User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Children and COVID: Weekly cases close out August with a second straight increase
New cases rose by 4.6% for the week of Aug. 26 to Sept. 1, following a week in which cases increased by almost 9%, as the second half of August basically reversed the two consecutive weeks of decreases during the first half of the month, based on the AAP/CHA data collected from state and territorial health departments.
Similar trends can be seen for emergency department visits, with the exception of children aged 0-11 years, whose ED visit rates have continued to fall since late July. Children aged 12-15, however, had a 7-day average of 4.4% of ED visits with diagnosed COVID on Aug. 25, compared with 3.1% for Aug. 12. Children aged 16-17 years were at 3.4% on Aug. 27, compared with 3.1% as late as Aug. 15, the Centers for Disease Control and Prevention reported.
Hospital admissions with confirmed COVID-19, reported only for children aged 0-17 years, also reflect the late-August trend of increased cases. New hospitalizations dropped from 0.46 per 100,000 population on July 30 to 0.40 per 100,000 on Aug. 19 but have since risen to 0.44 per 100,000 as of Aug. 27, the CDC said on its COVID Data Tracker.
Initial vaccinations, meanwhile, have declined since early August for all children, according to a separate report from the AAP. A look at CDC data for two specific days – the first and last Mondays of the month – shows that those aged under 5 received 12,982 doses on Aug. 1, compared with 5,824 doses on Aug. 29. Over that same time, initial vaccinations in 5- to 11-year-olds went from 9,058 to 2,879, while among those aged 12-17 they dropped from 4,245 to 1,226.
Cumulatively, 5.5% of all children under age 5 had received at least one dose and 1.3% were fully vaccinated by Aug. 30, compared with 38.1% and 30.7%, respectively, of those aged 5-11 and 70.7% and 60.5% of 12- to 17-year-olds, the CDC said.
New cases rose by 4.6% for the week of Aug. 26 to Sept. 1, following a week in which cases increased by almost 9%, as the second half of August basically reversed the two consecutive weeks of decreases during the first half of the month, based on the AAP/CHA data collected from state and territorial health departments.
Similar trends can be seen for emergency department visits, with the exception of children aged 0-11 years, whose ED visit rates have continued to fall since late July. Children aged 12-15, however, had a 7-day average of 4.4% of ED visits with diagnosed COVID on Aug. 25, compared with 3.1% for Aug. 12. Children aged 16-17 years were at 3.4% on Aug. 27, compared with 3.1% as late as Aug. 15, the Centers for Disease Control and Prevention reported.
Hospital admissions with confirmed COVID-19, reported only for children aged 0-17 years, also reflect the late-August trend of increased cases. New hospitalizations dropped from 0.46 per 100,000 population on July 30 to 0.40 per 100,000 on Aug. 19 but have since risen to 0.44 per 100,000 as of Aug. 27, the CDC said on its COVID Data Tracker.
Initial vaccinations, meanwhile, have declined since early August for all children, according to a separate report from the AAP. A look at CDC data for two specific days – the first and last Mondays of the month – shows that those aged under 5 received 12,982 doses on Aug. 1, compared with 5,824 doses on Aug. 29. Over that same time, initial vaccinations in 5- to 11-year-olds went from 9,058 to 2,879, while among those aged 12-17 they dropped from 4,245 to 1,226.
Cumulatively, 5.5% of all children under age 5 had received at least one dose and 1.3% were fully vaccinated by Aug. 30, compared with 38.1% and 30.7%, respectively, of those aged 5-11 and 70.7% and 60.5% of 12- to 17-year-olds, the CDC said.
New cases rose by 4.6% for the week of Aug. 26 to Sept. 1, following a week in which cases increased by almost 9%, as the second half of August basically reversed the two consecutive weeks of decreases during the first half of the month, based on the AAP/CHA data collected from state and territorial health departments.
Similar trends can be seen for emergency department visits, with the exception of children aged 0-11 years, whose ED visit rates have continued to fall since late July. Children aged 12-15, however, had a 7-day average of 4.4% of ED visits with diagnosed COVID on Aug. 25, compared with 3.1% for Aug. 12. Children aged 16-17 years were at 3.4% on Aug. 27, compared with 3.1% as late as Aug. 15, the Centers for Disease Control and Prevention reported.
Hospital admissions with confirmed COVID-19, reported only for children aged 0-17 years, also reflect the late-August trend of increased cases. New hospitalizations dropped from 0.46 per 100,000 population on July 30 to 0.40 per 100,000 on Aug. 19 but have since risen to 0.44 per 100,000 as of Aug. 27, the CDC said on its COVID Data Tracker.
Initial vaccinations, meanwhile, have declined since early August for all children, according to a separate report from the AAP. A look at CDC data for two specific days – the first and last Mondays of the month – shows that those aged under 5 received 12,982 doses on Aug. 1, compared with 5,824 doses on Aug. 29. Over that same time, initial vaccinations in 5- to 11-year-olds went from 9,058 to 2,879, while among those aged 12-17 they dropped from 4,245 to 1,226.
Cumulatively, 5.5% of all children under age 5 had received at least one dose and 1.3% were fully vaccinated by Aug. 30, compared with 38.1% and 30.7%, respectively, of those aged 5-11 and 70.7% and 60.5% of 12- to 17-year-olds, the CDC said.
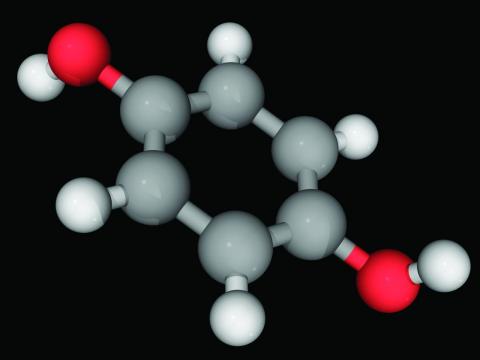
Reduced-lactose infant formula related to higher risk of obesity later
Doctors may want to advise parents against giving their infants lactose-reduced infant formula unless absolutely necessary, because doing so may be setting babies up for an increased risk of obesity in toddlerhood, new research shows.
Infants who drink infant formula instead of breast milk already carry an increased risk of obesity. But the new study, published in The American Journal of Clinical Nutrition, found a difference in types of formula and obesity outcomes for children.
Babies under 1 year who received lactose-reduced formula made partially of corn syrup solids were at a 10% greater risk (risk ratio, 1.10; 95% confidence interval, 1.02, 1.20; P = .02) of being obese by age 2 than infants who received regular cow’s milk formula.
“This is even another reason to not use a low-lactose formula,” said Mark R. Corkins, MD, division chief of pediatric gastroenterology, hepatology, and nutrition at the University of Tennessee Health Science Center, Memphis, who was not involved in the study. “Parents think if babies are fussy, or they spit up, they have lactose intolerance, but if you look at the actual numbers, lactose intolerance in infants is rare.”
Actual lactose intolerance in infancy is the result of a newborn receiving the same mutated gene from both parents, called congenital lactase deficiency, said Dr. Corkins.
“The reason the low-lactose formulas are even on the market is because parents want them, and they think their kid is lactose intolerant, but they are not,” Dr. Corkins said.
Researchers from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in southern California and the University of Southern California, Los Angeles, analyzed data from over 15,000 infants in southern California enrolled in WIC.
Records from infants born between Sept. 2012 and March 2016 were separated into two groups: infants that had stopped breastfeeding by month 3 and had started reduced-lactose formula and infants who received all other forms of formula. Over 80% of infants in both groups were Hispanic.
Infants who received the reduced-lactose formula with corn syrup solids were at an 8% increased risk of obesity by age 3 (RR = 1.08; 95% CI, 1.02, 1.15; P = .01), compared with children who received regular cow’s milk formula, and a 7% increased risk by age 4 (RR = 1.07; 95% CI; 1.01, 1.14; P = .01).
Tara Williams, MD, pediatrician and breastfeeding specialist associated with the Florida Chapter of American Academy of Pediatrics, said the findings should make pediatricians, parents, and others pause and consider what infant formulas contain.
She explained that babies who receive formula have higher obesity risk than babies who are breastfed overall. But research into the effects of different types of formula is relatively new. She said there may be a few reasons for the association between reduced-lactose, corn syrup solid formula and a higher risk of obesity.
“The addition of the corn syrup really starts to potentially teach that child to like sweet things,” Dr. Williams said, which in turn can lead to less healthy eating habits in childhood and adulthood.
Or, it may be that parents who tend to give their children lactose-reduced formula are less likely to be tolerant of fussy babies and end up feeding their babies more, Dr. Williams hypothesized.
In addition, emerging research shows corn syrup may act differently from other sugars in the gut microbiome and as it is metabolized in the liver, leading to weight gain.
Although parents make individual choices for what kind of formula to feed their infants, states play a large role in these choices. In 2018, 45% of babies in the United States were eligible for WIC, which is funded through the federal government but administered by states. State WIC programs request bids from formula manufacturers, and products chosen are then redeemed at retailers by parents.
“Now that we’re starting to see a signal that perhaps some formulas will have a potentially added risk of obesity for participants, states may say that when we’re helping mothers select among the formulas, we need to be very explicit about this additional risk,” said Christopher Anderson, PhD, MSPH, associate research scientist at the southern California Public Health Foundation Enterprises WIC and lead author of the study.
Dr. Williams said more research to do similar analyses in other populations is needed to draw cause and effect conclusions, while Dr. Corkins said he’d like to see more research into the amount of formula eaten and health connections to types of formula.
“We know as soon as you sign up for a baby registry at Target, you’re getting formula samples in the mail. You’re very aggressively marketed to; it’s a $55 billion industry,” Dr. Williams said. “And their goal is to sell their product – not to promote the health of infants. “This research certainly will cause us to pause and consider what we are feeding our infants in the United States and how we allow companies to market their products.”
Dr. Goran receives book royalties from Penguin Random House and is a scientific consultant for Yumi Foods and Else Nutrition. All other authors disclosed no conflicts of interest. Dr. Corkins reports working at a clinic that’s the site of a Takeda pharmaceutical research study. Dr. Williams reports no relevant financial relationships.
Doctors may want to advise parents against giving their infants lactose-reduced infant formula unless absolutely necessary, because doing so may be setting babies up for an increased risk of obesity in toddlerhood, new research shows.
Infants who drink infant formula instead of breast milk already carry an increased risk of obesity. But the new study, published in The American Journal of Clinical Nutrition, found a difference in types of formula and obesity outcomes for children.
Babies under 1 year who received lactose-reduced formula made partially of corn syrup solids were at a 10% greater risk (risk ratio, 1.10; 95% confidence interval, 1.02, 1.20; P = .02) of being obese by age 2 than infants who received regular cow’s milk formula.
“This is even another reason to not use a low-lactose formula,” said Mark R. Corkins, MD, division chief of pediatric gastroenterology, hepatology, and nutrition at the University of Tennessee Health Science Center, Memphis, who was not involved in the study. “Parents think if babies are fussy, or they spit up, they have lactose intolerance, but if you look at the actual numbers, lactose intolerance in infants is rare.”
Actual lactose intolerance in infancy is the result of a newborn receiving the same mutated gene from both parents, called congenital lactase deficiency, said Dr. Corkins.
“The reason the low-lactose formulas are even on the market is because parents want them, and they think their kid is lactose intolerant, but they are not,” Dr. Corkins said.
Researchers from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in southern California and the University of Southern California, Los Angeles, analyzed data from over 15,000 infants in southern California enrolled in WIC.
Records from infants born between Sept. 2012 and March 2016 were separated into two groups: infants that had stopped breastfeeding by month 3 and had started reduced-lactose formula and infants who received all other forms of formula. Over 80% of infants in both groups were Hispanic.
Infants who received the reduced-lactose formula with corn syrup solids were at an 8% increased risk of obesity by age 3 (RR = 1.08; 95% CI, 1.02, 1.15; P = .01), compared with children who received regular cow’s milk formula, and a 7% increased risk by age 4 (RR = 1.07; 95% CI; 1.01, 1.14; P = .01).
Tara Williams, MD, pediatrician and breastfeeding specialist associated with the Florida Chapter of American Academy of Pediatrics, said the findings should make pediatricians, parents, and others pause and consider what infant formulas contain.
She explained that babies who receive formula have higher obesity risk than babies who are breastfed overall. But research into the effects of different types of formula is relatively new. She said there may be a few reasons for the association between reduced-lactose, corn syrup solid formula and a higher risk of obesity.
“The addition of the corn syrup really starts to potentially teach that child to like sweet things,” Dr. Williams said, which in turn can lead to less healthy eating habits in childhood and adulthood.
Or, it may be that parents who tend to give their children lactose-reduced formula are less likely to be tolerant of fussy babies and end up feeding their babies more, Dr. Williams hypothesized.
In addition, emerging research shows corn syrup may act differently from other sugars in the gut microbiome and as it is metabolized in the liver, leading to weight gain.
Although parents make individual choices for what kind of formula to feed their infants, states play a large role in these choices. In 2018, 45% of babies in the United States were eligible for WIC, which is funded through the federal government but administered by states. State WIC programs request bids from formula manufacturers, and products chosen are then redeemed at retailers by parents.
“Now that we’re starting to see a signal that perhaps some formulas will have a potentially added risk of obesity for participants, states may say that when we’re helping mothers select among the formulas, we need to be very explicit about this additional risk,” said Christopher Anderson, PhD, MSPH, associate research scientist at the southern California Public Health Foundation Enterprises WIC and lead author of the study.
Dr. Williams said more research to do similar analyses in other populations is needed to draw cause and effect conclusions, while Dr. Corkins said he’d like to see more research into the amount of formula eaten and health connections to types of formula.
“We know as soon as you sign up for a baby registry at Target, you’re getting formula samples in the mail. You’re very aggressively marketed to; it’s a $55 billion industry,” Dr. Williams said. “And their goal is to sell their product – not to promote the health of infants. “This research certainly will cause us to pause and consider what we are feeding our infants in the United States and how we allow companies to market their products.”
Dr. Goran receives book royalties from Penguin Random House and is a scientific consultant for Yumi Foods and Else Nutrition. All other authors disclosed no conflicts of interest. Dr. Corkins reports working at a clinic that’s the site of a Takeda pharmaceutical research study. Dr. Williams reports no relevant financial relationships.
Doctors may want to advise parents against giving their infants lactose-reduced infant formula unless absolutely necessary, because doing so may be setting babies up for an increased risk of obesity in toddlerhood, new research shows.
Infants who drink infant formula instead of breast milk already carry an increased risk of obesity. But the new study, published in The American Journal of Clinical Nutrition, found a difference in types of formula and obesity outcomes for children.
Babies under 1 year who received lactose-reduced formula made partially of corn syrup solids were at a 10% greater risk (risk ratio, 1.10; 95% confidence interval, 1.02, 1.20; P = .02) of being obese by age 2 than infants who received regular cow’s milk formula.
