User login
Election gift for Florida? Trump poised to approve drug imports from Canada
Over the objections of drugmakers, the Trump administration is expected within weeks to finalize its plan that would allow states to import some prescription medicines from Canada.
Six states – Colorado, Florida, Maine, New Hampshire, New Mexico, and Vermont – have passed laws allowing them to seek federal approval to buy drugs from Canada to give their residents access to lower-cost medicines.
But industry observers say the drug importation proposal under review by the administration is squarely aimed at Florida – the most populous swing state in the November election. Trump’s support of the idea initially came at the urging of Florida Gov. Ron DeSantis, a close Republican ally.
The DeSantis administration is so confident Trump will move ahead with allowing drug importation that it put out a request June 30 for private companies to bid on a three-year, $30 million contract to run the program. It hopes to award the contract in December.
Industry experts say Florida is likely to be the first state to win federal approval for a drug importation plan – something that could occur before the November election.
“Approving Florida would feel like the politically astute thing to do,” said Mara Baer, a health consultant who has worked with Colorado on its importation proposal.
Ben England, CEO of FDAImports, a consulting firm in Glen Burnie, Maryland, said the OMB typically has 60 days to review final rules, although he expects this one could be completed before Nov. 3 and predicted there’s a small chance it could get finalized and Florida’s request approved by then. “It’s an election year, so I do see the current administration trying to use this as a talking point to say ‘Look what we’ve accomplished,’” he said.
Florida also makes sense because of the large number of retirees, who face high costs for medicines despite Medicare drug coverage.
The DeSantis administration did not respond to requests for comment.
Trump boasted about his importation plan during an October speech in The Villages, a large retirement community about 60 miles northwest of Orlando. “We will soon allow the safe and legal importation of prescription drugs from other countries, including the country of Canada, where, believe it or not, they pay much less money for the exact same drug,” Trump said, with DeSantis in attendance. “Stand up, Ron. Boy, he wants this so badly.”
The Food and Drug Administration released a detailed proposal last December and sought comments. A final plan was delivered Sept. 10 to the Office of Management and Budget for review, signaling it could be unveiled within weeks.
The proposal would regulate how states set up their own programs for importing drugs from Canada.
Prices are cheaper because Canada limits how much drugmakers can charge for medicines. The United States lets free markets dictate drug prices.
The pharmaceutical industry signaled it will likely sue the Trump administration if it goes forward with its importation plans, saying the plan violates several federal laws and the U.S. Constitution.
But the most stinging rebuke of the Trump importation plan came from the Canadian government, which said the proposal would make it harder for Canadian citizens to get drugs, putting their health at risk.
“Canada will employ all necessary measures to safeguard access for Canadians to needed drugs,” the Canadian government wrote in a letter to the FDA about the draft proposal. “The Canadian drug market and manufacturing capacity are too small to meet the demand of both Canadian and American consumers for prescription drugs.”
Without buy-in from Canada, any plan to import medicines is unlikely to succeed, officials said.
Ena Backus, director of Health Care Reform in Vermont, who has worked on setting up an importation program there, said states will need help from Canada. “Our state importation program relies on a willing partner in Canada,” she said.
For decades, Americans have been buying drugs from Canada for personal use — either by driving over the border, ordering medication on the Internet, or using storefronts that connect them to foreign pharmacies. Though illegal, the FDA has generally permitted purchases for individual use.
About 4 million Americans import lower-cost medicines for personal use each year, and about 20 million say they or someone in their household have done so because the prices are much lower in other countries, according to surveys.
The practice has been popular in Florida. More than a dozen storefronts across the state help consumers connect to pharmacies in Canada and other countries. Several cities, state and school districts in Florida help employees get drugs from Canada.
The administration’s proposal builds on a 2000 law that opened the door to allowing drug importation from Canada. But that provision could take effect only if the Health and Human Services secretary certified importation as safe, something that Democratic and Republican administrations have refused to do.
The drug industry for years has said allowing drugs to be imported from Canada would disrupt the nation’s supply chain and make it easier for unsafe or counterfeit medications to enter the market.
Trump, who made lowering prescription drug prices a signature promise in his 2016 campaign, has been eager to fulfill his pledge. In July 2019, at Trump’s direction, HHS Secretary Alex Azar said the federal government was “open for business” on drug importation, a year after calling drug importation a “gimmick.”
The administration envisions a system in which a Canadian-licensed wholesaler buys directly from a manufacturer for drugs approved for sale in Canada and exports the drugs to a U.S. wholesaler/importer under contract to a state.
Florida’s legislation – approved in 2019 – would set up two importation programs. The first would focus on getting drugs for state programs such as Medicaid, the Department of Corrections and county health departments. State officials said they expect the programs would save the state about $150 million annually.
The second program would be geared to the broader state population.
In response to the draft rule, the states seeking to start a drug importation program suggested changes to the administration’s proposal.
“Should the final rule not address these areas of concern, Colorado will struggle to find appropriate partners and realize significant savings for consumers,” Kim Bimestefer, executive director of the Colorado Department of Health Care Policy & Financing, told the FDA in March.
Among the state’s concerns is that it would be limited to using only one Canadian wholesaler, and without competition the state fears prices might not be as low as officials hoped. Bimestefer also noted that under the draft rule, the federal government would approve the importation program for only two years and states need a longer time frame to get buy-in from wholesalers and other partners.
Colorado officials estimate importing drugs from Canada could cut prices by 54% for cancer drugs and 75% for cardiac medicines. The state also noted the diabetes drug Jardiance costs $400 a month in the United States and sells for $85 in Canada.
Several states worry some of the most expensive drugs – including injectable and biologic medicines – were exempt from the federal rule. Those drug classes are not allowed to be imported under the 2000 law.
However, in an executive order in July, Trump said he would allow insulin to be imported if Azar determined it is required for emergency medical care. An HHS spokesman would not say whether Azar has done that.
Jane Horvath, a health policy consultant in College Park, Md., said the administration faces several challenges getting an importation program up and running, including possible opposition from the pharmaceutical industry and limits on classes of drugs that can be sold over the border.
“Despite the barriers, the programs are still quite worthwhile to pursue,” she said.
Maine’s top health official said the administration should work with the Canadian government to address Canada’s concerns. HHS officials refused to say whether such discussions have started.
Officials in Vermont, where the program would also include consumers covered by private insurance, remain hopeful.
“Given that we want to reduce the burden of health care costs on residents in our state, then it is important to pursue this option if there is a clear pathway forward,” Backus said.
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente. This story also ran on Miami Herald.
Over the objections of drugmakers, the Trump administration is expected within weeks to finalize its plan that would allow states to import some prescription medicines from Canada.
Six states – Colorado, Florida, Maine, New Hampshire, New Mexico, and Vermont – have passed laws allowing them to seek federal approval to buy drugs from Canada to give their residents access to lower-cost medicines.
But industry observers say the drug importation proposal under review by the administration is squarely aimed at Florida – the most populous swing state in the November election. Trump’s support of the idea initially came at the urging of Florida Gov. Ron DeSantis, a close Republican ally.
The DeSantis administration is so confident Trump will move ahead with allowing drug importation that it put out a request June 30 for private companies to bid on a three-year, $30 million contract to run the program. It hopes to award the contract in December.
Industry experts say Florida is likely to be the first state to win federal approval for a drug importation plan – something that could occur before the November election.
“Approving Florida would feel like the politically astute thing to do,” said Mara Baer, a health consultant who has worked with Colorado on its importation proposal.
Ben England, CEO of FDAImports, a consulting firm in Glen Burnie, Maryland, said the OMB typically has 60 days to review final rules, although he expects this one could be completed before Nov. 3 and predicted there’s a small chance it could get finalized and Florida’s request approved by then. “It’s an election year, so I do see the current administration trying to use this as a talking point to say ‘Look what we’ve accomplished,’” he said.
Florida also makes sense because of the large number of retirees, who face high costs for medicines despite Medicare drug coverage.
The DeSantis administration did not respond to requests for comment.
Trump boasted about his importation plan during an October speech in The Villages, a large retirement community about 60 miles northwest of Orlando. “We will soon allow the safe and legal importation of prescription drugs from other countries, including the country of Canada, where, believe it or not, they pay much less money for the exact same drug,” Trump said, with DeSantis in attendance. “Stand up, Ron. Boy, he wants this so badly.”
The Food and Drug Administration released a detailed proposal last December and sought comments. A final plan was delivered Sept. 10 to the Office of Management and Budget for review, signaling it could be unveiled within weeks.
The proposal would regulate how states set up their own programs for importing drugs from Canada.
Prices are cheaper because Canada limits how much drugmakers can charge for medicines. The United States lets free markets dictate drug prices.
The pharmaceutical industry signaled it will likely sue the Trump administration if it goes forward with its importation plans, saying the plan violates several federal laws and the U.S. Constitution.
But the most stinging rebuke of the Trump importation plan came from the Canadian government, which said the proposal would make it harder for Canadian citizens to get drugs, putting their health at risk.
“Canada will employ all necessary measures to safeguard access for Canadians to needed drugs,” the Canadian government wrote in a letter to the FDA about the draft proposal. “The Canadian drug market and manufacturing capacity are too small to meet the demand of both Canadian and American consumers for prescription drugs.”
Without buy-in from Canada, any plan to import medicines is unlikely to succeed, officials said.
Ena Backus, director of Health Care Reform in Vermont, who has worked on setting up an importation program there, said states will need help from Canada. “Our state importation program relies on a willing partner in Canada,” she said.
For decades, Americans have been buying drugs from Canada for personal use — either by driving over the border, ordering medication on the Internet, or using storefronts that connect them to foreign pharmacies. Though illegal, the FDA has generally permitted purchases for individual use.
About 4 million Americans import lower-cost medicines for personal use each year, and about 20 million say they or someone in their household have done so because the prices are much lower in other countries, according to surveys.
The practice has been popular in Florida. More than a dozen storefronts across the state help consumers connect to pharmacies in Canada and other countries. Several cities, state and school districts in Florida help employees get drugs from Canada.
The administration’s proposal builds on a 2000 law that opened the door to allowing drug importation from Canada. But that provision could take effect only if the Health and Human Services secretary certified importation as safe, something that Democratic and Republican administrations have refused to do.
The drug industry for years has said allowing drugs to be imported from Canada would disrupt the nation’s supply chain and make it easier for unsafe or counterfeit medications to enter the market.
Trump, who made lowering prescription drug prices a signature promise in his 2016 campaign, has been eager to fulfill his pledge. In July 2019, at Trump’s direction, HHS Secretary Alex Azar said the federal government was “open for business” on drug importation, a year after calling drug importation a “gimmick.”
The administration envisions a system in which a Canadian-licensed wholesaler buys directly from a manufacturer for drugs approved for sale in Canada and exports the drugs to a U.S. wholesaler/importer under contract to a state.
Florida’s legislation – approved in 2019 – would set up two importation programs. The first would focus on getting drugs for state programs such as Medicaid, the Department of Corrections and county health departments. State officials said they expect the programs would save the state about $150 million annually.
The second program would be geared to the broader state population.
In response to the draft rule, the states seeking to start a drug importation program suggested changes to the administration’s proposal.
“Should the final rule not address these areas of concern, Colorado will struggle to find appropriate partners and realize significant savings for consumers,” Kim Bimestefer, executive director of the Colorado Department of Health Care Policy & Financing, told the FDA in March.
Among the state’s concerns is that it would be limited to using only one Canadian wholesaler, and without competition the state fears prices might not be as low as officials hoped. Bimestefer also noted that under the draft rule, the federal government would approve the importation program for only two years and states need a longer time frame to get buy-in from wholesalers and other partners.
Colorado officials estimate importing drugs from Canada could cut prices by 54% for cancer drugs and 75% for cardiac medicines. The state also noted the diabetes drug Jardiance costs $400 a month in the United States and sells for $85 in Canada.
Several states worry some of the most expensive drugs – including injectable and biologic medicines – were exempt from the federal rule. Those drug classes are not allowed to be imported under the 2000 law.
However, in an executive order in July, Trump said he would allow insulin to be imported if Azar determined it is required for emergency medical care. An HHS spokesman would not say whether Azar has done that.
Jane Horvath, a health policy consultant in College Park, Md., said the administration faces several challenges getting an importation program up and running, including possible opposition from the pharmaceutical industry and limits on classes of drugs that can be sold over the border.
“Despite the barriers, the programs are still quite worthwhile to pursue,” she said.
Maine’s top health official said the administration should work with the Canadian government to address Canada’s concerns. HHS officials refused to say whether such discussions have started.
Officials in Vermont, where the program would also include consumers covered by private insurance, remain hopeful.
“Given that we want to reduce the burden of health care costs on residents in our state, then it is important to pursue this option if there is a clear pathway forward,” Backus said.
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente. This story also ran on Miami Herald.
Over the objections of drugmakers, the Trump administration is expected within weeks to finalize its plan that would allow states to import some prescription medicines from Canada.
Six states – Colorado, Florida, Maine, New Hampshire, New Mexico, and Vermont – have passed laws allowing them to seek federal approval to buy drugs from Canada to give their residents access to lower-cost medicines.
But industry observers say the drug importation proposal under review by the administration is squarely aimed at Florida – the most populous swing state in the November election. Trump’s support of the idea initially came at the urging of Florida Gov. Ron DeSantis, a close Republican ally.
The DeSantis administration is so confident Trump will move ahead with allowing drug importation that it put out a request June 30 for private companies to bid on a three-year, $30 million contract to run the program. It hopes to award the contract in December.
Industry experts say Florida is likely to be the first state to win federal approval for a drug importation plan – something that could occur before the November election.
“Approving Florida would feel like the politically astute thing to do,” said Mara Baer, a health consultant who has worked with Colorado on its importation proposal.
Ben England, CEO of FDAImports, a consulting firm in Glen Burnie, Maryland, said the OMB typically has 60 days to review final rules, although he expects this one could be completed before Nov. 3 and predicted there’s a small chance it could get finalized and Florida’s request approved by then. “It’s an election year, so I do see the current administration trying to use this as a talking point to say ‘Look what we’ve accomplished,’” he said.
Florida also makes sense because of the large number of retirees, who face high costs for medicines despite Medicare drug coverage.
The DeSantis administration did not respond to requests for comment.
Trump boasted about his importation plan during an October speech in The Villages, a large retirement community about 60 miles northwest of Orlando. “We will soon allow the safe and legal importation of prescription drugs from other countries, including the country of Canada, where, believe it or not, they pay much less money for the exact same drug,” Trump said, with DeSantis in attendance. “Stand up, Ron. Boy, he wants this so badly.”
The Food and Drug Administration released a detailed proposal last December and sought comments. A final plan was delivered Sept. 10 to the Office of Management and Budget for review, signaling it could be unveiled within weeks.
The proposal would regulate how states set up their own programs for importing drugs from Canada.
Prices are cheaper because Canada limits how much drugmakers can charge for medicines. The United States lets free markets dictate drug prices.
The pharmaceutical industry signaled it will likely sue the Trump administration if it goes forward with its importation plans, saying the plan violates several federal laws and the U.S. Constitution.
But the most stinging rebuke of the Trump importation plan came from the Canadian government, which said the proposal would make it harder for Canadian citizens to get drugs, putting their health at risk.
“Canada will employ all necessary measures to safeguard access for Canadians to needed drugs,” the Canadian government wrote in a letter to the FDA about the draft proposal. “The Canadian drug market and manufacturing capacity are too small to meet the demand of both Canadian and American consumers for prescription drugs.”
Without buy-in from Canada, any plan to import medicines is unlikely to succeed, officials said.
Ena Backus, director of Health Care Reform in Vermont, who has worked on setting up an importation program there, said states will need help from Canada. “Our state importation program relies on a willing partner in Canada,” she said.
For decades, Americans have been buying drugs from Canada for personal use — either by driving over the border, ordering medication on the Internet, or using storefronts that connect them to foreign pharmacies. Though illegal, the FDA has generally permitted purchases for individual use.
About 4 million Americans import lower-cost medicines for personal use each year, and about 20 million say they or someone in their household have done so because the prices are much lower in other countries, according to surveys.
The practice has been popular in Florida. More than a dozen storefronts across the state help consumers connect to pharmacies in Canada and other countries. Several cities, state and school districts in Florida help employees get drugs from Canada.
The administration’s proposal builds on a 2000 law that opened the door to allowing drug importation from Canada. But that provision could take effect only if the Health and Human Services secretary certified importation as safe, something that Democratic and Republican administrations have refused to do.
The drug industry for years has said allowing drugs to be imported from Canada would disrupt the nation’s supply chain and make it easier for unsafe or counterfeit medications to enter the market.
Trump, who made lowering prescription drug prices a signature promise in his 2016 campaign, has been eager to fulfill his pledge. In July 2019, at Trump’s direction, HHS Secretary Alex Azar said the federal government was “open for business” on drug importation, a year after calling drug importation a “gimmick.”
The administration envisions a system in which a Canadian-licensed wholesaler buys directly from a manufacturer for drugs approved for sale in Canada and exports the drugs to a U.S. wholesaler/importer under contract to a state.
Florida’s legislation – approved in 2019 – would set up two importation programs. The first would focus on getting drugs for state programs such as Medicaid, the Department of Corrections and county health departments. State officials said they expect the programs would save the state about $150 million annually.
The second program would be geared to the broader state population.
In response to the draft rule, the states seeking to start a drug importation program suggested changes to the administration’s proposal.
“Should the final rule not address these areas of concern, Colorado will struggle to find appropriate partners and realize significant savings for consumers,” Kim Bimestefer, executive director of the Colorado Department of Health Care Policy & Financing, told the FDA in March.
Among the state’s concerns is that it would be limited to using only one Canadian wholesaler, and without competition the state fears prices might not be as low as officials hoped. Bimestefer also noted that under the draft rule, the federal government would approve the importation program for only two years and states need a longer time frame to get buy-in from wholesalers and other partners.
Colorado officials estimate importing drugs from Canada could cut prices by 54% for cancer drugs and 75% for cardiac medicines. The state also noted the diabetes drug Jardiance costs $400 a month in the United States and sells for $85 in Canada.
Several states worry some of the most expensive drugs – including injectable and biologic medicines – were exempt from the federal rule. Those drug classes are not allowed to be imported under the 2000 law.
However, in an executive order in July, Trump said he would allow insulin to be imported if Azar determined it is required for emergency medical care. An HHS spokesman would not say whether Azar has done that.
Jane Horvath, a health policy consultant in College Park, Md., said the administration faces several challenges getting an importation program up and running, including possible opposition from the pharmaceutical industry and limits on classes of drugs that can be sold over the border.
“Despite the barriers, the programs are still quite worthwhile to pursue,” she said.
Maine’s top health official said the administration should work with the Canadian government to address Canada’s concerns. HHS officials refused to say whether such discussions have started.
Officials in Vermont, where the program would also include consumers covered by private insurance, remain hopeful.
“Given that we want to reduce the burden of health care costs on residents in our state, then it is important to pursue this option if there is a clear pathway forward,” Backus said.
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente. This story also ran on Miami Herald.
Many Americans still concerned about access to health care
according to the results of a survey conducted Aug. 7-26.
Nationally, 23.8% of respondents said that they were very concerned about being able to receive care during the pandemic, and another 27.4% said that they were somewhat concerned. Just under a quarter, 24.3%, said they were not very concerned, while 20.4% were not at all concerned, the COVID-19 Consortium for Understanding the Public’s Policy Preferences Across States reported after surveying 21,196 adults.
At the state level, Mississippi had the most adults (35.5%) who were very concerned about their access to care, followed by Texas (32.7%) and Nevada (32.4%). The residents of Montana were least likely (10.5%) to be very concerned, with Vermont next at 11.6% and Wyoming slightly higher at 13.8%. Montana also had the highest proportion of adults, 30.2%, who were not at all concerned, the consortium’s data show.
When asked about getting the coronavirus themselves, 67.8% of U.S. adults came down on the concerned side (33.3% somewhat and 34.5% very concerned) versus 30.8% who were not concerned (18.6% were not very concerned; 12.2% were not concerned at all.). Respondents’ concern was higher for their family members’ risk of getting coronavirus: 30.2% were somewhat concerned and 47.6% were very concerned, the consortium said.
Among many other topics, respondents were asked how closely they had followed recommended health guidelines in the last week, with the two extremes shown here:
- Avoiding contact with other people: 49.3% very closely, 4.8% not at all closely.
- Frequently washing hands: 74.7% very, 1.6% not at all.
- Disinfecting often-touched surfaces: 54.4% very, 4.3% not at all.
- Wearing a face mask in public: 75.7% very, 3.5% not at all.
The consortium is a joint project of the Network Science Institute of Northeastern University; the Shorenstein Center on Media, Politics, and Public Policy of Harvard University; Harvard Medical School; the School of Communication and Information at Rutgers University; and the department of political science at Northwestern University. The project is supported by grants from the National Science Foundation.
according to the results of a survey conducted Aug. 7-26.
Nationally, 23.8% of respondents said that they were very concerned about being able to receive care during the pandemic, and another 27.4% said that they were somewhat concerned. Just under a quarter, 24.3%, said they were not very concerned, while 20.4% were not at all concerned, the COVID-19 Consortium for Understanding the Public’s Policy Preferences Across States reported after surveying 21,196 adults.
At the state level, Mississippi had the most adults (35.5%) who were very concerned about their access to care, followed by Texas (32.7%) and Nevada (32.4%). The residents of Montana were least likely (10.5%) to be very concerned, with Vermont next at 11.6% and Wyoming slightly higher at 13.8%. Montana also had the highest proportion of adults, 30.2%, who were not at all concerned, the consortium’s data show.
When asked about getting the coronavirus themselves, 67.8% of U.S. adults came down on the concerned side (33.3% somewhat and 34.5% very concerned) versus 30.8% who were not concerned (18.6% were not very concerned; 12.2% were not concerned at all.). Respondents’ concern was higher for their family members’ risk of getting coronavirus: 30.2% were somewhat concerned and 47.6% were very concerned, the consortium said.
Among many other topics, respondents were asked how closely they had followed recommended health guidelines in the last week, with the two extremes shown here:
- Avoiding contact with other people: 49.3% very closely, 4.8% not at all closely.
- Frequently washing hands: 74.7% very, 1.6% not at all.
- Disinfecting often-touched surfaces: 54.4% very, 4.3% not at all.
- Wearing a face mask in public: 75.7% very, 3.5% not at all.
The consortium is a joint project of the Network Science Institute of Northeastern University; the Shorenstein Center on Media, Politics, and Public Policy of Harvard University; Harvard Medical School; the School of Communication and Information at Rutgers University; and the department of political science at Northwestern University. The project is supported by grants from the National Science Foundation.
according to the results of a survey conducted Aug. 7-26.
Nationally, 23.8% of respondents said that they were very concerned about being able to receive care during the pandemic, and another 27.4% said that they were somewhat concerned. Just under a quarter, 24.3%, said they were not very concerned, while 20.4% were not at all concerned, the COVID-19 Consortium for Understanding the Public’s Policy Preferences Across States reported after surveying 21,196 adults.
At the state level, Mississippi had the most adults (35.5%) who were very concerned about their access to care, followed by Texas (32.7%) and Nevada (32.4%). The residents of Montana were least likely (10.5%) to be very concerned, with Vermont next at 11.6% and Wyoming slightly higher at 13.8%. Montana also had the highest proportion of adults, 30.2%, who were not at all concerned, the consortium’s data show.
When asked about getting the coronavirus themselves, 67.8% of U.S. adults came down on the concerned side (33.3% somewhat and 34.5% very concerned) versus 30.8% who were not concerned (18.6% were not very concerned; 12.2% were not concerned at all.). Respondents’ concern was higher for their family members’ risk of getting coronavirus: 30.2% were somewhat concerned and 47.6% were very concerned, the consortium said.
Among many other topics, respondents were asked how closely they had followed recommended health guidelines in the last week, with the two extremes shown here:
- Avoiding contact with other people: 49.3% very closely, 4.8% not at all closely.
- Frequently washing hands: 74.7% very, 1.6% not at all.
- Disinfecting often-touched surfaces: 54.4% very, 4.3% not at all.
- Wearing a face mask in public: 75.7% very, 3.5% not at all.
The consortium is a joint project of the Network Science Institute of Northeastern University; the Shorenstein Center on Media, Politics, and Public Policy of Harvard University; Harvard Medical School; the School of Communication and Information at Rutgers University; and the department of political science at Northwestern University. The project is supported by grants from the National Science Foundation.
Even in a virtual environment, the Society of Gynecologic Surgeons delivers without a “glitch”
Earlier this year, I was honored to serve as the Scientific Program Chair for the 46th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). This year’s meeting was the first ever (and hopefully last) “virtual” scientific meeting, which consisted of a hybrid of prerecorded and live presentations. Although faculty and attendees were not able to be together physically, the essence of the lively SGS meetings came through loud and clear. We still had “discussants” comment on the oral presentations and ask questions of the presenters. These questions and answers were all done live—without a glitch! Many thanks to all who made this meeting possible.
In addition to the outstanding abstract and video presentations, there were 4 superb postgraduate courses:
- Mikio Nihira, MD, chaired “Enhanced recovery after surgery: Overcoming barriers to implementation.”
- Charles Hanes, MD, headed up “It’s all about the apex: The key to successful POP surgery.”
- Cara King, DO, MS, led “Total laparoscopic hysterectomy: Pushing the envelope.”
