User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
A new (old) drug joins the COVID fray, and guess what? It works
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
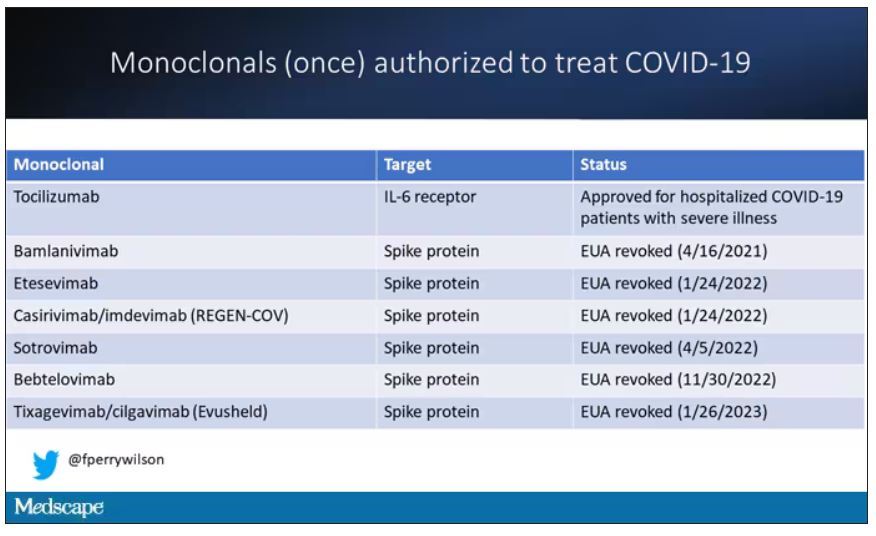
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.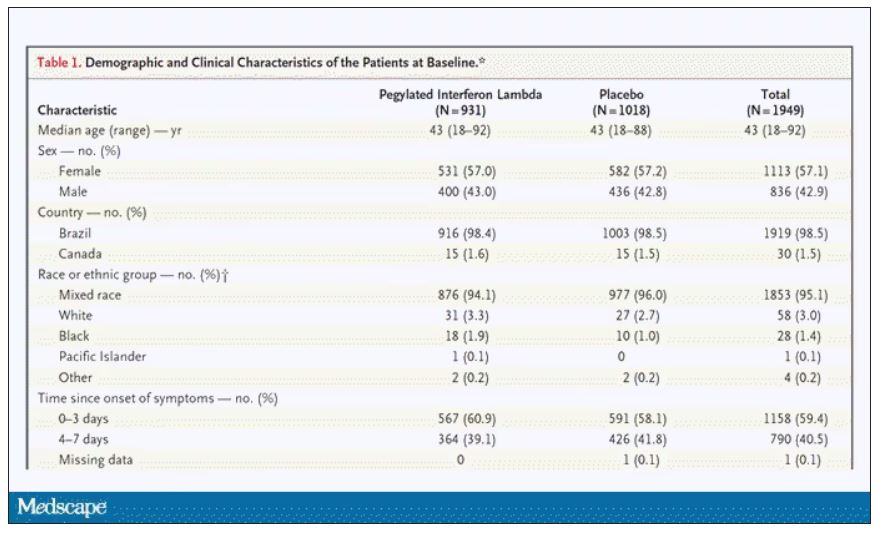
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.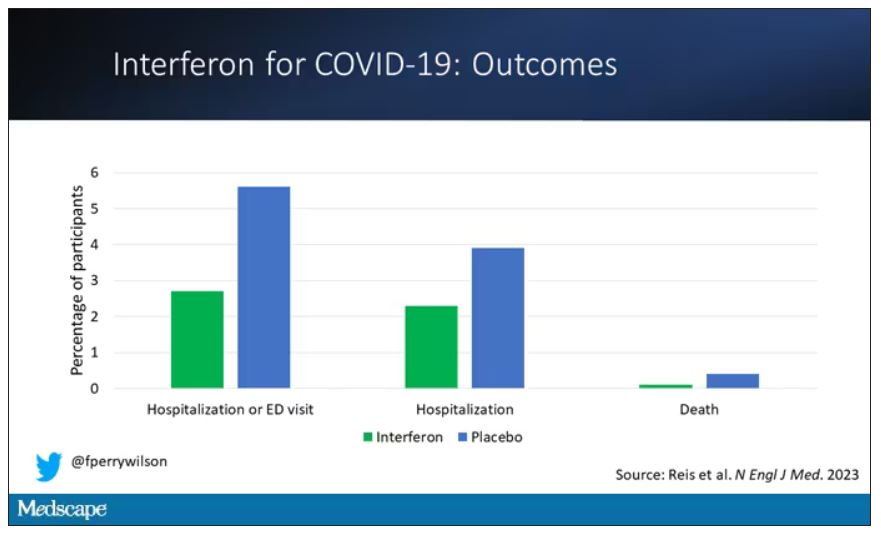
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.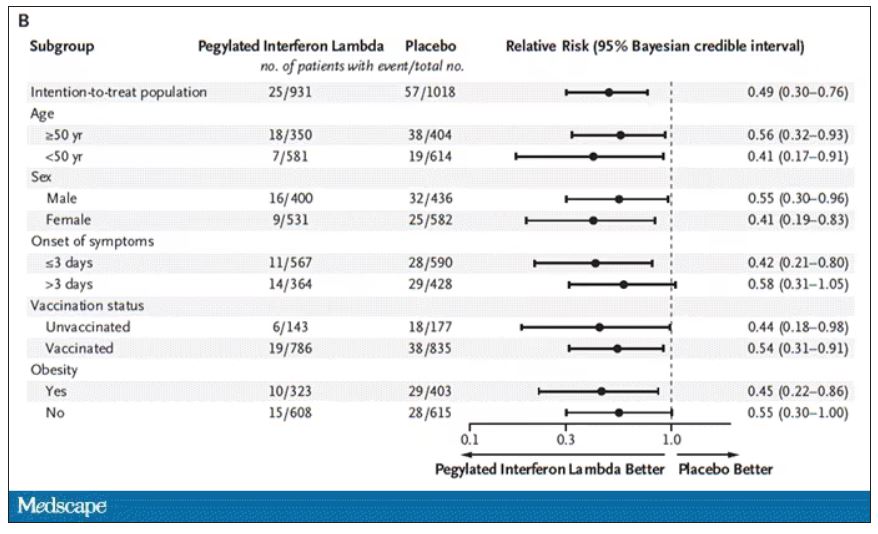
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.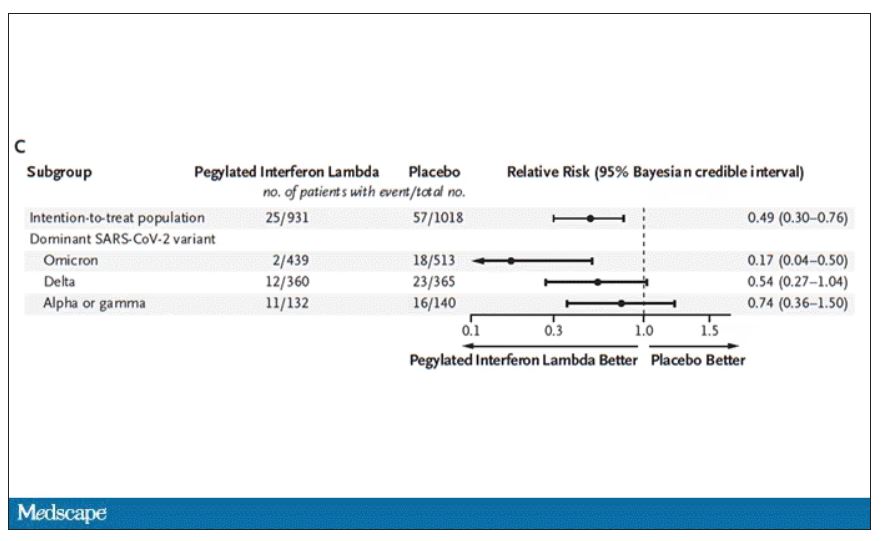
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.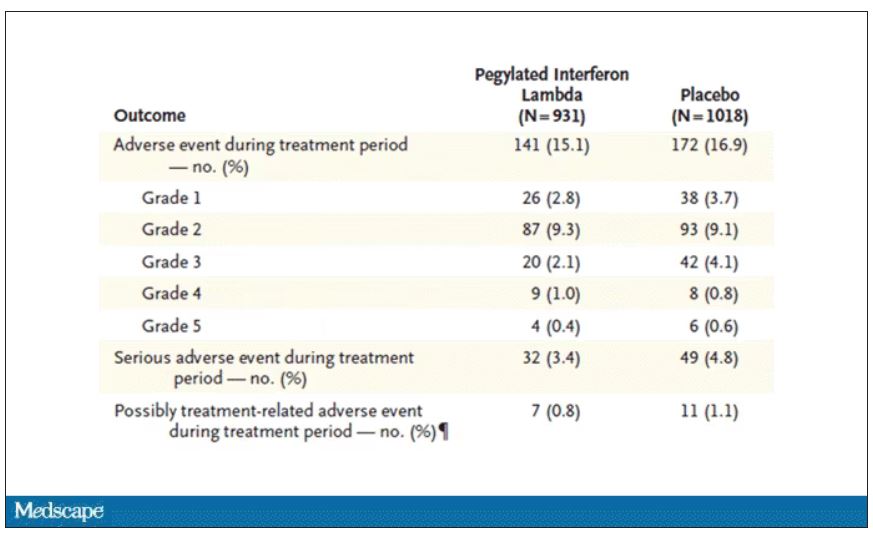
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
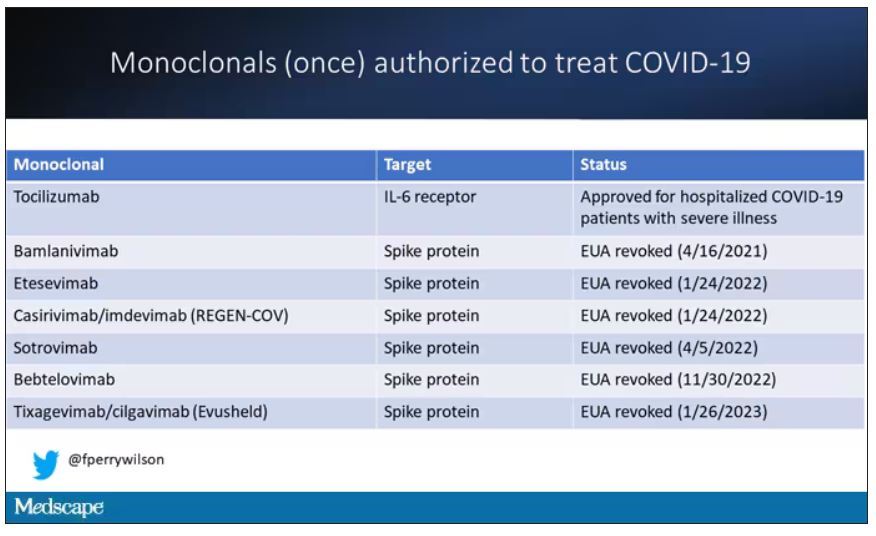
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.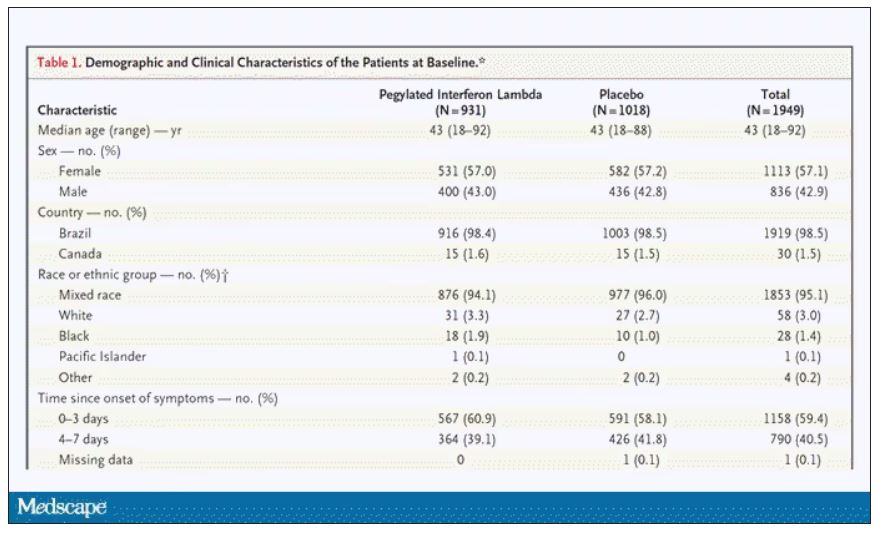
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.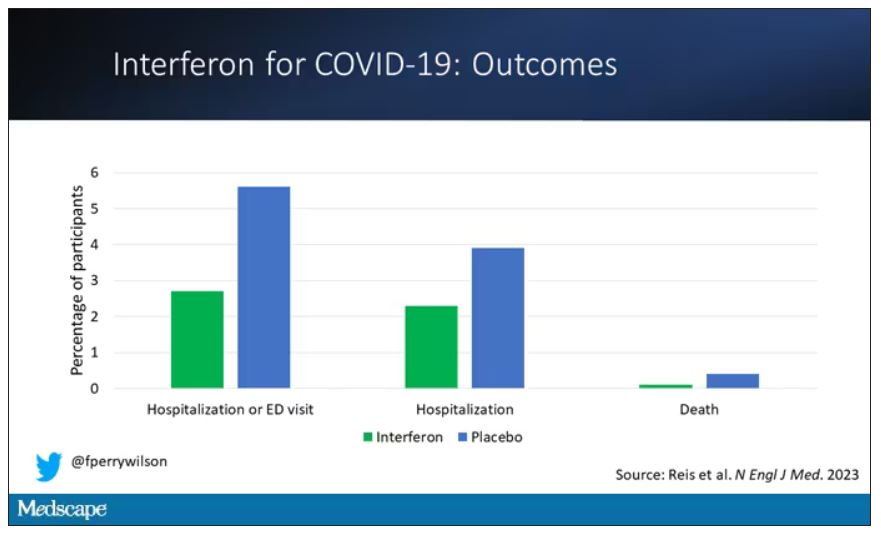
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.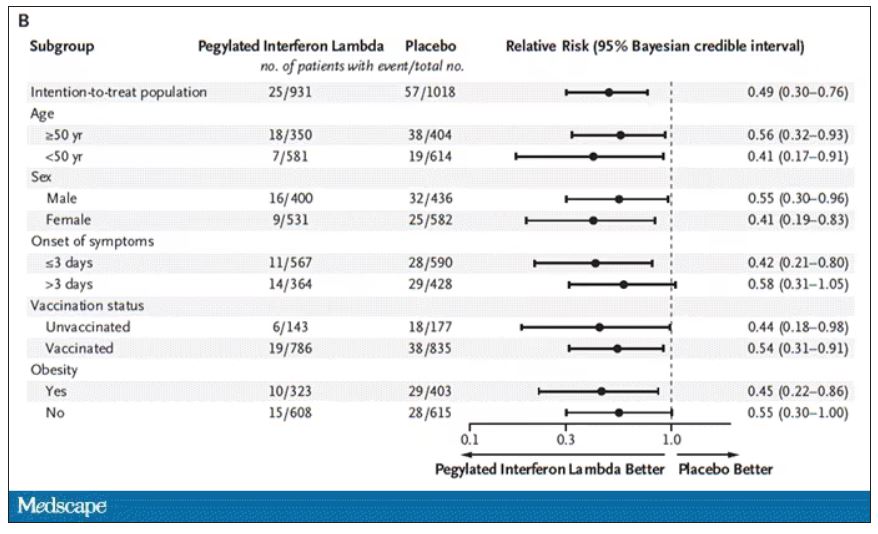
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.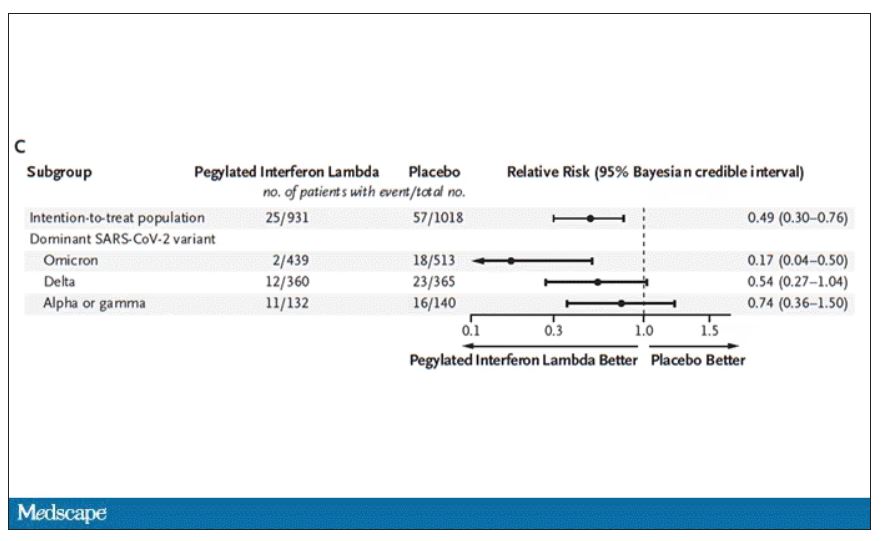
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.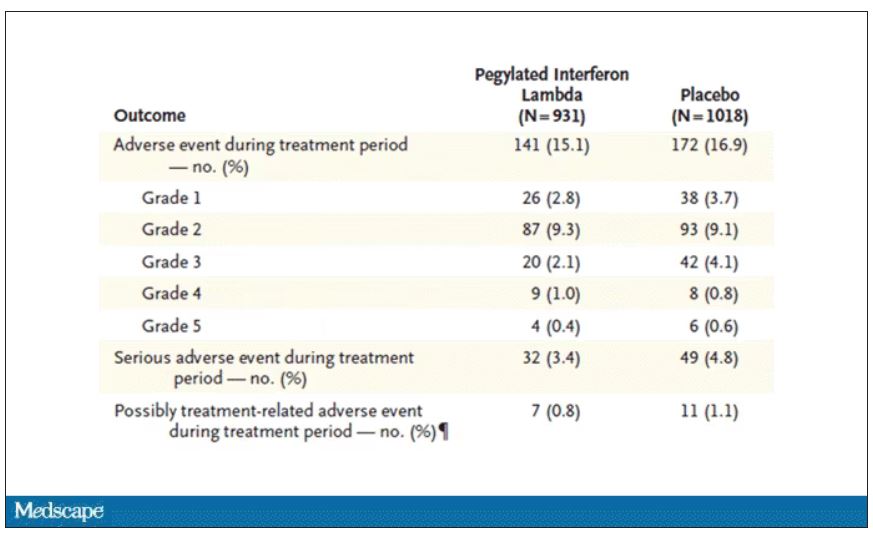
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
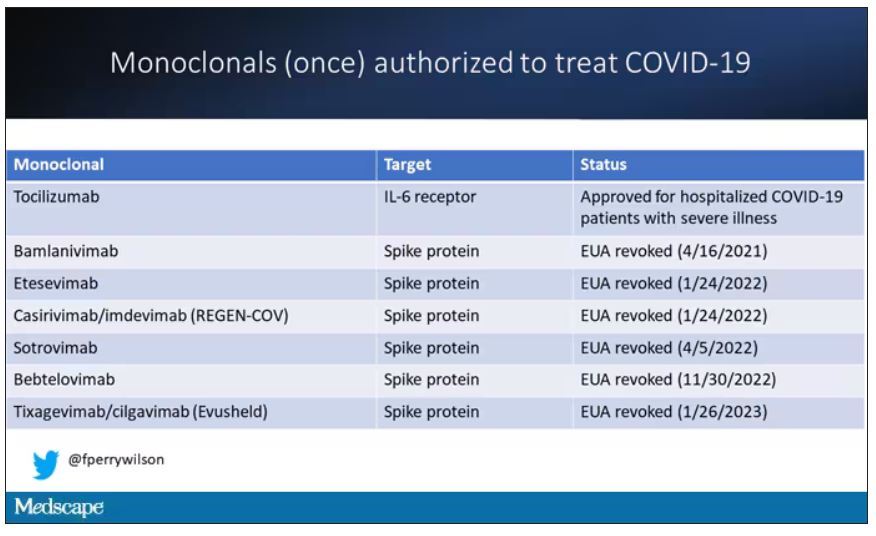
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.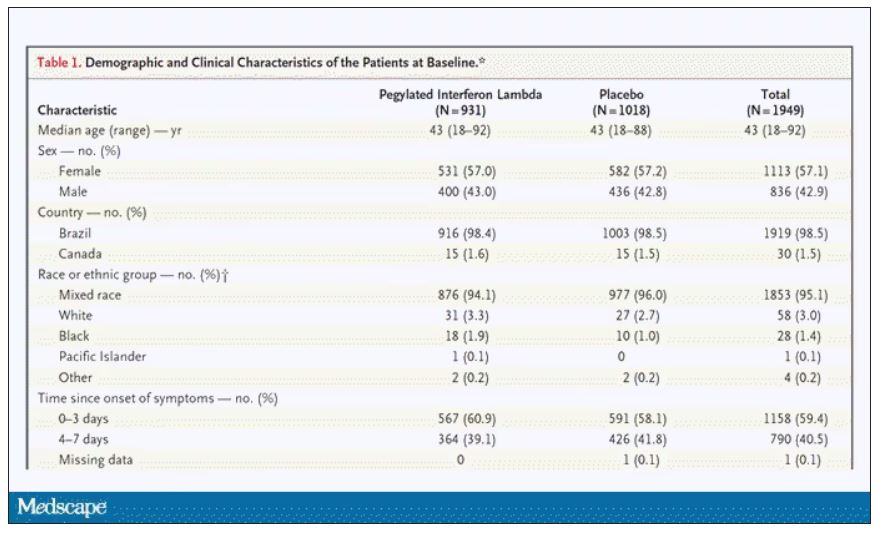
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.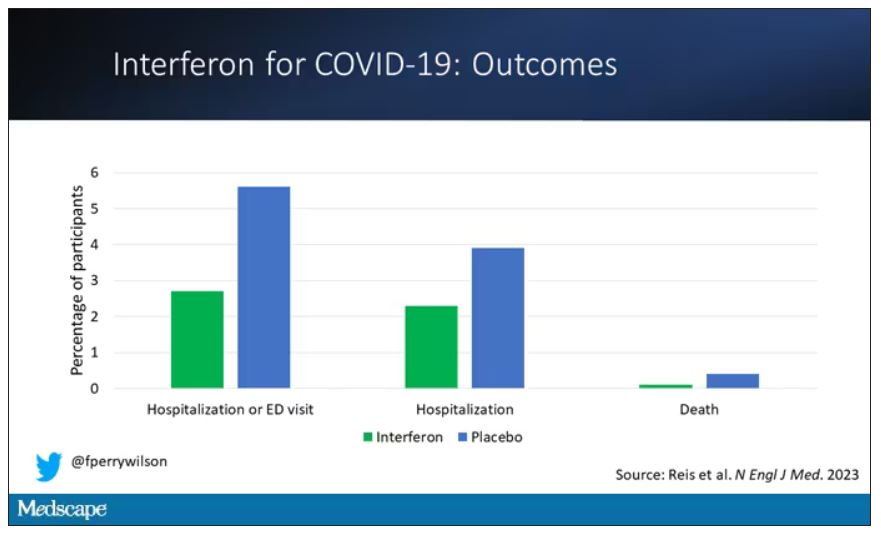
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.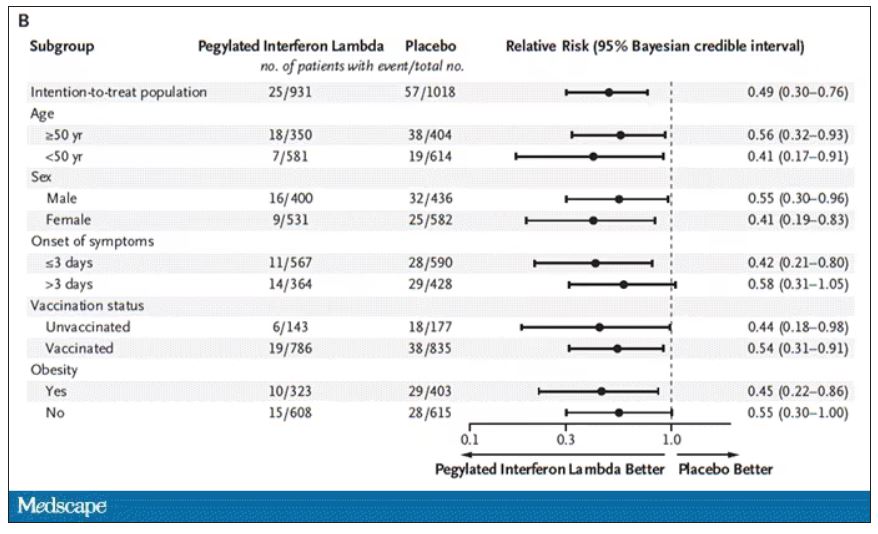
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.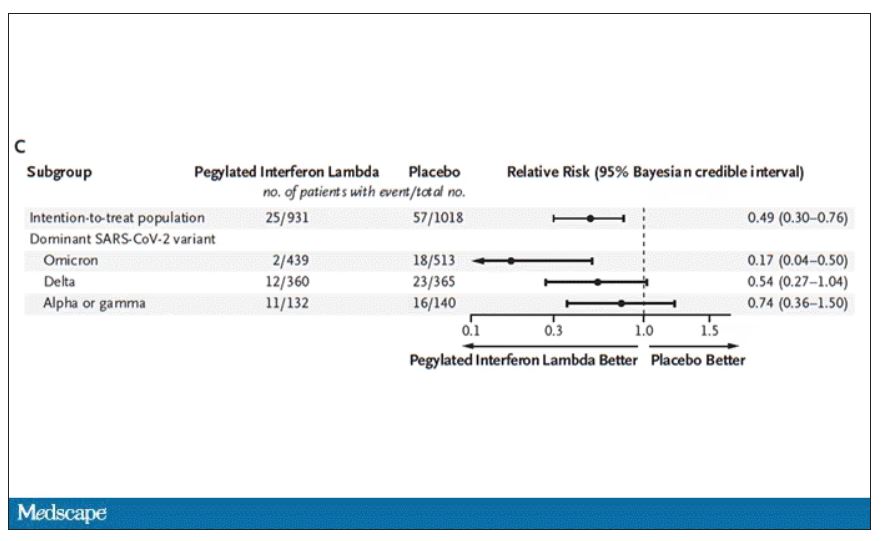
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.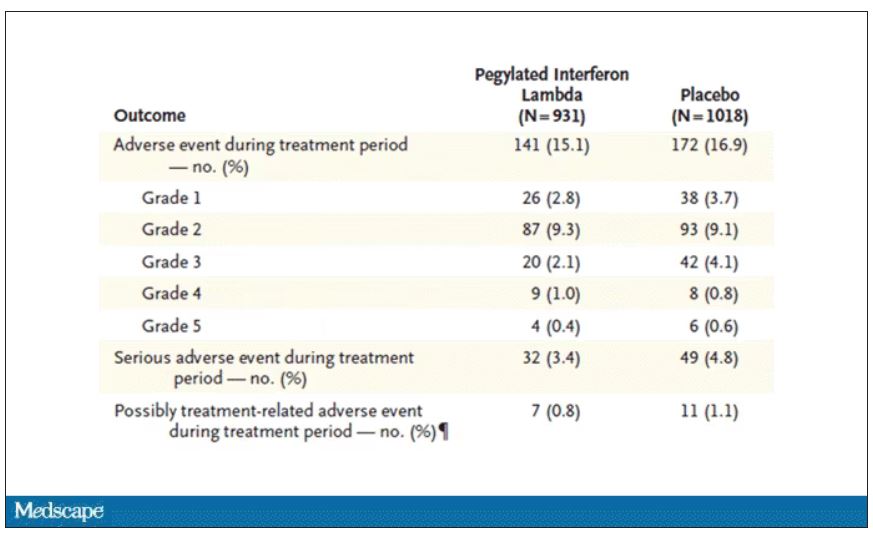
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Pound of flesh buys less prison time
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Maternal COVID-19 vaccine curbs infant infection
a new study shows.
Previous research has confirmed that COVID-19 neutralizing antibodies following maternal vaccination or maternal COVID-19 infection are present in umbilical cord blood, breast milk, and infant serum specimens, wrote Sarah C.J. Jorgensen, PharmD, MPH, of the University of Toronto, and colleagues in their article published in The BMJ.
In the study, the researchers identified maternal and newborn pairs using administrative databases from Canada. The study population included 8,809 infants aged younger than 6 months who were born between May 7, 2021, and March 31, 2022, and who underwent testing for COVID-19 between May 7, 2021, and September 5, 2022.
Maternal vaccination with the primary COVID-19 mRNA monovalent vaccine series was defined as two vaccine doses administered up to 14 days before delivery, with at least one of the doses after the conception date.
Maternal vaccination with the primary series plus one booster was defined as three doses administered up to 14 days before delivery, with at least one of these doses after the conception date.
The primary outcome was the presence of delta or omicron COVID-19 infection or hospital admission of the infants.
The study population included 99 COVID-19 cases with the delta variant (with 4,365 controls) and 1,501 cases with the omicron variant (with 4,847 controls).
Overall, the vaccine effectiveness of maternal doses was 95% against delta infection and 45% against omicron.
The effectiveness against hospital admission in cases of delta and omicron variants were 97% and 53%, respectively.
The effectiveness of three doses was 73% against omicron infant infection and 80% against omicron-related infant hospitalization. Data were not available for the effectiveness of three doses against the delta variant.
The effectiveness of two doses of vaccine against infant omicron infection was highest when mothers received the second dose during the third trimester of pregnancy, compared with during the first trimester or second trimester (53% vs. 47% and 53% vs. 37%, respectively).
Vaccine effectiveness with two doses against infant infection from omicron was highest in the first 8 weeks of life (57%), then decreased to 40% among infants after 16 weeks of age.
Although the study was not designed to assess the mechanism of action of the impact of maternal vaccination on infants, the current study results were consistent with other recent studies showing a reduction in infections and hospitalizations among infants whose mothers received COVID-19 vaccines during pregnancy, the researchers wrote in their discussion.
The findings were limited by several factors including the potential unmeasured confounders not available in databases, such as whether infants were breastfed, the researchers noted. Other limitations included a lack of data on home test results and the inability to assess the waning impact of the vaccine effectiveness against the delta variant because of the small number of delta cases, they said. However, the results suggest that the mRNA COVID-19 vaccine during pregnancy was moderately to highly effective for protection against omicron and delta infection and infection-related hospitalization – especially during the first 8 weeks of life.
Effectiveness is encouraging, but updates are needed
