User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Promising leads to crack long COVID discovered
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
Potential new neuromodulation treatment for migraines
Most people avoid smartphones when they have a migraine headache, but a noninvasive treatment for episodic migraines may change that.
that can help ease migraine pain.
Tina Montgomery, 58, has suffered from migraines since childhood and spent years looking for something to help manage them. Doctors consider her a “chronic” sufferer in that she has more than 14 migraines a month (fewer than 14 is considered “episodic”). Prescription antidepressants, anticonvulsants, and botulinum toxin shots as preventive treatments helped a little but not enough.
A few years ago, she found some relief using a new preventive injectable medication that targets a peptide known as CGRP, combined with an oral CGRP rescue medication, ubrogepant (Ubrelvy). However, by early 2021, Ms. Montgomery’s chronic migraines were back as she faced stress from the pandemic and her role as a caregiver for her aging parents.
“I was going through so much medication. I just didn’t feel good taking so much,” she said.
Looking for relief, she read about Nerivio, a wearable migraine treatment device that uses remote electrical neuromodulation (REN). She mentioned the device to her neurologist, and he agreed she might benefit from trying it out. Today, she uses the device whenever she feels a migraine may be imminent, she said.
“It really helps me stave off migraines I feel coming on and the milder ones where I would normally hesitate to use prescription medication because [insurance] limits the number of pills they give you in a month,” she said. “I follow through with the Nerivio treatment and usually find that my migraine doesn’t fully develop or is completely gone, and I don’t get a migraine at all.”
Taking it on the arm
The device works by stimulating nerves at the back of the arm right around the triceps. “Those nerve fibers relay information to the brain stem [so it can] work its magic and use the brain’s own natural mechanisms for reducing pain,” said Brian M. Grosberg, MD, director of the Hartford Healthcare Ayer Neuroscience Institute Headache Center, West Hartford, Conn.
These mechanisms are like a bait-and-switch for the brain, said Britany Klenofsky, MD, assistant professor of neurology, Icahn School of Medicine at Mount Sinai, New York. “You’re trying to stimulate pain somewhere else [on the body] to tell the brain to protect itself and release [the neurotransmitter] serotonin,” she said. “You do this by putting the device on your arm, an area that’s away from the head where the pain is actively occurring, turning the device on, and increasing the stimulation to a nearly painful stimulus.”
This pseudo pain prompts the brain to release serotonin, the feel-good hormone along with norepinephrine and noradrenaline. The device works best when it’s used as soon as a migraine starts, so patients should hook up Nerivio within the first 20-30 minutes of onset of pain, said Dr. Grosberg, who was an investigator on the double-blind treatment study that led to FDA clearance. If patients wait too long, the device may not work.
This is why as soon as Ms. Montgomery feels a migraine aura (there are six types of migraine auras, including visual changes and muscle weakness) that occurs right before a migraine strikes, she puts the device armband on her upper arm and launches its smartphone app. Then she turns on the device for a 45-minute treatment, which begins with what she characterizes as tingling and vibration sensations on her arm. She turns up the intensity of the sensations, which are mild electric currents, until they are well-felt but not painful.
Ms. Montgomery said she can use the device and multitask since there’s no need for her to lie down or sit in a darkened room. And since it is worn on the arm, she can wear it under a shirtsleeve while working or out in public without anyone noticing. She also uses the app’s migraine diary and guided meditation to help reduce the anxiety that often accompanies her migraines.
The device is approved for adolescents and adults and can be used for both episodic and chronic migraines. From an efficacy standpoint, the device provides relief about as well as a commonly used pharmaceutical class of drugs, triptans. About 37% of people with episodic migraine achieved complete freedom from pain 2 hours after their treatment. In addition, about two-thirds of people reported pain relief after 2 hours, which is better success than people find with many prescription and nonprescription drugs.
A separate study looked at acute treatment for chronic migraine sufferers and found nearly 60% of people using the device found relief and 21% said they were pain-free after 2 hours. Almost two-thirds of those who experienced pain relief were pain-free 24 hours after the treatment.
Finding the perfect patient
There are other FDA-cleared noninvasive devices to treat migraines. One device, CEFALY, is an external trigeminal nerve stimulation device that sits on the forehead. Another device, SpringTMS, uses transcranial magnetic stimulation on the back of the head. A third option, the gammaCore Sapphire, is placed on the neck to stimulate the vagus nerve. All three have been cleared by the FDA to work as preventive and acute treatments for migraine.
Theranica, the company that developed Nerivio, is trying to boost use of the device by allowing patients to get a prescription via telehealth visits with a physician.
The company, as well as the companies behind the other neuromodulation devices, are marketing their treatments to children ages 12 and up since nonpharmacologic options are often preferable for parents, said Thomas Berk, MD, a clinical associate professor in the division of headache at NYU Langone Health in New York.
Dr. Berk said the devices could be appealing for those people who don’t want or can’t take medication, such as pregnant women or those who don’t respond well to drugs. “[They] could also be used by somebody who needs something in addition to a medication,” he said.
For now, people like Ms. Montgomery say they are happy to have another tool in their migraine arsenal. “Overall, I’m taking less medication because I haven’t had to have my Ubrelvy refilled as often as I used to,” she said. “It’s really helped me manage changes and stresses in my life.”
A version of this article first appeared on Medscape.com.
Most people avoid smartphones when they have a migraine headache, but a noninvasive treatment for episodic migraines may change that.
that can help ease migraine pain.
Tina Montgomery, 58, has suffered from migraines since childhood and spent years looking for something to help manage them. Doctors consider her a “chronic” sufferer in that she has more than 14 migraines a month (fewer than 14 is considered “episodic”). Prescription antidepressants, anticonvulsants, and botulinum toxin shots as preventive treatments helped a little but not enough.
A few years ago, she found some relief using a new preventive injectable medication that targets a peptide known as CGRP, combined with an oral CGRP rescue medication, ubrogepant (Ubrelvy). However, by early 2021, Ms. Montgomery’s chronic migraines were back as she faced stress from the pandemic and her role as a caregiver for her aging parents.
“I was going through so much medication. I just didn’t feel good taking so much,” she said.
Looking for relief, she read about Nerivio, a wearable migraine treatment device that uses remote electrical neuromodulation (REN). She mentioned the device to her neurologist, and he agreed she might benefit from trying it out. Today, she uses the device whenever she feels a migraine may be imminent, she said.
“It really helps me stave off migraines I feel coming on and the milder ones where I would normally hesitate to use prescription medication because [insurance] limits the number of pills they give you in a month,” she said. “I follow through with the Nerivio treatment and usually find that my migraine doesn’t fully develop or is completely gone, and I don’t get a migraine at all.”
Taking it on the arm
The device works by stimulating nerves at the back of the arm right around the triceps. “Those nerve fibers relay information to the brain stem [so it can] work its magic and use the brain’s own natural mechanisms for reducing pain,” said Brian M. Grosberg, MD, director of the Hartford Healthcare Ayer Neuroscience Institute Headache Center, West Hartford, Conn.
These mechanisms are like a bait-and-switch for the brain, said Britany Klenofsky, MD, assistant professor of neurology, Icahn School of Medicine at Mount Sinai, New York. “You’re trying to stimulate pain somewhere else [on the body] to tell the brain to protect itself and release [the neurotransmitter] serotonin,” she said. “You do this by putting the device on your arm, an area that’s away from the head where the pain is actively occurring, turning the device on, and increasing the stimulation to a nearly painful stimulus.”
This pseudo pain prompts the brain to release serotonin, the feel-good hormone along with norepinephrine and noradrenaline. The device works best when it’s used as soon as a migraine starts, so patients should hook up Nerivio within the first 20-30 minutes of onset of pain, said Dr. Grosberg, who was an investigator on the double-blind treatment study that led to FDA clearance. If patients wait too long, the device may not work.
This is why as soon as Ms. Montgomery feels a migraine aura (there are six types of migraine auras, including visual changes and muscle weakness) that occurs right before a migraine strikes, she puts the device armband on her upper arm and launches its smartphone app. Then she turns on the device for a 45-minute treatment, which begins with what she characterizes as tingling and vibration sensations on her arm. She turns up the intensity of the sensations, which are mild electric currents, until they are well-felt but not painful.
Ms. Montgomery said she can use the device and multitask since there’s no need for her to lie down or sit in a darkened room. And since it is worn on the arm, she can wear it under a shirtsleeve while working or out in public without anyone noticing. She also uses the app’s migraine diary and guided meditation to help reduce the anxiety that often accompanies her migraines.
The device is approved for adolescents and adults and can be used for both episodic and chronic migraines. From an efficacy standpoint, the device provides relief about as well as a commonly used pharmaceutical class of drugs, triptans. About 37% of people with episodic migraine achieved complete freedom from pain 2 hours after their treatment. In addition, about two-thirds of people reported pain relief after 2 hours, which is better success than people find with many prescription and nonprescription drugs.
A separate study looked at acute treatment for chronic migraine sufferers and found nearly 60% of people using the device found relief and 21% said they were pain-free after 2 hours. Almost two-thirds of those who experienced pain relief were pain-free 24 hours after the treatment.
Finding the perfect patient
There are other FDA-cleared noninvasive devices to treat migraines. One device, CEFALY, is an external trigeminal nerve stimulation device that sits on the forehead. Another device, SpringTMS, uses transcranial magnetic stimulation on the back of the head. A third option, the gammaCore Sapphire, is placed on the neck to stimulate the vagus nerve. All three have been cleared by the FDA to work as preventive and acute treatments for migraine.
Theranica, the company that developed Nerivio, is trying to boost use of the device by allowing patients to get a prescription via telehealth visits with a physician.
The company, as well as the companies behind the other neuromodulation devices, are marketing their treatments to children ages 12 and up since nonpharmacologic options are often preferable for parents, said Thomas Berk, MD, a clinical associate professor in the division of headache at NYU Langone Health in New York.
Dr. Berk said the devices could be appealing for those people who don’t want or can’t take medication, such as pregnant women or those who don’t respond well to drugs. “[They] could also be used by somebody who needs something in addition to a medication,” he said.
For now, people like Ms. Montgomery say they are happy to have another tool in their migraine arsenal. “Overall, I’m taking less medication because I haven’t had to have my Ubrelvy refilled as often as I used to,” she said. “It’s really helped me manage changes and stresses in my life.”
A version of this article first appeared on Medscape.com.
Most people avoid smartphones when they have a migraine headache, but a noninvasive treatment for episodic migraines may change that.
that can help ease migraine pain.
Tina Montgomery, 58, has suffered from migraines since childhood and spent years looking for something to help manage them. Doctors consider her a “chronic” sufferer in that she has more than 14 migraines a month (fewer than 14 is considered “episodic”). Prescription antidepressants, anticonvulsants, and botulinum toxin shots as preventive treatments helped a little but not enough.
A few years ago, she found some relief using a new preventive injectable medication that targets a peptide known as CGRP, combined with an oral CGRP rescue medication, ubrogepant (Ubrelvy). However, by early 2021, Ms. Montgomery’s chronic migraines were back as she faced stress from the pandemic and her role as a caregiver for her aging parents.
“I was going through so much medication. I just didn’t feel good taking so much,” she said.
Looking for relief, she read about Nerivio, a wearable migraine treatment device that uses remote electrical neuromodulation (REN). She mentioned the device to her neurologist, and he agreed she might benefit from trying it out. Today, she uses the device whenever she feels a migraine may be imminent, she said.
“It really helps me stave off migraines I feel coming on and the milder ones where I would normally hesitate to use prescription medication because [insurance] limits the number of pills they give you in a month,” she said. “I follow through with the Nerivio treatment and usually find that my migraine doesn’t fully develop or is completely gone, and I don’t get a migraine at all.”
Taking it on the arm
The device works by stimulating nerves at the back of the arm right around the triceps. “Those nerve fibers relay information to the brain stem [so it can] work its magic and use the brain’s own natural mechanisms for reducing pain,” said Brian M. Grosberg, MD, director of the Hartford Healthcare Ayer Neuroscience Institute Headache Center, West Hartford, Conn.
These mechanisms are like a bait-and-switch for the brain, said Britany Klenofsky, MD, assistant professor of neurology, Icahn School of Medicine at Mount Sinai, New York. “You’re trying to stimulate pain somewhere else [on the body] to tell the brain to protect itself and release [the neurotransmitter] serotonin,” she said. “You do this by putting the device on your arm, an area that’s away from the head where the pain is actively occurring, turning the device on, and increasing the stimulation to a nearly painful stimulus.”
This pseudo pain prompts the brain to release serotonin, the feel-good hormone along with norepinephrine and noradrenaline. The device works best when it’s used as soon as a migraine starts, so patients should hook up Nerivio within the first 20-30 minutes of onset of pain, said Dr. Grosberg, who was an investigator on the double-blind treatment study that led to FDA clearance. If patients wait too long, the device may not work.
This is why as soon as Ms. Montgomery feels a migraine aura (there are six types of migraine auras, including visual changes and muscle weakness) that occurs right before a migraine strikes, she puts the device armband on her upper arm and launches its smartphone app. Then she turns on the device for a 45-minute treatment, which begins with what she characterizes as tingling and vibration sensations on her arm. She turns up the intensity of the sensations, which are mild electric currents, until they are well-felt but not painful.
Ms. Montgomery said she can use the device and multitask since there’s no need for her to lie down or sit in a darkened room. And since it is worn on the arm, she can wear it under a shirtsleeve while working or out in public without anyone noticing. She also uses the app’s migraine diary and guided meditation to help reduce the anxiety that often accompanies her migraines.
