User login
For MD-IQ use only
Daily Recap: Hospitalized COVID patients need MRIs; Americans vote for face masks
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Letter from the Board of Editors: Call to action (again)
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
The wave of the future
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Longtime CEO bids farewell to SHM
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
FDA approves new indications for pembrolizumab
The Food and Drug Administration recently announced two new types of cancer that can be treated by the anti–PD-1 antibody pembrolizumab.
The new indications expand the use of pembrolizumab (Keytruda) to include treatment of patients with unresectable or metastatic tumor mutational burden–high (TMB-H) solid tumors as well as patients with cutaneous squamous cell carcinoma (cSCC). The FDA announced the new indications just 8 days apart, on June 16 and June 24.
In addition, on June 29, the FDA approved a third new indication for pembrolizumab, this time as first-line treatment for patients with unresectable or metastatic microsatellite instability–high or mismatch repair–deficient colorectal cancer.
The new approvals add to a wide range of oncology indications for which pembrolizumab can be used.
Accelerated approval to treat solid tumors
The FDA granted accelerated approval for pembrolizumab to treat children and adults with unresectable or metastatic TMB-H solid tumors that progressed after previous treatment or in instances where there are no satisfactory alternative treatment options.
The tumor mutational burden must be confirmed by an FDA-approved test. To that end, the FDA approved the FoundationOneCDx assay, which is designed to help physicians determine which patients meet the threshold for TMB-H malignancies (10 or more mutations per megabase).
The efficacy of pembrolizumab in TMB-H solid tumors was investigated in 10 cohorts from the multicenter, open-label KEYNOTE-158 trial. Participants received 200 mg of pembrolizumab intravenously every 3 weeks until their disease progressed or they experienced unacceptable toxicity.
Within this population, 102 patients had tumors that met the TMB-H definition. In this group, the overall response rate was 29%, including a 25% partial response rate and a 4% complete response rate.
The median duration of response was not reached, but 57% of participants experienced a response lasting 12 months or longer, and 50% had a response lasting 24 months or longer.
The most common adverse events associated with pembrolizumab in this trial were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain. Pembrolizumab is associated with immune-mediated side effects, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and skin adverse reactions, the FDA noted.
Safety and efficacy of pembrolizumab in pediatric patients with TMB-H central nervous system cancers have not been established.
New option for recurrent or metastatic cSCC
Physicians treating patients with cSCC that is not curable by surgery or radiation now have pembrolizumab to consider as another treatment option.
The cSCC approval is based on results of the multicenter, open-label KEYNOTE-629 trial. The dosage regimen was 200 mg of pembrolizumab intravenously every 3 weeks until cancer progressed, unacceptable toxicity arose, or 24 months of treatment were completed.
The objective response rate was 34%, and the median duration of response was not reached.
Adverse events were similar to those occurring in patients who received pembrolizumab as a single agent in other clinical trials, the FDA noted.
The Food and Drug Administration recently announced two new types of cancer that can be treated by the anti–PD-1 antibody pembrolizumab.
The new indications expand the use of pembrolizumab (Keytruda) to include treatment of patients with unresectable or metastatic tumor mutational burden–high (TMB-H) solid tumors as well as patients with cutaneous squamous cell carcinoma (cSCC). The FDA announced the new indications just 8 days apart, on June 16 and June 24.
In addition, on June 29, the FDA approved a third new indication for pembrolizumab, this time as first-line treatment for patients with unresectable or metastatic microsatellite instability–high or mismatch repair–deficient colorectal cancer.
The new approvals add to a wide range of oncology indications for which pembrolizumab can be used.
Accelerated approval to treat solid tumors
The FDA granted accelerated approval for pembrolizumab to treat children and adults with unresectable or metastatic TMB-H solid tumors that progressed after previous treatment or in instances where there are no satisfactory alternative treatment options.
The tumor mutational burden must be confirmed by an FDA-approved test. To that end, the FDA approved the FoundationOneCDx assay, which is designed to help physicians determine which patients meet the threshold for TMB-H malignancies (10 or more mutations per megabase).
The efficacy of pembrolizumab in TMB-H solid tumors was investigated in 10 cohorts from the multicenter, open-label KEYNOTE-158 trial. Participants received 200 mg of pembrolizumab intravenously every 3 weeks until their disease progressed or they experienced unacceptable toxicity.
Within this population, 102 patients had tumors that met the TMB-H definition. In this group, the overall response rate was 29%, including a 25% partial response rate and a 4% complete response rate.
The median duration of response was not reached, but 57% of participants experienced a response lasting 12 months or longer, and 50% had a response lasting 24 months or longer.
The most common adverse events associated with pembrolizumab in this trial were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain. Pembrolizumab is associated with immune-mediated side effects, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and skin adverse reactions, the FDA noted.
Safety and efficacy of pembrolizumab in pediatric patients with TMB-H central nervous system cancers have not been established.
New option for recurrent or metastatic cSCC
Physicians treating patients with cSCC that is not curable by surgery or radiation now have pembrolizumab to consider as another treatment option.
The cSCC approval is based on results of the multicenter, open-label KEYNOTE-629 trial. The dosage regimen was 200 mg of pembrolizumab intravenously every 3 weeks until cancer progressed, unacceptable toxicity arose, or 24 months of treatment were completed.
The objective response rate was 34%, and the median duration of response was not reached.
Adverse events were similar to those occurring in patients who received pembrolizumab as a single agent in other clinical trials, the FDA noted.
The Food and Drug Administration recently announced two new types of cancer that can be treated by the anti–PD-1 antibody pembrolizumab.
The new indications expand the use of pembrolizumab (Keytruda) to include treatment of patients with unresectable or metastatic tumor mutational burden–high (TMB-H) solid tumors as well as patients with cutaneous squamous cell carcinoma (cSCC). The FDA announced the new indications just 8 days apart, on June 16 and June 24.
In addition, on June 29, the FDA approved a third new indication for pembrolizumab, this time as first-line treatment for patients with unresectable or metastatic microsatellite instability–high or mismatch repair–deficient colorectal cancer.
The new approvals add to a wide range of oncology indications for which pembrolizumab can be used.
Accelerated approval to treat solid tumors
The FDA granted accelerated approval for pembrolizumab to treat children and adults with unresectable or metastatic TMB-H solid tumors that progressed after previous treatment or in instances where there are no satisfactory alternative treatment options.
The tumor mutational burden must be confirmed by an FDA-approved test. To that end, the FDA approved the FoundationOneCDx assay, which is designed to help physicians determine which patients meet the threshold for TMB-H malignancies (10 or more mutations per megabase).
The efficacy of pembrolizumab in TMB-H solid tumors was investigated in 10 cohorts from the multicenter, open-label KEYNOTE-158 trial. Participants received 200 mg of pembrolizumab intravenously every 3 weeks until their disease progressed or they experienced unacceptable toxicity.
Within this population, 102 patients had tumors that met the TMB-H definition. In this group, the overall response rate was 29%, including a 25% partial response rate and a 4% complete response rate.
The median duration of response was not reached, but 57% of participants experienced a response lasting 12 months or longer, and 50% had a response lasting 24 months or longer.
The most common adverse events associated with pembrolizumab in this trial were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain. Pembrolizumab is associated with immune-mediated side effects, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and skin adverse reactions, the FDA noted.
Safety and efficacy of pembrolizumab in pediatric patients with TMB-H central nervous system cancers have not been established.
New option for recurrent or metastatic cSCC
Physicians treating patients with cSCC that is not curable by surgery or radiation now have pembrolizumab to consider as another treatment option.
The cSCC approval is based on results of the multicenter, open-label KEYNOTE-629 trial. The dosage regimen was 200 mg of pembrolizumab intravenously every 3 weeks until cancer progressed, unacceptable toxicity arose, or 24 months of treatment were completed.
The objective response rate was 34%, and the median duration of response was not reached.
Adverse events were similar to those occurring in patients who received pembrolizumab as a single agent in other clinical trials, the FDA noted.
Daily Recap: Docs are good at saving money; SARS-CoV-2 vaccine trials advance
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Many physicians live within their means and save
Although about two of five physicians report a net worth of between $1 million and $5 million, about half report that they are living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.
Net worth figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%). Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000. Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
Asked about saving habits, 43% of physicians reported they live below their means. Just 7% said they live above their means. How do they save money? Survey respondents reported putting bonus money into an investment account, putting extra money toward paying down the mortgage, and bringing lunch to work everyday.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic. Read more.
Phase 3 COVID-19 vaccine trials launching in July
There are now 120 Investigational New Drug applications to the Food and Drug Administration for a SARS-CoV-2 vaccine, and researchers at more than 70 companies across the globe are interested in making a vaccine, according to Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.” Read more.
FDA approves in-home breast cancer treatment
The Food and Drug Administration has approved a combination of subcutaneous breast cancer treatments that could be administered at home, following completion of chemotherapy.
The agency gave the green light to pertuzumab (Perjeta, Genentech/Roche), trastuzumab (Herceptin, Genentech/Roche) and hyaluronidase (Phesgo, Genentech/Roche), administered subcutaneously rather than intravenously, for the treatment of early and metastatic HER2-positive breast cancers.
Phesgo is initially used in combination with chemotherapy at an infusion center but could continue to be administered in a patient’s home by a qualified health care professional once chemotherapy is complete. Read more.
Could a visual tool aid migraine management?
A new visual tool aims to streamline patient-clinician communication about risk factors for progression from episodic to chronic migraines.
The tool is still just a prototype, but it could eventually synthesize patient responses to an integrated questionnaire and produce a chart illustrating where the patient stands with respect to a range of modifiable risk factors from depression to insomnia.
Physicians must see patients in short appointment periods, making it difficult to communicate all of the risk factors and behavioral characteristics that can contribute to risk of progression. “If you have a patient and you’re able to look at a visualization tool quickly and say: ‘Okay, my patient really is having insomnia and sleep issues,’ you can focus the session talking about sleep, cognitive-behavioral therapy for insomnia, and all the things we can help patients with,” lead researcher Ami Cuneo, MD, who is a headache fellow at the University of Washington, Seattle, said in an interview.
Dr. Cuneo presented a poster describing the concept at the virtual annual meeting of the American Headache Society. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
How racism contributes to the effects of SARS-CoV-2
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
Ignored by doctors, transgender people turn to DIY treatments
For the first 10 months of Christine’s gender transition, a progressive LGBT health clinic in Boston made getting on hormones easy. But after a year or so on estrogen and a testosterone-blocker, she found herself in financial trouble. She had just recently moved to the city, where she was unable to find a job, and her savings were starting to wear thin.
Finding employment as a transgender person, she says, was overwhelmingly difficult: “I was turned down for more jobs than I can count — 20 or 40 different positions in a couple of months.” She would land an interview, then wouldn’t hear back, she says, which she suspects happened because the company noticed she was “not like their other potential hires.”
Christine, a transgender woman, had been enrolled in the state’s Medicaid program, MassHealth, for four months, and her copay for hormone therapy was only $5. But without a job, she found herself torn between food, rent, and medication. For a while, she juggled all three expenses with donations from friends. But after several months, she felt guilty about asking for help and stopped treatment. (Undark has agreed to use only Christine's chosen name because she said she feared both online and in-person harassment for sharing her story.)
At first, Christine didn’t mind being off hormones. She marched in political protests alongside older trans people who assured her that starting and stopping hormones was a normal part of the trans experience. But eventually, Christine felt her body reverting back to the way it had been before her transition; her chest flattened and her fat moved from her hips to her stomach. She stopped wearing dresses and makeup.
“I wasn't looking at myself in the mirror anymore,” she says. “I existed for 10 months, and then I was gone.”
People who are visibly transgender often have trouble finding a job. Nearly a third live in poverty. Many don’t have health insurance, and those who do may have a plan that doesn’t cover hormones. Although testosterone and estrogen only cost $5 to $30 a month for patients with an insurance plan (and typically less than $100 per month for the uninsured), doctors often require consistent therapy and blood work, which ratchets up the cost. Even when trans people have the money, finding doctors willing to treat them can prove impossible. Trans people are also likely to have had bad experiences with the health care system and want to avoid it altogether.
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
But those solutions aren’t available to most people who are seeking DIY treatments right now. Many doctors aren’t even aware that DIY transitioning exists, although the few experts who are following the community aren’t surprised. Self-treatment is “the reality for most trans people in the world,” says Ayden Scheim, an epidemiologist focusing on transgender health at Drexel University who is trans himself.
