User login
‘War has changed’: CDC says Delta as contagious as chicken pox
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
COVID brings evolutionary virologists out of the shadows, into the fight
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
Becoming vaccine ambassadors: A new role for psychiatrists
After more than 600,000 deaths in the United States from the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), several safe and effective vaccines against the virus have become available. Vaccines are the most effective preventive measure against COVID-19 and the most promising way to achieve herd immunity to end the current pandemic. However, obstacles to reaching this goal include vaccine skepticism, structural barriers, or simple inertia to get vaccinated. These challenges provide opportunities for psychiatrists to use their medical knowledge and expertise, applying behavior management techniques such as motivational interviewing and nudging to encourage their patients to get vaccinated. In particular, marginalized patients with serious mental illness (SMI), who are subject to disproportionately high rates of COVID-19 infection and more severe outcomes,1 have much to gain if psychiatrists become involved in the COVID-19 vaccination campaign.
In this article, we define vaccine hesitancy and highlight what makes psychiatrists ideal vaccine ambassadors, given their unique skill set and longitudinal, trust-based connection with their patients. We expand on the particular vulnerabilities of patients with SMI, including structural barriers to vaccination that lead to health disparities and inequity. Finally, building on “The ABCs of successful vaccinations” framework published in
What is vaccine hesitancy?
The World Health Organization (WHO) defines vaccine hesitancy as a “delay in acceptance or refusal of vaccines despite availability of vaccine services.”3,4 Vaccine hesitancy occurs on a continuum ranging from uncertainty about accepting a vaccine to absolute refusal.4,5 It involves a complex decision-making process driven by contextual, individual, and social influences, and vaccine-specific issues.4 In the “3C” model developed by the WHO Strategic Advisory Group of Experts (SAGE) Working Group, vaccine hesitancy is influenced by confidence (trust in vaccines, in the health care system, and in policy makers), complacency (lower perceived risk), and convenience (availability, affordability, accessibility, language and health literacy, appeal of vaccination program).4
In 2019, the WHO named vaccine hesitancy as one of the top 10 global health threats.3 Hesitancy to receive COVID-19 vaccines may be particularly high because of their rapid development. In addition, the tumultuous political environment that often featured inconsistent messaging about the virus, its dangers, and its transmission since the early days of the pandemic created widespread public confusion and doubt as scientific understandings evolved. “Anti-vaxxer” movements that completely rejected vaccine efficacy disseminated misinformation online. Followers of these movements may have such extreme overvalued ideas that any effort to persuade them otherwise with scientific evidence will accomplish very little.6,7 Therefore, focusing on individuals who are “sitting on the fence” about getting vaccinated can be more productive because they represent a much larger group than those who adamantly refuse vaccines, and they may be more amenable to changing beliefs and behaviors.8
The US Census Bureau’s Household Pulse Survey asked, “How likely are you to accept the vaccine?”9 As of late June 2021, 11.4% of US adults reported they would “definitely not get a vaccine” or “probably not get a vaccine,” and that number increases to 16.9% when including those who are “unsure,” although there is wide geographical variability.10
A recent study in Denmark showed that willingness to receive the COVID-19 vaccine was slightly lower among patients with mental illness (84.8%) compared with the general population (89.5%).11 Given the small difference, vaccine hesitancy was not considered to be a major barrier for vaccination among patients with mental illness in Denmark. This is similar to the findings of a pre-pandemic study at a community mental health clinic in the United States involving other vaccinations, which suggested that 84% of patients with SMI perceived vaccinations as safe, effective, and important.12 In this clinic, identified barriers to vaccinations in general among patients with SMI included lack of awareness and knowledge (42.2%), accessibility (16.3%), personal cost (13.3%), fears about immunization (10.4%), and lack of recommendations by primary care providers (PCPs) (1.5%).12
It is critical to distinguish attitude-driven vaccine hesitancy from a lack of education and opportunity to receive a vaccine. Particularly disadvantaged communities may be mislabeled as “vaccine hesitant” when in fact they may not have the ability to be as proactive as other population groups (eg, difficulty scheduling appointments over the Internet).
Continue to: What makes psychiatrists ideal vaccine ambassadors?
What makes psychiatrists ideal vaccine ambassadors?
There are several reasons psychiatrists can be well-positioned to contribute to the success of vaccination campaigns (Table 1). These include their frequent contact with patients and their care teams, the high trust those patients have in them, and their medical expertise and skills in applied behavioral and social science techniques, including motivational interviewing and nudging. Vaccination efforts and outreach are more effective when led by the clinician with whom the patient has the most contact because resolving vaccine hesitancy is not a one-time discussion but requires ongoing communication, persistence, and consistency.13 Patients may contact their psychiatrists more frequently than their other clinicians, including PCPs. For this reason, psychiatrists can serve as the gateway to health care, particularly for patients with SMI.14 In addition, interruptions in nonemergency services caused by the COVID-19 pandemic may affect vaccine delivery because patients may have been unable to see their PCPs regularly during the pandemic.15
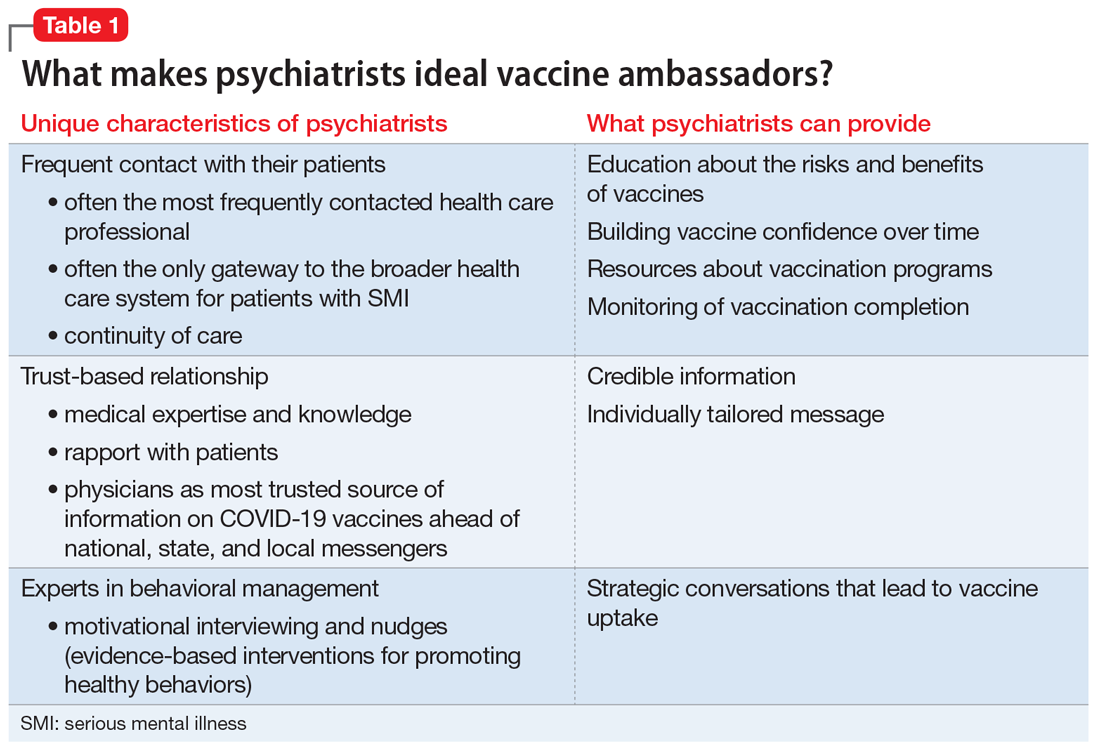
Psychiatrists’ medical expertise and their ability to develop rapport with their patients promote trust-building. Receiving credible information from a trusted source such as a patient’s psychiatrist can be impactful. A recent poll suggested that individual health care clinicians have been consistently identified as the most trusted sources for vaccine information, including for the COVID-19 vaccines.16 There is also higher trust when there is greater continuity of care both in terms of length of time the patient has known the clinician and the number of consultations,17 an inherent part of psychiatric practice. In addition, research has shown that patients trust their psychiatrists as much as they trust their general practitioners.18
Psychiatrists are experts in behavior change, promoting healthy behaviors through motivational interviewing and nudging. They also have experience with managing patients who hold overvalued ideas as well as dealing with uncertainty, given their scientific and medical training.
Motivational interviewing is a patient-centered, collaborative approach widely used by psychiatrists to treat unhealthy behaviors such as substance use. Clinicians elicit and strengthen the patient’s desire and motivation for change while respecting their autonomy. Instead of presenting persuasive facts, the clinician creates a welcoming, nonthreatening, safe environment by engaging patients in open dialogue, reflecting back the patients’ concerns with empathy, helping them realize contradictions in behavior, and supporting self-sufficiency.19 In a nonpsychiatric setting, studies have shown the effectiveness of motivational interviewing in increasing uptake of human papillomavirus vaccines and of pediatric vaccines.20
Nudging, which comes from behavioral economics and psychology, underscores the importance of structuring a choice architecture in changing the way people make their everyday decisions.21 Nudging still gives people a choice and respects autonomy, but it leads patients to more efficient and productive decision-making. Many nudges are based around giving good “default options” because people often do not make efforts to deviate from default options. In addition, social nudges are powerful, giving people a social reference point and normalizing certain behaviors.21 Psychiatrists have become skilled in nudging from working with patients with varying levels of insight and cognitive capabilities. That is, they give simple choices, prompts, and frequent feedback to reinforce “good” decisions and to discourage “bad” decisions.
Continue to: Managing overvalued ideas
Managing overvalued ideas. Psychiatrists are also well-versed in having discussions with patients who hold irrational beliefs (psychosis) or overvalued ideas. For example, psychiatrists frequently manage anorexia nervosa and hypochondria, which are rooted in overvalued ideas.7 While psychiatrists may not be able to directly confront the overvalued ideas, they can work around such ideas while waiting for more flexible moments. Similarly, managing patients with intense emotional commitment7 to commonly held anti-vaccination ideas may not be much different. Psychiatrists can work around resistance until patients may be less strongly attached to those overvalued ideas in instances when other techniques, such as motivational interviewing and nudging, may be more effective.
Managing uncertainty. Psychiatrists are experts in managing “not knowing” and uncertainty. Due to their medical scientific training, they are familiar with the process of science, and how understanding changes through trial and error. In contrast, most patients usually only see the end product (ie, a drug comes to market). Discussions with patients that acknowledge uncertainty and emphasize that changes in what is known are expected and appropriate as scientific knowledge evolves could help preempt skepticism when messages are updated.
Why do patients with SMI need more help?
SMI as a high-risk group. Patients with SMI are part of a “tragic” epidemiologic triad of agent-host-environment15 that places them at remarkably elevated risk for COVID-19 infection and more serious complications and death when infected.1 After age, a diagnosis of a schizophrenia spectrum disorder is the second largest predictor of mortality from COVID-19, with a 2.7-fold increase in mortality.22 This is how the elements of the triad come together: SARS-Cov-2 is a highly infectious agent affecting individuals who are vulnerable hosts because of their high frequency of medical comorbidities, including cardiovascular disease, type 2 diabetes, and respiratory tract diseases, which are all risk factors for worse outcomes due to COVID-19.23 In addition, SMI is associated with socioeconomic risk factors for SARS-Cov-2 infection, including poverty, homelessness, and crowded settings such as jails, group homes, hospitals, and shelters, which constitute ideal environments for high transmission of the virus.
Structural barriers to vaccination. Studies have suggested lower rates of vaccination among people with SMI for various other infectious diseases compared with the general population.12 For example, in 1 outpatient mental health setting, influenza vaccination rates were 24% to 28%, which was lower than the national vaccination rate of 40.9% for the same influenza season (2010 to 2011).24 More recently, a study in Israel examining the COVID-19 vaccination rate among >25,000 patients with schizophrenia suggested under-vaccination of this cohort. The results showed that the odds of getting the COVID-19 vaccination were significantly lower in the schizophrenia group compared with the general population (odds ratio = 0.80, 95% CI: 0.77 to 0.83).25
Patients with SMI encounter considerable system-level barriers to vaccinations in general, such as reduced access to health care due to cost and a lack of transportation,12 the digital divide given their reduced access to the internet and computers for information and scheduling,26 and lack of vaccination recommendations from their PCPs.12 Studies have also shown that patients with SMI often receive suboptimal medical care because of stigmatization and discrimination.27 They also have lower rates of preventive care utilization, seeking medical services only in times of crisis and seeking mental health services more often than physical health care.28-30
Continue to: Patients with SMI face...
Patients with SMI face additional individual challenges that impede vaccine uptake, such as lack of knowledge and awareness about the virus and vaccinations, general cognitive impairment, low digital literacy skills,31 low language literacy and educational attainment, baseline delusions, and negative symptoms such as apathy, avolition, and anhedonia.1 Thus, even if they overcome the external barriers and obtain vaccine-related information, these patients may experience difficulty in understanding the content and applying this information to their personal circumstances as a result of low health literacy.
How psychiatrists can help
The concept of using mental health care sites and trained clinicians to increase medical disease prevention is not new. The rigorously tested intervention model STIRR (Screen, Test, Immunize, Reduce risk, and Refer) uses co-located nurse practitioners in community mental health centers to provide risk assessment, counseling, and blood testing for hepatitis and HIV, as well as on-site vaccinations for hepatitis to patients dually diagnosed with SMI and substance use disorders.32
Prioritization of patients with SMI for vaccine eligibility does not directly lead to vaccine uptake. Patients with SMI need extra support from their primary point of health care contact, namely their psychiatrists. Psychiatrists may bring a set of specialized skills uniquely suited to this moment to address vaccine hesitancy and overall lack of vaccine resources and awareness. Freudenreich et al2 recently proposed “The ABCs of Successful Vaccinations” framework that psychiatrists can use in their interactions with patients to encourage vaccination by focusing on:
- attitudes towards vaccination
- barriers to vaccination
- completed vaccination series.
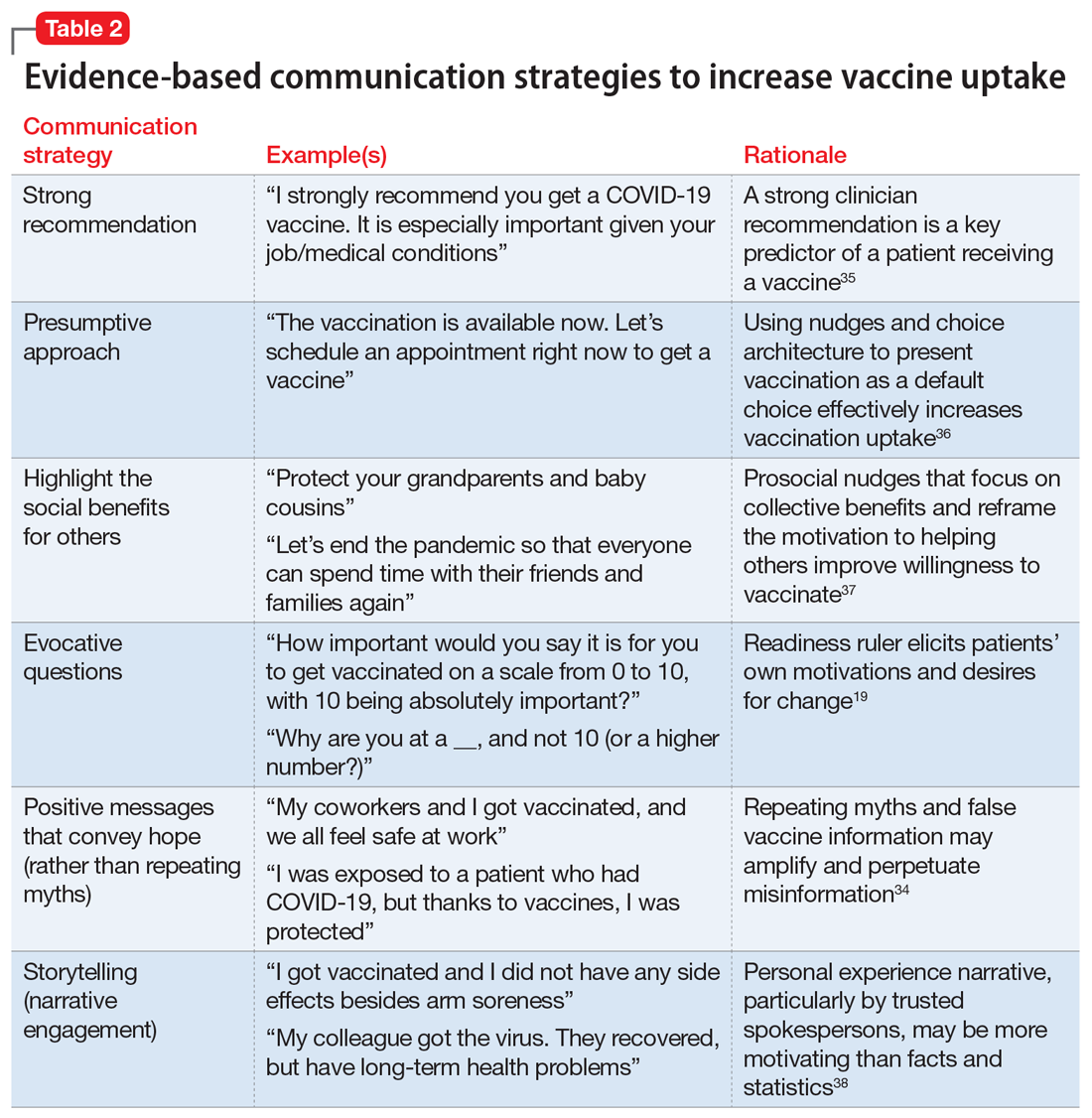
Understand attitudes toward vaccination. Decision-making may be an emotional and psychological experience that is informed by thoughts and feelings,34 and psychiatrists are uniquely positioned to tailor messages to individual patients by using motivational interviewing and applying nudging techniques.8 Given the large role of the pandemic in everyday life, it would be natural to address vaccine-related concerns in the course of routine rapport-building. Table 219,34-38 shows example phrases of COVID-19 vaccine messages that are based on communication strategies that have demonstrated success in health behavior domains (including vaccinations).39
Continue to: First, a strong recommendation...
First, a strong recommendation should be made using the presumptive approach.40 If vaccine hesitancy is detected, psychiatrists should next attempt to understand patients’ reasoning with open-ended questions to probe vaccine-related concerns. Motivational interviewing can then be used to target the fence sitters (rather than anti-vaxxers).6 Psychiatrists can also communicate with therapists about the need for further follow up on patients’ hesitancies.
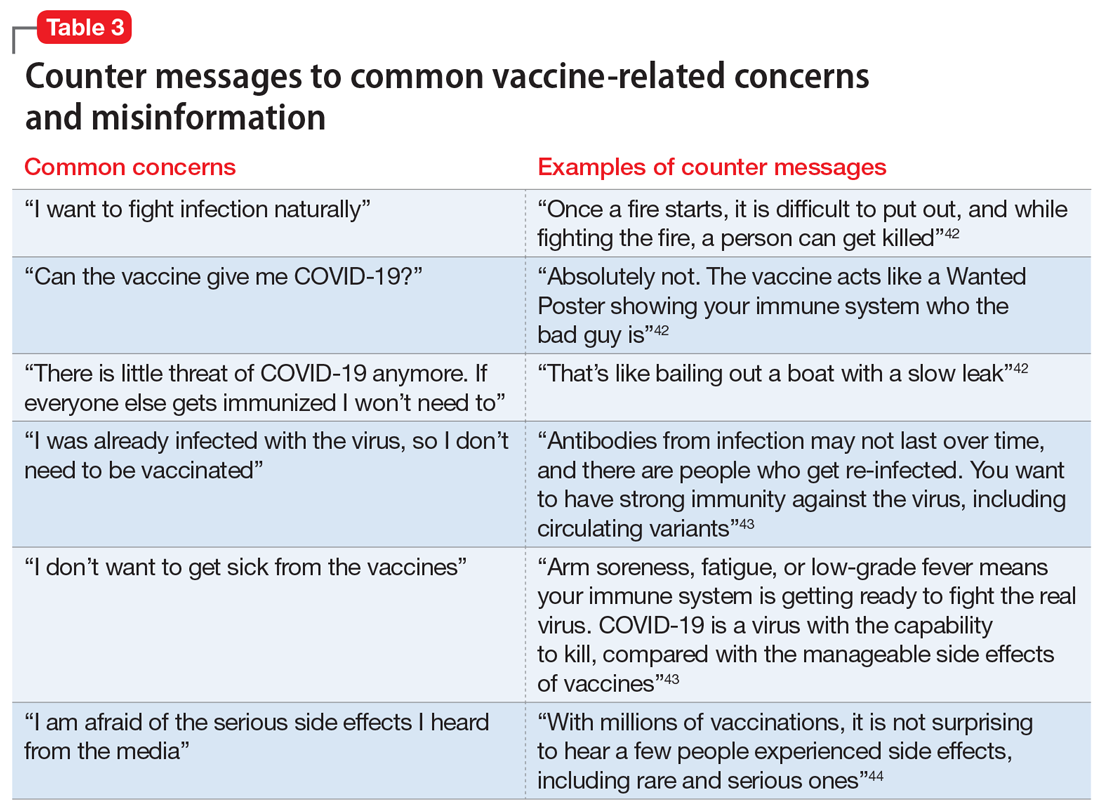
When assuring patients of vaccine safety and efficacy, it is helpful to explain the vaccine development process, including FDA approval, extensive clinical trials, monitoring, and the distribution process. Providing clear, transparent, accurate information about the risks and benefits of the vaccines is important, as well as monitoring misinformation and developing convincing counter messages that elicit positive emotions toward the vaccines.41 Examples of messages to counter common vaccine-related concerns and misinformation are shown in Table 3.42-44
Know the barriers to vaccination. The role of the psychiatrist is to help patients, particularly those with SMIs, overcome logistical barriers and address hesitancy, which are both essential for vaccine uptake. Psychiatrists can help identify actual barriers (eg, transportation, digital access for information and scheduling) and perceived barriers, improve information access, and help patients obtain self-efficacy to take the actions needed to get vaccinated, particularly by collaborating with and communicating these concerns to other social services (Table 4).41
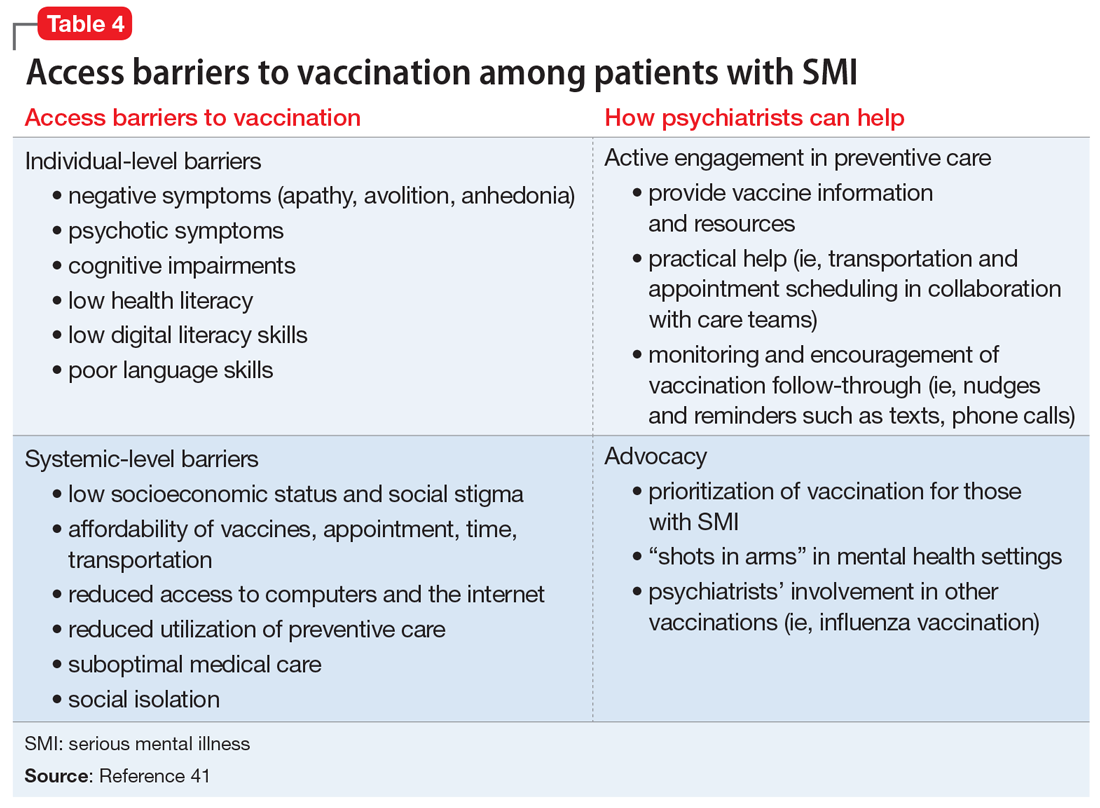
Monitor for vaccination series completion. Especially for vaccines that require more than a single dose over time, patients need more reminders, nudges, practical support, and encouragement to complete vaccination. A surprising degree of confusion regarding the timing of protection and benefit from the second COVID-19 injection (for the 2-injection vaccines) was uncovered in a recent survey of >1,000 US adults who had received their vaccinations in February 2021.45 Attentive monitoring of vaccination series completion by psychiatrists can thus increase the likelihood that a patient will follow through (Table 4).41 This can be as simple as asking about completion of the series during appointments, but further aided by communicating to the larger care team (social workers, care managers, care coordinators) when identifying that the patient may need further assistance.