The device is approved for adolescents and adults and can be used for both episodic and chronic migraines. From an efficacy standpoint, the device provides relief about as well as a commonly used pharmaceutical class of drugs, triptans. About 37% of people with episodic migraine achieved complete freedom from pain 2 hours after their treatment. In addition, about two-thirds of people reported pain relief after 2 hours, which is better success than people find with many prescription and nonprescription drugs.
A separate study looked at acute treatment for chronic migraine sufferers and found nearly 60% of people using the device found relief and 21% said they were pain-free after 2 hours. Almost two-thirds of those who experienced pain relief were pain-free 24 hours after the treatment.
Finding the perfect patient
There are other FDA-cleared noninvasive devices to treat migraines. One device, CEFALY, is an external trigeminal nerve stimulation device that sits on the forehead. Another device, SpringTMS, uses transcranial magnetic stimulation on the back of the head. A third option, the gammaCore Sapphire, is placed on the neck to stimulate the vagus nerve. All three have been cleared by the FDA to work as preventive and acute treatments for migraine.
Theranica, the company that developed Nerivio, is trying to boost use of the device by allowing patients to get a prescription via telehealth visits with a physician.
The company, as well as the companies behind the other neuromodulation devices, are marketing their treatments to children ages 12 and up since nonpharmacologic options are often preferable for parents, said Thomas Berk, MD, a clinical associate professor in the division of headache at NYU Langone Health in New York.
Dr. Berk said the devices could be appealing for those people who don’t want or can’t take medication, such as pregnant women or those who don’t respond well to drugs. “[They] could also be used by somebody who needs something in addition to a medication,” he said.
For now, people like Ms. Montgomery say they are happy to have another tool in their migraine arsenal. “Overall, I’m taking less medication because I haven’t had to have my Ubrelvy refilled as often as I used to,” she said. “It’s really helped me manage changes and stresses in my life.”
A version of this article first appeared on Medscape.com.
Endocrine Society and others to FDA: Restrict BPA
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
Cystic fibrosis in retreat, but still unbeaten
In 1938, the year that cystic fibrosis (CF) was first described clinically, four of five children born with the disease did not live past their first birthdays.
In 2019, the median age at death for patients enrolled in the Cystic Fibrosis Foundation (CFF) registry was 32 years, and the predicted life expectancy for patients with CF who were born from 2015 through 2019 was 46 years.
Those numbers reflect the remarkable progress made in the past 4 decades in the care of patients with CF, but also highlight the obstacles ahead, given that the predicted life expectancy for the overall U.S. population in 2019 (pre–COVID-19) was 78.9 years.
Julie Desch, MD, is a CF survivor who has beaten the odds and then some. At age 61, the retired surgical pathologist is a CF patient advocate, speaker, and a board member of the Cystic Fibrosis Research Institute, a not-for-profit organization that funds CF research and offers education, advocacy, and psychosocial support for persons with CF and their families and caregivers.
In an interview, Dr. Desch said that while there has been remarkable progress in her lifetime in the field of CF research and treatment, particularly in the development of drugs that modulate function of the underlying cause of approximately 90% of CF cases, there are still many CF patients who cannot benefit from these therapies.
“There are still 10% of people who don’t make a protein to be modified, so that’s a huge unmet need,” she said.
Genetic disorder
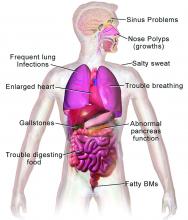
CF is a chronic autosomal recessive disorder with multiorgan and multisystem manifestations. It is caused by mutations in the CFTR gene, which codes for the protein CF transmembrane conductance regulator. CFTR controls transport of chloride ions across cell membranes, specifically the apical membrane of epithelial cells in tissues of the airways, intestinal tract, pancreas, kidneys, sweat glands, and the reproductive system, notably the vas deferens in males.
The F508 deletion (F508del) mutation is the most common, occurring in approximately 70% of persons with CF. It is a class 2-type protein processing mutation, leading to defects in cellular processing, protein stability, and chloride channel gating defects.
The CFTR protein also secretes bicarbonate to regulate the pH of airway surface liquid, and inhibits the epithelial sodium channel, which mediates passive sodium transport across apical membranes of sodium-absorbing epithelial cells in the kidneys, intestine, and airways.
CF typically presents with the buildup in the lungs of abnormally viscous and sticky mucus leading to frequent, severe infections, particularly with Pseudomonas aeruginosa, progressive lung damage and, prior to the development of effective disease management, to premature death. The phenotype often includes malnutrition due to malabsorption, and failure to thrive.
Diagnosis
In all 50 U.S. states and the District of Columbia, newborns are screened for CF with an assay for immunoreactive trypsinogen (IRT) an indirect marker for pancreatic injury that is elevated in serum in most newborns with CF, but also detected in premature infants or those delivered under stressful circumstances. In some states newborns are tested only for IRT, with a diagnosis confirmed with a sweat chloride test and/or a CFTR mutation panel.
Treatment
There is no cure for CF, but the discovery of the gene in 1989 by Canadian and U.S. investigators has led to life-prolonging therapeutic interventions, specifically the development of CFTR modulators.
CFTR modulators include potentiators such as ivacaftor (Kalydeco), and correctors such as lumacaftor and tezacaftor (available in the combination Orkambi), and most recently in the triple combination of elexacaftor, tezacaftor, and ivacaftor (Trikafta; ETI).
Neil Sweezey, MD, FRCPC, a CF expert at The Hospital for Sick Children (SickKids) in Toronto, told this news organization that the ideal therapy for CF, genetic correction of the underlying mutations, is still not feasible, but that CFTR modulators are a close second.
“For 90% of patients, the three-drug combination Trikafta has been shown to be quite safe, quite tolerable, and quite remarkably beneficial,” he said.
In a study reported at CHEST 2021 by investigators from Nationwide Children’s Hospital in Columbus, Ohio, 32 adults who were started on the triple combination had significantly improved in forced expiratory volume in 1 second (FEV1), gain in body mass index, decreased sweat chloride and decreased colonization by Pseudomonas species. In addition, patients had significant improvements in blood inflammatory markers.
Christopher H. Goss, MD, FCCP, professor of pulmonary critical care and sleep medicine and professor of pediatrics at the University of Washington in Seattle, agreed that with the availability of the triple combination, “these are extraordinary times. An astounding fact is that most patients have complete resolution of cough, and the exacerbation rates have just plummeted,” he said in an interview.
Some of the reductions in exacerbations may be attributable to the COVID-19 pandemic, he noted, because patients in isolation have less exposure to circulating respiratory viruses.
“But it has been miraculous, and the clinical effect is certainly still more astounding than the effects of ivacaftor, which was the first truly breakthrough drug. Weight goes up, well-being increases, and the population lung function has shifted up to better grade lung function, in the entire population,” he said.
In addition, the need for lung and heart transplantation has sharply declined.
“I had a patient who had decided to forgo transplantation, despite absolutely horrible lung function, and he’s now bowling and leading a very productive life, when before he had been preparing for end of life,” Dr. Goss said.
Dr. Sweezey emphasized that as with all medications, patients being started on the triple combination require close monitoring for potential adverse events that might require dose modification or, for a small number of patients, withdrawal.
Burden of care
CFTR modulators have reduced but not eliminated the need for some patients to have mucolytic therapy, which may include dornase alfa, a recombinant human deoxyribonuclease (DNase) that reduces the viscosity of lung secretions, hypertonic saline inhaled twice daily (for patients 12 and older), mannitol, and physical manipulations to help patients clear mucus. This can include both manual percussion and the use of devices for high-frequency chest wall oscillation.
The complex nature of CF often requires a combination of other therapies to address comorbidities. These therapies may include infection prophylaxis and treatment with antibiotics and antifungals, nutrition support, and therapy for CF-related complications, including gastrointestinal issues, liver diseases, diabetes, and osteopenia that may be related to poor nutrient absorption, chronic inflammation, or other sequelae of CF.
In addition, patients often require frequent CF care center visits – ideally a minimum of every 3 months – which can result in significant loss of work or school time.
“Outcomes for patients in the long run have been absolutely proven to be best if they’re followed in big, established, multidisciplinary well-organized CF centers,” Dr. Sweezey said. “In the United States and Canada if you’re looked after on a regular basis, which means quarterly, every 3 months – whether you need it or not, you really do need it – and if the patients are seen and assessed and checked every 3 months all of their lives, they have small changes caught early, whether it’s an infection you can slap down with medication or a nutrition problem that may be affecting a child’s growth and development.”
“We’re really kind of at a pivotal moment in CF, where we realize things are changing,” said A. Whitney Brown, MD, senior director for clinical affairs at the Cystic Fibrosis Foundation, and an adult CF and lung transplant physician in the Inova Advanced Lung Disease Program in Falls Church, Va.
“Patient needs and interest have evolved, because of the pandemic and because of the highly effective modulator therapy, but we want to take great effort to study it in a rigorous way, to make sure that as we are agile and adapt the care model, that we can maintain the same quality outcomes that we have traditionally done,” she said in an interview.
The Lancet Respiratory Medicine Commission on the future of CF care states that models of care “need to consider management approaches (including disease monitoring) to maintain health and delay lung transplantation, while minimizing the burden of care for patients and their families.”
‘A great problem to have’
One of the most significant changes in CF care has been the growing population of CF patients like Dr. Desch who are living well into adulthood, with some approaching Medicare eligibility.
With the advent of triple therapy and CFTR modulators being started earlier in life, lung function can be preserved, damage to other organs can be minimized, and life expectancy for patients with CF will continue to improve.
“We’re anticipating that there may be some needs in the aging CF population that are different than what we have historically had,” Dr. Brown said. “Will there be geriatric providers that need to become experts in CF care? That’s a great problem to have,” she said.
Dr. Goss agreed, noting that CF is steadily shifting from a near uniformly fatal disease to a chronic disorder that in many cases can be managed “with a complex regimen of novel drugs, much like HIV.”
He noted that there are multiple drug interactions with the triple combination, “so it’s really important that people don’t start a CF patient on a drug without consulting a pharmacist, because you can totally inactivate ETI, or augment it dramatically, and we’ve seen both happen.”
Cost and access
All experts interviewed for this article agreed that while the care of patients with CF has improved exponentially over the last few decades, there are still troubling inequities in care.
One of the largest impediments is the cost of care, with the triple combination costing more than $300,000 per year.
“Clearly patients aren’t paying that, but insurance companies are, and that’s causing all kinds of trickle-down effects that definitely affect patients. The patients like myself who are able to have insurance that covers it benefit, but there are so many people that don’t,” Dr. Desch said.
Dr. Sweezey noted that prior to the advent of ETI, patients with CF in Canada had better outcomes and longer life expectancy than did similar patients in the United States because of universal access to care and coordinated services under Canada’s health care system, compared with the highly fragmented and inefficient U.S. system. He added that the wider availability of ETI in the United States vs. Canada may begin to narrow that gap, however.
As noted before, there is a substantial proportion of patients – an estimated 10% – who have CFTR mutations that are not correctable by currently available CFTR modulators, and these patients are at significant risk for irreversible airway complications and lung damage.
In addition, although CF occurs most frequently among people of White ancestry, the disease does not respect distinctions of race or ethnicity.
“It’s not just [Whites] – a lot of people from different racial backgrounds, ethnic backgrounds, are not being diagnosed or are not being diagnosed soon enough to have effective care early enough,” Dr. Desch said.
That statement is supported by the Lancet Respiratory Medicine Commission on the future of cystic fibrosis care, whose members noted in 2019 that “epidemiological studies in the past 2 decades have shown that cystic fibrosis occurs and is more frequent than was previously thought in populations of non-European descent, and the disease is now recognized in many regions of the world.”
The commission members noted that the costs of adequate CF care may be beyond the reach of many patients in developing nations.
Still, if the substantial barriers of cost and access can be overcome, the future will continue to look brighter for patients with CF. As Dr. Sweezey put it: “There are studies that are pushing lower age limits for using these modulators, and as the evidence builds for the efficacy and safety at younger ages, I think all of us are hoping that we’ll end up being able to use either the current or future modulators to actually prevent trouble in CF, rather than trying to come along and fix it after it’s been there.”
Dr. Brown disclosed advisory board activity for Vertex that ended prior to her joining the CF Foundation. Dr. Desch, Dr. Goss, and Dr. Sweezey reported no relevant conflicts of interest.
In 1938, the year that cystic fibrosis (CF) was first described clinically, four of five children born with the disease did not live past their first birthdays.
In 2019, the median age at death for patients enrolled in the Cystic Fibrosis Foundation (CFF) registry was 32 years, and the predicted life expectancy for patients with CF who were born from 2015 through 2019 was 46 years.
Those numbers reflect the remarkable progress made in the past 4 decades in the care of patients with CF, but also highlight the obstacles ahead, given that the predicted life expectancy for the overall U.S. population in 2019 (pre–COVID-19) was 78.9 years.
Julie Desch, MD, is a CF survivor who has beaten the odds and then some. At age 61, the retired surgical pathologist is a CF patient advocate, speaker, and a board member of the Cystic Fibrosis Research Institute, a not-for-profit organization that funds CF research and offers education, advocacy, and psychosocial support for persons with CF and their families and caregivers.
In an interview, Dr. Desch said that while there has been remarkable progress in her lifetime in the field of CF research and treatment, particularly in the development of drugs that modulate function of the underlying cause of approximately 90% of CF cases, there are still many CF patients who cannot benefit from these therapies.
“There are still 10% of people who don’t make a protein to be modified, so that’s a huge unmet need,” she said.
