User login
Compound can inhibit metastasis in multiple myeloma
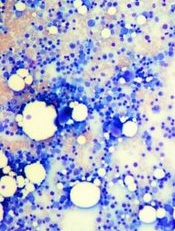
Credit: Daniel E. Sabath
A novel compound can prevent metastasis in mouse models of multiple myeloma (MM), according to research published in Cell Reports.
Investigators discovered that this compound, olaptesed pegol, can inhibit stromal cell-derived factor-1 (SDF-1), which attracts certain cells to new locations within the bone marrow.
By blocking the activity of SDF-1, olaptesed pegol renders the bone marrow uninviting to MM cells and prevents metastasis.
“Metastasis remains one of the most formidable complications we face as cancer researchers and physicians,” said study author Irene Ghobrial, MD, of the Dana-Farber Cancer Institute in Boston.
“Improvements in the treatment of metastatic cancers have, for the most part, not been nearly as dramatic as in primary disease.”
Dr Ghobrial and her colleagues studied MM because it is metastatic by nature. Myeloma cells originate in the bone marrow, depart for the bloodstream, and eventually return to the bones, where they form numerous colonies.
The team found that mice with advanced stages of MM had higher levels of SDF-1 at sites in the bones where metastasis had occurred.
“We reasoned that by neutralizing SDF-1, we could change the bone marrow environment to make it less receptive for multiple myeloma cells, reduce myeloma cells’ affinity for the marrow, and thereby inhibit the progression of the disease,” said Aldo Roccaro, MD, PhD, also of Dana-Farber.
Working with the German biotechnology company NOXXON Pharma, the investigators tested olaptesed pegol (a PEGylated mirror-image L-oligonucleotide), which binds to SDF-1.
The team found that olaptesed pegol modulates bone marrow niches and prevents MM cells from homing and engrafting to bone.
This slowed disease progression and prolonged survival in the animals, both compared to control mice and mice treated with AMD3100.
The investigators said it isn’t completely clear what becomes of the blood-borne MM cells that are prevented from metastasizing.
“We know that myeloma cells can’t survive for long if they’re circulating in the blood and can’t adhere to other tissue,” Dr Ghobrial said. “We saw no evidence that they had metastasized and begun to grow in other tissue either.”
“Our findings clearly document a therapeutic effect of olaptesed pegol in a mouse model of advanced myeloma. It is now being tested in a clinical trial of multiple myeloma patients, with more trials to come.” ![]()
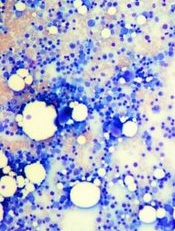
Credit: Daniel E. Sabath
A novel compound can prevent metastasis in mouse models of multiple myeloma (MM), according to research published in Cell Reports.
Investigators discovered that this compound, olaptesed pegol, can inhibit stromal cell-derived factor-1 (SDF-1), which attracts certain cells to new locations within the bone marrow.
By blocking the activity of SDF-1, olaptesed pegol renders the bone marrow uninviting to MM cells and prevents metastasis.
“Metastasis remains one of the most formidable complications we face as cancer researchers and physicians,” said study author Irene Ghobrial, MD, of the Dana-Farber Cancer Institute in Boston.
“Improvements in the treatment of metastatic cancers have, for the most part, not been nearly as dramatic as in primary disease.”
Dr Ghobrial and her colleagues studied MM because it is metastatic by nature. Myeloma cells originate in the bone marrow, depart for the bloodstream, and eventually return to the bones, where they form numerous colonies.
The team found that mice with advanced stages of MM had higher levels of SDF-1 at sites in the bones where metastasis had occurred.
“We reasoned that by neutralizing SDF-1, we could change the bone marrow environment to make it less receptive for multiple myeloma cells, reduce myeloma cells’ affinity for the marrow, and thereby inhibit the progression of the disease,” said Aldo Roccaro, MD, PhD, also of Dana-Farber.
Working with the German biotechnology company NOXXON Pharma, the investigators tested olaptesed pegol (a PEGylated mirror-image L-oligonucleotide), which binds to SDF-1.
The team found that olaptesed pegol modulates bone marrow niches and prevents MM cells from homing and engrafting to bone.
This slowed disease progression and prolonged survival in the animals, both compared to control mice and mice treated with AMD3100.
The investigators said it isn’t completely clear what becomes of the blood-borne MM cells that are prevented from metastasizing.
“We know that myeloma cells can’t survive for long if they’re circulating in the blood and can’t adhere to other tissue,” Dr Ghobrial said. “We saw no evidence that they had metastasized and begun to grow in other tissue either.”
“Our findings clearly document a therapeutic effect of olaptesed pegol in a mouse model of advanced myeloma. It is now being tested in a clinical trial of multiple myeloma patients, with more trials to come.” ![]()
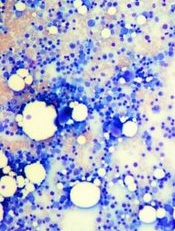
Credit: Daniel E. Sabath
A novel compound can prevent metastasis in mouse models of multiple myeloma (MM), according to research published in Cell Reports.
Investigators discovered that this compound, olaptesed pegol, can inhibit stromal cell-derived factor-1 (SDF-1), which attracts certain cells to new locations within the bone marrow.
By blocking the activity of SDF-1, olaptesed pegol renders the bone marrow uninviting to MM cells and prevents metastasis.
“Metastasis remains one of the most formidable complications we face as cancer researchers and physicians,” said study author Irene Ghobrial, MD, of the Dana-Farber Cancer Institute in Boston.
“Improvements in the treatment of metastatic cancers have, for the most part, not been nearly as dramatic as in primary disease.”
Dr Ghobrial and her colleagues studied MM because it is metastatic by nature. Myeloma cells originate in the bone marrow, depart for the bloodstream, and eventually return to the bones, where they form numerous colonies.
The team found that mice with advanced stages of MM had higher levels of SDF-1 at sites in the bones where metastasis had occurred.
“We reasoned that by neutralizing SDF-1, we could change the bone marrow environment to make it less receptive for multiple myeloma cells, reduce myeloma cells’ affinity for the marrow, and thereby inhibit the progression of the disease,” said Aldo Roccaro, MD, PhD, also of Dana-Farber.
Working with the German biotechnology company NOXXON Pharma, the investigators tested olaptesed pegol (a PEGylated mirror-image L-oligonucleotide), which binds to SDF-1.
The team found that olaptesed pegol modulates bone marrow niches and prevents MM cells from homing and engrafting to bone.
This slowed disease progression and prolonged survival in the animals, both compared to control mice and mice treated with AMD3100.
The investigators said it isn’t completely clear what becomes of the blood-borne MM cells that are prevented from metastasizing.
“We know that myeloma cells can’t survive for long if they’re circulating in the blood and can’t adhere to other tissue,” Dr Ghobrial said. “We saw no evidence that they had metastasized and begun to grow in other tissue either.”
“Our findings clearly document a therapeutic effect of olaptesed pegol in a mouse model of advanced myeloma. It is now being tested in a clinical trial of multiple myeloma patients, with more trials to come.” ![]()
Preventing cancer-related infection

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()
Pneumonia Guideline Therapy Outcomes
Community‐acquired pneumonia (CAP) is a common and serious infection in children. With more than 150,000 children requiring hospitalization annually, CAP is the fifth most prevalent and the second most costly diagnosis of all pediatric hospitalizations in the United States.[1, 2, 3]
In August 2011, the Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) published an evidence‐based guideline for the management of CAP in children. This guideline recommended that fully immunized children without underlying complications who require hospitalization receive an aminopenicillin as first‐line antibiotic therapy.[4] Additionally, the guideline recommends empirically adding a macrolide to an aminopenicillin when atypical pneumonia is a diagnostic consideration.
This recommendation was a substantial departure from practice for hospitals nationwide, as a multicenter study of children's hospitals (20052010) demonstrated that <10% of patients diagnosed with CAP received aminopenicillins as empiric therapy.[5] Since publication of the PIDS/IDSA guidelines, the use of aminopenicillins has increased significantly across institutions, but the majority of hospitalized patients still receive broad‐spectrum cephalosporin therapy for CAP.[6]
At baseline, 30% of patients hospitalized with CAP received guideline‐recommended antibiotic therapy at our institution. Through the use of quality‐improvement methods, the proportion of patients receiving guideline‐recommended therapy increased to 100%.[7] The objective of this study was to ensure that there were not unintended negative consequences to guideline implementation. Specifically, we sought to identify changes in length of stay (LOS), hospital costs, and treatment failures associated with use of guideline‐recommended antibiotic therapy for children hospitalized with uncomplicated CAP.
METHODS
Study Design and Study Population
This retrospective cohort study included children age 3 months to 18 years, hospitalized with CAP, between May 2, 2011 and July 30, 2012, at Cincinnati Children's Hospital Medical Center (CCHMC), a 512‐bed free‐standing children's hospital. The CCHMC Institutional Review Board approved this study with a waiver of informed consent.
Patients were eligible for inclusion if they were admitted to the hospital for inpatient or observation level care with a primary or secondary International Classification of Disease, 9th Revision discharge diagnosis code of pneumonia (480.02, 480.89, 481, 482.0, 482.30‐2, 482.41‐2, 482.83, 482.8990, 483.8, 484.3, 485, 486, 487.0) or effusion/empyema (510.0, 510.9, 511.01, 511.89, 513).[8] Patients with complex chronic conditions[9] were excluded. Medical records of eligible patients (n=260) were reviewed by 2 members of the study team to ensure that patients fell into the purview of the guideline. Patients who did not receive antibiotics (n=11) or for whom there was documented concern for aspiration (n=1) were excluded. Additionally, patients with immunodeficiency (n=1) or who had not received age‐appropriate vaccinations (n=2), and patients who required intensive care unit admission on presentation (n=17) or who had a complicated pneumonia, defined by presence of moderate or large pleural effusion at time of admission (n=8), were also excluded.[7] Finally, for patients with multiple pneumonia admissions, only the index visit was included; subsequent visits occurring within 30 days of discharge were considered readmissions.
Treatment Measure
The primary exposure of interest was empiric antibiotic therapy upon hospital admission. Antibiotic therapy was classified as guideline recommended or nonguideline recommended. Guideline‐recommended therapy was defined as follows:
- For children without drug allergies: ampicillin (200 mg/kg/day intravenously) or amoxicillin (90 mg/kg/day orally);
- For children with penicillin allergy: ceftriaxone (50100 mg/kg/day intravenously or intramuscularly) or cefdinir (14 mg/kg/day orally);
- For children with penicillin and cephalosporin allergy: clindamycin (40 mg/kg/day orally or intravenously); and
- Or azithromycin (10 mg/kg/day orally or intravenously on day 1) in combination with antibiotic category 1 or 2 or 3 above.
Outcome Measures
The primary outcomes examined were hospital LOS, total cost of hospitalization, and inpatient pharmacy costs. LOS was measured in hours and defined as the difference in time between departure from and arrival to the inpatient unit. Total cost of index hospitalization included both direct and indirect costs, obtained from the Centers for Medicare & Medicaid Services' Relative Value Units data for Current Procedural Terminology codes.[10]
Secondary outcomes included broadening of antibiotic therapy during the hospital course, pneumonia‐related emergency department (ED) revisits within 30 days, and pneumonia‐related inpatient readmissions within 30 days. Broadening of antibiotic therapy was defined as addition of a second antibiotic (eg, adding azithromycin on day 3 of hospitalization) or change in empiric antibiotic to a class with broader antimicrobial activity (eg, ampicillin to ceftriaxone) at any time during hospitalization. As our study population included only patients with uncomplicated pneumonia at the time of admission, this outcome was used to capture possible treatment failure. ED revisits and inpatient readmissions were reviewed by 3 investigators to identify pneumonia‐related visits. To encompass all possible treatment failures, all respiratory‐related complaints (eg, wheezing, respiratory distress) were considered as pneumonia‐related. Disagreements were resolved by group discussion.
Covariates
Severity of illness on presentation was evaluated using the Emergency Severity Index version 4,[11] abnormal vital signs on presentation (as defined by Pediatric Advanced Life Support age‐specific criteria[12]), and need for oxygen in the first 24 hours of hospitalization. Supplemental oxygen is administered for saturations <91% per protocol at our institution. The patient's highest Pediatric Early Warning Scale score[13] during hospitalization was used as a proxy for disease severity. Exam findings on presentation (eg, increased respiratory effort, rales, wheezing) were determined through chart review. Laboratory tests and radiologic imaging variables included complete blood cell count, blood culture, chest radiograph, chest ultrasound, and chest computed tomography. Abnormal white blood cell count was defined as <5000 or >15,000 cells/mL, the defined reference range for the CCHMC clinical laboratory.
Data Analysis
Continuous variables were described using median and interquartile range (IQR) and compared across groups using Wilcoxon rank sum test due to non‐normal distributions. Categorical variables were described by counts and frequencies and compared using the 2 test.
Multivariable linear regression analysis was performed to assess the independent effect of receipt of empiric guideline‐recommended antibiotic therapy on outcomes of LOS and costs while adjusting for covariates. As LOS and costs were non‐normally distributed, we logarithmically transformed these values to use as the dependent variables in our models. The resulting coefficients were back‐transformed to reflect the percent change in LOS and costs incurred between subjects who received empiric guideline therapy compared with those who did not.[14] Covariates were chosen a priori due to their clinical and biological relevance to the outcomes of LOS (eg, wheezing on presentation and need for supplemental oxygen), total cost of hospitalization (eg, LOS and need for repeat imaging), and inpatient pharmacy costs (eg, LOS and wheezing on presentation) (Table 1).
| Characteristic | Overall Cohort, n=220 | Guideline Therapy, n=166 | Nonguideline Therapy, n=54 | P Value |
|---|---|---|---|---|
| ||||
| Age, y, median (IQR) | 2.9 (1.36.3) | 2.5 (1.35.2) | 5.6 (2.38.8) | <0.01* |
| Male, no. (%) | 122 (55.5%) | 89 (53.6%) | 33 (61.1%) | 0.34 |
| Emergency Severity Index, no. (%) | 0.11 | |||
| 2 | 90 (40.9%) | 73 (44.0%) | 17 (31.5%) | |
| 3 | 116 (52.7%) | 85 (51.2%) | 31 (57.4%) | |
| 4 | 14 (6.4%) | 8 (4.8%) | 6 (11.1%) | |
| Abnormal vital signs on presentation, no. (%) | ||||
| Fever | 99 (45.0%) | 80 (48.2%) | 19 (35.2%) | 0.10 |
| Tachycardia | 100 (45.5%) | 76 (45.8%) | 24 (44.4%) | 0.86 |
| Tachypnea | 124 (56.4%) | 100 (60.2%) | 24 (44.4%) | 0.04* |
| Hypotension | 0 | 0 | 0 | |
| Hypoxia | 27 (12.3%) | 24 (14.5%) | 3 (5.6%) | 0.08 |
| Physical exam on presentation, no. (%) | ||||
| Increased respiratory effort | 146 (66.4%) | 111 (66.9%) | 35 (64.8%) | 0.78 |
| Distressed | 110 (50.0%) | 86 (51.8%) | 24 (44.4%) | 0.35 |
| Retraction | 103 (46.8%) | 81 (48.8%) | 22 (40.7%) | 0.30 |
| Grunting | 17 (7.7%) | 14 (8.4%) | 3 (5.6%) | 0.49 |
| Nasal flaring | 19 (8.6%) | 17 (10.2%) | 2 (3.7%) | 0.14 |
| Rales | 135 (61.4%) | 99 (59.6%) | 36 (66.7%) | 0.36 |
| Wheeze | 91 (41.4%) | 66 (39.8%) | 25 (46.3%) | 0.40 |
| Decreased breath sounds | 89 (40.5%) | 65 (39.2%) | 24 (44.4%) | 0.49 |
| Dehydration | 21 (9.6%) | 13 (7.8%) | 8 (14.8%) | 0.13 |
| PEWS 5 during admission, no. (%) | 43 (19.6%) | 34 (20.5%) | 9 (16.7%) | 0.54 |
| Oxygen requirement in first 24 hours, no. (%) | 114 (51.8%) | 90 (53.6%) | 24 (46.2%) | 0.35 |
| Complete blood count obtained, no. (%) | 99 (45.0%) | 72 (43.4%) | 27 (50.0%) | 0.40 |
| Abnormal white blood cell count | 35 (35.7%) | 23 (32.4%) | 12 (44.4%) | 0.27 |
| Blood culture obtained, no. (%) | 104 (47.3%) | 80 (48.2%) | 24 (44.4%) | 0.63 |
| Positive | 2 (1.9%) | 1 (1.3%) | 1 (4.2%) | 0.36 |
| Chest radiograph available, no. (%) | 214 (97.3%) | 161 (97.0%) | 53 (98.2%) | 0.65 |
| Infiltrate | 178 (83.2%) | 139 (86.3%) | 39 (73.6%) | 0.03* |
| Bilateral | 29 (16.3%) | 20 (14.4%) | 9 (23.1%) | 0.19 |
| Multilobar | 46 (25.8%) | 33 (23.7%) | 13 (33.3%) | 0.23 |
| Effusion | 24 (11.2%) | 16 (9.9%) | 8 (15.1%) | 0.30 |
| Additional imaging, no. (%) | ||||
| Repeat chest radiograph | 26 (11.8%) | 17 (10.2%) | 9 (16.7%) | 0.20 |
| Chest ultrasound | 4 (1.8%) | 3 (1.8%) | 1 (1.9%) | 0.98 |
| Chest CT | 2 (0.9%) | 1 (0.6%) | 1 (1.9%) | 0.40 |
| Antibiotic, no. (%) | <0.01* | |||
| Aminopenicillin | 140 (63.6%) | 140 (84.3%) | 0 (0%) | |
| Third‐generation cephalosporin | 37 (16.8%) | 8 (4.8%) | 29 (53.7%) | |
| Macrolide monotherapy | 18 (8.2%) | 0 (0%) | 18 (33.3%) | |
| Clindamycin | 2 (0.9%) | 1 (0.6%) | 1 (1.9%) | |
| Levofloxacin | 1 (0.5%) | 0 (0%) | 1 (1.9%) | |
| Aminopenicillin+macrolide | 16 (7.3%) | 16 (9.6%) | 0 (0%) | |
| Cephalosporin+macrolide | 6 (2.7%) | 1 (0.6%) | 5 (9.3%) | |
Secondary outcomes of broadened antibiotic therapy, ED revisits, and hospital readmissions were assessed using the Fisher exact test. Due to the small number of events, we were unable to evaluate these associations in models adjusted for potential confounders.
All analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC), and P values <0.05 were considered significant.
RESULTS
Of the 220 unique patients included, 122 (55%) were male. The median age was 2.9 years (IQR: 1.36.3 years). Empiric guideline‐recommended therapy was prescribed to 168 (76%) patients (Table 1). Aminopenicillins were the most common guideline‐recommended therapy, accounting for 84% of guideline‐recommended antibiotics. An additional 10% of patients received the guideline‐recommended combination therapy with an aminopenicillin and a macrolide. Nonguideline‐recommended therapy included third‐generation cephalosporin antibiotics (54%) and macrolide monotherapy (33%).
Those who received empiric guideline‐recommended antibiotic therapy were similar to those who received nonguideline‐recommended therapy with respect to sex, Emergency Severity Index, physical exam findings on presentation, oxygen requirement in the first 24 hours, abnormal laboratory findings, presence of effusion on chest radiograph, and need for additional imaging (Table 1). However, patients in the guideline‐recommended therapy group were significantly younger (median 2.5 years vs 5.6 years, P0.01), more likely to have elevated respiratory rate on presentation (60.2% vs 44.4%, P=0.04), and more likely to have an infiltrate on chest radiograph (86.3% vs 73.6%, P=0.03) (Table 1). Patients who received nonguideline‐recommended macrolide monotherapy had a median age of 7.4 years (IQR: 5.89.8 years).
