User login
For MD-IQ use only
Daily Recap: Healthy lifestyle may stave off dementia; Tentative evidence on marijuana for migraine
Here are the stories our MDedge editors across specialties think you need to know about today:
First reported U.S. case of COVID-19 linked to Guillain-Barré syndrome
The first official U.S. case of Guillain-Barré syndrome (GBS) associated with COVID-19 has been reported by neurologists from Allegheny General Hospital in Pittsburgh, further supporting a link between the virus and neurologic complications, including GBS.
Physicians in China reported the first case that initially presented as acute GBS. Subsequently, physicians in Italy reported five cases of GBS in association with COVID-19.
“This onset is similar to a case report of acute Zika virus infection with concurrent GBS suggesting a parainfectious complication,” first author Sandeep Rana, MD, and colleagues noted. Read more.
Five healthy lifestyle choices tied to dramatic cut in dementia risk
Combining four of five healthy lifestyle choices has been linked to up to a 60% reduced risk for Alzheimer’s dementia in new research that strengthens ties between healthy behaviors and lower dementia risk. “I hope this study will motivate people to engage in a healthy lifestyle by not smoking, being physically and cognitively active, and having a high-quality diet,” lead investigator Klodian Dhana, MD, PhD, said in an interview.
They defined a healthy lifestyle score on the basis of the following factors: not smoking; engaging in 150 min/wk or more of physical exercise; light to moderate alcohol consumption; consuming a high-quality Mediterranean-DASH Diet Intervention for Neurodegenerative Delay diet (upper 40%); and engaging in late-life cognitive activities.
“What needs to be determined is how early should we start ‘behaving.’ We should all aim to score four to five factors across our entire lifespan, but this is not always feasible. So, when is the time to behave? Also, what is the relative weight of each of these factors?” said Luca Giliberto, MD, PhD. Read more.
Marijuana for migraine? Some tentative evidence
Medical marijuana may have promise for managing headache pain, according to results from a small study conducted at the Jefferson Headache Center at Thomas Jefferson University. The researchers found general satisfaction with medical marijuana, more frequent use as an abortive medication rather than a preventative, and more than two-thirds using the inhaled form rather than oral.
“A lot of patients are interested in medical marijuana but don’t know how to integrate it into the therapy plan they already have – whether it should be just to treat bad headaches when they happen, or is it meant to be a preventive medicine they use every day? We have some data out there that it can be helpful, but not a lot of specific information to guide your recommendations,” said Jefferson headache fellow Claire Ceriani, MD, in an interview. Read more.
Inside Mercy’s mission to care for non-COVID patients in Los Angeles
When the hospital ship USNS Mercy departed San Diego’s Naval Station North Island on March 23, 2020, to support the Department of Defense efforts in Los Angeles during the coronavirus outbreak, Commander Erin Blevins remembers the crew’s excitement was palpable. “We normally do partnerships abroad and respond to tsunamis and earthquakes,” said Cdr. Blevins, MD, a pediatric hematologist-oncologist who served as director of medical services for the mission.
Between March 29 and May 15, about 1,071 medical personnel aboard the Mercy cared for 77 patients with an average age of 53 years who were referred from 11 Los Angeles area hospitals.
Care aboard the ship ranged from basic medical and surgical care to critical care and trauma. The most common procedures were cholecystectomies and orthopedic procedures, and the average length of stay was 4-5 days, according to Cdr. Blevins. Over the course of the mission, the medical professionals conducted 36 surgeries, 77 x-ray exams, 26 CT scans, and administered hundreds of ancillary studies ranging from routine labs to high-end x-rays and blood transfusion support. Special Feature.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
First reported U.S. case of COVID-19 linked to Guillain-Barré syndrome
The first official U.S. case of Guillain-Barré syndrome (GBS) associated with COVID-19 has been reported by neurologists from Allegheny General Hospital in Pittsburgh, further supporting a link between the virus and neurologic complications, including GBS.
Physicians in China reported the first case that initially presented as acute GBS. Subsequently, physicians in Italy reported five cases of GBS in association with COVID-19.
“This onset is similar to a case report of acute Zika virus infection with concurrent GBS suggesting a parainfectious complication,” first author Sandeep Rana, MD, and colleagues noted. Read more.
Five healthy lifestyle choices tied to dramatic cut in dementia risk
Combining four of five healthy lifestyle choices has been linked to up to a 60% reduced risk for Alzheimer’s dementia in new research that strengthens ties between healthy behaviors and lower dementia risk. “I hope this study will motivate people to engage in a healthy lifestyle by not smoking, being physically and cognitively active, and having a high-quality diet,” lead investigator Klodian Dhana, MD, PhD, said in an interview.
They defined a healthy lifestyle score on the basis of the following factors: not smoking; engaging in 150 min/wk or more of physical exercise; light to moderate alcohol consumption; consuming a high-quality Mediterranean-DASH Diet Intervention for Neurodegenerative Delay diet (upper 40%); and engaging in late-life cognitive activities.
“What needs to be determined is how early should we start ‘behaving.’ We should all aim to score four to five factors across our entire lifespan, but this is not always feasible. So, when is the time to behave? Also, what is the relative weight of each of these factors?” said Luca Giliberto, MD, PhD. Read more.
Marijuana for migraine? Some tentative evidence
Medical marijuana may have promise for managing headache pain, according to results from a small study conducted at the Jefferson Headache Center at Thomas Jefferson University. The researchers found general satisfaction with medical marijuana, more frequent use as an abortive medication rather than a preventative, and more than two-thirds using the inhaled form rather than oral.
“A lot of patients are interested in medical marijuana but don’t know how to integrate it into the therapy plan they already have – whether it should be just to treat bad headaches when they happen, or is it meant to be a preventive medicine they use every day? We have some data out there that it can be helpful, but not a lot of specific information to guide your recommendations,” said Jefferson headache fellow Claire Ceriani, MD, in an interview. Read more.
Inside Mercy’s mission to care for non-COVID patients in Los Angeles
When the hospital ship USNS Mercy departed San Diego’s Naval Station North Island on March 23, 2020, to support the Department of Defense efforts in Los Angeles during the coronavirus outbreak, Commander Erin Blevins remembers the crew’s excitement was palpable. “We normally do partnerships abroad and respond to tsunamis and earthquakes,” said Cdr. Blevins, MD, a pediatric hematologist-oncologist who served as director of medical services for the mission.
Between March 29 and May 15, about 1,071 medical personnel aboard the Mercy cared for 77 patients with an average age of 53 years who were referred from 11 Los Angeles area hospitals.
Care aboard the ship ranged from basic medical and surgical care to critical care and trauma. The most common procedures were cholecystectomies and orthopedic procedures, and the average length of stay was 4-5 days, according to Cdr. Blevins. Over the course of the mission, the medical professionals conducted 36 surgeries, 77 x-ray exams, 26 CT scans, and administered hundreds of ancillary studies ranging from routine labs to high-end x-rays and blood transfusion support. Special Feature.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
First reported U.S. case of COVID-19 linked to Guillain-Barré syndrome
The first official U.S. case of Guillain-Barré syndrome (GBS) associated with COVID-19 has been reported by neurologists from Allegheny General Hospital in Pittsburgh, further supporting a link between the virus and neurologic complications, including GBS.
Physicians in China reported the first case that initially presented as acute GBS. Subsequently, physicians in Italy reported five cases of GBS in association with COVID-19.
“This onset is similar to a case report of acute Zika virus infection with concurrent GBS suggesting a parainfectious complication,” first author Sandeep Rana, MD, and colleagues noted. Read more.
Five healthy lifestyle choices tied to dramatic cut in dementia risk
Combining four of five healthy lifestyle choices has been linked to up to a 60% reduced risk for Alzheimer’s dementia in new research that strengthens ties between healthy behaviors and lower dementia risk. “I hope this study will motivate people to engage in a healthy lifestyle by not smoking, being physically and cognitively active, and having a high-quality diet,” lead investigator Klodian Dhana, MD, PhD, said in an interview.
They defined a healthy lifestyle score on the basis of the following factors: not smoking; engaging in 150 min/wk or more of physical exercise; light to moderate alcohol consumption; consuming a high-quality Mediterranean-DASH Diet Intervention for Neurodegenerative Delay diet (upper 40%); and engaging in late-life cognitive activities.
“What needs to be determined is how early should we start ‘behaving.’ We should all aim to score four to five factors across our entire lifespan, but this is not always feasible. So, when is the time to behave? Also, what is the relative weight of each of these factors?” said Luca Giliberto, MD, PhD. Read more.
Marijuana for migraine? Some tentative evidence
Medical marijuana may have promise for managing headache pain, according to results from a small study conducted at the Jefferson Headache Center at Thomas Jefferson University. The researchers found general satisfaction with medical marijuana, more frequent use as an abortive medication rather than a preventative, and more than two-thirds using the inhaled form rather than oral.
“A lot of patients are interested in medical marijuana but don’t know how to integrate it into the therapy plan they already have – whether it should be just to treat bad headaches when they happen, or is it meant to be a preventive medicine they use every day? We have some data out there that it can be helpful, but not a lot of specific information to guide your recommendations,” said Jefferson headache fellow Claire Ceriani, MD, in an interview. Read more.
Inside Mercy’s mission to care for non-COVID patients in Los Angeles
When the hospital ship USNS Mercy departed San Diego’s Naval Station North Island on March 23, 2020, to support the Department of Defense efforts in Los Angeles during the coronavirus outbreak, Commander Erin Blevins remembers the crew’s excitement was palpable. “We normally do partnerships abroad and respond to tsunamis and earthquakes,” said Cdr. Blevins, MD, a pediatric hematologist-oncologist who served as director of medical services for the mission.
Between March 29 and May 15, about 1,071 medical personnel aboard the Mercy cared for 77 patients with an average age of 53 years who were referred from 11 Los Angeles area hospitals.
Care aboard the ship ranged from basic medical and surgical care to critical care and trauma. The most common procedures were cholecystectomies and orthopedic procedures, and the average length of stay was 4-5 days, according to Cdr. Blevins. Over the course of the mission, the medical professionals conducted 36 surgeries, 77 x-ray exams, 26 CT scans, and administered hundreds of ancillary studies ranging from routine labs to high-end x-rays and blood transfusion support. Special Feature.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Women thrive on baroreflex activation for heart failure
The striking gains in functional capacity and quality of life conferred by baroreflex activation therapy in patients with heart failure, as shown in the pivotal phase 3 clinical trial for this novel intervention, were at least as great in women as in men, JoAnn Lindenfeld, MD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
The results of the multicenter, prospective, randomized BeAT-HF trial led to marketing approval of the BaroStim Neo system for improvement in symptoms of heart failure with reduced ejection fraction (HFrEF) by the Food and Drug Administration in August 2019. Dr. Lindenfeld presented a fresh breakdown of the results by gender which showed, intriguingly, that the improvement in all study endpoints was consistently numerically greater in the women – sometimes startlingly so – although these gender differences in response didn’t achieve statistical significance. The 6-month randomized trial was underpowered for drawing definitive conclusions on that score, with a study population of only 53 women and 211 men. So the investigator remained circumspect.
“We think that what this study shows us is that women have at least equivalent improvement as men in this population. I don’t think we can conclude from this study yet that it’s better, but it’s certainly in all these parameters as least as good. And I think this is a population in which we’ve seen that improving symptoms and functional capacity is very important,” said Dr. Lindenfeld, professor of medicine and director of advanced heart failure/cardiac transplantation at Vanderbilt University, Nashville, Tenn.
The FDA approval was restricted to patients like those enrolled in BeAT-HF: that is, individuals with New York Heart Association functional class III heart failure, a left ventricular ejection fraction of 35% or less while on stable optimal medical therapy, and ineligibility for cardiac resynchronization therapy according to current guidelines. Seventy-eight percent of BeAT-HF participants had an implantable cardioverter-defibrillator.
