User login
NASH on the rise as a cause of liver transplants
Since 2004, there’s been almost a tripling of the number of nonalcoholic steatohepatitis patients waiting for liver transplants; the condition is now the second leading reason to be put on the waiting list in the United States, according to a study published in the March issue of Gastroenterology.*
Even so and for reasons that are not fully clear, adults with nonalcoholic steatohepatitis (NASH) are less likely to survive for 90 days on the wait list than are patients with alcoholic liver disease (ALD), and less likely to get a new liver within 90 days than are patients with ALD, hepatitis C virus (HCV), or a blend of both. For now, HCV remains the No. 1 reason for liver transplants in the United States (Gastroenterology 2014 Nov. 24 [doi: 10.1053/j.gastro.2014.11.039]).
“Our study provides valuable information about the changing epidemiology of chronic liver disease among wait-listed patients, and adds greatly to our understanding of the epidemiology of NASH in the United States,” the researchers wrote. The rapid rise in the prevalence of NASH is “a direct consequence of the worldwide obesity epidemic” as well as greater awareness of the condition. An expected decline in HCV-related cirrhosis due to effective antiviral therapy “will further contribute to the changing epidemiology of patients awaiting liver transplants in the United States,” said the authors, led by Dr. Robert Wong of the division of gastroenterology and hepatology at Highland Hospital, Oakland, Calif.
“Given the expected continued rise in the number of NASH patients awaiting liver transplant, additional research is needed to improve wait-list survival and ... outcomes among this cohort. In addition, the projection that overall donor availability will significantly diminish in the next 15-20 years emphasizes the need for additional research to improve liver transplant opportunities for NASH patients, including the option of living donor[s],” they said.
The researchers analyzed data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174; those with ALD increased by 45% from 1,400 to 2,024; and those with HCV increased by 14% from 2,887 to 3,291. Registrants with both HCV and ALD decreased by 9% from 880 to 803. NASH became the second-leading disease among liver transplant wait-list registrants in 2013.
Patients with ALD had a significantly higher Model for End-Stage Liver Disease (MELD) score at the time of registration than did others. However, after adjustment for MELD and other variables, patients with ALD were less likely to die within 90 days than were NASH patients (OR 0.77; 95% CI 0.67–0.89; P < .001). No difference was seen in wait-list mortality between NASH and HCV and HCV/ALD patients.
Compared with NASH, patients with HCV (OR 1.45; 95% CI 1.35–1.55; P < .001), ALD (OR 1.15; 95% CI: 1.06–1.24; P < .001), and HCV/ALD (OR 1.29; 95% CI 1.18–1.42; P < .001) were all significantly more likely to receive a liver after 3 months on the wait list.
A “potential explanation for these observations might be etiology-specific differences in disease progression, such that more aggressive etiologies (e.g., HCV or HCV/ALD) can have a more rapid rise in MELD score, receive liver transplant, and have lower wait-list mortality, and etiologies with less rapid progression (e.g., NASH) can have slower rise in MELD score over time, lower rates of LT, but no significant increase in wait-list mortality,” the investigators said.
Overall 1-year wait-list survival among NASH patients decreased from 42.8% in 2004-2008 to 25.6% in 2009-2013, and overall 1-year probability of receiving liver transplant among NASH patients also decreased from 42.1% in 2004-2008 to 39.6% in 2009-2013. The trends were similar for other etiologies, perhaps in part because there are more people waiting for a liver.
The authors said they have no financial conflicts to disclose.
*A change was made to the text on 3/12/2015.
Since 2004, there’s been almost a tripling of the number of nonalcoholic steatohepatitis patients waiting for liver transplants; the condition is now the second leading reason to be put on the waiting list in the United States, according to a study published in the March issue of Gastroenterology.*
Even so and for reasons that are not fully clear, adults with nonalcoholic steatohepatitis (NASH) are less likely to survive for 90 days on the wait list than are patients with alcoholic liver disease (ALD), and less likely to get a new liver within 90 days than are patients with ALD, hepatitis C virus (HCV), or a blend of both. For now, HCV remains the No. 1 reason for liver transplants in the United States (Gastroenterology 2014 Nov. 24 [doi: 10.1053/j.gastro.2014.11.039]).
“Our study provides valuable information about the changing epidemiology of chronic liver disease among wait-listed patients, and adds greatly to our understanding of the epidemiology of NASH in the United States,” the researchers wrote. The rapid rise in the prevalence of NASH is “a direct consequence of the worldwide obesity epidemic” as well as greater awareness of the condition. An expected decline in HCV-related cirrhosis due to effective antiviral therapy “will further contribute to the changing epidemiology of patients awaiting liver transplants in the United States,” said the authors, led by Dr. Robert Wong of the division of gastroenterology and hepatology at Highland Hospital, Oakland, Calif.
“Given the expected continued rise in the number of NASH patients awaiting liver transplant, additional research is needed to improve wait-list survival and ... outcomes among this cohort. In addition, the projection that overall donor availability will significantly diminish in the next 15-20 years emphasizes the need for additional research to improve liver transplant opportunities for NASH patients, including the option of living donor[s],” they said.
The researchers analyzed data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174; those with ALD increased by 45% from 1,400 to 2,024; and those with HCV increased by 14% from 2,887 to 3,291. Registrants with both HCV and ALD decreased by 9% from 880 to 803. NASH became the second-leading disease among liver transplant wait-list registrants in 2013.
Patients with ALD had a significantly higher Model for End-Stage Liver Disease (MELD) score at the time of registration than did others. However, after adjustment for MELD and other variables, patients with ALD were less likely to die within 90 days than were NASH patients (OR 0.77; 95% CI 0.67–0.89; P < .001). No difference was seen in wait-list mortality between NASH and HCV and HCV/ALD patients.
Compared with NASH, patients with HCV (OR 1.45; 95% CI 1.35–1.55; P < .001), ALD (OR 1.15; 95% CI: 1.06–1.24; P < .001), and HCV/ALD (OR 1.29; 95% CI 1.18–1.42; P < .001) were all significantly more likely to receive a liver after 3 months on the wait list.
A “potential explanation for these observations might be etiology-specific differences in disease progression, such that more aggressive etiologies (e.g., HCV or HCV/ALD) can have a more rapid rise in MELD score, receive liver transplant, and have lower wait-list mortality, and etiologies with less rapid progression (e.g., NASH) can have slower rise in MELD score over time, lower rates of LT, but no significant increase in wait-list mortality,” the investigators said.
Overall 1-year wait-list survival among NASH patients decreased from 42.8% in 2004-2008 to 25.6% in 2009-2013, and overall 1-year probability of receiving liver transplant among NASH patients also decreased from 42.1% in 2004-2008 to 39.6% in 2009-2013. The trends were similar for other etiologies, perhaps in part because there are more people waiting for a liver.
The authors said they have no financial conflicts to disclose.
*A change was made to the text on 3/12/2015.
Since 2004, there’s been almost a tripling of the number of nonalcoholic steatohepatitis patients waiting for liver transplants; the condition is now the second leading reason to be put on the waiting list in the United States, according to a study published in the March issue of Gastroenterology.*
Even so and for reasons that are not fully clear, adults with nonalcoholic steatohepatitis (NASH) are less likely to survive for 90 days on the wait list than are patients with alcoholic liver disease (ALD), and less likely to get a new liver within 90 days than are patients with ALD, hepatitis C virus (HCV), or a blend of both. For now, HCV remains the No. 1 reason for liver transplants in the United States (Gastroenterology 2014 Nov. 24 [doi: 10.1053/j.gastro.2014.11.039]).
“Our study provides valuable information about the changing epidemiology of chronic liver disease among wait-listed patients, and adds greatly to our understanding of the epidemiology of NASH in the United States,” the researchers wrote. The rapid rise in the prevalence of NASH is “a direct consequence of the worldwide obesity epidemic” as well as greater awareness of the condition. An expected decline in HCV-related cirrhosis due to effective antiviral therapy “will further contribute to the changing epidemiology of patients awaiting liver transplants in the United States,” said the authors, led by Dr. Robert Wong of the division of gastroenterology and hepatology at Highland Hospital, Oakland, Calif.
“Given the expected continued rise in the number of NASH patients awaiting liver transplant, additional research is needed to improve wait-list survival and ... outcomes among this cohort. In addition, the projection that overall donor availability will significantly diminish in the next 15-20 years emphasizes the need for additional research to improve liver transplant opportunities for NASH patients, including the option of living donor[s],” they said.
The researchers analyzed data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174; those with ALD increased by 45% from 1,400 to 2,024; and those with HCV increased by 14% from 2,887 to 3,291. Registrants with both HCV and ALD decreased by 9% from 880 to 803. NASH became the second-leading disease among liver transplant wait-list registrants in 2013.
Patients with ALD had a significantly higher Model for End-Stage Liver Disease (MELD) score at the time of registration than did others. However, after adjustment for MELD and other variables, patients with ALD were less likely to die within 90 days than were NASH patients (OR 0.77; 95% CI 0.67–0.89; P < .001). No difference was seen in wait-list mortality between NASH and HCV and HCV/ALD patients.
Compared with NASH, patients with HCV (OR 1.45; 95% CI 1.35–1.55; P < .001), ALD (OR 1.15; 95% CI: 1.06–1.24; P < .001), and HCV/ALD (OR 1.29; 95% CI 1.18–1.42; P < .001) were all significantly more likely to receive a liver after 3 months on the wait list.
A “potential explanation for these observations might be etiology-specific differences in disease progression, such that more aggressive etiologies (e.g., HCV or HCV/ALD) can have a more rapid rise in MELD score, receive liver transplant, and have lower wait-list mortality, and etiologies with less rapid progression (e.g., NASH) can have slower rise in MELD score over time, lower rates of LT, but no significant increase in wait-list mortality,” the investigators said.
Overall 1-year wait-list survival among NASH patients decreased from 42.8% in 2004-2008 to 25.6% in 2009-2013, and overall 1-year probability of receiving liver transplant among NASH patients also decreased from 42.1% in 2004-2008 to 39.6% in 2009-2013. The trends were similar for other etiologies, perhaps in part because there are more people waiting for a liver.
The authors said they have no financial conflicts to disclose.
*A change was made to the text on 3/12/2015.
FROM GASTROENTEROLOGY
Key clinical point: As the epidemiology of liver transplantation changes in the United States, more needs to be done to ensure good outcomes in NASH patients.
Major finding: From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174.
Data source: The United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
Disclosures: The authors said they have no relevant disclosures.
LISTEN NOW: SHM Launches a Patient Experience Committee
Advance Care Planning Among Patients with Heart Failure: A Review of Challenges and Approaches to Better Communication
From the Rand Corporation and UCLA Fielding School of Public Health, Santa Monica, CA (Dr. Ahluwalia) and University of Southern California, Leonard Davis School of Gerontology, Los Angeles, CA (Dr. Enguidanos).
Abstract
- Objective: To review the relevance of advance care planning to heart failure management, describe key advance care planning challenges, and provide clinicians with actionable guidance for engaging in advance care planning conversations.
- Methods: Review of the literature.
- Results: Although most patients with heart failure prefer to receive thorough and honest information about their health condition and prognosis, the unpredictability of the heart failure trajectory coupled with physician barriers including discomfort with emotionally-laden topics and difficulty identifying the “right” time to engage in advance care planning, and systems barriers such as inadequate clinic time and limited reimbursement, impede timely engagement in advance care planning discussions. Approaches to effective advance care planning communication include using open-ended questions to stimulate patient engagement, evaluating how much information the patient wants to ensure patient-centeredness, and using empathic language to demonstrate support and understanding. While successful models of advance care planning communication have been identified, replication is limited due to the resource intense nature of these approaches.
- Conclusion: Challenges to advance care planning discussions among patients with heart failure may be mitigated through the establishment of communication quality standards as well as guidelines promoting early and ongoing advance care planning discussions, as well as reimbursement for outpatient discussions.
Heart failure, a leading cause of death, disability, and health care costs in the United States, is an incurable and life-limiting illness that is becoming increasingly prevalent due to an aging population and improved life expectancy. Approximately 5.3 million Americans are currently living with heart failure [1], with more than 550,000 new cases diagnosed each year [2]. Heart failure disproportionately affects older adults; about 80% of all cases occur in persons aged 65 years or older [3], and heart failure is the leading cause of hospital admissions among older adults [4]. The burden and impact of heart failure peaks near the end of life; 80% of Medicare beneficiaries with heart failure are hospitalized in the last 6 months of life [5].
The Trajectory of Heart Failure
Patients with heart failure experience a highly variable, nonlinear clinical trajectory marked by progressive deterioration and frequent exacerbations requiring hospitalization [6]. Their prognosis, though uncertain, is poor, with reported 1-year mortality rates following a hospitalization between 30% and 50% and 5-year mortality as high as 75% [7–11], a survival rate worse than that of some cancers [12]. Patients with heart failure caused by ischemic heart disease are at high risk for sudden cardiac death, particularly at earlier stages of the disease, which can confound the ability to appropriately plan for the future [13]. Those who survive to more advanced stages of heart failure face worsening quality of life [14–16], driven by a high prevalence of fatigue, breathlessness, pain, and depression [17–24]. Indeed, patients with heart failure have a similar symptom burden to patients with advanced cancer [25]. Older adults with heart failure also have a high comorbidity burden that further complicates both symptomology and disease trajectory with implications for decision-making about life-prolonging heart failure therapies [26,27].
Advance Care Planning in Heart Failure
The unpredictable nature of heart failure makes it difficult for patients and families to plan and prepare for their future, yet it is this very uncertainty that makes advance care planning (ACP) so critical for heart failure patients. Clear and honest patient-clinician communication about ACP, including an exploration of patient values and goals for care in the context of prognostic information, is essential to patient-centered treatment decision-making [28]. This is particularly relevant in heart failure, where a range of high-intensity, invasive, and costly interventions are increasingly being applied (eg, ventricular assist devices) without equivalent attention to quality of life and patients’ long-term goals for care.
Patients with heart failure and their families face multiple complex treatment decisions along the trajectory of their illness, such as discontinuation of beta blockers among patients with refractory fluid overload or angiotensin-converting enzyme inhibitors in end-stage patients with symptomatic hypotension [29,30]. In end-stage heart failure patients, deactivation of an implantable cardiac defibrillator might be considered to avoid the pain and distress associated with repeated shocks. In contrast, other interventions such as cardiac resynchronization therapy and continuous inotropic infusion have quality of life benefits; continuation of these therapies may be appropriate even when discontinuing other interventions. Such decisions should be guided by a thorough understanding of the patient’s expressed preferences and values, ideally assessed early in the trajectory of the disease and continuously re-evaluated as the diseases progresses.
The American Heart Association supports early and regular patient-provider ACP discussions to guide heart failure patients’ future decision-making [31], and recommends that such discussions be initiated in the outpatient setting, prior to and in anticipation of clinical decline. ACP communication plays a critical role in enhancing patients’ understanding of their diagnosis, treatment, prognosis, and choices in end-of-life care [31]. ACP communication also helps the clinician to better understand the context within which patients and their caregivers might make health care decisions, including their values and preferences for care. Patient-provider discussions about ACP focused on understanding patient values and initiated early in the trajectory of serious illness can support future in-the-moment decision-making, and is likely more effective than asking patients to make specific treatment decisions in advance [32]. A growing body of rigorous research has shown that ACP communication is associated with greater preference-concordant care and congruence in patient-surrogate understanding of patient preferences, lower costs, and less aggressive care at the end of life [33–37].
Patient Preferences for ACP Communication
Most patients with heart failure and their caregivers want honest disclosure regarding prognosis and to receive information about the expected trajectory of their disease [38–41] as early as possible [38] to help them plan and prepare for their future. Patients and their caregivers prefer to have these conversations with their physician [38] or other provider most familiar with the patient and family [39]. Patients also express a preference for support with dealing with the uncertainty inherent to heart failure [39]. Although most patients and caregivers desire to receive clear and honest communication about their disease, it is important to note that patients may vary in the extent of information they prefer to receive about their heart failure, with some individuals preferring not to talk about the end of life and future care needs at all [39,42–44].
Challenges to ACP Communication in Heart Failure
Despite patient and caregiver preferences for ACP communication with their providers, evidence suggests such communication occurs infrequently [40,45] and that heart failure patients may lack important information about their prognosis and treatment options [40,44,46,47]. For example, patients may not recognize the terminal nature of heart failure, and may be unaware of the range of treatment options, including hospice, available to them. Evidence also demonstrates that ACP is infrequently discussed with their health care providers [40], resulting in these conversations being avoided or deferred until an emergent clinical situation [44,48] when hasty questions about treatment choices may yield uncertain and conflicting answers not representative of a patient’s underlying values.
The infrequent, late, and often lack of discussions about ACP are driven by several challenges. First, the uncertain trajectory of heart failure makes communication regarding “what to expect” difficult. Prognostication is an immense challenge in heart failure [40,49–52], making it harder to talk about end-of-life issues and hindering the ability of patients, caregivers and health care providers to plan and prepare for the future. It is often difficult for clinicians, who face the challenge of instilling hope in the face of truthful disclosure [53], to identify the “right time” to initiate such discussions.
Second, a lack of time, particularly during outpatient visits, impedes physician ability to have considered discussions about future care needs and preferences [32,54]. The U.S. health care system currently lacks financial reimbursement for these discussions, which poses a significant barrier to the integration of ACP conversations into routine clinical practice. Moreover, these conversations are lengthy and iterative [53]. ACP discussions that are focused on facilitating patient-centered decision-making ideally begin with a discussion of expected prognosis, followed by an exploration of patient preferences and values for health care, and then a review of treatment options to be considered in the context of those preferences. Often additional time is needed for completing advance directive documents or for charting key outcomes from these discussions. Clinicians today are frequently overloaded with addressing multiple medical issues during outpatient visits that leave little time for non-medical tasks such as ACP discussions. The lack of financial incentives to support in-depth discussions is a critical challenge in improving ACP.
Third, a lack of training in specialized communication skills, particularly focused on empathic and emotionally sensitive disclosure, may further hinder physicians from initiating frank discussions with their patients. ACP conversations are highly sensitive and fraught with emotional complexity, and clinicians understandably experience discomfort with breaking bad news [49,51,55] or with broader issues of decline and death [51,56,57]. Physicians tend to be most comfortable addressing cognitive aspects of communication; addressing the emotional needs of patients is harder. Medical school training teaches detachment in physician practice, perhaps as a way of coping with the sadness they regularly confront and in maintaining their ability to provide clinical care. In fact, physicians describe their most difficult encounters as those with the most negative expressed emotions and miss opportunities to respond with empathy [58–60], a critical skill in effective patient-physician communication that is associated with improved patient satisfaction [61,62]. While patients value good communication skills in their health care encounters, many providers feel they lack the necessary skills to lead effective ACP discussions [49,63].
Finally, information gaps with regards to heart failure contribute to delayed or absent conversations about planning for future care. Many heart failure patients have a limited understanding of their disease [32,40,44,55], particularly an inaccurate perception that heart failure is not a terminal and life-limiting illness [42,49,64]. Compounding this is the fact that even some health care providers are reluctant to acknowledge the terminal nature of heart failure [50,56]. Without frank acknowledgement of the terminal nature of heart failure, the initiation of discussions regarding end-of-life care will remain difficult if not impossible.
Approaches to ACP in Heart Failure
When Is the Right Time?
Given the complexity and unpredictable trajectory of heart failure, indicators of disease progression, including changes in health status and health service use, may serve as useful signals to help clinicians identify the appropriate time to initiate care planning discussions. Repeated hospital admissions for heart failure are strongly associated with increased mortality. In a sample of community heart failure patients [8], median survival after the first, second, and third hospitalization was 2.4, 1.4, and 1.0 years, respectively. In light of this, a patient with 1 or more hospitalizations in a 12-month period may be an appropriate candidate for an ACP conversation. Similarly, comorbidity in patients with heart failure may signal the relevance and need for discussions about future care. In a sample of Medicare beneficiaries with advanced heart failure, an increasing burden of comorbidity was associated with significantly higher mortality, as were certain conditions (COPD, CKD, dementia, depression) and combinations of conditions (eg, CKD and dementia) [26]. Davidson and colleagues [68] suggest a list of clinical indicators signaling the need for an ACP conversation, including any of the following:
- > 1 episodes of exacerbation of heart failure leading to hospital admission
- New York Heart Association Class IV heart failure
- Decline in function and mobility
- Unexplained weight loss
- Resting pulse rate greater than 100 beats/minute
- Raised serum creatinine (> 150 µmol/L)
- Low serum sodium (< 135 mmol/L)
- Low serum albumen (< 33 g/L)
- High dose of loop diuretic (eg, furosemide ≥ 160 mg daily)
Given the considerable complexity and multisystem nature of heart failure, none of these indicators alone can signal certainty about disease progression and consequent outcomes; however, they can serve as a useful heuristic for helping clinicians identify appropriate times to raise the topic of ACP with their patients.
What Do I Say? Structuring the Conversation
Heart failure patients and their caregivers may vary in their preferences for hearing information about their disease; therefore, it is critical to open any conversation about planning for future in the context of their illness by asking what and how much information is desired. This includes evaluating how involved in decision-making the patient wants to be. Previously suggested language includes [69,70]:
- Would you like to consider all the options, or my opinion about the options that fit best with what I know about you?
- Some people like to know everything about their disease and be involved in all decision making. Others do not want all the news and would rather the doctor talk to __________. Which kind of person are you? How involved do you want to be in these decisions?
- Would you like me to tell you the full details of your condition?
- If you prefer not to hear the details, is there someone in your family who you trust to receive this information?
After establishing the patient’s preferences for hearing different types of information and level of involvement in decision-making about their care, the ask-tell-ask model [69,71] provides a useful approach to communicating with patients and their families. The conversation generally begins by asking patients what he or she understands about their illness (eg, “What do you understand about your heart failure?”; “I want to make sure we’re on the same page; what have other doctors told you?”). Building on what the patient already knows, the clinician can then disclose new information, correct misunderstandings, or confirm impressions and expectations the patient might have. In this way, information is tailored to the patient’s understanding and aimed at addressing potential knowledge gaps, all within the context of their preferences. Finally, the clinician asks the patient to describe their new understanding and whether or not they have questions or concerns (eg, “To make sure I did a good job of explaining to you, can you tell me what you now know about your condition from our conversation?”; “I know I’ve covered a lot and I want to make sure I was clear. When you get home, how are you going to explain what I’ve told you to your spouse?”). This approach encourages communication and exchange between patient and physician. Additionally, expressions of concern promote relationship building and bonding between physician and patient.
Keeping the Conversation Going
ACP communication can cover a wide range of topics beyond disease and prognostic disclosure by the provider to the patient. A critical aspect of ACP conversations is an exploration of the patient’s values and preferences, which can be used to help contextualize treatment choices and subsequently guide in-the-moment decision-making [72]. Using open-ended questions throughout the conversation gives the patient an opportunity to reflect on and communicate their wishes and values and allows them to engage in the conversation on their own terms. Examples of discussion-stimulating questions include [69,73]:
- What concerns you most about your illness?
- How is treatment going for you (your family)?
- As you think about your illness, what is the best and worst that might happen?
- What are your greatest hopes about your health?
- What has been most difficult about this illness for you?
- Looking back at your life, what has been important to you?
- At this point, what is most important for you to do?
Language
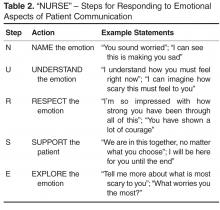
Central to this process is the use of empathic language to demonstrate support and understanding. An expression of empathy is also an appropriate way to acknowledge and share difficult emotions when it becomes hard to know where to take the conversation next. Quill and colleagues [74] suggest the following empathic responses to patients’ emotional expressions:
- I wish for that too
- It's unfortunate that things aren't different
- I am so sorry that this happened to you
- I understand how much you want that
- It must be very hard to accept the seriousness of this illness
Relatedly, the use of medical jargon in ACP conversations can increase the distance between patients and their providers, and may hinder patient understanding. Physicians may use technical language out of habit, or as an unconscious way to emotionally separate themselves from the task of delivering bad news. However, clear communication using layperson terms is the most effective approach to providing information necessary to patient-centered decision making. Explaining medical procedures in simple terms can improve understanding and help to build trust with the physician (eg, “We will perform an angioplasty – a procedure where a special tube with a balloon on the end of it is inserted into your artery to stretch it open. This will improve blood flow and relieve some of the symptoms you are currently experiencing”.)
Cultural Issues in Communication
There are various cultural issues to consider and address when conducting ACP discussions with heart failure patients and their families. Heart failure disproportionately affects certain racial and ethnic groups (eg, African Americans) [77–79], and effective management of heart failure depends on the provision of culturally sensitive information and facilitation of culturally informed self-care behaviors. There is evidence of cultural variation in preferences for information and role in decision-making. For example, most white and African-American patients prefer to be fully informed of their condition [80], whereas other cultures may focus on protecting the patient from difficult information in order to maintain hope [80–86]. Moreover, even in cultures where nondisclosure is preferred, patients may want to be told the truth in an indirect, euphemistic, or even nonverbal manner [80,87–89]. These complexities underscore the importance of taking a patient-centered approach to ACP communication, respecting individuality and autonomy while ultimately facilitating decision-making [90,91].
Are There Effective Training Programs for ACP Communication?
Effective communication skills are a critical component of ACP conversations between clinicians and their patients; however, most clinicians do not receive formal training in ACP communication and believe it to be a difficult task [92]. Strong evidence of the effectiveness of communication skills training has yet to be established, largely due to variation in the approach to training and the specification of relevant outcomes. For example, a systematic review of communication skills training courses found that some courses are effective at improving different types of communication skills related to providing support and gathering information, but these courses lacked effectiveness in improving patient satisfaction or provider burnout and distress [93]. Similarly, a range of approaches to teaching clinicians effective ACP communication skills early in their medical training have been identified [94], but considerable variation in quality preclude any conclusions from being drawn about their effectiveness.
Despite these challenges, there are some studies of communication skills training courses that have demonstrated the ability to increase providers’ use of empathic and facilitative communication (eg, use of open-ended questions) [58,95], and to increase self-efficacy and confidence among providers [96]. One particular teaching model that is increasingly used in cancer care is Oncotalk (http://depts.washington.edu/oncotalk/). Oncotalk has been shown to significantly increase clinical skills in giving bad news and facilitating the transition to palliative care. Building on this success, the program has expanded to training courses focused on the intensive care setting (http://depts.washington.edu/icutalk/) and geriatrics care [97–99]. It is important to note, however, that the considerable time and resource-intensive nature of communication training programs limits widespread implementation of any one approach into routine medical education. More attention to the type and structure of communication skills training programs are needed as well as scalable approaches to assist clinicians in developing effective ACP communication skills.
Policy Implications of ACP and Future Directions
There is growing recognition of the need to improve ACP among patients with seriously illness, including heart failure. In a recent Institute of Medicine (IOM) report, Dying in America [100], the need for clinician-patient communication about ACP was identified as a primary area of improvement. Recommendations include the establishment of communication quality standards as well as guidelines promoting early and ongoing ACP discussions. This is supported by recommendations from medical professional societies for an iterative model of ACP that follows the course of a serious illness [2,101]. At early stages of the illness, ACP might be focused on helping patients clarify their broad health care values and raise awareness of their disease and expected prognosis. As the condition progresses, ACP discussion might focus on exploring disease-specific treatment options within the context of previously expressed preferences, as well as identifying changes in patients’ values over time, particularly as they gain experience with their illness and health status changes [102]. In late stages of the disease, ACP might focus on documenting specific treatment choices (eg, DNR orders) and on exploring options such as palliative care, while also ensuring that patients and caregivers are appropriately prepared for imminent decline and death.
The IOM report also calls for payment reforms to include reimbursement for outpatient ACP discussions [100]. There is burgeoning national support for developing reimbursement models for ACP discussions. The American Medical Association has recently released current procedural terminology (CPT) codes for ACP services, a first step toward urging Medicare to consider reimbursement for ACP discussions with physicians.
Finally, the IOM report calls for improved education and training in ACP communication across all disciplines and specialties providing care to patients with serious illness. These recommendations bring national attention to the current limitations surrounding ACP discussions for those with serious illness, including heart failure. Further research is needed to identify methods and care models to address the gap in communication skills, processes, and policies.
Corresponding author: Sangeeta C. Ahluwalia, Rand Corporation, 1776 Main St., Santa Monica, CA, 90401, [email protected].
Financial disclosures: None.
Author contributions: conception and design, SCA, SE; analysis and interpretation of data, SCA, SE; drafting of article, SCA, SE; critical revision of the article, SCA, SE.
1. American Heart Association. Heart disease and stroke statistics—2008 update. [Internet]. Available at www.americanheart.org/downloadable/heart/1200078608862HS_Stats%202008.final.pdf.
2. Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult—summary article. Circulation 2005;112:1825–52.
3. Masoudi FA, Havranek EP, Krumholz HM. The burden of chronic congestive heart failure in older persons: magnitude and implications for policy and research. Heart Fail Rev 2002;7:9–16.
4. McMurray JJ PM. Heart failure. Lancet 2005;365:1877–89.
5. Unroe KT, Greiner MA, Hernandez AF, et al. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000-2007. Arch Intern Med 2011;171:196–203.
6. Lunney JR, Lynn J, Foley DJ, et al. Patterns of functional decline at the end of life. JAMA 2003;289:2387–92.
7. Ko D, Alter D, Austin P, et al. Life expectancy after an index hospitalization for patients with heart failure: A population-based study. Am Heart J 2008;155:324–31.
8. Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 2007;154:260–6.
9. Jong P, Vowinskel E, Liu PP, et al. Prognosis and determinants for survival in patients newly hospitalized for heart failure. Arch Intern Med 2002;162:1689-94.
10. Thom T, Haase N, Rodamond W, et al. Heart disease and stroke statistics- 2006 update. Circulation 2006;113:e85-e151.
11. Shahar E, Lee S, Kim J, et al. Hospitalized heart failure: Rates and long-term mortality. J Card Fail 2004;10:374–9.
12. Kirkpatrick JN, Guger CJ, Arnsdorf MF, et al. Advance directives in the cardiac care unit. Am Heart J 2007;154:477–81.
13. Orn S, Dickstein K. How do heart failure patients die? Eur Heart J. 2002;4(suppl D).
14. Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic disease and relation to functional variables. Heart 2002;87:235–41.
15. Steptoe A, Mohabir A, Mahon NG, et al. Health related quality of life and psychological wellbeing in patients with dilated cardiomyopathy. Heart 2000;83:645–50.
16. Johansson P, Agnebrink M, Dahlstrom U, et al. Measurement of health-related quality of life in chronic heart failure, form a nursing perspective--a review of the literature. Eur J Cardiovasc Nurs 2004;3:7–20.
