. The reality is that a physician will be judged for an inappropriate communication whether it’s found on their professional or personal site. Either posting could result in reputation damage, reprimands, medical license restrictions or revocations, and litigation. Nationally, medical boards now regularly deal with disciplinary actions for inappropriate social media activity. The best preventive measures include pausing before you post, check the veracity of what you are posting, place your post in context, and assess the tone of your post and the tone of the site that you are posting to. A perfect storm for disaster is that the material is not clearly evidence based and could be construed as “fake,” you are personally emotionally charged, and the site you are posting to is a known cauldron of emotion and fake news.
In summary, social media affords benefits in a health care setting but it comes with some baggage. However, the risks of a social media presence are largely instinctive. An initial starting point is pausing to consider, “Would I say/do this in a public venue where everybody could hear/see me?” If there is any concern, don’t post. Subsequently, conduct yourself on social media with meticulous attention to protecting confidentiality, avoiding any impression of creating a doctor-patient relationship, avoiding doctor-friend relationships, being aware of key legal, institutional, and professional society guidance, separating personal and professional activities, and maintaining professionalism.
Dr. Pappas is in the GI and hepatology section of the department of medicine at Baylor College of Medicine, Houston. He has no relevant conflicts of interest to disclose.
References
Attai DJ et al. Semin Hematol. 2017 Oct; 54(4): 198-204.
Bal BS et al. Clin Orthop Relat Res. 2019 Oct; 477(10): 2204-6.
Ekrem, D et al. 20111 Jun 6. https://www.kevinmd.com/2011/06/7-tips-avoid-hipaa-violations-social-media.html
Hallenbeck J. Doctor and Friend. 2005 Jun. https://journalofethics.ama-assn.org/article/doctor-and-friend/2005-06
Moses RE et al. Am J Gastroenterol. 2014 Aug;109(8):1128-32.
Understand its multifaceted importance
BY MOHAMMAD BILAL, MD, FACP
Merriam-Webster’s dictionary defines social media as “forms of electronic communication (such as websites for social networking and microblogging) through which users create online communities to share information, ideas, personal messages, and other content.” Over the last few years, there has been an increase in use of social media by medical professionals. Whether we like it or not, social media is here to stay. Patients use social media to look up information regarding their doctors, medical practices use it to promote the services they offer, institutions share their programs and initiatives, and doctors use it for education, to engage with like-minded colleagues, collaborate, spread awareness, network, and combat medical misinformation. Social media is now rapidly being used by gastroenterologists and hepatologists, as well as majority of professional GI organizations, and hashtags such as “#MedTwitter”, “#GITwitter,” and “#LiverTwitter” have developed into popular academic forums.1 Therefore, the impact of social media in GI is multifaceted and includes its role in medical education, promoting your practice or division, finding collaborations, building your network and establishing mentors and peer-mentors, disseminating your work, and building your brand.2
What is your goal?
Gastroenterologists could have one or more of the goals mentioned above for using social media. Determining the goals for social media use a priori will allow for determining which social media platform will be appropriate for you. Therefore, it is important to understand the users of various social media platforms. In 2017, Facebook was the highest used social media platform in all age groups, whereas Instagram was most popular amongst ages 18-29 years, while Twitter was used more commonly in ages 30-59 years as compared with Instagram. If your goal is to share scientific knowledge and literature with like-minded physicians and interact with leaders in the field, then Twitter may be ideal. If you want to connect with a younger, more diverse audience, Instagram might be a good option. While many physicians may have a Facebook account, this is often reserved for personal use. Many have separated of personal and professional social media use, although they do not need to exist in silos. Defining your goal with social media use will direct you to the best platform to reach your audience.
Medical education
The use of social media especially Twitter for medical education is continuously increasing. Several leaders in the field use “Tweetorials” as a means to educate others. Tweetorials are a collective set of tweets that systematically cover a specialized topic.3 Other educational forums such as @ScopingSundays, @MondayNightIBD, @IBDClub and @GIJournal provide structured platforms for GI focused discussion.4 @MondayNightIBD is also a source for official continued medical education. Other social media educational platforms include “Liver Fellow Network” which has wide variety of educational materials pertaining to hepatology. In addition, there is continuous opportunity to engage with leaders in the field and authors of published studies and guidelines. Several endoscopy educators have dedicated YouTube channels which have endless supply of educational videos.
Networking
As mentioned above, platforms such as #GITwitter and #LiverTwitter have become popular forums for engaging and connecting with like minded colleagues. Social media provides a space to share ideas and build collaborations with colleagues working on similar projects. The concept “#Twitter2Paper” has been proposed which signifies an idea that generated on Twitter and was eventually converted to a manuscript.5
Institutional, divisional, and practice promotion
Social media is a great tool to showcase the clinical, educational and scholarship services and efforts by programs, practices or divisions. During the COVID-19 pandemic, recruitment efforts at all stages were mainly shifted to virtual platforms, and social media was an instrumental way for programs to highlight their culture and initiatives. Prospective applicants can often refer to social media to get a better understanding of what the program offers. Similarly, if a new clinical service is being provided, targeted efforts can be made to ensure that patients are aware of the available services.
Patient education and combating misinformation
Several gastroenterologists also use social media to spread awareness regarding GI diseases. Instagram, Facebook, and TikTok are effective mediums where one can reach a wider audience. It is important for gastroenterologists to provide accurate information since there is a sea of misinformation available on the internet as well. Posts regarding colonoscopy and colon cancer awareness can help alleviate myths regarding role of colonoscopy. In addition, patient advocates use social media to provide peer support to others who deal with challenges related to chronic illnesses such as inflammatory bowel disease.
Sharing your work
Sharing your work on social media can help your work reach a broader audience. Studies have shown that work shared on social media has higher altmetric scores and can also lead to increased citations.
Diversity, equity, and inclusion
Social media offers a platform where one can promote or showcase their support for causes they believe in. The hashtag “#DiversityinGI” has been instrumental in promoting causes pertaining to diversity and inclusion in GI.
Pitfalls
As gastroenterologists continue to use social media, it is important to be mindful of potential pitfalls. The most critical aspect is to always remember that no post should intentionally or unintentionally violate HIPAA. It is advisable to know your institutional and state social media policies.
Social media is beaming with knowledge, education, science and inspiration. There are endless opportunities for professional and personal growth with effective and responsible use of social media. Its never to late to join the conversation.
Dr. Bilal is an assistant professor of medicine at the University of Minnesota, Minneapolis and an advanced endoscopist in the division of gastroenterology at Minneapolis VA Medical Center. He has no relevant conflicts of interest to disclose.
References
1. Mikolajczyk AE et al. Hepatol Commun. 2020 Jul 5;4(8):1229-33.
2. Bilal M and Oxentenko AS. Am J Gastroenterol. 2020 Oct;115(10):1549-52.
3. Breu AC. N Engl J Med. 2019 Sep 19;381(12):1097-8.
4. Bilal M et al. Nat Rev Gastroenterol Hepatol. 2021 Aug;18(8):519-20.
5. Pawlak KM et al. United European Gastroenterol J. 2021 Feb;9(1):129-32.
Dear colleagues,
Most of us engage with social media, whether actively tweeting, following friends on Facebook, or discussing TikTok videos with family. Many gastroenterologists leverage social media to build their professional brand and to reach a wider audience. Others remain wary of committing a social media faux paux or worry about patient confidentiality. In this Perspectives column, Dr. Stephen Chris Pappas and Dr. Mohammad Bilal discuss the risks and benefits of social media for the practicing gastroenterologist. Dr. Pappas has a unique perspective as a gastroenterologist who is also trained as a lawyer, and Dr. Bilal speaks from a wealth of experience leading educational activities on social media. We look forward to hearing your thoughts on Twitter @AGA_GIHN and by email at [email protected].
Gyanprakash A. Ketwaroo, MD, MSc, an associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Carefully consider the plentiful risks, concerns
BY STEPHEN CHRIS PAPPAS, MD, JD, FAASLD, FACLM
Social media for gastroenterologists comes with benefits accompanied by pesky risks. The risks are pesky like a mosquito bite: An itching bite is annoying, but getting malaria is serious. Managing your unprofessional tweet to salvage your reputation is going to be annoying. Disclosing a patient's identity on social media is going to be serious; you could find yourself fired, fined, reprimanded, and without hospital privileges, as happened recently to a Rhode Island physician. I divide the risks of social media into legal risks (for example, disclosing patient identity or inadvertently creating a doctor-patient relationship), risks of compromising ethical standards (for example, impairing the doctor-patient relationship), and mixed legal/ethics risks (for example, inappropriate Twitter banter disparaging individuals, promotion of “fake news”). Fortunately, these risks are intuitive and can be mitigated by attention to some simple principles.
