User login
For MD-IQ use only
Dodging potholes from cancer care to hospice transitions
I’m often in the position of caring for patients after they’ve stopped active cancer treatments, but before they’ve made the decision to enroll in hospice. They remain under my care until they feel emotionally ready, or until their care needs have escalated to the point in which hospice is unavoidable.
Jenny, a mom in her 50s with metastatic pancreatic cancer, stopped coming to the clinic. She lived about 40 minutes away from the clinic and was no longer receiving treatment. The car rides were painful and difficult for her. I held weekly video visits with her for 2 months before she eventually went to hospice and passed away. Before she died, she shared with me her sadness that her oncologist – who had taken care of her for 3 years – had “washed his hands of [me].” She rarely heard from him after their final conversation in the clinic when he informed her that she was no longer a candidate for further therapy. The sense of abandonment Jenny described was visceral and devastating. With her permission, I let her oncology team know how she felt and they reached out to her just 1 week before her death. After she died, her husband told me how meaningful it had been for the whole family to hear from Jenny’s oncologist who told them that she had done everything possible to fight her cancer and that “no stone was left unturned.” Her husband felt this final conversation provided Jenny with the closure she needed to pass away peacefully.
Transitioning from active therapy to symptom management
Switching gears from an all-out pursuit of active therapy to focusing on cancer symptoms is often a scary transition for patients and their families. The transition is often viewed as a movement away from hope and optimism to “giving up the fight.” Whether you agree with the warrior language or not, many patients still describe their journey in these terms and thus, experience enrollment in hospice as a sense of having failed.
The sense of failure can be compounded by feelings of abandonment by oncology providers when they are referred without much guidance or continuity through the hospice enrollment process. Unfortunately, the consequences of suboptimal hospice transitions can be damaging, especially for the mental health and well-being of the patient and their surviving loved ones.
When managed poorly, hospice transitions can easily lead to patient and family harm, which is a claim supported by research. A qualitative study published in 2019 included 92 caregivers of patients with terminal cancer. The authors found three common pathways for end-of-life transitions – a frictionless transition in which the patient and family are well prepared in advance by their oncologist; a more turbulent transition in which patient and family had direct conversations with their oncologist about the incurability of the disease and the lack of efficacy of further treatments, but were given no guidance on prognosis; and a third type of transition marked by abrupt shifts toward end-of-life care occurring in extremis and typically in the hospital.
In the latter two groups, caregivers felt their loved ones died very quickly after stopping treatment, taking them by surprise and leaving them rushing to put end-of-life care plans in place without much support from their oncologists. In the last group, caregivers shared they received their first prognostic information from the hospital or ICU doctor caring for their actively dying loved one, leaving them with a sense of anger and betrayal toward their oncologist for allowing them to be so ill-prepared.
A Japanese survey published in 2018 in The Oncologist of families of cancer patients who had passed away under hospice care over a 2-year period (2012-2014), found that about one-quarter felt abandoned by oncologists. Several factors that were associated with feeling either more or less abandonment. Spouses of patients, patients aged less than 60 years, and patients whose oncologists informed them that there was “nothing more to do” felt more abandoned by oncologists; whereas families for whom the oncologist provided reassurance about the trajectory of care, recommended hospice, and engaged with a palliative care team felt less abandoned by oncologists. Families who felt more abandoned had higher levels of depression and grief when measured with standardized instruments.
‘Don’t just put in the hospice order and walk away’
Fortunately, there are a few low-resource interventions that can improve the quality of care-to-hospice transitions and prevent the sense of abandonment felt by many patients and families.
First, don’t just put in the hospice order and walk away. Designate a staffer in your office to contact hospice directly, ensure all medical records are faxed and received, and update the patient and family on this progress throughout the transition. Taking care of details like these ensures the patient enrolls in hospice in a timely manner and reduces the chance the patient, who is likely to be quite sick at this point, will end up in the hospital despite your best efforts to get hospice involved.
Make sure the patient and family understand that you are still their oncologist and still available to them. If they want to continue care with you, have them name you as the “non–hospice-attending physician” so that you can continue to bill for telemedicine and office visits using the terminal diagnosis (with a billing modifier). This does not mean that you will be expected to manage the patient’s hospice problem list or respond to hospice nurse calls at 2 a.m. – the hospice doctor will still do this. It just ensures that patients do not receive a bill if you continue to see them.
If ongoing office or video visits are too much for the patient and family, consider assigning a member of your team to call the patient and family on a weekly basis to check in and offer support. A small 2018 pilot study aimed at improving communication found that when caregivers of advanced cancer patients transitioning to hospice received weekly supportive phone calls by a member of their oncology team (typically a nurse or nurse practitioner), they felt emotionally supported, had good continuity of care throughout the hospice enrollment, and appreciated the ability to have closure with their oncology team. In other words, a sense of abandonment was prevented and the patient-provider relationship was actually deepened through the transition.
These suggestions are not rocket science – they are simple, obvious ways to try to restore patient-centeredness to a transition that for providers can seem routine, but for patients and families is often the first time they have confronted the reality that death is approaching. That reality is terrifying and overwhelming. Patients and caregivers need our support more during hospice transitions than at any other point during their cancer journey – except perhaps at diagnosis.
As with Jenny, my patient who felt abandoned, all it took was a single call by her oncology team to restore the trust and heal the sense of feeling forsaken by the people who cared for her for years. Sometimes, even just one more phone call can feel like a lot to a chronically overburdened provider – but what a difference a simple call can make.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I’m often in the position of caring for patients after they’ve stopped active cancer treatments, but before they’ve made the decision to enroll in hospice. They remain under my care until they feel emotionally ready, or until their care needs have escalated to the point in which hospice is unavoidable.
Jenny, a mom in her 50s with metastatic pancreatic cancer, stopped coming to the clinic. She lived about 40 minutes away from the clinic and was no longer receiving treatment. The car rides were painful and difficult for her. I held weekly video visits with her for 2 months before she eventually went to hospice and passed away. Before she died, she shared with me her sadness that her oncologist – who had taken care of her for 3 years – had “washed his hands of [me].” She rarely heard from him after their final conversation in the clinic when he informed her that she was no longer a candidate for further therapy. The sense of abandonment Jenny described was visceral and devastating. With her permission, I let her oncology team know how she felt and they reached out to her just 1 week before her death. After she died, her husband told me how meaningful it had been for the whole family to hear from Jenny’s oncologist who told them that she had done everything possible to fight her cancer and that “no stone was left unturned.” Her husband felt this final conversation provided Jenny with the closure she needed to pass away peacefully.
Transitioning from active therapy to symptom management
Switching gears from an all-out pursuit of active therapy to focusing on cancer symptoms is often a scary transition for patients and their families. The transition is often viewed as a movement away from hope and optimism to “giving up the fight.” Whether you agree with the warrior language or not, many patients still describe their journey in these terms and thus, experience enrollment in hospice as a sense of having failed.
The sense of failure can be compounded by feelings of abandonment by oncology providers when they are referred without much guidance or continuity through the hospice enrollment process. Unfortunately, the consequences of suboptimal hospice transitions can be damaging, especially for the mental health and well-being of the patient and their surviving loved ones.
When managed poorly, hospice transitions can easily lead to patient and family harm, which is a claim supported by research. A qualitative study published in 2019 included 92 caregivers of patients with terminal cancer. The authors found three common pathways for end-of-life transitions – a frictionless transition in which the patient and family are well prepared in advance by their oncologist; a more turbulent transition in which patient and family had direct conversations with their oncologist about the incurability of the disease and the lack of efficacy of further treatments, but were given no guidance on prognosis; and a third type of transition marked by abrupt shifts toward end-of-life care occurring in extremis and typically in the hospital.
In the latter two groups, caregivers felt their loved ones died very quickly after stopping treatment, taking them by surprise and leaving them rushing to put end-of-life care plans in place without much support from their oncologists. In the last group, caregivers shared they received their first prognostic information from the hospital or ICU doctor caring for their actively dying loved one, leaving them with a sense of anger and betrayal toward their oncologist for allowing them to be so ill-prepared.
A Japanese survey published in 2018 in The Oncologist of families of cancer patients who had passed away under hospice care over a 2-year period (2012-2014), found that about one-quarter felt abandoned by oncologists. Several factors that were associated with feeling either more or less abandonment. Spouses of patients, patients aged less than 60 years, and patients whose oncologists informed them that there was “nothing more to do” felt more abandoned by oncologists; whereas families for whom the oncologist provided reassurance about the trajectory of care, recommended hospice, and engaged with a palliative care team felt less abandoned by oncologists. Families who felt more abandoned had higher levels of depression and grief when measured with standardized instruments.
‘Don’t just put in the hospice order and walk away’
Fortunately, there are a few low-resource interventions that can improve the quality of care-to-hospice transitions and prevent the sense of abandonment felt by many patients and families.
First, don’t just put in the hospice order and walk away. Designate a staffer in your office to contact hospice directly, ensure all medical records are faxed and received, and update the patient and family on this progress throughout the transition. Taking care of details like these ensures the patient enrolls in hospice in a timely manner and reduces the chance the patient, who is likely to be quite sick at this point, will end up in the hospital despite your best efforts to get hospice involved.
Make sure the patient and family understand that you are still their oncologist and still available to them. If they want to continue care with you, have them name you as the “non–hospice-attending physician” so that you can continue to bill for telemedicine and office visits using the terminal diagnosis (with a billing modifier). This does not mean that you will be expected to manage the patient’s hospice problem list or respond to hospice nurse calls at 2 a.m. – the hospice doctor will still do this. It just ensures that patients do not receive a bill if you continue to see them.
If ongoing office or video visits are too much for the patient and family, consider assigning a member of your team to call the patient and family on a weekly basis to check in and offer support. A small 2018 pilot study aimed at improving communication found that when caregivers of advanced cancer patients transitioning to hospice received weekly supportive phone calls by a member of their oncology team (typically a nurse or nurse practitioner), they felt emotionally supported, had good continuity of care throughout the hospice enrollment, and appreciated the ability to have closure with their oncology team. In other words, a sense of abandonment was prevented and the patient-provider relationship was actually deepened through the transition.
These suggestions are not rocket science – they are simple, obvious ways to try to restore patient-centeredness to a transition that for providers can seem routine, but for patients and families is often the first time they have confronted the reality that death is approaching. That reality is terrifying and overwhelming. Patients and caregivers need our support more during hospice transitions than at any other point during their cancer journey – except perhaps at diagnosis.
As with Jenny, my patient who felt abandoned, all it took was a single call by her oncology team to restore the trust and heal the sense of feeling forsaken by the people who cared for her for years. Sometimes, even just one more phone call can feel like a lot to a chronically overburdened provider – but what a difference a simple call can make.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I’m often in the position of caring for patients after they’ve stopped active cancer treatments, but before they’ve made the decision to enroll in hospice. They remain under my care until they feel emotionally ready, or until their care needs have escalated to the point in which hospice is unavoidable.
Jenny, a mom in her 50s with metastatic pancreatic cancer, stopped coming to the clinic. She lived about 40 minutes away from the clinic and was no longer receiving treatment. The car rides were painful and difficult for her. I held weekly video visits with her for 2 months before she eventually went to hospice and passed away. Before she died, she shared with me her sadness that her oncologist – who had taken care of her for 3 years – had “washed his hands of [me].” She rarely heard from him after their final conversation in the clinic when he informed her that she was no longer a candidate for further therapy. The sense of abandonment Jenny described was visceral and devastating. With her permission, I let her oncology team know how she felt and they reached out to her just 1 week before her death. After she died, her husband told me how meaningful it had been for the whole family to hear from Jenny’s oncologist who told them that she had done everything possible to fight her cancer and that “no stone was left unturned.” Her husband felt this final conversation provided Jenny with the closure she needed to pass away peacefully.
Transitioning from active therapy to symptom management
Switching gears from an all-out pursuit of active therapy to focusing on cancer symptoms is often a scary transition for patients and their families. The transition is often viewed as a movement away from hope and optimism to “giving up the fight.” Whether you agree with the warrior language or not, many patients still describe their journey in these terms and thus, experience enrollment in hospice as a sense of having failed.
The sense of failure can be compounded by feelings of abandonment by oncology providers when they are referred without much guidance or continuity through the hospice enrollment process. Unfortunately, the consequences of suboptimal hospice transitions can be damaging, especially for the mental health and well-being of the patient and their surviving loved ones.
When managed poorly, hospice transitions can easily lead to patient and family harm, which is a claim supported by research. A qualitative study published in 2019 included 92 caregivers of patients with terminal cancer. The authors found three common pathways for end-of-life transitions – a frictionless transition in which the patient and family are well prepared in advance by their oncologist; a more turbulent transition in which patient and family had direct conversations with their oncologist about the incurability of the disease and the lack of efficacy of further treatments, but were given no guidance on prognosis; and a third type of transition marked by abrupt shifts toward end-of-life care occurring in extremis and typically in the hospital.
In the latter two groups, caregivers felt their loved ones died very quickly after stopping treatment, taking them by surprise and leaving them rushing to put end-of-life care plans in place without much support from their oncologists. In the last group, caregivers shared they received their first prognostic information from the hospital or ICU doctor caring for their actively dying loved one, leaving them with a sense of anger and betrayal toward their oncologist for allowing them to be so ill-prepared.
A Japanese survey published in 2018 in The Oncologist of families of cancer patients who had passed away under hospice care over a 2-year period (2012-2014), found that about one-quarter felt abandoned by oncologists. Several factors that were associated with feeling either more or less abandonment. Spouses of patients, patients aged less than 60 years, and patients whose oncologists informed them that there was “nothing more to do” felt more abandoned by oncologists; whereas families for whom the oncologist provided reassurance about the trajectory of care, recommended hospice, and engaged with a palliative care team felt less abandoned by oncologists. Families who felt more abandoned had higher levels of depression and grief when measured with standardized instruments.
‘Don’t just put in the hospice order and walk away’
Fortunately, there are a few low-resource interventions that can improve the quality of care-to-hospice transitions and prevent the sense of abandonment felt by many patients and families.
First, don’t just put in the hospice order and walk away. Designate a staffer in your office to contact hospice directly, ensure all medical records are faxed and received, and update the patient and family on this progress throughout the transition. Taking care of details like these ensures the patient enrolls in hospice in a timely manner and reduces the chance the patient, who is likely to be quite sick at this point, will end up in the hospital despite your best efforts to get hospice involved.
Make sure the patient and family understand that you are still their oncologist and still available to them. If they want to continue care with you, have them name you as the “non–hospice-attending physician” so that you can continue to bill for telemedicine and office visits using the terminal diagnosis (with a billing modifier). This does not mean that you will be expected to manage the patient’s hospice problem list or respond to hospice nurse calls at 2 a.m. – the hospice doctor will still do this. It just ensures that patients do not receive a bill if you continue to see them.
If ongoing office or video visits are too much for the patient and family, consider assigning a member of your team to call the patient and family on a weekly basis to check in and offer support. A small 2018 pilot study aimed at improving communication found that when caregivers of advanced cancer patients transitioning to hospice received weekly supportive phone calls by a member of their oncology team (typically a nurse or nurse practitioner), they felt emotionally supported, had good continuity of care throughout the hospice enrollment, and appreciated the ability to have closure with their oncology team. In other words, a sense of abandonment was prevented and the patient-provider relationship was actually deepened through the transition.