17. Levenson J, McCarthy E, Lynn J, et al. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc 2000;48(Suppl 5):S101–S109.
18. Sullivan M, Levy W, Russo J, Spertus J. Depression and health status in patients with advanced heart failure: a prospective study in tertiary care. J Card Fail 2004;10:390–6.
19. Bekelman DB, Havranek EP, Becker DM, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail 2007;13:643–8.
20. Godfrey CM, Harrison MB, Friedberg E, et al. The symptom of pain in individuals recently hospitalized for heart failure. J Cardiovasc Nurs 2007;22:368–74.
21. McCarthy M, Lay M, Addington-Hall J. Dying from heart disease. J R Coll Physicians Lond 1996;30:325–8.
22. Norgren L SS. Symptoms experienced in the last six months of life in patients with end-stage heart failure. Eur J Cardiovasc Nurs 2003;2:213–7.
23. Zambroski CH, Moser DK, Bhat G, et al. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur J Cardiovasc Nurs 2005;4:198–206.
24. Walke LM, Byers AL, Tinetti ME, et al. Range and severity of symptoms over time among older adults wih chronic obstructive pulmonary disease and heart failure. Arch Intern Med 2007;167:2503–8.
25. Bekelman DB, Rumsfeld JS, Havranek EP, et al. Symptom burden, depression, and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med 2009;24:592–8.
26. Ahluwalia SC, Gross CP, Chaudhry SI, et al. Impact of comorbidity on mortality among older persons with advanced heart failure. J Gen Intern Med 2012;27:513–9.
27. Ahluwalia SC, Gross CP, Chaudhry SI, et al. Change in comorbidity prevalence with advancing age among persons with heart failure. J Gen Intern Med 2011;26:1145–51.
28. Corrigan JM, Donaldson MS, Kohn LT, et al. A new health system for the 21st century. crossing the quality chasm. Washington, DC: Institute of Medicine, National Academy of Sciences, National Academies Press; 2001.
29. Kirchhoff KT, Hammes BJ, Kehl KA, et al. Effect of a disease-specific advance care planning intervention on end-of-life care. J Am Geriatr Soc 2012;60:946–50.
30. Kirchhoff KT, Hammes BJ, Kehl KA, et al. Effect of a disease-specific planning intervention on surrogate understanding of patient goals for future medical treatment. J Am Geriatr Soc 2010;58:1233–40.
31. Janssen DJ, Engelberg RA, Wouters EF, Curtis JR. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns 2012;86:19–24.
32. Aldred H, Gott M, Gariballa S. Advanced heart failure: Impact on older patients and informal carers. J Adv Nurs 2005;49:116–24.
33. Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: Associations with end-of-life conversations. Arch Intern Med 2009;169:480–8.
34. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665–73.
35. Mack JW, Smith TJ. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. J Clin Oncol 2012;30:2715–7.
36. Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340:c1345.
37. Schwartz CE, Wheeler HB, Hammes B, et al. Early intervention in planning end-of-life care with ambulatory geriatric patients: results of a pilot trial. Arch Intern Med 2002;162:1611–8.
38. Caldwell PH, Arthur HM, Demers C. Preferences of patients with heart failure for prognosis communication. Can J Cardiol 2007;23:791–6.
39. Bekelman DB, Nowels Ct, Retrum JH, et al. Giving voice to patients’ and family caregivers’ needs in chronic heart failure: implications for palliative care programs. J Palliat Med 2011;14:1317–24.
40. Harding R, Selman L, Beynon T, et al. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 2008;36:149–56.
41. Strachan PH, Ross H, Dodek PM, et al. Mind the gap: opportunities for improving end-of-life care for patients with advanced heart failure. Can J Cardiol 2009;25:635–40.
42. Ågård A, Hermerén G, Herlitz J. When is a patient with heart failure adequately informed? A study of patients’ knowledge of and attitudes toward medical information. Heart Lung 2004;33:219–26.
43. Gott M, Small N, Barnes S, et al. Older people’s views of a good death in heart failure: implications for palliative care provision. Soc Sci Med 2008;67:1113–21.
44. Murray SA, Boyd K, Kendall M, et al. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ 2002;325:929.
45. Ahluwalia SC, Levin JR, Lorenz KA, et al. Missed opportunities for advance care planning communication during outpatient clinic visits. J Gen Intern Med 2012;27:445–51.
46. Rodriguez KL, Appelt CJ, Switzer GE, et al. “They diagnosed bad heart”: a qualitative exploration of patients’ knowledge about and experiences with heart failure. Heart Lung. 2008;37:257–65.
47. Remme WJ,McMurray JJ, Rauch B, et al. Public awareness of heart failure in Europe: first results from SHAPE. Eur Heart J 2005;22:2413e21.
48. Golin CE, Wenger NS, Liu H, et al. A prospective study of patient-physician communication about resuscitation. J Am Geriatr Soc 2000;48(5 Suppl):S52–60.
49. Selman L, Harding R, Beynon T, et al. Improving end of life care for patients with chronic heart failure: ‘let’s hope it’ll get better when I know in my heart of hearts it won’t’. Heart 2007;93:963–7.
50. Barnes S, Gott M, Payne S, et al. Communication in heart failure: Perspectives from older people and primary care professionals. Health Soc Care Comm 2006;14:482–90.
51. Brännström M, Ekman I, Norberg A, et al. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs 2006;5:295–302.
52. Barclay S, Momen N, Case-Upton S, et al. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e49–62.
53. Whitney SN, McCullough LB, Fruge E, et al. Beyond breaking bad news: the roles of hope and hopefulness. Cancer 2008;113:442–5.
54. Tung EE, North F. Advance care planning in the primary care setting: a comparison of attending staff and resident barriers. Am J Hosp Palliat Care 2009;26:456–63.
55. Boyd K, Murray S, Kendall M, et al. Living with advanced heart failure: A prospective, community based study of patients and their carers. Eur J Heart Fail 2004;6:585–91.
56. Borbasi S, Wotton K, Redden M, et al. Letting go: A qualitative study of acute care and community nurses’ perceptions of a ‘good’ versus a ‘bad’ death. Austr Crit Care 2005 2005;18:104–13.
57. Hanratty B, Hibbert D, Mair F, et al. Doctors’ perceptions of palliative care for heart failure: Focus group study. BMJ 2002;325:581–5.
58. Fallowfield L, Jenkins V, Farewell V, et al. Efficacy of a communication skills training model for oncologists: a randomized controlled trial. Lancet 2002;359:650–6.
59. Platt F, Keller V. Empathic communication: a teachable and learnable skill. J Gen Intern Med 1994;9:222–6.
60. Morse D, Edwardsen E, Gordon H. Missed opportunities for interval empathy in lung cancer communication. Arch Intern Med 2008;22;168:1853–8.
61. Epstein R, Hadee T, Carroll J, et al. “Could this be something serious?” reassurance, uncertainty, and empathy in response to patients’ expressions of worry. J Gen Intern Med 2007;22:1731–9.
62. Stewart M. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med 1984;19:
167–75.
63. Wotton K, Borbasi S, Redden M. When all else has failed. Nurses’ perception of factors influencing palliative care for patients with end-stage heart failure. J Cardiovasc Nurs 2005;20:18–25.
64. Willems DL, Hak A, Visser F, Van der Wal G. Thoughts of patients with advanced heart failure on dying. Palliat Med 2004;18:564–72.
65. Briggs L, Kirchhoff K, Hammes B, et al. Patient-centered advance care planning in special patient populations: a pilot study. J Prof Nurs 2004;20:47–58.
66. Hammes B, Rooney B. Death and EOL planning in one midwestern community. Arch Intern Med 1998;158:390.
67. Lilly C, DeMeo D, Sonna L, et al. An intensive communication intervention for the critically ill. Am J Med 2000;109:469–75.
68. Davidson P, Macdonald P, Newton P, et al. End stage heart failure patients: Palliative care in general practice. Aust Fam Physician 2010;39:920.
69. Goodlin S, Quill T, Arnold R. Communication and decision-making about prognosis in heart failure care. J Card Fail 2008;14:106–13.
70. Analysis of U.S. hospital palliative care programs 2010 snapshot. Center to Advance Palliative Care (CAPC). Accessed 24 Nov 2014 at www.capc.org/news-and-events/releases/analysis-of-us-hospital-palliative-care-programs-2010-snapshot.pdf.
71. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
72. Sudore RL, Fried TR, Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med 2010;153:256–61.
73. Lo B, Quill T, Tulsky J. Discussing palliative care with patients. Ann Intern Med 1999;130:744–9.
74. Quill T, Arnold R, Platt F. I wish things were different: Expressing wishes in response to loss, futility, and unrealistic hopes. Ann Intern Med 2001;135:551–5.
75. Pollak K, Arnold R, Jeffreys A, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;25:5748–52.
76. Back AL, Anderson WG, Bunch L, et al. Communication about cancer near the end of life. Cancer 2008;113(S7):1897–910.
77. Dries D, Exner D, Gersh B, et al. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999;340:609–16.
78. Alexander M, Grumbach K, Selby J, et al. Hospitalization for congestive heart failure. Explaining racial differences. JAMA 1995;274:1037–42.
79. Afzal A, Ananthasubramaniam K, Sharma N, et al. Racial differences in patients with heart failure. Clin Cardiol 1999;22:791–4.
80. Blackhall L, Murphy S, Frank G, et al. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274:820–5.
81. Huang X, Butow P, Meiser B, et al. Attitudes and information needs of chinese migrant cancer patients and their relatives. Aust N Z J Med 1999;29:207–13.
82. Tan T, Teo F, Wong K, et al. Cancer: to tell or not to tell? Singapore Med J 1993;34:202–3.
83. Gorgaki S, Kalaidopoulou O, Liarmakopoulos I, et al. Nurses’ attitudes toward truthful communication with patients with cancer. A Greek study. Cancer Nurs 2002;25:436–41.
84. Harris J, Shao J, Sugarman J. Disclosure of cancer diagnosis and prognosis in northern Tanzania. Soc Sci Med 2003;56:905–13.
85. Goldstein D, Thewes B, Butow P. Communicating in a multicultural society. II: Greek community attitudes towards cancer in Australia. Intern Med J 2002;32:289–96.
86. Beyene Y. Medical disclosure and refugees. Telling bad news to Ethiopian patients. West J Med 1992;157:328–32.
87. Matsumura S, Bito S, Liu H, et al. Acculturation of attitudes toward end-of-life care: A cross-cultural survey of Japanese Americans and Japanese. J Gen Intern Med 2002;17:531–9.
88. Yick AG, Gupta R. Chinese cultural dimensions of death, dying, and bereavement: Focus group findings. J Cult Divers 2002 Summer;9:32–42.
89. Frank G, Blackhall L, Murphy S, et al. Ambiguity and hope: Disclosure preferences of less acculturated elderly Mexican Americans concerning terminal cancer—A case story. Camb Q Healthc Ethics 2002;11:117–26.
90. Hern HJ, Koenig B, Moore L, et al. The difference that culture can make in end-of-life decisionmaking. Camb Q Healthc Ethics 1998;7:27–48.
91. Kagawa-Singer M, Kassim-Lakha S. A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes. Acad Med 2003;78:577–87.
92. Barnett MM, Fisher JD, Cooke H, et al. Breaking bad news: consultants’ experience, previous education, and views on educational format and timing. Med Educ 2007;41:947–56.
93. Moore P, Rivera Mercado S, Grez Artigues M, Lawrie T. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3CD003751.
94. Alelwani S, Ahmed Y. Medical training for communication of bad news: A literature review. J Educ Health Promot 2014;3
95. Delvaux N, Razavi D, Marchal S, et al. Effects of a 105 hour psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. Br J Cancer 2004;90:106–14.
96. Baile WF, Lenzi R, Kudelka AP, et al. Improving physician-patient communication in cancer care: Outcome of a workshop for oncologists. J Cancer Educ 1997;12:166–73.
97. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
98. Gelfman LP, Lindenberger E, Fernandez H, et al. The effectiveness of the Geritalk communication skills course: a real-time assessment of skill acquisition and deliberate practice. J Pain Sympt Manage 2014;48:738–44.
99. Kelley AS, Back AL, Arnold RM, et al. Geritalk: communication skills training for geriatric and palliative medicine fellows. J Am Geriatr Soc 2012;60:332–7.
100. Institute of Medicine. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: National Academies Press; 2014.
101. Allen LA, Stevenson LW, Grady KL, et al. Decision making in advanced heart failure: a scientific statement From the American Heart Association. Circulation 2012;125:1928–52.
102. Ditto PH, Jacobson JA, Smucker WD, et al. Context changes choices: a prospective study of the effects of hospitalization on life-sustaining treatment preferences. Med Decis Making 2006;26:313–22.
From the Rand Corporation and UCLA Fielding School of Public Health, Santa Monica, CA (Dr. Ahluwalia) and University of Southern California, Leonard Davis School of Gerontology, Los Angeles, CA (Dr. Enguidanos).
Abstract
- Objective: To review the relevance of advance care planning to heart failure management, describe key advance care planning challenges, and provide clinicians with actionable guidance for engaging in advance care planning conversations.
- Methods: Review of the literature.
- Results: Although most patients with heart failure prefer to receive thorough and honest information about their health condition and prognosis, the unpredictability of the heart failure trajectory coupled with physician barriers including discomfort with emotionally-laden topics and difficulty identifying the “right” time to engage in advance care planning, and systems barriers such as inadequate clinic time and limited reimbursement, impede timely engagement in advance care planning discussions. Approaches to effective advance care planning communication include using open-ended questions to stimulate patient engagement, evaluating how much information the patient wants to ensure patient-centeredness, and using empathic language to demonstrate support and understanding. While successful models of advance care planning communication have been identified, replication is limited due to the resource intense nature of these approaches.
- Conclusion: Challenges to advance care planning discussions among patients with heart failure may be mitigated through the establishment of communication quality standards as well as guidelines promoting early and ongoing advance care planning discussions, as well as reimbursement for outpatient discussions.
Heart failure, a leading cause of death, disability, and health care costs in the United States, is an incurable and life-limiting illness that is becoming increasingly prevalent due to an aging population and improved life expectancy. Approximately 5.3 million Americans are currently living with heart failure [1], with more than 550,000 new cases diagnosed each year [2]. Heart failure disproportionately affects older adults; about 80% of all cases occur in persons aged 65 years or older [3], and heart failure is the leading cause of hospital admissions among older adults [4]. The burden and impact of heart failure peaks near the end of life; 80% of Medicare beneficiaries with heart failure are hospitalized in the last 6 months of life [5].
The Trajectory of Heart Failure
Patients with heart failure experience a highly variable, nonlinear clinical trajectory marked by progressive deterioration and frequent exacerbations requiring hospitalization [6]. Their prognosis, though uncertain, is poor, with reported 1-year mortality rates following a hospitalization between 30% and 50% and 5-year mortality as high as 75% [7–11], a survival rate worse than that of some cancers [12]. Patients with heart failure caused by ischemic heart disease are at high risk for sudden cardiac death, particularly at earlier stages of the disease, which can confound the ability to appropriately plan for the future [13]. Those who survive to more advanced stages of heart failure face worsening quality of life [14–16], driven by a high prevalence of fatigue, breathlessness, pain, and depression [17–24]. Indeed, patients with heart failure have a similar symptom burden to patients with advanced cancer [25]. Older adults with heart failure also have a high comorbidity burden that further complicates both symptomology and disease trajectory with implications for decision-making about life-prolonging heart failure therapies [26,27].
Advance Care Planning in Heart Failure
The unpredictable nature of heart failure makes it difficult for patients and families to plan and prepare for their future, yet it is this very uncertainty that makes advance care planning (ACP) so critical for heart failure patients. Clear and honest patient-clinician communication about ACP, including an exploration of patient values and goals for care in the context of prognostic information, is essential to patient-centered treatment decision-making [28]. This is particularly relevant in heart failure, where a range of high-intensity, invasive, and costly interventions are increasingly being applied (eg, ventricular assist devices) without equivalent attention to quality of life and patients’ long-term goals for care.
Patients with heart failure and their families face multiple complex treatment decisions along the trajectory of their illness, such as discontinuation of beta blockers among patients with refractory fluid overload or angiotensin-converting enzyme inhibitors in end-stage patients with symptomatic hypotension [29,30]. In end-stage heart failure patients, deactivation of an implantable cardiac defibrillator might be considered to avoid the pain and distress associated with repeated shocks. In contrast, other interventions such as cardiac resynchronization therapy and continuous inotropic infusion have quality of life benefits; continuation of these therapies may be appropriate even when discontinuing other interventions. Such decisions should be guided by a thorough understanding of the patient’s expressed preferences and values, ideally assessed early in the trajectory of the disease and continuously re-evaluated as the diseases progresses.
The American Heart Association supports early and regular patient-provider ACP discussions to guide heart failure patients’ future decision-making [31], and recommends that such discussions be initiated in the outpatient setting, prior to and in anticipation of clinical decline. ACP communication plays a critical role in enhancing patients’ understanding of their diagnosis, treatment, prognosis, and choices in end-of-life care [31]. ACP communication also helps the clinician to better understand the context within which patients and their caregivers might make health care decisions, including their values and preferences for care. Patient-provider discussions about ACP focused on understanding patient values and initiated early in the trajectory of serious illness can support future in-the-moment decision-making, and is likely more effective than asking patients to make specific treatment decisions in advance [32]. A growing body of rigorous research has shown that ACP communication is associated with greater preference-concordant care and congruence in patient-surrogate understanding of patient preferences, lower costs, and less aggressive care at the end of life [33–37].
Patient Preferences for ACP Communication
Most patients with heart failure and their caregivers want honest disclosure regarding prognosis and to receive information about the expected trajectory of their disease [38–41] as early as possible [38] to help them plan and prepare for their future. Patients and their caregivers prefer to have these conversations with their physician [38] or other provider most familiar with the patient and family [39]. Patients also express a preference for support with dealing with the uncertainty inherent to heart failure [39]. Although most patients and caregivers desire to receive clear and honest communication about their disease, it is important to note that patients may vary in the extent of information they prefer to receive about their heart failure, with some individuals preferring not to talk about the end of life and future care needs at all [39,42–44].
Challenges to ACP Communication in Heart Failure
Despite patient and caregiver preferences for ACP communication with their providers, evidence suggests such communication occurs infrequently [40,45] and that heart failure patients may lack important information about their prognosis and treatment options [40,44,46,47]. For example, patients may not recognize the terminal nature of heart failure, and may be unaware of the range of treatment options, including hospice, available to them. Evidence also demonstrates that ACP is infrequently discussed with their health care providers [40], resulting in these conversations being avoided or deferred until an emergent clinical situation [44,48] when hasty questions about treatment choices may yield uncertain and conflicting answers not representative of a patient’s underlying values.
The infrequent, late, and often lack of discussions about ACP are driven by several challenges. First, the uncertain trajectory of heart failure makes communication regarding “what to expect” difficult. Prognostication is an immense challenge in heart failure [40,49–52], making it harder to talk about end-of-life issues and hindering the ability of patients, caregivers and health care providers to plan and prepare for the future. It is often difficult for clinicians, who face the challenge of instilling hope in the face of truthful disclosure [53], to identify the “right time” to initiate such discussions.
Second, a lack of time, particularly during outpatient visits, impedes physician ability to have considered discussions about future care needs and preferences [32,54]. The U.S. health care system currently lacks financial reimbursement for these discussions, which poses a significant barrier to the integration of ACP conversations into routine clinical practice. Moreover, these conversations are lengthy and iterative [53]. ACP discussions that are focused on facilitating patient-centered decision-making ideally begin with a discussion of expected prognosis, followed by an exploration of patient preferences and values for health care, and then a review of treatment options to be considered in the context of those preferences. Often additional time is needed for completing advance directive documents or for charting key outcomes from these discussions. Clinicians today are frequently overloaded with addressing multiple medical issues during outpatient visits that leave little time for non-medical tasks such as ACP discussions. The lack of financial incentives to support in-depth discussions is a critical challenge in improving ACP.
Third, a lack of training in specialized communication skills, particularly focused on empathic and emotionally sensitive disclosure, may further hinder physicians from initiating frank discussions with their patients. ACP conversations are highly sensitive and fraught with emotional complexity, and clinicians understandably experience discomfort with breaking bad news [49,51,55] or with broader issues of decline and death [51,56,57]. Physicians tend to be most comfortable addressing cognitive aspects of communication; addressing the emotional needs of patients is harder. Medical school training teaches detachment in physician practice, perhaps as a way of coping with the sadness they regularly confront and in maintaining their ability to provide clinical care. In fact, physicians describe their most difficult encounters as those with the most negative expressed emotions and miss opportunities to respond with empathy [58–60], a critical skill in effective patient-physician communication that is associated with improved patient satisfaction [61,62]. While patients value good communication skills in their health care encounters, many providers feel they lack the necessary skills to lead effective ACP discussions [49,63].
Finally, information gaps with regards to heart failure contribute to delayed or absent conversations about planning for future care. Many heart failure patients have a limited understanding of their disease [32,40,44,55], particularly an inaccurate perception that heart failure is not a terminal and life-limiting illness [42,49,64]. Compounding this is the fact that even some health care providers are reluctant to acknowledge the terminal nature of heart failure [50,56]. Without frank acknowledgement of the terminal nature of heart failure, the initiation of discussions regarding end-of-life care will remain difficult if not impossible.
Approaches to ACP in Heart Failure
When Is the Right Time?
Given the complexity and unpredictable trajectory of heart failure, indicators of disease progression, including changes in health status and health service use, may serve as useful signals to help clinicians identify the appropriate time to initiate care planning discussions. Repeated hospital admissions for heart failure are strongly associated with increased mortality. In a sample of community heart failure patients [8], median survival after the first, second, and third hospitalization was 2.4, 1.4, and 1.0 years, respectively. In light of this, a patient with 1 or more hospitalizations in a 12-month period may be an appropriate candidate for an ACP conversation. Similarly, comorbidity in patients with heart failure may signal the relevance and need for discussions about future care. In a sample of Medicare beneficiaries with advanced heart failure, an increasing burden of comorbidity was associated with significantly higher mortality, as were certain conditions (COPD, CKD, dementia, depression) and combinations of conditions (eg, CKD and dementia) [26]. Davidson and colleagues [68] suggest a list of clinical indicators signaling the need for an ACP conversation, including any of the following:
- > 1 episodes of exacerbation of heart failure leading to hospital admission
- New York Heart Association Class IV heart failure
- Decline in function and mobility
- Unexplained weight loss
- Resting pulse rate greater than 100 beats/minute
- Raised serum creatinine (> 150 µmol/L)
- Low serum sodium (< 135 mmol/L)
- Low serum albumen (< 33 g/L)
- High dose of loop diuretic (eg, furosemide ≥ 160 mg daily)
Given the considerable complexity and multisystem nature of heart failure, none of these indicators alone can signal certainty about disease progression and consequent outcomes; however, they can serve as a useful heuristic for helping clinicians identify appropriate times to raise the topic of ACP with their patients.
What Do I Say? Structuring the Conversation
Heart failure patients and their caregivers may vary in their preferences for hearing information about their disease; therefore, it is critical to open any conversation about planning for future in the context of their illness by asking what and how much information is desired. This includes evaluating how involved in decision-making the patient wants to be. Previously suggested language includes [69,70]:
- Would you like to consider all the options, or my opinion about the options that fit best with what I know about you?
- Some people like to know everything about their disease and be involved in all decision making. Others do not want all the news and would rather the doctor talk to __________. Which kind of person are you? How involved do you want to be in these decisions?
- Would you like me to tell you the full details of your condition?
- If you prefer not to hear the details, is there someone in your family who you trust to receive this information?
After establishing the patient’s preferences for hearing different types of information and level of involvement in decision-making about their care, the ask-tell-ask model [69,71] provides a useful approach to communicating with patients and their families. The conversation generally begins by asking patients what he or she understands about their illness (eg, “What do you understand about your heart failure?”; “I want to make sure we’re on the same page; what have other doctors told you?”). Building on what the patient already knows, the clinician can then disclose new information, correct misunderstandings, or confirm impressions and expectations the patient might have. In this way, information is tailored to the patient’s understanding and aimed at addressing potential knowledge gaps, all within the context of their preferences. Finally, the clinician asks the patient to describe their new understanding and whether or not they have questions or concerns (eg, “To make sure I did a good job of explaining to you, can you tell me what you now know about your condition from our conversation?”; “I know I’ve covered a lot and I want to make sure I was clear. When you get home, how are you going to explain what I’ve told you to your spouse?”). This approach encourages communication and exchange between patient and physician. Additionally, expressions of concern promote relationship building and bonding between physician and patient.
Keeping the Conversation Going
ACP communication can cover a wide range of topics beyond disease and prognostic disclosure by the provider to the patient. A critical aspect of ACP conversations is an exploration of the patient’s values and preferences, which can be used to help contextualize treatment choices and subsequently guide in-the-moment decision-making [72]. Using open-ended questions throughout the conversation gives the patient an opportunity to reflect on and communicate their wishes and values and allows them to engage in the conversation on their own terms. Examples of discussion-stimulating questions include [69,73]:
- What concerns you most about your illness?
- How is treatment going for you (your family)?
- As you think about your illness, what is the best and worst that might happen?
- What are your greatest hopes about your health?
- What has been most difficult about this illness for you?
- Looking back at your life, what has been important to you?
- At this point, what is most important for you to do?
Language
Central to this process is the use of empathic language to demonstrate support and understanding. An expression of empathy is also an appropriate way to acknowledge and share difficult emotions when it becomes hard to know where to take the conversation next. Quill and colleagues [74] suggest the following empathic responses to patients’ emotional expressions:
- I wish for that too
- It's unfortunate that things aren't different
- I am so sorry that this happened to you
- I understand how much you want that
- It must be very hard to accept the seriousness of this illness
Relatedly, the use of medical jargon in ACP conversations can increase the distance between patients and their providers, and may hinder patient understanding. Physicians may use technical language out of habit, or as an unconscious way to emotionally separate themselves from the task of delivering bad news. However, clear communication using layperson terms is the most effective approach to providing information necessary to patient-centered decision making. Explaining medical procedures in simple terms can improve understanding and help to build trust with the physician (eg, “We will perform an angioplasty – a procedure where a special tube with a balloon on the end of it is inserted into your artery to stretch it open. This will improve blood flow and relieve some of the symptoms you are currently experiencing”.)
Cultural Issues in Communication
There are various cultural issues to consider and address when conducting ACP discussions with heart failure patients and their families. Heart failure disproportionately affects certain racial and ethnic groups (eg, African Americans) [77–79], and effective management of heart failure depends on the provision of culturally sensitive information and facilitation of culturally informed self-care behaviors. There is evidence of cultural variation in preferences for information and role in decision-making. For example, most white and African-American patients prefer to be fully informed of their condition [80], whereas other cultures may focus on protecting the patient from difficult information in order to maintain hope [80–86]. Moreover, even in cultures where nondisclosure is preferred, patients may want to be told the truth in an indirect, euphemistic, or even nonverbal manner [80,87–89]. These complexities underscore the importance of taking a patient-centered approach to ACP communication, respecting individuality and autonomy while ultimately facilitating decision-making [90,91].
Are There Effective Training Programs for ACP Communication?
Effective communication skills are a critical component of ACP conversations between clinicians and their patients; however, most clinicians do not receive formal training in ACP communication and believe it to be a difficult task [92]. Strong evidence of the effectiveness of communication skills training has yet to be established, largely due to variation in the approach to training and the specification of relevant outcomes. For example, a systematic review of communication skills training courses found that some courses are effective at improving different types of communication skills related to providing support and gathering information, but these courses lacked effectiveness in improving patient satisfaction or provider burnout and distress [93]. Similarly, a range of approaches to teaching clinicians effective ACP communication skills early in their medical training have been identified [94], but considerable variation in quality preclude any conclusions from being drawn about their effectiveness.
Despite these challenges, there are some studies of communication skills training courses that have demonstrated the ability to increase providers’ use of empathic and facilitative communication (eg, use of open-ended questions) [58,95], and to increase self-efficacy and confidence among providers [96]. One particular teaching model that is increasingly used in cancer care is Oncotalk (http://depts.washington.edu/oncotalk/). Oncotalk has been shown to significantly increase clinical skills in giving bad news and facilitating the transition to palliative care. Building on this success, the program has expanded to training courses focused on the intensive care setting (http://depts.washington.edu/icutalk/) and geriatrics care [97–99]. It is important to note, however, that the considerable time and resource-intensive nature of communication training programs limits widespread implementation of any one approach into routine medical education. More attention to the type and structure of communication skills training programs are needed as well as scalable approaches to assist clinicians in developing effective ACP communication skills.
Policy Implications of ACP and Future Directions
There is growing recognition of the need to improve ACP among patients with seriously illness, including heart failure. In a recent Institute of Medicine (IOM) report, Dying in America [100], the need for clinician-patient communication about ACP was identified as a primary area of improvement. Recommendations include the establishment of communication quality standards as well as guidelines promoting early and ongoing ACP discussions. This is supported by recommendations from medical professional societies for an iterative model of ACP that follows the course of a serious illness [2,101]. At early stages of the illness, ACP might be focused on helping patients clarify their broad health care values and raise awareness of their disease and expected prognosis. As the condition progresses, ACP discussion might focus on exploring disease-specific treatment options within the context of previously expressed preferences, as well as identifying changes in patients’ values over time, particularly as they gain experience with their illness and health status changes [102]. In late stages of the disease, ACP might focus on documenting specific treatment choices (eg, DNR orders) and on exploring options such as palliative care, while also ensuring that patients and caregivers are appropriately prepared for imminent decline and death.
The IOM report also calls for payment reforms to include reimbursement for outpatient ACP discussions [100]. There is burgeoning national support for developing reimbursement models for ACP discussions. The American Medical Association has recently released current procedural terminology (CPT) codes for ACP services, a first step toward urging Medicare to consider reimbursement for ACP discussions with physicians.
Finally, the IOM report calls for improved education and training in ACP communication across all disciplines and specialties providing care to patients with serious illness. These recommendations bring national attention to the current limitations surrounding ACP discussions for those with serious illness, including heart failure. Further research is needed to identify methods and care models to address the gap in communication skills, processes, and policies.
Corresponding author: Sangeeta C. Ahluwalia, Rand Corporation, 1776 Main St., Santa Monica, CA, 90401, [email protected].
Financial disclosures: None.
Author contributions: conception and design, SCA, SE; analysis and interpretation of data, SCA, SE; drafting of article, SCA, SE; critical revision of the article, SCA, SE.
From the Rand Corporation and UCLA Fielding School of Public Health, Santa Monica, CA (Dr. Ahluwalia) and University of Southern California, Leonard Davis School of Gerontology, Los Angeles, CA (Dr. Enguidanos).