Disclosing a patient’s identity on social media is clearly in violation of privacy laws and other regulations. Since privacy compliance is drummed into us ad nauseum via annual compliance training, we could ask “how on earth could an inadvertent disclosure of identity occur?” We must remember that sites that are nominally termed “secure” may not be. As a general suggestion, I would regard social media of all types as open public forums with permanent postings. Even limited descriptions of a patient on social media may allow identification of the actual patient. The risk may be highest in smaller communities; in the past I assisted a small-town practitioner manage the fallout from inadvertently identifying a patient on his professional Facebook page by simply saying “I recently managed a 38-year-old pregnant woman with Crohn’s disease ...” That small amount of information allowed some members of his community to identify the specific patient. My suggestion would be to never talk about individual patients on social media. Phrase comments or questions generically; for example, “Crohn’s disease in pregnancy is managed with attention to ...”.
Another legal risk of social media engagement is to unknowingly create a patient-doctor relationship with a duty to treat, opening the door for exposure to malpractice litigation if something goes awry. A patient may interpret a social media interaction as establishing a patient-doctor relationship. While we think we know what defines a doctor-patient relationship, it’s not always clear and varies between jurisdictions. Indeed, a physician-patient relationship may not even be a necessary element of a claim for professional negligence (an issue shared with “curbside” consults). A recent court case in Minnesota ruled that a duty to care is established if “... it is reasonably foreseeable that the third party will rely on the physician’s acts and be harmed by a breach of the standard of care.” That case involved a telephone call, but you could see the standard easily morphing to apply to social media posts. Gastroenterologists should always talk about disease and treatment on social media in generic terms, preferably with appropriate caveats (for example, “Patients with cholestasis and intense itching may be treated with naloxone in selected cases after detailed assessment by a hepatologist”).
Impairing an established doctor-patient relationship by “friending” a patient on your personal Facebook risks a potential compromise of professional ethics, breaking the boundaries between profession and person for the gastroenterologist. The approach by most professional societies is that a “friend” on social media is equal to a friend in the real world; the same legal and ethical standards apply. Doctor-patient friendships may compromise objectivity, lead to preferential but not optimal therapy, and increase the risk of skirting around informed consent among other issues. Being friends on social media is discouraged, but not prohibited, by most professional societies and licensing bodies. In my opinion, that is sound advice. Over a career of more than 40 years, I have had patients who became friends, but only after I had transferred their care to another hepatologist.
More recently with escalating, aggressive, tones for social media communications, GI/hepatology practitioners must be aware of the serious risk of blurring their personal and professional online lives, particularly where Twitter is involved. The rapidity which people seem to want to reply to a tweet, the public and durable natures of a tweet, and the ability to significantly retweet and repost all spell potential disasters for the physician tweeting an inappropriate communication. Separation of personal and professional social media accounts is strongly encouraged but alone is not enough; you are never totally anonymous online. The reality is that a physician will be judged for an inappropriate communication whether it’s found on their professional or personal site. Either posting could result in reputation damage, reprimands, medical license restrictions or revocations, and litigation. Nationally, medical boards now regularly deal with disciplinary actions for inappropriate social media activity. The best preventive measures include pausing before you post, check the veracity of what you are posting, place your post in context, and assess the tone of your post and the tone of the site that you are posting to. A perfect storm for disaster is that the material is not clearly evidence based and could be construed as “fake,” you are personally emotionally charged, and the site you are posting to is a known cauldron of emotion and fake news.
In summary, social media affords benefits in a health care setting but it comes with some baggage. However, the risks of a social media presence are largely instinctive. An initial starting point is pausing to consider, “Would I say/do this in a public venue where everybody could hear/see me?” If there is any concern, don’t post. Subsequently, conduct yourself on social media with meticulous attention to protecting confidentiality, avoiding any impression of creating a doctor-patient relationship, avoiding doctor-friend relationships, being aware of key legal, institutional, and professional society guidance, separating personal and professional activities, and maintaining professionalism.
Dr. Pappas is in the GI and hepatology section of the department of medicine at Baylor College of Medicine, Houston. He has no relevant conflicts of interest to disclose.
References
Attai DJ et al. Semin Hematol. 2017 Oct; 54(4): 198-204.
Bal BS et al. Clin Orthop Relat Res. 2019 Oct; 477(10): 2204-6.
Ekrem, D et al. 20111 Jun 6. https://www.kevinmd.com/2011/06/7-tips-avoid-hipaa-violations-social-media.html
Hallenbeck J. Doctor and Friend. 2005 Jun. https://journalofethics.ama-assn.org/article/doctor-and-friend/2005-06
Moses RE et al. Am J Gastroenterol. 2014 Aug;109(8):1128-32.
Understand its multifaceted importance
BY MOHAMMAD BILAL, MD, FACP
Merriam-Webster’s dictionary defines social media as “forms of electronic communication (such as websites for social networking and microblogging) through which users create online communities to share information, ideas, personal messages, and other content.” Over the last few years, there has been an increase in use of social media by medical professionals. Whether we like it or not, social media is here to stay. Patients use social media to look up information regarding their doctors, medical practices use it to promote the services they offer, institutions share their programs and initiatives, and doctors use it for education, to engage with like-minded colleagues, collaborate, spread awareness, network, and combat medical misinformation. Social media is now rapidly being used by gastroenterologists and hepatologists, as well as majority of professional GI organizations, and hashtags such as “#MedTwitter”, “#GITwitter,” and “#LiverTwitter” have developed into popular academic forums.1 Therefore, the impact of social media in GI is multifaceted and includes its role in medical education, promoting your practice or division, finding collaborations, building your network and establishing mentors and peer-mentors, disseminating your work, and building your brand.2
What is your goal?
Gastroenterologists could have one or more of the goals mentioned above for using social media. Determining the goals for social media use a priori will allow for determining which social media platform will be appropriate for you. Therefore, it is important to understand the users of various social media platforms. In 2017, Facebook was the highest used social media platform in all age groups, whereas Instagram was most popular amongst ages 18-29 years, while Twitter was used more commonly in ages 30-59 years as compared with Instagram. If your goal is to share scientific knowledge and literature with like-minded physicians and interact with leaders in the field, then Twitter may be ideal. If you want to connect with a younger, more diverse audience, Instagram might be a good option. While many physicians may have a Facebook account, this is often reserved for personal use. Many have separated of personal and professional social media use, although they do not need to exist in silos. Defining your goal with social media use will direct you to the best platform to reach your audience.
Medical education
The use of social media especially Twitter for medical education is continuously increasing. Several leaders in the field use “Tweetorials” as a means to educate others. Tweetorials are a collective set of tweets that systematically cover a specialized topic.3 Other educational forums such as @ScopingSundays, @MondayNightIBD, @IBDClub and @GIJournal provide structured platforms for GI focused discussion.4 @MondayNightIBD is also a source for official continued medical education. Other social media educational platforms include “Liver Fellow Network” which has wide variety of educational materials pertaining to hepatology. In addition, there is continuous opportunity to engage with leaders in the field and authors of published studies and guidelines. Several endoscopy educators have dedicated YouTube channels which have endless supply of educational videos.
Networking
As mentioned above, platforms such as #GITwitter and #LiverTwitter have become popular forums for engaging and connecting with like minded colleagues. Social media provides a space to share ideas and build collaborations with colleagues working on similar projects. The concept “#Twitter2Paper” has been proposed which signifies an idea that generated on Twitter and was eventually converted to a manuscript.5
Institutional, divisional, and practice promotion
Social media is a great tool to showcase the clinical, educational and scholarship services and efforts by programs, practices or divisions. During the COVID-19 pandemic, recruitment efforts at all stages were mainly shifted to virtual platforms, and social media was an instrumental way for programs to highlight their culture and initiatives. Prospective applicants can often refer to social media to get a better understanding of what the program offers. Similarly, if a new clinical service is being provided, targeted efforts can be made to ensure that patients are aware of the available services.
Patient education and combating misinformation
Several gastroenterologists also use social media to spread awareness regarding GI diseases. Instagram, Facebook, and TikTok are effective mediums where one can reach a wider audience. It is important for gastroenterologists to provide accurate information since there is a sea of misinformation available on the internet as well. Posts regarding colonoscopy and colon cancer awareness can help alleviate myths regarding role of colonoscopy. In addition, patient advocates use social media to provide peer support to others who deal with challenges related to chronic illnesses such as inflammatory bowel disease.
Sharing your work
Sharing your work on social media can help your work reach a broader audience. Studies have shown that work shared on social media has higher altmetric scores and can also lead to increased citations.
Diversity, equity, and inclusion
Social media offers a platform where one can promote or showcase their support for causes they believe in. The hashtag “#DiversityinGI” has been instrumental in promoting causes pertaining to diversity and inclusion in GI.