- Vincent Lucente, MD, chaired “Transvaginal reconstructive pelvic surgery using graft augmentation post-FDA.”
Many special thanks to Dr. Lucente who transformed his course into a wonderful article for this special section of
One of our exceptional keynote speakers was Marc Beer (a serial entrepreneur and cofounder, chairman, and CEO of Renovia, Inc.), whose talk was entitled “A primer on medical device innovation—How to avoid common pitfalls while realizing your vision.” Mr. Beer has turned this topic into a unique article for this special section (see next month’s issue for Part 2).
Our TeLinde Lecture, entitled “Artificial intelligence in surgery,” was delivered by the dynamic Vicente Gracias, MD, professor of surgery at Robert Wood Johnson University Hospital, New Brunswick, New Jersey. We also held 2 live panel discussions that were very popular. The first, “Work-life balance and gynecologic surgery,” featured various perspectives from Drs. Kristie Green, Sally Huber, Catherine Matthews, and Charles Rardin. The second panel discussion, entitled “Understanding, managing, and benefiting from your e-presence,” by experts Heather Schueppert; Chief Marketing Officer at Unified Physician Management, Brad Bowman, MD; and Peter Lotze, MD. Both of these panel discussions are included in this special section as well.
I hope you enjoy the content of this special section of
Earlier this year, I was honored to serve as the Scientific Program Chair for the 46th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). This year’s meeting was the first ever (and hopefully last) “virtual” scientific meeting, which consisted of a hybrid of prerecorded and live presentations. Although faculty and attendees were not able to be together physically, the essence of the lively SGS meetings came through loud and clear. We still had “discussants” comment on the oral presentations and ask questions of the presenters. These questions and answers were all done live—without a glitch! Many thanks to all who made this meeting possible.
In addition to the outstanding abstract and video presentations, there were 4 superb postgraduate courses:
- Mikio Nihira, MD, chaired “Enhanced recovery after surgery: Overcoming barriers to implementation.”
- Charles Hanes, MD, headed up “It’s all about the apex: The key to successful POP surgery.”
- Cara King, DO, MS, led “Total laparoscopic hysterectomy: Pushing the envelope.”
- Vincent Lucente, MD, chaired “Transvaginal reconstructive pelvic surgery using graft augmentation post-FDA.”
Many special thanks to Dr. Lucente who transformed his course into a wonderful article for this special section of
One of our exceptional keynote speakers was Marc Beer (a serial entrepreneur and cofounder, chairman, and CEO of Renovia, Inc.), whose talk was entitled “A primer on medical device innovation—How to avoid common pitfalls while realizing your vision.” Mr. Beer has turned this topic into a unique article for this special section (see next month’s issue for Part 2).
Our TeLinde Lecture, entitled “Artificial intelligence in surgery,” was delivered by the dynamic Vicente Gracias, MD, professor of surgery at Robert Wood Johnson University Hospital, New Brunswick, New Jersey. We also held 2 live panel discussions that were very popular. The first, “Work-life balance and gynecologic surgery,” featured various perspectives from Drs. Kristie Green, Sally Huber, Catherine Matthews, and Charles Rardin. The second panel discussion, entitled “Understanding, managing, and benefiting from your e-presence,” by experts Heather Schueppert; Chief Marketing Officer at Unified Physician Management, Brad Bowman, MD; and Peter Lotze, MD. Both of these panel discussions are included in this special section as well.
I hope you enjoy the content of this special section of
Earlier this year, I was honored to serve as the Scientific Program Chair for the 46th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). This year’s meeting was the first ever (and hopefully last) “virtual” scientific meeting, which consisted of a hybrid of prerecorded and live presentations. Although faculty and attendees were not able to be together physically, the essence of the lively SGS meetings came through loud and clear. We still had “discussants” comment on the oral presentations and ask questions of the presenters. These questions and answers were all done live—without a glitch! Many thanks to all who made this meeting possible.
In addition to the outstanding abstract and video presentations, there were 4 superb postgraduate courses:
- Mikio Nihira, MD, chaired “Enhanced recovery after surgery: Overcoming barriers to implementation.”
- Charles Hanes, MD, headed up “It’s all about the apex: The key to successful POP surgery.”
- Cara King, DO, MS, led “Total laparoscopic hysterectomy: Pushing the envelope.”
- Vincent Lucente, MD, chaired “Transvaginal reconstructive pelvic surgery using graft augmentation post-FDA.”
Many special thanks to Dr. Lucente who transformed his course into a wonderful article for this special section of
One of our exceptional keynote speakers was Marc Beer (a serial entrepreneur and cofounder, chairman, and CEO of Renovia, Inc.), whose talk was entitled “A primer on medical device innovation—How to avoid common pitfalls while realizing your vision.” Mr. Beer has turned this topic into a unique article for this special section (see next month’s issue for Part 2).
Our TeLinde Lecture, entitled “Artificial intelligence in surgery,” was delivered by the dynamic Vicente Gracias, MD, professor of surgery at Robert Wood Johnson University Hospital, New Brunswick, New Jersey. We also held 2 live panel discussions that were very popular. The first, “Work-life balance and gynecologic surgery,” featured various perspectives from Drs. Kristie Green, Sally Huber, Catherine Matthews, and Charles Rardin. The second panel discussion, entitled “Understanding, managing, and benefiting from your e-presence,” by experts Heather Schueppert; Chief Marketing Officer at Unified Physician Management, Brad Bowman, MD; and Peter Lotze, MD. Both of these panel discussions are included in this special section as well.
I hope you enjoy the content of this special section of
Exorcising your ghosts
The COVID-19 pandemic has affected private medical practices on so many levels, not least of which is the loss of employees to illness, fear of illness, early retirement, and other reasons.
If you’re not hip to the slang, “ghosting” is the situation in which an employee disappears without any warning, notice, or explanation. It usually occurs after a candidate accepts a job offer, and you schedule their first day of work. That day dawns, but the new hire never arrives. Less commonly, an employee who has been with you for some time simply stops showing up and cannot be contacted.
Many employers think of ghosting as a relatively new phenomenon, and blame it on the irresponsibility of younger age groups – millennials, in particular. In fact, it has been an issue for many years across all age groups, and employers often share more of the responsibility than they think.
While total prevention is impossible, there are steps you can take as an employer to minimize ghosting in your practice.
- Your hiring process needs to be efficient. If you wait too long to schedule an interview with a promising candidate or to offer them the job, another job offer could lure them away. At the very least, a lengthy process or a lack of transparency may make the applicant apprehensive about accepting a job with you, particularly if other employers are pursuing them.
- Keep applicants in the loop. Follow up with every candidate; let them know where they are in your hiring process. Applicants who have no clue whether they have a shot at the job are going to start looking elsewhere. And make sure they know the job description and starting salary from the outset.
- Talk to new hires before their first day. Contact them personally to see if they have any questions or concerns, and let them know that you’re looking forward to their arrival.
- Once they start, make them feel welcome. An employee’s first few days on the job set the tone for the rest of the employment relationship. During this time, clearly communicate what the employee can expect from you and what you expect from them. Take time to discuss key issues, such as work schedules, timekeeping practices, how performance is measured, and dress codes. Introduce them to coworkers, and get them started shadowing more experienced staff members.
- Take a hard look at your supervision and your supervisors. Business people like to say that employees don’t quit their job, they quit their boss. If an employee quits – with or without notice – it may very well be because of a poor working relationship with you or the supervisor. To be effective, you and your supervisors need to be diligent in setting goals, managing performance, and applying workplace rules and policies. Numerous third-party companies provide training and guidance in these areas when needed.
- Recognize and reward. As I’ve written many times, positive feedback is a simple, low-cost way to improve employee retention. It demonstrates that you value an employee’s contributions and sets an excellent example for other employees. Effective recognition can come from anyone – including patients – and should be given openly. (Another old adage: “Praise publicly, criticize privately.”) It never hurts to catch an employee doing something right and acknowledge it.
- Don’t jump to conclusions. If a new hire or employee is absent without notice, don’t just assume you’ve been ghosted. There may be extenuating circumstances, such as an emergency or illness. In some states, an employee’s absence is protected under a law where the employee may not be required to provide advance notice, and taking adverse action could violate these laws. Establish procedures for attempting to contact absent employees, and make sure you’re complying with all applicable leave laws before taking any action.
If an employee does abandon their job, think before you act. Comply with all applicable laws. Act consistently with how you’ve handled similar situations in the past. Your attorney should be involved, especially if the decision involves termination. Notify the employee in writing. As with all employment decisions, keep adequate documentation in case the decision is ever challenged, or you need it to support future disciplinary decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no disclosures related to this column. Write to him at [email protected].
The COVID-19 pandemic has affected private medical practices on so many levels, not least of which is the loss of employees to illness, fear of illness, early retirement, and other reasons.
If you’re not hip to the slang, “ghosting” is the situation in which an employee disappears without any warning, notice, or explanation. It usually occurs after a candidate accepts a job offer, and you schedule their first day of work. That day dawns, but the new hire never arrives. Less commonly, an employee who has been with you for some time simply stops showing up and cannot be contacted.
Many employers think of ghosting as a relatively new phenomenon, and blame it on the irresponsibility of younger age groups – millennials, in particular. In fact, it has been an issue for many years across all age groups, and employers often share more of the responsibility than they think.
While total prevention is impossible, there are steps you can take as an employer to minimize ghosting in your practice.
- Your hiring process needs to be efficient. If you wait too long to schedule an interview with a promising candidate or to offer them the job, another job offer could lure them away. At the very least, a lengthy process or a lack of transparency may make the applicant apprehensive about accepting a job with you, particularly if other employers are pursuing them.
- Keep applicants in the loop. Follow up with every candidate; let them know where they are in your hiring process. Applicants who have no clue whether they have a shot at the job are going to start looking elsewhere. And make sure they know the job description and starting salary from the outset.
- Talk to new hires before their first day. Contact them personally to see if they have any questions or concerns, and let them know that you’re looking forward to their arrival.
- Once they start, make them feel welcome. An employee’s first few days on the job set the tone for the rest of the employment relationship. During this time, clearly communicate what the employee can expect from you and what you expect from them. Take time to discuss key issues, such as work schedules, timekeeping practices, how performance is measured, and dress codes. Introduce them to coworkers, and get them started shadowing more experienced staff members.
- Take a hard look at your supervision and your supervisors. Business people like to say that employees don’t quit their job, they quit their boss. If an employee quits – with or without notice – it may very well be because of a poor working relationship with you or the supervisor. To be effective, you and your supervisors need to be diligent in setting goals, managing performance, and applying workplace rules and policies. Numerous third-party companies provide training and guidance in these areas when needed.
- Recognize and reward. As I’ve written many times, positive feedback is a simple, low-cost way to improve employee retention. It demonstrates that you value an employee’s contributions and sets an excellent example for other employees. Effective recognition can come from anyone – including patients – and should be given openly. (Another old adage: “Praise publicly, criticize privately.”) It never hurts to catch an employee doing something right and acknowledge it.
- Don’t jump to conclusions. If a new hire or employee is absent without notice, don’t just assume you’ve been ghosted. There may be extenuating circumstances, such as an emergency or illness. In some states, an employee’s absence is protected under a law where the employee may not be required to provide advance notice, and taking adverse action could violate these laws. Establish procedures for attempting to contact absent employees, and make sure you’re complying with all applicable leave laws before taking any action.
If an employee does abandon their job, think before you act. Comply with all applicable laws. Act consistently with how you’ve handled similar situations in the past. Your attorney should be involved, especially if the decision involves termination. Notify the employee in writing. As with all employment decisions, keep adequate documentation in case the decision is ever challenged, or you need it to support future disciplinary decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no disclosures related to this column. Write to him at [email protected].
The COVID-19 pandemic has affected private medical practices on so many levels, not least of which is the loss of employees to illness, fear of illness, early retirement, and other reasons.
If you’re not hip to the slang, “ghosting” is the situation in which an employee disappears without any warning, notice, or explanation. It usually occurs after a candidate accepts a job offer, and you schedule their first day of work. That day dawns, but the new hire never arrives. Less commonly, an employee who has been with you for some time simply stops showing up and cannot be contacted.
Many employers think of ghosting as a relatively new phenomenon, and blame it on the irresponsibility of younger age groups – millennials, in particular. In fact, it has been an issue for many years across all age groups, and employers often share more of the responsibility than they think.
While total prevention is impossible, there are steps you can take as an employer to minimize ghosting in your practice.
- Your hiring process needs to be efficient. If you wait too long to schedule an interview with a promising candidate or to offer them the job, another job offer could lure them away. At the very least, a lengthy process or a lack of transparency may make the applicant apprehensive about accepting a job with you, particularly if other employers are pursuing them.
- Keep applicants in the loop. Follow up with every candidate; let them know where they are in your hiring process. Applicants who have no clue whether they have a shot at the job are going to start looking elsewhere. And make sure they know the job description and starting salary from the outset.
- Talk to new hires before their first day. Contact them personally to see if they have any questions or concerns, and let them know that you’re looking forward to their arrival.
- Once they start, make them feel welcome. An employee’s first few days on the job set the tone for the rest of the employment relationship. During this time, clearly communicate what the employee can expect from you and what you expect from them. Take time to discuss key issues, such as work schedules, timekeeping practices, how performance is measured, and dress codes. Introduce them to coworkers, and get them started shadowing more experienced staff members.
- Take a hard look at your supervision and your supervisors. Business people like to say that employees don’t quit their job, they quit their boss. If an employee quits – with or without notice – it may very well be because of a poor working relationship with you or the supervisor. To be effective, you and your supervisors need to be diligent in setting goals, managing performance, and applying workplace rules and policies. Numerous third-party companies provide training and guidance in these areas when needed.
- Recognize and reward. As I’ve written many times, positive feedback is a simple, low-cost way to improve employee retention. It demonstrates that you value an employee’s contributions and sets an excellent example for other employees. Effective recognition can come from anyone – including patients – and should be given openly. (Another old adage: “Praise publicly, criticize privately.”) It never hurts to catch an employee doing something right and acknowledge it.
- Don’t jump to conclusions. If a new hire or employee is absent without notice, don’t just assume you’ve been ghosted. There may be extenuating circumstances, such as an emergency or illness. In some states, an employee’s absence is protected under a law where the employee may not be required to provide advance notice, and taking adverse action could violate these laws. Establish procedures for attempting to contact absent employees, and make sure you’re complying with all applicable leave laws before taking any action.
If an employee does abandon their job, think before you act. Comply with all applicable laws. Act consistently with how you’ve handled similar situations in the past. Your attorney should be involved, especially if the decision involves termination. Notify the employee in writing. As with all employment decisions, keep adequate documentation in case the decision is ever challenged, or you need it to support future disciplinary decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no disclosures related to this column. Write to him at [email protected].
Studying in Dermatology Residency
Dermatology residency can feel like drinking from a firehose, in which one is bombarded with so much information that it is impossible to retain any content. This article provides an overview of available resources and a guide on how to tailor studying throughout one’s training.
Prior to Residency
There are several resources that provide an introduction to dermatology and are appropriate for all medical students, regardless of intended specialty. The American Academy of Dermatology offers a free basic dermatology curriculum (https://www.aad.org/member/education/residents/bdc), with a choice of a 2- or 4-week course consisting of modules such as skin examination, basic science of the skin, dermatologic therapies, and specific dermatologic conditions. VisualDx offers LearnDerm (https://www.visualdx.com/learnderm/), which includes a 5-part tutorial and quiz focused on the skin examination, morphology, and lesion distribution. Lookingbill and Marks’ Principles of Dermatology1 is a book at an appropriate level for a medical student to learn about the fundamentals of dermatology. These resources may be helpful for residents to review immediately before starting dermatology residency (toward the end of intern year for most).
First Year
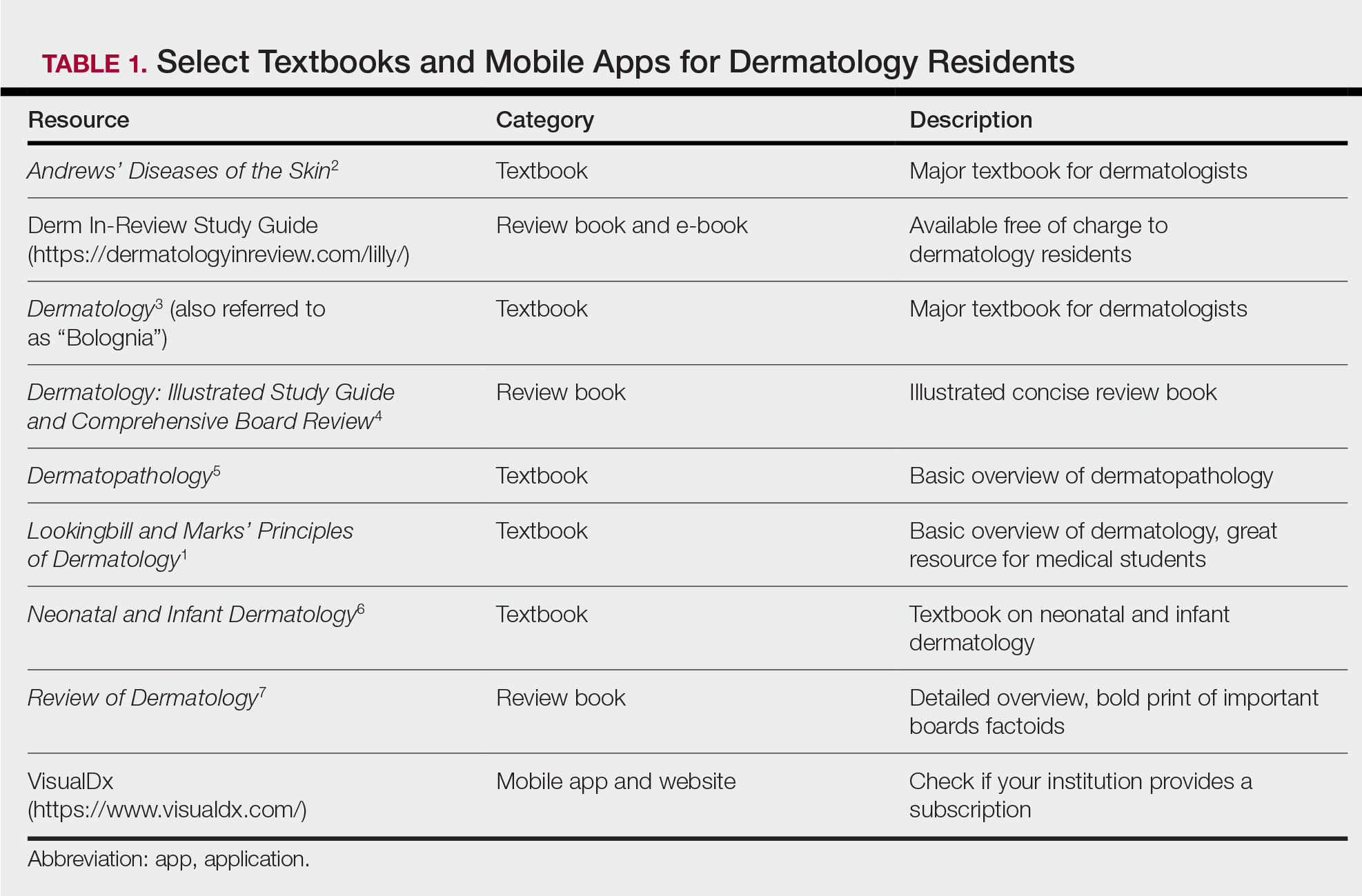
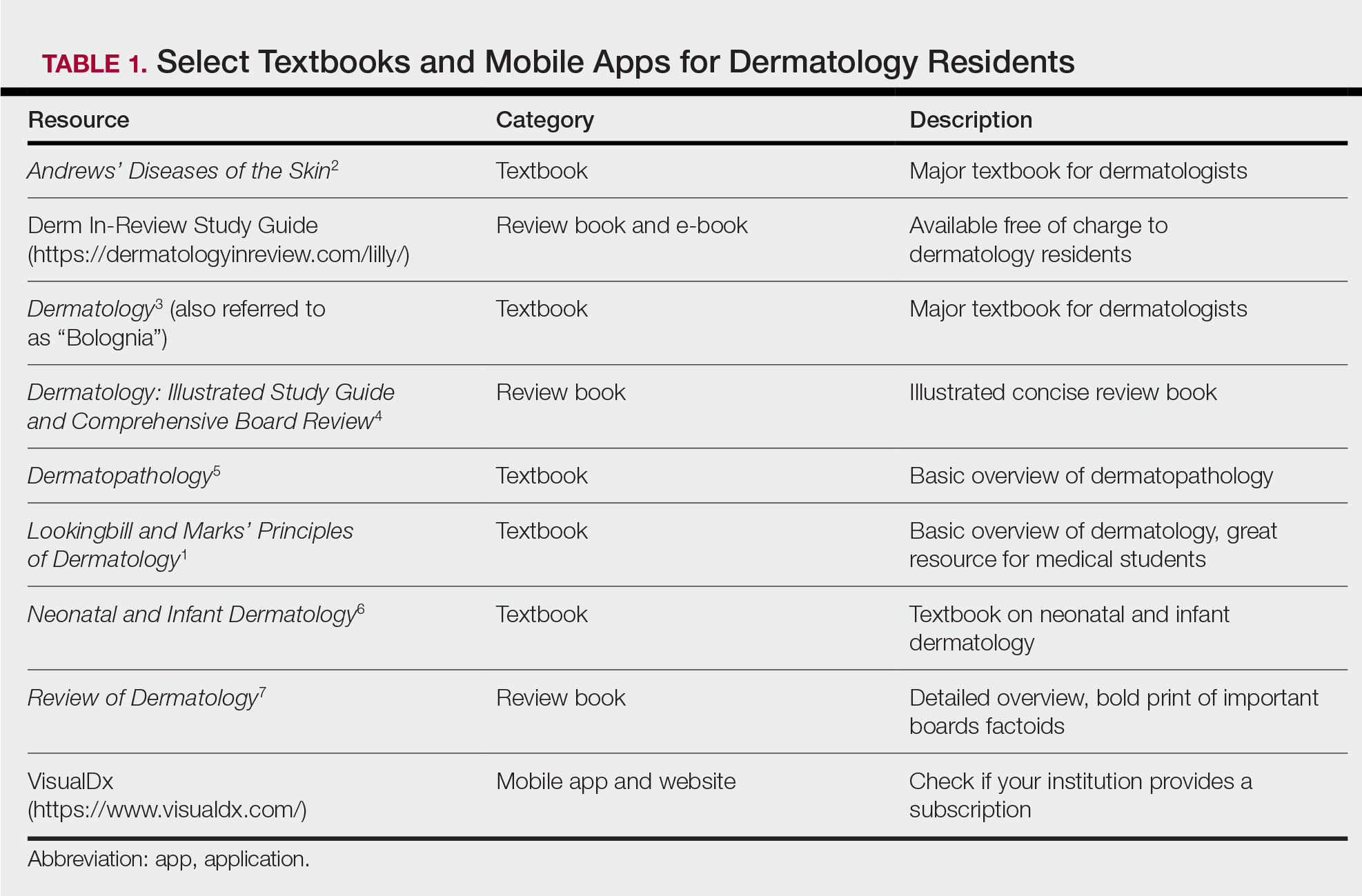
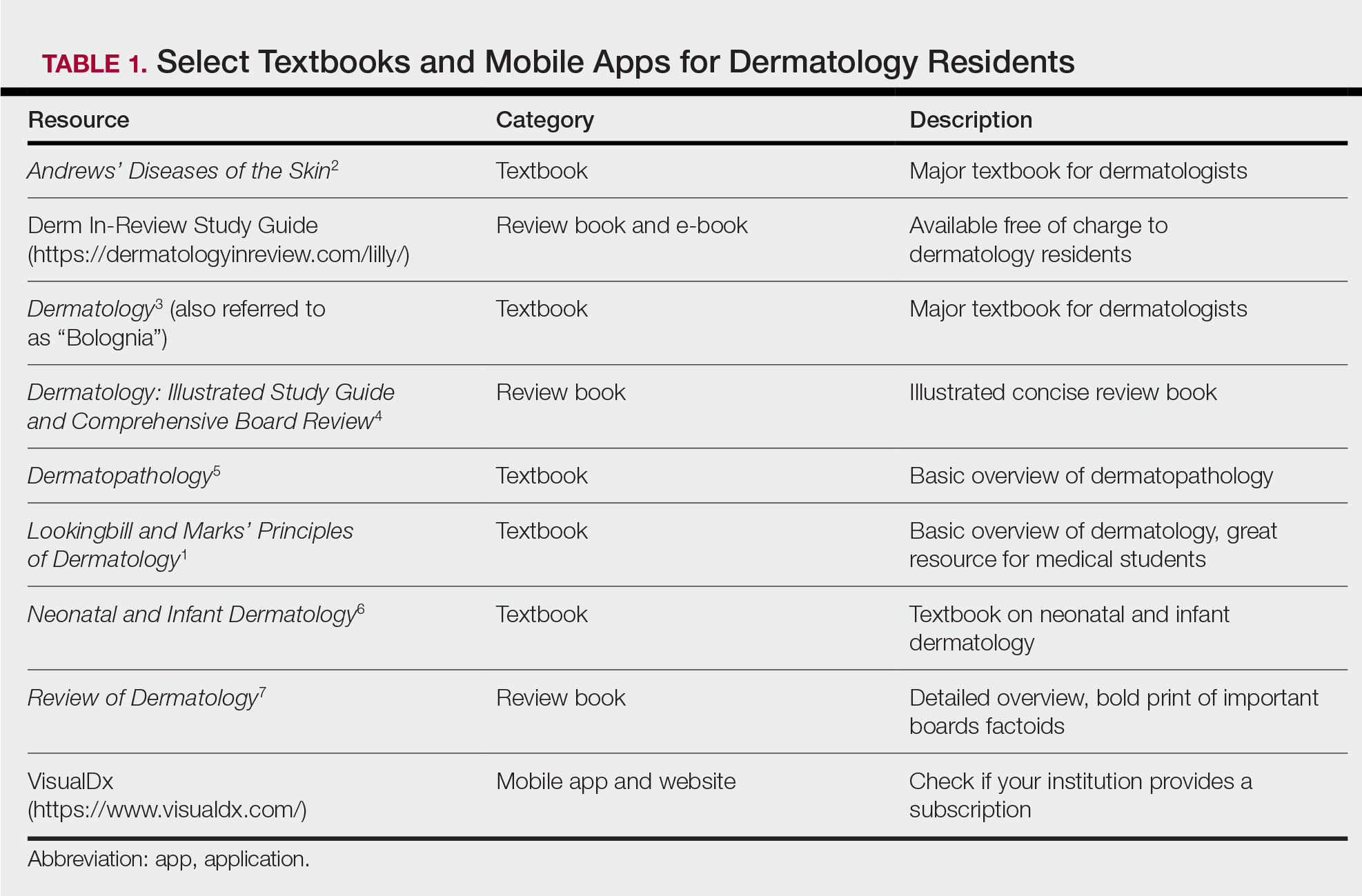
During the beginning of dermatology residency (postgraduate year [PGY] 2 for most), the fire hose of information feels most daunting. During this time, studying should focus on engendering a broad overview of dermatology. Most residencies maintain a textbook reading schedule, which provides a framework from which residents may structure their studying. Selection of a textbook tends to be program dependent. Even if the details of reading the textbook do not stick when reading it the first time, benefits include becoming familiar with what information one is expected to learn as a dermatologist and developing a strong foundation upon which one may continue to build. Based on my informal discussions with current residents, some reported that reading the textbook did not work well for them, citing too much minutiae in the textbooks and/or a preference for a more active learning approach. These residents instead focused on reading a review book for a broad overview, accompanied by a textbook or VisualDx when a more detailed reference is necessary. Table 1 provides a list of textbooks and mobile applications (apps) that residents may find helpful.
