User login
How federal budget cuts are affecting research

Credit: Rhoda Baer
A new report suggests recent budget cuts to federal health programs in the US have had some negative consequences for hematology researchers.
The Coalition for Health Funding, an alliance of more than 90 public health advocacy organizations, invited scientists, public health advocates, and others to share stories of how they have been hurt by the budget cuts.
The resulting report is titled “Faces of Austerity, How Budget Cuts Hurt America’s Health.”
It details the negative effects the cuts have had on scientific discovery and innovation, scientists and health practitioners, health and social services, and government programs designed to respond to health hazards and natural disasters.
Among the stories included in the report are 2 from members of the American Society of Hematology (ASH), who detail how a decade of flat funding for the National Institutes of Health (NIH) and a 5% budget cut in 2013 have shuttered labs and jeopardized tomorrow’s treatments.
“Most people I know have been affected,” said Debra Newman, PhD, an investigator at BloodCenter of Wisconsin in Milwaukee.
“Their research funding has decreased and, consequently, so has the size of their laboratories because they cannot afford to employ the same number of staff. Talented investigators have started to leave research and go on to other things because they can’t support a research operation without money to run it.”
The other ASH member story is that of Christopher Porter, MD, a pediatric hematologist/oncologist at Children’s Hospital Colorado in Aurora. Despite receiving an excellent score on an NIH grant application, Dr Porter was denied funding in 2013 amid budget cuts.
“My lab had been able to report exciting preliminary data, but we really needed supplemental funds to keep this project moving,” he said. “While our initial application to NIH scored high enough to have received funding in previous years, it was not within the current funding range.”
Drs Newman and Porter are among the first recipients of ASH Bridge Grants, awards first offered in 2012 for investigators who applied for competitive grants from NIH but were denied funding due to cuts. The awards are intended to “bridge” investigators to their next NIH grant.
While such supplementary grant funding programs are helpful, they cannot replace critical NIH funding that has been cut for hematology research, according to ASH.
“When biomedical research is under-funded, everybody loses,” said ASH President Linda J. Burns, MD, of the University of Minnesota.
“Scientists are forced to slow or suspend research because they no longer have the resources to continue searching for new treatments, and even cures, for some of the world’s deadliest diseases. We continue to urge Congress to support a balanced approach to deficit reduction that does not include further cuts to critical biomedical research and public health and safety programs.”
“Faces of Austerity” is available online at www.cutshurt.org. A related report, “Faces of Austerity: How Budget Cuts Have Made Us Sicker, Poorer, and Less Safe,” was published last November. ![]()

Credit: Rhoda Baer
A new report suggests recent budget cuts to federal health programs in the US have had some negative consequences for hematology researchers.
The Coalition for Health Funding, an alliance of more than 90 public health advocacy organizations, invited scientists, public health advocates, and others to share stories of how they have been hurt by the budget cuts.
The resulting report is titled “Faces of Austerity, How Budget Cuts Hurt America’s Health.”
It details the negative effects the cuts have had on scientific discovery and innovation, scientists and health practitioners, health and social services, and government programs designed to respond to health hazards and natural disasters.
Among the stories included in the report are 2 from members of the American Society of Hematology (ASH), who detail how a decade of flat funding for the National Institutes of Health (NIH) and a 5% budget cut in 2013 have shuttered labs and jeopardized tomorrow’s treatments.
“Most people I know have been affected,” said Debra Newman, PhD, an investigator at BloodCenter of Wisconsin in Milwaukee.
“Their research funding has decreased and, consequently, so has the size of their laboratories because they cannot afford to employ the same number of staff. Talented investigators have started to leave research and go on to other things because they can’t support a research operation without money to run it.”
The other ASH member story is that of Christopher Porter, MD, a pediatric hematologist/oncologist at Children’s Hospital Colorado in Aurora. Despite receiving an excellent score on an NIH grant application, Dr Porter was denied funding in 2013 amid budget cuts.
“My lab had been able to report exciting preliminary data, but we really needed supplemental funds to keep this project moving,” he said. “While our initial application to NIH scored high enough to have received funding in previous years, it was not within the current funding range.”
Drs Newman and Porter are among the first recipients of ASH Bridge Grants, awards first offered in 2012 for investigators who applied for competitive grants from NIH but were denied funding due to cuts. The awards are intended to “bridge” investigators to their next NIH grant.
While such supplementary grant funding programs are helpful, they cannot replace critical NIH funding that has been cut for hematology research, according to ASH.
“When biomedical research is under-funded, everybody loses,” said ASH President Linda J. Burns, MD, of the University of Minnesota.
“Scientists are forced to slow or suspend research because they no longer have the resources to continue searching for new treatments, and even cures, for some of the world’s deadliest diseases. We continue to urge Congress to support a balanced approach to deficit reduction that does not include further cuts to critical biomedical research and public health and safety programs.”
“Faces of Austerity” is available online at www.cutshurt.org. A related report, “Faces of Austerity: How Budget Cuts Have Made Us Sicker, Poorer, and Less Safe,” was published last November. ![]()

Credit: Rhoda Baer
A new report suggests recent budget cuts to federal health programs in the US have had some negative consequences for hematology researchers.
