User login
COVID-SAFE: Strategies for safeguarding your outpatient clinical practice against COVID-19
No question, the COVID-19 pandemic has been a challenging time for medical practices across the United States. Uncertainty remains regarding bringing patients and services back into our offices. One factor that distinguishes many ObGyn practices from other specialties is that our practices have remained open—in some form—since the beginning of the pandemic. In various parts of the country, gynecologic surgeries and routine office visits have been significantly reduced; however, deliveries and gynecologic emergencies have continued.
In this article, I suggest a framework of strategies and resources to provide insight for outpatient operations. Individual practices will vary across the nation depending on local conditions. Full practice capacity may take on a different look than it had prior to the pandemic, and there is opportunity to change the way we operate.
Strategy 1: Consult regulatory requirements frequently
As the local status of COVID-19 evolves quickly, it is essential to examine the frequently updated recommendations from regulatory agencies at the federal, state, and local levels. Clinical practices that function within health systems need to demonstrate alignment with hospital or university policies and procedures. The Centers for Disease Control and Prevention (CDC), Occupational Safety and Health Administration (OSHA), Centers for Medicare and Medicaid Services (CMS), and individual state departments of health provide dynamic resources that are easily accessible online.1-3
The American College of Obstetricians and Gynecologists (ACOG) continues to be an excellent medical society resource.4 Subspecialty organizations that provide up-to-date guidance include the Society for Maternal-Fetal Medicine (SMFM), Society of Gynecologic Surgeons (SGS), AAGL (American Association of Gynecologic Laparoscopists), American Society for Reproductive Medicine (ASRM), and Society of Gynecologic Oncology (SGO).5-9 These resources are updated as more information about COVID-19 emerges, and they may be modified to different local-regional conditions.
The professional liability insurance carrier is an important source of insight for a number of circumstances, including modifications to your office practice, such as returning to full-scope or part-time practice; operating outside normal clinical service arrangements (for example, assisting with emergency care); offering telehealth services; and adding extra hours or employees to accommodate the patient backlog. Business insurance coverage is a separate issue to consider. Reviewing the practice policy may protect your business from COVID-related liabilities.
Consulting with legal counselors can be helpful. They can assist with navigating various practice and personnel COVID-related changes, as well as developing a viable plan for patients who were previously insured pre–COVID-19 who are currently uninsured.
Continue to: Strategy 2: Reimagine schedule capacity...
Strategy 2: Reimagine schedule capacity
The waxing and waning of the COVID-19 crisis presents an opportunity to evaluate our office practices and make necessary and positive changes. The question becomes, do we operate our practices as usual or do we rethink our strategy for seeing patients and integrate lessons learned from the pandemic? Patients are deciding when they are comfortable to schedule elective surgeries and routine office encounters. This gives us the chance to break from the tradition of 100% in-person visits and change the way we care for women.
The coronavirus has accelerated the rise of telehealth/telemedicine and is, perhaps, a silver lining of the pandemic. Telehealth is a valuable tool for accessing health services when in-person visits are not possible. Evaluating and triaging patients for in-person versus telehealth visits is now a viable option for clinical practice and reduces exposure to COVID-19 infection.
Telemedicine is convenient, and clinicians can use it to counsel and screen for various health issues as well as to extend their reach to rural communities. Appropriate consent should be documented in the patient chart. As some areas continue to be without adequate access to WiFi, telephone contact also is currently acceptable. Telehealth does not replace the in-person visit but can be viewed as a complementary and supplementary service.
Consider a balance between telehealth and in-person visits by evaluating which visits can continue remotely and which can alternate with in-person visits. This offers tremendous flexibility and will expand delivery of essential health care to patients.10 Integrating telemedicine into clinical practice provides an additional benefit: It minimizes the exposure and transmission of COVID-19 to health care workers and patients and preserves supplies, including personal protective equipment (PPE).
Prioritize the backlog of patients who require follow-up testing, procedures, and surgeries. Communicate with patients that it is safe to be seen and important to not avoid routine and preventative visits that might reveal concerns or conditions that require treatment.
Strategy 3: Institute infection prevention and control measures
The importance of instituting and ensuring safety measures for office personnel and patients cannot be underestimated. Recently, a study from King’s College in London found that frontline health care workers with PPE still have 3 to 4 times the risk of contracting coronavirus compared with the general public.11 Health care systems should ensure adequate PPE availability and develop additional strategies to protect health care workers from COVID-19. We have to be fanatical about cleanliness and PPE. We have to be diligent about how we space ourselves and our patients. Consider adjusting workflows to ensure that visits can be conducted as quickly and safely as possible.
Communicating updated safety plans and processes are invaluable for both patients and health care workers. Patients want to be reassured that safety precautions are in place to keep the environment safe and clean. Additionally, privacy and confidentiality concerns should be addressed.
Consider a modified office schedule that can reduce the number of people in the office, person-to-person contact, and COVID-19 transmission. Social distancing is improved and PPE and other supplies are preserved.
Continue to: Employees can work on alternating days...
- Employees can work on alternating days or during different parts of the day.
- Administrative staff who do not need to be physically present in the office might work remotely.
- Expanding office hours (early morning, evening, and weekends) spreads patient visits throughout the day and minimizes high-volume in-person visits.
Institute a daily COVID-19 symptom attestation and temperature check for employees on arrival at work.
Health care personnel with symptoms of COVID-19 should be prioritized for SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) RNA testing with an approved nucleic acid or antigen detection assay. A negative result indicates that the person most likely did not have an active SARS-CoV-2 infection at the time the sample was collected. A second test for SARS-CoV-2 RNA may be performed at the discretion of the evaluating health care provider, particularly when a higher level of clinical suspicion for infection exists.
The return to work decision should be determined by an agreed on symptom-based approach to clearance. If needed on a case-by-case basis, a review can be performed with the individual’s health care provider.12
Require universal masking and appropriate protective equipment.
- All staff members, patients, and visitors must wear masks correctly in the facilities (except children under age 2).
- All clinical staff members must wear masks correctly and eye protection during every patient encounter.
Reconfigure the waiting room and patient flow.
- Configure waiting room furniture to reinforce 6 feet of physical distancing.
- Remove all books, magazines, and toys from all waiting areas.
- Laminate signage for display.
- Install plexiglass at the check-in desk to minimize virus transmission.
- If possible, ask patients to wait in their car until their appointment time or to go directly to their exam room on arrival if it is available.
- Implement virtual check-in and check-out so that patients reduce unnecessary contact with surfaces and staff.
- Limit a high volume of patients to maintain social distancing etiquette, avoid delays, and allow adequate cleaning time between patients.
- Permit visitors to accompany adult patients to their ambulatory appointments only if special assistance is required.
- Limit the number of staff members in the exam and treatment rooms and maintain at least 6 feet between people except during medical care activities.
- Consider patient flow in a one-way traffic pattern.
Focus on keeping the clinical practice clean. (Follow the instructions and disinfect with a registered disinfectant product that meets the US Environmental Protection Agency criteria for use against COVID-19.13)
- Clean waiting rooms and restrooms frequently.
- Coordinate patient appointments to allow for infection control measures.
- Frequently clean high-touch surfaces, including tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
- Clinicians and all medical staff members should wash their hands before and after interacting with patients.
- Clean and disinfect the exam and treatment rooms before and after each patient.
- Use products that are effective against a range of organisms and viruses, including the coronavirus that causes COVID-19.
- Place signs indicating that rooms have been cleaned; this will assure and comfort patients. Take credit for your infection control processes.
Keep abreast of isolation and precaution guidelines. Based on data available at the time of this article’s publication, the CDC recommends ending isolation and transmission-based precautions for most people with COVID-19 using a symptom-based strategy.14 This limits unnecessary prolonged isolation and use of laboratory testing resources.
Generally, repeat SARS-CoV-2 polymerase chain reaction (PCR) testing is not recommended for “COVID-19 recovered” patients. Specifically, those patients with a prior positive SARS-CoV-2 PCR test result and who have met criteria for isolation discontinuation do not need a follow-up PCR test. A test-based strategy to discontinue isolation and transmission-based precautions is required only for severely immunocompromised patients.15
Prepare for a future COVID-19 surge and review your emergency plan and responses and revise as needed. Review handling of the current pandemic and best practices plus areas of improvement.
Symptom-based criteria for discontinuing transmission-based precautions include the following:
Patients with mild to moderate illness, not severely immunocompromised:
- at least 10 days have passed since symptoms first appeared and
- at least 24 hours have passed since last fever without fever-reducing medications and
- symptoms (cough, shortness of breath) have improved.
Note: For patients who are not severely immunocompromised and are asymptomatic throughout their infection, transmission-based precautions may be discontinued when at least 10 days have passed since the date of their first positive viral diagnostic test.
Patients with severe to critical illness, severely immunocompromised:
- at least 20 days have passed since symptoms first appeared and
- at least 24 hours have passed since last fever without fever-reducing medications and
- symptoms (cough, shortness of breath) have improved.
Note: For patients who are severely immunocompromised and are asymptomatic throughout their infection, transmission-based precautions may be discontinued when at least 20 days have passed since the date of their first positive viral diagnostic test.
Continue to: Strategy 4: Implement frequent employee communication and care...
Strategy 4: Implement frequent employee communication and care
The safety and well-being of our health care workers and patients in our clinical practices is paramount. Continuing to communicate this message and developing and sharing a plan may ameliorate the obvious toll on mental and emotional well-being. Frequent and effective communication with your clinical team is vital to reinforce policies and protocols, eliminate silos, and reduce errors.
Practice communication and care with these approaches:
- Offer regular employee COVID-19 testing.
- Re-educate staff about infection control protocols to ensure buy-in.
- Communicate with staff about the plan to address staffing shortages.
- Implement regular employee team huddles that can address accomplishments, challenges, areas for improvement, and top priorities.
- Perform regular celebrations for staff appreciation.
- Address mental health and chronic stress and offer empathy and coping resources and services to staff and clinicians. This will have a valuable, long-term benefit.
Patient communication. As the COVID-19 pandemic continues and stay-at-home policies are in place, patients should be encouraged to seek medical care if they are ill or have acute or chronic conditions. Communicate regularly with patients and let them know that their safety and well-being is the top priority. Prior to in-person visits, inform them of the safety processes that are in place to protect them.
Fostering an honest clinician-patient relationship enhances communication. Despite these efforts, some patients may not be forthcoming about their COVID-19 symptoms, illness, exposure, or travel. Health care staff can be encouraged to set a tone of tolerance and compassion and treat everyone with universal precautions.
Rising to the challenges
During the coronavirus pandemic, ObGyns continue to safely care for pregnant women and also triage and treat women who require timely office care as well as emergency and cancer-related surgeries.
The COVID-19 environment rapidly changes depending on the practice location. The strategies described represent a compilation of resources from key organizations that hopefully will prove useful and can be shaped to fit your practice. Local and regional recommendations vary, and no one can predict the course of the virus.
Consider reviewing your contingency plans regularly. As we have learned over the last several months, there is a science to maintaining a COVID-SAFE environment.
Practice operations likely will change to adapt to new conditions. The pandemic has challenged us to evolve, and we have responded with new capabilities and resilience while we continue to deliver superior and compassionate care for women.
For additional strategies on how to safeguard your practice against COVID-19, see the box below. ●
Continue to: Additional strategies on how to safeguard your practice against COVID-19...
Strategy 5: Develop a resource plan for practice operations
Assess financial solvency. Because of the mitigation measures taken during the pandemic, physician practices of all sizes are facing financial hardships and instability. As the pandemic progresses, physicians in private practice and those employed by health systems may benefit from existing resources and pandemic relief to help navigate COVID-related challenges.
Frequent revision of your financial plan may safeguard cash flow in the event of fewer patient visits and elective surgeries. Many medical organizations, including ACOG, are advocating for financial relief, fair reimbursement for telehealth and in-person visits, and access to adequate PPE. ACOG provides updated information on practice management.1
The American Medical Association (AMA) has created resources for physician practices to assist in staying focused on business and financial operations. The AMA has provided a summary of the Health, Economic Assistance, Liability Protection and Schools Act (HEALS Act).2 This is the next proposed coronavirus relief fund package, which includes provisions that benefit physicians and physician practices.
Create a plan. Review available resources and establish processes to optimize your practice capacity during the ongoing COVID-19 pandemic. Develop a game plan for patient care with a phased approach to identify and address challenges. This planning will allow your practice to pivot in response to changing local COVID-19 conditions to help you anticipate and prepare for a future surge. Maintain and revise plans as the pandemic shifts. Thinking ahead avoids the need to navigate issues in real time. Communicating clearly and often with all members of the office staff and patients lets everyone know that their safety is the main priority.
Assess staffing for flexible coverage. Frequent needs assessment helps to determine the number of staff needed to maintain a safe work environment for the patient volume.
Staff shortages may occur because of COVID-19 exposure, personal or family member illness, or childcare constraints due to daycare or school availability. Staff readiness includes evaluating individual availability and willingness.
Staff members with health issues, including comorbidities and chronic medical conditions, may not be comfortable working. Nonclinical staff members with health concerns could work remotely, although some may not be able to work from home due to technology-related issues such as WiFi deficiencies.
The CDC has interim guidelines to assist employers with providing a safe workplace and employees with making the best health decisions for themselves and their families.3,4 The US Office of Personnel Management provides guidance for COVID-19–related leave and benefits for federal employees.5
To mitigate staff shortages, approaches include adjusting schedules, cross-training to perform the tasks of other positions, and hiring additional personnel. A needs assessment can help determine if existing personnel could be cross-trained for other purposes or if additional staff should be hired. Understanding the minimum number of staff required for safe and effective patient care will assist in planning for shortages as the pandemic progresses. Understanding the availability of external resources could be a critical part of an office contingency plan.6
Proactively manage your supply chain. The pandemic has caused global supply shortages. Solid supply chain management is crucial for practice operations. Take inventory of your PPE and various supplies and place orders in advance. Analyze cash flow and connect with vendors as well as local and state health agencies to understand available resources. Given ongoing PPE shortages, practices should consider preserving PPE and employ appropriate strategies for optimizing supplies of face masks.7
Certain medications and vaccines administered in the office setting may be outdated and need to be replaced. Office equipment that has not been used for several months will need to be tested. For equipment used in office electrosurgery procedures, certain safety measures can be taken to reduce the transmission of aerosolized viral particles to the health care team. While currently the risk is theoretical and more research is needed, this potential risk should be mitigated.8 Assessing availability of hospital and ambulance or transport services also is recommended as these may change depending on the local COVID-19 status.
Strategy 6: Establish and refine the patient screening process
Patients want reassurance that the health care environment is safe and that their well-being is a priority. In advance of a patient’s visit, relieve any anxiety by explaining the COVID-SAFE measures that your practice has taken.
For employee use, consider telephone and in-person scripting to ensure consistent messaging for patients.
Prescreening. At the time of appointment scheduling and on the day prior to the scheduled appointment, all patients should be screened for symptoms of COVID-19,9 fever, exposure within 14 days to someone newly diagnosed with COVID-19, and travel within 14 days from a foreign country or from a US state with a quarantine requirement.
Patients who screen positive for symptoms, exposure, or travel should be referred to a clinician. If possible, asymptomatic patients who report exposure or travel should have their in-person visit deferred until after the required 14-day quarantine.
Consider restricting visitors from accompanying adult patients to their appointment unless they are required for special assistance.
Arrival screening. At the time of presentation for the appointment, all patients and any accompanying visitors should be rescreened. The optimal location for arrival screening should be determined by the local operations team and the infection prevention and control program.
At presentation, all patients and visitors should appropriately don a surgical mask or other face covering. Patients and visitors should have their temperature checked on arrival. Patients who screen positive for symptoms, exposure to COVID-19, and/or travel should be referred to a clinician or the visit deferred and a telehealth visit considered.
Visitors who screen positive for symptoms, fever, or exposure to COVID-19 are not permitted to accompany the patient. Asymptomatic parents or guardians of pediatric patients may serve as support persons.
References
- American College of Obstetricians and Gynecologists. Financial support for physicians and practices during the COVID-19 pandemic. https://www.acog.org/practice -management/coding/coding-library/financial-support-for-physicians-and-practices-during-the-covid-19-pandemic. Accessed July 23, 2020.
- American Medical Association. HEALS Act: What physicians and medical students need to know. https://www.ama-assn.org/delivering-care/public-health/heals-act -what-physicians-and-medical-students-need-know. Accessed July 29, 2020.
- Centers for Disease Control and Prevention. Interim guidance for businesses and employers responding to coronavirus disease 2019 (COVID-19). https://www.cdc.gov /coronavirus/2019-ncov/community/guidance-business-response.html. Accessed July 12, 2020.
- Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with SARS-CoV-2 infection (interim guidance). https://www.cdc.gov /coronavirus/2019-ncov/hcp/return-to-work.html. Accessed July 20, 2020.
- US Office of Personnel Management. Questions and answers on human resources flexibilities and authorities for coronavirus disease 2019 (COVID-19). https://www .opm.gov/policy-data-oversight/covid-19/questions-and-answers-on-human-resources-flexibilities-and-authorities-for-coronavirus-disease-2019-covid-19.pdf. Accessed July 3, 2020.
- Centers for Disease Control and Prevention. Strategies to mitigate healthcare personnel staffing shortages. https://www.cdc.gov/coronavirus/2019-ncov/hcp /mitigating-staff-shortages.html. Accessed July 17, 2020.
- Centers for Disease Control and Prevention. Strategies for optimizing the supply of facemasks. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face -masks.html. Accessed July 3, 2020.
- Rahman S, Klebanoff J, Moawad G. Smoke evacuation in the age of COVID-19. Contemporary OB/GYN. July 2, 2020. https://www.contemporaryobgyn.net/view/smoke -evacuation-in-the-age-of-covid-19. Accessed July 3, 2020.
- Centers for Disease Control and Prevention. Symptoms of coronavirus. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed July 25, 2020.
- Centers for Disease Control and Prevention. Information for healthcare professionals about coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. Accessed July 22, 2020.
- US Department of Labor Occupational Safety and Health Administration. COVID-19 control and prevention: healthcare workers and employers. https://www.osha.gov/SLTC/covid-19/healthcare-workers.html. Accessed August 5, 2020.
- Centers for Medicare and Medicaid Services. COVID-19 resources for health care professionals and researchers. https://www.cms.gov/About-CMS/Agency-Information/OMH/resource-center/hcps-and-researchers. Accessed August 7, 2020.
- American College of Obstetricians and Gynecologists. COVID-19. https://www.acog.org/topics/covid-19. Accessed August 7, 2020.
- Society for Maternal-Fetal Medicine. Coronavirus (COVID-19). https://www.smfm.org/covid19. Accessed August 7, 2020.
- Society of Gynecologic Surgeons. Joint statement on re-introduction of hospital and office-based procedures in the COVID-19 climate for the practicing gynecologist. https://www.sgsonline.org/joint-statement-on-re-introduction-of-hospital-and-office-based-procedures-in-the-covid-19-climate. Accessed August 7, 2020.
- AAGL. COVID-19 articles, resources and webinars. https://www.aagl.org/covid-19/. Accessed August 7, 2020.
- American Society for Reproductive Medicine. COVID-19 updates and resources. https://www.asrm.org/news-and-publications/covid-19/. Accessed August 7, 2020.
- Society of Gynecologic Oncology. COVID-19 resources for health care practitioners. https://www.sgo.org/practice-management/covid-19/. Accessed August 7, 2020.
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html. Accessed July 3, 2020.
- Nguyen LH, Drew DA, Graham MS, et al; on behalf of the COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet. July 31, 2020. http://www.thelancet-press.com/embargo/hcwcovid.pdf. Accessed August 25, 2020.
- Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with SARS-CoV-2 infection (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html. Accessed July 20, 2020.
- US Environmental Protection Agency. List N: Disinfectants for use against SARS-CoV-2 (COVID-19). https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2-covid-19. Accessed August 24, 2020.
- Centers for Disease Control and Prevention. Duration of isolation and precautions for adults with COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Accessed July 23, 2020.
- Centers for Disease Control and Prevention. Discontinuation of transmission-based precautions and disposition of patients with COVID-19 in healthcare settings (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html#fn1. Accessed July 23, 2020.
No question, the COVID-19 pandemic has been a challenging time for medical practices across the United States. Uncertainty remains regarding bringing patients and services back into our offices. One factor that distinguishes many ObGyn practices from other specialties is that our practices have remained open—in some form—since the beginning of the pandemic. In various parts of the country, gynecologic surgeries and routine office visits have been significantly reduced; however, deliveries and gynecologic emergencies have continued.
In this article, I suggest a framework of strategies and resources to provide insight for outpatient operations. Individual practices will vary across the nation depending on local conditions. Full practice capacity may take on a different look than it had prior to the pandemic, and there is opportunity to change the way we operate.
Strategy 1: Consult regulatory requirements frequently
As the local status of COVID-19 evolves quickly, it is essential to examine the frequently updated recommendations from regulatory agencies at the federal, state, and local levels. Clinical practices that function within health systems need to demonstrate alignment with hospital or university policies and procedures. The Centers for Disease Control and Prevention (CDC), Occupational Safety and Health Administration (OSHA), Centers for Medicare and Medicaid Services (CMS), and individual state departments of health provide dynamic resources that are easily accessible online.1-3
The American College of Obstetricians and Gynecologists (ACOG) continues to be an excellent medical society resource.4 Subspecialty organizations that provide up-to-date guidance include the Society for Maternal-Fetal Medicine (SMFM), Society of Gynecologic Surgeons (SGS), AAGL (American Association of Gynecologic Laparoscopists), American Society for Reproductive Medicine (ASRM), and Society of Gynecologic Oncology (SGO).5-9 These resources are updated as more information about COVID-19 emerges, and they may be modified to different local-regional conditions.
The professional liability insurance carrier is an important source of insight for a number of circumstances, including modifications to your office practice, such as returning to full-scope or part-time practice; operating outside normal clinical service arrangements (for example, assisting with emergency care); offering telehealth services; and adding extra hours or employees to accommodate the patient backlog. Business insurance coverage is a separate issue to consider. Reviewing the practice policy may protect your business from COVID-related liabilities.
Consulting with legal counselors can be helpful. They can assist with navigating various practice and personnel COVID-related changes, as well as developing a viable plan for patients who were previously insured pre–COVID-19 who are currently uninsured.
Continue to: Strategy 2: Reimagine schedule capacity...
Strategy 2: Reimagine schedule capacity
The waxing and waning of the COVID-19 crisis presents an opportunity to evaluate our office practices and make necessary and positive changes. The question becomes, do we operate our practices as usual or do we rethink our strategy for seeing patients and integrate lessons learned from the pandemic? Patients are deciding when they are comfortable to schedule elective surgeries and routine office encounters. This gives us the chance to break from the tradition of 100% in-person visits and change the way we care for women.
The coronavirus has accelerated the rise of telehealth/telemedicine and is, perhaps, a silver lining of the pandemic. Telehealth is a valuable tool for accessing health services when in-person visits are not possible. Evaluating and triaging patients for in-person versus telehealth visits is now a viable option for clinical practice and reduces exposure to COVID-19 infection.
Telemedicine is convenient, and clinicians can use it to counsel and screen for various health issues as well as to extend their reach to rural communities. Appropriate consent should be documented in the patient chart. As some areas continue to be without adequate access to WiFi, telephone contact also is currently acceptable. Telehealth does not replace the in-person visit but can be viewed as a complementary and supplementary service.
Consider a balance between telehealth and in-person visits by evaluating which visits can continue remotely and which can alternate with in-person visits. This offers tremendous flexibility and will expand delivery of essential health care to patients.10 Integrating telemedicine into clinical practice provides an additional benefit: It minimizes the exposure and transmission of COVID-19 to health care workers and patients and preserves supplies, including personal protective equipment (PPE).
Prioritize the backlog of patients who require follow-up testing, procedures, and surgeries. Communicate with patients that it is safe to be seen and important to not avoid routine and preventative visits that might reveal concerns or conditions that require treatment.
Strategy 3: Institute infection prevention and control measures
The importance of instituting and ensuring safety measures for office personnel and patients cannot be underestimated. Recently, a study from King’s College in London found that frontline health care workers with PPE still have 3 to 4 times the risk of contracting coronavirus compared with the general public.11 Health care systems should ensure adequate PPE availability and develop additional strategies to protect health care workers from COVID-19. We have to be fanatical about cleanliness and PPE. We have to be diligent about how we space ourselves and our patients. Consider adjusting workflows to ensure that visits can be conducted as quickly and safely as possible.
Communicating updated safety plans and processes are invaluable for both patients and health care workers. Patients want to be reassured that safety precautions are in place to keep the environment safe and clean. Additionally, privacy and confidentiality concerns should be addressed.
Consider a modified office schedule that can reduce the number of people in the office, person-to-person contact, and COVID-19 transmission. Social distancing is improved and PPE and other supplies are preserved.
Continue to: Employees can work on alternating days...
- Employees can work on alternating days or during different parts of the day.
- Administrative staff who do not need to be physically present in the office might work remotely.
- Expanding office hours (early morning, evening, and weekends) spreads patient visits throughout the day and minimizes high-volume in-person visits.
Institute a daily COVID-19 symptom attestation and temperature check for employees on arrival at work.
Health care personnel with symptoms of COVID-19 should be prioritized for SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) RNA testing with an approved nucleic acid or antigen detection assay. A negative result indicates that the person most likely did not have an active SARS-CoV-2 infection at the time the sample was collected. A second test for SARS-CoV-2 RNA may be performed at the discretion of the evaluating health care provider, particularly when a higher level of clinical suspicion for infection exists.
The return to work decision should be determined by an agreed on symptom-based approach to clearance. If needed on a case-by-case basis, a review can be performed with the individual’s health care provider.12
Require universal masking and appropriate protective equipment.
- All staff members, patients, and visitors must wear masks correctly in the facilities (except children under age 2).
- All clinical staff members must wear masks correctly and eye protection during every patient encounter.
Reconfigure the waiting room and patient flow.
- Configure waiting room furniture to reinforce 6 feet of physical distancing.
- Remove all books, magazines, and toys from all waiting areas.
- Laminate signage for display.
- Install plexiglass at the check-in desk to minimize virus transmission.
- If possible, ask patients to wait in their car until their appointment time or to go directly to their exam room on arrival if it is available.
- Implement virtual check-in and check-out so that patients reduce unnecessary contact with surfaces and staff.
- Limit a high volume of patients to maintain social distancing etiquette, avoid delays, and allow adequate cleaning time between patients.
- Permit visitors to accompany adult patients to their ambulatory appointments only if special assistance is required.
- Limit the number of staff members in the exam and treatment rooms and maintain at least 6 feet between people except during medical care activities.
- Consider patient flow in a one-way traffic pattern.
Focus on keeping the clinical practice clean. (Follow the instructions and disinfect with a registered disinfectant product that meets the US Environmental Protection Agency criteria for use against COVID-19.13)
- Clean waiting rooms and restrooms frequently.
- Coordinate patient appointments to allow for infection control measures.
- Frequently clean high-touch surfaces, including tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
- Clinicians and all medical staff members should wash their hands before and after interacting with patients.
- Clean and disinfect the exam and treatment rooms before and after each patient.
- Use products that are effective against a range of organisms and viruses, including the coronavirus that causes COVID-19.
- Place signs indicating that rooms have been cleaned; this will assure and comfort patients. Take credit for your infection control processes.
Keep abreast of isolation and precaution guidelines. Based on data available at the time of this article’s publication, the CDC recommends ending isolation and transmission-based precautions for most people with COVID-19 using a symptom-based strategy.14 This limits unnecessary prolonged isolation and use of laboratory testing resources.
Generally, repeat SARS-CoV-2 polymerase chain reaction (PCR) testing is not recommended for “COVID-19 recovered” patients. Specifically, those patients with a prior positive SARS-CoV-2 PCR test result and who have met criteria for isolation discontinuation do not need a follow-up PCR test. A test-based strategy to discontinue isolation and transmission-based precautions is required only for severely immunocompromised patients.15
Prepare for a future COVID-19 surge and review your emergency plan and responses and revise as needed. Review handling of the current pandemic and best practices plus areas of improvement.
Symptom-based criteria for discontinuing transmission-based precautions include the following:
Patients with mild to moderate illness, not severely immunocompromised:
- at least 10 days have passed since symptoms first appeared and
- at least 24 hours have passed since last fever without fever-reducing medications and
- symptoms (cough, shortness of breath) have improved.
Note: For patients who are not severely immunocompromised and are asymptomatic throughout their infection, transmission-based precautions may be discontinued when at least 10 days have passed since the date of their first positive viral diagnostic test.
Patients with severe to critical illness, severely immunocompromised:
- at least 20 days have passed since symptoms first appeared and
- at least 24 hours have passed since last fever without fever-reducing medications and
- symptoms (cough, shortness of breath) have improved.
Note: For patients who are severely immunocompromised and are asymptomatic throughout their infection, transmission-based precautions may be discontinued when at least 20 days have passed since the date of their first positive viral diagnostic test.
Continue to: Strategy 4: Implement frequent employee communication and care...
Strategy 4: Implement frequent employee communication and care
The safety and well-being of our health care workers and patients in our clinical practices is paramount. Continuing to communicate this message and developing and sharing a plan may ameliorate the obvious toll on mental and emotional well-being. Frequent and effective communication with your clinical team is vital to reinforce policies and protocols, eliminate silos, and reduce errors.
Practice communication and care with these approaches:
- Offer regular employee COVID-19 testing.
- Re-educate staff about infection control protocols to ensure buy-in.
- Communicate with staff about the plan to address staffing shortages.
- Implement regular employee team huddles that can address accomplishments, challenges, areas for improvement, and top priorities.
- Perform regular celebrations for staff appreciation.
- Address mental health and chronic stress and offer empathy and coping resources and services to staff and clinicians. This will have a valuable, long-term benefit.
Patient communication. As the COVID-19 pandemic continues and stay-at-home policies are in place, patients should be encouraged to seek medical care if they are ill or have acute or chronic conditions. Communicate regularly with patients and let them know that their safety and well-being is the top priority. Prior to in-person visits, inform them of the safety processes that are in place to protect them.
Fostering an honest clinician-patient relationship enhances communication. Despite these efforts, some patients may not be forthcoming about their COVID-19 symptoms, illness, exposure, or travel. Health care staff can be encouraged to set a tone of tolerance and compassion and treat everyone with universal precautions.
Rising to the challenges
During the coronavirus pandemic, ObGyns continue to safely care for pregnant women and also triage and treat women who require timely office care as well as emergency and cancer-related surgeries.
The COVID-19 environment rapidly changes depending on the practice location. The strategies described represent a compilation of resources from key organizations that hopefully will prove useful and can be shaped to fit your practice. Local and regional recommendations vary, and no one can predict the course of the virus.
Consider reviewing your contingency plans regularly. As we have learned over the last several months, there is a science to maintaining a COVID-SAFE environment.
Practice operations likely will change to adapt to new conditions. The pandemic has challenged us to evolve, and we have responded with new capabilities and resilience while we continue to deliver superior and compassionate care for women.
For additional strategies on how to safeguard your practice against COVID-19, see the box below. ●
Continue to: Additional strategies on how to safeguard your practice against COVID-19...
Strategy 5: Develop a resource plan for practice operations
Assess financial solvency. Because of the mitigation measures taken during the pandemic, physician practices of all sizes are facing financial hardships and instability. As the pandemic progresses, physicians in private practice and those employed by health systems may benefit from existing resources and pandemic relief to help navigate COVID-related challenges.
Frequent revision of your financial plan may safeguard cash flow in the event of fewer patient visits and elective surgeries. Many medical organizations, including ACOG, are advocating for financial relief, fair reimbursement for telehealth and in-person visits, and access to adequate PPE. ACOG provides updated information on practice management.1
The American Medical Association (AMA) has created resources for physician practices to assist in staying focused on business and financial operations. The AMA has provided a summary of the Health, Economic Assistance, Liability Protection and Schools Act (HEALS Act).2 This is the next proposed coronavirus relief fund package, which includes provisions that benefit physicians and physician practices.
Create a plan. Review available resources and establish processes to optimize your practice capacity during the ongoing COVID-19 pandemic. Develop a game plan for patient care with a phased approach to identify and address challenges. This planning will allow your practice to pivot in response to changing local COVID-19 conditions to help you anticipate and prepare for a future surge. Maintain and revise plans as the pandemic shifts. Thinking ahead avoids the need to navigate issues in real time. Communicating clearly and often with all members of the office staff and patients lets everyone know that their safety is the main priority.
Assess staffing for flexible coverage. Frequent needs assessment helps to determine the number of staff needed to maintain a safe work environment for the patient volume.
Staff shortages may occur because of COVID-19 exposure, personal or family member illness, or childcare constraints due to daycare or school availability. Staff readiness includes evaluating individual availability and willingness.
Staff members with health issues, including comorbidities and chronic medical conditions, may not be comfortable working. Nonclinical staff members with health concerns could work remotely, although some may not be able to work from home due to technology-related issues such as WiFi deficiencies.
The CDC has interim guidelines to assist employers with providing a safe workplace and employees with making the best health decisions for themselves and their families.3,4 The US Office of Personnel Management provides guidance for COVID-19–related leave and benefits for federal employees.5
To mitigate staff shortages, approaches include adjusting schedules, cross-training to perform the tasks of other positions, and hiring additional personnel. A needs assessment can help determine if existing personnel could be cross-trained for other purposes or if additional staff should be hired. Understanding the minimum number of staff required for safe and effective patient care will assist in planning for shortages as the pandemic progresses. Understanding the availability of external resources could be a critical part of an office contingency plan.6
Proactively manage your supply chain. The pandemic has caused global supply shortages. Solid supply chain management is crucial for practice operations. Take inventory of your PPE and various supplies and place orders in advance. Analyze cash flow and connect with vendors as well as local and state health agencies to understand available resources. Given ongoing PPE shortages, practices should consider preserving PPE and employ appropriate strategies for optimizing supplies of face masks.7
Certain medications and vaccines administered in the office setting may be outdated and need to be replaced. Office equipment that has not been used for several months will need to be tested. For equipment used in office electrosurgery procedures, certain safety measures can be taken to reduce the transmission of aerosolized viral particles to the health care team. While currently the risk is theoretical and more research is needed, this potential risk should be mitigated.8 Assessing availability of hospital and ambulance or transport services also is recommended as these may change depending on the local COVID-19 status.
Strategy 6: Establish and refine the patient screening process
Patients want reassurance that the health care environment is safe and that their well-being is a priority. In advance of a patient’s visit, relieve any anxiety by explaining the COVID-SAFE measures that your practice has taken.
For employee use, consider telephone and in-person scripting to ensure consistent messaging for patients.
Prescreening. At the time of appointment scheduling and on the day prior to the scheduled appointment, all patients should be screened for symptoms of COVID-19,9 fever, exposure within 14 days to someone newly diagnosed with COVID-19, and travel within 14 days from a foreign country or from a US state with a quarantine requirement.
Patients who screen positive for symptoms, exposure, or travel should be referred to a clinician. If possible, asymptomatic patients who report exposure or travel should have their in-person visit deferred until after the required 14-day quarantine.
Consider restricting visitors from accompanying adult patients to their appointment unless they are required for special assistance.
Arrival screening. At the time of presentation for the appointment, all patients and any accompanying visitors should be rescreened. The optimal location for arrival screening should be determined by the local operations team and the infection prevention and control program.
At presentation, all patients and visitors should appropriately don a surgical mask or other face covering. Patients and visitors should have their temperature checked on arrival. Patients who screen positive for symptoms, exposure to COVID-19, and/or travel should be referred to a clinician or the visit deferred and a telehealth visit considered.
