User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Teen girls report record levels of sadness, sexual violence: CDC
Teenage girls are experiencing record high levels of sexual violence, and nearly three in five girls report feeling persistently sad or hopeless, according to a new report by the Centers for Disease Control and Prevention.
Nearly 70% of teens who identified as lesbian, bisexual, gay, or questioning (LGBQ+) report experiencing feelings of persistent sadness and hopeless, and nearly one in four (22%) LGBQ+ had attempted suicide in 2021, according to the report.
“High school should be a time for trailblazing, not trauma. These data show our kids need far more support to cope, hope, and thrive,” said Debra Houry, MD, MPH, the CDC’s acting principal deputy director, in a press release about the findings.
The new analysis looked at data from 2011 to 2021 from the CDC’s Youth Risk and Behavior Survey (YRBS), a semiannual analysis of the health behaviors of students in grades 9-12. The 2021 survey is the first YRBS conducted since the COVID-19 pandemic began and included 17,232 respondents.
Although the researchers saw signs of improvement in risky sexual behaviors and substance abuse, as well as fewer experiences of bullying, the analysis found youth mental health worsened over the past 10 years. This trend was particularly troubling for teenage girls: 57% said they felt persistently sad or hopeless in 2021, a 60% increase from a decade ago. By comparison, 29% of teenage boys reported feeling persistently sad or hopeless, compared with 21% in 2011.
Nearly one-third of girls (30%) reported seriously considering suicide, up from 19% in 2011. In teenage boys, serious thoughts of suicide increased from 13% to 14% from 2011 to 2021. The percentage of teenage girls who had attempted suicide in 2021 was 13%, nearly twice that of teenage boys (7%).
More than half of students with a same-sex partner (58%) reported seriously considering suicide, and 45% of LGBQ+ teens reported the same thoughts. One third of students with a same-sex partner reported attempting suicide in the past year.
The report did not have trend data on LGBQ+ students because of changes in survey methods. The 2021 survey did not have a question accessing gender identity, but this will be incorporated into future surveys, according to the researchers.
Hispanic and multiracial students were more likely to experience persistent feelings of sadness or hopelessness, compared with their peers, with 46% and 49%, respectively, reporting these feelings. From 2011-2021, the percentage of students reporting feelings of hopelessness increased in each racial and ethnic group. The percentage of Black, Hispanic, and White teens who seriously considered suicide also increased over the decade. (A different report released by the CDC on Feb. 10 found that the rate of suicide among Blacks in the United States aged 10-24 jumped 36.6% between 2018 and 2021, the largest increase for any racial or ethnic group.)
The survey also found an alarming spike in sexual violence toward teenage girls. Nearly one in five females (18%) experienced sexual violence in the past year, a 20% increase from 2017. More than 1 in 10 teen girls (14%) said they had been forced to have sex, according to the researchers.
Rates of sexual violence was even higher in LGBQ+ teens. Nearly two in five teens with a partner of the same sex (39%) experienced sexual violence, and 37% reported being sexually assaulted. More than one in five LGBQ+ teens (22%) had experienced sexual violence, and 20% said they had been forced to have sex, the report found.
Among racial and ethnic groups, American Indian and Alaskan Native and multiracial students were more likely to experience sexual violence. The percentage of White students reporting sexual violence increased from 2017 to 2021, but that trend was not observed in other racial and ethnic groups.
Delaney Ruston, MD, an internal medicine specialist in Seattle and creator of “Screenagers,” a 2016 documentary about how technology affects youth, said excessive exposure to social media can compound feelings of depression in teens – particularly, but not only, girls. “They can scroll and consume media for hours, and rather than do activities and have interactions that would help heal from depression symptoms, they stay stuck,” Ruston said in an interview. “As a primary care physician working with teens, this is an extremely common problem I see in my clinic.”
One approach that can help, Dr. Ruston added, is behavioral activation. “This is a strategy where you get them, usually with the support of other people, to do small activities that help to reset brain reward pathways so they start to experience doses of well-being and hope that eventually reverses the depression. Being stuck on screens prevents these healing actions from happening.”
The report also emphasized the importance of school-based services to support students and combat these troubling trends in worsening mental health. “Schools are the gateway to needed services for many young people,” the report stated. “Schools can provide health, behavioral, and mental health services directly or establish referral systems to connect to community sources of care.”
“Young people are experiencing a level of distress that calls on us to act with urgency and compassion,” Kathleen Ethier, PhD, director of the CDC’s division of adolescent and school health, added in a statement. “With the right programs and services in place, schools have the unique ability to help our youth flourish.”
A version of this article first appeared on Medscape.com.
Teenage girls are experiencing record high levels of sexual violence, and nearly three in five girls report feeling persistently sad or hopeless, according to a new report by the Centers for Disease Control and Prevention.
Nearly 70% of teens who identified as lesbian, bisexual, gay, or questioning (LGBQ+) report experiencing feelings of persistent sadness and hopeless, and nearly one in four (22%) LGBQ+ had attempted suicide in 2021, according to the report.
“High school should be a time for trailblazing, not trauma. These data show our kids need far more support to cope, hope, and thrive,” said Debra Houry, MD, MPH, the CDC’s acting principal deputy director, in a press release about the findings.
The new analysis looked at data from 2011 to 2021 from the CDC’s Youth Risk and Behavior Survey (YRBS), a semiannual analysis of the health behaviors of students in grades 9-12. The 2021 survey is the first YRBS conducted since the COVID-19 pandemic began and included 17,232 respondents.
Although the researchers saw signs of improvement in risky sexual behaviors and substance abuse, as well as fewer experiences of bullying, the analysis found youth mental health worsened over the past 10 years. This trend was particularly troubling for teenage girls: 57% said they felt persistently sad or hopeless in 2021, a 60% increase from a decade ago. By comparison, 29% of teenage boys reported feeling persistently sad or hopeless, compared with 21% in 2011.
Nearly one-third of girls (30%) reported seriously considering suicide, up from 19% in 2011. In teenage boys, serious thoughts of suicide increased from 13% to 14% from 2011 to 2021. The percentage of teenage girls who had attempted suicide in 2021 was 13%, nearly twice that of teenage boys (7%).
More than half of students with a same-sex partner (58%) reported seriously considering suicide, and 45% of LGBQ+ teens reported the same thoughts. One third of students with a same-sex partner reported attempting suicide in the past year.
The report did not have trend data on LGBQ+ students because of changes in survey methods. The 2021 survey did not have a question accessing gender identity, but this will be incorporated into future surveys, according to the researchers.
Hispanic and multiracial students were more likely to experience persistent feelings of sadness or hopelessness, compared with their peers, with 46% and 49%, respectively, reporting these feelings. From 2011-2021, the percentage of students reporting feelings of hopelessness increased in each racial and ethnic group. The percentage of Black, Hispanic, and White teens who seriously considered suicide also increased over the decade. (A different report released by the CDC on Feb. 10 found that the rate of suicide among Blacks in the United States aged 10-24 jumped 36.6% between 2018 and 2021, the largest increase for any racial or ethnic group.)
The survey also found an alarming spike in sexual violence toward teenage girls. Nearly one in five females (18%) experienced sexual violence in the past year, a 20% increase from 2017. More than 1 in 10 teen girls (14%) said they had been forced to have sex, according to the researchers.
Rates of sexual violence was even higher in LGBQ+ teens. Nearly two in five teens with a partner of the same sex (39%) experienced sexual violence, and 37% reported being sexually assaulted. More than one in five LGBQ+ teens (22%) had experienced sexual violence, and 20% said they had been forced to have sex, the report found.
Among racial and ethnic groups, American Indian and Alaskan Native and multiracial students were more likely to experience sexual violence. The percentage of White students reporting sexual violence increased from 2017 to 2021, but that trend was not observed in other racial and ethnic groups.
Delaney Ruston, MD, an internal medicine specialist in Seattle and creator of “Screenagers,” a 2016 documentary about how technology affects youth, said excessive exposure to social media can compound feelings of depression in teens – particularly, but not only, girls. “They can scroll and consume media for hours, and rather than do activities and have interactions that would help heal from depression symptoms, they stay stuck,” Ruston said in an interview. “As a primary care physician working with teens, this is an extremely common problem I see in my clinic.”
One approach that can help, Dr. Ruston added, is behavioral activation. “This is a strategy where you get them, usually with the support of other people, to do small activities that help to reset brain reward pathways so they start to experience doses of well-being and hope that eventually reverses the depression. Being stuck on screens prevents these healing actions from happening.”
The report also emphasized the importance of school-based services to support students and combat these troubling trends in worsening mental health. “Schools are the gateway to needed services for many young people,” the report stated. “Schools can provide health, behavioral, and mental health services directly or establish referral systems to connect to community sources of care.”
“Young people are experiencing a level of distress that calls on us to act with urgency and compassion,” Kathleen Ethier, PhD, director of the CDC’s division of adolescent and school health, added in a statement. “With the right programs and services in place, schools have the unique ability to help our youth flourish.”
A version of this article first appeared on Medscape.com.
Teenage girls are experiencing record high levels of sexual violence, and nearly three in five girls report feeling persistently sad or hopeless, according to a new report by the Centers for Disease Control and Prevention.
Nearly 70% of teens who identified as lesbian, bisexual, gay, or questioning (LGBQ+) report experiencing feelings of persistent sadness and hopeless, and nearly one in four (22%) LGBQ+ had attempted suicide in 2021, according to the report.
“High school should be a time for trailblazing, not trauma. These data show our kids need far more support to cope, hope, and thrive,” said Debra Houry, MD, MPH, the CDC’s acting principal deputy director, in a press release about the findings.
The new analysis looked at data from 2011 to 2021 from the CDC’s Youth Risk and Behavior Survey (YRBS), a semiannual analysis of the health behaviors of students in grades 9-12. The 2021 survey is the first YRBS conducted since the COVID-19 pandemic began and included 17,232 respondents.
Although the researchers saw signs of improvement in risky sexual behaviors and substance abuse, as well as fewer experiences of bullying, the analysis found youth mental health worsened over the past 10 years. This trend was particularly troubling for teenage girls: 57% said they felt persistently sad or hopeless in 2021, a 60% increase from a decade ago. By comparison, 29% of teenage boys reported feeling persistently sad or hopeless, compared with 21% in 2011.
Nearly one-third of girls (30%) reported seriously considering suicide, up from 19% in 2011. In teenage boys, serious thoughts of suicide increased from 13% to 14% from 2011 to 2021. The percentage of teenage girls who had attempted suicide in 2021 was 13%, nearly twice that of teenage boys (7%).
More than half of students with a same-sex partner (58%) reported seriously considering suicide, and 45% of LGBQ+ teens reported the same thoughts. One third of students with a same-sex partner reported attempting suicide in the past year.
The report did not have trend data on LGBQ+ students because of changes in survey methods. The 2021 survey did not have a question accessing gender identity, but this will be incorporated into future surveys, according to the researchers.
Hispanic and multiracial students were more likely to experience persistent feelings of sadness or hopelessness, compared with their peers, with 46% and 49%, respectively, reporting these feelings. From 2011-2021, the percentage of students reporting feelings of hopelessness increased in each racial and ethnic group. The percentage of Black, Hispanic, and White teens who seriously considered suicide also increased over the decade. (A different report released by the CDC on Feb. 10 found that the rate of suicide among Blacks in the United States aged 10-24 jumped 36.6% between 2018 and 2021, the largest increase for any racial or ethnic group.)
The survey also found an alarming spike in sexual violence toward teenage girls. Nearly one in five females (18%) experienced sexual violence in the past year, a 20% increase from 2017. More than 1 in 10 teen girls (14%) said they had been forced to have sex, according to the researchers.
Rates of sexual violence was even higher in LGBQ+ teens. Nearly two in five teens with a partner of the same sex (39%) experienced sexual violence, and 37% reported being sexually assaulted. More than one in five LGBQ+ teens (22%) had experienced sexual violence, and 20% said they had been forced to have sex, the report found.
Among racial and ethnic groups, American Indian and Alaskan Native and multiracial students were more likely to experience sexual violence. The percentage of White students reporting sexual violence increased from 2017 to 2021, but that trend was not observed in other racial and ethnic groups.
Delaney Ruston, MD, an internal medicine specialist in Seattle and creator of “Screenagers,” a 2016 documentary about how technology affects youth, said excessive exposure to social media can compound feelings of depression in teens – particularly, but not only, girls. “They can scroll and consume media for hours, and rather than do activities and have interactions that would help heal from depression symptoms, they stay stuck,” Ruston said in an interview. “As a primary care physician working with teens, this is an extremely common problem I see in my clinic.”
One approach that can help, Dr. Ruston added, is behavioral activation. “This is a strategy where you get them, usually with the support of other people, to do small activities that help to reset brain reward pathways so they start to experience doses of well-being and hope that eventually reverses the depression. Being stuck on screens prevents these healing actions from happening.”
The report also emphasized the importance of school-based services to support students and combat these troubling trends in worsening mental health. “Schools are the gateway to needed services for many young people,” the report stated. “Schools can provide health, behavioral, and mental health services directly or establish referral systems to connect to community sources of care.”
“Young people are experiencing a level of distress that calls on us to act with urgency and compassion,” Kathleen Ethier, PhD, director of the CDC’s division of adolescent and school health, added in a statement. “With the right programs and services in place, schools have the unique ability to help our youth flourish.”
A version of this article first appeared on Medscape.com.
Money can buy health but it may not be affordable
It is said that “Money cannot buy happiness.” But ask anyone who does not have it and you will find that money can buy security and freedom from many fears and aggravations. There are no guarantees, but the odds are better with resources than without them. Nations with higher per capita gross domestic product have longer life expectancies, have more freedom, and offer more opportunities for the favored subsets of their populations. The adage is that a rising tide lifts all boats.
It is also said that “Money cannot buy health.” That is also a half lie. Again, there is no guarantee that money can cure what ails you. But over the past 4 decades, modern medical care has added on average 3 years to the average American’s life expectancy. These gains in life expectancy came at a steep cost. The United States has been paying a luxurious, premium price for health care compared with similarly developed nations. When I started my career studying health economics 40 years ago, U.S. health care had increased from 6% of the gross domestic product, was passing 9%, and per my professors, appeared headed for 12% – at which point the predictions were that the sky would start falling. Costs continued to rise and for the past decade about 17% of the U.S. GDP has been going to health care before the pandemic blip.
U.S. life expectancy in the past 150 years nearly doubled. This was primarily due to public health measures rather than the small contributions of medical care for individuals. Life expectancy has mostly risen by reducing infant mortality and childhood mortality. The civil engineers who figured out how to get clean running water into cities and sewage out without the two intermingling have saved far more lives than all the doctors graduating from the medical schools. Better nutrition, better sanitation, vaccines, and, to a smaller extent, antibiotics, have all contributed worthy but lesser effects.
When it comes to individual behavior rather than public health measures, the biggest effect comes from advice physicians have been doling out for decades: Stop smoking, exercise, wear your seatbelt, and do not drink and drive. Over the past generation, medical technology added an incremental improvement to the life span (life expectancy once you attain age 60). This has occurred in cardiovascular health by treating high blood pressure, reducing stroke risk, and lowering hemoglobin A1c. Those measures added about 3 years to life span before the obesity epidemic, the opioid epidemic, and the COVID pandemic wiped out the gains. In round numbers, the price for those 3 extra years of life was about the earnings of working an extra 1-2 years in a lifetime. To share those benefits with everyone, the working stiff has to postpone retirement and work an extra 3 years.
Most recently, modern medicine has produced some very expensive therapies that can add months or years to the lives of people with certain diseases. These therapies may involve over $100,000 worth of marginally beneficial medication that statistically adds a few months to the lives of people with certain varieties of prostate, lung, and breast cancers. Similarly, treatments for chronic disease such as AIDS and cystic fibrosis may involve ongoing medication costs of $10,000 or $20,000 or more per year every year for a lifetime. There are even more extreme examples on the horizon. CAR T-cells and Aduhelm [aducanumab] have the potential to break the Medicare bank. Kaftrio [ivacaftor/tezacaftor/elexacaftor], for cystic fibrosis, is being offered only to wealthier countries.
Medical expenses are hard to analyze because the cited “cost” of many of these medications is like a manufacturer’s suggested retail price that few are actually paying. I am a highly educated consumer, and a physician, but various policies at insurance companies and at national chain pharmacies make it impossible for me to comparison shop for lower prices on my personal medicines. It is not just medications. Over the past 15 years, I have noticed that the “cost” charged for routine lab tests I get have also increased to be 300%-900% higher than what the lab ultimately gets paid by my insurance. It is a farce, and I am chagrined to have been a part of the medical system (managed care organizations, pharmacies, hospitals, and government) that concocted this Frankenstein’s monster of health care payments.
Communicating these issues to a polarized public will require leadership. It will also require better speech writing than the distorted story President Biden used to discuss insulin prices during the State of the Union address. The expensive insulin analogues in common use for diabetes are not the same insulin that was discovered a century ago. The newer medications do provide extra benefits. Assigning a fair value to those benefits is the real issue.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
It is said that “Money cannot buy happiness.” But ask anyone who does not have it and you will find that money can buy security and freedom from many fears and aggravations. There are no guarantees, but the odds are better with resources than without them. Nations with higher per capita gross domestic product have longer life expectancies, have more freedom, and offer more opportunities for the favored subsets of their populations. The adage is that a rising tide lifts all boats.
It is also said that “Money cannot buy health.” That is also a half lie. Again, there is no guarantee that money can cure what ails you. But over the past 4 decades, modern medical care has added on average 3 years to the average American’s life expectancy. These gains in life expectancy came at a steep cost. The United States has been paying a luxurious, premium price for health care compared with similarly developed nations. When I started my career studying health economics 40 years ago, U.S. health care had increased from 6% of the gross domestic product, was passing 9%, and per my professors, appeared headed for 12% – at which point the predictions were that the sky would start falling. Costs continued to rise and for the past decade about 17% of the U.S. GDP has been going to health care before the pandemic blip.
U.S. life expectancy in the past 150 years nearly doubled. This was primarily due to public health measures rather than the small contributions of medical care for individuals. Life expectancy has mostly risen by reducing infant mortality and childhood mortality. The civil engineers who figured out how to get clean running water into cities and sewage out without the two intermingling have saved far more lives than all the doctors graduating from the medical schools. Better nutrition, better sanitation, vaccines, and, to a smaller extent, antibiotics, have all contributed worthy but lesser effects.
