User login
For MD-IQ use only
Reading Chekhov on the Cancer Ward
Burnout and other forms of psychosocial distress are common among health care professionals necessitating measures to promote well-being and reduce burnout.1 Studies have shown that nonmedical reading is associated with low burnout and that small group study sections can promote wellness.2,3 Narrative medicine, which proposes a model for humane and effective medical practice, advocates for the necessity of narrative competence.
Short Story Club
Narrative competence is the ability to acknowledge, interpret, and act on the stories of others. The narrative skill of close reading also encourages reflective practice, equipping practitioners to better weather the tides of illness.4 In our case, we formed a short story club intervention to closely read, or read and reflect, on literary fiction. We explored how reading and reflecting would result in profound changes in thinking and feeling and noted different ways by which they can cause such well-being. We describe here the 7 ways in which stories led us to increase bonding, improve empathy, and promote meaning in medicine.
Slowing Down
The short story club helped to bond us together and increase our sense of meaning in medicine by slowing us down. One member of the group likened the experience to increasing the pixels in a painting, thereby improving the resolution and seeing more clearly. Another member mentioned the experience as a form of meditation in slowing down the brain, breathing in the story, and breathing out impressions. One story by Anatole Broyard emphasized the importance of slowing down and “brooding” over a patient.5 The author describes his experience as a prostate cancer patient, in which his body was treated but his story was ignored. He begged his doctors to pay more attention to his story to listen and to brood over him. This story was enlightening to us; we saw how desperate our patients are to tell their stories, and for us to hear their stories.
Mirrors and Windows
Another way reading and reflecting on short stories helped was by reflecting our practices to ourselves, as though looking into a mirror to see ourselves and out of a window to see others. We found that stories mirrored our own world and allowed us to discuss issues close to us without the embarrassment or stigma of owning the story. In one session we read “The Doctor’s Visit” by Anton Chekhov.6 Some of the members resonated with the doctor of this story who awkwardly attended to his lady patient whose son was dying of a brain tumor. The doctor was nervous, insecure, and unable to express any empathy. He was also the father of the child who was dying and refused to admit any responsibility. One member of the group stated that he could relate to the doctor’s insecurities and mentioned that he too felt insecure and even sometimes felt like an imposter. This led to a discussion of insecurities, ways to bolster self-confidence, and ways to accept and respect limitations. This was a conversation that may not have taken place without the story as anchor to discuss insecurities that we individually may not have been willing to admit to the group.
In a different session, we discussed the story “Interpreter of Maladies” by Jhumpa Lahiri in which a settled Indian American family returns to India to tour and learn about their heritage from a guide (the interpreter of maladies) who interpreted the culture for them.7 The family professed to be interested in knowing about the culture but could not concentrate: the wife stayed busy flirting with the guide and revealing outrageous secrets to him, the children were engrossed in their squabbles, and the father was essentially absent taking photographs as souvenirs instead of seeing the sites firsthand. Some of the members of the group were Indian American and could relate to the alienation from their home and nostalgia for their country, while others could relate to the same alienation, albeit from other cultures and countries. This allowed us to talk about deeply personal topics, without having to own the topic or reveal personal issues. The discussion led to a deep understanding and empathy for us and our colleagues knowing the pain of alienation that some of them felt but could not discuss.
The stories also served as windows into the world of others which enabled us to see and become the other. For example, in one session we reflected on “Babylon Revisited” by F. Scott Fitzgerald.8 In this story, an American man returns to Paris after the Great Depression and recalls his life as a young artist in the American artist expatriate community of Paris in the 1920s and 1930s. During that time, he partied, drank in excess, lost his wife to pneumonia (for which he was at least partially responsible), lost custody of his daughter, and lost his fortune. As he returned to Paris to try to reclaim his daughter, we feel his pain as he tries but fails to overcome chronic alcoholism, sexual indiscretions, and losses. This gave rise to discussion of losses in general as we became one with the main character. This increased our empathy for others in a way that could not have been possible without this short story as anchor.
In another session we reflected on “Hills Like White Elephants” by Ernest Hemingway, in which a man is waiting for a train while proposing his girlfriend get an abortion.9 She agonizes over her choices and makes no decision in this story. Yet, we the reader could “become” the woman in the story faced with hard choices of having a baby but losing the man she loves, or having an abortion and maybe losing him anyway. In becoming this woman, we could experience the complex emotions and feel an experience of the other.
Exploring the Taboo
A third aspect of the club was enabling discussion of controversial topics. There were topics that arose in the group which never would have arisen in clinical practice discussions. These had to do with the taboo topics such as romantic attachments to patients. We read “The Caves of Lascaux” and reflected on the story of a young doctor who becomes enamored and obsessed with his beautiful but dying patient.10 He becomes so obsessed with her that he almost abandons his wife, family, and stable livelihood to descend with her into the caves. This story gave rise to discussions about romantic attachment to patients and how to handle and extricate one from the situation. The senior doctors explained some of their relevant experiences and how they either transferred care or sought counseling to extricate themselves from a potentially dangerous situation, especially when they too fell under the spell of forbidden romance.
Moral Grounding
These sessions also served to define the moral basis of our own practice. Much of health care psychosocial distress is related to moral injury in which health care professionals do the wrong thing or fail to do the right thing at the right time, due to external pressures related to financial or other gains. Reading and reflecting put us face-to-face with moral dilemmas and let us find our moral grounding. In reading “The Haircut” by Ring Lardner, we explored the disruptive town scoundrel who harassed and tortured his friends and neighbors but in such outrageous ways that he was considered a comedian rather than an abuser.11 Despite his hurtful acts, the townspeople (including the narrator) considered him a clown and laughed at his racist and sexist statements as well as his tricks.He faced no consequences such as confrontation, until the end when fate caught up. This story gave rise to a discussion of how we handle unkind, racist, sexist, or other comments which are disguised as humor, and to what extent we tolerate such controversial behavior. Do we go along with the scoundrel and laugh, or do we confront such people and insist that they respect and honor other people? The story sensitized the group to the ways in which prejudice and racism or sexism can be masked as humor, and to consider our moral responsibilities in society.
In another session we read and reflected on “Three Questions” by Leo Tolstoy.12 In this story, a king travels to another territory but gets distracted by helping a neighbor in need, and thereby inadvertently and fortunately avoids the trap that had been devised to kill him. The author gives us his moral basis by asking and answering 3 questions: Who is the most important person? What is the most important thing to do? What is the most important thing to do now? His answers provided his moral grounding. We discussed our answers and the basis of our moral grounding, whether it be the injunction do no harm, the more complex religious backgrounds of our childhood, or otherwise.
Symbols and Metaphors
The practice of reading and reflecting also taught us symbols and metaphors. Symbols and metaphors are the essence of storytelling, and they provide keys to understanding people. We sought out and studied the metaphors and symbols in each of the stories we read. In “I Stood There Ironing”, a woman is ironing as she is being questioned by a social worker on the upbringing of her first daughter, and its impact on her psychosocial distress.13 The woman remembers the hardships in raising her daughter and her neglect and abuse of the child due to circumstances beyond her control. She keeps ironing back and forth as she recounts the ways in which she neglected her child. The ironing provides a metaphor for attempting to straighten out her life and for recognizing finally at the end of the story that the daughter should not be the dress, under which her iron is pressing. This gave rise to a discussion of metaphors in our lives and the meanings they carry.
Problem-solving Guide
A sixth way the reflections helped was by serving as a guide to solving our problems. Some of the stories we read resonated deeply with members of the group and provided guides to solving problems. In one meeting we discussed “Those Are as Brothers” by Nancy Hale, a story in which a Nazi concentration camp survivor finds refuge in a country home and develops a friendship with a survivor of an abusive marriage.14 Reading and reflecting on this story enabled us to see the impact of trauma on ourselves, our life choices, professions, ways of being, philosophies, and even on our next generation. The story was personal for several members of the group, some of whom were second-generation Holocaust survivors, and for one who admitted to severe trauma as a child. Discussing our backgrounds together, we empathized with each other and helped each other heal. The story also provided a guide to healing from trauma, as its title indicates: sharing stories together can be a way to heal. The solidarity of standing together, as brothers, heals. The concentration camp survivor was mistreated in his job, but the abuse trauma victim rushes to his defense and vows her friendship and support. This soothed his soul and healed his mind. The guidance is clear: we can do the same, find friends, treat them like brothers, support each other and heal.
Bonding Through Shared Experience
The final and possibly most important way in which the club helped was by serving as an adventure to bond group members together through shared experience. We believe that literature can capture imagination in extraordinary ways and provide an opportunity to undertake remarkable journeys. As such, together we traveled to the ends of the earth from the beginning to the end of time and beyond. We traveled through the hills of Africa, meandered in the streets of Russia and Poland, watched the racetracks in Italy, toured the Taj Mahal in India, and descended into the caves of Lascaux, all while working in Little Rock, Arkansas. We shared a wide array of experiences together, which allowed us to know ourselves and others better, to share stories, and to develop a common vision, common ground, and common culture.
Conclusions
Through reading and reflecting on stories, we bonded as a group, increased our empathy for each other and others, and found meaning in medicine. Other studies have shown that participation in small study groups promote physician well-being, improve job satisfaction, and decrease burnout.3 We synergized this effort by reading nonmedical stories on a consistent basis, hoping to gain resilience to psychosocial distress.3 We chose short stories rather than novels to minimize any stress from excess reading. Combining these interventions, small group studies and nonmedical reading, into a single intervention as is typical in the practice of narrative medicine may provide a way to improve team functioning.
This pilot study showed that it is possible to form short story clubs even in a busy oncology program and that such programs benefit participants in a variety of ways with no apparent adverse effects. Further research is needed to study the impact of reading and reflecting on medical work in small study groups in larger numbers of subjects and to evaluate their impact on burnout. Further study is also needed to develop narrative medicine curricula that best address the needs of particular subspecialties and to determine the optimal conditions for implementation.
Acknowledgments
The authors acknowledge Dr. Erick Messias for inspiring and encouraging this project at the University of Arkansas for Medical Sciences where he was Associate Dean for Faculty Affairs. He is presently Chair of Psychiatry and Behavioral Neuroscience at the St. Louis University School of Medicine, St. Louis, Missouri.
1. Messias E, Gathright MM, Freeman ES, et al. Differences in burnout prevalence between clinical professionals and biomedical scientists in an academic medical centre: a cross-sectional survey. BMJ Open. 2019;9(2):e023506. doi:10.1136/bmjopen-2018-023506
2. Marchalik D, Rodriguez A, Namath A, et al. The impact of non-medical reading on clinical burnout: a national survey of palliative care providers. Ann Palliat Med. 2019;8(4):428-435. doi:10.21037/apm.2019.05.02
3. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533. doi:10.1001/jamainternmed.2013.14387
4. Charon R. Narrative medicine: a model for empathy, reflection, profession, and tust. JAMA. 2001;286(15):1897–1902. doi:10.1001/jama.286.15.1897
5. Broyard A. Doctor Talk to Me. August 26, 1990. Accessed September 2021. https://www.nytimes.com/1990/08/26/magazine/doctor-talk-to-me.html
6. Chekhov A. A Doctor’s Visit,. In: Reynolds R, Stone J, eds. On Doctoring. Simon and Shuster;1995:50-59.
7. Lahiri J. Interpreter of Maladies. In: Lahiri J. Interpreter of Maladies. Mariner Books;2019.
8. Fitzgerald FS. Babylon Revisited. In: Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:62-81.
9. Hemingway E. Hills like White Elephants. In: Reynolds R, Stone J, eds. On Doctoring. Simon and Shuster;1995:108-111.
10. Karmel M. Caves of Lascaux. In: Ofri D, Staff of the Bellavue Literary Review, eds. The Best of the Bellevue Literary Review. Bellevue Literary Press;2008:168-174.
11. Lardner R. The Haircut. In Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:48-61.
12. Tolstoy L. The Three Questions. Accessed September 2021. https://www.plough.com/en/topics/culture/short-stories/the-three-questions
13. Olsen T. I Stand Here Ironing. In Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:173-180.
14. Hale N. Those Are as Brothers. In: Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:132-141.
Burnout and other forms of psychosocial distress are common among health care professionals necessitating measures to promote well-being and reduce burnout.1 Studies have shown that nonmedical reading is associated with low burnout and that small group study sections can promote wellness.2,3 Narrative medicine, which proposes a model for humane and effective medical practice, advocates for the necessity of narrative competence.
Short Story Club
Narrative competence is the ability to acknowledge, interpret, and act on the stories of others. The narrative skill of close reading also encourages reflective practice, equipping practitioners to better weather the tides of illness.4 In our case, we formed a short story club intervention to closely read, or read and reflect, on literary fiction. We explored how reading and reflecting would result in profound changes in thinking and feeling and noted different ways by which they can cause such well-being. We describe here the 7 ways in which stories led us to increase bonding, improve empathy, and promote meaning in medicine.
Slowing Down
The short story club helped to bond us together and increase our sense of meaning in medicine by slowing us down. One member of the group likened the experience to increasing the pixels in a painting, thereby improving the resolution and seeing more clearly. Another member mentioned the experience as a form of meditation in slowing down the brain, breathing in the story, and breathing out impressions. One story by Anatole Broyard emphasized the importance of slowing down and “brooding” over a patient.5 The author describes his experience as a prostate cancer patient, in which his body was treated but his story was ignored. He begged his doctors to pay more attention to his story to listen and to brood over him. This story was enlightening to us; we saw how desperate our patients are to tell their stories, and for us to hear their stories.
Mirrors and Windows
Another way reading and reflecting on short stories helped was by reflecting our practices to ourselves, as though looking into a mirror to see ourselves and out of a window to see others. We found that stories mirrored our own world and allowed us to discuss issues close to us without the embarrassment or stigma of owning the story. In one session we read “The Doctor’s Visit” by Anton Chekhov.6 Some of the members resonated with the doctor of this story who awkwardly attended to his lady patient whose son was dying of a brain tumor. The doctor was nervous, insecure, and unable to express any empathy. He was also the father of the child who was dying and refused to admit any responsibility. One member of the group stated that he could relate to the doctor’s insecurities and mentioned that he too felt insecure and even sometimes felt like an imposter. This led to a discussion of insecurities, ways to bolster self-confidence, and ways to accept and respect limitations. This was a conversation that may not have taken place without the story as anchor to discuss insecurities that we individually may not have been willing to admit to the group.
In a different session, we discussed the story “Interpreter of Maladies” by Jhumpa Lahiri in which a settled Indian American family returns to India to tour and learn about their heritage from a guide (the interpreter of maladies) who interpreted the culture for them.7 The family professed to be interested in knowing about the culture but could not concentrate: the wife stayed busy flirting with the guide and revealing outrageous secrets to him, the children were engrossed in their squabbles, and the father was essentially absent taking photographs as souvenirs instead of seeing the sites firsthand. Some of the members of the group were Indian American and could relate to the alienation from their home and nostalgia for their country, while others could relate to the same alienation, albeit from other cultures and countries. This allowed us to talk about deeply personal topics, without having to own the topic or reveal personal issues. The discussion led to a deep understanding and empathy for us and our colleagues knowing the pain of alienation that some of them felt but could not discuss.
The stories also served as windows into the world of others which enabled us to see and become the other. For example, in one session we reflected on “Babylon Revisited” by F. Scott Fitzgerald.8 In this story, an American man returns to Paris after the Great Depression and recalls his life as a young artist in the American artist expatriate community of Paris in the 1920s and 1930s. During that time, he partied, drank in excess, lost his wife to pneumonia (for which he was at least partially responsible), lost custody of his daughter, and lost his fortune. As he returned to Paris to try to reclaim his daughter, we feel his pain as he tries but fails to overcome chronic alcoholism, sexual indiscretions, and losses. This gave rise to discussion of losses in general as we became one with the main character. This increased our empathy for others in a way that could not have been possible without this short story as anchor.
