User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Black women weigh emerging risks of ‘creamy crack’ hair straighteners
Deanna Denham Hughes was stunned when she was diagnosed with ovarian cancer in 2022. She was only 32. She had no family history of cancer, and tests found no genetic link. Ms. Hughes wondered why she, an otherwise healthy Black mother of two, would develop a malignancy known as a “silent killer.”
After emergency surgery to remove the mass, along with her ovaries, uterus, fallopian tubes, and appendix, Ms. Hughes said, she saw an Instagram post in which a woman with uterine cancer linked her condition to chemical hair straighteners.
“I almost fell over,” she said from her home in Smyrna, Ga.
When Ms. Hughes was about 4, her mother began applying a chemical straightener, or relaxer, to her hair every 6-8 weeks. “It burned, and it smelled awful,” Ms. Hughes recalled. “But it was just part of our routine to ‘deal with my hair.’ ”
The routine continued until she went to college and met other Black women who wore their hair naturally. Soon, Ms. Hughes quit relaxers.
Social and economic pressures have long compelled Black girls and women to straighten their hair to conform to Eurocentric beauty standards. But chemical straighteners are stinky and costly and sometimes cause painful scalp burns. Mounting evidence now shows they could be a health hazard.
Relaxers can contain carcinogens, such as formaldehyde-releasing agents, phthalates, and other endocrine-disrupting compounds, according to National Institutes of Health studies. The compounds can mimic the body’s hormones and have been linked to breast, uterine, and ovarian cancers, studies show.
African American women’s often frequent and lifelong application of chemical relaxers to their hair and scalp might explain why hormone-related cancers kill disproportionately more Black than White women, say researchers and cancer doctors.
“What’s in these products is harmful,” said Tamarra James-Todd, PhD, an epidemiology professor at Harvard T.H. Chan School of Public Health, Boston, who has studied straightening products for the past 20 years.
She believes manufacturers, policymakers, and physicians should warn consumers that relaxers might cause cancer and other health problems.
But regulators have been slow to act, physicians have been reluctant to take up the cause, and racism continues to dictate fashion standards that make it tough for women to quit relaxers, products so addictive they’re known as “creamy crack.”
Michelle Obama straightened her hair when Barack Obama served as president because she believed Americans were “not ready” to see her in braids, the former first lady said after leaving the White House. The U.S. military still prohibited popular Black hairstyles such as dreadlocks and twists while the nation’s first Black president was in office.
California in 2019 became the first of nearly two dozen states to ban race-based hair discrimination. Last year, the U.S. House of Representatives passed similar legislation, known as the CROWN Act, for Creating a Respectful and Open World for Natural Hair. But the bill failed in the Senate.
The need for legislation underscores the challenges Black girls and women face at school and in the workplace.
“You have to pick your struggles,” said Atlanta-based surgical oncologist Ryland J. Gore, MD. She informs her breast cancer patients about the increased cancer risk from relaxers. Despite her knowledge, however, Dr. Gore continues to use chemical straighteners on her own hair, as she has since she was about 7 years old.
“Your hair tells a story,” she said.
In conversations with patients, Dr. Gore sometimes talks about how African American women once wove messages into their braids about the route to take on the Underground Railroad as they sought freedom from slavery.
“It’s just a deep discussion,” one that touches on culture, history, and research into current hairstyling practices, she said. “The data is out there. So patients should be warned, and then they can make a decision.”
The first hint of a connection between hair products and health issues surfaced in the 1990s. Doctors began seeing signs of sexual maturation in Black babies and young girls who developed breasts and pubic hair after using shampoo containing estrogen or placental extract. When the girls stopped using the shampoo, the hair and breast development receded, according to a study published in the journal Clinical Pediatrics in 1998.
Since then, Dr. James-Todd and other researchers have linked chemicals in hair products to a variety of health issues more prevalent among Black women – from early puberty to preterm birth, obesity, and diabetes.
In recent years, researchers have focused on a possible connection between ingredients in chemical relaxers and hormone-related cancers, like the one Ms. Hughes developed, which tend to be more aggressive and deadly in Black women.
A 2017 study found White women who used chemical relaxers were nearly twice as likely to develop breast cancer as those who did not use them. Because the vast majority of the Black study participants used relaxers, researchers could not effectively test the association in Black women, said lead author Adana Llanos, PhD, associate professor of epidemiology at Columbia University’s Mailman School of Public Health, New York.
Researchers did test it in 2020.
The so-called Sister Study, a landmark National Institute of Environmental Health Sciences investigation into the causes of breast cancer and related diseases, followed 50,000 U.S. women whose sisters had been diagnosed with breast cancer and who were cancer-free when they enrolled. Regardless of race, women who reported using relaxers in the prior year were 18% more likely to be diagnosed with breast cancer. Those who used relaxers at least every 5-8 weeks had a 31% higher breast cancer risk.
Nearly 75% of the Black sisters used relaxers in the prior year, compared with 3% of the non-Hispanic White sisters. Three-quarters of Black women self-reported using the straighteners as adolescents, and frequent use of chemical straighteners during adolescence raised the risk of premenopausal breast cancer, a 2021 NIH-funded study in the International Journal of Cancer found.
Another 2021 analysis of the Sister Study data showed sisters who self-reported that they frequently used relaxers or pressing products doubled their ovarian cancer risk. In 2022, another study found frequent use more than doubled uterine cancer risk.
After researchers discovered the link with uterine cancer, some called for policy changes and other measures to reduce exposure to chemical relaxers.
“It is time to intervene,” Dr. Llanos and her colleagues wrote in a Journal of the National Cancer Institute editorial accompanying the uterine cancer analysis. While acknowledging the need for more research, they issued a “call for action.”
No one can say that using permanent hair straighteners will give you cancer, Dr. Llanos said in an interview. “That’s not how cancer works,” she said, noting that some smokers never develop lung cancer, despite tobacco use being a known risk factor.
The body of research linking hair straighteners and cancer is more limited, said Dr. Llanos, who quit using chemical relaxers 15 years ago. But, she asked rhetorically, “Do we need to do the research for 50 more years to know that chemical relaxers are harmful?”
Charlotte R. Gamble, MD, a gynecological oncologist whose Washington, D.C., practice includes Black women with uterine and ovarian cancer, said she and her colleagues see the uterine cancer study findings as worthy of further exploration – but not yet worthy of discussion with patients.
“The jury’s out for me personally,” she said. “There’s so much more data that’s needed.”
Meanwhile, Dr. James-Todd and other researchers believe they have built a solid body of evidence.
“There are enough things we do know to begin taking action, developing interventions, providing useful information to clinicians and patients and the general public,” said Traci N. Bethea, PhD, assistant professor in the Office of Minority Health and Health Disparities Research at Georgetown University.
Responsibility for regulating personal-care products, including chemical hair straighteners and hair dyes – which also have been linked to hormone-related cancers – lies with the Food and Drug Administration. But the FDA does not subject personal-care products to the same approval process it uses for food and drugs. The FDA restricts only 11 categories of chemicals used in cosmetics, while concerns about health effects have prompted the European Union to restrict the use of at least 2,400 substances.
In March, Reps. Ayanna Pressley (D-Mass.) and Shontel Brown (D-Ohio) asked the FDA to investigate the potential health threat posed by chemical relaxers. An FDA representative said the agency would look into it.
Natural hairstyles are enjoying a resurgence among Black girls and women, but many continue to rely on the creamy crack, said Dede Teteh, DrPH, assistant professor of public health at Chapman University, Irvine, Calif.
She had her first straightening perm at 8 and has struggled to withdraw from relaxers as an adult, said Dr. Teteh, who now wears locs. Not long ago, she considered chemically straightening her hair for an academic job interview because she didn’t want her hair to “be a hindrance” when she appeared before White professors.
Dr. Teteh led “The Cost of Beauty,” a hair-health research project published in 2017. She and her team interviewed 91 Black women in Southern California. Some became “combative” at the idea of quitting relaxers and claimed “everything can cause cancer.”
Their reactions speak to the challenges Black women face in America, Dr. Teteh said.
“It’s not that people do not want to hear the information related to their health,” she said. “But they want people to share the information in a way that it’s really empathetic to the plight of being Black here in the United States.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
Deanna Denham Hughes was stunned when she was diagnosed with ovarian cancer in 2022. She was only 32. She had no family history of cancer, and tests found no genetic link. Ms. Hughes wondered why she, an otherwise healthy Black mother of two, would develop a malignancy known as a “silent killer.”
After emergency surgery to remove the mass, along with her ovaries, uterus, fallopian tubes, and appendix, Ms. Hughes said, she saw an Instagram post in which a woman with uterine cancer linked her condition to chemical hair straighteners.
“I almost fell over,” she said from her home in Smyrna, Ga.
When Ms. Hughes was about 4, her mother began applying a chemical straightener, or relaxer, to her hair every 6-8 weeks. “It burned, and it smelled awful,” Ms. Hughes recalled. “But it was just part of our routine to ‘deal with my hair.’ ”
The routine continued until she went to college and met other Black women who wore their hair naturally. Soon, Ms. Hughes quit relaxers.
Social and economic pressures have long compelled Black girls and women to straighten their hair to conform to Eurocentric beauty standards. But chemical straighteners are stinky and costly and sometimes cause painful scalp burns. Mounting evidence now shows they could be a health hazard.
Relaxers can contain carcinogens, such as formaldehyde-releasing agents, phthalates, and other endocrine-disrupting compounds, according to National Institutes of Health studies. The compounds can mimic the body’s hormones and have been linked to breast, uterine, and ovarian cancers, studies show.
African American women’s often frequent and lifelong application of chemical relaxers to their hair and scalp might explain why hormone-related cancers kill disproportionately more Black than White women, say researchers and cancer doctors.
“What’s in these products is harmful,” said Tamarra James-Todd, PhD, an epidemiology professor at Harvard T.H. Chan School of Public Health, Boston, who has studied straightening products for the past 20 years.
She believes manufacturers, policymakers, and physicians should warn consumers that relaxers might cause cancer and other health problems.
But regulators have been slow to act, physicians have been reluctant to take up the cause, and racism continues to dictate fashion standards that make it tough for women to quit relaxers, products so addictive they’re known as “creamy crack.”
Michelle Obama straightened her hair when Barack Obama served as president because she believed Americans were “not ready” to see her in braids, the former first lady said after leaving the White House. The U.S. military still prohibited popular Black hairstyles such as dreadlocks and twists while the nation’s first Black president was in office.
California in 2019 became the first of nearly two dozen states to ban race-based hair discrimination. Last year, the U.S. House of Representatives passed similar legislation, known as the CROWN Act, for Creating a Respectful and Open World for Natural Hair. But the bill failed in the Senate.
The need for legislation underscores the challenges Black girls and women face at school and in the workplace.
“You have to pick your struggles,” said Atlanta-based surgical oncologist Ryland J. Gore, MD. She informs her breast cancer patients about the increased cancer risk from relaxers. Despite her knowledge, however, Dr. Gore continues to use chemical straighteners on her own hair, as she has since she was about 7 years old.
“Your hair tells a story,” she said.
In conversations with patients, Dr. Gore sometimes talks about how African American women once wove messages into their braids about the route to take on the Underground Railroad as they sought freedom from slavery.
“It’s just a deep discussion,” one that touches on culture, history, and research into current hairstyling practices, she said. “The data is out there. So patients should be warned, and then they can make a decision.”
The first hint of a connection between hair products and health issues surfaced in the 1990s. Doctors began seeing signs of sexual maturation in Black babies and young girls who developed breasts and pubic hair after using shampoo containing estrogen or placental extract. When the girls stopped using the shampoo, the hair and breast development receded, according to a study published in the journal Clinical Pediatrics in 1998.
Since then, Dr. James-Todd and other researchers have linked chemicals in hair products to a variety of health issues more prevalent among Black women – from early puberty to preterm birth, obesity, and diabetes.
In recent years, researchers have focused on a possible connection between ingredients in chemical relaxers and hormone-related cancers, like the one Ms. Hughes developed, which tend to be more aggressive and deadly in Black women.
A 2017 study found White women who used chemical relaxers were nearly twice as likely to develop breast cancer as those who did not use them. Because the vast majority of the Black study participants used relaxers, researchers could not effectively test the association in Black women, said lead author Adana Llanos, PhD, associate professor of epidemiology at Columbia University’s Mailman School of Public Health, New York.
Researchers did test it in 2020.
The so-called Sister Study, a landmark National Institute of Environmental Health Sciences investigation into the causes of breast cancer and related diseases, followed 50,000 U.S. women whose sisters had been diagnosed with breast cancer and who were cancer-free when they enrolled. Regardless of race, women who reported using relaxers in the prior year were 18% more likely to be diagnosed with breast cancer. Those who used relaxers at least every 5-8 weeks had a 31% higher breast cancer risk.
Nearly 75% of the Black sisters used relaxers in the prior year, compared with 3% of the non-Hispanic White sisters. Three-quarters of Black women self-reported using the straighteners as adolescents, and frequent use of chemical straighteners during adolescence raised the risk of premenopausal breast cancer, a 2021 NIH-funded study in the International Journal of Cancer found.
Another 2021 analysis of the Sister Study data showed sisters who self-reported that they frequently used relaxers or pressing products doubled their ovarian cancer risk. In 2022, another study found frequent use more than doubled uterine cancer risk.
After researchers discovered the link with uterine cancer, some called for policy changes and other measures to reduce exposure to chemical relaxers.
“It is time to intervene,” Dr. Llanos and her colleagues wrote in a Journal of the National Cancer Institute editorial accompanying the uterine cancer analysis. While acknowledging the need for more research, they issued a “call for action.”
No one can say that using permanent hair straighteners will give you cancer, Dr. Llanos said in an interview. “That’s not how cancer works,” she said, noting that some smokers never develop lung cancer, despite tobacco use being a known risk factor.
The body of research linking hair straighteners and cancer is more limited, said Dr. Llanos, who quit using chemical relaxers 15 years ago. But, she asked rhetorically, “Do we need to do the research for 50 more years to know that chemical relaxers are harmful?”
Charlotte R. Gamble, MD, a gynecological oncologist whose Washington, D.C., practice includes Black women with uterine and ovarian cancer, said she and her colleagues see the uterine cancer study findings as worthy of further exploration – but not yet worthy of discussion with patients.
“The jury’s out for me personally,” she said. “There’s so much more data that’s needed.”
Meanwhile, Dr. James-Todd and other researchers believe they have built a solid body of evidence.
“There are enough things we do know to begin taking action, developing interventions, providing useful information to clinicians and patients and the general public,” said Traci N. Bethea, PhD, assistant professor in the Office of Minority Health and Health Disparities Research at Georgetown University.
Responsibility for regulating personal-care products, including chemical hair straighteners and hair dyes – which also have been linked to hormone-related cancers – lies with the Food and Drug Administration. But the FDA does not subject personal-care products to the same approval process it uses for food and drugs. The FDA restricts only 11 categories of chemicals used in cosmetics, while concerns about health effects have prompted the European Union to restrict the use of at least 2,400 substances.
In March, Reps. Ayanna Pressley (D-Mass.) and Shontel Brown (D-Ohio) asked the FDA to investigate the potential health threat posed by chemical relaxers. An FDA representative said the agency would look into it.
Natural hairstyles are enjoying a resurgence among Black girls and women, but many continue to rely on the creamy crack, said Dede Teteh, DrPH, assistant professor of public health at Chapman University, Irvine, Calif.
She had her first straightening perm at 8 and has struggled to withdraw from relaxers as an adult, said Dr. Teteh, who now wears locs. Not long ago, she considered chemically straightening her hair for an academic job interview because she didn’t want her hair to “be a hindrance” when she appeared before White professors.
Dr. Teteh led “The Cost of Beauty,” a hair-health research project published in 2017. She and her team interviewed 91 Black women in Southern California. Some became “combative” at the idea of quitting relaxers and claimed “everything can cause cancer.”
Their reactions speak to the challenges Black women face in America, Dr. Teteh said.
“It’s not that people do not want to hear the information related to their health,” she said. “But they want people to share the information in a way that it’s really empathetic to the plight of being Black here in the United States.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
Deanna Denham Hughes was stunned when she was diagnosed with ovarian cancer in 2022. She was only 32. She had no family history of cancer, and tests found no genetic link. Ms. Hughes wondered why she, an otherwise healthy Black mother of two, would develop a malignancy known as a “silent killer.”
After emergency surgery to remove the mass, along with her ovaries, uterus, fallopian tubes, and appendix, Ms. Hughes said, she saw an Instagram post in which a woman with uterine cancer linked her condition to chemical hair straighteners.
“I almost fell over,” she said from her home in Smyrna, Ga.
When Ms. Hughes was about 4, her mother began applying a chemical straightener, or relaxer, to her hair every 6-8 weeks. “It burned, and it smelled awful,” Ms. Hughes recalled. “But it was just part of our routine to ‘deal with my hair.’ ”
The routine continued until she went to college and met other Black women who wore their hair naturally. Soon, Ms. Hughes quit relaxers.
Social and economic pressures have long compelled Black girls and women to straighten their hair to conform to Eurocentric beauty standards. But chemical straighteners are stinky and costly and sometimes cause painful scalp burns. Mounting evidence now shows they could be a health hazard.
Relaxers can contain carcinogens, such as formaldehyde-releasing agents, phthalates, and other endocrine-disrupting compounds, according to National Institutes of Health studies. The compounds can mimic the body’s hormones and have been linked to breast, uterine, and ovarian cancers, studies show.
African American women’s often frequent and lifelong application of chemical relaxers to their hair and scalp might explain why hormone-related cancers kill disproportionately more Black than White women, say researchers and cancer doctors.
“What’s in these products is harmful,” said Tamarra James-Todd, PhD, an epidemiology professor at Harvard T.H. Chan School of Public Health, Boston, who has studied straightening products for the past 20 years.
She believes manufacturers, policymakers, and physicians should warn consumers that relaxers might cause cancer and other health problems.
But regulators have been slow to act, physicians have been reluctant to take up the cause, and racism continues to dictate fashion standards that make it tough for women to quit relaxers, products so addictive they’re known as “creamy crack.”
Michelle Obama straightened her hair when Barack Obama served as president because she believed Americans were “not ready” to see her in braids, the former first lady said after leaving the White House. The U.S. military still prohibited popular Black hairstyles such as dreadlocks and twists while the nation’s first Black president was in office.
California in 2019 became the first of nearly two dozen states to ban race-based hair discrimination. Last year, the U.S. House of Representatives passed similar legislation, known as the CROWN Act, for Creating a Respectful and Open World for Natural Hair. But the bill failed in the Senate.
The need for legislation underscores the challenges Black girls and women face at school and in the workplace.
“You have to pick your struggles,” said Atlanta-based surgical oncologist Ryland J. Gore, MD. She informs her breast cancer patients about the increased cancer risk from relaxers. Despite her knowledge, however, Dr. Gore continues to use chemical straighteners on her own hair, as she has since she was about 7 years old.
“Your hair tells a story,” she said.
In conversations with patients, Dr. Gore sometimes talks about how African American women once wove messages into their braids about the route to take on the Underground Railroad as they sought freedom from slavery.
“It’s just a deep discussion,” one that touches on culture, history, and research into current hairstyling practices, she said. “The data is out there. So patients should be warned, and then they can make a decision.”
The first hint of a connection between hair products and health issues surfaced in the 1990s. Doctors began seeing signs of sexual maturation in Black babies and young girls who developed breasts and pubic hair after using shampoo containing estrogen or placental extract. When the girls stopped using the shampoo, the hair and breast development receded, according to a study published in the journal Clinical Pediatrics in 1998.
Since then, Dr. James-Todd and other researchers have linked chemicals in hair products to a variety of health issues more prevalent among Black women – from early puberty to preterm birth, obesity, and diabetes.
In recent years, researchers have focused on a possible connection between ingredients in chemical relaxers and hormone-related cancers, like the one Ms. Hughes developed, which tend to be more aggressive and deadly in Black women.
A 2017 study found White women who used chemical relaxers were nearly twice as likely to develop breast cancer as those who did not use them. Because the vast majority of the Black study participants used relaxers, researchers could not effectively test the association in Black women, said lead author Adana Llanos, PhD, associate professor of epidemiology at Columbia University’s Mailman School of Public Health, New York.
Researchers did test it in 2020.
The so-called Sister Study, a landmark National Institute of Environmental Health Sciences investigation into the causes of breast cancer and related diseases, followed 50,000 U.S. women whose sisters had been diagnosed with breast cancer and who were cancer-free when they enrolled. Regardless of race, women who reported using relaxers in the prior year were 18% more likely to be diagnosed with breast cancer. Those who used relaxers at least every 5-8 weeks had a 31% higher breast cancer risk.
Nearly 75% of the Black sisters used relaxers in the prior year, compared with 3% of the non-Hispanic White sisters. Three-quarters of Black women self-reported using the straighteners as adolescents, and frequent use of chemical straighteners during adolescence raised the risk of premenopausal breast cancer, a 2021 NIH-funded study in the International Journal of Cancer found.
Another 2021 analysis of the Sister Study data showed sisters who self-reported that they frequently used relaxers or pressing products doubled their ovarian cancer risk. In 2022, another study found frequent use more than doubled uterine cancer risk.
After researchers discovered the link with uterine cancer, some called for policy changes and other measures to reduce exposure to chemical relaxers.
“It is time to intervene,” Dr. Llanos and her colleagues wrote in a Journal of the National Cancer Institute editorial accompanying the uterine cancer analysis. While acknowledging the need for more research, they issued a “call for action.”
No one can say that using permanent hair straighteners will give you cancer, Dr. Llanos said in an interview. “That’s not how cancer works,” she said, noting that some smokers never develop lung cancer, despite tobacco use being a known risk factor.
The body of research linking hair straighteners and cancer is more limited, said Dr. Llanos, who quit using chemical relaxers 15 years ago. But, she asked rhetorically, “Do we need to do the research for 50 more years to know that chemical relaxers are harmful?”
Charlotte R. Gamble, MD, a gynecological oncologist whose Washington, D.C., practice includes Black women with uterine and ovarian cancer, said she and her colleagues see the uterine cancer study findings as worthy of further exploration – but not yet worthy of discussion with patients.
“The jury’s out for me personally,” she said. “There’s so much more data that’s needed.”
Meanwhile, Dr. James-Todd and other researchers believe they have built a solid body of evidence.
“There are enough things we do know to begin taking action, developing interventions, providing useful information to clinicians and patients and the general public,” said Traci N. Bethea, PhD, assistant professor in the Office of Minority Health and Health Disparities Research at Georgetown University.
Responsibility for regulating personal-care products, including chemical hair straighteners and hair dyes – which also have been linked to hormone-related cancers – lies with the Food and Drug Administration. But the FDA does not subject personal-care products to the same approval process it uses for food and drugs. The FDA restricts only 11 categories of chemicals used in cosmetics, while concerns about health effects have prompted the European Union to restrict the use of at least 2,400 substances.
In March, Reps. Ayanna Pressley (D-Mass.) and Shontel Brown (D-Ohio) asked the FDA to investigate the potential health threat posed by chemical relaxers. An FDA representative said the agency would look into it.
Natural hairstyles are enjoying a resurgence among Black girls and women, but many continue to rely on the creamy crack, said Dede Teteh, DrPH, assistant professor of public health at Chapman University, Irvine, Calif.
She had her first straightening perm at 8 and has struggled to withdraw from relaxers as an adult, said Dr. Teteh, who now wears locs. Not long ago, she considered chemically straightening her hair for an academic job interview because she didn’t want her hair to “be a hindrance” when she appeared before White professors.
Dr. Teteh led “The Cost of Beauty,” a hair-health research project published in 2017. She and her team interviewed 91 Black women in Southern California. Some became “combative” at the idea of quitting relaxers and claimed “everything can cause cancer.”
Their reactions speak to the challenges Black women face in America, Dr. Teteh said.
“It’s not that people do not want to hear the information related to their health,” she said. “But they want people to share the information in a way that it’s really empathetic to the plight of being Black here in the United States.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
FDA approves first pill for postpartum depression
a condition that affects an estimated one in seven mothers in the United States.
The pill, zuranolone (Zurzuvae), is a neuroactive steroid that acts on GABAA receptors in the brain responsible for regulating mood, arousal, behavior, and cognition, according to Biogen, which, along with Sage Therapeutics, developed the product. The recommended dose for Zurzuvae is 50 mg taken once daily for 14 days, in the evening with a fatty meal, according to the FDA.
Postpartum depression often goes undiagnosed and untreated. Many mothers are hesitant to reveal their symptoms to family and clinicians, fearing they’ll be judged on their parenting. A 2017 study found that suicide accounted for roughly 5% of perinatal deaths among women in Canada, with most of those deaths occurring in the first 3 months in the year after giving birth.
“Postpartum depression is a serious and potentially life-threatening condition in which women experience sadness, guilt, worthlessness – even, in severe cases, thoughts of harming themselves or their child. And, because postpartum depression can disrupt the maternal-infant bond, it can also have consequences for the child’s physical and emotional development,” Tiffany R. Farchione, MD, director of the division of psychiatry at the FDA’s Center for Drug Evaluation and Research, said in a statement about the approval. “Having access to an oral medication will be a beneficial option for many of these women coping with extreme, and sometimes life-threatening, feelings.”
The other approved therapy for postpartum depression is the intravenous agent brexanolone (Zulresso; Sage). But the product requires prolonged infusions in hospital settings and costs $34,000.
FDA approval of Zurzuvae was based in part on data reported in a 2023 study in the American Journal of Psychiatry, which showed that the drug led to significantly greater improvement in depressive symptoms at 15 days compared with the placebo group. Improvements were observed on day 3, the earliest assessment, and were sustained at all subsequent visits during the treatment and follow-up period (through day 42).
Patients with anxiety who received the active drug experienced improvement in related symptoms compared with the patients who received a placebo.
The most common adverse events reported in the trial were somnolence and headaches. Weight gain, sexual dysfunction, withdrawal symptoms, and increased suicidal ideation or behavior were not observed.
The packaging for Zurzuvae will include a boxed warning noting that the drug can affect a user’s ability to drive and perform other potentially hazardous activities, possibly without their knowledge of the impairment, the FDA said. As a result, people who use Zurzuvae should not drive or operate heavy machinery for at least 12 hours after taking the pill.
A version of this article first appeared on Medscape.com.
a condition that affects an estimated one in seven mothers in the United States.
The pill, zuranolone (Zurzuvae), is a neuroactive steroid that acts on GABAA receptors in the brain responsible for regulating mood, arousal, behavior, and cognition, according to Biogen, which, along with Sage Therapeutics, developed the product. The recommended dose for Zurzuvae is 50 mg taken once daily for 14 days, in the evening with a fatty meal, according to the FDA.