The Coalition for Health Funding, an alliance of more than 90 public health advocacy organizations, invited scientists, public health advocates, and others to share stories of how they have been hurt by the budget cuts.
The resulting report is titled “Faces of Austerity, How Budget Cuts Hurt America’s Health.”
It details the negative effects the cuts have had on scientific discovery and innovation, scientists and health practitioners, health and social services, and government programs designed to respond to health hazards and natural disasters.
Among the stories included in the report are 2 from members of the American Society of Hematology (ASH), who detail how a decade of flat funding for the National Institutes of Health (NIH) and a 5% budget cut in 2013 have shuttered labs and jeopardized tomorrow’s treatments.
“Most people I know have been affected,” said Debra Newman, PhD, an investigator at BloodCenter of Wisconsin in Milwaukee.
“Their research funding has decreased and, consequently, so has the size of their laboratories because they cannot afford to employ the same number of staff. Talented investigators have started to leave research and go on to other things because they can’t support a research operation without money to run it.”
The other ASH member story is that of Christopher Porter, MD, a pediatric hematologist/oncologist at Children’s Hospital Colorado in Aurora. Despite receiving an excellent score on an NIH grant application, Dr Porter was denied funding in 2013 amid budget cuts.
“My lab had been able to report exciting preliminary data, but we really needed supplemental funds to keep this project moving,” he said. “While our initial application to NIH scored high enough to have received funding in previous years, it was not within the current funding range.”
Drs Newman and Porter are among the first recipients of ASH Bridge Grants, awards first offered in 2012 for investigators who applied for competitive grants from NIH but were denied funding due to cuts. The awards are intended to “bridge” investigators to their next NIH grant.
While such supplementary grant funding programs are helpful, they cannot replace critical NIH funding that has been cut for hematology research, according to ASH.
“When biomedical research is under-funded, everybody loses,” said ASH President Linda J. Burns, MD, of the University of Minnesota.
“Scientists are forced to slow or suspend research because they no longer have the resources to continue searching for new treatments, and even cures, for some of the world’s deadliest diseases. We continue to urge Congress to support a balanced approach to deficit reduction that does not include further cuts to critical biomedical research and public health and safety programs.”
“Faces of Austerity” is available online at www.cutshurt.org. A related report, “Faces of Austerity: How Budget Cuts Have Made Us Sicker, Poorer, and Less Safe,” was published last November. ![]()
Method forces cells to devour dying neighbors
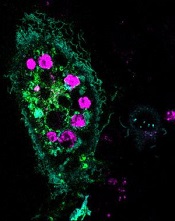
engulfed dying cells (purple)
Credit: Toru Komatsu
A two-pronged approach can prompt phagocytosis in inert cells, according to a paper published in Science Signaling.
Researchers manipulated HeLa cells, which typically cannot perform phagocytosis, by activating one protein inside the cells and expressing another protein on the cells’ surface. This forced the cells to engulf apoptotic Jurkat T cells.
So the researchers believe this technique could be used as a targeted therapy, with engineered cells consuming unwanted cells.
“Our goal is to build artificial cells programmed to eat up dangerous junk in the body, which could be anything from bacteria to the amyloid-beta plaques that cause Alzheimer’s to the body’s own rogue cancer cells,” said study author Takanari Inoue, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“By figuring out how to get normally inert cells to recognize and engulf dying cells, we’ve taken an important step in that direction.”
Dr Inoue and his colleagues set out to “strip down” phagocytosis, determining the minimum tools one cell needs to eat another. Their first task was to induce the HeLa cells to attach to nearby dying cells—apoptotic Jurkat T cells—by getting the right receptors to the HeLa cells’ surface.
The researchers knew that part of a receptor protein called MFG-E8 would recognize and stick to a distress signal on the surface of dying cells, and coaxing the HeLa cells to make the protein fragment was straightforward.
To get the fragment, termed C2, onto the outside of the cells, the team found a way to stick it to another protein that was bound for the cell’s surface, thus taking advantage of the cell’s own transportation system.
As a result, up to 6 apoptotic Jurkat T cells stuck to each HeLa cell. The bad news was that the HeLa cells weren’t actually eating the T cells.
Fortunately, the researchers already had an idea about what to try next. Previous research had shown that activating the Rac gene could cause a cell to engulf beads stuck to its surface.
Sure enough, the team found that HeLa cells with both surface C2 and activated Rac swallowed the apoptotic cells readily.
“We’ve shown it’s possible to endow ordinary cells with the power to do something unique: take on the role of a specialized macrophage,” Dr Inoue said.
He cautioned, however, that the researchers don’t believe the engulfed cells are being broken down. Getting the HeLa cells to finish the process of phagocytosis will be one of the group’s next steps. ![]()
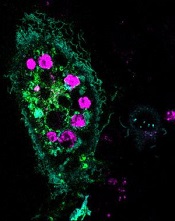
engulfed dying cells (purple)
Credit: Toru Komatsu
A two-pronged approach can prompt phagocytosis in inert cells, according to a paper published in Science Signaling.
Researchers manipulated HeLa cells, which typically cannot perform phagocytosis, by activating one protein inside the cells and expressing another protein on the cells’ surface. This forced the cells to engulf apoptotic Jurkat T cells.