In another session we reflected on “Hills Like White Elephants” by Ernest Hemingway, in which a man is waiting for a train while proposing his girlfriend get an abortion.9 She agonizes over her choices and makes no decision in this story. Yet, we the reader could “become” the woman in the story faced with hard choices of having a baby but losing the man she loves, or having an abortion and maybe losing him anyway. In becoming this woman, we could experience the complex emotions and feel an experience of the other.
Exploring the Taboo
A third aspect of the club was enabling discussion of controversial topics. There were topics that arose in the group which never would have arisen in clinical practice discussions. These had to do with the taboo topics such as romantic attachments to patients. We read “The Caves of Lascaux” and reflected on the story of a young doctor who becomes enamored and obsessed with his beautiful but dying patient.10 He becomes so obsessed with her that he almost abandons his wife, family, and stable livelihood to descend with her into the caves. This story gave rise to discussions about romantic attachment to patients and how to handle and extricate one from the situation. The senior doctors explained some of their relevant experiences and how they either transferred care or sought counseling to extricate themselves from a potentially dangerous situation, especially when they too fell under the spell of forbidden romance.
Moral Grounding
These sessions also served to define the moral basis of our own practice. Much of health care psychosocial distress is related to moral injury in which health care professionals do the wrong thing or fail to do the right thing at the right time, due to external pressures related to financial or other gains. Reading and reflecting put us face-to-face with moral dilemmas and let us find our moral grounding. In reading “The Haircut” by Ring Lardner, we explored the disruptive town scoundrel who harassed and tortured his friends and neighbors but in such outrageous ways that he was considered a comedian rather than an abuser.11 Despite his hurtful acts, the townspeople (including the narrator) considered him a clown and laughed at his racist and sexist statements as well as his tricks.He faced no consequences such as confrontation, until the end when fate caught up. This story gave rise to a discussion of how we handle unkind, racist, sexist, or other comments which are disguised as humor, and to what extent we tolerate such controversial behavior. Do we go along with the scoundrel and laugh, or do we confront such people and insist that they respect and honor other people? The story sensitized the group to the ways in which prejudice and racism or sexism can be masked as humor, and to consider our moral responsibilities in society.
In another session we read and reflected on “Three Questions” by Leo Tolstoy.12 In this story, a king travels to another territory but gets distracted by helping a neighbor in need, and thereby inadvertently and fortunately avoids the trap that had been devised to kill him. The author gives us his moral basis by asking and answering 3 questions: Who is the most important person? What is the most important thing to do? What is the most important thing to do now? His answers provided his moral grounding. We discussed our answers and the basis of our moral grounding, whether it be the injunction do no harm, the more complex religious backgrounds of our childhood, or otherwise.
Symbols and Metaphors
The practice of reading and reflecting also taught us symbols and metaphors. Symbols and metaphors are the essence of storytelling, and they provide keys to understanding people. We sought out and studied the metaphors and symbols in each of the stories we read. In “I Stood There Ironing”, a woman is ironing as she is being questioned by a social worker on the upbringing of her first daughter, and its impact on her psychosocial distress.13 The woman remembers the hardships in raising her daughter and her neglect and abuse of the child due to circumstances beyond her control. She keeps ironing back and forth as she recounts the ways in which she neglected her child. The ironing provides a metaphor for attempting to straighten out her life and for recognizing finally at the end of the story that the daughter should not be the dress, under which her iron is pressing. This gave rise to a discussion of metaphors in our lives and the meanings they carry.
Problem-solving Guide
A sixth way the reflections helped was by serving as a guide to solving our problems. Some of the stories we read resonated deeply with members of the group and provided guides to solving problems. In one meeting we discussed “Those Are as Brothers” by Nancy Hale, a story in which a Nazi concentration camp survivor finds refuge in a country home and develops a friendship with a survivor of an abusive marriage.14 Reading and reflecting on this story enabled us to see the impact of trauma on ourselves, our life choices, professions, ways of being, philosophies, and even on our next generation. The story was personal for several members of the group, some of whom were second-generation Holocaust survivors, and for one who admitted to severe trauma as a child. Discussing our backgrounds together, we empathized with each other and helped each other heal. The story also provided a guide to healing from trauma, as its title indicates: sharing stories together can be a way to heal. The solidarity of standing together, as brothers, heals. The concentration camp survivor was mistreated in his job, but the abuse trauma victim rushes to his defense and vows her friendship and support. This soothed his soul and healed his mind. The guidance is clear: we can do the same, find friends, treat them like brothers, support each other and heal.
Bonding Through Shared Experience
The final and possibly most important way in which the club helped was by serving as an adventure to bond group members together through shared experience. We believe that literature can capture imagination in extraordinary ways and provide an opportunity to undertake remarkable journeys. As such, together we traveled to the ends of the earth from the beginning to the end of time and beyond. We traveled through the hills of Africa, meandered in the streets of Russia and Poland, watched the racetracks in Italy, toured the Taj Mahal in India, and descended into the caves of Lascaux, all while working in Little Rock, Arkansas. We shared a wide array of experiences together, which allowed us to know ourselves and others better, to share stories, and to develop a common vision, common ground, and common culture.
Conclusions
Through reading and reflecting on stories, we bonded as a group, increased our empathy for each other and others, and found meaning in medicine. Other studies have shown that participation in small study groups promote physician well-being, improve job satisfaction, and decrease burnout.3 We synergized this effort by reading nonmedical stories on a consistent basis, hoping to gain resilience to psychosocial distress.3 We chose short stories rather than novels to minimize any stress from excess reading. Combining these interventions, small group studies and nonmedical reading, into a single intervention as is typical in the practice of narrative medicine may provide a way to improve team functioning.
This pilot study showed that it is possible to form short story clubs even in a busy oncology program and that such programs benefit participants in a variety of ways with no apparent adverse effects. Further research is needed to study the impact of reading and reflecting on medical work in small study groups in larger numbers of subjects and to evaluate their impact on burnout. Further study is also needed to develop narrative medicine curricula that best address the needs of particular subspecialties and to determine the optimal conditions for implementation.
Acknowledgments
The authors acknowledge Dr. Erick Messias for inspiring and encouraging this project at the University of Arkansas for Medical Sciences where he was Associate Dean for Faculty Affairs. He is presently Chair of Psychiatry and Behavioral Neuroscience at the St. Louis University School of Medicine, St. Louis, Missouri.
Burnout and other forms of psychosocial distress are common among health care professionals necessitating measures to promote well-being and reduce burnout.1 Studies have shown that nonmedical reading is associated with low burnout and that small group study sections can promote wellness.2,3 Narrative medicine, which proposes a model for humane and effective medical practice, advocates for the necessity of narrative competence.
Short Story Club
Narrative competence is the ability to acknowledge, interpret, and act on the stories of others. The narrative skill of close reading also encourages reflective practice, equipping practitioners to better weather the tides of illness.4 In our case, we formed a short story club intervention to closely read, or read and reflect, on literary fiction. We explored how reading and reflecting would result in profound changes in thinking and feeling and noted different ways by which they can cause such well-being. We describe here the 7 ways in which stories led us to increase bonding, improve empathy, and promote meaning in medicine.
Slowing Down
The short story club helped to bond us together and increase our sense of meaning in medicine by slowing us down. One member of the group likened the experience to increasing the pixels in a painting, thereby improving the resolution and seeing more clearly. Another member mentioned the experience as a form of meditation in slowing down the brain, breathing in the story, and breathing out impressions. One story by Anatole Broyard emphasized the importance of slowing down and “brooding” over a patient.5 The author describes his experience as a prostate cancer patient, in which his body was treated but his story was ignored. He begged his doctors to pay more attention to his story to listen and to brood over him. This story was enlightening to us; we saw how desperate our patients are to tell their stories, and for us to hear their stories.
Mirrors and Windows
Another way reading and reflecting on short stories helped was by reflecting our practices to ourselves, as though looking into a mirror to see ourselves and out of a window to see others. We found that stories mirrored our own world and allowed us to discuss issues close to us without the embarrassment or stigma of owning the story. In one session we read “The Doctor’s Visit” by Anton Chekhov.6 Some of the members resonated with the doctor of this story who awkwardly attended to his lady patient whose son was dying of a brain tumor. The doctor was nervous, insecure, and unable to express any empathy. He was also the father of the child who was dying and refused to admit any responsibility. One member of the group stated that he could relate to the doctor’s insecurities and mentioned that he too felt insecure and even sometimes felt like an imposter. This led to a discussion of insecurities, ways to bolster self-confidence, and ways to accept and respect limitations. This was a conversation that may not have taken place without the story as anchor to discuss insecurities that we individually may not have been willing to admit to the group.
In a different session, we discussed the story “Interpreter of Maladies” by Jhumpa Lahiri in which a settled Indian American family returns to India to tour and learn about their heritage from a guide (the interpreter of maladies) who interpreted the culture for them.7 The family professed to be interested in knowing about the culture but could not concentrate: the wife stayed busy flirting with the guide and revealing outrageous secrets to him, the children were engrossed in their squabbles, and the father was essentially absent taking photographs as souvenirs instead of seeing the sites firsthand. Some of the members of the group were Indian American and could relate to the alienation from their home and nostalgia for their country, while others could relate to the same alienation, albeit from other cultures and countries. This allowed us to talk about deeply personal topics, without having to own the topic or reveal personal issues. The discussion led to a deep understanding and empathy for us and our colleagues knowing the pain of alienation that some of them felt but could not discuss.
The stories also served as windows into the world of others which enabled us to see and become the other. For example, in one session we reflected on “Babylon Revisited” by F. Scott Fitzgerald.8 In this story, an American man returns to Paris after the Great Depression and recalls his life as a young artist in the American artist expatriate community of Paris in the 1920s and 1930s. During that time, he partied, drank in excess, lost his wife to pneumonia (for which he was at least partially responsible), lost custody of his daughter, and lost his fortune. As he returned to Paris to try to reclaim his daughter, we feel his pain as he tries but fails to overcome chronic alcoholism, sexual indiscretions, and losses. This gave rise to discussion of losses in general as we became one with the main character. This increased our empathy for others in a way that could not have been possible without this short story as anchor.
In another session we reflected on “Hills Like White Elephants” by Ernest Hemingway, in which a man is waiting for a train while proposing his girlfriend get an abortion.9 She agonizes over her choices and makes no decision in this story. Yet, we the reader could “become” the woman in the story faced with hard choices of having a baby but losing the man she loves, or having an abortion and maybe losing him anyway. In becoming this woman, we could experience the complex emotions and feel an experience of the other.
Exploring the Taboo
A third aspect of the club was enabling discussion of controversial topics. There were topics that arose in the group which never would have arisen in clinical practice discussions. These had to do with the taboo topics such as romantic attachments to patients. We read “The Caves of Lascaux” and reflected on the story of a young doctor who becomes enamored and obsessed with his beautiful but dying patient.10 He becomes so obsessed with her that he almost abandons his wife, family, and stable livelihood to descend with her into the caves. This story gave rise to discussions about romantic attachment to patients and how to handle and extricate one from the situation. The senior doctors explained some of their relevant experiences and how they either transferred care or sought counseling to extricate themselves from a potentially dangerous situation, especially when they too fell under the spell of forbidden romance.
Moral Grounding
These sessions also served to define the moral basis of our own practice. Much of health care psychosocial distress is related to moral injury in which health care professionals do the wrong thing or fail to do the right thing at the right time, due to external pressures related to financial or other gains. Reading and reflecting put us face-to-face with moral dilemmas and let us find our moral grounding. In reading “The Haircut” by Ring Lardner, we explored the disruptive town scoundrel who harassed and tortured his friends and neighbors but in such outrageous ways that he was considered a comedian rather than an abuser.11 Despite his hurtful acts, the townspeople (including the narrator) considered him a clown and laughed at his racist and sexist statements as well as his tricks.He faced no consequences such as confrontation, until the end when fate caught up. This story gave rise to a discussion of how we handle unkind, racist, sexist, or other comments which are disguised as humor, and to what extent we tolerate such controversial behavior. Do we go along with the scoundrel and laugh, or do we confront such people and insist that they respect and honor other people? The story sensitized the group to the ways in which prejudice and racism or sexism can be masked as humor, and to consider our moral responsibilities in society.
In another session we read and reflected on “Three Questions” by Leo Tolstoy.12 In this story, a king travels to another territory but gets distracted by helping a neighbor in need, and thereby inadvertently and fortunately avoids the trap that had been devised to kill him. The author gives us his moral basis by asking and answering 3 questions: Who is the most important person? What is the most important thing to do? What is the most important thing to do now? His answers provided his moral grounding. We discussed our answers and the basis of our moral grounding, whether it be the injunction do no harm, the more complex religious backgrounds of our childhood, or otherwise.
Symbols and Metaphors
The practice of reading and reflecting also taught us symbols and metaphors. Symbols and metaphors are the essence of storytelling, and they provide keys to understanding people. We sought out and studied the metaphors and symbols in each of the stories we read. In “I Stood There Ironing”, a woman is ironing as she is being questioned by a social worker on the upbringing of her first daughter, and its impact on her psychosocial distress.13 The woman remembers the hardships in raising her daughter and her neglect and abuse of the child due to circumstances beyond her control. She keeps ironing back and forth as she recounts the ways in which she neglected her child. The ironing provides a metaphor for attempting to straighten out her life and for recognizing finally at the end of the story that the daughter should not be the dress, under which her iron is pressing. This gave rise to a discussion of metaphors in our lives and the meanings they carry.
Problem-solving Guide
A sixth way the reflections helped was by serving as a guide to solving our problems. Some of the stories we read resonated deeply with members of the group and provided guides to solving problems. In one meeting we discussed “Those Are as Brothers” by Nancy Hale, a story in which a Nazi concentration camp survivor finds refuge in a country home and develops a friendship with a survivor of an abusive marriage.14 Reading and reflecting on this story enabled us to see the impact of trauma on ourselves, our life choices, professions, ways of being, philosophies, and even on our next generation. The story was personal for several members of the group, some of whom were second-generation Holocaust survivors, and for one who admitted to severe trauma as a child. Discussing our backgrounds together, we empathized with each other and helped each other heal. The story also provided a guide to healing from trauma, as its title indicates: sharing stories together can be a way to heal. The solidarity of standing together, as brothers, heals. The concentration camp survivor was mistreated in his job, but the abuse trauma victim rushes to his defense and vows her friendship and support. This soothed his soul and healed his mind. The guidance is clear: we can do the same, find friends, treat them like brothers, support each other and heal.
Bonding Through Shared Experience
The final and possibly most important way in which the club helped was by serving as an adventure to bond group members together through shared experience. We believe that literature can capture imagination in extraordinary ways and provide an opportunity to undertake remarkable journeys. As such, together we traveled to the ends of the earth from the beginning to the end of time and beyond. We traveled through the hills of Africa, meandered in the streets of Russia and Poland, watched the racetracks in Italy, toured the Taj Mahal in India, and descended into the caves of Lascaux, all while working in Little Rock, Arkansas. We shared a wide array of experiences together, which allowed us to know ourselves and others better, to share stories, and to develop a common vision, common ground, and common culture.
Conclusions
Through reading and reflecting on stories, we bonded as a group, increased our empathy for each other and others, and found meaning in medicine. Other studies have shown that participation in small study groups promote physician well-being, improve job satisfaction, and decrease burnout.3 We synergized this effort by reading nonmedical stories on a consistent basis, hoping to gain resilience to psychosocial distress.3 We chose short stories rather than novels to minimize any stress from excess reading. Combining these interventions, small group studies and nonmedical reading, into a single intervention as is typical in the practice of narrative medicine may provide a way to improve team functioning.
This pilot study showed that it is possible to form short story clubs even in a busy oncology program and that such programs benefit participants in a variety of ways with no apparent adverse effects. Further research is needed to study the impact of reading and reflecting on medical work in small study groups in larger numbers of subjects and to evaluate their impact on burnout. Further study is also needed to develop narrative medicine curricula that best address the needs of particular subspecialties and to determine the optimal conditions for implementation.
