User login
For MD-IQ use only
Antiaffirmative action paper blasted on Twitter now retracted
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
Immigrant hospitalist dilemma takes stage at HM20 Virtual
Manpreet Malik, MD, a hospitalist at Emory University, takes care of patients with COVID-19 at Grady Memorial Hospital in downtown Atlanta. Born in India but living in the United States for more than 10 years, he is awaiting permanent resident status. At the current pace of U.S. Citizenship and Immigration Services, that may be decades away.
Dr. Malik lives and works in the United States on an H-1B visa, which is based on employment in a specialty occupation. Although he has a job that he loves, his immigrant status, social life, and geographic location in the United States is, technically, entirely dependent on doing that job.
“For single-income families with doctors on visas, the pandemic brings anxiety and uncertainty about legal status in the U.S. in case the breadwinner gets sick, disabled or unemployed,” he said.
In a presentation to be given at the HM20 Virtual, hosted by the Society of Hospital Medicine, Dr. Malik will offer perspective on the current challenges facing immigrant hospitalists and health care workers, especially in a U.S. health care system stretched thin and one in which many health professionals born outside the United States are working on the front lines. These challenges should be motivation to make legislative changes to give these health care workers more stability, flexibility, and peace of mind, he said.
The talk – to be given along with HM20 course director Benji Mathews, MD, SFHM, and called “The Immigrant Hospitalist: Navigating the Uncertain Terrain During COVID-19” – will describe a long-standing issue and outline a path forward, the two physicians said.
“The objective of this talk is to really highlight the contributions of these physicians and health care workers and also to provide a call for action for our hospitalist colleagues. This talk paints a picture of what my family and thousands of the other immigrant health care worker families are going through,” Dr. Malik said.
Dr. Mathews said that many physicians do not have benefits they can fall back on should they fall ill. And without the jobs their visas are based on, they could face deportation.
“That’s extreme – but the pathway towards that is very much there,” said Dr. Mathews, who was born in the Middle East and immigrated to the United States, received a green card, and later his citizenship. He now advocates for immigrant health and immigrant health care workers.
Dr. Malik and Dr. Mathews recently published a perspective piece in the Journal of Hospital Medicine. In it, they pointed out that 16.4% of health care workers are immigrants, and 29% of physicians are immigrants. Among practicing hospitalists, 32% are international medical graduates. They called for reform to visa regulations to allow physicians who are immigrants to travel to areas where they are most needed during the pandemic, for extensions of visa deadlines, and exemption from future immigration bans or limitations. These measures would only bolster the health care workforce that is under such strain during the pandemic, they write. (J Hosp Med. 2020 Aug;15[8]:505-506)
Dr. Malik said that, even while under added personal strain caused by the uncertainty of the past several months, he has never questioned his decision to be a physician in the United States.
“Now, more than ever, there is a sense of purpose and a passion to make a difference for our patients,” he said.
“I think most of us get into medicine and become hospitalists because we want to care for people, because we want to serve, because we want to be able to take care of sick, hospitalized patients, and that can be anywhere in the world, whether you’re in India serving a population that you grew up with or whether you’re in the U.S. serving the population that are your neighbors, your friends, your community, or people that are vulnerable. You’re serving humanity, and that is the ultimate goal.”
SHM advocacy on immigration issues
SHM has been advocating for more equitable skilled-immigration system, recognizing that from visa-backlogs to per-country caps, unfair visa restrictions have limited the United States’ ability to adequately expand its health care workforce.
The Society has consistently advocated on Capitol Hill for visa and skilled-immigration reform and has championed several significant immigration bills, including the following:
The Fairness for High Skilled Immigrants Act
- This legislation will eliminate per-country caps on green cards and convert the system into a “first-come, first-serve” system. This will help ensure certain nationalize are not disproportionally impacted by excessive green card backlogs.
- This legislation has passed the House of Representatives. Send a message to your Senator asking them to cosponsor this legislation.
The Conrad State 30 Physician Reauthorization Act
- This legislation will renew the Conrad State 30 program, which allows physicians on a J-1 visa to remain in the United States if they work in an underserved region for a minimum of three years. This legislation also included additional employment protection claims.
The Healthcare Workforce Resilience Act
- This legislation will recapture 40,000 unused immigrant visas for foreign doctors (15,000) and nurses (25,000), as well as provide visas for their spouse and children.
- This legislation will only be in effect for the duration of the COVID-19 public health emergency.
To join SHM in supporting our immigrant clinicians, you can send a message to your representatives in support of these bills by visiting hospitalmedicine.org/takeaction.
Manpreet Malik, MD, a hospitalist at Emory University, takes care of patients with COVID-19 at Grady Memorial Hospital in downtown Atlanta. Born in India but living in the United States for more than 10 years, he is awaiting permanent resident status. At the current pace of U.S. Citizenship and Immigration Services, that may be decades away.
Dr. Malik lives and works in the United States on an H-1B visa, which is based on employment in a specialty occupation. Although he has a job that he loves, his immigrant status, social life, and geographic location in the United States is, technically, entirely dependent on doing that job.
“For single-income families with doctors on visas, the pandemic brings anxiety and uncertainty about legal status in the U.S. in case the breadwinner gets sick, disabled or unemployed,” he said.
In a presentation to be given at the HM20 Virtual, hosted by the Society of Hospital Medicine, Dr. Malik will offer perspective on the current challenges facing immigrant hospitalists and health care workers, especially in a U.S. health care system stretched thin and one in which many health professionals born outside the United States are working on the front lines. These challenges should be motivation to make legislative changes to give these health care workers more stability, flexibility, and peace of mind, he said.
The talk – to be given along with HM20 course director Benji Mathews, MD, SFHM, and called “The Immigrant Hospitalist: Navigating the Uncertain Terrain During COVID-19” – will describe a long-standing issue and outline a path forward, the two physicians said.
“The objective of this talk is to really highlight the contributions of these physicians and health care workers and also to provide a call for action for our hospitalist colleagues. This talk paints a picture of what my family and thousands of the other immigrant health care worker families are going through,” Dr. Malik said.
Dr. Mathews said that many physicians do not have benefits they can fall back on should they fall ill. And without the jobs their visas are based on, they could face deportation.
“That’s extreme – but the pathway towards that is very much there,” said Dr. Mathews, who was born in the Middle East and immigrated to the United States, received a green card, and later his citizenship. He now advocates for immigrant health and immigrant health care workers.
Dr. Malik and Dr. Mathews recently published a perspective piece in the Journal of Hospital Medicine. In it, they pointed out that 16.4% of health care workers are immigrants, and 29% of physicians are immigrants. Among practicing hospitalists, 32% are international medical graduates. They called for reform to visa regulations to allow physicians who are immigrants to travel to areas where they are most needed during the pandemic, for extensions of visa deadlines, and exemption from future immigration bans or limitations. These measures would only bolster the health care workforce that is under such strain during the pandemic, they write. (J Hosp Med. 2020 Aug;15[8]:505-506)
Dr. Malik said that, even while under added personal strain caused by the uncertainty of the past several months, he has never questioned his decision to be a physician in the United States.
“Now, more than ever, there is a sense of purpose and a passion to make a difference for our patients,” he said.
“I think most of us get into medicine and become hospitalists because we want to care for people, because we want to serve, because we want to be able to take care of sick, hospitalized patients, and that can be anywhere in the world, whether you’re in India serving a population that you grew up with or whether you’re in the U.S. serving the population that are your neighbors, your friends, your community, or people that are vulnerable. You’re serving humanity, and that is the ultimate goal.”
SHM advocacy on immigration issues
SHM has been advocating for more equitable skilled-immigration system, recognizing that from visa-backlogs to per-country caps, unfair visa restrictions have limited the United States’ ability to adequately expand its health care workforce.
The Society has consistently advocated on Capitol Hill for visa and skilled-immigration reform and has championed several significant immigration bills, including the following:
The Fairness for High Skilled Immigrants Act
- This legislation will eliminate per-country caps on green cards and convert the system into a “first-come, first-serve” system. This will help ensure certain nationalize are not disproportionally impacted by excessive green card backlogs.
- This legislation has passed the House of Representatives. Send a message to your Senator asking them to cosponsor this legislation.
The Conrad State 30 Physician Reauthorization Act
- This legislation will renew the Conrad State 30 program, which allows physicians on a J-1 visa to remain in the United States if they work in an underserved region for a minimum of three years. This legislation also included additional employment protection claims.
The Healthcare Workforce Resilience Act
- This legislation will recapture 40,000 unused immigrant visas for foreign doctors (15,000) and nurses (25,000), as well as provide visas for their spouse and children.
- This legislation will only be in effect for the duration of the COVID-19 public health emergency.
To join SHM in supporting our immigrant clinicians, you can send a message to your representatives in support of these bills by visiting hospitalmedicine.org/takeaction.
Manpreet Malik, MD, a hospitalist at Emory University, takes care of patients with COVID-19 at Grady Memorial Hospital in downtown Atlanta. Born in India but living in the United States for more than 10 years, he is awaiting permanent resident status. At the current pace of U.S. Citizenship and Immigration Services, that may be decades away.
Dr. Malik lives and works in the United States on an H-1B visa, which is based on employment in a specialty occupation. Although he has a job that he loves, his immigrant status, social life, and geographic location in the United States is, technically, entirely dependent on doing that job.
“For single-income families with doctors on visas, the pandemic brings anxiety and uncertainty about legal status in the U.S. in case the breadwinner gets sick, disabled or unemployed,” he said.
In a presentation to be given at the HM20 Virtual, hosted by the Society of Hospital Medicine, Dr. Malik will offer perspective on the current challenges facing immigrant hospitalists and health care workers, especially in a U.S. health care system stretched thin and one in which many health professionals born outside the United States are working on the front lines. These challenges should be motivation to make legislative changes to give these health care workers more stability, flexibility, and peace of mind, he said.
The talk – to be given along with HM20 course director Benji Mathews, MD, SFHM, and called “The Immigrant Hospitalist: Navigating the Uncertain Terrain During COVID-19” – will describe a long-standing issue and outline a path forward, the two physicians said.
“The objective of this talk is to really highlight the contributions of these physicians and health care workers and also to provide a call for action for our hospitalist colleagues. This talk paints a picture of what my family and thousands of the other immigrant health care worker families are going through,” Dr. Malik said.
Dr. Mathews said that many physicians do not have benefits they can fall back on should they fall ill. And without the jobs their visas are based on, they could face deportation.
“That’s extreme – but the pathway towards that is very much there,” said Dr. Mathews, who was born in the Middle East and immigrated to the United States, received a green card, and later his citizenship. He now advocates for immigrant health and immigrant health care workers.
Dr. Malik and Dr. Mathews recently published a perspective piece in the Journal of Hospital Medicine. In it, they pointed out that 16.4% of health care workers are immigrants, and 29% of physicians are immigrants. Among practicing hospitalists, 32% are international medical graduates. They called for reform to visa regulations to allow physicians who are immigrants to travel to areas where they are most needed during the pandemic, for extensions of visa deadlines, and exemption from future immigration bans or limitations. These measures would only bolster the health care workforce that is under such strain during the pandemic, they write. (J Hosp Med. 2020 Aug;15[8]:505-506)
Dr. Malik said that, even while under added personal strain caused by the uncertainty of the past several months, he has never questioned his decision to be a physician in the United States.
“Now, more than ever, there is a sense of purpose and a passion to make a difference for our patients,” he said.
“I think most of us get into medicine and become hospitalists because we want to care for people, because we want to serve, because we want to be able to take care of sick, hospitalized patients, and that can be anywhere in the world, whether you’re in India serving a population that you grew up with or whether you’re in the U.S. serving the population that are your neighbors, your friends, your community, or people that are vulnerable. You’re serving humanity, and that is the ultimate goal.”
SHM advocacy on immigration issues
SHM has been advocating for more equitable skilled-immigration system, recognizing that from visa-backlogs to per-country caps, unfair visa restrictions have limited the United States’ ability to adequately expand its health care workforce.
The Society has consistently advocated on Capitol Hill for visa and skilled-immigration reform and has championed several significant immigration bills, including the following:
The Fairness for High Skilled Immigrants Act
- This legislation will eliminate per-country caps on green cards and convert the system into a “first-come, first-serve” system. This will help ensure certain nationalize are not disproportionally impacted by excessive green card backlogs.
- This legislation has passed the House of Representatives. Send a message to your Senator asking them to cosponsor this legislation.
The Conrad State 30 Physician Reauthorization Act
- This legislation will renew the Conrad State 30 program, which allows physicians on a J-1 visa to remain in the United States if they work in an underserved region for a minimum of three years. This legislation also included additional employment protection claims.
The Healthcare Workforce Resilience Act
- This legislation will recapture 40,000 unused immigrant visas for foreign doctors (15,000) and nurses (25,000), as well as provide visas for their spouse and children.
- This legislation will only be in effect for the duration of the COVID-19 public health emergency.
To join SHM in supporting our immigrant clinicians, you can send a message to your representatives in support of these bills by visiting hospitalmedicine.org/takeaction.
HM20 Virtual: Experts to discuss structural racism in hospital medicine
Nathan Chomilo, MD, the Medicaid medical director for the state of Minnesota and assistant adjunct professor of pediatrics at the University of Minnesota, Minneapolis, was prepared to deliver a talk on structural racism in the U.S. health care system at Hospital Medicine 2020 meeting (HM20) in April 2020. But that changed in the COVID-19 era.
When the pandemic hit, the problems Dr. Chomilo was going to point out began to play out dramatically around the country: Black, Indigenous, and Latinx people – many of them under-insured; in high-exposure, frontline jobs; and already burdened with health comorbidities – are at a higher risk of contracting COVID-19 and dying from it.
He will now be giving his talk at HM20 Virtual in a session called “Structural Racism and Bias in Hospital Medicine During Two Pandemics,” with the powerful narrative of COVID-19 to get his message to sink in:
“It’s something that’s been going on since the start of our country,” said Dr. Chomilo, who is also a founding member of Minnesota Doctors for Health Equity. Physicians, he said, participated in upholding the institution of slavery by trying to describe the physical discrepancies between White people and non-White people.
Now, the way health care is provided in the United States fundamentally favors Whites over Black, Indigenous, and Latinx patients.
“We have a health care system here in the United States that is based on employer-sponsored insurance,” he said. “And who has had access to those jobs over the course of our country’s history has been mostly White people.” That impacts who is more at risk of contracting the virus, who is able to shelter in place, and who has the financial reserves to withstand furloughs and unemployment.
In a recent blog post in Health Affairs, Dr. Chomilo and his coauthors discussed articles from the New England Journal of Medicine and the Journal of the American Medical Association that try to offer an ethical framework for allocating scarce medical resources – such as intensive-care beds and ventilators – during the pandemic.
“Unfortunately, neither article acknowledged the structural racial inequities that inherently bias its proposals, nor did either piece adequately acknowledge how its care rationing plan might worsen already racially disparate health outcomes,” Dr. Chomilo and his coauthors wrote. For instance, the life expectancy of a White female in the United States is 81 years, compared with 72 years for Black males, and any allocation plan that prioritizes preserving years of life would automatically be tilted against black patients.
In his talk, Dr. Chomilo will also discuss how physicians can make a difference by looking at their own perceptions and habits and then start helping others and the systems in which they work.
“The first thing is, we have to look at ourselves,” he said.
In the same session, Benji Mathews, MD, SFHM – chief of hospital medicine at Regions Hospital in St. Paul, Minn., which is part of HealthPartners; associate professor of medicine at the University of Minnesota, Minneapolis; and the Annual Conference’s course director – said he will be discussing the way social inequities are “patterned by place” and how resources for staying healthy vary neighborhood to neighborhood. He will point to dense housing and multigenerational households as a chief driver of COVID-19 infection risk. People of color are often “first fired, last hired, and in the front lines of fire,” he said, and they are experiencing a more severe impact from the pandemic.
And he will get deeper into the other disparities that track along racial lines, such as insurance disparities. For instance, the percentage of African Americans on Medicaid is three times as high as the percentage of White, non-Hispanic patients, he said.
Dr. Mathews will also discuss race’s role in the biases that everyone has and how health care professionals might, with deliberate reflection, be able to reshape or mitigate their own biases and deliver care more equitably.
“The associations we have, and our biases, are not necessarily declared beliefs or even reflect our stances that we explicitly endorse – sometimes it comes through in our default stance, and generally favor our in-group,” he said. “These implicit biases are malleable, so that allows us some hope. There are some ways they can be unlearned or progressively acted upon with some coaching – some active, intentional development.”
Structural Racism and Bias in Hospital Medicine During Two Pandemics
Nathan Chomilo, MD, the Medicaid medical director for the state of Minnesota and assistant adjunct professor of pediatrics at the University of Minnesota, Minneapolis, was prepared to deliver a talk on structural racism in the U.S. health care system at Hospital Medicine 2020 meeting (HM20) in April 2020. But that changed in the COVID-19 era.
When the pandemic hit, the problems Dr. Chomilo was going to point out began to play out dramatically around the country: Black, Indigenous, and Latinx people – many of them under-insured; in high-exposure, frontline jobs; and already burdened with health comorbidities – are at a higher risk of contracting COVID-19 and dying from it.