When it comes to individual behavior rather than public health measures, the biggest effect comes from advice physicians have been doling out for decades: Stop smoking, exercise, wear your seatbelt, and do not drink and drive. Over the past generation, medical technology added an incremental improvement to the life span (life expectancy once you attain age 60). This has occurred in cardiovascular health by treating high blood pressure, reducing stroke risk, and lowering hemoglobin A1c. Those measures added about 3 years to life span before the obesity epidemic, the opioid epidemic, and the COVID pandemic wiped out the gains. In round numbers, the price for those 3 extra years of life was about the earnings of working an extra 1-2 years in a lifetime. To share those benefits with everyone, the working stiff has to postpone retirement and work an extra 3 years.
Most recently, modern medicine has produced some very expensive therapies that can add months or years to the lives of people with certain diseases. These therapies may involve over $100,000 worth of marginally beneficial medication that statistically adds a few months to the lives of people with certain varieties of prostate, lung, and breast cancers. Similarly, treatments for chronic disease such as AIDS and cystic fibrosis may involve ongoing medication costs of $10,000 or $20,000 or more per year every year for a lifetime. There are even more extreme examples on the horizon. CAR T-cells and Aduhelm [aducanumab] have the potential to break the Medicare bank. Kaftrio [ivacaftor/tezacaftor/elexacaftor], for cystic fibrosis, is being offered only to wealthier countries.
Medical expenses are hard to analyze because the cited “cost” of many of these medications is like a manufacturer’s suggested retail price that few are actually paying. I am a highly educated consumer, and a physician, but various policies at insurance companies and at national chain pharmacies make it impossible for me to comparison shop for lower prices on my personal medicines. It is not just medications. Over the past 15 years, I have noticed that the “cost” charged for routine lab tests I get have also increased to be 300%-900% higher than what the lab ultimately gets paid by my insurance. It is a farce, and I am chagrined to have been a part of the medical system (managed care organizations, pharmacies, hospitals, and government) that concocted this Frankenstein’s monster of health care payments.
Communicating these issues to a polarized public will require leadership. It will also require better speech writing than the distorted story President Biden used to discuss insulin prices during the State of the Union address. The expensive insulin analogues in common use for diabetes are not the same insulin that was discovered a century ago. The newer medications do provide extra benefits. Assigning a fair value to those benefits is the real issue.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
It is said that “Money cannot buy happiness.” But ask anyone who does not have it and you will find that money can buy security and freedom from many fears and aggravations. There are no guarantees, but the odds are better with resources than without them. Nations with higher per capita gross domestic product have longer life expectancies, have more freedom, and offer more opportunities for the favored subsets of their populations. The adage is that a rising tide lifts all boats.
It is also said that “Money cannot buy health.” That is also a half lie. Again, there is no guarantee that money can cure what ails you. But over the past 4 decades, modern medical care has added on average 3 years to the average American’s life expectancy. These gains in life expectancy came at a steep cost. The United States has been paying a luxurious, premium price for health care compared with similarly developed nations. When I started my career studying health economics 40 years ago, U.S. health care had increased from 6% of the gross domestic product, was passing 9%, and per my professors, appeared headed for 12% – at which point the predictions were that the sky would start falling. Costs continued to rise and for the past decade about 17% of the U.S. GDP has been going to health care before the pandemic blip.
U.S. life expectancy in the past 150 years nearly doubled. This was primarily due to public health measures rather than the small contributions of medical care for individuals. Life expectancy has mostly risen by reducing infant mortality and childhood mortality. The civil engineers who figured out how to get clean running water into cities and sewage out without the two intermingling have saved far more lives than all the doctors graduating from the medical schools. Better nutrition, better sanitation, vaccines, and, to a smaller extent, antibiotics, have all contributed worthy but lesser effects.
When it comes to individual behavior rather than public health measures, the biggest effect comes from advice physicians have been doling out for decades: Stop smoking, exercise, wear your seatbelt, and do not drink and drive. Over the past generation, medical technology added an incremental improvement to the life span (life expectancy once you attain age 60). This has occurred in cardiovascular health by treating high blood pressure, reducing stroke risk, and lowering hemoglobin A1c. Those measures added about 3 years to life span before the obesity epidemic, the opioid epidemic, and the COVID pandemic wiped out the gains. In round numbers, the price for those 3 extra years of life was about the earnings of working an extra 1-2 years in a lifetime. To share those benefits with everyone, the working stiff has to postpone retirement and work an extra 3 years.
Most recently, modern medicine has produced some very expensive therapies that can add months or years to the lives of people with certain diseases. These therapies may involve over $100,000 worth of marginally beneficial medication that statistically adds a few months to the lives of people with certain varieties of prostate, lung, and breast cancers. Similarly, treatments for chronic disease such as AIDS and cystic fibrosis may involve ongoing medication costs of $10,000 or $20,000 or more per year every year for a lifetime. There are even more extreme examples on the horizon. CAR T-cells and Aduhelm [aducanumab] have the potential to break the Medicare bank. Kaftrio [ivacaftor/tezacaftor/elexacaftor], for cystic fibrosis, is being offered only to wealthier countries.
Medical expenses are hard to analyze because the cited “cost” of many of these medications is like a manufacturer’s suggested retail price that few are actually paying. I am a highly educated consumer, and a physician, but various policies at insurance companies and at national chain pharmacies make it impossible for me to comparison shop for lower prices on my personal medicines. It is not just medications. Over the past 15 years, I have noticed that the “cost” charged for routine lab tests I get have also increased to be 300%-900% higher than what the lab ultimately gets paid by my insurance. It is a farce, and I am chagrined to have been a part of the medical system (managed care organizations, pharmacies, hospitals, and government) that concocted this Frankenstein’s monster of health care payments.
Communicating these issues to a polarized public will require leadership. It will also require better speech writing than the distorted story President Biden used to discuss insulin prices during the State of the Union address. The expensive insulin analogues in common use for diabetes are not the same insulin that was discovered a century ago. The newer medications do provide extra benefits. Assigning a fair value to those benefits is the real issue.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Expelled from high school, Alister Martin became a Harvard doc
It’s not often that a high school brawl with gang members sets you down a path to becoming a Harvard-trained doctor. But that’s exactly how Alister Martin’s life unfolded.
In retrospect, he should have seen the whole thing coming. That night at the party, his best friend was attacked by a gang member from a nearby high school. Martin was not in a gang but he jumped into the fray to defend his friend.
“I wanted to save the day, but that’s not what happened,” he says. “There were just too many of them.”
When his mother rushed to the hospital, he was so bruised and bloody that she couldn’t recognize him at first. Ever since he was a baby, she had done her best to shield him from the neighborhood where gang violence was a regular disruption. But it hadn’t worked.
“My high school had a zero-tolerance policy for gang violence,” Martin says, “so even though I wasn’t in a gang, I was kicked out.”
Now expelled from high school, his mother wanted him out of town, fearing gang retaliation, or that Martin might seek vengeance on the boy who had brutally beaten him. So, the biology teacher and single mom who worked numerous jobs to keep them afloat, came up with a plan to get him far away from any temptations.
Martin had loved tennis since middle school, when his 8th-grade math teacher, Billie Weise, also a tennis pro, got him a job as a court sweeper at an upscale tennis club nearby. He knew nothing then about tennis but would come to fall in love with the sport. To get her son out of town, Martin’s mother took out loans for $30,000 and sent him to a Florida tennis training camp.
After 6 months of training, Martin, who earned a GED degree while attending the camp, was offered a scholarship to play tennis at Rutgers University in New Brunswick, N.J. The transition to college was tough, however. He was nervous and felt out of place. “I could have died that first day. It became so obvious how poorly my high school education had prepared me for this.”
But the unease he felt was also motivating in a way. Worried about failure, “he locked himself in a room with another student and they studied day and night,” recalls Kamal Khan, director of the office for diversity and academic success at Rutgers. “I’ve never seen anything like it.”
And Martin displayed other attributes that would draw others to him – and later prove important in his career as a doctor. His ability to display empathy and interact with students and teachers separated him from his peers, Mr. Khan says. “There’re a lot of really smart students out there,” he says, “but not many who understand people like Martin.”
After graduating, he decided to pursue his dream of becoming a doctor. He’d wanted to be a doctor since he was 10 years old after his mom was diagnosed with metastatic breast cancer. He remembers overhearing a conversation she was having with a family friend about where he would go if she died.
“That’s when I knew it was serious,” he says.
Doctors saved her life, and it’s something he’ll never forget. But it wasn’t until his time at Rutgers that he finally had the confidence to think he could succeed in medical school.
Martin went on to attend Harvard Medical School and Harvard Kennedy School of Government as well as serving as chief resident at Brigham and Women’s Hospital. He was also a fellow at the White House in the Office of the Vice President and today, he’s an assistant professor at Harvard Medical School in Boston..
He is most at home in the emergency room at Massachusetts General Hospital, where he works as an emergency medical specialist. For him, the ER is the first line of defense for meeting the community’s health needs. Growing up in Neptune, the ER “was where poor folks got their care,” he says. His mom worked two jobs and when she got off work at 8 p.m. there was no pediatrician open. “When I was sick as a kid we always went to the emergency room,” he says.
While at Harvard, he also pursued a degree from the Kennedy School of Government, because of the huge role he feels that politics play in our health care system and especially in bringing care to impoverished communities. And since then he’s taken numerous steps to bridge the gap.
Addiction, for example, became an important issue for Martin, ever since a patient he encountered in his first week as an internist. She was a mom of two who had recently gotten surgery because she broke her ankle falling down the stairs at her child’s daycare, he says. Prescribed oxycodone, she feared she was becoming addicted and needed help. But at the time, there was nothing the ER could do.
“I remember that look in her eyes when we had to turn her away,” he says.
Martin has worked to change protocol at his hospital and others throughout the nation so they can be better set up to treat opioid addiction. He’s the founder of GetWaivered, an organization that trains doctors throughout the country to use evidence-based medicine to manage opioid addiction. In the U.S. doctors need what’s called a DEA X waiver to be able to prescribe buprenorphine to opioid-addicted patients. That means that currently only about 1% of all emergency room doctors nationwide have the waiver and without it, it’s impossible to help patients when they need it the most.
Shuhan He, MD, an internist with Martin at Massachusetts General Hospital who also works on the GetWaivered program, says Martin has a particular trait that helps him be successful.
“He’s a doer and when he sees a problem, he’s gonna try and fix it.”
A version of this article first appeared on Medscape.com.
It’s not often that a high school brawl with gang members sets you down a path to becoming a Harvard-trained doctor. But that’s exactly how Alister Martin’s life unfolded.
In retrospect, he should have seen the whole thing coming. That night at the party, his best friend was attacked by a gang member from a nearby high school. Martin was not in a gang but he jumped into the fray to defend his friend.
“I wanted to save the day, but that’s not what happened,” he says. “There were just too many of them.”
When his mother rushed to the hospital, he was so bruised and bloody that she couldn’t recognize him at first. Ever since he was a baby, she had done her best to shield him from the neighborhood where gang violence was a regular disruption. But it hadn’t worked.
“My high school had a zero-tolerance policy for gang violence,” Martin says, “so even though I wasn’t in a gang, I was kicked out.”
Now expelled from high school, his mother wanted him out of town, fearing gang retaliation, or that Martin might seek vengeance on the boy who had brutally beaten him. So, the biology teacher and single mom who worked numerous jobs to keep them afloat, came up with a plan to get him far away from any temptations.
Martin had loved tennis since middle school, when his 8th-grade math teacher, Billie Weise, also a tennis pro, got him a job as a court sweeper at an upscale tennis club nearby. He knew nothing then about tennis but would come to fall in love with the sport. To get her son out of town, Martin’s mother took out loans for $30,000 and sent him to a Florida tennis training camp.
After 6 months of training, Martin, who earned a GED degree while attending the camp, was offered a scholarship to play tennis at Rutgers University in New Brunswick, N.J. The transition to college was tough, however. He was nervous and felt out of place. “I could have died that first day. It became so obvious how poorly my high school education had prepared me for this.”
But the unease he felt was also motivating in a way. Worried about failure, “he locked himself in a room with another student and they studied day and night,” recalls Kamal Khan, director of the office for diversity and academic success at Rutgers. “I’ve never seen anything like it.”
And Martin displayed other attributes that would draw others to him – and later prove important in his career as a doctor. His ability to display empathy and interact with students and teachers separated him from his peers, Mr. Khan says. “There’re a lot of really smart students out there,” he says, “but not many who understand people like Martin.”
After graduating, he decided to pursue his dream of becoming a doctor. He’d wanted to be a doctor since he was 10 years old after his mom was diagnosed with metastatic breast cancer. He remembers overhearing a conversation she was having with a family friend about where he would go if she died.
“That’s when I knew it was serious,” he says.
Doctors saved her life, and it’s something he’ll never forget. But it wasn’t until his time at Rutgers that he finally had the confidence to think he could succeed in medical school.
Martin went on to attend Harvard Medical School and Harvard Kennedy School of Government as well as serving as chief resident at Brigham and Women’s Hospital. He was also a fellow at the White House in the Office of the Vice President and today, he’s an assistant professor at Harvard Medical School in Boston..
He is most at home in the emergency room at Massachusetts General Hospital, where he works as an emergency medical specialist. For him, the ER is the first line of defense for meeting the community’s health needs. Growing up in Neptune, the ER “was where poor folks got their care,” he says. His mom worked two jobs and when she got off work at 8 p.m. there was no pediatrician open. “When I was sick as a kid we always went to the emergency room,” he says.
While at Harvard, he also pursued a degree from the Kennedy School of Government, because of the huge role he feels that politics play in our health care system and especially in bringing care to impoverished communities. And since then he’s taken numerous steps to bridge the gap.
Addiction, for example, became an important issue for Martin, ever since a patient he encountered in his first week as an internist. She was a mom of two who had recently gotten surgery because she broke her ankle falling down the stairs at her child’s daycare, he says. Prescribed oxycodone, she feared she was becoming addicted and needed help. But at the time, there was nothing the ER could do.
“I remember that look in her eyes when we had to turn her away,” he says.
Martin has worked to change protocol at his hospital and others throughout the nation so they can be better set up to treat opioid addiction. He’s the founder of GetWaivered, an organization that trains doctors throughout the country to use evidence-based medicine to manage opioid addiction. In the U.S. doctors need what’s called a DEA X waiver to be able to prescribe buprenorphine to opioid-addicted patients. That means that currently only about 1% of all emergency room doctors nationwide have the waiver and without it, it’s impossible to help patients when they need it the most.
Shuhan He, MD, an internist with Martin at Massachusetts General Hospital who also works on the GetWaivered program, says Martin has a particular trait that helps him be successful.
“He’s a doer and when he sees a problem, he’s gonna try and fix it.”
A version of this article first appeared on Medscape.com.
It’s not often that a high school brawl with gang members sets you down a path to becoming a Harvard-trained doctor. But that’s exactly how Alister Martin’s life unfolded.
In retrospect, he should have seen the whole thing coming. That night at the party, his best friend was attacked by a gang member from a nearby high school. Martin was not in a gang but he jumped into the fray to defend his friend.
“I wanted to save the day, but that’s not what happened,” he says. “There were just too many of them.”
When his mother rushed to the hospital, he was so bruised and bloody that she couldn’t recognize him at first. Ever since he was a baby, she had done her best to shield him from the neighborhood where gang violence was a regular disruption. But it hadn’t worked.
“My high school had a zero-tolerance policy for gang violence,” Martin says, “so even though I wasn’t in a gang, I was kicked out.”
Now expelled from high school, his mother wanted him out of town, fearing gang retaliation, or that Martin might seek vengeance on the boy who had brutally beaten him. So, the biology teacher and single mom who worked numerous jobs to keep them afloat, came up with a plan to get him far away from any temptations.
Martin had loved tennis since middle school, when his 8th-grade math teacher, Billie Weise, also a tennis pro, got him a job as a court sweeper at an upscale tennis club nearby. He knew nothing then about tennis but would come to fall in love with the sport. To get her son out of town, Martin’s mother took out loans for $30,000 and sent him to a Florida tennis training camp.
After 6 months of training, Martin, who earned a GED degree while attending the camp, was offered a scholarship to play tennis at Rutgers University in New Brunswick, N.J. The transition to college was tough, however. He was nervous and felt out of place. “I could have died that first day. It became so obvious how poorly my high school education had prepared me for this.”
But the unease he felt was also motivating in a way. Worried about failure, “he locked himself in a room with another student and they studied day and night,” recalls Kamal Khan, director of the office for diversity and academic success at Rutgers. “I’ve never seen anything like it.”
And Martin displayed other attributes that would draw others to him – and later prove important in his career as a doctor. His ability to display empathy and interact with students and teachers separated him from his peers, Mr. Khan says. “There’re a lot of really smart students out there,” he says, “but not many who understand people like Martin.”
After graduating, he decided to pursue his dream of becoming a doctor. He’d wanted to be a doctor since he was 10 years old after his mom was diagnosed with metastatic breast cancer. He remembers overhearing a conversation she was having with a family friend about where he would go if she died.
“That’s when I knew it was serious,” he says.
Doctors saved her life, and it’s something he’ll never forget. But it wasn’t until his time at Rutgers that he finally had the confidence to think he could succeed in medical school.
Martin went on to attend Harvard Medical School and Harvard Kennedy School of Government as well as serving as chief resident at Brigham and Women’s Hospital. He was also a fellow at the White House in the Office of the Vice President and today, he’s an assistant professor at Harvard Medical School in Boston..
He is most at home in the emergency room at Massachusetts General Hospital, where he works as an emergency medical specialist. For him, the ER is the first line of defense for meeting the community’s health needs. Growing up in Neptune, the ER “was where poor folks got their care,” he says. His mom worked two jobs and when she got off work at 8 p.m. there was no pediatrician open. “When I was sick as a kid we always went to the emergency room,” he says.
While at Harvard, he also pursued a degree from the Kennedy School of Government, because of the huge role he feels that politics play in our health care system and especially in bringing care to impoverished communities. And since then he’s taken numerous steps to bridge the gap.