Abstract
- Objective: To review the relevance of advance care planning to heart failure management, describe key advance care planning challenges, and provide clinicians with actionable guidance for engaging in advance care planning conversations.
- Methods: Review of the literature.
- Results: Although most patients with heart failure prefer to receive thorough and honest information about their health condition and prognosis, the unpredictability of the heart failure trajectory coupled with physician barriers including discomfort with emotionally-laden topics and difficulty identifying the “right” time to engage in advance care planning, and systems barriers such as inadequate clinic time and limited reimbursement, impede timely engagement in advance care planning discussions. Approaches to effective advance care planning communication include using open-ended questions to stimulate patient engagement, evaluating how much information the patient wants to ensure patient-centeredness, and using empathic language to demonstrate support and understanding. While successful models of advance care planning communication have been identified, replication is limited due to the resource intense nature of these approaches.
- Conclusion: Challenges to advance care planning discussions among patients with heart failure may be mitigated through the establishment of communication quality standards as well as guidelines promoting early and ongoing advance care planning discussions, as well as reimbursement for outpatient discussions.
Heart failure, a leading cause of death, disability, and health care costs in the United States, is an incurable and life-limiting illness that is becoming increasingly prevalent due to an aging population and improved life expectancy. Approximately 5.3 million Americans are currently living with heart failure [1], with more than 550,000 new cases diagnosed each year [2]. Heart failure disproportionately affects older adults; about 80% of all cases occur in persons aged 65 years or older [3], and heart failure is the leading cause of hospital admissions among older adults [4]. The burden and impact of heart failure peaks near the end of life; 80% of Medicare beneficiaries with heart failure are hospitalized in the last 6 months of life [5].
The Trajectory of Heart Failure
Patients with heart failure experience a highly variable, nonlinear clinical trajectory marked by progressive deterioration and frequent exacerbations requiring hospitalization [6]. Their prognosis, though uncertain, is poor, with reported 1-year mortality rates following a hospitalization between 30% and 50% and 5-year mortality as high as 75% [7–11], a survival rate worse than that of some cancers [12]. Patients with heart failure caused by ischemic heart disease are at high risk for sudden cardiac death, particularly at earlier stages of the disease, which can confound the ability to appropriately plan for the future [13]. Those who survive to more advanced stages of heart failure face worsening quality of life [14–16], driven by a high prevalence of fatigue, breathlessness, pain, and depression [17–24]. Indeed, patients with heart failure have a similar symptom burden to patients with advanced cancer [25]. Older adults with heart failure also have a high comorbidity burden that further complicates both symptomology and disease trajectory with implications for decision-making about life-prolonging heart failure therapies [26,27].
Advance Care Planning in Heart Failure
The unpredictable nature of heart failure makes it difficult for patients and families to plan and prepare for their future, yet it is this very uncertainty that makes advance care planning (ACP) so critical for heart failure patients. Clear and honest patient-clinician communication about ACP, including an exploration of patient values and goals for care in the context of prognostic information, is essential to patient-centered treatment decision-making [28]. This is particularly relevant in heart failure, where a range of high-intensity, invasive, and costly interventions are increasingly being applied (eg, ventricular assist devices) without equivalent attention to quality of life and patients’ long-term goals for care.
Patients with heart failure and their families face multiple complex treatment decisions along the trajectory of their illness, such as discontinuation of beta blockers among patients with refractory fluid overload or angiotensin-converting enzyme inhibitors in end-stage patients with symptomatic hypotension [29,30]. In end-stage heart failure patients, deactivation of an implantable cardiac defibrillator might be considered to avoid the pain and distress associated with repeated shocks. In contrast, other interventions such as cardiac resynchronization therapy and continuous inotropic infusion have quality of life benefits; continuation of these therapies may be appropriate even when discontinuing other interventions. Such decisions should be guided by a thorough understanding of the patient’s expressed preferences and values, ideally assessed early in the trajectory of the disease and continuously re-evaluated as the diseases progresses.
The American Heart Association supports early and regular patient-provider ACP discussions to guide heart failure patients’ future decision-making [31], and recommends that such discussions be initiated in the outpatient setting, prior to and in anticipation of clinical decline. ACP communication plays a critical role in enhancing patients’ understanding of their diagnosis, treatment, prognosis, and choices in end-of-life care [31]. ACP communication also helps the clinician to better understand the context within which patients and their caregivers might make health care decisions, including their values and preferences for care. Patient-provider discussions about ACP focused on understanding patient values and initiated early in the trajectory of serious illness can support future in-the-moment decision-making, and is likely more effective than asking patients to make specific treatment decisions in advance [32]. A growing body of rigorous research has shown that ACP communication is associated with greater preference-concordant care and congruence in patient-surrogate understanding of patient preferences, lower costs, and less aggressive care at the end of life [33–37].
Patient Preferences for ACP Communication
Most patients with heart failure and their caregivers want honest disclosure regarding prognosis and to receive information about the expected trajectory of their disease [38–41] as early as possible [38] to help them plan and prepare for their future. Patients and their caregivers prefer to have these conversations with their physician [38] or other provider most familiar with the patient and family [39]. Patients also express a preference for support with dealing with the uncertainty inherent to heart failure [39]. Although most patients and caregivers desire to receive clear and honest communication about their disease, it is important to note that patients may vary in the extent of information they prefer to receive about their heart failure, with some individuals preferring not to talk about the end of life and future care needs at all [39,42–44].
Challenges to ACP Communication in Heart Failure
Despite patient and caregiver preferences for ACP communication with their providers, evidence suggests such communication occurs infrequently [40,45] and that heart failure patients may lack important information about their prognosis and treatment options [40,44,46,47]. For example, patients may not recognize the terminal nature of heart failure, and may be unaware of the range of treatment options, including hospice, available to them. Evidence also demonstrates that ACP is infrequently discussed with their health care providers [40], resulting in these conversations being avoided or deferred until an emergent clinical situation [44,48] when hasty questions about treatment choices may yield uncertain and conflicting answers not representative of a patient’s underlying values.
The infrequent, late, and often lack of discussions about ACP are driven by several challenges. First, the uncertain trajectory of heart failure makes communication regarding “what to expect” difficult. Prognostication is an immense challenge in heart failure [40,49–52], making it harder to talk about end-of-life issues and hindering the ability of patients, caregivers and health care providers to plan and prepare for the future. It is often difficult for clinicians, who face the challenge of instilling hope in the face of truthful disclosure [53], to identify the “right time” to initiate such discussions.
Second, a lack of time, particularly during outpatient visits, impedes physician ability to have considered discussions about future care needs and preferences [32,54]. The U.S. health care system currently lacks financial reimbursement for these discussions, which poses a significant barrier to the integration of ACP conversations into routine clinical practice. Moreover, these conversations are lengthy and iterative [53]. ACP discussions that are focused on facilitating patient-centered decision-making ideally begin with a discussion of expected prognosis, followed by an exploration of patient preferences and values for health care, and then a review of treatment options to be considered in the context of those preferences. Often additional time is needed for completing advance directive documents or for charting key outcomes from these discussions. Clinicians today are frequently overloaded with addressing multiple medical issues during outpatient visits that leave little time for non-medical tasks such as ACP discussions. The lack of financial incentives to support in-depth discussions is a critical challenge in improving ACP.
Third, a lack of training in specialized communication skills, particularly focused on empathic and emotionally sensitive disclosure, may further hinder physicians from initiating frank discussions with their patients. ACP conversations are highly sensitive and fraught with emotional complexity, and clinicians understandably experience discomfort with breaking bad news [49,51,55] or with broader issues of decline and death [51,56,57]. Physicians tend to be most comfortable addressing cognitive aspects of communication; addressing the emotional needs of patients is harder. Medical school training teaches detachment in physician practice, perhaps as a way of coping with the sadness they regularly confront and in maintaining their ability to provide clinical care. In fact, physicians describe their most difficult encounters as those with the most negative expressed emotions and miss opportunities to respond with empathy [58–60], a critical skill in effective patient-physician communication that is associated with improved patient satisfaction [61,62]. While patients value good communication skills in their health care encounters, many providers feel they lack the necessary skills to lead effective ACP discussions [49,63].
Finally, information gaps with regards to heart failure contribute to delayed or absent conversations about planning for future care. Many heart failure patients have a limited understanding of their disease [32,40,44,55], particularly an inaccurate perception that heart failure is not a terminal and life-limiting illness [42,49,64]. Compounding this is the fact that even some health care providers are reluctant to acknowledge the terminal nature of heart failure [50,56]. Without frank acknowledgement of the terminal nature of heart failure, the initiation of discussions regarding end-of-life care will remain difficult if not impossible.
Approaches to ACP in Heart Failure
When Is the Right Time?
Given the complexity and unpredictable trajectory of heart failure, indicators of disease progression, including changes in health status and health service use, may serve as useful signals to help clinicians identify the appropriate time to initiate care planning discussions. Repeated hospital admissions for heart failure are strongly associated with increased mortality. In a sample of community heart failure patients [8], median survival after the first, second, and third hospitalization was 2.4, 1.4, and 1.0 years, respectively. In light of this, a patient with 1 or more hospitalizations in a 12-month period may be an appropriate candidate for an ACP conversation. Similarly, comorbidity in patients with heart failure may signal the relevance and need for discussions about future care. In a sample of Medicare beneficiaries with advanced heart failure, an increasing burden of comorbidity was associated with significantly higher mortality, as were certain conditions (COPD, CKD, dementia, depression) and combinations of conditions (eg, CKD and dementia) [26]. Davidson and colleagues [68] suggest a list of clinical indicators signaling the need for an ACP conversation, including any of the following:
- > 1 episodes of exacerbation of heart failure leading to hospital admission
- New York Heart Association Class IV heart failure
- Decline in function and mobility
- Unexplained weight loss
- Resting pulse rate greater than 100 beats/minute
- Raised serum creatinine (> 150 µmol/L)
- Low serum sodium (< 135 mmol/L)
- Low serum albumen (< 33 g/L)
- High dose of loop diuretic (eg, furosemide ≥ 160 mg daily)
Given the considerable complexity and multisystem nature of heart failure, none of these indicators alone can signal certainty about disease progression and consequent outcomes; however, they can serve as a useful heuristic for helping clinicians identify appropriate times to raise the topic of ACP with their patients.
What Do I Say? Structuring the Conversation
Heart failure patients and their caregivers may vary in their preferences for hearing information about their disease; therefore, it is critical to open any conversation about planning for future in the context of their illness by asking what and how much information is desired. This includes evaluating how involved in decision-making the patient wants to be. Previously suggested language includes [69,70]:
- Would you like to consider all the options, or my opinion about the options that fit best with what I know about you?
- Some people like to know everything about their disease and be involved in all decision making. Others do not want all the news and would rather the doctor talk to __________. Which kind of person are you? How involved do you want to be in these decisions?
- Would you like me to tell you the full details of your condition?
- If you prefer not to hear the details, is there someone in your family who you trust to receive this information?
After establishing the patient’s preferences for hearing different types of information and level of involvement in decision-making about their care, the ask-tell-ask model [69,71] provides a useful approach to communicating with patients and their families. The conversation generally begins by asking patients what he or she understands about their illness (eg, “What do you understand about your heart failure?”; “I want to make sure we’re on the same page; what have other doctors told you?”). Building on what the patient already knows, the clinician can then disclose new information, correct misunderstandings, or confirm impressions and expectations the patient might have. In this way, information is tailored to the patient’s understanding and aimed at addressing potential knowledge gaps, all within the context of their preferences. Finally, the clinician asks the patient to describe their new understanding and whether or not they have questions or concerns (eg, “To make sure I did a good job of explaining to you, can you tell me what you now know about your condition from our conversation?”; “I know I’ve covered a lot and I want to make sure I was clear. When you get home, how are you going to explain what I’ve told you to your spouse?”). This approach encourages communication and exchange between patient and physician. Additionally, expressions of concern promote relationship building and bonding between physician and patient.
Keeping the Conversation Going
ACP communication can cover a wide range of topics beyond disease and prognostic disclosure by the provider to the patient. A critical aspect of ACP conversations is an exploration of the patient’s values and preferences, which can be used to help contextualize treatment choices and subsequently guide in-the-moment decision-making [72]. Using open-ended questions throughout the conversation gives the patient an opportunity to reflect on and communicate their wishes and values and allows them to engage in the conversation on their own terms. Examples of discussion-stimulating questions include [69,73]:
- What concerns you most about your illness?
- How is treatment going for you (your family)?
- As you think about your illness, what is the best and worst that might happen?
- What are your greatest hopes about your health?
- What has been most difficult about this illness for you?
- Looking back at your life, what has been important to you?
- At this point, what is most important for you to do?
Language
Central to this process is the use of empathic language to demonstrate support and understanding. An expression of empathy is also an appropriate way to acknowledge and share difficult emotions when it becomes hard to know where to take the conversation next. Quill and colleagues [74] suggest the following empathic responses to patients’ emotional expressions:
- I wish for that too
- It's unfortunate that things aren't different
- I am so sorry that this happened to you
- I understand how much you want that
- It must be very hard to accept the seriousness of this illness
Relatedly, the use of medical jargon in ACP conversations can increase the distance between patients and their providers, and may hinder patient understanding. Physicians may use technical language out of habit, or as an unconscious way to emotionally separate themselves from the task of delivering bad news. However, clear communication using layperson terms is the most effective approach to providing information necessary to patient-centered decision making. Explaining medical procedures in simple terms can improve understanding and help to build trust with the physician (eg, “We will perform an angioplasty – a procedure where a special tube with a balloon on the end of it is inserted into your artery to stretch it open. This will improve blood flow and relieve some of the symptoms you are currently experiencing”.)
Cultural Issues in Communication
There are various cultural issues to consider and address when conducting ACP discussions with heart failure patients and their families. Heart failure disproportionately affects certain racial and ethnic groups (eg, African Americans) [77–79], and effective management of heart failure depends on the provision of culturally sensitive information and facilitation of culturally informed self-care behaviors. There is evidence of cultural variation in preferences for information and role in decision-making. For example, most white and African-American patients prefer to be fully informed of their condition [80], whereas other cultures may focus on protecting the patient from difficult information in order to maintain hope [80–86]. Moreover, even in cultures where nondisclosure is preferred, patients may want to be told the truth in an indirect, euphemistic, or even nonverbal manner [80,87–89]. These complexities underscore the importance of taking a patient-centered approach to ACP communication, respecting individuality and autonomy while ultimately facilitating decision-making [90,91].
Are There Effective Training Programs for ACP Communication?
Effective communication skills are a critical component of ACP conversations between clinicians and their patients; however, most clinicians do not receive formal training in ACP communication and believe it to be a difficult task [92]. Strong evidence of the effectiveness of communication skills training has yet to be established, largely due to variation in the approach to training and the specification of relevant outcomes. For example, a systematic review of communication skills training courses found that some courses are effective at improving different types of communication skills related to providing support and gathering information, but these courses lacked effectiveness in improving patient satisfaction or provider burnout and distress [93]. Similarly, a range of approaches to teaching clinicians effective ACP communication skills early in their medical training have been identified [94], but considerable variation in quality preclude any conclusions from being drawn about their effectiveness.
Despite these challenges, there are some studies of communication skills training courses that have demonstrated the ability to increase providers’ use of empathic and facilitative communication (eg, use of open-ended questions) [58,95], and to increase self-efficacy and confidence among providers [96]. One particular teaching model that is increasingly used in cancer care is Oncotalk (http://depts.washington.edu/oncotalk/). Oncotalk has been shown to significantly increase clinical skills in giving bad news and facilitating the transition to palliative care. Building on this success, the program has expanded to training courses focused on the intensive care setting (http://depts.washington.edu/icutalk/) and geriatrics care [97–99]. It is important to note, however, that the considerable time and resource-intensive nature of communication training programs limits widespread implementation of any one approach into routine medical education. More attention to the type and structure of communication skills training programs are needed as well as scalable approaches to assist clinicians in developing effective ACP communication skills.
Policy Implications of ACP and Future Directions
There is growing recognition of the need to improve ACP among patients with seriously illness, including heart failure. In a recent Institute of Medicine (IOM) report, Dying in America [100], the need for clinician-patient communication about ACP was identified as a primary area of improvement. Recommendations include the establishment of communication quality standards as well as guidelines promoting early and ongoing ACP discussions. This is supported by recommendations from medical professional societies for an iterative model of ACP that follows the course of a serious illness [2,101]. At early stages of the illness, ACP might be focused on helping patients clarify their broad health care values and raise awareness of their disease and expected prognosis. As the condition progresses, ACP discussion might focus on exploring disease-specific treatment options within the context of previously expressed preferences, as well as identifying changes in patients’ values over time, particularly as they gain experience with their illness and health status changes [102]. In late stages of the disease, ACP might focus on documenting specific treatment choices (eg, DNR orders) and on exploring options such as palliative care, while also ensuring that patients and caregivers are appropriately prepared for imminent decline and death.
The IOM report also calls for payment reforms to include reimbursement for outpatient ACP discussions [100]. There is burgeoning national support for developing reimbursement models for ACP discussions. The American Medical Association has recently released current procedural terminology (CPT) codes for ACP services, a first step toward urging Medicare to consider reimbursement for ACP discussions with physicians.
Finally, the IOM report calls for improved education and training in ACP communication across all disciplines and specialties providing care to patients with serious illness. These recommendations bring national attention to the current limitations surrounding ACP discussions for those with serious illness, including heart failure. Further research is needed to identify methods and care models to address the gap in communication skills, processes, and policies.
Corresponding author: Sangeeta C. Ahluwalia, Rand Corporation, 1776 Main St., Santa Monica, CA, 90401, [email protected].
Financial disclosures: None.
Author contributions: conception and design, SCA, SE; analysis and interpretation of data, SCA, SE; drafting of article, SCA, SE; critical revision of the article, SCA, SE.
1. American Heart Association. Heart disease and stroke statistics—2008 update. [Internet]. Available at www.americanheart.org/downloadable/heart/1200078608862HS_Stats%202008.final.pdf.
2. Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult—summary article. Circulation 2005;112:1825–52.
3. Masoudi FA, Havranek EP, Krumholz HM. The burden of chronic congestive heart failure in older persons: magnitude and implications for policy and research. Heart Fail Rev 2002;7:9–16.
4. McMurray JJ PM. Heart failure. Lancet 2005;365:1877–89.
5. Unroe KT, Greiner MA, Hernandez AF, et al. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000-2007. Arch Intern Med 2011;171:196–203.
6. Lunney JR, Lynn J, Foley DJ, et al. Patterns of functional decline at the end of life. JAMA 2003;289:2387–92.
7. Ko D, Alter D, Austin P, et al. Life expectancy after an index hospitalization for patients with heart failure: A population-based study. Am Heart J 2008;155:324–31.
8. Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 2007;154:260–6.
9. Jong P, Vowinskel E, Liu PP, et al. Prognosis and determinants for survival in patients newly hospitalized for heart failure. Arch Intern Med 2002;162:1689-94.
10. Thom T, Haase N, Rodamond W, et al. Heart disease and stroke statistics- 2006 update. Circulation 2006;113:e85-e151.
11. Shahar E, Lee S, Kim J, et al. Hospitalized heart failure: Rates and long-term mortality. J Card Fail 2004;10:374–9.
12. Kirkpatrick JN, Guger CJ, Arnsdorf MF, et al. Advance directives in the cardiac care unit. Am Heart J 2007;154:477–81.
13. Orn S, Dickstein K. How do heart failure patients die? Eur Heart J. 2002;4(suppl D).
14. Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic disease and relation to functional variables. Heart 2002;87:235–41.
15. Steptoe A, Mohabir A, Mahon NG, et al. Health related quality of life and psychological wellbeing in patients with dilated cardiomyopathy. Heart 2000;83:645–50.
16. Johansson P, Agnebrink M, Dahlstrom U, et al. Measurement of health-related quality of life in chronic heart failure, form a nursing perspective--a review of the literature. Eur J Cardiovasc Nurs 2004;3:7–20.
17. Levenson J, McCarthy E, Lynn J, et al. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc 2000;48(Suppl 5):S101–S109.
18. Sullivan M, Levy W, Russo J, Spertus J. Depression and health status in patients with advanced heart failure: a prospective study in tertiary care. J Card Fail 2004;10:390–6.
19. Bekelman DB, Havranek EP, Becker DM, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail 2007;13:643–8.
20. Godfrey CM, Harrison MB, Friedberg E, et al. The symptom of pain in individuals recently hospitalized for heart failure. J Cardiovasc Nurs 2007;22:368–74.
21. McCarthy M, Lay M, Addington-Hall J. Dying from heart disease. J R Coll Physicians Lond 1996;30:325–8.
22. Norgren L SS. Symptoms experienced in the last six months of life in patients with end-stage heart failure. Eur J Cardiovasc Nurs 2003;2:213–7.
23. Zambroski CH, Moser DK, Bhat G, et al. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur J Cardiovasc Nurs 2005;4:198–206.
24. Walke LM, Byers AL, Tinetti ME, et al. Range and severity of symptoms over time among older adults wih chronic obstructive pulmonary disease and heart failure. Arch Intern Med 2007;167:2503–8.
25. Bekelman DB, Rumsfeld JS, Havranek EP, et al. Symptom burden, depression, and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med 2009;24:592–8.
26. Ahluwalia SC, Gross CP, Chaudhry SI, et al. Impact of comorbidity on mortality among older persons with advanced heart failure. J Gen Intern Med 2012;27:513–9.
27. Ahluwalia SC, Gross CP, Chaudhry SI, et al. Change in comorbidity prevalence with advancing age among persons with heart failure. J Gen Intern Med 2011;26:1145–51.
28. Corrigan JM, Donaldson MS, Kohn LT, et al. A new health system for the 21st century. crossing the quality chasm. Washington, DC: Institute of Medicine, National Academy of Sciences, National Academies Press; 2001.
29. Kirchhoff KT, Hammes BJ, Kehl KA, et al. Effect of a disease-specific advance care planning intervention on end-of-life care. J Am Geriatr Soc 2012;60:946–50.
30. Kirchhoff KT, Hammes BJ, Kehl KA, et al. Effect of a disease-specific planning intervention on surrogate understanding of patient goals for future medical treatment. J Am Geriatr Soc 2010;58:1233–40.
31. Janssen DJ, Engelberg RA, Wouters EF, Curtis JR. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns 2012;86:19–24.
32. Aldred H, Gott M, Gariballa S. Advanced heart failure: Impact on older patients and informal carers. J Adv Nurs 2005;49:116–24.
33. Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: Associations with end-of-life conversations. Arch Intern Med 2009;169:480–8.
34. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665–73.
35. Mack JW, Smith TJ. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. J Clin Oncol 2012;30:2715–7.
36. Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340:c1345.
37. Schwartz CE, Wheeler HB, Hammes B, et al. Early intervention in planning end-of-life care with ambulatory geriatric patients: results of a pilot trial. Arch Intern Med 2002;162:1611–8.
38. Caldwell PH, Arthur HM, Demers C. Preferences of patients with heart failure for prognosis communication. Can J Cardiol 2007;23:791–6.
39. Bekelman DB, Nowels Ct, Retrum JH, et al. Giving voice to patients’ and family caregivers’ needs in chronic heart failure: implications for palliative care programs. J Palliat Med 2011;14:1317–24.
40. Harding R, Selman L, Beynon T, et al. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 2008;36:149–56.
41. Strachan PH, Ross H, Dodek PM, et al. Mind the gap: opportunities for improving end-of-life care for patients with advanced heart failure. Can J Cardiol 2009;25:635–40.
42. Ågård A, Hermerén G, Herlitz J. When is a patient with heart failure adequately informed? A study of patients’ knowledge of and attitudes toward medical information. Heart Lung 2004;33:219–26.
43. Gott M, Small N, Barnes S, et al. Older people’s views of a good death in heart failure: implications for palliative care provision. Soc Sci Med 2008;67:1113–21.
44. Murray SA, Boyd K, Kendall M, et al. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ 2002;325:929.
45. Ahluwalia SC, Levin JR, Lorenz KA, et al. Missed opportunities for advance care planning communication during outpatient clinic visits. J Gen Intern Med 2012;27:445–51.
46. Rodriguez KL, Appelt CJ, Switzer GE, et al. “They diagnosed bad heart”: a qualitative exploration of patients’ knowledge about and experiences with heart failure. Heart Lung. 2008;37:257–65.
47. Remme WJ,McMurray JJ, Rauch B, et al. Public awareness of heart failure in Europe: first results from SHAPE. Eur Heart J 2005;22:2413e21.
48. Golin CE, Wenger NS, Liu H, et al. A prospective study of patient-physician communication about resuscitation. J Am Geriatr Soc 2000;48(5 Suppl):S52–60.
49. Selman L, Harding R, Beynon T, et al. Improving end of life care for patients with chronic heart failure: ‘let’s hope it’ll get better when I know in my heart of hearts it won’t’. Heart 2007;93:963–7.
50. Barnes S, Gott M, Payne S, et al. Communication in heart failure: Perspectives from older people and primary care professionals. Health Soc Care Comm 2006;14:482–90.
51. Brännström M, Ekman I, Norberg A, et al. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs 2006;5:295–302.
52. Barclay S, Momen N, Case-Upton S, et al. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e49–62.
53. Whitney SN, McCullough LB, Fruge E, et al. Beyond breaking bad news: the roles of hope and hopefulness. Cancer 2008;113:442–5.
54. Tung EE, North F. Advance care planning in the primary care setting: a comparison of attending staff and resident barriers. Am J Hosp Palliat Care 2009;26:456–63.
55. Boyd K, Murray S, Kendall M, et al. Living with advanced heart failure: A prospective, community based study of patients and their carers. Eur J Heart Fail 2004;6:585–91.
56. Borbasi S, Wotton K, Redden M, et al. Letting go: A qualitative study of acute care and community nurses’ perceptions of a ‘good’ versus a ‘bad’ death. Austr Crit Care 2005 2005;18:104–13.
57. Hanratty B, Hibbert D, Mair F, et al. Doctors’ perceptions of palliative care for heart failure: Focus group study. BMJ 2002;325:581–5.
58. Fallowfield L, Jenkins V, Farewell V, et al. Efficacy of a communication skills training model for oncologists: a randomized controlled trial. Lancet 2002;359:650–6.
59. Platt F, Keller V. Empathic communication: a teachable and learnable skill. J Gen Intern Med 1994;9:222–6.
60. Morse D, Edwardsen E, Gordon H. Missed opportunities for interval empathy in lung cancer communication. Arch Intern Med 2008;22;168:1853–8.
61. Epstein R, Hadee T, Carroll J, et al. “Could this be something serious?” reassurance, uncertainty, and empathy in response to patients’ expressions of worry. J Gen Intern Med 2007;22:1731–9.
62. Stewart M. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med 1984;19:
167–75.
63. Wotton K, Borbasi S, Redden M. When all else has failed. Nurses’ perception of factors influencing palliative care for patients with end-stage heart failure. J Cardiovasc Nurs 2005;20:18–25.
64. Willems DL, Hak A, Visser F, Van der Wal G. Thoughts of patients with advanced heart failure on dying. Palliat Med 2004;18:564–72.
65. Briggs L, Kirchhoff K, Hammes B, et al. Patient-centered advance care planning in special patient populations: a pilot study. J Prof Nurs 2004;20:47–58.
66. Hammes B, Rooney B. Death and EOL planning in one midwestern community. Arch Intern Med 1998;158:390.
67. Lilly C, DeMeo D, Sonna L, et al. An intensive communication intervention for the critically ill. Am J Med 2000;109:469–75.
68. Davidson P, Macdonald P, Newton P, et al. End stage heart failure patients: Palliative care in general practice. Aust Fam Physician 2010;39:920.
69. Goodlin S, Quill T, Arnold R. Communication and decision-making about prognosis in heart failure care. J Card Fail 2008;14:106–13.
70. Analysis of U.S. hospital palliative care programs 2010 snapshot. Center to Advance Palliative Care (CAPC). Accessed 24 Nov 2014 at www.capc.org/news-and-events/releases/analysis-of-us-hospital-palliative-care-programs-2010-snapshot.pdf.
71. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
72. Sudore RL, Fried TR, Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med 2010;153:256–61.
73. Lo B, Quill T, Tulsky J. Discussing palliative care with patients. Ann Intern Med 1999;130:744–9.
74. Quill T, Arnold R, Platt F. I wish things were different: Expressing wishes in response to loss, futility, and unrealistic hopes. Ann Intern Med 2001;135:551–5.
75. Pollak K, Arnold R, Jeffreys A, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;25:5748–52.
76. Back AL, Anderson WG, Bunch L, et al. Communication about cancer near the end of life. Cancer 2008;113(S7):1897–910.
77. Dries D, Exner D, Gersh B, et al. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999;340:609–16.
78. Alexander M, Grumbach K, Selby J, et al. Hospitalization for congestive heart failure. Explaining racial differences. JAMA 1995;274:1037–42.
79. Afzal A, Ananthasubramaniam K, Sharma N, et al. Racial differences in patients with heart failure. Clin Cardiol 1999;22:791–4.
80. Blackhall L, Murphy S, Frank G, et al. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274:820–5.
81. Huang X, Butow P, Meiser B, et al. Attitudes and information needs of chinese migrant cancer patients and their relatives. Aust N Z J Med 1999;29:207–13.
82. Tan T, Teo F, Wong K, et al. Cancer: to tell or not to tell? Singapore Med J 1993;34:202–3.
83. Gorgaki S, Kalaidopoulou O, Liarmakopoulos I, et al. Nurses’ attitudes toward truthful communication with patients with cancer. A Greek study. Cancer Nurs 2002;25:436–41.
84. Harris J, Shao J, Sugarman J. Disclosure of cancer diagnosis and prognosis in northern Tanzania. Soc Sci Med 2003;56:905–13.
85. Goldstein D, Thewes B, Butow P. Communicating in a multicultural society. II: Greek community attitudes towards cancer in Australia. Intern Med J 2002;32:289–96.
86. Beyene Y. Medical disclosure and refugees. Telling bad news to Ethiopian patients. West J Med 1992;157:328–32.
87. Matsumura S, Bito S, Liu H, et al. Acculturation of attitudes toward end-of-life care: A cross-cultural survey of Japanese Americans and Japanese. J Gen Intern Med 2002;17:531–9.
88. Yick AG, Gupta R. Chinese cultural dimensions of death, dying, and bereavement: Focus group findings. J Cult Divers 2002 Summer;9:32–42.
89. Frank G, Blackhall L, Murphy S, et al. Ambiguity and hope: Disclosure preferences of less acculturated elderly Mexican Americans concerning terminal cancer—A case story. Camb Q Healthc Ethics 2002;11:117–26.
90. Hern HJ, Koenig B, Moore L, et al. The difference that culture can make in end-of-life decisionmaking. Camb Q Healthc Ethics 1998;7:27–48.