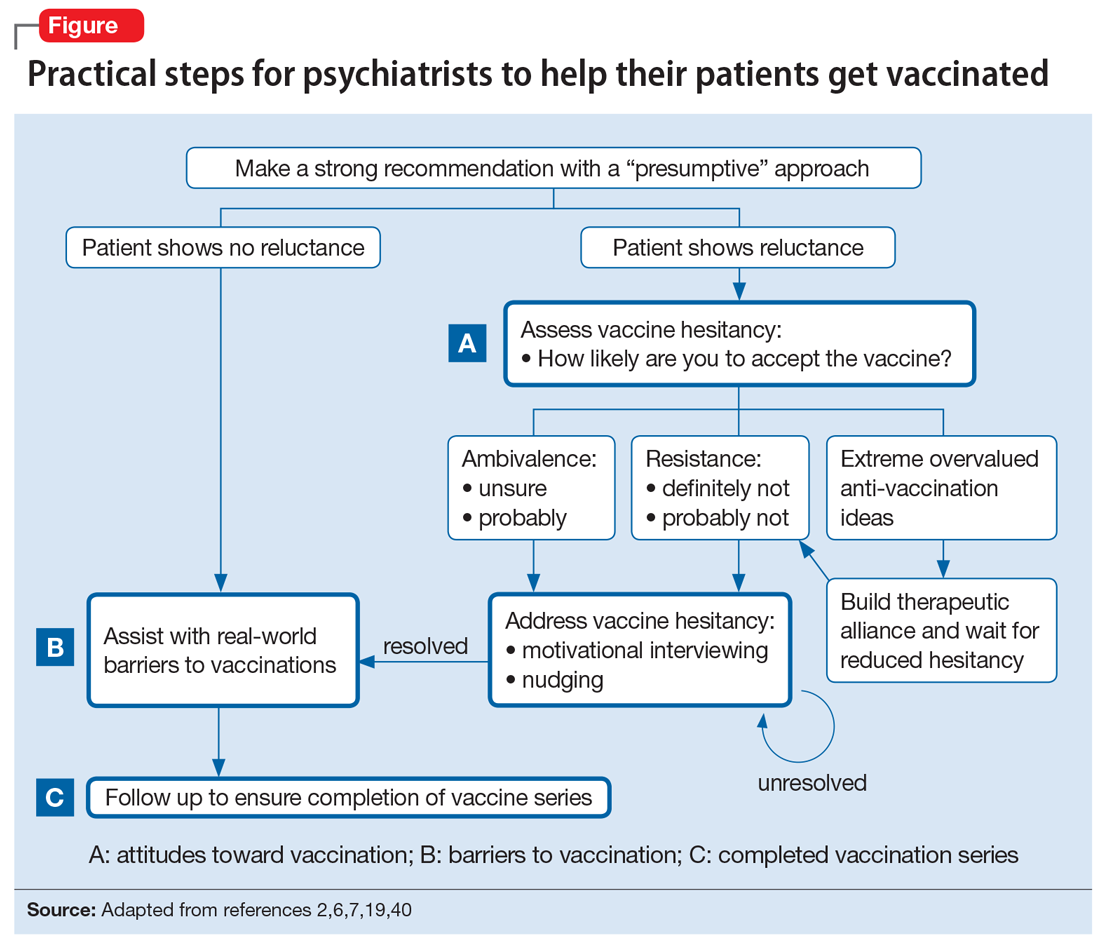
The Figure2,6,7,19,40 summarizes the steps that psychiatrists can take to help patients get vaccinated by assessing attitudes towards vaccination (vaccine hesitancy), helping to remove barriers to vaccination, and ensuring via patient follow-up that a vaccine series is completed.
Continue to: Active involvement is key
Active involvement is key
The active involvement of psychiatrists in COVID-19 vaccination efforts can protect patients from the virus, reduce health disparities among patients with SMI, and promote herd immunity, helping to end the pandemic. Psychiatry practices can serve as ideal platforms to deliver evidence-based COVID-19 vaccine information and encourage vaccine uptake, particularly for marginalized populations.
Vaccination programs in mental health practices can even be conceptualized as a moral mandate in the spirit of addressing distributive injustice. The population management challenges of individual-level barriers and follow-through could be dramatically reduced—if not nearly eliminated—through policy-level changes that allow vaccinations to be administered in places where patients with SMI are already engaged: that is, “shots in arms” in mental health settings. As noted, some studies have shown that mental health settings can play a key role in other preventive care campaigns, such as the annual influenza and hepatitis vaccinations, and thus the incorporation of preventive care need not be limited to just COVID-19 vaccination efforts.
The COVID-19 pandemic is an opportunity to rethink the role of psychiatrists and psychiatric offices and clinics in preventive health care. The health risks and disparities of patients with SMI require the proactive involvement of psychiatrists at both the level of their individual patients and at the federal and state levels to advocate for policy changes that can benefit these populations. Overall, psychiatrists occupy a special role within the medical establishment that enables them to uniquely advocate for patients with SMI and ensure they are not forgotten during the COVID-19 pandemic.
Bottom Line
Psychiatrists could apply behavior management techniques such as motivational interviewing and nudging to address vaccine hesitancy in their patients and move them to accepting the COVID-19 vaccination. This could be particularly valuable for patients with serious mental illness, who face increased risks from COVID-19 and additional barriers to getting vaccinated.
Related Resources
- American Psychiatric Association. APA coronavirus resources. https://www.psychiatry.org/psychiatrists/covid-19-Coronavirus
- Baddeley M. Behavioural economics: a very short introduction. Oxford University Press; 2017.
- Centers for Disease Control and Prevention. Vaccines for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html
- Chou W, Burgdorf C, Gaysynsky A, et al. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. National Institutes of Health. Published 2020. https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf
- Miller WR, Rollnick S. Motivational interviewing: helping people change. Guilford Press; 2012.
1. Mazereel V, Van Assche K, Detraux J, et al. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8(5):444-450.
2. Freudenreich O, Van Alphen MU, Lim C. The ABCs of successful vaccinations: a role for psychiatry. Current Psychiatry. 2021;20(3):48-50.
3. World Health Organization (WHO). Ten threats to global health in 2019. Accessed July 2, 2021. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
4. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4164.
5. McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550-1562.
6. Betsch C, Korn L, Holtmann C. Don’t try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci. 2015;112(49):E6725-E6726.
7. Rahman T, Hartz SM, Xiong W, et al. Extreme overvalued beliefs. J Am Acad Psychiatry Law. 2020;48(3):319-326.
8. Leask J. Target the fence-sitters. Nature. 2011;473(7348):443-445.
9. United States Census Bureau. Household Pulse Survey COVID-19 Vaccination Tracker. Updated June 30, 2021. Accessed July 2, 2021. https://www.census.gov/library/visualizations/interactive/household-pulse-survey-covid-19-vaccination-tracker.html
10. United States Census Bureau. Measuring household experiences during the coronavirus pandemic. Updated May 5, 2021. Accessed July 2, 2021. https://www.census.gov/data/experimental-data-products/household-pulse-survey.html
11. Jefsen OH, Kølbæk P, Gil Y, et al. COVID-19 vaccine willingness among patients with mental illness compared with the general population. Acta Neuropsychiatrica. 2021:1-24. doi:10.1017/neu.2021.15
12. Miles LW, Williams N, Luthy KE, et al. Adult vaccination rates in the mentally ill population: an outpatient improvement project. J Am Psychiatr Nurses Assoc. 2020;26(2):172-180.
13. Lewandowsky S, Ecker UK, Seifert CM, et al. Misinformation and its correction: continued influence and successful debiasing. Psychol Sci Public Interest. 2012;13(3):106-131.
14. Druss BG, Rosenheck RA. Locus of mental health treatment in an integrated service system. Psychiatr Serv. 2000;51(7):890-892.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-35.
16. Hamel L, Kirzinger A, Muñana C, et al. KFF COVID-19 vaccine monitor: December 2020. Accessed July 2, 2021. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/
17. Kai J, Crosland A. Perspectives of people with enduring mental ill health from a community-based qualitative study. Br J Gen Pract. 2001;51(470):730-736.
18. Mather G, Baker D, Laugharne R. Patient trust in psychiatrists. Psychosis. 2012;4(2):161-167.
19. Miller WR, Rollnick S. Motivational interviewing: helping people change. Guilford Press; 2012.
20. Reno JE, O’Leary S, Garrett K, et al. Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. J Health Commun. 2018;23(4):313-320.
21. Baddeley M. Behavioural economics: a very short introduction. Volume 505. Oxford University Press; 2017.
22. Nemani K, Li C, Olfson M, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380-386.
23. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52.
24. Lorenz RA, Norris MM, Norton LC, et al. Factors associated with influenza vaccination decisions among patients with mental illness. Int J Psychiatry Med. 2013;46(1):1-13.
25. Bitan DT. Patients with schizophrenia are under‐vaccinated for COVID‐19: a report from Israel. World Psychiatry. 2021;20(2):300.
26. Robotham D, Satkunanathan S, Doughty L, et al. Do we still have a digital divide in mental health? A five-year survey follow-up. J Med Internet Res. 2016;18(11):e309.
27. De Hert M, Cohen D, Bobes J, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10(2):138.
28. Carrà G, Bartoli F, Carretta D, et al. The prevalence of metabolic syndrome in people with severe mental illness: a mediation analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1739-1746.
29. Lin MT, Burgess JF, Carey K. The association between serious psychological distress and emergency department utilization among young adults in the USA. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):939-947.
30. DeCoux M. Acute versus primary care: the health care decision making process for individuals with severe mental illness. Issues Ment Health Nurs. 2005;26(9):935-951.
31. Hoffman L, Wisniewski H, Hays R, et al. Digital opportunities for outcomes in recovery services (DOORS): a pragmatic hands-on group approach toward increasing digital health and smartphone competencies, autonomy, relatedness, and alliance for those with serious mental illness. J Psychiatr Pract. 2020;26(2):80-88.
32. Rosenberg SD, Goldberg RW, Dixon LB, et al. Assessing the STIRR model of best practices for blood-borne infections of clients with severe mental illness. Psychiatr Serv. 2010;61(9):885-891.
33. Slade EP, Rosenberg S, Dixon LB, et al. Costs of a public health model to increase receipt of hepatitis-related services for persons with mental illness. Psychiatr Serv. 2013;64(2):127-133.
34. Brewer NT, Chapman GB, Rothman AJ, et al. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149-207.
35. Nabet B, Gable J, Eder J, et al. PolicyLab evidence to action brief: addressing vaccine hesitancy to protect children & communities against preventable diseases. Children’s Hospital of Philadelphia. Published Spring 2017. Accessed July 2, 2021. https://policylab.chop.edu/sites/default/files/pdf/publications/Addressing_Vaccine_Hesitancy.pdf
36. Opel DJ, Heritage J, Taylor JA, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037-1046.
37. Betsch C, Böhm R, Korn L, et al. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017;1(3):1-6.
38. Shen F, Sheer VC, Li R. Impact of narratives on persuasion in health communication: a meta-analysis. J Advert. 2015;44(2):105-113.
39. Parkerson N, Leader A. Vaccine hesitancy in the era of COVID. Population Health Leadership Series: PopTalk webinars. Paper 26. Published February 10, 2021. https://jdc.jefferson.edu/phlspoptalk/26/
40. Dempsey AF, O’Leary ST. Human papillomavirus vaccination: narrative review of studies on how providers’ vaccine communication affects attitudes and uptake. Acad Pediatr. 2018;18(2):S23-S27.
41. Chou W, Burgdorf C, Gaysynsky A, et al. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. National Institutes of Health. Published 2020. https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf
42. International Society for Vaccines and the MJH Life Sciences COVID-19 coalition. Building confidence in COVID-19 vaccination: a toolbox of talks from leaders in the field. March 9, 2021. https://globalmeet.webcasts.com/starthere.jsp?ei=1435659&tp_key=59ed660099
43. Centers for Disease Control and Prevention. Frequently asked questions about COVID-19 vaccination. Accessed July 2, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html
44. Singh BR, Gandharava S, Gandharva R. Covid-19 vaccines and community immunity. Infectious Diseases Research. 2021;2(1):5.
45. Goldfarb JL, Kreps S, Brownstein JS, et al. Beyond the first dose - Covid-19 vaccine follow-through and continued protective measures. N Engl J Med. 2021;85(2):101-103.
After more than 600,000 deaths in the United States from the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), several safe and effective vaccines against the virus have become available. Vaccines are the most effective preventive measure against COVID-19 and the most promising way to achieve herd immunity to end the current pandemic. However, obstacles to reaching this goal include vaccine skepticism, structural barriers, or simple inertia to get vaccinated. These challenges provide opportunities for psychiatrists to use their medical knowledge and expertise, applying behavior management techniques such as motivational interviewing and nudging to encourage their patients to get vaccinated. In particular, marginalized patients with serious mental illness (SMI), who are subject to disproportionately high rates of COVID-19 infection and more severe outcomes,1 have much to gain if psychiatrists become involved in the COVID-19 vaccination campaign.
In this article, we define vaccine hesitancy and highlight what makes psychiatrists ideal vaccine ambassadors, given their unique skill set and longitudinal, trust-based connection with their patients. We expand on the particular vulnerabilities of patients with SMI, including structural barriers to vaccination that lead to health disparities and inequity. Finally, building on “The ABCs of successful vaccinations” framework published in
What is vaccine hesitancy?
The World Health Organization (WHO) defines vaccine hesitancy as a “delay in acceptance or refusal of vaccines despite availability of vaccine services.”3,4 Vaccine hesitancy occurs on a continuum ranging from uncertainty about accepting a vaccine to absolute refusal.4,5 It involves a complex decision-making process driven by contextual, individual, and social influences, and vaccine-specific issues.4 In the “3C” model developed by the WHO Strategic Advisory Group of Experts (SAGE) Working Group, vaccine hesitancy is influenced by confidence (trust in vaccines, in the health care system, and in policy makers), complacency (lower perceived risk), and convenience (availability, affordability, accessibility, language and health literacy, appeal of vaccination program).4
In 2019, the WHO named vaccine hesitancy as one of the top 10 global health threats.3 Hesitancy to receive COVID-19 vaccines may be particularly high because of their rapid development. In addition, the tumultuous political environment that often featured inconsistent messaging about the virus, its dangers, and its transmission since the early days of the pandemic created widespread public confusion and doubt as scientific understandings evolved. “Anti-vaxxer” movements that completely rejected vaccine efficacy disseminated misinformation online. Followers of these movements may have such extreme overvalued ideas that any effort to persuade them otherwise with scientific evidence will accomplish very little.6,7 Therefore, focusing on individuals who are “sitting on the fence” about getting vaccinated can be more productive because they represent a much larger group than those who adamantly refuse vaccines, and they may be more amenable to changing beliefs and behaviors.8
The US Census Bureau’s Household Pulse Survey asked, “How likely are you to accept the vaccine?”9 As of late June 2021, 11.4% of US adults reported they would “definitely not get a vaccine” or “probably not get a vaccine,” and that number increases to 16.9% when including those who are “unsure,” although there is wide geographical variability.10
A recent study in Denmark showed that willingness to receive the COVID-19 vaccine was slightly lower among patients with mental illness (84.8%) compared with the general population (89.5%).11 Given the small difference, vaccine hesitancy was not considered to be a major barrier for vaccination among patients with mental illness in Denmark. This is similar to the findings of a pre-pandemic study at a community mental health clinic in the United States involving other vaccinations, which suggested that 84% of patients with SMI perceived vaccinations as safe, effective, and important.12 In this clinic, identified barriers to vaccinations in general among patients with SMI included lack of awareness and knowledge (42.2%), accessibility (16.3%), personal cost (13.3%), fears about immunization (10.4%), and lack of recommendations by primary care providers (PCPs) (1.5%).12
It is critical to distinguish attitude-driven vaccine hesitancy from a lack of education and opportunity to receive a vaccine. Particularly disadvantaged communities may be mislabeled as “vaccine hesitant” when in fact they may not have the ability to be as proactive as other population groups (eg, difficulty scheduling appointments over the Internet).
Continue to: What makes psychiatrists ideal vaccine ambassadors?
What makes psychiatrists ideal vaccine ambassadors?
There are several reasons psychiatrists can be well-positioned to contribute to the success of vaccination campaigns (Table 1). These include their frequent contact with patients and their care teams, the high trust those patients have in them, and their medical expertise and skills in applied behavioral and social science techniques, including motivational interviewing and nudging. Vaccination efforts and outreach are more effective when led by the clinician with whom the patient has the most contact because resolving vaccine hesitancy is not a one-time discussion but requires ongoing communication, persistence, and consistency.13 Patients may contact their psychiatrists more frequently than their other clinicians, including PCPs. For this reason, psychiatrists can serve as the gateway to health care, particularly for patients with SMI.14 In addition, interruptions in nonemergency services caused by the COVID-19 pandemic may affect vaccine delivery because patients may have been unable to see their PCPs regularly during the pandemic.15
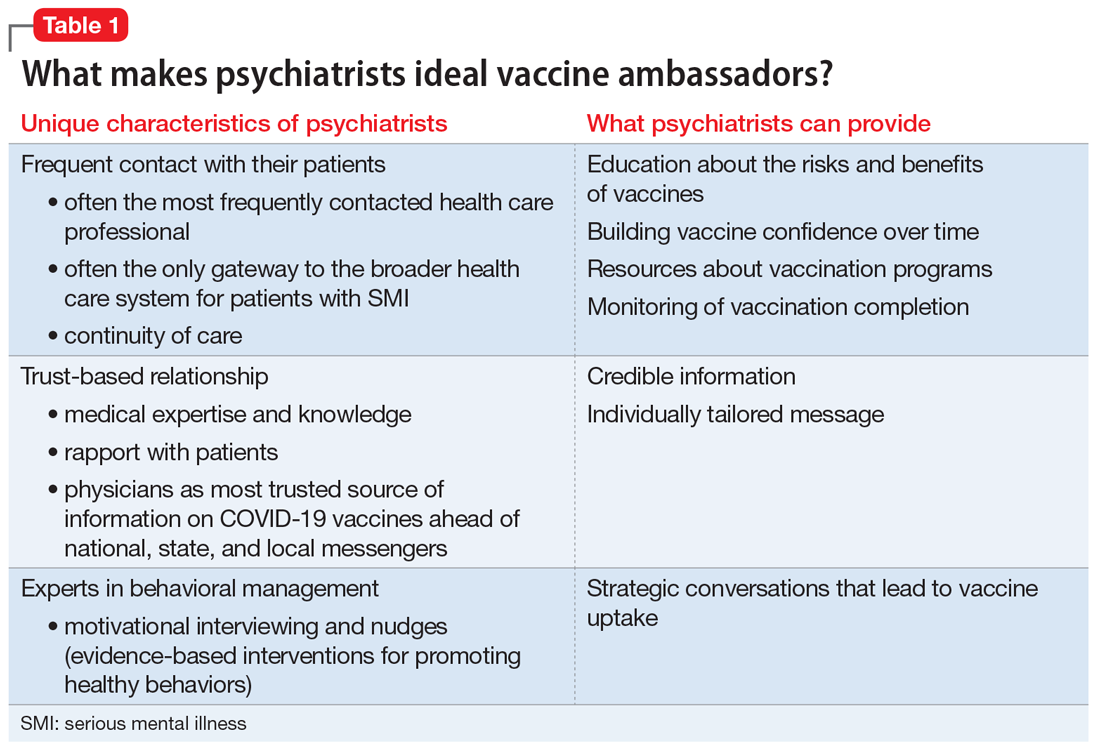
Psychiatrists’ medical expertise and their ability to develop rapport with their patients promote trust-building. Receiving credible information from a trusted source such as a patient’s psychiatrist can be impactful. A recent poll suggested that individual health care clinicians have been consistently identified as the most trusted sources for vaccine information, including for the COVID-19 vaccines.16 There is also higher trust when there is greater continuity of care both in terms of length of time the patient has known the clinician and the number of consultations,17 an inherent part of psychiatric practice. In addition, research has shown that patients trust their psychiatrists as much as they trust their general practitioners.18
Psychiatrists are experts in behavior change, promoting healthy behaviors through motivational interviewing and nudging. They also have experience with managing patients who hold overvalued ideas as well as dealing with uncertainty, given their scientific and medical training.
Motivational interviewing is a patient-centered, collaborative approach widely used by psychiatrists to treat unhealthy behaviors such as substance use. Clinicians elicit and strengthen the patient’s desire and motivation for change while respecting their autonomy. Instead of presenting persuasive facts, the clinician creates a welcoming, nonthreatening, safe environment by engaging patients in open dialogue, reflecting back the patients’ concerns with empathy, helping them realize contradictions in behavior, and supporting self-sufficiency.19 In a nonpsychiatric setting, studies have shown the effectiveness of motivational interviewing in increasing uptake of human papillomavirus vaccines and of pediatric vaccines.20
Nudging, which comes from behavioral economics and psychology, underscores the importance of structuring a choice architecture in changing the way people make their everyday decisions.21 Nudging still gives people a choice and respects autonomy, but it leads patients to more efficient and productive decision-making. Many nudges are based around giving good “default options” because people often do not make efforts to deviate from default options. In addition, social nudges are powerful, giving people a social reference point and normalizing certain behaviors.21 Psychiatrists have become skilled in nudging from working with patients with varying levels of insight and cognitive capabilities. That is, they give simple choices, prompts, and frequent feedback to reinforce “good” decisions and to discourage “bad” decisions.
Continue to: Managing overvalued ideas
Managing overvalued ideas. Psychiatrists are also well-versed in having discussions with patients who hold irrational beliefs (psychosis) or overvalued ideas. For example, psychiatrists frequently manage anorexia nervosa and hypochondria, which are rooted in overvalued ideas.7 While psychiatrists may not be able to directly confront the overvalued ideas, they can work around such ideas while waiting for more flexible moments. Similarly, managing patients with intense emotional commitment7 to commonly held anti-vaccination ideas may not be much different. Psychiatrists can work around resistance until patients may be less strongly attached to those overvalued ideas in instances when other techniques, such as motivational interviewing and nudging, may be more effective.
Managing uncertainty. Psychiatrists are experts in managing “not knowing” and uncertainty. Due to their medical scientific training, they are familiar with the process of science, and how understanding changes through trial and error. In contrast, most patients usually only see the end product (ie, a drug comes to market). Discussions with patients that acknowledge uncertainty and emphasize that changes in what is known are expected and appropriate as scientific knowledge evolves could help preempt skepticism when messages are updated.
Why do patients with SMI need more help?
SMI as a high-risk group. Patients with SMI are part of a “tragic” epidemiologic triad of agent-host-environment15 that places them at remarkably elevated risk for COVID-19 infection and more serious complications and death when infected.1 After age, a diagnosis of a schizophrenia spectrum disorder is the second largest predictor of mortality from COVID-19, with a 2.7-fold increase in mortality.22 This is how the elements of the triad come together: SARS-Cov-2 is a highly infectious agent affecting individuals who are vulnerable hosts because of their high frequency of medical comorbidities, including cardiovascular disease, type 2 diabetes, and respiratory tract diseases, which are all risk factors for worse outcomes due to COVID-19.23 In addition, SMI is associated with socioeconomic risk factors for SARS-Cov-2 infection, including poverty, homelessness, and crowded settings such as jails, group homes, hospitals, and shelters, which constitute ideal environments for high transmission of the virus.
Structural barriers to vaccination. Studies have suggested lower rates of vaccination among people with SMI for various other infectious diseases compared with the general population.12 For example, in 1 outpatient mental health setting, influenza vaccination rates were 24% to 28%, which was lower than the national vaccination rate of 40.9% for the same influenza season (2010 to 2011).24 More recently, a study in Israel examining the COVID-19 vaccination rate among >25,000 patients with schizophrenia suggested under-vaccination of this cohort. The results showed that the odds of getting the COVID-19 vaccination were significantly lower in the schizophrenia group compared with the general population (odds ratio = 0.80, 95% CI: 0.77 to 0.83).25
Patients with SMI encounter considerable system-level barriers to vaccinations in general, such as reduced access to health care due to cost and a lack of transportation,12 the digital divide given their reduced access to the internet and computers for information and scheduling,26 and lack of vaccination recommendations from their PCPs.12 Studies have also shown that patients with SMI often receive suboptimal medical care because of stigmatization and discrimination.27 They also have lower rates of preventive care utilization, seeking medical services only in times of crisis and seeking mental health services more often than physical health care.28-30
Continue to: Patients with SMI face...
Patients with SMI face additional individual challenges that impede vaccine uptake, such as lack of knowledge and awareness about the virus and vaccinations, general cognitive impairment, low digital literacy skills,31 low language literacy and educational attainment, baseline delusions, and negative symptoms such as apathy, avolition, and anhedonia.1 Thus, even if they overcome the external barriers and obtain vaccine-related information, these patients may experience difficulty in understanding the content and applying this information to their personal circumstances as a result of low health literacy.
