User login
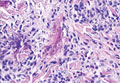
NICE recommends pixantrone for NHL

Credit: Bill Branson
Counter to its previous recommendations, the UK’s National Institute for Health and Care Excellence (NICE) is now supporting the use of pixantrone for certain patients with non-Hodgkin lymphoma (NHL).
In prior draft guidance documents, NICE said it could not recommend the antineoplastic agent for patients with relapsed or refractory NHL, due to concerns about efficacy and cost.
But now, in its final draft guidance, the agency has said pixantrone should be funded by the National Health Service to treat certain patients with B-cell NHL.
NICE is recommending pixantrone for patients with relapsed or refractory disease who have already received rituximab and are receiving their third- or fourth-line treatment.
The NICE guidance also says pixantrone can only be funded if the manufacturer, Cell Therapeutics, provides the drug at a discounted rate, as agreed between the manufacturer and the Department of Health.
“We are pleased that the manufacturer was able to provide a patient access scheme,” said Carole Longson, NICE Health Technology Evaluation Centre Director. “Pixantrone will be a useful addition to the treatment options available.”
Consultees now have until January 23, 2014, to appeal the draft recommendation. If no appeals are lodged, the final guidance should be published in February.
Clinical effectiveness
NICE’s current recommendations are based on the opinion of an independent appraisal committee. The committee considered data from the EXTEND PIX301 clinical trial. The committee said there are a number of uncertainties associated with this trial.
However, the group also said there was limited evidence suggesting that pixantrone works better than other available treatments for patients who had previously received rituximab and patients receiving third- or fourth-line treatment.
The EXTEND PIX301 trial enrolled 140 patients with aggressive B-cell lymphoma. Half of the patients were randomized to receive pixantrone and the other half to their physicians’ choice of treatment.
At the end of treatment, confirmed and unconfirmed response rates for the intent-to-treat population were significantly higher in the pixantrone arm than the comparator arm—20% and 5.7%, respectively (P=0.021). The same was true after 18 months of follow-up—24.3% and 7.1%, respectively (P=0.009).
The median progression-free survival was significantly longer in the pixantrone arm than the comparator arm—5.3 months and 2.6 months, respectively (P=0.005). But there was no significant difference in median overall survival—10.2 months and 7.6 months, respectively (P=0.251).
Cell Therapeutics also submitted results observed in 4 subgroups of patients with aggressive disease and in patients who had previously received rituximab. For detailed data from the trial, see pages 3 through 13 of the final draft guidance.
Cost-effectiveness
The appraisal committee said the manufacturer’s patient access scheme (the details of which are commercial-in-confidence) improved the cost-effectiveness of pixantrone.
The treatment would be cost-effective for patients who had previously received rituximab and patients receiving their third- or fourth-line treatment. The drug’s incremental cost-effectiveness ratio was estimated to be under £22,000 per quality adjusted life year gained for both groups.
According to the manufacturer, pixantrone costs £553.50 per 20 mL vial, excluding tax. The estimated cost of a course of treatment is £19,926.
The costs were calculated over 4 cycles using an average of 3 vials per dose and were based on the median length of treatment in the EXTEND PIX301 trial. Costs may vary in different settings because of negotiated discounts.
Marketing authorization
Pixantrone has conditional marketing authorization in the European Union as monotherapy for adults with relapsed or refractory NHL who have received at least 2 previous lines of treatment. However, the European Medicine’s Agency has noted that it is unclear whether pixantrone is effective as fifth-line or greater treatment in refractory patients.
The drug’s marketing authorization is linked to results of the phase 3 PIX306 trial, which is investigating pixantrone plus rituximab versus gemcitabine plus rituximab in patients with relapsed or refractory B-cell NHL who have previously received a rituximab-containing regimen. ![]()

Credit: Bill Branson
Counter to its previous recommendations, the UK’s National Institute for Health and Care Excellence (NICE) is now supporting the use of pixantrone for certain patients with non-Hodgkin lymphoma (NHL).
In prior draft guidance documents, NICE said it could not recommend the antineoplastic agent for patients with relapsed or refractory NHL, due to concerns about efficacy and cost.
But now, in its final draft guidance, the agency has said pixantrone should be funded by the National Health Service to treat certain patients with B-cell NHL.
NICE is recommending pixantrone for patients with relapsed or refractory disease who have already received rituximab and are receiving their third- or fourth-line treatment.
The NICE guidance also says pixantrone can only be funded if the manufacturer, Cell Therapeutics, provides the drug at a discounted rate, as agreed between the manufacturer and the Department of Health.
“We are pleased that the manufacturer was able to provide a patient access scheme,” said Carole Longson, NICE Health Technology Evaluation Centre Director. “Pixantrone will be a useful addition to the treatment options available.”
Consultees now have until January 23, 2014, to appeal the draft recommendation. If no appeals are lodged, the final guidance should be published in February.
Clinical effectiveness
NICE’s current recommendations are based on the opinion of an independent appraisal committee. The committee considered data from the EXTEND PIX301 clinical trial. The committee said there are a number of uncertainties associated with this trial.
However, the group also said there was limited evidence suggesting that pixantrone works better than other available treatments for patients who had previously received rituximab and patients receiving third- or fourth-line treatment.
The EXTEND PIX301 trial enrolled 140 patients with aggressive B-cell lymphoma. Half of the patients were randomized to receive pixantrone and the other half to their physicians’ choice of treatment.
At the end of treatment, confirmed and unconfirmed response rates for the intent-to-treat population were significantly higher in the pixantrone arm than the comparator arm—20% and 5.7%, respectively (P=0.021). The same was true after 18 months of follow-up—24.3% and 7.1%, respectively (P=0.009).
The median progression-free survival was significantly longer in the pixantrone arm than the comparator arm—5.3 months and 2.6 months, respectively (P=0.005). But there was no significant difference in median overall survival—10.2 months and 7.6 months, respectively (P=0.251).
Cell Therapeutics also submitted results observed in 4 subgroups of patients with aggressive disease and in patients who had previously received rituximab. For detailed data from the trial, see pages 3 through 13 of the final draft guidance.
Cost-effectiveness
The appraisal committee said the manufacturer’s patient access scheme (the details of which are commercial-in-confidence) improved the cost-effectiveness of pixantrone.
The treatment would be cost-effective for patients who had previously received rituximab and patients receiving their third- or fourth-line treatment. The drug’s incremental cost-effectiveness ratio was estimated to be under £22,000 per quality adjusted life year gained for both groups.
According to the manufacturer, pixantrone costs £553.50 per 20 mL vial, excluding tax. The estimated cost of a course of treatment is £19,926.
The costs were calculated over 4 cycles using an average of 3 vials per dose and were based on the median length of treatment in the EXTEND PIX301 trial. Costs may vary in different settings because of negotiated discounts.
Marketing authorization
Pixantrone has conditional marketing authorization in the European Union as monotherapy for adults with relapsed or refractory NHL who have received at least 2 previous lines of treatment. However, the European Medicine’s Agency has noted that it is unclear whether pixantrone is effective as fifth-line or greater treatment in refractory patients.
The drug’s marketing authorization is linked to results of the phase 3 PIX306 trial, which is investigating pixantrone plus rituximab versus gemcitabine plus rituximab in patients with relapsed or refractory B-cell NHL who have previously received a rituximab-containing regimen. ![]()

Credit: Bill Branson
Counter to its previous recommendations, the UK’s National Institute for Health and Care Excellence (NICE) is now supporting the use of pixantrone for certain patients with non-Hodgkin lymphoma (NHL).
In prior draft guidance documents, NICE said it could not recommend the antineoplastic agent for patients with relapsed or refractory NHL, due to concerns about efficacy and cost.
But now, in its final draft guidance, the agency has said pixantrone should be funded by the National Health Service to treat certain patients with B-cell NHL.
NICE is recommending pixantrone for patients with relapsed or refractory disease who have already received rituximab and are receiving their third- or fourth-line treatment.
The NICE guidance also says pixantrone can only be funded if the manufacturer, Cell Therapeutics, provides the drug at a discounted rate, as agreed between the manufacturer and the Department of Health.
“We are pleased that the manufacturer was able to provide a patient access scheme,” said Carole Longson, NICE Health Technology Evaluation Centre Director. “Pixantrone will be a useful addition to the treatment options available.”
Consultees now have until January 23, 2014, to appeal the draft recommendation. If no appeals are lodged, the final guidance should be published in February.
Clinical effectiveness
NICE’s current recommendations are based on the opinion of an independent appraisal committee. The committee considered data from the EXTEND PIX301 clinical trial. The committee said there are a number of uncertainties associated with this trial.
However, the group also said there was limited evidence suggesting that pixantrone works better than other available treatments for patients who had previously received rituximab and patients receiving third- or fourth-line treatment.
The EXTEND PIX301 trial enrolled 140 patients with aggressive B-cell lymphoma. Half of the patients were randomized to receive pixantrone and the other half to their physicians’ choice of treatment.
At the end of treatment, confirmed and unconfirmed response rates for the intent-to-treat population were significantly higher in the pixantrone arm than the comparator arm—20% and 5.7%, respectively (P=0.021). The same was true after 18 months of follow-up—24.3% and 7.1%, respectively (P=0.009).
The median progression-free survival was significantly longer in the pixantrone arm than the comparator arm—5.3 months and 2.6 months, respectively (P=0.005). But there was no significant difference in median overall survival—10.2 months and 7.6 months, respectively (P=0.251).
Cell Therapeutics also submitted results observed in 4 subgroups of patients with aggressive disease and in patients who had previously received rituximab. For detailed data from the trial, see pages 3 through 13 of the final draft guidance.
Cost-effectiveness
The appraisal committee said the manufacturer’s patient access scheme (the details of which are commercial-in-confidence) improved the cost-effectiveness of pixantrone.
The treatment would be cost-effective for patients who had previously received rituximab and patients receiving their third- or fourth-line treatment. The drug’s incremental cost-effectiveness ratio was estimated to be under £22,000 per quality adjusted life year gained for both groups.
According to the manufacturer, pixantrone costs £553.50 per 20 mL vial, excluding tax. The estimated cost of a course of treatment is £19,926.
The costs were calculated over 4 cycles using an average of 3 vials per dose and were based on the median length of treatment in the EXTEND PIX301 trial. Costs may vary in different settings because of negotiated discounts.
Marketing authorization
Pixantrone has conditional marketing authorization in the European Union as monotherapy for adults with relapsed or refractory NHL who have received at least 2 previous lines of treatment. However, the European Medicine’s Agency has noted that it is unclear whether pixantrone is effective as fifth-line or greater treatment in refractory patients.
The drug’s marketing authorization is linked to results of the phase 3 PIX306 trial, which is investigating pixantrone plus rituximab versus gemcitabine plus rituximab in patients with relapsed or refractory B-cell NHL who have previously received a rituximab-containing regimen. ![]()
Suicide on Medical Units
Suicide is the tenth leading cause of death in the United States,[1] resulting in the deaths of over 34,000 people each year.[2] In 2007, 165,997 individuals were hospitalized for self‐inflicted injuries, and 395,320 people were treated for self‐harm in emergency departments.[2] In 2003, the American Psychiatric Association reported that approximately 1500 suicides take place within hospital facilities in the United States each year.[3]
Although a number of studies have examined inpatient suicides that occurred on psychiatric units,[4, 5, 6, 7, 8] fewer have focused on suicides occurring on medical units. A Joint Commission review of inpatient suicide on medical/surgical units[9] found that 14.25% of all inpatient suicides occurred while the patient was on a medical unit, and now recommends that all hospitals identify individuals at risk for suicide, develop interventions for suicidal patients, and educate staff about the risk factors of suicide. Bostwick and Rackley[10] reviewed studies of suicide on medical/surgical units and found that few of the patients had histories of mental illness or suicidal ideation and recommend close attention to agitated patients, aggressively treating depression and pain, modifying the environment where possible, and observation of patients thought to be at risk. Wint and Alil[5] also report a high level of depression in patients who commit suicide in general hospitals and suggest that improved recognition of depression in general hospital patients will reduce suicide.
GOALS FOR THIS STUDY
Few studies have examined suicide on acute medical and surgical and intensive care units (ICUs), and there are no large studies conducted in the United States. The goal of this study was to describe suicide attempts and completions in the medical setting using Root Cause Analysis (RCA) reports of these events in the Veterans Health Administration (VHA).
METHODS
Study Design and Theoretical Model
This is an observational review of all RCA reports of suicide attempts or completions on the medical‐surgical wards and ICUs in the VHA system between December 1, 1999 (when the RCA system started) and December 31, 2012. The Committee for the Protection of Human Subjects, Dartmouth College considered this project exempt.
The VHA provides comprehensive healthcare services to over 6 million veterans across the United States through 152 VHA medical centers. Over the study period there were approximately 7,289,770 admissions to medical‐surgical wards and ICUs in the VHA (average number of admissions per year between 2000 and 2012=560,771.5, standard deviation=25,535.7).
The VHA National Center for Patient Safety RCA Program
Patient safety including the investigation of adverse events is coordinated by the National Center for Patient Safety (NCPS). The NCPS has instituted a systematic and structured RCA program to individually and collectively analyze adverse events.[11, 12]
RCA is a method for examining the underlying causes of an adverse event such as a hospital related death, surgical error, or suicide. The focus of an RCA is on the systemic and organizational factors that may have contributed to an adverse event.[11, 12] The RCA process within the VHA is conducted by multidisciplinary teams organized by the hospital's patient safety manager. In general, an RCA describes what happened, how it happened, and what should be done to avoid the same event happening again.[11]
Because of the focus on the system, the information contained in the RCA reports does not include detailed demographic data about the patients involved in the events. RCA reports that are submitted to NCPS include narrative descriptions of the event, all contributing factors, a final understanding of the event, and a specific action plan for addressing underlying causes of the event.
Analysis of RCA Reports
Our goal was to identify suicide attempts and completed suicides that occurred on acute care medical‐surgical wards or ICUs. The search was completed through use of event codes for suicide or suicide attempts entered in the RCA and through the use of natural language processing software to identify the terms related to suicide or suicide attempts anywhere in the RCA text (PolyAnalyst; Megaputer, Bloomington, IN).