These suggestions are not rocket science – they are simple, obvious ways to try to restore patient-centeredness to a transition that for providers can seem routine, but for patients and families is often the first time they have confronted the reality that death is approaching. That reality is terrifying and overwhelming. Patients and caregivers need our support more during hospice transitions than at any other point during their cancer journey – except perhaps at diagnosis.
As with Jenny, my patient who felt abandoned, all it took was a single call by her oncology team to restore the trust and heal the sense of feeling forsaken by the people who cared for her for years. Sometimes, even just one more phone call can feel like a lot to a chronically overburdened provider – but what a difference a simple call can make.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
Pick your sunscreen carefully: 75% don’t pass muster
Just in time for Memorial Day outings, a new report on sunscreens is out.
The news isn’t all sunny. , a nonprofit research and advocacy group that just issued its 16th annual Guide to Sunscreens.
In response, dermatologists, including the president of the American Academy of Dermatology, say that although some concerns have been raised about the safety of some sunscreen ingredients, sunscreens themselves remain an important tool in the fight against skin cancer. According to the Skin Cancer Foundation, 1 in 5 Americans will get skin cancer by age 70. Melanoma, the most deadly, has a 5-year survival rate of 99% if caught early.
2022 report
Overall, the Environmental Working Group found that about 1 in 4 sunscreens, or about 500 products, met their standards for providing adequate sun protection and avoiding ingredients linked to known health harms. Products meant for babies and children did slightly better, with about 1 in 3 meeting the standards. The group evaluated mineral sunscreens, also called physical sunscreens, and non-mineral sunscreens, also called chemical sunscreens. Mineral sunscreens contain zinc oxide or titanium dioxide and sit on the skin to deflect the sun’s rays. Chemical sunscreens, with ingredients such as oxybenzone or avobenzone, are partially absorbed into the skin.
Among the group’s concerns:
- The use of oxybenzone in the non-mineral sunscreens. About 30% of the non-mineral sunscreens have it, says Carla Burns, senior director for cosmetic science for the Environmental Working Group. Oxybenzone is a potential hormone disrupter and a skin sensitizer that may harm children and adults, she says. Some progress has been made, as the group found oxybenzone in 66% of the non-mineral sunscreens it reviewed in 2019. (The FDA is seeking more information on oxybenzone and many other sunscreen ingredients.)
- Contamination of sunscreens with benzene, which has been linked to leukemia and other blood disorders, according to the National Cancer Institute. But industry experts stress that that chemical is found in trace amounts in personal care products and does not pose a safety concern. “Benzene is a chemical that is ubiquitous in the environment and not an intentionally added ingredient in personal care products. People worldwide are exposed daily to benzene from indoor and outdoor sources, including air, drinking water, and food and beverages,” the Personal Care Products Council, an industry group, said in a statement.
- Protection from ultraviolet A (UVA) rays is often inadequate, according to research published last year by the Environmental Working Group.
Products on the ‘best’ list
The Environmental Working Group found that 282 recreational sunscreens met its criteria. Among them:
- Coral Safe Sunscreen Lotion, SPF 30
- Neutrogena Sheer Zinc Mineral Sunscreen Lotion, SPF 30
- Mad Hippie Facial Sunscreen Lotion, SPF 30+
The group chose 86 non-mineral sunscreens as better options, including:
- Alba Botanica Hawaiian Sunscreen Lotion, Aloe Vera, SPF 30
- Banana Boat Sport Ultra Sunscreen Stick, SPF 50+
- Black Girl Sunscreen Melanin Boosting Moisturizing Sunscreen Lotion, SPF 30
And 70 sunscreens made the kids’ best list, including:
- True Baby Everyday Play Sunscreen Lotion, SPF 30+
- Sun Biologic Kids’ Sunscreen Stick, SPF 30+
- Kiss My Face Organic Kids’ Defense Sunscreen Lotion, SPF 30
Industry response, FDA actions
In a statement, Alexandra Kowcz, chief scientist at the Personal Care Products Council, pointed out that “as part of a daily safe-sun regimen, sunscreen products help prevent sunburn and reduce skin cancer risk. It is unfortunate that as Americans spend more time outdoors, the Environmental Working Group’s (EWG) 2022 Guide to Sunscreens resorts to fear-mongering with misleading information that could keep consumers from using sunscreens altogether.”
The FDA has asked for more information about certain ingredients to further evaluate products, she says, and industry is working with the agency. The FDA says it is attempting to improve the quality, safety and effectiveness of over-the-counter sunscreen products. In September, 2021, the FDA issued a proposal for regulating OTC sunscreen products, as required under the CARES (Coronavirus Aid, Relief and Economic Security) Act. The effective date for the final order can’t be earlier than September 2022, the CARES Act says.
Dermatologists weigh in
“Every time something like this gets published, my patients come in hysterical,” says Michele Green, MD, a New York City dermatologist who reviewed the report for WebMD. She acknowledges that more research is needed on some sunscreen ingredients. “We really do not know the long-term consequence of oxybenzone,” she says.
Her advice: If her patients have melasma (a skin condition with brown patches on the face), she advises them to use both a chemical and a mineral sunscreen. “I don’t tell my patients in general not to use the chemical [sunscreens].”
For children, she says, the mineral sunscreens may be preferred. On her own children, who are teens, she uses the mineral sunscreens, due to possible concern about hormone disruption.
In a statement, Mark D. Kaufmann, MD, president of the American Academy of Dermatology, says that “sunscreen is an important part of a comprehensive sun protection strategy.”
Besides a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher for exposed skin, the academy recommends seeking shade and wearing sun-protective clothing to reduce skin cancer risk.
A version of this article first appeared on WebMD.com.
Just in time for Memorial Day outings, a new report on sunscreens is out.
The news isn’t all sunny. , a nonprofit research and advocacy group that just issued its 16th annual Guide to Sunscreens.
In response, dermatologists, including the president of the American Academy of Dermatology, say that although some concerns have been raised about the safety of some sunscreen ingredients, sunscreens themselves remain an important tool in the fight against skin cancer. According to the Skin Cancer Foundation, 1 in 5 Americans will get skin cancer by age 70. Melanoma, the most deadly, has a 5-year survival rate of 99% if caught early.
2022 report
Overall, the Environmental Working Group found that about 1 in 4 sunscreens, or about 500 products, met their standards for providing adequate sun protection and avoiding ingredients linked to known health harms. Products meant for babies and children did slightly better, with about 1 in 3 meeting the standards. The group evaluated mineral sunscreens, also called physical sunscreens, and non-mineral sunscreens, also called chemical sunscreens. Mineral sunscreens contain zinc oxide or titanium dioxide and sit on the skin to deflect the sun’s rays. Chemical sunscreens, with ingredients such as oxybenzone or avobenzone, are partially absorbed into the skin.
Among the group’s concerns:
- The use of oxybenzone in the non-mineral sunscreens. About 30% of the non-mineral sunscreens have it, says Carla Burns, senior director for cosmetic science for the Environmental Working Group. Oxybenzone is a potential hormone disrupter and a skin sensitizer that may harm children and adults, she says. Some progress has been made, as the group found oxybenzone in 66% of the non-mineral sunscreens it reviewed in 2019. (The FDA is seeking more information on oxybenzone and many other sunscreen ingredients.)
- Contamination of sunscreens with benzene, which has been linked to leukemia and other blood disorders, according to the National Cancer Institute. But industry experts stress that that chemical is found in trace amounts in personal care products and does not pose a safety concern. “Benzene is a chemical that is ubiquitous in the environment and not an intentionally added ingredient in personal care products. People worldwide are exposed daily to benzene from indoor and outdoor sources, including air, drinking water, and food and beverages,” the Personal Care Products Council, an industry group, said in a statement.
- Protection from ultraviolet A (UVA) rays is often inadequate, according to research published last year by the Environmental Working Group.
Products on the ‘best’ list
The Environmental Working Group found that 282 recreational sunscreens met its criteria. Among them:
- Coral Safe Sunscreen Lotion, SPF 30
- Neutrogena Sheer Zinc Mineral Sunscreen Lotion, SPF 30
- Mad Hippie Facial Sunscreen Lotion, SPF 30+
The group chose 86 non-mineral sunscreens as better options, including:
- Alba Botanica Hawaiian Sunscreen Lotion, Aloe Vera, SPF 30
- Banana Boat Sport Ultra Sunscreen Stick, SPF 50+
- Black Girl Sunscreen Melanin Boosting Moisturizing Sunscreen Lotion, SPF 30
And 70 sunscreens made the kids’ best list, including:
- True Baby Everyday Play Sunscreen Lotion, SPF 30+
- Sun Biologic Kids’ Sunscreen Stick, SPF 30+
- Kiss My Face Organic Kids’ Defense Sunscreen Lotion, SPF 30
Industry response, FDA actions
In a statement, Alexandra Kowcz, chief scientist at the Personal Care Products Council, pointed out that “as part of a daily safe-sun regimen, sunscreen products help prevent sunburn and reduce skin cancer risk. It is unfortunate that as Americans spend more time outdoors, the Environmental Working Group’s (EWG) 2022 Guide to Sunscreens resorts to fear-mongering with misleading information that could keep consumers from using sunscreens altogether.”
The FDA has asked for more information about certain ingredients to further evaluate products, she says, and industry is working with the agency. The FDA says it is attempting to improve the quality, safety and effectiveness of over-the-counter sunscreen products. In September, 2021, the FDA issued a proposal for regulating OTC sunscreen products, as required under the CARES (Coronavirus Aid, Relief and Economic Security) Act. The effective date for the final order can’t be earlier than September 2022, the CARES Act says.
Dermatologists weigh in
“Every time something like this gets published, my patients come in hysterical,” says Michele Green, MD, a New York City dermatologist who reviewed the report for WebMD. She acknowledges that more research is needed on some sunscreen ingredients. “We really do not know the long-term consequence of oxybenzone,” she says.
Her advice: If her patients have melasma (a skin condition with brown patches on the face), she advises them to use both a chemical and a mineral sunscreen. “I don’t tell my patients in general not to use the chemical [sunscreens].”
For children, she says, the mineral sunscreens may be preferred. On her own children, who are teens, she uses the mineral sunscreens, due to possible concern about hormone disruption.
In a statement, Mark D. Kaufmann, MD, president of the American Academy of Dermatology, says that “sunscreen is an important part of a comprehensive sun protection strategy.”
Besides a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher for exposed skin, the academy recommends seeking shade and wearing sun-protective clothing to reduce skin cancer risk.
A version of this article first appeared on WebMD.com.
Just in time for Memorial Day outings, a new report on sunscreens is out.
The news isn’t all sunny. , a nonprofit research and advocacy group that just issued its 16th annual Guide to Sunscreens.
In response, dermatologists, including the president of the American Academy of Dermatology, say that although some concerns have been raised about the safety of some sunscreen ingredients, sunscreens themselves remain an important tool in the fight against skin cancer. According to the Skin Cancer Foundation, 1 in 5 Americans will get skin cancer by age 70. Melanoma, the most deadly, has a 5-year survival rate of 99% if caught early.
2022 report
Overall, the Environmental Working Group found that about 1 in 4 sunscreens, or about 500 products, met their standards for providing adequate sun protection and avoiding ingredients linked to known health harms. Products meant for babies and children did slightly better, with about 1 in 3 meeting the standards. The group evaluated mineral sunscreens, also called physical sunscreens, and non-mineral sunscreens, also called chemical sunscreens. Mineral sunscreens contain zinc oxide or titanium dioxide and sit on the skin to deflect the sun’s rays. Chemical sunscreens, with ingredients such as oxybenzone or avobenzone, are partially absorbed into the skin.
Among the group’s concerns:
- The use of oxybenzone in the non-mineral sunscreens. About 30% of the non-mineral sunscreens have it, says Carla Burns, senior director for cosmetic science for the Environmental Working Group. Oxybenzone is a potential hormone disrupter and a skin sensitizer that may harm children and adults, she says. Some progress has been made, as the group found oxybenzone in 66% of the non-mineral sunscreens it reviewed in 2019. (The FDA is seeking more information on oxybenzone and many other sunscreen ingredients.)
- Contamination of sunscreens with benzene, which has been linked to leukemia and other blood disorders, according to the National Cancer Institute. But industry experts stress that that chemical is found in trace amounts in personal care products and does not pose a safety concern. “Benzene is a chemical that is ubiquitous in the environment and not an intentionally added ingredient in personal care products. People worldwide are exposed daily to benzene from indoor and outdoor sources, including air, drinking water, and food and beverages,” the Personal Care Products Council, an industry group, said in a statement.
- Protection from ultraviolet A (UVA) rays is often inadequate, according to research published last year by the Environmental Working Group.
Products on the ‘best’ list
The Environmental Working Group found that 282 recreational sunscreens met its criteria. Among them:
- Coral Safe Sunscreen Lotion, SPF 30
- Neutrogena Sheer Zinc Mineral Sunscreen Lotion, SPF 30
- Mad Hippie Facial Sunscreen Lotion, SPF 30+
The group chose 86 non-mineral sunscreens as better options, including:
- Alba Botanica Hawaiian Sunscreen Lotion, Aloe Vera, SPF 30
- Banana Boat Sport Ultra Sunscreen Stick, SPF 50+
- Black Girl Sunscreen Melanin Boosting Moisturizing Sunscreen Lotion, SPF 30
And 70 sunscreens made the kids’ best list, including:
- True Baby Everyday Play Sunscreen Lotion, SPF 30+
- Sun Biologic Kids’ Sunscreen Stick, SPF 30+
- Kiss My Face Organic Kids’ Defense Sunscreen Lotion, SPF 30
Industry response, FDA actions
In a statement, Alexandra Kowcz, chief scientist at the Personal Care Products Council, pointed out that “as part of a daily safe-sun regimen, sunscreen products help prevent sunburn and reduce skin cancer risk. It is unfortunate that as Americans spend more time outdoors, the Environmental Working Group’s (EWG) 2022 Guide to Sunscreens resorts to fear-mongering with misleading information that could keep consumers from using sunscreens altogether.”
The FDA has asked for more information about certain ingredients to further evaluate products, she says, and industry is working with the agency. The FDA says it is attempting to improve the quality, safety and effectiveness of over-the-counter sunscreen products. In September, 2021, the FDA issued a proposal for regulating OTC sunscreen products, as required under the CARES (Coronavirus Aid, Relief and Economic Security) Act. The effective date for the final order can’t be earlier than September 2022, the CARES Act says.
Dermatologists weigh in
“Every time something like this gets published, my patients come in hysterical,” says Michele Green, MD, a New York City dermatologist who reviewed the report for WebMD. She acknowledges that more research is needed on some sunscreen ingredients. “We really do not know the long-term consequence of oxybenzone,” she says.
Her advice: If her patients have melasma (a skin condition with brown patches on the face), she advises them to use both a chemical and a mineral sunscreen. “I don’t tell my patients in general not to use the chemical [sunscreens].”
For children, she says, the mineral sunscreens may be preferred. On her own children, who are teens, she uses the mineral sunscreens, due to possible concern about hormone disruption.