Postpartum depression often goes undiagnosed and untreated. Many mothers are hesitant to reveal their symptoms to family and clinicians, fearing they’ll be judged on their parenting. A 2017 study found that suicide accounted for roughly 5% of perinatal deaths among women in Canada, with most of those deaths occurring in the first 3 months in the year after giving birth.
“Postpartum depression is a serious and potentially life-threatening condition in which women experience sadness, guilt, worthlessness – even, in severe cases, thoughts of harming themselves or their child. And, because postpartum depression can disrupt the maternal-infant bond, it can also have consequences for the child’s physical and emotional development,” Tiffany R. Farchione, MD, director of the division of psychiatry at the FDA’s Center for Drug Evaluation and Research, said in a statement about the approval. “Having access to an oral medication will be a beneficial option for many of these women coping with extreme, and sometimes life-threatening, feelings.”
The other approved therapy for postpartum depression is the intravenous agent brexanolone (Zulresso; Sage). But the product requires prolonged infusions in hospital settings and costs $34,000.
FDA approval of Zurzuvae was based in part on data reported in a 2023 study in the American Journal of Psychiatry, which showed that the drug led to significantly greater improvement in depressive symptoms at 15 days compared with the placebo group. Improvements were observed on day 3, the earliest assessment, and were sustained at all subsequent visits during the treatment and follow-up period (through day 42).
Patients with anxiety who received the active drug experienced improvement in related symptoms compared with the patients who received a placebo.
The most common adverse events reported in the trial were somnolence and headaches. Weight gain, sexual dysfunction, withdrawal symptoms, and increased suicidal ideation or behavior were not observed.
The packaging for Zurzuvae will include a boxed warning noting that the drug can affect a user’s ability to drive and perform other potentially hazardous activities, possibly without their knowledge of the impairment, the FDA said. As a result, people who use Zurzuvae should not drive or operate heavy machinery for at least 12 hours after taking the pill.
A version of this article first appeared on Medscape.com.
a condition that affects an estimated one in seven mothers in the United States.
The pill, zuranolone (Zurzuvae), is a neuroactive steroid that acts on GABAA receptors in the brain responsible for regulating mood, arousal, behavior, and cognition, according to Biogen, which, along with Sage Therapeutics, developed the product. The recommended dose for Zurzuvae is 50 mg taken once daily for 14 days, in the evening with a fatty meal, according to the FDA.
Postpartum depression often goes undiagnosed and untreated. Many mothers are hesitant to reveal their symptoms to family and clinicians, fearing they’ll be judged on their parenting. A 2017 study found that suicide accounted for roughly 5% of perinatal deaths among women in Canada, with most of those deaths occurring in the first 3 months in the year after giving birth.
“Postpartum depression is a serious and potentially life-threatening condition in which women experience sadness, guilt, worthlessness – even, in severe cases, thoughts of harming themselves or their child. And, because postpartum depression can disrupt the maternal-infant bond, it can also have consequences for the child’s physical and emotional development,” Tiffany R. Farchione, MD, director of the division of psychiatry at the FDA’s Center for Drug Evaluation and Research, said in a statement about the approval. “Having access to an oral medication will be a beneficial option for many of these women coping with extreme, and sometimes life-threatening, feelings.”
The other approved therapy for postpartum depression is the intravenous agent brexanolone (Zulresso; Sage). But the product requires prolonged infusions in hospital settings and costs $34,000.
FDA approval of Zurzuvae was based in part on data reported in a 2023 study in the American Journal of Psychiatry, which showed that the drug led to significantly greater improvement in depressive symptoms at 15 days compared with the placebo group. Improvements were observed on day 3, the earliest assessment, and were sustained at all subsequent visits during the treatment and follow-up period (through day 42).
Patients with anxiety who received the active drug experienced improvement in related symptoms compared with the patients who received a placebo.
The most common adverse events reported in the trial were somnolence and headaches. Weight gain, sexual dysfunction, withdrawal symptoms, and increased suicidal ideation or behavior were not observed.
The packaging for Zurzuvae will include a boxed warning noting that the drug can affect a user’s ability to drive and perform other potentially hazardous activities, possibly without their knowledge of the impairment, the FDA said. As a result, people who use Zurzuvae should not drive or operate heavy machinery for at least 12 hours after taking the pill.
A version of this article first appeared on Medscape.com.
Trends in prepregnancy diabetes rates in the United States, 2016 -2021
Managing clinician burnout: Challenges and opportunities
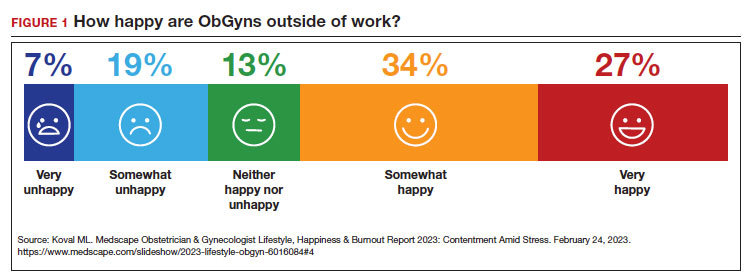
Physicians have some of the highest rates of burnout among all professions.1 Complicating matters is that clinicians (including residents)2 may avoid seeking treatment out of fear it will affect their license or privileges.3 In this article, we consider burnout in greater detail, as well as ways of successfully addressing the level of burnout in the profession (FIGURE 1), including steps individual practitioners, health care entities, and regulators should consider to reduce burnout and its harmful effects.
How burnout becomes a problem
Six general factors are commonly identified as leading to clinician career dissatisfaction and burnout:4
1. work overload
2. lack of autonomy and control
3. inadequate rewards, financial and otherwise
4. work-home schedules
5. perception of lack of fairness
6. values conflict between the clinician and employer (including a breakdown of professional community).
At the top of the list of causes of burnout is often “administrative and bureaucratic headaches.”5 More specifically, electronic health records (EHRs), including computerized order entry, is commonly cited as a major cause of burnout.6,7 According to some studies, clinicians spend as much as 49% of working time doing clerical work,8 and studies found the extension of work into home life.9
Increased measurement of performance metrics in health care services are a significant contributor to physician burnout.10 These include pressure to see more patients, perform more procedures, and respond quickly to patient requests (eg, through email).7 As we will see, medical malpractice cases, or the risk of such cases, have also played a role in burnout in some medical specialties.11 The pandemic also contributed, at least temporarily, to burnout.12,13
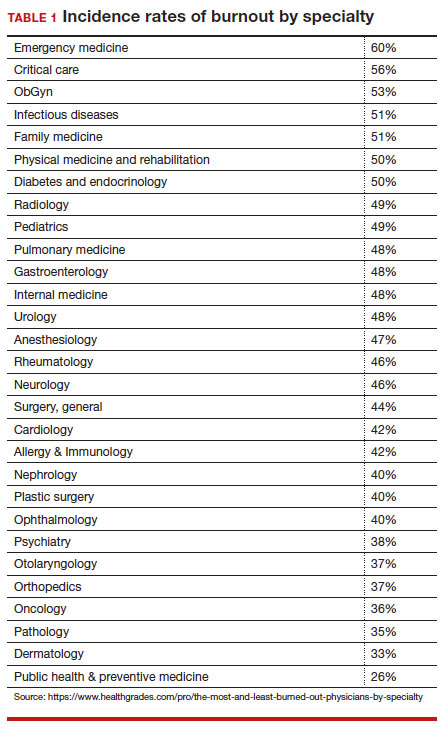
Rates of burnout among physicians are notably higher than among the general population14 or other professions.6 Although physicians have generally entered clinical practice with lower rates of burnout than the general population,15 The American College of Obstetricians and Gynecologists (ACOG) reports that 40% to 75% of ObGyns “experience some form of professional burnout.”16,17 Other source(s) cite that 53% of ObGyns report burnout (TABLE 1).
Code QD85
Burnout is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by 3 dimensions:
- feelings of energy depletion or exhaustion
- increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job
- a sense of ineffectiveness and lack of accomplishment. Burn-out refers specifically to phenomena in the occupational context and should not be applied to describe experiences in other areas of life. Exclusions to burnout diagnosis include adjustment disorder, disorders specifically associated with stress, anxiety or fear-related disorders, and mood disorders.
Reference
1. International Classification of Diseases Eleventh Revision (ICD-11). Geneva, Switzerland: World Health Organization; 2022.
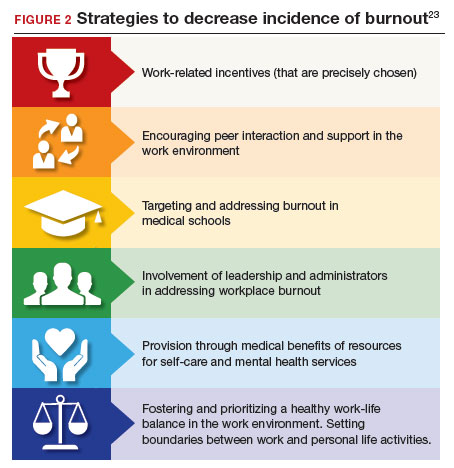
Burnout undoubtedly contributes to professionals leaving practice, leading to a significant shortage of ObGyns.18 It also raises several significant legal concerns. Despite the enormity and seriousness of the problem, there is considerable optimism and assurance that the epidemic of burnout is solvable on the individual, specialty, and profession-wide levels. ACOG and other organizations have made suggestions for physicians, the profession, and to health care institutions for reducing burnout.19 This is not to say that solutions are simple or easy for individual professionals or institutions, but they are within the reach of the profession (FIGURE 2).
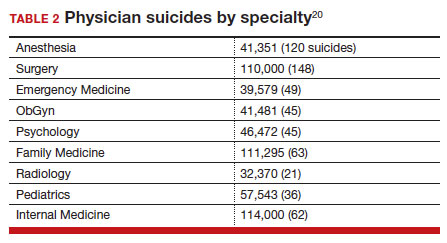
Suicide among health care professionals is one other concern (TABLE 2)20 and theoretically can stem from burnout, depression, and other psychosocial concerns.
Costs of clinician burnout
Burnout is endemic among health care providers, with numerous studies detailing the professional, emotional, and financial costs. Prior to the pandemic, one analysis of nationwide fiscal costs associated with burnout estimated an annual cost of $4.6B due to physician turnover and reduced clinical hours.21 The COVID-19 epidemic has by all accounts worsened rates of health care worker burnout, particularly for those in high patient-contact positions.22
Female clinicians appear to be differentially affected; in one recent study women reported symptoms of burnout at twice the rate of their male counterparts.23 Whether burnout rates will return to pre-pandemic levels remains an open question, but since burnout is frequently related to one’s own assessment of work-life balance, it is possible that a longer term shift in burnout rates associated with post-pandemic occupational attitudes will be observed.
Combining factors contribute to burnout
Burnout is a universal occupational hazard, but extant data suggest that physicians and other health care providers may be at higher risk. Among physicians, younger age, female gender, and front-line specialty status appear associated with higher burnout rates.24 Given that ObGyn physicians are overwhelmingly female (60% of physicians and 86% of residents),25,26 gender-related burnout factors exist alongside other specific occupational burnout risks. While gender parity has been achieved among health care providers, gender disparities persist in terms of those in leadership positions, compensation, and other factors.22
The smattering of evidence suggesting that ObGyns have higher rates of burnout than many other specialties is understandable given the unique legal challenges confronting ObGyn practice. This may be of special significance because ObGyn malpractice insurance rates are among the highest of all specialties.27 The overall shortage of ObGyns has been exacerbated by the demonstrated negative effects on training and workforce representation stemming from recent legislation that has the effect of criminalizing certain aspects of ObGyn practice;28 for instance, uncertainty regarding abortion regulations.
These negative effects are particularly heightened in states in which the law is in flux or where there are continuing efforts to substantially limit access to abortion. The efforts to increase civil and even criminal penalties related to abortion care challenge ObGyns’ professional practices, as legal rules are frequently changing. In some states, ObGyns may face additional workloads secondary to a flight of ObGyns from restrictive jurisdictions in addition to legal and professional repercussions. In a small study of 19 genetic counselors dealing with restrictive legislation in the state of Ohio,29 increased stress and burnout rates were identified as a consequence of practice uncertainties under this legislation. It is certain that other professionals working in reproductive health care are similarly affected.30
The programs provide individual resources to providers in distress, periodically survey initiatives at Stanford to assess burnout at the organizational level, and provide input designed to spur organizational change to reduce the burden of burnout. Ways that they build community and connections include:
- Live Story Rounds events (as told by Stanford Medicine physicians)
- Commensality Groups (facilitated small discussion groups built around tested evidence)
- Aim to increase sense of connection and collegiality among physicians and build comradery at work
- CME-accredited physician wellness forum, including annual doctor’s day events
Continue to: Assessment of burnout...
Assessment of burnout
Numerous scales for the assessment of burnout exist. Of these, the 22-item Maslach Burnout Inventory (MBI) is the best studied. The MBI is a well-investigated tool for assessing burnout. The MBI consists of 3 major subscales measuring overall burnout, emotional exhaustion, depersonalization, and low personal accomplishment. It exists in numerous forms. For instance, the MBI-HSS (MP), adapted for medical personnel, is available. However, the most commonly used form for assessing burnout in clinicians is the MBI-HHS (Human Services Survey); approximately 85% of all burnout studies examined in a recent meta-analysis used this survey version.31 As those authors commented, while burnout is a recognized phenomenon, a great deal of variability in study design, interpretation of subscale scores, and sample selection makes generalizations regarding burnout difficult to assess.
The MBI in various forms has been extensively used over the past 40 years to assess burnout amongst physicians and physicians in training. While not the only instrument designed to measure such factors, it is by far the most prevalent. Williamson and colleagues32 compared the MBI with several other measures of quality of life and found good correlation between the various instruments used, a finding replicated by other studies.33 Brady and colleagues compared item responses to the Stanford Professional Fulfillment Index and the Min-Z Single-item Burnout scale (a 1-item screening measure) to MBI’s Emotional Exhaustion and Depersonalization subscales. Basing their findings on a survey of more than 1,300 physicians, they found that all analyzed scales were significantly correlated with such adverse outcomes as depression, distress, or intent to leave the profession.
It is important to note that most surveys of clinician burnout were conducted prior to the pandemic. While the psychometric analyses of the MBI and other scales are likely still germane, observed rates of clinician burnout have likely increased. Thus, comparisons of pre- and post-pandemic studies should factor in an increase in the incidence and prevalence of burnout.
Management strategies
In general, there are several interventions for managing burnout34:
- individual-focused (including self-care and communications-skills workshops)
- mindfulness training
- yoga
- meditation
- organizational/structural (workload reduction, schedule realignment, teamwork training, and group-delivered stress management interventions)
- combination(s) of the above.
There is little evidence to suggest that any particular individual intervention (whether delivered in individual or group-based formats) is superior to any other in treating clinician burnout. A recent analysis of 24 studies employing mindfulness-based interventions demonstrated generally positive results for such interventions.35 Other studies have also found general support for mindfulness-based interventions, although mindfulness is often integrated with other stress-reduction techniques, such as meditation, yoga, and communication skills. Such interventions are nonspecific but generally effective.
An accumulation of evidence to date suggests that a combination of individual and organizational interventions is most effective in combatting clinician burnout. No individual intervention can be successful without addressing root causes, such as overscheduling, lack of organizational support, and the effect of restrictive legislation on practice.
Several large teaching hospitals have established programs to address physician and health care provider burnout. Notable among these is the Stanford University School of Medicine’s WellMD and WellPhD programs (https://wellmd.stanford.edu/about.html). These programs were described by Olson and colleagues36 as using a model focused on practice efficiency, organizational culture, and personal resilience to enhance physicians’ well-being. (See “Aspects of the WellMD and WellPhD programs from Stanford University.”)
A growing number of institutions have established burnout programs to support physicians experiencing work/life imbalances and other aspects of burnout.37 In general, these share common features of assessment, individual and/or group intervention, and organizational change. Fear of repercussion may be one factor preventing physicians from seeking individual treatment for burnout.38 Importantly, they emphasize the need for professional confidentiality when offering treatment to patients within organizational settings. Those authors also reported that a focus on organizational engagement may be an important factor in addressing burnout in female physicians, as they tend to report lower levels of organizational engagement.
Continue to: Legal considerations...
Legal considerations
Until recently, physician burnout “received little notice in the legal literature.”39 Although there have been burnout legal consequences in the past, the legal issues are now becoming more visible.40
Medical malpractice
A well-documented consequence of burnout is an increase in errors.14 Medical errors, of course, are at the heart of malpractice claims. Technically, malpractice is medical or professional negligence. It is the breach of a duty owed by the physician, or other provider, or organization (defendant) to the patient, which causes injury to the plaintiff/patient.41
“Medical error” is generally a meaningful deviation from the “standard of care” or accepted medical practice.42 Many medical errors do not cause injury to the patient; in those cases, the negligence does not result in liability. In instances in which the negligence causes harm, the clinician and health care facility may be subject to liability for that injury. Fortunately, however, for a variety of reasons, most harmful medical errors do not result in a medical malpractice claim or lawsuit. The absence of a good clinician-patient relationship is likely associated with an increased inclination of a patient to file a malpractice action.43Clinician burnout may, therefore, contribute to increased malpractice claims in two ways. First, burnout likely leads to increased medical errors, perhaps because burnout is associated with lower concentration, inattention, reduced cognitive vigilance, and fatigue.8,44 It may also lead to less time with patients, reduced patient empathy, and lower patient rapport, which may make injured patients more likely to file a claim or lawsuit.45 Because the relationshipbetween burnout and medical error is bidirectional, malpractice claims tend to increase burnout, which increases error. Given the time it takes to resolve most malpractice claims, the uncertainty of medical malpractice may be especially stressful for health care providers.46,47
Burnout is not a mitigating factor in malpractice. Our sympathies may go out to a professional suffering from burnout, but it does not excuse or reduce liability—it may, indeed, be an aggravating factor. Clinicians who can diagnose burnout and know its negative consequences but fail to deal with their own burnout may be demonstrating negligence if there has been harm to a patient related to the burnout.48
Institutional or corporate liability to patients
Health care institutions have obligations to avoid injury to patients. Just as poorly maintained medical equipment may harm patients, so may burned-out professionals. Therefore, institutions have some obligation to supervise and avoid the increased risks to patients posed by professionals suffering from burnout.
Respondeat superior and institutional negligence. Institutional liability may arise in two ways, the first through agency, or respondeat superior. That is, if the physician or other professional is an employee (or similar agent) of the health care institution, that institution is generally responsible for the physician’s negligence during the employment.49 Even if the physician is not an employee (for example, an independent contractor providing care or using the hospital facilities), the health care facility may be liable for the physician’s negligence.50 Liability may occur, for example, if the health care facility was aware that the physician was engaged in careless practice or was otherwise a risk to patients but the facility did not take steps to avoid those risks.51 The basis for liability is that the health care organization owes a duty to patients to take reasonable care to ensure that its facilities are not used to injure patients negligently.52 Just as it must take care that unqualified physicians are not granted privileges to practice, it also must take reasonable steps to protect patients when it is aware (through nurses or other agents) of a physician’s negligent practice.
In one case, for example, the court found liability where a staff member had “severe” burnout in a physician’s office and failed to read fetal monitoring strips. The physician was found negligent for relying on the staff member who was obviously making errors in interpretation of fetal distress.53
Continue to: Legal obligations of health care organizations to physicians and others...
Legal obligations of health care organizations to physicians and others
In addition to obligations to patients, health care organizations may have obligations to employees (and others) at risk for injury. For example, assume a patient is diagnosed with a highly contagious disease. The health care organization would be obligated to warn, and take reasonable steps to protect, the staff (employees and independent contractors) from being harmed from exposure to the disease. This principle may apply to coworkers of employees with significant burnout, thereby presenting a danger in the workplace. The liability issue is more difficult for employees experiencing job-related burnout themselves. Organizations generally compensate injured employees through no-fault workers’ compensation (an insurance-like system); for independent contractors, the liability is usually through a tort claim (negligence).54
In modern times, a focus has been on preventing those injuries, not just providing compensation after injuries have occurred. Notably, federal and state occupational health and safety laws (particularly the Occupational Safety and Health Administration [OSHA]) require most organizations (including those employing health care providers) to take steps to mitigate various kinds of worker injuries.55
Although these worker protections have commonly been applied to hospitals and other health care providers, burnout has not traditionally been a significant concern in federal or state OSHA enforcement. For example, no formal federal OSHA regulations govern work-related burnout. Regulators, including OSHA, are increasingly interested in burnout that may affect many employees. OSHA has several recommendations for reducing health care work burnout.56 The Surgeon General has expressed similar concerns.57 The federal government recently allocated $103 million from the American Rescue Plan to address burnout among health care workers.58 Also, OSHA appears to be increasing its oversight of healthcare-institution-worker injuries.55
Is burnout a “disability”?
The federal Americans with Disabilities Act (ADA) and similar state laws prohibit discrimination based on disability.59 A disability is defined as a “physical or mental impairment that substantially limits one or more major life activities” or “perceived as having such an impairment.”60 The initial issue is whether burnout is a “mental impairment.” As noted earlier, it is not officially a “medical condition.”61 To date, the United Nations has classified it as an “occupational phenomenon.”62 It may, therefore, not qualify under the ADA, even if it “interferes with a major life activity.” There is, however, some movement toward defining burnout as a mental condition. Even if defined as a disability, there would still be legal issues of how severe it must be to qualify as a disability and the proper accommodation. Apart from the legal definition of an ADA disability, as a practical matter it likely is in the best interest of health care facilities to provide accommodations that reduce burnout. A number of strategies to decrease the incidence of burnout include the role of health care systems (FIGURE 2).
In conclusion we look at several things that can be done to “treat” or reduce burnout. That effort requires the cooperation of physicians and other providers, health care facilities, training programs, licensing authorities, and professional organizations. See suggestions below.
Conclusion
There are many excellent suggestions for reducing burnout and improving patient care and practitioner satisfaction.63-65 We conclude with a summary of some of these suggestions for individual practitioners, health care organizations, the profession, and licensing. It is worth remembering, however, that it will require the efforts of each area to reduce burnout substantially.
For practitioners:
- Engage in quality coaching/therapy on mindfulness and stress management.
- Practice self-care, including exercise and relaxation techniques.
- Make work-life balance a priority.
- Take opportunities for collegial social and professional discussions.
- Prioritize (and periodically assess) your own professional satisfaction and burnout risk.
- Smile—enjoy a sense of humor (endorphins and cortisol).
For health care organizations:
- Urgently work with vendors and regulators to revise electronic health records to reduce their substantial impact on burnout.
- Reduce physicians’ time on clerical and administrative tasks (eg, by enhancing the use of quality AI, scribes, and automated notes from appointments. (This may increase the time they spend with patients.) Eliminate “pajama-time” charting.
- Provide various kinds of confidential professional counseling, therapy, and support related to burnout prevention and treatment, and avoid any penalty or stigma related to their use.
- Provide reasonable flexibility in scheduling.
- Routinely provide employees with information about burnout prevention and services.
- Appoint a wellness officer with authority to ensure the organization maximizes its prevention and treatment services.
- Constantly seek input from practitioners on how to improve the atmosphere for practice to maximize patient care and practitioner satisfaction.
- Provide ample professional and social opportunities for discussing and learning about work-life balance, resilience, intellectual stimulation, and career development.
For regulators, licensors, and professional organizations:
- Work with health care organizations and EHR vendors to substantially reduce the complexity, physician effort, and stress associated with those record systems. Streamlining should, in the future, be part of formally certifying EHR systems.
- Reduce the administrative burden on physicians by modifying complex regulations and using AI and other technology to the extent possible to obtain necessary reimbursement information.
- Eliminate unnecessary data gathering that requires practitioner time or attention.
- Licensing, educational, and certifying bodies should eliminate any questions regarding the diagnosis or treatment of mental health and focus on current (or very recent) impairments.
- Seek funding for research on burnout prevention and treatment.
Dr. H is a 58-year-old ObGyn who, after completing residency, went into solo practice. The practice grew, and Dr. H found it increasingly more challenging to cover, especially the obstetrics sector. Dr. H then merged the practice with a group of 3 other ObGyns. Their practice expanded, and began recruiting recent residency graduates. In time, the practice was bought out by the local hospital health care system. Dr. H was faced with complying with the rules and regulations of that health care system. The electronic health record (EHR) component proved challenging, as did the restrictions on staff hiring (and firing), but Dr. H did receive a paycheck each month and complied with it all. The health care system administrators had clear financial targets Dr. H was to meet each quarter, which created additional pressure. Dr. H used to love being an OB and providing excellent care for every patient, but that sense of accomplishment was being lost.
Dr. H increasingly found it difficult to focus because of mind wandering, especially in the operating room (OR). Thoughts occurred about retirement, the current challenges imposed by “the new way of practicing medicine” (more focused on financial productivity restraints and reimbursement), and EHR challenges. Then Dr. H’s attention would return to the OR case at hand. All of this resulted in considerable stress and emotional exhaustion, and sometimes a sense of being disconnected. A few times, colleagues or nurses had asked Dr. H if everything was “okay,” or if a break would help. Dr. H made more small errors than usual, but Dr. H’s self-assessment was “doing an adequate job.” Patient satisfaction scores (collected routinely by the health care system) declined over the last 9 months.
Six months ago, Dr. H finished doing a laparoscopic total hysterectomy and bilateral salpingo-oophorectomy and got into the right uterine artery. The estimated blood loss was 3,500 mL. Using minimally invasive techniques, Dr. H identified the bleeder and, with monopolar current, got everything under control. The patient went to the post-anesthesia care unit, and all appeared to be in order. Her vital signs were stable, and she was discharged home the same day.
The patient presented 1 week later with lower abdominal and right flank pain. Dr. H addressed the problem in the emergency department and admitted the patient for further evaluation and urology consultation. The right ureter was damaged and obstructed; ultimately, the urologist performed a psoas bladder hitch. The patient recovered slowly, lost several weeks of work, experienced significant pain, and had other disruptions and costs. Additional medical care related to the surgery is ongoing. A health care system committee asked Dr. H to explain the problem. Over the last 6 months, Dr. H’s frustration with practice and being tired and disconnected have increased.
Dr. H has received a letter from a law firm saying that he and the health care system are being sued for malpractice focused on an iatrogenic ureter injury. The letter names two very reputable experts who are prepared to testify that the patient’s injury resulted from clear negligence. Dr. H has told the malpractice carrier absolutely not to settle this case—it is “a sham— without merit.” The health care system has asked Dr. H to take a “burnout test.”