Data Processing
Each RCA report was coded for the location of the event, method of self‐harm, and root causes; where possible, we also coded medical diagnosis, reason for admission, history of suicidal behavior, age, and gender. The coding system was developed in a previous study of RCA reports of suicide.[13]
RESULTS
Our search resulted in 525 RCA reports of inpatient suicide attempts and completions. These were obtained from the 14,851 total RCA reports in the RCA dataset. Of the 525, we identified 50 cases that occurred while the patient was on the acute medical‐surgical unit (43 cases) or ICU (7 cases). Other cases occurred on mental health units, emergency department, or other areas of the hospital. Five cases were completed suicides, and 45 were suicide attempts. Based on the number of admissions per year reported above, the approximate rate of completed inpatient suicides on medical‐surgical and ICUs is 0.6 per million admissions. (For comparison, the rate of completed suicide on psychiatric units in the VA has been estimated to be 8.7 per million admissions.[14] Table 1 displays the admitting diagnosis and demographic data for those RCA reports that contained this information. The most common admitting diagnoses were alcohol detoxification and chest pain or rule out myocardial infarction (MI); note that 12 reports did not contain an admitting diagnosis. Table 2 displays the methods and root causes for the 50 cases; there were 118 root causes generated. The most common methods were cutting, overdose, and hanging; and the most common root causes were poor communication, need for staff training in suicide assessment, and need to improve suicide risk assessment.
| Medical‐Surgical | ICU | |||
|---|---|---|---|---|
| Attempts | Completions | Attempts | Completions | |
| ||||
| Admitting diagnosis, N=50 | ||||
| Alcohol detox | 3 | 2 | 2 | 0 |
| Chest pain or rule out MI | 5 | 0 | 0 | 0 |
| Delirium | 1 | 0 | 0 | 0 |
| Peripheral infection/cellulitis | 2 | 1 | 0 | 0 |
| Spine surgery or spine issue | 2 | 0 | 0 | 0 |
| Lung CA | 1 | 1 | 0 | 0 |
| Cystopy (bladder surgery) | 2 | 0 | 0 | 0 |
| Head and neck CA | 1 | 0 | 1 | 0 |
| Other | 4 | 0 | 0 | 0 |
| Respiratory (COPD) | 2 | 0 | 1 | 0 |
| Suicide attempt by overdose | 2 | 0 | 0 | 0 |
| Lung infection | 1 | 0 | 1 | 0 |
| CVA | 0 | 1 | 0 | 0 |
| Unknown | 12 | 0 | 2 | 0 |
| Demographics N =50 | ||||
| % male | 91.40% | 100% | 80% | NA |
| Average age, y | 56 | 53 | 47 | NA |
| History of suicidal thoughts or behaviors | 16 | 2 | 3 | 0 |
| Medical‐Surgical | ICU | |||
|---|---|---|---|---|
| Attempts | Completions | Attempts | Completions | |
| ||||
| Methods | ||||
| Cutting with a sharp object | 29% | 0% | 43% | None |
| Overdose | 26% | 20% | 0% | None |
| Hanging | 18% | 40% | 29% | None |
| Strangulation | 8% | 0% | 0% | None |
| Jumping | 5% | 0% | 14% | None |
| Asphyxiation | 8% | 0% | 0% | None |
| Removed lines or equipment | 5% | 0% | 14% | None |
| Gun shot | 0% | 40% | 0% | None |
| Column total | 100% | 100% | 100% | None |
| Root causes | ||||
| Poor communication between providers or services | 22% | 9% | 7% | None |
| Need for staff training in suicide assessment | 14% | 0% | 20% | None |
| Need to improve process of suicide assessment | 13% | 9% | 13% | None |
| Need for improvement of risk documentation | 9% | 0% | 7% | None |
| Physical environment is a risk factor | 7% | 0% | 20% | None |
| Contraband search needs improvement | 7% | 18% | 0% | None |
| Problems with treatment for suicidal patients | 7% | 27% | 7% | None |
| Not following existing policies | 5% | 0% | 0% | None |
| Medical assess or treatment delayed or incomplete | 5% | 0% | 0% | None |
| Easy access to medication for overdose | 4% | 9% | 0% | None |
| Stressed by medical/mental health/pain problems | 5% | 18% | 20% | None |
| Other root causes | 1% | 0% | 7% | None |
| No root cause | 1% | 9% | 0% | None |
| Column totals | 100% | 100% | 100% | None |
DISCUSSION
This study examined the specific systemic factors involved in suicide attempts and completions in medical‐surgical and intensive care units in a large, national hospital sample. Overall, the number of completed suicides over the 13‐year period was small (5 in total). The most common reason for admission was alcohol detoxification. Many patients going through alcohol detoxification experience agitation, which is a risk factor for suicide among medical patients.[10] This hypothesis is further supported by the fact that 2 of the 5 completed suicides were admitted for alcohol detoxification. Interestingly, only 2 of the patients who attempted suicide in the hospital were also admitted for medical conditions related to a prior suicide attempt. It is likely the case that patients admitted for a suicide attempt are closely watched throughout the admission and so may have fewer opportunities to repeat the suicide attempt.
The most common method of suicide attempts was cutting with a sharp object. However, cutting did not result in death, whereas overdose, hanging, and gunshot did. As a precaution, especially with patients with a known history of suicidal ideation, removing sharp objects such as razor blades and knives as well as extra medications is a reasonable first step. It may also be possible to create safer bathroom environments, at least in some medical rooms for potentially suicidal patients, which have break‐away shower curtains, sealed grab‐bars, and a general reduction of anchor points for hanging (see
As with other studies of RCAs,[15, 16] we found that problems communicating risk was the most common identified root cause for suicide attempts and completions. Problems communicating risk most often involved knowledge of suicide risk or specific suicide mitigation plans that were not shared by the treatment team or communicated during handoffs. Most frequently, this communication problem involved team members assessing a patient to be at high risk for suicide, but that information was not provided to other care team members. This root cause also included situations in which the treatment plan for suicide prevention was inadequately disseminated to the entire treatment team. It is critical that good systems are in place so that staff members have the time to communicate critical information about patients. In addition, the system should be standardized so that the same information is communicated each time there is a handoff. The lack of clear steps to mitigate suicide risk when a patient was identified at high risk was also a commonly cited root cause. The most extreme examples involved completed suicides occurring with a patient receiving 1‐on‐1 staffing. This 1‐on‐1 staffing did not include specific guidance for the sitters such as the need to remove personal items that could be used for self‐harm. We also saw that staff on medical units needed to learn more about risk factors for suicide and how to conduct a suicide assessment with their patients. Another root cause was the stress caused by the medical and psychiatric conditions of the patients. It is notable that no completed suicides occurred in ICUs, suggesting that closer observation and/or a higher level of medical incapacitation can reduce the risk of completed suicides.
To address these root causes, staff should be educated about risk factors for suicide, and standardized high‐risk for suicide order sets and checklists should be used to ensure staff execute the desired care processes and communicate them to all staff. In addition, specific training in suicide prevention should be provided to staff involved in 1‐on‐1 observation for high‐risk patients. Again, this may be aided by a checklist to help staff remember the protocol for what may be a low‐frequency event. A high risk suicide care process may include:
- Conducting contraband searches for items that could be used for self‐harm, modifying the environment of a small percentage of toilet rooms on medical floors to reduce anchor points for hanging. A high risk patient could then be moved to these rooms.
- Regular psychiatric input into the treatment plan.
- Discharge planning that includes attention to the potential for depression and suicidal ideation upon discharge.
Limitations
This study has several limitations. First, our data only contained suicide attempts and completions that were reported through our patient safety system in the VHA, and only completed suicides require an RCA, thus there are likely some events that were not included. Second, the RCA reports focus on the systemic vulnerabilities in medical‐surgical units and ICUs that may have contributed to the adverse event rather than the specific characteristics of the patients involved, so we do not have complete demographic information about these individual patients. Third, our sample was mostly male, so the results may not generalize well to units with a higher percentage of female patients.
These limitations notwithstanding, we know of no other study to present data on suicide attempts and completions in medical‐surgical and ICUs in a large national medical system.
Disclosures: This material is the result of work supported with resources and the use of facilities at the Department of Veterans Affairs National Center for Patient Safety at Ann Arbor, Michigan, and the Veterans Affairs Medical Centers, White River Junction, Vermont. The Research and Development Committee, White River Junction VA Medical Center approved this project, and the Committee for the Protection of Human Subjects, Dartmouth College considered this project exempt. The views expressed in this article do not necessarily represent the views of the Department of Veterans Affairs or the United States government. The authors report no conflicts of interest.
- Centers for Disease Control and Prevention. National Center for Injury and Prevention Control. WISQARS (Web‐based Injury Statistics Query and Reporting System). Available at: http://www.cdc.gov/injury/wisqars/index.html. Accessed September 27, 2012.
- Centers for Disease Control and Prevention. Suicide: facts at a glance. Available at: http://www.cdc.gov/ViolencePrevention/pdf/Suicide_DataSheet‐a.pdf. Accessed September 27, 2012.
- American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160:1–60.
- , . Inpatient suicide: preventing a common sentinel event. Gen Hosp Psychiatry. 2009;31:103–109.
- , . Suicidality in the general hospitalized patient. Hosp Physician. 2006;42(1):13–18.
- , , . Suicide inside: a systematic review of inpatient suicides. J Nervous and Ment Dis. 2010;198(5):315–328.
- , , . Environmental risk factors in hospital suicide. Suicide Life Threat Behav. 2004;34(4):448–453.
- , , . Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003;64(1):14–19.
- A follow‐up report on preventing suicide: focus on medical/surgical units and the emergency department. Sentinel Event Alert. 2010;(46):1–4.
- , . Completed suicide in medical/surgical patients: who is at risk? Curr Psychiatry Rep. 2007;9(3):242–246.
- , , , , , , et al. Developing and deploying a patient safety program in a large health care system: you can't fix what you don't know about. Jt Comm J Qual Improv. 2001;27:522–532.
- , . Developing a culture of safety in the Veterans Health Administration. Eff Clin Pract. 2007;3:270–276.
- , , , , . Actions and Implementation Strategies to Reduce Suicidal Events in the VHA. Jt Comm J on Qual and Safe. 2006:32(3):130–141.
- , , , et al. An examination of the effectiveness of a mental health environment of care checklist in reducing suicide on inpatient mental health units. Arch GenPsychiatry. 2012:69(6):588–592.
- , , , , . Helping elderly patients to avoid suicide: a review of case reports from a national Veterans Affairs database. J Nerv Ment Dis. 2013;201(1):12–16.
- , , , , . Suicide attempts and completions in the emergency department in Veterans Affairs hospitals. Emerg Med J. 2012;29(5):399–403.
Suicide is the tenth leading cause of death in the United States,[1] resulting in the deaths of over 34,000 people each year.[2] In 2007, 165,997 individuals were hospitalized for self‐inflicted injuries, and 395,320 people were treated for self‐harm in emergency departments.[2] In 2003, the American Psychiatric Association reported that approximately 1500 suicides take place within hospital facilities in the United States each year.[3]
Although a number of studies have examined inpatient suicides that occurred on psychiatric units,[4, 5, 6, 7, 8] fewer have focused on suicides occurring on medical units. A Joint Commission review of inpatient suicide on medical/surgical units[9] found that 14.25% of all inpatient suicides occurred while the patient was on a medical unit, and now recommends that all hospitals identify individuals at risk for suicide, develop interventions for suicidal patients, and educate staff about the risk factors of suicide. Bostwick and Rackley[10] reviewed studies of suicide on medical/surgical units and found that few of the patients had histories of mental illness or suicidal ideation and recommend close attention to agitated patients, aggressively treating depression and pain, modifying the environment where possible, and observation of patients thought to be at risk. Wint and Alil[5] also report a high level of depression in patients who commit suicide in general hospitals and suggest that improved recognition of depression in general hospital patients will reduce suicide.
GOALS FOR THIS STUDY
Few studies have examined suicide on acute medical and surgical and intensive care units (ICUs), and there are no large studies conducted in the United States. The goal of this study was to describe suicide attempts and completions in the medical setting using Root Cause Analysis (RCA) reports of these events in the Veterans Health Administration (VHA).
METHODS
Study Design and Theoretical Model
This is an observational review of all RCA reports of suicide attempts or completions on the medical‐surgical wards and ICUs in the VHA system between December 1, 1999 (when the RCA system started) and December 31, 2012. The Committee for the Protection of Human Subjects, Dartmouth College considered this project exempt.
The VHA provides comprehensive healthcare services to over 6 million veterans across the United States through 152 VHA medical centers. Over the study period there were approximately 7,289,770 admissions to medical‐surgical wards and ICUs in the VHA (average number of admissions per year between 2000 and 2012=560,771.5, standard deviation=25,535.7).
The VHA National Center for Patient Safety RCA Program
Patient safety including the investigation of adverse events is coordinated by the National Center for Patient Safety (NCPS). The NCPS has instituted a systematic and structured RCA program to individually and collectively analyze adverse events.[11, 12]
RCA is a method for examining the underlying causes of an adverse event such as a hospital related death, surgical error, or suicide. The focus of an RCA is on the systemic and organizational factors that may have contributed to an adverse event.[11, 12] The RCA process within the VHA is conducted by multidisciplinary teams organized by the hospital's patient safety manager. In general, an RCA describes what happened, how it happened, and what should be done to avoid the same event happening again.[11]
Because of the focus on the system, the information contained in the RCA reports does not include detailed demographic data about the patients involved in the events. RCA reports that are submitted to NCPS include narrative descriptions of the event, all contributing factors, a final understanding of the event, and a specific action plan for addressing underlying causes of the event.
Analysis of RCA Reports
Our goal was to identify suicide attempts and completed suicides that occurred on acute care medical‐surgical wards or ICUs. The search was completed through use of event codes for suicide or suicide attempts entered in the RCA and through the use of natural language processing software to identify the terms related to suicide or suicide attempts anywhere in the RCA text (PolyAnalyst; Megaputer, Bloomington, IN).