Addiction, for example, became an important issue for Martin, ever since a patient he encountered in his first week as an internist. She was a mom of two who had recently gotten surgery because she broke her ankle falling down the stairs at her child’s daycare, he says. Prescribed oxycodone, she feared she was becoming addicted and needed help. But at the time, there was nothing the ER could do.
“I remember that look in her eyes when we had to turn her away,” he says.
Martin has worked to change protocol at his hospital and others throughout the nation so they can be better set up to treat opioid addiction. He’s the founder of GetWaivered, an organization that trains doctors throughout the country to use evidence-based medicine to manage opioid addiction. In the U.S. doctors need what’s called a DEA X waiver to be able to prescribe buprenorphine to opioid-addicted patients. That means that currently only about 1% of all emergency room doctors nationwide have the waiver and without it, it’s impossible to help patients when they need it the most.
Shuhan He, MD, an internist with Martin at Massachusetts General Hospital who also works on the GetWaivered program, says Martin has a particular trait that helps him be successful.
“He’s a doer and when he sees a problem, he’s gonna try and fix it.”
A version of this article first appeared on Medscape.com.
Joint effort: CBD not just innocent bystander in weed
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.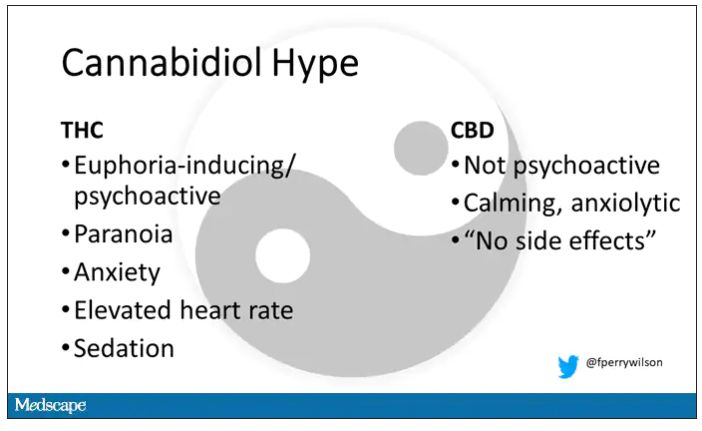
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.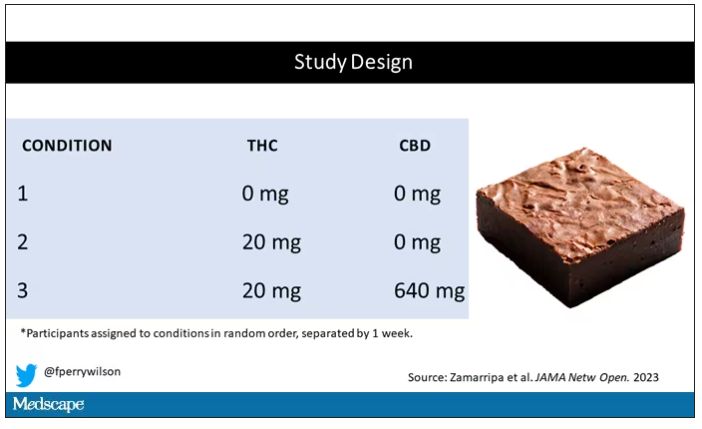
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.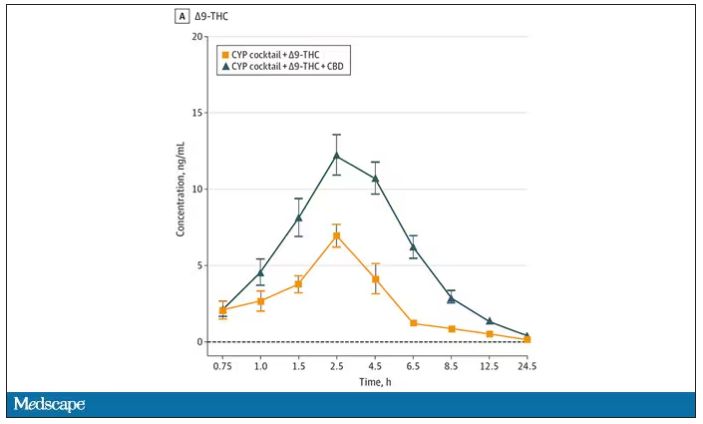
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.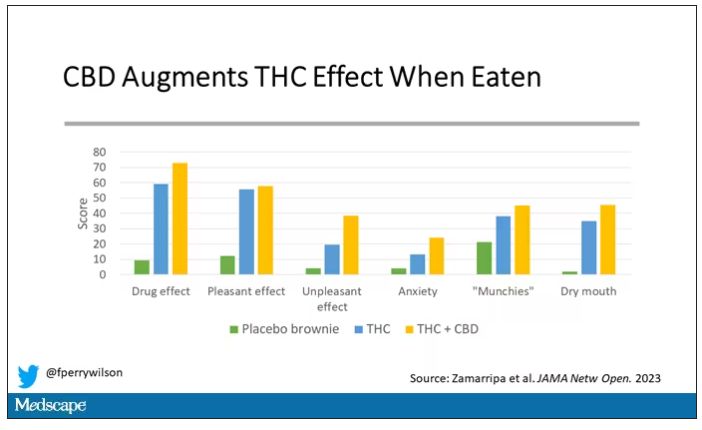
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.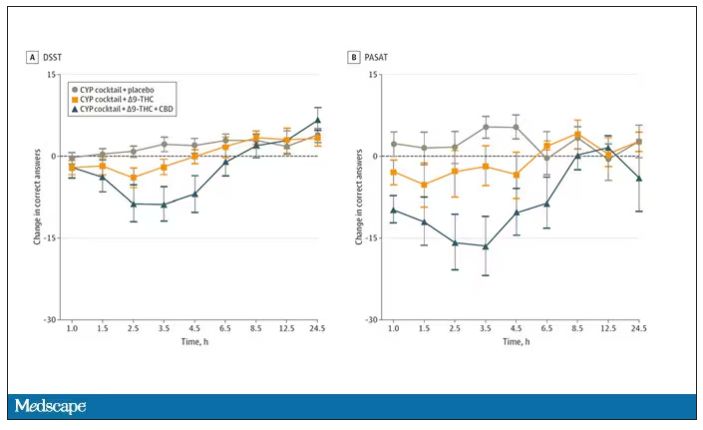
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.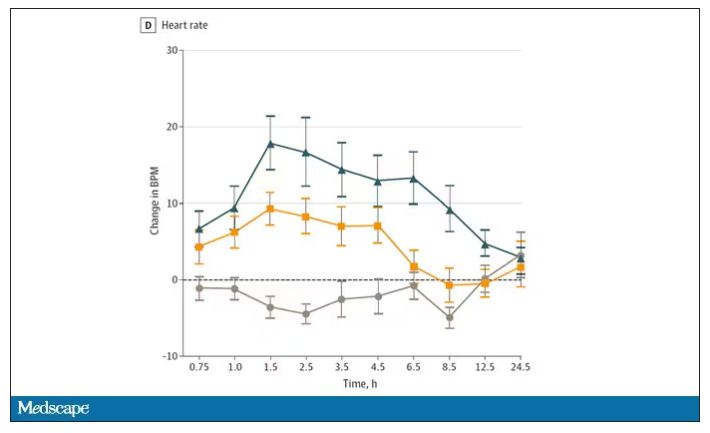
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.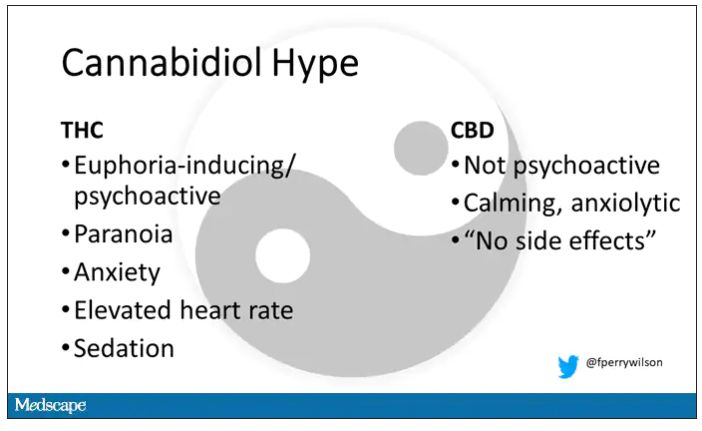
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.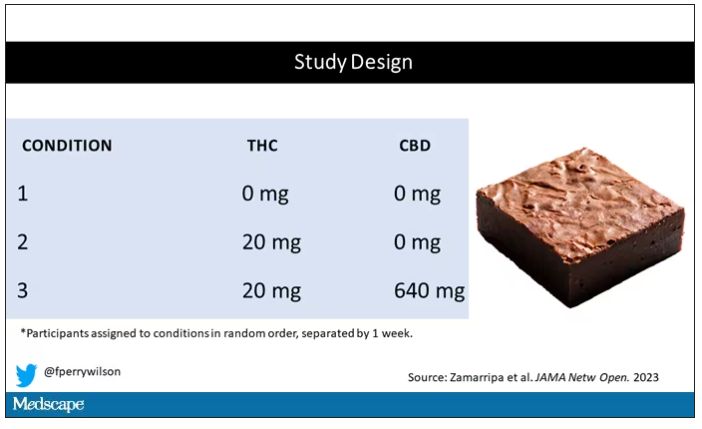
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.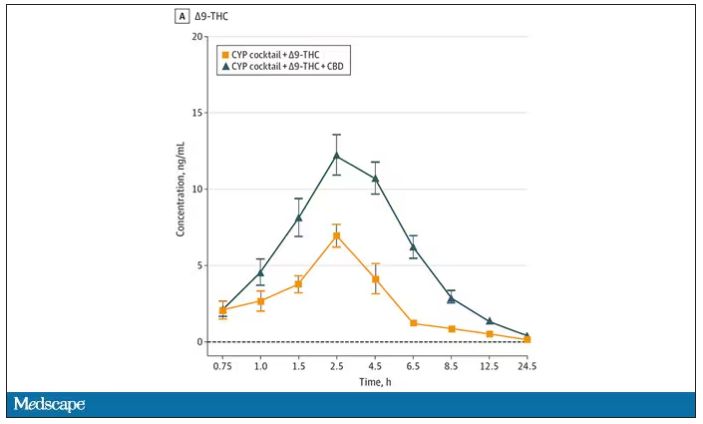
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.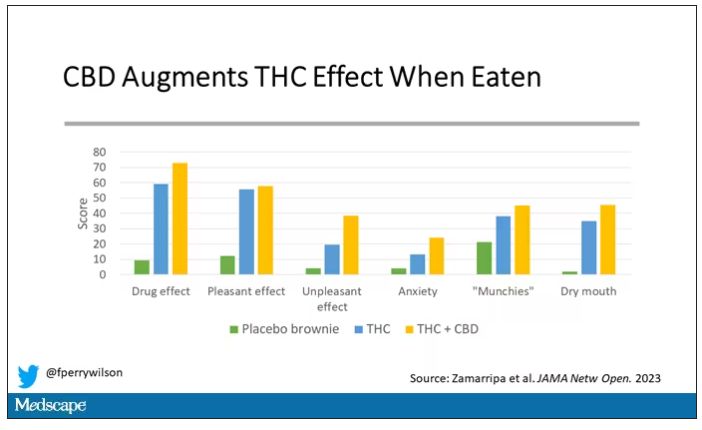
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.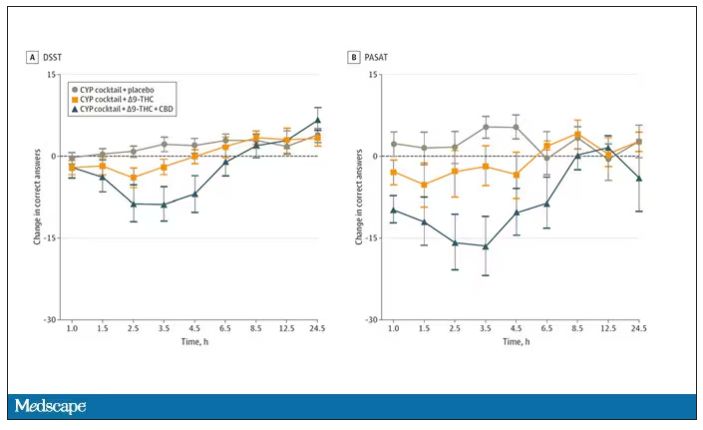
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.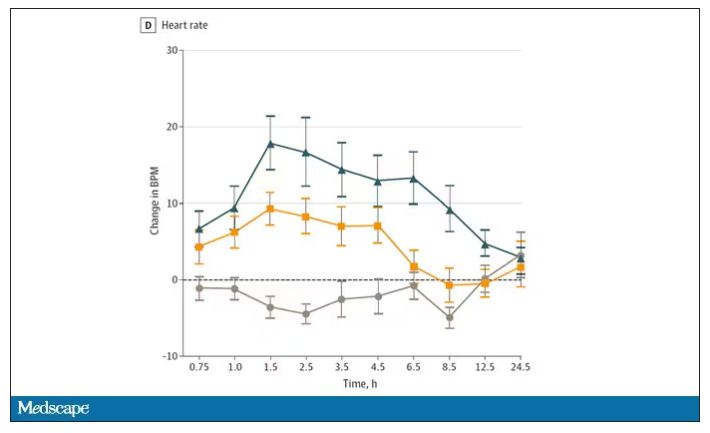
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
I visited a legal cannabis dispensary in Massachusetts a few years ago, mostly to see what the hype was about. There I was, knowing basically nothing about pot, as the gentle stoner behind the counter explained to me the differences between the various strains. Acapulco Gold is buoyant and energizing; Purple Kush is sleepy, relaxed, dissociative. Here’s a strain that makes you feel nostalgic; here’s one that helps you focus. It was as complicated and as oddly specific as a fancy wine tasting – and, I had a feeling, about as reliable.
It’s a plant, after all, and though delta-9-tetrahydrocannabinol (THC) is the chemical responsible for its euphoric effects, it is far from the only substance in there.
The second most important compound in cannabis is cannabidiol, and most people will tell you that CBD is the gentle yin to THC’s paranoiac yang. Hence your local ganja barista reminding you that, if you don›t want all those anxiety-inducing side effects of THC, grab a strain with a nice CBD balance.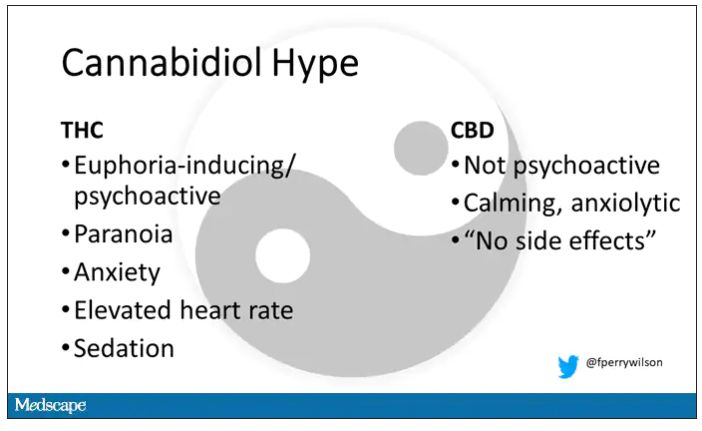
But is it true? A new study appearing in JAMA Network Open suggests, in fact, that it’s quite the opposite. This study is from Austin Zamarripa and colleagues, who clearly sit at the researcher cool kids table.
Eighteen adults who had abstained from marijuana use for at least a month participated in this trial (which is way more fun than anything we do in my lab at Yale). In random order, separated by at least a week, they ate some special brownies.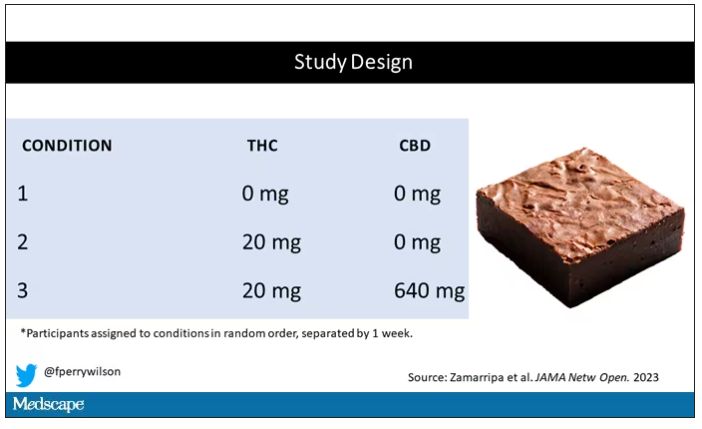
Condition one was a control brownie, condition two was a brownie containing 20 mg of THC, and condition three was a brownie containing 20 mg of THC and 640 mg of CBD. Participants were assigned each condition in random order, separated by at least a week.
A side note on doses for those of you who, like me, are not totally weed literate. A dose of 20 mg of THC is about a third of what you might find in a typical joint these days (though it’s about double the THC content of a joint in the ‘70s – I believe the technical term is “doobie”). And 640 mg of CBD is a decent dose, as 5 mg per kilogram is what some folks start with to achieve therapeutic effects.
Both THC and CBD interact with the cytochrome p450 system in the liver. This matters when you’re ingesting them instead of smoking them because you have first-pass metabolism to contend with. And, because of that p450 inhibition, it’s possible that CBD might actually increase the amount of THC that gets into your bloodstream from the brownie, or gummy, or pizza sauce, or whatever.