Acknowledgments
The authors acknowledge Dr. Erick Messias for inspiring and encouraging this project at the University of Arkansas for Medical Sciences where he was Associate Dean for Faculty Affairs. He is presently Chair of Psychiatry and Behavioral Neuroscience at the St. Louis University School of Medicine, St. Louis, Missouri.
1. Messias E, Gathright MM, Freeman ES, et al. Differences in burnout prevalence between clinical professionals and biomedical scientists in an academic medical centre: a cross-sectional survey. BMJ Open. 2019;9(2):e023506. doi:10.1136/bmjopen-2018-023506
2. Marchalik D, Rodriguez A, Namath A, et al. The impact of non-medical reading on clinical burnout: a national survey of palliative care providers. Ann Palliat Med. 2019;8(4):428-435. doi:10.21037/apm.2019.05.02
3. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533. doi:10.1001/jamainternmed.2013.14387
4. Charon R. Narrative medicine: a model for empathy, reflection, profession, and tust. JAMA. 2001;286(15):1897–1902. doi:10.1001/jama.286.15.1897
5. Broyard A. Doctor Talk to Me. August 26, 1990. Accessed September 2021. https://www.nytimes.com/1990/08/26/magazine/doctor-talk-to-me.html
6. Chekhov A. A Doctor’s Visit,. In: Reynolds R, Stone J, eds. On Doctoring. Simon and Shuster;1995:50-59.
7. Lahiri J. Interpreter of Maladies. In: Lahiri J. Interpreter of Maladies. Mariner Books;2019.
8. Fitzgerald FS. Babylon Revisited. In: Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:62-81.
9. Hemingway E. Hills like White Elephants. In: Reynolds R, Stone J, eds. On Doctoring. Simon and Shuster;1995:108-111.
10. Karmel M. Caves of Lascaux. In: Ofri D, Staff of the Bellavue Literary Review, eds. The Best of the Bellevue Literary Review. Bellevue Literary Press;2008:168-174.
11. Lardner R. The Haircut. In Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:48-61.
12. Tolstoy L. The Three Questions. Accessed September 2021. https://www.plough.com/en/topics/culture/short-stories/the-three-questions
13. Olsen T. I Stand Here Ironing. In Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:173-180.
14. Hale N. Those Are as Brothers. In: Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:132-141.
1. Messias E, Gathright MM, Freeman ES, et al. Differences in burnout prevalence between clinical professionals and biomedical scientists in an academic medical centre: a cross-sectional survey. BMJ Open. 2019;9(2):e023506. doi:10.1136/bmjopen-2018-023506
2. Marchalik D, Rodriguez A, Namath A, et al. The impact of non-medical reading on clinical burnout: a national survey of palliative care providers. Ann Palliat Med. 2019;8(4):428-435. doi:10.21037/apm.2019.05.02
3. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533. doi:10.1001/jamainternmed.2013.14387
4. Charon R. Narrative medicine: a model for empathy, reflection, profession, and tust. JAMA. 2001;286(15):1897–1902. doi:10.1001/jama.286.15.1897
5. Broyard A. Doctor Talk to Me. August 26, 1990. Accessed September 2021. https://www.nytimes.com/1990/08/26/magazine/doctor-talk-to-me.html
6. Chekhov A. A Doctor’s Visit,. In: Reynolds R, Stone J, eds. On Doctoring. Simon and Shuster;1995:50-59.
7. Lahiri J. Interpreter of Maladies. In: Lahiri J. Interpreter of Maladies. Mariner Books;2019.
8. Fitzgerald FS. Babylon Revisited. In: Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:62-81.
9. Hemingway E. Hills like White Elephants. In: Reynolds R, Stone J, eds. On Doctoring. Simon and Shuster;1995:108-111.
10. Karmel M. Caves of Lascaux. In: Ofri D, Staff of the Bellavue Literary Review, eds. The Best of the Bellevue Literary Review. Bellevue Literary Press;2008:168-174.
11. Lardner R. The Haircut. In Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:48-61.
12. Tolstoy L. The Three Questions. Accessed September 2021. https://www.plough.com/en/topics/culture/short-stories/the-three-questions
13. Olsen T. I Stand Here Ironing. In Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:173-180.
14. Hale N. Those Are as Brothers. In: Moore L, Pitlor H, eds. 100 Years of the Best American Short Stories. Houghton Mifflin Harcourt;2015:132-141.
‘Forever chemicals’ linked to liver damage
(NAFLD), say the authors of a comprehensive evidence review.
They found “consistent” evidence for PFAS hepatotoxicity from rodent studies. In addition, exposure to PFAS was found to be associated with markers of liver function in observational studies in people.
The review, published online in Environmental Health Perspectives, may be the first systematic analysis of PFAS exposure and liver damage.
Possible contributor to growing NAFLD epidemic
In their analysis, the authors included 85 rodent studies and 24 epidemiologic studies, primarily involving people from the United States and largely focusing on four “legacy” PFAS: perfluorooctanoic acid (PFOA), perfluorooctanesulfonic acid (PFOS), perfluorononanoic acid (PFNA), and perfluorohexanesulfonic acid (PFHxS).
Meta-analyses of human studies found that higher levels of alanine aminotransferase were significantly associated with exposure to three of the older chemicals – PFOA, PFOS, and PFNA.
The “positive” and “convincing” associations between exposure to these synthetic chemicals and higher ALT levels suggest that exposure may contribute to the growing NAFLD epidemic, the researchers write.
Exposure to one of the chemicals, PFOA, was also associated with higher aspartate aminotransferase and gamma-glutamyl transferase levels in people.
In rodents, exposure to these synthetic chemicals consistently resulted in higher ALT levels and steatosis.
“The mechanism is not well understood yet, but there are a few proposed theories,” first author Elizabeth Costello, MPH, PhD student, department of population and public health sciences, University of Southern California, Los Angeles, told this news organization.
“PFAS are similar to fatty acids in chemical structure, so it’s possible that they activate some of the same receptors or otherwise interfere with fat metabolism. This might lead to inflammation or fat accumulation in the liver,” Ms. Costello explained.
People widely exposed
PFAS are ubiquitous in the environment. They have been detected in the blood of most people and have been linked to a variety of health concerns. Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and even drinking water.
“We are exposed to PFAS in so many ways – through water, food, and products we use. It can be very difficult for individuals to control their own exposure,” Ms. Costello commented.
“At this point, it’s important to look for ways to remove PFAS from the environment and phase them out of our products and carefully consider the safety of any replacement chemicals,” she said.
Although most of the research to date has been limited to the four older PFAS (PFOA, PFOS, PFNA, and PFHxS), there are thousands of different PFAS chemicals.
“We don’t know very much about the effects of exposure to multiple PFAS at the same time or how newer replacement PFAS might affect liver disease or other health conditions,” Ms. Costello said.
Reached for comment, Lisa B. VanWagner, MD, with Northwestern University, Chicago, said this analysis is “very interesting,” but she is also “left wondering how we could do anything since it seems from my reading that these chemicals are ubiquitous and used regularly in the environment.”
Dr. VanWagner, who was not involved in the study, said the major limitation is the small number of human studies and the high heterogeneity between studies, “meaning it is hard to come to a firm conclusion about whether what has been observed in the animal studies does truly apply to humans.
“Overall, this study provides important proof of concept for future work to look more specifically at PFAS exposure, and more specific markers of fatty liver disease and liver damage, like liver biopsy, are needed in humans,” Dr. VanWagner said.
“If data accumulate showing that these chemicals do in fact contribute to fatty liver and worsening inflammation or liver damage as a result of exposure, then public health interventions to remove or reduce use of these chemicals could have wide-ranging public health effects,” Dr. VanWagner added.
Further research needed
The authors of an invited perspective published with the study say it underscores the “urgent need for further research and for immediate and reasonable public health action.”
“This work firmly puts PFAS exposure on the list of persistent pollutants, such as polychlorinated biphenyls, that cause hepatotoxicity and whose mechanism is linked to steatosis,” write Alan Ducatman, MD. MSc, with West Virginia University School of Public Health, Morgantown, and Suzanne Fenton, PhD, MS, with the National Institute of Environmental Health Sciences, Research Triangle Park, N.C.
They say other important questions raised by this review include whether individuals who are overweight or obese and those with diabetes are more susceptible to PFAS hepatoxicity, which “replacement” or emerging PFAS can cause liver damage, and whether high doses cause different kinds of liver toxicity than low doses.
“GenX, a current replacement [chemical] for PFOA, has shown significant hepatotoxicity in several recent experimental studies, suggesting it may not be a safe replacement,” they point out.
“A significant challenge will be deciding which of the multiple metabolic pathways altered by PFAS are most important and predictive for induction of liver damage and for progression of liver disease, so that emerging PFAS may be screened for hepatotoxicity prior to entering the market,” Dr. Ducatman and Dr. Fenton conclude.
Support for this research was provided by the National Institute of Environmental Health Science, part of the National Institutes of Health, and the U.S. Department of Agriculture National Institute of Food and Agriculture. Dr. Costello, Dr. VanWagner, Dr. Ducatman, and Dr. Fenton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(NAFLD), say the authors of a comprehensive evidence review.
They found “consistent” evidence for PFAS hepatotoxicity from rodent studies. In addition, exposure to PFAS was found to be associated with markers of liver function in observational studies in people.
The review, published online in Environmental Health Perspectives, may be the first systematic analysis of PFAS exposure and liver damage.
Possible contributor to growing NAFLD epidemic
In their analysis, the authors included 85 rodent studies and 24 epidemiologic studies, primarily involving people from the United States and largely focusing on four “legacy” PFAS: perfluorooctanoic acid (PFOA), perfluorooctanesulfonic acid (PFOS), perfluorononanoic acid (PFNA), and perfluorohexanesulfonic acid (PFHxS).
Meta-analyses of human studies found that higher levels of alanine aminotransferase were significantly associated with exposure to three of the older chemicals – PFOA, PFOS, and PFNA.
The “positive” and “convincing” associations between exposure to these synthetic chemicals and higher ALT levels suggest that exposure may contribute to the growing NAFLD epidemic, the researchers write.
Exposure to one of the chemicals, PFOA, was also associated with higher aspartate aminotransferase and gamma-glutamyl transferase levels in people.
In rodents, exposure to these synthetic chemicals consistently resulted in higher ALT levels and steatosis.
“The mechanism is not well understood yet, but there are a few proposed theories,” first author Elizabeth Costello, MPH, PhD student, department of population and public health sciences, University of Southern California, Los Angeles, told this news organization.
“PFAS are similar to fatty acids in chemical structure, so it’s possible that they activate some of the same receptors or otherwise interfere with fat metabolism. This might lead to inflammation or fat accumulation in the liver,” Ms. Costello explained.
People widely exposed
PFAS are ubiquitous in the environment. They have been detected in the blood of most people and have been linked to a variety of health concerns. Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and even drinking water.
“We are exposed to PFAS in so many ways – through water, food, and products we use. It can be very difficult for individuals to control their own exposure,” Ms. Costello commented.
“At this point, it’s important to look for ways to remove PFAS from the environment and phase them out of our products and carefully consider the safety of any replacement chemicals,” she said.
Although most of the research to date has been limited to the four older PFAS (PFOA, PFOS, PFNA, and PFHxS), there are thousands of different PFAS chemicals.
“We don’t know very much about the effects of exposure to multiple PFAS at the same time or how newer replacement PFAS might affect liver disease or other health conditions,” Ms. Costello said.
Reached for comment, Lisa B. VanWagner, MD, with Northwestern University, Chicago, said this analysis is “very interesting,” but she is also “left wondering how we could do anything since it seems from my reading that these chemicals are ubiquitous and used regularly in the environment.”
Dr. VanWagner, who was not involved in the study, said the major limitation is the small number of human studies and the high heterogeneity between studies, “meaning it is hard to come to a firm conclusion about whether what has been observed in the animal studies does truly apply to humans.
“Overall, this study provides important proof of concept for future work to look more specifically at PFAS exposure, and more specific markers of fatty liver disease and liver damage, like liver biopsy, are needed in humans,” Dr. VanWagner said.
“If data accumulate showing that these chemicals do in fact contribute to fatty liver and worsening inflammation or liver damage as a result of exposure, then public health interventions to remove or reduce use of these chemicals could have wide-ranging public health effects,” Dr. VanWagner added.
Further research needed
The authors of an invited perspective published with the study say it underscores the “urgent need for further research and for immediate and reasonable public health action.”
“This work firmly puts PFAS exposure on the list of persistent pollutants, such as polychlorinated biphenyls, that cause hepatotoxicity and whose mechanism is linked to steatosis,” write Alan Ducatman, MD. MSc, with West Virginia University School of Public Health, Morgantown, and Suzanne Fenton, PhD, MS, with the National Institute of Environmental Health Sciences, Research Triangle Park, N.C.
They say other important questions raised by this review include whether individuals who are overweight or obese and those with diabetes are more susceptible to PFAS hepatoxicity, which “replacement” or emerging PFAS can cause liver damage, and whether high doses cause different kinds of liver toxicity than low doses.
“GenX, a current replacement [chemical] for PFOA, has shown significant hepatotoxicity in several recent experimental studies, suggesting it may not be a safe replacement,” they point out.
“A significant challenge will be deciding which of the multiple metabolic pathways altered by PFAS are most important and predictive for induction of liver damage and for progression of liver disease, so that emerging PFAS may be screened for hepatotoxicity prior to entering the market,” Dr. Ducatman and Dr. Fenton conclude.
Support for this research was provided by the National Institute of Environmental Health Science, part of the National Institutes of Health, and the U.S. Department of Agriculture National Institute of Food and Agriculture. Dr. Costello, Dr. VanWagner, Dr. Ducatman, and Dr. Fenton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(NAFLD), say the authors of a comprehensive evidence review.
They found “consistent” evidence for PFAS hepatotoxicity from rodent studies. In addition, exposure to PFAS was found to be associated with markers of liver function in observational studies in people.
The review, published online in Environmental Health Perspectives, may be the first systematic analysis of PFAS exposure and liver damage.
Possible contributor to growing NAFLD epidemic
In their analysis, the authors included 85 rodent studies and 24 epidemiologic studies, primarily involving people from the United States and largely focusing on four “legacy” PFAS: perfluorooctanoic acid (PFOA), perfluorooctanesulfonic acid (PFOS), perfluorononanoic acid (PFNA), and perfluorohexanesulfonic acid (PFHxS).
Meta-analyses of human studies found that higher levels of alanine aminotransferase were significantly associated with exposure to three of the older chemicals – PFOA, PFOS, and PFNA.
The “positive” and “convincing” associations between exposure to these synthetic chemicals and higher ALT levels suggest that exposure may contribute to the growing NAFLD epidemic, the researchers write.
Exposure to one of the chemicals, PFOA, was also associated with higher aspartate aminotransferase and gamma-glutamyl transferase levels in people.
In rodents, exposure to these synthetic chemicals consistently resulted in higher ALT levels and steatosis.
“The mechanism is not well understood yet, but there are a few proposed theories,” first author Elizabeth Costello, MPH, PhD student, department of population and public health sciences, University of Southern California, Los Angeles, told this news organization.
“PFAS are similar to fatty acids in chemical structure, so it’s possible that they activate some of the same receptors or otherwise interfere with fat metabolism. This might lead to inflammation or fat accumulation in the liver,” Ms. Costello explained.
People widely exposed
PFAS are ubiquitous in the environment. They have been detected in the blood of most people and have been linked to a variety of health concerns. Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and even drinking water.
“We are exposed to PFAS in so many ways – through water, food, and products we use. It can be very difficult for individuals to control their own exposure,” Ms. Costello commented.
“At this point, it’s important to look for ways to remove PFAS from the environment and phase them out of our products and carefully consider the safety of any replacement chemicals,” she said.
Although most of the research to date has been limited to the four older PFAS (PFOA, PFOS, PFNA, and PFHxS), there are thousands of different PFAS chemicals.