Data Processing
Each RCA report was coded for the location of the event, method of self‐harm, and root causes; where possible, we also coded medical diagnosis, reason for admission, history of suicidal behavior, age, and gender. The coding system was developed in a previous study of RCA reports of suicide.[13]
RESULTS
Our search resulted in 525 RCA reports of inpatient suicide attempts and completions. These were obtained from the 14,851 total RCA reports in the RCA dataset. Of the 525, we identified 50 cases that occurred while the patient was on the acute medical‐surgical unit (43 cases) or ICU (7 cases). Other cases occurred on mental health units, emergency department, or other areas of the hospital. Five cases were completed suicides, and 45 were suicide attempts. Based on the number of admissions per year reported above, the approximate rate of completed inpatient suicides on medical‐surgical and ICUs is 0.6 per million admissions. (For comparison, the rate of completed suicide on psychiatric units in the VA has been estimated to be 8.7 per million admissions.[14] Table 1 displays the admitting diagnosis and demographic data for those RCA reports that contained this information. The most common admitting diagnoses were alcohol detoxification and chest pain or rule out myocardial infarction (MI); note that 12 reports did not contain an admitting diagnosis. Table 2 displays the methods and root causes for the 50 cases; there were 118 root causes generated. The most common methods were cutting, overdose, and hanging; and the most common root causes were poor communication, need for staff training in suicide assessment, and need to improve suicide risk assessment.
| Medical‐Surgical | ICU | |||
|---|---|---|---|---|
| Attempts | Completions | Attempts | Completions | |
| ||||
| Admitting diagnosis, N=50 | ||||
| Alcohol detox | 3 | 2 | 2 | 0 |
| Chest pain or rule out MI | 5 | 0 | 0 | 0 |
| Delirium | 1 | 0 | 0 | 0 |
| Peripheral infection/cellulitis | 2 | 1 | 0 | 0 |
| Spine surgery or spine issue | 2 | 0 | 0 | 0 |
| Lung CA | 1 | 1 | 0 | 0 |
| Cystopy (bladder surgery) | 2 | 0 | 0 | 0 |
| Head and neck CA | 1 | 0 | 1 | 0 |
| Other | 4 | 0 | 0 | 0 |
| Respiratory (COPD) | 2 | 0 | 1 | 0 |
| Suicide attempt by overdose | 2 | 0 | 0 | 0 |
| Lung infection | 1 | 0 | 1 | 0 |
| CVA | 0 | 1 | 0 | 0 |
| Unknown | 12 | 0 | 2 | 0 |
| Demographics N =50 | ||||
| % male | 91.40% | 100% | 80% | NA |
| Average age, y | 56 | 53 | 47 | NA |
| History of suicidal thoughts or behaviors | 16 | 2 | 3 | 0 |
| Medical‐Surgical | ICU | |||
|---|---|---|---|---|
| Attempts | Completions | Attempts | Completions | |
| ||||
| Methods | ||||
| Cutting with a sharp object | 29% | 0% | 43% | None |
| Overdose | 26% | 20% | 0% | None |
| Hanging | 18% | 40% | 29% | None |
| Strangulation | 8% | 0% | 0% | None |
| Jumping | 5% | 0% | 14% | None |
| Asphyxiation | 8% | 0% | 0% | None |
| Removed lines or equipment | 5% | 0% | 14% | None |
| Gun shot | 0% | 40% | 0% | None |
| Column total | 100% | 100% | 100% | None |
| Root causes | ||||
| Poor communication between providers or services | 22% | 9% | 7% | None |
| Need for staff training in suicide assessment | 14% | 0% | 20% | None |
| Need to improve process of suicide assessment | 13% | 9% | 13% | None |
| Need for improvement of risk documentation | 9% | 0% | 7% | None |
| Physical environment is a risk factor | 7% | 0% | 20% | None |
| Contraband search needs improvement | 7% | 18% | 0% | None |
| Problems with treatment for suicidal patients | 7% | 27% | 7% | None |
| Not following existing policies | 5% | 0% | 0% | None |
| Medical assess or treatment delayed or incomplete | 5% | 0% | 0% | None |
| Easy access to medication for overdose | 4% | 9% | 0% | None |
| Stressed by medical/mental health/pain problems | 5% | 18% | 20% | None |
| Other root causes | 1% | 0% | 7% | None |
| No root cause | 1% | 9% | 0% | None |
| Column totals | 100% | 100% | 100% | None |
DISCUSSION
This study examined the specific systemic factors involved in suicide attempts and completions in medical‐surgical and intensive care units in a large, national hospital sample. Overall, the number of completed suicides over the 13‐year period was small (5 in total). The most common reason for admission was alcohol detoxification. Many patients going through alcohol detoxification experience agitation, which is a risk factor for suicide among medical patients.[10] This hypothesis is further supported by the fact that 2 of the 5 completed suicides were admitted for alcohol detoxification. Interestingly, only 2 of the patients who attempted suicide in the hospital were also admitted for medical conditions related to a prior suicide attempt. It is likely the case that patients admitted for a suicide attempt are closely watched throughout the admission and so may have fewer opportunities to repeat the suicide attempt.
The most common method of suicide attempts was cutting with a sharp object. However, cutting did not result in death, whereas overdose, hanging, and gunshot did. As a precaution, especially with patients with a known history of suicidal ideation, removing sharp objects such as razor blades and knives as well as extra medications is a reasonable first step. It may also be possible to create safer bathroom environments, at least in some medical rooms for potentially suicidal patients, which have break‐away shower curtains, sealed grab‐bars, and a general reduction of anchor points for hanging (see
As with other studies of RCAs,[15, 16] we found that problems communicating risk was the most common identified root cause for suicide attempts and completions. Problems communicating risk most often involved knowledge of suicide risk or specific suicide mitigation plans that were not shared by the treatment team or communicated during handoffs. Most frequently, this communication problem involved team members assessing a patient to be at high risk for suicide, but that information was not provided to other care team members. This root cause also included situations in which the treatment plan for suicide prevention was inadequately disseminated to the entire treatment team. It is critical that good systems are in place so that staff members have the time to communicate critical information about patients. In addition, the system should be standardized so that the same information is communicated each time there is a handoff. The lack of clear steps to mitigate suicide risk when a patient was identified at high risk was also a commonly cited root cause. The most extreme examples involved completed suicides occurring with a patient receiving 1‐on‐1 staffing. This 1‐on‐1 staffing did not include specific guidance for the sitters such as the need to remove personal items that could be used for self‐harm. We also saw that staff on medical units needed to learn more about risk factors for suicide and how to conduct a suicide assessment with their patients. Another root cause was the stress caused by the medical and psychiatric conditions of the patients. It is notable that no completed suicides occurred in ICUs, suggesting that closer observation and/or a higher level of medical incapacitation can reduce the risk of completed suicides.
To address these root causes, staff should be educated about risk factors for suicide, and standardized high‐risk for suicide order sets and checklists should be used to ensure staff execute the desired care processes and communicate them to all staff. In addition, specific training in suicide prevention should be provided to staff involved in 1‐on‐1 observation for high‐risk patients. Again, this may be aided by a checklist to help staff remember the protocol for what may be a low‐frequency event. A high risk suicide care process may include:
- Conducting contraband searches for items that could be used for self‐harm, modifying the environment of a small percentage of toilet rooms on medical floors to reduce anchor points for hanging. A high risk patient could then be moved to these rooms.
- Regular psychiatric input into the treatment plan.
- Discharge planning that includes attention to the potential for depression and suicidal ideation upon discharge.
Limitations
This study has several limitations. First, our data only contained suicide attempts and completions that were reported through our patient safety system in the VHA, and only completed suicides require an RCA, thus there are likely some events that were not included. Second, the RCA reports focus on the systemic vulnerabilities in medical‐surgical units and ICUs that may have contributed to the adverse event rather than the specific characteristics of the patients involved, so we do not have complete demographic information about these individual patients. Third, our sample was mostly male, so the results may not generalize well to units with a higher percentage of female patients.
These limitations notwithstanding, we know of no other study to present data on suicide attempts and completions in medical‐surgical and ICUs in a large national medical system.
Disclosures: This material is the result of work supported with resources and the use of facilities at the Department of Veterans Affairs National Center for Patient Safety at Ann Arbor, Michigan, and the Veterans Affairs Medical Centers, White River Junction, Vermont. The Research and Development Committee, White River Junction VA Medical Center approved this project, and the Committee for the Protection of Human Subjects, Dartmouth College considered this project exempt. The views expressed in this article do not necessarily represent the views of the Department of Veterans Affairs or the United States government. The authors report no conflicts of interest.
Suicide is the tenth leading cause of death in the United States,[1] resulting in the deaths of over 34,000 people each year.[2] In 2007, 165,997 individuals were hospitalized for self‐inflicted injuries, and 395,320 people were treated for self‐harm in emergency departments.[2] In 2003, the American Psychiatric Association reported that approximately 1500 suicides take place within hospital facilities in the United States each year.[3]
Although a number of studies have examined inpatient suicides that occurred on psychiatric units,[4, 5, 6, 7, 8] fewer have focused on suicides occurring on medical units. A Joint Commission review of inpatient suicide on medical/surgical units[9] found that 14.25% of all inpatient suicides occurred while the patient was on a medical unit, and now recommends that all hospitals identify individuals at risk for suicide, develop interventions for suicidal patients, and educate staff about the risk factors of suicide. Bostwick and Rackley[10] reviewed studies of suicide on medical/surgical units and found that few of the patients had histories of mental illness or suicidal ideation and recommend close attention to agitated patients, aggressively treating depression and pain, modifying the environment where possible, and observation of patients thought to be at risk. Wint and Alil[5] also report a high level of depression in patients who commit suicide in general hospitals and suggest that improved recognition of depression in general hospital patients will reduce suicide.
GOALS FOR THIS STUDY
Few studies have examined suicide on acute medical and surgical and intensive care units (ICUs), and there are no large studies conducted in the United States. The goal of this study was to describe suicide attempts and completions in the medical setting using Root Cause Analysis (RCA) reports of these events in the Veterans Health Administration (VHA).
METHODS
Study Design and Theoretical Model
This is an observational review of all RCA reports of suicide attempts or completions on the medical‐surgical wards and ICUs in the VHA system between December 1, 1999 (when the RCA system started) and December 31, 2012. The Committee for the Protection of Human Subjects, Dartmouth College considered this project exempt.
The VHA provides comprehensive healthcare services to over 6 million veterans across the United States through 152 VHA medical centers. Over the study period there were approximately 7,289,770 admissions to medical‐surgical wards and ICUs in the VHA (average number of admissions per year between 2000 and 2012=560,771.5, standard deviation=25,535.7).
The VHA National Center for Patient Safety RCA Program
Patient safety including the investigation of adverse events is coordinated by the National Center for Patient Safety (NCPS). The NCPS has instituted a systematic and structured RCA program to individually and collectively analyze adverse events.[11, 12]
RCA is a method for examining the underlying causes of an adverse event such as a hospital related death, surgical error, or suicide. The focus of an RCA is on the systemic and organizational factors that may have contributed to an adverse event.[11, 12] The RCA process within the VHA is conducted by multidisciplinary teams organized by the hospital's patient safety manager. In general, an RCA describes what happened, how it happened, and what should be done to avoid the same event happening again.[11]
Because of the focus on the system, the information contained in the RCA reports does not include detailed demographic data about the patients involved in the events. RCA reports that are submitted to NCPS include narrative descriptions of the event, all contributing factors, a final understanding of the event, and a specific action plan for addressing underlying causes of the event.
Analysis of RCA Reports
Our goal was to identify suicide attempts and completed suicides that occurred on acute care medical‐surgical wards or ICUs. The search was completed through use of event codes for suicide or suicide attempts entered in the RCA and through the use of natural language processing software to identify the terms related to suicide or suicide attempts anywhere in the RCA text (PolyAnalyst; Megaputer, Bloomington, IN).
Data Processing
Each RCA report was coded for the location of the event, method of self‐harm, and root causes; where possible, we also coded medical diagnosis, reason for admission, history of suicidal behavior, age, and gender. The coding system was developed in a previous study of RCA reports of suicide.[13]
RESULTS
Our search resulted in 525 RCA reports of inpatient suicide attempts and completions. These were obtained from the 14,851 total RCA reports in the RCA dataset. Of the 525, we identified 50 cases that occurred while the patient was on the acute medical‐surgical unit (43 cases) or ICU (7 cases). Other cases occurred on mental health units, emergency department, or other areas of the hospital. Five cases were completed suicides, and 45 were suicide attempts. Based on the number of admissions per year reported above, the approximate rate of completed inpatient suicides on medical‐surgical and ICUs is 0.6 per million admissions. (For comparison, the rate of completed suicide on psychiatric units in the VA has been estimated to be 8.7 per million admissions.[14] Table 1 displays the admitting diagnosis and demographic data for those RCA reports that contained this information. The most common admitting diagnoses were alcohol detoxification and chest pain or rule out myocardial infarction (MI); note that 12 reports did not contain an admitting diagnosis. Table 2 displays the methods and root causes for the 50 cases; there were 118 root causes generated. The most common methods were cutting, overdose, and hanging; and the most common root causes were poor communication, need for staff training in suicide assessment, and need to improve suicide risk assessment.
| Medical‐Surgical | ICU | |||
|---|---|---|---|---|
| Attempts | Completions | Attempts | Completions | |
| ||||
| Admitting diagnosis, N=50 | ||||
| Alcohol detox | 3 | 2 | 2 | 0 |
| Chest pain or rule out MI | 5 | 0 | 0 | 0 |
| Delirium | 1 | 0 | 0 | 0 |
| Peripheral infection/cellulitis | 2 | 1 | 0 | 0 |
| Spine surgery or spine issue | 2 | 0 | 0 | 0 |
| Lung CA | 1 | 1 | 0 | 0 |
| Cystopy (bladder surgery) | 2 | 0 | 0 | 0 |
| Head and neck CA | 1 | 0 | 1 | 0 |
| Other | 4 | 0 | 0 | 0 |
| Respiratory (COPD) | 2 | 0 | 1 | 0 |
| Suicide attempt by overdose | 2 | 0 | 0 | 0 |
| Lung infection | 1 | 0 | 1 | 0 |
| CVA | 0 | 1 | 0 | 0 |
| Unknown | 12 | 0 | 2 | 0 |
| Demographics N =50 | ||||
| % male | 91.40% | 100% | 80% | NA |
| Average age, y | 56 | 53 | 47 | NA |
| History of suicidal thoughts or behaviors | 16 | 2 | 3 | 0 |
| Medical‐Surgical | ICU | |||
|---|---|---|---|---|
| Attempts | Completions | Attempts | Completions | |
| ||||
| Methods | ||||
| Cutting with a sharp object | 29% | 0% | 43% | None |
| Overdose | 26% | 20% | 0% | None |
| Hanging | 18% | 40% | 29% | None |
| Strangulation | 8% | 0% | 0% | None |
| Jumping | 5% | 0% | 14% | None |
| Asphyxiation | 8% | 0% | 0% | None |
| Removed lines or equipment | 5% | 0% | 14% | None |
| Gun shot | 0% | 40% | 0% | None |
| Column total | 100% | 100% | 100% | None |
| Root causes | ||||
| Poor communication between providers or services | 22% | 9% | 7% | None |
| Need for staff training in suicide assessment | 14% | 0% | 20% | None |
| Need to improve process of suicide assessment | 13% | 9% | 13% | None |
| Need for improvement of risk documentation | 9% | 0% | 7% | None |
| Physical environment is a risk factor | 7% | 0% | 20% | None |
| Contraband search needs improvement | 7% | 18% | 0% | None |
| Problems with treatment for suicidal patients | 7% | 27% | 7% | None |
| Not following existing policies | 5% | 0% | 0% | None |
| Medical assess or treatment delayed or incomplete | 5% | 0% | 0% | None |
| Easy access to medication for overdose | 4% | 9% | 0% | None |
| Stressed by medical/mental health/pain problems | 5% | 18% | 20% | None |
| Other root causes | 1% | 0% | 7% | None |
| No root cause | 1% | 9% | 0% | None |
| Column totals | 100% | 100% | 100% | None |
DISCUSSION
This study examined the specific systemic factors involved in suicide attempts and completions in medical‐surgical and intensive care units in a large, national hospital sample. Overall, the number of completed suicides over the 13‐year period was small (5 in total). The most common reason for admission was alcohol detoxification. Many patients going through alcohol detoxification experience agitation, which is a risk factor for suicide among medical patients.[10] This hypothesis is further supported by the fact that 2 of the 5 completed suicides were admitted for alcohol detoxification. Interestingly, only 2 of the patients who attempted suicide in the hospital were also admitted for medical conditions related to a prior suicide attempt. It is likely the case that patients admitted for a suicide attempt are closely watched throughout the admission and so may have fewer opportunities to repeat the suicide attempt.