Median hospital LOS for the total cohort was 1.3 days (IQR: 0.91.9 days) (Table 2). There were no differences in LOS between patients who received and did not receive guideline‐recommended therapy in the unadjusted or the adjusted model (Table 3).
| Outcome | Guideline Therapy, n=166 | Nonguideline Therapy, n=54 | P Value |
|---|---|---|---|
| |||
| Length of stay, d, median (IQR) | 1.3 (0.91.9) | 1.3 (0.92.0) | 0.74 |
| Total costs, median, (IQR) | $4118 ($2,647$6,004) | $4045 ($2,829$6,200) | 0.44 |
| Pharmacy total costs, median, (IQR) | $84 ($40$179) | $106 ($58$217) | 0.12 |
| Broadened therapy, no. (%) | 10 (6.0%) | 4 (7.4%) | 0.75 |
| Emergency department revisit, no. (%) | 7 (4.2%) | 2 (3.7%) | 1.00 |
| Readmission, no. (%) | 1 (0.6%) | 1 (1.9%) | 0.43 |
| Outcome | Unadjusted Coefficient (95% CI) | Adjusted Coefficient (95% CI) | Adjusted % Change in Outcome (95% CI)* |
|---|---|---|---|
| |||
| Length of stay | 0.06 (0.27 to 0.15) | 0.06 (0.25 to 0.12) | 5.8 (22.1 to 12.8) |
| Total costs | 0.18 (0.40 to 0.04) | 0.11 (0.32 to 0.09) | 10.9 (27.4 to 9.4) |
| Pharmacy total costs | 0.44 (0.46 to 0.02) | 0.16 (0.57 to 0.24) | 14.8 (43.4 to 27.1) |
Median total costs of the index hospitalization for the total cohort were $4097 (IQR: $2657$6054), with median inpatient pharmacy costs of $92 (IQR: $40$183) (Table 2). There were no differences in total or inpatient pharmacy costs for patients who received guideline‐recommended therapy compared with those who did not in unadjusted or adjusted analyses. Fourteen patients (6.4%) had antibiotic therapy broadened during hospitalization, 10 were initially prescribed guideline‐recommended therapy, and 4 were initially prescribed nonguideline‐recommended therapy (Table 4).
| Initial Therapy | Reasons for Antibiotic Change Identified From Chart Review |
|---|---|
| Guideline=10 | Ampicillin to ceftriaxone: |
| 1 patient with clinical worsening | |
| 1 patient with coincident urinary tract infection due to resistant organism | |
| 4 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of a macrolide: | |
| 3 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of clindamycin: | |
| 1 patient with clinical worsening | |
| Nonguideline=4 | Ceftriaxone to clindamycin: |
| 1 patient with clinical worsening | |
| Addition of a macrolide: | |
| 1 patient with clinical worsening | |
| 1 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of clindamycin: | |
| 1 patient with clinical worsening |
Of the 9 pneumonia‐related ED revisits within 30 days of discharge, 7 occurred in patients prescribed empiric guideline‐recommended therapy (Table 5). No ED revisit resulted in hospital readmission or antibiotic change related to pneumonia. Two ED revisits resulted in new antibiotic prescriptions for diagnoses other than pneumonia.
| Revisit | Initial Therapy | Day Postdischarge | Clinical Symptoms at Return Visit | Clinical Diagnosis | Antibiotic Prescription |
|---|---|---|---|---|---|
| |||||
| ED | Guideline | 3 | Poor oral intake and fever | Pneumonia | Continued prior antibiotic |
| ED | Guideline | 8 | Recurrent cough and fever | Resolving pneumonia | Continued prior antibiotic |
| ED | Guideline | 13 | Follow‐up | Resolved pneumonia | No further antibiotic |
| ED | Guideline | 16 | Increased work of breathing | Reactive airway disease | No antibiotic |
| ED | Guideline | 20 | Persistent cough | Viral illness | No antibiotic |
| ED | Guideline | 22 | Recurrent cough and congestion | Sinusitis | Augmentin |
| ED | Guideline | 26 | Increased work of breathing | Reactive airway disease | No antibiotic |
| ED | Nonguideline | 16 | Recurrent fever | Acute otitis media | Amoxicillin |
| ED | Nonguideline | 20 | Recurrent cough and fever | Viral illness | No antibiotic |
| Admission | Guideline | 3 | Increased work of breathing | Pneumonia | IV ampicillin |
| Admission | Nonguideline | 9 | Refusal to take oral clindamycin | Pneumonia | IV clindamycin |
Two patients were readmitted for a pneumonia‐related illness within 30 days of discharge; 1 had received guideline‐recommended therapy (Table 5). Both patients were directly admitted to the inpatient ward without an associated ED visit. Antibiotic class was not changed for either patient upon readmission, despite the decision to convert to intravenous form.
DISCUSSION
In this retrospective cohort study, patients who received empiric guideline‐recommended antibiotic therapy on admission for CAP had no difference in LOS, total cost of hospitalization, or inpatient pharmacy costs compared with those who received therapy that varied from guideline recommendations. Our study suggests that prescribing narrow‐spectrum therapy and, in some circumstances, combination therapy, as recommended by the 2011 PIDS/IDSA pneumonia guideline, did not result in negative unintended consequences.
In our study, children receiving guideline‐recommended therapy were younger, more likely to have elevated respiratory rate on presentation, and more likely to have an infiltrate on chest radiograph. We hypothesize the age difference is a reflection of common use of nonguideline macrolide monotherapy in the older, school‐age child, as macrolides are commonly used for coverage of Mycoplasma pneumonia in older children with CAP.[15] Children receiving macrolide monotherapy were older than those receiving guideline‐recommended therapy (median age of 7.4 years and 2.5 years, respectively). We also hypothesize that some providers may prescribe macrolide monotherapy to children deemed less ill than expected for CAP (eg, normal percutaneous oxygen saturation). This hypothesis is supported by the finding that 60% of patients who had a normal respiratory rate and received nonguideline therapy were prescribed macrolide monotherapy. We did control for the characteristics that varied between the two treatment groups in our models to eliminate potential confounding.
One prior study evaluated the effects of guideline implementation in CAP. In evaluation of a clinical practice guideline that recommended ampicillin as first‐line therapy for CAP, no significant difference was found following guideline introduction in the number of treatment failures (defined as the need to broaden therapy or development of complicated pneumonia within 48 hours or 30‐day inpatient readmission).[16] Our study builds on these findings by directly comparing outcomes between recipients of guideline and nonguideline therapy, which was not done in the prestudy or poststudy design of prior work.[16] We believe that classifying patients based on empiric therapy received rather than timing of guideline introduction thoroughly examines the effect of following guideline recommendations. Additionally, outcomes other than treatment failures were examined in our study including LOS, costs, and ED revisits.
Our results are similar to other observational studies that compared narrow‐ and broad‐spectrum antibiotics for children hospitalized with CAP. Using administrative data, Williams et al. found no significant difference in LOS or cost between narrow‐ and broad‐spectrum intravenous antibiotic recipients ages 6 months to 18 years at 43 children's hospitals.[17] Queen et al. compared narrow‐ and broad‐spectrum antibiotic therapy for children ages 2 months to 18 years at 4 children's hospitals.[18] Differences in average daily cost were not significant, but children who received narrow‐spectrum antibiotics had a significantly shorter LOS. Finally, an observational study of 319 Israeli children <2 years of age found no significant difference in duration of oxygen requirement, LOS, or need for change in antibiotic therapy between the 66 children prescribed aminopenicillins and the 253 children prescribed cefuroxime.[19] These studies suggest that prescribing narrow‐spectrum antimicrobial therapy, as per the guideline recommendations, results in similar outcomes to broad‐spectrum antimicrobial therapy.
Our study adds to prior studies that compared narrow‐ and broad‐spectrum therapy by comparing outcomes associated with guideline‐recommended therapy to nonguideline therapy. We considered antibiotic therapy as guideline recommended if appropriately chosen per the guideline, not just by simple classification of antibiotic. For example, the use of a cephalosporin in a patient with aminopenicillin allergy was considered guideline‐recommended therapy. We chose to classify the exposure of empiric antibiotic therapy in this manner to reflect true clinical application of the guideline, as not all children are able to receive aminopenicillins. Additionally, as our study stemmed from our prior improvement work aimed at increasing guideline adherent therapy,[7] we have a higher frequency of narrow‐spectrum antibiotic use than prior studies. In our study, almost two‐thirds of patients received narrow‐spectrum therapy, whereas narrow‐spectrum use in prior studies ranged from 10% to 33%.[17, 18, 19] Finally, we were able to confirm the diagnosis of pneumonia via medical record review and to adjust for severity of illness using clinical variables including vital signs, physical exam findings, and laboratory and radiologic study results.
This study must be interpreted in the context of several limitations. First, our study population was defined through discharge diagnosis codes, and therefore dependent on the accuracy of coding. However, we minimized potential for misclassification through use of a previously validated approach to identify patients with CAP and through medical record review to confirm the diagnosis. Second, we may be unable to detect very small differences in outcomes given limited power, specifically for outcomes of LOS, ED revisits, hospital readmissions, and need to broaden antibiotic therapy. Third, residual confounding may be present. Although we controlled for many clinical variables in our analyses, antibiotic prescribing practices may be influenced by unmeasured factors. The potential of system level confounding is mitigated by standardized care for patients with CAP at our institution. Prior system‐level changes using quality‐improvement science have resulted in a high level of adherence with guideline‐recommended antimicrobials as well as standardized medical discharge criteria.[7, 20] Additionally, nonmedical factors may influence LOS, limiting its use as an outcome measure. This limitation was minimized in our study by standardizing medical discharge criteria. Prior work at our institution demonstrated that the majority of patients, including those with CAP, were discharged within 2 hours of meeting medical discharge criteria.[20] Fourth, discharged patients who experienced adverse outcomes may have received care at a nearby adult emergency department or at their pediatrician's office. Although these events would not have been captured in our electronic health record, serious complications due to treatment failure (eg, empyema) would require hospitalization. As our hospital is the only children's hospital in the Greater Cincinnati metropolitan area, these patents would receive care at our institution. Therefore, any misclassification of revisits or readmissions is likely to be minimal. Finally, study patients were admitted to a large tertiary academic children's hospital, warranting further investigation to determine if these findings can be translated to smaller community settings.
In conclusion, receipt of guideline‐recommended antibiotic therapy for patients hospitalized with CAP was not associated with increases in LOS, total costs of hospitalization, or inpatient pharmacy costs. Our findings highlight the importance of changing antibiotic prescribing practices to reflect guideline recommendations, as there was no evidence of negative unintended consequences with our local practice change.
Acknowledgments
Disclosures: Dr. Ambroggio and Dr. Thomson were supported by funds from the NRSA T32HP10027‐14. Dr. Shah was supported by funds from NIAID K01A173729. The authors report no conflicts of interest.
- , , , , , . Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994–2007. Pediatrics. 2011;127(3):411–418.
- , , , , . National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126(2):204–213.
- , , , et al. Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166(12):1155–1164.
- , , , et al. The management of community‐acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25–e76.
- , , , et al. Variability in processes of care and outcomes among children hospitalized with community‐acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036–1041.
- , , , et al. Impact of IDSA/PIDS guidelines on treatment of community‐acquired pneumonia in hospitalized children. Clin Infect Dis. 2014;58(6):834–838.
- , , , et al. Quality improvement methods increase appropriate antibiotic prescribing for childhood pneumonia. Pediatrics. 2013;131(5):e1623–e1631.
- , , , et al. Identifying pediatric community‐acquired pneumonia hospitalizations: accuracy of administrative billing codes. JAMA Pediatr. 2013;167(9):851–858.
- , , , , , . Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):E99.
- Centers for Medicare 2011.
- , , , et al. Pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126(5):e1361–e1399.
- , , , , . Prospective evaluation of a pediatric inpatient early warning scoring system. J Spec Pediatr Nurs. 2009;14(2):79–85.
- , , , . Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. New York, NY: Springer; 2005.
- , , , , . Treatment of mycoplasma pneumonia: a systematic review. Pediatrics. 2014;133(6):1081–1090.
- , , , , , . Impact of a guideline on management of children hospitalized with community‐acquired pneumonia. Pediatrics. 2012;129(3):e597–e604.
- , , , et al. Narrow vs broad‐spectrum antimicrobial therapy for children hospitalized with pneumonia. Pediatrics. 2013;132(5):e1141–e1148.
- , , , et al. Comparative effectiveness of empiric antibiotics for community‐acquired pneumonia. Pediatrics. 2014;133(1):e23–e29.
- , , , et al. Antibiotic treatment of children with community‐acquired pneumonia: comparison of penicillin or ampicillin versus cefuroxime. Pediatr Pulmonol. 2013;48(1):52–58.
- , , , et al. Using quality improvement to optimise paediatric discharge efficiency. BMJ Qual Saf. 2014;23(5):428–436.
Community‐acquired pneumonia (CAP) is a common and serious infection in children. With more than 150,000 children requiring hospitalization annually, CAP is the fifth most prevalent and the second most costly diagnosis of all pediatric hospitalizations in the United States.[1, 2, 3]
In August 2011, the Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) published an evidence‐based guideline for the management of CAP in children. This guideline recommended that fully immunized children without underlying complications who require hospitalization receive an aminopenicillin as first‐line antibiotic therapy.[4] Additionally, the guideline recommends empirically adding a macrolide to an aminopenicillin when atypical pneumonia is a diagnostic consideration.
This recommendation was a substantial departure from practice for hospitals nationwide, as a multicenter study of children's hospitals (20052010) demonstrated that <10% of patients diagnosed with CAP received aminopenicillins as empiric therapy.[5] Since publication of the PIDS/IDSA guidelines, the use of aminopenicillins has increased significantly across institutions, but the majority of hospitalized patients still receive broad‐spectrum cephalosporin therapy for CAP.[6]
At baseline, 30% of patients hospitalized with CAP received guideline‐recommended antibiotic therapy at our institution. Through the use of quality‐improvement methods, the proportion of patients receiving guideline‐recommended therapy increased to 100%.[7] The objective of this study was to ensure that there were not unintended negative consequences to guideline implementation. Specifically, we sought to identify changes in length of stay (LOS), hospital costs, and treatment failures associated with use of guideline‐recommended antibiotic therapy for children hospitalized with uncomplicated CAP.
METHODS
Study Design and Study Population
This retrospective cohort study included children age 3 months to 18 years, hospitalized with CAP, between May 2, 2011 and July 30, 2012, at Cincinnati Children's Hospital Medical Center (CCHMC), a 512‐bed free‐standing children's hospital. The CCHMC Institutional Review Board approved this study with a waiver of informed consent.
Patients were eligible for inclusion if they were admitted to the hospital for inpatient or observation level care with a primary or secondary International Classification of Disease, 9th Revision discharge diagnosis code of pneumonia (480.02, 480.89, 481, 482.0, 482.30‐2, 482.41‐2, 482.83, 482.8990, 483.8, 484.3, 485, 486, 487.0) or effusion/empyema (510.0, 510.9, 511.01, 511.89, 513).[8] Patients with complex chronic conditions[9] were excluded. Medical records of eligible patients (n=260) were reviewed by 2 members of the study team to ensure that patients fell into the purview of the guideline. Patients who did not receive antibiotics (n=11) or for whom there was documented concern for aspiration (n=1) were excluded. Additionally, patients with immunodeficiency (n=1) or who had not received age‐appropriate vaccinations (n=2), and patients who required intensive care unit admission on presentation (n=17) or who had a complicated pneumonia, defined by presence of moderate or large pleural effusion at time of admission (n=8), were also excluded.[7] Finally, for patients with multiple pneumonia admissions, only the index visit was included; subsequent visits occurring within 30 days of discharge were considered readmissions.
Treatment Measure
The primary exposure of interest was empiric antibiotic therapy upon hospital admission. Antibiotic therapy was classified as guideline recommended or nonguideline recommended. Guideline‐recommended therapy was defined as follows:
- For children without drug allergies: ampicillin (200 mg/kg/day intravenously) or amoxicillin (90 mg/kg/day orally);
- For children with penicillin allergy: ceftriaxone (50100 mg/kg/day intravenously or intramuscularly) or cefdinir (14 mg/kg/day orally);
- For children with penicillin and cephalosporin allergy: clindamycin (40 mg/kg/day orally or intravenously); and
- Or azithromycin (10 mg/kg/day orally or intravenously on day 1) in combination with antibiotic category 1 or 2 or 3 above.
Outcome Measures
The primary outcomes examined were hospital LOS, total cost of hospitalization, and inpatient pharmacy costs. LOS was measured in hours and defined as the difference in time between departure from and arrival to the inpatient unit. Total cost of index hospitalization included both direct and indirect costs, obtained from the Centers for Medicare & Medicaid Services' Relative Value Units data for Current Procedural Terminology codes.[10]
Secondary outcomes included broadening of antibiotic therapy during the hospital course, pneumonia‐related emergency department (ED) revisits within 30 days, and pneumonia‐related inpatient readmissions within 30 days. Broadening of antibiotic therapy was defined as addition of a second antibiotic (eg, adding azithromycin on day 3 of hospitalization) or change in empiric antibiotic to a class with broader antimicrobial activity (eg, ampicillin to ceftriaxone) at any time during hospitalization. As our study population included only patients with uncomplicated pneumonia at the time of admission, this outcome was used to capture possible treatment failure. ED revisits and inpatient readmissions were reviewed by 3 investigators to identify pneumonia‐related visits. To encompass all possible treatment failures, all respiratory‐related complaints (eg, wheezing, respiratory distress) were considered as pneumonia‐related. Disagreements were resolved by group discussion.
Covariates
Severity of illness on presentation was evaluated using the Emergency Severity Index version 4,[11] abnormal vital signs on presentation (as defined by Pediatric Advanced Life Support age‐specific criteria[12]), and need for oxygen in the first 24 hours of hospitalization. Supplemental oxygen is administered for saturations <91% per protocol at our institution. The patient's highest Pediatric Early Warning Scale score[13] during hospitalization was used as a proxy for disease severity. Exam findings on presentation (eg, increased respiratory effort, rales, wheezing) were determined through chart review. Laboratory tests and radiologic imaging variables included complete blood cell count, blood culture, chest radiograph, chest ultrasound, and chest computed tomography. Abnormal white blood cell count was defined as <5000 or >15,000 cells/mL, the defined reference range for the CCHMC clinical laboratory.
Data Analysis
Continuous variables were described using median and interquartile range (IQR) and compared across groups using Wilcoxon rank sum test due to non‐normal distributions. Categorical variables were described by counts and frequencies and compared using the 2 test.