Let’s get to the results, starting with blood THC concentration. It’s not subtle. With CBD on board the THC concentration rises higher faster, with roughly double the area under the curve.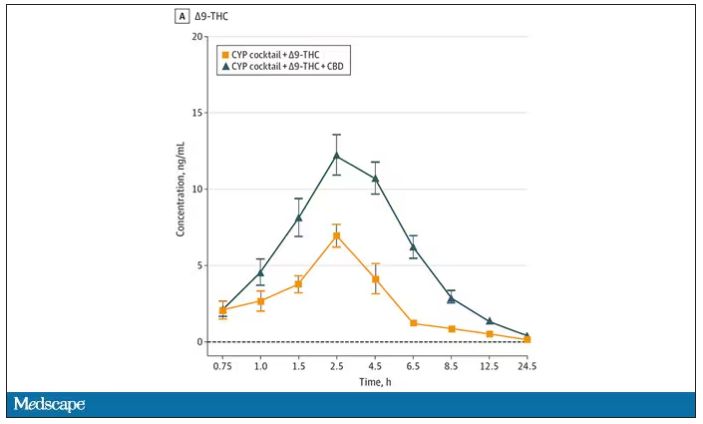
And, unsurprisingly, the subjective experience correlated with those higher levels. Individuals rated the “drug effect” higher with the combo. But, interestingly, the “pleasant” drug effect didn’t change much, while the unpleasant effects were substantially higher. No mitigation of THC anxiety here – quite the opposite. CBD made the anxiety worse.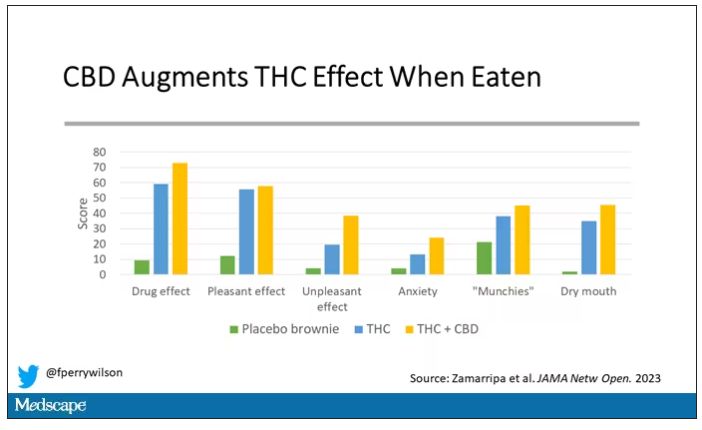
Cognitive effects were equally profound. Scores on a digit symbol substitution test and a paced serial addition task were all substantially worse when CBD was mixed with THC.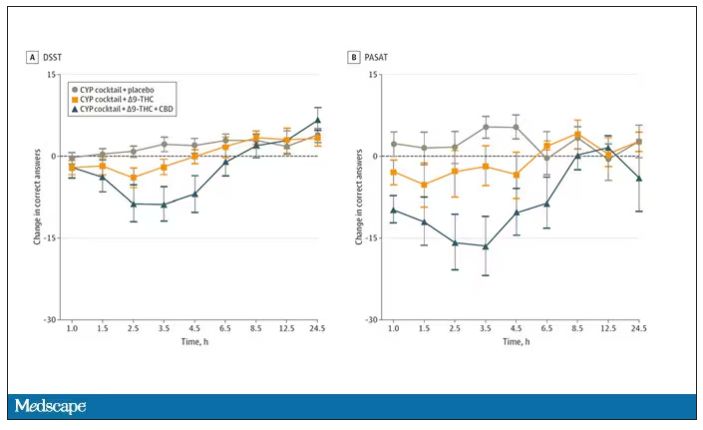
And for those of you who want some more objective measures, check out the heart rate. Despite the purported “calming” nature of CBD, heart rates were way higher when individuals were exposed to both chemicals.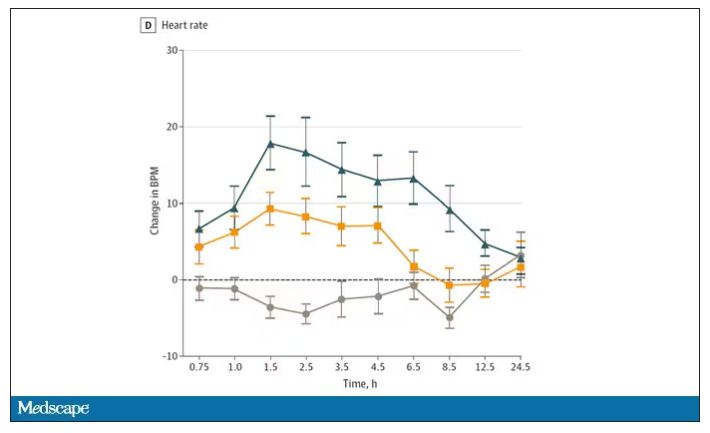
The picture here is quite clear, though the mechanism is not. At least when talking edibles, CBD enhances the effects of THC, and not necessarily for the better. It may be that CBD is competing with some of the proteins that metabolize THC, thus prolonging its effects. CBD may also directly inhibit those enzymes. But whatever the case, I think we can safely say the myth that CBD makes the effects of THC more mild or more tolerable is busted.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn.
A version of this article first appeared on Medscape.com.
New challenge for docs: End of COVID federal public health emergency
The Biden administration intends to end by May 11 certain COVID-19 emergency measures used to aid in the response to the pandemic, while many others will remain in place.
A separate declaration covers the Food and Drug Administration’s emergency use authorizations (EUAs) for COVID medicines and tests. That would not be affected by the May 11 deadline, the FDA said. In addition, Congress and state lawmakers have extended some COVID response measures.
The result is a patchwork of emergency COVID-19 measures with different end dates.
The American Medical Association and the American Academy of Family Physicians (AAFP) are assessing how best to advise their members about the end of the public health emergency.
Several waivers regarding copays and coverage and policies regarding controlled substances will expire, Claire Ernst, director of government affairs at the Medical Group Management Association, told this news organization.
The impact of the unwinding “will vary based on some factors, such as what state the practice resides in,” Ms. Ernst said. “Fortunately, Congress provided some predictability for practices by extending many of the telehealth waivers through the end of 2024.”
The AAFP told this news organization that it has joined several other groups in calling for the release of proposed Drug Enforcement Administration (DEA) regulations meant to permanently allow prescriptions of buprenorphine treatment for opioid use disorder via telehealth. The AAFP and other groups want to review these proposals and, if needed, urge the DEA to modify or finalize before there are any disruptions in access to medications for opioid use disorder.
Patients’ questions
Clinicians can expect to field patients’ questions about their insurance coverage and what they need to pay, said Nancy Foster, vice president for quality and patient safety policy at the American Hospital Association (AHA).
“Your doctor’s office, that clinic you typically get care at, that is the face of medicine to you,” Ms. Foster told this news organization. “Many doctors and their staff will be asked, ‘What’s happening with Medicaid?’ ‘What about my Medicare coverage?’ ‘Can I still access care in the same way that I did before?’ ”
Physicians will need to be ready to answers those question, or point patients to where they can get answers, Ms. Foster said.
For example, Medicaid will no longer cover postpartum care for some enrollees after giving birth, said Taylor Platt, health policy manager for the American College of Obstetricians and Gynecologists.
The federal response to the pandemic created “a de facto postpartum coverage extension for Medicaid enrollees,” which will be lost in some states, Ms. Platt told this news organization. However, 28 states and the District of Columbia have taken separate measures to extend postpartum coverage to 1 year.
“This coverage has been critical for postpartum individuals to address health needs like substance use and mental health treatment and chronic conditions,” Ms. Platt said.
States significantly changed Medicaid policy to expand access to care during the pandemic.
All 50 states and the District of Columbia, for example, expanded coverage or access to telehealth services in Medicaid during the pandemic, according to a Jan. 31 report from the Kaiser Family Foundation (KFF). These expansions expire under various deadlines, although most states have made or are planning to make some Medicaid telehealth flexibilities permanent, KFF said.
The KFF report notes that all states and the District of Columbia temporarily waived some aspects of state licensure requirements, so that clinicians with equivalent licenses in other states could practice via telehealth.
In some states, these waivers are still active and are tied to the end of the federal emergency declaration. In others, they expired, with some states allowing for long-term or permanent interstate telemedicine, KFF said. (The Federation of State Medical Boards has a detailed summary of these modifications.)
The end of free COVID vaccines, testing for some patients
The AAFP has also raised concerns about continued access to COVID-19 vaccines, particularly for uninsured adults. Ashish Jha, MD, MPH, the White House COVID-19 Response Coordinator, said in a tweet that this transition, however, wouldn’t happen until a few months after the public health emergency ends.
After those few months, there will be a transition from U.S. government–distributed vaccines and treatments to ones purchased through the regular health care system, the “way we do for every other vaccine and treatment,” Dr. Jha added.
But that raises the same kind of difficult questions that permeate U.S. health care, with a potential to keep COVID active, said Patricia Jackson, RN, president of the Association for Professionals in Infection Control and Epidemiology (APIC).
People who don’t have insurance may lose access to COVID testing and vaccines.
“Will that lead to increases in transmission? Who knows,” Ms. Jackson told this news organization. “We will have to see. There are some health equity issues that potentially arise.”
Future FDA actions
Biden’s May 11 deadline applies to emergency provisions made under a Section 319 declaration, which allow the Department of Health and Human Services to respond to crises.
But a separate flexibility, known as a Section 564 declaration, covers the FDA’s EUAs, which can remain in effect even as the other declarations end.
The best-known EUAs for the pandemic were used to bring COVID vaccines and treatments to market. Many of these have since been converted to normal approvals as companies presented more evidence to support the initial emergency approvals. In other cases, EUAs have been withdrawn owing to disappointing research results, changing virus strains, and evolving medical treatments.
The FDA also used many EUAs to cover new uses of ventilators and other hospital equipment and expand these supplies in response to the pandemic, said Mark Howell, AHA’s director of policy and patient safety.
The FDA should examine the EUAs issued during the pandemic to see what greater flexibilities might be used to deal with future serious shortages of critical supplies. International incidents such as the war in Ukraine show how fragile the supply chain can be. The FDA should consider its recent experience with EUAs to address this, Mr. Howell said.
“What do we do coming out of the pandemic? And how do we think about being more proactive in this space to ensure that our supply doesn’t bottleneck, that we continue to make sure that providers have access to supply that’s not only safe and effective, but that they can use?” Mr. Howell told this news organization.
Such planning might also help prepare the country for the next pandemic, which is a near certainty, APIC’s Ms. Jackson said. The nation needs a nimbler response to the next major outbreak of an infectious disease, she said.
“There is going to be a next time,” Ms. Jackson said. “We are going to have another pandemic.”
A version of this article first appeared on Medscape.com.
The Biden administration intends to end by May 11 certain COVID-19 emergency measures used to aid in the response to the pandemic, while many others will remain in place.
A separate declaration covers the Food and Drug Administration’s emergency use authorizations (EUAs) for COVID medicines and tests. That would not be affected by the May 11 deadline, the FDA said. In addition, Congress and state lawmakers have extended some COVID response measures.
The result is a patchwork of emergency COVID-19 measures with different end dates.
The American Medical Association and the American Academy of Family Physicians (AAFP) are assessing how best to advise their members about the end of the public health emergency.
Several waivers regarding copays and coverage and policies regarding controlled substances will expire, Claire Ernst, director of government affairs at the Medical Group Management Association, told this news organization.
The impact of the unwinding “will vary based on some factors, such as what state the practice resides in,” Ms. Ernst said. “Fortunately, Congress provided some predictability for practices by extending many of the telehealth waivers through the end of 2024.”
The AAFP told this news organization that it has joined several other groups in calling for the release of proposed Drug Enforcement Administration (DEA) regulations meant to permanently allow prescriptions of buprenorphine treatment for opioid use disorder via telehealth. The AAFP and other groups want to review these proposals and, if needed, urge the DEA to modify or finalize before there are any disruptions in access to medications for opioid use disorder.
Patients’ questions
Clinicians can expect to field patients’ questions about their insurance coverage and what they need to pay, said Nancy Foster, vice president for quality and patient safety policy at the American Hospital Association (AHA).
“Your doctor’s office, that clinic you typically get care at, that is the face of medicine to you,” Ms. Foster told this news organization. “Many doctors and their staff will be asked, ‘What’s happening with Medicaid?’ ‘What about my Medicare coverage?’ ‘Can I still access care in the same way that I did before?’ ”
Physicians will need to be ready to answers those question, or point patients to where they can get answers, Ms. Foster said.
For example, Medicaid will no longer cover postpartum care for some enrollees after giving birth, said Taylor Platt, health policy manager for the American College of Obstetricians and Gynecologists.
The federal response to the pandemic created “a de facto postpartum coverage extension for Medicaid enrollees,” which will be lost in some states, Ms. Platt told this news organization. However, 28 states and the District of Columbia have taken separate measures to extend postpartum coverage to 1 year.
“This coverage has been critical for postpartum individuals to address health needs like substance use and mental health treatment and chronic conditions,” Ms. Platt said.
States significantly changed Medicaid policy to expand access to care during the pandemic.
All 50 states and the District of Columbia, for example, expanded coverage or access to telehealth services in Medicaid during the pandemic, according to a Jan. 31 report from the Kaiser Family Foundation (KFF). These expansions expire under various deadlines, although most states have made or are planning to make some Medicaid telehealth flexibilities permanent, KFF said.
The KFF report notes that all states and the District of Columbia temporarily waived some aspects of state licensure requirements, so that clinicians with equivalent licenses in other states could practice via telehealth.
In some states, these waivers are still active and are tied to the end of the federal emergency declaration. In others, they expired, with some states allowing for long-term or permanent interstate telemedicine, KFF said. (The Federation of State Medical Boards has a detailed summary of these modifications.)
The end of free COVID vaccines, testing for some patients
The AAFP has also raised concerns about continued access to COVID-19 vaccines, particularly for uninsured adults. Ashish Jha, MD, MPH, the White House COVID-19 Response Coordinator, said in a tweet that this transition, however, wouldn’t happen until a few months after the public health emergency ends.
After those few months, there will be a transition from U.S. government–distributed vaccines and treatments to ones purchased through the regular health care system, the “way we do for every other vaccine and treatment,” Dr. Jha added.
But that raises the same kind of difficult questions that permeate U.S. health care, with a potential to keep COVID active, said Patricia Jackson, RN, president of the Association for Professionals in Infection Control and Epidemiology (APIC).
People who don’t have insurance may lose access to COVID testing and vaccines.
“Will that lead to increases in transmission? Who knows,” Ms. Jackson told this news organization. “We will have to see. There are some health equity issues that potentially arise.”
Future FDA actions
Biden’s May 11 deadline applies to emergency provisions made under a Section 319 declaration, which allow the Department of Health and Human Services to respond to crises.
But a separate flexibility, known as a Section 564 declaration, covers the FDA’s EUAs, which can remain in effect even as the other declarations end.
The best-known EUAs for the pandemic were used to bring COVID vaccines and treatments to market. Many of these have since been converted to normal approvals as companies presented more evidence to support the initial emergency approvals. In other cases, EUAs have been withdrawn owing to disappointing research results, changing virus strains, and evolving medical treatments.
The FDA also used many EUAs to cover new uses of ventilators and other hospital equipment and expand these supplies in response to the pandemic, said Mark Howell, AHA’s director of policy and patient safety.
The FDA should examine the EUAs issued during the pandemic to see what greater flexibilities might be used to deal with future serious shortages of critical supplies. International incidents such as the war in Ukraine show how fragile the supply chain can be. The FDA should consider its recent experience with EUAs to address this, Mr. Howell said.
“What do we do coming out of the pandemic? And how do we think about being more proactive in this space to ensure that our supply doesn’t bottleneck, that we continue to make sure that providers have access to supply that’s not only safe and effective, but that they can use?” Mr. Howell told this news organization.
Such planning might also help prepare the country for the next pandemic, which is a near certainty, APIC’s Ms. Jackson said. The nation needs a nimbler response to the next major outbreak of an infectious disease, she said.
“There is going to be a next time,” Ms. Jackson said. “We are going to have another pandemic.”
A version of this article first appeared on Medscape.com.
The Biden administration intends to end by May 11 certain COVID-19 emergency measures used to aid in the response to the pandemic, while many others will remain in place.
A separate declaration covers the Food and Drug Administration’s emergency use authorizations (EUAs) for COVID medicines and tests. That would not be affected by the May 11 deadline, the FDA said. In addition, Congress and state lawmakers have extended some COVID response measures.
The result is a patchwork of emergency COVID-19 measures with different end dates.
The American Medical Association and the American Academy of Family Physicians (AAFP) are assessing how best to advise their members about the end of the public health emergency.
Several waivers regarding copays and coverage and policies regarding controlled substances will expire, Claire Ernst, director of government affairs at the Medical Group Management Association, told this news organization.
The impact of the unwinding “will vary based on some factors, such as what state the practice resides in,” Ms. Ernst said. “Fortunately, Congress provided some predictability for practices by extending many of the telehealth waivers through the end of 2024.”
The AAFP told this news organization that it has joined several other groups in calling for the release of proposed Drug Enforcement Administration (DEA) regulations meant to permanently allow prescriptions of buprenorphine treatment for opioid use disorder via telehealth. The AAFP and other groups want to review these proposals and, if needed, urge the DEA to modify or finalize before there are any disruptions in access to medications for opioid use disorder.
Patients’ questions
Clinicians can expect to field patients’ questions about their insurance coverage and what they need to pay, said Nancy Foster, vice president for quality and patient safety policy at the American Hospital Association (AHA).
“Your doctor’s office, that clinic you typically get care at, that is the face of medicine to you,” Ms. Foster told this news organization. “Many doctors and their staff will be asked, ‘What’s happening with Medicaid?’ ‘What about my Medicare coverage?’ ‘Can I still access care in the same way that I did before?’ ”
Physicians will need to be ready to answers those question, or point patients to where they can get answers, Ms. Foster said.
For example, Medicaid will no longer cover postpartum care for some enrollees after giving birth, said Taylor Platt, health policy manager for the American College of Obstetricians and Gynecologists.
The federal response to the pandemic created “a de facto postpartum coverage extension for Medicaid enrollees,” which will be lost in some states, Ms. Platt told this news organization. However, 28 states and the District of Columbia have taken separate measures to extend postpartum coverage to 1 year.
“This coverage has been critical for postpartum individuals to address health needs like substance use and mental health treatment and chronic conditions,” Ms. Platt said.
States significantly changed Medicaid policy to expand access to care during the pandemic.
All 50 states and the District of Columbia, for example, expanded coverage or access to telehealth services in Medicaid during the pandemic, according to a Jan. 31 report from the Kaiser Family Foundation (KFF). These expansions expire under various deadlines, although most states have made or are planning to make some Medicaid telehealth flexibilities permanent, KFF said.