Participants were randomized to baroreflex activation therapy (BAT) plus optimal medical therapy or to optimal medical therapy alone. The three coprimary endpoints were change from baseline to 6 months in 6-minute hall walk distance (6MHW), scores on the Minnesota Living with Heart Failure Questionnaire (MLHF), and N-terminal pro-B-type natriuretic peptide (NT-proBNP).
In the overall study population, 6MHW increased by 60 m in the BAT group and decreased by 8 m in controls; MLHF scores dropped by 14 and 6 points, respectively; and NT-proBNP fell by an average of 25% with BAT while rising by 3% in controls.
Very often, just a 5-point reduction in MLHF score is considered a clinically meaningful improvement in quality of life, the cardiologist noted.
The gender-based analysis is where things got particularly interesting.
The investigators defined a clinically relevant response as a greater than 10% increase from baseline on the 6MHW, at least a one-class improvement in NYHA class, or a reduction of 5 points or more on the MLHF. Among subjects in the BAT group, 70% of women and 60% of men met the clinically relevant response standard in terms of 6MHW, as did 70% of women and 64% of men for improvement in NYHA class, and 78% of women and 66% of men for MLHF score.
Eighty-seven percent of women and 68% of men on BAT had a clinically relevant response on at least one of these endpoints, as did about 28% of controls. Moreover, 31% of women in the BAT group were clinically relevant responders on at least two endpoints, compared with 19% of BAT men and 4% and 9% of controls.
Women dominate super-responder category
In order to be classified as a super responder, a patient had to demonstrate a greater than 20% increase in 6MHW, improvement in NYHA class I status, or at least a 10-point improvement in MLHF score. Ninety-one percent of women on BAT achieved super-responder status for at least one of these endpoints, compared with 76% of men. Forty-three percent of women and 24% of men in the BAT group were super responders in at least two domains, as were 8% and 11% of female and male controls, Dr. Lindenfeld continued.
Discussant Ewa Anita Jankowska, MD, PhD, deemed the BeAT-HF results on the therapeutic benefits of this autonomic modulation strategy “quite convincing.”
“We need to acknowledge that in recent years we have been spoiled a bit by the huge trials in heart failure where the ultimate goal was a reduction in mortality. But I think this is the time when we should think about the patients who want to live – here, now – with a better life. Patients expect symptomatic benefits. There is a substantial group of patients who are symptomatic even though they receive quite extensive neurohormonal blockage and who are not suitable for CRT. This study demonstrates that, for this group of patients, BAT can bring really significant symptomatic benefits,” she said.
“If you think about a treatment that provides patients who are NYHA class III an increase in 6MHW of 60 meters, that’s really something. And 20% of patients went from NYHA class III to class I – that’s really something, too,” added Dr. Jankowska, professor of medicine and head of the laboratory of applied research on the cardiovascular system at Wroclaw (Poland) University.
How baroreflex activation therapy works
The BaroStim system consists of a 2-mm unipolar electrode on a 7-mm backer that is placed over the carotid sinus. It is supported by a small generator with a 4- to 5-year battery life implanted under the collarbone, along with radiofrequency telemetry capability and programming flexibility.
Stimulation of the carotid baroreceptor promotes an integrated autonomic nervous system response which enhances parasympathetic activity and inhibits sympathetic nervous system activity. The result, as shown in numerous earlier proof-of-concept studies, is a reduced heart rate, decreased ventricular remodeling, enhanced diuresis, increased vasodilation, a drop in elevated blood pressure, and decreased renin secretion – all achieved nonpharmacologically.
The study was sponsored by CVRx. Dr. Lindenfeld reported serving as a consultant to CVRx, Abbott, AstraZeneca, Boehringer Ingelheim, Edwards Lifesciences, Impulse Dynamics, and VWave.
The striking gains in functional capacity and quality of life conferred by baroreflex activation therapy in patients with heart failure, as shown in the pivotal phase 3 clinical trial for this novel intervention, were at least as great in women as in men, JoAnn Lindenfeld, MD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
The results of the multicenter, prospective, randomized BeAT-HF trial led to marketing approval of the BaroStim Neo system for improvement in symptoms of heart failure with reduced ejection fraction (HFrEF) by the Food and Drug Administration in August 2019. Dr. Lindenfeld presented a fresh breakdown of the results by gender which showed, intriguingly, that the improvement in all study endpoints was consistently numerically greater in the women – sometimes startlingly so – although these gender differences in response didn’t achieve statistical significance. The 6-month randomized trial was underpowered for drawing definitive conclusions on that score, with a study population of only 53 women and 211 men. So the investigator remained circumspect.
“We think that what this study shows us is that women have at least equivalent improvement as men in this population. I don’t think we can conclude from this study yet that it’s better, but it’s certainly in all these parameters as least as good. And I think this is a population in which we’ve seen that improving symptoms and functional capacity is very important,” said Dr. Lindenfeld, professor of medicine and director of advanced heart failure/cardiac transplantation at Vanderbilt University, Nashville, Tenn.
The FDA approval was restricted to patients like those enrolled in BeAT-HF: that is, individuals with New York Heart Association functional class III heart failure, a left ventricular ejection fraction of 35% or less while on stable optimal medical therapy, and ineligibility for cardiac resynchronization therapy according to current guidelines. Seventy-eight percent of BeAT-HF participants had an implantable cardioverter-defibrillator.
Participants were randomized to baroreflex activation therapy (BAT) plus optimal medical therapy or to optimal medical therapy alone. The three coprimary endpoints were change from baseline to 6 months in 6-minute hall walk distance (6MHW), scores on the Minnesota Living with Heart Failure Questionnaire (MLHF), and N-terminal pro-B-type natriuretic peptide (NT-proBNP).
In the overall study population, 6MHW increased by 60 m in the BAT group and decreased by 8 m in controls; MLHF scores dropped by 14 and 6 points, respectively; and NT-proBNP fell by an average of 25% with BAT while rising by 3% in controls.
Very often, just a 5-point reduction in MLHF score is considered a clinically meaningful improvement in quality of life, the cardiologist noted.
The gender-based analysis is where things got particularly interesting.
The investigators defined a clinically relevant response as a greater than 10% increase from baseline on the 6MHW, at least a one-class improvement in NYHA class, or a reduction of 5 points or more on the MLHF. Among subjects in the BAT group, 70% of women and 60% of men met the clinically relevant response standard in terms of 6MHW, as did 70% of women and 64% of men for improvement in NYHA class, and 78% of women and 66% of men for MLHF score.
Eighty-seven percent of women and 68% of men on BAT had a clinically relevant response on at least one of these endpoints, as did about 28% of controls. Moreover, 31% of women in the BAT group were clinically relevant responders on at least two endpoints, compared with 19% of BAT men and 4% and 9% of controls.
Women dominate super-responder category
In order to be classified as a super responder, a patient had to demonstrate a greater than 20% increase in 6MHW, improvement in NYHA class I status, or at least a 10-point improvement in MLHF score. Ninety-one percent of women on BAT achieved super-responder status for at least one of these endpoints, compared with 76% of men. Forty-three percent of women and 24% of men in the BAT group were super responders in at least two domains, as were 8% and 11% of female and male controls, Dr. Lindenfeld continued.
Discussant Ewa Anita Jankowska, MD, PhD, deemed the BeAT-HF results on the therapeutic benefits of this autonomic modulation strategy “quite convincing.”
“We need to acknowledge that in recent years we have been spoiled a bit by the huge trials in heart failure where the ultimate goal was a reduction in mortality. But I think this is the time when we should think about the patients who want to live – here, now – with a better life. Patients expect symptomatic benefits. There is a substantial group of patients who are symptomatic even though they receive quite extensive neurohormonal blockage and who are not suitable for CRT. This study demonstrates that, for this group of patients, BAT can bring really significant symptomatic benefits,” she said.
“If you think about a treatment that provides patients who are NYHA class III an increase in 6MHW of 60 meters, that’s really something. And 20% of patients went from NYHA class III to class I – that’s really something, too,” added Dr. Jankowska, professor of medicine and head of the laboratory of applied research on the cardiovascular system at Wroclaw (Poland) University.
How baroreflex activation therapy works
The BaroStim system consists of a 2-mm unipolar electrode on a 7-mm backer that is placed over the carotid sinus. It is supported by a small generator with a 4- to 5-year battery life implanted under the collarbone, along with radiofrequency telemetry capability and programming flexibility.
Stimulation of the carotid baroreceptor promotes an integrated autonomic nervous system response which enhances parasympathetic activity and inhibits sympathetic nervous system activity. The result, as shown in numerous earlier proof-of-concept studies, is a reduced heart rate, decreased ventricular remodeling, enhanced diuresis, increased vasodilation, a drop in elevated blood pressure, and decreased renin secretion – all achieved nonpharmacologically.
The study was sponsored by CVRx. Dr. Lindenfeld reported serving as a consultant to CVRx, Abbott, AstraZeneca, Boehringer Ingelheim, Edwards Lifesciences, Impulse Dynamics, and VWave.
The striking gains in functional capacity and quality of life conferred by baroreflex activation therapy in patients with heart failure, as shown in the pivotal phase 3 clinical trial for this novel intervention, were at least as great in women as in men, JoAnn Lindenfeld, MD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
The results of the multicenter, prospective, randomized BeAT-HF trial led to marketing approval of the BaroStim Neo system for improvement in symptoms of heart failure with reduced ejection fraction (HFrEF) by the Food and Drug Administration in August 2019. Dr. Lindenfeld presented a fresh breakdown of the results by gender which showed, intriguingly, that the improvement in all study endpoints was consistently numerically greater in the women – sometimes startlingly so – although these gender differences in response didn’t achieve statistical significance. The 6-month randomized trial was underpowered for drawing definitive conclusions on that score, with a study population of only 53 women and 211 men. So the investigator remained circumspect.
“We think that what this study shows us is that women have at least equivalent improvement as men in this population. I don’t think we can conclude from this study yet that it’s better, but it’s certainly in all these parameters as least as good. And I think this is a population in which we’ve seen that improving symptoms and functional capacity is very important,” said Dr. Lindenfeld, professor of medicine and director of advanced heart failure/cardiac transplantation at Vanderbilt University, Nashville, Tenn.
The FDA approval was restricted to patients like those enrolled in BeAT-HF: that is, individuals with New York Heart Association functional class III heart failure, a left ventricular ejection fraction of 35% or less while on stable optimal medical therapy, and ineligibility for cardiac resynchronization therapy according to current guidelines. Seventy-eight percent of BeAT-HF participants had an implantable cardioverter-defibrillator.
Participants were randomized to baroreflex activation therapy (BAT) plus optimal medical therapy or to optimal medical therapy alone. The three coprimary endpoints were change from baseline to 6 months in 6-minute hall walk distance (6MHW), scores on the Minnesota Living with Heart Failure Questionnaire (MLHF), and N-terminal pro-B-type natriuretic peptide (NT-proBNP).
In the overall study population, 6MHW increased by 60 m in the BAT group and decreased by 8 m in controls; MLHF scores dropped by 14 and 6 points, respectively; and NT-proBNP fell by an average of 25% with BAT while rising by 3% in controls.
Very often, just a 5-point reduction in MLHF score is considered a clinically meaningful improvement in quality of life, the cardiologist noted.
The gender-based analysis is where things got particularly interesting.
The investigators defined a clinically relevant response as a greater than 10% increase from baseline on the 6MHW, at least a one-class improvement in NYHA class, or a reduction of 5 points or more on the MLHF. Among subjects in the BAT group, 70% of women and 60% of men met the clinically relevant response standard in terms of 6MHW, as did 70% of women and 64% of men for improvement in NYHA class, and 78% of women and 66% of men for MLHF score.