91. Kagawa-Singer M, Kassim-Lakha S. A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes. Acad Med 2003;78:577–87.
92. Barnett MM, Fisher JD, Cooke H, et al. Breaking bad news: consultants’ experience, previous education, and views on educational format and timing. Med Educ 2007;41:947–56.
93. Moore P, Rivera Mercado S, Grez Artigues M, Lawrie T. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3CD003751.
94. Alelwani S, Ahmed Y. Medical training for communication of bad news: A literature review. J Educ Health Promot 2014;3
95. Delvaux N, Razavi D, Marchal S, et al. Effects of a 105 hour psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. Br J Cancer 2004;90:106–14.
96. Baile WF, Lenzi R, Kudelka AP, et al. Improving physician-patient communication in cancer care: Outcome of a workshop for oncologists. J Cancer Educ 1997;12:166–73.
97. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
98. Gelfman LP, Lindenberger E, Fernandez H, et al. The effectiveness of the Geritalk communication skills course: a real-time assessment of skill acquisition and deliberate practice. J Pain Sympt Manage 2014;48:738–44.
99. Kelley AS, Back AL, Arnold RM, et al. Geritalk: communication skills training for geriatric and palliative medicine fellows. J Am Geriatr Soc 2012;60:332–7.
100. Institute of Medicine. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: National Academies Press; 2014.
101. Allen LA, Stevenson LW, Grady KL, et al. Decision making in advanced heart failure: a scientific statement From the American Heart Association. Circulation 2012;125:1928–52.
102. Ditto PH, Jacobson JA, Smucker WD, et al. Context changes choices: a prospective study of the effects of hospitalization on life-sustaining treatment preferences. Med Decis Making 2006;26:313–22.
1. American Heart Association. Heart disease and stroke statistics—2008 update. [Internet]. Available at www.americanheart.org/downloadable/heart/1200078608862HS_Stats%202008.final.pdf.
2. Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult—summary article. Circulation 2005;112:1825–52.
3. Masoudi FA, Havranek EP, Krumholz HM. The burden of chronic congestive heart failure in older persons: magnitude and implications for policy and research. Heart Fail Rev 2002;7:9–16.
4. McMurray JJ PM. Heart failure. Lancet 2005;365:1877–89.
5. Unroe KT, Greiner MA, Hernandez AF, et al. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000-2007. Arch Intern Med 2011;171:196–203.
6. Lunney JR, Lynn J, Foley DJ, et al. Patterns of functional decline at the end of life. JAMA 2003;289:2387–92.
7. Ko D, Alter D, Austin P, et al. Life expectancy after an index hospitalization for patients with heart failure: A population-based study. Am Heart J 2008;155:324–31.
8. Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 2007;154:260–6.
9. Jong P, Vowinskel E, Liu PP, et al. Prognosis and determinants for survival in patients newly hospitalized for heart failure. Arch Intern Med 2002;162:1689-94.
10. Thom T, Haase N, Rodamond W, et al. Heart disease and stroke statistics- 2006 update. Circulation 2006;113:e85-e151.
11. Shahar E, Lee S, Kim J, et al. Hospitalized heart failure: Rates and long-term mortality. J Card Fail 2004;10:374–9.
12. Kirkpatrick JN, Guger CJ, Arnsdorf MF, et al. Advance directives in the cardiac care unit. Am Heart J 2007;154:477–81.
13. Orn S, Dickstein K. How do heart failure patients die? Eur Heart J. 2002;4(suppl D).
14. Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic disease and relation to functional variables. Heart 2002;87:235–41.
15. Steptoe A, Mohabir A, Mahon NG, et al. Health related quality of life and psychological wellbeing in patients with dilated cardiomyopathy. Heart 2000;83:645–50.
16. Johansson P, Agnebrink M, Dahlstrom U, et al. Measurement of health-related quality of life in chronic heart failure, form a nursing perspective--a review of the literature. Eur J Cardiovasc Nurs 2004;3:7–20.
17. Levenson J, McCarthy E, Lynn J, et al. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc 2000;48(Suppl 5):S101–S109.
18. Sullivan M, Levy W, Russo J, Spertus J. Depression and health status in patients with advanced heart failure: a prospective study in tertiary care. J Card Fail 2004;10:390–6.
19. Bekelman DB, Havranek EP, Becker DM, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail 2007;13:643–8.
20. Godfrey CM, Harrison MB, Friedberg E, et al. The symptom of pain in individuals recently hospitalized for heart failure. J Cardiovasc Nurs 2007;22:368–74.
21. McCarthy M, Lay M, Addington-Hall J. Dying from heart disease. J R Coll Physicians Lond 1996;30:325–8.
22. Norgren L SS. Symptoms experienced in the last six months of life in patients with end-stage heart failure. Eur J Cardiovasc Nurs 2003;2:213–7.
23. Zambroski CH, Moser DK, Bhat G, et al. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur J Cardiovasc Nurs 2005;4:198–206.
24. Walke LM, Byers AL, Tinetti ME, et al. Range and severity of symptoms over time among older adults wih chronic obstructive pulmonary disease and heart failure. Arch Intern Med 2007;167:2503–8.
25. Bekelman DB, Rumsfeld JS, Havranek EP, et al. Symptom burden, depression, and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med 2009;24:592–8.
26. Ahluwalia SC, Gross CP, Chaudhry SI, et al. Impact of comorbidity on mortality among older persons with advanced heart failure. J Gen Intern Med 2012;27:513–9.
27. Ahluwalia SC, Gross CP, Chaudhry SI, et al. Change in comorbidity prevalence with advancing age among persons with heart failure. J Gen Intern Med 2011;26:1145–51.
28. Corrigan JM, Donaldson MS, Kohn LT, et al. A new health system for the 21st century. crossing the quality chasm. Washington, DC: Institute of Medicine, National Academy of Sciences, National Academies Press; 2001.
29. Kirchhoff KT, Hammes BJ, Kehl KA, et al. Effect of a disease-specific advance care planning intervention on end-of-life care. J Am Geriatr Soc 2012;60:946–50.
30. Kirchhoff KT, Hammes BJ, Kehl KA, et al. Effect of a disease-specific planning intervention on surrogate understanding of patient goals for future medical treatment. J Am Geriatr Soc 2010;58:1233–40.
31. Janssen DJ, Engelberg RA, Wouters EF, Curtis JR. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns 2012;86:19–24.
32. Aldred H, Gott M, Gariballa S. Advanced heart failure: Impact on older patients and informal carers. J Adv Nurs 2005;49:116–24.
33. Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: Associations with end-of-life conversations. Arch Intern Med 2009;169:480–8.
34. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665–73.
35. Mack JW, Smith TJ. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. J Clin Oncol 2012;30:2715–7.
36. Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340:c1345.
37. Schwartz CE, Wheeler HB, Hammes B, et al. Early intervention in planning end-of-life care with ambulatory geriatric patients: results of a pilot trial. Arch Intern Med 2002;162:1611–8.
38. Caldwell PH, Arthur HM, Demers C. Preferences of patients with heart failure for prognosis communication. Can J Cardiol 2007;23:791–6.
39. Bekelman DB, Nowels Ct, Retrum JH, et al. Giving voice to patients’ and family caregivers’ needs in chronic heart failure: implications for palliative care programs. J Palliat Med 2011;14:1317–24.
40. Harding R, Selman L, Beynon T, et al. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 2008;36:149–56.
41. Strachan PH, Ross H, Dodek PM, et al. Mind the gap: opportunities for improving end-of-life care for patients with advanced heart failure. Can J Cardiol 2009;25:635–40.
42. Ågård A, Hermerén G, Herlitz J. When is a patient with heart failure adequately informed? A study of patients’ knowledge of and attitudes toward medical information. Heart Lung 2004;33:219–26.
43. Gott M, Small N, Barnes S, et al. Older people’s views of a good death in heart failure: implications for palliative care provision. Soc Sci Med 2008;67:1113–21.
44. Murray SA, Boyd K, Kendall M, et al. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ 2002;325:929.
45. Ahluwalia SC, Levin JR, Lorenz KA, et al. Missed opportunities for advance care planning communication during outpatient clinic visits. J Gen Intern Med 2012;27:445–51.
46. Rodriguez KL, Appelt CJ, Switzer GE, et al. “They diagnosed bad heart”: a qualitative exploration of patients’ knowledge about and experiences with heart failure. Heart Lung. 2008;37:257–65.
47. Remme WJ,McMurray JJ, Rauch B, et al. Public awareness of heart failure in Europe: first results from SHAPE. Eur Heart J 2005;22:2413e21.
48. Golin CE, Wenger NS, Liu H, et al. A prospective study of patient-physician communication about resuscitation. J Am Geriatr Soc 2000;48(5 Suppl):S52–60.
49. Selman L, Harding R, Beynon T, et al. Improving end of life care for patients with chronic heart failure: ‘let’s hope it’ll get better when I know in my heart of hearts it won’t’. Heart 2007;93:963–7.
50. Barnes S, Gott M, Payne S, et al. Communication in heart failure: Perspectives from older people and primary care professionals. Health Soc Care Comm 2006;14:482–90.
51. Brännström M, Ekman I, Norberg A, et al. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs 2006;5:295–302.
52. Barclay S, Momen N, Case-Upton S, et al. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e49–62.
53. Whitney SN, McCullough LB, Fruge E, et al. Beyond breaking bad news: the roles of hope and hopefulness. Cancer 2008;113:442–5.
54. Tung EE, North F. Advance care planning in the primary care setting: a comparison of attending staff and resident barriers. Am J Hosp Palliat Care 2009;26:456–63.
55. Boyd K, Murray S, Kendall M, et al. Living with advanced heart failure: A prospective, community based study of patients and their carers. Eur J Heart Fail 2004;6:585–91.
56. Borbasi S, Wotton K, Redden M, et al. Letting go: A qualitative study of acute care and community nurses’ perceptions of a ‘good’ versus a ‘bad’ death. Austr Crit Care 2005 2005;18:104–13.
57. Hanratty B, Hibbert D, Mair F, et al. Doctors’ perceptions of palliative care for heart failure: Focus group study. BMJ 2002;325:581–5.
58. Fallowfield L, Jenkins V, Farewell V, et al. Efficacy of a communication skills training model for oncologists: a randomized controlled trial. Lancet 2002;359:650–6.
59. Platt F, Keller V. Empathic communication: a teachable and learnable skill. J Gen Intern Med 1994;9:222–6.
60. Morse D, Edwardsen E, Gordon H. Missed opportunities for interval empathy in lung cancer communication. Arch Intern Med 2008;22;168:1853–8.
61. Epstein R, Hadee T, Carroll J, et al. “Could this be something serious?” reassurance, uncertainty, and empathy in response to patients’ expressions of worry. J Gen Intern Med 2007;22:1731–9.
62. Stewart M. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med 1984;19:
167–75.
63. Wotton K, Borbasi S, Redden M. When all else has failed. Nurses’ perception of factors influencing palliative care for patients with end-stage heart failure. J Cardiovasc Nurs 2005;20:18–25.
64. Willems DL, Hak A, Visser F, Van der Wal G. Thoughts of patients with advanced heart failure on dying. Palliat Med 2004;18:564–72.
65. Briggs L, Kirchhoff K, Hammes B, et al. Patient-centered advance care planning in special patient populations: a pilot study. J Prof Nurs 2004;20:47–58.
66. Hammes B, Rooney B. Death and EOL planning in one midwestern community. Arch Intern Med 1998;158:390.
67. Lilly C, DeMeo D, Sonna L, et al. An intensive communication intervention for the critically ill. Am J Med 2000;109:469–75.
68. Davidson P, Macdonald P, Newton P, et al. End stage heart failure patients: Palliative care in general practice. Aust Fam Physician 2010;39:920.
69. Goodlin S, Quill T, Arnold R. Communication and decision-making about prognosis in heart failure care. J Card Fail 2008;14:106–13.
70. Analysis of U.S. hospital palliative care programs 2010 snapshot. Center to Advance Palliative Care (CAPC). Accessed 24 Nov 2014 at www.capc.org/news-and-events/releases/analysis-of-us-hospital-palliative-care-programs-2010-snapshot.pdf.
71. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
72. Sudore RL, Fried TR, Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med 2010;153:256–61.
73. Lo B, Quill T, Tulsky J. Discussing palliative care with patients. Ann Intern Med 1999;130:744–9.
74. Quill T, Arnold R, Platt F. I wish things were different: Expressing wishes in response to loss, futility, and unrealistic hopes. Ann Intern Med 2001;135:551–5.
75. Pollak K, Arnold R, Jeffreys A, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;25:5748–52.
76. Back AL, Anderson WG, Bunch L, et al. Communication about cancer near the end of life. Cancer 2008;113(S7):1897–910.
77. Dries D, Exner D, Gersh B, et al. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999;340:609–16.
78. Alexander M, Grumbach K, Selby J, et al. Hospitalization for congestive heart failure. Explaining racial differences. JAMA 1995;274:1037–42.
79. Afzal A, Ananthasubramaniam K, Sharma N, et al. Racial differences in patients with heart failure. Clin Cardiol 1999;22:791–4.
80. Blackhall L, Murphy S, Frank G, et al. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274:820–5.
81. Huang X, Butow P, Meiser B, et al. Attitudes and information needs of chinese migrant cancer patients and their relatives. Aust N Z J Med 1999;29:207–13.
82. Tan T, Teo F, Wong K, et al. Cancer: to tell or not to tell? Singapore Med J 1993;34:202–3.
83. Gorgaki S, Kalaidopoulou O, Liarmakopoulos I, et al. Nurses’ attitudes toward truthful communication with patients with cancer. A Greek study. Cancer Nurs 2002;25:436–41.
84. Harris J, Shao J, Sugarman J. Disclosure of cancer diagnosis and prognosis in northern Tanzania. Soc Sci Med 2003;56:905–13.
85. Goldstein D, Thewes B, Butow P. Communicating in a multicultural society. II: Greek community attitudes towards cancer in Australia. Intern Med J 2002;32:289–96.
86. Beyene Y. Medical disclosure and refugees. Telling bad news to Ethiopian patients. West J Med 1992;157:328–32.
87. Matsumura S, Bito S, Liu H, et al. Acculturation of attitudes toward end-of-life care: A cross-cultural survey of Japanese Americans and Japanese. J Gen Intern Med 2002;17:531–9.
88. Yick AG, Gupta R. Chinese cultural dimensions of death, dying, and bereavement: Focus group findings. J Cult Divers 2002 Summer;9:32–42.
89. Frank G, Blackhall L, Murphy S, et al. Ambiguity and hope: Disclosure preferences of less acculturated elderly Mexican Americans concerning terminal cancer—A case story. Camb Q Healthc Ethics 2002;11:117–26.
90. Hern HJ, Koenig B, Moore L, et al. The difference that culture can make in end-of-life decisionmaking. Camb Q Healthc Ethics 1998;7:27–48.
91. Kagawa-Singer M, Kassim-Lakha S. A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes. Acad Med 2003;78:577–87.
92. Barnett MM, Fisher JD, Cooke H, et al. Breaking bad news: consultants’ experience, previous education, and views on educational format and timing. Med Educ 2007;41:947–56.
93. Moore P, Rivera Mercado S, Grez Artigues M, Lawrie T. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3CD003751.
94. Alelwani S, Ahmed Y. Medical training for communication of bad news: A literature review. J Educ Health Promot 2014;3
95. Delvaux N, Razavi D, Marchal S, et al. Effects of a 105 hour psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. Br J Cancer 2004;90:106–14.
96. Baile WF, Lenzi R, Kudelka AP, et al. Improving physician-patient communication in cancer care: Outcome of a workshop for oncologists. J Cancer Educ 1997;12:166–73.
97. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
98. Gelfman LP, Lindenberger E, Fernandez H, et al. The effectiveness of the Geritalk communication skills course: a real-time assessment of skill acquisition and deliberate practice. J Pain Sympt Manage 2014;48:738–44.
99. Kelley AS, Back AL, Arnold RM, et al. Geritalk: communication skills training for geriatric and palliative medicine fellows. J Am Geriatr Soc 2012;60:332–7.
100. Institute of Medicine. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: National Academies Press; 2014.
101. Allen LA, Stevenson LW, Grady KL, et al. Decision making in advanced heart failure: a scientific statement From the American Heart Association. Circulation 2012;125:1928–52.
102. Ditto PH, Jacobson JA, Smucker WD, et al. Context changes choices: a prospective study of the effects of hospitalization on life-sustaining treatment preferences. Med Decis Making 2006;26:313–22.
Abnormal Uterine Bleeding in Reproductive-Aged Women
From the University of Wisconsin School of Medicine and Public Health, Madison, WI.
Abstract
- Objective: To describe the contributing etiologies, common presentations, diagnosis, evaluation, and management of abnormal uterine bleeding (AUB).
- Methods: Review of the literature in the context of 3 cases.
- Results: AUB is one of the most common reasons that reproductive-aged women seek health care. The causes are varied, depending in large part on the age and life stage of the woman. Diagnosis requires a systematic approach that is driven by a thorough health history and review of presenting symptoms. Determining whether the bleeding is ovulatory or anovulatory is a central part of the evaluation. A methodical history, physical examination, and laboratory evaluation may enable the physician to rule out causes such as pregnancy and pregnancy-related disorders, medications, iatrogenic causes, systemic conditions, and obvious genital tract pathology.
- Conclusion: Clinicians must be knowledgeable about AUB and partner with women to develop appropriate, individualized treatment plans.
Abnormal vaginal bleeding is a common complaint in primary care. The prevalence of some type of abnormal bleeding is up to 30% among women of reproductive age [1].Over 18% of all gynecology outpatient visits in the United States are for menorrhagia alone [2].A retrospective analysis of medical expenditures data compared 1.4 million women with abnormal uterine bleeding to over 50 million women without abnormal bleeding. This study found that women with abnormal bleeding were more likely to be younger, Caucasian, and obese and had poorer physical and mental health quality of life scores [3].
The estimated direct and indirect costs of abnormal bleeding are $1 billion and $12 billion annually, respectively [4]. Indirect costs of abnormal bleeding include time off from work and cost of products to protect clothing from bleeding (eg, tampons and pads). Abnormal bleeding is also a common reason for women to be referred to gynecologists and is an indication for up to 25% of all gynecologic surgeries [5].
History Taking
Taking a menstrual history is an important step in determining whether the current bleeding pattern is normal or abnormal. Regularity of menstrual bleeding is clarified by asking about the frequency of the menses and their duration. Other important questions include age at menarche, presence of premenstrual syndrome symptoms, breast tenderness, cervical mucus changes, and amount of bleeding. An ovulatory cycle will usually include premenstrual symptoms whereas an anovulatory cycle will be random in its symptomatology. Women’s estimates of the amount of menstrual bleeding are notoriously inaccurate. Traditionally, more than 80 cc of menstrual blood loss per cycle is considered menorrhagia. However, women and their health care providers do not measure menstrual blood volume outside of study settings, and one study found that only half of women who presented with menorrhagia actually had more than 80 cc of blood loss [6]. There is movement toward use of more patient-centered measures to diagnose men-orrhagia, such as bleeding interfering with a woman’s daily activities, needing to wake up at night to change tampons or pads, or inability to exercise during menses. Anemia in the setting of menorrhagia by history is a less subjective way to diagnose menorrhagia.
Nomenclature and Differential Diagnosis
Differential diagnosis will vary based on symptomatology as well as age. Pregnancy is a possible cause of any type of abnormal bleeding in any woman of reproductive age (ie, after menarche and before menopause). Many systemic illnesses and medications can affect menstrual bleeding and should be included in a broad differential diagnosis of a presenting woman.
Case 1—Heavy Menstrual Bleeding
Initial Presentation
A 42-year-old woman presents reporting increasingly heavy, somewhat painful periods over the last 6 to 8 months. She experienced menarche at age 12 and has had regular, moderately heavy periods throughout her adult life. She denies any inter-menstrual bleeding.
What additional history should be obtained?
Heavy menstrual bleeding refers to abnormally heavy bleeding that occurs in an ovulatory, cyclical pattern. Women with anovulatory cycles can also have heavy bleeding as well, and distinguishing ovulatory vs anovulatory cycles is often the first step in the evaluation.
The initial evaluation of a woman presenting with heavy menstrual bleeding includes a detailed history and physical examination. The first goal of the history is to establish the severity of bleeding, including any symptoms of hemodynamically significant anemia such as dizziness or exertional dyspnea. Next, the clinician should determine whether the bleeding pattern is ovulatory or anovulatory. Ovulatory heavy menstrual bleeding is most often caused by structural lesions (leiomyomas, endometriosis, adenomyosis, cervical polyps, and endometrial polyps) or a coagulopathy (von Willebrand disease, anticoagulant use, etc). Less commonly, ovulatory heavy menstrual bleeding may be due to systemic illness (including thyroid disease, renal disease, and liver disease) or endometrial hyperplasia or carcinoma.
Once an ovulatory pattern is confirmed, a history of dysmenorrhea, pelvic pain, lower urinary tract symptoms, constipation, dyspareunia, or infertility should be elicited.
Further history taking should seek to identify any symptoms suggestive of thyroid, kidney, or liver disease,
What are key elements of the physical examination?
The physical examination should include visual inspection and palpation of the thyroid gland as well as an abdominal exam to evaluate for hepatosplenomegaly or lower abdominal tenderness or masses. Signs of anemia such as pallor should also be noted. The gynecologic exam should include visual inspection of the external genitalia, a bimanual exam, and a speculum exam. Cervical and endometrial polyps may be visible as masses at the cervical os or extending into the vaginal canal. An enlarged mobile uterus with irregular contours is consistent with leiomyomas [8].Endometriosis may manifest as tenderness, thickening, or nodularity of the uterine corpus, the vaginal canal, the uterosacral ligaments, or the adnexa. Endometriosis may also cause an asymmetric, fixed position of the uterus, the cervix, or the adnexa [9].Adenomyosis may cause diffuse moderate uterine enlargement with or without tenderness [10].Endometrial carcinoma may also cause uterine enlargement and/or immobility.
What laboratory testing should be performed?
What additional testing would be useful in narrowing the differential diagnosis?
If the physical examination and initial laboratory testing is nondiagnostic, the decision to initiate a trial of symptom management or proceed with further testing (imaging and/or tissue sampling) is based on risk of endometrial cancer, severity of symptoms, and patient preference. In many women, body habitus makes a confirmatory pelvic examination difficult, which may lower the threshold for obtaining a pelvic ultrasound.
Women with risk factors for endometrial cancer should undergo office-based endometrial biopsy as the first step in evaluation of heavy menstrual bleeding [7].Risk factors include older age (45 years and older), obesity (BMI > 30), diabetes mellitus, nulliparity, and history of chronic anovulation (eg, polycystic ovary syndrome). Pelvic ultrasound is the first step in the evaluation of women with an abnormal physical exam suggesting a structural lesion [7].If the physical exam is abnormal and the pelvic ultrasound is nondiagnostic, a hysteroscopy or saline-infusion sonohysterogram should be performed, as these tests are more sensitive for the detection of intracavitary lesions and submucosal fibroids [13].Most endometrial polyps will appear as a thickened or irregular endometrium on pelvic ultrasound, but be clearly delineated on sonohysterogram. Women who have a negative initial evaluation but then go on to have persistent bleeding despite a trial of therapy also require further evaluation.
Case Continued
The patient reports that her periods are regular, with a cycle length of 30 to 31 days. She usually notes some bloating and breast tenderness in the days leading up to onset of menses. She experiences lower abdominal cramping during days 1–3 of her period. This has worsened somewhat over the last year, and sometimes radiates to her low back. Her reproductive history is significant for 3 uncomplicated vaginal deliveries and 1 first trimester spontaneous abortion. She did not experience postpartum hemorrhage, and has no history of significant oropharyngeal bleeding or unexplained bruising. Her BMI is 23.3. Her physical exam is unremarkable, including a normal thyroid, abdominal, bimanual and speculum exam. Laboratory evaluation demonstrates a low-normal hemoglobin, hematocrit, and MCV. The TSH is normal and a urine pregnancy test is negative. She had a normal pap smear and HPV assay 2 years ago.
What is the most likely diagnosis?
What treatment is recommended?
Oral tranexamic acid is an anti-fibrinolytic that was recently approved by the FDA for treatment of menorrhagia or heavy menstrual bleeding. It has been used for many years to prevent bleeding during surgery and to treat bleeding disorders. It has been used for over 30 years to treat menorrhagia in Europe. It has a different mechanism of action than NSAIDs and hormonal contraceptives, and is therefore an appropriate alternative for women who cannot tolerate other medication options [16,17].Tranexamic acid is contraindicated in women with an elevated risk of thromboembolic disease.
For women who have insufficient response to medical management or for women who present with more severe symptoms, anemia, or prominent bulk-related symptoms due to fibroids, gynecologic referral should be made for consideration of surgical intervention. The preferred interventional approach to the treatment of uterine fibroid tumors depends upon the type of fibroid (eg submucosal, intramural, subserosal), the number of fibroids, desire for future childbearing, risk for surgical complications, and patient preference. Effective options include myomectomy, uterine artery embolization, endometrial ablation, and hysterectomy [18].
By contrast, good evidence supports the use of medication as first-line therapy for heavy menstrual bleeding when it occurs in the setting of endometriosis. Estrogen-progestin oral contraceptive pills, oral progestins, and depot medroxyprogesterone have all been demonstrated to be effective in decreasing pain [19,20].The levonorgestrel-releasing intrauterine system is also effective in decreasing pain due to endometriosis [21].
Women who do not respond to first-line therapy should be referred to a gynecologist for consideration of other treatment options. Effective second-line treatment options include oral danazol, intramuscular GnRH agonists, and surgical approaches such as laparoscopic ablation and/or excision of endometriosis implants [22].
A similar range of treatment options appears to be effective in the management of heavy menstrual bleeding due to adenomyosis. First-line therapies include oral NSAIDs, oral tranexamic acid, estrogen-progestin oral contraceptive pills, and the levonorgestrel-releasing intrauterine system [23,24].Women with an inadequate response to first-line treatment should be referred to a gynecologist for consideration definitive treatment with hysterectomy versus uterine artery embolization or a trial of a GnRH agonist [24].
For some women with heavy menstrual bleeding, no specific underlying cause is identified. Current evidence suggests that such patients may have disorders of local endometrial hemostasis leading to increased blood loss during otherwise normal menstrual cycles [25].The levonorgestrel-releasing intrauterine system may be the most effective medical therapy for heavy menstrual bleeding in the absence of a specific target lesion [26].For women wishing to avoid hormonal treatment, scheduled oral NSAIDs or oral tranexamic acid are inexpensive and effective options for reducing blood loss [27–29].Other medical treatment options include estrogen-progestin contraceptive pills, cyclic oral progestin, and depot medroxy-progesterone.
For patients who experience treatment failure with pharmaceutical therapy or who desire definitive treatment, both endometrial ablation and hysterectomy have been shown to be effective and associated with high rates of patient satisfaction [30].
Follow-up
The patient reports that she would like to avoid invasive testing if possible. Given her relatively low risk for endometrial cancer, she elects a trial of scheduled NSAIDs. Unfortunately, after a couple of cycles she reports that her heavy bleeding has not been well-controlled. A pelvic ultrasound demonstrates an anterior submucosal fibroid measuring 2.4 cm and a posterior intramural fibroid measuring 1.5 cm. She agrees to insertion of a levonorgestrel IUD and calls 6 months later to report a significant decrease in her bleeding.
Case 2—Anovulation
Initial Presentation
A 27-year-old female presents for pregnancy testing. She is 2 weeks late for her period. She and her husband are attempting pregnancy and she seems disappointed that the pregnancy test is negative. She is having trouble tracking her periods. Her cycles range from 24 to 45 days apart and often she skips cycles altogether. Her flow is scant at times but some months are heavy with soaking tampons/pads.
What are diagnostic considerations in evaluating this bleeding pattern?
Menstrual history can help differentiate between of ovulatory and anovulatory abnormal bleeding. Typically, anovulatory bleeding is marked by irregular or infrequent periods. Flow can be scant to excessive. Women experiencing anovulatory cycles may fail to notice common ovulation symptoms (thin watery cervical mucus) or pre-menstrual symptoms (breast tenderness) [31].
The International Federation of Gynecology and Obstetrics (FIGO) designates AUD-O as “abnormal uterine bleeding due to ovulatory dysfunction” or “anovulatory abnormal uterine bleeding” [7,31].In general, if women are having menses at regular cycles their bleeding is likely to be ovulatory.
Differential Diagnosis
Anovulatory bleeding may be physiologic. After menarche, the hypothalamic-pituitary-ovarian axis is immature. This may result in anovulatory cycles for 2 to 3 years. Women entering perimenopausal transition may also experience intermittent anovulation and subsequent abnormal uterine bleeding. Other physiologic examples include lactation and pregnancy [31].
Physical Examination
A thorough history will help to narrow the differential diagnosis. The physical exam can evaluate for other findings that indicate endocrine dysfunction such as low body weight, hirsutism, balding, acne, high blood pressure, obesity (especially centripetal fat distribution). Acanthosis nigricans is a sign of insulin resistance which is part of the pathophysiology of PCOS. The gynecologic exam is often unremarkable in AUB-O although a bimanual exam can reveal adnexal enlargement indicative of cystic ovaries. Of note, clitoromegally is not common in PCOS. This finding would increase the likelihood of other causes of hyperandrogenism [32].
What is the pathophysiologic basis for this patient’s bleeding pattern?
Pathophysiology of Anovulatory Bleeding
Anovulatory bleeding presumes that there is a normal anatomic and genetic makeup. For example, a woman without ovaries will be, by definition, anovulatory. Using current terminology anovulatory bleeding implies a disruption in the hypothalamic-pituitary-ovarian axis and is therefore primarily an endocrine disorder [31,33].
At the level of the ovary and uterus, anovulation results in prolonged estrogen effect on the endometrium. After ovulation, the corpus luteum produces progesterone which stops endometrial thickening and stabilizes the endometrium. Without ovulation, estrogen continues endometrial stimulation and excess proliferation of endometrial lining. The endometrium becomes unstable, undifferentiated, and sheds unpredictably. The blood vessels become larger, more tortuous and have increased fragility. The result is light or heavy menstrual bleeding, decreased frequency of periods but overall unpredictable menstrual bleeding [33].
Effects of Chronic Anovulation
Irregular cycles can be more than a mere inconvenience. Women who have anovulatory cycles associated with heavy menstrual bleeding are at risk for anemia. Anovulation that is a result of hyperandrogen state or other endocrine disorder has other health ramifications. Infertility and its treatment are common sequelae. Finally, over time, unopposed estrogen in anovulation increases the risk of endometrial hyperplasia, or cancer [7,34].