“This is even another reason to not use a low-lactose formula,” said Mark R. Corkins, MD, division chief of pediatric gastroenterology, hepatology, and nutrition at the University of Tennessee Health Science Center, Memphis, who was not involved in the study. “Parents think if babies are fussy, or they spit up, they have lactose intolerance, but if you look at the actual numbers, lactose intolerance in infants is rare.”
Actual lactose intolerance in infancy is the result of a newborn receiving the same mutated gene from both parents, called congenital lactase deficiency, said Dr. Corkins.
“The reason the low-lactose formulas are even on the market is because parents want them, and they think their kid is lactose intolerant, but they are not,” Dr. Corkins said.
Researchers from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in southern California and the University of Southern California, Los Angeles, analyzed data from over 15,000 infants in southern California enrolled in WIC.
Records from infants born between Sept. 2012 and March 2016 were separated into two groups: infants that had stopped breastfeeding by month 3 and had started reduced-lactose formula and infants who received all other forms of formula. Over 80% of infants in both groups were Hispanic.
Infants who received the reduced-lactose formula with corn syrup solids were at an 8% increased risk of obesity by age 3 (RR = 1.08; 95% CI, 1.02, 1.15; P = .01), compared with children who received regular cow’s milk formula, and a 7% increased risk by age 4 (RR = 1.07; 95% CI; 1.01, 1.14; P = .01).
Tara Williams, MD, pediatrician and breastfeeding specialist associated with the Florida Chapter of American Academy of Pediatrics, said the findings should make pediatricians, parents, and others pause and consider what infant formulas contain.
She explained that babies who receive formula have higher obesity risk than babies who are breastfed overall. But research into the effects of different types of formula is relatively new. She said there may be a few reasons for the association between reduced-lactose, corn syrup solid formula and a higher risk of obesity.
“The addition of the corn syrup really starts to potentially teach that child to like sweet things,” Dr. Williams said, which in turn can lead to less healthy eating habits in childhood and adulthood.
Or, it may be that parents who tend to give their children lactose-reduced formula are less likely to be tolerant of fussy babies and end up feeding their babies more, Dr. Williams hypothesized.
In addition, emerging research shows corn syrup may act differently from other sugars in the gut microbiome and as it is metabolized in the liver, leading to weight gain.
Although parents make individual choices for what kind of formula to feed their infants, states play a large role in these choices. In 2018, 45% of babies in the United States were eligible for WIC, which is funded through the federal government but administered by states. State WIC programs request bids from formula manufacturers, and products chosen are then redeemed at retailers by parents.
“Now that we’re starting to see a signal that perhaps some formulas will have a potentially added risk of obesity for participants, states may say that when we’re helping mothers select among the formulas, we need to be very explicit about this additional risk,” said Christopher Anderson, PhD, MSPH, associate research scientist at the southern California Public Health Foundation Enterprises WIC and lead author of the study.
Dr. Williams said more research to do similar analyses in other populations is needed to draw cause and effect conclusions, while Dr. Corkins said he’d like to see more research into the amount of formula eaten and health connections to types of formula.
“We know as soon as you sign up for a baby registry at Target, you’re getting formula samples in the mail. You’re very aggressively marketed to; it’s a $55 billion industry,” Dr. Williams said. “And their goal is to sell their product – not to promote the health of infants. “This research certainly will cause us to pause and consider what we are feeding our infants in the United States and how we allow companies to market their products.”
Dr. Goran receives book royalties from Penguin Random House and is a scientific consultant for Yumi Foods and Else Nutrition. All other authors disclosed no conflicts of interest. Dr. Corkins reports working at a clinic that’s the site of a Takeda pharmaceutical research study. Dr. Williams reports no relevant financial relationships.
FROM AMERICAN JOURNAL OF CLINICAL NUTRITION
WIC review finds broad benefits, knowledge gaps
How exactly the national program achieves these outcomes, however, remains unclear, and study quality shows room for improvement, reported co–lead authors Maya Venkataramani, MD, MPH and S. Michelle Ogunwole, MD, PhD of Johns Hopkins University, Baltimore, and colleagues.
The WIC program, which has been serving low-income women and young children since 1974, “provides supplemental foods, nutrition education and breastfeeding support, screening and referrals to medical and social services, and support for high-risk pregnancies,” the investigators wrote in Annals of Internal Medicine. The U.S. Food and Nutrition Service administers the program.
The authors conducted a systematic review of 20 observational studies aimed at determining the impacts of WIC participation on maternal, neonatal-birth, and infant-child health outcomes.
All studies included in the review began in or after 2009, when the WIC food package was revised to better address diet-related chronic diseases. For inclusion in the review, studies were required to have a WIC-eligible comparison group. Included research also evaluated the relationship between WIC participation and the prespecified health outcomes.
“We found only 20 studies that fulfilled our rigorous study inclusion criteria for these specific outcomes,” the investigators wrote. “In some areas, the evidence was absent, and in others, the strength of evidence (SOE) was moderate or low.”
Six outcome categories were assessed: maternal morbidity, maternal pregnancy outcomes, maternal health behaviors, maternal health care utilization, child morbidity, and childhood health care utilization. Of these, maternal health care utilization had the most robust body of evidence, while data from studies evaluating maternal morbidity and child morbidity were deemed insufficient.
Based on eligible studies, WIC participation was associated with reduced risks of insufficient weight gain in pregnancy, preterm birth, low infant birthweight, and infant mortality. Participation was also associated with an increased likelihood of infant and child health care utilization, such as routine immunizations.
Growing evidence should drive enrollment
“Growing evidence points to WIC as a way to reduce risk of preterm birth and other adverse outcomes,” said Laura Jelliffe-Pawlowski, PhD, MS, professor at the University of California, San Francisco and a director for the UCSF California Preterm Birth Initiative.
Dr. Jelliffe-Pawlowski, who conducted a California-based study included in the paper, said the review is noteworthy because it shows that WIC-associated benefits are observed across locations.
“It’s not just in California; it’s across the country,” she said. “It’s a national call to action – where there’s partnership between national-, state- and community-level WIC programs – to make WIC as accessible as possible, and reflect community wants and needs, so that more people enroll, and more people stay enrolled.”
Dr. Jelliffe-Pawlowski’s coauthor on the California study, Rita Hamad, MD, PhD, associate professor of family & community medicine at UCSF and associate director of the UCSF Center for Health Equity, encouraged health care providers to drive WIC enrollment, noting that, presently, only one in four eligible 4-year-olds participates.
“Physicians and other health care stakeholders can help patients benefit from this program by encouraging them to sign up, and even by providing sign-up support in the form of a social worker or other staff member,” Dr. Hamad said. “There is also literature on the types of interventions that improve take-up of safety net programs that providers can look to.”
Goals of future research
Optimizing WIC operations, however, is only half the battle, considering the evidence gaps revealed by the review.
“We still need stronger studies that use more rigorous study designs ... to provide more convincing evidence to policymakers, as well as more evidence on long-term impacts,” Dr. Hamad said. “We also need to better understand why take-up is low in these programs despite these potential health benefits. Then we can make sure that economically disadvantaged families receive the benefits for which they are eligible through interventions to improve participation rates.”
Ideally, WIC programs would receive additional funding for independent parties to evaluate health outcomes, according to Ashwini Lakshmanan, MD, MS, MPH, associate professor in the department of health systems science at Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, Calif.
Dr. Lakshmanan, who previously evaluated the benefits of WIC participation for high-risk infants, noted that randomized clinical trials would be unethical in this setting, yet data collection can still be “very conscientious and intentional,” with a focus on policy-shaping outcome metrics like immunizations and pediatric health care visits.
“The main point is thinking about it at the forefront, and not retrospectively,” Dr. Lakshmanan said.
Dr. Ogunwole, who led the present review, suggested in a written comment that future studies “could employ robust statistical methods (propensity matching, fixed effects models, etc.) to help reduce bias.”
She also recommended evaluating innovations in WIC programs; for example, adding a health coach, or conducting a cooking skills intervention.
Studies are also needed to better understand the various obstacles to WIC success, such as misconceptions about the program, discrimination, and barriers to enrollment, Dr. Ogunwole added.
“WIC enrollment has been decreasing for a number of years, and this was occurring prepandemic as well,” she said. “More work needs to be done to understand this issue.”
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators and interviewees disclosed no conflicts of interest.
How exactly the national program achieves these outcomes, however, remains unclear, and study quality shows room for improvement, reported co–lead authors Maya Venkataramani, MD, MPH and S. Michelle Ogunwole, MD, PhD of Johns Hopkins University, Baltimore, and colleagues.
The WIC program, which has been serving low-income women and young children since 1974, “provides supplemental foods, nutrition education and breastfeeding support, screening and referrals to medical and social services, and support for high-risk pregnancies,” the investigators wrote in Annals of Internal Medicine. The U.S. Food and Nutrition Service administers the program.
The authors conducted a systematic review of 20 observational studies aimed at determining the impacts of WIC participation on maternal, neonatal-birth, and infant-child health outcomes.
All studies included in the review began in or after 2009, when the WIC food package was revised to better address diet-related chronic diseases. For inclusion in the review, studies were required to have a WIC-eligible comparison group. Included research also evaluated the relationship between WIC participation and the prespecified health outcomes.
“We found only 20 studies that fulfilled our rigorous study inclusion criteria for these specific outcomes,” the investigators wrote. “In some areas, the evidence was absent, and in others, the strength of evidence (SOE) was moderate or low.”
Six outcome categories were assessed: maternal morbidity, maternal pregnancy outcomes, maternal health behaviors, maternal health care utilization, child morbidity, and childhood health care utilization. Of these, maternal health care utilization had the most robust body of evidence, while data from studies evaluating maternal morbidity and child morbidity were deemed insufficient.
Based on eligible studies, WIC participation was associated with reduced risks of insufficient weight gain in pregnancy, preterm birth, low infant birthweight, and infant mortality. Participation was also associated with an increased likelihood of infant and child health care utilization, such as routine immunizations.
Growing evidence should drive enrollment
“Growing evidence points to WIC as a way to reduce risk of preterm birth and other adverse outcomes,” said Laura Jelliffe-Pawlowski, PhD, MS, professor at the University of California, San Francisco and a director for the UCSF California Preterm Birth Initiative.
Dr. Jelliffe-Pawlowski, who conducted a California-based study included in the paper, said the review is noteworthy because it shows that WIC-associated benefits are observed across locations.
“It’s not just in California; it’s across the country,” she said. “It’s a national call to action – where there’s partnership between national-, state- and community-level WIC programs – to make WIC as accessible as possible, and reflect community wants and needs, so that more people enroll, and more people stay enrolled.”
Dr. Jelliffe-Pawlowski’s coauthor on the California study, Rita Hamad, MD, PhD, associate professor of family & community medicine at UCSF and associate director of the UCSF Center for Health Equity, encouraged health care providers to drive WIC enrollment, noting that, presently, only one in four eligible 4-year-olds participates.
“Physicians and other health care stakeholders can help patients benefit from this program by encouraging them to sign up, and even by providing sign-up support in the form of a social worker or other staff member,” Dr. Hamad said. “There is also literature on the types of interventions that improve take-up of safety net programs that providers can look to.”
Goals of future research
Optimizing WIC operations, however, is only half the battle, considering the evidence gaps revealed by the review.
“We still need stronger studies that use more rigorous study designs ... to provide more convincing evidence to policymakers, as well as more evidence on long-term impacts,” Dr. Hamad said. “We also need to better understand why take-up is low in these programs despite these potential health benefits. Then we can make sure that economically disadvantaged families receive the benefits for which they are eligible through interventions to improve participation rates.”
Ideally, WIC programs would receive additional funding for independent parties to evaluate health outcomes, according to Ashwini Lakshmanan, MD, MS, MPH, associate professor in the department of health systems science at Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, Calif.
Dr. Lakshmanan, who previously evaluated the benefits of WIC participation for high-risk infants, noted that randomized clinical trials would be unethical in this setting, yet data collection can still be “very conscientious and intentional,” with a focus on policy-shaping outcome metrics like immunizations and pediatric health care visits.
“The main point is thinking about it at the forefront, and not retrospectively,” Dr. Lakshmanan said.
Dr. Ogunwole, who led the present review, suggested in a written comment that future studies “could employ robust statistical methods (propensity matching, fixed effects models, etc.) to help reduce bias.”
She also recommended evaluating innovations in WIC programs; for example, adding a health coach, or conducting a cooking skills intervention.
Studies are also needed to better understand the various obstacles to WIC success, such as misconceptions about the program, discrimination, and barriers to enrollment, Dr. Ogunwole added.
“WIC enrollment has been decreasing for a number of years, and this was occurring prepandemic as well,” she said. “More work needs to be done to understand this issue.”
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators and interviewees disclosed no conflicts of interest.
How exactly the national program achieves these outcomes, however, remains unclear, and study quality shows room for improvement, reported co–lead authors Maya Venkataramani, MD, MPH and S. Michelle Ogunwole, MD, PhD of Johns Hopkins University, Baltimore, and colleagues.
The WIC program, which has been serving low-income women and young children since 1974, “provides supplemental foods, nutrition education and breastfeeding support, screening and referrals to medical and social services, and support for high-risk pregnancies,” the investigators wrote in Annals of Internal Medicine. The U.S. Food and Nutrition Service administers the program.
The authors conducted a systematic review of 20 observational studies aimed at determining the impacts of WIC participation on maternal, neonatal-birth, and infant-child health outcomes.
All studies included in the review began in or after 2009, when the WIC food package was revised to better address diet-related chronic diseases. For inclusion in the review, studies were required to have a WIC-eligible comparison group. Included research also evaluated the relationship between WIC participation and the prespecified health outcomes.
“We found only 20 studies that fulfilled our rigorous study inclusion criteria for these specific outcomes,” the investigators wrote. “In some areas, the evidence was absent, and in others, the strength of evidence (SOE) was moderate or low.”
Six outcome categories were assessed: maternal morbidity, maternal pregnancy outcomes, maternal health behaviors, maternal health care utilization, child morbidity, and childhood health care utilization. Of these, maternal health care utilization had the most robust body of evidence, while data from studies evaluating maternal morbidity and child morbidity were deemed insufficient.
Based on eligible studies, WIC participation was associated with reduced risks of insufficient weight gain in pregnancy, preterm birth, low infant birthweight, and infant mortality. Participation was also associated with an increased likelihood of infant and child health care utilization, such as routine immunizations.
Growing evidence should drive enrollment
“Growing evidence points to WIC as a way to reduce risk of preterm birth and other adverse outcomes,” said Laura Jelliffe-Pawlowski, PhD, MS, professor at the University of California, San Francisco and a director for the UCSF California Preterm Birth Initiative.
Dr. Jelliffe-Pawlowski, who conducted a California-based study included in the paper, said the review is noteworthy because it shows that WIC-associated benefits are observed across locations.
“It’s not just in California; it’s across the country,” she said. “It’s a national call to action – where there’s partnership between national-, state- and community-level WIC programs – to make WIC as accessible as possible, and reflect community wants and needs, so that more people enroll, and more people stay enrolled.”