Eighty-seven percent of women and 68% of men on BAT had a clinically relevant response on at least one of these endpoints, as did about 28% of controls. Moreover, 31% of women in the BAT group were clinically relevant responders on at least two endpoints, compared with 19% of BAT men and 4% and 9% of controls.
Women dominate super-responder category
In order to be classified as a super responder, a patient had to demonstrate a greater than 20% increase in 6MHW, improvement in NYHA class I status, or at least a 10-point improvement in MLHF score. Ninety-one percent of women on BAT achieved super-responder status for at least one of these endpoints, compared with 76% of men. Forty-three percent of women and 24% of men in the BAT group were super responders in at least two domains, as were 8% and 11% of female and male controls, Dr. Lindenfeld continued.
Discussant Ewa Anita Jankowska, MD, PhD, deemed the BeAT-HF results on the therapeutic benefits of this autonomic modulation strategy “quite convincing.”
“We need to acknowledge that in recent years we have been spoiled a bit by the huge trials in heart failure where the ultimate goal was a reduction in mortality. But I think this is the time when we should think about the patients who want to live – here, now – with a better life. Patients expect symptomatic benefits. There is a substantial group of patients who are symptomatic even though they receive quite extensive neurohormonal blockage and who are not suitable for CRT. This study demonstrates that, for this group of patients, BAT can bring really significant symptomatic benefits,” she said.
“If you think about a treatment that provides patients who are NYHA class III an increase in 6MHW of 60 meters, that’s really something. And 20% of patients went from NYHA class III to class I – that’s really something, too,” added Dr. Jankowska, professor of medicine and head of the laboratory of applied research on the cardiovascular system at Wroclaw (Poland) University.
How baroreflex activation therapy works
The BaroStim system consists of a 2-mm unipolar electrode on a 7-mm backer that is placed over the carotid sinus. It is supported by a small generator with a 4- to 5-year battery life implanted under the collarbone, along with radiofrequency telemetry capability and programming flexibility.
Stimulation of the carotid baroreceptor promotes an integrated autonomic nervous system response which enhances parasympathetic activity and inhibits sympathetic nervous system activity. The result, as shown in numerous earlier proof-of-concept studies, is a reduced heart rate, decreased ventricular remodeling, enhanced diuresis, increased vasodilation, a drop in elevated blood pressure, and decreased renin secretion – all achieved nonpharmacologically.
The study was sponsored by CVRx. Dr. Lindenfeld reported serving as a consultant to CVRx, Abbott, AstraZeneca, Boehringer Ingelheim, Edwards Lifesciences, Impulse Dynamics, and VWave.
FROM ESC HEART FAILURE 2020
Telehealth and medical liability
The COVID-19 pandemic has led to the rapid uptake of telehealth nationwide in primary care and specialty practices. Over the last few months many practices have actually performed more telehealth visits than traditional in-person visits. The use of telehealth, which had been increasing slowly for the last few years, accelerated rapidly during the pandemic. Long term, telehealth has the potential to increase access to primary care and specialists, and make follow-up easier for many patients, changing how health care is delivered to millions of patients throughout the world.
Since telehealth will be a regular part of our practices from now on, it is important for clinicians to recognize how telehealth visits are viewed in a legal arena.
As is often the case with technological advances, the law needs time to adapt. Will a health care provider treating a patient using telemedicine be held to the same standard of care applicable to an in-person encounter? Stated differently, will consideration be given to the obvious limitations imposed by a telemedicine exam?
Standard of care in medical malpractice cases
The central question in most medical malpractice cases is whether the provider complied with the generally accepted standard of care when evaluating, diagnosing, or treating a patient. This standard typically takes into consideration the provider’s particular specialty as well as all the circumstances surrounding the encounter.1 Medical providers, not state legislators, usually define the standard of care for medical professionals. In malpractice cases, medical experts explain the applicable standard of care to the jury and guide its determination of whether, in the particular case, the standard of care was met. In this way, the law has long recognized that the medical profession itself is best suited to establish the appropriate standards of care under any particular set of circumstances. This standard of care is often referred to as the “reasonable professional under the circumstances” standard of care.
Telemedicine standard of care
Despite the fact that the complex and often nebulous concept of standard of care has been traditionally left to the medical experts to define, state legislators and regulators throughout the nation have chosen to weigh in on this issue in the context of telemedicine. Most states with telemedicine regulations have followed the model policy adopted by the Federation of State Medical Boards in April 2014 which states that “[t]reatment and consultation recommendations made in an online setting … will be held to the same standards of appropriate practice as those in traditional (in-person) settings.”2 States that have adopted this model policy have effectively created a “legal fiction” requiring a jury to ignore the fact that the care was provided virtually by telemedicine technologies and instead assume that the physician treated the patient in person, i.e, applying an “in-person” standard of care. Hawaii appears to be the lone notable exception. Its telemedicine law recognizes that an in-person standard of care should not be applied if there was not a face-to-face visit.3
Proponents of the in-person telemedicine standard claim that it is necessary to ensure patient safety, thus justifying the “legal fiction.” Holding the provider to the in-person standard, it is argued, forces the physician to err on the side of caution and require an actual in-person encounter to ensure the advantages of sight, touch, and sense of things are fully available.4 This discourages the use of telemedicine and deprives the population of its many benefits.
Telemedicine can overcome geographical barriers, increase clinical support, improve health outcomes, reduce health care costs, encourage patient input, reduce travel, and foster continuity of care. The pandemic, which has significantly limited the ability of providers to see patients in person, only underscores the benefits of telemedicine.
The legislatively imposed in-person telemedicine standard of care should be replaced with the “reasonable professional under the circumstances” standard in order to fairly judge physicians’ care and promote overall population health. The “reasonable professional under the circumstances” standard has applied to physicians and other health care professionals outside of telemedicine for decades, and it has served the medical community and public well. It is unfortunate that legislators felt the need to weigh in and define a distinctly different standard of care for telemedicine than for the rest of medicine, as this may present unforeseen obstacles to the use of telemedicine.
The in-person telemedicine standard of care remains a significant barrier for long-term telemedicine. Eliminating this legal fiction has the potential to further expand physicians’ use of telemedicine and fulfill its promise of improving access to care and improving population health.
Mr. Horner (partner), Mr. Milewski (partner), and Mr. Gajer (associate) are attorneys with White and Williams. They specialize in defending health care providers in medical malpractice lawsuits and other health care–related matters. Dr. Skolnik is professor of family and community Medicine at the Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Follow Dr. Skolnik, and feel free to submit questions to him on Twitter: @neilskolnik. The authors have no financial conflicts related to the content of this piece.
References
1. Cowan v. Doering, 111 N.J. 451-62,.1988.
2. Model Policy For The Appropriate Use Of Telemedicine Technologies In The Practice Of Medicine. State Medical Boards Appropriate Regulation of Telemedicine. April 2014..
3. Haw. Rev. Stat. Ann. § 453-1.3(c).
4. Kaspar BJ. Iowa Law Review. 2014 Jan;99:839-59.
The COVID-19 pandemic has led to the rapid uptake of telehealth nationwide in primary care and specialty practices. Over the last few months many practices have actually performed more telehealth visits than traditional in-person visits. The use of telehealth, which had been increasing slowly for the last few years, accelerated rapidly during the pandemic. Long term, telehealth has the potential to increase access to primary care and specialists, and make follow-up easier for many patients, changing how health care is delivered to millions of patients throughout the world.
Since telehealth will be a regular part of our practices from now on, it is important for clinicians to recognize how telehealth visits are viewed in a legal arena.
As is often the case with technological advances, the law needs time to adapt. Will a health care provider treating a patient using telemedicine be held to the same standard of care applicable to an in-person encounter? Stated differently, will consideration be given to the obvious limitations imposed by a telemedicine exam?
Standard of care in medical malpractice cases
The central question in most medical malpractice cases is whether the provider complied with the generally accepted standard of care when evaluating, diagnosing, or treating a patient. This standard typically takes into consideration the provider’s particular specialty as well as all the circumstances surrounding the encounter.1 Medical providers, not state legislators, usually define the standard of care for medical professionals. In malpractice cases, medical experts explain the applicable standard of care to the jury and guide its determination of whether, in the particular case, the standard of care was met. In this way, the law has long recognized that the medical profession itself is best suited to establish the appropriate standards of care under any particular set of circumstances. This standard of care is often referred to as the “reasonable professional under the circumstances” standard of care.
Telemedicine standard of care
Despite the fact that the complex and often nebulous concept of standard of care has been traditionally left to the medical experts to define, state legislators and regulators throughout the nation have chosen to weigh in on this issue in the context of telemedicine. Most states with telemedicine regulations have followed the model policy adopted by the Federation of State Medical Boards in April 2014 which states that “[t]reatment and consultation recommendations made in an online setting … will be held to the same standards of appropriate practice as those in traditional (in-person) settings.”2 States that have adopted this model policy have effectively created a “legal fiction” requiring a jury to ignore the fact that the care was provided virtually by telemedicine technologies and instead assume that the physician treated the patient in person, i.e, applying an “in-person” standard of care. Hawaii appears to be the lone notable exception. Its telemedicine law recognizes that an in-person standard of care should not be applied if there was not a face-to-face visit.3
Proponents of the in-person telemedicine standard claim that it is necessary to ensure patient safety, thus justifying the “legal fiction.” Holding the provider to the in-person standard, it is argued, forces the physician to err on the side of caution and require an actual in-person encounter to ensure the advantages of sight, touch, and sense of things are fully available.4 This discourages the use of telemedicine and deprives the population of its many benefits.
Telemedicine can overcome geographical barriers, increase clinical support, improve health outcomes, reduce health care costs, encourage patient input, reduce travel, and foster continuity of care. The pandemic, which has significantly limited the ability of providers to see patients in person, only underscores the benefits of telemedicine.
The legislatively imposed in-person telemedicine standard of care should be replaced with the “reasonable professional under the circumstances” standard in order to fairly judge physicians’ care and promote overall population health. The “reasonable professional under the circumstances” standard has applied to physicians and other health care professionals outside of telemedicine for decades, and it has served the medical community and public well. It is unfortunate that legislators felt the need to weigh in and define a distinctly different standard of care for telemedicine than for the rest of medicine, as this may present unforeseen obstacles to the use of telemedicine.
The in-person telemedicine standard of care remains a significant barrier for long-term telemedicine. Eliminating this legal fiction has the potential to further expand physicians’ use of telemedicine and fulfill its promise of improving access to care and improving population health.
Mr. Horner (partner), Mr. Milewski (partner), and Mr. Gajer (associate) are attorneys with White and Williams. They specialize in defending health care providers in medical malpractice lawsuits and other health care–related matters. Dr. Skolnik is professor of family and community Medicine at the Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Follow Dr. Skolnik, and feel free to submit questions to him on Twitter: @neilskolnik. The authors have no financial conflicts related to the content of this piece.
References
1. Cowan v. Doering, 111 N.J. 451-62,.1988.
2. Model Policy For The Appropriate Use Of Telemedicine Technologies In The Practice Of Medicine. State Medical Boards Appropriate Regulation of Telemedicine. April 2014..
3. Haw. Rev. Stat. Ann. § 453-1.3(c).
4. Kaspar BJ. Iowa Law Review. 2014 Jan;99:839-59.
The COVID-19 pandemic has led to the rapid uptake of telehealth nationwide in primary care and specialty practices. Over the last few months many practices have actually performed more telehealth visits than traditional in-person visits. The use of telehealth, which had been increasing slowly for the last few years, accelerated rapidly during the pandemic. Long term, telehealth has the potential to increase access to primary care and specialists, and make follow-up easier for many patients, changing how health care is delivered to millions of patients throughout the world.