Pitfalls
As gastroenterologists continue to use social media, it is important to be mindful of potential pitfalls. The most critical aspect is to always remember that no post should intentionally or unintentionally violate HIPAA. It is advisable to know your institutional and state social media policies.
Social media is beaming with knowledge, education, science and inspiration. There are endless opportunities for professional and personal growth with effective and responsible use of social media. Its never to late to join the conversation.
Dr. Bilal is an assistant professor of medicine at the University of Minnesota, Minneapolis and an advanced endoscopist in the division of gastroenterology at Minneapolis VA Medical Center. He has no relevant conflicts of interest to disclose.
References
1. Mikolajczyk AE et al. Hepatol Commun. 2020 Jul 5;4(8):1229-33.
2. Bilal M and Oxentenko AS. Am J Gastroenterol. 2020 Oct;115(10):1549-52.
3. Breu AC. N Engl J Med. 2019 Sep 19;381(12):1097-8.
4. Bilal M et al. Nat Rev Gastroenterol Hepatol. 2021 Aug;18(8):519-20.
5. Pawlak KM et al. United European Gastroenterol J. 2021 Feb;9(1):129-32.
Dear colleagues,
Most of us engage with social media, whether actively tweeting, following friends on Facebook, or discussing TikTok videos with family. Many gastroenterologists leverage social media to build their professional brand and to reach a wider audience. Others remain wary of committing a social media faux paux or worry about patient confidentiality. In this Perspectives column, Dr. Stephen Chris Pappas and Dr. Mohammad Bilal discuss the risks and benefits of social media for the practicing gastroenterologist. Dr. Pappas has a unique perspective as a gastroenterologist who is also trained as a lawyer, and Dr. Bilal speaks from a wealth of experience leading educational activities on social media. We look forward to hearing your thoughts on Twitter @AGA_GIHN and by email at [email protected].
Gyanprakash A. Ketwaroo, MD, MSc, an associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Carefully consider the plentiful risks, concerns
BY STEPHEN CHRIS PAPPAS, MD, JD, FAASLD, FACLM
Social media for gastroenterologists comes with benefits accompanied by pesky risks. The risks are pesky like a mosquito bite: An itching bite is annoying, but getting malaria is serious. Managing your unprofessional tweet to salvage your reputation is going to be annoying. Disclosing a patient's identity on social media is going to be serious; you could find yourself fired, fined, reprimanded, and without hospital privileges, as happened recently to a Rhode Island physician. I divide the risks of social media into legal risks (for example, disclosing patient identity or inadvertently creating a doctor-patient relationship), risks of compromising ethical standards (for example, impairing the doctor-patient relationship), and mixed legal/ethics risks (for example, inappropriate Twitter banter disparaging individuals, promotion of “fake news”). Fortunately, these risks are intuitive and can be mitigated by attention to some simple principles.
Disclosing a patient’s identity on social media is clearly in violation of privacy laws and other regulations. Since privacy compliance is drummed into us ad nauseum via annual compliance training, we could ask “how on earth could an inadvertent disclosure of identity occur?” We must remember that sites that are nominally termed “secure” may not be. As a general suggestion, I would regard social media of all types as open public forums with permanent postings. Even limited descriptions of a patient on social media may allow identification of the actual patient. The risk may be highest in smaller communities; in the past I assisted a small-town practitioner manage the fallout from inadvertently identifying a patient on his professional Facebook page by simply saying “I recently managed a 38-year-old pregnant woman with Crohn’s disease ...” That small amount of information allowed some members of his community to identify the specific patient. My suggestion would be to never talk about individual patients on social media. Phrase comments or questions generically; for example, “Crohn’s disease in pregnancy is managed with attention to ...”.
Another legal risk of social media engagement is to unknowingly create a patient-doctor relationship with a duty to treat, opening the door for exposure to malpractice litigation if something goes awry. A patient may interpret a social media interaction as establishing a patient-doctor relationship. While we think we know what defines a doctor-patient relationship, it’s not always clear and varies between jurisdictions. Indeed, a physician-patient relationship may not even be a necessary element of a claim for professional negligence (an issue shared with “curbside” consults). A recent court case in Minnesota ruled that a duty to care is established if “... it is reasonably foreseeable that the third party will rely on the physician’s acts and be harmed by a breach of the standard of care.” That case involved a telephone call, but you could see the standard easily morphing to apply to social media posts. Gastroenterologists should always talk about disease and treatment on social media in generic terms, preferably with appropriate caveats (for example, “Patients with cholestasis and intense itching may be treated with naloxone in selected cases after detailed assessment by a hepatologist”).
Impairing an established doctor-patient relationship by “friending” a patient on your personal Facebook risks a potential compromise of professional ethics, breaking the boundaries between profession and person for the gastroenterologist. The approach by most professional societies is that a “friend” on social media is equal to a friend in the real world; the same legal and ethical standards apply. Doctor-patient friendships may compromise objectivity, lead to preferential but not optimal therapy, and increase the risk of skirting around informed consent among other issues. Being friends on social media is discouraged, but not prohibited, by most professional societies and licensing bodies. In my opinion, that is sound advice. Over a career of more than 40 years, I have had patients who became friends, but only after I had transferred their care to another hepatologist.
More recently with escalating, aggressive, tones for social media communications, GI/hepatology practitioners must be aware of the serious risk of blurring their personal and professional online lives, particularly where Twitter is involved. The rapidity which people seem to want to reply to a tweet, the public and durable natures of a tweet, and the ability to significantly retweet and repost all spell potential disasters for the physician tweeting an inappropriate communication. Separation of personal and professional social media accounts is strongly encouraged but alone is not enough; you are never totally anonymous online. The reality is that a physician will be judged for an inappropriate communication whether it’s found on their professional or personal site. Either posting could result in reputation damage, reprimands, medical license restrictions or revocations, and litigation. Nationally, medical boards now regularly deal with disciplinary actions for inappropriate social media activity. The best preventive measures include pausing before you post, check the veracity of what you are posting, place your post in context, and assess the tone of your post and the tone of the site that you are posting to. A perfect storm for disaster is that the material is not clearly evidence based and could be construed as “fake,” you are personally emotionally charged, and the site you are posting to is a known cauldron of emotion and fake news.
In summary, social media affords benefits in a health care setting but it comes with some baggage. However, the risks of a social media presence are largely instinctive. An initial starting point is pausing to consider, “Would I say/do this in a public venue where everybody could hear/see me?” If there is any concern, don’t post. Subsequently, conduct yourself on social media with meticulous attention to protecting confidentiality, avoiding any impression of creating a doctor-patient relationship, avoiding doctor-friend relationships, being aware of key legal, institutional, and professional society guidance, separating personal and professional activities, and maintaining professionalism.
Dr. Pappas is in the GI and hepatology section of the department of medicine at Baylor College of Medicine, Houston. He has no relevant conflicts of interest to disclose.
References
Attai DJ et al. Semin Hematol. 2017 Oct; 54(4): 198-204.
Bal BS et al. Clin Orthop Relat Res. 2019 Oct; 477(10): 2204-6.
Ekrem, D et al. 20111 Jun 6. https://www.kevinmd.com/2011/06/7-tips-avoid-hipaa-violations-social-media.html
Hallenbeck J. Doctor and Friend. 2005 Jun. https://journalofethics.ama-assn.org/article/doctor-and-friend/2005-06
Moses RE et al. Am J Gastroenterol. 2014 Aug;109(8):1128-32.
Understand its multifaceted importance
BY MOHAMMAD BILAL, MD, FACP
Merriam-Webster’s dictionary defines social media as “forms of electronic communication (such as websites for social networking and microblogging) through which users create online communities to share information, ideas, personal messages, and other content.” Over the last few years, there has been an increase in use of social media by medical professionals. Whether we like it or not, social media is here to stay. Patients use social media to look up information regarding their doctors, medical practices use it to promote the services they offer, institutions share their programs and initiatives, and doctors use it for education, to engage with like-minded colleagues, collaborate, spread awareness, network, and combat medical misinformation. Social media is now rapidly being used by gastroenterologists and hepatologists, as well as majority of professional GI organizations, and hashtags such as “#MedTwitter”, “#GITwitter,” and “#LiverTwitter” have developed into popular academic forums.1 Therefore, the impact of social media in GI is multifaceted and includes its role in medical education, promoting your practice or division, finding collaborations, building your network and establishing mentors and peer-mentors, disseminating your work, and building your brand.2
What is your goal?
