User login
Key Abstracts in Early Breast Cancer From ASCO 2023
Dr Harold J. Burstein, of the Dana-Farber Cancer Institute in Boston, Massachusetts, highlights key abstracts on early breast cancer from the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Dr Burstein first reports on exciting results from the phase 3 NATALEE trial, which compared adjuvant use of CDK4/6 inhibitor ribociclib plus endocrine therapy (ET) vs ET alone in patients with HR+/HER2- early breast cancer and found that the combination lowered risk for recurrence.
The results of NATALEE, together with the recent findings of the monarchE trial, provide strong evidence that the addition of a CDK4/6 inhibitor to ET is useful in the adjuvant setting. Dr Burstein suggests that these findings may point to an emerging treatment paradigm in HR+/HER2- patients, particularly those with higher-risk breast cancers.
Dr Burstein next discusses important data from the Early Breast Cancer Trialists Collaborative Group (EBCTCG). Their meta-analysis of 25 randomized trials on ovarian ablation in premenopausal women showed that ovarian ablation provided a substantial reduction in 15-year risk for recurrence and death.
Finally, Dr Burstein reports on data from an analysis of patients enrolled in the PENELOPE-B trial to assess the value of circulating tumor DNA (ctDNA) in predicting clinical relapse. Dr Burstein reports that the results indicated that ctDNA was a strong prognostic factor for disease recurrence.
--
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Institute Physician, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.
Dr Harold J. Burstein, of the Dana-Farber Cancer Institute in Boston, Massachusetts, highlights key abstracts on early breast cancer from the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Dr Burstein first reports on exciting results from the phase 3 NATALEE trial, which compared adjuvant use of CDK4/6 inhibitor ribociclib plus endocrine therapy (ET) vs ET alone in patients with HR+/HER2- early breast cancer and found that the combination lowered risk for recurrence.
The results of NATALEE, together with the recent findings of the monarchE trial, provide strong evidence that the addition of a CDK4/6 inhibitor to ET is useful in the adjuvant setting. Dr Burstein suggests that these findings may point to an emerging treatment paradigm in HR+/HER2- patients, particularly those with higher-risk breast cancers.
Dr Burstein next discusses important data from the Early Breast Cancer Trialists Collaborative Group (EBCTCG). Their meta-analysis of 25 randomized trials on ovarian ablation in premenopausal women showed that ovarian ablation provided a substantial reduction in 15-year risk for recurrence and death.
Finally, Dr Burstein reports on data from an analysis of patients enrolled in the PENELOPE-B trial to assess the value of circulating tumor DNA (ctDNA) in predicting clinical relapse. Dr Burstein reports that the results indicated that ctDNA was a strong prognostic factor for disease recurrence.
--
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Institute Physician, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.
Dr Harold J. Burstein, of the Dana-Farber Cancer Institute in Boston, Massachusetts, highlights key abstracts on early breast cancer from the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Dr Burstein first reports on exciting results from the phase 3 NATALEE trial, which compared adjuvant use of CDK4/6 inhibitor ribociclib plus endocrine therapy (ET) vs ET alone in patients with HR+/HER2- early breast cancer and found that the combination lowered risk for recurrence.
The results of NATALEE, together with the recent findings of the monarchE trial, provide strong evidence that the addition of a CDK4/6 inhibitor to ET is useful in the adjuvant setting. Dr Burstein suggests that these findings may point to an emerging treatment paradigm in HR+/HER2- patients, particularly those with higher-risk breast cancers.
Dr Burstein next discusses important data from the Early Breast Cancer Trialists Collaborative Group (EBCTCG). Their meta-analysis of 25 randomized trials on ovarian ablation in premenopausal women showed that ovarian ablation provided a substantial reduction in 15-year risk for recurrence and death.
Finally, Dr Burstein reports on data from an analysis of patients enrolled in the PENELOPE-B trial to assess the value of circulating tumor DNA (ctDNA) in predicting clinical relapse. Dr Burstein reports that the results indicated that ctDNA was a strong prognostic factor for disease recurrence.
--
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Institute Physician, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.

Low-calorie tastes sweeter with a little salt
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
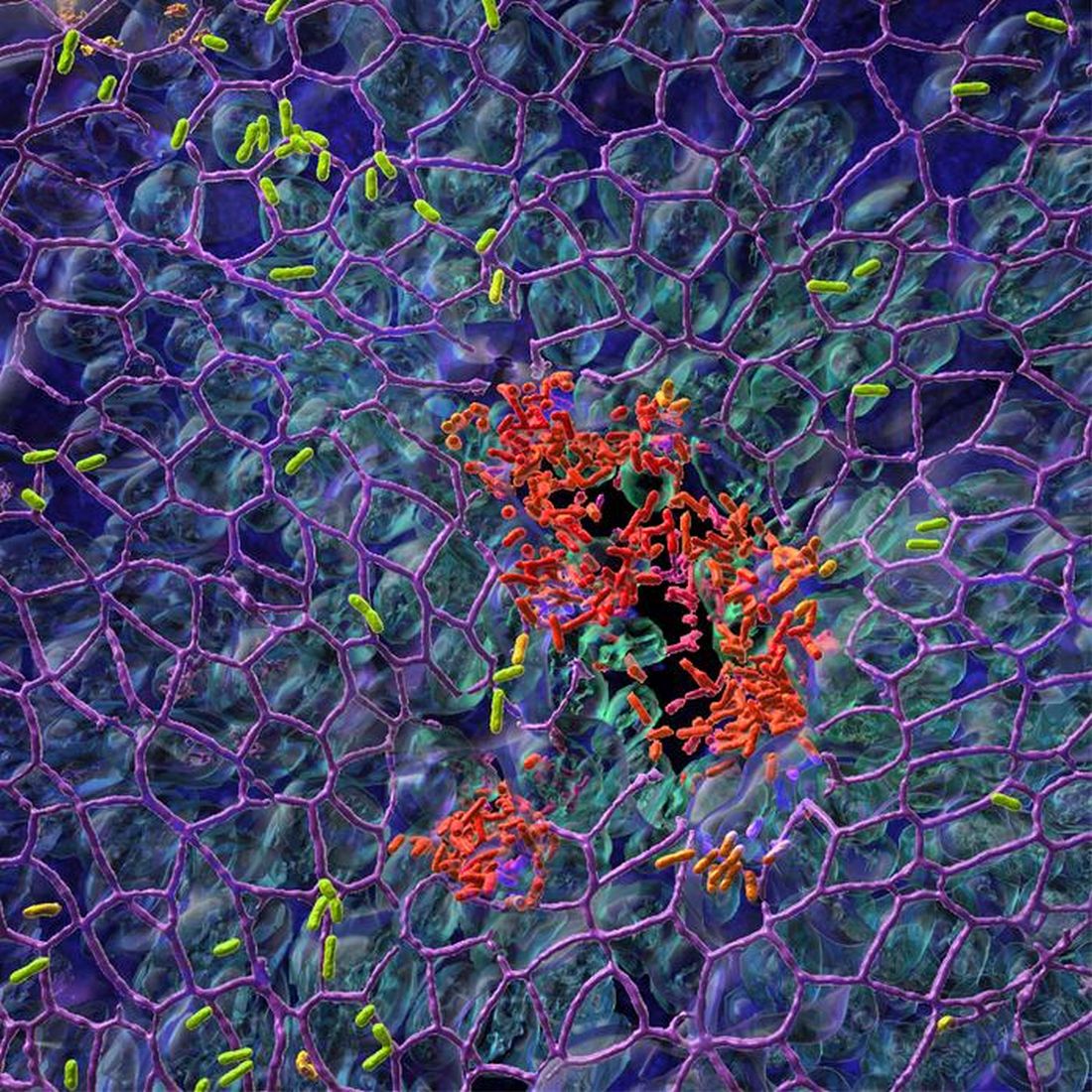
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Key Abstracts in Metastatic Breast Cancer From ASCO 2023
Dr Harold J. Burstein, of the Dana-Farber Cancer Institute in Boston, Massachusetts, presents key abstracts on metastatic breast cancer (mBC) from the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Dr Burstein first highlights results from the SONIA study, which compared endocrine therapy followed by a CDK4/6 inhibitor in the second-line with the use of a CDK4/6 inhibitor in the first line. Although the CDK4/6 inhibitor in first-line improved progression-free survival, overall survival remained unchanged.
Dr Burstein next discusses results from the CANKADO trial, which randomized patients with mBC to report symptoms via a smartphone app. The app users reported fewer adverse events and better quality of life.
Dr Burstein reports on the potentially practice-changing results of the X-7/7 trial comparing a fixed dose of capecitabine (7/7) with the standard dose (14/7). Although both dosing schedules showed similar overall survival results, the fixed dose was better tolerated.
Finally, Dr Burstein turns to advances in the use of antibody-drug conjugates (ADCs), starting with an update from the TROPiCS-02 study comparing sacituzumab govitecan (SG) with standard chemotherapy. The 12.75-month follow-up showed an overall survival benefit when using SG in third- or fourth-line treatment.
He also highlights phase 2 trial results with another ADC, HER3-DXd (patritumab deruxtecan), which showed significant response rates across a broad range of HER3 expression levels.
--
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Institute Physician, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.
Dr Harold J. Burstein, of the Dana-Farber Cancer Institute in Boston, Massachusetts, presents key abstracts on metastatic breast cancer (mBC) from the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Dr Burstein first highlights results from the SONIA study, which compared endocrine therapy followed by a CDK4/6 inhibitor in the second-line with the use of a CDK4/6 inhibitor in the first line. Although the CDK4/6 inhibitor in first-line improved progression-free survival, overall survival remained unchanged.
Dr Burstein next discusses results from the CANKADO trial, which randomized patients with mBC to report symptoms via a smartphone app. The app users reported fewer adverse events and better quality of life.
Dr Burstein reports on the potentially practice-changing results of the X-7/7 trial comparing a fixed dose of capecitabine (7/7) with the standard dose (14/7). Although both dosing schedules showed similar overall survival results, the fixed dose was better tolerated.
Finally, Dr Burstein turns to advances in the use of antibody-drug conjugates (ADCs), starting with an update from the TROPiCS-02 study comparing sacituzumab govitecan (SG) with standard chemotherapy. The 12.75-month follow-up showed an overall survival benefit when using SG in third- or fourth-line treatment.
He also highlights phase 2 trial results with another ADC, HER3-DXd (patritumab deruxtecan), which showed significant response rates across a broad range of HER3 expression levels.
--
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Institute Physician, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.
Dr Harold J. Burstein, of the Dana-Farber Cancer Institute in Boston, Massachusetts, presents key abstracts on metastatic breast cancer (mBC) from the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Dr Burstein first highlights results from the SONIA study, which compared endocrine therapy followed by a CDK4/6 inhibitor in the second-line with the use of a CDK4/6 inhibitor in the first line. Although the CDK4/6 inhibitor in first-line improved progression-free survival, overall survival remained unchanged.
Dr Burstein next discusses results from the CANKADO trial, which randomized patients with mBC to report symptoms via a smartphone app. The app users reported fewer adverse events and better quality of life.