The most common method of suicide attempts was cutting with a sharp object. However, cutting did not result in death, whereas overdose, hanging, and gunshot did. As a precaution, especially with patients with a known history of suicidal ideation, removing sharp objects such as razor blades and knives as well as extra medications is a reasonable first step. It may also be possible to create safer bathroom environments, at least in some medical rooms for potentially suicidal patients, which have break‐away shower curtains, sealed grab‐bars, and a general reduction of anchor points for hanging (see
As with other studies of RCAs,[15, 16] we found that problems communicating risk was the most common identified root cause for suicide attempts and completions. Problems communicating risk most often involved knowledge of suicide risk or specific suicide mitigation plans that were not shared by the treatment team or communicated during handoffs. Most frequently, this communication problem involved team members assessing a patient to be at high risk for suicide, but that information was not provided to other care team members. This root cause also included situations in which the treatment plan for suicide prevention was inadequately disseminated to the entire treatment team. It is critical that good systems are in place so that staff members have the time to communicate critical information about patients. In addition, the system should be standardized so that the same information is communicated each time there is a handoff. The lack of clear steps to mitigate suicide risk when a patient was identified at high risk was also a commonly cited root cause. The most extreme examples involved completed suicides occurring with a patient receiving 1‐on‐1 staffing. This 1‐on‐1 staffing did not include specific guidance for the sitters such as the need to remove personal items that could be used for self‐harm. We also saw that staff on medical units needed to learn more about risk factors for suicide and how to conduct a suicide assessment with their patients. Another root cause was the stress caused by the medical and psychiatric conditions of the patients. It is notable that no completed suicides occurred in ICUs, suggesting that closer observation and/or a higher level of medical incapacitation can reduce the risk of completed suicides.
To address these root causes, staff should be educated about risk factors for suicide, and standardized high‐risk for suicide order sets and checklists should be used to ensure staff execute the desired care processes and communicate them to all staff. In addition, specific training in suicide prevention should be provided to staff involved in 1‐on‐1 observation for high‐risk patients. Again, this may be aided by a checklist to help staff remember the protocol for what may be a low‐frequency event. A high risk suicide care process may include:
- Conducting contraband searches for items that could be used for self‐harm, modifying the environment of a small percentage of toilet rooms on medical floors to reduce anchor points for hanging. A high risk patient could then be moved to these rooms.
- Regular psychiatric input into the treatment plan.
- Discharge planning that includes attention to the potential for depression and suicidal ideation upon discharge.
Limitations
This study has several limitations. First, our data only contained suicide attempts and completions that were reported through our patient safety system in the VHA, and only completed suicides require an RCA, thus there are likely some events that were not included. Second, the RCA reports focus on the systemic vulnerabilities in medical‐surgical units and ICUs that may have contributed to the adverse event rather than the specific characteristics of the patients involved, so we do not have complete demographic information about these individual patients. Third, our sample was mostly male, so the results may not generalize well to units with a higher percentage of female patients.
These limitations notwithstanding, we know of no other study to present data on suicide attempts and completions in medical‐surgical and ICUs in a large national medical system.
Disclosures: This material is the result of work supported with resources and the use of facilities at the Department of Veterans Affairs National Center for Patient Safety at Ann Arbor, Michigan, and the Veterans Affairs Medical Centers, White River Junction, Vermont. The Research and Development Committee, White River Junction VA Medical Center approved this project, and the Committee for the Protection of Human Subjects, Dartmouth College considered this project exempt. The views expressed in this article do not necessarily represent the views of the Department of Veterans Affairs or the United States government. The authors report no conflicts of interest.
- Centers for Disease Control and Prevention. National Center for Injury and Prevention Control. WISQARS (Web‐based Injury Statistics Query and Reporting System). Available at: http://www.cdc.gov/injury/wisqars/index.html. Accessed September 27, 2012.
- Centers for Disease Control and Prevention. Suicide: facts at a glance. Available at: http://www.cdc.gov/ViolencePrevention/pdf/Suicide_DataSheet‐a.pdf. Accessed September 27, 2012.
- American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160:1–60.
- , . Inpatient suicide: preventing a common sentinel event. Gen Hosp Psychiatry. 2009;31:103–109.
- , . Suicidality in the general hospitalized patient. Hosp Physician. 2006;42(1):13–18.
- , , . Suicide inside: a systematic review of inpatient suicides. J Nervous and Ment Dis. 2010;198(5):315–328.
- , , . Environmental risk factors in hospital suicide. Suicide Life Threat Behav. 2004;34(4):448–453.
- , , . Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003;64(1):14–19.
- A follow‐up report on preventing suicide: focus on medical/surgical units and the emergency department. Sentinel Event Alert. 2010;(46):1–4.
- , . Completed suicide in medical/surgical patients: who is at risk? Curr Psychiatry Rep. 2007;9(3):242–246.
- , , , , , , et al. Developing and deploying a patient safety program in a large health care system: you can't fix what you don't know about. Jt Comm J Qual Improv. 2001;27:522–532.
- , . Developing a culture of safety in the Veterans Health Administration. Eff Clin Pract. 2007;3:270–276.
- , , , , . Actions and Implementation Strategies to Reduce Suicidal Events in the VHA. Jt Comm J on Qual and Safe. 2006:32(3):130–141.
- , , , et al. An examination of the effectiveness of a mental health environment of care checklist in reducing suicide on inpatient mental health units. Arch GenPsychiatry. 2012:69(6):588–592.
- , , , , . Helping elderly patients to avoid suicide: a review of case reports from a national Veterans Affairs database. J Nerv Ment Dis. 2013;201(1):12–16.
- , , , , . Suicide attempts and completions in the emergency department in Veterans Affairs hospitals. Emerg Med J. 2012;29(5):399–403.
- Centers for Disease Control and Prevention. National Center for Injury and Prevention Control. WISQARS (Web‐based Injury Statistics Query and Reporting System). Available at: http://www.cdc.gov/injury/wisqars/index.html. Accessed September 27, 2012.
- Centers for Disease Control and Prevention. Suicide: facts at a glance. Available at: http://www.cdc.gov/ViolencePrevention/pdf/Suicide_DataSheet‐a.pdf. Accessed September 27, 2012.
- American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160:1–60.
- , . Inpatient suicide: preventing a common sentinel event. Gen Hosp Psychiatry. 2009;31:103–109.
- , . Suicidality in the general hospitalized patient. Hosp Physician. 2006;42(1):13–18.
- , , . Suicide inside: a systematic review of inpatient suicides. J Nervous and Ment Dis. 2010;198(5):315–328.
- , , . Environmental risk factors in hospital suicide. Suicide Life Threat Behav. 2004;34(4):448–453.
- , , . Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003;64(1):14–19.
- A follow‐up report on preventing suicide: focus on medical/surgical units and the emergency department. Sentinel Event Alert. 2010;(46):1–4.
- , . Completed suicide in medical/surgical patients: who is at risk? Curr Psychiatry Rep. 2007;9(3):242–246.
- , , , , , , et al. Developing and deploying a patient safety program in a large health care system: you can't fix what you don't know about. Jt Comm J Qual Improv. 2001;27:522–532.
- , . Developing a culture of safety in the Veterans Health Administration. Eff Clin Pract. 2007;3:270–276.
- , , , , . Actions and Implementation Strategies to Reduce Suicidal Events in the VHA. Jt Comm J on Qual and Safe. 2006:32(3):130–141.
- , , , et al. An examination of the effectiveness of a mental health environment of care checklist in reducing suicide on inpatient mental health units. Arch GenPsychiatry. 2012:69(6):588–592.
- , , , , . Helping elderly patients to avoid suicide: a review of case reports from a national Veterans Affairs database. J Nerv Ment Dis. 2013;201(1):12–16.
- , , , , . Suicide attempts and completions in the emergency department in Veterans Affairs hospitals. Emerg Med J. 2012;29(5):399–403.
What's the appropriate lens to use in rigid cystoscopy to evaluate the bladder?
Dr. Gebhart says an angled lens is critical to viewing the bladder, but which angle is ideal?
When Dr. Gebhart surveyed attendees of the Pelvic Anatomy and Gynecology Symposium in Las Vegas, Nevada, in December 2013, as to which lens angle was the best option, the majority chose the 30-degree lens. Listen to why Dr. Gebhart recommends the 70-degree lens.
Dr. Gebhart says an angled lens is critical to viewing the bladder, but which angle is ideal?
When Dr. Gebhart surveyed attendees of the Pelvic Anatomy and Gynecology Symposium in Las Vegas, Nevada, in December 2013, as to which lens angle was the best option, the majority chose the 30-degree lens. Listen to why Dr. Gebhart recommends the 70-degree lens.
Dr. Gebhart says an angled lens is critical to viewing the bladder, but which angle is ideal?
When Dr. Gebhart surveyed attendees of the Pelvic Anatomy and Gynecology Symposium in Las Vegas, Nevada, in December 2013, as to which lens angle was the best option, the majority chose the 30-degree lens. Listen to why Dr. Gebhart recommends the 70-degree lens.
'JNC 8' guideline follows convoluted endgame
The federally funded program to produce a set of U.S. guidelines for hypertension management, a process more than 5 years in the making, came to an unusual end on December 18 when the members of what had already become the officially-disbanded JNC 8 panel published their conclusions and guideline.
No longer recognized or supported by the National Heart Lung and Blood Institute (NHLBI), the Federal agency that had organized the Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) panel in 2008, and unwilling to work with potential collaborating groups like the American Heart Association (AHA), the American College of Cardiology (ACC), or the American Society of Hypertension (ASH), the 17-person group that wound up identifying themselves as the “panel members appointed to the Eighth Joint National Committee (JNC 8).”
Call them JNC Ain’t.
The U.S. hypertension guidelines began veering off on an unexpected course last June, when Dr. Gary H. Gibbons, NHLBI director, announced that the agency was withdrawing from issuing guidelines itself and would instead collaborate with “partner organizations.”
In August, Dr. Gibbons, said that the AHA and ACC had reached an agreement with the agency to “spearhead” development of three sets of practice guidelines, for hypertension, cholesterol, and obesity. This agreement led to the release in November of the cholesterol and obesity guidelines under the auspices of the AHA and ACC, but instead of also releasing hypertension guidelines, the AHA and ACC as well as the NHLBI said that the process had fallen through and failed to produce guidelines.
According to Dr. Paul A. James, co-chair of the former JNC 8 panel and professor of family medicine at the University of Iowa in Iowa City, that’s because the panel members decided they weren’t comfortable with “the idea of shopping our guideline around prior to publication and getting an endorsement.” Now that the panel’s conclusions have been published “we hope to get active public review of our work; we invite people to analyze our process, and hopefully organizations will endorse our findings,” he said in an interview. “Our belief is that the approach we took, the transparent nature of our guideline development, and our release of it through JAMA will increase the credibility of our work.”
But others said that the panel’s break with the NHLBI and its inability to partner with any organization will inevitably affect how people view these recommendations, especially because parts are also clinically controversial.
“There was clear controversy when this guideline was circulated” while under review, said Dr. John M. Flack, professor and chief of medicine at Wayne State University in Detroit. “The biggest problem this committee has is that many experts with a very significant stake in the recommendations were excluded from the process of generating the guideline. That limits buy-in from key opinion leaders, which will be needed for the uptake of this guideline into clinical practice,” he said in an interview.
“Unlike the previous JNC reports, this one will be seen as interesting, but not as persuasive,” said Dr. Michael A. Weber, professor of medicine at the State University of New York Downstate Medical Center in Brooklyn. “I believe the AHA, ACC, and ASH had hoped to endorse these guidelines, but that wasn’t possible.”
ASH leaders had discussions with the JNC 8 panel last summer, but the two groups could not reach an agreement on how to use the panel’s work for management recommendations, said Dr. William B. White, ASH president and chief of hypertension and clinical pharmacology at the University of Connecticut in Farmington.
What ASH has since agreed to do is join with the AHA and ACC to produce evidence-based hypertension guidelines using NHLBI materials, Dr. White said in an interview. The planned guidelines will “use some of the evidence derived by the NHLBI’s methodology, but adding to it other clinical issues,” including blood pressure measurement. These groups also hope the guidelines development will receive participation from a primary-care society such as the American College of Physicians, he said.
“The ACC/AHA Task Force on Practice Guidelines has begun the process of developing the collaborative model to update the national hypertensive guidelines in partnership with the NHLBI, which will provide an updated systematic review informed by the relevant critical clinical questions. We are seeking appropriate partners to begin this work in early 2014. The writing group will draft recommendations, followed by a peer and stakeholder review process. Once the review process is complete the ACC/AHA and partnering organizations will publish the guidelines in 2015 for clinicians to follow as the national standard for hypertension prevention and treatment,” said a spokeswoman for the American College of Cardiology in a statement released on December 18.
Leaders from the AHA and ACC said that once it became clear several weeks ago that they would not be able to collaborate with the JNC 8 panel, they felt compelled to immediately develop some form of updated guidance on hypertensive management. That led to an AHA-ACC Science Advisory (J. Am. Coll. Card. 2013;doi:10.1016/j.jacc.2013.11.007) released on Nov. 15 in collaboration with the Centers for Disease Control and Prevention that endorsed the use of treatment algorithms when managing patients with hypertension.
“Because the JNC 8 panel chose not to be part of the AHA-ACC structure, we felt we needed to go forward to make sure that we had guidance that reflected the evidence,” said Dr. Kim A. Williams Sr., professor and head of cardiology at Rush University in Chicago, vice president of the ACC, and a member of the group that wrote the advisory. “We felt the need to have risk covered as best we could, and have some hypertension guidance out there, even if it is not a guideline,” he said in an interview.
“We felt that after the enormous progress forward with the other four guidelines” released on Nov. 12 by the AHA and ACC (Circulation 2013 [doi: 10.1161/01.cir.0000437738.63853.7a; doi: 10.1161/01.cir.0000437739.71477.ee; doi: 10.1161/01.cir.0000437740.48606.d1; doi: 10.1161/01.cir.0000437741.48606.98]) “there was some urgency” to provide guidance for hypertension too, said Dr. Mariell Jessup, professor and medical director of the Penn Heart and Vascular Center at the University of Pennsylvania in Philadelphia and president of the AHA, during a session on the new guidelines at the AHA Scientific Sessions in Dallas in November.