“We don’t know very much about the effects of exposure to multiple PFAS at the same time or how newer replacement PFAS might affect liver disease or other health conditions,” Ms. Costello said.
Reached for comment, Lisa B. VanWagner, MD, with Northwestern University, Chicago, said this analysis is “very interesting,” but she is also “left wondering how we could do anything since it seems from my reading that these chemicals are ubiquitous and used regularly in the environment.”
Dr. VanWagner, who was not involved in the study, said the major limitation is the small number of human studies and the high heterogeneity between studies, “meaning it is hard to come to a firm conclusion about whether what has been observed in the animal studies does truly apply to humans.
“Overall, this study provides important proof of concept for future work to look more specifically at PFAS exposure, and more specific markers of fatty liver disease and liver damage, like liver biopsy, are needed in humans,” Dr. VanWagner said.
“If data accumulate showing that these chemicals do in fact contribute to fatty liver and worsening inflammation or liver damage as a result of exposure, then public health interventions to remove or reduce use of these chemicals could have wide-ranging public health effects,” Dr. VanWagner added.
Further research needed
The authors of an invited perspective published with the study say it underscores the “urgent need for further research and for immediate and reasonable public health action.”
“This work firmly puts PFAS exposure on the list of persistent pollutants, such as polychlorinated biphenyls, that cause hepatotoxicity and whose mechanism is linked to steatosis,” write Alan Ducatman, MD. MSc, with West Virginia University School of Public Health, Morgantown, and Suzanne Fenton, PhD, MS, with the National Institute of Environmental Health Sciences, Research Triangle Park, N.C.
They say other important questions raised by this review include whether individuals who are overweight or obese and those with diabetes are more susceptible to PFAS hepatoxicity, which “replacement” or emerging PFAS can cause liver damage, and whether high doses cause different kinds of liver toxicity than low doses.
“GenX, a current replacement [chemical] for PFOA, has shown significant hepatotoxicity in several recent experimental studies, suggesting it may not be a safe replacement,” they point out.
“A significant challenge will be deciding which of the multiple metabolic pathways altered by PFAS are most important and predictive for induction of liver damage and for progression of liver disease, so that emerging PFAS may be screened for hepatotoxicity prior to entering the market,” Dr. Ducatman and Dr. Fenton conclude.
Support for this research was provided by the National Institute of Environmental Health Science, part of the National Institutes of Health, and the U.S. Department of Agriculture National Institute of Food and Agriculture. Dr. Costello, Dr. VanWagner, Dr. Ducatman, and Dr. Fenton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ENVIRONMENTAL HEALTH PERSPECTIVES
OIG Finds More Problems in the VA’s Problem-Prone EHR Rollout
Scheduling delays. Disappearing lab orders. Bad links for telehealth appointments. Erroneous medication dispensing. Time-consuming workarounds.
The rollout of the $16 billion electronic health record (EHR) system at the US Department of Veterans Affair (VA) has met some fairly large bumps in the past few years. And now, the VA Office of the Inspector General (OIG) has pronounced on a “range of allegations” at the Mann-Grandstaff VA Medical Center in Spokane, Washington, the first of several hospitals and clinics in the Pacific Northwest set to implement the new system.
VA Inspector General Michael Missal issued 3 reports in mid-March on how the “go-live” process was faring: one on medication management deficiencies, one on care coordination deficiencies, and one on technical issues.
The reports document the OIG’s “concerns” with the new process. According to the technical report, for instance, between October 2020 and March 2021, new EHR users placed more than 38,700 requests for assistance. Of those, 33% were closed without a documented resolution. The OIG also reviewed 210 tickets related to care coordination and found that 1% were closed without a documented resolution.
The OIG said EHR implementation had “created difficulties” for end users in 8 areas:
- Patient record flags, including failures to transfer flags and information related to patients at high risk for suicide;
- Data migration errors leading to inaccurate name, sex, and contact information;
- Scheduling process issues, such as delays in primary care scheduling;
- VA Video Connect problems, including inoperable and misdirected links;
- Referral management deficiencies, including lost or unaddressed referrals;
- Laboratory orders “disappearing” that affected workflow and tracking, and delayed results;
- Patient portal and secure messaging being inaccessible; and
- Documentation processes, including creating additional work and limiting the ability to correctly code patient diagnoses.
The OIG’s technical report identified 5 factors that contributed to the headaches: EHR usability problems, training deficits, interoperability challenges, post–go-live fixes and refinement needs, and problem-resolution process challenges.
The OIG did not identify any associated patient deaths during the inspection but says “future deployment of the new EHR without resolving deficiencies can increase risks to patient safety.”
The technological overhaul has been handled by Cerner. The VA initially awarded Cerner $113 million for EHR modernization, and in 2018 the company secured a 10-year, $10 billion contract to help the VA rebuild its system, similar to the way it did for the US Department of Defense (DoD) with MHS GENESIS. The Cerner DoD project, which has been called “the most lucrative electronic health record contract in history” was launched at the Fairchild Air Force Base in Spokane, Washington, in 2017, and is expected to be operational in more than half of military hospitals and clinics by the end of this year. In 2021, Cerner received an 18-month, $134.1 million task order to deploy the company’s EHR platform at VA medical centers.
This isn’t the first time the VA/Cerner EHR project has hit snags. In 2021, the VA scrapped the schedule, trading it for a 6-month pause after a strategic review ordered by VA Secretary Denis McDonough found problems with governance and management. McDonough told the Senate Veterans’ Affairs Committee that a 3-month internal review had found too many structural problems to warrant continuing the rollout. The sole-source contract with Cerner also raised concerns, as did the influence of 3 confidants of Present Trump on the process. Moreover, cost estimates kept growing—from $10 billion to $16 billion—in part because VA leaders during the Trump administration did not budget for technology and hospital upgrades to allow the new platform to work, according to an article in The Washington Post.
During the senate hearing, committee chair Sen. Jon Tester (D-MT) said, “There’s been damn little accountability. I hope Cerner’s watching this. If they’re not open to making a user-friendly health medical record, they ought to admit it so we can get the money back and start all over.” He told McDonough that the failures were “not all your fault—I don’t know if any of it is your fault.”
“It’s a lot of money you’ve entrusted to us,” McDonough told the committee. The serious problems, he said, were “on us.” He added, “We are taking swift and decisive action to incorporate the management rigor and enterprise jointness required for this program to deliver on its intended purpose: seamless excellence in VA care for veterans. VA’s first implementation of the [project] did not live up to that promise, either for our veterans or for our providers.”
He said he had ordered an overhaul that will include better training for clinical staff, more reliable testing and oversight of Cerner, and a leadership shake-up. He also said he had installed a patient safety team at the Spokane hospital.
Terry Adirim, MD, formerly with the DoD, took over the EHR program in January. In an interview, she said, “[W]e’ve made a substantial number of changes,” such as a new round of training for the hospital’s medical staff. “These deployments are really complex and they’re really hard,” Adirim said, noting that about half of digital medical records programs at private hospitals fail at first. She pointed to the revamped DoD program, which also had its flaws but is running much more smoothly. One of the issues, she said, is that many physicians did not realize that the Cerner system would differ so dramatically from VistA, the system it’s replacing.
The first installment of the rocky rollout left hospital staff confused and worn out. Sen. Patty Murphy (D-WA) said in 2021 that the Spokane staff had filed hundreds of reports of patient safety issues caused by the new system. “Patients are not getting accurate meds. Meds are sent to the wrong address. What used to take a few clicks is now a lot more complicated. Providers are burning out.”
A year later, in a statement, echoing her earlier comments, she said, “We need to put a pause on this rollout right now.”
But Adirim has said the VA is moving ahead with the rollout. The VA has added extra support staff and plans to have physicians from outside the hospital on hand in case things go wrong. According to the Washington Post, Deputy VA Secretary Donald Remy told the OIG that the VA is working to address the outstanding issues and hopes to resolve them by mid-May.
Meanwhile, the beleaguered project ran into another obstacle in early March, when computers went down at Mann-Grandstaff, leading to 20 hours of yet more confusion about medications and surgeries. The VA said the IT system outage also happened at Columbus, Ohio (another of the planned pilot spots). The system was back online the next day, with no known patient safety issues.
Eastern Washington Congresswoman Cathy McMorris Rodgers released a statement saying, “The shutdown of Mann-Grandstaff VA yesterday is another event in a series of challenges that the new electronic health record has created for staff and veterans at the facility. My understanding is that an update made to help the VA’s database for demographic data better communicate with the Cerner system was not performed correctly. Mann-Grandstaff leadership rightly took the system offline until the scope of the problem was understood, so no patients were harmed.”
However, Sen. Murphy called the technical failure “absolutely unacceptable.” In a more recent statement about the rollout, she said, “This is about patient safety and it needs to get fixed—period. VA needs to be upfront about issues like this in real time—Congress absolutely requires transparency when it comes to failures as serious as this. I should be hearing about this from local reporting first.”
If the high-quality care veterans deserve is uncertain at any point, she added, “the rollout should be delayed.” Again.
Scheduling delays. Disappearing lab orders. Bad links for telehealth appointments. Erroneous medication dispensing. Time-consuming workarounds.
The rollout of the $16 billion electronic health record (EHR) system at the US Department of Veterans Affair (VA) has met some fairly large bumps in the past few years. And now, the VA Office of the Inspector General (OIG) has pronounced on a “range of allegations” at the Mann-Grandstaff VA Medical Center in Spokane, Washington, the first of several hospitals and clinics in the Pacific Northwest set to implement the new system.
VA Inspector General Michael Missal issued 3 reports in mid-March on how the “go-live” process was faring: one on medication management deficiencies, one on care coordination deficiencies, and one on technical issues.
The reports document the OIG’s “concerns” with the new process. According to the technical report, for instance, between October 2020 and March 2021, new EHR users placed more than 38,700 requests for assistance. Of those, 33% were closed without a documented resolution. The OIG also reviewed 210 tickets related to care coordination and found that 1% were closed without a documented resolution.
The OIG said EHR implementation had “created difficulties” for end users in 8 areas:
- Patient record flags, including failures to transfer flags and information related to patients at high risk for suicide;
- Data migration errors leading to inaccurate name, sex, and contact information;
- Scheduling process issues, such as delays in primary care scheduling;
- VA Video Connect problems, including inoperable and misdirected links;
- Referral management deficiencies, including lost or unaddressed referrals;
- Laboratory orders “disappearing” that affected workflow and tracking, and delayed results;
- Patient portal and secure messaging being inaccessible; and
- Documentation processes, including creating additional work and limiting the ability to correctly code patient diagnoses.
The OIG’s technical report identified 5 factors that contributed to the headaches: EHR usability problems, training deficits, interoperability challenges, post–go-live fixes and refinement needs, and problem-resolution process challenges.
The OIG did not identify any associated patient deaths during the inspection but says “future deployment of the new EHR without resolving deficiencies can increase risks to patient safety.”
The technological overhaul has been handled by Cerner. The VA initially awarded Cerner $113 million for EHR modernization, and in 2018 the company secured a 10-year, $10 billion contract to help the VA rebuild its system, similar to the way it did for the US Department of Defense (DoD) with MHS GENESIS. The Cerner DoD project, which has been called “the most lucrative electronic health record contract in history” was launched at the Fairchild Air Force Base in Spokane, Washington, in 2017, and is expected to be operational in more than half of military hospitals and clinics by the end of this year. In 2021, Cerner received an 18-month, $134.1 million task order to deploy the company’s EHR platform at VA medical centers.
This isn’t the first time the VA/Cerner EHR project has hit snags. In 2021, the VA scrapped the schedule, trading it for a 6-month pause after a strategic review ordered by VA Secretary Denis McDonough found problems with governance and management. McDonough told the Senate Veterans’ Affairs Committee that a 3-month internal review had found too many structural problems to warrant continuing the rollout. The sole-source contract with Cerner also raised concerns, as did the influence of 3 confidants of Present Trump on the process. Moreover, cost estimates kept growing—from $10 billion to $16 billion—in part because VA leaders during the Trump administration did not budget for technology and hospital upgrades to allow the new platform to work, according to an article in The Washington Post.
During the senate hearing, committee chair Sen. Jon Tester (D-MT) said, “There’s been damn little accountability. I hope Cerner’s watching this. If they’re not open to making a user-friendly health medical record, they ought to admit it so we can get the money back and start all over.” He told McDonough that the failures were “not all your fault—I don’t know if any of it is your fault.”
“It’s a lot of money you’ve entrusted to us,” McDonough told the committee. The serious problems, he said, were “on us.” He added, “We are taking swift and decisive action to incorporate the management rigor and enterprise jointness required for this program to deliver on its intended purpose: seamless excellence in VA care for veterans. VA’s first implementation of the [project] did not live up to that promise, either for our veterans or for our providers.”
He said he had ordered an overhaul that will include better training for clinical staff, more reliable testing and oversight of Cerner, and a leadership shake-up. He also said he had installed a patient safety team at the Spokane hospital.
Terry Adirim, MD, formerly with the DoD, took over the EHR program in January. In an interview, she said, “[W]e’ve made a substantial number of changes,” such as a new round of training for the hospital’s medical staff. “These deployments are really complex and they’re really hard,” Adirim said, noting that about half of digital medical records programs at private hospitals fail at first. She pointed to the revamped DoD program, which also had its flaws but is running much more smoothly. One of the issues, she said, is that many physicians did not realize that the Cerner system would differ so dramatically from VistA, the system it’s replacing.
The first installment of the rocky rollout left hospital staff confused and worn out. Sen. Patty Murphy (D-WA) said in 2021 that the Spokane staff had filed hundreds of reports of patient safety issues caused by the new system. “Patients are not getting accurate meds. Meds are sent to the wrong address. What used to take a few clicks is now a lot more complicated. Providers are burning out.”
A year later, in a statement, echoing her earlier comments, she said, “We need to put a pause on this rollout right now.”
But Adirim has said the VA is moving ahead with the rollout. The VA has added extra support staff and plans to have physicians from outside the hospital on hand in case things go wrong. According to the Washington Post, Deputy VA Secretary Donald Remy told the OIG that the VA is working to address the outstanding issues and hopes to resolve them by mid-May.
Meanwhile, the beleaguered project ran into another obstacle in early March, when computers went down at Mann-Grandstaff, leading to 20 hours of yet more confusion about medications and surgeries. The VA said the IT system outage also happened at Columbus, Ohio (another of the planned pilot spots). The system was back online the next day, with no known patient safety issues.
Eastern Washington Congresswoman Cathy McMorris Rodgers released a statement saying, “The shutdown of Mann-Grandstaff VA yesterday is another event in a series of challenges that the new electronic health record has created for staff and veterans at the facility. My understanding is that an update made to help the VA’s database for demographic data better communicate with the Cerner system was not performed correctly. Mann-Grandstaff leadership rightly took the system offline until the scope of the problem was understood, so no patients were harmed.”
However, Sen. Murphy called the technical failure “absolutely unacceptable.” In a more recent statement about the rollout, she said, “This is about patient safety and it needs to get fixed—period. VA needs to be upfront about issues like this in real time—Congress absolutely requires transparency when it comes to failures as serious as this. I should be hearing about this from local reporting first.”
If the high-quality care veterans deserve is uncertain at any point, she added, “the rollout should be delayed.” Again.
Scheduling delays. Disappearing lab orders. Bad links for telehealth appointments. Erroneous medication dispensing. Time-consuming workarounds.
The rollout of the $16 billion electronic health record (EHR) system at the US Department of Veterans Affair (VA) has met some fairly large bumps in the past few years. And now, the VA Office of the Inspector General (OIG) has pronounced on a “range of allegations” at the Mann-Grandstaff VA Medical Center in Spokane, Washington, the first of several hospitals and clinics in the Pacific Northwest set to implement the new system.
VA Inspector General Michael Missal issued 3 reports in mid-March on how the “go-live” process was faring: one on medication management deficiencies, one on care coordination deficiencies, and one on technical issues.