Multivariable linear regression analysis was performed to assess the independent effect of receipt of empiric guideline‐recommended antibiotic therapy on outcomes of LOS and costs while adjusting for covariates. As LOS and costs were non‐normally distributed, we logarithmically transformed these values to use as the dependent variables in our models. The resulting coefficients were back‐transformed to reflect the percent change in LOS and costs incurred between subjects who received empiric guideline therapy compared with those who did not.[14] Covariates were chosen a priori due to their clinical and biological relevance to the outcomes of LOS (eg, wheezing on presentation and need for supplemental oxygen), total cost of hospitalization (eg, LOS and need for repeat imaging), and inpatient pharmacy costs (eg, LOS and wheezing on presentation) (Table 1).
| Characteristic | Overall Cohort, n=220 | Guideline Therapy, n=166 | Nonguideline Therapy, n=54 | P Value |
|---|---|---|---|---|
| ||||
| Age, y, median (IQR) | 2.9 (1.36.3) | 2.5 (1.35.2) | 5.6 (2.38.8) | <0.01* |
| Male, no. (%) | 122 (55.5%) | 89 (53.6%) | 33 (61.1%) | 0.34 |
| Emergency Severity Index, no. (%) | 0.11 | |||
| 2 | 90 (40.9%) | 73 (44.0%) | 17 (31.5%) | |
| 3 | 116 (52.7%) | 85 (51.2%) | 31 (57.4%) | |
| 4 | 14 (6.4%) | 8 (4.8%) | 6 (11.1%) | |
| Abnormal vital signs on presentation, no. (%) | ||||
| Fever | 99 (45.0%) | 80 (48.2%) | 19 (35.2%) | 0.10 |
| Tachycardia | 100 (45.5%) | 76 (45.8%) | 24 (44.4%) | 0.86 |
| Tachypnea | 124 (56.4%) | 100 (60.2%) | 24 (44.4%) | 0.04* |
| Hypotension | 0 | 0 | 0 | |
| Hypoxia | 27 (12.3%) | 24 (14.5%) | 3 (5.6%) | 0.08 |
| Physical exam on presentation, no. (%) | ||||
| Increased respiratory effort | 146 (66.4%) | 111 (66.9%) | 35 (64.8%) | 0.78 |
| Distressed | 110 (50.0%) | 86 (51.8%) | 24 (44.4%) | 0.35 |
| Retraction | 103 (46.8%) | 81 (48.8%) | 22 (40.7%) | 0.30 |
| Grunting | 17 (7.7%) | 14 (8.4%) | 3 (5.6%) | 0.49 |
| Nasal flaring | 19 (8.6%) | 17 (10.2%) | 2 (3.7%) | 0.14 |
| Rales | 135 (61.4%) | 99 (59.6%) | 36 (66.7%) | 0.36 |
| Wheeze | 91 (41.4%) | 66 (39.8%) | 25 (46.3%) | 0.40 |
| Decreased breath sounds | 89 (40.5%) | 65 (39.2%) | 24 (44.4%) | 0.49 |
| Dehydration | 21 (9.6%) | 13 (7.8%) | 8 (14.8%) | 0.13 |
| PEWS 5 during admission, no. (%) | 43 (19.6%) | 34 (20.5%) | 9 (16.7%) | 0.54 |
| Oxygen requirement in first 24 hours, no. (%) | 114 (51.8%) | 90 (53.6%) | 24 (46.2%) | 0.35 |
| Complete blood count obtained, no. (%) | 99 (45.0%) | 72 (43.4%) | 27 (50.0%) | 0.40 |
| Abnormal white blood cell count | 35 (35.7%) | 23 (32.4%) | 12 (44.4%) | 0.27 |
| Blood culture obtained, no. (%) | 104 (47.3%) | 80 (48.2%) | 24 (44.4%) | 0.63 |
| Positive | 2 (1.9%) | 1 (1.3%) | 1 (4.2%) | 0.36 |
| Chest radiograph available, no. (%) | 214 (97.3%) | 161 (97.0%) | 53 (98.2%) | 0.65 |
| Infiltrate | 178 (83.2%) | 139 (86.3%) | 39 (73.6%) | 0.03* |
| Bilateral | 29 (16.3%) | 20 (14.4%) | 9 (23.1%) | 0.19 |
| Multilobar | 46 (25.8%) | 33 (23.7%) | 13 (33.3%) | 0.23 |
| Effusion | 24 (11.2%) | 16 (9.9%) | 8 (15.1%) | 0.30 |
| Additional imaging, no. (%) | ||||
| Repeat chest radiograph | 26 (11.8%) | 17 (10.2%) | 9 (16.7%) | 0.20 |
| Chest ultrasound | 4 (1.8%) | 3 (1.8%) | 1 (1.9%) | 0.98 |
| Chest CT | 2 (0.9%) | 1 (0.6%) | 1 (1.9%) | 0.40 |
| Antibiotic, no. (%) | <0.01* | |||
| Aminopenicillin | 140 (63.6%) | 140 (84.3%) | 0 (0%) | |
| Third‐generation cephalosporin | 37 (16.8%) | 8 (4.8%) | 29 (53.7%) | |
| Macrolide monotherapy | 18 (8.2%) | 0 (0%) | 18 (33.3%) | |
| Clindamycin | 2 (0.9%) | 1 (0.6%) | 1 (1.9%) | |
| Levofloxacin | 1 (0.5%) | 0 (0%) | 1 (1.9%) | |
| Aminopenicillin+macrolide | 16 (7.3%) | 16 (9.6%) | 0 (0%) | |
| Cephalosporin+macrolide | 6 (2.7%) | 1 (0.6%) | 5 (9.3%) | |
Secondary outcomes of broadened antibiotic therapy, ED revisits, and hospital readmissions were assessed using the Fisher exact test. Due to the small number of events, we were unable to evaluate these associations in models adjusted for potential confounders.
All analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC), and P values <0.05 were considered significant.
RESULTS
Of the 220 unique patients included, 122 (55%) were male. The median age was 2.9 years (IQR: 1.36.3 years). Empiric guideline‐recommended therapy was prescribed to 168 (76%) patients (Table 1). Aminopenicillins were the most common guideline‐recommended therapy, accounting for 84% of guideline‐recommended antibiotics. An additional 10% of patients received the guideline‐recommended combination therapy with an aminopenicillin and a macrolide. Nonguideline‐recommended therapy included third‐generation cephalosporin antibiotics (54%) and macrolide monotherapy (33%).
Those who received empiric guideline‐recommended antibiotic therapy were similar to those who received nonguideline‐recommended therapy with respect to sex, Emergency Severity Index, physical exam findings on presentation, oxygen requirement in the first 24 hours, abnormal laboratory findings, presence of effusion on chest radiograph, and need for additional imaging (Table 1). However, patients in the guideline‐recommended therapy group were significantly younger (median 2.5 years vs 5.6 years, P0.01), more likely to have elevated respiratory rate on presentation (60.2% vs 44.4%, P=0.04), and more likely to have an infiltrate on chest radiograph (86.3% vs 73.6%, P=0.03) (Table 1). Patients who received nonguideline‐recommended macrolide monotherapy had a median age of 7.4 years (IQR: 5.89.8 years).
Median hospital LOS for the total cohort was 1.3 days (IQR: 0.91.9 days) (Table 2). There were no differences in LOS between patients who received and did not receive guideline‐recommended therapy in the unadjusted or the adjusted model (Table 3).
| Outcome | Guideline Therapy, n=166 | Nonguideline Therapy, n=54 | P Value |
|---|---|---|---|
| |||
| Length of stay, d, median (IQR) | 1.3 (0.91.9) | 1.3 (0.92.0) | 0.74 |
| Total costs, median, (IQR) | $4118 ($2,647$6,004) | $4045 ($2,829$6,200) | 0.44 |
| Pharmacy total costs, median, (IQR) | $84 ($40$179) | $106 ($58$217) | 0.12 |
| Broadened therapy, no. (%) | 10 (6.0%) | 4 (7.4%) | 0.75 |
| Emergency department revisit, no. (%) | 7 (4.2%) | 2 (3.7%) | 1.00 |
| Readmission, no. (%) | 1 (0.6%) | 1 (1.9%) | 0.43 |
| Outcome | Unadjusted Coefficient (95% CI) | Adjusted Coefficient (95% CI) | Adjusted % Change in Outcome (95% CI)* |
|---|---|---|---|
| |||
| Length of stay | 0.06 (0.27 to 0.15) | 0.06 (0.25 to 0.12) | 5.8 (22.1 to 12.8) |
| Total costs | 0.18 (0.40 to 0.04) | 0.11 (0.32 to 0.09) | 10.9 (27.4 to 9.4) |
| Pharmacy total costs | 0.44 (0.46 to 0.02) | 0.16 (0.57 to 0.24) | 14.8 (43.4 to 27.1) |
Median total costs of the index hospitalization for the total cohort were $4097 (IQR: $2657$6054), with median inpatient pharmacy costs of $92 (IQR: $40$183) (Table 2). There were no differences in total or inpatient pharmacy costs for patients who received guideline‐recommended therapy compared with those who did not in unadjusted or adjusted analyses. Fourteen patients (6.4%) had antibiotic therapy broadened during hospitalization, 10 were initially prescribed guideline‐recommended therapy, and 4 were initially prescribed nonguideline‐recommended therapy (Table 4).
| Initial Therapy | Reasons for Antibiotic Change Identified From Chart Review |
|---|---|
| Guideline=10 | Ampicillin to ceftriaxone: |
| 1 patient with clinical worsening | |
| 1 patient with coincident urinary tract infection due to resistant organism | |
| 4 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of a macrolide: | |
| 3 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of clindamycin: | |
| 1 patient with clinical worsening | |
| Nonguideline=4 | Ceftriaxone to clindamycin: |
| 1 patient with clinical worsening | |
| Addition of a macrolide: | |
| 1 patient with clinical worsening | |
| 1 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of clindamycin: | |
| 1 patient with clinical worsening |
Of the 9 pneumonia‐related ED revisits within 30 days of discharge, 7 occurred in patients prescribed empiric guideline‐recommended therapy (Table 5). No ED revisit resulted in hospital readmission or antibiotic change related to pneumonia. Two ED revisits resulted in new antibiotic prescriptions for diagnoses other than pneumonia.
| Revisit | Initial Therapy | Day Postdischarge | Clinical Symptoms at Return Visit | Clinical Diagnosis | Antibiotic Prescription |
|---|---|---|---|---|---|
| |||||
| ED | Guideline | 3 | Poor oral intake and fever | Pneumonia | Continued prior antibiotic |
| ED | Guideline | 8 | Recurrent cough and fever | Resolving pneumonia | Continued prior antibiotic |
| ED | Guideline | 13 | Follow‐up | Resolved pneumonia | No further antibiotic |
| ED | Guideline | 16 | Increased work of breathing | Reactive airway disease | No antibiotic |
| ED | Guideline | 20 | Persistent cough | Viral illness | No antibiotic |
| ED | Guideline | 22 | Recurrent cough and congestion | Sinusitis | Augmentin |
| ED | Guideline | 26 | Increased work of breathing | Reactive airway disease | No antibiotic |
| ED | Nonguideline | 16 | Recurrent fever | Acute otitis media | Amoxicillin |
| ED | Nonguideline | 20 | Recurrent cough and fever | Viral illness | No antibiotic |
| Admission | Guideline | 3 | Increased work of breathing | Pneumonia | IV ampicillin |
| Admission | Nonguideline | 9 | Refusal to take oral clindamycin | Pneumonia | IV clindamycin |
Two patients were readmitted for a pneumonia‐related illness within 30 days of discharge; 1 had received guideline‐recommended therapy (Table 5). Both patients were directly admitted to the inpatient ward without an associated ED visit. Antibiotic class was not changed for either patient upon readmission, despite the decision to convert to intravenous form.
DISCUSSION
In this retrospective cohort study, patients who received empiric guideline‐recommended antibiotic therapy on admission for CAP had no difference in LOS, total cost of hospitalization, or inpatient pharmacy costs compared with those who received therapy that varied from guideline recommendations. Our study suggests that prescribing narrow‐spectrum therapy and, in some circumstances, combination therapy, as recommended by the 2011 PIDS/IDSA pneumonia guideline, did not result in negative unintended consequences.
In our study, children receiving guideline‐recommended therapy were younger, more likely to have elevated respiratory rate on presentation, and more likely to have an infiltrate on chest radiograph. We hypothesize the age difference is a reflection of common use of nonguideline macrolide monotherapy in the older, school‐age child, as macrolides are commonly used for coverage of Mycoplasma pneumonia in older children with CAP.[15] Children receiving macrolide monotherapy were older than those receiving guideline‐recommended therapy (median age of 7.4 years and 2.5 years, respectively). We also hypothesize that some providers may prescribe macrolide monotherapy to children deemed less ill than expected for CAP (eg, normal percutaneous oxygen saturation). This hypothesis is supported by the finding that 60% of patients who had a normal respiratory rate and received nonguideline therapy were prescribed macrolide monotherapy. We did control for the characteristics that varied between the two treatment groups in our models to eliminate potential confounding.
One prior study evaluated the effects of guideline implementation in CAP. In evaluation of a clinical practice guideline that recommended ampicillin as first‐line therapy for CAP, no significant difference was found following guideline introduction in the number of treatment failures (defined as the need to broaden therapy or development of complicated pneumonia within 48 hours or 30‐day inpatient readmission).[16] Our study builds on these findings by directly comparing outcomes between recipients of guideline and nonguideline therapy, which was not done in the prestudy or poststudy design of prior work.[16] We believe that classifying patients based on empiric therapy received rather than timing of guideline introduction thoroughly examines the effect of following guideline recommendations. Additionally, outcomes other than treatment failures were examined in our study including LOS, costs, and ED revisits.
Our results are similar to other observational studies that compared narrow‐ and broad‐spectrum antibiotics for children hospitalized with CAP. Using administrative data, Williams et al. found no significant difference in LOS or cost between narrow‐ and broad‐spectrum intravenous antibiotic recipients ages 6 months to 18 years at 43 children's hospitals.[17] Queen et al. compared narrow‐ and broad‐spectrum antibiotic therapy for children ages 2 months to 18 years at 4 children's hospitals.[18] Differences in average daily cost were not significant, but children who received narrow‐spectrum antibiotics had a significantly shorter LOS. Finally, an observational study of 319 Israeli children <2 years of age found no significant difference in duration of oxygen requirement, LOS, or need for change in antibiotic therapy between the 66 children prescribed aminopenicillins and the 253 children prescribed cefuroxime.[19] These studies suggest that prescribing narrow‐spectrum antimicrobial therapy, as per the guideline recommendations, results in similar outcomes to broad‐spectrum antimicrobial therapy.
Our study adds to prior studies that compared narrow‐ and broad‐spectrum therapy by comparing outcomes associated with guideline‐recommended therapy to nonguideline therapy. We considered antibiotic therapy as guideline recommended if appropriately chosen per the guideline, not just by simple classification of antibiotic. For example, the use of a cephalosporin in a patient with aminopenicillin allergy was considered guideline‐recommended therapy. We chose to classify the exposure of empiric antibiotic therapy in this manner to reflect true clinical application of the guideline, as not all children are able to receive aminopenicillins. Additionally, as our study stemmed from our prior improvement work aimed at increasing guideline adherent therapy,[7] we have a higher frequency of narrow‐spectrum antibiotic use than prior studies. In our study, almost two‐thirds of patients received narrow‐spectrum therapy, whereas narrow‐spectrum use in prior studies ranged from 10% to 33%.[17, 18, 19] Finally, we were able to confirm the diagnosis of pneumonia via medical record review and to adjust for severity of illness using clinical variables including vital signs, physical exam findings, and laboratory and radiologic study results.
This study must be interpreted in the context of several limitations. First, our study population was defined through discharge diagnosis codes, and therefore dependent on the accuracy of coding. However, we minimized potential for misclassification through use of a previously validated approach to identify patients with CAP and through medical record review to confirm the diagnosis. Second, we may be unable to detect very small differences in outcomes given limited power, specifically for outcomes of LOS, ED revisits, hospital readmissions, and need to broaden antibiotic therapy. Third, residual confounding may be present. Although we controlled for many clinical variables in our analyses, antibiotic prescribing practices may be influenced by unmeasured factors. The potential of system level confounding is mitigated by standardized care for patients with CAP at our institution. Prior system‐level changes using quality‐improvement science have resulted in a high level of adherence with guideline‐recommended antimicrobials as well as standardized medical discharge criteria.[7, 20] Additionally, nonmedical factors may influence LOS, limiting its use as an outcome measure. This limitation was minimized in our study by standardizing medical discharge criteria. Prior work at our institution demonstrated that the majority of patients, including those with CAP, were discharged within 2 hours of meeting medical discharge criteria.[20] Fourth, discharged patients who experienced adverse outcomes may have received care at a nearby adult emergency department or at their pediatrician's office. Although these events would not have been captured in our electronic health record, serious complications due to treatment failure (eg, empyema) would require hospitalization. As our hospital is the only children's hospital in the Greater Cincinnati metropolitan area, these patents would receive care at our institution. Therefore, any misclassification of revisits or readmissions is likely to be minimal. Finally, study patients were admitted to a large tertiary academic children's hospital, warranting further investigation to determine if these findings can be translated to smaller community settings.
In conclusion, receipt of guideline‐recommended antibiotic therapy for patients hospitalized with CAP was not associated with increases in LOS, total costs of hospitalization, or inpatient pharmacy costs. Our findings highlight the importance of changing antibiotic prescribing practices to reflect guideline recommendations, as there was no evidence of negative unintended consequences with our local practice change.
Acknowledgments
Disclosures: Dr. Ambroggio and Dr. Thomson were supported by funds from the NRSA T32HP10027‐14. Dr. Shah was supported by funds from NIAID K01A173729. The authors report no conflicts of interest.
Community‐acquired pneumonia (CAP) is a common and serious infection in children. With more than 150,000 children requiring hospitalization annually, CAP is the fifth most prevalent and the second most costly diagnosis of all pediatric hospitalizations in the United States.[1, 2, 3]
In August 2011, the Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) published an evidence‐based guideline for the management of CAP in children. This guideline recommended that fully immunized children without underlying complications who require hospitalization receive an aminopenicillin as first‐line antibiotic therapy.[4] Additionally, the guideline recommends empirically adding a macrolide to an aminopenicillin when atypical pneumonia is a diagnostic consideration.
This recommendation was a substantial departure from practice for hospitals nationwide, as a multicenter study of children's hospitals (20052010) demonstrated that <10% of patients diagnosed with CAP received aminopenicillins as empiric therapy.[5] Since publication of the PIDS/IDSA guidelines, the use of aminopenicillins has increased significantly across institutions, but the majority of hospitalized patients still receive broad‐spectrum cephalosporin therapy for CAP.[6]
At baseline, 30% of patients hospitalized with CAP received guideline‐recommended antibiotic therapy at our institution. Through the use of quality‐improvement methods, the proportion of patients receiving guideline‐recommended therapy increased to 100%.[7] The objective of this study was to ensure that there were not unintended negative consequences to guideline implementation. Specifically, we sought to identify changes in length of stay (LOS), hospital costs, and treatment failures associated with use of guideline‐recommended antibiotic therapy for children hospitalized with uncomplicated CAP.
METHODS
Study Design and Study Population
This retrospective cohort study included children age 3 months to 18 years, hospitalized with CAP, between May 2, 2011 and July 30, 2012, at Cincinnati Children's Hospital Medical Center (CCHMC), a 512‐bed free‐standing children's hospital. The CCHMC Institutional Review Board approved this study with a waiver of informed consent.
Patients were eligible for inclusion if they were admitted to the hospital for inpatient or observation level care with a primary or secondary International Classification of Disease, 9th Revision discharge diagnosis code of pneumonia (480.02, 480.89, 481, 482.0, 482.30‐2, 482.41‐2, 482.83, 482.8990, 483.8, 484.3, 485, 486, 487.0) or effusion/empyema (510.0, 510.9, 511.01, 511.89, 513).[8] Patients with complex chronic conditions[9] were excluded. Medical records of eligible patients (n=260) were reviewed by 2 members of the study team to ensure that patients fell into the purview of the guideline. Patients who did not receive antibiotics (n=11) or for whom there was documented concern for aspiration (n=1) were excluded. Additionally, patients with immunodeficiency (n=1) or who had not received age‐appropriate vaccinations (n=2), and patients who required intensive care unit admission on presentation (n=17) or who had a complicated pneumonia, defined by presence of moderate or large pleural effusion at time of admission (n=8), were also excluded.[7] Finally, for patients with multiple pneumonia admissions, only the index visit was included; subsequent visits occurring within 30 days of discharge were considered readmissions.