First-year residents may begin their efforts in synthesizing this new knowledge base toward the end of the year in preparation for the BASIC examination. The American Board of Dermatology provides a content outline as well as sample questions on their website (https://www.abderm.org/residents-and-fellows/exam-of-the-future-information-center.aspx#content), which may be used to guide more focused studying efforts during the weeks leading up to the examination.
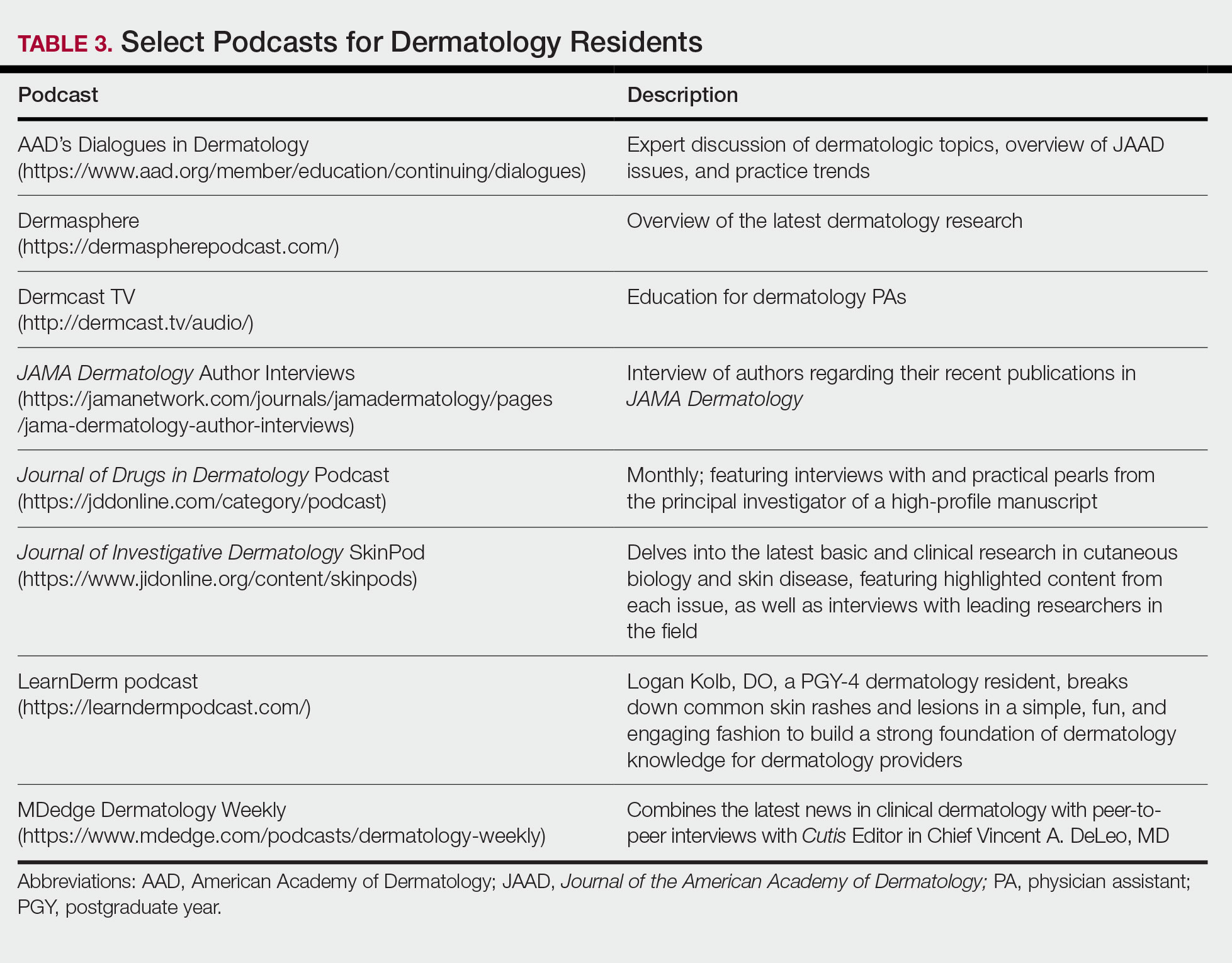
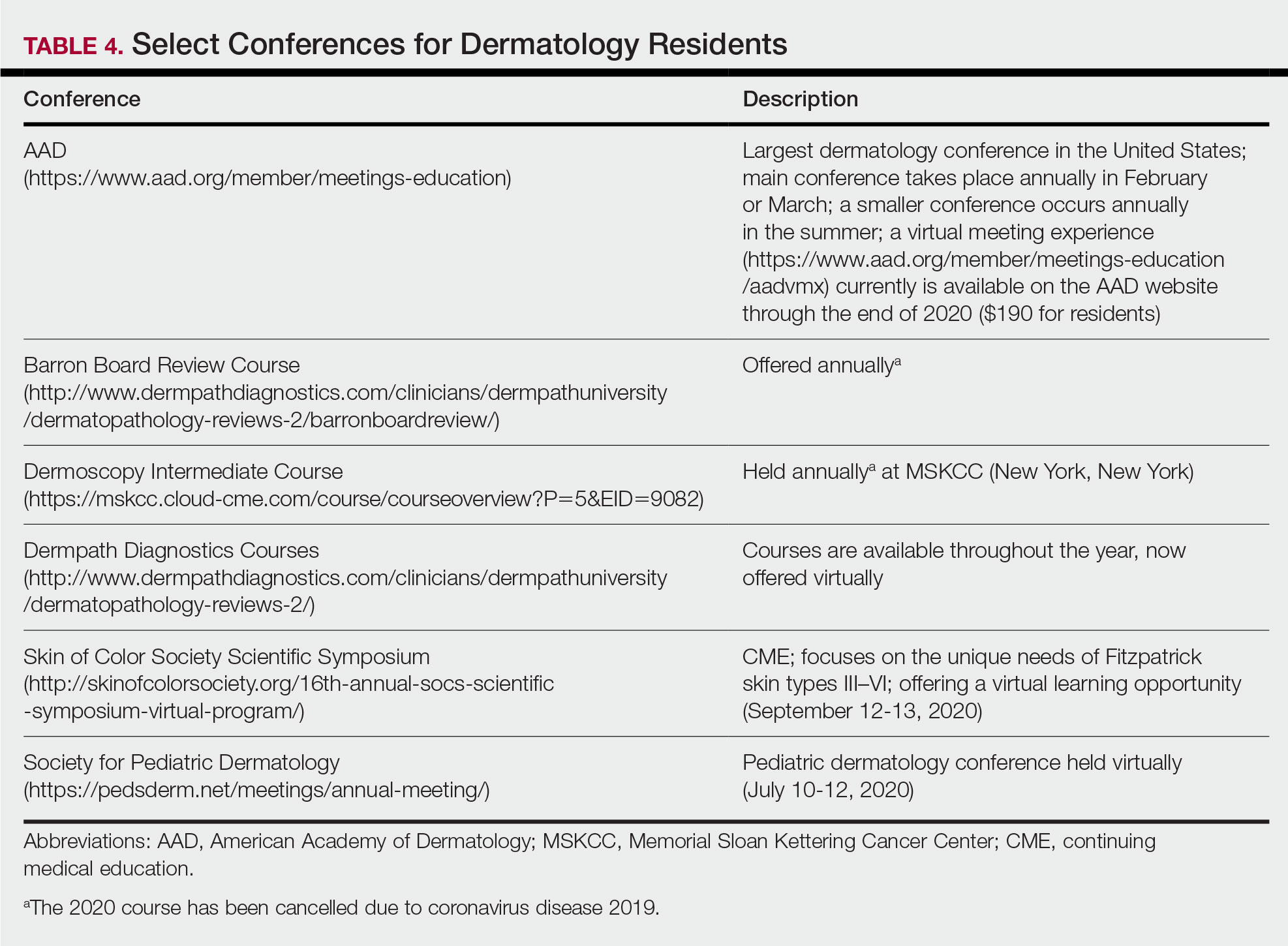
Second Year
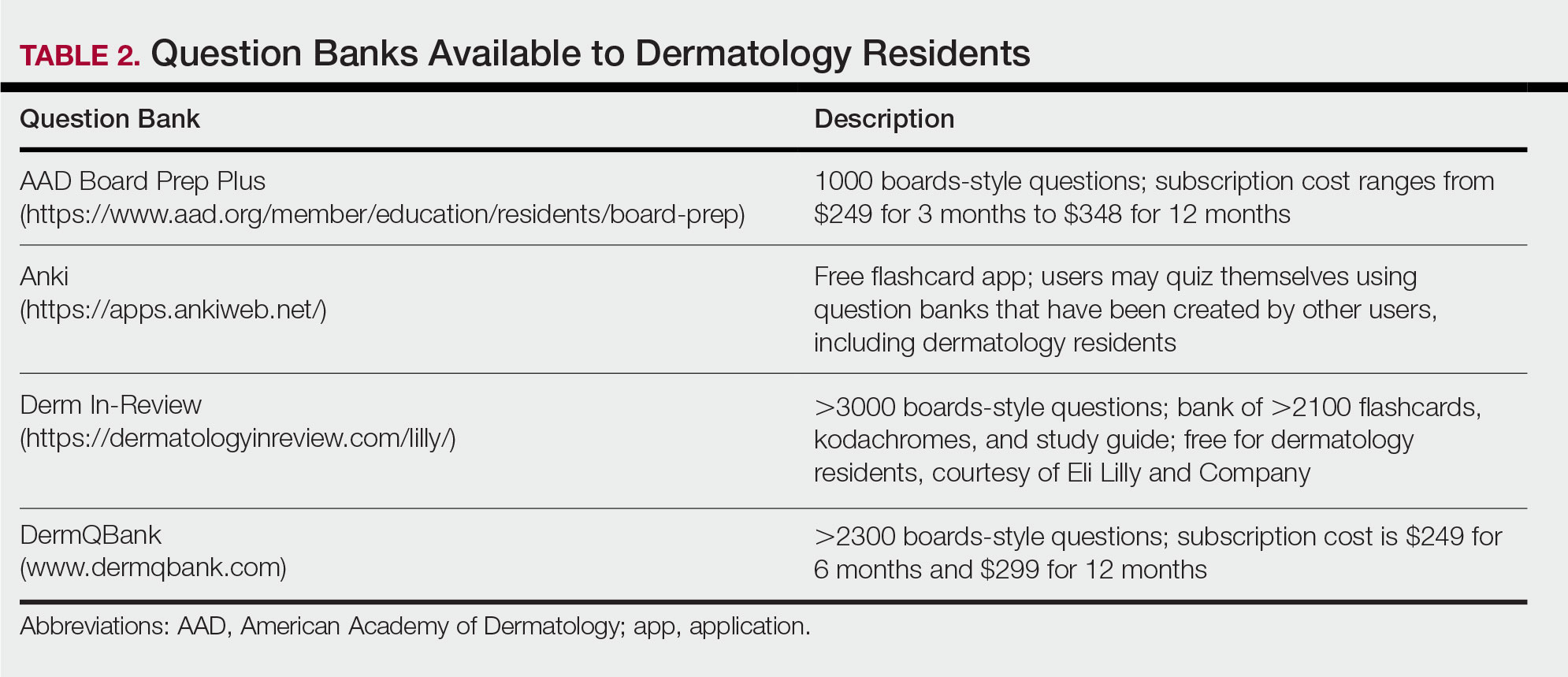
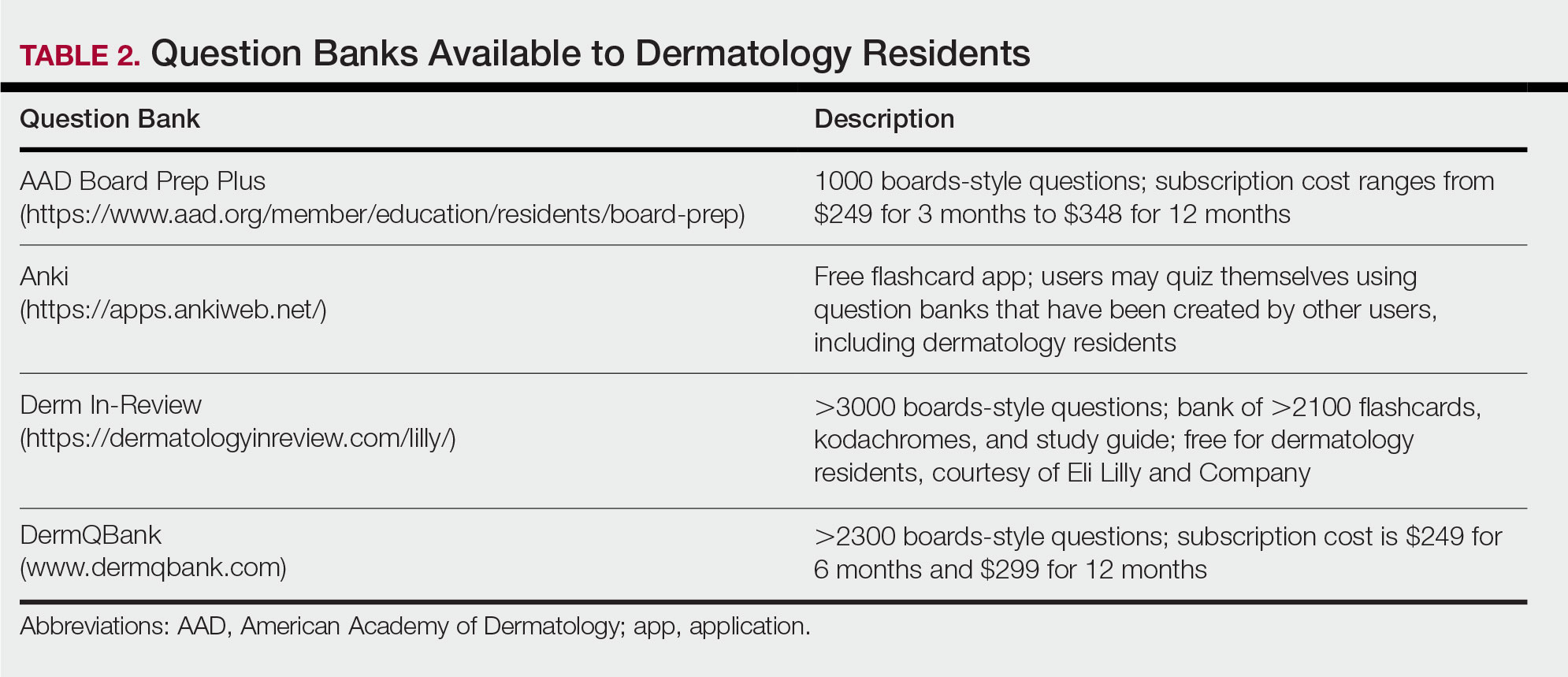
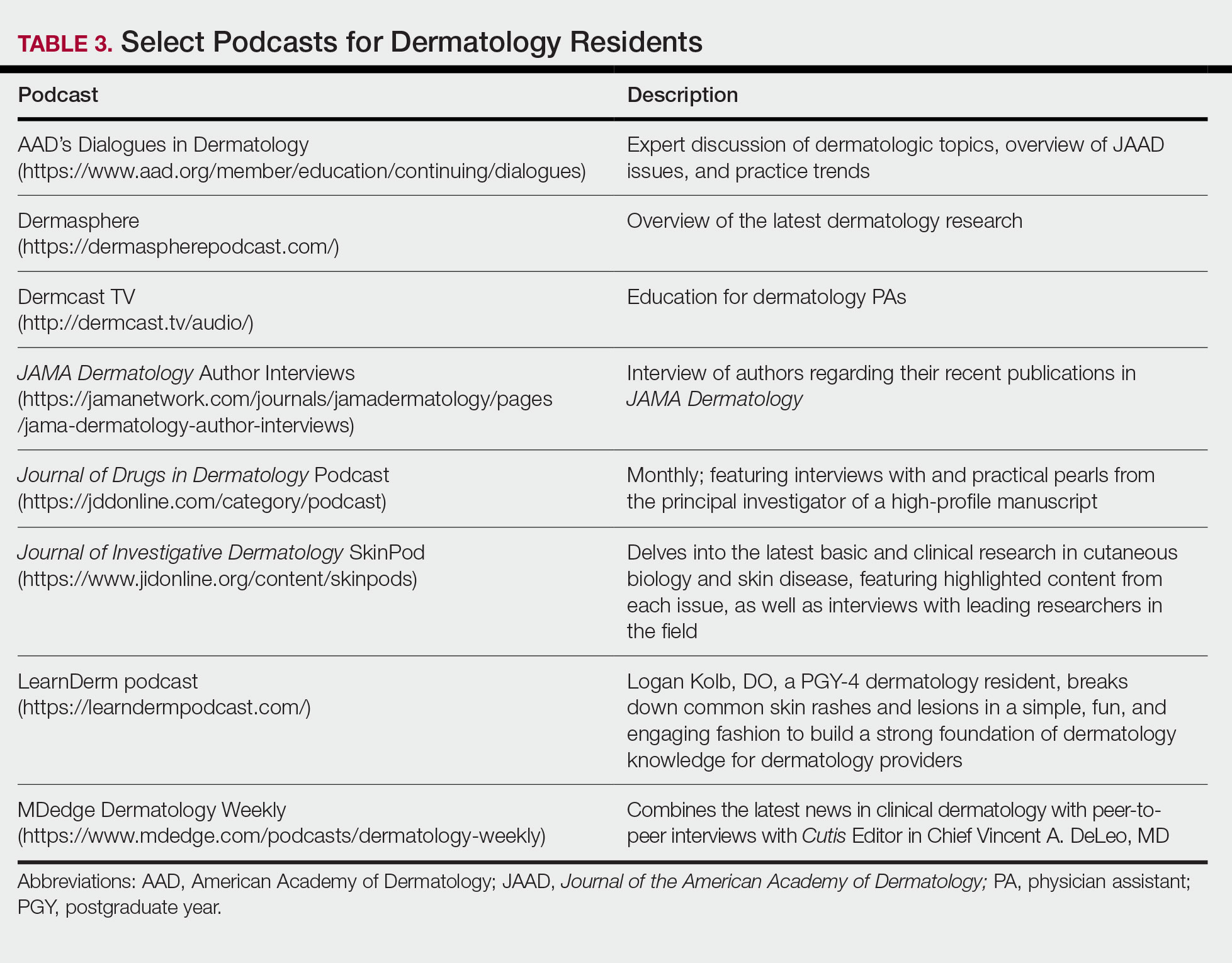
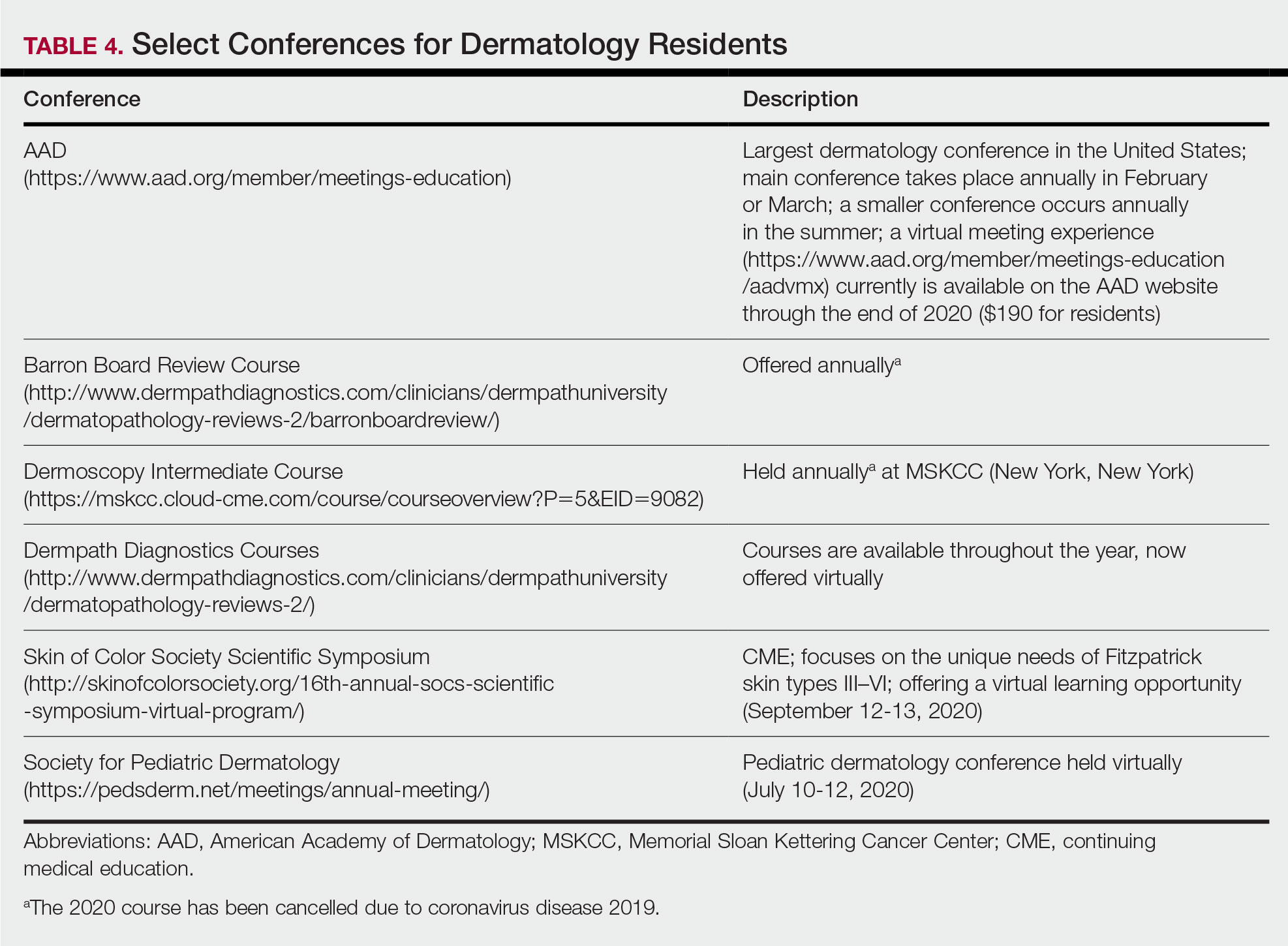
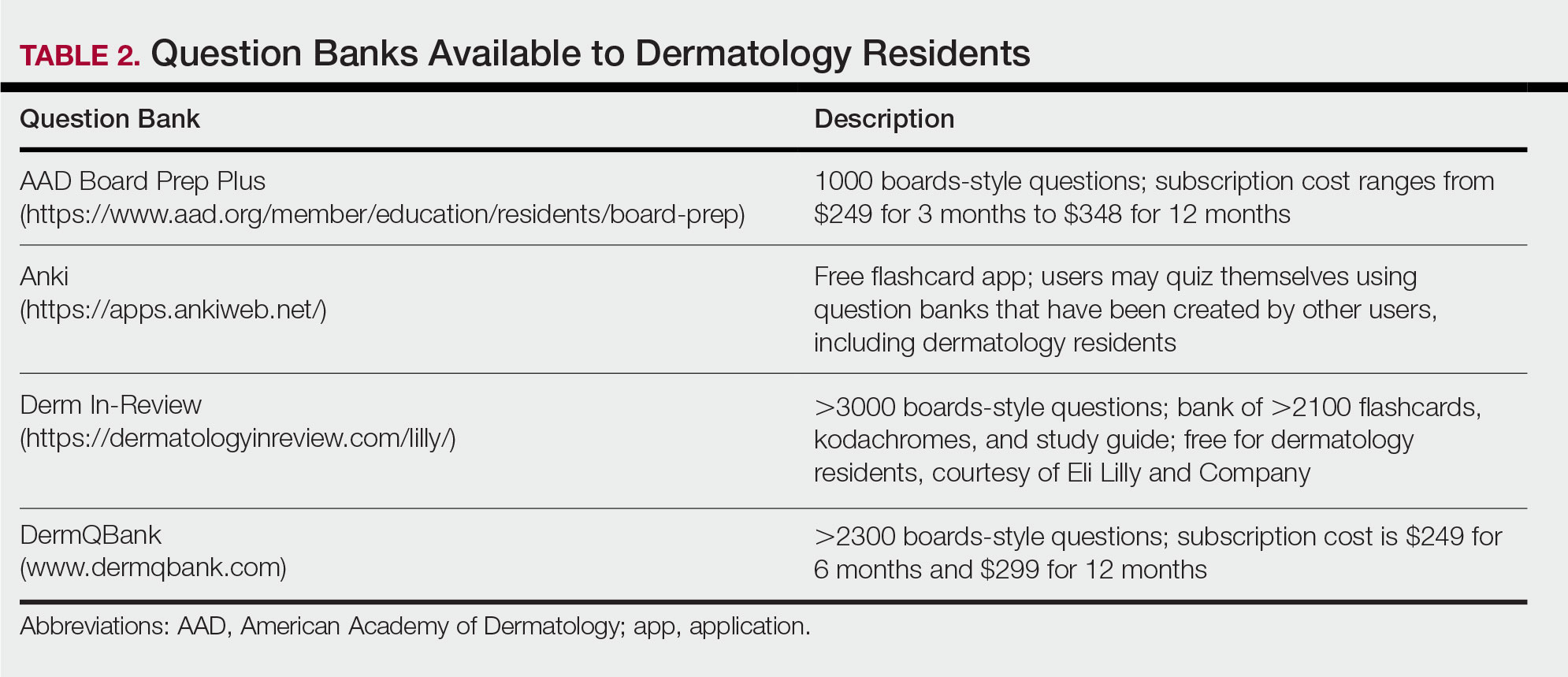
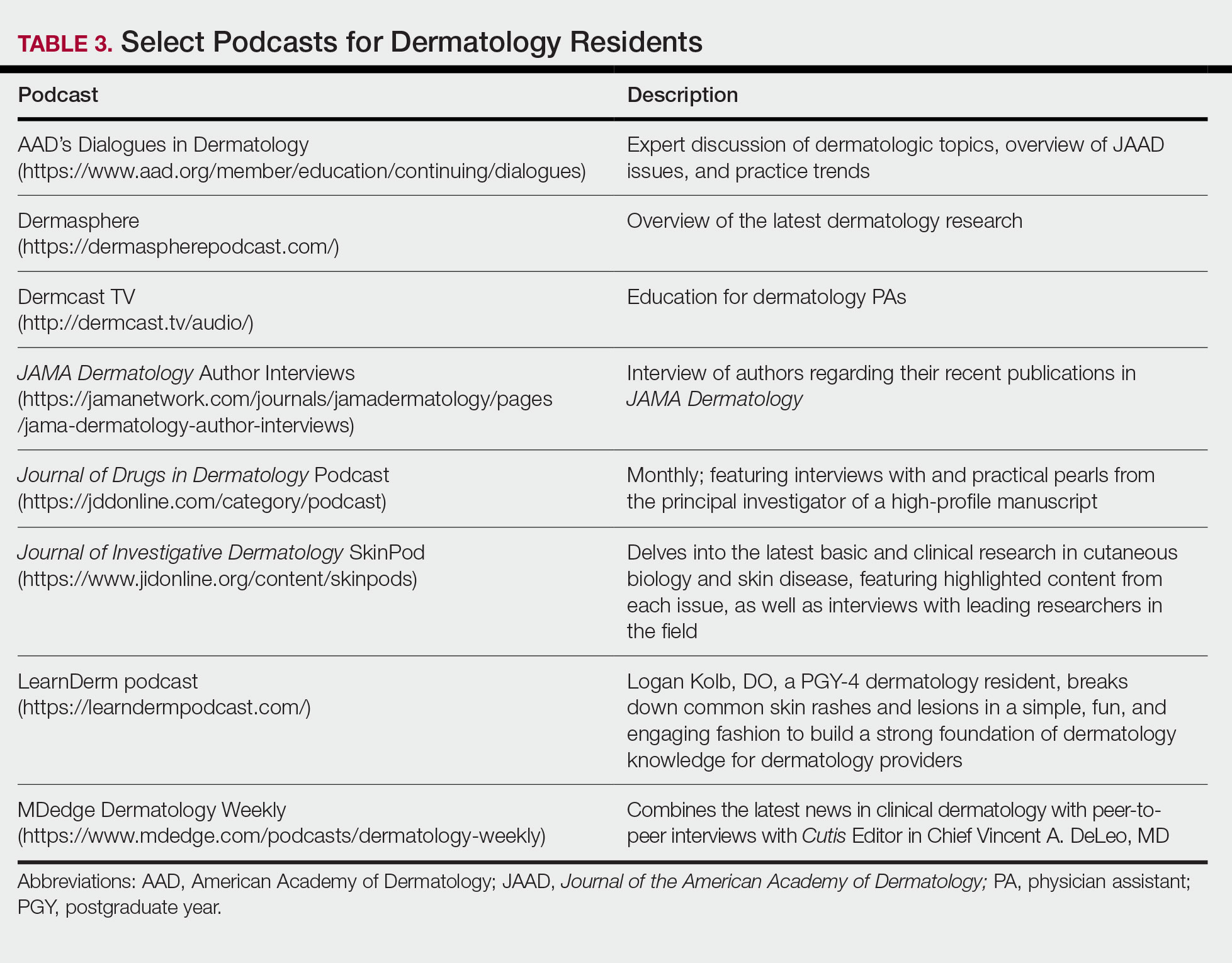
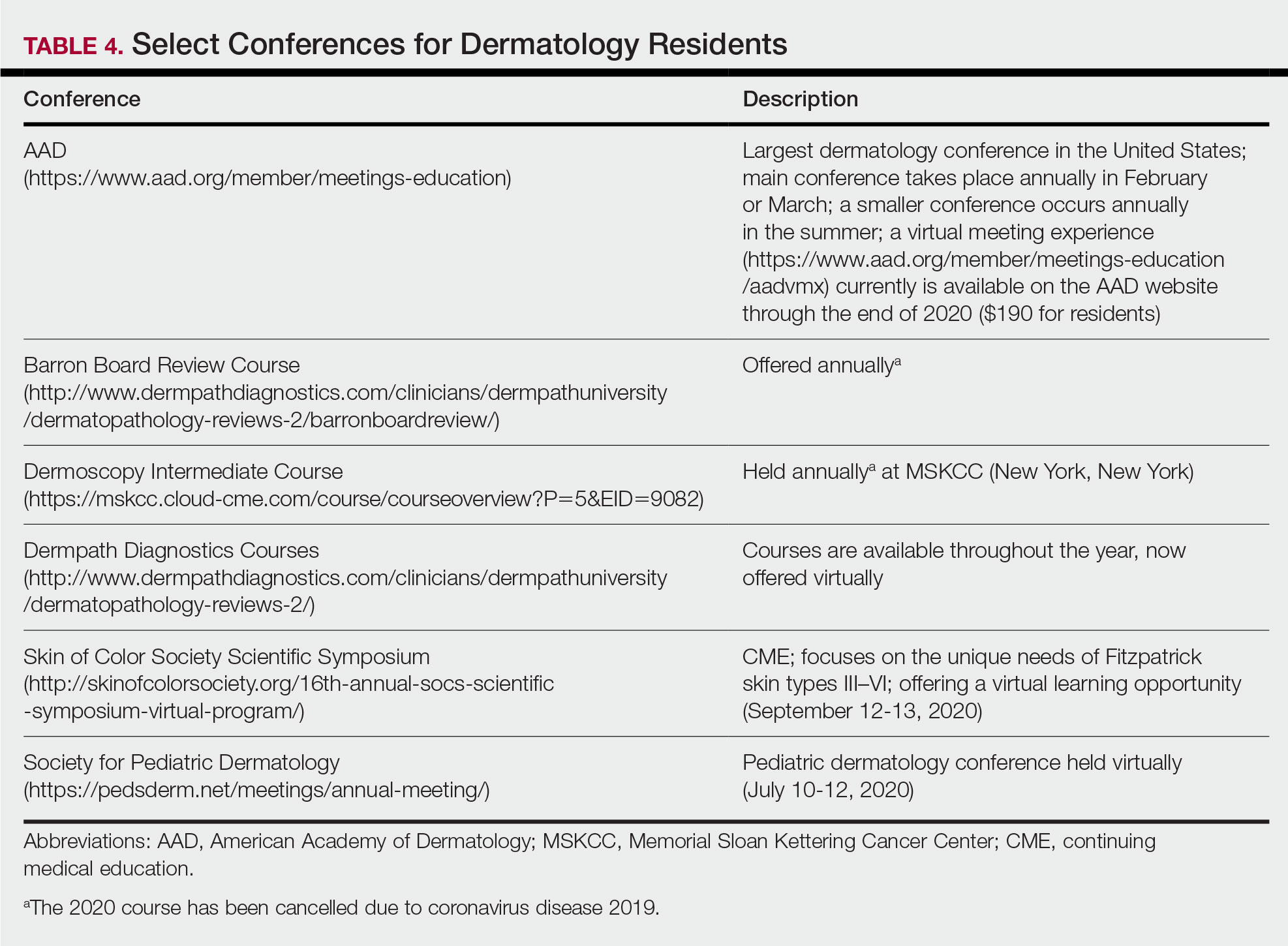
For second-year residents (PGY-3 for most) studying should focus on deepening and consolidating the broad foundation that was established during their first year. For many, this pursuit involves rereading the textbook chapters alongside more active learning measures, such as taking notes and quizzing oneself using flashcard apps and question banks (Table 2). Others may benefit from listening to podcasts (Table 3) or other sources utilizing audiovisual content, including attending conferences and other lectures virtually, which is becoming increasingly available in the setting of the coronavirus disease 2019 pandemic (Table 4). Because there are so many resources available to support these efforts, residents should be encouraged to try out a variety to determine what works best.
Toward the end of second year, studying may be tailored to preparing for the CORE examinations using the resources of one’s choice. Based on my discussions with current residents, a combination of reading review books, reviewing one’s personal notes, and quizzing through question banks and/or flashcard apps could be used.
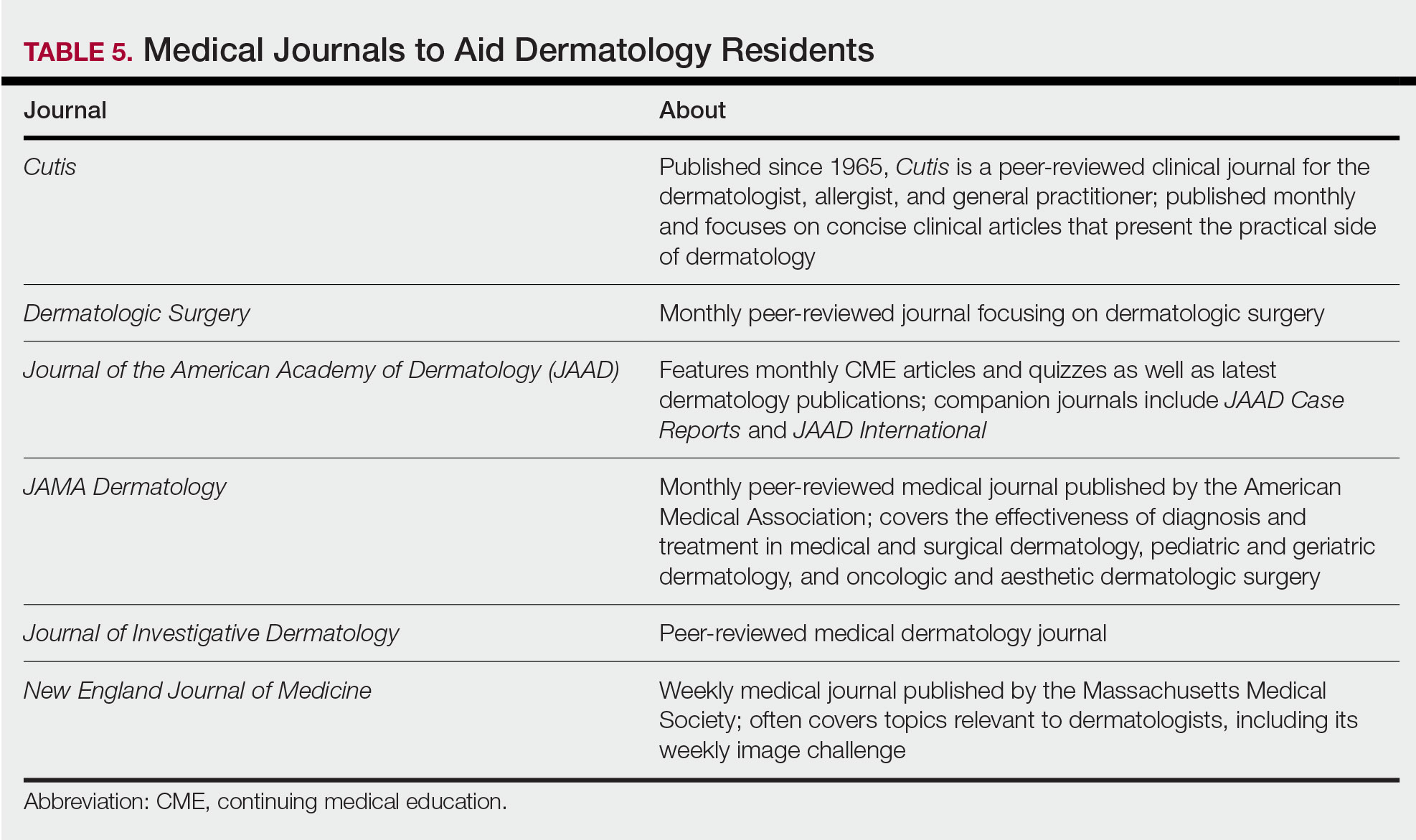
In addition to maintaining a consistent and organized study schedule, second-year residents should continue to read in depth on topics related to patients for whom they are caring and stay on top of the dermatology literature. Table 5 provides a list of medical journals that dermatology residents should aim to read. The Journal of the American Academy of Dermatology’s continuing medical education series (https://www.jaad.org/content/collection-cme) may be particularly helpful to residents. In this series, experts review a variety of dermatologic topics in depth paired with quiz questions.
Third Year
As a third-year resident (PGY-4 for most), studying should focus on deepening one’s knowledge base and beginning preparation for the boards examination. At this point, residents should stick to a limited selection of resources (ie, 1 textbook, 1 review book, 1 question bank) for in-depth study. More time should be spent on active learning, such as note-taking and question banks. Boards review courses historically have been available to dermatology residents, namely the Barron Board Review course and a plenary session at the American Academy of Dermatology Annual Conference (Table 4).
Consistent Habits
Studying strategies can and should differ throughout dermatology residency, though consistency is necessary throughout. It is helpful to plan study schedules in advance—yearly, monthly, weekly—and aim to stick to them as much as possible. Finding what works for each individual may take trial and error. For some, it may mean waking up early to study before work, whereas others may do better in the evenings. It also is helpful to utilize a combination of longer blocks of studying (ie, weekend days), with consistent shorter blocks of time during the week. Many residents also learn to take advantage of time spent commuting by listening to podcasts in the car or reading while on public transportation.
Final Thoughts
There are many resources available to support residents in their learning such as textbooks, journals, podcasts, flashcards, question banks, and more. The path to mastery will be individualized for each resident, likely using a unique combination of resources. The beginning of residency is a good time to explore a variety of resources to see what works best, whereas at the end studying becomes more targeted.
- Marks Jr JG, Miller JJ. Lookingbill and Marks’ Principles of Dermatology. 6th ed. China: Elsevier; 2019.
- James WD, Elston DM, Treat JR. Andrews’ Diseases of the Skin. 13th ed. China: Elsevier; 2019.
- Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018.
- Jain S. Dermatology: Illustrated Study Guide and Comprehensive Board Review. New York, NY: Springer; 2012.
- Elston DM, Ferringer T, Ko C, et al. Dermatopathology. 2nd ed. China: Elsevier Saunders; 2014.
