User login
Studies explain gene’s role in thrombosis, hemostasis

Credit: Kevin MacKenzie
Two preclinical studies provide new insight into the activity of STXBP5, a gene that has been linked to changes in von Willebrand factor (VWF).
One research group found evidence suggesting that STXBP5 regulates endothelial exocytosis and thrombosis.
Another group’s work indicated that STXBP5 is required for normal arterial hemostasis, as it contributes to platelet packaging and secretion.
Both studies appear in The Journal of Clinical Investigation.
Charles Lowenstein, MD, of the University of Rochester in New York, and his colleagues began their research with the theory that STXBP5 inhibits endothelial cell exocytosis.
The group found that STXBP5 is expressed in human endothelial cells, and reducing STXBP5 increases exocytosis of VWF and P-selectin.
STXBP5-knockout mice had higher levels of VWF in their plasma, increased P-selectin translocation, and more platelet-endothelial interactions. This suggests that defective STXBP5 is a risk factor for thrombosis.
However, STXBP5-knockout mice also exhibited prolonged bleeding and impaired thrombosis. They had defects in platelet secretion and activation as well.
Sidney (Wally) Whiteheart, PhD, of the University of Kentucky in Lexington, and his colleagues helped to explain these findings with their research.
The group showed that platelets lacking SXTBP5 failed to function correctly, and SXTBP5 was required for platelets to assist in normal clot formation. This suggests STXBP5 plays different roles in endothelial cells and platelets.
Specifically, the researchers found that STXBP5 interacts with core secretion machinery complexes and the platelet cytoskeleton.
And platelets from STXBP5-knockout mice exhibited defects in granule secretion. These platelets had altered granule cargo levels, despite having normal morphology and granule numbers.
Like Dr Lowenstein’s group, Dr Whiteheart and his colleagues observed dramatic bleeding and defective hemostasis in STXBP5-knockout mice. Transplant experiments suggested these defects were due to a loss of STXBP5 in bone marrow-derived cells. ![]()

Credit: Kevin MacKenzie
Two preclinical studies provide new insight into the activity of STXBP5, a gene that has been linked to changes in von Willebrand factor (VWF).
One research group found evidence suggesting that STXBP5 regulates endothelial exocytosis and thrombosis.
Another group’s work indicated that STXBP5 is required for normal arterial hemostasis, as it contributes to platelet packaging and secretion.
Both studies appear in The Journal of Clinical Investigation.
Charles Lowenstein, MD, of the University of Rochester in New York, and his colleagues began their research with the theory that STXBP5 inhibits endothelial cell exocytosis.
The group found that STXBP5 is expressed in human endothelial cells, and reducing STXBP5 increases exocytosis of VWF and P-selectin.
STXBP5-knockout mice had higher levels of VWF in their plasma, increased P-selectin translocation, and more platelet-endothelial interactions. This suggests that defective STXBP5 is a risk factor for thrombosis.
However, STXBP5-knockout mice also exhibited prolonged bleeding and impaired thrombosis. They had defects in platelet secretion and activation as well.
Sidney (Wally) Whiteheart, PhD, of the University of Kentucky in Lexington, and his colleagues helped to explain these findings with their research.
The group showed that platelets lacking SXTBP5 failed to function correctly, and SXTBP5 was required for platelets to assist in normal clot formation. This suggests STXBP5 plays different roles in endothelial cells and platelets.
Specifically, the researchers found that STXBP5 interacts with core secretion machinery complexes and the platelet cytoskeleton.
And platelets from STXBP5-knockout mice exhibited defects in granule secretion. These platelets had altered granule cargo levels, despite having normal morphology and granule numbers.
Like Dr Lowenstein’s group, Dr Whiteheart and his colleagues observed dramatic bleeding and defective hemostasis in STXBP5-knockout mice. Transplant experiments suggested these defects were due to a loss of STXBP5 in bone marrow-derived cells. ![]()

Credit: Kevin MacKenzie
Two preclinical studies provide new insight into the activity of STXBP5, a gene that has been linked to changes in von Willebrand factor (VWF).
One research group found evidence suggesting that STXBP5 regulates endothelial exocytosis and thrombosis.
Another group’s work indicated that STXBP5 is required for normal arterial hemostasis, as it contributes to platelet packaging and secretion.
Both studies appear in The Journal of Clinical Investigation.
Charles Lowenstein, MD, of the University of Rochester in New York, and his colleagues began their research with the theory that STXBP5 inhibits endothelial cell exocytosis.
The group found that STXBP5 is expressed in human endothelial cells, and reducing STXBP5 increases exocytosis of VWF and P-selectin.
STXBP5-knockout mice had higher levels of VWF in their plasma, increased P-selectin translocation, and more platelet-endothelial interactions. This suggests that defective STXBP5 is a risk factor for thrombosis.
However, STXBP5-knockout mice also exhibited prolonged bleeding and impaired thrombosis. They had defects in platelet secretion and activation as well.
Sidney (Wally) Whiteheart, PhD, of the University of Kentucky in Lexington, and his colleagues helped to explain these findings with their research.
The group showed that platelets lacking SXTBP5 failed to function correctly, and SXTBP5 was required for platelets to assist in normal clot formation. This suggests STXBP5 plays different roles in endothelial cells and platelets.
Specifically, the researchers found that STXBP5 interacts with core secretion machinery complexes and the platelet cytoskeleton.
And platelets from STXBP5-knockout mice exhibited defects in granule secretion. These platelets had altered granule cargo levels, despite having normal morphology and granule numbers.
Like Dr Lowenstein’s group, Dr Whiteheart and his colleagues observed dramatic bleeding and defective hemostasis in STXBP5-knockout mice. Transplant experiments suggested these defects were due to a loss of STXBP5 in bone marrow-derived cells. ![]()
Dr. Robert L. Barbieri’s Editor’s Picks September 2014
Editor in Chief Robert L. Barbieri, MD, provides an overview of three articles appearing in OBG Management’s September 2014 issue. Listen to his take on why these articles are of particular importance to women’s health professionals.
Access all of the articles in the September 2014 issue here.
Editor in Chief Robert L. Barbieri, MD, provides an overview of three articles appearing in OBG Management’s September 2014 issue. Listen to his take on why these articles are of particular importance to women’s health professionals.
Access all of the articles in the September 2014 issue here.
Editor in Chief Robert L. Barbieri, MD, provides an overview of three articles appearing in OBG Management’s September 2014 issue. Listen to his take on why these articles are of particular importance to women’s health professionals.
Access all of the articles in the September 2014 issue here.
Library can help cut cost of syringe pumps

Credit: Darren Baker
Researchers have published an open-source library of designs that could allow scientists to cut the cost of syringe pumps.
These syringe-pump designs can be made on a RepRap 3D printer for the cost of the plastic filament, and the designs are customizable.
“Not only have we designed a single syringe pump, we’ve designed all future syringe pumps,” said Joshua Pearce, PhD, of Michigan Technological University in Houghton.
“Scientists can customize the design of a pump for exactly what they are doing, just by changing a couple of numbers in the software.”
Dr Pearce and his colleagues described their work creating the library of designs in PLOS ONE. The hardware plans, designs, and source code for the pumps are available on Appropedia.
The library includes recipes for most parts of a syringe pump. Scientists will have to buy the small electric stepper motor that drives the liquid, some simple hardware, and the syringe itself.
The researchers also incorporated a low-cost, credit card-sized Raspberry Pi computer as a wireless controller.
“That way, you can link the syringe pump to the network, sit on a beach in Hawaii, and control your lab,” Dr Pearce said. “Plenty of people can have access, and you can run multiple experiments at the same time. Our entire single-pump system costs only $50 and can replace pumps that run between $250 and $2500.”
It costs more to make a double-pump system, about $120, but it replaces a commercial system that costs $5000.
And Dr Pearce believes someone will find a way to make the pumps even better.
“I’m sure someone will improve our designs and share their results with us and the rest of the community,” he said. “That’s the beauty and power of open source.” ![]()

Credit: Darren Baker
Researchers have published an open-source library of designs that could allow scientists to cut the cost of syringe pumps.
These syringe-pump designs can be made on a RepRap 3D printer for the cost of the plastic filament, and the designs are customizable.
“Not only have we designed a single syringe pump, we’ve designed all future syringe pumps,” said Joshua Pearce, PhD, of Michigan Technological University in Houghton.
“Scientists can customize the design of a pump for exactly what they are doing, just by changing a couple of numbers in the software.”
Dr Pearce and his colleagues described their work creating the library of designs in PLOS ONE. The hardware plans, designs, and source code for the pumps are available on Appropedia.
The library includes recipes for most parts of a syringe pump. Scientists will have to buy the small electric stepper motor that drives the liquid, some simple hardware, and the syringe itself.
The researchers also incorporated a low-cost, credit card-sized Raspberry Pi computer as a wireless controller.
“That way, you can link the syringe pump to the network, sit on a beach in Hawaii, and control your lab,” Dr Pearce said. “Plenty of people can have access, and you can run multiple experiments at the same time. Our entire single-pump system costs only $50 and can replace pumps that run between $250 and $2500.”
It costs more to make a double-pump system, about $120, but it replaces a commercial system that costs $5000.
And Dr Pearce believes someone will find a way to make the pumps even better.
“I’m sure someone will improve our designs and share their results with us and the rest of the community,” he said. “That’s the beauty and power of open source.” ![]()