Treatment Measure
The primary exposure of interest was empiric antibiotic therapy upon hospital admission. Antibiotic therapy was classified as guideline recommended or nonguideline recommended. Guideline‐recommended therapy was defined as follows:
- For children without drug allergies: ampicillin (200 mg/kg/day intravenously) or amoxicillin (90 mg/kg/day orally);
- For children with penicillin allergy: ceftriaxone (50100 mg/kg/day intravenously or intramuscularly) or cefdinir (14 mg/kg/day orally);
- For children with penicillin and cephalosporin allergy: clindamycin (40 mg/kg/day orally or intravenously); and
- Or azithromycin (10 mg/kg/day orally or intravenously on day 1) in combination with antibiotic category 1 or 2 or 3 above.
Outcome Measures
The primary outcomes examined were hospital LOS, total cost of hospitalization, and inpatient pharmacy costs. LOS was measured in hours and defined as the difference in time between departure from and arrival to the inpatient unit. Total cost of index hospitalization included both direct and indirect costs, obtained from the Centers for Medicare & Medicaid Services' Relative Value Units data for Current Procedural Terminology codes.[10]
Secondary outcomes included broadening of antibiotic therapy during the hospital course, pneumonia‐related emergency department (ED) revisits within 30 days, and pneumonia‐related inpatient readmissions within 30 days. Broadening of antibiotic therapy was defined as addition of a second antibiotic (eg, adding azithromycin on day 3 of hospitalization) or change in empiric antibiotic to a class with broader antimicrobial activity (eg, ampicillin to ceftriaxone) at any time during hospitalization. As our study population included only patients with uncomplicated pneumonia at the time of admission, this outcome was used to capture possible treatment failure. ED revisits and inpatient readmissions were reviewed by 3 investigators to identify pneumonia‐related visits. To encompass all possible treatment failures, all respiratory‐related complaints (eg, wheezing, respiratory distress) were considered as pneumonia‐related. Disagreements were resolved by group discussion.
Covariates
Severity of illness on presentation was evaluated using the Emergency Severity Index version 4,[11] abnormal vital signs on presentation (as defined by Pediatric Advanced Life Support age‐specific criteria[12]), and need for oxygen in the first 24 hours of hospitalization. Supplemental oxygen is administered for saturations <91% per protocol at our institution. The patient's highest Pediatric Early Warning Scale score[13] during hospitalization was used as a proxy for disease severity. Exam findings on presentation (eg, increased respiratory effort, rales, wheezing) were determined through chart review. Laboratory tests and radiologic imaging variables included complete blood cell count, blood culture, chest radiograph, chest ultrasound, and chest computed tomography. Abnormal white blood cell count was defined as <5000 or >15,000 cells/mL, the defined reference range for the CCHMC clinical laboratory.
Data Analysis
Continuous variables were described using median and interquartile range (IQR) and compared across groups using Wilcoxon rank sum test due to non‐normal distributions. Categorical variables were described by counts and frequencies and compared using the 2 test.
Multivariable linear regression analysis was performed to assess the independent effect of receipt of empiric guideline‐recommended antibiotic therapy on outcomes of LOS and costs while adjusting for covariates. As LOS and costs were non‐normally distributed, we logarithmically transformed these values to use as the dependent variables in our models. The resulting coefficients were back‐transformed to reflect the percent change in LOS and costs incurred between subjects who received empiric guideline therapy compared with those who did not.[14] Covariates were chosen a priori due to their clinical and biological relevance to the outcomes of LOS (eg, wheezing on presentation and need for supplemental oxygen), total cost of hospitalization (eg, LOS and need for repeat imaging), and inpatient pharmacy costs (eg, LOS and wheezing on presentation) (Table 1).
| Characteristic | Overall Cohort, n=220 | Guideline Therapy, n=166 | Nonguideline Therapy, n=54 | P Value |
|---|---|---|---|---|
| ||||
| Age, y, median (IQR) | 2.9 (1.36.3) | 2.5 (1.35.2) | 5.6 (2.38.8) | <0.01* |
| Male, no. (%) | 122 (55.5%) | 89 (53.6%) | 33 (61.1%) | 0.34 |
| Emergency Severity Index, no. (%) | 0.11 | |||
| 2 | 90 (40.9%) | 73 (44.0%) | 17 (31.5%) | |
| 3 | 116 (52.7%) | 85 (51.2%) | 31 (57.4%) | |
| 4 | 14 (6.4%) | 8 (4.8%) | 6 (11.1%) | |
| Abnormal vital signs on presentation, no. (%) | ||||
| Fever | 99 (45.0%) | 80 (48.2%) | 19 (35.2%) | 0.10 |
| Tachycardia | 100 (45.5%) | 76 (45.8%) | 24 (44.4%) | 0.86 |
| Tachypnea | 124 (56.4%) | 100 (60.2%) | 24 (44.4%) | 0.04* |
| Hypotension | 0 | 0 | 0 | |
| Hypoxia | 27 (12.3%) | 24 (14.5%) | 3 (5.6%) | 0.08 |
| Physical exam on presentation, no. (%) | ||||
| Increased respiratory effort | 146 (66.4%) | 111 (66.9%) | 35 (64.8%) | 0.78 |
| Distressed | 110 (50.0%) | 86 (51.8%) | 24 (44.4%) | 0.35 |
| Retraction | 103 (46.8%) | 81 (48.8%) | 22 (40.7%) | 0.30 |
| Grunting | 17 (7.7%) | 14 (8.4%) | 3 (5.6%) | 0.49 |
| Nasal flaring | 19 (8.6%) | 17 (10.2%) | 2 (3.7%) | 0.14 |
| Rales | 135 (61.4%) | 99 (59.6%) | 36 (66.7%) | 0.36 |
| Wheeze | 91 (41.4%) | 66 (39.8%) | 25 (46.3%) | 0.40 |
| Decreased breath sounds | 89 (40.5%) | 65 (39.2%) | 24 (44.4%) | 0.49 |
| Dehydration | 21 (9.6%) | 13 (7.8%) | 8 (14.8%) | 0.13 |
| PEWS 5 during admission, no. (%) | 43 (19.6%) | 34 (20.5%) | 9 (16.7%) | 0.54 |
| Oxygen requirement in first 24 hours, no. (%) | 114 (51.8%) | 90 (53.6%) | 24 (46.2%) | 0.35 |
| Complete blood count obtained, no. (%) | 99 (45.0%) | 72 (43.4%) | 27 (50.0%) | 0.40 |
| Abnormal white blood cell count | 35 (35.7%) | 23 (32.4%) | 12 (44.4%) | 0.27 |
| Blood culture obtained, no. (%) | 104 (47.3%) | 80 (48.2%) | 24 (44.4%) | 0.63 |
| Positive | 2 (1.9%) | 1 (1.3%) | 1 (4.2%) | 0.36 |
| Chest radiograph available, no. (%) | 214 (97.3%) | 161 (97.0%) | 53 (98.2%) | 0.65 |
| Infiltrate | 178 (83.2%) | 139 (86.3%) | 39 (73.6%) | 0.03* |
| Bilateral | 29 (16.3%) | 20 (14.4%) | 9 (23.1%) | 0.19 |
| Multilobar | 46 (25.8%) | 33 (23.7%) | 13 (33.3%) | 0.23 |
| Effusion | 24 (11.2%) | 16 (9.9%) | 8 (15.1%) | 0.30 |
| Additional imaging, no. (%) | ||||
| Repeat chest radiograph | 26 (11.8%) | 17 (10.2%) | 9 (16.7%) | 0.20 |
| Chest ultrasound | 4 (1.8%) | 3 (1.8%) | 1 (1.9%) | 0.98 |
| Chest CT | 2 (0.9%) | 1 (0.6%) | 1 (1.9%) | 0.40 |
| Antibiotic, no. (%) | <0.01* | |||
| Aminopenicillin | 140 (63.6%) | 140 (84.3%) | 0 (0%) | |
| Third‐generation cephalosporin | 37 (16.8%) | 8 (4.8%) | 29 (53.7%) | |
| Macrolide monotherapy | 18 (8.2%) | 0 (0%) | 18 (33.3%) | |
| Clindamycin | 2 (0.9%) | 1 (0.6%) | 1 (1.9%) | |
| Levofloxacin | 1 (0.5%) | 0 (0%) | 1 (1.9%) | |
| Aminopenicillin+macrolide | 16 (7.3%) | 16 (9.6%) | 0 (0%) | |
| Cephalosporin+macrolide | 6 (2.7%) | 1 (0.6%) | 5 (9.3%) | |
Secondary outcomes of broadened antibiotic therapy, ED revisits, and hospital readmissions were assessed using the Fisher exact test. Due to the small number of events, we were unable to evaluate these associations in models adjusted for potential confounders.
All analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC), and P values <0.05 were considered significant.
RESULTS
Of the 220 unique patients included, 122 (55%) were male. The median age was 2.9 years (IQR: 1.36.3 years). Empiric guideline‐recommended therapy was prescribed to 168 (76%) patients (Table 1). Aminopenicillins were the most common guideline‐recommended therapy, accounting for 84% of guideline‐recommended antibiotics. An additional 10% of patients received the guideline‐recommended combination therapy with an aminopenicillin and a macrolide. Nonguideline‐recommended therapy included third‐generation cephalosporin antibiotics (54%) and macrolide monotherapy (33%).
Those who received empiric guideline‐recommended antibiotic therapy were similar to those who received nonguideline‐recommended therapy with respect to sex, Emergency Severity Index, physical exam findings on presentation, oxygen requirement in the first 24 hours, abnormal laboratory findings, presence of effusion on chest radiograph, and need for additional imaging (Table 1). However, patients in the guideline‐recommended therapy group were significantly younger (median 2.5 years vs 5.6 years, P0.01), more likely to have elevated respiratory rate on presentation (60.2% vs 44.4%, P=0.04), and more likely to have an infiltrate on chest radiograph (86.3% vs 73.6%, P=0.03) (Table 1). Patients who received nonguideline‐recommended macrolide monotherapy had a median age of 7.4 years (IQR: 5.89.8 years).
Median hospital LOS for the total cohort was 1.3 days (IQR: 0.91.9 days) (Table 2). There were no differences in LOS between patients who received and did not receive guideline‐recommended therapy in the unadjusted or the adjusted model (Table 3).
| Outcome | Guideline Therapy, n=166 | Nonguideline Therapy, n=54 | P Value |
|---|---|---|---|
| |||
| Length of stay, d, median (IQR) | 1.3 (0.91.9) | 1.3 (0.92.0) | 0.74 |
| Total costs, median, (IQR) | $4118 ($2,647$6,004) | $4045 ($2,829$6,200) | 0.44 |
| Pharmacy total costs, median, (IQR) | $84 ($40$179) | $106 ($58$217) | 0.12 |
| Broadened therapy, no. (%) | 10 (6.0%) | 4 (7.4%) | 0.75 |
| Emergency department revisit, no. (%) | 7 (4.2%) | 2 (3.7%) | 1.00 |
| Readmission, no. (%) | 1 (0.6%) | 1 (1.9%) | 0.43 |
| Outcome | Unadjusted Coefficient (95% CI) | Adjusted Coefficient (95% CI) | Adjusted % Change in Outcome (95% CI)* |
|---|---|---|---|
| |||
| Length of stay | 0.06 (0.27 to 0.15) | 0.06 (0.25 to 0.12) | 5.8 (22.1 to 12.8) |
| Total costs | 0.18 (0.40 to 0.04) | 0.11 (0.32 to 0.09) | 10.9 (27.4 to 9.4) |
| Pharmacy total costs | 0.44 (0.46 to 0.02) | 0.16 (0.57 to 0.24) | 14.8 (43.4 to 27.1) |
Median total costs of the index hospitalization for the total cohort were $4097 (IQR: $2657$6054), with median inpatient pharmacy costs of $92 (IQR: $40$183) (Table 2). There were no differences in total or inpatient pharmacy costs for patients who received guideline‐recommended therapy compared with those who did not in unadjusted or adjusted analyses. Fourteen patients (6.4%) had antibiotic therapy broadened during hospitalization, 10 were initially prescribed guideline‐recommended therapy, and 4 were initially prescribed nonguideline‐recommended therapy (Table 4).
| Initial Therapy | Reasons for Antibiotic Change Identified From Chart Review |
|---|---|
| Guideline=10 | Ampicillin to ceftriaxone: |
| 1 patient with clinical worsening | |
| 1 patient with coincident urinary tract infection due to resistant organism | |
| 4 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of a macrolide: | |
| 3 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of clindamycin: | |
| 1 patient with clinical worsening | |
| Nonguideline=4 | Ceftriaxone to clindamycin: |
| 1 patient with clinical worsening | |
| Addition of a macrolide: | |
| 1 patient with clinical worsening | |
| 1 patients without evidence of clinical worsening or documentation of rationale | |
| Addition of clindamycin: | |
| 1 patient with clinical worsening |
Of the 9 pneumonia‐related ED revisits within 30 days of discharge, 7 occurred in patients prescribed empiric guideline‐recommended therapy (Table 5). No ED revisit resulted in hospital readmission or antibiotic change related to pneumonia. Two ED revisits resulted in new antibiotic prescriptions for diagnoses other than pneumonia.
| Revisit | Initial Therapy | Day Postdischarge | Clinical Symptoms at Return Visit | Clinical Diagnosis | Antibiotic Prescription |
|---|---|---|---|---|---|
| |||||
| ED | Guideline | 3 | Poor oral intake and fever | Pneumonia | Continued prior antibiotic |
| ED | Guideline | 8 | Recurrent cough and fever | Resolving pneumonia | Continued prior antibiotic |
| ED | Guideline | 13 | Follow‐up | Resolved pneumonia | No further antibiotic |
| ED | Guideline | 16 | Increased work of breathing | Reactive airway disease | No antibiotic |
| ED | Guideline | 20 | Persistent cough | Viral illness | No antibiotic |
| ED | Guideline | 22 | Recurrent cough and congestion | Sinusitis | Augmentin |
| ED | Guideline | 26 | Increased work of breathing | Reactive airway disease | No antibiotic |
| ED | Nonguideline | 16 | Recurrent fever | Acute otitis media | Amoxicillin |
| ED | Nonguideline | 20 | Recurrent cough and fever | Viral illness | No antibiotic |
| Admission | Guideline | 3 | Increased work of breathing | Pneumonia | IV ampicillin |
| Admission | Nonguideline | 9 | Refusal to take oral clindamycin | Pneumonia | IV clindamycin |
Two patients were readmitted for a pneumonia‐related illness within 30 days of discharge; 1 had received guideline‐recommended therapy (Table 5). Both patients were directly admitted to the inpatient ward without an associated ED visit. Antibiotic class was not changed for either patient upon readmission, despite the decision to convert to intravenous form.
DISCUSSION
In this retrospective cohort study, patients who received empiric guideline‐recommended antibiotic therapy on admission for CAP had no difference in LOS, total cost of hospitalization, or inpatient pharmacy costs compared with those who received therapy that varied from guideline recommendations. Our study suggests that prescribing narrow‐spectrum therapy and, in some circumstances, combination therapy, as recommended by the 2011 PIDS/IDSA pneumonia guideline, did not result in negative unintended consequences.
In our study, children receiving guideline‐recommended therapy were younger, more likely to have elevated respiratory rate on presentation, and more likely to have an infiltrate on chest radiograph. We hypothesize the age difference is a reflection of common use of nonguideline macrolide monotherapy in the older, school‐age child, as macrolides are commonly used for coverage of Mycoplasma pneumonia in older children with CAP.[15] Children receiving macrolide monotherapy were older than those receiving guideline‐recommended therapy (median age of 7.4 years and 2.5 years, respectively). We also hypothesize that some providers may prescribe macrolide monotherapy to children deemed less ill than expected for CAP (eg, normal percutaneous oxygen saturation). This hypothesis is supported by the finding that 60% of patients who had a normal respiratory rate and received nonguideline therapy were prescribed macrolide monotherapy. We did control for the characteristics that varied between the two treatment groups in our models to eliminate potential confounding.
One prior study evaluated the effects of guideline implementation in CAP. In evaluation of a clinical practice guideline that recommended ampicillin as first‐line therapy for CAP, no significant difference was found following guideline introduction in the number of treatment failures (defined as the need to broaden therapy or development of complicated pneumonia within 48 hours or 30‐day inpatient readmission).[16] Our study builds on these findings by directly comparing outcomes between recipients of guideline and nonguideline therapy, which was not done in the prestudy or poststudy design of prior work.[16] We believe that classifying patients based on empiric therapy received rather than timing of guideline introduction thoroughly examines the effect of following guideline recommendations. Additionally, outcomes other than treatment failures were examined in our study including LOS, costs, and ED revisits.
Our results are similar to other observational studies that compared narrow‐ and broad‐spectrum antibiotics for children hospitalized with CAP. Using administrative data, Williams et al. found no significant difference in LOS or cost between narrow‐ and broad‐spectrum intravenous antibiotic recipients ages 6 months to 18 years at 43 children's hospitals.[17] Queen et al. compared narrow‐ and broad‐spectrum antibiotic therapy for children ages 2 months to 18 years at 4 children's hospitals.[18] Differences in average daily cost were not significant, but children who received narrow‐spectrum antibiotics had a significantly shorter LOS. Finally, an observational study of 319 Israeli children <2 years of age found no significant difference in duration of oxygen requirement, LOS, or need for change in antibiotic therapy between the 66 children prescribed aminopenicillins and the 253 children prescribed cefuroxime.[19] These studies suggest that prescribing narrow‐spectrum antimicrobial therapy, as per the guideline recommendations, results in similar outcomes to broad‐spectrum antimicrobial therapy.
Our study adds to prior studies that compared narrow‐ and broad‐spectrum therapy by comparing outcomes associated with guideline‐recommended therapy to nonguideline therapy. We considered antibiotic therapy as guideline recommended if appropriately chosen per the guideline, not just by simple classification of antibiotic. For example, the use of a cephalosporin in a patient with aminopenicillin allergy was considered guideline‐recommended therapy. We chose to classify the exposure of empiric antibiotic therapy in this manner to reflect true clinical application of the guideline, as not all children are able to receive aminopenicillins. Additionally, as our study stemmed from our prior improvement work aimed at increasing guideline adherent therapy,[7] we have a higher frequency of narrow‐spectrum antibiotic use than prior studies. In our study, almost two‐thirds of patients received narrow‐spectrum therapy, whereas narrow‐spectrum use in prior studies ranged from 10% to 33%.[17, 18, 19] Finally, we were able to confirm the diagnosis of pneumonia via medical record review and to adjust for severity of illness using clinical variables including vital signs, physical exam findings, and laboratory and radiologic study results.