Gastroenterologists could have one or more of the goals mentioned above for using social media. Determining the goals for social media use a priori will allow for determining which social media platform will be appropriate for you. Therefore, it is important to understand the users of various social media platforms. In 2017, Facebook was the highest used social media platform in all age groups, whereas Instagram was most popular amongst ages 18-29 years, while Twitter was used more commonly in ages 30-59 years as compared with Instagram. If your goal is to share scientific knowledge and literature with like-minded physicians and interact with leaders in the field, then Twitter may be ideal. If you want to connect with a younger, more diverse audience, Instagram might be a good option. While many physicians may have a Facebook account, this is often reserved for personal use. Many have separated of personal and professional social media use, although they do not need to exist in silos. Defining your goal with social media use will direct you to the best platform to reach your audience.
Medical education
The use of social media especially Twitter for medical education is continuously increasing. Several leaders in the field use “Tweetorials” as a means to educate others. Tweetorials are a collective set of tweets that systematically cover a specialized topic.3 Other educational forums such as @ScopingSundays, @MondayNightIBD, @IBDClub and @GIJournal provide structured platforms for GI focused discussion.4 @MondayNightIBD is also a source for official continued medical education. Other social media educational platforms include “Liver Fellow Network” which has wide variety of educational materials pertaining to hepatology. In addition, there is continuous opportunity to engage with leaders in the field and authors of published studies and guidelines. Several endoscopy educators have dedicated YouTube channels which have endless supply of educational videos.
Networking
As mentioned above, platforms such as #GITwitter and #LiverTwitter have become popular forums for engaging and connecting with like minded colleagues. Social media provides a space to share ideas and build collaborations with colleagues working on similar projects. The concept “#Twitter2Paper” has been proposed which signifies an idea that generated on Twitter and was eventually converted to a manuscript.5
Institutional, divisional, and practice promotion
Social media is a great tool to showcase the clinical, educational and scholarship services and efforts by programs, practices or divisions. During the COVID-19 pandemic, recruitment efforts at all stages were mainly shifted to virtual platforms, and social media was an instrumental way for programs to highlight their culture and initiatives. Prospective applicants can often refer to social media to get a better understanding of what the program offers. Similarly, if a new clinical service is being provided, targeted efforts can be made to ensure that patients are aware of the available services.
Patient education and combating misinformation
Several gastroenterologists also use social media to spread awareness regarding GI diseases. Instagram, Facebook, and TikTok are effective mediums where one can reach a wider audience. It is important for gastroenterologists to provide accurate information since there is a sea of misinformation available on the internet as well. Posts regarding colonoscopy and colon cancer awareness can help alleviate myths regarding role of colonoscopy. In addition, patient advocates use social media to provide peer support to others who deal with challenges related to chronic illnesses such as inflammatory bowel disease.
Sharing your work
Sharing your work on social media can help your work reach a broader audience. Studies have shown that work shared on social media has higher altmetric scores and can also lead to increased citations.
Diversity, equity, and inclusion
Social media offers a platform where one can promote or showcase their support for causes they believe in. The hashtag “#DiversityinGI” has been instrumental in promoting causes pertaining to diversity and inclusion in GI.
Pitfalls
As gastroenterologists continue to use social media, it is important to be mindful of potential pitfalls. The most critical aspect is to always remember that no post should intentionally or unintentionally violate HIPAA. It is advisable to know your institutional and state social media policies.
Social media is beaming with knowledge, education, science and inspiration. There are endless opportunities for professional and personal growth with effective and responsible use of social media. Its never to late to join the conversation.
Dr. Bilal is an assistant professor of medicine at the University of Minnesota, Minneapolis and an advanced endoscopist in the division of gastroenterology at Minneapolis VA Medical Center. He has no relevant conflicts of interest to disclose.
References
1. Mikolajczyk AE et al. Hepatol Commun. 2020 Jul 5;4(8):1229-33.
2. Bilal M and Oxentenko AS. Am J Gastroenterol. 2020 Oct;115(10):1549-52.
3. Breu AC. N Engl J Med. 2019 Sep 19;381(12):1097-8.
4. Bilal M et al. Nat Rev Gastroenterol Hepatol. 2021 Aug;18(8):519-20.
5. Pawlak KM et al. United European Gastroenterol J. 2021 Feb;9(1):129-32.
The Ethical Implications of Dermatology Residents Treating Attending Physicians
Residents are confronted daily with situations in clinic that require a foundation in medical ethics to assist in decision-making. Attending physicians require health care services and at times may seek care from resident physicians. If the attending physician has direct oversight over the resident, however, the ethics of the resident treating them need to be addressed. Although patients have autonomy to choose whoever they want as a physician, nonmaleficence dictates that the resident may forego treatment due to concerns for providing suboptimal care; however, this same attending may be treated under specific circumstances. This column explores the ethical implications of both situations.
The Ethical Dilemma of Treating an Attending
Imagine this scenario: You are in your resident general dermatology clinic seeing patients with an attending overseeing your clinical decisions following each encounter. You look on your schedule and see that the next patient is one of your pediatric dermatology attendings for a total-body skin examination (TBSE). You have never treated a physician that oversees you, and you ponder whether you should perform the examination or fetch your attending to perform the encounter alone.
This conundrum then brings other questions to mind: Would changing the reason for the appointment (ie, an acute problem vs a TBSE) alter your decision as to whether or not you would treat this attending? Would the situation be different if this was an attending in a different department?
Ethics Curriculum for Residents
Medical providers face ethical dilemmas daily, and dermatologists and dermatology residents are not excluded. Dermatoethics can provide a framework for the best approach to this hypothetical situation. To equip residents with resources on ethics and a cognitive framework to approach similar situations, the American Board of Dermatology has created an ethics curriculum for residents to learn over their 3 years of training.1
One study that analyzed the ethical themes portrayed in essays by fourth-year medical students showed that the most common themes included autonomy, social justice, nonmaleficence, beneficence, honesty, and respect.2 These themes must be considered in different permutations throughout ethical conundrums.
In the situation of an attending physician who supervises a resident in another clinic voluntarily attending the resident clinic, the physician is aware of the resident’s skills and qualifications and knows that supervision is being provided by an attending physician, which allows informed consent to be made, as a study by Unruh et al3 shows. The patient’s autonomy allows them to choose their treating provider.
However, there are several reasons why the resident may be hesitant to enter the room. One concern may be that during a TBSE the provider usually examines the patient’s genitals, rectum, and breasts.4 Because the resident knows the individual personally, the patient and/or the provider may be uncomfortable checking these areas, leaving a portion of the examination unperformed. This neglect may harm the patient (eg, a genital melanoma is missed), violating the tenant of nonmaleficence.
The effect of the medical hierarchy also should be considered. The de facto hierarchy of attendings supervising residents, interns, and medical students, with each group having some oversight over the next, can have positive effects on education and appropriate patient management but also can prove to be detrimental to the patient and provider in some circumstances. Studies have shown that residents may be less willing to disagree with their superior’s opinions for fear of negative reactions and harmful effects on their future careers.5-7 The hierarchy of medicine also can affect a resident’s moral judgement by intimidating the practitioner to perform tasks or make diagnoses they may not wish to make.5,6,8,9 For example, the resident may send a prescription for a medication that the attending requested despite no clear indication of need. This mingling of patient and supervisor roles can result in a resident treating their attending physician inconsistently with their standard of care.
Navigating the Ethics of Treating Family Members
The American Medical Association Code of Medical Ethics Opinions on Patient-Physician Relationships highlights treating family members as an important ethical topic. Although most residents and attendings are not biologically related, a familial-style relationship exists in many dermatology programs between attendings and residents due to the close-knit nature of dermatology programs. Diagnostic and treatment accuracy may be diminished by the discomfort or disbelief that a condition could affect someone the resident cares about.10
The American Medical Association also states that a physician can treat family members in an emergency situation or for short-term minor problems. If these 2 exceptions were to be extrapolated to apply to situations involving residents and attendings in addition to family, there would be situations where a dermatology resident could ethically treat their attending physician.10 If the attending physician was worried about a problem that was deemed potentially life-threatening, such as a rapidly progressive bullous eruption concerning for Stevens-Johnson syndrome following the initiation of a new medication, and they wanted an urgent evaluation and biopsy, an ethicist could argue that urgent treatment is medically indicated as deferring treatment could have negative consequences on the patient’s health. In addition, if the attending found a splinter in their finger following yardwork and needed assistance in removal, this also could be treated by their resident, as it is minimally invasive and has a finite conclusion.
Treating Nonsupervisory Attendings
In the case of performing a TBSE on an attending from another specialty, it would be acceptable and less ethically ambiguous if no close personal relationship existed between the two practitioners, as this patient would have no direct oversight over the resident physician.