In a statement, Mark D. Kaufmann, MD, president of the American Academy of Dermatology, says that “sunscreen is an important part of a comprehensive sun protection strategy.”
Besides a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher for exposed skin, the academy recommends seeking shade and wearing sun-protective clothing to reduce skin cancer risk.
A version of this article first appeared on WebMD.com.
New toolkit offers help for climate change anxiety
These strategies include volunteering, building a community, discussing emotions with others, practicing mindfulness, and seeking therapy.
The toolkit, which was developed by nursing experts at the University of British Columbia in Vancouver, also offers reflection questions and a film with diverse voices for people to examine their values, emotions, and behaviors in relation to the environment.
“Many people have a hard time understanding the relationship between climate change and mental health and are experiencing high levels of stress about climate change,” Natania Abebe, MSN/MPH, RN, a registered nurse and graduate student at UBC who developed the toolkit, told this news organization.
“Youth, in particular, appear to have higher levels of consciousness regarding climate change because they’re the ones who are going to inherit the planet,” she said. “A big part of why they have mental health issues is that they feel trapped in sociopolitical structures that they didn’t agree to and didn’t necessarily create.”
The toolkit was published online on April 20.
Empowering agents for change
Ms. Abebe was inspired to create the toolkit after giving guest lectures on climate change and mental health as part of UBC’s Nursing 290 course. Her faculty advisor, Raluca Radu, MSN, a lecturer in the School of Nursing at UBC, developed the course in 2020 to teach students about the broad impacts of climate change on communities.
As the course has grown during the past 2 years, Ms. Abebe wanted to create a coping framework and engaging film for health educators to use with students, as well as for everyday people.
The toolkit includes contributions from three Canadian climate change experts, as well as six students from different backgrounds who have taken the course.
“I wanted to center the voices of youth and empower them to think they can be agents for change,” Ms. Abebe said. “I also wanted to highlight diverse voices and take a collaborative approach because climate change is such a big problem that we have to come together to address it.”
Ms. Abebe and Ms. Radu also noticed an increase in climate anxiety in recent years because of the pandemic, worldwide food and energy shortages, and extreme weather events that hit close to home, such as wildfires and floods in British Columbia.
“With the pandemic, people have been spending more time online and thinking about our world at large,” Ms. Abebe said. “At the same time that they’re thinking about it, climate change events are happening simultaneously – not in the future, but right now.”
Economic, social, and political shifts during the past 2 years have also prompted people to question standard practices and institutions, which has created an opportunity to discuss change, Ms. Radu told this news organization.
“It’s a pivotal time to question our values and highly consumerist society,” she said. “We’re at a point in time where, if we don’t take action, the planetary health will be in an irreversible state, and we won’t be able to turn back time and make changes.”
Our psyches and nature
The toolkit includes three main sections that feature video clips and reflective questions around eco-anxiety, eco-paralysis, and ecological grief.
In the first section, eco-anxiety is defined as a “chronic fear of environmental doom,” which could include anxiousness around the likelihood of a severe weather event because of ongoing news coverage and social media. The reflective questions prompt readers to discuss eco-anxiety in their life, work through their emotions, understand their beliefs and values, and determine how to use them to address climate change anxiety.
The second section defines eco-paralysis as the powerlessness that people may feel when they don’t believe they can do anything meaningful on an individual level to address climate change. Paralysis can look like apathy, complacency, or disengagement. The questions prompt readers to observe how paralysis may show up in their lives, explore the tension between individual versus collective responsibility, and consider ways to address their sense of helplessness about climate change.
In the third section, ecological grief centers around “experienced or anticipated ecological losses,” which could include the loss of species, ecosystems, and landscapes because of short- or long-term environmental change. The questions prompt readers to explore their feelings, beliefs, and values and feel empowered to address their ecological grief over climate change.
The toolkit also includes recommendations for books, journal articles, websites, podcasts, and meditations around mental health and climate change, as well as ways to get involved with others. For instance, health care practitioners can register with PaRx, a program in British Columbia that allows providers to prescribe time in nature to improve a client’s health. The program is being adopted across Canada, and people with a prescription can visit local and national parks, historic sites, and marine conservation areas for free.
“This is about recognizing that there is a connection between our psyches and nature, and by talking about it, we can name what we’re feeling,” Ms. Abebe said. “We can take action not only to handle our emotions, but also to live kinder and more sustainable lifestyles.”
Future work will need to focus on population-level approaches to climate change and mental health as well, including policy and financial support to address environmental changes directly.
“We need to start thinking beyond individualized approaches and focus on how to create supportive and resilient communities to respond to climate change,” Kiffer Card, PhD, executive director of the Mental Health and Climate Change Alliance and an assistant professor of health sciences at Simon Fraser University, Burnaby, B.C., told this news organization.
Dr. Card, who wasn’t involved in developing the toolkit, has researched recent trends around climate change anxiety in Canada and fielded questions from health care practitioners and mental health professionals who are looking for ways to help their patients.
“Communities need to be ready to stand up and respond to acute emergency disasters, and government leaders need to take this seriously,” he said. “Those who are experiencing climate anxiety now are the canaries in the coal mine for the severe weather events and consequences to come.”
The toolkit was developed with funding from the Alma Mater Society of the University of British Columbia, Vancouver. Ms. Abebe, Ms. Radu, and Dr. Card reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
These strategies include volunteering, building a community, discussing emotions with others, practicing mindfulness, and seeking therapy.
The toolkit, which was developed by nursing experts at the University of British Columbia in Vancouver, also offers reflection questions and a film with diverse voices for people to examine their values, emotions, and behaviors in relation to the environment.
“Many people have a hard time understanding the relationship between climate change and mental health and are experiencing high levels of stress about climate change,” Natania Abebe, MSN/MPH, RN, a registered nurse and graduate student at UBC who developed the toolkit, told this news organization.
“Youth, in particular, appear to have higher levels of consciousness regarding climate change because they’re the ones who are going to inherit the planet,” she said. “A big part of why they have mental health issues is that they feel trapped in sociopolitical structures that they didn’t agree to and didn’t necessarily create.”
The toolkit was published online on April 20.
Empowering agents for change
Ms. Abebe was inspired to create the toolkit after giving guest lectures on climate change and mental health as part of UBC’s Nursing 290 course. Her faculty advisor, Raluca Radu, MSN, a lecturer in the School of Nursing at UBC, developed the course in 2020 to teach students about the broad impacts of climate change on communities.
As the course has grown during the past 2 years, Ms. Abebe wanted to create a coping framework and engaging film for health educators to use with students, as well as for everyday people.
The toolkit includes contributions from three Canadian climate change experts, as well as six students from different backgrounds who have taken the course.
“I wanted to center the voices of youth and empower them to think they can be agents for change,” Ms. Abebe said. “I also wanted to highlight diverse voices and take a collaborative approach because climate change is such a big problem that we have to come together to address it.”
Ms. Abebe and Ms. Radu also noticed an increase in climate anxiety in recent years because of the pandemic, worldwide food and energy shortages, and extreme weather events that hit close to home, such as wildfires and floods in British Columbia.
“With the pandemic, people have been spending more time online and thinking about our world at large,” Ms. Abebe said. “At the same time that they’re thinking about it, climate change events are happening simultaneously – not in the future, but right now.”
Economic, social, and political shifts during the past 2 years have also prompted people to question standard practices and institutions, which has created an opportunity to discuss change, Ms. Radu told this news organization.
“It’s a pivotal time to question our values and highly consumerist society,” she said. “We’re at a point in time where, if we don’t take action, the planetary health will be in an irreversible state, and we won’t be able to turn back time and make changes.”
Our psyches and nature
The toolkit includes three main sections that feature video clips and reflective questions around eco-anxiety, eco-paralysis, and ecological grief.
In the first section, eco-anxiety is defined as a “chronic fear of environmental doom,” which could include anxiousness around the likelihood of a severe weather event because of ongoing news coverage and social media. The reflective questions prompt readers to discuss eco-anxiety in their life, work through their emotions, understand their beliefs and values, and determine how to use them to address climate change anxiety.
The second section defines eco-paralysis as the powerlessness that people may feel when they don’t believe they can do anything meaningful on an individual level to address climate change. Paralysis can look like apathy, complacency, or disengagement. The questions prompt readers to observe how paralysis may show up in their lives, explore the tension between individual versus collective responsibility, and consider ways to address their sense of helplessness about climate change.
In the third section, ecological grief centers around “experienced or anticipated ecological losses,” which could include the loss of species, ecosystems, and landscapes because of short- or long-term environmental change. The questions prompt readers to explore their feelings, beliefs, and values and feel empowered to address their ecological grief over climate change.
The toolkit also includes recommendations for books, journal articles, websites, podcasts, and meditations around mental health and climate change, as well as ways to get involved with others. For instance, health care practitioners can register with PaRx, a program in British Columbia that allows providers to prescribe time in nature to improve a client’s health. The program is being adopted across Canada, and people with a prescription can visit local and national parks, historic sites, and marine conservation areas for free.
“This is about recognizing that there is a connection between our psyches and nature, and by talking about it, we can name what we’re feeling,” Ms. Abebe said. “We can take action not only to handle our emotions, but also to live kinder and more sustainable lifestyles.”
Future work will need to focus on population-level approaches to climate change and mental health as well, including policy and financial support to address environmental changes directly.
“We need to start thinking beyond individualized approaches and focus on how to create supportive and resilient communities to respond to climate change,” Kiffer Card, PhD, executive director of the Mental Health and Climate Change Alliance and an assistant professor of health sciences at Simon Fraser University, Burnaby, B.C., told this news organization.
Dr. Card, who wasn’t involved in developing the toolkit, has researched recent trends around climate change anxiety in Canada and fielded questions from health care practitioners and mental health professionals who are looking for ways to help their patients.
“Communities need to be ready to stand up and respond to acute emergency disasters, and government leaders need to take this seriously,” he said. “Those who are experiencing climate anxiety now are the canaries in the coal mine for the severe weather events and consequences to come.”
The toolkit was developed with funding from the Alma Mater Society of the University of British Columbia, Vancouver. Ms. Abebe, Ms. Radu, and Dr. Card reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
These strategies include volunteering, building a community, discussing emotions with others, practicing mindfulness, and seeking therapy.
The toolkit, which was developed by nursing experts at the University of British Columbia in Vancouver, also offers reflection questions and a film with diverse voices for people to examine their values, emotions, and behaviors in relation to the environment.
“Many people have a hard time understanding the relationship between climate change and mental health and are experiencing high levels of stress about climate change,” Natania Abebe, MSN/MPH, RN, a registered nurse and graduate student at UBC who developed the toolkit, told this news organization.
“Youth, in particular, appear to have higher levels of consciousness regarding climate change because they’re the ones who are going to inherit the planet,” she said. “A big part of why they have mental health issues is that they feel trapped in sociopolitical structures that they didn’t agree to and didn’t necessarily create.”
The toolkit was published online on April 20.
Empowering agents for change
Ms. Abebe was inspired to create the toolkit after giving guest lectures on climate change and mental health as part of UBC’s Nursing 290 course. Her faculty advisor, Raluca Radu, MSN, a lecturer in the School of Nursing at UBC, developed the course in 2020 to teach students about the broad impacts of climate change on communities.
As the course has grown during the past 2 years, Ms. Abebe wanted to create a coping framework and engaging film for health educators to use with students, as well as for everyday people.
The toolkit includes contributions from three Canadian climate change experts, as well as six students from different backgrounds who have taken the course.
“I wanted to center the voices of youth and empower them to think they can be agents for change,” Ms. Abebe said. “I also wanted to highlight diverse voices and take a collaborative approach because climate change is such a big problem that we have to come together to address it.”
Ms. Abebe and Ms. Radu also noticed an increase in climate anxiety in recent years because of the pandemic, worldwide food and energy shortages, and extreme weather events that hit close to home, such as wildfires and floods in British Columbia.
“With the pandemic, people have been spending more time online and thinking about our world at large,” Ms. Abebe said. “At the same time that they’re thinking about it, climate change events are happening simultaneously – not in the future, but right now.”
Economic, social, and political shifts during the past 2 years have also prompted people to question standard practices and institutions, which has created an opportunity to discuss change, Ms. Radu told this news organization.
“It’s a pivotal time to question our values and highly consumerist society,” she said. “We’re at a point in time where, if we don’t take action, the planetary health will be in an irreversible state, and we won’t be able to turn back time and make changes.”
Our psyches and nature
The toolkit includes three main sections that feature video clips and reflective questions around eco-anxiety, eco-paralysis, and ecological grief.
In the first section, eco-anxiety is defined as a “chronic fear of environmental doom,” which could include anxiousness around the likelihood of a severe weather event because of ongoing news coverage and social media. The reflective questions prompt readers to discuss eco-anxiety in their life, work through their emotions, understand their beliefs and values, and determine how to use them to address climate change anxiety.
The second section defines eco-paralysis as the powerlessness that people may feel when they don’t believe they can do anything meaningful on an individual level to address climate change. Paralysis can look like apathy, complacency, or disengagement. The questions prompt readers to observe how paralysis may show up in their lives, explore the tension between individual versus collective responsibility, and consider ways to address their sense of helplessness about climate change.
In the third section, ecological grief centers around “experienced or anticipated ecological losses,” which could include the loss of species, ecosystems, and landscapes because of short- or long-term environmental change. The questions prompt readers to explore their feelings, beliefs, and values and feel empowered to address their ecological grief over climate change.
The toolkit also includes recommendations for books, journal articles, websites, podcasts, and meditations around mental health and climate change, as well as ways to get involved with others. For instance, health care practitioners can register with PaRx, a program in British Columbia that allows providers to prescribe time in nature to improve a client’s health. The program is being adopted across Canada, and people with a prescription can visit local and national parks, historic sites, and marine conservation areas for free.
“This is about recognizing that there is a connection between our psyches and nature, and by talking about it, we can name what we’re feeling,” Ms. Abebe said. “We can take action not only to handle our emotions, but also to live kinder and more sustainable lifestyles.”
Future work will need to focus on population-level approaches to climate change and mental health as well, including policy and financial support to address environmental changes directly.
“We need to start thinking beyond individualized approaches and focus on how to create supportive and resilient communities to respond to climate change,” Kiffer Card, PhD, executive director of the Mental Health and Climate Change Alliance and an assistant professor of health sciences at Simon Fraser University, Burnaby, B.C., told this news organization.
Dr. Card, who wasn’t involved in developing the toolkit, has researched recent trends around climate change anxiety in Canada and fielded questions from health care practitioners and mental health professionals who are looking for ways to help their patients.
“Communities need to be ready to stand up and respond to acute emergency disasters, and government leaders need to take this seriously,” he said. “Those who are experiencing climate anxiety now are the canaries in the coal mine for the severe weather events and consequences to come.”
The toolkit was developed with funding from the Alma Mater Society of the University of British Columbia, Vancouver. Ms. Abebe, Ms. Radu, and Dr. Card reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FDA approves two vonoprazan therapies for H. pylori eradication
: Voquezna Triple Pak (vonoprazan, amoxicillin, clarithromycin) and Voquezna Dual Pak (vonoprazan, amoxicillin), both from Phathom Pharmaceuticals.
Vonoprazan is an oral potassium-competitive acid blocker and “the first innovative acid suppressant from a new drug class approved in the United States in over 30 years,” the company said in a news release announcing the approval.