After Christine posted about her frustrations on Facebook, a trans friend offered a connection to a store in China that illicitly ships hormones to the United States. Christine didn’t follow up, not wanting to take the legal risk. But as time ticked by and job opportunities came and went, her mind started to change.
“I'm ready to throw all of this away and reach out to anyone — any underground black-market means — of getting what I need,” she thought after moving to the Cape. “If these systems put in place to help me have failed me over and over again, why would I go back to them?”
Transgender is an umbrella term that refers to a person who identifies with a gender that doesn’t match the one they were assigned at birth. For example, someone who has male written on their birth certificate, but who identifies as a woman, is a transgender woman. Many trans people experience distress over how their bodies relate to their gender identity, called gender dysphoria. But gender identity is deeply personal. A five o’clock shadow can spur an intense reaction in some trans women, for instance, while others may be fine with it.
To treat gender dysphoria, some trans people take sex hormones, spurring a sort of second puberty. Trans women — as well as people like Christine, who also identifies as nonbinary, meaning she doesn’t exclusively identify as being either a man or a woman — usually take estrogen with the testosterone-blocker spironolactone. Estrogen comes as a daily pill, by injection, or as a patch (recommended for women above the age of 40). The medications redistribute body fat, spur breast growth, decrease muscle mass, slow body hair growth, and shrink the testicles.
Transgender men and non-binary people who want to appear more traditionally masculine use testosterone, usually in the form of injections, which can be taken weekly, biweekly, or every three months depending on the medication. Others use a daily cream, gel, or patch applied to the skin. Testosterone therapy can redistribute body fat, increase strength, boost body hair growth, deepen the voice, stop menstruation, increase libido, and make the clitoris larger.
Some family members — especially those who are cisgender, which means their gender identity matches what they were assigned at birth — worry that people who are confused about their gender will begin hormones and accumulate permanent bodily changes before they realize they’re actually cisgender.
But many of the changes from taking hormones are reversible, and regret appears to be uncommon. Out of a group of nearly 3,400 trans people in the United Kingdom, only 16 regretted their gender transition, according to research presented at the 2019 biennial conference of the European Professional Association for Transgender Health. And although research on surgical transition is sparse, there are some hints that those who choose it are ultimately happy with the decision. According to a small 2018 study in Istanbul, post-operative trans people report a higher quality of life and fewer concerns about gender discrimination compared to those with dysphoria who haven’t had surgery.
And for trans people with dysphoria, hormones can be medically necessary. The treatments aren’t just cosmetic — transitioning literally saves lives, according to the American Academy of Pediatrics. In a 2019 review paper, researchers from the University of San Francisco found that hormone therapy is also linked to a higher quality of life and reduced anxiety and depression.
Despite the growing evidence that medical intervention can help, some trans people are wary of the health care system. According to the 2015 U.S. Transgender Survey, a third of trans people who saw a health care provider experienced mistreatment — from having to educate their doctor about transgender issues to being refused medical treatment to verbal abuse — and 23 percent avoided the doctor’s office because they feared mistreatment.
The health care system has a history of stigmatizing trans identity. Until recently, the World Health Organization and the American Psychiatric Association even considered it a mental disorder. And according to a 2015 study from researchers at the Lesbian, Gay, Bisexual, and Transgender Medical Education Research Group at the Stanford University School of Medicine, less than 35 percent of medical schools teach coursework related to transgender hormone therapy and surgery.
On June 12, the administration of President Donald J. Trump finalized a rule removing protections that had been put in place in 2016 to bar discrimination against transgender people by health care providers. Just three days later, the U.S. Supreme Court decided that the 1964 law that bans discrimination in the workplace based on sex, race, national origin, and religion also applies to sexual orientation and gender identity. While not directly touching on the new health care rule, some experts think the Supreme Court's decision may make legal challenges to it more likely to succeed.
Trans-friendly health care providers are rare, and booking an appointment can stretch out over many weeks. In England, for example, the average wait time from the referral to the first appointment is 18 months, according to an investigation by the BBC. Even those with hormone prescriptions face hurdles to get them filled. Scheim, who lived in Canada until recently, knows this firsthand. “As someone who just moved to the U.S., I’m keenly aware of the hoops one has to jump through,” he says.
“Even if it's theoretically possible to get a hormone prescription, and get it filled, and get it paid for, at a certain point people are going to want to go outside the system,” Scheim says. Navigating bureaucracy, being incorrectly identified — or misgendered — and facing outright transphobia from health care providers, he adds, “can just become too much for folks.”
Many of the health care barriers trans people face are amplified when it comes to surgery. Bottom surgery for trans feminine people, for example, costs about $25,000 and isn’t covered by most insurance plans in the U.S.
There are some signs that at least parts of the medical community have been rethinking their stance on transgender patients. “Clearly the medical professionals didn’t do the right thing. But things are changing now,” says Antonio Metastasio, a psychiatrist at the Camden and Islington NHS Foundation Trust in the U.K.
The Association of American Medical Colleges, for example, released their first curriculum guidelines for treating LGBT patients in 2014. In 2018, the American Academy of Pediatrics released a policy statement on transgender youth, encouraging gender-affirming models of treatment. And in 2019, the American College of Physicians released guidelines for primary care physicians on serving transgender patients.
The World Professional Association for Transgender Health (WPATH) — the international authority on transgender health care, according to a summary of clinical evidence on gender reassignment surgery prepared for the Centers for Medicare and Medicaid Services — has also changed its Standards of Care to make access to hormones easier. Previously, WPATH recommended that before a person could receive hormone treatment, they had to have “persistent, well-documented gender dysphoria,” as well as documented, real-life experiences covering at least three months. The newest guidelines, published in 2012, nix these stringent requirements, although they still strongly recommend mental health evaluations before allowing trans people to access gender-affirming medical care and require a referral letter from a mental health professional.
But the shift hasn’t stopped trans people from seeking DIY treatments.
Before Christine moved to Cape Cod, she secured about two weeks of estrogen from a trans friend. But she soon decided to end the DIY treatment and went off hormones for good. “I can only accept help for something like that for so long before I start to feel bad about it,” she says. “At that point, it was just like I gave up.”
But she didn’t give up for long. After the move, Christine tried to get back on hormones through a legitimate health care provider. First, she considered visiting a Planned Parenthood, but the closest one she could find was at least two hours away and she worried her old car couldn’t make the journey. Then she visited a local women’s health clinic. But she says they turned her away, refused to recognize her gender, and wouldn’t direct her to another provider or clinic. Instead of advice, Christine says, “I got ‘no, goodbye.’”
Left with few options and not wanting to take the risks of further DIY treatment, Christine accepted that she would be off hormones for the foreseeable future.
Many trans folks, however, start or extend their hormone use by turning to drugs that aren’t meant for transitioning, like birth control pills. Others buy hormones online, skirting the law to order from overseas pharmacies without a prescription. To figure out how best to take the drugs, people determine dosages from research online — they read academic literature, technical standards written for health care providers, or advice in blog posts and public forums like Reddit.
Then, they medicate themselves.
Metastasio is one of the few scientists who have studied the practice. He learned about it in 2014, when one of his transgender patients admitted they were taking non-prescribed hormones. Metastasio asked his colleagues if they’d heard similar stories, but none had. So he started asking all his trans patients about DIY hormones and tracked those who were involved in the practice, ultimately publishing a report of seven case studies in 2018.
While there isn’t a lot of other existing research on DIY hormone treatment, and some of it may be outdated, the available studies suggest it is fairly common and researchers may in fact be underestimating the prevalence of DIY hormone use because they miss people who avoid the medical system completely. In 2014, researchers in the U.K. found that at the time of their first gender clinic visit, 17 percent of transgender people were already taking hormones that they had bought online or from a friend. In Canada, a quarter of trans people on hormones had self-medicated, according to a 2013 study in the American Journal of Public Health. And in a survey of trans people in Washington, D.C. in 2000, 58 percent said they used non-prescribed hormones.
People cite all sorts of reasons for ordering the drugs online or acquiring them by other means. In addition to distrust of doctors and a lack of insurance or access to health care, some simply don’t want to endure long waits for medications. That’s the case for Emma, a trans woman in college in the Netherlands, where it can take two to three years to receive a physician prescription. (Emma is only using her first name to avoid online harassment, which she says she’s experienced in the past.)
As for surgery, far fewer people turn to DIY versions compared to those who try hormones. A 2012 study in the Journal of Sexual Medicine reported that only 109 cases of self-castration or self-mutilation of the genitals appear in the scientific literature, and not all are related to gender identity. “But one is too many,” Scheim says. “No one should be in a position where they feel like they need to do that.”
The individual cases reveal a practice that is dangerous and devastating. In Hangzhou, China, a 30-year-old transgender woman feared rejection from her family, so she hid her true gender, according to a 2019 Amnesty International report. She also tried to transition in secret. At first, the woman tried putting ice on her genitals to stop them from functioning. When that didn’t work, she booked an appointment with a black-market surgeon, but the doctor was arrested before her session. She attempted surgery on herself, the report says, and after losing a profuse amount of blood, hailed a taxi to the emergency room. There, she asked the doctor to tell her family she had been in an accident.
When it comes to self-surgery, the dangers of DIY transitioning are obvious. The dangers of DIY hormones are more far-ranging, from “not ideal to serious,” Scheim says. Some DIY users take a more-is-better approach, but taking too much testosterone too quickly can fry the vocal cords. Even buying hormones from an online pharmacy is risky. In 2010, more than half of all treatments from illicit websites — not only of hormones, but of any drug — were counterfeit, according to a bulletin from the World Health Organization.
Still, Charley isn’t worried about the legitimacy of the drugs he’s taking. The packaging his estrogen comes in matches what he would get from a pharmacy with a doctor’s prescription, he says. He’s also unconcerned about the side effects. “I just did a metric century” — a 100-kilometer bike ride — “in under four hours and walked away from it feeling great. I’m healthy,” he says. “So, yeah, there might be a few side effects. But I know where the local hospital is.”
Yet waiting to see if a seemingly minor side effect leads to a health emergency may mean a patient gets help too late. “I don’t want to say that the risks are incredibly high and there is a high mortality,” Metastasio says. “I am saying, though, that this is a procedure best to be monitored.” Metastasio and others recommend seeing a doctor regularly to catch any health issues that arise as quickly as possible.
But even when doctors prescribe the drugs, the risks are unclear because of a lack of research on trans health, says Scheim: “There’s so much we don’t know about hormone use.”
Researchers do know a little bit, though. Even when a doctor weighs in on the proper dosages, there is an increased risk of heart attack. Taking testosterone increases the chances of developing acne, headaches and migraines, and anger and irritability, according to the Trans Care Project, a program of the Transcend Transgender Support and Education Society and Vancouver Coastal Health’s Transgender Health Program in Canada. Testosterone also increases the risk of having abnormally high levels of red blood cells, or polycythemia, which thickens the blood and can lead to clotting. Meanwhile, studies suggest estrogen can up the risk for breast cancer, stroke, blood clots, gallstones, and a range of heart issues. And the most common testosterone-blocker, spironolactone, can cause dehydration and weaken the kidneys.
All of these risks make it especially important for trans people to have the support of a medical provider, Metastasio says. Specialists are in short supply, but general practitioners and family doctors should be able to fill the gap. After all, they already sign off on the hormone medications for cisgender people for birth control and conditions such as menopause and male pattern baldness — which come with similar side effects and warnings as when trans people use them.
Some doctors have already realized the connection. “People can increasingly get hormone therapy from their pre-existing family doctor,” Scheim says, “which is really ideal because people should be able to have a sort of continuity of health care.”
Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City, would like to see more of this. Treating gender dysphoria, she says, should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” she says. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.”
Another way to increase access to hormones is through informed consent, a system which received a green light from the newest WPATH guidelines. That’s how Christine received her hormones from Fenway Health before she moved from Boston to Cape Cod. Under informed consent, if someone has a blood test to assess personal health risks of treatment, they can receive a diagnosis of gender dysphoria, sign off on knowing the risks and benefits of hormone therapy, and get a prescription — all in one day.
And Jaime Lynn Gilmour, a trans woman using the full name she chose to match her gender identity, turned to informed consent after struggling to find DIY hormones. In 2017, Jaime realized she was trans while serving in the military, and says she felt she had to keep her gender a secret. When her service ended, she was ready to start taking hormones right away. So she tried to find them online, but her order wouldn’t go through on three different websites. Instead, she visited a Planned Parenthood clinic. After blood work and a few questions, she walked out with three months of estrogen and spironolactone.