How psychiatrists can help
The concept of using mental health care sites and trained clinicians to increase medical disease prevention is not new. The rigorously tested intervention model STIRR (Screen, Test, Immunize, Reduce risk, and Refer) uses co-located nurse practitioners in community mental health centers to provide risk assessment, counseling, and blood testing for hepatitis and HIV, as well as on-site vaccinations for hepatitis to patients dually diagnosed with SMI and substance use disorders.32
Prioritization of patients with SMI for vaccine eligibility does not directly lead to vaccine uptake. Patients with SMI need extra support from their primary point of health care contact, namely their psychiatrists. Psychiatrists may bring a set of specialized skills uniquely suited to this moment to address vaccine hesitancy and overall lack of vaccine resources and awareness. Freudenreich et al2 recently proposed “The ABCs of Successful Vaccinations” framework that psychiatrists can use in their interactions with patients to encourage vaccination by focusing on:
- attitudes towards vaccination
- barriers to vaccination
- completed vaccination series.
Understand attitudes toward vaccination. Decision-making may be an emotional and psychological experience that is informed by thoughts and feelings,34 and psychiatrists are uniquely positioned to tailor messages to individual patients by using motivational interviewing and applying nudging techniques.8 Given the large role of the pandemic in everyday life, it would be natural to address vaccine-related concerns in the course of routine rapport-building. Table 219,34-38 shows example phrases of COVID-19 vaccine messages that are based on communication strategies that have demonstrated success in health behavior domains (including vaccinations).39
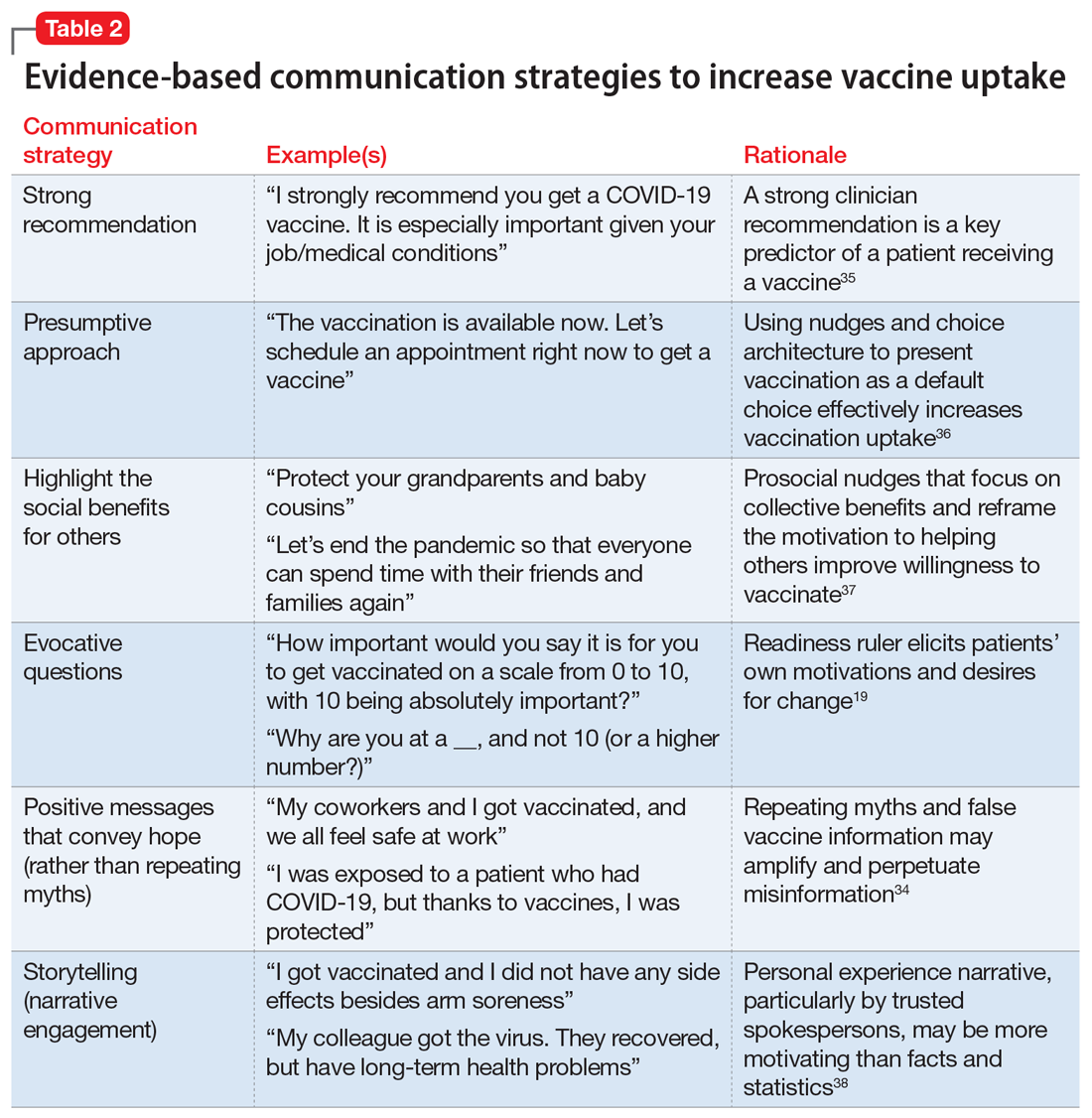
Continue to: First, a strong recommendation...
First, a strong recommendation should be made using the presumptive approach.40 If vaccine hesitancy is detected, psychiatrists should next attempt to understand patients’ reasoning with open-ended questions to probe vaccine-related concerns. Motivational interviewing can then be used to target the fence sitters (rather than anti-vaxxers).6 Psychiatrists can also communicate with therapists about the need for further follow up on patients’ hesitancies.
When assuring patients of vaccine safety and efficacy, it is helpful to explain the vaccine development process, including FDA approval, extensive clinical trials, monitoring, and the distribution process. Providing clear, transparent, accurate information about the risks and benefits of the vaccines is important, as well as monitoring misinformation and developing convincing counter messages that elicit positive emotions toward the vaccines.41 Examples of messages to counter common vaccine-related concerns and misinformation are shown in Table 3.42-44
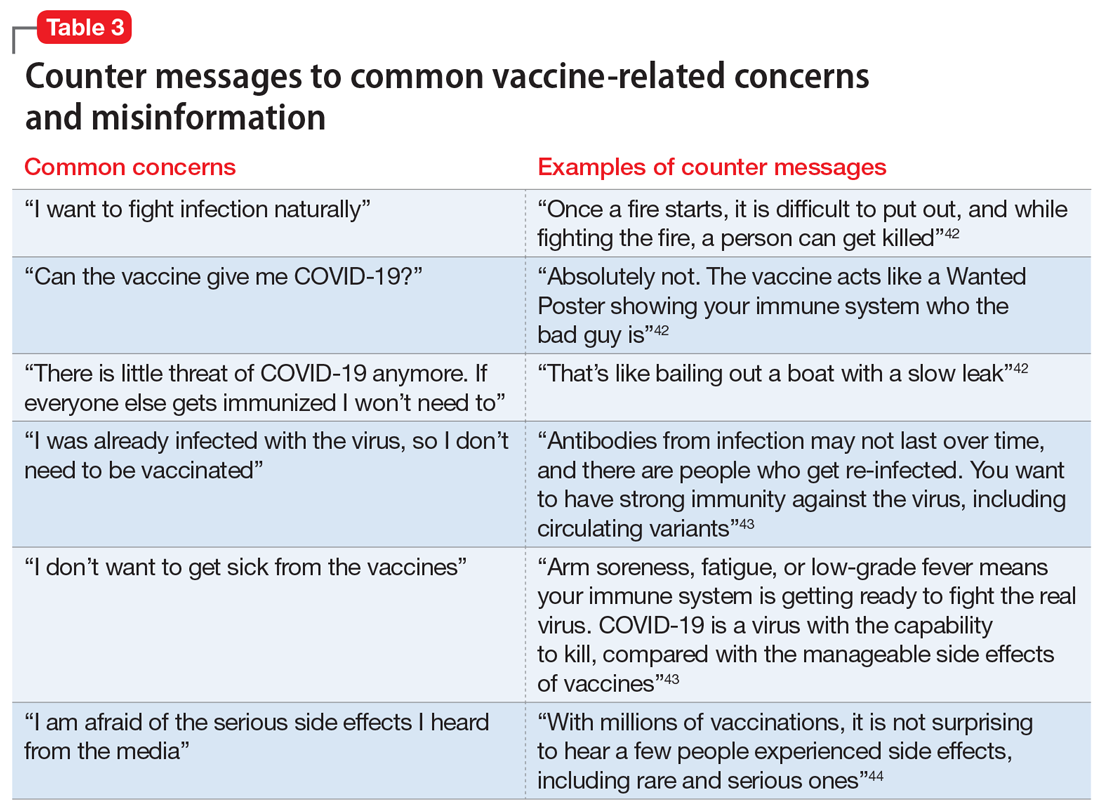
Know the barriers to vaccination. The role of the psychiatrist is to help patients, particularly those with SMIs, overcome logistical barriers and address hesitancy, which are both essential for vaccine uptake. Psychiatrists can help identify actual barriers (eg, transportation, digital access for information and scheduling) and perceived barriers, improve information access, and help patients obtain self-efficacy to take the actions needed to get vaccinated, particularly by collaborating with and communicating these concerns to other social services (Table 4).41
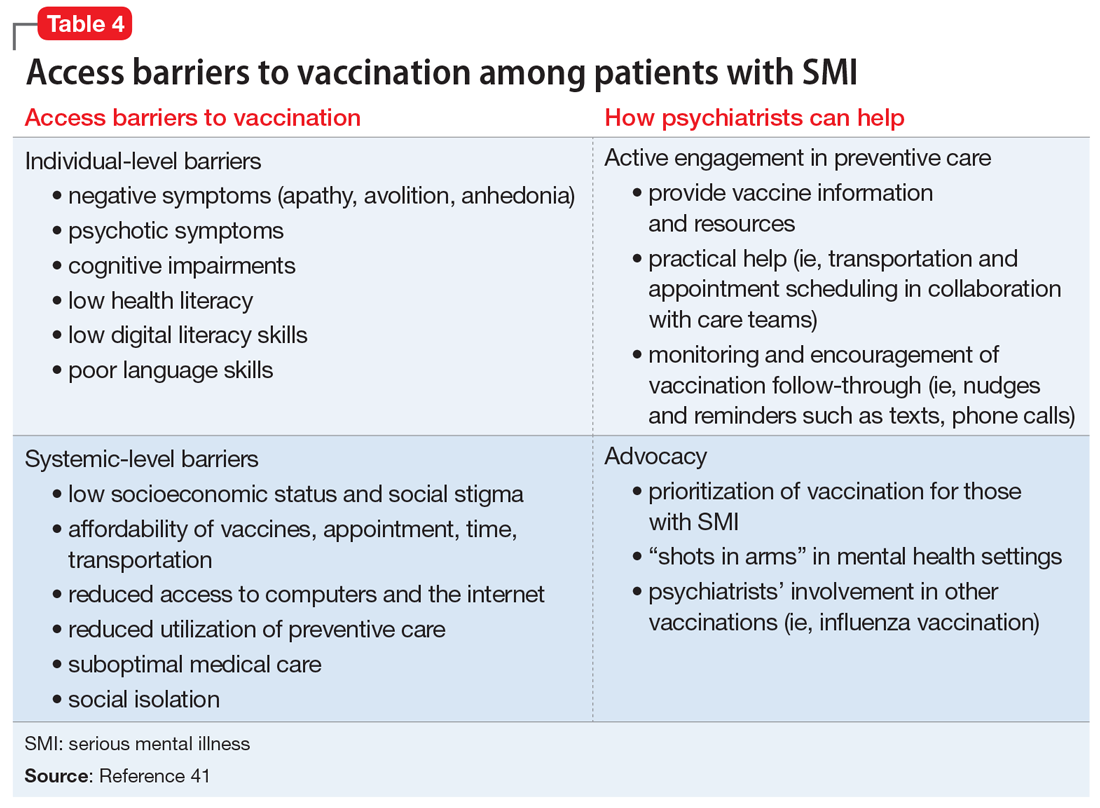
Monitor for vaccination series completion. Especially for vaccines that require more than a single dose over time, patients need more reminders, nudges, practical support, and encouragement to complete vaccination. A surprising degree of confusion regarding the timing of protection and benefit from the second COVID-19 injection (for the 2-injection vaccines) was uncovered in a recent survey of >1,000 US adults who had received their vaccinations in February 2021.45 Attentive monitoring of vaccination series completion by psychiatrists can thus increase the likelihood that a patient will follow through (Table 4).41 This can be as simple as asking about completion of the series during appointments, but further aided by communicating to the larger care team (social workers, care managers, care coordinators) when identifying that the patient may need further assistance.
The Figure2,6,7,19,40 summarizes the steps that psychiatrists can take to help patients get vaccinated by assessing attitudes towards vaccination (vaccine hesitancy), helping to remove barriers to vaccination, and ensuring via patient follow-up that a vaccine series is completed.
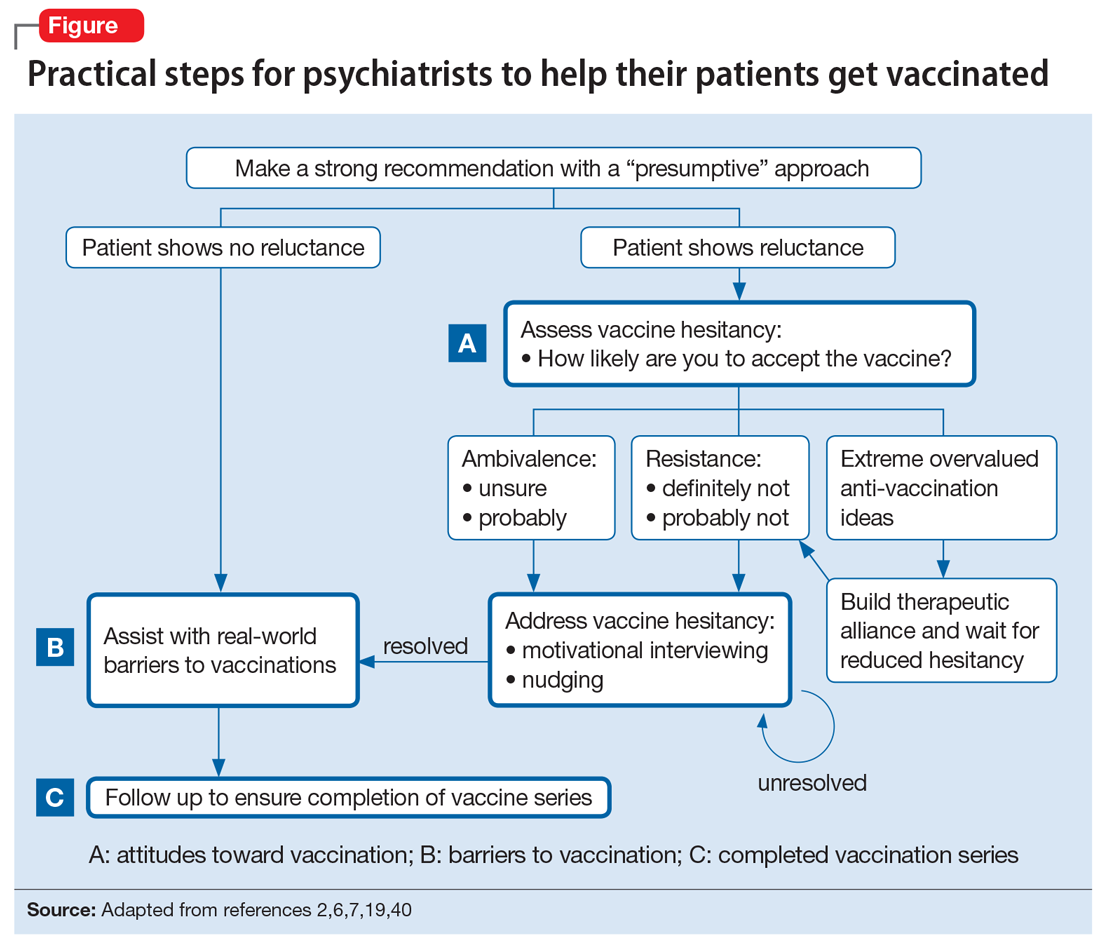
Continue to: Active involvement is key
Active involvement is key
The active involvement of psychiatrists in COVID-19 vaccination efforts can protect patients from the virus, reduce health disparities among patients with SMI, and promote herd immunity, helping to end the pandemic. Psychiatry practices can serve as ideal platforms to deliver evidence-based COVID-19 vaccine information and encourage vaccine uptake, particularly for marginalized populations.
Vaccination programs in mental health practices can even be conceptualized as a moral mandate in the spirit of addressing distributive injustice. The population management challenges of individual-level barriers and follow-through could be dramatically reduced—if not nearly eliminated—through policy-level changes that allow vaccinations to be administered in places where patients with SMI are already engaged: that is, “shots in arms” in mental health settings. As noted, some studies have shown that mental health settings can play a key role in other preventive care campaigns, such as the annual influenza and hepatitis vaccinations, and thus the incorporation of preventive care need not be limited to just COVID-19 vaccination efforts.
The COVID-19 pandemic is an opportunity to rethink the role of psychiatrists and psychiatric offices and clinics in preventive health care. The health risks and disparities of patients with SMI require the proactive involvement of psychiatrists at both the level of their individual patients and at the federal and state levels to advocate for policy changes that can benefit these populations. Overall, psychiatrists occupy a special role within the medical establishment that enables them to uniquely advocate for patients with SMI and ensure they are not forgotten during the COVID-19 pandemic.
Bottom Line
Psychiatrists could apply behavior management techniques such as motivational interviewing and nudging to address vaccine hesitancy in their patients and move them to accepting the COVID-19 vaccination. This could be particularly valuable for patients with serious mental illness, who face increased risks from COVID-19 and additional barriers to getting vaccinated.
Related Resources
- American Psychiatric Association. APA coronavirus resources. https://www.psychiatry.org/psychiatrists/covid-19-Coronavirus
- Baddeley M. Behavioural economics: a very short introduction. Oxford University Press; 2017.
- Centers for Disease Control and Prevention. Vaccines for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html
- Chou W, Burgdorf C, Gaysynsky A, et al. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. National Institutes of Health. Published 2020. https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf
- Miller WR, Rollnick S. Motivational interviewing: helping people change. Guilford Press; 2012.
After more than 600,000 deaths in the United States from the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), several safe and effective vaccines against the virus have become available. Vaccines are the most effective preventive measure against COVID-19 and the most promising way to achieve herd immunity to end the current pandemic. However, obstacles to reaching this goal include vaccine skepticism, structural barriers, or simple inertia to get vaccinated. These challenges provide opportunities for psychiatrists to use their medical knowledge and expertise, applying behavior management techniques such as motivational interviewing and nudging to encourage their patients to get vaccinated. In particular, marginalized patients with serious mental illness (SMI), who are subject to disproportionately high rates of COVID-19 infection and more severe outcomes,1 have much to gain if psychiatrists become involved in the COVID-19 vaccination campaign.
In this article, we define vaccine hesitancy and highlight what makes psychiatrists ideal vaccine ambassadors, given their unique skill set and longitudinal, trust-based connection with their patients. We expand on the particular vulnerabilities of patients with SMI, including structural barriers to vaccination that lead to health disparities and inequity. Finally, building on “The ABCs of successful vaccinations” framework published in
What is vaccine hesitancy?
The World Health Organization (WHO) defines vaccine hesitancy as a “delay in acceptance or refusal of vaccines despite availability of vaccine services.”3,4 Vaccine hesitancy occurs on a continuum ranging from uncertainty about accepting a vaccine to absolute refusal.4,5 It involves a complex decision-making process driven by contextual, individual, and social influences, and vaccine-specific issues.4 In the “3C” model developed by the WHO Strategic Advisory Group of Experts (SAGE) Working Group, vaccine hesitancy is influenced by confidence (trust in vaccines, in the health care system, and in policy makers), complacency (lower perceived risk), and convenience (availability, affordability, accessibility, language and health literacy, appeal of vaccination program).4
In 2019, the WHO named vaccine hesitancy as one of the top 10 global health threats.3 Hesitancy to receive COVID-19 vaccines may be particularly high because of their rapid development. In addition, the tumultuous political environment that often featured inconsistent messaging about the virus, its dangers, and its transmission since the early days of the pandemic created widespread public confusion and doubt as scientific understandings evolved. “Anti-vaxxer” movements that completely rejected vaccine efficacy disseminated misinformation online. Followers of these movements may have such extreme overvalued ideas that any effort to persuade them otherwise with scientific evidence will accomplish very little.6,7 Therefore, focusing on individuals who are “sitting on the fence” about getting vaccinated can be more productive because they represent a much larger group than those who adamantly refuse vaccines, and they may be more amenable to changing beliefs and behaviors.8
The US Census Bureau’s Household Pulse Survey asked, “How likely are you to accept the vaccine?”9 As of late June 2021, 11.4% of US adults reported they would “definitely not get a vaccine” or “probably not get a vaccine,” and that number increases to 16.9% when including those who are “unsure,” although there is wide geographical variability.10
A recent study in Denmark showed that willingness to receive the COVID-19 vaccine was slightly lower among patients with mental illness (84.8%) compared with the general population (89.5%).11 Given the small difference, vaccine hesitancy was not considered to be a major barrier for vaccination among patients with mental illness in Denmark. This is similar to the findings of a pre-pandemic study at a community mental health clinic in the United States involving other vaccinations, which suggested that 84% of patients with SMI perceived vaccinations as safe, effective, and important.12 In this clinic, identified barriers to vaccinations in general among patients with SMI included lack of awareness and knowledge (42.2%), accessibility (16.3%), personal cost (13.3%), fears about immunization (10.4%), and lack of recommendations by primary care providers (PCPs) (1.5%).12
It is critical to distinguish attitude-driven vaccine hesitancy from a lack of education and opportunity to receive a vaccine. Particularly disadvantaged communities may be mislabeled as “vaccine hesitant” when in fact they may not have the ability to be as proactive as other population groups (eg, difficulty scheduling appointments over the Internet).
Continue to: What makes psychiatrists ideal vaccine ambassadors?
What makes psychiatrists ideal vaccine ambassadors?
There are several reasons psychiatrists can be well-positioned to contribute to the success of vaccination campaigns (Table 1). These include their frequent contact with patients and their care teams, the high trust those patients have in them, and their medical expertise and skills in applied behavioral and social science techniques, including motivational interviewing and nudging. Vaccination efforts and outreach are more effective when led by the clinician with whom the patient has the most contact because resolving vaccine hesitancy is not a one-time discussion but requires ongoing communication, persistence, and consistency.13 Patients may contact their psychiatrists more frequently than their other clinicians, including PCPs. For this reason, psychiatrists can serve as the gateway to health care, particularly for patients with SMI.14 In addition, interruptions in nonemergency services caused by the COVID-19 pandemic may affect vaccine delivery because patients may have been unable to see their PCPs regularly during the pandemic.15
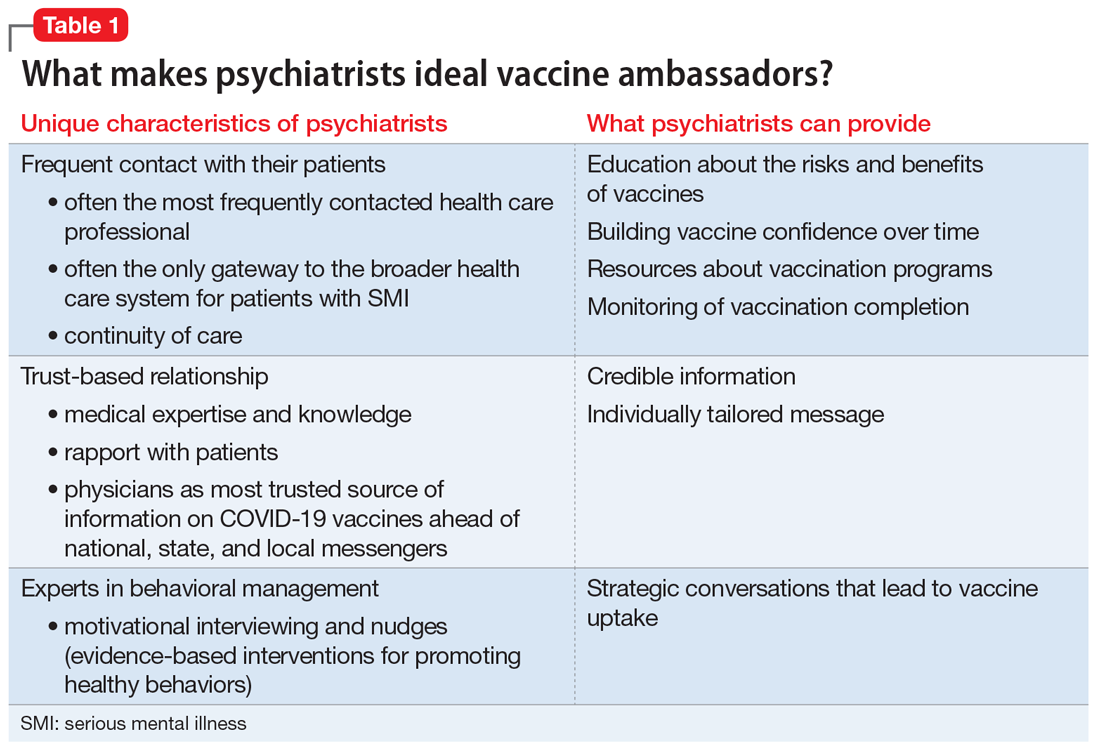
Psychiatrists’ medical expertise and their ability to develop rapport with their patients promote trust-building. Receiving credible information from a trusted source such as a patient’s psychiatrist can be impactful. A recent poll suggested that individual health care clinicians have been consistently identified as the most trusted sources for vaccine information, including for the COVID-19 vaccines.16 There is also higher trust when there is greater continuity of care both in terms of length of time the patient has known the clinician and the number of consultations,17 an inherent part of psychiatric practice. In addition, research has shown that patients trust their psychiatrists as much as they trust their general practitioners.18
Psychiatrists are experts in behavior change, promoting healthy behaviors through motivational interviewing and nudging. They also have experience with managing patients who hold overvalued ideas as well as dealing with uncertainty, given their scientific and medical training.
