User login
Online support tool improves AD self-management
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ISAD 2022
Children and COVID: Weekly cases can’t sustain downward trend
New COVID-19 cases in children inched up in late October, just 1 week after dipping to their lowest level in more than a year, and some measures of pediatric emergency visits and hospital admissions rose as well.
There was an 8% increase in the number of cases for the week of Oct. 21-27, compared with the previous week, but this week’s total was still below 25,000, and the overall trend since the beginning of September is still one of decline, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.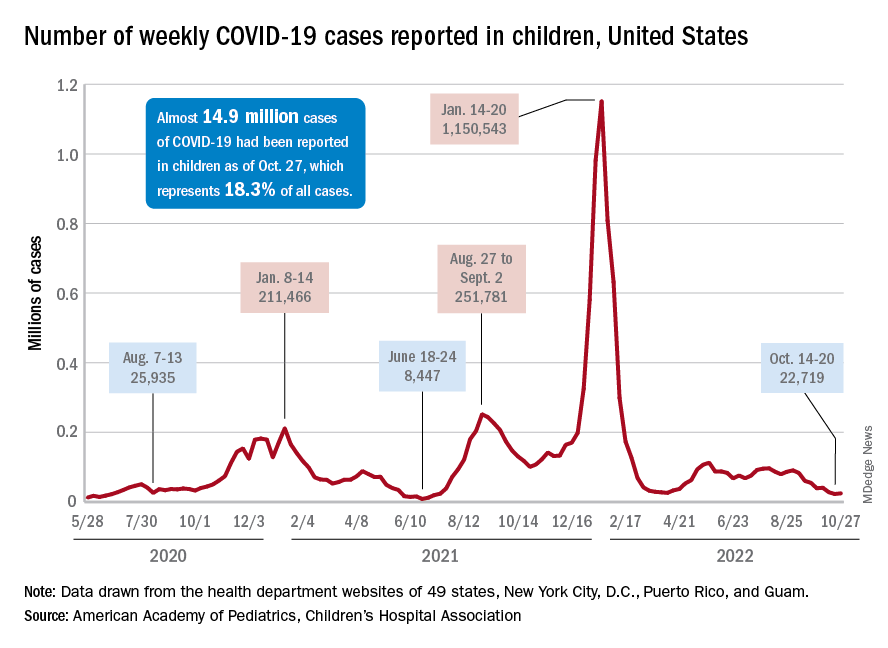
A similar increase can be seen for hospitalizations with confirmed COVID. The rate for children aged 0-17 years fell from 0.44 admissions per 100,000 population at the end of August to 0.16 per 100,000 on Oct. 23. Hospitalizations have since ticked up to 0.17 per 100,000, according to the Centers for Disease Control and Prevention.
Emergency department visits with diagnosed COVID among children aged 16-17 years, as a percentage of all ED visits, rose from 0.6% on Oct. 21 to 0.8% on Oct. 26. ED visits for 12- to 15-year-olds rose from 0.6% to 0.7% at about the same time, with both increases coming after declines that started in late August. No such increase has occurred yet among children aged 0-11 years, the CDC reported on its COVID Data Tracker.
One small milestone reached in the past week involved the proportion of all COVID cases that have occurred in children. The total number of child cases as of Oct. 27 was almost 14.9 million, which represents 18.3% of cases in all Americans, according to the AAP and CHA. That figure had been sitting at 18.4% since mid-August after reaching as high as 19.0% during the spring.
The CDC puts total COVID-related hospital admissions for children aged 0-17 at 163,588 since Aug. 1, 2020, which is 3.0% of all U.S. admissions. Total pediatric deaths number 1,843, or just about 0.2% of all COVID-related fatalities since the start of the pandemic, the CDC data show.
The latest vaccination figures show that 71.3% of children aged 12-17 years have received at least one dose, as have 38.8% of 5- to 11-year-olds, 8.4% of 2- to 4-year-olds, and 5.5% of those under age 2. Full vaccination by age group looks like this: 60.9% (12-17 years), 31.7% (5-11 years), 3.7% (2-4 years), and 2.1% (<2 years), the CDC reported. Almost 30% of children aged 12-17 have gotten a first booster dose, as have 16% of 5- to 11-year-olds.
New COVID-19 cases in children inched up in late October, just 1 week after dipping to their lowest level in more than a year, and some measures of pediatric emergency visits and hospital admissions rose as well.
There was an 8% increase in the number of cases for the week of Oct. 21-27, compared with the previous week, but this week’s total was still below 25,000, and the overall trend since the beginning of September is still one of decline, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.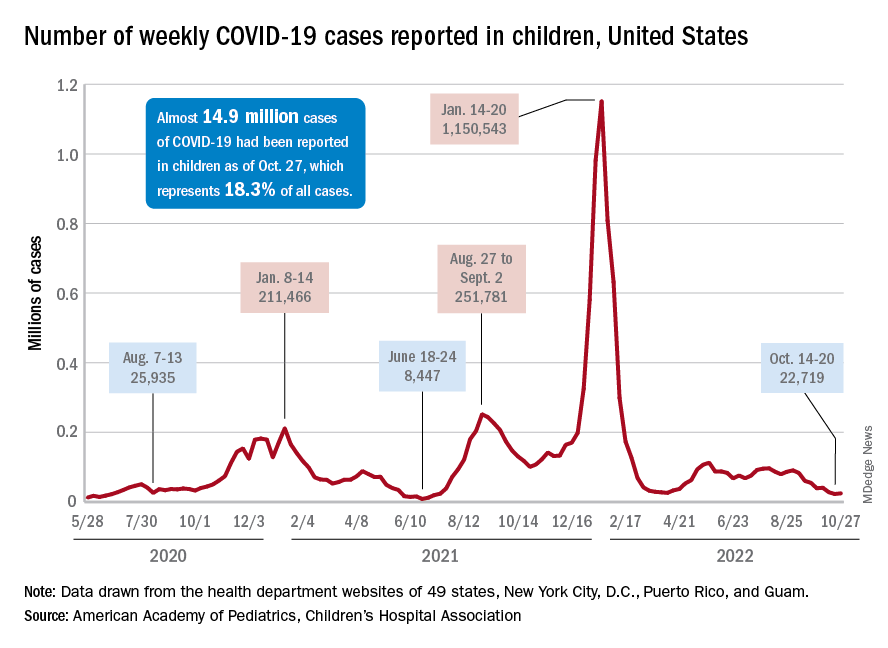
A similar increase can be seen for hospitalizations with confirmed COVID. The rate for children aged 0-17 years fell from 0.44 admissions per 100,000 population at the end of August to 0.16 per 100,000 on Oct. 23. Hospitalizations have since ticked up to 0.17 per 100,000, according to the Centers for Disease Control and Prevention.
Emergency department visits with diagnosed COVID among children aged 16-17 years, as a percentage of all ED visits, rose from 0.6% on Oct. 21 to 0.8% on Oct. 26. ED visits for 12- to 15-year-olds rose from 0.6% to 0.7% at about the same time, with both increases coming after declines that started in late August. No such increase has occurred yet among children aged 0-11 years, the CDC reported on its COVID Data Tracker.
One small milestone reached in the past week involved the proportion of all COVID cases that have occurred in children. The total number of child cases as of Oct. 27 was almost 14.9 million, which represents 18.3% of cases in all Americans, according to the AAP and CHA. That figure had been sitting at 18.4% since mid-August after reaching as high as 19.0% during the spring.
The CDC puts total COVID-related hospital admissions for children aged 0-17 at 163,588 since Aug. 1, 2020, which is 3.0% of all U.S. admissions. Total pediatric deaths number 1,843, or just about 0.2% of all COVID-related fatalities since the start of the pandemic, the CDC data show.
The latest vaccination figures show that 71.3% of children aged 12-17 years have received at least one dose, as have 38.8% of 5- to 11-year-olds, 8.4% of 2- to 4-year-olds, and 5.5% of those under age 2. Full vaccination by age group looks like this: 60.9% (12-17 years), 31.7% (5-11 years), 3.7% (2-4 years), and 2.1% (<2 years), the CDC reported. Almost 30% of children aged 12-17 have gotten a first booster dose, as have 16% of 5- to 11-year-olds.
New COVID-19 cases in children inched up in late October, just 1 week after dipping to their lowest level in more than a year, and some measures of pediatric emergency visits and hospital admissions rose as well.
There was an 8% increase in the number of cases for the week of Oct. 21-27, compared with the previous week, but this week’s total was still below 25,000, and the overall trend since the beginning of September is still one of decline, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.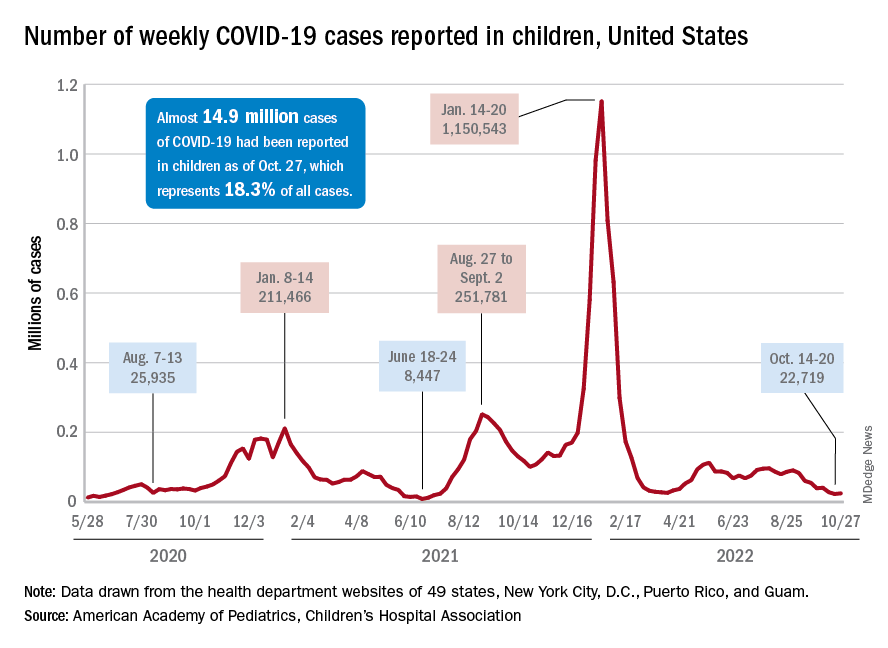
A similar increase can be seen for hospitalizations with confirmed COVID. The rate for children aged 0-17 years fell from 0.44 admissions per 100,000 population at the end of August to 0.16 per 100,000 on Oct. 23. Hospitalizations have since ticked up to 0.17 per 100,000, according to the Centers for Disease Control and Prevention.
Emergency department visits with diagnosed COVID among children aged 16-17 years, as a percentage of all ED visits, rose from 0.6% on Oct. 21 to 0.8% on Oct. 26. ED visits for 12- to 15-year-olds rose from 0.6% to 0.7% at about the same time, with both increases coming after declines that started in late August. No such increase has occurred yet among children aged 0-11 years, the CDC reported on its COVID Data Tracker.
One small milestone reached in the past week involved the proportion of all COVID cases that have occurred in children. The total number of child cases as of Oct. 27 was almost 14.9 million, which represents 18.3% of cases in all Americans, according to the AAP and CHA. That figure had been sitting at 18.4% since mid-August after reaching as high as 19.0% during the spring.
The CDC puts total COVID-related hospital admissions for children aged 0-17 at 163,588 since Aug. 1, 2020, which is 3.0% of all U.S. admissions. Total pediatric deaths number 1,843, or just about 0.2% of all COVID-related fatalities since the start of the pandemic, the CDC data show.
The latest vaccination figures show that 71.3% of children aged 12-17 years have received at least one dose, as have 38.8% of 5- to 11-year-olds, 8.4% of 2- to 4-year-olds, and 5.5% of those under age 2. Full vaccination by age group looks like this: 60.9% (12-17 years), 31.7% (5-11 years), 3.7% (2-4 years), and 2.1% (<2 years), the CDC reported. Almost 30% of children aged 12-17 have gotten a first booster dose, as have 16% of 5- to 11-year-olds.
Scientists identify new genetic links to dyslexia
Dyslexia occurs in 5%-17% of the general population, depending on the diagnostic criteria, and has been linked with speech and language disorders, as well as ADHD, Catherine Doust, PhD, of the University of Edinburgh and colleagues wrote.
However, previous studies of the genetics of dyslexia are limited, corresponding author Michelle Luciano, PhD, said in an interview. “So much progress has been made in understanding the genetics of behavior and health, but only a small genomewide study of dyslexia existed before ours.”
Currently, genetic testing for dyslexia alone is not done.
“You couldn’t order a genetic test for dyslexia unless it were part of another genetic panel,” according to Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y.
There are also known associations with some genes and autism, but none are definitive, and testing requires a workup of which a genetic panel may be a part. Such tests are expensive, and rarely covered by insurance, the pediatrician explained.
Experts recommend genetic screening for every child with developmental delay, but most insurance won’t cover it, Dr. Lessin continued.
In the new genomewide association study published in Nature Genetics, the researchers reviewed data from 51,800 adults aged 18 years and older with a self-reported dyslexia diagnosis and 1,087,070 controls. All study participants are enrolled in ongoing research with 23andMe, the personal genetics company.
The researchers investigated the genetic correlations with reading and related skills and evaluated evidence for genes previously associated with dyslexia. The mean ages of the dyslexia cases and controls were 49.6 years and 51.7 years, respectively.
The researchers identified 42 independent genetic variants (genomewide significant loci) associated with dyslexia; 15 of these loci were in genes previously associated with cognitive ability and educational attainment, and 27 were newly identified as specifically associated with dyslexia. The researchers further determined that 12 of the newly identified genes were associated with proficiency in reading and spelling in English and European languages, and 1 in a Chinese-language population.
A polygenic risk score is a way to characterize an individual’s risk of developing a disease, based on the total number of genetic changes related to the disease; the researchers used this score to validate their results. Dyslexia polygenic scores were used to predict reading and spelling in additional population-based and reading disorder–enriched samples outside of the study population; these genetic measures explained up to 6% of variance in reading traits, the researchers noted. Ultimately, these scores may be a tool to help identify children with a predisposition for dyslexia so reading skills support can begin early.
The researchers also found that many of the genes associated with dyslexia are also associated with ADHD, (24% of dyslexia patients reporting ADHD vs. 9% of controls), and with a moderate correlation, which suggests possible shared genetic components for deficits in working memory and attention.
The study findings were limited by the inability to prove causality, and by the potential bias in the study sample, but were strengthened by the large study population, the researchers noted.
Potential implications for reading and spelling
“We were surprised that none of the previous dyslexia candidate genes were genomewide significant in our study; all of our discoveries were in new genes that had not been previously implicated in dyslexia,” Dr. Luciano said in an interview. “Some of these genes have been found to be associated with general cognitive ability, but most were novel and may represent genes specifically related to cognitive processes dominant in reading and spelling.
“We were also surprised that there was little genetic correlation (or overlap) with brain MRI variables, given that brain regions have been linked to reading skill. This suggests that the link is environmental in origin,” she added.
“Our results do not directly feed into clinical practice,” said Dr. Luciano. However, “the moderate genetic overlap with ADHD suggests that broader assessments of behavior are important when a child presents with dyslexia, as co-occurrence with other conditions might influence the intervention chosen. Asking about family history of dyslexia might also help in identification.
With more research, genetic studies may find a place in the clinical setting, said Dr. Luciano.
“As genomewide association studies become larger and the findings more stable, genetic information might be used as an adjunct to what is known about the child’s environment and their performance on standardized tests of reading. The key advantage of genetic information is that it could allow much earlier identification of children who would benefit from extra learning support,” she said.
More research is needed to understand the interaction between genes and the environment, Dr. Luciano said. “It is essential that we understand what environmental learning support can minimize genetic predisposition to dyslexia.”
Too soon for clinical utility
The study findings are an important foundation for additional research, but not yet clinically useful, Dr. Lessin said in an interview.
“Dyslexia is a tough diagnosis,” that requires assessment by a developmental pediatrician or a pediatric neurologist and these specialists are often not accessible to many parents, Dr. Lessin noted.
In the current study, the researchers found a number of genes potentially associated with dyslexia, but the study does not prove causality, he emphasized. The findings simply mean that some of these genes may have something to do with dyslexia, and further research might identify a genetic cause.
“No one is going to make a diagnosis of dyslexia based on genes just yet,” said Dr. Lessin. In the meantime, clinicians should be aware that good research is being conducted, and that the genetic foundations for dyslexia are being explored.
Lead author Dr. Doust and corresponding author Dr. Luciano had no financial conflicts to disclose. Several coauthors disclosed support from the Max Planck Society (Germany), the National Natural Science Foundation of China, Funds for Humanities and Social Sciences Research of the Ministry of Education, and General Project of Shaanxi Natural Science Basic Research Program. Two coauthors are employed by and hold stock or stock options in 23andMe. Dr. Lessin had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
Dyslexia occurs in 5%-17% of the general population, depending on the diagnostic criteria, and has been linked with speech and language disorders, as well as ADHD, Catherine Doust, PhD, of the University of Edinburgh and colleagues wrote.
However, previous studies of the genetics of dyslexia are limited, corresponding author Michelle Luciano, PhD, said in an interview. “So much progress has been made in understanding the genetics of behavior and health, but only a small genomewide study of dyslexia existed before ours.”
Currently, genetic testing for dyslexia alone is not done.
“You couldn’t order a genetic test for dyslexia unless it were part of another genetic panel,” according to Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y.
There are also known associations with some genes and autism, but none are definitive, and testing requires a workup of which a genetic panel may be a part. Such tests are expensive, and rarely covered by insurance, the pediatrician explained.
Experts recommend genetic screening for every child with developmental delay, but most insurance won’t cover it, Dr. Lessin continued.
In the new genomewide association study published in Nature Genetics, the researchers reviewed data from 51,800 adults aged 18 years and older with a self-reported dyslexia diagnosis and 1,087,070 controls. All study participants are enrolled in ongoing research with 23andMe, the personal genetics company.