Case Continued
The patient reports menarche at age 12. Her periods were irregular for the first 1–2 years but became more regular after that. She has been taking combination oral contraceptives since the age of 20 to prevent pregnancy. She stopped this 1 year ago and she and her husband began actively trying to conceive 6 months ago. Her family history is notable for diabetes and hypertension in her father. Her mother had heavy periods leading up to menopause and had a hysterectomy with no malignancy at the age of 47. She has a BMI of 33; blood pressure is mildly elevated at 134/84 mm Hg. She has oily skin and acne along her chin and neck. She has mild hirsutism of her face. Otherwise her skin is normal appearing. She has an elevated waist circumference of 35 inches. The remainder of her exam is normal.
What is the likely diagnosis?
Women with PCOS are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, type 2 diabetes and cardiovascular disease, endometrial cancer, and infertility. Women with PCOS who become pregnant have increased risk of pregnancy complications such as hypertensive disorders and gestational diabetes.
What tests are indicated in this patient?
Appropriate laboratory testing is often determined based on findings in the history and physical as well as the patient’s age. Anovulation in the first 18 months to 3 years after menarche is common and testing for pregnancy, infection, and anemia are often sufficient. Menorrhagia in adolescents warrants testing for bleeding disorders as well [7].Within 3 years of menarche, menstrual cycles should become more regular. Persistent anovulatory cycles increase the likelihood of pathologic causes and warrant additional evaluation. Pregnancy testing, thyroid stimulation hormone and prolactin levels are recommended first line evaluation [7,32,34].If PCOS is suspected an ultrasound can be performed but as noted above, polycystic ovaries are not required to make the diagnosis after adolescence.
Additional testing includes testosterone levels to look for androgen secreting tumors. Late onset congenital adrenal hyperplasia is an uncommon cause of hyperandrogenism but is more common in women of Ashkenazi Jewish descent and those with a family history [34].Morning hydroxyprogesterone can be performed to evaluate for this. If women exhibit abrupt change in menstrual pattern and other signs of cortisol excess (hypertension, abdominal striae) 24-hour urine cortisol can detect Cushing’s syndrome [34].
In patients with PCOS, additional testing to evaluate for medical comorbidities is recommended. This includes screening for diabetes, dyslipidemia, and liver dysfunction.
Case Continued
The patient’s prolactin and TSH are normal. Tests for diabetes are normal. Her LDL is elevated to 162, triglycerides are 200, and her HDL is 38. The physician informs her that she meets criteria for PCOS and also that she has obesity and metabolic syndrome.
What factors should be considered when making treatment recommendations for this patient?
Treatment for anovulation is guided by the goals of therapy. Since anovulation is an endocrine abnormality, medical treatment is first line [31].If secondary causes are diagnosed, these should be treated first. Other goals of treatment can include reducing amount and irregularity of menstruation, provide contraception, increasing ovulation in women with desired fertility, and reducing androgenic sequelae such as acne and hirsutism.
When treating the irregular or heavy bleeding associated with anovulation, first-line treatment is exogenous hormone. This can be in the form of combined estrogen/progesterone formulations (pill, patch, and ring). Medroxyprogesterone (medroxyprogesterone acetate 5–10 mg daily) taken 10 to 14 days per month is another option. Standard consideration for medical eligibility in prescribing these agents should be considered (see U.S. medical eligibility criteria for contraceptive use available at www.cdc.gov/reproductivehealth/unintendedpregnancy/usmec.htm). Combined formulations offer contraception, while cyclic progesterone does not. Both offer cyclic withdrawal bleeding. A Cochrane review did not find any RCTs comparing one to the other and therefore either are reasonable options [36].The levonorgestrel IUD is effective at treating AUB as well [31].Women may still experience intermittent vaginal bleeding or amenorrhea so it is less likely to result in cyclic withdrawal bleeding.
All of the above treatments provide the additional benefit of thinning the endometrium and preventing unopposed estrogen effect. This provides further protection the endometrial hyperplasia with chronic anovulatory cycles and unopposed estrogen [31].
In women with PCOS and associated metabolic conditions, first-line treatment is weight loss and other lifestyle interventions to improve or prevent other sequelae of the condition. Weight loss has been shown to reduce circulating androgen levels and increase ovulation. It has been shown to reduce glucose and lipid levels and hirsutism. Pregnancy rates increase as well. Weight loss achieved through medications and gastric bypass has similar effects. There is no special diet that has been shown to be more effective than another [32]. As little as a 5% weight reduction from baseline can improve PCOS symptoms [34,35].
Metformin is also commonly added to lifestyle modifications in women with PCOS to reduce risks for developing diabetes. There is little high quality evidence of added benefit above lifestyle modifications [34].Statin therapy can be considered in women with hyperlipidemia and PCOS [32].
For women with PCOS who desire to conceive, treatment should target increased ovulation. Pre-conception counseling and lifestyle modifications are again first line [32].Ovulation induction interventions carry increased risk of multiple gestation. For ovulation induction, clomiphene citrate is first line therapy. Metformin is commonly used as noted above to improve comorbidities associated with PCOS and can increase ovulation compared to placebo [37].However, RCTs do not support its use as first-line treatment of infertility treatment in PCOS. Clomiphene is 3 times more effective than metformin alone [32].
Medications can improve but often do not resolve hirsutism in women with PCOS. Combined hormonal contraceptives are commonly used off-label and no one type of pill has been shown to be superior. Anti-androgens are also off-label but empirically used. They can also improve lipid and other metabolic variables. They are all teratogenic and therefore should not be used in women who desire conception, and be used with effective contraceptives. Spironolactone is an androgen receptor antagonist. It takes months for effect. Some women will have improved menstrual frequency with this medication as well. Often adjunctive therapy such as eflornithine facial cream or laser therapy or a combination is needed to further treat hirsutism [32,35,38].
Follow-up
After discussion, the patient decides to adopt therapeutic lifestyle changes. She desires to get pregnant and does not opt for hormonal contraceptives at this time. She sees a nutritionist and begins calorie restriction and exercise. Three months later she has lost 20 pounds and feels “healthier.” Her lipid panel shows LDL of 125 and HDL of 43. Her triglycerides are now 160. Her blood pressure in the office is 118/78 mm Hg. She has lost “inches” around her middle. She has had more regular periods as well. She is still not pregnant so the physician asks her to begin tracking ovulation with cervical mucus evaluation and basal body temperature prior to considering further infertility evaluations. Three months after that she misses a period but is pleased to report a positive home pregnancy test.
Case 3—Breakthough Bleeding On Combined Hormonal Contraceptives
A 28-year-old G0P0 in a monogamous relationship presents to her physician. She has been on oral contraceptive pills for 8 years. For the last 3 years she has been taking the pills on an extended cycle schedule. She normally takes an active pill daily for 3 cycles of pills (9 weeks), and then takes a 7-day pill-free week when she gets a menstrual period. This had been working fine until the last 6 months. She has noticed breakthrough spotting up to 2 weeks at a time during the 2nd and 3rd pack of pills.
What is the approach to evaluation and treatment in this patient?
Bleeding in Women on Combined Hormonal Contraception
Many women are now using combined hormonal contraceptives on different schedules. Extended-cycle contraception has been shown to be as effective as the traditional 21/7 schedule of active pills/pill-free week. The FDA has approved several packaged extended-cycle contraceptives. Extended-cycle contraception decreases overall number of bleeding days and improves many menstrual-related symptoms [39].Breakthrough bleeding is the most common side effect of extended cycle contraception. It is classified as AUB-I (abnormal uterine bleeding—iatrogenic). It is most common in the first few months of use, and decreases as use continues. Up to 86% of women will have unscheduled bleeding during the first 3 months of use of extended cycle contraception, but this bleedingdecreases as use continues [40].
There is no consensus as to the underlying mechanism causing this abnormal bleeding. Most clinicians believe that it is related to the balance of estrogen/progestin in each combined hormonal contraceptive. Each woman reacts differently to this combination, making it difficult to predict who will have abnormal bleeding. In women who are beginning an extended-cycle regimen, reassurance is sufficient. Most abnormal bleeding will normalize within the first 2 to 3 months. Missed pills and smoking are consistently related to breakthrough bleeding in women who take combined oral contraceptive pills [41].In women who have previously had stable bleeding patterns and who present with new breakthrough bleeding, evaluation for secondary causes of bleeding may be considered (ie, urine hCG, TSH, STI cultures, evaluation for cervical cancer screening). A pelvic examination may help determine a possible secondary cause of bleeding, but is not necessary.
Treatment of unscheduled bleeding in women on extended-cycle contraception includes shortening the hormone-free interval and adding medications for prevention/treatment of bleeding episodes. The 7-day hormone-free interval in the context of low-dose hormonal contraception may be too long. One study demonstrated that a 7-day hormone-free interval was associated with a lack of pituitary-ovarian suppression, follicular development, and possible ovulation [42].A systematic review found that shortened hormone-free intervals decreased the amount of unscheduled bleeding [39].A small RCT (65 women) of continuous contraceptive ring users found that the group that removed the ring for 4 days during an episode of unscheduled bleeding, and then reinserted it had overall reduction in unscheduled bleeding [43].Some clinicians will also recommend trying a different pill formlation or a different schedule. There is no evidence to support this recommendation, but it can be helpful in some women.
Low-dose doxycycline (40 mg daily) for prevention of unscheduled bleeding shows promise [44].This low- dose doxycycline is also helpful to prevent more unscheduled bleeding in extended-cycle oral contraceptive users [44].However, an RCT found that traditional-dose doxycline (100 mg BID) taken for 5 days at the onset of a bleeding episode, did not decrease the amount or length of unscheduled bleeding [40].Neither estrogen dose [45]nor progestin dose [45]affected bleeding patterns. There is some suggestion based on a small study that women on pills with norethindrone may have less unscheduled bleeding than those who are on pills with levonorgestrel, but more research needs to be done before clinicians change practice [46].A Cochrane review looked at one small study that suggested third-generation progestins had more favorable bleeding profiles than second-generation progestins [47].
Follow-up
The physician investigates for secondary causes of the bleeding. The patient’s urine hCG, TSH, and prolactin levels are all normal. No fibroids or polyps are seen on ultrasound. The physician and patient discuss treatment options, including a low-dose doxycycline pill to help minimize bleeding, trying a different pill formulation, or use of naproxen during the bleeding episodes, but the patient does not want to take 2 pills every day. After further discussion, the patient decides she would like to change to the contraceptive ring with the plan of removing the ring for 4 days at the onset of any unscheduled bleeding. In a phone call 6 months later, the patient states that her unscheduled bleeding has been controlled.
Corresponding author: Sarina Schrager, MD, MS, Dept. of Family Medicine, University of Wisconsin School of Medicine and Public Health, 1100 Delaplaine Ct., Madison, WI 53715, [email protected].
1. Singh S, Best C, Dunn S, et al; Society of Obstetricians and Gynaecologists of Canada. Abnormal uterine bleeding in pre-menopausal women. J Obstet Gynaecol Can 2013 May;35:473-9.
2. Nicholson WR, Ellison SA, Grason H, Powe NR. Patterns of ambulatory care use for gynecologic conditions: a national study. Am J Ob Gyn 2001;184:523-30.
3. Matteson KA, Raker CA, Clark MA, Frick KD. Abnormal uterine bleeding, health status, and usual source of medical care: analyses using the medical expenditures panel survey. J Wom Health 2013;22:959-65.
4. Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health 2007;10:183-94.
5. Goodman A. Abnormal genital tract bleeding. Clin Cornerstone 2000;3:25-35.
6. Higham JM, Shaw RW. Clinical associations with objective menstrual blood volume. Eur J Obstet Gynecol Reprod Biol 1999;82:73-6.
7. ACOG Practice Bulletin No. 128. Diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol 2012;120:197-206.
8. Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril 2007; 87:725-736.
9. Ballard KD, Seaman HE, de Vries CS, Wright JT. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study—Part 1. BJOG 2008;115:1382-91.
10. Benagiano G, Habiba M, Brosens I. The pathophysiology of uterine adenomyosis: an update. Fertil Steril 2012;98(3):572-9.
11. Krassas GE, Pontikides N, Kaltsas T, et al. Disturbances of menstruation in hypothyroidism. Clin Endocrinol 1999;50:655-9.
12. Knol HM, Mulder AB, Bogchelman DH, et al. The prevalence of underlying bleeding disorders in patients with heavy menstrual bleeding with and without gynecologic abnormalities. Am J Obstet Gynecol 2013;209:202.e1-7.
13. Kelekci S, Kaya E, Alan M, et al. Comparison of transvaginal sonography, saline infusion sonography, and office hysteroscopy in reproductive-aged women with or without abnormal uterine bleeding. Fertil Steril 2005;84:682–6.
14. Zapata LB, Whiteman MK, Tepper NK, et al. Intrauterine device use among women with uterine fibroids: a systematic review. Contraception 2010;82:41-55.
15. Sangkomkamhang US, Lumbiganon P, Laopaiboon M, Mol BWJ. Progestogens or progestogen-releasing intrauterine systems for uterine fibroids. Cochrane Database Systematic Rev 2013, Issue 2.
16. Phillip CS. Antifibrinolytics in women with menorrhagia. Thrombosis Research 2011;127(Sup 3):S113-S115.
17. Hrometz SL. Oral modified release tranexamic acid for heavy menstrual bleeding. Ann Pharmacother 2012;46:1047-53.
18. NICE clinical guidelines. Heavy menstrual bleeding. London: National Institute for Health and Care Excellence.
19. Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD001019.
20. Brown J, Kives S, Akhtar M. Progestagens and anti-progestagens for pain associated with endometriosis. Cochrane Database Syst Rev. 2012 Mar 14;3:CD002122.
21. Management of endometriosis. Practice Bulletin No. 114. American College of Obstetricians and Gynecologists. Obstet Gynecol 2010;116:223-36.
22. B. Brown J, Farquhar C. Endometriosis: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews 2014, Issue 3.
23. Farquhar C, Brosens I. Medical and surgical management of adenomyosis. Best Pract Res Clin Obstet Gynaecol 2006 Aug;20:603-16.
24. Sheng J, Zhang WY, Zhang JP, Lu D. The LNG-IUS study on adenomyosis: a 3-year follow-up study on the efficacy and side effects of the use of levonorgestrel intrauterine system for the treatment of dysmenorrhea associated with adenomyosis. Contraception 2009;79:189-93.
25. Munro MG, Critchley HO, Broder MS, Fraser IS. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. FIGO Working Group on Menstrual Disorders. Int J Gynaecol Obstet 2011;113:3–13.
26. Gupta J, Kai J, Middleton L, et al. Levonorgestrel intrauterine system versus medical therapy for menorrhagia. N Engl J Med 2013;368:128-37.
27. Lethaby A, Duckitt K, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database System Rev 2013;1: CD000400.
28. Naoulou BB, MC Ming C Tsai. Efficacy of tranexamic acid in the treatment of idiopathic and non-functional heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand 2012;91:529-37.
29. Lukes AS, Moore KA, Muse KN, et al. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol 2010;116:865-75.
30. Fergusson RJ, Lethaby A, Shepperd, S, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding Cochrane Database System Rev 2013;11:CD000329.
31. ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin 136. Management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstet Gynecol 2013;122:176-85.
32. ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin. Polycystic ovary syndrome. Obstet Gynecol 2009;114 :936-49.
33. Livinstone M, Fraser IS. Mechanisms of abnormal uterine bleeding. Human Reproduction Update 2002;8:60-67.
34. Setji TL, Brown AJ. Polycystic ovary syndrome: diagnosis and treatment. Am J Med 2007;120: 128-132.
35. Cahill D. PCOS. Clinical Evidence. BMJ Publishing Group. 2009;01:1-45.
36. Hickey M, Higam JM, Fraser I. Progestogens with our without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Reviews 2012;9:CD001895.
37. Nothinagle M, Scott-Taylor J. Does metformin improve clinical features of polycystic ovary syndrome? Cochrane for clinicians: putting evidence into practice. Am Fam Physician 2003;68:2163-4.
38. Brown J, Farquhar C, Beck J, Boothroyd C, Hughes E. Clomiphene and anti-oestrogens for ovulation induction in PCOS. Cochrane Database Systematic Rev 2009;(4): CD002249.
39. Godfrey EM, Whiteman MK, Curtis KM. Treatment of unscheduled bleeding in women using extended- or continuous-use combined hormonal contraception: a systematic review. Contraception 2013;87:567-75.
40. Kaneshiro B, Edelman A, Carlson N, et al. Treatment of unscheduled bleeding in continuous oral contraceptive users with doxycycline: a randomized controlled trial. Obstet &Gynecol 2010;115 :1141-9.
41. Grossman MP, Nakajima SP. Menstrual cycle bleeding patterns in smokers. Contraception 2006;73:562-5.
42. Schlaff WD, Lynch Am, Hughes HD, et al. Manipulation of the pill-free interval in oral contraceptive pill users: the effects on follicular suppression. Am J Obstet Gynecol 2004;190:943-51.
43. Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring. Obstet Gynecol 2008;112:563-71.
44. Kaneshiro B, Edelman A, Carlson NE, et al. A randomized controlled trial of subantimicrobial-dose doxycycline to prevent unscheduled bleeding with continuous oral contraceptive pill use. Contraception 2012;85:351-8.
45. Kaneshiro B, Edelman A, Carlson NE, et al. Unscheduled bleeding with continuous oral contraceptive pills: a comparison of progestin dose. Contraception 2012;86:22-
46. Edelman AB, Koontz SL, Nichols MD, Jensen JT. Continuous oral contraceptives: are bleeding patterns dependent on the hormones given? Obstet Gynecol 2006;107:657-65.
47. Lawrie TA, Helmerhorst FM, Maitra NK, et al. Types of progestogens in combined oral contraception: effectiveness and side-effects. Cochrane Database Syst Rev 2011; (5):CD0004681.
From the University of Wisconsin School of Medicine and Public Health, Madison, WI.
Abstract
- Objective: To describe the contributing etiologies, common presentations, diagnosis, evaluation, and management of abnormal uterine bleeding (AUB).
- Methods: Review of the literature in the context of 3 cases.
- Results: AUB is one of the most common reasons that reproductive-aged women seek health care. The causes are varied, depending in large part on the age and life stage of the woman. Diagnosis requires a systematic approach that is driven by a thorough health history and review of presenting symptoms. Determining whether the bleeding is ovulatory or anovulatory is a central part of the evaluation. A methodical history, physical examination, and laboratory evaluation may enable the physician to rule out causes such as pregnancy and pregnancy-related disorders, medications, iatrogenic causes, systemic conditions, and obvious genital tract pathology.
- Conclusion: Clinicians must be knowledgeable about AUB and partner with women to develop appropriate, individualized treatment plans.
Abnormal vaginal bleeding is a common complaint in primary care. The prevalence of some type of abnormal bleeding is up to 30% among women of reproductive age [1].Over 18% of all gynecology outpatient visits in the United States are for menorrhagia alone [2].A retrospective analysis of medical expenditures data compared 1.4 million women with abnormal uterine bleeding to over 50 million women without abnormal bleeding. This study found that women with abnormal bleeding were more likely to be younger, Caucasian, and obese and had poorer physical and mental health quality of life scores [3].
The estimated direct and indirect costs of abnormal bleeding are $1 billion and $12 billion annually, respectively [4]. Indirect costs of abnormal bleeding include time off from work and cost of products to protect clothing from bleeding (eg, tampons and pads). Abnormal bleeding is also a common reason for women to be referred to gynecologists and is an indication for up to 25% of all gynecologic surgeries [5].
History Taking
Taking a menstrual history is an important step in determining whether the current bleeding pattern is normal or abnormal. Regularity of menstrual bleeding is clarified by asking about the frequency of the menses and their duration. Other important questions include age at menarche, presence of premenstrual syndrome symptoms, breast tenderness, cervical mucus changes, and amount of bleeding. An ovulatory cycle will usually include premenstrual symptoms whereas an anovulatory cycle will be random in its symptomatology. Women’s estimates of the amount of menstrual bleeding are notoriously inaccurate. Traditionally, more than 80 cc of menstrual blood loss per cycle is considered menorrhagia. However, women and their health care providers do not measure menstrual blood volume outside of study settings, and one study found that only half of women who presented with menorrhagia actually had more than 80 cc of blood loss [6]. There is movement toward use of more patient-centered measures to diagnose men-orrhagia, such as bleeding interfering with a woman’s daily activities, needing to wake up at night to change tampons or pads, or inability to exercise during menses. Anemia in the setting of menorrhagia by history is a less subjective way to diagnose menorrhagia.
Nomenclature and Differential Diagnosis
Differential diagnosis will vary based on symptomatology as well as age. Pregnancy is a possible cause of any type of abnormal bleeding in any woman of reproductive age (ie, after menarche and before menopause). Many systemic illnesses and medications can affect menstrual bleeding and should be included in a broad differential diagnosis of a presenting woman.
Case 1—Heavy Menstrual Bleeding
Initial Presentation
A 42-year-old woman presents reporting increasingly heavy, somewhat painful periods over the last 6 to 8 months. She experienced menarche at age 12 and has had regular, moderately heavy periods throughout her adult life. She denies any inter-menstrual bleeding.
What additional history should be obtained?
Heavy menstrual bleeding refers to abnormally heavy bleeding that occurs in an ovulatory, cyclical pattern. Women with anovulatory cycles can also have heavy bleeding as well, and distinguishing ovulatory vs anovulatory cycles is often the first step in the evaluation.
The initial evaluation of a woman presenting with heavy menstrual bleeding includes a detailed history and physical examination. The first goal of the history is to establish the severity of bleeding, including any symptoms of hemodynamically significant anemia such as dizziness or exertional dyspnea. Next, the clinician should determine whether the bleeding pattern is ovulatory or anovulatory. Ovulatory heavy menstrual bleeding is most often caused by structural lesions (leiomyomas, endometriosis, adenomyosis, cervical polyps, and endometrial polyps) or a coagulopathy (von Willebrand disease, anticoagulant use, etc). Less commonly, ovulatory heavy menstrual bleeding may be due to systemic illness (including thyroid disease, renal disease, and liver disease) or endometrial hyperplasia or carcinoma.
Once an ovulatory pattern is confirmed, a history of dysmenorrhea, pelvic pain, lower urinary tract symptoms, constipation, dyspareunia, or infertility should be elicited.
Further history taking should seek to identify any symptoms suggestive of thyroid, kidney, or liver disease,
What are key elements of the physical examination?
The physical examination should include visual inspection and palpation of the thyroid gland as well as an abdominal exam to evaluate for hepatosplenomegaly or lower abdominal tenderness or masses. Signs of anemia such as pallor should also be noted. The gynecologic exam should include visual inspection of the external genitalia, a bimanual exam, and a speculum exam. Cervical and endometrial polyps may be visible as masses at the cervical os or extending into the vaginal canal. An enlarged mobile uterus with irregular contours is consistent with leiomyomas [8].Endometriosis may manifest as tenderness, thickening, or nodularity of the uterine corpus, the vaginal canal, the uterosacral ligaments, or the adnexa. Endometriosis may also cause an asymmetric, fixed position of the uterus, the cervix, or the adnexa [9].Adenomyosis may cause diffuse moderate uterine enlargement with or without tenderness [10].Endometrial carcinoma may also cause uterine enlargement and/or immobility.
What laboratory testing should be performed?
What additional testing would be useful in narrowing the differential diagnosis?
If the physical examination and initial laboratory testing is nondiagnostic, the decision to initiate a trial of symptom management or proceed with further testing (imaging and/or tissue sampling) is based on risk of endometrial cancer, severity of symptoms, and patient preference. In many women, body habitus makes a confirmatory pelvic examination difficult, which may lower the threshold for obtaining a pelvic ultrasound.
Women with risk factors for endometrial cancer should undergo office-based endometrial biopsy as the first step in evaluation of heavy menstrual bleeding [7].Risk factors include older age (45 years and older), obesity (BMI > 30), diabetes mellitus, nulliparity, and history of chronic anovulation (eg, polycystic ovary syndrome). Pelvic ultrasound is the first step in the evaluation of women with an abnormal physical exam suggesting a structural lesion [7].If the physical exam is abnormal and the pelvic ultrasound is nondiagnostic, a hysteroscopy or saline-infusion sonohysterogram should be performed, as these tests are more sensitive for the detection of intracavitary lesions and submucosal fibroids [13].Most endometrial polyps will appear as a thickened or irregular endometrium on pelvic ultrasound, but be clearly delineated on sonohysterogram. Women who have a negative initial evaluation but then go on to have persistent bleeding despite a trial of therapy also require further evaluation.
Case Continued
The patient reports that her periods are regular, with a cycle length of 30 to 31 days. She usually notes some bloating and breast tenderness in the days leading up to onset of menses. She experiences lower abdominal cramping during days 1–3 of her period. This has worsened somewhat over the last year, and sometimes radiates to her low back. Her reproductive history is significant for 3 uncomplicated vaginal deliveries and 1 first trimester spontaneous abortion. She did not experience postpartum hemorrhage, and has no history of significant oropharyngeal bleeding or unexplained bruising. Her BMI is 23.3. Her physical exam is unremarkable, including a normal thyroid, abdominal, bimanual and speculum exam. Laboratory evaluation demonstrates a low-normal hemoglobin, hematocrit, and MCV. The TSH is normal and a urine pregnancy test is negative. She had a normal pap smear and HPV assay 2 years ago.
What is the most likely diagnosis?
What treatment is recommended?
Oral tranexamic acid is an anti-fibrinolytic that was recently approved by the FDA for treatment of menorrhagia or heavy menstrual bleeding. It has been used for many years to prevent bleeding during surgery and to treat bleeding disorders. It has been used for over 30 years to treat menorrhagia in Europe. It has a different mechanism of action than NSAIDs and hormonal contraceptives, and is therefore an appropriate alternative for women who cannot tolerate other medication options [16,17].Tranexamic acid is contraindicated in women with an elevated risk of thromboembolic disease.
For women who have insufficient response to medical management or for women who present with more severe symptoms, anemia, or prominent bulk-related symptoms due to fibroids, gynecologic referral should be made for consideration of surgical intervention. The preferred interventional approach to the treatment of uterine fibroid tumors depends upon the type of fibroid (eg submucosal, intramural, subserosal), the number of fibroids, desire for future childbearing, risk for surgical complications, and patient preference. Effective options include myomectomy, uterine artery embolization, endometrial ablation, and hysterectomy [18].
By contrast, good evidence supports the use of medication as first-line therapy for heavy menstrual bleeding when it occurs in the setting of endometriosis. Estrogen-progestin oral contraceptive pills, oral progestins, and depot medroxyprogesterone have all been demonstrated to be effective in decreasing pain [19,20].The levonorgestrel-releasing intrauterine system is also effective in decreasing pain due to endometriosis [21].
Women who do not respond to first-line therapy should be referred to a gynecologist for consideration of other treatment options. Effective second-line treatment options include oral danazol, intramuscular GnRH agonists, and surgical approaches such as laparoscopic ablation and/or excision of endometriosis implants [22].
A similar range of treatment options appears to be effective in the management of heavy menstrual bleeding due to adenomyosis. First-line therapies include oral NSAIDs, oral tranexamic acid, estrogen-progestin oral contraceptive pills, and the levonorgestrel-releasing intrauterine system [23,24].Women with an inadequate response to first-line treatment should be referred to a gynecologist for consideration definitive treatment with hysterectomy versus uterine artery embolization or a trial of a GnRH agonist [24].
For some women with heavy menstrual bleeding, no specific underlying cause is identified. Current evidence suggests that such patients may have disorders of local endometrial hemostasis leading to increased blood loss during otherwise normal menstrual cycles [25].The levonorgestrel-releasing intrauterine system may be the most effective medical therapy for heavy menstrual bleeding in the absence of a specific target lesion [26].For women wishing to avoid hormonal treatment, scheduled oral NSAIDs or oral tranexamic acid are inexpensive and effective options for reducing blood loss [27–29].Other medical treatment options include estrogen-progestin contraceptive pills, cyclic oral progestin, and depot medroxy-progesterone.
For patients who experience treatment failure with pharmaceutical therapy or who desire definitive treatment, both endometrial ablation and hysterectomy have been shown to be effective and associated with high rates of patient satisfaction [30].
Follow-up
The patient reports that she would like to avoid invasive testing if possible. Given her relatively low risk for endometrial cancer, she elects a trial of scheduled NSAIDs. Unfortunately, after a couple of cycles she reports that her heavy bleeding has not been well-controlled. A pelvic ultrasound demonstrates an anterior submucosal fibroid measuring 2.4 cm and a posterior intramural fibroid measuring 1.5 cm. She agrees to insertion of a levonorgestrel IUD and calls 6 months later to report a significant decrease in her bleeding.
Case 2—Anovulation
Initial Presentation
A 27-year-old female presents for pregnancy testing. She is 2 weeks late for her period. She and her husband are attempting pregnancy and she seems disappointed that the pregnancy test is negative. She is having trouble tracking her periods. Her cycles range from 24 to 45 days apart and often she skips cycles altogether. Her flow is scant at times but some months are heavy with soaking tampons/pads.
What are diagnostic considerations in evaluating this bleeding pattern?
Menstrual history can help differentiate between of ovulatory and anovulatory abnormal bleeding. Typically, anovulatory bleeding is marked by irregular or infrequent periods. Flow can be scant to excessive. Women experiencing anovulatory cycles may fail to notice common ovulation symptoms (thin watery cervical mucus) or pre-menstrual symptoms (breast tenderness) [31].
The International Federation of Gynecology and Obstetrics (FIGO) designates AUD-O as “abnormal uterine bleeding due to ovulatory dysfunction” or “anovulatory abnormal uterine bleeding” [7,31].In general, if women are having menses at regular cycles their bleeding is likely to be ovulatory.
Differential Diagnosis
Anovulatory bleeding may be physiologic. After menarche, the hypothalamic-pituitary-ovarian axis is immature. This may result in anovulatory cycles for 2 to 3 years. Women entering perimenopausal transition may also experience intermittent anovulation and subsequent abnormal uterine bleeding. Other physiologic examples include lactation and pregnancy [31].
Physical Examination
A thorough history will help to narrow the differential diagnosis. The physical exam can evaluate for other findings that indicate endocrine dysfunction such as low body weight, hirsutism, balding, acne, high blood pressure, obesity (especially centripetal fat distribution). Acanthosis nigricans is a sign of insulin resistance which is part of the pathophysiology of PCOS. The gynecologic exam is often unremarkable in AUB-O although a bimanual exam can reveal adnexal enlargement indicative of cystic ovaries. Of note, clitoromegally is not common in PCOS. This finding would increase the likelihood of other causes of hyperandrogenism [32].
What is the pathophysiologic basis for this patient’s bleeding pattern?
Pathophysiology of Anovulatory Bleeding
Anovulatory bleeding presumes that there is a normal anatomic and genetic makeup. For example, a woman without ovaries will be, by definition, anovulatory. Using current terminology anovulatory bleeding implies a disruption in the hypothalamic-pituitary-ovarian axis and is therefore primarily an endocrine disorder [31,33].