So the researchers believe this technique could be used as a targeted therapy, with engineered cells consuming unwanted cells.
“Our goal is to build artificial cells programmed to eat up dangerous junk in the body, which could be anything from bacteria to the amyloid-beta plaques that cause Alzheimer’s to the body’s own rogue cancer cells,” said study author Takanari Inoue, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“By figuring out how to get normally inert cells to recognize and engulf dying cells, we’ve taken an important step in that direction.”
Dr Inoue and his colleagues set out to “strip down” phagocytosis, determining the minimum tools one cell needs to eat another. Their first task was to induce the HeLa cells to attach to nearby dying cells—apoptotic Jurkat T cells—by getting the right receptors to the HeLa cells’ surface.
The researchers knew that part of a receptor protein called MFG-E8 would recognize and stick to a distress signal on the surface of dying cells, and coaxing the HeLa cells to make the protein fragment was straightforward.
To get the fragment, termed C2, onto the outside of the cells, the team found a way to stick it to another protein that was bound for the cell’s surface, thus taking advantage of the cell’s own transportation system.
As a result, up to 6 apoptotic Jurkat T cells stuck to each HeLa cell. The bad news was that the HeLa cells weren’t actually eating the T cells.
Fortunately, the researchers already had an idea about what to try next. Previous research had shown that activating the Rac gene could cause a cell to engulf beads stuck to its surface.
Sure enough, the team found that HeLa cells with both surface C2 and activated Rac swallowed the apoptotic cells readily.
“We’ve shown it’s possible to endow ordinary cells with the power to do something unique: take on the role of a specialized macrophage,” Dr Inoue said.
He cautioned, however, that the researchers don’t believe the engulfed cells are being broken down. Getting the HeLa cells to finish the process of phagocytosis will be one of the group’s next steps. ![]()
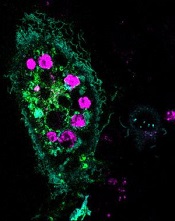
engulfed dying cells (purple)
Credit: Toru Komatsu
A two-pronged approach can prompt phagocytosis in inert cells, according to a paper published in Science Signaling.
Researchers manipulated HeLa cells, which typically cannot perform phagocytosis, by activating one protein inside the cells and expressing another protein on the cells’ surface. This forced the cells to engulf apoptotic Jurkat T cells.
So the researchers believe this technique could be used as a targeted therapy, with engineered cells consuming unwanted cells.
“Our goal is to build artificial cells programmed to eat up dangerous junk in the body, which could be anything from bacteria to the amyloid-beta plaques that cause Alzheimer’s to the body’s own rogue cancer cells,” said study author Takanari Inoue, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“By figuring out how to get normally inert cells to recognize and engulf dying cells, we’ve taken an important step in that direction.”
Dr Inoue and his colleagues set out to “strip down” phagocytosis, determining the minimum tools one cell needs to eat another. Their first task was to induce the HeLa cells to attach to nearby dying cells—apoptotic Jurkat T cells—by getting the right receptors to the HeLa cells’ surface.
The researchers knew that part of a receptor protein called MFG-E8 would recognize and stick to a distress signal on the surface of dying cells, and coaxing the HeLa cells to make the protein fragment was straightforward.
To get the fragment, termed C2, onto the outside of the cells, the team found a way to stick it to another protein that was bound for the cell’s surface, thus taking advantage of the cell’s own transportation system.
As a result, up to 6 apoptotic Jurkat T cells stuck to each HeLa cell. The bad news was that the HeLa cells weren’t actually eating the T cells.
Fortunately, the researchers already had an idea about what to try next. Previous research had shown that activating the Rac gene could cause a cell to engulf beads stuck to its surface.
Sure enough, the team found that HeLa cells with both surface C2 and activated Rac swallowed the apoptotic cells readily.
“We’ve shown it’s possible to endow ordinary cells with the power to do something unique: take on the role of a specialized macrophage,” Dr Inoue said.
He cautioned, however, that the researchers don’t believe the engulfed cells are being broken down. Getting the HeLa cells to finish the process of phagocytosis will be one of the group’s next steps. ![]()
Technique allows for early cancer diagnosis

Credit: Максим Кукушкин
Immunosignaturing can allow for early detection of multiple myeloma and a range of other cancers, according to research published in PNAS.
Immunosignaturing involves profiling the entire population of antibodies circulating in the blood at a given time.
The method allowed researchers to distinguish 14 separate diseases, including 12 cancers, from one another and from healthy controls. The specificity was greater than 98% for each diagnosis.
“For years, we’ve seen remarkable results from immunosignatures, but introducing the technology to the scientific community has required a lot of patience,” said study author Phillip Stafford, PhD, of Arizona State University in Tempe.
The technique relies on a microarray consisting of thousands of random sequence peptides, imprinted on a glass slide. When a tiny droplet of blood (less than a microliter is needed) is spread across the microarray, antibodies in the blood selectively bind with individual peptides, forming a portrait of immune activity—an immunosignature.
Because the peptide sequences are random and not related to any naturally occurring disease antigens, the immunosignatures are “disease agnostic,” which means a single platform is potentially applicable to multiple disease types.