Dr. Jelliffe-Pawlowski’s coauthor on the California study, Rita Hamad, MD, PhD, associate professor of family & community medicine at UCSF and associate director of the UCSF Center for Health Equity, encouraged health care providers to drive WIC enrollment, noting that, presently, only one in four eligible 4-year-olds participates.
“Physicians and other health care stakeholders can help patients benefit from this program by encouraging them to sign up, and even by providing sign-up support in the form of a social worker or other staff member,” Dr. Hamad said. “There is also literature on the types of interventions that improve take-up of safety net programs that providers can look to.”
Goals of future research
Optimizing WIC operations, however, is only half the battle, considering the evidence gaps revealed by the review.
“We still need stronger studies that use more rigorous study designs ... to provide more convincing evidence to policymakers, as well as more evidence on long-term impacts,” Dr. Hamad said. “We also need to better understand why take-up is low in these programs despite these potential health benefits. Then we can make sure that economically disadvantaged families receive the benefits for which they are eligible through interventions to improve participation rates.”
Ideally, WIC programs would receive additional funding for independent parties to evaluate health outcomes, according to Ashwini Lakshmanan, MD, MS, MPH, associate professor in the department of health systems science at Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, Calif.
Dr. Lakshmanan, who previously evaluated the benefits of WIC participation for high-risk infants, noted that randomized clinical trials would be unethical in this setting, yet data collection can still be “very conscientious and intentional,” with a focus on policy-shaping outcome metrics like immunizations and pediatric health care visits.
“The main point is thinking about it at the forefront, and not retrospectively,” Dr. Lakshmanan said.
Dr. Ogunwole, who led the present review, suggested in a written comment that future studies “could employ robust statistical methods (propensity matching, fixed effects models, etc.) to help reduce bias.”
She also recommended evaluating innovations in WIC programs; for example, adding a health coach, or conducting a cooking skills intervention.
Studies are also needed to better understand the various obstacles to WIC success, such as misconceptions about the program, discrimination, and barriers to enrollment, Dr. Ogunwole added.
“WIC enrollment has been decreasing for a number of years, and this was occurring prepandemic as well,” she said. “More work needs to be done to understand this issue.”
The study was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health & Human Services. The investigators and interviewees disclosed no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Robots better than humans at detecting mental well-being issues in children
Robots can be better at detecting mental well-being issues in children than parent-reported or self-reported testing, say U.K. researchers.
The researchers behind a new study, presented at the 31st IEEE International Conference on Robot & Human Interactive Communication (RO-MAN) in Naples, Italy, have suggested that robots could be a useful addition to traditional methods of mental health assessment.
“There are times when traditional methods aren’t able to catch mental well-being lapses in children, as sometimes the changes are incredibly subtle,” said Nida Itrat Abbasi, a PhD student at Cambridge (England) Affective Computing and Robotics Group, University of Cambridge, and the study’s first author. “We wanted to see whether robots might be able to help with this process,” she explained.
The authors highlighted how, during the COVID-19 pandemic, home schooling, financial pressures, and isolation from peers and friends impacted the mental health of many children. Even before the pandemic however, anxiety and depression among children in the United Kingdom has been on the rise, but the resources and support to address mental well-being are severely limited.
Children engage with robots
For their study the research team – which comprised roboticists, computer scientists, and psychiatrists from the University of Cambridge – enrolled 28 participants between ages 8 and 13 years. While being observed from an adjacent room by a parent or guardian, along with members of the research team, the participants took part in a one-to-one 45-minute session with a Nao robot – a humanoid robot about 60 cm tall – that administered a series of standard psychological questionnaires to assess the mental well-being of each participant.
Participants interacted with the robot throughout the session by speaking with it or by touching sensors on the robot’s hands and feet. Additional sensors tracked participants’ heartbeat, head, and eye movements during the session.
Professor Hatice Gunes, affective intelligence and robotics laboratory, department of computer science, University of Cambridge, said: “Children are quite tactile, and they’re drawn to technology. If they’re using a screen-based tool, they’re withdrawn from the physical world,” she said. “But robots are perfect because they’re in the physical world – they’re more interactive, so the children are more engaged.”
Prior to each session the children and their parent or guardian completed standard online questionnaires to assess each child’s mental well-being.
During each session, the robot performed four different tasks:
- Asked open-ended questions about happy and sad memories over the last week.
- Administered the Short Mood and Feelings Questionnaire (SMFQ).
- Administered a picture task inspired by the Children’s Apperception Test (CAT), where children are asked to answer questions related to pictures shown.
- Administered the Revised Children’s Anxiety and Depression Scale (RCADS) for generalized anxiety, panic disorder, and low mood.
Following the SMFQ children were divided into three different groups according to how likely they were to be struggling with their mental well-being.
The researchers found that children with varying levels of well-being concerns interacted differently with the robot. For children that might not be experiencing mental well-being–related problems, the researchers found that interacting with the robot led to more positive response ratings to the questionnaires. However, for children that might be experiencing well-being–related concerns, the robot may have enabled them to divulge their true feelings and experiences, leading to more negative response ratings to the questionnaire.
Robots an addition not a replacement
“Since the robot we use is child-sized, and completely nonthreatening, children might see the robot as a confidant – they feel like they won’t get into trouble if they share secrets with it,” said Ms. Abbasi. “Other researchers have found that children are more likely to divulge private information – like that they’re being bullied, for example – to a robot than they would be to an adult,” she said.
Study participants all said they “enjoyed talking with the robot,” commented the authors, who added that, “the children were willing to confide in the robot, in some cases sharing information with the robot that they had not yet shared via the standard assessment method of online or in-person questionnaires.”
This is the first time that robots have been used to assess mental well-being in children, the researchers pointed out. “Robots could be a useful addition to traditional methods of mental health assessment,” they said, though they emphasized that robots are “not intended to be a substitute for professional mental health support.”
“We don’t have any intention of replacing psychologists or other mental health professionals with robots, since their expertise far surpasses anything a robot can do,” said Dr. Micol Spitale, affective computing and robotics laboratory, University of Cambridge, and study coauthor. “However, our work suggests that robots could be a useful tool in helping children to open up and share things they might not be comfortable sharing at first.”
The researchers say that they hope to expand their survey in future by including more participants and following them over time. They are also investigating whether similar results could be achieved if children interact with the robot via video chat.
A version of this article first appeared on Medscape UK.
Robots can be better at detecting mental well-being issues in children than parent-reported or self-reported testing, say U.K. researchers.
The researchers behind a new study, presented at the 31st IEEE International Conference on Robot & Human Interactive Communication (RO-MAN) in Naples, Italy, have suggested that robots could be a useful addition to traditional methods of mental health assessment.
“There are times when traditional methods aren’t able to catch mental well-being lapses in children, as sometimes the changes are incredibly subtle,” said Nida Itrat Abbasi, a PhD student at Cambridge (England) Affective Computing and Robotics Group, University of Cambridge, and the study’s first author. “We wanted to see whether robots might be able to help with this process,” she explained.
The authors highlighted how, during the COVID-19 pandemic, home schooling, financial pressures, and isolation from peers and friends impacted the mental health of many children. Even before the pandemic however, anxiety and depression among children in the United Kingdom has been on the rise, but the resources and support to address mental well-being are severely limited.
Children engage with robots
For their study the research team – which comprised roboticists, computer scientists, and psychiatrists from the University of Cambridge – enrolled 28 participants between ages 8 and 13 years. While being observed from an adjacent room by a parent or guardian, along with members of the research team, the participants took part in a one-to-one 45-minute session with a Nao robot – a humanoid robot about 60 cm tall – that administered a series of standard psychological questionnaires to assess the mental well-being of each participant.
Participants interacted with the robot throughout the session by speaking with it or by touching sensors on the robot’s hands and feet. Additional sensors tracked participants’ heartbeat, head, and eye movements during the session.
Professor Hatice Gunes, affective intelligence and robotics laboratory, department of computer science, University of Cambridge, said: “Children are quite tactile, and they’re drawn to technology. If they’re using a screen-based tool, they’re withdrawn from the physical world,” she said. “But robots are perfect because they’re in the physical world – they’re more interactive, so the children are more engaged.”
Prior to each session the children and their parent or guardian completed standard online questionnaires to assess each child’s mental well-being.
During each session, the robot performed four different tasks:
- Asked open-ended questions about happy and sad memories over the last week.
- Administered the Short Mood and Feelings Questionnaire (SMFQ).
- Administered a picture task inspired by the Children’s Apperception Test (CAT), where children are asked to answer questions related to pictures shown.
- Administered the Revised Children’s Anxiety and Depression Scale (RCADS) for generalized anxiety, panic disorder, and low mood.
Following the SMFQ children were divided into three different groups according to how likely they were to be struggling with their mental well-being.
The researchers found that children with varying levels of well-being concerns interacted differently with the robot. For children that might not be experiencing mental well-being–related problems, the researchers found that interacting with the robot led to more positive response ratings to the questionnaires. However, for children that might be experiencing well-being–related concerns, the robot may have enabled them to divulge their true feelings and experiences, leading to more negative response ratings to the questionnaire.
Robots an addition not a replacement
“Since the robot we use is child-sized, and completely nonthreatening, children might see the robot as a confidant – they feel like they won’t get into trouble if they share secrets with it,” said Ms. Abbasi. “Other researchers have found that children are more likely to divulge private information – like that they’re being bullied, for example – to a robot than they would be to an adult,” she said.
Study participants all said they “enjoyed talking with the robot,” commented the authors, who added that, “the children were willing to confide in the robot, in some cases sharing information with the robot that they had not yet shared via the standard assessment method of online or in-person questionnaires.”
This is the first time that robots have been used to assess mental well-being in children, the researchers pointed out. “Robots could be a useful addition to traditional methods of mental health assessment,” they said, though they emphasized that robots are “not intended to be a substitute for professional mental health support.”
“We don’t have any intention of replacing psychologists or other mental health professionals with robots, since their expertise far surpasses anything a robot can do,” said Dr. Micol Spitale, affective computing and robotics laboratory, University of Cambridge, and study coauthor. “However, our work suggests that robots could be a useful tool in helping children to open up and share things they might not be comfortable sharing at first.”
The researchers say that they hope to expand their survey in future by including more participants and following them over time. They are also investigating whether similar results could be achieved if children interact with the robot via video chat.
A version of this article first appeared on Medscape UK.
Robots can be better at detecting mental well-being issues in children than parent-reported or self-reported testing, say U.K. researchers.
The researchers behind a new study, presented at the 31st IEEE International Conference on Robot & Human Interactive Communication (RO-MAN) in Naples, Italy, have suggested that robots could be a useful addition to traditional methods of mental health assessment.
“There are times when traditional methods aren’t able to catch mental well-being lapses in children, as sometimes the changes are incredibly subtle,” said Nida Itrat Abbasi, a PhD student at Cambridge (England) Affective Computing and Robotics Group, University of Cambridge, and the study’s first author. “We wanted to see whether robots might be able to help with this process,” she explained.
The authors highlighted how, during the COVID-19 pandemic, home schooling, financial pressures, and isolation from peers and friends impacted the mental health of many children. Even before the pandemic however, anxiety and depression among children in the United Kingdom has been on the rise, but the resources and support to address mental well-being are severely limited.
Children engage with robots
For their study the research team – which comprised roboticists, computer scientists, and psychiatrists from the University of Cambridge – enrolled 28 participants between ages 8 and 13 years. While being observed from an adjacent room by a parent or guardian, along with members of the research team, the participants took part in a one-to-one 45-minute session with a Nao robot – a humanoid robot about 60 cm tall – that administered a series of standard psychological questionnaires to assess the mental well-being of each participant.
Participants interacted with the robot throughout the session by speaking with it or by touching sensors on the robot’s hands and feet. Additional sensors tracked participants’ heartbeat, head, and eye movements during the session.
Professor Hatice Gunes, affective intelligence and robotics laboratory, department of computer science, University of Cambridge, said: “Children are quite tactile, and they’re drawn to technology. If they’re using a screen-based tool, they’re withdrawn from the physical world,” she said. “But robots are perfect because they’re in the physical world – they’re more interactive, so the children are more engaged.”
Prior to each session the children and their parent or guardian completed standard online questionnaires to assess each child’s mental well-being.
During each session, the robot performed four different tasks:
- Asked open-ended questions about happy and sad memories over the last week.
- Administered the Short Mood and Feelings Questionnaire (SMFQ).
- Administered a picture task inspired by the Children’s Apperception Test (CAT), where children are asked to answer questions related to pictures shown.
- Administered the Revised Children’s Anxiety and Depression Scale (RCADS) for generalized anxiety, panic disorder, and low mood.
Following the SMFQ children were divided into three different groups according to how likely they were to be struggling with their mental well-being.
The researchers found that children with varying levels of well-being concerns interacted differently with the robot. For children that might not be experiencing mental well-being–related problems, the researchers found that interacting with the robot led to more positive response ratings to the questionnaires. However, for children that might be experiencing well-being–related concerns, the robot may have enabled them to divulge their true feelings and experiences, leading to more negative response ratings to the questionnaire.
Robots an addition not a replacement
“Since the robot we use is child-sized, and completely nonthreatening, children might see the robot as a confidant – they feel like they won’t get into trouble if they share secrets with it,” said Ms. Abbasi. “Other researchers have found that children are more likely to divulge private information – like that they’re being bullied, for example – to a robot than they would be to an adult,” she said.
Study participants all said they “enjoyed talking with the robot,” commented the authors, who added that, “the children were willing to confide in the robot, in some cases sharing information with the robot that they had not yet shared via the standard assessment method of online or in-person questionnaires.”
This is the first time that robots have been used to assess mental well-being in children, the researchers pointed out. “Robots could be a useful addition to traditional methods of mental health assessment,” they said, though they emphasized that robots are “not intended to be a substitute for professional mental health support.”
“We don’t have any intention of replacing psychologists or other mental health professionals with robots, since their expertise far surpasses anything a robot can do,” said Dr. Micol Spitale, affective computing and robotics laboratory, University of Cambridge, and study coauthor. “However, our work suggests that robots could be a useful tool in helping children to open up and share things they might not be comfortable sharing at first.”
The researchers say that they hope to expand their survey in future by including more participants and following them over time. They are also investigating whether similar results could be achieved if children interact with the robot via video chat.
A version of this article first appeared on Medscape UK.
Dolutegravir in pregnant patients with HIV showed more viral suppression at delivery vs. other treatments
“Dolutegravir is increasingly used in pregnancy in the United States,” Kunjal Patel, DSc, one of the investigators, said in an interview. “While its effectiveness and safety in pregnancy have been compared to efavirenz in previous studies, including three randomized trials, efavirenz isn’t really used in the United States and Europe for treatment of HIV; it is mainly used in Africa,” she said. Therefore, it was important to compare dolutegravir use in pregnancy to the other antiretroviral regimens that are listed as being preferred for use in pregnancy in the U.S., including atazanavir/ritonavir, darunavir/ritonavir, and raltegravir, and others often used in the U.S. and Europe, she said.