Genetic disorder
CF is a chronic autosomal recessive disorder with multiorgan and multisystem manifestations. It is caused by mutations in the CFTR gene, which codes for the protein CF transmembrane conductance regulator. CFTR controls transport of chloride ions across cell membranes, specifically the apical membrane of epithelial cells in tissues of the airways, intestinal tract, pancreas, kidneys, sweat glands, and the reproductive system, notably the vas deferens in males.
The F508 deletion (F508del) mutation is the most common, occurring in approximately 70% of persons with CF. It is a class 2-type protein processing mutation, leading to defects in cellular processing, protein stability, and chloride channel gating defects.
The CFTR protein also secretes bicarbonate to regulate the pH of airway surface liquid, and inhibits the epithelial sodium channel, which mediates passive sodium transport across apical membranes of sodium-absorbing epithelial cells in the kidneys, intestine, and airways.
CF typically presents with the buildup in the lungs of abnormally viscous and sticky mucus leading to frequent, severe infections, particularly with Pseudomonas aeruginosa, progressive lung damage and, prior to the development of effective disease management, to premature death. The phenotype often includes malnutrition due to malabsorption, and failure to thrive.
Diagnosis
In all 50 U.S. states and the District of Columbia, newborns are screened for CF with an assay for immunoreactive trypsinogen (IRT) an indirect marker for pancreatic injury that is elevated in serum in most newborns with CF, but also detected in premature infants or those delivered under stressful circumstances. In some states newborns are tested only for IRT, with a diagnosis confirmed with a sweat chloride test and/or a CFTR mutation panel.
Treatment
There is no cure for CF, but the discovery of the gene in 1989 by Canadian and U.S. investigators has led to life-prolonging therapeutic interventions, specifically the development of CFTR modulators.
CFTR modulators include potentiators such as ivacaftor (Kalydeco), and correctors such as lumacaftor and tezacaftor (available in the combination Orkambi), and most recently in the triple combination of elexacaftor, tezacaftor, and ivacaftor (Trikafta; ETI).
Neil Sweezey, MD, FRCPC, a CF expert at The Hospital for Sick Children (SickKids) in Toronto, told this news organization that the ideal therapy for CF, genetic correction of the underlying mutations, is still not feasible, but that CFTR modulators are a close second.
“For 90% of patients, the three-drug combination Trikafta has been shown to be quite safe, quite tolerable, and quite remarkably beneficial,” he said.
In a study reported at CHEST 2021 by investigators from Nationwide Children’s Hospital in Columbus, Ohio, 32 adults who were started on the triple combination had significantly improved in forced expiratory volume in 1 second (FEV1), gain in body mass index, decreased sweat chloride and decreased colonization by Pseudomonas species. In addition, patients had significant improvements in blood inflammatory markers.
Christopher H. Goss, MD, FCCP, professor of pulmonary critical care and sleep medicine and professor of pediatrics at the University of Washington in Seattle, agreed that with the availability of the triple combination, “these are extraordinary times. An astounding fact is that most patients have complete resolution of cough, and the exacerbation rates have just plummeted,” he said in an interview.
Some of the reductions in exacerbations may be attributable to the COVID-19 pandemic, he noted, because patients in isolation have less exposure to circulating respiratory viruses.
“But it has been miraculous, and the clinical effect is certainly still more astounding than the effects of ivacaftor, which was the first truly breakthrough drug. Weight goes up, well-being increases, and the population lung function has shifted up to better grade lung function, in the entire population,” he said.
In addition, the need for lung and heart transplantation has sharply declined.
“I had a patient who had decided to forgo transplantation, despite absolutely horrible lung function, and he’s now bowling and leading a very productive life, when before he had been preparing for end of life,” Dr. Goss said.
Dr. Sweezey emphasized that as with all medications, patients being started on the triple combination require close monitoring for potential adverse events that might require dose modification or, for a small number of patients, withdrawal.
Burden of care
CFTR modulators have reduced but not eliminated the need for some patients to have mucolytic therapy, which may include dornase alfa, a recombinant human deoxyribonuclease (DNase) that reduces the viscosity of lung secretions, hypertonic saline inhaled twice daily (for patients 12 and older), mannitol, and physical manipulations to help patients clear mucus. This can include both manual percussion and the use of devices for high-frequency chest wall oscillation.
The complex nature of CF often requires a combination of other therapies to address comorbidities. These therapies may include infection prophylaxis and treatment with antibiotics and antifungals, nutrition support, and therapy for CF-related complications, including gastrointestinal issues, liver diseases, diabetes, and osteopenia that may be related to poor nutrient absorption, chronic inflammation, or other sequelae of CF.
In addition, patients often require frequent CF care center visits – ideally a minimum of every 3 months – which can result in significant loss of work or school time.
“Outcomes for patients in the long run have been absolutely proven to be best if they’re followed in big, established, multidisciplinary well-organized CF centers,” Dr. Sweezey said. “In the United States and Canada if you’re looked after on a regular basis, which means quarterly, every 3 months – whether you need it or not, you really do need it – and if the patients are seen and assessed and checked every 3 months all of their lives, they have small changes caught early, whether it’s an infection you can slap down with medication or a nutrition problem that may be affecting a child’s growth and development.”
“We’re really kind of at a pivotal moment in CF, where we realize things are changing,” said A. Whitney Brown, MD, senior director for clinical affairs at the Cystic Fibrosis Foundation, and an adult CF and lung transplant physician in the Inova Advanced Lung Disease Program in Falls Church, Va.
“Patient needs and interest have evolved, because of the pandemic and because of the highly effective modulator therapy, but we want to take great effort to study it in a rigorous way, to make sure that as we are agile and adapt the care model, that we can maintain the same quality outcomes that we have traditionally done,” she said in an interview.
The Lancet Respiratory Medicine Commission on the future of CF care states that models of care “need to consider management approaches (including disease monitoring) to maintain health and delay lung transplantation, while minimizing the burden of care for patients and their families.”
‘A great problem to have’
One of the most significant changes in CF care has been the growing population of CF patients like Dr. Desch who are living well into adulthood, with some approaching Medicare eligibility.
With the advent of triple therapy and CFTR modulators being started earlier in life, lung function can be preserved, damage to other organs can be minimized, and life expectancy for patients with CF will continue to improve.
“We’re anticipating that there may be some needs in the aging CF population that are different than what we have historically had,” Dr. Brown said. “Will there be geriatric providers that need to become experts in CF care? That’s a great problem to have,” she said.
Dr. Goss agreed, noting that CF is steadily shifting from a near uniformly fatal disease to a chronic disorder that in many cases can be managed “with a complex regimen of novel drugs, much like HIV.”
He noted that there are multiple drug interactions with the triple combination, “so it’s really important that people don’t start a CF patient on a drug without consulting a pharmacist, because you can totally inactivate ETI, or augment it dramatically, and we’ve seen both happen.”
Cost and access
All experts interviewed for this article agreed that while the care of patients with CF has improved exponentially over the last few decades, there are still troubling inequities in care.
One of the largest impediments is the cost of care, with the triple combination costing more than $300,000 per year.
“Clearly patients aren’t paying that, but insurance companies are, and that’s causing all kinds of trickle-down effects that definitely affect patients. The patients like myself who are able to have insurance that covers it benefit, but there are so many people that don’t,” Dr. Desch said.
Dr. Sweezey noted that prior to the advent of ETI, patients with CF in Canada had better outcomes and longer life expectancy than did similar patients in the United States because of universal access to care and coordinated services under Canada’s health care system, compared with the highly fragmented and inefficient U.S. system. He added that the wider availability of ETI in the United States vs. Canada may begin to narrow that gap, however.
As noted before, there is a substantial proportion of patients – an estimated 10% – who have CFTR mutations that are not correctable by currently available CFTR modulators, and these patients are at significant risk for irreversible airway complications and lung damage.
In addition, although CF occurs most frequently among people of White ancestry, the disease does not respect distinctions of race or ethnicity.
“It’s not just [Whites] – a lot of people from different racial backgrounds, ethnic backgrounds, are not being diagnosed or are not being diagnosed soon enough to have effective care early enough,” Dr. Desch said.
That statement is supported by the Lancet Respiratory Medicine Commission on the future of cystic fibrosis care, whose members noted in 2019 that “epidemiological studies in the past 2 decades have shown that cystic fibrosis occurs and is more frequent than was previously thought in populations of non-European descent, and the disease is now recognized in many regions of the world.”
The commission members noted that the costs of adequate CF care may be beyond the reach of many patients in developing nations.
Still, if the substantial barriers of cost and access can be overcome, the future will continue to look brighter for patients with CF. As Dr. Sweezey put it: “There are studies that are pushing lower age limits for using these modulators, and as the evidence builds for the efficacy and safety at younger ages, I think all of us are hoping that we’ll end up being able to use either the current or future modulators to actually prevent trouble in CF, rather than trying to come along and fix it after it’s been there.”
Dr. Brown disclosed advisory board activity for Vertex that ended prior to her joining the CF Foundation. Dr. Desch, Dr. Goss, and Dr. Sweezey reported no relevant conflicts of interest.
In 1938, the year that cystic fibrosis (CF) was first described clinically, four of five children born with the disease did not live past their first birthdays.
In 2019, the median age at death for patients enrolled in the Cystic Fibrosis Foundation (CFF) registry was 32 years, and the predicted life expectancy for patients with CF who were born from 2015 through 2019 was 46 years.
Those numbers reflect the remarkable progress made in the past 4 decades in the care of patients with CF, but also highlight the obstacles ahead, given that the predicted life expectancy for the overall U.S. population in 2019 (pre–COVID-19) was 78.9 years.
Julie Desch, MD, is a CF survivor who has beaten the odds and then some. At age 61, the retired surgical pathologist is a CF patient advocate, speaker, and a board member of the Cystic Fibrosis Research Institute, a not-for-profit organization that funds CF research and offers education, advocacy, and psychosocial support for persons with CF and their families and caregivers.
In an interview, Dr. Desch said that while there has been remarkable progress in her lifetime in the field of CF research and treatment, particularly in the development of drugs that modulate function of the underlying cause of approximately 90% of CF cases, there are still many CF patients who cannot benefit from these therapies.
“There are still 10% of people who don’t make a protein to be modified, so that’s a huge unmet need,” she said.
Genetic disorder
CF is a chronic autosomal recessive disorder with multiorgan and multisystem manifestations. It is caused by mutations in the CFTR gene, which codes for the protein CF transmembrane conductance regulator. CFTR controls transport of chloride ions across cell membranes, specifically the apical membrane of epithelial cells in tissues of the airways, intestinal tract, pancreas, kidneys, sweat glands, and the reproductive system, notably the vas deferens in males.
The F508 deletion (F508del) mutation is the most common, occurring in approximately 70% of persons with CF. It is a class 2-type protein processing mutation, leading to defects in cellular processing, protein stability, and chloride channel gating defects.
The CFTR protein also secretes bicarbonate to regulate the pH of airway surface liquid, and inhibits the epithelial sodium channel, which mediates passive sodium transport across apical membranes of sodium-absorbing epithelial cells in the kidneys, intestine, and airways.
CF typically presents with the buildup in the lungs of abnormally viscous and sticky mucus leading to frequent, severe infections, particularly with Pseudomonas aeruginosa, progressive lung damage and, prior to the development of effective disease management, to premature death. The phenotype often includes malnutrition due to malabsorption, and failure to thrive.
Diagnosis
In all 50 U.S. states and the District of Columbia, newborns are screened for CF with an assay for immunoreactive trypsinogen (IRT) an indirect marker for pancreatic injury that is elevated in serum in most newborns with CF, but also detected in premature infants or those delivered under stressful circumstances. In some states newborns are tested only for IRT, with a diagnosis confirmed with a sweat chloride test and/or a CFTR mutation panel.
Treatment
There is no cure for CF, but the discovery of the gene in 1989 by Canadian and U.S. investigators has led to life-prolonging therapeutic interventions, specifically the development of CFTR modulators.
CFTR modulators include potentiators such as ivacaftor (Kalydeco), and correctors such as lumacaftor and tezacaftor (available in the combination Orkambi), and most recently in the triple combination of elexacaftor, tezacaftor, and ivacaftor (Trikafta; ETI).
Neil Sweezey, MD, FRCPC, a CF expert at The Hospital for Sick Children (SickKids) in Toronto, told this news organization that the ideal therapy for CF, genetic correction of the underlying mutations, is still not feasible, but that CFTR modulators are a close second.
“For 90% of patients, the three-drug combination Trikafta has been shown to be quite safe, quite tolerable, and quite remarkably beneficial,” he said.
In a study reported at CHEST 2021 by investigators from Nationwide Children’s Hospital in Columbus, Ohio, 32 adults who were started on the triple combination had significantly improved in forced expiratory volume in 1 second (FEV1), gain in body mass index, decreased sweat chloride and decreased colonization by Pseudomonas species. In addition, patients had significant improvements in blood inflammatory markers.
Christopher H. Goss, MD, FCCP, professor of pulmonary critical care and sleep medicine and professor of pediatrics at the University of Washington in Seattle, agreed that with the availability of the triple combination, “these are extraordinary times. An astounding fact is that most patients have complete resolution of cough, and the exacerbation rates have just plummeted,” he said in an interview.
Some of the reductions in exacerbations may be attributable to the COVID-19 pandemic, he noted, because patients in isolation have less exposure to circulating respiratory viruses.