With their research, Dr Stafford and his colleagues put this claim to the test. The team first “trained” the system to calibrate results and establish reference immunosignatures using 20 samples each from 5 cancer patient cohorts, along with 20 non-cancer patients.
Once reference immunosignatures were established, the researchers tested the technique in a blind evaluation of 120 independent samples covering the same diseases. The results demonstrated 95% accuracy.
To further assess the diagnostic power of immunosignaturing, the team tested more than 1500 historical samples comprising 14 different diseases. This included 12 cancers, such as breast, brain, and multiple myeloma.
The average diagnostic accuracy of immunosignaturing was greater than 98% for each diagnosis, which suggests the method is suitable for the simultaneous classification of multiple diseases.
In a pairwise test against healthy control samples, multiple myeloma samples displayed the most significantly different peptides by t test. Of the top 100 peptides selected in this way, only breast cancer showed no overlap with any other disease.
Nevertheless, the researchers were able to distinguish the 14 separate diseases from one another, as well as from healthy controls, through immunosignatures.
Dr Stafford and his colleagues said these results suggest that immunosignatures provide an attractive means of capturing disease complexity. They offer a marked improvement over traditional methods in which one-to-one molecular recognition events are measured and a small number of analytes can be evaluated.
Furthermore, the technology is flexible in terms of handling and processing, the team said. A dried sample of blood, collected on filter paper and mailed to a study facility, can be used to generate an immunosignature.
The researchers also pointed out that the microarray chip used for this study contains 10,000 imprinted peptides, and this allows for enhanced sensitivity, owing to the large number of different possible signals elicited.
However, a significant improvement in immunosignaturing sensitivity and accuracy might be achieved through new chip technology. The team is currently developing a chip imprinted with more than 100,000 peptides. ![]()

Credit: Максим Кукушкин
Immunosignaturing can allow for early detection of multiple myeloma and a range of other cancers, according to research published in PNAS.
Immunosignaturing involves profiling the entire population of antibodies circulating in the blood at a given time.
The method allowed researchers to distinguish 14 separate diseases, including 12 cancers, from one another and from healthy controls. The specificity was greater than 98% for each diagnosis.
“For years, we’ve seen remarkable results from immunosignatures, but introducing the technology to the scientific community has required a lot of patience,” said study author Phillip Stafford, PhD, of Arizona State University in Tempe.
The technique relies on a microarray consisting of thousands of random sequence peptides, imprinted on a glass slide. When a tiny droplet of blood (less than a microliter is needed) is spread across the microarray, antibodies in the blood selectively bind with individual peptides, forming a portrait of immune activity—an immunosignature.
Because the peptide sequences are random and not related to any naturally occurring disease antigens, the immunosignatures are “disease agnostic,” which means a single platform is potentially applicable to multiple disease types.
With their research, Dr Stafford and his colleagues put this claim to the test. The team first “trained” the system to calibrate results and establish reference immunosignatures using 20 samples each from 5 cancer patient cohorts, along with 20 non-cancer patients.
Once reference immunosignatures were established, the researchers tested the technique in a blind evaluation of 120 independent samples covering the same diseases. The results demonstrated 95% accuracy.
To further assess the diagnostic power of immunosignaturing, the team tested more than 1500 historical samples comprising 14 different diseases. This included 12 cancers, such as breast, brain, and multiple myeloma.
The average diagnostic accuracy of immunosignaturing was greater than 98% for each diagnosis, which suggests the method is suitable for the simultaneous classification of multiple diseases.
In a pairwise test against healthy control samples, multiple myeloma samples displayed the most significantly different peptides by t test. Of the top 100 peptides selected in this way, only breast cancer showed no overlap with any other disease.
Nevertheless, the researchers were able to distinguish the 14 separate diseases from one another, as well as from healthy controls, through immunosignatures.
Dr Stafford and his colleagues said these results suggest that immunosignatures provide an attractive means of capturing disease complexity. They offer a marked improvement over traditional methods in which one-to-one molecular recognition events are measured and a small number of analytes can be evaluated.
Furthermore, the technology is flexible in terms of handling and processing, the team said. A dried sample of blood, collected on filter paper and mailed to a study facility, can be used to generate an immunosignature.
The researchers also pointed out that the microarray chip used for this study contains 10,000 imprinted peptides, and this allows for enhanced sensitivity, owing to the large number of different possible signals elicited.
However, a significant improvement in immunosignaturing sensitivity and accuracy might be achieved through new chip technology. The team is currently developing a chip imprinted with more than 100,000 peptides. ![]()

Credit: Максим Кукушкин
Immunosignaturing can allow for early detection of multiple myeloma and a range of other cancers, according to research published in PNAS.
Immunosignaturing involves profiling the entire population of antibodies circulating in the blood at a given time.
The method allowed researchers to distinguish 14 separate diseases, including 12 cancers, from one another and from healthy controls. The specificity was greater than 98% for each diagnosis.
“For years, we’ve seen remarkable results from immunosignatures, but introducing the technology to the scientific community has required a lot of patience,” said study author Phillip Stafford, PhD, of Arizona State University in Tempe.
The technique relies on a microarray consisting of thousands of random sequence peptides, imprinted on a glass slide. When a tiny droplet of blood (less than a microliter is needed) is spread across the microarray, antibodies in the blood selectively bind with individual peptides, forming a portrait of immune activity—an immunosignature.