He will now be giving his talk at HM20 Virtual in a session called “Structural Racism and Bias in Hospital Medicine During Two Pandemics,” with the powerful narrative of COVID-19 to get his message to sink in:
“It’s something that’s been going on since the start of our country,” said Dr. Chomilo, who is also a founding member of Minnesota Doctors for Health Equity. Physicians, he said, participated in upholding the institution of slavery by trying to describe the physical discrepancies between White people and non-White people.
Now, the way health care is provided in the United States fundamentally favors Whites over Black, Indigenous, and Latinx patients.
“We have a health care system here in the United States that is based on employer-sponsored insurance,” he said. “And who has had access to those jobs over the course of our country’s history has been mostly White people.” That impacts who is more at risk of contracting the virus, who is able to shelter in place, and who has the financial reserves to withstand furloughs and unemployment.
In a recent blog post in Health Affairs, Dr. Chomilo and his coauthors discussed articles from the New England Journal of Medicine and the Journal of the American Medical Association that try to offer an ethical framework for allocating scarce medical resources – such as intensive-care beds and ventilators – during the pandemic.
“Unfortunately, neither article acknowledged the structural racial inequities that inherently bias its proposals, nor did either piece adequately acknowledge how its care rationing plan might worsen already racially disparate health outcomes,” Dr. Chomilo and his coauthors wrote. For instance, the life expectancy of a White female in the United States is 81 years, compared with 72 years for Black males, and any allocation plan that prioritizes preserving years of life would automatically be tilted against black patients.
In his talk, Dr. Chomilo will also discuss how physicians can make a difference by looking at their own perceptions and habits and then start helping others and the systems in which they work.
“The first thing is, we have to look at ourselves,” he said.
In the same session, Benji Mathews, MD, SFHM – chief of hospital medicine at Regions Hospital in St. Paul, Minn., which is part of HealthPartners; associate professor of medicine at the University of Minnesota, Minneapolis; and the Annual Conference’s course director – said he will be discussing the way social inequities are “patterned by place” and how resources for staying healthy vary neighborhood to neighborhood. He will point to dense housing and multigenerational households as a chief driver of COVID-19 infection risk. People of color are often “first fired, last hired, and in the front lines of fire,” he said, and they are experiencing a more severe impact from the pandemic.
And he will get deeper into the other disparities that track along racial lines, such as insurance disparities. For instance, the percentage of African Americans on Medicaid is three times as high as the percentage of White, non-Hispanic patients, he said.
Dr. Mathews will also discuss race’s role in the biases that everyone has and how health care professionals might, with deliberate reflection, be able to reshape or mitigate their own biases and deliver care more equitably.
“The associations we have, and our biases, are not necessarily declared beliefs or even reflect our stances that we explicitly endorse – sometimes it comes through in our default stance, and generally favor our in-group,” he said. “These implicit biases are malleable, so that allows us some hope. There are some ways they can be unlearned or progressively acted upon with some coaching – some active, intentional development.”
Structural Racism and Bias in Hospital Medicine During Two Pandemics
Nathan Chomilo, MD, the Medicaid medical director for the state of Minnesota and assistant adjunct professor of pediatrics at the University of Minnesota, Minneapolis, was prepared to deliver a talk on structural racism in the U.S. health care system at Hospital Medicine 2020 meeting (HM20) in April 2020. But that changed in the COVID-19 era.
When the pandemic hit, the problems Dr. Chomilo was going to point out began to play out dramatically around the country: Black, Indigenous, and Latinx people – many of them under-insured; in high-exposure, frontline jobs; and already burdened with health comorbidities – are at a higher risk of contracting COVID-19 and dying from it.
He will now be giving his talk at HM20 Virtual in a session called “Structural Racism and Bias in Hospital Medicine During Two Pandemics,” with the powerful narrative of COVID-19 to get his message to sink in:
“It’s something that’s been going on since the start of our country,” said Dr. Chomilo, who is also a founding member of Minnesota Doctors for Health Equity. Physicians, he said, participated in upholding the institution of slavery by trying to describe the physical discrepancies between White people and non-White people.
Now, the way health care is provided in the United States fundamentally favors Whites over Black, Indigenous, and Latinx patients.
“We have a health care system here in the United States that is based on employer-sponsored insurance,” he said. “And who has had access to those jobs over the course of our country’s history has been mostly White people.” That impacts who is more at risk of contracting the virus, who is able to shelter in place, and who has the financial reserves to withstand furloughs and unemployment.
In a recent blog post in Health Affairs, Dr. Chomilo and his coauthors discussed articles from the New England Journal of Medicine and the Journal of the American Medical Association that try to offer an ethical framework for allocating scarce medical resources – such as intensive-care beds and ventilators – during the pandemic.
“Unfortunately, neither article acknowledged the structural racial inequities that inherently bias its proposals, nor did either piece adequately acknowledge how its care rationing plan might worsen already racially disparate health outcomes,” Dr. Chomilo and his coauthors wrote. For instance, the life expectancy of a White female in the United States is 81 years, compared with 72 years for Black males, and any allocation plan that prioritizes preserving years of life would automatically be tilted against black patients.
In his talk, Dr. Chomilo will also discuss how physicians can make a difference by looking at their own perceptions and habits and then start helping others and the systems in which they work.
“The first thing is, we have to look at ourselves,” he said.
In the same session, Benji Mathews, MD, SFHM – chief of hospital medicine at Regions Hospital in St. Paul, Minn., which is part of HealthPartners; associate professor of medicine at the University of Minnesota, Minneapolis; and the Annual Conference’s course director – said he will be discussing the way social inequities are “patterned by place” and how resources for staying healthy vary neighborhood to neighborhood. He will point to dense housing and multigenerational households as a chief driver of COVID-19 infection risk. People of color are often “first fired, last hired, and in the front lines of fire,” he said, and they are experiencing a more severe impact from the pandemic.
And he will get deeper into the other disparities that track along racial lines, such as insurance disparities. For instance, the percentage of African Americans on Medicaid is three times as high as the percentage of White, non-Hispanic patients, he said.
Dr. Mathews will also discuss race’s role in the biases that everyone has and how health care professionals might, with deliberate reflection, be able to reshape or mitigate their own biases and deliver care more equitably.
“The associations we have, and our biases, are not necessarily declared beliefs or even reflect our stances that we explicitly endorse – sometimes it comes through in our default stance, and generally favor our in-group,” he said. “These implicit biases are malleable, so that allows us some hope. There are some ways they can be unlearned or progressively acted upon with some coaching – some active, intentional development.”
Structural Racism and Bias in Hospital Medicine During Two Pandemics
Dermatology atlas will profile disease in all skin types
An atlas that displays the unique nuances between different skin types across the spectrum of dermatologic disease is scheduled for release this coming winter.
Available as an e-book or physical text, Dermatologists need to know what skin diseases look like on all types of skin, said Adam Friedman, MD, who is developing this e-book with Misty Eleryan, MD, MS.
From the SARS-CoV-2 pandemic, multiple nonviral pandemics have rapidly emerged, “most notably the persistent and well-masked racism that maintains disparities in all facets of life, from economics to health care,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview.
In dermatology, “clear disparities in workforce representation and trainee/practitioner education have become more apparent than ever before,” he added.
The project is a collaboration of George Washington University and education publishers Sanova Works and Educational Testing & Assessment Systems.
As a person of color who recently completed her residency in dermatology at George Washington University, Dr. Eleryan had noticed a lack of diversity in photos of common dermatoses. This can contribute to misdiagnoses and delays in treatment in patients of color, Dr. Eleryan, who is now a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, said in an interview.
“We recognized the gap, which is the lack of diversity/variation of skin tones in our dermatology textbooks and atlases,” she added.
The project was several years in the making, Dr. Friedman said. To do this right, “you need resources, funding, and a collaborative and galvanized team of experts.” That involved coordinating with several medical publishers and amassing a team of medical photographers and an expert panel that will assist in evaluating and securing difficult-to-access clinical images.
The atlas is one of several initiatives in the dermatology field to address racial disparities in patient care.
Noticing similar information gaps about clinical presentations in darker skin, a medical student in the United Kingdom, Malone Mukwende, created “Mind the Gap,” a handbook that presents side-by-side images of diseases and illnesses in light and dark skin. This project “highlights how far behind we are, that a medical student with minimal dermatology exposure and experience not only recognized the need but was ready to do something about it,” Dr. Friedman noted.
Others in the field have spotlighted disparities in the medical literature. The SARS-CoV-2 pandemic has especially brought this out, Graeme M. Lipper, MD wrote in a recent editorial for this news organization.
He referred to a literature review of 46 articles describing COVID-19–associated skin manifestations, which included mostly (92%) images in patients with skin types I-III (92%) and none in patients with skin types V or VI.
“These investigators have identified a damning lack of images of COVID-19–associated skin manifestations in patients with darker skin,” added Dr. Lipper, an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital.
For now, Dr. Friedman said that the atlas won’t contain a specific section on COVID-19 skin manifestations, although viral-associated skin reactions like morbilliform eruptions, urticaria, and retiform purpura will be displayed. Overall, the atlas will address 60-70 skin conditions.
Physicians who fail to educate themselves on the variations of skin conditions in all skin types may potentially harm patients of color, Dr. Eleryan said. As Dr. Lipper noted in his editorial, nearly half of all dermatologists feel they haven’t had adequate exposure to diseases in skin of color.
“Our atlas will fill that void and hopefully assist in closing the gap in health disparities among patients of color, who are often misdiagnosed or rendered diagnoses very late in the disease process,” Dr. Eleryan said.
An atlas that displays the unique nuances between different skin types across the spectrum of dermatologic disease is scheduled for release this coming winter.
Available as an e-book or physical text, Dermatologists need to know what skin diseases look like on all types of skin, said Adam Friedman, MD, who is developing this e-book with Misty Eleryan, MD, MS.
From the SARS-CoV-2 pandemic, multiple nonviral pandemics have rapidly emerged, “most notably the persistent and well-masked racism that maintains disparities in all facets of life, from economics to health care,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview.
In dermatology, “clear disparities in workforce representation and trainee/practitioner education have become more apparent than ever before,” he added.
The project is a collaboration of George Washington University and education publishers Sanova Works and Educational Testing & Assessment Systems.
As a person of color who recently completed her residency in dermatology at George Washington University, Dr. Eleryan had noticed a lack of diversity in photos of common dermatoses. This can contribute to misdiagnoses and delays in treatment in patients of color, Dr. Eleryan, who is now a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, said in an interview.
“We recognized the gap, which is the lack of diversity/variation of skin tones in our dermatology textbooks and atlases,” she added.
The project was several years in the making, Dr. Friedman said. To do this right, “you need resources, funding, and a collaborative and galvanized team of experts.” That involved coordinating with several medical publishers and amassing a team of medical photographers and an expert panel that will assist in evaluating and securing difficult-to-access clinical images.
The atlas is one of several initiatives in the dermatology field to address racial disparities in patient care.
Noticing similar information gaps about clinical presentations in darker skin, a medical student in the United Kingdom, Malone Mukwende, created “Mind the Gap,” a handbook that presents side-by-side images of diseases and illnesses in light and dark skin. This project “highlights how far behind we are, that a medical student with minimal dermatology exposure and experience not only recognized the need but was ready to do something about it,” Dr. Friedman noted.
Others in the field have spotlighted disparities in the medical literature. The SARS-CoV-2 pandemic has especially brought this out, Graeme M. Lipper, MD wrote in a recent editorial for this news organization.
He referred to a literature review of 46 articles describing COVID-19–associated skin manifestations, which included mostly (92%) images in patients with skin types I-III (92%) and none in patients with skin types V or VI.
“These investigators have identified a damning lack of images of COVID-19–associated skin manifestations in patients with darker skin,” added Dr. Lipper, an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital.
For now, Dr. Friedman said that the atlas won’t contain a specific section on COVID-19 skin manifestations, although viral-associated skin reactions like morbilliform eruptions, urticaria, and retiform purpura will be displayed. Overall, the atlas will address 60-70 skin conditions.
Physicians who fail to educate themselves on the variations of skin conditions in all skin types may potentially harm patients of color, Dr. Eleryan said. As Dr. Lipper noted in his editorial, nearly half of all dermatologists feel they haven’t had adequate exposure to diseases in skin of color.
“Our atlas will fill that void and hopefully assist in closing the gap in health disparities among patients of color, who are often misdiagnosed or rendered diagnoses very late in the disease process,” Dr. Eleryan said.
An atlas that displays the unique nuances between different skin types across the spectrum of dermatologic disease is scheduled for release this coming winter.
Available as an e-book or physical text, Dermatologists need to know what skin diseases look like on all types of skin, said Adam Friedman, MD, who is developing this e-book with Misty Eleryan, MD, MS.
From the SARS-CoV-2 pandemic, multiple nonviral pandemics have rapidly emerged, “most notably the persistent and well-masked racism that maintains disparities in all facets of life, from economics to health care,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview.
In dermatology, “clear disparities in workforce representation and trainee/practitioner education have become more apparent than ever before,” he added.
The project is a collaboration of George Washington University and education publishers Sanova Works and Educational Testing & Assessment Systems.
As a person of color who recently completed her residency in dermatology at George Washington University, Dr. Eleryan had noticed a lack of diversity in photos of common dermatoses. This can contribute to misdiagnoses and delays in treatment in patients of color, Dr. Eleryan, who is now a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, said in an interview.
“We recognized the gap, which is the lack of diversity/variation of skin tones in our dermatology textbooks and atlases,” she added.
The project was several years in the making, Dr. Friedman said. To do this right, “you need resources, funding, and a collaborative and galvanized team of experts.” That involved coordinating with several medical publishers and amassing a team of medical photographers and an expert panel that will assist in evaluating and securing difficult-to-access clinical images.
The atlas is one of several initiatives in the dermatology field to address racial disparities in patient care.
Noticing similar information gaps about clinical presentations in darker skin, a medical student in the United Kingdom, Malone Mukwende, created “Mind the Gap,” a handbook that presents side-by-side images of diseases and illnesses in light and dark skin. This project “highlights how far behind we are, that a medical student with minimal dermatology exposure and experience not only recognized the need but was ready to do something about it,” Dr. Friedman noted.
Others in the field have spotlighted disparities in the medical literature. The SARS-CoV-2 pandemic has especially brought this out, Graeme M. Lipper, MD wrote in a recent editorial for this news organization.
He referred to a literature review of 46 articles describing COVID-19–associated skin manifestations, which included mostly (92%) images in patients with skin types I-III (92%) and none in patients with skin types V or VI.
“These investigators have identified a damning lack of images of COVID-19–associated skin manifestations in patients with darker skin,” added Dr. Lipper, an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital.
For now, Dr. Friedman said that the atlas won’t contain a specific section on COVID-19 skin manifestations, although viral-associated skin reactions like morbilliform eruptions, urticaria, and retiform purpura will be displayed. Overall, the atlas will address 60-70 skin conditions.
Physicians who fail to educate themselves on the variations of skin conditions in all skin types may potentially harm patients of color, Dr. Eleryan said. As Dr. Lipper noted in his editorial, nearly half of all dermatologists feel they haven’t had adequate exposure to diseases in skin of color.
“Our atlas will fill that void and hopefully assist in closing the gap in health disparities among patients of color, who are often misdiagnosed or rendered diagnoses very late in the disease process,” Dr. Eleryan said.
Welcome to HM20 Virtual
Welcome to the HM20 virtual conference! We’re glad to have you join us to virtually experience sessions from our most popular SHM annual conference tracks including Rapid Fire, Clinical Updates, and High-Value Care! We also have added some new timely topics given our current times that you won’t want to miss. We encourage you to engage with the larger community via social media at #HM20Virtual.
HM20 in San Diego, scheduled originally for April 2020, was trending to be the highest in-person attended SHM annual conference with a fantastic line-up of offerings. Unfortunately, then came our pandemic, or pandemics. In mid-March, the Society of Hospital Medicine board of directors concluded that it was impossible for SHM to move forward with Hospital Medicine 2020 in San Diego because of the continued spread of COVID-19. Canceling the in-person conference during this unprecedented time was the right thing to do. I have valued the SHM leadership team and the larger SHM community for their support in being even more engaged on the front lines and with each other across our world during this time.
The COVID-19 pandemic has created a systemic challenge for health care systems across the nation. As hospitalists continue to be on the front lines of care and also innovations, organizations have leveraged telemedicine to support their patients, protect their clinicians, and conserve scarce resources. It is hospital medicine that has been on the front lines of change and adaptations and have led in this pandemic in many organizations across the nation and the world.
Unfortunately, known health disparities have also been amplified and there came an acute worsening of the chronic issues in this nation. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home. Armaud Arbery was shot and killed by armed neighbors while running through a neighborhood in Brunswick, Ga. Then on May 25, 5 miles from where I call home here in the Twin Cities in Minnesota, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after police kneeled on his neck for over 8 minutes. This pandemic has also shaken up the status quo and laid bare a lot of our country’s long and deep-seated issues – from massive economic inequities to ongoing racial disparities to immigration concerns. It’s woken a lot of our valued hospitalists to the fact that the old ways of doing things just don’t work.