The reports document the OIG’s “concerns” with the new process. According to the technical report, for instance, between October 2020 and March 2021, new EHR users placed more than 38,700 requests for assistance. Of those, 33% were closed without a documented resolution. The OIG also reviewed 210 tickets related to care coordination and found that 1% were closed without a documented resolution.
The OIG said EHR implementation had “created difficulties” for end users in 8 areas:
- Patient record flags, including failures to transfer flags and information related to patients at high risk for suicide;
- Data migration errors leading to inaccurate name, sex, and contact information;
- Scheduling process issues, such as delays in primary care scheduling;
- VA Video Connect problems, including inoperable and misdirected links;
- Referral management deficiencies, including lost or unaddressed referrals;
- Laboratory orders “disappearing” that affected workflow and tracking, and delayed results;
- Patient portal and secure messaging being inaccessible; and
- Documentation processes, including creating additional work and limiting the ability to correctly code patient diagnoses.
The OIG’s technical report identified 5 factors that contributed to the headaches: EHR usability problems, training deficits, interoperability challenges, post–go-live fixes and refinement needs, and problem-resolution process challenges.
The OIG did not identify any associated patient deaths during the inspection but says “future deployment of the new EHR without resolving deficiencies can increase risks to patient safety.”
The technological overhaul has been handled by Cerner. The VA initially awarded Cerner $113 million for EHR modernization, and in 2018 the company secured a 10-year, $10 billion contract to help the VA rebuild its system, similar to the way it did for the US Department of Defense (DoD) with MHS GENESIS. The Cerner DoD project, which has been called “the most lucrative electronic health record contract in history” was launched at the Fairchild Air Force Base in Spokane, Washington, in 2017, and is expected to be operational in more than half of military hospitals and clinics by the end of this year. In 2021, Cerner received an 18-month, $134.1 million task order to deploy the company’s EHR platform at VA medical centers.
This isn’t the first time the VA/Cerner EHR project has hit snags. In 2021, the VA scrapped the schedule, trading it for a 6-month pause after a strategic review ordered by VA Secretary Denis McDonough found problems with governance and management. McDonough told the Senate Veterans’ Affairs Committee that a 3-month internal review had found too many structural problems to warrant continuing the rollout. The sole-source contract with Cerner also raised concerns, as did the influence of 3 confidants of Present Trump on the process. Moreover, cost estimates kept growing—from $10 billion to $16 billion—in part because VA leaders during the Trump administration did not budget for technology and hospital upgrades to allow the new platform to work, according to an article in The Washington Post.
During the senate hearing, committee chair Sen. Jon Tester (D-MT) said, “There’s been damn little accountability. I hope Cerner’s watching this. If they’re not open to making a user-friendly health medical record, they ought to admit it so we can get the money back and start all over.” He told McDonough that the failures were “not all your fault—I don’t know if any of it is your fault.”
“It’s a lot of money you’ve entrusted to us,” McDonough told the committee. The serious problems, he said, were “on us.” He added, “We are taking swift and decisive action to incorporate the management rigor and enterprise jointness required for this program to deliver on its intended purpose: seamless excellence in VA care for veterans. VA’s first implementation of the [project] did not live up to that promise, either for our veterans or for our providers.”
He said he had ordered an overhaul that will include better training for clinical staff, more reliable testing and oversight of Cerner, and a leadership shake-up. He also said he had installed a patient safety team at the Spokane hospital.
Terry Adirim, MD, formerly with the DoD, took over the EHR program in January. In an interview, she said, “[W]e’ve made a substantial number of changes,” such as a new round of training for the hospital’s medical staff. “These deployments are really complex and they’re really hard,” Adirim said, noting that about half of digital medical records programs at private hospitals fail at first. She pointed to the revamped DoD program, which also had its flaws but is running much more smoothly. One of the issues, she said, is that many physicians did not realize that the Cerner system would differ so dramatically from VistA, the system it’s replacing.
The first installment of the rocky rollout left hospital staff confused and worn out. Sen. Patty Murphy (D-WA) said in 2021 that the Spokane staff had filed hundreds of reports of patient safety issues caused by the new system. “Patients are not getting accurate meds. Meds are sent to the wrong address. What used to take a few clicks is now a lot more complicated. Providers are burning out.”
A year later, in a statement, echoing her earlier comments, she said, “We need to put a pause on this rollout right now.”
But Adirim has said the VA is moving ahead with the rollout. The VA has added extra support staff and plans to have physicians from outside the hospital on hand in case things go wrong. According to the Washington Post, Deputy VA Secretary Donald Remy told the OIG that the VA is working to address the outstanding issues and hopes to resolve them by mid-May.
Meanwhile, the beleaguered project ran into another obstacle in early March, when computers went down at Mann-Grandstaff, leading to 20 hours of yet more confusion about medications and surgeries. The VA said the IT system outage also happened at Columbus, Ohio (another of the planned pilot spots). The system was back online the next day, with no known patient safety issues.
Eastern Washington Congresswoman Cathy McMorris Rodgers released a statement saying, “The shutdown of Mann-Grandstaff VA yesterday is another event in a series of challenges that the new electronic health record has created for staff and veterans at the facility. My understanding is that an update made to help the VA’s database for demographic data better communicate with the Cerner system was not performed correctly. Mann-Grandstaff leadership rightly took the system offline until the scope of the problem was understood, so no patients were harmed.”
However, Sen. Murphy called the technical failure “absolutely unacceptable.” In a more recent statement about the rollout, she said, “This is about patient safety and it needs to get fixed—period. VA needs to be upfront about issues like this in real time—Congress absolutely requires transparency when it comes to failures as serious as this. I should be hearing about this from local reporting first.”
If the high-quality care veterans deserve is uncertain at any point, she added, “the rollout should be delayed.” Again.
San Diego, here we come
I attended my inaugural Digestive Disease Week® (DDW) in Orlando in 2013 as a first-year fellow, both excited and somewhat intimidated to be giving my first oral abstract presentation on an international stage. At that time, the only familiar faces at the conference were my co-fellows and faculty, along with a few welcoming faces from the fellowship interview trail. My attendings, on the other hand, couldn’t walk more than 100 feet in the conference hall without bumping into a smiling colleague! Now nearly a decade later, I am pleased to say that there are many more familiar faces in the crowd as I walk the halls of DDW. Each May, I look forward to meeting up with friends and colleagues across the country and the world while learning from an outstanding group of GI thought-leaders. While the COVID pandemic has disrupted this annual tradition in recent years, for the first time since 2019 those who feel comfortable will convene in San Diego to see old colleagues and meet new ones, learn about exciting, practice-changing innovations in our field, and enjoy the California sunshine. For those who cannot travel, robust DDW virtual offerings are planned as well.
A quick look at the 2022 conference schedule reveals an astonishing 3,300 oral abstract and poster presentations, 400 original lectures, and a variety of professional networking events on the agenda. The conference weekend will open with the AGA Post-Graduate Course, which offers a great opportunity to efficiently brush up on your clinical knowledge, guided by leading experts in the field. Monday, May 23 will feature the AGA Presidential Plenary, with AGA Institute President John Inadomi, MD, AGAF, and an exciting lineup of speakers discussing how best to address health care disparities impacting our patients and outlining AGA’s recent efforts to promote diversity, equity, and inclusion in our field. While it is nearly impossible to attend all sessions of interest during this whirlwind 4-day conference, you can rely on GI & Hepatology News to bring you key conference highlights over the coming months to ensure you don’t miss a beat!
Megan A. Adams, MD, JD, MSc
I attended my inaugural Digestive Disease Week® (DDW) in Orlando in 2013 as a first-year fellow, both excited and somewhat intimidated to be giving my first oral abstract presentation on an international stage. At that time, the only familiar faces at the conference were my co-fellows and faculty, along with a few welcoming faces from the fellowship interview trail. My attendings, on the other hand, couldn’t walk more than 100 feet in the conference hall without bumping into a smiling colleague! Now nearly a decade later, I am pleased to say that there are many more familiar faces in the crowd as I walk the halls of DDW. Each May, I look forward to meeting up with friends and colleagues across the country and the world while learning from an outstanding group of GI thought-leaders. While the COVID pandemic has disrupted this annual tradition in recent years, for the first time since 2019 those who feel comfortable will convene in San Diego to see old colleagues and meet new ones, learn about exciting, practice-changing innovations in our field, and enjoy the California sunshine. For those who cannot travel, robust DDW virtual offerings are planned as well.
A quick look at the 2022 conference schedule reveals an astonishing 3,300 oral abstract and poster presentations, 400 original lectures, and a variety of professional networking events on the agenda. The conference weekend will open with the AGA Post-Graduate Course, which offers a great opportunity to efficiently brush up on your clinical knowledge, guided by leading experts in the field. Monday, May 23 will feature the AGA Presidential Plenary, with AGA Institute President John Inadomi, MD, AGAF, and an exciting lineup of speakers discussing how best to address health care disparities impacting our patients and outlining AGA’s recent efforts to promote diversity, equity, and inclusion in our field. While it is nearly impossible to attend all sessions of interest during this whirlwind 4-day conference, you can rely on GI & Hepatology News to bring you key conference highlights over the coming months to ensure you don’t miss a beat!
Megan A. Adams, MD, JD, MSc
I attended my inaugural Digestive Disease Week® (DDW) in Orlando in 2013 as a first-year fellow, both excited and somewhat intimidated to be giving my first oral abstract presentation on an international stage. At that time, the only familiar faces at the conference were my co-fellows and faculty, along with a few welcoming faces from the fellowship interview trail. My attendings, on the other hand, couldn’t walk more than 100 feet in the conference hall without bumping into a smiling colleague! Now nearly a decade later, I am pleased to say that there are many more familiar faces in the crowd as I walk the halls of DDW. Each May, I look forward to meeting up with friends and colleagues across the country and the world while learning from an outstanding group of GI thought-leaders. While the COVID pandemic has disrupted this annual tradition in recent years, for the first time since 2019 those who feel comfortable will convene in San Diego to see old colleagues and meet new ones, learn about exciting, practice-changing innovations in our field, and enjoy the California sunshine. For those who cannot travel, robust DDW virtual offerings are planned as well.
A quick look at the 2022 conference schedule reveals an astonishing 3,300 oral abstract and poster presentations, 400 original lectures, and a variety of professional networking events on the agenda. The conference weekend will open with the AGA Post-Graduate Course, which offers a great opportunity to efficiently brush up on your clinical knowledge, guided by leading experts in the field. Monday, May 23 will feature the AGA Presidential Plenary, with AGA Institute President John Inadomi, MD, AGAF, and an exciting lineup of speakers discussing how best to address health care disparities impacting our patients and outlining AGA’s recent efforts to promote diversity, equity, and inclusion in our field. While it is nearly impossible to attend all sessions of interest during this whirlwind 4-day conference, you can rely on GI & Hepatology News to bring you key conference highlights over the coming months to ensure you don’t miss a beat!
Megan A. Adams, MD, JD, MSc
How to communicate effectively with patients when tension is high
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
AT INTERNAL MEDICINE 2022
Homelessness seems to have greater link to death than common diseases, says physician
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
REPORTING FROM INTERNAL MEDICINE 2022
What's your diagnosis?
Answer: Colonic Malakoplakia.
Histopathologic examination of the biopsy specimens revealed nodular mixed inflammatory cells and infiltration of the epithelioid histiocytes in lamina propria (Figure D; stain: hematoxylin and eosin; original magnification 40×). The histiocytes showed foamy and eosinophilic cytoplasm (Figure E, arrow) and some of them had a targetoid appearance (Figure E, arrow head; stain: hematoxylin and eosin; original magnification 200×). Von Kossa stains highlighted the targetoid structures in the histiocytes (Figure F, Michaelis-Gutmann bodies). The granular cytoplasm of the histiocytes was positive on periodic acid-Schiff stain (Figure G). Based on these findings, the patient was diagnosed with colonic malakoplakia.
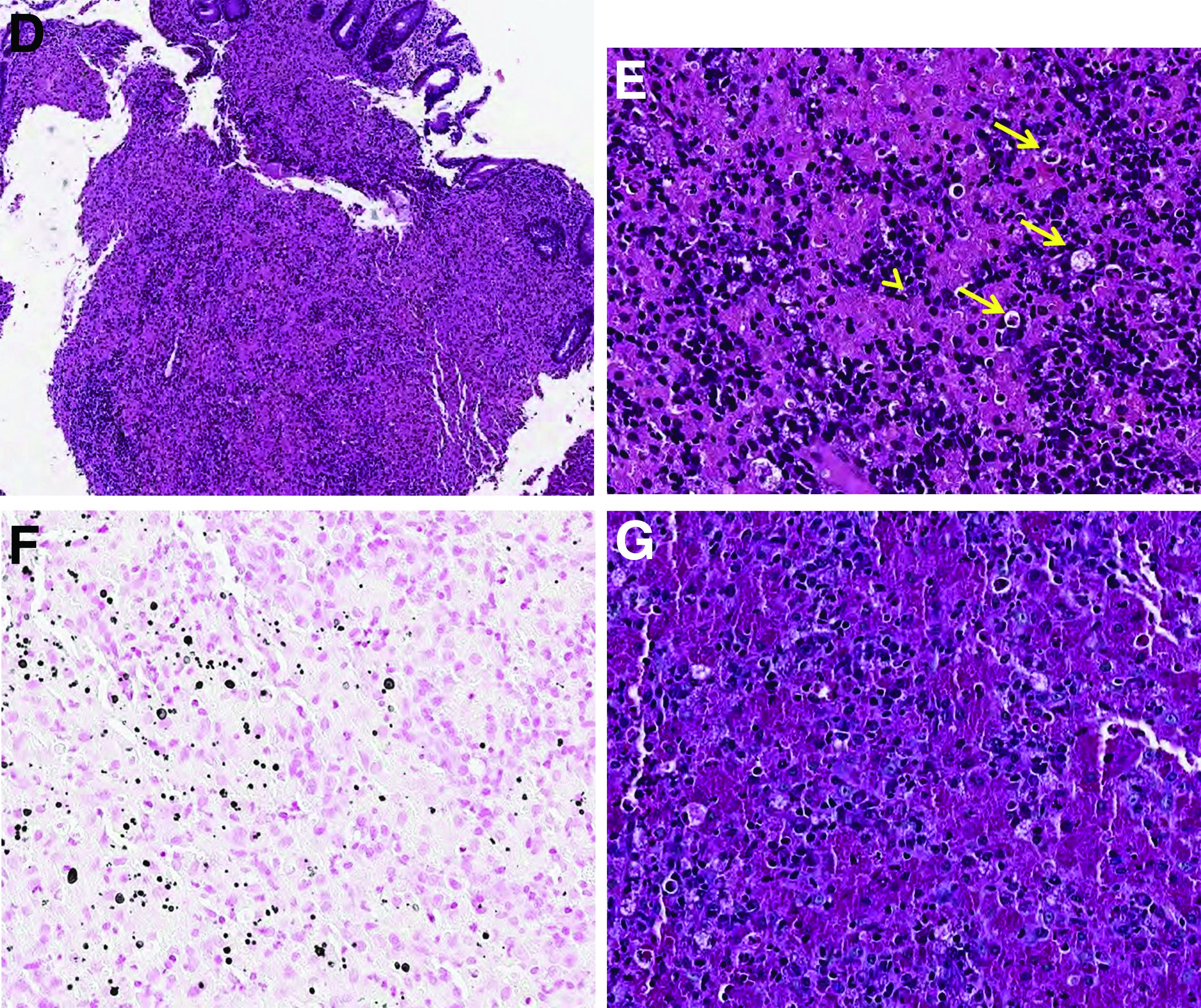
Malakoplakia is an uncommon, chronic, granulomatous inflammatory disease. It most commonly affects the urinary tract and gastrointestinal tract, but may occur at any anatomic site. Malakoplakia of the gastrointestinal tract are seen most frequently in the rectum, sigmoid, and right colon.1 It is diagnosed by the characteristic histologic feature of accumulated histiocytes with abundant eosinophilic granular cytoplasm containing basophilic inclusions, consistent with Michaelis-Gutmann bodies. Although the exact etiology and pathogenesis of malakoplakia are unclear, it seems to originate from an acquired defect in the intracellular destruction of phagocytosed bacteria, usually associated with Escherichia coli, Klebsiella, and Mycobacterium.2 It can have various causes, such as immunosuppression, malignant neoplasms, systemic diseases, and genetic diseases. Clinical manifestation of colonic malakoplakia is diverse, ranging from asymptomatic to malaise, fever, abdominal pain, diarrhea, hematochezia, and intestinal obstruction. Granulomatous reaction of malakoplakia generates the endoscopic appearance of lesions, which ranges from plaques to nodules and yellow-brown masses. In the early stage, malakoplakia commonly presents as soft yellow to tan mucosal plaques endoscopically, as seen in our case (Figure A). As the disease progresses in the later stage, malakoplakia presents as raised, grey to tan polypoid lesions of various sizes with peripheral hyperemia and a central depressed area, as seen in our case (Figure B).3 Owing to this endoscopic morphology, colonic malakoplakia may be misdiagnosed as atypical lymphoma, familial adenomatous polyposis, and metastatic carcinoma. To date, the natural course of malakoplakia of the colon is unclear, and no guidelines for treatment, treatment methods, duration of treatment, or surveillance are currently available. However, treatment of malakoplakia is essential to reduce immunosuppression and includes antibiotics with intracellular action and choline agonists that replenish the decreased cyclic 3’, 5’-guanosine monophosphate levels. In summary, although malakoplakia of the colon is very rare, it should be considered in the differential diagnosis of polypoid colonic lesions, especially in immunocompromised or malnourished patients.