Credit: Darren Baker
Researchers have published an open-source library of designs that could allow scientists to cut the cost of syringe pumps.
These syringe-pump designs can be made on a RepRap 3D printer for the cost of the plastic filament, and the designs are customizable.
“Not only have we designed a single syringe pump, we’ve designed all future syringe pumps,” said Joshua Pearce, PhD, of Michigan Technological University in Houghton.
“Scientists can customize the design of a pump for exactly what they are doing, just by changing a couple of numbers in the software.”
Dr Pearce and his colleagues described their work creating the library of designs in PLOS ONE. The hardware plans, designs, and source code for the pumps are available on Appropedia.
The library includes recipes for most parts of a syringe pump. Scientists will have to buy the small electric stepper motor that drives the liquid, some simple hardware, and the syringe itself.
The researchers also incorporated a low-cost, credit card-sized Raspberry Pi computer as a wireless controller.
“That way, you can link the syringe pump to the network, sit on a beach in Hawaii, and control your lab,” Dr Pearce said. “Plenty of people can have access, and you can run multiple experiments at the same time. Our entire single-pump system costs only $50 and can replace pumps that run between $250 and $2500.”
It costs more to make a double-pump system, about $120, but it replaces a commercial system that costs $5000.
And Dr Pearce believes someone will find a way to make the pumps even better.
“I’m sure someone will improve our designs and share their results with us and the rest of the community,” he said. “That’s the beauty and power of open source.” ![]()
Idelalisib approved to treat CLL, FL in EU

The European Commission has granted marketing authorization for the PI3K delta inhibitor idelalisib (Zydelig) to treat chronic lymphocytic leukemia (CLL) and follicular lymphoma (FL) in the European Union.
The drug is now approved for use in combination with rituximab for CLL patients who have received at least 1 prior therapy or as first-line treatment in CLL patients who have 17p deletion or TP53 mutation and are not eligible for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for FL patients who were refractory to 2 prior lines of treatment.
These approvals are based on data from 2 clinical trials—Study 116 and Study 101-09.
Study 116: Idelalisib in CLL
This phase 3 trial was stopped early because idelalisib had a significant impact on progression-free survival.
The study included 220 CLL patients who could not receive chemotherapy. Half were randomized to receive idelalisib plus rituximab, and the other half were randomized to rituximab plus placebo.
Patients in the rituximab-idelalisib arm had a much higher overall response rate than patients in the rituximab-placebo arm—81% and 13%, respectively (P<0.001). There were no complete responses.
At 24 weeks, the rate of progression-free survival was 93% in the rituximab-idelalisib arm and 46% in the rituximab-placebo arm (P<0.001). The median progression-free survival was 5.5 months in the rituximab-placebo arm and not reached in the rituximab-idelalisib arm (P<0.001).
At 12 months, the overall survival rate was 92% in the rituximab-idelalisib arm and 80% in the rituximab-placebo arm (P=0.02).
Most adverse events, in either treatment arm, were grade 2 or lower. The most common events in the rituximab-idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the rituximab-placebo arm, the most common events were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious adverse events in the rituximab-idelalisib arm than in the rituximab-placebo arm—40% and 35%, respectively. The most frequent serious events were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Study 101-09: Idelalisib in FL
This phase 2 trial enrolled 125 patients with indolent non-Hodgkin lymphoma who were refractory to rituximab and chemotherapy containing an alkylating agent. Patients received idelalisib monotherapy.
Of the 72 subjects with FL, 54% achieved a response, and 8% had a complete response. The median duration of response was not reached (range, 0-14.8 months).
Improvements in survival or disease-related symptoms have not been established.
In all patients, the most common grade 3 or higher adverse events were neutropenia (27%), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
Idelalisib is under development by Gilead Sciences. The drug is already approved in the US for the aforementioned indications, as well as to treat small lymphocytic lymphoma. ![]()

The European Commission has granted marketing authorization for the PI3K delta inhibitor idelalisib (Zydelig) to treat chronic lymphocytic leukemia (CLL) and follicular lymphoma (FL) in the European Union.
The drug is now approved for use in combination with rituximab for CLL patients who have received at least 1 prior therapy or as first-line treatment in CLL patients who have 17p deletion or TP53 mutation and are not eligible for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for FL patients who were refractory to 2 prior lines of treatment.
These approvals are based on data from 2 clinical trials—Study 116 and Study 101-09.
Study 116: Idelalisib in CLL
This phase 3 trial was stopped early because idelalisib had a significant impact on progression-free survival.
The study included 220 CLL patients who could not receive chemotherapy. Half were randomized to receive idelalisib plus rituximab, and the other half were randomized to rituximab plus placebo.
Patients in the rituximab-idelalisib arm had a much higher overall response rate than patients in the rituximab-placebo arm—81% and 13%, respectively (P<0.001). There were no complete responses.
At 24 weeks, the rate of progression-free survival was 93% in the rituximab-idelalisib arm and 46% in the rituximab-placebo arm (P<0.001). The median progression-free survival was 5.5 months in the rituximab-placebo arm and not reached in the rituximab-idelalisib arm (P<0.001).
At 12 months, the overall survival rate was 92% in the rituximab-idelalisib arm and 80% in the rituximab-placebo arm (P=0.02).
Most adverse events, in either treatment arm, were grade 2 or lower. The most common events in the rituximab-idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the rituximab-placebo arm, the most common events were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious adverse events in the rituximab-idelalisib arm than in the rituximab-placebo arm—40% and 35%, respectively. The most frequent serious events were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Study 101-09: Idelalisib in FL
This phase 2 trial enrolled 125 patients with indolent non-Hodgkin lymphoma who were refractory to rituximab and chemotherapy containing an alkylating agent. Patients received idelalisib monotherapy.
Of the 72 subjects with FL, 54% achieved a response, and 8% had a complete response. The median duration of response was not reached (range, 0-14.8 months).
Improvements in survival or disease-related symptoms have not been established.
In all patients, the most common grade 3 or higher adverse events were neutropenia (27%), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
Idelalisib is under development by Gilead Sciences. The drug is already approved in the US for the aforementioned indications, as well as to treat small lymphocytic lymphoma. ![]()