I’m grateful our society has taken steps to speak into these timely topics, and to share via publications, Twitter chats, advocacy items, and more! I want to encourage all of us to use the immense network of our hospitalist communities to comfort each other, learn, grow, and engage. We have not achieved big changes by ourselves. We’ve created valued offerings and innovative changes, and we’ve led on the front lines, in policies and procedures, by doing it together. Meaningful change requires allies in a common cause. We stand with our black and brown brothers and sisters who are particularly attuned to injustice, inequality, and struggle. We in hospital medicine stand up with many others who are struggling, our African American, Latin American, Native American, immigrant, LGBTQ+ communities. This intersection of the crisis of the COVID-19 pandemic and the racism pandemic have led us to a pivotal point in the arc of change and justice. I invite you to comfort each other, learn from each other, and act together in this community. To this end we have included timely resources in our HM20 virtual offering on these topics.
This year has been a big transition year. Not only did 2020 usher in a new decade, along with COVID-19 and our double pandemic, SHM has also had important transitions within its senior leadership. We say farewell to Larry Wellikson, MD, who has been at the helm of SHM since the beginning. On behalf of this annual conference, we want to celebrate and thank you, Larry, for your years of dedication and service to SHM. You have taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team may gather under a bigger tent for education, community, and for the betterment of care for our patients.
We extend a welcome to Eric Howell, MD, who succeeds Dr. Wellikson as SHM’s CEO. We also welcome Danielle Scheurer, MD, as the new SHM president, succeeding the great leadership offered this past year by Christopher Frost, MD. In addition, Jerome C. Siy, MD, was voted president-elect, Dr. Rachel Thompson, MD, was elected treasurer, Kris Rehm, MD, was voted secretary, and Darlene Tad-y, MD, was elected to the board of directors. We welcome these new officers.
HM20 Virtual will consist of prerecorded on-demand sessions that can be viewed at your convenience as well as live Q&A and attendee networking that will take place during specific dates/times. A few of the top-rated sessions from our historically popular tracks include: Update in Clinical Practice Guidelines, Antibiotics Made Ridiculously Simple, Getting to Know Oncology Emergencies, Inpatient Pain Management in the Era of the Opioid Epidemic, Updates in Heart Failure, and Hyponatremia: Don’t Drink the Water. Additionally, we have some of our perennial favorites including the Update in Hospital Medicine and Top Pediatric Articles of 2019. There will be COVID-19 specific content from expertise throughout the nation focusing on care pathways, clinical updates, telemedicine, point-of-care ultrasound, and more! To view the HM20 Virtual Opening Session and discover what you can expect in this educational experience, click here.
The Journal of Hospital Medicine has had a large presence in our meetings for many years. We are grateful for Samir Shah, MD, and his leadership during this double pandemic, for identifying areas where we can advance the field responsibly in the face of relatively limited evidence, and rapidly evolving news. As part of his commitment, all JHM articles related to COVID-19 and published during the pandemic are open access. A pre-COVID goal that has been realized during the pandemic was to bring more of the journal into our annual conference and the conference contents into the journal. We are proud to say this has been a great collaboration, particularly during this pandemic, and much thanks to Dr. Shah’s leadership for highlighting timely pieces. Kimberly Manning, MD, had an especially powerful piece on the topic of racism and our double pandemic, and she is a featured speaker during our HM20 Virtual offering, under the same title as her article: “When Grief and Crises Intersect: Perspectives of a Black Physician in the Time of Two Pandemics.” Additionally, Manpreet Malik, MD, and I will be copresenting on a timely topic about the “Immigrant Hospitalist during COVID-19.”
Aside from these sessions for HM20 Virtual, the real can’t miss(es) for the conference are the Research, Innovations, and Clinical Vignette (RIV) posters sessions. I am grateful for the leadership of Stephanie Mueller, MD, who served as chair for this year’s RIV. This unique year has led to the hosting of a virtual poster competition with judging and the opening of a virtual gallery. We are so pleased to be able to share and highlight the work of many of learners and staff hospitalists! I love that a hospitalist on one side of the country can help provide pearls on a case, an innovation, or a research idea that can help improve diagnosis for a patient at the other side of the country. Keep an eye on SHM’s social media and the presentation by Dr. Mueller for announcements of the winners.
A favorite reason many of us attend the annual conference is for the people and community. We wanted to keep this value as we shifted to a virtual offering. Networking will occur through a variety of offerings including Simulive sessions and Special Interest Forums. Simulive sessions will run for 3 weeks from August 11 to August 27. For those of you new to the term, Simulive may sound like a made-up word, but it is an actual amalgamation of a prerecorded webinar and a live interaction (simulated + live = Simulive). Simulive allows the faculty to sit in on their prerecorded session and interact with the audience via the chat feature during the live scheduled recording and spend time afterwards for a live Q&A from the audience.
There will also be over 20 Special Interest Forums hosted in the evenings after these Simulive sessions have concluded to give you a chance to connect with individuals, share experiences, and have meaningful discussions that can directly impact your practice. Samples of the forums include: Diversity and Inclusion, Rural Hospital Medicine, Pediatrics, NP/PA, Perioperative and Comanagement, Health Information Technology, and Point of Care Ultrasound! Take a look at the HM20 registration page for further information. You will receive direct information on how to attend. We encourage you to join!
HM20 also features a virtual 5K! Whether you run on a treadmill or jog in your neighborhood or local park, you can participate in HM20’s Virtual Fun Run or Walk. To participate, simply run your 5K during the weeks of HM20 Virtual and when you’re done, fill out our form to log your time. We encourage you to post a picture on social media as well with #HM20Virtual. You’ll also receive a certificate of completion at the close of HM20 Virtual.
All HM20 Virtual sessions will be available as on-demand after August 31. HM20 virtual offers more than 60 CME hours and over 35 MOC hours that you can claim at your convenience! That’s the most amount of CME and MOC ever offered at SHM for an event! This conference would not be possible without the tireless and relentless effort of SHM staff and leadership, our terrific speakers and faculty, and all the volunteer committee members of SHM. A huge thanks to the Annual Conference Committee who had the charge to develop the content for the Annual Conference, including topics, speakers, and learning objectives. I am grateful to have had the opportunity to serve on this committee for the past 7 years and to lead HM20 this year. Thanks to Brittany Evans, Hayleigh Lawrence, and Michelle Kann for their valued support this past year from an SHM staff perspective; to my assistant course director, Dan Steinberg, MD; and to the immediate past course director, Dustin Smith, MD, for their support.
Once again, we are excited to have you join, and we hope this conference elevates your education in hospital medicine, advances your career, stimulates innovative thinking, and provides you with enduring networking opportunities. We sincerely thank you for attending HM20 Virtual. Welcome!
Dr. Mathews is chief of hospital medicine at Regions Hospital, HealthPartners in St. Paul, Minn., an associate professor at the University of Minnesota, Minneapolis, and course director of HM20.
Welcome to the HM20 virtual conference! We’re glad to have you join us to virtually experience sessions from our most popular SHM annual conference tracks including Rapid Fire, Clinical Updates, and High-Value Care! We also have added some new timely topics given our current times that you won’t want to miss. We encourage you to engage with the larger community via social media at #HM20Virtual.
HM20 in San Diego, scheduled originally for April 2020, was trending to be the highest in-person attended SHM annual conference with a fantastic line-up of offerings. Unfortunately, then came our pandemic, or pandemics. In mid-March, the Society of Hospital Medicine board of directors concluded that it was impossible for SHM to move forward with Hospital Medicine 2020 in San Diego because of the continued spread of COVID-19. Canceling the in-person conference during this unprecedented time was the right thing to do. I have valued the SHM leadership team and the larger SHM community for their support in being even more engaged on the front lines and with each other across our world during this time.
The COVID-19 pandemic has created a systemic challenge for health care systems across the nation. As hospitalists continue to be on the front lines of care and also innovations, organizations have leveraged telemedicine to support their patients, protect their clinicians, and conserve scarce resources. It is hospital medicine that has been on the front lines of change and adaptations and have led in this pandemic in many organizations across the nation and the world.
Unfortunately, known health disparities have also been amplified and there came an acute worsening of the chronic issues in this nation. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home. Armaud Arbery was shot and killed by armed neighbors while running through a neighborhood in Brunswick, Ga. Then on May 25, 5 miles from where I call home here in the Twin Cities in Minnesota, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after police kneeled on his neck for over 8 minutes. This pandemic has also shaken up the status quo and laid bare a lot of our country’s long and deep-seated issues – from massive economic inequities to ongoing racial disparities to immigration concerns. It’s woken a lot of our valued hospitalists to the fact that the old ways of doing things just don’t work.
I’m grateful our society has taken steps to speak into these timely topics, and to share via publications, Twitter chats, advocacy items, and more! I want to encourage all of us to use the immense network of our hospitalist communities to comfort each other, learn, grow, and engage. We have not achieved big changes by ourselves. We’ve created valued offerings and innovative changes, and we’ve led on the front lines, in policies and procedures, by doing it together. Meaningful change requires allies in a common cause. We stand with our black and brown brothers and sisters who are particularly attuned to injustice, inequality, and struggle. We in hospital medicine stand up with many others who are struggling, our African American, Latin American, Native American, immigrant, LGBTQ+ communities. This intersection of the crisis of the COVID-19 pandemic and the racism pandemic have led us to a pivotal point in the arc of change and justice. I invite you to comfort each other, learn from each other, and act together in this community. To this end we have included timely resources in our HM20 virtual offering on these topics.
This year has been a big transition year. Not only did 2020 usher in a new decade, along with COVID-19 and our double pandemic, SHM has also had important transitions within its senior leadership. We say farewell to Larry Wellikson, MD, who has been at the helm of SHM since the beginning. On behalf of this annual conference, we want to celebrate and thank you, Larry, for your years of dedication and service to SHM. You have taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team may gather under a bigger tent for education, community, and for the betterment of care for our patients.
We extend a welcome to Eric Howell, MD, who succeeds Dr. Wellikson as SHM’s CEO. We also welcome Danielle Scheurer, MD, as the new SHM president, succeeding the great leadership offered this past year by Christopher Frost, MD. In addition, Jerome C. Siy, MD, was voted president-elect, Dr. Rachel Thompson, MD, was elected treasurer, Kris Rehm, MD, was voted secretary, and Darlene Tad-y, MD, was elected to the board of directors. We welcome these new officers.
HM20 Virtual will consist of prerecorded on-demand sessions that can be viewed at your convenience as well as live Q&A and attendee networking that will take place during specific dates/times. A few of the top-rated sessions from our historically popular tracks include: Update in Clinical Practice Guidelines, Antibiotics Made Ridiculously Simple, Getting to Know Oncology Emergencies, Inpatient Pain Management in the Era of the Opioid Epidemic, Updates in Heart Failure, and Hyponatremia: Don’t Drink the Water. Additionally, we have some of our perennial favorites including the Update in Hospital Medicine and Top Pediatric Articles of 2019. There will be COVID-19 specific content from expertise throughout the nation focusing on care pathways, clinical updates, telemedicine, point-of-care ultrasound, and more! To view the HM20 Virtual Opening Session and discover what you can expect in this educational experience, click here.
The Journal of Hospital Medicine has had a large presence in our meetings for many years. We are grateful for Samir Shah, MD, and his leadership during this double pandemic, for identifying areas where we can advance the field responsibly in the face of relatively limited evidence, and rapidly evolving news. As part of his commitment, all JHM articles related to COVID-19 and published during the pandemic are open access. A pre-COVID goal that has been realized during the pandemic was to bring more of the journal into our annual conference and the conference contents into the journal. We are proud to say this has been a great collaboration, particularly during this pandemic, and much thanks to Dr. Shah’s leadership for highlighting timely pieces. Kimberly Manning, MD, had an especially powerful piece on the topic of racism and our double pandemic, and she is a featured speaker during our HM20 Virtual offering, under the same title as her article: “When Grief and Crises Intersect: Perspectives of a Black Physician in the Time of Two Pandemics.” Additionally, Manpreet Malik, MD, and I will be copresenting on a timely topic about the “Immigrant Hospitalist during COVID-19.”
Aside from these sessions for HM20 Virtual, the real can’t miss(es) for the conference are the Research, Innovations, and Clinical Vignette (RIV) posters sessions. I am grateful for the leadership of Stephanie Mueller, MD, who served as chair for this year’s RIV. This unique year has led to the hosting of a virtual poster competition with judging and the opening of a virtual gallery. We are so pleased to be able to share and highlight the work of many of learners and staff hospitalists! I love that a hospitalist on one side of the country can help provide pearls on a case, an innovation, or a research idea that can help improve diagnosis for a patient at the other side of the country. Keep an eye on SHM’s social media and the presentation by Dr. Mueller for announcements of the winners.
A favorite reason many of us attend the annual conference is for the people and community. We wanted to keep this value as we shifted to a virtual offering. Networking will occur through a variety of offerings including Simulive sessions and Special Interest Forums. Simulive sessions will run for 3 weeks from August 11 to August 27. For those of you new to the term, Simulive may sound like a made-up word, but it is an actual amalgamation of a prerecorded webinar and a live interaction (simulated + live = Simulive). Simulive allows the faculty to sit in on their prerecorded session and interact with the audience via the chat feature during the live scheduled recording and spend time afterwards for a live Q&A from the audience.
There will also be over 20 Special Interest Forums hosted in the evenings after these Simulive sessions have concluded to give you a chance to connect with individuals, share experiences, and have meaningful discussions that can directly impact your practice. Samples of the forums include: Diversity and Inclusion, Rural Hospital Medicine, Pediatrics, NP/PA, Perioperative and Comanagement, Health Information Technology, and Point of Care Ultrasound! Take a look at the HM20 registration page for further information. You will receive direct information on how to attend. We encourage you to join!
HM20 also features a virtual 5K! Whether you run on a treadmill or jog in your neighborhood or local park, you can participate in HM20’s Virtual Fun Run or Walk. To participate, simply run your 5K during the weeks of HM20 Virtual and when you’re done, fill out our form to log your time. We encourage you to post a picture on social media as well with #HM20Virtual. You’ll also receive a certificate of completion at the close of HM20 Virtual.
All HM20 Virtual sessions will be available as on-demand after August 31. HM20 virtual offers more than 60 CME hours and over 35 MOC hours that you can claim at your convenience! That’s the most amount of CME and MOC ever offered at SHM for an event! This conference would not be possible without the tireless and relentless effort of SHM staff and leadership, our terrific speakers and faculty, and all the volunteer committee members of SHM. A huge thanks to the Annual Conference Committee who had the charge to develop the content for the Annual Conference, including topics, speakers, and learning objectives. I am grateful to have had the opportunity to serve on this committee for the past 7 years and to lead HM20 this year. Thanks to Brittany Evans, Hayleigh Lawrence, and Michelle Kann for their valued support this past year from an SHM staff perspective; to my assistant course director, Dan Steinberg, MD; and to the immediate past course director, Dustin Smith, MD, for their support.
Once again, we are excited to have you join, and we hope this conference elevates your education in hospital medicine, advances your career, stimulates innovative thinking, and provides you with enduring networking opportunities. We sincerely thank you for attending HM20 Virtual. Welcome!
Dr. Mathews is chief of hospital medicine at Regions Hospital, HealthPartners in St. Paul, Minn., an associate professor at the University of Minnesota, Minneapolis, and course director of HM20.
Welcome to the HM20 virtual conference! We’re glad to have you join us to virtually experience sessions from our most popular SHM annual conference tracks including Rapid Fire, Clinical Updates, and High-Value Care! We also have added some new timely topics given our current times that you won’t want to miss. We encourage you to engage with the larger community via social media at #HM20Virtual.
HM20 in San Diego, scheduled originally for April 2020, was trending to be the highest in-person attended SHM annual conference with a fantastic line-up of offerings. Unfortunately, then came our pandemic, or pandemics. In mid-March, the Society of Hospital Medicine board of directors concluded that it was impossible for SHM to move forward with Hospital Medicine 2020 in San Diego because of the continued spread of COVID-19. Canceling the in-person conference during this unprecedented time was the right thing to do. I have valued the SHM leadership team and the larger SHM community for their support in being even more engaged on the front lines and with each other across our world during this time.
The COVID-19 pandemic has created a systemic challenge for health care systems across the nation. As hospitalists continue to be on the front lines of care and also innovations, organizations have leveraged telemedicine to support their patients, protect their clinicians, and conserve scarce resources. It is hospital medicine that has been on the front lines of change and adaptations and have led in this pandemic in many organizations across the nation and the world.
Unfortunately, known health disparities have also been amplified and there came an acute worsening of the chronic issues in this nation. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home. Armaud Arbery was shot and killed by armed neighbors while running through a neighborhood in Brunswick, Ga. Then on May 25, 5 miles from where I call home here in the Twin Cities in Minnesota, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after police kneeled on his neck for over 8 minutes. This pandemic has also shaken up the status quo and laid bare a lot of our country’s long and deep-seated issues – from massive economic inequities to ongoing racial disparities to immigration concerns. It’s woken a lot of our valued hospitalists to the fact that the old ways of doing things just don’t work.