Legal considerations
Dr. H exhibits relatively clear signs of professional burnout. The fact that there was a bad outcome while Dr. H was experiencing burnout is not proof of negligence (or, breach of duty of care to the patient). Nor is it a defense or mitigation to any malpractice that occurred.
In the malpractice case, the plaintiff will have the burden of proving that Dr. H’s treatment was negligent in that it fell below the standard of care. Even if it was a medical error, the question is whether it was negligence. If the patient/plaintiff, using expert witnesses, can prove that Dr. H fell below the standard of care that caused injury, Dr. H may be liable for the resulting extra costs, loss of income, and pain and suffering resulting from the negligent care.
The health care system likely will also be responsible for Dr. H’s negligence, either through respondeat superior (for example, if Dr. H is an employee) or for its own negligence. The case for its negligence is that the nurses and assistants had repeatedly seen him making errors and becoming disengaged (to the extent that they asked Dr. H if “everything is okay” or if a break would help). Furthermore, Dr. H’s patient satisfaction scores have been declining for several months. The plaintiff will argue that Dr. H exhibited classic burnout symptoms with the attendant risks of medical errors. However, the health care system did not take action to protect patients or to assist Dr. H. In short, one way or another, there is some likelihood that the health care system may also be liable if patient injuries are found to have been caused by negligence.
At this point, the health care system also faces the question of how to work with Dr. H in the future. The most pressing question is whether or not to allow Dr. H to continue practicing. If, as it appears, Dr. H is dealing with burnout, the pressure of the malpractice claim could well increase the probability of other medical mistakes. The institution has asked Dr. H to take a burnout test, but it is unclear where things go if the test (as likely) demonstrates significant burnout. This is a counseling and human relations question, at least as much as a legal issue, and the institution should probably proceed in that way—which is, trying to understand and support Dr. H and determining what can be done to address the burnout. At the same time, the system must reasonably assess Dr. H’s fitness to continue practicing as the matters are resolved. Almost everyone shares the goal to provide every individual and corporate opportunity for Dr. H to deal with burnout issues and return to successful practice.
Dr. H will be represented in the malpractice case by counsel provided through the insurance carrier. However, Dr. H would be well advised to retain a trusted and knowledgeable personal attorney. For example, the instruction not to consider settlement is likely misguided, but Dr. H needs to talk with an attorney that Dr. H has chosen and trusts. In addition, the attorney can help guide Dr. H through a rational process of dealing with the health care system, putting the practice in order, and considering the options for the future.
The health care system should reconsider its processes to deal with burnout to ensure the quality of care, patient satisfaction, professional retention, and economic stability. Several burnoutresponse programs have had success in achieving these goals.
What’s the Verdict?
Dr. H received good mental health, legal, and professional advice. As a result, an out of court settlement was reached following pretrial discovery. Dr. H has continued consultation regarding burnout and has returned to productive practice.
- Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clinic Proceed. 2019;94:1681-1694.
- Smith R, Rayburn W. Burnout in obstetrician-gynecologists. Its prevalence, identification, prevention, and reversal. Obstet Gynecol Clin North Am. 2021;48:231-245. https://doi. org/10.1016/j.ogc.2021.06.003
- Patti MG, Schlottmann F, Sarr MG. The problem of burnout among surgeons. JAMA Surg. 2018;153:403-404. doi:10.1001 /jamasurg.2018.0047
- Carrau D, Janis JE. Physician burnout: solutions for individuals and organizations. Plastic and Reconstructive Surgery Global Open. 2021;91-97.
- Southwick R. The key to fixing physician burnout is the workplace not the worker. Contemporary Ob/Gyn. March 13, 2023.
- Patel RS, Bachu R, Adikey A, et al. Factors related to physician burnout and its consequences: a review. Behav Sciences. 2018;8:98.
- Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clinic Proceed. 2020;95:476-487.
- Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017;317:901-902. doi:10.1001/jama.2017.0076
- Ommaya AK, Cipriano PF, Hoyt DB, et al. Care-centered clinical documentation in the digital environment: Solutions to alleviate burnout. National Academy of Medicine Perspectives. 2018.
- Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;382:2485-2487. Discussion Paper, National Academy of Medicine. Accessed July 21, 2023. https://nam .edu/care
- Ji YD, Robertson FC, Patel NA, et al. Assessment of risk factors for suicide among US health care professionals. JAMA Surg. 2020;155:713-721. centered-clinical-documentation-digital -environment-solutions-alleviate-burnout/
- Shanafelt TD, West CP, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clinic Proceed. 2022;97:2248-2258.
- Herber-Valdez C, Kupesic-Plavsic S. Satisfaction and shortfall of OB-GYN physicians and radiologists. J. Ultrasound Obstet Gynecol. 2021;15:387-392.
- Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. National Academy of Medicine Perspectives. Accessed July 5, 2017. https://iuhcpe.org/file_manager/1501524077-Burnout -Among-Health-Care-Professionals-A-Call-to-Explore-and -Address-This-Underrecognized-Threat.pdf
- Olson KD. Physician burnout—a leading indicator of health system performance? Mayo Clinic Proceed. 2017;92: 1608-1611.
- American College of Obstetricians and Gynecologists. Why obgyns are burning out. October 28, 2019. Accessed July 21, 2023. https://www.acog.org/news/news-articles/2019/10/why-ob -gyns-are-burning-out#:~:text=A%202017%20report%20 by%20the,exhaustion%20or%20lack%20of%20motivation
- Peckham C. National physician burnout & depression report 2018. Medscape. January 17, 2018. https://nap. nationalacademies.org/catalog/25521/taking-action -against-clinician-burnout-a-systems-approach-to -professional
- Marsa L. Labor pains: The OB-GYN shortage. AAMC News. Nov. 15, 2018. Accessed July 21, 2023. https://www.aamc.org /news-insights/labor-pains-ob-gyn-shortage
- American College of Obstetricians and Gynecologists. Coping with the stress of medical professional liability litigation. ACOG Committee Opinion. February 2005;309:453454. Accessed July 21, 2023. https://www.acog.org/clinical /clinical-guidance/committee-opinion/articles/2013/01 /coping-with-the-stress-of-medical-professional-liability -litigation
- Reith TP. Burnout in United States healthcare professionals: a narrative review. Cureus. 2018;10:e3681. doi: 10.7759 /cureus.3681
- Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;4:784-790.
- Sullivan D, Sullivan V, Weatherspoon D, et al. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs Clin North Am. 2022;57:79-99. doi: 10.1016 /j.cnur.2021.11.006
- Chandawarkar A, Chaparro JD. Burnout in clinicians. Curr Prob Pediatr Adolesc Health Care. 2021;51:101-104. https ://doi.org/10.1016/j.cppeds.2021.101104
- Brady KJS, Sheldrick RC, Ni P, et al. Examining the measurement equivalence of the Maslach Burnout Inventory across age, gender, and specialty groups in US physicians. J Patient-Reported Outcomes. 2021;5.
- Association of American Medical Colleges. Physician Specialty Data Report—Active Physicians by Sex and Specialty, 2021. Accessed June 19, 2023. https://www.aamc .org/data-reports/workforce/data/active-physicians-sex -specialty-2021
- Association of American Medical Colleges. Physician Specialty Data Report—ACGME Residents and Fellows by Sex and Specialty, 2021. Accessed June 19, 2023. https://www .aamc.org/data-reports/workforce/data/acgme-residents -fellows-sex-and-specialty-2021
- Painter LM, Biggans KA, Turner CT. Risk managementobstetrics and gynecology perspective. Clin Obstet Gynecol. 2023;66:331-341. DOI:10.1097/GRF.0000000000000775
- Darney BG, Boniface E, Liberty A. Assessing the effect of abortion restrictions. Obstetr Gynecol. 2023;141:233-235.
- Heuerman AC, Bessett D, Antommaria AHM, et al. Experiences of reproductive genetic counselors with abortion regulations in Ohio. J Genet Counseling. 2022;31:641-652.
- Brandi K, Gill P. Abortion restrictions threaten all reproductive health care clinicians. Am J Public Health. 2023;113:384-385.
- Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131-1150. doi: 10.1001/jama.2018.1277
- Williamson K, Lank PM, Cheema N, et al. Comparing the Maslach Burnout Inventory to other well-being instruments in emergency medicine residents. J Graduate Med Education. 2018;532-536. DOI: http://dx.doi.org/10.4300 /JGME-D-18-00155.1
- Brady KJS, Sheldrick RC, Ni P, et al. Establishing crosswalks between common measures of burnout in US physicians. J Gen Intern Med. 2022;37:777-784.
- Zhang X, Song Y, Jiang T, et al. Interventions to reduce burnout of physicians and nurses: an overview of systematic reviews and meta-analyses. Medicine (Baltimore). 2020;26:e20992. DOI: 10.1097/MD.0000000000020992
- Scheepers RA, Emke H, Ronald M, et al. The impact of mindfulness-based interventions on doctors’ well-being and performance: a systematic review. Med Education. 2020;54:138-149. https://doi.org/10.1111/medu.14020
- Olson K, Marchalik D, Farley H, et al. Organizational strategies to reduce physician burnout and improve professional fulfillment. Curr Prob Pediatr Adolesc Health Care. 2019;49:12. https://doi.org/10.1016/j.cppeds.2019.100664
- Berry LL, Awdish RLA, Swensen SJ. 5 ways to restore depleted health care workers. Harvard Business Rev. February 11, 2022.
- Sullivan AB, Hersh CM, Rensel M, et al. Leadership inequity, burnout, and lower engagement of women in medicine. J Health Serv Psychol. 2023;49:33-39.
- Hoffman S. Healing the healers: legal remedies for physician burnout. Yale J Health Policy Law Ethics. 2018;18:56-113.
- Federation of State Medical Boards. Physician wellness and burnout: report and recommendations of the workgroup on physician wellness and burnout. (Policy adopted by FSMB). April 2018. Accessed July 21, 2023. https://www.fsmb.org /siteassets/advocacy/policies/policy-on-wellness-and -burnout.pdf
- Robinson C, Kettering C, Sanfilippo JS. Medical malpractice lawsuits. Clin Obstet Gynecol. 2023;66:256-260. DOI: https ://doi.org/10.1097/GRF.0000000000000777
- Gittler GJ, Goldstein EJ. The elements of medical malpractice: an overview. Clin Infect Dis. 1996;23:1152-1155.
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467:339-347.
- Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clinic Proceed. 2018;93: 1571-1580.
- Sundholm B. Elevating physician-patient relationships in the shadow of metric mania. Drexel L Rev. 2020;12:287-330.
- Ghaith S, Campbell RL, Pollock JR, et al. Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. Healthcare. 2022;10:1328.
- Muller TM, Warsi S. Litigation culture causing burnout in American physicians. Trauma Mental Health Report. April 9, 2021.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. 2015:60;26-28, 30.
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. Southern Med J. 2002;95.5:545-549. DOI 10.1097/00007611-200295050-00018
- Levin H. Hospital vicarious liability for negligence by independent contractor physicians: new rule for new times. Univ Illinois Law Rev. 2005:1291-1332.
- Darling v Charleston Hospital, 33 Ill. 2d 326, 211 N.E.2d 253 (Ill. 1965).
- Dangel R. Hospital liability for physician malpractice. Ohio State Law J. 1986;47:1077-1098.
- Reffitt v Hajjar, 892 S.W.2d 599, 605 (Ky. Ct. App. 1994).
- McMichael BJ. Malpractice. In Laws of Medicine: Core Legal Aspects for the Healthcare Professional. New York, NY: Springer International; 2022:129-150.
- Occupational Safety and Health Administration. Worker safety in hospitals: caring for our caregivers. Accessed June 8, 2023. https://www.osha.gov/hospitals
- Occupational Safety and Health Administration. Workplace stress. Accessed June 8, 2023. https://www.osha.gov /workplace-stress/understanding-the-problem
- U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. Addressing health worker burnout. Accessed July 21, 2023. https://www.hhs.gov/sites/default/files/health -worker-wellbeing-advisory.pdf
- Department of Health & Human Services. Biden-Harris administration awards $103 Million in American Rescue Plan funds to reduce burnout and promote mental health and wellness among health care workforce. January 20, 2022. Accessed July 24, 2023. https://www.hhs.gov/about /news/2022/01/20/biden-harris-administration-awards -103-million-american-rescue-plan-funds-reduce-burnout -promote-mental-health-wellness-among-health-care -workforce.html
- Rothstein LF, Irzyk J. Disabilities and the Law. 4th ed. Toronto, Canada: Thompson Reuters; 2023.
- Department of Labor. Guide to disability rights laws. February 28, 2020. Accessed July 24, 2023. https://www .ada.gov/resources/disability-rights-guide/#:~:text=An%20 individual%20with%20a%20disability%20is%20defined%20 by%20the%20ADA,as%20having%20such%20an%20 impairment
- Nadon L, De Beer LT, Morin AJS. Should burnout be conceptualized as a mental disorder? Behavioral Sci. 2022;12:82.
- World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases. May 28, 2019. Accessed July 21, 2023. https://www.who.int/news /item/28-05-2019-burn-out-an-occupational-phenomenon -international-classification-of-diseases
- Hoffman S. Physician burnout: why legal and regulatory systems may need to step in. The Conversation. July 9, 2019. https://theconversation.com/physician-burnout-why-legal -and-regulatory-systems-may-need-to-step-in-119705
- Jha A, Iliff A, Chaoi A, et al. A crisis in healthcare: a call to action on physician burnout. Harvard Global Health Institute. 2019. Accessed July 21, 2023. https://www.massmed.org /Publications/Research,-Studies,-and-Reports/Physician -Burnout-Report-2018/
- Arnsten AF, Shanafelt T. Physician distress and burnout: the neurobiological perspective. Mayo Clin Proceed. 2021;96:763-769.
Physicians have some of the highest rates of burnout among all professions.1 Complicating matters is that clinicians (including residents)2 may avoid seeking treatment out of fear it will affect their license or privileges.3 In this article, we consider burnout in greater detail, as well as ways of successfully addressing the level of burnout in the profession (FIGURE 1), including steps individual practitioners, health care entities, and regulators should consider to reduce burnout and its harmful effects.
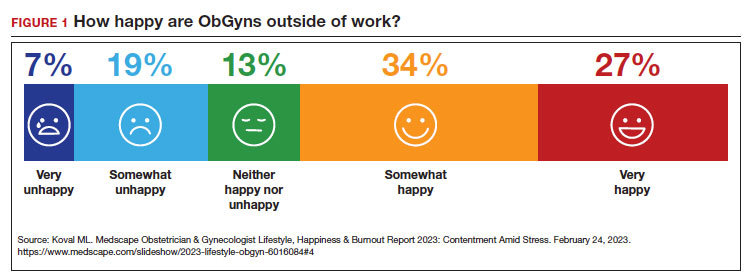
How burnout becomes a problem
Six general factors are commonly identified as leading to clinician career dissatisfaction and burnout:4
1. work overload
2. lack of autonomy and control
3. inadequate rewards, financial and otherwise
4. work-home schedules
5. perception of lack of fairness
6. values conflict between the clinician and employer (including a breakdown of professional community).
At the top of the list of causes of burnout is often “administrative and bureaucratic headaches.”5 More specifically, electronic health records (EHRs), including computerized order entry, is commonly cited as a major cause of burnout.6,7 According to some studies, clinicians spend as much as 49% of working time doing clerical work,8 and studies found the extension of work into home life.9
Increased measurement of performance metrics in health care services are a significant contributor to physician burnout.10 These include pressure to see more patients, perform more procedures, and respond quickly to patient requests (eg, through email).7 As we will see, medical malpractice cases, or the risk of such cases, have also played a role in burnout in some medical specialties.11 The pandemic also contributed, at least temporarily, to burnout.12,13
Rates of burnout among physicians are notably higher than among the general population14 or other professions.6 Although physicians have generally entered clinical practice with lower rates of burnout than the general population,15 The American College of Obstetricians and Gynecologists (ACOG) reports that 40% to 75% of ObGyns “experience some form of professional burnout.”16,17 Other source(s) cite that 53% of ObGyns report burnout (TABLE 1).
Code QD85
Burnout is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by 3 dimensions:
- feelings of energy depletion or exhaustion
- increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job
- a sense of ineffectiveness and lack of accomplishment. Burn-out refers specifically to phenomena in the occupational context and should not be applied to describe experiences in other areas of life. Exclusions to burnout diagnosis include adjustment disorder, disorders specifically associated with stress, anxiety or fear-related disorders, and mood disorders.
Reference
1. International Classification of Diseases Eleventh Revision (ICD-11). Geneva, Switzerland: World Health Organization; 2022.
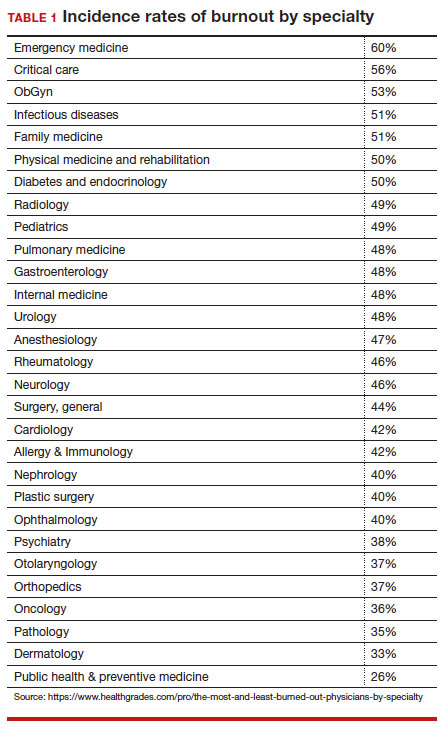
Burnout undoubtedly contributes to professionals leaving practice, leading to a significant shortage of ObGyns.18 It also raises several significant legal concerns. Despite the enormity and seriousness of the problem, there is considerable optimism and assurance that the epidemic of burnout is solvable on the individual, specialty, and profession-wide levels. ACOG and other organizations have made suggestions for physicians, the profession, and to health care institutions for reducing burnout.19 This is not to say that solutions are simple or easy for individual professionals or institutions, but they are within the reach of the profession (FIGURE 2).
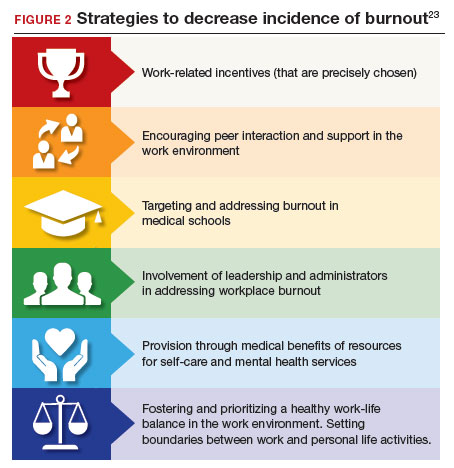
Suicide among health care professionals is one other concern (TABLE 2)20 and theoretically can stem from burnout, depression, and other psychosocial concerns.
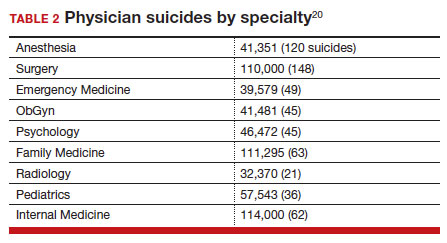
Costs of clinician burnout
Burnout is endemic among health care providers, with numerous studies detailing the professional, emotional, and financial costs. Prior to the pandemic, one analysis of nationwide fiscal costs associated with burnout estimated an annual cost of $4.6B due to physician turnover and reduced clinical hours.21 The COVID-19 epidemic has by all accounts worsened rates of health care worker burnout, particularly for those in high patient-contact positions.22
Female clinicians appear to be differentially affected; in one recent study women reported symptoms of burnout at twice the rate of their male counterparts.23 Whether burnout rates will return to pre-pandemic levels remains an open question, but since burnout is frequently related to one’s own assessment of work-life balance, it is possible that a longer term shift in burnout rates associated with post-pandemic occupational attitudes will be observed.
Combining factors contribute to burnout
Burnout is a universal occupational hazard, but extant data suggest that physicians and other health care providers may be at higher risk. Among physicians, younger age, female gender, and front-line specialty status appear associated with higher burnout rates.24 Given that ObGyn physicians are overwhelmingly female (60% of physicians and 86% of residents),25,26 gender-related burnout factors exist alongside other specific occupational burnout risks. While gender parity has been achieved among health care providers, gender disparities persist in terms of those in leadership positions, compensation, and other factors.22
The smattering of evidence suggesting that ObGyns have higher rates of burnout than many other specialties is understandable given the unique legal challenges confronting ObGyn practice. This may be of special significance because ObGyn malpractice insurance rates are among the highest of all specialties.27 The overall shortage of ObGyns has been exacerbated by the demonstrated negative effects on training and workforce representation stemming from recent legislation that has the effect of criminalizing certain aspects of ObGyn practice;28 for instance, uncertainty regarding abortion regulations.
These negative effects are particularly heightened in states in which the law is in flux or where there are continuing efforts to substantially limit access to abortion. The efforts to increase civil and even criminal penalties related to abortion care challenge ObGyns’ professional practices, as legal rules are frequently changing. In some states, ObGyns may face additional workloads secondary to a flight of ObGyns from restrictive jurisdictions in addition to legal and professional repercussions. In a small study of 19 genetic counselors dealing with restrictive legislation in the state of Ohio,29 increased stress and burnout rates were identified as a consequence of practice uncertainties under this legislation. It is certain that other professionals working in reproductive health care are similarly affected.30
The programs provide individual resources to providers in distress, periodically survey initiatives at Stanford to assess burnout at the organizational level, and provide input designed to spur organizational change to reduce the burden of burnout. Ways that they build community and connections include:
- Live Story Rounds events (as told by Stanford Medicine physicians)
- Commensality Groups (facilitated small discussion groups built around tested evidence)
- Aim to increase sense of connection and collegiality among physicians and build comradery at work
- CME-accredited physician wellness forum, including annual doctor’s day events
Continue to: Assessment of burnout...
Assessment of burnout
Numerous scales for the assessment of burnout exist. Of these, the 22-item Maslach Burnout Inventory (MBI) is the best studied. The MBI is a well-investigated tool for assessing burnout. The MBI consists of 3 major subscales measuring overall burnout, emotional exhaustion, depersonalization, and low personal accomplishment. It exists in numerous forms. For instance, the MBI-HSS (MP), adapted for medical personnel, is available. However, the most commonly used form for assessing burnout in clinicians is the MBI-HHS (Human Services Survey); approximately 85% of all burnout studies examined in a recent meta-analysis used this survey version.31 As those authors commented, while burnout is a recognized phenomenon, a great deal of variability in study design, interpretation of subscale scores, and sample selection makes generalizations regarding burnout difficult to assess.
The MBI in various forms has been extensively used over the past 40 years to assess burnout amongst physicians and physicians in training. While not the only instrument designed to measure such factors, it is by far the most prevalent. Williamson and colleagues32 compared the MBI with several other measures of quality of life and found good correlation between the various instruments used, a finding replicated by other studies.33 Brady and colleagues compared item responses to the Stanford Professional Fulfillment Index and the Min-Z Single-item Burnout scale (a 1-item screening measure) to MBI’s Emotional Exhaustion and Depersonalization subscales. Basing their findings on a survey of more than 1,300 physicians, they found that all analyzed scales were significantly correlated with such adverse outcomes as depression, distress, or intent to leave the profession.
It is important to note that most surveys of clinician burnout were conducted prior to the pandemic. While the psychometric analyses of the MBI and other scales are likely still germane, observed rates of clinician burnout have likely increased. Thus, comparisons of pre- and post-pandemic studies should factor in an increase in the incidence and prevalence of burnout.
Management strategies
In general, there are several interventions for managing burnout34:
- individual-focused (including self-care and communications-skills workshops)
- mindfulness training
- yoga
- meditation
- organizational/structural (workload reduction, schedule realignment, teamwork training, and group-delivered stress management interventions)
- combination(s) of the above.
There is little evidence to suggest that any particular individual intervention (whether delivered in individual or group-based formats) is superior to any other in treating clinician burnout. A recent analysis of 24 studies employing mindfulness-based interventions demonstrated generally positive results for such interventions.35 Other studies have also found general support for mindfulness-based interventions, although mindfulness is often integrated with other stress-reduction techniques, such as meditation, yoga, and communication skills. Such interventions are nonspecific but generally effective.
An accumulation of evidence to date suggests that a combination of individual and organizational interventions is most effective in combatting clinician burnout. No individual intervention can be successful without addressing root causes, such as overscheduling, lack of organizational support, and the effect of restrictive legislation on practice.
Several large teaching hospitals have established programs to address physician and health care provider burnout. Notable among these is the Stanford University School of Medicine’s WellMD and WellPhD programs (https://wellmd.stanford.edu/about.html). These programs were described by Olson and colleagues36 as using a model focused on practice efficiency, organizational culture, and personal resilience to enhance physicians’ well-being. (See “Aspects of the WellMD and WellPhD programs from Stanford University.”)
A growing number of institutions have established burnout programs to support physicians experiencing work/life imbalances and other aspects of burnout.37 In general, these share common features of assessment, individual and/or group intervention, and organizational change. Fear of repercussion may be one factor preventing physicians from seeking individual treatment for burnout.38 Importantly, they emphasize the need for professional confidentiality when offering treatment to patients within organizational settings. Those authors also reported that a focus on organizational engagement may be an important factor in addressing burnout in female physicians, as they tend to report lower levels of organizational engagement.
Continue to: Legal considerations...
Legal considerations
Until recently, physician burnout “received little notice in the legal literature.”39 Although there have been burnout legal consequences in the past, the legal issues are now becoming more visible.40
Medical malpractice
A well-documented consequence of burnout is an increase in errors.14 Medical errors, of course, are at the heart of malpractice claims. Technically, malpractice is medical or professional negligence. It is the breach of a duty owed by the physician, or other provider, or organization (defendant) to the patient, which causes injury to the plaintiff/patient.41
“Medical error” is generally a meaningful deviation from the “standard of care” or accepted medical practice.42 Many medical errors do not cause injury to the patient; in those cases, the negligence does not result in liability. In instances in which the negligence causes harm, the clinician and health care facility may be subject to liability for that injury. Fortunately, however, for a variety of reasons, most harmful medical errors do not result in a medical malpractice claim or lawsuit. The absence of a good clinician-patient relationship is likely associated with an increased inclination of a patient to file a malpractice action.43Clinician burnout may, therefore, contribute to increased malpractice claims in two ways. First, burnout likely leads to increased medical errors, perhaps because burnout is associated with lower concentration, inattention, reduced cognitive vigilance, and fatigue.8,44 It may also lead to less time with patients, reduced patient empathy, and lower patient rapport, which may make injured patients more likely to file a claim or lawsuit.45 Because the relationshipbetween burnout and medical error is bidirectional, malpractice claims tend to increase burnout, which increases error. Given the time it takes to resolve most malpractice claims, the uncertainty of medical malpractice may be especially stressful for health care providers.46,47
Burnout is not a mitigating factor in malpractice. Our sympathies may go out to a professional suffering from burnout, but it does not excuse or reduce liability—it may, indeed, be an aggravating factor. Clinicians who can diagnose burnout and know its negative consequences but fail to deal with their own burnout may be demonstrating negligence if there has been harm to a patient related to the burnout.48
Institutional or corporate liability to patients
Health care institutions have obligations to avoid injury to patients. Just as poorly maintained medical equipment may harm patients, so may burned-out professionals. Therefore, institutions have some obligation to supervise and avoid the increased risks to patients posed by professionals suffering from burnout.