The European Commission has granted marketing authorization for the PI3K delta inhibitor idelalisib (Zydelig) to treat chronic lymphocytic leukemia (CLL) and follicular lymphoma (FL) in the European Union.
The drug is now approved for use in combination with rituximab for CLL patients who have received at least 1 prior therapy or as first-line treatment in CLL patients who have 17p deletion or TP53 mutation and are not eligible for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for FL patients who were refractory to 2 prior lines of treatment.
These approvals are based on data from 2 clinical trials—Study 116 and Study 101-09.
Study 116: Idelalisib in CLL
This phase 3 trial was stopped early because idelalisib had a significant impact on progression-free survival.
The study included 220 CLL patients who could not receive chemotherapy. Half were randomized to receive idelalisib plus rituximab, and the other half were randomized to rituximab plus placebo.
Patients in the rituximab-idelalisib arm had a much higher overall response rate than patients in the rituximab-placebo arm—81% and 13%, respectively (P<0.001). There were no complete responses.
At 24 weeks, the rate of progression-free survival was 93% in the rituximab-idelalisib arm and 46% in the rituximab-placebo arm (P<0.001). The median progression-free survival was 5.5 months in the rituximab-placebo arm and not reached in the rituximab-idelalisib arm (P<0.001).
At 12 months, the overall survival rate was 92% in the rituximab-idelalisib arm and 80% in the rituximab-placebo arm (P=0.02).
Most adverse events, in either treatment arm, were grade 2 or lower. The most common events in the rituximab-idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the rituximab-placebo arm, the most common events were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious adverse events in the rituximab-idelalisib arm than in the rituximab-placebo arm—40% and 35%, respectively. The most frequent serious events were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Study 101-09: Idelalisib in FL
This phase 2 trial enrolled 125 patients with indolent non-Hodgkin lymphoma who were refractory to rituximab and chemotherapy containing an alkylating agent. Patients received idelalisib monotherapy.
Of the 72 subjects with FL, 54% achieved a response, and 8% had a complete response. The median duration of response was not reached (range, 0-14.8 months).
Improvements in survival or disease-related symptoms have not been established.
In all patients, the most common grade 3 or higher adverse events were neutropenia (27%), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
Idelalisib is under development by Gilead Sciences. The drug is already approved in the US for the aforementioned indications, as well as to treat small lymphocytic lymphoma. ![]()
Targeting the Kidneys to Improve Glycemic Control
A 37-year-old woman with a history of papillary carcinoma (status post total thyroidectomy 12 years ago, with negative recurrence) presents for a check-up. She also has polycystic ovarian syndrome (PCOS) with obesity and is taking metformin XR (one 500-mg tablet bid). Her visit is uneventful, and she leaves the office with an order for labwork.
Results indicate normal thyroid function and negative thyroglobulin. However, her serum glucose level is 350 mg/dL, so the patient is called and informed of the result. She denies polyphagia, polydipsia, and polyuria. Repeat blood work confirms overt hyperglycemia (320 mg/dL) with an A1C of 13%, undetectable C-peptide, and negative glutamic acid decarboxylase 65 (GAD65) and islet cell antibodies.
She is advised to increase her metformin dose (to two 500-mg tablets bid) and is started on insulin detemir (20 U every evening), with instructions to increase the latter by three units every two to three days until a target fasting glucose level of 100 to 140 mg/dL is achieved. She is also advised to follow a low-carbohydrate diet and increase her exercise.
The patient returns in two weeks for follow-up. She remains asymptomatic and has now increased her insulin detemir to 34 U bid (she started splitting the dosage after it reached 50 U/d). However, her glucose is still in the low 200s in the morning and the high 200s during the day (after lunch and dinner).
Her overt hyperglycemia is most likely a result of her longstanding insulin resistance, essential lack of b-cell function, and PCOS-associated obesity. Once diabetes from autoimmunity is ruled out by laboratory findings (negative antibodies) and clinical assessment (classic metabolic syndrome features), we focus on her glycemic control.
Even with nearly 70 U/d of insulin, the patient’s glycemic improvement is disappointing, suggesting significant insulin resistance and glucose toxicity. Living in an era with numerous classes of antidiabetic medications, we have lengthy discussions on treatment options. Canagliflozin, recently (at the time) approved, is included. The patient is interested in this new medication, and it is a reasonable choice to get her out of the glucotoxic phase.
After a discussion of benefits and potential adverse effects, she is placed on canagliflozin 100 mg/d. Her glucose log in one week shows fasting glucose values in the range of 140 to 160 mg/dL and postprandial glucose values in the 180s. As a result, she lowers her insulin to 25 U bid. Her renal panel shows a potassium level of 4.3 mEq/L (reference range, 3.5 to 5.3) and a glomerular filtration rate (GFR) of 103 mL/min/1.73 m2. She is advised to further increase her canagliflozin to 300 mg and slowly titrate her insulin down as needed, with a target fasting glucose level of 80 to 110 mg/dL and a postprandial target of 100 to 140 mg/dL.
What are SGLT2 inhibitors, and how do they work?
What are SGLT2 inhibitors, and how do they work?
Sodium-GLucose co-Transporter 2 (SGLT2) inhibitors are a new class of antihyperglycemic agent. The first, canagliflozin, was approved by the FDA in March 2013, followed by dapagliflozin (January 2014) and empagliflozin (August 2014).
As glucose is filtered through the nephrons of the kidney, about 90% is reabsorbed via SGLT2 in the proximal tubule (SGLT1 is responsible for the remaining 10%) so that glucose calories are not eliminated through urine.1 In a healthy person, the renal glucose threshold is about 180 mg/dL.1 When blood glucose exceeds this level, glucose is excreted into the urine. However, in diabetic patients, this threshold is higher due to the up-regulation of SGLT2s (and other glucose transporters), which worsens hyperglycemia.1 SGLT2 inhibitors will reset the threshold, which in turn will increase glucosuria and thereby lower serum glucose.1
SGLT2 inhibitors lower A1C by about 0.7% to 0.8%.2 Independent of other mechanisms such as the degree of b-cell function or insulin resistance, these agents can be used regardless of the duration of diabetes3 if the GFR is intact (≥ 45 mL/min/1.73 m2 for canagliflozin and empagliflozin, ≥ 60 mL/min/ 1.73 m2 for dapagliflozin).4,5
What are the risks and benefits associated with these agents?
What are the risks and benefits associated with these agents?
Modest weight loss is seen with the use of SGLT2 inhibitors. Initial weight loss is believed to be related to volume loss, but more sustained weight loss is thought to be from loss of fat mass.6 This is not surprising, as excreting glucose means excreting calories through urine.
Risk for hypoglycemia is extremely low, which makes this therapeutic class an attractive option. However, caution should be exercised when SGLT2 inhibitors are combined with other agents known to cause hypoglycemia (sulfonylureas and insulin).6
The most common adverse effect is genital mycotic infection. Women with a history of recurrent genital mycotic infection and uncircumcised men are at the greatest risk.6
Due to increased glycosuria, which results in an osmotic diuresis, modest blood pressure improvement has been seen (3 to 4 mm Hg systolic and 1 to 2 mm Hg diastolic7,8) in patients taking SGLT2 inhibitors, which is an additional benefit for hypertensive diabetic patients.6 On the other hand, use of SGLT2 inhibitors can also cause dehydration and volume depletion and can raise serum creatinine in patients who are already taking diuretics (particularly loop diuretics).6 Drug tolerance and adherence can be improved by advising patients to expect transient increased urination (approximately 135 to 350 mL/d increase from baseline5,9) and emphasizing the importance of good hydration and maintaining good genital hygiene.
A slight increase in LDL cholesterol was seen in clinical trials of the SGLT2 inhibitors, although this phenomenon is poorly understood. However, HDL cholesterol increased as well, maintaining the LDL:HDL ratio.6 No long-term cardiovascular outcome data are available at this time; as with any new antidiabetic medication, postmarketing studies, as required by the FDA, are currently ongoing.6
What are the options in this therapeutic category, and how are they distinct?
What are the options in this therapeutic category, and how are they distinct?
As mentioned previously, there are currently three SGLT2 inhibitors on the market: canagliflozin, dapagliflozin, and empagliflozin. There are subtle clinical differences among these three agents, which might direct the clinician’s choice.
First, canagliflozin is available in dosages of 100 and 300 mg. The starting dosage is 100 mg, which can be titrated to 300 mg in patients with a GFR ≥ 60 mL/min/1.73 m2 who require a greater glucose-lowering effect. Those with a GFR < 60 mL/min/1.73 m2 but ≥ 45 mL/min/1.73 m2 are limited to the 100-mg dosage. Dapagliflozin is available in 5-mg and 10-mg dosages, the former being the starting dosage. But dapagliflozin is not recommended in patients whose GFR is < 60 mL/min/1.73 m2.4
Empagliflozin is available in dosages of 10 and 25 mg. The starting dosage of 10 mg can be increased to 25 mg if the patient has not achieved his/her target glucose level. Either can be used in patients with a GFR ≥ 45 mL/min/1.73 m2.5
Second, hyperkalemia was seen in patients taking canagliflozin but not in those taking dapagliflozin or empagliflozin. Therefore, serum potassium should be monitored and caution used, especially when patients are being treated with potassium-sparing diuretics and/or ACE inhibitors or angiotensin II receptor blockers.6
Third, dapagliflozin carries a warning for bladder cancer, as higher rates of newly diagnosed bladder cancer were seen with this drug compared with placebo or comparator drugs (0.17% vs 0.03%, respectively).4 However, this finding may have resulted from a randomization imbalance of patients in the study, and further research is needed to clarify this risk.6 It is not recommended that dapagliflozin be used in patients with active or a history of bladder cancer at this time.
With these agents, there is a paradoxical rise in glucagon that increases endogenous glucose production from the liver.10 The mechanism is poorly understood, but it might be due to the body’s compensatory (survival) mechanism to “make up” the loss of glucose through urine by increasing hepatic gluconeogenesis.
Using an incretin agent, such as dipeptidyl peptidase 4 (DPP-4) inhibitors or glucagon-like peptide 1 (GLP-1) receptor agonists, in conjunction with an SGLT2 inhibitor, has been suggested as a way to potentiate the glucose-lowering effect, as it may attenuate the paradoxical rise in glucagon.10 Since the incretin class is weight neutral (DPP-4 inhibitors) or associated with weight loss (GLP-1 agonists), using incretins with SGLT2 inhibitors might produce more significant weight loss, which has numerous additional benefits for diabetic patients.
SGLT2 inhibitors are currently approved as an adjunct to diet and exercise for patients with type 2 diabetes. They are not approved for those with type 1 diabetes, although the mechanism of action of these drugs (which is independent of the b-cell function) might make them effective in this population. Active pilot studies of this patient population are in progress.11
Conclusion
In summary, SGLT2 inhibitors are an exciting new class of antidiabetic medication that offers a unique mechanism to lower serum glucose. It is the only medication that will actually remove glucose from the body; by contrast, all other existing antidiabetic medications move glucose within the body (to liver, fat, muscle, etc).
There is no curative medication for diabetes. But with an increasing diabetic population and an emphasis on individualizing antihyperglycemic regimens, we always welcome medications with novel mechanisms of action. Due to SLGT2 inhibitors’ recent approval, however, short-term and long-term adverse effects are unknown, and ongoing postmarketing surveillance should be closely followed.
References
1. Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782-790.
2. Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
3. Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care. 2009;32:1656-1662.
4. Taylor JR. Dapagliflozin offers differences from other SGLT2 inhibitors. Endocrine Today. May 2014.
5. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2014.
6. Bakris G, Fonseca VA, Peters AL, Wysham CH. Clinical perspectives on the role of the kidney in the pathophysiology of T2DM: emerging options for treatment [video series]. 2013. www.thedoctorschannel.com/view/the-kid ney-in-t2dm-cme-part-1/. Accessed September 12, 2014.
7. Vercruysse F. Efficacy and safety of canagliflozin in subjects with type 2 diabetes mellitus inadequately controlled with metformin plus sulphonylurea over 52 weeks [abstract 934]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
8. Hach T. Empagliflozin improves glycaemic parameters and cardiovascular risk factors in patients with type 2 diabetes: pooled data from four pivotal phase III trials [abstract 943]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
9. List JF, Woo V, Morales E, et al. Sodium-glucose co-transport inhibition with dapagliflozin in type 2 diabetes mellitus. Diabetes Care. 2009;32(4):650-657.
10. Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(5):2287.
11. Perkins BA, Cherney DZ, Partridge H, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480-1483.
A 37-year-old woman with a history of papillary carcinoma (status post total thyroidectomy 12 years ago, with negative recurrence) presents for a check-up. She also has polycystic ovarian syndrome (PCOS) with obesity and is taking metformin XR (one 500-mg tablet bid). Her visit is uneventful, and she leaves the office with an order for labwork.
Results indicate normal thyroid function and negative thyroglobulin. However, her serum glucose level is 350 mg/dL, so the patient is called and informed of the result. She denies polyphagia, polydipsia, and polyuria. Repeat blood work confirms overt hyperglycemia (320 mg/dL) with an A1C of 13%, undetectable C-peptide, and negative glutamic acid decarboxylase 65 (GAD65) and islet cell antibodies.
She is advised to increase her metformin dose (to two 500-mg tablets bid) and is started on insulin detemir (20 U every evening), with instructions to increase the latter by three units every two to three days until a target fasting glucose level of 100 to 140 mg/dL is achieved. She is also advised to follow a low-carbohydrate diet and increase her exercise.
The patient returns in two weeks for follow-up. She remains asymptomatic and has now increased her insulin detemir to 34 U bid (she started splitting the dosage after it reached 50 U/d). However, her glucose is still in the low 200s in the morning and the high 200s during the day (after lunch and dinner).
Her overt hyperglycemia is most likely a result of her longstanding insulin resistance, essential lack of b-cell function, and PCOS-associated obesity. Once diabetes from autoimmunity is ruled out by laboratory findings (negative antibodies) and clinical assessment (classic metabolic syndrome features), we focus on her glycemic control.
Even with nearly 70 U/d of insulin, the patient’s glycemic improvement is disappointing, suggesting significant insulin resistance and glucose toxicity. Living in an era with numerous classes of antidiabetic medications, we have lengthy discussions on treatment options. Canagliflozin, recently (at the time) approved, is included. The patient is interested in this new medication, and it is a reasonable choice to get her out of the glucotoxic phase.
After a discussion of benefits and potential adverse effects, she is placed on canagliflozin 100 mg/d. Her glucose log in one week shows fasting glucose values in the range of 140 to 160 mg/dL and postprandial glucose values in the 180s. As a result, she lowers her insulin to 25 U bid. Her renal panel shows a potassium level of 4.3 mEq/L (reference range, 3.5 to 5.3) and a glomerular filtration rate (GFR) of 103 mL/min/1.73 m2. She is advised to further increase her canagliflozin to 300 mg and slowly titrate her insulin down as needed, with a target fasting glucose level of 80 to 110 mg/dL and a postprandial target of 100 to 140 mg/dL.
What are SGLT2 inhibitors, and how do they work?
What are SGLT2 inhibitors, and how do they work?
Sodium-GLucose co-Transporter 2 (SGLT2) inhibitors are a new class of antihyperglycemic agent. The first, canagliflozin, was approved by the FDA in March 2013, followed by dapagliflozin (January 2014) and empagliflozin (August 2014).
As glucose is filtered through the nephrons of the kidney, about 90% is reabsorbed via SGLT2 in the proximal tubule (SGLT1 is responsible for the remaining 10%) so that glucose calories are not eliminated through urine.1 In a healthy person, the renal glucose threshold is about 180 mg/dL.1 When blood glucose exceeds this level, glucose is excreted into the urine. However, in diabetic patients, this threshold is higher due to the up-regulation of SGLT2s (and other glucose transporters), which worsens hyperglycemia.1 SGLT2 inhibitors will reset the threshold, which in turn will increase glucosuria and thereby lower serum glucose.1
SGLT2 inhibitors lower A1C by about 0.7% to 0.8%.2 Independent of other mechanisms such as the degree of b-cell function or insulin resistance, these agents can be used regardless of the duration of diabetes3 if the GFR is intact (≥ 45 mL/min/1.73 m2 for canagliflozin and empagliflozin, ≥ 60 mL/min/ 1.73 m2 for dapagliflozin).4,5
What are the risks and benefits associated with these agents?
What are the risks and benefits associated with these agents?
Modest weight loss is seen with the use of SGLT2 inhibitors. Initial weight loss is believed to be related to volume loss, but more sustained weight loss is thought to be from loss of fat mass.6 This is not surprising, as excreting glucose means excreting calories through urine.
Risk for hypoglycemia is extremely low, which makes this therapeutic class an attractive option. However, caution should be exercised when SGLT2 inhibitors are combined with other agents known to cause hypoglycemia (sulfonylureas and insulin).6
The most common adverse effect is genital mycotic infection. Women with a history of recurrent genital mycotic infection and uncircumcised men are at the greatest risk.6
Due to increased glycosuria, which results in an osmotic diuresis, modest blood pressure improvement has been seen (3 to 4 mm Hg systolic and 1 to 2 mm Hg diastolic7,8) in patients taking SGLT2 inhibitors, which is an additional benefit for hypertensive diabetic patients.6 On the other hand, use of SGLT2 inhibitors can also cause dehydration and volume depletion and can raise serum creatinine in patients who are already taking diuretics (particularly loop diuretics).6 Drug tolerance and adherence can be improved by advising patients to expect transient increased urination (approximately 135 to 350 mL/d increase from baseline5,9) and emphasizing the importance of good hydration and maintaining good genital hygiene.
A slight increase in LDL cholesterol was seen in clinical trials of the SGLT2 inhibitors, although this phenomenon is poorly understood. However, HDL cholesterol increased as well, maintaining the LDL:HDL ratio.6 No long-term cardiovascular outcome data are available at this time; as with any new antidiabetic medication, postmarketing studies, as required by the FDA, are currently ongoing.6
What are the options in this therapeutic category, and how are they distinct?
What are the options in this therapeutic category, and how are they distinct?
As mentioned previously, there are currently three SGLT2 inhibitors on the market: canagliflozin, dapagliflozin, and empagliflozin. There are subtle clinical differences among these three agents, which might direct the clinician’s choice.
First, canagliflozin is available in dosages of 100 and 300 mg. The starting dosage is 100 mg, which can be titrated to 300 mg in patients with a GFR ≥ 60 mL/min/1.73 m2 who require a greater glucose-lowering effect. Those with a GFR < 60 mL/min/1.73 m2 but ≥ 45 mL/min/1.73 m2 are limited to the 100-mg dosage. Dapagliflozin is available in 5-mg and 10-mg dosages, the former being the starting dosage. But dapagliflozin is not recommended in patients whose GFR is < 60 mL/min/1.73 m2.4
Empagliflozin is available in dosages of 10 and 25 mg. The starting dosage of 10 mg can be increased to 25 mg if the patient has not achieved his/her target glucose level. Either can be used in patients with a GFR ≥ 45 mL/min/1.73 m2.5
Second, hyperkalemia was seen in patients taking canagliflozin but not in those taking dapagliflozin or empagliflozin. Therefore, serum potassium should be monitored and caution used, especially when patients are being treated with potassium-sparing diuretics and/or ACE inhibitors or angiotensin II receptor blockers.6
Third, dapagliflozin carries a warning for bladder cancer, as higher rates of newly diagnosed bladder cancer were seen with this drug compared with placebo or comparator drugs (0.17% vs 0.03%, respectively).4 However, this finding may have resulted from a randomization imbalance of patients in the study, and further research is needed to clarify this risk.6 It is not recommended that dapagliflozin be used in patients with active or a history of bladder cancer at this time.
With these agents, there is a paradoxical rise in glucagon that increases endogenous glucose production from the liver.10 The mechanism is poorly understood, but it might be due to the body’s compensatory (survival) mechanism to “make up” the loss of glucose through urine by increasing hepatic gluconeogenesis.
Using an incretin agent, such as dipeptidyl peptidase 4 (DPP-4) inhibitors or glucagon-like peptide 1 (GLP-1) receptor agonists, in conjunction with an SGLT2 inhibitor, has been suggested as a way to potentiate the glucose-lowering effect, as it may attenuate the paradoxical rise in glucagon.10 Since the incretin class is weight neutral (DPP-4 inhibitors) or associated with weight loss (GLP-1 agonists), using incretins with SGLT2 inhibitors might produce more significant weight loss, which has numerous additional benefits for diabetic patients.
SGLT2 inhibitors are currently approved as an adjunct to diet and exercise for patients with type 2 diabetes. They are not approved for those with type 1 diabetes, although the mechanism of action of these drugs (which is independent of the b-cell function) might make them effective in this population. Active pilot studies of this patient population are in progress.11
Conclusion
In summary, SGLT2 inhibitors are an exciting new class of antidiabetic medication that offers a unique mechanism to lower serum glucose. It is the only medication that will actually remove glucose from the body; by contrast, all other existing antidiabetic medications move glucose within the body (to liver, fat, muscle, etc).
There is no curative medication for diabetes. But with an increasing diabetic population and an emphasis on individualizing antihyperglycemic regimens, we always welcome medications with novel mechanisms of action. Due to SLGT2 inhibitors’ recent approval, however, short-term and long-term adverse effects are unknown, and ongoing postmarketing surveillance should be closely followed.
References
1. Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782-790.
2. Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
3. Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care. 2009;32:1656-1662.
4. Taylor JR. Dapagliflozin offers differences from other SGLT2 inhibitors. Endocrine Today. May 2014.
5. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2014.
6. Bakris G, Fonseca VA, Peters AL, Wysham CH. Clinical perspectives on the role of the kidney in the pathophysiology of T2DM: emerging options for treatment [video series]. 2013. www.thedoctorschannel.com/view/the-kid ney-in-t2dm-cme-part-1/. Accessed September 12, 2014.
7. Vercruysse F. Efficacy and safety of canagliflozin in subjects with type 2 diabetes mellitus inadequately controlled with metformin plus sulphonylurea over 52 weeks [abstract 934]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
8. Hach T. Empagliflozin improves glycaemic parameters and cardiovascular risk factors in patients with type 2 diabetes: pooled data from four pivotal phase III trials [abstract 943]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
9. List JF, Woo V, Morales E, et al. Sodium-glucose co-transport inhibition with dapagliflozin in type 2 diabetes mellitus. Diabetes Care. 2009;32(4):650-657.
10. Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(5):2287.
11. Perkins BA, Cherney DZ, Partridge H, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480-1483.
A 37-year-old woman with a history of papillary carcinoma (status post total thyroidectomy 12 years ago, with negative recurrence) presents for a check-up. She also has polycystic ovarian syndrome (PCOS) with obesity and is taking metformin XR (one 500-mg tablet bid). Her visit is uneventful, and she leaves the office with an order for labwork.
Results indicate normal thyroid function and negative thyroglobulin. However, her serum glucose level is 350 mg/dL, so the patient is called and informed of the result. She denies polyphagia, polydipsia, and polyuria. Repeat blood work confirms overt hyperglycemia (320 mg/dL) with an A1C of 13%, undetectable C-peptide, and negative glutamic acid decarboxylase 65 (GAD65) and islet cell antibodies.
She is advised to increase her metformin dose (to two 500-mg tablets bid) and is started on insulin detemir (20 U every evening), with instructions to increase the latter by three units every two to three days until a target fasting glucose level of 100 to 140 mg/dL is achieved. She is also advised to follow a low-carbohydrate diet and increase her exercise.
The patient returns in two weeks for follow-up. She remains asymptomatic and has now increased her insulin detemir to 34 U bid (she started splitting the dosage after it reached 50 U/d). However, her glucose is still in the low 200s in the morning and the high 200s during the day (after lunch and dinner).
Her overt hyperglycemia is most likely a result of her longstanding insulin resistance, essential lack of b-cell function, and PCOS-associated obesity. Once diabetes from autoimmunity is ruled out by laboratory findings (negative antibodies) and clinical assessment (classic metabolic syndrome features), we focus on her glycemic control.
Even with nearly 70 U/d of insulin, the patient’s glycemic improvement is disappointing, suggesting significant insulin resistance and glucose toxicity. Living in an era with numerous classes of antidiabetic medications, we have lengthy discussions on treatment options. Canagliflozin, recently (at the time) approved, is included. The patient is interested in this new medication, and it is a reasonable choice to get her out of the glucotoxic phase.
After a discussion of benefits and potential adverse effects, she is placed on canagliflozin 100 mg/d. Her glucose log in one week shows fasting glucose values in the range of 140 to 160 mg/dL and postprandial glucose values in the 180s. As a result, she lowers her insulin to 25 U bid. Her renal panel shows a potassium level of 4.3 mEq/L (reference range, 3.5 to 5.3) and a glomerular filtration rate (GFR) of 103 mL/min/1.73 m2. She is advised to further increase her canagliflozin to 300 mg and slowly titrate her insulin down as needed, with a target fasting glucose level of 80 to 110 mg/dL and a postprandial target of 100 to 140 mg/dL.
What are SGLT2 inhibitors, and how do they work?
What are SGLT2 inhibitors, and how do they work?
Sodium-GLucose co-Transporter 2 (SGLT2) inhibitors are a new class of antihyperglycemic agent. The first, canagliflozin, was approved by the FDA in March 2013, followed by dapagliflozin (January 2014) and empagliflozin (August 2014).
As glucose is filtered through the nephrons of the kidney, about 90% is reabsorbed via SGLT2 in the proximal tubule (SGLT1 is responsible for the remaining 10%) so that glucose calories are not eliminated through urine.1 In a healthy person, the renal glucose threshold is about 180 mg/dL.1 When blood glucose exceeds this level, glucose is excreted into the urine. However, in diabetic patients, this threshold is higher due to the up-regulation of SGLT2s (and other glucose transporters), which worsens hyperglycemia.1 SGLT2 inhibitors will reset the threshold, which in turn will increase glucosuria and thereby lower serum glucose.1
SGLT2 inhibitors lower A1C by about 0.7% to 0.8%.2 Independent of other mechanisms such as the degree of b-cell function or insulin resistance, these agents can be used regardless of the duration of diabetes3 if the GFR is intact (≥ 45 mL/min/1.73 m2 for canagliflozin and empagliflozin, ≥ 60 mL/min/ 1.73 m2 for dapagliflozin).4,5
What are the risks and benefits associated with these agents?
What are the risks and benefits associated with these agents?
Modest weight loss is seen with the use of SGLT2 inhibitors. Initial weight loss is believed to be related to volume loss, but more sustained weight loss is thought to be from loss of fat mass.6 This is not surprising, as excreting glucose means excreting calories through urine.
Risk for hypoglycemia is extremely low, which makes this therapeutic class an attractive option. However, caution should be exercised when SGLT2 inhibitors are combined with other agents known to cause hypoglycemia (sulfonylureas and insulin).6
The most common adverse effect is genital mycotic infection. Women with a history of recurrent genital mycotic infection and uncircumcised men are at the greatest risk.6
Due to increased glycosuria, which results in an osmotic diuresis, modest blood pressure improvement has been seen (3 to 4 mm Hg systolic and 1 to 2 mm Hg diastolic7,8) in patients taking SGLT2 inhibitors, which is an additional benefit for hypertensive diabetic patients.6 On the other hand, use of SGLT2 inhibitors can also cause dehydration and volume depletion and can raise serum creatinine in patients who are already taking diuretics (particularly loop diuretics).6 Drug tolerance and adherence can be improved by advising patients to expect transient increased urination (approximately 135 to 350 mL/d increase from baseline5,9) and emphasizing the importance of good hydration and maintaining good genital hygiene.
A slight increase in LDL cholesterol was seen in clinical trials of the SGLT2 inhibitors, although this phenomenon is poorly understood. However, HDL cholesterol increased as well, maintaining the LDL:HDL ratio.6 No long-term cardiovascular outcome data are available at this time; as with any new antidiabetic medication, postmarketing studies, as required by the FDA, are currently ongoing.6
What are the options in this therapeutic category, and how are they distinct?
What are the options in this therapeutic category, and how are they distinct?
As mentioned previously, there are currently three SGLT2 inhibitors on the market: canagliflozin, dapagliflozin, and empagliflozin. There are subtle clinical differences among these three agents, which might direct the clinician’s choice.
First, canagliflozin is available in dosages of 100 and 300 mg. The starting dosage is 100 mg, which can be titrated to 300 mg in patients with a GFR ≥ 60 mL/min/1.73 m2 who require a greater glucose-lowering effect. Those with a GFR < 60 mL/min/1.73 m2 but ≥ 45 mL/min/1.73 m2 are limited to the 100-mg dosage. Dapagliflozin is available in 5-mg and 10-mg dosages, the former being the starting dosage. But dapagliflozin is not recommended in patients whose GFR is < 60 mL/min/1.73 m2.4
Empagliflozin is available in dosages of 10 and 25 mg. The starting dosage of 10 mg can be increased to 25 mg if the patient has not achieved his/her target glucose level. Either can be used in patients with a GFR ≥ 45 mL/min/1.73 m2.5
Second, hyperkalemia was seen in patients taking canagliflozin but not in those taking dapagliflozin or empagliflozin. Therefore, serum potassium should be monitored and caution used, especially when patients are being treated with potassium-sparing diuretics and/or ACE inhibitors or angiotensin II receptor blockers.6
Third, dapagliflozin carries a warning for bladder cancer, as higher rates of newly diagnosed bladder cancer were seen with this drug compared with placebo or comparator drugs (0.17% vs 0.03%, respectively).4 However, this finding may have resulted from a randomization imbalance of patients in the study, and further research is needed to clarify this risk.6 It is not recommended that dapagliflozin be used in patients with active or a history of bladder cancer at this time.
With these agents, there is a paradoxical rise in glucagon that increases endogenous glucose production from the liver.10 The mechanism is poorly understood, but it might be due to the body’s compensatory (survival) mechanism to “make up” the loss of glucose through urine by increasing hepatic gluconeogenesis.
Using an incretin agent, such as dipeptidyl peptidase 4 (DPP-4) inhibitors or glucagon-like peptide 1 (GLP-1) receptor agonists, in conjunction with an SGLT2 inhibitor, has been suggested as a way to potentiate the glucose-lowering effect, as it may attenuate the paradoxical rise in glucagon.10 Since the incretin class is weight neutral (DPP-4 inhibitors) or associated with weight loss (GLP-1 agonists), using incretins with SGLT2 inhibitors might produce more significant weight loss, which has numerous additional benefits for diabetic patients.
SGLT2 inhibitors are currently approved as an adjunct to diet and exercise for patients with type 2 diabetes. They are not approved for those with type 1 diabetes, although the mechanism of action of these drugs (which is independent of the b-cell function) might make them effective in this population. Active pilot studies of this patient population are in progress.11
Conclusion
In summary, SGLT2 inhibitors are an exciting new class of antidiabetic medication that offers a unique mechanism to lower serum glucose. It is the only medication that will actually remove glucose from the body; by contrast, all other existing antidiabetic medications move glucose within the body (to liver, fat, muscle, etc).
There is no curative medication for diabetes. But with an increasing diabetic population and an emphasis on individualizing antihyperglycemic regimens, we always welcome medications with novel mechanisms of action. Due to SLGT2 inhibitors’ recent approval, however, short-term and long-term adverse effects are unknown, and ongoing postmarketing surveillance should be closely followed.
References
1. Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782-790.
2. Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
3. Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care. 2009;32:1656-1662.
4. Taylor JR. Dapagliflozin offers differences from other SGLT2 inhibitors. Endocrine Today. May 2014.
5. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2014.
6. Bakris G, Fonseca VA, Peters AL, Wysham CH. Clinical perspectives on the role of the kidney in the pathophysiology of T2DM: emerging options for treatment [video series]. 2013. www.thedoctorschannel.com/view/the-kid ney-in-t2dm-cme-part-1/. Accessed September 12, 2014.
7. Vercruysse F. Efficacy and safety of canagliflozin in subjects with type 2 diabetes mellitus inadequately controlled with metformin plus sulphonylurea over 52 weeks [abstract 934]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
8. Hach T. Empagliflozin improves glycaemic parameters and cardiovascular risk factors in patients with type 2 diabetes: pooled data from four pivotal phase III trials [abstract 943]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
9. List JF, Woo V, Morales E, et al. Sodium-glucose co-transport inhibition with dapagliflozin in type 2 diabetes mellitus. Diabetes Care. 2009;32(4):650-657.
10. Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(5):2287.
11. Perkins BA, Cherney DZ, Partridge H, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480-1483.
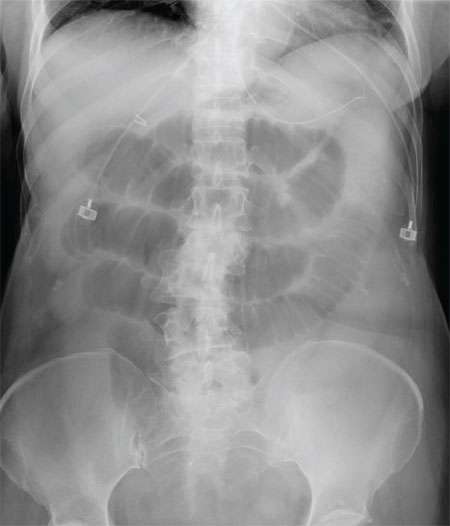
Nausea, Vomiting, and Worsening Pain
ANSWER
The radiograph shows multiple stacked dilated loops of small bowel. The colon does not appear distended. (A nasogastric tube is also present, and there are degenerative changes in the spine.) Such a finding is typically associated with at least a partial small bowel obstruction, since no definite air fluid levels are noted.
The patient was admitted and made npo. Nasogastric decompression was started, and general surgery consultation was obtained.
ANSWER
The radiograph shows multiple stacked dilated loops of small bowel. The colon does not appear distended. (A nasogastric tube is also present, and there are degenerative changes in the spine.) Such a finding is typically associated with at least a partial small bowel obstruction, since no definite air fluid levels are noted.
The patient was admitted and made npo. Nasogastric decompression was started, and general surgery consultation was obtained.
ANSWER
The radiograph shows multiple stacked dilated loops of small bowel. The colon does not appear distended. (A nasogastric tube is also present, and there are degenerative changes in the spine.) Such a finding is typically associated with at least a partial small bowel obstruction, since no definite air fluid levels are noted.
The patient was admitted and made npo. Nasogastric decompression was started, and general surgery consultation was obtained.