The KFF report notes that all states and the District of Columbia temporarily waived some aspects of state licensure requirements, so that clinicians with equivalent licenses in other states could practice via telehealth.
In some states, these waivers are still active and are tied to the end of the federal emergency declaration. In others, they expired, with some states allowing for long-term or permanent interstate telemedicine, KFF said. (The Federation of State Medical Boards has a detailed summary of these modifications.)
The end of free COVID vaccines, testing for some patients
The AAFP has also raised concerns about continued access to COVID-19 vaccines, particularly for uninsured adults. Ashish Jha, MD, MPH, the White House COVID-19 Response Coordinator, said in a tweet that this transition, however, wouldn’t happen until a few months after the public health emergency ends.
After those few months, there will be a transition from U.S. government–distributed vaccines and treatments to ones purchased through the regular health care system, the “way we do for every other vaccine and treatment,” Dr. Jha added.
But that raises the same kind of difficult questions that permeate U.S. health care, with a potential to keep COVID active, said Patricia Jackson, RN, president of the Association for Professionals in Infection Control and Epidemiology (APIC).
People who don’t have insurance may lose access to COVID testing and vaccines.
“Will that lead to increases in transmission? Who knows,” Ms. Jackson told this news organization. “We will have to see. There are some health equity issues that potentially arise.”
Future FDA actions
Biden’s May 11 deadline applies to emergency provisions made under a Section 319 declaration, which allow the Department of Health and Human Services to respond to crises.
But a separate flexibility, known as a Section 564 declaration, covers the FDA’s EUAs, which can remain in effect even as the other declarations end.
The best-known EUAs for the pandemic were used to bring COVID vaccines and treatments to market. Many of these have since been converted to normal approvals as companies presented more evidence to support the initial emergency approvals. In other cases, EUAs have been withdrawn owing to disappointing research results, changing virus strains, and evolving medical treatments.
The FDA also used many EUAs to cover new uses of ventilators and other hospital equipment and expand these supplies in response to the pandemic, said Mark Howell, AHA’s director of policy and patient safety.
The FDA should examine the EUAs issued during the pandemic to see what greater flexibilities might be used to deal with future serious shortages of critical supplies. International incidents such as the war in Ukraine show how fragile the supply chain can be. The FDA should consider its recent experience with EUAs to address this, Mr. Howell said.
“What do we do coming out of the pandemic? And how do we think about being more proactive in this space to ensure that our supply doesn’t bottleneck, that we continue to make sure that providers have access to supply that’s not only safe and effective, but that they can use?” Mr. Howell told this news organization.
Such planning might also help prepare the country for the next pandemic, which is a near certainty, APIC’s Ms. Jackson said. The nation needs a nimbler response to the next major outbreak of an infectious disease, she said.
“There is going to be a next time,” Ms. Jackson said. “We are going to have another pandemic.”
A version of this article first appeared on Medscape.com.
The 5-year survival rate for pancreatic cancer is increasing
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
John Whyte, MD: Hello, I’m Dr. John Whyte, the Chief Medical Officer of WebMD. One of those cancers was pancreatic cancer, which historically has had a very low survival rate. What’s going on here? Are we doing better with diagnosis, treatment, a combination?
Joining me today is Dr. Lynn Matrisian. She is PanCAN’s chief science officer. Dr. Matrisian, thanks for joining me today. It’s great to see you.
Lynn Matrisian, PhD, MBA: Great to be here. Thank you.
Dr. Whyte: Well, tell me what your first reaction was when you saw the recent data from the American Cancer Society. What one word would you use?
Dr. Matrisian: Hopeful. I think hopeful in general that survival rates are increasing, not for all cancers, but for many cancers. We continue to make progress. Research is making a difference. And we’re making progress against cancer in general.
Dr. Whyte: You’re passionate, as our viewers know, about pancreatic cancer. And that’s been one of the hardest cancers to treat, and one of the lowest survival rates. But there’s some encouraging news that we saw, didn’t we?
Dr. Matrisian: Yes. So the 5-year survival rate for pancreatic cancer went up a whole percentage. It’s at 12% now. And what’s really good is it was at 11% last year. It was at 10% the year before. So that’s 2 years in a row that we’ve had an increase in the 5-year survival rate for pancreatic cancer. So we’re hopeful that’s a trajectory that we can really capitalize on is how fast we’re making progress in this disease.
Dr. Whyte: I want to put it into context, Lynn. Because some people might be thinking, 1%? Like you’re excited about 1%? That doesn’t seem that much. But correct me if I’m wrong. A one percentage point increase means 641 more loved ones will enjoy life’s moments, as you put it, 5 years after their diagnosis that otherwise wouldn’t have. What does that practically mean to viewers?
Dr. Matrisian: That means that more than 600 people in the United States will hug a loved one 5 years after that diagnosis of pancreatic cancer. It is a very deadly disease. But we’re going to, by continuing to make progress, it gives those moments to those people. And it means that we’re making progress against the disease in general.
Dr. Whyte: So even 1%, and 1% each year, does have value.
Dr. Matrisian: It has a lot of value.
Dr. Whyte: What’s driving this improvement? Is it better screening? And we’re not so great still in screening a pancreatic cancer. Is it the innovation in cancer treatments? What do you think is accounting for what we hope is this trajectory of increases in 5-year survival?
Dr. Matrisian: Right, so the nice thing the reason that we like looking at 5-year survival rates is because it takes into account all of those things. And we have actually made progress in all of those things. So by looking at those that are diagnosed with pancreatic cancer in general as a whole, and looking at their survival, we are looking at better treatments. People who are getting pancreatic cancer later are living longer as a result of better treatments.
But it’s not just that. It’s also, if you’re diagnosed earlier, your 5-year survival rate is higher. More people who are diagnosed early live to five years than those that are diagnosed later. So within that statistic, there are more people who are diagnosed earlier. And those people also live longer. So it takes into account all of those things, which is why we really like to look at that five-year survival rate for a disease like pancreatic cancer.
Dr. Whyte: Where are we on screening? Because we always want to catch people early. That gives them that greatest chance of survival. Have we made much improvements there? And if we have, what are they?
Dr. Matrisian: Well we have made improvements there are more people that are now diagnosed with localized disease than there were 20 years ago. So that is increasing. And we’re still doing it really by being aware of the symptoms right now. Being aware that kind of chronic indigestion, lower back pain that won’t go away, these are signs and symptoms. And especially things like jaundice ...
Dr. Whyte: That yellow color that they might see.
Dr. Matrisian: Yes, that yellow colors in your eye, that’s a really important symptom that would certainly send people to the doctor in order to look at this. So some of it is being more aware and finding the disease earlier. But what we’re really hoping for is some sort of blood test or some sort of other way of looking through medical records and identifying those people that need to go and be checked.
Dr. Whyte: Now we chatted about that almost two years ago. So tell me the progress that we’ve made. How are we doing?
Dr. Matrisian: Yeah, well there’s a number of companies now that have blood tests that are available. They still need more work. They still need more studies to really understand how good they are at finding pancreatic cancer early. But we didn’t have them a couple of years ago. And so it’s really a very exciting time in the field, that there’s companies that were taking advantage of research for many years and actually turning it into a commercial product that is available for people to check.
Dr. Whyte: And then what about treatments? More treatment options today than there were just a few years ago, but still a lot of progress to be made. So when we talk about even 12% 5-year survival, we’d love to see it much more. And you talk about, I don’t want to misquote, so correct me if I’m wrong. Your goal is 20%. Five-year survival by 2030. That’s not too far. So, Lynn, how are we going to get there?
Dr. Matrisian: Okay, well this is our mission. And that’s exactly our goal, 20% by 2030. So we’ve got some work to do. And we are working at both fronts. You’re right, we need better treatments. And so we’ve set up a clinical trial platform where we can look at a lot of different treatments much more efficiently, much faster, kind of taking advantage of an infrastructure to do that. And that’s called Precision Promise. And we’re excited about that as a way to get new treatments for advanced pancreatic cancer.
And then we’re also working on the early detection end. We think an important symptom of pancreatic cancer that isn’t often recognized is new onset diabetes, sudden diabetes in those over 50 where that person did not have diabetes before. So it’s new, looks like type 2 diabetes, but it’s actually caused by pancreatic cancer.
And so we have an initiative, The Early Detection Initiative, that is taking advantage of that. And seeing if we image people right away based on that symptom, can we find pancreatic cancer early? So we think it’s important to look both at trying to diagnose it earlier, as well as trying to treat it better for advanced disease.
Dr. Whyte: Yeah. You know, at WebMD we’re always trying to empower people with better information so they can also become advocates for their health. You’re an expert in advocacy on pancreatic cancer. So what’s your advice to listeners as to how they become good advocates for themselves or advocates in general for loved ones who have pancreatic cancer?
Dr. Matrisian: Yeah. Yeah. Well certainly, knowledge is power. And so the real thing to do is to call the Pancreatic Cancer Action Network. This is what we do. We stay up on the most current information. We have very experienced case managers who can help navigate the complexities of pancreatic cancer at every stage of the journey.
Or if you have questions about pancreatic cancer, call PanCAN. Go to PanCAN.org and give us a call. Because it’s really that knowledge, knowing what it is that you need to get more knowledge about, how to advocate for yourself is very important in a disease, in any disease, but in particular a disease like pancreatic cancer.
Dr. Whyte: And I don’t want to dismiss the progress that we’ve made, that you’ve just referenced in terms of the increased survival. But there’s still a long way to go. We need a lot more dollars for research. We need a lot more clinical trials to take place. What’s your message to a viewer who’s been diagnosed with pancreatic cancer or a loved one? What’s your message, Lynn, today for them?
Dr. Matrisian: Well, first, get as much knowledge as you can. Call PanCAN, and let us help you help your loved one. But then help us. Let’s do research. Let’s do more research. Let’s understand this disease better so we can make those kinds of progress in both treatment and early detection.
And PanCAN works very hard at understanding the disease and setting up research programs that are going to make a difference, that are going to get us to that aggressive goal of 20% survival by 2030. So there is a lot of things that can be done, raise awareness to your friends and neighbors about the disease, lots of things that will help this whole field.
Dr. Whyte: What’s your feeling on second opinions? Given that this can be a difficult cancer to treat, given that there’s emerging therapies that are always developing, when you have a diagnosis of pancreatic cancer, is it important to consider getting a second opinion?
Dr. Matrisian: Yes. Yes, it is. And our case managers will help with that process. We do think it’s important.
Dr. Whyte: Because sometimes, Lynn, people just want to get started, right? Get it out of me. Get treatment. And sometimes getting a second opinion, doing some genomic testing can take time. So what’s your response to that?
Dr. Matrisian: Yeah. Yeah. Well we say, your care team is very important. Who is on your care team, and it may take a little time to find the right people on your care team. But that is an incredibly important step. Sometimes it’s not just one person. Sometimes you need more than one doctor, more than one nurse, more than one type of specialty to help you deal with this. And taking the time to do that is incredibly important.
Yes, you need to – you do need to act. But act smart. And do it with knowledge. Do it really understanding what your options are, and advocate for yourself.
Dr. Whyte: And surround yourself as you reference with that right care team for you, because that’s the most important thing when you have any type of cancer diagnosis. Dr. Lynn Matrisian, I want to thank you for taking time today.
Dr. Matrisian: Thank you so much, John.
A version of this article first appeared on Medscape.com.
Doctors are disappearing from emergency departments as hospitals look to cut costs
She didn’t know much about miscarriage, but this seemed like one.
In the emergency department, she was examined then sent home, she said. She went back when her cramping became excruciating. Then home again. It ultimately took three trips to the ED on 3 consecutive days, generating three separate bills, before she saw a doctor who looked at her blood work and confirmed her fears.
“At the time I wasn’t thinking, ‘Oh, I need to see a doctor,’ ” Ms. Valle recalled. “But when you think about it, it’s like, ‘Well, dang – why didn’t I see a doctor?’ ” It’s unclear whether the repeat visits were due to delays in seeing a physician, but the experience worried her. And she’s still paying the bills.
The hospital declined to discuss Ms. Valle’s care, citing patient privacy. But 17 months before her 3-day ordeal, Tennova had outsourced its emergency departments to American Physician Partners, a medical staffing company owned by private equity investors. APP employs fewer doctors in its EDs as one of its cost-saving initiatives to increase earnings, according to a confidential company document obtained by KHN and NPR.
This staffing strategy has permeated hospitals, and particularly emergency departments, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once their domain, doctors are increasingly being replaced by nurse practitioners and physician assistants, collectively known as “midlevel practitioners,” who can perform many of the same duties and generate much of the same revenue for less than half of the pay.
“APP has numerous cost saving initiatives underway as part of the Company’s continual focus on cost optimization,” the document says, including a “shift of staffing” between doctors and midlevel practitioners.
In a statement to KHN, American Physician Partners said this strategy is a way to ensure all EDs remain fully staffed, calling it a “blended model” that allows doctors, nurse practitioners, and physician assistants “to provide care to their fullest potential.”
Critics of this strategy say the quest to save money results in treatment meted out by someone with far less training than a physician, leaving patients vulnerable to misdiagnoses, higher medical bills, and inadequate care. And these fears are bolstered by evidence that suggests dropping doctors from EDs may not be good for patients.
A working paper, published in October by the National Bureau of Economic Research, analyzed roughly 1.1 million visits to 44 EDs throughout the Veterans Health Administration, where nurse practitioners can treat patients without oversight from doctors.
Researchers found that treatment by a nurse practitioner resulted on average in a 7% increase in cost of care and an 11% increase in length of stay, extending patients’ time in the ED by minutes for minor visits and hours for longer ones. These gaps widened among patients with more severe diagnoses, the study said, but could be somewhat mitigated by nurse practitioners with more experience.
The study also found that ED patients treated by a nurse practitioner were 20% more likely to be readmitted to the hospital for a preventable reason within 30 days, although the overall risk of readmission remained very small.
Yiqun Chen, PhD, who is an assistant professor of economics at the University of Illinois at Chicago and coauthored the study, said these findings are not an indictment of nurse practitioners in the ED. Instead, she said, she hopes the study will guide how to best deploy nurse practitioners: in treatment of simpler patients or circumstances when no doctor is available.
“It’s not just a simple question of if we can substitute physicians with nurse practitioners or not,” Dr. Chen said. “It depends on how we use them. If we just use them as independent providers, especially ... for relatively complicated patients, it doesn’t seem to be a very good use.”
Dr. Chen’s research echoes smaller studies, like one from The Harvey L. Neiman Health Policy Institute that found nonphysician practitioners in EDs were associated with a 5.3% increase in imaging, which could unnecessarily increase bills for patients. Separately, a study at the Hattiesburg Clinic in Mississippi found that midlevel practitioners in primary care – not in the emergency department – increased the out-of-pocket costs to patients while also leading to worse performance on 9 of 10 quality-of-care metrics, including cancer screenings and vaccination rates.
But definitive evidence remains elusive that replacing ER doctors with nonphysicians has a negative impact on patients, said Cameron Gettel, MD, an assistant professor of emergency medicine at Yale University, New Haven, Conn. Private equity investment and the use of midlevel practitioners rose in lockstep in the ED, Dr. Gettel said, and in the absence of game-changing research, the pattern will likely continue.
“Worse patient outcomes haven’t really been shown across the board,” he said. “And I think until that is shown, then they will continue to play an increasing role.”
For private equity, dropping ED docs is a “simple equation”
Private equity companies pool money from wealthy investors to buy their way into various industries, often slashing spending and seeking to flip businesses in 3 to 7 years. While this business model is a proven moneymaker on Wall Street, it raises concerns in health care, where critics worry the pressure to turn big profits will influence life-or-death decisions that were once left solely to medical professionals.
Nearly $1 trillion in private equity funds have gone into almost 8,000 health care transactions over the past decade, according to industry tracker PitchBook, including buying into medical staffing companies that many hospitals hire to manage their emergency departments.
Two firms dominate the ED staffing industry: TeamHealth, bought by private equity firm Blackstone in 2016, and Envision Healthcare, bought by KKR in 2018. Trying to undercut these staffing giants is American Physician Partners, a rapidly expanding company that runs EDs in at least 17 states and is 50% owned by private equity firm BBH Capital Partners.
These staffing companies have been among the most aggressive in replacing doctors to cut costs, said Robert McNamara, MD, a founder of the American Academy of Emergency Medicine and chair of emergency medicine at Temple University, Philadelphia.
“It’s a relatively simple equation,” Dr. McNamara said. “Their No. 1 expense is the board-certified emergency physician. So they are going to want to keep that expense as low as possible.”
Not everyone sees the trend of private equity in ED staffing in a negative light. Jennifer Orozco, president of the American Academy of Physician Associates, which represents physician assistants, said even if the change – to use more nonphysician providers – is driven by the staffing firms’ desire to make more money, patients are still well served by a team approach that includes nurse practitioners and physician assistants.
“Though I see that shift, it’s not about profits at the end of the day,” Ms. Orozco said. “It’s about the patient.”
The “shift” is nearly invisible to patients because hospitals rarely promote branding from their ED staffing firms and there is little public documentation of private equity investments.
Arthur Smolensky, MD, a Tennessee emergency medicine specialist attempting to measure private equity’s intrusion into EDs, said his review of hospital job postings and employment contracts in 14 major metropolitan areas found that 43% of ED patients were seen in EDs staffed by companies with nonphysician owners, nearly all of whom are private equity investors.
Dr. Smolensky hopes to publish his full study, expanding to 55 metro areas, later this year. But this research will merely quantify what many doctors already know: The ED has changed. Demoralized by an increased focus on profit, and wary of a looming surplus of emergency medicine residents because there are fewer jobs to fill, many experienced doctors are leaving the ED on their own, he said.
“Most of us didn’t go into medicine to supervise an army of people that are not as well trained as we are,” Dr. Smolensky said. “We want to take care of patients.”
“I guess we’re the first guinea pigs for our ER”
Joshua Allen, a nurse practitioner at a small Kentucky hospital, snaked a rubber hose through a rack of pork ribs to practice inserting a chest tube to fix a collapsed lung.
It was 2020, and American Physician Partners was restructuring the ED where Mr. Allen worked, reducing shifts from two doctors to one. Once Mr. Allen had placed 10 tubes under a doctor’s supervision, he would be allowed to do it on his own.