The effectiveness of maternal vaccination to prevent COVID-19 infection and related hospitalizations in infants is promising, especially since those younger than 6 months have no other source of vaccine protection against COVID-19 infection, wrote Dana Danino, MD, of Soroka University Medical Center, Israel, and Ilan Youngster, MD, of Shamir Medical Center, Israel, in an accompanying editorial also published in The BMJ.
They also noted that maternal vaccination during pregnancy is an established method of protecting infants from infections such as influenza and pertussis.
Data from previous studies show that most infants whose mothers were vaccinated against COVID-19 during pregnancy retained maternal antibodies at 6 months, “but evidence for protection against neonatal COVID-19 infection has been deficient,” they said.
The current study findings support the value of vaccination during pregnancy, and the findings were strengthened by the large study population, the editorialists wrote. However, whether the same effectiveness holds for other COVID-19 strains such as BQ.1, BQ.1.1, BF.7, XBB, and XBB.1 remains unknown, they said.
Other areas in need of exploration include the optimal timing of vaccination during pregnancy, the protective effects of a bivalent mRNA vaccine (vs. the primary monovalent vaccine in the current study), and the potential benefits of additional boosters, they added.
“Although Jorgenson and colleagues’ study reinforces the value of maternal vaccination against COVID-19 during pregnancy, more studies are needed to better inform vaccination recommendations in an evolving landscape of new SARS-CoV-2 strains and novel vaccines,” the editorialists concluded.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-term Care; the study also received funding from the Canadian Immunization Research Network and the Public Health Agency of Canada. Dr. Jorgensen and the editorialists had no financial conflicts to disclose.
*This article was updated on 3/2/2023.
a new study shows.
Previous research has confirmed that COVID-19 neutralizing antibodies following maternal vaccination or maternal COVID-19 infection are present in umbilical cord blood, breast milk, and infant serum specimens, wrote Sarah C.J. Jorgensen, PharmD, MPH, of the University of Toronto, and colleagues in their article published in The BMJ.
In the study, the researchers identified maternal and newborn pairs using administrative databases from Canada. The study population included 8,809 infants aged younger than 6 months who were born between May 7, 2021, and March 31, 2022, and who underwent testing for COVID-19 between May 7, 2021, and September 5, 2022.
Maternal vaccination with the primary COVID-19 mRNA monovalent vaccine series was defined as two vaccine doses administered up to 14 days before delivery, with at least one of the doses after the conception date.
Maternal vaccination with the primary series plus one booster was defined as three doses administered up to 14 days before delivery, with at least one of these doses after the conception date.
The primary outcome was the presence of delta or omicron COVID-19 infection or hospital admission of the infants.
The study population included 99 COVID-19 cases with the delta variant (with 4,365 controls) and 1,501 cases with the omicron variant (with 4,847 controls).
Overall, the vaccine effectiveness of maternal doses was 95% against delta infection and 45% against omicron.
The effectiveness against hospital admission in cases of delta and omicron variants were 97% and 53%, respectively.
The effectiveness of three doses was 73% against omicron infant infection and 80% against omicron-related infant hospitalization. Data were not available for the effectiveness of three doses against the delta variant.
The effectiveness of two doses of vaccine against infant omicron infection was highest when mothers received the second dose during the third trimester of pregnancy, compared with during the first trimester or second trimester (53% vs. 47% and 53% vs. 37%, respectively).
Vaccine effectiveness with two doses against infant infection from omicron was highest in the first 8 weeks of life (57%), then decreased to 40% among infants after 16 weeks of age.
Although the study was not designed to assess the mechanism of action of the impact of maternal vaccination on infants, the current study results were consistent with other recent studies showing a reduction in infections and hospitalizations among infants whose mothers received COVID-19 vaccines during pregnancy, the researchers wrote in their discussion.
The findings were limited by several factors including the potential unmeasured confounders not available in databases, such as whether infants were breastfed, the researchers noted. Other limitations included a lack of data on home test results and the inability to assess the waning impact of the vaccine effectiveness against the delta variant because of the small number of delta cases, they said. However, the results suggest that the mRNA COVID-19 vaccine during pregnancy was moderately to highly effective for protection against omicron and delta infection and infection-related hospitalization – especially during the first 8 weeks of life.
Effectiveness is encouraging, but updates are needed
The effectiveness of maternal vaccination to prevent COVID-19 infection and related hospitalizations in infants is promising, especially since those younger than 6 months have no other source of vaccine protection against COVID-19 infection, wrote Dana Danino, MD, of Soroka University Medical Center, Israel, and Ilan Youngster, MD, of Shamir Medical Center, Israel, in an accompanying editorial also published in The BMJ.