The researchers investigated the genetic correlations with reading and related skills and evaluated evidence for genes previously associated with dyslexia. The mean ages of the dyslexia cases and controls were 49.6 years and 51.7 years, respectively.
The researchers identified 42 independent genetic variants (genomewide significant loci) associated with dyslexia; 15 of these loci were in genes previously associated with cognitive ability and educational attainment, and 27 were newly identified as specifically associated with dyslexia. The researchers further determined that 12 of the newly identified genes were associated with proficiency in reading and spelling in English and European languages, and 1 in a Chinese-language population.
A polygenic risk score is a way to characterize an individual’s risk of developing a disease, based on the total number of genetic changes related to the disease; the researchers used this score to validate their results. Dyslexia polygenic scores were used to predict reading and spelling in additional population-based and reading disorder–enriched samples outside of the study population; these genetic measures explained up to 6% of variance in reading traits, the researchers noted. Ultimately, these scores may be a tool to help identify children with a predisposition for dyslexia so reading skills support can begin early.
The researchers also found that many of the genes associated with dyslexia are also associated with ADHD, (24% of dyslexia patients reporting ADHD vs. 9% of controls), and with a moderate correlation, which suggests possible shared genetic components for deficits in working memory and attention.
The study findings were limited by the inability to prove causality, and by the potential bias in the study sample, but were strengthened by the large study population, the researchers noted.
Potential implications for reading and spelling
“We were surprised that none of the previous dyslexia candidate genes were genomewide significant in our study; all of our discoveries were in new genes that had not been previously implicated in dyslexia,” Dr. Luciano said in an interview. “Some of these genes have been found to be associated with general cognitive ability, but most were novel and may represent genes specifically related to cognitive processes dominant in reading and spelling.
“We were also surprised that there was little genetic correlation (or overlap) with brain MRI variables, given that brain regions have been linked to reading skill. This suggests that the link is environmental in origin,” she added.
“Our results do not directly feed into clinical practice,” said Dr. Luciano. However, “the moderate genetic overlap with ADHD suggests that broader assessments of behavior are important when a child presents with dyslexia, as co-occurrence with other conditions might influence the intervention chosen. Asking about family history of dyslexia might also help in identification.
With more research, genetic studies may find a place in the clinical setting, said Dr. Luciano.
“As genomewide association studies become larger and the findings more stable, genetic information might be used as an adjunct to what is known about the child’s environment and their performance on standardized tests of reading. The key advantage of genetic information is that it could allow much earlier identification of children who would benefit from extra learning support,” she said.
More research is needed to understand the interaction between genes and the environment, Dr. Luciano said. “It is essential that we understand what environmental learning support can minimize genetic predisposition to dyslexia.”
Too soon for clinical utility
The study findings are an important foundation for additional research, but not yet clinically useful, Dr. Lessin said in an interview.
“Dyslexia is a tough diagnosis,” that requires assessment by a developmental pediatrician or a pediatric neurologist and these specialists are often not accessible to many parents, Dr. Lessin noted.
In the current study, the researchers found a number of genes potentially associated with dyslexia, but the study does not prove causality, he emphasized. The findings simply mean that some of these genes may have something to do with dyslexia, and further research might identify a genetic cause.
“No one is going to make a diagnosis of dyslexia based on genes just yet,” said Dr. Lessin. In the meantime, clinicians should be aware that good research is being conducted, and that the genetic foundations for dyslexia are being explored.
Lead author Dr. Doust and corresponding author Dr. Luciano had no financial conflicts to disclose. Several coauthors disclosed support from the Max Planck Society (Germany), the National Natural Science Foundation of China, Funds for Humanities and Social Sciences Research of the Ministry of Education, and General Project of Shaanxi Natural Science Basic Research Program. Two coauthors are employed by and hold stock or stock options in 23andMe. Dr. Lessin had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
Dyslexia occurs in 5%-17% of the general population, depending on the diagnostic criteria, and has been linked with speech and language disorders, as well as ADHD, Catherine Doust, PhD, of the University of Edinburgh and colleagues wrote.
However, previous studies of the genetics of dyslexia are limited, corresponding author Michelle Luciano, PhD, said in an interview. “So much progress has been made in understanding the genetics of behavior and health, but only a small genomewide study of dyslexia existed before ours.”
Currently, genetic testing for dyslexia alone is not done.
“You couldn’t order a genetic test for dyslexia unless it were part of another genetic panel,” according to Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y.
There are also known associations with some genes and autism, but none are definitive, and testing requires a workup of which a genetic panel may be a part. Such tests are expensive, and rarely covered by insurance, the pediatrician explained.
Experts recommend genetic screening for every child with developmental delay, but most insurance won’t cover it, Dr. Lessin continued.
In the new genomewide association study published in Nature Genetics, the researchers reviewed data from 51,800 adults aged 18 years and older with a self-reported dyslexia diagnosis and 1,087,070 controls. All study participants are enrolled in ongoing research with 23andMe, the personal genetics company.
The researchers investigated the genetic correlations with reading and related skills and evaluated evidence for genes previously associated with dyslexia. The mean ages of the dyslexia cases and controls were 49.6 years and 51.7 years, respectively.
The researchers identified 42 independent genetic variants (genomewide significant loci) associated with dyslexia; 15 of these loci were in genes previously associated with cognitive ability and educational attainment, and 27 were newly identified as specifically associated with dyslexia. The researchers further determined that 12 of the newly identified genes were associated with proficiency in reading and spelling in English and European languages, and 1 in a Chinese-language population.
A polygenic risk score is a way to characterize an individual’s risk of developing a disease, based on the total number of genetic changes related to the disease; the researchers used this score to validate their results. Dyslexia polygenic scores were used to predict reading and spelling in additional population-based and reading disorder–enriched samples outside of the study population; these genetic measures explained up to 6% of variance in reading traits, the researchers noted. Ultimately, these scores may be a tool to help identify children with a predisposition for dyslexia so reading skills support can begin early.
The researchers also found that many of the genes associated with dyslexia are also associated with ADHD, (24% of dyslexia patients reporting ADHD vs. 9% of controls), and with a moderate correlation, which suggests possible shared genetic components for deficits in working memory and attention.
The study findings were limited by the inability to prove causality, and by the potential bias in the study sample, but were strengthened by the large study population, the researchers noted.
Potential implications for reading and spelling
“We were surprised that none of the previous dyslexia candidate genes were genomewide significant in our study; all of our discoveries were in new genes that had not been previously implicated in dyslexia,” Dr. Luciano said in an interview. “Some of these genes have been found to be associated with general cognitive ability, but most were novel and may represent genes specifically related to cognitive processes dominant in reading and spelling.
“We were also surprised that there was little genetic correlation (or overlap) with brain MRI variables, given that brain regions have been linked to reading skill. This suggests that the link is environmental in origin,” she added.
“Our results do not directly feed into clinical practice,” said Dr. Luciano. However, “the moderate genetic overlap with ADHD suggests that broader assessments of behavior are important when a child presents with dyslexia, as co-occurrence with other conditions might influence the intervention chosen. Asking about family history of dyslexia might also help in identification.
With more research, genetic studies may find a place in the clinical setting, said Dr. Luciano.
“As genomewide association studies become larger and the findings more stable, genetic information might be used as an adjunct to what is known about the child’s environment and their performance on standardized tests of reading. The key advantage of genetic information is that it could allow much earlier identification of children who would benefit from extra learning support,” she said.
More research is needed to understand the interaction between genes and the environment, Dr. Luciano said. “It is essential that we understand what environmental learning support can minimize genetic predisposition to dyslexia.”
Too soon for clinical utility
The study findings are an important foundation for additional research, but not yet clinically useful, Dr. Lessin said in an interview.
“Dyslexia is a tough diagnosis,” that requires assessment by a developmental pediatrician or a pediatric neurologist and these specialists are often not accessible to many parents, Dr. Lessin noted.
In the current study, the researchers found a number of genes potentially associated with dyslexia, but the study does not prove causality, he emphasized. The findings simply mean that some of these genes may have something to do with dyslexia, and further research might identify a genetic cause.
“No one is going to make a diagnosis of dyslexia based on genes just yet,” said Dr. Lessin. In the meantime, clinicians should be aware that good research is being conducted, and that the genetic foundations for dyslexia are being explored.
Lead author Dr. Doust and corresponding author Dr. Luciano had no financial conflicts to disclose. Several coauthors disclosed support from the Max Planck Society (Germany), the National Natural Science Foundation of China, Funds for Humanities and Social Sciences Research of the Ministry of Education, and General Project of Shaanxi Natural Science Basic Research Program. Two coauthors are employed by and hold stock or stock options in 23andMe. Dr. Lessin had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
FROM NATURE GENETICS
Itchy Red-Brown Spots on a Child
The Diagnosis: Maculopapular Cutaneous Mastocytosis (Urticaria Pigmentosa)
A stroke test revealed urtication at the exact traumatized site (Figure). A skin biopsy performed 2 years prior by another physician in the same hospital had revealed mast cell infiltration of virtually the entire dermis. The diagnosis was then firmly established as maculopapular cutaneous mastocytosis (CM)(also known as urticaria pigmentosa) with both the pathology results and a confirmative stroke test, and no additional biopsy was attempted. Serum IgE and tryptase levels were within the reference range. General recommendations about the avoidance of trigger factors were given to the family, and a new-generation H1 blocker antihistaminic syrup was prescribed for flushing, itching, and urtication.

Mastocytosis is a canopy term for a heterogeneous group of disorders caused by clonal proliferation and accumulation of abnormal mast cells within the skin and visceral organs (ie, bone marrow, liver, spleen, lymph nodes, gastrointestinal tract). Cutaneous mastocytosis, the skin-restricted variant, is by far the most common form of childhood mastocytosis (90% of mastocytosis cases in children)1 and generally appears within the first 2 years of life.1-7 Pediatric CM usually is a benign and transient disease with an excellent prognosis and a negligible risk for systemic involvement.2,3,5
The pathogenesis of CM in children is obscure1; however, somatic or germline gain-of-function mutations of the c-KIT proto-oncogene, which encodes KIT (ie, a tyrosine kinase membrane receptor for stem cell factor), may account for most pediatric CM phenotypes.1,3,6 Activating c-KIT mutations leads to constitutive activation of the KIT receptor (expressed on the surface membrane of mast cells) and instigates autonomous (stem cell factor– independent) clonal proliferation, enhanced survival, and accumulation of mast cells.2
Maculopapular CM is the most common clinical form of CM.2,4,5 In children, maculopapular CM usually presents with polymorphous red-brown lesions of varying sizes and types—macule, papule, plaque, or nodule—on the torso and extremities.1-5 The distribution may be widespread and rarely is almost universal, as in our patient.2 Darier sign typically is positive, with a wheal and flare developing upon stroking or rubbing 1 or several lesions.1-6 The lesions gradually involute and often spontaneously regress at the time of puberty.1-3,5-7
The clinical signs and symptoms of mastocytosis are not only related to mast cell infiltration but also to mast cell activation within the tissues. The release of intracellular mediators from activated mast cells may have local and/or systemic consequences.4,7 Erythema, edema, flushing, pruritus, urticaria, blistering, and dermatographism are among the local cutaneous symptoms of mast cell activation.2-4,7 Systemic symptoms are rare in childhood CM and consist of wheezing, shortness of breath, nausea, vomiting, reflux, abdominal cramping, diarrhea, tachycardia, hypotension, syncope, anaphylaxis, and cyanotic spells.1-7 An elevated serum tryptase level is an indicator of both mast cell burden and risk for mast cell activation in the skin.4,7
Treatment of pediatric CM is conservative and symptomatic.3 Prevention of mediator release may be accomplished through avoidance of trigger factors.1 Alleviation of mediator-related symptoms might be attained using H1 and H2 histamine receptor blockers, oral cromolyn sodium, leukotriene antagonists, and epinephrine autoinjectors.1-3,5 Short-term topical or oral corticosteroids; calcineurin inhibitors (eg, pimecrolimus, tacrolimus); phototherapy; psoralen plus UVA; omalizumab; and innovative agents such as topical miltefosine, nemolizumab (an IL-31 antagonist), kinase inhibitors such as midostaurin, and tyrosine kinase inhibitors such as imatinib and masitinib may be tried in refractory or extensive pediatric CM.1,2,5,6
Although several disorders in childhood may present with red-brown macules and papules, Darier sign is unique to cutaneous mastocytosis. A biopsy also will be helpful in establishing the definitive diagnosis.
Histiocytosis X (also referred to as Langerhans cell histiocytosis) is the most common proliferative histiocytic disorder. Cutaneous lesions are polymorphic and consist of seborrheic involvement of the scalp with yellow, scaly or crusted papules; eroded patches; pustules; vesicles; petechiae; purpura; or red to purplish papules on the groin, abdomen, back, or chest.8
LEOPARD syndrome (also known as Noonan syndrome with multiple lentigines) is an acronym denoting lentigines (multiple), electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of the genitalia, retarded growth, and deafness (sensorineural). The disorder is caused by a genetic mutation involving the PTPN11 gene and currently is categorized under the canopy of RASopathies. Cutaneous findings consist of lentiginous and café-au-lait macules and patches.9
Neurofibromatosis is a genetic disorder with a plethora of cutaneous and systemic manifestations. The type 1 variant that constitutes more than 95% of cases is caused by mutations in the neurofibromin gene. The main cutaneous findings include café-au-lait macules, freckling in axillary and inguinal locations (Crowe sign), and neurofibromas. These lesions may present as macules, patches, papules, or nodules.10
Xanthoma disseminatum is a rare sporadic proliferative histiocyte disorder involving the skin and mucosa. The disorder may be a harbinger of diabetes insipidus. Cutaneous lesions consist of asymptomatic, symmetrical, discrete, erythematous to yellow-brown papules and nodules.11
- Sandru F, Petca RC, Costescu M, et al. Cutaneous mastocytosis in childhood: update from the literature. J Clin Med. 2021;10:1474. doi:10.3390/jcm10071474
- Lange M, Hartmann K, Carter MC, et al. Molecular background, clinical features and management of pediatric mastocytosis: status 2021. Int J Mol Sci. 2021;22:2586. doi:10.3390/ijms22052586
- Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12:259-270. doi:10.2165/11588890-000000000-00000
- Nedoszytko B, Arock M, Lyons JJ, et al. Clinical impact of inherited and acquired genetic variants in mastocytosis. Int J Mol Sci. 2021;22:411. doi:10.3390/ijms22010411
- Nemat K, Abraham S. Cutaneous mastocytosis in childhood. Allergol Select. 2022;6:1-10. doi:10.5414/ALX02304E
- Giona F. Pediatric mastocytosis: an update. Mediterr J Hematol Infect Dis. 2021;13:E2021069. doi:10.4084/MJHID.2021.069
- Brockow K, Plata-Nazar K, Lange M, et al. Mediator-related symptoms and anaphylaxis in children with mastocytosis. Int J Mol Sci. 2021;22:2684. doi:10.3390/ijms22052684
- Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21: 328-334.
- García-Gil MF, Álvarez-Salafranca M, Valero-Torres A, et al. Melanoma in Noonan syndrome with multiple lentigines (LEOPARD syndrome): a new case. Actas Dermosifiliogr (Engl Ed). 2020;111:619-621.
- Ozarslan B, Russo T, Argenziano G, et al. Cutaneous findings in neurofibromatosis type 1. Cancers (Basel). 2021;13:463.
- Behra A, Sa DK, Naik R, et al. A rare case of persistent xanthoma disseminatum without any systemic involvement. Indian J Dermatol. 2020;65:239-241.
The Diagnosis: Maculopapular Cutaneous Mastocytosis (Urticaria Pigmentosa)
A stroke test revealed urtication at the exact traumatized site (Figure). A skin biopsy performed 2 years prior by another physician in the same hospital had revealed mast cell infiltration of virtually the entire dermis. The diagnosis was then firmly established as maculopapular cutaneous mastocytosis (CM)(also known as urticaria pigmentosa) with both the pathology results and a confirmative stroke test, and no additional biopsy was attempted. Serum IgE and tryptase levels were within the reference range. General recommendations about the avoidance of trigger factors were given to the family, and a new-generation H1 blocker antihistaminic syrup was prescribed for flushing, itching, and urtication.

Mastocytosis is a canopy term for a heterogeneous group of disorders caused by clonal proliferation and accumulation of abnormal mast cells within the skin and visceral organs (ie, bone marrow, liver, spleen, lymph nodes, gastrointestinal tract). Cutaneous mastocytosis, the skin-restricted variant, is by far the most common form of childhood mastocytosis (90% of mastocytosis cases in children)1 and generally appears within the first 2 years of life.1-7 Pediatric CM usually is a benign and transient disease with an excellent prognosis and a negligible risk for systemic involvement.2,3,5
The pathogenesis of CM in children is obscure1; however, somatic or germline gain-of-function mutations of the c-KIT proto-oncogene, which encodes KIT (ie, a tyrosine kinase membrane receptor for stem cell factor), may account for most pediatric CM phenotypes.1,3,6 Activating c-KIT mutations leads to constitutive activation of the KIT receptor (expressed on the surface membrane of mast cells) and instigates autonomous (stem cell factor– independent) clonal proliferation, enhanced survival, and accumulation of mast cells.2
Maculopapular CM is the most common clinical form of CM.2,4,5 In children, maculopapular CM usually presents with polymorphous red-brown lesions of varying sizes and types—macule, papule, plaque, or nodule—on the torso and extremities.1-5 The distribution may be widespread and rarely is almost universal, as in our patient.2 Darier sign typically is positive, with a wheal and flare developing upon stroking or rubbing 1 or several lesions.1-6 The lesions gradually involute and often spontaneously regress at the time of puberty.1-3,5-7
The clinical signs and symptoms of mastocytosis are not only related to mast cell infiltration but also to mast cell activation within the tissues. The release of intracellular mediators from activated mast cells may have local and/or systemic consequences.4,7 Erythema, edema, flushing, pruritus, urticaria, blistering, and dermatographism are among the local cutaneous symptoms of mast cell activation.2-4,7 Systemic symptoms are rare in childhood CM and consist of wheezing, shortness of breath, nausea, vomiting, reflux, abdominal cramping, diarrhea, tachycardia, hypotension, syncope, anaphylaxis, and cyanotic spells.1-7 An elevated serum tryptase level is an indicator of both mast cell burden and risk for mast cell activation in the skin.4,7
Treatment of pediatric CM is conservative and symptomatic.3 Prevention of mediator release may be accomplished through avoidance of trigger factors.1 Alleviation of mediator-related symptoms might be attained using H1 and H2 histamine receptor blockers, oral cromolyn sodium, leukotriene antagonists, and epinephrine autoinjectors.1-3,5 Short-term topical or oral corticosteroids; calcineurin inhibitors (eg, pimecrolimus, tacrolimus); phototherapy; psoralen plus UVA; omalizumab; and innovative agents such as topical miltefosine, nemolizumab (an IL-31 antagonist), kinase inhibitors such as midostaurin, and tyrosine kinase inhibitors such as imatinib and masitinib may be tried in refractory or extensive pediatric CM.1,2,5,6
Although several disorders in childhood may present with red-brown macules and papules, Darier sign is unique to cutaneous mastocytosis. A biopsy also will be helpful in establishing the definitive diagnosis.