I’m grateful our society has taken steps to speak into these timely topics, and to share via publications, Twitter chats, advocacy items, and more! I want to encourage all of us to use the immense network of our hospitalist communities to comfort each other, learn, grow, and engage. We have not achieved big changes by ourselves. We’ve created valued offerings and innovative changes, and we’ve led on the front lines, in policies and procedures, by doing it together. Meaningful change requires allies in a common cause. We stand with our black and brown brothers and sisters who are particularly attuned to injustice, inequality, and struggle. We in hospital medicine stand up with many others who are struggling, our African American, Latin American, Native American, immigrant, LGBTQ+ communities. This intersection of the crisis of the COVID-19 pandemic and the racism pandemic have led us to a pivotal point in the arc of change and justice. I invite you to comfort each other, learn from each other, and act together in this community. To this end we have included timely resources in our HM20 virtual offering on these topics.
This year has been a big transition year. Not only did 2020 usher in a new decade, along with COVID-19 and our double pandemic, SHM has also had important transitions within its senior leadership. We say farewell to Larry Wellikson, MD, who has been at the helm of SHM since the beginning. On behalf of this annual conference, we want to celebrate and thank you, Larry, for your years of dedication and service to SHM. You have taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team may gather under a bigger tent for education, community, and for the betterment of care for our patients.
We extend a welcome to Eric Howell, MD, who succeeds Dr. Wellikson as SHM’s CEO. We also welcome Danielle Scheurer, MD, as the new SHM president, succeeding the great leadership offered this past year by Christopher Frost, MD. In addition, Jerome C. Siy, MD, was voted president-elect, Dr. Rachel Thompson, MD, was elected treasurer, Kris Rehm, MD, was voted secretary, and Darlene Tad-y, MD, was elected to the board of directors. We welcome these new officers.
HM20 Virtual will consist of prerecorded on-demand sessions that can be viewed at your convenience as well as live Q&A and attendee networking that will take place during specific dates/times. A few of the top-rated sessions from our historically popular tracks include: Update in Clinical Practice Guidelines, Antibiotics Made Ridiculously Simple, Getting to Know Oncology Emergencies, Inpatient Pain Management in the Era of the Opioid Epidemic, Updates in Heart Failure, and Hyponatremia: Don’t Drink the Water. Additionally, we have some of our perennial favorites including the Update in Hospital Medicine and Top Pediatric Articles of 2019. There will be COVID-19 specific content from expertise throughout the nation focusing on care pathways, clinical updates, telemedicine, point-of-care ultrasound, and more! To view the HM20 Virtual Opening Session and discover what you can expect in this educational experience, click here.
The Journal of Hospital Medicine has had a large presence in our meetings for many years. We are grateful for Samir Shah, MD, and his leadership during this double pandemic, for identifying areas where we can advance the field responsibly in the face of relatively limited evidence, and rapidly evolving news. As part of his commitment, all JHM articles related to COVID-19 and published during the pandemic are open access. A pre-COVID goal that has been realized during the pandemic was to bring more of the journal into our annual conference and the conference contents into the journal. We are proud to say this has been a great collaboration, particularly during this pandemic, and much thanks to Dr. Shah’s leadership for highlighting timely pieces. Kimberly Manning, MD, had an especially powerful piece on the topic of racism and our double pandemic, and she is a featured speaker during our HM20 Virtual offering, under the same title as her article: “When Grief and Crises Intersect: Perspectives of a Black Physician in the Time of Two Pandemics.” Additionally, Manpreet Malik, MD, and I will be copresenting on a timely topic about the “Immigrant Hospitalist during COVID-19.”
Aside from these sessions for HM20 Virtual, the real can’t miss(es) for the conference are the Research, Innovations, and Clinical Vignette (RIV) posters sessions. I am grateful for the leadership of Stephanie Mueller, MD, who served as chair for this year’s RIV. This unique year has led to the hosting of a virtual poster competition with judging and the opening of a virtual gallery. We are so pleased to be able to share and highlight the work of many of learners and staff hospitalists! I love that a hospitalist on one side of the country can help provide pearls on a case, an innovation, or a research idea that can help improve diagnosis for a patient at the other side of the country. Keep an eye on SHM’s social media and the presentation by Dr. Mueller for announcements of the winners.
A favorite reason many of us attend the annual conference is for the people and community. We wanted to keep this value as we shifted to a virtual offering. Networking will occur through a variety of offerings including Simulive sessions and Special Interest Forums. Simulive sessions will run for 3 weeks from August 11 to August 27. For those of you new to the term, Simulive may sound like a made-up word, but it is an actual amalgamation of a prerecorded webinar and a live interaction (simulated + live = Simulive). Simulive allows the faculty to sit in on their prerecorded session and interact with the audience via the chat feature during the live scheduled recording and spend time afterwards for a live Q&A from the audience.
There will also be over 20 Special Interest Forums hosted in the evenings after these Simulive sessions have concluded to give you a chance to connect with individuals, share experiences, and have meaningful discussions that can directly impact your practice. Samples of the forums include: Diversity and Inclusion, Rural Hospital Medicine, Pediatrics, NP/PA, Perioperative and Comanagement, Health Information Technology, and Point of Care Ultrasound! Take a look at the HM20 registration page for further information. You will receive direct information on how to attend. We encourage you to join!
HM20 also features a virtual 5K! Whether you run on a treadmill or jog in your neighborhood or local park, you can participate in HM20’s Virtual Fun Run or Walk. To participate, simply run your 5K during the weeks of HM20 Virtual and when you’re done, fill out our form to log your time. We encourage you to post a picture on social media as well with #HM20Virtual. You’ll also receive a certificate of completion at the close of HM20 Virtual.
All HM20 Virtual sessions will be available as on-demand after August 31. HM20 virtual offers more than 60 CME hours and over 35 MOC hours that you can claim at your convenience! That’s the most amount of CME and MOC ever offered at SHM for an event! This conference would not be possible without the tireless and relentless effort of SHM staff and leadership, our terrific speakers and faculty, and all the volunteer committee members of SHM. A huge thanks to the Annual Conference Committee who had the charge to develop the content for the Annual Conference, including topics, speakers, and learning objectives. I am grateful to have had the opportunity to serve on this committee for the past 7 years and to lead HM20 this year. Thanks to Brittany Evans, Hayleigh Lawrence, and Michelle Kann for their valued support this past year from an SHM staff perspective; to my assistant course director, Dan Steinberg, MD; and to the immediate past course director, Dustin Smith, MD, for their support.
Once again, we are excited to have you join, and we hope this conference elevates your education in hospital medicine, advances your career, stimulates innovative thinking, and provides you with enduring networking opportunities. We sincerely thank you for attending HM20 Virtual. Welcome!
Dr. Mathews is chief of hospital medicine at Regions Hospital, HealthPartners in St. Paul, Minn., an associate professor at the University of Minnesota, Minneapolis, and course director of HM20.
AHA on cannabis: No evidence of heart benefits, but potential harms
Evidence for a link between cannabis use and cardiovascular health remains unsupported, and the potential risks outweigh any potential benefits, according to a scientific statement from the American Heart Association.
The increased legalization of cannabis and cannabis products in the United States has driven medical professionals to evaluate the safety and efficacy of cannabis in relation to health conditions, wrote Robert L. Page II, PharmD, of the University of Colorado, Aurora, and colleagues.
In a statement published in Circulation, the researchers noted that although cannabis has been shown to relieve pain and other symptoms in certain conditions, clinicians in the United States have been limited from studying its health effects because of federal law restrictions. “Cannabis remains a schedule I controlled substance, deeming no accepted medical use, a high potential for abuse, and an unacceptable safety profile,” the researchers wrote.
The statement addresses issues with the use of cannabis by individuals with cardiovascular disease or those at increased risk. Observational studies have shown no cardiovascular benefits associated with cannabis, the writers noted. The most common chemicals in cannabis include THC (tetrahydrocannabinolic acid) and CBD (cannabidiol).
Some research has shown associations between CBD cardiovascular features including lower blood pressure and reduced inflammation, the writers noted. However, THC, the component of cannabis associated with a “high” or intoxication, has been associated with heart rhythm abnormalities. The writers cited data suggesting an increased risk of heart attacks, atrial fibrillation and heart failure, although more research is needed.
The statement outlines common cannabis formulations including plant-based, extracts, crystalline forms, edible products, and tinctures. In addition, the statement notes that synthetic cannabis products are marketed and used in the United States without subject to regulation.
“Over the past 5 years, we have seen a surge in cannabis use, particularly during the COVID-19 pandemic here in Colorado, especially among adolescents and young adults,” Dr. Page said in an interview. Because of the surge, health care practitioners need to familiarize themselves with not only the benefits, but risks associated with cannabis use regardless of the formulation,” he said. As heart disease remains a leading cause of death in the United States, understanding the cardiovascular risks associated with cannabis is crucial at this time.
Dr. Page noted that popular attitudes about cannabis could pose risks to users’ cardiovascular health. “One leading misconception about cannabis is because it is ‘natural’ it must be safe,” Dr. Page said. “As with all medications, cannabis has side effects, some of which can be cardiovascular in nature,” he said. “Significant drug-drug interactions can occur as CBD and THC, both found in cannabis, inhibit CYP3A4, which metabolizes a large number of medications used to treat many cardiovascular conditions,” he noted.
“Unfortunately, much of the published data is observational in nature due to the federal restrictions on cannabis as a schedule I drug,” said Dr. Page. “Nonetheless, safety signals have emerged regarding cannabis use and adverse cardiovascular outcomes, including myocardial infarction, heart failure, and atrial fibrillation. Carefully designed prospective short- and long-term studies regarding cannabis use and cardiovascular safety are needed,” he emphasized.
Areas in particular need of additional research include the cardiovascular effects of cannabis in several vulnerable populations such as adolescents, older adults, pregnant women, transplant recipients, and those with underlying cardiovascular disease, said Dr. Page.
“Nonetheless, based on the safety signals described within this Clinical Science Statement, an open discussion regarding the risks of using cannabis needs to occur between patient and health care providers,” he said. “Furthermore, patients must be transparent regarding their cannabis use with their cardiologist and primary care provider. The cannabis story will continue to evolve and is a rapidly moving/changing target,” he said.
“Whether cannabis use is a definitive risk factor for cardiovascular disease as with tobacco use is still unknown, and both acute and long-term studies are desperately needed to address this issue,” he said.
Dr. Page had no relevant financial conflicts to disclose.
SOURCE: Page et al. Circulation. 2020 Aug 5. doi: 10.1161/CIR.0000000000000883.
Evidence for a link between cannabis use and cardiovascular health remains unsupported, and the potential risks outweigh any potential benefits, according to a scientific statement from the American Heart Association.
The increased legalization of cannabis and cannabis products in the United States has driven medical professionals to evaluate the safety and efficacy of cannabis in relation to health conditions, wrote Robert L. Page II, PharmD, of the University of Colorado, Aurora, and colleagues.
In a statement published in Circulation, the researchers noted that although cannabis has been shown to relieve pain and other symptoms in certain conditions, clinicians in the United States have been limited from studying its health effects because of federal law restrictions. “Cannabis remains a schedule I controlled substance, deeming no accepted medical use, a high potential for abuse, and an unacceptable safety profile,” the researchers wrote.
The statement addresses issues with the use of cannabis by individuals with cardiovascular disease or those at increased risk. Observational studies have shown no cardiovascular benefits associated with cannabis, the writers noted. The most common chemicals in cannabis include THC (tetrahydrocannabinolic acid) and CBD (cannabidiol).
Some research has shown associations between CBD cardiovascular features including lower blood pressure and reduced inflammation, the writers noted. However, THC, the component of cannabis associated with a “high” or intoxication, has been associated with heart rhythm abnormalities. The writers cited data suggesting an increased risk of heart attacks, atrial fibrillation and heart failure, although more research is needed.
The statement outlines common cannabis formulations including plant-based, extracts, crystalline forms, edible products, and tinctures. In addition, the statement notes that synthetic cannabis products are marketed and used in the United States without subject to regulation.
“Over the past 5 years, we have seen a surge in cannabis use, particularly during the COVID-19 pandemic here in Colorado, especially among adolescents and young adults,” Dr. Page said in an interview. Because of the surge, health care practitioners need to familiarize themselves with not only the benefits, but risks associated with cannabis use regardless of the formulation,” he said. As heart disease remains a leading cause of death in the United States, understanding the cardiovascular risks associated with cannabis is crucial at this time.
Dr. Page noted that popular attitudes about cannabis could pose risks to users’ cardiovascular health. “One leading misconception about cannabis is because it is ‘natural’ it must be safe,” Dr. Page said. “As with all medications, cannabis has side effects, some of which can be cardiovascular in nature,” he said. “Significant drug-drug interactions can occur as CBD and THC, both found in cannabis, inhibit CYP3A4, which metabolizes a large number of medications used to treat many cardiovascular conditions,” he noted.
“Unfortunately, much of the published data is observational in nature due to the federal restrictions on cannabis as a schedule I drug,” said Dr. Page. “Nonetheless, safety signals have emerged regarding cannabis use and adverse cardiovascular outcomes, including myocardial infarction, heart failure, and atrial fibrillation. Carefully designed prospective short- and long-term studies regarding cannabis use and cardiovascular safety are needed,” he emphasized.
Areas in particular need of additional research include the cardiovascular effects of cannabis in several vulnerable populations such as adolescents, older adults, pregnant women, transplant recipients, and those with underlying cardiovascular disease, said Dr. Page.
“Nonetheless, based on the safety signals described within this Clinical Science Statement, an open discussion regarding the risks of using cannabis needs to occur between patient and health care providers,” he said. “Furthermore, patients must be transparent regarding their cannabis use with their cardiologist and primary care provider. The cannabis story will continue to evolve and is a rapidly moving/changing target,” he said.
“Whether cannabis use is a definitive risk factor for cardiovascular disease as with tobacco use is still unknown, and both acute and long-term studies are desperately needed to address this issue,” he said.
Dr. Page had no relevant financial conflicts to disclose.
SOURCE: Page et al. Circulation. 2020 Aug 5. doi: 10.1161/CIR.0000000000000883.
Evidence for a link between cannabis use and cardiovascular health remains unsupported, and the potential risks outweigh any potential benefits, according to a scientific statement from the American Heart Association.
The increased legalization of cannabis and cannabis products in the United States has driven medical professionals to evaluate the safety and efficacy of cannabis in relation to health conditions, wrote Robert L. Page II, PharmD, of the University of Colorado, Aurora, and colleagues.
In a statement published in Circulation, the researchers noted that although cannabis has been shown to relieve pain and other symptoms in certain conditions, clinicians in the United States have been limited from studying its health effects because of federal law restrictions. “Cannabis remains a schedule I controlled substance, deeming no accepted medical use, a high potential for abuse, and an unacceptable safety profile,” the researchers wrote.
The statement addresses issues with the use of cannabis by individuals with cardiovascular disease or those at increased risk. Observational studies have shown no cardiovascular benefits associated with cannabis, the writers noted. The most common chemicals in cannabis include THC (tetrahydrocannabinolic acid) and CBD (cannabidiol).
Some research has shown associations between CBD cardiovascular features including lower blood pressure and reduced inflammation, the writers noted. However, THC, the component of cannabis associated with a “high” or intoxication, has been associated with heart rhythm abnormalities. The writers cited data suggesting an increased risk of heart attacks, atrial fibrillation and heart failure, although more research is needed.
The statement outlines common cannabis formulations including plant-based, extracts, crystalline forms, edible products, and tinctures. In addition, the statement notes that synthetic cannabis products are marketed and used in the United States without subject to regulation.
“Over the past 5 years, we have seen a surge in cannabis use, particularly during the COVID-19 pandemic here in Colorado, especially among adolescents and young adults,” Dr. Page said in an interview. Because of the surge, health care practitioners need to familiarize themselves with not only the benefits, but risks associated with cannabis use regardless of the formulation,” he said. As heart disease remains a leading cause of death in the United States, understanding the cardiovascular risks associated with cannabis is crucial at this time.
Dr. Page noted that popular attitudes about cannabis could pose risks to users’ cardiovascular health. “One leading misconception about cannabis is because it is ‘natural’ it must be safe,” Dr. Page said. “As with all medications, cannabis has side effects, some of which can be cardiovascular in nature,” he said. “Significant drug-drug interactions can occur as CBD and THC, both found in cannabis, inhibit CYP3A4, which metabolizes a large number of medications used to treat many cardiovascular conditions,” he noted.
“Unfortunately, much of the published data is observational in nature due to the federal restrictions on cannabis as a schedule I drug,” said Dr. Page. “Nonetheless, safety signals have emerged regarding cannabis use and adverse cardiovascular outcomes, including myocardial infarction, heart failure, and atrial fibrillation. Carefully designed prospective short- and long-term studies regarding cannabis use and cardiovascular safety are needed,” he emphasized.