They also noted that maternal vaccination during pregnancy is an established method of protecting infants from infections such as influenza and pertussis.
Data from previous studies show that most infants whose mothers were vaccinated against COVID-19 during pregnancy retained maternal antibodies at 6 months, “but evidence for protection against neonatal COVID-19 infection has been deficient,” they said.
The current study findings support the value of vaccination during pregnancy, and the findings were strengthened by the large study population, the editorialists wrote. However, whether the same effectiveness holds for other COVID-19 strains such as BQ.1, BQ.1.1, BF.7, XBB, and XBB.1 remains unknown, they said.
Other areas in need of exploration include the optimal timing of vaccination during pregnancy, the protective effects of a bivalent mRNA vaccine (vs. the primary monovalent vaccine in the current study), and the potential benefits of additional boosters, they added.
“Although Jorgenson and colleagues’ study reinforces the value of maternal vaccination against COVID-19 during pregnancy, more studies are needed to better inform vaccination recommendations in an evolving landscape of new SARS-CoV-2 strains and novel vaccines,” the editorialists concluded.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-term Care; the study also received funding from the Canadian Immunization Research Network and the Public Health Agency of Canada. Dr. Jorgensen and the editorialists had no financial conflicts to disclose.
*This article was updated on 3/2/2023.
a new study shows.
Previous research has confirmed that COVID-19 neutralizing antibodies following maternal vaccination or maternal COVID-19 infection are present in umbilical cord blood, breast milk, and infant serum specimens, wrote Sarah C.J. Jorgensen, PharmD, MPH, of the University of Toronto, and colleagues in their article published in The BMJ.
In the study, the researchers identified maternal and newborn pairs using administrative databases from Canada. The study population included 8,809 infants aged younger than 6 months who were born between May 7, 2021, and March 31, 2022, and who underwent testing for COVID-19 between May 7, 2021, and September 5, 2022.
Maternal vaccination with the primary COVID-19 mRNA monovalent vaccine series was defined as two vaccine doses administered up to 14 days before delivery, with at least one of the doses after the conception date.
Maternal vaccination with the primary series plus one booster was defined as three doses administered up to 14 days before delivery, with at least one of these doses after the conception date.
The primary outcome was the presence of delta or omicron COVID-19 infection or hospital admission of the infants.
The study population included 99 COVID-19 cases with the delta variant (with 4,365 controls) and 1,501 cases with the omicron variant (with 4,847 controls).
Overall, the vaccine effectiveness of maternal doses was 95% against delta infection and 45% against omicron.
The effectiveness against hospital admission in cases of delta and omicron variants were 97% and 53%, respectively.
The effectiveness of three doses was 73% against omicron infant infection and 80% against omicron-related infant hospitalization. Data were not available for the effectiveness of three doses against the delta variant.
The effectiveness of two doses of vaccine against infant omicron infection was highest when mothers received the second dose during the third trimester of pregnancy, compared with during the first trimester or second trimester (53% vs. 47% and 53% vs. 37%, respectively).
Vaccine effectiveness with two doses against infant infection from omicron was highest in the first 8 weeks of life (57%), then decreased to 40% among infants after 16 weeks of age.
Although the study was not designed to assess the mechanism of action of the impact of maternal vaccination on infants, the current study results were consistent with other recent studies showing a reduction in infections and hospitalizations among infants whose mothers received COVID-19 vaccines during pregnancy, the researchers wrote in their discussion.
The findings were limited by several factors including the potential unmeasured confounders not available in databases, such as whether infants were breastfed, the researchers noted. Other limitations included a lack of data on home test results and the inability to assess the waning impact of the vaccine effectiveness against the delta variant because of the small number of delta cases, they said. However, the results suggest that the mRNA COVID-19 vaccine during pregnancy was moderately to highly effective for protection against omicron and delta infection and infection-related hospitalization – especially during the first 8 weeks of life.
Effectiveness is encouraging, but updates are needed
The effectiveness of maternal vaccination to prevent COVID-19 infection and related hospitalizations in infants is promising, especially since those younger than 6 months have no other source of vaccine protection against COVID-19 infection, wrote Dana Danino, MD, of Soroka University Medical Center, Israel, and Ilan Youngster, MD, of Shamir Medical Center, Israel, in an accompanying editorial also published in The BMJ.
They also noted that maternal vaccination during pregnancy is an established method of protecting infants from infections such as influenza and pertussis.
Data from previous studies show that most infants whose mothers were vaccinated against COVID-19 during pregnancy retained maternal antibodies at 6 months, “but evidence for protection against neonatal COVID-19 infection has been deficient,” they said.
The current study findings support the value of vaccination during pregnancy, and the findings were strengthened by the large study population, the editorialists wrote. However, whether the same effectiveness holds for other COVID-19 strains such as BQ.1, BQ.1.1, BF.7, XBB, and XBB.1 remains unknown, they said.
Other areas in need of exploration include the optimal timing of vaccination during pregnancy, the protective effects of a bivalent mRNA vaccine (vs. the primary monovalent vaccine in the current study), and the potential benefits of additional boosters, they added.
“Although Jorgenson and colleagues’ study reinforces the value of maternal vaccination against COVID-19 during pregnancy, more studies are needed to better inform vaccination recommendations in an evolving landscape of new SARS-CoV-2 strains and novel vaccines,” the editorialists concluded.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-term Care; the study also received funding from the Canadian Immunization Research Network and the Public Health Agency of Canada. Dr. Jorgensen and the editorialists had no financial conflicts to disclose.
*This article was updated on 3/2/2023.
FROM THE BMJ
IVF-conceived children show strong developmental performance
In vitro fertilization has been around long enough that researchers can now compare developmental and academic achievements between these children and peers at school age.
Amber Kennedy, MBBS, and colleagues did just that. They found little difference in these milestones between a total of 11,059 IVF-conceived children and 401,654 spontaneously conceived children in a new study.
“Parents considering IVF and health care professionals can be reassured that the school age developmental and educational outcomes of IVF-conceived children are equivalent to their peers,” said Dr. Kennedy, lead author and obstetrician and gynecologist at Mercy Hospital for Women at the University of Melbourne.
The findings were published online in PLOS Medicine.
“Overall, we know that children born through IVF are doing fine in terms of health, but also emotionally and cognitively. So I wasn’t surprised. I live in this world,” said Ariadna Cymet Lanski, PsyD, chair of the American Society for Reproductive Medicine Mental Health Professional Group, who was not affiliated with the study.
Some previous researchers linked conception via IVF to an increased risk of congenital abnormalities, autism spectrum disorder, developmental delay, and intellectual disability.
Asked why the current study did not find increased risks, Dr. Kennedy said, “Our population included a relatively recent birth cohort, which may explain some differences from previous studies as IVF practices have evolved over time.”
An estimated 8 million people worldwide have been conceived through IVF since the first birth in 1978, the researchers said. In Australia, this has grown from 2% of births in the year 2000 to now nearly 5% or 1 in 20 live births, Dr. Kennedy noted. “Consequently, it is important to understand the longer-term outcomes for this population of children.”
Along with senior author Anthea Lindquist, MBBS, Dr. Kennedy and colleagues studied 585,659 single births in Victoria, Australia, between 2005 and 2014. They did not include multiple births such as twins or triplets.
The investigators compared 4,697 children conceived via IVF and 168,503 others conceived spontaneously using a standard developmental measure, the Australian Early Developmental Census (AEDC). They also assessed 8,976 children in the IVF group and 333,335 other children on a standard educational measure, the National Assessment Program–Literacy and Numeracy (NAPLAN).
For example, the developmental census measures developmental vulnerability. Dr. Kennedy and colleagues found a 0.3% difference in favor of IVF-conceived children, which statistically was no different than zero.
Similarly, the researchers reported that IVF conception had essentially no effect on overall the literacy score, with an adjusted average difference of 0.03.
Dr. Lanski said the results should be reassuring for people considering IVF. “I can see the value of the study.” The findings “probably brings a lot of comfort ... if you want to build a family, and medically this is what’s recommended.”
Not all IVF techniques are the same, and the researchers want to take a deeper dive to evaluate any distinctions among them. For example, Dr. Kennedy said, “We plan to investigate the same school-aged outcomes after specific IVF-associated techniques.”
A version of this article first appeared on WebMD.com.
In vitro fertilization has been around long enough that researchers can now compare developmental and academic achievements between these children and peers at school age.
Amber Kennedy, MBBS, and colleagues did just that. They found little difference in these milestones between a total of 11,059 IVF-conceived children and 401,654 spontaneously conceived children in a new study.
“Parents considering IVF and health care professionals can be reassured that the school age developmental and educational outcomes of IVF-conceived children are equivalent to their peers,” said Dr. Kennedy, lead author and obstetrician and gynecologist at Mercy Hospital for Women at the University of Melbourne.
The findings were published online in PLOS Medicine.
“Overall, we know that children born through IVF are doing fine in terms of health, but also emotionally and cognitively. So I wasn’t surprised. I live in this world,” said Ariadna Cymet Lanski, PsyD, chair of the American Society for Reproductive Medicine Mental Health Professional Group, who was not affiliated with the study.
Some previous researchers linked conception via IVF to an increased risk of congenital abnormalities, autism spectrum disorder, developmental delay, and intellectual disability.
Asked why the current study did not find increased risks, Dr. Kennedy said, “Our population included a relatively recent birth cohort, which may explain some differences from previous studies as IVF practices have evolved over time.”
An estimated 8 million people worldwide have been conceived through IVF since the first birth in 1978, the researchers said. In Australia, this has grown from 2% of births in the year 2000 to now nearly 5% or 1 in 20 live births, Dr. Kennedy noted. “Consequently, it is important to understand the longer-term outcomes for this population of children.”
Along with senior author Anthea Lindquist, MBBS, Dr. Kennedy and colleagues studied 585,659 single births in Victoria, Australia, between 2005 and 2014. They did not include multiple births such as twins or triplets.
The investigators compared 4,697 children conceived via IVF and 168,503 others conceived spontaneously using a standard developmental measure, the Australian Early Developmental Census (AEDC). They also assessed 8,976 children in the IVF group and 333,335 other children on a standard educational measure, the National Assessment Program–Literacy and Numeracy (NAPLAN).
For example, the developmental census measures developmental vulnerability. Dr. Kennedy and colleagues found a 0.3% difference in favor of IVF-conceived children, which statistically was no different than zero.
Similarly, the researchers reported that IVF conception had essentially no effect on overall the literacy score, with an adjusted average difference of 0.03.
Dr. Lanski said the results should be reassuring for people considering IVF. “I can see the value of the study.” The findings “probably brings a lot of comfort ... if you want to build a family, and medically this is what’s recommended.”
Not all IVF techniques are the same, and the researchers want to take a deeper dive to evaluate any distinctions among them. For example, Dr. Kennedy said, “We plan to investigate the same school-aged outcomes after specific IVF-associated techniques.”
A version of this article first appeared on WebMD.com.
In vitro fertilization has been around long enough that researchers can now compare developmental and academic achievements between these children and peers at school age.
Amber Kennedy, MBBS, and colleagues did just that. They found little difference in these milestones between a total of 11,059 IVF-conceived children and 401,654 spontaneously conceived children in a new study.
“Parents considering IVF and health care professionals can be reassured that the school age developmental and educational outcomes of IVF-conceived children are equivalent to their peers,” said Dr. Kennedy, lead author and obstetrician and gynecologist at Mercy Hospital for Women at the University of Melbourne.
The findings were published online in PLOS Medicine.
“Overall, we know that children born through IVF are doing fine in terms of health, but also emotionally and cognitively. So I wasn’t surprised. I live in this world,” said Ariadna Cymet Lanski, PsyD, chair of the American Society for Reproductive Medicine Mental Health Professional Group, who was not affiliated with the study.
Some previous researchers linked conception via IVF to an increased risk of congenital abnormalities, autism spectrum disorder, developmental delay, and intellectual disability.
Asked why the current study did not find increased risks, Dr. Kennedy said, “Our population included a relatively recent birth cohort, which may explain some differences from previous studies as IVF practices have evolved over time.”
An estimated 8 million people worldwide have been conceived through IVF since the first birth in 1978, the researchers said. In Australia, this has grown from 2% of births in the year 2000 to now nearly 5% or 1 in 20 live births, Dr. Kennedy noted. “Consequently, it is important to understand the longer-term outcomes for this population of children.”
Along with senior author Anthea Lindquist, MBBS, Dr. Kennedy and colleagues studied 585,659 single births in Victoria, Australia, between 2005 and 2014. They did not include multiple births such as twins or triplets.
The investigators compared 4,697 children conceived via IVF and 168,503 others conceived spontaneously using a standard developmental measure, the Australian Early Developmental Census (AEDC). They also assessed 8,976 children in the IVF group and 333,335 other children on a standard educational measure, the National Assessment Program–Literacy and Numeracy (NAPLAN).
For example, the developmental census measures developmental vulnerability. Dr. Kennedy and colleagues found a 0.3% difference in favor of IVF-conceived children, which statistically was no different than zero.
Similarly, the researchers reported that IVF conception had essentially no effect on overall the literacy score, with an adjusted average difference of 0.03.
Dr. Lanski said the results should be reassuring for people considering IVF. “I can see the value of the study.” The findings “probably brings a lot of comfort ... if you want to build a family, and medically this is what’s recommended.”
Not all IVF techniques are the same, and the researchers want to take a deeper dive to evaluate any distinctions among them. For example, Dr. Kennedy said, “We plan to investigate the same school-aged outcomes after specific IVF-associated techniques.”
A version of this article first appeared on WebMD.com.
FROM PLOS MEDICINE
Study documents link between preadolescent acne and elevated BMI
The that used age- and sex-matched controls.
The investigators also identified “a potential association” with precocious puberty that they said “should be considered, especially among those presenting [with acne] under 8 or 9 years old.” The study was published in Pediatric Dermatology .
Senior author Megha M. Tollefson, MD, and coauthors used resources of the Rochester Epidemiology Project to identify all residents of Olmstead County, Minn., who were diagnosed with acne between the ages of 7 and 12 years during 2010-2018. They then randomly selected two age and sex-matched community controls in order to evaluate the relationship of preadolescent acne and BMI.
They confirmed 643 acne cases, and calculated an annual age- and sex-adjusted incidence rate for ages 7-12 of 58 per 10,000 person-years (95% confidence interval, 53.5-62.5). The incidence rate was significantly higher in females than males (89.2 vs. 28.2 per 10,000 person-years; P < .001), and it significantly increased with age (incidence rates of 4.3, 24.4, and 144.3 per 10,000 person-years among those ages 7-8, 9-10, and 11-12 years, respectively).
The median BMI percentile among children with acne was significantly higher than those without an acne diagnosis (75.0 vs. 65.0; P <.001). They also were much more likely to be obese: 16.7% of the children with acne had a BMI in at least the 95th percentile, compared with 12.2% among controls with no acne diagnosis (P = .01). (The qualifying 581 acne cases for this analysis had BMIs recorded within 8 months of the index data, in addition to not having pre-existing acne-relevant endocrine disorders.)
“High BMI is a strong risk factor for acne development and severity in adults, but until now pediatric studies have revealed mixed information ... [and have been] largely retrospective reviews without controls,” Dr. Tollefson, professor of pediatrics and dermatology at the Mayo Clinic, Rochester, Minn., and colleagues wrote.
‘Valuable’ data
Leah Lalor, MD, a pediatric dermatologist not involved with the research, said she is happy to see it. “It’s really valuable,” she said in an interview. “It’s actually the first study that gives us incidence data for preadolescent acne. We all have [had our estimates], but this study quantifies it ... and it will set the stage for further studies of preadolescents in the future.”
The study also documents that “girls are more likely to present to the clinic with acne, and to do so at younger ages, which we’ve suspected and which makes physiologic sense since girls tend to go through puberty earlier than boys,” said Dr. Lalor, assistant professor of dermatology and pediatrics at the Medical College of Wisconsin and the Children’s Wisconsin Clinics, both in Milwaukee. “And most interestingly, it really reveals that BMI is higher among preadolescents with acne than those without.”
The important caveat, she emphasized, is that the study population in Olmstead County, Minn. has a relatively higher level of education, wealth, and employment than the rest of the United States.
The investigators also found that use of systemic acne medications increased with increasing BMI (odds ratio, 1.43 per 5 kg/m2 increase in BMI; 95% CI, 1.07-1.92; P = .015). Approximately 5% of underweight or normal children were prescribed systemic acne medications, compared with 8.1% of overweight children, and 10.3% of those who were obese – data that suggest that most preadolescents with acne had mild to moderate disease and that more severe acne may be associated with increasing BMI percentiles, the authors wrote.
Approximately 4% of the 643 preadolescents with acne were diagnosed with an acne-relevant endocrine disorder prior to or at the time of acne diagnosis – most commonly precocious puberty. Of the 24 diagnoses of precocious puberty, 22 were in females, with a mean age at diagnosis of 7.3 years.
Puberty before age 8 in girls and 9 in boys is classified as precocious puberty. “Thus, a thorough review of systems and exam should be done in this population [with acne] to look for precocious puberty with a low threshold for systemic evaluation if indicated,” the authors wrote, also noting that 19 or the 482 female patients with acne were subsequently diagnosed with polycystic ovary syndrome.
Dr. Lalor said she “automatically” refers children with acne who are younger than 7 for an endocrine workup, but not necessarily children ages 7, 8, or 9 because “that’s considered within the normal realm of starting to get some acne.” Acne in the context of other symptoms such as body odor, hair, or thelarche may prompt referral in these ages, however, she said.
Future research
Obesity may influence preadolescent acne development through its effect on puberty, as overweight and obese girls achieve puberty earlier than those with normal BMI. And “insulin resistance, which may be related to obesity, has been implicated with inducing or worsening acne potentially related to shifts in IGF-1 [insulin-like growth factor 1] signaling and hyperandrogenemia,” Dr. Tollefson and colleagues wrote. Nutrition is also a possible confounder in the study.