But Goldstein says even informed consent doesn’t go far enough: “If I have someone who's diabetic, I don't make them sign a document eliciting their informed consent before starting insulin.”
For trans people, hormone treatments “are life-saving therapies,” Goldstein adds, “and we shouldn’t delay or stigmatize.”
For now Christine still lives with her parents in Cape Cod. She’s also still off hormones. But she found a job. After she stashes a bit more cash in the bank, she plans to move closer to Boston and find a physician.
Despite the positive shifts in her life, it’s been a difficult few months. After moving to Cape Cod, Christine lost most of her social life and support system — particularly since her parents don’t understand or accept her gender identity. Though she has reconnected with a few friends in the past several weeks, she says she’s in a tough place emotionally. In public, she typically dresses and styles herself to look more masculine to avoid rude stares, and she is experiencing self-hatred that she fears won’t go away when she restarts treatment. Transitioning again isn’t going to be easy, as she explained to Undark in a private message on Facebook: “I've been beaten down enough that now I don't wanna get back up most of the time.”
Even worse is the fear that she might not be able to restart treatment at all. Earlier this year, Christine suffered two health emergencies within the span of a week, in which she says her blood pressure spiked, potentially causing organ damage. Christine has had one similar episode in the past and her family has a history of heart issues.
Christine may not be able to get back on estrogen despite the hard work she’s done to be able to afford it, she says, since it can increase the risk of heart attack and stroke. Because she has so far resisted trying DIY treatments again, she may have saved herself from additional health problems.
But Christine doesn’t see it that way. “Even if it was unsafe, even if I risked health concerns making myself a guinea pig, I wish I followed through,” she wrote. “Being off hormones is hell. And now that I face potentially never taking them again, I wish I had.”
Tara Santora is a science journalist based out of Denver. They have written for Psychology Today, Live Science, Fatherly, Audubon, and more.
This article was originally published on Undark. Read the original article.

For the first 10 months of Christine’s gender transition, a progressive LGBT health clinic in Boston made getting on hormones easy. But after a year or so on estrogen and a testosterone-blocker, she found herself in financial trouble. She had just recently moved to the city, where she was unable to find a job, and her savings were starting to wear thin.
Finding employment as a transgender person, she says, was overwhelmingly difficult: “I was turned down for more jobs than I can count — 20 or 40 different positions in a couple of months.” She would land an interview, then wouldn’t hear back, she says, which she suspects happened because the company noticed she was “not like their other potential hires.”
Christine, a transgender woman, had been enrolled in the state’s Medicaid program, MassHealth, for four months, and her copay for hormone therapy was only $5. But without a job, she found herself torn between food, rent, and medication. For a while, she juggled all three expenses with donations from friends. But after several months, she felt guilty about asking for help and stopped treatment. (Undark has agreed to use only Christine's chosen name because she said she feared both online and in-person harassment for sharing her story.)
At first, Christine didn’t mind being off hormones. She marched in political protests alongside older trans people who assured her that starting and stopping hormones was a normal part of the trans experience. But eventually, Christine felt her body reverting back to the way it had been before her transition; her chest flattened and her fat moved from her hips to her stomach. She stopped wearing dresses and makeup.
“I wasn't looking at myself in the mirror anymore,” she says. “I existed for 10 months, and then I was gone.”
People who are visibly transgender often have trouble finding a job. Nearly a third live in poverty. Many don’t have health insurance, and those who do may have a plan that doesn’t cover hormones. Although testosterone and estrogen only cost $5 to $30 a month for patients with an insurance plan (and typically less than $100 per month for the uninsured), doctors often require consistent therapy and blood work, which ratchets up the cost. Even when trans people have the money, finding doctors willing to treat them can prove impossible. Trans people are also likely to have had bad experiences with the health care system and want to avoid it altogether.
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
But those solutions aren’t available to most people who are seeking DIY treatments right now. Many doctors aren’t even aware that DIY transitioning exists, although the few experts who are following the community aren’t surprised. Self-treatment is “the reality for most trans people in the world,” says Ayden Scheim, an epidemiologist focusing on transgender health at Drexel University who is trans himself.
After Christine posted about her frustrations on Facebook, a trans friend offered a connection to a store in China that illicitly ships hormones to the United States. Christine didn’t follow up, not wanting to take the legal risk. But as time ticked by and job opportunities came and went, her mind started to change.
“I'm ready to throw all of this away and reach out to anyone — any underground black-market means — of getting what I need,” she thought after moving to the Cape. “If these systems put in place to help me have failed me over and over again, why would I go back to them?”
Transgender is an umbrella term that refers to a person who identifies with a gender that doesn’t match the one they were assigned at birth. For example, someone who has male written on their birth certificate, but who identifies as a woman, is a transgender woman. Many trans people experience distress over how their bodies relate to their gender identity, called gender dysphoria. But gender identity is deeply personal. A five o’clock shadow can spur an intense reaction in some trans women, for instance, while others may be fine with it.
To treat gender dysphoria, some trans people take sex hormones, spurring a sort of second puberty. Trans women — as well as people like Christine, who also identifies as nonbinary, meaning she doesn’t exclusively identify as being either a man or a woman — usually take estrogen with the testosterone-blocker spironolactone. Estrogen comes as a daily pill, by injection, or as a patch (recommended for women above the age of 40). The medications redistribute body fat, spur breast growth, decrease muscle mass, slow body hair growth, and shrink the testicles.
Transgender men and non-binary people who want to appear more traditionally masculine use testosterone, usually in the form of injections, which can be taken weekly, biweekly, or every three months depending on the medication. Others use a daily cream, gel, or patch applied to the skin. Testosterone therapy can redistribute body fat, increase strength, boost body hair growth, deepen the voice, stop menstruation, increase libido, and make the clitoris larger.
Some family members — especially those who are cisgender, which means their gender identity matches what they were assigned at birth — worry that people who are confused about their gender will begin hormones and accumulate permanent bodily changes before they realize they’re actually cisgender.
But many of the changes from taking hormones are reversible, and regret appears to be uncommon. Out of a group of nearly 3,400 trans people in the United Kingdom, only 16 regretted their gender transition, according to research presented at the 2019 biennial conference of the European Professional Association for Transgender Health. And although research on surgical transition is sparse, there are some hints that those who choose it are ultimately happy with the decision. According to a small 2018 study in Istanbul, post-operative trans people report a higher quality of life and fewer concerns about gender discrimination compared to those with dysphoria who haven’t had surgery.
And for trans people with dysphoria, hormones can be medically necessary. The treatments aren’t just cosmetic — transitioning literally saves lives, according to the American Academy of Pediatrics. In a 2019 review paper, researchers from the University of San Francisco found that hormone therapy is also linked to a higher quality of life and reduced anxiety and depression.
Despite the growing evidence that medical intervention can help, some trans people are wary of the health care system. According to the 2015 U.S. Transgender Survey, a third of trans people who saw a health care provider experienced mistreatment — from having to educate their doctor about transgender issues to being refused medical treatment to verbal abuse — and 23 percent avoided the doctor’s office because they feared mistreatment.
The health care system has a history of stigmatizing trans identity. Until recently, the World Health Organization and the American Psychiatric Association even considered it a mental disorder. And according to a 2015 study from researchers at the Lesbian, Gay, Bisexual, and Transgender Medical Education Research Group at the Stanford University School of Medicine, less than 35 percent of medical schools teach coursework related to transgender hormone therapy and surgery.
On June 12, the administration of President Donald J. Trump finalized a rule removing protections that had been put in place in 2016 to bar discrimination against transgender people by health care providers. Just three days later, the U.S. Supreme Court decided that the 1964 law that bans discrimination in the workplace based on sex, race, national origin, and religion also applies to sexual orientation and gender identity. While not directly touching on the new health care rule, some experts think the Supreme Court's decision may make legal challenges to it more likely to succeed.
Trans-friendly health care providers are rare, and booking an appointment can stretch out over many weeks. In England, for example, the average wait time from the referral to the first appointment is 18 months, according to an investigation by the BBC. Even those with hormone prescriptions face hurdles to get them filled. Scheim, who lived in Canada until recently, knows this firsthand. “As someone who just moved to the U.S., I’m keenly aware of the hoops one has to jump through,” he says.
“Even if it's theoretically possible to get a hormone prescription, and get it filled, and get it paid for, at a certain point people are going to want to go outside the system,” Scheim says. Navigating bureaucracy, being incorrectly identified — or misgendered — and facing outright transphobia from health care providers, he adds, “can just become too much for folks.”
Many of the health care barriers trans people face are amplified when it comes to surgery. Bottom surgery for trans feminine people, for example, costs about $25,000 and isn’t covered by most insurance plans in the U.S.
There are some signs that at least parts of the medical community have been rethinking their stance on transgender patients. “Clearly the medical professionals didn’t do the right thing. But things are changing now,” says Antonio Metastasio, a psychiatrist at the Camden and Islington NHS Foundation Trust in the U.K.
The Association of American Medical Colleges, for example, released their first curriculum guidelines for treating LGBT patients in 2014. In 2018, the American Academy of Pediatrics released a policy statement on transgender youth, encouraging gender-affirming models of treatment. And in 2019, the American College of Physicians released guidelines for primary care physicians on serving transgender patients.
The World Professional Association for Transgender Health (WPATH) — the international authority on transgender health care, according to a summary of clinical evidence on gender reassignment surgery prepared for the Centers for Medicare and Medicaid Services — has also changed its Standards of Care to make access to hormones easier. Previously, WPATH recommended that before a person could receive hormone treatment, they had to have “persistent, well-documented gender dysphoria,” as well as documented, real-life experiences covering at least three months. The newest guidelines, published in 2012, nix these stringent requirements, although they still strongly recommend mental health evaluations before allowing trans people to access gender-affirming medical care and require a referral letter from a mental health professional.
But the shift hasn’t stopped trans people from seeking DIY treatments.
Before Christine moved to Cape Cod, she secured about two weeks of estrogen from a trans friend. But she soon decided to end the DIY treatment and went off hormones for good. “I can only accept help for something like that for so long before I start to feel bad about it,” she says. “At that point, it was just like I gave up.”
But she didn’t give up for long. After the move, Christine tried to get back on hormones through a legitimate health care provider. First, she considered visiting a Planned Parenthood, but the closest one she could find was at least two hours away and she worried her old car couldn’t make the journey. Then she visited a local women’s health clinic. But she says they turned her away, refused to recognize her gender, and wouldn’t direct her to another provider or clinic. Instead of advice, Christine says, “I got ‘no, goodbye.’”
Left with few options and not wanting to take the risks of further DIY treatment, Christine accepted that she would be off hormones for the foreseeable future.
Many trans folks, however, start or extend their hormone use by turning to drugs that aren’t meant for transitioning, like birth control pills. Others buy hormones online, skirting the law to order from overseas pharmacies without a prescription. To figure out how best to take the drugs, people determine dosages from research online — they read academic literature, technical standards written for health care providers, or advice in blog posts and public forums like Reddit.
Then, they medicate themselves.
Metastasio is one of the few scientists who have studied the practice. He learned about it in 2014, when one of his transgender patients admitted they were taking non-prescribed hormones. Metastasio asked his colleagues if they’d heard similar stories, but none had. So he started asking all his trans patients about DIY hormones and tracked those who were involved in the practice, ultimately publishing a report of seven case studies in 2018.
While there isn’t a lot of other existing research on DIY hormone treatment, and some of it may be outdated, the available studies suggest it is fairly common and researchers may in fact be underestimating the prevalence of DIY hormone use because they miss people who avoid the medical system completely. In 2014, researchers in the U.K. found that at the time of their first gender clinic visit, 17 percent of transgender people were already taking hormones that they had bought online or from a friend. In Canada, a quarter of trans people on hormones had self-medicated, according to a 2013 study in the American Journal of Public Health. And in a survey of trans people in Washington, D.C. in 2000, 58 percent said they used non-prescribed hormones.
People cite all sorts of reasons for ordering the drugs online or acquiring them by other means. In addition to distrust of doctors and a lack of insurance or access to health care, some simply don’t want to endure long waits for medications. That’s the case for Emma, a trans woman in college in the Netherlands, where it can take two to three years to receive a physician prescription. (Emma is only using her first name to avoid online harassment, which she says she’s experienced in the past.)