Areas in particular need of additional research include the cardiovascular effects of cannabis in several vulnerable populations such as adolescents, older adults, pregnant women, transplant recipients, and those with underlying cardiovascular disease, said Dr. Page.
“Nonetheless, based on the safety signals described within this Clinical Science Statement, an open discussion regarding the risks of using cannabis needs to occur between patient and health care providers,” he said. “Furthermore, patients must be transparent regarding their cannabis use with their cardiologist and primary care provider. The cannabis story will continue to evolve and is a rapidly moving/changing target,” he said.
“Whether cannabis use is a definitive risk factor for cardiovascular disease as with tobacco use is still unknown, and both acute and long-term studies are desperately needed to address this issue,” he said.
Dr. Page had no relevant financial conflicts to disclose.
SOURCE: Page et al. Circulation. 2020 Aug 5. doi: 10.1161/CIR.0000000000000883.
FROM CIRCULATION
Order errors not reduced with limiting number of open records
Background: An estimated 600,000 patients in U.S. hospitals had an order placed in their record that was meant for another patient in 2016. The Office of the National Coordinator for Health Information Technology and the Joint Commission recommend that EHRs limit the number of open records to one at a time based on expert opinion only. There is wide variation in the number of open records allowed among EHRs across the United States currently.
Study design: Randomized clinical trial.
Setting: Large health system in New York.
Synopsis: There were 3,356 clinicians (inpatient, outpatient, ED) randomized in a 1:1 ratio into either a restricted group (one open record at a time) or an unrestricted group (up to four open records at a time). In this study, 12,140,298 orders, in 4,486,631 order sessions, were analyzed with the Wrong-Patient Retract-and-Reorder (RAR) measure to identify wrong-patient orders. The proportion of wrong-patient order sessions were 90.7 vs. 88.0 per 100,000 order sessions for the restricted versus unrestricted groups (odds ratio, 1.03; 95% confidence interval, 0.90-1.20). There were no statistically significant differences in wrong-patient order sessions between the restricted and unrestricted groups in any clinical setting examined (inpatient, outpatient, ED).
Despite the ability to have up to four open records at one time in the unrestricted group, 66% of the order sessions were completed with only one record open in that group. This limited the power of the study to detect a difference in risk of order errors between the restricted and unrestricted groups.
Bottom line: Limiting clinicians to only one open record did not reduce the proportion of wrong-patient orders, compared with allowing up to four open records concurrently.
Citation: Adelman JS et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: A randomized clinical trial. JAMA. 2019;32(18):1780-7.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Background: An estimated 600,000 patients in U.S. hospitals had an order placed in their record that was meant for another patient in 2016. The Office of the National Coordinator for Health Information Technology and the Joint Commission recommend that EHRs limit the number of open records to one at a time based on expert opinion only. There is wide variation in the number of open records allowed among EHRs across the United States currently.
Study design: Randomized clinical trial.
Setting: Large health system in New York.
Synopsis: There were 3,356 clinicians (inpatient, outpatient, ED) randomized in a 1:1 ratio into either a restricted group (one open record at a time) or an unrestricted group (up to four open records at a time). In this study, 12,140,298 orders, in 4,486,631 order sessions, were analyzed with the Wrong-Patient Retract-and-Reorder (RAR) measure to identify wrong-patient orders. The proportion of wrong-patient order sessions were 90.7 vs. 88.0 per 100,000 order sessions for the restricted versus unrestricted groups (odds ratio, 1.03; 95% confidence interval, 0.90-1.20). There were no statistically significant differences in wrong-patient order sessions between the restricted and unrestricted groups in any clinical setting examined (inpatient, outpatient, ED).
Despite the ability to have up to four open records at one time in the unrestricted group, 66% of the order sessions were completed with only one record open in that group. This limited the power of the study to detect a difference in risk of order errors between the restricted and unrestricted groups.
Bottom line: Limiting clinicians to only one open record did not reduce the proportion of wrong-patient orders, compared with allowing up to four open records concurrently.
Citation: Adelman JS et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: A randomized clinical trial. JAMA. 2019;32(18):1780-7.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Background: An estimated 600,000 patients in U.S. hospitals had an order placed in their record that was meant for another patient in 2016. The Office of the National Coordinator for Health Information Technology and the Joint Commission recommend that EHRs limit the number of open records to one at a time based on expert opinion only. There is wide variation in the number of open records allowed among EHRs across the United States currently.
Study design: Randomized clinical trial.
Setting: Large health system in New York.
Synopsis: There were 3,356 clinicians (inpatient, outpatient, ED) randomized in a 1:1 ratio into either a restricted group (one open record at a time) or an unrestricted group (up to four open records at a time). In this study, 12,140,298 orders, in 4,486,631 order sessions, were analyzed with the Wrong-Patient Retract-and-Reorder (RAR) measure to identify wrong-patient orders. The proportion of wrong-patient order sessions were 90.7 vs. 88.0 per 100,000 order sessions for the restricted versus unrestricted groups (odds ratio, 1.03; 95% confidence interval, 0.90-1.20). There were no statistically significant differences in wrong-patient order sessions between the restricted and unrestricted groups in any clinical setting examined (inpatient, outpatient, ED).
Despite the ability to have up to four open records at one time in the unrestricted group, 66% of the order sessions were completed with only one record open in that group. This limited the power of the study to detect a difference in risk of order errors between the restricted and unrestricted groups.
Bottom line: Limiting clinicians to only one open record did not reduce the proportion of wrong-patient orders, compared with allowing up to four open records concurrently.
Citation: Adelman JS et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: A randomized clinical trial. JAMA. 2019;32(18):1780-7.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
New topicals for excessive sweating are in sight
Safe and effective of novel agents presented at the virtual annual meeting of the American Academy of Dermatology.
Both investigational topical anticholinergic agents – 5% sofpironium bromide (SPB) gel and 1% glycopyrronium bromide (GPB) cream – met all of the efficacy and safety endpoints required by the Food and Drug Administration.
Primary axillary hyperhidrosis, or symmetrical bilateral excessive armpit sweating, has a prevalence worldwide of 1%-16%, with 5%-6% the most frequently cited numbers. The condition has a strong adverse impact on quality of life. Primary axillary hyperhidrosis is not caused by a disorder of the sweat glands; rather, it’s actually a dysregulation of the autonomic nervous system leading to disproportionate sweating, explained Christoph Abels, MD, PhD, medical director at Dr. August Wolff in Bielefeld, Germany.
“What’s surprising is that more than 50% of patients do not receive appropriate treatment, very likely due to lack of awareness or embarrassment,” he added.
Also, many patients are put off by the systemic side effects of the oral anticholinergic agents, which are the current off-label treatment mainstay for patients with moderate or severe disease, according to Tomoko Fujimoto, MD, PhD, director of Ikebukuro Nishiguchi Fukurou Dermatology, near Tokyo.
Sofpironium bromide gel
Dr. Fujimoto presented the results of a phase 3, double-blind, multicenter, 6-week, vehicle-controlled clinical trial conducted in 281 Japanese patients with moderate to severe primary axillary hyperhidrosis as defined by a baseline score of 3 or 4 on the 4-point Hyperhidrosis Disease Severity Scale (HDSS). Participants were randomized to self-application of 5% SPB gel or its vehicle once daily before bedtime.
Sofpironium bromide blocks the cholinergic response mediated by the M3 muscarinic receptor subtype expressed on eccrine sweat glands, thereby inhibiting sweating. The drug then undergoes breakdown into an inactive metabolite after reaching the blood.
An important aspect of both SPB gel and GPB cream is that these agents are rolled onto the axillae using a dedicated applicator. Patients never touch the medications with their hands, thus avoiding accidental exposure to the mucous membranes. This largely prevents problems with mydriasis and blurred vision as anticholinergic side effects, which has been an issue with glycopyrronium tosylate topical cloth wipes (Qbrexza), the first FDA-approved treatment for primary axillary hyperhidrosis.
The primary endpoint in the Japanese study was at least a 1-point improvement on the HDSS plus at least a 50% reduction in gravimetric sweat production between baseline and week 6. This composite outcome was achieved in 53.9% of patients in the active treatment arm, compared with 36.4% of controls.
The secondary endpoint consisting of a week-6 HDSS score of 1 or 2 – that is, underarm sweating that’s either never noticeable or is tolerable – occurred in 60.3% of the sofpironium bromide group and 47.9% of controls, a between-group difference that achieved statistical significance by week 2, when the rates were 46.8% and 28.2%.
The reduction in total gravimetric weight of axillary sweat from a mean baseline of 227 mg collected over 5 minutes was also significantly greater in the SPB group: a decrease of 157.6 mg, compared with 127.6 mg in controls; a between-group difference that also was significant by week 2. The mean Dermatology Life Quality Index score dropped by 6.8 points in the active-treatment arm from a baseline of 11.3, a significant improvement over the mean 4.5-point drop in controls.
A new 5-point measure of subjective symptoms of primary axillary hyperhidrosis – the Hyperhidrosis Disease Severity Measure–Axilla (HDSM-Ax) – improved by 1.41 points in the SPB group, significantly better than the 0.93 points in vehicle-treated controls. About 48% of patients on SBP experienced at least a 1.5-point reduction on the HDSM-Ax, compared with 26% of controls.
Regarding safety, there was a 2% incidence of application-site itch or scale in the SBP group. Anticholinergic side effects consisted of a single case of mydriasis, another of constipation, and two complaints of thirst, all mild, none resulting in treatment discontinuation. There were no reports of headache or blurred vision.
“These results indicate that the safety risks of sofpironium bromide can be considered small and controllable,” Dr. Fujimoto said. “Moreover, sofpironium bromide is a topical agent that patients can use by themselves, so it is highly convenient, unlike, say, botulinum toxin type A injections.”
Glycopyrronium bromide cream
Following on the heels of a recently published dose-ranging study (Br J Dermatol. 2020 Jan;182[1]:229-231), Dr. Abels presented the 4-week outcomes of a phase 3a, double-blind, randomized, five-country trial of once-daily 1% GPB cream or placebo in 171 patients with moderate or severe primary axillary hyperhidrosis. A phase 3b, open-label, 72-week, long-term safety trial is ongoing in 516 patients.
The primary endpoint of the 4-week trial was the reduction in gravimetric sweat production from day 1 to day 29. A reduction of 50% or more was documented in 57.5% of the patients on GBP and 34.5% of controls. A 75% or greater reduction occurred in 32.2% of the active-treatment group and 16.7% of those on placebo. And a decrease of at least 90% was seen in 23% of patients on topical GBP, compared with 9.5% of controls. All these between-group differences were significant.
The FDA now requires a quality of life measurement as a coprimary endpoint in phase 3 hyperhidrosis studies, and the phase 3 GBP trial also served as the successful validation study for a new patient-reported quality of life instrument designed specifically for this purpose. The new tool, known as the Hyperhydrosis Quality of Life questionnaire (HidroQol), proved much more sensitive than the HDSS or DLQI for evaluating clinical improvement in response to treatment (Br J Dermatol. 2020 Jun 8. doi: 10.1111/bjd.19300).
Initial results from the long-term phase 3b safety study should be available this fall on the first 100 patients followed on topical GBP for 1 year and for 300 followed for 6 months, Dr. Abels said.
Dr. Fujimoto reported serving as a paid consultant to and speaker for Kaken Pharmaceutical, which is developing SBP gel with Brickell Biotech. Dr. Abels is an employee of the company that is developing GPB cream.
Safe and effective of novel agents presented at the virtual annual meeting of the American Academy of Dermatology.
Both investigational topical anticholinergic agents – 5% sofpironium bromide (SPB) gel and 1% glycopyrronium bromide (GPB) cream – met all of the efficacy and safety endpoints required by the Food and Drug Administration.
Primary axillary hyperhidrosis, or symmetrical bilateral excessive armpit sweating, has a prevalence worldwide of 1%-16%, with 5%-6% the most frequently cited numbers. The condition has a strong adverse impact on quality of life. Primary axillary hyperhidrosis is not caused by a disorder of the sweat glands; rather, it’s actually a dysregulation of the autonomic nervous system leading to disproportionate sweating, explained Christoph Abels, MD, PhD, medical director at Dr. August Wolff in Bielefeld, Germany.
“What’s surprising is that more than 50% of patients do not receive appropriate treatment, very likely due to lack of awareness or embarrassment,” he added.
Also, many patients are put off by the systemic side effects of the oral anticholinergic agents, which are the current off-label treatment mainstay for patients with moderate or severe disease, according to Tomoko Fujimoto, MD, PhD, director of Ikebukuro Nishiguchi Fukurou Dermatology, near Tokyo.
Sofpironium bromide gel
Dr. Fujimoto presented the results of a phase 3, double-blind, multicenter, 6-week, vehicle-controlled clinical trial conducted in 281 Japanese patients with moderate to severe primary axillary hyperhidrosis as defined by a baseline score of 3 or 4 on the 4-point Hyperhidrosis Disease Severity Scale (HDSS). Participants were randomized to self-application of 5% SPB gel or its vehicle once daily before bedtime.
Sofpironium bromide blocks the cholinergic response mediated by the M3 muscarinic receptor subtype expressed on eccrine sweat glands, thereby inhibiting sweating. The drug then undergoes breakdown into an inactive metabolite after reaching the blood.
An important aspect of both SPB gel and GPB cream is that these agents are rolled onto the axillae using a dedicated applicator. Patients never touch the medications with their hands, thus avoiding accidental exposure to the mucous membranes. This largely prevents problems with mydriasis and blurred vision as anticholinergic side effects, which has been an issue with glycopyrronium tosylate topical cloth wipes (Qbrexza), the first FDA-approved treatment for primary axillary hyperhidrosis.
The primary endpoint in the Japanese study was at least a 1-point improvement on the HDSS plus at least a 50% reduction in gravimetric sweat production between baseline and week 6. This composite outcome was achieved in 53.9% of patients in the active treatment arm, compared with 36.4% of controls.
The secondary endpoint consisting of a week-6 HDSS score of 1 or 2 – that is, underarm sweating that’s either never noticeable or is tolerable – occurred in 60.3% of the sofpironium bromide group and 47.9% of controls, a between-group difference that achieved statistical significance by week 2, when the rates were 46.8% and 28.2%.
The reduction in total gravimetric weight of axillary sweat from a mean baseline of 227 mg collected over 5 minutes was also significantly greater in the SPB group: a decrease of 157.6 mg, compared with 127.6 mg in controls; a between-group difference that also was significant by week 2. The mean Dermatology Life Quality Index score dropped by 6.8 points in the active-treatment arm from a baseline of 11.3, a significant improvement over the mean 4.5-point drop in controls.
A new 5-point measure of subjective symptoms of primary axillary hyperhidrosis – the Hyperhidrosis Disease Severity Measure–Axilla (HDSM-Ax) – improved by 1.41 points in the SPB group, significantly better than the 0.93 points in vehicle-treated controls. About 48% of patients on SBP experienced at least a 1.5-point reduction on the HDSM-Ax, compared with 26% of controls.
Regarding safety, there was a 2% incidence of application-site itch or scale in the SBP group. Anticholinergic side effects consisted of a single case of mydriasis, another of constipation, and two complaints of thirst, all mild, none resulting in treatment discontinuation. There were no reports of headache or blurred vision.
“These results indicate that the safety risks of sofpironium bromide can be considered small and controllable,” Dr. Fujimoto said. “Moreover, sofpironium bromide is a topical agent that patients can use by themselves, so it is highly convenient, unlike, say, botulinum toxin type A injections.”
Glycopyrronium bromide cream
Following on the heels of a recently published dose-ranging study (Br J Dermatol. 2020 Jan;182[1]:229-231), Dr. Abels presented the 4-week outcomes of a phase 3a, double-blind, randomized, five-country trial of once-daily 1% GPB cream or placebo in 171 patients with moderate or severe primary axillary hyperhidrosis. A phase 3b, open-label, 72-week, long-term safety trial is ongoing in 516 patients.
The primary endpoint of the 4-week trial was the reduction in gravimetric sweat production from day 1 to day 29. A reduction of 50% or more was documented in 57.5% of the patients on GBP and 34.5% of controls. A 75% or greater reduction occurred in 32.2% of the active-treatment group and 16.7% of those on placebo. And a decrease of at least 90% was seen in 23% of patients on topical GBP, compared with 9.5% of controls. All these between-group differences were significant.
The FDA now requires a quality of life measurement as a coprimary endpoint in phase 3 hyperhidrosis studies, and the phase 3 GBP trial also served as the successful validation study for a new patient-reported quality of life instrument designed specifically for this purpose. The new tool, known as the Hyperhydrosis Quality of Life questionnaire (HidroQol), proved much more sensitive than the HDSS or DLQI for evaluating clinical improvement in response to treatment (Br J Dermatol. 2020 Jun 8. doi: 10.1111/bjd.19300).
Initial results from the long-term phase 3b safety study should be available this fall on the first 100 patients followed on topical GBP for 1 year and for 300 followed for 6 months, Dr. Abels said.
Dr. Fujimoto reported serving as a paid consultant to and speaker for Kaken Pharmaceutical, which is developing SBP gel with Brickell Biotech. Dr. Abels is an employee of the company that is developing GPB cream.