“But it has been miraculous, and the clinical effect is certainly still more astounding than the effects of ivacaftor, which was the first truly breakthrough drug. Weight goes up, well-being increases, and the population lung function has shifted up to better grade lung function, in the entire population,” he said.
In addition, the need for lung and heart transplantation has sharply declined.
“I had a patient who had decided to forgo transplantation, despite absolutely horrible lung function, and he’s now bowling and leading a very productive life, when before he had been preparing for end of life,” Dr. Goss said.
Dr. Sweezey emphasized that as with all medications, patients being started on the triple combination require close monitoring for potential adverse events that might require dose modification or, for a small number of patients, withdrawal.
Burden of care
CFTR modulators have reduced but not eliminated the need for some patients to have mucolytic therapy, which may include dornase alfa, a recombinant human deoxyribonuclease (DNase) that reduces the viscosity of lung secretions, hypertonic saline inhaled twice daily (for patients 12 and older), mannitol, and physical manipulations to help patients clear mucus. This can include both manual percussion and the use of devices for high-frequency chest wall oscillation.
The complex nature of CF often requires a combination of other therapies to address comorbidities. These therapies may include infection prophylaxis and treatment with antibiotics and antifungals, nutrition support, and therapy for CF-related complications, including gastrointestinal issues, liver diseases, diabetes, and osteopenia that may be related to poor nutrient absorption, chronic inflammation, or other sequelae of CF.
In addition, patients often require frequent CF care center visits – ideally a minimum of every 3 months – which can result in significant loss of work or school time.
“Outcomes for patients in the long run have been absolutely proven to be best if they’re followed in big, established, multidisciplinary well-organized CF centers,” Dr. Sweezey said. “In the United States and Canada if you’re looked after on a regular basis, which means quarterly, every 3 months – whether you need it or not, you really do need it – and if the patients are seen and assessed and checked every 3 months all of their lives, they have small changes caught early, whether it’s an infection you can slap down with medication or a nutrition problem that may be affecting a child’s growth and development.”
“We’re really kind of at a pivotal moment in CF, where we realize things are changing,” said A. Whitney Brown, MD, senior director for clinical affairs at the Cystic Fibrosis Foundation, and an adult CF and lung transplant physician in the Inova Advanced Lung Disease Program in Falls Church, Va.
“Patient needs and interest have evolved, because of the pandemic and because of the highly effective modulator therapy, but we want to take great effort to study it in a rigorous way, to make sure that as we are agile and adapt the care model, that we can maintain the same quality outcomes that we have traditionally done,” she said in an interview.
The Lancet Respiratory Medicine Commission on the future of CF care states that models of care “need to consider management approaches (including disease monitoring) to maintain health and delay lung transplantation, while minimizing the burden of care for patients and their families.”
‘A great problem to have’
One of the most significant changes in CF care has been the growing population of CF patients like Dr. Desch who are living well into adulthood, with some approaching Medicare eligibility.
With the advent of triple therapy and CFTR modulators being started earlier in life, lung function can be preserved, damage to other organs can be minimized, and life expectancy for patients with CF will continue to improve.
“We’re anticipating that there may be some needs in the aging CF population that are different than what we have historically had,” Dr. Brown said. “Will there be geriatric providers that need to become experts in CF care? That’s a great problem to have,” she said.
Dr. Goss agreed, noting that CF is steadily shifting from a near uniformly fatal disease to a chronic disorder that in many cases can be managed “with a complex regimen of novel drugs, much like HIV.”
He noted that there are multiple drug interactions with the triple combination, “so it’s really important that people don’t start a CF patient on a drug without consulting a pharmacist, because you can totally inactivate ETI, or augment it dramatically, and we’ve seen both happen.”
Cost and access
All experts interviewed for this article agreed that while the care of patients with CF has improved exponentially over the last few decades, there are still troubling inequities in care.
One of the largest impediments is the cost of care, with the triple combination costing more than $300,000 per year.
“Clearly patients aren’t paying that, but insurance companies are, and that’s causing all kinds of trickle-down effects that definitely affect patients. The patients like myself who are able to have insurance that covers it benefit, but there are so many people that don’t,” Dr. Desch said.
Dr. Sweezey noted that prior to the advent of ETI, patients with CF in Canada had better outcomes and longer life expectancy than did similar patients in the United States because of universal access to care and coordinated services under Canada’s health care system, compared with the highly fragmented and inefficient U.S. system. He added that the wider availability of ETI in the United States vs. Canada may begin to narrow that gap, however.
As noted before, there is a substantial proportion of patients – an estimated 10% – who have CFTR mutations that are not correctable by currently available CFTR modulators, and these patients are at significant risk for irreversible airway complications and lung damage.
In addition, although CF occurs most frequently among people of White ancestry, the disease does not respect distinctions of race or ethnicity.
“It’s not just [Whites] – a lot of people from different racial backgrounds, ethnic backgrounds, are not being diagnosed or are not being diagnosed soon enough to have effective care early enough,” Dr. Desch said.
That statement is supported by the Lancet Respiratory Medicine Commission on the future of cystic fibrosis care, whose members noted in 2019 that “epidemiological studies in the past 2 decades have shown that cystic fibrosis occurs and is more frequent than was previously thought in populations of non-European descent, and the disease is now recognized in many regions of the world.”
The commission members noted that the costs of adequate CF care may be beyond the reach of many patients in developing nations.
Still, if the substantial barriers of cost and access can be overcome, the future will continue to look brighter for patients with CF. As Dr. Sweezey put it: “There are studies that are pushing lower age limits for using these modulators, and as the evidence builds for the efficacy and safety at younger ages, I think all of us are hoping that we’ll end up being able to use either the current or future modulators to actually prevent trouble in CF, rather than trying to come along and fix it after it’s been there.”
Dr. Brown disclosed advisory board activity for Vertex that ended prior to her joining the CF Foundation. Dr. Desch, Dr. Goss, and Dr. Sweezey reported no relevant conflicts of interest.
USDA announces stricter standards for school nutrition
The U.S. Department of Agriculture has announced new changes to school nutrition standards for the next 2 school years, which will reinstate health goals that were rolled back during the Trump administration.
The Biden administration is also tightening rules for fat and salt content in foods after restrictions were eased during the pandemic, according to the Washington Post.
“Nutritious school meals give America’s children the foundation for successful, healthy lives,” Tom Vilsack, the U.S. agriculture secretary, said in a statement on Feb. 4.
“We applaud schools’ heroic efforts throughout the challenges of this pandemic to continue serving kids the most nutritious meals possible,” he said. “The standards we’re putting in place of the next 2 school years will help schools transition to a future that builds on the tremendous strides they’ve made improving school meal nutrition over the past decade.”
For the 2022-2023 school year, schools and childcare providers will be required to offer low-fat or nonfat unflavored milks and limit the fat in sweet flavored milks. In addition, at least 80% of the grains served during school breakfasts and lunches each week must be considered rich in whole grains.
For the 2023-2024 school year, the weekly sodium limit for school lunches will be decreased by 10%.
The changes mark a shift from the Trump administration, which eased policies on whole grains, nonfat milk, and sodium, the newspaper reported. Then the pandemic forced additional changes as school districts scrambled to package meals for students. The USDA granted extra flexibility and eased some guidelines to ensure that children could be fed while schools were closed or focused on remote learning.
Now the USDA is updating the nutrition standards to “give schools clear expectations for gradual transition from current pandemic operations to more nutritious meals,” Stacy Dean, the USDA’s deputy undersecretary for food, nutrition, and consumer services, told reporters.
The Biden administration’s changes represent a shift back to Obama-era nutrition standards from 2012, according to the Post. But some nutrition advocates have said the new changes don’t address enough issues, such as added sugars. Fruit and vegetable requirements, for instance, will remain the same as the 2012 standards.
That said, some advocates have said the transition could be tough as schools move out of pandemic-era protocols. The School Nutrition Association, which represents school food service manufacturers and professionals, has urged Congress to provide additional support and waiver extensions for the next school year.
“School nutrition professionals are frantic just trying to get enough food on the tray for our students amid relentless supply chain disruptions and labor shortages,” Beth Wallace, the association’s president, told the Washington Post.
The shift will likely require a balancing act and slow transition. The USDA has been consulting with stakeholders for months to determine how to move toward stricter school nutrition standards while also acknowledging the pandemic, supply chain disruptions, and labor shortages.
“This approach is really going to help move forward the nutrition of the meals and allows the schools to continue to function effectively,” Geri Henchy, director of nutrition policy at the Food Research and Action Center, told the Post.
“Schools can’t make big changes at this point because of the supply chain and staffing,” she said. “They have a lot of waivers at this point that are helping them, and this balances the needs of all the different sectors.”
The USDA plans to issue a proposed rule in fall 2022 to update nutrition standards for the future, the department said in its announcement, which would be finalized for the 2024-2025 school year.
A version of this article first appeared on WebMD.com.
The U.S. Department of Agriculture has announced new changes to school nutrition standards for the next 2 school years, which will reinstate health goals that were rolled back during the Trump administration.
The Biden administration is also tightening rules for fat and salt content in foods after restrictions were eased during the pandemic, according to the Washington Post.
“Nutritious school meals give America’s children the foundation for successful, healthy lives,” Tom Vilsack, the U.S. agriculture secretary, said in a statement on Feb. 4.
“We applaud schools’ heroic efforts throughout the challenges of this pandemic to continue serving kids the most nutritious meals possible,” he said. “The standards we’re putting in place of the next 2 school years will help schools transition to a future that builds on the tremendous strides they’ve made improving school meal nutrition over the past decade.”
For the 2022-2023 school year, schools and childcare providers will be required to offer low-fat or nonfat unflavored milks and limit the fat in sweet flavored milks. In addition, at least 80% of the grains served during school breakfasts and lunches each week must be considered rich in whole grains.
For the 2023-2024 school year, the weekly sodium limit for school lunches will be decreased by 10%.
The changes mark a shift from the Trump administration, which eased policies on whole grains, nonfat milk, and sodium, the newspaper reported. Then the pandemic forced additional changes as school districts scrambled to package meals for students. The USDA granted extra flexibility and eased some guidelines to ensure that children could be fed while schools were closed or focused on remote learning.
Now the USDA is updating the nutrition standards to “give schools clear expectations for gradual transition from current pandemic operations to more nutritious meals,” Stacy Dean, the USDA’s deputy undersecretary for food, nutrition, and consumer services, told reporters.
The Biden administration’s changes represent a shift back to Obama-era nutrition standards from 2012, according to the Post. But some nutrition advocates have said the new changes don’t address enough issues, such as added sugars. Fruit and vegetable requirements, for instance, will remain the same as the 2012 standards.
That said, some advocates have said the transition could be tough as schools move out of pandemic-era protocols. The School Nutrition Association, which represents school food service manufacturers and professionals, has urged Congress to provide additional support and waiver extensions for the next school year.
“School nutrition professionals are frantic just trying to get enough food on the tray for our students amid relentless supply chain disruptions and labor shortages,” Beth Wallace, the association’s president, told the Washington Post.
The shift will likely require a balancing act and slow transition. The USDA has been consulting with stakeholders for months to determine how to move toward stricter school nutrition standards while also acknowledging the pandemic, supply chain disruptions, and labor shortages.
“This approach is really going to help move forward the nutrition of the meals and allows the schools to continue to function effectively,” Geri Henchy, director of nutrition policy at the Food Research and Action Center, told the Post.
“Schools can’t make big changes at this point because of the supply chain and staffing,” she said. “They have a lot of waivers at this point that are helping them, and this balances the needs of all the different sectors.”
The USDA plans to issue a proposed rule in fall 2022 to update nutrition standards for the future, the department said in its announcement, which would be finalized for the 2024-2025 school year.
A version of this article first appeared on WebMD.com.
The U.S. Department of Agriculture has announced new changes to school nutrition standards for the next 2 school years, which will reinstate health goals that were rolled back during the Trump administration.
The Biden administration is also tightening rules for fat and salt content in foods after restrictions were eased during the pandemic, according to the Washington Post.
“Nutritious school meals give America’s children the foundation for successful, healthy lives,” Tom Vilsack, the U.S. agriculture secretary, said in a statement on Feb. 4.
“We applaud schools’ heroic efforts throughout the challenges of this pandemic to continue serving kids the most nutritious meals possible,” he said. “The standards we’re putting in place of the next 2 school years will help schools transition to a future that builds on the tremendous strides they’ve made improving school meal nutrition over the past decade.”
For the 2022-2023 school year, schools and childcare providers will be required to offer low-fat or nonfat unflavored milks and limit the fat in sweet flavored milks. In addition, at least 80% of the grains served during school breakfasts and lunches each week must be considered rich in whole grains.
For the 2023-2024 school year, the weekly sodium limit for school lunches will be decreased by 10%.
The changes mark a shift from the Trump administration, which eased policies on whole grains, nonfat milk, and sodium, the newspaper reported. Then the pandemic forced additional changes as school districts scrambled to package meals for students. The USDA granted extra flexibility and eased some guidelines to ensure that children could be fed while schools were closed or focused on remote learning.
Now the USDA is updating the nutrition standards to “give schools clear expectations for gradual transition from current pandemic operations to more nutritious meals,” Stacy Dean, the USDA’s deputy undersecretary for food, nutrition, and consumer services, told reporters.
The Biden administration’s changes represent a shift back to Obama-era nutrition standards from 2012, according to the Post. But some nutrition advocates have said the new changes don’t address enough issues, such as added sugars. Fruit and vegetable requirements, for instance, will remain the same as the 2012 standards.