“I guess we’re the first guinea pigs for our ER,” he said. “If we do have a major trauma and multiple victims come in, there’s only one doctor there. ... We need to be prepared.”
Mr. Allen is one of many midlevel practitioners finding work in emergency departments. Nurse practitioners and physician assistants are among the fastest-growing occupations in the nation, according to the U.S. Bureau of Labor Statistics.
Generally, they have master’s degrees and receive several years of specialized schooling but have significantly less training than doctors. Many are permitted to diagnose patients and prescribe medication with little or no supervision from a doctor, although limitations vary by state.
The Neiman Institute found that the share of ED visits in which a midlevel practitioner was the main clinician increased by more than 172% between 2005 and 2020. Another study, in the Journal of Emergency Medicine, reported that if trends continue there may be equal numbers of midlevel practitioners and doctors in EDs by 2030.
There is little mystery as to why. Federal data shows emergency medicine doctors are paid about $310,000 a year on average, while nurse practitioners and physician assistants earn less than $120,000. Generally, hospitals can bill for care by a midlevel practitioner at 85% the rate of a doctor while paying them less than half as much.
Private equity can make millions in the gap.
For example, Envision once encouraged EDs to employ “the least expensive resource” and treat up to 35% of patients with midlevel practitioners, according to a 2017 PowerPoint presentation. The presentation drew scorn on social media and disappeared from Envision’s website.
Envision declined a request for a phone interview. In a written statement to KHN, spokesperson Aliese Polk said the company does not direct its physician leaders on how to care for patients and called the presentation a “concept guide” that does not represent current views.
American Physician Partners touted roughly the same staffing strategy in 2021 in response to the No Surprises Act, which threatened the company’s profits by outlawing surprise medical bills. In its confidential pitch to lenders, the company estimated it could cut almost $6 million by shifting more staffing from physicians to midlevel practitioners.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
She didn’t know much about miscarriage, but this seemed like one.
In the emergency department, she was examined then sent home, she said. She went back when her cramping became excruciating. Then home again. It ultimately took three trips to the ED on 3 consecutive days, generating three separate bills, before she saw a doctor who looked at her blood work and confirmed her fears.
“At the time I wasn’t thinking, ‘Oh, I need to see a doctor,’ ” Ms. Valle recalled. “But when you think about it, it’s like, ‘Well, dang – why didn’t I see a doctor?’ ” It’s unclear whether the repeat visits were due to delays in seeing a physician, but the experience worried her. And she’s still paying the bills.
The hospital declined to discuss Ms. Valle’s care, citing patient privacy. But 17 months before her 3-day ordeal, Tennova had outsourced its emergency departments to American Physician Partners, a medical staffing company owned by private equity investors. APP employs fewer doctors in its EDs as one of its cost-saving initiatives to increase earnings, according to a confidential company document obtained by KHN and NPR.
This staffing strategy has permeated hospitals, and particularly emergency departments, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once their domain, doctors are increasingly being replaced by nurse practitioners and physician assistants, collectively known as “midlevel practitioners,” who can perform many of the same duties and generate much of the same revenue for less than half of the pay.
“APP has numerous cost saving initiatives underway as part of the Company’s continual focus on cost optimization,” the document says, including a “shift of staffing” between doctors and midlevel practitioners.
In a statement to KHN, American Physician Partners said this strategy is a way to ensure all EDs remain fully staffed, calling it a “blended model” that allows doctors, nurse practitioners, and physician assistants “to provide care to their fullest potential.”
Critics of this strategy say the quest to save money results in treatment meted out by someone with far less training than a physician, leaving patients vulnerable to misdiagnoses, higher medical bills, and inadequate care. And these fears are bolstered by evidence that suggests dropping doctors from EDs may not be good for patients.
A working paper, published in October by the National Bureau of Economic Research, analyzed roughly 1.1 million visits to 44 EDs throughout the Veterans Health Administration, where nurse practitioners can treat patients without oversight from doctors.
Researchers found that treatment by a nurse practitioner resulted on average in a 7% increase in cost of care and an 11% increase in length of stay, extending patients’ time in the ED by minutes for minor visits and hours for longer ones. These gaps widened among patients with more severe diagnoses, the study said, but could be somewhat mitigated by nurse practitioners with more experience.
The study also found that ED patients treated by a nurse practitioner were 20% more likely to be readmitted to the hospital for a preventable reason within 30 days, although the overall risk of readmission remained very small.
Yiqun Chen, PhD, who is an assistant professor of economics at the University of Illinois at Chicago and coauthored the study, said these findings are not an indictment of nurse practitioners in the ED. Instead, she said, she hopes the study will guide how to best deploy nurse practitioners: in treatment of simpler patients or circumstances when no doctor is available.
“It’s not just a simple question of if we can substitute physicians with nurse practitioners or not,” Dr. Chen said. “It depends on how we use them. If we just use them as independent providers, especially ... for relatively complicated patients, it doesn’t seem to be a very good use.”
Dr. Chen’s research echoes smaller studies, like one from The Harvey L. Neiman Health Policy Institute that found nonphysician practitioners in EDs were associated with a 5.3% increase in imaging, which could unnecessarily increase bills for patients. Separately, a study at the Hattiesburg Clinic in Mississippi found that midlevel practitioners in primary care – not in the emergency department – increased the out-of-pocket costs to patients while also leading to worse performance on 9 of 10 quality-of-care metrics, including cancer screenings and vaccination rates.
But definitive evidence remains elusive that replacing ER doctors with nonphysicians has a negative impact on patients, said Cameron Gettel, MD, an assistant professor of emergency medicine at Yale University, New Haven, Conn. Private equity investment and the use of midlevel practitioners rose in lockstep in the ED, Dr. Gettel said, and in the absence of game-changing research, the pattern will likely continue.
“Worse patient outcomes haven’t really been shown across the board,” he said. “And I think until that is shown, then they will continue to play an increasing role.”
For private equity, dropping ED docs is a “simple equation”
Private equity companies pool money from wealthy investors to buy their way into various industries, often slashing spending and seeking to flip businesses in 3 to 7 years. While this business model is a proven moneymaker on Wall Street, it raises concerns in health care, where critics worry the pressure to turn big profits will influence life-or-death decisions that were once left solely to medical professionals.
Nearly $1 trillion in private equity funds have gone into almost 8,000 health care transactions over the past decade, according to industry tracker PitchBook, including buying into medical staffing companies that many hospitals hire to manage their emergency departments.
Two firms dominate the ED staffing industry: TeamHealth, bought by private equity firm Blackstone in 2016, and Envision Healthcare, bought by KKR in 2018. Trying to undercut these staffing giants is American Physician Partners, a rapidly expanding company that runs EDs in at least 17 states and is 50% owned by private equity firm BBH Capital Partners.
These staffing companies have been among the most aggressive in replacing doctors to cut costs, said Robert McNamara, MD, a founder of the American Academy of Emergency Medicine and chair of emergency medicine at Temple University, Philadelphia.
“It’s a relatively simple equation,” Dr. McNamara said. “Their No. 1 expense is the board-certified emergency physician. So they are going to want to keep that expense as low as possible.”
Not everyone sees the trend of private equity in ED staffing in a negative light. Jennifer Orozco, president of the American Academy of Physician Associates, which represents physician assistants, said even if the change – to use more nonphysician providers – is driven by the staffing firms’ desire to make more money, patients are still well served by a team approach that includes nurse practitioners and physician assistants.
“Though I see that shift, it’s not about profits at the end of the day,” Ms. Orozco said. “It’s about the patient.”
The “shift” is nearly invisible to patients because hospitals rarely promote branding from their ED staffing firms and there is little public documentation of private equity investments.
Arthur Smolensky, MD, a Tennessee emergency medicine specialist attempting to measure private equity’s intrusion into EDs, said his review of hospital job postings and employment contracts in 14 major metropolitan areas found that 43% of ED patients were seen in EDs staffed by companies with nonphysician owners, nearly all of whom are private equity investors.
Dr. Smolensky hopes to publish his full study, expanding to 55 metro areas, later this year. But this research will merely quantify what many doctors already know: The ED has changed. Demoralized by an increased focus on profit, and wary of a looming surplus of emergency medicine residents because there are fewer jobs to fill, many experienced doctors are leaving the ED on their own, he said.
“Most of us didn’t go into medicine to supervise an army of people that are not as well trained as we are,” Dr. Smolensky said. “We want to take care of patients.”
“I guess we’re the first guinea pigs for our ER”
Joshua Allen, a nurse practitioner at a small Kentucky hospital, snaked a rubber hose through a rack of pork ribs to practice inserting a chest tube to fix a collapsed lung.
It was 2020, and American Physician Partners was restructuring the ED where Mr. Allen worked, reducing shifts from two doctors to one. Once Mr. Allen had placed 10 tubes under a doctor’s supervision, he would be allowed to do it on his own.
“I guess we’re the first guinea pigs for our ER,” he said. “If we do have a major trauma and multiple victims come in, there’s only one doctor there. ... We need to be prepared.”
Mr. Allen is one of many midlevel practitioners finding work in emergency departments. Nurse practitioners and physician assistants are among the fastest-growing occupations in the nation, according to the U.S. Bureau of Labor Statistics.
Generally, they have master’s degrees and receive several years of specialized schooling but have significantly less training than doctors. Many are permitted to diagnose patients and prescribe medication with little or no supervision from a doctor, although limitations vary by state.
The Neiman Institute found that the share of ED visits in which a midlevel practitioner was the main clinician increased by more than 172% between 2005 and 2020. Another study, in the Journal of Emergency Medicine, reported that if trends continue there may be equal numbers of midlevel practitioners and doctors in EDs by 2030.
There is little mystery as to why. Federal data shows emergency medicine doctors are paid about $310,000 a year on average, while nurse practitioners and physician assistants earn less than $120,000. Generally, hospitals can bill for care by a midlevel practitioner at 85% the rate of a doctor while paying them less than half as much.
Private equity can make millions in the gap.
For example, Envision once encouraged EDs to employ “the least expensive resource” and treat up to 35% of patients with midlevel practitioners, according to a 2017 PowerPoint presentation. The presentation drew scorn on social media and disappeared from Envision’s website.
Envision declined a request for a phone interview. In a written statement to KHN, spokesperson Aliese Polk said the company does not direct its physician leaders on how to care for patients and called the presentation a “concept guide” that does not represent current views.
American Physician Partners touted roughly the same staffing strategy in 2021 in response to the No Surprises Act, which threatened the company’s profits by outlawing surprise medical bills. In its confidential pitch to lenders, the company estimated it could cut almost $6 million by shifting more staffing from physicians to midlevel practitioners.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
She didn’t know much about miscarriage, but this seemed like one.
In the emergency department, she was examined then sent home, she said. She went back when her cramping became excruciating. Then home again. It ultimately took three trips to the ED on 3 consecutive days, generating three separate bills, before she saw a doctor who looked at her blood work and confirmed her fears.
“At the time I wasn’t thinking, ‘Oh, I need to see a doctor,’ ” Ms. Valle recalled. “But when you think about it, it’s like, ‘Well, dang – why didn’t I see a doctor?’ ” It’s unclear whether the repeat visits were due to delays in seeing a physician, but the experience worried her. And she’s still paying the bills.
The hospital declined to discuss Ms. Valle’s care, citing patient privacy. But 17 months before her 3-day ordeal, Tennova had outsourced its emergency departments to American Physician Partners, a medical staffing company owned by private equity investors. APP employs fewer doctors in its EDs as one of its cost-saving initiatives to increase earnings, according to a confidential company document obtained by KHN and NPR.
This staffing strategy has permeated hospitals, and particularly emergency departments, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once their domain, doctors are increasingly being replaced by nurse practitioners and physician assistants, collectively known as “midlevel practitioners,” who can perform many of the same duties and generate much of the same revenue for less than half of the pay.
“APP has numerous cost saving initiatives underway as part of the Company’s continual focus on cost optimization,” the document says, including a “shift of staffing” between doctors and midlevel practitioners.
In a statement to KHN, American Physician Partners said this strategy is a way to ensure all EDs remain fully staffed, calling it a “blended model” that allows doctors, nurse practitioners, and physician assistants “to provide care to their fullest potential.”
Critics of this strategy say the quest to save money results in treatment meted out by someone with far less training than a physician, leaving patients vulnerable to misdiagnoses, higher medical bills, and inadequate care. And these fears are bolstered by evidence that suggests dropping doctors from EDs may not be good for patients.
A working paper, published in October by the National Bureau of Economic Research, analyzed roughly 1.1 million visits to 44 EDs throughout the Veterans Health Administration, where nurse practitioners can treat patients without oversight from doctors.
Researchers found that treatment by a nurse practitioner resulted on average in a 7% increase in cost of care and an 11% increase in length of stay, extending patients’ time in the ED by minutes for minor visits and hours for longer ones. These gaps widened among patients with more severe diagnoses, the study said, but could be somewhat mitigated by nurse practitioners with more experience.
The study also found that ED patients treated by a nurse practitioner were 20% more likely to be readmitted to the hospital for a preventable reason within 30 days, although the overall risk of readmission remained very small.
Yiqun Chen, PhD, who is an assistant professor of economics at the University of Illinois at Chicago and coauthored the study, said these findings are not an indictment of nurse practitioners in the ED. Instead, she said, she hopes the study will guide how to best deploy nurse practitioners: in treatment of simpler patients or circumstances when no doctor is available.
“It’s not just a simple question of if we can substitute physicians with nurse practitioners or not,” Dr. Chen said. “It depends on how we use them. If we just use them as independent providers, especially ... for relatively complicated patients, it doesn’t seem to be a very good use.”
Dr. Chen’s research echoes smaller studies, like one from The Harvey L. Neiman Health Policy Institute that found nonphysician practitioners in EDs were associated with a 5.3% increase in imaging, which could unnecessarily increase bills for patients. Separately, a study at the Hattiesburg Clinic in Mississippi found that midlevel practitioners in primary care – not in the emergency department – increased the out-of-pocket costs to patients while also leading to worse performance on 9 of 10 quality-of-care metrics, including cancer screenings and vaccination rates.
But definitive evidence remains elusive that replacing ER doctors with nonphysicians has a negative impact on patients, said Cameron Gettel, MD, an assistant professor of emergency medicine at Yale University, New Haven, Conn. Private equity investment and the use of midlevel practitioners rose in lockstep in the ED, Dr. Gettel said, and in the absence of game-changing research, the pattern will likely continue.
“Worse patient outcomes haven’t really been shown across the board,” he said. “And I think until that is shown, then they will continue to play an increasing role.”
For private equity, dropping ED docs is a “simple equation”
Private equity companies pool money from wealthy investors to buy their way into various industries, often slashing spending and seeking to flip businesses in 3 to 7 years. While this business model is a proven moneymaker on Wall Street, it raises concerns in health care, where critics worry the pressure to turn big profits will influence life-or-death decisions that were once left solely to medical professionals.
Nearly $1 trillion in private equity funds have gone into almost 8,000 health care transactions over the past decade, according to industry tracker PitchBook, including buying into medical staffing companies that many hospitals hire to manage their emergency departments.
Two firms dominate the ED staffing industry: TeamHealth, bought by private equity firm Blackstone in 2016, and Envision Healthcare, bought by KKR in 2018. Trying to undercut these staffing giants is American Physician Partners, a rapidly expanding company that runs EDs in at least 17 states and is 50% owned by private equity firm BBH Capital Partners.
These staffing companies have been among the most aggressive in replacing doctors to cut costs, said Robert McNamara, MD, a founder of the American Academy of Emergency Medicine and chair of emergency medicine at Temple University, Philadelphia.
“It’s a relatively simple equation,” Dr. McNamara said. “Their No. 1 expense is the board-certified emergency physician. So they are going to want to keep that expense as low as possible.”
Not everyone sees the trend of private equity in ED staffing in a negative light. Jennifer Orozco, president of the American Academy of Physician Associates, which represents physician assistants, said even if the change – to use more nonphysician providers – is driven by the staffing firms’ desire to make more money, patients are still well served by a team approach that includes nurse practitioners and physician assistants.
“Though I see that shift, it’s not about profits at the end of the day,” Ms. Orozco said. “It’s about the patient.”
The “shift” is nearly invisible to patients because hospitals rarely promote branding from their ED staffing firms and there is little public documentation of private equity investments.
Arthur Smolensky, MD, a Tennessee emergency medicine specialist attempting to measure private equity’s intrusion into EDs, said his review of hospital job postings and employment contracts in 14 major metropolitan areas found that 43% of ED patients were seen in EDs staffed by companies with nonphysician owners, nearly all of whom are private equity investors.
Dr. Smolensky hopes to publish his full study, expanding to 55 metro areas, later this year. But this research will merely quantify what many doctors already know: The ED has changed. Demoralized by an increased focus on profit, and wary of a looming surplus of emergency medicine residents because there are fewer jobs to fill, many experienced doctors are leaving the ED on their own, he said.
“Most of us didn’t go into medicine to supervise an army of people that are not as well trained as we are,” Dr. Smolensky said. “We want to take care of patients.”
“I guess we’re the first guinea pigs for our ER”
Joshua Allen, a nurse practitioner at a small Kentucky hospital, snaked a rubber hose through a rack of pork ribs to practice inserting a chest tube to fix a collapsed lung.
It was 2020, and American Physician Partners was restructuring the ED where Mr. Allen worked, reducing shifts from two doctors to one. Once Mr. Allen had placed 10 tubes under a doctor’s supervision, he would be allowed to do it on his own.
“I guess we’re the first guinea pigs for our ER,” he said. “If we do have a major trauma and multiple victims come in, there’s only one doctor there. ... We need to be prepared.”
Mr. Allen is one of many midlevel practitioners finding work in emergency departments. Nurse practitioners and physician assistants are among the fastest-growing occupations in the nation, according to the U.S. Bureau of Labor Statistics.
Generally, they have master’s degrees and receive several years of specialized schooling but have significantly less training than doctors. Many are permitted to diagnose patients and prescribe medication with little or no supervision from a doctor, although limitations vary by state.
The Neiman Institute found that the share of ED visits in which a midlevel practitioner was the main clinician increased by more than 172% between 2005 and 2020. Another study, in the Journal of Emergency Medicine, reported that if trends continue there may be equal numbers of midlevel practitioners and doctors in EDs by 2030.