Since telehealth will be a regular part of our practices from now on, it is important for clinicians to recognize how telehealth visits are viewed in a legal arena.
As is often the case with technological advances, the law needs time to adapt. Will a health care provider treating a patient using telemedicine be held to the same standard of care applicable to an in-person encounter? Stated differently, will consideration be given to the obvious limitations imposed by a telemedicine exam?
Standard of care in medical malpractice cases
The central question in most medical malpractice cases is whether the provider complied with the generally accepted standard of care when evaluating, diagnosing, or treating a patient. This standard typically takes into consideration the provider’s particular specialty as well as all the circumstances surrounding the encounter.1 Medical providers, not state legislators, usually define the standard of care for medical professionals. In malpractice cases, medical experts explain the applicable standard of care to the jury and guide its determination of whether, in the particular case, the standard of care was met. In this way, the law has long recognized that the medical profession itself is best suited to establish the appropriate standards of care under any particular set of circumstances. This standard of care is often referred to as the “reasonable professional under the circumstances” standard of care.
Telemedicine standard of care
Despite the fact that the complex and often nebulous concept of standard of care has been traditionally left to the medical experts to define, state legislators and regulators throughout the nation have chosen to weigh in on this issue in the context of telemedicine. Most states with telemedicine regulations have followed the model policy adopted by the Federation of State Medical Boards in April 2014 which states that “[t]reatment and consultation recommendations made in an online setting … will be held to the same standards of appropriate practice as those in traditional (in-person) settings.”2 States that have adopted this model policy have effectively created a “legal fiction” requiring a jury to ignore the fact that the care was provided virtually by telemedicine technologies and instead assume that the physician treated the patient in person, i.e, applying an “in-person” standard of care. Hawaii appears to be the lone notable exception. Its telemedicine law recognizes that an in-person standard of care should not be applied if there was not a face-to-face visit.3
Proponents of the in-person telemedicine standard claim that it is necessary to ensure patient safety, thus justifying the “legal fiction.” Holding the provider to the in-person standard, it is argued, forces the physician to err on the side of caution and require an actual in-person encounter to ensure the advantages of sight, touch, and sense of things are fully available.4 This discourages the use of telemedicine and deprives the population of its many benefits.
Telemedicine can overcome geographical barriers, increase clinical support, improve health outcomes, reduce health care costs, encourage patient input, reduce travel, and foster continuity of care. The pandemic, which has significantly limited the ability of providers to see patients in person, only underscores the benefits of telemedicine.
The legislatively imposed in-person telemedicine standard of care should be replaced with the “reasonable professional under the circumstances” standard in order to fairly judge physicians’ care and promote overall population health. The “reasonable professional under the circumstances” standard has applied to physicians and other health care professionals outside of telemedicine for decades, and it has served the medical community and public well. It is unfortunate that legislators felt the need to weigh in and define a distinctly different standard of care for telemedicine than for the rest of medicine, as this may present unforeseen obstacles to the use of telemedicine.
The in-person telemedicine standard of care remains a significant barrier for long-term telemedicine. Eliminating this legal fiction has the potential to further expand physicians’ use of telemedicine and fulfill its promise of improving access to care and improving population health.
Mr. Horner (partner), Mr. Milewski (partner), and Mr. Gajer (associate) are attorneys with White and Williams. They specialize in defending health care providers in medical malpractice lawsuits and other health care–related matters. Dr. Skolnik is professor of family and community Medicine at the Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Follow Dr. Skolnik, and feel free to submit questions to him on Twitter: @neilskolnik. The authors have no financial conflicts related to the content of this piece.
References
1. Cowan v. Doering, 111 N.J. 451-62,.1988.
2. Model Policy For The Appropriate Use Of Telemedicine Technologies In The Practice Of Medicine. State Medical Boards Appropriate Regulation of Telemedicine. April 2014..
3. Haw. Rev. Stat. Ann. § 453-1.3(c).
4. Kaspar BJ. Iowa Law Review. 2014 Jan;99:839-59.
Daily Recap: ED visits for life-threatening conditions plummet; COVID-19 imaging strategies for kids
Here are the stories our MDedge editors across specialties think you need to know about today:
ED visits drop for life-threatening conditions
Emergency department visits for myocardial infarction, stroke, and hyperglycemic crisis dropped substantially in the 10 weeks after COVID-19 was declared a national emergency, according to new research from the Centers for Disease Control and Prevention.
Compared with the 10-week period from Jan. 5 to March 14, ED visits were down by 23% for MI, 20% for stroke, and 10% for hyperglycemic crisis from March 15 to May 23.
“A short-term decline of this magnitude … is biologically implausible for MI and stroke, especially for older adults, and unlikely for hyperglycemic crisis, and the finding suggests that patients with these conditions either could not access care or were delaying or avoiding seeking care during the early pandemic period,” the researchers wrote in the Morbidity and Mortality Weekly Report. Read more.
Expert recommendations for pediatric COVID-19 imaging
A team of pulmonologists has synthesized the clinical and imaging characteristics of COVID-19 in children, and has issued recommendations for ordering imaging studies in suspected cases of the infection.
Current recommendations from the American College of Radiology (ACR) do not include chest computed tomography (CT) or chest radiography (CXR) as an upfront test to diagnose pediatric COVID-19, but the tests may still have a role in clinical monitoring, especially in patients with a moderate to severe disease course. The potential benefits of utilizing radiologic evaluation – such as establishing a baseline for monitoring disease progression – must be balanced with potential drawbacks, including radiation exposure and reduced availability of imaging resources owing to necessary cleaning and air turnover time.
Based on the most recent international guidelines for pediatric COVID-19 patient management, the authors developed an algorithm for performing imaging studies in suspected cases of COVID-19 pneumonia. The purpose of the tool is to support clinical decision-making around the utilization of CXR and CT to evaluate pediatric COVID-19 pneumonia. “The step by step algorithm addresses the selection, sequence and timing of imaging studies with multiple images illustrating key findings of COVID-19 pneumonia in the pediatric age group,” said Mary Cataletto, MD, of NYU Langone Health in Mineola, N.Y. Read more.
Cortisol levels on COVID-19 admission may be a marker of severity
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to the hospital have a substantially increased risk of dying, according to new study findings.
Researchers assessed 535 patients admitted to major London hospitals. Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing or a strong clinical and radiological suspicion, despite a negative test. Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus and as of May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%).
Measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” said Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said. Read more.
Normal-weight prediabetes patients can benefit from lifestyle changes
Adults of normal weight with prediabetes may derive at least as much benefit from lifestyle health coaching programs as adults who are overweight or obese, results of a recent nonrandomized, real-world study show.
Fasting plasma glucose (FPG) normalized in about 63% of prediabetic adults with normal body mass index (BMI) participating in a personalized coaching program that emphasized exercise, nutrition, and weight management. In contrast, FPG normalized in about 52% of overweight and 44% of obese prediabetic individuals participating in the program.
“It is interesting to note that, although the normal weight group lost the least amount of weight, they still benefited from the lifestyle health coaching program... having a resultant greatest decrease in fasting plasma glucose and normalization to a range of someone without prediabetes,” said researcher Mandy Salmon, MS, a medical student at the University of Pennsylvania, Philadelphia. She presented the findings at the virtual annual scientific sessions of the American Diabetes Association. Read more.
Diabetes-related amputations rise in older adults
The recent resurgence in diabetes-related lower-extremity amputations in the United States is not limited to younger adults, according to the author of a recent study that documents similar increases among an older population of Medicare beneficiaries.
While the rate of amputations fell among these older adults from 2000 to 2009, it increased significantly from 2009 to 2017, albeit at a “less severe rate” than recently reported in younger populations, according to study investigator Jessica Harding, PhD, an assistant professor in the department of surgery at Emory University, Atlanta. Dr. Harding reported the results at the virtual annual scientific sessions of the American Diabetes Association.
The rate of nontraumatic lower extremity amputation (NLEA) was ticking upward by more than 1% per year over the 2009-2017 period. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
ED visits drop for life-threatening conditions
Emergency department visits for myocardial infarction, stroke, and hyperglycemic crisis dropped substantially in the 10 weeks after COVID-19 was declared a national emergency, according to new research from the Centers for Disease Control and Prevention.
Compared with the 10-week period from Jan. 5 to March 14, ED visits were down by 23% for MI, 20% for stroke, and 10% for hyperglycemic crisis from March 15 to May 23.
“A short-term decline of this magnitude … is biologically implausible for MI and stroke, especially for older adults, and unlikely for hyperglycemic crisis, and the finding suggests that patients with these conditions either could not access care or were delaying or avoiding seeking care during the early pandemic period,” the researchers wrote in the Morbidity and Mortality Weekly Report. Read more.
Expert recommendations for pediatric COVID-19 imaging
A team of pulmonologists has synthesized the clinical and imaging characteristics of COVID-19 in children, and has issued recommendations for ordering imaging studies in suspected cases of the infection.
Current recommendations from the American College of Radiology (ACR) do not include chest computed tomography (CT) or chest radiography (CXR) as an upfront test to diagnose pediatric COVID-19, but the tests may still have a role in clinical monitoring, especially in patients with a moderate to severe disease course. The potential benefits of utilizing radiologic evaluation – such as establishing a baseline for monitoring disease progression – must be balanced with potential drawbacks, including radiation exposure and reduced availability of imaging resources owing to necessary cleaning and air turnover time.
Based on the most recent international guidelines for pediatric COVID-19 patient management, the authors developed an algorithm for performing imaging studies in suspected cases of COVID-19 pneumonia. The purpose of the tool is to support clinical decision-making around the utilization of CXR and CT to evaluate pediatric COVID-19 pneumonia. “The step by step algorithm addresses the selection, sequence and timing of imaging studies with multiple images illustrating key findings of COVID-19 pneumonia in the pediatric age group,” said Mary Cataletto, MD, of NYU Langone Health in Mineola, N.Y. Read more.
Cortisol levels on COVID-19 admission may be a marker of severity
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to the hospital have a substantially increased risk of dying, according to new study findings.
Researchers assessed 535 patients admitted to major London hospitals. Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing or a strong clinical and radiological suspicion, despite a negative test. Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus and as of May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%).
Measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” said Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said. Read more.
Normal-weight prediabetes patients can benefit from lifestyle changes
Adults of normal weight with prediabetes may derive at least as much benefit from lifestyle health coaching programs as adults who are overweight or obese, results of a recent nonrandomized, real-world study show.
Fasting plasma glucose (FPG) normalized in about 63% of prediabetic adults with normal body mass index (BMI) participating in a personalized coaching program that emphasized exercise, nutrition, and weight management. In contrast, FPG normalized in about 52% of overweight and 44% of obese prediabetic individuals participating in the program.
“It is interesting to note that, although the normal weight group lost the least amount of weight, they still benefited from the lifestyle health coaching program... having a resultant greatest decrease in fasting plasma glucose and normalization to a range of someone without prediabetes,” said researcher Mandy Salmon, MS, a medical student at the University of Pennsylvania, Philadelphia. She presented the findings at the virtual annual scientific sessions of the American Diabetes Association. Read more.
Diabetes-related amputations rise in older adults
The recent resurgence in diabetes-related lower-extremity amputations in the United States is not limited to younger adults, according to the author of a recent study that documents similar increases among an older population of Medicare beneficiaries.
While the rate of amputations fell among these older adults from 2000 to 2009, it increased significantly from 2009 to 2017, albeit at a “less severe rate” than recently reported in younger populations, according to study investigator Jessica Harding, PhD, an assistant professor in the department of surgery at Emory University, Atlanta. Dr. Harding reported the results at the virtual annual scientific sessions of the American Diabetes Association.