The potential this now presents for the AHA and ACC to produce unified U.S. guidelines for all aspects of cardiovascular disease risk, integrating the assessment and treatment of hypertension, cholesterol, and obesity, is a positive development, said Dr. Eric D. Peterson, professor of medicine at Duke University in Durham, N.C. He was also hopeful that this new collaboration will draw in groups like ASH and the American College of Physicians to represent the interests of subspecialists and primary-care physicians. “Ideally you want consensus on where you’re trying to get blood pressure” that cuts across all strata of U.S. medicine, he said.
Dr. James, Dr. White, Dr. Jessup, Dr. Williams and Dr. Peterson said that they had no disclosures. Dr. Flack said that he has been a consultant to Novartis, Medtronic, and Back Beat Hypertension and received funding from Novartis and Medtronic. Dr. Weber said that he has been a consultant to Novartis, Takeda, and Forest.
[email protected]
On Twitter @mitchelzoler
**UPDATED Jan. 4, 2014
The federally funded program to produce a set of U.S. guidelines for hypertension management, a process more than 5 years in the making, came to an unusual end on December 18 when the members of what had already become the officially-disbanded JNC 8 panel published their conclusions and guideline.
No longer recognized or supported by the National Heart Lung and Blood Institute (NHLBI), the Federal agency that had organized the Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) panel in 2008, and unwilling to work with potential collaborating groups like the American Heart Association (AHA), the American College of Cardiology (ACC), or the American Society of Hypertension (ASH), the 17-person group that wound up identifying themselves as the “panel members appointed to the Eighth Joint National Committee (JNC 8).”
Call them JNC Ain’t.
The U.S. hypertension guidelines began veering off on an unexpected course last June, when Dr. Gary H. Gibbons, NHLBI director, announced that the agency was withdrawing from issuing guidelines itself and would instead collaborate with “partner organizations.”
In August, Dr. Gibbons, said that the AHA and ACC had reached an agreement with the agency to “spearhead” development of three sets of practice guidelines, for hypertension, cholesterol, and obesity. This agreement led to the release in November of the cholesterol and obesity guidelines under the auspices of the AHA and ACC, but instead of also releasing hypertension guidelines, the AHA and ACC as well as the NHLBI said that the process had fallen through and failed to produce guidelines.
According to Dr. Paul A. James, co-chair of the former JNC 8 panel and professor of family medicine at the University of Iowa in Iowa City, that’s because the panel members decided they weren’t comfortable with “the idea of shopping our guideline around prior to publication and getting an endorsement.” Now that the panel’s conclusions have been published “we hope to get active public review of our work; we invite people to analyze our process, and hopefully organizations will endorse our findings,” he said in an interview. “Our belief is that the approach we took, the transparent nature of our guideline development, and our release of it through JAMA will increase the credibility of our work.”
But others said that the panel’s break with the NHLBI and its inability to partner with any organization will inevitably affect how people view these recommendations, especially because parts are also clinically controversial.
“There was clear controversy when this guideline was circulated” while under review, said Dr. John M. Flack, professor and chief of medicine at Wayne State University in Detroit. “The biggest problem this committee has is that many experts with a very significant stake in the recommendations were excluded from the process of generating the guideline. That limits buy-in from key opinion leaders, which will be needed for the uptake of this guideline into clinical practice,” he said in an interview.
“Unlike the previous JNC reports, this one will be seen as interesting, but not as persuasive,” said Dr. Michael A. Weber, professor of medicine at the State University of New York Downstate Medical Center in Brooklyn. “I believe the AHA, ACC, and ASH had hoped to endorse these guidelines, but that wasn’t possible.”
ASH leaders had discussions with the JNC 8 panel last summer, but the two groups could not reach an agreement on how to use the panel’s work for management recommendations, said Dr. William B. White, ASH president and chief of hypertension and clinical pharmacology at the University of Connecticut in Farmington.
What ASH has since agreed to do is join with the AHA and ACC to produce evidence-based hypertension guidelines using NHLBI materials, Dr. White said in an interview. The planned guidelines will “use some of the evidence derived by the NHLBI’s methodology, but adding to it other clinical issues,” including blood pressure measurement. These groups also hope the guidelines development will receive participation from a primary-care society such as the American College of Physicians, he said.
“The ACC/AHA Task Force on Practice Guidelines has begun the process of developing the collaborative model to update the national hypertensive guidelines in partnership with the NHLBI, which will provide an updated systematic review informed by the relevant critical clinical questions. We are seeking appropriate partners to begin this work in early 2014. The writing group will draft recommendations, followed by a peer and stakeholder review process. Once the review process is complete the ACC/AHA and partnering organizations will publish the guidelines in 2015 for clinicians to follow as the national standard for hypertension prevention and treatment,” said a spokeswoman for the American College of Cardiology in a statement released on December 18.
Leaders from the AHA and ACC said that once it became clear several weeks ago that they would not be able to collaborate with the JNC 8 panel, they felt compelled to immediately develop some form of updated guidance on hypertensive management. That led to an AHA-ACC Science Advisory (J. Am. Coll. Card. 2013;doi:10.1016/j.jacc.2013.11.007) released on Nov. 15 in collaboration with the Centers for Disease Control and Prevention that endorsed the use of treatment algorithms when managing patients with hypertension.
“Because the JNC 8 panel chose not to be part of the AHA-ACC structure, we felt we needed to go forward to make sure that we had guidance that reflected the evidence,” said Dr. Kim A. Williams Sr., professor and head of cardiology at Rush University in Chicago, vice president of the ACC, and a member of the group that wrote the advisory. “We felt the need to have risk covered as best we could, and have some hypertension guidance out there, even if it is not a guideline,” he said in an interview.
“We felt that after the enormous progress forward with the other four guidelines” released on Nov. 12 by the AHA and ACC (Circulation 2013 [doi: 10.1161/01.cir.0000437738.63853.7a; doi: 10.1161/01.cir.0000437739.71477.ee; doi: 10.1161/01.cir.0000437740.48606.d1; doi: 10.1161/01.cir.0000437741.48606.98]) “there was some urgency” to provide guidance for hypertension too, said Dr. Mariell Jessup, professor and medical director of the Penn Heart and Vascular Center at the University of Pennsylvania in Philadelphia and president of the AHA, during a session on the new guidelines at the AHA Scientific Sessions in Dallas in November.
The potential this now presents for the AHA and ACC to produce unified U.S. guidelines for all aspects of cardiovascular disease risk, integrating the assessment and treatment of hypertension, cholesterol, and obesity, is a positive development, said Dr. Eric D. Peterson, professor of medicine at Duke University in Durham, N.C. He was also hopeful that this new collaboration will draw in groups like ASH and the American College of Physicians to represent the interests of subspecialists and primary-care physicians. “Ideally you want consensus on where you’re trying to get blood pressure” that cuts across all strata of U.S. medicine, he said.
Dr. James, Dr. White, Dr. Jessup, Dr. Williams and Dr. Peterson said that they had no disclosures. Dr. Flack said that he has been a consultant to Novartis, Medtronic, and Back Beat Hypertension and received funding from Novartis and Medtronic. Dr. Weber said that he has been a consultant to Novartis, Takeda, and Forest.
[email protected]
On Twitter @mitchelzoler
**UPDATED Jan. 4, 2014
The federally funded program to produce a set of U.S. guidelines for hypertension management, a process more than 5 years in the making, came to an unusual end on December 18 when the members of what had already become the officially-disbanded JNC 8 panel published their conclusions and guideline.
No longer recognized or supported by the National Heart Lung and Blood Institute (NHLBI), the Federal agency that had organized the Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) panel in 2008, and unwilling to work with potential collaborating groups like the American Heart Association (AHA), the American College of Cardiology (ACC), or the American Society of Hypertension (ASH), the 17-person group that wound up identifying themselves as the “panel members appointed to the Eighth Joint National Committee (JNC 8).”
Call them JNC Ain’t.
The U.S. hypertension guidelines began veering off on an unexpected course last June, when Dr. Gary H. Gibbons, NHLBI director, announced that the agency was withdrawing from issuing guidelines itself and would instead collaborate with “partner organizations.”
In August, Dr. Gibbons, said that the AHA and ACC had reached an agreement with the agency to “spearhead” development of three sets of practice guidelines, for hypertension, cholesterol, and obesity. This agreement led to the release in November of the cholesterol and obesity guidelines under the auspices of the AHA and ACC, but instead of also releasing hypertension guidelines, the AHA and ACC as well as the NHLBI said that the process had fallen through and failed to produce guidelines.
According to Dr. Paul A. James, co-chair of the former JNC 8 panel and professor of family medicine at the University of Iowa in Iowa City, that’s because the panel members decided they weren’t comfortable with “the idea of shopping our guideline around prior to publication and getting an endorsement.” Now that the panel’s conclusions have been published “we hope to get active public review of our work; we invite people to analyze our process, and hopefully organizations will endorse our findings,” he said in an interview. “Our belief is that the approach we took, the transparent nature of our guideline development, and our release of it through JAMA will increase the credibility of our work.”
But others said that the panel’s break with the NHLBI and its inability to partner with any organization will inevitably affect how people view these recommendations, especially because parts are also clinically controversial.
“There was clear controversy when this guideline was circulated” while under review, said Dr. John M. Flack, professor and chief of medicine at Wayne State University in Detroit. “The biggest problem this committee has is that many experts with a very significant stake in the recommendations were excluded from the process of generating the guideline. That limits buy-in from key opinion leaders, which will be needed for the uptake of this guideline into clinical practice,” he said in an interview.
“Unlike the previous JNC reports, this one will be seen as interesting, but not as persuasive,” said Dr. Michael A. Weber, professor of medicine at the State University of New York Downstate Medical Center in Brooklyn. “I believe the AHA, ACC, and ASH had hoped to endorse these guidelines, but that wasn’t possible.”
ASH leaders had discussions with the JNC 8 panel last summer, but the two groups could not reach an agreement on how to use the panel’s work for management recommendations, said Dr. William B. White, ASH president and chief of hypertension and clinical pharmacology at the University of Connecticut in Farmington.
What ASH has since agreed to do is join with the AHA and ACC to produce evidence-based hypertension guidelines using NHLBI materials, Dr. White said in an interview. The planned guidelines will “use some of the evidence derived by the NHLBI’s methodology, but adding to it other clinical issues,” including blood pressure measurement. These groups also hope the guidelines development will receive participation from a primary-care society such as the American College of Physicians, he said.
“The ACC/AHA Task Force on Practice Guidelines has begun the process of developing the collaborative model to update the national hypertensive guidelines in partnership with the NHLBI, which will provide an updated systematic review informed by the relevant critical clinical questions. We are seeking appropriate partners to begin this work in early 2014. The writing group will draft recommendations, followed by a peer and stakeholder review process. Once the review process is complete the ACC/AHA and partnering organizations will publish the guidelines in 2015 for clinicians to follow as the national standard for hypertension prevention and treatment,” said a spokeswoman for the American College of Cardiology in a statement released on December 18.
Leaders from the AHA and ACC said that once it became clear several weeks ago that they would not be able to collaborate with the JNC 8 panel, they felt compelled to immediately develop some form of updated guidance on hypertensive management. That led to an AHA-ACC Science Advisory (J. Am. Coll. Card. 2013;doi:10.1016/j.jacc.2013.11.007) released on Nov. 15 in collaboration with the Centers for Disease Control and Prevention that endorsed the use of treatment algorithms when managing patients with hypertension.
“Because the JNC 8 panel chose not to be part of the AHA-ACC structure, we felt we needed to go forward to make sure that we had guidance that reflected the evidence,” said Dr. Kim A. Williams Sr., professor and head of cardiology at Rush University in Chicago, vice president of the ACC, and a member of the group that wrote the advisory. “We felt the need to have risk covered as best we could, and have some hypertension guidance out there, even if it is not a guideline,” he said in an interview.
“We felt that after the enormous progress forward with the other four guidelines” released on Nov. 12 by the AHA and ACC (Circulation 2013 [doi: 10.1161/01.cir.0000437738.63853.7a; doi: 10.1161/01.cir.0000437739.71477.ee; doi: 10.1161/01.cir.0000437740.48606.d1; doi: 10.1161/01.cir.0000437741.48606.98]) “there was some urgency” to provide guidance for hypertension too, said Dr. Mariell Jessup, professor and medical director of the Penn Heart and Vascular Center at the University of Pennsylvania in Philadelphia and president of the AHA, during a session on the new guidelines at the AHA Scientific Sessions in Dallas in November.
The potential this now presents for the AHA and ACC to produce unified U.S. guidelines for all aspects of cardiovascular disease risk, integrating the assessment and treatment of hypertension, cholesterol, and obesity, is a positive development, said Dr. Eric D. Peterson, professor of medicine at Duke University in Durham, N.C. He was also hopeful that this new collaboration will draw in groups like ASH and the American College of Physicians to represent the interests of subspecialists and primary-care physicians. “Ideally you want consensus on where you’re trying to get blood pressure” that cuts across all strata of U.S. medicine, he said.
Dr. James, Dr. White, Dr. Jessup, Dr. Williams and Dr. Peterson said that they had no disclosures. Dr. Flack said that he has been a consultant to Novartis, Medtronic, and Back Beat Hypertension and received funding from Novartis and Medtronic. Dr. Weber said that he has been a consultant to Novartis, Takeda, and Forest.
[email protected]
On Twitter @mitchelzoler
**UPDATED Jan. 4, 2014
Routinely screen relatives when thoracic aortic aneurysm disease presents before age 60
DALLAS – Routine screening is warranted for the first-degree relatives of patients who present with thoracic aortic disease before age 60 years in the absence of predisposing conditions such as hypertension, Marfan syndrome, or bicuspid aortic valve, Dr. Elizabeth N. Robertson said at the American Heart Association scientific sessions.
"We’ve shown that screening of first-degree relatives for familial thoracic aortic aneurysm disease is essential, as we detected an average of two additional affected individuals per initial patient," noted Dr. Robertson of Royal Prince Alfred Hospital in Camperdown, Australia.

Thoracic aortic aneurysm and dissection (TAAD) is more common than previously recognized. It accounted for one in seven cases of thoracic aortic disease in a series of 1,276 patients who presented with thoracic aortic disease to the tertiary center during a recent 12-year period.
TAAD is an asymptomatic progressive dilatation of the thoracic aorta characterized by cystic medial necrosis. It has no evident predisposing cause. It can occur sporadically or in a familial form, which has been linked to multiple gene mutations transmitted in autosomal dominant fashion in large family studies. Unlike Marfan syndrome, Ehler-Danlos syndrome, and other genetic causes of thoracic aortic disease, TAAD has no characteristic external physical features. The clinical signs of TAAD are minimal and nonpathognomonic: an aortic flow murmur or a prominent A2 second heart sound.
"The most common first indication of a problem is occurrence of aortic dissection, by which time it’s often too late," she said.