- Eichenfield LF, Frieden IJ, eds. Neonatal and Infant Dermatology. London, England: Saunders; 2015.
- Alikhan A, Hocker TLH, eds. Review of Dermatology. China: Elsevier; 2017.
Dermatology residency can feel like drinking from a firehose, in which one is bombarded with so much information that it is impossible to retain any content. This article provides an overview of available resources and a guide on how to tailor studying throughout one’s training.
Prior to Residency
There are several resources that provide an introduction to dermatology and are appropriate for all medical students, regardless of intended specialty. The American Academy of Dermatology offers a free basic dermatology curriculum (https://www.aad.org/member/education/residents/bdc), with a choice of a 2- or 4-week course consisting of modules such as skin examination, basic science of the skin, dermatologic therapies, and specific dermatologic conditions. VisualDx offers LearnDerm (https://www.visualdx.com/learnderm/), which includes a 5-part tutorial and quiz focused on the skin examination, morphology, and lesion distribution. Lookingbill and Marks’ Principles of Dermatology1 is a book at an appropriate level for a medical student to learn about the fundamentals of dermatology. These resources may be helpful for residents to review immediately before starting dermatology residency (toward the end of intern year for most).
First Year
During the beginning of dermatology residency (postgraduate year [PGY] 2 for most), the fire hose of information feels most daunting. During this time, studying should focus on engendering a broad overview of dermatology. Most residencies maintain a textbook reading schedule, which provides a framework from which residents may structure their studying. Selection of a textbook tends to be program dependent. Even if the details of reading the textbook do not stick when reading it the first time, benefits include becoming familiar with what information one is expected to learn as a dermatologist and developing a strong foundation upon which one may continue to build. Based on my informal discussions with current residents, some reported that reading the textbook did not work well for them, citing too much minutiae in the textbooks and/or a preference for a more active learning approach. These residents instead focused on reading a review book for a broad overview, accompanied by a textbook or VisualDx when a more detailed reference is necessary. Table 1 provides a list of textbooks and mobile applications (apps) that residents may find helpful.
First-year residents may begin their efforts in synthesizing this new knowledge base toward the end of the year in preparation for the BASIC examination. The American Board of Dermatology provides a content outline as well as sample questions on their website (https://www.abderm.org/residents-and-fellows/exam-of-the-future-information-center.aspx#content), which may be used to guide more focused studying efforts during the weeks leading up to the examination.
Second Year
For second-year residents (PGY-3 for most) studying should focus on deepening and consolidating the broad foundation that was established during their first year. For many, this pursuit involves rereading the textbook chapters alongside more active learning measures, such as taking notes and quizzing oneself using flashcard apps and question banks (Table 2). Others may benefit from listening to podcasts (Table 3) or other sources utilizing audiovisual content, including attending conferences and other lectures virtually, which is becoming increasingly available in the setting of the coronavirus disease 2019 pandemic (Table 4). Because there are so many resources available to support these efforts, residents should be encouraged to try out a variety to determine what works best.
Toward the end of second year, studying may be tailored to preparing for the CORE examinations using the resources of one’s choice. Based on my discussions with current residents, a combination of reading review books, reviewing one’s personal notes, and quizzing through question banks and/or flashcard apps could be used.
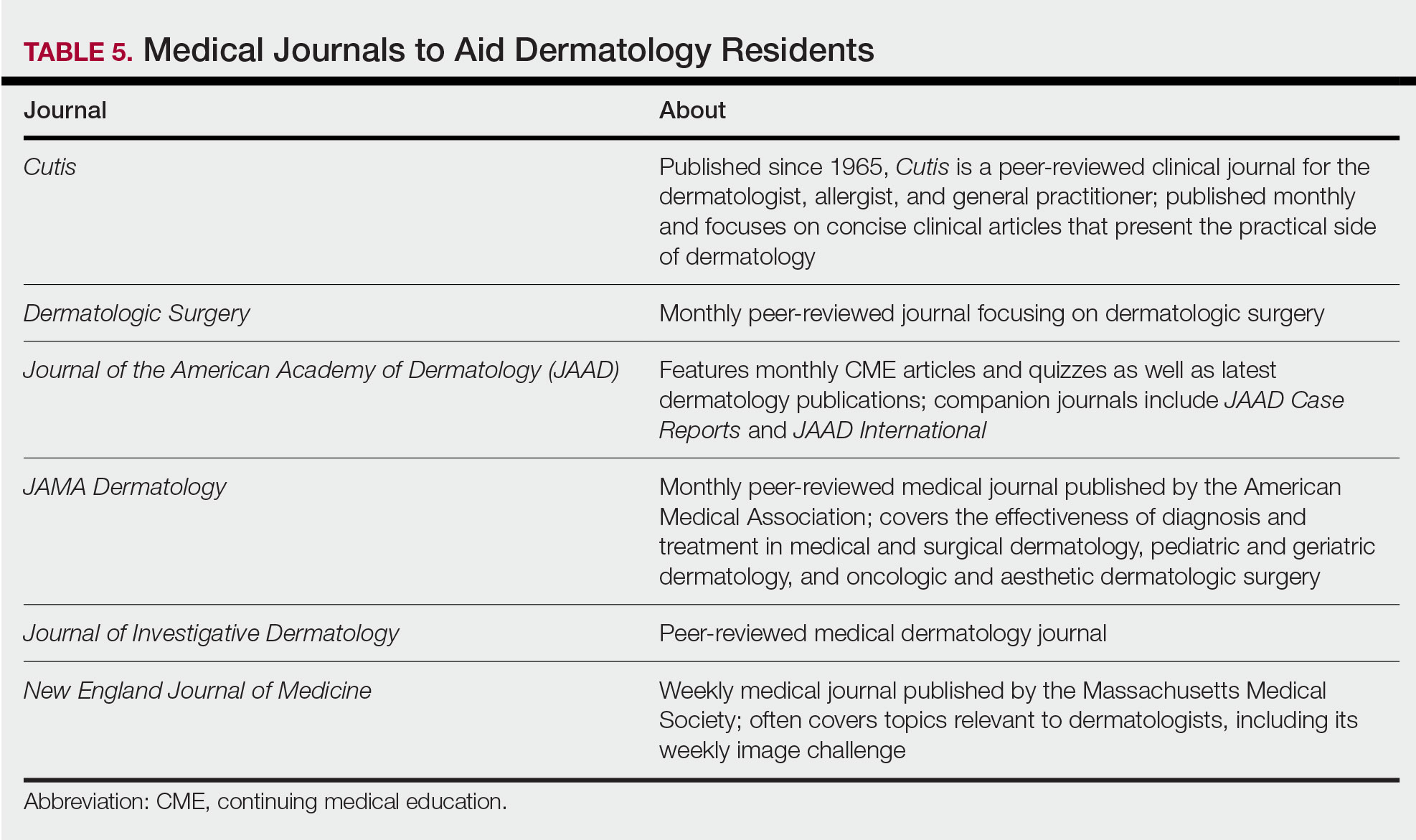
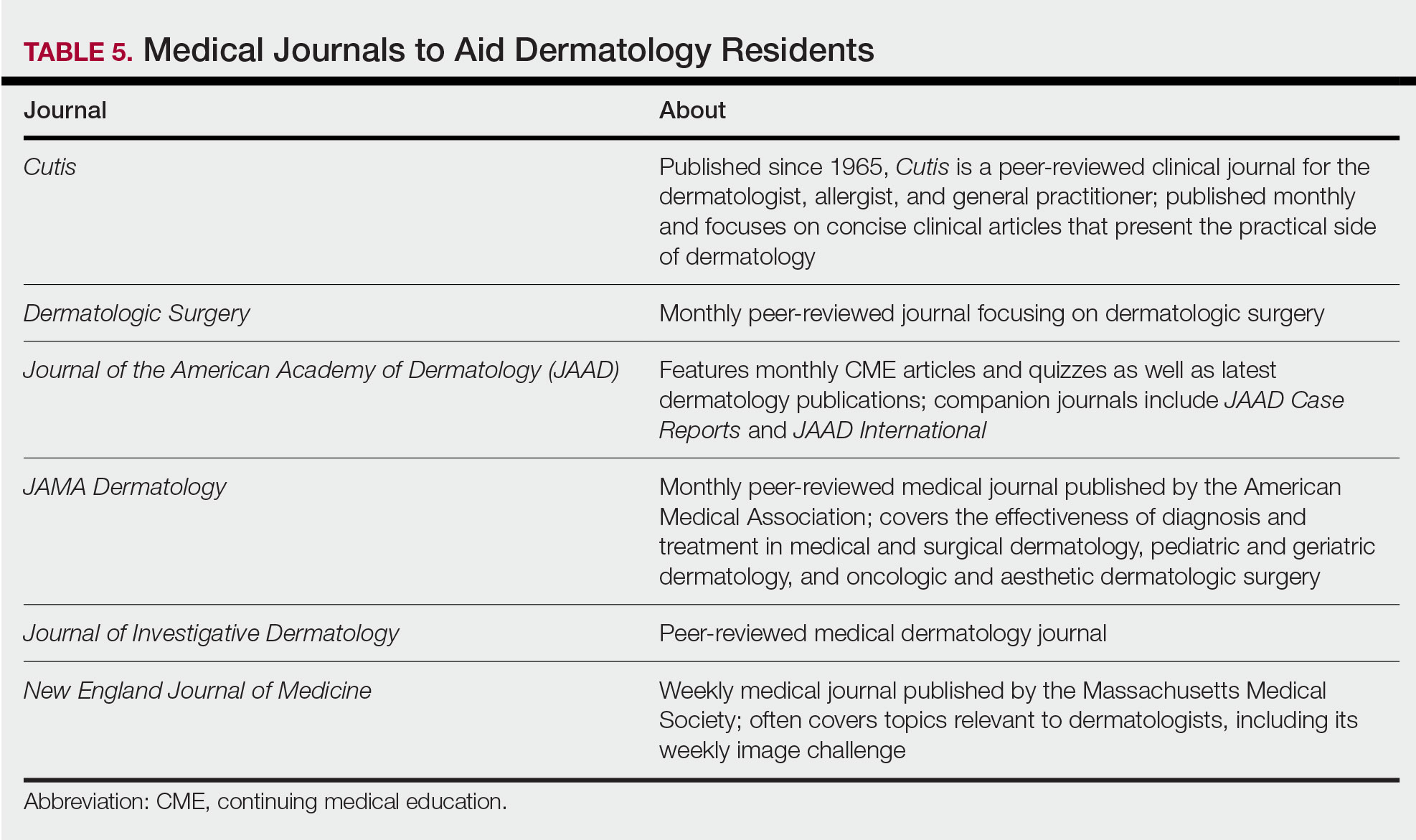
In addition to maintaining a consistent and organized study schedule, second-year residents should continue to read in depth on topics related to patients for whom they are caring and stay on top of the dermatology literature. Table 5 provides a list of medical journals that dermatology residents should aim to read. The Journal of the American Academy of Dermatology’s continuing medical education series (https://www.jaad.org/content/collection-cme) may be particularly helpful to residents. In this series, experts review a variety of dermatologic topics in depth paired with quiz questions.