“Patients and families have long felt that certain foods or practices contribute to acne, though this has been difficult to prove,” Dr. Lalor said. “We know that excess skim milk seems to contribute ... and there’s a correlation between high glycemic load diets [and acne].”
Assessing dietary habits in conjunction with BMI, and acne incidence and severity, would be valuable. So would research to determine “if decreasing the BMI percentile [in children with acne] would improve or prevent acne, without doing any acne treatments,” she said.
The study was supported by the National Institute on Aging and the Rochester Epidemiology Project. The authors reported no conflicts of interest. Dr. Lalor also reported no conflicts of interest.
The that used age- and sex-matched controls.
The investigators also identified “a potential association” with precocious puberty that they said “should be considered, especially among those presenting [with acne] under 8 or 9 years old.” The study was published in Pediatric Dermatology .
Senior author Megha M. Tollefson, MD, and coauthors used resources of the Rochester Epidemiology Project to identify all residents of Olmstead County, Minn., who were diagnosed with acne between the ages of 7 and 12 years during 2010-2018. They then randomly selected two age and sex-matched community controls in order to evaluate the relationship of preadolescent acne and BMI.
They confirmed 643 acne cases, and calculated an annual age- and sex-adjusted incidence rate for ages 7-12 of 58 per 10,000 person-years (95% confidence interval, 53.5-62.5). The incidence rate was significantly higher in females than males (89.2 vs. 28.2 per 10,000 person-years; P < .001), and it significantly increased with age (incidence rates of 4.3, 24.4, and 144.3 per 10,000 person-years among those ages 7-8, 9-10, and 11-12 years, respectively).
The median BMI percentile among children with acne was significantly higher than those without an acne diagnosis (75.0 vs. 65.0; P <.001). They also were much more likely to be obese: 16.7% of the children with acne had a BMI in at least the 95th percentile, compared with 12.2% among controls with no acne diagnosis (P = .01). (The qualifying 581 acne cases for this analysis had BMIs recorded within 8 months of the index data, in addition to not having pre-existing acne-relevant endocrine disorders.)
“High BMI is a strong risk factor for acne development and severity in adults, but until now pediatric studies have revealed mixed information ... [and have been] largely retrospective reviews without controls,” Dr. Tollefson, professor of pediatrics and dermatology at the Mayo Clinic, Rochester, Minn., and colleagues wrote.
‘Valuable’ data
Leah Lalor, MD, a pediatric dermatologist not involved with the research, said she is happy to see it. “It’s really valuable,” she said in an interview. “It’s actually the first study that gives us incidence data for preadolescent acne. We all have [had our estimates], but this study quantifies it ... and it will set the stage for further studies of preadolescents in the future.”
The study also documents that “girls are more likely to present to the clinic with acne, and to do so at younger ages, which we’ve suspected and which makes physiologic sense since girls tend to go through puberty earlier than boys,” said Dr. Lalor, assistant professor of dermatology and pediatrics at the Medical College of Wisconsin and the Children’s Wisconsin Clinics, both in Milwaukee. “And most interestingly, it really reveals that BMI is higher among preadolescents with acne than those without.”
The important caveat, she emphasized, is that the study population in Olmstead County, Minn. has a relatively higher level of education, wealth, and employment than the rest of the United States.
The investigators also found that use of systemic acne medications increased with increasing BMI (odds ratio, 1.43 per 5 kg/m2 increase in BMI; 95% CI, 1.07-1.92; P = .015). Approximately 5% of underweight or normal children were prescribed systemic acne medications, compared with 8.1% of overweight children, and 10.3% of those who were obese – data that suggest that most preadolescents with acne had mild to moderate disease and that more severe acne may be associated with increasing BMI percentiles, the authors wrote.
Approximately 4% of the 643 preadolescents with acne were diagnosed with an acne-relevant endocrine disorder prior to or at the time of acne diagnosis – most commonly precocious puberty. Of the 24 diagnoses of precocious puberty, 22 were in females, with a mean age at diagnosis of 7.3 years.
Puberty before age 8 in girls and 9 in boys is classified as precocious puberty. “Thus, a thorough review of systems and exam should be done in this population [with acne] to look for precocious puberty with a low threshold for systemic evaluation if indicated,” the authors wrote, also noting that 19 or the 482 female patients with acne were subsequently diagnosed with polycystic ovary syndrome.
Dr. Lalor said she “automatically” refers children with acne who are younger than 7 for an endocrine workup, but not necessarily children ages 7, 8, or 9 because “that’s considered within the normal realm of starting to get some acne.” Acne in the context of other symptoms such as body odor, hair, or thelarche may prompt referral in these ages, however, she said.
Future research
Obesity may influence preadolescent acne development through its effect on puberty, as overweight and obese girls achieve puberty earlier than those with normal BMI. And “insulin resistance, which may be related to obesity, has been implicated with inducing or worsening acne potentially related to shifts in IGF-1 [insulin-like growth factor 1] signaling and hyperandrogenemia,” Dr. Tollefson and colleagues wrote. Nutrition is also a possible confounder in the study.
“Patients and families have long felt that certain foods or practices contribute to acne, though this has been difficult to prove,” Dr. Lalor said. “We know that excess skim milk seems to contribute ... and there’s a correlation between high glycemic load diets [and acne].”
Assessing dietary habits in conjunction with BMI, and acne incidence and severity, would be valuable. So would research to determine “if decreasing the BMI percentile [in children with acne] would improve or prevent acne, without doing any acne treatments,” she said.
The study was supported by the National Institute on Aging and the Rochester Epidemiology Project. The authors reported no conflicts of interest. Dr. Lalor also reported no conflicts of interest.
The that used age- and sex-matched controls.
The investigators also identified “a potential association” with precocious puberty that they said “should be considered, especially among those presenting [with acne] under 8 or 9 years old.” The study was published in Pediatric Dermatology .
Senior author Megha M. Tollefson, MD, and coauthors used resources of the Rochester Epidemiology Project to identify all residents of Olmstead County, Minn., who were diagnosed with acne between the ages of 7 and 12 years during 2010-2018. They then randomly selected two age and sex-matched community controls in order to evaluate the relationship of preadolescent acne and BMI.
They confirmed 643 acne cases, and calculated an annual age- and sex-adjusted incidence rate for ages 7-12 of 58 per 10,000 person-years (95% confidence interval, 53.5-62.5). The incidence rate was significantly higher in females than males (89.2 vs. 28.2 per 10,000 person-years; P < .001), and it significantly increased with age (incidence rates of 4.3, 24.4, and 144.3 per 10,000 person-years among those ages 7-8, 9-10, and 11-12 years, respectively).
The median BMI percentile among children with acne was significantly higher than those without an acne diagnosis (75.0 vs. 65.0; P <.001). They also were much more likely to be obese: 16.7% of the children with acne had a BMI in at least the 95th percentile, compared with 12.2% among controls with no acne diagnosis (P = .01). (The qualifying 581 acne cases for this analysis had BMIs recorded within 8 months of the index data, in addition to not having pre-existing acne-relevant endocrine disorders.)
“High BMI is a strong risk factor for acne development and severity in adults, but until now pediatric studies have revealed mixed information ... [and have been] largely retrospective reviews without controls,” Dr. Tollefson, professor of pediatrics and dermatology at the Mayo Clinic, Rochester, Minn., and colleagues wrote.
‘Valuable’ data
Leah Lalor, MD, a pediatric dermatologist not involved with the research, said she is happy to see it. “It’s really valuable,” she said in an interview. “It’s actually the first study that gives us incidence data for preadolescent acne. We all have [had our estimates], but this study quantifies it ... and it will set the stage for further studies of preadolescents in the future.”
The study also documents that “girls are more likely to present to the clinic with acne, and to do so at younger ages, which we’ve suspected and which makes physiologic sense since girls tend to go through puberty earlier than boys,” said Dr. Lalor, assistant professor of dermatology and pediatrics at the Medical College of Wisconsin and the Children’s Wisconsin Clinics, both in Milwaukee. “And most interestingly, it really reveals that BMI is higher among preadolescents with acne than those without.”
The important caveat, she emphasized, is that the study population in Olmstead County, Minn. has a relatively higher level of education, wealth, and employment than the rest of the United States.
The investigators also found that use of systemic acne medications increased with increasing BMI (odds ratio, 1.43 per 5 kg/m2 increase in BMI; 95% CI, 1.07-1.92; P = .015). Approximately 5% of underweight or normal children were prescribed systemic acne medications, compared with 8.1% of overweight children, and 10.3% of those who were obese – data that suggest that most preadolescents with acne had mild to moderate disease and that more severe acne may be associated with increasing BMI percentiles, the authors wrote.
Approximately 4% of the 643 preadolescents with acne were diagnosed with an acne-relevant endocrine disorder prior to or at the time of acne diagnosis – most commonly precocious puberty. Of the 24 diagnoses of precocious puberty, 22 were in females, with a mean age at diagnosis of 7.3 years.
Puberty before age 8 in girls and 9 in boys is classified as precocious puberty. “Thus, a thorough review of systems and exam should be done in this population [with acne] to look for precocious puberty with a low threshold for systemic evaluation if indicated,” the authors wrote, also noting that 19 or the 482 female patients with acne were subsequently diagnosed with polycystic ovary syndrome.
Dr. Lalor said she “automatically” refers children with acne who are younger than 7 for an endocrine workup, but not necessarily children ages 7, 8, or 9 because “that’s considered within the normal realm of starting to get some acne.” Acne in the context of other symptoms such as body odor, hair, or thelarche may prompt referral in these ages, however, she said.
Future research
Obesity may influence preadolescent acne development through its effect on puberty, as overweight and obese girls achieve puberty earlier than those with normal BMI. And “insulin resistance, which may be related to obesity, has been implicated with inducing or worsening acne potentially related to shifts in IGF-1 [insulin-like growth factor 1] signaling and hyperandrogenemia,” Dr. Tollefson and colleagues wrote. Nutrition is also a possible confounder in the study.
“Patients and families have long felt that certain foods or practices contribute to acne, though this has been difficult to prove,” Dr. Lalor said. “We know that excess skim milk seems to contribute ... and there’s a correlation between high glycemic load diets [and acne].”
Assessing dietary habits in conjunction with BMI, and acne incidence and severity, would be valuable. So would research to determine “if decreasing the BMI percentile [in children with acne] would improve or prevent acne, without doing any acne treatments,” she said.
The study was supported by the National Institute on Aging and the Rochester Epidemiology Project. The authors reported no conflicts of interest. Dr. Lalor also reported no conflicts of interest.
FROM PEDIATRIC DERMATOLOGY
Can pediatricians’ offices be urgent care centers again?
If you live in a suburban or semirural community you have seen at least one urgent care center open up in the last decade. They now number nearly 12,000 nationwide and are growing in number at a 7% rate. Urgent care center patient volume surged during the pandemic and an industry trade group reports it has risen 60% since 2019 (Meyerson N. Why urgent care centers are popping up everywhere. CNN Business. 2023 Jan 28).
According to a report on the CNN Business website, this growth is the result of “convenience, gaps in primary care, high costs of emergency room visits, and increased investment by health systems and equity groups.” Initially, these centers were generally staffed by physicians (70% in 2009) but as of 2022 this number has fallen to 16%. While there are conflicting data to support the claim that urgent care centers are overprescribing, it is pretty clear that their presence in a community encourages fragmented care and weakens established provider-patient relationships. One study has shown that although urgent care centers can prevent a costly emergency room visit ($1,649/visit) this advantage is offset by urgent care cost of more than $6,000.
In the same CNN report, Susan Kressly MD, chair of the AAP’s Private Payer Advocacy Advisory Committee, said: “There’s a need to keep up with society’s demand for quick turnaround, on-demand services that can’t be supported by underfunded primary care.”
Her observation suggests that there is an accelerating demand for timely primary care services. From my perch here in semirural Maine, I don’t see an increasing or unreasonable demand for timeliness by patients and families. Two decades ago, the practice I was in offered evening and weekend morning office hours and call-in times when patientsor parents could speak directly to a physician. These avenues of accessibility have disappeared community wide.
Back in the 1990s “the medical home” was all the buzz. We were encouraged to be the first and primary place to go for a broad range of preventive and responsive care. One-stop shopping at its best. Now it’s “knock, knock ... is anybody home?” Not if it’s getting dark, or it’s the weekend, or you have a minor injury. “Please call the urgent care center.”
I will admit that our dedicated call-in times were unusual and probably not sustainable for most practices. But, most practices back then would see children with acute illness and minor scrapes and trauma on a same-day basis. We dressed burns, splinted joints, and closed minor lacerations. What has changed to create the void that urgent care centers see as an opportunity to make money?
One explanation is the difficulty in finding folks (both providers and support people) who are willing to work a schedule that includes evenings and weekends. One study predicts that there will be a shortfall of 55,000 primary care physicians in the next decade, regardless of their work-life balance preferences. Sometimes it is a lack of creativity and foresight in creating flexible booking schedules that include ample time for patient- and parent-friendly same-day appointments. Minor injuries and skin problems can usually be managed quickly and effectively by an experienced clinician. Unquestionably, one of the big changes has been the shift in the patient mix leaning more toward time-consuming mental health complaints, which make it more difficult to leave open same-day slots. Restoring pediatricians’ offices to their former role as urgent care centers will require training not just more primary care physicians but also mental health consultants and providers.
First, we must decide that we want to become a real medical home that answers to a knock with a receptive response at almost any hour. By failing to accept the challenge of seeing our patients in a timely manner for their minor problems we will continue to fragment their care and threaten to make our relationship with them increasingly irrelevant.
It will mean rethinking how we schedule ourselves and our offices. It may require taking a hard look at how we spend our professional time. For example are annual checkups a must for every child at every age? Are all follow-up visits equally important? Would a phone call be just as effective? Most of all it will require adopting a mindset that we want to be complete physicians for our patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
If you live in a suburban or semirural community you have seen at least one urgent care center open up in the last decade. They now number nearly 12,000 nationwide and are growing in number at a 7% rate. Urgent care center patient volume surged during the pandemic and an industry trade group reports it has risen 60% since 2019 (Meyerson N. Why urgent care centers are popping up everywhere. CNN Business. 2023 Jan 28).
According to a report on the CNN Business website, this growth is the result of “convenience, gaps in primary care, high costs of emergency room visits, and increased investment by health systems and equity groups.” Initially, these centers were generally staffed by physicians (70% in 2009) but as of 2022 this number has fallen to 16%. While there are conflicting data to support the claim that urgent care centers are overprescribing, it is pretty clear that their presence in a community encourages fragmented care and weakens established provider-patient relationships. One study has shown that although urgent care centers can prevent a costly emergency room visit ($1,649/visit) this advantage is offset by urgent care cost of more than $6,000.
In the same CNN report, Susan Kressly MD, chair of the AAP’s Private Payer Advocacy Advisory Committee, said: “There’s a need to keep up with society’s demand for quick turnaround, on-demand services that can’t be supported by underfunded primary care.”
Her observation suggests that there is an accelerating demand for timely primary care services. From my perch here in semirural Maine, I don’t see an increasing or unreasonable demand for timeliness by patients and families. Two decades ago, the practice I was in offered evening and weekend morning office hours and call-in times when patientsor parents could speak directly to a physician. These avenues of accessibility have disappeared community wide.
Back in the 1990s “the medical home” was all the buzz. We were encouraged to be the first and primary place to go for a broad range of preventive and responsive care. One-stop shopping at its best. Now it’s “knock, knock ... is anybody home?” Not if it’s getting dark, or it’s the weekend, or you have a minor injury. “Please call the urgent care center.”
I will admit that our dedicated call-in times were unusual and probably not sustainable for most practices. But, most practices back then would see children with acute illness and minor scrapes and trauma on a same-day basis. We dressed burns, splinted joints, and closed minor lacerations. What has changed to create the void that urgent care centers see as an opportunity to make money?
One explanation is the difficulty in finding folks (both providers and support people) who are willing to work a schedule that includes evenings and weekends. One study predicts that there will be a shortfall of 55,000 primary care physicians in the next decade, regardless of their work-life balance preferences. Sometimes it is a lack of creativity and foresight in creating flexible booking schedules that include ample time for patient- and parent-friendly same-day appointments. Minor injuries and skin problems can usually be managed quickly and effectively by an experienced clinician. Unquestionably, one of the big changes has been the shift in the patient mix leaning more toward time-consuming mental health complaints, which make it more difficult to leave open same-day slots. Restoring pediatricians’ offices to their former role as urgent care centers will require training not just more primary care physicians but also mental health consultants and providers.
First, we must decide that we want to become a real medical home that answers to a knock with a receptive response at almost any hour. By failing to accept the challenge of seeing our patients in a timely manner for their minor problems we will continue to fragment their care and threaten to make our relationship with them increasingly irrelevant.
It will mean rethinking how we schedule ourselves and our offices. It may require taking a hard look at how we spend our professional time. For example are annual checkups a must for every child at every age? Are all follow-up visits equally important? Would a phone call be just as effective? Most of all it will require adopting a mindset that we want to be complete physicians for our patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
If you live in a suburban or semirural community you have seen at least one urgent care center open up in the last decade. They now number nearly 12,000 nationwide and are growing in number at a 7% rate. Urgent care center patient volume surged during the pandemic and an industry trade group reports it has risen 60% since 2019 (Meyerson N. Why urgent care centers are popping up everywhere. CNN Business. 2023 Jan 28).
According to a report on the CNN Business website, this growth is the result of “convenience, gaps in primary care, high costs of emergency room visits, and increased investment by health systems and equity groups.” Initially, these centers were generally staffed by physicians (70% in 2009) but as of 2022 this number has fallen to 16%. While there are conflicting data to support the claim that urgent care centers are overprescribing, it is pretty clear that their presence in a community encourages fragmented care and weakens established provider-patient relationships. One study has shown that although urgent care centers can prevent a costly emergency room visit ($1,649/visit) this advantage is offset by urgent care cost of more than $6,000.