Final Thoughts
Each situation that residents face may carry ethical implications with perspectives from the patient, provider, and bystanders. The above scenarios highlight specific instances that a dermatology resident may face and provide insight into how they may approach the situations. At the same time, it is important to remember that every situation is different and requires a unique approach. Fortunately,physicians—specifically dermatologists—are provided many resources to help navigate challenging scenarios.
Acknowledgments—The author thanks Jane M. Grant-Kels, MD (Farmington, Connecticut), for reviewing this paper and providing feedback to improve its content, as well as Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and article.
- Dermatoethics. American Board of Dermatology website. Accessed August 9, 2022. https://www.abderm.org/residents-and-fellows/dermatoethics
- House JB, Theyyunni N, Barnosky AR, et al. Understanding ethical dilemmas in the emergency department: views from medical students’ essays. J Emerg Med. 2015;48:492-498.
- Unruh KP, Dhulipala SC, Holt GE. Patient understanding of the role of the orthopedic resident. J Surg Educ. 2013;70:345-349.
- Grandhi R, Grant-Kels JM. Naked and vulnerable: the ethics of chaperoning full-body skin examinations. J Am Acad Dermatol. 2017;76:1221-1223.
- Salehi PP, Jacobs D, Suhail-Sindhu T, et al. Consequences of medical hierarchy on medical students, residents, and medical education in otolaryngology. Otolaryngol Head Neck Surg. 2020;163:906-914.
- Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school: a descriptive review of student case reflections. Am J Surg. 2009;197:107-112.
- Troughton R, Mariano V, Campbell A, et al. Understanding determinants of infection control practices in surgery: the role of shared ownership and team hierarchy. Antimicrob Resist Infect Control. 2019;8:116.
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg. 2008;43:986-993.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ. 2008;42:733-741.
- Chapter 1. opinions on patient-physician relationships. American Medical Association website. Accessed on August 9, 2022. https://www.ama-assn.org/system/files/code-of-medical-ethics-chapter-1.pdf
Residents are confronted daily with situations in clinic that require a foundation in medical ethics to assist in decision-making. Attending physicians require health care services and at times may seek care from resident physicians. If the attending physician has direct oversight over the resident, however, the ethics of the resident treating them need to be addressed. Although patients have autonomy to choose whoever they want as a physician, nonmaleficence dictates that the resident may forego treatment due to concerns for providing suboptimal care; however, this same attending may be treated under specific circumstances. This column explores the ethical implications of both situations.
The Ethical Dilemma of Treating an Attending
Imagine this scenario: You are in your resident general dermatology clinic seeing patients with an attending overseeing your clinical decisions following each encounter. You look on your schedule and see that the next patient is one of your pediatric dermatology attendings for a total-body skin examination (TBSE). You have never treated a physician that oversees you, and you ponder whether you should perform the examination or fetch your attending to perform the encounter alone.
This conundrum then brings other questions to mind: Would changing the reason for the appointment (ie, an acute problem vs a TBSE) alter your decision as to whether or not you would treat this attending? Would the situation be different if this was an attending in a different department?
Ethics Curriculum for Residents
Medical providers face ethical dilemmas daily, and dermatologists and dermatology residents are not excluded. Dermatoethics can provide a framework for the best approach to this hypothetical situation. To equip residents with resources on ethics and a cognitive framework to approach similar situations, the American Board of Dermatology has created an ethics curriculum for residents to learn over their 3 years of training.1
One study that analyzed the ethical themes portrayed in essays by fourth-year medical students showed that the most common themes included autonomy, social justice, nonmaleficence, beneficence, honesty, and respect.2 These themes must be considered in different permutations throughout ethical conundrums.
In the situation of an attending physician who supervises a resident in another clinic voluntarily attending the resident clinic, the physician is aware of the resident’s skills and qualifications and knows that supervision is being provided by an attending physician, which allows informed consent to be made, as a study by Unruh et al3 shows. The patient’s autonomy allows them to choose their treating provider.
However, there are several reasons why the resident may be hesitant to enter the room. One concern may be that during a TBSE the provider usually examines the patient’s genitals, rectum, and breasts.4 Because the resident knows the individual personally, the patient and/or the provider may be uncomfortable checking these areas, leaving a portion of the examination unperformed. This neglect may harm the patient (eg, a genital melanoma is missed), violating the tenant of nonmaleficence.
The effect of the medical hierarchy also should be considered. The de facto hierarchy of attendings supervising residents, interns, and medical students, with each group having some oversight over the next, can have positive effects on education and appropriate patient management but also can prove to be detrimental to the patient and provider in some circumstances. Studies have shown that residents may be less willing to disagree with their superior’s opinions for fear of negative reactions and harmful effects on their future careers.5-7 The hierarchy of medicine also can affect a resident’s moral judgement by intimidating the practitioner to perform tasks or make diagnoses they may not wish to make.5,6,8,9 For example, the resident may send a prescription for a medication that the attending requested despite no clear indication of need. This mingling of patient and supervisor roles can result in a resident treating their attending physician inconsistently with their standard of care.
Navigating the Ethics of Treating Family Members
The American Medical Association Code of Medical Ethics Opinions on Patient-Physician Relationships highlights treating family members as an important ethical topic. Although most residents and attendings are not biologically related, a familial-style relationship exists in many dermatology programs between attendings and residents due to the close-knit nature of dermatology programs. Diagnostic and treatment accuracy may be diminished by the discomfort or disbelief that a condition could affect someone the resident cares about.10
The American Medical Association also states that a physician can treat family members in an emergency situation or for short-term minor problems. If these 2 exceptions were to be extrapolated to apply to situations involving residents and attendings in addition to family, there would be situations where a dermatology resident could ethically treat their attending physician.10 If the attending physician was worried about a problem that was deemed potentially life-threatening, such as a rapidly progressive bullous eruption concerning for Stevens-Johnson syndrome following the initiation of a new medication, and they wanted an urgent evaluation and biopsy, an ethicist could argue that urgent treatment is medically indicated as deferring treatment could have negative consequences on the patient’s health. In addition, if the attending found a splinter in their finger following yardwork and needed assistance in removal, this also could be treated by their resident, as it is minimally invasive and has a finite conclusion.
Treating Nonsupervisory Attendings
In the case of performing a TBSE on an attending from another specialty, it would be acceptable and less ethically ambiguous if no close personal relationship existed between the two practitioners, as this patient would have no direct oversight over the resident physician.
Final Thoughts
Each situation that residents face may carry ethical implications with perspectives from the patient, provider, and bystanders. The above scenarios highlight specific instances that a dermatology resident may face and provide insight into how they may approach the situations. At the same time, it is important to remember that every situation is different and requires a unique approach. Fortunately,physicians—specifically dermatologists—are provided many resources to help navigate challenging scenarios.
Acknowledgments—The author thanks Jane M. Grant-Kels, MD (Farmington, Connecticut), for reviewing this paper and providing feedback to improve its content, as well as Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and article.
Residents are confronted daily with situations in clinic that require a foundation in medical ethics to assist in decision-making. Attending physicians require health care services and at times may seek care from resident physicians. If the attending physician has direct oversight over the resident, however, the ethics of the resident treating them need to be addressed. Although patients have autonomy to choose whoever they want as a physician, nonmaleficence dictates that the resident may forego treatment due to concerns for providing suboptimal care; however, this same attending may be treated under specific circumstances. This column explores the ethical implications of both situations.
The Ethical Dilemma of Treating an Attending
Imagine this scenario: You are in your resident general dermatology clinic seeing patients with an attending overseeing your clinical decisions following each encounter. You look on your schedule and see that the next patient is one of your pediatric dermatology attendings for a total-body skin examination (TBSE). You have never treated a physician that oversees you, and you ponder whether you should perform the examination or fetch your attending to perform the encounter alone.
This conundrum then brings other questions to mind: Would changing the reason for the appointment (ie, an acute problem vs a TBSE) alter your decision as to whether or not you would treat this attending? Would the situation be different if this was an attending in a different department?
Ethics Curriculum for Residents
Medical providers face ethical dilemmas daily, and dermatologists and dermatology residents are not excluded. Dermatoethics can provide a framework for the best approach to this hypothetical situation. To equip residents with resources on ethics and a cognitive framework to approach similar situations, the American Board of Dermatology has created an ethics curriculum for residents to learn over their 3 years of training.1
One study that analyzed the ethical themes portrayed in essays by fourth-year medical students showed that the most common themes included autonomy, social justice, nonmaleficence, beneficence, honesty, and respect.2 These themes must be considered in different permutations throughout ethical conundrums.
In the situation of an attending physician who supervises a resident in another clinic voluntarily attending the resident clinic, the physician is aware of the resident’s skills and qualifications and knows that supervision is being provided by an attending physician, which allows informed consent to be made, as a study by Unruh et al3 shows. The patient’s autonomy allows them to choose their treating provider.