At the level of the ovary and uterus, anovulation results in prolonged estrogen effect on the endometrium. After ovulation, the corpus luteum produces progesterone which stops endometrial thickening and stabilizes the endometrium. Without ovulation, estrogen continues endometrial stimulation and excess proliferation of endometrial lining. The endometrium becomes unstable, undifferentiated, and sheds unpredictably. The blood vessels become larger, more tortuous and have increased fragility. The result is light or heavy menstrual bleeding, decreased frequency of periods but overall unpredictable menstrual bleeding [33].
Effects of Chronic Anovulation
Irregular cycles can be more than a mere inconvenience. Women who have anovulatory cycles associated with heavy menstrual bleeding are at risk for anemia. Anovulation that is a result of hyperandrogen state or other endocrine disorder has other health ramifications. Infertility and its treatment are common sequelae. Finally, over time, unopposed estrogen in anovulation increases the risk of endometrial hyperplasia, or cancer [7,34].
Case Continued
The patient reports menarche at age 12. Her periods were irregular for the first 1–2 years but became more regular after that. She has been taking combination oral contraceptives since the age of 20 to prevent pregnancy. She stopped this 1 year ago and she and her husband began actively trying to conceive 6 months ago. Her family history is notable for diabetes and hypertension in her father. Her mother had heavy periods leading up to menopause and had a hysterectomy with no malignancy at the age of 47. She has a BMI of 33; blood pressure is mildly elevated at 134/84 mm Hg. She has oily skin and acne along her chin and neck. She has mild hirsutism of her face. Otherwise her skin is normal appearing. She has an elevated waist circumference of 35 inches. The remainder of her exam is normal.
What is the likely diagnosis?
Women with PCOS are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, type 2 diabetes and cardiovascular disease, endometrial cancer, and infertility. Women with PCOS who become pregnant have increased risk of pregnancy complications such as hypertensive disorders and gestational diabetes.
What tests are indicated in this patient?
Appropriate laboratory testing is often determined based on findings in the history and physical as well as the patient’s age. Anovulation in the first 18 months to 3 years after menarche is common and testing for pregnancy, infection, and anemia are often sufficient. Menorrhagia in adolescents warrants testing for bleeding disorders as well [7].Within 3 years of menarche, menstrual cycles should become more regular. Persistent anovulatory cycles increase the likelihood of pathologic causes and warrant additional evaluation. Pregnancy testing, thyroid stimulation hormone and prolactin levels are recommended first line evaluation [7,32,34].If PCOS is suspected an ultrasound can be performed but as noted above, polycystic ovaries are not required to make the diagnosis after adolescence.
Additional testing includes testosterone levels to look for androgen secreting tumors. Late onset congenital adrenal hyperplasia is an uncommon cause of hyperandrogenism but is more common in women of Ashkenazi Jewish descent and those with a family history [34].Morning hydroxyprogesterone can be performed to evaluate for this. If women exhibit abrupt change in menstrual pattern and other signs of cortisol excess (hypertension, abdominal striae) 24-hour urine cortisol can detect Cushing’s syndrome [34].
In patients with PCOS, additional testing to evaluate for medical comorbidities is recommended. This includes screening for diabetes, dyslipidemia, and liver dysfunction.
Case Continued
The patient’s prolactin and TSH are normal. Tests for diabetes are normal. Her LDL is elevated to 162, triglycerides are 200, and her HDL is 38. The physician informs her that she meets criteria for PCOS and also that she has obesity and metabolic syndrome.
What factors should be considered when making treatment recommendations for this patient?
Treatment for anovulation is guided by the goals of therapy. Since anovulation is an endocrine abnormality, medical treatment is first line [31].If secondary causes are diagnosed, these should be treated first. Other goals of treatment can include reducing amount and irregularity of menstruation, provide contraception, increasing ovulation in women with desired fertility, and reducing androgenic sequelae such as acne and hirsutism.
When treating the irregular or heavy bleeding associated with anovulation, first-line treatment is exogenous hormone. This can be in the form of combined estrogen/progesterone formulations (pill, patch, and ring). Medroxyprogesterone (medroxyprogesterone acetate 5–10 mg daily) taken 10 to 14 days per month is another option. Standard consideration for medical eligibility in prescribing these agents should be considered (see U.S. medical eligibility criteria for contraceptive use available at www.cdc.gov/reproductivehealth/unintendedpregnancy/usmec.htm). Combined formulations offer contraception, while cyclic progesterone does not. Both offer cyclic withdrawal bleeding. A Cochrane review did not find any RCTs comparing one to the other and therefore either are reasonable options [36].The levonorgestrel IUD is effective at treating AUB as well [31].Women may still experience intermittent vaginal bleeding or amenorrhea so it is less likely to result in cyclic withdrawal bleeding.
All of the above treatments provide the additional benefit of thinning the endometrium and preventing unopposed estrogen effect. This provides further protection the endometrial hyperplasia with chronic anovulatory cycles and unopposed estrogen [31].
In women with PCOS and associated metabolic conditions, first-line treatment is weight loss and other lifestyle interventions to improve or prevent other sequelae of the condition. Weight loss has been shown to reduce circulating androgen levels and increase ovulation. It has been shown to reduce glucose and lipid levels and hirsutism. Pregnancy rates increase as well. Weight loss achieved through medications and gastric bypass has similar effects. There is no special diet that has been shown to be more effective than another [32]. As little as a 5% weight reduction from baseline can improve PCOS symptoms [34,35].
Metformin is also commonly added to lifestyle modifications in women with PCOS to reduce risks for developing diabetes. There is little high quality evidence of added benefit above lifestyle modifications [34].Statin therapy can be considered in women with hyperlipidemia and PCOS [32].
For women with PCOS who desire to conceive, treatment should target increased ovulation. Pre-conception counseling and lifestyle modifications are again first line [32].Ovulation induction interventions carry increased risk of multiple gestation. For ovulation induction, clomiphene citrate is first line therapy. Metformin is commonly used as noted above to improve comorbidities associated with PCOS and can increase ovulation compared to placebo [37].However, RCTs do not support its use as first-line treatment of infertility treatment in PCOS. Clomiphene is 3 times more effective than metformin alone [32].
Medications can improve but often do not resolve hirsutism in women with PCOS. Combined hormonal contraceptives are commonly used off-label and no one type of pill has been shown to be superior. Anti-androgens are also off-label but empirically used. They can also improve lipid and other metabolic variables. They are all teratogenic and therefore should not be used in women who desire conception, and be used with effective contraceptives. Spironolactone is an androgen receptor antagonist. It takes months for effect. Some women will have improved menstrual frequency with this medication as well. Often adjunctive therapy such as eflornithine facial cream or laser therapy or a combination is needed to further treat hirsutism [32,35,38].
Follow-up
After discussion, the patient decides to adopt therapeutic lifestyle changes. She desires to get pregnant and does not opt for hormonal contraceptives at this time. She sees a nutritionist and begins calorie restriction and exercise. Three months later she has lost 20 pounds and feels “healthier.” Her lipid panel shows LDL of 125 and HDL of 43. Her triglycerides are now 160. Her blood pressure in the office is 118/78 mm Hg. She has lost “inches” around her middle. She has had more regular periods as well. She is still not pregnant so the physician asks her to begin tracking ovulation with cervical mucus evaluation and basal body temperature prior to considering further infertility evaluations. Three months after that she misses a period but is pleased to report a positive home pregnancy test.
Case 3—Breakthough Bleeding On Combined Hormonal Contraceptives
A 28-year-old G0P0 in a monogamous relationship presents to her physician. She has been on oral contraceptive pills for 8 years. For the last 3 years she has been taking the pills on an extended cycle schedule. She normally takes an active pill daily for 3 cycles of pills (9 weeks), and then takes a 7-day pill-free week when she gets a menstrual period. This had been working fine until the last 6 months. She has noticed breakthrough spotting up to 2 weeks at a time during the 2nd and 3rd pack of pills.
What is the approach to evaluation and treatment in this patient?
Bleeding in Women on Combined Hormonal Contraception
Many women are now using combined hormonal contraceptives on different schedules. Extended-cycle contraception has been shown to be as effective as the traditional 21/7 schedule of active pills/pill-free week. The FDA has approved several packaged extended-cycle contraceptives. Extended-cycle contraception decreases overall number of bleeding days and improves many menstrual-related symptoms [39].Breakthrough bleeding is the most common side effect of extended cycle contraception. It is classified as AUB-I (abnormal uterine bleeding—iatrogenic). It is most common in the first few months of use, and decreases as use continues. Up to 86% of women will have unscheduled bleeding during the first 3 months of use of extended cycle contraception, but this bleedingdecreases as use continues [40].
There is no consensus as to the underlying mechanism causing this abnormal bleeding. Most clinicians believe that it is related to the balance of estrogen/progestin in each combined hormonal contraceptive. Each woman reacts differently to this combination, making it difficult to predict who will have abnormal bleeding. In women who are beginning an extended-cycle regimen, reassurance is sufficient. Most abnormal bleeding will normalize within the first 2 to 3 months. Missed pills and smoking are consistently related to breakthrough bleeding in women who take combined oral contraceptive pills [41].In women who have previously had stable bleeding patterns and who present with new breakthrough bleeding, evaluation for secondary causes of bleeding may be considered (ie, urine hCG, TSH, STI cultures, evaluation for cervical cancer screening). A pelvic examination may help determine a possible secondary cause of bleeding, but is not necessary.
Treatment of unscheduled bleeding in women on extended-cycle contraception includes shortening the hormone-free interval and adding medications for prevention/treatment of bleeding episodes. The 7-day hormone-free interval in the context of low-dose hormonal contraception may be too long. One study demonstrated that a 7-day hormone-free interval was associated with a lack of pituitary-ovarian suppression, follicular development, and possible ovulation [42].A systematic review found that shortened hormone-free intervals decreased the amount of unscheduled bleeding [39].A small RCT (65 women) of continuous contraceptive ring users found that the group that removed the ring for 4 days during an episode of unscheduled bleeding, and then reinserted it had overall reduction in unscheduled bleeding [43].Some clinicians will also recommend trying a different pill formlation or a different schedule. There is no evidence to support this recommendation, but it can be helpful in some women.
Low-dose doxycycline (40 mg daily) for prevention of unscheduled bleeding shows promise [44].This low- dose doxycycline is also helpful to prevent more unscheduled bleeding in extended-cycle oral contraceptive users [44].However, an RCT found that traditional-dose doxycline (100 mg BID) taken for 5 days at the onset of a bleeding episode, did not decrease the amount or length of unscheduled bleeding [40].Neither estrogen dose [45]nor progestin dose [45]affected bleeding patterns. There is some suggestion based on a small study that women on pills with norethindrone may have less unscheduled bleeding than those who are on pills with levonorgestrel, but more research needs to be done before clinicians change practice [46].A Cochrane review looked at one small study that suggested third-generation progestins had more favorable bleeding profiles than second-generation progestins [47].
Follow-up
The physician investigates for secondary causes of the bleeding. The patient’s urine hCG, TSH, and prolactin levels are all normal. No fibroids or polyps are seen on ultrasound. The physician and patient discuss treatment options, including a low-dose doxycycline pill to help minimize bleeding, trying a different pill formulation, or use of naproxen during the bleeding episodes, but the patient does not want to take 2 pills every day. After further discussion, the patient decides she would like to change to the contraceptive ring with the plan of removing the ring for 4 days at the onset of any unscheduled bleeding. In a phone call 6 months later, the patient states that her unscheduled bleeding has been controlled.
Corresponding author: Sarina Schrager, MD, MS, Dept. of Family Medicine, University of Wisconsin School of Medicine and Public Health, 1100 Delaplaine Ct., Madison, WI 53715, [email protected].
From the University of Wisconsin School of Medicine and Public Health, Madison, WI.
Abstract
- Objective: To describe the contributing etiologies, common presentations, diagnosis, evaluation, and management of abnormal uterine bleeding (AUB).
- Methods: Review of the literature in the context of 3 cases.
- Results: AUB is one of the most common reasons that reproductive-aged women seek health care. The causes are varied, depending in large part on the age and life stage of the woman. Diagnosis requires a systematic approach that is driven by a thorough health history and review of presenting symptoms. Determining whether the bleeding is ovulatory or anovulatory is a central part of the evaluation. A methodical history, physical examination, and laboratory evaluation may enable the physician to rule out causes such as pregnancy and pregnancy-related disorders, medications, iatrogenic causes, systemic conditions, and obvious genital tract pathology.
- Conclusion: Clinicians must be knowledgeable about AUB and partner with women to develop appropriate, individualized treatment plans.
Abnormal vaginal bleeding is a common complaint in primary care. The prevalence of some type of abnormal bleeding is up to 30% among women of reproductive age [1].Over 18% of all gynecology outpatient visits in the United States are for menorrhagia alone [2].A retrospective analysis of medical expenditures data compared 1.4 million women with abnormal uterine bleeding to over 50 million women without abnormal bleeding. This study found that women with abnormal bleeding were more likely to be younger, Caucasian, and obese and had poorer physical and mental health quality of life scores [3].
The estimated direct and indirect costs of abnormal bleeding are $1 billion and $12 billion annually, respectively [4]. Indirect costs of abnormal bleeding include time off from work and cost of products to protect clothing from bleeding (eg, tampons and pads). Abnormal bleeding is also a common reason for women to be referred to gynecologists and is an indication for up to 25% of all gynecologic surgeries [5].
History Taking
Taking a menstrual history is an important step in determining whether the current bleeding pattern is normal or abnormal. Regularity of menstrual bleeding is clarified by asking about the frequency of the menses and their duration. Other important questions include age at menarche, presence of premenstrual syndrome symptoms, breast tenderness, cervical mucus changes, and amount of bleeding. An ovulatory cycle will usually include premenstrual symptoms whereas an anovulatory cycle will be random in its symptomatology. Women’s estimates of the amount of menstrual bleeding are notoriously inaccurate. Traditionally, more than 80 cc of menstrual blood loss per cycle is considered menorrhagia. However, women and their health care providers do not measure menstrual blood volume outside of study settings, and one study found that only half of women who presented with menorrhagia actually had more than 80 cc of blood loss [6]. There is movement toward use of more patient-centered measures to diagnose men-orrhagia, such as bleeding interfering with a woman’s daily activities, needing to wake up at night to change tampons or pads, or inability to exercise during menses. Anemia in the setting of menorrhagia by history is a less subjective way to diagnose menorrhagia.
Nomenclature and Differential Diagnosis
Differential diagnosis will vary based on symptomatology as well as age. Pregnancy is a possible cause of any type of abnormal bleeding in any woman of reproductive age (ie, after menarche and before menopause). Many systemic illnesses and medications can affect menstrual bleeding and should be included in a broad differential diagnosis of a presenting woman.
Case 1—Heavy Menstrual Bleeding
Initial Presentation
A 42-year-old woman presents reporting increasingly heavy, somewhat painful periods over the last 6 to 8 months. She experienced menarche at age 12 and has had regular, moderately heavy periods throughout her adult life. She denies any inter-menstrual bleeding.
What additional history should be obtained?
Heavy menstrual bleeding refers to abnormally heavy bleeding that occurs in an ovulatory, cyclical pattern. Women with anovulatory cycles can also have heavy bleeding as well, and distinguishing ovulatory vs anovulatory cycles is often the first step in the evaluation.
The initial evaluation of a woman presenting with heavy menstrual bleeding includes a detailed history and physical examination. The first goal of the history is to establish the severity of bleeding, including any symptoms of hemodynamically significant anemia such as dizziness or exertional dyspnea. Next, the clinician should determine whether the bleeding pattern is ovulatory or anovulatory. Ovulatory heavy menstrual bleeding is most often caused by structural lesions (leiomyomas, endometriosis, adenomyosis, cervical polyps, and endometrial polyps) or a coagulopathy (von Willebrand disease, anticoagulant use, etc). Less commonly, ovulatory heavy menstrual bleeding may be due to systemic illness (including thyroid disease, renal disease, and liver disease) or endometrial hyperplasia or carcinoma.
Once an ovulatory pattern is confirmed, a history of dysmenorrhea, pelvic pain, lower urinary tract symptoms, constipation, dyspareunia, or infertility should be elicited.
Further history taking should seek to identify any symptoms suggestive of thyroid, kidney, or liver disease,
What are key elements of the physical examination?
The physical examination should include visual inspection and palpation of the thyroid gland as well as an abdominal exam to evaluate for hepatosplenomegaly or lower abdominal tenderness or masses. Signs of anemia such as pallor should also be noted. The gynecologic exam should include visual inspection of the external genitalia, a bimanual exam, and a speculum exam. Cervical and endometrial polyps may be visible as masses at the cervical os or extending into the vaginal canal. An enlarged mobile uterus with irregular contours is consistent with leiomyomas [8].Endometriosis may manifest as tenderness, thickening, or nodularity of the uterine corpus, the vaginal canal, the uterosacral ligaments, or the adnexa. Endometriosis may also cause an asymmetric, fixed position of the uterus, the cervix, or the adnexa [9].Adenomyosis may cause diffuse moderate uterine enlargement with or without tenderness [10].Endometrial carcinoma may also cause uterine enlargement and/or immobility.
What laboratory testing should be performed?
What additional testing would be useful in narrowing the differential diagnosis?
If the physical examination and initial laboratory testing is nondiagnostic, the decision to initiate a trial of symptom management or proceed with further testing (imaging and/or tissue sampling) is based on risk of endometrial cancer, severity of symptoms, and patient preference. In many women, body habitus makes a confirmatory pelvic examination difficult, which may lower the threshold for obtaining a pelvic ultrasound.
Women with risk factors for endometrial cancer should undergo office-based endometrial biopsy as the first step in evaluation of heavy menstrual bleeding [7].Risk factors include older age (45 years and older), obesity (BMI > 30), diabetes mellitus, nulliparity, and history of chronic anovulation (eg, polycystic ovary syndrome). Pelvic ultrasound is the first step in the evaluation of women with an abnormal physical exam suggesting a structural lesion [7].If the physical exam is abnormal and the pelvic ultrasound is nondiagnostic, a hysteroscopy or saline-infusion sonohysterogram should be performed, as these tests are more sensitive for the detection of intracavitary lesions and submucosal fibroids [13].Most endometrial polyps will appear as a thickened or irregular endometrium on pelvic ultrasound, but be clearly delineated on sonohysterogram. Women who have a negative initial evaluation but then go on to have persistent bleeding despite a trial of therapy also require further evaluation.
Case Continued
The patient reports that her periods are regular, with a cycle length of 30 to 31 days. She usually notes some bloating and breast tenderness in the days leading up to onset of menses. She experiences lower abdominal cramping during days 1–3 of her period. This has worsened somewhat over the last year, and sometimes radiates to her low back. Her reproductive history is significant for 3 uncomplicated vaginal deliveries and 1 first trimester spontaneous abortion. She did not experience postpartum hemorrhage, and has no history of significant oropharyngeal bleeding or unexplained bruising. Her BMI is 23.3. Her physical exam is unremarkable, including a normal thyroid, abdominal, bimanual and speculum exam. Laboratory evaluation demonstrates a low-normal hemoglobin, hematocrit, and MCV. The TSH is normal and a urine pregnancy test is negative. She had a normal pap smear and HPV assay 2 years ago.
What is the most likely diagnosis?
What treatment is recommended?
Oral tranexamic acid is an anti-fibrinolytic that was recently approved by the FDA for treatment of menorrhagia or heavy menstrual bleeding. It has been used for many years to prevent bleeding during surgery and to treat bleeding disorders. It has been used for over 30 years to treat menorrhagia in Europe. It has a different mechanism of action than NSAIDs and hormonal contraceptives, and is therefore an appropriate alternative for women who cannot tolerate other medication options [16,17].Tranexamic acid is contraindicated in women with an elevated risk of thromboembolic disease.
For women who have insufficient response to medical management or for women who present with more severe symptoms, anemia, or prominent bulk-related symptoms due to fibroids, gynecologic referral should be made for consideration of surgical intervention. The preferred interventional approach to the treatment of uterine fibroid tumors depends upon the type of fibroid (eg submucosal, intramural, subserosal), the number of fibroids, desire for future childbearing, risk for surgical complications, and patient preference. Effective options include myomectomy, uterine artery embolization, endometrial ablation, and hysterectomy [18].
By contrast, good evidence supports the use of medication as first-line therapy for heavy menstrual bleeding when it occurs in the setting of endometriosis. Estrogen-progestin oral contraceptive pills, oral progestins, and depot medroxyprogesterone have all been demonstrated to be effective in decreasing pain [19,20].The levonorgestrel-releasing intrauterine system is also effective in decreasing pain due to endometriosis [21].
Women who do not respond to first-line therapy should be referred to a gynecologist for consideration of other treatment options. Effective second-line treatment options include oral danazol, intramuscular GnRH agonists, and surgical approaches such as laparoscopic ablation and/or excision of endometriosis implants [22].
A similar range of treatment options appears to be effective in the management of heavy menstrual bleeding due to adenomyosis. First-line therapies include oral NSAIDs, oral tranexamic acid, estrogen-progestin oral contraceptive pills, and the levonorgestrel-releasing intrauterine system [23,24].Women with an inadequate response to first-line treatment should be referred to a gynecologist for consideration definitive treatment with hysterectomy versus uterine artery embolization or a trial of a GnRH agonist [24].
For some women with heavy menstrual bleeding, no specific underlying cause is identified. Current evidence suggests that such patients may have disorders of local endometrial hemostasis leading to increased blood loss during otherwise normal menstrual cycles [25].The levonorgestrel-releasing intrauterine system may be the most effective medical therapy for heavy menstrual bleeding in the absence of a specific target lesion [26].For women wishing to avoid hormonal treatment, scheduled oral NSAIDs or oral tranexamic acid are inexpensive and effective options for reducing blood loss [27–29].Other medical treatment options include estrogen-progestin contraceptive pills, cyclic oral progestin, and depot medroxy-progesterone.
For patients who experience treatment failure with pharmaceutical therapy or who desire definitive treatment, both endometrial ablation and hysterectomy have been shown to be effective and associated with high rates of patient satisfaction [30].
Follow-up
The patient reports that she would like to avoid invasive testing if possible. Given her relatively low risk for endometrial cancer, she elects a trial of scheduled NSAIDs. Unfortunately, after a couple of cycles she reports that her heavy bleeding has not been well-controlled. A pelvic ultrasound demonstrates an anterior submucosal fibroid measuring 2.4 cm and a posterior intramural fibroid measuring 1.5 cm. She agrees to insertion of a levonorgestrel IUD and calls 6 months later to report a significant decrease in her bleeding.
Case 2—Anovulation
Initial Presentation
A 27-year-old female presents for pregnancy testing. She is 2 weeks late for her period. She and her husband are attempting pregnancy and she seems disappointed that the pregnancy test is negative. She is having trouble tracking her periods. Her cycles range from 24 to 45 days apart and often she skips cycles altogether. Her flow is scant at times but some months are heavy with soaking tampons/pads.
What are diagnostic considerations in evaluating this bleeding pattern?
Menstrual history can help differentiate between of ovulatory and anovulatory abnormal bleeding. Typically, anovulatory bleeding is marked by irregular or infrequent periods. Flow can be scant to excessive. Women experiencing anovulatory cycles may fail to notice common ovulation symptoms (thin watery cervical mucus) or pre-menstrual symptoms (breast tenderness) [31].
The International Federation of Gynecology and Obstetrics (FIGO) designates AUD-O as “abnormal uterine bleeding due to ovulatory dysfunction” or “anovulatory abnormal uterine bleeding” [7,31].In general, if women are having menses at regular cycles their bleeding is likely to be ovulatory.
Differential Diagnosis
Anovulatory bleeding may be physiologic. After menarche, the hypothalamic-pituitary-ovarian axis is immature. This may result in anovulatory cycles for 2 to 3 years. Women entering perimenopausal transition may also experience intermittent anovulation and subsequent abnormal uterine bleeding. Other physiologic examples include lactation and pregnancy [31].
Physical Examination
A thorough history will help to narrow the differential diagnosis. The physical exam can evaluate for other findings that indicate endocrine dysfunction such as low body weight, hirsutism, balding, acne, high blood pressure, obesity (especially centripetal fat distribution). Acanthosis nigricans is a sign of insulin resistance which is part of the pathophysiology of PCOS. The gynecologic exam is often unremarkable in AUB-O although a bimanual exam can reveal adnexal enlargement indicative of cystic ovaries. Of note, clitoromegally is not common in PCOS. This finding would increase the likelihood of other causes of hyperandrogenism [32].
What is the pathophysiologic basis for this patient’s bleeding pattern?
Pathophysiology of Anovulatory Bleeding
Anovulatory bleeding presumes that there is a normal anatomic and genetic makeup. For example, a woman without ovaries will be, by definition, anovulatory. Using current terminology anovulatory bleeding implies a disruption in the hypothalamic-pituitary-ovarian axis and is therefore primarily an endocrine disorder [31,33].
At the level of the ovary and uterus, anovulation results in prolonged estrogen effect on the endometrium. After ovulation, the corpus luteum produces progesterone which stops endometrial thickening and stabilizes the endometrium. Without ovulation, estrogen continues endometrial stimulation and excess proliferation of endometrial lining. The endometrium becomes unstable, undifferentiated, and sheds unpredictably. The blood vessels become larger, more tortuous and have increased fragility. The result is light or heavy menstrual bleeding, decreased frequency of periods but overall unpredictable menstrual bleeding [33].
Effects of Chronic Anovulation
Irregular cycles can be more than a mere inconvenience. Women who have anovulatory cycles associated with heavy menstrual bleeding are at risk for anemia. Anovulation that is a result of hyperandrogen state or other endocrine disorder has other health ramifications. Infertility and its treatment are common sequelae. Finally, over time, unopposed estrogen in anovulation increases the risk of endometrial hyperplasia, or cancer [7,34].
Case Continued
The patient reports menarche at age 12. Her periods were irregular for the first 1–2 years but became more regular after that. She has been taking combination oral contraceptives since the age of 20 to prevent pregnancy. She stopped this 1 year ago and she and her husband began actively trying to conceive 6 months ago. Her family history is notable for diabetes and hypertension in her father. Her mother had heavy periods leading up to menopause and had a hysterectomy with no malignancy at the age of 47. She has a BMI of 33; blood pressure is mildly elevated at 134/84 mm Hg. She has oily skin and acne along her chin and neck. She has mild hirsutism of her face. Otherwise her skin is normal appearing. She has an elevated waist circumference of 35 inches. The remainder of her exam is normal.
What is the likely diagnosis?
Women with PCOS are at increased risk for metabolic syndrome, nonalcoholic fatty liver disease, type 2 diabetes and cardiovascular disease, endometrial cancer, and infertility. Women with PCOS who become pregnant have increased risk of pregnancy complications such as hypertensive disorders and gestational diabetes.
What tests are indicated in this patient?
Appropriate laboratory testing is often determined based on findings in the history and physical as well as the patient’s age. Anovulation in the first 18 months to 3 years after menarche is common and testing for pregnancy, infection, and anemia are often sufficient. Menorrhagia in adolescents warrants testing for bleeding disorders as well [7].Within 3 years of menarche, menstrual cycles should become more regular. Persistent anovulatory cycles increase the likelihood of pathologic causes and warrant additional evaluation. Pregnancy testing, thyroid stimulation hormone and prolactin levels are recommended first line evaluation [7,32,34].If PCOS is suspected an ultrasound can be performed but as noted above, polycystic ovaries are not required to make the diagnosis after adolescence.
Additional testing includes testosterone levels to look for androgen secreting tumors. Late onset congenital adrenal hyperplasia is an uncommon cause of hyperandrogenism but is more common in women of Ashkenazi Jewish descent and those with a family history [34].Morning hydroxyprogesterone can be performed to evaluate for this. If women exhibit abrupt change in menstrual pattern and other signs of cortisol excess (hypertension, abdominal striae) 24-hour urine cortisol can detect Cushing’s syndrome [34].
In patients with PCOS, additional testing to evaluate for medical comorbidities is recommended. This includes screening for diabetes, dyslipidemia, and liver dysfunction.
Case Continued
The patient’s prolactin and TSH are normal. Tests for diabetes are normal. Her LDL is elevated to 162, triglycerides are 200, and her HDL is 38. The physician informs her that she meets criteria for PCOS and also that she has obesity and metabolic syndrome.
What factors should be considered when making treatment recommendations for this patient?
Treatment for anovulation is guided by the goals of therapy. Since anovulation is an endocrine abnormality, medical treatment is first line [31].If secondary causes are diagnosed, these should be treated first. Other goals of treatment can include reducing amount and irregularity of menstruation, provide contraception, increasing ovulation in women with desired fertility, and reducing androgenic sequelae such as acne and hirsutism.
When treating the irregular or heavy bleeding associated with anovulation, first-line treatment is exogenous hormone. This can be in the form of combined estrogen/progesterone formulations (pill, patch, and ring). Medroxyprogesterone (medroxyprogesterone acetate 5–10 mg daily) taken 10 to 14 days per month is another option. Standard consideration for medical eligibility in prescribing these agents should be considered (see U.S. medical eligibility criteria for contraceptive use available at www.cdc.gov/reproductivehealth/unintendedpregnancy/usmec.htm). Combined formulations offer contraception, while cyclic progesterone does not. Both offer cyclic withdrawal bleeding. A Cochrane review did not find any RCTs comparing one to the other and therefore either are reasonable options [36].The levonorgestrel IUD is effective at treating AUB as well [31].Women may still experience intermittent vaginal bleeding or amenorrhea so it is less likely to result in cyclic withdrawal bleeding.
All of the above treatments provide the additional benefit of thinning the endometrium and preventing unopposed estrogen effect. This provides further protection the endometrial hyperplasia with chronic anovulatory cycles and unopposed estrogen [31].
In women with PCOS and associated metabolic conditions, first-line treatment is weight loss and other lifestyle interventions to improve or prevent other sequelae of the condition. Weight loss has been shown to reduce circulating androgen levels and increase ovulation. It has been shown to reduce glucose and lipid levels and hirsutism. Pregnancy rates increase as well. Weight loss achieved through medications and gastric bypass has similar effects. There is no special diet that has been shown to be more effective than another [32]. As little as a 5% weight reduction from baseline can improve PCOS symptoms [34,35].
Metformin is also commonly added to lifestyle modifications in women with PCOS to reduce risks for developing diabetes. There is little high quality evidence of added benefit above lifestyle modifications [34].Statin therapy can be considered in women with hyperlipidemia and PCOS [32].