Motivational interviewing is a patient-centered, collaborative approach widely used by psychiatrists to treat unhealthy behaviors such as substance use. Clinicians elicit and strengthen the patient’s desire and motivation for change while respecting their autonomy. Instead of presenting persuasive facts, the clinician creates a welcoming, nonthreatening, safe environment by engaging patients in open dialogue, reflecting back the patients’ concerns with empathy, helping them realize contradictions in behavior, and supporting self-sufficiency.19 In a nonpsychiatric setting, studies have shown the effectiveness of motivational interviewing in increasing uptake of human papillomavirus vaccines and of pediatric vaccines.20
Nudging, which comes from behavioral economics and psychology, underscores the importance of structuring a choice architecture in changing the way people make their everyday decisions.21 Nudging still gives people a choice and respects autonomy, but it leads patients to more efficient and productive decision-making. Many nudges are based around giving good “default options” because people often do not make efforts to deviate from default options. In addition, social nudges are powerful, giving people a social reference point and normalizing certain behaviors.21 Psychiatrists have become skilled in nudging from working with patients with varying levels of insight and cognitive capabilities. That is, they give simple choices, prompts, and frequent feedback to reinforce “good” decisions and to discourage “bad” decisions.
Continue to: Managing overvalued ideas
Managing overvalued ideas. Psychiatrists are also well-versed in having discussions with patients who hold irrational beliefs (psychosis) or overvalued ideas. For example, psychiatrists frequently manage anorexia nervosa and hypochondria, which are rooted in overvalued ideas.7 While psychiatrists may not be able to directly confront the overvalued ideas, they can work around such ideas while waiting for more flexible moments. Similarly, managing patients with intense emotional commitment7 to commonly held anti-vaccination ideas may not be much different. Psychiatrists can work around resistance until patients may be less strongly attached to those overvalued ideas in instances when other techniques, such as motivational interviewing and nudging, may be more effective.
Managing uncertainty. Psychiatrists are experts in managing “not knowing” and uncertainty. Due to their medical scientific training, they are familiar with the process of science, and how understanding changes through trial and error. In contrast, most patients usually only see the end product (ie, a drug comes to market). Discussions with patients that acknowledge uncertainty and emphasize that changes in what is known are expected and appropriate as scientific knowledge evolves could help preempt skepticism when messages are updated.
Why do patients with SMI need more help?
SMI as a high-risk group. Patients with SMI are part of a “tragic” epidemiologic triad of agent-host-environment15 that places them at remarkably elevated risk for COVID-19 infection and more serious complications and death when infected.1 After age, a diagnosis of a schizophrenia spectrum disorder is the second largest predictor of mortality from COVID-19, with a 2.7-fold increase in mortality.22 This is how the elements of the triad come together: SARS-Cov-2 is a highly infectious agent affecting individuals who are vulnerable hosts because of their high frequency of medical comorbidities, including cardiovascular disease, type 2 diabetes, and respiratory tract diseases, which are all risk factors for worse outcomes due to COVID-19.23 In addition, SMI is associated with socioeconomic risk factors for SARS-Cov-2 infection, including poverty, homelessness, and crowded settings such as jails, group homes, hospitals, and shelters, which constitute ideal environments for high transmission of the virus.
Structural barriers to vaccination. Studies have suggested lower rates of vaccination among people with SMI for various other infectious diseases compared with the general population.12 For example, in 1 outpatient mental health setting, influenza vaccination rates were 24% to 28%, which was lower than the national vaccination rate of 40.9% for the same influenza season (2010 to 2011).24 More recently, a study in Israel examining the COVID-19 vaccination rate among >25,000 patients with schizophrenia suggested under-vaccination of this cohort. The results showed that the odds of getting the COVID-19 vaccination were significantly lower in the schizophrenia group compared with the general population (odds ratio = 0.80, 95% CI: 0.77 to 0.83).25
Patients with SMI encounter considerable system-level barriers to vaccinations in general, such as reduced access to health care due to cost and a lack of transportation,12 the digital divide given their reduced access to the internet and computers for information and scheduling,26 and lack of vaccination recommendations from their PCPs.12 Studies have also shown that patients with SMI often receive suboptimal medical care because of stigmatization and discrimination.27 They also have lower rates of preventive care utilization, seeking medical services only in times of crisis and seeking mental health services more often than physical health care.28-30
Continue to: Patients with SMI face...
Patients with SMI face additional individual challenges that impede vaccine uptake, such as lack of knowledge and awareness about the virus and vaccinations, general cognitive impairment, low digital literacy skills,31 low language literacy and educational attainment, baseline delusions, and negative symptoms such as apathy, avolition, and anhedonia.1 Thus, even if they overcome the external barriers and obtain vaccine-related information, these patients may experience difficulty in understanding the content and applying this information to their personal circumstances as a result of low health literacy.
How psychiatrists can help
The concept of using mental health care sites and trained clinicians to increase medical disease prevention is not new. The rigorously tested intervention model STIRR (Screen, Test, Immunize, Reduce risk, and Refer) uses co-located nurse practitioners in community mental health centers to provide risk assessment, counseling, and blood testing for hepatitis and HIV, as well as on-site vaccinations for hepatitis to patients dually diagnosed with SMI and substance use disorders.32
Prioritization of patients with SMI for vaccine eligibility does not directly lead to vaccine uptake. Patients with SMI need extra support from their primary point of health care contact, namely their psychiatrists. Psychiatrists may bring a set of specialized skills uniquely suited to this moment to address vaccine hesitancy and overall lack of vaccine resources and awareness. Freudenreich et al2 recently proposed “The ABCs of Successful Vaccinations” framework that psychiatrists can use in their interactions with patients to encourage vaccination by focusing on:
- attitudes towards vaccination
- barriers to vaccination
- completed vaccination series.
Understand attitudes toward vaccination. Decision-making may be an emotional and psychological experience that is informed by thoughts and feelings,34 and psychiatrists are uniquely positioned to tailor messages to individual patients by using motivational interviewing and applying nudging techniques.8 Given the large role of the pandemic in everyday life, it would be natural to address vaccine-related concerns in the course of routine rapport-building. Table 219,34-38 shows example phrases of COVID-19 vaccine messages that are based on communication strategies that have demonstrated success in health behavior domains (including vaccinations).39
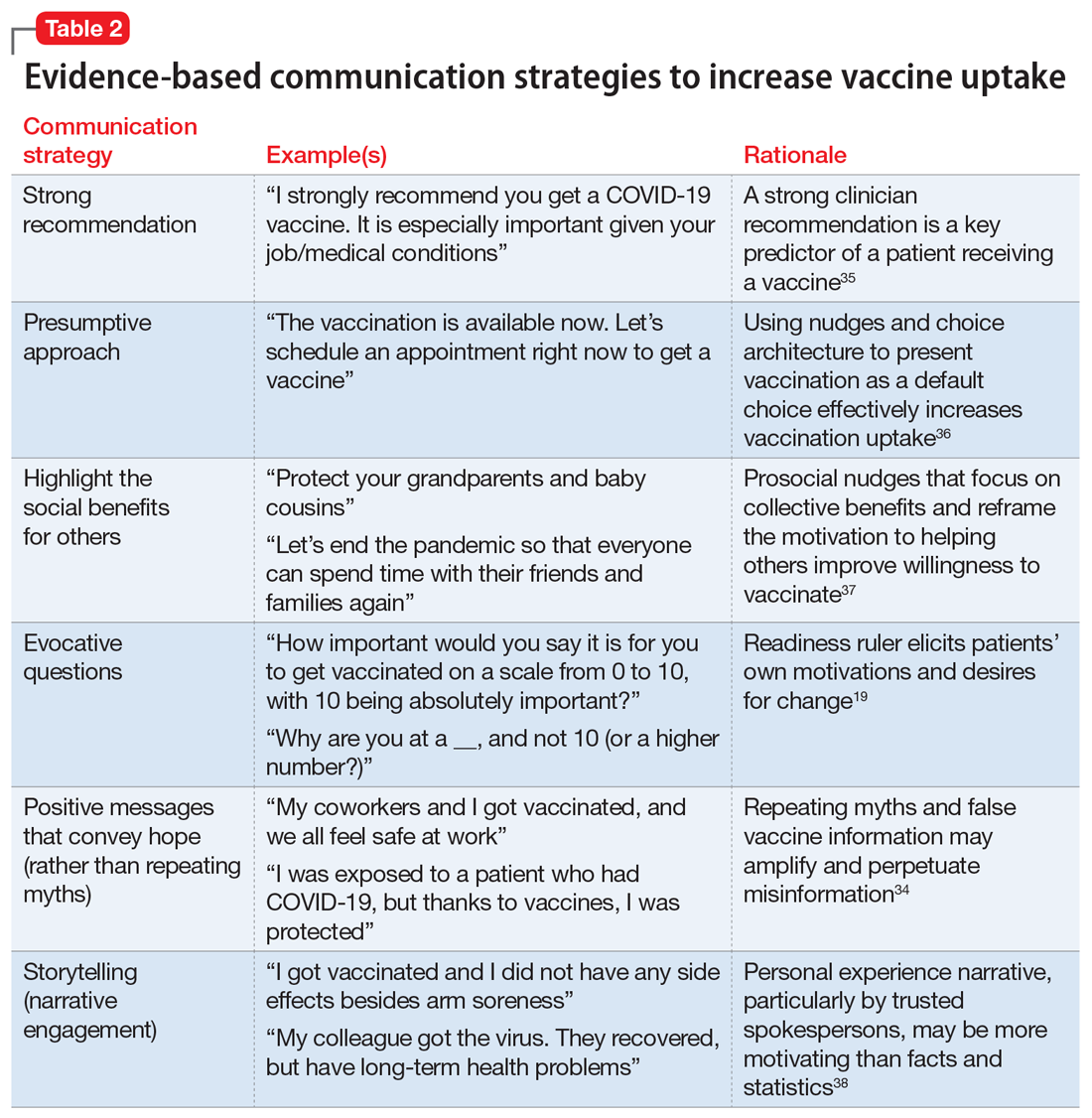
Continue to: First, a strong recommendation...
First, a strong recommendation should be made using the presumptive approach.40 If vaccine hesitancy is detected, psychiatrists should next attempt to understand patients’ reasoning with open-ended questions to probe vaccine-related concerns. Motivational interviewing can then be used to target the fence sitters (rather than anti-vaxxers).6 Psychiatrists can also communicate with therapists about the need for further follow up on patients’ hesitancies.
When assuring patients of vaccine safety and efficacy, it is helpful to explain the vaccine development process, including FDA approval, extensive clinical trials, monitoring, and the distribution process. Providing clear, transparent, accurate information about the risks and benefits of the vaccines is important, as well as monitoring misinformation and developing convincing counter messages that elicit positive emotions toward the vaccines.41 Examples of messages to counter common vaccine-related concerns and misinformation are shown in Table 3.42-44
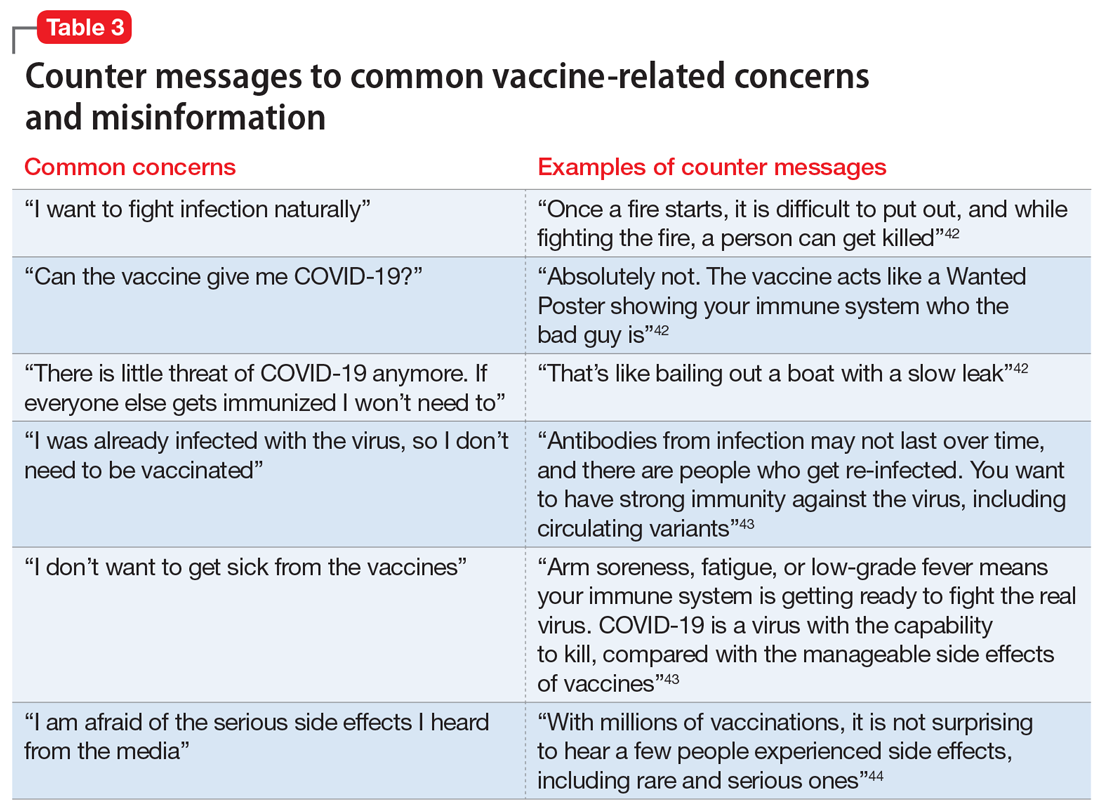
Know the barriers to vaccination. The role of the psychiatrist is to help patients, particularly those with SMIs, overcome logistical barriers and address hesitancy, which are both essential for vaccine uptake. Psychiatrists can help identify actual barriers (eg, transportation, digital access for information and scheduling) and perceived barriers, improve information access, and help patients obtain self-efficacy to take the actions needed to get vaccinated, particularly by collaborating with and communicating these concerns to other social services (Table 4).41
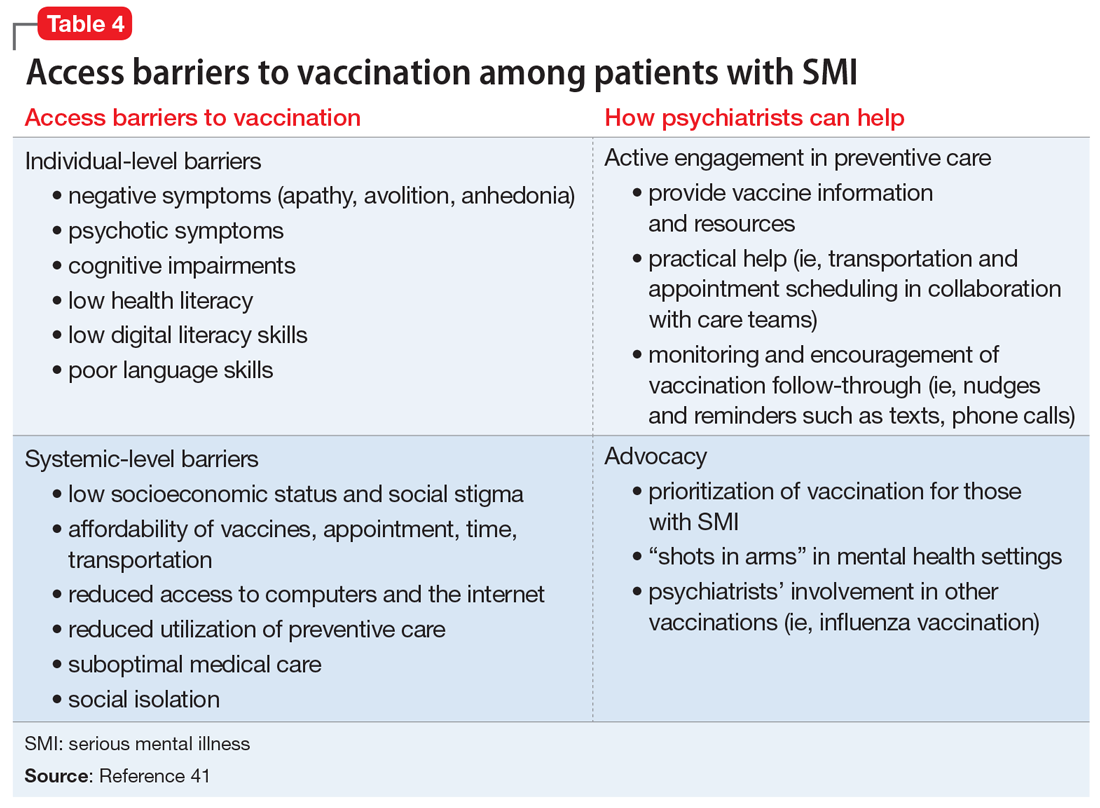
Monitor for vaccination series completion. Especially for vaccines that require more than a single dose over time, patients need more reminders, nudges, practical support, and encouragement to complete vaccination. A surprising degree of confusion regarding the timing of protection and benefit from the second COVID-19 injection (for the 2-injection vaccines) was uncovered in a recent survey of >1,000 US adults who had received their vaccinations in February 2021.45 Attentive monitoring of vaccination series completion by psychiatrists can thus increase the likelihood that a patient will follow through (Table 4).41 This can be as simple as asking about completion of the series during appointments, but further aided by communicating to the larger care team (social workers, care managers, care coordinators) when identifying that the patient may need further assistance.
The Figure2,6,7,19,40 summarizes the steps that psychiatrists can take to help patients get vaccinated by assessing attitudes towards vaccination (vaccine hesitancy), helping to remove barriers to vaccination, and ensuring via patient follow-up that a vaccine series is completed.
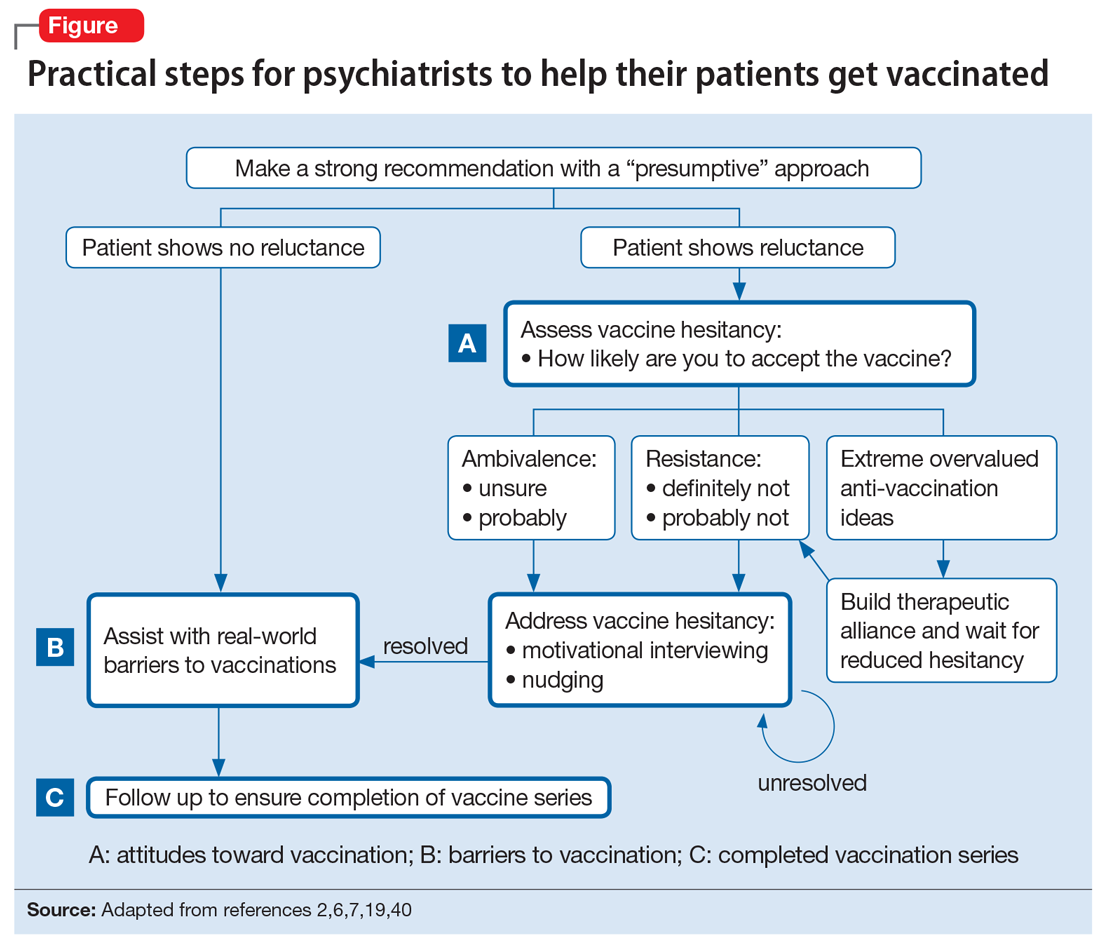
Continue to: Active involvement is key
Active involvement is key
The active involvement of psychiatrists in COVID-19 vaccination efforts can protect patients from the virus, reduce health disparities among patients with SMI, and promote herd immunity, helping to end the pandemic. Psychiatry practices can serve as ideal platforms to deliver evidence-based COVID-19 vaccine information and encourage vaccine uptake, particularly for marginalized populations.
Vaccination programs in mental health practices can even be conceptualized as a moral mandate in the spirit of addressing distributive injustice. The population management challenges of individual-level barriers and follow-through could be dramatically reduced—if not nearly eliminated—through policy-level changes that allow vaccinations to be administered in places where patients with SMI are already engaged: that is, “shots in arms” in mental health settings. As noted, some studies have shown that mental health settings can play a key role in other preventive care campaigns, such as the annual influenza and hepatitis vaccinations, and thus the incorporation of preventive care need not be limited to just COVID-19 vaccination efforts.
The COVID-19 pandemic is an opportunity to rethink the role of psychiatrists and psychiatric offices and clinics in preventive health care. The health risks and disparities of patients with SMI require the proactive involvement of psychiatrists at both the level of their individual patients and at the federal and state levels to advocate for policy changes that can benefit these populations. Overall, psychiatrists occupy a special role within the medical establishment that enables them to uniquely advocate for patients with SMI and ensure they are not forgotten during the COVID-19 pandemic.
Bottom Line
Psychiatrists could apply behavior management techniques such as motivational interviewing and nudging to address vaccine hesitancy in their patients and move them to accepting the COVID-19 vaccination. This could be particularly valuable for patients with serious mental illness, who face increased risks from COVID-19 and additional barriers to getting vaccinated.
Related Resources
- American Psychiatric Association. APA coronavirus resources. https://www.psychiatry.org/psychiatrists/covid-19-Coronavirus
- Baddeley M. Behavioural economics: a very short introduction. Oxford University Press; 2017.
- Centers for Disease Control and Prevention. Vaccines for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html
- Chou W, Burgdorf C, Gaysynsky A, et al. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. National Institutes of Health. Published 2020. https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf
- Miller WR, Rollnick S. Motivational interviewing: helping people change. Guilford Press; 2012.
1. Mazereel V, Van Assche K, Detraux J, et al. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8(5):444-450.
2. Freudenreich O, Van Alphen MU, Lim C. The ABCs of successful vaccinations: a role for psychiatry. Current Psychiatry. 2021;20(3):48-50.
3. World Health Organization (WHO). Ten threats to global health in 2019. Accessed July 2, 2021. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
4. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4164.
5. McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550-1562.
6. Betsch C, Korn L, Holtmann C. Don’t try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci. 2015;112(49):E6725-E6726.