Dr. Robertson and her coinvestigators did a retrospective review of 1,276 patients who presented with thoracic aortic disease at the Royal Prince Alfred Hospital cardiovascular myopathy service during 2000-2012. TAAD was seen in 178. TAAD was defined as aortic dilatation or dissection before age 60 years with no predisposing condition and with confirmation of cystic medial necrosis whenever possible. TAAD was sporadic in 93 patients. The other 85 had familial TAAD based upon their history of having one or more affected family members. Screening was offered to all first-degree relatives of the patients with familial TAAD.
Two-dimensional echocardiographic screening of 383 first-degree family members identified an additional 181 affected individuals, bringing the total study population with familial TAAD to 266. When the screened patients were added to the 93 patients with sporadic TAAD, thoracic aortic aneurysm and dissection became the second most common cause of thoracic aortic dilatation or dissection seen at the hospital during the study period.
The median age at diagnosis was 46 years both in the sporadic and familial TAAD groups. However, the detection rate was steady from the teen years through old age, underscoring the importance of surveillance of younger at-risk individuals. Most of the at-risk population was male, 73% of the familial and 86% of the sporadic cases. The aortic diameter at diagnosis varied, but it was 50 mm or greater in 25% of the subjects in the familial and sporadic groups. Under current guidelines, this measure warrants semi-urgent surgical intervention.
Of the first-degree relatives identified through screening, 26% experienced aortic dissection, as did more than 60% of the initial 85 probands with familial TAAD. The familial phenotype appears to be more aggressive: 40% of patients with familial TAAD who had an aortic dissection died as a result, compared with less than 15% of patients with sporadic TAAD who had aortic dissection.
Dissection in patients with familial TAAD frequently occurred at smaller aortic diameters, including less than 40 mm. Dr. Robertson noted this width would not typically be flagged as a problematic in routine screening.
The rate of progression of dilatation in patients with familial TAAD was 0.5 mm per year, which is roughly half the rate typically seen in patients with Marfan syndrome, according to Dr. Robertson.
Session cochair Dr. Brendan M. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston, called Dr. Robertson’s study "fascinating" and thanked her for bringing to his attention a serious and relatively common condition he was hitherto unaware of. Given that aortic size is age-, gender-, and body surface area–dependent, what’s the best threshold aortic diameter in defining a positive screening test in first-degree relatives?, he asked.
Because of those associations, Dr. Robertson replied, the best definition of a positive screening test is a Z score greater than 2, rather than simply relying upon a given aortic diameter measurement.
Dr. Robertson’s study was conducted free of commercial support. She reported having no financial conflicts of interest.
DALLAS – Routine screening is warranted for the first-degree relatives of patients who present with thoracic aortic disease before age 60 years in the absence of predisposing conditions such as hypertension, Marfan syndrome, or bicuspid aortic valve, Dr. Elizabeth N. Robertson said at the American Heart Association scientific sessions.
"We’ve shown that screening of first-degree relatives for familial thoracic aortic aneurysm disease is essential, as we detected an average of two additional affected individuals per initial patient," noted Dr. Robertson of Royal Prince Alfred Hospital in Camperdown, Australia.

Thoracic aortic aneurysm and dissection (TAAD) is more common than previously recognized. It accounted for one in seven cases of thoracic aortic disease in a series of 1,276 patients who presented with thoracic aortic disease to the tertiary center during a recent 12-year period.
TAAD is an asymptomatic progressive dilatation of the thoracic aorta characterized by cystic medial necrosis. It has no evident predisposing cause. It can occur sporadically or in a familial form, which has been linked to multiple gene mutations transmitted in autosomal dominant fashion in large family studies. Unlike Marfan syndrome, Ehler-Danlos syndrome, and other genetic causes of thoracic aortic disease, TAAD has no characteristic external physical features. The clinical signs of TAAD are minimal and nonpathognomonic: an aortic flow murmur or a prominent A2 second heart sound.
"The most common first indication of a problem is occurrence of aortic dissection, by which time it’s often too late," she said.
Dr. Robertson and her coinvestigators did a retrospective review of 1,276 patients who presented with thoracic aortic disease at the Royal Prince Alfred Hospital cardiovascular myopathy service during 2000-2012. TAAD was seen in 178. TAAD was defined as aortic dilatation or dissection before age 60 years with no predisposing condition and with confirmation of cystic medial necrosis whenever possible. TAAD was sporadic in 93 patients. The other 85 had familial TAAD based upon their history of having one or more affected family members. Screening was offered to all first-degree relatives of the patients with familial TAAD.
Two-dimensional echocardiographic screening of 383 first-degree family members identified an additional 181 affected individuals, bringing the total study population with familial TAAD to 266. When the screened patients were added to the 93 patients with sporadic TAAD, thoracic aortic aneurysm and dissection became the second most common cause of thoracic aortic dilatation or dissection seen at the hospital during the study period.
The median age at diagnosis was 46 years both in the sporadic and familial TAAD groups. However, the detection rate was steady from the teen years through old age, underscoring the importance of surveillance of younger at-risk individuals. Most of the at-risk population was male, 73% of the familial and 86% of the sporadic cases. The aortic diameter at diagnosis varied, but it was 50 mm or greater in 25% of the subjects in the familial and sporadic groups. Under current guidelines, this measure warrants semi-urgent surgical intervention.
Of the first-degree relatives identified through screening, 26% experienced aortic dissection, as did more than 60% of the initial 85 probands with familial TAAD. The familial phenotype appears to be more aggressive: 40% of patients with familial TAAD who had an aortic dissection died as a result, compared with less than 15% of patients with sporadic TAAD who had aortic dissection.
Dissection in patients with familial TAAD frequently occurred at smaller aortic diameters, including less than 40 mm. Dr. Robertson noted this width would not typically be flagged as a problematic in routine screening.
The rate of progression of dilatation in patients with familial TAAD was 0.5 mm per year, which is roughly half the rate typically seen in patients with Marfan syndrome, according to Dr. Robertson.
Session cochair Dr. Brendan M. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston, called Dr. Robertson’s study "fascinating" and thanked her for bringing to his attention a serious and relatively common condition he was hitherto unaware of. Given that aortic size is age-, gender-, and body surface area–dependent, what’s the best threshold aortic diameter in defining a positive screening test in first-degree relatives?, he asked.
Because of those associations, Dr. Robertson replied, the best definition of a positive screening test is a Z score greater than 2, rather than simply relying upon a given aortic diameter measurement.
Dr. Robertson’s study was conducted free of commercial support. She reported having no financial conflicts of interest.
DALLAS – Routine screening is warranted for the first-degree relatives of patients who present with thoracic aortic disease before age 60 years in the absence of predisposing conditions such as hypertension, Marfan syndrome, or bicuspid aortic valve, Dr. Elizabeth N. Robertson said at the American Heart Association scientific sessions.
"We’ve shown that screening of first-degree relatives for familial thoracic aortic aneurysm disease is essential, as we detected an average of two additional affected individuals per initial patient," noted Dr. Robertson of Royal Prince Alfred Hospital in Camperdown, Australia.

Thoracic aortic aneurysm and dissection (TAAD) is more common than previously recognized. It accounted for one in seven cases of thoracic aortic disease in a series of 1,276 patients who presented with thoracic aortic disease to the tertiary center during a recent 12-year period.
TAAD is an asymptomatic progressive dilatation of the thoracic aorta characterized by cystic medial necrosis. It has no evident predisposing cause. It can occur sporadically or in a familial form, which has been linked to multiple gene mutations transmitted in autosomal dominant fashion in large family studies. Unlike Marfan syndrome, Ehler-Danlos syndrome, and other genetic causes of thoracic aortic disease, TAAD has no characteristic external physical features. The clinical signs of TAAD are minimal and nonpathognomonic: an aortic flow murmur or a prominent A2 second heart sound.
"The most common first indication of a problem is occurrence of aortic dissection, by which time it’s often too late," she said.
Dr. Robertson and her coinvestigators did a retrospective review of 1,276 patients who presented with thoracic aortic disease at the Royal Prince Alfred Hospital cardiovascular myopathy service during 2000-2012. TAAD was seen in 178. TAAD was defined as aortic dilatation or dissection before age 60 years with no predisposing condition and with confirmation of cystic medial necrosis whenever possible. TAAD was sporadic in 93 patients. The other 85 had familial TAAD based upon their history of having one or more affected family members. Screening was offered to all first-degree relatives of the patients with familial TAAD.
Two-dimensional echocardiographic screening of 383 first-degree family members identified an additional 181 affected individuals, bringing the total study population with familial TAAD to 266. When the screened patients were added to the 93 patients with sporadic TAAD, thoracic aortic aneurysm and dissection became the second most common cause of thoracic aortic dilatation or dissection seen at the hospital during the study period.
The median age at diagnosis was 46 years both in the sporadic and familial TAAD groups. However, the detection rate was steady from the teen years through old age, underscoring the importance of surveillance of younger at-risk individuals. Most of the at-risk population was male, 73% of the familial and 86% of the sporadic cases. The aortic diameter at diagnosis varied, but it was 50 mm or greater in 25% of the subjects in the familial and sporadic groups. Under current guidelines, this measure warrants semi-urgent surgical intervention.
Of the first-degree relatives identified through screening, 26% experienced aortic dissection, as did more than 60% of the initial 85 probands with familial TAAD. The familial phenotype appears to be more aggressive: 40% of patients with familial TAAD who had an aortic dissection died as a result, compared with less than 15% of patients with sporadic TAAD who had aortic dissection.
Dissection in patients with familial TAAD frequently occurred at smaller aortic diameters, including less than 40 mm. Dr. Robertson noted this width would not typically be flagged as a problematic in routine screening.
The rate of progression of dilatation in patients with familial TAAD was 0.5 mm per year, which is roughly half the rate typically seen in patients with Marfan syndrome, according to Dr. Robertson.
Session cochair Dr. Brendan M. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston, called Dr. Robertson’s study "fascinating" and thanked her for bringing to his attention a serious and relatively common condition he was hitherto unaware of. Given that aortic size is age-, gender-, and body surface area–dependent, what’s the best threshold aortic diameter in defining a positive screening test in first-degree relatives?, he asked.
Because of those associations, Dr. Robertson replied, the best definition of a positive screening test is a Z score greater than 2, rather than simply relying upon a given aortic diameter measurement.
Dr. Robertson’s study was conducted free of commercial support. She reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: One in seven patients presenting with thoracic aortic disease in a large series had thoracic aortic aneurysm and dissection, or TAAD, an under-recognized, asymptomatic condition characterized by cystic medial necrosis and a strong genetic component.
Data source: This was a review of 1,276 patients who presented to a tertiary center with thoracic aortic disease. Systemic screening of first-degree relatives of patients with familial TAAD turned up two additional cases per proband.
Disclosures: The study was conducted free of commercial support. The presenter reported having no financial conflicts.
Mohs surgery site, not type, predicts risk of suture contamination
CHICAGO – Bacterial contamination of sutures is surprisingly common, and periorificial sites have a suture contamination rate of nearly 100%, according to a study of sutures collected during Mohs micrographic surgeries in 182 patients.
There’s no direct correlation between suture contamination and surgery site infection, said Dr. Jeremy Sunseri of Brown University, Providence, R.I., who presented the unpublished study at the annual meeting of the American Society of Dermatologic Surgery. However, knowing the risk factors for suture contamination can help reduce the risk of infections and potential antibiotic overuse, he noted.
"For instance, the use of antibiotic-coated sutures in high-risk contamination sites, or variations on draping techniques in these areas, may prove beneficial," Dr. Sunseri noted.
The investigators removed 338 sutures directly from their sterile surgery sites, and placed them in Petri dishes with a growth medium used for the isolation of gram-positive organisms.
They further classified the sutures based on anatomic locations (17), type of surgical closure (5), and suture type (7).
More than 57% of all sutures had bacterial growth, and almost all of those collected from the nose, mouth/lip, eye/orbit were contaminated.
Sutures collected from the scalp, neck, trunk, and upper and lower extremities had significantly lower risk of contamination, ranging from 0% to 20%, with the exception of the groin, which showed a 100% contamination rate.
Sutures from flap repairs were the most frequently contaminated (71%). Sutures collected from complex closures also had a relatively high rate of contamination (68%).
Sutures from intermediate repairs had a contamination rate of 47%, while grafts, purse string closures, and incomplete closures had a 44% rate.
Staphylococci were the most commonly identified bacteria, notably isolates of of Propionibacterium acnes, Corynebacterium sp., and Rothia dentocariosa.
There were no significant differences in the contamination rates of the seven different types of sutures studied.
"The take-home message is that the suture is long and patients are dirty, so be careful where you put that suture," Dr. Sunseri said during his presentation.
Dr. Sunseri had no financial conflicts to disclose.
On Twitter @NaseemSMiller
CHICAGO – Bacterial contamination of sutures is surprisingly common, and periorificial sites have a suture contamination rate of nearly 100%, according to a study of sutures collected during Mohs micrographic surgeries in 182 patients.
There’s no direct correlation between suture contamination and surgery site infection, said Dr. Jeremy Sunseri of Brown University, Providence, R.I., who presented the unpublished study at the annual meeting of the American Society of Dermatologic Surgery. However, knowing the risk factors for suture contamination can help reduce the risk of infections and potential antibiotic overuse, he noted.
"For instance, the use of antibiotic-coated sutures in high-risk contamination sites, or variations on draping techniques in these areas, may prove beneficial," Dr. Sunseri noted.
The investigators removed 338 sutures directly from their sterile surgery sites, and placed them in Petri dishes with a growth medium used for the isolation of gram-positive organisms.
They further classified the sutures based on anatomic locations (17), type of surgical closure (5), and suture type (7).
More than 57% of all sutures had bacterial growth, and almost all of those collected from the nose, mouth/lip, eye/orbit were contaminated.
Sutures collected from the scalp, neck, trunk, and upper and lower extremities had significantly lower risk of contamination, ranging from 0% to 20%, with the exception of the groin, which showed a 100% contamination rate.
Sutures from flap repairs were the most frequently contaminated (71%). Sutures collected from complex closures also had a relatively high rate of contamination (68%).
Sutures from intermediate repairs had a contamination rate of 47%, while grafts, purse string closures, and incomplete closures had a 44% rate.
Staphylococci were the most commonly identified bacteria, notably isolates of of Propionibacterium acnes, Corynebacterium sp., and Rothia dentocariosa.
There were no significant differences in the contamination rates of the seven different types of sutures studied.
"The take-home message is that the suture is long and patients are dirty, so be careful where you put that suture," Dr. Sunseri said during his presentation.
Dr. Sunseri had no financial conflicts to disclose.
On Twitter @NaseemSMiller
CHICAGO – Bacterial contamination of sutures is surprisingly common, and periorificial sites have a suture contamination rate of nearly 100%, according to a study of sutures collected during Mohs micrographic surgeries in 182 patients.