Third Year
As a third-year resident (PGY-4 for most), studying should focus on deepening one’s knowledge base and beginning preparation for the boards examination. At this point, residents should stick to a limited selection of resources (ie, 1 textbook, 1 review book, 1 question bank) for in-depth study. More time should be spent on active learning, such as note-taking and question banks. Boards review courses historically have been available to dermatology residents, namely the Barron Board Review course and a plenary session at the American Academy of Dermatology Annual Conference (Table 4).
Consistent Habits
Studying strategies can and should differ throughout dermatology residency, though consistency is necessary throughout. It is helpful to plan study schedules in advance—yearly, monthly, weekly—and aim to stick to them as much as possible. Finding what works for each individual may take trial and error. For some, it may mean waking up early to study before work, whereas others may do better in the evenings. It also is helpful to utilize a combination of longer blocks of studying (ie, weekend days), with consistent shorter blocks of time during the week. Many residents also learn to take advantage of time spent commuting by listening to podcasts in the car or reading while on public transportation.
Final Thoughts
There are many resources available to support residents in their learning such as textbooks, journals, podcasts, flashcards, question banks, and more. The path to mastery will be individualized for each resident, likely using a unique combination of resources. The beginning of residency is a good time to explore a variety of resources to see what works best, whereas at the end studying becomes more targeted.
Dermatology residency can feel like drinking from a firehose, in which one is bombarded with so much information that it is impossible to retain any content. This article provides an overview of available resources and a guide on how to tailor studying throughout one’s training.
Prior to Residency
There are several resources that provide an introduction to dermatology and are appropriate for all medical students, regardless of intended specialty. The American Academy of Dermatology offers a free basic dermatology curriculum (https://www.aad.org/member/education/residents/bdc), with a choice of a 2- or 4-week course consisting of modules such as skin examination, basic science of the skin, dermatologic therapies, and specific dermatologic conditions. VisualDx offers LearnDerm (https://www.visualdx.com/learnderm/), which includes a 5-part tutorial and quiz focused on the skin examination, morphology, and lesion distribution. Lookingbill and Marks’ Principles of Dermatology1 is a book at an appropriate level for a medical student to learn about the fundamentals of dermatology. These resources may be helpful for residents to review immediately before starting dermatology residency (toward the end of intern year for most).
First Year
During the beginning of dermatology residency (postgraduate year [PGY] 2 for most), the fire hose of information feels most daunting. During this time, studying should focus on engendering a broad overview of dermatology. Most residencies maintain a textbook reading schedule, which provides a framework from which residents may structure their studying. Selection of a textbook tends to be program dependent. Even if the details of reading the textbook do not stick when reading it the first time, benefits include becoming familiar with what information one is expected to learn as a dermatologist and developing a strong foundation upon which one may continue to build. Based on my informal discussions with current residents, some reported that reading the textbook did not work well for them, citing too much minutiae in the textbooks and/or a preference for a more active learning approach. These residents instead focused on reading a review book for a broad overview, accompanied by a textbook or VisualDx when a more detailed reference is necessary. Table 1 provides a list of textbooks and mobile applications (apps) that residents may find helpful.
First-year residents may begin their efforts in synthesizing this new knowledge base toward the end of the year in preparation for the BASIC examination. The American Board of Dermatology provides a content outline as well as sample questions on their website (https://www.abderm.org/residents-and-fellows/exam-of-the-future-information-center.aspx#content), which may be used to guide more focused studying efforts during the weeks leading up to the examination.
Second Year
For second-year residents (PGY-3 for most) studying should focus on deepening and consolidating the broad foundation that was established during their first year. For many, this pursuit involves rereading the textbook chapters alongside more active learning measures, such as taking notes and quizzing oneself using flashcard apps and question banks (Table 2). Others may benefit from listening to podcasts (Table 3) or other sources utilizing audiovisual content, including attending conferences and other lectures virtually, which is becoming increasingly available in the setting of the coronavirus disease 2019 pandemic (Table 4). Because there are so many resources available to support these efforts, residents should be encouraged to try out a variety to determine what works best.
Toward the end of second year, studying may be tailored to preparing for the CORE examinations using the resources of one’s choice. Based on my discussions with current residents, a combination of reading review books, reviewing one’s personal notes, and quizzing through question banks and/or flashcard apps could be used.
In addition to maintaining a consistent and organized study schedule, second-year residents should continue to read in depth on topics related to patients for whom they are caring and stay on top of the dermatology literature. Table 5 provides a list of medical journals that dermatology residents should aim to read. The Journal of the American Academy of Dermatology’s continuing medical education series (https://www.jaad.org/content/collection-cme) may be particularly helpful to residents. In this series, experts review a variety of dermatologic topics in depth paired with quiz questions.
Third Year
As a third-year resident (PGY-4 for most), studying should focus on deepening one’s knowledge base and beginning preparation for the boards examination. At this point, residents should stick to a limited selection of resources (ie, 1 textbook, 1 review book, 1 question bank) for in-depth study. More time should be spent on active learning, such as note-taking and question banks. Boards review courses historically have been available to dermatology residents, namely the Barron Board Review course and a plenary session at the American Academy of Dermatology Annual Conference (Table 4).
Consistent Habits
Studying strategies can and should differ throughout dermatology residency, though consistency is necessary throughout. It is helpful to plan study schedules in advance—yearly, monthly, weekly—and aim to stick to them as much as possible. Finding what works for each individual may take trial and error. For some, it may mean waking up early to study before work, whereas others may do better in the evenings. It also is helpful to utilize a combination of longer blocks of studying (ie, weekend days), with consistent shorter blocks of time during the week. Many residents also learn to take advantage of time spent commuting by listening to podcasts in the car or reading while on public transportation.
Final Thoughts
There are many resources available to support residents in their learning such as textbooks, journals, podcasts, flashcards, question banks, and more. The path to mastery will be individualized for each resident, likely using a unique combination of resources. The beginning of residency is a good time to explore a variety of resources to see what works best, whereas at the end studying becomes more targeted.
- Marks Jr JG, Miller JJ. Lookingbill and Marks’ Principles of Dermatology. 6th ed. China: Elsevier; 2019.
- James WD, Elston DM, Treat JR. Andrews’ Diseases of the Skin. 13th ed. China: Elsevier; 2019.
- Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018.
- Jain S. Dermatology: Illustrated Study Guide and Comprehensive Board Review. New York, NY: Springer; 2012.
- Elston DM, Ferringer T, Ko C, et al. Dermatopathology. 2nd ed. China: Elsevier Saunders; 2014.
- Eichenfield LF, Frieden IJ, eds. Neonatal and Infant Dermatology. London, England: Saunders; 2015.
- Alikhan A, Hocker TLH, eds. Review of Dermatology. China: Elsevier; 2017.
- Marks Jr JG, Miller JJ. Lookingbill and Marks’ Principles of Dermatology. 6th ed. China: Elsevier; 2019.
- James WD, Elston DM, Treat JR. Andrews’ Diseases of the Skin. 13th ed. China: Elsevier; 2019.
- Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018.
- Jain S. Dermatology: Illustrated Study Guide and Comprehensive Board Review. New York, NY: Springer; 2012.
- Elston DM, Ferringer T, Ko C, et al. Dermatopathology. 2nd ed. China: Elsevier Saunders; 2014.
- Eichenfield LF, Frieden IJ, eds. Neonatal and Infant Dermatology. London, England: Saunders; 2015.
- Alikhan A, Hocker TLH, eds. Review of Dermatology. China: Elsevier; 2017.
Resident Pearls
- Independent study is a large component of dermatology residency.
- Consistent habits and a tailored approach will support optimal learning for each dermatology resident.
- The beginning of residency is a good time to explore a variety of resources to see what works best. Toward the end of residency, as studying becomes more targeted, residents may benefit from sticking to the resources with which they are most comfortable.
Physician income drops, burnout spikes globally in pandemic
according to the results of a Medscape survey.
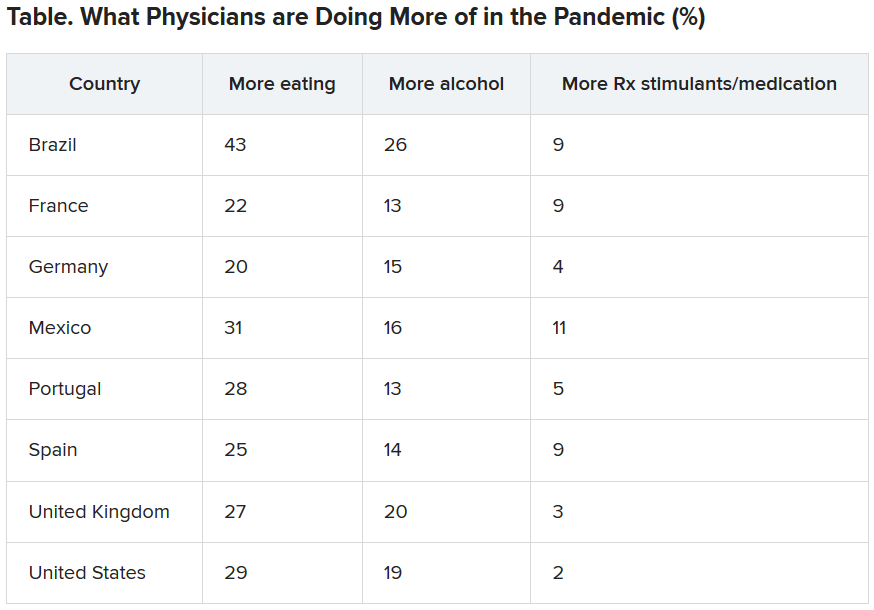
More than 7,500 physicians – nearly 5,000 in the United States, and others in Brazil, France, Germany, Mexico, Portugal, Spain, and the United Kingdom – responded to questions about their struggles to save patients and how the pandemic has changed their income and their lives at home and at work.
The pain was evident in this response from an emergency medicine physician in Spain: “It has been the worst time in my life ever, in both my personal and professional life.”
Conversely, some reported positive effects.
An internist in Brazil wrote: “I feel more proud of my career than ever before.”
One quarter of U.S. physicians considering earlier retirement
Physicians in the United States were asked what career changes, if any, they were considering in light of their experience with COVID-19. Although a little more than half (51%) said they were not planning any changes, 25% answered, “retiring earlier than previously planned,” and 12% answered, “a career change away from medicine.”
The number of physicians reporting an income drop was highest in Brazil (63% reported a drop), followed by the United States (62%), Mexico (56%), Portugal (49%), Germany (42%), France (41%), and Spain (31%). The question was not asked in the United Kingdom survey.
In the United States, the size of the drop has been substantial: 9% lost 76%-100% of their income; 14% lost 51%-75%; 28% lost 26%-50%; 33% lost 11%-25%; and 15% lost 1%-10%.
The U.S. specialists with the largest drop in income were ophthalmologists, who lost 51%, followed by allergists (46%), plastic surgeons (46%), and otolaryngologists (45%).
“I’m looking for a new profession due to economic impact,” an otolaryngologist in the United States said. “We are at risk while essentially using our private savings to keep our practice solvent.”
More than half of U.S. physicians (54%) have personally treated patients with COVID-19. Percentages were higher in France, Spain, and the United Kingdom (percentages ranged from 60%-68%).
The United States led all eight countries in treating patients with COVID-19 via telemedicine, at 26%. Germany had the lowest telemedicine percentage, at 10%.
Burnout intensifies
About two thirds of US physicians (64%) said that burnout had intensified during the crisis (70% of female physicians and 61% of male physicians said it had).
Many factors are feeding the burnout.
A critical care physician in the United States responded, “It is terrible to see people arriving at their rooms and assuming they were going to die soon; to see people saying goodbye to their families before dying or before being intubated.”
In all eight countries, a substantial percentage of physicians reported they “sometimes, often or always” treated patients with COVID-19 without the proper personal protective equipment. Spain had by far the largest percentage who answered that way (67%), followed by France (45%), Mexico (40%), the United Kingdom (34%), Brazil and Germany (28% each); and the United States and Portugal (23% each).
A U.S. rheumatologist wrote: “The fact that we were sent to take care of infectious patients without proper protection equipment made me feel we were betrayed in this fight.”
Sense of duty to volunteer to treat COVID-19 patients varied substantially among countries, from 69% who felt that way in Spain to 40% in Brazil. Half (50%) in the United States felt that way.
“Altruism must take second place where a real and present threat exists to my own personal existence,” one U.S. internist wrote.
Numbers personally infected
One fifth of physicians in Spain and the United Kingdom had personally been infected with the virus. Brazil, France, and Mexico had the next highest numbers, with 13%-15% of physicians infected; 5%-6% in the United States, Germany, and Portugal said they had been infected.
The percentage of physicians who reported that immediate family members had been infected ranged from 25% in Spain to 6% in Portugal. Among US physicians, 9% reported that family members had been diagnosed with COVID-19.
In the United States, 44% of respondents who had family living with them at home during the pandemic reported that relationships at home were more stressed because of stay-at-home guidelines and social distancing. Almost half (47%) said there had been no change, and 9% said relationships were less stressed.
Eating is coping mechanism of choice
Physicians were asked what they were doing more of during the pandemic, and food seemed to be the top source of comfort in all eight countries.
Loneliness reports differ across globe
Portugal had the highest percentage (51%) of physicians reporting increased loneliness. Next were Brazil (48%), the United States (46%), the United Kingdom (42%), France (41%), Spain and Mexico (40% each), and Germany (32%).
All eight countries lacked workplace activities to help physicians with grief. More than half (55%) of U.K. physicians reported having such activities available at their workplace, whereas only 25% of physicians in Germany did; 12%-24% of respondents across the countries were unsure about the offerings.
This article first appeared on Medscape.com.
according to the results of a Medscape survey.
More than 7,500 physicians – nearly 5,000 in the United States, and others in Brazil, France, Germany, Mexico, Portugal, Spain, and the United Kingdom – responded to questions about their struggles to save patients and how the pandemic has changed their income and their lives at home and at work.
The pain was evident in this response from an emergency medicine physician in Spain: “It has been the worst time in my life ever, in both my personal and professional life.”
Conversely, some reported positive effects.
An internist in Brazil wrote: “I feel more proud of my career than ever before.”
One quarter of U.S. physicians considering earlier retirement
Physicians in the United States were asked what career changes, if any, they were considering in light of their experience with COVID-19. Although a little more than half (51%) said they were not planning any changes, 25% answered, “retiring earlier than previously planned,” and 12% answered, “a career change away from medicine.”
The number of physicians reporting an income drop was highest in Brazil (63% reported a drop), followed by the United States (62%), Mexico (56%), Portugal (49%), Germany (42%), France (41%), and Spain (31%). The question was not asked in the United Kingdom survey.
In the United States, the size of the drop has been substantial: 9% lost 76%-100% of their income; 14% lost 51%-75%; 28% lost 26%-50%; 33% lost 11%-25%; and 15% lost 1%-10%.
The U.S. specialists with the largest drop in income were ophthalmologists, who lost 51%, followed by allergists (46%), plastic surgeons (46%), and otolaryngologists (45%).
“I’m looking for a new profession due to economic impact,” an otolaryngologist in the United States said. “We are at risk while essentially using our private savings to keep our practice solvent.”
More than half of U.S. physicians (54%) have personally treated patients with COVID-19. Percentages were higher in France, Spain, and the United Kingdom (percentages ranged from 60%-68%).
The United States led all eight countries in treating patients with COVID-19 via telemedicine, at 26%. Germany had the lowest telemedicine percentage, at 10%.
Burnout intensifies
About two thirds of US physicians (64%) said that burnout had intensified during the crisis (70% of female physicians and 61% of male physicians said it had).
Many factors are feeding the burnout.
A critical care physician in the United States responded, “It is terrible to see people arriving at their rooms and assuming they were going to die soon; to see people saying goodbye to their families before dying or before being intubated.”
In all eight countries, a substantial percentage of physicians reported they “sometimes, often or always” treated patients with COVID-19 without the proper personal protective equipment. Spain had by far the largest percentage who answered that way (67%), followed by France (45%), Mexico (40%), the United Kingdom (34%), Brazil and Germany (28% each); and the United States and Portugal (23% each).
A U.S. rheumatologist wrote: “The fact that we were sent to take care of infectious patients without proper protection equipment made me feel we were betrayed in this fight.”
Sense of duty to volunteer to treat COVID-19 patients varied substantially among countries, from 69% who felt that way in Spain to 40% in Brazil. Half (50%) in the United States felt that way.
“Altruism must take second place where a real and present threat exists to my own personal existence,” one U.S. internist wrote.
Numbers personally infected
One fifth of physicians in Spain and the United Kingdom had personally been infected with the virus. Brazil, France, and Mexico had the next highest numbers, with 13%-15% of physicians infected; 5%-6% in the United States, Germany, and Portugal said they had been infected.
The percentage of physicians who reported that immediate family members had been infected ranged from 25% in Spain to 6% in Portugal. Among US physicians, 9% reported that family members had been diagnosed with COVID-19.
In the United States, 44% of respondents who had family living with them at home during the pandemic reported that relationships at home were more stressed because of stay-at-home guidelines and social distancing. Almost half (47%) said there had been no change, and 9% said relationships were less stressed.
Eating is coping mechanism of choice
Physicians were asked what they were doing more of during the pandemic, and food seemed to be the top source of comfort in all eight countries.
Loneliness reports differ across globe
Portugal had the highest percentage (51%) of physicians reporting increased loneliness. Next were Brazil (48%), the United States (46%), the United Kingdom (42%), France (41%), Spain and Mexico (40% each), and Germany (32%).
All eight countries lacked workplace activities to help physicians with grief. More than half (55%) of U.K. physicians reported having such activities available at their workplace, whereas only 25% of physicians in Germany did; 12%-24% of respondents across the countries were unsure about the offerings.
This article first appeared on Medscape.com.
according to the results of a Medscape survey.
More than 7,500 physicians – nearly 5,000 in the United States, and others in Brazil, France, Germany, Mexico, Portugal, Spain, and the United Kingdom – responded to questions about their struggles to save patients and how the pandemic has changed their income and their lives at home and at work.
The pain was evident in this response from an emergency medicine physician in Spain: “It has been the worst time in my life ever, in both my personal and professional life.”
Conversely, some reported positive effects.
An internist in Brazil wrote: “I feel more proud of my career than ever before.”
One quarter of U.S. physicians considering earlier retirement
Physicians in the United States were asked what career changes, if any, they were considering in light of their experience with COVID-19. Although a little more than half (51%) said they were not planning any changes, 25% answered, “retiring earlier than previously planned,” and 12% answered, “a career change away from medicine.”
The number of physicians reporting an income drop was highest in Brazil (63% reported a drop), followed by the United States (62%), Mexico (56%), Portugal (49%), Germany (42%), France (41%), and Spain (31%). The question was not asked in the United Kingdom survey.
In the United States, the size of the drop has been substantial: 9% lost 76%-100% of their income; 14% lost 51%-75%; 28% lost 26%-50%; 33% lost 11%-25%; and 15% lost 1%-10%.
The U.S. specialists with the largest drop in income were ophthalmologists, who lost 51%, followed by allergists (46%), plastic surgeons (46%), and otolaryngologists (45%).
“I’m looking for a new profession due to economic impact,” an otolaryngologist in the United States said. “We are at risk while essentially using our private savings to keep our practice solvent.”
More than half of U.S. physicians (54%) have personally treated patients with COVID-19. Percentages were higher in France, Spain, and the United Kingdom (percentages ranged from 60%-68%).
The United States led all eight countries in treating patients with COVID-19 via telemedicine, at 26%. Germany had the lowest telemedicine percentage, at 10%.
Burnout intensifies
About two thirds of US physicians (64%) said that burnout had intensified during the crisis (70% of female physicians and 61% of male physicians said it had).
Many factors are feeding the burnout.
A critical care physician in the United States responded, “It is terrible to see people arriving at their rooms and assuming they were going to die soon; to see people saying goodbye to their families before dying or before being intubated.”
In all eight countries, a substantial percentage of physicians reported they “sometimes, often or always” treated patients with COVID-19 without the proper personal protective equipment. Spain had by far the largest percentage who answered that way (67%), followed by France (45%), Mexico (40%), the United Kingdom (34%), Brazil and Germany (28% each); and the United States and Portugal (23% each).
A U.S. rheumatologist wrote: “The fact that we were sent to take care of infectious patients without proper protection equipment made me feel we were betrayed in this fight.”
Sense of duty to volunteer to treat COVID-19 patients varied substantially among countries, from 69% who felt that way in Spain to 40% in Brazil. Half (50%) in the United States felt that way.
“Altruism must take second place where a real and present threat exists to my own personal existence,” one U.S. internist wrote.
Numbers personally infected
One fifth of physicians in Spain and the United Kingdom had personally been infected with the virus. Brazil, France, and Mexico had the next highest numbers, with 13%-15% of physicians infected; 5%-6% in the United States, Germany, and Portugal said they had been infected.
The percentage of physicians who reported that immediate family members had been infected ranged from 25% in Spain to 6% in Portugal. Among US physicians, 9% reported that family members had been diagnosed with COVID-19.
In the United States, 44% of respondents who had family living with them at home during the pandemic reported that relationships at home were more stressed because of stay-at-home guidelines and social distancing. Almost half (47%) said there had been no change, and 9% said relationships were less stressed.
Eating is coping mechanism of choice
Physicians were asked what they were doing more of during the pandemic, and food seemed to be the top source of comfort in all eight countries.
Loneliness reports differ across globe
Portugal had the highest percentage (51%) of physicians reporting increased loneliness. Next were Brazil (48%), the United States (46%), the United Kingdom (42%), France (41%), Spain and Mexico (40% each), and Germany (32%).
All eight countries lacked workplace activities to help physicians with grief. More than half (55%) of U.K. physicians reported having such activities available at their workplace, whereas only 25% of physicians in Germany did; 12%-24% of respondents across the countries were unsure about the offerings.
This article first appeared on Medscape.com.
The march of immunotherapy continues at ESMO 2020
The use of immunotherapy for upper gastrointestinal tumors and renal cancer, ALK- and EGFR-targeted agents in non–small cell lung cancer (NSCLC), and the next step in personalized prostate cancer management will all be subjects of headlining presentations at the ESMO Virtual Congress 2020.
The conference will, like so many other major events, be held online this year because of the COVID-19 pandemic.
John B. Haanen, PhD, ESMO 2020 scientific chair, who is from the Netherlands Cancer Institute, Amsterdam, the Netherlands, told Medscape Medical News that, because the congress is being held online this year, fewer abstracts were submitted; nevertheless, “We were very happy to see ... that the quality was very good.”
The number of submissions was not the only problem the organizing committee had to face in transforming the ESMO Congress into a virtual meeting.