“The approval of Voquezna treatment regimens offers physicians and patients two therapeutic options that showed superior eradication rates compared to proton pump inhibitor-based (PPI) lansoprazole triple therapy in the overall patient population in a pivotal trial,” Terrie Curran, president and CEO of Phathom Pharmaceuticals, said in the release.
“H. pylori eradication rates continue to decline in part due to antibiotic resistance, inadequate acid suppression, and complex treatment regimens, resulting in treatment failures and complications for patients,” Ms. Curran noted.
“New therapies that have the potential to address the limitations of current treatments are needed, and we look forward to bringing these innovative vonoprazan-based treatment options to the millions of H pylori sufferers in the United States,” Ms. Curran said.
FDA approval of vonoprazan triple and dual therapy was based on safety and efficacy data from the phase 3 PHALCON-HP trial involving 1,046 patients.
As earlier reported, both treatment regimens were noninferior to PPI-based triple therapy (lansoprazole with amoxicillin and clarithromycin) in patients with H. pylori strains that were not resistant to clarithromycin or amoxicillin at baseline.
In this analysis, the eradication rate was 78.8% with PPI-based triple therapy, compared with 84.7% with vonoprazan triple therapy and 78.5% with vonoprazan dual therapy.
Vonoprazan triple and dual therapy were both superior to PPI-based triple therapy among all patients, including patients with clarithromycin-resistant H. pylori.
Among patients with clarithromycin-resistant H. pylori, 31.9% achieved eradication with PPI triple therapy, compared with 65.8% with vonoprazan triple therapy and 69.6% with vonoprazan dual therapy.
Among all patients, 68.5% achieved eradication with PPI triple therapy, 80.8% with vonoprazan triple therapy and 77.2% with vonoprazan dual therapy.
Adverse event rates for the vonoprazan-based regimens were comparable to lansoprazole triple therapy. Full prescribing information is available online.
“As a practicing physician, I am excited about the potential of two novel, first-line H. pylori treatment options,” William D. Chey, MD, chief of gastroenterology & hepatology at the University of Michigan, Ann Arbor, said in the news release.
“I believe the added flexibility of having two additional effective therapies, including a dual therapy option that does not contain clarithromycin, offers the potential to improve clinical outcomes in patients with H. pylori infection,” Dr. Chey added.
The company expects to launch both products in the third quarter of 2022. Both treatment regimens will be supplied in convenient blister packs to help promote compliance.
A version of this article first appeared on Medscape.com.
: Voquezna Triple Pak (vonoprazan, amoxicillin, clarithromycin) and Voquezna Dual Pak (vonoprazan, amoxicillin), both from Phathom Pharmaceuticals.
Vonoprazan is an oral potassium-competitive acid blocker and “the first innovative acid suppressant from a new drug class approved in the United States in over 30 years,” the company said in a news release announcing the approval.
“The approval of Voquezna treatment regimens offers physicians and patients two therapeutic options that showed superior eradication rates compared to proton pump inhibitor-based (PPI) lansoprazole triple therapy in the overall patient population in a pivotal trial,” Terrie Curran, president and CEO of Phathom Pharmaceuticals, said in the release.
“H. pylori eradication rates continue to decline in part due to antibiotic resistance, inadequate acid suppression, and complex treatment regimens, resulting in treatment failures and complications for patients,” Ms. Curran noted.
“New therapies that have the potential to address the limitations of current treatments are needed, and we look forward to bringing these innovative vonoprazan-based treatment options to the millions of H pylori sufferers in the United States,” Ms. Curran said.
FDA approval of vonoprazan triple and dual therapy was based on safety and efficacy data from the phase 3 PHALCON-HP trial involving 1,046 patients.
As earlier reported, both treatment regimens were noninferior to PPI-based triple therapy (lansoprazole with amoxicillin and clarithromycin) in patients with H. pylori strains that were not resistant to clarithromycin or amoxicillin at baseline.
In this analysis, the eradication rate was 78.8% with PPI-based triple therapy, compared with 84.7% with vonoprazan triple therapy and 78.5% with vonoprazan dual therapy.
Vonoprazan triple and dual therapy were both superior to PPI-based triple therapy among all patients, including patients with clarithromycin-resistant H. pylori.
Among patients with clarithromycin-resistant H. pylori, 31.9% achieved eradication with PPI triple therapy, compared with 65.8% with vonoprazan triple therapy and 69.6% with vonoprazan dual therapy.
Among all patients, 68.5% achieved eradication with PPI triple therapy, 80.8% with vonoprazan triple therapy and 77.2% with vonoprazan dual therapy.
Adverse event rates for the vonoprazan-based regimens were comparable to lansoprazole triple therapy. Full prescribing information is available online.
“As a practicing physician, I am excited about the potential of two novel, first-line H. pylori treatment options,” William D. Chey, MD, chief of gastroenterology & hepatology at the University of Michigan, Ann Arbor, said in the news release.
“I believe the added flexibility of having two additional effective therapies, including a dual therapy option that does not contain clarithromycin, offers the potential to improve clinical outcomes in patients with H. pylori infection,” Dr. Chey added.
The company expects to launch both products in the third quarter of 2022. Both treatment regimens will be supplied in convenient blister packs to help promote compliance.
A version of this article first appeared on Medscape.com.
: Voquezna Triple Pak (vonoprazan, amoxicillin, clarithromycin) and Voquezna Dual Pak (vonoprazan, amoxicillin), both from Phathom Pharmaceuticals.
Vonoprazan is an oral potassium-competitive acid blocker and “the first innovative acid suppressant from a new drug class approved in the United States in over 30 years,” the company said in a news release announcing the approval.
“The approval of Voquezna treatment regimens offers physicians and patients two therapeutic options that showed superior eradication rates compared to proton pump inhibitor-based (PPI) lansoprazole triple therapy in the overall patient population in a pivotal trial,” Terrie Curran, president and CEO of Phathom Pharmaceuticals, said in the release.
“H. pylori eradication rates continue to decline in part due to antibiotic resistance, inadequate acid suppression, and complex treatment regimens, resulting in treatment failures and complications for patients,” Ms. Curran noted.
“New therapies that have the potential to address the limitations of current treatments are needed, and we look forward to bringing these innovative vonoprazan-based treatment options to the millions of H pylori sufferers in the United States,” Ms. Curran said.
FDA approval of vonoprazan triple and dual therapy was based on safety and efficacy data from the phase 3 PHALCON-HP trial involving 1,046 patients.
As earlier reported, both treatment regimens were noninferior to PPI-based triple therapy (lansoprazole with amoxicillin and clarithromycin) in patients with H. pylori strains that were not resistant to clarithromycin or amoxicillin at baseline.
In this analysis, the eradication rate was 78.8% with PPI-based triple therapy, compared with 84.7% with vonoprazan triple therapy and 78.5% with vonoprazan dual therapy.
Vonoprazan triple and dual therapy were both superior to PPI-based triple therapy among all patients, including patients with clarithromycin-resistant H. pylori.
Among patients with clarithromycin-resistant H. pylori, 31.9% achieved eradication with PPI triple therapy, compared with 65.8% with vonoprazan triple therapy and 69.6% with vonoprazan dual therapy.
Among all patients, 68.5% achieved eradication with PPI triple therapy, 80.8% with vonoprazan triple therapy and 77.2% with vonoprazan dual therapy.
Adverse event rates for the vonoprazan-based regimens were comparable to lansoprazole triple therapy. Full prescribing information is available online.
“As a practicing physician, I am excited about the potential of two novel, first-line H. pylori treatment options,” William D. Chey, MD, chief of gastroenterology & hepatology at the University of Michigan, Ann Arbor, said in the news release.
“I believe the added flexibility of having two additional effective therapies, including a dual therapy option that does not contain clarithromycin, offers the potential to improve clinical outcomes in patients with H. pylori infection,” Dr. Chey added.
The company expects to launch both products in the third quarter of 2022. Both treatment regimens will be supplied in convenient blister packs to help promote compliance.
A version of this article first appeared on Medscape.com.
Restoring dignity to sex trafficking survivors, one tattoo removal at a time
SAN DIEGO – , according to the results of an online survey evaluating the need for and impact of tattoo removal in this population.
Sex trafficking involves the use of force, fraud, or coercion to compel another person to engage in commercial sex acts, and traffickers often brand their victims with tattoos that convey ownership, including tattoos of names, symbols, and barcodes. According to data from Polaris, a nonprofit organization that works to combat and prevent sex and labor trafficking in the United States, 16,658 sex trafficking victims were identified in the country in 2020, but tens of thousands go unreported.
“Given the inherently covert nature of this crime, it is difficult to determine exact statistics,” Emily L. Guo, MD, a cosmetic dermatologic surgery fellow at the Dermatology and Laser Surgery Center in Houston, said during a clinical abstract session at the annual meeting of the American Society for Laser Medicine and Surgery. “We have been working with sex trafficking survivors local to our practice in Houston providing pro bono tattoo removal, and we’ve observed how impactful that is in their recovery. We wanted to see if there was a national need for support of these survivors, allowing them to reclaim their lives.”
In collaboration with Elizabeth Kream, MD, a dermatology resident at the University of Illinois at Chicago, and Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center and the current ASLMS president, Dr. Guo conducted an online needs and impact survey regarding laser removal of branding tattoos. With assistance from the National Trafficking Sheltered Alliance, the researchers distributed the survey to U.S. organizations that support sex trafficking survivors. Representatives from 40 organizations responded to the survey. Most were based in the South (45%), followed by the West (20%) and Midwest (20%), and the Northeast (15%).
“On average, these programs support 81 survivors per year, which translates into 3,240 victims per year,” Dr. Guo said. Survey respondents estimated that 47% of sex trafficking survivors had branding tattoos. Of those, 67% were in a stable situation that would make it possible to undergo tattoo removal.
On a scale of 1 to 10 with 10 being the highest, “pro bono removal of branding tattoos received a survivor impact recovery score of 9.2 by these respondents,” Dr. Guo said. “Breaking down these numbers, there are at least 1,200 survivors per year who would benefit from tattoo removal during recovery. Qualitative responses to our survey echoed the same messages: There is a great need and a large impact for pro bono tattoo removal.”
For example, one survey respondent wrote, “Thank you for being willing to remove tattoos, allowing them to feel as though they are no longer owned by their trafficker.” Another wrote, “Erasing or revising the mark of her trafficker is a critical part of every survivor’s recovery journey.”
Sometimes branding tattoos are placed in highly visible locations. One sex trafficking survivor presented to Dr. Guo with a large dark blue tattoo above an eyebrow. “She shared with me that because the tattoo was so highly visible, nobody would offer her a job,” Dr. Guo said. Another survivor had her trafficker’s initial tattooed on her left ring finger. Yet another had a large tattoo on her forearm branded with her trafficker’s name as well as the word cash, “indicating that she is source of money for him,” she said, noting that on average, one sex trafficking victim generates about $100,000 per year for their trafficker.
Although there has been work published on recognition of branding tattoos in the medical community, including the difficulty in differentiating branding tattoos from voluntary tattoos, Dr. Friedman said that there have not been any studies evaluating the need and impact of laser branding tattoo removal in the recovery of sex trafficking survivors. Findings from the current survey “illuminate that the removal of branding tattoos is highly impactful on recovery and may be preferred over tattoo cover-ups,” Dr. Friedman told this news organization.
“Furthermore, survivors frequently move during their recovery process, so a national partnership is essential to allowing survivors to continue the removal process wherever they may be.”
The findings support a proposed ASLMS campaign that intends to connect sex trafficking survivors with board-certified physicians for pro bono removal of branding tattoos. “This will not only aid in survivors’ recovery, but this work will also be beneficial to allow for an avenue to create a repository of sex trafficking tattoo images to improve branding tattoo identification competency among health care providers,” Dr. Friedman said.
He acknowledged certain limitations of the survey, including the fact that “thorough and exact data collection regarding human trafficking is challenging given the inherently covert and underground nature of this crime.” In addition, the study involved surveying organizations supporting sex trafficking survivors rather than the survivors themselves. However, he noted, “we felt for this initial study we wanted to be sensitive to the survivors.”
In an interview at the meeting, one of the session moderators, Oge Onwudiwe, MD, a dermatologist who practices at AllPhases Dermatology in Alexandria, Va., said that pro bono laser removal of branding tattoos “is something that a lot of us can work on and do, and have an impact on. There’s no reason why we shouldn’t help. I can only imagine the psychological impact of having a daily reminder of that [in the form of a branding tattoo]. That’s like PTSD every day almost. You have a trigger there.”
Another session moderator, Eliot Battle, MD, CEO of Cultura Dermatology and Laser Center in Washington, is a board member of Innocents at Risk, a nonprofit that works to fight child exploitation and human trafficking. With pro bono laser removal of a branded tattoo, “this is not just a cosmetic correction you’re making,” Dr. Battle said. “It’s so much deeper than that. It changes people’s lives.”
The researchers and Dr. Onwudiwe reported having no financial disclosures. Dr. Battle disclosed that he conducts research for Cynosure, and has received discounts from Cynosure, Cutera, Solta Medical, Lumenis, Be Inc., and Sciton.
SAN DIEGO – , according to the results of an online survey evaluating the need for and impact of tattoo removal in this population.
Sex trafficking involves the use of force, fraud, or coercion to compel another person to engage in commercial sex acts, and traffickers often brand their victims with tattoos that convey ownership, including tattoos of names, symbols, and barcodes. According to data from Polaris, a nonprofit organization that works to combat and prevent sex and labor trafficking in the United States, 16,658 sex trafficking victims were identified in the country in 2020, but tens of thousands go unreported.
“Given the inherently covert nature of this crime, it is difficult to determine exact statistics,” Emily L. Guo, MD, a cosmetic dermatologic surgery fellow at the Dermatology and Laser Surgery Center in Houston, said during a clinical abstract session at the annual meeting of the American Society for Laser Medicine and Surgery. “We have been working with sex trafficking survivors local to our practice in Houston providing pro bono tattoo removal, and we’ve observed how impactful that is in their recovery. We wanted to see if there was a national need for support of these survivors, allowing them to reclaim their lives.”
In collaboration with Elizabeth Kream, MD, a dermatology resident at the University of Illinois at Chicago, and Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center and the current ASLMS president, Dr. Guo conducted an online needs and impact survey regarding laser removal of branding tattoos. With assistance from the National Trafficking Sheltered Alliance, the researchers distributed the survey to U.S. organizations that support sex trafficking survivors. Representatives from 40 organizations responded to the survey. Most were based in the South (45%), followed by the West (20%) and Midwest (20%), and the Northeast (15%).
“On average, these programs support 81 survivors per year, which translates into 3,240 victims per year,” Dr. Guo said. Survey respondents estimated that 47% of sex trafficking survivors had branding tattoos. Of those, 67% were in a stable situation that would make it possible to undergo tattoo removal.
On a scale of 1 to 10 with 10 being the highest, “pro bono removal of branding tattoos received a survivor impact recovery score of 9.2 by these respondents,” Dr. Guo said. “Breaking down these numbers, there are at least 1,200 survivors per year who would benefit from tattoo removal during recovery. Qualitative responses to our survey echoed the same messages: There is a great need and a large impact for pro bono tattoo removal.”