In the study published in the New England Journal of Medicine, Dr. Patel, of Harvard T.H. Chan School of Public Health, Boston, and colleagues analyzed data from kids enrolled in the Surveillance and Monitoring for ART Toxicities Dynamic (SMARTT) cohort. This group is part of an ongoing research project focused on evaluating ART toxicities during pregnancy in children who were exposed to HIV perinatally but not infected. It included pregnancies from 2007 until January 2020 that involved use of the ARTs listed.
The study population of 1,257 pregnancies with observed birth outcomes included 120 individuals with an initial ART of dolutegravir (DTG), 464 started on atazanavir–ritonavir (ATV/r), 185 on darunavir–ritonavir (DRV/r), 243 on oral rilpivirine (RPV), 86 on raltegravir (RAL), and 159 on elvitegravir–cobicistat (EVG/c). In approximately half of the pregnancies (51%), ART was started before conception, and the initial ART was changed in 27%.
The primary outcomes were viral suppression at delivery, and adverse birth outcomes, including preterm and very preterm birth, low and very low birth weight, and neonatal death within 14 days.
The median age of the patients at conception was 29 years, and 66% were non-Hispanic Black, representative of persons with HIV of childbearing age in the United States, the researchers noted. Overall, 96.7% of the patients who received dolutegravir showed viral suppression at delivery, compared to 90.1% for darunavir–ritonavir, 89.8% for elvitegravir–cobicistat, 89.2% for raltegravir, and 84.0% for atazanavir–ritonavir.
“We expected that dolutegravir to be similar with regards to viral suppression at delivery compared to raltegravir so were surprised that we observed less viral suppression with raltegravir compared to dolutegravir,” Dr. Patel said in an interview. “Our results may be due to the higher pill burden and lower barrier to resistance with RAL compared to dolutegravir, but we did not assess adherence or resistance in our study,” she noted.
Across ART regimens, the observed risks of preterm birth ranged from 13.6% to 17.6%, risks of low birth weight ranged from 11.9% to 16.7%, and risks of being small for gestational age ranged from 9.1% to 12.5%. For the composite of any adverse birth outcome and any severe adverse birth outcome, the observed risks ranged from 22.6% to 27.9% and 0% to 4.2%, respectively.
A total of 20 very preterm births, including 15 infants with very low birth weight, occurred across patients receiving all ART regimens, and no neonatal deaths occurred. The researchers found no apparent patterns of differences in the observed risk of adverse birth outcomes across all groups related to the timing of ART initiation in pregnancy, but the risks were greater among those who began the drugs during pregnancy compared to those who began before conception.
“Our results confirm the recommendation of DTG as “preferred” in U.S. perinatal guidelines, and provide evidence suggesting ATV/r and RAL provides lower HIV viral suppression at delivery compared to DTG, and support DRV/r as a reasonable alternative when DTG use is not feasible,” Dr. Patel said in an interview.
“With regards to next steps, we are interested in comparing the effectiveness and safety of dolutegravir-based regimens that include tenofovir alafenamide (TAF) vs. tenofovir disoproxil fumarate (TDF) in our U.S. setting,” she said.
The study findings were limited by several factors including the lack of data on predictors of preterm birth and low birth weight, such as previous preterm birth and prepregnancy body mass index, the researchers noted.
However, the results indicate that other common ARTs provide less HIV viral suppression at delivery than dolutegravir, with similar adverse birth outcomes; the results also support darunavir–ritonavir as a reasonable alternative when dolutegravir use is not feasible, as it showed the next highest level of viral suppression after dolutegravir, the researchers concluded.
Findings fill a key research gap
The current study is important given the limited data on effectiveness and outcomes in pregnancy with the use of contemporary HIV regimens in the United States, Martina L. Badell, MD, a maternal-fetal medicine specialist at Emory University, Atlanta, said in an interview.
“Pregnancy is still among exclusion criteria for most drug studies,” said Dr. Badell, who was not involved in the current study. “Dolutegravir-based ART is first line in the U.S. today because of its effectiveness, lower side effects, and higher barrier to resistance; therefore understanding the benefits and birth outcomes in pregnancy is critical,” she explained.
Dr. Badell said she was not surprised by the study findings. “However it is very reassuring to see in a large observational study comparing the dolutegravir regimens to other contemporary regimens in pregnancy, such a high level of viral suppression and no increased risk of adverse perinatal outcomes,” she said.
The study findings will impact clinical practice by reaffirming patient counseling regarding the use of dolutegravir in pregnancy, said Dr. Badell. “The use of ART in pregnancy is complex given the number of drug choices, whether the patient was on ART prior to pregnancy or initiated during pregnancy, and the various factors other than ART that affect perinatal outcomes, such as preterm birth and congenital anomalies, she explained.
The finding that the risk of adverse outcomes was higher for those who initiated ART during pregnancy vs. those who were already on ARTs when they became pregnant contradicts some previous research, said Dr. Badell. But this is “reassuring, as we highly recommend ART with viral suppression prior to pregnancy or to start as early as possible in pregnancy.”
Adverse birth outcomes can be affected by many variables such as age, substance abuse, prior adverse birth outcome and other factors, and larger studies that control for these variables will allow better evaluation of the effect of the ART drugs, Dr. Badell added.
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, along with the Office of the Director, National Institutes of Health; National Institute of Dental and Craniofacial Research; National Institute of Allergy and Infectious Diseases; National Institute of Neurological Disorders and Stroke; National Institute on Deafness and Other Communication Disorders; National Institute of Mental Health; National Institute on Drug Abuse; National Cancer Institute; National Institute on Alcohol Abuse and Alcoholism; and National Heart, Lung, and Blood Institute through cooperative agreements with the Harvard T.H. Chan School of Public Health and the Tulane University School of Medicine.
The researchers and Dr. Badell had no financial conflicts to disclose.
“Dolutegravir is increasingly used in pregnancy in the United States,” Kunjal Patel, DSc, one of the investigators, said in an interview. “While its effectiveness and safety in pregnancy have been compared to efavirenz in previous studies, including three randomized trials, efavirenz isn’t really used in the United States and Europe for treatment of HIV; it is mainly used in Africa,” she said. Therefore, it was important to compare dolutegravir use in pregnancy to the other antiretroviral regimens that are listed as being preferred for use in pregnancy in the U.S., including atazanavir/ritonavir, darunavir/ritonavir, and raltegravir, and others often used in the U.S. and Europe, she said.
In the study published in the New England Journal of Medicine, Dr. Patel, of Harvard T.H. Chan School of Public Health, Boston, and colleagues analyzed data from kids enrolled in the Surveillance and Monitoring for ART Toxicities Dynamic (SMARTT) cohort. This group is part of an ongoing research project focused on evaluating ART toxicities during pregnancy in children who were exposed to HIV perinatally but not infected. It included pregnancies from 2007 until January 2020 that involved use of the ARTs listed.
The study population of 1,257 pregnancies with observed birth outcomes included 120 individuals with an initial ART of dolutegravir (DTG), 464 started on atazanavir–ritonavir (ATV/r), 185 on darunavir–ritonavir (DRV/r), 243 on oral rilpivirine (RPV), 86 on raltegravir (RAL), and 159 on elvitegravir–cobicistat (EVG/c). In approximately half of the pregnancies (51%), ART was started before conception, and the initial ART was changed in 27%.
The primary outcomes were viral suppression at delivery, and adverse birth outcomes, including preterm and very preterm birth, low and very low birth weight, and neonatal death within 14 days.
The median age of the patients at conception was 29 years, and 66% were non-Hispanic Black, representative of persons with HIV of childbearing age in the United States, the researchers noted. Overall, 96.7% of the patients who received dolutegravir showed viral suppression at delivery, compared to 90.1% for darunavir–ritonavir, 89.8% for elvitegravir–cobicistat, 89.2% for raltegravir, and 84.0% for atazanavir–ritonavir.
“We expected that dolutegravir to be similar with regards to viral suppression at delivery compared to raltegravir so were surprised that we observed less viral suppression with raltegravir compared to dolutegravir,” Dr. Patel said in an interview. “Our results may be due to the higher pill burden and lower barrier to resistance with RAL compared to dolutegravir, but we did not assess adherence or resistance in our study,” she noted.
Across ART regimens, the observed risks of preterm birth ranged from 13.6% to 17.6%, risks of low birth weight ranged from 11.9% to 16.7%, and risks of being small for gestational age ranged from 9.1% to 12.5%. For the composite of any adverse birth outcome and any severe adverse birth outcome, the observed risks ranged from 22.6% to 27.9% and 0% to 4.2%, respectively.
A total of 20 very preterm births, including 15 infants with very low birth weight, occurred across patients receiving all ART regimens, and no neonatal deaths occurred. The researchers found no apparent patterns of differences in the observed risk of adverse birth outcomes across all groups related to the timing of ART initiation in pregnancy, but the risks were greater among those who began the drugs during pregnancy compared to those who began before conception.
“Our results confirm the recommendation of DTG as “preferred” in U.S. perinatal guidelines, and provide evidence suggesting ATV/r and RAL provides lower HIV viral suppression at delivery compared to DTG, and support DRV/r as a reasonable alternative when DTG use is not feasible,” Dr. Patel said in an interview.
“With regards to next steps, we are interested in comparing the effectiveness and safety of dolutegravir-based regimens that include tenofovir alafenamide (TAF) vs. tenofovir disoproxil fumarate (TDF) in our U.S. setting,” she said.
The study findings were limited by several factors including the lack of data on predictors of preterm birth and low birth weight, such as previous preterm birth and prepregnancy body mass index, the researchers noted.
However, the results indicate that other common ARTs provide less HIV viral suppression at delivery than dolutegravir, with similar adverse birth outcomes; the results also support darunavir–ritonavir as a reasonable alternative when dolutegravir use is not feasible, as it showed the next highest level of viral suppression after dolutegravir, the researchers concluded.
Findings fill a key research gap
The current study is important given the limited data on effectiveness and outcomes in pregnancy with the use of contemporary HIV regimens in the United States, Martina L. Badell, MD, a maternal-fetal medicine specialist at Emory University, Atlanta, said in an interview.
“Pregnancy is still among exclusion criteria for most drug studies,” said Dr. Badell, who was not involved in the current study. “Dolutegravir-based ART is first line in the U.S. today because of its effectiveness, lower side effects, and higher barrier to resistance; therefore understanding the benefits and birth outcomes in pregnancy is critical,” she explained.
Dr. Badell said she was not surprised by the study findings. “However it is very reassuring to see in a large observational study comparing the dolutegravir regimens to other contemporary regimens in pregnancy, such a high level of viral suppression and no increased risk of adverse perinatal outcomes,” she said.
The study findings will impact clinical practice by reaffirming patient counseling regarding the use of dolutegravir in pregnancy, said Dr. Badell. “The use of ART in pregnancy is complex given the number of drug choices, whether the patient was on ART prior to pregnancy or initiated during pregnancy, and the various factors other than ART that affect perinatal outcomes, such as preterm birth and congenital anomalies, she explained.
The finding that the risk of adverse outcomes was higher for those who initiated ART during pregnancy vs. those who were already on ARTs when they became pregnant contradicts some previous research, said Dr. Badell. But this is “reassuring, as we highly recommend ART with viral suppression prior to pregnancy or to start as early as possible in pregnancy.”
Adverse birth outcomes can be affected by many variables such as age, substance abuse, prior adverse birth outcome and other factors, and larger studies that control for these variables will allow better evaluation of the effect of the ART drugs, Dr. Badell added.
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, along with the Office of the Director, National Institutes of Health; National Institute of Dental and Craniofacial Research; National Institute of Allergy and Infectious Diseases; National Institute of Neurological Disorders and Stroke; National Institute on Deafness and Other Communication Disorders; National Institute of Mental Health; National Institute on Drug Abuse; National Cancer Institute; National Institute on Alcohol Abuse and Alcoholism; and National Heart, Lung, and Blood Institute through cooperative agreements with the Harvard T.H. Chan School of Public Health and the Tulane University School of Medicine.
The researchers and Dr. Badell had no financial conflicts to disclose.
“Dolutegravir is increasingly used in pregnancy in the United States,” Kunjal Patel, DSc, one of the investigators, said in an interview. “While its effectiveness and safety in pregnancy have been compared to efavirenz in previous studies, including three randomized trials, efavirenz isn’t really used in the United States and Europe for treatment of HIV; it is mainly used in Africa,” she said. Therefore, it was important to compare dolutegravir use in pregnancy to the other antiretroviral regimens that are listed as being preferred for use in pregnancy in the U.S., including atazanavir/ritonavir, darunavir/ritonavir, and raltegravir, and others often used in the U.S. and Europe, she said.
In the study published in the New England Journal of Medicine, Dr. Patel, of Harvard T.H. Chan School of Public Health, Boston, and colleagues analyzed data from kids enrolled in the Surveillance and Monitoring for ART Toxicities Dynamic (SMARTT) cohort. This group is part of an ongoing research project focused on evaluating ART toxicities during pregnancy in children who were exposed to HIV perinatally but not infected. It included pregnancies from 2007 until January 2020 that involved use of the ARTs listed.
The study population of 1,257 pregnancies with observed birth outcomes included 120 individuals with an initial ART of dolutegravir (DTG), 464 started on atazanavir–ritonavir (ATV/r), 185 on darunavir–ritonavir (DRV/r), 243 on oral rilpivirine (RPV), 86 on raltegravir (RAL), and 159 on elvitegravir–cobicistat (EVG/c). In approximately half of the pregnancies (51%), ART was started before conception, and the initial ART was changed in 27%.
The primary outcomes were viral suppression at delivery, and adverse birth outcomes, including preterm and very preterm birth, low and very low birth weight, and neonatal death within 14 days.
The median age of the patients at conception was 29 years, and 66% were non-Hispanic Black, representative of persons with HIV of childbearing age in the United States, the researchers noted. Overall, 96.7% of the patients who received dolutegravir showed viral suppression at delivery, compared to 90.1% for darunavir–ritonavir, 89.8% for elvitegravir–cobicistat, 89.2% for raltegravir, and 84.0% for atazanavir–ritonavir.
“We expected that dolutegravir to be similar with regards to viral suppression at delivery compared to raltegravir so were surprised that we observed less viral suppression with raltegravir compared to dolutegravir,” Dr. Patel said in an interview. “Our results may be due to the higher pill burden and lower barrier to resistance with RAL compared to dolutegravir, but we did not assess adherence or resistance in our study,” she noted.
Across ART regimens, the observed risks of preterm birth ranged from 13.6% to 17.6%, risks of low birth weight ranged from 11.9% to 16.7%, and risks of being small for gestational age ranged from 9.1% to 12.5%. For the composite of any adverse birth outcome and any severe adverse birth outcome, the observed risks ranged from 22.6% to 27.9% and 0% to 4.2%, respectively.