Histiocytosis X (also referred to as Langerhans cell histiocytosis) is the most common proliferative histiocytic disorder. Cutaneous lesions are polymorphic and consist of seborrheic involvement of the scalp with yellow, scaly or crusted papules; eroded patches; pustules; vesicles; petechiae; purpura; or red to purplish papules on the groin, abdomen, back, or chest.8
LEOPARD syndrome (also known as Noonan syndrome with multiple lentigines) is an acronym denoting lentigines (multiple), electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of the genitalia, retarded growth, and deafness (sensorineural). The disorder is caused by a genetic mutation involving the PTPN11 gene and currently is categorized under the canopy of RASopathies. Cutaneous findings consist of lentiginous and café-au-lait macules and patches.9
Neurofibromatosis is a genetic disorder with a plethora of cutaneous and systemic manifestations. The type 1 variant that constitutes more than 95% of cases is caused by mutations in the neurofibromin gene. The main cutaneous findings include café-au-lait macules, freckling in axillary and inguinal locations (Crowe sign), and neurofibromas. These lesions may present as macules, patches, papules, or nodules.10
Xanthoma disseminatum is a rare sporadic proliferative histiocyte disorder involving the skin and mucosa. The disorder may be a harbinger of diabetes insipidus. Cutaneous lesions consist of asymptomatic, symmetrical, discrete, erythematous to yellow-brown papules and nodules.11
The Diagnosis: Maculopapular Cutaneous Mastocytosis (Urticaria Pigmentosa)
A stroke test revealed urtication at the exact traumatized site (Figure). A skin biopsy performed 2 years prior by another physician in the same hospital had revealed mast cell infiltration of virtually the entire dermis. The diagnosis was then firmly established as maculopapular cutaneous mastocytosis (CM)(also known as urticaria pigmentosa) with both the pathology results and a confirmative stroke test, and no additional biopsy was attempted. Serum IgE and tryptase levels were within the reference range. General recommendations about the avoidance of trigger factors were given to the family, and a new-generation H1 blocker antihistaminic syrup was prescribed for flushing, itching, and urtication.

Mastocytosis is a canopy term for a heterogeneous group of disorders caused by clonal proliferation and accumulation of abnormal mast cells within the skin and visceral organs (ie, bone marrow, liver, spleen, lymph nodes, gastrointestinal tract). Cutaneous mastocytosis, the skin-restricted variant, is by far the most common form of childhood mastocytosis (90% of mastocytosis cases in children)1 and generally appears within the first 2 years of life.1-7 Pediatric CM usually is a benign and transient disease with an excellent prognosis and a negligible risk for systemic involvement.2,3,5
The pathogenesis of CM in children is obscure1; however, somatic or germline gain-of-function mutations of the c-KIT proto-oncogene, which encodes KIT (ie, a tyrosine kinase membrane receptor for stem cell factor), may account for most pediatric CM phenotypes.1,3,6 Activating c-KIT mutations leads to constitutive activation of the KIT receptor (expressed on the surface membrane of mast cells) and instigates autonomous (stem cell factor– independent) clonal proliferation, enhanced survival, and accumulation of mast cells.2
Maculopapular CM is the most common clinical form of CM.2,4,5 In children, maculopapular CM usually presents with polymorphous red-brown lesions of varying sizes and types—macule, papule, plaque, or nodule—on the torso and extremities.1-5 The distribution may be widespread and rarely is almost universal, as in our patient.2 Darier sign typically is positive, with a wheal and flare developing upon stroking or rubbing 1 or several lesions.1-6 The lesions gradually involute and often spontaneously regress at the time of puberty.1-3,5-7
The clinical signs and symptoms of mastocytosis are not only related to mast cell infiltration but also to mast cell activation within the tissues. The release of intracellular mediators from activated mast cells may have local and/or systemic consequences.4,7 Erythema, edema, flushing, pruritus, urticaria, blistering, and dermatographism are among the local cutaneous symptoms of mast cell activation.2-4,7 Systemic symptoms are rare in childhood CM and consist of wheezing, shortness of breath, nausea, vomiting, reflux, abdominal cramping, diarrhea, tachycardia, hypotension, syncope, anaphylaxis, and cyanotic spells.1-7 An elevated serum tryptase level is an indicator of both mast cell burden and risk for mast cell activation in the skin.4,7
Treatment of pediatric CM is conservative and symptomatic.3 Prevention of mediator release may be accomplished through avoidance of trigger factors.1 Alleviation of mediator-related symptoms might be attained using H1 and H2 histamine receptor blockers, oral cromolyn sodium, leukotriene antagonists, and epinephrine autoinjectors.1-3,5 Short-term topical or oral corticosteroids; calcineurin inhibitors (eg, pimecrolimus, tacrolimus); phototherapy; psoralen plus UVA; omalizumab; and innovative agents such as topical miltefosine, nemolizumab (an IL-31 antagonist), kinase inhibitors such as midostaurin, and tyrosine kinase inhibitors such as imatinib and masitinib may be tried in refractory or extensive pediatric CM.1,2,5,6
Although several disorders in childhood may present with red-brown macules and papules, Darier sign is unique to cutaneous mastocytosis. A biopsy also will be helpful in establishing the definitive diagnosis.
Histiocytosis X (also referred to as Langerhans cell histiocytosis) is the most common proliferative histiocytic disorder. Cutaneous lesions are polymorphic and consist of seborrheic involvement of the scalp with yellow, scaly or crusted papules; eroded patches; pustules; vesicles; petechiae; purpura; or red to purplish papules on the groin, abdomen, back, or chest.8
LEOPARD syndrome (also known as Noonan syndrome with multiple lentigines) is an acronym denoting lentigines (multiple), electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of the genitalia, retarded growth, and deafness (sensorineural). The disorder is caused by a genetic mutation involving the PTPN11 gene and currently is categorized under the canopy of RASopathies. Cutaneous findings consist of lentiginous and café-au-lait macules and patches.9
Neurofibromatosis is a genetic disorder with a plethora of cutaneous and systemic manifestations. The type 1 variant that constitutes more than 95% of cases is caused by mutations in the neurofibromin gene. The main cutaneous findings include café-au-lait macules, freckling in axillary and inguinal locations (Crowe sign), and neurofibromas. These lesions may present as macules, patches, papules, or nodules.10
Xanthoma disseminatum is a rare sporadic proliferative histiocyte disorder involving the skin and mucosa. The disorder may be a harbinger of diabetes insipidus. Cutaneous lesions consist of asymptomatic, symmetrical, discrete, erythematous to yellow-brown papules and nodules.11
- Sandru F, Petca RC, Costescu M, et al. Cutaneous mastocytosis in childhood: update from the literature. J Clin Med. 2021;10:1474. doi:10.3390/jcm10071474
- Lange M, Hartmann K, Carter MC, et al. Molecular background, clinical features and management of pediatric mastocytosis: status 2021. Int J Mol Sci. 2021;22:2586. doi:10.3390/ijms22052586
- Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12:259-270. doi:10.2165/11588890-000000000-00000
- Nedoszytko B, Arock M, Lyons JJ, et al. Clinical impact of inherited and acquired genetic variants in mastocytosis. Int J Mol Sci. 2021;22:411. doi:10.3390/ijms22010411
- Nemat K, Abraham S. Cutaneous mastocytosis in childhood. Allergol Select. 2022;6:1-10. doi:10.5414/ALX02304E
- Giona F. Pediatric mastocytosis: an update. Mediterr J Hematol Infect Dis. 2021;13:E2021069. doi:10.4084/MJHID.2021.069
- Brockow K, Plata-Nazar K, Lange M, et al. Mediator-related symptoms and anaphylaxis in children with mastocytosis. Int J Mol Sci. 2021;22:2684. doi:10.3390/ijms22052684
- Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21: 328-334.
- García-Gil MF, Álvarez-Salafranca M, Valero-Torres A, et al. Melanoma in Noonan syndrome with multiple lentigines (LEOPARD syndrome): a new case. Actas Dermosifiliogr (Engl Ed). 2020;111:619-621.
- Ozarslan B, Russo T, Argenziano G, et al. Cutaneous findings in neurofibromatosis type 1. Cancers (Basel). 2021;13:463.
- Behra A, Sa DK, Naik R, et al. A rare case of persistent xanthoma disseminatum without any systemic involvement. Indian J Dermatol. 2020;65:239-241.
- Sandru F, Petca RC, Costescu M, et al. Cutaneous mastocytosis in childhood: update from the literature. J Clin Med. 2021;10:1474. doi:10.3390/jcm10071474
- Lange M, Hartmann K, Carter MC, et al. Molecular background, clinical features and management of pediatric mastocytosis: status 2021. Int J Mol Sci. 2021;22:2586. doi:10.3390/ijms22052586
- Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12:259-270. doi:10.2165/11588890-000000000-00000
- Nedoszytko B, Arock M, Lyons JJ, et al. Clinical impact of inherited and acquired genetic variants in mastocytosis. Int J Mol Sci. 2021;22:411. doi:10.3390/ijms22010411
- Nemat K, Abraham S. Cutaneous mastocytosis in childhood. Allergol Select. 2022;6:1-10. doi:10.5414/ALX02304E
- Giona F. Pediatric mastocytosis: an update. Mediterr J Hematol Infect Dis. 2021;13:E2021069. doi:10.4084/MJHID.2021.069
- Brockow K, Plata-Nazar K, Lange M, et al. Mediator-related symptoms and anaphylaxis in children with mastocytosis. Int J Mol Sci. 2021;22:2684. doi:10.3390/ijms22052684
- Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21: 328-334.
- García-Gil MF, Álvarez-Salafranca M, Valero-Torres A, et al. Melanoma in Noonan syndrome with multiple lentigines (LEOPARD syndrome): a new case. Actas Dermosifiliogr (Engl Ed). 2020;111:619-621.
- Ozarslan B, Russo T, Argenziano G, et al. Cutaneous findings in neurofibromatosis type 1. Cancers (Basel). 2021;13:463.
- Behra A, Sa DK, Naik R, et al. A rare case of persistent xanthoma disseminatum without any systemic involvement. Indian J Dermatol. 2020;65:239-241.
A 5-year-old boy presented with red-brown spots diffusely spread over the body that were present since birth. There were no subjective symptoms, except for rare instances of flushing, itching, and urtication following hot baths and abrasive scrubs. Dermatologic examination revealed widespread brown polymorphic macules and papules of varying sizes on the forehead, neck, torso, and extremities. Physical examination was otherwise normal.

Incorporating positive psychiatry with children and adolescents
The principles and practices of positive psychiatry are especially well-suited for work with children, adolescents, and families. Positive psychiatry is “the science and practice of psychiatry that seeks to understand and promote well-being through assessments and interventions aimed at enhancing positive psychosocial factors among people who have or are at risk for developing mental or physical illnesses.”1 The concept sprung from the momentum of positive psychology, which originated from Seligman et al.2 Importantly, the standards and techniques of positive psychiatry are designed as an enhancement, perhaps even as a completion, of more traditional psychiatry, rather than an alternative.3 They come from an acknowledgment that to be most effective as a mental health professional, it is important for clinicians to be experts in the full range of mental functioning.4,5
For most clinicians currently practicing “traditional” child and adolescent psychiatry, adapting at least some of the principles of positive psychiatry within one’s routine practice will not necessarily involve a radical transformation of thought or effort. Indeed, upon hearing about positive psychiatry principles, many nonprofessionals express surprise that this is not already considered routine practice. This article briefly outlines some of the basic tenets of positive child psychiatry and describes practical initial steps that can be readily incorporated into one’s day-to-day approach.
Defining pediatric positive psychiatry
There remains a fair amount of discussion and debate regarding what positive psychiatry is and isn’t, and how it fits into routine practice. While there is no official doctrine as to what “counts” as the practice of positive psychiatry, one can arguably divide most of its interventions into 2 main areas. The first is paying additional clinical attention to behaviors commonly associated with wellness or health promotion in youth. These include domains such as exercise, sleep habits, an authoritative parenting style, screen limits, and nutrition. The second area relates to specific techniques or procedures designed to cultivate positive emotions and mindsets; these often are referred to as positive psychology interventions (PPIs).6 Examples include gratitude exercises, practicing forgiveness, and activities that build optimism and hope. Many of the latter procedures share poorly defined boundaries with “tried and true” cognitive-behavioral therapy techniques, while others are more distinct to positive psychology and psychiatry. For both health promotion and PPIs, the goal of these interventions is to go beyond response and even remission for a patient to actual mental well-being, which is a construct that has also proven to be somewhat elusive and difficult to define. One well-described model by Seligman7 that has been gaining traction is the PERMA model, which breaks down well-being into 5 main components: positive emotions, engagement, relationships, meaning, and accomplishment.
Positive psychiatry: The evidence base
One myth about positive psychiatry is that it involves the pursuit of fringe and scientifically suspect techniques that have fallen under the expanding umbrella of “wellness.” Sadly, numerous unscientific and ineffective remedies have been widely promoted under the guise of wellness, leaving many families and clinicians uncertain about which areas have a solid evidence base and which are scientifically on shakier ground. While the lines delineating what are often referred to as PPI and more traditional psychotherapeutic techniques are blurry, there is increasing evidence supporting the use of PPI.8 A recent meta-analysis indicated that these techniques have larger effect sizes for children and young adults compared to older adults.9 More research, however, is needed, particularly for youth with diagnosable mental health conditions and for younger children.10
The evidence supporting the role of wellness and health promotion in preventing and treating pediatric mental health conditions has a quite robust research base. For example, a recent randomized controlled trial found greater reductions in multiple areas of emotional-behavior problems in children treated in a primary care setting with a wellness and health promotion model (the Vermont Family Based Approach) compared to those in a control condition.11 Another study examining the course of attention-deficit/hyperactivity disorder (ADHD) showed a 62% reduction of diagnosis among children who met 7 of 9 health promotion recommendations in areas such as nutrition, physical activity, and screen time, compared to those who met just 1 to 3 of these recommendations.12 Techniques such as mindfulness also have been found to be useful for adolescents with anxiety disorders.13 While a full review of the evidence is beyond the scope of this article, it is fair to say that many health promotion areas (such as exercise, nutrition, sleep habits, positive parenting skills, and some types of mindfulness) have strong scientific support—arguably at a level that is comparable to or even exceeds that of the off-label use of many psychiatric medications. The American Academy of Child and Adolescent Psychiatry has published a brief document that summarizes many age-related health promotion recommendations.14 The studies that underlie many of these recommendations contradict the misperception that wellness activities are only for already healthy individuals who want to become healthier, and show their utility for patients with more significant and chronic mental health conditions.
Incorporating core principles of positive psychiatry
Table 1 summarizes the core principles of positive child and adolescent psychiatry. There is no official procedure or certification one must complete to be considered a “positive psychiatrist,” and the term itself is somewhat debatable. Incorporating many of the principles of positive psychiatry into one’s daily routine does not necessitate a practice overhaul, and clinicians can integrate as many of these ideas as they deem clinically appropriate. That said, some adjustments to one’s perspective, approach, and workflow are likely needed, and the practice of positive psychiatry is arguably difficult to accomplish within the common “med check” model that emphasizes high volumes of short appointments that focus primarily on symptoms and adverse effects of medications.

Contrary to another misconception about positive psychiatry, working within a positive psychiatry framework does not involve encouraging patients to “put on a happy face” and ignore the very real suffering and trauma that many of them have experienced. Further, adhering to positive psychiatry does not entail abandoning the use of psychopharmacology (although careful prescribing is generally recommended) or applying gimmicks to superficially cover a person’s emotional pain.
Continue to: Rather, incorporating positive psychiatry...
Rather, incorporating positive psychiatry is best viewed as the creation of a supplementary toolbox that allows clinicians an expanded set of focus areas that can be used along with traditional psychotherapy and pharmacotherapy to help patients achieve a more robust and sustained response to treatment.4,5,15 The positive psychiatrist looks beyond the individual to examine a youth’s entire environment, and beyond areas of challenge to assess strengths, hopes, and aspirations.16 While many of these values are already in the formal description of a child psychiatrist, these priorities can take a back seat when trying to get through a busy day. For some, being a positive child psychiatrist means prescribing exercise rather than a sleep medication, assessing a child’s character strengths in addition to their behavioral challenges, or discussing the concept of parental warmth and how a struggling mother or father can replenish their tank when it feels like there is little left to give. It can mean reading literature on subjects such as happiness and optimal parenting practices in addition to depression and child maltreatment, and seeing oneself as an expert in mental health rather than just mental illness.