However, there are several reasons why the resident may be hesitant to enter the room. One concern may be that during a TBSE the provider usually examines the patient’s genitals, rectum, and breasts.4 Because the resident knows the individual personally, the patient and/or the provider may be uncomfortable checking these areas, leaving a portion of the examination unperformed. This neglect may harm the patient (eg, a genital melanoma is missed), violating the tenant of nonmaleficence.
The effect of the medical hierarchy also should be considered. The de facto hierarchy of attendings supervising residents, interns, and medical students, with each group having some oversight over the next, can have positive effects on education and appropriate patient management but also can prove to be detrimental to the patient and provider in some circumstances. Studies have shown that residents may be less willing to disagree with their superior’s opinions for fear of negative reactions and harmful effects on their future careers.5-7 The hierarchy of medicine also can affect a resident’s moral judgement by intimidating the practitioner to perform tasks or make diagnoses they may not wish to make.5,6,8,9 For example, the resident may send a prescription for a medication that the attending requested despite no clear indication of need. This mingling of patient and supervisor roles can result in a resident treating their attending physician inconsistently with their standard of care.
Navigating the Ethics of Treating Family Members
The American Medical Association Code of Medical Ethics Opinions on Patient-Physician Relationships highlights treating family members as an important ethical topic. Although most residents and attendings are not biologically related, a familial-style relationship exists in many dermatology programs between attendings and residents due to the close-knit nature of dermatology programs. Diagnostic and treatment accuracy may be diminished by the discomfort or disbelief that a condition could affect someone the resident cares about.10
The American Medical Association also states that a physician can treat family members in an emergency situation or for short-term minor problems. If these 2 exceptions were to be extrapolated to apply to situations involving residents and attendings in addition to family, there would be situations where a dermatology resident could ethically treat their attending physician.10 If the attending physician was worried about a problem that was deemed potentially life-threatening, such as a rapidly progressive bullous eruption concerning for Stevens-Johnson syndrome following the initiation of a new medication, and they wanted an urgent evaluation and biopsy, an ethicist could argue that urgent treatment is medically indicated as deferring treatment could have negative consequences on the patient’s health. In addition, if the attending found a splinter in their finger following yardwork and needed assistance in removal, this also could be treated by their resident, as it is minimally invasive and has a finite conclusion.
Treating Nonsupervisory Attendings
In the case of performing a TBSE on an attending from another specialty, it would be acceptable and less ethically ambiguous if no close personal relationship existed between the two practitioners, as this patient would have no direct oversight over the resident physician.
Final Thoughts
Each situation that residents face may carry ethical implications with perspectives from the patient, provider, and bystanders. The above scenarios highlight specific instances that a dermatology resident may face and provide insight into how they may approach the situations. At the same time, it is important to remember that every situation is different and requires a unique approach. Fortunately,physicians—specifically dermatologists—are provided many resources to help navigate challenging scenarios.
Acknowledgments—The author thanks Jane M. Grant-Kels, MD (Farmington, Connecticut), for reviewing this paper and providing feedback to improve its content, as well as Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and article.
- Dermatoethics. American Board of Dermatology website. Accessed August 9, 2022. https://www.abderm.org/residents-and-fellows/dermatoethics
- House JB, Theyyunni N, Barnosky AR, et al. Understanding ethical dilemmas in the emergency department: views from medical students’ essays. J Emerg Med. 2015;48:492-498.
- Unruh KP, Dhulipala SC, Holt GE. Patient understanding of the role of the orthopedic resident. J Surg Educ. 2013;70:345-349.
- Grandhi R, Grant-Kels JM. Naked and vulnerable: the ethics of chaperoning full-body skin examinations. J Am Acad Dermatol. 2017;76:1221-1223.
- Salehi PP, Jacobs D, Suhail-Sindhu T, et al. Consequences of medical hierarchy on medical students, residents, and medical education in otolaryngology. Otolaryngol Head Neck Surg. 2020;163:906-914.
- Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school: a descriptive review of student case reflections. Am J Surg. 2009;197:107-112.
- Troughton R, Mariano V, Campbell A, et al. Understanding determinants of infection control practices in surgery: the role of shared ownership and team hierarchy. Antimicrob Resist Infect Control. 2019;8:116.
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg. 2008;43:986-993.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ. 2008;42:733-741.
- Chapter 1. opinions on patient-physician relationships. American Medical Association website. Accessed on August 9, 2022. https://www.ama-assn.org/system/files/code-of-medical-ethics-chapter-1.pdf
- Dermatoethics. American Board of Dermatology website. Accessed August 9, 2022. https://www.abderm.org/residents-and-fellows/dermatoethics
- House JB, Theyyunni N, Barnosky AR, et al. Understanding ethical dilemmas in the emergency department: views from medical students’ essays. J Emerg Med. 2015;48:492-498.
- Unruh KP, Dhulipala SC, Holt GE. Patient understanding of the role of the orthopedic resident. J Surg Educ. 2013;70:345-349.
- Grandhi R, Grant-Kels JM. Naked and vulnerable: the ethics of chaperoning full-body skin examinations. J Am Acad Dermatol. 2017;76:1221-1223.
- Salehi PP, Jacobs D, Suhail-Sindhu T, et al. Consequences of medical hierarchy on medical students, residents, and medical education in otolaryngology. Otolaryngol Head Neck Surg. 2020;163:906-914.
- Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school: a descriptive review of student case reflections. Am J Surg. 2009;197:107-112.
- Troughton R, Mariano V, Campbell A, et al. Understanding determinants of infection control practices in surgery: the role of shared ownership and team hierarchy. Antimicrob Resist Infect Control. 2019;8:116.
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg. 2008;43:986-993.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ. 2008;42:733-741.
- Chapter 1. opinions on patient-physician relationships. American Medical Association website. Accessed on August 9, 2022. https://www.ama-assn.org/system/files/code-of-medical-ethics-chapter-1.pdf
Resident Pearls
- Dermatology residents should not perform total-body skin examinations on or provide long-term care to attending physicians that directly oversee them.
- Residents should only provide care to their attending physicians if the attending’s life is in imminent danger from delay of treatment or if it is a self-limited, minor problem.
Dermatologists and the Aging Eye: Visual Performance in Physicians
The years start coming and they don’t stop coming.
Smash Mouth, “All Star”
Dermatologists, similar to everyone else, are subject to the inevitable: aging. More than 80% of the US population develops presbyopia, an age-related reduction in visual acuity, in their lifetime. The most common cause of refractive error in adults, presbyopia can contribute to reduced professional productivity, and individuals with uncorrected presbyopia face an estimated 8-fold increase in difficulty performing demanding near-vision tasks.1
As specialists who rely heavily on visual assessment, dermatologists likely are aware of presbyopia, seeking care as appropriate; however, visual correction is not one size fits all, and identifying effective job-specific adjustments may require considerable trial and error. To this end, if visual correction may be needed by a large majority of dermatologists at some point, why do we not have specialized recommendations to guide the corrective process according to the individual’s defect and type of practice within the specialty? Do we need resources for dermatologists concerning ophthalmologic wellness and key warning signs of visual acuity deficits and other ocular complications?
These matters are difficult to address, made more so by the lack of data examining correctable visual impairment (CVI) in dermatology. The basis for discussion is clear; however, visual skills are highly relevant to the practice of dermatology, and age-related visual changes often are inevitable. This article will provide an overview of CVI in related disciplines and the importance of understanding CVI and corrective options in dermatology.
CVI Across Medical Disciplines
Other predominantly visual medical specialties such as pathology, radiology, and surgery have initiated research evaluating the impact of CVI on their respective practices, although consistent data still are limited. Much of the work surrounding CVI in medicine can be identified in surgery and its subspecialties. A 2020 study by Tuna et al2 found that uncorrected myopia with greater than 1.75 diopter, hyperopia regardless of grade, and presbyopia with greater than 1.25 diopter correlated with reduced surgical performance when using the Da Vinci robotic system. A 2002 report by Wanzel et al3 was among the first of many studies to demonstrate the importance of visuospatial ability in surgical success. In radiology, Krupinski et al4 demonstrated reduced accuracy in detecting pulmonary nodules that correlated with increased myopia and decreased accommodation secondary to visual strain.
Most reports examining CVI across medical disciplines are primarily conversational or observational, with some utilizing surveys to assess the prevalence of CVI and the opinions of physicians in the field. For example, in a survey of 93 pathologists in Turkey, 93.5% (87/93) reported at least 1 type of refractive error. Eyeglasses were the most common form of correction (64.5% [60/93]); of those, 33.3% (31/93) reported using eyeglasses during microscopy.5
The importance of visual ability in other highly visual specialties suggests that parallels can be drawn to similar practices in dermatology. Detection of cutaneous lesions might be affected by changes in vision, similar to detection of pulmonary lesions in radiology. Likewise, dermatologic surgeons might experience a similar reduction in surgical performance due to impaired visual acuity or visuospatial ability.