They were unable to fit the scientific and educational programs together and so have had to split them over two consecutive weekends. Moreover, many of the sessions were highly interactive and needed to be either adapted or omitted.
“So the program is somewhat different,” Haanen said. He noted that “the presentations were also made shorter, especially on the educational sessions, because...we can’t expect people to sit behind screens for hours listening to long presentations.”
He added: “That was out of the question.”
Haanen is nevertheless hopeful that the virtual meeting will be “very exciting.”
Solange Peters, MD, PhD, ESMO president, who is also affiliated with the Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland, said in a press conference that it was a “sacrifice” to move ESMO 2020 online and that “there were very sad moments” when deciding on the content.
However, there were some benefits from the change.
She said that all of the ESMO meetings this year have seen “huge” increases in the number of attendees and the geographical span or reach of each of the conferences.
“So suddenly you also realize that, what is one of the missions of ESMO being to convey education globally ... was probably better reached, better achieved with the virtual format,” she commented.
Presidential symposia
Turning to the program, Haanen first picked out the third presidential symposium, which will be held on Monday, September 21. This will focus entirely on upper gastrointestinal tumors in both the adjuvant and metastatic setting.
He said that in recent years, “very little progress has been made” in this area, with treatment mostly consisting of chemotherapy and chemoradiotherapy.
However, this year’s presentations will explore the addition of immunotherapy either to chemotherapy or as an adjuvant treatment following completion of standard-of-care treatment for local disease.
Haanen said that the results will be “very interesting ... and may change current practice,” something that “is very important for both doctors and their patients.”
On Saturday, September 19, the first presidential symposium will include two presentations on lung cancer that Haanen said will offer some “exciting new [results] that I am sure will change clinical practice.”
One will be on the CROWN phase 3 trial comparing lorlatinib and crizotinib in the first-line treatment of patients with advanced ALK-positive NSCLC.
The other will present results on central nervous system disease recurrence from the ADAURA phase 3 trial of osimertinib adjuvant therapy in patients with resected EGFR-mutated NSCLC.
The same session will also see new data in advanced renal cell carcinoma from CheckMate 9ER, in which the c-Met and VEGFR2 inhibitor cabozantinib (Cabometyx) was combined with nivolumab (Opdivo) and compared to sunitinib (Sutent) in untreated patients.
“Last year, there were already some exciting results of the combination of axitinib [Inlyta], either with pembrolizumab [Keytruda] or with avelumab [Bavencio]...in the first-line setting in metastatic clear cell renal cell cancer,” Hannen said.
“Clearly there was a survival advantage over the standard of care, sunitinib,” he added.
This year, not only will efficacy data from CheckMate 9ER be presented but also quality-of-life results.
“That’s very important, because what everybody is afraid of is that, by adding drugs, you always get more impact on the quality of life, but you will see that the quality-of-life results are very exciting,” he said.
The second presidential symposium will feature studies on prostate cancer, notably the phase 3 IPATential150 trial of abiraterone (Zytiga) plus either ipatasertib or placebo in metastatic castration-resistant prostate cancer.
Ipatasertib targets Akt, and Haanen said that “by adding it to, let’s say, standard-of-care treatment ... the question of course of will be, Does that have a better outcome?”
He believes the results will be a “very nice illustration” that prostate cancer management is heading in the direction of personalized treatment.
Alongside the presidential symposia, there will be a number of proffered paper sessions on the latest results in all aspects of oncology, including results from the ASCENT trial in triple-negative breast cancer, as well as a dedicated COVID-19 track.
Haanen said that the ESMO Virtual Congress 2020, coming after the AACR and ASCO annual meetings, has the “advantage” of being able to present the latest outcomes of patients treated with chemotherapy and immunotherapy against the backdrop of the pandemic.
This will include a study from the ESMO Resilience Task Force on the impact of COVID-19 on oncology professionals both in terms of their personal distress and burnout and their job performance.
“I think that is very important,” Haanen said, “especially because the whole thing with COVID-19 is not yet over, and everybody is preparing for a second wave in the fall and winter.
“It may help us give us clues on how we can protect ourselves or each other to prevent burnout or other problems that we as healthcare caregivers face in this difficult period.”
Next year
For next year, Peters remains hopeful that the ESMO 2021 meeting will take place as planned in Paris.
She anticipates that, indeed, ESMO meetings will be able to take place from spring next year.
This will depend on a vaccine for COVID-19 becoming widely available, although oncologists in some countries may still not be able to travel.
This means “starting probably with hybrid formats, with some of the faculty being on site and some not, [and] the same thing for the attendees,” Peters said.
She suggested that, for ESMO Congress 2021 to work as an on-site meeting, it will require at least half or two-thirds of the originally anticipated number of attendees.
“I hope that Paris next year will happen,” Peters said, adding that it “will probably happen with less attendees – that’s fine, but [still] with a large number of faculty and attendees.”
The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The use of immunotherapy for upper gastrointestinal tumors and renal cancer, ALK- and EGFR-targeted agents in non–small cell lung cancer (NSCLC), and the next step in personalized prostate cancer management will all be subjects of headlining presentations at the ESMO Virtual Congress 2020.
The conference will, like so many other major events, be held online this year because of the COVID-19 pandemic.
John B. Haanen, PhD, ESMO 2020 scientific chair, who is from the Netherlands Cancer Institute, Amsterdam, the Netherlands, told Medscape Medical News that, because the congress is being held online this year, fewer abstracts were submitted; nevertheless, “We were very happy to see ... that the quality was very good.”
The number of submissions was not the only problem the organizing committee had to face in transforming the ESMO Congress into a virtual meeting.
They were unable to fit the scientific and educational programs together and so have had to split them over two consecutive weekends. Moreover, many of the sessions were highly interactive and needed to be either adapted or omitted.
“So the program is somewhat different,” Haanen said. He noted that “the presentations were also made shorter, especially on the educational sessions, because...we can’t expect people to sit behind screens for hours listening to long presentations.”
He added: “That was out of the question.”
Haanen is nevertheless hopeful that the virtual meeting will be “very exciting.”
Solange Peters, MD, PhD, ESMO president, who is also affiliated with the Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland, said in a press conference that it was a “sacrifice” to move ESMO 2020 online and that “there were very sad moments” when deciding on the content.
However, there were some benefits from the change.
She said that all of the ESMO meetings this year have seen “huge” increases in the number of attendees and the geographical span or reach of each of the conferences.
“So suddenly you also realize that, what is one of the missions of ESMO being to convey education globally ... was probably better reached, better achieved with the virtual format,” she commented.
Presidential symposia
Turning to the program, Haanen first picked out the third presidential symposium, which will be held on Monday, September 21. This will focus entirely on upper gastrointestinal tumors in both the adjuvant and metastatic setting.
He said that in recent years, “very little progress has been made” in this area, with treatment mostly consisting of chemotherapy and chemoradiotherapy.
However, this year’s presentations will explore the addition of immunotherapy either to chemotherapy or as an adjuvant treatment following completion of standard-of-care treatment for local disease.
Haanen said that the results will be “very interesting ... and may change current practice,” something that “is very important for both doctors and their patients.”
On Saturday, September 19, the first presidential symposium will include two presentations on lung cancer that Haanen said will offer some “exciting new [results] that I am sure will change clinical practice.”
One will be on the CROWN phase 3 trial comparing lorlatinib and crizotinib in the first-line treatment of patients with advanced ALK-positive NSCLC.
The other will present results on central nervous system disease recurrence from the ADAURA phase 3 trial of osimertinib adjuvant therapy in patients with resected EGFR-mutated NSCLC.
The same session will also see new data in advanced renal cell carcinoma from CheckMate 9ER, in which the c-Met and VEGFR2 inhibitor cabozantinib (Cabometyx) was combined with nivolumab (Opdivo) and compared to sunitinib (Sutent) in untreated patients.
“Last year, there were already some exciting results of the combination of axitinib [Inlyta], either with pembrolizumab [Keytruda] or with avelumab [Bavencio]...in the first-line setting in metastatic clear cell renal cell cancer,” Hannen said.
“Clearly there was a survival advantage over the standard of care, sunitinib,” he added.
This year, not only will efficacy data from CheckMate 9ER be presented but also quality-of-life results.
“That’s very important, because what everybody is afraid of is that, by adding drugs, you always get more impact on the quality of life, but you will see that the quality-of-life results are very exciting,” he said.
The second presidential symposium will feature studies on prostate cancer, notably the phase 3 IPATential150 trial of abiraterone (Zytiga) plus either ipatasertib or placebo in metastatic castration-resistant prostate cancer.
Ipatasertib targets Akt, and Haanen said that “by adding it to, let’s say, standard-of-care treatment ... the question of course of will be, Does that have a better outcome?”
He believes the results will be a “very nice illustration” that prostate cancer management is heading in the direction of personalized treatment.
Alongside the presidential symposia, there will be a number of proffered paper sessions on the latest results in all aspects of oncology, including results from the ASCENT trial in triple-negative breast cancer, as well as a dedicated COVID-19 track.
Haanen said that the ESMO Virtual Congress 2020, coming after the AACR and ASCO annual meetings, has the “advantage” of being able to present the latest outcomes of patients treated with chemotherapy and immunotherapy against the backdrop of the pandemic.
This will include a study from the ESMO Resilience Task Force on the impact of COVID-19 on oncology professionals both in terms of their personal distress and burnout and their job performance.
“I think that is very important,” Haanen said, “especially because the whole thing with COVID-19 is not yet over, and everybody is preparing for a second wave in the fall and winter.
“It may help us give us clues on how we can protect ourselves or each other to prevent burnout or other problems that we as healthcare caregivers face in this difficult period.”
Next year
For next year, Peters remains hopeful that the ESMO 2021 meeting will take place as planned in Paris.
She anticipates that, indeed, ESMO meetings will be able to take place from spring next year.
This will depend on a vaccine for COVID-19 becoming widely available, although oncologists in some countries may still not be able to travel.
This means “starting probably with hybrid formats, with some of the faculty being on site and some not, [and] the same thing for the attendees,” Peters said.
She suggested that, for ESMO Congress 2021 to work as an on-site meeting, it will require at least half or two-thirds of the originally anticipated number of attendees.
“I hope that Paris next year will happen,” Peters said, adding that it “will probably happen with less attendees – that’s fine, but [still] with a large number of faculty and attendees.”
The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The use of immunotherapy for upper gastrointestinal tumors and renal cancer, ALK- and EGFR-targeted agents in non–small cell lung cancer (NSCLC), and the next step in personalized prostate cancer management will all be subjects of headlining presentations at the ESMO Virtual Congress 2020.
The conference will, like so many other major events, be held online this year because of the COVID-19 pandemic.
John B. Haanen, PhD, ESMO 2020 scientific chair, who is from the Netherlands Cancer Institute, Amsterdam, the Netherlands, told Medscape Medical News that, because the congress is being held online this year, fewer abstracts were submitted; nevertheless, “We were very happy to see ... that the quality was very good.”
The number of submissions was not the only problem the organizing committee had to face in transforming the ESMO Congress into a virtual meeting.
They were unable to fit the scientific and educational programs together and so have had to split them over two consecutive weekends. Moreover, many of the sessions were highly interactive and needed to be either adapted or omitted.
“So the program is somewhat different,” Haanen said. He noted that “the presentations were also made shorter, especially on the educational sessions, because...we can’t expect people to sit behind screens for hours listening to long presentations.”
He added: “That was out of the question.”
Haanen is nevertheless hopeful that the virtual meeting will be “very exciting.”
Solange Peters, MD, PhD, ESMO president, who is also affiliated with the Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland, said in a press conference that it was a “sacrifice” to move ESMO 2020 online and that “there were very sad moments” when deciding on the content.
However, there were some benefits from the change.
She said that all of the ESMO meetings this year have seen “huge” increases in the number of attendees and the geographical span or reach of each of the conferences.
“So suddenly you also realize that, what is one of the missions of ESMO being to convey education globally ... was probably better reached, better achieved with the virtual format,” she commented.
Presidential symposia
Turning to the program, Haanen first picked out the third presidential symposium, which will be held on Monday, September 21. This will focus entirely on upper gastrointestinal tumors in both the adjuvant and metastatic setting.
He said that in recent years, “very little progress has been made” in this area, with treatment mostly consisting of chemotherapy and chemoradiotherapy.
However, this year’s presentations will explore the addition of immunotherapy either to chemotherapy or as an adjuvant treatment following completion of standard-of-care treatment for local disease.
Haanen said that the results will be “very interesting ... and may change current practice,” something that “is very important for both doctors and their patients.”
On Saturday, September 19, the first presidential symposium will include two presentations on lung cancer that Haanen said will offer some “exciting new [results] that I am sure will change clinical practice.”
One will be on the CROWN phase 3 trial comparing lorlatinib and crizotinib in the first-line treatment of patients with advanced ALK-positive NSCLC.
The other will present results on central nervous system disease recurrence from the ADAURA phase 3 trial of osimertinib adjuvant therapy in patients with resected EGFR-mutated NSCLC.
The same session will also see new data in advanced renal cell carcinoma from CheckMate 9ER, in which the c-Met and VEGFR2 inhibitor cabozantinib (Cabometyx) was combined with nivolumab (Opdivo) and compared to sunitinib (Sutent) in untreated patients.
“Last year, there were already some exciting results of the combination of axitinib [Inlyta], either with pembrolizumab [Keytruda] or with avelumab [Bavencio]...in the first-line setting in metastatic clear cell renal cell cancer,” Hannen said.
“Clearly there was a survival advantage over the standard of care, sunitinib,” he added.
This year, not only will efficacy data from CheckMate 9ER be presented but also quality-of-life results.
“That’s very important, because what everybody is afraid of is that, by adding drugs, you always get more impact on the quality of life, but you will see that the quality-of-life results are very exciting,” he said.
The second presidential symposium will feature studies on prostate cancer, notably the phase 3 IPATential150 trial of abiraterone (Zytiga) plus either ipatasertib or placebo in metastatic castration-resistant prostate cancer.
Ipatasertib targets Akt, and Haanen said that “by adding it to, let’s say, standard-of-care treatment ... the question of course of will be, Does that have a better outcome?”
He believes the results will be a “very nice illustration” that prostate cancer management is heading in the direction of personalized treatment.
Alongside the presidential symposia, there will be a number of proffered paper sessions on the latest results in all aspects of oncology, including results from the ASCENT trial in triple-negative breast cancer, as well as a dedicated COVID-19 track.
Haanen said that the ESMO Virtual Congress 2020, coming after the AACR and ASCO annual meetings, has the “advantage” of being able to present the latest outcomes of patients treated with chemotherapy and immunotherapy against the backdrop of the pandemic.
This will include a study from the ESMO Resilience Task Force on the impact of COVID-19 on oncology professionals both in terms of their personal distress and burnout and their job performance.
“I think that is very important,” Haanen said, “especially because the whole thing with COVID-19 is not yet over, and everybody is preparing for a second wave in the fall and winter.
“It may help us give us clues on how we can protect ourselves or each other to prevent burnout or other problems that we as healthcare caregivers face in this difficult period.”
Next year
For next year, Peters remains hopeful that the ESMO 2021 meeting will take place as planned in Paris.
She anticipates that, indeed, ESMO meetings will be able to take place from spring next year.
This will depend on a vaccine for COVID-19 becoming widely available, although oncologists in some countries may still not be able to travel.
This means “starting probably with hybrid formats, with some of the faculty being on site and some not, [and] the same thing for the attendees,” Peters said.
She suggested that, for ESMO Congress 2021 to work as an on-site meeting, it will require at least half or two-thirds of the originally anticipated number of attendees.
“I hope that Paris next year will happen,” Peters said, adding that it “will probably happen with less attendees – that’s fine, but [still] with a large number of faculty and attendees.”
The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
FROM ESMO 2020
New billing code for added COVID practice expense
The American Medical Association on Sept. 8 announced that a new code, 99072, is intended to cover additional supplies, materials, and clinical staff time over and above those usually included in an office visit when performed during a declared public health emergency, as defined by law, attributable to respiratory-transmitted infectious disease, the AMA said in a release.
Fifty national medical specialty societies and other organizations worked with the AMA’s Specialty Society RVS Update Committee over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency. It has submitted recommendations to the Centers for Medicare & Medicaid Services seeking to persuade the federal agencies to recognize the new 99072 payment code.
The intention is to recognize the extra expenses involved in steps now routinely taken to reduce the risk for COVID transmission from office visits, Current Procedural Terminology Editorial Panel Chair Mark S. Synovec, MD, said in an interview. Some practices have adapted by having staff screen patients before they enter offices and making arrangements to keep patients at a safe distance from others during their visits, he said.
“Everyone’s life has significantly changed because of COVID and the health care system has dramatically changed,” Dr. Synovec said. “It was pretty clear that the status quo was not going to work.”
Physician practices will welcome this change, said Veronica Bradley, CPC, a senior industry adviser to the Medical Group Management Association. An office visit that in the past may have involved only basic infection control measures, such as donning a pair of gloves, now may involve clinicians taking the time to put on more extensive protective gear, she said.
“Now they are taking a heck of a lot more precautions, and there’s more time and more supplies being consumed,” Ms. Bradley said in an interview.
Code looks ahead to future use
The AMA explained how this new code differs from CPT code 99070, which is typically reported for supplies and materials that may be used or provided to patients during an office visit.
The new 99072 code applies only during declared public health emergencies and applies only to additional items required to support “a safe in-person provision” of evaluation, treatment, and procedures, the AMA said.
“These items contrast with those typically reported with code 99070, which focuses on additional supplies provided over and above those usually included with a specific service, such as drugs, intravenous catheters, or trays,” the AMA said.
The CPT panel sought to structure the new code for covering COVID practice expenses so that it could not be abused, and also looked ahead to the future, Dr. Synovec said.
“It’s a code that you would put on during a public health emergency as defined by law that would be related to a respiratory-transmitted infectious disease. Obviously we meant it for SARS-CoV-2,” he said. “Hopefully we can go another 100 years before we have another pandemic, but we also wanted to prepare something where if we have another airborne respiratory virus that requires additional practice expenses as seen this time, it would be available for use.”
The AMA also announced a second addition, CPT code 86413, that anticipates greater use of quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) provided by laboratory tests reported by other CPT codes.
More information is available on the AMA website.
A version of this article originally appeared on Medscape.com.
The American Medical Association on Sept. 8 announced that a new code, 99072, is intended to cover additional supplies, materials, and clinical staff time over and above those usually included in an office visit when performed during a declared public health emergency, as defined by law, attributable to respiratory-transmitted infectious disease, the AMA said in a release.
Fifty national medical specialty societies and other organizations worked with the AMA’s Specialty Society RVS Update Committee over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency. It has submitted recommendations to the Centers for Medicare & Medicaid Services seeking to persuade the federal agencies to recognize the new 99072 payment code.
The intention is to recognize the extra expenses involved in steps now routinely taken to reduce the risk for COVID transmission from office visits, Current Procedural Terminology Editorial Panel Chair Mark S. Synovec, MD, said in an interview. Some practices have adapted by having staff screen patients before they enter offices and making arrangements to keep patients at a safe distance from others during their visits, he said.
“Everyone’s life has significantly changed because of COVID and the health care system has dramatically changed,” Dr. Synovec said. “It was pretty clear that the status quo was not going to work.”
Physician practices will welcome this change, said Veronica Bradley, CPC, a senior industry adviser to the Medical Group Management Association. An office visit that in the past may have involved only basic infection control measures, such as donning a pair of gloves, now may involve clinicians taking the time to put on more extensive protective gear, she said.
“Now they are taking a heck of a lot more precautions, and there’s more time and more supplies being consumed,” Ms. Bradley said in an interview.
Code looks ahead to future use
The AMA explained how this new code differs from CPT code 99070, which is typically reported for supplies and materials that may be used or provided to patients during an office visit.
The new 99072 code applies only during declared public health emergencies and applies only to additional items required to support “a safe in-person provision” of evaluation, treatment, and procedures, the AMA said.
“These items contrast with those typically reported with code 99070, which focuses on additional supplies provided over and above those usually included with a specific service, such as drugs, intravenous catheters, or trays,” the AMA said.
The CPT panel sought to structure the new code for covering COVID practice expenses so that it could not be abused, and also looked ahead to the future, Dr. Synovec said.
“It’s a code that you would put on during a public health emergency as defined by law that would be related to a respiratory-transmitted infectious disease. Obviously we meant it for SARS-CoV-2,” he said. “Hopefully we can go another 100 years before we have another pandemic, but we also wanted to prepare something where if we have another airborne respiratory virus that requires additional practice expenses as seen this time, it would be available for use.”
The AMA also announced a second addition, CPT code 86413, that anticipates greater use of quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) provided by laboratory tests reported by other CPT codes.
More information is available on the AMA website.
A version of this article originally appeared on Medscape.com.
The American Medical Association on Sept. 8 announced that a new code, 99072, is intended to cover additional supplies, materials, and clinical staff time over and above those usually included in an office visit when performed during a declared public health emergency, as defined by law, attributable to respiratory-transmitted infectious disease, the AMA said in a release.
Fifty national medical specialty societies and other organizations worked with the AMA’s Specialty Society RVS Update Committee over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency. It has submitted recommendations to the Centers for Medicare & Medicaid Services seeking to persuade the federal agencies to recognize the new 99072 payment code.
The intention is to recognize the extra expenses involved in steps now routinely taken to reduce the risk for COVID transmission from office visits, Current Procedural Terminology Editorial Panel Chair Mark S. Synovec, MD, said in an interview. Some practices have adapted by having staff screen patients before they enter offices and making arrangements to keep patients at a safe distance from others during their visits, he said.
“Everyone’s life has significantly changed because of COVID and the health care system has dramatically changed,” Dr. Synovec said. “It was pretty clear that the status quo was not going to work.”
Physician practices will welcome this change, said Veronica Bradley, CPC, a senior industry adviser to the Medical Group Management Association. An office visit that in the past may have involved only basic infection control measures, such as donning a pair of gloves, now may involve clinicians taking the time to put on more extensive protective gear, she said.
“Now they are taking a heck of a lot more precautions, and there’s more time and more supplies being consumed,” Ms. Bradley said in an interview.
Code looks ahead to future use
The AMA explained how this new code differs from CPT code 99070, which is typically reported for supplies and materials that may be used or provided to patients during an office visit.
The new 99072 code applies only during declared public health emergencies and applies only to additional items required to support “a safe in-person provision” of evaluation, treatment, and procedures, the AMA said.
“These items contrast with those typically reported with code 99070, which focuses on additional supplies provided over and above those usually included with a specific service, such as drugs, intravenous catheters, or trays,” the AMA said.
The CPT panel sought to structure the new code for covering COVID practice expenses so that it could not be abused, and also looked ahead to the future, Dr. Synovec said.
“It’s a code that you would put on during a public health emergency as defined by law that would be related to a respiratory-transmitted infectious disease. Obviously we meant it for SARS-CoV-2,” he said. “Hopefully we can go another 100 years before we have another pandemic, but we also wanted to prepare something where if we have another airborne respiratory virus that requires additional practice expenses as seen this time, it would be available for use.”
The AMA also announced a second addition, CPT code 86413, that anticipates greater use of quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) provided by laboratory tests reported by other CPT codes.
More information is available on the AMA website.
A version of this article originally appeared on Medscape.com.
Use of 3D Technology to Support Dermatologists Returning to Practice Amid COVID-19
Coronavirus disease 2019 (COVID-19) has spread across all 7 continents, including 185 countries, and infected more than 21.9 million individuals worldwide as of August 18, 2020, according to the Johns Hopkins Coronavirus Resource Center. It has strained our health care system and affected all specialties, including dermatology. Dermatologists have taken important safety measures by canceling/deferring elective and nonemergency procedures and diagnosing/treating patients via telemedicine. Many residents and attending dermatologists have volunteered to care for COVID-19 inpatients and donated
N95 masks are necessary during the COVID-19 pandemic because they effectively filter at least 95% of 0.3-μm airborne particles and provide adequate face seals.1 3-Dimensional imaging integrated with 3D printers can be used to scan precise facial parameters (eg, jawline, nose) and account for facial hair density and length to produce comfortable tailored N95 masks and face seals.1,2 3-Dimensional printing utilizes robotics and
Face shields offer an additional layer of safety for the face and mucosae and also may provide longevity for N95 masks. Using synthetic polymers such as polycarbonate and polyethylene, 3D printers can be used to construct face shields via fused deposition modeling.1 These face shields may be worn over N95 masks and then can be sanitized and reused.
Mohs surgeons and staff may be at particularly high risk for COVID-19 infection due to their close proximity to the face during surgery, use of cautery, and prolonged time spent with patients while taking layers and suturing.

As dermatologists reopen and ramp up practice volume, there will be increased PPE requirements. Using 3D technology and imaging to produce N95 masks, face shields, and face coverings, we can offer effective diagnosis and treatment while optimizing safety for dermatologists, staff, and patients.
- Ishack S, Lipner SR. Applications of 3D printing technology to address COVID-19-related supply shortages [published online April 21, 2020]. Am J Med. 2020;133:771-773.
- Cai M, Li H, Shen S, et al. Customized design and 3D printing of face seal for an N95 filtering facepiece respirator. J Occup Environ Hyg. 2018;3:226-234.
- Ishack S, Lipner SR. A review of 3-dimensional skin bioprinting techniques: applications, approaches, and trends [published online March 17, 2020]. Dermatol Surg. doi:10.1097/DSS.0000000000002378.