Visitors who screen positive for symptoms, fever, or exposure to COVID-19 are not permitted to accompany the patient. Asymptomatic parents or guardians of pediatric patients may serve as support persons.
References
- American College of Obstetricians and Gynecologists. Financial support for physicians and practices during the COVID-19 pandemic. https://www.acog.org/practice -management/coding/coding-library/financial-support-for-physicians-and-practices-during-the-covid-19-pandemic. Accessed July 23, 2020.
- American Medical Association. HEALS Act: What physicians and medical students need to know. https://www.ama-assn.org/delivering-care/public-health/heals-act -what-physicians-and-medical-students-need-know. Accessed July 29, 2020.
- Centers for Disease Control and Prevention. Interim guidance for businesses and employers responding to coronavirus disease 2019 (COVID-19). https://www.cdc.gov /coronavirus/2019-ncov/community/guidance-business-response.html. Accessed July 12, 2020.
- Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with SARS-CoV-2 infection (interim guidance). https://www.cdc.gov /coronavirus/2019-ncov/hcp/return-to-work.html. Accessed July 20, 2020.
- US Office of Personnel Management. Questions and answers on human resources flexibilities and authorities for coronavirus disease 2019 (COVID-19). https://www .opm.gov/policy-data-oversight/covid-19/questions-and-answers-on-human-resources-flexibilities-and-authorities-for-coronavirus-disease-2019-covid-19.pdf. Accessed July 3, 2020.
- Centers for Disease Control and Prevention. Strategies to mitigate healthcare personnel staffing shortages. https://www.cdc.gov/coronavirus/2019-ncov/hcp /mitigating-staff-shortages.html. Accessed July 17, 2020.
- Centers for Disease Control and Prevention. Strategies for optimizing the supply of facemasks. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face -masks.html. Accessed July 3, 2020.
- Rahman S, Klebanoff J, Moawad G. Smoke evacuation in the age of COVID-19. Contemporary OB/GYN. July 2, 2020. https://www.contemporaryobgyn.net/view/smoke -evacuation-in-the-age-of-covid-19. Accessed July 3, 2020.
- Centers for Disease Control and Prevention. Symptoms of coronavirus. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed July 25, 2020.
No question, the COVID-19 pandemic has been a challenging time for medical practices across the United States. Uncertainty remains regarding bringing patients and services back into our offices. One factor that distinguishes many ObGyn practices from other specialties is that our practices have remained open—in some form—since the beginning of the pandemic. In various parts of the country, gynecologic surgeries and routine office visits have been significantly reduced; however, deliveries and gynecologic emergencies have continued.
In this article, I suggest a framework of strategies and resources to provide insight for outpatient operations. Individual practices will vary across the nation depending on local conditions. Full practice capacity may take on a different look than it had prior to the pandemic, and there is opportunity to change the way we operate.
Strategy 1: Consult regulatory requirements frequently
As the local status of COVID-19 evolves quickly, it is essential to examine the frequently updated recommendations from regulatory agencies at the federal, state, and local levels. Clinical practices that function within health systems need to demonstrate alignment with hospital or university policies and procedures. The Centers for Disease Control and Prevention (CDC), Occupational Safety and Health Administration (OSHA), Centers for Medicare and Medicaid Services (CMS), and individual state departments of health provide dynamic resources that are easily accessible online.1-3
The American College of Obstetricians and Gynecologists (ACOG) continues to be an excellent medical society resource.4 Subspecialty organizations that provide up-to-date guidance include the Society for Maternal-Fetal Medicine (SMFM), Society of Gynecologic Surgeons (SGS), AAGL (American Association of Gynecologic Laparoscopists), American Society for Reproductive Medicine (ASRM), and Society of Gynecologic Oncology (SGO).5-9 These resources are updated as more information about COVID-19 emerges, and they may be modified to different local-regional conditions.
The professional liability insurance carrier is an important source of insight for a number of circumstances, including modifications to your office practice, such as returning to full-scope or part-time practice; operating outside normal clinical service arrangements (for example, assisting with emergency care); offering telehealth services; and adding extra hours or employees to accommodate the patient backlog. Business insurance coverage is a separate issue to consider. Reviewing the practice policy may protect your business from COVID-related liabilities.
Consulting with legal counselors can be helpful. They can assist with navigating various practice and personnel COVID-related changes, as well as developing a viable plan for patients who were previously insured pre–COVID-19 who are currently uninsured.
Continue to: Strategy 2: Reimagine schedule capacity...
Strategy 2: Reimagine schedule capacity
The waxing and waning of the COVID-19 crisis presents an opportunity to evaluate our office practices and make necessary and positive changes. The question becomes, do we operate our practices as usual or do we rethink our strategy for seeing patients and integrate lessons learned from the pandemic? Patients are deciding when they are comfortable to schedule elective surgeries and routine office encounters. This gives us the chance to break from the tradition of 100% in-person visits and change the way we care for women.
The coronavirus has accelerated the rise of telehealth/telemedicine and is, perhaps, a silver lining of the pandemic. Telehealth is a valuable tool for accessing health services when in-person visits are not possible. Evaluating and triaging patients for in-person versus telehealth visits is now a viable option for clinical practice and reduces exposure to COVID-19 infection.
Telemedicine is convenient, and clinicians can use it to counsel and screen for various health issues as well as to extend their reach to rural communities. Appropriate consent should be documented in the patient chart. As some areas continue to be without adequate access to WiFi, telephone contact also is currently acceptable. Telehealth does not replace the in-person visit but can be viewed as a complementary and supplementary service.
Consider a balance between telehealth and in-person visits by evaluating which visits can continue remotely and which can alternate with in-person visits. This offers tremendous flexibility and will expand delivery of essential health care to patients.10 Integrating telemedicine into clinical practice provides an additional benefit: It minimizes the exposure and transmission of COVID-19 to health care workers and patients and preserves supplies, including personal protective equipment (PPE).
Prioritize the backlog of patients who require follow-up testing, procedures, and surgeries. Communicate with patients that it is safe to be seen and important to not avoid routine and preventative visits that might reveal concerns or conditions that require treatment.
Strategy 3: Institute infection prevention and control measures
The importance of instituting and ensuring safety measures for office personnel and patients cannot be underestimated. Recently, a study from King’s College in London found that frontline health care workers with PPE still have 3 to 4 times the risk of contracting coronavirus compared with the general public.11 Health care systems should ensure adequate PPE availability and develop additional strategies to protect health care workers from COVID-19. We have to be fanatical about cleanliness and PPE. We have to be diligent about how we space ourselves and our patients. Consider adjusting workflows to ensure that visits can be conducted as quickly and safely as possible.
Communicating updated safety plans and processes are invaluable for both patients and health care workers. Patients want to be reassured that safety precautions are in place to keep the environment safe and clean. Additionally, privacy and confidentiality concerns should be addressed.
Consider a modified office schedule that can reduce the number of people in the office, person-to-person contact, and COVID-19 transmission. Social distancing is improved and PPE and other supplies are preserved.
Continue to: Employees can work on alternating days...
- Employees can work on alternating days or during different parts of the day.
- Administrative staff who do not need to be physically present in the office might work remotely.
- Expanding office hours (early morning, evening, and weekends) spreads patient visits throughout the day and minimizes high-volume in-person visits.
Institute a daily COVID-19 symptom attestation and temperature check for employees on arrival at work.
Health care personnel with symptoms of COVID-19 should be prioritized for SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) RNA testing with an approved nucleic acid or antigen detection assay. A negative result indicates that the person most likely did not have an active SARS-CoV-2 infection at the time the sample was collected. A second test for SARS-CoV-2 RNA may be performed at the discretion of the evaluating health care provider, particularly when a higher level of clinical suspicion for infection exists.
The return to work decision should be determined by an agreed on symptom-based approach to clearance. If needed on a case-by-case basis, a review can be performed with the individual’s health care provider.12
Require universal masking and appropriate protective equipment.
- All staff members, patients, and visitors must wear masks correctly in the facilities (except children under age 2).
- All clinical staff members must wear masks correctly and eye protection during every patient encounter.
Reconfigure the waiting room and patient flow.
- Configure waiting room furniture to reinforce 6 feet of physical distancing.
- Remove all books, magazines, and toys from all waiting areas.
- Laminate signage for display.
- Install plexiglass at the check-in desk to minimize virus transmission.
- If possible, ask patients to wait in their car until their appointment time or to go directly to their exam room on arrival if it is available.
- Implement virtual check-in and check-out so that patients reduce unnecessary contact with surfaces and staff.
- Limit a high volume of patients to maintain social distancing etiquette, avoid delays, and allow adequate cleaning time between patients.
- Permit visitors to accompany adult patients to their ambulatory appointments only if special assistance is required.
- Limit the number of staff members in the exam and treatment rooms and maintain at least 6 feet between people except during medical care activities.
- Consider patient flow in a one-way traffic pattern.
Focus on keeping the clinical practice clean. (Follow the instructions and disinfect with a registered disinfectant product that meets the US Environmental Protection Agency criteria for use against COVID-19.13)
- Clean waiting rooms and restrooms frequently.
- Coordinate patient appointments to allow for infection control measures.
- Frequently clean high-touch surfaces, including tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
- Clinicians and all medical staff members should wash their hands before and after interacting with patients.
- Clean and disinfect the exam and treatment rooms before and after each patient.
- Use products that are effective against a range of organisms and viruses, including the coronavirus that causes COVID-19.
- Place signs indicating that rooms have been cleaned; this will assure and comfort patients. Take credit for your infection control processes.
Keep abreast of isolation and precaution guidelines. Based on data available at the time of this article’s publication, the CDC recommends ending isolation and transmission-based precautions for most people with COVID-19 using a symptom-based strategy.14 This limits unnecessary prolonged isolation and use of laboratory testing resources.
Generally, repeat SARS-CoV-2 polymerase chain reaction (PCR) testing is not recommended for “COVID-19 recovered” patients. Specifically, those patients with a prior positive SARS-CoV-2 PCR test result and who have met criteria for isolation discontinuation do not need a follow-up PCR test. A test-based strategy to discontinue isolation and transmission-based precautions is required only for severely immunocompromised patients.15
Prepare for a future COVID-19 surge and review your emergency plan and responses and revise as needed. Review handling of the current pandemic and best practices plus areas of improvement.
Symptom-based criteria for discontinuing transmission-based precautions include the following:
Patients with mild to moderate illness, not severely immunocompromised:
- at least 10 days have passed since symptoms first appeared and
- at least 24 hours have passed since last fever without fever-reducing medications and
- symptoms (cough, shortness of breath) have improved.
Note: For patients who are not severely immunocompromised and are asymptomatic throughout their infection, transmission-based precautions may be discontinued when at least 10 days have passed since the date of their first positive viral diagnostic test.
Patients with severe to critical illness, severely immunocompromised:
- at least 20 days have passed since symptoms first appeared and
- at least 24 hours have passed since last fever without fever-reducing medications and
- symptoms (cough, shortness of breath) have improved.
Note: For patients who are severely immunocompromised and are asymptomatic throughout their infection, transmission-based precautions may be discontinued when at least 20 days have passed since the date of their first positive viral diagnostic test.
Continue to: Strategy 4: Implement frequent employee communication and care...
Strategy 4: Implement frequent employee communication and care
The safety and well-being of our health care workers and patients in our clinical practices is paramount. Continuing to communicate this message and developing and sharing a plan may ameliorate the obvious toll on mental and emotional well-being. Frequent and effective communication with your clinical team is vital to reinforce policies and protocols, eliminate silos, and reduce errors.
Practice communication and care with these approaches:
- Offer regular employee COVID-19 testing.
- Re-educate staff about infection control protocols to ensure buy-in.
- Communicate with staff about the plan to address staffing shortages.
- Implement regular employee team huddles that can address accomplishments, challenges, areas for improvement, and top priorities.
- Perform regular celebrations for staff appreciation.
- Address mental health and chronic stress and offer empathy and coping resources and services to staff and clinicians. This will have a valuable, long-term benefit.
Patient communication. As the COVID-19 pandemic continues and stay-at-home policies are in place, patients should be encouraged to seek medical care if they are ill or have acute or chronic conditions. Communicate regularly with patients and let them know that their safety and well-being is the top priority. Prior to in-person visits, inform them of the safety processes that are in place to protect them.
Fostering an honest clinician-patient relationship enhances communication. Despite these efforts, some patients may not be forthcoming about their COVID-19 symptoms, illness, exposure, or travel. Health care staff can be encouraged to set a tone of tolerance and compassion and treat everyone with universal precautions.
Rising to the challenges
During the coronavirus pandemic, ObGyns continue to safely care for pregnant women and also triage and treat women who require timely office care as well as emergency and cancer-related surgeries.
The COVID-19 environment rapidly changes depending on the practice location. The strategies described represent a compilation of resources from key organizations that hopefully will prove useful and can be shaped to fit your practice. Local and regional recommendations vary, and no one can predict the course of the virus.
Consider reviewing your contingency plans regularly. As we have learned over the last several months, there is a science to maintaining a COVID-SAFE environment.
Practice operations likely will change to adapt to new conditions. The pandemic has challenged us to evolve, and we have responded with new capabilities and resilience while we continue to deliver superior and compassionate care for women.
For additional strategies on how to safeguard your practice against COVID-19, see the box below. ●
Continue to: Additional strategies on how to safeguard your practice against COVID-19...
Strategy 5: Develop a resource plan for practice operations
Assess financial solvency. Because of the mitigation measures taken during the pandemic, physician practices of all sizes are facing financial hardships and instability. As the pandemic progresses, physicians in private practice and those employed by health systems may benefit from existing resources and pandemic relief to help navigate COVID-related challenges.
Frequent revision of your financial plan may safeguard cash flow in the event of fewer patient visits and elective surgeries. Many medical organizations, including ACOG, are advocating for financial relief, fair reimbursement for telehealth and in-person visits, and access to adequate PPE. ACOG provides updated information on practice management.1
The American Medical Association (AMA) has created resources for physician practices to assist in staying focused on business and financial operations. The AMA has provided a summary of the Health, Economic Assistance, Liability Protection and Schools Act (HEALS Act).2 This is the next proposed coronavirus relief fund package, which includes provisions that benefit physicians and physician practices.
Create a plan. Review available resources and establish processes to optimize your practice capacity during the ongoing COVID-19 pandemic. Develop a game plan for patient care with a phased approach to identify and address challenges. This planning will allow your practice to pivot in response to changing local COVID-19 conditions to help you anticipate and prepare for a future surge. Maintain and revise plans as the pandemic shifts. Thinking ahead avoids the need to navigate issues in real time. Communicating clearly and often with all members of the office staff and patients lets everyone know that their safety is the main priority.
Assess staffing for flexible coverage. Frequent needs assessment helps to determine the number of staff needed to maintain a safe work environment for the patient volume.
Staff shortages may occur because of COVID-19 exposure, personal or family member illness, or childcare constraints due to daycare or school availability. Staff readiness includes evaluating individual availability and willingness.
Staff members with health issues, including comorbidities and chronic medical conditions, may not be comfortable working. Nonclinical staff members with health concerns could work remotely, although some may not be able to work from home due to technology-related issues such as WiFi deficiencies.
The CDC has interim guidelines to assist employers with providing a safe workplace and employees with making the best health decisions for themselves and their families.3,4 The US Office of Personnel Management provides guidance for COVID-19–related leave and benefits for federal employees.5
To mitigate staff shortages, approaches include adjusting schedules, cross-training to perform the tasks of other positions, and hiring additional personnel. A needs assessment can help determine if existing personnel could be cross-trained for other purposes or if additional staff should be hired. Understanding the minimum number of staff required for safe and effective patient care will assist in planning for shortages as the pandemic progresses. Understanding the availability of external resources could be a critical part of an office contingency plan.6
Proactively manage your supply chain. The pandemic has caused global supply shortages. Solid supply chain management is crucial for practice operations. Take inventory of your PPE and various supplies and place orders in advance. Analyze cash flow and connect with vendors as well as local and state health agencies to understand available resources. Given ongoing PPE shortages, practices should consider preserving PPE and employ appropriate strategies for optimizing supplies of face masks.7
Certain medications and vaccines administered in the office setting may be outdated and need to be replaced. Office equipment that has not been used for several months will need to be tested. For equipment used in office electrosurgery procedures, certain safety measures can be taken to reduce the transmission of aerosolized viral particles to the health care team. While currently the risk is theoretical and more research is needed, this potential risk should be mitigated.8 Assessing availability of hospital and ambulance or transport services also is recommended as these may change depending on the local COVID-19 status.
Strategy 6: Establish and refine the patient screening process
Patients want reassurance that the health care environment is safe and that their well-being is a priority. In advance of a patient’s visit, relieve any anxiety by explaining the COVID-SAFE measures that your practice has taken.
For employee use, consider telephone and in-person scripting to ensure consistent messaging for patients.
Prescreening. At the time of appointment scheduling and on the day prior to the scheduled appointment, all patients should be screened for symptoms of COVID-19,9 fever, exposure within 14 days to someone newly diagnosed with COVID-19, and travel within 14 days from a foreign country or from a US state with a quarantine requirement.
Patients who screen positive for symptoms, exposure, or travel should be referred to a clinician. If possible, asymptomatic patients who report exposure or travel should have their in-person visit deferred until after the required 14-day quarantine.
Consider restricting visitors from accompanying adult patients to their appointment unless they are required for special assistance.
Arrival screening. At the time of presentation for the appointment, all patients and any accompanying visitors should be rescreened. The optimal location for arrival screening should be determined by the local operations team and the infection prevention and control program.
At presentation, all patients and visitors should appropriately don a surgical mask or other face covering. Patients and visitors should have their temperature checked on arrival. Patients who screen positive for symptoms, exposure to COVID-19, and/or travel should be referred to a clinician or the visit deferred and a telehealth visit considered.
Visitors who screen positive for symptoms, fever, or exposure to COVID-19 are not permitted to accompany the patient. Asymptomatic parents or guardians of pediatric patients may serve as support persons.
References
- American College of Obstetricians and Gynecologists. Financial support for physicians and practices during the COVID-19 pandemic. https://www.acog.org/practice -management/coding/coding-library/financial-support-for-physicians-and-practices-during-the-covid-19-pandemic. Accessed July 23, 2020.
- American Medical Association. HEALS Act: What physicians and medical students need to know. https://www.ama-assn.org/delivering-care/public-health/heals-act -what-physicians-and-medical-students-need-know. Accessed July 29, 2020.
- Centers for Disease Control and Prevention. Interim guidance for businesses and employers responding to coronavirus disease 2019 (COVID-19). https://www.cdc.gov /coronavirus/2019-ncov/community/guidance-business-response.html. Accessed July 12, 2020.
- Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with SARS-CoV-2 infection (interim guidance). https://www.cdc.gov /coronavirus/2019-ncov/hcp/return-to-work.html. Accessed July 20, 2020.
- US Office of Personnel Management. Questions and answers on human resources flexibilities and authorities for coronavirus disease 2019 (COVID-19). https://www .opm.gov/policy-data-oversight/covid-19/questions-and-answers-on-human-resources-flexibilities-and-authorities-for-coronavirus-disease-2019-covid-19.pdf. Accessed July 3, 2020.
- Centers for Disease Control and Prevention. Strategies to mitigate healthcare personnel staffing shortages. https://www.cdc.gov/coronavirus/2019-ncov/hcp /mitigating-staff-shortages.html. Accessed July 17, 2020.
- Centers for Disease Control and Prevention. Strategies for optimizing the supply of facemasks. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face -masks.html. Accessed July 3, 2020.
- Rahman S, Klebanoff J, Moawad G. Smoke evacuation in the age of COVID-19. Contemporary OB/GYN. July 2, 2020. https://www.contemporaryobgyn.net/view/smoke -evacuation-in-the-age-of-covid-19. Accessed July 3, 2020.
- Centers for Disease Control and Prevention. Symptoms of coronavirus. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed July 25, 2020.
- Centers for Disease Control and Prevention. Information for healthcare professionals about coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. Accessed July 22, 2020.
- US Department of Labor Occupational Safety and Health Administration. COVID-19 control and prevention: healthcare workers and employers. https://www.osha.gov/SLTC/covid-19/healthcare-workers.html. Accessed August 5, 2020.
- Centers for Medicare and Medicaid Services. COVID-19 resources for health care professionals and researchers. https://www.cms.gov/About-CMS/Agency-Information/OMH/resource-center/hcps-and-researchers. Accessed August 7, 2020.
- American College of Obstetricians and Gynecologists. COVID-19. https://www.acog.org/topics/covid-19. Accessed August 7, 2020.
- Society for Maternal-Fetal Medicine. Coronavirus (COVID-19). https://www.smfm.org/covid19. Accessed August 7, 2020.
- Society of Gynecologic Surgeons. Joint statement on re-introduction of hospital and office-based procedures in the COVID-19 climate for the practicing gynecologist. https://www.sgsonline.org/joint-statement-on-re-introduction-of-hospital-and-office-based-procedures-in-the-covid-19-climate. Accessed August 7, 2020.
- AAGL. COVID-19 articles, resources and webinars. https://www.aagl.org/covid-19/. Accessed August 7, 2020.
- American Society for Reproductive Medicine. COVID-19 updates and resources. https://www.asrm.org/news-and-publications/covid-19/. Accessed August 7, 2020.
- Society of Gynecologic Oncology. COVID-19 resources for health care practitioners. https://www.sgo.org/practice-management/covid-19/. Accessed August 7, 2020.
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html. Accessed July 3, 2020.
- Nguyen LH, Drew DA, Graham MS, et al; on behalf of the COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet. July 31, 2020. http://www.thelancet-press.com/embargo/hcwcovid.pdf. Accessed August 25, 2020.
- Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with SARS-CoV-2 infection (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html. Accessed July 20, 2020.
- US Environmental Protection Agency. List N: Disinfectants for use against SARS-CoV-2 (COVID-19). https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2-covid-19. Accessed August 24, 2020.
- Centers for Disease Control and Prevention. Duration of isolation and precautions for adults with COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Accessed July 23, 2020.
- Centers for Disease Control and Prevention. Discontinuation of transmission-based precautions and disposition of patients with COVID-19 in healthcare settings (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html#fn1. Accessed July 23, 2020.
- Centers for Disease Control and Prevention. Information for healthcare professionals about coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. Accessed July 22, 2020.
- US Department of Labor Occupational Safety and Health Administration. COVID-19 control and prevention: healthcare workers and employers. https://www.osha.gov/SLTC/covid-19/healthcare-workers.html. Accessed August 5, 2020.
- Centers for Medicare and Medicaid Services. COVID-19 resources for health care professionals and researchers. https://www.cms.gov/About-CMS/Agency-Information/OMH/resource-center/hcps-and-researchers. Accessed August 7, 2020.
- American College of Obstetricians and Gynecologists. COVID-19. https://www.acog.org/topics/covid-19. Accessed August 7, 2020.
- Society for Maternal-Fetal Medicine. Coronavirus (COVID-19). https://www.smfm.org/covid19. Accessed August 7, 2020.
- Society of Gynecologic Surgeons. Joint statement on re-introduction of hospital and office-based procedures in the COVID-19 climate for the practicing gynecologist. https://www.sgsonline.org/joint-statement-on-re-introduction-of-hospital-and-office-based-procedures-in-the-covid-19-climate. Accessed August 7, 2020.
- AAGL. COVID-19 articles, resources and webinars. https://www.aagl.org/covid-19/. Accessed August 7, 2020.
- American Society for Reproductive Medicine. COVID-19 updates and resources. https://www.asrm.org/news-and-publications/covid-19/. Accessed August 7, 2020.
- Society of Gynecologic Oncology. COVID-19 resources for health care practitioners. https://www.sgo.org/practice-management/covid-19/. Accessed August 7, 2020.
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html. Accessed July 3, 2020.
- Nguyen LH, Drew DA, Graham MS, et al; on behalf of the COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet. July 31, 2020. http://www.thelancet-press.com/embargo/hcwcovid.pdf. Accessed August 25, 2020.
- Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with SARS-CoV-2 infection (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html. Accessed July 20, 2020.
- US Environmental Protection Agency. List N: Disinfectants for use against SARS-CoV-2 (COVID-19). https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2-covid-19. Accessed August 24, 2020.
- Centers for Disease Control and Prevention. Duration of isolation and precautions for adults with COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Accessed July 23, 2020.
- Centers for Disease Control and Prevention. Discontinuation of transmission-based precautions and disposition of patients with COVID-19 in healthcare settings (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html#fn1. Accessed July 23, 2020.
Major changes in Medicare billing are planned for January 2021: Some specialties fare better than others
The Centers for Medicare and Medicaid Services (CMS) finalized an increase in the relative value of evaluation and management (E/M) service codes effective January 1, 2021, which results in an overall decrease in the payment for procedural services in the Medicare program. (Due to the mandate for budget neutrality, an increase in relative value units [RVUs] for E/M resulted in a large decrease in the conversion factor—the number of dollars per RVU). This has increased payments for endocrinologists, rheumatologists, and family medicine clinicians and decreased payments for radiologists, pathologists, and surgeons.
In a major win for physicians, CMS proposes to simplify documentation requirements for billing and focus on the complexity of the medical decision making (MDM) or the total time needed to care for the patient on the date of the service as the foundation for determining the relative value of the service. Therefore, there is no more counting bullets—ie, we don’t have to perform a comprehensive physical exam or review of systems to achieve a high level code! Prior to this change, time was only available for coding purposes when counseling and coordination of care was the predominant service (>50%), and only face-to-face time with the patient was considered. Effective January 1, for office and other outpatient services, total time on the calendar date of the encounter will be used. This acknowledges the intensity and value of non–face-to-face work.
Acting through CMS, the federal government influences greatly the US health care system. CMS is an agency in the Department of Health and Human Services that administers the Medicare program and partners with state governments to administer the Health Insurance Exchanges, Medicaid, and the Children’s Health Insurance programs (CHIP).1 In addition, CMS is responsible for enforcing quality care standards in long-term care facilities and clinical laboratories and the implementation of the Health Insurance Portability and Accountability Act.1
In January, CMS plans the following major changes to coding and documentation2,3:
- Selection of the level of E/M service will no longer require documentation of bullet points in the history, physical exam, and MDM. The simplified system allows physicians and qualified health care professionals to code either by total time (both face-to-face and non–face-to-face) on the date of the encounter or by level of MDM.
- For established office patients, 5 levels of office-based evaluation and management services will be retained. CMS had initially proposed to reduce the number of office-based E/M codes from 5 to 3, combining code levels 2, 3, and 4 into 1 code.4 However, after receiving feedback from professional societies and the public, CMS abandoned the plan for radical simplification of coding levels.2,3 Implementation of their proposal would have resulted in the same payment for treatment of a hang nail as for a complex gyn patient with multiple medical problems. Both patient advocacy groups and professional societies argued that incentives originally were misaligned.
- For new office patients, since both 99201 and 99202 require straightforward MDM, the level 1 code (99201) has been eliminated, reducing the number of code levels from 5 to 4.
- History and physical exam will no longer be used to determine code level for office E/M codes. These elements will be required only as medically appropriate. This means that documentation review will no longer focus on “bean counting” the elements in the history and physical exam.
- Following a reassessment of the actual time required to provide E/M services in real-life practice, CMS plans to markedly increase the relative value of office visits for established patients and modestly increase the relative value of office visits for new patients. CMS operates under the principle of “neutral budgeting,” meaning that an increase of the relative value of E/M codes will result in a decrease in the payment for procedural codes. The actual RVUs for procedural services do not change; however, budget neutrality requires a decrease in the dollar conversion factor. The proposed changes will increase the payment for E/M services and decrease payments for procedural services.
Continue to: Refocusing practice on MDM complexity...
Refocusing practice on MDM complexity
The practice of medicine is a calling with great rewards. Prominent among those rewards are improving the health of women, children, and the community, developing deep and trusting relationships with patients, families, and clinical colleagues. The practice of medicine is also replete with a host of punishing administrative burdens, including prior authorizations, clunky electronic medical records, poorly designed quality metrics that are applied to clinicians, and billing compliance rules that emphasize the repetitive documentation of clinical information with minimal value.
Some of the most irritating aspects of medical practice are the CMS rules governing medical record documentation required for billing ambulatory office visits. Current coding compliance focuses on counting the number of systems reviewed in the review of systems; the documentation of past history, social history, and family history; the number of organs and organ elements examined during the physical examination; and the complexity of MDM.
In January 2021, CMS plans to adopt new Current Procedural Terminology (CPT) code descriptors for the office and other outpatient E/M services that sunset most of the “bean-counting” metrics and emphasize the importance of the complexity of MDM in guiding selection of a correct code.2 Beginning in January 2021, clinicians will have the option of selecting an E/M code level based on the total amount of time required to provide the office visit service or the complexity of MDM. When selecting a code level based on MDM the new guidance emphasizes the importance of reviewing notes from other clinicians, reviewing test results, ordering of tests, and discussing and coordinating the care of the patient with other treating physicians. These changes reflect a better understanding of what is most important in good medical practice, promoting better patient care. TABLES 1 and 2 provide the initial guidance from CMS concerning selection of E/M code level based on time and MDM, respectively.2 The guidance for using MDM to select an E/M code level is likely to evolve following implementation, so stay tuned. When using MDM to select a code, 2 of the 3 general categories are required to select that level of service.
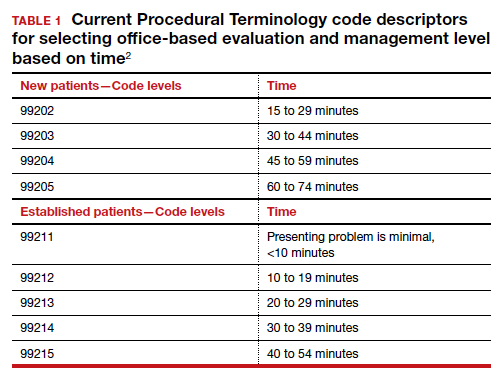
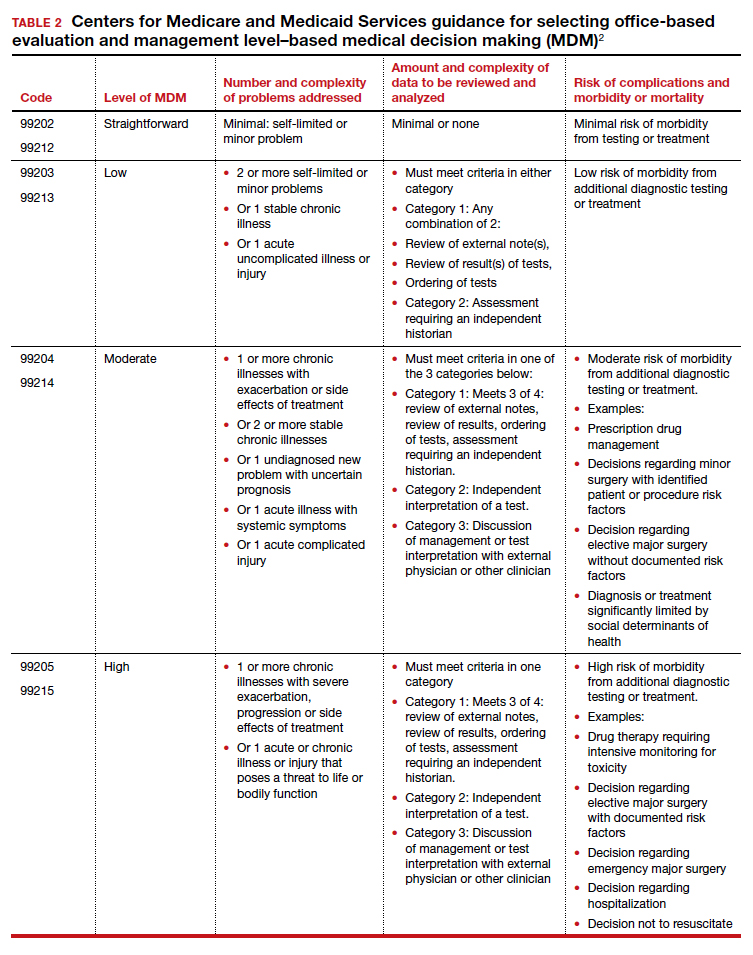
Increase in the valuation of office-based E/M services
The Medicare Physician Fee Schedule uses a resource-based relative value system to determine time and intensity of the work of clinical practice. This system recognizes 3 major factors that influence the resources required to provide a service:
- work of the clinician
- practice expense for technical components
- cost of professional liability insurance.
Many primary care professional associations have long contended that CMS has undervalued office-based E/M services relative to procedures, resulting in the devaluing of primary care practice. After the CPT code descriptors were updated by the CPT editorial panel, 52 specialty societies surveyed their members to provide inputs to CMS on the time and intensity of the office and other outpatient E/M codes as currently practiced. The American Medical Association’s Specialty Society Resource-Based Relative Value Scale Update Committee (RUC) reviewed the surveys and provided new inputs via open comment to CMS. CMS has responded to this feedback with a review of the intensity of clinical work required to provide an ambulatory visit service. In response to the review, CMS proposes to accept the recommendations of the RUC representing the house of medicine and increase the work and practice expense relative value assigned to new and established office visit codes. Overall, the combination of changes in relative values assigned for the work of the clinician and the expense of practice, increases the total value of office-based E/M codes for new patients by 7% to 14% and for established patients from 28% to 46% (see supplemental table in the sidebar at the end of this article).
Continue to: Decreased payments for procedural services...
Decreased payments for procedural services
Medicare is required to offset increased payment in one arena of health care delivery with decreased payment in other arenas of care, thereby achieving “budget-neutrality.” As detailed above, CMS plans to increase Medicare payments for office-based E/M services. Payment for services is calculated by multiplying the total RVUs for a particular service by a “conversion factor” (ie, number of dollars per RVU). To achieve budget-neutrality, CMS has proposed substantially reducing the conversion factor for 2021 (from $36.09 to $32.26), which will effectively decrease Medicare payments for procedural services since their RVUs have not changed. While the AMA RUC and many specialty societies continue to strongly advocate for the E/M work RVU increases to be included in the E/M components of 10- and 90-day global services, CMS has proposed to implement them only for “stand alone” E/M services.
Organizations are lobbying to delay or prevent the planned decrease in conversion factor, which results in substantial declines in payment for procedural services. (See "What do the Medicare billing changes mean for the Obstetrical Bundled services?" at the end of this article.) Due to the economic and clinical practice challenges caused by the coronavirus disease 2019 (COVID-19) pandemic it would be best if CMS did not reduce payments to physicians who are experts in procedural health care, thereby avoiding the risk of reduced access to these vital services.
If the current CMS changes in payment are implemented, endocrinologists, rheumatologists, and family physicians will have an increase in payment, and radiologists, pathologists, and surgeons will have a decrease in payment (TABLE 3).6 Obstetrics and gynecology is projected to have an 8% increase in Medicare payment. However, if an obstetrician-gynecologist derives most of their Medicare payments from surgical procedures, they are likely to have a decrease in payment from Medicare. Other payers will be incorporating the new coding structure for 2021; however, their payment structures and conversion factors are likely to vary. It is important to note that the RVUs for procedures have not changed. The budget neutrality adjustment resulted in a much lower conversion factor and therefore a decrease in payment for those specialties whose RVUs did not increase.