In the same CNN report, Susan Kressly MD, chair of the AAP’s Private Payer Advocacy Advisory Committee, said: “There’s a need to keep up with society’s demand for quick turnaround, on-demand services that can’t be supported by underfunded primary care.”
Her observation suggests that there is an accelerating demand for timely primary care services. From my perch here in semirural Maine, I don’t see an increasing or unreasonable demand for timeliness by patients and families. Two decades ago, the practice I was in offered evening and weekend morning office hours and call-in times when patientsor parents could speak directly to a physician. These avenues of accessibility have disappeared community wide.
Back in the 1990s “the medical home” was all the buzz. We were encouraged to be the first and primary place to go for a broad range of preventive and responsive care. One-stop shopping at its best. Now it’s “knock, knock ... is anybody home?” Not if it’s getting dark, or it’s the weekend, or you have a minor injury. “Please call the urgent care center.”
I will admit that our dedicated call-in times were unusual and probably not sustainable for most practices. But, most practices back then would see children with acute illness and minor scrapes and trauma on a same-day basis. We dressed burns, splinted joints, and closed minor lacerations. What has changed to create the void that urgent care centers see as an opportunity to make money?
One explanation is the difficulty in finding folks (both providers and support people) who are willing to work a schedule that includes evenings and weekends. One study predicts that there will be a shortfall of 55,000 primary care physicians in the next decade, regardless of their work-life balance preferences. Sometimes it is a lack of creativity and foresight in creating flexible booking schedules that include ample time for patient- and parent-friendly same-day appointments. Minor injuries and skin problems can usually be managed quickly and effectively by an experienced clinician. Unquestionably, one of the big changes has been the shift in the patient mix leaning more toward time-consuming mental health complaints, which make it more difficult to leave open same-day slots. Restoring pediatricians’ offices to their former role as urgent care centers will require training not just more primary care physicians but also mental health consultants and providers.
First, we must decide that we want to become a real medical home that answers to a knock with a receptive response at almost any hour. By failing to accept the challenge of seeing our patients in a timely manner for their minor problems we will continue to fragment their care and threaten to make our relationship with them increasingly irrelevant.
It will mean rethinking how we schedule ourselves and our offices. It may require taking a hard look at how we spend our professional time. For example are annual checkups a must for every child at every age? Are all follow-up visits equally important? Would a phone call be just as effective? Most of all it will require adopting a mindset that we want to be complete physicians for our patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Acute cardiac events common during COVID hospitalization
particularly among those with underlying heart disease, and are associated with more severe disease outcomes, a new study suggests.
“We expected to see acute cardiac events occurring among adults hospitalized with COVID-19 but were surprised by how frequently they occurred,” Rebecca C. Woodruff, PhD, MPH, of the U.S. Centers for Disease Control and Prevention, Atlanta, told this news organization.
Overall, she said, “about 1 in 10 adults experienced an acute cardiac event – including heart attacks and acute heart failure – while hospitalized with COVID-19, and this included people with no preexisting heart disease.”
However, she added, “about a quarter of those with underlying heart disease had an acute cardiac event. These patients tended to experience more severe disease outcomes relative to patients hospitalized with COVID-19 who did not experience an acute cardiac event.”
The findings might be relevant to hospitalizations for other viral diseases, “though we can’t say for sure,” she noted. “This study was modeled off a previous study conducted before the COVID-19 pandemic among adults hospitalized with influenza. About 11.7% of [those] adults experienced an acute cardiac event, which was a similar percentage as what we found among patients hospitalized with COVID-19.”
The study was published online in the Journal of the American College of Cardiology.
Underlying cardiac disease key
Dr. Woodruff and colleagues analyzed medical records on a probability sample of 8,460 adults hospitalized with SARS-CoV-2 infection identified from 99 U.S. counties in 14 U.S. states (about 10% of the United States population) from January to November 2021.
Among participants, 11.4% had an acute cardiac event during their hospitalization. The median age was 69 years; 56.5% were men; 48.7%, non-Hispanic White; 33.6%, non-Hispanic Black; 7.4%, Hispanic; and 7.1%, non-Hispanic Asian or Pacific Islander.
As indicated, the prevalence was higher among those with underlying cardiac disease (23.4%), compared with those without (6.2%).
Acute ischemic heart disease (5.5%) and acute heart failure (5.4%) were the most prevalent events; 0.3% of participants had acute myocarditis or pericarditis.
Risk factors varied, depending on underlying cardiac disease status. Those who experienced one or more acute cardiac events had a greater risk for intensive care unit admission (adjusted risk ratio,1.9) and in-hospital death (aRR, 1.7) versus those who did not.
In multivariable analyses, the risk of experiencing acute heart failure was significantly greater among men (aRR, 1.5) and among those with a history of congestive heart failure (aRR, 13.5), atrial fibrillation (aRR, 1.6) or hypertension (aRR,1.3).
Among patients who experienced one or more acute cardiac events, 39.2% required an intensive care unit stay for a median of 5 days. Approximately 22.4% required invasive mechanical ventilation or extracorporeal membrane oxygenation, and 21.1% died while hospitalized.
“Persons at greater risk for experiencing acute cardiac events during COVID-19–associated hospitalizations might benefit from more intensive clinical evaluation and monitoring during hospitalization,” the authors conclude.
The team currently is taking a closer look at acute myocarditis among patients hospitalized with COVID-19, Dr. Woodruff said. Preliminary results were presented at the 2022 annual scientific sessions of the American Heart Association and a paper is forthcoming.
Contemporary data needed
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said the findings mirror his team’s clinical experience in 2020 and 2021 and echo what was seen in the AHA COVID registry: that is, a 0.3% rate of myocarditis.
“The major caveat is that [the findings] may not be generalizable to contemporary COVID infection, both due to changing viral variants and higher levels of immunity in the population,” he said.
“Rates of COVID hospitalization are markedly lower with the current dominant variants, and we would expect the cardiac risk to be lower as well. I would like to see more contemporary data with current variants, particularly focused on higher risk patients with cardiovascular disease,” Dr. de Lemos added.
In a related editorial, George A. Mensa, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Md., and colleagues suggest that the broader impact of the COVID-19 pandemic on human health remains “incompletely examined.”
“The impact of COVID-19 on cardiovascular mortality, in particular, appears to have varied widely, with no large increases seen in a number of the most developed countries but marked increases in hypertensive heart disease mortality seen in the United States in 2021,” they conclude. “The potential contribution of COVID-19 to these deaths, either directly or indirectly, remains to be determined.”
No commercial funding or relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
particularly among those with underlying heart disease, and are associated with more severe disease outcomes, a new study suggests.
“We expected to see acute cardiac events occurring among adults hospitalized with COVID-19 but were surprised by how frequently they occurred,” Rebecca C. Woodruff, PhD, MPH, of the U.S. Centers for Disease Control and Prevention, Atlanta, told this news organization.
Overall, she said, “about 1 in 10 adults experienced an acute cardiac event – including heart attacks and acute heart failure – while hospitalized with COVID-19, and this included people with no preexisting heart disease.”
However, she added, “about a quarter of those with underlying heart disease had an acute cardiac event. These patients tended to experience more severe disease outcomes relative to patients hospitalized with COVID-19 who did not experience an acute cardiac event.”
The findings might be relevant to hospitalizations for other viral diseases, “though we can’t say for sure,” she noted. “This study was modeled off a previous study conducted before the COVID-19 pandemic among adults hospitalized with influenza. About 11.7% of [those] adults experienced an acute cardiac event, which was a similar percentage as what we found among patients hospitalized with COVID-19.”
The study was published online in the Journal of the American College of Cardiology.
Underlying cardiac disease key
Dr. Woodruff and colleagues analyzed medical records on a probability sample of 8,460 adults hospitalized with SARS-CoV-2 infection identified from 99 U.S. counties in 14 U.S. states (about 10% of the United States population) from January to November 2021.
Among participants, 11.4% had an acute cardiac event during their hospitalization. The median age was 69 years; 56.5% were men; 48.7%, non-Hispanic White; 33.6%, non-Hispanic Black; 7.4%, Hispanic; and 7.1%, non-Hispanic Asian or Pacific Islander.
As indicated, the prevalence was higher among those with underlying cardiac disease (23.4%), compared with those without (6.2%).
Acute ischemic heart disease (5.5%) and acute heart failure (5.4%) were the most prevalent events; 0.3% of participants had acute myocarditis or pericarditis.
Risk factors varied, depending on underlying cardiac disease status. Those who experienced one or more acute cardiac events had a greater risk for intensive care unit admission (adjusted risk ratio,1.9) and in-hospital death (aRR, 1.7) versus those who did not.
In multivariable analyses, the risk of experiencing acute heart failure was significantly greater among men (aRR, 1.5) and among those with a history of congestive heart failure (aRR, 13.5), atrial fibrillation (aRR, 1.6) or hypertension (aRR,1.3).
Among patients who experienced one or more acute cardiac events, 39.2% required an intensive care unit stay for a median of 5 days. Approximately 22.4% required invasive mechanical ventilation or extracorporeal membrane oxygenation, and 21.1% died while hospitalized.
“Persons at greater risk for experiencing acute cardiac events during COVID-19–associated hospitalizations might benefit from more intensive clinical evaluation and monitoring during hospitalization,” the authors conclude.
The team currently is taking a closer look at acute myocarditis among patients hospitalized with COVID-19, Dr. Woodruff said. Preliminary results were presented at the 2022 annual scientific sessions of the American Heart Association and a paper is forthcoming.
Contemporary data needed
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said the findings mirror his team’s clinical experience in 2020 and 2021 and echo what was seen in the AHA COVID registry: that is, a 0.3% rate of myocarditis.
“The major caveat is that [the findings] may not be generalizable to contemporary COVID infection, both due to changing viral variants and higher levels of immunity in the population,” he said.
“Rates of COVID hospitalization are markedly lower with the current dominant variants, and we would expect the cardiac risk to be lower as well. I would like to see more contemporary data with current variants, particularly focused on higher risk patients with cardiovascular disease,” Dr. de Lemos added.
In a related editorial, George A. Mensa, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Md., and colleagues suggest that the broader impact of the COVID-19 pandemic on human health remains “incompletely examined.”
“The impact of COVID-19 on cardiovascular mortality, in particular, appears to have varied widely, with no large increases seen in a number of the most developed countries but marked increases in hypertensive heart disease mortality seen in the United States in 2021,” they conclude. “The potential contribution of COVID-19 to these deaths, either directly or indirectly, remains to be determined.”
No commercial funding or relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
particularly among those with underlying heart disease, and are associated with more severe disease outcomes, a new study suggests.
“We expected to see acute cardiac events occurring among adults hospitalized with COVID-19 but were surprised by how frequently they occurred,” Rebecca C. Woodruff, PhD, MPH, of the U.S. Centers for Disease Control and Prevention, Atlanta, told this news organization.
Overall, she said, “about 1 in 10 adults experienced an acute cardiac event – including heart attacks and acute heart failure – while hospitalized with COVID-19, and this included people with no preexisting heart disease.”
However, she added, “about a quarter of those with underlying heart disease had an acute cardiac event. These patients tended to experience more severe disease outcomes relative to patients hospitalized with COVID-19 who did not experience an acute cardiac event.”
The findings might be relevant to hospitalizations for other viral diseases, “though we can’t say for sure,” she noted. “This study was modeled off a previous study conducted before the COVID-19 pandemic among adults hospitalized with influenza. About 11.7% of [those] adults experienced an acute cardiac event, which was a similar percentage as what we found among patients hospitalized with COVID-19.”
The study was published online in the Journal of the American College of Cardiology.
Underlying cardiac disease key
Dr. Woodruff and colleagues analyzed medical records on a probability sample of 8,460 adults hospitalized with SARS-CoV-2 infection identified from 99 U.S. counties in 14 U.S. states (about 10% of the United States population) from January to November 2021.
Among participants, 11.4% had an acute cardiac event during their hospitalization. The median age was 69 years; 56.5% were men; 48.7%, non-Hispanic White; 33.6%, non-Hispanic Black; 7.4%, Hispanic; and 7.1%, non-Hispanic Asian or Pacific Islander.
As indicated, the prevalence was higher among those with underlying cardiac disease (23.4%), compared with those without (6.2%).
Acute ischemic heart disease (5.5%) and acute heart failure (5.4%) were the most prevalent events; 0.3% of participants had acute myocarditis or pericarditis.
Risk factors varied, depending on underlying cardiac disease status. Those who experienced one or more acute cardiac events had a greater risk for intensive care unit admission (adjusted risk ratio,1.9) and in-hospital death (aRR, 1.7) versus those who did not.
In multivariable analyses, the risk of experiencing acute heart failure was significantly greater among men (aRR, 1.5) and among those with a history of congestive heart failure (aRR, 13.5), atrial fibrillation (aRR, 1.6) or hypertension (aRR,1.3).
Among patients who experienced one or more acute cardiac events, 39.2% required an intensive care unit stay for a median of 5 days. Approximately 22.4% required invasive mechanical ventilation or extracorporeal membrane oxygenation, and 21.1% died while hospitalized.
“Persons at greater risk for experiencing acute cardiac events during COVID-19–associated hospitalizations might benefit from more intensive clinical evaluation and monitoring during hospitalization,” the authors conclude.
The team currently is taking a closer look at acute myocarditis among patients hospitalized with COVID-19, Dr. Woodruff said. Preliminary results were presented at the 2022 annual scientific sessions of the American Heart Association and a paper is forthcoming.
Contemporary data needed
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said the findings mirror his team’s clinical experience in 2020 and 2021 and echo what was seen in the AHA COVID registry: that is, a 0.3% rate of myocarditis.
“The major caveat is that [the findings] may not be generalizable to contemporary COVID infection, both due to changing viral variants and higher levels of immunity in the population,” he said.
“Rates of COVID hospitalization are markedly lower with the current dominant variants, and we would expect the cardiac risk to be lower as well. I would like to see more contemporary data with current variants, particularly focused on higher risk patients with cardiovascular disease,” Dr. de Lemos added.
In a related editorial, George A. Mensa, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Md., and colleagues suggest that the broader impact of the COVID-19 pandemic on human health remains “incompletely examined.”
“The impact of COVID-19 on cardiovascular mortality, in particular, appears to have varied widely, with no large increases seen in a number of the most developed countries but marked increases in hypertensive heart disease mortality seen in the United States in 2021,” they conclude. “The potential contribution of COVID-19 to these deaths, either directly or indirectly, remains to be determined.”
No commercial funding or relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
What is the psychological cost of performing CPR?
One year ago, as the sun was setting on a late fall day, Andrés Snitcofsky, a 40-year-old designer from Buenos Aires, Argentina, heard harrowing cries for help. It was the niece and the wife of one of his neighbors: a man in his 60s who the women had found “passed out” in the bedroom. “I did CPR for 5 minutes straight until a friend of the victim came in and asked me to stop, telling me that the man had probably been dead for 2 or 3 hours already. But I had no idea because I’d never seen a dead body before,” Mr. Snitcofsky told this news organization. A few minutes later, the ambulance arrived. The doctor confirmed that there was nothing more that could be done.
Mr. Snitcofsky went home. Nobody had asked for his name or address or phone number. … And it wasn’t because they already knew who he was. In fact, there wasn’t any sort of relationship there. Mr. Snitcofsky had only known his neighbors by sight. His actions that day, however, “did not come without a cost. It took me weeks – months, actually – to put myself together again,” he said. The things he saw, the things he heard, everything about that night played over and over in his head. “I had trouble sleeping. I would play out different scenarios in my head. I questioned myself. I second-guessed myself, criticized myself. It’s like some taboo subject. There’s no one to share the experience with, no one who gets it. But with time, I was able to process the event.
“For 2 months, I talked to my psychologist about it all,” he continued. “That really helped me a lot. In addition to therapy, I reached out to a couple I know – they’re both physicians – and to a firefighter who teaches CPR. Their insight and guidance allowed me to get to a point where I was able to understand that what I did was a good thing and that what I did was all that could have been done. But anyone who finds themselves in the position of having to do CPR – they’re going to be affected in many, many ways. It goes beyond the euphoria of seeing a person come back to life. Of that, I’m quite certain.”
We’ve all seen campaigns encouraging people to learn CPR and to be prepared if the need arises. But in training the public (and even health care professionals), not much, if anything, is said about the “collateral damage”: the psychological and emotional consequences of carrying out the procedure. These especially come into play when you don’t know whether the person survived, when your efforts weren’t able to reverse the sudden cardiac arrest, or when the person you gave CPR to was a loved one – a case that may entail immediate therapeutic interventions to minimize or prevent the risk of suffering long-lasting trauma.
In May 2020, popular American activist and educator Kristin Flanary saw someone suffering cardiac arrest. She stepped in and started doing CPR. And she continued doing CPR … for 10 long minutes. The person she was trying to save was her 34-year-old husband, ophthalmologist and comedian Will Flanary. On Twitter, where she’s known as Lady Glaucomflecken, Ms. Flanary recently shared the following message, putting the topic of CPR and automated external defibrillator training front and center.
“Yes, everyone should learn #CPRandAED. But if we are going to ask people to perform such a brutal task, it’s imperative that we also provide them with the info and resources they need to process it mentally and emotionally. It’s traumatic and life changing. It’s irresponsible and unethical to ask people to help in such a brutal and traumatic way and then neglect to help them in return.” In less than a month, the tweet has racked up over 200,000 views.