Safe and effective of novel agents presented at the virtual annual meeting of the American Academy of Dermatology.
Both investigational topical anticholinergic agents – 5% sofpironium bromide (SPB) gel and 1% glycopyrronium bromide (GPB) cream – met all of the efficacy and safety endpoints required by the Food and Drug Administration.
Primary axillary hyperhidrosis, or symmetrical bilateral excessive armpit sweating, has a prevalence worldwide of 1%-16%, with 5%-6% the most frequently cited numbers. The condition has a strong adverse impact on quality of life. Primary axillary hyperhidrosis is not caused by a disorder of the sweat glands; rather, it’s actually a dysregulation of the autonomic nervous system leading to disproportionate sweating, explained Christoph Abels, MD, PhD, medical director at Dr. August Wolff in Bielefeld, Germany.
“What’s surprising is that more than 50% of patients do not receive appropriate treatment, very likely due to lack of awareness or embarrassment,” he added.
Also, many patients are put off by the systemic side effects of the oral anticholinergic agents, which are the current off-label treatment mainstay for patients with moderate or severe disease, according to Tomoko Fujimoto, MD, PhD, director of Ikebukuro Nishiguchi Fukurou Dermatology, near Tokyo.
Sofpironium bromide gel
Dr. Fujimoto presented the results of a phase 3, double-blind, multicenter, 6-week, vehicle-controlled clinical trial conducted in 281 Japanese patients with moderate to severe primary axillary hyperhidrosis as defined by a baseline score of 3 or 4 on the 4-point Hyperhidrosis Disease Severity Scale (HDSS). Participants were randomized to self-application of 5% SPB gel or its vehicle once daily before bedtime.
Sofpironium bromide blocks the cholinergic response mediated by the M3 muscarinic receptor subtype expressed on eccrine sweat glands, thereby inhibiting sweating. The drug then undergoes breakdown into an inactive metabolite after reaching the blood.
An important aspect of both SPB gel and GPB cream is that these agents are rolled onto the axillae using a dedicated applicator. Patients never touch the medications with their hands, thus avoiding accidental exposure to the mucous membranes. This largely prevents problems with mydriasis and blurred vision as anticholinergic side effects, which has been an issue with glycopyrronium tosylate topical cloth wipes (Qbrexza), the first FDA-approved treatment for primary axillary hyperhidrosis.
The primary endpoint in the Japanese study was at least a 1-point improvement on the HDSS plus at least a 50% reduction in gravimetric sweat production between baseline and week 6. This composite outcome was achieved in 53.9% of patients in the active treatment arm, compared with 36.4% of controls.
The secondary endpoint consisting of a week-6 HDSS score of 1 or 2 – that is, underarm sweating that’s either never noticeable or is tolerable – occurred in 60.3% of the sofpironium bromide group and 47.9% of controls, a between-group difference that achieved statistical significance by week 2, when the rates were 46.8% and 28.2%.
The reduction in total gravimetric weight of axillary sweat from a mean baseline of 227 mg collected over 5 minutes was also significantly greater in the SPB group: a decrease of 157.6 mg, compared with 127.6 mg in controls; a between-group difference that also was significant by week 2. The mean Dermatology Life Quality Index score dropped by 6.8 points in the active-treatment arm from a baseline of 11.3, a significant improvement over the mean 4.5-point drop in controls.
A new 5-point measure of subjective symptoms of primary axillary hyperhidrosis – the Hyperhidrosis Disease Severity Measure–Axilla (HDSM-Ax) – improved by 1.41 points in the SPB group, significantly better than the 0.93 points in vehicle-treated controls. About 48% of patients on SBP experienced at least a 1.5-point reduction on the HDSM-Ax, compared with 26% of controls.
Regarding safety, there was a 2% incidence of application-site itch or scale in the SBP group. Anticholinergic side effects consisted of a single case of mydriasis, another of constipation, and two complaints of thirst, all mild, none resulting in treatment discontinuation. There were no reports of headache or blurred vision.
“These results indicate that the safety risks of sofpironium bromide can be considered small and controllable,” Dr. Fujimoto said. “Moreover, sofpironium bromide is a topical agent that patients can use by themselves, so it is highly convenient, unlike, say, botulinum toxin type A injections.”
Glycopyrronium bromide cream
Following on the heels of a recently published dose-ranging study (Br J Dermatol. 2020 Jan;182[1]:229-231), Dr. Abels presented the 4-week outcomes of a phase 3a, double-blind, randomized, five-country trial of once-daily 1% GPB cream or placebo in 171 patients with moderate or severe primary axillary hyperhidrosis. A phase 3b, open-label, 72-week, long-term safety trial is ongoing in 516 patients.
The primary endpoint of the 4-week trial was the reduction in gravimetric sweat production from day 1 to day 29. A reduction of 50% or more was documented in 57.5% of the patients on GBP and 34.5% of controls. A 75% or greater reduction occurred in 32.2% of the active-treatment group and 16.7% of those on placebo. And a decrease of at least 90% was seen in 23% of patients on topical GBP, compared with 9.5% of controls. All these between-group differences were significant.
The FDA now requires a quality of life measurement as a coprimary endpoint in phase 3 hyperhidrosis studies, and the phase 3 GBP trial also served as the successful validation study for a new patient-reported quality of life instrument designed specifically for this purpose. The new tool, known as the Hyperhydrosis Quality of Life questionnaire (HidroQol), proved much more sensitive than the HDSS or DLQI for evaluating clinical improvement in response to treatment (Br J Dermatol. 2020 Jun 8. doi: 10.1111/bjd.19300).
Initial results from the long-term phase 3b safety study should be available this fall on the first 100 patients followed on topical GBP for 1 year and for 300 followed for 6 months, Dr. Abels said.
Dr. Fujimoto reported serving as a paid consultant to and speaker for Kaken Pharmaceutical, which is developing SBP gel with Brickell Biotech. Dr. Abels is an employee of the company that is developing GPB cream.
FROM AAD 20
Painful Hemorrhagic Erosions
The Diagnosis: Kaposi Varicelliform Eruption (Eczema Herpeticum)
Polymerase chain reaction confirmed presence of herpes simplex virus (HSV) type 1, and the patient was started on intravenous acyclovir (10 mg/kg every 8 hours). Diagnosis was further supported by histopathologic examination with confirmatory immunohistochemistry (Figure 1). The patient's anemia and thrombocytopenia also were attributed to widespread HSV infection.
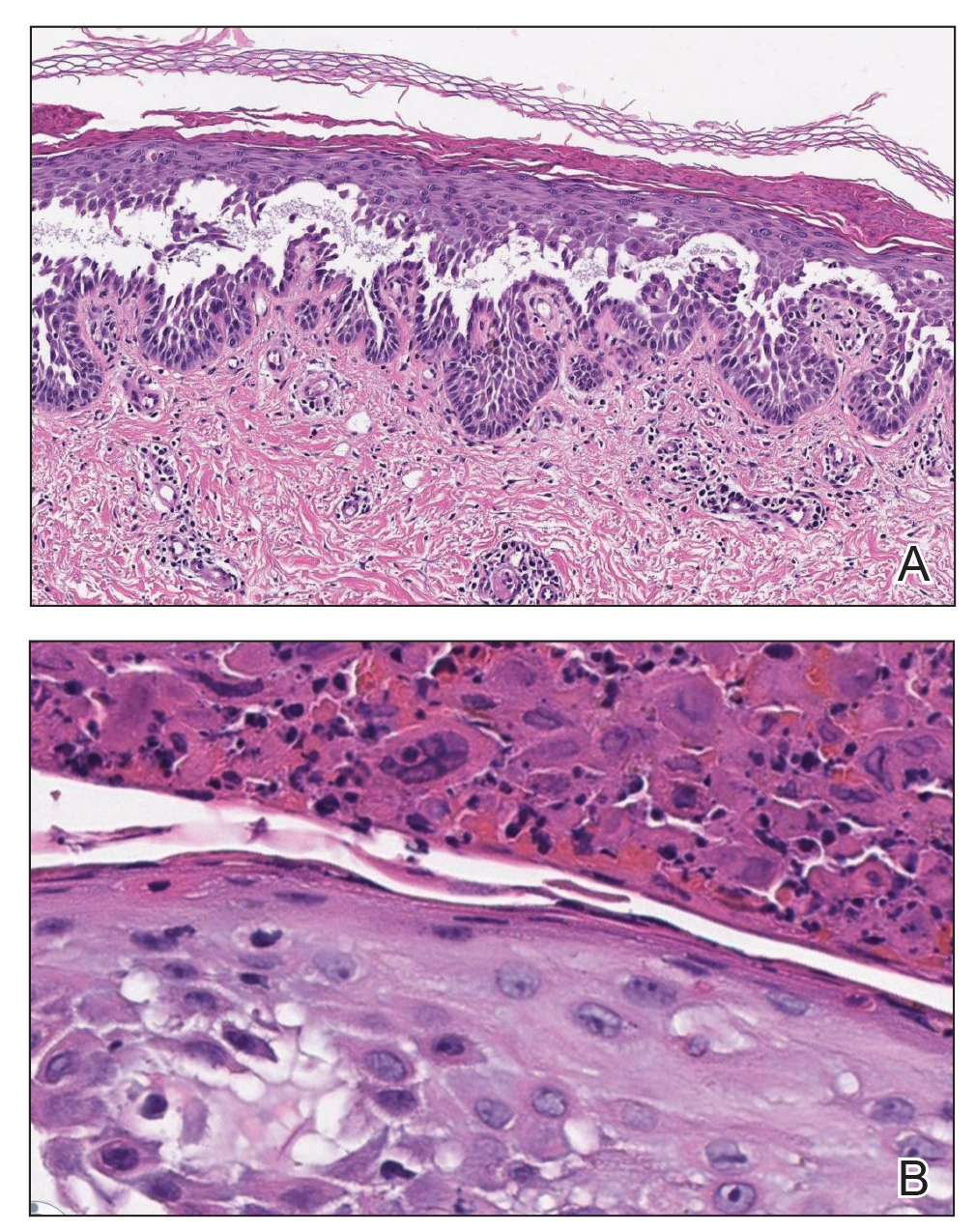
Approximately 8 hours after the patient was started on acyclovir, he developed increasing tremors, confusion, and impaired speech. Lumbar puncture confirmed the presence of HSV-1 in the cerebrospinal fluid. Despite ongoing intravenous antiviral therapy, he required intubation 6 days after hospitalization due to impaired mental status and myoclonic jerking. He remained intubated, unresponsive, and in critical condition for 9 days before he gradually began to demonstrate cognitive recovery. He subsequently was weaned off the ventilator, his mental status returned to normal, and his skin rash slowly resolved (Figure 2).

Hailey-Hailey disease (HHD), also known as familial benign chronic pemphigus, is a rare autosomal-dominant condition first described by Howard and Hugh Hailey in 1939.1 It is a chronic blistering process characterized by epidermal fragility, often manifesting as macerated fissured erosions in areas exposed to heat and friction (eg, axillae, groin). Hailey-Hailey disease results from a defective calcium transporter (ATP2C1 gene), leading to impaired keratinocyte adhesion.2
Eczema herpeticum refers to the dissemination of herpes infection to areas of compromised skin barrier. Although originally used to describe HSV infection in patients with atopic dermatitis, eczema herpeticum has been described in various conditions that affect the skin barrier function, including Darier disease, ichthyosis vulgaris, pemphigus foliaceus, pemphigus vulgaris, and mycosis fungoides, among others.3 When applied to skin conditions other than atopic dermatitis, it sometimes is referred to as Kaposi varicelliform eruption.2
Hailey-Hailey disease commonly is complicated by a bacterial or fungal infection, including impetigo, tinea, or candidiasis. The first case of HHD complicated by HSV infection was reported in 1973.4 A PubMed search of articles indexed for MEDLINE using the terms benign familial pemphigus AND herpes, Hailey-Hailey AND herpes, Hailey-Hailey AND eczema herpeticum, Hailey-Hailey AND Kaposi varicelliform eruption, and Hailey-Hailey herpeticum revealed 15 cases of HHD complicated by eczema herpeticum.4-6 Herpes simplex virus encephalitis is a rare and life-threatening complication of eczema herpeticum.7,8 We report a case of HSV encephalitis resulting from eczema herpeticum in a patient with HHD.
The clinical differential includes a flare of the patient's known HHD, secondary bacterial or fungal infection, or a superimposed viral infection (eg, HSV, zoster). Histologic evidence of herpetic infection would be absent in an uncomplicated flare of HHD. Impetigo is a superficial bacterial infection that can present in 2 clinical forms: a vesiculopustular type and less commonly a bullous type. It is caused by Staphylococcus aureus in most cases. In multiple myeloma with cutaneous dissemination, a monoclonal proliferation of plasma cells would be evident. Lastly, tinea corporis is caused by dermatophytes that can be seen on hematoxylin and eosin or periodic acid-Schiff staining.
The diagnosis of eczema herpeticum in a patient with HHD should be considered in patients who present with grouped vesicles or hemorrhagic or punched-out erosions in areas of pre-existing HHD. The diagnosis can be confirmed by Tzanck smear, viral culture, polymerase chain reaction, or histopathology (with or without immunohistochemistry).1,2,6 When eczema herpeticum is suspected, prompt antiviral administration is imperative to limit life-threatening systemic spread.
- Hailey J, Hailey H. Familial benign chronic pemphigus. Arch Dermatol. 1939;39:679-685.
- de Aquino Paulo Filho T, deFreitas YK, da Nóbrega MT, et al. Hailey-Hailey disease associated with herpetic eczema-the value of the Tzanck smear test. Dermatol Pract Concept. 2014;4:29-31.
- Flint ID, Spencer DM, Wilkin JK. Eczema herpeticum in association with familial benign chronic pemphigus. J Am Acad Dermatol. 1993;28(2, pt 1):257-259.
- Leppard B, Delaney TJ, Sanderson KV. Chronic benign familial pemphigus. induction of lesions by Herpesvirus hominis. Br J Dermatol. 1973;88:609-613.
- Lee GH, Kim YM, Lee SY, et al. A case of eczema herpeticum with Hailey-Hailey disease. Ann Dermatol. 2009;21:311-314.
- Zamperetti M, Pichler M, Perino F, et al. Ein fall von morbus Hailey-Hailey in verbindung mit einem eczema herpeticatum. J Dtsch Dermatol Ges. 2016;14:1035-1038.
- Ingrand D, Briquet I, Babinet JM, et al. Eczema herpeticum of the child. an unusual manifestation of herpes simplex virus infection. Clin Pediatr (Phila). 1985;24:660-663.
- Finlow C, Thomas J. Disseminated herpes simplex virus: a case of eczema herpeticum causing viral encephalitis. J R Coll Physicians Edinb. 2018;48:36-39.
The Diagnosis: Kaposi Varicelliform Eruption (Eczema Herpeticum)
Polymerase chain reaction confirmed presence of herpes simplex virus (HSV) type 1, and the patient was started on intravenous acyclovir (10 mg/kg every 8 hours). Diagnosis was further supported by histopathologic examination with confirmatory immunohistochemistry (Figure 1). The patient's anemia and thrombocytopenia also were attributed to widespread HSV infection.