Dr Burstein reports on the potentially practice-changing results of the X-7/7 trial comparing a fixed dose of capecitabine (7/7) with the standard dose (14/7). Although both dosing schedules showed similar overall survival results, the fixed dose was better tolerated.
Finally, Dr Burstein turns to advances in the use of antibody-drug conjugates (ADCs), starting with an update from the TROPiCS-02 study comparing sacituzumab govitecan (SG) with standard chemotherapy. The 12.75-month follow-up showed an overall survival benefit when using SG in third- or fourth-line treatment.
He also highlights phase 2 trial results with another ADC, HER3-DXd (patritumab deruxtecan), which showed significant response rates across a broad range of HER3 expression levels.
--
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Institute Physician, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.

Observation recommended as first-line therapy in select cases of primary spontaneous pneumothorax
Observation should be considered the first-line treatment of choice in appropriately selected primary spontaneous pneumothorax patients, according to a review comparing observation alone with aspiration or chest tube placement.
Observation was the dominant choice, based on economic modeling showing it to offer both the highest utility and the lowest cost, according to the review, published in CHEST, which encompassed 20 years of relevant publications.
, Gilgamesh Eamer, MD, MSc, FRCSC, of Children’s Hospital of Eastern Ontario, Ottawa, and colleagues wrote. They pointed to recent studies suggesting equivalent or improved outcomes with simple observation in appropriately selected patients. The authors asked, “What management strategy derives the most utility for patients given the cost and morbidity of chest tube placement, hospital admission, surgical intervention and the risk of recurrence of primary spontaneous pneumothorax.”
Primary spontaneous pneumothorax, which leads to progressive pulmonary collapse and respiratory compromise, is thought to be attributable to rupture of air-containing blisters (or bullae) formed under the visceral pleura of the lung, according to the researchers. They stated that, while prior systematic reviews have examined various primary spontaneous pneumothorax management techniques, no reviews encompass more recently published high-quality studies comparing aspiration to other interventions such as observation or Heimlich valve devices.
The authors identified 22 articles for systematic review and meta-analysis after screening an initial list of 5,179 potentially relevant articles (Jan. 1, 2000 to April 10, 2020). They compared observation, needle aspiration, and chest tube placement, and created an economic model for these three treatment pathways based on Canadian medical cost data. The primary outcome measure was resolution following the initial intervention. Secondary outcomes included primary spontaneous pneumothorax recurrence, length of hospital stay, and treatment complications.
The analysis revealed that, compared with observation, chest tube and aspiration had higher resolution without additional intervention (relative risk for chest tube, 0.81; P < .01; RR for aspiration, 0.73; P < .01). Compared with a chest tube, observation and aspiration had shorter length of stay (mean difference for observation, 5.17; P < .01): (MD for aspiration, 2.72; P < .01).
Two-year recurrence rates did not differ between management strategies. Cost utility modeling found a cost of $14,658 (Canadian dollars [CAD] with 1.2535 = 1 US dollar) for chest tube placement, $13,126 CAD for aspiration, and $6,408 CAD for observation.
The utility (a measure including both quantity and quality of life) for each management arm was 0.77 for CT placement, 0.79 for aspiration, and 0.82 for observation. “The observation arm dominates the other two arms meaning it results in a more desirable (higher) utility with lower cost and results in a negative ICER [incremental cost-effectiveness ratio],” the authors stated.
They observed further that it is not typical for a medical intervention to improve patient outcomes, compared with standard care, and at the same time to bring costs down. “Given this, and the increasing evidence that observation is safe and effective in appropriately selected patients presenting with primary spontaneous pneumothorax,” they concluded that “observation should be considered in all patients presenting with primary spontaneous pneumothorax who meet predefined criteria.” They added that, because aspiration is favored over chest tube placement, it should be considered second-line therapy in well-selected primary spontaneous pneumothorax patients presenting with recurrence or who have failed a trial of observation.
“This review sheds light on ‘less is better’ for primary spontaneous pneumothorax management,” commented Dharani K. Narendra, MD, of the department of medicine, Baylor College of Medicine, Houston. “It allows clinicians to utilize a ‘wait approach’ versus invasive treatment. Interestingly, recurrence was lower in the observation group.” She said further, in an interview, “In general we assume that if no intervention is done, there is higher chance of recurrence. However, this meta-analysis reveals that is not the case; there is no difference in recurrence of pneumothorax in all groups and fewer complications in the observation group. The invasive treatments such as aspiration or chest tube are risky as they have more complications like pain, bleeding, injury to surrounding structures, etc.”
Neither Dr. Eamer nor Dr. Narendra reported any conflicts of interest. The study was self-funded.
Observation should be considered the first-line treatment of choice in appropriately selected primary spontaneous pneumothorax patients, according to a review comparing observation alone with aspiration or chest tube placement.
Observation was the dominant choice, based on economic modeling showing it to offer both the highest utility and the lowest cost, according to the review, published in CHEST, which encompassed 20 years of relevant publications.
, Gilgamesh Eamer, MD, MSc, FRCSC, of Children’s Hospital of Eastern Ontario, Ottawa, and colleagues wrote. They pointed to recent studies suggesting equivalent or improved outcomes with simple observation in appropriately selected patients. The authors asked, “What management strategy derives the most utility for patients given the cost and morbidity of chest tube placement, hospital admission, surgical intervention and the risk of recurrence of primary spontaneous pneumothorax.”
Primary spontaneous pneumothorax, which leads to progressive pulmonary collapse and respiratory compromise, is thought to be attributable to rupture of air-containing blisters (or bullae) formed under the visceral pleura of the lung, according to the researchers. They stated that, while prior systematic reviews have examined various primary spontaneous pneumothorax management techniques, no reviews encompass more recently published high-quality studies comparing aspiration to other interventions such as observation or Heimlich valve devices.
The authors identified 22 articles for systematic review and meta-analysis after screening an initial list of 5,179 potentially relevant articles (Jan. 1, 2000 to April 10, 2020). They compared observation, needle aspiration, and chest tube placement, and created an economic model for these three treatment pathways based on Canadian medical cost data. The primary outcome measure was resolution following the initial intervention. Secondary outcomes included primary spontaneous pneumothorax recurrence, length of hospital stay, and treatment complications.
The analysis revealed that, compared with observation, chest tube and aspiration had higher resolution without additional intervention (relative risk for chest tube, 0.81; P < .01; RR for aspiration, 0.73; P < .01). Compared with a chest tube, observation and aspiration had shorter length of stay (mean difference for observation, 5.17; P < .01): (MD for aspiration, 2.72; P < .01).
Two-year recurrence rates did not differ between management strategies. Cost utility modeling found a cost of $14,658 (Canadian dollars [CAD] with 1.2535 = 1 US dollar) for chest tube placement, $13,126 CAD for aspiration, and $6,408 CAD for observation.
The utility (a measure including both quantity and quality of life) for each management arm was 0.77 for CT placement, 0.79 for aspiration, and 0.82 for observation. “The observation arm dominates the other two arms meaning it results in a more desirable (higher) utility with lower cost and results in a negative ICER [incremental cost-effectiveness ratio],” the authors stated.
They observed further that it is not typical for a medical intervention to improve patient outcomes, compared with standard care, and at the same time to bring costs down. “Given this, and the increasing evidence that observation is safe and effective in appropriately selected patients presenting with primary spontaneous pneumothorax,” they concluded that “observation should be considered in all patients presenting with primary spontaneous pneumothorax who meet predefined criteria.” They added that, because aspiration is favored over chest tube placement, it should be considered second-line therapy in well-selected primary spontaneous pneumothorax patients presenting with recurrence or who have failed a trial of observation.
“This review sheds light on ‘less is better’ for primary spontaneous pneumothorax management,” commented Dharani K. Narendra, MD, of the department of medicine, Baylor College of Medicine, Houston. “It allows clinicians to utilize a ‘wait approach’ versus invasive treatment. Interestingly, recurrence was lower in the observation group.” She said further, in an interview, “In general we assume that if no intervention is done, there is higher chance of recurrence. However, this meta-analysis reveals that is not the case; there is no difference in recurrence of pneumothorax in all groups and fewer complications in the observation group. The invasive treatments such as aspiration or chest tube are risky as they have more complications like pain, bleeding, injury to surrounding structures, etc.”
Neither Dr. Eamer nor Dr. Narendra reported any conflicts of interest. The study was self-funded.
Observation should be considered the first-line treatment of choice in appropriately selected primary spontaneous pneumothorax patients, according to a review comparing observation alone with aspiration or chest tube placement.
Observation was the dominant choice, based on economic modeling showing it to offer both the highest utility and the lowest cost, according to the review, published in CHEST, which encompassed 20 years of relevant publications.
, Gilgamesh Eamer, MD, MSc, FRCSC, of Children’s Hospital of Eastern Ontario, Ottawa, and colleagues wrote. They pointed to recent studies suggesting equivalent or improved outcomes with simple observation in appropriately selected patients. The authors asked, “What management strategy derives the most utility for patients given the cost and morbidity of chest tube placement, hospital admission, surgical intervention and the risk of recurrence of primary spontaneous pneumothorax.”
Primary spontaneous pneumothorax, which leads to progressive pulmonary collapse and respiratory compromise, is thought to be attributable to rupture of air-containing blisters (or bullae) formed under the visceral pleura of the lung, according to the researchers. They stated that, while prior systematic reviews have examined various primary spontaneous pneumothorax management techniques, no reviews encompass more recently published high-quality studies comparing aspiration to other interventions such as observation or Heimlich valve devices.
The authors identified 22 articles for systematic review and meta-analysis after screening an initial list of 5,179 potentially relevant articles (Jan. 1, 2000 to April 10, 2020). They compared observation, needle aspiration, and chest tube placement, and created an economic model for these three treatment pathways based on Canadian medical cost data. The primary outcome measure was resolution following the initial intervention. Secondary outcomes included primary spontaneous pneumothorax recurrence, length of hospital stay, and treatment complications.
The analysis revealed that, compared with observation, chest tube and aspiration had higher resolution without additional intervention (relative risk for chest tube, 0.81; P < .01; RR for aspiration, 0.73; P < .01). Compared with a chest tube, observation and aspiration had shorter length of stay (mean difference for observation, 5.17; P < .01): (MD for aspiration, 2.72; P < .01).
Two-year recurrence rates did not differ between management strategies. Cost utility modeling found a cost of $14,658 (Canadian dollars [CAD] with 1.2535 = 1 US dollar) for chest tube placement, $13,126 CAD for aspiration, and $6,408 CAD for observation.
The utility (a measure including both quantity and quality of life) for each management arm was 0.77 for CT placement, 0.79 for aspiration, and 0.82 for observation. “The observation arm dominates the other two arms meaning it results in a more desirable (higher) utility with lower cost and results in a negative ICER [incremental cost-effectiveness ratio],” the authors stated.