The rate of nontraumatic lower extremity amputation (NLEA) was ticking upward by more than 1% per year over the 2009-2017 period. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
ED visits drop for life-threatening conditions
Emergency department visits for myocardial infarction, stroke, and hyperglycemic crisis dropped substantially in the 10 weeks after COVID-19 was declared a national emergency, according to new research from the Centers for Disease Control and Prevention.
Compared with the 10-week period from Jan. 5 to March 14, ED visits were down by 23% for MI, 20% for stroke, and 10% for hyperglycemic crisis from March 15 to May 23.
“A short-term decline of this magnitude … is biologically implausible for MI and stroke, especially for older adults, and unlikely for hyperglycemic crisis, and the finding suggests that patients with these conditions either could not access care or were delaying or avoiding seeking care during the early pandemic period,” the researchers wrote in the Morbidity and Mortality Weekly Report. Read more.
Expert recommendations for pediatric COVID-19 imaging
A team of pulmonologists has synthesized the clinical and imaging characteristics of COVID-19 in children, and has issued recommendations for ordering imaging studies in suspected cases of the infection.
Current recommendations from the American College of Radiology (ACR) do not include chest computed tomography (CT) or chest radiography (CXR) as an upfront test to diagnose pediatric COVID-19, but the tests may still have a role in clinical monitoring, especially in patients with a moderate to severe disease course. The potential benefits of utilizing radiologic evaluation – such as establishing a baseline for monitoring disease progression – must be balanced with potential drawbacks, including radiation exposure and reduced availability of imaging resources owing to necessary cleaning and air turnover time.
Based on the most recent international guidelines for pediatric COVID-19 patient management, the authors developed an algorithm for performing imaging studies in suspected cases of COVID-19 pneumonia. The purpose of the tool is to support clinical decision-making around the utilization of CXR and CT to evaluate pediatric COVID-19 pneumonia. “The step by step algorithm addresses the selection, sequence and timing of imaging studies with multiple images illustrating key findings of COVID-19 pneumonia in the pediatric age group,” said Mary Cataletto, MD, of NYU Langone Health in Mineola, N.Y. Read more.
Cortisol levels on COVID-19 admission may be a marker of severity
Patients with COVID-19 who have high levels of the steroid hormone cortisol on admission to the hospital have a substantially increased risk of dying, according to new study findings.
Researchers assessed 535 patients admitted to major London hospitals. Of these, 403 patients were diagnosed with COVID-19 based on a positive result on real-time polymerase chain reaction testing or a strong clinical and radiological suspicion, despite a negative test. Mean cortisol concentrations in patients with COVID-19 were significantly higher than those not diagnosed with the virus and as of May 8, significantly more patients with COVID-19 died than those without (27.8% vs 6.8%).
Measuring cortisol on admission is potentially “another simple marker to use alongside oxygen saturation levels to help us identify which patients need to be admitted immediately, and which may not,” said Waljit S. Dhillo, MBBS, PhD, head of the division of diabetes, endocrinology and metabolism at Imperial College London.
“Having an early indicator of which patients may deteriorate more quickly will help us with providing the best level of care as quickly as possible. In addition, we can also take cortisol levels into account when we are working out how best to treat our patients,” he said. Read more.
Normal-weight prediabetes patients can benefit from lifestyle changes
Adults of normal weight with prediabetes may derive at least as much benefit from lifestyle health coaching programs as adults who are overweight or obese, results of a recent nonrandomized, real-world study show.
Fasting plasma glucose (FPG) normalized in about 63% of prediabetic adults with normal body mass index (BMI) participating in a personalized coaching program that emphasized exercise, nutrition, and weight management. In contrast, FPG normalized in about 52% of overweight and 44% of obese prediabetic individuals participating in the program.
“It is interesting to note that, although the normal weight group lost the least amount of weight, they still benefited from the lifestyle health coaching program... having a resultant greatest decrease in fasting plasma glucose and normalization to a range of someone without prediabetes,” said researcher Mandy Salmon, MS, a medical student at the University of Pennsylvania, Philadelphia. She presented the findings at the virtual annual scientific sessions of the American Diabetes Association. Read more.
Diabetes-related amputations rise in older adults
The recent resurgence in diabetes-related lower-extremity amputations in the United States is not limited to younger adults, according to the author of a recent study that documents similar increases among an older population of Medicare beneficiaries.
While the rate of amputations fell among these older adults from 2000 to 2009, it increased significantly from 2009 to 2017, albeit at a “less severe rate” than recently reported in younger populations, according to study investigator Jessica Harding, PhD, an assistant professor in the department of surgery at Emory University, Atlanta. Dr. Harding reported the results at the virtual annual scientific sessions of the American Diabetes Association.
The rate of nontraumatic lower extremity amputation (NLEA) was ticking upward by more than 1% per year over the 2009-2017 period. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Daily Recap: Headache as COVID evolution predictor; psoriasis drug treats canker sores
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
The plague of racism in our society
Here we are, faced with history in real time. A plague upon a plague. A new one and a longstanding one. COVID-19 and racial injustice. Both are plagues upon our medical house, and it’s time for some spring cleaning.
Initially, COVID-19 concerns brought news of an infection coming for anyone and everyone. Like the Black Death, it was supposedly “the great equalizer,” the “Triumph of Death,” regardless of station in life.
Yet, as the COVID-19 story unfurls, it is clear that minorities are disproportionately affected, just as they always seem to be. In Chicago, for example, African Americans make up 70% of the COVID-19 deaths, yet only 29% of the population. Similar results have been found in Milwaukee and Louisiana, and other parts of the country. As an article in the Journal of Law and the Biosciences indicated, “These racial and ethnic disparities in COVID-19 infections and deaths are a result of historical and current practices of racism that cause disparities in exposure, susceptibility and treatment.”
People of color are disproportionately affected, an outcome of racial health disparities. And these disparities are a public health crisis, sitting in the living room of our house. Disparities continue to exist in national infant mortality, maternal health, and deaths from premature heart disease and stroke. They exist in access to care and are playing out in real time during this pandemic.
COVID-19 and racial injustice, in addition to being sociological and economic crises, are both public health crises that are plaguing African American communities. Consider the case of police violence as a public health issue. Black males are three times more likely to be killed by police than are non-Hispanic white males.
This is a dying room in our medical house, with our patient lying alongside a history of medicine littered with racial injustice, telling us, “I can’t breathe.”
As professionals, we must run to that patient. Professionalism bears the pillars of our ethical principles of primacy of patient welfare, patient autonomy, and social justice. We work hard on the first two. Medical errors, quality improvement, communication, patient safety. All important. But we too often dance, or sit silently, about the third.
Here is an excerpt from “Moral choices for today’s physician”, by Donald M. Berwick, MD:
“The work of a physician as healer cannot stop at the door of an office, the threshold of an operating room, or the front gate of a hospital. The rescue of a society and the restoration of a political ethos that remembers to heal have become the physician’s jobs, too. Professional silence in the face of social injustice is wrong.”
It is chilling to see the great institutions of health care, hospitals, physician groups, and scientific bodies assume that the seat of bystander is available. That seat is gone. To try to avoid the political fray through silence is impossible because silence is now political. Either engage or assist the harm. There is no third choice.
Dr. Berwick echoed the words of Rev. Dr. Martin Luther King Jr., from 1959, in Birmingham, Ala.:
“If you fail to act now, history will have to record that the greatest tragedy of this period of social transition was not the strident clamor of the bad people, but the appalling silence of the good people.”
I have this space to write and speak up, and I urge many of you to do the same. Write to your local newspaper. Share your stories. Listen to others. Engage with your society. Create the space in your practice, your group, your hospital, your department for listening, learning, relearning, educating, and acting.
It’s not easy speaking up and speaking out. Yet, this is our foundation, our call, our professional obligation. We must remember George Floyd, Breonna Taylor, Sandra Bland, Eric Garner, Tamir Rice, Trayvon Martin, and too many others. To recognize the humanity behind the injustices, and to call out their names.
This is lesson 101 on the wards. It’s not the heart failure in bed 1 or the sepsis in bed 2, but the mother, brother, father, and sister who seek out just care. Humanity reaching out their hand, and we must grab it.
I came to medicine for the compassion, for the love, for the comforting hand offered to our patients. That compassion, by definition, requires action.
In his book “Altruism: The Power of Compassion to Change Yourself and the World,” Matthieu Ricard wrote “If compassion without wisdom is blind, compassion without action is hypocritical.”
Silence is inaction. Let’s act.
Dr. Messler is the executive director, quality initiatives, at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared first at SHM’s official blog The Hospital Leader.
Here we are, faced with history in real time. A plague upon a plague. A new one and a longstanding one. COVID-19 and racial injustice. Both are plagues upon our medical house, and it’s time for some spring cleaning.
Initially, COVID-19 concerns brought news of an infection coming for anyone and everyone. Like the Black Death, it was supposedly “the great equalizer,” the “Triumph of Death,” regardless of station in life.
Yet, as the COVID-19 story unfurls, it is clear that minorities are disproportionately affected, just as they always seem to be. In Chicago, for example, African Americans make up 70% of the COVID-19 deaths, yet only 29% of the population. Similar results have been found in Milwaukee and Louisiana, and other parts of the country. As an article in the Journal of Law and the Biosciences indicated, “These racial and ethnic disparities in COVID-19 infections and deaths are a result of historical and current practices of racism that cause disparities in exposure, susceptibility and treatment.”
People of color are disproportionately affected, an outcome of racial health disparities. And these disparities are a public health crisis, sitting in the living room of our house. Disparities continue to exist in national infant mortality, maternal health, and deaths from premature heart disease and stroke. They exist in access to care and are playing out in real time during this pandemic.
COVID-19 and racial injustice, in addition to being sociological and economic crises, are both public health crises that are plaguing African American communities. Consider the case of police violence as a public health issue. Black males are three times more likely to be killed by police than are non-Hispanic white males.
This is a dying room in our medical house, with our patient lying alongside a history of medicine littered with racial injustice, telling us, “I can’t breathe.”
As professionals, we must run to that patient. Professionalism bears the pillars of our ethical principles of primacy of patient welfare, patient autonomy, and social justice. We work hard on the first two. Medical errors, quality improvement, communication, patient safety. All important. But we too often dance, or sit silently, about the third.
Here is an excerpt from “Moral choices for today’s physician”, by Donald M. Berwick, MD:
“The work of a physician as healer cannot stop at the door of an office, the threshold of an operating room, or the front gate of a hospital. The rescue of a society and the restoration of a political ethos that remembers to heal have become the physician’s jobs, too. Professional silence in the face of social injustice is wrong.”
It is chilling to see the great institutions of health care, hospitals, physician groups, and scientific bodies assume that the seat of bystander is available. That seat is gone. To try to avoid the political fray through silence is impossible because silence is now political. Either engage or assist the harm. There is no third choice.
Dr. Berwick echoed the words of Rev. Dr. Martin Luther King Jr., from 1959, in Birmingham, Ala.:
“If you fail to act now, history will have to record that the greatest tragedy of this period of social transition was not the strident clamor of the bad people, but the appalling silence of the good people.”
I have this space to write and speak up, and I urge many of you to do the same. Write to your local newspaper. Share your stories. Listen to others. Engage with your society. Create the space in your practice, your group, your hospital, your department for listening, learning, relearning, educating, and acting.
It’s not easy speaking up and speaking out. Yet, this is our foundation, our call, our professional obligation. We must remember George Floyd, Breonna Taylor, Sandra Bland, Eric Garner, Tamir Rice, Trayvon Martin, and too many others. To recognize the humanity behind the injustices, and to call out their names.
This is lesson 101 on the wards. It’s not the heart failure in bed 1 or the sepsis in bed 2, but the mother, brother, father, and sister who seek out just care. Humanity reaching out their hand, and we must grab it.