That said, some advocates have said the transition could be tough as schools move out of pandemic-era protocols. The School Nutrition Association, which represents school food service manufacturers and professionals, has urged Congress to provide additional support and waiver extensions for the next school year.
“School nutrition professionals are frantic just trying to get enough food on the tray for our students amid relentless supply chain disruptions and labor shortages,” Beth Wallace, the association’s president, told the Washington Post.
The shift will likely require a balancing act and slow transition. The USDA has been consulting with stakeholders for months to determine how to move toward stricter school nutrition standards while also acknowledging the pandemic, supply chain disruptions, and labor shortages.
“This approach is really going to help move forward the nutrition of the meals and allows the schools to continue to function effectively,” Geri Henchy, director of nutrition policy at the Food Research and Action Center, told the Post.
“Schools can’t make big changes at this point because of the supply chain and staffing,” she said. “They have a lot of waivers at this point that are helping them, and this balances the needs of all the different sectors.”
The USDA plans to issue a proposed rule in fall 2022 to update nutrition standards for the future, the department said in its announcement, which would be finalized for the 2024-2025 school year.
A version of this article first appeared on WebMD.com.
Children and COVID: New cases down again, but still ‘extremely high’
The indication of an Omicron decline has become a trend: New cases of COVID-19 in children were down for a second consecutive week in the United States, according to the American Academy of Pediatrics and the Children’s Hospital Association.
but the nearly 632,000 cases reported were down by 22% from the previous week and by 45% from what appears to be the peak of the Omicron surge during the week of Jan. 14-20, the AAP/CHA data show.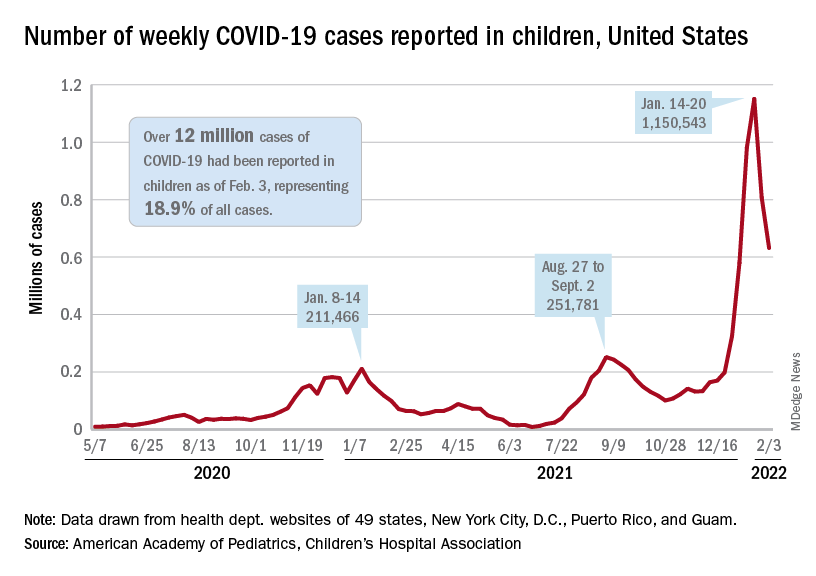
To put the effect of the Delta and Omicron variants into some sort of perspective, the total number of COVID-19 cases among children passed 5 million at the beginning of September 2021, about a year and a half into the pandemic. In the last 5 months, the cumulative count has more than doubled and now stands at 12 million, the AAP and CHA said in their weekly COVID report.
Hospital admissions and emergency department visits followed the same downward trend over the last week. The rate of new hospitalizations fell to 0.81 per 100,000 children aged 0-17 years as of Feb. 2 (down from a peak of 1.25 per 100,000 on Jan. 15), and ED visits with diagnosed COVID-19 dropped to 1.8% (peak was 14.1%), 1.9% (peak was 14.3%), and 3.4% (peak was 14%) of all visits for children aged 16-17, 12-15, and 0-11 years, respectively, the Centers for Disease Control and Prevention reported.
The vaccination response
The surge of infections brought about by the Omicron variant, however, did not translate into increased vaccination, at least for the youngest eligible children. Vaccine initiation rose slightly among children aged 5-11 in early and mid-January but, by early February, new vaccinations had declined to their lowest point since approval in early November of 2021, the AAP said in its weekly COVID vaccination report.
As a result, the 5- to 11-year-olds are well behind the pace set by those aged 12-15 for the first 3 months of their vaccination experience. Through the first 13 weeks after the COVID vaccine was approved for children aged 12-15 in early May, 44.5% had received at least one dose and 32.3% were fully vaccinated. Among children aged 5-11, the corresponding figures through 13 weeks were 31% and 22.5%, according to CDC data.
The vaccination reaction to Omicron was somewhat more robust for children aged 12-17, compared with the younger group, but initiations dropped at the same time that new cases began to decline. In terms of total volume, the response among 12- to 17-year-olds was much smaller than that seen in July and August of 2021 as the Delta surge was hitting the United States, the AAP vaccination report shows.
All those vaccinations add up to this: Over 16.8 million children aged 12-17 and almost 9 million aged 5-11 had received at least one dose of vaccine as of Feb. 7, which works out to 66.6% of the older group and 31.2% of the younger cohort. Almost 14.3 million (56.4%) of those aged 12-17 are fully vaccinated, as are 6.6 million (22.9%) of the 5- to 11-year-olds, the CDC said on its COVID Data Tracker.
The indication of an Omicron decline has become a trend: New cases of COVID-19 in children were down for a second consecutive week in the United States, according to the American Academy of Pediatrics and the Children’s Hospital Association.
but the nearly 632,000 cases reported were down by 22% from the previous week and by 45% from what appears to be the peak of the Omicron surge during the week of Jan. 14-20, the AAP/CHA data show.
To put the effect of the Delta and Omicron variants into some sort of perspective, the total number of COVID-19 cases among children passed 5 million at the beginning of September 2021, about a year and a half into the pandemic. In the last 5 months, the cumulative count has more than doubled and now stands at 12 million, the AAP and CHA said in their weekly COVID report.
Hospital admissions and emergency department visits followed the same downward trend over the last week. The rate of new hospitalizations fell to 0.81 per 100,000 children aged 0-17 years as of Feb. 2 (down from a peak of 1.25 per 100,000 on Jan. 15), and ED visits with diagnosed COVID-19 dropped to 1.8% (peak was 14.1%), 1.9% (peak was 14.3%), and 3.4% (peak was 14%) of all visits for children aged 16-17, 12-15, and 0-11 years, respectively, the Centers for Disease Control and Prevention reported.
The vaccination response
The surge of infections brought about by the Omicron variant, however, did not translate into increased vaccination, at least for the youngest eligible children. Vaccine initiation rose slightly among children aged 5-11 in early and mid-January but, by early February, new vaccinations had declined to their lowest point since approval in early November of 2021, the AAP said in its weekly COVID vaccination report.
As a result, the 5- to 11-year-olds are well behind the pace set by those aged 12-15 for the first 3 months of their vaccination experience. Through the first 13 weeks after the COVID vaccine was approved for children aged 12-15 in early May, 44.5% had received at least one dose and 32.3% were fully vaccinated. Among children aged 5-11, the corresponding figures through 13 weeks were 31% and 22.5%, according to CDC data.
The vaccination reaction to Omicron was somewhat more robust for children aged 12-17, compared with the younger group, but initiations dropped at the same time that new cases began to decline. In terms of total volume, the response among 12- to 17-year-olds was much smaller than that seen in July and August of 2021 as the Delta surge was hitting the United States, the AAP vaccination report shows.
All those vaccinations add up to this: Over 16.8 million children aged 12-17 and almost 9 million aged 5-11 had received at least one dose of vaccine as of Feb. 7, which works out to 66.6% of the older group and 31.2% of the younger cohort. Almost 14.3 million (56.4%) of those aged 12-17 are fully vaccinated, as are 6.6 million (22.9%) of the 5- to 11-year-olds, the CDC said on its COVID Data Tracker.
The indication of an Omicron decline has become a trend: New cases of COVID-19 in children were down for a second consecutive week in the United States, according to the American Academy of Pediatrics and the Children’s Hospital Association.
but the nearly 632,000 cases reported were down by 22% from the previous week and by 45% from what appears to be the peak of the Omicron surge during the week of Jan. 14-20, the AAP/CHA data show.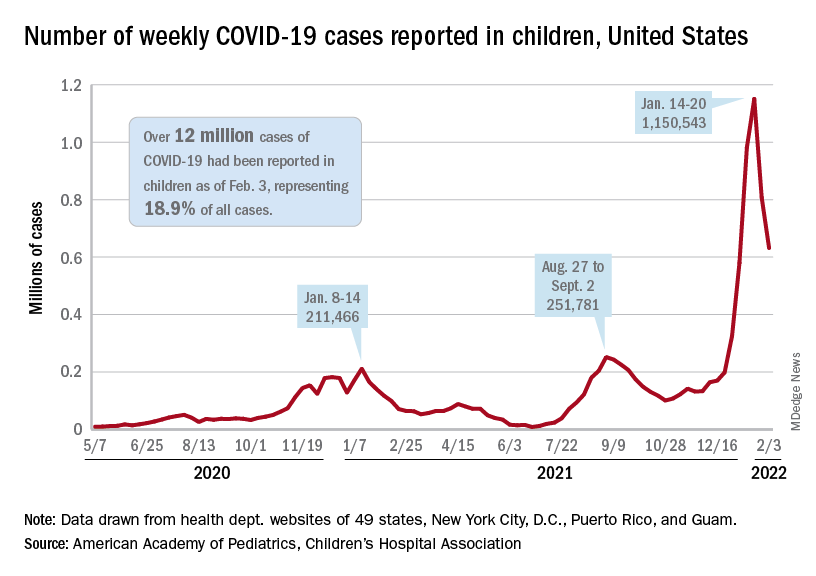
To put the effect of the Delta and Omicron variants into some sort of perspective, the total number of COVID-19 cases among children passed 5 million at the beginning of September 2021, about a year and a half into the pandemic. In the last 5 months, the cumulative count has more than doubled and now stands at 12 million, the AAP and CHA said in their weekly COVID report.
Hospital admissions and emergency department visits followed the same downward trend over the last week. The rate of new hospitalizations fell to 0.81 per 100,000 children aged 0-17 years as of Feb. 2 (down from a peak of 1.25 per 100,000 on Jan. 15), and ED visits with diagnosed COVID-19 dropped to 1.8% (peak was 14.1%), 1.9% (peak was 14.3%), and 3.4% (peak was 14%) of all visits for children aged 16-17, 12-15, and 0-11 years, respectively, the Centers for Disease Control and Prevention reported.
The vaccination response
The surge of infections brought about by the Omicron variant, however, did not translate into increased vaccination, at least for the youngest eligible children. Vaccine initiation rose slightly among children aged 5-11 in early and mid-January but, by early February, new vaccinations had declined to their lowest point since approval in early November of 2021, the AAP said in its weekly COVID vaccination report.
As a result, the 5- to 11-year-olds are well behind the pace set by those aged 12-15 for the first 3 months of their vaccination experience. Through the first 13 weeks after the COVID vaccine was approved for children aged 12-15 in early May, 44.5% had received at least one dose and 32.3% were fully vaccinated. Among children aged 5-11, the corresponding figures through 13 weeks were 31% and 22.5%, according to CDC data.
The vaccination reaction to Omicron was somewhat more robust for children aged 12-17, compared with the younger group, but initiations dropped at the same time that new cases began to decline. In terms of total volume, the response among 12- to 17-year-olds was much smaller than that seen in July and August of 2021 as the Delta surge was hitting the United States, the AAP vaccination report shows.
All those vaccinations add up to this: Over 16.8 million children aged 12-17 and almost 9 million aged 5-11 had received at least one dose of vaccine as of Feb. 7, which works out to 66.6% of the older group and 31.2% of the younger cohort. Almost 14.3 million (56.4%) of those aged 12-17 are fully vaccinated, as are 6.6 million (22.9%) of the 5- to 11-year-olds, the CDC said on its COVID Data Tracker.
Picture warnings on sugary drinks could help fight childhood obesity
Sugary beverages – juice, soda, decadent lattes, sports drinks, and more – are the leading source of both calories and added sugar in the American diet, according to the Harvard T. H. Chan School of Public Health. But new research published in PLoS Medicine has found that
The new study, from researchers at the University of North Carolina at Chapel Hill, found that parents were 17% less likely to buy sugary drinks for their children when the beverages had the graphical – and graphic – warnings on the products.
The researchers turned a laboratory setting into a “minimart,” and parents were told to choose one drink and snack for their children, along with one household item (to disguise the purpose of the study).
Some parents were presented with sweetened drinks with images on the products reflecting type 2 diabetes and heart damage. Others were shown sugary drinks with a barcode label and no picture warning.
Forty-five percent of parents chose sugary drinks for their children when the products had no picture warning, but only 28% of parents chose sugary beverages with the cautionary images.
“When people make choices about what food to buy, they are juggling dozens of factors, like taste, cost, and advertising, and are looking at many products at once,” said Lindsey Smith Taillie, PhD, a nutrition researcher and the senior author of the paper.
“Showing that warnings can cut through the noise of everything else that’s happening in a food store is powerful evidence that they would help reduce sugary drink purchases in the real world.”
Children are particularly prone to overindulging on sugar, largely due to companies’ frequent marketing displays of pleasurable-looking and seemingly “thirst-quenching” sweet beverages.
Drink packaging also can be misleading.
Fruits and vegetables displayed on the front of many beverages often lead parents to buy what they believe are “healthy” options, when these drinks could be packed with sugar, according to a study published online Jan. 22 in the journal Appetite.