As for surgery, far fewer people turn to DIY versions compared to those who try hormones. A 2012 study in the Journal of Sexual Medicine reported that only 109 cases of self-castration or self-mutilation of the genitals appear in the scientific literature, and not all are related to gender identity. “But one is too many,” Scheim says. “No one should be in a position where they feel like they need to do that.”
The individual cases reveal a practice that is dangerous and devastating. In Hangzhou, China, a 30-year-old transgender woman feared rejection from her family, so she hid her true gender, according to a 2019 Amnesty International report. She also tried to transition in secret. At first, the woman tried putting ice on her genitals to stop them from functioning. When that didn’t work, she booked an appointment with a black-market surgeon, but the doctor was arrested before her session. She attempted surgery on herself, the report says, and after losing a profuse amount of blood, hailed a taxi to the emergency room. There, she asked the doctor to tell her family she had been in an accident.
When it comes to self-surgery, the dangers of DIY transitioning are obvious. The dangers of DIY hormones are more far-ranging, from “not ideal to serious,” Scheim says. Some DIY users take a more-is-better approach, but taking too much testosterone too quickly can fry the vocal cords. Even buying hormones from an online pharmacy is risky. In 2010, more than half of all treatments from illicit websites — not only of hormones, but of any drug — were counterfeit, according to a bulletin from the World Health Organization.
Still, Charley isn’t worried about the legitimacy of the drugs he’s taking. The packaging his estrogen comes in matches what he would get from a pharmacy with a doctor’s prescription, he says. He’s also unconcerned about the side effects. “I just did a metric century” — a 100-kilometer bike ride — “in under four hours and walked away from it feeling great. I’m healthy,” he says. “So, yeah, there might be a few side effects. But I know where the local hospital is.”
Yet waiting to see if a seemingly minor side effect leads to a health emergency may mean a patient gets help too late. “I don’t want to say that the risks are incredibly high and there is a high mortality,” Metastasio says. “I am saying, though, that this is a procedure best to be monitored.” Metastasio and others recommend seeing a doctor regularly to catch any health issues that arise as quickly as possible.
But even when doctors prescribe the drugs, the risks are unclear because of a lack of research on trans health, says Scheim: “There’s so much we don’t know about hormone use.”
Researchers do know a little bit, though. Even when a doctor weighs in on the proper dosages, there is an increased risk of heart attack. Taking testosterone increases the chances of developing acne, headaches and migraines, and anger and irritability, according to the Trans Care Project, a program of the Transcend Transgender Support and Education Society and Vancouver Coastal Health’s Transgender Health Program in Canada. Testosterone also increases the risk of having abnormally high levels of red blood cells, or polycythemia, which thickens the blood and can lead to clotting. Meanwhile, studies suggest estrogen can up the risk for breast cancer, stroke, blood clots, gallstones, and a range of heart issues. And the most common testosterone-blocker, spironolactone, can cause dehydration and weaken the kidneys.
All of these risks make it especially important for trans people to have the support of a medical provider, Metastasio says. Specialists are in short supply, but general practitioners and family doctors should be able to fill the gap. After all, they already sign off on the hormone medications for cisgender people for birth control and conditions such as menopause and male pattern baldness — which come with similar side effects and warnings as when trans people use them.
Some doctors have already realized the connection. “People can increasingly get hormone therapy from their pre-existing family doctor,” Scheim says, “which is really ideal because people should be able to have a sort of continuity of health care.”
Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City, would like to see more of this. Treating gender dysphoria, she says, should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” she says. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.”
Another way to increase access to hormones is through informed consent, a system which received a green light from the newest WPATH guidelines. That’s how Christine received her hormones from Fenway Health before she moved from Boston to Cape Cod. Under informed consent, if someone has a blood test to assess personal health risks of treatment, they can receive a diagnosis of gender dysphoria, sign off on knowing the risks and benefits of hormone therapy, and get a prescription — all in one day.
And Jaime Lynn Gilmour, a trans woman using the full name she chose to match her gender identity, turned to informed consent after struggling to find DIY hormones. In 2017, Jaime realized she was trans while serving in the military, and says she felt she had to keep her gender a secret. When her service ended, she was ready to start taking hormones right away. So she tried to find them online, but her order wouldn’t go through on three different websites. Instead, she visited a Planned Parenthood clinic. After blood work and a few questions, she walked out with three months of estrogen and spironolactone.
But Goldstein says even informed consent doesn’t go far enough: “If I have someone who's diabetic, I don't make them sign a document eliciting their informed consent before starting insulin.”
For trans people, hormone treatments “are life-saving therapies,” Goldstein adds, “and we shouldn’t delay or stigmatize.”
For now Christine still lives with her parents in Cape Cod. She’s also still off hormones. But she found a job. After she stashes a bit more cash in the bank, she plans to move closer to Boston and find a physician.
Despite the positive shifts in her life, it’s been a difficult few months. After moving to Cape Cod, Christine lost most of her social life and support system — particularly since her parents don’t understand or accept her gender identity. Though she has reconnected with a few friends in the past several weeks, she says she’s in a tough place emotionally. In public, she typically dresses and styles herself to look more masculine to avoid rude stares, and she is experiencing self-hatred that she fears won’t go away when she restarts treatment. Transitioning again isn’t going to be easy, as she explained to Undark in a private message on Facebook: “I've been beaten down enough that now I don't wanna get back up most of the time.”
Even worse is the fear that she might not be able to restart treatment at all. Earlier this year, Christine suffered two health emergencies within the span of a week, in which she says her blood pressure spiked, potentially causing organ damage. Christine has had one similar episode in the past and her family has a history of heart issues.
Christine may not be able to get back on estrogen despite the hard work she’s done to be able to afford it, she says, since it can increase the risk of heart attack and stroke. Because she has so far resisted trying DIY treatments again, she may have saved herself from additional health problems.
But Christine doesn’t see it that way. “Even if it was unsafe, even if I risked health concerns making myself a guinea pig, I wish I followed through,” she wrote. “Being off hormones is hell. And now that I face potentially never taking them again, I wish I had.”
Tara Santora is a science journalist based out of Denver. They have written for Psychology Today, Live Science, Fatherly, Audubon, and more.
This article was originally published on Undark. Read the original article.

For the first 10 months of Christine’s gender transition, a progressive LGBT health clinic in Boston made getting on hormones easy. But after a year or so on estrogen and a testosterone-blocker, she found herself in financial trouble. She had just recently moved to the city, where she was unable to find a job, and her savings were starting to wear thin.
Finding employment as a transgender person, she says, was overwhelmingly difficult: “I was turned down for more jobs than I can count — 20 or 40 different positions in a couple of months.” She would land an interview, then wouldn’t hear back, she says, which she suspects happened because the company noticed she was “not like their other potential hires.”
Christine, a transgender woman, had been enrolled in the state’s Medicaid program, MassHealth, for four months, and her copay for hormone therapy was only $5. But without a job, she found herself torn between food, rent, and medication. For a while, she juggled all three expenses with donations from friends. But after several months, she felt guilty about asking for help and stopped treatment. (Undark has agreed to use only Christine's chosen name because she said she feared both online and in-person harassment for sharing her story.)
At first, Christine didn’t mind being off hormones. She marched in political protests alongside older trans people who assured her that starting and stopping hormones was a normal part of the trans experience. But eventually, Christine felt her body reverting back to the way it had been before her transition; her chest flattened and her fat moved from her hips to her stomach. She stopped wearing dresses and makeup.
“I wasn't looking at myself in the mirror anymore,” she says. “I existed for 10 months, and then I was gone.”
People who are visibly transgender often have trouble finding a job. Nearly a third live in poverty. Many don’t have health insurance, and those who do may have a plan that doesn’t cover hormones. Although testosterone and estrogen only cost $5 to $30 a month for patients with an insurance plan (and typically less than $100 per month for the uninsured), doctors often require consistent therapy and blood work, which ratchets up the cost. Even when trans people have the money, finding doctors willing to treat them can prove impossible. Trans people are also likely to have had bad experiences with the health care system and want to avoid it altogether.
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
But those solutions aren’t available to most people who are seeking DIY treatments right now. Many doctors aren’t even aware that DIY transitioning exists, although the few experts who are following the community aren’t surprised. Self-treatment is “the reality for most trans people in the world,” says Ayden Scheim, an epidemiologist focusing on transgender health at Drexel University who is trans himself.
After Christine posted about her frustrations on Facebook, a trans friend offered a connection to a store in China that illicitly ships hormones to the United States. Christine didn’t follow up, not wanting to take the legal risk. But as time ticked by and job opportunities came and went, her mind started to change.
“I'm ready to throw all of this away and reach out to anyone — any underground black-market means — of getting what I need,” she thought after moving to the Cape. “If these systems put in place to help me have failed me over and over again, why would I go back to them?”
Transgender is an umbrella term that refers to a person who identifies with a gender that doesn’t match the one they were assigned at birth. For example, someone who has male written on their birth certificate, but who identifies as a woman, is a transgender woman. Many trans people experience distress over how their bodies relate to their gender identity, called gender dysphoria. But gender identity is deeply personal. A five o’clock shadow can spur an intense reaction in some trans women, for instance, while others may be fine with it.
To treat gender dysphoria, some trans people take sex hormones, spurring a sort of second puberty. Trans women — as well as people like Christine, who also identifies as nonbinary, meaning she doesn’t exclusively identify as being either a man or a woman — usually take estrogen with the testosterone-blocker spironolactone. Estrogen comes as a daily pill, by injection, or as a patch (recommended for women above the age of 40). The medications redistribute body fat, spur breast growth, decrease muscle mass, slow body hair growth, and shrink the testicles.
Transgender men and non-binary people who want to appear more traditionally masculine use testosterone, usually in the form of injections, which can be taken weekly, biweekly, or every three months depending on the medication. Others use a daily cream, gel, or patch applied to the skin. Testosterone therapy can redistribute body fat, increase strength, boost body hair growth, deepen the voice, stop menstruation, increase libido, and make the clitoris larger.
Some family members — especially those who are cisgender, which means their gender identity matches what they were assigned at birth — worry that people who are confused about their gender will begin hormones and accumulate permanent bodily changes before they realize they’re actually cisgender.
But many of the changes from taking hormones are reversible, and regret appears to be uncommon. Out of a group of nearly 3,400 trans people in the United Kingdom, only 16 regretted their gender transition, according to research presented at the 2019 biennial conference of the European Professional Association for Transgender Health. And although research on surgical transition is sparse, there are some hints that those who choose it are ultimately happy with the decision. According to a small 2018 study in Istanbul, post-operative trans people report a higher quality of life and fewer concerns about gender discrimination compared to those with dysphoria who haven’t had surgery.
And for trans people with dysphoria, hormones can be medically necessary. The treatments aren’t just cosmetic — transitioning literally saves lives, according to the American Academy of Pediatrics. In a 2019 review paper, researchers from the University of San Francisco found that hormone therapy is also linked to a higher quality of life and reduced anxiety and depression.
Despite the growing evidence that medical intervention can help, some trans people are wary of the health care system. According to the 2015 U.S. Transgender Survey, a third of trans people who saw a health care provider experienced mistreatment — from having to educate their doctor about transgender issues to being refused medical treatment to verbal abuse — and 23 percent avoided the doctor’s office because they feared mistreatment.
The health care system has a history of stigmatizing trans identity. Until recently, the World Health Organization and the American Psychiatric Association even considered it a mental disorder. And according to a 2015 study from researchers at the Lesbian, Gay, Bisexual, and Transgender Medical Education Research Group at the Stanford University School of Medicine, less than 35 percent of medical schools teach coursework related to transgender hormone therapy and surgery.
On June 12, the administration of President Donald J. Trump finalized a rule removing protections that had been put in place in 2016 to bar discrimination against transgender people by health care providers. Just three days later, the U.S. Supreme Court decided that the 1964 law that bans discrimination in the workplace based on sex, race, national origin, and religion also applies to sexual orientation and gender identity. While not directly touching on the new health care rule, some experts think the Supreme Court's decision may make legal challenges to it more likely to succeed.
Trans-friendly health care providers are rare, and booking an appointment can stretch out over many weeks. In England, for example, the average wait time from the referral to the first appointment is 18 months, according to an investigation by the BBC. Even those with hormone prescriptions face hurdles to get them filled. Scheim, who lived in Canada until recently, knows this firsthand. “As someone who just moved to the U.S., I’m keenly aware of the hoops one has to jump through,” he says.