The Importance of Visual Performancein Dermatology
With presbyopia often becoming clinically apparent at approximately 40 years of age,1,6 CVI has the potential to be present for much of a dermatologist’s career. Responsibility falls on the individual practitioner to recognize their visual deficit and seek appropriate optometric or ophthalmologic care. It should be emphasized that there are many effective avenues to correct refractive error, most of which can functionally restore an individual’s vision; however, each option prioritizes different visual attributes (eg, contrast, depth perception, clarity) that have varying degrees of importance in particular areas of dermatologic practice. For example, in addition to visual acuity, dermatologic surgeons might require optimized depth perception, whereas dermatologists performing detailed visual inspection or dermoscopy might instead require optimized contrast sensitivity and acuity. At present, the literature is silent on guiding dermatologists in selecting corrective approaches that enhance the visual characteristics most important for their practice. Lack of research and direction surrounding which visual correction techniques are best suited for individual tasks risks inaccurate and nonspecific conversations with our eye care providers. Focused educated dialogues about visual needs would streamline the process of finding appropriate correction, thereby reducing unnecessary trial and error. As each dermatologic subspecialty might require a unique subset of visual skills, the conceivable benefit of dermatology-specific visual correction resources is evident.
Additionally (although beyond the scope of this commentary), guidance on how a dermatologist should increase their awareness and approach to more serious ophthalmologic conditions—including retinal tear or detachment, age-related macular degeneration, and glaucoma—also would serve as a valuable resource. Overall, prompt identification of visual changes and educated discussions surrounding their correction would allow for optimization based on the required skill set and would improve overall outcomes.
Final Thoughts
Age-related visual changes are a highly prevalent and normal process that carry the potential to impact clinical practice. Fortunately, there are multiple corrective mechanisms that can functionally restore an individual’s eyesight. However, there are no resources to guide dermatologists in seeking specialty-specific correction centered on their daily tasks, which places the responsibility for such correction on the individual. This is a circumstance in which the task at hand is clear, yet we continue to individually reinvent the wheel. We should consider this an opportunity to work together with our optometry and ophthalmology colleagues to create centralized resources that assist dermatologists in navigating age-related visual changes.
Acknowledgments—The authors thank Delaney Stratton, DNP, FNP-BC (Tucson, Arizona); J. Daniel Twelker, OD, PhD (Tucson, Arizona); and Julia Freeman, MD (Pittsburgh, Pennsylvania), for their contributions to the manuscript, as well as Susan M. Swetter, MD (Palo Alto, California) for reviewing and providing feedback.
- Berdahl J, Bala C, Dhariwal M, et al. Patient and economic burden of presbyopia: a systematic literature review. Clin Ophthalmol. 2020;14:3439-3450. doi:10.2147/OPTH.S269597
- Tuna MB, Kilavuzoglu AE, Mourmouris P, et al. Impact of refractive errors on Da Vinci SI robotic system. JSLS. 2020;24:e2020.00031. doi:10.4293/JSLS.2020.00031
- Wanzel KR, Hamstra SJ, Anastakis DJ, et al. Effect of visual-spatial ability on learning of spatially-complex surgical skills. Lancet. 2002;359:230-231. doi:10.1016/S0140-6736(02)07441-X
- Krupinski EA, Berbaum KS, Caldwell RT, et al. Do long radiology workdays affect nodule detection in dynamic CT interpretation? J Am Coll Radiol. 2012;9:191-198. doi:10.1016/j.jacr.2011.11.013
- Akman O, Kösemehmetog˘lu K. Ocular diseases among pathologists and pathologists’ perceptions on ocular diseases: a survey study. Turk Patoloji Derg. 2015;31:194-199. doi:10.5146/tjpath.2015.01326
- Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111-1119. doi:10.1001/archopht.126.8.1111
The years start coming and they don’t stop coming.
Smash Mouth, “All Star”
Dermatologists, similar to everyone else, are subject to the inevitable: aging. More than 80% of the US population develops presbyopia, an age-related reduction in visual acuity, in their lifetime. The most common cause of refractive error in adults, presbyopia can contribute to reduced professional productivity, and individuals with uncorrected presbyopia face an estimated 8-fold increase in difficulty performing demanding near-vision tasks.1
As specialists who rely heavily on visual assessment, dermatologists likely are aware of presbyopia, seeking care as appropriate; however, visual correction is not one size fits all, and identifying effective job-specific adjustments may require considerable trial and error. To this end, if visual correction may be needed by a large majority of dermatologists at some point, why do we not have specialized recommendations to guide the corrective process according to the individual’s defect and type of practice within the specialty? Do we need resources for dermatologists concerning ophthalmologic wellness and key warning signs of visual acuity deficits and other ocular complications?
These matters are difficult to address, made more so by the lack of data examining correctable visual impairment (CVI) in dermatology. The basis for discussion is clear; however, visual skills are highly relevant to the practice of dermatology, and age-related visual changes often are inevitable. This article will provide an overview of CVI in related disciplines and the importance of understanding CVI and corrective options in dermatology.
CVI Across Medical Disciplines
Other predominantly visual medical specialties such as pathology, radiology, and surgery have initiated research evaluating the impact of CVI on their respective practices, although consistent data still are limited. Much of the work surrounding CVI in medicine can be identified in surgery and its subspecialties. A 2020 study by Tuna et al2 found that uncorrected myopia with greater than 1.75 diopter, hyperopia regardless of grade, and presbyopia with greater than 1.25 diopter correlated with reduced surgical performance when using the Da Vinci robotic system. A 2002 report by Wanzel et al3 was among the first of many studies to demonstrate the importance of visuospatial ability in surgical success. In radiology, Krupinski et al4 demonstrated reduced accuracy in detecting pulmonary nodules that correlated with increased myopia and decreased accommodation secondary to visual strain.
Most reports examining CVI across medical disciplines are primarily conversational or observational, with some utilizing surveys to assess the prevalence of CVI and the opinions of physicians in the field. For example, in a survey of 93 pathologists in Turkey, 93.5% (87/93) reported at least 1 type of refractive error. Eyeglasses were the most common form of correction (64.5% [60/93]); of those, 33.3% (31/93) reported using eyeglasses during microscopy.5
The importance of visual ability in other highly visual specialties suggests that parallels can be drawn to similar practices in dermatology. Detection of cutaneous lesions might be affected by changes in vision, similar to detection of pulmonary lesions in radiology. Likewise, dermatologic surgeons might experience a similar reduction in surgical performance due to impaired visual acuity or visuospatial ability.
The Importance of Visual Performancein Dermatology
With presbyopia often becoming clinically apparent at approximately 40 years of age,1,6 CVI has the potential to be present for much of a dermatologist’s career. Responsibility falls on the individual practitioner to recognize their visual deficit and seek appropriate optometric or ophthalmologic care. It should be emphasized that there are many effective avenues to correct refractive error, most of which can functionally restore an individual’s vision; however, each option prioritizes different visual attributes (eg, contrast, depth perception, clarity) that have varying degrees of importance in particular areas of dermatologic practice. For example, in addition to visual acuity, dermatologic surgeons might require optimized depth perception, whereas dermatologists performing detailed visual inspection or dermoscopy might instead require optimized contrast sensitivity and acuity. At present, the literature is silent on guiding dermatologists in selecting corrective approaches that enhance the visual characteristics most important for their practice. Lack of research and direction surrounding which visual correction techniques are best suited for individual tasks risks inaccurate and nonspecific conversations with our eye care providers. Focused educated dialogues about visual needs would streamline the process of finding appropriate correction, thereby reducing unnecessary trial and error. As each dermatologic subspecialty might require a unique subset of visual skills, the conceivable benefit of dermatology-specific visual correction resources is evident.
Additionally (although beyond the scope of this commentary), guidance on how a dermatologist should increase their awareness and approach to more serious ophthalmologic conditions—including retinal tear or detachment, age-related macular degeneration, and glaucoma—also would serve as a valuable resource. Overall, prompt identification of visual changes and educated discussions surrounding their correction would allow for optimization based on the required skill set and would improve overall outcomes.
Final Thoughts
Age-related visual changes are a highly prevalent and normal process that carry the potential to impact clinical practice. Fortunately, there are multiple corrective mechanisms that can functionally restore an individual’s eyesight. However, there are no resources to guide dermatologists in seeking specialty-specific correction centered on their daily tasks, which places the responsibility for such correction on the individual. This is a circumstance in which the task at hand is clear, yet we continue to individually reinvent the wheel. We should consider this an opportunity to work together with our optometry and ophthalmology colleagues to create centralized resources that assist dermatologists in navigating age-related visual changes.