A total of 20 very preterm births, including 15 infants with very low birth weight, occurred across patients receiving all ART regimens, and no neonatal deaths occurred. The researchers found no apparent patterns of differences in the observed risk of adverse birth outcomes across all groups related to the timing of ART initiation in pregnancy, but the risks were greater among those who began the drugs during pregnancy compared to those who began before conception.
“Our results confirm the recommendation of DTG as “preferred” in U.S. perinatal guidelines, and provide evidence suggesting ATV/r and RAL provides lower HIV viral suppression at delivery compared to DTG, and support DRV/r as a reasonable alternative when DTG use is not feasible,” Dr. Patel said in an interview.
“With regards to next steps, we are interested in comparing the effectiveness and safety of dolutegravir-based regimens that include tenofovir alafenamide (TAF) vs. tenofovir disoproxil fumarate (TDF) in our U.S. setting,” she said.
The study findings were limited by several factors including the lack of data on predictors of preterm birth and low birth weight, such as previous preterm birth and prepregnancy body mass index, the researchers noted.
However, the results indicate that other common ARTs provide less HIV viral suppression at delivery than dolutegravir, with similar adverse birth outcomes; the results also support darunavir–ritonavir as a reasonable alternative when dolutegravir use is not feasible, as it showed the next highest level of viral suppression after dolutegravir, the researchers concluded.
Findings fill a key research gap
The current study is important given the limited data on effectiveness and outcomes in pregnancy with the use of contemporary HIV regimens in the United States, Martina L. Badell, MD, a maternal-fetal medicine specialist at Emory University, Atlanta, said in an interview.
“Pregnancy is still among exclusion criteria for most drug studies,” said Dr. Badell, who was not involved in the current study. “Dolutegravir-based ART is first line in the U.S. today because of its effectiveness, lower side effects, and higher barrier to resistance; therefore understanding the benefits and birth outcomes in pregnancy is critical,” she explained.
Dr. Badell said she was not surprised by the study findings. “However it is very reassuring to see in a large observational study comparing the dolutegravir regimens to other contemporary regimens in pregnancy, such a high level of viral suppression and no increased risk of adverse perinatal outcomes,” she said.
The study findings will impact clinical practice by reaffirming patient counseling regarding the use of dolutegravir in pregnancy, said Dr. Badell. “The use of ART in pregnancy is complex given the number of drug choices, whether the patient was on ART prior to pregnancy or initiated during pregnancy, and the various factors other than ART that affect perinatal outcomes, such as preterm birth and congenital anomalies, she explained.
The finding that the risk of adverse outcomes was higher for those who initiated ART during pregnancy vs. those who were already on ARTs when they became pregnant contradicts some previous research, said Dr. Badell. But this is “reassuring, as we highly recommend ART with viral suppression prior to pregnancy or to start as early as possible in pregnancy.”
Adverse birth outcomes can be affected by many variables such as age, substance abuse, prior adverse birth outcome and other factors, and larger studies that control for these variables will allow better evaluation of the effect of the ART drugs, Dr. Badell added.
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, along with the Office of the Director, National Institutes of Health; National Institute of Dental and Craniofacial Research; National Institute of Allergy and Infectious Diseases; National Institute of Neurological Disorders and Stroke; National Institute on Deafness and Other Communication Disorders; National Institute of Mental Health; National Institute on Drug Abuse; National Cancer Institute; National Institute on Alcohol Abuse and Alcoholism; and National Heart, Lung, and Blood Institute through cooperative agreements with the Harvard T.H. Chan School of Public Health and the Tulane University School of Medicine.
The researchers and Dr. Badell had no financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
CDC gives final approval to Omicron COVID-19 vaccine boosters
The Centers for Disease Control and Prevention on Sept. 1 approved the use of vaccines designed to target both Omicron and the older variants of the coronavirus, a step that may aid a goal of a widespread immunization campaign before winter arrives in the United States.
The CDC’s Advisory Committee on Immunization Practices voted 13-1 on two separate questions. One sought the panel’s backing for the use of a single dose of a new version of the Pfizer COVID-19 vaccines for people aged 12 and older. The second question dealt with a single dose of the reworked Moderna vaccine for people aged 18 and older.
The federal government wants to speed use of revamped COVID-19 shots, which the Food and Drug Administration on Sept. 1 cleared for use in the United States. Hours later, CDC Director Rochelle Walensky, MD, agreed with the panel’s recommendation.
“The updated COVID-19 boosters are formulated to better protect against the most recently circulating COVID-19 variant,” Dr. Walensky said in a statement. “They can help restore protection that has waned since previous vaccination and were designed to provide broader protection against newer variants. This recommendation followed a comprehensive scientific evaluation and robust scientific discussion. If you are eligible, there is no bad time to get your COVID-19 booster and I strongly encourage you to receive it.”
The FDA vote on Aug. 31 expanded the emergency use authorization EUA for both Moderna and Pfizer’s original COVID-19 vaccines. The new products are also called “updated boosters.” Both contain two mRNA components of SARS-CoV-2 virus, one of the original strain and another that is found in the BA.4 and BA.5 strains of the Omicron variant, the FDA said.
Basically, the FDA cleared the way for these new boosters after it relied heavily on results of certain blood tests that suggested an immune response boost from the new formulas, plus 18 months of mostly safe use of the original versions of the shots.
What neither the FDA nor the CDC has, however, is evidence from studies in humans on how well these new vaccines work or whether they are as safe as the originals. But the FDA did consider clinical evidence for the older shots and results from studies on the new boosters that were done in mice.
ACIP Committee member Pablo Sanchez, MD, of Ohio State University was the sole “no” vote on each question.
“It’s a new vaccine, it’s a new platform. There’s a lot of hesitancy already. We need the human data,” Dr. Sanchez said.
Dr. Sanchez did not doubt that the newer versions of the vaccine would prove safe.
“I personally am in the age group where I’m at high risk and I’m almost sure that I will receive it,” Dr. Sanchez said. “I just feel that this was a bit premature, and I wish that we had seen that data. Having said that, I am comfortable that the vaccine will likely be safe like the others.”
Dr. Sanchez was not alone in raising concerns about backing new COVID-19 shots for which there is not direct clinical evidence from human studies.
Committee member Sarah Long, MD, of Drexel University in Philadelphia, said during the discussion she would “reluctantly” vote in favor of the updated vaccines. She said she believes they will have the potential to reduce hospitalizations and even deaths, even with questions remaining about the data.
Dr. Long joined other committee members in pointing to the approach to updating flu vaccines as a model. In an attempt to keep ahead of influenza, companies seek to defeat new strains through tweaks to their FDA-approved vaccines. There is not much clinical information available about these revised products, Dr. Long said. She compared it to remodeling an existing home.
“It is the same scaffolding, part of the same roof, we’re just putting in some dormers and windows,” with the revisions to the flu vaccine, she said.
Earlier in the day, committee member Jamie Loehr, MD, of Cayuga Family Medicine in Ithaca, N.Y., also used changes to the annual flu shots as the model for advancing COVID-19 shots.
“So after thinking about it, I am comfortable even though we don’t have human data,” he said.
There were several questions during the meeting about why the FDA had not convened a meeting of its Vaccines and Related Biological Products Advisory Committee (regarding these specific bivalent vaccines). Typically, the FDA committee of advisers considers new vaccines before the agency authorizes their use. In this case, however, the agency acted on its own.
The FDA said the committee considered the new, bivalent COVID-19 boosters in earlier meetings and that was enough outside feedback.
But holding a meeting of advisers on these specific products could have helped build public confidence in these medicines, Dorit Reiss, PhD, of the University of California Hastings College of Law, said during the public comment session of the CDC advisers’ meeting.
“We could wish the vaccines were more effective against infection, but they’re safe and they prevent hospitalization and death,” she said.
The Department of Health and Human Services anticipated the backing of ACIP. The Administration for Strategic Preparedness and Response on Aug. 31 began distributing “millions of doses of the updated booster to tens of thousands of sites nationwide,” Jason Roos, PhD, chief operating officer for HHS Coordination Operations and Response Element, wrote in a blog.
“These boosters will be available at tens of thousands of vaccination sites ... including local pharmacies, their physicians’ offices, and vaccine centers operated by state and local health officials,”Dr. Roos wrote.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention on Sept. 1 approved the use of vaccines designed to target both Omicron and the older variants of the coronavirus, a step that may aid a goal of a widespread immunization campaign before winter arrives in the United States.
The CDC’s Advisory Committee on Immunization Practices voted 13-1 on two separate questions. One sought the panel’s backing for the use of a single dose of a new version of the Pfizer COVID-19 vaccines for people aged 12 and older. The second question dealt with a single dose of the reworked Moderna vaccine for people aged 18 and older.
The federal government wants to speed use of revamped COVID-19 shots, which the Food and Drug Administration on Sept. 1 cleared for use in the United States. Hours later, CDC Director Rochelle Walensky, MD, agreed with the panel’s recommendation.
“The updated COVID-19 boosters are formulated to better protect against the most recently circulating COVID-19 variant,” Dr. Walensky said in a statement. “They can help restore protection that has waned since previous vaccination and were designed to provide broader protection against newer variants. This recommendation followed a comprehensive scientific evaluation and robust scientific discussion. If you are eligible, there is no bad time to get your COVID-19 booster and I strongly encourage you to receive it.”
The FDA vote on Aug. 31 expanded the emergency use authorization EUA for both Moderna and Pfizer’s original COVID-19 vaccines. The new products are also called “updated boosters.” Both contain two mRNA components of SARS-CoV-2 virus, one of the original strain and another that is found in the BA.4 and BA.5 strains of the Omicron variant, the FDA said.
Basically, the FDA cleared the way for these new boosters after it relied heavily on results of certain blood tests that suggested an immune response boost from the new formulas, plus 18 months of mostly safe use of the original versions of the shots.
What neither the FDA nor the CDC has, however, is evidence from studies in humans on how well these new vaccines work or whether they are as safe as the originals. But the FDA did consider clinical evidence for the older shots and results from studies on the new boosters that were done in mice.
ACIP Committee member Pablo Sanchez, MD, of Ohio State University was the sole “no” vote on each question.
“It’s a new vaccine, it’s a new platform. There’s a lot of hesitancy already. We need the human data,” Dr. Sanchez said.
Dr. Sanchez did not doubt that the newer versions of the vaccine would prove safe.
“I personally am in the age group where I’m at high risk and I’m almost sure that I will receive it,” Dr. Sanchez said. “I just feel that this was a bit premature, and I wish that we had seen that data. Having said that, I am comfortable that the vaccine will likely be safe like the others.”
Dr. Sanchez was not alone in raising concerns about backing new COVID-19 shots for which there is not direct clinical evidence from human studies.
Committee member Sarah Long, MD, of Drexel University in Philadelphia, said during the discussion she would “reluctantly” vote in favor of the updated vaccines. She said she believes they will have the potential to reduce hospitalizations and even deaths, even with questions remaining about the data.
Dr. Long joined other committee members in pointing to the approach to updating flu vaccines as a model. In an attempt to keep ahead of influenza, companies seek to defeat new strains through tweaks to their FDA-approved vaccines. There is not much clinical information available about these revised products, Dr. Long said. She compared it to remodeling an existing home.
“It is the same scaffolding, part of the same roof, we’re just putting in some dormers and windows,” with the revisions to the flu vaccine, she said.
Earlier in the day, committee member Jamie Loehr, MD, of Cayuga Family Medicine in Ithaca, N.Y., also used changes to the annual flu shots as the model for advancing COVID-19 shots.
“So after thinking about it, I am comfortable even though we don’t have human data,” he said.
There were several questions during the meeting about why the FDA had not convened a meeting of its Vaccines and Related Biological Products Advisory Committee (regarding these specific bivalent vaccines). Typically, the FDA committee of advisers considers new vaccines before the agency authorizes their use. In this case, however, the agency acted on its own.
The FDA said the committee considered the new, bivalent COVID-19 boosters in earlier meetings and that was enough outside feedback.
But holding a meeting of advisers on these specific products could have helped build public confidence in these medicines, Dorit Reiss, PhD, of the University of California Hastings College of Law, said during the public comment session of the CDC advisers’ meeting.
“We could wish the vaccines were more effective against infection, but they’re safe and they prevent hospitalization and death,” she said.
The Department of Health and Human Services anticipated the backing of ACIP. The Administration for Strategic Preparedness and Response on Aug. 31 began distributing “millions of doses of the updated booster to tens of thousands of sites nationwide,” Jason Roos, PhD, chief operating officer for HHS Coordination Operations and Response Element, wrote in a blog.
“These boosters will be available at tens of thousands of vaccination sites ... including local pharmacies, their physicians’ offices, and vaccine centers operated by state and local health officials,”Dr. Roos wrote.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention on Sept. 1 approved the use of vaccines designed to target both Omicron and the older variants of the coronavirus, a step that may aid a goal of a widespread immunization campaign before winter arrives in the United States.
The CDC’s Advisory Committee on Immunization Practices voted 13-1 on two separate questions. One sought the panel’s backing for the use of a single dose of a new version of the Pfizer COVID-19 vaccines for people aged 12 and older. The second question dealt with a single dose of the reworked Moderna vaccine for people aged 18 and older.
The federal government wants to speed use of revamped COVID-19 shots, which the Food and Drug Administration on Sept. 1 cleared for use in the United States. Hours later, CDC Director Rochelle Walensky, MD, agreed with the panel’s recommendation.
“The updated COVID-19 boosters are formulated to better protect against the most recently circulating COVID-19 variant,” Dr. Walensky said in a statement. “They can help restore protection that has waned since previous vaccination and were designed to provide broader protection against newer variants. This recommendation followed a comprehensive scientific evaluation and robust scientific discussion. If you are eligible, there is no bad time to get your COVID-19 booster and I strongly encourage you to receive it.”
The FDA vote on Aug. 31 expanded the emergency use authorization EUA for both Moderna and Pfizer’s original COVID-19 vaccines. The new products are also called “updated boosters.” Both contain two mRNA components of SARS-CoV-2 virus, one of the original strain and another that is found in the BA.4 and BA.5 strains of the Omicron variant, the FDA said.
Basically, the FDA cleared the way for these new boosters after it relied heavily on results of certain blood tests that suggested an immune response boost from the new formulas, plus 18 months of mostly safe use of the original versions of the shots.
What neither the FDA nor the CDC has, however, is evidence from studies in humans on how well these new vaccines work or whether they are as safe as the originals. But the FDA did consider clinical evidence for the older shots and results from studies on the new boosters that were done in mice.
ACIP Committee member Pablo Sanchez, MD, of Ohio State University was the sole “no” vote on each question.
“It’s a new vaccine, it’s a new platform. There’s a lot of hesitancy already. We need the human data,” Dr. Sanchez said.
Dr. Sanchez did not doubt that the newer versions of the vaccine would prove safe.
“I personally am in the age group where I’m at high risk and I’m almost sure that I will receive it,” Dr. Sanchez said. “I just feel that this was a bit premature, and I wish that we had seen that data. Having said that, I am comfortable that the vaccine will likely be safe like the others.”