7. Rahman T, Hartz SM, Xiong W, et al. Extreme overvalued beliefs. J Am Acad Psychiatry Law. 2020;48(3):319-326.
8. Leask J. Target the fence-sitters. Nature. 2011;473(7348):443-445.
9. United States Census Bureau. Household Pulse Survey COVID-19 Vaccination Tracker. Updated June 30, 2021. Accessed July 2, 2021. https://www.census.gov/library/visualizations/interactive/household-pulse-survey-covid-19-vaccination-tracker.html
10. United States Census Bureau. Measuring household experiences during the coronavirus pandemic. Updated May 5, 2021. Accessed July 2, 2021. https://www.census.gov/data/experimental-data-products/household-pulse-survey.html
11. Jefsen OH, Kølbæk P, Gil Y, et al. COVID-19 vaccine willingness among patients with mental illness compared with the general population. Acta Neuropsychiatrica. 2021:1-24. doi:10.1017/neu.2021.15
12. Miles LW, Williams N, Luthy KE, et al. Adult vaccination rates in the mentally ill population: an outpatient improvement project. J Am Psychiatr Nurses Assoc. 2020;26(2):172-180.
13. Lewandowsky S, Ecker UK, Seifert CM, et al. Misinformation and its correction: continued influence and successful debiasing. Psychol Sci Public Interest. 2012;13(3):106-131.
14. Druss BG, Rosenheck RA. Locus of mental health treatment in an integrated service system. Psychiatr Serv. 2000;51(7):890-892.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-35.
16. Hamel L, Kirzinger A, Muñana C, et al. KFF COVID-19 vaccine monitor: December 2020. Accessed July 2, 2021. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/
17. Kai J, Crosland A. Perspectives of people with enduring mental ill health from a community-based qualitative study. Br J Gen Pract. 2001;51(470):730-736.
18. Mather G, Baker D, Laugharne R. Patient trust in psychiatrists. Psychosis. 2012;4(2):161-167.
19. Miller WR, Rollnick S. Motivational interviewing: helping people change. Guilford Press; 2012.
20. Reno JE, O’Leary S, Garrett K, et al. Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. J Health Commun. 2018;23(4):313-320.
21. Baddeley M. Behavioural economics: a very short introduction. Volume 505. Oxford University Press; 2017.
22. Nemani K, Li C, Olfson M, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380-386.
23. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52.
24. Lorenz RA, Norris MM, Norton LC, et al. Factors associated with influenza vaccination decisions among patients with mental illness. Int J Psychiatry Med. 2013;46(1):1-13.
25. Bitan DT. Patients with schizophrenia are under‐vaccinated for COVID‐19: a report from Israel. World Psychiatry. 2021;20(2):300.
26. Robotham D, Satkunanathan S, Doughty L, et al. Do we still have a digital divide in mental health? A five-year survey follow-up. J Med Internet Res. 2016;18(11):e309.
27. De Hert M, Cohen D, Bobes J, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10(2):138.
28. Carrà G, Bartoli F, Carretta D, et al. The prevalence of metabolic syndrome in people with severe mental illness: a mediation analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1739-1746.
29. Lin MT, Burgess JF, Carey K. The association between serious psychological distress and emergency department utilization among young adults in the USA. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):939-947.
30. DeCoux M. Acute versus primary care: the health care decision making process for individuals with severe mental illness. Issues Ment Health Nurs. 2005;26(9):935-951.
31. Hoffman L, Wisniewski H, Hays R, et al. Digital opportunities for outcomes in recovery services (DOORS): a pragmatic hands-on group approach toward increasing digital health and smartphone competencies, autonomy, relatedness, and alliance for those with serious mental illness. J Psychiatr Pract. 2020;26(2):80-88.
32. Rosenberg SD, Goldberg RW, Dixon LB, et al. Assessing the STIRR model of best practices for blood-borne infections of clients with severe mental illness. Psychiatr Serv. 2010;61(9):885-891.
33. Slade EP, Rosenberg S, Dixon LB, et al. Costs of a public health model to increase receipt of hepatitis-related services for persons with mental illness. Psychiatr Serv. 2013;64(2):127-133.
34. Brewer NT, Chapman GB, Rothman AJ, et al. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149-207.
35. Nabet B, Gable J, Eder J, et al. PolicyLab evidence to action brief: addressing vaccine hesitancy to protect children & communities against preventable diseases. Children’s Hospital of Philadelphia. Published Spring 2017. Accessed July 2, 2021. https://policylab.chop.edu/sites/default/files/pdf/publications/Addressing_Vaccine_Hesitancy.pdf
36. Opel DJ, Heritage J, Taylor JA, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037-1046.
37. Betsch C, Böhm R, Korn L, et al. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017;1(3):1-6.
38. Shen F, Sheer VC, Li R. Impact of narratives on persuasion in health communication: a meta-analysis. J Advert. 2015;44(2):105-113.
39. Parkerson N, Leader A. Vaccine hesitancy in the era of COVID. Population Health Leadership Series: PopTalk webinars. Paper 26. Published February 10, 2021. https://jdc.jefferson.edu/phlspoptalk/26/
40. Dempsey AF, O’Leary ST. Human papillomavirus vaccination: narrative review of studies on how providers’ vaccine communication affects attitudes and uptake. Acad Pediatr. 2018;18(2):S23-S27.
41. Chou W, Burgdorf C, Gaysynsky A, et al. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. National Institutes of Health. Published 2020. https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf
42. International Society for Vaccines and the MJH Life Sciences COVID-19 coalition. Building confidence in COVID-19 vaccination: a toolbox of talks from leaders in the field. March 9, 2021. https://globalmeet.webcasts.com/starthere.jsp?ei=1435659&tp_key=59ed660099
43. Centers for Disease Control and Prevention. Frequently asked questions about COVID-19 vaccination. Accessed July 2, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html
44. Singh BR, Gandharava S, Gandharva R. Covid-19 vaccines and community immunity. Infectious Diseases Research. 2021;2(1):5.
45. Goldfarb JL, Kreps S, Brownstein JS, et al. Beyond the first dose - Covid-19 vaccine follow-through and continued protective measures. N Engl J Med. 2021;85(2):101-103.
1. Mazereel V, Van Assche K, Detraux J, et al. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8(5):444-450.
2. Freudenreich O, Van Alphen MU, Lim C. The ABCs of successful vaccinations: a role for psychiatry. Current Psychiatry. 2021;20(3):48-50.
3. World Health Organization (WHO). Ten threats to global health in 2019. Accessed July 2, 2021. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
4. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4164.
5. McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550-1562.
6. Betsch C, Korn L, Holtmann C. Don’t try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci. 2015;112(49):E6725-E6726.
7. Rahman T, Hartz SM, Xiong W, et al. Extreme overvalued beliefs. J Am Acad Psychiatry Law. 2020;48(3):319-326.
8. Leask J. Target the fence-sitters. Nature. 2011;473(7348):443-445.
9. United States Census Bureau. Household Pulse Survey COVID-19 Vaccination Tracker. Updated June 30, 2021. Accessed July 2, 2021. https://www.census.gov/library/visualizations/interactive/household-pulse-survey-covid-19-vaccination-tracker.html
10. United States Census Bureau. Measuring household experiences during the coronavirus pandemic. Updated May 5, 2021. Accessed July 2, 2021. https://www.census.gov/data/experimental-data-products/household-pulse-survey.html
11. Jefsen OH, Kølbæk P, Gil Y, et al. COVID-19 vaccine willingness among patients with mental illness compared with the general population. Acta Neuropsychiatrica. 2021:1-24. doi:10.1017/neu.2021.15
12. Miles LW, Williams N, Luthy KE, et al. Adult vaccination rates in the mentally ill population: an outpatient improvement project. J Am Psychiatr Nurses Assoc. 2020;26(2):172-180.
13. Lewandowsky S, Ecker UK, Seifert CM, et al. Misinformation and its correction: continued influence and successful debiasing. Psychol Sci Public Interest. 2012;13(3):106-131.
14. Druss BG, Rosenheck RA. Locus of mental health treatment in an integrated service system. Psychiatr Serv. 2000;51(7):890-892.
15. Freudenreich O, Kontos N, Querques J. COVID-19 and patients with serious mental illness. Current Psychiatry. 2020;19(9):24-35.
16. Hamel L, Kirzinger A, Muñana C, et al. KFF COVID-19 vaccine monitor: December 2020. Accessed July 2, 2021. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/
17. Kai J, Crosland A. Perspectives of people with enduring mental ill health from a community-based qualitative study. Br J Gen Pract. 2001;51(470):730-736.
18. Mather G, Baker D, Laugharne R. Patient trust in psychiatrists. Psychosis. 2012;4(2):161-167.
19. Miller WR, Rollnick S. Motivational interviewing: helping people change. Guilford Press; 2012.
20. Reno JE, O’Leary S, Garrett K, et al. Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. J Health Commun. 2018;23(4):313-320.
21. Baddeley M. Behavioural economics: a very short introduction. Volume 505. Oxford University Press; 2017.
22. Nemani K, Li C, Olfson M, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380-386.
23. De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52.
24. Lorenz RA, Norris MM, Norton LC, et al. Factors associated with influenza vaccination decisions among patients with mental illness. Int J Psychiatry Med. 2013;46(1):1-13.
25. Bitan DT. Patients with schizophrenia are under‐vaccinated for COVID‐19: a report from Israel. World Psychiatry. 2021;20(2):300.
26. Robotham D, Satkunanathan S, Doughty L, et al. Do we still have a digital divide in mental health? A five-year survey follow-up. J Med Internet Res. 2016;18(11):e309.
27. De Hert M, Cohen D, Bobes J, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10(2):138.
28. Carrà G, Bartoli F, Carretta D, et al. The prevalence of metabolic syndrome in people with severe mental illness: a mediation analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1739-1746.
29. Lin MT, Burgess JF, Carey K. The association between serious psychological distress and emergency department utilization among young adults in the USA. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):939-947.
30. DeCoux M. Acute versus primary care: the health care decision making process for individuals with severe mental illness. Issues Ment Health Nurs. 2005;26(9):935-951.
31. Hoffman L, Wisniewski H, Hays R, et al. Digital opportunities for outcomes in recovery services (DOORS): a pragmatic hands-on group approach toward increasing digital health and smartphone competencies, autonomy, relatedness, and alliance for those with serious mental illness. J Psychiatr Pract. 2020;26(2):80-88.
32. Rosenberg SD, Goldberg RW, Dixon LB, et al. Assessing the STIRR model of best practices for blood-borne infections of clients with severe mental illness. Psychiatr Serv. 2010;61(9):885-891.
33. Slade EP, Rosenberg S, Dixon LB, et al. Costs of a public health model to increase receipt of hepatitis-related services for persons with mental illness. Psychiatr Serv. 2013;64(2):127-133.
34. Brewer NT, Chapman GB, Rothman AJ, et al. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149-207.
35. Nabet B, Gable J, Eder J, et al. PolicyLab evidence to action brief: addressing vaccine hesitancy to protect children & communities against preventable diseases. Children’s Hospital of Philadelphia. Published Spring 2017. Accessed July 2, 2021. https://policylab.chop.edu/sites/default/files/pdf/publications/Addressing_Vaccine_Hesitancy.pdf
36. Opel DJ, Heritage J, Taylor JA, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037-1046.
37. Betsch C, Böhm R, Korn L, et al. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017;1(3):1-6.
38. Shen F, Sheer VC, Li R. Impact of narratives on persuasion in health communication: a meta-analysis. J Advert. 2015;44(2):105-113.
39. Parkerson N, Leader A. Vaccine hesitancy in the era of COVID. Population Health Leadership Series: PopTalk webinars. Paper 26. Published February 10, 2021. https://jdc.jefferson.edu/phlspoptalk/26/
40. Dempsey AF, O’Leary ST. Human papillomavirus vaccination: narrative review of studies on how providers’ vaccine communication affects attitudes and uptake. Acad Pediatr. 2018;18(2):S23-S27.
41. Chou W, Burgdorf C, Gaysynsky A, et al. COVID-19 vaccination communication: applying behavioral and social science to address vaccine hesitancy and foster vaccine confidence. National Institutes of Health. Published 2020. https://obssr.od.nih.gov/sites/obssr/files/inline-files/OBSSR_VaccineWhitePaper_FINAL_508.pdf
42. International Society for Vaccines and the MJH Life Sciences COVID-19 coalition. Building confidence in COVID-19 vaccination: a toolbox of talks from leaders in the field. March 9, 2021. https://globalmeet.webcasts.com/starthere.jsp?ei=1435659&tp_key=59ed660099
43. Centers for Disease Control and Prevention. Frequently asked questions about COVID-19 vaccination. Accessed July 2, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html
44. Singh BR, Gandharava S, Gandharva R. Covid-19 vaccines and community immunity. Infectious Diseases Research. 2021;2(1):5.
45. Goldfarb JL, Kreps S, Brownstein JS, et al. Beyond the first dose - Covid-19 vaccine follow-through and continued protective measures. N Engl J Med. 2021;85(2):101-103.
Doctors’ offices may be hot spot for transmission of respiratory infections
Prior research has examined the issue of hospital-acquired infections. A 2014 study published in the New England Journal of Medicine, for example, found that 4% of hospitalized patients acquired a health care–associated infection during their stay. Furthermore, the Centers for Disease Control and Prevention estimates that, on any given day, one in 31 hospital patients has at least one health care–associated infection. However, researchers for the new study, published in Health Affairs, said evidence about the risk of acquiring respiratory viral infections in medical office settings is limited.
“Hospital-acquired infections has been a problem for a while,” study author Hannah Neprash, PhD, of the department of health policy and management at the University of Minnesota School of Public Health, Minneapolis, said in an interview. “However, there’s never been a similar study of whether a similar phenomenon happens in physician offices. This is especially relevant now when we’re dealing with respiratory infections.”
Methods and results
For the new study, Dr. Neprash and her colleagues analyzed deidentified billing and scheduling data from 2016-2017 for 105,462,600 outpatient visits that occurred at 6,709 office-based primary care practices. They used the World Health Organization case definition for influenzalike illness “to capture cases in which the physician may suspect this illness even if a specific diagnosis code was not present.” Their control conditions included exposure to urinary tract infections and back pain.
Doctor visits were considered unexposed if they were scheduled to start at least 90 minutes before the first influenzalike illness visit of the day. They were considered exposed if they were scheduled to start at the same time or after the first influenzalike illness visit of the day at that practice.
Researchers quantified whether exposed patients were more likely to return with a similar illness in the next 2 weeks, compared with nonexposed patients seen earlier in the day
They found that 2.7 patients per 1,000 returned within 2 weeks with an influenzalike illness.
Patients were more likely to return with influenzalike illness if their visit occurred after an influenzalike illness visit versus before, the researchers said.
The authors of the paper said their new research highlights the importance of infection control in health care settings, including outpatient offices.
Where did the exposure occur?
Diego Hijano, MD, MSc, pediatric infectious disease specialist at St. Jude’s Children’s Research Hospital, Memphis, Tenn., said he was not surprised by the findings, but noted that it’s hard to say if the exposure to influenzalike illnesses happened in the office or in the community.
“If you start to see individuals with influenza in your office it’s because [there’s influenza] in the community,” Dr. Hijano explained. “So that means that you will have more patients coming in with influenza.”
To reduce the transmission of infections, Dr. Neprash suggested that doctors’ offices follow the CDC guidelines for indoor conduct, which include masking, washing hands, and “taking appropriate infection control measures.”
So potentially masking within offices is a way to minimize transmission between whatever people are there to be seen when it’s contagious, Dr. Neprash said.
“Telehealth really took off in 2020 and it’s unclear what the state of telehealth will be going forward. [These findings] suggest that there’s a patient safety argument for continuing to enable primary care physicians to provide visits either by phone or by video,” he added.
Dr. Hijano thinks it would be helpful for doctors to separate patients with respiratory illnesses from those without respiratory illnesses.
Driver of transmissions
Dr. Neprash suggested that another driver of these transmissions could be doctors not washing their hands, which is a “notorious issue,” and Dr. Hijano agreed with that statement.
“We did know that the hands of physicians and nurses and care providers are the main driver of infections in the health care setting,” Dr. Hijano explained. “I mean, washing your hands properly between encounters is the single best way that any given health care provider can prevent the spread of infections.”
“We have a unique opportunity with COVID-19 to change how these clinics are operating now,” Dr. Hijano said. “Many clinics are actually asking patients to call ahead of time if you have symptoms of a respiratory illness that could be contagious, and those who are not are still mandating the use of mask and physical distance in the waiting areas and limiting the amount of number of patients in any given hour. So I think that those are really big practices that would kind of make an impact in respiratory illness in terms of decreasing transmission in clinics.”
The authors, who had no conflicts of interest said their hope is that their study will help inform policy for reopening outpatient care settings. Dr. Hijano, who was not involved in the study also had no conflicts.
Prior research has examined the issue of hospital-acquired infections. A 2014 study published in the New England Journal of Medicine, for example, found that 4% of hospitalized patients acquired a health care–associated infection during their stay. Furthermore, the Centers for Disease Control and Prevention estimates that, on any given day, one in 31 hospital patients has at least one health care–associated infection. However, researchers for the new study, published in Health Affairs, said evidence about the risk of acquiring respiratory viral infections in medical office settings is limited.
“Hospital-acquired infections has been a problem for a while,” study author Hannah Neprash, PhD, of the department of health policy and management at the University of Minnesota School of Public Health, Minneapolis, said in an interview. “However, there’s never been a similar study of whether a similar phenomenon happens in physician offices. This is especially relevant now when we’re dealing with respiratory infections.”
Methods and results
For the new study, Dr. Neprash and her colleagues analyzed deidentified billing and scheduling data from 2016-2017 for 105,462,600 outpatient visits that occurred at 6,709 office-based primary care practices. They used the World Health Organization case definition for influenzalike illness “to capture cases in which the physician may suspect this illness even if a specific diagnosis code was not present.” Their control conditions included exposure to urinary tract infections and back pain.
Doctor visits were considered unexposed if they were scheduled to start at least 90 minutes before the first influenzalike illness visit of the day. They were considered exposed if they were scheduled to start at the same time or after the first influenzalike illness visit of the day at that practice.
Researchers quantified whether exposed patients were more likely to return with a similar illness in the next 2 weeks, compared with nonexposed patients seen earlier in the day
They found that 2.7 patients per 1,000 returned within 2 weeks with an influenzalike illness.
Patients were more likely to return with influenzalike illness if their visit occurred after an influenzalike illness visit versus before, the researchers said.
The authors of the paper said their new research highlights the importance of infection control in health care settings, including outpatient offices.
Where did the exposure occur?
Diego Hijano, MD, MSc, pediatric infectious disease specialist at St. Jude’s Children’s Research Hospital, Memphis, Tenn., said he was not surprised by the findings, but noted that it’s hard to say if the exposure to influenzalike illnesses happened in the office or in the community.
“If you start to see individuals with influenza in your office it’s because [there’s influenza] in the community,” Dr. Hijano explained. “So that means that you will have more patients coming in with influenza.”
To reduce the transmission of infections, Dr. Neprash suggested that doctors’ offices follow the CDC guidelines for indoor conduct, which include masking, washing hands, and “taking appropriate infection control measures.”
So potentially masking within offices is a way to minimize transmission between whatever people are there to be seen when it’s contagious, Dr. Neprash said.
“Telehealth really took off in 2020 and it’s unclear what the state of telehealth will be going forward. [These findings] suggest that there’s a patient safety argument for continuing to enable primary care physicians to provide visits either by phone or by video,” he added.
Dr. Hijano thinks it would be helpful for doctors to separate patients with respiratory illnesses from those without respiratory illnesses.
Driver of transmissions
Dr. Neprash suggested that another driver of these transmissions could be doctors not washing their hands, which is a “notorious issue,” and Dr. Hijano agreed with that statement.
“We did know that the hands of physicians and nurses and care providers are the main driver of infections in the health care setting,” Dr. Hijano explained. “I mean, washing your hands properly between encounters is the single best way that any given health care provider can prevent the spread of infections.”
“We have a unique opportunity with COVID-19 to change how these clinics are operating now,” Dr. Hijano said. “Many clinics are actually asking patients to call ahead of time if you have symptoms of a respiratory illness that could be contagious, and those who are not are still mandating the use of mask and physical distance in the waiting areas and limiting the amount of number of patients in any given hour. So I think that those are really big practices that would kind of make an impact in respiratory illness in terms of decreasing transmission in clinics.”
The authors, who had no conflicts of interest said their hope is that their study will help inform policy for reopening outpatient care settings. Dr. Hijano, who was not involved in the study also had no conflicts.
Prior research has examined the issue of hospital-acquired infections. A 2014 study published in the New England Journal of Medicine, for example, found that 4% of hospitalized patients acquired a health care–associated infection during their stay. Furthermore, the Centers for Disease Control and Prevention estimates that, on any given day, one in 31 hospital patients has at least one health care–associated infection. However, researchers for the new study, published in Health Affairs, said evidence about the risk of acquiring respiratory viral infections in medical office settings is limited.
“Hospital-acquired infections has been a problem for a while,” study author Hannah Neprash, PhD, of the department of health policy and management at the University of Minnesota School of Public Health, Minneapolis, said in an interview. “However, there’s never been a similar study of whether a similar phenomenon happens in physician offices. This is especially relevant now when we’re dealing with respiratory infections.”
Methods and results
For the new study, Dr. Neprash and her colleagues analyzed deidentified billing and scheduling data from 2016-2017 for 105,462,600 outpatient visits that occurred at 6,709 office-based primary care practices. They used the World Health Organization case definition for influenzalike illness “to capture cases in which the physician may suspect this illness even if a specific diagnosis code was not present.” Their control conditions included exposure to urinary tract infections and back pain.
Doctor visits were considered unexposed if they were scheduled to start at least 90 minutes before the first influenzalike illness visit of the day. They were considered exposed if they were scheduled to start at the same time or after the first influenzalike illness visit of the day at that practice.
Researchers quantified whether exposed patients were more likely to return with a similar illness in the next 2 weeks, compared with nonexposed patients seen earlier in the day
They found that 2.7 patients per 1,000 returned within 2 weeks with an influenzalike illness.
Patients were more likely to return with influenzalike illness if their visit occurred after an influenzalike illness visit versus before, the researchers said.
The authors of the paper said their new research highlights the importance of infection control in health care settings, including outpatient offices.
Where did the exposure occur?
Diego Hijano, MD, MSc, pediatric infectious disease specialist at St. Jude’s Children’s Research Hospital, Memphis, Tenn., said he was not surprised by the findings, but noted that it’s hard to say if the exposure to influenzalike illnesses happened in the office or in the community.
“If you start to see individuals with influenza in your office it’s because [there’s influenza] in the community,” Dr. Hijano explained. “So that means that you will have more patients coming in with influenza.”
To reduce the transmission of infections, Dr. Neprash suggested that doctors’ offices follow the CDC guidelines for indoor conduct, which include masking, washing hands, and “taking appropriate infection control measures.”
So potentially masking within offices is a way to minimize transmission between whatever people are there to be seen when it’s contagious, Dr. Neprash said.
“Telehealth really took off in 2020 and it’s unclear what the state of telehealth will be going forward. [These findings] suggest that there’s a patient safety argument for continuing to enable primary care physicians to provide visits either by phone or by video,” he added.
Dr. Hijano thinks it would be helpful for doctors to separate patients with respiratory illnesses from those without respiratory illnesses.
Driver of transmissions
Dr. Neprash suggested that another driver of these transmissions could be doctors not washing their hands, which is a “notorious issue,” and Dr. Hijano agreed with that statement.
“We did know that the hands of physicians and nurses and care providers are the main driver of infections in the health care setting,” Dr. Hijano explained. “I mean, washing your hands properly between encounters is the single best way that any given health care provider can prevent the spread of infections.”
“We have a unique opportunity with COVID-19 to change how these clinics are operating now,” Dr. Hijano said. “Many clinics are actually asking patients to call ahead of time if you have symptoms of a respiratory illness that could be contagious, and those who are not are still mandating the use of mask and physical distance in the waiting areas and limiting the amount of number of patients in any given hour. So I think that those are really big practices that would kind of make an impact in respiratory illness in terms of decreasing transmission in clinics.”
The authors, who had no conflicts of interest said their hope is that their study will help inform policy for reopening outpatient care settings. Dr. Hijano, who was not involved in the study also had no conflicts.
FROM HEALTH AFFAIRS
Hospital disaster preparation confronts COVID
Hospitalist groups should have disaster response plans
Jason Persoff, MD, SFHM, now a hospitalist at University of Colorado Hospital in Aurora and an amateur storm chaser, got a close look at how natural disasters can impact hospital care when a tornado destroyed St. John’s Regional Medical Center in Joplin, Mo., on May 22, 2011.
He and a colleague who had been following the storm responded to injuries on the highway before reporting for a long day’s service at the other hospital in Joplin, Freeman Hospital West, caring for patients transferred from St. John’s on an impromptu unit without access to their medical records.
“During my medical training, I had done emergency medicine as an EMT, so I was interested in how the system responds to emergencies,” he explained. “At Joplin I learned how it feels when the boots on the ground in a crisis are not connected to an incident command structure.” Another thing he learned was the essential role for hospitalists in a hospital’s response to a crisis – and thus the need to involve them well in advance in the hospital’s planning for future emergencies.