A 75-year-old woman presents to the emergency department with a three-day history of abdominal pain. She does not recall eating anything unusual. She reports having nausea and vomiting and states that her pain is progressively worsening. Her medical history is significant for hypertension. Surgical history is significant for previous cholecystectomy and total abdominal hysterectomy. She is afebrile, and her vital signs are within normal limits. Her abdomen is soft and diffusely tender, with slightly decreased bowel sounds. No rebound or guarding is present. The rest of her physical examination overall is within normal limits. During the exam, she experiences a couple episodes of bilious vomiting. You order some laboratory studies as well as an abdominal radiograph (shown). What is your impression?
Inspiring Americans
With the understanding that healing after war is a long-term process, Welcome Back Veterans (http://www.welcomebackveterans.org), founded by Major League Baseball Charities, the nonprofit McCormick Foundation, and the charitable Entertainment Industry Foundation, was created to “inspire Americans to reach out and help our returning veterans and their families.”
Welcome Back Veterans offers resources on PTSD, including an overview and related statistics, a detailed symptoms list, treatment information, support group names and phone numbers, and a reading list of books on PTSD, all vetted by the organization.
Highlighted veteran stories are posted in the Latest News, which are also accessible via e-mail sign-ups and RSS feeds. A robust list of family resources is available, as well as many inspiring active-duty military personnel and veteran videos.
In addition to the online resources provided for free on the website, Welcome Back Veterans is funding programs at various institutions throughout the U.S. The McCormick Foundation donation page may be accessed directly through
the homepage of Welcome Back Veterans.
With the understanding that healing after war is a long-term process, Welcome Back Veterans (http://www.welcomebackveterans.org), founded by Major League Baseball Charities, the nonprofit McCormick Foundation, and the charitable Entertainment Industry Foundation, was created to “inspire Americans to reach out and help our returning veterans and their families.”
Welcome Back Veterans offers resources on PTSD, including an overview and related statistics, a detailed symptoms list, treatment information, support group names and phone numbers, and a reading list of books on PTSD, all vetted by the organization.
Highlighted veteran stories are posted in the Latest News, which are also accessible via e-mail sign-ups and RSS feeds. A robust list of family resources is available, as well as many inspiring active-duty military personnel and veteran videos.
In addition to the online resources provided for free on the website, Welcome Back Veterans is funding programs at various institutions throughout the U.S. The McCormick Foundation donation page may be accessed directly through
the homepage of Welcome Back Veterans.
With the understanding that healing after war is a long-term process, Welcome Back Veterans (http://www.welcomebackveterans.org), founded by Major League Baseball Charities, the nonprofit McCormick Foundation, and the charitable Entertainment Industry Foundation, was created to “inspire Americans to reach out and help our returning veterans and their families.”
Welcome Back Veterans offers resources on PTSD, including an overview and related statistics, a detailed symptoms list, treatment information, support group names and phone numbers, and a reading list of books on PTSD, all vetted by the organization.
Highlighted veteran stories are posted in the Latest News, which are also accessible via e-mail sign-ups and RSS feeds. A robust list of family resources is available, as well as many inspiring active-duty military personnel and veteran videos.
In addition to the online resources provided for free on the website, Welcome Back Veterans is funding programs at various institutions throughout the U.S. The McCormick Foundation donation page may be accessed directly through
the homepage of Welcome Back Veterans.
Molecule enables ‘robust’ expansion of cord blood cells