This study must be interpreted in the context of several limitations. First, our study population was defined through discharge diagnosis codes, and therefore dependent on the accuracy of coding. However, we minimized potential for misclassification through use of a previously validated approach to identify patients with CAP and through medical record review to confirm the diagnosis. Second, we may be unable to detect very small differences in outcomes given limited power, specifically for outcomes of LOS, ED revisits, hospital readmissions, and need to broaden antibiotic therapy. Third, residual confounding may be present. Although we controlled for many clinical variables in our analyses, antibiotic prescribing practices may be influenced by unmeasured factors. The potential of system level confounding is mitigated by standardized care for patients with CAP at our institution. Prior system‐level changes using quality‐improvement science have resulted in a high level of adherence with guideline‐recommended antimicrobials as well as standardized medical discharge criteria.[7, 20] Additionally, nonmedical factors may influence LOS, limiting its use as an outcome measure. This limitation was minimized in our study by standardizing medical discharge criteria. Prior work at our institution demonstrated that the majority of patients, including those with CAP, were discharged within 2 hours of meeting medical discharge criteria.[20] Fourth, discharged patients who experienced adverse outcomes may have received care at a nearby adult emergency department or at their pediatrician's office. Although these events would not have been captured in our electronic health record, serious complications due to treatment failure (eg, empyema) would require hospitalization. As our hospital is the only children's hospital in the Greater Cincinnati metropolitan area, these patents would receive care at our institution. Therefore, any misclassification of revisits or readmissions is likely to be minimal. Finally, study patients were admitted to a large tertiary academic children's hospital, warranting further investigation to determine if these findings can be translated to smaller community settings.
In conclusion, receipt of guideline‐recommended antibiotic therapy for patients hospitalized with CAP was not associated with increases in LOS, total costs of hospitalization, or inpatient pharmacy costs. Our findings highlight the importance of changing antibiotic prescribing practices to reflect guideline recommendations, as there was no evidence of negative unintended consequences with our local practice change.
Acknowledgments
Disclosures: Dr. Ambroggio and Dr. Thomson were supported by funds from the NRSA T32HP10027‐14. Dr. Shah was supported by funds from NIAID K01A173729. The authors report no conflicts of interest.
- , , , , , . Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994–2007. Pediatrics. 2011;127(3):411–418.
- , , , , . National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126(2):204–213.
- , , , et al. Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166(12):1155–1164.
- , , , et al. The management of community‐acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25–e76.
- , , , et al. Variability in processes of care and outcomes among children hospitalized with community‐acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036–1041.
- , , , et al. Impact of IDSA/PIDS guidelines on treatment of community‐acquired pneumonia in hospitalized children. Clin Infect Dis. 2014;58(6):834–838.
- , , , et al. Quality improvement methods increase appropriate antibiotic prescribing for childhood pneumonia. Pediatrics. 2013;131(5):e1623–e1631.
- , , , et al. Identifying pediatric community‐acquired pneumonia hospitalizations: accuracy of administrative billing codes. JAMA Pediatr. 2013;167(9):851–858.
- , , , , , . Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):E99.
- Centers for Medicare 2011.
- , , , et al. Pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126(5):e1361–e1399.
- , , , , . Prospective evaluation of a pediatric inpatient early warning scoring system. J Spec Pediatr Nurs. 2009;14(2):79–85.
- , , , . Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. New York, NY: Springer; 2005.
- , , , , . Treatment of mycoplasma pneumonia: a systematic review. Pediatrics. 2014;133(6):1081–1090.
- , , , , , . Impact of a guideline on management of children hospitalized with community‐acquired pneumonia. Pediatrics. 2012;129(3):e597–e604.
- , , , et al. Narrow vs broad‐spectrum antimicrobial therapy for children hospitalized with pneumonia. Pediatrics. 2013;132(5):e1141–e1148.
- , , , et al. Comparative effectiveness of empiric antibiotics for community‐acquired pneumonia. Pediatrics. 2014;133(1):e23–e29.
- , , , et al. Antibiotic treatment of children with community‐acquired pneumonia: comparison of penicillin or ampicillin versus cefuroxime. Pediatr Pulmonol. 2013;48(1):52–58.
- , , , et al. Using quality improvement to optimise paediatric discharge efficiency. BMJ Qual Saf. 2014;23(5):428–436.
- , , , , , . Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994–2007. Pediatrics. 2011;127(3):411–418.
- , , , , . National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126(2):204–213.
- , , , et al. Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166(12):1155–1164.
- , , , et al. The management of community‐acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25–e76.
- , , , et al. Variability in processes of care and outcomes among children hospitalized with community‐acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036–1041.
- , , , et al. Impact of IDSA/PIDS guidelines on treatment of community‐acquired pneumonia in hospitalized children. Clin Infect Dis. 2014;58(6):834–838.
- , , , et al. Quality improvement methods increase appropriate antibiotic prescribing for childhood pneumonia. Pediatrics. 2013;131(5):e1623–e1631.
- , , , et al. Identifying pediatric community‐acquired pneumonia hospitalizations: accuracy of administrative billing codes. JAMA Pediatr. 2013;167(9):851–858.
- , , , , , . Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):E99.
- Centers for Medicare 2011.
- , , , et al. Pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126(5):e1361–e1399.
- , , , , . Prospective evaluation of a pediatric inpatient early warning scoring system. J Spec Pediatr Nurs. 2009;14(2):79–85.
- , , , . Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. New York, NY: Springer; 2005.
- , , , , . Treatment of mycoplasma pneumonia: a systematic review. Pediatrics. 2014;133(6):1081–1090.
- , , , , , . Impact of a guideline on management of children hospitalized with community‐acquired pneumonia. Pediatrics. 2012;129(3):e597–e604.
- , , , et al. Narrow vs broad‐spectrum antimicrobial therapy for children hospitalized with pneumonia. Pediatrics. 2013;132(5):e1141–e1148.
- , , , et al. Comparative effectiveness of empiric antibiotics for community‐acquired pneumonia. Pediatrics. 2014;133(1):e23–e29.
- , , , et al. Antibiotic treatment of children with community‐acquired pneumonia: comparison of penicillin or ampicillin versus cefuroxime. Pediatr Pulmonol. 2013;48(1):52–58.
- , , , et al. Using quality improvement to optimise paediatric discharge efficiency. BMJ Qual Saf. 2014;23(5):428–436.
© 2014 Society of Hospital Medicine
Memory problems more common in psychogenic nonepileptic seizures plus PTSD
Individuals suffering from psychogenic nonepileptic seizures with posttraumatic stress disorder have significant verbal and visual memory impairments, and a greater likelihood of a history of substance abuse than individuals without PTSD, even if those individuals have a history of trauma, investigators have found in a case-control study.
“Up to 90% of patients with PNESs [psychogenic nonepileptic seizures] have been reported to have histories of significant traumatic experiences, with particularly high instances of childhood sexual and physical abuse, compared with control groups and the general population,” wrote Lorna Myers, Ph.D., of the Northeast Regional Epilepsy Group, New York, and her associates.
Those with psychogenic nonepileptic seizures and PTSD had the highest rates of psychiatric medication use, substance abuse, history of rape, and history of physical abuse, compared with individuals who had psychogenic nonepileptic seizures without a diagnosis of PTSD but with a history of trauma, and individuals with psychogenic nonepileptic seizures and no history of trauma, according to the study (Epilepsy & Behavior 2014;37:82-6).
Investigators for the study – which enrolled 17 people with psychogenic nonepileptic seizures and PTSD, 29 people with psychogenic nonepileptic seizures and a history of trauma but no PTSD, and 17 individuals with psychogenic nonepileptic seizures but no PTSD or trauma history – also found that those with psychogenic nonepileptic seizures and PTSD scored lowest in delayed narrative memory, and showed the highest scores for self-perceived verbal memory, visuospatial memory, and overall Memory Complaints Inventory.
Dr. Myers and her associates cited several limitations. For example, they did not collect data on the patients’ ethnic or racial backgrounds, which suggests that information on “PNES pathology and neuropsychological functions” might have been missed.
The authors declared no conflicts of interest.
Individuals suffering from psychogenic nonepileptic seizures with posttraumatic stress disorder have significant verbal and visual memory impairments, and a greater likelihood of a history of substance abuse than individuals without PTSD, even if those individuals have a history of trauma, investigators have found in a case-control study.
“Up to 90% of patients with PNESs [psychogenic nonepileptic seizures] have been reported to have histories of significant traumatic experiences, with particularly high instances of childhood sexual and physical abuse, compared with control groups and the general population,” wrote Lorna Myers, Ph.D., of the Northeast Regional Epilepsy Group, New York, and her associates.
Those with psychogenic nonepileptic seizures and PTSD had the highest rates of psychiatric medication use, substance abuse, history of rape, and history of physical abuse, compared with individuals who had psychogenic nonepileptic seizures without a diagnosis of PTSD but with a history of trauma, and individuals with psychogenic nonepileptic seizures and no history of trauma, according to the study (Epilepsy & Behavior 2014;37:82-6).
Investigators for the study – which enrolled 17 people with psychogenic nonepileptic seizures and PTSD, 29 people with psychogenic nonepileptic seizures and a history of trauma but no PTSD, and 17 individuals with psychogenic nonepileptic seizures but no PTSD or trauma history – also found that those with psychogenic nonepileptic seizures and PTSD scored lowest in delayed narrative memory, and showed the highest scores for self-perceived verbal memory, visuospatial memory, and overall Memory Complaints Inventory.
Dr. Myers and her associates cited several limitations. For example, they did not collect data on the patients’ ethnic or racial backgrounds, which suggests that information on “PNES pathology and neuropsychological functions” might have been missed.
The authors declared no conflicts of interest.
Individuals suffering from psychogenic nonepileptic seizures with posttraumatic stress disorder have significant verbal and visual memory impairments, and a greater likelihood of a history of substance abuse than individuals without PTSD, even if those individuals have a history of trauma, investigators have found in a case-control study.
“Up to 90% of patients with PNESs [psychogenic nonepileptic seizures] have been reported to have histories of significant traumatic experiences, with particularly high instances of childhood sexual and physical abuse, compared with control groups and the general population,” wrote Lorna Myers, Ph.D., of the Northeast Regional Epilepsy Group, New York, and her associates.
Those with psychogenic nonepileptic seizures and PTSD had the highest rates of psychiatric medication use, substance abuse, history of rape, and history of physical abuse, compared with individuals who had psychogenic nonepileptic seizures without a diagnosis of PTSD but with a history of trauma, and individuals with psychogenic nonepileptic seizures and no history of trauma, according to the study (Epilepsy & Behavior 2014;37:82-6).
Investigators for the study – which enrolled 17 people with psychogenic nonepileptic seizures and PTSD, 29 people with psychogenic nonepileptic seizures and a history of trauma but no PTSD, and 17 individuals with psychogenic nonepileptic seizures but no PTSD or trauma history – also found that those with psychogenic nonepileptic seizures and PTSD scored lowest in delayed narrative memory, and showed the highest scores for self-perceived verbal memory, visuospatial memory, and overall Memory Complaints Inventory.
Dr. Myers and her associates cited several limitations. For example, they did not collect data on the patients’ ethnic or racial backgrounds, which suggests that information on “PNES pathology and neuropsychological functions” might have been missed.
The authors declared no conflicts of interest.
FROM EPILEPSY & BEHAVIOR
Key clinical point: Individuals with psychogenic nonepileptic seizures and PTSD have worse memory problems and higher rates of substance abuse.
Major finding: Substance abuse, memory problems, and history of trauma were more likely in psychogenic nonepileptic seizures plus PTSD than without PTSD.
Data source: Case-control study among 17 people with psychogenic nonepileptic seizures and PTSD, 29 people with psychogenic nonepileptic seizures and a history of trauma but no PTSD, and 17 individuals with psychogenic nonepileptic seizures but no PTSD or trauma history.
Disclosures: The authors declared no conflicts of interest.
BEST PRACTICES IN: Infant Feeding
Medical Education Library
A Best Practices Supplement to Pediatric News®. This supplement was sponsored by Perrigo Nutritionals.
Topics
- Introduction
- Store Brands and Advertised Brands
- FDA Regulation of Formula
- Formula Selection
- The Problem of Infant Formula Dilution
- Is Switching Formula Safe?
- Conclusion
Faculty/Faculty Disclosure
Joel R. Rosh, MD
Director, Pediatric
Gastroenterology
Goryeb Children’s
Hospital/Atlantic Health
Morristown, NJ
Professor of Pediatrics
Icahn School of Medicine
at Mount Sinai
New York, NY
Dr. Rosh discloses that he is on an advisory board for Perrigo Nutritionals.
Medical Education Library
A Best Practices Supplement to Pediatric News®. This supplement was sponsored by Perrigo Nutritionals.
Topics
- Introduction
- Store Brands and Advertised Brands
- FDA Regulation of Formula
- Formula Selection
- The Problem of Infant Formula Dilution
- Is Switching Formula Safe?
- Conclusion
Faculty/Faculty Disclosure
Joel R. Rosh, MD
Director, Pediatric
Gastroenterology
Goryeb Children’s
Hospital/Atlantic Health
Morristown, NJ
Professor of Pediatrics
Icahn School of Medicine
at Mount Sinai
New York, NY
Dr. Rosh discloses that he is on an advisory board for Perrigo Nutritionals.
Medical Education Library
A Best Practices Supplement to Pediatric News®. This supplement was sponsored by Perrigo Nutritionals.
Topics
- Introduction
- Store Brands and Advertised Brands
- FDA Regulation of Formula
- Formula Selection
- The Problem of Infant Formula Dilution
- Is Switching Formula Safe?
- Conclusion
Faculty/Faculty Disclosure
Joel R. Rosh, MD
Director, Pediatric
Gastroenterology
Goryeb Children’s
Hospital/Atlantic Health
Morristown, NJ
Professor of Pediatrics
Icahn School of Medicine
at Mount Sinai
New York, NY
Dr. Rosh discloses that he is on an advisory board for Perrigo Nutritionals.
How can I get training in working with families?
In the late-20th century, family therapy was a new therapeutic modality. It was an exciting time! Family therapy and the application of systems principles to families was considered “thinking outside the box.” Different schools of family therapy were developed, usually based in an academic center and led by a charismatic leader, often a psychiatrist.
Today, with the rise in the popularity of psychopharmacology and the promise of biological interventions, there are fewer opportunities for family systems training within psychiatric residency programs. In order to receive family systems training, a psychiatrist may decide to enroll in an independent family training institute, such as the Ackerman Institute for the Family in New York. However, there are still some psychiatric residency programs that consider learning to work with families to be an essential psychotherapeutic skill.
Psychiatric training in family therapy
Dr. Ellen Berman, president of the Association of Family Psychiatrists, recently asked family psychiatrists to indicate psychiatric residency programs offering family systems training. Nine programs were identified. Here is a description of each program and contact information:
• Albert Einstein College of Medicine, New York
“We have a well-established and extensive Family Studies program that is part of the department of psychiatry at Albert Einstein College of Medicine and is well integrated into the residency training program. All residents in the 4 years of the training program at Montefiore Medical Center and Bronx (N.Y.) Psychiatric Center as well as child fellows receive supervision in couples and family therapy, courses, seminars, electives, and more. Faculty and residents have presented different innovative projects related to family and systems at national conferences and have written papers on their clinical work.”
– Contact: [email protected], Director of Family Studies, department of psychiatry, Albert Einstein College of Medicine.
• McGill University, Montreal
“We have a very active family therapy community in Montreal, with [Dr.] Herta Guttman as our pioneer. At the Jewish General [Hospital] department of psychiatry, we run an [American Association for Marriage and Family Therapy]–accredited postgraduate certificate couple and family therapy program. This program primarily trains community mental health practitioners (social workers, psychologists, etc.), however, we have had psychiatrists take this course. This year, we are training our first Couple and Family Fellow (child psychiatrist) through the department of psychiatry.
In McGill Psychiatry, we have a new family skills teaching module in the McGill Resident Diploma Program. We will provide 3 hours of teaching in the R1 year (basic concepts). In the R2 and R3 years, residents receive training on a range of family therapy topics. The curriculum was inspired by the Group for the Advancement of Psychiatry curriculum. Dr. Nick Casacalenda spearheaded this initiative. There are 3 hours of family teaching in the diploma course module: gender, social, and cultural aspects of psychiatry, and 6 hours in the child psychiatry module.”
– Contact: Sharon Bond, Ph.D.; School of Social Work; Director, Couple and Family Therapy Program.
• NYU School of Medicine
“I am the director of service at the Roberto Clemente Center in the Lower East Side (now East Village) in Manhattan. The center is part of the departments of mental health of both Gouverneur [Healthcare Services] and Bellevue. We have an academic affiliation with New York University School of Medicine. The center was started about 30 years ago by a psychologist, Jaime Inclan, Ph.D. He was initially was trained by [Dr.] Salvador Minuchin. As a family clinic embedded in the community, we mostly serve minority underserved populations. We provide primary health and mental health services. We have been providing for decades training to medical students, psychology interns, and social work students.”
– Contact: Dr. Miguel Vilaro-Colon, Clinical Assistant Professor of Psychiatry, NYU School of Medicine.
• Stanford (Calif.) University
“Our 4-year training program in couples and family therapy begins with didactics and family meetings (inpatient) in the first year; didactics and opportunities for a couples and family therapy clinical elective as [postgraduate year]-2s; live case observation in the family therapy program at the [Veterans Affairs] Palo Alto Health Care System, as well as an intensive seminar at Stanford during the PGY-3 year, and supervised outpatient clinical work in Stanford’s Couples and Family Therapy Clinic during the PGY-3 and PGY-4 years. Residents who are interested in child and adolescent psychiatry can focus their PGY-3 rotation on family cases with a child/adolescent focus. An earlier version of this training sequence is described in program for residents is described in ‘A Model for Reintegrating Couples and Family Therapy Training in Psychiatric Residency Programs’ ” (Acad. Psychiatry 2008;32:81-6).
– Contact: Douglas S. Rait, Ph.D., Chief, Couples and Family Therapy Clinic, Clinical Professor of Psychiatry & Behavioral Sciences, Stanford University.
• University of Pennsylvania Perlman School of Medicine
“The Center for Couples and Adult Families in the department of psychiatry includes a didactic program for residents spanning all 4 years and supervision in PGY-3 and 4. Residents help run multifamily psychoeducation groups in the bipolar clinic, and see couples and families in their outpatient clinics. Our focus is on family inclusion and family psychoeducation for all patients when possible, with couple and adult family therapy when appropriate. Our curriculum is on our website As the clinical director, I work closely with Ellen Berman, who founded the center 5 years ago.”
– Contact: Jacqueline Hudak, Ph.D., LMFT, Center for Couples and Adult Families, Department of Psychiatry, Perelman School of Medicine.
• Mount Sinai Beth Israel, New York The Family Center for Bipolar provides services to patients with bipolar disorder “within the context of the family.” In addition, Dr. Igor Galynker, who runs the center, gives a series of lectures on family inclusion. The center also has a formal training program in family therapy run by Haya Mermelstein, CSW.
– Contact: Dr. Igor Galynker, professor of psychiatry, Icahn School of Medicine at Mount Sinai; director, the Family Center for Bipolar Disorder; Associate Chairman, Department Of Psychiatry and Behavioral Sciences.
• Brown University, Providence, R.I.
“We have a formal Family Therapy Training Program in the department of psychiatry at Brown University, based at Rhode Island Hospital.”
– Contact: Dr. Gabor I. Keitner, Associate Chief of Psychiatry, Rhode Island and Miriam Hospitals; Professor, Department of Psychiatry, Brown University.
• University of Rochester, Institute for the Family
“An emphasis on family is embedded in all of our training. The residents have a formal didactic curriculum and participate in family care and family research. Many of the residents fast track into a child fellowship, which has an extensive program in family therapy.
– Contact: Dr. [email protected], Director of Psychiatry Residency Education, University of Rochester Medical Center.
• University of Colorado Denver
“Our department offers a unique psychotherapy scholar track. The mission of this track is to offer advanced psychotherapy training to a subgroup of psychiatric residents, within an adult general residency program, who wish to learn and do psychotherapy. Within this track we offer extensive family therapy training. The family therapy component consists of didactics and direct supervision. It runs through the 4 years of residency. There are several experienced family therapists on the faculty who supervise in this program.”