“Disaster preparation – when done right – helps you ‘herd cats’ in a crisis situation,” he said. “The tornado and its wake served as defining moments for me. I used them as the impetus to improve health care’s response to disasters.” Part of that commitment was to help hospitalists understand their part in emergency preparation.1
Dr. Persoff is now the assistant medical director of emergency preparedness at University of Colorado Hospital. He also helped to create a position called physician support supervisor, which is filled by physicians who have held leadership positions in a hospital to help coordinate the disparate needs of all clinicians in a crisis and facilitate rapid response.2
But then along came the COVID pandemic – which in many locales around the world was unprecedented in scope. Dr. Persoff said his hospital was fairly well prepared, after a decade of engagement with emergency planning. It drew on experience with H1N1, also known as swine flu, and the Ebola virus, which killed 11,323 people, primarily in West Africa, from 2013 to 2016, as models. In a matter of days, the CU division of hospital medicine was able to modify and deploy its existing disaster plans to quickly respond to an influx of COVID patients.3
“Basically, what we set out to do was to treat COVID patients as if they were Ebola patients, cordoning them off in a small area of the hospital. That was naive of us,” he said. “We weren’t able to grasp the scale at the outset. It does defy the imagination – how the hospital could fill up with just one type of patient.”
What is disaster planning?
Emergency preparation for hospitals emerged as a recognized medical specialization in the 1970s. Initially it was largely considered the realm of emergency physicians, trauma services, or critical care doctors. Resources such as the World Health Organization, the Federal Emergency Management Agency, and similar groups recommend an all-hazards approach, a broad and flexible strategy for managing emergencies that could include natural disasters – earthquakes, storms, tornadoes, or wildfires – or human-caused events, such as mass shootings or terrorist attacks. The Joint Commission requires accredited hospitals to conduct several disaster drills annually.
The U.S. Hospital Preparedness Program was created in 2002 to enhance the ability of hospitals and health systems to prepare for and respond to bioterrorism attacks on civilians and other public health emergencies, including natural disasters and pandemics. It offers a foundation for national preparedness and a primary source of federal funding for health care system preparedness. The hospital, at the heart of the health care system, is expected to receive the injured and infected, because patients know they can obtain care there.
One of the fundamental tools for crisis response is the incident command system (ICS), which spells out how to quickly establish a command structure and assign responsibility for key tasks as well as overall leadership. The National Incident Management System organizes emergency management across all government levels and the private sector to ensure that the most pressing needs are met and precious resources are used without duplication. ICS is a standardized approach to command, control, and coordination of emergency response using a common hierarchy recognized across organizations, with advance training in how it should be deployed.
A crisis like never before
Nearly every hospital or health system goes through drills for an emergency, said Hassan Khouli, MD, chair of the department of critical care medicine at the Cleveland Clinic, and coauthor of an article in the journal Chest last year outlining 10 principles of emergency preparedness derived from its experience with the COVID pandemic.4 Some of these include: don’t wait; engage a variety of stakeholders; identify sources of truth; and prioritize hospital employees’ safety and well-being.
Part of the preparation is doing table-top exercises, with case scenarios or actual situations presented, working with clinicians on brainstorming and identifying opportunities for improvement, Dr. Khouli said. “These drills are so important, regardless of what the disaster turns out to be. We’ve done that over the years. We are a large health system, very process and detail oriented. Our emergency incident command structure was activated before we saw our first COVID patient,” he said.
“This was a crisis like never before, with huge amounts of uncertainty,” he noted. “But I believe the Cleveland Clinic system did very well, measured by outcomes such as surveys of health care teams across the system, which gave us reassuring results, and clinical outcomes with lower ICU and hospital mortality rates.”
Christopher Whinney, MD, SFHM, department chair of hospital medicine at Cleveland Clinic, said hospitalists worked hand in hand with the health system’s incident command structure and took responsibility for managing non-ICU COVID patients at six hospitals in the system.
“Hospitalists had a place at the table, and we collaborated well with incident command, enterprise redeployment committees, and emergency and critical care colleagues,” he noted. Hospitalists were on the leadership team for a number of planning meetings, and key stakeholders for bringing information back to their groups.
“First thing we did was to look at our workforce. The challenge was how to respond to up to a hundred COVID admissions per day – how to mobilize providers and build surge teams that incorporated primary care providers and medical trainees. We onboarded 200 providers to do hospital care within 60 days,” he said.
“We realized that communication with patients and families was a big part of the challenge, so we assigned people with good communication skills to fill this role. While we were fortunate not to get the terrible surges they had in other places, we felt we were prepared for the worst.”
Challenges of surge capacity
Every disaster is different, said Srikant Polepalli, MD, associate hospitalist medical director for Staten Island University Hospital in New York, part of the Northwell Health system. He brought the experience of being part of the response to Superstorm Sandy in October 2012 to the COVID pandemic.
“Specifically for hospitalists, the biggest challenge is working on surge capacity for a sudden influx of patients,” he said. “But with Northwell as our umbrella, we can triage and load-balance to move patients from hospital to hospital as needed. With the pandemic, we started with one COVID unit and then expanded to fill the entire hospital.”
Dr. Polepalli was appointed medical director for a temporary field hospital installed at South Beach Psychiatric Center, also in Staten Island. “We were able to acquire help and bring in people ranging from hospitalists to ER physicians, travel nurses, operation managers and the National Guard. Our command center did a phenomenal job of allocating and obtaining resources. It helped to have a structure that was already established and to rely on the resources of the health system,” Dr. Polepalli said. Not every hospital has a structure like Northwell’s.
“We’re not out of the pandemic yet, but we’ll continue with disaster drills and planning,” he said. “We must continue to adapt and have converted our temporary facilities to COVID testing centers, antibody infusion centers, and vaccination centers.”
For Alfred Burger, MD, SFHM, a hospitalist at Mount Sinai’s Beth Israel campus in New York, hospital medicine, now in its maturing phase, is still feeling its way through hospital and health care system transformation.
“My group is an academic, multicampus hospitalist group employed by the hospital system. When I meet other hospitalists at SHM conferences, whether they come from privately owned, corporately owned, or contracted models, they vary widely in terms of how involved the hospitalists are in crisis planning and their ability to respond to crises. At large academic medical centers like ours, one or more doctors is tasked with being involved in preparing for the next disaster,” he said.
“I think we responded the best we could, although it was difficult as we lost many patients to COVID. We were trying to save lives using the tools we knew from treating pneumonias and other forms of acute inflammatory lung injuries. We used every bit of our training in situations where no one had the right answers. But disasters teach us how to be flexible and pivot on the fly, and what to do when things don’t go our way.”
What is disaster response?
Medical response to a disaster essentially boils down to three main things: stuff, staff, and space, Dr. Persoff said. Those are the cornerstones of an emergency plan.
“There is not a hazard that exists that you can’t take an all-hazards approach to dealing with fundamental realities on the ground. No plan can be comprehensive enough to deal with all the intricacies of an emergency. But many plans can have the bones of a response that will allow you to face adverse circumstances,” he said.
“We actually became quite efficient early on in the pandemic, able to adapt in the moment. We were able to build an effective bridge between workers on the ground and our incident command structure, which seemed to reduce a lot of stress and create situational awareness. We implemented ICS as soon as we heard that China was building a COVID hospital, back in February of 2020.”
When one thinks about mass trauma, such as a 747 crash, Dr. Persoff said, the need is to treat burn victims and trauma victims in large numbers. At that point, the ED downstairs is filled with medical patients. Hospital medicine can rapidly admit those patients to clear out room in the ED. Surgeons are also dedicated to rapidly treating those patients, but what about patients who are on the floor following their surgeries? Hospitalists can offer consultations or primary management so the surgeons can stay in the OR, and the same in the ICU, while safely discharging hospitalized patients in a timely manner to make room for incoming patients.
“The lessons of COVID have been hard-taught and hard-earned. No good plan survives contact with the enemy,” he said. “But I think we’ll be better prepared for the next pandemic.”
Maria Frank, MD, FACP, SFHM, a hospitalist at Denver Health who chairs SHM’s Disaster Management Special Interest Group, says she got the bug for disaster preparation during postresidency training as an internist in emergency medicine. “I’m also the medical director for our biocontainment unit, created for infections like Ebola.” SHM’s SIG, which has 150 members, is now writing a review article on disaster planning for the field.
“I got a call on Dec. 27, 2019, about this new pneumonia, and they said, ‘We don’t know what it is, but it’s a coronavirus,’” she recalled. “When I got off the phone, I said, ‘Let’s make sure our response plan works and we have enough of everything on hand.’” Dr. Frank said she was expecting something more like SARS (severe acute respiratory syndrome). “When they called the public health emergency of international concern for COVID, I was at a Centers for Disease Control and Prevention meeting in Atlanta. It really wasn’t a surprise for us.”
All hospitals plan for disasters, although they use different names and have different levels of commitment, Dr. Frank said. What’s not consistent is the participation of hospitalists. “Even when a disaster is 100% trauma related, consider a hospital like mine that has at least four times as many hospitalists as surgeons at any given time. The hospitalists need to take overall management for the patients who aren’t actually in the operating room.”
Time to debrief
Dr. Frank recommends debriefing on the hospital’s and the hospitalist group’s experience with COVID. “Look at the biggest challenges your group faced. Was it staffing, or time off, or the need for day care? Was it burnout, lack of knowledge, lack of [personal protective equipment]?” Each hospital could use its own COVID experience to work on identifying the challenges and the problems, she said. “I’d encourage each department and division to do this exercise individually. Then come together to find common ground with other departments in the hospital.”
This debriefing exercise isn’t just for doctors – it’s also for nurses, environmental services, security, and many other departments, she said. “COVID showed us how crisis response is a group effort. What will bring us together is to learn the challenges each of us faced. It was amazing to see hospitalists doing what they do best.” Post pandemic, hospitalists should also consider getting involved in research and publications, in order to share their lessons.
“One of the things we learned is that hospitalists are very versatile,” Dr. Frank added. But it’s also good for the group to have members specialize, for example, in biocontainment. “We are experts in discharging patients, in patient flow and operations, in coordinating complex medical care. So we would naturally take the lead in, for example, opening a geographic unit or collaborating with other specialists to create innovative models. That’s our job. It’s essential that we’re involved well in advance.”
COVID may be a once-in-a-lifetime experience, but there will be other disasters to come, she said. “If your hospital doesn’t have a disaster plan for hospitalists, get involved in establishing one. Each hospitalist group should have its own response plan. Talk to your peers at other hospitals, and get involved at the institutional level. I’m happy to share our plan; just contact me.” Readers can contact Dr. Frank at [email protected].
References
1. Persoff J et al. The role of hospital medicine in emergency preparedness: A framework for hospitalist leadership in disaster preparedness, response and recovery. J Hosp Med. 2018 Oct;13(10):713-7. doi: 10.12788/jhm.3073.
2. Persoff J et al. Expanding the hospital incident command system with a physician-centric role during a pandemic: The role of the physician clinical support supervisor. J Hosp Adm. 2020;9(3):7-10. doi: 10.5430/jha.v9n3p7.
3. Bowden K et al. Harnessing the power of hospitalists in operational disaster planning: COVID-19. J Gen Intern Med. 2020 Sep;35(9):273-7. doi: 10.1007/s11606-020-05952-6.
4. Orsini E et al. Lessons on outbreak preparedness from the Cleveland Clinic. Chest. 2020;158(5):2090-6. doi: 10.1016/j.chest.2020.06.009.
Hospitalist groups should have disaster response plans
Hospitalist groups should have disaster response plans
Jason Persoff, MD, SFHM, now a hospitalist at University of Colorado Hospital in Aurora and an amateur storm chaser, got a close look at how natural disasters can impact hospital care when a tornado destroyed St. John’s Regional Medical Center in Joplin, Mo., on May 22, 2011.
He and a colleague who had been following the storm responded to injuries on the highway before reporting for a long day’s service at the other hospital in Joplin, Freeman Hospital West, caring for patients transferred from St. John’s on an impromptu unit without access to their medical records.
“During my medical training, I had done emergency medicine as an EMT, so I was interested in how the system responds to emergencies,” he explained. “At Joplin I learned how it feels when the boots on the ground in a crisis are not connected to an incident command structure.” Another thing he learned was the essential role for hospitalists in a hospital’s response to a crisis – and thus the need to involve them well in advance in the hospital’s planning for future emergencies.
“Disaster preparation – when done right – helps you ‘herd cats’ in a crisis situation,” he said. “The tornado and its wake served as defining moments for me. I used them as the impetus to improve health care’s response to disasters.” Part of that commitment was to help hospitalists understand their part in emergency preparation.1
Dr. Persoff is now the assistant medical director of emergency preparedness at University of Colorado Hospital. He also helped to create a position called physician support supervisor, which is filled by physicians who have held leadership positions in a hospital to help coordinate the disparate needs of all clinicians in a crisis and facilitate rapid response.2
But then along came the COVID pandemic – which in many locales around the world was unprecedented in scope. Dr. Persoff said his hospital was fairly well prepared, after a decade of engagement with emergency planning. It drew on experience with H1N1, also known as swine flu, and the Ebola virus, which killed 11,323 people, primarily in West Africa, from 2013 to 2016, as models. In a matter of days, the CU division of hospital medicine was able to modify and deploy its existing disaster plans to quickly respond to an influx of COVID patients.3
“Basically, what we set out to do was to treat COVID patients as if they were Ebola patients, cordoning them off in a small area of the hospital. That was naive of us,” he said. “We weren’t able to grasp the scale at the outset. It does defy the imagination – how the hospital could fill up with just one type of patient.”
What is disaster planning?
Emergency preparation for hospitals emerged as a recognized medical specialization in the 1970s. Initially it was largely considered the realm of emergency physicians, trauma services, or critical care doctors. Resources such as the World Health Organization, the Federal Emergency Management Agency, and similar groups recommend an all-hazards approach, a broad and flexible strategy for managing emergencies that could include natural disasters – earthquakes, storms, tornadoes, or wildfires – or human-caused events, such as mass shootings or terrorist attacks. The Joint Commission requires accredited hospitals to conduct several disaster drills annually.
The U.S. Hospital Preparedness Program was created in 2002 to enhance the ability of hospitals and health systems to prepare for and respond to bioterrorism attacks on civilians and other public health emergencies, including natural disasters and pandemics. It offers a foundation for national preparedness and a primary source of federal funding for health care system preparedness. The hospital, at the heart of the health care system, is expected to receive the injured and infected, because patients know they can obtain care there.
One of the fundamental tools for crisis response is the incident command system (ICS), which spells out how to quickly establish a command structure and assign responsibility for key tasks as well as overall leadership. The National Incident Management System organizes emergency management across all government levels and the private sector to ensure that the most pressing needs are met and precious resources are used without duplication. ICS is a standardized approach to command, control, and coordination of emergency response using a common hierarchy recognized across organizations, with advance training in how it should be deployed.
A crisis like never before
Nearly every hospital or health system goes through drills for an emergency, said Hassan Khouli, MD, chair of the department of critical care medicine at the Cleveland Clinic, and coauthor of an article in the journal Chest last year outlining 10 principles of emergency preparedness derived from its experience with the COVID pandemic.4 Some of these include: don’t wait; engage a variety of stakeholders; identify sources of truth; and prioritize hospital employees’ safety and well-being.
Part of the preparation is doing table-top exercises, with case scenarios or actual situations presented, working with clinicians on brainstorming and identifying opportunities for improvement, Dr. Khouli said. “These drills are so important, regardless of what the disaster turns out to be. We’ve done that over the years. We are a large health system, very process and detail oriented. Our emergency incident command structure was activated before we saw our first COVID patient,” he said.
“This was a crisis like never before, with huge amounts of uncertainty,” he noted. “But I believe the Cleveland Clinic system did very well, measured by outcomes such as surveys of health care teams across the system, which gave us reassuring results, and clinical outcomes with lower ICU and hospital mortality rates.”
Christopher Whinney, MD, SFHM, department chair of hospital medicine at Cleveland Clinic, said hospitalists worked hand in hand with the health system’s incident command structure and took responsibility for managing non-ICU COVID patients at six hospitals in the system.
“Hospitalists had a place at the table, and we collaborated well with incident command, enterprise redeployment committees, and emergency and critical care colleagues,” he noted. Hospitalists were on the leadership team for a number of planning meetings, and key stakeholders for bringing information back to their groups.
“First thing we did was to look at our workforce. The challenge was how to respond to up to a hundred COVID admissions per day – how to mobilize providers and build surge teams that incorporated primary care providers and medical trainees. We onboarded 200 providers to do hospital care within 60 days,” he said.
“We realized that communication with patients and families was a big part of the challenge, so we assigned people with good communication skills to fill this role. While we were fortunate not to get the terrible surges they had in other places, we felt we were prepared for the worst.”
Challenges of surge capacity
Every disaster is different, said Srikant Polepalli, MD, associate hospitalist medical director for Staten Island University Hospital in New York, part of the Northwell Health system. He brought the experience of being part of the response to Superstorm Sandy in October 2012 to the COVID pandemic.
“Specifically for hospitalists, the biggest challenge is working on surge capacity for a sudden influx of patients,” he said. “But with Northwell as our umbrella, we can triage and load-balance to move patients from hospital to hospital as needed. With the pandemic, we started with one COVID unit and then expanded to fill the entire hospital.”
Dr. Polepalli was appointed medical director for a temporary field hospital installed at South Beach Psychiatric Center, also in Staten Island. “We were able to acquire help and bring in people ranging from hospitalists to ER physicians, travel nurses, operation managers and the National Guard. Our command center did a phenomenal job of allocating and obtaining resources. It helped to have a structure that was already established and to rely on the resources of the health system,” Dr. Polepalli said. Not every hospital has a structure like Northwell’s.
“We’re not out of the pandemic yet, but we’ll continue with disaster drills and planning,” he said. “We must continue to adapt and have converted our temporary facilities to COVID testing centers, antibody infusion centers, and vaccination centers.”
For Alfred Burger, MD, SFHM, a hospitalist at Mount Sinai’s Beth Israel campus in New York, hospital medicine, now in its maturing phase, is still feeling its way through hospital and health care system transformation.
“My group is an academic, multicampus hospitalist group employed by the hospital system. When I meet other hospitalists at SHM conferences, whether they come from privately owned, corporately owned, or contracted models, they vary widely in terms of how involved the hospitalists are in crisis planning and their ability to respond to crises. At large academic medical centers like ours, one or more doctors is tasked with being involved in preparing for the next disaster,” he said.
“I think we responded the best we could, although it was difficult as we lost many patients to COVID. We were trying to save lives using the tools we knew from treating pneumonias and other forms of acute inflammatory lung injuries. We used every bit of our training in situations where no one had the right answers. But disasters teach us how to be flexible and pivot on the fly, and what to do when things don’t go our way.”
What is disaster response?
Medical response to a disaster essentially boils down to three main things: stuff, staff, and space, Dr. Persoff said. Those are the cornerstones of an emergency plan.
“There is not a hazard that exists that you can’t take an all-hazards approach to dealing with fundamental realities on the ground. No plan can be comprehensive enough to deal with all the intricacies of an emergency. But many plans can have the bones of a response that will allow you to face adverse circumstances,” he said.
“We actually became quite efficient early on in the pandemic, able to adapt in the moment. We were able to build an effective bridge between workers on the ground and our incident command structure, which seemed to reduce a lot of stress and create situational awareness. We implemented ICS as soon as we heard that China was building a COVID hospital, back in February of 2020.”
When one thinks about mass trauma, such as a 747 crash, Dr. Persoff said, the need is to treat burn victims and trauma victims in large numbers. At that point, the ED downstairs is filled with medical patients. Hospital medicine can rapidly admit those patients to clear out room in the ED. Surgeons are also dedicated to rapidly treating those patients, but what about patients who are on the floor following their surgeries? Hospitalists can offer consultations or primary management so the surgeons can stay in the OR, and the same in the ICU, while safely discharging hospitalized patients in a timely manner to make room for incoming patients.
“The lessons of COVID have been hard-taught and hard-earned. No good plan survives contact with the enemy,” he said. “But I think we’ll be better prepared for the next pandemic.”
Maria Frank, MD, FACP, SFHM, a hospitalist at Denver Health who chairs SHM’s Disaster Management Special Interest Group, says she got the bug for disaster preparation during postresidency training as an internist in emergency medicine. “I’m also the medical director for our biocontainment unit, created for infections like Ebola.” SHM’s SIG, which has 150 members, is now writing a review article on disaster planning for the field.
“I got a call on Dec. 27, 2019, about this new pneumonia, and they said, ‘We don’t know what it is, but it’s a coronavirus,’” she recalled. “When I got off the phone, I said, ‘Let’s make sure our response plan works and we have enough of everything on hand.’” Dr. Frank said she was expecting something more like SARS (severe acute respiratory syndrome). “When they called the public health emergency of international concern for COVID, I was at a Centers for Disease Control and Prevention meeting in Atlanta. It really wasn’t a surprise for us.”
All hospitals plan for disasters, although they use different names and have different levels of commitment, Dr. Frank said. What’s not consistent is the participation of hospitalists. “Even when a disaster is 100% trauma related, consider a hospital like mine that has at least four times as many hospitalists as surgeons at any given time. The hospitalists need to take overall management for the patients who aren’t actually in the operating room.”
Time to debrief
Dr. Frank recommends debriefing on the hospital’s and the hospitalist group’s experience with COVID. “Look at the biggest challenges your group faced. Was it staffing, or time off, or the need for day care? Was it burnout, lack of knowledge, lack of [personal protective equipment]?” Each hospital could use its own COVID experience to work on identifying the challenges and the problems, she said. “I’d encourage each department and division to do this exercise individually. Then come together to find common ground with other departments in the hospital.”
This debriefing exercise isn’t just for doctors – it’s also for nurses, environmental services, security, and many other departments, she said. “COVID showed us how crisis response is a group effort. What will bring us together is to learn the challenges each of us faced. It was amazing to see hospitalists doing what they do best.” Post pandemic, hospitalists should also consider getting involved in research and publications, in order to share their lessons.
“One of the things we learned is that hospitalists are very versatile,” Dr. Frank added. But it’s also good for the group to have members specialize, for example, in biocontainment. “We are experts in discharging patients, in patient flow and operations, in coordinating complex medical care. So we would naturally take the lead in, for example, opening a geographic unit or collaborating with other specialists to create innovative models. That’s our job. It’s essential that we’re involved well in advance.”
COVID may be a once-in-a-lifetime experience, but there will be other disasters to come, she said. “If your hospital doesn’t have a disaster plan for hospitalists, get involved in establishing one. Each hospitalist group should have its own response plan. Talk to your peers at other hospitals, and get involved at the institutional level. I’m happy to share our plan; just contact me.” Readers can contact Dr. Frank at [email protected].
References
1. Persoff J et al. The role of hospital medicine in emergency preparedness: A framework for hospitalist leadership in disaster preparedness, response and recovery. J Hosp Med. 2018 Oct;13(10):713-7. doi: 10.12788/jhm.3073.
2. Persoff J et al. Expanding the hospital incident command system with a physician-centric role during a pandemic: The role of the physician clinical support supervisor. J Hosp Adm. 2020;9(3):7-10. doi: 10.5430/jha.v9n3p7.
3. Bowden K et al. Harnessing the power of hospitalists in operational disaster planning: COVID-19. J Gen Intern Med. 2020 Sep;35(9):273-7. doi: 10.1007/s11606-020-05952-6.
4. Orsini E et al. Lessons on outbreak preparedness from the Cleveland Clinic. Chest. 2020;158(5):2090-6. doi: 10.1016/j.chest.2020.06.009.
Jason Persoff, MD, SFHM, now a hospitalist at University of Colorado Hospital in Aurora and an amateur storm chaser, got a close look at how natural disasters can impact hospital care when a tornado destroyed St. John’s Regional Medical Center in Joplin, Mo., on May 22, 2011.
He and a colleague who had been following the storm responded to injuries on the highway before reporting for a long day’s service at the other hospital in Joplin, Freeman Hospital West, caring for patients transferred from St. John’s on an impromptu unit without access to their medical records.
“During my medical training, I had done emergency medicine as an EMT, so I was interested in how the system responds to emergencies,” he explained. “At Joplin I learned how it feels when the boots on the ground in a crisis are not connected to an incident command structure.” Another thing he learned was the essential role for hospitalists in a hospital’s response to a crisis – and thus the need to involve them well in advance in the hospital’s planning for future emergencies.
“Disaster preparation – when done right – helps you ‘herd cats’ in a crisis situation,” he said. “The tornado and its wake served as defining moments for me. I used them as the impetus to improve health care’s response to disasters.” Part of that commitment was to help hospitalists understand their part in emergency preparation.1
Dr. Persoff is now the assistant medical director of emergency preparedness at University of Colorado Hospital. He also helped to create a position called physician support supervisor, which is filled by physicians who have held leadership positions in a hospital to help coordinate the disparate needs of all clinicians in a crisis and facilitate rapid response.2
But then along came the COVID pandemic – which in many locales around the world was unprecedented in scope. Dr. Persoff said his hospital was fairly well prepared, after a decade of engagement with emergency planning. It drew on experience with H1N1, also known as swine flu, and the Ebola virus, which killed 11,323 people, primarily in West Africa, from 2013 to 2016, as models. In a matter of days, the CU division of hospital medicine was able to modify and deploy its existing disaster plans to quickly respond to an influx of COVID patients.3
“Basically, what we set out to do was to treat COVID patients as if they were Ebola patients, cordoning them off in a small area of the hospital. That was naive of us,” he said. “We weren’t able to grasp the scale at the outset. It does defy the imagination – how the hospital could fill up with just one type of patient.”