Dr. Sanchez was not alone in raising concerns about backing new COVID-19 shots for which there is not direct clinical evidence from human studies.
Committee member Sarah Long, MD, of Drexel University in Philadelphia, said during the discussion she would “reluctantly” vote in favor of the updated vaccines. She said she believes they will have the potential to reduce hospitalizations and even deaths, even with questions remaining about the data.
Dr. Long joined other committee members in pointing to the approach to updating flu vaccines as a model. In an attempt to keep ahead of influenza, companies seek to defeat new strains through tweaks to their FDA-approved vaccines. There is not much clinical information available about these revised products, Dr. Long said. She compared it to remodeling an existing home.
“It is the same scaffolding, part of the same roof, we’re just putting in some dormers and windows,” with the revisions to the flu vaccine, she said.
Earlier in the day, committee member Jamie Loehr, MD, of Cayuga Family Medicine in Ithaca, N.Y., also used changes to the annual flu shots as the model for advancing COVID-19 shots.
“So after thinking about it, I am comfortable even though we don’t have human data,” he said.
There were several questions during the meeting about why the FDA had not convened a meeting of its Vaccines and Related Biological Products Advisory Committee (regarding these specific bivalent vaccines). Typically, the FDA committee of advisers considers new vaccines before the agency authorizes their use. In this case, however, the agency acted on its own.
The FDA said the committee considered the new, bivalent COVID-19 boosters in earlier meetings and that was enough outside feedback.
But holding a meeting of advisers on these specific products could have helped build public confidence in these medicines, Dorit Reiss, PhD, of the University of California Hastings College of Law, said during the public comment session of the CDC advisers’ meeting.
“We could wish the vaccines were more effective against infection, but they’re safe and they prevent hospitalization and death,” she said.
The Department of Health and Human Services anticipated the backing of ACIP. The Administration for Strategic Preparedness and Response on Aug. 31 began distributing “millions of doses of the updated booster to tens of thousands of sites nationwide,” Jason Roos, PhD, chief operating officer for HHS Coordination Operations and Response Element, wrote in a blog.
“These boosters will be available at tens of thousands of vaccination sites ... including local pharmacies, their physicians’ offices, and vaccine centers operated by state and local health officials,”Dr. Roos wrote.
A version of this article first appeared on WebMD.com.
Alcohol warning labels need updates to reflect harms: NEJM
The current labeling, which has not changed for 30 years, focuses on risks during pregnancy and with operating machinery and includes a vague statement that alcohol “may cause health problems.”
This is “so understated that it borders on being misleading,” the two researchers argued.
The science related to the use of alcohol has moved on, and there is now firm evidence of harm. Alcohol has been classified by the International Agency for Research on Cancer (IARC) as a group 1 carcinogen and has been linked to an increased risk of many types of cancer. Drinking alcohol has also been linked to a wide range of other diseases, from liver disease to pancreatitis to some types of heart disease, the authors noted.
Yet the general public is mostly unaware of the most serious health risks that are associated with alcohol consumption, they pointed out.
“We believe Americans deserve the opportunity to make well-informed decisions about their alcohol consumption,” said Anna H. Grummon, PhD, of the Harvard T. H. Chan School of Public Health, Boston, and Marissa G. Hall, PhD, of the University of North Carolina at Chapel Hill.
“Designing and adopting new alcohol warning labels should therefore be a research and policy priority,” they added.
The two researchers set out their arguments in a perspective article published in The New England Journal of Medicine.
“Alcohol consumption and its associated harms are reaching a crisis point in the United States,” they pointed out.
It now accounts for more than 140,000 deaths per year in the United States, according to the latest data from the Centers for Disease Control and Prevention. The COVID-19 pandemic has made the problem even worse – there was a 25% increase in alcohol-related deaths during 2020.
New, well-designed warning labels on alcohol is a common sense strategy for providing consumers with information and reducing the burden of alcohol-related harm, the authors suggested.
Warning Labels Prominently Displayed
Warning labels are most effective when they are prominently displayed, when they include pictures of some type, and when the messages alternate so as to avoid any one message from becoming “stale,” the authors noted. This approach has worked well with cigarette packs. This type of warning has increased smoking quit rates in comparison with smaller, side-of-pack, text-only warning labels.
There is some evidence that this type of labeling can be effective for alcohol. When large, pictorial warnings about cancer risk were temporarily added to the front of alcohol containers in some stores in Yukon, Canada, alcohol sales declined by 6%-10%, they pointed out.
However, pressure from the alcohol industry led to changes in the Yukon project, and while a general health warning remains, the label about increased cancer risk was removed.
The alcohol industry has tried to suppress efforts to educate the public, and this has created problems in conveying health information to consumers, the authors noted. The industry spends more than $1 billion each year to market its products in the United States.
The authors caution that without government intervention, the alcohol industry has little incentive to communicate the risks.
Some companies even link their products to health campaigns, such as selling pink ribbon–themed alcoholic drinks during October to promote their efforts to raise funds for breast cancer research, despite compelling evidence linking alcohol to an increased risk of breast cancer.
Petition at Congress calling for new labels
This is not the first call for a change in the warning labels on alcohol.
Last year, a number of medical groups petitioned Congress for a new cancer-specific warning label to be displayed on all alcoholic beverages.
The petition was signed by the American Society of Clinical Oncology (ASCO), the American Institute for Cancer Research (AICR), and Breast Cancer Prevention Partners, in collaboration with the American Public Health Association, the Consumer Federation of America, the Center for Science in the Public Interest, Alcohol Justice, and the U.S. Alcohol Policy Alliance.
They are advocating for a label that would say: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
That petition is still pending, Melissa Maitin-Shepard, MPP, policy expert at the AICR, said in an interview.
In addition, the AICR is “working to advocate for the addition of a cancer warning label to alcoholic beverages through multiple channels,” she said. “Given the strong evidence linking alcohol use with at least six types of cancer – and low awareness of the alcohol and cancer connection – there is a tremendous need to educate the public about alcohol and cancer risk.”
Noelle K. LoConte, MD, associate professor of medicine at the University of Wisconsin, Madison, who is the lead author of ASCO’s statement on alcohol and cancer risk, emphasized that there is no doubt that alcohol is a carcinogen, that it causes about 5% of cancers globally, and that its use has increased during the pandemic.
“Initiatives that raise awareness around this issue could help generate more public support for policies that limit alcohol access and thereby decrease the number of alcohol-associated cancers,” she said. “In ASCO’s statement on alcohol and cancer, we recommend several key strategies to reduce high-risk alcohol consumption, including limiting youth access to alcohol, giving municipalities more control over alcohol outlet density and points of sale, and increasing taxes on alcohol.”
However, she also had a small criticism of one point in the NEJM article. It shows a sample infographic that lists gastric cancer as being caused by alcohol. “But as of today, gastric cancer is not on the IARC list of alcohol-associated cancers,” she said. “I think this brings to mind one critical point, that these warning labels have to contain scientifically established facts.”
Dr. Grummon and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The current labeling, which has not changed for 30 years, focuses on risks during pregnancy and with operating machinery and includes a vague statement that alcohol “may cause health problems.”
This is “so understated that it borders on being misleading,” the two researchers argued.
The science related to the use of alcohol has moved on, and there is now firm evidence of harm. Alcohol has been classified by the International Agency for Research on Cancer (IARC) as a group 1 carcinogen and has been linked to an increased risk of many types of cancer. Drinking alcohol has also been linked to a wide range of other diseases, from liver disease to pancreatitis to some types of heart disease, the authors noted.
Yet the general public is mostly unaware of the most serious health risks that are associated with alcohol consumption, they pointed out.
“We believe Americans deserve the opportunity to make well-informed decisions about their alcohol consumption,” said Anna H. Grummon, PhD, of the Harvard T. H. Chan School of Public Health, Boston, and Marissa G. Hall, PhD, of the University of North Carolina at Chapel Hill.
“Designing and adopting new alcohol warning labels should therefore be a research and policy priority,” they added.
The two researchers set out their arguments in a perspective article published in The New England Journal of Medicine.
“Alcohol consumption and its associated harms are reaching a crisis point in the United States,” they pointed out.
It now accounts for more than 140,000 deaths per year in the United States, according to the latest data from the Centers for Disease Control and Prevention. The COVID-19 pandemic has made the problem even worse – there was a 25% increase in alcohol-related deaths during 2020.
New, well-designed warning labels on alcohol is a common sense strategy for providing consumers with information and reducing the burden of alcohol-related harm, the authors suggested.
Warning Labels Prominently Displayed
Warning labels are most effective when they are prominently displayed, when they include pictures of some type, and when the messages alternate so as to avoid any one message from becoming “stale,” the authors noted. This approach has worked well with cigarette packs. This type of warning has increased smoking quit rates in comparison with smaller, side-of-pack, text-only warning labels.
There is some evidence that this type of labeling can be effective for alcohol. When large, pictorial warnings about cancer risk were temporarily added to the front of alcohol containers in some stores in Yukon, Canada, alcohol sales declined by 6%-10%, they pointed out.
However, pressure from the alcohol industry led to changes in the Yukon project, and while a general health warning remains, the label about increased cancer risk was removed.
The alcohol industry has tried to suppress efforts to educate the public, and this has created problems in conveying health information to consumers, the authors noted. The industry spends more than $1 billion each year to market its products in the United States.
The authors caution that without government intervention, the alcohol industry has little incentive to communicate the risks.
Some companies even link their products to health campaigns, such as selling pink ribbon–themed alcoholic drinks during October to promote their efforts to raise funds for breast cancer research, despite compelling evidence linking alcohol to an increased risk of breast cancer.
Petition at Congress calling for new labels
This is not the first call for a change in the warning labels on alcohol.
Last year, a number of medical groups petitioned Congress for a new cancer-specific warning label to be displayed on all alcoholic beverages.
The petition was signed by the American Society of Clinical Oncology (ASCO), the American Institute for Cancer Research (AICR), and Breast Cancer Prevention Partners, in collaboration with the American Public Health Association, the Consumer Federation of America, the Center for Science in the Public Interest, Alcohol Justice, and the U.S. Alcohol Policy Alliance.
They are advocating for a label that would say: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
That petition is still pending, Melissa Maitin-Shepard, MPP, policy expert at the AICR, said in an interview.
In addition, the AICR is “working to advocate for the addition of a cancer warning label to alcoholic beverages through multiple channels,” she said. “Given the strong evidence linking alcohol use with at least six types of cancer – and low awareness of the alcohol and cancer connection – there is a tremendous need to educate the public about alcohol and cancer risk.”
Noelle K. LoConte, MD, associate professor of medicine at the University of Wisconsin, Madison, who is the lead author of ASCO’s statement on alcohol and cancer risk, emphasized that there is no doubt that alcohol is a carcinogen, that it causes about 5% of cancers globally, and that its use has increased during the pandemic.
“Initiatives that raise awareness around this issue could help generate more public support for policies that limit alcohol access and thereby decrease the number of alcohol-associated cancers,” she said. “In ASCO’s statement on alcohol and cancer, we recommend several key strategies to reduce high-risk alcohol consumption, including limiting youth access to alcohol, giving municipalities more control over alcohol outlet density and points of sale, and increasing taxes on alcohol.”
However, she also had a small criticism of one point in the NEJM article. It shows a sample infographic that lists gastric cancer as being caused by alcohol. “But as of today, gastric cancer is not on the IARC list of alcohol-associated cancers,” she said. “I think this brings to mind one critical point, that these warning labels have to contain scientifically established facts.”
Dr. Grummon and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The current labeling, which has not changed for 30 years, focuses on risks during pregnancy and with operating machinery and includes a vague statement that alcohol “may cause health problems.”
This is “so understated that it borders on being misleading,” the two researchers argued.
The science related to the use of alcohol has moved on, and there is now firm evidence of harm. Alcohol has been classified by the International Agency for Research on Cancer (IARC) as a group 1 carcinogen and has been linked to an increased risk of many types of cancer. Drinking alcohol has also been linked to a wide range of other diseases, from liver disease to pancreatitis to some types of heart disease, the authors noted.
Yet the general public is mostly unaware of the most serious health risks that are associated with alcohol consumption, they pointed out.
“We believe Americans deserve the opportunity to make well-informed decisions about their alcohol consumption,” said Anna H. Grummon, PhD, of the Harvard T. H. Chan School of Public Health, Boston, and Marissa G. Hall, PhD, of the University of North Carolina at Chapel Hill.
“Designing and adopting new alcohol warning labels should therefore be a research and policy priority,” they added.
The two researchers set out their arguments in a perspective article published in The New England Journal of Medicine.
“Alcohol consumption and its associated harms are reaching a crisis point in the United States,” they pointed out.
It now accounts for more than 140,000 deaths per year in the United States, according to the latest data from the Centers for Disease Control and Prevention. The COVID-19 pandemic has made the problem even worse – there was a 25% increase in alcohol-related deaths during 2020.
New, well-designed warning labels on alcohol is a common sense strategy for providing consumers with information and reducing the burden of alcohol-related harm, the authors suggested.
Warning Labels Prominently Displayed
Warning labels are most effective when they are prominently displayed, when they include pictures of some type, and when the messages alternate so as to avoid any one message from becoming “stale,” the authors noted. This approach has worked well with cigarette packs. This type of warning has increased smoking quit rates in comparison with smaller, side-of-pack, text-only warning labels.
There is some evidence that this type of labeling can be effective for alcohol. When large, pictorial warnings about cancer risk were temporarily added to the front of alcohol containers in some stores in Yukon, Canada, alcohol sales declined by 6%-10%, they pointed out.
However, pressure from the alcohol industry led to changes in the Yukon project, and while a general health warning remains, the label about increased cancer risk was removed.
The alcohol industry has tried to suppress efforts to educate the public, and this has created problems in conveying health information to consumers, the authors noted. The industry spends more than $1 billion each year to market its products in the United States.
The authors caution that without government intervention, the alcohol industry has little incentive to communicate the risks.
Some companies even link their products to health campaigns, such as selling pink ribbon–themed alcoholic drinks during October to promote their efforts to raise funds for breast cancer research, despite compelling evidence linking alcohol to an increased risk of breast cancer.
Petition at Congress calling for new labels
This is not the first call for a change in the warning labels on alcohol.
Last year, a number of medical groups petitioned Congress for a new cancer-specific warning label to be displayed on all alcoholic beverages.
The petition was signed by the American Society of Clinical Oncology (ASCO), the American Institute for Cancer Research (AICR), and Breast Cancer Prevention Partners, in collaboration with the American Public Health Association, the Consumer Federation of America, the Center for Science in the Public Interest, Alcohol Justice, and the U.S. Alcohol Policy Alliance.
They are advocating for a label that would say: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
That petition is still pending, Melissa Maitin-Shepard, MPP, policy expert at the AICR, said in an interview.
In addition, the AICR is “working to advocate for the addition of a cancer warning label to alcoholic beverages through multiple channels,” she said. “Given the strong evidence linking alcohol use with at least six types of cancer – and low awareness of the alcohol and cancer connection – there is a tremendous need to educate the public about alcohol and cancer risk.”