Because the peptide sequences are random and not related to any naturally occurring disease antigens, the immunosignatures are “disease agnostic,” which means a single platform is potentially applicable to multiple disease types.
With their research, Dr Stafford and his colleagues put this claim to the test. The team first “trained” the system to calibrate results and establish reference immunosignatures using 20 samples each from 5 cancer patient cohorts, along with 20 non-cancer patients.
Once reference immunosignatures were established, the researchers tested the technique in a blind evaluation of 120 independent samples covering the same diseases. The results demonstrated 95% accuracy.
To further assess the diagnostic power of immunosignaturing, the team tested more than 1500 historical samples comprising 14 different diseases. This included 12 cancers, such as breast, brain, and multiple myeloma.
The average diagnostic accuracy of immunosignaturing was greater than 98% for each diagnosis, which suggests the method is suitable for the simultaneous classification of multiple diseases.
In a pairwise test against healthy control samples, multiple myeloma samples displayed the most significantly different peptides by t test. Of the top 100 peptides selected in this way, only breast cancer showed no overlap with any other disease.
Nevertheless, the researchers were able to distinguish the 14 separate diseases from one another, as well as from healthy controls, through immunosignatures.
Dr Stafford and his colleagues said these results suggest that immunosignatures provide an attractive means of capturing disease complexity. They offer a marked improvement over traditional methods in which one-to-one molecular recognition events are measured and a small number of analytes can be evaluated.
Furthermore, the technology is flexible in terms of handling and processing, the team said. A dried sample of blood, collected on filter paper and mailed to a study facility, can be used to generate an immunosignature.
The researchers also pointed out that the microarray chip used for this study contains 10,000 imprinted peptides, and this allows for enhanced sensitivity, owing to the large number of different possible signals elicited.
However, a significant improvement in immunosignaturing sensitivity and accuracy might be achieved through new chip technology. The team is currently developing a chip imprinted with more than 100,000 peptides. ![]()
From the Vascular Community
Baylor Vascular Fellows 50th Anniversary
On May 20, alumni and friends of Baylor University Medical Center’s vascular fellowship program gathered to celebrate the 50th anniversary of the program and commemorate the man who created it, Dr. Jesse Thompson. Dr. Thompson, who passed away in 2008, was a founding editor for the Journal of Vascular Surgery and president of the Society of Vascular Surgery.
In 1964, he established the country’s second vascular fellowship program at Baylor. Since then, approximately 100 vascular surgeons have received their training in this program. Its alumni include Dr. Larry Hollier, Dr. Hugh Trout, and Dr. Jonathan Towne.
The reunion was held at the Dallas Country Club with more than 140 in attendance, including Dr. Thompson’s children and grandchildren. The program’s first, middle, and last (i.e., most recent) fellows also attended. The following day Baylor hosted the Jesse E. Thompson, MD Lectureship and Speaker Symposium.
Dr. Spence Taylor was the visiting professor, delivering an address entitled "Surgeons as Leaders: Lessons Learned While Building a Medical School."
In Memoriam: Dr. John J. Bergan
Vascular pioneer Dr. John J. Bergan died June 11, 2014. Dr. Bergan began his career as a clinical assistant in surgery at Northwestern University Medical School. He served as the chief of the Division of Transplantation at Northwestern University Medical School from 1969 to 1976. When the Division of Vascular Surgery was formed in 1976, Dr. Bergan was appointed as the first division chief. Along with Dr. James Yao, Dr. Bergan established one of the earliest clinical vascular fellowship programs that same year, at Northwestern. In 1989, Dr. Bergan left Northwestern for southern California.
Dr. Bergan was instrumental in founding and developing many new societies and publications, including Midwestern Vascular Surgical Society. He also participated in the development of many practice guidelines including a method for data retrieval using computer programming and guidelines for venous disease diagnosis and treatment. He served as president of numerous societies, including SVS and the American Venous Forum.
We are truly grateful for all that he has contributed, and he will be sorely missed.
–Dr. Mark Eskandari
Baylor Vascular Fellows 50th Anniversary
On May 20, alumni and friends of Baylor University Medical Center’s vascular fellowship program gathered to celebrate the 50th anniversary of the program and commemorate the man who created it, Dr. Jesse Thompson. Dr. Thompson, who passed away in 2008, was a founding editor for the Journal of Vascular Surgery and president of the Society of Vascular Surgery.
In 1964, he established the country’s second vascular fellowship program at Baylor. Since then, approximately 100 vascular surgeons have received their training in this program. Its alumni include Dr. Larry Hollier, Dr. Hugh Trout, and Dr. Jonathan Towne.
The reunion was held at the Dallas Country Club with more than 140 in attendance, including Dr. Thompson’s children and grandchildren. The program’s first, middle, and last (i.e., most recent) fellows also attended. The following day Baylor hosted the Jesse E. Thompson, MD Lectureship and Speaker Symposium.
Dr. Spence Taylor was the visiting professor, delivering an address entitled "Surgeons as Leaders: Lessons Learned While Building a Medical School."