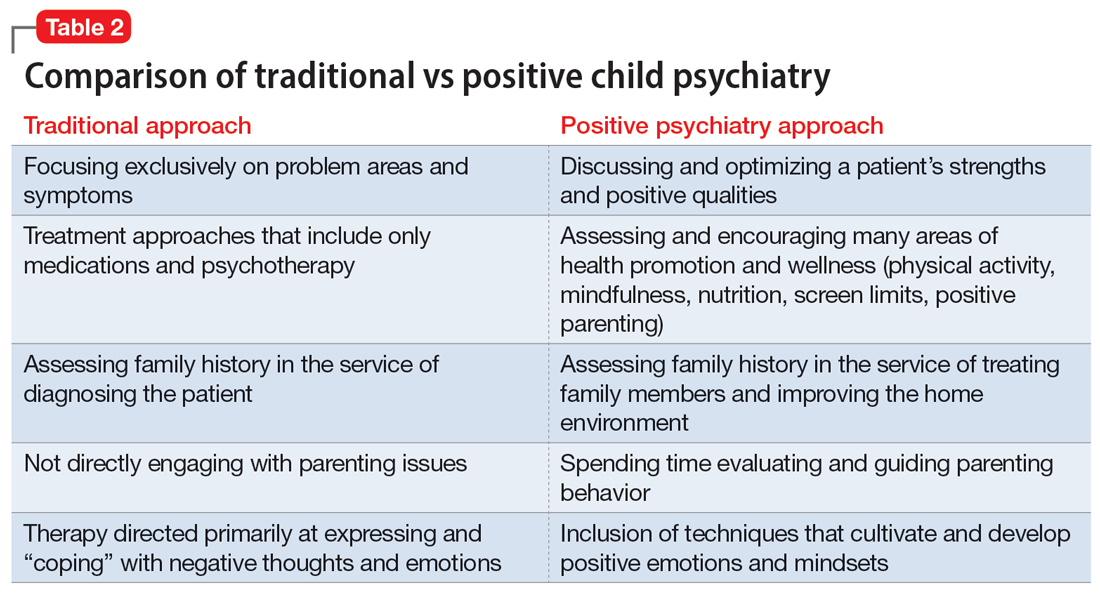
I have published a previous case example of positive psychiatry.17 Here I provide a brief vignette to further illustrate these concepts, and to compare traditional vs positive child psychiatry (Table 2).
CASE REPORT
Tyler, age 7, presents to a child and adolescent psychiatrist for refractory ADHD problems, continued defiance, and aggressive outbursts. Approximately 1 year ago, Tyler’s pediatrician had diagnosed him with fairly classic ADHD symptoms and prescribed long-acting methylphenidate. Tyler’s attention has improved somewhat at school, but there remains a significant degree of conflict and dysregulation at home. Tyler remains easily frustrated and is often very negative. The pediatrician is looking for additional treatment recommendations.
Traditional approach
The child psychiatrist assesses Tyler and gathers data from the patient, his parents, and his school. She confirms the diagnosis of ADHD, but in reviewing other potential conditions also discovers that Tyler meets DSM-5 criteria for oppositional defiant disorder. The clinician suspects there may also be a co-occurring learning disability and notices that Tyler has chronic difficulties getting to sleep. She also hypothesizes the stimulant medication is wearing off at about the time Tyler gets home from school. The psychiatrist recommends adding an immediate-release formulation of methylphenidate upon return from school, melatonin at night, a school psychoeducational assessment, and behavioral therapy for Tyler and his parents to focus on his disrespectful and oppositional behavior.
Three months later, there has been incremental improvement with the additional medication and a school individualized education plan. Tyler is also working with a therapist, who does some play therapy with Tyler and works on helping his parents create incentives for prosocial behavior, but progress has been slow and the amount of improvement in this area is minimal. Further, the initial positive effect of the melatonin on sleep has waned lately, and the parents now ask about “something stronger.”
Continue to: Positive psychiatry approach
Positive psychiatry approach
In addition to assessing problem areas and DSM-5 criteria, the psychiatrist assesses a number of other domains. She finds that most of the interaction between Tyler and his parents are negative to the point that his parents often just stay out of his way. She also discovers that Tyler does little in the way of structured activities and spends most of his time at home playing video games, sometimes well into the evening. He gets little to no physical activity outside of school. He also is a very selective eater and often skips breakfast entirely due to the usually chaotic home scene in the morning. A brief mental health screen of the parents further reveals that the mother would also likely meet criteria for ADHD, and the father may be experiencing depression.
The psychiatrist prescribes an additional immediate-release formulation stimulant for the afternoon but holds off on prescribing sleep medication. Instead, she discusses a plan in which Tyler can earn his screen time by reading or exercising, and urges the parents to do some regular physical activity together. She discusses the findings of her screenings of the parents and helps them get a more thorough assessment. She also encourages more family time and introduces them to the “rose, thorn, bud” exercise where each family member discusses a success, challenge, and opportunity of the day.
Three months later, Tyler’s attention and negativity have decreased. His increased physical activity has helped his sleep, and ADHD treatment for the mother has made the mornings much smoother, allowing Tyler to eat a regular breakfast. Both improvements contribute further to Tyler’s improved attention during the day. Challenges remain, but the increased positive family experiences are helping the parents feel less depleted. As a result, they engage with Tyler more productively, and he has responded with more confidence and enthusiasm.
A natural extension of traditional work
The principles and practices associated with positive psychiatry represent a natural and highly needed extension of traditional work within child and adolescent psychiatry. Its emphasis on health promotion activities, family functioning, parental mental health, and utilization of strengths align closely with the growing scientific knowledge base that supports the complex interplay between the many genetic and environmental factors that underlie mental and physical health across the lifespan. For most psychiatrists, incorporating these important concepts and approaches will not require a radical transformation of one’s outlook or methodology, although some adjustments to practice and knowledge base augmentations are often needed. Clinicians interested in supplementing their skill set and working toward becoming an expert in the full range of mental functioning are encouraged to begin taking some of the steps outlined in this article to further their proficiency in the emerging discipline of positive psychiatry.
Bottom Line
Positive psychiatry is an important development that complements traditional approaches to child and adolescent mental health treatment through health promotion and cultivation of positive emotions and qualities. Incorporating it into routine practice is well within reach.
Related Resources
- Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015.
- Positive Psychology Center. University of Pennsylvania School of Arts and Sciences. https://ppc.sas.upenn.edu/
- Rettew DC. Building healthy brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
Drug Brand Names
Methylphenidate extended-release • Concerta, Ritalin LA
1. Jeste DV, Palmer BW. Introduction: What is positive psychiatry? In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:1-16.
2. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5-14.
3. Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76:675-683.
4. Rettew DC. Better than better: the new focus on well-being in child psychiatry. Child Adolesc Psychiatr Clin N Am. 2019;28:127-135.
5. Rettew DC. Positive child psychiatry. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:285-304.
6. Parks AC, Kleiman EM, Kashdan TB, et al. Positive psychotherapeutic and behavioral interventions. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:147-165.
7. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon & Shuster; 2012.
8. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042-1054.
9. Carr A, Cullen K, Keeney C, et al. Effectiveness of positive psychology interventions: a systematic review and meta-analysis. J Pos Psychol. 2021:16:749-769.
10. Benoit V, Gabola P. Effects of positive psychology interventions on the well-being of young children: a systematic literature review. Int J Environ Res Public Health. 2021;18:12065.
11. Ivanova MY, Hall A, Weinberger S, et al. The Vermont family based approach in primary care pediatrics: effects on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. Child Psychiatry Hum Dev. Published online March 4, 2022. doi: 10.1007/s10578-022-01329-4
12. Lowen OK, Maximova K, Ekwaru JP, et al. Adherence to life-style recommendations and attention-deficit/hyperactivity disorder. Psychosom Med. 2020;82:305-315.
13. Zhou X, Guo J, et al. Effects of mindfulness-based stress reduction on anxiety symptoms in young people: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113002.
14. Rettew DC. Building health brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. Accessed May 11, 2022. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
15. Pustilnik S. Adapting well-being into outpatient child psychiatry. Child Adolesc Psychiatry Clin N Am. 2019;28:221-235.
16. Schlechter AD, O’Brien KH, Stewart C. The positive assessment: a model for integrating well-being and strengths-based approaches into the child and adolescent psychiatry clinical evaluation. Child Adolesc Psychiatry Clin N Am. 2019;28:157-169.
17. Rettew DC. A family- and wellness-based approach to child emotional-behavioral problems. In: RF Summers, Jeste DV, eds. Positive Psychiatry: A Casebook. American Psychiatric Association Publishing; 2019:29-44.
The principles and practices of positive psychiatry are especially well-suited for work with children, adolescents, and families. Positive psychiatry is “the science and practice of psychiatry that seeks to understand and promote well-being through assessments and interventions aimed at enhancing positive psychosocial factors among people who have or are at risk for developing mental or physical illnesses.”1 The concept sprung from the momentum of positive psychology, which originated from Seligman et al.2 Importantly, the standards and techniques of positive psychiatry are designed as an enhancement, perhaps even as a completion, of more traditional psychiatry, rather than an alternative.3 They come from an acknowledgment that to be most effective as a mental health professional, it is important for clinicians to be experts in the full range of mental functioning.4,5
For most clinicians currently practicing “traditional” child and adolescent psychiatry, adapting at least some of the principles of positive psychiatry within one’s routine practice will not necessarily involve a radical transformation of thought or effort. Indeed, upon hearing about positive psychiatry principles, many nonprofessionals express surprise that this is not already considered routine practice. This article briefly outlines some of the basic tenets of positive child psychiatry and describes practical initial steps that can be readily incorporated into one’s day-to-day approach.
Defining pediatric positive psychiatry
There remains a fair amount of discussion and debate regarding what positive psychiatry is and isn’t, and how it fits into routine practice. While there is no official doctrine as to what “counts” as the practice of positive psychiatry, one can arguably divide most of its interventions into 2 main areas. The first is paying additional clinical attention to behaviors commonly associated with wellness or health promotion in youth. These include domains such as exercise, sleep habits, an authoritative parenting style, screen limits, and nutrition. The second area relates to specific techniques or procedures designed to cultivate positive emotions and mindsets; these often are referred to as positive psychology interventions (PPIs).6 Examples include gratitude exercises, practicing forgiveness, and activities that build optimism and hope. Many of the latter procedures share poorly defined boundaries with “tried and true” cognitive-behavioral therapy techniques, while others are more distinct to positive psychology and psychiatry. For both health promotion and PPIs, the goal of these interventions is to go beyond response and even remission for a patient to actual mental well-being, which is a construct that has also proven to be somewhat elusive and difficult to define. One well-described model by Seligman7 that has been gaining traction is the PERMA model, which breaks down well-being into 5 main components: positive emotions, engagement, relationships, meaning, and accomplishment.
Positive psychiatry: The evidence base
One myth about positive psychiatry is that it involves the pursuit of fringe and scientifically suspect techniques that have fallen under the expanding umbrella of “wellness.” Sadly, numerous unscientific and ineffective remedies have been widely promoted under the guise of wellness, leaving many families and clinicians uncertain about which areas have a solid evidence base and which are scientifically on shakier ground. While the lines delineating what are often referred to as PPI and more traditional psychotherapeutic techniques are blurry, there is increasing evidence supporting the use of PPI.8 A recent meta-analysis indicated that these techniques have larger effect sizes for children and young adults compared to older adults.9 More research, however, is needed, particularly for youth with diagnosable mental health conditions and for younger children.10
The evidence supporting the role of wellness and health promotion in preventing and treating pediatric mental health conditions has a quite robust research base. For example, a recent randomized controlled trial found greater reductions in multiple areas of emotional-behavior problems in children treated in a primary care setting with a wellness and health promotion model (the Vermont Family Based Approach) compared to those in a control condition.11 Another study examining the course of attention-deficit/hyperactivity disorder (ADHD) showed a 62% reduction of diagnosis among children who met 7 of 9 health promotion recommendations in areas such as nutrition, physical activity, and screen time, compared to those who met just 1 to 3 of these recommendations.12 Techniques such as mindfulness also have been found to be useful for adolescents with anxiety disorders.13 While a full review of the evidence is beyond the scope of this article, it is fair to say that many health promotion areas (such as exercise, nutrition, sleep habits, positive parenting skills, and some types of mindfulness) have strong scientific support—arguably at a level that is comparable to or even exceeds that of the off-label use of many psychiatric medications. The American Academy of Child and Adolescent Psychiatry has published a brief document that summarizes many age-related health promotion recommendations.14 The studies that underlie many of these recommendations contradict the misperception that wellness activities are only for already healthy individuals who want to become healthier, and show their utility for patients with more significant and chronic mental health conditions.
Incorporating core principles of positive psychiatry
Table 1 summarizes the core principles of positive child and adolescent psychiatry. There is no official procedure or certification one must complete to be considered a “positive psychiatrist,” and the term itself is somewhat debatable. Incorporating many of the principles of positive psychiatry into one’s daily routine does not necessitate a practice overhaul, and clinicians can integrate as many of these ideas as they deem clinically appropriate. That said, some adjustments to one’s perspective, approach, and workflow are likely needed, and the practice of positive psychiatry is arguably difficult to accomplish within the common “med check” model that emphasizes high volumes of short appointments that focus primarily on symptoms and adverse effects of medications.

Contrary to another misconception about positive psychiatry, working within a positive psychiatry framework does not involve encouraging patients to “put on a happy face” and ignore the very real suffering and trauma that many of them have experienced. Further, adhering to positive psychiatry does not entail abandoning the use of psychopharmacology (although careful prescribing is generally recommended) or applying gimmicks to superficially cover a person’s emotional pain.
Continue to: Rather, incorporating positive psychiatry...
Rather, incorporating positive psychiatry is best viewed as the creation of a supplementary toolbox that allows clinicians an expanded set of focus areas that can be used along with traditional psychotherapy and pharmacotherapy to help patients achieve a more robust and sustained response to treatment.4,5,15 The positive psychiatrist looks beyond the individual to examine a youth’s entire environment, and beyond areas of challenge to assess strengths, hopes, and aspirations.16 While many of these values are already in the formal description of a child psychiatrist, these priorities can take a back seat when trying to get through a busy day. For some, being a positive child psychiatrist means prescribing exercise rather than a sleep medication, assessing a child’s character strengths in addition to their behavioral challenges, or discussing the concept of parental warmth and how a struggling mother or father can replenish their tank when it feels like there is little left to give. It can mean reading literature on subjects such as happiness and optimal parenting practices in addition to depression and child maltreatment, and seeing oneself as an expert in mental health rather than just mental illness.
I have published a previous case example of positive psychiatry.17 Here I provide a brief vignette to further illustrate these concepts, and to compare traditional vs positive child psychiatry (Table 2).
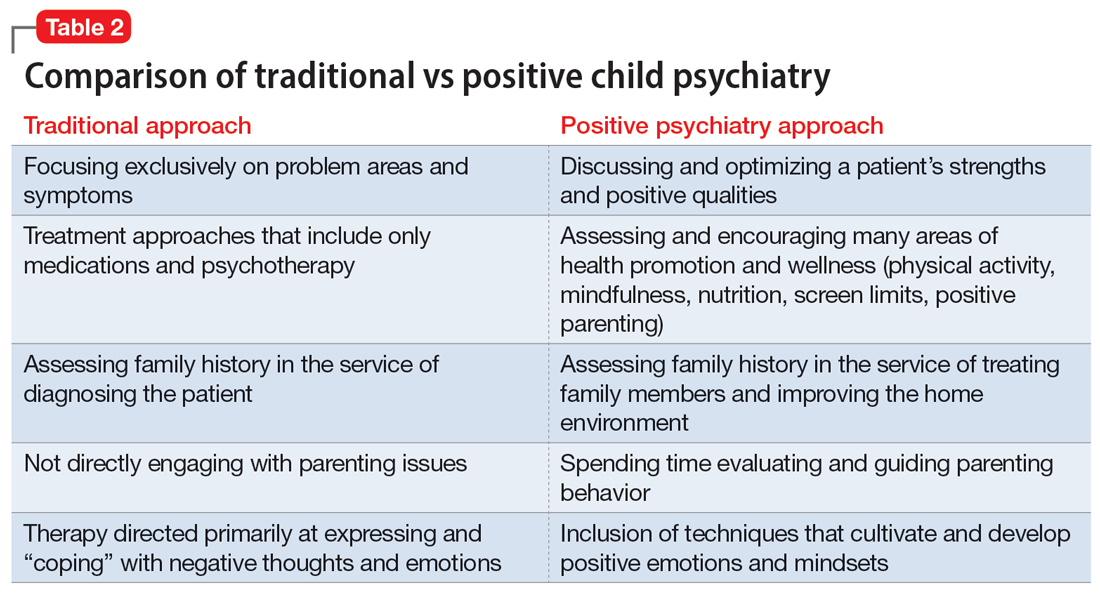
CASE REPORT
Tyler, age 7, presents to a child and adolescent psychiatrist for refractory ADHD problems, continued defiance, and aggressive outbursts. Approximately 1 year ago, Tyler’s pediatrician had diagnosed him with fairly classic ADHD symptoms and prescribed long-acting methylphenidate. Tyler’s attention has improved somewhat at school, but there remains a significant degree of conflict and dysregulation at home. Tyler remains easily frustrated and is often very negative. The pediatrician is looking for additional treatment recommendations.
Traditional approach
The child psychiatrist assesses Tyler and gathers data from the patient, his parents, and his school. She confirms the diagnosis of ADHD, but in reviewing other potential conditions also discovers that Tyler meets DSM-5 criteria for oppositional defiant disorder. The clinician suspects there may also be a co-occurring learning disability and notices that Tyler has chronic difficulties getting to sleep. She also hypothesizes the stimulant medication is wearing off at about the time Tyler gets home from school. The psychiatrist recommends adding an immediate-release formulation of methylphenidate upon return from school, melatonin at night, a school psychoeducational assessment, and behavioral therapy for Tyler and his parents to focus on his disrespectful and oppositional behavior.
Three months later, there has been incremental improvement with the additional medication and a school individualized education plan. Tyler is also working with a therapist, who does some play therapy with Tyler and works on helping his parents create incentives for prosocial behavior, but progress has been slow and the amount of improvement in this area is minimal. Further, the initial positive effect of the melatonin on sleep has waned lately, and the parents now ask about “something stronger.”
Continue to: Positive psychiatry approach
Positive psychiatry approach
In addition to assessing problem areas and DSM-5 criteria, the psychiatrist assesses a number of other domains. She finds that most of the interaction between Tyler and his parents are negative to the point that his parents often just stay out of his way. She also discovers that Tyler does little in the way of structured activities and spends most of his time at home playing video games, sometimes well into the evening. He gets little to no physical activity outside of school. He also is a very selective eater and often skips breakfast entirely due to the usually chaotic home scene in the morning. A brief mental health screen of the parents further reveals that the mother would also likely meet criteria for ADHD, and the father may be experiencing depression.