Doing one’s duty
There are many people who work to promote CPR and strengthen the other links in the chain of survival for out-of-hospital sudden cardiac arrest, such as prompt access to and delivery of early defibrillation. According to them, any negative psychological impact of intervening is temporary and, when compared with the satisfaction of having done one’s duty, quite insignificant – even if the efforts to save a person’s life are not successful.
“In 99.9% of cases, people who have performed CPR feel a sense of satisfaction, even happiness, knowing that they’ve helped. The individuals I’ve spoken with, I’ve never heard any of them say that they felt worse after the event or that they needed to see a psychologist,” said Mario Fitz Maurice, MD, director of the Arrhythmia Council of the Argentine Society of Cardiology and head of Electrophysiology at Rivadavia Hospital in Buenos Aires. He went on to tell this news organization, “Of course, some degree of fear, sadness, or melancholy can remain afterward. But it seems to me, and there are reports saying as much, that, in the end, what stands out in the person’s mind is the fact that they tried to save a life. And for them, there’s joy in knowing this.”
Dr. Fitz Maurice, who is also the director of the National Arrhythmia Institute in Buenos Aires, pointed out that the kind of person who takes CPR classes “has a profile that’s going to allow them to be psychologically involved; they’re the caring person, the one who’s ready and willing to help people.” And he added that, at his hospital, if they can identify the individuals or first responders who have done CPR on a patient, the protocol is to always contact them to offer psychological care and assistance. “But in 99% of cases, they don’t even understand why we’re calling them, they’re extremely happy to have taken part.”
Some studies, though, paint a much different picture, one that shows that providing CPR can be emotionally challenging and have consequences in terms of one’s family and work life. A qualitative study published in 2016 looked into the experiences of 20 lay rescuers in Norway – five were health educated – who had provided CPR to 18 out-of-hospital cardiac arrest (OHCA) victims, 66% of whom survived. The time from experiencing the OHCA incident to participating in the interview ranged from 6 days to 13 years (median 5.5 years). Several participants reported the OHCA incident as a “shocking and terrifying” experience. Tiredness, exhaustion, confusion, and feeling alone about the OHCA experience were individual reactions that could vary in time from days to months. Anxiety and insomnia were also experienced following the incident.
Some lay rescuers described the influence on work and family life, and a few of them described deep sorrow, even several years after the incident. Overall, they reported repetitive self-criticism regarding whether they could have carried out anything else to achieve a better outcome for the cardiac arrest victim. All of them wanted to be informed about the outcome. And four of the lay rescuers needed professional counseling to process the OHCA experience.
In 2020, another qualitative study was conducted, this time in Taiwan. There were nine participants, none of whom were health professionals. Each had provided initial CPR and defibrillation with AED in public locations. Event-to-interview duration was within 1 year and 1-2 years. The major findings from the study were the following:
- The lay rescuers possessed helping traits and high motivation.
- The lay rescuers reported certain aspects of rescue reality that differed much from prior training and expectations, including difficulty in the depth of chest compression, and uncertainties in real emergency situations.
- The lay rescuers gained positive personal fulfillment in sharing their experience and receiving positive feedback from others, and were willing to help next time, although they experienced a short-term negative psychological impact from the event. “Measures should be taken to increase [a] layperson’s confidence and situation awareness, to reduce training-reality discrepancy, and to build up a support system to avoid negative psychological effects.” This was the conclusion of the study team, which was led by Matthew Huei-Ming Ma, MD, PhD. A professor in the department of emergency medicine at National Taiwan University in Taipei, he is also on the board of directors of the Resuscitation Council of Asia.
Potential trauma
In recalling his experience, Mr. Snitcofsky said, “The hardest part of it all was the moment that I stopped giving CPR, that moment of letting go. This became the image that kept coming back to me, the traumatic moment I hadn’t thought about.”
Psychiatrist Daniel Mosca, MD, is the founder and former president of the Argentine Society of Trauma Psychology. He is also the coordinator of the human factors team at the City of Buenos Aires Emergency Medical Care System. “Any event has the potential to be traumatic, all the more so when it’s an event where you come face to face with death and uncertainty. But how a rescuer reacts will depend on their psychological makeup.” Of the individuals who were held for months or years in the jungle as hostages of the Revolutionary Armed Forces of Colombia, “only” half developed symptoms of posttraumatic stress disorder.
Dr. Mosca believes that a comment by Frank Ochberg, MD, speaks to this finding. “In many cases, peritraumatic symptoms are a normal person’s normal response to an abnormal situation.” For a lot of people who have found themselves having to perform CPR, the symptoms associated with the initial acute stress reaction will resolve on their own in 30-90 days. “But if this doesn’t happen, and those symptoms persist, psychotherapeutic or pharmacological intervention will be necessary,” he noted.
“In CPR classes, it would be good for the instructors to talk about the warning signs that people should look out for in themselves and their fellow rescuers. So, for example, insomnia, anxiety, a heightened state of alertness, feeling disconnected from reality,” Dr. Mosca told this news organization.
“Another thing that can help rescuers is letting them know what happened to the person they gave CPR to. This way, they can get closure,” suggested Manlio Márquez Murillo, MD, a cardiologist and electrophysiologist in Mexico. He is also the coordinator of the Alliance Against Sudden Cardiac Death at the Interamerican Society of Cardiology.
“Medical and nursing societies would have to develop a brief protocol or performance standard. The goal would be to ensure that rescuers are asked for their contact information and that someone gets in touch to debrief them and to offer them care. Next would come the treatment part, to resolve any remaining aftereffects,” said in an interview.
For example, a three-stage Lay Responder Support Model (LRSM) was developed and implemented as part of a lay responder support program established in 2014 by the Peel Regional Council in Ontario. The LRSM identifies and engages individuals who witnessed or participated directly or indirectly in an OHCA, inviting them to participate in a debriefing session facilitated by a trained practitioner. Held 24-48 hours post event, the debriefing allows lay responders to contextualize their reaction to the event. The conversation also serves as an opportunity for them to fully articulate their concerns, questions, and thoughts. The facilitator can communicate stress reduction techniques and address psychological first aid needs as they emerge. Approximately 1 week post event, a secondary follow-up occurs. If the lay responder communicates a continuing struggle with symptoms impacting and interfering with everyday life, the facilitator offers a coordinated or facilitated referral for mental health support.
In an article published in the Journal of Cardiac Failure. Ms. Flanary speaks about the three kinds of language that anyone who was either forced to or inspired to perform CPR can use to help process their trauma: words that explain what happened, words that name (eg, “forgotten patients”), and words that validate the experience and allow the person to articulate their feelings. The tools and technologies that organizations and health care professionals provide can help the healing process. Empathy and compassion, too, have a place.
But there are virtually no standardized and proactive initiatives of this kind in much of the world, including Latin America. So, most people who just happened to be in the right place at the right time find that they have to navigate the “after” part all on their own.
Other obstacles
Dr. Márquez Murillo finds it unfortunate that countries in the region have yet to enact “Good Samaritan” laws. If individuals render aid to someone suffering cardiac arrest, then these laws would ensure that they will not be held liable in any way. This is the case in Argentina and Uruguay. So, the fear of things turning into a legal matter may be holding people back from taking action; that fear could also create additional stress for those who end up stepping in to help.
Even with the legal safeguards, exceptional circumstances may arise where rescuers find themselves facing unexpected emotional challenges. In Argentina, Virginia Pérez Antonelli, the 17-year-old who tried in vain to save the life of Fernando Báez Sosa, had to testify at the trial of the eight defendants accused of brutally beating him in January 2020. The press, the public – the attention of an entire country – was focused on her. She had to respond to the defense attorneys who were able to ask whether she was sure that she performed the CPR maneuvers correctly. And a few weeks ago, a medical examiner hired by the defense suggested that “the CPR may have made the situation worse” for the victim. An indignant Dr. Fitz Maurice responded on Twitter: “CPR SAVES LIVES!! Let’s not let a CHEAP AND BASELESS argument destroy all the work that’s been done…!”
Of course, there are consequences that are beyond our control and others that can, in fact, be anticipated and planned for. Dr. Fitz Maurice brought up a preventive approach: Make CPR second nature, teach it in schools, help people overcome their fears. “Cardiac deaths are 200 times more frequent than deaths resulting from fires – and we practice fire drills a lot more than we practice CPR,” he told this news organization. In a society where there is widespread training on the procedure, where people regularly practice the technique, those who have had the experience of giving someone CPR will feel less alone, will be better understood by others.
“On the other hand, beyond the initial impact and the lack of a formal support system, the medium- and long-term outcome for those who acted is also psychologically and emotionally favorable,” said Jorge Bombau, MD, an obstetrician/gynecologist in Buenos Aires. After Dr. Bombau’s 14-year-old son Beltrán suddenly died during a school sports tournament, Dr. Bombau became a prominent advocate spreading the word about CPR.
“I don’t know anyone who regrets doing CPR,” he told this news organization. “There may be a brief period when the person feels distressed or depressed, when they have trouble sleeping. But it’s been proven that doing a good deed improves one’s mood. And what better deed is there than trying to save someone’s life? Whether their efforts were successful or in vain, that person has, at the end of the day, done something meaningful and worthwhile.”
Mr. Snitcofsky shares this sentiment. For several months now, he’s been feeling he’s “in a good place.” And he’s been actively promoting CPR on social media. As he recently posted on Twitter, “I’m here to retweet everything that has to do with getting us all to become familiar with how to do CPR and working up the courage to do it. The training takes no more than a few hours.
“I want to know that, if I ever have an out-of-hospital sudden cardiac arrest, there will be neighbors, friends, or family members around who know how to do CPR. Every person who knows how to do CPR can persuade others, and those of us who’ve had to do CPR in real life are even better candidates for persuading others. And if one day a person ends up needing CPR, I want to step in again and make up for lost time. Here’s hoping it’ll do the job,” he concluded.
It’s the same for Matías Alonso, a journalist in Buenos Aires. On New Year’s Eve 15 years ago, he was at a family dinner when, a few minutes before midnight, he found himself giving CPR to his stepmother’s father. “Unfortunately, he passed away, but I continued doing CPR on him until the ambulance arrived. For some time, I felt a little guilty for not taking charge of the situation from the beginning, and because I had this idea in my head that more people pulled through and recovered. But afterwards, they really thanked me a lot. And that helped me realize that I’d done something. I didn’t stand still when faced with the inevitability of death. I understood that it was good to have tried,” Mr. Alonso told this news organization. “And next time … hopefully there won’t be a next time … but I’m more prepared, and I now know how I can do better.”
Mr. Alonso, Mr. Snitcofsky, Dr. Fitz Maurice, Dr. Mosca, Dr. Bombau, and Dr. Márquez Murillo disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from Medscape Spanish.
One year ago, as the sun was setting on a late fall day, Andrés Snitcofsky, a 40-year-old designer from Buenos Aires, Argentina, heard harrowing cries for help. It was the niece and the wife of one of his neighbors: a man in his 60s who the women had found “passed out” in the bedroom. “I did CPR for 5 minutes straight until a friend of the victim came in and asked me to stop, telling me that the man had probably been dead for 2 or 3 hours already. But I had no idea because I’d never seen a dead body before,” Mr. Snitcofsky told this news organization. A few minutes later, the ambulance arrived. The doctor confirmed that there was nothing more that could be done.
Mr. Snitcofsky went home. Nobody had asked for his name or address or phone number. … And it wasn’t because they already knew who he was. In fact, there wasn’t any sort of relationship there. Mr. Snitcofsky had only known his neighbors by sight. His actions that day, however, “did not come without a cost. It took me weeks – months, actually – to put myself together again,” he said. The things he saw, the things he heard, everything about that night played over and over in his head. “I had trouble sleeping. I would play out different scenarios in my head. I questioned myself. I second-guessed myself, criticized myself. It’s like some taboo subject. There’s no one to share the experience with, no one who gets it. But with time, I was able to process the event.
“For 2 months, I talked to my psychologist about it all,” he continued. “That really helped me a lot. In addition to therapy, I reached out to a couple I know – they’re both physicians – and to a firefighter who teaches CPR. Their insight and guidance allowed me to get to a point where I was able to understand that what I did was a good thing and that what I did was all that could have been done. But anyone who finds themselves in the position of having to do CPR – they’re going to be affected in many, many ways. It goes beyond the euphoria of seeing a person come back to life. Of that, I’m quite certain.”
We’ve all seen campaigns encouraging people to learn CPR and to be prepared if the need arises. But in training the public (and even health care professionals), not much, if anything, is said about the “collateral damage”: the psychological and emotional consequences of carrying out the procedure. These especially come into play when you don’t know whether the person survived, when your efforts weren’t able to reverse the sudden cardiac arrest, or when the person you gave CPR to was a loved one – a case that may entail immediate therapeutic interventions to minimize or prevent the risk of suffering long-lasting trauma.
In May 2020, popular American activist and educator Kristin Flanary saw someone suffering cardiac arrest. She stepped in and started doing CPR. And she continued doing CPR … for 10 long minutes. The person she was trying to save was her 34-year-old husband, ophthalmologist and comedian Will Flanary. On Twitter, where she’s known as Lady Glaucomflecken, Ms. Flanary recently shared the following message, putting the topic of CPR and automated external defibrillator training front and center.
“Yes, everyone should learn #CPRandAED. But if we are going to ask people to perform such a brutal task, it’s imperative that we also provide them with the info and resources they need to process it mentally and emotionally. It’s traumatic and life changing. It’s irresponsible and unethical to ask people to help in such a brutal and traumatic way and then neglect to help them in return.” In less than a month, the tweet has racked up over 200,000 views.
Doing one’s duty
There are many people who work to promote CPR and strengthen the other links in the chain of survival for out-of-hospital sudden cardiac arrest, such as prompt access to and delivery of early defibrillation. According to them, any negative psychological impact of intervening is temporary and, when compared with the satisfaction of having done one’s duty, quite insignificant – even if the efforts to save a person’s life are not successful.
“In 99.9% of cases, people who have performed CPR feel a sense of satisfaction, even happiness, knowing that they’ve helped. The individuals I’ve spoken with, I’ve never heard any of them say that they felt worse after the event or that they needed to see a psychologist,” said Mario Fitz Maurice, MD, director of the Arrhythmia Council of the Argentine Society of Cardiology and head of Electrophysiology at Rivadavia Hospital in Buenos Aires. He went on to tell this news organization, “Of course, some degree of fear, sadness, or melancholy can remain afterward. But it seems to me, and there are reports saying as much, that, in the end, what stands out in the person’s mind is the fact that they tried to save a life. And for them, there’s joy in knowing this.”
Dr. Fitz Maurice, who is also the director of the National Arrhythmia Institute in Buenos Aires, pointed out that the kind of person who takes CPR classes “has a profile that’s going to allow them to be psychologically involved; they’re the caring person, the one who’s ready and willing to help people.” And he added that, at his hospital, if they can identify the individuals or first responders who have done CPR on a patient, the protocol is to always contact them to offer psychological care and assistance. “But in 99% of cases, they don’t even understand why we’re calling them, they’re extremely happy to have taken part.”
Some studies, though, paint a much different picture, one that shows that providing CPR can be emotionally challenging and have consequences in terms of one’s family and work life. A qualitative study published in 2016 looked into the experiences of 20 lay rescuers in Norway – five were health educated – who had provided CPR to 18 out-of-hospital cardiac arrest (OHCA) victims, 66% of whom survived. The time from experiencing the OHCA incident to participating in the interview ranged from 6 days to 13 years (median 5.5 years). Several participants reported the OHCA incident as a “shocking and terrifying” experience. Tiredness, exhaustion, confusion, and feeling alone about the OHCA experience were individual reactions that could vary in time from days to months. Anxiety and insomnia were also experienced following the incident.
Some lay rescuers described the influence on work and family life, and a few of them described deep sorrow, even several years after the incident. Overall, they reported repetitive self-criticism regarding whether they could have carried out anything else to achieve a better outcome for the cardiac arrest victim. All of them wanted to be informed about the outcome. And four of the lay rescuers needed professional counseling to process the OHCA experience.
In 2020, another qualitative study was conducted, this time in Taiwan. There were nine participants, none of whom were health professionals. Each had provided initial CPR and defibrillation with AED in public locations. Event-to-interview duration was within 1 year and 1-2 years. The major findings from the study were the following:
- The lay rescuers possessed helping traits and high motivation.
- The lay rescuers reported certain aspects of rescue reality that differed much from prior training and expectations, including difficulty in the depth of chest compression, and uncertainties in real emergency situations.
- The lay rescuers gained positive personal fulfillment in sharing their experience and receiving positive feedback from others, and were willing to help next time, although they experienced a short-term negative psychological impact from the event. “Measures should be taken to increase [a] layperson’s confidence and situation awareness, to reduce training-reality discrepancy, and to build up a support system to avoid negative psychological effects.” This was the conclusion of the study team, which was led by Matthew Huei-Ming Ma, MD, PhD. A professor in the department of emergency medicine at National Taiwan University in Taipei, he is also on the board of directors of the Resuscitation Council of Asia.
Potential trauma
In recalling his experience, Mr. Snitcofsky said, “The hardest part of it all was the moment that I stopped giving CPR, that moment of letting go. This became the image that kept coming back to me, the traumatic moment I hadn’t thought about.”
Psychiatrist Daniel Mosca, MD, is the founder and former president of the Argentine Society of Trauma Psychology. He is also the coordinator of the human factors team at the City of Buenos Aires Emergency Medical Care System. “Any event has the potential to be traumatic, all the more so when it’s an event where you come face to face with death and uncertainty. But how a rescuer reacts will depend on their psychological makeup.” Of the individuals who were held for months or years in the jungle as hostages of the Revolutionary Armed Forces of Colombia, “only” half developed symptoms of posttraumatic stress disorder.
Dr. Mosca believes that a comment by Frank Ochberg, MD, speaks to this finding. “In many cases, peritraumatic symptoms are a normal person’s normal response to an abnormal situation.” For a lot of people who have found themselves having to perform CPR, the symptoms associated with the initial acute stress reaction will resolve on their own in 30-90 days. “But if this doesn’t happen, and those symptoms persist, psychotherapeutic or pharmacological intervention will be necessary,” he noted.