Credit: NHS
Investigators say they have identified a molecule that allows for robust ex vivo expansion of human cord blood (CB) cells.
CB cells expanded with this molecule, known as UM171, were capable of human hematopoietic reconstitution in NSG mice, an effect that lasted more than 6 months.
The researchers believe UM171 acts by enhancing the long-term-hematopoietic stem cell (LT-HSC) self-renewal machinery independently of AhR suppression.
Guy Sauvageau, MD, PhD, of the University of Montreal in Quebec, Canada, and his colleagues identified UM171 and described the discovery in Science.
The team first screened a library of 5280 low-molecular-weight compounds looking for those with the ability to expand human CD34+CD45RA- mobilized peripheral blood cells, which are enriched in LT-HSCs.
They got 7 hits, and only 2 of these—UM729 and UM118428—did not suppress the AhR pathway. The researchers selected UM729 for further characterization and optimization because it demonstrated superior activity in expanding CD34+CD45RA- cells.
The investigators analyzed more than 300 newly synthesized analogs of UM729 and identified one that was 10 to 20 times more potent than UM729. That compound was UM171.
UM171 could expand CD34+CD45RA- cells at concentrations of 17 nM to 19 nM. The highest expansion of multipotent progenitors and long-term culture-initiating cells occurred on day 12.
The effect of UM171 required its constant presence in the media, and the compound lacked direct mitogenic activity. UM171 did not affect the division rate of phenotypically primitive cell populations.
The researchers compared UM171 to SR1 (a compound known to promote self-renewal of HSCs) in fed-batch culture. They found that frequencies of CD34+ CB cells were similar in cultures containing SR1 and those containing UM171. But CD34+CD45RA- cells were more abundant with UM171 (P<0.005).
The team then evaluated LT-HSC populations. Twenty weeks after CD34+ CB cells were transplanted into mice, LT-HSC frequencies were similar in mice that received control and SR1-expanded cells. But LT-HSC frequencies were 13-fold higher in the mice that received UM171-expanded cells.
Next, the investigators assessed human hematopoietic reconstitution in NSG mice transplanted with fresh or expanded cells. They observed 2 patterns of reconstitution. One was from predominantly lymphomyeloid LT-HSCs that occurred with high cell doses in most conditions.
And the other was from LT-HSCs that display a lymphoid-deficient differentiation phenotype mostly observed with UM171 treatment, with or without SR1. However, UM171 did not negatively affect B lymphopoiesis or the frequency or number of lymphomyeloid LT-HSCs.
The impact of UM171 on LT-HSCs was preserved at 30 weeks post-transplant. And myeloid cell output was slightly augmented, a phenomenon that has been observed with normal, unexpanded cells.
The researchers also transplanted UM171-treated LT-HSC populations into secondary recipients. And they found the cells were still competent, but they had no advantage over unmanipulated CD34+ cells.
A clinical study of UM171 and a new type of bioreactor developed for stem cell culture is set to begin this December. The cells will be expanded at Maisonneuve-Rosemont Hospital, and grafts will be distributed to patients in Montreal, Quebec City, and Vancouver. The investigators expect tangible results will be available in December 2015. ![]()