“Even if it's theoretically possible to get a hormone prescription, and get it filled, and get it paid for, at a certain point people are going to want to go outside the system,” Scheim says. Navigating bureaucracy, being incorrectly identified — or misgendered — and facing outright transphobia from health care providers, he adds, “can just become too much for folks.”
Many of the health care barriers trans people face are amplified when it comes to surgery. Bottom surgery for trans feminine people, for example, costs about $25,000 and isn’t covered by most insurance plans in the U.S.
There are some signs that at least parts of the medical community have been rethinking their stance on transgender patients. “Clearly the medical professionals didn’t do the right thing. But things are changing now,” says Antonio Metastasio, a psychiatrist at the Camden and Islington NHS Foundation Trust in the U.K.
The Association of American Medical Colleges, for example, released their first curriculum guidelines for treating LGBT patients in 2014. In 2018, the American Academy of Pediatrics released a policy statement on transgender youth, encouraging gender-affirming models of treatment. And in 2019, the American College of Physicians released guidelines for primary care physicians on serving transgender patients.
The World Professional Association for Transgender Health (WPATH) — the international authority on transgender health care, according to a summary of clinical evidence on gender reassignment surgery prepared for the Centers for Medicare and Medicaid Services — has also changed its Standards of Care to make access to hormones easier. Previously, WPATH recommended that before a person could receive hormone treatment, they had to have “persistent, well-documented gender dysphoria,” as well as documented, real-life experiences covering at least three months. The newest guidelines, published in 2012, nix these stringent requirements, although they still strongly recommend mental health evaluations before allowing trans people to access gender-affirming medical care and require a referral letter from a mental health professional.
But the shift hasn’t stopped trans people from seeking DIY treatments.
Before Christine moved to Cape Cod, she secured about two weeks of estrogen from a trans friend. But she soon decided to end the DIY treatment and went off hormones for good. “I can only accept help for something like that for so long before I start to feel bad about it,” she says. “At that point, it was just like I gave up.”
But she didn’t give up for long. After the move, Christine tried to get back on hormones through a legitimate health care provider. First, she considered visiting a Planned Parenthood, but the closest one she could find was at least two hours away and she worried her old car couldn’t make the journey. Then she visited a local women’s health clinic. But she says they turned her away, refused to recognize her gender, and wouldn’t direct her to another provider or clinic. Instead of advice, Christine says, “I got ‘no, goodbye.’”
Left with few options and not wanting to take the risks of further DIY treatment, Christine accepted that she would be off hormones for the foreseeable future.
Many trans folks, however, start or extend their hormone use by turning to drugs that aren’t meant for transitioning, like birth control pills. Others buy hormones online, skirting the law to order from overseas pharmacies without a prescription. To figure out how best to take the drugs, people determine dosages from research online — they read academic literature, technical standards written for health care providers, or advice in blog posts and public forums like Reddit.
Then, they medicate themselves.
Metastasio is one of the few scientists who have studied the practice. He learned about it in 2014, when one of his transgender patients admitted they were taking non-prescribed hormones. Metastasio asked his colleagues if they’d heard similar stories, but none had. So he started asking all his trans patients about DIY hormones and tracked those who were involved in the practice, ultimately publishing a report of seven case studies in 2018.
While there isn’t a lot of other existing research on DIY hormone treatment, and some of it may be outdated, the available studies suggest it is fairly common and researchers may in fact be underestimating the prevalence of DIY hormone use because they miss people who avoid the medical system completely. In 2014, researchers in the U.K. found that at the time of their first gender clinic visit, 17 percent of transgender people were already taking hormones that they had bought online or from a friend. In Canada, a quarter of trans people on hormones had self-medicated, according to a 2013 study in the American Journal of Public Health. And in a survey of trans people in Washington, D.C. in 2000, 58 percent said they used non-prescribed hormones.
People cite all sorts of reasons for ordering the drugs online or acquiring them by other means. In addition to distrust of doctors and a lack of insurance or access to health care, some simply don’t want to endure long waits for medications. That’s the case for Emma, a trans woman in college in the Netherlands, where it can take two to three years to receive a physician prescription. (Emma is only using her first name to avoid online harassment, which she says she’s experienced in the past.)
As for surgery, far fewer people turn to DIY versions compared to those who try hormones. A 2012 study in the Journal of Sexual Medicine reported that only 109 cases of self-castration or self-mutilation of the genitals appear in the scientific literature, and not all are related to gender identity. “But one is too many,” Scheim says. “No one should be in a position where they feel like they need to do that.”
The individual cases reveal a practice that is dangerous and devastating. In Hangzhou, China, a 30-year-old transgender woman feared rejection from her family, so she hid her true gender, according to a 2019 Amnesty International report. She also tried to transition in secret. At first, the woman tried putting ice on her genitals to stop them from functioning. When that didn’t work, she booked an appointment with a black-market surgeon, but the doctor was arrested before her session. She attempted surgery on herself, the report says, and after losing a profuse amount of blood, hailed a taxi to the emergency room. There, she asked the doctor to tell her family she had been in an accident.
When it comes to self-surgery, the dangers of DIY transitioning are obvious. The dangers of DIY hormones are more far-ranging, from “not ideal to serious,” Scheim says. Some DIY users take a more-is-better approach, but taking too much testosterone too quickly can fry the vocal cords. Even buying hormones from an online pharmacy is risky. In 2010, more than half of all treatments from illicit websites — not only of hormones, but of any drug — were counterfeit, according to a bulletin from the World Health Organization.
Still, Charley isn’t worried about the legitimacy of the drugs he’s taking. The packaging his estrogen comes in matches what he would get from a pharmacy with a doctor’s prescription, he says. He’s also unconcerned about the side effects. “I just did a metric century” — a 100-kilometer bike ride — “in under four hours and walked away from it feeling great. I’m healthy,” he says. “So, yeah, there might be a few side effects. But I know where the local hospital is.”
Yet waiting to see if a seemingly minor side effect leads to a health emergency may mean a patient gets help too late. “I don’t want to say that the risks are incredibly high and there is a high mortality,” Metastasio says. “I am saying, though, that this is a procedure best to be monitored.” Metastasio and others recommend seeing a doctor regularly to catch any health issues that arise as quickly as possible.
But even when doctors prescribe the drugs, the risks are unclear because of a lack of research on trans health, says Scheim: “There’s so much we don’t know about hormone use.”
Researchers do know a little bit, though. Even when a doctor weighs in on the proper dosages, there is an increased risk of heart attack. Taking testosterone increases the chances of developing acne, headaches and migraines, and anger and irritability, according to the Trans Care Project, a program of the Transcend Transgender Support and Education Society and Vancouver Coastal Health’s Transgender Health Program in Canada. Testosterone also increases the risk of having abnormally high levels of red blood cells, or polycythemia, which thickens the blood and can lead to clotting. Meanwhile, studies suggest estrogen can up the risk for breast cancer, stroke, blood clots, gallstones, and a range of heart issues. And the most common testosterone-blocker, spironolactone, can cause dehydration and weaken the kidneys.
All of these risks make it especially important for trans people to have the support of a medical provider, Metastasio says. Specialists are in short supply, but general practitioners and family doctors should be able to fill the gap. After all, they already sign off on the hormone medications for cisgender people for birth control and conditions such as menopause and male pattern baldness — which come with similar side effects and warnings as when trans people use them.
Some doctors have already realized the connection. “People can increasingly get hormone therapy from their pre-existing family doctor,” Scheim says, “which is really ideal because people should be able to have a sort of continuity of health care.”
Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City, would like to see more of this. Treating gender dysphoria, she says, should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” she says. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.”
Another way to increase access to hormones is through informed consent, a system which received a green light from the newest WPATH guidelines. That’s how Christine received her hormones from Fenway Health before she moved from Boston to Cape Cod. Under informed consent, if someone has a blood test to assess personal health risks of treatment, they can receive a diagnosis of gender dysphoria, sign off on knowing the risks and benefits of hormone therapy, and get a prescription — all in one day.
And Jaime Lynn Gilmour, a trans woman using the full name she chose to match her gender identity, turned to informed consent after struggling to find DIY hormones. In 2017, Jaime realized she was trans while serving in the military, and says she felt she had to keep her gender a secret. When her service ended, she was ready to start taking hormones right away. So she tried to find them online, but her order wouldn’t go through on three different websites. Instead, she visited a Planned Parenthood clinic. After blood work and a few questions, she walked out with three months of estrogen and spironolactone.
But Goldstein says even informed consent doesn’t go far enough: “If I have someone who's diabetic, I don't make them sign a document eliciting their informed consent before starting insulin.”
For trans people, hormone treatments “are life-saving therapies,” Goldstein adds, “and we shouldn’t delay or stigmatize.”
For now Christine still lives with her parents in Cape Cod. She’s also still off hormones. But she found a job. After she stashes a bit more cash in the bank, she plans to move closer to Boston and find a physician.
Despite the positive shifts in her life, it’s been a difficult few months. After moving to Cape Cod, Christine lost most of her social life and support system — particularly since her parents don’t understand or accept her gender identity. Though she has reconnected with a few friends in the past several weeks, she says she’s in a tough place emotionally. In public, she typically dresses and styles herself to look more masculine to avoid rude stares, and she is experiencing self-hatred that she fears won’t go away when she restarts treatment. Transitioning again isn’t going to be easy, as she explained to Undark in a private message on Facebook: “I've been beaten down enough that now I don't wanna get back up most of the time.”
Even worse is the fear that she might not be able to restart treatment at all. Earlier this year, Christine suffered two health emergencies within the span of a week, in which she says her blood pressure spiked, potentially causing organ damage. Christine has had one similar episode in the past and her family has a history of heart issues.
Christine may not be able to get back on estrogen despite the hard work she’s done to be able to afford it, she says, since it can increase the risk of heart attack and stroke. Because she has so far resisted trying DIY treatments again, she may have saved herself from additional health problems.
But Christine doesn’t see it that way. “Even if it was unsafe, even if I risked health concerns making myself a guinea pig, I wish I followed through,” she wrote. “Being off hormones is hell. And now that I face potentially never taking them again, I wish I had.”
Tara Santora is a science journalist based out of Denver. They have written for Psychology Today, Live Science, Fatherly, Audubon, and more.
This article was originally published on Undark. Read the original article.

Daily Recap: COVID-19 care delays mean excess cancer deaths; flu vaccine recommendations
Here are the stories our MDedge editors across specialties think you need to know about today:
COVID-related care delays mean excess cancer deaths
There could be 10,000 excess deaths from breast and colorectal cancer over the next 10 years as a result of missed screenings, delays in diagnosis, and reductions in oncology care caused by the COVID-19 pandemic, according to predictions generated by a National Cancer Institute model.
The number of excess deaths per year would peak in the next year or two, likely sooner for colorectal cancer than for breast cancer.
In an editorial published June 19 in Science, NCI Director Norman “Ned” Sharpless, MD, highlighted the modeling. In an interview, he pointed out that this analysis is conservative because the researchers evaluated only two types of cancer. They chose breast and colorectal cancer because these are common cancers – accounting for about one-sixth of all cancers – with relatively high screening rates.
“We didn’t model other cancer types, but we have no reason to think that we’re not going to see the same thing with other types of malignancies,” he said. “That is a significant amount of excess mortality.” Read more.
Diabetes control in U.S. youth has worsened over time
Glycemic control among youth with diabetes is no better today than it was in 2002 and in some subgroups it’s worse, according to data reported at the virtual American Diabetes Association scientific sessions. This finding comes despite the increased availability of diabetes technology, newer therapies, and more aggressive recommended blood glucose targets.
A particularly striking data point was seen among youth who had type 2 diabetes for 10 years or more: average A1c skyrocketed from 7.9% in 2008-2013 to 10.1% in 2014-2019. The numbers were small, 25 patients in the earlier cohort and 149 patients in the later, yet the difference was still statistically significant.
“Our finding that current youth and young adults with diabetes are not demonstrating improved glycemic control, compared to earlier cohorts in the SEARCH study, was surprising given how the landscape of diabetes management has changed dramatically over the past decade,” Faisal S. Malik, MD, of the University of Washington, Seattle, and Seattle Children’s Research Institute, said in an interview. Read more.