- Banerjee SS, Burbine S, Shivaprakash NK, et al. 3D-printable PP/SEBS thermoplastic elastomeric blends: preparation and properties [published online February 17, 2019]. Polymers (Basel). doi:10.3390/polym11020347.
- Chuah SY, Attia ABE, Long V. Structural and functional 3D mapping of skin tumours with non-invasive multispectral optoacoustic tomography [published online November 2, 2016]. Skin Res Technol. 2017;23:221-226.
Coronavirus disease 2019 (COVID-19) has spread across all 7 continents, including 185 countries, and infected more than 21.9 million individuals worldwide as of August 18, 2020, according to the Johns Hopkins Coronavirus Resource Center. It has strained our health care system and affected all specialties, including dermatology. Dermatologists have taken important safety measures by canceling/deferring elective and nonemergency procedures and diagnosing/treating patients via telemedicine. Many residents and attending dermatologists have volunteered to care for COVID-19 inpatients and donated
N95 masks are necessary during the COVID-19 pandemic because they effectively filter at least 95% of 0.3-μm airborne particles and provide adequate face seals.1 3-Dimensional imaging integrated with 3D printers can be used to scan precise facial parameters (eg, jawline, nose) and account for facial hair density and length to produce comfortable tailored N95 masks and face seals.1,2 3-Dimensional printing utilizes robotics and
Face shields offer an additional layer of safety for the face and mucosae and also may provide longevity for N95 masks. Using synthetic polymers such as polycarbonate and polyethylene, 3D printers can be used to construct face shields via fused deposition modeling.1 These face shields may be worn over N95 masks and then can be sanitized and reused.
Mohs surgeons and staff may be at particularly high risk for COVID-19 infection due to their close proximity to the face during surgery, use of cautery, and prolonged time spent with patients while taking layers and suturing.

As dermatologists reopen and ramp up practice volume, there will be increased PPE requirements. Using 3D technology and imaging to produce N95 masks, face shields, and face coverings, we can offer effective diagnosis and treatment while optimizing safety for dermatologists, staff, and patients.
Coronavirus disease 2019 (COVID-19) has spread across all 7 continents, including 185 countries, and infected more than 21.9 million individuals worldwide as of August 18, 2020, according to the Johns Hopkins Coronavirus Resource Center. It has strained our health care system and affected all specialties, including dermatology. Dermatologists have taken important safety measures by canceling/deferring elective and nonemergency procedures and diagnosing/treating patients via telemedicine. Many residents and attending dermatologists have volunteered to care for COVID-19 inpatients and donated
N95 masks are necessary during the COVID-19 pandemic because they effectively filter at least 95% of 0.3-μm airborne particles and provide adequate face seals.1 3-Dimensional imaging integrated with 3D printers can be used to scan precise facial parameters (eg, jawline, nose) and account for facial hair density and length to produce comfortable tailored N95 masks and face seals.1,2 3-Dimensional printing utilizes robotics and
Face shields offer an additional layer of safety for the face and mucosae and also may provide longevity for N95 masks. Using synthetic polymers such as polycarbonate and polyethylene, 3D printers can be used to construct face shields via fused deposition modeling.1 These face shields may be worn over N95 masks and then can be sanitized and reused.
Mohs surgeons and staff may be at particularly high risk for COVID-19 infection due to their close proximity to the face during surgery, use of cautery, and prolonged time spent with patients while taking layers and suturing.

As dermatologists reopen and ramp up practice volume, there will be increased PPE requirements. Using 3D technology and imaging to produce N95 masks, face shields, and face coverings, we can offer effective diagnosis and treatment while optimizing safety for dermatologists, staff, and patients.
- Ishack S, Lipner SR. Applications of 3D printing technology to address COVID-19-related supply shortages [published online April 21, 2020]. Am J Med. 2020;133:771-773.
- Cai M, Li H, Shen S, et al. Customized design and 3D printing of face seal for an N95 filtering facepiece respirator. J Occup Environ Hyg. 2018;3:226-234.
- Ishack S, Lipner SR. A review of 3-dimensional skin bioprinting techniques: applications, approaches, and trends [published online March 17, 2020]. Dermatol Surg. doi:10.1097/DSS.0000000000002378.
- Banerjee SS, Burbine S, Shivaprakash NK, et al. 3D-printable PP/SEBS thermoplastic elastomeric blends: preparation and properties [published online February 17, 2019]. Polymers (Basel). doi:10.3390/polym11020347.
- Chuah SY, Attia ABE, Long V. Structural and functional 3D mapping of skin tumours with non-invasive multispectral optoacoustic tomography [published online November 2, 2016]. Skin Res Technol. 2017;23:221-226.
- Ishack S, Lipner SR. Applications of 3D printing technology to address COVID-19-related supply shortages [published online April 21, 2020]. Am J Med. 2020;133:771-773.
- Cai M, Li H, Shen S, et al. Customized design and 3D printing of face seal for an N95 filtering facepiece respirator. J Occup Environ Hyg. 2018;3:226-234.
- Ishack S, Lipner SR. A review of 3-dimensional skin bioprinting techniques: applications, approaches, and trends [published online March 17, 2020]. Dermatol Surg. doi:10.1097/DSS.0000000000002378.
- Banerjee SS, Burbine S, Shivaprakash NK, et al. 3D-printable PP/SEBS thermoplastic elastomeric blends: preparation and properties [published online February 17, 2019]. Polymers (Basel). doi:10.3390/polym11020347.
- Chuah SY, Attia ABE, Long V. Structural and functional 3D mapping of skin tumours with non-invasive multispectral optoacoustic tomography [published online November 2, 2016]. Skin Res Technol. 2017;23:221-226.
Practice Points
- Coronavirus disease 19 has overwhelmed our health care system and affected all specialties, including dermatology.
- There are concerns about shortages of personal protective equipment to safely care for patients.
- 3-Dimensional imaging and printing technologies can be harnessed to create face coverings and face shields for the dermatology outpatient setting.
How to build your identity as a physician online
To have a thriving business in today’s world, a functioning website is crucial to the overall business health. For a medical practice in general, and for its physicians specifically, it is one of the first steps for maintaining a practice. But to grow that practice, it is crucial to take the steps beyond just having a website. Growth requires website optimization for search engines, an expanding referral base, and the knowledge to use web tools and social media at your disposal to promote the practice and its physicians. In this roundtable, several marketing experts and web-savvy physicians discuss using available tools to best position and grow a practice.
Choosing a web upgrade
Patrick J. Culligan, MD: Peter, can you start us off by describing your relationship with Heather, and how your practice benefitted from her expertise?
Peter M. Lotze, MD: Sure. I am a urogynecologist in the competitive market of pelvic reconstructive surgery in Houston, Texas. Within that market, my main approach was to reach out to other physicians to refer patients to my practice. It generally would work, but took increasingly greater amounts of time to call these physicians up, write them letters, and maintain relationships. I felt that the large, national practice group that I am in did not have a significant web presence optimized to promote my practice, which makes it difficult for patients seeking your services to find you in their search for a doctor. It is helpful for patients to be able to understand from your website who you are, what you do, and what their experience may be like.
Glaring to me was that a web search specific for me or things that I do, would not produce our company’s results until page 2 or more on Google. This can be devastating for a practice because most people don’t go past the first page, and you can end up with fewer self-referrals, which should be a significant portion of new patients to your practice. I knew I needed guidance; I knew of Heather’s expertise given her exceptional past work building marketing strategies.
Digital go-tos for marketing
Heather Schueppert: Yes, I was pleased to work with Dr. Lotze, and at the time was a marketing consultant for practices such as his. But gone are the days of printed material—brochures, pamphlets, or even billboards—to effectively promote a business, or in this case, a practice. What still withstands the test of time, however, as the number 1 marketing referral source is word of mouth—from your trusted friend, family member, or coworker.
It is now proven that the number 2 most trusted form of advertising, the most persuasive and the most motivating, is online marketing.1 It is the “digital word of mouth”—the review. Patients are actively online, and a strong digital presence is critical to provide that direct value to retain and grow your patient base.
Continue to: Foundations of private practice reach out...
Foundations of private practice reach out
There are 3 important areas that I consider the foundation of any private practice marketing strategy (TABLE). First is an updated website that is search engine optimized (SEO). You can’t just set it and forget it, it needs to be an updated website. The algorithms for search engines are changing constantly to try to make it as fair and relevant as possible for patients or consumers to find the businesses they are searching for online.
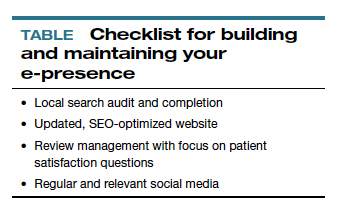
The second area is review management, and for a physician, or even a care center, to do this on your own is a daunting task. It is a critical component, however, to making sure that your reputation out there, that online word of mouth, is as high a star rating as possible.
The third component is local search, which is basically a form of SEO that helps businesses show up in relevant local searches. We are all familiar with the search, “find a restaurant near me,” anything that pushes those search engines to find something local.
Those are what I call the effective triad: that updated website, the review management, and the local search, and all of these are tied together. I think Dr. Lotze and his practice did these effectively well, and I believe that he achieved his goals for the longer term.
Review/reputation management
Dr. Culligan: Brad, is there something that doctors may not know about Healthgrades, and are there opportunities to take full advantage of this physician-rating site?
Brad Bowman, MD: I agree with everything that Dr. Lotze and Heather have said. Start with yourself—what is it that you want to be, the one thing you want to stand for? Get your own marketing, your website right, then, the point is, once you do all that and you are number 1 in SEO, you are still only going to get about 25% of the people looking for you by name to come to your website. The other 75% are going to look at all the other different sites that are out there to provide information to consumers. So the question becomes what do you do with all these other third-party sites? Healthgrades is the most comprehensive and has the highest traffic of the third-party “find a doctor” sites. In 2020, half of all Americans who go to a doctor will use Healthgrades at some point to help select and connect with that doctor.
Physicians have their focus on the quality of the care they provide. Patients, however, focus on the quality of the entire health care experience. Did I get better? How long did I have to wait? Was the office staff helpful? Scarily enough, we still spend more time shopping for a refrigerator or mattress than we do shopping for a doctor. We still tend to think that all doctors are the same. It is the reality of how we have been trained by our insurance companies and by the health care system. That is why getting your marketing right and getting what is it that you want to be known for out there is important, so that you can get the types of patients you want.
Listings management is very important. Make sure that you are findable everywhere. There are services that will do this: Doctor.com, Reputation.com, and many others. They can help you make sure you get all your basic materials right: addresses, phone numbers, your picture. Because 75% of people are going to end up on third-party websites, if your phone number is wrong there, you could lose that patient.
Then the second piece of working with third-party sites is reputation management. Physician reviews are not a bad thing, they are the new word of mouth, as Heather pointed out. Most (80%) of the reviews are going to be positive. The others will be negative, and that is okay. It is important that you get at least 1 or 2 reviews on all the different sites. We know from Healthgrades.com that going from zero reviews to 1 review will increase your call volume by 60%. If you have the choice between 2 physicians and one practice looks like people have been there before, you will go to that one.
You can learn from reviews as well, consumers provide valid feedback. Best practice is to respond to every positive and negative review. Thank them, indicate that you have listened to them, and address any concerns as necessary.
Continue to: Dr. Lotze...
Dr. Lotze: As an example, one of the paramount things that Heather introduced me to was the third party I use to run my website. That company sends a HIPAA-compliant review out to each patient we have seen that day and gives them the opportunity to rate our services and leave comments. If a patient brings up a concern, we can respond immediately, which is important. Patients appreciate feeling that they have been heard. Typically, communicating with a patient will turn the 3-star review into a 5-star as she follows up with the practice.
Ms. Schueppert: Timeliness is important. And just to mention, there certainly is a time commitment to this (and it is a marathon versus a sprint) and there is some financial investment to get it going, but it could truly be detrimental to a practice if you decide not to do anything at all.
Dr. Bowman: Agencies can really help with the time commitment.
Handling bad reviews
Dr. Culligan: What about that person who seems to have it out for you, perhaps giving you multiple bad reviews?
Dr. Bowman: I have seen this before. At Healthgrades, we recently analyzed 8.4 million patient reviews to see what people wrote about.2 The first thing they will talk about is quality of care as they see it. Did I get better or not? You can’t “fix” every patient; there will be some that you cannot help. The next thing patients comment on is bedside manner. With negative reviews, you will see more comments about the office staff.2
A single negative review actually helps make the positive ones look more credible. But if you do believe someone is trolling you, we can flag it and will investigate to the best of our ability. (Different sites likely have different editorial policies.) For example, we look at the IP addresses of all reviews, and if multiple reviews are coming from the same location, we would only let one through, overwriting the previous review from that address.
Patients just want to be heard. We have seen people change their views, based on how their review is handled and responded to.
Dr. Lotze: Is there a response by the physician that you think tends to work better in terms of resolving the issue that can minimize a perceived caustic reaction to a patient’s criticism?
Dr. Bowman: First, just like with any stressful situation, take a deep breath and respond when you feel like you can be constructive. When you do respond, be gracious. Thank them for their feedback. Make sure you reference something about their concern: “I understand that you had to wait longer than you would have liked.” Acknowledge the problem they reference, and then just apologize: “I’m sorry we didn’t meet your expectations.” Then, if they waited too long for example, “We have a new system where no one should have to wait more than 30 minutes….” You can respond privately or publically. Generally, public responses are better as it shows other consumers that you are willing to listen and consider their point of view.
Continue to: The next phase at Healthgrades...
The next phase at Healthgrades
Dr. Culligan: Do you see changes to the way physician-rating sites are working now? Are we going to stay status quo over the next 10 years, or do you see frontiers in how your site is going to develop?
Dr. Bowman: For Healthgrades, we rely on quantitative and objective measures, not just the qualitative. We are investing heavily right now in trying to help consumers understand what are the relative volumes of different procedures or different patient types that each individual doctor sees. Orthopedics is an easy example—if you have a knee problem, you want to go to someone who specializes in knees. Our job is to help consumers easily identify, “This is a shoulder doctor, this is a knee doctor, and this is why that matters.”
In the meantime, as a physician, you can always go into our site and state your care philosophy, identifying what is the sort of patient that you like to treat. Transparency is good for everyone, and especially physicians. It helps the right patient show up for you, and it helps you do a better job providing referrals.
Social media: Avoid pitfalls, and use it to your benefit
Dr. Lotze: Branding was one of the things that I was confused about, and Heather really helped me out. As physicians, we put ourselves out there on our websites, which we try to make professional sources of information for patients. But patients often want to see what else they can find out about us, including Healthgrades and social media. I think the thing that is important to know with social media is that it is a place where people learn about you as a person. Your social media should be another avenue of promotion. Whether it is your personal or professional Facebook page, people are going to see those sites. You have an opportunity to promote yourself as a good physician and a good person with a wholesome practice that you want people to come to. If a physician is posting questionable things about themselves on any kind of social media, it could be perceived as inappropriate by the patient. That can impact how patients think of you as a person, and how they are going to grade you. If people lose sight of who you are due to a questionable social media posting, everything else (SEO, the website) can be for naught.
Dr. Culligan: What are the most important social media tools to invest your time in?
Ms. Schueppert: Before anybody jumps into social media, I firmly recommend that you make sure your local search and your Google 3-pack is set up—which is basically a method Google uses to display the top 3 results on its listings page. Then make sure you have a review management system in place. Make sure you have that updated website. Those are the foundational elements. Once you have that going, social media is the next added layer to that digital presence.
I usually recommend LinkedIn. It is huge because you are staying in contact with your colleagues, that business-to-business type of connection. It remains a way for physicians to set themselves up as experts in their level of specialty.
From there, it’s either Instagram or Facebook. If you are serving more of the younger generations, the millennials and younger, then Instagram is the way to go. If you are focusing on your 40+, 50+, they are going to be far more on Facebook.
Continue to: Dr. Lotze...
Dr. Lotze: For me, a Facebook page was a great place to start. The cost of those Google ads—the first things we see at the top of a Google search in their own separate box—is significant. If a practice has that kind of money to invest, great; it is an instant way to be first on the page during a search. But there are more cost-effective ways of doing that, especially as you are getting your name out. Facebook provides, at a smaller cost, promotion of whatever it is that you are seeking to promote. You can find people within a certain zip code, for instance, and use a Facebook ad campaign that can drive people to your Facebook page—which should have both routinely updated new posts and a link to your website. The posts should be interesting topics relevant to the patients you wish to treat (avoiding personal stories or controversial discussions). You can put a post together, or you can have a third-party service do this. People who follow your page will get reminders of you and your practice with each new post. As your page followers increase, your Facebook rank will improve, and your page will more likely be discovered by Facebook searches for your services. With an added link to your office practice website, those patients go straight to your site without getting lost in the noise of Google search results.
For Instagram, a short video or an interesting picture, along with a brief statement, are the essentials. You can add a single link. Marketing here is by direct messaging or having patients going to your website through a link. Instagram, like Facebook, offers analytics to help show you what your audience likes to read about, improving the quality of your posts and increasing number of followers.
YouTube is the number 2 search engine behind Google. A Google search for your field of medicine may be filled with pages of competitors. However, YouTube has a much lower volume of competing practices, making it easier for patients to find you. The only downside to YouTube is that it will list your video along with other competing videos, which can draw attention away from your practice.
If you want to promote your website or practice with video, using a company such as Vimeo is a better choice compared with YouTube, as YouTube gets credit for video views—which improves YouTube’s SEO and not your own website. Vimeo allows for your website to get credit each time the video is watched. Regardless of where you place your videos, make them short and to the point, with links to your website. Videos only need to be long enough to get your message across and stimulate interest in your practice.
If you can have a blog on your website, it also will help with SEO. What a search engine like Google wants to see is that a patient is on your web page and looking at something for at least 60 seconds. If so, the website is deemed to have information that is relevant, improving your SEO ranking.
Finally, Twitter also can be used for getting messaging out and for branding. The problem with it is that many people go to Twitter to follow a Hollywood celebrity, a sports star, or are looking for mass communication. There is less interest on Twitter for physician outreach.
Continue to: Measuring ROI...
Measuring ROI
Dr. Culligan: What’s the best way to track your return on investment?
Dr. Lotze: First for me was to find out what didn’t work in the office and fix that before really promoting my practice. It’s about the global experience for a patient, as Brad mentioned. As a marketing expert, Heather met with me to understand my goals. She then called my office as a patient to set up an appointment and went through that entire office experience. We identified issues needing improvement.
The next step was to develop a working relationship with my webmaster—someone who can help manage Internet image and SEO. Together, you will develop goals for what the SEO should promote specific to your practice. Once a good SEO program is in place, your website’s ranking will go up—although it can take a minimum of 6 months to see a significant increase. To help understand your website’s performance, your webmaster should provide you with reports on your site’s analytics.
As you go through this process, it is great to have a marketing expert to be the point person. You will work closely together for a while, but eventually you can back off over time. The time and expense you invest on the front end have huge rewards on the back end. Currently, I still spend a reasonable amount of money every month. I have a high self-referral base because of these efforts, however, which results in more patient surgeries and easily covers my expenses. It is money well invested. My website traffic increased by 268% over 2 years (FIGURE). I’ll propose that currently more than half of my patients are self-referrals due to online marketing.
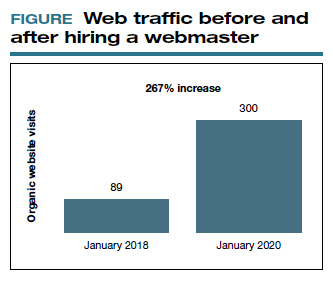
Ms. Schueppert: The only thing I would add is training your front staff. They are checking people in, taking appointments, checking your patients out. Have them be mindful that there are campaigns going on, whether it is a social media push, or a new video that went on the website. They can ask, “How did you hear about us?” when a new patient calls.
Dr. Bowman: Unless you are a large university hospital, where the analytics get significantly more advanced in terms of measuring return on investment (ROI), I think you should just be looking at your schedule and looking at your monthly billings and seeing how they change over time. You can calculate how much a new patient is worth because you can figure out how many patients you have and how much you bill and what your profits are.
Dr. Culligan: For those of us who are hospital employees, you can try to convince the hospital that you can do a detailed ROI analysis, or you can just look at it like (say it’s $3,000 per month), how many surgeries does this project have to generate before the hospital makes that back? The answer is a fraction of 1 case.
Thank you to all of you for your expertise on this roundtable.
- Anderson A. Online reviews vs. word of mouth: Which one is more important. https://www.revlocal.com/blog/reviewandreputationmanagement/onlinereviewsvswordofmouthwhichoneismoreimportant. Accessed July 17, 2020.
- 2020 Patient sentiment report. Healthgrades; Medical Group Management Association. https://www.healthgrades.com/content /patientsentimentreport. Accessed July 17, 2020
To have a thriving business in today’s world, a functioning website is crucial to the overall business health. For a medical practice in general, and for its physicians specifically, it is one of the first steps for maintaining a practice. But to grow that practice, it is crucial to take the steps beyond just having a website. Growth requires website optimization for search engines, an expanding referral base, and the knowledge to use web tools and social media at your disposal to promote the practice and its physicians. In this roundtable, several marketing experts and web-savvy physicians discuss using available tools to best position and grow a practice.
Choosing a web upgrade
Patrick J. Culligan, MD: Peter, can you start us off by describing your relationship with Heather, and how your practice benefitted from her expertise?
Peter M. Lotze, MD: Sure. I am a urogynecologist in the competitive market of pelvic reconstructive surgery in Houston, Texas. Within that market, my main approach was to reach out to other physicians to refer patients to my practice. It generally would work, but took increasingly greater amounts of time to call these physicians up, write them letters, and maintain relationships. I felt that the large, national practice group that I am in did not have a significant web presence optimized to promote my practice, which makes it difficult for patients seeking your services to find you in their search for a doctor. It is helpful for patients to be able to understand from your website who you are, what you do, and what their experience may be like.
Glaring to me was that a web search specific for me or things that I do, would not produce our company’s results until page 2 or more on Google. This can be devastating for a practice because most people don’t go past the first page, and you can end up with fewer self-referrals, which should be a significant portion of new patients to your practice. I knew I needed guidance; I knew of Heather’s expertise given her exceptional past work building marketing strategies.
Digital go-tos for marketing
Heather Schueppert: Yes, I was pleased to work with Dr. Lotze, and at the time was a marketing consultant for practices such as his. But gone are the days of printed material—brochures, pamphlets, or even billboards—to effectively promote a business, or in this case, a practice. What still withstands the test of time, however, as the number 1 marketing referral source is word of mouth—from your trusted friend, family member, or coworker.
It is now proven that the number 2 most trusted form of advertising, the most persuasive and the most motivating, is online marketing.1 It is the “digital word of mouth”—the review. Patients are actively online, and a strong digital presence is critical to provide that direct value to retain and grow your patient base.
Continue to: Foundations of private practice reach out...
Foundations of private practice reach out
There are 3 important areas that I consider the foundation of any private practice marketing strategy (TABLE). First is an updated website that is search engine optimized (SEO). You can’t just set it and forget it, it needs to be an updated website. The algorithms for search engines are changing constantly to try to make it as fair and relevant as possible for patients or consumers to find the businesses they are searching for online.
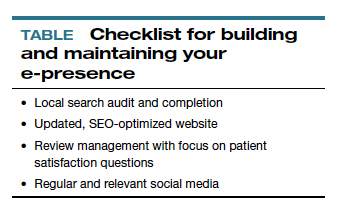
The second area is review management, and for a physician, or even a care center, to do this on your own is a daunting task. It is a critical component, however, to making sure that your reputation out there, that online word of mouth, is as high a star rating as possible.
The third component is local search, which is basically a form of SEO that helps businesses show up in relevant local searches. We are all familiar with the search, “find a restaurant near me,” anything that pushes those search engines to find something local.
Those are what I call the effective triad: that updated website, the review management, and the local search, and all of these are tied together. I think Dr. Lotze and his practice did these effectively well, and I believe that he achieved his goals for the longer term.
Review/reputation management
Dr. Culligan: Brad, is there something that doctors may not know about Healthgrades, and are there opportunities to take full advantage of this physician-rating site?
Brad Bowman, MD: I agree with everything that Dr. Lotze and Heather have said. Start with yourself—what is it that you want to be, the one thing you want to stand for? Get your own marketing, your website right, then, the point is, once you do all that and you are number 1 in SEO, you are still only going to get about 25% of the people looking for you by name to come to your website. The other 75% are going to look at all the other different sites that are out there to provide information to consumers. So the question becomes what do you do with all these other third-party sites? Healthgrades is the most comprehensive and has the highest traffic of the third-party “find a doctor” sites. In 2020, half of all Americans who go to a doctor will use Healthgrades at some point to help select and connect with that doctor.
Physicians have their focus on the quality of the care they provide. Patients, however, focus on the quality of the entire health care experience. Did I get better? How long did I have to wait? Was the office staff helpful? Scarily enough, we still spend more time shopping for a refrigerator or mattress than we do shopping for a doctor. We still tend to think that all doctors are the same. It is the reality of how we have been trained by our insurance companies and by the health care system. That is why getting your marketing right and getting what is it that you want to be known for out there is important, so that you can get the types of patients you want.