References
1. Cipolletta L et al. Gastrointest Endosc. 1995 Mar;41(3):255-8.
2. Berney T et al. Transpl Int. 1999;12(4):293-6.
3. Weinrach DM et al. Arch Pathol Lab Med. 2004 Oct;128(10):e133-4.
Answer: Colonic Malakoplakia.
Histopathologic examination of the biopsy specimens revealed nodular mixed inflammatory cells and infiltration of the epithelioid histiocytes in lamina propria (Figure D; stain: hematoxylin and eosin; original magnification 40×). The histiocytes showed foamy and eosinophilic cytoplasm (Figure E, arrow) and some of them had a targetoid appearance (Figure E, arrow head; stain: hematoxylin and eosin; original magnification 200×). Von Kossa stains highlighted the targetoid structures in the histiocytes (Figure F, Michaelis-Gutmann bodies). The granular cytoplasm of the histiocytes was positive on periodic acid-Schiff stain (Figure G). Based on these findings, the patient was diagnosed with colonic malakoplakia.
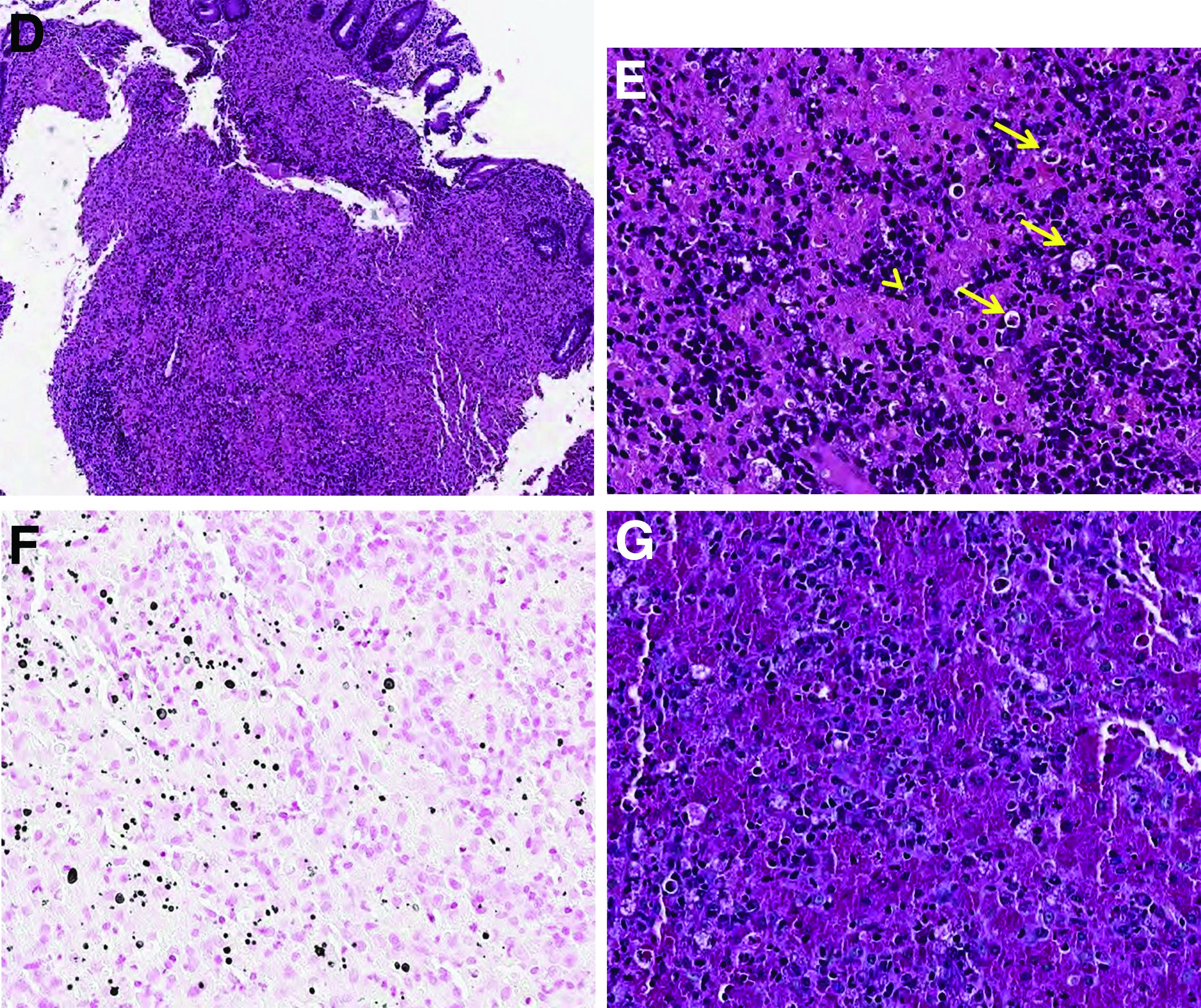
Malakoplakia is an uncommon, chronic, granulomatous inflammatory disease. It most commonly affects the urinary tract and gastrointestinal tract, but may occur at any anatomic site. Malakoplakia of the gastrointestinal tract are seen most frequently in the rectum, sigmoid, and right colon.1 It is diagnosed by the characteristic histologic feature of accumulated histiocytes with abundant eosinophilic granular cytoplasm containing basophilic inclusions, consistent with Michaelis-Gutmann bodies. Although the exact etiology and pathogenesis of malakoplakia are unclear, it seems to originate from an acquired defect in the intracellular destruction of phagocytosed bacteria, usually associated with Escherichia coli, Klebsiella, and Mycobacterium.2 It can have various causes, such as immunosuppression, malignant neoplasms, systemic diseases, and genetic diseases. Clinical manifestation of colonic malakoplakia is diverse, ranging from asymptomatic to malaise, fever, abdominal pain, diarrhea, hematochezia, and intestinal obstruction. Granulomatous reaction of malakoplakia generates the endoscopic appearance of lesions, which ranges from plaques to nodules and yellow-brown masses. In the early stage, malakoplakia commonly presents as soft yellow to tan mucosal plaques endoscopically, as seen in our case (Figure A). As the disease progresses in the later stage, malakoplakia presents as raised, grey to tan polypoid lesions of various sizes with peripheral hyperemia and a central depressed area, as seen in our case (Figure B).3 Owing to this endoscopic morphology, colonic malakoplakia may be misdiagnosed as atypical lymphoma, familial adenomatous polyposis, and metastatic carcinoma. To date, the natural course of malakoplakia of the colon is unclear, and no guidelines for treatment, treatment methods, duration of treatment, or surveillance are currently available. However, treatment of malakoplakia is essential to reduce immunosuppression and includes antibiotics with intracellular action and choline agonists that replenish the decreased cyclic 3’, 5’-guanosine monophosphate levels. In summary, although malakoplakia of the colon is very rare, it should be considered in the differential diagnosis of polypoid colonic lesions, especially in immunocompromised or malnourished patients.
References
1. Cipolletta L et al. Gastrointest Endosc. 1995 Mar;41(3):255-8.
2. Berney T et al. Transpl Int. 1999;12(4):293-6.
3. Weinrach DM et al. Arch Pathol Lab Med. 2004 Oct;128(10):e133-4.
Answer: Colonic Malakoplakia.
Histopathologic examination of the biopsy specimens revealed nodular mixed inflammatory cells and infiltration of the epithelioid histiocytes in lamina propria (Figure D; stain: hematoxylin and eosin; original magnification 40×). The histiocytes showed foamy and eosinophilic cytoplasm (Figure E, arrow) and some of them had a targetoid appearance (Figure E, arrow head; stain: hematoxylin and eosin; original magnification 200×). Von Kossa stains highlighted the targetoid structures in the histiocytes (Figure F, Michaelis-Gutmann bodies). The granular cytoplasm of the histiocytes was positive on periodic acid-Schiff stain (Figure G). Based on these findings, the patient was diagnosed with colonic malakoplakia.
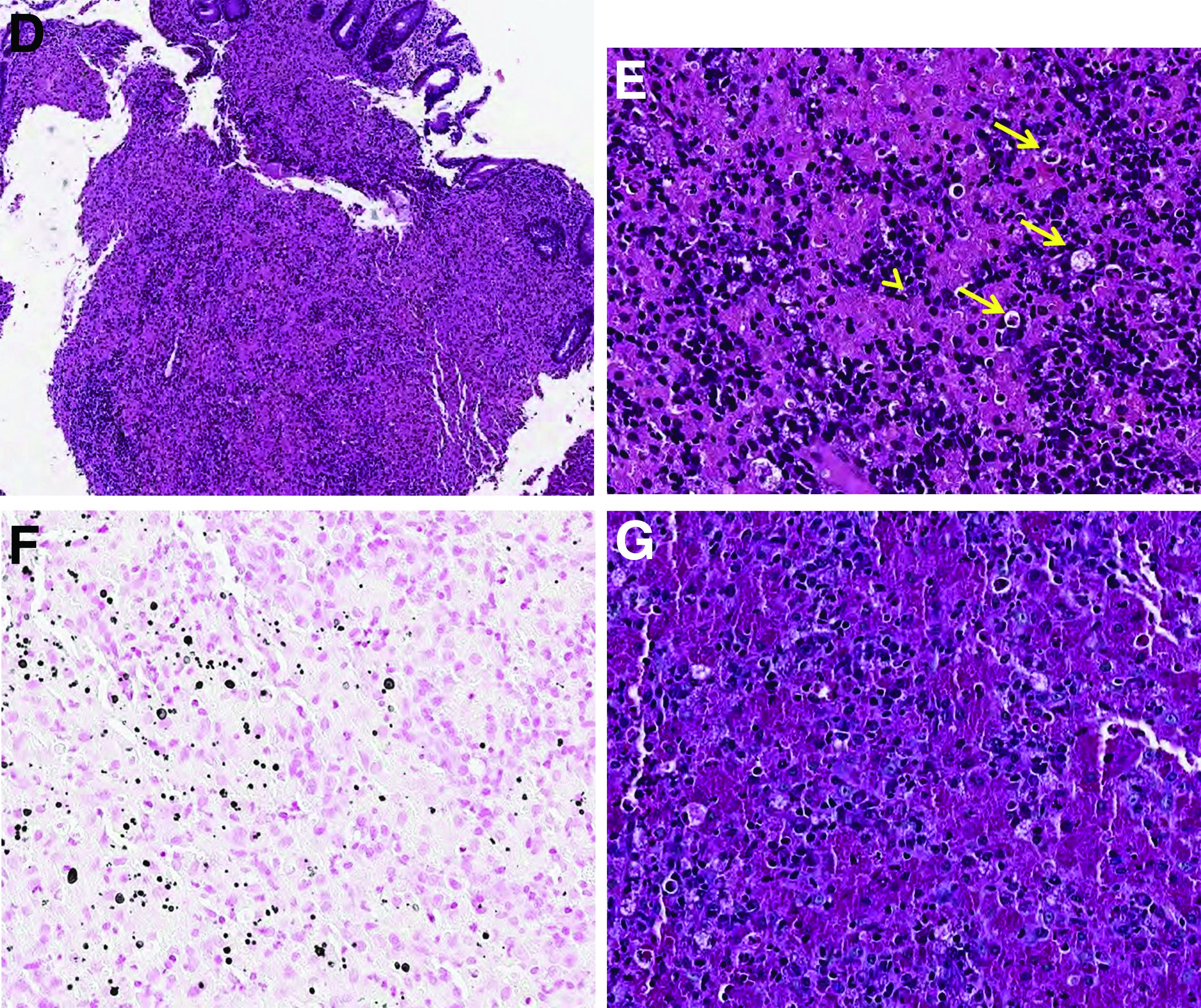
Malakoplakia is an uncommon, chronic, granulomatous inflammatory disease. It most commonly affects the urinary tract and gastrointestinal tract, but may occur at any anatomic site. Malakoplakia of the gastrointestinal tract are seen most frequently in the rectum, sigmoid, and right colon.1 It is diagnosed by the characteristic histologic feature of accumulated histiocytes with abundant eosinophilic granular cytoplasm containing basophilic inclusions, consistent with Michaelis-Gutmann bodies. Although the exact etiology and pathogenesis of malakoplakia are unclear, it seems to originate from an acquired defect in the intracellular destruction of phagocytosed bacteria, usually associated with Escherichia coli, Klebsiella, and Mycobacterium.2 It can have various causes, such as immunosuppression, malignant neoplasms, systemic diseases, and genetic diseases. Clinical manifestation of colonic malakoplakia is diverse, ranging from asymptomatic to malaise, fever, abdominal pain, diarrhea, hematochezia, and intestinal obstruction. Granulomatous reaction of malakoplakia generates the endoscopic appearance of lesions, which ranges from plaques to nodules and yellow-brown masses. In the early stage, malakoplakia commonly presents as soft yellow to tan mucosal plaques endoscopically, as seen in our case (Figure A). As the disease progresses in the later stage, malakoplakia presents as raised, grey to tan polypoid lesions of various sizes with peripheral hyperemia and a central depressed area, as seen in our case (Figure B).3 Owing to this endoscopic morphology, colonic malakoplakia may be misdiagnosed as atypical lymphoma, familial adenomatous polyposis, and metastatic carcinoma. To date, the natural course of malakoplakia of the colon is unclear, and no guidelines for treatment, treatment methods, duration of treatment, or surveillance are currently available. However, treatment of malakoplakia is essential to reduce immunosuppression and includes antibiotics with intracellular action and choline agonists that replenish the decreased cyclic 3’, 5’-guanosine monophosphate levels. In summary, although malakoplakia of the colon is very rare, it should be considered in the differential diagnosis of polypoid colonic lesions, especially in immunocompromised or malnourished patients.