CDC advisors approve flu vaccine recommendations for 2020-2021
A pair of new vaccines for adults aged 65 years and older will be available for the 2020-2021 flu season – Fluzone high-dose quadrivalent, which replaces the trivalent Fluzone high-dose and Fluad quadrivalent (Seqirus), according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
At a virtual meeting on June 24, the committee voted unanimously to approve the vaccine recommendations for annual influenza immunization of all individuals aged 6 months and older. They also voted to accept some guidance and language changes to the recommendations. Read more.
How can we better engage black men as patients?
In a new commentary, Kevin M. Simon, MD, seeks to answer a key question: “How do psychiatrists and other mental health clinicians better engage men of color?” Dr. Simon, a psychiatrist at Boston Children’s Hospital, recommends creating a comfortable environment, allowing for storytelling, assuring confidentiality, being aware of nonverbal language, and being respectful.
“Those on the front lines providing mental health services should understand black men’s mental health from an ecological perspective. Beyond the emotional burden that mental illness imposes on the individual, there are more considerable interpersonal and societal implications for the state of black men’s mental health. As such, in our full capacity like other men, black men play an essential role within families, churches, neighborhoods, and organizations,” Dr. Simon wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
COVID-related care delays mean excess cancer deaths
There could be 10,000 excess deaths from breast and colorectal cancer over the next 10 years as a result of missed screenings, delays in diagnosis, and reductions in oncology care caused by the COVID-19 pandemic, according to predictions generated by a National Cancer Institute model.
The number of excess deaths per year would peak in the next year or two, likely sooner for colorectal cancer than for breast cancer.
In an editorial published June 19 in Science, NCI Director Norman “Ned” Sharpless, MD, highlighted the modeling. In an interview, he pointed out that this analysis is conservative because the researchers evaluated only two types of cancer. They chose breast and colorectal cancer because these are common cancers – accounting for about one-sixth of all cancers – with relatively high screening rates.
“We didn’t model other cancer types, but we have no reason to think that we’re not going to see the same thing with other types of malignancies,” he said. “That is a significant amount of excess mortality.” Read more.
Diabetes control in U.S. youth has worsened over time
Glycemic control among youth with diabetes is no better today than it was in 2002 and in some subgroups it’s worse, according to data reported at the virtual American Diabetes Association scientific sessions. This finding comes despite the increased availability of diabetes technology, newer therapies, and more aggressive recommended blood glucose targets.
A particularly striking data point was seen among youth who had type 2 diabetes for 10 years or more: average A1c skyrocketed from 7.9% in 2008-2013 to 10.1% in 2014-2019. The numbers were small, 25 patients in the earlier cohort and 149 patients in the later, yet the difference was still statistically significant.
“Our finding that current youth and young adults with diabetes are not demonstrating improved glycemic control, compared to earlier cohorts in the SEARCH study, was surprising given how the landscape of diabetes management has changed dramatically over the past decade,” Faisal S. Malik, MD, of the University of Washington, Seattle, and Seattle Children’s Research Institute, said in an interview. Read more.
CDC advisors approve flu vaccine recommendations for 2020-2021
A pair of new vaccines for adults aged 65 years and older will be available for the 2020-2021 flu season – Fluzone high-dose quadrivalent, which replaces the trivalent Fluzone high-dose and Fluad quadrivalent (Seqirus), according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
At a virtual meeting on June 24, the committee voted unanimously to approve the vaccine recommendations for annual influenza immunization of all individuals aged 6 months and older. They also voted to accept some guidance and language changes to the recommendations. Read more.
How can we better engage black men as patients?
In a new commentary, Kevin M. Simon, MD, seeks to answer a key question: “How do psychiatrists and other mental health clinicians better engage men of color?” Dr. Simon, a psychiatrist at Boston Children’s Hospital, recommends creating a comfortable environment, allowing for storytelling, assuring confidentiality, being aware of nonverbal language, and being respectful.
“Those on the front lines providing mental health services should understand black men’s mental health from an ecological perspective. Beyond the emotional burden that mental illness imposes on the individual, there are more considerable interpersonal and societal implications for the state of black men’s mental health. As such, in our full capacity like other men, black men play an essential role within families, churches, neighborhoods, and organizations,” Dr. Simon wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
COVID-related care delays mean excess cancer deaths
There could be 10,000 excess deaths from breast and colorectal cancer over the next 10 years as a result of missed screenings, delays in diagnosis, and reductions in oncology care caused by the COVID-19 pandemic, according to predictions generated by a National Cancer Institute model.
The number of excess deaths per year would peak in the next year or two, likely sooner for colorectal cancer than for breast cancer.
In an editorial published June 19 in Science, NCI Director Norman “Ned” Sharpless, MD, highlighted the modeling. In an interview, he pointed out that this analysis is conservative because the researchers evaluated only two types of cancer. They chose breast and colorectal cancer because these are common cancers – accounting for about one-sixth of all cancers – with relatively high screening rates.
“We didn’t model other cancer types, but we have no reason to think that we’re not going to see the same thing with other types of malignancies,” he said. “That is a significant amount of excess mortality.” Read more.
Diabetes control in U.S. youth has worsened over time
Glycemic control among youth with diabetes is no better today than it was in 2002 and in some subgroups it’s worse, according to data reported at the virtual American Diabetes Association scientific sessions. This finding comes despite the increased availability of diabetes technology, newer therapies, and more aggressive recommended blood glucose targets.
A particularly striking data point was seen among youth who had type 2 diabetes for 10 years or more: average A1c skyrocketed from 7.9% in 2008-2013 to 10.1% in 2014-2019. The numbers were small, 25 patients in the earlier cohort and 149 patients in the later, yet the difference was still statistically significant.
“Our finding that current youth and young adults with diabetes are not demonstrating improved glycemic control, compared to earlier cohorts in the SEARCH study, was surprising given how the landscape of diabetes management has changed dramatically over the past decade,” Faisal S. Malik, MD, of the University of Washington, Seattle, and Seattle Children’s Research Institute, said in an interview. Read more.
CDC advisors approve flu vaccine recommendations for 2020-2021
A pair of new vaccines for adults aged 65 years and older will be available for the 2020-2021 flu season – Fluzone high-dose quadrivalent, which replaces the trivalent Fluzone high-dose and Fluad quadrivalent (Seqirus), according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
At a virtual meeting on June 24, the committee voted unanimously to approve the vaccine recommendations for annual influenza immunization of all individuals aged 6 months and older. They also voted to accept some guidance and language changes to the recommendations. Read more.
How can we better engage black men as patients?
In a new commentary, Kevin M. Simon, MD, seeks to answer a key question: “How do psychiatrists and other mental health clinicians better engage men of color?” Dr. Simon, a psychiatrist at Boston Children’s Hospital, recommends creating a comfortable environment, allowing for storytelling, assuring confidentiality, being aware of nonverbal language, and being respectful.
“Those on the front lines providing mental health services should understand black men’s mental health from an ecological perspective. Beyond the emotional burden that mental illness imposes on the individual, there are more considerable interpersonal and societal implications for the state of black men’s mental health. As such, in our full capacity like other men, black men play an essential role within families, churches, neighborhoods, and organizations,” Dr. Simon wrote. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Erythematous Plaques on a Tattoo
The Diagnosis: Epidermodysplasia Verruciformis
Histopathologic examination demonstrated acanthosis and coarse hypergranulosis with enlarged keratinocytes exhibiting blue cytoplasmic discoloration (Figure), which was suggestive of acquired epidermodysplasia verruciformis (EV).
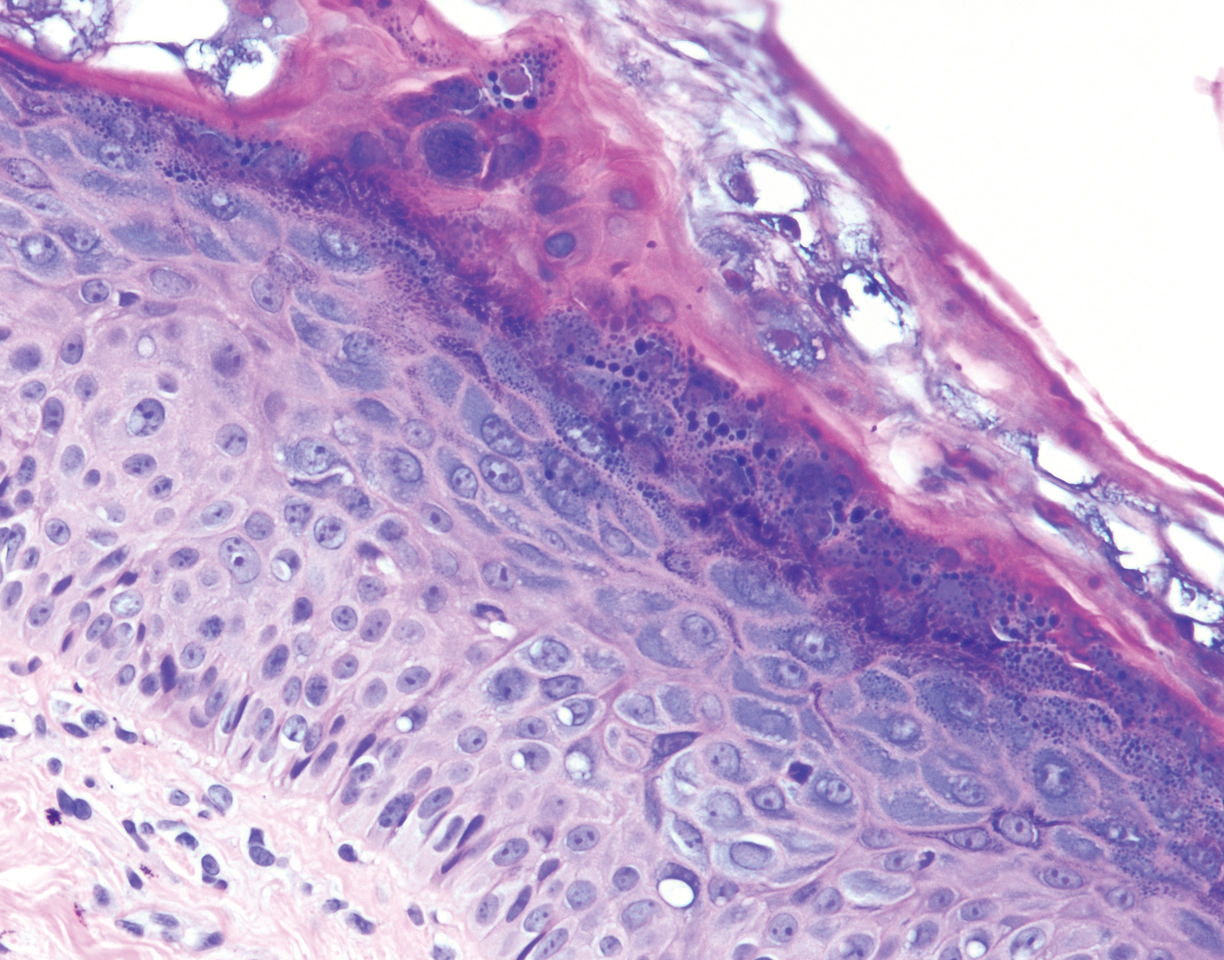
Acquired EV is a rare dermatologic condition associated with specific human papillomavirus (HPV) types that presents with recalcitrant lesions most commonly in the setting of immunosuppression.1 The most common HPV types associated with EV are HPV-5 and -8, but associations with HPV-3, -9, -10, -12, -14, -15, -17, -19 to -25, -36 to -38, -47, and -50 also have been reported.1,2 Acquired EV has been identified in individuals with human immunodeficiency virus, as well as in immunosuppressed patients with organ transplantation, Hodgkin lymphoma, systemic lupus erythematosus, and IgM deficiency, and in patients taking immunosuppressive medications such as tumor necrosis factor α inhibitors.1,3 The diagnosis is clinicopathological with potential polymerase chain reaction studies to identify underlying HPV types.