For example, one survey respondent wrote, “Thank you for being willing to remove tattoos, allowing them to feel as though they are no longer owned by their trafficker.” Another wrote, “Erasing or revising the mark of her trafficker is a critical part of every survivor’s recovery journey.”
Sometimes branding tattoos are placed in highly visible locations. One sex trafficking survivor presented to Dr. Guo with a large dark blue tattoo above an eyebrow. “She shared with me that because the tattoo was so highly visible, nobody would offer her a job,” Dr. Guo said. Another survivor had her trafficker’s initial tattooed on her left ring finger. Yet another had a large tattoo on her forearm branded with her trafficker’s name as well as the word cash, “indicating that she is source of money for him,” she said, noting that on average, one sex trafficking victim generates about $100,000 per year for their trafficker.
Although there has been work published on recognition of branding tattoos in the medical community, including the difficulty in differentiating branding tattoos from voluntary tattoos, Dr. Friedman said that there have not been any studies evaluating the need and impact of laser branding tattoo removal in the recovery of sex trafficking survivors. Findings from the current survey “illuminate that the removal of branding tattoos is highly impactful on recovery and may be preferred over tattoo cover-ups,” Dr. Friedman told this news organization.
“Furthermore, survivors frequently move during their recovery process, so a national partnership is essential to allowing survivors to continue the removal process wherever they may be.”
The findings support a proposed ASLMS campaign that intends to connect sex trafficking survivors with board-certified physicians for pro bono removal of branding tattoos. “This will not only aid in survivors’ recovery, but this work will also be beneficial to allow for an avenue to create a repository of sex trafficking tattoo images to improve branding tattoo identification competency among health care providers,” Dr. Friedman said.
He acknowledged certain limitations of the survey, including the fact that “thorough and exact data collection regarding human trafficking is challenging given the inherently covert and underground nature of this crime.” In addition, the study involved surveying organizations supporting sex trafficking survivors rather than the survivors themselves. However, he noted, “we felt for this initial study we wanted to be sensitive to the survivors.”
In an interview at the meeting, one of the session moderators, Oge Onwudiwe, MD, a dermatologist who practices at AllPhases Dermatology in Alexandria, Va., said that pro bono laser removal of branding tattoos “is something that a lot of us can work on and do, and have an impact on. There’s no reason why we shouldn’t help. I can only imagine the psychological impact of having a daily reminder of that [in the form of a branding tattoo]. That’s like PTSD every day almost. You have a trigger there.”
Another session moderator, Eliot Battle, MD, CEO of Cultura Dermatology and Laser Center in Washington, is a board member of Innocents at Risk, a nonprofit that works to fight child exploitation and human trafficking. With pro bono laser removal of a branded tattoo, “this is not just a cosmetic correction you’re making,” Dr. Battle said. “It’s so much deeper than that. It changes people’s lives.”
The researchers and Dr. Onwudiwe reported having no financial disclosures. Dr. Battle disclosed that he conducts research for Cynosure, and has received discounts from Cynosure, Cutera, Solta Medical, Lumenis, Be Inc., and Sciton.
SAN DIEGO – , according to the results of an online survey evaluating the need for and impact of tattoo removal in this population.
Sex trafficking involves the use of force, fraud, or coercion to compel another person to engage in commercial sex acts, and traffickers often brand their victims with tattoos that convey ownership, including tattoos of names, symbols, and barcodes. According to data from Polaris, a nonprofit organization that works to combat and prevent sex and labor trafficking in the United States, 16,658 sex trafficking victims were identified in the country in 2020, but tens of thousands go unreported.
“Given the inherently covert nature of this crime, it is difficult to determine exact statistics,” Emily L. Guo, MD, a cosmetic dermatologic surgery fellow at the Dermatology and Laser Surgery Center in Houston, said during a clinical abstract session at the annual meeting of the American Society for Laser Medicine and Surgery. “We have been working with sex trafficking survivors local to our practice in Houston providing pro bono tattoo removal, and we’ve observed how impactful that is in their recovery. We wanted to see if there was a national need for support of these survivors, allowing them to reclaim their lives.”
In collaboration with Elizabeth Kream, MD, a dermatology resident at the University of Illinois at Chicago, and Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center and the current ASLMS president, Dr. Guo conducted an online needs and impact survey regarding laser removal of branding tattoos. With assistance from the National Trafficking Sheltered Alliance, the researchers distributed the survey to U.S. organizations that support sex trafficking survivors. Representatives from 40 organizations responded to the survey. Most were based in the South (45%), followed by the West (20%) and Midwest (20%), and the Northeast (15%).
“On average, these programs support 81 survivors per year, which translates into 3,240 victims per year,” Dr. Guo said. Survey respondents estimated that 47% of sex trafficking survivors had branding tattoos. Of those, 67% were in a stable situation that would make it possible to undergo tattoo removal.
On a scale of 1 to 10 with 10 being the highest, “pro bono removal of branding tattoos received a survivor impact recovery score of 9.2 by these respondents,” Dr. Guo said. “Breaking down these numbers, there are at least 1,200 survivors per year who would benefit from tattoo removal during recovery. Qualitative responses to our survey echoed the same messages: There is a great need and a large impact for pro bono tattoo removal.”
For example, one survey respondent wrote, “Thank you for being willing to remove tattoos, allowing them to feel as though they are no longer owned by their trafficker.” Another wrote, “Erasing or revising the mark of her trafficker is a critical part of every survivor’s recovery journey.”
Sometimes branding tattoos are placed in highly visible locations. One sex trafficking survivor presented to Dr. Guo with a large dark blue tattoo above an eyebrow. “She shared with me that because the tattoo was so highly visible, nobody would offer her a job,” Dr. Guo said. Another survivor had her trafficker’s initial tattooed on her left ring finger. Yet another had a large tattoo on her forearm branded with her trafficker’s name as well as the word cash, “indicating that she is source of money for him,” she said, noting that on average, one sex trafficking victim generates about $100,000 per year for their trafficker.
Although there has been work published on recognition of branding tattoos in the medical community, including the difficulty in differentiating branding tattoos from voluntary tattoos, Dr. Friedman said that there have not been any studies evaluating the need and impact of laser branding tattoo removal in the recovery of sex trafficking survivors. Findings from the current survey “illuminate that the removal of branding tattoos is highly impactful on recovery and may be preferred over tattoo cover-ups,” Dr. Friedman told this news organization.
“Furthermore, survivors frequently move during their recovery process, so a national partnership is essential to allowing survivors to continue the removal process wherever they may be.”
The findings support a proposed ASLMS campaign that intends to connect sex trafficking survivors with board-certified physicians for pro bono removal of branding tattoos. “This will not only aid in survivors’ recovery, but this work will also be beneficial to allow for an avenue to create a repository of sex trafficking tattoo images to improve branding tattoo identification competency among health care providers,” Dr. Friedman said.
He acknowledged certain limitations of the survey, including the fact that “thorough and exact data collection regarding human trafficking is challenging given the inherently covert and underground nature of this crime.” In addition, the study involved surveying organizations supporting sex trafficking survivors rather than the survivors themselves. However, he noted, “we felt for this initial study we wanted to be sensitive to the survivors.”
In an interview at the meeting, one of the session moderators, Oge Onwudiwe, MD, a dermatologist who practices at AllPhases Dermatology in Alexandria, Va., said that pro bono laser removal of branding tattoos “is something that a lot of us can work on and do, and have an impact on. There’s no reason why we shouldn’t help. I can only imagine the psychological impact of having a daily reminder of that [in the form of a branding tattoo]. That’s like PTSD every day almost. You have a trigger there.”
Another session moderator, Eliot Battle, MD, CEO of Cultura Dermatology and Laser Center in Washington, is a board member of Innocents at Risk, a nonprofit that works to fight child exploitation and human trafficking. With pro bono laser removal of a branded tattoo, “this is not just a cosmetic correction you’re making,” Dr. Battle said. “It’s so much deeper than that. It changes people’s lives.”
The researchers and Dr. Onwudiwe reported having no financial disclosures. Dr. Battle disclosed that he conducts research for Cynosure, and has received discounts from Cynosure, Cutera, Solta Medical, Lumenis, Be Inc., and Sciton.
AT ASLMS 2022
Bone, breath, heart, guts: Eight essential papers in primary care
1. Adding a New Medication Versus Maximizing Dose to Intensify Hypertension Treatment in Older Adults: A Retrospective Observational Study
Roughly one in three adults with hypertension have inadequate blood pressure control, and clinicians have two options for intensifying treatment: “The dose of the current drug regimen can be maximized, or a new drug can be added,” said deputy editor Christina C. Wee, MD, MPH, at the annual meeting of the American College of Physicians.
Data from randomized controlled trials suggest treatment with lower doses of combination therapy may be more effective, with fewer side effects – although the best strategy in older adults remains unclear.
To answer that question, researchers conducted a large-scale, population-based, retrospective cohort study, and observational data were used to emulate a target trial with two groups: new medication and maximizing dose.
The cohort comprised people aged 65 years or older with hypertension and was limited to those with a systolic blood pressure of 130 mm Hg or higher. Two intensification approaches were used: adding a new medication, defined as a total dose increase with a new medication; and maximizing dose, defined as a total dose increase without new medication.
A total of 178,562 patients were included in the study, and 45,575 (25.5%) had intensification by adding a new medication and 132,987 (74.5%) by maximizing dose.
“Both produced systolic blood pressure reduction with a slight advantage in the ‘add a new medication’ group,” Dr. Wee said. “That group reduced their systolic blood pressure by over 4.5 points as compared to 3.8 points in the maximized [dose] group.”
At 12 months the results were similar, but only 50% of patients in the new medication group were able to sustain that strategy, compared with two-thirds of patients who had their dose increased.
“This suggests that, in older adults, adding a new antihypertensive medication versus maximizing dosing of existing regimen is less common, only minimally more effective, and less sustainable,” Dr. Wee said. “Maximizing dose of antihypertensive medication is a reasonable approach [and] may be easier to sustain.”
2. Cost-Effectiveness of Screening Mammography Beyond Age 75 Years: A Cost-Effectiveness Analysis
The U.S. Preventive Services Task Force recommends biennial screening mammograms through the age of 74 years, and a meta-analysis of randomized controlled trials suggests mortality is reduced among women with at least a 10-year life expectancy, Dr. Wee said.
However, whether screening beyond age 75 years is cost effective, especially among women with comorbidities, is unclear.
To address that question, researchers estimated benefits, harms, and cost-effectiveness of extending mammography to age 80, 85, or 90 years according to comorbidity burden, using data from the Surveillance, Epidemiology, and End Results program and the Breast Cancer Surveillance Consortium.
The results showed that extending annual mammography beyond age 75 years was not cost effective, but biennial mammography was. “It was cost effective to age 80 regardless of baseline comorbidity score, but it averted only small, absolute numbers of breast cancer deaths – especially for women with comorbidities,” Dr. Wee said. “It was not cost effective beyond age 80.”
3. Prediction of End-Stage Kidney Disease Using Estimated Glomerular Filtration Rate With and Without Race: A Prospective Cohort Study
Estimated glomerular filtration rate (eGFR) is associated with end-stage kidney disease (ESKD) and is used to make dialysis and transplant decisions. “However, the accuracy of using eGFR alone has been questioned and, previously, some eGFR equations included a correction for race and this has been quite controversial,” Dr. Wee said. “And just last year, the Chronic Kidney Disease Epidemiology Collaboration released their new equations, removing the adjustment for race.”
The study authors posed two questions:
- How well does eGFR alone predict risk of ESKD, compared with Kidney Function Risk Equation (KFRE)?
- Does using different eGFR equations affect performance of either eGFR alone or KFRE in predicting the risk of ESKD?
During a maximum 16 years of follow-up, 856 participants (n = 3,873) developed ESKD. Across all eGFR equations, the KFRE score was superior for predicting 2-year incidence of end-stage kidney disease, compared with eGFR alone.
“KFRE score better predicted 2-year risk of ESKD than eGFR alone regardless of eGFR equations used,” Dr. Wee said. “Correcting eGFR equations for race did not improve performance and validates recent guidelines.”
4. Comparative Fracture Risk During Osteoporosis Drug Holidays After Long-Term Risedronate Versus Alendronate Therapy: A Propensity Score-Matched Cohort Study
The study looked at the comparative risks of drug holidays after long-term (≥ 3 years) risedronate versus alendronate therapy in a cohort of individuals aged 66 years or older. The primary outcome was hip fracture within 3 years after a 120-day ascertainment period.
The cohort included 25,077 propensity score–matched pairs (81% female) with a mean age of 81 years. Hip fracture rates were higher among risedronate than alendronate drug holidays, although this association was attenuated when any fracture was included as the outcome.
Overall, risedronate treatment before a drug holiday was associated with an 18% greater risk of hip fractures than alendronate, and this relative increase translated to a small absolute increase of 0.6%.
“These differences primarily manifested after 24 months, but given these small differences, I’m not sure if we need to change our current management strategy,” Dr. Wee said. “But further study is warranted.”
5. The Effects of Four Doses of Vitamin D Supplements on Falls in Older Adults: A Response-Adaptive, Randomized Clinical Trial
This study assessed the effects of four doses of vitamin D3 supplements on the risk of falls.
The cohort included 688 participants, aged 70 years and older, with an elevated fall risk and a serum 25-hydroxyvitamin D level of 25-72.5 nmol/L. The intervention was 200 (control), 1,000, 2,000, or 4,000 IU of vitamin D3 per day.
“Their results showed that supplementation at doses of 1,000 IU/day or higher did not prevent falls compared with 200 IU/day,” said deputy editor Stephanie Chang, MD, MPH. “Several analyses raised safety concerns about vitamin D3 doses of 1,000 IU/day or higher.”
6. Postdiagnosis Smoking Cessation and Reduced Risk for Lung Cancer Progression and Mortality: A Prospective Cohort Study
This study sought to determine if quitting smoking after a diagnosis of lung cancer reduced the risk for disease progression and mortality. Researchers prospectively analyzed patients with non–small cell lung cancer (NSCLC) who were recruited between 2007 and 2016 and followed annually through 2020. The cohort comprised 517 current smokers who were diagnosed with early-stage (IA-IIIA) NSCLC.
The adjusted median overall survival time was 21.6 months higher among patients who quit smoking versus those who continued smoking, and a higher 5-year overall and progression-free survival were observed among patients who quit than those who continued smoking. After adjusting for confounders, smoking cessation remained associated with a lower risk for all-cause mortality, cancer-specific mortality, and disease progression.
7. Acute Consumption of Alcohol and Discrete Atrial Fibrillation Events
This study sought to determine if alcohol consumption heightened the risk for an episode of atrial fibrillation (AFib). The cohort included 100 individuals with paroxysmal AFib who were fitted with a continuous electrocardiogram monitor and an ankle-worn transdermal ethanol sensor for 4 weeks. Real-time documentation of each alcoholic drink consumed was self-recorded and finger-stick blood tests for phosphatidylethanol were used to corroborate ascertainments of drinking events.
Phosphatidylethanol testing correlated with the number of real-time recorded drinks and with the transdermal alcohol sensor. Consuming one alcoholic drink was associated with a twofold increased risk of AFib over the next 4 hours. The risk rose threefold with the consumption of two drinks.