Credit: NHS
Investigators say they have identified a molecule that allows for robust ex vivo expansion of human cord blood (CB) cells.
CB cells expanded with this molecule, known as UM171, were capable of human hematopoietic reconstitution in NSG mice, an effect that lasted more than 6 months.
The researchers believe UM171 acts by enhancing the long-term-hematopoietic stem cell (LT-HSC) self-renewal machinery independently of AhR suppression.
Guy Sauvageau, MD, PhD, of the University of Montreal in Quebec, Canada, and his colleagues identified UM171 and described the discovery in Science.
The team first screened a library of 5280 low-molecular-weight compounds looking for those with the ability to expand human CD34+CD45RA- mobilized peripheral blood cells, which are enriched in LT-HSCs.
They got 7 hits, and only 2 of these—UM729 and UM118428—did not suppress the AhR pathway. The researchers selected UM729 for further characterization and optimization because it demonstrated superior activity in expanding CD34+CD45RA- cells.
The investigators analyzed more than 300 newly synthesized analogs of UM729 and identified one that was 10 to 20 times more potent than UM729. That compound was UM171.
UM171 could expand CD34+CD45RA- cells at concentrations of 17 nM to 19 nM. The highest expansion of multipotent progenitors and long-term culture-initiating cells occurred on day 12.
The effect of UM171 required its constant presence in the media, and the compound lacked direct mitogenic activity. UM171 did not affect the division rate of phenotypically primitive cell populations.
The researchers compared UM171 to SR1 (a compound known to promote self-renewal of HSCs) in fed-batch culture. They found that frequencies of CD34+ CB cells were similar in cultures containing SR1 and those containing UM171. But CD34+CD45RA- cells were more abundant with UM171 (P<0.005).
The team then evaluated LT-HSC populations. Twenty weeks after CD34+ CB cells were transplanted into mice, LT-HSC frequencies were similar in mice that received control and SR1-expanded cells. But LT-HSC frequencies were 13-fold higher in the mice that received UM171-expanded cells.
Next, the investigators assessed human hematopoietic reconstitution in NSG mice transplanted with fresh or expanded cells. They observed 2 patterns of reconstitution. One was from predominantly lymphomyeloid LT-HSCs that occurred with high cell doses in most conditions.
And the other was from LT-HSCs that display a lymphoid-deficient differentiation phenotype mostly observed with UM171 treatment, with or without SR1. However, UM171 did not negatively affect B lymphopoiesis or the frequency or number of lymphomyeloid LT-HSCs.
The impact of UM171 on LT-HSCs was preserved at 30 weeks post-transplant. And myeloid cell output was slightly augmented, a phenomenon that has been observed with normal, unexpanded cells.
The researchers also transplanted UM171-treated LT-HSC populations into secondary recipients. And they found the cells were still competent, but they had no advantage over unmanipulated CD34+ cells.
A clinical study of UM171 and a new type of bioreactor developed for stem cell culture is set to begin this December. The cells will be expanded at Maisonneuve-Rosemont Hospital, and grafts will be distributed to patients in Montreal, Quebec City, and Vancouver. The investigators expect tangible results will be available in December 2015. ![]()