They observed further that it is not typical for a medical intervention to improve patient outcomes, compared with standard care, and at the same time to bring costs down. “Given this, and the increasing evidence that observation is safe and effective in appropriately selected patients presenting with primary spontaneous pneumothorax,” they concluded that “observation should be considered in all patients presenting with primary spontaneous pneumothorax who meet predefined criteria.” They added that, because aspiration is favored over chest tube placement, it should be considered second-line therapy in well-selected primary spontaneous pneumothorax patients presenting with recurrence or who have failed a trial of observation.
“This review sheds light on ‘less is better’ for primary spontaneous pneumothorax management,” commented Dharani K. Narendra, MD, of the department of medicine, Baylor College of Medicine, Houston. “It allows clinicians to utilize a ‘wait approach’ versus invasive treatment. Interestingly, recurrence was lower in the observation group.” She said further, in an interview, “In general we assume that if no intervention is done, there is higher chance of recurrence. However, this meta-analysis reveals that is not the case; there is no difference in recurrence of pneumothorax in all groups and fewer complications in the observation group. The invasive treatments such as aspiration or chest tube are risky as they have more complications like pain, bleeding, injury to surrounding structures, etc.”
Neither Dr. Eamer nor Dr. Narendra reported any conflicts of interest. The study was self-funded.
FROM CHEST
Scripts surge for desiccated thyroid extract to treat hypothyroidism
new research has found.
Nationwide MarketScan claims data reveal that, among first-time thyroid hormone prescriptions, those for DTE rose from 5.4% in 2010 to 10.2% in 2020. At the same time, prescriptions for first-line levothyroxine dropped from 91.8% to 87.2%. Prescriptions for liothyronine (LT3), primarily in combination with levothyroxine, remained at about 2% throughout the decade.
The nonlevothyroxine therapies were more commonly prescribed in the West and Southwestern United States, while levothyroxine monotherapy was more frequent in the Northwest and upper Midwest, and also in states with higher densities of primary care physicians and endocrinologists.
The magnitude of this shift in first-line treatment was unexpected.
“We were frankly quite surprised to see that difference in just 10 years,” lead author Matthew Ettleson, MD, of the University of Chicago, said in an interview.
Asked to comment, session moderator Elizabeth N. Pearce, MD, professor of medicine at Boston University Medical Center, said she also found the dramatic shift to DTE surprising.
“It’s unclear why since there hasn’t been a shift in the science or in the guidelines over the last decade. ... I think we need to understand better what is driving this, who the patients are who are seeking it out, and which providers are the primary drivers of these prescriptions,” she said.
Dr. Ettleson presented the findings at the annual meeting of the Endocrine Society. The results were simultaneously published in the Journal of Clinical Endocrinology and Metabolism.
Why the increase in desiccated thyroid extract?
Current guidelines by the American Thyroid Association recommend levothyroxine, a synthetic form of thyroxine (T4) monotherapy, as the standard of care for treating hypothyroidism. However, approximately 10%-20% of levothyroxine-treated patients report bothersome symptoms despite normalization of thyroid-stimulating hormone (TSH) levels.
In 2021, the ATA, along with European and British thyroid societies, issued a consensus statement noting that new trials of triiodothyronine (T3)/T4 combination therapy were “justified.”
However, the MarketScan data were gathered before that statement came out, which doesn’t mention desiccated thyroid extract, “so that’s a bit of a head-scratcher,” Ettleson said.
He said one possibility may be the existence of online materials saying negative things about levothyroxine, so that “people who are just learning about hypothyroidism might already be primed to think about alternative treatments.” Moreover, some patients may view DTE as more “natural” than levothyroxine.
Dr. Ettleson also noted that the distinct geographic variation “didn’t seem random. ... So not only was there a doubling overall but there’s a variation in practice patterns across the country. I don’t have an explanation for that, but I think it’s important to recognize in the medical community that there are these big differences.”
Endocrinologists not as keen to prescribe DTE or T3
Residence in a state with higher endocrinologist density (3.0/100,000 population) was associated with a decreased likelihood of receiving T3 (adjusted odds ratio, 0.33; P < .001) or DTE therapy (aOR, 0.18; P < .001).
Residence in large central metro zones was associated with an increased likelihood of receiving T3 (aOR, 1.32; P < .001) or DTE therapy (aOR, 1.05; P < .008, respectively).
Dr. Pearce observed: “I don’t see DTE in Boston. It’s mostly in the South and Southwest.”
She said she doubted that endocrinologists were the primary prescribers of DTE, as many endocrinologists are “wary” of the pig thyroid–derived product because its T4 to T3 ratio is about 4:1, in contrast to the ratio in humans of 13-14:1.
Thus, DTE contains a much higher proportion of the active hormone T3. It is also much shorter acting, with a half-life of a few hours, compared to a few days for T4, she explained.
“We don’t really know what long-term safety effects are but it’s probably a less physiologic way of dosing thyroid hormone than ... either levothyroxine or levothyroxine in combination with a lower T3 proportion,” she said.
Just trying to understand
Dr. Ettleson emphasized that the goal of his research wasn’t to reverse the trend but to better understand it.
Nonetheless, he also noted, “now that we know there are more patients taking DTE, we need to start looking at rates of atrial fibrillation, fracture, heart failure, and other possible outcomes in this population and compare them with levothyroxine and nonthyroid populations to make sure that it is as safe as levothyroxine.”
“There are no data to suggest increased risk, especially if TSH is monitored and stays in the normal range, but there’s very little data for over 5 or 10 years on DTE-treated patients. We need the data,” he emphasized.
Meanwhile, he’s working on a survey of endocrinologists and non-endocrinologists to ask if they’ve prescribed DTE, and if so, why, and whether it’s because patients asked for it. “There’s a lot more work to be done, but I think it’s exciting. It’s important to see how patients are being treated in the real world ... and understand why it’s happening and what the outcomes are.”
Dr. Ettleson and Dr. Pearce have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research has found.
Nationwide MarketScan claims data reveal that, among first-time thyroid hormone prescriptions, those for DTE rose from 5.4% in 2010 to 10.2% in 2020. At the same time, prescriptions for first-line levothyroxine dropped from 91.8% to 87.2%. Prescriptions for liothyronine (LT3), primarily in combination with levothyroxine, remained at about 2% throughout the decade.
The nonlevothyroxine therapies were more commonly prescribed in the West and Southwestern United States, while levothyroxine monotherapy was more frequent in the Northwest and upper Midwest, and also in states with higher densities of primary care physicians and endocrinologists.
The magnitude of this shift in first-line treatment was unexpected.
“We were frankly quite surprised to see that difference in just 10 years,” lead author Matthew Ettleson, MD, of the University of Chicago, said in an interview.
Asked to comment, session moderator Elizabeth N. Pearce, MD, professor of medicine at Boston University Medical Center, said she also found the dramatic shift to DTE surprising.
“It’s unclear why since there hasn’t been a shift in the science or in the guidelines over the last decade. ... I think we need to understand better what is driving this, who the patients are who are seeking it out, and which providers are the primary drivers of these prescriptions,” she said.
Dr. Ettleson presented the findings at the annual meeting of the Endocrine Society. The results were simultaneously published in the Journal of Clinical Endocrinology and Metabolism.
Why the increase in desiccated thyroid extract?
Current guidelines by the American Thyroid Association recommend levothyroxine, a synthetic form of thyroxine (T4) monotherapy, as the standard of care for treating hypothyroidism. However, approximately 10%-20% of levothyroxine-treated patients report bothersome symptoms despite normalization of thyroid-stimulating hormone (TSH) levels.
In 2021, the ATA, along with European and British thyroid societies, issued a consensus statement noting that new trials of triiodothyronine (T3)/T4 combination therapy were “justified.”
However, the MarketScan data were gathered before that statement came out, which doesn’t mention desiccated thyroid extract, “so that’s a bit of a head-scratcher,” Ettleson said.
He said one possibility may be the existence of online materials saying negative things about levothyroxine, so that “people who are just learning about hypothyroidism might already be primed to think about alternative treatments.” Moreover, some patients may view DTE as more “natural” than levothyroxine.
Dr. Ettleson also noted that the distinct geographic variation “didn’t seem random. ... So not only was there a doubling overall but there’s a variation in practice patterns across the country. I don’t have an explanation for that, but I think it’s important to recognize in the medical community that there are these big differences.”
Endocrinologists not as keen to prescribe DTE or T3
Residence in a state with higher endocrinologist density (3.0/100,000 population) was associated with a decreased likelihood of receiving T3 (adjusted odds ratio, 0.33; P < .001) or DTE therapy (aOR, 0.18; P < .001).
Residence in large central metro zones was associated with an increased likelihood of receiving T3 (aOR, 1.32; P < .001) or DTE therapy (aOR, 1.05; P < .008, respectively).
Dr. Pearce observed: “I don’t see DTE in Boston. It’s mostly in the South and Southwest.”
She said she doubted that endocrinologists were the primary prescribers of DTE, as many endocrinologists are “wary” of the pig thyroid–derived product because its T4 to T3 ratio is about 4:1, in contrast to the ratio in humans of 13-14:1.
Thus, DTE contains a much higher proportion of the active hormone T3. It is also much shorter acting, with a half-life of a few hours, compared to a few days for T4, she explained.
“We don’t really know what long-term safety effects are but it’s probably a less physiologic way of dosing thyroid hormone than ... either levothyroxine or levothyroxine in combination with a lower T3 proportion,” she said.
Just trying to understand
Dr. Ettleson emphasized that the goal of his research wasn’t to reverse the trend but to better understand it.
Nonetheless, he also noted, “now that we know there are more patients taking DTE, we need to start looking at rates of atrial fibrillation, fracture, heart failure, and other possible outcomes in this population and compare them with levothyroxine and nonthyroid populations to make sure that it is as safe as levothyroxine.”
“There are no data to suggest increased risk, especially if TSH is monitored and stays in the normal range, but there’s very little data for over 5 or 10 years on DTE-treated patients. We need the data,” he emphasized.
Meanwhile, he’s working on a survey of endocrinologists and non-endocrinologists to ask if they’ve prescribed DTE, and if so, why, and whether it’s because patients asked for it. “There’s a lot more work to be done, but I think it’s exciting. It’s important to see how patients are being treated in the real world ... and understand why it’s happening and what the outcomes are.”
Dr. Ettleson and Dr. Pearce have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research has found.
Nationwide MarketScan claims data reveal that, among first-time thyroid hormone prescriptions, those for DTE rose from 5.4% in 2010 to 10.2% in 2020. At the same time, prescriptions for first-line levothyroxine dropped from 91.8% to 87.2%. Prescriptions for liothyronine (LT3), primarily in combination with levothyroxine, remained at about 2% throughout the decade.
The nonlevothyroxine therapies were more commonly prescribed in the West and Southwestern United States, while levothyroxine monotherapy was more frequent in the Northwest and upper Midwest, and also in states with higher densities of primary care physicians and endocrinologists.
The magnitude of this shift in first-line treatment was unexpected.
“We were frankly quite surprised to see that difference in just 10 years,” lead author Matthew Ettleson, MD, of the University of Chicago, said in an interview.