There’s no direct correlation between suture contamination and surgery site infection, said Dr. Jeremy Sunseri of Brown University, Providence, R.I., who presented the unpublished study at the annual meeting of the American Society of Dermatologic Surgery. However, knowing the risk factors for suture contamination can help reduce the risk of infections and potential antibiotic overuse, he noted.
"For instance, the use of antibiotic-coated sutures in high-risk contamination sites, or variations on draping techniques in these areas, may prove beneficial," Dr. Sunseri noted.
The investigators removed 338 sutures directly from their sterile surgery sites, and placed them in Petri dishes with a growth medium used for the isolation of gram-positive organisms.
They further classified the sutures based on anatomic locations (17), type of surgical closure (5), and suture type (7).
More than 57% of all sutures had bacterial growth, and almost all of those collected from the nose, mouth/lip, eye/orbit were contaminated.
Sutures collected from the scalp, neck, trunk, and upper and lower extremities had significantly lower risk of contamination, ranging from 0% to 20%, with the exception of the groin, which showed a 100% contamination rate.
Sutures from flap repairs were the most frequently contaminated (71%). Sutures collected from complex closures also had a relatively high rate of contamination (68%).
Sutures from intermediate repairs had a contamination rate of 47%, while grafts, purse string closures, and incomplete closures had a 44% rate.
Staphylococci were the most commonly identified bacteria, notably isolates of of Propionibacterium acnes, Corynebacterium sp., and Rothia dentocariosa.
There were no significant differences in the contamination rates of the seven different types of sutures studied.
"The take-home message is that the suture is long and patients are dirty, so be careful where you put that suture," Dr. Sunseri said during his presentation.
Dr. Sunseri had no financial conflicts to disclose.
On Twitter @NaseemSMiller
AT THE ASDS ANNUAL MEETING
Major finding: Nearly 100% of sutures removed from periorificial surfaces showed bacterial contamination.
Data source: Analysis of bacterial growth from 338 sutures removed directly from the sterile surgery site in 182 patients.
Disclosures: Dr. Sunseri had no financial conflicts to disclose.
Wells Syndrome
Consensus Recommendations From the American Acne & Rosacea Society on the Management of Rosacea, Part 3: A Status Report on Systemic Therapies
Psychoanalytic theory and the young child
I recently ran into a colleague who asked me whether I was still writing my column. I said yes and that I was currently writing an article on Selma H. Fraiberg. His response, "You don’t hear that name very much anymore," disappointed me. I responded by saying whenever a colleague, friend, or family member is having a baby, I send them a copy of "The Magic Years" with a clear statement that both parents must read it. It is clearly the best book on child rearing ever written in my opinion.
Ms. Fraiberg, creator of "The Magic Years," was a master’s in social work–trained psychoanalyst affiliated with the department of psychiatry at the University of California, San Francisco, who translated numerous concepts about babies, parents, and the first few years of life with wonderful examples of the type of incidents that every parent faces. She was highly regarded 50 years ago and received a great deal of praise for her book. But, at that time, there was a lot of prejudice against nonmedical degree psychoanalysts, and her book was not regarded as highly as I believe it should have been.
When I was a resident, I was required to read "The Magic Years," understand it, and be able to discuss it. Our teachers were concerned that we were busy being residents but also having children, and we really had to understand child rearing so that we could serve as resources for our residents and our analytic trainees.
Ms. Fraiberg translated psychoanalytic theory into child-rearing guidance in the book by looking at three age ranges: the first 18 months, 18 months to 3 years, and 3-6 years. Some of the examples are still fresh today, even though the book was published originally in 1959.
Dr. T. Berry Brazelton, the renowned pediatrician, wrote an introduction to the 50th anniversary of the book (New York: Scribner, 2008) saying that Ms. Fraiberg "makes each stage of emotional and mental development come alive!" I agree wholeheartedly. Furthermore, I would say that the concepts in the book can inform psychiatrists in our efforts to help our patients. After all, raising children (and growing up) is fraught with pitfalls. As Freud said early in his career, there are three impossible professions: governing nations, raising children, and psychoanalysis.
How the magic unfolds
Parents are often confused by things that children do or say, imaginary friends and animals – frustrating the child by pointing out reality when the child needs that imaginary friend or animal to survive. To the child, these imaginary friends and animals are not silly at all. A good example is what a niece of Ms. Fraiberg’s called the "Laughing Tiger."
Her niece, who was 2 years, 8 months old at the time, created the Laughing Tiger and many other imaginary companions at a time when she was afraid of ferocious animals. The niece’s "imaginary tiger gives her a kind of control over a danger which earlier had left her helpless and anxious," Ms. Fraiberg wrote. Instead of viewing this companion as problematic, it makes more sense to see this use of imagination as a healthy sign. Indeed, the child "can maintain his human ties and his good contact with reality while he maintains his imaginary world," she writes. "Moreover, it can be demonstrated that the child’s contact with the real world is strengthened by his periodic excursions into fantasy."
Virtually every chapter of the book is filled with insights that explain how young children interpret their world, which makes it invaluable for new parents. As we all know too well, the pitfalls in raising a child and growing up are many. I have not referred back to it for personal reasons in recent years. After all, my children are 54, 52, and 50 years old. But my wife and I did make very liberal use of the book throughout the years – while all of our friends were using Dr. Spock to help them navigate the waters of child rearing.
Mastering fear
Ms. Fraiberg gently guides the reader in an understanding of the child’s developing mind, why they cry, why they have tantrums, why they use imagination and how to help mom deal with the child’s anxiety. Take the example of a 2-year-old who was afraid of the family vacuum cleaner. Some young children control their fear of what must seem like loud monsters to them by learning to control the switch. But this toddler, who was known for his tendency to carry around a pocket-size screwdriver, was not satisfied with that solution. He had another idea: "Tiny screws and wheels were removed and lost in this frantic search," Ms. Fraiberg wrote. "...Finally, this limping monster issued its dying croak and succumbed without giving up its secret."
After a couple of years, the youngster’s "drive to investigate" was motivated by factors other than anxiety. Instead, he found investigation, discovery, and reconstruction to be pleasures in themselves. Interestingly, this child grew up to be a physicist.
There are many lessons here for psychoanalysts and our patients. One is that children experience things in which adults have no conscious memory. This means that we can help patients become better parents if we can get them to empathize with the child’s fears and frustrations.
Attachment, active handling
Ms. Fraiberg tells the story of an infant who developed an extremely severe sleep disturbance when she was 8 months old. Around 11 p.m. nightly, the infant woke up screaming, despite her parents’ efforts to calm her down. When her parents checked on her, the baby clung to her mother.
The episodes started after the baby woke up one night when the parents were out and had left her in the care of a babysitter. These meltdowns came in contrast to the child’s earlier reactions to her parents’ absence: "She never seemed to mind before if she wakened and saw a babysitter instead of us," Ms. Fraiberg quotes the parents as saying. "We just didn’t expect anything like this." What might explain this sudden new reaction?
"We know that the attachment to the mother is especially strong at this stage of development and a strange face may disturb the child at this age, even when encountered in the daytime," she writes. "The reaction to the strange face, as we have seen, is an indication of the discrimination of the mother as a person and the recognition of her as the person who gives satisfactions and protection. The stranger’s face that appears when mother’s face is expected produces anxiety because it symbolizes the absence or loss of the mother."
As you can see from that scenario, Ms. Fraiberg lets the mother know how essential she is and how early the child is distressed by the mother’s disappearance. In general, some people argue that they have to go on with their lives and that the baby will have to learn to be away from their mothers. We have to help our patients understand that the learning process is a burden for the infant. Some kids take a long time to learn how to separate from mom. Ms. Fraiberg helped the baby under discussion overcome her anxiety through nursery games in which her mother would hide her face one minute and return the next. She said the game allowed the baby to "work out the problem in her waking hours so that gradually the sleep disturbance disappeared."
Ms. Fraiberg also applies psychoanalytic theory to explain why a 9-month-old with a healthy appetite stopped eating and went on what she calls a "food strike" that lasted for 3 days. The child’s mother – who wanted the meals to be neat and orderly events – had been feeding the baby. So what brought the strike to an end?
One day the child’s father took over the feeding, and to the parents’ surprise, the baby started eating again. The mother immediately blamed herself, but the child’s behavior had nothing to do with her, per se. When the baby’s father tried to feed him, he grabbed the spoon and "plastered his face with strained carrots. Papa seemed quite unconcerned." When the baby turned his cup upside down, allowing his milk to spill all over the floor, the father took the messiness in stride.
This scenario was in stark contrast to those that emerged when the baby’s mother was in charge. When the baby tried to snatch the spoon from his mother, she got an extra spoon. When he tried to play with his milk cup, she moved it out of reach. As soon as the baby’s father allowed him to have freedom in feeding himself, the strike ended.
The explanation for the baby’s behavior changes is rooted in child development theory, Ms. Fraiberg writes. "...A certain amount of active handling of objects is absolutely necessary for the child in discovering and learning about the world around him," she says.
The period of 18 months to 3 years is dominated by words. If the child wishes something, he will use whatever words he has learned up until then, not knowing that they might not have any relationship to what he’s wishing for. If he wants something, he demands it or screams. He does not have language that is precise in any way. He uses words that he hopes will satisfy his wishes.
When the child acquires the word "bye-bye," he "begins to take the departures of his parents with more grace." The acquisition of language also makes it possible for the child to show more self-control and plays a role in the formation of his conscience.
I consider myself a developmental psychiatrist, an area in which child development is essential to all therapeutic engagement. Much can be learned about the patient if we know about his childhood and parents. I often see the patient doing to his child what his parents did to him. Patients are always shocked when I point this out to them, and the process of understanding how they got to where they are occurs. I call it therapeutic living. The book is so important because it tries to help parents learn how to handle tough developmental moments and periods. The section on toilet training is classic.
Please read "The Magic Years," and get your colleagues and students to read it as well. Ms. Fraiberg was a true master of the analytic method.
Dr. Fink is a psychiatrist and consultant, and professor of psychiatry at Temple University, Philadelphia.
I recently ran into a colleague who asked me whether I was still writing my column. I said yes and that I was currently writing an article on Selma H. Fraiberg. His response, "You don’t hear that name very much anymore," disappointed me. I responded by saying whenever a colleague, friend, or family member is having a baby, I send them a copy of "The Magic Years" with a clear statement that both parents must read it. It is clearly the best book on child rearing ever written in my opinion.
Ms. Fraiberg, creator of "The Magic Years," was a master’s in social work–trained psychoanalyst affiliated with the department of psychiatry at the University of California, San Francisco, who translated numerous concepts about babies, parents, and the first few years of life with wonderful examples of the type of incidents that every parent faces. She was highly regarded 50 years ago and received a great deal of praise for her book. But, at that time, there was a lot of prejudice against nonmedical degree psychoanalysts, and her book was not regarded as highly as I believe it should have been.
When I was a resident, I was required to read "The Magic Years," understand it, and be able to discuss it. Our teachers were concerned that we were busy being residents but also having children, and we really had to understand child rearing so that we could serve as resources for our residents and our analytic trainees.
Ms. Fraiberg translated psychoanalytic theory into child-rearing guidance in the book by looking at three age ranges: the first 18 months, 18 months to 3 years, and 3-6 years. Some of the examples are still fresh today, even though the book was published originally in 1959.
Dr. T. Berry Brazelton, the renowned pediatrician, wrote an introduction to the 50th anniversary of the book (New York: Scribner, 2008) saying that Ms. Fraiberg "makes each stage of emotional and mental development come alive!" I agree wholeheartedly. Furthermore, I would say that the concepts in the book can inform psychiatrists in our efforts to help our patients. After all, raising children (and growing up) is fraught with pitfalls. As Freud said early in his career, there are three impossible professions: governing nations, raising children, and psychoanalysis.
How the magic unfolds
Parents are often confused by things that children do or say, imaginary friends and animals – frustrating the child by pointing out reality when the child needs that imaginary friend or animal to survive. To the child, these imaginary friends and animals are not silly at all. A good example is what a niece of Ms. Fraiberg’s called the "Laughing Tiger."
Her niece, who was 2 years, 8 months old at the time, created the Laughing Tiger and many other imaginary companions at a time when she was afraid of ferocious animals. The niece’s "imaginary tiger gives her a kind of control over a danger which earlier had left her helpless and anxious," Ms. Fraiberg wrote. Instead of viewing this companion as problematic, it makes more sense to see this use of imagination as a healthy sign. Indeed, the child "can maintain his human ties and his good contact with reality while he maintains his imaginary world," she writes. "Moreover, it can be demonstrated that the child’s contact with the real world is strengthened by his periodic excursions into fantasy."
Virtually every chapter of the book is filled with insights that explain how young children interpret their world, which makes it invaluable for new parents. As we all know too well, the pitfalls in raising a child and growing up are many. I have not referred back to it for personal reasons in recent years. After all, my children are 54, 52, and 50 years old. But my wife and I did make very liberal use of the book throughout the years – while all of our friends were using Dr. Spock to help them navigate the waters of child rearing.
Mastering fear
Ms. Fraiberg gently guides the reader in an understanding of the child’s developing mind, why they cry, why they have tantrums, why they use imagination and how to help mom deal with the child’s anxiety. Take the example of a 2-year-old who was afraid of the family vacuum cleaner. Some young children control their fear of what must seem like loud monsters to them by learning to control the switch. But this toddler, who was known for his tendency to carry around a pocket-size screwdriver, was not satisfied with that solution. He had another idea: "Tiny screws and wheels were removed and lost in this frantic search," Ms. Fraiberg wrote. "...Finally, this limping monster issued its dying croak and succumbed without giving up its secret."
After a couple of years, the youngster’s "drive to investigate" was motivated by factors other than anxiety. Instead, he found investigation, discovery, and reconstruction to be pleasures in themselves. Interestingly, this child grew up to be a physicist.
There are many lessons here for psychoanalysts and our patients. One is that children experience things in which adults have no conscious memory. This means that we can help patients become better parents if we can get them to empathize with the child’s fears and frustrations.
Attachment, active handling
Ms. Fraiberg tells the story of an infant who developed an extremely severe sleep disturbance when she was 8 months old. Around 11 p.m. nightly, the infant woke up screaming, despite her parents’ efforts to calm her down. When her parents checked on her, the baby clung to her mother.
The episodes started after the baby woke up one night when the parents were out and had left her in the care of a babysitter. These meltdowns came in contrast to the child’s earlier reactions to her parents’ absence: "She never seemed to mind before if she wakened and saw a babysitter instead of us," Ms. Fraiberg quotes the parents as saying. "We just didn’t expect anything like this." What might explain this sudden new reaction?
"We know that the attachment to the mother is especially strong at this stage of development and a strange face may disturb the child at this age, even when encountered in the daytime," she writes. "The reaction to the strange face, as we have seen, is an indication of the discrimination of the mother as a person and the recognition of her as the person who gives satisfactions and protection. The stranger’s face that appears when mother’s face is expected produces anxiety because it symbolizes the absence or loss of the mother."