In Memoriam: Dr. John J. Bergan
Vascular pioneer Dr. John J. Bergan died June 11, 2014. Dr. Bergan began his career as a clinical assistant in surgery at Northwestern University Medical School. He served as the chief of the Division of Transplantation at Northwestern University Medical School from 1969 to 1976. When the Division of Vascular Surgery was formed in 1976, Dr. Bergan was appointed as the first division chief. Along with Dr. James Yao, Dr. Bergan established one of the earliest clinical vascular fellowship programs that same year, at Northwestern. In 1989, Dr. Bergan left Northwestern for southern California.
Dr. Bergan was instrumental in founding and developing many new societies and publications, including Midwestern Vascular Surgical Society. He also participated in the development of many practice guidelines including a method for data retrieval using computer programming and guidelines for venous disease diagnosis and treatment. He served as president of numerous societies, including SVS and the American Venous Forum.
We are truly grateful for all that he has contributed, and he will be sorely missed.
–Dr. Mark Eskandari
Baylor Vascular Fellows 50th Anniversary
On May 20, alumni and friends of Baylor University Medical Center’s vascular fellowship program gathered to celebrate the 50th anniversary of the program and commemorate the man who created it, Dr. Jesse Thompson. Dr. Thompson, who passed away in 2008, was a founding editor for the Journal of Vascular Surgery and president of the Society of Vascular Surgery.
In 1964, he established the country’s second vascular fellowship program at Baylor. Since then, approximately 100 vascular surgeons have received their training in this program. Its alumni include Dr. Larry Hollier, Dr. Hugh Trout, and Dr. Jonathan Towne.
The reunion was held at the Dallas Country Club with more than 140 in attendance, including Dr. Thompson’s children and grandchildren. The program’s first, middle, and last (i.e., most recent) fellows also attended. The following day Baylor hosted the Jesse E. Thompson, MD Lectureship and Speaker Symposium.
Dr. Spence Taylor was the visiting professor, delivering an address entitled "Surgeons as Leaders: Lessons Learned While Building a Medical School."
In Memoriam: Dr. John J. Bergan
Vascular pioneer Dr. John J. Bergan died June 11, 2014. Dr. Bergan began his career as a clinical assistant in surgery at Northwestern University Medical School. He served as the chief of the Division of Transplantation at Northwestern University Medical School from 1969 to 1976. When the Division of Vascular Surgery was formed in 1976, Dr. Bergan was appointed as the first division chief. Along with Dr. James Yao, Dr. Bergan established one of the earliest clinical vascular fellowship programs that same year, at Northwestern. In 1989, Dr. Bergan left Northwestern for southern California.
Dr. Bergan was instrumental in founding and developing many new societies and publications, including Midwestern Vascular Surgical Society. He also participated in the development of many practice guidelines including a method for data retrieval using computer programming and guidelines for venous disease diagnosis and treatment. He served as president of numerous societies, including SVS and the American Venous Forum.
We are truly grateful for all that he has contributed, and he will be sorely missed.
–Dr. Mark Eskandari
Asymptomatic carotid stenosis tied to mental decline
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
Fetal growth restriction may be underestimated in obese patients
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Recurrent Multidrug Resistant Urinary Tract Infections in Geriatric Patients
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
A novel method of blood cell production

stem cells to form endothelium
(green), then blood cells (red)
Credit: Irina Elcheva
and Akhilesh Kumar
Researchers have reported a new method for creating human blood cells in the lab, and they believe the approach is safer and more reliable than its predecessors.
The team determined how blood cells are made at the earliest stages of development; namely, 2 genetic programs are responsible for turning pluripotent stem cells into blood cells.
This discovery gave the researchers the tools to make an array of blood cells themselves, using transcription factors.
“This is the first demonstration of the production of different kinds of cells from human pluripotent stem cells using transcription factors,” said Igor Slukvin, MD, PhD, of the University of Wisconsin-Madison.
He and his colleagues described this method in Nature Communications.
During development, blood cells emerge in the aorta. There, blood cells, including hematopoietic stem cells, are generated by budding from hemogenic endothelial cells.
Dr Slukvin and his colleagues found that 2 distinct groups of transcription factors—pan-myeloid (ETV2 and GATA2) and erythro-megakaryocytic (GATA2 and TAL1)—directly convert human pluripotent stem cells into hemogenic endothelial cells.
These cells then develop into blood cells with pan-myeloid or erythro-megakaryocytic potential.
“By overexpressing just 2 transcription factors, we can, in the laboratory dish, reproduce the sequence of events we see in the embryo,” Dr Slukvin said.
Furthermore, the method could produce blood cells in abundance. For every million stem cells, the researchers were able to produce 30 million blood cells.
The team noted that a critical aspect of this work is the use of modified messenger RNA to direct stem cells toward particular developmental fates.
This approach makes it possible to induce cells without introducing any genetic artifacts. So this method of blood cell production is safer than other methods, according to the researchers.
“You can do it without a virus, and genome integrity is not affected,” Dr Slukvin noted.
He added that his group is still working on a method for producing hematopoietic stem cells in the lab.
“We still don’t know how to do that,” he said. “But our new approach to making blood cells will give us an opportunity to model their development in a dish and identify novel hematopoietic stem cell factors.” ![]()

stem cells to form endothelium
(green), then blood cells (red)
Credit: Irina Elcheva
and Akhilesh Kumar
Researchers have reported a new method for creating human blood cells in the lab, and they believe the approach is safer and more reliable than its predecessors.