“There is evidence of dose-response relationship with higher risk with more drinks,” Dr. Chang said. “Even one drink may predispose to an acute episode of AF[ib] in those so predisposed.”
8. Evaluation and Management After Acute Left-Sided Colonic Diverticulitis: A Systematic Review
Management of uncomplicated diverticulitis is usually conservative and includes bowel rest and fluids. However, uncertainty remains about the role of hospitalization and antibiotics, Dr. Chang said. The new review included 51 studies looking at colonoscopy, nonsurgical treatments, and elective surgery for patients with diverticulitis.
It was unclear if patients with recent acute diverticulitis are at increased risk for colorectal cancer, although those with complicated diverticulitis do appear to be at a higher risk of the disease. Treatment with mesalamine was shown to be ineffective in preventing recurrence, and other nonsurgical treatments lacked adequate evidence.
As for surgery, elective procedures reduce recurrence in patients with prior complicated or smoldering or frequently recurrent diverticulitis, but it is unclear which of these patients may benefit most.
“The ACP recommends initial management without antibiotics,” said Dr. Chang, adding that other questions need to be addressed, such as inpatient versus outpatient management and elective surgery after an acute episode.
Dr. Wee and Dr. Chang disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
1. Adding a New Medication Versus Maximizing Dose to Intensify Hypertension Treatment in Older Adults: A Retrospective Observational Study
Roughly one in three adults with hypertension have inadequate blood pressure control, and clinicians have two options for intensifying treatment: “The dose of the current drug regimen can be maximized, or a new drug can be added,” said deputy editor Christina C. Wee, MD, MPH, at the annual meeting of the American College of Physicians.
Data from randomized controlled trials suggest treatment with lower doses of combination therapy may be more effective, with fewer side effects – although the best strategy in older adults remains unclear.
To answer that question, researchers conducted a large-scale, population-based, retrospective cohort study, and observational data were used to emulate a target trial with two groups: new medication and maximizing dose.
The cohort comprised people aged 65 years or older with hypertension and was limited to those with a systolic blood pressure of 130 mm Hg or higher. Two intensification approaches were used: adding a new medication, defined as a total dose increase with a new medication; and maximizing dose, defined as a total dose increase without new medication.
A total of 178,562 patients were included in the study, and 45,575 (25.5%) had intensification by adding a new medication and 132,987 (74.5%) by maximizing dose.
“Both produced systolic blood pressure reduction with a slight advantage in the ‘add a new medication’ group,” Dr. Wee said. “That group reduced their systolic blood pressure by over 4.5 points as compared to 3.8 points in the maximized [dose] group.”
At 12 months the results were similar, but only 50% of patients in the new medication group were able to sustain that strategy, compared with two-thirds of patients who had their dose increased.
“This suggests that, in older adults, adding a new antihypertensive medication versus maximizing dosing of existing regimen is less common, only minimally more effective, and less sustainable,” Dr. Wee said. “Maximizing dose of antihypertensive medication is a reasonable approach [and] may be easier to sustain.”
2. Cost-Effectiveness of Screening Mammography Beyond Age 75 Years: A Cost-Effectiveness Analysis
The U.S. Preventive Services Task Force recommends biennial screening mammograms through the age of 74 years, and a meta-analysis of randomized controlled trials suggests mortality is reduced among women with at least a 10-year life expectancy, Dr. Wee said.
However, whether screening beyond age 75 years is cost effective, especially among women with comorbidities, is unclear.
To address that question, researchers estimated benefits, harms, and cost-effectiveness of extending mammography to age 80, 85, or 90 years according to comorbidity burden, using data from the Surveillance, Epidemiology, and End Results program and the Breast Cancer Surveillance Consortium.
The results showed that extending annual mammography beyond age 75 years was not cost effective, but biennial mammography was. “It was cost effective to age 80 regardless of baseline comorbidity score, but it averted only small, absolute numbers of breast cancer deaths – especially for women with comorbidities,” Dr. Wee said. “It was not cost effective beyond age 80.”
3. Prediction of End-Stage Kidney Disease Using Estimated Glomerular Filtration Rate With and Without Race: A Prospective Cohort Study
Estimated glomerular filtration rate (eGFR) is associated with end-stage kidney disease (ESKD) and is used to make dialysis and transplant decisions. “However, the accuracy of using eGFR alone has been questioned and, previously, some eGFR equations included a correction for race and this has been quite controversial,” Dr. Wee said. “And just last year, the Chronic Kidney Disease Epidemiology Collaboration released their new equations, removing the adjustment for race.”
The study authors posed two questions:
- How well does eGFR alone predict risk of ESKD, compared with Kidney Function Risk Equation (KFRE)?
- Does using different eGFR equations affect performance of either eGFR alone or KFRE in predicting the risk of ESKD?
During a maximum 16 years of follow-up, 856 participants (n = 3,873) developed ESKD. Across all eGFR equations, the KFRE score was superior for predicting 2-year incidence of end-stage kidney disease, compared with eGFR alone.
“KFRE score better predicted 2-year risk of ESKD than eGFR alone regardless of eGFR equations used,” Dr. Wee said. “Correcting eGFR equations for race did not improve performance and validates recent guidelines.”
4. Comparative Fracture Risk During Osteoporosis Drug Holidays After Long-Term Risedronate Versus Alendronate Therapy: A Propensity Score-Matched Cohort Study
The study looked at the comparative risks of drug holidays after long-term (≥ 3 years) risedronate versus alendronate therapy in a cohort of individuals aged 66 years or older. The primary outcome was hip fracture within 3 years after a 120-day ascertainment period.
The cohort included 25,077 propensity score–matched pairs (81% female) with a mean age of 81 years. Hip fracture rates were higher among risedronate than alendronate drug holidays, although this association was attenuated when any fracture was included as the outcome.
Overall, risedronate treatment before a drug holiday was associated with an 18% greater risk of hip fractures than alendronate, and this relative increase translated to a small absolute increase of 0.6%.
“These differences primarily manifested after 24 months, but given these small differences, I’m not sure if we need to change our current management strategy,” Dr. Wee said. “But further study is warranted.”
5. The Effects of Four Doses of Vitamin D Supplements on Falls in Older Adults: A Response-Adaptive, Randomized Clinical Trial
This study assessed the effects of four doses of vitamin D3 supplements on the risk of falls.
The cohort included 688 participants, aged 70 years and older, with an elevated fall risk and a serum 25-hydroxyvitamin D level of 25-72.5 nmol/L. The intervention was 200 (control), 1,000, 2,000, or 4,000 IU of vitamin D3 per day.
“Their results showed that supplementation at doses of 1,000 IU/day or higher did not prevent falls compared with 200 IU/day,” said deputy editor Stephanie Chang, MD, MPH. “Several analyses raised safety concerns about vitamin D3 doses of 1,000 IU/day or higher.”
6. Postdiagnosis Smoking Cessation and Reduced Risk for Lung Cancer Progression and Mortality: A Prospective Cohort Study
This study sought to determine if quitting smoking after a diagnosis of lung cancer reduced the risk for disease progression and mortality. Researchers prospectively analyzed patients with non–small cell lung cancer (NSCLC) who were recruited between 2007 and 2016 and followed annually through 2020. The cohort comprised 517 current smokers who were diagnosed with early-stage (IA-IIIA) NSCLC.
The adjusted median overall survival time was 21.6 months higher among patients who quit smoking versus those who continued smoking, and a higher 5-year overall and progression-free survival were observed among patients who quit than those who continued smoking. After adjusting for confounders, smoking cessation remained associated with a lower risk for all-cause mortality, cancer-specific mortality, and disease progression.
7. Acute Consumption of Alcohol and Discrete Atrial Fibrillation Events
This study sought to determine if alcohol consumption heightened the risk for an episode of atrial fibrillation (AFib). The cohort included 100 individuals with paroxysmal AFib who were fitted with a continuous electrocardiogram monitor and an ankle-worn transdermal ethanol sensor for 4 weeks. Real-time documentation of each alcoholic drink consumed was self-recorded and finger-stick blood tests for phosphatidylethanol were used to corroborate ascertainments of drinking events.
Phosphatidylethanol testing correlated with the number of real-time recorded drinks and with the transdermal alcohol sensor. Consuming one alcoholic drink was associated with a twofold increased risk of AFib over the next 4 hours. The risk rose threefold with the consumption of two drinks.
“There is evidence of dose-response relationship with higher risk with more drinks,” Dr. Chang said. “Even one drink may predispose to an acute episode of AF[ib] in those so predisposed.”
8. Evaluation and Management After Acute Left-Sided Colonic Diverticulitis: A Systematic Review
Management of uncomplicated diverticulitis is usually conservative and includes bowel rest and fluids. However, uncertainty remains about the role of hospitalization and antibiotics, Dr. Chang said. The new review included 51 studies looking at colonoscopy, nonsurgical treatments, and elective surgery for patients with diverticulitis.
It was unclear if patients with recent acute diverticulitis are at increased risk for colorectal cancer, although those with complicated diverticulitis do appear to be at a higher risk of the disease. Treatment with mesalamine was shown to be ineffective in preventing recurrence, and other nonsurgical treatments lacked adequate evidence.
As for surgery, elective procedures reduce recurrence in patients with prior complicated or smoldering or frequently recurrent diverticulitis, but it is unclear which of these patients may benefit most.
“The ACP recommends initial management without antibiotics,” said Dr. Chang, adding that other questions need to be addressed, such as inpatient versus outpatient management and elective surgery after an acute episode.
Dr. Wee and Dr. Chang disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
1. Adding a New Medication Versus Maximizing Dose to Intensify Hypertension Treatment in Older Adults: A Retrospective Observational Study
Roughly one in three adults with hypertension have inadequate blood pressure control, and clinicians have two options for intensifying treatment: “The dose of the current drug regimen can be maximized, or a new drug can be added,” said deputy editor Christina C. Wee, MD, MPH, at the annual meeting of the American College of Physicians.
Data from randomized controlled trials suggest treatment with lower doses of combination therapy may be more effective, with fewer side effects – although the best strategy in older adults remains unclear.
To answer that question, researchers conducted a large-scale, population-based, retrospective cohort study, and observational data were used to emulate a target trial with two groups: new medication and maximizing dose.
The cohort comprised people aged 65 years or older with hypertension and was limited to those with a systolic blood pressure of 130 mm Hg or higher. Two intensification approaches were used: adding a new medication, defined as a total dose increase with a new medication; and maximizing dose, defined as a total dose increase without new medication.
A total of 178,562 patients were included in the study, and 45,575 (25.5%) had intensification by adding a new medication and 132,987 (74.5%) by maximizing dose.
“Both produced systolic blood pressure reduction with a slight advantage in the ‘add a new medication’ group,” Dr. Wee said. “That group reduced their systolic blood pressure by over 4.5 points as compared to 3.8 points in the maximized [dose] group.”
At 12 months the results were similar, but only 50% of patients in the new medication group were able to sustain that strategy, compared with two-thirds of patients who had their dose increased.
“This suggests that, in older adults, adding a new antihypertensive medication versus maximizing dosing of existing regimen is less common, only minimally more effective, and less sustainable,” Dr. Wee said. “Maximizing dose of antihypertensive medication is a reasonable approach [and] may be easier to sustain.”
2. Cost-Effectiveness of Screening Mammography Beyond Age 75 Years: A Cost-Effectiveness Analysis
The U.S. Preventive Services Task Force recommends biennial screening mammograms through the age of 74 years, and a meta-analysis of randomized controlled trials suggests mortality is reduced among women with at least a 10-year life expectancy, Dr. Wee said.
However, whether screening beyond age 75 years is cost effective, especially among women with comorbidities, is unclear.
To address that question, researchers estimated benefits, harms, and cost-effectiveness of extending mammography to age 80, 85, or 90 years according to comorbidity burden, using data from the Surveillance, Epidemiology, and End Results program and the Breast Cancer Surveillance Consortium.
The results showed that extending annual mammography beyond age 75 years was not cost effective, but biennial mammography was. “It was cost effective to age 80 regardless of baseline comorbidity score, but it averted only small, absolute numbers of breast cancer deaths – especially for women with comorbidities,” Dr. Wee said. “It was not cost effective beyond age 80.”
3. Prediction of End-Stage Kidney Disease Using Estimated Glomerular Filtration Rate With and Without Race: A Prospective Cohort Study
Estimated glomerular filtration rate (eGFR) is associated with end-stage kidney disease (ESKD) and is used to make dialysis and transplant decisions. “However, the accuracy of using eGFR alone has been questioned and, previously, some eGFR equations included a correction for race and this has been quite controversial,” Dr. Wee said. “And just last year, the Chronic Kidney Disease Epidemiology Collaboration released their new equations, removing the adjustment for race.”
The study authors posed two questions:
- How well does eGFR alone predict risk of ESKD, compared with Kidney Function Risk Equation (KFRE)?
- Does using different eGFR equations affect performance of either eGFR alone or KFRE in predicting the risk of ESKD?
During a maximum 16 years of follow-up, 856 participants (n = 3,873) developed ESKD. Across all eGFR equations, the KFRE score was superior for predicting 2-year incidence of end-stage kidney disease, compared with eGFR alone.
“KFRE score better predicted 2-year risk of ESKD than eGFR alone regardless of eGFR equations used,” Dr. Wee said. “Correcting eGFR equations for race did not improve performance and validates recent guidelines.”
4. Comparative Fracture Risk During Osteoporosis Drug Holidays After Long-Term Risedronate Versus Alendronate Therapy: A Propensity Score-Matched Cohort Study
The study looked at the comparative risks of drug holidays after long-term (≥ 3 years) risedronate versus alendronate therapy in a cohort of individuals aged 66 years or older. The primary outcome was hip fracture within 3 years after a 120-day ascertainment period.
The cohort included 25,077 propensity score–matched pairs (81% female) with a mean age of 81 years. Hip fracture rates were higher among risedronate than alendronate drug holidays, although this association was attenuated when any fracture was included as the outcome.
Overall, risedronate treatment before a drug holiday was associated with an 18% greater risk of hip fractures than alendronate, and this relative increase translated to a small absolute increase of 0.6%.
“These differences primarily manifested after 24 months, but given these small differences, I’m not sure if we need to change our current management strategy,” Dr. Wee said. “But further study is warranted.”
5. The Effects of Four Doses of Vitamin D Supplements on Falls in Older Adults: A Response-Adaptive, Randomized Clinical Trial
This study assessed the effects of four doses of vitamin D3 supplements on the risk of falls.
The cohort included 688 participants, aged 70 years and older, with an elevated fall risk and a serum 25-hydroxyvitamin D level of 25-72.5 nmol/L. The intervention was 200 (control), 1,000, 2,000, or 4,000 IU of vitamin D3 per day.
“Their results showed that supplementation at doses of 1,000 IU/day or higher did not prevent falls compared with 200 IU/day,” said deputy editor Stephanie Chang, MD, MPH. “Several analyses raised safety concerns about vitamin D3 doses of 1,000 IU/day or higher.”