Noelle K. LoConte, MD, associate professor of medicine at the University of Wisconsin, Madison, who is the lead author of ASCO’s statement on alcohol and cancer risk, emphasized that there is no doubt that alcohol is a carcinogen, that it causes about 5% of cancers globally, and that its use has increased during the pandemic.
“Initiatives that raise awareness around this issue could help generate more public support for policies that limit alcohol access and thereby decrease the number of alcohol-associated cancers,” she said. “In ASCO’s statement on alcohol and cancer, we recommend several key strategies to reduce high-risk alcohol consumption, including limiting youth access to alcohol, giving municipalities more control over alcohol outlet density and points of sale, and increasing taxes on alcohol.”
However, she also had a small criticism of one point in the NEJM article. It shows a sample infographic that lists gastric cancer as being caused by alcohol. “But as of today, gastric cancer is not on the IARC list of alcohol-associated cancers,” she said. “I think this brings to mind one critical point, that these warning labels have to contain scientifically established facts.”
Dr. Grummon and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Real medical news: Many teens trust fake medical news
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
Many young kids with COVID may show no symptoms
BY WILL PASS
Just 14% of adults who tested positive for SARS-CoV-2 were asymptomatic, versus 37% of children aged 0-4 years, in the paper. This raises concern that parents, childcare providers, and preschools may be underestimating infection in seemingly healthy young kids who have been exposed to COVID, wrote lead author Ruth A. Karron, MD, and colleagues in JAMA Network Open.
Methods
The new research involved 690 individuals from 175 households in Maryland who were monitored closely between November 2020 and October 2021. Every week for 8 months, participants completed online symptom checks and underwent PCR testing using nasal swabs, with symptomatic individuals submitting additional swabs for analysis.
“What was different about our study [compared with previous studies] was the intensity of our collection, and the fact that we collected specimens from asymptomatic people,” said Dr. Karron, a pediatrician and professor in the department of international health, Johns Hopkins University, Baltimore, in an interview. “You shed more virus earlier in the infection than later, and the fact that we were sampling every single week meant that we could pick up those early infections.”
The study also stands out for its focus on young children, Dr. Karron said. Enrollment required all households to have at least one child aged 0-4 years, so 256 out of 690 participants (37.1%) were in this youngest age group. The remainder of the population consisted of 100 older children aged 5-17 years (14.5%) and 334 adults aged 18-74 years (48.4%).
Children 4 and under more than twice as likely to be asymptomatic
By the end of the study, 51 participants had tested positive for SARS-CoV-2, among whom 14 had no symptoms. A closer look showed that children 0-4 years of age who contracted COVID were more than twice as likely to be asymptomatic as infected adults (36.8% vs. 14.3%).
The relationship between symptoms and viral load also differed between adults and young children.
While adults with high viral loads – suggesting greater contagiousness – typically had more severe COVID symptoms, no correlation was found in young kids, meaning children with mild or no symptoms could still be highly contagious.
Dr. Karron said these findings should help parents and other stakeholders make better-informed decisions based on known risks. She recommended testing young, asymptomatic children for COVID if they have been exposed to infected individuals, then acting accordingly based on the results.
“If a family is infected with the virus, and the 2-year-old is asymptomatic, and people are thinking about a visit to elderly grandparents who may be frail, one shouldn’t assume that the 2-year-old is uninfected,” Dr. Karron said. “That child should be tested along with other family members.”
Testing should also be considered for young children exposed to COVID at childcare facilities, she added.
But not every expert consulted for this piece shared these opinions of Dr. Karron.
“I question whether that effort is worth it,” said Dean Blumberg, MD, professor and chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, Calif.
He noted that recent Food and Drug Administration guidance for COVID testing calls for three negative at-home antigen tests to confirm lack of infection.
“That would take 4 days to get those tests done,” he said. “So, it’s a lot of testing. It’s a lot of record keeping, it’s inconvenient, it’s uncomfortable to be tested, and I just question whether it’s worth that effort.”
Applicability of findings to today questioned
Dr. Blumberg also questioned whether the study, which was completed almost a year ago, reflects the current pandemic landscape.
“At the time this study was done, it was predominantly Delta [variant instead of Omicron],” Dr. Blumberg said. “The other issue [with the study] is that … most of the children didn’t have preexisting immunity, so you have to take that into account.”
Preexisting immunity – whether from exposure or vaccination – could lower viral loads, so asymptomatic children today really could be less contagious than they were when the study was done, according to Dr. Blumberg. Kids without symptoms are also less likely to spread the virus, because they aren’t coughing or sneezing, he added.
Sara R. Kim, MD, and Janet A. Englund, MD, of the Seattle Children’s Research Institute, University of Washington, said it’s challenging to know how applicable the findings are, although they sided more with the investigators than Dr. Blumberg.
“Given the higher rate of transmissibility and infectivity of the Omicron variant, it is difficult to make direct associations between findings reported during this study period and those present in the current era during which the Omicron variant is circulating,” they wrote in an accompanying editorial. “However, the higher rates of asymptomatic infection observed among children in this study are likely to be consistent with those observed for current and future viral variants.”
Although the experts offered different interpretations of the findings, they shared similar perspectives on vaccination.
“The most important thing that parents can do is get their kids vaccinated, be vaccinated themselves, and have everybody in the household vaccinated and up to date for all doses that are indicated,” Dr. Blumberg said.
Dr. Karron noted that vaccination will be increasingly important in the coming months.
“Summer is ending; school is starting,” she said. “We’re going to be in large groups indoors again very soon. To keep young children safe, I think it’s really important for them to get vaccinated.”
The study was funded by the CDC. The investigators disclosed no other relationships. Dr. Englund disclosed relationships with AstraZeneca, GlaxoSmithKline, Merck, and others. Dr. Kim and Dr. Blumberg disclosed no relevant conflicts of interest.
BY WILL PASS
Just 14% of adults who tested positive for SARS-CoV-2 were asymptomatic, versus 37% of children aged 0-4 years, in the paper. This raises concern that parents, childcare providers, and preschools may be underestimating infection in seemingly healthy young kids who have been exposed to COVID, wrote lead author Ruth A. Karron, MD, and colleagues in JAMA Network Open.
Methods
The new research involved 690 individuals from 175 households in Maryland who were monitored closely between November 2020 and October 2021. Every week for 8 months, participants completed online symptom checks and underwent PCR testing using nasal swabs, with symptomatic individuals submitting additional swabs for analysis.
“What was different about our study [compared with previous studies] was the intensity of our collection, and the fact that we collected specimens from asymptomatic people,” said Dr. Karron, a pediatrician and professor in the department of international health, Johns Hopkins University, Baltimore, in an interview. “You shed more virus earlier in the infection than later, and the fact that we were sampling every single week meant that we could pick up those early infections.”
The study also stands out for its focus on young children, Dr. Karron said. Enrollment required all households to have at least one child aged 0-4 years, so 256 out of 690 participants (37.1%) were in this youngest age group. The remainder of the population consisted of 100 older children aged 5-17 years (14.5%) and 334 adults aged 18-74 years (48.4%).
Children 4 and under more than twice as likely to be asymptomatic
By the end of the study, 51 participants had tested positive for SARS-CoV-2, among whom 14 had no symptoms. A closer look showed that children 0-4 years of age who contracted COVID were more than twice as likely to be asymptomatic as infected adults (36.8% vs. 14.3%).
The relationship between symptoms and viral load also differed between adults and young children.
While adults with high viral loads – suggesting greater contagiousness – typically had more severe COVID symptoms, no correlation was found in young kids, meaning children with mild or no symptoms could still be highly contagious.
Dr. Karron said these findings should help parents and other stakeholders make better-informed decisions based on known risks. She recommended testing young, asymptomatic children for COVID if they have been exposed to infected individuals, then acting accordingly based on the results.
“If a family is infected with the virus, and the 2-year-old is asymptomatic, and people are thinking about a visit to elderly grandparents who may be frail, one shouldn’t assume that the 2-year-old is uninfected,” Dr. Karron said. “That child should be tested along with other family members.”
Testing should also be considered for young children exposed to COVID at childcare facilities, she added.
But not every expert consulted for this piece shared these opinions of Dr. Karron.
“I question whether that effort is worth it,” said Dean Blumberg, MD, professor and chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, Calif.
He noted that recent Food and Drug Administration guidance for COVID testing calls for three negative at-home antigen tests to confirm lack of infection.
“That would take 4 days to get those tests done,” he said. “So, it’s a lot of testing. It’s a lot of record keeping, it’s inconvenient, it’s uncomfortable to be tested, and I just question whether it’s worth that effort.”
Applicability of findings to today questioned
Dr. Blumberg also questioned whether the study, which was completed almost a year ago, reflects the current pandemic landscape.
“At the time this study was done, it was predominantly Delta [variant instead of Omicron],” Dr. Blumberg said. “The other issue [with the study] is that … most of the children didn’t have preexisting immunity, so you have to take that into account.”
Preexisting immunity – whether from exposure or vaccination – could lower viral loads, so asymptomatic children today really could be less contagious than they were when the study was done, according to Dr. Blumberg. Kids without symptoms are also less likely to spread the virus, because they aren’t coughing or sneezing, he added.
Sara R. Kim, MD, and Janet A. Englund, MD, of the Seattle Children’s Research Institute, University of Washington, said it’s challenging to know how applicable the findings are, although they sided more with the investigators than Dr. Blumberg.
“Given the higher rate of transmissibility and infectivity of the Omicron variant, it is difficult to make direct associations between findings reported during this study period and those present in the current era during which the Omicron variant is circulating,” they wrote in an accompanying editorial. “However, the higher rates of asymptomatic infection observed among children in this study are likely to be consistent with those observed for current and future viral variants.”
Although the experts offered different interpretations of the findings, they shared similar perspectives on vaccination.
“The most important thing that parents can do is get their kids vaccinated, be vaccinated themselves, and have everybody in the household vaccinated and up to date for all doses that are indicated,” Dr. Blumberg said.
Dr. Karron noted that vaccination will be increasingly important in the coming months.
“Summer is ending; school is starting,” she said. “We’re going to be in large groups indoors again very soon. To keep young children safe, I think it’s really important for them to get vaccinated.”
The study was funded by the CDC. The investigators disclosed no other relationships. Dr. Englund disclosed relationships with AstraZeneca, GlaxoSmithKline, Merck, and others. Dr. Kim and Dr. Blumberg disclosed no relevant conflicts of interest.
BY WILL PASS
Just 14% of adults who tested positive for SARS-CoV-2 were asymptomatic, versus 37% of children aged 0-4 years, in the paper. This raises concern that parents, childcare providers, and preschools may be underestimating infection in seemingly healthy young kids who have been exposed to COVID, wrote lead author Ruth A. Karron, MD, and colleagues in JAMA Network Open.
Methods
The new research involved 690 individuals from 175 households in Maryland who were monitored closely between November 2020 and October 2021. Every week for 8 months, participants completed online symptom checks and underwent PCR testing using nasal swabs, with symptomatic individuals submitting additional swabs for analysis.
“What was different about our study [compared with previous studies] was the intensity of our collection, and the fact that we collected specimens from asymptomatic people,” said Dr. Karron, a pediatrician and professor in the department of international health, Johns Hopkins University, Baltimore, in an interview. “You shed more virus earlier in the infection than later, and the fact that we were sampling every single week meant that we could pick up those early infections.”
The study also stands out for its focus on young children, Dr. Karron said. Enrollment required all households to have at least one child aged 0-4 years, so 256 out of 690 participants (37.1%) were in this youngest age group. The remainder of the population consisted of 100 older children aged 5-17 years (14.5%) and 334 adults aged 18-74 years (48.4%).
Children 4 and under more than twice as likely to be asymptomatic
By the end of the study, 51 participants had tested positive for SARS-CoV-2, among whom 14 had no symptoms. A closer look showed that children 0-4 years of age who contracted COVID were more than twice as likely to be asymptomatic as infected adults (36.8% vs. 14.3%).
The relationship between symptoms and viral load also differed between adults and young children.
While adults with high viral loads – suggesting greater contagiousness – typically had more severe COVID symptoms, no correlation was found in young kids, meaning children with mild or no symptoms could still be highly contagious.
Dr. Karron said these findings should help parents and other stakeholders make better-informed decisions based on known risks. She recommended testing young, asymptomatic children for COVID if they have been exposed to infected individuals, then acting accordingly based on the results.
“If a family is infected with the virus, and the 2-year-old is asymptomatic, and people are thinking about a visit to elderly grandparents who may be frail, one shouldn’t assume that the 2-year-old is uninfected,” Dr. Karron said. “That child should be tested along with other family members.”
Testing should also be considered for young children exposed to COVID at childcare facilities, she added.
But not every expert consulted for this piece shared these opinions of Dr. Karron.
“I question whether that effort is worth it,” said Dean Blumberg, MD, professor and chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, Calif.
He noted that recent Food and Drug Administration guidance for COVID testing calls for three negative at-home antigen tests to confirm lack of infection.
“That would take 4 days to get those tests done,” he said. “So, it’s a lot of testing. It’s a lot of record keeping, it’s inconvenient, it’s uncomfortable to be tested, and I just question whether it’s worth that effort.”
Applicability of findings to today questioned
Dr. Blumberg also questioned whether the study, which was completed almost a year ago, reflects the current pandemic landscape.
“At the time this study was done, it was predominantly Delta [variant instead of Omicron],” Dr. Blumberg said. “The other issue [with the study] is that … most of the children didn’t have preexisting immunity, so you have to take that into account.”
Preexisting immunity – whether from exposure or vaccination – could lower viral loads, so asymptomatic children today really could be less contagious than they were when the study was done, according to Dr. Blumberg. Kids without symptoms are also less likely to spread the virus, because they aren’t coughing or sneezing, he added.
Sara R. Kim, MD, and Janet A. Englund, MD, of the Seattle Children’s Research Institute, University of Washington, said it’s challenging to know how applicable the findings are, although they sided more with the investigators than Dr. Blumberg.
“Given the higher rate of transmissibility and infectivity of the Omicron variant, it is difficult to make direct associations between findings reported during this study period and those present in the current era during which the Omicron variant is circulating,” they wrote in an accompanying editorial. “However, the higher rates of asymptomatic infection observed among children in this study are likely to be consistent with those observed for current and future viral variants.”
Although the experts offered different interpretations of the findings, they shared similar perspectives on vaccination.
“The most important thing that parents can do is get their kids vaccinated, be vaccinated themselves, and have everybody in the household vaccinated and up to date for all doses that are indicated,” Dr. Blumberg said.
Dr. Karron noted that vaccination will be increasingly important in the coming months.
“Summer is ending; school is starting,” she said. “We’re going to be in large groups indoors again very soon. To keep young children safe, I think it’s really important for them to get vaccinated.”
The study was funded by the CDC. The investigators disclosed no other relationships. Dr. Englund disclosed relationships with AstraZeneca, GlaxoSmithKline, Merck, and others. Dr. Kim and Dr. Blumberg disclosed no relevant conflicts of interest.