Asked to comment, session moderator Elizabeth N. Pearce, MD, professor of medicine at Boston University Medical Center, said she also found the dramatic shift to DTE surprising.
“It’s unclear why since there hasn’t been a shift in the science or in the guidelines over the last decade. ... I think we need to understand better what is driving this, who the patients are who are seeking it out, and which providers are the primary drivers of these prescriptions,” she said.
Dr. Ettleson presented the findings at the annual meeting of the Endocrine Society. The results were simultaneously published in the Journal of Clinical Endocrinology and Metabolism.
Why the increase in desiccated thyroid extract?
Current guidelines by the American Thyroid Association recommend levothyroxine, a synthetic form of thyroxine (T4) monotherapy, as the standard of care for treating hypothyroidism. However, approximately 10%-20% of levothyroxine-treated patients report bothersome symptoms despite normalization of thyroid-stimulating hormone (TSH) levels.
In 2021, the ATA, along with European and British thyroid societies, issued a consensus statement noting that new trials of triiodothyronine (T3)/T4 combination therapy were “justified.”
However, the MarketScan data were gathered before that statement came out, which doesn’t mention desiccated thyroid extract, “so that’s a bit of a head-scratcher,” Ettleson said.
He said one possibility may be the existence of online materials saying negative things about levothyroxine, so that “people who are just learning about hypothyroidism might already be primed to think about alternative treatments.” Moreover, some patients may view DTE as more “natural” than levothyroxine.
Dr. Ettleson also noted that the distinct geographic variation “didn’t seem random. ... So not only was there a doubling overall but there’s a variation in practice patterns across the country. I don’t have an explanation for that, but I think it’s important to recognize in the medical community that there are these big differences.”
Endocrinologists not as keen to prescribe DTE or T3
Residence in a state with higher endocrinologist density (3.0/100,000 population) was associated with a decreased likelihood of receiving T3 (adjusted odds ratio, 0.33; P < .001) or DTE therapy (aOR, 0.18; P < .001).
Residence in large central metro zones was associated with an increased likelihood of receiving T3 (aOR, 1.32; P < .001) or DTE therapy (aOR, 1.05; P < .008, respectively).
Dr. Pearce observed: “I don’t see DTE in Boston. It’s mostly in the South and Southwest.”
She said she doubted that endocrinologists were the primary prescribers of DTE, as many endocrinologists are “wary” of the pig thyroid–derived product because its T4 to T3 ratio is about 4:1, in contrast to the ratio in humans of 13-14:1.
Thus, DTE contains a much higher proportion of the active hormone T3. It is also much shorter acting, with a half-life of a few hours, compared to a few days for T4, she explained.
“We don’t really know what long-term safety effects are but it’s probably a less physiologic way of dosing thyroid hormone than ... either levothyroxine or levothyroxine in combination with a lower T3 proportion,” she said.
Just trying to understand
Dr. Ettleson emphasized that the goal of his research wasn’t to reverse the trend but to better understand it.
Nonetheless, he also noted, “now that we know there are more patients taking DTE, we need to start looking at rates of atrial fibrillation, fracture, heart failure, and other possible outcomes in this population and compare them with levothyroxine and nonthyroid populations to make sure that it is as safe as levothyroxine.”
“There are no data to suggest increased risk, especially if TSH is monitored and stays in the normal range, but there’s very little data for over 5 or 10 years on DTE-treated patients. We need the data,” he emphasized.
Meanwhile, he’s working on a survey of endocrinologists and non-endocrinologists to ask if they’ve prescribed DTE, and if so, why, and whether it’s because patients asked for it. “There’s a lot more work to be done, but I think it’s exciting. It’s important to see how patients are being treated in the real world ... and understand why it’s happening and what the outcomes are.”
Dr. Ettleson and Dr. Pearce have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ENDO 2023
Proteomics reveals potential targets for drug-resistant TB
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Proposal to cap Part B pay on some drugs draws opposition
An influential panel proposed capping Medicare Part B pay for some drugs, arguing this would remove financial incentives to use more costly medicines when there are less expensive equivalents.
Medical groups have objected to both this recommendation from the Medicare Payment Advisory Commission (MedPAC) and the panel’s underlying premise. MedPAC said financial as well as clinical factors can come into play in clinicians’ choices of drugs for patients.
In an interview, Christina Downey, MD, chair of the Government Affairs Committee of the American College of Rheumatology, said physicians in her field cannot switch patients’ medicines to try to make a profit.
“Patients only respond to the drugs that they respond to,” Dr. Downey said. “It’s frankly very insulting to say that physicians just force patients to go on medicines that are going to make them a bunch of money.”
In a June report to Congress, MedPAC recommended reducing the add-on payment for many drugs given in hospitals and clinics, which are thus covered by Part B, as part of a package of suggestions for addressing rising costs. Part B drug spending grew about 9% annually between 2009 and 2021, rising from $15.4 billion to $42.9 billion, MedPAC said.
Medicare’s current Part B drug pricing model starts with the reported average sales price (ASP) and then adds about 4.3% or 6%, depending on current budget-sequester law, to the cost of medicines.
MedPAC members voted 17-0 in April in favor of a general recommendation to revise the Part B payment approach. In the June report, MedPAC fleshes out this idea. It mentions a model in which the add-on Part B payment would be the lesser of either 6% of the ASP, 3% plus $24, or $220.
The majority of Part B drug administrations are for very low-priced drugs, MedPAC said. But for some of the more costly ones, annual prices can be more than $400,000 per patient, and future launch prices may be even higher for certain types of products, such as gene therapies, MedPAC said.
“There is no evidence that the costs of a drug’s administration are proportionate to the price of the drug,” MedPAC said.
Concerns about how well Medicare covers the cost of drug administration should be addressed through other pathways, such as the American Medical
Association’s Specialty Society Relative Value Scale Update Committee (RUC), MedPAC said. AMA’s RUC advises the Centers for Medicare & Medicaid Services on the physician fee schedule.
Congress is not obliged to act on or to even consider MedPAC’s work. In general, lawmakers and CMS often pay heed to the panel’s recommendations, sometimes incorporating them into new policy.
But this new MedPAC Part B recommendation has drawn strong opposition, similar to the response to a 2016 CMS plan to cut the Part B add-on payment. That plan, which CMS later abandoned, would have cut the markup on Part B drugs to 2.5% and added a flat fee to cover administration costs.
Why not focus on PBMs instead?
The timing of the MedPAC recommendation is poor, given that CMS already is trying to implement the Inflation Reduction Act and create a new system of direct Medicare drug price negotiations, as ordered by Congress, said Madelaine A. Feldman, MD, a rheumatologist based in New Orleans.
A better approach for lowering drug prices would be to focus more on the operations of pharmacy benefit managers (PBMs), said Dr. Feldman, who also is vice president for advocacy and government affairs for the Coalition of State Rheumatology Organizations. A pending bipartisan Senate bill, for example, would prohibit PBM compensation based on the price of a drug as a condition of entering into a contract with a Medicare Part D plan.
Congress needs to take steps to unlink the profits of PBMs from higher drug prices, Dr. Feldman said.
“Until that happens, we can put all the lipstick we want on this big pig, but it’s not going to really fix the problem,” she said.
Reduced pay for drugs acquired through 340B program?
In an interview about the new MedPAC proposal, Ted Okon, executive director of the Community Oncology Alliance, urged renewed attention to what he sees as unintended consequences of the 340B discount drug program.
Under this program, certain hospitals can acquire drugs at steeply reduced prices, but they are not obliged to share those discounts with patients. Hospitals that participate in the 340B program can gain funds when patients and their insurers, including Medicare, pay more for the medicines hospitals and other organizations acquired with the 340B discount. Hospitals say they use the money from the 340B program to expand resources in their communities.
But rapid growth of the program in recent years has led to questions, especially about the role of contract pharmacies that manage the program. Congress created the 340B program in 1992 as a workaround to then new rules on Medicaid drug coverage.
In 2021, participating hospitals and clinics and organizations purchased about $44 billion worth of medicines through the 340B drug program. This was an increase of 16% from the previous year, according to a report from the nonprofit Commonwealth Fund. The number of sites, including hospitals and pharmacies, enrolled in the 340B program rose from 8,100 in 2000 to 50,000 by 2020, the report said.
MedPAC in 2016 urged CMS to reduce the amount Medicare pays for drugs acquired through the 340B program. CMS did so during the Trump administration, a policy later defended by the Biden administration.
But the U.S. Supreme Court last year said Medicare erred in its approach to making this cut, as earlier reported. Federal law required that the Department of Health and Human Services conduct a survey to support such a step, and HHS did not do this, the court said. CMS thus was ordered to return Medicare to the ASP+6% payment model for drugs purchased through the 340B discount program.
In the June report, though, MedPAC stuck by its 2016 recommendation that Medicare reduce its payments for drugs purchased through the 340B discount program despite this setback.
“We continue to believe that this approach is appropriate, and the specific level of payment reduction could be considered further as newer data become available,” MedPAC said.
Hospital, PhRMA split
Hospitals would certainly contest any renewed bid by CMS to drop Medicare’s pay for drugs purchased through the 340B program. The American Hospital Association objected to the MedPAC proposal regarding the add-on payment in Part B drug pricing.
MedPAC commissioners discussed this idea at a January meeting, prompting a February letter from the AHA to the panel. Like Dr. Feldman, AHA said it would be “premature” to launch into a revision of Part B drug pricing while the impact of the IRA on drug prices was still unclear.
AHA also noted that a reduction in Part B drug reimbursement would “shift the responsibility for the rapid increase in drug prices away from drug manufacturers, and instead places the burden on hospitals and patients.”
But the AHA gave a much warmer reception to another proposal MedPAC considered this year and that it included in its June report, which is a plan to address the high cost of certain drugs of as yet unconfirmed clinical benefit.
In April, the AHA said it supports a move toward a “value-based approach” in certain cases in which first-in-class medicines are sold under U.S. Food and Drug Administration’s accelerated approvals. Medicare could then cap payment for such drugs that have excessively high launch prices and uncertain clinical benefit, AHA said.
In the June report, MedPAC recommended that Medicare be able to place such a limit on Part B payments in certain cases, including ones in which companies do not meet FDA deadlines for postmarketing confirmatory trials.
The Pharmaceutical Research and Manufacturers of America (PhRMA) objected to this proposed change. The trade group for drugmakers said the FDA often revises and extends enrollment milestones for pending confirmatory trials when companies hit snags, such as challenges in enrolling patients, PhRMA said.
Reducing Part B payment for drugs for which confirmatory trials have been delayed would have a “disproportionate impact” on smaller and rural communities, where independent practices struggle to keep their doors open as it is, PhRMA spokeswoman Nicole Longo wrote in a blog post.
“If physicians can’t afford to administer a medicine, then they won’t and that means their patients won’t have access to them either,” Ms. Longo wrote.
A version of this article first appeared on Medscape.com.
An influential panel proposed capping Medicare Part B pay for some drugs, arguing this would remove financial incentives to use more costly medicines when there are less expensive equivalents.