“In CPR classes, it would be good for the instructors to talk about the warning signs that people should look out for in themselves and their fellow rescuers. So, for example, insomnia, anxiety, a heightened state of alertness, feeling disconnected from reality,” Dr. Mosca told this news organization.
“Another thing that can help rescuers is letting them know what happened to the person they gave CPR to. This way, they can get closure,” suggested Manlio Márquez Murillo, MD, a cardiologist and electrophysiologist in Mexico. He is also the coordinator of the Alliance Against Sudden Cardiac Death at the Interamerican Society of Cardiology.
“Medical and nursing societies would have to develop a brief protocol or performance standard. The goal would be to ensure that rescuers are asked for their contact information and that someone gets in touch to debrief them and to offer them care. Next would come the treatment part, to resolve any remaining aftereffects,” said in an interview.
For example, a three-stage Lay Responder Support Model (LRSM) was developed and implemented as part of a lay responder support program established in 2014 by the Peel Regional Council in Ontario. The LRSM identifies and engages individuals who witnessed or participated directly or indirectly in an OHCA, inviting them to participate in a debriefing session facilitated by a trained practitioner. Held 24-48 hours post event, the debriefing allows lay responders to contextualize their reaction to the event. The conversation also serves as an opportunity for them to fully articulate their concerns, questions, and thoughts. The facilitator can communicate stress reduction techniques and address psychological first aid needs as they emerge. Approximately 1 week post event, a secondary follow-up occurs. If the lay responder communicates a continuing struggle with symptoms impacting and interfering with everyday life, the facilitator offers a coordinated or facilitated referral for mental health support.
In an article published in the Journal of Cardiac Failure. Ms. Flanary speaks about the three kinds of language that anyone who was either forced to or inspired to perform CPR can use to help process their trauma: words that explain what happened, words that name (eg, “forgotten patients”), and words that validate the experience and allow the person to articulate their feelings. The tools and technologies that organizations and health care professionals provide can help the healing process. Empathy and compassion, too, have a place.
But there are virtually no standardized and proactive initiatives of this kind in much of the world, including Latin America. So, most people who just happened to be in the right place at the right time find that they have to navigate the “after” part all on their own.
Other obstacles
Dr. Márquez Murillo finds it unfortunate that countries in the region have yet to enact “Good Samaritan” laws. If individuals render aid to someone suffering cardiac arrest, then these laws would ensure that they will not be held liable in any way. This is the case in Argentina and Uruguay. So, the fear of things turning into a legal matter may be holding people back from taking action; that fear could also create additional stress for those who end up stepping in to help.
Even with the legal safeguards, exceptional circumstances may arise where rescuers find themselves facing unexpected emotional challenges. In Argentina, Virginia Pérez Antonelli, the 17-year-old who tried in vain to save the life of Fernando Báez Sosa, had to testify at the trial of the eight defendants accused of brutally beating him in January 2020. The press, the public – the attention of an entire country – was focused on her. She had to respond to the defense attorneys who were able to ask whether she was sure that she performed the CPR maneuvers correctly. And a few weeks ago, a medical examiner hired by the defense suggested that “the CPR may have made the situation worse” for the victim. An indignant Dr. Fitz Maurice responded on Twitter: “CPR SAVES LIVES!! Let’s not let a CHEAP AND BASELESS argument destroy all the work that’s been done…!”
Of course, there are consequences that are beyond our control and others that can, in fact, be anticipated and planned for. Dr. Fitz Maurice brought up a preventive approach: Make CPR second nature, teach it in schools, help people overcome their fears. “Cardiac deaths are 200 times more frequent than deaths resulting from fires – and we practice fire drills a lot more than we practice CPR,” he told this news organization. In a society where there is widespread training on the procedure, where people regularly practice the technique, those who have had the experience of giving someone CPR will feel less alone, will be better understood by others.
“On the other hand, beyond the initial impact and the lack of a formal support system, the medium- and long-term outcome for those who acted is also psychologically and emotionally favorable,” said Jorge Bombau, MD, an obstetrician/gynecologist in Buenos Aires. After Dr. Bombau’s 14-year-old son Beltrán suddenly died during a school sports tournament, Dr. Bombau became a prominent advocate spreading the word about CPR.
“I don’t know anyone who regrets doing CPR,” he told this news organization. “There may be a brief period when the person feels distressed or depressed, when they have trouble sleeping. But it’s been proven that doing a good deed improves one’s mood. And what better deed is there than trying to save someone’s life? Whether their efforts were successful or in vain, that person has, at the end of the day, done something meaningful and worthwhile.”
Mr. Snitcofsky shares this sentiment. For several months now, he’s been feeling he’s “in a good place.” And he’s been actively promoting CPR on social media. As he recently posted on Twitter, “I’m here to retweet everything that has to do with getting us all to become familiar with how to do CPR and working up the courage to do it. The training takes no more than a few hours.
“I want to know that, if I ever have an out-of-hospital sudden cardiac arrest, there will be neighbors, friends, or family members around who know how to do CPR. Every person who knows how to do CPR can persuade others, and those of us who’ve had to do CPR in real life are even better candidates for persuading others. And if one day a person ends up needing CPR, I want to step in again and make up for lost time. Here’s hoping it’ll do the job,” he concluded.
It’s the same for Matías Alonso, a journalist in Buenos Aires. On New Year’s Eve 15 years ago, he was at a family dinner when, a few minutes before midnight, he found himself giving CPR to his stepmother’s father. “Unfortunately, he passed away, but I continued doing CPR on him until the ambulance arrived. For some time, I felt a little guilty for not taking charge of the situation from the beginning, and because I had this idea in my head that more people pulled through and recovered. But afterwards, they really thanked me a lot. And that helped me realize that I’d done something. I didn’t stand still when faced with the inevitability of death. I understood that it was good to have tried,” Mr. Alonso told this news organization. “And next time … hopefully there won’t be a next time … but I’m more prepared, and I now know how I can do better.”
Mr. Alonso, Mr. Snitcofsky, Dr. Fitz Maurice, Dr. Mosca, Dr. Bombau, and Dr. Márquez Murillo disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from Medscape Spanish.
One year ago, as the sun was setting on a late fall day, Andrés Snitcofsky, a 40-year-old designer from Buenos Aires, Argentina, heard harrowing cries for help. It was the niece and the wife of one of his neighbors: a man in his 60s who the women had found “passed out” in the bedroom. “I did CPR for 5 minutes straight until a friend of the victim came in and asked me to stop, telling me that the man had probably been dead for 2 or 3 hours already. But I had no idea because I’d never seen a dead body before,” Mr. Snitcofsky told this news organization. A few minutes later, the ambulance arrived. The doctor confirmed that there was nothing more that could be done.
Mr. Snitcofsky went home. Nobody had asked for his name or address or phone number. … And it wasn’t because they already knew who he was. In fact, there wasn’t any sort of relationship there. Mr. Snitcofsky had only known his neighbors by sight. His actions that day, however, “did not come without a cost. It took me weeks – months, actually – to put myself together again,” he said. The things he saw, the things he heard, everything about that night played over and over in his head. “I had trouble sleeping. I would play out different scenarios in my head. I questioned myself. I second-guessed myself, criticized myself. It’s like some taboo subject. There’s no one to share the experience with, no one who gets it. But with time, I was able to process the event.
“For 2 months, I talked to my psychologist about it all,” he continued. “That really helped me a lot. In addition to therapy, I reached out to a couple I know – they’re both physicians – and to a firefighter who teaches CPR. Their insight and guidance allowed me to get to a point where I was able to understand that what I did was a good thing and that what I did was all that could have been done. But anyone who finds themselves in the position of having to do CPR – they’re going to be affected in many, many ways. It goes beyond the euphoria of seeing a person come back to life. Of that, I’m quite certain.”
We’ve all seen campaigns encouraging people to learn CPR and to be prepared if the need arises. But in training the public (and even health care professionals), not much, if anything, is said about the “collateral damage”: the psychological and emotional consequences of carrying out the procedure. These especially come into play when you don’t know whether the person survived, when your efforts weren’t able to reverse the sudden cardiac arrest, or when the person you gave CPR to was a loved one – a case that may entail immediate therapeutic interventions to minimize or prevent the risk of suffering long-lasting trauma.
In May 2020, popular American activist and educator Kristin Flanary saw someone suffering cardiac arrest. She stepped in and started doing CPR. And she continued doing CPR … for 10 long minutes. The person she was trying to save was her 34-year-old husband, ophthalmologist and comedian Will Flanary. On Twitter, where she’s known as Lady Glaucomflecken, Ms. Flanary recently shared the following message, putting the topic of CPR and automated external defibrillator training front and center.
“Yes, everyone should learn #CPRandAED. But if we are going to ask people to perform such a brutal task, it’s imperative that we also provide them with the info and resources they need to process it mentally and emotionally. It’s traumatic and life changing. It’s irresponsible and unethical to ask people to help in such a brutal and traumatic way and then neglect to help them in return.” In less than a month, the tweet has racked up over 200,000 views.
Doing one’s duty
There are many people who work to promote CPR and strengthen the other links in the chain of survival for out-of-hospital sudden cardiac arrest, such as prompt access to and delivery of early defibrillation. According to them, any negative psychological impact of intervening is temporary and, when compared with the satisfaction of having done one’s duty, quite insignificant – even if the efforts to save a person’s life are not successful.
“In 99.9% of cases, people who have performed CPR feel a sense of satisfaction, even happiness, knowing that they’ve helped. The individuals I’ve spoken with, I’ve never heard any of them say that they felt worse after the event or that they needed to see a psychologist,” said Mario Fitz Maurice, MD, director of the Arrhythmia Council of the Argentine Society of Cardiology and head of Electrophysiology at Rivadavia Hospital in Buenos Aires. He went on to tell this news organization, “Of course, some degree of fear, sadness, or melancholy can remain afterward. But it seems to me, and there are reports saying as much, that, in the end, what stands out in the person’s mind is the fact that they tried to save a life. And for them, there’s joy in knowing this.”
Dr. Fitz Maurice, who is also the director of the National Arrhythmia Institute in Buenos Aires, pointed out that the kind of person who takes CPR classes “has a profile that’s going to allow them to be psychologically involved; they’re the caring person, the one who’s ready and willing to help people.” And he added that, at his hospital, if they can identify the individuals or first responders who have done CPR on a patient, the protocol is to always contact them to offer psychological care and assistance. “But in 99% of cases, they don’t even understand why we’re calling them, they’re extremely happy to have taken part.”
Some studies, though, paint a much different picture, one that shows that providing CPR can be emotionally challenging and have consequences in terms of one’s family and work life. A qualitative study published in 2016 looked into the experiences of 20 lay rescuers in Norway – five were health educated – who had provided CPR to 18 out-of-hospital cardiac arrest (OHCA) victims, 66% of whom survived. The time from experiencing the OHCA incident to participating in the interview ranged from 6 days to 13 years (median 5.5 years). Several participants reported the OHCA incident as a “shocking and terrifying” experience. Tiredness, exhaustion, confusion, and feeling alone about the OHCA experience were individual reactions that could vary in time from days to months. Anxiety and insomnia were also experienced following the incident.
Some lay rescuers described the influence on work and family life, and a few of them described deep sorrow, even several years after the incident. Overall, they reported repetitive self-criticism regarding whether they could have carried out anything else to achieve a better outcome for the cardiac arrest victim. All of them wanted to be informed about the outcome. And four of the lay rescuers needed professional counseling to process the OHCA experience.
In 2020, another qualitative study was conducted, this time in Taiwan. There were nine participants, none of whom were health professionals. Each had provided initial CPR and defibrillation with AED in public locations. Event-to-interview duration was within 1 year and 1-2 years. The major findings from the study were the following:
- The lay rescuers possessed helping traits and high motivation.
- The lay rescuers reported certain aspects of rescue reality that differed much from prior training and expectations, including difficulty in the depth of chest compression, and uncertainties in real emergency situations.
- The lay rescuers gained positive personal fulfillment in sharing their experience and receiving positive feedback from others, and were willing to help next time, although they experienced a short-term negative psychological impact from the event. “Measures should be taken to increase [a] layperson’s confidence and situation awareness, to reduce training-reality discrepancy, and to build up a support system to avoid negative psychological effects.” This was the conclusion of the study team, which was led by Matthew Huei-Ming Ma, MD, PhD. A professor in the department of emergency medicine at National Taiwan University in Taipei, he is also on the board of directors of the Resuscitation Council of Asia.
Potential trauma
In recalling his experience, Mr. Snitcofsky said, “The hardest part of it all was the moment that I stopped giving CPR, that moment of letting go. This became the image that kept coming back to me, the traumatic moment I hadn’t thought about.”
Psychiatrist Daniel Mosca, MD, is the founder and former president of the Argentine Society of Trauma Psychology. He is also the coordinator of the human factors team at the City of Buenos Aires Emergency Medical Care System. “Any event has the potential to be traumatic, all the more so when it’s an event where you come face to face with death and uncertainty. But how a rescuer reacts will depend on their psychological makeup.” Of the individuals who were held for months or years in the jungle as hostages of the Revolutionary Armed Forces of Colombia, “only” half developed symptoms of posttraumatic stress disorder.
Dr. Mosca believes that a comment by Frank Ochberg, MD, speaks to this finding. “In many cases, peritraumatic symptoms are a normal person’s normal response to an abnormal situation.” For a lot of people who have found themselves having to perform CPR, the symptoms associated with the initial acute stress reaction will resolve on their own in 30-90 days. “But if this doesn’t happen, and those symptoms persist, psychotherapeutic or pharmacological intervention will be necessary,” he noted.
“In CPR classes, it would be good for the instructors to talk about the warning signs that people should look out for in themselves and their fellow rescuers. So, for example, insomnia, anxiety, a heightened state of alertness, feeling disconnected from reality,” Dr. Mosca told this news organization.
“Another thing that can help rescuers is letting them know what happened to the person they gave CPR to. This way, they can get closure,” suggested Manlio Márquez Murillo, MD, a cardiologist and electrophysiologist in Mexico. He is also the coordinator of the Alliance Against Sudden Cardiac Death at the Interamerican Society of Cardiology.
“Medical and nursing societies would have to develop a brief protocol or performance standard. The goal would be to ensure that rescuers are asked for their contact information and that someone gets in touch to debrief them and to offer them care. Next would come the treatment part, to resolve any remaining aftereffects,” said in an interview.
For example, a three-stage Lay Responder Support Model (LRSM) was developed and implemented as part of a lay responder support program established in 2014 by the Peel Regional Council in Ontario. The LRSM identifies and engages individuals who witnessed or participated directly or indirectly in an OHCA, inviting them to participate in a debriefing session facilitated by a trained practitioner. Held 24-48 hours post event, the debriefing allows lay responders to contextualize their reaction to the event. The conversation also serves as an opportunity for them to fully articulate their concerns, questions, and thoughts. The facilitator can communicate stress reduction techniques and address psychological first aid needs as they emerge. Approximately 1 week post event, a secondary follow-up occurs. If the lay responder communicates a continuing struggle with symptoms impacting and interfering with everyday life, the facilitator offers a coordinated or facilitated referral for mental health support.
In an article published in the Journal of Cardiac Failure. Ms. Flanary speaks about the three kinds of language that anyone who was either forced to or inspired to perform CPR can use to help process their trauma: words that explain what happened, words that name (eg, “forgotten patients”), and words that validate the experience and allow the person to articulate their feelings. The tools and technologies that organizations and health care professionals provide can help the healing process. Empathy and compassion, too, have a place.
But there are virtually no standardized and proactive initiatives of this kind in much of the world, including Latin America. So, most people who just happened to be in the right place at the right time find that they have to navigate the “after” part all on their own.
Other obstacles
Dr. Márquez Murillo finds it unfortunate that countries in the region have yet to enact “Good Samaritan” laws. If individuals render aid to someone suffering cardiac arrest, then these laws would ensure that they will not be held liable in any way. This is the case in Argentina and Uruguay. So, the fear of things turning into a legal matter may be holding people back from taking action; that fear could also create additional stress for those who end up stepping in to help.
Even with the legal safeguards, exceptional circumstances may arise where rescuers find themselves facing unexpected emotional challenges. In Argentina, Virginia Pérez Antonelli, the 17-year-old who tried in vain to save the life of Fernando Báez Sosa, had to testify at the trial of the eight defendants accused of brutally beating him in January 2020. The press, the public – the attention of an entire country – was focused on her. She had to respond to the defense attorneys who were able to ask whether she was sure that she performed the CPR maneuvers correctly. And a few weeks ago, a medical examiner hired by the defense suggested that “the CPR may have made the situation worse” for the victim. An indignant Dr. Fitz Maurice responded on Twitter: “CPR SAVES LIVES!! Let’s not let a CHEAP AND BASELESS argument destroy all the work that’s been done…!”
Of course, there are consequences that are beyond our control and others that can, in fact, be anticipated and planned for. Dr. Fitz Maurice brought up a preventive approach: Make CPR second nature, teach it in schools, help people overcome their fears. “Cardiac deaths are 200 times more frequent than deaths resulting from fires – and we practice fire drills a lot more than we practice CPR,” he told this news organization. In a society where there is widespread training on the procedure, where people regularly practice the technique, those who have had the experience of giving someone CPR will feel less alone, will be better understood by others.
“On the other hand, beyond the initial impact and the lack of a formal support system, the medium- and long-term outcome for those who acted is also psychologically and emotionally favorable,” said Jorge Bombau, MD, an obstetrician/gynecologist in Buenos Aires. After Dr. Bombau’s 14-year-old son Beltrán suddenly died during a school sports tournament, Dr. Bombau became a prominent advocate spreading the word about CPR.