The psychiatrist prescribes an additional immediate-release formulation stimulant for the afternoon but holds off on prescribing sleep medication. Instead, she discusses a plan in which Tyler can earn his screen time by reading or exercising, and urges the parents to do some regular physical activity together. She discusses the findings of her screenings of the parents and helps them get a more thorough assessment. She also encourages more family time and introduces them to the “rose, thorn, bud” exercise where each family member discusses a success, challenge, and opportunity of the day.
Three months later, Tyler’s attention and negativity have decreased. His increased physical activity has helped his sleep, and ADHD treatment for the mother has made the mornings much smoother, allowing Tyler to eat a regular breakfast. Both improvements contribute further to Tyler’s improved attention during the day. Challenges remain, but the increased positive family experiences are helping the parents feel less depleted. As a result, they engage with Tyler more productively, and he has responded with more confidence and enthusiasm.
A natural extension of traditional work
The principles and practices associated with positive psychiatry represent a natural and highly needed extension of traditional work within child and adolescent psychiatry. Its emphasis on health promotion activities, family functioning, parental mental health, and utilization of strengths align closely with the growing scientific knowledge base that supports the complex interplay between the many genetic and environmental factors that underlie mental and physical health across the lifespan. For most psychiatrists, incorporating these important concepts and approaches will not require a radical transformation of one’s outlook or methodology, although some adjustments to practice and knowledge base augmentations are often needed. Clinicians interested in supplementing their skill set and working toward becoming an expert in the full range of mental functioning are encouraged to begin taking some of the steps outlined in this article to further their proficiency in the emerging discipline of positive psychiatry.
Bottom Line
Positive psychiatry is an important development that complements traditional approaches to child and adolescent mental health treatment through health promotion and cultivation of positive emotions and qualities. Incorporating it into routine practice is well within reach.
Related Resources
- Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015.
- Positive Psychology Center. University of Pennsylvania School of Arts and Sciences. https://ppc.sas.upenn.edu/
- Rettew DC. Building healthy brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
Drug Brand Names
Methylphenidate extended-release • Concerta, Ritalin LA
The principles and practices of positive psychiatry are especially well-suited for work with children, adolescents, and families. Positive psychiatry is “the science and practice of psychiatry that seeks to understand and promote well-being through assessments and interventions aimed at enhancing positive psychosocial factors among people who have or are at risk for developing mental or physical illnesses.”1 The concept sprung from the momentum of positive psychology, which originated from Seligman et al.2 Importantly, the standards and techniques of positive psychiatry are designed as an enhancement, perhaps even as a completion, of more traditional psychiatry, rather than an alternative.3 They come from an acknowledgment that to be most effective as a mental health professional, it is important for clinicians to be experts in the full range of mental functioning.4,5
For most clinicians currently practicing “traditional” child and adolescent psychiatry, adapting at least some of the principles of positive psychiatry within one’s routine practice will not necessarily involve a radical transformation of thought or effort. Indeed, upon hearing about positive psychiatry principles, many nonprofessionals express surprise that this is not already considered routine practice. This article briefly outlines some of the basic tenets of positive child psychiatry and describes practical initial steps that can be readily incorporated into one’s day-to-day approach.
Defining pediatric positive psychiatry
There remains a fair amount of discussion and debate regarding what positive psychiatry is and isn’t, and how it fits into routine practice. While there is no official doctrine as to what “counts” as the practice of positive psychiatry, one can arguably divide most of its interventions into 2 main areas. The first is paying additional clinical attention to behaviors commonly associated with wellness or health promotion in youth. These include domains such as exercise, sleep habits, an authoritative parenting style, screen limits, and nutrition. The second area relates to specific techniques or procedures designed to cultivate positive emotions and mindsets; these often are referred to as positive psychology interventions (PPIs).6 Examples include gratitude exercises, practicing forgiveness, and activities that build optimism and hope. Many of the latter procedures share poorly defined boundaries with “tried and true” cognitive-behavioral therapy techniques, while others are more distinct to positive psychology and psychiatry. For both health promotion and PPIs, the goal of these interventions is to go beyond response and even remission for a patient to actual mental well-being, which is a construct that has also proven to be somewhat elusive and difficult to define. One well-described model by Seligman7 that has been gaining traction is the PERMA model, which breaks down well-being into 5 main components: positive emotions, engagement, relationships, meaning, and accomplishment.
Positive psychiatry: The evidence base
One myth about positive psychiatry is that it involves the pursuit of fringe and scientifically suspect techniques that have fallen under the expanding umbrella of “wellness.” Sadly, numerous unscientific and ineffective remedies have been widely promoted under the guise of wellness, leaving many families and clinicians uncertain about which areas have a solid evidence base and which are scientifically on shakier ground. While the lines delineating what are often referred to as PPI and more traditional psychotherapeutic techniques are blurry, there is increasing evidence supporting the use of PPI.8 A recent meta-analysis indicated that these techniques have larger effect sizes for children and young adults compared to older adults.9 More research, however, is needed, particularly for youth with diagnosable mental health conditions and for younger children.10
The evidence supporting the role of wellness and health promotion in preventing and treating pediatric mental health conditions has a quite robust research base. For example, a recent randomized controlled trial found greater reductions in multiple areas of emotional-behavior problems in children treated in a primary care setting with a wellness and health promotion model (the Vermont Family Based Approach) compared to those in a control condition.11 Another study examining the course of attention-deficit/hyperactivity disorder (ADHD) showed a 62% reduction of diagnosis among children who met 7 of 9 health promotion recommendations in areas such as nutrition, physical activity, and screen time, compared to those who met just 1 to 3 of these recommendations.12 Techniques such as mindfulness also have been found to be useful for adolescents with anxiety disorders.13 While a full review of the evidence is beyond the scope of this article, it is fair to say that many health promotion areas (such as exercise, nutrition, sleep habits, positive parenting skills, and some types of mindfulness) have strong scientific support—arguably at a level that is comparable to or even exceeds that of the off-label use of many psychiatric medications. The American Academy of Child and Adolescent Psychiatry has published a brief document that summarizes many age-related health promotion recommendations.14 The studies that underlie many of these recommendations contradict the misperception that wellness activities are only for already healthy individuals who want to become healthier, and show their utility for patients with more significant and chronic mental health conditions.
Incorporating core principles of positive psychiatry
Table 1 summarizes the core principles of positive child and adolescent psychiatry. There is no official procedure or certification one must complete to be considered a “positive psychiatrist,” and the term itself is somewhat debatable. Incorporating many of the principles of positive psychiatry into one’s daily routine does not necessitate a practice overhaul, and clinicians can integrate as many of these ideas as they deem clinically appropriate. That said, some adjustments to one’s perspective, approach, and workflow are likely needed, and the practice of positive psychiatry is arguably difficult to accomplish within the common “med check” model that emphasizes high volumes of short appointments that focus primarily on symptoms and adverse effects of medications.

Contrary to another misconception about positive psychiatry, working within a positive psychiatry framework does not involve encouraging patients to “put on a happy face” and ignore the very real suffering and trauma that many of them have experienced. Further, adhering to positive psychiatry does not entail abandoning the use of psychopharmacology (although careful prescribing is generally recommended) or applying gimmicks to superficially cover a person’s emotional pain.
Continue to: Rather, incorporating positive psychiatry...
Rather, incorporating positive psychiatry is best viewed as the creation of a supplementary toolbox that allows clinicians an expanded set of focus areas that can be used along with traditional psychotherapy and pharmacotherapy to help patients achieve a more robust and sustained response to treatment.4,5,15 The positive psychiatrist looks beyond the individual to examine a youth’s entire environment, and beyond areas of challenge to assess strengths, hopes, and aspirations.16 While many of these values are already in the formal description of a child psychiatrist, these priorities can take a back seat when trying to get through a busy day. For some, being a positive child psychiatrist means prescribing exercise rather than a sleep medication, assessing a child’s character strengths in addition to their behavioral challenges, or discussing the concept of parental warmth and how a struggling mother or father can replenish their tank when it feels like there is little left to give. It can mean reading literature on subjects such as happiness and optimal parenting practices in addition to depression and child maltreatment, and seeing oneself as an expert in mental health rather than just mental illness.
I have published a previous case example of positive psychiatry.17 Here I provide a brief vignette to further illustrate these concepts, and to compare traditional vs positive child psychiatry (Table 2).
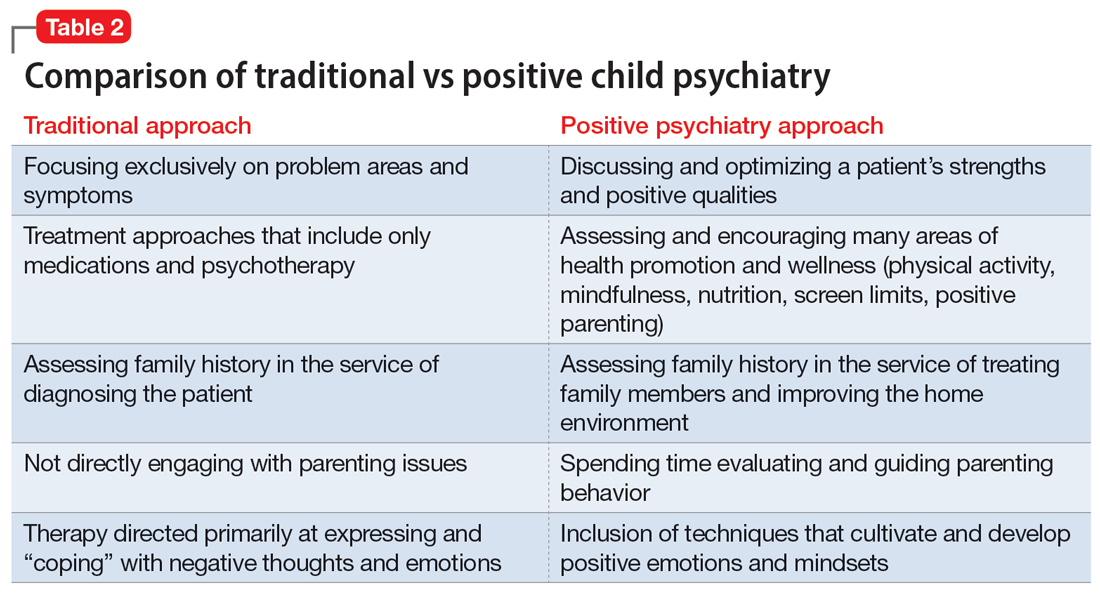
CASE REPORT
Tyler, age 7, presents to a child and adolescent psychiatrist for refractory ADHD problems, continued defiance, and aggressive outbursts. Approximately 1 year ago, Tyler’s pediatrician had diagnosed him with fairly classic ADHD symptoms and prescribed long-acting methylphenidate. Tyler’s attention has improved somewhat at school, but there remains a significant degree of conflict and dysregulation at home. Tyler remains easily frustrated and is often very negative. The pediatrician is looking for additional treatment recommendations.
Traditional approach
The child psychiatrist assesses Tyler and gathers data from the patient, his parents, and his school. She confirms the diagnosis of ADHD, but in reviewing other potential conditions also discovers that Tyler meets DSM-5 criteria for oppositional defiant disorder. The clinician suspects there may also be a co-occurring learning disability and notices that Tyler has chronic difficulties getting to sleep. She also hypothesizes the stimulant medication is wearing off at about the time Tyler gets home from school. The psychiatrist recommends adding an immediate-release formulation of methylphenidate upon return from school, melatonin at night, a school psychoeducational assessment, and behavioral therapy for Tyler and his parents to focus on his disrespectful and oppositional behavior.
Three months later, there has been incremental improvement with the additional medication and a school individualized education plan. Tyler is also working with a therapist, who does some play therapy with Tyler and works on helping his parents create incentives for prosocial behavior, but progress has been slow and the amount of improvement in this area is minimal. Further, the initial positive effect of the melatonin on sleep has waned lately, and the parents now ask about “something stronger.”
Continue to: Positive psychiatry approach
Positive psychiatry approach
In addition to assessing problem areas and DSM-5 criteria, the psychiatrist assesses a number of other domains. She finds that most of the interaction between Tyler and his parents are negative to the point that his parents often just stay out of his way. She also discovers that Tyler does little in the way of structured activities and spends most of his time at home playing video games, sometimes well into the evening. He gets little to no physical activity outside of school. He also is a very selective eater and often skips breakfast entirely due to the usually chaotic home scene in the morning. A brief mental health screen of the parents further reveals that the mother would also likely meet criteria for ADHD, and the father may be experiencing depression.
The psychiatrist prescribes an additional immediate-release formulation stimulant for the afternoon but holds off on prescribing sleep medication. Instead, she discusses a plan in which Tyler can earn his screen time by reading or exercising, and urges the parents to do some regular physical activity together. She discusses the findings of her screenings of the parents and helps them get a more thorough assessment. She also encourages more family time and introduces them to the “rose, thorn, bud” exercise where each family member discusses a success, challenge, and opportunity of the day.
Three months later, Tyler’s attention and negativity have decreased. His increased physical activity has helped his sleep, and ADHD treatment for the mother has made the mornings much smoother, allowing Tyler to eat a regular breakfast. Both improvements contribute further to Tyler’s improved attention during the day. Challenges remain, but the increased positive family experiences are helping the parents feel less depleted. As a result, they engage with Tyler more productively, and he has responded with more confidence and enthusiasm.
A natural extension of traditional work
The principles and practices associated with positive psychiatry represent a natural and highly needed extension of traditional work within child and adolescent psychiatry. Its emphasis on health promotion activities, family functioning, parental mental health, and utilization of strengths align closely with the growing scientific knowledge base that supports the complex interplay between the many genetic and environmental factors that underlie mental and physical health across the lifespan. For most psychiatrists, incorporating these important concepts and approaches will not require a radical transformation of one’s outlook or methodology, although some adjustments to practice and knowledge base augmentations are often needed. Clinicians interested in supplementing their skill set and working toward becoming an expert in the full range of mental functioning are encouraged to begin taking some of the steps outlined in this article to further their proficiency in the emerging discipline of positive psychiatry.
Bottom Line
Positive psychiatry is an important development that complements traditional approaches to child and adolescent mental health treatment through health promotion and cultivation of positive emotions and qualities. Incorporating it into routine practice is well within reach.
Related Resources
- Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015.
- Positive Psychology Center. University of Pennsylvania School of Arts and Sciences. https://ppc.sas.upenn.edu/
- Rettew DC. Building healthy brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
Drug Brand Names
Methylphenidate extended-release • Concerta, Ritalin LA
1. Jeste DV, Palmer BW. Introduction: What is positive psychiatry? In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:1-16.
2. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5-14.
3. Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76:675-683.
4. Rettew DC. Better than better: the new focus on well-being in child psychiatry. Child Adolesc Psychiatr Clin N Am. 2019;28:127-135.
5. Rettew DC. Positive child psychiatry. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:285-304.
6. Parks AC, Kleiman EM, Kashdan TB, et al. Positive psychotherapeutic and behavioral interventions. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:147-165.
7. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon & Shuster; 2012.
8. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042-1054.
9. Carr A, Cullen K, Keeney C, et al. Effectiveness of positive psychology interventions: a systematic review and meta-analysis. J Pos Psychol. 2021:16:749-769.
10. Benoit V, Gabola P. Effects of positive psychology interventions on the well-being of young children: a systematic literature review. Int J Environ Res Public Health. 2021;18:12065.
11. Ivanova MY, Hall A, Weinberger S, et al. The Vermont family based approach in primary care pediatrics: effects on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. Child Psychiatry Hum Dev. Published online March 4, 2022. doi: 10.1007/s10578-022-01329-4
12. Lowen OK, Maximova K, Ekwaru JP, et al. Adherence to life-style recommendations and attention-deficit/hyperactivity disorder. Psychosom Med. 2020;82:305-315.
13. Zhou X, Guo J, et al. Effects of mindfulness-based stress reduction on anxiety symptoms in young people: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113002.
14. Rettew DC. Building health brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. Accessed May 11, 2022. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
15. Pustilnik S. Adapting well-being into outpatient child psychiatry. Child Adolesc Psychiatry Clin N Am. 2019;28:221-235.
16. Schlechter AD, O’Brien KH, Stewart C. The positive assessment: a model for integrating well-being and strengths-based approaches into the child and adolescent psychiatry clinical evaluation. Child Adolesc Psychiatry Clin N Am. 2019;28:157-169.
17. Rettew DC. A family- and wellness-based approach to child emotional-behavioral problems. In: RF Summers, Jeste DV, eds. Positive Psychiatry: A Casebook. American Psychiatric Association Publishing; 2019:29-44.
1. Jeste DV, Palmer BW. Introduction: What is positive psychiatry? In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:1-16.
2. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5-14.
3. Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76:675-683.
4. Rettew DC. Better than better: the new focus on well-being in child psychiatry. Child Adolesc Psychiatr Clin N Am. 2019;28:127-135.
5. Rettew DC. Positive child psychiatry. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:285-304.
6. Parks AC, Kleiman EM, Kashdan TB, et al. Positive psychotherapeutic and behavioral interventions. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:147-165.
7. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon & Shuster; 2012.
8. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042-1054.
9. Carr A, Cullen K, Keeney C, et al. Effectiveness of positive psychology interventions: a systematic review and meta-analysis. J Pos Psychol. 2021:16:749-769.
10. Benoit V, Gabola P. Effects of positive psychology interventions on the well-being of young children: a systematic literature review. Int J Environ Res Public Health. 2021;18:12065.
11. Ivanova MY, Hall A, Weinberger S, et al. The Vermont family based approach in primary care pediatrics: effects on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. Child Psychiatry Hum Dev. Published online March 4, 2022. doi: 10.1007/s10578-022-01329-4
12. Lowen OK, Maximova K, Ekwaru JP, et al. Adherence to life-style recommendations and attention-deficit/hyperactivity disorder. Psychosom Med. 2020;82:305-315.