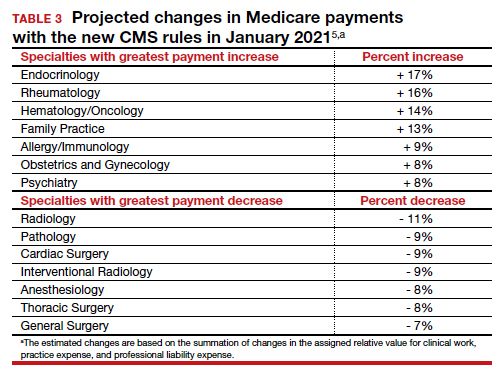
Bottom line
Working through the Medicare, Medicaid, and CHIP programs, CMS can influence greatly the practice of medicine including medical record documentation practices and payment rates for every clinical service. CMS proposes to end the onerous “bean counting” approach to billing compliance and refocus on the complexity of MDM as the foundation for selecting a billing code level. This change is long overdue, valuing the effective management of complex patients in office practice. Hopefully, CMS will reverse the planned reduction in the payment for procedural services, preserving patient access to important health care services. ●
The CY 2020 Medicare Physician Fee Schedule Final Rule was published electronically in the Federal Register on November 1, 2019. This final rule aligns the evaluation and management (E/M) coding and payment with changes recommended by the Current Procedural Terminology (CPT) Editorial Panel and American Medical Association’s (AMA) Specialty Society Resource-Based Relative Value Scale Update Committee (RUC) for office/outpatient E/M visits. Unfortunately, the Centers for Medicare and Medicaid Services (CMS) did not agree with the RUC, AMA, and specialty societies that the E/M payment changes should be applicable across all global services that incorporate E/M visits—despite the fact that the values proposed by the RUC incorporated survey data from 52 specialties, representing most of medicine (including those specialties that predominantly perform procedures). Specifically, CMS expressed the view that the number of E/M visits within the 10- and 90-day global codes, as well as the maternity care bundle, were difficult to validate; therefore, the increased values would not be distributed to those procedural services.
Many professional societies expressed significant concerns about the resulting budget neutrality adjustments that would occur effective January 2021. The great news for ObGyns is that the American College of Obstetricians and Gynecologists (ACOG) was able to respond directly to CMS’s concerns with data to support the number of prenatal visits within the Obstetrical Bundle. Tapping into a de-identified, cloud-based data set of prenatal records—representing more than 1,100 obstetric providers with close to 30,000 recently completed pregnancies—ACOG was able to document both a mean and median number of prenatal visits across a broad geographic, payer, and patient demographic that supported the 13 prenatal visits in the Obstetrical Bundle.
With ACOG’s advocacy and ability to provide data to CMS, the proposed physician fee schedule rule for 2021 has proposed to incorporate the E/M increased reimbursement into the prenatal care codes. Now we urge the CMS to finalize this proposal. Although Medicare pays for a tiny number of pregnancies annually, we hope that all payers, including Medicaid and managed care plans, will agree with this acknowledgement of the increased work of evaluation and management that obstetricians provide during prenatal care. Join ACOG in telling CMS to finalize their proposal to increase the values of the global obstetric codes: https://acog.quorum.us/campaign/28579/.
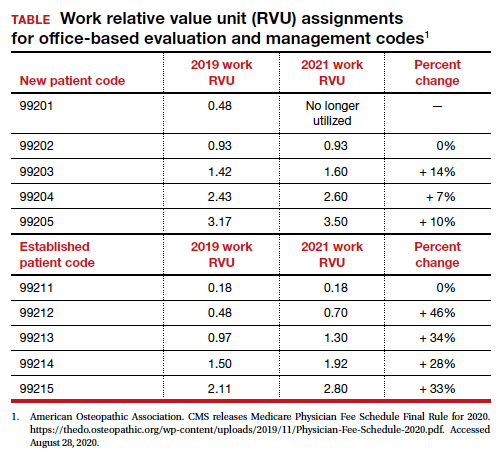
- Centers for Medicare and Medicaid Services. https://www.cms.gov/. Accessed August 28, 2020.
- American Medical Association. CPT Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes. 2019. https://www.ama-assn.org /system/files/2019-06/cpt-office-prolonged-svs -code-changes.pdf. Accessed August 28, 2020.
- The American Academy of Family Physicians. Family medicine updates. Ann Fam Med. 2020;18:84-85. doi: 10.1370/afm.2508.
- Centers for Medicare and Medicaid Services. Final policy, payment and quality provisions changes to the Medicare Physician Fee Schedule for calendar year 2019. November 1, 2018. https://www.cms.gov/newsroom/fact-sheets /final-policy-payment-and-quality-provisionschanges-medicare-physician-fee-schedulecalendar-year. Accessed August 28, 2020.
- Department of Health and Human Services; Centers for Medicare and Medicaid Services. 42 CFR Parts 410, 414, 415, 423, 424, and 425. Federal Register. 2020;85(159). https://www.govinfo.gov /content/pkg/FR-2020-08-17/pdf/2020-17127 .pdf. Accessed August 28, 2020.
The Centers for Medicare and Medicaid Services (CMS) finalized an increase in the relative value of evaluation and management (E/M) service codes effective January 1, 2021, which results in an overall decrease in the payment for procedural services in the Medicare program. (Due to the mandate for budget neutrality, an increase in relative value units [RVUs] for E/M resulted in a large decrease in the conversion factor—the number of dollars per RVU). This has increased payments for endocrinologists, rheumatologists, and family medicine clinicians and decreased payments for radiologists, pathologists, and surgeons.
In a major win for physicians, CMS proposes to simplify documentation requirements for billing and focus on the complexity of the medical decision making (MDM) or the total time needed to care for the patient on the date of the service as the foundation for determining the relative value of the service. Therefore, there is no more counting bullets—ie, we don’t have to perform a comprehensive physical exam or review of systems to achieve a high level code! Prior to this change, time was only available for coding purposes when counseling and coordination of care was the predominant service (>50%), and only face-to-face time with the patient was considered. Effective January 1, for office and other outpatient services, total time on the calendar date of the encounter will be used. This acknowledges the intensity and value of non–face-to-face work.
Acting through CMS, the federal government influences greatly the US health care system. CMS is an agency in the Department of Health and Human Services that administers the Medicare program and partners with state governments to administer the Health Insurance Exchanges, Medicaid, and the Children’s Health Insurance programs (CHIP).1 In addition, CMS is responsible for enforcing quality care standards in long-term care facilities and clinical laboratories and the implementation of the Health Insurance Portability and Accountability Act.1
In January, CMS plans the following major changes to coding and documentation2,3:
- Selection of the level of E/M service will no longer require documentation of bullet points in the history, physical exam, and MDM. The simplified system allows physicians and qualified health care professionals to code either by total time (both face-to-face and non–face-to-face) on the date of the encounter or by level of MDM.
- For established office patients, 5 levels of office-based evaluation and management services will be retained. CMS had initially proposed to reduce the number of office-based E/M codes from 5 to 3, combining code levels 2, 3, and 4 into 1 code.4 However, after receiving feedback from professional societies and the public, CMS abandoned the plan for radical simplification of coding levels.2,3 Implementation of their proposal would have resulted in the same payment for treatment of a hang nail as for a complex gyn patient with multiple medical problems. Both patient advocacy groups and professional societies argued that incentives originally were misaligned.
- For new office patients, since both 99201 and 99202 require straightforward MDM, the level 1 code (99201) has been eliminated, reducing the number of code levels from 5 to 4.
- History and physical exam will no longer be used to determine code level for office E/M codes. These elements will be required only as medically appropriate. This means that documentation review will no longer focus on “bean counting” the elements in the history and physical exam.
- Following a reassessment of the actual time required to provide E/M services in real-life practice, CMS plans to markedly increase the relative value of office visits for established patients and modestly increase the relative value of office visits for new patients. CMS operates under the principle of “neutral budgeting,” meaning that an increase of the relative value of E/M codes will result in a decrease in the payment for procedural codes. The actual RVUs for procedural services do not change; however, budget neutrality requires a decrease in the dollar conversion factor. The proposed changes will increase the payment for E/M services and decrease payments for procedural services.
Continue to: Refocusing practice on MDM complexity...
Refocusing practice on MDM complexity
The practice of medicine is a calling with great rewards. Prominent among those rewards are improving the health of women, children, and the community, developing deep and trusting relationships with patients, families, and clinical colleagues. The practice of medicine is also replete with a host of punishing administrative burdens, including prior authorizations, clunky electronic medical records, poorly designed quality metrics that are applied to clinicians, and billing compliance rules that emphasize the repetitive documentation of clinical information with minimal value.
Some of the most irritating aspects of medical practice are the CMS rules governing medical record documentation required for billing ambulatory office visits. Current coding compliance focuses on counting the number of systems reviewed in the review of systems; the documentation of past history, social history, and family history; the number of organs and organ elements examined during the physical examination; and the complexity of MDM.
In January 2021, CMS plans to adopt new Current Procedural Terminology (CPT) code descriptors for the office and other outpatient E/M services that sunset most of the “bean-counting” metrics and emphasize the importance of the complexity of MDM in guiding selection of a correct code.2 Beginning in January 2021, clinicians will have the option of selecting an E/M code level based on the total amount of time required to provide the office visit service or the complexity of MDM. When selecting a code level based on MDM the new guidance emphasizes the importance of reviewing notes from other clinicians, reviewing test results, ordering of tests, and discussing and coordinating the care of the patient with other treating physicians. These changes reflect a better understanding of what is most important in good medical practice, promoting better patient care. TABLES 1 and 2 provide the initial guidance from CMS concerning selection of E/M code level based on time and MDM, respectively.2 The guidance for using MDM to select an E/M code level is likely to evolve following implementation, so stay tuned. When using MDM to select a code, 2 of the 3 general categories are required to select that level of service.
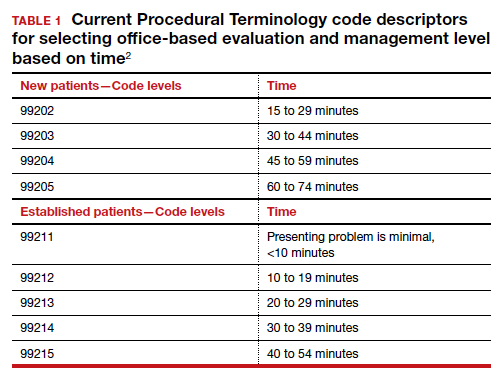
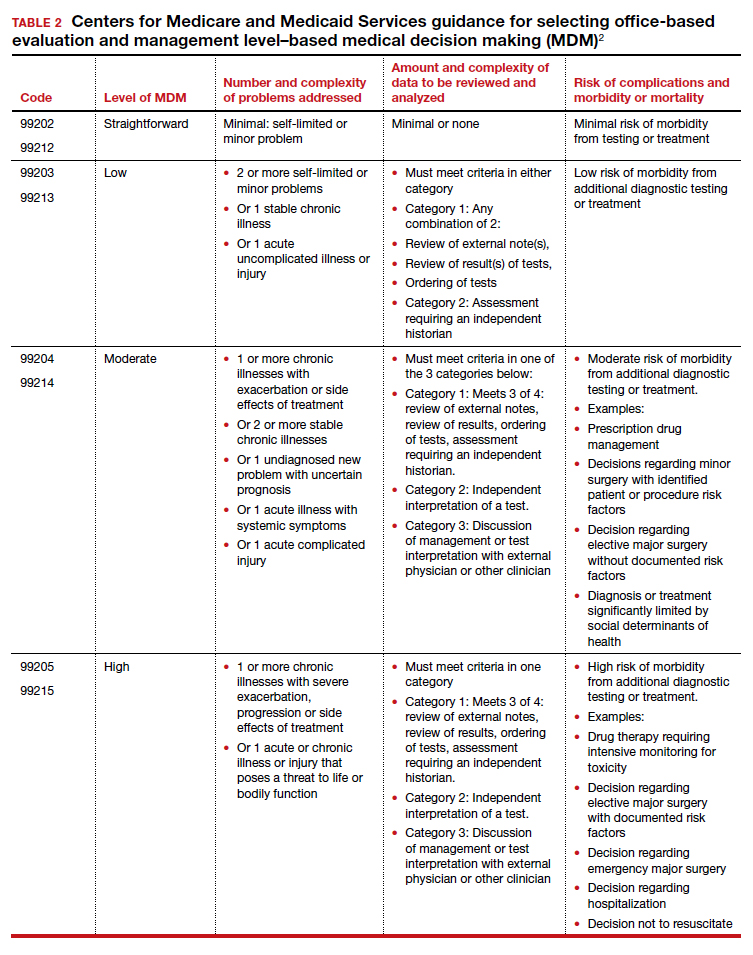
Increase in the valuation of office-based E/M services
The Medicare Physician Fee Schedule uses a resource-based relative value system to determine time and intensity of the work of clinical practice. This system recognizes 3 major factors that influence the resources required to provide a service:
- work of the clinician
- practice expense for technical components
- cost of professional liability insurance.
Many primary care professional associations have long contended that CMS has undervalued office-based E/M services relative to procedures, resulting in the devaluing of primary care practice. After the CPT code descriptors were updated by the CPT editorial panel, 52 specialty societies surveyed their members to provide inputs to CMS on the time and intensity of the office and other outpatient E/M codes as currently practiced. The American Medical Association’s Specialty Society Resource-Based Relative Value Scale Update Committee (RUC) reviewed the surveys and provided new inputs via open comment to CMS. CMS has responded to this feedback with a review of the intensity of clinical work required to provide an ambulatory visit service. In response to the review, CMS proposes to accept the recommendations of the RUC representing the house of medicine and increase the work and practice expense relative value assigned to new and established office visit codes. Overall, the combination of changes in relative values assigned for the work of the clinician and the expense of practice, increases the total value of office-based E/M codes for new patients by 7% to 14% and for established patients from 28% to 46% (see supplemental table in the sidebar at the end of this article).
Continue to: Decreased payments for procedural services...
Decreased payments for procedural services
Medicare is required to offset increased payment in one arena of health care delivery with decreased payment in other arenas of care, thereby achieving “budget-neutrality.” As detailed above, CMS plans to increase Medicare payments for office-based E/M services. Payment for services is calculated by multiplying the total RVUs for a particular service by a “conversion factor” (ie, number of dollars per RVU). To achieve budget-neutrality, CMS has proposed substantially reducing the conversion factor for 2021 (from $36.09 to $32.26), which will effectively decrease Medicare payments for procedural services since their RVUs have not changed. While the AMA RUC and many specialty societies continue to strongly advocate for the E/M work RVU increases to be included in the E/M components of 10- and 90-day global services, CMS has proposed to implement them only for “stand alone” E/M services.
Organizations are lobbying to delay or prevent the planned decrease in conversion factor, which results in substantial declines in payment for procedural services. (See "What do the Medicare billing changes mean for the Obstetrical Bundled services?" at the end of this article.) Due to the economic and clinical practice challenges caused by the coronavirus disease 2019 (COVID-19) pandemic it would be best if CMS did not reduce payments to physicians who are experts in procedural health care, thereby avoiding the risk of reduced access to these vital services.
If the current CMS changes in payment are implemented, endocrinologists, rheumatologists, and family physicians will have an increase in payment, and radiologists, pathologists, and surgeons will have a decrease in payment (TABLE 3).6 Obstetrics and gynecology is projected to have an 8% increase in Medicare payment. However, if an obstetrician-gynecologist derives most of their Medicare payments from surgical procedures, they are likely to have a decrease in payment from Medicare. Other payers will be incorporating the new coding structure for 2021; however, their payment structures and conversion factors are likely to vary. It is important to note that the RVUs for procedures have not changed. The budget neutrality adjustment resulted in a much lower conversion factor and therefore a decrease in payment for those specialties whose RVUs did not increase.
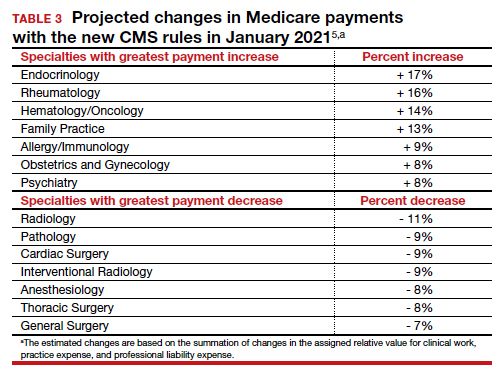
Bottom line
Working through the Medicare, Medicaid, and CHIP programs, CMS can influence greatly the practice of medicine including medical record documentation practices and payment rates for every clinical service. CMS proposes to end the onerous “bean counting” approach to billing compliance and refocus on the complexity of MDM as the foundation for selecting a billing code level. This change is long overdue, valuing the effective management of complex patients in office practice. Hopefully, CMS will reverse the planned reduction in the payment for procedural services, preserving patient access to important health care services. ●
The CY 2020 Medicare Physician Fee Schedule Final Rule was published electronically in the Federal Register on November 1, 2019. This final rule aligns the evaluation and management (E/M) coding and payment with changes recommended by the Current Procedural Terminology (CPT) Editorial Panel and American Medical Association’s (AMA) Specialty Society Resource-Based Relative Value Scale Update Committee (RUC) for office/outpatient E/M visits. Unfortunately, the Centers for Medicare and Medicaid Services (CMS) did not agree with the RUC, AMA, and specialty societies that the E/M payment changes should be applicable across all global services that incorporate E/M visits—despite the fact that the values proposed by the RUC incorporated survey data from 52 specialties, representing most of medicine (including those specialties that predominantly perform procedures). Specifically, CMS expressed the view that the number of E/M visits within the 10- and 90-day global codes, as well as the maternity care bundle, were difficult to validate; therefore, the increased values would not be distributed to those procedural services.
Many professional societies expressed significant concerns about the resulting budget neutrality adjustments that would occur effective January 2021. The great news for ObGyns is that the American College of Obstetricians and Gynecologists (ACOG) was able to respond directly to CMS’s concerns with data to support the number of prenatal visits within the Obstetrical Bundle. Tapping into a de-identified, cloud-based data set of prenatal records—representing more than 1,100 obstetric providers with close to 30,000 recently completed pregnancies—ACOG was able to document both a mean and median number of prenatal visits across a broad geographic, payer, and patient demographic that supported the 13 prenatal visits in the Obstetrical Bundle.
With ACOG’s advocacy and ability to provide data to CMS, the proposed physician fee schedule rule for 2021 has proposed to incorporate the E/M increased reimbursement into the prenatal care codes. Now we urge the CMS to finalize this proposal. Although Medicare pays for a tiny number of pregnancies annually, we hope that all payers, including Medicaid and managed care plans, will agree with this acknowledgement of the increased work of evaluation and management that obstetricians provide during prenatal care. Join ACOG in telling CMS to finalize their proposal to increase the values of the global obstetric codes: https://acog.quorum.us/campaign/28579/.
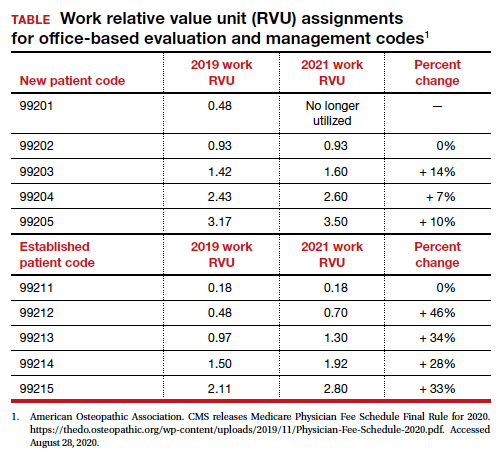
The Centers for Medicare and Medicaid Services (CMS) finalized an increase in the relative value of evaluation and management (E/M) service codes effective January 1, 2021, which results in an overall decrease in the payment for procedural services in the Medicare program. (Due to the mandate for budget neutrality, an increase in relative value units [RVUs] for E/M resulted in a large decrease in the conversion factor—the number of dollars per RVU). This has increased payments for endocrinologists, rheumatologists, and family medicine clinicians and decreased payments for radiologists, pathologists, and surgeons.
In a major win for physicians, CMS proposes to simplify documentation requirements for billing and focus on the complexity of the medical decision making (MDM) or the total time needed to care for the patient on the date of the service as the foundation for determining the relative value of the service. Therefore, there is no more counting bullets—ie, we don’t have to perform a comprehensive physical exam or review of systems to achieve a high level code! Prior to this change, time was only available for coding purposes when counseling and coordination of care was the predominant service (>50%), and only face-to-face time with the patient was considered. Effective January 1, for office and other outpatient services, total time on the calendar date of the encounter will be used. This acknowledges the intensity and value of non–face-to-face work.
Acting through CMS, the federal government influences greatly the US health care system. CMS is an agency in the Department of Health and Human Services that administers the Medicare program and partners with state governments to administer the Health Insurance Exchanges, Medicaid, and the Children’s Health Insurance programs (CHIP).1 In addition, CMS is responsible for enforcing quality care standards in long-term care facilities and clinical laboratories and the implementation of the Health Insurance Portability and Accountability Act.1
In January, CMS plans the following major changes to coding and documentation2,3:
- Selection of the level of E/M service will no longer require documentation of bullet points in the history, physical exam, and MDM. The simplified system allows physicians and qualified health care professionals to code either by total time (both face-to-face and non–face-to-face) on the date of the encounter or by level of MDM.
- For established office patients, 5 levels of office-based evaluation and management services will be retained. CMS had initially proposed to reduce the number of office-based E/M codes from 5 to 3, combining code levels 2, 3, and 4 into 1 code.4 However, after receiving feedback from professional societies and the public, CMS abandoned the plan for radical simplification of coding levels.2,3 Implementation of their proposal would have resulted in the same payment for treatment of a hang nail as for a complex gyn patient with multiple medical problems. Both patient advocacy groups and professional societies argued that incentives originally were misaligned.
- For new office patients, since both 99201 and 99202 require straightforward MDM, the level 1 code (99201) has been eliminated, reducing the number of code levels from 5 to 4.
- History and physical exam will no longer be used to determine code level for office E/M codes. These elements will be required only as medically appropriate. This means that documentation review will no longer focus on “bean counting” the elements in the history and physical exam.
- Following a reassessment of the actual time required to provide E/M services in real-life practice, CMS plans to markedly increase the relative value of office visits for established patients and modestly increase the relative value of office visits for new patients. CMS operates under the principle of “neutral budgeting,” meaning that an increase of the relative value of E/M codes will result in a decrease in the payment for procedural codes. The actual RVUs for procedural services do not change; however, budget neutrality requires a decrease in the dollar conversion factor. The proposed changes will increase the payment for E/M services and decrease payments for procedural services.
Continue to: Refocusing practice on MDM complexity...
Refocusing practice on MDM complexity
The practice of medicine is a calling with great rewards. Prominent among those rewards are improving the health of women, children, and the community, developing deep and trusting relationships with patients, families, and clinical colleagues. The practice of medicine is also replete with a host of punishing administrative burdens, including prior authorizations, clunky electronic medical records, poorly designed quality metrics that are applied to clinicians, and billing compliance rules that emphasize the repetitive documentation of clinical information with minimal value.
Some of the most irritating aspects of medical practice are the CMS rules governing medical record documentation required for billing ambulatory office visits. Current coding compliance focuses on counting the number of systems reviewed in the review of systems; the documentation of past history, social history, and family history; the number of organs and organ elements examined during the physical examination; and the complexity of MDM.
In January 2021, CMS plans to adopt new Current Procedural Terminology (CPT) code descriptors for the office and other outpatient E/M services that sunset most of the “bean-counting” metrics and emphasize the importance of the complexity of MDM in guiding selection of a correct code.2 Beginning in January 2021, clinicians will have the option of selecting an E/M code level based on the total amount of time required to provide the office visit service or the complexity of MDM. When selecting a code level based on MDM the new guidance emphasizes the importance of reviewing notes from other clinicians, reviewing test results, ordering of tests, and discussing and coordinating the care of the patient with other treating physicians. These changes reflect a better understanding of what is most important in good medical practice, promoting better patient care. TABLES 1 and 2 provide the initial guidance from CMS concerning selection of E/M code level based on time and MDM, respectively.2 The guidance for using MDM to select an E/M code level is likely to evolve following implementation, so stay tuned. When using MDM to select a code, 2 of the 3 general categories are required to select that level of service.
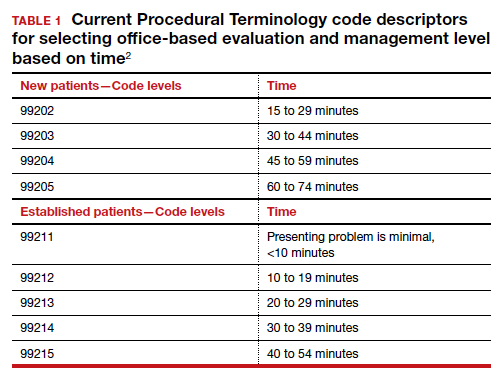
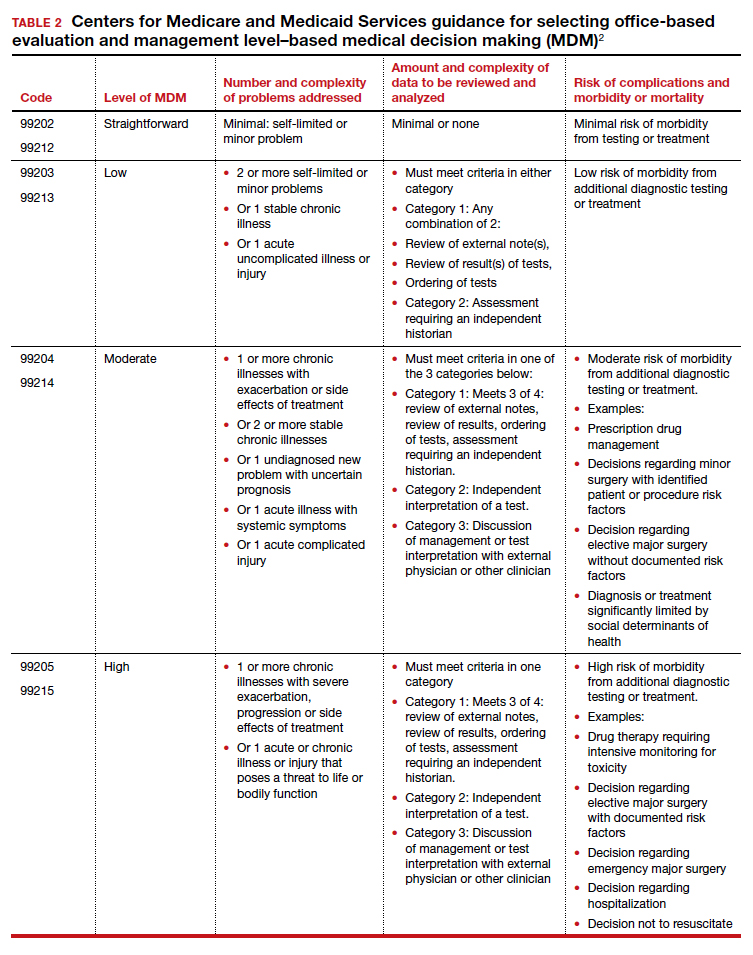
Increase in the valuation of office-based E/M services
The Medicare Physician Fee Schedule uses a resource-based relative value system to determine time and intensity of the work of clinical practice. This system recognizes 3 major factors that influence the resources required to provide a service:
- work of the clinician
- practice expense for technical components
- cost of professional liability insurance.
Many primary care professional associations have long contended that CMS has undervalued office-based E/M services relative to procedures, resulting in the devaluing of primary care practice. After the CPT code descriptors were updated by the CPT editorial panel, 52 specialty societies surveyed their members to provide inputs to CMS on the time and intensity of the office and other outpatient E/M codes as currently practiced. The American Medical Association’s Specialty Society Resource-Based Relative Value Scale Update Committee (RUC) reviewed the surveys and provided new inputs via open comment to CMS. CMS has responded to this feedback with a review of the intensity of clinical work required to provide an ambulatory visit service. In response to the review, CMS proposes to accept the recommendations of the RUC representing the house of medicine and increase the work and practice expense relative value assigned to new and established office visit codes. Overall, the combination of changes in relative values assigned for the work of the clinician and the expense of practice, increases the total value of office-based E/M codes for new patients by 7% to 14% and for established patients from 28% to 46% (see supplemental table in the sidebar at the end of this article).
Continue to: Decreased payments for procedural services...
Decreased payments for procedural services
Medicare is required to offset increased payment in one arena of health care delivery with decreased payment in other arenas of care, thereby achieving “budget-neutrality.” As detailed above, CMS plans to increase Medicare payments for office-based E/M services. Payment for services is calculated by multiplying the total RVUs for a particular service by a “conversion factor” (ie, number of dollars per RVU). To achieve budget-neutrality, CMS has proposed substantially reducing the conversion factor for 2021 (from $36.09 to $32.26), which will effectively decrease Medicare payments for procedural services since their RVUs have not changed. While the AMA RUC and many specialty societies continue to strongly advocate for the E/M work RVU increases to be included in the E/M components of 10- and 90-day global services, CMS has proposed to implement them only for “stand alone” E/M services.
Organizations are lobbying to delay or prevent the planned decrease in conversion factor, which results in substantial declines in payment for procedural services. (See "What do the Medicare billing changes mean for the Obstetrical Bundled services?" at the end of this article.) Due to the economic and clinical practice challenges caused by the coronavirus disease 2019 (COVID-19) pandemic it would be best if CMS did not reduce payments to physicians who are experts in procedural health care, thereby avoiding the risk of reduced access to these vital services.
If the current CMS changes in payment are implemented, endocrinologists, rheumatologists, and family physicians will have an increase in payment, and radiologists, pathologists, and surgeons will have a decrease in payment (TABLE 3).6 Obstetrics and gynecology is projected to have an 8% increase in Medicare payment. However, if an obstetrician-gynecologist derives most of their Medicare payments from surgical procedures, they are likely to have a decrease in payment from Medicare. Other payers will be incorporating the new coding structure for 2021; however, their payment structures and conversion factors are likely to vary. It is important to note that the RVUs for procedures have not changed. The budget neutrality adjustment resulted in a much lower conversion factor and therefore a decrease in payment for those specialties whose RVUs did not increase.
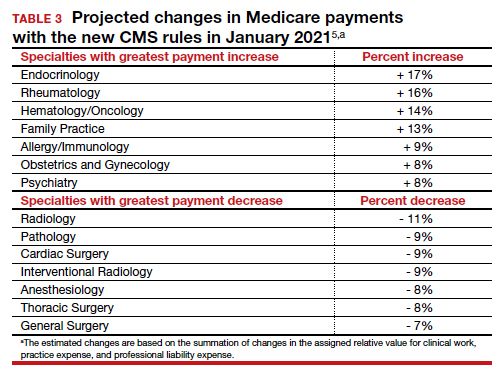
Bottom line
Working through the Medicare, Medicaid, and CHIP programs, CMS can influence greatly the practice of medicine including medical record documentation practices and payment rates for every clinical service. CMS proposes to end the onerous “bean counting” approach to billing compliance and refocus on the complexity of MDM as the foundation for selecting a billing code level. This change is long overdue, valuing the effective management of complex patients in office practice. Hopefully, CMS will reverse the planned reduction in the payment for procedural services, preserving patient access to important health care services. ●
The CY 2020 Medicare Physician Fee Schedule Final Rule was published electronically in the Federal Register on November 1, 2019. This final rule aligns the evaluation and management (E/M) coding and payment with changes recommended by the Current Procedural Terminology (CPT) Editorial Panel and American Medical Association’s (AMA) Specialty Society Resource-Based Relative Value Scale Update Committee (RUC) for office/outpatient E/M visits. Unfortunately, the Centers for Medicare and Medicaid Services (CMS) did not agree with the RUC, AMA, and specialty societies that the E/M payment changes should be applicable across all global services that incorporate E/M visits—despite the fact that the values proposed by the RUC incorporated survey data from 52 specialties, representing most of medicine (including those specialties that predominantly perform procedures). Specifically, CMS expressed the view that the number of E/M visits within the 10- and 90-day global codes, as well as the maternity care bundle, were difficult to validate; therefore, the increased values would not be distributed to those procedural services.
Many professional societies expressed significant concerns about the resulting budget neutrality adjustments that would occur effective January 2021. The great news for ObGyns is that the American College of Obstetricians and Gynecologists (ACOG) was able to respond directly to CMS’s concerns with data to support the number of prenatal visits within the Obstetrical Bundle. Tapping into a de-identified, cloud-based data set of prenatal records—representing more than 1,100 obstetric providers with close to 30,000 recently completed pregnancies—ACOG was able to document both a mean and median number of prenatal visits across a broad geographic, payer, and patient demographic that supported the 13 prenatal visits in the Obstetrical Bundle.
With ACOG’s advocacy and ability to provide data to CMS, the proposed physician fee schedule rule for 2021 has proposed to incorporate the E/M increased reimbursement into the prenatal care codes. Now we urge the CMS to finalize this proposal. Although Medicare pays for a tiny number of pregnancies annually, we hope that all payers, including Medicaid and managed care plans, will agree with this acknowledgement of the increased work of evaluation and management that obstetricians provide during prenatal care. Join ACOG in telling CMS to finalize their proposal to increase the values of the global obstetric codes: https://acog.quorum.us/campaign/28579/.
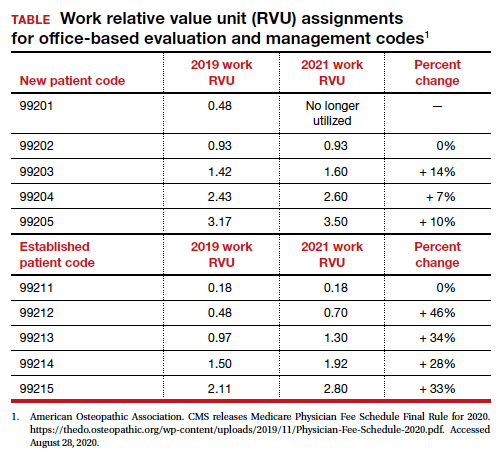
- Centers for Medicare and Medicaid Services. https://www.cms.gov/. Accessed August 28, 2020.
- American Medical Association. CPT Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes. 2019. https://www.ama-assn.org /system/files/2019-06/cpt-office-prolonged-svs -code-changes.pdf. Accessed August 28, 2020.
- The American Academy of Family Physicians. Family medicine updates. Ann Fam Med. 2020;18:84-85. doi: 10.1370/afm.2508.
- Centers for Medicare and Medicaid Services. Final policy, payment and quality provisions changes to the Medicare Physician Fee Schedule for calendar year 2019. November 1, 2018. https://www.cms.gov/newsroom/fact-sheets /final-policy-payment-and-quality-provisionschanges-medicare-physician-fee-schedulecalendar-year. Accessed August 28, 2020.
- Department of Health and Human Services; Centers for Medicare and Medicaid Services. 42 CFR Parts 410, 414, 415, 423, 424, and 425. Federal Register. 2020;85(159). https://www.govinfo.gov /content/pkg/FR-2020-08-17/pdf/2020-17127 .pdf. Accessed August 28, 2020.
- Centers for Medicare and Medicaid Services. https://www.cms.gov/. Accessed August 28, 2020.
- American Medical Association. CPT Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes. 2019. https://www.ama-assn.org /system/files/2019-06/cpt-office-prolonged-svs -code-changes.pdf. Accessed August 28, 2020.
- The American Academy of Family Physicians. Family medicine updates. Ann Fam Med. 2020;18:84-85. doi: 10.1370/afm.2508.
- Centers for Medicare and Medicaid Services. Final policy, payment and quality provisions changes to the Medicare Physician Fee Schedule for calendar year 2019. November 1, 2018. https://www.cms.gov/newsroom/fact-sheets /final-policy-payment-and-quality-provisionschanges-medicare-physician-fee-schedulecalendar-year. Accessed August 28, 2020.
- Department of Health and Human Services; Centers for Medicare and Medicaid Services. 42 CFR Parts 410, 414, 415, 423, 424, and 425. Federal Register. 2020;85(159). https://www.govinfo.gov /content/pkg/FR-2020-08-17/pdf/2020-17127 .pdf. Accessed August 28, 2020.