What is disaster planning?
Emergency preparation for hospitals emerged as a recognized medical specialization in the 1970s. Initially it was largely considered the realm of emergency physicians, trauma services, or critical care doctors. Resources such as the World Health Organization, the Federal Emergency Management Agency, and similar groups recommend an all-hazards approach, a broad and flexible strategy for managing emergencies that could include natural disasters – earthquakes, storms, tornadoes, or wildfires – or human-caused events, such as mass shootings or terrorist attacks. The Joint Commission requires accredited hospitals to conduct several disaster drills annually.
The U.S. Hospital Preparedness Program was created in 2002 to enhance the ability of hospitals and health systems to prepare for and respond to bioterrorism attacks on civilians and other public health emergencies, including natural disasters and pandemics. It offers a foundation for national preparedness and a primary source of federal funding for health care system preparedness. The hospital, at the heart of the health care system, is expected to receive the injured and infected, because patients know they can obtain care there.
One of the fundamental tools for crisis response is the incident command system (ICS), which spells out how to quickly establish a command structure and assign responsibility for key tasks as well as overall leadership. The National Incident Management System organizes emergency management across all government levels and the private sector to ensure that the most pressing needs are met and precious resources are used without duplication. ICS is a standardized approach to command, control, and coordination of emergency response using a common hierarchy recognized across organizations, with advance training in how it should be deployed.
A crisis like never before
Nearly every hospital or health system goes through drills for an emergency, said Hassan Khouli, MD, chair of the department of critical care medicine at the Cleveland Clinic, and coauthor of an article in the journal Chest last year outlining 10 principles of emergency preparedness derived from its experience with the COVID pandemic.4 Some of these include: don’t wait; engage a variety of stakeholders; identify sources of truth; and prioritize hospital employees’ safety and well-being.
Part of the preparation is doing table-top exercises, with case scenarios or actual situations presented, working with clinicians on brainstorming and identifying opportunities for improvement, Dr. Khouli said. “These drills are so important, regardless of what the disaster turns out to be. We’ve done that over the years. We are a large health system, very process and detail oriented. Our emergency incident command structure was activated before we saw our first COVID patient,” he said.
“This was a crisis like never before, with huge amounts of uncertainty,” he noted. “But I believe the Cleveland Clinic system did very well, measured by outcomes such as surveys of health care teams across the system, which gave us reassuring results, and clinical outcomes with lower ICU and hospital mortality rates.”
Christopher Whinney, MD, SFHM, department chair of hospital medicine at Cleveland Clinic, said hospitalists worked hand in hand with the health system’s incident command structure and took responsibility for managing non-ICU COVID patients at six hospitals in the system.
“Hospitalists had a place at the table, and we collaborated well with incident command, enterprise redeployment committees, and emergency and critical care colleagues,” he noted. Hospitalists were on the leadership team for a number of planning meetings, and key stakeholders for bringing information back to their groups.
“First thing we did was to look at our workforce. The challenge was how to respond to up to a hundred COVID admissions per day – how to mobilize providers and build surge teams that incorporated primary care providers and medical trainees. We onboarded 200 providers to do hospital care within 60 days,” he said.
“We realized that communication with patients and families was a big part of the challenge, so we assigned people with good communication skills to fill this role. While we were fortunate not to get the terrible surges they had in other places, we felt we were prepared for the worst.”
Challenges of surge capacity
Every disaster is different, said Srikant Polepalli, MD, associate hospitalist medical director for Staten Island University Hospital in New York, part of the Northwell Health system. He brought the experience of being part of the response to Superstorm Sandy in October 2012 to the COVID pandemic.
“Specifically for hospitalists, the biggest challenge is working on surge capacity for a sudden influx of patients,” he said. “But with Northwell as our umbrella, we can triage and load-balance to move patients from hospital to hospital as needed. With the pandemic, we started with one COVID unit and then expanded to fill the entire hospital.”
Dr. Polepalli was appointed medical director for a temporary field hospital installed at South Beach Psychiatric Center, also in Staten Island. “We were able to acquire help and bring in people ranging from hospitalists to ER physicians, travel nurses, operation managers and the National Guard. Our command center did a phenomenal job of allocating and obtaining resources. It helped to have a structure that was already established and to rely on the resources of the health system,” Dr. Polepalli said. Not every hospital has a structure like Northwell’s.
“We’re not out of the pandemic yet, but we’ll continue with disaster drills and planning,” he said. “We must continue to adapt and have converted our temporary facilities to COVID testing centers, antibody infusion centers, and vaccination centers.”
For Alfred Burger, MD, SFHM, a hospitalist at Mount Sinai’s Beth Israel campus in New York, hospital medicine, now in its maturing phase, is still feeling its way through hospital and health care system transformation.
“My group is an academic, multicampus hospitalist group employed by the hospital system. When I meet other hospitalists at SHM conferences, whether they come from privately owned, corporately owned, or contracted models, they vary widely in terms of how involved the hospitalists are in crisis planning and their ability to respond to crises. At large academic medical centers like ours, one or more doctors is tasked with being involved in preparing for the next disaster,” he said.
“I think we responded the best we could, although it was difficult as we lost many patients to COVID. We were trying to save lives using the tools we knew from treating pneumonias and other forms of acute inflammatory lung injuries. We used every bit of our training in situations where no one had the right answers. But disasters teach us how to be flexible and pivot on the fly, and what to do when things don’t go our way.”
What is disaster response?
Medical response to a disaster essentially boils down to three main things: stuff, staff, and space, Dr. Persoff said. Those are the cornerstones of an emergency plan.
“There is not a hazard that exists that you can’t take an all-hazards approach to dealing with fundamental realities on the ground. No plan can be comprehensive enough to deal with all the intricacies of an emergency. But many plans can have the bones of a response that will allow you to face adverse circumstances,” he said.
“We actually became quite efficient early on in the pandemic, able to adapt in the moment. We were able to build an effective bridge between workers on the ground and our incident command structure, which seemed to reduce a lot of stress and create situational awareness. We implemented ICS as soon as we heard that China was building a COVID hospital, back in February of 2020.”
When one thinks about mass trauma, such as a 747 crash, Dr. Persoff said, the need is to treat burn victims and trauma victims in large numbers. At that point, the ED downstairs is filled with medical patients. Hospital medicine can rapidly admit those patients to clear out room in the ED. Surgeons are also dedicated to rapidly treating those patients, but what about patients who are on the floor following their surgeries? Hospitalists can offer consultations or primary management so the surgeons can stay in the OR, and the same in the ICU, while safely discharging hospitalized patients in a timely manner to make room for incoming patients.
“The lessons of COVID have been hard-taught and hard-earned. No good plan survives contact with the enemy,” he said. “But I think we’ll be better prepared for the next pandemic.”
Maria Frank, MD, FACP, SFHM, a hospitalist at Denver Health who chairs SHM’s Disaster Management Special Interest Group, says she got the bug for disaster preparation during postresidency training as an internist in emergency medicine. “I’m also the medical director for our biocontainment unit, created for infections like Ebola.” SHM’s SIG, which has 150 members, is now writing a review article on disaster planning for the field.
“I got a call on Dec. 27, 2019, about this new pneumonia, and they said, ‘We don’t know what it is, but it’s a coronavirus,’” she recalled. “When I got off the phone, I said, ‘Let’s make sure our response plan works and we have enough of everything on hand.’” Dr. Frank said she was expecting something more like SARS (severe acute respiratory syndrome). “When they called the public health emergency of international concern for COVID, I was at a Centers for Disease Control and Prevention meeting in Atlanta. It really wasn’t a surprise for us.”
All hospitals plan for disasters, although they use different names and have different levels of commitment, Dr. Frank said. What’s not consistent is the participation of hospitalists. “Even when a disaster is 100% trauma related, consider a hospital like mine that has at least four times as many hospitalists as surgeons at any given time. The hospitalists need to take overall management for the patients who aren’t actually in the operating room.”
Time to debrief
Dr. Frank recommends debriefing on the hospital’s and the hospitalist group’s experience with COVID. “Look at the biggest challenges your group faced. Was it staffing, or time off, or the need for day care? Was it burnout, lack of knowledge, lack of [personal protective equipment]?” Each hospital could use its own COVID experience to work on identifying the challenges and the problems, she said. “I’d encourage each department and division to do this exercise individually. Then come together to find common ground with other departments in the hospital.”
This debriefing exercise isn’t just for doctors – it’s also for nurses, environmental services, security, and many other departments, she said. “COVID showed us how crisis response is a group effort. What will bring us together is to learn the challenges each of us faced. It was amazing to see hospitalists doing what they do best.” Post pandemic, hospitalists should also consider getting involved in research and publications, in order to share their lessons.
“One of the things we learned is that hospitalists are very versatile,” Dr. Frank added. But it’s also good for the group to have members specialize, for example, in biocontainment. “We are experts in discharging patients, in patient flow and operations, in coordinating complex medical care. So we would naturally take the lead in, for example, opening a geographic unit or collaborating with other specialists to create innovative models. That’s our job. It’s essential that we’re involved well in advance.”
COVID may be a once-in-a-lifetime experience, but there will be other disasters to come, she said. “If your hospital doesn’t have a disaster plan for hospitalists, get involved in establishing one. Each hospitalist group should have its own response plan. Talk to your peers at other hospitals, and get involved at the institutional level. I’m happy to share our plan; just contact me.” Readers can contact Dr. Frank at [email protected].
References
1. Persoff J et al. The role of hospital medicine in emergency preparedness: A framework for hospitalist leadership in disaster preparedness, response and recovery. J Hosp Med. 2018 Oct;13(10):713-7. doi: 10.12788/jhm.3073.
2. Persoff J et al. Expanding the hospital incident command system with a physician-centric role during a pandemic: The role of the physician clinical support supervisor. J Hosp Adm. 2020;9(3):7-10. doi: 10.5430/jha.v9n3p7.
3. Bowden K et al. Harnessing the power of hospitalists in operational disaster planning: COVID-19. J Gen Intern Med. 2020 Sep;35(9):273-7. doi: 10.1007/s11606-020-05952-6.
4. Orsini E et al. Lessons on outbreak preparedness from the Cleveland Clinic. Chest. 2020;158(5):2090-6. doi: 10.1016/j.chest.2020.06.009.
CDC to show vaccinated people infected with Delta remain contagious
and infect others, the New York Times reported on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the New York Times said. The bottom line is that the CDC data shows people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on Jul 29 that the CDC’s updated mask guidance followed an outbreak on Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
A version of this article first appeared on Medscape.com.
and infect others, the New York Times reported on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the New York Times said. The bottom line is that the CDC data shows people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on Jul 29 that the CDC’s updated mask guidance followed an outbreak on Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
A version of this article first appeared on Medscape.com.
and infect others, the New York Times reported on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the New York Times said. The bottom line is that the CDC data shows people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on Jul 29 that the CDC’s updated mask guidance followed an outbreak on Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
A version of this article first appeared on Medscape.com.
COVID-19, hearings on Jan. 6 attack reignite interest in PTSD
After Sept. 11, 2001, and the subsequent long war in Iraq and Afghanistan, both mental health providers and the general public focused on posttraumatic stress disorder (PTSD). However, after almost 20 years of war and the COVID-19 epidemic, attention waned away from military service members and PTSD.
COVID-19–related PTSD and the hearings on the Jan. 6 attack on the Capitol have reignited interest in PTSD diagnosis and treatment. Testimony from police officers at the House select committee hearing about their experiences during the assault and PTSD was harrowing. One of the police officers had also served in Iraq, perhaps leading to “layered PTSD” – symptoms from war abroad and at home.
Thus, I thought a brief review of updates about diagnosis and treatment would be useful. Note: These are my opinions based on my extensive experience and do not represent the official opinion of my employer (MedStar Health).
PTSD was first classified as a disorder in 1980, based mainly on the experiences of military service members in Vietnam, as well as sexual assault victims and disaster survivors. Readers may look elsewhere for a fuller history of the disorder.
However, in brief, we have evolved from strict reliance on a variety of symptoms in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to a more global determination of the experience of trauma and related symptoms of distress. We still rely for diagnosis on trauma-related anxiety and depression symptoms, such as nightmare, flashbacks, numbness, and disassociation.
Treatment has evolved. Patients may benefit from treatment even if they do not meet all the PTSD criteria. As many of my colleagues who treat patients have said, “if it smells like PTSD, treat it like PTSD.”
What is the most effective treatment? The literature declares that evidence-based treatments include two selective serotonin reuptake inhibitors (Zoloft and Paxil) and several psychotherapies. The psychotherapies include cognitive-behavioral therapies, exposure therapy, and EMDR (eye movement desensitization reprocessing).
The problem is that many patients cannot tolerate these therapies. SSRIs do have side effects, the most distressing being sexual dysfunction. Many service members do not enter the psychotherapies, or they drop out of trials, because they cannot tolerate the reimagining of their trauma.
I now counsel patients about the “three buckets” of treatment. The first bucket is medication, which as a psychiatrist is what I focus on. The second bucket is psychotherapy as discussed above. The third bucket is “everything else.”
“Everything else” includes a variety of methods the patients can use to reduce symptoms of anxiety, depression, and PTSD symptoms: exercising; deep breathing through the nose; doing yoga; doing meditation; playing or working with animals; gardening; and engaging in other activities that “self sooth.” I also recommend always doing “small acts of kindness” for others. I myself contribute to food banks and bring cookies or watermelons to the staff at my hospital.
Why is this approach useful? A menu of options gives control back to the patient. It provides activities that can reduce anxiety. Thinking about caring for others helps patients get out of their own “swamp of distress.”
We do live in very difficult times. We’re coping with COVID-19 Delta variant, attacks on the Capitol, and gun violence. I have not yet mentioned climate change, which is extremely frightening to many of us. So all providers need to be aware of all the strategies at our disposal to treat anxiety, depression, and PTSD.
Dr. Ritchie is chair of psychiatry at Medstar Washington (D.C.) Hospital Center. She has no conflicts of interest.
After Sept. 11, 2001, and the subsequent long war in Iraq and Afghanistan, both mental health providers and the general public focused on posttraumatic stress disorder (PTSD). However, after almost 20 years of war and the COVID-19 epidemic, attention waned away from military service members and PTSD.
COVID-19–related PTSD and the hearings on the Jan. 6 attack on the Capitol have reignited interest in PTSD diagnosis and treatment. Testimony from police officers at the House select committee hearing about their experiences during the assault and PTSD was harrowing. One of the police officers had also served in Iraq, perhaps leading to “layered PTSD” – symptoms from war abroad and at home.
Thus, I thought a brief review of updates about diagnosis and treatment would be useful. Note: These are my opinions based on my extensive experience and do not represent the official opinion of my employer (MedStar Health).
PTSD was first classified as a disorder in 1980, based mainly on the experiences of military service members in Vietnam, as well as sexual assault victims and disaster survivors. Readers may look elsewhere for a fuller history of the disorder.
However, in brief, we have evolved from strict reliance on a variety of symptoms in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to a more global determination of the experience of trauma and related symptoms of distress. We still rely for diagnosis on trauma-related anxiety and depression symptoms, such as nightmare, flashbacks, numbness, and disassociation.
Treatment has evolved. Patients may benefit from treatment even if they do not meet all the PTSD criteria. As many of my colleagues who treat patients have said, “if it smells like PTSD, treat it like PTSD.”
What is the most effective treatment? The literature declares that evidence-based treatments include two selective serotonin reuptake inhibitors (Zoloft and Paxil) and several psychotherapies. The psychotherapies include cognitive-behavioral therapies, exposure therapy, and EMDR (eye movement desensitization reprocessing).
The problem is that many patients cannot tolerate these therapies. SSRIs do have side effects, the most distressing being sexual dysfunction. Many service members do not enter the psychotherapies, or they drop out of trials, because they cannot tolerate the reimagining of their trauma.
I now counsel patients about the “three buckets” of treatment. The first bucket is medication, which as a psychiatrist is what I focus on. The second bucket is psychotherapy as discussed above. The third bucket is “everything else.”
“Everything else” includes a variety of methods the patients can use to reduce symptoms of anxiety, depression, and PTSD symptoms: exercising; deep breathing through the nose; doing yoga; doing meditation; playing or working with animals; gardening; and engaging in other activities that “self sooth.” I also recommend always doing “small acts of kindness” for others. I myself contribute to food banks and bring cookies or watermelons to the staff at my hospital.
Why is this approach useful? A menu of options gives control back to the patient. It provides activities that can reduce anxiety. Thinking about caring for others helps patients get out of their own “swamp of distress.”
We do live in very difficult times. We’re coping with COVID-19 Delta variant, attacks on the Capitol, and gun violence. I have not yet mentioned climate change, which is extremely frightening to many of us. So all providers need to be aware of all the strategies at our disposal to treat anxiety, depression, and PTSD.
Dr. Ritchie is chair of psychiatry at Medstar Washington (D.C.) Hospital Center. She has no conflicts of interest.
After Sept. 11, 2001, and the subsequent long war in Iraq and Afghanistan, both mental health providers and the general public focused on posttraumatic stress disorder (PTSD). However, after almost 20 years of war and the COVID-19 epidemic, attention waned away from military service members and PTSD.
COVID-19–related PTSD and the hearings on the Jan. 6 attack on the Capitol have reignited interest in PTSD diagnosis and treatment. Testimony from police officers at the House select committee hearing about their experiences during the assault and PTSD was harrowing. One of the police officers had also served in Iraq, perhaps leading to “layered PTSD” – symptoms from war abroad and at home.
Thus, I thought a brief review of updates about diagnosis and treatment would be useful. Note: These are my opinions based on my extensive experience and do not represent the official opinion of my employer (MedStar Health).
PTSD was first classified as a disorder in 1980, based mainly on the experiences of military service members in Vietnam, as well as sexual assault victims and disaster survivors. Readers may look elsewhere for a fuller history of the disorder.
However, in brief, we have evolved from strict reliance on a variety of symptoms in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to a more global determination of the experience of trauma and related symptoms of distress. We still rely for diagnosis on trauma-related anxiety and depression symptoms, such as nightmare, flashbacks, numbness, and disassociation.
Treatment has evolved. Patients may benefit from treatment even if they do not meet all the PTSD criteria. As many of my colleagues who treat patients have said, “if it smells like PTSD, treat it like PTSD.”
What is the most effective treatment? The literature declares that evidence-based treatments include two selective serotonin reuptake inhibitors (Zoloft and Paxil) and several psychotherapies. The psychotherapies include cognitive-behavioral therapies, exposure therapy, and EMDR (eye movement desensitization reprocessing).
The problem is that many patients cannot tolerate these therapies. SSRIs do have side effects, the most distressing being sexual dysfunction. Many service members do not enter the psychotherapies, or they drop out of trials, because they cannot tolerate the reimagining of their trauma.
I now counsel patients about the “three buckets” of treatment. The first bucket is medication, which as a psychiatrist is what I focus on. The second bucket is psychotherapy as discussed above. The third bucket is “everything else.”
“Everything else” includes a variety of methods the patients can use to reduce symptoms of anxiety, depression, and PTSD symptoms: exercising; deep breathing through the nose; doing yoga; doing meditation; playing or working with animals; gardening; and engaging in other activities that “self sooth.” I also recommend always doing “small acts of kindness” for others. I myself contribute to food banks and bring cookies or watermelons to the staff at my hospital.
Why is this approach useful? A menu of options gives control back to the patient. It provides activities that can reduce anxiety. Thinking about caring for others helps patients get out of their own “swamp of distress.”
We do live in very difficult times. We’re coping with COVID-19 Delta variant, attacks on the Capitol, and gun violence. I have not yet mentioned climate change, which is extremely frightening to many of us. So all providers need to be aware of all the strategies at our disposal to treat anxiety, depression, and PTSD.
Dr. Ritchie is chair of psychiatry at Medstar Washington (D.C.) Hospital Center. She has no conflicts of interest.
‘A few mutations away’: The threat of a vaccine-proof variant
The Centers for Disease Control and Prevention Director Rochelle Walensky, MD, MPH, made a dire prediction during a media briefing this week that, if we weren’t already living within the reality of the COVID-19 pandemic, would sound more like a pitch for a movie about a dystopian future.
“For the amount of virus circulating in this country right now largely among unvaccinated people, the largest concern that we in public health and science are worried about is that the virus … [becomes] a very transmissible virus that has the potential to evade our vaccines in terms of how it protects us from severe disease and death,” Dr. Walensky told reporters on July 27.
A new, more elusive variant could be “just a few mutations away,” she said.
“That’s a very prescient comment,” Lewis Nelson, MD, professor and clinical chair of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School in Newark, told this news organization.
“We’ve gone through a few mutations already that have been named, and each one of them gets a little more transmissible,” he said. “That’s normal, natural selection and what you would expect to happen as viruses mutate from one strain to another.”
“What we’ve mostly seen this virus do is evolve to become more infectious,” said Stuart Ray, MD, when also asked to comment. “That is the remarkable feature of Delta – that it is so infectious.”
He said that the SARS-CoV-2 has evolved largely as expected, at least so far. “The potential for this virus to mutate has been something that has been a concern from early on.”
“The viral evolution is a bit like a ticking clock. The more we allow infections to occur, the more likely changes will occur. When we have lots of people infected, we give more chances to the virus to diversify and then adapt to selective pressures,” said Dr. Ray, vice-chair of medicine for data integrity and analytics and professor in the division of infectious diseases at Johns Hopkins School of Medicine in Baltimore.
Dr. Nelson said.
If this occurs, he added, “we will have an ineffective vaccine, essentially. And we’ll be back to where we were last March with a brand-new disease.”
Technology to the rescue?
The flexibility of mRNA vaccines is one potential solution. These vaccines could be more easily and quickly adapted to respond to a new, more vaccine-elusive variant.
“That’s absolutely reassuring,” Dr. Nelson said. For example, if a mutation changes the spike protein and vaccines no longer recognize it, a manufacturer could identify the new protein and incorporate that in a new mRNA vaccine.
“The problem is that some people are not taking the current vaccine,” he added. “I’m not sure what is going to make them take the next vaccine.”
Nothing appears certain
When asked how likely a new strain of SARS-CoV-2 could emerge that gets around vaccine protection, Dr. Nelson said, “I think [what] we’ve learned so far there is no way to predict anything” about this pandemic.
“The best way to prevent the virus from mutating is to prevent hosts, people, from getting sick with it,” he said. “That’s why it’s so important people should get immunized and wear masks.”
Both Dr. Nelson and Dr. Ray pointed out that it is in the best interest of the virus to evolve to be more transmissible and spread to more people. In contrast, a virus that causes people to get so sick that they isolate or die, thus halting transmission, works against viruses surviving evolutionarily.
Some viruses also mutate to become milder over time, but that has not been the case with SARS-CoV-2, Dr. Ray said.
Mutations not the only concern
Viruses have another mechanism that produces new strains, and it works even more quickly than mutations. Recombination, as it’s known, can occur when a person is infected with two different strains of the same virus. If the two versions enter the same cell, the viruses can swap genetic material and produce a third, altogether different strain.
Recombination has already been seen with influenza strains, where H and N genetic segments are swapped to yield H1N1, H1N2, and H3N2 versions of the flu, for example.
“In the early days of SARS-CoV-2 there was so little diversity that recombination did not matter,” Dr. Ray said. However, there are now distinct lineages of the virus circulating globally. If two of these lineages swap segments “this would make a very new viral sequence in one step without having to mutate to gain those differences.”
“The more diverse the strains that are circulating, the bigger a possibility this is,” Dr. Ray said.
Protected, for now
Dr. Walensky’s sober warning came at the same time the CDC released new guidance calling for the wearing of masks indoors in schools and in any location in the country where COVID-19 cases surpass 50 people per 100,000, also known as substantial or high transmission areas.
On a positive note, Dr. Walensky said: “Right now, fortunately, we are not there. The vaccines operate really well in protecting us from severe disease and death.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention Director Rochelle Walensky, MD, MPH, made a dire prediction during a media briefing this week that, if we weren’t already living within the reality of the COVID-19 pandemic, would sound more like a pitch for a movie about a dystopian future.
“For the amount of virus circulating in this country right now largely among unvaccinated people, the largest concern that we in public health and science are worried about is that the virus … [becomes] a very transmissible virus that has the potential to evade our vaccines in terms of how it protects us from severe disease and death,” Dr. Walensky told reporters on July 27.
A new, more elusive variant could be “just a few mutations away,” she said.
“That’s a very prescient comment,” Lewis Nelson, MD, professor and clinical chair of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School in Newark, told this news organization.
“We’ve gone through a few mutations already that have been named, and each one of them gets a little more transmissible,” he said. “That’s normal, natural selection and what you would expect to happen as viruses mutate from one strain to another.”
“What we’ve mostly seen this virus do is evolve to become more infectious,” said Stuart Ray, MD, when also asked to comment. “That is the remarkable feature of Delta – that it is so infectious.”