6. Postdiagnosis Smoking Cessation and Reduced Risk for Lung Cancer Progression and Mortality: A Prospective Cohort Study
This study sought to determine if quitting smoking after a diagnosis of lung cancer reduced the risk for disease progression and mortality. Researchers prospectively analyzed patients with non–small cell lung cancer (NSCLC) who were recruited between 2007 and 2016 and followed annually through 2020. The cohort comprised 517 current smokers who were diagnosed with early-stage (IA-IIIA) NSCLC.
The adjusted median overall survival time was 21.6 months higher among patients who quit smoking versus those who continued smoking, and a higher 5-year overall and progression-free survival were observed among patients who quit than those who continued smoking. After adjusting for confounders, smoking cessation remained associated with a lower risk for all-cause mortality, cancer-specific mortality, and disease progression.
7. Acute Consumption of Alcohol and Discrete Atrial Fibrillation Events
This study sought to determine if alcohol consumption heightened the risk for an episode of atrial fibrillation (AFib). The cohort included 100 individuals with paroxysmal AFib who were fitted with a continuous electrocardiogram monitor and an ankle-worn transdermal ethanol sensor for 4 weeks. Real-time documentation of each alcoholic drink consumed was self-recorded and finger-stick blood tests for phosphatidylethanol were used to corroborate ascertainments of drinking events.
Phosphatidylethanol testing correlated with the number of real-time recorded drinks and with the transdermal alcohol sensor. Consuming one alcoholic drink was associated with a twofold increased risk of AFib over the next 4 hours. The risk rose threefold with the consumption of two drinks.
“There is evidence of dose-response relationship with higher risk with more drinks,” Dr. Chang said. “Even one drink may predispose to an acute episode of AF[ib] in those so predisposed.”
8. Evaluation and Management After Acute Left-Sided Colonic Diverticulitis: A Systematic Review
Management of uncomplicated diverticulitis is usually conservative and includes bowel rest and fluids. However, uncertainty remains about the role of hospitalization and antibiotics, Dr. Chang said. The new review included 51 studies looking at colonoscopy, nonsurgical treatments, and elective surgery for patients with diverticulitis.
It was unclear if patients with recent acute diverticulitis are at increased risk for colorectal cancer, although those with complicated diverticulitis do appear to be at a higher risk of the disease. Treatment with mesalamine was shown to be ineffective in preventing recurrence, and other nonsurgical treatments lacked adequate evidence.
As for surgery, elective procedures reduce recurrence in patients with prior complicated or smoldering or frequently recurrent diverticulitis, but it is unclear which of these patients may benefit most.
“The ACP recommends initial management without antibiotics,” said Dr. Chang, adding that other questions need to be addressed, such as inpatient versus outpatient management and elective surgery after an acute episode.
Dr. Wee and Dr. Chang disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM INTERNAL MEDICINE 2022
Study provides new analysis of isotretinoin and risk for adverse neuropsychiatric outcomes
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
The use of , in a large retrospective cohort study published in the British Journal of Dermatology.
Although severe neuropsychiatric effects associated with isotretinoin therapy in patients with acne have been reported, “the evidence base ... is mixed and inconclusive,” and many studies are small, Seena Fazel, MBChB, MD, of the department of psychiatry, Oxford University, England, and co-authors write in the study.
The study results suggest that isotretinoin is conferring protection against adverse neuropsychiatric outcomes, particularly when compared with using oral antibiotics to treat acne, Dr. Fazel, professor of forensic psychiatry at Oxford University and the study’s senior author, said in an interview.
In the study, the investigators reviewed electronic health records (2013-2019) from a primarily United States–based dataset (TriNetX) of patients with acne aged 12-27 who had been followed for up to 1 year after their prescriptions had been dispensed.
There were four arms: those prescribed isotretinoin (30,866), oral antibiotics (44,748), topical anti-acne treatments (108,367), and those who had not been prescribed any acne treatment (78,666). The primary outcomes were diagnoses of a neuropsychiatric disorder (psychotic, mood, anxiety, personality, behavioral, and sleep disorders; and non-fatal self-harm) within one year of being prescribed treatment.
After using propensity score matching to adjust for confounders at baseline, the investigators determined that the odds ratio for any incident neuropsychiatric outcomes among patients with acne treated with isotretinoin was 0.80 (95% confidence interval, 0.74-0.87), compared with patients on oral antibiotics; 0.94 (95% CI, 0.87-1.02), compared with patients on topical anti-acne medications; and 1.06 (95% CI, 0.97-1.16), compared with those without a prescription for anti-acne medicines.
Side effects of isotretinoin – such as headache, dry mouth, and fatigue – were higher among those on isotretinoin than in the other three groups.
The authors concluded that isotretinoin was not independently linked to excess adverse neuropsychiatric outcomes at a population level. “We observed a consistent association between increasing acne severity as indicated by anti-acne treatment options and incidence of adverse neuropsychiatric outcomes, but the findings showed that isotretinoin exposure did not add to the risk of neuropsychiatric adverse outcomes over and above what was associated with oral antibiotics,” they write.
Isotretinoin treatment “appeared to mitigate the excess neuropsychiatric risk associated with recalcitrant moderate-to-severe acne,” they add.
The dermatology community has been interested in the impact isotretinoin has on mental health, and “I think clinically, they see that people get better on isotretinoin and their mental health improves,” Dr. Fazel told this news organization.
Asked to comment on the study results, John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic, Brigham and Women’s Hospital, Boston, commended the investigators for the design of the trial.
“One of the strengths of this study is that they use a technique called propensity-score matching, where you try to make the groups of patients similar with respect to their other characteristics to minimize the risks of confounding and bias in the study, which I think is a real strength,” he told this news organization. “The other thing that they do, which I think is a strength, is to think about the impact of acne severity on these outcomes, because we know acne itself is associated with depression and risk for suicide and other neuropsychiatric outcomes.”
Including a cohort of patients who had acne and received oral antibiotics for comparison “is a nice way to address the potential for confounding by severity and confounding by indication,” Dr. Barbieri said. “Those who get antibiotics usually have more severe acne. They may not have it as severely as those who get isotretinoin, but it is a nice approach to account for background levels of depression and neuropsychiatric outcomes in patients with acne. I think that is a real strength of the study. This is one of the best studies to have looked at this question.”
However, although the study found that isotretinoin decreased the excess psychiatric risk associated with refractory moderate-to-severe acne, it does not rule out the possibility that individuals may experience an adverse psychiatric outcome while on isotretinoin, Dr. Barbieri said.
“While I think on a population level, we absolutely can feel reassured by these data, I do think there are individual patients who have idiosyncratic, unpredictable reactions to isotretinoin where they have mood changes, whether it be irritability, depression, or other mood changes,” he cautioned. “Given the association of acne itself with mental health comorbidities, it is important to screen for comorbidities such as depression in all patients with acne.”
The study was funded by the Wellcome Trust, which provided Dr. Fazel and the first author with financial support for the study. One author is an employee of TriNetX; the other authors had no relevant disclosures. Dr. Barbieri reported no financial disclosures. He is cochair of the AAD’s Acne Guidelines Workgroup and associate editor at JAMA Dermatology.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Fecal transfer could be the transplant of youth
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Fecal matter may be in the fountain of youth
Yes, you read that headline correctly. New research by scientists at Quadram Institute and the University of East Anglia, both in Norwich, England, supports the claim that transferring fecal microbes might actually have some positive effects on reversing the aging process in the eyes, brain, and gut.
How do they know? Mice, of course. In the study, scientists took the gut microbes from older mice and transferred them into the younger mince. The young mice displayed inflamed signs of aging in their guts, brains, and eyes, which, we all know, decline in function as we age. What happens is a chronic inflammation of cells as we get older that can be found in the brain or gut that leads to a degenerative state over time.
When the older mice received the gut microbes from younger mice, the investigators saw the reverse: Gut, brain, and eye functionality improved. In a way, minimizing the inflammation.
There’s tons of research out there that suggests gut health is the key to a healthy life, but this study points directly to an improvement in brain and vision functionality as a result of the transfer.
Now, we’re not insinuating you get a poo transfer as you reach old age. And the shift to human studies on microbiota replacement therapy is still in the works. But this definitely is a topic to watch and could be a game changer in the age-old quest to bottle youth or at least improve quality of life as we age.
For now, the scientists did find some connections between the beneficial bacteria in the transplants and the human diet that could have similar effects, like changes in the metabolism of certain fats and vitamin that could have effects on the inflammatory cells in the eye and brain.
The more you know!
It’s not lying, it’s preemptive truth
Lying is bad. Bold statement, we know, but a true one. After all, God spent an entire commandment telling people not to do the whole bearing false witness thing, and God is generally known for not joking around. He’s a pretty serious dude.
In case you’ve been wandering around the desert for a while and haven’t had wifi, we have a bit of a misinformation problem these days. People lie all the time about a lot of things, and a lot of people believe the lies. According to new research, however, there are also a lot of people who recognize the lies but accept them anyway because they believe that the lies will become true in the future.
Imagine the following scenario: A friend gets a job he’s not qualified for because he listed a skill he doesn’t have. That’s bad, right? And the people the researchers interviewed agreed, at least initially. But when informed that our friend is planning on obtaining the skill in summer classes in the near future, the study participants became far more willing to excuse the initial lie.
A friend jumping the gun on training he doesn’t have yet is fairly innocuous as far as lying goes, but as the researchers found, this willingness to forgive lies because they could become true extends far further. For example, millions of people do not vote illegally in U.S. elections, nor do White people get approved for mortgages at rates 300% higher than minorities, but when asked to imagine scenarios in which those statements could be true, study participants were less likely to condemn the lie and prevent it from spreading further, especially if their political viewpoints aligned with the respective falsehood.
It seems, then, that while we may aspire to not tell lies, we take after another guy with magic powers who spent too much time in the desert: “What I told you was true, from a certain point of view.”
It tastes like feng shui, but it’s not
You know about biomes. You’ve read about various microbiomes. Allow us to introduce you to the envirome,
The envirome “includes all the natural and man-made elements of our environment throughout the lifespan, notably the built environment,” said Robert Schneider, dean of the College of Integrative Medicine at Maharishi International University. Located in – you guessed it – Fairfield, Iowa, and home of the Fighting Transcendentalists. MAHARISHI RULES!
[Editor’s note: You made that up, right? Well, it really is in Iowa, but they don’t seem to have an athletic program.]
In an effort to maximize the envirome’s potential to improve quality of life, Dr. Schneider and his associates systematically integrated the principles of Maharishi Vastu architecture (MVA) into a comprehensive building system. MVA is “a holistic wellness architectural system that aligns buildings with nature’s intelligence, creating balanced, orderly, and integrated living environments with the goal of improving occupants’ lives,” the university explained in a written statement.
Since “modern medicine now recognizes the powerful effects of the ‘envirome’ on health,” Dr. Schneider said in that statement, the researchers reviewed 40 years’ worth of published studies on MVA’s benefits – an analysis that appears in Global Advances in Health and Medicine.
As far as our homes are concerned, here are some of the things MVA says we should be doing:
- The headboard of a bed should be oriented to the east or south when you sleep. This will improve mental health.
- While sitting at a desk or work area, a person should face east or north to improve brain coherence.
- The main entrance of a house should face east because morning light is superior to afternoon light.
And you were worried about feng shui. Well, forget feng shui. Feng shui is for amateurs. MVA is the way to go. MVA is the GOAT. MAHARISHI RULES!
Don’t let FOMI lead to antibiotic overuse
Is fear of missing an infection – call it “FOMI” – leading you to overprescribe antibiotics to your patients?
Inappropriate use of antibiotics can result in adverse events and toxicity, superinfections such as Clostridioides difficile and Methicillin-resistant Staphylococcus aureus, excess mortality and costs, and resistance to the drugs.
All that has been well-known for years, and antibiotic resistance has become a leading public health concern. So why are physicians continuing to overprescribe the drugs?
Speaking at the 2022 annual Internal Medicine Meeting of the American College of Physicians, James “Brad” Cutrell, MD, medical director of antimicrobial stewardship, University of Texas Southwestern Medical Center, Dallas, said clinicians in the United States and elsewhere appear to be falling into a three-part fallacy when it comes to using the drugs: fear of “missing an infection,” coupled with patient expectations that they will leave the office with a prescription and combined with an overemphasis on the potential benefit to the individual at the expense of the risk to society of antibiotic resistance.
Antibiotics are the only drugs that lose their efficacy for all patients over time the more they are used. “For example, if I give a beta blocker to a patient, it’s not going to affect other patients down the road,” Dr. Cutrell said. “It’s not going to lose its efficacy.”
“What we need in medicine is a new culture around antibiotic use,” Dr. Cutrell added. “We need more respect for the dangers of antibiotic misuse and to have confidence in [their] benefits and when they can be used wisely.”
Rampant misuse
Outpatient prescriptions account for at least 60% of antibiotic use in the United States. The rate is even higher in other countries, Dr. Cutrell said during a presentation at the 2022 annual Internal Medicine Meeting of the American College of Physicians.
“About 10% of adult visits and 20% of pediatric visits will result in an antibiotic prescription,” said Dr. Cutrell, noting that prescribing patterns vary widely across the country, with as much as a three-fold difference in some locations. But at least 30% of outpatient antibiotic prescriptions are inappropriately ordered, he said.
“When we look at acute respiratory infections, upwards of 50% are not indicated at all,” he said. Imagine, he added, if the same error rate applied to other medical practices: “What if surgeons were only right 50% of the time, or if the oncologist was only giving the right treatment 50% of the time?”
The most recent Antibiotic Threats Report from the U.S. Centers for Disease Control and Prevention estimated that antibiotic-resistant bacteria and fungi cause more than 2.8 million infections and about 36,000 deaths annually in the United States alone.
How to be a better steward
The core elements for antimicrobial stewardship in the outpatient setting, according to Dr. Cutrell, include making a commitment to optimize prescribing, implementing at least one policy or practice to improve prescribing, monitoring prescribing practices and offering feedback to clinicians, and educating both patients and clinicians.
All that is similar to in-patient stewardship, he said, but outpatient clinicians face a few unique challenges. “Patients are lower acuity, and there is less diagnostic data, and program resources and time are more limited,” he said. Patient satisfaction is also a major driver, and it is also more difficult to measure and track ambulatory antibiotic use.
Interventions have been identified, however, that can help improve stewardship. One is auditing and feedback with peers. “Another [is] commitment posters, which can be placed around the clinic, and that helps set the culture,” he said. “Clinical education and practice guidelines are also important.”
Clinicians should also:
- Observe antibiotic best practices
- Optimize antibiotic selection and dosing
- Practice effective diagnostic stewardship
- Use the shortest duration of therapy necessary
- Avoid antibiotics for inappropriate indications
- Educate patients on when antibiotics are needed
- Follow and become good antibiotic stewardship mentors
“Multiple antibiotic stewardship interventions are effective, particularly those focused on behavioral interventions,” Dr. Cutrell said. “Every provider should follow antibiotic ‘best practices’ and other simple steps to prescribe antibiotics more wisely and to improve patient care.”
Dr. Cutrell reported financial relationships with Gilead Sciences and Regeneron Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Is fear of missing an infection – call it “FOMI” – leading you to overprescribe antibiotics to your patients?
Inappropriate use of antibiotics can result in adverse events and toxicity, superinfections such as Clostridioides difficile and Methicillin-resistant Staphylococcus aureus, excess mortality and costs, and resistance to the drugs.