Lifting the restrictions on mifepristone during COVID-19: A step in the right direction
Mifepristone is a safe, effective, and well-tolerated medication for managing miscarriage and for medical abortion when combined with misoprostol.1,2 Since the US Food and Drug Administration (FDA) approved its use in 2000, more than 4 million women have used this medication.3 The combination of mifepristone with misoprostol was used for 39% of all US abortions in 2017.4 Approximately 10% of all clinically recognized pregnancies end in miscarriages, and many are safely managed with either misoprostol alone or with the combination of mifepristone and misoprostol.5
The issue
The prescription and distribution of mifepristone is highly regulated by the FDA via requirements outlined in the Risk Evaluation and Mitigation Strategies (REMS) drug safety program. The FDA may determine a REMS is necessary for a specific drug to ensure the benefits of a drug outweigh the potential risks. A REMS may include an informative package insert for patients, follow-up communication to prescribers—including letters, safety protocols or recommended laboratory tests, or Elements to Assure Safe Use (ETASU). ETASU are types of REMS that are placed on medications that have significant potential for serious adverse effects, and without such restrictions FDA approval would be rescinded.
Are mifepristone requirements fairly applied?
The 3 ETASU restrictions on the distribution of mifepristone are in-person dispensation, prescriber certification, and patient signatures on special forms.6 The in-person dispensing requirement is applied to only 16 other medications (one of which is Mifeprex, the brand version of mifepristone), and Mifeprex/mifepristone are the only ones deemed safe for self-administration—meaning that patients receive the drug from a clinic but then may take it at a site of their choosing. The prescriber certification requirement places expectations on providers to account for distribution of doses and keep records of serial numbers (in effect, having clinicians act as both physician and pharmacist, as most medications are distributed and recorded in pharmacies). The patient form was recommended for elimination in 2016 due to its duplicative information and burden on patients—a recommendation that was then overruled by the FDA commissioner.7
These 3 requirements placed on mifepristone specifically target dosages for use related to abortions and miscarriages. Mifepristone is used to treat other medical conditions, with much higher doses, without the same restrictions—in fact, the FDA has allowed much higher doses of mifepristone to be mailed directly to a patient when prescribed for different disorders. The American College of Obstetricians and Gynecologists (ACOG) has long opposed the burdensome REMS requirements on mifepristone for reproductive health indications.8
Arguments regarding the safety of mifepristone must be understood in the context of how the medication is taken, and the unique difference with other medications that must be administered by physicians or in health care facilities. Mifepristone is self-administered, and the desired effect—evacuation of uterine contents—typically occurs after a patient takes the accompanying medication misoprostol, which is some 24 to 72 hours later. This timeframe makes it highly unlikely that any patient would be in the presence of their provider at the time of medication effect, thus an in-person dispensing requirement has no medical bearing on the outcome of the health of the patient.
REMS changes during the COVID-19 pandemic
The coronavirus disease 2019 (COVID-19) pandemic has necessarily changed the structure of REMS and ETASU requirements for many medications, with changes made in order to mitigate viral transmission through the limitation of unnecessary visits to clinics or hospitals. The FDA announced in March of 2020 that it would not enforce pre-prescription requirements, such as laboratory or magnetic resonance imaging results, for many medications (including those more toxic than mifepristone), and that it would lift the requirement for in-person dispensation of several medications.9 Also in March 2020 the Department of Health and Human Services Secretary (HHS) and the Drug Enforcement Agency (DEA) activated a “telemedicine exception” to allow physicians to use telemedicine to satisfy mandatory requirements for prescribing controlled substances, including opioids.10
Despite repeated pleas from organizations, individuals, and physician groups, the FDA continued to enforce the REMS/ETASU for mifepristone as the pandemic decimated communities. Importantly, the pandemic has not had an equal effect on all communities, and the disparities highlighted in outcomes as related to COVID-19 are also reflected in disparities to access to reproductive choices.11 By enforcing REMS/ETASU for mifepristone during a global pandemic, the FDA has placed additional burden on women and people who menstruate. As offices and clinics have closed, and as many jobs have evaporated, additional barriers have emerged, such as lack of childcare, fewer transportation options, and decreased clinic appointments.
As the pandemic continues to affect communities in the United States, ACOG has issued guidance recommending assessment for eligibility for medical abortion remotely, and has encouraged the use of telemedicine and other remote interactions for its members and patients to limit transmission of the virus.
The lawsuit
On May 27, 2020, the American Civil Liberties Union (ACLU) (on behalf of ACOG, the Council of University Chairs of Obstetrics and Gynecology, New York State Academy of Family Physicians, SisterSong, and Honor MacNaughton, MD) filed a civil action against the FDA and HHS challenging the requirement for in-person dispensing of mifepristone and associated ETASU requirements during the COVID-19 pandemic. The plaintiffs sought this injunction based on the claim that these restrictions during the pandemic infringe on the constitutional rights to patients’ privacy and liberty and to equal protection of the law as protected by the Due Process Clause of the Fifth Amendment. Additionally, the ACLU and other organizations said these unnecessary restrictions place patients, providers, and staff at unnecessary risk of viral exposure amidst a global pandemic.
The verdict
On July 13, 2020, a federal court granted the preliminary injunction to suspend FDA’s enforcement of the in-person requirements of mifepristone for abortion during the COVID-19 pandemic. The court denied the motion for suspension of in-person restrictions as applied to miscarriage management. The preliminary injunction applies nationwide without geographic limitation. It will remain in effect until the end of the litigation or for 30 days following the expiration of the public health emergency.
What the outcome means
This injunction is a step in the right direction for patients and providers to allow for autonomy and clinical practice guided by clinician expertise. However, this ruling remains narrow. Patients must be counseled about mifepristone via telemedicine and sign a Patient Agreement Form, which must be returned electronically or by mail. Patients must receive a copy of the mifepristone medication guide, and dispensing of mifepristone must still be conducted by or under the supervision of a certified provider. The medication may not be dispensed by retail pharmacies, thus requiring providers to arrange for mailing of prescriptions to patients. Given state-based legal statutes regarding mailing of medications, this injunction may not lead to an immediate increase in access to care. In addition, patients seeking management for miscarriage must go to clinic to have mifepristone dispensed and thus risk exposure to viral transmission.
What now?
The regulation of mifepristone—in spite of excellent safety and specifically for the narrow purpose of administration in the setting of abortion and miscarriage care—is by definition a discriminatory practice against patients and providers. As clinicians, we are duty-bound to speak out against injustices to our practices and our patients. At a local level, we can work to implement safe practices in the setting of this injunction and continue to work on a national level to ensure this injunction becomes permanent and with more broad scope to eliminate all of the REMS requirements for mifepristone.
ACTION ITEMS
- Act locally! Are you an abortion provider? Contact your local ACLU (find them here) or lawyer in your area for assistance navigating the legal landscape to prescribe after this injunction.
- Act statewide! Press candidates in your state to stand up for science and data. Support legislative acts and bills that address combating discriminatory regulations.
- Act nationally! The President is responsible for appointing the Commissioner of the FDA and the Secretary of Health and Human Services (with Senate advice and consent). Who we elect matters. Seek out opportunities to become involved in increasing access to and awareness of voter registration and Election Day, and speak out against voter suppression. Make sure you are registered to vote here and check your area to review new recommendations amidst the pandemic.
- American College of Obstetricians and Gynecologists. Practice bulletin number 143: medical management of first trimester abortion. Obstet Gynecol. 2014;123:676-692.
- Schreiber CA, Crenin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170.
- Danco Laboratories. Mifeprex effectiveness and advantages. https://www.earlyoptionpill.com/is-mifeprex-right-for-me/effectiveness-advantages/ Accessed August 2, 2020.
- Jones RK, Witwer E, Jerman J. Abortion incidence and service availability in the United States, 2017. September 2019. https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Practice bulletin no. 150: early pregnancy loss. Obstet Gynecol. 2015;125:1258-1267.
- US Food and Drug Administration. Risk evaluation and mitigation strategy (REMS) single shared system for mifepristone 200 mg. April 2019. https://www.accessdata.fda.gov/drugsatfda_docs/rems/Mifepristone_2019_04_11_REMS_Full.pdf. Accessed September 10, 2020.
- US Food and Drug Administration; Center for Drug Evaluation and Research. 2016 REMS Review, Summary Review 25. March 29, 2016. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/020687Orig1s020SumR.pdf. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Improving access to mifepristone for reproductive health indications. June 2018. https://www.acog.org/clinical-information/policy-and-position-statements/position-statements/2018/improving-access-to-mifepristone-for-reproductive-health-indications. Accessed August 2, 2020.
- US Food and Drug Administration. Policy for certain REMS requirements during the COVID-19 public health emergency: guidance for industry and health care professionals. March 2020. https://www.fda.gov/media/136317/download. Accessed September 10, 2020.
- US Department of Justice. US Drug Enforcement Administration. COVID-19 Information Page, Telemedicine. https://www.deadiversion.usdoj.gov/coronavirus.html#TELE. Accessed May 25, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019: health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Updated July 24, 2020. Accessed September 10, 2020.
Mifepristone is a safe, effective, and well-tolerated medication for managing miscarriage and for medical abortion when combined with misoprostol.1,2 Since the US Food and Drug Administration (FDA) approved its use in 2000, more than 4 million women have used this medication.3 The combination of mifepristone with misoprostol was used for 39% of all US abortions in 2017.4 Approximately 10% of all clinically recognized pregnancies end in miscarriages, and many are safely managed with either misoprostol alone or with the combination of mifepristone and misoprostol.5
The issue
The prescription and distribution of mifepristone is highly regulated by the FDA via requirements outlined in the Risk Evaluation and Mitigation Strategies (REMS) drug safety program. The FDA may determine a REMS is necessary for a specific drug to ensure the benefits of a drug outweigh the potential risks. A REMS may include an informative package insert for patients, follow-up communication to prescribers—including letters, safety protocols or recommended laboratory tests, or Elements to Assure Safe Use (ETASU). ETASU are types of REMS that are placed on medications that have significant potential for serious adverse effects, and without such restrictions FDA approval would be rescinded.
Are mifepristone requirements fairly applied?
The 3 ETASU restrictions on the distribution of mifepristone are in-person dispensation, prescriber certification, and patient signatures on special forms.6 The in-person dispensing requirement is applied to only 16 other medications (one of which is Mifeprex, the brand version of mifepristone), and Mifeprex/mifepristone are the only ones deemed safe for self-administration—meaning that patients receive the drug from a clinic but then may take it at a site of their choosing. The prescriber certification requirement places expectations on providers to account for distribution of doses and keep records of serial numbers (in effect, having clinicians act as both physician and pharmacist, as most medications are distributed and recorded in pharmacies). The patient form was recommended for elimination in 2016 due to its duplicative information and burden on patients—a recommendation that was then overruled by the FDA commissioner.7
These 3 requirements placed on mifepristone specifically target dosages for use related to abortions and miscarriages. Mifepristone is used to treat other medical conditions, with much higher doses, without the same restrictions—in fact, the FDA has allowed much higher doses of mifepristone to be mailed directly to a patient when prescribed for different disorders. The American College of Obstetricians and Gynecologists (ACOG) has long opposed the burdensome REMS requirements on mifepristone for reproductive health indications.8
Arguments regarding the safety of mifepristone must be understood in the context of how the medication is taken, and the unique difference with other medications that must be administered by physicians or in health care facilities. Mifepristone is self-administered, and the desired effect—evacuation of uterine contents—typically occurs after a patient takes the accompanying medication misoprostol, which is some 24 to 72 hours later. This timeframe makes it highly unlikely that any patient would be in the presence of their provider at the time of medication effect, thus an in-person dispensing requirement has no medical bearing on the outcome of the health of the patient.
REMS changes during the COVID-19 pandemic
The coronavirus disease 2019 (COVID-19) pandemic has necessarily changed the structure of REMS and ETASU requirements for many medications, with changes made in order to mitigate viral transmission through the limitation of unnecessary visits to clinics or hospitals. The FDA announced in March of 2020 that it would not enforce pre-prescription requirements, such as laboratory or magnetic resonance imaging results, for many medications (including those more toxic than mifepristone), and that it would lift the requirement for in-person dispensation of several medications.9 Also in March 2020 the Department of Health and Human Services Secretary (HHS) and the Drug Enforcement Agency (DEA) activated a “telemedicine exception” to allow physicians to use telemedicine to satisfy mandatory requirements for prescribing controlled substances, including opioids.10
Despite repeated pleas from organizations, individuals, and physician groups, the FDA continued to enforce the REMS/ETASU for mifepristone as the pandemic decimated communities. Importantly, the pandemic has not had an equal effect on all communities, and the disparities highlighted in outcomes as related to COVID-19 are also reflected in disparities to access to reproductive choices.11 By enforcing REMS/ETASU for mifepristone during a global pandemic, the FDA has placed additional burden on women and people who menstruate. As offices and clinics have closed, and as many jobs have evaporated, additional barriers have emerged, such as lack of childcare, fewer transportation options, and decreased clinic appointments.
As the pandemic continues to affect communities in the United States, ACOG has issued guidance recommending assessment for eligibility for medical abortion remotely, and has encouraged the use of telemedicine and other remote interactions for its members and patients to limit transmission of the virus.
The lawsuit
On May 27, 2020, the American Civil Liberties Union (ACLU) (on behalf of ACOG, the Council of University Chairs of Obstetrics and Gynecology, New York State Academy of Family Physicians, SisterSong, and Honor MacNaughton, MD) filed a civil action against the FDA and HHS challenging the requirement for in-person dispensing of mifepristone and associated ETASU requirements during the COVID-19 pandemic. The plaintiffs sought this injunction based on the claim that these restrictions during the pandemic infringe on the constitutional rights to patients’ privacy and liberty and to equal protection of the law as protected by the Due Process Clause of the Fifth Amendment. Additionally, the ACLU and other organizations said these unnecessary restrictions place patients, providers, and staff at unnecessary risk of viral exposure amidst a global pandemic.
The verdict
On July 13, 2020, a federal court granted the preliminary injunction to suspend FDA’s enforcement of the in-person requirements of mifepristone for abortion during the COVID-19 pandemic. The court denied the motion for suspension of in-person restrictions as applied to miscarriage management. The preliminary injunction applies nationwide without geographic limitation. It will remain in effect until the end of the litigation or for 30 days following the expiration of the public health emergency.
What the outcome means
This injunction is a step in the right direction for patients and providers to allow for autonomy and clinical practice guided by clinician expertise. However, this ruling remains narrow. Patients must be counseled about mifepristone via telemedicine and sign a Patient Agreement Form, which must be returned electronically or by mail. Patients must receive a copy of the mifepristone medication guide, and dispensing of mifepristone must still be conducted by or under the supervision of a certified provider. The medication may not be dispensed by retail pharmacies, thus requiring providers to arrange for mailing of prescriptions to patients. Given state-based legal statutes regarding mailing of medications, this injunction may not lead to an immediate increase in access to care. In addition, patients seeking management for miscarriage must go to clinic to have mifepristone dispensed and thus risk exposure to viral transmission.
What now?
The regulation of mifepristone—in spite of excellent safety and specifically for the narrow purpose of administration in the setting of abortion and miscarriage care—is by definition a discriminatory practice against patients and providers. As clinicians, we are duty-bound to speak out against injustices to our practices and our patients. At a local level, we can work to implement safe practices in the setting of this injunction and continue to work on a national level to ensure this injunction becomes permanent and with more broad scope to eliminate all of the REMS requirements for mifepristone.
ACTION ITEMS
- Act locally! Are you an abortion provider? Contact your local ACLU (find them here) or lawyer in your area for assistance navigating the legal landscape to prescribe after this injunction.
- Act statewide! Press candidates in your state to stand up for science and data. Support legislative acts and bills that address combating discriminatory regulations.
- Act nationally! The President is responsible for appointing the Commissioner of the FDA and the Secretary of Health and Human Services (with Senate advice and consent). Who we elect matters. Seek out opportunities to become involved in increasing access to and awareness of voter registration and Election Day, and speak out against voter suppression. Make sure you are registered to vote here and check your area to review new recommendations amidst the pandemic.
Mifepristone is a safe, effective, and well-tolerated medication for managing miscarriage and for medical abortion when combined with misoprostol.1,2 Since the US Food and Drug Administration (FDA) approved its use in 2000, more than 4 million women have used this medication.3 The combination of mifepristone with misoprostol was used for 39% of all US abortions in 2017.4 Approximately 10% of all clinically recognized pregnancies end in miscarriages, and many are safely managed with either misoprostol alone or with the combination of mifepristone and misoprostol.5
The issue
The prescription and distribution of mifepristone is highly regulated by the FDA via requirements outlined in the Risk Evaluation and Mitigation Strategies (REMS) drug safety program. The FDA may determine a REMS is necessary for a specific drug to ensure the benefits of a drug outweigh the potential risks. A REMS may include an informative package insert for patients, follow-up communication to prescribers—including letters, safety protocols or recommended laboratory tests, or Elements to Assure Safe Use (ETASU). ETASU are types of REMS that are placed on medications that have significant potential for serious adverse effects, and without such restrictions FDA approval would be rescinded.
Are mifepristone requirements fairly applied?
The 3 ETASU restrictions on the distribution of mifepristone are in-person dispensation, prescriber certification, and patient signatures on special forms.6 The in-person dispensing requirement is applied to only 16 other medications (one of which is Mifeprex, the brand version of mifepristone), and Mifeprex/mifepristone are the only ones deemed safe for self-administration—meaning that patients receive the drug from a clinic but then may take it at a site of their choosing. The prescriber certification requirement places expectations on providers to account for distribution of doses and keep records of serial numbers (in effect, having clinicians act as both physician and pharmacist, as most medications are distributed and recorded in pharmacies). The patient form was recommended for elimination in 2016 due to its duplicative information and burden on patients—a recommendation that was then overruled by the FDA commissioner.7
These 3 requirements placed on mifepristone specifically target dosages for use related to abortions and miscarriages. Mifepristone is used to treat other medical conditions, with much higher doses, without the same restrictions—in fact, the FDA has allowed much higher doses of mifepristone to be mailed directly to a patient when prescribed for different disorders. The American College of Obstetricians and Gynecologists (ACOG) has long opposed the burdensome REMS requirements on mifepristone for reproductive health indications.8
Arguments regarding the safety of mifepristone must be understood in the context of how the medication is taken, and the unique difference with other medications that must be administered by physicians or in health care facilities. Mifepristone is self-administered, and the desired effect—evacuation of uterine contents—typically occurs after a patient takes the accompanying medication misoprostol, which is some 24 to 72 hours later. This timeframe makes it highly unlikely that any patient would be in the presence of their provider at the time of medication effect, thus an in-person dispensing requirement has no medical bearing on the outcome of the health of the patient.
REMS changes during the COVID-19 pandemic
The coronavirus disease 2019 (COVID-19) pandemic has necessarily changed the structure of REMS and ETASU requirements for many medications, with changes made in order to mitigate viral transmission through the limitation of unnecessary visits to clinics or hospitals. The FDA announced in March of 2020 that it would not enforce pre-prescription requirements, such as laboratory or magnetic resonance imaging results, for many medications (including those more toxic than mifepristone), and that it would lift the requirement for in-person dispensation of several medications.9 Also in March 2020 the Department of Health and Human Services Secretary (HHS) and the Drug Enforcement Agency (DEA) activated a “telemedicine exception” to allow physicians to use telemedicine to satisfy mandatory requirements for prescribing controlled substances, including opioids.10
Despite repeated pleas from organizations, individuals, and physician groups, the FDA continued to enforce the REMS/ETASU for mifepristone as the pandemic decimated communities. Importantly, the pandemic has not had an equal effect on all communities, and the disparities highlighted in outcomes as related to COVID-19 are also reflected in disparities to access to reproductive choices.11 By enforcing REMS/ETASU for mifepristone during a global pandemic, the FDA has placed additional burden on women and people who menstruate. As offices and clinics have closed, and as many jobs have evaporated, additional barriers have emerged, such as lack of childcare, fewer transportation options, and decreased clinic appointments.
As the pandemic continues to affect communities in the United States, ACOG has issued guidance recommending assessment for eligibility for medical abortion remotely, and has encouraged the use of telemedicine and other remote interactions for its members and patients to limit transmission of the virus.
The lawsuit
On May 27, 2020, the American Civil Liberties Union (ACLU) (on behalf of ACOG, the Council of University Chairs of Obstetrics and Gynecology, New York State Academy of Family Physicians, SisterSong, and Honor MacNaughton, MD) filed a civil action against the FDA and HHS challenging the requirement for in-person dispensing of mifepristone and associated ETASU requirements during the COVID-19 pandemic. The plaintiffs sought this injunction based on the claim that these restrictions during the pandemic infringe on the constitutional rights to patients’ privacy and liberty and to equal protection of the law as protected by the Due Process Clause of the Fifth Amendment. Additionally, the ACLU and other organizations said these unnecessary restrictions place patients, providers, and staff at unnecessary risk of viral exposure amidst a global pandemic.
The verdict
On July 13, 2020, a federal court granted the preliminary injunction to suspend FDA’s enforcement of the in-person requirements of mifepristone for abortion during the COVID-19 pandemic. The court denied the motion for suspension of in-person restrictions as applied to miscarriage management. The preliminary injunction applies nationwide without geographic limitation. It will remain in effect until the end of the litigation or for 30 days following the expiration of the public health emergency.
What the outcome means
This injunction is a step in the right direction for patients and providers to allow for autonomy and clinical practice guided by clinician expertise. However, this ruling remains narrow. Patients must be counseled about mifepristone via telemedicine and sign a Patient Agreement Form, which must be returned electronically or by mail. Patients must receive a copy of the mifepristone medication guide, and dispensing of mifepristone must still be conducted by or under the supervision of a certified provider. The medication may not be dispensed by retail pharmacies, thus requiring providers to arrange for mailing of prescriptions to patients. Given state-based legal statutes regarding mailing of medications, this injunction may not lead to an immediate increase in access to care. In addition, patients seeking management for miscarriage must go to clinic to have mifepristone dispensed and thus risk exposure to viral transmission.
What now?
The regulation of mifepristone—in spite of excellent safety and specifically for the narrow purpose of administration in the setting of abortion and miscarriage care—is by definition a discriminatory practice against patients and providers. As clinicians, we are duty-bound to speak out against injustices to our practices and our patients. At a local level, we can work to implement safe practices in the setting of this injunction and continue to work on a national level to ensure this injunction becomes permanent and with more broad scope to eliminate all of the REMS requirements for mifepristone.
ACTION ITEMS
- Act locally! Are you an abortion provider? Contact your local ACLU (find them here) or lawyer in your area for assistance navigating the legal landscape to prescribe after this injunction.
- Act statewide! Press candidates in your state to stand up for science and data. Support legislative acts and bills that address combating discriminatory regulations.
- Act nationally! The President is responsible for appointing the Commissioner of the FDA and the Secretary of Health and Human Services (with Senate advice and consent). Who we elect matters. Seek out opportunities to become involved in increasing access to and awareness of voter registration and Election Day, and speak out against voter suppression. Make sure you are registered to vote here and check your area to review new recommendations amidst the pandemic.
- American College of Obstetricians and Gynecologists. Practice bulletin number 143: medical management of first trimester abortion. Obstet Gynecol. 2014;123:676-692.
- Schreiber CA, Crenin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170.
- Danco Laboratories. Mifeprex effectiveness and advantages. https://www.earlyoptionpill.com/is-mifeprex-right-for-me/effectiveness-advantages/ Accessed August 2, 2020.
- Jones RK, Witwer E, Jerman J. Abortion incidence and service availability in the United States, 2017. September 2019. https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Practice bulletin no. 150: early pregnancy loss. Obstet Gynecol. 2015;125:1258-1267.
- US Food and Drug Administration. Risk evaluation and mitigation strategy (REMS) single shared system for mifepristone 200 mg. April 2019. https://www.accessdata.fda.gov/drugsatfda_docs/rems/Mifepristone_2019_04_11_REMS_Full.pdf. Accessed September 10, 2020.
- US Food and Drug Administration; Center for Drug Evaluation and Research. 2016 REMS Review, Summary Review 25. March 29, 2016. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/020687Orig1s020SumR.pdf. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Improving access to mifepristone for reproductive health indications. June 2018. https://www.acog.org/clinical-information/policy-and-position-statements/position-statements/2018/improving-access-to-mifepristone-for-reproductive-health-indications. Accessed August 2, 2020.
- US Food and Drug Administration. Policy for certain REMS requirements during the COVID-19 public health emergency: guidance for industry and health care professionals. March 2020. https://www.fda.gov/media/136317/download. Accessed September 10, 2020.
- US Department of Justice. US Drug Enforcement Administration. COVID-19 Information Page, Telemedicine. https://www.deadiversion.usdoj.gov/coronavirus.html#TELE. Accessed May 25, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019: health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Updated July 24, 2020. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Practice bulletin number 143: medical management of first trimester abortion. Obstet Gynecol. 2014;123:676-692.
- Schreiber CA, Crenin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170.
- Danco Laboratories. Mifeprex effectiveness and advantages. https://www.earlyoptionpill.com/is-mifeprex-right-for-me/effectiveness-advantages/ Accessed August 2, 2020.
- Jones RK, Witwer E, Jerman J. Abortion incidence and service availability in the United States, 2017. September 2019. https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Practice bulletin no. 150: early pregnancy loss. Obstet Gynecol. 2015;125:1258-1267.
- US Food and Drug Administration. Risk evaluation and mitigation strategy (REMS) single shared system for mifepristone 200 mg. April 2019. https://www.accessdata.fda.gov/drugsatfda_docs/rems/Mifepristone_2019_04_11_REMS_Full.pdf. Accessed September 10, 2020.
- US Food and Drug Administration; Center for Drug Evaluation and Research. 2016 REMS Review, Summary Review 25. March 29, 2016. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/020687Orig1s020SumR.pdf. Accessed September 10, 2020.
- American College of Obstetricians and Gynecologists. Improving access to mifepristone for reproductive health indications. June 2018. https://www.acog.org/clinical-information/policy-and-position-statements/position-statements/2018/improving-access-to-mifepristone-for-reproductive-health-indications. Accessed August 2, 2020.
- US Food and Drug Administration. Policy for certain REMS requirements during the COVID-19 public health emergency: guidance for industry and health care professionals. March 2020. https://www.fda.gov/media/136317/download. Accessed September 10, 2020.
- US Department of Justice. US Drug Enforcement Administration. COVID-19 Information Page, Telemedicine. https://www.deadiversion.usdoj.gov/coronavirus.html#TELE. Accessed May 25, 2020.
- Centers for Disease Control and Prevention. Coronavirus disease 2019: health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Updated July 24, 2020. Accessed September 10, 2020.
COVID-19: New guidance to stem mental health crisis in frontline HCPs
A new review offers fresh guidance to help stem the mental health toll of the COVID-19 pandemic on frontline clinicians.
Investigators gathered practice guidelines and resources from a wide range of health care organizations and professional societies to develop a conceptual framework of mental health support for health care professionals (HCPs) caring for COVID-19 patients.
“Support needs to be deployed in multiple dimensions – including individual, organizational, and societal levels – and include training in resilience, stress reduction, emotional awareness, and self-care strategies,” lead author Rachel Schwartz, PhD, health services researcher, Stanford (Calif.) University, said in an interview.
The review was published Aug. 21 in the Annals of Internal Medicine.
An opportune moment
Coauthor Rebecca Margolis, DO, director of well-being in the division of medical education and faculty development, Children’s Hospital of Los Angeles, said that this is “an opportune moment to look at how we treat frontline providers in this country.”
Studies of previous pandemics have shown heightened distress in HCPs, even years after the pandemic, and the unique challenges posed by the COVID-19 pandemic surpass those of previous pandemics, Dr. Margolis said in an interview.
Dr. Schwartz, Dr. Margolis, and coauthors Uma Anand, PhD, LP, and Jina Sinskey, MD, met through the Collaborative for Healing and Renewal in Medicine network, a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians.
“We were brought together on a conference call in March, when things were particularly bad in New York, and started looking to see what resources we could get to frontline providers who were suffering. It was great to lean on each other and stand on the shoulders of colleagues in New York, who were the ones we learned from on these calls,” said Dr. Margolis.
The authors recommended addressing clinicians’ basic practical needs, including ensuring essentials like meals and transportation, establishing a “well-being area” within hospitals for staff to rest, and providing well-stocked living quarters so clinicians can safely quarantine from family, as well as personal protective equipment and child care.
Clinicians are often asked to “assume new professional roles to meet evolving needs” during a pandemic, which can increase stress. The authors recommended targeted training, assessment of clinician skills before redeployment to a new clinical role, and clear communication practices around redeployment.
Recognition from hospital and government leaders improves morale and supports clinicians’ ability to continue delivering care. Leadership should “leverage communication strategies to provide clinicians with up-to-date information and reassurance,” they wrote.
‘Uniquely isolated’
Dr. Margolis noted that
“My colleagues feel a sense of moral injury, putting their lives on the line at work, performing the most perilous job, and their kids can’t hang out with other kids, which just puts salt on the wound,” she said.
Additional sources of moral injury are deciding which patients should receive life support in the event of inadequate resources and bearing witness to, or enforcing, policies that lead to patients dying alone.
Leaders should encourage clinicians to “seek informal support from colleagues, managers, or chaplains” and to “provide rapid access to professional help,” the authors noted.
Furthermore, they contended that leaders should “proactively and routinely monitor the psychological well-being of their teams,” since guilt and shame often prevent clinicians from disclosing feelings of moral injury.
“Being provided with routine mental health support should be normalized and it should be part of the job – not only during COVID-19 but in general,” Dr. Schwartz said.
‘Battle buddies’
Dr. Margolis recommended the “battle buddy” model for mutual peer support.
Dr. Anand, a mental health clinician at Mayo Medical School, Rochester, Minn., elaborated.
“We connect residents with each other, and they form pairs to support each other and watch for warning signs such as withdrawal from colleagues, being frequently tearful, not showing up at work or showing up late, missing assignments, making mistakes at work, increased use of alcohol, or verbalizing serious concerns,” Dr. Anand said.
If the buddy shows any of these warning signs, he or she can be directed to appropriate resources to get help.
Since the pandemic has interfered with the ability to connect with colleagues and family members, attention should be paid to addressing the social support needs of clinicians.
Dr. Anand suggested that clinicians maintain contact with counselors, friends, and family, even if they cannot be together in person and must connect “virtually.”
Resilience and strength training are “key” components of reducing clinician distress, but trainings as well as processing groups and support workshops should be offered during protected time, Dr. Margolis advised, since it can be burdensome for clinicians to wake up early or stay late to attend these sessions.
Leaders and administrators should “model self-care and well-being,” she noted. For example, sending emails to clinicians late at night or on weekends creates an expectation of a rapid reply, which leads to additional pressure for the clinician.
“This is of the most powerful unspoken curricula we can develop,” Dr. Margolis emphasized.
Self-care critical
Marcus S. Shaker, MD, MSc, associate professor of pediatrics, medicine, and community and family medicine, Children’s Hospital at Dartmouth-Hitchcock in Lebanon, N.H., and Geisel School of Medicine at Dartmouth, Hanover, N.H., said the study was “a much appreciated, timely reminder of the importance of clinician wellness.”
Moreover, “without self-care, our ability to help our patients withers. This article provides a useful conceptual framework for individuals and organizations to provide the right care at the right time in these unprecedented times,” said Dr. Shaker, who was not involved with the study.
The authors agreed, stating that clinicians “require proactive psychological protection specifically because they are a population known for putting others’ needs before their own.”
They recommended several resources for HCPs, including the Physician Support Line; Headspace, a mindfulness Web-based app for reducing stress and anxiety; the National Suicide Prevention Lifeline; and the Crisis Text Line.
The authors and Dr. Shaker disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new review offers fresh guidance to help stem the mental health toll of the COVID-19 pandemic on frontline clinicians.
Investigators gathered practice guidelines and resources from a wide range of health care organizations and professional societies to develop a conceptual framework of mental health support for health care professionals (HCPs) caring for COVID-19 patients.
“Support needs to be deployed in multiple dimensions – including individual, organizational, and societal levels – and include training in resilience, stress reduction, emotional awareness, and self-care strategies,” lead author Rachel Schwartz, PhD, health services researcher, Stanford (Calif.) University, said in an interview.
The review was published Aug. 21 in the Annals of Internal Medicine.
An opportune moment
Coauthor Rebecca Margolis, DO, director of well-being in the division of medical education and faculty development, Children’s Hospital of Los Angeles, said that this is “an opportune moment to look at how we treat frontline providers in this country.”
Studies of previous pandemics have shown heightened distress in HCPs, even years after the pandemic, and the unique challenges posed by the COVID-19 pandemic surpass those of previous pandemics, Dr. Margolis said in an interview.
Dr. Schwartz, Dr. Margolis, and coauthors Uma Anand, PhD, LP, and Jina Sinskey, MD, met through the Collaborative for Healing and Renewal in Medicine network, a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians.
“We were brought together on a conference call in March, when things were particularly bad in New York, and started looking to see what resources we could get to frontline providers who were suffering. It was great to lean on each other and stand on the shoulders of colleagues in New York, who were the ones we learned from on these calls,” said Dr. Margolis.
The authors recommended addressing clinicians’ basic practical needs, including ensuring essentials like meals and transportation, establishing a “well-being area” within hospitals for staff to rest, and providing well-stocked living quarters so clinicians can safely quarantine from family, as well as personal protective equipment and child care.
Clinicians are often asked to “assume new professional roles to meet evolving needs” during a pandemic, which can increase stress. The authors recommended targeted training, assessment of clinician skills before redeployment to a new clinical role, and clear communication practices around redeployment.
Recognition from hospital and government leaders improves morale and supports clinicians’ ability to continue delivering care. Leadership should “leverage communication strategies to provide clinicians with up-to-date information and reassurance,” they wrote.
‘Uniquely isolated’
Dr. Margolis noted that
“My colleagues feel a sense of moral injury, putting their lives on the line at work, performing the most perilous job, and their kids can’t hang out with other kids, which just puts salt on the wound,” she said.
Additional sources of moral injury are deciding which patients should receive life support in the event of inadequate resources and bearing witness to, or enforcing, policies that lead to patients dying alone.
Leaders should encourage clinicians to “seek informal support from colleagues, managers, or chaplains” and to “provide rapid access to professional help,” the authors noted.
Furthermore, they contended that leaders should “proactively and routinely monitor the psychological well-being of their teams,” since guilt and shame often prevent clinicians from disclosing feelings of moral injury.
“Being provided with routine mental health support should be normalized and it should be part of the job – not only during COVID-19 but in general,” Dr. Schwartz said.
‘Battle buddies’
Dr. Margolis recommended the “battle buddy” model for mutual peer support.
Dr. Anand, a mental health clinician at Mayo Medical School, Rochester, Minn., elaborated.
“We connect residents with each other, and they form pairs to support each other and watch for warning signs such as withdrawal from colleagues, being frequently tearful, not showing up at work or showing up late, missing assignments, making mistakes at work, increased use of alcohol, or verbalizing serious concerns,” Dr. Anand said.
If the buddy shows any of these warning signs, he or she can be directed to appropriate resources to get help.
Since the pandemic has interfered with the ability to connect with colleagues and family members, attention should be paid to addressing the social support needs of clinicians.
Dr. Anand suggested that clinicians maintain contact with counselors, friends, and family, even if they cannot be together in person and must connect “virtually.”
Resilience and strength training are “key” components of reducing clinician distress, but trainings as well as processing groups and support workshops should be offered during protected time, Dr. Margolis advised, since it can be burdensome for clinicians to wake up early or stay late to attend these sessions.