There is little mystery as to why. Federal data shows emergency medicine doctors are paid about $310,000 a year on average, while nurse practitioners and physician assistants earn less than $120,000. Generally, hospitals can bill for care by a midlevel practitioner at 85% the rate of a doctor while paying them less than half as much.
Private equity can make millions in the gap.
For example, Envision once encouraged EDs to employ “the least expensive resource” and treat up to 35% of patients with midlevel practitioners, according to a 2017 PowerPoint presentation. The presentation drew scorn on social media and disappeared from Envision’s website.
Envision declined a request for a phone interview. In a written statement to KHN, spokesperson Aliese Polk said the company does not direct its physician leaders on how to care for patients and called the presentation a “concept guide” that does not represent current views.
American Physician Partners touted roughly the same staffing strategy in 2021 in response to the No Surprises Act, which threatened the company’s profits by outlawing surprise medical bills. In its confidential pitch to lenders, the company estimated it could cut almost $6 million by shifting more staffing from physicians to midlevel practitioners.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
New report says suicide rates rising among young Black people
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Antenatal corticosteroids: Fresh answers to old questions
Giving corticosteroids to pregnant women at risk for preterm birth before 34 weeks of gestational age has been the standard of care since the 1990s, but a few scenarios for their use remain up for debate. Two studies presented this week at the 2023 meeting sponsored by the Society for Maternal–Fetal Medicine provided some fresh insight into the practice that could help clinicians better manage pregnant patients.
Neurodevelopmental outcomes in late preterm
First, should antenatal corticosteroids (ACS) be given to mothers who present with late preterm labor, defined as 34-36 weeks’ gestational age?
A landmark randomized clinical trial published in 2016 demonstrated that use of ACS in mothers in late preterm labor reduced severe respiratory complications. That practice has largely been adopted by clinicians. The only downside, according to the researchers, was that infants whose mothers received steroid therapy were more likely to develop hypoglycemia. The condition is self-limiting, but studies have raised concern about the potential long-term risk of neurocognitive or psychological outcomes in infants with hypoglycemia.
Cynthia Gyamfi-Bannerman, MD, MSc, endowed chair and professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, led the 2016 study. Her team was unable to secure funding for their originally planned follow-up study of the infants 2 years later. But once the American College of Obstetricians and Gynecologists endorsed the practice and more women received ACS in the late preterm period, Dr. Gyamfi-Bannerman and her colleagues felt the need to “follow up the infants just to see what the outcomes are from a neurodevelopmental standpoint,” she said.
Dr. Gyamfi-Bannerman and colleagues recruited children older than age 6 from the original trial whose parents were willing to have them participate in a follow-up study. A total of 949 from the initial 2,831 cohort completed cognitive testing and received assessments for cerebral palsy, social impairment within the autism spectrum, and behavioral and emotional problems.
At the SMFM conference, Dr. Gyamfi-Bannerman reported no differences in the primary outcome of cognitive function between those whose mothers had received a single course of betamethasone and those who did not, or any differences in rates of the other outcomes.
Kathy Zhang-Rutledge, MD, a maternal-fetal medicine specialist who practices with Obstetrix Maternal Fetal Medicine Group of Houston, part of Pediatrix Medical Group, said she was glad to see a study that addressed the potential long-term adverse events associated with ACS in the late preterm period.
“Having this pretty large study – with really good neurological testing results – should help reassure clinicians that this is something they should consider adopting in their practice,” Dr. Zhang-Rutledge said.
Are boosters better?
The second unresolved question was if a repeat course of ACS should be administered when a woman at risk for preterm birth receives a course of steroids but does not deliver in the following 7 days.
Any benefits to the initial course of ACS wear off after a week. As a result, clinicians often give booster courses 7 days after the first dose if the infant is likely to be delivered in the following week. A 2009 study showed this approach may protect infants from respiratory problems, but data on long-term outcomes have been weak.
ACOG guidelines say to “consider” a booster dose in women who are less than 34 weeks’ gestation at risk for preterm delivery within 7 days.
The exception is when the mother already has experienced preterm prelabor rupture of membranes (PPROM), because ACS may increase the risk for infection for both mother and child. ACOG doesn’t take a stand on use of booster doses for PPROM, citing a lack of data to show that potential benefits outweigh the potential risks of this approach.
A recent multicenter, double-blinded, randomized clinical trial attempted to fill that void in knowledge. Between 2016 and 2022, 194 women with PPROM and gestational age less than 32 weeks who had received an initial ACS course at least 7 days prior to randomization received a booster course of ACS or saline placebo.
“Our primary outcome was designed to be like the prior rescue study (in 2009) that we did with patients with intact membranes,” said Andrew Combs, MD, PhD, a maternal-fetal medicine specialist at Pediatrix Medical Group in Sunrise, Fla., who participated in the earlier study. “It was a composite of neonatal morbidity that was any one of a variety of outcomes including respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, and neonatal death.”
The primary outcome occurred in 64% of women who received booster ACS and 66% with placebo (odds ratio, 0.82; 95% confidence interval, 0.43-1.57), according to Dr. Combs, who presented the findings at SMFM.
Although the study was not powered to detect significant differences in specific outcomes, the rate of neonatal sepsis was not higher in the ACS group, suggesting that ACS may be safe if membranes have ruptured, the researchers reported. But because the booster course of ACS did not prevent respiratory morbidity, clinicians may wonder what to do with the findings.
Niraj Chavan, MD, an associate professor in the department of obstetrics, gynecology, and women’s health at Saint Louis University, said he was unsure how the study would affect clinical practice.
The relatively small sample number of patients prevented analysis of specific outcomes and subgroup analyses of important variables such as race, ethnicity, gestational age, and other comorbid conditions in the mothers, he said. So clinicians still must weigh potential risks and benefits on a case-by-case basis.
“You have to think about it in buckets,” he said, “One is conditions that would increase the risk for neonatal morbidity. The other is the risk for infection, both for the mom and the baby.”
But for Dr. Combs, the interpretation of the findings was simpler: “We concluded that there’s no indication to give a booster course of steroids after a week has elapsed in patients with ruptured membranes.”
The study presented by Dr. Gyamfi-Bannerman was funded by the National Institute of Child Health and Human Development. The study presented by Dr. Combs was funded by MEDNAX Center for Research, Education, and Quality, which in 2022 was renamed Pediatrix Center for Research, Education,and Quality. Dr. Combs is an employee of Pediatrix Medical Group but has no conflicts of interest. Dr. Gyamfi-Bannerman, Dr. Zhang-Rutledge, and Dr. Chavan report no relevant financial relationships.
Ann Thomas is a pediatrician and epidemiologist in Portland, Ore.
A version of this article originally appeared on Medscape.com.
Giving corticosteroids to pregnant women at risk for preterm birth before 34 weeks of gestational age has been the standard of care since the 1990s, but a few scenarios for their use remain up for debate. Two studies presented this week at the 2023 meeting sponsored by the Society for Maternal–Fetal Medicine provided some fresh insight into the practice that could help clinicians better manage pregnant patients.
Neurodevelopmental outcomes in late preterm
First, should antenatal corticosteroids (ACS) be given to mothers who present with late preterm labor, defined as 34-36 weeks’ gestational age?
A landmark randomized clinical trial published in 2016 demonstrated that use of ACS in mothers in late preterm labor reduced severe respiratory complications. That practice has largely been adopted by clinicians. The only downside, according to the researchers, was that infants whose mothers received steroid therapy were more likely to develop hypoglycemia. The condition is self-limiting, but studies have raised concern about the potential long-term risk of neurocognitive or psychological outcomes in infants with hypoglycemia.
Cynthia Gyamfi-Bannerman, MD, MSc, endowed chair and professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, led the 2016 study. Her team was unable to secure funding for their originally planned follow-up study of the infants 2 years later. But once the American College of Obstetricians and Gynecologists endorsed the practice and more women received ACS in the late preterm period, Dr. Gyamfi-Bannerman and her colleagues felt the need to “follow up the infants just to see what the outcomes are from a neurodevelopmental standpoint,” she said.
Dr. Gyamfi-Bannerman and colleagues recruited children older than age 6 from the original trial whose parents were willing to have them participate in a follow-up study. A total of 949 from the initial 2,831 cohort completed cognitive testing and received assessments for cerebral palsy, social impairment within the autism spectrum, and behavioral and emotional problems.
At the SMFM conference, Dr. Gyamfi-Bannerman reported no differences in the primary outcome of cognitive function between those whose mothers had received a single course of betamethasone and those who did not, or any differences in rates of the other outcomes.
Kathy Zhang-Rutledge, MD, a maternal-fetal medicine specialist who practices with Obstetrix Maternal Fetal Medicine Group of Houston, part of Pediatrix Medical Group, said she was glad to see a study that addressed the potential long-term adverse events associated with ACS in the late preterm period.
“Having this pretty large study – with really good neurological testing results – should help reassure clinicians that this is something they should consider adopting in their practice,” Dr. Zhang-Rutledge said.
Are boosters better?
The second unresolved question was if a repeat course of ACS should be administered when a woman at risk for preterm birth receives a course of steroids but does not deliver in the following 7 days.
Any benefits to the initial course of ACS wear off after a week. As a result, clinicians often give booster courses 7 days after the first dose if the infant is likely to be delivered in the following week. A 2009 study showed this approach may protect infants from respiratory problems, but data on long-term outcomes have been weak.
ACOG guidelines say to “consider” a booster dose in women who are less than 34 weeks’ gestation at risk for preterm delivery within 7 days.
The exception is when the mother already has experienced preterm prelabor rupture of membranes (PPROM), because ACS may increase the risk for infection for both mother and child. ACOG doesn’t take a stand on use of booster doses for PPROM, citing a lack of data to show that potential benefits outweigh the potential risks of this approach.
A recent multicenter, double-blinded, randomized clinical trial attempted to fill that void in knowledge. Between 2016 and 2022, 194 women with PPROM and gestational age less than 32 weeks who had received an initial ACS course at least 7 days prior to randomization received a booster course of ACS or saline placebo.
“Our primary outcome was designed to be like the prior rescue study (in 2009) that we did with patients with intact membranes,” said Andrew Combs, MD, PhD, a maternal-fetal medicine specialist at Pediatrix Medical Group in Sunrise, Fla., who participated in the earlier study. “It was a composite of neonatal morbidity that was any one of a variety of outcomes including respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, and neonatal death.”
The primary outcome occurred in 64% of women who received booster ACS and 66% with placebo (odds ratio, 0.82; 95% confidence interval, 0.43-1.57), according to Dr. Combs, who presented the findings at SMFM.
Although the study was not powered to detect significant differences in specific outcomes, the rate of neonatal sepsis was not higher in the ACS group, suggesting that ACS may be safe if membranes have ruptured, the researchers reported. But because the booster course of ACS did not prevent respiratory morbidity, clinicians may wonder what to do with the findings.
Niraj Chavan, MD, an associate professor in the department of obstetrics, gynecology, and women’s health at Saint Louis University, said he was unsure how the study would affect clinical practice.
The relatively small sample number of patients prevented analysis of specific outcomes and subgroup analyses of important variables such as race, ethnicity, gestational age, and other comorbid conditions in the mothers, he said. So clinicians still must weigh potential risks and benefits on a case-by-case basis.
“You have to think about it in buckets,” he said, “One is conditions that would increase the risk for neonatal morbidity. The other is the risk for infection, both for the mom and the baby.”
But for Dr. Combs, the interpretation of the findings was simpler: “We concluded that there’s no indication to give a booster course of steroids after a week has elapsed in patients with ruptured membranes.”
The study presented by Dr. Gyamfi-Bannerman was funded by the National Institute of Child Health and Human Development. The study presented by Dr. Combs was funded by MEDNAX Center for Research, Education, and Quality, which in 2022 was renamed Pediatrix Center for Research, Education,and Quality. Dr. Combs is an employee of Pediatrix Medical Group but has no conflicts of interest. Dr. Gyamfi-Bannerman, Dr. Zhang-Rutledge, and Dr. Chavan report no relevant financial relationships.
Ann Thomas is a pediatrician and epidemiologist in Portland, Ore.
A version of this article originally appeared on Medscape.com.
Giving corticosteroids to pregnant women at risk for preterm birth before 34 weeks of gestational age has been the standard of care since the 1990s, but a few scenarios for their use remain up for debate. Two studies presented this week at the 2023 meeting sponsored by the Society for Maternal–Fetal Medicine provided some fresh insight into the practice that could help clinicians better manage pregnant patients.
Neurodevelopmental outcomes in late preterm
First, should antenatal corticosteroids (ACS) be given to mothers who present with late preterm labor, defined as 34-36 weeks’ gestational age?
A landmark randomized clinical trial published in 2016 demonstrated that use of ACS in mothers in late preterm labor reduced severe respiratory complications. That practice has largely been adopted by clinicians. The only downside, according to the researchers, was that infants whose mothers received steroid therapy were more likely to develop hypoglycemia. The condition is self-limiting, but studies have raised concern about the potential long-term risk of neurocognitive or psychological outcomes in infants with hypoglycemia.
Cynthia Gyamfi-Bannerman, MD, MSc, endowed chair and professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Diego, led the 2016 study. Her team was unable to secure funding for their originally planned follow-up study of the infants 2 years later. But once the American College of Obstetricians and Gynecologists endorsed the practice and more women received ACS in the late preterm period, Dr. Gyamfi-Bannerman and her colleagues felt the need to “follow up the infants just to see what the outcomes are from a neurodevelopmental standpoint,” she said.
Dr. Gyamfi-Bannerman and colleagues recruited children older than age 6 from the original trial whose parents were willing to have them participate in a follow-up study. A total of 949 from the initial 2,831 cohort completed cognitive testing and received assessments for cerebral palsy, social impairment within the autism spectrum, and behavioral and emotional problems.
At the SMFM conference, Dr. Gyamfi-Bannerman reported no differences in the primary outcome of cognitive function between those whose mothers had received a single course of betamethasone and those who did not, or any differences in rates of the other outcomes.
Kathy Zhang-Rutledge, MD, a maternal-fetal medicine specialist who practices with Obstetrix Maternal Fetal Medicine Group of Houston, part of Pediatrix Medical Group, said she was glad to see a study that addressed the potential long-term adverse events associated with ACS in the late preterm period.
“Having this pretty large study – with really good neurological testing results – should help reassure clinicians that this is something they should consider adopting in their practice,” Dr. Zhang-Rutledge said.
Are boosters better?
The second unresolved question was if a repeat course of ACS should be administered when a woman at risk for preterm birth receives a course of steroids but does not deliver in the following 7 days.
Any benefits to the initial course of ACS wear off after a week. As a result, clinicians often give booster courses 7 days after the first dose if the infant is likely to be delivered in the following week. A 2009 study showed this approach may protect infants from respiratory problems, but data on long-term outcomes have been weak.
ACOG guidelines say to “consider” a booster dose in women who are less than 34 weeks’ gestation at risk for preterm delivery within 7 days.
The exception is when the mother already has experienced preterm prelabor rupture of membranes (PPROM), because ACS may increase the risk for infection for both mother and child. ACOG doesn’t take a stand on use of booster doses for PPROM, citing a lack of data to show that potential benefits outweigh the potential risks of this approach.
A recent multicenter, double-blinded, randomized clinical trial attempted to fill that void in knowledge. Between 2016 and 2022, 194 women with PPROM and gestational age less than 32 weeks who had received an initial ACS course at least 7 days prior to randomization received a booster course of ACS or saline placebo.
“Our primary outcome was designed to be like the prior rescue study (in 2009) that we did with patients with intact membranes,” said Andrew Combs, MD, PhD, a maternal-fetal medicine specialist at Pediatrix Medical Group in Sunrise, Fla., who participated in the earlier study. “It was a composite of neonatal morbidity that was any one of a variety of outcomes including respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, and neonatal death.”
The primary outcome occurred in 64% of women who received booster ACS and 66% with placebo (odds ratio, 0.82; 95% confidence interval, 0.43-1.57), according to Dr. Combs, who presented the findings at SMFM.
Although the study was not powered to detect significant differences in specific outcomes, the rate of neonatal sepsis was not higher in the ACS group, suggesting that ACS may be safe if membranes have ruptured, the researchers reported. But because the booster course of ACS did not prevent respiratory morbidity, clinicians may wonder what to do with the findings.
Niraj Chavan, MD, an associate professor in the department of obstetrics, gynecology, and women’s health at Saint Louis University, said he was unsure how the study would affect clinical practice.
The relatively small sample number of patients prevented analysis of specific outcomes and subgroup analyses of important variables such as race, ethnicity, gestational age, and other comorbid conditions in the mothers, he said. So clinicians still must weigh potential risks and benefits on a case-by-case basis.
“You have to think about it in buckets,” he said, “One is conditions that would increase the risk for neonatal morbidity. The other is the risk for infection, both for the mom and the baby.”
But for Dr. Combs, the interpretation of the findings was simpler: “We concluded that there’s no indication to give a booster course of steroids after a week has elapsed in patients with ruptured membranes.”
The study presented by Dr. Gyamfi-Bannerman was funded by the National Institute of Child Health and Human Development. The study presented by Dr. Combs was funded by MEDNAX Center for Research, Education, and Quality, which in 2022 was renamed Pediatrix Center for Research, Education,and Quality. Dr. Combs is an employee of Pediatrix Medical Group but has no conflicts of interest. Dr. Gyamfi-Bannerman, Dr. Zhang-Rutledge, and Dr. Chavan report no relevant financial relationships.
Ann Thomas is a pediatrician and epidemiologist in Portland, Ore.
A version of this article originally appeared on Medscape.com.
FROM THE PREGNANCY MEETING
Isothiazolinone contact allergy up in North America, down in Europe
, a trend that is likely driven by regulatory differences, a retrospective cohort study suggests.
“Between 2009 to 2018, the global burden of isothiazolinone allergy showed divergent trends between North American and European countries,” lead study author Margo J. Reeder, MD, of the University of Wisconsin in Madison and her colleagues write. The study was published online in JAMA Dermatology.
Isothiazolinone contact allergy peaked in Europe in 2013-2014 before gradually decreasing, they found. The prevalence of isothiazolinone allergy steadily increased in North America during the study period. “Earlier and more stringent regulation of MI [methylisothiazolinone] in Europe is associated with these divergent trends,” they write.