All that has been well-known for years, and antibiotic resistance has become a leading public health concern. So why are physicians continuing to overprescribe the drugs?
Speaking at the 2022 annual Internal Medicine Meeting of the American College of Physicians, James “Brad” Cutrell, MD, medical director of antimicrobial stewardship, University of Texas Southwestern Medical Center, Dallas, said clinicians in the United States and elsewhere appear to be falling into a three-part fallacy when it comes to using the drugs: fear of “missing an infection,” coupled with patient expectations that they will leave the office with a prescription and combined with an overemphasis on the potential benefit to the individual at the expense of the risk to society of antibiotic resistance.
Antibiotics are the only drugs that lose their efficacy for all patients over time the more they are used. “For example, if I give a beta blocker to a patient, it’s not going to affect other patients down the road,” Dr. Cutrell said. “It’s not going to lose its efficacy.”
“What we need in medicine is a new culture around antibiotic use,” Dr. Cutrell added. “We need more respect for the dangers of antibiotic misuse and to have confidence in [their] benefits and when they can be used wisely.”
Rampant misuse
Outpatient prescriptions account for at least 60% of antibiotic use in the United States. The rate is even higher in other countries, Dr. Cutrell said during a presentation at the 2022 annual Internal Medicine Meeting of the American College of Physicians.
“About 10% of adult visits and 20% of pediatric visits will result in an antibiotic prescription,” said Dr. Cutrell, noting that prescribing patterns vary widely across the country, with as much as a three-fold difference in some locations. But at least 30% of outpatient antibiotic prescriptions are inappropriately ordered, he said.
“When we look at acute respiratory infections, upwards of 50% are not indicated at all,” he said. Imagine, he added, if the same error rate applied to other medical practices: “What if surgeons were only right 50% of the time, or if the oncologist was only giving the right treatment 50% of the time?”
The most recent Antibiotic Threats Report from the U.S. Centers for Disease Control and Prevention estimated that antibiotic-resistant bacteria and fungi cause more than 2.8 million infections and about 36,000 deaths annually in the United States alone.
How to be a better steward
The core elements for antimicrobial stewardship in the outpatient setting, according to Dr. Cutrell, include making a commitment to optimize prescribing, implementing at least one policy or practice to improve prescribing, monitoring prescribing practices and offering feedback to clinicians, and educating both patients and clinicians.
All that is similar to in-patient stewardship, he said, but outpatient clinicians face a few unique challenges. “Patients are lower acuity, and there is less diagnostic data, and program resources and time are more limited,” he said. Patient satisfaction is also a major driver, and it is also more difficult to measure and track ambulatory antibiotic use.
Interventions have been identified, however, that can help improve stewardship. One is auditing and feedback with peers. “Another [is] commitment posters, which can be placed around the clinic, and that helps set the culture,” he said. “Clinical education and practice guidelines are also important.”
Clinicians should also:
- Observe antibiotic best practices
- Optimize antibiotic selection and dosing
- Practice effective diagnostic stewardship
- Use the shortest duration of therapy necessary
- Avoid antibiotics for inappropriate indications
- Educate patients on when antibiotics are needed
- Follow and become good antibiotic stewardship mentors
“Multiple antibiotic stewardship interventions are effective, particularly those focused on behavioral interventions,” Dr. Cutrell said. “Every provider should follow antibiotic ‘best practices’ and other simple steps to prescribe antibiotics more wisely and to improve patient care.”
Dr. Cutrell reported financial relationships with Gilead Sciences and Regeneron Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Is fear of missing an infection – call it “FOMI” – leading you to overprescribe antibiotics to your patients?
Inappropriate use of antibiotics can result in adverse events and toxicity, superinfections such as Clostridioides difficile and Methicillin-resistant Staphylococcus aureus, excess mortality and costs, and resistance to the drugs.
All that has been well-known for years, and antibiotic resistance has become a leading public health concern. So why are physicians continuing to overprescribe the drugs?
Speaking at the 2022 annual Internal Medicine Meeting of the American College of Physicians, James “Brad” Cutrell, MD, medical director of antimicrobial stewardship, University of Texas Southwestern Medical Center, Dallas, said clinicians in the United States and elsewhere appear to be falling into a three-part fallacy when it comes to using the drugs: fear of “missing an infection,” coupled with patient expectations that they will leave the office with a prescription and combined with an overemphasis on the potential benefit to the individual at the expense of the risk to society of antibiotic resistance.
Antibiotics are the only drugs that lose their efficacy for all patients over time the more they are used. “For example, if I give a beta blocker to a patient, it’s not going to affect other patients down the road,” Dr. Cutrell said. “It’s not going to lose its efficacy.”
“What we need in medicine is a new culture around antibiotic use,” Dr. Cutrell added. “We need more respect for the dangers of antibiotic misuse and to have confidence in [their] benefits and when they can be used wisely.”
Rampant misuse
Outpatient prescriptions account for at least 60% of antibiotic use in the United States. The rate is even higher in other countries, Dr. Cutrell said during a presentation at the 2022 annual Internal Medicine Meeting of the American College of Physicians.
“About 10% of adult visits and 20% of pediatric visits will result in an antibiotic prescription,” said Dr. Cutrell, noting that prescribing patterns vary widely across the country, with as much as a three-fold difference in some locations. But at least 30% of outpatient antibiotic prescriptions are inappropriately ordered, he said.
“When we look at acute respiratory infections, upwards of 50% are not indicated at all,” he said. Imagine, he added, if the same error rate applied to other medical practices: “What if surgeons were only right 50% of the time, or if the oncologist was only giving the right treatment 50% of the time?”
The most recent Antibiotic Threats Report from the U.S. Centers for Disease Control and Prevention estimated that antibiotic-resistant bacteria and fungi cause more than 2.8 million infections and about 36,000 deaths annually in the United States alone.
How to be a better steward
The core elements for antimicrobial stewardship in the outpatient setting, according to Dr. Cutrell, include making a commitment to optimize prescribing, implementing at least one policy or practice to improve prescribing, monitoring prescribing practices and offering feedback to clinicians, and educating both patients and clinicians.
All that is similar to in-patient stewardship, he said, but outpatient clinicians face a few unique challenges. “Patients are lower acuity, and there is less diagnostic data, and program resources and time are more limited,” he said. Patient satisfaction is also a major driver, and it is also more difficult to measure and track ambulatory antibiotic use.
Interventions have been identified, however, that can help improve stewardship. One is auditing and feedback with peers. “Another [is] commitment posters, which can be placed around the clinic, and that helps set the culture,” he said. “Clinical education and practice guidelines are also important.”
Clinicians should also:
- Observe antibiotic best practices
- Optimize antibiotic selection and dosing
- Practice effective diagnostic stewardship
- Use the shortest duration of therapy necessary
- Avoid antibiotics for inappropriate indications
- Educate patients on when antibiotics are needed
- Follow and become good antibiotic stewardship mentors
“Multiple antibiotic stewardship interventions are effective, particularly those focused on behavioral interventions,” Dr. Cutrell said. “Every provider should follow antibiotic ‘best practices’ and other simple steps to prescribe antibiotics more wisely and to improve patient care.”
Dr. Cutrell reported financial relationships with Gilead Sciences and Regeneron Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM INTERNAL MEDICINE 2022
Burnout ‘highly prevalent’ in psychiatrists across the globe
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.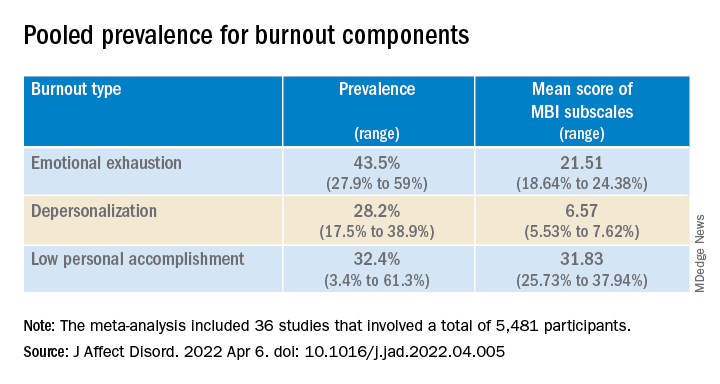
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.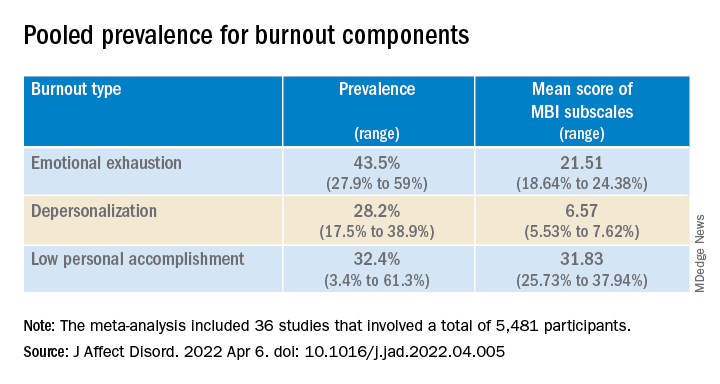
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Burnout in psychiatrists is “highly prevalent” across the globe, new research shows.
In a review and meta-analysis of 36 studies and more than 5,000 psychiatrists in European countries, as well as the United States, Australia, New Zealand, India, Turkey, and Thailand,
“Our review showed that regardless of the identification method of burnout, its prevalence among psychiatrists is high and ranges from 25% to 50%,” lead author Kirill Bykov, MD, a PhD candidate at the Peoples’ Friendship University of Russia (RUDN University), Moscow, Russian Federation, told this news organization.
There was a “high heterogeneity of studies in terms of statistics, screening methods, burnout definitions, and cutoff points in the included studies, which necessitates the unification of future research methodology, but not to the detriment of the development of the theoretical background,” Dr. Bykov said.
The findings were published online in the Journal of Affective Disorders.
‘Unresolved problem’
Although burnout is a serious and prevalent problem among health care workers, little research has focused on burnout in mental health workers compared with other professionals, the investigators noted.
A previous systematic review and meta-analysis that focused specifically on burnout in psychiatrists was limited by methodologic concerns, including that the only burnout screening instrument used in the included studies was the full-length (22-item) MBI.
The current researchers surmised that “the integration of different empirical studies of psychiatrists’ burnout prevalence [remained] an unresolved problem.”
Dr. Bykov noted the current review was “investigator-initiated” and was a part of his PhD dissertation.
“Studying the works devoted to the burnout of psychiatrists, I drew attention to the varying prevalence rates of this phenomenon among them. This prompted me to conduct a systematic review of the literature and summarize the available data,” he said.
Unlike the previous review, the current one “does not contain restrictions regarding the place of research, publication language, covered burnout concepts, definitions, and screening instruments. Thus, its results will be helpful for practitioners and scientists around the world,” Dr. Bykov added.
Among the inclusion criteria was that a study should be empirical and quantitative, contain at least 20 practicing psychiatrists as participants, use a valid and reliable burnout screening instrument, have at least one burnout metric extractable specifically with regard to psychiatrists, and have a national survey or a response rate among psychiatrists of 20% or greater.
Qualitative or review articles or studies consisting of psychiatric trainees (such as medical students or residents) or nonpracticing psychiatrists were excluded.
Pooled prevalence
The researchers included 36 studies that comprised 5,481 participants (51.3% were women; mean age, 46.7 years). All studies had from 20 to 1,157 participants. They were employed in an array of settings in 19 countries.
In 22 studies, survey years ranged from 1996 to 2018; 14 studies did not report the year of data collection.
Most studies (75%) used some version of the MBI, and 19 studies used the full-length 22-item MBI Human Service Survey (MBI-HSS) . The survey rates emotional exhaustion (EE), depersonalization (DP), and low personal achievement (PA) on a 7-point Likert scale from 0 (“never”) to 6 (“almost every day”).
Other instruments included the CBI, the 16-item Oldenburg Burnout Inventory, the 21-item Tedium Measure, the 30-item Professional Quality of Life measure, the Rohland et al. Single-Item Measure of Self-Perceived Burnout, and the 21-item Brief Burnout Questionnaire.
Only three studies were free of methodologic limitations. The remaining 33 studies had some problems, such as not reporting the response rate or comparability between responders and nonresponders.
Results showed that the overall prevalence of burnout, as measured by the MBI and the CBI, was 25.9% (range, 11.1%-40.75%) and 50.3% (range, 30.9%-69.8%), respectively.
The pooled prevalence for burnout components is shown in the table.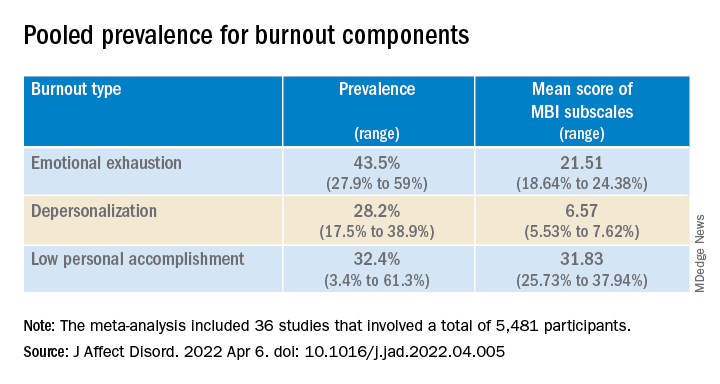
European psychiatrists had lower EE scores (20.82; 95% confidence interval, 7.24-4.41) compared with their non-European counterparts (24.99; 95% CI, 23.05-26.94; P = .045).
‘Carry the hope’
In a comment, Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness (NAMI), said she was surprised the burnout numbers weren’t higher.
Many colleagues she interacts with “have been experiencing pretty significant burnout that has only been exacerbated by the pandemic and ever-growing demand for mental health providers, and there aren’t enough to meet that demand,” said Dr. Crawford, a psychiatrist at Boston Medical Center’s Outpatient Child and Adolescent Psychiatry Clinic and at Codman Square Health Center. She was not involved with the current research.
Dr. Crawford noted that much of the data was from Europeans. Speaking to the experience of U.S.-based psychiatrists, she said there is a “greater appreciation for what we do as mental health providers, due to the growing conversations around mental health and normalizing mental health conditions.”
On the other hand, there is “a lack of parity in reimbursement rates. Although the general public values mental health, the medical system doesn’t value mental health providers in the same way as physicians in other specialties,” Dr. Crawford said. Feeling devalued can contribute to burnout, she added.
One way to counter burnout is to remember “that our role is to carry the hope. We can be hopeful for the patient that the treatment will work or the medications can provide some relief,” Dr. Crawford noted.
Psychiatrists “may need to hold on tightly to that hope because we may not receive that instant gratification from the patient or receive praise or see the change from the patient during that time, which can be challenging,” she said.
“But it’s important for us to keep in mind that, even in that moment when the patient can’t see it, we can work alongside the patient to create the vision of hope and what it will look like in the future,” said Dr. Crawford.
In the 2022 Medscape Psychiatrist Lifestyle, Happiness & Burnout Report, an annual online survey of Medscape member physicians, 47% of respondents reported burnout – which was up from 42% the previous year.
The investigators received no funding for this work. They and Dr. Crawford report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF AFFECTIVE DISORDERS