“I don’t know anyone who regrets doing CPR,” he told this news organization. “There may be a brief period when the person feels distressed or depressed, when they have trouble sleeping. But it’s been proven that doing a good deed improves one’s mood. And what better deed is there than trying to save someone’s life? Whether their efforts were successful or in vain, that person has, at the end of the day, done something meaningful and worthwhile.”
Mr. Snitcofsky shares this sentiment. For several months now, he’s been feeling he’s “in a good place.” And he’s been actively promoting CPR on social media. As he recently posted on Twitter, “I’m here to retweet everything that has to do with getting us all to become familiar with how to do CPR and working up the courage to do it. The training takes no more than a few hours.
“I want to know that, if I ever have an out-of-hospital sudden cardiac arrest, there will be neighbors, friends, or family members around who know how to do CPR. Every person who knows how to do CPR can persuade others, and those of us who’ve had to do CPR in real life are even better candidates for persuading others. And if one day a person ends up needing CPR, I want to step in again and make up for lost time. Here’s hoping it’ll do the job,” he concluded.
It’s the same for Matías Alonso, a journalist in Buenos Aires. On New Year’s Eve 15 years ago, he was at a family dinner when, a few minutes before midnight, he found himself giving CPR to his stepmother’s father. “Unfortunately, he passed away, but I continued doing CPR on him until the ambulance arrived. For some time, I felt a little guilty for not taking charge of the situation from the beginning, and because I had this idea in my head that more people pulled through and recovered. But afterwards, they really thanked me a lot. And that helped me realize that I’d done something. I didn’t stand still when faced with the inevitability of death. I understood that it was good to have tried,” Mr. Alonso told this news organization. “And next time … hopefully there won’t be a next time … but I’m more prepared, and I now know how I can do better.”
Mr. Alonso, Mr. Snitcofsky, Dr. Fitz Maurice, Dr. Mosca, Dr. Bombau, and Dr. Márquez Murillo disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from Medscape Spanish.
We don’t lose our keys (or other things) as much as we think
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
Can’t find your keys? Misplaced your glasses? No clue where you parked your car?
We all lose things from time to time. And we’ve all heard the standard-issue advice: Picture when you had the object last. Despite this common experience,
“It is well known that we have massive recognition memory for objects,” says study coauthor Jeremy Wolfe, PhD, a professor of ophthalmology and radiology at Harvard Medical School, Boston. In other words, we’re good at recognizing objects we’ve seen before. “For example, after viewing 100 objects for 2-3 seconds each, observers can discriminate those 100 old images from 100 new ones with well over 80% accuracy.”
But remembering what your keys look like won’t necessarily help you find them. “We often want to know when and where we saw [an object],” Dr. Wolfe says. “So our goal was to measure these spatial and temporal memories.”
In a series of experiments, reported in Current Biology, Wolfe and colleagues asked people in the study to remember objects placed on a grid. They viewed 300 objects (pictures of things like a vase, a wedding dress, camo pants, a wet suit) and were asked to recall each one and where it had been located on the grid.
About a third of the people remembered 100 or more locations, by choosing either the correct square on the grid or one directly next to it. Another third remembered between 50 and 100, and the rest remembered less than 50.
Results would likely be even better in the real world “because no one gives up and decides ‘I can’t remember where anything is. I will just guess in this silly experiment,’ ” Dr. Wolfe says.
Later, they were shown items one at a time and asked to click on a time line to indicate when they had seen them. Between 60% and 80% of the time, they identified when they had seen an object within 10% of the correct time. That’s a lot better than the 40% they would have achieved by guessing.
The findings build on previous research and expand our understanding of memory, Dr. Wolfe says. “We knew that people could remember where some things were located. However, no one had tried to quantify that memory,” he says.
But wait: If we’re so good at remembering the where and when, why do we struggle to locate lost objects so much? Chances are, we don’t. We just feel that way because we tend to focus on the fails and overlook the many wins.
“This [study] is showing us something about how we come to know where hundreds of things are in our world,” Dr. Wolfe says. “We tend to notice when this fails – ‘where are my keys?’ – but on a normal day, you are successfully tapping a massive memory on a regular basis.”
Next, the researchers plan to investigate whether spatial and temporal memories are correlated – if you’re good at one, are you good at the other? So far, “that correlation looks rather weak,” Dr. Wolfe says.
A version of this article first appeared on WebMD.com.
FROM CURRENT BIOLOGY
Parents driving the ‘talk’ supports healthy sexual behaviors in GBQ teens and young adults
When it comes to sexual health education in the United States, one thing is abundantly clear: It’s a messy patchwork of programs, topics, and criteria. Only 29 states and the District of Columbia currently mandate sexual health education. Sixteen states have an abstinence-only curriculum, whereas 13 do not require that instruction be age-appropriate, inclusive, medically accurate, or evidence-based/informed. And this is just the tip of the iceberg, according to a 2022 report issued by the Sex Ed for Social Change organization.
Parents should take an inclusive approach to sex communication and create a safe space for discussing sex and sexual orientation, said almost all (96.7%) of male young adults who participated in a qualitative study. This would help reinforce acceptance and parents could possibly serve as a proxy for children who’ve not yet disclosed their sexual orientation. Yet, few parents are equipped or prepared to have these meaningful conversations with gay, bisexual, queer, or gender-diverse children, despite the fact that they are especially vulnerable to poor sexual health outcomes, bullying, abuse, and mental health challenges, as well as high-risk sexual behaviors.
“Parents are sexual socialization agents,” Dalmacio Dennis Flores, PhD, ACRN, assistant professor of nursing at the University of Pennsylvania, Philadelphia, told this news organization. “It’s through the information that they convey, the way that they normalize rituals and expectations, that they inform young people of all of societal expectations or roles they’ll be fulfilling in the future.”
Dr. Flores is lead author of a study published in the Journal of Adolescent Health. He and his colleagues collected perspectives on comprehensive, inclusive, and age-appropriate parent-child sex communications from 30 GBQ adolescent males aged 15-20 years who were already “out” to their parents. Participants were asked to sort through 28 preprinted note cards containing broad sexual health topics (for instance, human anatomy, dating, sexually transmitted infections) as well as topics theoretically specific to GBQ individuals (for example, anal sex), and were asked to add additional topics that they felt were missing. They were then directed to recommend topics along with ideal timing (that is, elementary, middle, or high school) for these conversations.
Study findings also underscored the importance of initiating comprehensive sexuality talks as early as elementary school age – namely to start preparing GBQ children for inevitable adversities that they were likely to encounter later in life, as well as to form building blocks for more mature, in-depth discussions during high school.
Importantly, these recommendations generally align with those aimed at heterosexual youth.
“When we refer to topics for elementary school, they are general parameters of what kids might be interested in or want to hear more about; it’s not planting a seed,” explained Dr. Flores.
Eva Goldfarb, PhD, LHD, MA, professor of public health at Montclair (N.J.) State University, agreed. “We always talk about (in sex education) to follow young people’s lead. If your child is asking you a question, they deserve a response,” said Dr. Goldfarb, who wasn’t involved in the study. “It doesn’t mean you have to give a detailed- level explanation but if they’re asking about it, it means that they are thinking about it. But it’s really important for all young people to know all of this information.”
Along those lines, participants deemed that fundamental issues about bodies (for example, human anatomy, reproduction), different sexual orientations, and an introduction to foundational issues (like privacy, peer or social pressure, sexual abuse) would help elementary-aged children to normalize discussions about sex, anatomy, and sexual orientation.
Middle school conversations were ideally more in-depth to reflect the time when young people are beginning to explore and accept their social and sexual identities. Topics of discussion might include types of sexual intercourse (anal, oral, and vaginal), health promotion strategies (abstinence, condoms, and contraception), possible adverse outcomes of condomless intercourse (HIV, STIs), considerations about engaging in sexual intercourse (including readiness, negotiating boundaries, virginity), and interpersonal safety (for instance, sexting, alcohol/drugs/chemsex, sexual coercion, and partner abuse/violence).
Finally, high school age recommendations focused on socio-relational topics (such as hook-up culture, technology/online dating, and multiple or concurrent sex partners), which are most relevant during a time when adolescents are most prone to experimentation and risk-taking.
Acknowledging that the study approach was novel, Dr. Flores noted that hearing about these topics from the youth perspective allowed parents to prepare. “Communication is better when it’s anticipated vs. reactive,” he said.
Last but not least, clinicians also have an important role in supporting these conversations.
“We’ve always looked at sex communication as a dyadic process, as a parent bestowing wisdom on a child who doesn’t have that knowledge yet. But it can be a triadic model,” said Dr. Flores. “Providers can encourage parents to ask if a child is dating or is familiar with ways to protect themselves or provide consent, and act as a resource exclusively to troubleshoot emergent issues.”
This study was funded by the National Institutes of Health. The study also received supplementary funding from the Surgeon General C. Everett Koop HIV/AIDS Research Award. Dr. Flores and Dr. Goldfarb report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
When it comes to sexual health education in the United States, one thing is abundantly clear: It’s a messy patchwork of programs, topics, and criteria. Only 29 states and the District of Columbia currently mandate sexual health education. Sixteen states have an abstinence-only curriculum, whereas 13 do not require that instruction be age-appropriate, inclusive, medically accurate, or evidence-based/informed. And this is just the tip of the iceberg, according to a 2022 report issued by the Sex Ed for Social Change organization.
Parents should take an inclusive approach to sex communication and create a safe space for discussing sex and sexual orientation, said almost all (96.7%) of male young adults who participated in a qualitative study. This would help reinforce acceptance and parents could possibly serve as a proxy for children who’ve not yet disclosed their sexual orientation. Yet, few parents are equipped or prepared to have these meaningful conversations with gay, bisexual, queer, or gender-diverse children, despite the fact that they are especially vulnerable to poor sexual health outcomes, bullying, abuse, and mental health challenges, as well as high-risk sexual behaviors.
“Parents are sexual socialization agents,” Dalmacio Dennis Flores, PhD, ACRN, assistant professor of nursing at the University of Pennsylvania, Philadelphia, told this news organization. “It’s through the information that they convey, the way that they normalize rituals and expectations, that they inform young people of all of societal expectations or roles they’ll be fulfilling in the future.”
Dr. Flores is lead author of a study published in the Journal of Adolescent Health. He and his colleagues collected perspectives on comprehensive, inclusive, and age-appropriate parent-child sex communications from 30 GBQ adolescent males aged 15-20 years who were already “out” to their parents. Participants were asked to sort through 28 preprinted note cards containing broad sexual health topics (for instance, human anatomy, dating, sexually transmitted infections) as well as topics theoretically specific to GBQ individuals (for example, anal sex), and were asked to add additional topics that they felt were missing. They were then directed to recommend topics along with ideal timing (that is, elementary, middle, or high school) for these conversations.
Study findings also underscored the importance of initiating comprehensive sexuality talks as early as elementary school age – namely to start preparing GBQ children for inevitable adversities that they were likely to encounter later in life, as well as to form building blocks for more mature, in-depth discussions during high school.
Importantly, these recommendations generally align with those aimed at heterosexual youth.
“When we refer to topics for elementary school, they are general parameters of what kids might be interested in or want to hear more about; it’s not planting a seed,” explained Dr. Flores.
Eva Goldfarb, PhD, LHD, MA, professor of public health at Montclair (N.J.) State University, agreed. “We always talk about (in sex education) to follow young people’s lead. If your child is asking you a question, they deserve a response,” said Dr. Goldfarb, who wasn’t involved in the study. “It doesn’t mean you have to give a detailed- level explanation but if they’re asking about it, it means that they are thinking about it. But it’s really important for all young people to know all of this information.”
Along those lines, participants deemed that fundamental issues about bodies (for example, human anatomy, reproduction), different sexual orientations, and an introduction to foundational issues (like privacy, peer or social pressure, sexual abuse) would help elementary-aged children to normalize discussions about sex, anatomy, and sexual orientation.
Middle school conversations were ideally more in-depth to reflect the time when young people are beginning to explore and accept their social and sexual identities. Topics of discussion might include types of sexual intercourse (anal, oral, and vaginal), health promotion strategies (abstinence, condoms, and contraception), possible adverse outcomes of condomless intercourse (HIV, STIs), considerations about engaging in sexual intercourse (including readiness, negotiating boundaries, virginity), and interpersonal safety (for instance, sexting, alcohol/drugs/chemsex, sexual coercion, and partner abuse/violence).
Finally, high school age recommendations focused on socio-relational topics (such as hook-up culture, technology/online dating, and multiple or concurrent sex partners), which are most relevant during a time when adolescents are most prone to experimentation and risk-taking.
Acknowledging that the study approach was novel, Dr. Flores noted that hearing about these topics from the youth perspective allowed parents to prepare. “Communication is better when it’s anticipated vs. reactive,” he said.
Last but not least, clinicians also have an important role in supporting these conversations.
“We’ve always looked at sex communication as a dyadic process, as a parent bestowing wisdom on a child who doesn’t have that knowledge yet. But it can be a triadic model,” said Dr. Flores. “Providers can encourage parents to ask if a child is dating or is familiar with ways to protect themselves or provide consent, and act as a resource exclusively to troubleshoot emergent issues.”
This study was funded by the National Institutes of Health. The study also received supplementary funding from the Surgeon General C. Everett Koop HIV/AIDS Research Award. Dr. Flores and Dr. Goldfarb report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
When it comes to sexual health education in the United States, one thing is abundantly clear: It’s a messy patchwork of programs, topics, and criteria. Only 29 states and the District of Columbia currently mandate sexual health education. Sixteen states have an abstinence-only curriculum, whereas 13 do not require that instruction be age-appropriate, inclusive, medically accurate, or evidence-based/informed. And this is just the tip of the iceberg, according to a 2022 report issued by the Sex Ed for Social Change organization.
Parents should take an inclusive approach to sex communication and create a safe space for discussing sex and sexual orientation, said almost all (96.7%) of male young adults who participated in a qualitative study. This would help reinforce acceptance and parents could possibly serve as a proxy for children who’ve not yet disclosed their sexual orientation. Yet, few parents are equipped or prepared to have these meaningful conversations with gay, bisexual, queer, or gender-diverse children, despite the fact that they are especially vulnerable to poor sexual health outcomes, bullying, abuse, and mental health challenges, as well as high-risk sexual behaviors.
“Parents are sexual socialization agents,” Dalmacio Dennis Flores, PhD, ACRN, assistant professor of nursing at the University of Pennsylvania, Philadelphia, told this news organization. “It’s through the information that they convey, the way that they normalize rituals and expectations, that they inform young people of all of societal expectations or roles they’ll be fulfilling in the future.”
Dr. Flores is lead author of a study published in the Journal of Adolescent Health. He and his colleagues collected perspectives on comprehensive, inclusive, and age-appropriate parent-child sex communications from 30 GBQ adolescent males aged 15-20 years who were already “out” to their parents. Participants were asked to sort through 28 preprinted note cards containing broad sexual health topics (for instance, human anatomy, dating, sexually transmitted infections) as well as topics theoretically specific to GBQ individuals (for example, anal sex), and were asked to add additional topics that they felt were missing. They were then directed to recommend topics along with ideal timing (that is, elementary, middle, or high school) for these conversations.
Study findings also underscored the importance of initiating comprehensive sexuality talks as early as elementary school age – namely to start preparing GBQ children for inevitable adversities that they were likely to encounter later in life, as well as to form building blocks for more mature, in-depth discussions during high school.
Importantly, these recommendations generally align with those aimed at heterosexual youth.
“When we refer to topics for elementary school, they are general parameters of what kids might be interested in or want to hear more about; it’s not planting a seed,” explained Dr. Flores.
Eva Goldfarb, PhD, LHD, MA, professor of public health at Montclair (N.J.) State University, agreed. “We always talk about (in sex education) to follow young people’s lead. If your child is asking you a question, they deserve a response,” said Dr. Goldfarb, who wasn’t involved in the study. “It doesn’t mean you have to give a detailed- level explanation but if they’re asking about it, it means that they are thinking about it. But it’s really important for all young people to know all of this information.”
Along those lines, participants deemed that fundamental issues about bodies (for example, human anatomy, reproduction), different sexual orientations, and an introduction to foundational issues (like privacy, peer or social pressure, sexual abuse) would help elementary-aged children to normalize discussions about sex, anatomy, and sexual orientation.
Middle school conversations were ideally more in-depth to reflect the time when young people are beginning to explore and accept their social and sexual identities. Topics of discussion might include types of sexual intercourse (anal, oral, and vaginal), health promotion strategies (abstinence, condoms, and contraception), possible adverse outcomes of condomless intercourse (HIV, STIs), considerations about engaging in sexual intercourse (including readiness, negotiating boundaries, virginity), and interpersonal safety (for instance, sexting, alcohol/drugs/chemsex, sexual coercion, and partner abuse/violence).
Finally, high school age recommendations focused on socio-relational topics (such as hook-up culture, technology/online dating, and multiple or concurrent sex partners), which are most relevant during a time when adolescents are most prone to experimentation and risk-taking.
Acknowledging that the study approach was novel, Dr. Flores noted that hearing about these topics from the youth perspective allowed parents to prepare. “Communication is better when it’s anticipated vs. reactive,” he said.
Last but not least, clinicians also have an important role in supporting these conversations.
“We’ve always looked at sex communication as a dyadic process, as a parent bestowing wisdom on a child who doesn’t have that knowledge yet. But it can be a triadic model,” said Dr. Flores. “Providers can encourage parents to ask if a child is dating or is familiar with ways to protect themselves or provide consent, and act as a resource exclusively to troubleshoot emergent issues.”
This study was funded by the National Institutes of Health. The study also received supplementary funding from the Surgeon General C. Everett Koop HIV/AIDS Research Award. Dr. Flores and Dr. Goldfarb report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.