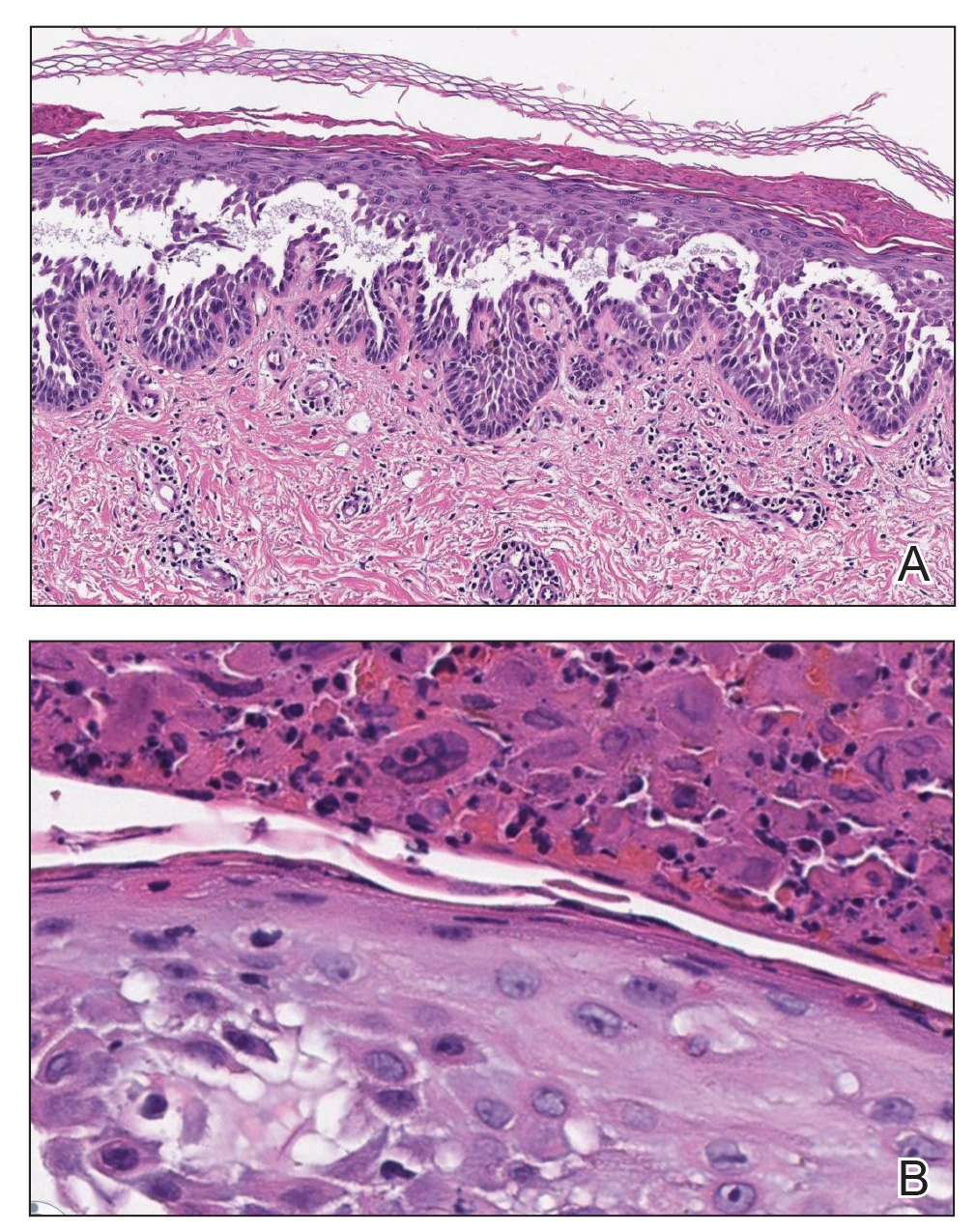
Approximately 8 hours after the patient was started on acyclovir, he developed increasing tremors, confusion, and impaired speech. Lumbar puncture confirmed the presence of HSV-1 in the cerebrospinal fluid. Despite ongoing intravenous antiviral therapy, he required intubation 6 days after hospitalization due to impaired mental status and myoclonic jerking. He remained intubated, unresponsive, and in critical condition for 9 days before he gradually began to demonstrate cognitive recovery. He subsequently was weaned off the ventilator, his mental status returned to normal, and his skin rash slowly resolved (Figure 2).

Hailey-Hailey disease (HHD), also known as familial benign chronic pemphigus, is a rare autosomal-dominant condition first described by Howard and Hugh Hailey in 1939.1 It is a chronic blistering process characterized by epidermal fragility, often manifesting as macerated fissured erosions in areas exposed to heat and friction (eg, axillae, groin). Hailey-Hailey disease results from a defective calcium transporter (ATP2C1 gene), leading to impaired keratinocyte adhesion.2
Eczema herpeticum refers to the dissemination of herpes infection to areas of compromised skin barrier. Although originally used to describe HSV infection in patients with atopic dermatitis, eczema herpeticum has been described in various conditions that affect the skin barrier function, including Darier disease, ichthyosis vulgaris, pemphigus foliaceus, pemphigus vulgaris, and mycosis fungoides, among others.3 When applied to skin conditions other than atopic dermatitis, it sometimes is referred to as Kaposi varicelliform eruption.2
Hailey-Hailey disease commonly is complicated by a bacterial or fungal infection, including impetigo, tinea, or candidiasis. The first case of HHD complicated by HSV infection was reported in 1973.4 A PubMed search of articles indexed for MEDLINE using the terms benign familial pemphigus AND herpes, Hailey-Hailey AND herpes, Hailey-Hailey AND eczema herpeticum, Hailey-Hailey AND Kaposi varicelliform eruption, and Hailey-Hailey herpeticum revealed 15 cases of HHD complicated by eczema herpeticum.4-6 Herpes simplex virus encephalitis is a rare and life-threatening complication of eczema herpeticum.7,8 We report a case of HSV encephalitis resulting from eczema herpeticum in a patient with HHD.
The clinical differential includes a flare of the patient's known HHD, secondary bacterial or fungal infection, or a superimposed viral infection (eg, HSV, zoster). Histologic evidence of herpetic infection would be absent in an uncomplicated flare of HHD. Impetigo is a superficial bacterial infection that can present in 2 clinical forms: a vesiculopustular type and less commonly a bullous type. It is caused by Staphylococcus aureus in most cases. In multiple myeloma with cutaneous dissemination, a monoclonal proliferation of plasma cells would be evident. Lastly, tinea corporis is caused by dermatophytes that can be seen on hematoxylin and eosin or periodic acid-Schiff staining.
The diagnosis of eczema herpeticum in a patient with HHD should be considered in patients who present with grouped vesicles or hemorrhagic or punched-out erosions in areas of pre-existing HHD. The diagnosis can be confirmed by Tzanck smear, viral culture, polymerase chain reaction, or histopathology (with or without immunohistochemistry).1,2,6 When eczema herpeticum is suspected, prompt antiviral administration is imperative to limit life-threatening systemic spread.
The Diagnosis: Kaposi Varicelliform Eruption (Eczema Herpeticum)
Polymerase chain reaction confirmed presence of herpes simplex virus (HSV) type 1, and the patient was started on intravenous acyclovir (10 mg/kg every 8 hours). Diagnosis was further supported by histopathologic examination with confirmatory immunohistochemistry (Figure 1). The patient's anemia and thrombocytopenia also were attributed to widespread HSV infection.
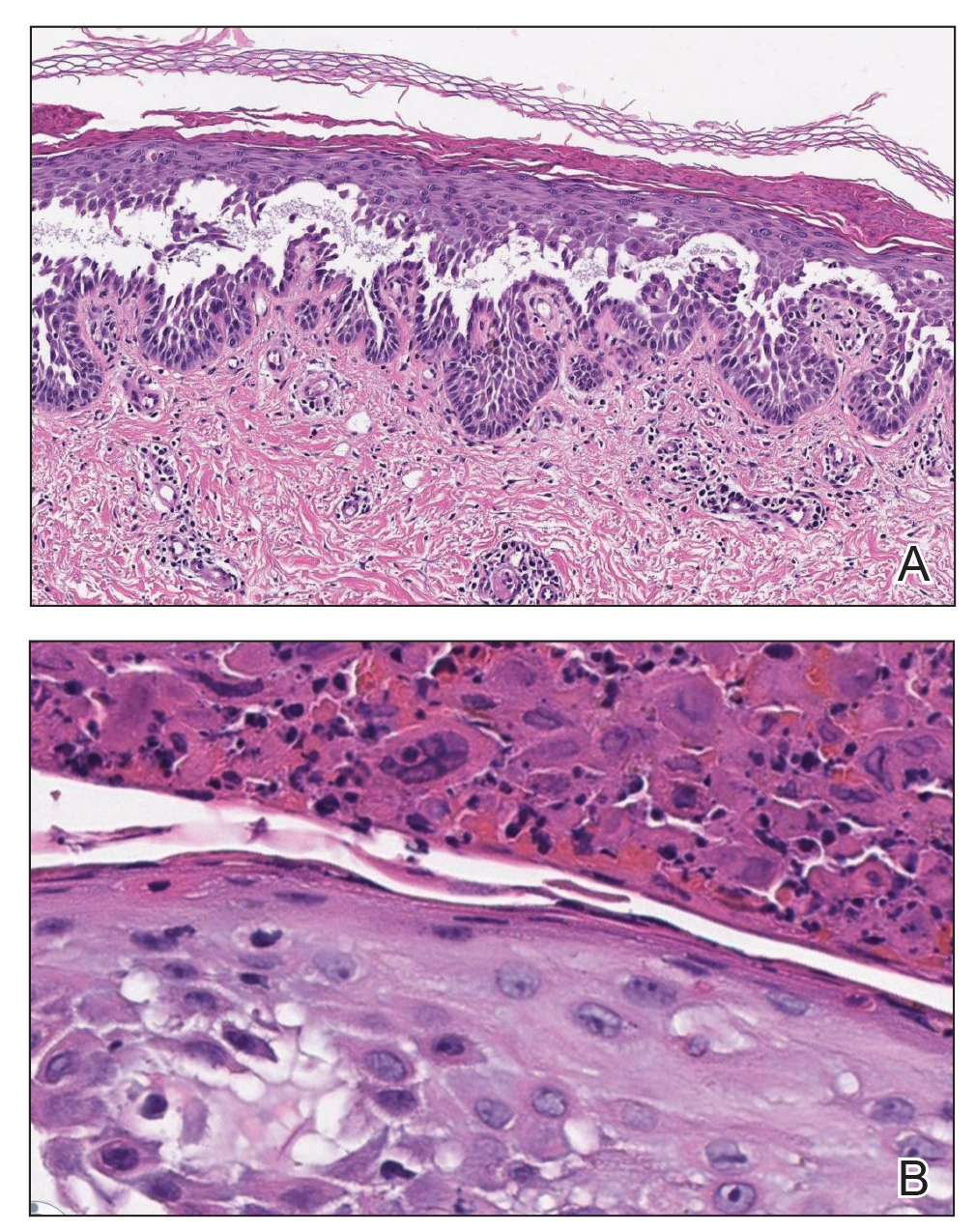
Approximately 8 hours after the patient was started on acyclovir, he developed increasing tremors, confusion, and impaired speech. Lumbar puncture confirmed the presence of HSV-1 in the cerebrospinal fluid. Despite ongoing intravenous antiviral therapy, he required intubation 6 days after hospitalization due to impaired mental status and myoclonic jerking. He remained intubated, unresponsive, and in critical condition for 9 days before he gradually began to demonstrate cognitive recovery. He subsequently was weaned off the ventilator, his mental status returned to normal, and his skin rash slowly resolved (Figure 2).

Hailey-Hailey disease (HHD), also known as familial benign chronic pemphigus, is a rare autosomal-dominant condition first described by Howard and Hugh Hailey in 1939.1 It is a chronic blistering process characterized by epidermal fragility, often manifesting as macerated fissured erosions in areas exposed to heat and friction (eg, axillae, groin). Hailey-Hailey disease results from a defective calcium transporter (ATP2C1 gene), leading to impaired keratinocyte adhesion.2
Eczema herpeticum refers to the dissemination of herpes infection to areas of compromised skin barrier. Although originally used to describe HSV infection in patients with atopic dermatitis, eczema herpeticum has been described in various conditions that affect the skin barrier function, including Darier disease, ichthyosis vulgaris, pemphigus foliaceus, pemphigus vulgaris, and mycosis fungoides, among others.3 When applied to skin conditions other than atopic dermatitis, it sometimes is referred to as Kaposi varicelliform eruption.2
Hailey-Hailey disease commonly is complicated by a bacterial or fungal infection, including impetigo, tinea, or candidiasis. The first case of HHD complicated by HSV infection was reported in 1973.4 A PubMed search of articles indexed for MEDLINE using the terms benign familial pemphigus AND herpes, Hailey-Hailey AND herpes, Hailey-Hailey AND eczema herpeticum, Hailey-Hailey AND Kaposi varicelliform eruption, and Hailey-Hailey herpeticum revealed 15 cases of HHD complicated by eczema herpeticum.4-6 Herpes simplex virus encephalitis is a rare and life-threatening complication of eczema herpeticum.7,8 We report a case of HSV encephalitis resulting from eczema herpeticum in a patient with HHD.
The clinical differential includes a flare of the patient's known HHD, secondary bacterial or fungal infection, or a superimposed viral infection (eg, HSV, zoster). Histologic evidence of herpetic infection would be absent in an uncomplicated flare of HHD. Impetigo is a superficial bacterial infection that can present in 2 clinical forms: a vesiculopustular type and less commonly a bullous type. It is caused by Staphylococcus aureus in most cases. In multiple myeloma with cutaneous dissemination, a monoclonal proliferation of plasma cells would be evident. Lastly, tinea corporis is caused by dermatophytes that can be seen on hematoxylin and eosin or periodic acid-Schiff staining.
The diagnosis of eczema herpeticum in a patient with HHD should be considered in patients who present with grouped vesicles or hemorrhagic or punched-out erosions in areas of pre-existing HHD. The diagnosis can be confirmed by Tzanck smear, viral culture, polymerase chain reaction, or histopathology (with or without immunohistochemistry).1,2,6 When eczema herpeticum is suspected, prompt antiviral administration is imperative to limit life-threatening systemic spread.
- Hailey J, Hailey H. Familial benign chronic pemphigus. Arch Dermatol. 1939;39:679-685.
- de Aquino Paulo Filho T, deFreitas YK, da Nóbrega MT, et al. Hailey-Hailey disease associated with herpetic eczema-the value of the Tzanck smear test. Dermatol Pract Concept. 2014;4:29-31.
- Flint ID, Spencer DM, Wilkin JK. Eczema herpeticum in association with familial benign chronic pemphigus. J Am Acad Dermatol. 1993;28(2, pt 1):257-259.
- Leppard B, Delaney TJ, Sanderson KV. Chronic benign familial pemphigus. induction of lesions by Herpesvirus hominis. Br J Dermatol. 1973;88:609-613.
- Lee GH, Kim YM, Lee SY, et al. A case of eczema herpeticum with Hailey-Hailey disease. Ann Dermatol. 2009;21:311-314.
- Zamperetti M, Pichler M, Perino F, et al. Ein fall von morbus Hailey-Hailey in verbindung mit einem eczema herpeticatum. J Dtsch Dermatol Ges. 2016;14:1035-1038.
- Ingrand D, Briquet I, Babinet JM, et al. Eczema herpeticum of the child. an unusual manifestation of herpes simplex virus infection. Clin Pediatr (Phila). 1985;24:660-663.
- Finlow C, Thomas J. Disseminated herpes simplex virus: a case of eczema herpeticum causing viral encephalitis. J R Coll Physicians Edinb. 2018;48:36-39.
- Hailey J, Hailey H. Familial benign chronic pemphigus. Arch Dermatol. 1939;39:679-685.
- de Aquino Paulo Filho T, deFreitas YK, da Nóbrega MT, et al. Hailey-Hailey disease associated with herpetic eczema-the value of the Tzanck smear test. Dermatol Pract Concept. 2014;4:29-31.
- Flint ID, Spencer DM, Wilkin JK. Eczema herpeticum in association with familial benign chronic pemphigus. J Am Acad Dermatol. 1993;28(2, pt 1):257-259.
- Leppard B, Delaney TJ, Sanderson KV. Chronic benign familial pemphigus. induction of lesions by Herpesvirus hominis. Br J Dermatol. 1973;88:609-613.
- Lee GH, Kim YM, Lee SY, et al. A case of eczema herpeticum with Hailey-Hailey disease. Ann Dermatol. 2009;21:311-314.
- Zamperetti M, Pichler M, Perino F, et al. Ein fall von morbus Hailey-Hailey in verbindung mit einem eczema herpeticatum. J Dtsch Dermatol Ges. 2016;14:1035-1038.
- Ingrand D, Briquet I, Babinet JM, et al. Eczema herpeticum of the child. an unusual manifestation of herpes simplex virus infection. Clin Pediatr (Phila). 1985;24:660-663.
- Finlow C, Thomas J. Disseminated herpes simplex virus: a case of eczema herpeticum causing viral encephalitis. J R Coll Physicians Edinb. 2018;48:36-39.


A 62-year-old man with a long-standing history (>40 years) of Hailey-Hailey disease was admitted from an outside hospital due to anemia (hemoglobin, 8.6 g/dL [reference range, 14.0–17.5 g/dL]), thrombocytopenia (platelets, 7×103 /µL [reference range, 150–350×103 /µL]), and worsening skin rash. The patient reported that his Hailey-Hailey disease worsened abruptly 1 month prior to admission and had progressed steadily since then. He described the rash as painful, especially with movement. Over the preceding month, he had been treated with topical triamcinolone, topical diphenhydramine, oral prednisone, fluconazole, and oral clindamycin, all without improvement. The skin lesions continued to worsen and persistently bled; he then presented to our institution for further care.
Physical examination demonstrated widespread shallow erosions with hemorrhagic drainage and crusting located on the lower back, chest, abdomen (top), axillae (bottom), groin, arms, and legs. No vesicles or pustules were noted. The patient had no cognitive dysfunction or focal neurologic deficits. A punch biopsy was performed.
Urine screen as part of triple test improves ID of adrenal cancer
A strategy that includes a urine steroid test along with imaging characteristics and tumor size criteria can significantly improve the challenging diagnosis of adrenocortical cancer, helping to avoid unnecessary, and often unsuccessful, further imaging and even surgery, new research shows.
“A triple-test strategy of tumor diameter, imaging characteristics, and urine steroid metabolomics improves detection of adrenocortical carcinoma, which could shorten time to surgery for patients with ... carcinoma and help to avoid unnecessary surgery in patients with benign tumors,” the authors say in research published online July 23 in The Lancet Diabetes & Endocrinology.