Respondeat superior and institutional negligence. Institutional liability may arise in two ways, the first through agency, or respondeat superior. That is, if the physician or other professional is an employee (or similar agent) of the health care institution, that institution is generally responsible for the physician’s negligence during the employment.49 Even if the physician is not an employee (for example, an independent contractor providing care or using the hospital facilities), the health care facility may be liable for the physician’s negligence.50 Liability may occur, for example, if the health care facility was aware that the physician was engaged in careless practice or was otherwise a risk to patients but the facility did not take steps to avoid those risks.51 The basis for liability is that the health care organization owes a duty to patients to take reasonable care to ensure that its facilities are not used to injure patients negligently.52 Just as it must take care that unqualified physicians are not granted privileges to practice, it also must take reasonable steps to protect patients when it is aware (through nurses or other agents) of a physician’s negligent practice.
In one case, for example, the court found liability where a staff member had “severe” burnout in a physician’s office and failed to read fetal monitoring strips. The physician was found negligent for relying on the staff member who was obviously making errors in interpretation of fetal distress.53
Continue to: Legal obligations of health care organizations to physicians and others...
Legal obligations of health care organizations to physicians and others
In addition to obligations to patients, health care organizations may have obligations to employees (and others) at risk for injury. For example, assume a patient is diagnosed with a highly contagious disease. The health care organization would be obligated to warn, and take reasonable steps to protect, the staff (employees and independent contractors) from being harmed from exposure to the disease. This principle may apply to coworkers of employees with significant burnout, thereby presenting a danger in the workplace. The liability issue is more difficult for employees experiencing job-related burnout themselves. Organizations generally compensate injured employees through no-fault workers’ compensation (an insurance-like system); for independent contractors, the liability is usually through a tort claim (negligence).54
In modern times, a focus has been on preventing those injuries, not just providing compensation after injuries have occurred. Notably, federal and state occupational health and safety laws (particularly the Occupational Safety and Health Administration [OSHA]) require most organizations (including those employing health care providers) to take steps to mitigate various kinds of worker injuries.55
Although these worker protections have commonly been applied to hospitals and other health care providers, burnout has not traditionally been a significant concern in federal or state OSHA enforcement. For example, no formal federal OSHA regulations govern work-related burnout. Regulators, including OSHA, are increasingly interested in burnout that may affect many employees. OSHA has several recommendations for reducing health care work burnout.56 The Surgeon General has expressed similar concerns.57 The federal government recently allocated $103 million from the American Rescue Plan to address burnout among health care workers.58 Also, OSHA appears to be increasing its oversight of healthcare-institution-worker injuries.55
Is burnout a “disability”?
The federal Americans with Disabilities Act (ADA) and similar state laws prohibit discrimination based on disability.59 A disability is defined as a “physical or mental impairment that substantially limits one or more major life activities” or “perceived as having such an impairment.”60 The initial issue is whether burnout is a “mental impairment.” As noted earlier, it is not officially a “medical condition.”61 To date, the United Nations has classified it as an “occupational phenomenon.”62 It may, therefore, not qualify under the ADA, even if it “interferes with a major life activity.” There is, however, some movement toward defining burnout as a mental condition. Even if defined as a disability, there would still be legal issues of how severe it must be to qualify as a disability and the proper accommodation. Apart from the legal definition of an ADA disability, as a practical matter it likely is in the best interest of health care facilities to provide accommodations that reduce burnout. A number of strategies to decrease the incidence of burnout include the role of health care systems (FIGURE 2).
In conclusion we look at several things that can be done to “treat” or reduce burnout. That effort requires the cooperation of physicians and other providers, health care facilities, training programs, licensing authorities, and professional organizations. See suggestions below.
Conclusion
There are many excellent suggestions for reducing burnout and improving patient care and practitioner satisfaction.63-65 We conclude with a summary of some of these suggestions for individual practitioners, health care organizations, the profession, and licensing. It is worth remembering, however, that it will require the efforts of each area to reduce burnout substantially.
For practitioners:
- Engage in quality coaching/therapy on mindfulness and stress management.
- Practice self-care, including exercise and relaxation techniques.
- Make work-life balance a priority.
- Take opportunities for collegial social and professional discussions.
- Prioritize (and periodically assess) your own professional satisfaction and burnout risk.
- Smile—enjoy a sense of humor (endorphins and cortisol).
For health care organizations:
- Urgently work with vendors and regulators to revise electronic health records to reduce their substantial impact on burnout.
- Reduce physicians’ time on clerical and administrative tasks (eg, by enhancing the use of quality AI, scribes, and automated notes from appointments. (This may increase the time they spend with patients.) Eliminate “pajama-time” charting.
- Provide various kinds of confidential professional counseling, therapy, and support related to burnout prevention and treatment, and avoid any penalty or stigma related to their use.
- Provide reasonable flexibility in scheduling.
- Routinely provide employees with information about burnout prevention and services.
- Appoint a wellness officer with authority to ensure the organization maximizes its prevention and treatment services.
- Constantly seek input from practitioners on how to improve the atmosphere for practice to maximize patient care and practitioner satisfaction.
- Provide ample professional and social opportunities for discussing and learning about work-life balance, resilience, intellectual stimulation, and career development.
For regulators, licensors, and professional organizations:
- Work with health care organizations and EHR vendors to substantially reduce the complexity, physician effort, and stress associated with those record systems. Streamlining should, in the future, be part of formally certifying EHR systems.
- Reduce the administrative burden on physicians by modifying complex regulations and using AI and other technology to the extent possible to obtain necessary reimbursement information.
- Eliminate unnecessary data gathering that requires practitioner time or attention.
- Licensing, educational, and certifying bodies should eliminate any questions regarding the diagnosis or treatment of mental health and focus on current (or very recent) impairments.
- Seek funding for research on burnout prevention and treatment.
Dr. H is a 58-year-old ObGyn who, after completing residency, went into solo practice. The practice grew, and Dr. H found it increasingly more challenging to cover, especially the obstetrics sector. Dr. H then merged the practice with a group of 3 other ObGyns. Their practice expanded, and began recruiting recent residency graduates. In time, the practice was bought out by the local hospital health care system. Dr. H was faced with complying with the rules and regulations of that health care system. The electronic health record (EHR) component proved challenging, as did the restrictions on staff hiring (and firing), but Dr. H did receive a paycheck each month and complied with it all. The health care system administrators had clear financial targets Dr. H was to meet each quarter, which created additional pressure. Dr. H used to love being an OB and providing excellent care for every patient, but that sense of accomplishment was being lost.
Dr. H increasingly found it difficult to focus because of mind wandering, especially in the operating room (OR). Thoughts occurred about retirement, the current challenges imposed by “the new way of practicing medicine” (more focused on financial productivity restraints and reimbursement), and EHR challenges. Then Dr. H’s attention would return to the OR case at hand. All of this resulted in considerable stress and emotional exhaustion, and sometimes a sense of being disconnected. A few times, colleagues or nurses had asked Dr. H if everything was “okay,” or if a break would help. Dr. H made more small errors than usual, but Dr. H’s self-assessment was “doing an adequate job.” Patient satisfaction scores (collected routinely by the health care system) declined over the last 9 months.
Six months ago, Dr. H finished doing a laparoscopic total hysterectomy and bilateral salpingo-oophorectomy and got into the right uterine artery. The estimated blood loss was 3,500 mL. Using minimally invasive techniques, Dr. H identified the bleeder and, with monopolar current, got everything under control. The patient went to the post-anesthesia care unit, and all appeared to be in order. Her vital signs were stable, and she was discharged home the same day.
The patient presented 1 week later with lower abdominal and right flank pain. Dr. H addressed the problem in the emergency department and admitted the patient for further evaluation and urology consultation. The right ureter was damaged and obstructed; ultimately, the urologist performed a psoas bladder hitch. The patient recovered slowly, lost several weeks of work, experienced significant pain, and had other disruptions and costs. Additional medical care related to the surgery is ongoing. A health care system committee asked Dr. H to explain the problem. Over the last 6 months, Dr. H’s frustration with practice and being tired and disconnected have increased.
Dr. H has received a letter from a law firm saying that he and the health care system are being sued for malpractice focused on an iatrogenic ureter injury. The letter names two very reputable experts who are prepared to testify that the patient’s injury resulted from clear negligence. Dr. H has told the malpractice carrier absolutely not to settle this case—it is “a sham— without merit.” The health care system has asked Dr. H to take a “burnout test.”
Legal considerations
Dr. H exhibits relatively clear signs of professional burnout. The fact that there was a bad outcome while Dr. H was experiencing burnout is not proof of negligence (or, breach of duty of care to the patient). Nor is it a defense or mitigation to any malpractice that occurred.
In the malpractice case, the plaintiff will have the burden of proving that Dr. H’s treatment was negligent in that it fell below the standard of care. Even if it was a medical error, the question is whether it was negligence. If the patient/plaintiff, using expert witnesses, can prove that Dr. H fell below the standard of care that caused injury, Dr. H may be liable for the resulting extra costs, loss of income, and pain and suffering resulting from the negligent care.
The health care system likely will also be responsible for Dr. H’s negligence, either through respondeat superior (for example, if Dr. H is an employee) or for its own negligence. The case for its negligence is that the nurses and assistants had repeatedly seen him making errors and becoming disengaged (to the extent that they asked Dr. H if “everything is okay” or if a break would help). Furthermore, Dr. H’s patient satisfaction scores have been declining for several months. The plaintiff will argue that Dr. H exhibited classic burnout symptoms with the attendant risks of medical errors. However, the health care system did not take action to protect patients or to assist Dr. H. In short, one way or another, there is some likelihood that the health care system may also be liable if patient injuries are found to have been caused by negligence.
At this point, the health care system also faces the question of how to work with Dr. H in the future. The most pressing question is whether or not to allow Dr. H to continue practicing. If, as it appears, Dr. H is dealing with burnout, the pressure of the malpractice claim could well increase the probability of other medical mistakes. The institution has asked Dr. H to take a burnout test, but it is unclear where things go if the test (as likely) demonstrates significant burnout. This is a counseling and human relations question, at least as much as a legal issue, and the institution should probably proceed in that way—which is, trying to understand and support Dr. H and determining what can be done to address the burnout. At the same time, the system must reasonably assess Dr. H’s fitness to continue practicing as the matters are resolved. Almost everyone shares the goal to provide every individual and corporate opportunity for Dr. H to deal with burnout issues and return to successful practice.
Dr. H will be represented in the malpractice case by counsel provided through the insurance carrier. However, Dr. H would be well advised to retain a trusted and knowledgeable personal attorney. For example, the instruction not to consider settlement is likely misguided, but Dr. H needs to talk with an attorney that Dr. H has chosen and trusts. In addition, the attorney can help guide Dr. H through a rational process of dealing with the health care system, putting the practice in order, and considering the options for the future.
The health care system should reconsider its processes to deal with burnout to ensure the quality of care, patient satisfaction, professional retention, and economic stability. Several burnoutresponse programs have had success in achieving these goals.
What’s the Verdict?
Dr. H received good mental health, legal, and professional advice. As a result, an out of court settlement was reached following pretrial discovery. Dr. H has continued consultation regarding burnout and has returned to productive practice.
Physicians have some of the highest rates of burnout among all professions.1 Complicating matters is that clinicians (including residents)2 may avoid seeking treatment out of fear it will affect their license or privileges.3 In this article, we consider burnout in greater detail, as well as ways of successfully addressing the level of burnout in the profession (FIGURE 1), including steps individual practitioners, health care entities, and regulators should consider to reduce burnout and its harmful effects.
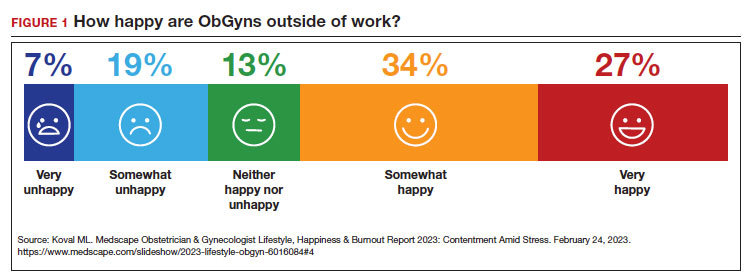
How burnout becomes a problem
Six general factors are commonly identified as leading to clinician career dissatisfaction and burnout:4
1. work overload
2. lack of autonomy and control
3. inadequate rewards, financial and otherwise
4. work-home schedules
5. perception of lack of fairness
6. values conflict between the clinician and employer (including a breakdown of professional community).
At the top of the list of causes of burnout is often “administrative and bureaucratic headaches.”5 More specifically, electronic health records (EHRs), including computerized order entry, is commonly cited as a major cause of burnout.6,7 According to some studies, clinicians spend as much as 49% of working time doing clerical work,8 and studies found the extension of work into home life.9
Increased measurement of performance metrics in health care services are a significant contributor to physician burnout.10 These include pressure to see more patients, perform more procedures, and respond quickly to patient requests (eg, through email).7 As we will see, medical malpractice cases, or the risk of such cases, have also played a role in burnout in some medical specialties.11 The pandemic also contributed, at least temporarily, to burnout.12,13
Rates of burnout among physicians are notably higher than among the general population14 or other professions.6 Although physicians have generally entered clinical practice with lower rates of burnout than the general population,15 The American College of Obstetricians and Gynecologists (ACOG) reports that 40% to 75% of ObGyns “experience some form of professional burnout.”16,17 Other source(s) cite that 53% of ObGyns report burnout (TABLE 1).
Code QD85
Burnout is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by 3 dimensions:
- feelings of energy depletion or exhaustion
- increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job
- a sense of ineffectiveness and lack of accomplishment. Burn-out refers specifically to phenomena in the occupational context and should not be applied to describe experiences in other areas of life. Exclusions to burnout diagnosis include adjustment disorder, disorders specifically associated with stress, anxiety or fear-related disorders, and mood disorders.
Reference
1. International Classification of Diseases Eleventh Revision (ICD-11). Geneva, Switzerland: World Health Organization; 2022.
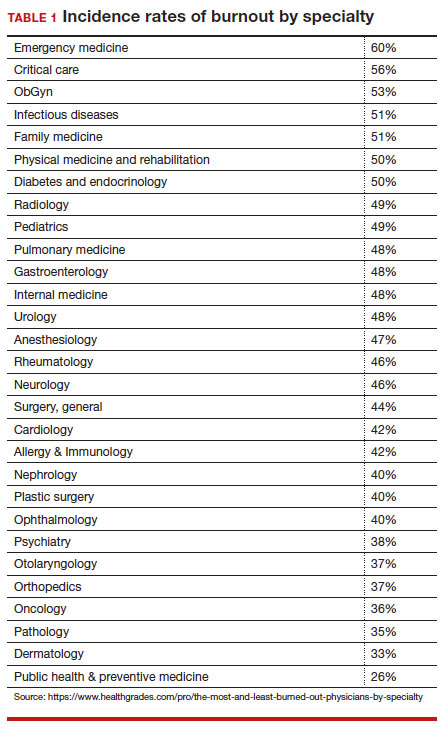
Burnout undoubtedly contributes to professionals leaving practice, leading to a significant shortage of ObGyns.18 It also raises several significant legal concerns. Despite the enormity and seriousness of the problem, there is considerable optimism and assurance that the epidemic of burnout is solvable on the individual, specialty, and profession-wide levels. ACOG and other organizations have made suggestions for physicians, the profession, and to health care institutions for reducing burnout.19 This is not to say that solutions are simple or easy for individual professionals or institutions, but they are within the reach of the profession (FIGURE 2).
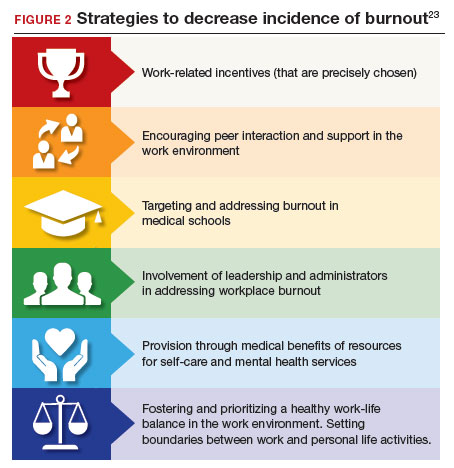
Suicide among health care professionals is one other concern (TABLE 2)20 and theoretically can stem from burnout, depression, and other psychosocial concerns.
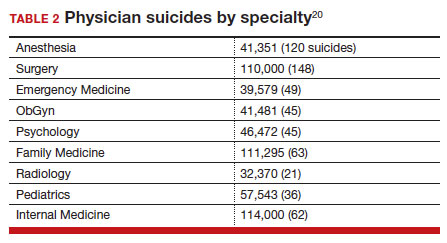
Costs of clinician burnout
Burnout is endemic among health care providers, with numerous studies detailing the professional, emotional, and financial costs. Prior to the pandemic, one analysis of nationwide fiscal costs associated with burnout estimated an annual cost of $4.6B due to physician turnover and reduced clinical hours.21 The COVID-19 epidemic has by all accounts worsened rates of health care worker burnout, particularly for those in high patient-contact positions.22
Female clinicians appear to be differentially affected; in one recent study women reported symptoms of burnout at twice the rate of their male counterparts.23 Whether burnout rates will return to pre-pandemic levels remains an open question, but since burnout is frequently related to one’s own assessment of work-life balance, it is possible that a longer term shift in burnout rates associated with post-pandemic occupational attitudes will be observed.
Combining factors contribute to burnout
Burnout is a universal occupational hazard, but extant data suggest that physicians and other health care providers may be at higher risk. Among physicians, younger age, female gender, and front-line specialty status appear associated with higher burnout rates.24 Given that ObGyn physicians are overwhelmingly female (60% of physicians and 86% of residents),25,26 gender-related burnout factors exist alongside other specific occupational burnout risks. While gender parity has been achieved among health care providers, gender disparities persist in terms of those in leadership positions, compensation, and other factors.22
The smattering of evidence suggesting that ObGyns have higher rates of burnout than many other specialties is understandable given the unique legal challenges confronting ObGyn practice. This may be of special significance because ObGyn malpractice insurance rates are among the highest of all specialties.27 The overall shortage of ObGyns has been exacerbated by the demonstrated negative effects on training and workforce representation stemming from recent legislation that has the effect of criminalizing certain aspects of ObGyn practice;28 for instance, uncertainty regarding abortion regulations.
These negative effects are particularly heightened in states in which the law is in flux or where there are continuing efforts to substantially limit access to abortion. The efforts to increase civil and even criminal penalties related to abortion care challenge ObGyns’ professional practices, as legal rules are frequently changing. In some states, ObGyns may face additional workloads secondary to a flight of ObGyns from restrictive jurisdictions in addition to legal and professional repercussions. In a small study of 19 genetic counselors dealing with restrictive legislation in the state of Ohio,29 increased stress and burnout rates were identified as a consequence of practice uncertainties under this legislation. It is certain that other professionals working in reproductive health care are similarly affected.30
The programs provide individual resources to providers in distress, periodically survey initiatives at Stanford to assess burnout at the organizational level, and provide input designed to spur organizational change to reduce the burden of burnout. Ways that they build community and connections include:
- Live Story Rounds events (as told by Stanford Medicine physicians)
- Commensality Groups (facilitated small discussion groups built around tested evidence)
- Aim to increase sense of connection and collegiality among physicians and build comradery at work
- CME-accredited physician wellness forum, including annual doctor’s day events
Continue to: Assessment of burnout...
Assessment of burnout
Numerous scales for the assessment of burnout exist. Of these, the 22-item Maslach Burnout Inventory (MBI) is the best studied. The MBI is a well-investigated tool for assessing burnout. The MBI consists of 3 major subscales measuring overall burnout, emotional exhaustion, depersonalization, and low personal accomplishment. It exists in numerous forms. For instance, the MBI-HSS (MP), adapted for medical personnel, is available. However, the most commonly used form for assessing burnout in clinicians is the MBI-HHS (Human Services Survey); approximately 85% of all burnout studies examined in a recent meta-analysis used this survey version.31 As those authors commented, while burnout is a recognized phenomenon, a great deal of variability in study design, interpretation of subscale scores, and sample selection makes generalizations regarding burnout difficult to assess.
The MBI in various forms has been extensively used over the past 40 years to assess burnout amongst physicians and physicians in training. While not the only instrument designed to measure such factors, it is by far the most prevalent. Williamson and colleagues32 compared the MBI with several other measures of quality of life and found good correlation between the various instruments used, a finding replicated by other studies.33 Brady and colleagues compared item responses to the Stanford Professional Fulfillment Index and the Min-Z Single-item Burnout scale (a 1-item screening measure) to MBI’s Emotional Exhaustion and Depersonalization subscales. Basing their findings on a survey of more than 1,300 physicians, they found that all analyzed scales were significantly correlated with such adverse outcomes as depression, distress, or intent to leave the profession.
It is important to note that most surveys of clinician burnout were conducted prior to the pandemic. While the psychometric analyses of the MBI and other scales are likely still germane, observed rates of clinician burnout have likely increased. Thus, comparisons of pre- and post-pandemic studies should factor in an increase in the incidence and prevalence of burnout.
Management strategies
In general, there are several interventions for managing burnout34:
- individual-focused (including self-care and communications-skills workshops)
- mindfulness training
- yoga
- meditation
- organizational/structural (workload reduction, schedule realignment, teamwork training, and group-delivered stress management interventions)
- combination(s) of the above.
There is little evidence to suggest that any particular individual intervention (whether delivered in individual or group-based formats) is superior to any other in treating clinician burnout. A recent analysis of 24 studies employing mindfulness-based interventions demonstrated generally positive results for such interventions.35 Other studies have also found general support for mindfulness-based interventions, although mindfulness is often integrated with other stress-reduction techniques, such as meditation, yoga, and communication skills. Such interventions are nonspecific but generally effective.
An accumulation of evidence to date suggests that a combination of individual and organizational interventions is most effective in combatting clinician burnout. No individual intervention can be successful without addressing root causes, such as overscheduling, lack of organizational support, and the effect of restrictive legislation on practice.
Several large teaching hospitals have established programs to address physician and health care provider burnout. Notable among these is the Stanford University School of Medicine’s WellMD and WellPhD programs (https://wellmd.stanford.edu/about.html). These programs were described by Olson and colleagues36 as using a model focused on practice efficiency, organizational culture, and personal resilience to enhance physicians’ well-being. (See “Aspects of the WellMD and WellPhD programs from Stanford University.”)
A growing number of institutions have established burnout programs to support physicians experiencing work/life imbalances and other aspects of burnout.37 In general, these share common features of assessment, individual and/or group intervention, and organizational change. Fear of repercussion may be one factor preventing physicians from seeking individual treatment for burnout.38 Importantly, they emphasize the need for professional confidentiality when offering treatment to patients within organizational settings. Those authors also reported that a focus on organizational engagement may be an important factor in addressing burnout in female physicians, as they tend to report lower levels of organizational engagement.
Continue to: Legal considerations...
Legal considerations
Until recently, physician burnout “received little notice in the legal literature.”39 Although there have been burnout legal consequences in the past, the legal issues are now becoming more visible.40
Medical malpractice
A well-documented consequence of burnout is an increase in errors.14 Medical errors, of course, are at the heart of malpractice claims. Technically, malpractice is medical or professional negligence. It is the breach of a duty owed by the physician, or other provider, or organization (defendant) to the patient, which causes injury to the plaintiff/patient.41
“Medical error” is generally a meaningful deviation from the “standard of care” or accepted medical practice.42 Many medical errors do not cause injury to the patient; in those cases, the negligence does not result in liability. In instances in which the negligence causes harm, the clinician and health care facility may be subject to liability for that injury. Fortunately, however, for a variety of reasons, most harmful medical errors do not result in a medical malpractice claim or lawsuit. The absence of a good clinician-patient relationship is likely associated with an increased inclination of a patient to file a malpractice action.43Clinician burnout may, therefore, contribute to increased malpractice claims in two ways. First, burnout likely leads to increased medical errors, perhaps because burnout is associated with lower concentration, inattention, reduced cognitive vigilance, and fatigue.8,44 It may also lead to less time with patients, reduced patient empathy, and lower patient rapport, which may make injured patients more likely to file a claim or lawsuit.45 Because the relationshipbetween burnout and medical error is bidirectional, malpractice claims tend to increase burnout, which increases error. Given the time it takes to resolve most malpractice claims, the uncertainty of medical malpractice may be especially stressful for health care providers.46,47
Burnout is not a mitigating factor in malpractice. Our sympathies may go out to a professional suffering from burnout, but it does not excuse or reduce liability—it may, indeed, be an aggravating factor. Clinicians who can diagnose burnout and know its negative consequences but fail to deal with their own burnout may be demonstrating negligence if there has been harm to a patient related to the burnout.48
Institutional or corporate liability to patients
Health care institutions have obligations to avoid injury to patients. Just as poorly maintained medical equipment may harm patients, so may burned-out professionals. Therefore, institutions have some obligation to supervise and avoid the increased risks to patients posed by professionals suffering from burnout.
Respondeat superior and institutional negligence. Institutional liability may arise in two ways, the first through agency, or respondeat superior. That is, if the physician or other professional is an employee (or similar agent) of the health care institution, that institution is generally responsible for the physician’s negligence during the employment.49 Even if the physician is not an employee (for example, an independent contractor providing care or using the hospital facilities), the health care facility may be liable for the physician’s negligence.50 Liability may occur, for example, if the health care facility was aware that the physician was engaged in careless practice or was otherwise a risk to patients but the facility did not take steps to avoid those risks.51 The basis for liability is that the health care organization owes a duty to patients to take reasonable care to ensure that its facilities are not used to injure patients negligently.52 Just as it must take care that unqualified physicians are not granted privileges to practice, it also must take reasonable steps to protect patients when it is aware (through nurses or other agents) of a physician’s negligent practice.