Leaders and administrators should “model self-care and well-being,” she noted. For example, sending emails to clinicians late at night or on weekends creates an expectation of a rapid reply, which leads to additional pressure for the clinician.
“This is of the most powerful unspoken curricula we can develop,” Dr. Margolis emphasized.
Self-care critical
Marcus S. Shaker, MD, MSc, associate professor of pediatrics, medicine, and community and family medicine, Children’s Hospital at Dartmouth-Hitchcock in Lebanon, N.H., and Geisel School of Medicine at Dartmouth, Hanover, N.H., said the study was “a much appreciated, timely reminder of the importance of clinician wellness.”
Moreover, “without self-care, our ability to help our patients withers. This article provides a useful conceptual framework for individuals and organizations to provide the right care at the right time in these unprecedented times,” said Dr. Shaker, who was not involved with the study.
The authors agreed, stating that clinicians “require proactive psychological protection specifically because they are a population known for putting others’ needs before their own.”
They recommended several resources for HCPs, including the Physician Support Line; Headspace, a mindfulness Web-based app for reducing stress and anxiety; the National Suicide Prevention Lifeline; and the Crisis Text Line.
The authors and Dr. Shaker disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new review offers fresh guidance to help stem the mental health toll of the COVID-19 pandemic on frontline clinicians.
Investigators gathered practice guidelines and resources from a wide range of health care organizations and professional societies to develop a conceptual framework of mental health support for health care professionals (HCPs) caring for COVID-19 patients.
“Support needs to be deployed in multiple dimensions – including individual, organizational, and societal levels – and include training in resilience, stress reduction, emotional awareness, and self-care strategies,” lead author Rachel Schwartz, PhD, health services researcher, Stanford (Calif.) University, said in an interview.
The review was published Aug. 21 in the Annals of Internal Medicine.
An opportune moment
Coauthor Rebecca Margolis, DO, director of well-being in the division of medical education and faculty development, Children’s Hospital of Los Angeles, said that this is “an opportune moment to look at how we treat frontline providers in this country.”
Studies of previous pandemics have shown heightened distress in HCPs, even years after the pandemic, and the unique challenges posed by the COVID-19 pandemic surpass those of previous pandemics, Dr. Margolis said in an interview.
Dr. Schwartz, Dr. Margolis, and coauthors Uma Anand, PhD, LP, and Jina Sinskey, MD, met through the Collaborative for Healing and Renewal in Medicine network, a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians.
“We were brought together on a conference call in March, when things were particularly bad in New York, and started looking to see what resources we could get to frontline providers who were suffering. It was great to lean on each other and stand on the shoulders of colleagues in New York, who were the ones we learned from on these calls,” said Dr. Margolis.
The authors recommended addressing clinicians’ basic practical needs, including ensuring essentials like meals and transportation, establishing a “well-being area” within hospitals for staff to rest, and providing well-stocked living quarters so clinicians can safely quarantine from family, as well as personal protective equipment and child care.
Clinicians are often asked to “assume new professional roles to meet evolving needs” during a pandemic, which can increase stress. The authors recommended targeted training, assessment of clinician skills before redeployment to a new clinical role, and clear communication practices around redeployment.
Recognition from hospital and government leaders improves morale and supports clinicians’ ability to continue delivering care. Leadership should “leverage communication strategies to provide clinicians with up-to-date information and reassurance,” they wrote.
‘Uniquely isolated’
Dr. Margolis noted that
“My colleagues feel a sense of moral injury, putting their lives on the line at work, performing the most perilous job, and their kids can’t hang out with other kids, which just puts salt on the wound,” she said.
Additional sources of moral injury are deciding which patients should receive life support in the event of inadequate resources and bearing witness to, or enforcing, policies that lead to patients dying alone.
Leaders should encourage clinicians to “seek informal support from colleagues, managers, or chaplains” and to “provide rapid access to professional help,” the authors noted.
Furthermore, they contended that leaders should “proactively and routinely monitor the psychological well-being of their teams,” since guilt and shame often prevent clinicians from disclosing feelings of moral injury.
“Being provided with routine mental health support should be normalized and it should be part of the job – not only during COVID-19 but in general,” Dr. Schwartz said.
‘Battle buddies’
Dr. Margolis recommended the “battle buddy” model for mutual peer support.
Dr. Anand, a mental health clinician at Mayo Medical School, Rochester, Minn., elaborated.
“We connect residents with each other, and they form pairs to support each other and watch for warning signs such as withdrawal from colleagues, being frequently tearful, not showing up at work or showing up late, missing assignments, making mistakes at work, increased use of alcohol, or verbalizing serious concerns,” Dr. Anand said.
If the buddy shows any of these warning signs, he or she can be directed to appropriate resources to get help.
Since the pandemic has interfered with the ability to connect with colleagues and family members, attention should be paid to addressing the social support needs of clinicians.
Dr. Anand suggested that clinicians maintain contact with counselors, friends, and family, even if they cannot be together in person and must connect “virtually.”
Resilience and strength training are “key” components of reducing clinician distress, but trainings as well as processing groups and support workshops should be offered during protected time, Dr. Margolis advised, since it can be burdensome for clinicians to wake up early or stay late to attend these sessions.
Leaders and administrators should “model self-care and well-being,” she noted. For example, sending emails to clinicians late at night or on weekends creates an expectation of a rapid reply, which leads to additional pressure for the clinician.
“This is of the most powerful unspoken curricula we can develop,” Dr. Margolis emphasized.
Self-care critical
Marcus S. Shaker, MD, MSc, associate professor of pediatrics, medicine, and community and family medicine, Children’s Hospital at Dartmouth-Hitchcock in Lebanon, N.H., and Geisel School of Medicine at Dartmouth, Hanover, N.H., said the study was “a much appreciated, timely reminder of the importance of clinician wellness.”
Moreover, “without self-care, our ability to help our patients withers. This article provides a useful conceptual framework for individuals and organizations to provide the right care at the right time in these unprecedented times,” said Dr. Shaker, who was not involved with the study.
The authors agreed, stating that clinicians “require proactive psychological protection specifically because they are a population known for putting others’ needs before their own.”
They recommended several resources for HCPs, including the Physician Support Line; Headspace, a mindfulness Web-based app for reducing stress and anxiety; the National Suicide Prevention Lifeline; and the Crisis Text Line.
The authors and Dr. Shaker disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Hysteroscopy and COVID-19: Have recommended techniques changed due to the pandemic?
The emergence of the coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19) in December 2019, has resulted in a global pandemic that has challenged the medical community and will continue to represent a public health emergency for the next several months.1 It has rapidly spread globally, infecting many individuals in an unprecedented rate of infection and worldwide reach. On March 11, 2020, the World Health Organization designated COVID-19 as a pandemic. While the majority of infected individuals are asymptomatic or develop only mild symptoms, some have an unfortunate clinical course resulting in multi-organ failure and death.2
It is accepted that the virus mainly spreads during close contact and via respiratory droplets.3 The average time from infection to onset of symptoms ranges from 2 to 14 days, with an average of 5 days.4 Recommended measures to prevent the spread of the infection include social distancing (at least 6 feet from others), meticulous hand hygiene, and wearing a mask covering the mouth and nose when in public.5 Aiming to mitigate the risk of viral dissemination for patients and health care providers, and to preserve hospital resources, all nonessential medical interventions were initially suspended. Recently, the American College of Surgeons in a joint statement with 9 women’s health care societies have provided recommendations on how to resume clinical activities as we recover from the pandemic.6
As we reinitiate clinical activities, gynecologists have been alerted of the potential risk of viral dissemination during gynecologic minimally invasive surgical procedures due to the presence of the virus in blood, stool, and the potential risk of aerosolization of the virus, especially when using smoke-generating devices.7,8 This risk is not limited to intubation and extubation of the airway during anesthesia; the risk also presents itself during other aerosol-generating procedures, such as laparoscopy or robotic surgery.9,10
Hysteroscopy is considered the gold standard procedure for the diagnosis and management of intrauterine pathologies.11 It is frequently performed in an office setting without the use of anesthesia.11,12 It is usually well tolerated, with only a few patients reporting discomfort.12 It allows for immediate treatment (using the “see and treat” approach) while avoiding not only the risk of anesthesia, as stated, but also the need for intubation—which has a high risk of droplet contamination in COVID-19–infected individuals.13
Is there risk of viral dissemination during hysteroscopic procedures?
The novel and rapidly changing nature of the COVID-19 pandemic present many challenges to the gynecologist. Significant concerns have been raised regarding potential risk of viral dissemination during laparoscopic surgery due to aerosolization of viral particles and the presence of the virus in blood and the gastrointestinal tract of infected patients.7 Diagnostic, and some simple, hysteroscopic procedures are commonly performed in an outpatient setting, with the patient awake. Complex hysteroscopic interventions, however, are generally performed in the operating room, typically with the use of general anesthesia. Hysteroscopy has the theoretical risks of viral dissemination when performed in COVID-19–positive patients. Two important questions must be addressed to better understand the potential risk of COVID-19 viral dissemination during hysteroscopic procedures.
Continue to: 1. Is the virus present in the vaginal fluid of women infected with COVID-19?...
1. Is the virus present in the vaginal fluid of women infected with COVID-19?
Recent studies have confirmed the presence of viral particles in urine, feces, blood, and tears in addition to the respiratory tract in patients infected with COVID-19.3,14,15 The presence of the SARS-CoV-2 virus in the female genital system is currently unknown. Previous studies, of other epidemic viral infections, have demonstrated the presence of the virus in the female genital tract in affected patients of Zika virus and Ebola.16,17 However, 2 recent studies have failed to demonstrate the presence of the SARS-CoV-2 virus in the vaginal fluid of pregnant14 and not pregnant18 women with severe COVID-19 infection.
2. Is there risk of viral dissemination during hysteroscopy if using electrosurgery?
There are significant concerns with possible risk of COVID-19 transmission to health care providers in direct contact with infected patients during minimally invasive gynecologic procedures due to direct contamination and aerosolization of the virus.10,19 Current data on COVID-19 transmission during surgery are limited. However, it is important to recognize that viral aerosolization has been documented with other viral diseases, such as human papillomavirus and hepatitis B.20 A recent report called for awareness in the surgical community about the potential risks of COVID-19 viral dissemination during laparoscopic surgery. Among other recommendations, international experts advised minimizing the use of electrosurgery to reduce the creation of surgical plume, decreasing the pneumoperitoneum pressure to minimum levels, and using suction devices in a closed system.21 Although these preventive measures apply to laparoscopic surgery, it is important to consider that hysteroscopy is performed in a unique environment.
During hysteroscopy the uterine cavity is distended with a liquid medium (normal saline or electrolyte-free solutions); this is opposed to gynecologic laparoscopy, in which the peritoneal cavity is distended with carbon dioxide.22 The smoke produced with the use of hysteroscopic electrosurgical instruments generates bubbles that are immediately cooled down to the temperature of the distention media and subsequently dissolve into it. Therefore, there are no bubbles generated during hysteroscopic surgery that are subsequently released into the air. This results in a low risk for viral dissemination during hysteroscopic procedures. Nevertheless, the necessary precautions to minimize the risk of COVID-19 transmission during hysteroscopic intervention are extremely important.
Recommendations for hysteroscopic procedures during the COVID-19 pandemic
We provide our overall recommendations for hysteroscopy, as well as those specific to the office and hospital setting.
Recommendations: General
Limit hysteroscopic procedures to COVID-19–negative patients and to those patients in whom delaying the procedure could result in adverse clinical outcomes.23
Universally screen for potential COVID-19 infection. When possible, a phone interview to triage patients based on their symptoms and infection exposure status should take place before the patient arrives to the health care center. Patients with suspected or confirmed COVID-19 infection who require immediate evaluation should be directed to COVID-19–designated emergency areas.
Universally test for SARS-CoV-2 before procedures performed in the operating room (OR). Using nasopharyngeal swabs for the detection of viral RNA, employing molecular methods such as polymerase chain reaction (PCR), within 48 to 72 hours prior to all OR hysteroscopic procedures is strongly recommended. Adopting this testing strategy will aid to identify asymptomatic SARS-CoV-2‒infected patients, allowing to defer the procedure, if possible, among patients testing positive. If tests are limited, testing only patients scheduled for hysteroscopic procedures in which general or regional anesthesia will be required is acceptable.
Universal SARS-CoV-2 testing of patients undergoing in-office hysteroscopic diagnostic or minor operative procedures without the use of anesthesia is not required.
Limit the presence of a companion. It is understood that visitor policies may vary at the discretion of each institution’s guidelines. Children and individuals over the age of 60 years should not be granted access to the center. Companions will be subjected to the same screening criteria as patients.
Provide for social distancing and other precautionary measures. If more than one patient is scheduled to be at the facility at the same time, ensure that the facility provides adequate space to allow the appropriate social distancing recommendations between patients. Hand sanitizers and facemasks should be available for patients and companions.
Provide PPE for clinicians. All health care providers in close contact with the patient must wear personal protective equipment (PPE), which includes an apron and gown, a surgical mask, eye protection, and gloves. Health care providers should wear PPE deemed appropriate by their regulatory institutions following their local and national guidelines during clinical patient interactions.
Restrict surgical attendees to vital personnel. The participation of learners by physical presence in the office or operating room should be restricted.
Continue to: Recommendations: Office setting...
Recommendations: Office setting
Preprocedural recommendations
- Advise patients to come to the office alone. If the patient requires a companion, a maximum of one adult companion under the age of 60 should be accepted.
- Limit the number of health care team members present in the procedure room.
Intraprocedural recommendations
- Choose the appropriate device(s) that will allow for an effective and fast procedure.
- Use the recommended PPE for all clinicians.
- Limit the movement of staff members in and out of the procedure room.
Postprocedure recommendations
- When more than one case is scheduled to be performed in the same procedure room, allow enough time in between cases to grant a thorough OR decontamination.
- Allow for patients to recover from the procedure in the same room as the procedure took place in order to avoid potential contamination of multiple rooms.
- Expedite patient discharge.
- Follow up after the procedure by phone or telemedicine.
- Use standard endoscope disinfection procedures, as they are effective and should not be modified.
Continue to: Recommendations: Operating room setting...
Recommendations: Operating room setting
Preprocedural recommendations
- Perform adequate patient screening for potential COVID-19 infection. (Screening should be independent of symptoms and not be limited to those with clinical symptoms.)
- Limit the number of health care team members in the operating procedure room.
- To minimize unnecessary staff exposure, have surgeons and staff not needed for intubation remain outside the OR until intubation is completed and leave the OR before extubation.
Intraprocedure recommendations
- Limit personnel in the OR to a minimum.
- Staff should not enter or leave the room during the procedure.
- When possible, use conscious sedation or regional anesthesia to avoid the risk of viral dissemination at the time of intubation/extubation.
- Choose the device that will allow an effective and fast procedure.
- Favor non–smoke-generating devices, such as hysteroscopic scissors, graspers, and tissue retrieval systems.
- Connect active suction to the outflow, especially when using smoke-generating instruments, to facilitate the extraction of surgical smoke.
Postprocedure recommendations
- When more than one case is scheduled to be performed in the same room, allow enough time in between cases to grant a thorough OR decontamination.
- Expedite postprocedure recovery and patient discharge.
- After completion of the procedure, staff should remove scrubs and change into clean clothing.
- Use standard endoscope disinfection procedures, as they are effective and should not be modified.
Conclusions
The COVID-19 pandemic has caused a global health emergency. Our knowledge of this devastating virus is constantly evolving as we continue to fight this overwhelming disease. Theoretical risk of “viral” dissemination is considered extremely low, or negligible, during hysterosocopy. Hysteroscopic procedures in COVID-19–positive patients with life-threatening conditions or in patients in whom delaying the procedure could worsen outcomes should be performed taking appropriate measures. Patients who test negative for COVID-19 (confirmed by PCR) and require hysteroscopic procedures, should be treated using universal precautions. ●
- Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25:e936-e945.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. February 24, 2020. doi:10.1001/jama.2020.2648.
- Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843-1844.
- Yu F, Yan L, Wang N, et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020;71:793-798.
- Prem K, Liu Y, Russell TW, et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261-e270.
- American College of Surgeons, American Society of Aesthesiologists, Association of periOperative Registered Nurses, American Hospital Association. Joint Statement: Roadmap for resuming elective surgery after COVID-19 pandemic. April 16, 2020. https://www.aorn.org/guidelines/aorn-support/roadmap-for-resuming-elective-surgery-after-covid-19. Accessed August 27, 2020.
- Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386-389.
- Mowbray NG, Ansell J, Horwood J, et al. Safe management of surgical smoke in the age of COVID-19. Br J Surg. May 3, 2020. doi: 10.1002/bjs.11679.
- Cohen SL, Liu G, Abrao M, et al. Perspectives on surgery in the time of COVID-19: safety first. J Minim Invasive Gynecol. 2020;27:792-793.
- COVID-19: protecting health-care workers. Lancet. 2020;395:922.
- Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199-208.
- Cicinelli E. Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol. 2010;17:703-708.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568-576.
- Aslan MM, Yuvaci HU, Köse O, et al. SARS-CoV-2 is not present in the vaginal fluid of pregnant women with COVID-19. J Matern Fetal Neonatal Med. 2020:1-3. doi: 10.1080/14767058.2020.1793318.
- Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92:833-840.
- Prisant N, Bujan L, Benichou H, et al. Zika virus in the female genital tract. Lancet Infect Dis. 2016;16:1000-1001.
- Rodriguez LL, De Roo A, Guimard Y, et al. Persistence and genetic stability of Ebola virus during the outbreak in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis. 1999;179 Suppl 1:S170-S176.
- Qiu L, Liu X, Xiao M, et al. SARS-CoV-2 is not detectable in the vaginal fluid of women with severe COVID-19 infection. Clin Infect Dis. 2020;71:813-817.
- Brat GA, Hersey S, Chhabra K, et al. Protecting surgical teams during the COVID-19 outbreak: a narrative review and clinical considerations. Ann Surg. April 17, 2020. doi: 10.1097/SLA.0000000000003926.
- Kwak HD, Kim SH, Seo YS, et al. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73:857-863.
- Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020;272:e5-e6.
- Catena U. Surgical smoke in hysteroscopic surgery: does it really matter in COVID-19 times? Facts Views Vis Obgyn. 2020;12:67-68.
- Carugno J, Di Spiezio Sardo A, Alonso L, et al. COVID-19 pandemic. Impact on hysteroscopic procedures: a consensus statement from the Global Congress of Hysteroscopy Scientific Committee. J Minim Invasive Gynecol. 2020;27:988-992.
The emergence of the coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19) in December 2019, has resulted in a global pandemic that has challenged the medical community and will continue to represent a public health emergency for the next several months.1 It has rapidly spread globally, infecting many individuals in an unprecedented rate of infection and worldwide reach. On March 11, 2020, the World Health Organization designated COVID-19 as a pandemic. While the majority of infected individuals are asymptomatic or develop only mild symptoms, some have an unfortunate clinical course resulting in multi-organ failure and death.2
It is accepted that the virus mainly spreads during close contact and via respiratory droplets.3 The average time from infection to onset of symptoms ranges from 2 to 14 days, with an average of 5 days.4 Recommended measures to prevent the spread of the infection include social distancing (at least 6 feet from others), meticulous hand hygiene, and wearing a mask covering the mouth and nose when in public.5 Aiming to mitigate the risk of viral dissemination for patients and health care providers, and to preserve hospital resources, all nonessential medical interventions were initially suspended. Recently, the American College of Surgeons in a joint statement with 9 women’s health care societies have provided recommendations on how to resume clinical activities as we recover from the pandemic.6
As we reinitiate clinical activities, gynecologists have been alerted of the potential risk of viral dissemination during gynecologic minimally invasive surgical procedures due to the presence of the virus in blood, stool, and the potential risk of aerosolization of the virus, especially when using smoke-generating devices.7,8 This risk is not limited to intubation and extubation of the airway during anesthesia; the risk also presents itself during other aerosol-generating procedures, such as laparoscopy or robotic surgery.9,10
Hysteroscopy is considered the gold standard procedure for the diagnosis and management of intrauterine pathologies.11 It is frequently performed in an office setting without the use of anesthesia.11,12 It is usually well tolerated, with only a few patients reporting discomfort.12 It allows for immediate treatment (using the “see and treat” approach) while avoiding not only the risk of anesthesia, as stated, but also the need for intubation—which has a high risk of droplet contamination in COVID-19–infected individuals.13
Is there risk of viral dissemination during hysteroscopic procedures?
The novel and rapidly changing nature of the COVID-19 pandemic present many challenges to the gynecologist. Significant concerns have been raised regarding potential risk of viral dissemination during laparoscopic surgery due to aerosolization of viral particles and the presence of the virus in blood and the gastrointestinal tract of infected patients.7 Diagnostic, and some simple, hysteroscopic procedures are commonly performed in an outpatient setting, with the patient awake. Complex hysteroscopic interventions, however, are generally performed in the operating room, typically with the use of general anesthesia. Hysteroscopy has the theoretical risks of viral dissemination when performed in COVID-19–positive patients. Two important questions must be addressed to better understand the potential risk of COVID-19 viral dissemination during hysteroscopic procedures.
Continue to: 1. Is the virus present in the vaginal fluid of women infected with COVID-19?...
1. Is the virus present in the vaginal fluid of women infected with COVID-19?
Recent studies have confirmed the presence of viral particles in urine, feces, blood, and tears in addition to the respiratory tract in patients infected with COVID-19.3,14,15 The presence of the SARS-CoV-2 virus in the female genital system is currently unknown. Previous studies, of other epidemic viral infections, have demonstrated the presence of the virus in the female genital tract in affected patients of Zika virus and Ebola.16,17 However, 2 recent studies have failed to demonstrate the presence of the SARS-CoV-2 virus in the vaginal fluid of pregnant14 and not pregnant18 women with severe COVID-19 infection.
2. Is there risk of viral dissemination during hysteroscopy if using electrosurgery?
There are significant concerns with possible risk of COVID-19 transmission to health care providers in direct contact with infected patients during minimally invasive gynecologic procedures due to direct contamination and aerosolization of the virus.10,19 Current data on COVID-19 transmission during surgery are limited. However, it is important to recognize that viral aerosolization has been documented with other viral diseases, such as human papillomavirus and hepatitis B.20 A recent report called for awareness in the surgical community about the potential risks of COVID-19 viral dissemination during laparoscopic surgery. Among other recommendations, international experts advised minimizing the use of electrosurgery to reduce the creation of surgical plume, decreasing the pneumoperitoneum pressure to minimum levels, and using suction devices in a closed system.21 Although these preventive measures apply to laparoscopic surgery, it is important to consider that hysteroscopy is performed in a unique environment.
During hysteroscopy the uterine cavity is distended with a liquid medium (normal saline or electrolyte-free solutions); this is opposed to gynecologic laparoscopy, in which the peritoneal cavity is distended with carbon dioxide.22 The smoke produced with the use of hysteroscopic electrosurgical instruments generates bubbles that are immediately cooled down to the temperature of the distention media and subsequently dissolve into it. Therefore, there are no bubbles generated during hysteroscopic surgery that are subsequently released into the air. This results in a low risk for viral dissemination during hysteroscopic procedures. Nevertheless, the necessary precautions to minimize the risk of COVID-19 transmission during hysteroscopic intervention are extremely important.
Recommendations for hysteroscopic procedures during the COVID-19 pandemic
We provide our overall recommendations for hysteroscopy, as well as those specific to the office and hospital setting.
Recommendations: General
Limit hysteroscopic procedures to COVID-19–negative patients and to those patients in whom delaying the procedure could result in adverse clinical outcomes.23
Universally screen for potential COVID-19 infection. When possible, a phone interview to triage patients based on their symptoms and infection exposure status should take place before the patient arrives to the health care center. Patients with suspected or confirmed COVID-19 infection who require immediate evaluation should be directed to COVID-19–designated emergency areas.
Universally test for SARS-CoV-2 before procedures performed in the operating room (OR). Using nasopharyngeal swabs for the detection of viral RNA, employing molecular methods such as polymerase chain reaction (PCR), within 48 to 72 hours prior to all OR hysteroscopic procedures is strongly recommended. Adopting this testing strategy will aid to identify asymptomatic SARS-CoV-2‒infected patients, allowing to defer the procedure, if possible, among patients testing positive. If tests are limited, testing only patients scheduled for hysteroscopic procedures in which general or regional anesthesia will be required is acceptable.
Universal SARS-CoV-2 testing of patients undergoing in-office hysteroscopic diagnostic or minor operative procedures without the use of anesthesia is not required.
Limit the presence of a companion. It is understood that visitor policies may vary at the discretion of each institution’s guidelines. Children and individuals over the age of 60 years should not be granted access to the center. Companions will be subjected to the same screening criteria as patients.
Provide for social distancing and other precautionary measures. If more than one patient is scheduled to be at the facility at the same time, ensure that the facility provides adequate space to allow the appropriate social distancing recommendations between patients. Hand sanitizers and facemasks should be available for patients and companions.
Provide PPE for clinicians. All health care providers in close contact with the patient must wear personal protective equipment (PPE), which includes an apron and gown, a surgical mask, eye protection, and gloves. Health care providers should wear PPE deemed appropriate by their regulatory institutions following their local and national guidelines during clinical patient interactions.
Restrict surgical attendees to vital personnel. The participation of learners by physical presence in the office or operating room should be restricted.
Continue to: Recommendations: Office setting...
Recommendations: Office setting
Preprocedural recommendations
- Advise patients to come to the office alone. If the patient requires a companion, a maximum of one adult companion under the age of 60 should be accepted.
- Limit the number of health care team members present in the procedure room.
Intraprocedural recommendations
- Choose the appropriate device(s) that will allow for an effective and fast procedure.
- Use the recommended PPE for all clinicians.
- Limit the movement of staff members in and out of the procedure room.
Postprocedure recommendations
- When more than one case is scheduled to be performed in the same procedure room, allow enough time in between cases to grant a thorough OR decontamination.
- Allow for patients to recover from the procedure in the same room as the procedure took place in order to avoid potential contamination of multiple rooms.
- Expedite patient discharge.
- Follow up after the procedure by phone or telemedicine.
- Use standard endoscope disinfection procedures, as they are effective and should not be modified.
Continue to: Recommendations: Operating room setting...
Recommendations: Operating room setting
Preprocedural recommendations
- Perform adequate patient screening for potential COVID-19 infection. (Screening should be independent of symptoms and not be limited to those with clinical symptoms.)
- Limit the number of health care team members in the operating procedure room.
- To minimize unnecessary staff exposure, have surgeons and staff not needed for intubation remain outside the OR until intubation is completed and leave the OR before extubation.
Intraprocedure recommendations
- Limit personnel in the OR to a minimum.
- Staff should not enter or leave the room during the procedure.
- When possible, use conscious sedation or regional anesthesia to avoid the risk of viral dissemination at the time of intubation/extubation.
- Choose the device that will allow an effective and fast procedure.
- Favor non–smoke-generating devices, such as hysteroscopic scissors, graspers, and tissue retrieval systems.
- Connect active suction to the outflow, especially when using smoke-generating instruments, to facilitate the extraction of surgical smoke.
Postprocedure recommendations
- When more than one case is scheduled to be performed in the same room, allow enough time in between cases to grant a thorough OR decontamination.
- Expedite postprocedure recovery and patient discharge.
- After completion of the procedure, staff should remove scrubs and change into clean clothing.
- Use standard endoscope disinfection procedures, as they are effective and should not be modified.
Conclusions
The COVID-19 pandemic has caused a global health emergency. Our knowledge of this devastating virus is constantly evolving as we continue to fight this overwhelming disease. Theoretical risk of “viral” dissemination is considered extremely low, or negligible, during hysterosocopy. Hysteroscopic procedures in COVID-19–positive patients with life-threatening conditions or in patients in whom delaying the procedure could worsen outcomes should be performed taking appropriate measures. Patients who test negative for COVID-19 (confirmed by PCR) and require hysteroscopic procedures, should be treated using universal precautions. ●
The emergence of the coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19) in December 2019, has resulted in a global pandemic that has challenged the medical community and will continue to represent a public health emergency for the next several months.1 It has rapidly spread globally, infecting many individuals in an unprecedented rate of infection and worldwide reach. On March 11, 2020, the World Health Organization designated COVID-19 as a pandemic. While the majority of infected individuals are asymptomatic or develop only mild symptoms, some have an unfortunate clinical course resulting in multi-organ failure and death.2
It is accepted that the virus mainly spreads during close contact and via respiratory droplets.3 The average time from infection to onset of symptoms ranges from 2 to 14 days, with an average of 5 days.4 Recommended measures to prevent the spread of the infection include social distancing (at least 6 feet from others), meticulous hand hygiene, and wearing a mask covering the mouth and nose when in public.5 Aiming to mitigate the risk of viral dissemination for patients and health care providers, and to preserve hospital resources, all nonessential medical interventions were initially suspended. Recently, the American College of Surgeons in a joint statement with 9 women’s health care societies have provided recommendations on how to resume clinical activities as we recover from the pandemic.6
As we reinitiate clinical activities, gynecologists have been alerted of the potential risk of viral dissemination during gynecologic minimally invasive surgical procedures due to the presence of the virus in blood, stool, and the potential risk of aerosolization of the virus, especially when using smoke-generating devices.7,8 This risk is not limited to intubation and extubation of the airway during anesthesia; the risk also presents itself during other aerosol-generating procedures, such as laparoscopy or robotic surgery.9,10
Hysteroscopy is considered the gold standard procedure for the diagnosis and management of intrauterine pathologies.11 It is frequently performed in an office setting without the use of anesthesia.11,12 It is usually well tolerated, with only a few patients reporting discomfort.12 It allows for immediate treatment (using the “see and treat” approach) while avoiding not only the risk of anesthesia, as stated, but also the need for intubation—which has a high risk of droplet contamination in COVID-19–infected individuals.13
Is there risk of viral dissemination during hysteroscopic procedures?
The novel and rapidly changing nature of the COVID-19 pandemic present many challenges to the gynecologist. Significant concerns have been raised regarding potential risk of viral dissemination during laparoscopic surgery due to aerosolization of viral particles and the presence of the virus in blood and the gastrointestinal tract of infected patients.7 Diagnostic, and some simple, hysteroscopic procedures are commonly performed in an outpatient setting, with the patient awake. Complex hysteroscopic interventions, however, are generally performed in the operating room, typically with the use of general anesthesia. Hysteroscopy has the theoretical risks of viral dissemination when performed in COVID-19–positive patients. Two important questions must be addressed to better understand the potential risk of COVID-19 viral dissemination during hysteroscopic procedures.
Continue to: 1. Is the virus present in the vaginal fluid of women infected with COVID-19?...
1. Is the virus present in the vaginal fluid of women infected with COVID-19?
Recent studies have confirmed the presence of viral particles in urine, feces, blood, and tears in addition to the respiratory tract in patients infected with COVID-19.3,14,15 The presence of the SARS-CoV-2 virus in the female genital system is currently unknown. Previous studies, of other epidemic viral infections, have demonstrated the presence of the virus in the female genital tract in affected patients of Zika virus and Ebola.16,17 However, 2 recent studies have failed to demonstrate the presence of the SARS-CoV-2 virus in the vaginal fluid of pregnant14 and not pregnant18 women with severe COVID-19 infection.
2. Is there risk of viral dissemination during hysteroscopy if using electrosurgery?
There are significant concerns with possible risk of COVID-19 transmission to health care providers in direct contact with infected patients during minimally invasive gynecologic procedures due to direct contamination and aerosolization of the virus.10,19 Current data on COVID-19 transmission during surgery are limited. However, it is important to recognize that viral aerosolization has been documented with other viral diseases, such as human papillomavirus and hepatitis B.20 A recent report called for awareness in the surgical community about the potential risks of COVID-19 viral dissemination during laparoscopic surgery. Among other recommendations, international experts advised minimizing the use of electrosurgery to reduce the creation of surgical plume, decreasing the pneumoperitoneum pressure to minimum levels, and using suction devices in a closed system.21 Although these preventive measures apply to laparoscopic surgery, it is important to consider that hysteroscopy is performed in a unique environment.
During hysteroscopy the uterine cavity is distended with a liquid medium (normal saline or electrolyte-free solutions); this is opposed to gynecologic laparoscopy, in which the peritoneal cavity is distended with carbon dioxide.22 The smoke produced with the use of hysteroscopic electrosurgical instruments generates bubbles that are immediately cooled down to the temperature of the distention media and subsequently dissolve into it. Therefore, there are no bubbles generated during hysteroscopic surgery that are subsequently released into the air. This results in a low risk for viral dissemination during hysteroscopic procedures. Nevertheless, the necessary precautions to minimize the risk of COVID-19 transmission during hysteroscopic intervention are extremely important.
Recommendations for hysteroscopic procedures during the COVID-19 pandemic
We provide our overall recommendations for hysteroscopy, as well as those specific to the office and hospital setting.
Recommendations: General
Limit hysteroscopic procedures to COVID-19–negative patients and to those patients in whom delaying the procedure could result in adverse clinical outcomes.23
Universally screen for potential COVID-19 infection. When possible, a phone interview to triage patients based on their symptoms and infection exposure status should take place before the patient arrives to the health care center. Patients with suspected or confirmed COVID-19 infection who require immediate evaluation should be directed to COVID-19–designated emergency areas.
Universally test for SARS-CoV-2 before procedures performed in the operating room (OR). Using nasopharyngeal swabs for the detection of viral RNA, employing molecular methods such as polymerase chain reaction (PCR), within 48 to 72 hours prior to all OR hysteroscopic procedures is strongly recommended. Adopting this testing strategy will aid to identify asymptomatic SARS-CoV-2‒infected patients, allowing to defer the procedure, if possible, among patients testing positive. If tests are limited, testing only patients scheduled for hysteroscopic procedures in which general or regional anesthesia will be required is acceptable.
Universal SARS-CoV-2 testing of patients undergoing in-office hysteroscopic diagnostic or minor operative procedures without the use of anesthesia is not required.
Limit the presence of a companion. It is understood that visitor policies may vary at the discretion of each institution’s guidelines. Children and individuals over the age of 60 years should not be granted access to the center. Companions will be subjected to the same screening criteria as patients.
Provide for social distancing and other precautionary measures. If more than one patient is scheduled to be at the facility at the same time, ensure that the facility provides adequate space to allow the appropriate social distancing recommendations between patients. Hand sanitizers and facemasks should be available for patients and companions.
Provide PPE for clinicians. All health care providers in close contact with the patient must wear personal protective equipment (PPE), which includes an apron and gown, a surgical mask, eye protection, and gloves. Health care providers should wear PPE deemed appropriate by their regulatory institutions following their local and national guidelines during clinical patient interactions.
Restrict surgical attendees to vital personnel. The participation of learners by physical presence in the office or operating room should be restricted.
Continue to: Recommendations: Office setting...
Recommendations: Office setting
Preprocedural recommendations
- Advise patients to come to the office alone. If the patient requires a companion, a maximum of one adult companion under the age of 60 should be accepted.
- Limit the number of health care team members present in the procedure room.
Intraprocedural recommendations
- Choose the appropriate device(s) that will allow for an effective and fast procedure.
- Use the recommended PPE for all clinicians.
- Limit the movement of staff members in and out of the procedure room.
Postprocedure recommendations
- When more than one case is scheduled to be performed in the same procedure room, allow enough time in between cases to grant a thorough OR decontamination.
- Allow for patients to recover from the procedure in the same room as the procedure took place in order to avoid potential contamination of multiple rooms.
- Expedite patient discharge.
- Follow up after the procedure by phone or telemedicine.
- Use standard endoscope disinfection procedures, as they are effective and should not be modified.
Continue to: Recommendations: Operating room setting...