Parents are often “doing the best with what information they have,” so more education about nutrition, through picture warning labels, for example, would make a difference, said Caroline Fausel, a paleo food blogger, podcaster, and author of “Prep, Cook, Freeze: A Paleo Meal Planning Cookbook.”
Healthier choices on the rise
The American Beverage Association, an industry trade group, shared the current steps that major companies are taking to help lower Americans’ sugar intake.
Pepsi, Coca-Cola, and Keurig Dr Pepper joined forces in 2014 to create the Balance Calories Initiative, which aims to reduce beverage calories in the national diet.
Coca-Cola now offers 250 beverages with zero to low calories, and Keurig Dr Pepper has 158 products with 40 calories or less. Pepsi sells 7.5-ounce mini-cans, along with various other sizes, to encourage portion control.
“Beverage companies are fully transparent about the calories and sugar in our products, and we are offering more choices with less sugar than ever before,” William Dermody, vice president of media and public affairs for the American Beverage Association, said in a statement. “We agree that too much sugar is not good for anyone, and clear information about beverages is most helpful to consumers.”
Other big companies also are taking strides to lower sugar content in their products.
Kraft Heinz, which owns the popular line of Capri Sun drinks, has publicly shared its efforts to ramp up the nutritional value of its products.
The company has a goal to slash 60 million pounds of total sugar in Kraft Heinz products globally by 2025.
“As more people become aware of the harm that excessive sugar can cause in the body, my hope is that they continue to choose healthier alternatives,” Ms. Fausel said.
Creating new patterns
For children who consume sweetened juices and sodas regularly, the transition to healthier options might be challenging at first.
“Change can involve tantrums and unhappiness, and right now parents are at their max living pandemic parenting life,” said Jennifer Anderson, a registered dietitian and CEO of Kids Eat in Color, LLC, a resource for improving child nutrition and health through innovative education, meal plans, and tools. “Kids can get used to having sugary drinks, and they don’t want to give them up.”
One way to help make the switch is by having only water and milk as options while children are up and about, a technique that works particularly well for younger children, she said.
“This sort of ‘quiet restriction’ helps kids learn to love the healthier option without feeling deprived,” Ms. Anderson said. “They will eventually learn about juice, soda, chocolate milk, sports drinks, and more, but you can let them learn about those foods at a slower pace when you rarely or don’t serve them at home.”
The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sugary beverages – juice, soda, decadent lattes, sports drinks, and more – are the leading source of both calories and added sugar in the American diet, according to the Harvard T. H. Chan School of Public Health. But new research published in PLoS Medicine has found that
The new study, from researchers at the University of North Carolina at Chapel Hill, found that parents were 17% less likely to buy sugary drinks for their children when the beverages had the graphical – and graphic – warnings on the products.
The researchers turned a laboratory setting into a “minimart,” and parents were told to choose one drink and snack for their children, along with one household item (to disguise the purpose of the study).
Some parents were presented with sweetened drinks with images on the products reflecting type 2 diabetes and heart damage. Others were shown sugary drinks with a barcode label and no picture warning.
Forty-five percent of parents chose sugary drinks for their children when the products had no picture warning, but only 28% of parents chose sugary beverages with the cautionary images.
“When people make choices about what food to buy, they are juggling dozens of factors, like taste, cost, and advertising, and are looking at many products at once,” said Lindsey Smith Taillie, PhD, a nutrition researcher and the senior author of the paper.
“Showing that warnings can cut through the noise of everything else that’s happening in a food store is powerful evidence that they would help reduce sugary drink purchases in the real world.”
Children are particularly prone to overindulging on sugar, largely due to companies’ frequent marketing displays of pleasurable-looking and seemingly “thirst-quenching” sweet beverages.
Drink packaging also can be misleading.
Fruits and vegetables displayed on the front of many beverages often lead parents to buy what they believe are “healthy” options, when these drinks could be packed with sugar, according to a study published online Jan. 22 in the journal Appetite.
Parents are often “doing the best with what information they have,” so more education about nutrition, through picture warning labels, for example, would make a difference, said Caroline Fausel, a paleo food blogger, podcaster, and author of “Prep, Cook, Freeze: A Paleo Meal Planning Cookbook.”
Healthier choices on the rise
The American Beverage Association, an industry trade group, shared the current steps that major companies are taking to help lower Americans’ sugar intake.
Pepsi, Coca-Cola, and Keurig Dr Pepper joined forces in 2014 to create the Balance Calories Initiative, which aims to reduce beverage calories in the national diet.
Coca-Cola now offers 250 beverages with zero to low calories, and Keurig Dr Pepper has 158 products with 40 calories or less. Pepsi sells 7.5-ounce mini-cans, along with various other sizes, to encourage portion control.
“Beverage companies are fully transparent about the calories and sugar in our products, and we are offering more choices with less sugar than ever before,” William Dermody, vice president of media and public affairs for the American Beverage Association, said in a statement. “We agree that too much sugar is not good for anyone, and clear information about beverages is most helpful to consumers.”
Other big companies also are taking strides to lower sugar content in their products.
Kraft Heinz, which owns the popular line of Capri Sun drinks, has publicly shared its efforts to ramp up the nutritional value of its products.
The company has a goal to slash 60 million pounds of total sugar in Kraft Heinz products globally by 2025.
“As more people become aware of the harm that excessive sugar can cause in the body, my hope is that they continue to choose healthier alternatives,” Ms. Fausel said.
Creating new patterns
For children who consume sweetened juices and sodas regularly, the transition to healthier options might be challenging at first.
“Change can involve tantrums and unhappiness, and right now parents are at their max living pandemic parenting life,” said Jennifer Anderson, a registered dietitian and CEO of Kids Eat in Color, LLC, a resource for improving child nutrition and health through innovative education, meal plans, and tools. “Kids can get used to having sugary drinks, and they don’t want to give them up.”
One way to help make the switch is by having only water and milk as options while children are up and about, a technique that works particularly well for younger children, she said.
“This sort of ‘quiet restriction’ helps kids learn to love the healthier option without feeling deprived,” Ms. Anderson said. “They will eventually learn about juice, soda, chocolate milk, sports drinks, and more, but you can let them learn about those foods at a slower pace when you rarely or don’t serve them at home.”
The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sugary beverages – juice, soda, decadent lattes, sports drinks, and more – are the leading source of both calories and added sugar in the American diet, according to the Harvard T. H. Chan School of Public Health. But new research published in PLoS Medicine has found that
The new study, from researchers at the University of North Carolina at Chapel Hill, found that parents were 17% less likely to buy sugary drinks for their children when the beverages had the graphical – and graphic – warnings on the products.
The researchers turned a laboratory setting into a “minimart,” and parents were told to choose one drink and snack for their children, along with one household item (to disguise the purpose of the study).
Some parents were presented with sweetened drinks with images on the products reflecting type 2 diabetes and heart damage. Others were shown sugary drinks with a barcode label and no picture warning.
Forty-five percent of parents chose sugary drinks for their children when the products had no picture warning, but only 28% of parents chose sugary beverages with the cautionary images.
“When people make choices about what food to buy, they are juggling dozens of factors, like taste, cost, and advertising, and are looking at many products at once,” said Lindsey Smith Taillie, PhD, a nutrition researcher and the senior author of the paper.
“Showing that warnings can cut through the noise of everything else that’s happening in a food store is powerful evidence that they would help reduce sugary drink purchases in the real world.”
Children are particularly prone to overindulging on sugar, largely due to companies’ frequent marketing displays of pleasurable-looking and seemingly “thirst-quenching” sweet beverages.
Drink packaging also can be misleading.
Fruits and vegetables displayed on the front of many beverages often lead parents to buy what they believe are “healthy” options, when these drinks could be packed with sugar, according to a study published online Jan. 22 in the journal Appetite.
Parents are often “doing the best with what information they have,” so more education about nutrition, through picture warning labels, for example, would make a difference, said Caroline Fausel, a paleo food blogger, podcaster, and author of “Prep, Cook, Freeze: A Paleo Meal Planning Cookbook.”
Healthier choices on the rise
The American Beverage Association, an industry trade group, shared the current steps that major companies are taking to help lower Americans’ sugar intake.
Pepsi, Coca-Cola, and Keurig Dr Pepper joined forces in 2014 to create the Balance Calories Initiative, which aims to reduce beverage calories in the national diet.
Coca-Cola now offers 250 beverages with zero to low calories, and Keurig Dr Pepper has 158 products with 40 calories or less. Pepsi sells 7.5-ounce mini-cans, along with various other sizes, to encourage portion control.
“Beverage companies are fully transparent about the calories and sugar in our products, and we are offering more choices with less sugar than ever before,” William Dermody, vice president of media and public affairs for the American Beverage Association, said in a statement. “We agree that too much sugar is not good for anyone, and clear information about beverages is most helpful to consumers.”
Other big companies also are taking strides to lower sugar content in their products.
Kraft Heinz, which owns the popular line of Capri Sun drinks, has publicly shared its efforts to ramp up the nutritional value of its products.
The company has a goal to slash 60 million pounds of total sugar in Kraft Heinz products globally by 2025.
“As more people become aware of the harm that excessive sugar can cause in the body, my hope is that they continue to choose healthier alternatives,” Ms. Fausel said.
Creating new patterns
For children who consume sweetened juices and sodas regularly, the transition to healthier options might be challenging at first.
“Change can involve tantrums and unhappiness, and right now parents are at their max living pandemic parenting life,” said Jennifer Anderson, a registered dietitian and CEO of Kids Eat in Color, LLC, a resource for improving child nutrition and health through innovative education, meal plans, and tools. “Kids can get used to having sugary drinks, and they don’t want to give them up.”
One way to help make the switch is by having only water and milk as options while children are up and about, a technique that works particularly well for younger children, she said.
“This sort of ‘quiet restriction’ helps kids learn to love the healthier option without feeling deprived,” Ms. Anderson said. “They will eventually learn about juice, soda, chocolate milk, sports drinks, and more, but you can let them learn about those foods at a slower pace when you rarely or don’t serve them at home.”
The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE
Absolute increase in Kawasaki CV risk remains small in long-term follow-up
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
FROM THE ANNUAL MEETING OF THE CANADIAN RHEUMATOLOGY ASSOCIATION
Q&A: Long COVID symptoms, management, and where we’re headed
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Referrals to gender clinics in Sweden drop after media coverage
Media coverage of transgender health care judged to be “negative” was associated with a drop of around 30% in referral rates to gender identity clinics in Sweden among young people under age 19, a new study indicates.
Malin Indremo, MS, from the department of neuroscience, Uppsala (Sweden) University, and colleagues explored the effect of the documentaries, “The Trans Train and Teenage Girls,” which they explain was a “Swedish public service television show” representing “investigative journalism.” The two-part documentary series was aired in Sweden in April 2019 and October 2019, respectively, and is now available in English on YouTube.
In their article, published online in JAMA Network Open, the authors said they consider “The Trans Train” programs to be “negative” media coverage because the “documentaries addressed the distinct increase among adolescents referred to gender identity clinics in recent years. Two young adults who regretted their transition and parents of transgender individuals who questioned the clinics’ assessments of their children were interviewed, and concerns were raised about whether gender-confirming treatments are based on sufficient scientific evidence.”
The programs, they suggest, may have influenced and jeopardized young transgender individuals’ access to transgender-specific health care.
Stella O’Malley, a U.K.-based psychotherapist specializing in transgender care and executive director of Genspect, an international organization that provides support to the parents of young people who are questioning their gender, expressed her disappointment with the study’s conclusions.
“I’m really surprised and disappointed that the researchers believe that negative coverage is the reason for a drop in referrals when it is more accurate to say that the information provided by ‘The Trans Train’ documentaries was concerning and suggests that further critical analysis and a review needs to be carried out on the clinics in question,” she said in an interview.
Ms. O’Malley herself made a documentary for Channel 4 in the United Kingdom, broadcast in 2018, called: “Trans Kids: It’s Time to Talk.”
Rapidly increasing numbers of youth, especially girls, question gender
As Ms. Indremo and coauthors explained – and as has been widely reported by this news organization – “the number of referrals to gender identity clinics have rapidly increased worldwide” in recent years, and this “has been especially prominent in adolescents and young adults.”
In addition, they acknowledged, “there has been a shift in gender ratio, with a preponderance toward individuals who were assigned female at birth (AFAB).”
This was the topic of “The Trans Train” programs, and in fact, following their broadcast, Ms. Indremo and colleagues noted that “an intense debate in national media [in Sweden] arose from the documentaries.”
Their research aimed to explore the association between both “positive” and “negative” media coverage and the number of referrals to gender identity clinics for young people (under aged 19) respectively. Data from the six gender clinics in Sweden were included between January 2017 and December 2019.
In the period studied, the clinics received 1,784 referrals, including 613 referrals in 2017, 663 referrals in 2018, and 508 referrals in 2019.
From the age-specific data that included 1,674 referrals, 359 individuals (21.4%) were younger than 13 years and 1,315 individuals (78.6%) were aged 13-18 years. From the assigned sex-specific data that included 1,435 referrals, 1,034 individuals (72.1%) were AFAB and 401 individuals (27.9%) were assigned male at birth (AMAB). Information on sex assigned at birth was lacking from one clinic, which was excluded from the analysis.
When they examined data for the 3 months following the airing of the first part of “The Trans Train” documentary series (in April 2019), they found that referrals to gender clinics fell by 25.4% overall, compared with the 3 months before part 1 was screened. Specifically, they fell by 25.3% for young people aged 13-18 years and by 32.2% for those born female.