In one case, for example, the court found liability where a staff member had “severe” burnout in a physician’s office and failed to read fetal monitoring strips. The physician was found negligent for relying on the staff member who was obviously making errors in interpretation of fetal distress.53
Continue to: Legal obligations of health care organizations to physicians and others...
Legal obligations of health care organizations to physicians and others
In addition to obligations to patients, health care organizations may have obligations to employees (and others) at risk for injury. For example, assume a patient is diagnosed with a highly contagious disease. The health care organization would be obligated to warn, and take reasonable steps to protect, the staff (employees and independent contractors) from being harmed from exposure to the disease. This principle may apply to coworkers of employees with significant burnout, thereby presenting a danger in the workplace. The liability issue is more difficult for employees experiencing job-related burnout themselves. Organizations generally compensate injured employees through no-fault workers’ compensation (an insurance-like system); for independent contractors, the liability is usually through a tort claim (negligence).54
In modern times, a focus has been on preventing those injuries, not just providing compensation after injuries have occurred. Notably, federal and state occupational health and safety laws (particularly the Occupational Safety and Health Administration [OSHA]) require most organizations (including those employing health care providers) to take steps to mitigate various kinds of worker injuries.55
Although these worker protections have commonly been applied to hospitals and other health care providers, burnout has not traditionally been a significant concern in federal or state OSHA enforcement. For example, no formal federal OSHA regulations govern work-related burnout. Regulators, including OSHA, are increasingly interested in burnout that may affect many employees. OSHA has several recommendations for reducing health care work burnout.56 The Surgeon General has expressed similar concerns.57 The federal government recently allocated $103 million from the American Rescue Plan to address burnout among health care workers.58 Also, OSHA appears to be increasing its oversight of healthcare-institution-worker injuries.55
Is burnout a “disability”?
The federal Americans with Disabilities Act (ADA) and similar state laws prohibit discrimination based on disability.59 A disability is defined as a “physical or mental impairment that substantially limits one or more major life activities” or “perceived as having such an impairment.”60 The initial issue is whether burnout is a “mental impairment.” As noted earlier, it is not officially a “medical condition.”61 To date, the United Nations has classified it as an “occupational phenomenon.”62 It may, therefore, not qualify under the ADA, even if it “interferes with a major life activity.” There is, however, some movement toward defining burnout as a mental condition. Even if defined as a disability, there would still be legal issues of how severe it must be to qualify as a disability and the proper accommodation. Apart from the legal definition of an ADA disability, as a practical matter it likely is in the best interest of health care facilities to provide accommodations that reduce burnout. A number of strategies to decrease the incidence of burnout include the role of health care systems (FIGURE 2).
In conclusion we look at several things that can be done to “treat” or reduce burnout. That effort requires the cooperation of physicians and other providers, health care facilities, training programs, licensing authorities, and professional organizations. See suggestions below.
Conclusion
There are many excellent suggestions for reducing burnout and improving patient care and practitioner satisfaction.63-65 We conclude with a summary of some of these suggestions for individual practitioners, health care organizations, the profession, and licensing. It is worth remembering, however, that it will require the efforts of each area to reduce burnout substantially.
For practitioners:
- Engage in quality coaching/therapy on mindfulness and stress management.
- Practice self-care, including exercise and relaxation techniques.
- Make work-life balance a priority.
- Take opportunities for collegial social and professional discussions.
- Prioritize (and periodically assess) your own professional satisfaction and burnout risk.
- Smile—enjoy a sense of humor (endorphins and cortisol).
For health care organizations:
- Urgently work with vendors and regulators to revise electronic health records to reduce their substantial impact on burnout.
- Reduce physicians’ time on clerical and administrative tasks (eg, by enhancing the use of quality AI, scribes, and automated notes from appointments. (This may increase the time they spend with patients.) Eliminate “pajama-time” charting.
- Provide various kinds of confidential professional counseling, therapy, and support related to burnout prevention and treatment, and avoid any penalty or stigma related to their use.
- Provide reasonable flexibility in scheduling.
- Routinely provide employees with information about burnout prevention and services.
- Appoint a wellness officer with authority to ensure the organization maximizes its prevention and treatment services.
- Constantly seek input from practitioners on how to improve the atmosphere for practice to maximize patient care and practitioner satisfaction.
- Provide ample professional and social opportunities for discussing and learning about work-life balance, resilience, intellectual stimulation, and career development.
For regulators, licensors, and professional organizations:
- Work with health care organizations and EHR vendors to substantially reduce the complexity, physician effort, and stress associated with those record systems. Streamlining should, in the future, be part of formally certifying EHR systems.
- Reduce the administrative burden on physicians by modifying complex regulations and using AI and other technology to the extent possible to obtain necessary reimbursement information.
- Eliminate unnecessary data gathering that requires practitioner time or attention.
- Licensing, educational, and certifying bodies should eliminate any questions regarding the diagnosis or treatment of mental health and focus on current (or very recent) impairments.
- Seek funding for research on burnout prevention and treatment.
Dr. H is a 58-year-old ObGyn who, after completing residency, went into solo practice. The practice grew, and Dr. H found it increasingly more challenging to cover, especially the obstetrics sector. Dr. H then merged the practice with a group of 3 other ObGyns. Their practice expanded, and began recruiting recent residency graduates. In time, the practice was bought out by the local hospital health care system. Dr. H was faced with complying with the rules and regulations of that health care system. The electronic health record (EHR) component proved challenging, as did the restrictions on staff hiring (and firing), but Dr. H did receive a paycheck each month and complied with it all. The health care system administrators had clear financial targets Dr. H was to meet each quarter, which created additional pressure. Dr. H used to love being an OB and providing excellent care for every patient, but that sense of accomplishment was being lost.
Dr. H increasingly found it difficult to focus because of mind wandering, especially in the operating room (OR). Thoughts occurred about retirement, the current challenges imposed by “the new way of practicing medicine” (more focused on financial productivity restraints and reimbursement), and EHR challenges. Then Dr. H’s attention would return to the OR case at hand. All of this resulted in considerable stress and emotional exhaustion, and sometimes a sense of being disconnected. A few times, colleagues or nurses had asked Dr. H if everything was “okay,” or if a break would help. Dr. H made more small errors than usual, but Dr. H’s self-assessment was “doing an adequate job.” Patient satisfaction scores (collected routinely by the health care system) declined over the last 9 months.
Six months ago, Dr. H finished doing a laparoscopic total hysterectomy and bilateral salpingo-oophorectomy and got into the right uterine artery. The estimated blood loss was 3,500 mL. Using minimally invasive techniques, Dr. H identified the bleeder and, with monopolar current, got everything under control. The patient went to the post-anesthesia care unit, and all appeared to be in order. Her vital signs were stable, and she was discharged home the same day.
The patient presented 1 week later with lower abdominal and right flank pain. Dr. H addressed the problem in the emergency department and admitted the patient for further evaluation and urology consultation. The right ureter was damaged and obstructed; ultimately, the urologist performed a psoas bladder hitch. The patient recovered slowly, lost several weeks of work, experienced significant pain, and had other disruptions and costs. Additional medical care related to the surgery is ongoing. A health care system committee asked Dr. H to explain the problem. Over the last 6 months, Dr. H’s frustration with practice and being tired and disconnected have increased.
Dr. H has received a letter from a law firm saying that he and the health care system are being sued for malpractice focused on an iatrogenic ureter injury. The letter names two very reputable experts who are prepared to testify that the patient’s injury resulted from clear negligence. Dr. H has told the malpractice carrier absolutely not to settle this case—it is “a sham— without merit.” The health care system has asked Dr. H to take a “burnout test.”
Legal considerations
Dr. H exhibits relatively clear signs of professional burnout. The fact that there was a bad outcome while Dr. H was experiencing burnout is not proof of negligence (or, breach of duty of care to the patient). Nor is it a defense or mitigation to any malpractice that occurred.
In the malpractice case, the plaintiff will have the burden of proving that Dr. H’s treatment was negligent in that it fell below the standard of care. Even if it was a medical error, the question is whether it was negligence. If the patient/plaintiff, using expert witnesses, can prove that Dr. H fell below the standard of care that caused injury, Dr. H may be liable for the resulting extra costs, loss of income, and pain and suffering resulting from the negligent care.
The health care system likely will also be responsible for Dr. H’s negligence, either through respondeat superior (for example, if Dr. H is an employee) or for its own negligence. The case for its negligence is that the nurses and assistants had repeatedly seen him making errors and becoming disengaged (to the extent that they asked Dr. H if “everything is okay” or if a break would help). Furthermore, Dr. H’s patient satisfaction scores have been declining for several months. The plaintiff will argue that Dr. H exhibited classic burnout symptoms with the attendant risks of medical errors. However, the health care system did not take action to protect patients or to assist Dr. H. In short, one way or another, there is some likelihood that the health care system may also be liable if patient injuries are found to have been caused by negligence.
At this point, the health care system also faces the question of how to work with Dr. H in the future. The most pressing question is whether or not to allow Dr. H to continue practicing. If, as it appears, Dr. H is dealing with burnout, the pressure of the malpractice claim could well increase the probability of other medical mistakes. The institution has asked Dr. H to take a burnout test, but it is unclear where things go if the test (as likely) demonstrates significant burnout. This is a counseling and human relations question, at least as much as a legal issue, and the institution should probably proceed in that way—which is, trying to understand and support Dr. H and determining what can be done to address the burnout. At the same time, the system must reasonably assess Dr. H’s fitness to continue practicing as the matters are resolved. Almost everyone shares the goal to provide every individual and corporate opportunity for Dr. H to deal with burnout issues and return to successful practice.
Dr. H will be represented in the malpractice case by counsel provided through the insurance carrier. However, Dr. H would be well advised to retain a trusted and knowledgeable personal attorney. For example, the instruction not to consider settlement is likely misguided, but Dr. H needs to talk with an attorney that Dr. H has chosen and trusts. In addition, the attorney can help guide Dr. H through a rational process of dealing with the health care system, putting the practice in order, and considering the options for the future.
The health care system should reconsider its processes to deal with burnout to ensure the quality of care, patient satisfaction, professional retention, and economic stability. Several burnoutresponse programs have had success in achieving these goals.
What’s the Verdict?
Dr. H received good mental health, legal, and professional advice. As a result, an out of court settlement was reached following pretrial discovery. Dr. H has continued consultation regarding burnout and has returned to productive practice.
- Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clinic Proceed. 2019;94:1681-1694.
- Smith R, Rayburn W. Burnout in obstetrician-gynecologists. Its prevalence, identification, prevention, and reversal. Obstet Gynecol Clin North Am. 2021;48:231-245. https://doi. org/10.1016/j.ogc.2021.06.003
- Patti MG, Schlottmann F, Sarr MG. The problem of burnout among surgeons. JAMA Surg. 2018;153:403-404. doi:10.1001 /jamasurg.2018.0047
- Carrau D, Janis JE. Physician burnout: solutions for individuals and organizations. Plastic and Reconstructive Surgery Global Open. 2021;91-97.
- Southwick R. The key to fixing physician burnout is the workplace not the worker. Contemporary Ob/Gyn. March 13, 2023.
- Patel RS, Bachu R, Adikey A, et al. Factors related to physician burnout and its consequences: a review. Behav Sciences. 2018;8:98.
- Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clinic Proceed. 2020;95:476-487.
- Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017;317:901-902. doi:10.1001/jama.2017.0076
- Ommaya AK, Cipriano PF, Hoyt DB, et al. Care-centered clinical documentation in the digital environment: Solutions to alleviate burnout. National Academy of Medicine Perspectives. 2018.
- Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;382:2485-2487. Discussion Paper, National Academy of Medicine. Accessed July 21, 2023. https://nam .edu/care
- Ji YD, Robertson FC, Patel NA, et al. Assessment of risk factors for suicide among US health care professionals. JAMA Surg. 2020;155:713-721. centered-clinical-documentation-digital -environment-solutions-alleviate-burnout/
- Shanafelt TD, West CP, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clinic Proceed. 2022;97:2248-2258.
- Herber-Valdez C, Kupesic-Plavsic S. Satisfaction and shortfall of OB-GYN physicians and radiologists. J. Ultrasound Obstet Gynecol. 2021;15:387-392.
- Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. National Academy of Medicine Perspectives. Accessed July 5, 2017. https://iuhcpe.org/file_manager/1501524077-Burnout -Among-Health-Care-Professionals-A-Call-to-Explore-and -Address-This-Underrecognized-Threat.pdf
- Olson KD. Physician burnout—a leading indicator of health system performance? Mayo Clinic Proceed. 2017;92: 1608-1611.
- American College of Obstetricians and Gynecologists. Why obgyns are burning out. October 28, 2019. Accessed July 21, 2023. https://www.acog.org/news/news-articles/2019/10/why-ob -gyns-are-burning-out#:~:text=A%202017%20report%20 by%20the,exhaustion%20or%20lack%20of%20motivation
- Peckham C. National physician burnout & depression report 2018. Medscape. January 17, 2018. https://nap. nationalacademies.org/catalog/25521/taking-action -against-clinician-burnout-a-systems-approach-to -professional
- Marsa L. Labor pains: The OB-GYN shortage. AAMC News. Nov. 15, 2018. Accessed July 21, 2023. https://www.aamc.org /news-insights/labor-pains-ob-gyn-shortage
- American College of Obstetricians and Gynecologists. Coping with the stress of medical professional liability litigation. ACOG Committee Opinion. February 2005;309:453454. Accessed July 21, 2023. https://www.acog.org/clinical /clinical-guidance/committee-opinion/articles/2013/01 /coping-with-the-stress-of-medical-professional-liability -litigation
- Reith TP. Burnout in United States healthcare professionals: a narrative review. Cureus. 2018;10:e3681. doi: 10.7759 /cureus.3681
- Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;4:784-790.
- Sullivan D, Sullivan V, Weatherspoon D, et al. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs Clin North Am. 2022;57:79-99. doi: 10.1016 /j.cnur.2021.11.006
- Chandawarkar A, Chaparro JD. Burnout in clinicians. Curr Prob Pediatr Adolesc Health Care. 2021;51:101-104. https ://doi.org/10.1016/j.cppeds.2021.101104
- Brady KJS, Sheldrick RC, Ni P, et al. Examining the measurement equivalence of the Maslach Burnout Inventory across age, gender, and specialty groups in US physicians. J Patient-Reported Outcomes. 2021;5.
- Association of American Medical Colleges. Physician Specialty Data Report—Active Physicians by Sex and Specialty, 2021. Accessed June 19, 2023. https://www.aamc .org/data-reports/workforce/data/active-physicians-sex -specialty-2021
- Association of American Medical Colleges. Physician Specialty Data Report—ACGME Residents and Fellows by Sex and Specialty, 2021. Accessed June 19, 2023. https://www .aamc.org/data-reports/workforce/data/acgme-residents -fellows-sex-and-specialty-2021
- Painter LM, Biggans KA, Turner CT. Risk managementobstetrics and gynecology perspective. Clin Obstet Gynecol. 2023;66:331-341. DOI:10.1097/GRF.0000000000000775
- Darney BG, Boniface E, Liberty A. Assessing the effect of abortion restrictions. Obstetr Gynecol. 2023;141:233-235.
- Heuerman AC, Bessett D, Antommaria AHM, et al. Experiences of reproductive genetic counselors with abortion regulations in Ohio. J Genet Counseling. 2022;31:641-652.
- Brandi K, Gill P. Abortion restrictions threaten all reproductive health care clinicians. Am J Public Health. 2023;113:384-385.
- Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131-1150. doi: 10.1001/jama.2018.1277
- Williamson K, Lank PM, Cheema N, et al. Comparing the Maslach Burnout Inventory to other well-being instruments in emergency medicine residents. J Graduate Med Education. 2018;532-536. DOI: http://dx.doi.org/10.4300 /JGME-D-18-00155.1
- Brady KJS, Sheldrick RC, Ni P, et al. Establishing crosswalks between common measures of burnout in US physicians. J Gen Intern Med. 2022;37:777-784.
- Zhang X, Song Y, Jiang T, et al. Interventions to reduce burnout of physicians and nurses: an overview of systematic reviews and meta-analyses. Medicine (Baltimore). 2020;26:e20992. DOI: 10.1097/MD.0000000000020992
- Scheepers RA, Emke H, Ronald M, et al. The impact of mindfulness-based interventions on doctors’ well-being and performance: a systematic review. Med Education. 2020;54:138-149. https://doi.org/10.1111/medu.14020
- Olson K, Marchalik D, Farley H, et al. Organizational strategies to reduce physician burnout and improve professional fulfillment. Curr Prob Pediatr Adolesc Health Care. 2019;49:12. https://doi.org/10.1016/j.cppeds.2019.100664
- Berry LL, Awdish RLA, Swensen SJ. 5 ways to restore depleted health care workers. Harvard Business Rev. February 11, 2022.
- Sullivan AB, Hersh CM, Rensel M, et al. Leadership inequity, burnout, and lower engagement of women in medicine. J Health Serv Psychol. 2023;49:33-39.
- Hoffman S. Healing the healers: legal remedies for physician burnout. Yale J Health Policy Law Ethics. 2018;18:56-113.
- Federation of State Medical Boards. Physician wellness and burnout: report and recommendations of the workgroup on physician wellness and burnout. (Policy adopted by FSMB). April 2018. Accessed July 21, 2023. https://www.fsmb.org /siteassets/advocacy/policies/policy-on-wellness-and -burnout.pdf
- Robinson C, Kettering C, Sanfilippo JS. Medical malpractice lawsuits. Clin Obstet Gynecol. 2023;66:256-260. DOI: https ://doi.org/10.1097/GRF.0000000000000777
- Gittler GJ, Goldstein EJ. The elements of medical malpractice: an overview. Clin Infect Dis. 1996;23:1152-1155.
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467:339-347.
- Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clinic Proceed. 2018;93: 1571-1580.
- Sundholm B. Elevating physician-patient relationships in the shadow of metric mania. Drexel L Rev. 2020;12:287-330.
- Ghaith S, Campbell RL, Pollock JR, et al. Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. Healthcare. 2022;10:1328.
- Muller TM, Warsi S. Litigation culture causing burnout in American physicians. Trauma Mental Health Report. April 9, 2021.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. 2015:60;26-28, 30.
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. Southern Med J. 2002;95.5:545-549. DOI 10.1097/00007611-200295050-00018
- Levin H. Hospital vicarious liability for negligence by independent contractor physicians: new rule for new times. Univ Illinois Law Rev. 2005:1291-1332.
- Darling v Charleston Hospital, 33 Ill. 2d 326, 211 N.E.2d 253 (Ill. 1965).
- Dangel R. Hospital liability for physician malpractice. Ohio State Law J. 1986;47:1077-1098.
- Reffitt v Hajjar, 892 S.W.2d 599, 605 (Ky. Ct. App. 1994).
- McMichael BJ. Malpractice. In Laws of Medicine: Core Legal Aspects for the Healthcare Professional. New York, NY: Springer International; 2022:129-150.
- Occupational Safety and Health Administration. Worker safety in hospitals: caring for our caregivers. Accessed June 8, 2023. https://www.osha.gov/hospitals
- Occupational Safety and Health Administration. Workplace stress. Accessed June 8, 2023. https://www.osha.gov /workplace-stress/understanding-the-problem
- U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. Addressing health worker burnout. Accessed July 21, 2023. https://www.hhs.gov/sites/default/files/health -worker-wellbeing-advisory.pdf
- Department of Health & Human Services. Biden-Harris administration awards $103 Million in American Rescue Plan funds to reduce burnout and promote mental health and wellness among health care workforce. January 20, 2022. Accessed July 24, 2023. https://www.hhs.gov/about /news/2022/01/20/biden-harris-administration-awards -103-million-american-rescue-plan-funds-reduce-burnout -promote-mental-health-wellness-among-health-care -workforce.html
- Rothstein LF, Irzyk J. Disabilities and the Law. 4th ed. Toronto, Canada: Thompson Reuters; 2023.
- Department of Labor. Guide to disability rights laws. February 28, 2020. Accessed July 24, 2023. https://www .ada.gov/resources/disability-rights-guide/#:~:text=An%20 individual%20with%20a%20disability%20is%20defined%20 by%20the%20ADA,as%20having%20such%20an%20 impairment
- Nadon L, De Beer LT, Morin AJS. Should burnout be conceptualized as a mental disorder? Behavioral Sci. 2022;12:82.
- World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases. May 28, 2019. Accessed July 21, 2023. https://www.who.int/news /item/28-05-2019-burn-out-an-occupational-phenomenon -international-classification-of-diseases
- Hoffman S. Physician burnout: why legal and regulatory systems may need to step in. The Conversation. July 9, 2019. https://theconversation.com/physician-burnout-why-legal -and-regulatory-systems-may-need-to-step-in-119705
- Jha A, Iliff A, Chaoi A, et al. A crisis in healthcare: a call to action on physician burnout. Harvard Global Health Institute. 2019. Accessed July 21, 2023. https://www.massmed.org /Publications/Research,-Studies,-and-Reports/Physician -Burnout-Report-2018/
- Arnsten AF, Shanafelt T. Physician distress and burnout: the neurobiological perspective. Mayo Clin Proceed. 2021;96:763-769.
- Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clinic Proceed. 2019;94:1681-1694.
- Smith R, Rayburn W. Burnout in obstetrician-gynecologists. Its prevalence, identification, prevention, and reversal. Obstet Gynecol Clin North Am. 2021;48:231-245. https://doi. org/10.1016/j.ogc.2021.06.003
- Patti MG, Schlottmann F, Sarr MG. The problem of burnout among surgeons. JAMA Surg. 2018;153:403-404. doi:10.1001 /jamasurg.2018.0047
- Carrau D, Janis JE. Physician burnout: solutions for individuals and organizations. Plastic and Reconstructive Surgery Global Open. 2021;91-97.
- Southwick R. The key to fixing physician burnout is the workplace not the worker. Contemporary Ob/Gyn. March 13, 2023.
- Patel RS, Bachu R, Adikey A, et al. Factors related to physician burnout and its consequences: a review. Behav Sciences. 2018;8:98.
- Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clinic Proceed. 2020;95:476-487.
- Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017;317:901-902. doi:10.1001/jama.2017.0076
- Ommaya AK, Cipriano PF, Hoyt DB, et al. Care-centered clinical documentation in the digital environment: Solutions to alleviate burnout. National Academy of Medicine Perspectives. 2018.
- Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;382:2485-2487. Discussion Paper, National Academy of Medicine. Accessed July 21, 2023. https://nam .edu/care
- Ji YD, Robertson FC, Patel NA, et al. Assessment of risk factors for suicide among US health care professionals. JAMA Surg. 2020;155:713-721. centered-clinical-documentation-digital -environment-solutions-alleviate-burnout/
- Shanafelt TD, West CP, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clinic Proceed. 2022;97:2248-2258.
- Herber-Valdez C, Kupesic-Plavsic S. Satisfaction and shortfall of OB-GYN physicians and radiologists. J. Ultrasound Obstet Gynecol. 2021;15:387-392.
- Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. National Academy of Medicine Perspectives. Accessed July 5, 2017. https://iuhcpe.org/file_manager/1501524077-Burnout -Among-Health-Care-Professionals-A-Call-to-Explore-and -Address-This-Underrecognized-Threat.pdf
- Olson KD. Physician burnout—a leading indicator of health system performance? Mayo Clinic Proceed. 2017;92: 1608-1611.
- American College of Obstetricians and Gynecologists. Why obgyns are burning out. October 28, 2019. Accessed July 21, 2023. https://www.acog.org/news/news-articles/2019/10/why-ob -gyns-are-burning-out#:~:text=A%202017%20report%20 by%20the,exhaustion%20or%20lack%20of%20motivation
- Peckham C. National physician burnout & depression report 2018. Medscape. January 17, 2018. https://nap. nationalacademies.org/catalog/25521/taking-action -against-clinician-burnout-a-systems-approach-to -professional
- Marsa L. Labor pains: The OB-GYN shortage. AAMC News. Nov. 15, 2018. Accessed July 21, 2023. https://www.aamc.org /news-insights/labor-pains-ob-gyn-shortage
- American College of Obstetricians and Gynecologists. Coping with the stress of medical professional liability litigation. ACOG Committee Opinion. February 2005;309:453454. Accessed July 21, 2023. https://www.acog.org/clinical /clinical-guidance/committee-opinion/articles/2013/01 /coping-with-the-stress-of-medical-professional-liability -litigation
- Reith TP. Burnout in United States healthcare professionals: a narrative review. Cureus. 2018;10:e3681. doi: 10.7759 /cureus.3681
- Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;4:784-790.
- Sullivan D, Sullivan V, Weatherspoon D, et al. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs Clin North Am. 2022;57:79-99. doi: 10.1016 /j.cnur.2021.11.006
- Chandawarkar A, Chaparro JD. Burnout in clinicians. Curr Prob Pediatr Adolesc Health Care. 2021;51:101-104. https ://doi.org/10.1016/j.cppeds.2021.101104
- Brady KJS, Sheldrick RC, Ni P, et al. Examining the measurement equivalence of the Maslach Burnout Inventory across age, gender, and specialty groups in US physicians. J Patient-Reported Outcomes. 2021;5.
- Association of American Medical Colleges. Physician Specialty Data Report—Active Physicians by Sex and Specialty, 2021. Accessed June 19, 2023. https://www.aamc .org/data-reports/workforce/data/active-physicians-sex -specialty-2021
- Association of American Medical Colleges. Physician Specialty Data Report—ACGME Residents and Fellows by Sex and Specialty, 2021. Accessed June 19, 2023. https://www .aamc.org/data-reports/workforce/data/acgme-residents -fellows-sex-and-specialty-2021
- Painter LM, Biggans KA, Turner CT. Risk managementobstetrics and gynecology perspective. Clin Obstet Gynecol. 2023;66:331-341. DOI:10.1097/GRF.0000000000000775
- Darney BG, Boniface E, Liberty A. Assessing the effect of abortion restrictions. Obstetr Gynecol. 2023;141:233-235.
- Heuerman AC, Bessett D, Antommaria AHM, et al. Experiences of reproductive genetic counselors with abortion regulations in Ohio. J Genet Counseling. 2022;31:641-652.
- Brandi K, Gill P. Abortion restrictions threaten all reproductive health care clinicians. Am J Public Health. 2023;113:384-385.
- Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131-1150. doi: 10.1001/jama.2018.1277
- Williamson K, Lank PM, Cheema N, et al. Comparing the Maslach Burnout Inventory to other well-being instruments in emergency medicine residents. J Graduate Med Education. 2018;532-536. DOI: http://dx.doi.org/10.4300 /JGME-D-18-00155.1
- Brady KJS, Sheldrick RC, Ni P, et al. Establishing crosswalks between common measures of burnout in US physicians. J Gen Intern Med. 2022;37:777-784.