I came to medicine for the compassion, for the love, for the comforting hand offered to our patients. That compassion, by definition, requires action.
In his book “Altruism: The Power of Compassion to Change Yourself and the World,” Matthieu Ricard wrote “If compassion without wisdom is blind, compassion without action is hypocritical.”
Silence is inaction. Let’s act.
Dr. Messler is the executive director, quality initiatives, at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared first at SHM’s official blog The Hospital Leader.
Here we are, faced with history in real time. A plague upon a plague. A new one and a longstanding one. COVID-19 and racial injustice. Both are plagues upon our medical house, and it’s time for some spring cleaning.
Initially, COVID-19 concerns brought news of an infection coming for anyone and everyone. Like the Black Death, it was supposedly “the great equalizer,” the “Triumph of Death,” regardless of station in life.
Yet, as the COVID-19 story unfurls, it is clear that minorities are disproportionately affected, just as they always seem to be. In Chicago, for example, African Americans make up 70% of the COVID-19 deaths, yet only 29% of the population. Similar results have been found in Milwaukee and Louisiana, and other parts of the country. As an article in the Journal of Law and the Biosciences indicated, “These racial and ethnic disparities in COVID-19 infections and deaths are a result of historical and current practices of racism that cause disparities in exposure, susceptibility and treatment.”
People of color are disproportionately affected, an outcome of racial health disparities. And these disparities are a public health crisis, sitting in the living room of our house. Disparities continue to exist in national infant mortality, maternal health, and deaths from premature heart disease and stroke. They exist in access to care and are playing out in real time during this pandemic.
COVID-19 and racial injustice, in addition to being sociological and economic crises, are both public health crises that are plaguing African American communities. Consider the case of police violence as a public health issue. Black males are three times more likely to be killed by police than are non-Hispanic white males.
This is a dying room in our medical house, with our patient lying alongside a history of medicine littered with racial injustice, telling us, “I can’t breathe.”
As professionals, we must run to that patient. Professionalism bears the pillars of our ethical principles of primacy of patient welfare, patient autonomy, and social justice. We work hard on the first two. Medical errors, quality improvement, communication, patient safety. All important. But we too often dance, or sit silently, about the third.
Here is an excerpt from “Moral choices for today’s physician”, by Donald M. Berwick, MD:
“The work of a physician as healer cannot stop at the door of an office, the threshold of an operating room, or the front gate of a hospital. The rescue of a society and the restoration of a political ethos that remembers to heal have become the physician’s jobs, too. Professional silence in the face of social injustice is wrong.”
It is chilling to see the great institutions of health care, hospitals, physician groups, and scientific bodies assume that the seat of bystander is available. That seat is gone. To try to avoid the political fray through silence is impossible because silence is now political. Either engage or assist the harm. There is no third choice.
Dr. Berwick echoed the words of Rev. Dr. Martin Luther King Jr., from 1959, in Birmingham, Ala.:
“If you fail to act now, history will have to record that the greatest tragedy of this period of social transition was not the strident clamor of the bad people, but the appalling silence of the good people.”
I have this space to write and speak up, and I urge many of you to do the same. Write to your local newspaper. Share your stories. Listen to others. Engage with your society. Create the space in your practice, your group, your hospital, your department for listening, learning, relearning, educating, and acting.
It’s not easy speaking up and speaking out. Yet, this is our foundation, our call, our professional obligation. We must remember George Floyd, Breonna Taylor, Sandra Bland, Eric Garner, Tamir Rice, Trayvon Martin, and too many others. To recognize the humanity behind the injustices, and to call out their names.
This is lesson 101 on the wards. It’s not the heart failure in bed 1 or the sepsis in bed 2, but the mother, brother, father, and sister who seek out just care. Humanity reaching out their hand, and we must grab it.
I came to medicine for the compassion, for the love, for the comforting hand offered to our patients. That compassion, by definition, requires action.
In his book “Altruism: The Power of Compassion to Change Yourself and the World,” Matthieu Ricard wrote “If compassion without wisdom is blind, compassion without action is hypocritical.”
Silence is inaction. Let’s act.
Dr. Messler is the executive director, quality initiatives, at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared first at SHM’s official blog The Hospital Leader.
Pilot study shows apremilast effective for severe recurrent canker sores
showed.
“Canker sores [aphthous ulcers] are very common, yet are often not well managed as the diagnosis is not always correctly made,” lead study author Alison J. Bruce, MB, ChB, said in an interview following the virtual annual meeting of the American Academy of Dermatology. “They’re often mistaken for herpes infection and therefore treated with antiviral therapy. Of the available therapies, several have common side effects or require lab monitoring or are not uniformly effective.”
In their poster abstract, Dr. Bruce, of the division of dermatology at the Mayo Clinic, Jacksonville, Fla., and colleagues noted that, while no principal etiology has been established for recurrent aphthous stomatitis (RAS), immune up-regulation plays a role in the pathogenesis of the condition. “Attacks of RAS may be precipitated by local trauma, stress, food intake, drugs, hormonal changes and vitamin and trace element deficiencies,” they wrote. “Local and systemic conditions and genetic, immunological and microbial factors all may play a role in the pathogenesis.”
Apremilast, a phosphodiesterase-4 inhibitor, down-regulates inflammatory response by modulating expression of tumor necrosis factor–alpha; interferon-gamma; and interleukin-2, IL-12, IL-17, and IL-23. It is approved by the Food and Drug Administration for treating plaque psoriasis and psoriatic arthritis, and in July 2019, was approved for treating ulcers associated with Behçet’s disease, in adults.*
For the pilot study, the researchers enrolled 15 patients with RAS to receive apremilast 30 mg twice daily for 15 weeks after 1 week titration. To be eligible for the trial, patients must have had monthly oral ulcers in preceding 6 months, at least two ulcers in previous 4 weeks prior to enrollment at baseline, at least three ulcers during flares, inadequate control with topical therapy, and no evidence of systemic disease. They excluded patients on immune-modulating therapy or systemic steroids, pregnant or breastfeeding women, those with a systemic infection, those with a history of recurrent bacterial, viral, fungal, or mycobacterial infection, those with a history of depression, as well as those with a known malignancy or vitamin deficiencies. Patients were assessed monthly, evaluating number of ulcers, visual analog pain scale, physician’s global assessment and Chronic Oral Mucosal Disease Questionnaire (COMDQ).
Dr. Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. That patient had considerable reduction in number, size, and duration of oral ulcers. Remission in all patients was sustained during 16 weeks of treatment. COMDQ responses improved considerably from baseline to week 8, and this was continued until week 16.
“Onset of response [to apremilast] was rapid,” Dr. Bruce said. “For many other therapies, patients are counseled that [they] may take several weeks to become effective. Response was also dramatic. Almost all patients had complete remission from their ulcers, compared with other therapies where oftentimes reduction or attenuation is achieved, as opposed to complete resolution. There was a suggestion that a lower dose [of apremilast] may still be effective. This adds to our ‘toolbox’ of therapeutic options.”
The most common adverse effects were nausea/vomiting and headache, but these were mild and tolerable and generally resolved by week 4.
The researchers acknowledged certain limitations of the study, including its small sample size. “The challenge will most likely be insurance coverage,” Dr. Bruce said. “This is unfortunate, as it would be ideal to offer a safe treatment without the need for monitoring.”
The investigator-initiated study was supported by Celgene. The researchers reported having no financial disclosures.
SOURCE: Bruce AJ et al. AAD 20, Abstract 17701.
*Correction 6/23/2020: An earlier version of this story misstated the approved indications for apremilast.
showed.
“Canker sores [aphthous ulcers] are very common, yet are often not well managed as the diagnosis is not always correctly made,” lead study author Alison J. Bruce, MB, ChB, said in an interview following the virtual annual meeting of the American Academy of Dermatology. “They’re often mistaken for herpes infection and therefore treated with antiviral therapy. Of the available therapies, several have common side effects or require lab monitoring or are not uniformly effective.”
In their poster abstract, Dr. Bruce, of the division of dermatology at the Mayo Clinic, Jacksonville, Fla., and colleagues noted that, while no principal etiology has been established for recurrent aphthous stomatitis (RAS), immune up-regulation plays a role in the pathogenesis of the condition. “Attacks of RAS may be precipitated by local trauma, stress, food intake, drugs, hormonal changes and vitamin and trace element deficiencies,” they wrote. “Local and systemic conditions and genetic, immunological and microbial factors all may play a role in the pathogenesis.”
Apremilast, a phosphodiesterase-4 inhibitor, down-regulates inflammatory response by modulating expression of tumor necrosis factor–alpha; interferon-gamma; and interleukin-2, IL-12, IL-17, and IL-23. It is approved by the Food and Drug Administration for treating plaque psoriasis and psoriatic arthritis, and in July 2019, was approved for treating ulcers associated with Behçet’s disease, in adults.*
For the pilot study, the researchers enrolled 15 patients with RAS to receive apremilast 30 mg twice daily for 15 weeks after 1 week titration. To be eligible for the trial, patients must have had monthly oral ulcers in preceding 6 months, at least two ulcers in previous 4 weeks prior to enrollment at baseline, at least three ulcers during flares, inadequate control with topical therapy, and no evidence of systemic disease. They excluded patients on immune-modulating therapy or systemic steroids, pregnant or breastfeeding women, those with a systemic infection, those with a history of recurrent bacterial, viral, fungal, or mycobacterial infection, those with a history of depression, as well as those with a known malignancy or vitamin deficiencies. Patients were assessed monthly, evaluating number of ulcers, visual analog pain scale, physician’s global assessment and Chronic Oral Mucosal Disease Questionnaire (COMDQ).
Dr. Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. That patient had considerable reduction in number, size, and duration of oral ulcers. Remission in all patients was sustained during 16 weeks of treatment. COMDQ responses improved considerably from baseline to week 8, and this was continued until week 16.
“Onset of response [to apremilast] was rapid,” Dr. Bruce said. “For many other therapies, patients are counseled that [they] may take several weeks to become effective. Response was also dramatic. Almost all patients had complete remission from their ulcers, compared with other therapies where oftentimes reduction or attenuation is achieved, as opposed to complete resolution. There was a suggestion that a lower dose [of apremilast] may still be effective. This adds to our ‘toolbox’ of therapeutic options.”
The most common adverse effects were nausea/vomiting and headache, but these were mild and tolerable and generally resolved by week 4.
The researchers acknowledged certain limitations of the study, including its small sample size. “The challenge will most likely be insurance coverage,” Dr. Bruce said. “This is unfortunate, as it would be ideal to offer a safe treatment without the need for monitoring.”
The investigator-initiated study was supported by Celgene. The researchers reported having no financial disclosures.
SOURCE: Bruce AJ et al. AAD 20, Abstract 17701.
*Correction 6/23/2020: An earlier version of this story misstated the approved indications for apremilast.
showed.
“Canker sores [aphthous ulcers] are very common, yet are often not well managed as the diagnosis is not always correctly made,” lead study author Alison J. Bruce, MB, ChB, said in an interview following the virtual annual meeting of the American Academy of Dermatology. “They’re often mistaken for herpes infection and therefore treated with antiviral therapy. Of the available therapies, several have common side effects or require lab monitoring or are not uniformly effective.”
In their poster abstract, Dr. Bruce, of the division of dermatology at the Mayo Clinic, Jacksonville, Fla., and colleagues noted that, while no principal etiology has been established for recurrent aphthous stomatitis (RAS), immune up-regulation plays a role in the pathogenesis of the condition. “Attacks of RAS may be precipitated by local trauma, stress, food intake, drugs, hormonal changes and vitamin and trace element deficiencies,” they wrote. “Local and systemic conditions and genetic, immunological and microbial factors all may play a role in the pathogenesis.”