References
1. Cipolletta L et al. Gastrointest Endosc. 1995 Mar;41(3):255-8.
2. Berney T et al. Transpl Int. 1999;12(4):293-6.
3. Weinrach DM et al. Arch Pathol Lab Med. 2004 Oct;128(10):e133-4.
A 60-year-old man with C3 tetraplegia was referred to our department for evaluation of abdominal pain and hematochezia. He was diagnosed with adrenal insufficiency 5 years prior and has been taking low-dose prednisolone (7.5 mg) once a day. One year before presentation, he complained of intermittent loose, mucoid stool and abdominal pain. Sigmoidoscopy revealed multiple small yellowish plaques in the sigmoid colon (Figure A). However, symptoms improved without any treatment, and he was discharged from the rehabilitation department. He was readmitted for respiratory rehabilitation owing to dyspnea. On hospital day 4, he complained of abdominal pain and passing loose stool with foul odor 4-5 times a day. On hospital day 7, the abdominal pain worsened, and hematochezia occurred.
On physical examination, he was hemodynamically stable and afebrile. The abdomen was soft with mild tenderness on palpation in the periumbilical area without peritoneal signs. Laboratory studies were notable with a hemoglobin level of 10.7 g/dL, total protein of 4.09 g/dL, and albumin of 2.21 g/dL. Inflammatory marker (C-reactive protein) was mildly elevated to 1.83 mg/dL. Serology for human immunodeficiency virus was negative. Tumor markers, such as carcinoembryonic antigen, carbohydrate antigenic determinant, and alpha-fetoprotein, were within the normal range. Antineutrophil cytoplasmic antibody was negative, and rheumatic factor was within the normal range. Findings from stool for acid-fast bacillus and Clostridioides difficile toxin were negative; no pathogens were cultured, and no parasites were identified.
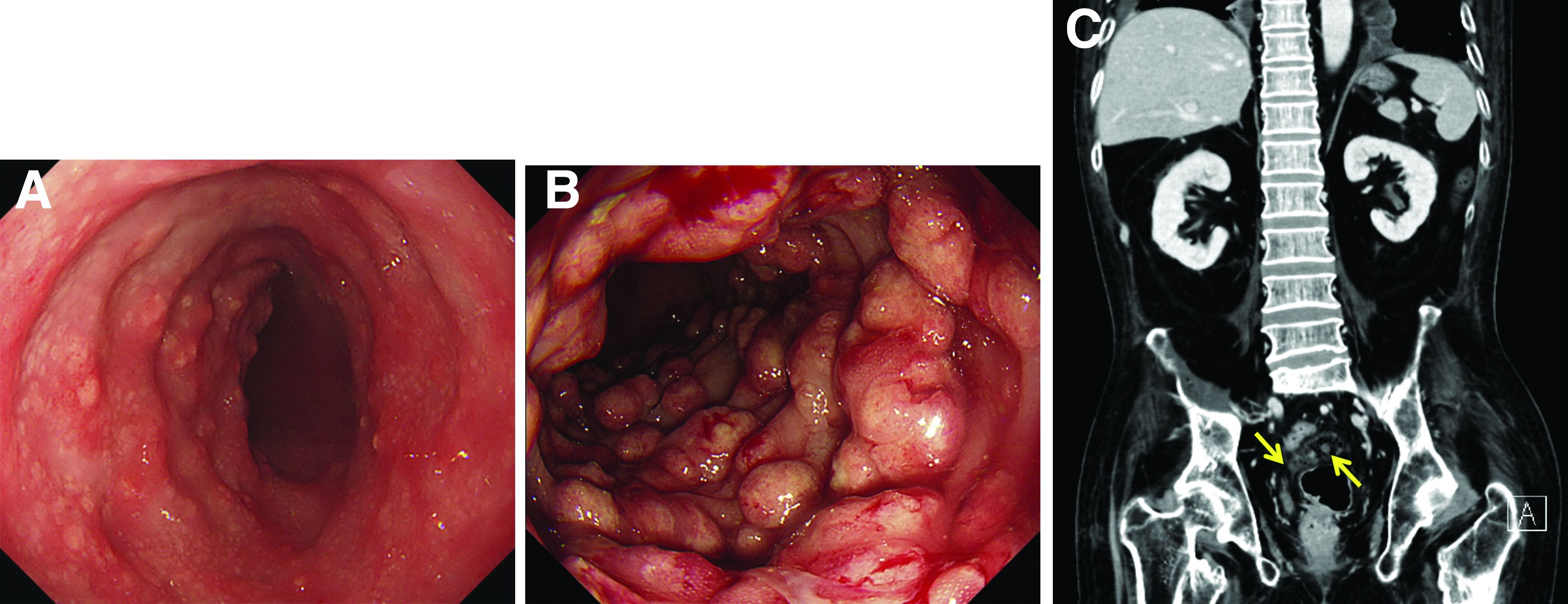
Sigmoidoscopy revealed diverse, multiple polypoid lesions (3-10 mm) with erythema, edema, and friability surrounding the entire lumen on the sigmoid colon (Figure B). The number and size of the polypoid lesions increased compared with the endoscopic findings obtained 1 year prior. The lesions easily bled on contact. Multiple biopsies of different sites were taken. An abdominal computed tomography scan showed multiple polyps of <1 cm that were confined to the sigmoid colon (Figure C, arrow).
Based on this information, what is the most likely diagnosis?
Previously published in Gastroenterology (2020 Feb;158[3]:482-4).
Three symptoms suggest higher risk for self-injury in cancer
, according to a Canadian study.
In a population-based, case-control study, each of these symptoms was associated with an increase of at least 60% in the risk for NFSI in the following 180 days, the investigators report.
“Clinicians should know that self-injury is a real problem after a cancer diagnosis,” lead investigator Julie Hallet, MD, an associate scientist at Sunnybrook Health Sciences Centre in Toronto, told this news organization.
Self-injury “does not necessarily represent an attempted suicide,” she added. “While our data do not allow us to know what the intent was, we know from other work that the repercussions of distress in patients with cancer are much broader than suicide. Self-injury can be a means to cope with psychological difficulties for some patients, without intent for suicide.”
The study was published online in JAMA Oncology.
Nine common symptoms
The study included adults who were diagnosed with cancer between Jan. 1, 2007, and March 31, 2019, and had completed the Edmonton Symptom Assessment System (ESAS) evaluation within 36 months of their index cancer diagnosis. ESAS evaluates nine common cancer-associated symptoms, including pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath, on a patient-reported scale of 0 (absence of symptom) to 10 (worst possible symptom).
The analysis included 406 patients who had visited an emergency department for an NFSI within 180 days of their ESAS evaluation, as well as 1,624 matched control patients with cancer who did not have an NFSI. Case patients and control patients were matched according to age at cancer diagnosis, sex, prior self-injury within 5 years of being diagnosed with cancer, and cancer type. Nonmatched covariates included psychiatric illness and therapy received before NFSI, comorbidity burden, material deprivation, and cancer stage.
Toward tailored intervention
A higher proportion of case patients than control patients reported moderate to severe scores for all nine ESAS symptoms. In an adjusted analysis, moderate to severe anxiety (odds ratio, 1.61), depression (OR, 1.66), and shortness of breath (OR, 1.65) were independently associated with higher odds of subsequent NFSI. Each 10-point increase in total ESAS score also was associated with increased risk (OR, 1.51).
“These findings are important to enhance the use of screening ESAS scores to better support patients,” say the authors. “Scores from ESAS assessments can be used to identify patients at higher risk of NFSI, indicating higher level of distress, and help direct tailored assessment and intervention.”
In prior work, Dr. Hallet’s group showed that NFSI occurs in 3 of every 1,000 patients with cancer. NFSI is more frequent among younger patients and those with a history of prior mental illness. “Identifying patients at risk in clinical practice requires you to inquire about a patient’s prior history, identify high symptom scores and ask about them, and trigger intervention pathways when risk is identified,” said Dr. Hallet.
“For example, a young patient with head and neck cancer and a prior history of mental illness who reports high scores for anxiety and drowsiness would be at high risk of self-injury,” she added. Such a patient should be referred to psycho-oncology, psychiatry, or social work. “To facilitate this, we are working on prognostic scores that can be integrated in clinical practice, such as an electronic medical record, to flag patients at risk,” said Dr. Hallet. “Future work will also need to identify the optimal care pathways for at-risk patients.”
Self-injury vs. suicidality
Commenting on the study for this news organization, Madeline Li, MD, PhD, a psychiatrist and clinician-scientist at Toronto’s Princess Margaret Cancer Centre, said that the findings are “underwhelming” because they tell us what is already known – that “NFSI is associated with distress, and cancer is a stressor.” It would have been more interesting to ask how to distinguish patients at risk for suicide from those at risk for self-harm without suicide, she added.
“The way these authors formulated NFSI included both self-harm intent and suicidal intent,” she explained. The researchers compared patients who were at risk for these two types of events with patients without NFSI. “When we see self-harm without suicidal intent in the emergency room, it’s mostly people making cries for help,” said Dr. Li. “These are people who cut their wrists or take small overdoses on purpose without the intent to die. It would have been more interesting to see if there are different risk factors for people who are just going to self-harm vs. those who are actually going to attempt suicide.”
The study’s identification of risk factors for NSFI is important because “it does tell us that when there’s anxiety, depression, and shortness of breath, we should pay attention to these patients and do something about it,” said Dr. Li. Still, research in cancer psychiatry needs to shift its focus from identifying and addressing existing risk factors to preventing them from developing, she added.
“We need to move earlier and provide emotional and mental health support to cancer patients to prevent them from becoming suicidal, rather than intervening when somebody already is,” Dr. Li concluded.
The study was funded by the Hanna Research Award from the division of surgical oncology at the Odette Cancer Centre–Sunnybrook Health Sciences Centre and by a Sunnybrook Health Sciences Centre Alternate Funding Plan Innovation grant. It was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Dr. Hallet has received personal fees from Ipsen Biopharmaceuticals Canada and AAA outside the submitted work. Dr. Li reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a Canadian study.
In a population-based, case-control study, each of these symptoms was associated with an increase of at least 60% in the risk for NFSI in the following 180 days, the investigators report.
“Clinicians should know that self-injury is a real problem after a cancer diagnosis,” lead investigator Julie Hallet, MD, an associate scientist at Sunnybrook Health Sciences Centre in Toronto, told this news organization.
Self-injury “does not necessarily represent an attempted suicide,” she added. “While our data do not allow us to know what the intent was, we know from other work that the repercussions of distress in patients with cancer are much broader than suicide. Self-injury can be a means to cope with psychological difficulties for some patients, without intent for suicide.”
The study was published online in JAMA Oncology.
Nine common symptoms
The study included adults who were diagnosed with cancer between Jan. 1, 2007, and March 31, 2019, and had completed the Edmonton Symptom Assessment System (ESAS) evaluation within 36 months of their index cancer diagnosis. ESAS evaluates nine common cancer-associated symptoms, including pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath, on a patient-reported scale of 0 (absence of symptom) to 10 (worst possible symptom).
The analysis included 406 patients who had visited an emergency department for an NFSI within 180 days of their ESAS evaluation, as well as 1,624 matched control patients with cancer who did not have an NFSI. Case patients and control patients were matched according to age at cancer diagnosis, sex, prior self-injury within 5 years of being diagnosed with cancer, and cancer type. Nonmatched covariates included psychiatric illness and therapy received before NFSI, comorbidity burden, material deprivation, and cancer stage.
Toward tailored intervention
A higher proportion of case patients than control patients reported moderate to severe scores for all nine ESAS symptoms. In an adjusted analysis, moderate to severe anxiety (odds ratio, 1.61), depression (OR, 1.66), and shortness of breath (OR, 1.65) were independently associated with higher odds of subsequent NFSI. Each 10-point increase in total ESAS score also was associated with increased risk (OR, 1.51).
“These findings are important to enhance the use of screening ESAS scores to better support patients,” say the authors. “Scores from ESAS assessments can be used to identify patients at higher risk of NFSI, indicating higher level of distress, and help direct tailored assessment and intervention.”
In prior work, Dr. Hallet’s group showed that NFSI occurs in 3 of every 1,000 patients with cancer. NFSI is more frequent among younger patients and those with a history of prior mental illness. “Identifying patients at risk in clinical practice requires you to inquire about a patient’s prior history, identify high symptom scores and ask about them, and trigger intervention pathways when risk is identified,” said Dr. Hallet.
“For example, a young patient with head and neck cancer and a prior history of mental illness who reports high scores for anxiety and drowsiness would be at high risk of self-injury,” she added. Such a patient should be referred to psycho-oncology, psychiatry, or social work. “To facilitate this, we are working on prognostic scores that can be integrated in clinical practice, such as an electronic medical record, to flag patients at risk,” said Dr. Hallet. “Future work will also need to identify the optimal care pathways for at-risk patients.”
Self-injury vs. suicidality
Commenting on the study for this news organization, Madeline Li, MD, PhD, a psychiatrist and clinician-scientist at Toronto’s Princess Margaret Cancer Centre, said that the findings are “underwhelming” because they tell us what is already known – that “NFSI is associated with distress, and cancer is a stressor.” It would have been more interesting to ask how to distinguish patients at risk for suicide from those at risk for self-harm without suicide, she added.
“The way these authors formulated NFSI included both self-harm intent and suicidal intent,” she explained. The researchers compared patients who were at risk for these two types of events with patients without NFSI. “When we see self-harm without suicidal intent in the emergency room, it’s mostly people making cries for help,” said Dr. Li. “These are people who cut their wrists or take small overdoses on purpose without the intent to die. It would have been more interesting to see if there are different risk factors for people who are just going to self-harm vs. those who are actually going to attempt suicide.”
The study’s identification of risk factors for NSFI is important because “it does tell us that when there’s anxiety, depression, and shortness of breath, we should pay attention to these patients and do something about it,” said Dr. Li. Still, research in cancer psychiatry needs to shift its focus from identifying and addressing existing risk factors to preventing them from developing, she added.
“We need to move earlier and provide emotional and mental health support to cancer patients to prevent them from becoming suicidal, rather than intervening when somebody already is,” Dr. Li concluded.
The study was funded by the Hanna Research Award from the division of surgical oncology at the Odette Cancer Centre–Sunnybrook Health Sciences Centre and by a Sunnybrook Health Sciences Centre Alternate Funding Plan Innovation grant. It was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Dr. Hallet has received personal fees from Ipsen Biopharmaceuticals Canada and AAA outside the submitted work. Dr. Li reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a Canadian study.
In a population-based, case-control study, each of these symptoms was associated with an increase of at least 60% in the risk for NFSI in the following 180 days, the investigators report.
“Clinicians should know that self-injury is a real problem after a cancer diagnosis,” lead investigator Julie Hallet, MD, an associate scientist at Sunnybrook Health Sciences Centre in Toronto, told this news organization.
Self-injury “does not necessarily represent an attempted suicide,” she added. “While our data do not allow us to know what the intent was, we know from other work that the repercussions of distress in patients with cancer are much broader than suicide. Self-injury can be a means to cope with psychological difficulties for some patients, without intent for suicide.”
The study was published online in JAMA Oncology.
Nine common symptoms
The study included adults who were diagnosed with cancer between Jan. 1, 2007, and March 31, 2019, and had completed the Edmonton Symptom Assessment System (ESAS) evaluation within 36 months of their index cancer diagnosis. ESAS evaluates nine common cancer-associated symptoms, including pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath, on a patient-reported scale of 0 (absence of symptom) to 10 (worst possible symptom).
The analysis included 406 patients who had visited an emergency department for an NFSI within 180 days of their ESAS evaluation, as well as 1,624 matched control patients with cancer who did not have an NFSI. Case patients and control patients were matched according to age at cancer diagnosis, sex, prior self-injury within 5 years of being diagnosed with cancer, and cancer type. Nonmatched covariates included psychiatric illness and therapy received before NFSI, comorbidity burden, material deprivation, and cancer stage.
Toward tailored intervention
A higher proportion of case patients than control patients reported moderate to severe scores for all nine ESAS symptoms. In an adjusted analysis, moderate to severe anxiety (odds ratio, 1.61), depression (OR, 1.66), and shortness of breath (OR, 1.65) were independently associated with higher odds of subsequent NFSI. Each 10-point increase in total ESAS score also was associated with increased risk (OR, 1.51).