FROM JAMA NETWORK OPEN
Hydroquinone, found in skin-lightening agents worldwide, linked with increased skin cancer risk
an analysis of records from a large research database suggests.
In the study, hydroquinone use was associated with an approximately threefold increase for skin cancer risk, coauthor Brittany Miles, a fourth-year medical student at the University of Texas Medical Branch at Galveston’s John Sealy School of Medicine, told this news organization. “The magnitude of the risk was surprising. Increased risk should be disclosed to patients considering hydroquinone treatment.”
The results of the study were presented in a poster at the annual meeting of the Society for Investigative Dermatology.
Hydroquinone (multiple brand names), a tyrosinase inhibitor used worldwide for skin lightening because of its inhibition of melanin production, was once considered “generally safe and effective” by the Food and Drug Administration, the authors wrote.
The compound’s use in over-the-counter products in the United States has been restricted based on suspicion of carcinogenicity, but few human studies have been conducted. In April, the FDA issued warning letters to 12 companies that sold hydroquinone in concentrations not generally recognized as safe and effective, because of other concerns including rashes, facial swelling, and ochronosis (skin discoloration).
Ms. Miles and her coauthor, Michael Wilkerson, MD, professor and chair of the department of dermatology at UTMB, analyzed data from TriNetX, the medical research database of anonymized medical record information from 61 million patients in 57 large health care organizations, almost all of them in the United States.
The researchers created two cohorts of patients aged 15 years and older with no prior diagnosis of skin cancer: one group had been treated with hydroquinone (medication code 5509 in the TriNetX system), and the other had not been exposed to the drug. Using ICD-10 codes for melanoma, nonmelanoma skin cancer, and all skin cancers, they investigated which groups of people were likely to develop these cancers.
They found that hydroquinone exposure was linked with a significant increase in melanoma (relative risk, 3.0; 95% confidence interval, 1.704-5.281; P < .0001), nonmelanoma skin cancers (RR, 3.6; 95%; CI, 2.815-4.561; P < .0001), and all reported skin cancers combined (relative risk, 3.4; 95% CI, 2.731-4.268; P < .0001)
While “the source of the data and the number of patients in the study are significant strengths,” Ms. Miles said, “the inability to determine how long and how consistently the patients used hydroquinone is likely the biggest weakness.”
Skin lightening is big business and more research is needed
“The U.S. market for skin-lightening agents was approximately 330 million dollars in 2021, and 330,000 prescriptions containing hydroquinone were dispensed in 2019,” Ms. Miles said.
Valencia D. Thomas, MD, professor in the department of dermatology of the University of Texas MD Anderson Cancer Center, Houston, said in an email that over-the-counter skin-lightening products containing low-concentration hydroquinone are in widespread use and are commonly used in populations of color.
“Hydroquinone preparations in higher concentrations are unfortunately also available in the United States,” added Dr. Thomas, who was not involved in the study and referred to the FDA warning letter issued in April.
Only one hydroquinone-containing medication – Tri-Luma at 4% concentration, used to treat melasma – is currently FDA-approved, she said.
The data in the study do not show an increased risk for skin cancer with hydroquinone exposure, but do show “an increased risk of cancer in the TriNetX medication code 5509 hydroquinone exposure group, which does not prove causation,” Dr. Thomas commented.
“Because ‘hydroquinone exposure’ is not defined, it is unclear how TriNetX identified the hydroquinone exposure cohort,” she noted. “Does ‘exposure’ count prescriptions written and potentially not used, the use of hydroquinone products of high concentration not approved by the FDA, or the use of over-the-counter hydroquinone products?
“The strength of this study is its size,” Dr. Thomas acknowledged. “This study is a wonderful starting point to further investigate the ‘hydroquinone exposure’ cohort to determine if hydroquinone is a driver of cancer, or if hydroquinone is itself a confounder.”
These results highlight the need to examine the social determinants of health that may explain increased risk for cancer, including race, geography, and poverty, she added.
“Given the global consumption of hydroquinone, multinational collaboration investigating hydroquinone and cancer data will likely be needed to provide insight into this continuing question,” Dr. Thomas advised.
Christiane Querfeld, MD, PhD, associate professor of dermatology and dermatopathology at City of Hope in Duarte, Calif., agreed that the occurrence of skin cancer following use of hydroquinone is largely understudied.
“The findings have a huge impact on how we counsel and monitor future patients,” Dr. Querfeld, who also was not involved in the study, said in an email. “There may be a trade-off at the start of treatment: Get rid of melasma but develop a skin cancer or melanoma with potentially severe outcomes.
“It remains to be seen if there is a higher incidence of skin cancer following use of hydroquinone or other voluntary bleaching and depigmentation remedies in ethnic groups such as African American or Hispanic patient populations, who have historically been at low risk of developing skin cancer,” she added. “It also remains to be seen if increased risk is due to direct effects or to indirect effects on already-photodamaged skin.
“These data are critical, and I am sure this will open further investigations to study effects in more detail,” Dr. Querfeld said.
The study authors, Dr. Thomas, and Dr. Querfeld reported no relevant financial relationships. The study did not receive external funding.
A version of this article first appeared on Medscape.com.
an analysis of records from a large research database suggests.
In the study, hydroquinone use was associated with an approximately threefold increase for skin cancer risk, coauthor Brittany Miles, a fourth-year medical student at the University of Texas Medical Branch at Galveston’s John Sealy School of Medicine, told this news organization. “The magnitude of the risk was surprising. Increased risk should be disclosed to patients considering hydroquinone treatment.”
The results of the study were presented in a poster at the annual meeting of the Society for Investigative Dermatology.
Hydroquinone (multiple brand names), a tyrosinase inhibitor used worldwide for skin lightening because of its inhibition of melanin production, was once considered “generally safe and effective” by the Food and Drug Administration, the authors wrote.
The compound’s use in over-the-counter products in the United States has been restricted based on suspicion of carcinogenicity, but few human studies have been conducted. In April, the FDA issued warning letters to 12 companies that sold hydroquinone in concentrations not generally recognized as safe and effective, because of other concerns including rashes, facial swelling, and ochronosis (skin discoloration).
Ms. Miles and her coauthor, Michael Wilkerson, MD, professor and chair of the department of dermatology at UTMB, analyzed data from TriNetX, the medical research database of anonymized medical record information from 61 million patients in 57 large health care organizations, almost all of them in the United States.
The researchers created two cohorts of patients aged 15 years and older with no prior diagnosis of skin cancer: one group had been treated with hydroquinone (medication code 5509 in the TriNetX system), and the other had not been exposed to the drug. Using ICD-10 codes for melanoma, nonmelanoma skin cancer, and all skin cancers, they investigated which groups of people were likely to develop these cancers.
They found that hydroquinone exposure was linked with a significant increase in melanoma (relative risk, 3.0; 95% confidence interval, 1.704-5.281; P < .0001), nonmelanoma skin cancers (RR, 3.6; 95%; CI, 2.815-4.561; P < .0001), and all reported skin cancers combined (relative risk, 3.4; 95% CI, 2.731-4.268; P < .0001)
While “the source of the data and the number of patients in the study are significant strengths,” Ms. Miles said, “the inability to determine how long and how consistently the patients used hydroquinone is likely the biggest weakness.”
Skin lightening is big business and more research is needed
“The U.S. market for skin-lightening agents was approximately 330 million dollars in 2021, and 330,000 prescriptions containing hydroquinone were dispensed in 2019,” Ms. Miles said.
Valencia D. Thomas, MD, professor in the department of dermatology of the University of Texas MD Anderson Cancer Center, Houston, said in an email that over-the-counter skin-lightening products containing low-concentration hydroquinone are in widespread use and are commonly used in populations of color.
“Hydroquinone preparations in higher concentrations are unfortunately also available in the United States,” added Dr. Thomas, who was not involved in the study and referred to the FDA warning letter issued in April.
Only one hydroquinone-containing medication – Tri-Luma at 4% concentration, used to treat melasma – is currently FDA-approved, she said.
The data in the study do not show an increased risk for skin cancer with hydroquinone exposure, but do show “an increased risk of cancer in the TriNetX medication code 5509 hydroquinone exposure group, which does not prove causation,” Dr. Thomas commented.
“Because ‘hydroquinone exposure’ is not defined, it is unclear how TriNetX identified the hydroquinone exposure cohort,” she noted. “Does ‘exposure’ count prescriptions written and potentially not used, the use of hydroquinone products of high concentration not approved by the FDA, or the use of over-the-counter hydroquinone products?
“The strength of this study is its size,” Dr. Thomas acknowledged. “This study is a wonderful starting point to further investigate the ‘hydroquinone exposure’ cohort to determine if hydroquinone is a driver of cancer, or if hydroquinone is itself a confounder.”
These results highlight the need to examine the social determinants of health that may explain increased risk for cancer, including race, geography, and poverty, she added.
“Given the global consumption of hydroquinone, multinational collaboration investigating hydroquinone and cancer data will likely be needed to provide insight into this continuing question,” Dr. Thomas advised.
Christiane Querfeld, MD, PhD, associate professor of dermatology and dermatopathology at City of Hope in Duarte, Calif., agreed that the occurrence of skin cancer following use of hydroquinone is largely understudied.
“The findings have a huge impact on how we counsel and monitor future patients,” Dr. Querfeld, who also was not involved in the study, said in an email. “There may be a trade-off at the start of treatment: Get rid of melasma but develop a skin cancer or melanoma with potentially severe outcomes.
“It remains to be seen if there is a higher incidence of skin cancer following use of hydroquinone or other voluntary bleaching and depigmentation remedies in ethnic groups such as African American or Hispanic patient populations, who have historically been at low risk of developing skin cancer,” she added. “It also remains to be seen if increased risk is due to direct effects or to indirect effects on already-photodamaged skin.
“These data are critical, and I am sure this will open further investigations to study effects in more detail,” Dr. Querfeld said.
The study authors, Dr. Thomas, and Dr. Querfeld reported no relevant financial relationships. The study did not receive external funding.
A version of this article first appeared on Medscape.com.
an analysis of records from a large research database suggests.
In the study, hydroquinone use was associated with an approximately threefold increase for skin cancer risk, coauthor Brittany Miles, a fourth-year medical student at the University of Texas Medical Branch at Galveston’s John Sealy School of Medicine, told this news organization. “The magnitude of the risk was surprising. Increased risk should be disclosed to patients considering hydroquinone treatment.”
The results of the study were presented in a poster at the annual meeting of the Society for Investigative Dermatology.
Hydroquinone (multiple brand names), a tyrosinase inhibitor used worldwide for skin lightening because of its inhibition of melanin production, was once considered “generally safe and effective” by the Food and Drug Administration, the authors wrote.
The compound’s use in over-the-counter products in the United States has been restricted based on suspicion of carcinogenicity, but few human studies have been conducted. In April, the FDA issued warning letters to 12 companies that sold hydroquinone in concentrations not generally recognized as safe and effective, because of other concerns including rashes, facial swelling, and ochronosis (skin discoloration).
Ms. Miles and her coauthor, Michael Wilkerson, MD, professor and chair of the department of dermatology at UTMB, analyzed data from TriNetX, the medical research database of anonymized medical record information from 61 million patients in 57 large health care organizations, almost all of them in the United States.
The researchers created two cohorts of patients aged 15 years and older with no prior diagnosis of skin cancer: one group had been treated with hydroquinone (medication code 5509 in the TriNetX system), and the other had not been exposed to the drug. Using ICD-10 codes for melanoma, nonmelanoma skin cancer, and all skin cancers, they investigated which groups of people were likely to develop these cancers.
They found that hydroquinone exposure was linked with a significant increase in melanoma (relative risk, 3.0; 95% confidence interval, 1.704-5.281; P < .0001), nonmelanoma skin cancers (RR, 3.6; 95%; CI, 2.815-4.561; P < .0001), and all reported skin cancers combined (relative risk, 3.4; 95% CI, 2.731-4.268; P < .0001)
While “the source of the data and the number of patients in the study are significant strengths,” Ms. Miles said, “the inability to determine how long and how consistently the patients used hydroquinone is likely the biggest weakness.”
Skin lightening is big business and more research is needed
“The U.S. market for skin-lightening agents was approximately 330 million dollars in 2021, and 330,000 prescriptions containing hydroquinone were dispensed in 2019,” Ms. Miles said.
Valencia D. Thomas, MD, professor in the department of dermatology of the University of Texas MD Anderson Cancer Center, Houston, said in an email that over-the-counter skin-lightening products containing low-concentration hydroquinone are in widespread use and are commonly used in populations of color.
“Hydroquinone preparations in higher concentrations are unfortunately also available in the United States,” added Dr. Thomas, who was not involved in the study and referred to the FDA warning letter issued in April.
Only one hydroquinone-containing medication – Tri-Luma at 4% concentration, used to treat melasma – is currently FDA-approved, she said.
The data in the study do not show an increased risk for skin cancer with hydroquinone exposure, but do show “an increased risk of cancer in the TriNetX medication code 5509 hydroquinone exposure group, which does not prove causation,” Dr. Thomas commented.
“Because ‘hydroquinone exposure’ is not defined, it is unclear how TriNetX identified the hydroquinone exposure cohort,” she noted. “Does ‘exposure’ count prescriptions written and potentially not used, the use of hydroquinone products of high concentration not approved by the FDA, or the use of over-the-counter hydroquinone products?
“The strength of this study is its size,” Dr. Thomas acknowledged. “This study is a wonderful starting point to further investigate the ‘hydroquinone exposure’ cohort to determine if hydroquinone is a driver of cancer, or if hydroquinone is itself a confounder.”
These results highlight the need to examine the social determinants of health that may explain increased risk for cancer, including race, geography, and poverty, she added.
“Given the global consumption of hydroquinone, multinational collaboration investigating hydroquinone and cancer data will likely be needed to provide insight into this continuing question,” Dr. Thomas advised.
Christiane Querfeld, MD, PhD, associate professor of dermatology and dermatopathology at City of Hope in Duarte, Calif., agreed that the occurrence of skin cancer following use of hydroquinone is largely understudied.
“The findings have a huge impact on how we counsel and monitor future patients,” Dr. Querfeld, who also was not involved in the study, said in an email. “There may be a trade-off at the start of treatment: Get rid of melasma but develop a skin cancer or melanoma with potentially severe outcomes.
“It remains to be seen if there is a higher incidence of skin cancer following use of hydroquinone or other voluntary bleaching and depigmentation remedies in ethnic groups such as African American or Hispanic patient populations, who have historically been at low risk of developing skin cancer,” she added. “It also remains to be seen if increased risk is due to direct effects or to indirect effects on already-photodamaged skin.
“These data are critical, and I am sure this will open further investigations to study effects in more detail,” Dr. Querfeld said.
The study authors, Dr. Thomas, and Dr. Querfeld reported no relevant financial relationships. The study did not receive external funding.
A version of this article first appeared on Medscape.com.
FROM SID 2022