The team determined how blood cells are made at the earliest stages of development; namely, 2 genetic programs are responsible for turning pluripotent stem cells into blood cells.
This discovery gave the researchers the tools to make an array of blood cells themselves, using transcription factors.
“This is the first demonstration of the production of different kinds of cells from human pluripotent stem cells using transcription factors,” said Igor Slukvin, MD, PhD, of the University of Wisconsin-Madison.
He and his colleagues described this method in Nature Communications.
During development, blood cells emerge in the aorta. There, blood cells, including hematopoietic stem cells, are generated by budding from hemogenic endothelial cells.
Dr Slukvin and his colleagues found that 2 distinct groups of transcription factors—pan-myeloid (ETV2 and GATA2) and erythro-megakaryocytic (GATA2 and TAL1)—directly convert human pluripotent stem cells into hemogenic endothelial cells.
These cells then develop into blood cells with pan-myeloid or erythro-megakaryocytic potential.
“By overexpressing just 2 transcription factors, we can, in the laboratory dish, reproduce the sequence of events we see in the embryo,” Dr Slukvin said.
Furthermore, the method could produce blood cells in abundance. For every million stem cells, the researchers were able to produce 30 million blood cells.
The team noted that a critical aspect of this work is the use of modified messenger RNA to direct stem cells toward particular developmental fates.
This approach makes it possible to induce cells without introducing any genetic artifacts. So this method of blood cell production is safer than other methods, according to the researchers.
“You can do it without a virus, and genome integrity is not affected,” Dr Slukvin noted.
He added that his group is still working on a method for producing hematopoietic stem cells in the lab.
“We still don’t know how to do that,” he said. “But our new approach to making blood cells will give us an opportunity to model their development in a dish and identify novel hematopoietic stem cell factors.” ![]()

stem cells to form endothelium
(green), then blood cells (red)
Credit: Irina Elcheva
and Akhilesh Kumar
Researchers have reported a new method for creating human blood cells in the lab, and they believe the approach is safer and more reliable than its predecessors.
The team determined how blood cells are made at the earliest stages of development; namely, 2 genetic programs are responsible for turning pluripotent stem cells into blood cells.
This discovery gave the researchers the tools to make an array of blood cells themselves, using transcription factors.
“This is the first demonstration of the production of different kinds of cells from human pluripotent stem cells using transcription factors,” said Igor Slukvin, MD, PhD, of the University of Wisconsin-Madison.
He and his colleagues described this method in Nature Communications.
During development, blood cells emerge in the aorta. There, blood cells, including hematopoietic stem cells, are generated by budding from hemogenic endothelial cells.
Dr Slukvin and his colleagues found that 2 distinct groups of transcription factors—pan-myeloid (ETV2 and GATA2) and erythro-megakaryocytic (GATA2 and TAL1)—directly convert human pluripotent stem cells into hemogenic endothelial cells.
These cells then develop into blood cells with pan-myeloid or erythro-megakaryocytic potential.
“By overexpressing just 2 transcription factors, we can, in the laboratory dish, reproduce the sequence of events we see in the embryo,” Dr Slukvin said.
Furthermore, the method could produce blood cells in abundance. For every million stem cells, the researchers were able to produce 30 million blood cells.
The team noted that a critical aspect of this work is the use of modified messenger RNA to direct stem cells toward particular developmental fates.
This approach makes it possible to induce cells without introducing any genetic artifacts. So this method of blood cell production is safer than other methods, according to the researchers.
“You can do it without a virus, and genome integrity is not affected,” Dr Slukvin noted.
He added that his group is still working on a method for producing hematopoietic stem cells in the lab.
“We still don’t know how to do that,” he said. “But our new approach to making blood cells will give us an opportunity to model their development in a dish and identify novel hematopoietic stem cell factors.” ![]()
What Can We Do to Prevent Alzheimer Disease?
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
FDA warns of non-sterile drugs

Credit: Bill Branson
The US Food and Drug Administration (FDA) is alerting healthcare professionals not to use sterile drugs produced by Unique Pharmaceuticals Ltd., as they may be contaminated.
Healthcare professionals should immediately check their medical supplies and quarantine any sterile drug products from Unique Pharmaceuticals, a compounding outsourcing facility in Temple, Texas.
Administration of a non-sterile product may result in serious infection or death.
Unique Pharmaceuticals’ products were distributed nationwide. Most of the product labels include: “Unique Pharmaceuticals, Temple TX USA 76502.”
FDA investigators conducted 2 recent inspections of the Unique Pharmaceuticals facility and observed unsanitary conditions that resulted in a lack of sterility assurance.
The inspections revealed sterility failures in several lots of products intended to be sterile, recurring environmental contamination problems, and poor sterile production practices.
The FDA previously asked the company to recall all non-expired lots of sterile drug products, but the company refused to do so. The FDA has now issued a formal request for Unique Pharmaceuticals to recall all non-expired lots of its sterile products currently on the market.
The FDA has also asked the company to cease sterile compounding operations until sufficient corrections are made at its facility. Unique Pharmaceuticals has refused this request as well.