Medical groups have objected to both this recommendation from the Medicare Payment Advisory Commission (MedPAC) and the panel’s underlying premise. MedPAC said financial as well as clinical factors can come into play in clinicians’ choices of drugs for patients.
In an interview, Christina Downey, MD, chair of the Government Affairs Committee of the American College of Rheumatology, said physicians in her field cannot switch patients’ medicines to try to make a profit.
“Patients only respond to the drugs that they respond to,” Dr. Downey said. “It’s frankly very insulting to say that physicians just force patients to go on medicines that are going to make them a bunch of money.”
In a June report to Congress, MedPAC recommended reducing the add-on payment for many drugs given in hospitals and clinics, which are thus covered by Part B, as part of a package of suggestions for addressing rising costs. Part B drug spending grew about 9% annually between 2009 and 2021, rising from $15.4 billion to $42.9 billion, MedPAC said.
Medicare’s current Part B drug pricing model starts with the reported average sales price (ASP) and then adds about 4.3% or 6%, depending on current budget-sequester law, to the cost of medicines.
MedPAC members voted 17-0 in April in favor of a general recommendation to revise the Part B payment approach. In the June report, MedPAC fleshes out this idea. It mentions a model in which the add-on Part B payment would be the lesser of either 6% of the ASP, 3% plus $24, or $220.
The majority of Part B drug administrations are for very low-priced drugs, MedPAC said. But for some of the more costly ones, annual prices can be more than $400,000 per patient, and future launch prices may be even higher for certain types of products, such as gene therapies, MedPAC said.
“There is no evidence that the costs of a drug’s administration are proportionate to the price of the drug,” MedPAC said.
Concerns about how well Medicare covers the cost of drug administration should be addressed through other pathways, such as the American Medical
Association’s Specialty Society Relative Value Scale Update Committee (RUC), MedPAC said. AMA’s RUC advises the Centers for Medicare & Medicaid Services on the physician fee schedule.
Congress is not obliged to act on or to even consider MedPAC’s work. In general, lawmakers and CMS often pay heed to the panel’s recommendations, sometimes incorporating them into new policy.
But this new MedPAC Part B recommendation has drawn strong opposition, similar to the response to a 2016 CMS plan to cut the Part B add-on payment. That plan, which CMS later abandoned, would have cut the markup on Part B drugs to 2.5% and added a flat fee to cover administration costs.
Why not focus on PBMs instead?
The timing of the MedPAC recommendation is poor, given that CMS already is trying to implement the Inflation Reduction Act and create a new system of direct Medicare drug price negotiations, as ordered by Congress, said Madelaine A. Feldman, MD, a rheumatologist based in New Orleans.
A better approach for lowering drug prices would be to focus more on the operations of pharmacy benefit managers (PBMs), said Dr. Feldman, who also is vice president for advocacy and government affairs for the Coalition of State Rheumatology Organizations. A pending bipartisan Senate bill, for example, would prohibit PBM compensation based on the price of a drug as a condition of entering into a contract with a Medicare Part D plan.
Congress needs to take steps to unlink the profits of PBMs from higher drug prices, Dr. Feldman said.
“Until that happens, we can put all the lipstick we want on this big pig, but it’s not going to really fix the problem,” she said.
Reduced pay for drugs acquired through 340B program?
In an interview about the new MedPAC proposal, Ted Okon, executive director of the Community Oncology Alliance, urged renewed attention to what he sees as unintended consequences of the 340B discount drug program.
Under this program, certain hospitals can acquire drugs at steeply reduced prices, but they are not obliged to share those discounts with patients. Hospitals that participate in the 340B program can gain funds when patients and their insurers, including Medicare, pay more for the medicines hospitals and other organizations acquired with the 340B discount. Hospitals say they use the money from the 340B program to expand resources in their communities.
But rapid growth of the program in recent years has led to questions, especially about the role of contract pharmacies that manage the program. Congress created the 340B program in 1992 as a workaround to then new rules on Medicaid drug coverage.
In 2021, participating hospitals and clinics and organizations purchased about $44 billion worth of medicines through the 340B drug program. This was an increase of 16% from the previous year, according to a report from the nonprofit Commonwealth Fund. The number of sites, including hospitals and pharmacies, enrolled in the 340B program rose from 8,100 in 2000 to 50,000 by 2020, the report said.
MedPAC in 2016 urged CMS to reduce the amount Medicare pays for drugs acquired through the 340B program. CMS did so during the Trump administration, a policy later defended by the Biden administration.
But the U.S. Supreme Court last year said Medicare erred in its approach to making this cut, as earlier reported. Federal law required that the Department of Health and Human Services conduct a survey to support such a step, and HHS did not do this, the court said. CMS thus was ordered to return Medicare to the ASP+6% payment model for drugs purchased through the 340B discount program.
In the June report, though, MedPAC stuck by its 2016 recommendation that Medicare reduce its payments for drugs purchased through the 340B discount program despite this setback.
“We continue to believe that this approach is appropriate, and the specific level of payment reduction could be considered further as newer data become available,” MedPAC said.
Hospital, PhRMA split
Hospitals would certainly contest any renewed bid by CMS to drop Medicare’s pay for drugs purchased through the 340B program. The American Hospital Association objected to the MedPAC proposal regarding the add-on payment in Part B drug pricing.
MedPAC commissioners discussed this idea at a January meeting, prompting a February letter from the AHA to the panel. Like Dr. Feldman, AHA said it would be “premature” to launch into a revision of Part B drug pricing while the impact of the IRA on drug prices was still unclear.
AHA also noted that a reduction in Part B drug reimbursement would “shift the responsibility for the rapid increase in drug prices away from drug manufacturers, and instead places the burden on hospitals and patients.”
But the AHA gave a much warmer reception to another proposal MedPAC considered this year and that it included in its June report, which is a plan to address the high cost of certain drugs of as yet unconfirmed clinical benefit.
In April, the AHA said it supports a move toward a “value-based approach” in certain cases in which first-in-class medicines are sold under U.S. Food and Drug Administration’s accelerated approvals. Medicare could then cap payment for such drugs that have excessively high launch prices and uncertain clinical benefit, AHA said.
In the June report, MedPAC recommended that Medicare be able to place such a limit on Part B payments in certain cases, including ones in which companies do not meet FDA deadlines for postmarketing confirmatory trials.
The Pharmaceutical Research and Manufacturers of America (PhRMA) objected to this proposed change. The trade group for drugmakers said the FDA often revises and extends enrollment milestones for pending confirmatory trials when companies hit snags, such as challenges in enrolling patients, PhRMA said.
Reducing Part B payment for drugs for which confirmatory trials have been delayed would have a “disproportionate impact” on smaller and rural communities, where independent practices struggle to keep their doors open as it is, PhRMA spokeswoman Nicole Longo wrote in a blog post.
“If physicians can’t afford to administer a medicine, then they won’t and that means their patients won’t have access to them either,” Ms. Longo wrote.
A version of this article first appeared on Medscape.com.
An influential panel proposed capping Medicare Part B pay for some drugs, arguing this would remove financial incentives to use more costly medicines when there are less expensive equivalents.
Medical groups have objected to both this recommendation from the Medicare Payment Advisory Commission (MedPAC) and the panel’s underlying premise. MedPAC said financial as well as clinical factors can come into play in clinicians’ choices of drugs for patients.
In an interview, Christina Downey, MD, chair of the Government Affairs Committee of the American College of Rheumatology, said physicians in her field cannot switch patients’ medicines to try to make a profit.
“Patients only respond to the drugs that they respond to,” Dr. Downey said. “It’s frankly very insulting to say that physicians just force patients to go on medicines that are going to make them a bunch of money.”
In a June report to Congress, MedPAC recommended reducing the add-on payment for many drugs given in hospitals and clinics, which are thus covered by Part B, as part of a package of suggestions for addressing rising costs. Part B drug spending grew about 9% annually between 2009 and 2021, rising from $15.4 billion to $42.9 billion, MedPAC said.
Medicare’s current Part B drug pricing model starts with the reported average sales price (ASP) and then adds about 4.3% or 6%, depending on current budget-sequester law, to the cost of medicines.
MedPAC members voted 17-0 in April in favor of a general recommendation to revise the Part B payment approach. In the June report, MedPAC fleshes out this idea. It mentions a model in which the add-on Part B payment would be the lesser of either 6% of the ASP, 3% plus $24, or $220.
The majority of Part B drug administrations are for very low-priced drugs, MedPAC said. But for some of the more costly ones, annual prices can be more than $400,000 per patient, and future launch prices may be even higher for certain types of products, such as gene therapies, MedPAC said.
“There is no evidence that the costs of a drug’s administration are proportionate to the price of the drug,” MedPAC said.
Concerns about how well Medicare covers the cost of drug administration should be addressed through other pathways, such as the American Medical
Association’s Specialty Society Relative Value Scale Update Committee (RUC), MedPAC said. AMA’s RUC advises the Centers for Medicare & Medicaid Services on the physician fee schedule.
Congress is not obliged to act on or to even consider MedPAC’s work. In general, lawmakers and CMS often pay heed to the panel’s recommendations, sometimes incorporating them into new policy.
But this new MedPAC Part B recommendation has drawn strong opposition, similar to the response to a 2016 CMS plan to cut the Part B add-on payment. That plan, which CMS later abandoned, would have cut the markup on Part B drugs to 2.5% and added a flat fee to cover administration costs.
Why not focus on PBMs instead?
The timing of the MedPAC recommendation is poor, given that CMS already is trying to implement the Inflation Reduction Act and create a new system of direct Medicare drug price negotiations, as ordered by Congress, said Madelaine A. Feldman, MD, a rheumatologist based in New Orleans.
A better approach for lowering drug prices would be to focus more on the operations of pharmacy benefit managers (PBMs), said Dr. Feldman, who also is vice president for advocacy and government affairs for the Coalition of State Rheumatology Organizations. A pending bipartisan Senate bill, for example, would prohibit PBM compensation based on the price of a drug as a condition of entering into a contract with a Medicare Part D plan.
Congress needs to take steps to unlink the profits of PBMs from higher drug prices, Dr. Feldman said.
“Until that happens, we can put all the lipstick we want on this big pig, but it’s not going to really fix the problem,” she said.
Reduced pay for drugs acquired through 340B program?
In an interview about the new MedPAC proposal, Ted Okon, executive director of the Community Oncology Alliance, urged renewed attention to what he sees as unintended consequences of the 340B discount drug program.
Under this program, certain hospitals can acquire drugs at steeply reduced prices, but they are not obliged to share those discounts with patients. Hospitals that participate in the 340B program can gain funds when patients and their insurers, including Medicare, pay more for the medicines hospitals and other organizations acquired with the 340B discount. Hospitals say they use the money from the 340B program to expand resources in their communities.
But rapid growth of the program in recent years has led to questions, especially about the role of contract pharmacies that manage the program. Congress created the 340B program in 1992 as a workaround to then new rules on Medicaid drug coverage.