The triple-test strategy can be expected to make its way into international guidelines, notes joint lead author Irina Bancos, MD, an associate professor of endocrinology at the Mayo Clinic, Rochester, Minn., in a press statement issued by the University of Birmingham (England), which also had a number of researchers involved in the study.
“The findings of this study will feed into the next international guidelines on the management of adrenal tumors and the implementation of the new test will hopefully improve the overall outlook for patients diagnosed with adrenal tumors,” Dr. Bancos emphasized.
More imaging has led to detection of more adrenal tumors
Advances in CT and MRI imaging have increased the ability to detect adrenal incidentalomas, which are now picked up on about 5% of scans, and the widespread use of imaging has compounded the prevalence of such findings, particularly in older people.
Adrenocortical carcinomas represent only about 2%-12% of adrenal incidentalomas, but the prognosis is very poor, and early detection and surgery can improve outcomes, so findings of any adrenal tumor typically trigger additional multimodal imaging to rule out malignancy.
Evidence is lacking on the accuracy of imaging in determining whether such masses are truly cancerous, or benign, and such procedures add costs, as well as expose patients to radiation that may ultimately have no benefit. However, a previous proof-of-concept study from the same authors did show that the presence of excess adrenal steroid hormones in the urine is a key indicator of adrenal tumors, and other research has supported the findings.
All three tests together give best predictive value: EURINE-ACT
To further validate this work, the authors conducted the EURINE-ACT trial, a prospective 14-center study that is the first of its kind to evaluate the efficacy of a screening strategy for adrenocortical carcinoma that combines urine steroid profiling with tumor size and imaging characteristics.
The study of 2,017 participants with newly diagnosed adrenal masses, recruited from January 2011 to July 2016 from specialist centers in 11 different countries, assessed the diagnostic accuracy of three components: maximum tumor diameter (≥4 cm vs. <4 cm), imaging characteristics (positive vs. negative), and urine steroid metabolomics (low, medium, or high risk of adrenocortical carcinoma), separately and in combination.
Of the patients, 98 (4.9%) had adrenocortical carcinoma confirmed clinically, histopathologically, or biochemically.
Tumors with diameters of 4 cm or larger were identified in 488 patients (24.2%) and were observed in the vast majority of patients with adrenocortical carcinoma (96 of 98), for a positive predictive value (PPV) of 19.7%.
Likewise, the PPV for imaging characteristics was 19.7%. However, increasing the unenhanced CT tumor attenuation threshold to 20 Hounsfield units (HU) from the recommended 10 HU increased specificity for adrenocortical carcinoma (80.0% vs. 64.0%) while maintaining sensitivity (99.0% vs. 100.0%).
Comparatively, a urine steroid metabolomics result suggesting a high risk of adrenocortical carcinoma had a PPV of 34.6%.
A total of 106 patients (5.3%) met the criteria for all three measures, and the PPV for all three was 76.4%.
Using the criteria, 70 patients (3.5%) were classified as being at moderate risk of adrenocortical carcinoma and 1,841 (91.3%) at low risk, for a negative predictive value (NPV) of 99.7%.
“Use of radiation-free, noninvasive urine steroid metabolomics has a higher PPV than two standard imaging tests, and best performance was seen with the combination of all three tests,” the authors state.
Limit urine test to patients with larger tumors
They note that the use of the combined diagnostic strategy would have led to additional imaging in only 488 (24.2%) of the study’s 2,017 patients, compared with the 2,737 scans that were actually conducted before reaching a diagnostic decision.
“Implementation of urine steroid metabolomics in the routine diagnostic assessment of newly discovered adrenal masses could reduce the number of imaging procedures required to diagnose adrenocortical carcinoma and avoid unnecessary surgery of benign adrenal tumors, potentially yielding beneficial effects with respect to patient burden and health care costs,” they stress.
And regarding imaging parameters, “we also showed that using a cutoff of 20 HU for unenhanced CT tumor attenuation increases the accuracy of imaging characteristic assessment for exclusion of adrenocortical carcinoma, compared with the currently recommended cutoff of 10 HU, which has immediate implications for clinical practice,” they emphasize.
In an accompanying editorial, Adina F. Turcu, MD, of the division of metabolism, endocrinology, and diabetes, University of Michigan, Ann Arbor, and Axel K. Walch, MD, of the Helmholtz Zentrum München–German Research Centre for Environmental Health, agree. “The introduction of urine steroid metabolomics into routine clinical practice would provide major advantages,” they state.
However, they point out that, although the overall negative predictive value of the test was excellent, the specificity was weak.
“Thus, urine steroid metabolomics should be limited to patients who have adrenal nodules larger than 4 cm and have qualitative imaging characteristics suggestive of malignancy,” say Dr. Turcu and Dr. Walch.
The EURINE-ACT study results suggest this subgroup would represent roughly only 12% of all patients with adrenal incidentalomas, they add.
Issues that remain to be addressed with regard to the implementation of the screening strategy include how to best respond to patients who are classified as having intermediate or moderate risk of malignancy, and whether the diagnostic value of steroid metabolomics could be refined by adding analytes or parameters, the editorialists conclude.
The study was funded by the European Commission, U.K. Medical Research Council, Wellcome Trust, U.K. National Institute for Health Research, U.S. National Institutes of Health, the Claire Khan Trust Fund at University Hospitals Birmingham Charities, and the Mayo Clinic Foundation for Medical Education and Research.
A version of this article originally appeared on Medscape.com.
A strategy that includes a urine steroid test along with imaging characteristics and tumor size criteria can significantly improve the challenging diagnosis of adrenocortical cancer, helping to avoid unnecessary, and often unsuccessful, further imaging and even surgery, new research shows.
“A triple-test strategy of tumor diameter, imaging characteristics, and urine steroid metabolomics improves detection of adrenocortical carcinoma, which could shorten time to surgery for patients with ... carcinoma and help to avoid unnecessary surgery in patients with benign tumors,” the authors say in research published online July 23 in The Lancet Diabetes & Endocrinology.
The triple-test strategy can be expected to make its way into international guidelines, notes joint lead author Irina Bancos, MD, an associate professor of endocrinology at the Mayo Clinic, Rochester, Minn., in a press statement issued by the University of Birmingham (England), which also had a number of researchers involved in the study.
“The findings of this study will feed into the next international guidelines on the management of adrenal tumors and the implementation of the new test will hopefully improve the overall outlook for patients diagnosed with adrenal tumors,” Dr. Bancos emphasized.
More imaging has led to detection of more adrenal tumors
Advances in CT and MRI imaging have increased the ability to detect adrenal incidentalomas, which are now picked up on about 5% of scans, and the widespread use of imaging has compounded the prevalence of such findings, particularly in older people.
Adrenocortical carcinomas represent only about 2%-12% of adrenal incidentalomas, but the prognosis is very poor, and early detection and surgery can improve outcomes, so findings of any adrenal tumor typically trigger additional multimodal imaging to rule out malignancy.
Evidence is lacking on the accuracy of imaging in determining whether such masses are truly cancerous, or benign, and such procedures add costs, as well as expose patients to radiation that may ultimately have no benefit. However, a previous proof-of-concept study from the same authors did show that the presence of excess adrenal steroid hormones in the urine is a key indicator of adrenal tumors, and other research has supported the findings.
All three tests together give best predictive value: EURINE-ACT
To further validate this work, the authors conducted the EURINE-ACT trial, a prospective 14-center study that is the first of its kind to evaluate the efficacy of a screening strategy for adrenocortical carcinoma that combines urine steroid profiling with tumor size and imaging characteristics.
The study of 2,017 participants with newly diagnosed adrenal masses, recruited from January 2011 to July 2016 from specialist centers in 11 different countries, assessed the diagnostic accuracy of three components: maximum tumor diameter (≥4 cm vs. <4 cm), imaging characteristics (positive vs. negative), and urine steroid metabolomics (low, medium, or high risk of adrenocortical carcinoma), separately and in combination.
Of the patients, 98 (4.9%) had adrenocortical carcinoma confirmed clinically, histopathologically, or biochemically.
Tumors with diameters of 4 cm or larger were identified in 488 patients (24.2%) and were observed in the vast majority of patients with adrenocortical carcinoma (96 of 98), for a positive predictive value (PPV) of 19.7%.
Likewise, the PPV for imaging characteristics was 19.7%. However, increasing the unenhanced CT tumor attenuation threshold to 20 Hounsfield units (HU) from the recommended 10 HU increased specificity for adrenocortical carcinoma (80.0% vs. 64.0%) while maintaining sensitivity (99.0% vs. 100.0%).
Comparatively, a urine steroid metabolomics result suggesting a high risk of adrenocortical carcinoma had a PPV of 34.6%.
A total of 106 patients (5.3%) met the criteria for all three measures, and the PPV for all three was 76.4%.
Using the criteria, 70 patients (3.5%) were classified as being at moderate risk of adrenocortical carcinoma and 1,841 (91.3%) at low risk, for a negative predictive value (NPV) of 99.7%.
“Use of radiation-free, noninvasive urine steroid metabolomics has a higher PPV than two standard imaging tests, and best performance was seen with the combination of all three tests,” the authors state.
Limit urine test to patients with larger tumors
They note that the use of the combined diagnostic strategy would have led to additional imaging in only 488 (24.2%) of the study’s 2,017 patients, compared with the 2,737 scans that were actually conducted before reaching a diagnostic decision.
“Implementation of urine steroid metabolomics in the routine diagnostic assessment of newly discovered adrenal masses could reduce the number of imaging procedures required to diagnose adrenocortical carcinoma and avoid unnecessary surgery of benign adrenal tumors, potentially yielding beneficial effects with respect to patient burden and health care costs,” they stress.
And regarding imaging parameters, “we also showed that using a cutoff of 20 HU for unenhanced CT tumor attenuation increases the accuracy of imaging characteristic assessment for exclusion of adrenocortical carcinoma, compared with the currently recommended cutoff of 10 HU, which has immediate implications for clinical practice,” they emphasize.
In an accompanying editorial, Adina F. Turcu, MD, of the division of metabolism, endocrinology, and diabetes, University of Michigan, Ann Arbor, and Axel K. Walch, MD, of the Helmholtz Zentrum München–German Research Centre for Environmental Health, agree. “The introduction of urine steroid metabolomics into routine clinical practice would provide major advantages,” they state.
However, they point out that, although the overall negative predictive value of the test was excellent, the specificity was weak.
“Thus, urine steroid metabolomics should be limited to patients who have adrenal nodules larger than 4 cm and have qualitative imaging characteristics suggestive of malignancy,” say Dr. Turcu and Dr. Walch.
The EURINE-ACT study results suggest this subgroup would represent roughly only 12% of all patients with adrenal incidentalomas, they add.
Issues that remain to be addressed with regard to the implementation of the screening strategy include how to best respond to patients who are classified as having intermediate or moderate risk of malignancy, and whether the diagnostic value of steroid metabolomics could be refined by adding analytes or parameters, the editorialists conclude.
The study was funded by the European Commission, U.K. Medical Research Council, Wellcome Trust, U.K. National Institute for Health Research, U.S. National Institutes of Health, the Claire Khan Trust Fund at University Hospitals Birmingham Charities, and the Mayo Clinic Foundation for Medical Education and Research.
A version of this article originally appeared on Medscape.com.
A strategy that includes a urine steroid test along with imaging characteristics and tumor size criteria can significantly improve the challenging diagnosis of adrenocortical cancer, helping to avoid unnecessary, and often unsuccessful, further imaging and even surgery, new research shows.
“A triple-test strategy of tumor diameter, imaging characteristics, and urine steroid metabolomics improves detection of adrenocortical carcinoma, which could shorten time to surgery for patients with ... carcinoma and help to avoid unnecessary surgery in patients with benign tumors,” the authors say in research published online July 23 in The Lancet Diabetes & Endocrinology.
The triple-test strategy can be expected to make its way into international guidelines, notes joint lead author Irina Bancos, MD, an associate professor of endocrinology at the Mayo Clinic, Rochester, Minn., in a press statement issued by the University of Birmingham (England), which also had a number of researchers involved in the study.
“The findings of this study will feed into the next international guidelines on the management of adrenal tumors and the implementation of the new test will hopefully improve the overall outlook for patients diagnosed with adrenal tumors,” Dr. Bancos emphasized.
More imaging has led to detection of more adrenal tumors
Advances in CT and MRI imaging have increased the ability to detect adrenal incidentalomas, which are now picked up on about 5% of scans, and the widespread use of imaging has compounded the prevalence of such findings, particularly in older people.
Adrenocortical carcinomas represent only about 2%-12% of adrenal incidentalomas, but the prognosis is very poor, and early detection and surgery can improve outcomes, so findings of any adrenal tumor typically trigger additional multimodal imaging to rule out malignancy.
Evidence is lacking on the accuracy of imaging in determining whether such masses are truly cancerous, or benign, and such procedures add costs, as well as expose patients to radiation that may ultimately have no benefit. However, a previous proof-of-concept study from the same authors did show that the presence of excess adrenal steroid hormones in the urine is a key indicator of adrenal tumors, and other research has supported the findings.
All three tests together give best predictive value: EURINE-ACT
To further validate this work, the authors conducted the EURINE-ACT trial, a prospective 14-center study that is the first of its kind to evaluate the efficacy of a screening strategy for adrenocortical carcinoma that combines urine steroid profiling with tumor size and imaging characteristics.
The study of 2,017 participants with newly diagnosed adrenal masses, recruited from January 2011 to July 2016 from specialist centers in 11 different countries, assessed the diagnostic accuracy of three components: maximum tumor diameter (≥4 cm vs. <4 cm), imaging characteristics (positive vs. negative), and urine steroid metabolomics (low, medium, or high risk of adrenocortical carcinoma), separately and in combination.
Of the patients, 98 (4.9%) had adrenocortical carcinoma confirmed clinically, histopathologically, or biochemically.
Tumors with diameters of 4 cm or larger were identified in 488 patients (24.2%) and were observed in the vast majority of patients with adrenocortical carcinoma (96 of 98), for a positive predictive value (PPV) of 19.7%.
Likewise, the PPV for imaging characteristics was 19.7%. However, increasing the unenhanced CT tumor attenuation threshold to 20 Hounsfield units (HU) from the recommended 10 HU increased specificity for adrenocortical carcinoma (80.0% vs. 64.0%) while maintaining sensitivity (99.0% vs. 100.0%).
Comparatively, a urine steroid metabolomics result suggesting a high risk of adrenocortical carcinoma had a PPV of 34.6%.
A total of 106 patients (5.3%) met the criteria for all three measures, and the PPV for all three was 76.4%.
Using the criteria, 70 patients (3.5%) were classified as being at moderate risk of adrenocortical carcinoma and 1,841 (91.3%) at low risk, for a negative predictive value (NPV) of 99.7%.
“Use of radiation-free, noninvasive urine steroid metabolomics has a higher PPV than two standard imaging tests, and best performance was seen with the combination of all three tests,” the authors state.
Limit urine test to patients with larger tumors
They note that the use of the combined diagnostic strategy would have led to additional imaging in only 488 (24.2%) of the study’s 2,017 patients, compared with the 2,737 scans that were actually conducted before reaching a diagnostic decision.
“Implementation of urine steroid metabolomics in the routine diagnostic assessment of newly discovered adrenal masses could reduce the number of imaging procedures required to diagnose adrenocortical carcinoma and avoid unnecessary surgery of benign adrenal tumors, potentially yielding beneficial effects with respect to patient burden and health care costs,” they stress.
And regarding imaging parameters, “we also showed that using a cutoff of 20 HU for unenhanced CT tumor attenuation increases the accuracy of imaging characteristic assessment for exclusion of adrenocortical carcinoma, compared with the currently recommended cutoff of 10 HU, which has immediate implications for clinical practice,” they emphasize.
In an accompanying editorial, Adina F. Turcu, MD, of the division of metabolism, endocrinology, and diabetes, University of Michigan, Ann Arbor, and Axel K. Walch, MD, of the Helmholtz Zentrum München–German Research Centre for Environmental Health, agree. “The introduction of urine steroid metabolomics into routine clinical practice would provide major advantages,” they state.
However, they point out that, although the overall negative predictive value of the test was excellent, the specificity was weak.
“Thus, urine steroid metabolomics should be limited to patients who have adrenal nodules larger than 4 cm and have qualitative imaging characteristics suggestive of malignancy,” say Dr. Turcu and Dr. Walch.
The EURINE-ACT study results suggest this subgroup would represent roughly only 12% of all patients with adrenal incidentalomas, they add.
Issues that remain to be addressed with regard to the implementation of the screening strategy include how to best respond to patients who are classified as having intermediate or moderate risk of malignancy, and whether the diagnostic value of steroid metabolomics could be refined by adding analytes or parameters, the editorialists conclude.
The study was funded by the European Commission, U.K. Medical Research Council, Wellcome Trust, U.K. National Institute for Health Research, U.S. National Institutes of Health, the Claire Khan Trust Fund at University Hospitals Birmingham Charities, and the Mayo Clinic Foundation for Medical Education and Research.
A version of this article originally appeared on Medscape.com.