13. Zhou X, Guo J, et al. Effects of mindfulness-based stress reduction on anxiety symptoms in young people: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113002.
14. Rettew DC. Building health brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. Accessed May 11, 2022. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
15. Pustilnik S. Adapting well-being into outpatient child psychiatry. Child Adolesc Psychiatry Clin N Am. 2019;28:221-235.
16. Schlechter AD, O’Brien KH, Stewart C. The positive assessment: a model for integrating well-being and strengths-based approaches into the child and adolescent psychiatry clinical evaluation. Child Adolesc Psychiatry Clin N Am. 2019;28:157-169.
17. Rettew DC. A family- and wellness-based approach to child emotional-behavioral problems. In: RF Summers, Jeste DV, eds. Positive Psychiatry: A Casebook. American Psychiatric Association Publishing; 2019:29-44.
Strategies to treat food allergy with oral immunotherapy
according to a new review.
In OIT, a patient who is allergic to a specific food consumes increasing amounts of the allergen over time to reduce their risk for allergic reaction.
“OIT is an elective, usually noncurative procedure with inherent risks that require families to function as amateur medical professionals. Preparing them for this role is essential to protect patients and ensure the long-term success of this life-changing procedure,” lead author Douglas P. Mack, MD, MSc, a pediatric allergy, asthma, and immunology specialist at McMaster University in Hamilton, Ont., and colleagues write in Clinical & Experimental Allergy.
From strict avoidance to desensitization
Food allergy treatment has traditionally involved avoiding accidental exposure that may lead to anaphylaxis and providing rescue medication. In recent years, OIT “has been recommended by several guidelines as a primary option,” Dr. Mack and coauthors write. And with the “approval by European and USA regulators of [peanut allergen powder] Palforzia [Aimmune Therapeutics], there are now commercial and noncommercial forms of OIT available for use in several countries.”
They advise physicians to take a proactive, educational, supportive approach to patients and their families throughout the therapy.
“Ultimately, the decision to pursue OIT or continue avoidance strategies remains the responsibility of the family and the patients,” they write. “Some families may not be prepared for the role that they have to play in actively managing their child’s food allergy treatment.”
Strategies to overcome OIT challenges
Reviewing the literature about OIT for food allergy, the authors suggest various strategies physicians can use to help OIT patients and their families prepare for and overcome common treatment-related challenges.
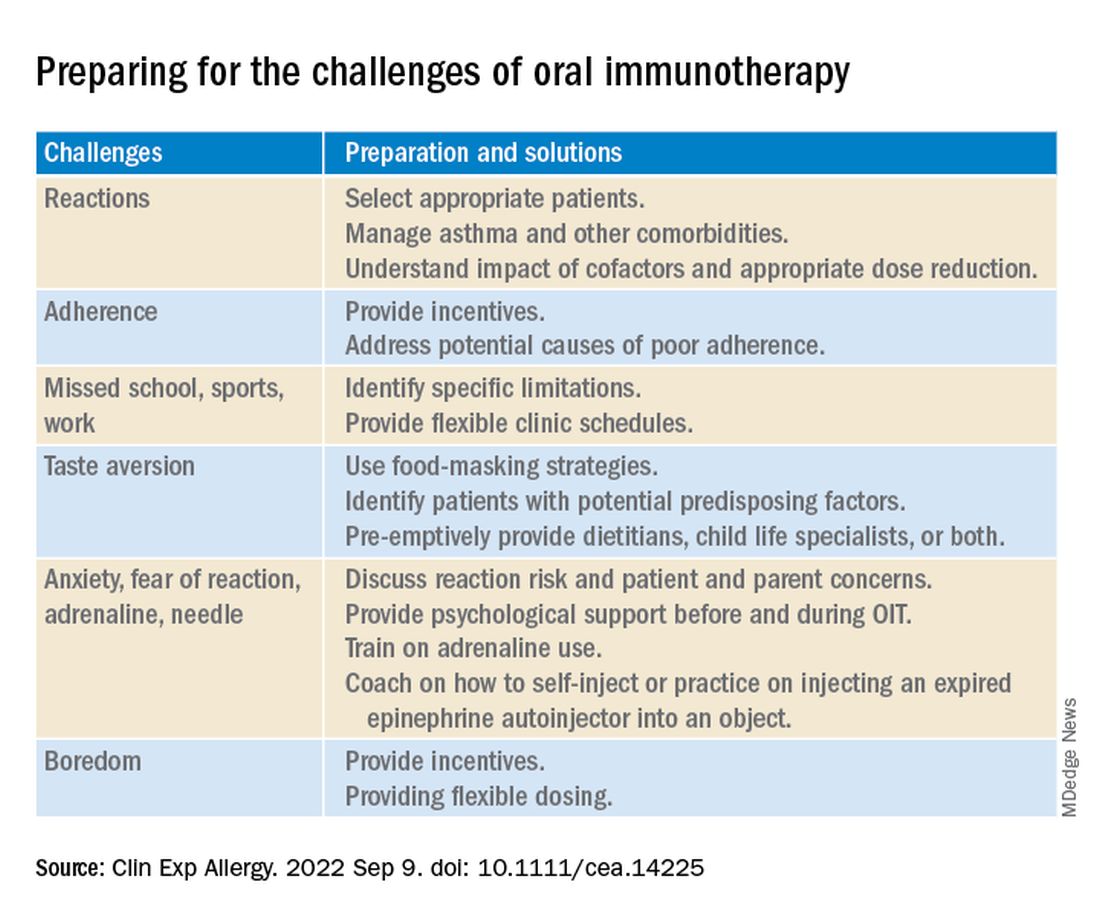
Two experts welcome the report
Rita Kachru, MD, a specialist in allergy and immunology and a codirector of the food allergy program at UCLA Health in Los Angeles, called this “an excellent report about a wonderful, individualized option in food allergy management.
“The authors did an excellent job delineating OIT terminology, outlining the goals, risks, and benefits of OIT, noting that it’s not a cure, and emphasizing the crucial importance of discussions with each family throughout the process,” Dr. Kachru, who was not involved in developing the report, told this news organization.
“I thoroughly agree with their assessment,” she added. “The more you do OIT research and clinical care, the more you realize the pitfalls, the benefits, and the importance of patient goals and family dynamics. Discussing the goals, risks, benefits, and alternatives to OIT in detail with the family is crucial so they fully understand the process.”
Basil M. Kahwash, MD, an allergy, pulmonary, and critical care medicine specialist at Vanderbilt University Medical Center in Nashville, Tenn., said that providers in the immunology community have been discussing OIT for years and that he welcomes the well-written report that summarizes the evidence.
“It’s important to periodically summarize the evidence, as well as the consensus expert opinion about the evidence, so we may better inform our colleagues and patients,” said Dr. Kahwash, who was not involved in developing the report. “The authors are well-known experts in our field who have experience with OIT and with reviewing the evidence of food allergy.
“OIT can be a fantastic option for some patients, especially those who are very highly motivated and understand the process from start to finish. But OIT is not the best option for every child, and it’s not much of an option for adults,” he explained. “Patients need to be chosen carefully and understand the level of motivation required to safely follow through with the treatment.
“The report will hopefully affect patient care positively and allow patients to understand the limitations around OIT when they consider their candidacy for it,” he added. “In most cases, OIT patients will still need to avoid the allergen, but if a small amount accidentally gets into their food, they probably won’t have a very severe reaction to it.”
Dr. Kahwash would like to see data on patients who have seen long-term remission with OIT.
“Clearly, some patients benefit from OIT. What differentiates patients who benefit from OIT from those who do not?” he asked. “In the future, we need to consider possible biomarkers of patients who are and who aren’t good candidates for OIT.
“Regardless of OIT’s limitations, the potential for desensitization rather than strict avoidance represents a big step in the evolution of food allergy treatment,” Dr. Kahwash noted.
No funding details were provided. Dr. Mack and three coauthors report financial relationships with Aimmune. Aimmune Therapeutics is the manufacturer of Palforzia OIT (AR101 powder provided in capsules and sachets). Most coauthors also report financial relationships with other pharmaceutical companies. The full list can be found with the original article. Dr. Kachru was an investigator in the PALISADES clinical trial of AR101. Dr. Kahwash reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new review.
In OIT, a patient who is allergic to a specific food consumes increasing amounts of the allergen over time to reduce their risk for allergic reaction.
“OIT is an elective, usually noncurative procedure with inherent risks that require families to function as amateur medical professionals. Preparing them for this role is essential to protect patients and ensure the long-term success of this life-changing procedure,” lead author Douglas P. Mack, MD, MSc, a pediatric allergy, asthma, and immunology specialist at McMaster University in Hamilton, Ont., and colleagues write in Clinical & Experimental Allergy.
From strict avoidance to desensitization
Food allergy treatment has traditionally involved avoiding accidental exposure that may lead to anaphylaxis and providing rescue medication. In recent years, OIT “has been recommended by several guidelines as a primary option,” Dr. Mack and coauthors write. And with the “approval by European and USA regulators of [peanut allergen powder] Palforzia [Aimmune Therapeutics], there are now commercial and noncommercial forms of OIT available for use in several countries.”
They advise physicians to take a proactive, educational, supportive approach to patients and their families throughout the therapy.
“Ultimately, the decision to pursue OIT or continue avoidance strategies remains the responsibility of the family and the patients,” they write. “Some families may not be prepared for the role that they have to play in actively managing their child’s food allergy treatment.”
Strategies to overcome OIT challenges
Reviewing the literature about OIT for food allergy, the authors suggest various strategies physicians can use to help OIT patients and their families prepare for and overcome common treatment-related challenges.
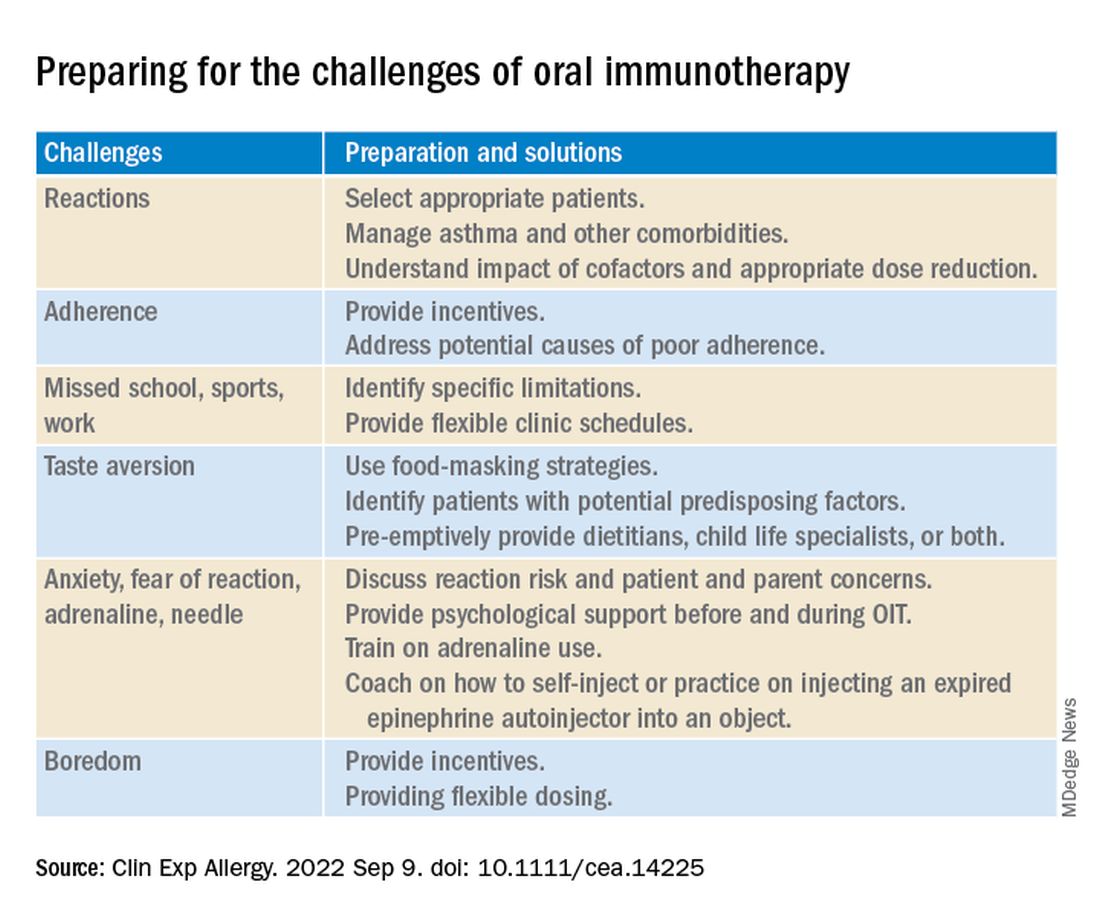
Two experts welcome the report
Rita Kachru, MD, a specialist in allergy and immunology and a codirector of the food allergy program at UCLA Health in Los Angeles, called this “an excellent report about a wonderful, individualized option in food allergy management.
“The authors did an excellent job delineating OIT terminology, outlining the goals, risks, and benefits of OIT, noting that it’s not a cure, and emphasizing the crucial importance of discussions with each family throughout the process,” Dr. Kachru, who was not involved in developing the report, told this news organization.
“I thoroughly agree with their assessment,” she added. “The more you do OIT research and clinical care, the more you realize the pitfalls, the benefits, and the importance of patient goals and family dynamics. Discussing the goals, risks, benefits, and alternatives to OIT in detail with the family is crucial so they fully understand the process.”
Basil M. Kahwash, MD, an allergy, pulmonary, and critical care medicine specialist at Vanderbilt University Medical Center in Nashville, Tenn., said that providers in the immunology community have been discussing OIT for years and that he welcomes the well-written report that summarizes the evidence.
“It’s important to periodically summarize the evidence, as well as the consensus expert opinion about the evidence, so we may better inform our colleagues and patients,” said Dr. Kahwash, who was not involved in developing the report. “The authors are well-known experts in our field who have experience with OIT and with reviewing the evidence of food allergy.
“OIT can be a fantastic option for some patients, especially those who are very highly motivated and understand the process from start to finish. But OIT is not the best option for every child, and it’s not much of an option for adults,” he explained. “Patients need to be chosen carefully and understand the level of motivation required to safely follow through with the treatment.
“The report will hopefully affect patient care positively and allow patients to understand the limitations around OIT when they consider their candidacy for it,” he added. “In most cases, OIT patients will still need to avoid the allergen, but if a small amount accidentally gets into their food, they probably won’t have a very severe reaction to it.”
Dr. Kahwash would like to see data on patients who have seen long-term remission with OIT.
“Clearly, some patients benefit from OIT. What differentiates patients who benefit from OIT from those who do not?” he asked. “In the future, we need to consider possible biomarkers of patients who are and who aren’t good candidates for OIT.
“Regardless of OIT’s limitations, the potential for desensitization rather than strict avoidance represents a big step in the evolution of food allergy treatment,” Dr. Kahwash noted.
No funding details were provided. Dr. Mack and three coauthors report financial relationships with Aimmune. Aimmune Therapeutics is the manufacturer of Palforzia OIT (AR101 powder provided in capsules and sachets). Most coauthors also report financial relationships with other pharmaceutical companies. The full list can be found with the original article. Dr. Kachru was an investigator in the PALISADES clinical trial of AR101. Dr. Kahwash reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new review.
In OIT, a patient who is allergic to a specific food consumes increasing amounts of the allergen over time to reduce their risk for allergic reaction.
“OIT is an elective, usually noncurative procedure with inherent risks that require families to function as amateur medical professionals. Preparing them for this role is essential to protect patients and ensure the long-term success of this life-changing procedure,” lead author Douglas P. Mack, MD, MSc, a pediatric allergy, asthma, and immunology specialist at McMaster University in Hamilton, Ont., and colleagues write in Clinical & Experimental Allergy.
From strict avoidance to desensitization
Food allergy treatment has traditionally involved avoiding accidental exposure that may lead to anaphylaxis and providing rescue medication. In recent years, OIT “has been recommended by several guidelines as a primary option,” Dr. Mack and coauthors write. And with the “approval by European and USA regulators of [peanut allergen powder] Palforzia [Aimmune Therapeutics], there are now commercial and noncommercial forms of OIT available for use in several countries.”
They advise physicians to take a proactive, educational, supportive approach to patients and their families throughout the therapy.
“Ultimately, the decision to pursue OIT or continue avoidance strategies remains the responsibility of the family and the patients,” they write. “Some families may not be prepared for the role that they have to play in actively managing their child’s food allergy treatment.”
Strategies to overcome OIT challenges
Reviewing the literature about OIT for food allergy, the authors suggest various strategies physicians can use to help OIT patients and their families prepare for and overcome common treatment-related challenges.