Recommendations: Operating room setting
Preprocedural recommendations
- Perform adequate patient screening for potential COVID-19 infection. (Screening should be independent of symptoms and not be limited to those with clinical symptoms.)
- Limit the number of health care team members in the operating procedure room.
- To minimize unnecessary staff exposure, have surgeons and staff not needed for intubation remain outside the OR until intubation is completed and leave the OR before extubation.
Intraprocedure recommendations
- Limit personnel in the OR to a minimum.
- Staff should not enter or leave the room during the procedure.
- When possible, use conscious sedation or regional anesthesia to avoid the risk of viral dissemination at the time of intubation/extubation.
- Choose the device that will allow an effective and fast procedure.
- Favor non–smoke-generating devices, such as hysteroscopic scissors, graspers, and tissue retrieval systems.
- Connect active suction to the outflow, especially when using smoke-generating instruments, to facilitate the extraction of surgical smoke.
Postprocedure recommendations
- When more than one case is scheduled to be performed in the same room, allow enough time in between cases to grant a thorough OR decontamination.
- Expedite postprocedure recovery and patient discharge.
- After completion of the procedure, staff should remove scrubs and change into clean clothing.
- Use standard endoscope disinfection procedures, as they are effective and should not be modified.
Conclusions
The COVID-19 pandemic has caused a global health emergency. Our knowledge of this devastating virus is constantly evolving as we continue to fight this overwhelming disease. Theoretical risk of “viral” dissemination is considered extremely low, or negligible, during hysterosocopy. Hysteroscopic procedures in COVID-19–positive patients with life-threatening conditions or in patients in whom delaying the procedure could worsen outcomes should be performed taking appropriate measures. Patients who test negative for COVID-19 (confirmed by PCR) and require hysteroscopic procedures, should be treated using universal precautions. ●
- Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25:e936-e945.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. February 24, 2020. doi:10.1001/jama.2020.2648.
- Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843-1844.
- Yu F, Yan L, Wang N, et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020;71:793-798.
- Prem K, Liu Y, Russell TW, et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261-e270.
- American College of Surgeons, American Society of Aesthesiologists, Association of periOperative Registered Nurses, American Hospital Association. Joint Statement: Roadmap for resuming elective surgery after COVID-19 pandemic. April 16, 2020. https://www.aorn.org/guidelines/aorn-support/roadmap-for-resuming-elective-surgery-after-covid-19. Accessed August 27, 2020.
- Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386-389.
- Mowbray NG, Ansell J, Horwood J, et al. Safe management of surgical smoke in the age of COVID-19. Br J Surg. May 3, 2020. doi: 10.1002/bjs.11679.
- Cohen SL, Liu G, Abrao M, et al. Perspectives on surgery in the time of COVID-19: safety first. J Minim Invasive Gynecol. 2020;27:792-793.
- COVID-19: protecting health-care workers. Lancet. 2020;395:922.
- Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199-208.
- Cicinelli E. Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol. 2010;17:703-708.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568-576.
- Aslan MM, Yuvaci HU, Köse O, et al. SARS-CoV-2 is not present in the vaginal fluid of pregnant women with COVID-19. J Matern Fetal Neonatal Med. 2020:1-3. doi: 10.1080/14767058.2020.1793318.
- Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92:833-840.
- Prisant N, Bujan L, Benichou H, et al. Zika virus in the female genital tract. Lancet Infect Dis. 2016;16:1000-1001.
- Rodriguez LL, De Roo A, Guimard Y, et al. Persistence and genetic stability of Ebola virus during the outbreak in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis. 1999;179 Suppl 1:S170-S176.
- Qiu L, Liu X, Xiao M, et al. SARS-CoV-2 is not detectable in the vaginal fluid of women with severe COVID-19 infection. Clin Infect Dis. 2020;71:813-817.
- Brat GA, Hersey S, Chhabra K, et al. Protecting surgical teams during the COVID-19 outbreak: a narrative review and clinical considerations. Ann Surg. April 17, 2020. doi: 10.1097/SLA.0000000000003926.
- Kwak HD, Kim SH, Seo YS, et al. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73:857-863.
- Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020;272:e5-e6.
- Catena U. Surgical smoke in hysteroscopic surgery: does it really matter in COVID-19 times? Facts Views Vis Obgyn. 2020;12:67-68.
- Carugno J, Di Spiezio Sardo A, Alonso L, et al. COVID-19 pandemic. Impact on hysteroscopic procedures: a consensus statement from the Global Congress of Hysteroscopy Scientific Committee. J Minim Invasive Gynecol. 2020;27:988-992.
- Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25:e936-e945.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. February 24, 2020. doi:10.1001/jama.2020.2648.
- Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843-1844.
- Yu F, Yan L, Wang N, et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020;71:793-798.
- Prem K, Liu Y, Russell TW, et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261-e270.
- American College of Surgeons, American Society of Aesthesiologists, Association of periOperative Registered Nurses, American Hospital Association. Joint Statement: Roadmap for resuming elective surgery after COVID-19 pandemic. April 16, 2020. https://www.aorn.org/guidelines/aorn-support/roadmap-for-resuming-elective-surgery-after-covid-19. Accessed August 27, 2020.
- Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386-389.
- Mowbray NG, Ansell J, Horwood J, et al. Safe management of surgical smoke in the age of COVID-19. Br J Surg. May 3, 2020. doi: 10.1002/bjs.11679.
- Cohen SL, Liu G, Abrao M, et al. Perspectives on surgery in the time of COVID-19: safety first. J Minim Invasive Gynecol. 2020;27:792-793.
- COVID-19: protecting health-care workers. Lancet. 2020;395:922.
- Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199-208.
- Cicinelli E. Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol. 2010;17:703-708.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568-576.
- Aslan MM, Yuvaci HU, Köse O, et al. SARS-CoV-2 is not present in the vaginal fluid of pregnant women with COVID-19. J Matern Fetal Neonatal Med. 2020:1-3. doi: 10.1080/14767058.2020.1793318.
- Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92:833-840.
- Prisant N, Bujan L, Benichou H, et al. Zika virus in the female genital tract. Lancet Infect Dis. 2016;16:1000-1001.
- Rodriguez LL, De Roo A, Guimard Y, et al. Persistence and genetic stability of Ebola virus during the outbreak in Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis. 1999;179 Suppl 1:S170-S176.
- Qiu L, Liu X, Xiao M, et al. SARS-CoV-2 is not detectable in the vaginal fluid of women with severe COVID-19 infection. Clin Infect Dis. 2020;71:813-817.
- Brat GA, Hersey S, Chhabra K, et al. Protecting surgical teams during the COVID-19 outbreak: a narrative review and clinical considerations. Ann Surg. April 17, 2020. doi: 10.1097/SLA.0000000000003926.
- Kwak HD, Kim SH, Seo YS, et al. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73:857-863.
- Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020;272:e5-e6.
- Catena U. Surgical smoke in hysteroscopic surgery: does it really matter in COVID-19 times? Facts Views Vis Obgyn. 2020;12:67-68.
- Carugno J, Di Spiezio Sardo A, Alonso L, et al. COVID-19 pandemic. Impact on hysteroscopic procedures: a consensus statement from the Global Congress of Hysteroscopy Scientific Committee. J Minim Invasive Gynecol. 2020;27:988-992.
HHS plan to improve rural health focuses on better broadband, telehealth services
Even before the coronavirus pandemic reached into the nation’s less-populated regions, rural Americans were sicker, poorer, and older than the rest of the country. Hospitals are shuttering at record rates, and health care experts have long called for changes.
The new plan, released by the Department of Health & Human Services Secretary Alex M. Azar, II, acknowledges the gaps in health care and other problems facing rural America. It lists a litany of projects and directives, with many already underway or announced within federal agencies.
“We cannot just tinker around the edges of a rural healthcare system that has struggled for too long,” Azar said in a prepared statement.
Yet, that is exactly what experts say the administration continues to do.
“They tinker around the edges,” said Tommy Barnhart, former president of the National Rural Health Association. And he added, “there’s a lot of political hype” that has happened under President Trump, as well as previous presidents.
In the past few months, rural health care has increasingly become a focus for Mr. Trump, whose polling numbers are souring as COVID-19 kills hundreds of Americans every day, drives down restaurant demand for some farm products, and spreads through meatpacking plants. Rural states including Iowa and the Dakotas are reporting the latest surges in cases.
This announcement comes in response to Mr. Trump’s executive order last month calling for improved rural health and telehealth access. Earlier this week, three federal agencies also announced they would team up to address gaps in rural broadband service – a key need because large portions of the plan seek to expand telehealth.
The plan is more than 70 pages long and the word “telehealth” appears more than 90 times, with a focus on projects across HHS, including the Health Resources and Services Administration and the Centers for Medicare & Medicaid Services.
Mr. Barnhart said CMS has passed some public health emergency waivers since the beginning of the pandemic that helped rural facilities get more funding, including one that specifically was designed to provide additional money for telehealth services. However, those waivers are set to expire when the coronavirus emergency ends. Officials have not yet set a date for when the federal emergency will end.
Andrew Jay Schwartzman, senior counselor to the Benton Institute for Broadband & Society, a private foundation that works to ensure greater Internet access, said there are multiple challenges with implementing telehealth across the nation. Many initiatives for robust telehealth programs need fast bandwidth, yet getting the money and setting up the necessary infrastructure is very difficult, he said.
“It will be a long time before this kind of technology will be readily available to much of the country,” he said.
Ge Bai, associate professor of accounting and health policy at Johns Hopkins University in Baltimore, noted that telehealth was short on funding in the HHS initiative. However, she said, the focus on telehealth, as well as a proposed shift in payment for small rural hospitals and changing workforce licensing requirements, had good potential.
“We are so close to the election that this is probably more of a messaging issue to cater to rural residents,” Ms. Bai said. “But it doesn’t matter who will be president. This report will give the next administration useful guidance.”
The American Hospital Association, representing 5,000 hospitals nationwide, sent a letter to Mr. Trump last week recommending a host of steps the administration could take. As of late Thursday, AHA was still reviewing the HHS plan but said it was “encouraged by the increased attention on rural health care.”
Buried within the HHS announcement are technical initiatives, such as a contract to help clinics and hospitals integrate care, and detailed efforts to address gaps in care, including a proposal to increase funding for school-based mental health programs in the president’s 2021 budget.
A senior HHS official said that, while some actions have been taken in recent months to improve rural health — such as the $11 billion provided to rural hospitals through coronavirus relief funding — more is needed.
“We’re putting our stake in the ground that the time for talk is over,” he said. “We’re going to move forward.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Even before the coronavirus pandemic reached into the nation’s less-populated regions, rural Americans were sicker, poorer, and older than the rest of the country. Hospitals are shuttering at record rates, and health care experts have long called for changes.
The new plan, released by the Department of Health & Human Services Secretary Alex M. Azar, II, acknowledges the gaps in health care and other problems facing rural America. It lists a litany of projects and directives, with many already underway or announced within federal agencies.
“We cannot just tinker around the edges of a rural healthcare system that has struggled for too long,” Azar said in a prepared statement.
Yet, that is exactly what experts say the administration continues to do.
“They tinker around the edges,” said Tommy Barnhart, former president of the National Rural Health Association. And he added, “there’s a lot of political hype” that has happened under President Trump, as well as previous presidents.
In the past few months, rural health care has increasingly become a focus for Mr. Trump, whose polling numbers are souring as COVID-19 kills hundreds of Americans every day, drives down restaurant demand for some farm products, and spreads through meatpacking plants. Rural states including Iowa and the Dakotas are reporting the latest surges in cases.
This announcement comes in response to Mr. Trump’s executive order last month calling for improved rural health and telehealth access. Earlier this week, three federal agencies also announced they would team up to address gaps in rural broadband service – a key need because large portions of the plan seek to expand telehealth.
The plan is more than 70 pages long and the word “telehealth” appears more than 90 times, with a focus on projects across HHS, including the Health Resources and Services Administration and the Centers for Medicare & Medicaid Services.
Mr. Barnhart said CMS has passed some public health emergency waivers since the beginning of the pandemic that helped rural facilities get more funding, including one that specifically was designed to provide additional money for telehealth services. However, those waivers are set to expire when the coronavirus emergency ends. Officials have not yet set a date for when the federal emergency will end.
Andrew Jay Schwartzman, senior counselor to the Benton Institute for Broadband & Society, a private foundation that works to ensure greater Internet access, said there are multiple challenges with implementing telehealth across the nation. Many initiatives for robust telehealth programs need fast bandwidth, yet getting the money and setting up the necessary infrastructure is very difficult, he said.
“It will be a long time before this kind of technology will be readily available to much of the country,” he said.
Ge Bai, associate professor of accounting and health policy at Johns Hopkins University in Baltimore, noted that telehealth was short on funding in the HHS initiative. However, she said, the focus on telehealth, as well as a proposed shift in payment for small rural hospitals and changing workforce licensing requirements, had good potential.
“We are so close to the election that this is probably more of a messaging issue to cater to rural residents,” Ms. Bai said. “But it doesn’t matter who will be president. This report will give the next administration useful guidance.”
The American Hospital Association, representing 5,000 hospitals nationwide, sent a letter to Mr. Trump last week recommending a host of steps the administration could take. As of late Thursday, AHA was still reviewing the HHS plan but said it was “encouraged by the increased attention on rural health care.”
Buried within the HHS announcement are technical initiatives, such as a contract to help clinics and hospitals integrate care, and detailed efforts to address gaps in care, including a proposal to increase funding for school-based mental health programs in the president’s 2021 budget.
A senior HHS official said that, while some actions have been taken in recent months to improve rural health — such as the $11 billion provided to rural hospitals through coronavirus relief funding — more is needed.
“We’re putting our stake in the ground that the time for talk is over,” he said. “We’re going to move forward.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Even before the coronavirus pandemic reached into the nation’s less-populated regions, rural Americans were sicker, poorer, and older than the rest of the country. Hospitals are shuttering at record rates, and health care experts have long called for changes.
The new plan, released by the Department of Health & Human Services Secretary Alex M. Azar, II, acknowledges the gaps in health care and other problems facing rural America. It lists a litany of projects and directives, with many already underway or announced within federal agencies.
“We cannot just tinker around the edges of a rural healthcare system that has struggled for too long,” Azar said in a prepared statement.
Yet, that is exactly what experts say the administration continues to do.
“They tinker around the edges,” said Tommy Barnhart, former president of the National Rural Health Association. And he added, “there’s a lot of political hype” that has happened under President Trump, as well as previous presidents.
In the past few months, rural health care has increasingly become a focus for Mr. Trump, whose polling numbers are souring as COVID-19 kills hundreds of Americans every day, drives down restaurant demand for some farm products, and spreads through meatpacking plants. Rural states including Iowa and the Dakotas are reporting the latest surges in cases.
This announcement comes in response to Mr. Trump’s executive order last month calling for improved rural health and telehealth access. Earlier this week, three federal agencies also announced they would team up to address gaps in rural broadband service – a key need because large portions of the plan seek to expand telehealth.
The plan is more than 70 pages long and the word “telehealth” appears more than 90 times, with a focus on projects across HHS, including the Health Resources and Services Administration and the Centers for Medicare & Medicaid Services.
Mr. Barnhart said CMS has passed some public health emergency waivers since the beginning of the pandemic that helped rural facilities get more funding, including one that specifically was designed to provide additional money for telehealth services. However, those waivers are set to expire when the coronavirus emergency ends. Officials have not yet set a date for when the federal emergency will end.
Andrew Jay Schwartzman, senior counselor to the Benton Institute for Broadband & Society, a private foundation that works to ensure greater Internet access, said there are multiple challenges with implementing telehealth across the nation. Many initiatives for robust telehealth programs need fast bandwidth, yet getting the money and setting up the necessary infrastructure is very difficult, he said.
“It will be a long time before this kind of technology will be readily available to much of the country,” he said.
Ge Bai, associate professor of accounting and health policy at Johns Hopkins University in Baltimore, noted that telehealth was short on funding in the HHS initiative. However, she said, the focus on telehealth, as well as a proposed shift in payment for small rural hospitals and changing workforce licensing requirements, had good potential.
“We are so close to the election that this is probably more of a messaging issue to cater to rural residents,” Ms. Bai said. “But it doesn’t matter who will be president. This report will give the next administration useful guidance.”
The American Hospital Association, representing 5,000 hospitals nationwide, sent a letter to Mr. Trump last week recommending a host of steps the administration could take. As of late Thursday, AHA was still reviewing the HHS plan but said it was “encouraged by the increased attention on rural health care.”
Buried within the HHS announcement are technical initiatives, such as a contract to help clinics and hospitals integrate care, and detailed efforts to address gaps in care, including a proposal to increase funding for school-based mental health programs in the president’s 2021 budget.
A senior HHS official said that, while some actions have been taken in recent months to improve rural health — such as the $11 billion provided to rural hospitals through coronavirus relief funding — more is needed.
“We’re putting our stake in the ground that the time for talk is over,” he said. “We’re going to move forward.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Ten ways docs are cutting costs and saving money
“Some of our physician clients have seen their income decrease by as much as 50%,” says Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minnesota. “Many physicians had previously figured that whatever financial obligations they had wouldn’t be a problem because whatever amount they were making would continue, and if there were a decline it would be gradual.” However, assumption is now creating financial strain for many doctors.
Vikram Tarugu, MD, a gastroenterologist and CEO of Detox of South Florida in Okeechobee, Florida, says he has watched his budget for years, but has become even more careful with his spending in the past few months.
“It has helped me a lot to adjust to the new normal when it comes to the financial side of things,” Dr. Tarugu said. “Patients aren’t coming in as much as they used to, so my income has really been affected.”
Primary care physicians have seen a 55% decrease in revenue and a 20%-30% decrease in patient volume as a result of COVID-19. The impact has been even more severe for specialists. Even for physicians whose practices remain busy and whose family members haven’t lost their jobs or income, broader concerns about the economy may be reason enough for physicians to adopt cost-cutting measures.
In Medscape’s Physician Compensation Report 2020, we asked physicians to share their best cost-cutting tips. Many illustrate the lengths to which physicians are going to conserve money.
Here’s a look at some of the advice they shared, along with guidance from experts on how to make it work for you:
1. Create a written budget, even if you think it’s pointless.
Physicians said their most important piece of advice includes the following: “Use a formal budget to track progress,” “write out a budget,” “plan intermittent/large expenses in advance,” “Make sure all expenses are paid before you spend on leisure.”
Nearly 7 in 10 physicians say they have a budget for personal expenses, yet only one-quarter of those who do have a formal, written budget. Writing out a spending plan is key to being intentional about your spending, making sure that you’re living within your means, and identifying areas in which you may be able to cut back.
“Financial planning is all about cash flow, and everybody should know the amount of money coming in, how much is going out, and the difference between the two,” says Amy Guerich, a partner with Stepp & Rothwell, a Kansas City–based financial planning firm. “That’s important in good times, but it’s even more important now when we see physicians taking pay cuts.”
Many physicians have found that budget apps or software programs are easier to work with than anticipated; some even walk you through the process of creating a budget. To get the most out of the apps, you’ll need to check them regularly and make changes based on their data.
“Sometimes there’s this false belief that just by signing up, you are automatically going to be better at budgeting,” says Scott Snider, CFP, a certified financial planner and partner with Mellen Money Management in Ponte Vedra Beach, Florida. “Basically, these apps are a great way to identify problem areas of spending. We have a tendency as humans to underestimate how much we spend on things like Starbucks, dining out, and Amazon shopping.”
One of the doctors’ tips that requires the most willpower is to “pay all expenses before spending on leisure.” That’s because we live in an instant gratification world, and want everything right away, Ms. Guerich said.
“I also think there’s an element of ‘keeping up with the Joneses’ and pressure associated with this profession,” she said. “The stereotype is that physicians are high-income earners so ‘We should be able to do that’ or ‘Mom and dad are doctors, so they can afford it.’ “
Creating and then revisiting your budget progress on a monthly or quarterly basis can give you a feeling of accomplishment and keep you motivated to stay with it.
Keep in mind that budgeting is a continual process rather than a singular event, and you’ll likely adjust it over time as your income and goals change.
2. Save more as you earn more.
Respondents to our Physician Compensation Report gave the following recommendations: “Pay yourself first,” “I put half of my bonus into an investment account no matter how much it is,” “I allocate extra money and put it into a savings account.”
Dr. Greenwald said, “I have a rule that every client needs to be saving 20% of their gross income toward retirement, including whatever the employer is putting in.”
Putting a portion of every paycheck into savings is key to making progress toward financial goals. Start by building an emergency fund with at least 3-6 months’ worth of expenses in it and making sure you’re saving at least enough for retirement to get any potential employer match.
Mr. Snider suggests increasing the percentage you save every time you get a raise.
“The thought behind that strategy is that when a doctor receives a pay raise – even if it’s just a cost-of-living raise of 3% – an extra 1% saved doesn’t reduce their take-home pay year-over-year,” he says. “In fact, they still take home more money, and they save more money. Win-win.”
3. Focus on paying down your debt.
Physicians told us how they were working to pay down debt with the following recommendations: “Accelerate debt reduction,” “I make additional principal payment to our home mortgage,” “We are aggressively attacking our remaining student loans.”
Reducing or eliminating debt is key to increasing cash flow, which can make it easier to meet all of your other financial goals. One-quarter of physicians have credit card debt, which typically carries interest rates higher than other types of debt, making it far more expensive. Focus on paying off such high-interest debt first, before moving on to other types of debt such as auto loans, student loans, or a mortgage.
“Credit card debt and any unsecured debt should be paid before anything else,” Mr. Snider says. “Getting rid of those high interest rates should be a priority. And that type of debt has less flexible terms than student debt.”
4. Great opportunity to take advantage of record-low interest rates.
Physicians said that, to save money, they are recommending the following: “Consolidating student debt into our mortgage,” “Accelerating payments of the principle on our mortgage,” “Making sure we have an affordable mortgage.”
With interest rates at an all-time low, even those who’ve recently refinanced might see significant savings by refinancing again. Given the associated fees, it typically makes sense to refinance if you can reduce your mortgage rate by at least a point, and you’re planning to stay in the home for at least 5 years.
“Depending on how much lower your rate is, refinancing can make a big difference in your monthly payments,” Ms. Guerich said. “For physicians who might need an emergency reserve but don’t have cash on hand, a HELOC [Home Equity Line of Credit] is a great way to accomplish that.”
5. Be wary of credit cards dangers; use cards wisely.
Physician respondents recommended the following: “Use 0% interest offers on credit cards,” “Only have one card and pay it off every month,” “Never carry over balance.”
Nearly 80% of physicians have three or more credit cards, with 18% reporting that they have seven or more. When used wisely, credit cards can be an important tool for managing finances. Many credit cards come with tools that can help with budgeting, and credit cards rewards and perks can offer real value to users. That said, rewards typically are not valuable enough to offset the cost of interest on balances (or the associated damage to your credit score) that aren’t paid off each month.
“If you’re paying a high rate on credit card balances that carry over every month, regardless of your income, that could be a symptom that you may be spending more than you should,” says Dan Keady, a CFP and chief financial planning strategist at financial services firm TIAA.
6. Give less to Uncle Sam: Keep it for yourself.
Physicians said that they do the following: “Maximize tax-free/deferred savings (401k, HSA, etc.),” “Give to charity to reduce tax,” “Use pre-tax dollars for childcare and healthcare.”
Not only does saving in workplace retirement accounts help you build your nest egg, but it also reduces the amount that you have to pay in taxes in a given year. Physicians should also take advantage of other ways to reduce their income for tax purposes, such as saving money in a health savings account or flexible savings account.
The 401(k) or 403(b) contribution limit for this year is $19,500 ($26,000) for those age 50 years and older. Self-employed physicians can save even more money via a Simplified Employee Pension (SEP) IRA, says Ms. Guerich said. They can save up to 25% of compensation, up to $57,000 in 2020.
7. Automate everything and spare yourself the headache.
Physicians said the following: “Designate money from your paycheck directly to tax deferred and taxable accounts automatically,” “Use automatic payment for credit card balance monthly,” “Automate your savings.”
You probably already automate your 401(k) contributions, but you can also automate bill payments, emergency savings contributions and other financial tasks. For busy physicians, this can make it easier to stick to your financial plan and achieve your goals.
“The older you get, the busier you get, said Mr. Snider says. “Automation can definitely help with that. But make sure you are checking in quarterly to make sure that everything is still in line with your plan. The problem with automation is when you forget about it completely and just let everything sit there.”
8. Save separately for big purchases.
Sometimes it’s the big major expenses that can start to derail a budget. Physicians told us the following tactics for large purchases: “We buy affordable cars and take budget vacations,” “I buy used cars,” “We save in advance for new cars and only buy cars with cash.”
The decision of which car to purchase or where to go on a family vacation is a personal one, and some physicians take great enjoyment and pride in driving a luxury vehicle or traveling to exotic locales. The key, experts say, is to factor the cost of that car into the rest of your budget, and make sure that it’s not preventing you from achieving other financial goals.
“I don’t like to judge or tell clients how they should spend their money,” said Andrew Musbach, a certified financial planner and cofounder of MD Wealth Management in Chelsea, Mich. “Some people like cars, we have clients that have two planes, others want a second house or like to travel. Each person has their own interest where they may spend more relative to other people, but as long as they are meeting their savings targets, I encourage them to spend their money and enjoy what they enjoy most, guilt free.”
Mr. Snider suggests setting up a savings account separate from emergency or retirement accounts to set aside money if you have a goal for a large future purchase, such as a boat or a second home.
“That way, the funds don’t get commingled, and it’s explicitly clear whether or not the doctor is on target,” he says. “It also prevents them from treating their emergency savings account as an ATM machine.”
9. Start saving for college when the kids are little.
Respondents said the following: “We are buying less to save for the kids’ college education,” “We set up direct deposit into college and retirement savings plans,” “We have a 529 account for college savings.”
Helping pay for their children’s college education is an important financial goal for many physicians. The earlier that you start saving, the less you’ll have to save overall, thanks to compound interest. State 529 accounts are often a good place to start, especially if your state offers a tax incentive for doing so.
Mr. Snider recommends that physicians start small, with an initial investment of $1,000 per month and $100 per month contributions. Assuming a 7% rate of return and 17 years’ worth of savings, this would generate just over $42,000. (Note, current typical rates of return are less than 7%).
“Ideally, as other goals are accomplished and personal debt gets paid off, the doctor is ramping up their savings to have at least 50% of college expenses covered from their 529 college savings,” he says.
10. Watch out for the temptation of impulse purchases.
Physicians said the following: “Avoid impulse purchases,” “Avoid impulse shopping, make a list for the store and stick to it,” “Wait to buy things on sale.”
Nothing wrecks a budget like an impulse buy. More than half (54%) of U.S. shoppers have admitted to spending $100 or more on an impulse purchase. And 20% of shoppers have spent at least $1,000 on an impulse buy. Avoid buyers’ remorse by waiting a few days to make large purchase decisions or by limiting your unplanned spending to a certain dollar amount within your budget.
Online shopping may be a particular temptation. Dr. Tarugu, the Florida gastroenterologist, has focused on reducing those impulse buys as well, deleting all online shopping apps from his and his family’s phones.
“You won’t notice how much you have ordered online until it arrives at your doorstep,” he said. “It’s really important to keep it at bay.”
Mr. Keady, the TIAA chief planning strategist, recommended this tactic: Calculate the number of patients (or hours) you’d need to see in order to earn the cash required to make the purchase.
“Then, in a mindful way, figure out the amount of value derived from the purchase,” he said.
A version of this article originally appeared on Medscape.com.
“Some of our physician clients have seen their income decrease by as much as 50%,” says Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minnesota. “Many physicians had previously figured that whatever financial obligations they had wouldn’t be a problem because whatever amount they were making would continue, and if there were a decline it would be gradual.” However, assumption is now creating financial strain for many doctors.
Vikram Tarugu, MD, a gastroenterologist and CEO of Detox of South Florida in Okeechobee, Florida, says he has watched his budget for years, but has become even more careful with his spending in the past few months.
“It has helped me a lot to adjust to the new normal when it comes to the financial side of things,” Dr. Tarugu said. “Patients aren’t coming in as much as they used to, so my income has really been affected.”
Primary care physicians have seen a 55% decrease in revenue and a 20%-30% decrease in patient volume as a result of COVID-19. The impact has been even more severe for specialists. Even for physicians whose practices remain busy and whose family members haven’t lost their jobs or income, broader concerns about the economy may be reason enough for physicians to adopt cost-cutting measures.
In Medscape’s Physician Compensation Report 2020, we asked physicians to share their best cost-cutting tips. Many illustrate the lengths to which physicians are going to conserve money.
Here’s a look at some of the advice they shared, along with guidance from experts on how to make it work for you:
1. Create a written budget, even if you think it’s pointless.
Physicians said their most important piece of advice includes the following: “Use a formal budget to track progress,” “write out a budget,” “plan intermittent/large expenses in advance,” “Make sure all expenses are paid before you spend on leisure.”
Nearly 7 in 10 physicians say they have a budget for personal expenses, yet only one-quarter of those who do have a formal, written budget. Writing out a spending plan is key to being intentional about your spending, making sure that you’re living within your means, and identifying areas in which you may be able to cut back.
“Financial planning is all about cash flow, and everybody should know the amount of money coming in, how much is going out, and the difference between the two,” says Amy Guerich, a partner with Stepp & Rothwell, a Kansas City–based financial planning firm. “That’s important in good times, but it’s even more important now when we see physicians taking pay cuts.”
Many physicians have found that budget apps or software programs are easier to work with than anticipated; some even walk you through the process of creating a budget. To get the most out of the apps, you’ll need to check them regularly and make changes based on their data.
“Sometimes there’s this false belief that just by signing up, you are automatically going to be better at budgeting,” says Scott Snider, CFP, a certified financial planner and partner with Mellen Money Management in Ponte Vedra Beach, Florida. “Basically, these apps are a great way to identify problem areas of spending. We have a tendency as humans to underestimate how much we spend on things like Starbucks, dining out, and Amazon shopping.”
One of the doctors’ tips that requires the most willpower is to “pay all expenses before spending on leisure.” That’s because we live in an instant gratification world, and want everything right away, Ms. Guerich said.
“I also think there’s an element of ‘keeping up with the Joneses’ and pressure associated with this profession,” she said. “The stereotype is that physicians are high-income earners so ‘We should be able to do that’ or ‘Mom and dad are doctors, so they can afford it.’ “
Creating and then revisiting your budget progress on a monthly or quarterly basis can give you a feeling of accomplishment and keep you motivated to stay with it.
Keep in mind that budgeting is a continual process rather than a singular event, and you’ll likely adjust it over time as your income and goals change.
2. Save more as you earn more.
Respondents to our Physician Compensation Report gave the following recommendations: “Pay yourself first,” “I put half of my bonus into an investment account no matter how much it is,” “I allocate extra money and put it into a savings account.”
Dr. Greenwald said, “I have a rule that every client needs to be saving 20% of their gross income toward retirement, including whatever the employer is putting in.”
Putting a portion of every paycheck into savings is key to making progress toward financial goals. Start by building an emergency fund with at least 3-6 months’ worth of expenses in it and making sure you’re saving at least enough for retirement to get any potential employer match.
Mr. Snider suggests increasing the percentage you save every time you get a raise.
“The thought behind that strategy is that when a doctor receives a pay raise – even if it’s just a cost-of-living raise of 3% – an extra 1% saved doesn’t reduce their take-home pay year-over-year,” he says. “In fact, they still take home more money, and they save more money. Win-win.”
3. Focus on paying down your debt.
Physicians told us how they were working to pay down debt with the following recommendations: “Accelerate debt reduction,” “I make additional principal payment to our home mortgage,” “We are aggressively attacking our remaining student loans.”
Reducing or eliminating debt is key to increasing cash flow, which can make it easier to meet all of your other financial goals. One-quarter of physicians have credit card debt, which typically carries interest rates higher than other types of debt, making it far more expensive. Focus on paying off such high-interest debt first, before moving on to other types of debt such as auto loans, student loans, or a mortgage.
“Credit card debt and any unsecured debt should be paid before anything else,” Mr. Snider says. “Getting rid of those high interest rates should be a priority. And that type of debt has less flexible terms than student debt.”
4. Great opportunity to take advantage of record-low interest rates.
Physicians said that, to save money, they are recommending the following: “Consolidating student debt into our mortgage,” “Accelerating payments of the principle on our mortgage,” “Making sure we have an affordable mortgage.”
With interest rates at an all-time low, even those who’ve recently refinanced might see significant savings by refinancing again. Given the associated fees, it typically makes sense to refinance if you can reduce your mortgage rate by at least a point, and you’re planning to stay in the home for at least 5 years.
“Depending on how much lower your rate is, refinancing can make a big difference in your monthly payments,” Ms. Guerich said. “For physicians who might need an emergency reserve but don’t have cash on hand, a HELOC [Home Equity Line of Credit] is a great way to accomplish that.”
5. Be wary of credit cards dangers; use cards wisely.
Physician respondents recommended the following: “Use 0% interest offers on credit cards,” “Only have one card and pay it off every month,” “Never carry over balance.”
Nearly 80% of physicians have three or more credit cards, with 18% reporting that they have seven or more. When used wisely, credit cards can be an important tool for managing finances. Many credit cards come with tools that can help with budgeting, and credit cards rewards and perks can offer real value to users. That said, rewards typically are not valuable enough to offset the cost of interest on balances (or the associated damage to your credit score) that aren’t paid off each month.
“If you’re paying a high rate on credit card balances that carry over every month, regardless of your income, that could be a symptom that you may be spending more than you should,” says Dan Keady, a CFP and chief financial planning strategist at financial services firm TIAA.
6. Give less to Uncle Sam: Keep it for yourself.
Physicians said that they do the following: “Maximize tax-free/deferred savings (401k, HSA, etc.),” “Give to charity to reduce tax,” “Use pre-tax dollars for childcare and healthcare.”
Not only does saving in workplace retirement accounts help you build your nest egg, but it also reduces the amount that you have to pay in taxes in a given year. Physicians should also take advantage of other ways to reduce their income for tax purposes, such as saving money in a health savings account or flexible savings account.
The 401(k) or 403(b) contribution limit for this year is $19,500 ($26,000) for those age 50 years and older. Self-employed physicians can save even more money via a Simplified Employee Pension (SEP) IRA, says Ms. Guerich said. They can save up to 25% of compensation, up to $57,000 in 2020.
7. Automate everything and spare yourself the headache.
Physicians said the following: “Designate money from your paycheck directly to tax deferred and taxable accounts automatically,” “Use automatic payment for credit card balance monthly,” “Automate your savings.”
You probably already automate your 401(k) contributions, but you can also automate bill payments, emergency savings contributions and other financial tasks. For busy physicians, this can make it easier to stick to your financial plan and achieve your goals.
“The older you get, the busier you get, said Mr. Snider says. “Automation can definitely help with that. But make sure you are checking in quarterly to make sure that everything is still in line with your plan. The problem with automation is when you forget about it completely and just let everything sit there.”
8. Save separately for big purchases.
Sometimes it’s the big major expenses that can start to derail a budget. Physicians told us the following tactics for large purchases: “We buy affordable cars and take budget vacations,” “I buy used cars,” “We save in advance for new cars and only buy cars with cash.”
The decision of which car to purchase or where to go on a family vacation is a personal one, and some physicians take great enjoyment and pride in driving a luxury vehicle or traveling to exotic locales. The key, experts say, is to factor the cost of that car into the rest of your budget, and make sure that it’s not preventing you from achieving other financial goals.
“I don’t like to judge or tell clients how they should spend their money,” said Andrew Musbach, a certified financial planner and cofounder of MD Wealth Management in Chelsea, Mich. “Some people like cars, we have clients that have two planes, others want a second house or like to travel. Each person has their own interest where they may spend more relative to other people, but as long as they are meeting their savings targets, I encourage them to spend their money and enjoy what they enjoy most, guilt free.”