He said that the SARS-CoV-2 has evolved largely as expected, at least so far. “The potential for this virus to mutate has been something that has been a concern from early on.”
“The viral evolution is a bit like a ticking clock. The more we allow infections to occur, the more likely changes will occur. When we have lots of people infected, we give more chances to the virus to diversify and then adapt to selective pressures,” said Dr. Ray, vice-chair of medicine for data integrity and analytics and professor in the division of infectious diseases at Johns Hopkins School of Medicine in Baltimore.
Dr. Nelson said.
If this occurs, he added, “we will have an ineffective vaccine, essentially. And we’ll be back to where we were last March with a brand-new disease.”
Technology to the rescue?
The flexibility of mRNA vaccines is one potential solution. These vaccines could be more easily and quickly adapted to respond to a new, more vaccine-elusive variant.
“That’s absolutely reassuring,” Dr. Nelson said. For example, if a mutation changes the spike protein and vaccines no longer recognize it, a manufacturer could identify the new protein and incorporate that in a new mRNA vaccine.
“The problem is that some people are not taking the current vaccine,” he added. “I’m not sure what is going to make them take the next vaccine.”
Nothing appears certain
When asked how likely a new strain of SARS-CoV-2 could emerge that gets around vaccine protection, Dr. Nelson said, “I think [what] we’ve learned so far there is no way to predict anything” about this pandemic.
“The best way to prevent the virus from mutating is to prevent hosts, people, from getting sick with it,” he said. “That’s why it’s so important people should get immunized and wear masks.”
Both Dr. Nelson and Dr. Ray pointed out that it is in the best interest of the virus to evolve to be more transmissible and spread to more people. In contrast, a virus that causes people to get so sick that they isolate or die, thus halting transmission, works against viruses surviving evolutionarily.
Some viruses also mutate to become milder over time, but that has not been the case with SARS-CoV-2, Dr. Ray said.
Mutations not the only concern
Viruses have another mechanism that produces new strains, and it works even more quickly than mutations. Recombination, as it’s known, can occur when a person is infected with two different strains of the same virus. If the two versions enter the same cell, the viruses can swap genetic material and produce a third, altogether different strain.
Recombination has already been seen with influenza strains, where H and N genetic segments are swapped to yield H1N1, H1N2, and H3N2 versions of the flu, for example.
“In the early days of SARS-CoV-2 there was so little diversity that recombination did not matter,” Dr. Ray said. However, there are now distinct lineages of the virus circulating globally. If two of these lineages swap segments “this would make a very new viral sequence in one step without having to mutate to gain those differences.”
“The more diverse the strains that are circulating, the bigger a possibility this is,” Dr. Ray said.
Protected, for now
Dr. Walensky’s sober warning came at the same time the CDC released new guidance calling for the wearing of masks indoors in schools and in any location in the country where COVID-19 cases surpass 50 people per 100,000, also known as substantial or high transmission areas.
On a positive note, Dr. Walensky said: “Right now, fortunately, we are not there. The vaccines operate really well in protecting us from severe disease and death.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention Director Rochelle Walensky, MD, MPH, made a dire prediction during a media briefing this week that, if we weren’t already living within the reality of the COVID-19 pandemic, would sound more like a pitch for a movie about a dystopian future.
“For the amount of virus circulating in this country right now largely among unvaccinated people, the largest concern that we in public health and science are worried about is that the virus … [becomes] a very transmissible virus that has the potential to evade our vaccines in terms of how it protects us from severe disease and death,” Dr. Walensky told reporters on July 27.
A new, more elusive variant could be “just a few mutations away,” she said.
“That’s a very prescient comment,” Lewis Nelson, MD, professor and clinical chair of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School in Newark, told this news organization.
“We’ve gone through a few mutations already that have been named, and each one of them gets a little more transmissible,” he said. “That’s normal, natural selection and what you would expect to happen as viruses mutate from one strain to another.”
“What we’ve mostly seen this virus do is evolve to become more infectious,” said Stuart Ray, MD, when also asked to comment. “That is the remarkable feature of Delta – that it is so infectious.”
He said that the SARS-CoV-2 has evolved largely as expected, at least so far. “The potential for this virus to mutate has been something that has been a concern from early on.”
“The viral evolution is a bit like a ticking clock. The more we allow infections to occur, the more likely changes will occur. When we have lots of people infected, we give more chances to the virus to diversify and then adapt to selective pressures,” said Dr. Ray, vice-chair of medicine for data integrity and analytics and professor in the division of infectious diseases at Johns Hopkins School of Medicine in Baltimore.
Dr. Nelson said.
If this occurs, he added, “we will have an ineffective vaccine, essentially. And we’ll be back to where we were last March with a brand-new disease.”
Technology to the rescue?
The flexibility of mRNA vaccines is one potential solution. These vaccines could be more easily and quickly adapted to respond to a new, more vaccine-elusive variant.
“That’s absolutely reassuring,” Dr. Nelson said. For example, if a mutation changes the spike protein and vaccines no longer recognize it, a manufacturer could identify the new protein and incorporate that in a new mRNA vaccine.
“The problem is that some people are not taking the current vaccine,” he added. “I’m not sure what is going to make them take the next vaccine.”
Nothing appears certain
When asked how likely a new strain of SARS-CoV-2 could emerge that gets around vaccine protection, Dr. Nelson said, “I think [what] we’ve learned so far there is no way to predict anything” about this pandemic.
“The best way to prevent the virus from mutating is to prevent hosts, people, from getting sick with it,” he said. “That’s why it’s so important people should get immunized and wear masks.”
Both Dr. Nelson and Dr. Ray pointed out that it is in the best interest of the virus to evolve to be more transmissible and spread to more people. In contrast, a virus that causes people to get so sick that they isolate or die, thus halting transmission, works against viruses surviving evolutionarily.
Some viruses also mutate to become milder over time, but that has not been the case with SARS-CoV-2, Dr. Ray said.
Mutations not the only concern
Viruses have another mechanism that produces new strains, and it works even more quickly than mutations. Recombination, as it’s known, can occur when a person is infected with two different strains of the same virus. If the two versions enter the same cell, the viruses can swap genetic material and produce a third, altogether different strain.
Recombination has already been seen with influenza strains, where H and N genetic segments are swapped to yield H1N1, H1N2, and H3N2 versions of the flu, for example.
“In the early days of SARS-CoV-2 there was so little diversity that recombination did not matter,” Dr. Ray said. However, there are now distinct lineages of the virus circulating globally. If two of these lineages swap segments “this would make a very new viral sequence in one step without having to mutate to gain those differences.”
“The more diverse the strains that are circulating, the bigger a possibility this is,” Dr. Ray said.
Protected, for now
Dr. Walensky’s sober warning came at the same time the CDC released new guidance calling for the wearing of masks indoors in schools and in any location in the country where COVID-19 cases surpass 50 people per 100,000, also known as substantial or high transmission areas.
On a positive note, Dr. Walensky said: “Right now, fortunately, we are not there. The vaccines operate really well in protecting us from severe disease and death.”
A version of this article first appeared on Medscape.com.
Vaccinated people infected with Delta remain contagious
, The New York Times reported late on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the Times said. The bottom line is that the CDC data show people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on July 29 that the CDC’s updated mask guidance followed an outbreak in Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
, The New York Times reported late on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the Times said. The bottom line is that the CDC data show people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on July 29 that the CDC’s updated mask guidance followed an outbreak in Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
, The New York Times reported late on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the Times said. The bottom line is that the CDC data show people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on July 29 that the CDC’s updated mask guidance followed an outbreak in Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
I Never Wanted To Be a Hero
I have been in the business of medicine for more than 15 years and I will never forget the initial surge of the COVID-19 pandemic in Massachusetts.
As a hospitalist, I admitted patients infected with COVID-19, followed them on the floor, and, since I had some experience working in an intensive care unit (ICU), was assigned to cover a “COVID ICU.” This wing of the hospital used to be a fancy orthopedic floor that our institution was lucky enough to have. So began the most life-changing experience in my career as a physician.
In this role, we witness death more than any of us would care to discuss. It comes with the territory, and we never expected this to change once COVID hit. However, so many patients succumbed to this disease, especially during the first surge, which made it difficult to handle emotionally. Patients that fell ill initially stayed isolated at home, optimistic they would turn the corner only to enter the hospital a week later after their conditioned worsened. After requiring a couple of liters of supplemental oxygen in the emergency room, they eventually ended up on a high flow nasal cannula in just a matter of hours.
Patients slowly got sicker and felt more helpless as the days passed, leading us to prescribe drugs that eventually proved to have no benefit. We checked countless inflammatory markers, most of which we were not even sure what to do with. Many times, we hosted a family meeting via FaceTime, holding a patient’s hand in one hand and an iPad in the other to discuss goals of care. Too often, a dark cloud hung over these discussions, a realization that there was not much else we could do.
I have always felt that helping someone have a decent and peaceful death is important, especially when the prognosis is grim, and that patient is suffering. But the sheer number of times this happened during the initial surge of the pandemic was difficult to handle. It felt like I had more of those discussions in 3 months than I did during my entire career as a hospitalist.
We helped plenty of people get better, with some heading home in a week. They thanked us, painted rocks and the sidewalks in front of the hospital displaying messages of gratitude, and sent lunches. Others, though, left the hospital 2 months later with a tube in their stomach so they could receive some form of nutrition and another in their neck to help them breathe.
These struggles were by no means special to me; other hospitalists around the world faced similar situations at one point or another during the pandemic. Working overtime, coming home late, exhausted, undressing in the garage, trying to be there for my 3 kids who were full of energy after a whole day of Zoom and doing the usual kid stuff. My house used to have strict rules about screen time. No more.
The summer months provided a bit of a COVID break, with only 1 or 2 infected patients entering my care. We went to outdoor restaurants and tried to get our lives back to “normal.” As the weather turned cold, however, things went south again. This time no more hydroxychloroquine, a drug used to fight malaria but also treat other autoimmune diseases, as it was proven eventually over many studies that it is not helpful and was potentially harmful. We instead shifted our focus to remdesivir—an antiviral drug that displayed some benefits—tocilizumab, and dexamethasone, anti-inflammatory drugs with the latter providing some positive outcomes on mortality.
Patient survival rates improved slightly, likely due to a combination of factors. We were more experienced at fighting the disease, which led to things in the hospital not being as chaotic and more time available to spend with the patients. Personal protective equipment (PPE) and tests were more readily available, and the population getting hit by the disease changed slightly with fewer elderly people from nursing homes falling ill because of social distancing, other safety measures, or having already fought the disease. Our attention turned instead to more young people that had returned to work and their social lives.
The arrival of the vaccines brought considerable relief. I remember a few decades ago debating and sometimes fighting with friends and family over who was better: Iron Man or Spider-Man. Now I found myself having the same conversation about the Pfizer and Moderna COVID vaccines.
Summer 2021 holds significantly more promise. Most of the adult population is getting vaccinated, and I am very hopeful that we are approaching the end of this nightmare. In June, our office received word that we could remove our masks if we were fully vaccinated. It felt weird, but represented another sign that things are improving. I took my kids to the mall and removed my mask. It felt odd considering how that little blue thing became part of me during the pandemic. It also felt strange to not prescribe a single dose of remdesivir for an entire month.
It feels good—and normal—to care for the patients that we neglected for a year. It has been a needed boost to see patients return to their health care providers for their colonoscopy screenings, mammograms, and managing chronic problems like coronary artery disease, congestive heart failure, or receiving chemotherapy.
I learned plenty from this pandemic and hope I am not alone. I learned to be humble. We started with a drug that was harmful, moved on to a drug that is probably neutral and eventually were able to come up with a drug that seems to decrease mortality at least in some COVID patients. I learned it is fine to try new therapies based on the best data in the hope they result in positive clinical outcomes. However, it is critical that we all keep an eye on the rapidly evolving literature and adjust our behavior accordingly.
I also learned, or relearned, that if people are desperate enough, they will drink bleach to see if it works. Others are convinced that the purpose of vaccination is to inject a microchip allowing ourselves to be tracked by some higher power. I learned that we must take the first step to prepare for the next pandemic by having a decent reserve of PPE.
It is clear synthetic messenger RNA (mRNA) technology is here to stay, and I believe it has a huge potential to change many areas of medicine. mRNA vaccines proved to be much faster to develop and probably much easier to change as the pathogen, in this case coronavirus, changes.
The technology could be used against a variety of infectious diseases to make vaccines against malaria, tuberculosis, HIV, or hepatitis. It can also be very useful for faster vaccine development needed in future possible pandemics such as influenza, Ebola, or severe acute respiratory syndrome. It may also be used for cancer treatment.
As John P. Cooke, MD, PhD, the medical director for the Center of RNA Therapeutics Program at the Houston Methodist Research Institute, said, “Most vaccines today are still viral vaccines – they are inactivated virus, so it’s potentially infectious and you have to have virus on hand. With mRNA, you’re just writing code which is going to tell the cell to make a viral protein – one part of a viral protein to stimulate an immune response. And, here’s the wonderful thing, you don’t even need the virus in hand, just its DNA code.”1
Corresponding author: Dragos Vesbianu, MD, Attending Hospitalist, Newton-Wellesley Hospital, 2014 Washington St, Newton, MA 02462; [email protected].
Financial dislosures: None.
1. Houston Methodist. Messenger RNA – the Therapy of the Future. Newswise. November 16, 2020. Accessed June 25, 2021. https://www.newswise.com/coronavirus/messenger-rna-the-therapy-of-the-future/
I have been in the business of medicine for more than 15 years and I will never forget the initial surge of the COVID-19 pandemic in Massachusetts.
As a hospitalist, I admitted patients infected with COVID-19, followed them on the floor, and, since I had some experience working in an intensive care unit (ICU), was assigned to cover a “COVID ICU.” This wing of the hospital used to be a fancy orthopedic floor that our institution was lucky enough to have. So began the most life-changing experience in my career as a physician.
In this role, we witness death more than any of us would care to discuss. It comes with the territory, and we never expected this to change once COVID hit. However, so many patients succumbed to this disease, especially during the first surge, which made it difficult to handle emotionally. Patients that fell ill initially stayed isolated at home, optimistic they would turn the corner only to enter the hospital a week later after their conditioned worsened. After requiring a couple of liters of supplemental oxygen in the emergency room, they eventually ended up on a high flow nasal cannula in just a matter of hours.
Patients slowly got sicker and felt more helpless as the days passed, leading us to prescribe drugs that eventually proved to have no benefit. We checked countless inflammatory markers, most of which we were not even sure what to do with. Many times, we hosted a family meeting via FaceTime, holding a patient’s hand in one hand and an iPad in the other to discuss goals of care. Too often, a dark cloud hung over these discussions, a realization that there was not much else we could do.
I have always felt that helping someone have a decent and peaceful death is important, especially when the prognosis is grim, and that patient is suffering. But the sheer number of times this happened during the initial surge of the pandemic was difficult to handle. It felt like I had more of those discussions in 3 months than I did during my entire career as a hospitalist.
We helped plenty of people get better, with some heading home in a week. They thanked us, painted rocks and the sidewalks in front of the hospital displaying messages of gratitude, and sent lunches. Others, though, left the hospital 2 months later with a tube in their stomach so they could receive some form of nutrition and another in their neck to help them breathe.
These struggles were by no means special to me; other hospitalists around the world faced similar situations at one point or another during the pandemic. Working overtime, coming home late, exhausted, undressing in the garage, trying to be there for my 3 kids who were full of energy after a whole day of Zoom and doing the usual kid stuff. My house used to have strict rules about screen time. No more.
The summer months provided a bit of a COVID break, with only 1 or 2 infected patients entering my care. We went to outdoor restaurants and tried to get our lives back to “normal.” As the weather turned cold, however, things went south again. This time no more hydroxychloroquine, a drug used to fight malaria but also treat other autoimmune diseases, as it was proven eventually over many studies that it is not helpful and was potentially harmful. We instead shifted our focus to remdesivir—an antiviral drug that displayed some benefits—tocilizumab, and dexamethasone, anti-inflammatory drugs with the latter providing some positive outcomes on mortality.
Patient survival rates improved slightly, likely due to a combination of factors. We were more experienced at fighting the disease, which led to things in the hospital not being as chaotic and more time available to spend with the patients. Personal protective equipment (PPE) and tests were more readily available, and the population getting hit by the disease changed slightly with fewer elderly people from nursing homes falling ill because of social distancing, other safety measures, or having already fought the disease. Our attention turned instead to more young people that had returned to work and their social lives.
The arrival of the vaccines brought considerable relief. I remember a few decades ago debating and sometimes fighting with friends and family over who was better: Iron Man or Spider-Man. Now I found myself having the same conversation about the Pfizer and Moderna COVID vaccines.
Summer 2021 holds significantly more promise. Most of the adult population is getting vaccinated, and I am very hopeful that we are approaching the end of this nightmare. In June, our office received word that we could remove our masks if we were fully vaccinated. It felt weird, but represented another sign that things are improving. I took my kids to the mall and removed my mask. It felt odd considering how that little blue thing became part of me during the pandemic. It also felt strange to not prescribe a single dose of remdesivir for an entire month.
It feels good—and normal—to care for the patients that we neglected for a year. It has been a needed boost to see patients return to their health care providers for their colonoscopy screenings, mammograms, and managing chronic problems like coronary artery disease, congestive heart failure, or receiving chemotherapy.
I learned plenty from this pandemic and hope I am not alone. I learned to be humble. We started with a drug that was harmful, moved on to a drug that is probably neutral and eventually were able to come up with a drug that seems to decrease mortality at least in some COVID patients. I learned it is fine to try new therapies based on the best data in the hope they result in positive clinical outcomes. However, it is critical that we all keep an eye on the rapidly evolving literature and adjust our behavior accordingly.
I also learned, or relearned, that if people are desperate enough, they will drink bleach to see if it works. Others are convinced that the purpose of vaccination is to inject a microchip allowing ourselves to be tracked by some higher power. I learned that we must take the first step to prepare for the next pandemic by having a decent reserve of PPE.
It is clear synthetic messenger RNA (mRNA) technology is here to stay, and I believe it has a huge potential to change many areas of medicine. mRNA vaccines proved to be much faster to develop and probably much easier to change as the pathogen, in this case coronavirus, changes.
The technology could be used against a variety of infectious diseases to make vaccines against malaria, tuberculosis, HIV, or hepatitis. It can also be very useful for faster vaccine development needed in future possible pandemics such as influenza, Ebola, or severe acute respiratory syndrome. It may also be used for cancer treatment.
As John P. Cooke, MD, PhD, the medical director for the Center of RNA Therapeutics Program at the Houston Methodist Research Institute, said, “Most vaccines today are still viral vaccines – they are inactivated virus, so it’s potentially infectious and you have to have virus on hand. With mRNA, you’re just writing code which is going to tell the cell to make a viral protein – one part of a viral protein to stimulate an immune response. And, here’s the wonderful thing, you don’t even need the virus in hand, just its DNA code.”1
Corresponding author: Dragos Vesbianu, MD, Attending Hospitalist, Newton-Wellesley Hospital, 2014 Washington St, Newton, MA 02462; [email protected].
Financial dislosures: None.
I have been in the business of medicine for more than 15 years and I will never forget the initial surge of the COVID-19 pandemic in Massachusetts.
As a hospitalist, I admitted patients infected with COVID-19, followed them on the floor, and, since I had some experience working in an intensive care unit (ICU), was assigned to cover a “COVID ICU.” This wing of the hospital used to be a fancy orthopedic floor that our institution was lucky enough to have. So began the most life-changing experience in my career as a physician.
In this role, we witness death more than any of us would care to discuss. It comes with the territory, and we never expected this to change once COVID hit. However, so many patients succumbed to this disease, especially during the first surge, which made it difficult to handle emotionally. Patients that fell ill initially stayed isolated at home, optimistic they would turn the corner only to enter the hospital a week later after their conditioned worsened. After requiring a couple of liters of supplemental oxygen in the emergency room, they eventually ended up on a high flow nasal cannula in just a matter of hours.
Patients slowly got sicker and felt more helpless as the days passed, leading us to prescribe drugs that eventually proved to have no benefit. We checked countless inflammatory markers, most of which we were not even sure what to do with. Many times, we hosted a family meeting via FaceTime, holding a patient’s hand in one hand and an iPad in the other to discuss goals of care. Too often, a dark cloud hung over these discussions, a realization that there was not much else we could do.
I have always felt that helping someone have a decent and peaceful death is important, especially when the prognosis is grim, and that patient is suffering. But the sheer number of times this happened during the initial surge of the pandemic was difficult to handle. It felt like I had more of those discussions in 3 months than I did during my entire career as a hospitalist.
We helped plenty of people get better, with some heading home in a week. They thanked us, painted rocks and the sidewalks in front of the hospital displaying messages of gratitude, and sent lunches. Others, though, left the hospital 2 months later with a tube in their stomach so they could receive some form of nutrition and another in their neck to help them breathe.
These struggles were by no means special to me; other hospitalists around the world faced similar situations at one point or another during the pandemic. Working overtime, coming home late, exhausted, undressing in the garage, trying to be there for my 3 kids who were full of energy after a whole day of Zoom and doing the usual kid stuff. My house used to have strict rules about screen time. No more.
The summer months provided a bit of a COVID break, with only 1 or 2 infected patients entering my care. We went to outdoor restaurants and tried to get our lives back to “normal.” As the weather turned cold, however, things went south again. This time no more hydroxychloroquine, a drug used to fight malaria but also treat other autoimmune diseases, as it was proven eventually over many studies that it is not helpful and was potentially harmful. We instead shifted our focus to remdesivir—an antiviral drug that displayed some benefits—tocilizumab, and dexamethasone, anti-inflammatory drugs with the latter providing some positive outcomes on mortality.
Patient survival rates improved slightly, likely due to a combination of factors. We were more experienced at fighting the disease, which led to things in the hospital not being as chaotic and more time available to spend with the patients. Personal protective equipment (PPE) and tests were more readily available, and the population getting hit by the disease changed slightly with fewer elderly people from nursing homes falling ill because of social distancing, other safety measures, or having already fought the disease. Our attention turned instead to more young people that had returned to work and their social lives.
The arrival of the vaccines brought considerable relief. I remember a few decades ago debating and sometimes fighting with friends and family over who was better: Iron Man or Spider-Man. Now I found myself having the same conversation about the Pfizer and Moderna COVID vaccines.
Summer 2021 holds significantly more promise. Most of the adult population is getting vaccinated, and I am very hopeful that we are approaching the end of this nightmare. In June, our office received word that we could remove our masks if we were fully vaccinated. It felt weird, but represented another sign that things are improving. I took my kids to the mall and removed my mask. It felt odd considering how that little blue thing became part of me during the pandemic. It also felt strange to not prescribe a single dose of remdesivir for an entire month.
It feels good—and normal—to care for the patients that we neglected for a year. It has been a needed boost to see patients return to their health care providers for their colonoscopy screenings, mammograms, and managing chronic problems like coronary artery disease, congestive heart failure, or receiving chemotherapy.
I learned plenty from this pandemic and hope I am not alone. I learned to be humble. We started with a drug that was harmful, moved on to a drug that is probably neutral and eventually were able to come up with a drug that seems to decrease mortality at least in some COVID patients. I learned it is fine to try new therapies based on the best data in the hope they result in positive clinical outcomes. However, it is critical that we all keep an eye on the rapidly evolving literature and adjust our behavior accordingly.
I also learned, or relearned, that if people are desperate enough, they will drink bleach to see if it works. Others are convinced that the purpose of vaccination is to inject a microchip allowing ourselves to be tracked by some higher power. I learned that we must take the first step to prepare for the next pandemic by having a decent reserve of PPE.
It is clear synthetic messenger RNA (mRNA) technology is here to stay, and I believe it has a huge potential to change many areas of medicine. mRNA vaccines proved to be much faster to develop and probably much easier to change as the pathogen, in this case coronavirus, changes.
The technology could be used against a variety of infectious diseases to make vaccines against malaria, tuberculosis, HIV, or hepatitis. It can also be very useful for faster vaccine development needed in future possible pandemics such as influenza, Ebola, or severe acute respiratory syndrome. It may also be used for cancer treatment.
As John P. Cooke, MD, PhD, the medical director for the Center of RNA Therapeutics Program at the Houston Methodist Research Institute, said, “Most vaccines today are still viral vaccines – they are inactivated virus, so it’s potentially infectious and you have to have virus on hand. With mRNA, you’re just writing code which is going to tell the cell to make a viral protein – one part of a viral protein to stimulate an immune response. And, here’s the wonderful thing, you don’t even need the virus in hand, just its DNA code.”1
Corresponding author: Dragos Vesbianu, MD, Attending Hospitalist, Newton-Wellesley Hospital, 2014 Washington St, Newton, MA 02462; [email protected].
Financial dislosures: None.
1. Houston Methodist. Messenger RNA – the Therapy of the Future. Newswise. November 16, 2020. Accessed June 25, 2021. https://www.newswise.com/coronavirus/messenger-rna-the-therapy-of-the-future/
1. Houston Methodist. Messenger RNA – the Therapy of the Future. Newswise. November 16, 2020. Accessed June 25, 2021. https://www.newswise.com/coronavirus/messenger-rna-the-therapy-of-the-future/