Apremilast, a phosphodiesterase-4 inhibitor, down-regulates inflammatory response by modulating expression of tumor necrosis factor–alpha; interferon-gamma; and interleukin-2, IL-12, IL-17, and IL-23. It is approved by the Food and Drug Administration for treating plaque psoriasis and psoriatic arthritis, and in July 2019, was approved for treating ulcers associated with Behçet’s disease, in adults.*
For the pilot study, the researchers enrolled 15 patients with RAS to receive apremilast 30 mg twice daily for 15 weeks after 1 week titration. To be eligible for the trial, patients must have had monthly oral ulcers in preceding 6 months, at least two ulcers in previous 4 weeks prior to enrollment at baseline, at least three ulcers during flares, inadequate control with topical therapy, and no evidence of systemic disease. They excluded patients on immune-modulating therapy or systemic steroids, pregnant or breastfeeding women, those with a systemic infection, those with a history of recurrent bacterial, viral, fungal, or mycobacterial infection, those with a history of depression, as well as those with a known malignancy or vitamin deficiencies. Patients were assessed monthly, evaluating number of ulcers, visual analog pain scale, physician’s global assessment and Chronic Oral Mucosal Disease Questionnaire (COMDQ).
Dr. Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. That patient had considerable reduction in number, size, and duration of oral ulcers. Remission in all patients was sustained during 16 weeks of treatment. COMDQ responses improved considerably from baseline to week 8, and this was continued until week 16.
“Onset of response [to apremilast] was rapid,” Dr. Bruce said. “For many other therapies, patients are counseled that [they] may take several weeks to become effective. Response was also dramatic. Almost all patients had complete remission from their ulcers, compared with other therapies where oftentimes reduction or attenuation is achieved, as opposed to complete resolution. There was a suggestion that a lower dose [of apremilast] may still be effective. This adds to our ‘toolbox’ of therapeutic options.”
The most common adverse effects were nausea/vomiting and headache, but these were mild and tolerable and generally resolved by week 4.
The researchers acknowledged certain limitations of the study, including its small sample size. “The challenge will most likely be insurance coverage,” Dr. Bruce said. “This is unfortunate, as it would be ideal to offer a safe treatment without the need for monitoring.”
The investigator-initiated study was supported by Celgene. The researchers reported having no financial disclosures.
SOURCE: Bruce AJ et al. AAD 20, Abstract 17701.
*Correction 6/23/2020: An earlier version of this story misstated the approved indications for apremilast.
FROM AAD 20
Daily Recap: From hospitalist to ‘COVIDist’; Systolic BP -- How low should you go?
Here are the stories our MDedge editors across specialties think you need to know about today:
A ‘Fraternity of People Who Are Struggling’
Kathleen Ronan spent a week in a New Jersey hospital, including 5 days in the ICU, battling the novel coronavirus.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, 51, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article. “It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, researchers have documented what they call post–intensive care syndrome (PICS) — a constellation of physical, cognitive, and psychiatric symptoms that result from an ICU stay. Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her. Read more.
The evolution of ‘COVIDists’
At the start of the pandemic earlier this year hospitalists at Baystate Health in Western Massachusetts realized the necessity of a new model of care for COVID-19 patients. Challenges included a massive surge of COVID-19 patients, a limited supply of PPE, an inadequate number of intensivists for managing the anticipated ventilated patients, and the potential of losing some of our workforce if they became infected. Hospitalists there came up with an elaborate plan to manage the disease burden and the strain on resources effectively.
A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them. The group underwent rapid training in various treatment protocols and ongoing clinical trials.
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. Read more.
How low should you go?
Cardiovascular risk continues to reduce as systolic blood pressure decreases right down to levels as low as 90 mm Hg, according to a new study.
Researchers analyzed data from a cohort of 1,457 participants (mean age, 58 years) who did not have any traditional cardiovascular risk factors and had a systolic blood pressure level between 90 and 129 mm Hg at baseline. Results showed that, during a mean follow-up of 14.5 years, there was an increase in traditional cardiovascular risk factors, coronary artery calcium, and incident cardiovascular events with increasing systolic blood pressure levels.
“We modeled systolic blood pressure on a continuous scale and saw the risk increasing in a linear fashion as blood pressure increased and this occurred right down to 90 mm Hg. We didn’t see any nadir or J-point where there may be an increased risk at lower pressures,” said lead author Seamus Whelton, MD, assistant professor of medicine at the division of cardiology at Johns Hopkins Medicine, Baltimore.
“From an individual level we can now say that in healthy individuals, a systolic pressure in the 90s is not too low. It is a positive thing. And it is recommended to try and keep systolic pressure at these levels if possible by maintaining a healthy lifestyle,” Dr. Whelton said in an interview. Read more.
Asthma tops spending on avoidable pediatric inpatient stays
Asthma costs nearly equaled potentially avoidable hospital bills for diabetes, gastroenteritis, and UTIs combined in a study of in-patient stays among children aged 3 months to 17 years.
Indeed, hospital charges for the treatment of children with asthma made up nearly half of all potentially avoidable pediatric inpatient costs in 2017, according to the Agency for Healthcare Research and Quality.
The cost of potentially avoidable visits for asthma that year was $278 million, versus $284 million combined for the other three conditions, Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, reported in an AHRQ statistical brief.
The state inpatient databases of the AHRQ’s Healthcare Cost and Utilization Project included 1.4 million inpatient stays among children aged 3 months to 17 years in 2017, of which 8% (108,300) were deemed potentially preventable.
Rates of potentially avoidable stays for asthma (159 per 100,000 population), gastroenteritis (90 per 100,000), and UTIs (41 per 100,000) were highest for children aged 0-4 years and generally decreased with age, but diabetes stays increased with age, rising from 12 per 100,000 in children aged 5-9 years to 38 per 100,000 for those 15-17 years old, the researchers said. Read more.
Adding monoclonal antibodies to Botox for migraine prevention
Adjunctive preventive therapy with a calcitonin gene–related peptide monoclonal antibody (CGRP-mAb) medication is safe and effective in patients with chronic migraine who have only achieved a partial response to onabotulinumtoxinA (Botox) treatment.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed. Three CGRP-mAbs have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. Patients treated with Botox had been excluded from these earlier trials, however. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
A ‘Fraternity of People Who Are Struggling’
Kathleen Ronan spent a week in a New Jersey hospital, including 5 days in the ICU, battling the novel coronavirus.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, 51, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article. “It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, researchers have documented what they call post–intensive care syndrome (PICS) — a constellation of physical, cognitive, and psychiatric symptoms that result from an ICU stay. Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her. Read more.
The evolution of ‘COVIDists’
At the start of the pandemic earlier this year hospitalists at Baystate Health in Western Massachusetts realized the necessity of a new model of care for COVID-19 patients. Challenges included a massive surge of COVID-19 patients, a limited supply of PPE, an inadequate number of intensivists for managing the anticipated ventilated patients, and the potential of losing some of our workforce if they became infected. Hospitalists there came up with an elaborate plan to manage the disease burden and the strain on resources effectively.
A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them. The group underwent rapid training in various treatment protocols and ongoing clinical trials.
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. Read more.
How low should you go?
Cardiovascular risk continues to reduce as systolic blood pressure decreases right down to levels as low as 90 mm Hg, according to a new study.
Researchers analyzed data from a cohort of 1,457 participants (mean age, 58 years) who did not have any traditional cardiovascular risk factors and had a systolic blood pressure level between 90 and 129 mm Hg at baseline. Results showed that, during a mean follow-up of 14.5 years, there was an increase in traditional cardiovascular risk factors, coronary artery calcium, and incident cardiovascular events with increasing systolic blood pressure levels.
“We modeled systolic blood pressure on a continuous scale and saw the risk increasing in a linear fashion as blood pressure increased and this occurred right down to 90 mm Hg. We didn’t see any nadir or J-point where there may be an increased risk at lower pressures,” said lead author Seamus Whelton, MD, assistant professor of medicine at the division of cardiology at Johns Hopkins Medicine, Baltimore.
“From an individual level we can now say that in healthy individuals, a systolic pressure in the 90s is not too low. It is a positive thing. And it is recommended to try and keep systolic pressure at these levels if possible by maintaining a healthy lifestyle,” Dr. Whelton said in an interview. Read more.
Asthma tops spending on avoidable pediatric inpatient stays
Asthma costs nearly equaled potentially avoidable hospital bills for diabetes, gastroenteritis, and UTIs combined in a study of in-patient stays among children aged 3 months to 17 years.
Indeed, hospital charges for the treatment of children with asthma made up nearly half of all potentially avoidable pediatric inpatient costs in 2017, according to the Agency for Healthcare Research and Quality.
The cost of potentially avoidable visits for asthma that year was $278 million, versus $284 million combined for the other three conditions, Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, reported in an AHRQ statistical brief.
The state inpatient databases of the AHRQ’s Healthcare Cost and Utilization Project included 1.4 million inpatient stays among children aged 3 months to 17 years in 2017, of which 8% (108,300) were deemed potentially preventable.
Rates of potentially avoidable stays for asthma (159 per 100,000 population), gastroenteritis (90 per 100,000), and UTIs (41 per 100,000) were highest for children aged 0-4 years and generally decreased with age, but diabetes stays increased with age, rising from 12 per 100,000 in children aged 5-9 years to 38 per 100,000 for those 15-17 years old, the researchers said. Read more.
Adding monoclonal antibodies to Botox for migraine prevention
Adjunctive preventive therapy with a calcitonin gene–related peptide monoclonal antibody (CGRP-mAb) medication is safe and effective in patients with chronic migraine who have only achieved a partial response to onabotulinumtoxinA (Botox) treatment.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed. Three CGRP-mAbs have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. Patients treated with Botox had been excluded from these earlier trials, however. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
A ‘Fraternity of People Who Are Struggling’
Kathleen Ronan spent a week in a New Jersey hospital, including 5 days in the ICU, battling the novel coronavirus.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, 51, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article. “It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, researchers have documented what they call post–intensive care syndrome (PICS) — a constellation of physical, cognitive, and psychiatric symptoms that result from an ICU stay. Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her. Read more.
The evolution of ‘COVIDists’
At the start of the pandemic earlier this year hospitalists at Baystate Health in Western Massachusetts realized the necessity of a new model of care for COVID-19 patients. Challenges included a massive surge of COVID-19 patients, a limited supply of PPE, an inadequate number of intensivists for managing the anticipated ventilated patients, and the potential of losing some of our workforce if they became infected. Hospitalists there came up with an elaborate plan to manage the disease burden and the strain on resources effectively.
A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them. The group underwent rapid training in various treatment protocols and ongoing clinical trials.
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. Read more.
How low should you go?
Cardiovascular risk continues to reduce as systolic blood pressure decreases right down to levels as low as 90 mm Hg, according to a new study.
Researchers analyzed data from a cohort of 1,457 participants (mean age, 58 years) who did not have any traditional cardiovascular risk factors and had a systolic blood pressure level between 90 and 129 mm Hg at baseline. Results showed that, during a mean follow-up of 14.5 years, there was an increase in traditional cardiovascular risk factors, coronary artery calcium, and incident cardiovascular events with increasing systolic blood pressure levels.
“We modeled systolic blood pressure on a continuous scale and saw the risk increasing in a linear fashion as blood pressure increased and this occurred right down to 90 mm Hg. We didn’t see any nadir or J-point where there may be an increased risk at lower pressures,” said lead author Seamus Whelton, MD, assistant professor of medicine at the division of cardiology at Johns Hopkins Medicine, Baltimore.
“From an individual level we can now say that in healthy individuals, a systolic pressure in the 90s is not too low. It is a positive thing. And it is recommended to try and keep systolic pressure at these levels if possible by maintaining a healthy lifestyle,” Dr. Whelton said in an interview. Read more.