To date, the FDA is not aware of reports of illness associated with the use of Unique Pharmaceuticals’ products.
Patients who have received any drug product produced by Unique Pharmaceuticals and have concerns should contact their healthcare professional.
Professionals and consumers may report adverse events or quality problems associated with the use of Unique Pharmaceuticals’ products to the FDA’s MedWatch Adverse Event Reporting Program.
Unique Pharmaceuticals is registered under section 503B of the Federal Food, Drug, and Cosmetic Act (FDCA) as an outsourcing facility. The Drug Quality and Security Act, signed into law on November 27, 2013, added a new section 503B to the FDCA. Under section 503B, a compounder can elect to become an outsourcing facility.
Outsourcing facilities must comply with current good manufacturing practice requirements, will be subject to inspection by the FDA according to a risk-based schedule, and must meet certain other requirements, such as reporting adverse events and providing the FDA with certain information about the products they compound. ![]()

Credit: Bill Branson
The US Food and Drug Administration (FDA) is alerting healthcare professionals not to use sterile drugs produced by Unique Pharmaceuticals Ltd., as they may be contaminated.
Healthcare professionals should immediately check their medical supplies and quarantine any sterile drug products from Unique Pharmaceuticals, a compounding outsourcing facility in Temple, Texas.
Administration of a non-sterile product may result in serious infection or death.
Unique Pharmaceuticals’ products were distributed nationwide. Most of the product labels include: “Unique Pharmaceuticals, Temple TX USA 76502.”
FDA investigators conducted 2 recent inspections of the Unique Pharmaceuticals facility and observed unsanitary conditions that resulted in a lack of sterility assurance.
The inspections revealed sterility failures in several lots of products intended to be sterile, recurring environmental contamination problems, and poor sterile production practices.
The FDA previously asked the company to recall all non-expired lots of sterile drug products, but the company refused to do so. The FDA has now issued a formal request for Unique Pharmaceuticals to recall all non-expired lots of its sterile products currently on the market.
The FDA has also asked the company to cease sterile compounding operations until sufficient corrections are made at its facility. Unique Pharmaceuticals has refused this request as well.
To date, the FDA is not aware of reports of illness associated with the use of Unique Pharmaceuticals’ products.
Patients who have received any drug product produced by Unique Pharmaceuticals and have concerns should contact their healthcare professional.
Professionals and consumers may report adverse events or quality problems associated with the use of Unique Pharmaceuticals’ products to the FDA’s MedWatch Adverse Event Reporting Program.
Unique Pharmaceuticals is registered under section 503B of the Federal Food, Drug, and Cosmetic Act (FDCA) as an outsourcing facility. The Drug Quality and Security Act, signed into law on November 27, 2013, added a new section 503B to the FDCA. Under section 503B, a compounder can elect to become an outsourcing facility.
Outsourcing facilities must comply with current good manufacturing practice requirements, will be subject to inspection by the FDA according to a risk-based schedule, and must meet certain other requirements, such as reporting adverse events and providing the FDA with certain information about the products they compound. ![]()

Credit: Bill Branson
The US Food and Drug Administration (FDA) is alerting healthcare professionals not to use sterile drugs produced by Unique Pharmaceuticals Ltd., as they may be contaminated.
Healthcare professionals should immediately check their medical supplies and quarantine any sterile drug products from Unique Pharmaceuticals, a compounding outsourcing facility in Temple, Texas.
Administration of a non-sterile product may result in serious infection or death.
Unique Pharmaceuticals’ products were distributed nationwide. Most of the product labels include: “Unique Pharmaceuticals, Temple TX USA 76502.”
FDA investigators conducted 2 recent inspections of the Unique Pharmaceuticals facility and observed unsanitary conditions that resulted in a lack of sterility assurance.
The inspections revealed sterility failures in several lots of products intended to be sterile, recurring environmental contamination problems, and poor sterile production practices.
The FDA previously asked the company to recall all non-expired lots of sterile drug products, but the company refused to do so. The FDA has now issued a formal request for Unique Pharmaceuticals to recall all non-expired lots of its sterile products currently on the market.
The FDA has also asked the company to cease sterile compounding operations until sufficient corrections are made at its facility. Unique Pharmaceuticals has refused this request as well.
To date, the FDA is not aware of reports of illness associated with the use of Unique Pharmaceuticals’ products.
Patients who have received any drug product produced by Unique Pharmaceuticals and have concerns should contact their healthcare professional.
Professionals and consumers may report adverse events or quality problems associated with the use of Unique Pharmaceuticals’ products to the FDA’s MedWatch Adverse Event Reporting Program.
Unique Pharmaceuticals is registered under section 503B of the Federal Food, Drug, and Cosmetic Act (FDCA) as an outsourcing facility. The Drug Quality and Security Act, signed into law on November 27, 2013, added a new section 503B to the FDCA. Under section 503B, a compounder can elect to become an outsourcing facility.
Outsourcing facilities must comply with current good manufacturing practice requirements, will be subject to inspection by the FDA according to a risk-based schedule, and must meet certain other requirements, such as reporting adverse events and providing the FDA with certain information about the products they compound. ![]()