– Contact: Dr. [email protected], Vice Chair, Department of Psychiatry.
A multidisciplinary field
Family systems training occurs in other disciplines: psychology, social work, and marriage and family therapy (MFT) programs. The number of MFT programs across the United States is large, reflecting the demand for family systems therapists.
Psychologists with a special interest in family therapy belong to the American Psychological Association’s Division 43. Division 43 supports family-oriented clinical and scientific activities as well as education and public policy, a journal called the Journal of Family Psychology, and a quarterly newsletter called The Family Psychologist. Many psychologists are trained in family therapy work in primary care settings. The current president of American Psychological Association, Nadine J. Kaslow, Ph.D., is a family therapist who helps underserved and underprivileged populations receive culturally competent, evidence-based, biopsychosocially oriented mental health services.
Social Workers are required to take two exams: one to be “licensed” as an LCSW (licensed clinical social worker) after graduation with a master’s degree. After 3,000 hours of supervised clinical practice, social worker takes second exam for independent licensure LICSW (licensed independent clinical social worker).
Social work schools have a course or two in family therapy. After graduation, students may choose to specialize in couples and family therapy. Like psychiatric and psychological training programs, there is wide variation in the amount of family therapy taught in schools of social work.
Marriage and family therapists (MFTs) have their own organization, the American Association for Marriage and Family Therapy (AAMFT). This organization’s training is specific to families and couples. Members are required to be supervised in clinical practice for 2 years. AAMFT produces the Journal of Marital and Family Therapy. The AAMFT website also lists accredited programs in the United States and Canada.
Two American journals in this area are interdisciplinary: Family Process and Families, Systems & Health. Family Process has broad representation on its board from all disciplines and has a strong focus on family systems research and social justice. Family Process aims to support emerging researchers and clinicians worldwide, and periodically offers grants. Families, Systems & Health is multidisciplinary with a focus on research and clinical practice in medical illness, and health psychology.
The American Family Therapy Academy (AFTA) is the only organization that is interdisciplinary. Founded in 1977, AFTA’s objectives include “the advancement of theories, therapies, research, and professional education that regard the family as a unit in a social context, to make information about family therapy available to practitioners in other fields of knowledge and to the public and to foster collaboration among the medical, psychological, social, legal, and other professions that serve families and the science and practice of family therapy.”
AFTA is outspoken on issues that affect families. For example, its Immigration Position Statement addresses the negative impact of U.S. immigration policy on families and children. AFTA has strong views about the DSM-5, stating that “the current revision of the DSM continues a long history of ignoring research and excluding vital contributions of nonpsychiatric mental health disciplines resulting in invalid diagnostic categories and treatment protocols. The DSM is dominant in determining mental health diagnosis and treatment and is more harmful than helpful in delineating best practices.” The next AFTA conference is in June 2015, and the theme is “Global Ecologies: Connections among Self, Families, Communities, and Cultures.”
Family therapy has grown from a small group of interested academics, mostly psychiatrists, to a large group of interdisciplinary professionals. Today, psychiatrists have less access to family systems training than in previous decades but can still access training. In addition to attending conferences, psychiatrists interested in this area might see whether training programs would accept them into their courses.
For those psychiatrists who have not had formal training during residency training, this review of programs is a good starting point for seeking family systems training.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of the recently published book Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals (New York: Routledge, 2013).
In the late-20th century, family therapy was a new therapeutic modality. It was an exciting time! Family therapy and the application of systems principles to families was considered “thinking outside the box.” Different schools of family therapy were developed, usually based in an academic center and led by a charismatic leader, often a psychiatrist.
Today, with the rise in the popularity of psychopharmacology and the promise of biological interventions, there are fewer opportunities for family systems training within psychiatric residency programs. In order to receive family systems training, a psychiatrist may decide to enroll in an independent family training institute, such as the Ackerman Institute for the Family in New York. However, there are still some psychiatric residency programs that consider learning to work with families to be an essential psychotherapeutic skill.
Psychiatric training in family therapy
Dr. Ellen Berman, president of the Association of Family Psychiatrists, recently asked family psychiatrists to indicate psychiatric residency programs offering family systems training. Nine programs were identified. Here is a description of each program and contact information:
• Albert Einstein College of Medicine, New York
“We have a well-established and extensive Family Studies program that is part of the department of psychiatry at Albert Einstein College of Medicine and is well integrated into the residency training program. All residents in the 4 years of the training program at Montefiore Medical Center and Bronx (N.Y.) Psychiatric Center as well as child fellows receive supervision in couples and family therapy, courses, seminars, electives, and more. Faculty and residents have presented different innovative projects related to family and systems at national conferences and have written papers on their clinical work.”
– Contact: [email protected], Director of Family Studies, department of psychiatry, Albert Einstein College of Medicine.
• McGill University, Montreal
“We have a very active family therapy community in Montreal, with [Dr.] Herta Guttman as our pioneer. At the Jewish General [Hospital] department of psychiatry, we run an [American Association for Marriage and Family Therapy]–accredited postgraduate certificate couple and family therapy program. This program primarily trains community mental health practitioners (social workers, psychologists, etc.), however, we have had psychiatrists take this course. This year, we are training our first Couple and Family Fellow (child psychiatrist) through the department of psychiatry.
In McGill Psychiatry, we have a new family skills teaching module in the McGill Resident Diploma Program. We will provide 3 hours of teaching in the R1 year (basic concepts). In the R2 and R3 years, residents receive training on a range of family therapy topics. The curriculum was inspired by the Group for the Advancement of Psychiatry curriculum. Dr. Nick Casacalenda spearheaded this initiative. There are 3 hours of family teaching in the diploma course module: gender, social, and cultural aspects of psychiatry, and 6 hours in the child psychiatry module.”
– Contact: Sharon Bond, Ph.D.; School of Social Work; Director, Couple and Family Therapy Program.
• NYU School of Medicine
“I am the director of service at the Roberto Clemente Center in the Lower East Side (now East Village) in Manhattan. The center is part of the departments of mental health of both Gouverneur [Healthcare Services] and Bellevue. We have an academic affiliation with New York University School of Medicine. The center was started about 30 years ago by a psychologist, Jaime Inclan, Ph.D. He was initially was trained by [Dr.] Salvador Minuchin. As a family clinic embedded in the community, we mostly serve minority underserved populations. We provide primary health and mental health services. We have been providing for decades training to medical students, psychology interns, and social work students.”
– Contact: Dr. Miguel Vilaro-Colon, Clinical Assistant Professor of Psychiatry, NYU School of Medicine.
• Stanford (Calif.) University
“Our 4-year training program in couples and family therapy begins with didactics and family meetings (inpatient) in the first year; didactics and opportunities for a couples and family therapy clinical elective as [postgraduate year]-2s; live case observation in the family therapy program at the [Veterans Affairs] Palo Alto Health Care System, as well as an intensive seminar at Stanford during the PGY-3 year, and supervised outpatient clinical work in Stanford’s Couples and Family Therapy Clinic during the PGY-3 and PGY-4 years. Residents who are interested in child and adolescent psychiatry can focus their PGY-3 rotation on family cases with a child/adolescent focus. An earlier version of this training sequence is described in program for residents is described in ‘A Model for Reintegrating Couples and Family Therapy Training in Psychiatric Residency Programs’ ” (Acad. Psychiatry 2008;32:81-6).
– Contact: Douglas S. Rait, Ph.D., Chief, Couples and Family Therapy Clinic, Clinical Professor of Psychiatry & Behavioral Sciences, Stanford University.
• University of Pennsylvania Perlman School of Medicine
“The Center for Couples and Adult Families in the department of psychiatry includes a didactic program for residents spanning all 4 years and supervision in PGY-3 and 4. Residents help run multifamily psychoeducation groups in the bipolar clinic, and see couples and families in their outpatient clinics. Our focus is on family inclusion and family psychoeducation for all patients when possible, with couple and adult family therapy when appropriate. Our curriculum is on our website As the clinical director, I work closely with Ellen Berman, who founded the center 5 years ago.”
– Contact: Jacqueline Hudak, Ph.D., LMFT, Center for Couples and Adult Families, Department of Psychiatry, Perelman School of Medicine.
• Mount Sinai Beth Israel, New York The Family Center for Bipolar provides services to patients with bipolar disorder “within the context of the family.” In addition, Dr. Igor Galynker, who runs the center, gives a series of lectures on family inclusion. The center also has a formal training program in family therapy run by Haya Mermelstein, CSW.
– Contact: Dr. Igor Galynker, professor of psychiatry, Icahn School of Medicine at Mount Sinai; director, the Family Center for Bipolar Disorder; Associate Chairman, Department Of Psychiatry and Behavioral Sciences.
• Brown University, Providence, R.I.
“We have a formal Family Therapy Training Program in the department of psychiatry at Brown University, based at Rhode Island Hospital.”
– Contact: Dr. Gabor I. Keitner, Associate Chief of Psychiatry, Rhode Island and Miriam Hospitals; Professor, Department of Psychiatry, Brown University.
• University of Rochester, Institute for the Family
“An emphasis on family is embedded in all of our training. The residents have a formal didactic curriculum and participate in family care and family research. Many of the residents fast track into a child fellowship, which has an extensive program in family therapy.
– Contact: Dr. [email protected], Director of Psychiatry Residency Education, University of Rochester Medical Center.
• University of Colorado Denver
“Our department offers a unique psychotherapy scholar track. The mission of this track is to offer advanced psychotherapy training to a subgroup of psychiatric residents, within an adult general residency program, who wish to learn and do psychotherapy. Within this track we offer extensive family therapy training. The family therapy component consists of didactics and direct supervision. It runs through the 4 years of residency. There are several experienced family therapists on the faculty who supervise in this program.”
– Contact: Dr. [email protected], Vice Chair, Department of Psychiatry.
A multidisciplinary field
Family systems training occurs in other disciplines: psychology, social work, and marriage and family therapy (MFT) programs. The number of MFT programs across the United States is large, reflecting the demand for family systems therapists.
Psychologists with a special interest in family therapy belong to the American Psychological Association’s Division 43. Division 43 supports family-oriented clinical and scientific activities as well as education and public policy, a journal called the Journal of Family Psychology, and a quarterly newsletter called The Family Psychologist. Many psychologists are trained in family therapy work in primary care settings. The current president of American Psychological Association, Nadine J. Kaslow, Ph.D., is a family therapist who helps underserved and underprivileged populations receive culturally competent, evidence-based, biopsychosocially oriented mental health services.
Social Workers are required to take two exams: one to be “licensed” as an LCSW (licensed clinical social worker) after graduation with a master’s degree. After 3,000 hours of supervised clinical practice, social worker takes second exam for independent licensure LICSW (licensed independent clinical social worker).
Social work schools have a course or two in family therapy. After graduation, students may choose to specialize in couples and family therapy. Like psychiatric and psychological training programs, there is wide variation in the amount of family therapy taught in schools of social work.
Marriage and family therapists (MFTs) have their own organization, the American Association for Marriage and Family Therapy (AAMFT). This organization’s training is specific to families and couples. Members are required to be supervised in clinical practice for 2 years. AAMFT produces the Journal of Marital and Family Therapy. The AAMFT website also lists accredited programs in the United States and Canada.
Two American journals in this area are interdisciplinary: Family Process and Families, Systems & Health. Family Process has broad representation on its board from all disciplines and has a strong focus on family systems research and social justice. Family Process aims to support emerging researchers and clinicians worldwide, and periodically offers grants. Families, Systems & Health is multidisciplinary with a focus on research and clinical practice in medical illness, and health psychology.
The American Family Therapy Academy (AFTA) is the only organization that is interdisciplinary. Founded in 1977, AFTA’s objectives include “the advancement of theories, therapies, research, and professional education that regard the family as a unit in a social context, to make information about family therapy available to practitioners in other fields of knowledge and to the public and to foster collaboration among the medical, psychological, social, legal, and other professions that serve families and the science and practice of family therapy.”
AFTA is outspoken on issues that affect families. For example, its Immigration Position Statement addresses the negative impact of U.S. immigration policy on families and children. AFTA has strong views about the DSM-5, stating that “the current revision of the DSM continues a long history of ignoring research and excluding vital contributions of nonpsychiatric mental health disciplines resulting in invalid diagnostic categories and treatment protocols. The DSM is dominant in determining mental health diagnosis and treatment and is more harmful than helpful in delineating best practices.” The next AFTA conference is in June 2015, and the theme is “Global Ecologies: Connections among Self, Families, Communities, and Cultures.”
Family therapy has grown from a small group of interested academics, mostly psychiatrists, to a large group of interdisciplinary professionals. Today, psychiatrists have less access to family systems training than in previous decades but can still access training. In addition to attending conferences, psychiatrists interested in this area might see whether training programs would accept them into their courses.
For those psychiatrists who have not had formal training during residency training, this review of programs is a good starting point for seeking family systems training.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of the recently published book Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals (New York: Routledge, 2013).
In the late-20th century, family therapy was a new therapeutic modality. It was an exciting time! Family therapy and the application of systems principles to families was considered “thinking outside the box.” Different schools of family therapy were developed, usually based in an academic center and led by a charismatic leader, often a psychiatrist.
Today, with the rise in the popularity of psychopharmacology and the promise of biological interventions, there are fewer opportunities for family systems training within psychiatric residency programs. In order to receive family systems training, a psychiatrist may decide to enroll in an independent family training institute, such as the Ackerman Institute for the Family in New York. However, there are still some psychiatric residency programs that consider learning to work with families to be an essential psychotherapeutic skill.
Psychiatric training in family therapy
Dr. Ellen Berman, president of the Association of Family Psychiatrists, recently asked family psychiatrists to indicate psychiatric residency programs offering family systems training. Nine programs were identified. Here is a description of each program and contact information:
• Albert Einstein College of Medicine, New York
“We have a well-established and extensive Family Studies program that is part of the department of psychiatry at Albert Einstein College of Medicine and is well integrated into the residency training program. All residents in the 4 years of the training program at Montefiore Medical Center and Bronx (N.Y.) Psychiatric Center as well as child fellows receive supervision in couples and family therapy, courses, seminars, electives, and more. Faculty and residents have presented different innovative projects related to family and systems at national conferences and have written papers on their clinical work.”
– Contact: [email protected], Director of Family Studies, department of psychiatry, Albert Einstein College of Medicine.
• McGill University, Montreal
“We have a very active family therapy community in Montreal, with [Dr.] Herta Guttman as our pioneer. At the Jewish General [Hospital] department of psychiatry, we run an [American Association for Marriage and Family Therapy]–accredited postgraduate certificate couple and family therapy program. This program primarily trains community mental health practitioners (social workers, psychologists, etc.), however, we have had psychiatrists take this course. This year, we are training our first Couple and Family Fellow (child psychiatrist) through the department of psychiatry.
In McGill Psychiatry, we have a new family skills teaching module in the McGill Resident Diploma Program. We will provide 3 hours of teaching in the R1 year (basic concepts). In the R2 and R3 years, residents receive training on a range of family therapy topics. The curriculum was inspired by the Group for the Advancement of Psychiatry curriculum. Dr. Nick Casacalenda spearheaded this initiative. There are 3 hours of family teaching in the diploma course module: gender, social, and cultural aspects of psychiatry, and 6 hours in the child psychiatry module.”
– Contact: Sharon Bond, Ph.D.; School of Social Work; Director, Couple and Family Therapy Program.
• NYU School of Medicine
“I am the director of service at the Roberto Clemente Center in the Lower East Side (now East Village) in Manhattan. The center is part of the departments of mental health of both Gouverneur [Healthcare Services] and Bellevue. We have an academic affiliation with New York University School of Medicine. The center was started about 30 years ago by a psychologist, Jaime Inclan, Ph.D. He was initially was trained by [Dr.] Salvador Minuchin. As a family clinic embedded in the community, we mostly serve minority underserved populations. We provide primary health and mental health services. We have been providing for decades training to medical students, psychology interns, and social work students.”
– Contact: Dr. Miguel Vilaro-Colon, Clinical Assistant Professor of Psychiatry, NYU School of Medicine.
• Stanford (Calif.) University
“Our 4-year training program in couples and family therapy begins with didactics and family meetings (inpatient) in the first year; didactics and opportunities for a couples and family therapy clinical elective as [postgraduate year]-2s; live case observation in the family therapy program at the [Veterans Affairs] Palo Alto Health Care System, as well as an intensive seminar at Stanford during the PGY-3 year, and supervised outpatient clinical work in Stanford’s Couples and Family Therapy Clinic during the PGY-3 and PGY-4 years. Residents who are interested in child and adolescent psychiatry can focus their PGY-3 rotation on family cases with a child/adolescent focus. An earlier version of this training sequence is described in program for residents is described in ‘A Model for Reintegrating Couples and Family Therapy Training in Psychiatric Residency Programs’ ” (Acad. Psychiatry 2008;32:81-6).
– Contact: Douglas S. Rait, Ph.D., Chief, Couples and Family Therapy Clinic, Clinical Professor of Psychiatry & Behavioral Sciences, Stanford University.
• University of Pennsylvania Perlman School of Medicine
“The Center for Couples and Adult Families in the department of psychiatry includes a didactic program for residents spanning all 4 years and supervision in PGY-3 and 4. Residents help run multifamily psychoeducation groups in the bipolar clinic, and see couples and families in their outpatient clinics. Our focus is on family inclusion and family psychoeducation for all patients when possible, with couple and adult family therapy when appropriate. Our curriculum is on our website As the clinical director, I work closely with Ellen Berman, who founded the center 5 years ago.”
– Contact: Jacqueline Hudak, Ph.D., LMFT, Center for Couples and Adult Families, Department of Psychiatry, Perelman School of Medicine.
• Mount Sinai Beth Israel, New York The Family Center for Bipolar provides services to patients with bipolar disorder “within the context of the family.” In addition, Dr. Igor Galynker, who runs the center, gives a series of lectures on family inclusion. The center also has a formal training program in family therapy run by Haya Mermelstein, CSW.
– Contact: Dr. Igor Galynker, professor of psychiatry, Icahn School of Medicine at Mount Sinai; director, the Family Center for Bipolar Disorder; Associate Chairman, Department Of Psychiatry and Behavioral Sciences.
• Brown University, Providence, R.I.
“We have a formal Family Therapy Training Program in the department of psychiatry at Brown University, based at Rhode Island Hospital.”
– Contact: Dr. Gabor I. Keitner, Associate Chief of Psychiatry, Rhode Island and Miriam Hospitals; Professor, Department of Psychiatry, Brown University.
• University of Rochester, Institute for the Family
“An emphasis on family is embedded in all of our training. The residents have a formal didactic curriculum and participate in family care and family research. Many of the residents fast track into a child fellowship, which has an extensive program in family therapy.
– Contact: Dr. [email protected], Director of Psychiatry Residency Education, University of Rochester Medical Center.
• University of Colorado Denver
“Our department offers a unique psychotherapy scholar track. The mission of this track is to offer advanced psychotherapy training to a subgroup of psychiatric residents, within an adult general residency program, who wish to learn and do psychotherapy. Within this track we offer extensive family therapy training. The family therapy component consists of didactics and direct supervision. It runs through the 4 years of residency. There are several experienced family therapists on the faculty who supervise in this program.”
– Contact: Dr. [email protected], Vice Chair, Department of Psychiatry.
A multidisciplinary field
Family systems training occurs in other disciplines: psychology, social work, and marriage and family therapy (MFT) programs. The number of MFT programs across the United States is large, reflecting the demand for family systems therapists.
Psychologists with a special interest in family therapy belong to the American Psychological Association’s Division 43. Division 43 supports family-oriented clinical and scientific activities as well as education and public policy, a journal called the Journal of Family Psychology, and a quarterly newsletter called The Family Psychologist. Many psychologists are trained in family therapy work in primary care settings. The current president of American Psychological Association, Nadine J. Kaslow, Ph.D., is a family therapist who helps underserved and underprivileged populations receive culturally competent, evidence-based, biopsychosocially oriented mental health services.
Social Workers are required to take two exams: one to be “licensed” as an LCSW (licensed clinical social worker) after graduation with a master’s degree. After 3,000 hours of supervised clinical practice, social worker takes second exam for independent licensure LICSW (licensed independent clinical social worker).
Social work schools have a course or two in family therapy. After graduation, students may choose to specialize in couples and family therapy. Like psychiatric and psychological training programs, there is wide variation in the amount of family therapy taught in schools of social work.
Marriage and family therapists (MFTs) have their own organization, the American Association for Marriage and Family Therapy (AAMFT). This organization’s training is specific to families and couples. Members are required to be supervised in clinical practice for 2 years. AAMFT produces the Journal of Marital and Family Therapy. The AAMFT website also lists accredited programs in the United States and Canada.
Two American journals in this area are interdisciplinary: Family Process and Families, Systems & Health. Family Process has broad representation on its board from all disciplines and has a strong focus on family systems research and social justice. Family Process aims to support emerging researchers and clinicians worldwide, and periodically offers grants. Families, Systems & Health is multidisciplinary with a focus on research and clinical practice in medical illness, and health psychology.
The American Family Therapy Academy (AFTA) is the only organization that is interdisciplinary. Founded in 1977, AFTA’s objectives include “the advancement of theories, therapies, research, and professional education that regard the family as a unit in a social context, to make information about family therapy available to practitioners in other fields of knowledge and to the public and to foster collaboration among the medical, psychological, social, legal, and other professions that serve families and the science and practice of family therapy.”
AFTA is outspoken on issues that affect families. For example, its Immigration Position Statement addresses the negative impact of U.S. immigration policy on families and children. AFTA has strong views about the DSM-5, stating that “the current revision of the DSM continues a long history of ignoring research and excluding vital contributions of nonpsychiatric mental health disciplines resulting in invalid diagnostic categories and treatment protocols. The DSM is dominant in determining mental health diagnosis and treatment and is more harmful than helpful in delineating best practices.” The next AFTA conference is in June 2015, and the theme is “Global Ecologies: Connections among Self, Families, Communities, and Cultures.”
Family therapy has grown from a small group of interested academics, mostly psychiatrists, to a large group of interdisciplinary professionals. Today, psychiatrists have less access to family systems training than in previous decades but can still access training. In addition to attending conferences, psychiatrists interested in this area might see whether training programs would accept them into their courses.
For those psychiatrists who have not had formal training during residency training, this review of programs is a good starting point for seeking family systems training.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of the recently published book Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals (New York: Routledge, 2013).
Speaker offers alternatives for sustainable TKI use in CML
NEW YORK—If any oncology drugs warrant a high price, BCR-ABL tyrosine kinase inhibitors (TKIs) could make a strong case, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
TKIs have revolutionized the therapeutic landscape in chronic myeloid leukemia (CML), said Neil P. Shah, MD, PhD, of the UCSF
Helen Diller Family Comprehensive Cancer Center in San Francisco.
Five-year overall survival is 93% in CML patients treated with imatinib. And 80,000 people are estimated to be living with CML in 2014, a number that is expected to double by 2035.
Yet the increase in life expectancy places a burden on the healthcare system, Dr Shah said, particularly since the price of BCR-ABL TKIs has risen dramatically.
A year of imatinib therapy circa 2001 cost approximately $30,000, and by 2013, approximately $92,000. Second-generation (2G) TKIs cost even more, at about $115,000 annually, and the third-generation TKI ponatinib costs about $138,000 annually.
Confounding the financial picture will be the advent of generic imatinib, which will be available in the US in early 2016.
Generic imatinib will, presumably, be less expensive than the brand-name drug. However, it is not clear whether it will be as effective or what impact it will have on the 2G and 3G TKIs.
With all that in mind, Dr Shah provided some options for maximizing therapeutic outcomes in a fiscally responsible manner.
He based his potential solutions on evidence-based premises. First, imatinib is a highly active therapy for many chronic-phase CML patients. The 8-year update of the IRIS study shows that 53% of patients sustain complete cytogenetic remission (CCyR) with imatinib.
Second, patients who are likely to do well on TKI therapy can be identified early based on their BCR-ABL PCR levels after 3 months of therapy.
This important 3-month milestone has been incorporated into the NCCN guidelines. Patients who achieve BCR-ABL/ABL levels of 10% or less have a significantly better overall survival than those who have levels greater than 10%.
Third, the ENESTnd and DASISION studies demonstrated that nilotinib and dasatinib elicit achievement of important treatment milestones (PCR<10% at 3 months and CCyR after 12 months) in a significantly higher proportion of patients than imatinib. But to date, neither agent has produced a significant improvement in overall survival.
And fourth, while nilotinib and dasatinib have an undisputable clinical benefit over imatinib in terms of transformation to accelerated phase/blast crisis (AP/BC), these agents cost between $23,000 and $31,000 more than imatinib for an annual course of treatment.
Dr Shah calculated that to achieve approximately 10 fewer AP/BC transformations over 5 years, approximately 300 patients would need to be treated at an additional cost of $37.5 million. This equates to $3.75 million in additional costs for 1 transformation event spared over 5 years.
“We do have to keep in mind transformation events are not cheap,” he said. “So when these happen, patients need to be hospitalized for chemotherapy, typically, or they have to go to allogeneic stem cell transplantation.”
So Dr Shah proffered 3 potential approaches for fiscally sustainable TKI use.
The first approach would be to initiate imatinib in most, if not all, chronic-phase CML patients. If they achieve BCR-ABL levels <10% at 3 months or partial CyR after 12 months, then continue imatinib. If not, switch to a 2G TKI.
Dr Shah noted that 40% to 60% of patients will have a deep, durable response to imatinib.
The second approach would be to initiate 2G TKIs in newly diagnosed patients. And when they achieve CCyR or major molecular response (MMR), enroll them in a clinical trial.
These trials could investigate a switch to imatinib, use of a lower dose of the 2G TKI, a switch to interferon-alfa, the addition of a CYP3A4 inhibitor (such as grapefruit) and a lower dose, or another investigational option.
And the third approach would be to initiate imatinib or an approved 2G TKI in newly diagnosed patients. When they achieve targeted molecular remission, enroll them in a treatment-discontinuation trial.
Dr Shah pointed out that in the STIM study, 61% of patients remained in complete molecular remission 60 months after discontinuing imatinib, and 40% experienced treatment-free survival.
Taking into account the cost of imatinib and the number of months without treatment, STIM investigators estimated the savings to be €4,587,500, or approximately $6 to $7 million.
Patients who relapsed 6 to 9 months after discontinuing imatinib tended to respond well to a rechallenge with imatinib. But Dr Shah cautioned that, at present, discontinuation should only be performed in the context of a clinical trial. ![]()
NEW YORK—If any oncology drugs warrant a high price, BCR-ABL tyrosine kinase inhibitors (TKIs) could make a strong case, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
TKIs have revolutionized the therapeutic landscape in chronic myeloid leukemia (CML), said Neil P. Shah, MD, PhD, of the UCSF
Helen Diller Family Comprehensive Cancer Center in San Francisco.
Five-year overall survival is 93% in CML patients treated with imatinib. And 80,000 people are estimated to be living with CML in 2014, a number that is expected to double by 2035.
Yet the increase in life expectancy places a burden on the healthcare system, Dr Shah said, particularly since the price of BCR-ABL TKIs has risen dramatically.
A year of imatinib therapy circa 2001 cost approximately $30,000, and by 2013, approximately $92,000. Second-generation (2G) TKIs cost even more, at about $115,000 annually, and the third-generation TKI ponatinib costs about $138,000 annually.
Confounding the financial picture will be the advent of generic imatinib, which will be available in the US in early 2016.
Generic imatinib will, presumably, be less expensive than the brand-name drug. However, it is not clear whether it will be as effective or what impact it will have on the 2G and 3G TKIs.
With all that in mind, Dr Shah provided some options for maximizing therapeutic outcomes in a fiscally responsible manner.
He based his potential solutions on evidence-based premises. First, imatinib is a highly active therapy for many chronic-phase CML patients. The 8-year update of the IRIS study shows that 53% of patients sustain complete cytogenetic remission (CCyR) with imatinib.
Second, patients who are likely to do well on TKI therapy can be identified early based on their BCR-ABL PCR levels after 3 months of therapy.
This important 3-month milestone has been incorporated into the NCCN guidelines. Patients who achieve BCR-ABL/ABL levels of 10% or less have a significantly better overall survival than those who have levels greater than 10%.
Third, the ENESTnd and DASISION studies demonstrated that nilotinib and dasatinib elicit achievement of important treatment milestones (PCR<10% at 3 months and CCyR after 12 months) in a significantly higher proportion of patients than imatinib. But to date, neither agent has produced a significant improvement in overall survival.
And fourth, while nilotinib and dasatinib have an undisputable clinical benefit over imatinib in terms of transformation to accelerated phase/blast crisis (AP/BC), these agents cost between $23,000 and $31,000 more than imatinib for an annual course of treatment.
Dr Shah calculated that to achieve approximately 10 fewer AP/BC transformations over 5 years, approximately 300 patients would need to be treated at an additional cost of $37.5 million. This equates to $3.75 million in additional costs for 1 transformation event spared over 5 years.
“We do have to keep in mind transformation events are not cheap,” he said. “So when these happen, patients need to be hospitalized for chemotherapy, typically, or they have to go to allogeneic stem cell transplantation.”
So Dr Shah proffered 3 potential approaches for fiscally sustainable TKI use.
The first approach would be to initiate imatinib in most, if not all, chronic-phase CML patients. If they achieve BCR-ABL levels <10% at 3 months or partial CyR after 12 months, then continue imatinib. If not, switch to a 2G TKI.
Dr Shah noted that 40% to 60% of patients will have a deep, durable response to imatinib.
The second approach would be to initiate 2G TKIs in newly diagnosed patients. And when they achieve CCyR or major molecular response (MMR), enroll them in a clinical trial.
These trials could investigate a switch to imatinib, use of a lower dose of the 2G TKI, a switch to interferon-alfa, the addition of a CYP3A4 inhibitor (such as grapefruit) and a lower dose, or another investigational option.
And the third approach would be to initiate imatinib or an approved 2G TKI in newly diagnosed patients. When they achieve targeted molecular remission, enroll them in a treatment-discontinuation trial.
Dr Shah pointed out that in the STIM study, 61% of patients remained in complete molecular remission 60 months after discontinuing imatinib, and 40% experienced treatment-free survival.
Taking into account the cost of imatinib and the number of months without treatment, STIM investigators estimated the savings to be €4,587,500, or approximately $6 to $7 million.
Patients who relapsed 6 to 9 months after discontinuing imatinib tended to respond well to a rechallenge with imatinib. But Dr Shah cautioned that, at present, discontinuation should only be performed in the context of a clinical trial. ![]()
NEW YORK—If any oncology drugs warrant a high price, BCR-ABL tyrosine kinase inhibitors (TKIs) could make a strong case, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
TKIs have revolutionized the therapeutic landscape in chronic myeloid leukemia (CML), said Neil P. Shah, MD, PhD, of the UCSF
Helen Diller Family Comprehensive Cancer Center in San Francisco.
Five-year overall survival is 93% in CML patients treated with imatinib. And 80,000 people are estimated to be living with CML in 2014, a number that is expected to double by 2035.
Yet the increase in life expectancy places a burden on the healthcare system, Dr Shah said, particularly since the price of BCR-ABL TKIs has risen dramatically.
A year of imatinib therapy circa 2001 cost approximately $30,000, and by 2013, approximately $92,000. Second-generation (2G) TKIs cost even more, at about $115,000 annually, and the third-generation TKI ponatinib costs about $138,000 annually.
Confounding the financial picture will be the advent of generic imatinib, which will be available in the US in early 2016.
Generic imatinib will, presumably, be less expensive than the brand-name drug. However, it is not clear whether it will be as effective or what impact it will have on the 2G and 3G TKIs.
With all that in mind, Dr Shah provided some options for maximizing therapeutic outcomes in a fiscally responsible manner.
He based his potential solutions on evidence-based premises. First, imatinib is a highly active therapy for many chronic-phase CML patients. The 8-year update of the IRIS study shows that 53% of patients sustain complete cytogenetic remission (CCyR) with imatinib.
Second, patients who are likely to do well on TKI therapy can be identified early based on their BCR-ABL PCR levels after 3 months of therapy.
This important 3-month milestone has been incorporated into the NCCN guidelines. Patients who achieve BCR-ABL/ABL levels of 10% or less have a significantly better overall survival than those who have levels greater than 10%.
Third, the ENESTnd and DASISION studies demonstrated that nilotinib and dasatinib elicit achievement of important treatment milestones (PCR<10% at 3 months and CCyR after 12 months) in a significantly higher proportion of patients than imatinib. But to date, neither agent has produced a significant improvement in overall survival.
And fourth, while nilotinib and dasatinib have an undisputable clinical benefit over imatinib in terms of transformation to accelerated phase/blast crisis (AP/BC), these agents cost between $23,000 and $31,000 more than imatinib for an annual course of treatment.
Dr Shah calculated that to achieve approximately 10 fewer AP/BC transformations over 5 years, approximately 300 patients would need to be treated at an additional cost of $37.5 million. This equates to $3.75 million in additional costs for 1 transformation event spared over 5 years.
“We do have to keep in mind transformation events are not cheap,” he said. “So when these happen, patients need to be hospitalized for chemotherapy, typically, or they have to go to allogeneic stem cell transplantation.”
So Dr Shah proffered 3 potential approaches for fiscally sustainable TKI use.
The first approach would be to initiate imatinib in most, if not all, chronic-phase CML patients. If they achieve BCR-ABL levels <10% at 3 months or partial CyR after 12 months, then continue imatinib. If not, switch to a 2G TKI.
Dr Shah noted that 40% to 60% of patients will have a deep, durable response to imatinib.
The second approach would be to initiate 2G TKIs in newly diagnosed patients. And when they achieve CCyR or major molecular response (MMR), enroll them in a clinical trial.
These trials could investigate a switch to imatinib, use of a lower dose of the 2G TKI, a switch to interferon-alfa, the addition of a CYP3A4 inhibitor (such as grapefruit) and a lower dose, or another investigational option.
And the third approach would be to initiate imatinib or an approved 2G TKI in newly diagnosed patients. When they achieve targeted molecular remission, enroll them in a treatment-discontinuation trial.
Dr Shah pointed out that in the STIM study, 61% of patients remained in complete molecular remission 60 months after discontinuing imatinib, and 40% experienced treatment-free survival.
Taking into account the cost of imatinib and the number of months without treatment, STIM investigators estimated the savings to be €4,587,500, or approximately $6 to $7 million.
Patients who relapsed 6 to 9 months after discontinuing imatinib tended to respond well to a rechallenge with imatinib. But Dr Shah cautioned that, at present, discontinuation should only be performed in the context of a clinical trial. ![]()
The Immunization Community
The Immunization Action Coalition (IAC) works in cadence with the Centers for Disease Control and Prevention (CDC) to offer health care professionals in both the public and private sectors the most up-to-date immunization information available in one retrievable location. This well established website, http://www.immunize.org, serves more than 14,000 visitors every day.
Talking About Vaccines provides research and guidelines by an assortment of nationally recognized institutions, including the IAC, CDC, and many others in response to common concerns.
Within Clinic Resources, users can access how-to documents on providing vaccines at a clinic or nontraditional setting. Also available are patient and staff handouts, including indexed vaccines (eg, human papillomavirus and tetanus) and topics such as needle safety.
The Immunization Action Coalition (IAC) works in cadence with the Centers for Disease Control and Prevention (CDC) to offer health care professionals in both the public and private sectors the most up-to-date immunization information available in one retrievable location. This well established website, http://www.immunize.org, serves more than 14,000 visitors every day.
Talking About Vaccines provides research and guidelines by an assortment of nationally recognized institutions, including the IAC, CDC, and many others in response to common concerns.
Within Clinic Resources, users can access how-to documents on providing vaccines at a clinic or nontraditional setting. Also available are patient and staff handouts, including indexed vaccines (eg, human papillomavirus and tetanus) and topics such as needle safety.
The Immunization Action Coalition (IAC) works in cadence with the Centers for Disease Control and Prevention (CDC) to offer health care professionals in both the public and private sectors the most up-to-date immunization information available in one retrievable location. This well established website, http://www.immunize.org, serves more than 14,000 visitors every day.
Talking About Vaccines provides research and guidelines by an assortment of nationally recognized institutions, including the IAC, CDC, and many others in response to common concerns.
Within Clinic Resources, users can access how-to documents on providing vaccines at a clinic or nontraditional setting. Also available are patient and staff handouts, including indexed vaccines (eg, human papillomavirus and tetanus) and topics such as needle safety.
Split decision on role of upfront transplant in MM

Credit: Chad McNeeley
NEW YORK—A debate on the pros and cons of upfront transplant in symptomatic multiple myeloma (MM) yielded a split decision from the audience during the NCCN 9th Annual Congress: Hematologic Malignancies.
Sergio Giralt, MD, of Memorial Sloan Kettering Cancer Center in New York, argued for upfront transplant, pointing out that long-term MM survivors have transplant as upfront therapy.
Kenneth Anderson, MD, of Dana Farber/Brigham and Women’s Cancer Center in Boston, took the stance that, in the past 10 years, there has been a
revolution in novel therapies that has significantly improved survival in MM.
For upfront transplant
Dr Giralt cited the 36-month follow-up of the E4A03 landmark analysis of patients who went off therapy after 4 cycles of lenalidomide/dexamethasone to pursue early stem cell transplant and those who continued treatment until disease progression.
Regardless of whether the patients were younger than 65 years or between 65 and 70, the patients who had an early transplant had superior progression-free survival (PFS) and overall survival (OS) compared to those who did not.
Dr Giralt added that bortezomib should be a component of induction therapy prior to autologous stem cell transplant (ASCT). Even though there is no survival benefit with bortezomib-based regimens, he said, there is significant improvement in PFS, as shown in a meta-analysis of phase 3 European studies.
The E4A03 landmark study also determined that the more intense the treatment, the better the outcome. So patients with double ASCT had a significantly longer PFS than patients who only had a single transplant.
This held true for OS as well, and included patients with 17p deletion and/or t(4;14) who failed to achieve complete remission after bortezomib-based induction regimens.
An analysis of 27,987 MM patients with a median age of 68 years (range, 19 to 90) revealed that of the patients who survived 10 years or more, 16.5% had ASCT as part of their initial therapy.
Dr Giralt concluded that the preponderance of evidence supports high-dose melphalan and ASCT as upfront consolidation therapy for MM. And until results of randomized trials investigating combination therapies are reported, melphalan consolidation should be considered the standard of care for all eligible patients with MM.
Against upfront transplant
Dr Anderson countered with data showing limited or no improvement in survival with ASCT, including evidence from studies by Attal, Fermand, Blade, Child, and Barlogie.
ASCT confers only modest PFS advantage, he said, showing results of the Barlogie study in which patients undergoing ASCT had a 25-month PFS, compared with a 21-month PFS with VBMCP (vincristine, carmustine, melphalan, cyclophosphamide, and prednisone).
“In the last 10 to 15 years, there has been a revolution in myeloma,” Dr Anderson said. “We have a lot of novel agents here today, and we have even more coming. It’s a hugely exciting time.”
Dr Anderson pointed out that since the introduction of novel agents, survival has improved between 2006 and 2010, compared to the period between 2001 and 2005, and particularly in patients older than 65 years (P=0.001).
Transplant has also changed, he said. Novel therapies have been integrated into the transplant paradigm, either before, as induction and consolidation therapy, or after, as maintenance. He indicated that this begs the question as to whether we really need the transplant component.
There has also been unprecedented use of triplets in combination therapy, Dr Anderson said, resulting in overall response rates upwards of 90%. For example, carfilzomib in combination with lenalidomide and dexamethasone prompted an overall response rate of 94%, with a stringent complete response (CR), CR, and near CR of 53%.
“It’s a new day in myeloma,” he said. “It’s taken us a long time, but we’re worrying about minimal residual disease (MRD) now. We’re worried about getting to the endpoint of 1 myeloma cell in 1 million normal cells.”
The point is, he added, that with novel therapies, such as carfilzomib, lenalidomide, and dexamethasone, patients who achieve a complete response can become MRD negative, suggesting an unprecedented extent of response without transplant.
MRD negativity may also be accomplished with oral agents, such as ixazomib. The depth of response with ixazomib increases over the course of treatment, with 27% achieving stringent CR or CR with a median duration of response of 13.8 months, and 82% of patients attaining MRD-negative status.
“In the absence of transplant,” Dr Anderson said, “this is an unprecedented response.”
Dr Anderson also pointed out that in the era of novel agents, there is no difference in outcome between early or delayed transplant. The 4-year OS in transplant-eligible patients who received initial therapy with lenalidomide was 80%, regardless of the timing of ASCT.
And in one trial, patients who received a delayed transplant fared better in OS than those transplanted early.
Dr Anderson said there is a parallel, international phase 3 study underway (IFM/DFCI2009) that will provide an answer to the debate on upfront transplant in the not-too-distant future. ![]()

Credit: Chad McNeeley
NEW YORK—A debate on the pros and cons of upfront transplant in symptomatic multiple myeloma (MM) yielded a split decision from the audience during the NCCN 9th Annual Congress: Hematologic Malignancies.
Sergio Giralt, MD, of Memorial Sloan Kettering Cancer Center in New York, argued for upfront transplant, pointing out that long-term MM survivors have transplant as upfront therapy.
Kenneth Anderson, MD, of Dana Farber/Brigham and Women’s Cancer Center in Boston, took the stance that, in the past 10 years, there has been a
revolution in novel therapies that has significantly improved survival in MM.
For upfront transplant
Dr Giralt cited the 36-month follow-up of the E4A03 landmark analysis of patients who went off therapy after 4 cycles of lenalidomide/dexamethasone to pursue early stem cell transplant and those who continued treatment until disease progression.
Regardless of whether the patients were younger than 65 years or between 65 and 70, the patients who had an early transplant had superior progression-free survival (PFS) and overall survival (OS) compared to those who did not.
Dr Giralt added that bortezomib should be a component of induction therapy prior to autologous stem cell transplant (ASCT). Even though there is no survival benefit with bortezomib-based regimens, he said, there is significant improvement in PFS, as shown in a meta-analysis of phase 3 European studies.
The E4A03 landmark study also determined that the more intense the treatment, the better the outcome. So patients with double ASCT had a significantly longer PFS than patients who only had a single transplant.
This held true for OS as well, and included patients with 17p deletion and/or t(4;14) who failed to achieve complete remission after bortezomib-based induction regimens.
An analysis of 27,987 MM patients with a median age of 68 years (range, 19 to 90) revealed that of the patients who survived 10 years or more, 16.5% had ASCT as part of their initial therapy.
Dr Giralt concluded that the preponderance of evidence supports high-dose melphalan and ASCT as upfront consolidation therapy for MM. And until results of randomized trials investigating combination therapies are reported, melphalan consolidation should be considered the standard of care for all eligible patients with MM.
Against upfront transplant
Dr Anderson countered with data showing limited or no improvement in survival with ASCT, including evidence from studies by Attal, Fermand, Blade, Child, and Barlogie.
ASCT confers only modest PFS advantage, he said, showing results of the Barlogie study in which patients undergoing ASCT had a 25-month PFS, compared with a 21-month PFS with VBMCP (vincristine, carmustine, melphalan, cyclophosphamide, and prednisone).
“In the last 10 to 15 years, there has been a revolution in myeloma,” Dr Anderson said. “We have a lot of novel agents here today, and we have even more coming. It’s a hugely exciting time.”
Dr Anderson pointed out that since the introduction of novel agents, survival has improved between 2006 and 2010, compared to the period between 2001 and 2005, and particularly in patients older than 65 years (P=0.001).
Transplant has also changed, he said. Novel therapies have been integrated into the transplant paradigm, either before, as induction and consolidation therapy, or after, as maintenance. He indicated that this begs the question as to whether we really need the transplant component.
There has also been unprecedented use of triplets in combination therapy, Dr Anderson said, resulting in overall response rates upwards of 90%. For example, carfilzomib in combination with lenalidomide and dexamethasone prompted an overall response rate of 94%, with a stringent complete response (CR), CR, and near CR of 53%.
“It’s a new day in myeloma,” he said. “It’s taken us a long time, but we’re worrying about minimal residual disease (MRD) now. We’re worried about getting to the endpoint of 1 myeloma cell in 1 million normal cells.”
The point is, he added, that with novel therapies, such as carfilzomib, lenalidomide, and dexamethasone, patients who achieve a complete response can become MRD negative, suggesting an unprecedented extent of response without transplant.
MRD negativity may also be accomplished with oral agents, such as ixazomib. The depth of response with ixazomib increases over the course of treatment, with 27% achieving stringent CR or CR with a median duration of response of 13.8 months, and 82% of patients attaining MRD-negative status.
“In the absence of transplant,” Dr Anderson said, “this is an unprecedented response.”
Dr Anderson also pointed out that in the era of novel agents, there is no difference in outcome between early or delayed transplant. The 4-year OS in transplant-eligible patients who received initial therapy with lenalidomide was 80%, regardless of the timing of ASCT.
And in one trial, patients who received a delayed transplant fared better in OS than those transplanted early.
Dr Anderson said there is a parallel, international phase 3 study underway (IFM/DFCI2009) that will provide an answer to the debate on upfront transplant in the not-too-distant future. ![]()

Credit: Chad McNeeley
NEW YORK—A debate on the pros and cons of upfront transplant in symptomatic multiple myeloma (MM) yielded a split decision from the audience during the NCCN 9th Annual Congress: Hematologic Malignancies.
Sergio Giralt, MD, of Memorial Sloan Kettering Cancer Center in New York, argued for upfront transplant, pointing out that long-term MM survivors have transplant as upfront therapy.
Kenneth Anderson, MD, of Dana Farber/Brigham and Women’s Cancer Center in Boston, took the stance that, in the past 10 years, there has been a
revolution in novel therapies that has significantly improved survival in MM.
For upfront transplant
Dr Giralt cited the 36-month follow-up of the E4A03 landmark analysis of patients who went off therapy after 4 cycles of lenalidomide/dexamethasone to pursue early stem cell transplant and those who continued treatment until disease progression.
Regardless of whether the patients were younger than 65 years or between 65 and 70, the patients who had an early transplant had superior progression-free survival (PFS) and overall survival (OS) compared to those who did not.
Dr Giralt added that bortezomib should be a component of induction therapy prior to autologous stem cell transplant (ASCT). Even though there is no survival benefit with bortezomib-based regimens, he said, there is significant improvement in PFS, as shown in a meta-analysis of phase 3 European studies.
The E4A03 landmark study also determined that the more intense the treatment, the better the outcome. So patients with double ASCT had a significantly longer PFS than patients who only had a single transplant.
This held true for OS as well, and included patients with 17p deletion and/or t(4;14) who failed to achieve complete remission after bortezomib-based induction regimens.
An analysis of 27,987 MM patients with a median age of 68 years (range, 19 to 90) revealed that of the patients who survived 10 years or more, 16.5% had ASCT as part of their initial therapy.
Dr Giralt concluded that the preponderance of evidence supports high-dose melphalan and ASCT as upfront consolidation therapy for MM. And until results of randomized trials investigating combination therapies are reported, melphalan consolidation should be considered the standard of care for all eligible patients with MM.
Against upfront transplant
Dr Anderson countered with data showing limited or no improvement in survival with ASCT, including evidence from studies by Attal, Fermand, Blade, Child, and Barlogie.
ASCT confers only modest PFS advantage, he said, showing results of the Barlogie study in which patients undergoing ASCT had a 25-month PFS, compared with a 21-month PFS with VBMCP (vincristine, carmustine, melphalan, cyclophosphamide, and prednisone).
“In the last 10 to 15 years, there has been a revolution in myeloma,” Dr Anderson said. “We have a lot of novel agents here today, and we have even more coming. It’s a hugely exciting time.”
Dr Anderson pointed out that since the introduction of novel agents, survival has improved between 2006 and 2010, compared to the period between 2001 and 2005, and particularly in patients older than 65 years (P=0.001).
Transplant has also changed, he said. Novel therapies have been integrated into the transplant paradigm, either before, as induction and consolidation therapy, or after, as maintenance. He indicated that this begs the question as to whether we really need the transplant component.
There has also been unprecedented use of triplets in combination therapy, Dr Anderson said, resulting in overall response rates upwards of 90%. For example, carfilzomib in combination with lenalidomide and dexamethasone prompted an overall response rate of 94%, with a stringent complete response (CR), CR, and near CR of 53%.
“It’s a new day in myeloma,” he said. “It’s taken us a long time, but we’re worrying about minimal residual disease (MRD) now. We’re worried about getting to the endpoint of 1 myeloma cell in 1 million normal cells.”
The point is, he added, that with novel therapies, such as carfilzomib, lenalidomide, and dexamethasone, patients who achieve a complete response can become MRD negative, suggesting an unprecedented extent of response without transplant.
MRD negativity may also be accomplished with oral agents, such as ixazomib. The depth of response with ixazomib increases over the course of treatment, with 27% achieving stringent CR or CR with a median duration of response of 13.8 months, and 82% of patients attaining MRD-negative status.
“In the absence of transplant,” Dr Anderson said, “this is an unprecedented response.”
Dr Anderson also pointed out that in the era of novel agents, there is no difference in outcome between early or delayed transplant. The 4-year OS in transplant-eligible patients who received initial therapy with lenalidomide was 80%, regardless of the timing of ASCT.
And in one trial, patients who received a delayed transplant fared better in OS than those transplanted early.
Dr Anderson said there is a parallel, international phase 3 study underway (IFM/DFCI2009) that will provide an answer to the debate on upfront transplant in the not-too-distant future. ![]()
Drug could treat a range of blood cancers

PHILADELPHIA—A drug that targets the ribosome may be active in a broad range of hematologic malignancies, researchers say.
The drug, CX-5461, inhibits the protein RNA polymerase I (Pol I), which is consistently upregulated in hematologic and other cancers.
CX-5461 significantly prolonged survival in mouse models of refractory acute myeloid leukemia (AML) and multiple myeloma (MM). It also synergized with everolimus to extend survival in mice with B-cell lymphoma.
Furthermore, the drug did not elicit severe adverse effects.
“We were excited to find that therapeutic doses of CX-5461 had little effect on normal cells in our experiments,” said Ross D. Hannan, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia,
“Prior to these studies, few people would have guessed that such a therapeutic window could be obtained by targeting a so-called house-keeping protein that is essential to all cells for survival.”
Dr Hannan and his colleagues presented these findings in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The researchers previously showed that cancer cells are much more dependent on ribosome biogenesis than normal cells. And blocking the accelerated reading of ribosomal genes in mice—using CX5461—can cause lymphoma and leukemia cells to die, while sparing normal cells.
With their latest research, the group expanded upon these findings by testing CX-5461 in MLL-driven AML, V*κ-Myc-driven MM, and Eμ-Myc lymphoma.
They found that CX-5461 improved overall survival in MLL/ENL Nras leukemic mice, compared to placebo and standard therapy. The median survival was 17 days for vehicle-treated mice, 21 days for mice treated with cytarabine and doxorubicin, and 36 days for mice that received CX-5461 (P<0.0001 for vehicle vs CX-5461).
CX-5461 treated MLL-driven AML by inducing apoptosis, delaying cell-cycle progression, and promoting differentiation.
The researchers also found the therapeutic benefit of CX-5461 is not p53-dependent, which contradicts their previous findings. Human AML cell lines and primary patient samples were sensitive to CX-5461 independent of p53 status.
And MLL/ENL Nras p53-/- leukemic mice had significantly prolonged survival when treated with CX-5461, compared to vehicle-treated controls. The median survival was 11 days and 24 days, respectively (P<0.0001).
Likewise, CX-5461 significantly prolonged survival in mice bearing V*κ-Myc MM. The median survival was 103.5 days for controls and 175 days for mice that received CX-5461 (P<0.0001).
Finally, the researchers showed that CX-5461 synergizes with everolimus to treat Eμ-Myc lymphoma. The median survival was 15 days in control mice, 18 days in mice that received everolimus, 32 days in mice treated with CX-5461, and 54 days in mice that received both drugs (P<0.0001 for CX-5461 vs the combination).
“These results provide further rationale for the first-in-human phase 1 clinical trial that we initiated in July 2013 testing CX-5461 for patients with advanced hematological malignancies, including AML and multiple myeloma,” Dr Hannan said.
His group’s preclinical research was funded by the National Health and Medical Research Council, Australia; the Leukaemia Foundation of Australia; and Cancer Council Victoria, Melbourne, Australia. Senhwa Biosciences, the makers of CX-5461, provided the drug. ![]()

PHILADELPHIA—A drug that targets the ribosome may be active in a broad range of hematologic malignancies, researchers say.
The drug, CX-5461, inhibits the protein RNA polymerase I (Pol I), which is consistently upregulated in hematologic and other cancers.
CX-5461 significantly prolonged survival in mouse models of refractory acute myeloid leukemia (AML) and multiple myeloma (MM). It also synergized with everolimus to extend survival in mice with B-cell lymphoma.
Furthermore, the drug did not elicit severe adverse effects.
“We were excited to find that therapeutic doses of CX-5461 had little effect on normal cells in our experiments,” said Ross D. Hannan, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia,
“Prior to these studies, few people would have guessed that such a therapeutic window could be obtained by targeting a so-called house-keeping protein that is essential to all cells for survival.”
Dr Hannan and his colleagues presented these findings in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The researchers previously showed that cancer cells are much more dependent on ribosome biogenesis than normal cells. And blocking the accelerated reading of ribosomal genes in mice—using CX5461—can cause lymphoma and leukemia cells to die, while sparing normal cells.
With their latest research, the group expanded upon these findings by testing CX-5461 in MLL-driven AML, V*κ-Myc-driven MM, and Eμ-Myc lymphoma.
They found that CX-5461 improved overall survival in MLL/ENL Nras leukemic mice, compared to placebo and standard therapy. The median survival was 17 days for vehicle-treated mice, 21 days for mice treated with cytarabine and doxorubicin, and 36 days for mice that received CX-5461 (P<0.0001 for vehicle vs CX-5461).
CX-5461 treated MLL-driven AML by inducing apoptosis, delaying cell-cycle progression, and promoting differentiation.
The researchers also found the therapeutic benefit of CX-5461 is not p53-dependent, which contradicts their previous findings. Human AML cell lines and primary patient samples were sensitive to CX-5461 independent of p53 status.
And MLL/ENL Nras p53-/- leukemic mice had significantly prolonged survival when treated with CX-5461, compared to vehicle-treated controls. The median survival was 11 days and 24 days, respectively (P<0.0001).
Likewise, CX-5461 significantly prolonged survival in mice bearing V*κ-Myc MM. The median survival was 103.5 days for controls and 175 days for mice that received CX-5461 (P<0.0001).
Finally, the researchers showed that CX-5461 synergizes with everolimus to treat Eμ-Myc lymphoma. The median survival was 15 days in control mice, 18 days in mice that received everolimus, 32 days in mice treated with CX-5461, and 54 days in mice that received both drugs (P<0.0001 for CX-5461 vs the combination).
“These results provide further rationale for the first-in-human phase 1 clinical trial that we initiated in July 2013 testing CX-5461 for patients with advanced hematological malignancies, including AML and multiple myeloma,” Dr Hannan said.
His group’s preclinical research was funded by the National Health and Medical Research Council, Australia; the Leukaemia Foundation of Australia; and Cancer Council Victoria, Melbourne, Australia. Senhwa Biosciences, the makers of CX-5461, provided the drug. ![]()

PHILADELPHIA—A drug that targets the ribosome may be active in a broad range of hematologic malignancies, researchers say.
The drug, CX-5461, inhibits the protein RNA polymerase I (Pol I), which is consistently upregulated in hematologic and other cancers.
CX-5461 significantly prolonged survival in mouse models of refractory acute myeloid leukemia (AML) and multiple myeloma (MM). It also synergized with everolimus to extend survival in mice with B-cell lymphoma.
Furthermore, the drug did not elicit severe adverse effects.
“We were excited to find that therapeutic doses of CX-5461 had little effect on normal cells in our experiments,” said Ross D. Hannan, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia,
“Prior to these studies, few people would have guessed that such a therapeutic window could be obtained by targeting a so-called house-keeping protein that is essential to all cells for survival.”
Dr Hannan and his colleagues presented these findings in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
The researchers previously showed that cancer cells are much more dependent on ribosome biogenesis than normal cells. And blocking the accelerated reading of ribosomal genes in mice—using CX5461—can cause lymphoma and leukemia cells to die, while sparing normal cells.
With their latest research, the group expanded upon these findings by testing CX-5461 in MLL-driven AML, V*κ-Myc-driven MM, and Eμ-Myc lymphoma.
They found that CX-5461 improved overall survival in MLL/ENL Nras leukemic mice, compared to placebo and standard therapy. The median survival was 17 days for vehicle-treated mice, 21 days for mice treated with cytarabine and doxorubicin, and 36 days for mice that received CX-5461 (P<0.0001 for vehicle vs CX-5461).
CX-5461 treated MLL-driven AML by inducing apoptosis, delaying cell-cycle progression, and promoting differentiation.
The researchers also found the therapeutic benefit of CX-5461 is not p53-dependent, which contradicts their previous findings. Human AML cell lines and primary patient samples were sensitive to CX-5461 independent of p53 status.
And MLL/ENL Nras p53-/- leukemic mice had significantly prolonged survival when treated with CX-5461, compared to vehicle-treated controls. The median survival was 11 days and 24 days, respectively (P<0.0001).
Likewise, CX-5461 significantly prolonged survival in mice bearing V*κ-Myc MM. The median survival was 103.5 days for controls and 175 days for mice that received CX-5461 (P<0.0001).
Finally, the researchers showed that CX-5461 synergizes with everolimus to treat Eμ-Myc lymphoma. The median survival was 15 days in control mice, 18 days in mice that received everolimus, 32 days in mice treated with CX-5461, and 54 days in mice that received both drugs (P<0.0001 for CX-5461 vs the combination).
“These results provide further rationale for the first-in-human phase 1 clinical trial that we initiated in July 2013 testing CX-5461 for patients with advanced hematological malignancies, including AML and multiple myeloma,” Dr Hannan said.
His group’s preclinical research was funded by the National Health and Medical Research Council, Australia; the Leukaemia Foundation of Australia; and Cancer Council Victoria, Melbourne, Australia. Senhwa Biosciences, the makers of CX-5461, provided the drug. ![]()