Mr. Snider suggests setting up a savings account separate from emergency or retirement accounts to set aside money if you have a goal for a large future purchase, such as a boat or a second home.
“That way, the funds don’t get commingled, and it’s explicitly clear whether or not the doctor is on target,” he says. “It also prevents them from treating their emergency savings account as an ATM machine.”
9. Start saving for college when the kids are little.
Respondents said the following: “We are buying less to save for the kids’ college education,” “We set up direct deposit into college and retirement savings plans,” “We have a 529 account for college savings.”
Helping pay for their children’s college education is an important financial goal for many physicians. The earlier that you start saving, the less you’ll have to save overall, thanks to compound interest. State 529 accounts are often a good place to start, especially if your state offers a tax incentive for doing so.
Mr. Snider recommends that physicians start small, with an initial investment of $1,000 per month and $100 per month contributions. Assuming a 7% rate of return and 17 years’ worth of savings, this would generate just over $42,000. (Note, current typical rates of return are less than 7%).
“Ideally, as other goals are accomplished and personal debt gets paid off, the doctor is ramping up their savings to have at least 50% of college expenses covered from their 529 college savings,” he says.
10. Watch out for the temptation of impulse purchases.
Physicians said the following: “Avoid impulse purchases,” “Avoid impulse shopping, make a list for the store and stick to it,” “Wait to buy things on sale.”
Nothing wrecks a budget like an impulse buy. More than half (54%) of U.S. shoppers have admitted to spending $100 or more on an impulse purchase. And 20% of shoppers have spent at least $1,000 on an impulse buy. Avoid buyers’ remorse by waiting a few days to make large purchase decisions or by limiting your unplanned spending to a certain dollar amount within your budget.
Online shopping may be a particular temptation. Dr. Tarugu, the Florida gastroenterologist, has focused on reducing those impulse buys as well, deleting all online shopping apps from his and his family’s phones.
“You won’t notice how much you have ordered online until it arrives at your doorstep,” he said. “It’s really important to keep it at bay.”
Mr. Keady, the TIAA chief planning strategist, recommended this tactic: Calculate the number of patients (or hours) you’d need to see in order to earn the cash required to make the purchase.
“Then, in a mindful way, figure out the amount of value derived from the purchase,” he said.
A version of this article originally appeared on Medscape.com.
“Some of our physician clients have seen their income decrease by as much as 50%,” says Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minnesota. “Many physicians had previously figured that whatever financial obligations they had wouldn’t be a problem because whatever amount they were making would continue, and if there were a decline it would be gradual.” However, assumption is now creating financial strain for many doctors.
Vikram Tarugu, MD, a gastroenterologist and CEO of Detox of South Florida in Okeechobee, Florida, says he has watched his budget for years, but has become even more careful with his spending in the past few months.
“It has helped me a lot to adjust to the new normal when it comes to the financial side of things,” Dr. Tarugu said. “Patients aren’t coming in as much as they used to, so my income has really been affected.”
Primary care physicians have seen a 55% decrease in revenue and a 20%-30% decrease in patient volume as a result of COVID-19. The impact has been even more severe for specialists. Even for physicians whose practices remain busy and whose family members haven’t lost their jobs or income, broader concerns about the economy may be reason enough for physicians to adopt cost-cutting measures.
In Medscape’s Physician Compensation Report 2020, we asked physicians to share their best cost-cutting tips. Many illustrate the lengths to which physicians are going to conserve money.
Here’s a look at some of the advice they shared, along with guidance from experts on how to make it work for you:
1. Create a written budget, even if you think it’s pointless.
Physicians said their most important piece of advice includes the following: “Use a formal budget to track progress,” “write out a budget,” “plan intermittent/large expenses in advance,” “Make sure all expenses are paid before you spend on leisure.”
Nearly 7 in 10 physicians say they have a budget for personal expenses, yet only one-quarter of those who do have a formal, written budget. Writing out a spending plan is key to being intentional about your spending, making sure that you’re living within your means, and identifying areas in which you may be able to cut back.
“Financial planning is all about cash flow, and everybody should know the amount of money coming in, how much is going out, and the difference between the two,” says Amy Guerich, a partner with Stepp & Rothwell, a Kansas City–based financial planning firm. “That’s important in good times, but it’s even more important now when we see physicians taking pay cuts.”
Many physicians have found that budget apps or software programs are easier to work with than anticipated; some even walk you through the process of creating a budget. To get the most out of the apps, you’ll need to check them regularly and make changes based on their data.
“Sometimes there’s this false belief that just by signing up, you are automatically going to be better at budgeting,” says Scott Snider, CFP, a certified financial planner and partner with Mellen Money Management in Ponte Vedra Beach, Florida. “Basically, these apps are a great way to identify problem areas of spending. We have a tendency as humans to underestimate how much we spend on things like Starbucks, dining out, and Amazon shopping.”
One of the doctors’ tips that requires the most willpower is to “pay all expenses before spending on leisure.” That’s because we live in an instant gratification world, and want everything right away, Ms. Guerich said.
“I also think there’s an element of ‘keeping up with the Joneses’ and pressure associated with this profession,” she said. “The stereotype is that physicians are high-income earners so ‘We should be able to do that’ or ‘Mom and dad are doctors, so they can afford it.’ “
Creating and then revisiting your budget progress on a monthly or quarterly basis can give you a feeling of accomplishment and keep you motivated to stay with it.
Keep in mind that budgeting is a continual process rather than a singular event, and you’ll likely adjust it over time as your income and goals change.
2. Save more as you earn more.
Respondents to our Physician Compensation Report gave the following recommendations: “Pay yourself first,” “I put half of my bonus into an investment account no matter how much it is,” “I allocate extra money and put it into a savings account.”
Dr. Greenwald said, “I have a rule that every client needs to be saving 20% of their gross income toward retirement, including whatever the employer is putting in.”
Putting a portion of every paycheck into savings is key to making progress toward financial goals. Start by building an emergency fund with at least 3-6 months’ worth of expenses in it and making sure you’re saving at least enough for retirement to get any potential employer match.
Mr. Snider suggests increasing the percentage you save every time you get a raise.
“The thought behind that strategy is that when a doctor receives a pay raise – even if it’s just a cost-of-living raise of 3% – an extra 1% saved doesn’t reduce their take-home pay year-over-year,” he says. “In fact, they still take home more money, and they save more money. Win-win.”
3. Focus on paying down your debt.
Physicians told us how they were working to pay down debt with the following recommendations: “Accelerate debt reduction,” “I make additional principal payment to our home mortgage,” “We are aggressively attacking our remaining student loans.”
Reducing or eliminating debt is key to increasing cash flow, which can make it easier to meet all of your other financial goals. One-quarter of physicians have credit card debt, which typically carries interest rates higher than other types of debt, making it far more expensive. Focus on paying off such high-interest debt first, before moving on to other types of debt such as auto loans, student loans, or a mortgage.
“Credit card debt and any unsecured debt should be paid before anything else,” Mr. Snider says. “Getting rid of those high interest rates should be a priority. And that type of debt has less flexible terms than student debt.”
4. Great opportunity to take advantage of record-low interest rates.
Physicians said that, to save money, they are recommending the following: “Consolidating student debt into our mortgage,” “Accelerating payments of the principle on our mortgage,” “Making sure we have an affordable mortgage.”
With interest rates at an all-time low, even those who’ve recently refinanced might see significant savings by refinancing again. Given the associated fees, it typically makes sense to refinance if you can reduce your mortgage rate by at least a point, and you’re planning to stay in the home for at least 5 years.
“Depending on how much lower your rate is, refinancing can make a big difference in your monthly payments,” Ms. Guerich said. “For physicians who might need an emergency reserve but don’t have cash on hand, a HELOC [Home Equity Line of Credit] is a great way to accomplish that.”
5. Be wary of credit cards dangers; use cards wisely.
Physician respondents recommended the following: “Use 0% interest offers on credit cards,” “Only have one card and pay it off every month,” “Never carry over balance.”
Nearly 80% of physicians have three or more credit cards, with 18% reporting that they have seven or more. When used wisely, credit cards can be an important tool for managing finances. Many credit cards come with tools that can help with budgeting, and credit cards rewards and perks can offer real value to users. That said, rewards typically are not valuable enough to offset the cost of interest on balances (or the associated damage to your credit score) that aren’t paid off each month.
“If you’re paying a high rate on credit card balances that carry over every month, regardless of your income, that could be a symptom that you may be spending more than you should,” says Dan Keady, a CFP and chief financial planning strategist at financial services firm TIAA.
6. Give less to Uncle Sam: Keep it for yourself.
Physicians said that they do the following: “Maximize tax-free/deferred savings (401k, HSA, etc.),” “Give to charity to reduce tax,” “Use pre-tax dollars for childcare and healthcare.”
Not only does saving in workplace retirement accounts help you build your nest egg, but it also reduces the amount that you have to pay in taxes in a given year. Physicians should also take advantage of other ways to reduce their income for tax purposes, such as saving money in a health savings account or flexible savings account.
The 401(k) or 403(b) contribution limit for this year is $19,500 ($26,000) for those age 50 years and older. Self-employed physicians can save even more money via a Simplified Employee Pension (SEP) IRA, says Ms. Guerich said. They can save up to 25% of compensation, up to $57,000 in 2020.
7. Automate everything and spare yourself the headache.
Physicians said the following: “Designate money from your paycheck directly to tax deferred and taxable accounts automatically,” “Use automatic payment for credit card balance monthly,” “Automate your savings.”
You probably already automate your 401(k) contributions, but you can also automate bill payments, emergency savings contributions and other financial tasks. For busy physicians, this can make it easier to stick to your financial plan and achieve your goals.
“The older you get, the busier you get, said Mr. Snider says. “Automation can definitely help with that. But make sure you are checking in quarterly to make sure that everything is still in line with your plan. The problem with automation is when you forget about it completely and just let everything sit there.”
8. Save separately for big purchases.
Sometimes it’s the big major expenses that can start to derail a budget. Physicians told us the following tactics for large purchases: “We buy affordable cars and take budget vacations,” “I buy used cars,” “We save in advance for new cars and only buy cars with cash.”
The decision of which car to purchase or where to go on a family vacation is a personal one, and some physicians take great enjoyment and pride in driving a luxury vehicle or traveling to exotic locales. The key, experts say, is to factor the cost of that car into the rest of your budget, and make sure that it’s not preventing you from achieving other financial goals.
“I don’t like to judge or tell clients how they should spend their money,” said Andrew Musbach, a certified financial planner and cofounder of MD Wealth Management in Chelsea, Mich. “Some people like cars, we have clients that have two planes, others want a second house or like to travel. Each person has their own interest where they may spend more relative to other people, but as long as they are meeting their savings targets, I encourage them to spend their money and enjoy what they enjoy most, guilt free.”
Mr. Snider suggests setting up a savings account separate from emergency or retirement accounts to set aside money if you have a goal for a large future purchase, such as a boat or a second home.
“That way, the funds don’t get commingled, and it’s explicitly clear whether or not the doctor is on target,” he says. “It also prevents them from treating their emergency savings account as an ATM machine.”
9. Start saving for college when the kids are little.
Respondents said the following: “We are buying less to save for the kids’ college education,” “We set up direct deposit into college and retirement savings plans,” “We have a 529 account for college savings.”
Helping pay for their children’s college education is an important financial goal for many physicians. The earlier that you start saving, the less you’ll have to save overall, thanks to compound interest. State 529 accounts are often a good place to start, especially if your state offers a tax incentive for doing so.
Mr. Snider recommends that physicians start small, with an initial investment of $1,000 per month and $100 per month contributions. Assuming a 7% rate of return and 17 years’ worth of savings, this would generate just over $42,000. (Note, current typical rates of return are less than 7%).
“Ideally, as other goals are accomplished and personal debt gets paid off, the doctor is ramping up their savings to have at least 50% of college expenses covered from their 529 college savings,” he says.
10. Watch out for the temptation of impulse purchases.
Physicians said the following: “Avoid impulse purchases,” “Avoid impulse shopping, make a list for the store and stick to it,” “Wait to buy things on sale.”
Nothing wrecks a budget like an impulse buy. More than half (54%) of U.S. shoppers have admitted to spending $100 or more on an impulse purchase. And 20% of shoppers have spent at least $1,000 on an impulse buy. Avoid buyers’ remorse by waiting a few days to make large purchase decisions or by limiting your unplanned spending to a certain dollar amount within your budget.
Online shopping may be a particular temptation. Dr. Tarugu, the Florida gastroenterologist, has focused on reducing those impulse buys as well, deleting all online shopping apps from his and his family’s phones.
“You won’t notice how much you have ordered online until it arrives at your doorstep,” he said. “It’s really important to keep it at bay.”
Mr. Keady, the TIAA chief planning strategist, recommended this tactic: Calculate the number of patients (or hours) you’d need to see in order to earn the cash required to make the purchase.
“Then, in a mindful way, figure out the amount of value derived from the purchase,” he said.
A version of this article originally appeared on Medscape.com.
Who’s better off: Employed or self-employed physicians?
Self-employed physicians have the highest salaries, largest homes, and greatest wealth – yet they feel the least fairly compensated, according to an analysis of data from over 17,000 physicians.
A new examination of survey responses from the Medscape Physician Compensation Report 2020, which included information about income, job satisfaction, and more, compared responses from self-employed physicians, independent contractors, and employed physicians.
Income and wealth, benefits, and job satisfaction were compared. From the results of the questionnaire, self-employed physicians stand out among their peers across all categories: They enjoy greater income, wealth, and benefits and appear to be more satisfied by their choice of practice.
“The survey confirms that self-employed is the most satisfying, although the trend in health care is to take employed positions,” said Robert Scroggins, JD, CPA, certified health care business consultant with ScrogginsGreer, Cincinnati. “Doctors who become employees primarily do that to escape the management responsibilities for the practice. It seems to be more a decision to get away from something than to go toward something.”
The financial and work picture for self-employed physicians
Self-employed physicians reported the largest salaries for 2019 (average, $360,752), followed by independent contractors ($336,005). Employees reported the lowest average salary ($297,332).
The largest percentage of self-employed physicians (46%) work in an office-based group practice, followed by those in office-based solo practices (30%). Almost two-thirds of self-employed respondents are owners and 37% are partners.
Self-employed physicians are more likely to be older than 45 years; 79% fall into that age bracket, compared with 57% of employees and 70% of independent contractors.
Self-employed physicians reported the highest levels of wealth among their peers. About 44% of self-employed respondents declared a net wealth of over $2 million, compared with 25% of employees. Only 6% of contractors and employed physicians reported a net wealth of over $5 million, compared with 13% of self-employed physicians.
Self-employed physicians also managed their personal expenses slightly differently. They were more likely to pool their income with their spouse in a common account used for bills and expenses, regardless of how much they each earned (63% of self-employed respondents, compared with 58% of employees and 50% of independent contractors).
Perhaps unsurprisingly, self-employed physicians also reported having the largest homes, with an average square footage of 3,629 square feet, compared with 3,023 square feet for employees and 2,984 square feet for independent contractors. Self-employed physicians’ mortgages (average, $240,389) were similar to those of employed physicians’ mortgages but were higher than those of independent contractors’ mortgages (average, $213,740).
Self-employed physicians were also most likely to highly appraise their own performance: Half of all self-employed respondents felt “very satisfied” with their job performance, compared with 40% of employees and 44% of independent contractors.
When asked what they consider to be the most rewarding aspect of their job, self-employed physicians were more likely to choose gratitude and patient relationships than their peers (32%, compared with 26% of employees and 19% of independent contractors).
Despite their higher net wealth and larger salaries, self-employed physicians were least likely to feel fairly compensated; 49% of self-employed physicians said they did not feel fairly compensated for their work, compared with 40% of employees and 40% of independent contractors.
“Self-employed physicians may be better compensated than others of the same specialty who are employees, so some of that may be perception,” said Mr. Scroggins. “Or they feel they should be compensated to a far greater degree than those who are employed.”
Self-employed physicians were also more likely to respond that they would choose the same practice setting again, though across all three categories, fewer than 50% of respondents would do so: 34% of self-employed physicians, compared with 29% of employees and 28% of independent contractors.
The financial and work picture for employed physicians
About a third (32%) of employed physician respondents work in hospitals; 28% work in private practices.
Employed physicians were most likely to report a salary increase from 2018 to 2019: 74%, compared with 45% of self-employed and 52% of independent contractors.
As for declines in income, self-employed physicians and independent contractors suffered a comparable loss, with 13% and 12% of them, respectively, reporting salary cuts greater than 10%. Decreases of up to 10% were felt mostly by the self-employed, with 17% experiencing such cuts, compared with 7% of employees and 10% of independent contractors.
In contrast, employees were the least likely of the three categories to have incurred large financial losses over the past year: 77% of employed respondents indicated that they had not experienced any significant financial losses in the past year, compared with 63% of self-employed physicians and 63% of independent contractors. They were also least likely to have made any investments at all over the past year – 21% of employees reported having made none at all in 2019, compared to 11% of self-employed physicians and 16% of independent contractors.
The financial and work picture for independent contractors
Just over half (52%) of all independent contractors who responded to our questionnaire work in hospitals, 15% work in group practices, 9% work in outpatient clinics, and just 2% work in solo practices.
Independent contractors were less likely than their peers to have received employment benefits such as health insurance, malpractice coverage, and paid time off. They were also less likely to be saving for retirement. Almost half (45%) of independent contractors said they received no employment benefits at all, compared to 20% of self-employed physicians and just 8% of employees.
What’s more, 27% of independent contractors do not currently put money into a 401(k) retirement account or tax-deferred college savings account on a regular basis, compared with 16% of self-employed physicians and 8% of employees. Similarly, they were less likely to put money into a taxable savings account (39% responded that they do not, compared with 32% of self-employed physicians and 27% of employees).
“Net worth and retirement funding findings do line up with what I’ve observed,” said Mr. Scroggins. “Those who have independent practices as opposed to working for a hospital do tend to more heavily fund retirement plan accounts, which is typically the biggest driver of building net worth.”
Despite the lack of retirement planning, independent contractors were more likely than their peers to derive satisfaction from making money at a job they like (18%, compared with 12% of employees and 11% of self-employed physicians). They’re also far more likely to be in emergency medicine (22% of independent contractors, compared with 3% of self-employed and 5% of employees) or psychiatry (11% of independent contractors, compared with 5% of self-employed and 6% of employees).
Among the three categories of physicians, independent contractors were least likely to say that they would choose the same practice setting again. Across all three categories, fewer than 50% of respondents would do so: 34% of self-employed physicians, compared with 29% of employees and 28% of independent contractors.
Physicians who are considering leaving their own practice for a hospital setting should do so with caution and fully understand what they are getting into, said Mr. Scroggins. “If they’re just looking at compensation, they also should be looking very carefully at retirement plan benefits. If that’s their main method of saving and building net worth, then that’s a dramatic difference.”
And of course, there’s always the intangible value of feeling connected to a practice and its patients: “Physicians got into this line of work to treat patients and help people become healthier, and in hospitals they end up being more disconnected from their patients,” Mr. Scroggins said. “That’s a big factor as well.”
Editor’s note: Only differences that are statistically significant at a 95% confidence level between categories of employment have been included. Of the 13,893 responses included in this analysis, 3,860 physicians identified as self-employed, 9,262 as employees, and 772 as independent contractors.
A version of this article originally appeared on Medscape.com.
Self-employed physicians have the highest salaries, largest homes, and greatest wealth – yet they feel the least fairly compensated, according to an analysis of data from over 17,000 physicians.
A new examination of survey responses from the Medscape Physician Compensation Report 2020, which included information about income, job satisfaction, and more, compared responses from self-employed physicians, independent contractors, and employed physicians.
Income and wealth, benefits, and job satisfaction were compared. From the results of the questionnaire, self-employed physicians stand out among their peers across all categories: They enjoy greater income, wealth, and benefits and appear to be more satisfied by their choice of practice.
“The survey confirms that self-employed is the most satisfying, although the trend in health care is to take employed positions,” said Robert Scroggins, JD, CPA, certified health care business consultant with ScrogginsGreer, Cincinnati. “Doctors who become employees primarily do that to escape the management responsibilities for the practice. It seems to be more a decision to get away from something than to go toward something.”
The financial and work picture for self-employed physicians
Self-employed physicians reported the largest salaries for 2019 (average, $360,752), followed by independent contractors ($336,005). Employees reported the lowest average salary ($297,332).
The largest percentage of self-employed physicians (46%) work in an office-based group practice, followed by those in office-based solo practices (30%). Almost two-thirds of self-employed respondents are owners and 37% are partners.
Self-employed physicians are more likely to be older than 45 years; 79% fall into that age bracket, compared with 57% of employees and 70% of independent contractors.
Self-employed physicians reported the highest levels of wealth among their peers. About 44% of self-employed respondents declared a net wealth of over $2 million, compared with 25% of employees. Only 6% of contractors and employed physicians reported a net wealth of over $5 million, compared with 13% of self-employed physicians.
Self-employed physicians also managed their personal expenses slightly differently. They were more likely to pool their income with their spouse in a common account used for bills and expenses, regardless of how much they each earned (63% of self-employed respondents, compared with 58% of employees and 50% of independent contractors).
Perhaps unsurprisingly, self-employed physicians also reported having the largest homes, with an average square footage of 3,629 square feet, compared with 3,023 square feet for employees and 2,984 square feet for independent contractors. Self-employed physicians’ mortgages (average, $240,389) were similar to those of employed physicians’ mortgages but were higher than those of independent contractors’ mortgages (average, $213,740).
Self-employed physicians were also most likely to highly appraise their own performance: Half of all self-employed respondents felt “very satisfied” with their job performance, compared with 40% of employees and 44% of independent contractors.
When asked what they consider to be the most rewarding aspect of their job, self-employed physicians were more likely to choose gratitude and patient relationships than their peers (32%, compared with 26% of employees and 19% of independent contractors).
Despite their higher net wealth and larger salaries, self-employed physicians were least likely to feel fairly compensated; 49% of self-employed physicians said they did not feel fairly compensated for their work, compared with 40% of employees and 40% of independent contractors.
“Self-employed physicians may be better compensated than others of the same specialty who are employees, so some of that may be perception,” said Mr. Scroggins. “Or they feel they should be compensated to a far greater degree than those who are employed.”
Self-employed physicians were also more likely to respond that they would choose the same practice setting again, though across all three categories, fewer than 50% of respondents would do so: 34% of self-employed physicians, compared with 29% of employees and 28% of independent contractors.
The financial and work picture for employed physicians
About a third (32%) of employed physician respondents work in hospitals; 28% work in private practices.
Employed physicians were most likely to report a salary increase from 2018 to 2019: 74%, compared with 45% of self-employed and 52% of independent contractors.
As for declines in income, self-employed physicians and independent contractors suffered a comparable loss, with 13% and 12% of them, respectively, reporting salary cuts greater than 10%. Decreases of up to 10% were felt mostly by the self-employed, with 17% experiencing such cuts, compared with 7% of employees and 10% of independent contractors.
In contrast, employees were the least likely of the three categories to have incurred large financial losses over the past year: 77% of employed respondents indicated that they had not experienced any significant financial losses in the past year, compared with 63% of self-employed physicians and 63% of independent contractors. They were also least likely to have made any investments at all over the past year – 21% of employees reported having made none at all in 2019, compared to 11% of self-employed physicians and 16% of independent contractors.
The financial and work picture for independent contractors
Just over half (52%) of all independent contractors who responded to our questionnaire work in hospitals, 15% work in group practices, 9% work in outpatient clinics, and just 2% work in solo practices.
Independent contractors were less likely than their peers to have received employment benefits such as health insurance, malpractice coverage, and paid time off. They were also less likely to be saving for retirement. Almost half (45%) of independent contractors said they received no employment benefits at all, compared to 20% of self-employed physicians and just 8% of employees.
What’s more, 27% of independent contractors do not currently put money into a 401(k) retirement account or tax-deferred college savings account on a regular basis, compared with 16% of self-employed physicians and 8% of employees. Similarly, they were less likely to put money into a taxable savings account (39% responded that they do not, compared with 32% of self-employed physicians and 27% of employees).
“Net worth and retirement funding findings do line up with what I’ve observed,” said Mr. Scroggins. “Those who have independent practices as opposed to working for a hospital do tend to more heavily fund retirement plan accounts, which is typically the biggest driver of building net worth.”
Despite the lack of retirement planning, independent contractors were more likely than their peers to derive satisfaction from making money at a job they like (18%, compared with 12% of employees and 11% of self-employed physicians). They’re also far more likely to be in emergency medicine (22% of independent contractors, compared with 3% of self-employed and 5% of employees) or psychiatry (11% of independent contractors, compared with 5% of self-employed and 6% of employees).
Among the three categories of physicians, independent contractors were least likely to say that they would choose the same practice setting again. Across all three categories, fewer than 50% of respondents would do so: 34% of self-employed physicians, compared with 29% of employees and 28% of independent contractors.
Physicians who are considering leaving their own practice for a hospital setting should do so with caution and fully understand what they are getting into, said Mr. Scroggins. “If they’re just looking at compensation, they also should be looking very carefully at retirement plan benefits. If that’s their main method of saving and building net worth, then that’s a dramatic difference.”
And of course, there’s always the intangible value of feeling connected to a practice and its patients: “Physicians got into this line of work to treat patients and help people become healthier, and in hospitals they end up being more disconnected from their patients,” Mr. Scroggins said. “That’s a big factor as well.”
Editor’s note: Only differences that are statistically significant at a 95% confidence level between categories of employment have been included. Of the 13,893 responses included in this analysis, 3,860 physicians identified as self-employed, 9,262 as employees, and 772 as independent contractors.
A version of this article originally appeared on Medscape.com.
Self-employed physicians have the highest salaries, largest homes, and greatest wealth – yet they feel the least fairly compensated, according to an analysis of data from over 17,000 physicians.
A new examination of survey responses from the Medscape Physician Compensation Report 2020, which included information about income, job satisfaction, and more, compared responses from self-employed physicians, independent contractors, and employed physicians.
Income and wealth, benefits, and job satisfaction were compared. From the results of the questionnaire, self-employed physicians stand out among their peers across all categories: They enjoy greater income, wealth, and benefits and appear to be more satisfied by their choice of practice.
“The survey confirms that self-employed is the most satisfying, although the trend in health care is to take employed positions,” said Robert Scroggins, JD, CPA, certified health care business consultant with ScrogginsGreer, Cincinnati. “Doctors who become employees primarily do that to escape the management responsibilities for the practice. It seems to be more a decision to get away from something than to go toward something.”
The financial and work picture for self-employed physicians
Self-employed physicians reported the largest salaries for 2019 (average, $360,752), followed by independent contractors ($336,005). Employees reported the lowest average salary ($297,332).
The largest percentage of self-employed physicians (46%) work in an office-based group practice, followed by those in office-based solo practices (30%). Almost two-thirds of self-employed respondents are owners and 37% are partners.
Self-employed physicians are more likely to be older than 45 years; 79% fall into that age bracket, compared with 57% of employees and 70% of independent contractors.
Self-employed physicians reported the highest levels of wealth among their peers. About 44% of self-employed respondents declared a net wealth of over $2 million, compared with 25% of employees. Only 6% of contractors and employed physicians reported a net wealth of over $5 million, compared with 13% of self-employed physicians.
Self-employed physicians also managed their personal expenses slightly differently. They were more likely to pool their income with their spouse in a common account used for bills and expenses, regardless of how much they each earned (63% of self-employed respondents, compared with 58% of employees and 50% of independent contractors).
Perhaps unsurprisingly, self-employed physicians also reported having the largest homes, with an average square footage of 3,629 square feet, compared with 3,023 square feet for employees and 2,984 square feet for independent contractors. Self-employed physicians’ mortgages (average, $240,389) were similar to those of employed physicians’ mortgages but were higher than those of independent contractors’ mortgages (average, $213,740).
Self-employed physicians were also most likely to highly appraise their own performance: Half of all self-employed respondents felt “very satisfied” with their job performance, compared with 40% of employees and 44% of independent contractors.
When asked what they consider to be the most rewarding aspect of their job, self-employed physicians were more likely to choose gratitude and patient relationships than their peers (32%, compared with 26% of employees and 19% of independent contractors).
Despite their higher net wealth and larger salaries, self-employed physicians were least likely to feel fairly compensated; 49% of self-employed physicians said they did not feel fairly compensated for their work, compared with 40% of employees and 40% of independent contractors.
“Self-employed physicians may be better compensated than others of the same specialty who are employees, so some of that may be perception,” said Mr. Scroggins. “Or they feel they should be compensated to a far greater degree than those who are employed.”
Self-employed physicians were also more likely to respond that they would choose the same practice setting again, though across all three categories, fewer than 50% of respondents would do so: 34% of self-employed physicians, compared with 29% of employees and 28% of independent contractors.
The financial and work picture for employed physicians
About a third (32%) of employed physician respondents work in hospitals; 28% work in private practices.
Employed physicians were most likely to report a salary increase from 2018 to 2019: 74%, compared with 45% of self-employed and 52% of independent contractors.
As for declines in income, self-employed physicians and independent contractors suffered a comparable loss, with 13% and 12% of them, respectively, reporting salary cuts greater than 10%. Decreases of up to 10% were felt mostly by the self-employed, with 17% experiencing such cuts, compared with 7% of employees and 10% of independent contractors.
In contrast, employees were the least likely of the three categories to have incurred large financial losses over the past year: 77% of employed respondents indicated that they had not experienced any significant financial losses in the past year, compared with 63% of self-employed physicians and 63% of independent contractors. They were also least likely to have made any investments at all over the past year – 21% of employees reported having made none at all in 2019, compared to 11% of self-employed physicians and 16% of independent contractors.
The financial and work picture for independent contractors
Just over half (52%) of all independent contractors who responded to our questionnaire work in hospitals, 15% work in group practices, 9% work in outpatient clinics, and just 2% work in solo practices.
Independent contractors were less likely than their peers to have received employment benefits such as health insurance, malpractice coverage, and paid time off. They were also less likely to be saving for retirement. Almost half (45%) of independent contractors said they received no employment benefits at all, compared to 20% of self-employed physicians and just 8% of employees.
What’s more, 27% of independent contractors do not currently put money into a 401(k) retirement account or tax-deferred college savings account on a regular basis, compared with 16% of self-employed physicians and 8% of employees. Similarly, they were less likely to put money into a taxable savings account (39% responded that they do not, compared with 32% of self-employed physicians and 27% of employees).
“Net worth and retirement funding findings do line up with what I’ve observed,” said Mr. Scroggins. “Those who have independent practices as opposed to working for a hospital do tend to more heavily fund retirement plan accounts, which is typically the biggest driver of building net worth.”
Despite the lack of retirement planning, independent contractors were more likely than their peers to derive satisfaction from making money at a job they like (18%, compared with 12% of employees and 11% of self-employed physicians). They’re also far more likely to be in emergency medicine (22% of independent contractors, compared with 3% of self-employed and 5% of employees) or psychiatry (11% of independent contractors, compared with 5% of self-employed and 6% of employees).
Among the three categories of physicians, independent contractors were least likely to say that they would choose the same practice setting again. Across all three categories, fewer than 50% of respondents would do so: 34% of self-employed physicians, compared with 29% of employees and 28% of independent contractors.
Physicians who are considering leaving their own practice for a hospital setting should do so with caution and fully understand what they are getting into, said Mr. Scroggins. “If they’re just looking at compensation, they also should be looking very carefully at retirement plan benefits. If that’s their main method of saving and building net worth, then that’s a dramatic difference.”
And of course, there’s always the intangible value of feeling connected to a practice and its patients: “Physicians got into this line of work to treat patients and help people become healthier, and in hospitals they end up being more disconnected from their patients,” Mr. Scroggins said. “That’s a big factor as well.”
Editor’s note: Only differences that are statistically significant at a 95% confidence level between categories of employment have been included. Of the 13,893 responses included in this analysis, 3,860 physicians identified as self-employed, 9,262 as employees, and 772 as independent contractors.
A version of this article originally appeared on Medscape.com.
Three malpractice risks of video visits
During a telemedicine visit with his physician, a 62-year-old obese patient with an ankle injury reported new swelling of his leg. Three weeks had passed since the man visited an emergency department, where he underwent surgery and had a cast applied to the wound. The physician, during the telemedicine visit, advised the patient to elevate his leg and see an orthopedist within 24 hours. A Doppler ultrasound was ordered for 12:30 p.m. that same day.
The patient never made it to the appointment. He became unresponsive and went into full arrest hours later. His death fueled a lawsuit by his family that claimed failure to diagnose and treat deep venous thrombosis. The family contended the providers involved should have referred the patient to care immediately during the video visit.
The case, which comes from the claims database of national medical liability insurer The Doctors Company, illustrates the legal risks that can stem from video visits with patients, says Richard Cahill, JD, vice president and associate general counsel for The Doctors Company.
“By evaluating the patient remotely, the physician failed to appreciate the often subtle nuances of the clinical presentation, which undoubtedly could have been more accurately assessed in the office setting, and would probably have led to more urgent evaluation and intervention, thereby likely preventing the unfortunate and otherwise avoidable result,” said Mr. Cahill.
According to a Harris poll, 42% of Americans reported using video visits during the pandemic, a trend that is likely to continue as practices reopen and virtual care becomes the norm. But as physicians conduct more video visits, so grows their risk for lawsuits associated with the technology.
“We probably will see more malpractice suits filed the more telehealth is used,” said Mei Wa Kwong, JD, executive director of the Center for Connected Health Policy. “It’s a numbers game. The more it’s used, the higher likelihood that lawsuits occur.”
Three problems in not being able to touch the patient
1. The primary challenge with video visits “is the inability to directly observe and lay hands on the patient,” says Jonathan Einbinder, MD, assistant vice president of analytics for CRICO, a medical liability insurer based in Boston.
said Dr. Einbinder, a practicing internist.
Such incomplete pictures can lead to diagnostic errors and the potential for lawsuits, as demonstrated by a recent CRICO analysis. Of 106 telemedicine-related claims from 2014 to 2018, 66% were diagnosis related, according to the analysis of claims from CRICO’s national database. Twelve percent of the telemedicine-related claims were associated with surgical treatment, 11% were related to medical treatment, and 5% were associated with medication issues. A smaller number of claims resulted from patient monitoring, ob.gyn. care, and safety and security.
Another analysis by The Doctors Company similarly determined that diagnostic errors are the most common allegation in telemedicine-related claims. In the study of 28 telemedicine-related claims from The Doctors’ database, 71% were diagnosis related, 11% were associated with mismanagement of treatment, and 7% were related to improper management of a surgical patient. Other allegations included improper performance of treatment or procedure and improper performance of surgery.
“Because a ‘typical’ exam can’t be done, there is the potential to miss things,” said David L. Feldman, MD, chief medical officer for The Doctors Company Group. “A subtlety, perhaps a lump that can’t be seen but only felt, and only by an experienced examiner, for example, may be missed.”
2. Documentation dangers also loom, said William Sullivan, DO, JD, an emergency physician and an attorney who specializes in health care. The legal risk lies in documenting a video visit in the same way the doctor would document an in-person visit, he explained.
“Investigation into a potential lawsuit begins when there is some type of bad outcome related to medical care,” Dr. Sullivan explained. “To determine whether the lawsuit has merit, patients/attorneys review the medical records to retrospectively determine the potential cause of the bad outcome. If the documentation reflects an examination that could not have been performed, a lawyer might be more likely to pursue a case, and it would be more difficult to defend the care provided.”