Listings management is very important. Make sure that you are findable everywhere. There are services that will do this: Doctor.com, Reputation.com, and many others. They can help you make sure you get all your basic materials right: addresses, phone numbers, your picture. Because 75% of people are going to end up on third-party websites, if your phone number is wrong there, you could lose that patient.
Then the second piece of working with third-party sites is reputation management. Physician reviews are not a bad thing, they are the new word of mouth, as Heather pointed out. Most (80%) of the reviews are going to be positive. The others will be negative, and that is okay. It is important that you get at least 1 or 2 reviews on all the different sites. We know from Healthgrades.com that going from zero reviews to 1 review will increase your call volume by 60%. If you have the choice between 2 physicians and one practice looks like people have been there before, you will go to that one.
You can learn from reviews as well, consumers provide valid feedback. Best practice is to respond to every positive and negative review. Thank them, indicate that you have listened to them, and address any concerns as necessary.
Continue to: Dr. Lotze...
Dr. Lotze: As an example, one of the paramount things that Heather introduced me to was the third party I use to run my website. That company sends a HIPAA-compliant review out to each patient we have seen that day and gives them the opportunity to rate our services and leave comments. If a patient brings up a concern, we can respond immediately, which is important. Patients appreciate feeling that they have been heard. Typically, communicating with a patient will turn the 3-star review into a 5-star as she follows up with the practice.
Ms. Schueppert: Timeliness is important. And just to mention, there certainly is a time commitment to this (and it is a marathon versus a sprint) and there is some financial investment to get it going, but it could truly be detrimental to a practice if you decide not to do anything at all.
Dr. Bowman: Agencies can really help with the time commitment.
Handling bad reviews
Dr. Culligan: What about that person who seems to have it out for you, perhaps giving you multiple bad reviews?
Dr. Bowman: I have seen this before. At Healthgrades, we recently analyzed 8.4 million patient reviews to see what people wrote about.2 The first thing they will talk about is quality of care as they see it. Did I get better or not? You can’t “fix” every patient; there will be some that you cannot help. The next thing patients comment on is bedside manner. With negative reviews, you will see more comments about the office staff.2
A single negative review actually helps make the positive ones look more credible. But if you do believe someone is trolling you, we can flag it and will investigate to the best of our ability. (Different sites likely have different editorial policies.) For example, we look at the IP addresses of all reviews, and if multiple reviews are coming from the same location, we would only let one through, overwriting the previous review from that address.
Patients just want to be heard. We have seen people change their views, based on how their review is handled and responded to.
Dr. Lotze: Is there a response by the physician that you think tends to work better in terms of resolving the issue that can minimize a perceived caustic reaction to a patient’s criticism?
Dr. Bowman: First, just like with any stressful situation, take a deep breath and respond when you feel like you can be constructive. When you do respond, be gracious. Thank them for their feedback. Make sure you reference something about their concern: “I understand that you had to wait longer than you would have liked.” Acknowledge the problem they reference, and then just apologize: “I’m sorry we didn’t meet your expectations.” Then, if they waited too long for example, “We have a new system where no one should have to wait more than 30 minutes….” You can respond privately or publically. Generally, public responses are better as it shows other consumers that you are willing to listen and consider their point of view.
Continue to: The next phase at Healthgrades...
The next phase at Healthgrades
Dr. Culligan: Do you see changes to the way physician-rating sites are working now? Are we going to stay status quo over the next 10 years, or do you see frontiers in how your site is going to develop?
Dr. Bowman: For Healthgrades, we rely on quantitative and objective measures, not just the qualitative. We are investing heavily right now in trying to help consumers understand what are the relative volumes of different procedures or different patient types that each individual doctor sees. Orthopedics is an easy example—if you have a knee problem, you want to go to someone who specializes in knees. Our job is to help consumers easily identify, “This is a shoulder doctor, this is a knee doctor, and this is why that matters.”
In the meantime, as a physician, you can always go into our site and state your care philosophy, identifying what is the sort of patient that you like to treat. Transparency is good for everyone, and especially physicians. It helps the right patient show up for you, and it helps you do a better job providing referrals.
Social media: Avoid pitfalls, and use it to your benefit
Dr. Lotze: Branding was one of the things that I was confused about, and Heather really helped me out. As physicians, we put ourselves out there on our websites, which we try to make professional sources of information for patients. But patients often want to see what else they can find out about us, including Healthgrades and social media. I think the thing that is important to know with social media is that it is a place where people learn about you as a person. Your social media should be another avenue of promotion. Whether it is your personal or professional Facebook page, people are going to see those sites. You have an opportunity to promote yourself as a good physician and a good person with a wholesome practice that you want people to come to. If a physician is posting questionable things about themselves on any kind of social media, it could be perceived as inappropriate by the patient. That can impact how patients think of you as a person, and how they are going to grade you. If people lose sight of who you are due to a questionable social media posting, everything else (SEO, the website) can be for naught.
Dr. Culligan: What are the most important social media tools to invest your time in?
Ms. Schueppert: Before anybody jumps into social media, I firmly recommend that you make sure your local search and your Google 3-pack is set up—which is basically a method Google uses to display the top 3 results on its listings page. Then make sure you have a review management system in place. Make sure you have that updated website. Those are the foundational elements. Once you have that going, social media is the next added layer to that digital presence.
I usually recommend LinkedIn. It is huge because you are staying in contact with your colleagues, that business-to-business type of connection. It remains a way for physicians to set themselves up as experts in their level of specialty.
From there, it’s either Instagram or Facebook. If you are serving more of the younger generations, the millennials and younger, then Instagram is the way to go. If you are focusing on your 40+, 50+, they are going to be far more on Facebook.
Continue to: Dr. Lotze...
Dr. Lotze: For me, a Facebook page was a great place to start. The cost of those Google ads—the first things we see at the top of a Google search in their own separate box—is significant. If a practice has that kind of money to invest, great; it is an instant way to be first on the page during a search. But there are more cost-effective ways of doing that, especially as you are getting your name out. Facebook provides, at a smaller cost, promotion of whatever it is that you are seeking to promote. You can find people within a certain zip code, for instance, and use a Facebook ad campaign that can drive people to your Facebook page—which should have both routinely updated new posts and a link to your website. The posts should be interesting topics relevant to the patients you wish to treat (avoiding personal stories or controversial discussions). You can put a post together, or you can have a third-party service do this. People who follow your page will get reminders of you and your practice with each new post. As your page followers increase, your Facebook rank will improve, and your page will more likely be discovered by Facebook searches for your services. With an added link to your office practice website, those patients go straight to your site without getting lost in the noise of Google search results.
For Instagram, a short video or an interesting picture, along with a brief statement, are the essentials. You can add a single link. Marketing here is by direct messaging or having patients going to your website through a link. Instagram, like Facebook, offers analytics to help show you what your audience likes to read about, improving the quality of your posts and increasing number of followers.
YouTube is the number 2 search engine behind Google. A Google search for your field of medicine may be filled with pages of competitors. However, YouTube has a much lower volume of competing practices, making it easier for patients to find you. The only downside to YouTube is that it will list your video along with other competing videos, which can draw attention away from your practice.
If you want to promote your website or practice with video, using a company such as Vimeo is a better choice compared with YouTube, as YouTube gets credit for video views—which improves YouTube’s SEO and not your own website. Vimeo allows for your website to get credit each time the video is watched. Regardless of where you place your videos, make them short and to the point, with links to your website. Videos only need to be long enough to get your message across and stimulate interest in your practice.
If you can have a blog on your website, it also will help with SEO. What a search engine like Google wants to see is that a patient is on your web page and looking at something for at least 60 seconds. If so, the website is deemed to have information that is relevant, improving your SEO ranking.
Finally, Twitter also can be used for getting messaging out and for branding. The problem with it is that many people go to Twitter to follow a Hollywood celebrity, a sports star, or are looking for mass communication. There is less interest on Twitter for physician outreach.
Continue to: Measuring ROI...
Measuring ROI
Dr. Culligan: What’s the best way to track your return on investment?
Dr. Lotze: First for me was to find out what didn’t work in the office and fix that before really promoting my practice. It’s about the global experience for a patient, as Brad mentioned. As a marketing expert, Heather met with me to understand my goals. She then called my office as a patient to set up an appointment and went through that entire office experience. We identified issues needing improvement.
The next step was to develop a working relationship with my webmaster—someone who can help manage Internet image and SEO. Together, you will develop goals for what the SEO should promote specific to your practice. Once a good SEO program is in place, your website’s ranking will go up—although it can take a minimum of 6 months to see a significant increase. To help understand your website’s performance, your webmaster should provide you with reports on your site’s analytics.
As you go through this process, it is great to have a marketing expert to be the point person. You will work closely together for a while, but eventually you can back off over time. The time and expense you invest on the front end have huge rewards on the back end. Currently, I still spend a reasonable amount of money every month. I have a high self-referral base because of these efforts, however, which results in more patient surgeries and easily covers my expenses. It is money well invested. My website traffic increased by 268% over 2 years (FIGURE). I’ll propose that currently more than half of my patients are self-referrals due to online marketing.
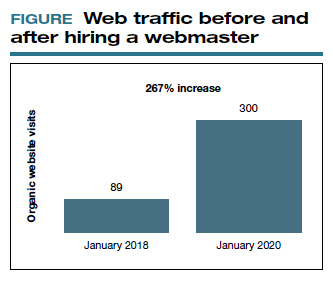
Ms. Schueppert: The only thing I would add is training your front staff. They are checking people in, taking appointments, checking your patients out. Have them be mindful that there are campaigns going on, whether it is a social media push, or a new video that went on the website. They can ask, “How did you hear about us?” when a new patient calls.
Dr. Bowman: Unless you are a large university hospital, where the analytics get significantly more advanced in terms of measuring return on investment (ROI), I think you should just be looking at your schedule and looking at your monthly billings and seeing how they change over time. You can calculate how much a new patient is worth because you can figure out how many patients you have and how much you bill and what your profits are.
Dr. Culligan: For those of us who are hospital employees, you can try to convince the hospital that you can do a detailed ROI analysis, or you can just look at it like (say it’s $3,000 per month), how many surgeries does this project have to generate before the hospital makes that back? The answer is a fraction of 1 case.
Thank you to all of you for your expertise on this roundtable.
To have a thriving business in today’s world, a functioning website is crucial to the overall business health. For a medical practice in general, and for its physicians specifically, it is one of the first steps for maintaining a practice. But to grow that practice, it is crucial to take the steps beyond just having a website. Growth requires website optimization for search engines, an expanding referral base, and the knowledge to use web tools and social media at your disposal to promote the practice and its physicians. In this roundtable, several marketing experts and web-savvy physicians discuss using available tools to best position and grow a practice.
Choosing a web upgrade
Patrick J. Culligan, MD: Peter, can you start us off by describing your relationship with Heather, and how your practice benefitted from her expertise?
Peter M. Lotze, MD: Sure. I am a urogynecologist in the competitive market of pelvic reconstructive surgery in Houston, Texas. Within that market, my main approach was to reach out to other physicians to refer patients to my practice. It generally would work, but took increasingly greater amounts of time to call these physicians up, write them letters, and maintain relationships. I felt that the large, national practice group that I am in did not have a significant web presence optimized to promote my practice, which makes it difficult for patients seeking your services to find you in their search for a doctor. It is helpful for patients to be able to understand from your website who you are, what you do, and what their experience may be like.
Glaring to me was that a web search specific for me or things that I do, would not produce our company’s results until page 2 or more on Google. This can be devastating for a practice because most people don’t go past the first page, and you can end up with fewer self-referrals, which should be a significant portion of new patients to your practice. I knew I needed guidance; I knew of Heather’s expertise given her exceptional past work building marketing strategies.
Digital go-tos for marketing
Heather Schueppert: Yes, I was pleased to work with Dr. Lotze, and at the time was a marketing consultant for practices such as his. But gone are the days of printed material—brochures, pamphlets, or even billboards—to effectively promote a business, or in this case, a practice. What still withstands the test of time, however, as the number 1 marketing referral source is word of mouth—from your trusted friend, family member, or coworker.
It is now proven that the number 2 most trusted form of advertising, the most persuasive and the most motivating, is online marketing.1 It is the “digital word of mouth”—the review. Patients are actively online, and a strong digital presence is critical to provide that direct value to retain and grow your patient base.
Continue to: Foundations of private practice reach out...
Foundations of private practice reach out
There are 3 important areas that I consider the foundation of any private practice marketing strategy (TABLE). First is an updated website that is search engine optimized (SEO). You can’t just set it and forget it, it needs to be an updated website. The algorithms for search engines are changing constantly to try to make it as fair and relevant as possible for patients or consumers to find the businesses they are searching for online.
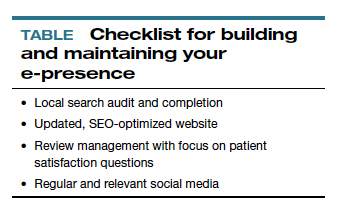
The second area is review management, and for a physician, or even a care center, to do this on your own is a daunting task. It is a critical component, however, to making sure that your reputation out there, that online word of mouth, is as high a star rating as possible.
The third component is local search, which is basically a form of SEO that helps businesses show up in relevant local searches. We are all familiar with the search, “find a restaurant near me,” anything that pushes those search engines to find something local.
Those are what I call the effective triad: that updated website, the review management, and the local search, and all of these are tied together. I think Dr. Lotze and his practice did these effectively well, and I believe that he achieved his goals for the longer term.
Review/reputation management
Dr. Culligan: Brad, is there something that doctors may not know about Healthgrades, and are there opportunities to take full advantage of this physician-rating site?
Brad Bowman, MD: I agree with everything that Dr. Lotze and Heather have said. Start with yourself—what is it that you want to be, the one thing you want to stand for? Get your own marketing, your website right, then, the point is, once you do all that and you are number 1 in SEO, you are still only going to get about 25% of the people looking for you by name to come to your website. The other 75% are going to look at all the other different sites that are out there to provide information to consumers. So the question becomes what do you do with all these other third-party sites? Healthgrades is the most comprehensive and has the highest traffic of the third-party “find a doctor” sites. In 2020, half of all Americans who go to a doctor will use Healthgrades at some point to help select and connect with that doctor.
Physicians have their focus on the quality of the care they provide. Patients, however, focus on the quality of the entire health care experience. Did I get better? How long did I have to wait? Was the office staff helpful? Scarily enough, we still spend more time shopping for a refrigerator or mattress than we do shopping for a doctor. We still tend to think that all doctors are the same. It is the reality of how we have been trained by our insurance companies and by the health care system. That is why getting your marketing right and getting what is it that you want to be known for out there is important, so that you can get the types of patients you want.
Listings management is very important. Make sure that you are findable everywhere. There are services that will do this: Doctor.com, Reputation.com, and many others. They can help you make sure you get all your basic materials right: addresses, phone numbers, your picture. Because 75% of people are going to end up on third-party websites, if your phone number is wrong there, you could lose that patient.
Then the second piece of working with third-party sites is reputation management. Physician reviews are not a bad thing, they are the new word of mouth, as Heather pointed out. Most (80%) of the reviews are going to be positive. The others will be negative, and that is okay. It is important that you get at least 1 or 2 reviews on all the different sites. We know from Healthgrades.com that going from zero reviews to 1 review will increase your call volume by 60%. If you have the choice between 2 physicians and one practice looks like people have been there before, you will go to that one.
You can learn from reviews as well, consumers provide valid feedback. Best practice is to respond to every positive and negative review. Thank them, indicate that you have listened to them, and address any concerns as necessary.
Continue to: Dr. Lotze...
Dr. Lotze: As an example, one of the paramount things that Heather introduced me to was the third party I use to run my website. That company sends a HIPAA-compliant review out to each patient we have seen that day and gives them the opportunity to rate our services and leave comments. If a patient brings up a concern, we can respond immediately, which is important. Patients appreciate feeling that they have been heard. Typically, communicating with a patient will turn the 3-star review into a 5-star as she follows up with the practice.
Ms. Schueppert: Timeliness is important. And just to mention, there certainly is a time commitment to this (and it is a marathon versus a sprint) and there is some financial investment to get it going, but it could truly be detrimental to a practice if you decide not to do anything at all.
Dr. Bowman: Agencies can really help with the time commitment.
Handling bad reviews
Dr. Culligan: What about that person who seems to have it out for you, perhaps giving you multiple bad reviews?
Dr. Bowman: I have seen this before. At Healthgrades, we recently analyzed 8.4 million patient reviews to see what people wrote about.2 The first thing they will talk about is quality of care as they see it. Did I get better or not? You can’t “fix” every patient; there will be some that you cannot help. The next thing patients comment on is bedside manner. With negative reviews, you will see more comments about the office staff.2
A single negative review actually helps make the positive ones look more credible. But if you do believe someone is trolling you, we can flag it and will investigate to the best of our ability. (Different sites likely have different editorial policies.) For example, we look at the IP addresses of all reviews, and if multiple reviews are coming from the same location, we would only let one through, overwriting the previous review from that address.
Patients just want to be heard. We have seen people change their views, based on how their review is handled and responded to.
Dr. Lotze: Is there a response by the physician that you think tends to work better in terms of resolving the issue that can minimize a perceived caustic reaction to a patient’s criticism?
Dr. Bowman: First, just like with any stressful situation, take a deep breath and respond when you feel like you can be constructive. When you do respond, be gracious. Thank them for their feedback. Make sure you reference something about their concern: “I understand that you had to wait longer than you would have liked.” Acknowledge the problem they reference, and then just apologize: “I’m sorry we didn’t meet your expectations.” Then, if they waited too long for example, “We have a new system where no one should have to wait more than 30 minutes….” You can respond privately or publically. Generally, public responses are better as it shows other consumers that you are willing to listen and consider their point of view.
Continue to: The next phase at Healthgrades...
The next phase at Healthgrades
Dr. Culligan: Do you see changes to the way physician-rating sites are working now? Are we going to stay status quo over the next 10 years, or do you see frontiers in how your site is going to develop?
Dr. Bowman: For Healthgrades, we rely on quantitative and objective measures, not just the qualitative. We are investing heavily right now in trying to help consumers understand what are the relative volumes of different procedures or different patient types that each individual doctor sees. Orthopedics is an easy example—if you have a knee problem, you want to go to someone who specializes in knees. Our job is to help consumers easily identify, “This is a shoulder doctor, this is a knee doctor, and this is why that matters.”
In the meantime, as a physician, you can always go into our site and state your care philosophy, identifying what is the sort of patient that you like to treat. Transparency is good for everyone, and especially physicians. It helps the right patient show up for you, and it helps you do a better job providing referrals.
Social media: Avoid pitfalls, and use it to your benefit
Dr. Lotze: Branding was one of the things that I was confused about, and Heather really helped me out. As physicians, we put ourselves out there on our websites, which we try to make professional sources of information for patients. But patients often want to see what else they can find out about us, including Healthgrades and social media. I think the thing that is important to know with social media is that it is a place where people learn about you as a person. Your social media should be another avenue of promotion. Whether it is your personal or professional Facebook page, people are going to see those sites. You have an opportunity to promote yourself as a good physician and a good person with a wholesome practice that you want people to come to. If a physician is posting questionable things about themselves on any kind of social media, it could be perceived as inappropriate by the patient. That can impact how patients think of you as a person, and how they are going to grade you. If people lose sight of who you are due to a questionable social media posting, everything else (SEO, the website) can be for naught.
Dr. Culligan: What are the most important social media tools to invest your time in?
Ms. Schueppert: Before anybody jumps into social media, I firmly recommend that you make sure your local search and your Google 3-pack is set up—which is basically a method Google uses to display the top 3 results on its listings page. Then make sure you have a review management system in place. Make sure you have that updated website. Those are the foundational elements. Once you have that going, social media is the next added layer to that digital presence.
I usually recommend LinkedIn. It is huge because you are staying in contact with your colleagues, that business-to-business type of connection. It remains a way for physicians to set themselves up as experts in their level of specialty.
From there, it’s either Instagram or Facebook. If you are serving more of the younger generations, the millennials and younger, then Instagram is the way to go. If you are focusing on your 40+, 50+, they are going to be far more on Facebook.
Continue to: Dr. Lotze...
Dr. Lotze: For me, a Facebook page was a great place to start. The cost of those Google ads—the first things we see at the top of a Google search in their own separate box—is significant. If a practice has that kind of money to invest, great; it is an instant way to be first on the page during a search. But there are more cost-effective ways of doing that, especially as you are getting your name out. Facebook provides, at a smaller cost, promotion of whatever it is that you are seeking to promote. You can find people within a certain zip code, for instance, and use a Facebook ad campaign that can drive people to your Facebook page—which should have both routinely updated new posts and a link to your website. The posts should be interesting topics relevant to the patients you wish to treat (avoiding personal stories or controversial discussions). You can put a post together, or you can have a third-party service do this. People who follow your page will get reminders of you and your practice with each new post. As your page followers increase, your Facebook rank will improve, and your page will more likely be discovered by Facebook searches for your services. With an added link to your office practice website, those patients go straight to your site without getting lost in the noise of Google search results.
For Instagram, a short video or an interesting picture, along with a brief statement, are the essentials. You can add a single link. Marketing here is by direct messaging or having patients going to your website through a link. Instagram, like Facebook, offers analytics to help show you what your audience likes to read about, improving the quality of your posts and increasing number of followers.
YouTube is the number 2 search engine behind Google. A Google search for your field of medicine may be filled with pages of competitors. However, YouTube has a much lower volume of competing practices, making it easier for patients to find you. The only downside to YouTube is that it will list your video along with other competing videos, which can draw attention away from your practice.
If you want to promote your website or practice with video, using a company such as Vimeo is a better choice compared with YouTube, as YouTube gets credit for video views—which improves YouTube’s SEO and not your own website. Vimeo allows for your website to get credit each time the video is watched. Regardless of where you place your videos, make them short and to the point, with links to your website. Videos only need to be long enough to get your message across and stimulate interest in your practice.
If you can have a blog on your website, it also will help with SEO. What a search engine like Google wants to see is that a patient is on your web page and looking at something for at least 60 seconds. If so, the website is deemed to have information that is relevant, improving your SEO ranking.
Finally, Twitter also can be used for getting messaging out and for branding. The problem with it is that many people go to Twitter to follow a Hollywood celebrity, a sports star, or are looking for mass communication. There is less interest on Twitter for physician outreach.
Continue to: Measuring ROI...
Measuring ROI
Dr. Culligan: What’s the best way to track your return on investment?
Dr. Lotze: First for me was to find out what didn’t work in the office and fix that before really promoting my practice. It’s about the global experience for a patient, as Brad mentioned. As a marketing expert, Heather met with me to understand my goals. She then called my office as a patient to set up an appointment and went through that entire office experience. We identified issues needing improvement.
The next step was to develop a working relationship with my webmaster—someone who can help manage Internet image and SEO. Together, you will develop goals for what the SEO should promote specific to your practice. Once a good SEO program is in place, your website’s ranking will go up—although it can take a minimum of 6 months to see a significant increase. To help understand your website’s performance, your webmaster should provide you with reports on your site’s analytics.
As you go through this process, it is great to have a marketing expert to be the point person. You will work closely together for a while, but eventually you can back off over time. The time and expense you invest on the front end have huge rewards on the back end. Currently, I still spend a reasonable amount of money every month. I have a high self-referral base because of these efforts, however, which results in more patient surgeries and easily covers my expenses. It is money well invested. My website traffic increased by 268% over 2 years (FIGURE). I’ll propose that currently more than half of my patients are self-referrals due to online marketing.
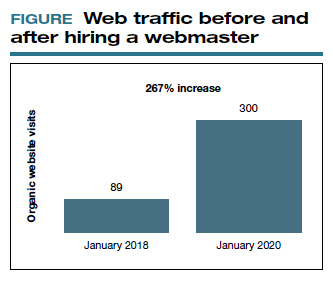
Ms. Schueppert: The only thing I would add is training your front staff. They are checking people in, taking appointments, checking your patients out. Have them be mindful that there are campaigns going on, whether it is a social media push, or a new video that went on the website. They can ask, “How did you hear about us?” when a new patient calls.
Dr. Bowman: Unless you are a large university hospital, where the analytics get significantly more advanced in terms of measuring return on investment (ROI), I think you should just be looking at your schedule and looking at your monthly billings and seeing how they change over time. You can calculate how much a new patient is worth because you can figure out how many patients you have and how much you bill and what your profits are.
Dr. Culligan: For those of us who are hospital employees, you can try to convince the hospital that you can do a detailed ROI analysis, or you can just look at it like (say it’s $3,000 per month), how many surgeries does this project have to generate before the hospital makes that back? The answer is a fraction of 1 case.
Thank you to all of you for your expertise on this roundtable.
- Anderson A. Online reviews vs. word of mouth: Which one is more important. https://www.revlocal.com/blog/reviewandreputationmanagement/onlinereviewsvswordofmouthwhichoneismoreimportant. Accessed July 17, 2020.
- 2020 Patient sentiment report. Healthgrades; Medical Group Management Association. https://www.healthgrades.com/content /patientsentimentreport. Accessed July 17, 2020
- Anderson A. Online reviews vs. word of mouth: Which one is more important. https://www.revlocal.com/blog/reviewandreputationmanagement/onlinereviewsvswordofmouthwhichoneismoreimportant. Accessed July 17, 2020.
- 2020 Patient sentiment report. Healthgrades; Medical Group Management Association. https://www.healthgrades.com/content /patientsentimentreport. Accessed July 17, 2020