Credit: NHS
Investigators say they have identified a molecule that allows for robust ex vivo expansion of human cord blood (CB) cells.
CB cells expanded with this molecule, known as UM171, were capable of human hematopoietic reconstitution in NSG mice, an effect that lasted more than 6 months.
The researchers believe UM171 acts by enhancing the long-term-hematopoietic stem cell (LT-HSC) self-renewal machinery independently of AhR suppression.
Guy Sauvageau, MD, PhD, of the University of Montreal in Quebec, Canada, and his colleagues identified UM171 and described the discovery in Science.
The team first screened a library of 5280 low-molecular-weight compounds looking for those with the ability to expand human CD34+CD45RA- mobilized peripheral blood cells, which are enriched in LT-HSCs.
They got 7 hits, and only 2 of these—UM729 and UM118428—did not suppress the AhR pathway. The researchers selected UM729 for further characterization and optimization because it demonstrated superior activity in expanding CD34+CD45RA- cells.
The investigators analyzed more than 300 newly synthesized analogs of UM729 and identified one that was 10 to 20 times more potent than UM729. That compound was UM171.
UM171 could expand CD34+CD45RA- cells at concentrations of 17 nM to 19 nM. The highest expansion of multipotent progenitors and long-term culture-initiating cells occurred on day 12.
The effect of UM171 required its constant presence in the media, and the compound lacked direct mitogenic activity. UM171 did not affect the division rate of phenotypically primitive cell populations.
The researchers compared UM171 to SR1 (a compound known to promote self-renewal of HSCs) in fed-batch culture. They found that frequencies of CD34+ CB cells were similar in cultures containing SR1 and those containing UM171. But CD34+CD45RA- cells were more abundant with UM171 (P<0.005).
The team then evaluated LT-HSC populations. Twenty weeks after CD34+ CB cells were transplanted into mice, LT-HSC frequencies were similar in mice that received control and SR1-expanded cells. But LT-HSC frequencies were 13-fold higher in the mice that received UM171-expanded cells.
Next, the investigators assessed human hematopoietic reconstitution in NSG mice transplanted with fresh or expanded cells. They observed 2 patterns of reconstitution. One was from predominantly lymphomyeloid LT-HSCs that occurred with high cell doses in most conditions.
And the other was from LT-HSCs that display a lymphoid-deficient differentiation phenotype mostly observed with UM171 treatment, with or without SR1. However, UM171 did not negatively affect B lymphopoiesis or the frequency or number of lymphomyeloid LT-HSCs.
The impact of UM171 on LT-HSCs was preserved at 30 weeks post-transplant. And myeloid cell output was slightly augmented, a phenomenon that has been observed with normal, unexpanded cells.
The researchers also transplanted UM171-treated LT-HSC populations into secondary recipients. And they found the cells were still competent, but they had no advantage over unmanipulated CD34+ cells.
A clinical study of UM171 and a new type of bioreactor developed for stem cell culture is set to begin this December. The cells will be expanded at Maisonneuve-Rosemont Hospital, and grafts will be distributed to patients in Montreal, Quebec City, and Vancouver. The investigators expect tangible results will be available in December 2015. ![]()
Predicting chemo drugs’ effects on male fertility

Credit: Rhoda Baer
A mathematical formula may help physicians predict which cancer survivors are likely to have normal sperm production following chemotherapy with alkylating agents.
Researchers developed the formula to calculate survivors’ cumulative treatment exposure to alkylating agents as a cyclophosphamide-equivalent dose (CED).
The team used this formula to evaluate a cohort of cancer survivors and found that CEDs of 4 g/m2 or less were associated with normal sperm concentrations.
An account of this research was published in The Lancet Oncology.
“Based on these results, we would recommend pretreatment fertility preservation be offered, whenever clinically possible, to any male whose projected treatment is expected to include a cyclophosphamide-equivalent dose greater than 4 g/m2,” said study author Daniel Green, MD, of St Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Green and his colleagues had studied 214 male survivors of childhood cancer who had a median age of 29. Subjects had received cyclophosphamide and other alkylating agents, but their treatment did not include radiation.
The researchers performed semen analysis in the survivors a median of 21 years from their diagnosis. The analysis showed that 47.6% of survivors had normal sperm concentrations (at least 15 million per milliliter), 27.6% had low sperm counts, and 24.8% produced no sperm.
To determine the impact of alkylating agents on the survivors’ sperm production, the researchers calculated each survivor’s cumulative treatment exposure as a CED.
They did this using the following formula: CED (mg/m2)= 1.0 (cumulative cyclophosphamide dose [mg/m2]) + 0.244 (cumulative ifosfamide dose [mg/m2]) + 0.857 (cumulative procarbazine dose [mg/m2]) + 14.286 (cumulative chlorambucil dose [mg/m2]) + 15.0 (cumulative carmustine dose [mg/m2]) + 16.0 (cumulative lomustine dose [mg/m2]) + 40 (cumulative melphalan dose [mg/m2]) + 50 (cumulative thiotepa dose [mg/m2]) + 100 cumulative chlormethine dose [mg/m2]) + 8.823 (cumulative busulfan dose [mg/m2]).
The researchers could not identify a uniformly safe or toxic dose of these drugs, but they found that survivor sperm concentrations generally decreased as cumulative exposure to alkylating agents increased.
And CEDs of 4 g/m2 or less were associated with normal sperm concentrations. Almost 89% of survivors whose CED was 4 g/m2 or less had a normal sperm count. Their sperm were also more likely than sperm from other survivors to look and behave normally.
Dr Green did note that, although a lower cumulative dose of alkylating agents was associated with normal sperm production, outcomes for individual patients were unpredictable and varied. ![]()

Credit: Rhoda Baer
A mathematical formula may help physicians predict which cancer survivors are likely to have normal sperm production following chemotherapy with alkylating agents.
Researchers developed the formula to calculate survivors’ cumulative treatment exposure to alkylating agents as a cyclophosphamide-equivalent dose (CED).
The team used this formula to evaluate a cohort of cancer survivors and found that CEDs of 4 g/m2 or less were associated with normal sperm concentrations.
An account of this research was published in The Lancet Oncology.
“Based on these results, we would recommend pretreatment fertility preservation be offered, whenever clinically possible, to any male whose projected treatment is expected to include a cyclophosphamide-equivalent dose greater than 4 g/m2,” said study author Daniel Green, MD, of St Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Green and his colleagues had studied 214 male survivors of childhood cancer who had a median age of 29. Subjects had received cyclophosphamide and other alkylating agents, but their treatment did not include radiation.
The researchers performed semen analysis in the survivors a median of 21 years from their diagnosis. The analysis showed that 47.6% of survivors had normal sperm concentrations (at least 15 million per milliliter), 27.6% had low sperm counts, and 24.8% produced no sperm.
To determine the impact of alkylating agents on the survivors’ sperm production, the researchers calculated each survivor’s cumulative treatment exposure as a CED.
They did this using the following formula: CED (mg/m2)= 1.0 (cumulative cyclophosphamide dose [mg/m2]) + 0.244 (cumulative ifosfamide dose [mg/m2]) + 0.857 (cumulative procarbazine dose [mg/m2]) + 14.286 (cumulative chlorambucil dose [mg/m2]) + 15.0 (cumulative carmustine dose [mg/m2]) + 16.0 (cumulative lomustine dose [mg/m2]) + 40 (cumulative melphalan dose [mg/m2]) + 50 (cumulative thiotepa dose [mg/m2]) + 100 cumulative chlormethine dose [mg/m2]) + 8.823 (cumulative busulfan dose [mg/m2]).
The researchers could not identify a uniformly safe or toxic dose of these drugs, but they found that survivor sperm concentrations generally decreased as cumulative exposure to alkylating agents increased.
And CEDs of 4 g/m2 or less were associated with normal sperm concentrations. Almost 89% of survivors whose CED was 4 g/m2 or less had a normal sperm count. Their sperm were also more likely than sperm from other survivors to look and behave normally.
Dr Green did note that, although a lower cumulative dose of alkylating agents was associated with normal sperm production, outcomes for individual patients were unpredictable and varied. ![]()