- Zhang X, Song Y, Jiang T, et al. Interventions to reduce burnout of physicians and nurses: an overview of systematic reviews and meta-analyses. Medicine (Baltimore). 2020;26:e20992. DOI: 10.1097/MD.0000000000020992
- Scheepers RA, Emke H, Ronald M, et al. The impact of mindfulness-based interventions on doctors’ well-being and performance: a systematic review. Med Education. 2020;54:138-149. https://doi.org/10.1111/medu.14020
- Olson K, Marchalik D, Farley H, et al. Organizational strategies to reduce physician burnout and improve professional fulfillment. Curr Prob Pediatr Adolesc Health Care. 2019;49:12. https://doi.org/10.1016/j.cppeds.2019.100664
- Berry LL, Awdish RLA, Swensen SJ. 5 ways to restore depleted health care workers. Harvard Business Rev. February 11, 2022.
- Sullivan AB, Hersh CM, Rensel M, et al. Leadership inequity, burnout, and lower engagement of women in medicine. J Health Serv Psychol. 2023;49:33-39.
- Hoffman S. Healing the healers: legal remedies for physician burnout. Yale J Health Policy Law Ethics. 2018;18:56-113.
- Federation of State Medical Boards. Physician wellness and burnout: report and recommendations of the workgroup on physician wellness and burnout. (Policy adopted by FSMB). April 2018. Accessed July 21, 2023. https://www.fsmb.org /siteassets/advocacy/policies/policy-on-wellness-and -burnout.pdf
- Robinson C, Kettering C, Sanfilippo JS. Medical malpractice lawsuits. Clin Obstet Gynecol. 2023;66:256-260. DOI: https ://doi.org/10.1097/GRF.0000000000000777
- Gittler GJ, Goldstein EJ. The elements of medical malpractice: an overview. Clin Infect Dis. 1996;23:1152-1155.
- Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467:339-347.
- Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clinic Proceed. 2018;93: 1571-1580.
- Sundholm B. Elevating physician-patient relationships in the shadow of metric mania. Drexel L Rev. 2020;12:287-330.
- Ghaith S, Campbell RL, Pollock JR, et al. Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. Healthcare. 2022;10:1328.
- Muller TM, Warsi S. Litigation culture causing burnout in American physicians. Trauma Mental Health Report. April 9, 2021.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. 2015:60;26-28, 30.
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. Southern Med J. 2002;95.5:545-549. DOI 10.1097/00007611-200295050-00018
- Levin H. Hospital vicarious liability for negligence by independent contractor physicians: new rule for new times. Univ Illinois Law Rev. 2005:1291-1332.
- Darling v Charleston Hospital, 33 Ill. 2d 326, 211 N.E.2d 253 (Ill. 1965).
- Dangel R. Hospital liability for physician malpractice. Ohio State Law J. 1986;47:1077-1098.
- Reffitt v Hajjar, 892 S.W.2d 599, 605 (Ky. Ct. App. 1994).
- McMichael BJ. Malpractice. In Laws of Medicine: Core Legal Aspects for the Healthcare Professional. New York, NY: Springer International; 2022:129-150.
- Occupational Safety and Health Administration. Worker safety in hospitals: caring for our caregivers. Accessed June 8, 2023. https://www.osha.gov/hospitals
- Occupational Safety and Health Administration. Workplace stress. Accessed June 8, 2023. https://www.osha.gov /workplace-stress/understanding-the-problem
- U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. Addressing health worker burnout. Accessed July 21, 2023. https://www.hhs.gov/sites/default/files/health -worker-wellbeing-advisory.pdf
- Department of Health & Human Services. Biden-Harris administration awards $103 Million in American Rescue Plan funds to reduce burnout and promote mental health and wellness among health care workforce. January 20, 2022. Accessed July 24, 2023. https://www.hhs.gov/about /news/2022/01/20/biden-harris-administration-awards -103-million-american-rescue-plan-funds-reduce-burnout -promote-mental-health-wellness-among-health-care -workforce.html
- Rothstein LF, Irzyk J. Disabilities and the Law. 4th ed. Toronto, Canada: Thompson Reuters; 2023.
- Department of Labor. Guide to disability rights laws. February 28, 2020. Accessed July 24, 2023. https://www .ada.gov/resources/disability-rights-guide/#:~:text=An%20 individual%20with%20a%20disability%20is%20defined%20 by%20the%20ADA,as%20having%20such%20an%20 impairment
- Nadon L, De Beer LT, Morin AJS. Should burnout be conceptualized as a mental disorder? Behavioral Sci. 2022;12:82.
- World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases. May 28, 2019. Accessed July 21, 2023. https://www.who.int/news /item/28-05-2019-burn-out-an-occupational-phenomenon -international-classification-of-diseases
- Hoffman S. Physician burnout: why legal and regulatory systems may need to step in. The Conversation. July 9, 2019. https://theconversation.com/physician-burnout-why-legal -and-regulatory-systems-may-need-to-step-in-119705
- Jha A, Iliff A, Chaoi A, et al. A crisis in healthcare: a call to action on physician burnout. Harvard Global Health Institute. 2019. Accessed July 21, 2023. https://www.massmed.org /Publications/Research,-Studies,-and-Reports/Physician -Burnout-Report-2018/
- Arnsten AF, Shanafelt T. Physician distress and burnout: the neurobiological perspective. Mayo Clin Proceed. 2021;96:763-769.
Recurrent pregnancy loss and inherited thrombophilias: Does low molecular weight heparin improve the live birth rate?
Quenby S, Booth K, Hiller L, et al; ALIFE2 Block Writing Committee and ALIFE2 Investigators. Heparin for women with recurrent miscarriage and inherited thrombophilia (ALIFE2): an international open-label, randomised controlled trial. Lancet. 2023;402:54-61. doi:10.1016/S0140-6736(23)00693-1.
EXPERT COMMENTARY
“Follow the evidence to where it leads, even if the conclusion is uncomfortable.”
—Steven James, author
Women with RPL have endured overzealous evaluations and management despite a lack of proven efficacy. From alloimmune testing that results in paternal leukocyte immunization1 and the long-entrusted metroplasty for a septate uterus recently put under fire2 to the “hammer and nail” approach of preimplantation genetic testing for embryo aneuploid screening,3 patients have been subjected to unsubstantiated treatments.
While the evaluation of RPL has evolved, guidelines from the American Society for Reproductive Medicine (ASRM), American College of Obstetricians and Gynecologists (ACOG), and Royal College of Obstetricians and Gynaecologists (RCOG) do not recommend testing for inherited thrombophilias outside of a history for venous thromboembolism.4-6 These 3 societies support treating acquired thrombophilias that represent the antiphospholipid antibody syndrome.
Citing insufficient evidence for reducing adverse pregnancy outcomes, ACOG recommends the use of prophylactic- or intermediate-dose LMWH or unfractionated heparin (UFH) for patients with “high-risk” thrombophilias only to prevent venous thromboembolism during pregnancy and continuing postpartum.4 (High-risk thrombophilias are defined as factor V Leiden homozygosity, prothrombin gene G20210A mutation homozygosity, heterozygosity for both factor V Leiden homozygosity and prothrombin gene G20210A mutation, or an antithrombin deficiency.4)
To determine the impact of LMWH treatment versus no treatment on live birth rate, Quenby and colleagues conducted a prospective randomized controlled trial of women with RPL and inherited thrombophilias (the ALIFE2 trial). This was a follow-up to their 2010 randomized controlled trial that demonstrated no effect of LMWH with low-dose aspirin versus low-dose aspirin alone compared with placebo in women with unexplained RPL.7
 PHOTO: BETAVERSO/SHUTTERSTOCK
PHOTO: BETAVERSO/SHUTTERSTOCK

Continue to: Details of the study...
Details of the study
The ALIFE2 study took place over 8 years and involved 5 countries, including the United States, with the 2 main centers in the Netherlands and the United Kingdom. Women eligible for the study were aged 18 to 42 years, had an inherited thrombophilia (confirmed by 2 tests), experienced recurrent miscarriages (2 or more consecutive miscarriages, nonconsecutive miscarriages, or intrauterine fetal deaths, irrespective of gestational age), and were less than 7 weeks’ estimated gestational age. Study patients were randomly allocated with a positive pregnancy test to either surveillance or LMWH treatment, which was continued throughout pregnancy.
The primary outcome was live birth rate, and secondary outcomes were a history of miscarriage, ectopic pregnancy, and obstetric complications. A total of 164 women were allocated to LMWH plus standard care, and 162 women to standard care alone. LMWH was shown to be safe without major/minor bleeding or maternal heparin-induced thrombocytopenia.
The statistical calculation was by “intention to treat,” which considers all enrolled participants, including those who dropped out of the study, as opposed to a “per protocol” analysis in which only patients who completed the study were analyzed.
Results. Primary outcome data were available for 320 participants. Of the 162 women in the LMWH-treated group, 116 (72%) had live birth rates, as did 112 (71%) of 158 in the standard care group. There was no significant difference between groups (OR, 1.04; 95% CI, 0.64–1.68).
Study strengths and limitations
The outcome of the ALIFE2 study is consistent with that of a Cochrane review that found insufficient evidence for improved live birth rate in patients with RPL and inherited thrombophilias treated with LMWH versus low-dose aspirin. Of their review of the studies at low risk of bias, only 1 was placebo controlled.8
This study by Quenby and colleagues was well designed and ensured a sufficient number of enrolled participants to comply with their power analysis. However, by beginning LMWH at 7 weeks’ gestation, patients may not have received a therapeutic benefit as opposed to initiation of treatment with a positive pregnancy test. The authors did not describe when testing for thrombophilias occurred or explain the protocol and reason for repeat testing.
Study limitations included a deviation from protocol in the standard care group, which was the initiation of LMWH after 7 weeks’ gestation. In the standard care group, 30 participants received LMWH, 18 of whom started heparin treatment before 12 weeks of gestation. The other 12 participants received LMWH after 12 weeks’ gestation, and 6 of those 12 started after 28 weeks’ gestation, since they were determined to need LMWH for thromboprophylaxis according to RCOG guidelines. While this had the potential to influence outcomes, only 18 of 162 (11%) patients were involved.
The authors did not define RPL based on a clinical versus a biochemical pregnancy loss as the latter is more common and is without agreed upon criteria for testing. Additionally, a lack of patient masking to medication could play an undetermined role in affecting the outcome. ●
This elegant, and vital, randomized controlled trial provides double take-home messages: There is no value in testing for inherited thrombophilias in RPL, as they occur in a similar prevalence in the general population, and there is no significant difference in live birth rate from LMWH treatment in women with RPL and inherited thrombophilias compared with surveillance. Consequently, the increased cost of medication and testing can be averted.
MARK P. TROLICE, MD, MBA
- Wong LF, Porter TF, Scott JR. Immunotherapy for recurrent miscarriage. Cochrane Database Syst Rev. 2014; CD000112. doi:10.1002/14651858.CD000112
- Trolice MP. The septate uterus and metroplasty—another dogma under siege. Fertil Steril. 2021;116:693-694. doi:10.1016/j.fertnstert.2021.06.063
- Dahdouh EM, Balayla J, Garcia-Velasco JA, et al. PGT-A for recurrent pregnancy loss: evidence is growing but the issue is not resolved. Hum Reprod. 2021;36:2805-2806. doi:10.1093 /humrep/deab194
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 197: inherited thrombophilias in pregnancy. Obstet Gynecol. 2018;132:e18-e34. doi:10.1097 /AOG.0000000000002703
- Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98:1103-1111. doi:10.1016/j.fertnstert.2012.06.048
- Regan L, Rai R, Saravelos S, et al; Royal College of Obstetricians and Gynaecologists. Recurrent Miscarriage Green‐top Guideline No. 17. BJOG. June 19, 2023. doi:10.1111/1471 -0528.17515
- Kaandorp SP, Goddijn M, van der Post JA, et al. Aspirin plus heparin or aspirin alone in women with recurrent miscarriage. N Engl J Med. 2010;362:1586-1596. doi:10.1056 /NEJMoa1000641
- de Jong PG, Kaandorp S, Di Nisio M, et al. Aspirin and/or heparin for women with unexplained recurrent miscarriage with or without inherited thrombophilia. Cochrane Database Syst Rev. 2014;CD004734. doi:10.1002/14651858.CD004734 .pub4
Quenby S, Booth K, Hiller L, et al; ALIFE2 Block Writing Committee and ALIFE2 Investigators. Heparin for women with recurrent miscarriage and inherited thrombophilia (ALIFE2): an international open-label, randomised controlled trial. Lancet. 2023;402:54-61. doi:10.1016/S0140-6736(23)00693-1.
EXPERT COMMENTARY
“Follow the evidence to where it leads, even if the conclusion is uncomfortable.”
—Steven James, author
Women with RPL have endured overzealous evaluations and management despite a lack of proven efficacy. From alloimmune testing that results in paternal leukocyte immunization1 and the long-entrusted metroplasty for a septate uterus recently put under fire2 to the “hammer and nail” approach of preimplantation genetic testing for embryo aneuploid screening,3 patients have been subjected to unsubstantiated treatments.
While the evaluation of RPL has evolved, guidelines from the American Society for Reproductive Medicine (ASRM), American College of Obstetricians and Gynecologists (ACOG), and Royal College of Obstetricians and Gynaecologists (RCOG) do not recommend testing for inherited thrombophilias outside of a history for venous thromboembolism.4-6 These 3 societies support treating acquired thrombophilias that represent the antiphospholipid antibody syndrome.
Citing insufficient evidence for reducing adverse pregnancy outcomes, ACOG recommends the use of prophylactic- or intermediate-dose LMWH or unfractionated heparin (UFH) for patients with “high-risk” thrombophilias only to prevent venous thromboembolism during pregnancy and continuing postpartum.4 (High-risk thrombophilias are defined as factor V Leiden homozygosity, prothrombin gene G20210A mutation homozygosity, heterozygosity for both factor V Leiden homozygosity and prothrombin gene G20210A mutation, or an antithrombin deficiency.4)
To determine the impact of LMWH treatment versus no treatment on live birth rate, Quenby and colleagues conducted a prospective randomized controlled trial of women with RPL and inherited thrombophilias (the ALIFE2 trial). This was a follow-up to their 2010 randomized controlled trial that demonstrated no effect of LMWH with low-dose aspirin versus low-dose aspirin alone compared with placebo in women with unexplained RPL.7
 PHOTO: BETAVERSO/SHUTTERSTOCK
PHOTO: BETAVERSO/SHUTTERSTOCK

Continue to: Details of the study...
Details of the study
The ALIFE2 study took place over 8 years and involved 5 countries, including the United States, with the 2 main centers in the Netherlands and the United Kingdom. Women eligible for the study were aged 18 to 42 years, had an inherited thrombophilia (confirmed by 2 tests), experienced recurrent miscarriages (2 or more consecutive miscarriages, nonconsecutive miscarriages, or intrauterine fetal deaths, irrespective of gestational age), and were less than 7 weeks’ estimated gestational age. Study patients were randomly allocated with a positive pregnancy test to either surveillance or LMWH treatment, which was continued throughout pregnancy.
The primary outcome was live birth rate, and secondary outcomes were a history of miscarriage, ectopic pregnancy, and obstetric complications. A total of 164 women were allocated to LMWH plus standard care, and 162 women to standard care alone. LMWH was shown to be safe without major/minor bleeding or maternal heparin-induced thrombocytopenia.
The statistical calculation was by “intention to treat,” which considers all enrolled participants, including those who dropped out of the study, as opposed to a “per protocol” analysis in which only patients who completed the study were analyzed.
Results. Primary outcome data were available for 320 participants. Of the 162 women in the LMWH-treated group, 116 (72%) had live birth rates, as did 112 (71%) of 158 in the standard care group. There was no significant difference between groups (OR, 1.04; 95% CI, 0.64–1.68).
Study strengths and limitations
The outcome of the ALIFE2 study is consistent with that of a Cochrane review that found insufficient evidence for improved live birth rate in patients with RPL and inherited thrombophilias treated with LMWH versus low-dose aspirin. Of their review of the studies at low risk of bias, only 1 was placebo controlled.8
This study by Quenby and colleagues was well designed and ensured a sufficient number of enrolled participants to comply with their power analysis. However, by beginning LMWH at 7 weeks’ gestation, patients may not have received a therapeutic benefit as opposed to initiation of treatment with a positive pregnancy test. The authors did not describe when testing for thrombophilias occurred or explain the protocol and reason for repeat testing.
Study limitations included a deviation from protocol in the standard care group, which was the initiation of LMWH after 7 weeks’ gestation. In the standard care group, 30 participants received LMWH, 18 of whom started heparin treatment before 12 weeks of gestation. The other 12 participants received LMWH after 12 weeks’ gestation, and 6 of those 12 started after 28 weeks’ gestation, since they were determined to need LMWH for thromboprophylaxis according to RCOG guidelines. While this had the potential to influence outcomes, only 18 of 162 (11%) patients were involved.
The authors did not define RPL based on a clinical versus a biochemical pregnancy loss as the latter is more common and is without agreed upon criteria for testing. Additionally, a lack of patient masking to medication could play an undetermined role in affecting the outcome. ●
This elegant, and vital, randomized controlled trial provides double take-home messages: There is no value in testing for inherited thrombophilias in RPL, as they occur in a similar prevalence in the general population, and there is no significant difference in live birth rate from LMWH treatment in women with RPL and inherited thrombophilias compared with surveillance. Consequently, the increased cost of medication and testing can be averted.
MARK P. TROLICE, MD, MBA
Quenby S, Booth K, Hiller L, et al; ALIFE2 Block Writing Committee and ALIFE2 Investigators. Heparin for women with recurrent miscarriage and inherited thrombophilia (ALIFE2): an international open-label, randomised controlled trial. Lancet. 2023;402:54-61. doi:10.1016/S0140-6736(23)00693-1.
EXPERT COMMENTARY
“Follow the evidence to where it leads, even if the conclusion is uncomfortable.”
—Steven James, author
Women with RPL have endured overzealous evaluations and management despite a lack of proven efficacy. From alloimmune testing that results in paternal leukocyte immunization1 and the long-entrusted metroplasty for a septate uterus recently put under fire2 to the “hammer and nail” approach of preimplantation genetic testing for embryo aneuploid screening,3 patients have been subjected to unsubstantiated treatments.
While the evaluation of RPL has evolved, guidelines from the American Society for Reproductive Medicine (ASRM), American College of Obstetricians and Gynecologists (ACOG), and Royal College of Obstetricians and Gynaecologists (RCOG) do not recommend testing for inherited thrombophilias outside of a history for venous thromboembolism.4-6 These 3 societies support treating acquired thrombophilias that represent the antiphospholipid antibody syndrome.
Citing insufficient evidence for reducing adverse pregnancy outcomes, ACOG recommends the use of prophylactic- or intermediate-dose LMWH or unfractionated heparin (UFH) for patients with “high-risk” thrombophilias only to prevent venous thromboembolism during pregnancy and continuing postpartum.4 (High-risk thrombophilias are defined as factor V Leiden homozygosity, prothrombin gene G20210A mutation homozygosity, heterozygosity for both factor V Leiden homozygosity and prothrombin gene G20210A mutation, or an antithrombin deficiency.4)
To determine the impact of LMWH treatment versus no treatment on live birth rate, Quenby and colleagues conducted a prospective randomized controlled trial of women with RPL and inherited thrombophilias (the ALIFE2 trial). This was a follow-up to their 2010 randomized controlled trial that demonstrated no effect of LMWH with low-dose aspirin versus low-dose aspirin alone compared with placebo in women with unexplained RPL.7
 PHOTO: BETAVERSO/SHUTTERSTOCK
PHOTO: BETAVERSO/SHUTTERSTOCK

Continue to: Details of the study...
Details of the study
The ALIFE2 study took place over 8 years and involved 5 countries, including the United States, with the 2 main centers in the Netherlands and the United Kingdom. Women eligible for the study were aged 18 to 42 years, had an inherited thrombophilia (confirmed by 2 tests), experienced recurrent miscarriages (2 or more consecutive miscarriages, nonconsecutive miscarriages, or intrauterine fetal deaths, irrespective of gestational age), and were less than 7 weeks’ estimated gestational age. Study patients were randomly allocated with a positive pregnancy test to either surveillance or LMWH treatment, which was continued throughout pregnancy.
The primary outcome was live birth rate, and secondary outcomes were a history of miscarriage, ectopic pregnancy, and obstetric complications. A total of 164 women were allocated to LMWH plus standard care, and 162 women to standard care alone. LMWH was shown to be safe without major/minor bleeding or maternal heparin-induced thrombocytopenia.
The statistical calculation was by “intention to treat,” which considers all enrolled participants, including those who dropped out of the study, as opposed to a “per protocol” analysis in which only patients who completed the study were analyzed.
Results. Primary outcome data were available for 320 participants. Of the 162 women in the LMWH-treated group, 116 (72%) had live birth rates, as did 112 (71%) of 158 in the standard care group. There was no significant difference between groups (OR, 1.04; 95% CI, 0.64–1.68).
Study strengths and limitations
The outcome of the ALIFE2 study is consistent with that of a Cochrane review that found insufficient evidence for improved live birth rate in patients with RPL and inherited thrombophilias treated with LMWH versus low-dose aspirin. Of their review of the studies at low risk of bias, only 1 was placebo controlled.8
This study by Quenby and colleagues was well designed and ensured a sufficient number of enrolled participants to comply with their power analysis. However, by beginning LMWH at 7 weeks’ gestation, patients may not have received a therapeutic benefit as opposed to initiation of treatment with a positive pregnancy test. The authors did not describe when testing for thrombophilias occurred or explain the protocol and reason for repeat testing.
Study limitations included a deviation from protocol in the standard care group, which was the initiation of LMWH after 7 weeks’ gestation. In the standard care group, 30 participants received LMWH, 18 of whom started heparin treatment before 12 weeks of gestation. The other 12 participants received LMWH after 12 weeks’ gestation, and 6 of those 12 started after 28 weeks’ gestation, since they were determined to need LMWH for thromboprophylaxis according to RCOG guidelines. While this had the potential to influence outcomes, only 18 of 162 (11%) patients were involved.
The authors did not define RPL based on a clinical versus a biochemical pregnancy loss as the latter is more common and is without agreed upon criteria for testing. Additionally, a lack of patient masking to medication could play an undetermined role in affecting the outcome. ●
This elegant, and vital, randomized controlled trial provides double take-home messages: There is no value in testing for inherited thrombophilias in RPL, as they occur in a similar prevalence in the general population, and there is no significant difference in live birth rate from LMWH treatment in women with RPL and inherited thrombophilias compared with surveillance. Consequently, the increased cost of medication and testing can be averted.
MARK P. TROLICE, MD, MBA
- Wong LF, Porter TF, Scott JR. Immunotherapy for recurrent miscarriage. Cochrane Database Syst Rev. 2014; CD000112. doi:10.1002/14651858.CD000112
- Trolice MP. The septate uterus and metroplasty—another dogma under siege. Fertil Steril. 2021;116:693-694. doi:10.1016/j.fertnstert.2021.06.063
- Dahdouh EM, Balayla J, Garcia-Velasco JA, et al. PGT-A for recurrent pregnancy loss: evidence is growing but the issue is not resolved. Hum Reprod. 2021;36:2805-2806. doi:10.1093 /humrep/deab194
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 197: inherited thrombophilias in pregnancy. Obstet Gynecol. 2018;132:e18-e34. doi:10.1097 /AOG.0000000000002703
- Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98:1103-1111. doi:10.1016/j.fertnstert.2012.06.048
- Regan L, Rai R, Saravelos S, et al; Royal College of Obstetricians and Gynaecologists. Recurrent Miscarriage Green‐top Guideline No. 17. BJOG. June 19, 2023. doi:10.1111/1471 -0528.17515
- Kaandorp SP, Goddijn M, van der Post JA, et al. Aspirin plus heparin or aspirin alone in women with recurrent miscarriage. N Engl J Med. 2010;362:1586-1596. doi:10.1056 /NEJMoa1000641
- de Jong PG, Kaandorp S, Di Nisio M, et al. Aspirin and/or heparin for women with unexplained recurrent miscarriage with or without inherited thrombophilia. Cochrane Database Syst Rev. 2014;CD004734. doi:10.1002/14651858.CD004734 .pub4
- Wong LF, Porter TF, Scott JR. Immunotherapy for recurrent miscarriage. Cochrane Database Syst Rev. 2014; CD000112. doi:10.1002/14651858.CD000112
- Trolice MP. The septate uterus and metroplasty—another dogma under siege. Fertil Steril. 2021;116:693-694. doi:10.1016/j.fertnstert.2021.06.063
- Dahdouh EM, Balayla J, Garcia-Velasco JA, et al. PGT-A for recurrent pregnancy loss: evidence is growing but the issue is not resolved. Hum Reprod. 2021;36:2805-2806. doi:10.1093 /humrep/deab194
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 197: inherited thrombophilias in pregnancy. Obstet Gynecol. 2018;132:e18-e34. doi:10.1097 /AOG.0000000000002703
- Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98:1103-1111. doi:10.1016/j.fertnstert.2012.06.048
- Regan L, Rai R, Saravelos S, et al; Royal College of Obstetricians and Gynaecologists. Recurrent Miscarriage Green‐top Guideline No. 17. BJOG. June 19, 2023. doi:10.1111/1471 -0528.17515
- Kaandorp SP, Goddijn M, van der Post JA, et al. Aspirin plus heparin or aspirin alone in women with recurrent miscarriage. N Engl J Med. 2010;362:1586-1596. doi:10.1056 /NEJMoa1000641
- de Jong PG, Kaandorp S, Di Nisio M, et al. Aspirin and/or heparin for women with unexplained recurrent miscarriage with or without inherited thrombophilia. Cochrane Database Syst Rev. 2014;CD004734. doi:10.1002/14651858.CD004734 .pub4
U.S. maternal mortality crisis grows, yet deaths seem preventable
On June 2, 2019, 35-year-old Anne Hutchinson gave birth to her first child, Lillian. There were no problems with the pregnancy or the birth at Fairview Hospital, which is part of the Cleveland Clinic system.
But 2 days after the birth, she had shortness of breath and couldn’t lie down and breathe.
“My mom’s a nurse, and she was like, ‘You need to go to the hospital immediately,’” Ms. Hutchinson said. When she was admitted to the hospital, there were suddenly “10 doctors in the room.”
Ms. Hutchinson was diagnosed with peripartum cardiomyopathy, a weakness of the heart muscle. She had heart failure. The seriousness of heart failure is measured by the ejection fraction, or the percentage of blood the heart pumps out. Normal is 50%-70%. Ms. Hutchinson’s ejection fraction was 20%.