In 2021, participating hospitals and clinics and organizations purchased about $44 billion worth of medicines through the 340B drug program. This was an increase of 16% from the previous year, according to a report from the nonprofit Commonwealth Fund. The number of sites, including hospitals and pharmacies, enrolled in the 340B program rose from 8,100 in 2000 to 50,000 by 2020, the report said.
MedPAC in 2016 urged CMS to reduce the amount Medicare pays for drugs acquired through the 340B program. CMS did so during the Trump administration, a policy later defended by the Biden administration.
But the U.S. Supreme Court last year said Medicare erred in its approach to making this cut, as earlier reported. Federal law required that the Department of Health and Human Services conduct a survey to support such a step, and HHS did not do this, the court said. CMS thus was ordered to return Medicare to the ASP+6% payment model for drugs purchased through the 340B discount program.
In the June report, though, MedPAC stuck by its 2016 recommendation that Medicare reduce its payments for drugs purchased through the 340B discount program despite this setback.
“We continue to believe that this approach is appropriate, and the specific level of payment reduction could be considered further as newer data become available,” MedPAC said.
Hospital, PhRMA split
Hospitals would certainly contest any renewed bid by CMS to drop Medicare’s pay for drugs purchased through the 340B program. The American Hospital Association objected to the MedPAC proposal regarding the add-on payment in Part B drug pricing.
MedPAC commissioners discussed this idea at a January meeting, prompting a February letter from the AHA to the panel. Like Dr. Feldman, AHA said it would be “premature” to launch into a revision of Part B drug pricing while the impact of the IRA on drug prices was still unclear.
AHA also noted that a reduction in Part B drug reimbursement would “shift the responsibility for the rapid increase in drug prices away from drug manufacturers, and instead places the burden on hospitals and patients.”
But the AHA gave a much warmer reception to another proposal MedPAC considered this year and that it included in its June report, which is a plan to address the high cost of certain drugs of as yet unconfirmed clinical benefit.
In April, the AHA said it supports a move toward a “value-based approach” in certain cases in which first-in-class medicines are sold under U.S. Food and Drug Administration’s accelerated approvals. Medicare could then cap payment for such drugs that have excessively high launch prices and uncertain clinical benefit, AHA said.
In the June report, MedPAC recommended that Medicare be able to place such a limit on Part B payments in certain cases, including ones in which companies do not meet FDA deadlines for postmarketing confirmatory trials.
The Pharmaceutical Research and Manufacturers of America (PhRMA) objected to this proposed change. The trade group for drugmakers said the FDA often revises and extends enrollment milestones for pending confirmatory trials when companies hit snags, such as challenges in enrolling patients, PhRMA said.
Reducing Part B payment for drugs for which confirmatory trials have been delayed would have a “disproportionate impact” on smaller and rural communities, where independent practices struggle to keep their doors open as it is, PhRMA spokeswoman Nicole Longo wrote in a blog post.
“If physicians can’t afford to administer a medicine, then they won’t and that means their patients won’t have access to them either,” Ms. Longo wrote.
A version of this article first appeared on Medscape.com.
New AGA CPU focuses on gastric peroral endoscopic myotomy for gastroparesis
Authored by Mouen A. Khashab, MD, director of therapeutic endoscopy at Johns Hopkins Medicine, Baltimore; Andrew Y. Wang, MD, AGAF, chief of interventional endoscopy, University of Virginia, Charlottesville; and, Qiang Cai, MD, PhD, chief of gastroenterology, Ochsner LSU Health Shreveport (La.), the update covers patient selection, procedural considerations, adverse events (AEs), and other topics.
“G-POEM is being performed worldwide to treat patients with refractory gastroparesis,” the investigators wrote in Gastroenterology). “G-POEM is an overall safe procedure with high technical success rates, particularly when performed by an endoscopist experienced in third-space endoscopy. Even if the durable clinical success of G-POEM is in the 50% to 60% range, this represents a huge clinical benefit to patients with refractory gastroparesis, which is a disease associated with substantial morbidity, poor quality of life, and a paucity of safe and effective treatments.”
The authors listed treatment alternatives, noting how associated clinical data have fallen short.
“Although endoscopic pyloric balloon dilation, intrapyloric botulinum toxin injection, gastric electrical stimulation, and transpyloric stenting have been used in patients [with gastroparesis] who have not responded to medical therapy, published studies concerning these therapies have been inconsistent, shown no benefit, or lacked methodologic rigor,” they wrote.
Patient selection
G-POEM should be considered in patients with medically refractory gastroparesis due to diabetes, prior surgery, or idiopathic causes. Candidates should undergo endoscopy to confirm no mechanical obstruction, as well as a solid-phase gastric emptying scan to confirm delayed emptying, with ideal candidates showing at least 20% retention at 4 hours, as this threshold has been linked with better clinical outcomes.
G-POEM is most beneficial when moderate to severe symptoms are present, the investigators wrote, particularly vomiting and nausea. The Gastroparesis Cardinal Symptom Index (GCSI) can be used to determine severity, with a score greater than 2 indicating moderate to severe presentation.
Procedural considerations
The CPU offers detailed procedural considerations, including preparation and equipment, technical guidance, and postprocedural strategy.
“G-POEM should only be performed by interventional endoscopists with expertise or training in third-space endoscopy,” Dr. Khashab and colleagues wrote. “Although experience in endoscopic submucosal dissection (ESD) is not mandatory before performing G-POEM, it likely shortens the learning curve.”
Equipment minimums are also described, including “a high-definition gastroscope, with a waterjet, affixed with a clear distal cap” and “a modern electrosurgical generator capable of modulating power based on tissue resistance and circuit impedance.”
While G-POEM is typically performed via a greater-curvature approach, similar outcomes have been documented for a lesser-curvature approach, Dr. Khashab and colleagues wrote. This alternative technique may increase difficulty of pyloromyotomy, they added.
Postprocedural care may involve an overnight stay, according to the update, with an upper GI study on the subsequent day to ensure no contrast leakage, though this is not mandatory.
Adverse events
“G-POEM is generally safe when performed by trained and/or experienced endoscopists, and AEs are uncommon,” the investigators wrote. “However, serious AEs can occur and have been reported.”
Reported AEs include capnoperitoneum, inadvertent mucosotomy, thermal-mucosal injury, abdominal pain, bleeding, gastric ulceration, and dumping syndrome.
Insurance companies called to action
After reviewing emerging data, the authors suggested the time has come to consider G-POEM as a routine, evidence-based procedure that deserves appropriate reimbursement by financial stakeholders.
“Many insurers still consider G-POEM investigational and refuse to cover this procedure for patients with medically refractory gastroparesis,” they wrote. “As the safety and clinical effectiveness of G-POEM is now well supported, insurance companies and payors should cover G-POEM for patients with significant gastroparesis.”
The clinical practice update was commissioned and approved by the American Gastroenterological Association. The investigators disclosed relationships with Boston Scientific, Medtronic, and Olympus, among others.
Authored by Mouen A. Khashab, MD, director of therapeutic endoscopy at Johns Hopkins Medicine, Baltimore; Andrew Y. Wang, MD, AGAF, chief of interventional endoscopy, University of Virginia, Charlottesville; and, Qiang Cai, MD, PhD, chief of gastroenterology, Ochsner LSU Health Shreveport (La.), the update covers patient selection, procedural considerations, adverse events (AEs), and other topics.
“G-POEM is being performed worldwide to treat patients with refractory gastroparesis,” the investigators wrote in Gastroenterology). “G-POEM is an overall safe procedure with high technical success rates, particularly when performed by an endoscopist experienced in third-space endoscopy. Even if the durable clinical success of G-POEM is in the 50% to 60% range, this represents a huge clinical benefit to patients with refractory gastroparesis, which is a disease associated with substantial morbidity, poor quality of life, and a paucity of safe and effective treatments.”
The authors listed treatment alternatives, noting how associated clinical data have fallen short.
“Although endoscopic pyloric balloon dilation, intrapyloric botulinum toxin injection, gastric electrical stimulation, and transpyloric stenting have been used in patients [with gastroparesis] who have not responded to medical therapy, published studies concerning these therapies have been inconsistent, shown no benefit, or lacked methodologic rigor,” they wrote.
Patient selection
G-POEM should be considered in patients with medically refractory gastroparesis due to diabetes, prior surgery, or idiopathic causes. Candidates should undergo endoscopy to confirm no mechanical obstruction, as well as a solid-phase gastric emptying scan to confirm delayed emptying, with ideal candidates showing at least 20% retention at 4 hours, as this threshold has been linked with better clinical outcomes.
G-POEM is most beneficial when moderate to severe symptoms are present, the investigators wrote, particularly vomiting and nausea. The Gastroparesis Cardinal Symptom Index (GCSI) can be used to determine severity, with a score greater than 2 indicating moderate to severe presentation.
Procedural considerations
The CPU offers detailed procedural considerations, including preparation and equipment, technical guidance, and postprocedural strategy.
“G-POEM should only be performed by interventional endoscopists with expertise or training in third-space endoscopy,” Dr. Khashab and colleagues wrote. “Although experience in endoscopic submucosal dissection (ESD) is not mandatory before performing G-POEM, it likely shortens the learning curve.”
Equipment minimums are also described, including “a high-definition gastroscope, with a waterjet, affixed with a clear distal cap” and “a modern electrosurgical generator capable of modulating power based on tissue resistance and circuit impedance.”
While G-POEM is typically performed via a greater-curvature approach, similar outcomes have been documented for a lesser-curvature approach, Dr. Khashab and colleagues wrote. This alternative technique may increase difficulty of pyloromyotomy, they added.
Postprocedural care may involve an overnight stay, according to the update, with an upper GI study on the subsequent day to ensure no contrast leakage, though this is not mandatory.
Adverse events
“G-POEM is generally safe when performed by trained and/or experienced endoscopists, and AEs are uncommon,” the investigators wrote. “However, serious AEs can occur and have been reported.”
Reported AEs include capnoperitoneum, inadvertent mucosotomy, thermal-mucosal injury, abdominal pain, bleeding, gastric ulceration, and dumping syndrome.
Insurance companies called to action
After reviewing emerging data, the authors suggested the time has come to consider G-POEM as a routine, evidence-based procedure that deserves appropriate reimbursement by financial stakeholders.
“Many insurers still consider G-POEM investigational and refuse to cover this procedure for patients with medically refractory gastroparesis,” they wrote. “As the safety and clinical effectiveness of G-POEM is now well supported, insurance companies and payors should cover G-POEM for patients with significant gastroparesis.”
The clinical practice update was commissioned and approved by the American Gastroenterological Association. The investigators disclosed relationships with Boston Scientific, Medtronic, and Olympus, among others.
Authored by Mouen A. Khashab, MD, director of therapeutic endoscopy at Johns Hopkins Medicine, Baltimore; Andrew Y. Wang, MD, AGAF, chief of interventional endoscopy, University of Virginia, Charlottesville; and, Qiang Cai, MD, PhD, chief of gastroenterology, Ochsner LSU Health Shreveport (La.), the update covers patient selection, procedural considerations, adverse events (AEs), and other topics.