Credit: Rhoda Baer
A mathematical formula may help physicians predict which cancer survivors are likely to have normal sperm production following chemotherapy with alkylating agents.
Researchers developed the formula to calculate survivors’ cumulative treatment exposure to alkylating agents as a cyclophosphamide-equivalent dose (CED).
The team used this formula to evaluate a cohort of cancer survivors and found that CEDs of 4 g/m2 or less were associated with normal sperm concentrations.
An account of this research was published in The Lancet Oncology.
“Based on these results, we would recommend pretreatment fertility preservation be offered, whenever clinically possible, to any male whose projected treatment is expected to include a cyclophosphamide-equivalent dose greater than 4 g/m2,” said study author Daniel Green, MD, of St Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Green and his colleagues had studied 214 male survivors of childhood cancer who had a median age of 29. Subjects had received cyclophosphamide and other alkylating agents, but their treatment did not include radiation.
The researchers performed semen analysis in the survivors a median of 21 years from their diagnosis. The analysis showed that 47.6% of survivors had normal sperm concentrations (at least 15 million per milliliter), 27.6% had low sperm counts, and 24.8% produced no sperm.
To determine the impact of alkylating agents on the survivors’ sperm production, the researchers calculated each survivor’s cumulative treatment exposure as a CED.
They did this using the following formula: CED (mg/m2)= 1.0 (cumulative cyclophosphamide dose [mg/m2]) + 0.244 (cumulative ifosfamide dose [mg/m2]) + 0.857 (cumulative procarbazine dose [mg/m2]) + 14.286 (cumulative chlorambucil dose [mg/m2]) + 15.0 (cumulative carmustine dose [mg/m2]) + 16.0 (cumulative lomustine dose [mg/m2]) + 40 (cumulative melphalan dose [mg/m2]) + 50 (cumulative thiotepa dose [mg/m2]) + 100 cumulative chlormethine dose [mg/m2]) + 8.823 (cumulative busulfan dose [mg/m2]).
The researchers could not identify a uniformly safe or toxic dose of these drugs, but they found that survivor sperm concentrations generally decreased as cumulative exposure to alkylating agents increased.
And CEDs of 4 g/m2 or less were associated with normal sperm concentrations. Almost 89% of survivors whose CED was 4 g/m2 or less had a normal sperm count. Their sperm were also more likely than sperm from other survivors to look and behave normally.
Dr Green did note that, although a lower cumulative dose of alkylating agents was associated with normal sperm production, outcomes for individual patients were unpredictable and varied. ![]()
Disrupting equilibrium to fight AML

Credit: Lance Liotta
Understanding the relationship between mutated and wild-type genes could lead to new therapies for acute myeloid leukemia (AML), according to researchers.
The group discovered that RUNX1/ETO, generated by the chromosomal translocation t(8;21), regulates a leukemia-propagating transcriptional network via a dynamic equilibrium with RUNX1.
But depleting RUNX1/ETO prompts the formation of a transcriptional network that promotes myeloid differentiation.
Constanze Bonifer, PhD, of the University of Birmingham in the UK, and her colleagues detailed this work in Cell Reports.
The researchers likened normal hematopoiesis to a production line, with genes acting as regulators to control each step of blood formation. When a mutation occurs in the relevant regulator genes, the finely balanced order of the production line is disrupted, with drastic consequences.
Using digital footprinting and chromatin immunoprecipitation sequencing, the team showed that RUNX1/ETO switches off hundreds of other genes, many of them regulators themselves. As a consequence of the drastically altered production line, normal blood formation cannot happen, and leukemic cells form.
“Understanding how these rogue regulators operate is essential,” Dr Bonifer said. “[T]hese leukemic cells have one mutated gene and one unchanged one that would make the normal regulator. What happens in the leukemic cell is fundamentally a battle for supremacy between the two regulators, and the mutated one wins much of the time.”
“This is compounded by the normal regulator, which tries to compensate for defeat, and, in doing so, changes the output of genes that would be otherwise unaffected by the abnormal regulator. Quite simply, the result is a real mess. The cells are confused and can’t develop into mature blood cells.”
More specifically, the researchers found that the transcriptional program underlying leukemic propagation is regulated by a dynamic equilibrium between RUNX1/ETO and RUNX1 complexes.
Disrupting this equilibrium in t(8;21) cells by depleting RUNX1/ETO led to a global redistribution of transcription factor complexes within pre-existing open chromatin. And this prompted the formation of a transcriptional network that drives myeloid differentiation.
“If targeting [RUNX1/ETO] can reverse the changes it is making to the cellular production line, then it would ultimately point towards new avenues for a more precise treatment of leukemia,” said study author Olaf Heidenreich, PhD, of Newcastle University in the UK.
“Knowing that the production line can be restored to normal function gives us real hope. Of course, that is much easier to do in the lab than it is in the human body. But now we know how this works, we can look to deliver inhibitors to those mutated regulators. Creating one that works is the next step we have to overcome.” ![]()

Credit: Lance Liotta
Understanding the relationship between mutated and wild-type genes could lead to new therapies for acute myeloid leukemia (AML), according to researchers.
The group discovered that RUNX1/ETO, generated by the chromosomal translocation t(8;21), regulates a leukemia-propagating transcriptional network via a dynamic equilibrium with RUNX1.
But depleting RUNX1/ETO prompts the formation of a transcriptional network that promotes myeloid differentiation.
Constanze Bonifer, PhD, of the University of Birmingham in the UK, and her colleagues detailed this work in Cell Reports.
The researchers likened normal hematopoiesis to a production line, with genes acting as regulators to control each step of blood formation. When a mutation occurs in the relevant regulator genes, the finely balanced order of the production line is disrupted, with drastic consequences.
Using digital footprinting and chromatin immunoprecipitation sequencing, the team showed that RUNX1/ETO switches off hundreds of other genes, many of them regulators themselves. As a consequence of the drastically altered production line, normal blood formation cannot happen, and leukemic cells form.
“Understanding how these rogue regulators operate is essential,” Dr Bonifer said. “[T]hese leukemic cells have one mutated gene and one unchanged one that would make the normal regulator. What happens in the leukemic cell is fundamentally a battle for supremacy between the two regulators, and the mutated one wins much of the time.”
“This is compounded by the normal regulator, which tries to compensate for defeat, and, in doing so, changes the output of genes that would be otherwise unaffected by the abnormal regulator. Quite simply, the result is a real mess. The cells are confused and can’t develop into mature blood cells.”
More specifically, the researchers found that the transcriptional program underlying leukemic propagation is regulated by a dynamic equilibrium between RUNX1/ETO and RUNX1 complexes.
Disrupting this equilibrium in t(8;21) cells by depleting RUNX1/ETO led to a global redistribution of transcription factor complexes within pre-existing open chromatin. And this prompted the formation of a transcriptional network that drives myeloid differentiation.
“If targeting [RUNX1/ETO] can reverse the changes it is making to the cellular production line, then it would ultimately point towards new avenues for a more precise treatment of leukemia,” said study author Olaf Heidenreich, PhD, of Newcastle University in the UK.
“Knowing that the production line can be restored to normal function gives us real hope. Of course, that is much easier to do in the lab than it is in the human body. But now we know how this works, we can look to deliver inhibitors to those mutated regulators. Creating one that works is the next step we have to overcome.” ![]()

Credit: Lance Liotta
Understanding the relationship between mutated and wild-type genes could lead to new therapies for acute myeloid leukemia (AML), according to researchers.
The group discovered that RUNX1/ETO, generated by the chromosomal translocation t(8;21), regulates a leukemia-propagating transcriptional network via a dynamic equilibrium with RUNX1.
But depleting RUNX1/ETO prompts the formation of a transcriptional network that promotes myeloid differentiation.
Constanze Bonifer, PhD, of the University of Birmingham in the UK, and her colleagues detailed this work in Cell Reports.
The researchers likened normal hematopoiesis to a production line, with genes acting as regulators to control each step of blood formation. When a mutation occurs in the relevant regulator genes, the finely balanced order of the production line is disrupted, with drastic consequences.
Using digital footprinting and chromatin immunoprecipitation sequencing, the team showed that RUNX1/ETO switches off hundreds of other genes, many of them regulators themselves. As a consequence of the drastically altered production line, normal blood formation cannot happen, and leukemic cells form.
“Understanding how these rogue regulators operate is essential,” Dr Bonifer said. “[T]hese leukemic cells have one mutated gene and one unchanged one that would make the normal regulator. What happens in the leukemic cell is fundamentally a battle for supremacy between the two regulators, and the mutated one wins much of the time.”
“This is compounded by the normal regulator, which tries to compensate for defeat, and, in doing so, changes the output of genes that would be otherwise unaffected by the abnormal regulator. Quite simply, the result is a real mess. The cells are confused and can’t develop into mature blood cells.”
More specifically, the researchers found that the transcriptional program underlying leukemic propagation is regulated by a dynamic equilibrium between RUNX1/ETO and RUNX1 complexes.
Disrupting this equilibrium in t(8;21) cells by depleting RUNX1/ETO led to a global redistribution of transcription factor complexes within pre-existing open chromatin. And this prompted the formation of a transcriptional network that drives myeloid differentiation.
“If targeting [RUNX1/ETO] can reverse the changes it is making to the cellular production line, then it would ultimately point towards new avenues for a more precise treatment of leukemia,” said study author Olaf Heidenreich, PhD, of Newcastle University in the UK.
“Knowing that the production line can be restored to normal function gives us real hope. Of course, that is much easier to do in the lab than it is in the human body. But now we know how this works, we can look to deliver inhibitors to those mutated regulators. Creating one that works is the next step we have to overcome.” ![]()