She was put on medication, left the hospital after 5 days, and her ejection fraction eventually rose to 35%. But she was still at risk for sudden cardiac death.
“The cardiologist said to me, ‘You probably can’t have any more children.’ My heart did not bounce back,” Ms. Hutchinson said.
By the end of 2019, her cardiologist determined that she needed an internal cardiac defibrillator, which monitors the heartbeat and delivers electric shocks to restore the heart’s normal rhythm when needed.
By 2020, when Ms. Hutchinson’s ejection fraction was near normal, she decided that she wanted another child.
“I had a daughter. She was beautiful and amazing. But I felt like I wanted to have a sibling for her,” she says. Yet when her cardiologist at Fairview Hospital heard the plan, she told her getting pregnant again “would be like Russian roulette.”
Ms. Hutchinson is one of a growing number of women whose medical condition puts them at high risk of death during and after giving birth. An estimated 30% of maternal deaths in the United States result from cardiovascular disease – a problem that has become more common with increases in diabetes and obesity.
And, in some women, hypertension can develop suddenly during pregnancy. This is called preeclampsia and is increasing in the United States, particularly in Black women. In rare cases, it can become the life-threatening condition eclampsia, with seizures and death.
Three-time Olympic medalist and world champion sprinter Tori Bowie was found dead in June of apparent complications of pregnancy. The medical examiner’s office in Orange County, Fla., said she was believed to have been in her 8th month of pregnancy and may have died of eclampsia.
Heart conditions in pregnant women are one of a long list of reasons why the United States has the highest maternal mortality rate of any developed country. But the risk is marked by significant racial differences, with death rates three times higher in Black women, compared with White women.
What troubles many experts is that it is estimated that 80% of these deaths are preventable.
“That is a ridiculous number,” said Melissa A. Simon, MD, MPH, director of the Center for Health Equity Transformation at Northwestern Medicine in Evanston, Ill.. “For a health care system in a country that is so high-resourced and high-income, for 8 out of 10 deaths for moms who are pregnant [to be preventable], that’s absolutely unacceptable.”
Pregnant women are not only at risk of death from cardiovascular complications, but other types of problems, including hemorrhage, thrombotic embolism, and infection.
But experts now are focusing attention on nonmedical reasons for maternal mortality, such as racial disparities and the fundamental issue of whether women are telling doctors about their symptoms but are not being heard.
The government has acknowledged the depth of this problem with the Centers for Disease Control and Prevention’s “Hear Her” campaign, which includes videos of women who describe how their health professionals did not take their concerns seriously.
In one such video, a woman named Sanari says 2 days after the birth of her second child, she started developing soreness.
“By day 3, it just didn’t feel right. I asked the nurses, explained my symptoms and that I was having crazy pains, and they assured me it was just gas,” she says on the video.
Sanari described how she started to have odorous discharge and ended up in an emergency room at a different hospital. Health care providers found a large abscess on her uterus.
“I’m glad I didn’t stop at no, and I’m glad someone finally heard me – someone finally listened to me,” she said.
“Hear Her” featured another woman named Lindsay, who had preeclampsia in her first pregnancy and began to get symptoms during her second pregnancy.
She describes how she voiced her concerns to her doctors, saying, “sometimes it would be, ‘Oh, you’re pregnant and your feet are supposed to swell. … It’s just fine.’ But I didn’t feel fine.”
The campaign aims to raise awareness of warning signs that require fast medical attention to prevent pregnancy-related deaths.
But Shanna Cox, associate director of the CDC’s Division of Reproductive Health, said the agency has collected many stories of women who died or nearly died because their concerns were not being addressed properly.
Ms. Cox says another part of the campaign “is really focused on health care providers and listening … to their patients, providing that respectful patient-centered care to be sure that all their concerns are addressed.”
And some experts believe the thinking has shifted even more dramatically.
“We’ve moved from beyond the days of blaming the individual, the birth person, or the woman, to say you haven’t done this, you haven’t come into health care, you are not taking care of yourself, you aren’t keeping your appointments,” says Laurie Zephyrin, MD, MPH, vice president of the Commonwealth Fund, a private foundation in New York dedicated to improving health care.
Dr. Zephyrin says the health care system falls short of providing equitable, quality care. “There’s data that shows Black people receive worse care than White people for about 40% of quality measures,” she said.
These disparities have led to the formation of organizations like National Birth Equity Collaborative, an advocacy group in New Orleans working to improve maternal care for Black patients.
Carmen Green, vice president of research and strategy, said institutional racism has been embedded into some health care providers.
“They have this hierarchy that teaches them they have to manage, they have to control, they have to direct the medical experience, and that is just not how birthing works,” she said.
She used the example of the birth experience as a car ride, where the mothers have been in the backseat with the doctor driving. “We want the birthing person in the driving seat and want [them] to be respected as a person who is deciding where that destination is going,” Ms. Green said.
She says health providers often “blame the mamas” based on assumptions, stereotypes, and biases against low-income people.
So how is American medicine responding to the medical and social causes of maternal mortality?
This news organization surveyed 10 medical centers ranked by U.S. News & World Report as the country’s top facilities for obstetrics. They were asked what programs they had and studies they had done to try to reduce maternal mortality, improve racial disparities, and target cardiovascular causes of maternal mortality.
One of the most extensive programs was founded at the Stanford School of Medicine in Stanford, Calif., in 2006. The California Maternal Quality Care Collaborative includes 200 hospitals in the state committed to ending preventable maternal mortality and racial disparities.
Nine hospitals in the collaborative have started programs to reduce hemorrhages, manage high blood pressure disorders, and reduce the rate of cesarean deliveries. All are important reasons for maternal mortality.
These programs helped bring about a 62% reduction in California’s maternal mortality rate from 2006 to 2016. And 2023 figures show that California has the lowest maternal mortality rate of any state.
Alabama has the sixth highest rate of maternal mortality in the nation. The University of Alabama at Birmingham wants to address the racial disparities in maternal mortality with a cooperative called the P3 EQUATE Network.
The network is part of a $20 million program by the American Heart Association to gain greater understanding of the disproportionate effect of maternal mortality on Black and Native American people.
The program works with pregnant and postpartum women “to discover ways to reduce racism and social problems that contribute to poor health outcomes.”
In addition to collaborative efforts, the survey found maternal mortality programs at all the top medical centers.
NewYork-Presbyterian Hospital has a Mothers Center that provides specialized care to pregnant women with complications.
The University of Chicago Medical Center established a program called “Systematic Treatment and Management of Postpartum Hypertension” that includes patient and staff education, standardized hospital discharge instructions, and a follow-up in a postpartum hypertension clinic.
A 2021 study found that the program had helped increase the number of postpartum women who correctly follow blood pressure control guidance.
A program called MOMS Navigation at Northwell Health in Long Island, N.Y., provides support to high-risk mothers. The program decreased 30-day readmission rates for all patients by 50% and for Black birthing patients by 60%. Reducing readmission is an important measure for reducing complications.
Vanderbilt University Medical Center in Nashville has what it calls the first-of-its-kind educational podcasts Healthy Mom Healthy Baby, where 30% of the content is devoted to health disparities.
And several centers, including Brigham and Women’s Hospital in Boston and NewYork-Presbyterian, make sure mothers have access to doulas – professional support people trained in the needs of the family during pregnancy and childbirth.
The survey found that 9 of the 10 centers have obstetric programs devoted to cardiac care, including the University of Chicago, Stanford Medicine, UCLA, and the Cleveland Clinic.
But the survey results raise the question: How can we have these programs and research at our best obstetrics centers devoted to reducing maternal mortality and have the highest rate of all developed countries?
“Maternal mortality largely falls on pregnant and birthing persons who do not intersect with, nor are touched, by the best obstetrical care centers in the country,” Dr. Simon said.
Unfortunately, she said, the pregnant people who face “high maternal mortality rates … face all the access-to-care barriers and do not have the privilege of birthing or accessing care at top centers.”
Anne Hutchinson believed going to a top center – the Cleveland Clinic – would give her a good chance of safely delivering a second child.
Karlee Hoffman, DO, a cardiologist in the hospital’s cardio-obstetric high-risk clinic, said Ms. Hutchinson “came to me, she was determined to have another child, and she said, ‘Please help me do this. I’m doing it regardless. So, I would really like your support in moving forward,’” Dr. Hoffman recalls.
Ms. Hutchinson said Cleveland Clinic doctors told her she had a 20%-30% chance of peripartum cardiomyopathy again if she had a second child. If that happened, the risks “ranged from mild decompensation of my heart function to death,“ she said.
Ms. Hutchinson and her husband decided to go ahead with the pregnancy. Her parents cried when they found out. But Ms. Hutchinson says she was confident in the cardio obstetric team at Cleveland Clinic.
Her fertility medicine raised the possibility of multiple births, which would be a definite threat to her life. Her heart failure medicine, Entresto, could not be used during pregnancy, so her doctors put her on older medicines.
She got pregnant in June 2022 and developed gestational diabetes, which can affect pregnancy because of raised blood sugar. Another potential risk. She was carefully monitored by the specialists and hospitalized once.
At 37 weeks, she was induced and had a forceps delivery. On Feb. 15, 2023, her second daughter, Charlotte, was born.
Ms. Hutchinson was asked to write about how she felt when she delivered Charlotte:
“I am not sure how to put into words the love, joy, and elation that I felt holding Charlotte for the first time. As I write this, I have tears of joy in my eyes thinking of that moment. I had prayed for her for so long and after being told I couldn’t or shouldn’t have any more children.”
“I felt that Charlotte and I were forever bonded in triumph from that moment on. We did it and made it out alive! And our family was now complete. I have so much joy watching the love that is growing between Charlotte and Lillian. Life is truly amazing, and I am forever grateful to have them.”
A version of this article first appeared on WebMD.com.
On June 2, 2019, 35-year-old Anne Hutchinson gave birth to her first child, Lillian. There were no problems with the pregnancy or the birth at Fairview Hospital, which is part of the Cleveland Clinic system.
But 2 days after the birth, she had shortness of breath and couldn’t lie down and breathe.
“My mom’s a nurse, and she was like, ‘You need to go to the hospital immediately,’” Ms. Hutchinson said. When she was admitted to the hospital, there were suddenly “10 doctors in the room.”
Ms. Hutchinson was diagnosed with peripartum cardiomyopathy, a weakness of the heart muscle. She had heart failure. The seriousness of heart failure is measured by the ejection fraction, or the percentage of blood the heart pumps out. Normal is 50%-70%. Ms. Hutchinson’s ejection fraction was 20%.
She was put on medication, left the hospital after 5 days, and her ejection fraction eventually rose to 35%. But she was still at risk for sudden cardiac death.
“The cardiologist said to me, ‘You probably can’t have any more children.’ My heart did not bounce back,” Ms. Hutchinson said.
By the end of 2019, her cardiologist determined that she needed an internal cardiac defibrillator, which monitors the heartbeat and delivers electric shocks to restore the heart’s normal rhythm when needed.
By 2020, when Ms. Hutchinson’s ejection fraction was near normal, she decided that she wanted another child.
“I had a daughter. She was beautiful and amazing. But I felt like I wanted to have a sibling for her,” she says. Yet when her cardiologist at Fairview Hospital heard the plan, she told her getting pregnant again “would be like Russian roulette.”
Ms. Hutchinson is one of a growing number of women whose medical condition puts them at high risk of death during and after giving birth. An estimated 30% of maternal deaths in the United States result from cardiovascular disease – a problem that has become more common with increases in diabetes and obesity.
And, in some women, hypertension can develop suddenly during pregnancy. This is called preeclampsia and is increasing in the United States, particularly in Black women. In rare cases, it can become the life-threatening condition eclampsia, with seizures and death.
Three-time Olympic medalist and world champion sprinter Tori Bowie was found dead in June of apparent complications of pregnancy. The medical examiner’s office in Orange County, Fla., said she was believed to have been in her 8th month of pregnancy and may have died of eclampsia.
Heart conditions in pregnant women are one of a long list of reasons why the United States has the highest maternal mortality rate of any developed country. But the risk is marked by significant racial differences, with death rates three times higher in Black women, compared with White women.
What troubles many experts is that it is estimated that 80% of these deaths are preventable.
“That is a ridiculous number,” said Melissa A. Simon, MD, MPH, director of the Center for Health Equity Transformation at Northwestern Medicine in Evanston, Ill.. “For a health care system in a country that is so high-resourced and high-income, for 8 out of 10 deaths for moms who are pregnant [to be preventable], that’s absolutely unacceptable.”
Pregnant women are not only at risk of death from cardiovascular complications, but other types of problems, including hemorrhage, thrombotic embolism, and infection.
But experts now are focusing attention on nonmedical reasons for maternal mortality, such as racial disparities and the fundamental issue of whether women are telling doctors about their symptoms but are not being heard.
The government has acknowledged the depth of this problem with the Centers for Disease Control and Prevention’s “Hear Her” campaign, which includes videos of women who describe how their health professionals did not take their concerns seriously.
In one such video, a woman named Sanari says 2 days after the birth of her second child, she started developing soreness.
“By day 3, it just didn’t feel right. I asked the nurses, explained my symptoms and that I was having crazy pains, and they assured me it was just gas,” she says on the video.
Sanari described how she started to have odorous discharge and ended up in an emergency room at a different hospital. Health care providers found a large abscess on her uterus.
“I’m glad I didn’t stop at no, and I’m glad someone finally heard me – someone finally listened to me,” she said.
“Hear Her” featured another woman named Lindsay, who had preeclampsia in her first pregnancy and began to get symptoms during her second pregnancy.
She describes how she voiced her concerns to her doctors, saying, “sometimes it would be, ‘Oh, you’re pregnant and your feet are supposed to swell. … It’s just fine.’ But I didn’t feel fine.”
The campaign aims to raise awareness of warning signs that require fast medical attention to prevent pregnancy-related deaths.
But Shanna Cox, associate director of the CDC’s Division of Reproductive Health, said the agency has collected many stories of women who died or nearly died because their concerns were not being addressed properly.
Ms. Cox says another part of the campaign “is really focused on health care providers and listening … to their patients, providing that respectful patient-centered care to be sure that all their concerns are addressed.”
And some experts believe the thinking has shifted even more dramatically.
“We’ve moved from beyond the days of blaming the individual, the birth person, or the woman, to say you haven’t done this, you haven’t come into health care, you are not taking care of yourself, you aren’t keeping your appointments,” says Laurie Zephyrin, MD, MPH, vice president of the Commonwealth Fund, a private foundation in New York dedicated to improving health care.
Dr. Zephyrin says the health care system falls short of providing equitable, quality care. “There’s data that shows Black people receive worse care than White people for about 40% of quality measures,” she said.
These disparities have led to the formation of organizations like National Birth Equity Collaborative, an advocacy group in New Orleans working to improve maternal care for Black patients.
Carmen Green, vice president of research and strategy, said institutional racism has been embedded into some health care providers.
“They have this hierarchy that teaches them they have to manage, they have to control, they have to direct the medical experience, and that is just not how birthing works,” she said.
She used the example of the birth experience as a car ride, where the mothers have been in the backseat with the doctor driving. “We want the birthing person in the driving seat and want [them] to be respected as a person who is deciding where that destination is going,” Ms. Green said.
She says health providers often “blame the mamas” based on assumptions, stereotypes, and biases against low-income people.
So how is American medicine responding to the medical and social causes of maternal mortality?
This news organization surveyed 10 medical centers ranked by U.S. News & World Report as the country’s top facilities for obstetrics. They were asked what programs they had and studies they had done to try to reduce maternal mortality, improve racial disparities, and target cardiovascular causes of maternal mortality.
One of the most extensive programs was founded at the Stanford School of Medicine in Stanford, Calif., in 2006. The California Maternal Quality Care Collaborative includes 200 hospitals in the state committed to ending preventable maternal mortality and racial disparities.
Nine hospitals in the collaborative have started programs to reduce hemorrhages, manage high blood pressure disorders, and reduce the rate of cesarean deliveries. All are important reasons for maternal mortality.
These programs helped bring about a 62% reduction in California’s maternal mortality rate from 2006 to 2016. And 2023 figures show that California has the lowest maternal mortality rate of any state.
Alabama has the sixth highest rate of maternal mortality in the nation. The University of Alabama at Birmingham wants to address the racial disparities in maternal mortality with a cooperative called the P3 EQUATE Network.
The network is part of a $20 million program by the American Heart Association to gain greater understanding of the disproportionate effect of maternal mortality on Black and Native American people.
The program works with pregnant and postpartum women “to discover ways to reduce racism and social problems that contribute to poor health outcomes.”
In addition to collaborative efforts, the survey found maternal mortality programs at all the top medical centers.
NewYork-Presbyterian Hospital has a Mothers Center that provides specialized care to pregnant women with complications.
The University of Chicago Medical Center established a program called “Systematic Treatment and Management of Postpartum Hypertension” that includes patient and staff education, standardized hospital discharge instructions, and a follow-up in a postpartum hypertension clinic.
A 2021 study found that the program had helped increase the number of postpartum women who correctly follow blood pressure control guidance.
A program called MOMS Navigation at Northwell Health in Long Island, N.Y., provides support to high-risk mothers. The program decreased 30-day readmission rates for all patients by 50% and for Black birthing patients by 60%. Reducing readmission is an important measure for reducing complications.
Vanderbilt University Medical Center in Nashville has what it calls the first-of-its-kind educational podcasts Healthy Mom Healthy Baby, where 30% of the content is devoted to health disparities.
And several centers, including Brigham and Women’s Hospital in Boston and NewYork-Presbyterian, make sure mothers have access to doulas – professional support people trained in the needs of the family during pregnancy and childbirth.
The survey found that 9 of the 10 centers have obstetric programs devoted to cardiac care, including the University of Chicago, Stanford Medicine, UCLA, and the Cleveland Clinic.
But the survey results raise the question: How can we have these programs and research at our best obstetrics centers devoted to reducing maternal mortality and have the highest rate of all developed countries?
“Maternal mortality largely falls on pregnant and birthing persons who do not intersect with, nor are touched, by the best obstetrical care centers in the country,” Dr. Simon said.
Unfortunately, she said, the pregnant people who face “high maternal mortality rates … face all the access-to-care barriers and do not have the privilege of birthing or accessing care at top centers.”
Anne Hutchinson believed going to a top center – the Cleveland Clinic – would give her a good chance of safely delivering a second child.
Karlee Hoffman, DO, a cardiologist in the hospital’s cardio-obstetric high-risk clinic, said Ms. Hutchinson “came to me, she was determined to have another child, and she said, ‘Please help me do this. I’m doing it regardless. So, I would really like your support in moving forward,’” Dr. Hoffman recalls.
Ms. Hutchinson said Cleveland Clinic doctors told her she had a 20%-30% chance of peripartum cardiomyopathy again if she had a second child. If that happened, the risks “ranged from mild decompensation of my heart function to death,“ she said.
Ms. Hutchinson and her husband decided to go ahead with the pregnancy. Her parents cried when they found out. But Ms. Hutchinson says she was confident in the cardio obstetric team at Cleveland Clinic.
Her fertility medicine raised the possibility of multiple births, which would be a definite threat to her life. Her heart failure medicine, Entresto, could not be used during pregnancy, so her doctors put her on older medicines.
She got pregnant in June 2022 and developed gestational diabetes, which can affect pregnancy because of raised blood sugar. Another potential risk. She was carefully monitored by the specialists and hospitalized once.
At 37 weeks, she was induced and had a forceps delivery. On Feb. 15, 2023, her second daughter, Charlotte, was born.
Ms. Hutchinson was asked to write about how she felt when she delivered Charlotte:
“I am not sure how to put into words the love, joy, and elation that I felt holding Charlotte for the first time. As I write this, I have tears of joy in my eyes thinking of that moment. I had prayed for her for so long and after being told I couldn’t or shouldn’t have any more children.”
“I felt that Charlotte and I were forever bonded in triumph from that moment on. We did it and made it out alive! And our family was now complete. I have so much joy watching the love that is growing between Charlotte and Lillian. Life is truly amazing, and I am forever grateful to have them.”
A version of this article first appeared on WebMD.com.
On June 2, 2019, 35-year-old Anne Hutchinson gave birth to her first child, Lillian. There were no problems with the pregnancy or the birth at Fairview Hospital, which is part of the Cleveland Clinic system.
But 2 days after the birth, she had shortness of breath and couldn’t lie down and breathe.
“My mom’s a nurse, and she was like, ‘You need to go to the hospital immediately,’” Ms. Hutchinson said. When she was admitted to the hospital, there were suddenly “10 doctors in the room.”
Ms. Hutchinson was diagnosed with peripartum cardiomyopathy, a weakness of the heart muscle. She had heart failure. The seriousness of heart failure is measured by the ejection fraction, or the percentage of blood the heart pumps out. Normal is 50%-70%. Ms. Hutchinson’s ejection fraction was 20%.
She was put on medication, left the hospital after 5 days, and her ejection fraction eventually rose to 35%. But she was still at risk for sudden cardiac death.
“The cardiologist said to me, ‘You probably can’t have any more children.’ My heart did not bounce back,” Ms. Hutchinson said.
By the end of 2019, her cardiologist determined that she needed an internal cardiac defibrillator, which monitors the heartbeat and delivers electric shocks to restore the heart’s normal rhythm when needed.
By 2020, when Ms. Hutchinson’s ejection fraction was near normal, she decided that she wanted another child.
“I had a daughter. She was beautiful and amazing. But I felt like I wanted to have a sibling for her,” she says. Yet when her cardiologist at Fairview Hospital heard the plan, she told her getting pregnant again “would be like Russian roulette.”
Ms. Hutchinson is one of a growing number of women whose medical condition puts them at high risk of death during and after giving birth. An estimated 30% of maternal deaths in the United States result from cardiovascular disease – a problem that has become more common with increases in diabetes and obesity.
And, in some women, hypertension can develop suddenly during pregnancy. This is called preeclampsia and is increasing in the United States, particularly in Black women. In rare cases, it can become the life-threatening condition eclampsia, with seizures and death.
Three-time Olympic medalist and world champion sprinter Tori Bowie was found dead in June of apparent complications of pregnancy. The medical examiner’s office in Orange County, Fla., said she was believed to have been in her 8th month of pregnancy and may have died of eclampsia.
Heart conditions in pregnant women are one of a long list of reasons why the United States has the highest maternal mortality rate of any developed country. But the risk is marked by significant racial differences, with death rates three times higher in Black women, compared with White women.
What troubles many experts is that it is estimated that 80% of these deaths are preventable.
“That is a ridiculous number,” said Melissa A. Simon, MD, MPH, director of the Center for Health Equity Transformation at Northwestern Medicine in Evanston, Ill.. “For a health care system in a country that is so high-resourced and high-income, for 8 out of 10 deaths for moms who are pregnant [to be preventable], that’s absolutely unacceptable.”
Pregnant women are not only at risk of death from cardiovascular complications, but other types of problems, including hemorrhage, thrombotic embolism, and infection.
But experts now are focusing attention on nonmedical reasons for maternal mortality, such as racial disparities and the fundamental issue of whether women are telling doctors about their symptoms but are not being heard.
The government has acknowledged the depth of this problem with the Centers for Disease Control and Prevention’s “Hear Her” campaign, which includes videos of women who describe how their health professionals did not take their concerns seriously.
In one such video, a woman named Sanari says 2 days after the birth of her second child, she started developing soreness.
“By day 3, it just didn’t feel right. I asked the nurses, explained my symptoms and that I was having crazy pains, and they assured me it was just gas,” she says on the video.
Sanari described how she started to have odorous discharge and ended up in an emergency room at a different hospital. Health care providers found a large abscess on her uterus.
“I’m glad I didn’t stop at no, and I’m glad someone finally heard me – someone finally listened to me,” she said.
“Hear Her” featured another woman named Lindsay, who had preeclampsia in her first pregnancy and began to get symptoms during her second pregnancy.
She describes how she voiced her concerns to her doctors, saying, “sometimes it would be, ‘Oh, you’re pregnant and your feet are supposed to swell. … It’s just fine.’ But I didn’t feel fine.”
The campaign aims to raise awareness of warning signs that require fast medical attention to prevent pregnancy-related deaths.
But Shanna Cox, associate director of the CDC’s Division of Reproductive Health, said the agency has collected many stories of women who died or nearly died because their concerns were not being addressed properly.
Ms. Cox says another part of the campaign “is really focused on health care providers and listening … to their patients, providing that respectful patient-centered care to be sure that all their concerns are addressed.”
And some experts believe the thinking has shifted even more dramatically.
“We’ve moved from beyond the days of blaming the individual, the birth person, or the woman, to say you haven’t done this, you haven’t come into health care, you are not taking care of yourself, you aren’t keeping your appointments,” says Laurie Zephyrin, MD, MPH, vice president of the Commonwealth Fund, a private foundation in New York dedicated to improving health care.
Dr. Zephyrin says the health care system falls short of providing equitable, quality care. “There’s data that shows Black people receive worse care than White people for about 40% of quality measures,” she said.
These disparities have led to the formation of organizations like National Birth Equity Collaborative, an advocacy group in New Orleans working to improve maternal care for Black patients.
Carmen Green, vice president of research and strategy, said institutional racism has been embedded into some health care providers.
“They have this hierarchy that teaches them they have to manage, they have to control, they have to direct the medical experience, and that is just not how birthing works,” she said.
She used the example of the birth experience as a car ride, where the mothers have been in the backseat with the doctor driving. “We want the birthing person in the driving seat and want [them] to be respected as a person who is deciding where that destination is going,” Ms. Green said.
She says health providers often “blame the mamas” based on assumptions, stereotypes, and biases against low-income people.
So how is American medicine responding to the medical and social causes of maternal mortality?
This news organization surveyed 10 medical centers ranked by U.S. News & World Report as the country’s top facilities for obstetrics. They were asked what programs they had and studies they had done to try to reduce maternal mortality, improve racial disparities, and target cardiovascular causes of maternal mortality.
One of the most extensive programs was founded at the Stanford School of Medicine in Stanford, Calif., in 2006. The California Maternal Quality Care Collaborative includes 200 hospitals in the state committed to ending preventable maternal mortality and racial disparities.
Nine hospitals in the collaborative have started programs to reduce hemorrhages, manage high blood pressure disorders, and reduce the rate of cesarean deliveries. All are important reasons for maternal mortality.
These programs helped bring about a 62% reduction in California’s maternal mortality rate from 2006 to 2016. And 2023 figures show that California has the lowest maternal mortality rate of any state.
Alabama has the sixth highest rate of maternal mortality in the nation. The University of Alabama at Birmingham wants to address the racial disparities in maternal mortality with a cooperative called the P3 EQUATE Network.