Asthma tops spending on avoidable pediatric inpatient stays
Asthma costs nearly equaled potentially avoidable hospital bills for diabetes, gastroenteritis, and UTIs combined in a study of in-patient stays among children aged 3 months to 17 years.
Indeed, hospital charges for the treatment of children with asthma made up nearly half of all potentially avoidable pediatric inpatient costs in 2017, according to the Agency for Healthcare Research and Quality.
The cost of potentially avoidable visits for asthma that year was $278 million, versus $284 million combined for the other three conditions, Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, reported in an AHRQ statistical brief.
The state inpatient databases of the AHRQ’s Healthcare Cost and Utilization Project included 1.4 million inpatient stays among children aged 3 months to 17 years in 2017, of which 8% (108,300) were deemed potentially preventable.
Rates of potentially avoidable stays for asthma (159 per 100,000 population), gastroenteritis (90 per 100,000), and UTIs (41 per 100,000) were highest for children aged 0-4 years and generally decreased with age, but diabetes stays increased with age, rising from 12 per 100,000 in children aged 5-9 years to 38 per 100,000 for those 15-17 years old, the researchers said. Read more.
Adding monoclonal antibodies to Botox for migraine prevention
Adjunctive preventive therapy with a calcitonin gene–related peptide monoclonal antibody (CGRP-mAb) medication is safe and effective in patients with chronic migraine who have only achieved a partial response to onabotulinumtoxinA (Botox) treatment.
Investigators found the CGRP-mAbs significantly reduced the number of headache days and pain severity with adverse event rates similar to those reported in previous trials of these medications.
Although Botox is associated with significant clinical improvement in chronic migraine, it often fails to adequately control headache frequency and additional medications are needed. Three CGRP-mAbs have recently been approved for migraine prevention, with results from clinical trials demonstrating they are effective for both chronic and episodic migraine. Patients treated with Botox had been excluded from these earlier trials, however. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
‘I can’t breathe’: Health inequity and state-sanctioned violence
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
ID dermatology: Advancements, but new challenges, over 50 years
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”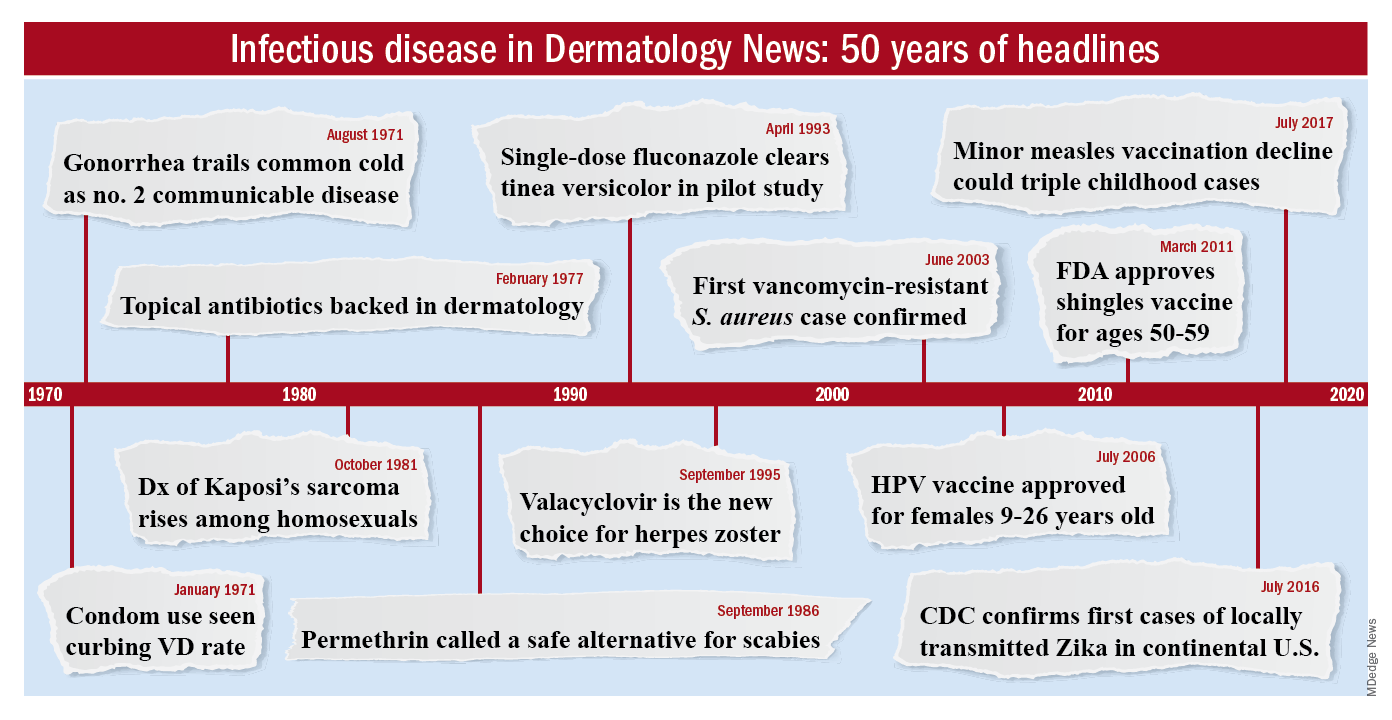
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”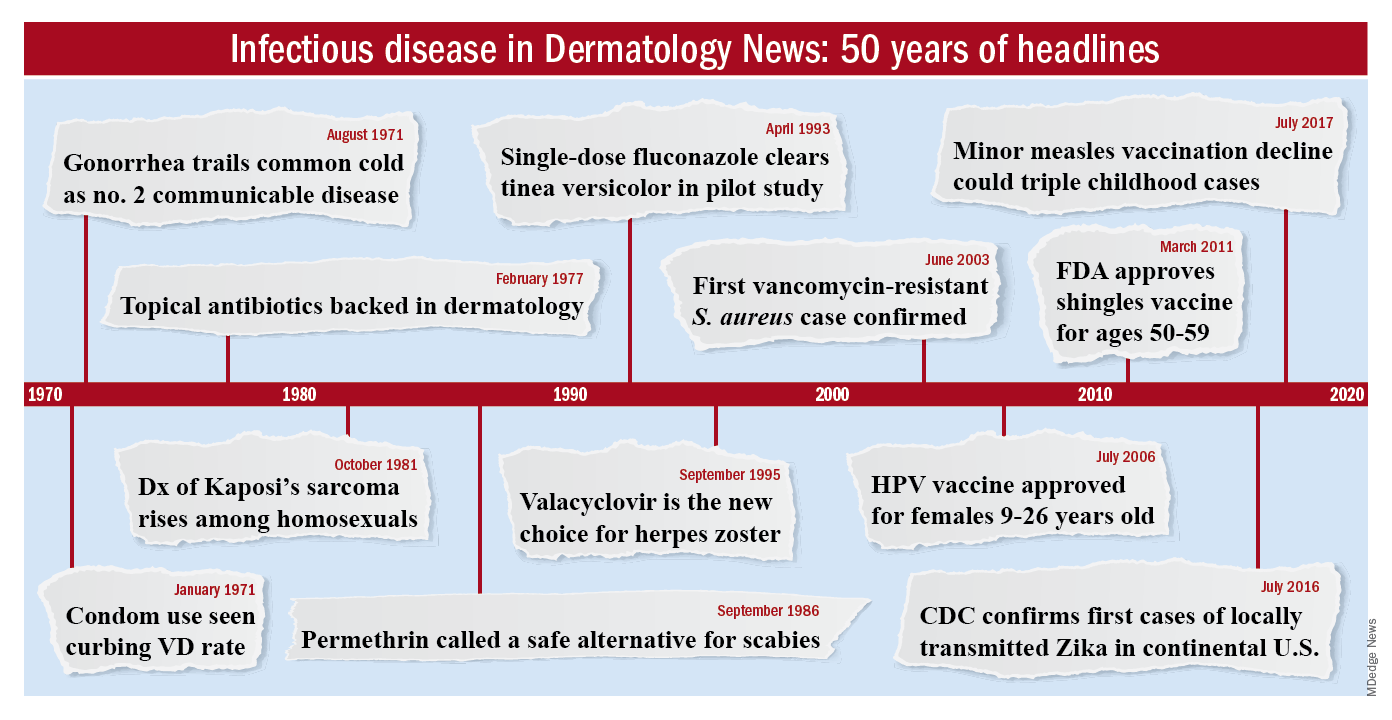
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”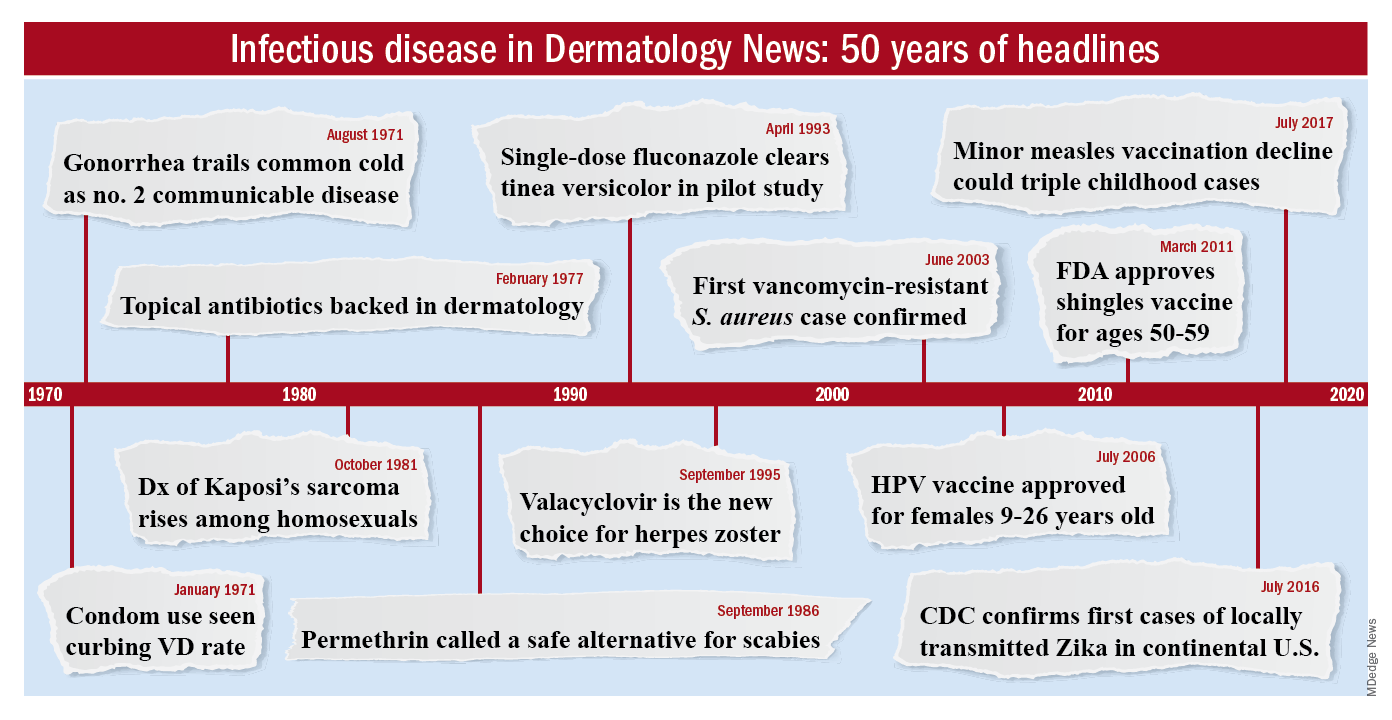
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
