In the extended analyses of 6 months following part 1, a decrease of total referrals by 30.7% was observed, while referrals for AFAB individuals decreased by 37.4% and referrals for individuals aged 13-18 years decreased by 27.7%. A decrease of referrals by 41.7% for children aged younger than 13 years was observed in the 6-month analysis, as well as a decrease of 8.2% among AMAB individuals.
“The Trans Train” documentaries, Ms. Indremo and colleagues said, “were criticized for being negatively biased and giving an oversimplified picture of transgender health care.”
Did the nature of the trans train documentaries influence referrals?
In an invited commentary published in JAMA Network Open, Ken C. Pang, PhD, from the Murdoch Children’s Research Institute, Melbourne, and colleagues noted: “Although the mechanisms underlying this decrease [in referrals] were not formally explored in their study, the authors reasonably speculated that both parents and referring health professionals may have been less likely to support a child or adolescent’s attendance at a specialist pediatric gender clinic following the documentaries.”
Dr. Pang and colleagues went on to say it is “the ... responsibility of media organizations in ensuring that stories depicting health care for transgender and gender diverse (TGD) young people are fair, balanced, nuanced, and accurate.”
Often, media reports have “fallen short of these standards and lacked the voices of TGD young people who have benefited from gender-affirming care or the perspectives of health professionals with expertise in providing such care,” they added.
“For example, some [media reports] have suggested that the growing number of referrals to such clinics is not owing to greater awareness of gender diversity and empowerment of TGD young people but is instead being driven by other factors such as peer influence, while others have warned that the use of gender-affirming hormonal interventions in TGD young people represents an undue risk,” they continue.
Ms. Indremo and colleagues didn’t see any drop-in referrals after the second part of the series, aired in October 2019, but they say this was likely because referrals were “already lowered” by the airing of the first part of the documentaries.
Nor did they see an increase in referrals following what they say was a “positive” media event in the form of a story about a professional Swedish handball player who announced the decision to quit his career to seek care for gender dysphoria.
“One may assume that a single news event is not significant enough to influence referral counts,” they suggested, noting also that Sweden represents “a society where there is already a relatively high level of awareness of gender identity issues.”
“Our results point to a differential association of media attention depending on the tone of the media content,” they observed.
Dr. Pang and coauthors noted it would be “helpful to examine whether similar media coverage in other countries has been associated with similar decreases in referral numbers and whether particular types of media stories are more prone to having this association.”
Parents and doctors debate treatment of gender dysphoria
In Sweden, custodians’ permission as well as custodians’ help is needed for minors to access care for gender dysphoria, said Ms. Indremo and coauthors. “It is possible that the content of the documentaries contributed to a higher custodian barrier to having their children referred for assessment, believing it may not be in the best interest of their child. This would highly impact young transgender individuals’ possibilities to access care.”
They also acknowledge that health care practitioners who refer young people to specialist clinics might also have been influenced by the documentaries, noting “some commentators argued that all treatments for gender dysphoria be stopped, and that ‘all health care given at the gender identity clinics was an experiment lacking scientific basis.’ ”
In April 2021, Angela Sämfjord, MD, child and adolescent psychiatrist at Sahlgrenska University Hospital, Gothenburg, Sweden, who started a child and adolescent clinic – the Lundstrom Gender Clinic – told this news organization she had reevaluated her approach even prior to “The Trans Train” documentaries and had resigned in 2018 because of her own fears about the lack of evidence for hormonal and surgical treatments of youth with gender dysphoria.
Following the debate that ensued after the airing of “The Trans Train” programs, the Swedish National Board of Health and Welfare published new recommendations in March 2021, which reflected a significant change in direction for the evaluation of gender dysphoria in minors, emphasizing the requirement for a thorough mental health assessment.
And in May 2021, Karolinska Children’s Hospital, which houses one of the leading gender identity clinics in Sweden, announced it would stop the routine medical treatment of children with gender dysphoria under the age of 18, which meant a total ban on the prescribing of puberty blockers and cross-sex hormones to minors. Such treatment could henceforth only be carried out within the setting of a clinical trial approved by the EPM (Ethical Review Agency/Swedish Institutional Review Board), it said.
The remaining five gender identity clinics in Sweden decided upon their own rules, but in general, they have become much more cautious regarding medical treatment of minors within the past year. Also, there is a desire in Sweden to reduce the number of gender identity clinics for minors from the current six to perhaps a maximum of three nationwide.
However, neither Ms. Indremo and colleagues nor Dr. Pang and colleagues mentioned the subsequent change to the Swedish NBHW recommendations on evaluation of gender dysphoria in minors in JAMA articles.
New NBHW recommendations about medical treatment of gender dysphoria with puberty blockers and cross-sex hormones for minors were due to be issued in 2021 but have been delayed.
Debate in other countries
Sweden is not alone in discussing this issue. In 2020, Finland became the first country in the world to issue new guidelines that concluded there is a lack of quality evidence to support the use of hormonal interventions in adolescents with gender dysphoria.
This issue has been hotly debated in the United Kingdom – not least with the Keira Bell court case and two National Institute for Health and Clinical Excellence evidence reviews concluding there is a lack of data to support the use of puberty-blocking agents and “cross-sex” hormones in youth with gender dysphoria.
And a number of U.S. states are attempting to outlaw the medical and surgical treatment of gender dysphoria in minors. Even health care professionals who have been treating young people with gender dysphoria for years – some of whom are transgender themselves – have started to speak out and are questioning what they call “sloppy care” given to many such youth.
Indeed, a recent survey shows that detransitioners – individuals who suffer from gender dysphoria, transition to the opposite sex but then regret their decision and detransition – are getting short shrift when it comes to care, with over half of the 100 surveyed saying they feel they did not receive adequate evaluation from a doctor or mental health professional before starting to transition.
And new draft standards of care for treating people with gender dysphoria by the World Professional Association for Transgender Health have drawn criticism from experts.
‘First do no harm’
In their conclusion, Dr. Pang and coauthors said that, with respect to the media coverage of young people with gender dysphoria, “who are, after all, one of the most vulnerable subgroups within our society, perhaps our media should recall one of the core tenets of health care and ensure their stories ‘first, do no harm.’”
However, in a commentary recently published in Child and Adolescent Mental Health, Alison Clayton, MBBS, from the University of Melbourne, and coauthors again pointed out that evidence reviews of the use of puberty blockers in young people with gender dysphoria show “there is very low certainty of the benefits of puberty blockers, an unknown risk of harm, and there is need for more rigorous research.”
“The clinically prudent thing to do, if we aim to ‘first, do no harm,’ is to proceed with extreme caution, especially given the rapidly rising case numbers and novel gender dysphoria presentations,” Clayton and colleagues concluded.
Ms. Indremo and coauthors reported no relevant financial relationships. Dr. Pang reported being a member of the Australian Professional Association for Trans Health and its research committee. One commentary coauthor has reported being a member of WPATH.
A version of this article first appeared on Medscape.com.
Media coverage of transgender health care judged to be “negative” was associated with a drop of around 30% in referral rates to gender identity clinics in Sweden among young people under age 19, a new study indicates.
Malin Indremo, MS, from the department of neuroscience, Uppsala (Sweden) University, and colleagues explored the effect of the documentaries, “The Trans Train and Teenage Girls,” which they explain was a “Swedish public service television show” representing “investigative journalism.” The two-part documentary series was aired in Sweden in April 2019 and October 2019, respectively, and is now available in English on YouTube.
In their article, published online in JAMA Network Open, the authors said they consider “The Trans Train” programs to be “negative” media coverage because the “documentaries addressed the distinct increase among adolescents referred to gender identity clinics in recent years. Two young adults who regretted their transition and parents of transgender individuals who questioned the clinics’ assessments of their children were interviewed, and concerns were raised about whether gender-confirming treatments are based on sufficient scientific evidence.”
The programs, they suggest, may have influenced and jeopardized young transgender individuals’ access to transgender-specific health care.
Stella O’Malley, a U.K.-based psychotherapist specializing in transgender care and executive director of Genspect, an international organization that provides support to the parents of young people who are questioning their gender, expressed her disappointment with the study’s conclusions.
“I’m really surprised and disappointed that the researchers believe that negative coverage is the reason for a drop in referrals when it is more accurate to say that the information provided by ‘The Trans Train’ documentaries was concerning and suggests that further critical analysis and a review needs to be carried out on the clinics in question,” she said in an interview.
Ms. O’Malley herself made a documentary for Channel 4 in the United Kingdom, broadcast in 2018, called: “Trans Kids: It’s Time to Talk.”
Rapidly increasing numbers of youth, especially girls, question gender
As Ms. Indremo and coauthors explained – and as has been widely reported by this news organization – “the number of referrals to gender identity clinics have rapidly increased worldwide” in recent years, and this “has been especially prominent in adolescents and young adults.”
In addition, they acknowledged, “there has been a shift in gender ratio, with a preponderance toward individuals who were assigned female at birth (AFAB).”
This was the topic of “The Trans Train” programs, and in fact, following their broadcast, Ms. Indremo and colleagues noted that “an intense debate in national media [in Sweden] arose from the documentaries.”
Their research aimed to explore the association between both “positive” and “negative” media coverage and the number of referrals to gender identity clinics for young people (under aged 19) respectively. Data from the six gender clinics in Sweden were included between January 2017 and December 2019.
In the period studied, the clinics received 1,784 referrals, including 613 referrals in 2017, 663 referrals in 2018, and 508 referrals in 2019.
From the age-specific data that included 1,674 referrals, 359 individuals (21.4%) were younger than 13 years and 1,315 individuals (78.6%) were aged 13-18 years. From the assigned sex-specific data that included 1,435 referrals, 1,034 individuals (72.1%) were AFAB and 401 individuals (27.9%) were assigned male at birth (AMAB). Information on sex assigned at birth was lacking from one clinic, which was excluded from the analysis.
When they examined data for the 3 months following the airing of the first part of “The Trans Train” documentary series (in April 2019), they found that referrals to gender clinics fell by 25.4% overall, compared with the 3 months before part 1 was screened. Specifically, they fell by 25.3% for young people aged 13-18 years and by 32.2% for those born female.
In the extended analyses of 6 months following part 1, a decrease of total referrals by 30.7% was observed, while referrals for AFAB individuals decreased by 37.4% and referrals for individuals aged 13-18 years decreased by 27.7%. A decrease of referrals by 41.7% for children aged younger than 13 years was observed in the 6-month analysis, as well as a decrease of 8.2% among AMAB individuals.
“The Trans Train” documentaries, Ms. Indremo and colleagues said, “were criticized for being negatively biased and giving an oversimplified picture of transgender health care.”
Did the nature of the trans train documentaries influence referrals?
In an invited commentary published in JAMA Network Open, Ken C. Pang, PhD, from the Murdoch Children’s Research Institute, Melbourne, and colleagues noted: “Although the mechanisms underlying this decrease [in referrals] were not formally explored in their study, the authors reasonably speculated that both parents and referring health professionals may have been less likely to support a child or adolescent’s attendance at a specialist pediatric gender clinic following the documentaries.”
Dr. Pang and colleagues went on to say it is “the ... responsibility of media organizations in ensuring that stories depicting health care for transgender and gender diverse (TGD) young people are fair, balanced, nuanced, and accurate.”
Often, media reports have “fallen short of these standards and lacked the voices of TGD young people who have benefited from gender-affirming care or the perspectives of health professionals with expertise in providing such care,” they added.
“For example, some [media reports] have suggested that the growing number of referrals to such clinics is not owing to greater awareness of gender diversity and empowerment of TGD young people but is instead being driven by other factors such as peer influence, while others have warned that the use of gender-affirming hormonal interventions in TGD young people represents an undue risk,” they continue.
Ms. Indremo and colleagues didn’t see any drop-in referrals after the second part of the series, aired in October 2019, but they say this was likely because referrals were “already lowered” by the airing of the first part of the documentaries.
Nor did they see an increase in referrals following what they say was a “positive” media event in the form of a story about a professional Swedish handball player who announced the decision to quit his career to seek care for gender dysphoria.
“One may assume that a single news event is not significant enough to influence referral counts,” they suggested, noting also that Sweden represents “a society where there is already a relatively high level of awareness of gender identity issues.”
“Our results point to a differential association of media attention depending on the tone of the media content,” they observed.
Dr. Pang and coauthors noted it would be “helpful to examine whether similar media coverage in other countries has been associated with similar decreases in referral numbers and whether particular types of media stories are more prone to having this association.”
Parents and doctors debate treatment of gender dysphoria
In Sweden, custodians’ permission as well as custodians’ help is needed for minors to access care for gender dysphoria, said Ms. Indremo and coauthors. “It is possible that the content of the documentaries contributed to a higher custodian barrier to having their children referred for assessment, believing it may not be in the best interest of their child. This would highly impact young transgender individuals’ possibilities to access care.”
They also acknowledge that health care practitioners who refer young people to specialist clinics might also have been influenced by the documentaries, noting “some commentators argued that all treatments for gender dysphoria be stopped, and that ‘all health care given at the gender identity clinics was an experiment lacking scientific basis.’ ”
In April 2021, Angela Sämfjord, MD, child and adolescent psychiatrist at Sahlgrenska University Hospital, Gothenburg, Sweden, who started a child and adolescent clinic – the Lundstrom Gender Clinic – told this news organization she had reevaluated her approach even prior to “The Trans Train” documentaries and had resigned in 2018 because of her own fears about the lack of evidence for hormonal and surgical treatments of youth with gender dysphoria.