The network is part of a $20 million program by the American Heart Association to gain greater understanding of the disproportionate effect of maternal mortality on Black and Native American people.
The program works with pregnant and postpartum women “to discover ways to reduce racism and social problems that contribute to poor health outcomes.”
In addition to collaborative efforts, the survey found maternal mortality programs at all the top medical centers.
NewYork-Presbyterian Hospital has a Mothers Center that provides specialized care to pregnant women with complications.
The University of Chicago Medical Center established a program called “Systematic Treatment and Management of Postpartum Hypertension” that includes patient and staff education, standardized hospital discharge instructions, and a follow-up in a postpartum hypertension clinic.
A 2021 study found that the program had helped increase the number of postpartum women who correctly follow blood pressure control guidance.
A program called MOMS Navigation at Northwell Health in Long Island, N.Y., provides support to high-risk mothers. The program decreased 30-day readmission rates for all patients by 50% and for Black birthing patients by 60%. Reducing readmission is an important measure for reducing complications.
Vanderbilt University Medical Center in Nashville has what it calls the first-of-its-kind educational podcasts Healthy Mom Healthy Baby, where 30% of the content is devoted to health disparities.
And several centers, including Brigham and Women’s Hospital in Boston and NewYork-Presbyterian, make sure mothers have access to doulas – professional support people trained in the needs of the family during pregnancy and childbirth.
The survey found that 9 of the 10 centers have obstetric programs devoted to cardiac care, including the University of Chicago, Stanford Medicine, UCLA, and the Cleveland Clinic.
But the survey results raise the question: How can we have these programs and research at our best obstetrics centers devoted to reducing maternal mortality and have the highest rate of all developed countries?
“Maternal mortality largely falls on pregnant and birthing persons who do not intersect with, nor are touched, by the best obstetrical care centers in the country,” Dr. Simon said.
Unfortunately, she said, the pregnant people who face “high maternal mortality rates … face all the access-to-care barriers and do not have the privilege of birthing or accessing care at top centers.”
Anne Hutchinson believed going to a top center – the Cleveland Clinic – would give her a good chance of safely delivering a second child.
Karlee Hoffman, DO, a cardiologist in the hospital’s cardio-obstetric high-risk clinic, said Ms. Hutchinson “came to me, she was determined to have another child, and she said, ‘Please help me do this. I’m doing it regardless. So, I would really like your support in moving forward,’” Dr. Hoffman recalls.
Ms. Hutchinson said Cleveland Clinic doctors told her she had a 20%-30% chance of peripartum cardiomyopathy again if she had a second child. If that happened, the risks “ranged from mild decompensation of my heart function to death,“ she said.
Ms. Hutchinson and her husband decided to go ahead with the pregnancy. Her parents cried when they found out. But Ms. Hutchinson says she was confident in the cardio obstetric team at Cleveland Clinic.
Her fertility medicine raised the possibility of multiple births, which would be a definite threat to her life. Her heart failure medicine, Entresto, could not be used during pregnancy, so her doctors put her on older medicines.
She got pregnant in June 2022 and developed gestational diabetes, which can affect pregnancy because of raised blood sugar. Another potential risk. She was carefully monitored by the specialists and hospitalized once.
At 37 weeks, she was induced and had a forceps delivery. On Feb. 15, 2023, her second daughter, Charlotte, was born.
Ms. Hutchinson was asked to write about how she felt when she delivered Charlotte:
“I am not sure how to put into words the love, joy, and elation that I felt holding Charlotte for the first time. As I write this, I have tears of joy in my eyes thinking of that moment. I had prayed for her for so long and after being told I couldn’t or shouldn’t have any more children.”
“I felt that Charlotte and I were forever bonded in triumph from that moment on. We did it and made it out alive! And our family was now complete. I have so much joy watching the love that is growing between Charlotte and Lillian. Life is truly amazing, and I am forever grateful to have them.”
A version of this article first appeared on WebMD.com.
Medical students are skipping class lectures: Does it matter?
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
Long COVID disability court battles just ‘tip of iceberg’
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
Offering HPV vaccine at age 9 linked to greater series completion
BALTIMORE – , according to a retrospective cohort study of commercially insured youth presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. The research was published ahead of print in Human Vaccines and Immunotherapeutics.
Changing attitudes
“These findings are novel because they emphasize starting at age 9, and that is different than prior studies that emphasize bundling of these vaccines,” Kevin Ault, MD, professor and chair of the department of obstetrics and gynecology at Western Michigan University Homer Stryker MD School of Medicine and a former member of the CDC’s Advisory Committee on Immunization Practices, said in an interview.
Dr. Ault was not involved in the study but noted that these findings support the AAP’s recommendation to start the HPV vaccine series at age 9. The Centers for Disease Control and Prevention currently recommends giving the first dose of the HPV vaccine at ages 11-12, at the same time as the Tdap and meningitis vaccines. This recommendation to “bundle” the HPV vaccine with the Tdap and meningitis vaccines aims to facilitate provider-family discussion about the HPV vaccine, ideally reducing parent hesitancy and concerns about the vaccines. Multiple studies have shown improved HPV vaccine uptake when providers offer the HPV vaccine at the same time as the Tdap and meningococcal vaccines.
However, shifts in parents’ attitudes have occurred toward the HPV vaccine since those studies on bundling: Concerns about sexual activity have receded while concerns about safety remain high. The American Academy of Pediatrics and the American Cancer Society both advise starting the HPV vaccine series at age 9, based on evidence showing that more children complete the series when they get the first shot before age 11 compared to getting it at 11 or 12.
“The bundling was really to vaccinate people by the age of 13, thinking that onset of sexual activity was after that,” study author Sidika Kajtezovic, MD, a resident at Boston Medical Center and Boston University Obstetrics and Gynecology, said in an interview. But Dr. Kajtezovic said she delivers babies for 13-year-old patients. “Kids are having sex sooner or sooner.” It’s also clear that using the bundling strategy is not making up the entire gap right now: Ninety percent of children are getting the meningococcal vaccine while only 49% are getting the HPV vaccine, Dr. Kajtezovic pointed out. “There’s a disconnect happening there, even with the bundling,” she said.
Debundling vaccines
Dr. Kajtezovic and her colleagues used a national database of employee-sponsored health insurance to analyze the records of 100,857 children who were continuously enrolled in a plan from age 9 in 2015 to age 13 in 2019. They calculated the odds of children completing the HPV vaccine series based on whether they started the series before, at the same time as, or after the Tdap vaccination.
Youth who received the HPV vaccine before their Tdap vaccine had 38% greater odds of completing the series – getting both doses – than did those who received the HPV vaccine at the same time as the Tdap vaccine. Meanwhile, in line with prior evidence, those who got the first HPV dose after their Tdap were less likely – 68% lower odds – to complete the two- or three-dose (if starting above age 14) series.
The researchers identified several other factors that were linked to completing the HPV vaccine series. Females had greater odds than did males of completing the series, as did those living in urban, rather than rural, areas. Other factors associated with completing the series included living in the Northeast United States and receiving primary care from a pediatrician rather than a family medicine physician.
Timing is important
“I am encouraged by the findings of this study,” Dr. Ault said in an interview. “However, I would have liked the authors to expand the age range a bit higher. There are data that continuing to discuss the HPV vaccine with parents and teens will increase uptake into the later teen years.”
One challenge is that research shows attendance at primary care visits declines in older adolescence. Since there is no second Tdap or meningitis shot, families need to return for the second HPV vaccine dose after those shots, though they could get the second dose at the same time as other two vaccines if they receive the first dose before age 11. There’s also evidence suggesting that providers find conversations about the HPV vaccine easier when sexual activity is not the focus.
“I often feel that, before a child reaches adolescence, they’re almost, in a way, not sexualized yet, so talking about cancer prevention for an 8- or 9-year-old sometimes sounds a little different to patients versus protecting your 12-year-old, who’s starting to go through adolescence and developing breasts” and other signs of puberty, Dr. Kajtezovic said. Keeping the focus of HPV vaccine discussions on cancer prevention also allows providers to point out the protection against anal cancer, vulvar cancer, vaginal cancer, and head and neck cancer. “They are horrible, and even if they’re treatable, they’re often very hard to treat at an advanced stage,” Dr. Kajtezovic said. “The surgery required is so life disabling and disfiguring.”
The HPV Roundtable advises continuing bundling at practices having success with it but encourages practices to consider earlier vaccination if their uptake is lagging. Quality improvement initiatives, such as earlier electronic medical record prompts and multi-level interventions in pediatric practices, have shown substantial increases in HPV vaccine uptake at 9 and 10 years old. One survey in 2021 found that one in five primary care providers already routinely recommend the HPV vaccine at ages 9-10, and nearly half of others would consider doing so.
“My hope is in the next few years, when [the CDC] refreshes their vaccine recommendations, that they will either unbundle it or move the bar a few years earlier so that you can initiate it to encourage earlier initiation,” Dr. Kajtezovic said.
Dr. Ault had no other disclosures besides prior service on ACIP. Dr. Kajtezovic had no disclosures.
BALTIMORE – , according to a retrospective cohort study of commercially insured youth presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. The research was published ahead of print in Human Vaccines and Immunotherapeutics.
Changing attitudes
“These findings are novel because they emphasize starting at age 9, and that is different than prior studies that emphasize bundling of these vaccines,” Kevin Ault, MD, professor and chair of the department of obstetrics and gynecology at Western Michigan University Homer Stryker MD School of Medicine and a former member of the CDC’s Advisory Committee on Immunization Practices, said in an interview.
Dr. Ault was not involved in the study but noted that these findings support the AAP’s recommendation to start the HPV vaccine series at age 9. The Centers for Disease Control and Prevention currently recommends giving the first dose of the HPV vaccine at ages 11-12, at the same time as the Tdap and meningitis vaccines. This recommendation to “bundle” the HPV vaccine with the Tdap and meningitis vaccines aims to facilitate provider-family discussion about the HPV vaccine, ideally reducing parent hesitancy and concerns about the vaccines. Multiple studies have shown improved HPV vaccine uptake when providers offer the HPV vaccine at the same time as the Tdap and meningococcal vaccines.
However, shifts in parents’ attitudes have occurred toward the HPV vaccine since those studies on bundling: Concerns about sexual activity have receded while concerns about safety remain high. The American Academy of Pediatrics and the American Cancer Society both advise starting the HPV vaccine series at age 9, based on evidence showing that more children complete the series when they get the first shot before age 11 compared to getting it at 11 or 12.
“The bundling was really to vaccinate people by the age of 13, thinking that onset of sexual activity was after that,” study author Sidika Kajtezovic, MD, a resident at Boston Medical Center and Boston University Obstetrics and Gynecology, said in an interview. But Dr. Kajtezovic said she delivers babies for 13-year-old patients. “Kids are having sex sooner or sooner.” It’s also clear that using the bundling strategy is not making up the entire gap right now: Ninety percent of children are getting the meningococcal vaccine while only 49% are getting the HPV vaccine, Dr. Kajtezovic pointed out. “There’s a disconnect happening there, even with the bundling,” she said.
Debundling vaccines
Dr. Kajtezovic and her colleagues used a national database of employee-sponsored health insurance to analyze the records of 100,857 children who were continuously enrolled in a plan from age 9 in 2015 to age 13 in 2019. They calculated the odds of children completing the HPV vaccine series based on whether they started the series before, at the same time as, or after the Tdap vaccination.
Youth who received the HPV vaccine before their Tdap vaccine had 38% greater odds of completing the series – getting both doses – than did those who received the HPV vaccine at the same time as the Tdap vaccine. Meanwhile, in line with prior evidence, those who got the first HPV dose after their Tdap were less likely – 68% lower odds – to complete the two- or three-dose (if starting above age 14) series.
The researchers identified several other factors that were linked to completing the HPV vaccine series. Females had greater odds than did males of completing the series, as did those living in urban, rather than rural, areas. Other factors associated with completing the series included living in the Northeast United States and receiving primary care from a pediatrician rather than a family medicine physician.
Timing is important
“I am encouraged by the findings of this study,” Dr. Ault said in an interview. “However, I would have liked the authors to expand the age range a bit higher. There are data that continuing to discuss the HPV vaccine with parents and teens will increase uptake into the later teen years.”
One challenge is that research shows attendance at primary care visits declines in older adolescence. Since there is no second Tdap or meningitis shot, families need to return for the second HPV vaccine dose after those shots, though they could get the second dose at the same time as other two vaccines if they receive the first dose before age 11. There’s also evidence suggesting that providers find conversations about the HPV vaccine easier when sexual activity is not the focus.
“I often feel that, before a child reaches adolescence, they’re almost, in a way, not sexualized yet, so talking about cancer prevention for an 8- or 9-year-old sometimes sounds a little different to patients versus protecting your 12-year-old, who’s starting to go through adolescence and developing breasts” and other signs of puberty, Dr. Kajtezovic said. Keeping the focus of HPV vaccine discussions on cancer prevention also allows providers to point out the protection against anal cancer, vulvar cancer, vaginal cancer, and head and neck cancer. “They are horrible, and even if they’re treatable, they’re often very hard to treat at an advanced stage,” Dr. Kajtezovic said. “The surgery required is so life disabling and disfiguring.”
The HPV Roundtable advises continuing bundling at practices having success with it but encourages practices to consider earlier vaccination if their uptake is lagging. Quality improvement initiatives, such as earlier electronic medical record prompts and multi-level interventions in pediatric practices, have shown substantial increases in HPV vaccine uptake at 9 and 10 years old. One survey in 2021 found that one in five primary care providers already routinely recommend the HPV vaccine at ages 9-10, and nearly half of others would consider doing so.
“My hope is in the next few years, when [the CDC] refreshes their vaccine recommendations, that they will either unbundle it or move the bar a few years earlier so that you can initiate it to encourage earlier initiation,” Dr. Kajtezovic said.
Dr. Ault had no other disclosures besides prior service on ACIP. Dr. Kajtezovic had no disclosures.
BALTIMORE – , according to a retrospective cohort study of commercially insured youth presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. The research was published ahead of print in Human Vaccines and Immunotherapeutics.
Changing attitudes
“These findings are novel because they emphasize starting at age 9, and that is different than prior studies that emphasize bundling of these vaccines,” Kevin Ault, MD, professor and chair of the department of obstetrics and gynecology at Western Michigan University Homer Stryker MD School of Medicine and a former member of the CDC’s Advisory Committee on Immunization Practices, said in an interview.
Dr. Ault was not involved in the study but noted that these findings support the AAP’s recommendation to start the HPV vaccine series at age 9. The Centers for Disease Control and Prevention currently recommends giving the first dose of the HPV vaccine at ages 11-12, at the same time as the Tdap and meningitis vaccines. This recommendation to “bundle” the HPV vaccine with the Tdap and meningitis vaccines aims to facilitate provider-family discussion about the HPV vaccine, ideally reducing parent hesitancy and concerns about the vaccines. Multiple studies have shown improved HPV vaccine uptake when providers offer the HPV vaccine at the same time as the Tdap and meningococcal vaccines.
However, shifts in parents’ attitudes have occurred toward the HPV vaccine since those studies on bundling: Concerns about sexual activity have receded while concerns about safety remain high. The American Academy of Pediatrics and the American Cancer Society both advise starting the HPV vaccine series at age 9, based on evidence showing that more children complete the series when they get the first shot before age 11 compared to getting it at 11 or 12.
“The bundling was really to vaccinate people by the age of 13, thinking that onset of sexual activity was after that,” study author Sidika Kajtezovic, MD, a resident at Boston Medical Center and Boston University Obstetrics and Gynecology, said in an interview. But Dr. Kajtezovic said she delivers babies for 13-year-old patients. “Kids are having sex sooner or sooner.” It’s also clear that using the bundling strategy is not making up the entire gap right now: Ninety percent of children are getting the meningococcal vaccine while only 49% are getting the HPV vaccine, Dr. Kajtezovic pointed out. “There’s a disconnect happening there, even with the bundling,” she said.
Debundling vaccines
Dr. Kajtezovic and her colleagues used a national database of employee-sponsored health insurance to analyze the records of 100,857 children who were continuously enrolled in a plan from age 9 in 2015 to age 13 in 2019. They calculated the odds of children completing the HPV vaccine series based on whether they started the series before, at the same time as, or after the Tdap vaccination.
Youth who received the HPV vaccine before their Tdap vaccine had 38% greater odds of completing the series – getting both doses – than did those who received the HPV vaccine at the same time as the Tdap vaccine. Meanwhile, in line with prior evidence, those who got the first HPV dose after their Tdap were less likely – 68% lower odds – to complete the two- or three-dose (if starting above age 14) series.
The researchers identified several other factors that were linked to completing the HPV vaccine series. Females had greater odds than did males of completing the series, as did those living in urban, rather than rural, areas. Other factors associated with completing the series included living in the Northeast United States and receiving primary care from a pediatrician rather than a family medicine physician.
Timing is important
“I am encouraged by the findings of this study,” Dr. Ault said in an interview. “However, I would have liked the authors to expand the age range a bit higher. There are data that continuing to discuss the HPV vaccine with parents and teens will increase uptake into the later teen years.”
One challenge is that research shows attendance at primary care visits declines in older adolescence. Since there is no second Tdap or meningitis shot, families need to return for the second HPV vaccine dose after those shots, though they could get the second dose at the same time as other two vaccines if they receive the first dose before age 11. There’s also evidence suggesting that providers find conversations about the HPV vaccine easier when sexual activity is not the focus.
“I often feel that, before a child reaches adolescence, they’re almost, in a way, not sexualized yet, so talking about cancer prevention for an 8- or 9-year-old sometimes sounds a little different to patients versus protecting your 12-year-old, who’s starting to go through adolescence and developing breasts” and other signs of puberty, Dr. Kajtezovic said. Keeping the focus of HPV vaccine discussions on cancer prevention also allows providers to point out the protection against anal cancer, vulvar cancer, vaginal cancer, and head and neck cancer. “They are horrible, and even if they’re treatable, they’re often very hard to treat at an advanced stage,” Dr. Kajtezovic said. “The surgery required is so life disabling and disfiguring.”
The HPV Roundtable advises continuing bundling at practices having success with it but encourages practices to consider earlier vaccination if their uptake is lagging. Quality improvement initiatives, such as earlier electronic medical record prompts and multi-level interventions in pediatric practices, have shown substantial increases in HPV vaccine uptake at 9 and 10 years old. One survey in 2021 found that one in five primary care providers already routinely recommend the HPV vaccine at ages 9-10, and nearly half of others would consider doing so.
“My hope is in the next few years, when [the CDC] refreshes their vaccine recommendations, that they will either unbundle it or move the bar a few years earlier so that you can initiate it to encourage earlier initiation,” Dr. Kajtezovic said.
Dr. Ault had no other disclosures besides prior service on ACIP. Dr. Kajtezovic had no disclosures.
AT ACOG 2023
Folic acid supplementation for birth defects reaffirmed
Taking folic acid supplements before conception and in the first trimester of pregnancy continues to be a major line of defense against neural tube defects.
In a statement published in JAMA, the U.S. Preventive Services Task Force recommended that all people planning on becoming pregnant or who could become pregnant take a daily supplement of 0.4-0.8 mg (400-800 mcg) of folic acid to prevent neural tube defects.
The task force also found that folic acid is not associated with maternal cancer or autism, which were the concerns of some researchers. The current findings regarding potential harm align with earlier evidence examining possible risks.
The recommendation also aligns with previous recommendations from the USPSTF and is supported by 12 more recent observational studies. Neural tube defects occur in an estimated 3,000 pregnancies per year.
Folic acid deficiency is common due to diet, impaired folate metabolism, and poor nutrient uptake as a result of medications or bariatric surgery.
“As much as we’ve been trying to get the word out there, we still need to get it out there even more,” Wanda Nicholson, MD, MPH, MBA, vice chair of the USPSTF, told this news organization. “It’s so simple and straightforward and can be so impactful for the health of the baby.”
Neural tube formation occurs 26-28 days after fertilization. Folic acid supplementation is essential for all people who may become pregnant, considering half of the pregnancies in the United States are unplanned, according to the USPSTF.
“In many cases, neural tube formation has already occurred, or not occurred appropriately, before someone realizes that they’re pregnant,” Dr. Nicholson said. “That’s why it’s so important to start taking folic acid one month prior to conception if you’re planning on becoming pregnant, and if you’re capable of being pregnant but not planning pregnancy, yes, we’re advocating that you also proceed with folic acid supplementation.”
Primary care physicians play a key role in patient education and ensuring that all patients receive adequate folic acid, according to Spencer McClelland, MD, an obstetrician-gynecologist at Denver Health, who was not involved in the statement. Dr. McClelland advised that clinicians recommend patients who are or could get pregnant take a multivitamin, because most brands will contain the recommended dosage of folic acid.
“There’s some confusion about folic acid,” he said. “Many patients know that they should be on a prenatal vitamin, but most don’t know that the reason we’re recommending a prenatal vitamin is almost entirely because of the value of folic acid, and everything else in the prenatal vitamin is kind of icing on the cake.”
For patients trying to get pregnant, the risk for neural tube defects “is one of many examples of the importance of preconception counseling,” Dr. McClelland said.
Dr. Nicholson noted that the recommended 0.4-0.8 mg of folic acid per day is for patients without heightened deficiency due to medications or bariatric surgery. At-risk patients should receive counseling from their physician to determine the correct amount to take.
The authors report no conflicts of interest, financial or otherwise.
A version of this article first appeared on Medscape.com.
Taking folic acid supplements before conception and in the first trimester of pregnancy continues to be a major line of defense against neural tube defects.
In a statement published in JAMA, the U.S. Preventive Services Task Force recommended that all people planning on becoming pregnant or who could become pregnant take a daily supplement of 0.4-0.8 mg (400-800 mcg) of folic acid to prevent neural tube defects.
The task force also found that folic acid is not associated with maternal cancer or autism, which were the concerns of some researchers. The current findings regarding potential harm align with earlier evidence examining possible risks.
The recommendation also aligns with previous recommendations from the USPSTF and is supported by 12 more recent observational studies. Neural tube defects occur in an estimated 3,000 pregnancies per year.
Folic acid deficiency is common due to diet, impaired folate metabolism, and poor nutrient uptake as a result of medications or bariatric surgery.
“As much as we’ve been trying to get the word out there, we still need to get it out there even more,” Wanda Nicholson, MD, MPH, MBA, vice chair of the USPSTF, told this news organization. “It’s so simple and straightforward and can be so impactful for the health of the baby.”
Neural tube formation occurs 26-28 days after fertilization. Folic acid supplementation is essential for all people who may become pregnant, considering half of the pregnancies in the United States are unplanned, according to the USPSTF.
“In many cases, neural tube formation has already occurred, or not occurred appropriately, before someone realizes that they’re pregnant,” Dr. Nicholson said. “That’s why it’s so important to start taking folic acid one month prior to conception if you’re planning on becoming pregnant, and if you’re capable of being pregnant but not planning pregnancy, yes, we’re advocating that you also proceed with folic acid supplementation.”
Primary care physicians play a key role in patient education and ensuring that all patients receive adequate folic acid, according to Spencer McClelland, MD, an obstetrician-gynecologist at Denver Health, who was not involved in the statement. Dr. McClelland advised that clinicians recommend patients who are or could get pregnant take a multivitamin, because most brands will contain the recommended dosage of folic acid.
“There’s some confusion about folic acid,” he said. “Many patients know that they should be on a prenatal vitamin, but most don’t know that the reason we’re recommending a prenatal vitamin is almost entirely because of the value of folic acid, and everything else in the prenatal vitamin is kind of icing on the cake.”
For patients trying to get pregnant, the risk for neural tube defects “is one of many examples of the importance of preconception counseling,” Dr. McClelland said.
Dr. Nicholson noted that the recommended 0.4-0.8 mg of folic acid per day is for patients without heightened deficiency due to medications or bariatric surgery. At-risk patients should receive counseling from their physician to determine the correct amount to take.
The authors report no conflicts of interest, financial or otherwise.
A version of this article first appeared on Medscape.com.
Taking folic acid supplements before conception and in the first trimester of pregnancy continues to be a major line of defense against neural tube defects.
In a statement published in JAMA, the U.S. Preventive Services Task Force recommended that all people planning on becoming pregnant or who could become pregnant take a daily supplement of 0.4-0.8 mg (400-800 mcg) of folic acid to prevent neural tube defects.
The task force also found that folic acid is not associated with maternal cancer or autism, which were the concerns of some researchers. The current findings regarding potential harm align with earlier evidence examining possible risks.
The recommendation also aligns with previous recommendations from the USPSTF and is supported by 12 more recent observational studies. Neural tube defects occur in an estimated 3,000 pregnancies per year.
Folic acid deficiency is common due to diet, impaired folate metabolism, and poor nutrient uptake as a result of medications or bariatric surgery.
“As much as we’ve been trying to get the word out there, we still need to get it out there even more,” Wanda Nicholson, MD, MPH, MBA, vice chair of the USPSTF, told this news organization. “It’s so simple and straightforward and can be so impactful for the health of the baby.”
Neural tube formation occurs 26-28 days after fertilization. Folic acid supplementation is essential for all people who may become pregnant, considering half of the pregnancies in the United States are unplanned, according to the USPSTF.
“In many cases, neural tube formation has already occurred, or not occurred appropriately, before someone realizes that they’re pregnant,” Dr. Nicholson said. “That’s why it’s so important to start taking folic acid one month prior to conception if you’re planning on becoming pregnant, and if you’re capable of being pregnant but not planning pregnancy, yes, we’re advocating that you also proceed with folic acid supplementation.”
Primary care physicians play a key role in patient education and ensuring that all patients receive adequate folic acid, according to Spencer McClelland, MD, an obstetrician-gynecologist at Denver Health, who was not involved in the statement. Dr. McClelland advised that clinicians recommend patients who are or could get pregnant take a multivitamin, because most brands will contain the recommended dosage of folic acid.
“There’s some confusion about folic acid,” he said. “Many patients know that they should be on a prenatal vitamin, but most don’t know that the reason we’re recommending a prenatal vitamin is almost entirely because of the value of folic acid, and everything else in the prenatal vitamin is kind of icing on the cake.”
For patients trying to get pregnant, the risk for neural tube defects “is one of many examples of the importance of preconception counseling,” Dr. McClelland said.
Dr. Nicholson noted that the recommended 0.4-0.8 mg of folic acid per day is for patients without heightened deficiency due to medications or bariatric surgery. At-risk patients should receive counseling from their physician to determine the correct amount to take.
The authors report no conflicts of interest, financial or otherwise.
A version of this article first appeared on Medscape.com.
FROM JAMA