“G-POEM is being performed worldwide to treat patients with refractory gastroparesis,” the investigators wrote in Gastroenterology). “G-POEM is an overall safe procedure with high technical success rates, particularly when performed by an endoscopist experienced in third-space endoscopy. Even if the durable clinical success of G-POEM is in the 50% to 60% range, this represents a huge clinical benefit to patients with refractory gastroparesis, which is a disease associated with substantial morbidity, poor quality of life, and a paucity of safe and effective treatments.”
The authors listed treatment alternatives, noting how associated clinical data have fallen short.
“Although endoscopic pyloric balloon dilation, intrapyloric botulinum toxin injection, gastric electrical stimulation, and transpyloric stenting have been used in patients [with gastroparesis] who have not responded to medical therapy, published studies concerning these therapies have been inconsistent, shown no benefit, or lacked methodologic rigor,” they wrote.
Patient selection
G-POEM should be considered in patients with medically refractory gastroparesis due to diabetes, prior surgery, or idiopathic causes. Candidates should undergo endoscopy to confirm no mechanical obstruction, as well as a solid-phase gastric emptying scan to confirm delayed emptying, with ideal candidates showing at least 20% retention at 4 hours, as this threshold has been linked with better clinical outcomes.
G-POEM is most beneficial when moderate to severe symptoms are present, the investigators wrote, particularly vomiting and nausea. The Gastroparesis Cardinal Symptom Index (GCSI) can be used to determine severity, with a score greater than 2 indicating moderate to severe presentation.
Procedural considerations
The CPU offers detailed procedural considerations, including preparation and equipment, technical guidance, and postprocedural strategy.
“G-POEM should only be performed by interventional endoscopists with expertise or training in third-space endoscopy,” Dr. Khashab and colleagues wrote. “Although experience in endoscopic submucosal dissection (ESD) is not mandatory before performing G-POEM, it likely shortens the learning curve.”
Equipment minimums are also described, including “a high-definition gastroscope, with a waterjet, affixed with a clear distal cap” and “a modern electrosurgical generator capable of modulating power based on tissue resistance and circuit impedance.”
While G-POEM is typically performed via a greater-curvature approach, similar outcomes have been documented for a lesser-curvature approach, Dr. Khashab and colleagues wrote. This alternative technique may increase difficulty of pyloromyotomy, they added.
Postprocedural care may involve an overnight stay, according to the update, with an upper GI study on the subsequent day to ensure no contrast leakage, though this is not mandatory.
Adverse events
“G-POEM is generally safe when performed by trained and/or experienced endoscopists, and AEs are uncommon,” the investigators wrote. “However, serious AEs can occur and have been reported.”
Reported AEs include capnoperitoneum, inadvertent mucosotomy, thermal-mucosal injury, abdominal pain, bleeding, gastric ulceration, and dumping syndrome.
Insurance companies called to action
After reviewing emerging data, the authors suggested the time has come to consider G-POEM as a routine, evidence-based procedure that deserves appropriate reimbursement by financial stakeholders.
“Many insurers still consider G-POEM investigational and refuse to cover this procedure for patients with medically refractory gastroparesis,” they wrote. “As the safety and clinical effectiveness of G-POEM is now well supported, insurance companies and payors should cover G-POEM for patients with significant gastroparesis.”
The clinical practice update was commissioned and approved by the American Gastroenterological Association. The investigators disclosed relationships with Boston Scientific, Medtronic, and Olympus, among others.
FROM GASTROENTEROLOGY
How not to establish rapport with your patient
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
1. Stride confidently into the room to greet your 84-year-old female patient.
2. Introduce yourself saying, “Hi, I’m Dr. Jeff Benabio.”
3. Extend your clenched fist toward her chest and wait for her to reciprocate.
4. Smile awkwardly behind your mask while you wait.
5. Advise that you are doing a fist bump instead of a handshake to prevent the spread of viruses.
6. Wait.
7. Explain that she can bump, also known as “dap,” you back by extending her clenched fist and bumping into yours.
8. Wait a bit more.
9. Lower your fist and pat her on the shoulder with your left hand. Do so gently so it doesn’t seem like you just did a quick right jab followed by a left hook.
10. Sit down diffidently and pray that you can help her so this office visit is not an utter disaster.
It seemed a good idea for 2020: Let’s stop shaking hands while we wait out this viral apocalypse. Sensible, but entering a patient room and just sitting down didn’t work. It felt cold, impolite – this isn’t the DMV. In medicine, a complete stranger has to trust us to get naked, tell intimate secrets, even be stuck by needles all within minutes of meeting. We needed a trust-building substitute greeting.
There was the Muslim hand-on-my-heart greeting. Or the Hindu “namaste” or Buddhist “amituofo” folded hands. Or perhaps the paternalistic shoulder pat? I went with the fist bump. With some of my partner docs, my old MBA squad, my neighbor, the fist bump felt natural, reciprocated without hesitation. But it fails with many patients. To understand why, it’s helpful to know the history of the fist bump, also known as the dap.
Dap is an acronym for Dignity And Pride. It’s a variation of a handshake that originated among Black soldiers in the Vietnam war as a means of showing fraternity and establishing connectedness. In Vietnam, 30% of the combat battalions were Black. Marginalized in the military and at home, they created a greeting that was meaningful and unique. The dap was a series of shakes, bumps, slaps, and hugs that was symbolic. It was a means of showing respect and humility, that no one is above others, that I’ve got your back and you’ve got mine. It was a powerful recognition of humanity and effective means of personal connection. It spread from the Black community to the general population and it exists still today. The choreographed pregame handshake you see so many NBA players engage in is a descendant of the dap. Like many rituals, it reinforces bonds with those who are your people, your team, those you trust.
The more generalized version is the simple fist bump. It is widely used, notably by President Obama, and in the appropriate circumstance, will almost always be reciprocated. But it doesn’t work well to create trust with a stranger. With a patient for example, you are not showing them respect for some accomplishment. Nor are we connecting with them as a member of your team. Unless this is a patient whom you’ve seen many times before, a fist bump attempt might be met with “are you serious?” In fact, a survey done in 2016 asking infectious disease professionals what they thought of fist bumps as a greeting, very few replied it was a good idea. Most felt it was unprofessional. Not to mention that a fist bump does not symbolize an agreement in the way that a handshake does (and has done since at least the 9th century BC).
With COVID waning and masks doffed, I’ve found myself back to handshaking. Yes, I sanitize before and after, another ritual that has symbolic as well as practical significance. I get fewer sideways glances from my geriatric patients for sure. But I do still offer a little dap for my liquid nitrogen–survivor kids and for the occasional fellow Gen Xer. “Wonder Twin powers, activate!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Systemic JIA and AOSD are the same disease, EULAR says
Systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD) should be grouped into one disease, Still’s disease, according to new diagnosis and treatment recommendations presented at the annual European Congress of Rheumatology.
The recommendations, made in collaboration with EULAR and the Pediatric Rheumatology European Society, emphasized that the ultimate treatment target for Still’s disease should be drug-free remission in all patients and that macrophage activation syndrome (MAS) should be identified and treated as soon as possible.
The task force focused on MAS because despite effective, innovative therapies, “we continued to see MAS,” said presenter Bruno Fautrel, MD, Pitié-Salpêtrière University Hospital, Paris. “We have to be very concerned about this potential complication.”
Dr. Fautrel copresented the recommendations with Fabrizio De Benedetti, MD, PhD, head of the division of rheumatology, Bambino Gesù Hospital, Rome.
Diagnosis
Dr. Fautrel noted that the cutoff age of 16 that differentiates sJIA and AOSD is “arbitrary.” There are some differences in age: The frequency of the disease is higher in young children, but it plateaus in young adults. Children under 18 months old are also far more likely to develop MAS.
To diagnose and treat Still’s disease, the recommendations state that clinicians should consider four criteria:
- A fever spiking at or above 39° C (102.2° F) for at least 7 days.
- A transient rash, preferentially on the trunk, that coincides with fever spikes, rash is typically erythematous but other rashes, like urticaria, can be consistent with the diagnosis.
- Some musculoskeletal involvement is common, involving arthralgia/myalgia.
- High levels of inflammation identified by neutrophilic leukocytosis, increased serum C-reactive protein (CRP), and ferritin.
Dr. Fautrel noted that, while arthritis can be present, it is not necessary to make a diagnosis. In pediatrics, “arthritis is likely to happen after a few weeks of the evolution of the disease,” and waiting for arthritis to develop can lead to diagnostic delay, “which is a problem.”
For individuals with suspected Still’s disease, NSAIDs can be used as a “bridging therapy” before the diagnosis is confirmed.
Treatment
The recommendations emphasized that treatment and therapeutic strategy “should be based on shared decision-making between the parents/patients and the treating team,” with the ultimate goal of drug-free remission.
To achieve this goal, the document outlines time-based targets for clinically inactive disease (CID). At 4 weeks, patients should have no fever, reduction of active or swollen joint count by more than 50%, a normal CRP level, and a rating of less than 20 on a visual analog scale of 0-100. At 3 months, patients should maintain clinically inactive disease with a glucocorticoid dose of less than 0.1 or 0.2 mg/kg per day. At 6 months, CID should be maintained without glucocorticoids.
While the authors of the recommendations noted that glucocorticoids are efficacious, their long-term use should be avoided because of safety issues. An interleukin-1 or IL-6 inhibitor should be prioritized and initiated as soon as possible after diagnosis.
Patients should maintain CID between 3 and 6 months before tapering off biologics.
The recommendations are congruent with the 2021 American College of Rheumatology’s guidelines for sJIA, noted Karen Onel, MD, pediatric rheumatologist, Hospital for Special Surgery, New York, and the principle investigator for the ACR guidelines. One main difference is that the EULAR recommendations included time lines for treatment targets, while the ACR’s did not.
“It’s great to have these time lines in there,” she said in an interview, though there are still some unknowns. “We don’t actually know what the tapering frequency should be,” she said, “but these are definitely goals that we need to explore and see how they evolve.”
MAS and lung complications
The EULAR recommendations also touched on two concerning complications, particularly in children: MAS and lung disease. According to the document, MAS should be considered in patients with Still’s disease with these symptoms: fever, splenomegaly, elevated serum ferritin, low cell counts, abnormal liver function tests, elevated serum triglycerides, and intravascular activation of coagulation. The MAS 2016 criteria can also be used to facilitate diagnosis.
“MAS treatment must include high-dose glucocorticoids,” the document states. “In addition, treatments including anakinra, ciclosporin, and/or interferon-gamma inhibitors should be considered as a part of initial therapy.”
The recommendations also addressed the risk for lung disease, “which is an emerging issue, particularly in children, that the physician should be very well aware of,” Dr. De Benedetti said. This complication can arise at any time point of the disease, he added.