For women with PCOS who desire to conceive, treatment should target increased ovulation. Pre-conception counseling and lifestyle modifications are again first line [32].Ovulation induction interventions carry increased risk of multiple gestation. For ovulation induction, clomiphene citrate is first line therapy. Metformin is commonly used as noted above to improve comorbidities associated with PCOS and can increase ovulation compared to placebo [37].However, RCTs do not support its use as first-line treatment of infertility treatment in PCOS. Clomiphene is 3 times more effective than metformin alone [32].
Medications can improve but often do not resolve hirsutism in women with PCOS. Combined hormonal contraceptives are commonly used off-label and no one type of pill has been shown to be superior. Anti-androgens are also off-label but empirically used. They can also improve lipid and other metabolic variables. They are all teratogenic and therefore should not be used in women who desire conception, and be used with effective contraceptives. Spironolactone is an androgen receptor antagonist. It takes months for effect. Some women will have improved menstrual frequency with this medication as well. Often adjunctive therapy such as eflornithine facial cream or laser therapy or a combination is needed to further treat hirsutism [32,35,38].
Follow-up
After discussion, the patient decides to adopt therapeutic lifestyle changes. She desires to get pregnant and does not opt for hormonal contraceptives at this time. She sees a nutritionist and begins calorie restriction and exercise. Three months later she has lost 20 pounds and feels “healthier.” Her lipid panel shows LDL of 125 and HDL of 43. Her triglycerides are now 160. Her blood pressure in the office is 118/78 mm Hg. She has lost “inches” around her middle. She has had more regular periods as well. She is still not pregnant so the physician asks her to begin tracking ovulation with cervical mucus evaluation and basal body temperature prior to considering further infertility evaluations. Three months after that she misses a period but is pleased to report a positive home pregnancy test.
Case 3—Breakthough Bleeding On Combined Hormonal Contraceptives
A 28-year-old G0P0 in a monogamous relationship presents to her physician. She has been on oral contraceptive pills for 8 years. For the last 3 years she has been taking the pills on an extended cycle schedule. She normally takes an active pill daily for 3 cycles of pills (9 weeks), and then takes a 7-day pill-free week when she gets a menstrual period. This had been working fine until the last 6 months. She has noticed breakthrough spotting up to 2 weeks at a time during the 2nd and 3rd pack of pills.
What is the approach to evaluation and treatment in this patient?
Bleeding in Women on Combined Hormonal Contraception
Many women are now using combined hormonal contraceptives on different schedules. Extended-cycle contraception has been shown to be as effective as the traditional 21/7 schedule of active pills/pill-free week. The FDA has approved several packaged extended-cycle contraceptives. Extended-cycle contraception decreases overall number of bleeding days and improves many menstrual-related symptoms [39].Breakthrough bleeding is the most common side effect of extended cycle contraception. It is classified as AUB-I (abnormal uterine bleeding—iatrogenic). It is most common in the first few months of use, and decreases as use continues. Up to 86% of women will have unscheduled bleeding during the first 3 months of use of extended cycle contraception, but this bleedingdecreases as use continues [40].
There is no consensus as to the underlying mechanism causing this abnormal bleeding. Most clinicians believe that it is related to the balance of estrogen/progestin in each combined hormonal contraceptive. Each woman reacts differently to this combination, making it difficult to predict who will have abnormal bleeding. In women who are beginning an extended-cycle regimen, reassurance is sufficient. Most abnormal bleeding will normalize within the first 2 to 3 months. Missed pills and smoking are consistently related to breakthrough bleeding in women who take combined oral contraceptive pills [41].In women who have previously had stable bleeding patterns and who present with new breakthrough bleeding, evaluation for secondary causes of bleeding may be considered (ie, urine hCG, TSH, STI cultures, evaluation for cervical cancer screening). A pelvic examination may help determine a possible secondary cause of bleeding, but is not necessary.
Treatment of unscheduled bleeding in women on extended-cycle contraception includes shortening the hormone-free interval and adding medications for prevention/treatment of bleeding episodes. The 7-day hormone-free interval in the context of low-dose hormonal contraception may be too long. One study demonstrated that a 7-day hormone-free interval was associated with a lack of pituitary-ovarian suppression, follicular development, and possible ovulation [42].A systematic review found that shortened hormone-free intervals decreased the amount of unscheduled bleeding [39].A small RCT (65 women) of continuous contraceptive ring users found that the group that removed the ring for 4 days during an episode of unscheduled bleeding, and then reinserted it had overall reduction in unscheduled bleeding [43].Some clinicians will also recommend trying a different pill formlation or a different schedule. There is no evidence to support this recommendation, but it can be helpful in some women.
Low-dose doxycycline (40 mg daily) for prevention of unscheduled bleeding shows promise [44].This low- dose doxycycline is also helpful to prevent more unscheduled bleeding in extended-cycle oral contraceptive users [44].However, an RCT found that traditional-dose doxycline (100 mg BID) taken for 5 days at the onset of a bleeding episode, did not decrease the amount or length of unscheduled bleeding [40].Neither estrogen dose [45]nor progestin dose [45]affected bleeding patterns. There is some suggestion based on a small study that women on pills with norethindrone may have less unscheduled bleeding than those who are on pills with levonorgestrel, but more research needs to be done before clinicians change practice [46].A Cochrane review looked at one small study that suggested third-generation progestins had more favorable bleeding profiles than second-generation progestins [47].
Follow-up
The physician investigates for secondary causes of the bleeding. The patient’s urine hCG, TSH, and prolactin levels are all normal. No fibroids or polyps are seen on ultrasound. The physician and patient discuss treatment options, including a low-dose doxycycline pill to help minimize bleeding, trying a different pill formulation, or use of naproxen during the bleeding episodes, but the patient does not want to take 2 pills every day. After further discussion, the patient decides she would like to change to the contraceptive ring with the plan of removing the ring for 4 days at the onset of any unscheduled bleeding. In a phone call 6 months later, the patient states that her unscheduled bleeding has been controlled.
Corresponding author: Sarina Schrager, MD, MS, Dept. of Family Medicine, University of Wisconsin School of Medicine and Public Health, 1100 Delaplaine Ct., Madison, WI 53715, [email protected].
1. Singh S, Best C, Dunn S, et al; Society of Obstetricians and Gynaecologists of Canada. Abnormal uterine bleeding in pre-menopausal women. J Obstet Gynaecol Can 2013 May;35:473-9.
2. Nicholson WR, Ellison SA, Grason H, Powe NR. Patterns of ambulatory care use for gynecologic conditions: a national study. Am J Ob Gyn 2001;184:523-30.
3. Matteson KA, Raker CA, Clark MA, Frick KD. Abnormal uterine bleeding, health status, and usual source of medical care: analyses using the medical expenditures panel survey. J Wom Health 2013;22:959-65.
4. Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health 2007;10:183-94.
5. Goodman A. Abnormal genital tract bleeding. Clin Cornerstone 2000;3:25-35.
6. Higham JM, Shaw RW. Clinical associations with objective menstrual blood volume. Eur J Obstet Gynecol Reprod Biol 1999;82:73-6.
7. ACOG Practice Bulletin No. 128. Diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol 2012;120:197-206.
8. Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril 2007; 87:725-736.
9. Ballard KD, Seaman HE, de Vries CS, Wright JT. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study—Part 1. BJOG 2008;115:1382-91.
10. Benagiano G, Habiba M, Brosens I. The pathophysiology of uterine adenomyosis: an update. Fertil Steril 2012;98(3):572-9.
11. Krassas GE, Pontikides N, Kaltsas T, et al. Disturbances of menstruation in hypothyroidism. Clin Endocrinol 1999;50:655-9.
12. Knol HM, Mulder AB, Bogchelman DH, et al. The prevalence of underlying bleeding disorders in patients with heavy menstrual bleeding with and without gynecologic abnormalities. Am J Obstet Gynecol 2013;209:202.e1-7.
13. Kelekci S, Kaya E, Alan M, et al. Comparison of transvaginal sonography, saline infusion sonography, and office hysteroscopy in reproductive-aged women with or without abnormal uterine bleeding. Fertil Steril 2005;84:682–6.
14. Zapata LB, Whiteman MK, Tepper NK, et al. Intrauterine device use among women with uterine fibroids: a systematic review. Contraception 2010;82:41-55.
15. Sangkomkamhang US, Lumbiganon P, Laopaiboon M, Mol BWJ. Progestogens or progestogen-releasing intrauterine systems for uterine fibroids. Cochrane Database Systematic Rev 2013, Issue 2.
16. Phillip CS. Antifibrinolytics in women with menorrhagia. Thrombosis Research 2011;127(Sup 3):S113-S115.
17. Hrometz SL. Oral modified release tranexamic acid for heavy menstrual bleeding. Ann Pharmacother 2012;46:1047-53.
18. NICE clinical guidelines. Heavy menstrual bleeding. London: National Institute for Health and Care Excellence.
19. Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD001019.
20. Brown J, Kives S, Akhtar M. Progestagens and anti-progestagens for pain associated with endometriosis. Cochrane Database Syst Rev. 2012 Mar 14;3:CD002122.
21. Management of endometriosis. Practice Bulletin No. 114. American College of Obstetricians and Gynecologists. Obstet Gynecol 2010;116:223-36.
22. B. Brown J, Farquhar C. Endometriosis: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews 2014, Issue 3.
23. Farquhar C, Brosens I. Medical and surgical management of adenomyosis. Best Pract Res Clin Obstet Gynaecol 2006 Aug;20:603-16.
24. Sheng J, Zhang WY, Zhang JP, Lu D. The LNG-IUS study on adenomyosis: a 3-year follow-up study on the efficacy and side effects of the use of levonorgestrel intrauterine system for the treatment of dysmenorrhea associated with adenomyosis. Contraception 2009;79:189-93.
25. Munro MG, Critchley HO, Broder MS, Fraser IS. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. FIGO Working Group on Menstrual Disorders. Int J Gynaecol Obstet 2011;113:3–13.
26. Gupta J, Kai J, Middleton L, et al. Levonorgestrel intrauterine system versus medical therapy for menorrhagia. N Engl J Med 2013;368:128-37.
27. Lethaby A, Duckitt K, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database System Rev 2013;1: CD000400.
28. Naoulou BB, MC Ming C Tsai. Efficacy of tranexamic acid in the treatment of idiopathic and non-functional heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand 2012;91:529-37.
29. Lukes AS, Moore KA, Muse KN, et al. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol 2010;116:865-75.
30. Fergusson RJ, Lethaby A, Shepperd, S, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding Cochrane Database System Rev 2013;11:CD000329.
31. ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin 136. Management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstet Gynecol 2013;122:176-85.
32. ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin. Polycystic ovary syndrome. Obstet Gynecol 2009;114 :936-49.
33. Livinstone M, Fraser IS. Mechanisms of abnormal uterine bleeding. Human Reproduction Update 2002;8:60-67.
34. Setji TL, Brown AJ. Polycystic ovary syndrome: diagnosis and treatment. Am J Med 2007;120: 128-132.
35. Cahill D. PCOS. Clinical Evidence. BMJ Publishing Group. 2009;01:1-45.
36. Hickey M, Higam JM, Fraser I. Progestogens with our without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Reviews 2012;9:CD001895.
37. Nothinagle M, Scott-Taylor J. Does metformin improve clinical features of polycystic ovary syndrome? Cochrane for clinicians: putting evidence into practice. Am Fam Physician 2003;68:2163-4.
38. Brown J, Farquhar C, Beck J, Boothroyd C, Hughes E. Clomiphene and anti-oestrogens for ovulation induction in PCOS. Cochrane Database Systematic Rev 2009;(4): CD002249.
39. Godfrey EM, Whiteman MK, Curtis KM. Treatment of unscheduled bleeding in women using extended- or continuous-use combined hormonal contraception: a systematic review. Contraception 2013;87:567-75.
40. Kaneshiro B, Edelman A, Carlson N, et al. Treatment of unscheduled bleeding in continuous oral contraceptive users with doxycycline: a randomized controlled trial. Obstet &Gynecol 2010;115 :1141-9.
41. Grossman MP, Nakajima SP. Menstrual cycle bleeding patterns in smokers. Contraception 2006;73:562-5.
42. Schlaff WD, Lynch Am, Hughes HD, et al. Manipulation of the pill-free interval in oral contraceptive pill users: the effects on follicular suppression. Am J Obstet Gynecol 2004;190:943-51.
43. Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring. Obstet Gynecol 2008;112:563-71.
44. Kaneshiro B, Edelman A, Carlson NE, et al. A randomized controlled trial of subantimicrobial-dose doxycycline to prevent unscheduled bleeding with continuous oral contraceptive pill use. Contraception 2012;85:351-8.
45. Kaneshiro B, Edelman A, Carlson NE, et al. Unscheduled bleeding with continuous oral contraceptive pills: a comparison of progestin dose. Contraception 2012;86:22-
46. Edelman AB, Koontz SL, Nichols MD, Jensen JT. Continuous oral contraceptives: are bleeding patterns dependent on the hormones given? Obstet Gynecol 2006;107:657-65.
47. Lawrie TA, Helmerhorst FM, Maitra NK, et al. Types of progestogens in combined oral contraception: effectiveness and side-effects. Cochrane Database Syst Rev 2011; (5):CD0004681.
1. Singh S, Best C, Dunn S, et al; Society of Obstetricians and Gynaecologists of Canada. Abnormal uterine bleeding in pre-menopausal women. J Obstet Gynaecol Can 2013 May;35:473-9.
2. Nicholson WR, Ellison SA, Grason H, Powe NR. Patterns of ambulatory care use for gynecologic conditions: a national study. Am J Ob Gyn 2001;184:523-30.
3. Matteson KA, Raker CA, Clark MA, Frick KD. Abnormal uterine bleeding, health status, and usual source of medical care: analyses using the medical expenditures panel survey. J Wom Health 2013;22:959-65.
4. Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health 2007;10:183-94.
5. Goodman A. Abnormal genital tract bleeding. Clin Cornerstone 2000;3:25-35.
6. Higham JM, Shaw RW. Clinical associations with objective menstrual blood volume. Eur J Obstet Gynecol Reprod Biol 1999;82:73-6.
7. ACOG Practice Bulletin No. 128. Diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol 2012;120:197-206.
8. Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril 2007; 87:725-736.
9. Ballard KD, Seaman HE, de Vries CS, Wright JT. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study—Part 1. BJOG 2008;115:1382-91.
10. Benagiano G, Habiba M, Brosens I. The pathophysiology of uterine adenomyosis: an update. Fertil Steril 2012;98(3):572-9.
11. Krassas GE, Pontikides N, Kaltsas T, et al. Disturbances of menstruation in hypothyroidism. Clin Endocrinol 1999;50:655-9.
12. Knol HM, Mulder AB, Bogchelman DH, et al. The prevalence of underlying bleeding disorders in patients with heavy menstrual bleeding with and without gynecologic abnormalities. Am J Obstet Gynecol 2013;209:202.e1-7.
13. Kelekci S, Kaya E, Alan M, et al. Comparison of transvaginal sonography, saline infusion sonography, and office hysteroscopy in reproductive-aged women with or without abnormal uterine bleeding. Fertil Steril 2005;84:682–6.
14. Zapata LB, Whiteman MK, Tepper NK, et al. Intrauterine device use among women with uterine fibroids: a systematic review. Contraception 2010;82:41-55.
15. Sangkomkamhang US, Lumbiganon P, Laopaiboon M, Mol BWJ. Progestogens or progestogen-releasing intrauterine systems for uterine fibroids. Cochrane Database Systematic Rev 2013, Issue 2.
16. Phillip CS. Antifibrinolytics in women with menorrhagia. Thrombosis Research 2011;127(Sup 3):S113-S115.
17. Hrometz SL. Oral modified release tranexamic acid for heavy menstrual bleeding. Ann Pharmacother 2012;46:1047-53.
18. NICE clinical guidelines. Heavy menstrual bleeding. London: National Institute for Health and Care Excellence.
19. Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD001019.
20. Brown J, Kives S, Akhtar M. Progestagens and anti-progestagens for pain associated with endometriosis. Cochrane Database Syst Rev. 2012 Mar 14;3:CD002122.
21. Management of endometriosis. Practice Bulletin No. 114. American College of Obstetricians and Gynecologists. Obstet Gynecol 2010;116:223-36.
22. B. Brown J, Farquhar C. Endometriosis: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews 2014, Issue 3.
23. Farquhar C, Brosens I. Medical and surgical management of adenomyosis. Best Pract Res Clin Obstet Gynaecol 2006 Aug;20:603-16.
24. Sheng J, Zhang WY, Zhang JP, Lu D. The LNG-IUS study on adenomyosis: a 3-year follow-up study on the efficacy and side effects of the use of levonorgestrel intrauterine system for the treatment of dysmenorrhea associated with adenomyosis. Contraception 2009;79:189-93.
25. Munro MG, Critchley HO, Broder MS, Fraser IS. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. FIGO Working Group on Menstrual Disorders. Int J Gynaecol Obstet 2011;113:3–13.
26. Gupta J, Kai J, Middleton L, et al. Levonorgestrel intrauterine system versus medical therapy for menorrhagia. N Engl J Med 2013;368:128-37.
27. Lethaby A, Duckitt K, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database System Rev 2013;1: CD000400.
28. Naoulou BB, MC Ming C Tsai. Efficacy of tranexamic acid in the treatment of idiopathic and non-functional heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand 2012;91:529-37.
29. Lukes AS, Moore KA, Muse KN, et al. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol 2010;116:865-75.
30. Fergusson RJ, Lethaby A, Shepperd, S, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding Cochrane Database System Rev 2013;11:CD000329.
31. ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin 136. Management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstet Gynecol 2013;122:176-85.
32. ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin. Polycystic ovary syndrome. Obstet Gynecol 2009;114 :936-49.
33. Livinstone M, Fraser IS. Mechanisms of abnormal uterine bleeding. Human Reproduction Update 2002;8:60-67.
34. Setji TL, Brown AJ. Polycystic ovary syndrome: diagnosis and treatment. Am J Med 2007;120: 128-132.
35. Cahill D. PCOS. Clinical Evidence. BMJ Publishing Group. 2009;01:1-45.
36. Hickey M, Higam JM, Fraser I. Progestogens with our without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Reviews 2012;9:CD001895.
37. Nothinagle M, Scott-Taylor J. Does metformin improve clinical features of polycystic ovary syndrome? Cochrane for clinicians: putting evidence into practice. Am Fam Physician 2003;68:2163-4.
38. Brown J, Farquhar C, Beck J, Boothroyd C, Hughes E. Clomiphene and anti-oestrogens for ovulation induction in PCOS. Cochrane Database Systematic Rev 2009;(4): CD002249.
39. Godfrey EM, Whiteman MK, Curtis KM. Treatment of unscheduled bleeding in women using extended- or continuous-use combined hormonal contraception: a systematic review. Contraception 2013;87:567-75.
40. Kaneshiro B, Edelman A, Carlson N, et al. Treatment of unscheduled bleeding in continuous oral contraceptive users with doxycycline: a randomized controlled trial. Obstet &Gynecol 2010;115 :1141-9.
41. Grossman MP, Nakajima SP. Menstrual cycle bleeding patterns in smokers. Contraception 2006;73:562-5.
42. Schlaff WD, Lynch Am, Hughes HD, et al. Manipulation of the pill-free interval in oral contraceptive pill users: the effects on follicular suppression. Am J Obstet Gynecol 2004;190:943-51.
43. Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring. Obstet Gynecol 2008;112:563-71.
44. Kaneshiro B, Edelman A, Carlson NE, et al. A randomized controlled trial of subantimicrobial-dose doxycycline to prevent unscheduled bleeding with continuous oral contraceptive pill use. Contraception 2012;85:351-8.
45. Kaneshiro B, Edelman A, Carlson NE, et al. Unscheduled bleeding with continuous oral contraceptive pills: a comparison of progestin dose. Contraception 2012;86:22-
46. Edelman AB, Koontz SL, Nichols MD, Jensen JT. Continuous oral contraceptives: are bleeding patterns dependent on the hormones given? Obstet Gynecol 2006;107:657-65.
47. Lawrie TA, Helmerhorst FM, Maitra NK, et al. Types of progestogens in combined oral contraception: effectiveness and side-effects. Cochrane Database Syst Rev 2011; (5):CD0004681.
Improved Safety Event Reporting in Outpatient, Nonacademic Practices with an Anonymous, Nonpunitive Approach
From Novant Health and Novant Health Medical Group, Winston-Salem, NC.
Abstract
- Objective: To evaluate the effect of an educational intervention with regular audit and feedback on reporting of patient safety events in a nonacademic, community practice setting with an established reporting system.
- Methods: A quasi-experimental with comparator design was used to compare a 6-practice collaborative group with a 27-practice comparator group with regard to safety event reporting rates. Baseline data were collected for a 12-month period followed by recruitment of 6 practices (3 family medicine, 2 pediatric, and 1 general surgery). An educational intervention was carried out with each, and this was followed by monthly audit and regular written and in-person feedback. Practice-level comparisons were made with specialty- and size-matched practices for the 6 practices in the collaborative group.
- Results: In the 12-month period following the intervention in March 2013, the 6 practices reported 175 patient safety events compared with only 19 events in the previous 12-month period. Each practice at least doubled reporting rates, and 5 of the 6 significantly increased rates. In contrast, rates for comparator practices were unchanged, with 84 events reported for the pre-intervention period and 81 for the post-intervention period. Event classification and types of events reported were different in the collaborative practices compared with the comparators for the post-intervention period. For the collaborative group, near miss events predominated as did diagnostic testing and communication event types.
- Conclusion: An initial educational session stressing anonymous, voluntary safety event reporting together with monthly audit and feedback and a focus on developing a nonpunitive environment can significantly enhance reporting of safety events.
Multiple challenges in the outpatient setting make establishing a culture of safety and improving care delivery more difficult than for inpatient settings. In the outpatient setting, care is often inaccessible, not well coordinated between providers and between facilities and providers, and delivered in many locations. It may also involve multiple sites and providers for a single patient, may require multiple visits in a single location, and can be provided by phone, email, mail, video, or in person [1]. Errors and adverse events may take long periods of time to become apparent and are more often errors of omission compared with those in the inpatient setting [2].
Incident reporting systems are considered important in improving patient safety [3], and their limitations and value have recently been reviewed [4]. However, limited research has been conducted on medical errors in ambulatory care, and even less is available on optimal monitoring and reporting strategies [5–12].Reporting in our system is time-consuming (about 15 minutes for entry of a single report), is not tailored for outpatient practices, may be considered potentially punitive (staff may believe that reporting may place themselves at risk for performance downgrade or other actions), and marked under-reporting of safety events was suspected. Most but not all of the suggested characteristics considered important for hospital-based reporting systems are fulfilled in our ambulatory reporting system [13].
Several academic groups have reported much improved reporting and a much better understanding of the types of errors occurring in their respective outpatient settings [14–16]. The most compelling model includes a voluntary, nonpunitive, anonymous reporting approach and a multidisciplinary practice-specific team to analyze reported errors and to enact change through a continuous quality improvement process [14,15].
We implemented a project to significantly improve reporting of safety events in an outpatient, nonacademic 6-practice collaborative by using education, monthly audit, and regular feedback.
Methods
Setting
Novant Health Medical Group is a consortium of over 380 clinic sites, nearly 1300 physicians, and over 500 advanced practice clinicians. Clinic locations are found in Virginia, North Carolina, and South Carolina. Medical group members partner with physicians and staff in 15 hospitals in these geographic locations. Novant Health utilizes Epic (Epic Systems, Verona, WI) as an electronic health record. Safety event reporting is accomplished electronically in a single software program (VIncident, Verge Solutions, Mt. Pleasant, SC), used for all patients in our integrated care system (inpatient and outpatient facilities).
Intervention
Two of the authors (HWC and TC) met in March 2013 with the lead physician, practice manager, and patient safety coach at each clinic for approximately 1 hour. We discussed current reporting practice, delivered education for the safety event compendium, and detailed an anonymous, voluntary, and nonpunitive approach (stressing the use of the term “safety event” and not “error”) to reporting using a single page, 8-question paper report about the event. The report was not to be signed by the person completing the event data with placement in a drop box for later collection and electronic reporting as per usual practice in the clinic. We agreed that clinic leaders would stress to staff and providers that the initiative was nonpunitive and anonymous and that the goal was to report all known safety events, as an improvement project.
Patient safety coaches were selected for each of the 6 practices by the manager. Patient safety coaches are volunteer clinical or nonclinical staff members whose role is to observe, model, and reinforce pre-established patient safety behaviors and use of error prevention tools among peers and providers. Training requirements include an initial 2-hour training session in which they learn fundamentals of patient safety science, high reliability principles, coaching techniques for team accountability, and concepts for continuous quality improvement. Additionally, they attend monthly meetings where patient safety concepts are discussed in greater detail and best practices are shared. Following this training, each clinic’s staff was educated on the project, a process improvement team (lead physician, manager, and patient safety coach) was constituted, and the project was begun in April 2013. In quarter 3 of 2013, each practice team selected a quality improvement project based upon reported safety events in their clinic. We asked our medical group risk managers to continue event discussion with practice managers as usual, as each event is discussed briefly after a report is made.
We audited reports monthly and provided feedback to the practice team with a written report at the end of each 3-month period starting in June 2013 and ending in June 2014 (5 reports). Individual on-site visits to meet and discuss progress were completed in September 2013 and March 2014, in addition to the initial visit in March 2013.
Evaluation
We compared reported monthly safety events for each of the 6 practices and for the 6-practice collaborative in the aggregate for the 12-month pre-intervention period (April 2012 through March 2013) and post-intervention period (April 2013 through March 2014). Each practice was compared with 3 specialty- and size (number of providers)-matched practices, none of whom received education or feedback on reporting or had patient safety coaches in the practice. In addition, for each of the 3 family medicine practices in the collaborative, we matched 1:3 other family medicine practices for specialty, size, and presence of a designated and trained patient safety coach. For the duration of the project, only 50 of 380 practices in the medical group had a trained patient safety coach.
The rate of safety events reported (ie, number of safety events reported/number of patient encounters) was compared for the 2 time periods using Poisson regression or zero-inflated Poisson regression. SASenterprise guide5.1 was used for all analyses. A P value of < 0.05 was considered statistically significant. The protocol was reviewed by the institutional review board of Novant Health Presbyterian Medical Center and a waiver for informed written consent was granted.
Results
To control for the presence of patient safety coaches in practices, the 3 family medicine clinics (clinics 4 through 6, Figure 2) were each matched 1:3 for size (number of providers) and specialty (other family medicine clinics), also with a patient safety coach. While the rates were significantly increased for the 3 collaborative family medicine clinics (P < 0.001), only 1 of the comparators clinic’s rate changed significantly (0.2 or 1/44,580 to 1.3 or 6/45,157), and this change was marginally significant (P = 0.048). This practice was the only one of the 27 comparator clinics to demonstrate any increased rate.
Discussion
In our nonacademic community practices, patient safety reporting rates improved following an initial educational session stressing anonymous, voluntary safety event reporting together with monthly audit and feedback. Our findings corroborate those of others in academic ambulatory settings, who found that an emphasis on patient safety reporting, particularly if an anonymous approach is taken in a nonpunitive atmosphere, can significantly increase the reporting of patient safety events [14–16]. We demonstrated marked under-reporting and stability of patient safety event reporting throughout our ambulatory practice group and a 10-fold increase in reporting among the 6-practice collaborative.
An unexpected finding was that with the exception of 1 practice, we found no increased reporting in comparator practices that had a patient safety coach. Additionally, we noted that general surgery practices report (or experience) very few ambulatory safety events, as a total of 4 events were reported for all 4 general surgery practices in 18 months.
We chose a quasi-experimental with a comparison group and pre-test/post-test design since randomization of practices was not feasible [17]. We used a 2-year period to control for any seasonal trends and to allow time after the intervention to see if meaningful improvement in reporting over time would continue. We attempted to address the potential for nonequivalence in the comparison group by matching for specialty and size of practice.
There are several limitations to this study. Bias in the selection of collaborative practices may have occurred since each had a proven leader, and this may have led to more rapid adoption and utilization of this reporting approach. Also, our findings may not be generalizable to other integrated health systems given the unique approaches to patient safety culture development and the disparate nature of reporting systems. In addition, with our study design we could not be certain that anonymous reporting was a key factor in the increase in reporting rates, but de-briefing interviews indicated that both anonymous reporting and declaring a nonpunitive, supportive approach in each practice was important to enhanced reporting.
We expect increased reporting to decline over time without consistent feedback, as has been demonstrated in other studies [18], and we will continue to monitor rates over time.
As our current reporting system requires considerable reporter time for data input and discussion with risk managers, is not specifically configured for ambulatory reporting, is considered by staff and providers potentially punitive, and marked under-reporting is clear, we have proposed moving to a new system that is more user-friendly, ambulatory-focused, and has a provision for anonymous reporting.
Presented in part at the Institute for Healthcare Improvement 15th Annual International Summit on Improving Patient Care in the Office Practice and the Community, Washington DC, March 2014.
Acknowledgements: We gratefully acknowledge the work of collaborative practice team members, including Christopher Isenhour MD, Janet White, Shelby Carlyle, Mark Tillotson MD, Maria Migliaccio, Melanie Trapp, Jennifer Ochs, Gary DeRosa MD, Margarete Hinkle, Scott Wagner, Kelly Schetselaar, Timothy Eichenbrenner MD, Sandy Hite, Jamie Shelton, Raymond Swetenburg MD, James Lye MD, Kelly Morrison, Jan Rapisardo, Jane Moss, Rhett Brown MD, Dorothy Hedrick, Camille Farmer, and William Anderson, MS, for assistance with analysis.
Corresponding author: Herbert Clegg, MD, 108 Providence Road, Charlotte NC, 28207, [email protected].
Financial disclosures: None.
1. Tang N, Meyer GS. Ambulatory patient safety: The time is now. Arch Intern Med 2010;170:1487–9.
2. Ghandi TK, Lee TH. Patient safety beyond the hospital. N Engl J Med 2010;363:1001–3.
3. Institute of Medicine. To err is human: Building a safer health system. Washington DC: National Academies Press; 1999.
4. Pham JC, Girard T, Pronovost PJ. What to do with healthcare incident reporting systems. J Public Health Res 2013;2:e27.
5. Elder NC, Dovey SM. Classification of medical errors and preventable adverse events in primary care: A synthesis of the literature. J Fam Pract 2002;51:927–32.
6. Mohr JJ, Lannon CM, Thoma KA, et al. Learning from errors in ambulatory pediatrics. In: Henriksen K, Battles JB, Marks ES, et al, editors. Advances in patient safety: from research to implementation. Washington, DC: Agency for Healthcare Research and Quality; 2005: 355–68. Available at www.ahrq.gov//downloads/pub/advances/vol1/Mohr.pdf.
7. Phillips RL, Dovey SM, Graham D, et al. Learning from different lenses: reports of medical errors in primary care by clinicians, staff, and patients. J Patient Saf 2006;2:140–6.