As you can see from that scenario, Ms. Fraiberg lets the mother know how essential she is and how early the child is distressed by the mother’s disappearance. In general, some people argue that they have to go on with their lives and that the baby will have to learn to be away from their mothers. We have to help our patients understand that the learning process is a burden for the infant. Some kids take a long time to learn how to separate from mom. Ms. Fraiberg helped the baby under discussion overcome her anxiety through nursery games in which her mother would hide her face one minute and return the next. She said the game allowed the baby to "work out the problem in her waking hours so that gradually the sleep disturbance disappeared."
Ms. Fraiberg also applies psychoanalytic theory to explain why a 9-month-old with a healthy appetite stopped eating and went on what she calls a "food strike" that lasted for 3 days. The child’s mother – who wanted the meals to be neat and orderly events – had been feeding the baby. So what brought the strike to an end?
One day the child’s father took over the feeding, and to the parents’ surprise, the baby started eating again. The mother immediately blamed herself, but the child’s behavior had nothing to do with her, per se. When the baby’s father tried to feed him, he grabbed the spoon and "plastered his face with strained carrots. Papa seemed quite unconcerned." When the baby turned his cup upside down, allowing his milk to spill all over the floor, the father took the messiness in stride.
This scenario was in stark contrast to those that emerged when the baby’s mother was in charge. When the baby tried to snatch the spoon from his mother, she got an extra spoon. When he tried to play with his milk cup, she moved it out of reach. As soon as the baby’s father allowed him to have freedom in feeding himself, the strike ended.
The explanation for the baby’s behavior changes is rooted in child development theory, Ms. Fraiberg writes. "...A certain amount of active handling of objects is absolutely necessary for the child in discovering and learning about the world around him," she says.
The period of 18 months to 3 years is dominated by words. If the child wishes something, he will use whatever words he has learned up until then, not knowing that they might not have any relationship to what he’s wishing for. If he wants something, he demands it or screams. He does not have language that is precise in any way. He uses words that he hopes will satisfy his wishes.
When the child acquires the word "bye-bye," he "begins to take the departures of his parents with more grace." The acquisition of language also makes it possible for the child to show more self-control and plays a role in the formation of his conscience.
I consider myself a developmental psychiatrist, an area in which child development is essential to all therapeutic engagement. Much can be learned about the patient if we know about his childhood and parents. I often see the patient doing to his child what his parents did to him. Patients are always shocked when I point this out to them, and the process of understanding how they got to where they are occurs. I call it therapeutic living. The book is so important because it tries to help parents learn how to handle tough developmental moments and periods. The section on toilet training is classic.
Please read "The Magic Years," and get your colleagues and students to read it as well. Ms. Fraiberg was a true master of the analytic method.
Dr. Fink is a psychiatrist and consultant, and professor of psychiatry at Temple University, Philadelphia.
I recently ran into a colleague who asked me whether I was still writing my column. I said yes and that I was currently writing an article on Selma H. Fraiberg. His response, "You don’t hear that name very much anymore," disappointed me. I responded by saying whenever a colleague, friend, or family member is having a baby, I send them a copy of "The Magic Years" with a clear statement that both parents must read it. It is clearly the best book on child rearing ever written in my opinion.
Ms. Fraiberg, creator of "The Magic Years," was a master’s in social work–trained psychoanalyst affiliated with the department of psychiatry at the University of California, San Francisco, who translated numerous concepts about babies, parents, and the first few years of life with wonderful examples of the type of incidents that every parent faces. She was highly regarded 50 years ago and received a great deal of praise for her book. But, at that time, there was a lot of prejudice against nonmedical degree psychoanalysts, and her book was not regarded as highly as I believe it should have been.
When I was a resident, I was required to read "The Magic Years," understand it, and be able to discuss it. Our teachers were concerned that we were busy being residents but also having children, and we really had to understand child rearing so that we could serve as resources for our residents and our analytic trainees.
Ms. Fraiberg translated psychoanalytic theory into child-rearing guidance in the book by looking at three age ranges: the first 18 months, 18 months to 3 years, and 3-6 years. Some of the examples are still fresh today, even though the book was published originally in 1959.
Dr. T. Berry Brazelton, the renowned pediatrician, wrote an introduction to the 50th anniversary of the book (New York: Scribner, 2008) saying that Ms. Fraiberg "makes each stage of emotional and mental development come alive!" I agree wholeheartedly. Furthermore, I would say that the concepts in the book can inform psychiatrists in our efforts to help our patients. After all, raising children (and growing up) is fraught with pitfalls. As Freud said early in his career, there are three impossible professions: governing nations, raising children, and psychoanalysis.
How the magic unfolds
Parents are often confused by things that children do or say, imaginary friends and animals – frustrating the child by pointing out reality when the child needs that imaginary friend or animal to survive. To the child, these imaginary friends and animals are not silly at all. A good example is what a niece of Ms. Fraiberg’s called the "Laughing Tiger."
Her niece, who was 2 years, 8 months old at the time, created the Laughing Tiger and many other imaginary companions at a time when she was afraid of ferocious animals. The niece’s "imaginary tiger gives her a kind of control over a danger which earlier had left her helpless and anxious," Ms. Fraiberg wrote. Instead of viewing this companion as problematic, it makes more sense to see this use of imagination as a healthy sign. Indeed, the child "can maintain his human ties and his good contact with reality while he maintains his imaginary world," she writes. "Moreover, it can be demonstrated that the child’s contact with the real world is strengthened by his periodic excursions into fantasy."
Virtually every chapter of the book is filled with insights that explain how young children interpret their world, which makes it invaluable for new parents. As we all know too well, the pitfalls in raising a child and growing up are many. I have not referred back to it for personal reasons in recent years. After all, my children are 54, 52, and 50 years old. But my wife and I did make very liberal use of the book throughout the years – while all of our friends were using Dr. Spock to help them navigate the waters of child rearing.
Mastering fear
Ms. Fraiberg gently guides the reader in an understanding of the child’s developing mind, why they cry, why they have tantrums, why they use imagination and how to help mom deal with the child’s anxiety. Take the example of a 2-year-old who was afraid of the family vacuum cleaner. Some young children control their fear of what must seem like loud monsters to them by learning to control the switch. But this toddler, who was known for his tendency to carry around a pocket-size screwdriver, was not satisfied with that solution. He had another idea: "Tiny screws and wheels were removed and lost in this frantic search," Ms. Fraiberg wrote. "...Finally, this limping monster issued its dying croak and succumbed without giving up its secret."
After a couple of years, the youngster’s "drive to investigate" was motivated by factors other than anxiety. Instead, he found investigation, discovery, and reconstruction to be pleasures in themselves. Interestingly, this child grew up to be a physicist.
There are many lessons here for psychoanalysts and our patients. One is that children experience things in which adults have no conscious memory. This means that we can help patients become better parents if we can get them to empathize with the child’s fears and frustrations.
Attachment, active handling
Ms. Fraiberg tells the story of an infant who developed an extremely severe sleep disturbance when she was 8 months old. Around 11 p.m. nightly, the infant woke up screaming, despite her parents’ efforts to calm her down. When her parents checked on her, the baby clung to her mother.
The episodes started after the baby woke up one night when the parents were out and had left her in the care of a babysitter. These meltdowns came in contrast to the child’s earlier reactions to her parents’ absence: "She never seemed to mind before if she wakened and saw a babysitter instead of us," Ms. Fraiberg quotes the parents as saying. "We just didn’t expect anything like this." What might explain this sudden new reaction?
"We know that the attachment to the mother is especially strong at this stage of development and a strange face may disturb the child at this age, even when encountered in the daytime," she writes. "The reaction to the strange face, as we have seen, is an indication of the discrimination of the mother as a person and the recognition of her as the person who gives satisfactions and protection. The stranger’s face that appears when mother’s face is expected produces anxiety because it symbolizes the absence or loss of the mother."
As you can see from that scenario, Ms. Fraiberg lets the mother know how essential she is and how early the child is distressed by the mother’s disappearance. In general, some people argue that they have to go on with their lives and that the baby will have to learn to be away from their mothers. We have to help our patients understand that the learning process is a burden for the infant. Some kids take a long time to learn how to separate from mom. Ms. Fraiberg helped the baby under discussion overcome her anxiety through nursery games in which her mother would hide her face one minute and return the next. She said the game allowed the baby to "work out the problem in her waking hours so that gradually the sleep disturbance disappeared."
Ms. Fraiberg also applies psychoanalytic theory to explain why a 9-month-old with a healthy appetite stopped eating and went on what she calls a "food strike" that lasted for 3 days. The child’s mother – who wanted the meals to be neat and orderly events – had been feeding the baby. So what brought the strike to an end?
One day the child’s father took over the feeding, and to the parents’ surprise, the baby started eating again. The mother immediately blamed herself, but the child’s behavior had nothing to do with her, per se. When the baby’s father tried to feed him, he grabbed the spoon and "plastered his face with strained carrots. Papa seemed quite unconcerned." When the baby turned his cup upside down, allowing his milk to spill all over the floor, the father took the messiness in stride.
This scenario was in stark contrast to those that emerged when the baby’s mother was in charge. When the baby tried to snatch the spoon from his mother, she got an extra spoon. When he tried to play with his milk cup, she moved it out of reach. As soon as the baby’s father allowed him to have freedom in feeding himself, the strike ended.
The explanation for the baby’s behavior changes is rooted in child development theory, Ms. Fraiberg writes. "...A certain amount of active handling of objects is absolutely necessary for the child in discovering and learning about the world around him," she says.
The period of 18 months to 3 years is dominated by words. If the child wishes something, he will use whatever words he has learned up until then, not knowing that they might not have any relationship to what he’s wishing for. If he wants something, he demands it or screams. He does not have language that is precise in any way. He uses words that he hopes will satisfy his wishes.
When the child acquires the word "bye-bye," he "begins to take the departures of his parents with more grace." The acquisition of language also makes it possible for the child to show more self-control and plays a role in the formation of his conscience.
I consider myself a developmental psychiatrist, an area in which child development is essential to all therapeutic engagement. Much can be learned about the patient if we know about his childhood and parents. I often see the patient doing to his child what his parents did to him. Patients are always shocked when I point this out to them, and the process of understanding how they got to where they are occurs. I call it therapeutic living. The book is so important because it tries to help parents learn how to handle tough developmental moments and periods. The section on toilet training is classic.
Please read "The Magic Years," and get your colleagues and students to read it as well. Ms. Fraiberg was a true master of the analytic method.
Dr. Fink is a psychiatrist and consultant, and professor of psychiatry at Temple University, Philadelphia.
Resident Handoff Program Reduces Medical Errors at Pediatric Hospital
A standardized handoff program can reduce medical errors and can be replicated at hospitals across the country, says the lead researcher of a new study published in JAMA.
Researchers reviewed the medical literature for successful handoff-intervention programs that they could teach to residents and senior interns working within two units at Boston Children’s Hospital. They ultimately settled on a bundle that included standardized communication and handoff training, a verbal mnemonic to help staff members remember what information to pass off to the next team, and a handoff structure that involved junior and senior physicians meeting in a quiet room to discuss the handoff. In addition, on one unit, residents used a computerized tool linked to the electronic medical record that made it easier for them to pass along important information about the patient.
The analysis included 642 handoffs that occurred before the intervention and 613 that happened afterwards. Researchers found that medical errors decreased from 33.8 per 100 admissions (95% CI, 27.3–40.3) prior to the intervention to 18.3 per 100 admissions (95% CI, 14.7–21.9; P?P=0.04).
Amy Starmer, MD, MPH, associate scientific researcher at Boston Children’s Hospital and lecturer in pediatrics at Harvard Medical School in Boston, says that when implementing an intervention program, it’s important to involve staff from all levels of the hospital.
“We thought carefully about who should be able to make transformational change happen,” says Dr. Starmer. “That included resident program directors, educators, attending physicians who help observe the residents, and senior administrative people in the hospital who knew this was going on and were supportive. Even the technology team was able to devote programming support and resources to allow the development of a computerized tool.”
Visit our website for more information on hospital handoff programs.
A standardized handoff program can reduce medical errors and can be replicated at hospitals across the country, says the lead researcher of a new study published in JAMA.
Researchers reviewed the medical literature for successful handoff-intervention programs that they could teach to residents and senior interns working within two units at Boston Children’s Hospital. They ultimately settled on a bundle that included standardized communication and handoff training, a verbal mnemonic to help staff members remember what information to pass off to the next team, and a handoff structure that involved junior and senior physicians meeting in a quiet room to discuss the handoff. In addition, on one unit, residents used a computerized tool linked to the electronic medical record that made it easier for them to pass along important information about the patient.
The analysis included 642 handoffs that occurred before the intervention and 613 that happened afterwards. Researchers found that medical errors decreased from 33.8 per 100 admissions (95% CI, 27.3–40.3) prior to the intervention to 18.3 per 100 admissions (95% CI, 14.7–21.9; P?P=0.04).
Amy Starmer, MD, MPH, associate scientific researcher at Boston Children’s Hospital and lecturer in pediatrics at Harvard Medical School in Boston, says that when implementing an intervention program, it’s important to involve staff from all levels of the hospital.
“We thought carefully about who should be able to make transformational change happen,” says Dr. Starmer. “That included resident program directors, educators, attending physicians who help observe the residents, and senior administrative people in the hospital who knew this was going on and were supportive. Even the technology team was able to devote programming support and resources to allow the development of a computerized tool.”
Visit our website for more information on hospital handoff programs.
A standardized handoff program can reduce medical errors and can be replicated at hospitals across the country, says the lead researcher of a new study published in JAMA.
Researchers reviewed the medical literature for successful handoff-intervention programs that they could teach to residents and senior interns working within two units at Boston Children’s Hospital. They ultimately settled on a bundle that included standardized communication and handoff training, a verbal mnemonic to help staff members remember what information to pass off to the next team, and a handoff structure that involved junior and senior physicians meeting in a quiet room to discuss the handoff. In addition, on one unit, residents used a computerized tool linked to the electronic medical record that made it easier for them to pass along important information about the patient.
The analysis included 642 handoffs that occurred before the intervention and 613 that happened afterwards. Researchers found that medical errors decreased from 33.8 per 100 admissions (95% CI, 27.3–40.3) prior to the intervention to 18.3 per 100 admissions (95% CI, 14.7–21.9; P?P=0.04).
Amy Starmer, MD, MPH, associate scientific researcher at Boston Children’s Hospital and lecturer in pediatrics at Harvard Medical School in Boston, says that when implementing an intervention program, it’s important to involve staff from all levels of the hospital.
“We thought carefully about who should be able to make transformational change happen,” says Dr. Starmer. “That included resident program directors, educators, attending physicians who help observe the residents, and senior administrative people in the hospital who knew this was going on and were supportive. Even the technology team was able to devote programming support and resources to allow the development of a computerized tool.”
Visit our website for more information on hospital handoff programs.