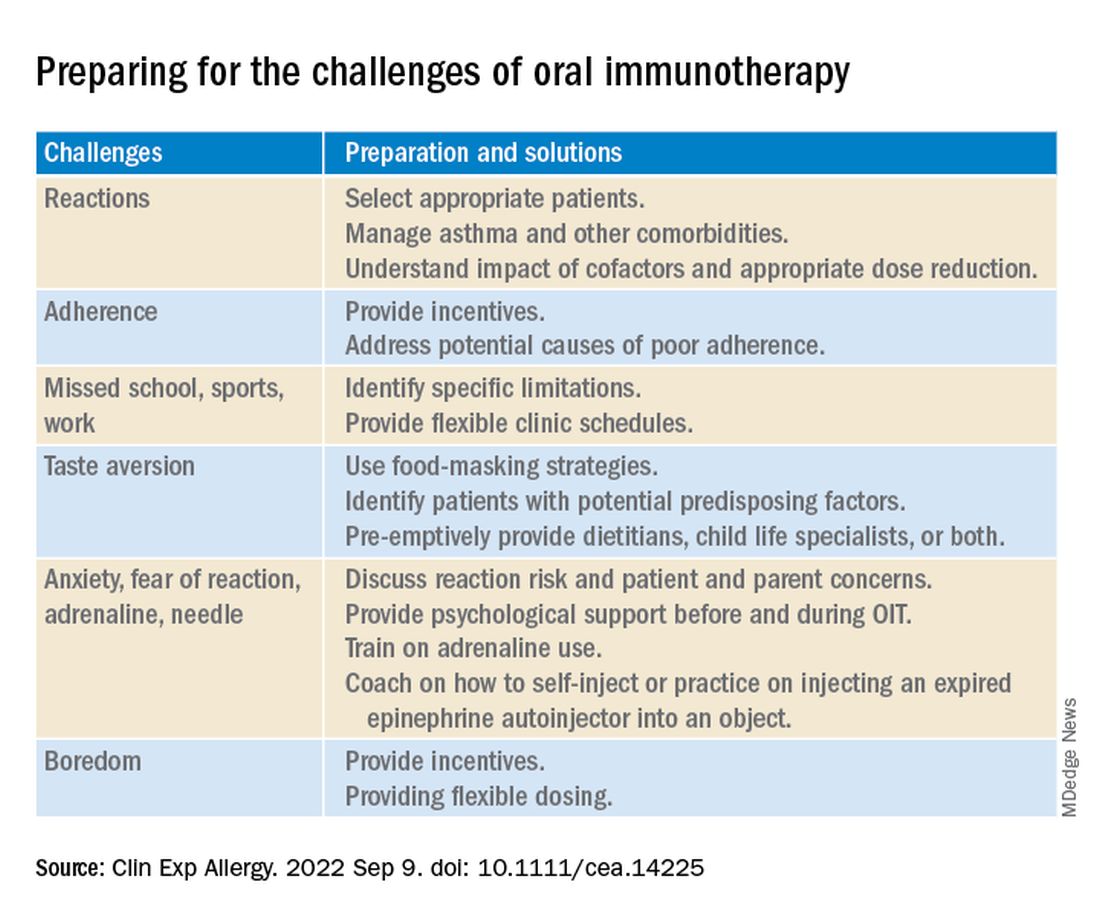
Two experts welcome the report
Rita Kachru, MD, a specialist in allergy and immunology and a codirector of the food allergy program at UCLA Health in Los Angeles, called this “an excellent report about a wonderful, individualized option in food allergy management.
“The authors did an excellent job delineating OIT terminology, outlining the goals, risks, and benefits of OIT, noting that it’s not a cure, and emphasizing the crucial importance of discussions with each family throughout the process,” Dr. Kachru, who was not involved in developing the report, told this news organization.
“I thoroughly agree with their assessment,” she added. “The more you do OIT research and clinical care, the more you realize the pitfalls, the benefits, and the importance of patient goals and family dynamics. Discussing the goals, risks, benefits, and alternatives to OIT in detail with the family is crucial so they fully understand the process.”
Basil M. Kahwash, MD, an allergy, pulmonary, and critical care medicine specialist at Vanderbilt University Medical Center in Nashville, Tenn., said that providers in the immunology community have been discussing OIT for years and that he welcomes the well-written report that summarizes the evidence.
“It’s important to periodically summarize the evidence, as well as the consensus expert opinion about the evidence, so we may better inform our colleagues and patients,” said Dr. Kahwash, who was not involved in developing the report. “The authors are well-known experts in our field who have experience with OIT and with reviewing the evidence of food allergy.
“OIT can be a fantastic option for some patients, especially those who are very highly motivated and understand the process from start to finish. But OIT is not the best option for every child, and it’s not much of an option for adults,” he explained. “Patients need to be chosen carefully and understand the level of motivation required to safely follow through with the treatment.
“The report will hopefully affect patient care positively and allow patients to understand the limitations around OIT when they consider their candidacy for it,” he added. “In most cases, OIT patients will still need to avoid the allergen, but if a small amount accidentally gets into their food, they probably won’t have a very severe reaction to it.”
Dr. Kahwash would like to see data on patients who have seen long-term remission with OIT.
“Clearly, some patients benefit from OIT. What differentiates patients who benefit from OIT from those who do not?” he asked. “In the future, we need to consider possible biomarkers of patients who are and who aren’t good candidates for OIT.
“Regardless of OIT’s limitations, the potential for desensitization rather than strict avoidance represents a big step in the evolution of food allergy treatment,” Dr. Kahwash noted.
No funding details were provided. Dr. Mack and three coauthors report financial relationships with Aimmune. Aimmune Therapeutics is the manufacturer of Palforzia OIT (AR101 powder provided in capsules and sachets). Most coauthors also report financial relationships with other pharmaceutical companies. The full list can be found with the original article. Dr. Kachru was an investigator in the PALISADES clinical trial of AR101. Dr. Kahwash reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL & EXPERIMENTAL ALLERGY
Younger doctors call for more attention to patients with disabilities
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
Understanding of capillary malformation characteristics continue to evolve
INDIANAPOLIS – The way Maria C. Garzon, MD, sees it,
“The challenge is, we also use that term to describe a diagnosis,” Dr. Garzon, professor of dermatology and pediatrics at Columbia University, New York, said at the annual meeting of the Society for Pediatric Dermatology. “We have imperfect terminology. We use many different terms like capillary nevi and vascular stain. Instead of port wine stain, we now use the term port wine birthmark, and old terms like nevus flammeus are still used. This leads to diagnostic confusion, and it’s a barrier to developing care guidelines.”
Some capillary malformations, she noted, are benign and fade away while others can cause disfigurement or herald significant medical issues.
Histologically, she continued, not all capillary malformations are composed of capillaries. “Some are composed of postcapillary venules,” she said. “There are also mixed type capillary malformations that include lymphatic tissue, and the capillary malformation of capillary malformation-arteriovenous malformation (CM-AVM) syndrome shares histologic features of evolving AVMs as opposed to classic port wine birthmarks.”
The most recent International Society for the Study of Vascular Anomalies Classification of Vascular Anomalies was published in 2018 and is currently being updated. Other proposed clinical classifications have been published, including one that is diagnosis-specific and includes 20 different types of capillary malformations (J Eur Acad Dermatol Venereol. 2015 29[12]:2295-305, Pediatr Dermatol. 2016;33[6]:570-84).
“There are also syndromic classifications. Another question relates to the role of genomics: Are we ready for a classification that’s based purely on genetic variants, or do we need to incorporate it into existing classifications?” Dr. Garzon said. “Novel testing technologies using cell-free DNA and digital droplet PCR may be used in the future to establish diagnoses.” Genetic variants are found within capillary malformations, and they tend to be associated with three major pathways: the RAS-MAPK/ERK pathway, the PI3K/Akt/mTOR pathway, and the G protein pathway.
The type of capillary malformation that dermatologists and pediatricians most commonly see is nevus simplex, which occurs in 20%-82% of neonates. Other terms used include angel’s kiss, stork bite, salmon patch, nevus flammeus simplex, fading vascular stain, medial telangiectatic nevus, and butterfly mark. “It’s important to differentiate this from a port wine birthmark,” Dr. Garzon said. “This can be challenging when the birthmark is a darker red color. I have cared for patients who were initially thought to have nevus simplex and later found to have Sturge-Weber syndrome.”
Typical locations of nevus simplex include the central forehead/glabella, eyelids, the nape of the neck, scalp (parietal and occipital), nose, lip area (including philtrum), and the back (lumbosacral area and upper back). Most lesions fade/disappear without treatment (J Am Acad Dermatol. 2020;63[5]:805-14). Rare genetic syndromes associated with exaggerated nevus simplex complex include macrocephaly-capillary malformation syndrome and Beckwith-Wiedemann syndrome, “which tells us that this is a heterogeneous group of patients,” she said.
Dr. Garzon added that it’s “incredibly common” to see an eczema flare occurring within a nevus simplex on the nape of the neck. These patients will have a patch of atopic dermatitis that doesn’t get better. “Beneath it is their nevus simplex,” she said. “Remind parents that even after treating the eczema, the pink patch is not going to go away” (Pediatr Rep. 2021;13[1]:131-4).
Meanwhile, the classic port wine birthmark is usually congenital, uniform, and darker red in color. It darkens with maturity and the pattern will correlate with embryonic vasculature. “I am very wary of acquired port wine lesions,” she added. “It’s been described with trauma-related lesions, but early morphea can also mimic a port wine birthmark. You will see this if you’re practicing pediatric dermatology.”
Nearly a decade ago researchers established a link between port wine birthmarks and genetic variants in the GNAQ gene. “We see this in GNA11 as well,” Dr. Garzon said. “These changes are found in isolated port wine stains, and in Sturge-Weber syndrome. We now know that GNAQ drives the formation of large blood vessels through angiopoietin-2,” she noted (Arterioscler Throm Vasc Biol. 2022;42[1]:e27-43).
In general, studies that have examined genotype-phenotype correlations have demonstrated that the classic port wine birthmark is associated with GNAQ while GNA11 variants can be associated with a more reticulated pattern. “But this is not as clearcut as it seems,” she said. Investigators of a recent study showed an association between hypertension and renal anomalies in patients with skin capillary malformations and mosaic GNAQ or GNA11 variants. “This is a new finding,” she said. “Investigators are working to understand this association.”
Port wine birthmarks with the highest risk of Sturge-Weber syndrome include those that involve the forehead, upper eyelid, the midline frontonasal area, the hemifacial area, and median sites. “Patients who have this should be evaluated at birth,” Dr. Garzon said. “You should not delay for 2 months. They should be evaluated by ophthalmology and neurology early.”
The other morphologies commonly seen are “geographic” well-demarcated capillary malformations, which are dark in color. These lesions can be seen in conditions that are associated with genetic variants in PIK3CA (PROS) and include classic Klippel-Trenaunay syndrome, CLOVES (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, scoliosis/skeletal and spinal) syndrome, and CLAPO (capillary malformation of the lower lip, lymphatic malformation of the face and neck, asymmetry of the face and limbs, and partial or generalized overgrowth) syndrome.
“Reticulated stains are much more heterogeneous,” Dr. Garzon said. “They can be localized or widespread. When you see a patient with a widespread reticulated capillary malformation, think about diffuse capillary malformation with overgrowth (DCMO). This condition is clinically and genetically heterogenous with the affected tissue of some patients showing variants in GNA11 while others have variants in PIK3CA. Therefore, a thorough examination at presentation and long-term follow-up is very important.”
Dr. Garzon disclosed that she is a member of the executive board for the International Society for the Study of Vascular Anomalies.
INDIANAPOLIS – The way Maria C. Garzon, MD, sees it,
“The challenge is, we also use that term to describe a diagnosis,” Dr. Garzon, professor of dermatology and pediatrics at Columbia University, New York, said at the annual meeting of the Society for Pediatric Dermatology. “We have imperfect terminology. We use many different terms like capillary nevi and vascular stain. Instead of port wine stain, we now use the term port wine birthmark, and old terms like nevus flammeus are still used. This leads to diagnostic confusion, and it’s a barrier to developing care guidelines.”
Some capillary malformations, she noted, are benign and fade away while others can cause disfigurement or herald significant medical issues.
Histologically, she continued, not all capillary malformations are composed of capillaries. “Some are composed of postcapillary venules,” she said. “There are also mixed type capillary malformations that include lymphatic tissue, and the capillary malformation of capillary malformation-arteriovenous malformation (CM-AVM) syndrome shares histologic features of evolving AVMs as opposed to classic port wine birthmarks.”
The most recent International Society for the Study of Vascular Anomalies Classification of Vascular Anomalies was published in 2018 and is currently being updated. Other proposed clinical classifications have been published, including one that is diagnosis-specific and includes 20 different types of capillary malformations (J Eur Acad Dermatol Venereol. 2015 29[12]:2295-305, Pediatr Dermatol. 2016;33[6]:570-84).
“There are also syndromic classifications. Another question relates to the role of genomics: Are we ready for a classification that’s based purely on genetic variants, or do we need to incorporate it into existing classifications?” Dr. Garzon said. “Novel testing technologies using cell-free DNA and digital droplet PCR may be used in the future to establish diagnoses.” Genetic variants are found within capillary malformations, and they tend to be associated with three major pathways: the RAS-MAPK/ERK pathway, the PI3K/Akt/mTOR pathway, and the G protein pathway.
The type of capillary malformation that dermatologists and pediatricians most commonly see is nevus simplex, which occurs in 20%-82% of neonates. Other terms used include angel’s kiss, stork bite, salmon patch, nevus flammeus simplex, fading vascular stain, medial telangiectatic nevus, and butterfly mark. “It’s important to differentiate this from a port wine birthmark,” Dr. Garzon said. “This can be challenging when the birthmark is a darker red color. I have cared for patients who were initially thought to have nevus simplex and later found to have Sturge-Weber syndrome.”
Typical locations of nevus simplex include the central forehead/glabella, eyelids, the nape of the neck, scalp (parietal and occipital), nose, lip area (including philtrum), and the back (lumbosacral area and upper back). Most lesions fade/disappear without treatment (J Am Acad Dermatol. 2020;63[5]:805-14). Rare genetic syndromes associated with exaggerated nevus simplex complex include macrocephaly-capillary malformation syndrome and Beckwith-Wiedemann syndrome, “which tells us that this is a heterogeneous group of patients,” she said.
Dr. Garzon added that it’s “incredibly common” to see an eczema flare occurring within a nevus simplex on the nape of the neck. These patients will have a patch of atopic dermatitis that doesn’t get better. “Beneath it is their nevus simplex,” she said. “Remind parents that even after treating the eczema, the pink patch is not going to go away” (Pediatr Rep. 2021;13[1]:131-4).
Meanwhile, the classic port wine birthmark is usually congenital, uniform, and darker red in color. It darkens with maturity and the pattern will correlate with embryonic vasculature. “I am very wary of acquired port wine lesions,” she added. “It’s been described with trauma-related lesions, but early morphea can also mimic a port wine birthmark. You will see this if you’re practicing pediatric dermatology.”
Nearly a decade ago researchers established a link between port wine birthmarks and genetic variants in the GNAQ gene. “We see this in GNA11 as well,” Dr. Garzon said. “These changes are found in isolated port wine stains, and in Sturge-Weber syndrome. We now know that GNAQ drives the formation of large blood vessels through angiopoietin-2,” she noted (Arterioscler Throm Vasc Biol. 2022;42[1]:e27-43).
In general, studies that have examined genotype-phenotype correlations have demonstrated that the classic port wine birthmark is associated with GNAQ while GNA11 variants can be associated with a more reticulated pattern. “But this is not as clearcut as it seems,” she said. Investigators of a recent study showed an association between hypertension and renal anomalies in patients with skin capillary malformations and mosaic GNAQ or GNA11 variants. “This is a new finding,” she said. “Investigators are working to understand this association.”
Port wine birthmarks with the highest risk of Sturge-Weber syndrome include those that involve the forehead, upper eyelid, the midline frontonasal area, the hemifacial area, and median sites. “Patients who have this should be evaluated at birth,” Dr. Garzon said. “You should not delay for 2 months. They should be evaluated by ophthalmology and neurology early.”
The other morphologies commonly seen are “geographic” well-demarcated capillary malformations, which are dark in color. These lesions can be seen in conditions that are associated with genetic variants in PIK3CA (PROS) and include classic Klippel-Trenaunay syndrome, CLOVES (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, scoliosis/skeletal and spinal) syndrome, and CLAPO (capillary malformation of the lower lip, lymphatic malformation of the face and neck, asymmetry of the face and limbs, and partial or generalized overgrowth) syndrome.
“Reticulated stains are much more heterogeneous,” Dr. Garzon said. “They can be localized or widespread. When you see a patient with a widespread reticulated capillary malformation, think about diffuse capillary malformation with overgrowth (DCMO). This condition is clinically and genetically heterogenous with the affected tissue of some patients showing variants in GNA11 while others have variants in PIK3CA. Therefore, a thorough examination at presentation and long-term follow-up is very important.”
Dr. Garzon disclosed that she is a member of the executive board for the International Society for the Study of Vascular Anomalies.
INDIANAPOLIS – The way Maria C. Garzon, MD, sees it,
“The challenge is, we also use that term to describe a diagnosis,” Dr. Garzon, professor of dermatology and pediatrics at Columbia University, New York, said at the annual meeting of the Society for Pediatric Dermatology. “We have imperfect terminology. We use many different terms like capillary nevi and vascular stain. Instead of port wine stain, we now use the term port wine birthmark, and old terms like nevus flammeus are still used. This leads to diagnostic confusion, and it’s a barrier to developing care guidelines.”
Some capillary malformations, she noted, are benign and fade away while others can cause disfigurement or herald significant medical issues.
Histologically, she continued, not all capillary malformations are composed of capillaries. “Some are composed of postcapillary venules,” she said. “There are also mixed type capillary malformations that include lymphatic tissue, and the capillary malformation of capillary malformation-arteriovenous malformation (CM-AVM) syndrome shares histologic features of evolving AVMs as opposed to classic port wine birthmarks.”
The most recent International Society for the Study of Vascular Anomalies Classification of Vascular Anomalies was published in 2018 and is currently being updated. Other proposed clinical classifications have been published, including one that is diagnosis-specific and includes 20 different types of capillary malformations (J Eur Acad Dermatol Venereol. 2015 29[12]:2295-305, Pediatr Dermatol. 2016;33[6]:570-84).
“There are also syndromic classifications. Another question relates to the role of genomics: Are we ready for a classification that’s based purely on genetic variants, or do we need to incorporate it into existing classifications?” Dr. Garzon said. “Novel testing technologies using cell-free DNA and digital droplet PCR may be used in the future to establish diagnoses.” Genetic variants are found within capillary malformations, and they tend to be associated with three major pathways: the RAS-MAPK/ERK pathway, the PI3K/Akt/mTOR pathway, and the G protein pathway.
The type of capillary malformation that dermatologists and pediatricians most commonly see is nevus simplex, which occurs in 20%-82% of neonates. Other terms used include angel’s kiss, stork bite, salmon patch, nevus flammeus simplex, fading vascular stain, medial telangiectatic nevus, and butterfly mark. “It’s important to differentiate this from a port wine birthmark,” Dr. Garzon said. “This can be challenging when the birthmark is a darker red color. I have cared for patients who were initially thought to have nevus simplex and later found to have Sturge-Weber syndrome.”