Following the debate that ensued after the airing of “The Trans Train” programs, the Swedish National Board of Health and Welfare published new recommendations in March 2021, which reflected a significant change in direction for the evaluation of gender dysphoria in minors, emphasizing the requirement for a thorough mental health assessment.
And in May 2021, Karolinska Children’s Hospital, which houses one of the leading gender identity clinics in Sweden, announced it would stop the routine medical treatment of children with gender dysphoria under the age of 18, which meant a total ban on the prescribing of puberty blockers and cross-sex hormones to minors. Such treatment could henceforth only be carried out within the setting of a clinical trial approved by the EPM (Ethical Review Agency/Swedish Institutional Review Board), it said.
The remaining five gender identity clinics in Sweden decided upon their own rules, but in general, they have become much more cautious regarding medical treatment of minors within the past year. Also, there is a desire in Sweden to reduce the number of gender identity clinics for minors from the current six to perhaps a maximum of three nationwide.
However, neither Ms. Indremo and colleagues nor Dr. Pang and colleagues mentioned the subsequent change to the Swedish NBHW recommendations on evaluation of gender dysphoria in minors in JAMA articles.
New NBHW recommendations about medical treatment of gender dysphoria with puberty blockers and cross-sex hormones for minors were due to be issued in 2021 but have been delayed.
Debate in other countries
Sweden is not alone in discussing this issue. In 2020, Finland became the first country in the world to issue new guidelines that concluded there is a lack of quality evidence to support the use of hormonal interventions in adolescents with gender dysphoria.
This issue has been hotly debated in the United Kingdom – not least with the Keira Bell court case and two National Institute for Health and Clinical Excellence evidence reviews concluding there is a lack of data to support the use of puberty-blocking agents and “cross-sex” hormones in youth with gender dysphoria.
And a number of U.S. states are attempting to outlaw the medical and surgical treatment of gender dysphoria in minors. Even health care professionals who have been treating young people with gender dysphoria for years – some of whom are transgender themselves – have started to speak out and are questioning what they call “sloppy care” given to many such youth.
Indeed, a recent survey shows that detransitioners – individuals who suffer from gender dysphoria, transition to the opposite sex but then regret their decision and detransition – are getting short shrift when it comes to care, with over half of the 100 surveyed saying they feel they did not receive adequate evaluation from a doctor or mental health professional before starting to transition.
And new draft standards of care for treating people with gender dysphoria by the World Professional Association for Transgender Health have drawn criticism from experts.
‘First do no harm’
In their conclusion, Dr. Pang and coauthors said that, with respect to the media coverage of young people with gender dysphoria, “who are, after all, one of the most vulnerable subgroups within our society, perhaps our media should recall one of the core tenets of health care and ensure their stories ‘first, do no harm.’”
However, in a commentary recently published in Child and Adolescent Mental Health, Alison Clayton, MBBS, from the University of Melbourne, and coauthors again pointed out that evidence reviews of the use of puberty blockers in young people with gender dysphoria show “there is very low certainty of the benefits of puberty blockers, an unknown risk of harm, and there is need for more rigorous research.”
“The clinically prudent thing to do, if we aim to ‘first, do no harm,’ is to proceed with extreme caution, especially given the rapidly rising case numbers and novel gender dysphoria presentations,” Clayton and colleagues concluded.
Ms. Indremo and coauthors reported no relevant financial relationships. Dr. Pang reported being a member of the Australian Professional Association for Trans Health and its research committee. One commentary coauthor has reported being a member of WPATH.
A version of this article first appeared on Medscape.com.
Media coverage of transgender health care judged to be “negative” was associated with a drop of around 30% in referral rates to gender identity clinics in Sweden among young people under age 19, a new study indicates.
Malin Indremo, MS, from the department of neuroscience, Uppsala (Sweden) University, and colleagues explored the effect of the documentaries, “The Trans Train and Teenage Girls,” which they explain was a “Swedish public service television show” representing “investigative journalism.” The two-part documentary series was aired in Sweden in April 2019 and October 2019, respectively, and is now available in English on YouTube.
In their article, published online in JAMA Network Open, the authors said they consider “The Trans Train” programs to be “negative” media coverage because the “documentaries addressed the distinct increase among adolescents referred to gender identity clinics in recent years. Two young adults who regretted their transition and parents of transgender individuals who questioned the clinics’ assessments of their children were interviewed, and concerns were raised about whether gender-confirming treatments are based on sufficient scientific evidence.”
The programs, they suggest, may have influenced and jeopardized young transgender individuals’ access to transgender-specific health care.
Stella O’Malley, a U.K.-based psychotherapist specializing in transgender care and executive director of Genspect, an international organization that provides support to the parents of young people who are questioning their gender, expressed her disappointment with the study’s conclusions.
“I’m really surprised and disappointed that the researchers believe that negative coverage is the reason for a drop in referrals when it is more accurate to say that the information provided by ‘The Trans Train’ documentaries was concerning and suggests that further critical analysis and a review needs to be carried out on the clinics in question,” she said in an interview.
Ms. O’Malley herself made a documentary for Channel 4 in the United Kingdom, broadcast in 2018, called: “Trans Kids: It’s Time to Talk.”
Rapidly increasing numbers of youth, especially girls, question gender
As Ms. Indremo and coauthors explained – and as has been widely reported by this news organization – “the number of referrals to gender identity clinics have rapidly increased worldwide” in recent years, and this “has been especially prominent in adolescents and young adults.”
In addition, they acknowledged, “there has been a shift in gender ratio, with a preponderance toward individuals who were assigned female at birth (AFAB).”
This was the topic of “The Trans Train” programs, and in fact, following their broadcast, Ms. Indremo and colleagues noted that “an intense debate in national media [in Sweden] arose from the documentaries.”
Their research aimed to explore the association between both “positive” and “negative” media coverage and the number of referrals to gender identity clinics for young people (under aged 19) respectively. Data from the six gender clinics in Sweden were included between January 2017 and December 2019.
In the period studied, the clinics received 1,784 referrals, including 613 referrals in 2017, 663 referrals in 2018, and 508 referrals in 2019.
From the age-specific data that included 1,674 referrals, 359 individuals (21.4%) were younger than 13 years and 1,315 individuals (78.6%) were aged 13-18 years. From the assigned sex-specific data that included 1,435 referrals, 1,034 individuals (72.1%) were AFAB and 401 individuals (27.9%) were assigned male at birth (AMAB). Information on sex assigned at birth was lacking from one clinic, which was excluded from the analysis.
When they examined data for the 3 months following the airing of the first part of “The Trans Train” documentary series (in April 2019), they found that referrals to gender clinics fell by 25.4% overall, compared with the 3 months before part 1 was screened. Specifically, they fell by 25.3% for young people aged 13-18 years and by 32.2% for those born female.
In the extended analyses of 6 months following part 1, a decrease of total referrals by 30.7% was observed, while referrals for AFAB individuals decreased by 37.4% and referrals for individuals aged 13-18 years decreased by 27.7%. A decrease of referrals by 41.7% for children aged younger than 13 years was observed in the 6-month analysis, as well as a decrease of 8.2% among AMAB individuals.
“The Trans Train” documentaries, Ms. Indremo and colleagues said, “were criticized for being negatively biased and giving an oversimplified picture of transgender health care.”
Did the nature of the trans train documentaries influence referrals?
In an invited commentary published in JAMA Network Open, Ken C. Pang, PhD, from the Murdoch Children’s Research Institute, Melbourne, and colleagues noted: “Although the mechanisms underlying this decrease [in referrals] were not formally explored in their study, the authors reasonably speculated that both parents and referring health professionals may have been less likely to support a child or adolescent’s attendance at a specialist pediatric gender clinic following the documentaries.”
Dr. Pang and colleagues went on to say it is “the ... responsibility of media organizations in ensuring that stories depicting health care for transgender and gender diverse (TGD) young people are fair, balanced, nuanced, and accurate.”
Often, media reports have “fallen short of these standards and lacked the voices of TGD young people who have benefited from gender-affirming care or the perspectives of health professionals with expertise in providing such care,” they added.
“For example, some [media reports] have suggested that the growing number of referrals to such clinics is not owing to greater awareness of gender diversity and empowerment of TGD young people but is instead being driven by other factors such as peer influence, while others have warned that the use of gender-affirming hormonal interventions in TGD young people represents an undue risk,” they continue.
Ms. Indremo and colleagues didn’t see any drop-in referrals after the second part of the series, aired in October 2019, but they say this was likely because referrals were “already lowered” by the airing of the first part of the documentaries.
Nor did they see an increase in referrals following what they say was a “positive” media event in the form of a story about a professional Swedish handball player who announced the decision to quit his career to seek care for gender dysphoria.
“One may assume that a single news event is not significant enough to influence referral counts,” they suggested, noting also that Sweden represents “a society where there is already a relatively high level of awareness of gender identity issues.”
“Our results point to a differential association of media attention depending on the tone of the media content,” they observed.
Dr. Pang and coauthors noted it would be “helpful to examine whether similar media coverage in other countries has been associated with similar decreases in referral numbers and whether particular types of media stories are more prone to having this association.”
Parents and doctors debate treatment of gender dysphoria
In Sweden, custodians’ permission as well as custodians’ help is needed for minors to access care for gender dysphoria, said Ms. Indremo and coauthors. “It is possible that the content of the documentaries contributed to a higher custodian barrier to having their children referred for assessment, believing it may not be in the best interest of their child. This would highly impact young transgender individuals’ possibilities to access care.”
They also acknowledge that health care practitioners who refer young people to specialist clinics might also have been influenced by the documentaries, noting “some commentators argued that all treatments for gender dysphoria be stopped, and that ‘all health care given at the gender identity clinics was an experiment lacking scientific basis.’ ”
In April 2021, Angela Sämfjord, MD, child and adolescent psychiatrist at Sahlgrenska University Hospital, Gothenburg, Sweden, who started a child and adolescent clinic – the Lundstrom Gender Clinic – told this news organization she had reevaluated her approach even prior to “The Trans Train” documentaries and had resigned in 2018 because of her own fears about the lack of evidence for hormonal and surgical treatments of youth with gender dysphoria.
Following the debate that ensued after the airing of “The Trans Train” programs, the Swedish National Board of Health and Welfare published new recommendations in March 2021, which reflected a significant change in direction for the evaluation of gender dysphoria in minors, emphasizing the requirement for a thorough mental health assessment.
And in May 2021, Karolinska Children’s Hospital, which houses one of the leading gender identity clinics in Sweden, announced it would stop the routine medical treatment of children with gender dysphoria under the age of 18, which meant a total ban on the prescribing of puberty blockers and cross-sex hormones to minors. Such treatment could henceforth only be carried out within the setting of a clinical trial approved by the EPM (Ethical Review Agency/Swedish Institutional Review Board), it said.
The remaining five gender identity clinics in Sweden decided upon their own rules, but in general, they have become much more cautious regarding medical treatment of minors within the past year. Also, there is a desire in Sweden to reduce the number of gender identity clinics for minors from the current six to perhaps a maximum of three nationwide.
However, neither Ms. Indremo and colleagues nor Dr. Pang and colleagues mentioned the subsequent change to the Swedish NBHW recommendations on evaluation of gender dysphoria in minors in JAMA articles.
New NBHW recommendations about medical treatment of gender dysphoria with puberty blockers and cross-sex hormones for minors were due to be issued in 2021 but have been delayed.
Debate in other countries
Sweden is not alone in discussing this issue. In 2020, Finland became the first country in the world to issue new guidelines that concluded there is a lack of quality evidence to support the use of hormonal interventions in adolescents with gender dysphoria.
This issue has been hotly debated in the United Kingdom – not least with the Keira Bell court case and two National Institute for Health and Clinical Excellence evidence reviews concluding there is a lack of data to support the use of puberty-blocking agents and “cross-sex” hormones in youth with gender dysphoria.
And a number of U.S. states are attempting to outlaw the medical and surgical treatment of gender dysphoria in minors. Even health care professionals who have been treating young people with gender dysphoria for years – some of whom are transgender themselves – have started to speak out and are questioning what they call “sloppy care” given to many such youth.
Indeed, a recent survey shows that detransitioners – individuals who suffer from gender dysphoria, transition to the opposite sex but then regret their decision and detransition – are getting short shrift when it comes to care, with over half of the 100 surveyed saying they feel they did not receive adequate evaluation from a doctor or mental health professional before starting to transition.
And new draft standards of care for treating people with gender dysphoria by the World Professional Association for Transgender Health have drawn criticism from experts.
‘First do no harm’
In their conclusion, Dr. Pang and coauthors said that, with respect to the media coverage of young people with gender dysphoria, “who are, after all, one of the most vulnerable subgroups within our society, perhaps our media should recall one of the core tenets of health care and ensure their stories ‘first, do no harm.’”
However, in a commentary recently published in Child and Adolescent Mental Health, Alison Clayton, MBBS, from the University of Melbourne, and coauthors again pointed out that evidence reviews of the use of puberty blockers in young people with gender dysphoria show “there is very low certainty of the benefits of puberty blockers, an unknown risk of harm, and there is need for more rigorous research.”
“The clinically prudent thing to do, if we aim to ‘first, do no harm,’ is to proceed with extreme caution, especially given the rapidly rising case numbers and novel gender dysphoria presentations,” Clayton and colleagues concluded.
Ms. Indremo and coauthors reported no relevant financial relationships. Dr. Pang reported being a member of the Australian Professional Association for Trans Health and its research committee. One commentary coauthor has reported being a member of WPATH.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN