User login
EC approves bortezomib for MCL

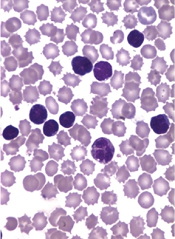
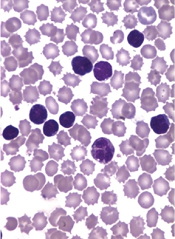
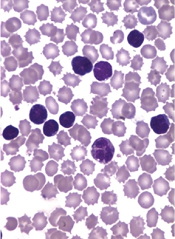
Photo courtesy of Millennium
The European Commission (EC) has approved bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) in whom hematopoietic stem cell transplant (HSCT) is considered unsuitable.
Now, bortezomib can be marketed for this indication in all 28 countries of the European Union (EU).
Bortezomib is already approved in the EU to treat multiple myeloma (MM), either as monotherapy or in combination with other agents.
The EC’s approval of bortezomib in MCL is based on data from a phase 3 study known as LYM-3002.
This randomized trial included 487 patients with newly diagnosed MCL who were ineligible, or not considered, for HSCT. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AEs) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
About bortezomib
Bortezomib works by reversibly interrupting the normal working of cell proteasomes, inducing cancerous cells to stop growing and die.
In addition to the new MCL indication, the drug is approved in the EU to treat various stages of MM. It’s approved in combination with melphalan and prednisone to treat previously untreated adults with MM who are unsuitable for high-dose chemotherapy with HSCT.
Bortezomib is also approved in combination with dexamethasone, or with dexamethasone plus thalidomide, to treat previously untreated MM patients set to receive high-dose chemotherapy followed by HSCT.
And the drug is approved as monotherapy or in combination with pegylated liposomal doxorubicin or dexamethasone to treat adults with MM whose disease has progressed after at least one other treatment and who have already had, or cannot undergo, HSCT.
Bortezomib is approved in more than 90 countries and has been used to treat more than 550,000 patients worldwide.
The product is co-developed by Millennium, the Takeda Oncology Company, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, and Janssen Pharmaceutical Companies.
Millennium is responsible for commercialization in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world. Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote the drug in Japan. ![]()

Photo courtesy of Millennium
The European Commission (EC) has approved bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) in whom hematopoietic stem cell transplant (HSCT) is considered unsuitable.
Now, bortezomib can be marketed for this indication in all 28 countries of the European Union (EU).
Bortezomib is already approved in the EU to treat multiple myeloma (MM), either as monotherapy or in combination with other agents.
The EC’s approval of bortezomib in MCL is based on data from a phase 3 study known as LYM-3002.
This randomized trial included 487 patients with newly diagnosed MCL who were ineligible, or not considered, for HSCT. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AEs) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
About bortezomib
Bortezomib works by reversibly interrupting the normal working of cell proteasomes, inducing cancerous cells to stop growing and die.
In addition to the new MCL indication, the drug is approved in the EU to treat various stages of MM. It’s approved in combination with melphalan and prednisone to treat previously untreated adults with MM who are unsuitable for high-dose chemotherapy with HSCT.
Bortezomib is also approved in combination with dexamethasone, or with dexamethasone plus thalidomide, to treat previously untreated MM patients set to receive high-dose chemotherapy followed by HSCT.
And the drug is approved as monotherapy or in combination with pegylated liposomal doxorubicin or dexamethasone to treat adults with MM whose disease has progressed after at least one other treatment and who have already had, or cannot undergo, HSCT.
Bortezomib is approved in more than 90 countries and has been used to treat more than 550,000 patients worldwide.
The product is co-developed by Millennium, the Takeda Oncology Company, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, and Janssen Pharmaceutical Companies.
Millennium is responsible for commercialization in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world. Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote the drug in Japan. ![]()

Photo courtesy of Millennium
The European Commission (EC) has approved bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) in whom hematopoietic stem cell transplant (HSCT) is considered unsuitable.
Now, bortezomib can be marketed for this indication in all 28 countries of the European Union (EU).
Bortezomib is already approved in the EU to treat multiple myeloma (MM), either as monotherapy or in combination with other agents.
The EC’s approval of bortezomib in MCL is based on data from a phase 3 study known as LYM-3002.
This randomized trial included 487 patients with newly diagnosed MCL who were ineligible, or not considered, for HSCT. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AEs) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
About bortezomib
Bortezomib works by reversibly interrupting the normal working of cell proteasomes, inducing cancerous cells to stop growing and die.
In addition to the new MCL indication, the drug is approved in the EU to treat various stages of MM. It’s approved in combination with melphalan and prednisone to treat previously untreated adults with MM who are unsuitable for high-dose chemotherapy with HSCT.
Bortezomib is also approved in combination with dexamethasone, or with dexamethasone plus thalidomide, to treat previously untreated MM patients set to receive high-dose chemotherapy followed by HSCT.
And the drug is approved as monotherapy or in combination with pegylated liposomal doxorubicin or dexamethasone to treat adults with MM whose disease has progressed after at least one other treatment and who have already had, or cannot undergo, HSCT.
Bortezomib is approved in more than 90 countries and has been used to treat more than 550,000 patients worldwide.
The product is co-developed by Millennium, the Takeda Oncology Company, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, and Janssen Pharmaceutical Companies.
Millennium is responsible for commercialization in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world. Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote the drug in Japan. ![]()
AUDIO: Training broadens psychotherapy in primary care
NEW YORK– The REACH Institute trains primary care clinicians to include more mental health assessment and management in their practices, Dr. Lawrence V. Amsel said during an interview at the psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
Many primary care clinicians don’t feel adequately trained to interview patients, guage their mental status, and then act on the findings by treatment or referral. But over the past decade, psychiatrists have developed and validated several tools that are appropriate for a primary care practice, said Dr. Amsel, a clinical psychiatrist at Columbia University in New York, and a faculty member of the REACH Institute, a New York–based nonprofit focused on disseminating mental health skills to primary care clinicians, teachers, parents, and others. The program also tries to make clinicians comfortable prescribing psychiatric medications and links them with psychiatrists who can provide consultations when needed.
“It’s kind of like a psychiatrist extender,” when a psychiatrist consults with several primary care clinicians, which allows for improved psychiatric care of many more patients, he said.
Dr. Amsel is on the faculty of the REACH Institute.
On Twitter@mitchelzoler
NEW YORK– The REACH Institute trains primary care clinicians to include more mental health assessment and management in their practices, Dr. Lawrence V. Amsel said during an interview at the psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
Many primary care clinicians don’t feel adequately trained to interview patients, guage their mental status, and then act on the findings by treatment or referral. But over the past decade, psychiatrists have developed and validated several tools that are appropriate for a primary care practice, said Dr. Amsel, a clinical psychiatrist at Columbia University in New York, and a faculty member of the REACH Institute, a New York–based nonprofit focused on disseminating mental health skills to primary care clinicians, teachers, parents, and others. The program also tries to make clinicians comfortable prescribing psychiatric medications and links them with psychiatrists who can provide consultations when needed.
“It’s kind of like a psychiatrist extender,” when a psychiatrist consults with several primary care clinicians, which allows for improved psychiatric care of many more patients, he said.
Dr. Amsel is on the faculty of the REACH Institute.
On Twitter@mitchelzoler
NEW YORK– The REACH Institute trains primary care clinicians to include more mental health assessment and management in their practices, Dr. Lawrence V. Amsel said during an interview at the psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
Many primary care clinicians don’t feel adequately trained to interview patients, guage their mental status, and then act on the findings by treatment or referral. But over the past decade, psychiatrists have developed and validated several tools that are appropriate for a primary care practice, said Dr. Amsel, a clinical psychiatrist at Columbia University in New York, and a faculty member of the REACH Institute, a New York–based nonprofit focused on disseminating mental health skills to primary care clinicians, teachers, parents, and others. The program also tries to make clinicians comfortable prescribing psychiatric medications and links them with psychiatrists who can provide consultations when needed.
“It’s kind of like a psychiatrist extender,” when a psychiatrist consults with several primary care clinicians, which allows for improved psychiatric care of many more patients, he said.
Dr. Amsel is on the faculty of the REACH Institute.
On Twitter@mitchelzoler
EXPERT ANALYSIS FROM THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
Treating VTE in patients with gynecologic malignancies
Rudolph Virchow clearly demonstrated the association between malignancy and venous thromboembolic events. VTE – deep vein thrombosis and pulmonary embolism – affect between 15% and 38% of patients with gynecologic malignancies after surgery.
The rate of pulmonary embolism (PE) in this patient population can be as high as 6.8%, with the case fatality rate being 11%-12% (Obstet. Gynecol. 2012;119:155-67). Other factors associated with the development of VTE include prior VTE, older age, African American race, prolonged operative time, obesity, and prior radiation therapy (Obstet. Gynecol. 1987;69:146-50). The risk of VTE in women undergoing gynecologic surgery is quadrupled in the presence of malignancy(Obstet. Gynecol. 2006;107:666-71) and these patients are twice as likely to die from a VTE compared to matched controls (Gynecol. Oncol. 2007;106:439-45).
Additionally, cancer patients are typically older, have longer and more complex surgeries, and the presence of a pelvic mass further contributes to venous stasis (Obstet. Gynecol. 2012;119:155-67).
Although the treatment of VTE is fairly similar between patients with malignancy and those without cancer, treatment of a VTE in patients with cancer can be further complicated by higher VTE recurrence rates and increased risk of bleeding. Furthermore, issues related to the malignant disease process such as prognosis, presence and location of metastasis, and life expectancy should be taken into consideration when managing VTE in this patient population.
Generally, in the setting of an acute or recurrent VTE, initial therapy with a parenteral anticoagulant (heparin or low-molecular-weight heparins [LMWH]) should be immediately instituted in patients with a gynecologic malignancy, unless there is evidence of active bleeding or any other contraindication for the use of an anticoagulant.
Other factors associated with cancer such as immobilization, the presence of metastases, and impaired renal function with a creatinine clearance less than 30 mL/min, may increase the risk of bleeding complications but are not absolute contraindications to anticoagulation (Thromb. Haemost. 2008;100:435-9). The initial treatment phase, which last for 5-10 days, is then followed by a longer treatment phase lasting 3-6 months.
In the majority of cases, LMWH is the preferred agent for both the initial and prolonged treatment phase assuming adequate renal function. Based on evidence from a meta-analysis of 16 randomized controlled trials in cancer patients receiving initial anticoagulation for VTE, LMWH is associated with a 30% reduction in mortality without an increased risk of bleeding in comparison to unfractionated heparin (Cochrane Database. Syst. Rev. 2014;6:CD006649).
When compared with the vitamin K antagonist warfarin, LMWH appears to be associated with a significantly reduced rate of recurrent VTE (hazard ratio, 0.47; 95% confidence interval 0.32-0.71). However, this was not associated with a survival advantage (N. Engl. J. Med. 2003;349:146-53).
There are no trials comparing the different formulations of LMWH. In our practice, we routinely use the LMWH enoxaparin dosed at 1 mg/kg subcutaneously twice daily. Other well-studied LMWHs include dalteparin and tinzaparin.
LMWHs are primarily renally excreted, thus, in patients with compromised renal function, the biological half-life of the medication may be prolonged, leading to potential bleeding complications. The majority of LMWH trials excluded patients with creatinine clearance less than 30 mL/min, therefore, in patients with compromised renal function, one option would be to decrease the daily dose by as much as 50% and closely monitor antifactor XA levels. Alternatively, the use of unfractionated heparin in the acute setting followed by warfarin with close monitoring of the patient’s international normalized ratio could prove less cumbersome and ultimately safer for these patients. However, given the limitations of the currently available data we would not recommend the routine use of newer oral anticoagulation agents.
Patients with a malignancy are at increased risk for the development of a recurrent VTE even in the setting of anticoagulation. Some of the risks factors for this phenomenon include presence of central venous catheters, interruption of therapy for procedures, and immobilization. In cases of recurrent VTE, consideration should be given to extending the duration of treatment beyond the initial planned 3-6 months. Other patients that may benefit from extended therapy include those with continued immobility or active cancer burden.
LMWH is also the preferred agent for extended therapy based on very limited evidence from experimental studies suggesting that LMWH may have antineoplastic effects and thus a survival advantage. However, in the setting of a recurrent VTE, there is very limited data on which to base the choice of extended treatment. Options include switching the therapeutic agent, increasing the dose or frequency of administration, or placement of an inferior vena cava filter. Consultation with a hematologist may also be warranted in this and more complicated scenarios.
Ultimately, LMWH appears to be the best available therapy for patients with a gynecologic malignancy. However, the decision to anticoagulate should be carefully planned out, taking into consideration the individual patient’s disease burden and associated comorbidities in order to select the most appropriate treatment option.
Dr. Roque is a fellow in the gynecologic oncology program at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and a professor in the division of gynecologic oncology at the university. Dr. Roque and Dr. Clarke-Pearson said they had no relevant financial disclosures.
Rudolph Virchow clearly demonstrated the association between malignancy and venous thromboembolic events. VTE – deep vein thrombosis and pulmonary embolism – affect between 15% and 38% of patients with gynecologic malignancies after surgery.
The rate of pulmonary embolism (PE) in this patient population can be as high as 6.8%, with the case fatality rate being 11%-12% (Obstet. Gynecol. 2012;119:155-67). Other factors associated with the development of VTE include prior VTE, older age, African American race, prolonged operative time, obesity, and prior radiation therapy (Obstet. Gynecol. 1987;69:146-50). The risk of VTE in women undergoing gynecologic surgery is quadrupled in the presence of malignancy(Obstet. Gynecol. 2006;107:666-71) and these patients are twice as likely to die from a VTE compared to matched controls (Gynecol. Oncol. 2007;106:439-45).
Additionally, cancer patients are typically older, have longer and more complex surgeries, and the presence of a pelvic mass further contributes to venous stasis (Obstet. Gynecol. 2012;119:155-67).
Although the treatment of VTE is fairly similar between patients with malignancy and those without cancer, treatment of a VTE in patients with cancer can be further complicated by higher VTE recurrence rates and increased risk of bleeding. Furthermore, issues related to the malignant disease process such as prognosis, presence and location of metastasis, and life expectancy should be taken into consideration when managing VTE in this patient population.
Generally, in the setting of an acute or recurrent VTE, initial therapy with a parenteral anticoagulant (heparin or low-molecular-weight heparins [LMWH]) should be immediately instituted in patients with a gynecologic malignancy, unless there is evidence of active bleeding or any other contraindication for the use of an anticoagulant.
Other factors associated with cancer such as immobilization, the presence of metastases, and impaired renal function with a creatinine clearance less than 30 mL/min, may increase the risk of bleeding complications but are not absolute contraindications to anticoagulation (Thromb. Haemost. 2008;100:435-9). The initial treatment phase, which last for 5-10 days, is then followed by a longer treatment phase lasting 3-6 months.
In the majority of cases, LMWH is the preferred agent for both the initial and prolonged treatment phase assuming adequate renal function. Based on evidence from a meta-analysis of 16 randomized controlled trials in cancer patients receiving initial anticoagulation for VTE, LMWH is associated with a 30% reduction in mortality without an increased risk of bleeding in comparison to unfractionated heparin (Cochrane Database. Syst. Rev. 2014;6:CD006649).
When compared with the vitamin K antagonist warfarin, LMWH appears to be associated with a significantly reduced rate of recurrent VTE (hazard ratio, 0.47; 95% confidence interval 0.32-0.71). However, this was not associated with a survival advantage (N. Engl. J. Med. 2003;349:146-53).
There are no trials comparing the different formulations of LMWH. In our practice, we routinely use the LMWH enoxaparin dosed at 1 mg/kg subcutaneously twice daily. Other well-studied LMWHs include dalteparin and tinzaparin.
LMWHs are primarily renally excreted, thus, in patients with compromised renal function, the biological half-life of the medication may be prolonged, leading to potential bleeding complications. The majority of LMWH trials excluded patients with creatinine clearance less than 30 mL/min, therefore, in patients with compromised renal function, one option would be to decrease the daily dose by as much as 50% and closely monitor antifactor XA levels. Alternatively, the use of unfractionated heparin in the acute setting followed by warfarin with close monitoring of the patient’s international normalized ratio could prove less cumbersome and ultimately safer for these patients. However, given the limitations of the currently available data we would not recommend the routine use of newer oral anticoagulation agents.
Patients with a malignancy are at increased risk for the development of a recurrent VTE even in the setting of anticoagulation. Some of the risks factors for this phenomenon include presence of central venous catheters, interruption of therapy for procedures, and immobilization. In cases of recurrent VTE, consideration should be given to extending the duration of treatment beyond the initial planned 3-6 months. Other patients that may benefit from extended therapy include those with continued immobility or active cancer burden.
LMWH is also the preferred agent for extended therapy based on very limited evidence from experimental studies suggesting that LMWH may have antineoplastic effects and thus a survival advantage. However, in the setting of a recurrent VTE, there is very limited data on which to base the choice of extended treatment. Options include switching the therapeutic agent, increasing the dose or frequency of administration, or placement of an inferior vena cava filter. Consultation with a hematologist may also be warranted in this and more complicated scenarios.
Ultimately, LMWH appears to be the best available therapy for patients with a gynecologic malignancy. However, the decision to anticoagulate should be carefully planned out, taking into consideration the individual patient’s disease burden and associated comorbidities in order to select the most appropriate treatment option.
Dr. Roque is a fellow in the gynecologic oncology program at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and a professor in the division of gynecologic oncology at the university. Dr. Roque and Dr. Clarke-Pearson said they had no relevant financial disclosures.
Rudolph Virchow clearly demonstrated the association between malignancy and venous thromboembolic events. VTE – deep vein thrombosis and pulmonary embolism – affect between 15% and 38% of patients with gynecologic malignancies after surgery.
The rate of pulmonary embolism (PE) in this patient population can be as high as 6.8%, with the case fatality rate being 11%-12% (Obstet. Gynecol. 2012;119:155-67). Other factors associated with the development of VTE include prior VTE, older age, African American race, prolonged operative time, obesity, and prior radiation therapy (Obstet. Gynecol. 1987;69:146-50). The risk of VTE in women undergoing gynecologic surgery is quadrupled in the presence of malignancy(Obstet. Gynecol. 2006;107:666-71) and these patients are twice as likely to die from a VTE compared to matched controls (Gynecol. Oncol. 2007;106:439-45).
Additionally, cancer patients are typically older, have longer and more complex surgeries, and the presence of a pelvic mass further contributes to venous stasis (Obstet. Gynecol. 2012;119:155-67).
Although the treatment of VTE is fairly similar between patients with malignancy and those without cancer, treatment of a VTE in patients with cancer can be further complicated by higher VTE recurrence rates and increased risk of bleeding. Furthermore, issues related to the malignant disease process such as prognosis, presence and location of metastasis, and life expectancy should be taken into consideration when managing VTE in this patient population.
Generally, in the setting of an acute or recurrent VTE, initial therapy with a parenteral anticoagulant (heparin or low-molecular-weight heparins [LMWH]) should be immediately instituted in patients with a gynecologic malignancy, unless there is evidence of active bleeding or any other contraindication for the use of an anticoagulant.
Other factors associated with cancer such as immobilization, the presence of metastases, and impaired renal function with a creatinine clearance less than 30 mL/min, may increase the risk of bleeding complications but are not absolute contraindications to anticoagulation (Thromb. Haemost. 2008;100:435-9). The initial treatment phase, which last for 5-10 days, is then followed by a longer treatment phase lasting 3-6 months.
In the majority of cases, LMWH is the preferred agent for both the initial and prolonged treatment phase assuming adequate renal function. Based on evidence from a meta-analysis of 16 randomized controlled trials in cancer patients receiving initial anticoagulation for VTE, LMWH is associated with a 30% reduction in mortality without an increased risk of bleeding in comparison to unfractionated heparin (Cochrane Database. Syst. Rev. 2014;6:CD006649).
When compared with the vitamin K antagonist warfarin, LMWH appears to be associated with a significantly reduced rate of recurrent VTE (hazard ratio, 0.47; 95% confidence interval 0.32-0.71). However, this was not associated with a survival advantage (N. Engl. J. Med. 2003;349:146-53).
There are no trials comparing the different formulations of LMWH. In our practice, we routinely use the LMWH enoxaparin dosed at 1 mg/kg subcutaneously twice daily. Other well-studied LMWHs include dalteparin and tinzaparin.
LMWHs are primarily renally excreted, thus, in patients with compromised renal function, the biological half-life of the medication may be prolonged, leading to potential bleeding complications. The majority of LMWH trials excluded patients with creatinine clearance less than 30 mL/min, therefore, in patients with compromised renal function, one option would be to decrease the daily dose by as much as 50% and closely monitor antifactor XA levels. Alternatively, the use of unfractionated heparin in the acute setting followed by warfarin with close monitoring of the patient’s international normalized ratio could prove less cumbersome and ultimately safer for these patients. However, given the limitations of the currently available data we would not recommend the routine use of newer oral anticoagulation agents.
Patients with a malignancy are at increased risk for the development of a recurrent VTE even in the setting of anticoagulation. Some of the risks factors for this phenomenon include presence of central venous catheters, interruption of therapy for procedures, and immobilization. In cases of recurrent VTE, consideration should be given to extending the duration of treatment beyond the initial planned 3-6 months. Other patients that may benefit from extended therapy include those with continued immobility or active cancer burden.
LMWH is also the preferred agent for extended therapy based on very limited evidence from experimental studies suggesting that LMWH may have antineoplastic effects and thus a survival advantage. However, in the setting of a recurrent VTE, there is very limited data on which to base the choice of extended treatment. Options include switching the therapeutic agent, increasing the dose or frequency of administration, or placement of an inferior vena cava filter. Consultation with a hematologist may also be warranted in this and more complicated scenarios.
Ultimately, LMWH appears to be the best available therapy for patients with a gynecologic malignancy. However, the decision to anticoagulate should be carefully planned out, taking into consideration the individual patient’s disease burden and associated comorbidities in order to select the most appropriate treatment option.
Dr. Roque is a fellow in the gynecologic oncology program at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and a professor in the division of gynecologic oncology at the university. Dr. Roque and Dr. Clarke-Pearson said they had no relevant financial disclosures.
Program fosters psychotherapy in primary care practices
NEW YORK – Making primary care clinicians comfortable performing basic mental health diagnoses and management is vital for adequately treating U.S. patients with psychiatric disorders, Dr. Lawrence V. Amsel said at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
In many parts of the United States there are “far fewer mental health practitioners than are needed.” Training primary care clinicians so that they are willing to do more mental health work can help address this issue, said Dr. Amsel, a clinical psychiatrist at Columbia University in New York and a faculty member of the REACH Institute, a New York–based nonprofit focused on disseminating mental health skills to primary care clinicians, teachers, parents, and others. “It’s like producing psychiatric extenders.” By consulting with a broad range of primary care clinicians, a psychiatrist can take care of a lot more kids than usual in a single psychiatric practice,” Dr. Amsel said.
But encouraging primary care providers to become more active in mental health diagnosis and management is not easy. “Most prescriptions for mental health indications are now written by primary care clinicians, but they often describe themselves as uncomfortable prescribing these medications and not adequately trained,” Dr. Amsel said in an interview.
“Their main anxiety comes from making the wrong diagnosis and then doing harm” as a consequence of their error, he explained during his talk at the meeting. Training by the REACH curriculum highlights the role of well-validated tools now available for refining assessment of a patient and boosting confidence in the diagnosis. This includes instruments like the Pediatric Symptom Checklist and the Mental Status Exam. “Reliable and validated tools are available to improve identification and assessment of mental health problems that can be used efficiently in clinical practice,” Dr. Amsel said.
Another aspect to mental health management that often troubles primary care clinicians is doubt about their knowledge and ability to safely and effectively prescribe psychiatric medications. The REACH Institute curriculum tells clinicians to focus on each patient’s primary diagnosis and treat that first, and whenever possible to use medications that are evidence based, with good supporting documentation from double-blind, randomized, controlled trials.
“We recommend that clinicians get a summary slide of the evidence that they can show to patients or family members if necessary to make clear that there is a scientific basis for the treatment and that it is based on facts and data rather than on opinion,” he said.
Training for primary care clinicians also emphasizes that management goes beyond drug treatment and also must include a psychosocial plan for each patient.
Members of the health care system have begun to “recognize that mental health is responsible for much if not most disability. Until now, this importance had not been recognized. Now that it is being recognized, I think people will develop systems that increase the capacity for identifying children with mental health issues and provide them with improved care,” Dr. Amsel said.
Dr. Amsel had no disclosures aside from his work for the REACH Institute.
On Twitter @mitchelzoler
NEW YORK – Making primary care clinicians comfortable performing basic mental health diagnoses and management is vital for adequately treating U.S. patients with psychiatric disorders, Dr. Lawrence V. Amsel said at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
In many parts of the United States there are “far fewer mental health practitioners than are needed.” Training primary care clinicians so that they are willing to do more mental health work can help address this issue, said Dr. Amsel, a clinical psychiatrist at Columbia University in New York and a faculty member of the REACH Institute, a New York–based nonprofit focused on disseminating mental health skills to primary care clinicians, teachers, parents, and others. “It’s like producing psychiatric extenders.” By consulting with a broad range of primary care clinicians, a psychiatrist can take care of a lot more kids than usual in a single psychiatric practice,” Dr. Amsel said.
But encouraging primary care providers to become more active in mental health diagnosis and management is not easy. “Most prescriptions for mental health indications are now written by primary care clinicians, but they often describe themselves as uncomfortable prescribing these medications and not adequately trained,” Dr. Amsel said in an interview.
“Their main anxiety comes from making the wrong diagnosis and then doing harm” as a consequence of their error, he explained during his talk at the meeting. Training by the REACH curriculum highlights the role of well-validated tools now available for refining assessment of a patient and boosting confidence in the diagnosis. This includes instruments like the Pediatric Symptom Checklist and the Mental Status Exam. “Reliable and validated tools are available to improve identification and assessment of mental health problems that can be used efficiently in clinical practice,” Dr. Amsel said.
Another aspect to mental health management that often troubles primary care clinicians is doubt about their knowledge and ability to safely and effectively prescribe psychiatric medications. The REACH Institute curriculum tells clinicians to focus on each patient’s primary diagnosis and treat that first, and whenever possible to use medications that are evidence based, with good supporting documentation from double-blind, randomized, controlled trials.
“We recommend that clinicians get a summary slide of the evidence that they can show to patients or family members if necessary to make clear that there is a scientific basis for the treatment and that it is based on facts and data rather than on opinion,” he said.
Training for primary care clinicians also emphasizes that management goes beyond drug treatment and also must include a psychosocial plan for each patient.
Members of the health care system have begun to “recognize that mental health is responsible for much if not most disability. Until now, this importance had not been recognized. Now that it is being recognized, I think people will develop systems that increase the capacity for identifying children with mental health issues and provide them with improved care,” Dr. Amsel said.
Dr. Amsel had no disclosures aside from his work for the REACH Institute.
On Twitter @mitchelzoler
NEW YORK – Making primary care clinicians comfortable performing basic mental health diagnoses and management is vital for adequately treating U.S. patients with psychiatric disorders, Dr. Lawrence V. Amsel said at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
In many parts of the United States there are “far fewer mental health practitioners than are needed.” Training primary care clinicians so that they are willing to do more mental health work can help address this issue, said Dr. Amsel, a clinical psychiatrist at Columbia University in New York and a faculty member of the REACH Institute, a New York–based nonprofit focused on disseminating mental health skills to primary care clinicians, teachers, parents, and others. “It’s like producing psychiatric extenders.” By consulting with a broad range of primary care clinicians, a psychiatrist can take care of a lot more kids than usual in a single psychiatric practice,” Dr. Amsel said.
But encouraging primary care providers to become more active in mental health diagnosis and management is not easy. “Most prescriptions for mental health indications are now written by primary care clinicians, but they often describe themselves as uncomfortable prescribing these medications and not adequately trained,” Dr. Amsel said in an interview.
“Their main anxiety comes from making the wrong diagnosis and then doing harm” as a consequence of their error, he explained during his talk at the meeting. Training by the REACH curriculum highlights the role of well-validated tools now available for refining assessment of a patient and boosting confidence in the diagnosis. This includes instruments like the Pediatric Symptom Checklist and the Mental Status Exam. “Reliable and validated tools are available to improve identification and assessment of mental health problems that can be used efficiently in clinical practice,” Dr. Amsel said.
Another aspect to mental health management that often troubles primary care clinicians is doubt about their knowledge and ability to safely and effectively prescribe psychiatric medications. The REACH Institute curriculum tells clinicians to focus on each patient’s primary diagnosis and treat that first, and whenever possible to use medications that are evidence based, with good supporting documentation from double-blind, randomized, controlled trials.
“We recommend that clinicians get a summary slide of the evidence that they can show to patients or family members if necessary to make clear that there is a scientific basis for the treatment and that it is based on facts and data rather than on opinion,” he said.
Training for primary care clinicians also emphasizes that management goes beyond drug treatment and also must include a psychosocial plan for each patient.
Members of the health care system have begun to “recognize that mental health is responsible for much if not most disability. Until now, this importance had not been recognized. Now that it is being recognized, I think people will develop systems that increase the capacity for identifying children with mental health issues and provide them with improved care,” Dr. Amsel said.
Dr. Amsel had no disclosures aside from his work for the REACH Institute.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
Aggressiveness of CLL linked to genetic variability

The genetic variability of chronic lymphocytic leukemia (CLL) appears to predict its aggressiveness, according to a study published in Genome Medicine.
Investigators found evidence suggesting that greater variability in gene expression is associated with more aggressive disease.
The team analyzed gene expression in two cohorts of CLL patients—those with IgVH mutations and a good prognosis and those with unmutated CLL who have more aggressive disease.
The researchers examined 70 mutated and 52 unmutated CLL samples, as well as 20 control samples taken from healthy individuals.
Unmutated, aggressive CLL showed increased gene expression variability across individuals, whereas gene expression variability was lower in less aggressive, mutated CLL.
The investigators validated these observations by comparing them against a second sample group consisting of 24 mutated and 36 unmutated CLL samples.
The results suggested that CLL aggressiveness is specifically determined by a set of 500 genes showing increased expression variability across individuals. The genes are involved in processes such as adaptation to the environment, cell death, tumor growth, and drug resistance.
“Our conclusion is that the coefficient of variation for gene expression in CLL efficiently predicts its aggressiveness,” said study author Alfonso Valencia, PhD, of Centro Nacional de Investigaciones Oncologicas (CNIO) in Madrid, Spain.
“More importantly, if further research confirms these findings, a classifier based on the measurement of gene expression variability could be created to predict the disease subtype of CLL patients.”
The researchers said their next step is to discover the mechanisms responsible for the high levels of expression variability for a given gene across individuals.
Understanding the mechanisms underlying this phenomenon is of crucial relevance for oncology research, the investigators said, as it is linked to tumor heterogeneity, a key feature of cancer progression and drug resistance.
The greater the genetic variability in a tumor, the better it will adapt to its environment, and the more probabilities for this tumor to spread, develop resistance to cancer therapies, and metastasize to distant organs. ![]()

The genetic variability of chronic lymphocytic leukemia (CLL) appears to predict its aggressiveness, according to a study published in Genome Medicine.
Investigators found evidence suggesting that greater variability in gene expression is associated with more aggressive disease.
The team analyzed gene expression in two cohorts of CLL patients—those with IgVH mutations and a good prognosis and those with unmutated CLL who have more aggressive disease.
The researchers examined 70 mutated and 52 unmutated CLL samples, as well as 20 control samples taken from healthy individuals.
Unmutated, aggressive CLL showed increased gene expression variability across individuals, whereas gene expression variability was lower in less aggressive, mutated CLL.
The investigators validated these observations by comparing them against a second sample group consisting of 24 mutated and 36 unmutated CLL samples.
The results suggested that CLL aggressiveness is specifically determined by a set of 500 genes showing increased expression variability across individuals. The genes are involved in processes such as adaptation to the environment, cell death, tumor growth, and drug resistance.
“Our conclusion is that the coefficient of variation for gene expression in CLL efficiently predicts its aggressiveness,” said study author Alfonso Valencia, PhD, of Centro Nacional de Investigaciones Oncologicas (CNIO) in Madrid, Spain.
“More importantly, if further research confirms these findings, a classifier based on the measurement of gene expression variability could be created to predict the disease subtype of CLL patients.”
The researchers said their next step is to discover the mechanisms responsible for the high levels of expression variability for a given gene across individuals.
Understanding the mechanisms underlying this phenomenon is of crucial relevance for oncology research, the investigators said, as it is linked to tumor heterogeneity, a key feature of cancer progression and drug resistance.
The greater the genetic variability in a tumor, the better it will adapt to its environment, and the more probabilities for this tumor to spread, develop resistance to cancer therapies, and metastasize to distant organs. ![]()

The genetic variability of chronic lymphocytic leukemia (CLL) appears to predict its aggressiveness, according to a study published in Genome Medicine.
Investigators found evidence suggesting that greater variability in gene expression is associated with more aggressive disease.
The team analyzed gene expression in two cohorts of CLL patients—those with IgVH mutations and a good prognosis and those with unmutated CLL who have more aggressive disease.
The researchers examined 70 mutated and 52 unmutated CLL samples, as well as 20 control samples taken from healthy individuals.
Unmutated, aggressive CLL showed increased gene expression variability across individuals, whereas gene expression variability was lower in less aggressive, mutated CLL.
The investigators validated these observations by comparing them against a second sample group consisting of 24 mutated and 36 unmutated CLL samples.
The results suggested that CLL aggressiveness is specifically determined by a set of 500 genes showing increased expression variability across individuals. The genes are involved in processes such as adaptation to the environment, cell death, tumor growth, and drug resistance.
“Our conclusion is that the coefficient of variation for gene expression in CLL efficiently predicts its aggressiveness,” said study author Alfonso Valencia, PhD, of Centro Nacional de Investigaciones Oncologicas (CNIO) in Madrid, Spain.
“More importantly, if further research confirms these findings, a classifier based on the measurement of gene expression variability could be created to predict the disease subtype of CLL patients.”
The researchers said their next step is to discover the mechanisms responsible for the high levels of expression variability for a given gene across individuals.
Understanding the mechanisms underlying this phenomenon is of crucial relevance for oncology research, the investigators said, as it is linked to tumor heterogeneity, a key feature of cancer progression and drug resistance.
The greater the genetic variability in a tumor, the better it will adapt to its environment, and the more probabilities for this tumor to spread, develop resistance to cancer therapies, and metastasize to distant organs. ![]()
Risk of HBV reactivation ‘underappreciated’

Credit: CDC
Reactivation of the hepatitis B virus (HBV) may be more of a risk than we anticipated, investigators have reported in Hepatology.
Their research indicates that HBV reactivation is associated with the use of chemotherapy, high-dose corticosteroids, biologics targeting tumor necrosis factor-alpha (TNF-α), and agents that aren’t really considered immunosuppressive.
HBV reactivation is also fairly common after organ transplant and hematopoietic stem cell transplant (HSCT).
As reactivation of HBV can be fatal, the study authors suggest routine screening of HBV in all patients prior to the start of these treatments.
The researchers noted that, in September 2013, the US Food and Drug Administration (FDA) issued a Drug Safety Communication in an attempt to decrease the risk of HBV reactivation. The communication advised healthcare professionals to screen patients for HBV prior to the administration of ofatumumab or rituximab.
“[T]his may be just the tip of the iceberg,” said Adrian Di Bisceglie, MD, of Saint Louis University School of Medicine in Missouri.
“Our research suggests that the issue of HBV reactivation may be an underappreciated clinical challenge that extends well beyond the use of just two anti-CD20 medications.”
After a systematic literature review, Dr Di Bisceglie and his colleagues identified 504 studies pertaining to reactivation of HBV.
The investigators reviewed 14 studies in which the antiviral agent lamivudine was used to prevent HBV reactivation in HBsAg-positive patients receiving chemotherapy. Among patients who did not receive lamivudine, HBV reactivation occurred in 32%. Thirteen percent of patients experienced liver failure, and 7% died.
The researchers also looked at patients undergoing HSCT. In one study, 61 patients had resolved HBV infection before HSCT. But 12 of these patients (20%) developed reverse seroconversion (reappearance of HBsAg in a person who was HBsAg-negative, anti-HBc-positive prior to HSCT).
The cumulative probability of reverse seroconversion was 9% a year after HSCT, 21.7% at 2 years, and 42.9% at 4 years.
The investigators also noted that high-dose corticosteroids carry a significant risk of HBV reactivation, both as part of combination treatment for malignancies and when used alone to treat benign conditions.
In addition, the researchers found data showing that HBV reactivation has occurred with antitumor agents that are not thought to be particularly immunosuppressive, such as imatinib and thalidomide. The team said this raises questions about the mechanisms by which drugs are causing HBV reactivation.
The investigators also looked at data from 257 patients with active or recovered HBV infection who received treatment with biological therapies targeting TNF-α.
Forty-two percent of the patients had elevations in serum aminotransferase levels, 39% had reappearance of HBV DNA, 16% had signs and symptoms of liver disease, and 5% died of liver failure.
HBV reactivation was more frequent among patients receiving infliximab than etanercept. It was 7-fold higher among patients who were HBsAg-positive (38%) than those who were HBsAg-negative but anti-HBc-positive (5%).
While it remains unclear how HBV reactivation occurs, experts believe a loss of immune control over viral replication may trigger the process.
“Further study and cooperation between various medical disciplines will help broaden understanding of HBV reactivation,” Dr Di Bisceglie concluded. ![]()

Credit: CDC
Reactivation of the hepatitis B virus (HBV) may be more of a risk than we anticipated, investigators have reported in Hepatology.
Their research indicates that HBV reactivation is associated with the use of chemotherapy, high-dose corticosteroids, biologics targeting tumor necrosis factor-alpha (TNF-α), and agents that aren’t really considered immunosuppressive.
HBV reactivation is also fairly common after organ transplant and hematopoietic stem cell transplant (HSCT).
As reactivation of HBV can be fatal, the study authors suggest routine screening of HBV in all patients prior to the start of these treatments.
The researchers noted that, in September 2013, the US Food and Drug Administration (FDA) issued a Drug Safety Communication in an attempt to decrease the risk of HBV reactivation. The communication advised healthcare professionals to screen patients for HBV prior to the administration of ofatumumab or rituximab.
“[T]his may be just the tip of the iceberg,” said Adrian Di Bisceglie, MD, of Saint Louis University School of Medicine in Missouri.
“Our research suggests that the issue of HBV reactivation may be an underappreciated clinical challenge that extends well beyond the use of just two anti-CD20 medications.”
After a systematic literature review, Dr Di Bisceglie and his colleagues identified 504 studies pertaining to reactivation of HBV.
The investigators reviewed 14 studies in which the antiviral agent lamivudine was used to prevent HBV reactivation in HBsAg-positive patients receiving chemotherapy. Among patients who did not receive lamivudine, HBV reactivation occurred in 32%. Thirteen percent of patients experienced liver failure, and 7% died.
The researchers also looked at patients undergoing HSCT. In one study, 61 patients had resolved HBV infection before HSCT. But 12 of these patients (20%) developed reverse seroconversion (reappearance of HBsAg in a person who was HBsAg-negative, anti-HBc-positive prior to HSCT).
The cumulative probability of reverse seroconversion was 9% a year after HSCT, 21.7% at 2 years, and 42.9% at 4 years.
The investigators also noted that high-dose corticosteroids carry a significant risk of HBV reactivation, both as part of combination treatment for malignancies and when used alone to treat benign conditions.
In addition, the researchers found data showing that HBV reactivation has occurred with antitumor agents that are not thought to be particularly immunosuppressive, such as imatinib and thalidomide. The team said this raises questions about the mechanisms by which drugs are causing HBV reactivation.
The investigators also looked at data from 257 patients with active or recovered HBV infection who received treatment with biological therapies targeting TNF-α.
Forty-two percent of the patients had elevations in serum aminotransferase levels, 39% had reappearance of HBV DNA, 16% had signs and symptoms of liver disease, and 5% died of liver failure.
HBV reactivation was more frequent among patients receiving infliximab than etanercept. It was 7-fold higher among patients who were HBsAg-positive (38%) than those who were HBsAg-negative but anti-HBc-positive (5%).
While it remains unclear how HBV reactivation occurs, experts believe a loss of immune control over viral replication may trigger the process.
“Further study and cooperation between various medical disciplines will help broaden understanding of HBV reactivation,” Dr Di Bisceglie concluded. ![]()

Credit: CDC
Reactivation of the hepatitis B virus (HBV) may be more of a risk than we anticipated, investigators have reported in Hepatology.
Their research indicates that HBV reactivation is associated with the use of chemotherapy, high-dose corticosteroids, biologics targeting tumor necrosis factor-alpha (TNF-α), and agents that aren’t really considered immunosuppressive.
HBV reactivation is also fairly common after organ transplant and hematopoietic stem cell transplant (HSCT).
As reactivation of HBV can be fatal, the study authors suggest routine screening of HBV in all patients prior to the start of these treatments.
The researchers noted that, in September 2013, the US Food and Drug Administration (FDA) issued a Drug Safety Communication in an attempt to decrease the risk of HBV reactivation. The communication advised healthcare professionals to screen patients for HBV prior to the administration of ofatumumab or rituximab.
“[T]his may be just the tip of the iceberg,” said Adrian Di Bisceglie, MD, of Saint Louis University School of Medicine in Missouri.
“Our research suggests that the issue of HBV reactivation may be an underappreciated clinical challenge that extends well beyond the use of just two anti-CD20 medications.”
After a systematic literature review, Dr Di Bisceglie and his colleagues identified 504 studies pertaining to reactivation of HBV.
The investigators reviewed 14 studies in which the antiviral agent lamivudine was used to prevent HBV reactivation in HBsAg-positive patients receiving chemotherapy. Among patients who did not receive lamivudine, HBV reactivation occurred in 32%. Thirteen percent of patients experienced liver failure, and 7% died.
The researchers also looked at patients undergoing HSCT. In one study, 61 patients had resolved HBV infection before HSCT. But 12 of these patients (20%) developed reverse seroconversion (reappearance of HBsAg in a person who was HBsAg-negative, anti-HBc-positive prior to HSCT).
The cumulative probability of reverse seroconversion was 9% a year after HSCT, 21.7% at 2 years, and 42.9% at 4 years.
The investigators also noted that high-dose corticosteroids carry a significant risk of HBV reactivation, both as part of combination treatment for malignancies and when used alone to treat benign conditions.
In addition, the researchers found data showing that HBV reactivation has occurred with antitumor agents that are not thought to be particularly immunosuppressive, such as imatinib and thalidomide. The team said this raises questions about the mechanisms by which drugs are causing HBV reactivation.
The investigators also looked at data from 257 patients with active or recovered HBV infection who received treatment with biological therapies targeting TNF-α.
Forty-two percent of the patients had elevations in serum aminotransferase levels, 39% had reappearance of HBV DNA, 16% had signs and symptoms of liver disease, and 5% died of liver failure.
HBV reactivation was more frequent among patients receiving infliximab than etanercept. It was 7-fold higher among patients who were HBsAg-positive (38%) than those who were HBsAg-negative but anti-HBc-positive (5%).
While it remains unclear how HBV reactivation occurs, experts believe a loss of immune control over viral replication may trigger the process.
“Further study and cooperation between various medical disciplines will help broaden understanding of HBV reactivation,” Dr Di Bisceglie concluded. ![]()
Vaccine gets orphan designation for ATLL
The European Medicines Agency (EMA) has granted orphan drug designation for a therapeutic vaccine candidate known as THV02 to treat adult T-cell leukemia/lymphoma (ATLL).
THV02 is an experimental treatment composed of 2 lentiviral vectors to be used in a prime/boost regimen in ATLL patients infected by the HTLV-1 virus.
Both investigational drugs encode the same antigens, derived from 4 proteins of the HTLV-1 virus.
THV02 is intended to induce an immune response against HTLV antigens born by ATLL with the aim of enabling the patients’ immune system to fight leukemic cells.
Preclinical evaluation has suggested that THV02 is safe, and the vaccine has presented an “unprecedented” immunogenicity profile in several models, according to THERAVECTYS, the company developing THV02.
“Preclinical immunogenicity results obtained to date are very promising, and we are really excited by the prospect of bringing a safe and better-tolerated alternative to patients who are desperately in need of a treatment,” said Déborah Revaud, the senior scientist in charge of developing THV02.
The EMA grants orphan designation to drugs in development intended for the treatment, prevention, or diagnosis of life-threatening or chronically debilitating diseases occurring in fewer than 5 in 10,000 people.
The designation allows sponsors to benefit from an accelerated development process, financial incentives, and a 10-year period of market exclusivity once the drug is on the market.
“We are extremely pleased that the European Medicines Agency has granted an orphan drug status to our vaccine candidate against ATLL,” said Emmanuelle Sabbah-Petrover, PhD, head of regulatory affairs at THERAVECTYS.
“We expect to recruit our first patients towards the end of Q3 2015 in Europe and advance further developments in the US and in Japan in 2016.”
Should THV02 demonstrate a convincing safety and efficacy profile during its development against ATLL, THERAVECTYS said it will consider developing the vaccine for HTLV-related infections as treatment and possibly as prophylaxis. ![]()
The European Medicines Agency (EMA) has granted orphan drug designation for a therapeutic vaccine candidate known as THV02 to treat adult T-cell leukemia/lymphoma (ATLL).
THV02 is an experimental treatment composed of 2 lentiviral vectors to be used in a prime/boost regimen in ATLL patients infected by the HTLV-1 virus.
Both investigational drugs encode the same antigens, derived from 4 proteins of the HTLV-1 virus.
THV02 is intended to induce an immune response against HTLV antigens born by ATLL with the aim of enabling the patients’ immune system to fight leukemic cells.
Preclinical evaluation has suggested that THV02 is safe, and the vaccine has presented an “unprecedented” immunogenicity profile in several models, according to THERAVECTYS, the company developing THV02.
“Preclinical immunogenicity results obtained to date are very promising, and we are really excited by the prospect of bringing a safe and better-tolerated alternative to patients who are desperately in need of a treatment,” said Déborah Revaud, the senior scientist in charge of developing THV02.
The EMA grants orphan designation to drugs in development intended for the treatment, prevention, or diagnosis of life-threatening or chronically debilitating diseases occurring in fewer than 5 in 10,000 people.
The designation allows sponsors to benefit from an accelerated development process, financial incentives, and a 10-year period of market exclusivity once the drug is on the market.
“We are extremely pleased that the European Medicines Agency has granted an orphan drug status to our vaccine candidate against ATLL,” said Emmanuelle Sabbah-Petrover, PhD, head of regulatory affairs at THERAVECTYS.
“We expect to recruit our first patients towards the end of Q3 2015 in Europe and advance further developments in the US and in Japan in 2016.”
Should THV02 demonstrate a convincing safety and efficacy profile during its development against ATLL, THERAVECTYS said it will consider developing the vaccine for HTLV-related infections as treatment and possibly as prophylaxis. ![]()
The European Medicines Agency (EMA) has granted orphan drug designation for a therapeutic vaccine candidate known as THV02 to treat adult T-cell leukemia/lymphoma (ATLL).
THV02 is an experimental treatment composed of 2 lentiviral vectors to be used in a prime/boost regimen in ATLL patients infected by the HTLV-1 virus.
Both investigational drugs encode the same antigens, derived from 4 proteins of the HTLV-1 virus.
THV02 is intended to induce an immune response against HTLV antigens born by ATLL with the aim of enabling the patients’ immune system to fight leukemic cells.
Preclinical evaluation has suggested that THV02 is safe, and the vaccine has presented an “unprecedented” immunogenicity profile in several models, according to THERAVECTYS, the company developing THV02.
“Preclinical immunogenicity results obtained to date are very promising, and we are really excited by the prospect of bringing a safe and better-tolerated alternative to patients who are desperately in need of a treatment,” said Déborah Revaud, the senior scientist in charge of developing THV02.
The EMA grants orphan designation to drugs in development intended for the treatment, prevention, or diagnosis of life-threatening or chronically debilitating diseases occurring in fewer than 5 in 10,000 people.
The designation allows sponsors to benefit from an accelerated development process, financial incentives, and a 10-year period of market exclusivity once the drug is on the market.
“We are extremely pleased that the European Medicines Agency has granted an orphan drug status to our vaccine candidate against ATLL,” said Emmanuelle Sabbah-Petrover, PhD, head of regulatory affairs at THERAVECTYS.
“We expect to recruit our first patients towards the end of Q3 2015 in Europe and advance further developments in the US and in Japan in 2016.”
Should THV02 demonstrate a convincing safety and efficacy profile during its development against ATLL, THERAVECTYS said it will consider developing the vaccine for HTLV-related infections as treatment and possibly as prophylaxis. ![]()
Team creates new cells for modeling malaria

infection in iPSC-derived liver
cells 8 days after infection
Credit: Shengyong Ng et al.
Researchers say they’ve found a way to grow liver-like cells from induced pluripotent stem cells (iPSCs).
The liver-like cells can be infected with several strains of the malaria parasite and respond to existing drugs the same way mature human liver cells do.
The new cells, described in Stem Cell Reports, could allow scientists to test drugs on cells from people with different genetic backgrounds, who may respond differently to malaria infection and treatment.
Modeling infection
Until now, malaria researchers have not had many reliable ways to test new drugs in liver tissue.
“What’s historically been done is people have tried to make do with the systems that were available,” said study author Sangeeta Bhatia, MD, PhD, of the Massachusetts Institute of Technology in Cambridge.
In 2013, Dr Bhatia and her colleagues showed they could model malaria infection in hepatocytes from human donors. However, this generates only a limited supply from each donor, and not all of the cells work well for drug studies.
The researchers then turned to iPSCs, which can be generated from human skin cells by adding reprogramming factors. To create liver cells, the researchers added a series of growth factors, including hepatocyte growth factor, to the iPSCs.
The team generated these cells in 2012 and used them to model infection of hepatitis C. However, these cells, known as hepatocyte-like cells, did not seem to be as mature as real adult liver cells.
In the current study, the researchers found these cells could be infected with several strains of malaria. But, initially, the cells did not respond to drugs in the same way as adult liver cells.
In particular, they were not sensitive to primaquine, which works only if cells have a certain set of drug-metabolism enzymes found in mature liver cells.
To induce the cells to become more mature and turn on these metabolic enzymes, the researchers added a molecule they had identified in a previous study. This compound, which the researchers call a “maturin,” stimulated the cells to turn on those enzymes, which made them sensitive to primaquine.
Toward better drugs
The team is now working with the nonprofit foundation Medical Malaria Ventures to test about 10 potential malaria drugs that are in the pipeline, first using adult donor liver cells and then the hepatocyte-like cells generated in this study.
These cells could also prove useful to help identify new drug targets, the researchers said. In this study, they found the liver-like cells can be infected with malaria when they are still in the equivalent of fetal stages of development, when they become hepatoblasts, which are precursors to hepatocytes.
In future studies, the researchers plan to investigate which genes get turned on when the cells become susceptible to infection, which may suggest new targets for malaria drugs.
They also hope to compare the genes needed for malaria infection with those needed for hepatitis infection, in hopes of identifying common pathways to target for both diseases. ![]()

infection in iPSC-derived liver
cells 8 days after infection
Credit: Shengyong Ng et al.
Researchers say they’ve found a way to grow liver-like cells from induced pluripotent stem cells (iPSCs).
The liver-like cells can be infected with several strains of the malaria parasite and respond to existing drugs the same way mature human liver cells do.
The new cells, described in Stem Cell Reports, could allow scientists to test drugs on cells from people with different genetic backgrounds, who may respond differently to malaria infection and treatment.
Modeling infection
Until now, malaria researchers have not had many reliable ways to test new drugs in liver tissue.
“What’s historically been done is people have tried to make do with the systems that were available,” said study author Sangeeta Bhatia, MD, PhD, of the Massachusetts Institute of Technology in Cambridge.
In 2013, Dr Bhatia and her colleagues showed they could model malaria infection in hepatocytes from human donors. However, this generates only a limited supply from each donor, and not all of the cells work well for drug studies.
The researchers then turned to iPSCs, which can be generated from human skin cells by adding reprogramming factors. To create liver cells, the researchers added a series of growth factors, including hepatocyte growth factor, to the iPSCs.
The team generated these cells in 2012 and used them to model infection of hepatitis C. However, these cells, known as hepatocyte-like cells, did not seem to be as mature as real adult liver cells.
In the current study, the researchers found these cells could be infected with several strains of malaria. But, initially, the cells did not respond to drugs in the same way as adult liver cells.
In particular, they were not sensitive to primaquine, which works only if cells have a certain set of drug-metabolism enzymes found in mature liver cells.
To induce the cells to become more mature and turn on these metabolic enzymes, the researchers added a molecule they had identified in a previous study. This compound, which the researchers call a “maturin,” stimulated the cells to turn on those enzymes, which made them sensitive to primaquine.
Toward better drugs
The team is now working with the nonprofit foundation Medical Malaria Ventures to test about 10 potential malaria drugs that are in the pipeline, first using adult donor liver cells and then the hepatocyte-like cells generated in this study.
These cells could also prove useful to help identify new drug targets, the researchers said. In this study, they found the liver-like cells can be infected with malaria when they are still in the equivalent of fetal stages of development, when they become hepatoblasts, which are precursors to hepatocytes.
In future studies, the researchers plan to investigate which genes get turned on when the cells become susceptible to infection, which may suggest new targets for malaria drugs.
They also hope to compare the genes needed for malaria infection with those needed for hepatitis infection, in hopes of identifying common pathways to target for both diseases. ![]()

infection in iPSC-derived liver
cells 8 days after infection
Credit: Shengyong Ng et al.
Researchers say they’ve found a way to grow liver-like cells from induced pluripotent stem cells (iPSCs).
The liver-like cells can be infected with several strains of the malaria parasite and respond to existing drugs the same way mature human liver cells do.
The new cells, described in Stem Cell Reports, could allow scientists to test drugs on cells from people with different genetic backgrounds, who may respond differently to malaria infection and treatment.
Modeling infection
Until now, malaria researchers have not had many reliable ways to test new drugs in liver tissue.
“What’s historically been done is people have tried to make do with the systems that were available,” said study author Sangeeta Bhatia, MD, PhD, of the Massachusetts Institute of Technology in Cambridge.
In 2013, Dr Bhatia and her colleagues showed they could model malaria infection in hepatocytes from human donors. However, this generates only a limited supply from each donor, and not all of the cells work well for drug studies.
The researchers then turned to iPSCs, which can be generated from human skin cells by adding reprogramming factors. To create liver cells, the researchers added a series of growth factors, including hepatocyte growth factor, to the iPSCs.
The team generated these cells in 2012 and used them to model infection of hepatitis C. However, these cells, known as hepatocyte-like cells, did not seem to be as mature as real adult liver cells.
In the current study, the researchers found these cells could be infected with several strains of malaria. But, initially, the cells did not respond to drugs in the same way as adult liver cells.
In particular, they were not sensitive to primaquine, which works only if cells have a certain set of drug-metabolism enzymes found in mature liver cells.
To induce the cells to become more mature and turn on these metabolic enzymes, the researchers added a molecule they had identified in a previous study. This compound, which the researchers call a “maturin,” stimulated the cells to turn on those enzymes, which made them sensitive to primaquine.
Toward better drugs
The team is now working with the nonprofit foundation Medical Malaria Ventures to test about 10 potential malaria drugs that are in the pipeline, first using adult donor liver cells and then the hepatocyte-like cells generated in this study.
These cells could also prove useful to help identify new drug targets, the researchers said. In this study, they found the liver-like cells can be infected with malaria when they are still in the equivalent of fetal stages of development, when they become hepatoblasts, which are precursors to hepatocytes.
In future studies, the researchers plan to investigate which genes get turned on when the cells become susceptible to infection, which may suggest new targets for malaria drugs.
They also hope to compare the genes needed for malaria infection with those needed for hepatitis infection, in hopes of identifying common pathways to target for both diseases. ![]()
Neurological Rare Disease Special Report
Click here to download the PDF.
Click here to download the PDF.
Click here to download the PDF.
Weight Loss Achieved with Medication Can Delay Onset of Type 2 Diabetes in At-Risk Individuals
Study Overview
Objective. To determine the effect of phentermine and topiramate extended release (PHEN/TPM ER) treatment on progression to type 2 diabetes and/or cardiometabolic disease in subjects with prediabetes and/or metabolic syndrome (MetS) at baseline.
Design. Sub-group analysis of a larger double-blind, randomized, placebo-controlled trial of PHEN/TPM ER in overweight and obese adults.
Setting and participants. The larger study had 2 phases —a 56-week weight loss trial (CONQUER, n = 866), followed by an extension of the drug trial out to 108 weeks (SEQUEL, n = 675) in a sub-group of CONQUER participants. The CONQUER trial, based at 93 U.S. centers, enrolled overweight or obese patients with at least 2 obesity-related comorbidities and randomly assigned them to receive either placebo or PHEN/TPM ER at a lower (7.5 mg/46 mg) or higher (15 mg/92 mg) daily dose. All 3 groups also received lifestyle modification counseling that included an evidence-based diet and exercise curriculum. Participants received study drug and lifestyle counseling in the setting of monthly visits during the 60- (CONQUER) or 108-week (SEQUEL) follow-up period.
The analyses presented in this paper focus on the 475 participants who completed both CONQUER and SEQUEL and who were characterized as pre-diabetic or as having the metabolic syndrome (MetS) at baseline. Pre-diabetes was defined as having a blood glucose level of 100–125 mg/dL or higher while fasting, or 140–199 mg/dL after an oral glucose tolerance test (GTT). MetS was characterized in participants who displayed 3 or more of the following at baseline: waist circumference ≥ 102 cm in men or 88 cm in women; triglycerides ≥ 150 mg/dL or on a lipid-lowering medication; HDL < 40 mg/dL in men or < 50 mg/dL in women; systolic BP ≥ 130 mm Hg or diastolic BP ≥ 85 mm Hg (or on antihypertensive); and fasting glucose ≥ 100 mg/dL or on treatment for elevated glucose.
Main outcome measures. The primary outcome for this study was percent weight loss at 108 weeks of follow-up (or early termination). Secondary outcomes included cardiometabolic changes, such as development of type 2 diabetes and changes in lipid measures, blood pressure, and waist circumference. These were assessed at baseline, week 56, and week 108 (or at early termination). Rates of progression to type 2 diabetes were compared between the treatment groups using chi-square testing. Intention-to-treat (ITT) ANCOVA analysis was performed with multiple imputation techniques to address missing data, as well as with an alternative analysis using last observation carried forward.
Results. The study arms were similar with respect to baseline characteristics. Average age was 51 years in the high dose PHEN/TPM ER arm and 52 in the other arms. Over half (65%) of participants were women and 86% were Caucasian. Mean BMI was 36 kg/m2 (class II obesity). Over half of participants were on antihypertensive medications at baseline but with well-controlled blood pressure (mean 128/80 mm Hg). Of the 475 people in this analysis, 316 met criteria for prediabetes, 451 for MetS, and 292 for both prediabetes and MetS.
Weight loss at 2 years was significantly greater in subjects taking PHEN/TPM ER (10.9% in the lower dose group, 12.1% in the higher dose group) compared to those taking placebo (2.5%) (P < 0.001). Mirroring weight loss results, type 2 diabetes incidence was also significantly lower in the drug treatment arms than in the placebo arm at 2 years after randomization—annualized incidence was 6.1% for placebo vs. 1.8% for lower-dose drug and 1.3% for higher-dose drug (P < 0.05). Greater weight loss was associated with greater decrease in diabetes incidence across all 3 arms of the study. Those persons who did not achieve at least a 5% weight loss at 2 years had the highest annualized risk of developing diabetes (6.3%), compared with a 0.9% risk among those who lost at least 15% of their weight. Improvements in other cardiometabolic parameters, including HDL, triglycerides, waist circumference, and insulin sensitivity index, was more common among the PHEN/TPM ER participants compared with placebo. Blood pressure decreased slightly for all 3 groups and there was no significant difference between the drug arms and the placebo arm.
Discontinuation of study medication occurred in all 3 groups (3.1% in placebo, 6.1% in lower-dose medication, and 5.5% in higher-dose medication), with serious adverse events in 5%, 7%, and 8.5%, respectively. There were no deaths.
Conclusion. PHEN/TPM ER administered over a 2-year period significantly improved weight loss and decreased progression to type 2 diabetes relative to placebo in a group of at-risk participants.
Commentary
Diabetes and related cardiometabolic disease are major contributors to morbidity and mortality in adults. With the exception of invasive treatments such as bariatric surgery, reversal of diabetes once it is established has proven quite difficult [1,2], and thus there is an increased emphasis from the public health and medical communities on preventing the development of this disease in the first place. Complicating the picture, recently broadened criteria for pre-diabetes will likely result in a very large number of these at-risk individuals being identified [3,4]. Although intensive lifestyle interventions resulting in a 5% to 7% weight loss among pre-diabetics have been shown to delay progression to diabetes [5], the translation of these programs into real-world settings has, so far, shown less promise than the original randomized trials might have indicated [4]. Although there is ongoing work to try to improve results and uptake in community-based lifestyle intervention programs, for many patients and clinicians these resource-intensive programs currently prove difficult to do well on a large scale.
Alternative methods of helping patients achieve and maintain that critical > 5% weight loss are desperately needed, not only for preventing diabetes, but also for impacting the numerous other risks associated with obesity. This particular trial capitalized on the notion that it is probably successful weight loss, not the intervention format used to achieve that weight loss, which drives decreased diabetes risk. This study was a sub-analysis of a larger randomized trial, and many of the strengths of that larger study are therefore reflected in this paper. Participants and study staff were blinded to treatment arm with the use of placebo, a very important strength when adverse reactions and drug intolerances need to be measured. Furthermore, this likely equalized motivation to comply with the lifestyle recommendations across the treatment arms—this might not have been the case if patients were aware that they were or were not receiving study drug. Another key strength of the study is its duration. PHEN/TPM ER is unique in that it is approved by the FDA for long-term use. Whereas many studies of weight loss show maximum intervention effect at about 6 months followed by weight regain, this study showed sustained weight loss up to 2 years after starting therapy, presumably because participants could actually continue the therapy for the full 2 years. Most importantly, the intervention itself (medication plus low-intensity lifestyle counseling) is likely highly replicable in clinical practice.
There are some important limitations to consider when interpreting the results from this study. First, the participants analyzed in this paper were comprised entirely of people who had already participated in a full year of the parent study and therefore probably represent a sub-group that might have been experiencing greater success as a result of their participation, potentially generating an overly optimistic estimate of weight loss and health effect for all of the groups relative to what might be seen in a general population. This feature of the design also limits this study’s ability to comment on drug intolerance or early adverse reactions—those who didn’t stick with the pills for at least a year would not have been included in these analyses. In terms of generalizability, although the infrastructure required from a clinical standpoint is much lower for an intervention like this (prescribing a medication) compared to an intensive lifestyle intervention, these drugs are still costly, and many insurers/providers may not offer them on formulary. Thus, to realize the long-term benefits of sustained weight loss, patients may need to face significant out-of-pocket costs, which may limit uptake of this therapy to those with financial means. For this and other reasons, it will be important to do future studies looking at how quickly weight is re-gained once people stop taking the medication. Another threat to generalizability is the racial makeup of the participants—the vast majority of them were non-Hispanic white. Furthermore, although a majority of the participants had hypertension, it was well-controlled in all (a prerequisite for taking the medication), and it is unclear whether in a real-world patient population hypertension would be adequately controlled in a large number of patients.
Another issue to consider when looking at the use of weight loss medications for prevention of diabetes is the relative risk of prolonged medication use compared with the risk for developing diabetes. Clearly, for obese patients who are interested in losing weight for other reasons, prevention of diabetes is a wonderful side effect of achieving that goal. However, it is worth noting that even in the highest-risk group of participants in this study (those who lost < 5% of weight), the annualized risk of developing diabetes was about 6% (< 20% cumulative risk projected over 3 years). Compare this to the 7% to 8% serious adverse event rate observed in those on drug therapy. Although the medication did reduce annualized diabetes risk significantly, the vast majority of people in all the arms did not develop diabetes during follow-up. This drives home the point that our current categorization of pre-diabetes is far from perfect in identifying people who are at imminent risk of becoming diabetic, and reinforces the notion that any treatment we provide to them in the name of diabetes prevention should be free from risk of harm. Rather than applying a long-term medication with potentially harmful side effects to a large group of at-risk patients, more research is needed to provide tools for clinicians to think carefully about which of their patients are truly at highest risk of going on to develop diabetes in the near future.
Applications for Clinical Practice
Although clinicians ought not use PHEN/TPM ER exclusively for diabetes prevention based on the results from this trial, delay of diabetes onset is a possible and important benefit of the use of PHEN/TPM ER in obese patients, provided that they are willing to also make and sustain lifestyle changes in order to lose a clinically significant amount of weight.
—Kristina Lewis, MD, MPH
1. Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012;308:2489-96.
2. Arterburn DE, O’Connor PJ. A look ahead at the future of diabetes prevention and treatment. JAMA 2012;308:2517–8.
3. Yudkin JS, Montori VM. The epidemic of pre-diabetes: the medicine and the politics. BMJ. 2014;349:g4485.
4. Kahn R, Davidson MB. The reality of type 2 diabetes prevention. Diabetes care 2014;37:943-9.
5. Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–86.
Study Overview
Objective. To determine the effect of phentermine and topiramate extended release (PHEN/TPM ER) treatment on progression to type 2 diabetes and/or cardiometabolic disease in subjects with prediabetes and/or metabolic syndrome (MetS) at baseline.
Design. Sub-group analysis of a larger double-blind, randomized, placebo-controlled trial of PHEN/TPM ER in overweight and obese adults.
Setting and participants. The larger study had 2 phases —a 56-week weight loss trial (CONQUER, n = 866), followed by an extension of the drug trial out to 108 weeks (SEQUEL, n = 675) in a sub-group of CONQUER participants. The CONQUER trial, based at 93 U.S. centers, enrolled overweight or obese patients with at least 2 obesity-related comorbidities and randomly assigned them to receive either placebo or PHEN/TPM ER at a lower (7.5 mg/46 mg) or higher (15 mg/92 mg) daily dose. All 3 groups also received lifestyle modification counseling that included an evidence-based diet and exercise curriculum. Participants received study drug and lifestyle counseling in the setting of monthly visits during the 60- (CONQUER) or 108-week (SEQUEL) follow-up period.
The analyses presented in this paper focus on the 475 participants who completed both CONQUER and SEQUEL and who were characterized as pre-diabetic or as having the metabolic syndrome (MetS) at baseline. Pre-diabetes was defined as having a blood glucose level of 100–125 mg/dL or higher while fasting, or 140–199 mg/dL after an oral glucose tolerance test (GTT). MetS was characterized in participants who displayed 3 or more of the following at baseline: waist circumference ≥ 102 cm in men or 88 cm in women; triglycerides ≥ 150 mg/dL or on a lipid-lowering medication; HDL < 40 mg/dL in men or < 50 mg/dL in women; systolic BP ≥ 130 mm Hg or diastolic BP ≥ 85 mm Hg (or on antihypertensive); and fasting glucose ≥ 100 mg/dL or on treatment for elevated glucose.
Main outcome measures. The primary outcome for this study was percent weight loss at 108 weeks of follow-up (or early termination). Secondary outcomes included cardiometabolic changes, such as development of type 2 diabetes and changes in lipid measures, blood pressure, and waist circumference. These were assessed at baseline, week 56, and week 108 (or at early termination). Rates of progression to type 2 diabetes were compared between the treatment groups using chi-square testing. Intention-to-treat (ITT) ANCOVA analysis was performed with multiple imputation techniques to address missing data, as well as with an alternative analysis using last observation carried forward.
Results. The study arms were similar with respect to baseline characteristics. Average age was 51 years in the high dose PHEN/TPM ER arm and 52 in the other arms. Over half (65%) of participants were women and 86% were Caucasian. Mean BMI was 36 kg/m2 (class II obesity). Over half of participants were on antihypertensive medications at baseline but with well-controlled blood pressure (mean 128/80 mm Hg). Of the 475 people in this analysis, 316 met criteria for prediabetes, 451 for MetS, and 292 for both prediabetes and MetS.
Weight loss at 2 years was significantly greater in subjects taking PHEN/TPM ER (10.9% in the lower dose group, 12.1% in the higher dose group) compared to those taking placebo (2.5%) (P < 0.001). Mirroring weight loss results, type 2 diabetes incidence was also significantly lower in the drug treatment arms than in the placebo arm at 2 years after randomization—annualized incidence was 6.1% for placebo vs. 1.8% for lower-dose drug and 1.3% for higher-dose drug (P < 0.05). Greater weight loss was associated with greater decrease in diabetes incidence across all 3 arms of the study. Those persons who did not achieve at least a 5% weight loss at 2 years had the highest annualized risk of developing diabetes (6.3%), compared with a 0.9% risk among those who lost at least 15% of their weight. Improvements in other cardiometabolic parameters, including HDL, triglycerides, waist circumference, and insulin sensitivity index, was more common among the PHEN/TPM ER participants compared with placebo. Blood pressure decreased slightly for all 3 groups and there was no significant difference between the drug arms and the placebo arm.
Discontinuation of study medication occurred in all 3 groups (3.1% in placebo, 6.1% in lower-dose medication, and 5.5% in higher-dose medication), with serious adverse events in 5%, 7%, and 8.5%, respectively. There were no deaths.
Conclusion. PHEN/TPM ER administered over a 2-year period significantly improved weight loss and decreased progression to type 2 diabetes relative to placebo in a group of at-risk participants.
Commentary
Diabetes and related cardiometabolic disease are major contributors to morbidity and mortality in adults. With the exception of invasive treatments such as bariatric surgery, reversal of diabetes once it is established has proven quite difficult [1,2], and thus there is an increased emphasis from the public health and medical communities on preventing the development of this disease in the first place. Complicating the picture, recently broadened criteria for pre-diabetes will likely result in a very large number of these at-risk individuals being identified [3,4]. Although intensive lifestyle interventions resulting in a 5% to 7% weight loss among pre-diabetics have been shown to delay progression to diabetes [5], the translation of these programs into real-world settings has, so far, shown less promise than the original randomized trials might have indicated [4]. Although there is ongoing work to try to improve results and uptake in community-based lifestyle intervention programs, for many patients and clinicians these resource-intensive programs currently prove difficult to do well on a large scale.
Alternative methods of helping patients achieve and maintain that critical > 5% weight loss are desperately needed, not only for preventing diabetes, but also for impacting the numerous other risks associated with obesity. This particular trial capitalized on the notion that it is probably successful weight loss, not the intervention format used to achieve that weight loss, which drives decreased diabetes risk. This study was a sub-analysis of a larger randomized trial, and many of the strengths of that larger study are therefore reflected in this paper. Participants and study staff were blinded to treatment arm with the use of placebo, a very important strength when adverse reactions and drug intolerances need to be measured. Furthermore, this likely equalized motivation to comply with the lifestyle recommendations across the treatment arms—this might not have been the case if patients were aware that they were or were not receiving study drug. Another key strength of the study is its duration. PHEN/TPM ER is unique in that it is approved by the FDA for long-term use. Whereas many studies of weight loss show maximum intervention effect at about 6 months followed by weight regain, this study showed sustained weight loss up to 2 years after starting therapy, presumably because participants could actually continue the therapy for the full 2 years. Most importantly, the intervention itself (medication plus low-intensity lifestyle counseling) is likely highly replicable in clinical practice.
There are some important limitations to consider when interpreting the results from this study. First, the participants analyzed in this paper were comprised entirely of people who had already participated in a full year of the parent study and therefore probably represent a sub-group that might have been experiencing greater success as a result of their participation, potentially generating an overly optimistic estimate of weight loss and health effect for all of the groups relative to what might be seen in a general population. This feature of the design also limits this study’s ability to comment on drug intolerance or early adverse reactions—those who didn’t stick with the pills for at least a year would not have been included in these analyses. In terms of generalizability, although the infrastructure required from a clinical standpoint is much lower for an intervention like this (prescribing a medication) compared to an intensive lifestyle intervention, these drugs are still costly, and many insurers/providers may not offer them on formulary. Thus, to realize the long-term benefits of sustained weight loss, patients may need to face significant out-of-pocket costs, which may limit uptake of this therapy to those with financial means. For this and other reasons, it will be important to do future studies looking at how quickly weight is re-gained once people stop taking the medication. Another threat to generalizability is the racial makeup of the participants—the vast majority of them were non-Hispanic white. Furthermore, although a majority of the participants had hypertension, it was well-controlled in all (a prerequisite for taking the medication), and it is unclear whether in a real-world patient population hypertension would be adequately controlled in a large number of patients.
Another issue to consider when looking at the use of weight loss medications for prevention of diabetes is the relative risk of prolonged medication use compared with the risk for developing diabetes. Clearly, for obese patients who are interested in losing weight for other reasons, prevention of diabetes is a wonderful side effect of achieving that goal. However, it is worth noting that even in the highest-risk group of participants in this study (those who lost < 5% of weight), the annualized risk of developing diabetes was about 6% (< 20% cumulative risk projected over 3 years). Compare this to the 7% to 8% serious adverse event rate observed in those on drug therapy. Although the medication did reduce annualized diabetes risk significantly, the vast majority of people in all the arms did not develop diabetes during follow-up. This drives home the point that our current categorization of pre-diabetes is far from perfect in identifying people who are at imminent risk of becoming diabetic, and reinforces the notion that any treatment we provide to them in the name of diabetes prevention should be free from risk of harm. Rather than applying a long-term medication with potentially harmful side effects to a large group of at-risk patients, more research is needed to provide tools for clinicians to think carefully about which of their patients are truly at highest risk of going on to develop diabetes in the near future.
Applications for Clinical Practice
Although clinicians ought not use PHEN/TPM ER exclusively for diabetes prevention based on the results from this trial, delay of diabetes onset is a possible and important benefit of the use of PHEN/TPM ER in obese patients, provided that they are willing to also make and sustain lifestyle changes in order to lose a clinically significant amount of weight.
—Kristina Lewis, MD, MPH
Study Overview
Objective. To determine the effect of phentermine and topiramate extended release (PHEN/TPM ER) treatment on progression to type 2 diabetes and/or cardiometabolic disease in subjects with prediabetes and/or metabolic syndrome (MetS) at baseline.
Design. Sub-group analysis of a larger double-blind, randomized, placebo-controlled trial of PHEN/TPM ER in overweight and obese adults.
Setting and participants. The larger study had 2 phases —a 56-week weight loss trial (CONQUER, n = 866), followed by an extension of the drug trial out to 108 weeks (SEQUEL, n = 675) in a sub-group of CONQUER participants. The CONQUER trial, based at 93 U.S. centers, enrolled overweight or obese patients with at least 2 obesity-related comorbidities and randomly assigned them to receive either placebo or PHEN/TPM ER at a lower (7.5 mg/46 mg) or higher (15 mg/92 mg) daily dose. All 3 groups also received lifestyle modification counseling that included an evidence-based diet and exercise curriculum. Participants received study drug and lifestyle counseling in the setting of monthly visits during the 60- (CONQUER) or 108-week (SEQUEL) follow-up period.
The analyses presented in this paper focus on the 475 participants who completed both CONQUER and SEQUEL and who were characterized as pre-diabetic or as having the metabolic syndrome (MetS) at baseline. Pre-diabetes was defined as having a blood glucose level of 100–125 mg/dL or higher while fasting, or 140–199 mg/dL after an oral glucose tolerance test (GTT). MetS was characterized in participants who displayed 3 or more of the following at baseline: waist circumference ≥ 102 cm in men or 88 cm in women; triglycerides ≥ 150 mg/dL or on a lipid-lowering medication; HDL < 40 mg/dL in men or < 50 mg/dL in women; systolic BP ≥ 130 mm Hg or diastolic BP ≥ 85 mm Hg (or on antihypertensive); and fasting glucose ≥ 100 mg/dL or on treatment for elevated glucose.
Main outcome measures. The primary outcome for this study was percent weight loss at 108 weeks of follow-up (or early termination). Secondary outcomes included cardiometabolic changes, such as development of type 2 diabetes and changes in lipid measures, blood pressure, and waist circumference. These were assessed at baseline, week 56, and week 108 (or at early termination). Rates of progression to type 2 diabetes were compared between the treatment groups using chi-square testing. Intention-to-treat (ITT) ANCOVA analysis was performed with multiple imputation techniques to address missing data, as well as with an alternative analysis using last observation carried forward.
Results. The study arms were similar with respect to baseline characteristics. Average age was 51 years in the high dose PHEN/TPM ER arm and 52 in the other arms. Over half (65%) of participants were women and 86% were Caucasian. Mean BMI was 36 kg/m2 (class II obesity). Over half of participants were on antihypertensive medications at baseline but with well-controlled blood pressure (mean 128/80 mm Hg). Of the 475 people in this analysis, 316 met criteria for prediabetes, 451 for MetS, and 292 for both prediabetes and MetS.
Weight loss at 2 years was significantly greater in subjects taking PHEN/TPM ER (10.9% in the lower dose group, 12.1% in the higher dose group) compared to those taking placebo (2.5%) (P < 0.001). Mirroring weight loss results, type 2 diabetes incidence was also significantly lower in the drug treatment arms than in the placebo arm at 2 years after randomization—annualized incidence was 6.1% for placebo vs. 1.8% for lower-dose drug and 1.3% for higher-dose drug (P < 0.05). Greater weight loss was associated with greater decrease in diabetes incidence across all 3 arms of the study. Those persons who did not achieve at least a 5% weight loss at 2 years had the highest annualized risk of developing diabetes (6.3%), compared with a 0.9% risk among those who lost at least 15% of their weight. Improvements in other cardiometabolic parameters, including HDL, triglycerides, waist circumference, and insulin sensitivity index, was more common among the PHEN/TPM ER participants compared with placebo. Blood pressure decreased slightly for all 3 groups and there was no significant difference between the drug arms and the placebo arm.
Discontinuation of study medication occurred in all 3 groups (3.1% in placebo, 6.1% in lower-dose medication, and 5.5% in higher-dose medication), with serious adverse events in 5%, 7%, and 8.5%, respectively. There were no deaths.
Conclusion. PHEN/TPM ER administered over a 2-year period significantly improved weight loss and decreased progression to type 2 diabetes relative to placebo in a group of at-risk participants.
Commentary
Diabetes and related cardiometabolic disease are major contributors to morbidity and mortality in adults. With the exception of invasive treatments such as bariatric surgery, reversal of diabetes once it is established has proven quite difficult [1,2], and thus there is an increased emphasis from the public health and medical communities on preventing the development of this disease in the first place. Complicating the picture, recently broadened criteria for pre-diabetes will likely result in a very large number of these at-risk individuals being identified [3,4]. Although intensive lifestyle interventions resulting in a 5% to 7% weight loss among pre-diabetics have been shown to delay progression to diabetes [5], the translation of these programs into real-world settings has, so far, shown less promise than the original randomized trials might have indicated [4]. Although there is ongoing work to try to improve results and uptake in community-based lifestyle intervention programs, for many patients and clinicians these resource-intensive programs currently prove difficult to do well on a large scale.
Alternative methods of helping patients achieve and maintain that critical > 5% weight loss are desperately needed, not only for preventing diabetes, but also for impacting the numerous other risks associated with obesity. This particular trial capitalized on the notion that it is probably successful weight loss, not the intervention format used to achieve that weight loss, which drives decreased diabetes risk. This study was a sub-analysis of a larger randomized trial, and many of the strengths of that larger study are therefore reflected in this paper. Participants and study staff were blinded to treatment arm with the use of placebo, a very important strength when adverse reactions and drug intolerances need to be measured. Furthermore, this likely equalized motivation to comply with the lifestyle recommendations across the treatment arms—this might not have been the case if patients were aware that they were or were not receiving study drug. Another key strength of the study is its duration. PHEN/TPM ER is unique in that it is approved by the FDA for long-term use. Whereas many studies of weight loss show maximum intervention effect at about 6 months followed by weight regain, this study showed sustained weight loss up to 2 years after starting therapy, presumably because participants could actually continue the therapy for the full 2 years. Most importantly, the intervention itself (medication plus low-intensity lifestyle counseling) is likely highly replicable in clinical practice.
There are some important limitations to consider when interpreting the results from this study. First, the participants analyzed in this paper were comprised entirely of people who had already participated in a full year of the parent study and therefore probably represent a sub-group that might have been experiencing greater success as a result of their participation, potentially generating an overly optimistic estimate of weight loss and health effect for all of the groups relative to what might be seen in a general population. This feature of the design also limits this study’s ability to comment on drug intolerance or early adverse reactions—those who didn’t stick with the pills for at least a year would not have been included in these analyses. In terms of generalizability, although the infrastructure required from a clinical standpoint is much lower for an intervention like this (prescribing a medication) compared to an intensive lifestyle intervention, these drugs are still costly, and many insurers/providers may not offer them on formulary. Thus, to realize the long-term benefits of sustained weight loss, patients may need to face significant out-of-pocket costs, which may limit uptake of this therapy to those with financial means. For this and other reasons, it will be important to do future studies looking at how quickly weight is re-gained once people stop taking the medication. Another threat to generalizability is the racial makeup of the participants—the vast majority of them were non-Hispanic white. Furthermore, although a majority of the participants had hypertension, it was well-controlled in all (a prerequisite for taking the medication), and it is unclear whether in a real-world patient population hypertension would be adequately controlled in a large number of patients.
Another issue to consider when looking at the use of weight loss medications for prevention of diabetes is the relative risk of prolonged medication use compared with the risk for developing diabetes. Clearly, for obese patients who are interested in losing weight for other reasons, prevention of diabetes is a wonderful side effect of achieving that goal. However, it is worth noting that even in the highest-risk group of participants in this study (those who lost < 5% of weight), the annualized risk of developing diabetes was about 6% (< 20% cumulative risk projected over 3 years). Compare this to the 7% to 8% serious adverse event rate observed in those on drug therapy. Although the medication did reduce annualized diabetes risk significantly, the vast majority of people in all the arms did not develop diabetes during follow-up. This drives home the point that our current categorization of pre-diabetes is far from perfect in identifying people who are at imminent risk of becoming diabetic, and reinforces the notion that any treatment we provide to them in the name of diabetes prevention should be free from risk of harm. Rather than applying a long-term medication with potentially harmful side effects to a large group of at-risk patients, more research is needed to provide tools for clinicians to think carefully about which of their patients are truly at highest risk of going on to develop diabetes in the near future.
Applications for Clinical Practice
Although clinicians ought not use PHEN/TPM ER exclusively for diabetes prevention based on the results from this trial, delay of diabetes onset is a possible and important benefit of the use of PHEN/TPM ER in obese patients, provided that they are willing to also make and sustain lifestyle changes in order to lose a clinically significant amount of weight.
—Kristina Lewis, MD, MPH
1. Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012;308:2489-96.
2. Arterburn DE, O’Connor PJ. A look ahead at the future of diabetes prevention and treatment. JAMA 2012;308:2517–8.
3. Yudkin JS, Montori VM. The epidemic of pre-diabetes: the medicine and the politics. BMJ. 2014;349:g4485.
4. Kahn R, Davidson MB. The reality of type 2 diabetes prevention. Diabetes care 2014;37:943-9.
5. Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–86.
1. Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012;308:2489-96.
2. Arterburn DE, O’Connor PJ. A look ahead at the future of diabetes prevention and treatment. JAMA 2012;308:2517–8.
3. Yudkin JS, Montori VM. The epidemic of pre-diabetes: the medicine and the politics. BMJ. 2014;349:g4485.
4. Kahn R, Davidson MB. The reality of type 2 diabetes prevention. Diabetes care 2014;37:943-9.
5. Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–86.