The document advised actively screening for lung disease by searching for clinical symptoms such as digital clubbing, persistent cough, and shortness of breath. Pulmonary function tests like pulse oximetry and diffusing capacity of the lungs for carbon monoxide may also be used, but these standard lung function tests are very difficult to do in children under 6 years old, Dr. De Benedetti noted. The recommendations advise performing high-resolution CT in “any patients with clinical concerns.”
“We have lowered the threshold for CT scan because of the emerging features of this lung disease that may actually be lethal and therefore require prompt attention,” Dr. De Benedetti noted.
The recommendations for lung disease are “broad,” as there is still much to learn about the risk for lung disease in a small portion of sJIA patients, Dr. Onel said.
“There’s a lot that we are trying to work out about this; exactly how to screen, who to screen, what to do, who to treat, and how to treat really remains unclear,” she said. “We absolutely agree that this is a major, major issue that we need to come to some sort of agreement upon, but we’re just not there yet.”
Dr. De Benedetti, Dr. Fautrel, and Dr. Onel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD) should be grouped into one disease, Still’s disease, according to new diagnosis and treatment recommendations presented at the annual European Congress of Rheumatology.
The recommendations, made in collaboration with EULAR and the Pediatric Rheumatology European Society, emphasized that the ultimate treatment target for Still’s disease should be drug-free remission in all patients and that macrophage activation syndrome (MAS) should be identified and treated as soon as possible.
The task force focused on MAS because despite effective, innovative therapies, “we continued to see MAS,” said presenter Bruno Fautrel, MD, Pitié-Salpêtrière University Hospital, Paris. “We have to be very concerned about this potential complication.”
Dr. Fautrel copresented the recommendations with Fabrizio De Benedetti, MD, PhD, head of the division of rheumatology, Bambino Gesù Hospital, Rome.
Diagnosis
Dr. Fautrel noted that the cutoff age of 16 that differentiates sJIA and AOSD is “arbitrary.” There are some differences in age: The frequency of the disease is higher in young children, but it plateaus in young adults. Children under 18 months old are also far more likely to develop MAS.
To diagnose and treat Still’s disease, the recommendations state that clinicians should consider four criteria:
- A fever spiking at or above 39° C (102.2° F) for at least 7 days.
- A transient rash, preferentially on the trunk, that coincides with fever spikes, rash is typically erythematous but other rashes, like urticaria, can be consistent with the diagnosis.
- Some musculoskeletal involvement is common, involving arthralgia/myalgia.
- High levels of inflammation identified by neutrophilic leukocytosis, increased serum C-reactive protein (CRP), and ferritin.
Dr. Fautrel noted that, while arthritis can be present, it is not necessary to make a diagnosis. In pediatrics, “arthritis is likely to happen after a few weeks of the evolution of the disease,” and waiting for arthritis to develop can lead to diagnostic delay, “which is a problem.”
For individuals with suspected Still’s disease, NSAIDs can be used as a “bridging therapy” before the diagnosis is confirmed.
Treatment
The recommendations emphasized that treatment and therapeutic strategy “should be based on shared decision-making between the parents/patients and the treating team,” with the ultimate goal of drug-free remission.
To achieve this goal, the document outlines time-based targets for clinically inactive disease (CID). At 4 weeks, patients should have no fever, reduction of active or swollen joint count by more than 50%, a normal CRP level, and a rating of less than 20 on a visual analog scale of 0-100. At 3 months, patients should maintain clinically inactive disease with a glucocorticoid dose of less than 0.1 or 0.2 mg/kg per day. At 6 months, CID should be maintained without glucocorticoids.
While the authors of the recommendations noted that glucocorticoids are efficacious, their long-term use should be avoided because of safety issues. An interleukin-1 or IL-6 inhibitor should be prioritized and initiated as soon as possible after diagnosis.
Patients should maintain CID between 3 and 6 months before tapering off biologics.
The recommendations are congruent with the 2021 American College of Rheumatology’s guidelines for sJIA, noted Karen Onel, MD, pediatric rheumatologist, Hospital for Special Surgery, New York, and the principle investigator for the ACR guidelines. One main difference is that the EULAR recommendations included time lines for treatment targets, while the ACR’s did not.
“It’s great to have these time lines in there,” she said in an interview, though there are still some unknowns. “We don’t actually know what the tapering frequency should be,” she said, “but these are definitely goals that we need to explore and see how they evolve.”
MAS and lung complications
The EULAR recommendations also touched on two concerning complications, particularly in children: MAS and lung disease. According to the document, MAS should be considered in patients with Still’s disease with these symptoms: fever, splenomegaly, elevated serum ferritin, low cell counts, abnormal liver function tests, elevated serum triglycerides, and intravascular activation of coagulation. The MAS 2016 criteria can also be used to facilitate diagnosis.
“MAS treatment must include high-dose glucocorticoids,” the document states. “In addition, treatments including anakinra, ciclosporin, and/or interferon-gamma inhibitors should be considered as a part of initial therapy.”
The recommendations also addressed the risk for lung disease, “which is an emerging issue, particularly in children, that the physician should be very well aware of,” Dr. De Benedetti said. This complication can arise at any time point of the disease, he added.
The document advised actively screening for lung disease by searching for clinical symptoms such as digital clubbing, persistent cough, and shortness of breath. Pulmonary function tests like pulse oximetry and diffusing capacity of the lungs for carbon monoxide may also be used, but these standard lung function tests are very difficult to do in children under 6 years old, Dr. De Benedetti noted. The recommendations advise performing high-resolution CT in “any patients with clinical concerns.”
“We have lowered the threshold for CT scan because of the emerging features of this lung disease that may actually be lethal and therefore require prompt attention,” Dr. De Benedetti noted.
The recommendations for lung disease are “broad,” as there is still much to learn about the risk for lung disease in a small portion of sJIA patients, Dr. Onel said.
“There’s a lot that we are trying to work out about this; exactly how to screen, who to screen, what to do, who to treat, and how to treat really remains unclear,” she said. “We absolutely agree that this is a major, major issue that we need to come to some sort of agreement upon, but we’re just not there yet.”
Dr. De Benedetti, Dr. Fautrel, and Dr. Onel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD) should be grouped into one disease, Still’s disease, according to new diagnosis and treatment recommendations presented at the annual European Congress of Rheumatology.
The recommendations, made in collaboration with EULAR and the Pediatric Rheumatology European Society, emphasized that the ultimate treatment target for Still’s disease should be drug-free remission in all patients and that macrophage activation syndrome (MAS) should be identified and treated as soon as possible.
The task force focused on MAS because despite effective, innovative therapies, “we continued to see MAS,” said presenter Bruno Fautrel, MD, Pitié-Salpêtrière University Hospital, Paris. “We have to be very concerned about this potential complication.”
Dr. Fautrel copresented the recommendations with Fabrizio De Benedetti, MD, PhD, head of the division of rheumatology, Bambino Gesù Hospital, Rome.
Diagnosis
Dr. Fautrel noted that the cutoff age of 16 that differentiates sJIA and AOSD is “arbitrary.” There are some differences in age: The frequency of the disease is higher in young children, but it plateaus in young adults. Children under 18 months old are also far more likely to develop MAS.
To diagnose and treat Still’s disease, the recommendations state that clinicians should consider four criteria:
- A fever spiking at or above 39° C (102.2° F) for at least 7 days.
- A transient rash, preferentially on the trunk, that coincides with fever spikes, rash is typically erythematous but other rashes, like urticaria, can be consistent with the diagnosis.
- Some musculoskeletal involvement is common, involving arthralgia/myalgia.
- High levels of inflammation identified by neutrophilic leukocytosis, increased serum C-reactive protein (CRP), and ferritin.
Dr. Fautrel noted that, while arthritis can be present, it is not necessary to make a diagnosis. In pediatrics, “arthritis is likely to happen after a few weeks of the evolution of the disease,” and waiting for arthritis to develop can lead to diagnostic delay, “which is a problem.”
For individuals with suspected Still’s disease, NSAIDs can be used as a “bridging therapy” before the diagnosis is confirmed.
Treatment
The recommendations emphasized that treatment and therapeutic strategy “should be based on shared decision-making between the parents/patients and the treating team,” with the ultimate goal of drug-free remission.
To achieve this goal, the document outlines time-based targets for clinically inactive disease (CID). At 4 weeks, patients should have no fever, reduction of active or swollen joint count by more than 50%, a normal CRP level, and a rating of less than 20 on a visual analog scale of 0-100. At 3 months, patients should maintain clinically inactive disease with a glucocorticoid dose of less than 0.1 or 0.2 mg/kg per day. At 6 months, CID should be maintained without glucocorticoids.
While the authors of the recommendations noted that glucocorticoids are efficacious, their long-term use should be avoided because of safety issues. An interleukin-1 or IL-6 inhibitor should be prioritized and initiated as soon as possible after diagnosis.
Patients should maintain CID between 3 and 6 months before tapering off biologics.
The recommendations are congruent with the 2021 American College of Rheumatology’s guidelines for sJIA, noted Karen Onel, MD, pediatric rheumatologist, Hospital for Special Surgery, New York, and the principle investigator for the ACR guidelines. One main difference is that the EULAR recommendations included time lines for treatment targets, while the ACR’s did not.
“It’s great to have these time lines in there,” she said in an interview, though there are still some unknowns. “We don’t actually know what the tapering frequency should be,” she said, “but these are definitely goals that we need to explore and see how they evolve.”
MAS and lung complications
The EULAR recommendations also touched on two concerning complications, particularly in children: MAS and lung disease. According to the document, MAS should be considered in patients with Still’s disease with these symptoms: fever, splenomegaly, elevated serum ferritin, low cell counts, abnormal liver function tests, elevated serum triglycerides, and intravascular activation of coagulation. The MAS 2016 criteria can also be used to facilitate diagnosis.
“MAS treatment must include high-dose glucocorticoids,” the document states. “In addition, treatments including anakinra, ciclosporin, and/or interferon-gamma inhibitors should be considered as a part of initial therapy.”
The recommendations also addressed the risk for lung disease, “which is an emerging issue, particularly in children, that the physician should be very well aware of,” Dr. De Benedetti said. This complication can arise at any time point of the disease, he added.
The document advised actively screening for lung disease by searching for clinical symptoms such as digital clubbing, persistent cough, and shortness of breath. Pulmonary function tests like pulse oximetry and diffusing capacity of the lungs for carbon monoxide may also be used, but these standard lung function tests are very difficult to do in children under 6 years old, Dr. De Benedetti noted. The recommendations advise performing high-resolution CT in “any patients with clinical concerns.”
“We have lowered the threshold for CT scan because of the emerging features of this lung disease that may actually be lethal and therefore require prompt attention,” Dr. De Benedetti noted.
The recommendations for lung disease are “broad,” as there is still much to learn about the risk for lung disease in a small portion of sJIA patients, Dr. Onel said.
“There’s a lot that we are trying to work out about this; exactly how to screen, who to screen, what to do, who to treat, and how to treat really remains unclear,” she said. “We absolutely agree that this is a major, major issue that we need to come to some sort of agreement upon, but we’re just not there yet.”
Dr. De Benedetti, Dr. Fautrel, and Dr. Onel disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EULAR 2023