Acknowledgments—The authors thank Delaney Stratton, DNP, FNP-BC (Tucson, Arizona); J. Daniel Twelker, OD, PhD (Tucson, Arizona); and Julia Freeman, MD (Pittsburgh, Pennsylvania), for their contributions to the manuscript, as well as Susan M. Swetter, MD (Palo Alto, California) for reviewing and providing feedback.
The years start coming and they don’t stop coming.
Smash Mouth, “All Star”
Dermatologists, similar to everyone else, are subject to the inevitable: aging. More than 80% of the US population develops presbyopia, an age-related reduction in visual acuity, in their lifetime. The most common cause of refractive error in adults, presbyopia can contribute to reduced professional productivity, and individuals with uncorrected presbyopia face an estimated 8-fold increase in difficulty performing demanding near-vision tasks.1
As specialists who rely heavily on visual assessment, dermatologists likely are aware of presbyopia, seeking care as appropriate; however, visual correction is not one size fits all, and identifying effective job-specific adjustments may require considerable trial and error. To this end, if visual correction may be needed by a large majority of dermatologists at some point, why do we not have specialized recommendations to guide the corrective process according to the individual’s defect and type of practice within the specialty? Do we need resources for dermatologists concerning ophthalmologic wellness and key warning signs of visual acuity deficits and other ocular complications?
These matters are difficult to address, made more so by the lack of data examining correctable visual impairment (CVI) in dermatology. The basis for discussion is clear; however, visual skills are highly relevant to the practice of dermatology, and age-related visual changes often are inevitable. This article will provide an overview of CVI in related disciplines and the importance of understanding CVI and corrective options in dermatology.
CVI Across Medical Disciplines
Other predominantly visual medical specialties such as pathology, radiology, and surgery have initiated research evaluating the impact of CVI on their respective practices, although consistent data still are limited. Much of the work surrounding CVI in medicine can be identified in surgery and its subspecialties. A 2020 study by Tuna et al2 found that uncorrected myopia with greater than 1.75 diopter, hyperopia regardless of grade, and presbyopia with greater than 1.25 diopter correlated with reduced surgical performance when using the Da Vinci robotic system. A 2002 report by Wanzel et al3 was among the first of many studies to demonstrate the importance of visuospatial ability in surgical success. In radiology, Krupinski et al4 demonstrated reduced accuracy in detecting pulmonary nodules that correlated with increased myopia and decreased accommodation secondary to visual strain.
Most reports examining CVI across medical disciplines are primarily conversational or observational, with some utilizing surveys to assess the prevalence of CVI and the opinions of physicians in the field. For example, in a survey of 93 pathologists in Turkey, 93.5% (87/93) reported at least 1 type of refractive error. Eyeglasses were the most common form of correction (64.5% [60/93]); of those, 33.3% (31/93) reported using eyeglasses during microscopy.5
The importance of visual ability in other highly visual specialties suggests that parallels can be drawn to similar practices in dermatology. Detection of cutaneous lesions might be affected by changes in vision, similar to detection of pulmonary lesions in radiology. Likewise, dermatologic surgeons might experience a similar reduction in surgical performance due to impaired visual acuity or visuospatial ability.
The Importance of Visual Performancein Dermatology
With presbyopia often becoming clinically apparent at approximately 40 years of age,1,6 CVI has the potential to be present for much of a dermatologist’s career. Responsibility falls on the individual practitioner to recognize their visual deficit and seek appropriate optometric or ophthalmologic care. It should be emphasized that there are many effective avenues to correct refractive error, most of which can functionally restore an individual’s vision; however, each option prioritizes different visual attributes (eg, contrast, depth perception, clarity) that have varying degrees of importance in particular areas of dermatologic practice. For example, in addition to visual acuity, dermatologic surgeons might require optimized depth perception, whereas dermatologists performing detailed visual inspection or dermoscopy might instead require optimized contrast sensitivity and acuity. At present, the literature is silent on guiding dermatologists in selecting corrective approaches that enhance the visual characteristics most important for their practice. Lack of research and direction surrounding which visual correction techniques are best suited for individual tasks risks inaccurate and nonspecific conversations with our eye care providers. Focused educated dialogues about visual needs would streamline the process of finding appropriate correction, thereby reducing unnecessary trial and error. As each dermatologic subspecialty might require a unique subset of visual skills, the conceivable benefit of dermatology-specific visual correction resources is evident.
Additionally (although beyond the scope of this commentary), guidance on how a dermatologist should increase their awareness and approach to more serious ophthalmologic conditions—including retinal tear or detachment, age-related macular degeneration, and glaucoma—also would serve as a valuable resource. Overall, prompt identification of visual changes and educated discussions surrounding their correction would allow for optimization based on the required skill set and would improve overall outcomes.
Final Thoughts
Age-related visual changes are a highly prevalent and normal process that carry the potential to impact clinical practice. Fortunately, there are multiple corrective mechanisms that can functionally restore an individual’s eyesight. However, there are no resources to guide dermatologists in seeking specialty-specific correction centered on their daily tasks, which places the responsibility for such correction on the individual. This is a circumstance in which the task at hand is clear, yet we continue to individually reinvent the wheel. We should consider this an opportunity to work together with our optometry and ophthalmology colleagues to create centralized resources that assist dermatologists in navigating age-related visual changes.
Acknowledgments—The authors thank Delaney Stratton, DNP, FNP-BC (Tucson, Arizona); J. Daniel Twelker, OD, PhD (Tucson, Arizona); and Julia Freeman, MD (Pittsburgh, Pennsylvania), for their contributions to the manuscript, as well as Susan M. Swetter, MD (Palo Alto, California) for reviewing and providing feedback.
- Berdahl J, Bala C, Dhariwal M, et al. Patient and economic burden of presbyopia: a systematic literature review. Clin Ophthalmol. 2020;14:3439-3450. doi:10.2147/OPTH.S269597
- Tuna MB, Kilavuzoglu AE, Mourmouris P, et al. Impact of refractive errors on Da Vinci SI robotic system. JSLS. 2020;24:e2020.00031. doi:10.4293/JSLS.2020.00031
- Wanzel KR, Hamstra SJ, Anastakis DJ, et al. Effect of visual-spatial ability on learning of spatially-complex surgical skills. Lancet. 2002;359:230-231. doi:10.1016/S0140-6736(02)07441-X
- Krupinski EA, Berbaum KS, Caldwell RT, et al. Do long radiology workdays affect nodule detection in dynamic CT interpretation? J Am Coll Radiol. 2012;9:191-198. doi:10.1016/j.jacr.2011.11.013
- Akman O, Kösemehmetog˘lu K. Ocular diseases among pathologists and pathologists’ perceptions on ocular diseases: a survey study. Turk Patoloji Derg. 2015;31:194-199. doi:10.5146/tjpath.2015.01326
- Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111-1119. doi:10.1001/archopht.126.8.1111
- Berdahl J, Bala C, Dhariwal M, et al. Patient and economic burden of presbyopia: a systematic literature review. Clin Ophthalmol. 2020;14:3439-3450. doi:10.2147/OPTH.S269597
- Tuna MB, Kilavuzoglu AE, Mourmouris P, et al. Impact of refractive errors on Da Vinci SI robotic system. JSLS. 2020;24:e2020.00031. doi:10.4293/JSLS.2020.00031
- Wanzel KR, Hamstra SJ, Anastakis DJ, et al. Effect of visual-spatial ability on learning of spatially-complex surgical skills. Lancet. 2002;359:230-231. doi:10.1016/S0140-6736(02)07441-X
- Krupinski EA, Berbaum KS, Caldwell RT, et al. Do long radiology workdays affect nodule detection in dynamic CT interpretation? J Am Coll Radiol. 2012;9:191-198. doi:10.1016/j.jacr.2011.11.013
- Akman O, Kösemehmetog˘lu K. Ocular diseases among pathologists and pathologists’ perceptions on ocular diseases: a survey study. Turk Patoloji Derg. 2015;31:194-199. doi:10.5146/tjpath.2015.01326
- Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111-1119. doi:10.1001/archopht.126.8.1111
Practice Points
- With presbyopia becoming clinically apparent starting at 40 years of age, dermatologists should be vigilant for correctable visual impairment.
- Although many corrective options exist, more research is needed to understand whether dermatologic subspecialties are better suited to specific options.
- As a specialty, we should consider standardized visual correction guidance.
Which state had the lowest primary cesarean delivery rate (15.5%) in 2021?
[polldaddy:11183184]
[polldaddy:11183184]
[polldaddy:11183184]
‘Medical Methuselahs’: Treating the growing population of centenarians
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.