Acquired EV presents as hypopigmented to red, tinea versicolor-like macules or as verrucous, flat-topped papules on the trunk, arms, and/or legs.4 Histopathology reveals viral epidermal cytopathic changes, blue cytoplasm, and coarse hypogranulosis.4
There is no standardized treatment regimen for acquired EV, and no single approach has proven to yield an efficacious clinical outcome. Topical treatment options include steroids, retinoids, immunomodulators, cryotherapy, and electrosurgery, whereas retinoids or interferon alfa have been used as oral systemic therapy. Photodynamic therapy also has been shown to improve symptoms.3 Combination therapy such as interferon alfa with zidovudine or imiquimod with oral isotretinoin has shown better results than any single treatment.4 Due to the underlying HPV infection and its role in promotion of skin cancer development, lesions can characteristically undergo malignant transformations into Bowen disease but most commonly invasive squamous cell carcinoma (SCC), with initial lesions preferentially affecting sun-exposed areas due to the synergistic effect of UV light with EV-HPV lesions. The EV-HPV strains 5, 8, and 41 carry the highest oncogenic potential.5 Little is known of the true incidence of oncogenicity for acquired EV. Regardless, consistent sun protection and lifelong clinical examinations are critical for prognosis.5
The differential diagnosis of EV presenting in a tattoo includes allergic contact dermatitis, cutaneous sarcoidosis, pityriasis versicolor, and SCC. The pathology is critical to differentiate between these entities. The most frequently reported skin reactions to tattoo ink include inflammatory diseases (eg, allergic contact dermatitis, granulomatous reaction) or infectious diseases (eg, bacterial, viral, fungal).6 Allergic contact dermatitis, typically red pigment, is a common tattoo reaction. The most common histologic feature, however, is spongiosis, which results from intercellular edema. It often is limited to the lower epidermis but may affect the upper layers if the reaction is severe.7 Cutaneous sarcoidosis is a great masquerader that can present in various ways; however, its salient features on pathology are noncaseating granuloma involving the basal cell layer and epithelioid granuloma consisting of Langerhans giant cells.8 Although pityriasis versicolor can present in young immunocompromised adults, histologically salient features are the presence of both spores and hyphae in the stratum corneum.9 Although immunosuppression is a known risk factor for SCC, it is characterized histologically by hyperkeratosis, parakeratosis, and acanthosis with thickened and elongated rete ridges. Scattered atypical cells and frequent mitoses are present.10
- Schultz B, Nguyen CV, Jacobson-Dunlop E. Acquired epidermodysplasia verruciformis in setting of tumor necrosis factor-α inhibitor therapy. J Am Acad Dermatol Case Rep. 2018;4:805-807.
- DeVilliers EM, Fauquet C, Brocker TR, et al. Classification of papillomaviruses. Virology. 2004;324:17-27.
- Zampetti A, Giurdanella F, Manco S, et al. Acquired epidermodysplasia verruciformis: a comprehensive review and a proposal for treatment. Dermatol Surg. 2013;39:974-980.
- Henley JK, Hossler EW. Acquired epidermodysplasia verruciformis occurring in a renal transplant recipient. Cutis. 2017;99:E9-E12.
- Berk DR, Bruckner AL, Lu D. Epidermodysplasia verruciform-like lesions in an HIV patient. Dermatol Online J. 2009;15:1.
- Napolitano M, Megna M, Cappello M, et al. Skin diseases and tattoos: a five-year experience. G Ital Dermatol Venereol. 2018;153:644-648.
- Nixon RL, Mowad CM, Marks JG Jr. Allergic contact dermatitis. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:242-259.
- Ferringer T. Granulomatous and histiocytic diseases. In: Elston DM, Ferringer T, Ko C, et al, eds. Dermatopathology. 3rd ed. China: Elsevier; 2019:175-176.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:1329-1346.
- Soyer HP, Rigel DS, McMeniman E. Actinic keratosis, basal cell carcinoma, and squamous cell carcinoma. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:1887-1884.
The Diagnosis: Epidermodysplasia Verruciformis
Histopathologic examination demonstrated acanthosis and coarse hypergranulosis with enlarged keratinocytes exhibiting blue cytoplasmic discoloration (Figure), which was suggestive of acquired epidermodysplasia verruciformis (EV).
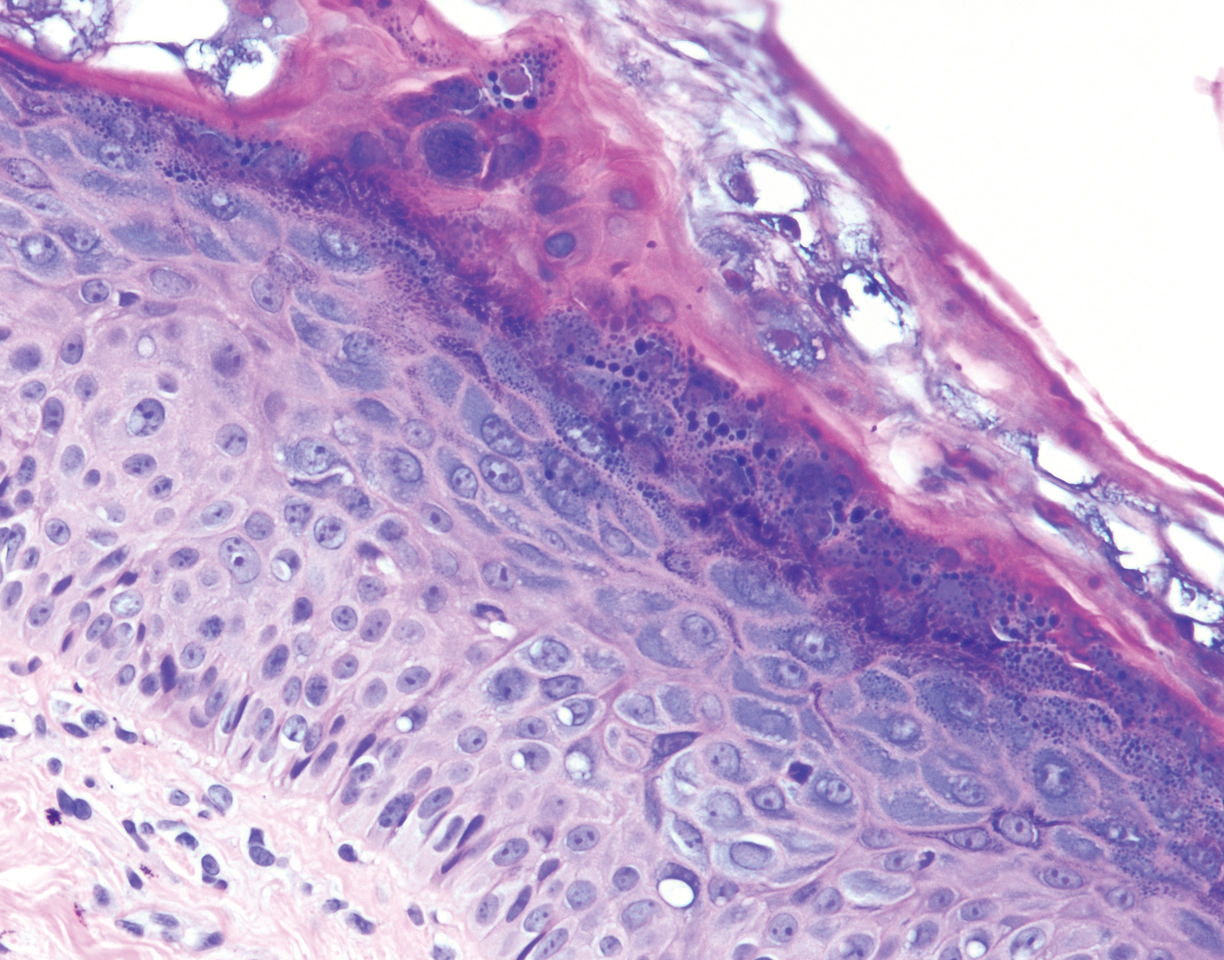
Acquired EV is a rare dermatologic condition associated with specific human papillomavirus (HPV) types that presents with recalcitrant lesions most commonly in the setting of immunosuppression.1 The most common HPV types associated with EV are HPV-5 and -8, but associations with HPV-3, -9, -10, -12, -14, -15, -17, -19 to -25, -36 to -38, -47, and -50 also have been reported.1,2 Acquired EV has been identified in individuals with human immunodeficiency virus, as well as in immunosuppressed patients with organ transplantation, Hodgkin lymphoma, systemic lupus erythematosus, and IgM deficiency, and in patients taking immunosuppressive medications such as tumor necrosis factor α inhibitors.1,3 The diagnosis is clinicopathological with potential polymerase chain reaction studies to identify underlying HPV types.
Acquired EV presents as hypopigmented to red, tinea versicolor-like macules or as verrucous, flat-topped papules on the trunk, arms, and/or legs.4 Histopathology reveals viral epidermal cytopathic changes, blue cytoplasm, and coarse hypogranulosis.4
There is no standardized treatment regimen for acquired EV, and no single approach has proven to yield an efficacious clinical outcome. Topical treatment options include steroids, retinoids, immunomodulators, cryotherapy, and electrosurgery, whereas retinoids or interferon alfa have been used as oral systemic therapy. Photodynamic therapy also has been shown to improve symptoms.3 Combination therapy such as interferon alfa with zidovudine or imiquimod with oral isotretinoin has shown better results than any single treatment.4 Due to the underlying HPV infection and its role in promotion of skin cancer development, lesions can characteristically undergo malignant transformations into Bowen disease but most commonly invasive squamous cell carcinoma (SCC), with initial lesions preferentially affecting sun-exposed areas due to the synergistic effect of UV light with EV-HPV lesions. The EV-HPV strains 5, 8, and 41 carry the highest oncogenic potential.5 Little is known of the true incidence of oncogenicity for acquired EV. Regardless, consistent sun protection and lifelong clinical examinations are critical for prognosis.5
The differential diagnosis of EV presenting in a tattoo includes allergic contact dermatitis, cutaneous sarcoidosis, pityriasis versicolor, and SCC. The pathology is critical to differentiate between these entities. The most frequently reported skin reactions to tattoo ink include inflammatory diseases (eg, allergic contact dermatitis, granulomatous reaction) or infectious diseases (eg, bacterial, viral, fungal).6 Allergic contact dermatitis, typically red pigment, is a common tattoo reaction. The most common histologic feature, however, is spongiosis, which results from intercellular edema. It often is limited to the lower epidermis but may affect the upper layers if the reaction is severe.7 Cutaneous sarcoidosis is a great masquerader that can present in various ways; however, its salient features on pathology are noncaseating granuloma involving the basal cell layer and epithelioid granuloma consisting of Langerhans giant cells.8 Although pityriasis versicolor can present in young immunocompromised adults, histologically salient features are the presence of both spores and hyphae in the stratum corneum.9 Although immunosuppression is a known risk factor for SCC, it is characterized histologically by hyperkeratosis, parakeratosis, and acanthosis with thickened and elongated rete ridges. Scattered atypical cells and frequent mitoses are present.10
The Diagnosis: Epidermodysplasia Verruciformis
Histopathologic examination demonstrated acanthosis and coarse hypergranulosis with enlarged keratinocytes exhibiting blue cytoplasmic discoloration (Figure), which was suggestive of acquired epidermodysplasia verruciformis (EV).