Common ingredients worldwide
Isothiazolinone preservatives, which are added to personal and industrial products, cause allergic contact dermatitis worldwide, the authors write. The preservatives are found in a wide range of leave-on and rinse-off water-based personal care products, such as shampoo and other hair products, dishwashing liquid, face cream, body lotion, shower gel, liquid soap, and wet wipes, as well as in water-based paint.
A mixture of methylchloroisothiazolinone (MCI) and MI has been used to prevent microbial growth in products since the 1980s. In 2005, U.S. and European regulators approved MI alone at higher concentrations as a preservative in personal care products. Coupled with consumer concerns about other preservatives, such as parabens (a rare allergen), use of MI in personal care products increased, the authors write.
Subsequently, researchers reported a global increase in the prevalence of contact allergy to isothiazolinones, the authors write. Regulatory restrictions on MI in personal care products were implemented in 2013 in Europe and in 2015 in Canada but not in the United States.
Patch test data reveal latest trends
To compare prevalence trends of allergic contact allergy to MI and sensitization to the MCI/MI mixture in North America and in Europe, Dr. Reeder and her colleagues compared the prevalence of positive patch test reactions to MCI/MI and to MI alone in North America and in Europe between 2009 and 2018.
They analyzed data from the North American Contact Dermatitis Group (NACDG), the European Surveillance System on Contact Allergies (ESSCA), and the Information Network of Departments of Dermatology (IVDK) in 2-year intervals. The data came from patients who had been patch tested at referral patch test clinics in North America and Europe.
Over the decade, the study sites conducted patch testing for 226,161 patients for MCI/MI and 118,779 for MI. Most data came from Europe. The researchers found the following:
- In Europe, isothiazolinone allergy peaked in 2013 and 2014; MCI/MI positivity reached 7.6% (ESSCA) and 5.4% (IVDK) before decreasing to 4.4% (ESSCA) and 3.2% (IVDK) in 2017-2018.
- In North America, MCI/MI positivity rose steadily from 2.5% in 2009-2010 to 10.8% in 2017-2018.
- In Europe, there were 5.5% (ESSCA) and 3.4% (IVDK) positive reactions to MI, compared with 15% (NACDG) in North America in 2017-2018.
Divergent contact allergy trends linked to regulatory approaches
The downward trend of isothiazolinone allergy in Europe after its peak in 2013 and 2014 may have been due in part, the authors explain, to a memo released in 2013 by Cosmetics Europe after it and the European Society of Contact Dermatitis reviewed reports of increased contact allergy to MI. The memo urged companies to remove MI from leave-on products.
Later that year, the European Union’s Scientific Committee on Consumer Safety advised omitting MI from leave-on consumer personal care products and moved to restrict the ingredient in rinse-off products to less than 15 ppm. The recommendation took effect in 2015.
That year, Canada banned the use of MCI/MI in leave-on products but allowed MI alone in leave-on products until 2018. The total concentration of MI and MCI in wash-off products was limited to less than 15 ppm.
The authors add that, to their knowledge, the U.S. government does not restrict the use of MCI/MI or MI.
Policy implications for contact allergy
MI is still widely used in “countless products,” including shampoos, skin cleansers, dishwashing and laundry detergents, paints, and adhesives, Daniel W. Shaw, MD, associate professor of dermatology at the University of California, San Diego, told this news organization by email.
“Exact figures between the U.S. and Europe are difficult to compare due to differing patch test concentrations, but the overall trends strongly suggest that stricter and earlier regulation in Europe resulted in lower MI allergy prevalence there than in the U.S.,” added Dr. Shaw, who was not involved in the study.
Steven R. Feldman, MD, PhD, professor of dermatology at Wake Forest University in Winston-Salem, N.C., said by email that accurate information on allergic reaction prevalence is difficult to find.
“The NACDG, ESSCA, and IVDK databases may contain the best data available, but the data depend on people who get patch tested and are not directly informative of the allergy rates in the general population,” added Dr. Feldman, who was not involved in the study.
“The great majority of people in the population may not be allergic,” he said. “For those with itchy rashes, getting patch tested or avoiding products with preservatives may be prudent. Broad regulations, however, should consider the overall risks and benefits in the population, and this particular study does not fully capture those issues.”
“This study shows that government regulations are important to limit consumer exposure to common allergens, especially to the concentrations used in personal care products,” Kelly Tyler, MD, associate professor of dermatology at the Ohio State University Wexner Medical Center in Columbus, noted by email. She was not involved in the study.
She advised clinicians to ask their patients who may have allergic contact dermatitis whether they have been exposed to products containing these compounds.
“All personal care products in the store contain preservatives, and their maximum concentrations should be limited,” she advised. “The Expert Panel for Cosmetic Ingredient Safety should establish stricter guidelines for MI use in personal care products, especially given the findings of this study.”
Has MI contact allergy in North America peaked?
“In the U.S., MI has not been banned from leave-on skin-care products, but recently, its use has markedly decreased,” Dr. Shaw commented. “Hopefully, the prevalence of MI contact allergy will also begin to decrease.”
New evidence is promising. In a related study published online in Dermatology, Joel G. DeKoven, MD, MHSc, FRCPC, of the University of Toronto and his colleagues reported the NACDG 2019-2020 patch test results for MI in North America. They found that 13.8% of patients tested positive for MI.
“For the first time, MI positivity did not increase between reporting periods,” they conclude. “The epidemic of MI contact allergy in North America may have reached a plateau.”
Information regarding funding for the study was not provided. Dr. Reeder has financial relationships with the American Contact Dermatitis Society and a publishing company. Several coauthors have financial relationships with the pharmaceutical industry. Dr. Tyler, Dr. Shaw, and Dr. Feldman report no relevant financial relationship.
A version of this article first appeared on Medscape.com.
, a trend that is likely driven by regulatory differences, a retrospective cohort study suggests.
“Between 2009 to 2018, the global burden of isothiazolinone allergy showed divergent trends between North American and European countries,” lead study author Margo J. Reeder, MD, of the University of Wisconsin in Madison and her colleagues write. The study was published online in JAMA Dermatology.
Isothiazolinone contact allergy peaked in Europe in 2013-2014 before gradually decreasing, they found. The prevalence of isothiazolinone allergy steadily increased in North America during the study period. “Earlier and more stringent regulation of MI [methylisothiazolinone] in Europe is associated with these divergent trends,” they write.
Common ingredients worldwide
Isothiazolinone preservatives, which are added to personal and industrial products, cause allergic contact dermatitis worldwide, the authors write. The preservatives are found in a wide range of leave-on and rinse-off water-based personal care products, such as shampoo and other hair products, dishwashing liquid, face cream, body lotion, shower gel, liquid soap, and wet wipes, as well as in water-based paint.
A mixture of methylchloroisothiazolinone (MCI) and MI has been used to prevent microbial growth in products since the 1980s. In 2005, U.S. and European regulators approved MI alone at higher concentrations as a preservative in personal care products. Coupled with consumer concerns about other preservatives, such as parabens (a rare allergen), use of MI in personal care products increased, the authors write.
Subsequently, researchers reported a global increase in the prevalence of contact allergy to isothiazolinones, the authors write. Regulatory restrictions on MI in personal care products were implemented in 2013 in Europe and in 2015 in Canada but not in the United States.
Patch test data reveal latest trends
To compare prevalence trends of allergic contact allergy to MI and sensitization to the MCI/MI mixture in North America and in Europe, Dr. Reeder and her colleagues compared the prevalence of positive patch test reactions to MCI/MI and to MI alone in North America and in Europe between 2009 and 2018.
They analyzed data from the North American Contact Dermatitis Group (NACDG), the European Surveillance System on Contact Allergies (ESSCA), and the Information Network of Departments of Dermatology (IVDK) in 2-year intervals. The data came from patients who had been patch tested at referral patch test clinics in North America and Europe.
Over the decade, the study sites conducted patch testing for 226,161 patients for MCI/MI and 118,779 for MI. Most data came from Europe. The researchers found the following:
- In Europe, isothiazolinone allergy peaked in 2013 and 2014; MCI/MI positivity reached 7.6% (ESSCA) and 5.4% (IVDK) before decreasing to 4.4% (ESSCA) and 3.2% (IVDK) in 2017-2018.
- In North America, MCI/MI positivity rose steadily from 2.5% in 2009-2010 to 10.8% in 2017-2018.
- In Europe, there were 5.5% (ESSCA) and 3.4% (IVDK) positive reactions to MI, compared with 15% (NACDG) in North America in 2017-2018.
Divergent contact allergy trends linked to regulatory approaches
The downward trend of isothiazolinone allergy in Europe after its peak in 2013 and 2014 may have been due in part, the authors explain, to a memo released in 2013 by Cosmetics Europe after it and the European Society of Contact Dermatitis reviewed reports of increased contact allergy to MI. The memo urged companies to remove MI from leave-on products.
Later that year, the European Union’s Scientific Committee on Consumer Safety advised omitting MI from leave-on consumer personal care products and moved to restrict the ingredient in rinse-off products to less than 15 ppm. The recommendation took effect in 2015.
That year, Canada banned the use of MCI/MI in leave-on products but allowed MI alone in leave-on products until 2018. The total concentration of MI and MCI in wash-off products was limited to less than 15 ppm.
The authors add that, to their knowledge, the U.S. government does not restrict the use of MCI/MI or MI.
Policy implications for contact allergy
MI is still widely used in “countless products,” including shampoos, skin cleansers, dishwashing and laundry detergents, paints, and adhesives, Daniel W. Shaw, MD, associate professor of dermatology at the University of California, San Diego, told this news organization by email.
“Exact figures between the U.S. and Europe are difficult to compare due to differing patch test concentrations, but the overall trends strongly suggest that stricter and earlier regulation in Europe resulted in lower MI allergy prevalence there than in the U.S.,” added Dr. Shaw, who was not involved in the study.
Steven R. Feldman, MD, PhD, professor of dermatology at Wake Forest University in Winston-Salem, N.C., said by email that accurate information on allergic reaction prevalence is difficult to find.
“The NACDG, ESSCA, and IVDK databases may contain the best data available, but the data depend on people who get patch tested and are not directly informative of the allergy rates in the general population,” added Dr. Feldman, who was not involved in the study.
“The great majority of people in the population may not be allergic,” he said. “For those with itchy rashes, getting patch tested or avoiding products with preservatives may be prudent. Broad regulations, however, should consider the overall risks and benefits in the population, and this particular study does not fully capture those issues.”
“This study shows that government regulations are important to limit consumer exposure to common allergens, especially to the concentrations used in personal care products,” Kelly Tyler, MD, associate professor of dermatology at the Ohio State University Wexner Medical Center in Columbus, noted by email. She was not involved in the study.
She advised clinicians to ask their patients who may have allergic contact dermatitis whether they have been exposed to products containing these compounds.
“All personal care products in the store contain preservatives, and their maximum concentrations should be limited,” she advised. “The Expert Panel for Cosmetic Ingredient Safety should establish stricter guidelines for MI use in personal care products, especially given the findings of this study.”
Has MI contact allergy in North America peaked?
“In the U.S., MI has not been banned from leave-on skin-care products, but recently, its use has markedly decreased,” Dr. Shaw commented. “Hopefully, the prevalence of MI contact allergy will also begin to decrease.”
New evidence is promising. In a related study published online in Dermatology, Joel G. DeKoven, MD, MHSc, FRCPC, of the University of Toronto and his colleagues reported the NACDG 2019-2020 patch test results for MI in North America. They found that 13.8% of patients tested positive for MI.
“For the first time, MI positivity did not increase between reporting periods,” they conclude. “The epidemic of MI contact allergy in North America may have reached a plateau.”
Information regarding funding for the study was not provided. Dr. Reeder has financial relationships with the American Contact Dermatitis Society and a publishing company. Several coauthors have financial relationships with the pharmaceutical industry. Dr. Tyler, Dr. Shaw, and Dr. Feldman report no relevant financial relationship.
A version of this article first appeared on Medscape.com.
, a trend that is likely driven by regulatory differences, a retrospective cohort study suggests.
“Between 2009 to 2018, the global burden of isothiazolinone allergy showed divergent trends between North American and European countries,” lead study author Margo J. Reeder, MD, of the University of Wisconsin in Madison and her colleagues write. The study was published online in JAMA Dermatology.
Isothiazolinone contact allergy peaked in Europe in 2013-2014 before gradually decreasing, they found. The prevalence of isothiazolinone allergy steadily increased in North America during the study period. “Earlier and more stringent regulation of MI [methylisothiazolinone] in Europe is associated with these divergent trends,” they write.
Common ingredients worldwide
Isothiazolinone preservatives, which are added to personal and industrial products, cause allergic contact dermatitis worldwide, the authors write. The preservatives are found in a wide range of leave-on and rinse-off water-based personal care products, such as shampoo and other hair products, dishwashing liquid, face cream, body lotion, shower gel, liquid soap, and wet wipes, as well as in water-based paint.
A mixture of methylchloroisothiazolinone (MCI) and MI has been used to prevent microbial growth in products since the 1980s. In 2005, U.S. and European regulators approved MI alone at higher concentrations as a preservative in personal care products. Coupled with consumer concerns about other preservatives, such as parabens (a rare allergen), use of MI in personal care products increased, the authors write.
Subsequently, researchers reported a global increase in the prevalence of contact allergy to isothiazolinones, the authors write. Regulatory restrictions on MI in personal care products were implemented in 2013 in Europe and in 2015 in Canada but not in the United States.
Patch test data reveal latest trends
To compare prevalence trends of allergic contact allergy to MI and sensitization to the MCI/MI mixture in North America and in Europe, Dr. Reeder and her colleagues compared the prevalence of positive patch test reactions to MCI/MI and to MI alone in North America and in Europe between 2009 and 2018.
They analyzed data from the North American Contact Dermatitis Group (NACDG), the European Surveillance System on Contact Allergies (ESSCA), and the Information Network of Departments of Dermatology (IVDK) in 2-year intervals. The data came from patients who had been patch tested at referral patch test clinics in North America and Europe.
Over the decade, the study sites conducted patch testing for 226,161 patients for MCI/MI and 118,779 for MI. Most data came from Europe. The researchers found the following:
- In Europe, isothiazolinone allergy peaked in 2013 and 2014; MCI/MI positivity reached 7.6% (ESSCA) and 5.4% (IVDK) before decreasing to 4.4% (ESSCA) and 3.2% (IVDK) in 2017-2018.
- In North America, MCI/MI positivity rose steadily from 2.5% in 2009-2010 to 10.8% in 2017-2018.
- In Europe, there were 5.5% (ESSCA) and 3.4% (IVDK) positive reactions to MI, compared with 15% (NACDG) in North America in 2017-2018.
Divergent contact allergy trends linked to regulatory approaches
The downward trend of isothiazolinone allergy in Europe after its peak in 2013 and 2014 may have been due in part, the authors explain, to a memo released in 2013 by Cosmetics Europe after it and the European Society of Contact Dermatitis reviewed reports of increased contact allergy to MI. The memo urged companies to remove MI from leave-on products.
Later that year, the European Union’s Scientific Committee on Consumer Safety advised omitting MI from leave-on consumer personal care products and moved to restrict the ingredient in rinse-off products to less than 15 ppm. The recommendation took effect in 2015.
That year, Canada banned the use of MCI/MI in leave-on products but allowed MI alone in leave-on products until 2018. The total concentration of MI and MCI in wash-off products was limited to less than 15 ppm.
The authors add that, to their knowledge, the U.S. government does not restrict the use of MCI/MI or MI.
Policy implications for contact allergy
MI is still widely used in “countless products,” including shampoos, skin cleansers, dishwashing and laundry detergents, paints, and adhesives, Daniel W. Shaw, MD, associate professor of dermatology at the University of California, San Diego, told this news organization by email.
“Exact figures between the U.S. and Europe are difficult to compare due to differing patch test concentrations, but the overall trends strongly suggest that stricter and earlier regulation in Europe resulted in lower MI allergy prevalence there than in the U.S.,” added Dr. Shaw, who was not involved in the study.
Steven R. Feldman, MD, PhD, professor of dermatology at Wake Forest University in Winston-Salem, N.C., said by email that accurate information on allergic reaction prevalence is difficult to find.
“The NACDG, ESSCA, and IVDK databases may contain the best data available, but the data depend on people who get patch tested and are not directly informative of the allergy rates in the general population,” added Dr. Feldman, who was not involved in the study.
“The great majority of people in the population may not be allergic,” he said. “For those with itchy rashes, getting patch tested or avoiding products with preservatives may be prudent. Broad regulations, however, should consider the overall risks and benefits in the population, and this particular study does not fully capture those issues.”
“This study shows that government regulations are important to limit consumer exposure to common allergens, especially to the concentrations used in personal care products,” Kelly Tyler, MD, associate professor of dermatology at the Ohio State University Wexner Medical Center in Columbus, noted by email. She was not involved in the study.
She advised clinicians to ask their patients who may have allergic contact dermatitis whether they have been exposed to products containing these compounds.
“All personal care products in the store contain preservatives, and their maximum concentrations should be limited,” she advised. “The Expert Panel for Cosmetic Ingredient Safety should establish stricter guidelines for MI use in personal care products, especially given the findings of this study.”
Has MI contact allergy in North America peaked?
“In the U.S., MI has not been banned from leave-on skin-care products, but recently, its use has markedly decreased,” Dr. Shaw commented. “Hopefully, the prevalence of MI contact allergy will also begin to decrease.”
New evidence is promising. In a related study published online in Dermatology, Joel G. DeKoven, MD, MHSc, FRCPC, of the University of Toronto and his colleagues reported the NACDG 2019-2020 patch test results for MI in North America. They found that 13.8% of patients tested positive for MI.
“For the first time, MI positivity did not increase between reporting periods,” they conclude. “The epidemic of MI contact allergy in North America may have reached a plateau.”
Information regarding funding for the study was not provided. Dr. Reeder has financial relationships with the American Contact Dermatitis Society and a publishing company. Several coauthors have financial relationships with the pharmaceutical industry. Dr. Tyler, Dr. Shaw, and Dr. Feldman report no relevant financial relationship.
A version of this article first appeared on Medscape.com.