“These findings are important to enhance the use of screening ESAS scores to better support patients,” say the authors. “Scores from ESAS assessments can be used to identify patients at higher risk of NFSI, indicating higher level of distress, and help direct tailored assessment and intervention.”
In prior work, Dr. Hallet’s group showed that NFSI occurs in 3 of every 1,000 patients with cancer. NFSI is more frequent among younger patients and those with a history of prior mental illness. “Identifying patients at risk in clinical practice requires you to inquire about a patient’s prior history, identify high symptom scores and ask about them, and trigger intervention pathways when risk is identified,” said Dr. Hallet.
“For example, a young patient with head and neck cancer and a prior history of mental illness who reports high scores for anxiety and drowsiness would be at high risk of self-injury,” she added. Such a patient should be referred to psycho-oncology, psychiatry, or social work. “To facilitate this, we are working on prognostic scores that can be integrated in clinical practice, such as an electronic medical record, to flag patients at risk,” said Dr. Hallet. “Future work will also need to identify the optimal care pathways for at-risk patients.”
Self-injury vs. suicidality
Commenting on the study for this news organization, Madeline Li, MD, PhD, a psychiatrist and clinician-scientist at Toronto’s Princess Margaret Cancer Centre, said that the findings are “underwhelming” because they tell us what is already known – that “NFSI is associated with distress, and cancer is a stressor.” It would have been more interesting to ask how to distinguish patients at risk for suicide from those at risk for self-harm without suicide, she added.
“The way these authors formulated NFSI included both self-harm intent and suicidal intent,” she explained. The researchers compared patients who were at risk for these two types of events with patients without NFSI. “When we see self-harm without suicidal intent in the emergency room, it’s mostly people making cries for help,” said Dr. Li. “These are people who cut their wrists or take small overdoses on purpose without the intent to die. It would have been more interesting to see if there are different risk factors for people who are just going to self-harm vs. those who are actually going to attempt suicide.”
The study’s identification of risk factors for NSFI is important because “it does tell us that when there’s anxiety, depression, and shortness of breath, we should pay attention to these patients and do something about it,” said Dr. Li. Still, research in cancer psychiatry needs to shift its focus from identifying and addressing existing risk factors to preventing them from developing, she added.
“We need to move earlier and provide emotional and mental health support to cancer patients to prevent them from becoming suicidal, rather than intervening when somebody already is,” Dr. Li concluded.
The study was funded by the Hanna Research Award from the division of surgical oncology at the Odette Cancer Centre–Sunnybrook Health Sciences Centre and by a Sunnybrook Health Sciences Centre Alternate Funding Plan Innovation grant. It was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Dr. Hallet has received personal fees from Ipsen Biopharmaceuticals Canada and AAA outside the submitted work. Dr. Li reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
It’s time to shame the fat shamers
Fat shaming doesn’t work. If it did, obesity as we know it wouldn’t exist because if the one thing society ensures isn’t lacking for people with obesity, it’s shame. We know that fat shaming doesn’t lead to weight loss and that it’s actually correlated with weight gain: More shame leads to more gain (Puhl and Suh; Sutin and Terracciano; Tomiyama et al).
Shaming and weight stigma have far more concerning associations than weight gain. People who report experiencing more weight stigma have an increased risk for depression, anxiety, low self-esteem, poor body image, substance abuse, suicidality, unhealthy eating behaviors, disordered eating, increased caloric intake, exercise avoidance, decreased exercise motivation potentially due to heightened cortisol reactivity, elevated C-reactive protein, and elevated blood pressure.
Meanwhile, people with obesity – likely in part owing to negative weight-biased experiences in health care – are reluctant to discuss weight with their health care providers and are less likely to seek care at all for any conditions. When care is sought, people with obesity are more likely to receive substandard treatment, including receiving fewer preventive health screenings, decreased health education, and decreased time spent in appointments.
Remember that obesity is not a conscious choice
A fact that is conveniently forgotten by those who are most prone to fat shaming is that obesity, like every chronic noncommunicable disease, isn’t a choice that is consciously made by patients.
And yes, though there are lifestyle means that might affect weight, there are lifestyle means that might affect all chronic diseases – yet obesity is the only one we seem to moralize about. It’s also worth noting that other chronic diseases’ lifestyle levers tend not to be governed by thousands of genes and dozens of hormones; those trying to “lifestyle” their way out of obesity are swimming against strong physiologic currents that influence our most seminally important survival drive: eating.
But forgetting about physiologic currents, there is also staggering privilege associated with intentional perpetual behavior change around food and fitness in the name of health.
Whereas medicine and the world are right and quick to embrace the fights against racism, sexism, and homophobia, the push to confront weight bias is far rarer, despite the fact that it’s been shown to be rampant among health care professionals.
Protecting the rights of people with obesity
Perhaps though, times are changing. Movements are popping up to protect the rights of people with obesity while combating hate.
Of note, Brazil seems to have embraced a campaign to fight gordofobia — the Portuguese term used to describe weight-based discrimination. For instance, laws are being passed to ensure appropriate seating is supplied in schools for children with obesity, an annual day was formalized to promote the rights of people with obesity, preferential seating is provided on subways for people with obesity, and fines have been levied against at least one comedian for making fat jokes on the grounds of the state’s duty to protect minorities.
We need to take this fight to medicine. Given the incredibly depressing prevalence of weight bias among trainees, medical schools and residency programs should ensure countering weight bias is not only part of the curriculum but that it’s explicitly examined. National medical licensing examinations should include weight bias as well.
Though we’re closer than ever before to widely effective treatment options for obesity, it’s likely to still be decades before pharmaceutical options to treat obesity are as effective, accepted, and encouraged as medications to treat hypertension, dyslipidemia, diabetes, and more are today.
If you’re curious about your own implicit weight biases, consider taking Harvard’s Implicit Association Test for Weight. You might also want to take a few moments and review the Strategies to Overcome and Prevent Obesity Alliances’ Weight Can’t Wait guide for advice on the management of obesity in primary care.
Treat patients with obesity the same as you would those with any chronic condition.
Also, consider your physical office space. Do you have chairs suitable for patients with obesity (wide base and with arms to help patients rise)? A scale that measures up to high weights that’s in a private location? Appropriately sized blood pressure cuffs?
If not,
Examples include the family doctor who hadn’t checked my patient’s blood pressure in over a decade because he couldn’t be bothered buying an appropriately sized blood pressure cuff. Or the fertility doctor who told one of my patients that perhaps her weight reflected God’s will that she does not have children.
Finally, if reading this article about treating people with obesity the same as you would patients with other chronic, noncommunicable, lifestyle responsive diseases made you angry, there’s a great chance that you’re part of the problem.
Dr. Freedhoff, is associate professor of family medicine at the University of Ottawa and medical director of the Bariatric Medical Institute, a nonsurgical weight management center. He is one of Canada’s most outspoken obesity experts and the author of The Diet Fix: Why Diets Fail and How to Make Yours Work. He has disclosed the following: He served as a director, officer, partner, employee, adviser, consultant, or trustee for Bariatric Medical Institute and Constant Health; has received research grant from Novo Nordisk, and has publicly shared opinions via Weighty Matters and social media. A version of this article first appeared on Medscape.com.
Fat shaming doesn’t work. If it did, obesity as we know it wouldn’t exist because if the one thing society ensures isn’t lacking for people with obesity, it’s shame. We know that fat shaming doesn’t lead to weight loss and that it’s actually correlated with weight gain: More shame leads to more gain (Puhl and Suh; Sutin and Terracciano; Tomiyama et al).
Shaming and weight stigma have far more concerning associations than weight gain. People who report experiencing more weight stigma have an increased risk for depression, anxiety, low self-esteem, poor body image, substance abuse, suicidality, unhealthy eating behaviors, disordered eating, increased caloric intake, exercise avoidance, decreased exercise motivation potentially due to heightened cortisol reactivity, elevated C-reactive protein, and elevated blood pressure.
Meanwhile, people with obesity – likely in part owing to negative weight-biased experiences in health care – are reluctant to discuss weight with their health care providers and are less likely to seek care at all for any conditions. When care is sought, people with obesity are more likely to receive substandard treatment, including receiving fewer preventive health screenings, decreased health education, and decreased time spent in appointments.
Remember that obesity is not a conscious choice
A fact that is conveniently forgotten by those who are most prone to fat shaming is that obesity, like every chronic noncommunicable disease, isn’t a choice that is consciously made by patients.
And yes, though there are lifestyle means that might affect weight, there are lifestyle means that might affect all chronic diseases – yet obesity is the only one we seem to moralize about. It’s also worth noting that other chronic diseases’ lifestyle levers tend not to be governed by thousands of genes and dozens of hormones; those trying to “lifestyle” their way out of obesity are swimming against strong physiologic currents that influence our most seminally important survival drive: eating.
But forgetting about physiologic currents, there is also staggering privilege associated with intentional perpetual behavior change around food and fitness in the name of health.
Whereas medicine and the world are right and quick to embrace the fights against racism, sexism, and homophobia, the push to confront weight bias is far rarer, despite the fact that it’s been shown to be rampant among health care professionals.
Protecting the rights of people with obesity
Perhaps though, times are changing. Movements are popping up to protect the rights of people with obesity while combating hate.
Of note, Brazil seems to have embraced a campaign to fight gordofobia — the Portuguese term used to describe weight-based discrimination. For instance, laws are being passed to ensure appropriate seating is supplied in schools for children with obesity, an annual day was formalized to promote the rights of people with obesity, preferential seating is provided on subways for people with obesity, and fines have been levied against at least one comedian for making fat jokes on the grounds of the state’s duty to protect minorities.
We need to take this fight to medicine. Given the incredibly depressing prevalence of weight bias among trainees, medical schools and residency programs should ensure countering weight bias is not only part of the curriculum but that it’s explicitly examined. National medical licensing examinations should include weight bias as well.
Though we’re closer than ever before to widely effective treatment options for obesity, it’s likely to still be decades before pharmaceutical options to treat obesity are as effective, accepted, and encouraged as medications to treat hypertension, dyslipidemia, diabetes, and more are today.
If you’re curious about your own implicit weight biases, consider taking Harvard’s Implicit Association Test for Weight. You might also want to take a few moments and review the Strategies to Overcome and Prevent Obesity Alliances’ Weight Can’t Wait guide for advice on the management of obesity in primary care.
Treat patients with obesity the same as you would those with any chronic condition.
Also, consider your physical office space. Do you have chairs suitable for patients with obesity (wide base and with arms to help patients rise)? A scale that measures up to high weights that’s in a private location? Appropriately sized blood pressure cuffs?
If not,
Examples include the family doctor who hadn’t checked my patient’s blood pressure in over a decade because he couldn’t be bothered buying an appropriately sized blood pressure cuff. Or the fertility doctor who told one of my patients that perhaps her weight reflected God’s will that she does not have children.
Finally, if reading this article about treating people with obesity the same as you would patients with other chronic, noncommunicable, lifestyle responsive diseases made you angry, there’s a great chance that you’re part of the problem.
Dr. Freedhoff, is associate professor of family medicine at the University of Ottawa and medical director of the Bariatric Medical Institute, a nonsurgical weight management center. He is one of Canada’s most outspoken obesity experts and the author of The Diet Fix: Why Diets Fail and How to Make Yours Work. He has disclosed the following: He served as a director, officer, partner, employee, adviser, consultant, or trustee for Bariatric Medical Institute and Constant Health; has received research grant from Novo Nordisk, and has publicly shared opinions via Weighty Matters and social media. A version of this article first appeared on Medscape.com.
Fat shaming doesn’t work. If it did, obesity as we know it wouldn’t exist because if the one thing society ensures isn’t lacking for people with obesity, it’s shame. We know that fat shaming doesn’t lead to weight loss and that it’s actually correlated with weight gain: More shame leads to more gain (Puhl and Suh; Sutin and Terracciano; Tomiyama et al).
Shaming and weight stigma have far more concerning associations than weight gain. People who report experiencing more weight stigma have an increased risk for depression, anxiety, low self-esteem, poor body image, substance abuse, suicidality, unhealthy eating behaviors, disordered eating, increased caloric intake, exercise avoidance, decreased exercise motivation potentially due to heightened cortisol reactivity, elevated C-reactive protein, and elevated blood pressure.
Meanwhile, people with obesity – likely in part owing to negative weight-biased experiences in health care – are reluctant to discuss weight with their health care providers and are less likely to seek care at all for any conditions. When care is sought, people with obesity are more likely to receive substandard treatment, including receiving fewer preventive health screenings, decreased health education, and decreased time spent in appointments.
Remember that obesity is not a conscious choice
A fact that is conveniently forgotten by those who are most prone to fat shaming is that obesity, like every chronic noncommunicable disease, isn’t a choice that is consciously made by patients.
And yes, though there are lifestyle means that might affect weight, there are lifestyle means that might affect all chronic diseases – yet obesity is the only one we seem to moralize about. It’s also worth noting that other chronic diseases’ lifestyle levers tend not to be governed by thousands of genes and dozens of hormones; those trying to “lifestyle” their way out of obesity are swimming against strong physiologic currents that influence our most seminally important survival drive: eating.
But forgetting about physiologic currents, there is also staggering privilege associated with intentional perpetual behavior change around food and fitness in the name of health.
Whereas medicine and the world are right and quick to embrace the fights against racism, sexism, and homophobia, the push to confront weight bias is far rarer, despite the fact that it’s been shown to be rampant among health care professionals.
Protecting the rights of people with obesity
Perhaps though, times are changing. Movements are popping up to protect the rights of people with obesity while combating hate.
Of note, Brazil seems to have embraced a campaign to fight gordofobia — the Portuguese term used to describe weight-based discrimination. For instance, laws are being passed to ensure appropriate seating is supplied in schools for children with obesity, an annual day was formalized to promote the rights of people with obesity, preferential seating is provided on subways for people with obesity, and fines have been levied against at least one comedian for making fat jokes on the grounds of the state’s duty to protect minorities.
We need to take this fight to medicine. Given the incredibly depressing prevalence of weight bias among trainees, medical schools and residency programs should ensure countering weight bias is not only part of the curriculum but that it’s explicitly examined. National medical licensing examinations should include weight bias as well.
Though we’re closer than ever before to widely effective treatment options for obesity, it’s likely to still be decades before pharmaceutical options to treat obesity are as effective, accepted, and encouraged as medications to treat hypertension, dyslipidemia, diabetes, and more are today.
If you’re curious about your own implicit weight biases, consider taking Harvard’s Implicit Association Test for Weight. You might also want to take a few moments and review the Strategies to Overcome and Prevent Obesity Alliances’ Weight Can’t Wait guide for advice on the management of obesity in primary care.
Treat patients with obesity the same as you would those with any chronic condition.
Also, consider your physical office space. Do you have chairs suitable for patients with obesity (wide base and with arms to help patients rise)? A scale that measures up to high weights that’s in a private location? Appropriately sized blood pressure cuffs?
If not,
Examples include the family doctor who hadn’t checked my patient’s blood pressure in over a decade because he couldn’t be bothered buying an appropriately sized blood pressure cuff. Or the fertility doctor who told one of my patients that perhaps her weight reflected God’s will that she does not have children.
Finally, if reading this article about treating people with obesity the same as you would patients with other chronic, noncommunicable, lifestyle responsive diseases made you angry, there’s a great chance that you’re part of the problem.
Dr. Freedhoff, is associate professor of family medicine at the University of Ottawa and medical director of the Bariatric Medical Institute, a nonsurgical weight management center. He is one of Canada’s most outspoken obesity experts and the author of The Diet Fix: Why Diets Fail and How to Make Yours Work. He has disclosed the following: He served as a director, officer, partner, employee, adviser, consultant, or trustee for Bariatric Medical Institute and Constant Health; has received research grant from Novo Nordisk, and has publicly shared opinions via Weighty Matters and social media. A version of this article first appeared on Medscape.com.
How to address social determinants of health, according to expert panel
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
AT INTERNAL MEDICINE 2022