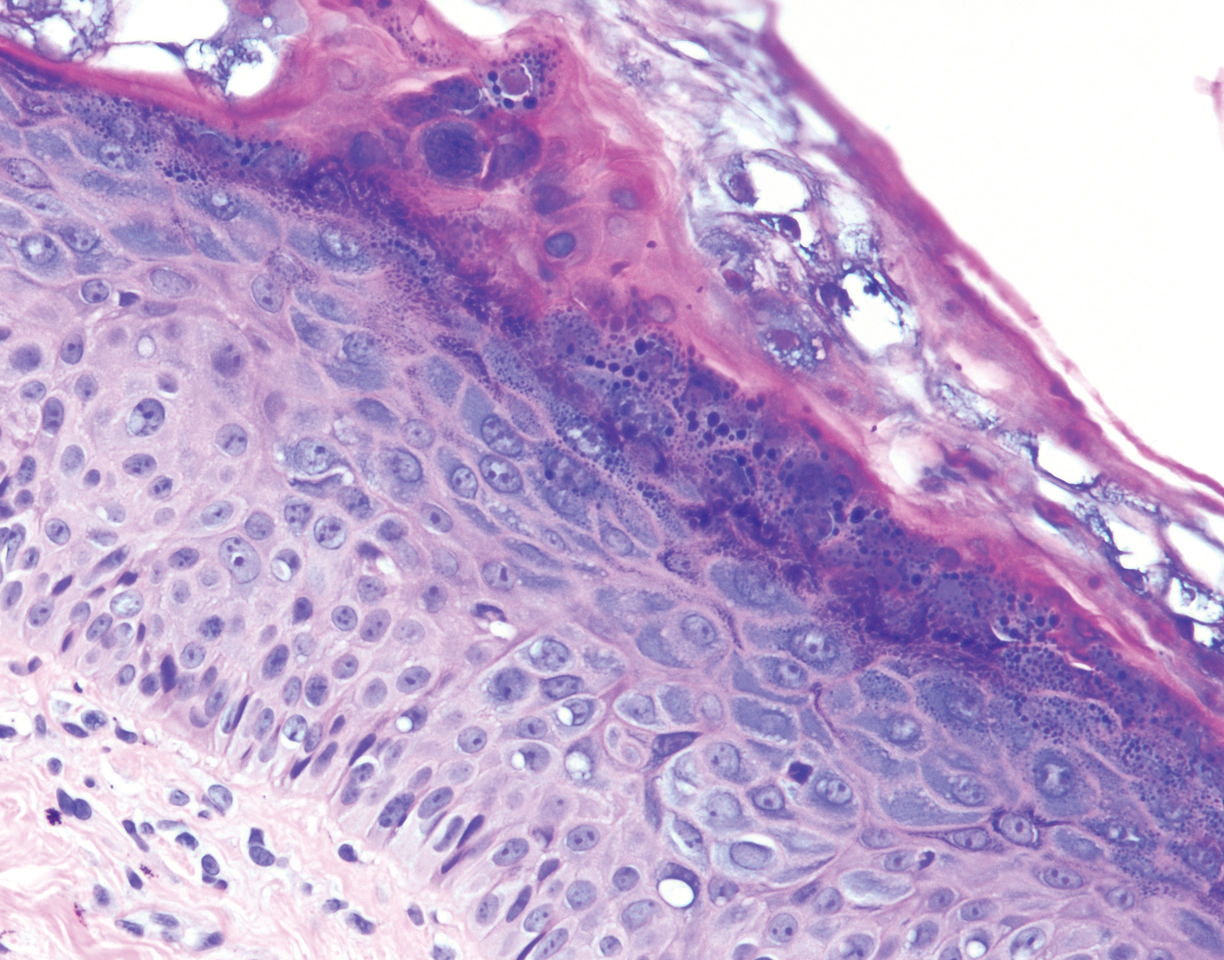
Acquired EV is a rare dermatologic condition associated with specific human papillomavirus (HPV) types that presents with recalcitrant lesions most commonly in the setting of immunosuppression.1 The most common HPV types associated with EV are HPV-5 and -8, but associations with HPV-3, -9, -10, -12, -14, -15, -17, -19 to -25, -36 to -38, -47, and -50 also have been reported.1,2 Acquired EV has been identified in individuals with human immunodeficiency virus, as well as in immunosuppressed patients with organ transplantation, Hodgkin lymphoma, systemic lupus erythematosus, and IgM deficiency, and in patients taking immunosuppressive medications such as tumor necrosis factor α inhibitors.1,3 The diagnosis is clinicopathological with potential polymerase chain reaction studies to identify underlying HPV types.
Acquired EV presents as hypopigmented to red, tinea versicolor-like macules or as verrucous, flat-topped papules on the trunk, arms, and/or legs.4 Histopathology reveals viral epidermal cytopathic changes, blue cytoplasm, and coarse hypogranulosis.4
There is no standardized treatment regimen for acquired EV, and no single approach has proven to yield an efficacious clinical outcome. Topical treatment options include steroids, retinoids, immunomodulators, cryotherapy, and electrosurgery, whereas retinoids or interferon alfa have been used as oral systemic therapy. Photodynamic therapy also has been shown to improve symptoms.3 Combination therapy such as interferon alfa with zidovudine or imiquimod with oral isotretinoin has shown better results than any single treatment.4 Due to the underlying HPV infection and its role in promotion of skin cancer development, lesions can characteristically undergo malignant transformations into Bowen disease but most commonly invasive squamous cell carcinoma (SCC), with initial lesions preferentially affecting sun-exposed areas due to the synergistic effect of UV light with EV-HPV lesions. The EV-HPV strains 5, 8, and 41 carry the highest oncogenic potential.5 Little is known of the true incidence of oncogenicity for acquired EV. Regardless, consistent sun protection and lifelong clinical examinations are critical for prognosis.5
The differential diagnosis of EV presenting in a tattoo includes allergic contact dermatitis, cutaneous sarcoidosis, pityriasis versicolor, and SCC. The pathology is critical to differentiate between these entities. The most frequently reported skin reactions to tattoo ink include inflammatory diseases (eg, allergic contact dermatitis, granulomatous reaction) or infectious diseases (eg, bacterial, viral, fungal).6 Allergic contact dermatitis, typically red pigment, is a common tattoo reaction. The most common histologic feature, however, is spongiosis, which results from intercellular edema. It often is limited to the lower epidermis but may affect the upper layers if the reaction is severe.7 Cutaneous sarcoidosis is a great masquerader that can present in various ways; however, its salient features on pathology are noncaseating granuloma involving the basal cell layer and epithelioid granuloma consisting of Langerhans giant cells.8 Although pityriasis versicolor can present in young immunocompromised adults, histologically salient features are the presence of both spores and hyphae in the stratum corneum.9 Although immunosuppression is a known risk factor for SCC, it is characterized histologically by hyperkeratosis, parakeratosis, and acanthosis with thickened and elongated rete ridges. Scattered atypical cells and frequent mitoses are present.10
- Schultz B, Nguyen CV, Jacobson-Dunlop E. Acquired epidermodysplasia verruciformis in setting of tumor necrosis factor-α inhibitor therapy. J Am Acad Dermatol Case Rep. 2018;4:805-807.
- DeVilliers EM, Fauquet C, Brocker TR, et al. Classification of papillomaviruses. Virology. 2004;324:17-27.
- Zampetti A, Giurdanella F, Manco S, et al. Acquired epidermodysplasia verruciformis: a comprehensive review and a proposal for treatment. Dermatol Surg. 2013;39:974-980.
- Henley JK, Hossler EW. Acquired epidermodysplasia verruciformis occurring in a renal transplant recipient. Cutis. 2017;99:E9-E12.
- Berk DR, Bruckner AL, Lu D. Epidermodysplasia verruciform-like lesions in an HIV patient. Dermatol Online J. 2009;15:1.
- Napolitano M, Megna M, Cappello M, et al. Skin diseases and tattoos: a five-year experience. G Ital Dermatol Venereol. 2018;153:644-648.
- Nixon RL, Mowad CM, Marks JG Jr. Allergic contact dermatitis. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:242-259.
- Ferringer T. Granulomatous and histiocytic diseases. In: Elston DM, Ferringer T, Ko C, et al, eds. Dermatopathology. 3rd ed. China: Elsevier; 2019:175-176.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:1329-1346.
- Soyer HP, Rigel DS, McMeniman E. Actinic keratosis, basal cell carcinoma, and squamous cell carcinoma. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:1887-1884.
- Schultz B, Nguyen CV, Jacobson-Dunlop E. Acquired epidermodysplasia verruciformis in setting of tumor necrosis factor-α inhibitor therapy. J Am Acad Dermatol Case Rep. 2018;4:805-807.
- DeVilliers EM, Fauquet C, Brocker TR, et al. Classification of papillomaviruses. Virology. 2004;324:17-27.
- Zampetti A, Giurdanella F, Manco S, et al. Acquired epidermodysplasia verruciformis: a comprehensive review and a proposal for treatment. Dermatol Surg. 2013;39:974-980.
- Henley JK, Hossler EW. Acquired epidermodysplasia verruciformis occurring in a renal transplant recipient. Cutis. 2017;99:E9-E12.
- Berk DR, Bruckner AL, Lu D. Epidermodysplasia verruciform-like lesions in an HIV patient. Dermatol Online J. 2009;15:1.
- Napolitano M, Megna M, Cappello M, et al. Skin diseases and tattoos: a five-year experience. G Ital Dermatol Venereol. 2018;153:644-648.
- Nixon RL, Mowad CM, Marks JG Jr. Allergic contact dermatitis. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:242-259.
- Ferringer T. Granulomatous and histiocytic diseases. In: Elston DM, Ferringer T, Ko C, et al, eds. Dermatopathology. 3rd ed. China: Elsevier; 2019:175-176.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:1329-1346.
- Soyer HP, Rigel DS, McMeniman E. Actinic keratosis, basal cell carcinoma, and squamous cell carcinoma. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2018:1887-1884.
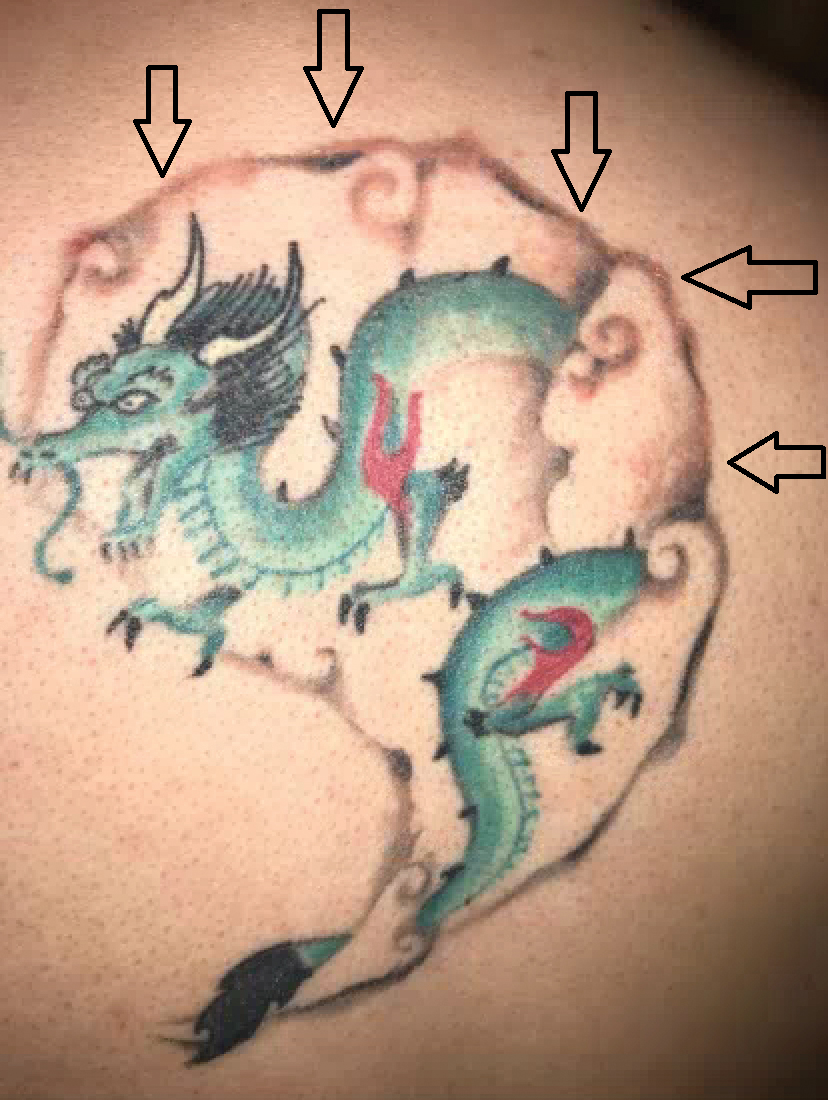
A 29-year-old man presented with increased redness, dryness, and pruritus at the periphery of a tattoo (arrows) on the upper back of 4 months' duration. He was diagnosed with human immunodeficiency virus 8 months prior to presentation and had a history of cystic fibrosis, eczema, and genital molluscum contagiosum. Laboratory analysis 1 month prior revealed a CD4 count of 42 cells/mm3 (reference range, 500-1200 cells/mm3), and the viral load was 2388 copies/mL (reference range, 20-10,000,000 copies/mL). Physical examination revealed multiple erythematous, eczematous, linear plaques along the dark gray lines of the tattoo. A 1.1.2 ×0.7.2 ×0.1-cm shave biopsy specimen was obtained. After the biopsy, tretinoin cream 0.1% and betamethasone dipropionate ointment 0.05% were prescribed to be alternately applied on the tattoo lesions until resolution.
SHM responds to racism in the United States
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.