Typical locations of nevus simplex include the central forehead/glabella, eyelids, the nape of the neck, scalp (parietal and occipital), nose, lip area (including philtrum), and the back (lumbosacral area and upper back). Most lesions fade/disappear without treatment (J Am Acad Dermatol. 2020;63[5]:805-14). Rare genetic syndromes associated with exaggerated nevus simplex complex include macrocephaly-capillary malformation syndrome and Beckwith-Wiedemann syndrome, “which tells us that this is a heterogeneous group of patients,” she said.
Dr. Garzon added that it’s “incredibly common” to see an eczema flare occurring within a nevus simplex on the nape of the neck. These patients will have a patch of atopic dermatitis that doesn’t get better. “Beneath it is their nevus simplex,” she said. “Remind parents that even after treating the eczema, the pink patch is not going to go away” (Pediatr Rep. 2021;13[1]:131-4).
Meanwhile, the classic port wine birthmark is usually congenital, uniform, and darker red in color. It darkens with maturity and the pattern will correlate with embryonic vasculature. “I am very wary of acquired port wine lesions,” she added. “It’s been described with trauma-related lesions, but early morphea can also mimic a port wine birthmark. You will see this if you’re practicing pediatric dermatology.”
Nearly a decade ago researchers established a link between port wine birthmarks and genetic variants in the GNAQ gene. “We see this in GNA11 as well,” Dr. Garzon said. “These changes are found in isolated port wine stains, and in Sturge-Weber syndrome. We now know that GNAQ drives the formation of large blood vessels through angiopoietin-2,” she noted (Arterioscler Throm Vasc Biol. 2022;42[1]:e27-43).
In general, studies that have examined genotype-phenotype correlations have demonstrated that the classic port wine birthmark is associated with GNAQ while GNA11 variants can be associated with a more reticulated pattern. “But this is not as clearcut as it seems,” she said. Investigators of a recent study showed an association between hypertension and renal anomalies in patients with skin capillary malformations and mosaic GNAQ or GNA11 variants. “This is a new finding,” she said. “Investigators are working to understand this association.”
Port wine birthmarks with the highest risk of Sturge-Weber syndrome include those that involve the forehead, upper eyelid, the midline frontonasal area, the hemifacial area, and median sites. “Patients who have this should be evaluated at birth,” Dr. Garzon said. “You should not delay for 2 months. They should be evaluated by ophthalmology and neurology early.”
The other morphologies commonly seen are “geographic” well-demarcated capillary malformations, which are dark in color. These lesions can be seen in conditions that are associated with genetic variants in PIK3CA (PROS) and include classic Klippel-Trenaunay syndrome, CLOVES (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, scoliosis/skeletal and spinal) syndrome, and CLAPO (capillary malformation of the lower lip, lymphatic malformation of the face and neck, asymmetry of the face and limbs, and partial or generalized overgrowth) syndrome.
“Reticulated stains are much more heterogeneous,” Dr. Garzon said. “They can be localized or widespread. When you see a patient with a widespread reticulated capillary malformation, think about diffuse capillary malformation with overgrowth (DCMO). This condition is clinically and genetically heterogenous with the affected tissue of some patients showing variants in GNA11 while others have variants in PIK3CA. Therefore, a thorough examination at presentation and long-term follow-up is very important.”
Dr. Garzon disclosed that she is a member of the executive board for the International Society for the Study of Vascular Anomalies.
AT SPD 2022
New EU guidelines: Individualize care for thyroid cancer in kids
Comprehensive evaluation, multidisciplinary care, individualized treatment, and ongoing follow-up are all key to the management of pediatric thyroid nodules and differentiated thyroid carcinoma (DTC), according to the first European guidelines for this rare disease.
The guidelines were recently published in the European Thyroid Journal.
Lead author Chantal A. Lebbink told this news organization one of the key takeaways for clinicians is that management of pediatric thyroid nodules and DTC is «challenging and cannot be captured in a one-size-fits-all model.”
She also underlined the need for a “multidisciplinary approach in pediatric thyroid cancer expertise centers.”
Above all, Ms. Lebbink, who is a PhD student in the department of pediatric endocrinology, Wilhelmina Children’s Hospital, Utrecht, the Netherlands, said that pediatric DTC “is not adult DTC in a small person; it has different genetics and a different clinical behavior.”
The authors noted that DTC may be a rare disease, but its worldwide incidence is rising. It has several histologic subtypes, although the “vast majority” of cases are papillary thyroid carcinoma.
Crucially, there are “important differences” between adult and pediatric DTC in terms of their clinical, molecular, and pathologic characteristics, with pediatric patients commonly presenting with more advanced disease with greater lymph node involvement, distant metastases, and multifocal disease.
“However, despite the aggressive presentation, the overall survival rates are excellent,” Ms. Lebbink said.
There are also differences in genetic alterations between adult and pediatric patients. RET-PTC and NTRK fusions are more common in pediatric patients, while mutations in BRAF V600E and RAS point mutations are less frequent.
First European guidelines on thyroid cancer, thyroid nodules in children
Despite these differences, and the existence of U.S. guidelines, until now there have been no European recommendations on the management of pediatric thyroid nodules and DTC.
The European Thyroid Association therefore convened a panel of experts in pediatric and adult endocrinology, pathology, endocrine surgery, nuclear medicine, clinical genetics, and oncology, and tasked them with looking at diagnostics and staging, treatment, and follow-up.
The 2015 American Thyroid Association pediatric guideline was used as framework for the European guideline, with the expert panel identifying areas of discordance and outstanding clinical questions (Thyroid. 2015 Jul;25[7]:716-59).
To answer these questions, they searched PubMed and identified 3,251 studies, of which 45 studies met the inclusion criteria. From this they developed a comprehensive set of recommendations. These include that a child with suspected or proven cancer be referred to an experienced multidisciplinary team and their likely benefit from higher- versus lower-intensity treatment be established.
In addition, children should undergo a preoperative evaluation, with neck palpation, comprehensive neck ultrasonography, and laboratory work-up as a minimum, with further testing suggested in case of a family history or extensive disease.
Total thyroidectomy is the recommended treatment, although the authors call for further studies to assess the impact of limited surgery, and they suggest that prophylactic central lymph node dissection be reserved for advanced cases.
Crucially, all children “should be operated on by high-volume pediatric thyroid cancer surgeons with experience in pediatric thyroid cancer and who are embedded in a center with expertise in the management of DTC,” they wrote.
RAI therapy recommended for all children, in contrast to ATA guidelines
Radioactive iodine (I-131) therapy is recommended for all children following total thyroidectomy, with treatment following an individual patient-based approach.
This differs slightly from the ATA guidelines, which recommend against radioactive iodine (RAI) therapy for children with low-risk differentiated thyroid cancer that is mostly confined to the thyroid (N0 or minimal N1a disease). A study presented at the recent 2022 annual meeting of the ATA found that such children who were spared RAI showed no increases in risk of remission compared with those who did receive it.
The ETA guidelines then go on to recommend that children should be followed up with thyroid-stimulating hormone monitoring and suppression to low-normal levels, as well as serum thyroglobulin measurement and neck ultrasound, although other imaging modalities are not recommended.
In children with persistent or recurrent cervical disease, “surgery or I-131 therapy are indicated depending on the size, tumor load, and degree of progression,” and the authors said that cases of radioactive refractory disease should be “thoroughly investigated.”
Patients should also be counseled on the risk of the late effects of treatment for DTC and undergo monitoring, with follow-up continued for at least 10 years. Any subsequent follow-up should be “the result of shared decision-making between the physician and the patient.”
Evidence for molecular testing is scarce
Ms. Lebbink said that developing the guidelines nevertheless revealed a series of gaps in current knowledge, notably that the evidence for molecular testing “and the clinical implications in the preoperative stage are scarce.”
Specifically, the “positive and negative predictive value of molecular testing in fine needle biopsy specimen for the presence of DTC in a thyroid nodule must be further investigated.»
She also said that there has been a shift towards less aggressive treatment, due to a reluctance to performed prophylactic central neck dissection, and to offer I-131 therapy after surgery.
“However, before less aggressive treatment could be recommended,” Ms. Lebbink said, “it first must be investigated if there are differences in outcomes,” such as recurrence rates, disease-free survival rates, and survival rates between patients who do and do not receive the treatments.
No funding was declared. One author has reported relationships with Sanofi, AstraZeneca, Bayer, and GE. No other relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Comprehensive evaluation, multidisciplinary care, individualized treatment, and ongoing follow-up are all key to the management of pediatric thyroid nodules and differentiated thyroid carcinoma (DTC), according to the first European guidelines for this rare disease.
The guidelines were recently published in the European Thyroid Journal.
Lead author Chantal A. Lebbink told this news organization one of the key takeaways for clinicians is that management of pediatric thyroid nodules and DTC is «challenging and cannot be captured in a one-size-fits-all model.”
She also underlined the need for a “multidisciplinary approach in pediatric thyroid cancer expertise centers.”
Above all, Ms. Lebbink, who is a PhD student in the department of pediatric endocrinology, Wilhelmina Children’s Hospital, Utrecht, the Netherlands, said that pediatric DTC “is not adult DTC in a small person; it has different genetics and a different clinical behavior.”
The authors noted that DTC may be a rare disease, but its worldwide incidence is rising. It has several histologic subtypes, although the “vast majority” of cases are papillary thyroid carcinoma.
Crucially, there are “important differences” between adult and pediatric DTC in terms of their clinical, molecular, and pathologic characteristics, with pediatric patients commonly presenting with more advanced disease with greater lymph node involvement, distant metastases, and multifocal disease.
“However, despite the aggressive presentation, the overall survival rates are excellent,” Ms. Lebbink said.
There are also differences in genetic alterations between adult and pediatric patients. RET-PTC and NTRK fusions are more common in pediatric patients, while mutations in BRAF V600E and RAS point mutations are less frequent.
First European guidelines on thyroid cancer, thyroid nodules in children
Despite these differences, and the existence of U.S. guidelines, until now there have been no European recommendations on the management of pediatric thyroid nodules and DTC.
The European Thyroid Association therefore convened a panel of experts in pediatric and adult endocrinology, pathology, endocrine surgery, nuclear medicine, clinical genetics, and oncology, and tasked them with looking at diagnostics and staging, treatment, and follow-up.
The 2015 American Thyroid Association pediatric guideline was used as framework for the European guideline, with the expert panel identifying areas of discordance and outstanding clinical questions (Thyroid. 2015 Jul;25[7]:716-59).
To answer these questions, they searched PubMed and identified 3,251 studies, of which 45 studies met the inclusion criteria. From this they developed a comprehensive set of recommendations. These include that a child with suspected or proven cancer be referred to an experienced multidisciplinary team and their likely benefit from higher- versus lower-intensity treatment be established.
In addition, children should undergo a preoperative evaluation, with neck palpation, comprehensive neck ultrasonography, and laboratory work-up as a minimum, with further testing suggested in case of a family history or extensive disease.
Total thyroidectomy is the recommended treatment, although the authors call for further studies to assess the impact of limited surgery, and they suggest that prophylactic central lymph node dissection be reserved for advanced cases.
Crucially, all children “should be operated on by high-volume pediatric thyroid cancer surgeons with experience in pediatric thyroid cancer and who are embedded in a center with expertise in the management of DTC,” they wrote.
RAI therapy recommended for all children, in contrast to ATA guidelines
Radioactive iodine (I-131) therapy is recommended for all children following total thyroidectomy, with treatment following an individual patient-based approach.
This differs slightly from the ATA guidelines, which recommend against radioactive iodine (RAI) therapy for children with low-risk differentiated thyroid cancer that is mostly confined to the thyroid (N0 or minimal N1a disease). A study presented at the recent 2022 annual meeting of the ATA found that such children who were spared RAI showed no increases in risk of remission compared with those who did receive it.
The ETA guidelines then go on to recommend that children should be followed up with thyroid-stimulating hormone monitoring and suppression to low-normal levels, as well as serum thyroglobulin measurement and neck ultrasound, although other imaging modalities are not recommended.
In children with persistent or recurrent cervical disease, “surgery or I-131 therapy are indicated depending on the size, tumor load, and degree of progression,” and the authors said that cases of radioactive refractory disease should be “thoroughly investigated.”
Patients should also be counseled on the risk of the late effects of treatment for DTC and undergo monitoring, with follow-up continued for at least 10 years. Any subsequent follow-up should be “the result of shared decision-making between the physician and the patient.”
Evidence for molecular testing is scarce
Ms. Lebbink said that developing the guidelines nevertheless revealed a series of gaps in current knowledge, notably that the evidence for molecular testing “and the clinical implications in the preoperative stage are scarce.”
Specifically, the “positive and negative predictive value of molecular testing in fine needle biopsy specimen for the presence of DTC in a thyroid nodule must be further investigated.»
She also said that there has been a shift towards less aggressive treatment, due to a reluctance to performed prophylactic central neck dissection, and to offer I-131 therapy after surgery.
“However, before less aggressive treatment could be recommended,” Ms. Lebbink said, “it first must be investigated if there are differences in outcomes,” such as recurrence rates, disease-free survival rates, and survival rates between patients who do and do not receive the treatments.
No funding was declared. One author has reported relationships with Sanofi, AstraZeneca, Bayer, and GE. No other relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Comprehensive evaluation, multidisciplinary care, individualized treatment, and ongoing follow-up are all key to the management of pediatric thyroid nodules and differentiated thyroid carcinoma (DTC), according to the first European guidelines for this rare disease.
The guidelines were recently published in the European Thyroid Journal.
Lead author Chantal A. Lebbink told this news organization one of the key takeaways for clinicians is that management of pediatric thyroid nodules and DTC is «challenging and cannot be captured in a one-size-fits-all model.”
She also underlined the need for a “multidisciplinary approach in pediatric thyroid cancer expertise centers.”
Above all, Ms. Lebbink, who is a PhD student in the department of pediatric endocrinology, Wilhelmina Children’s Hospital, Utrecht, the Netherlands, said that pediatric DTC “is not adult DTC in a small person; it has different genetics and a different clinical behavior.”
The authors noted that DTC may be a rare disease, but its worldwide incidence is rising. It has several histologic subtypes, although the “vast majority” of cases are papillary thyroid carcinoma.
Crucially, there are “important differences” between adult and pediatric DTC in terms of their clinical, molecular, and pathologic characteristics, with pediatric patients commonly presenting with more advanced disease with greater lymph node involvement, distant metastases, and multifocal disease.
“However, despite the aggressive presentation, the overall survival rates are excellent,” Ms. Lebbink said.
There are also differences in genetic alterations between adult and pediatric patients. RET-PTC and NTRK fusions are more common in pediatric patients, while mutations in BRAF V600E and RAS point mutations are less frequent.
First European guidelines on thyroid cancer, thyroid nodules in children
Despite these differences, and the existence of U.S. guidelines, until now there have been no European recommendations on the management of pediatric thyroid nodules and DTC.
The European Thyroid Association therefore convened a panel of experts in pediatric and adult endocrinology, pathology, endocrine surgery, nuclear medicine, clinical genetics, and oncology, and tasked them with looking at diagnostics and staging, treatment, and follow-up.
The 2015 American Thyroid Association pediatric guideline was used as framework for the European guideline, with the expert panel identifying areas of discordance and outstanding clinical questions (Thyroid. 2015 Jul;25[7]:716-59).
To answer these questions, they searched PubMed and identified 3,251 studies, of which 45 studies met the inclusion criteria. From this they developed a comprehensive set of recommendations. These include that a child with suspected or proven cancer be referred to an experienced multidisciplinary team and their likely benefit from higher- versus lower-intensity treatment be established.
In addition, children should undergo a preoperative evaluation, with neck palpation, comprehensive neck ultrasonography, and laboratory work-up as a minimum, with further testing suggested in case of a family history or extensive disease.
Total thyroidectomy is the recommended treatment, although the authors call for further studies to assess the impact of limited surgery, and they suggest that prophylactic central lymph node dissection be reserved for advanced cases.
Crucially, all children “should be operated on by high-volume pediatric thyroid cancer surgeons with experience in pediatric thyroid cancer and who are embedded in a center with expertise in the management of DTC,” they wrote.
RAI therapy recommended for all children, in contrast to ATA guidelines
Radioactive iodine (I-131) therapy is recommended for all children following total thyroidectomy, with treatment following an individual patient-based approach.
This differs slightly from the ATA guidelines, which recommend against radioactive iodine (RAI) therapy for children with low-risk differentiated thyroid cancer that is mostly confined to the thyroid (N0 or minimal N1a disease). A study presented at the recent 2022 annual meeting of the ATA found that such children who were spared RAI showed no increases in risk of remission compared with those who did receive it.
The ETA guidelines then go on to recommend that children should be followed up with thyroid-stimulating hormone monitoring and suppression to low-normal levels, as well as serum thyroglobulin measurement and neck ultrasound, although other imaging modalities are not recommended.
In children with persistent or recurrent cervical disease, “surgery or I-131 therapy are indicated depending on the size, tumor load, and degree of progression,” and the authors said that cases of radioactive refractory disease should be “thoroughly investigated.”
Patients should also be counseled on the risk of the late effects of treatment for DTC and undergo monitoring, with follow-up continued for at least 10 years. Any subsequent follow-up should be “the result of shared decision-making between the physician and the patient.”
Evidence for molecular testing is scarce
Ms. Lebbink said that developing the guidelines nevertheless revealed a series of gaps in current knowledge, notably that the evidence for molecular testing “and the clinical implications in the preoperative stage are scarce.”
Specifically, the “positive and negative predictive value of molecular testing in fine needle biopsy specimen for the presence of DTC in a thyroid nodule must be further investigated.»
She also said that there has been a shift towards less aggressive treatment, due to a reluctance to performed prophylactic central neck dissection, and to offer I-131 therapy after surgery.
“However, before less aggressive treatment could be recommended,” Ms. Lebbink said, “it first must be investigated if there are differences in outcomes,” such as recurrence rates, disease-free survival rates, and survival rates between patients who do and do not receive the treatments.
No funding was declared. One author has reported relationships with Sanofi, AstraZeneca, Bayer, and GE. No other relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM THE EUROPEAN THYROID JOURNAL
Has the pandemic affected babies’ brain development?
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
FROM JAMA NETWORK OPEN