Dr. Sullivan provided this example: During a video visit, a patient complains of acute onset weakness. The physician documents that the patient’s heart has a “regular rate and rhythm,” and “muscle strength is equal bilaterally.” The following day, the patient’s weakness continues, and the patient goes to the emergency department where he is diagnosed with stroke. An EKG in the ED shows that the patient is in atrial fibrillation.
“The telehealth provider would have a difficult time explaining how it was determined that the patient had normal muscle strength and a normal heart rhythm over a video visit the day before,” Dr. Sullivan said. “A lawyer in a subsequent malpractice case would present the provider as careless and would argue that if the provider had only sent the patient to the emergency department after the telehealth visit instead of documenting exam findings that couldn’t have been performed, the patient could have been successfully treated for the stroke.”
3. Poorly executed informed consent can also give rise to a lawsuit. This includes informed consent regarding the use of telehealth as the accepted modality for the visit rather than traditional on-site evaluations, as well as preprocedure informed consent.
“Inadequate and/or poorly documented informed consent can result in a claim for medical battery,” Mr. Cahill said.
A medical battery allegation refers to the alleged treatment or touching of a patient’s body without that person’s consent. As the AMA Journal of Ethics explains, a patient’s consent must be given, either expressly or implicitly, before a physician may legally “interfere” with the physical body of the patient.
Ideally, the informed consent process is undertaken during a first in-person visit, before virtual visits begin, Dr. Feldman said.
“There is a lot that a patient has to understand when a visit is done virtually, which is part of the informed consent process,” Dr. Feldman said. “The pandemic has forced some physicians to do their first visit virtually, and this makes the process of informing patients more onerous. It is not a simple matter of converting an in-person office practice to a remote office practice. The work flows are different, so there are definitely legal concerns as it relates to privacy and cybersecurity to name a few.”
Waivers may be weak protection
Since the pandemic started, a number of states have enacted emergency malpractice protections to shield health professionals from lawsuits. Some protections, such as those in Massachusetts, offer immunity to health professionals who provide general care to patients during the COVID-19 emergency, in addition to treatment of COVID-19 patients. Other protections, like those in Connecticut, apply specifically to care provided in support of the state’s pandemic response.
Whether that immunity applies both to in-person visits and video visits during the pandemic is not certain, said J. Richard Moore, JD, a medical liability defense attorney based in Indianapolis. Indiana’s immunity statute for example, does not make a specific provision for telehealth, he said.
“My best prediction is that if considered by the courts, the immunity would be applied to telehealth services, so long as they are being provided ‘in response to the emergency,’ which is the scope of the immunity,” he said. “I would not consider telehealth physicians to be either more or less protected than in-person providers.”
Regulatory scrutiny for telehealth providers has also been relaxed in response to COVID-19, but experts warn not to rely on the temporary shields for ultimate protection.
In March, the U.S. Department of Health and Human Service’s Office of Civil Rights (OCR) eased enforcement actions for noncompliance with Health Insurance Portability and Accountability Act requirements in connection with the good faith provision of telehealth during the COVID-19 health crisis. Under the notice, health providers can use popular applications such as Apple FaceTime, Facebook Messenger, Zoom, or Google Hangouts, to offer telehealth care without risk that OCR will impose fines or penalties for HIPAA violations.
But once the current health care emergency is mitigated, the waivers will likely be withdrawn, and enforcement actions will probably resume, Mr. Cahill said.
“It is recommended that, to avoid potential problems going forward, practitioners use due diligence and undertake best efforts to obey existing privacy and security requirements, including the use of technology that satisfies compliance regulations, despite the waiver by OCR,” he said.
In addition, a majority of states have relaxed state-specific rules for practicing telehealth and loosened licensure requirements during the pandemic. At least 47 states have issued waivers to alter in-state licensure requirements for telemedicine in response to COVID-19, according to the Federation of State Medical Boards. Most of the waivers allow physicians licensed in other states to provide care in states where they do not hold licenses, and some enable doctors to treat patients without first having had an in-person evaluation.
But at least for now, these are temporary changes, reminds Amy Lerman, JD, a health care attorney based in Washington, who specializes in telehealth and corporate compliance. Given the current pandemic environment, a significant concern is that physicians new to the telemedicine space are reacting only to the most recent rules established in the context of the pandemic, Ms. Lerman said.
“As previously noted, the recent developments are temporary in nature – states and various federal agencies have been pretty clear in setting this temporal boundary,” she said. “It is not advisable for providers to build telepractice models around temporary sets of rules.
“Furthermore, the recent developments are not necessarily comprehensive relative to all of the state-specific and other requirements that telemedicine providers are otherwise expected to follow, so relying only on the most recent guidance may cause providers to create telepractice models that have key gaps with respect to regulatory compliance.”
How you can avoid a lawsuit
As businesses reopen and practices resume treatments, physicians should weigh the choice between in-person care and video visits very carefully, said Joseph Kvedar, MD, president of the American Telemedicine Association and a dermatology professor at Harvard Medical School, Boston.
“We have to be very thoughtful about quality in this current phase, where we are doing what I call a hybrid model,” he said. “Some services are offered by telehealth and some require patients to come into the doctor’s office. We have to be very thoughtful about what types of care we determine to be appropriate for telehealth, and that has to be based on clinical quality. And if it is, it should follow that we’ll have low incidence of liability claims.”
Data should be at the center of that conclusion, Dr. Kvedar advises.
“Think about what data is needed to make a therapeutic or diagnostic decision,” he said. “If a health care provider can gather the information needed without touching the patient, then the provider is probably on safe, solid ground making that decision via a telehealth interaction. If the patient can come into the doctor’s office, and the provider deems it necessary to see the patient in person and touch the patient in order to make that clinical decision, then the patient should come in.”
An important step to preventing liability is also having strong telehealth systems and protocols in place and the necessary support to carry them out, said Dr. Einbinder of medical liability insurer CRICO.
For example, Dr. Einbinder, who practices in a 12-doctor internal medicine group, said when he finishes a virtual visit, he enters any orders into the electronic health record. Some of the orders will result in notifications to Dr. Einbinder if they are not executed, such as a referral appointment or a procedure that was not completed.
“I also can forward my orders to a front desk pool that is responsible for making sure things get done,” he said. “And, in our hospital system, we have good case management for complex patients and population management for a variety of chronic conditions. These represent additional safety nets.”
Another liability safeguard is sending patients a “visit summary” after each virtual visit, Dr. Sullivan said. This could be in the form of an email or a text that includes a brief template including items such as diagnosis, recommendations, follow-up, and a reminder to contact the doctor or go to the emergency department if symptoms worsen or new problems develop.
“Patients tend to remember about half of what physicians tell them and half of the information patients do remember is incorrect,” he said. “Consider a few sentences in an e-mail or text message as a substitute for the after-visit instructions from an office visit to enhance patient understanding. There are several inexpensive programs/services that allow text messages to be sent from a computer using a separate dedicated phone number and pretty much every patient has a cell phone to receive the instructions.”
Dr. Sullivan suggests having a documentation template specifically for telehealth visits. He also recommends the inclusion an “informed refusal of care” in the record when necessary. Dr. Sullivan’s wife, a family physician, has encountered several patients who fear contracting COVID-19 and who have refused her recommendations for in-person visits, he said. In such cases, he said it’s a good idea to document that the patient decided to forgo the recommendations given.
“If a patient suffers a bad outcome because of a failure to seek an in-person exam, a short note in the patient’s chart would help to establish that the lack of a follow-up physical exam was the patient’s informed decision, not due to some alleged negligence of the medical provider,” he said.
Concerning informed consent, Dr. Feldman says at a minimum physicians should discuss the following with patients:
- Names and credentials of staff participating.
- The right to stop or refuse treatment by telemedicine.
- Technology that will be used.
- Privacy and security risks.
- Technology-specific risks and permission to bill.
- Alternative care in case of an emergency or technology malfunction.
- Any state-specific requirements.
“Physicians can ensure they have a strong informed consent process during video visits by taking the time to cover these points at the beginning of the first visit, and being sure the patient understands and agrees to these,” Dr. Sullivan explained. “Ideally, this conversation can be recorded for future reference if necessary or at a minimum documented in the medical record.”
Consider these extra precautions
Mr. Cahill advises that practitioners be especially mindful of their “web-side manner” and the setting in which they are communicating with virtual patients to promote confidentiality, professionalism, and uninterrupted interactions.
“Use of a headset in a quiet home office is advisable,” he said. “Physicians must also be cognizant of their physical appearance and the background behind them when the visit includes both audio and visual capability. For ‘face-to-face’ telehealth encounters, it is recommended that a white lab jacket be worn as the appropriate attire; coat and tie are unnecessary.”
Some patients may need to be reminded of the need for confidentiality during a video visit, Mr. Moore added. Physicians are typically in a position to ensure confidentiality, but some patients may not understand how to protect their privacy on their end.
“If the physician sees on the screen or hears from an audio connection that there are other people around who may be able to overhear what is communicated, the physician probably has some responsibility to remind the patient that she or he may want to go to a more private place, close the door, etc.,” he said. “While I think a claim against a physician on this basis would be pretty weak, it is still a good practice for the physician to be cognizant of those kinds of concerns even if the patient is not.”
Finally, for physicians who set up telehealth operability during the pandemic – possibly in a hurry – consider using your actual case data to take a look backward, said Ms. Lerman, the Washington-based health care attorney. Reviewing the data can help determine whether you’re in compliance with relevant state laws, she said.
“If, for example, a provider set up telehealth operations during the pandemic and can see that most of [the] patients are based in a single state, or a small group of states, it is worthwhile to take [the] time and become familiar with the telemedicine laws in those states,” she said. “If there are modifications that need to be made, it may be easier to make them incrementally before the telehealth operations grow any larger in scope.”
A version of this article originally appeared on Medscape.com.
During a telemedicine visit with his physician, a 62-year-old obese patient with an ankle injury reported new swelling of his leg. Three weeks had passed since the man visited an emergency department, where he underwent surgery and had a cast applied to the wound. The physician, during the telemedicine visit, advised the patient to elevate his leg and see an orthopedist within 24 hours. A Doppler ultrasound was ordered for 12:30 p.m. that same day.
The patient never made it to the appointment. He became unresponsive and went into full arrest hours later. His death fueled a lawsuit by his family that claimed failure to diagnose and treat deep venous thrombosis. The family contended the providers involved should have referred the patient to care immediately during the video visit.
The case, which comes from the claims database of national medical liability insurer The Doctors Company, illustrates the legal risks that can stem from video visits with patients, says Richard Cahill, JD, vice president and associate general counsel for The Doctors Company.
“By evaluating the patient remotely, the physician failed to appreciate the often subtle nuances of the clinical presentation, which undoubtedly could have been more accurately assessed in the office setting, and would probably have led to more urgent evaluation and intervention, thereby likely preventing the unfortunate and otherwise avoidable result,” said Mr. Cahill.
According to a Harris poll, 42% of Americans reported using video visits during the pandemic, a trend that is likely to continue as practices reopen and virtual care becomes the norm. But as physicians conduct more video visits, so grows their risk for lawsuits associated with the technology.
“We probably will see more malpractice suits filed the more telehealth is used,” said Mei Wa Kwong, JD, executive director of the Center for Connected Health Policy. “It’s a numbers game. The more it’s used, the higher likelihood that lawsuits occur.”
Three problems in not being able to touch the patient
1. The primary challenge with video visits “is the inability to directly observe and lay hands on the patient,” says Jonathan Einbinder, MD, assistant vice president of analytics for CRICO, a medical liability insurer based in Boston.
said Dr. Einbinder, a practicing internist.
Such incomplete pictures can lead to diagnostic errors and the potential for lawsuits, as demonstrated by a recent CRICO analysis. Of 106 telemedicine-related claims from 2014 to 2018, 66% were diagnosis related, according to the analysis of claims from CRICO’s national database. Twelve percent of the telemedicine-related claims were associated with surgical treatment, 11% were related to medical treatment, and 5% were associated with medication issues. A smaller number of claims resulted from patient monitoring, ob.gyn. care, and safety and security.
Another analysis by The Doctors Company similarly determined that diagnostic errors are the most common allegation in telemedicine-related claims. In the study of 28 telemedicine-related claims from The Doctors’ database, 71% were diagnosis related, 11% were associated with mismanagement of treatment, and 7% were related to improper management of a surgical patient. Other allegations included improper performance of treatment or procedure and improper performance of surgery.
“Because a ‘typical’ exam can’t be done, there is the potential to miss things,” said David L. Feldman, MD, chief medical officer for The Doctors Company Group. “A subtlety, perhaps a lump that can’t be seen but only felt, and only by an experienced examiner, for example, may be missed.”
2. Documentation dangers also loom, said William Sullivan, DO, JD, an emergency physician and an attorney who specializes in health care. The legal risk lies in documenting a video visit in the same way the doctor would document an in-person visit, he explained.
“Investigation into a potential lawsuit begins when there is some type of bad outcome related to medical care,” Dr. Sullivan explained. “To determine whether the lawsuit has merit, patients/attorneys review the medical records to retrospectively determine the potential cause of the bad outcome. If the documentation reflects an examination that could not have been performed, a lawyer might be more likely to pursue a case, and it would be more difficult to defend the care provided.”
Dr. Sullivan provided this example: During a video visit, a patient complains of acute onset weakness. The physician documents that the patient’s heart has a “regular rate and rhythm,” and “muscle strength is equal bilaterally.” The following day, the patient’s weakness continues, and the patient goes to the emergency department where he is diagnosed with stroke. An EKG in the ED shows that the patient is in atrial fibrillation.
“The telehealth provider would have a difficult time explaining how it was determined that the patient had normal muscle strength and a normal heart rhythm over a video visit the day before,” Dr. Sullivan said. “A lawyer in a subsequent malpractice case would present the provider as careless and would argue that if the provider had only sent the patient to the emergency department after the telehealth visit instead of documenting exam findings that couldn’t have been performed, the patient could have been successfully treated for the stroke.”
3. Poorly executed informed consent can also give rise to a lawsuit. This includes informed consent regarding the use of telehealth as the accepted modality for the visit rather than traditional on-site evaluations, as well as preprocedure informed consent.
“Inadequate and/or poorly documented informed consent can result in a claim for medical battery,” Mr. Cahill said.
A medical battery allegation refers to the alleged treatment or touching of a patient’s body without that person’s consent. As the AMA Journal of Ethics explains, a patient’s consent must be given, either expressly or implicitly, before a physician may legally “interfere” with the physical body of the patient.
Ideally, the informed consent process is undertaken during a first in-person visit, before virtual visits begin, Dr. Feldman said.
“There is a lot that a patient has to understand when a visit is done virtually, which is part of the informed consent process,” Dr. Feldman said. “The pandemic has forced some physicians to do their first visit virtually, and this makes the process of informing patients more onerous. It is not a simple matter of converting an in-person office practice to a remote office practice. The work flows are different, so there are definitely legal concerns as it relates to privacy and cybersecurity to name a few.”
Waivers may be weak protection
Since the pandemic started, a number of states have enacted emergency malpractice protections to shield health professionals from lawsuits. Some protections, such as those in Massachusetts, offer immunity to health professionals who provide general care to patients during the COVID-19 emergency, in addition to treatment of COVID-19 patients. Other protections, like those in Connecticut, apply specifically to care provided in support of the state’s pandemic response.
Whether that immunity applies both to in-person visits and video visits during the pandemic is not certain, said J. Richard Moore, JD, a medical liability defense attorney based in Indianapolis. Indiana’s immunity statute for example, does not make a specific provision for telehealth, he said.
“My best prediction is that if considered by the courts, the immunity would be applied to telehealth services, so long as they are being provided ‘in response to the emergency,’ which is the scope of the immunity,” he said. “I would not consider telehealth physicians to be either more or less protected than in-person providers.”
Regulatory scrutiny for telehealth providers has also been relaxed in response to COVID-19, but experts warn not to rely on the temporary shields for ultimate protection.
In March, the U.S. Department of Health and Human Service’s Office of Civil Rights (OCR) eased enforcement actions for noncompliance with Health Insurance Portability and Accountability Act requirements in connection with the good faith provision of telehealth during the COVID-19 health crisis. Under the notice, health providers can use popular applications such as Apple FaceTime, Facebook Messenger, Zoom, or Google Hangouts, to offer telehealth care without risk that OCR will impose fines or penalties for HIPAA violations.
But once the current health care emergency is mitigated, the waivers will likely be withdrawn, and enforcement actions will probably resume, Mr. Cahill said.
“It is recommended that, to avoid potential problems going forward, practitioners use due diligence and undertake best efforts to obey existing privacy and security requirements, including the use of technology that satisfies compliance regulations, despite the waiver by OCR,” he said.
In addition, a majority of states have relaxed state-specific rules for practicing telehealth and loosened licensure requirements during the pandemic. At least 47 states have issued waivers to alter in-state licensure requirements for telemedicine in response to COVID-19, according to the Federation of State Medical Boards. Most of the waivers allow physicians licensed in other states to provide care in states where they do not hold licenses, and some enable doctors to treat patients without first having had an in-person evaluation.
But at least for now, these are temporary changes, reminds Amy Lerman, JD, a health care attorney based in Washington, who specializes in telehealth and corporate compliance. Given the current pandemic environment, a significant concern is that physicians new to the telemedicine space are reacting only to the most recent rules established in the context of the pandemic, Ms. Lerman said.
“As previously noted, the recent developments are temporary in nature – states and various federal agencies have been pretty clear in setting this temporal boundary,” she said. “It is not advisable for providers to build telepractice models around temporary sets of rules.
“Furthermore, the recent developments are not necessarily comprehensive relative to all of the state-specific and other requirements that telemedicine providers are otherwise expected to follow, so relying only on the most recent guidance may cause providers to create telepractice models that have key gaps with respect to regulatory compliance.”
How you can avoid a lawsuit
As businesses reopen and practices resume treatments, physicians should weigh the choice between in-person care and video visits very carefully, said Joseph Kvedar, MD, president of the American Telemedicine Association and a dermatology professor at Harvard Medical School, Boston.
“We have to be very thoughtful about quality in this current phase, where we are doing what I call a hybrid model,” he said. “Some services are offered by telehealth and some require patients to come into the doctor’s office. We have to be very thoughtful about what types of care we determine to be appropriate for telehealth, and that has to be based on clinical quality. And if it is, it should follow that we’ll have low incidence of liability claims.”
Data should be at the center of that conclusion, Dr. Kvedar advises.
“Think about what data is needed to make a therapeutic or diagnostic decision,” he said. “If a health care provider can gather the information needed without touching the patient, then the provider is probably on safe, solid ground making that decision via a telehealth interaction. If the patient can come into the doctor’s office, and the provider deems it necessary to see the patient in person and touch the patient in order to make that clinical decision, then the patient should come in.”
An important step to preventing liability is also having strong telehealth systems and protocols in place and the necessary support to carry them out, said Dr. Einbinder of medical liability insurer CRICO.
For example, Dr. Einbinder, who practices in a 12-doctor internal medicine group, said when he finishes a virtual visit, he enters any orders into the electronic health record. Some of the orders will result in notifications to Dr. Einbinder if they are not executed, such as a referral appointment or a procedure that was not completed.
“I also can forward my orders to a front desk pool that is responsible for making sure things get done,” he said. “And, in our hospital system, we have good case management for complex patients and population management for a variety of chronic conditions. These represent additional safety nets.”
Another liability safeguard is sending patients a “visit summary” after each virtual visit, Dr. Sullivan said. This could be in the form of an email or a text that includes a brief template including items such as diagnosis, recommendations, follow-up, and a reminder to contact the doctor or go to the emergency department if symptoms worsen or new problems develop.
“Patients tend to remember about half of what physicians tell them and half of the information patients do remember is incorrect,” he said. “Consider a few sentences in an e-mail or text message as a substitute for the after-visit instructions from an office visit to enhance patient understanding. There are several inexpensive programs/services that allow text messages to be sent from a computer using a separate dedicated phone number and pretty much every patient has a cell phone to receive the instructions.”
Dr. Sullivan suggests having a documentation template specifically for telehealth visits. He also recommends the inclusion an “informed refusal of care” in the record when necessary. Dr. Sullivan’s wife, a family physician, has encountered several patients who fear contracting COVID-19 and who have refused her recommendations for in-person visits, he said. In such cases, he said it’s a good idea to document that the patient decided to forgo the recommendations given.
“If a patient suffers a bad outcome because of a failure to seek an in-person exam, a short note in the patient’s chart would help to establish that the lack of a follow-up physical exam was the patient’s informed decision, not due to some alleged negligence of the medical provider,” he said.
Concerning informed consent, Dr. Feldman says at a minimum physicians should discuss the following with patients:
- Names and credentials of staff participating.
- The right to stop or refuse treatment by telemedicine.
- Technology that will be used.
- Privacy and security risks.
- Technology-specific risks and permission to bill.
- Alternative care in case of an emergency or technology malfunction.
- Any state-specific requirements.
“Physicians can ensure they have a strong informed consent process during video visits by taking the time to cover these points at the beginning of the first visit, and being sure the patient understands and agrees to these,” Dr. Sullivan explained. “Ideally, this conversation can be recorded for future reference if necessary or at a minimum documented in the medical record.”
Consider these extra precautions
Mr. Cahill advises that practitioners be especially mindful of their “web-side manner” and the setting in which they are communicating with virtual patients to promote confidentiality, professionalism, and uninterrupted interactions.
“Use of a headset in a quiet home office is advisable,” he said. “Physicians must also be cognizant of their physical appearance and the background behind them when the visit includes both audio and visual capability. For ‘face-to-face’ telehealth encounters, it is recommended that a white lab jacket be worn as the appropriate attire; coat and tie are unnecessary.”
Some patients may need to be reminded of the need for confidentiality during a video visit, Mr. Moore added. Physicians are typically in a position to ensure confidentiality, but some patients may not understand how to protect their privacy on their end.
“If the physician sees on the screen or hears from an audio connection that there are other people around who may be able to overhear what is communicated, the physician probably has some responsibility to remind the patient that she or he may want to go to a more private place, close the door, etc.,” he said. “While I think a claim against a physician on this basis would be pretty weak, it is still a good practice for the physician to be cognizant of those kinds of concerns even if the patient is not.”
Finally, for physicians who set up telehealth operability during the pandemic – possibly in a hurry – consider using your actual case data to take a look backward, said Ms. Lerman, the Washington-based health care attorney. Reviewing the data can help determine whether you’re in compliance with relevant state laws, she said.
“If, for example, a provider set up telehealth operations during the pandemic and can see that most of [the] patients are based in a single state, or a small group of states, it is worthwhile to take [the] time and become familiar with the telemedicine laws in those states,” she said. “If there are modifications that need to be made, it may be easier to make them incrementally before the telehealth operations grow any larger in scope.”
A version of this article originally appeared on Medscape.com.
During a telemedicine visit with his physician, a 62-year-old obese patient with an ankle injury reported new swelling of his leg. Three weeks had passed since the man visited an emergency department, where he underwent surgery and had a cast applied to the wound. The physician, during the telemedicine visit, advised the patient to elevate his leg and see an orthopedist within 24 hours. A Doppler ultrasound was ordered for 12:30 p.m. that same day.
The patient never made it to the appointment. He became unresponsive and went into full arrest hours later. His death fueled a lawsuit by his family that claimed failure to diagnose and treat deep venous thrombosis. The family contended the providers involved should have referred the patient to care immediately during the video visit.
The case, which comes from the claims database of national medical liability insurer The Doctors Company, illustrates the legal risks that can stem from video visits with patients, says Richard Cahill, JD, vice president and associate general counsel for The Doctors Company.
“By evaluating the patient remotely, the physician failed to appreciate the often subtle nuances of the clinical presentation, which undoubtedly could have been more accurately assessed in the office setting, and would probably have led to more urgent evaluation and intervention, thereby likely preventing the unfortunate and otherwise avoidable result,” said Mr. Cahill.
According to a Harris poll, 42% of Americans reported using video visits during the pandemic, a trend that is likely to continue as practices reopen and virtual care becomes the norm. But as physicians conduct more video visits, so grows their risk for lawsuits associated with the technology.
“We probably will see more malpractice suits filed the more telehealth is used,” said Mei Wa Kwong, JD, executive director of the Center for Connected Health Policy. “It’s a numbers game. The more it’s used, the higher likelihood that lawsuits occur.”
Three problems in not being able to touch the patient
1. The primary challenge with video visits “is the inability to directly observe and lay hands on the patient,” says Jonathan Einbinder, MD, assistant vice president of analytics for CRICO, a medical liability insurer based in Boston.
said Dr. Einbinder, a practicing internist.
Such incomplete pictures can lead to diagnostic errors and the potential for lawsuits, as demonstrated by a recent CRICO analysis. Of 106 telemedicine-related claims from 2014 to 2018, 66% were diagnosis related, according to the analysis of claims from CRICO’s national database. Twelve percent of the telemedicine-related claims were associated with surgical treatment, 11% were related to medical treatment, and 5% were associated with medication issues. A smaller number of claims resulted from patient monitoring, ob.gyn. care, and safety and security.
Another analysis by The Doctors Company similarly determined that diagnostic errors are the most common allegation in telemedicine-related claims. In the study of 28 telemedicine-related claims from The Doctors’ database, 71% were diagnosis related, 11% were associated with mismanagement of treatment, and 7% were related to improper management of a surgical patient. Other allegations included improper performance of treatment or procedure and improper performance of surgery.
“Because a ‘typical’ exam can’t be done, there is the potential to miss things,” said David L. Feldman, MD, chief medical officer for The Doctors Company Group. “A subtlety, perhaps a lump that can’t be seen but only felt, and only by an experienced examiner, for example, may be missed.”
2. Documentation dangers also loom, said William Sullivan, DO, JD, an emergency physician and an attorney who specializes in health care. The legal risk lies in documenting a video visit in the same way the doctor would document an in-person visit, he explained.
“Investigation into a potential lawsuit begins when there is some type of bad outcome related to medical care,” Dr. Sullivan explained. “To determine whether the lawsuit has merit, patients/attorneys review the medical records to retrospectively determine the potential cause of the bad outcome. If the documentation reflects an examination that could not have been performed, a lawyer might be more likely to pursue a case, and it would be more difficult to defend the care provided.”
Dr. Sullivan provided this example: During a video visit, a patient complains of acute onset weakness. The physician documents that the patient’s heart has a “regular rate and rhythm,” and “muscle strength is equal bilaterally.” The following day, the patient’s weakness continues, and the patient goes to the emergency department where he is diagnosed with stroke. An EKG in the ED shows that the patient is in atrial fibrillation.
“The telehealth provider would have a difficult time explaining how it was determined that the patient had normal muscle strength and a normal heart rhythm over a video visit the day before,” Dr. Sullivan said. “A lawyer in a subsequent malpractice case would present the provider as careless and would argue that if the provider had only sent the patient to the emergency department after the telehealth visit instead of documenting exam findings that couldn’t have been performed, the patient could have been successfully treated for the stroke.”
3. Poorly executed informed consent can also give rise to a lawsuit. This includes informed consent regarding the use of telehealth as the accepted modality for the visit rather than traditional on-site evaluations, as well as preprocedure informed consent.
“Inadequate and/or poorly documented informed consent can result in a claim for medical battery,” Mr. Cahill said.
A medical battery allegation refers to the alleged treatment or touching of a patient’s body without that person’s consent. As the AMA Journal of Ethics explains, a patient’s consent must be given, either expressly or implicitly, before a physician may legally “interfere” with the physical body of the patient.
Ideally, the informed consent process is undertaken during a first in-person visit, before virtual visits begin, Dr. Feldman said.
“There is a lot that a patient has to understand when a visit is done virtually, which is part of the informed consent process,” Dr. Feldman said. “The pandemic has forced some physicians to do their first visit virtually, and this makes the process of informing patients more onerous. It is not a simple matter of converting an in-person office practice to a remote office practice. The work flows are different, so there are definitely legal concerns as it relates to privacy and cybersecurity to name a few.”
Waivers may be weak protection
Since the pandemic started, a number of states have enacted emergency malpractice protections to shield health professionals from lawsuits. Some protections, such as those in Massachusetts, offer immunity to health professionals who provide general care to patients during the COVID-19 emergency, in addition to treatment of COVID-19 patients. Other protections, like those in Connecticut, apply specifically to care provided in support of the state’s pandemic response.
Whether that immunity applies both to in-person visits and video visits during the pandemic is not certain, said J. Richard Moore, JD, a medical liability defense attorney based in Indianapolis. Indiana’s immunity statute for example, does not make a specific provision for telehealth, he said.
“My best prediction is that if considered by the courts, the immunity would be applied to telehealth services, so long as they are being provided ‘in response to the emergency,’ which is the scope of the immunity,” he said. “I would not consider telehealth physicians to be either more or less protected than in-person providers.”
Regulatory scrutiny for telehealth providers has also been relaxed in response to COVID-19, but experts warn not to rely on the temporary shields for ultimate protection.
In March, the U.S. Department of Health and Human Service’s Office of Civil Rights (OCR) eased enforcement actions for noncompliance with Health Insurance Portability and Accountability Act requirements in connection with the good faith provision of telehealth during the COVID-19 health crisis. Under the notice, health providers can use popular applications such as Apple FaceTime, Facebook Messenger, Zoom, or Google Hangouts, to offer telehealth care without risk that OCR will impose fines or penalties for HIPAA violations.
But once the current health care emergency is mitigated, the waivers will likely be withdrawn, and enforcement actions will probably resume, Mr. Cahill said.
“It is recommended that, to avoid potential problems going forward, practitioners use due diligence and undertake best efforts to obey existing privacy and security requirements, including the use of technology that satisfies compliance regulations, despite the waiver by OCR,” he said.
In addition, a majority of states have relaxed state-specific rules for practicing telehealth and loosened licensure requirements during the pandemic. At least 47 states have issued waivers to alter in-state licensure requirements for telemedicine in response to COVID-19, according to the Federation of State Medical Boards. Most of the waivers allow physicians licensed in other states to provide care in states where they do not hold licenses, and some enable doctors to treat patients without first having had an in-person evaluation.
But at least for now, these are temporary changes, reminds Amy Lerman, JD, a health care attorney based in Washington, who specializes in telehealth and corporate compliance. Given the current pandemic environment, a significant concern is that physicians new to the telemedicine space are reacting only to the most recent rules established in the context of the pandemic, Ms. Lerman said.
“As previously noted, the recent developments are temporary in nature – states and various federal agencies have been pretty clear in setting this temporal boundary,” she said. “It is not advisable for providers to build telepractice models around temporary sets of rules.
“Furthermore, the recent developments are not necessarily comprehensive relative to all of the state-specific and other requirements that telemedicine providers are otherwise expected to follow, so relying only on the most recent guidance may cause providers to create telepractice models that have key gaps with respect to regulatory compliance.”
How you can avoid a lawsuit
As businesses reopen and practices resume treatments, physicians should weigh the choice between in-person care and video visits very carefully, said Joseph Kvedar, MD, president of the American Telemedicine Association and a dermatology professor at Harvard Medical School, Boston.
“We have to be very thoughtful about quality in this current phase, where we are doing what I call a hybrid model,” he said. “Some services are offered by telehealth and some require patients to come into the doctor’s office. We have to be very thoughtful about what types of care we determine to be appropriate for telehealth, and that has to be based on clinical quality. And if it is, it should follow that we’ll have low incidence of liability claims.”
Data should be at the center of that conclusion, Dr. Kvedar advises.
“Think about what data is needed to make a therapeutic or diagnostic decision,” he said. “If a health care provider can gather the information needed without touching the patient, then the provider is probably on safe, solid ground making that decision via a telehealth interaction. If the patient can come into the doctor’s office, and the provider deems it necessary to see the patient in person and touch the patient in order to make that clinical decision, then the patient should come in.”
An important step to preventing liability is also having strong telehealth systems and protocols in place and the necessary support to carry them out, said Dr. Einbinder of medical liability insurer CRICO.
For example, Dr. Einbinder, who practices in a 12-doctor internal medicine group, said when he finishes a virtual visit, he enters any orders into the electronic health record. Some of the orders will result in notifications to Dr. Einbinder if they are not executed, such as a referral appointment or a procedure that was not completed.
“I also can forward my orders to a front desk pool that is responsible for making sure things get done,” he said. “And, in our hospital system, we have good case management for complex patients and population management for a variety of chronic conditions. These represent additional safety nets.”
Another liability safeguard is sending patients a “visit summary” after each virtual visit, Dr. Sullivan said. This could be in the form of an email or a text that includes a brief template including items such as diagnosis, recommendations, follow-up, and a reminder to contact the doctor or go to the emergency department if symptoms worsen or new problems develop.
“Patients tend to remember about half of what physicians tell them and half of the information patients do remember is incorrect,” he said. “Consider a few sentences in an e-mail or text message as a substitute for the after-visit instructions from an office visit to enhance patient understanding. There are several inexpensive programs/services that allow text messages to be sent from a computer using a separate dedicated phone number and pretty much every patient has a cell phone to receive the instructions.”
Dr. Sullivan suggests having a documentation template specifically for telehealth visits. He also recommends the inclusion an “informed refusal of care” in the record when necessary. Dr. Sullivan’s wife, a family physician, has encountered several patients who fear contracting COVID-19 and who have refused her recommendations for in-person visits, he said. In such cases, he said it’s a good idea to document that the patient decided to forgo the recommendations given.
“If a patient suffers a bad outcome because of a failure to seek an in-person exam, a short note in the patient’s chart would help to establish that the lack of a follow-up physical exam was the patient’s informed decision, not due to some alleged negligence of the medical provider,” he said.
Concerning informed consent, Dr. Feldman says at a minimum physicians should discuss the following with patients:
- Names and credentials of staff participating.
- The right to stop or refuse treatment by telemedicine.
- Technology that will be used.
- Privacy and security risks.
- Technology-specific risks and permission to bill.
- Alternative care in case of an emergency or technology malfunction.
- Any state-specific requirements.
“Physicians can ensure they have a strong informed consent process during video visits by taking the time to cover these points at the beginning of the first visit, and being sure the patient understands and agrees to these,” Dr. Sullivan explained. “Ideally, this conversation can be recorded for future reference if necessary or at a minimum documented in the medical record.”
Consider these extra precautions
Mr. Cahill advises that practitioners be especially mindful of their “web-side manner” and the setting in which they are communicating with virtual patients to promote confidentiality, professionalism, and uninterrupted interactions.
“Use of a headset in a quiet home office is advisable,” he said. “Physicians must also be cognizant of their physical appearance and the background behind them when the visit includes both audio and visual capability. For ‘face-to-face’ telehealth encounters, it is recommended that a white lab jacket be worn as the appropriate attire; coat and tie are unnecessary.”
Some patients may need to be reminded of the need for confidentiality during a video visit, Mr. Moore added. Physicians are typically in a position to ensure confidentiality, but some patients may not understand how to protect their privacy on their end.
“If the physician sees on the screen or hears from an audio connection that there are other people around who may be able to overhear what is communicated, the physician probably has some responsibility to remind the patient that she or he may want to go to a more private place, close the door, etc.,” he said. “While I think a claim against a physician on this basis would be pretty weak, it is still a good practice for the physician to be cognizant of those kinds of concerns even if the patient is not.”
Finally, for physicians who set up telehealth operability during the pandemic – possibly in a hurry – consider using your actual case data to take a look backward, said Ms. Lerman, the Washington-based health care attorney. Reviewing the data can help determine whether you’re in compliance with relevant state laws, she said.
“If, for example, a provider set up telehealth operations during the pandemic and can see that most of [the] patients are based in a single state, or a small group of states, it is worthwhile to take [the] time and become familiar with the telemedicine laws in those states,” she said. “If there are modifications that need to be made, it may be easier to make them incrementally before the telehealth operations grow any larger in scope.”
A version of this article originally appeared on Medscape.com.
The joys of telemedicine
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].