8. Singh H, Thomas EJ, Khan MM, Peterson LA. Identifying diagnostic errors in primary care using an electronic screening algorithm. Arch Intern Med 2007;167:302–8.
9. Rappaport DI, Collins B, Koster A, et al. Implementing medication reconciliation in outpatient pediatrics. Pediatrics 2011;128:e1600-e1607.
10. Bishop TF, Ryan AK, Casalino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA 2011;305:2427–31.
11. Wynia MK, Classen DC. Improving ambulatory patient safety. Learning from the last decade, moving ahead in the next. JAMA 2011;306:2504–5.
12. Neuspiel DR, Stubbs EH. Patient safety in ambulatory care. Pediatr Clin North Am 2012;59:1341–54.
13. Leape LL. Patient safety. Reporting of adverse events. N Engl J Med 2002;347:1633–8.
14. Neuspiel DR, Stubbs EH, Liggin L. Improving reporting of outpatient medical errors. Pediatrics 2011;128:e1608–e1613.
15. Neuspiel DR, Gizman M, Harewood C. Improving error reporting in ambulatory pediatrics with team approach. In: Henriksen K, Battles JB, Keyes MA, et al, editors. Advances in patient safety: new directions and alternative approaches. Vol 1. Agency for Healthcare Research and Quality; 2008. Available at www.ncbi.nlm.nih.gov/books/NBK43643/.
16. Plews-Ogan ML, Nadkarni MM, Forren S, et al. Patient safety in the ambulatory setting: a clinician-based approach. J Gen Intern Med 2004;19:719–25.
17. Harris AD, McGregor JC, Perencevich EN, et al. The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inform Assoc 2006;13:16–23.
18. Gerber JS, Prasad PA, Fiks AG, et al. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA 2014;312:2569–70.
From Novant Health and Novant Health Medical Group, Winston-Salem, NC.
Abstract
- Objective: To evaluate the effect of an educational intervention with regular audit and feedback on reporting of patient safety events in a nonacademic, community practice setting with an established reporting system.
- Methods: A quasi-experimental with comparator design was used to compare a 6-practice collaborative group with a 27-practice comparator group with regard to safety event reporting rates. Baseline data were collected for a 12-month period followed by recruitment of 6 practices (3 family medicine, 2 pediatric, and 1 general surgery). An educational intervention was carried out with each, and this was followed by monthly audit and regular written and in-person feedback. Practice-level comparisons were made with specialty- and size-matched practices for the 6 practices in the collaborative group.
- Results: In the 12-month period following the intervention in March 2013, the 6 practices reported 175 patient safety events compared with only 19 events in the previous 12-month period. Each practice at least doubled reporting rates, and 5 of the 6 significantly increased rates. In contrast, rates for comparator practices were unchanged, with 84 events reported for the pre-intervention period and 81 for the post-intervention period. Event classification and types of events reported were different in the collaborative practices compared with the comparators for the post-intervention period. For the collaborative group, near miss events predominated as did diagnostic testing and communication event types.
- Conclusion: An initial educational session stressing anonymous, voluntary safety event reporting together with monthly audit and feedback and a focus on developing a nonpunitive environment can significantly enhance reporting of safety events.
Multiple challenges in the outpatient setting make establishing a culture of safety and improving care delivery more difficult than for inpatient settings. In the outpatient setting, care is often inaccessible, not well coordinated between providers and between facilities and providers, and delivered in many locations. It may also involve multiple sites and providers for a single patient, may require multiple visits in a single location, and can be provided by phone, email, mail, video, or in person [1]. Errors and adverse events may take long periods of time to become apparent and are more often errors of omission compared with those in the inpatient setting [2].
Incident reporting systems are considered important in improving patient safety [3], and their limitations and value have recently been reviewed [4]. However, limited research has been conducted on medical errors in ambulatory care, and even less is available on optimal monitoring and reporting strategies [5–12].Reporting in our system is time-consuming (about 15 minutes for entry of a single report), is not tailored for outpatient practices, may be considered potentially punitive (staff may believe that reporting may place themselves at risk for performance downgrade or other actions), and marked under-reporting of safety events was suspected. Most but not all of the suggested characteristics considered important for hospital-based reporting systems are fulfilled in our ambulatory reporting system [13].
Several academic groups have reported much improved reporting and a much better understanding of the types of errors occurring in their respective outpatient settings [14–16]. The most compelling model includes a voluntary, nonpunitive, anonymous reporting approach and a multidisciplinary practice-specific team to analyze reported errors and to enact change through a continuous quality improvement process [14,15].
We implemented a project to significantly improve reporting of safety events in an outpatient, nonacademic 6-practice collaborative by using education, monthly audit, and regular feedback.
Methods
Setting
Novant Health Medical Group is a consortium of over 380 clinic sites, nearly 1300 physicians, and over 500 advanced practice clinicians. Clinic locations are found in Virginia, North Carolina, and South Carolina. Medical group members partner with physicians and staff in 15 hospitals in these geographic locations. Novant Health utilizes Epic (Epic Systems, Verona, WI) as an electronic health record. Safety event reporting is accomplished electronically in a single software program (VIncident, Verge Solutions, Mt. Pleasant, SC), used for all patients in our integrated care system (inpatient and outpatient facilities).
Intervention
Two of the authors (HWC and TC) met in March 2013 with the lead physician, practice manager, and patient safety coach at each clinic for approximately 1 hour. We discussed current reporting practice, delivered education for the safety event compendium, and detailed an anonymous, voluntary, and nonpunitive approach (stressing the use of the term “safety event” and not “error”) to reporting using a single page, 8-question paper report about the event. The report was not to be signed by the person completing the event data with placement in a drop box for later collection and electronic reporting as per usual practice in the clinic. We agreed that clinic leaders would stress to staff and providers that the initiative was nonpunitive and anonymous and that the goal was to report all known safety events, as an improvement project.
Patient safety coaches were selected for each of the 6 practices by the manager. Patient safety coaches are volunteer clinical or nonclinical staff members whose role is to observe, model, and reinforce pre-established patient safety behaviors and use of error prevention tools among peers and providers. Training requirements include an initial 2-hour training session in which they learn fundamentals of patient safety science, high reliability principles, coaching techniques for team accountability, and concepts for continuous quality improvement. Additionally, they attend monthly meetings where patient safety concepts are discussed in greater detail and best practices are shared. Following this training, each clinic’s staff was educated on the project, a process improvement team (lead physician, manager, and patient safety coach) was constituted, and the project was begun in April 2013. In quarter 3 of 2013, each practice team selected a quality improvement project based upon reported safety events in their clinic. We asked our medical group risk managers to continue event discussion with practice managers as usual, as each event is discussed briefly after a report is made.
We audited reports monthly and provided feedback to the practice team with a written report at the end of each 3-month period starting in June 2013 and ending in June 2014 (5 reports). Individual on-site visits to meet and discuss progress were completed in September 2013 and March 2014, in addition to the initial visit in March 2013.
Evaluation
We compared reported monthly safety events for each of the 6 practices and for the 6-practice collaborative in the aggregate for the 12-month pre-intervention period (April 2012 through March 2013) and post-intervention period (April 2013 through March 2014). Each practice was compared with 3 specialty- and size (number of providers)-matched practices, none of whom received education or feedback on reporting or had patient safety coaches in the practice. In addition, for each of the 3 family medicine practices in the collaborative, we matched 1:3 other family medicine practices for specialty, size, and presence of a designated and trained patient safety coach. For the duration of the project, only 50 of 380 practices in the medical group had a trained patient safety coach.
The rate of safety events reported (ie, number of safety events reported/number of patient encounters) was compared for the 2 time periods using Poisson regression or zero-inflated Poisson regression. SASenterprise guide5.1 was used for all analyses. A P value of < 0.05 was considered statistically significant. The protocol was reviewed by the institutional review board of Novant Health Presbyterian Medical Center and a waiver for informed written consent was granted.
Results
To control for the presence of patient safety coaches in practices, the 3 family medicine clinics (clinics 4 through 6, Figure 2) were each matched 1:3 for size (number of providers) and specialty (other family medicine clinics), also with a patient safety coach. While the rates were significantly increased for the 3 collaborative family medicine clinics (P < 0.001), only 1 of the comparators clinic’s rate changed significantly (0.2 or 1/44,580 to 1.3 or 6/45,157), and this change was marginally significant (P = 0.048). This practice was the only one of the 27 comparator clinics to demonstrate any increased rate.
Discussion
In our nonacademic community practices, patient safety reporting rates improved following an initial educational session stressing anonymous, voluntary safety event reporting together with monthly audit and feedback. Our findings corroborate those of others in academic ambulatory settings, who found that an emphasis on patient safety reporting, particularly if an anonymous approach is taken in a nonpunitive atmosphere, can significantly increase the reporting of patient safety events [14–16]. We demonstrated marked under-reporting and stability of patient safety event reporting throughout our ambulatory practice group and a 10-fold increase in reporting among the 6-practice collaborative.
An unexpected finding was that with the exception of 1 practice, we found no increased reporting in comparator practices that had a patient safety coach. Additionally, we noted that general surgery practices report (or experience) very few ambulatory safety events, as a total of 4 events were reported for all 4 general surgery practices in 18 months.
We chose a quasi-experimental with a comparison group and pre-test/post-test design since randomization of practices was not feasible [17]. We used a 2-year period to control for any seasonal trends and to allow time after the intervention to see if meaningful improvement in reporting over time would continue. We attempted to address the potential for nonequivalence in the comparison group by matching for specialty and size of practice.
There are several limitations to this study. Bias in the selection of collaborative practices may have occurred since each had a proven leader, and this may have led to more rapid adoption and utilization of this reporting approach. Also, our findings may not be generalizable to other integrated health systems given the unique approaches to patient safety culture development and the disparate nature of reporting systems. In addition, with our study design we could not be certain that anonymous reporting was a key factor in the increase in reporting rates, but de-briefing interviews indicated that both anonymous reporting and declaring a nonpunitive, supportive approach in each practice was important to enhanced reporting.
We expect increased reporting to decline over time without consistent feedback, as has been demonstrated in other studies [18], and we will continue to monitor rates over time.
As our current reporting system requires considerable reporter time for data input and discussion with risk managers, is not specifically configured for ambulatory reporting, is considered by staff and providers potentially punitive, and marked under-reporting is clear, we have proposed moving to a new system that is more user-friendly, ambulatory-focused, and has a provision for anonymous reporting.
Presented in part at the Institute for Healthcare Improvement 15th Annual International Summit on Improving Patient Care in the Office Practice and the Community, Washington DC, March 2014.
Acknowledgements: We gratefully acknowledge the work of collaborative practice team members, including Christopher Isenhour MD, Janet White, Shelby Carlyle, Mark Tillotson MD, Maria Migliaccio, Melanie Trapp, Jennifer Ochs, Gary DeRosa MD, Margarete Hinkle, Scott Wagner, Kelly Schetselaar, Timothy Eichenbrenner MD, Sandy Hite, Jamie Shelton, Raymond Swetenburg MD, James Lye MD, Kelly Morrison, Jan Rapisardo, Jane Moss, Rhett Brown MD, Dorothy Hedrick, Camille Farmer, and William Anderson, MS, for assistance with analysis.
Corresponding author: Herbert Clegg, MD, 108 Providence Road, Charlotte NC, 28207, [email protected].
Financial disclosures: None.
From Novant Health and Novant Health Medical Group, Winston-Salem, NC.
Abstract
- Objective: To evaluate the effect of an educational intervention with regular audit and feedback on reporting of patient safety events in a nonacademic, community practice setting with an established reporting system.
- Methods: A quasi-experimental with comparator design was used to compare a 6-practice collaborative group with a 27-practice comparator group with regard to safety event reporting rates. Baseline data were collected for a 12-month period followed by recruitment of 6 practices (3 family medicine, 2 pediatric, and 1 general surgery). An educational intervention was carried out with each, and this was followed by monthly audit and regular written and in-person feedback. Practice-level comparisons were made with specialty- and size-matched practices for the 6 practices in the collaborative group.
- Results: In the 12-month period following the intervention in March 2013, the 6 practices reported 175 patient safety events compared with only 19 events in the previous 12-month period. Each practice at least doubled reporting rates, and 5 of the 6 significantly increased rates. In contrast, rates for comparator practices were unchanged, with 84 events reported for the pre-intervention period and 81 for the post-intervention period. Event classification and types of events reported were different in the collaborative practices compared with the comparators for the post-intervention period. For the collaborative group, near miss events predominated as did diagnostic testing and communication event types.
- Conclusion: An initial educational session stressing anonymous, voluntary safety event reporting together with monthly audit and feedback and a focus on developing a nonpunitive environment can significantly enhance reporting of safety events.
Multiple challenges in the outpatient setting make establishing a culture of safety and improving care delivery more difficult than for inpatient settings. In the outpatient setting, care is often inaccessible, not well coordinated between providers and between facilities and providers, and delivered in many locations. It may also involve multiple sites and providers for a single patient, may require multiple visits in a single location, and can be provided by phone, email, mail, video, or in person [1]. Errors and adverse events may take long periods of time to become apparent and are more often errors of omission compared with those in the inpatient setting [2].
Incident reporting systems are considered important in improving patient safety [3], and their limitations and value have recently been reviewed [4]. However, limited research has been conducted on medical errors in ambulatory care, and even less is available on optimal monitoring and reporting strategies [5–12].Reporting in our system is time-consuming (about 15 minutes for entry of a single report), is not tailored for outpatient practices, may be considered potentially punitive (staff may believe that reporting may place themselves at risk for performance downgrade or other actions), and marked under-reporting of safety events was suspected. Most but not all of the suggested characteristics considered important for hospital-based reporting systems are fulfilled in our ambulatory reporting system [13].
Several academic groups have reported much improved reporting and a much better understanding of the types of errors occurring in their respective outpatient settings [14–16]. The most compelling model includes a voluntary, nonpunitive, anonymous reporting approach and a multidisciplinary practice-specific team to analyze reported errors and to enact change through a continuous quality improvement process [14,15].
We implemented a project to significantly improve reporting of safety events in an outpatient, nonacademic 6-practice collaborative by using education, monthly audit, and regular feedback.
Methods
Setting
Novant Health Medical Group is a consortium of over 380 clinic sites, nearly 1300 physicians, and over 500 advanced practice clinicians. Clinic locations are found in Virginia, North Carolina, and South Carolina. Medical group members partner with physicians and staff in 15 hospitals in these geographic locations. Novant Health utilizes Epic (Epic Systems, Verona, WI) as an electronic health record. Safety event reporting is accomplished electronically in a single software program (VIncident, Verge Solutions, Mt. Pleasant, SC), used for all patients in our integrated care system (inpatient and outpatient facilities).
Intervention
Two of the authors (HWC and TC) met in March 2013 with the lead physician, practice manager, and patient safety coach at each clinic for approximately 1 hour. We discussed current reporting practice, delivered education for the safety event compendium, and detailed an anonymous, voluntary, and nonpunitive approach (stressing the use of the term “safety event” and not “error”) to reporting using a single page, 8-question paper report about the event. The report was not to be signed by the person completing the event data with placement in a drop box for later collection and electronic reporting as per usual practice in the clinic. We agreed that clinic leaders would stress to staff and providers that the initiative was nonpunitive and anonymous and that the goal was to report all known safety events, as an improvement project.
Patient safety coaches were selected for each of the 6 practices by the manager. Patient safety coaches are volunteer clinical or nonclinical staff members whose role is to observe, model, and reinforce pre-established patient safety behaviors and use of error prevention tools among peers and providers. Training requirements include an initial 2-hour training session in which they learn fundamentals of patient safety science, high reliability principles, coaching techniques for team accountability, and concepts for continuous quality improvement. Additionally, they attend monthly meetings where patient safety concepts are discussed in greater detail and best practices are shared. Following this training, each clinic’s staff was educated on the project, a process improvement team (lead physician, manager, and patient safety coach) was constituted, and the project was begun in April 2013. In quarter 3 of 2013, each practice team selected a quality improvement project based upon reported safety events in their clinic. We asked our medical group risk managers to continue event discussion with practice managers as usual, as each event is discussed briefly after a report is made.
We audited reports monthly and provided feedback to the practice team with a written report at the end of each 3-month period starting in June 2013 and ending in June 2014 (5 reports). Individual on-site visits to meet and discuss progress were completed in September 2013 and March 2014, in addition to the initial visit in March 2013.
Evaluation
We compared reported monthly safety events for each of the 6 practices and for the 6-practice collaborative in the aggregate for the 12-month pre-intervention period (April 2012 through March 2013) and post-intervention period (April 2013 through March 2014). Each practice was compared with 3 specialty- and size (number of providers)-matched practices, none of whom received education or feedback on reporting or had patient safety coaches in the practice. In addition, for each of the 3 family medicine practices in the collaborative, we matched 1:3 other family medicine practices for specialty, size, and presence of a designated and trained patient safety coach. For the duration of the project, only 50 of 380 practices in the medical group had a trained patient safety coach.
The rate of safety events reported (ie, number of safety events reported/number of patient encounters) was compared for the 2 time periods using Poisson regression or zero-inflated Poisson regression. SASenterprise guide5.1 was used for all analyses. A P value of < 0.05 was considered statistically significant. The protocol was reviewed by the institutional review board of Novant Health Presbyterian Medical Center and a waiver for informed written consent was granted.
Results
To control for the presence of patient safety coaches in practices, the 3 family medicine clinics (clinics 4 through 6, Figure 2) were each matched 1:3 for size (number of providers) and specialty (other family medicine clinics), also with a patient safety coach. While the rates were significantly increased for the 3 collaborative family medicine clinics (P < 0.001), only 1 of the comparators clinic’s rate changed significantly (0.2 or 1/44,580 to 1.3 or 6/45,157), and this change was marginally significant (P = 0.048). This practice was the only one of the 27 comparator clinics to demonstrate any increased rate.
Discussion
In our nonacademic community practices, patient safety reporting rates improved following an initial educational session stressing anonymous, voluntary safety event reporting together with monthly audit and feedback. Our findings corroborate those of others in academic ambulatory settings, who found that an emphasis on patient safety reporting, particularly if an anonymous approach is taken in a nonpunitive atmosphere, can significantly increase the reporting of patient safety events [14–16]. We demonstrated marked under-reporting and stability of patient safety event reporting throughout our ambulatory practice group and a 10-fold increase in reporting among the 6-practice collaborative.
An unexpected finding was that with the exception of 1 practice, we found no increased reporting in comparator practices that had a patient safety coach. Additionally, we noted that general surgery practices report (or experience) very few ambulatory safety events, as a total of 4 events were reported for all 4 general surgery practices in 18 months.
We chose a quasi-experimental with a comparison group and pre-test/post-test design since randomization of practices was not feasible [17]. We used a 2-year period to control for any seasonal trends and to allow time after the intervention to see if meaningful improvement in reporting over time would continue. We attempted to address the potential for nonequivalence in the comparison group by matching for specialty and size of practice.
There are several limitations to this study. Bias in the selection of collaborative practices may have occurred since each had a proven leader, and this may have led to more rapid adoption and utilization of this reporting approach. Also, our findings may not be generalizable to other integrated health systems given the unique approaches to patient safety culture development and the disparate nature of reporting systems. In addition, with our study design we could not be certain that anonymous reporting was a key factor in the increase in reporting rates, but de-briefing interviews indicated that both anonymous reporting and declaring a nonpunitive, supportive approach in each practice was important to enhanced reporting.
We expect increased reporting to decline over time without consistent feedback, as has been demonstrated in other studies [18], and we will continue to monitor rates over time.
As our current reporting system requires considerable reporter time for data input and discussion with risk managers, is not specifically configured for ambulatory reporting, is considered by staff and providers potentially punitive, and marked under-reporting is clear, we have proposed moving to a new system that is more user-friendly, ambulatory-focused, and has a provision for anonymous reporting.
Presented in part at the Institute for Healthcare Improvement 15th Annual International Summit on Improving Patient Care in the Office Practice and the Community, Washington DC, March 2014.
Acknowledgements: We gratefully acknowledge the work of collaborative practice team members, including Christopher Isenhour MD, Janet White, Shelby Carlyle, Mark Tillotson MD, Maria Migliaccio, Melanie Trapp, Jennifer Ochs, Gary DeRosa MD, Margarete Hinkle, Scott Wagner, Kelly Schetselaar, Timothy Eichenbrenner MD, Sandy Hite, Jamie Shelton, Raymond Swetenburg MD, James Lye MD, Kelly Morrison, Jan Rapisardo, Jane Moss, Rhett Brown MD, Dorothy Hedrick, Camille Farmer, and William Anderson, MS, for assistance with analysis.
Corresponding author: Herbert Clegg, MD, 108 Providence Road, Charlotte NC, 28207, [email protected].
Financial disclosures: None.
1. Tang N, Meyer GS. Ambulatory patient safety: The time is now. Arch Intern Med 2010;170:1487–9.
2. Ghandi TK, Lee TH. Patient safety beyond the hospital. N Engl J Med 2010;363:1001–3.
3. Institute of Medicine. To err is human: Building a safer health system. Washington DC: National Academies Press; 1999.
4. Pham JC, Girard T, Pronovost PJ. What to do with healthcare incident reporting systems. J Public Health Res 2013;2:e27.
5. Elder NC, Dovey SM. Classification of medical errors and preventable adverse events in primary care: A synthesis of the literature. J Fam Pract 2002;51:927–32.
6. Mohr JJ, Lannon CM, Thoma KA, et al. Learning from errors in ambulatory pediatrics. In: Henriksen K, Battles JB, Marks ES, et al, editors. Advances in patient safety: from research to implementation. Washington, DC: Agency for Healthcare Research and Quality; 2005: 355–68. Available at www.ahrq.gov//downloads/pub/advances/vol1/Mohr.pdf.
7. Phillips RL, Dovey SM, Graham D, et al. Learning from different lenses: reports of medical errors in primary care by clinicians, staff, and patients. J Patient Saf 2006;2:140–6.
8. Singh H, Thomas EJ, Khan MM, Peterson LA. Identifying diagnostic errors in primary care using an electronic screening algorithm. Arch Intern Med 2007;167:302–8.
9. Rappaport DI, Collins B, Koster A, et al. Implementing medication reconciliation in outpatient pediatrics. Pediatrics 2011;128:e1600-e1607.
10. Bishop TF, Ryan AK, Casalino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA 2011;305:2427–31.
11. Wynia MK, Classen DC. Improving ambulatory patient safety. Learning from the last decade, moving ahead in the next. JAMA 2011;306:2504–5.
12. Neuspiel DR, Stubbs EH. Patient safety in ambulatory care. Pediatr Clin North Am 2012;59:1341–54.
13. Leape LL. Patient safety. Reporting of adverse events. N Engl J Med 2002;347:1633–8.
14. Neuspiel DR, Stubbs EH, Liggin L. Improving reporting of outpatient medical errors. Pediatrics 2011;128:e1608–e1613.
15. Neuspiel DR, Gizman M, Harewood C. Improving error reporting in ambulatory pediatrics with team approach. In: Henriksen K, Battles JB, Keyes MA, et al, editors. Advances in patient safety: new directions and alternative approaches. Vol 1. Agency for Healthcare Research and Quality; 2008. Available at www.ncbi.nlm.nih.gov/books/NBK43643/.
16. Plews-Ogan ML, Nadkarni MM, Forren S, et al. Patient safety in the ambulatory setting: a clinician-based approach. J Gen Intern Med 2004;19:719–25.
17. Harris AD, McGregor JC, Perencevich EN, et al. The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inform Assoc 2006;13:16–23.
18. Gerber JS, Prasad PA, Fiks AG, et al. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA 2014;312:2569–70.
1. Tang N, Meyer GS. Ambulatory patient safety: The time is now. Arch Intern Med 2010;170:1487–9.
2. Ghandi TK, Lee TH. Patient safety beyond the hospital. N Engl J Med 2010;363:1001–3.
3. Institute of Medicine. To err is human: Building a safer health system. Washington DC: National Academies Press; 1999.
4. Pham JC, Girard T, Pronovost PJ. What to do with healthcare incident reporting systems. J Public Health Res 2013;2:e27.
5. Elder NC, Dovey SM. Classification of medical errors and preventable adverse events in primary care: A synthesis of the literature. J Fam Pract 2002;51:927–32.
6. Mohr JJ, Lannon CM, Thoma KA, et al. Learning from errors in ambulatory pediatrics. In: Henriksen K, Battles JB, Marks ES, et al, editors. Advances in patient safety: from research to implementation. Washington, DC: Agency for Healthcare Research and Quality; 2005: 355–68. Available at www.ahrq.gov//downloads/pub/advances/vol1/Mohr.pdf.
7. Phillips RL, Dovey SM, Graham D, et al. Learning from different lenses: reports of medical errors in primary care by clinicians, staff, and patients. J Patient Saf 2006;2:140–6.
8. Singh H, Thomas EJ, Khan MM, Peterson LA. Identifying diagnostic errors in primary care using an electronic screening algorithm. Arch Intern Med 2007;167:302–8.
9. Rappaport DI, Collins B, Koster A, et al. Implementing medication reconciliation in outpatient pediatrics. Pediatrics 2011;128:e1600-e1607.
10. Bishop TF, Ryan AK, Casalino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA 2011;305:2427–31.
11. Wynia MK, Classen DC. Improving ambulatory patient safety. Learning from the last decade, moving ahead in the next. JAMA 2011;306:2504–5.
12. Neuspiel DR, Stubbs EH. Patient safety in ambulatory care. Pediatr Clin North Am 2012;59:1341–54.
13. Leape LL. Patient safety. Reporting of adverse events. N Engl J Med 2002;347:1633–8.
14. Neuspiel DR, Stubbs EH, Liggin L. Improving reporting of outpatient medical errors. Pediatrics 2011;128:e1608–e1613.
15. Neuspiel DR, Gizman M, Harewood C. Improving error reporting in ambulatory pediatrics with team approach. In: Henriksen K, Battles JB, Keyes MA, et al, editors. Advances in patient safety: new directions and alternative approaches. Vol 1. Agency for Healthcare Research and Quality; 2008. Available at www.ncbi.nlm.nih.gov/books/NBK43643/.
16. Plews-Ogan ML, Nadkarni MM, Forren S, et al. Patient safety in the ambulatory setting: a clinician-based approach. J Gen Intern Med 2004;19:719–25.
17. Harris AD, McGregor JC, Perencevich EN, et al. The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inform Assoc 2006;13:16–23.
18. Gerber JS, Prasad PA, Fiks AG, et al. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA 2014;312:2569–70.
Outcomes of Treatment with Recombinant Tissue Plasminogen Activator in Patients Age 80 Years and Older Presenting with Acute Ischemic Stroke
From Summa Health System, Akron, OH.
Abstract
- Background: Ischemic stroke is a major cause of morbidity and mortality for patients ≥ 80 years old. The use of intravenous recombinant tissue plasminogen activator (tPA) in patients ≥ 80 years for treatment of ischemic stroke remains controversial.
- Objective: To examine outcomes in patients ≥ 80 years old who received tPA in our institution.
- Methods: This was a retrospective cohort study at a community-based certified acute stroke center. Individuals age ≥ 80 years evaluated emergently for acute neurologic changes consistent with ischemic stroke were included (n = 184). The comparison groups within this sample were patients who received tPA versus with those who did not because they came to the ED outside of the treatment window. Outcome measures included length of stay, symptomatic intracerebral hemorrhage (ICH), discharge disposition, and in-hospital death
- Results: 38 patients (20.7%) received tPA. 50 patients (27.2%) presented outside of treatment windows and were included in comparative analysis. There was no difference between groups in age (P = 0.26) or initial National Institute of Health Stroke Scale (P = 0.598). One patient (2.6%) who received tPA developed symptomatic ICH. Those receiving tPA were more likely to be discharged to acute rehabilitation hospitals (P = 0.012) and less likely to experience in hospital death (P = 0.048).
- Conclusion: At this institution, the use of tPA in patients ≥ 80 years old is not associated with increased mortality or risk of symptomatic ICH. Those who received tPA were more likely to be discharged to acute rehabilitation hospitals, suggesting greater potential for functional recovery.
Acute ischemic stroke is a major cause of morbidity and mortality in patients 80 years or older. Though less than 5% of the United States population is over the age of 80 [1], studies have shown that up to one-third of patients presenting with ischemic stroke are ≥ 80 years old [2] and among first-time strokes, a third occur in those ≥ 80 [3]. Older adults present with worse symptoms associated with ischemic stroke as measured by the National Institutes of Health Stroke Scale (NIHSS) compared with younger (< 80 years) counterparts [4]. Older patients are more likely to be discharged to a location other than home [5]. Older age is associated with higher hospital, 30-day, and 1-year mortality [3,5,6]. Patients ≥ 80 are significantly more likely to die in the hospital compared to younger patients, 11.7% to 23.6% vs 5.1%, respectively [3,7].
The Food and Drug Administration (FDA) approved the use of intravenous recombinant tissue plasminogen activator (tPA) in 1996 for the treatment of ischemic stroke [8]. Studies evaluating the safety and efficacy of tPA in ischemic stroke excluded or underrepresented patients ≥ 80 [8,9]. The use of tPA in those ≥ 80 has not been shown consistently to improve outcomes [6,10,11]. Post-hoc analysis of the National Institute of Neurologic Disorders and Stroke (NINDS) study did not show worse outcomes or harms to older adults treated with tPA [12]. Likewise, data from the International Stroke Treatment (IST-3) collaborative group show that treatment with tPA up to 6 hours from the onset of symptoms improves outcomes in the elderly [13]. Use of tPA in the oldest adults remains controversial due to perceived higher risk of symptomatic intracerebral hemorrhage (ICH). Published data suggest overall ICH risk of 4.3% to 6.4% across all age-groups [9,14,15].Studies have failed to demonstrate an increased risk in the oldest adults [4,10,16,17], though they may have higher mortality rates associated with ICH [15]. Despite this, trends suggest increasing use of tPA in those ≥ 80 over the past decade [2]. Along with primary data from NINDS [12] and IST-3 [13], a meta-analysis conducted in 2014 suggests that regardless of age, patients have improved outcomes with tPA [18].With the increasing age of the population, effective treatment of strokes in patients ≥ 80 will continue to be an important clinical and research endeavor.
This study evaluates the outcomes of clinical use of tPA for treatment of patients ≥ 80 years old who present to a community-based certified stroke center with ischemic stroke.
Methods
The study setting was a 540-bed acute care hospital that is a community-based certified stroke center. This study was deemed nonhuman subjects research by the institutional review board as the goal was to evaluate processes and outcomes of this institution’s stroke team in treating a subgroup of patients according to clinically accepted practice (quality improvement initiative). All patients presenting to the emergency department (ED) between 1 January 2011 and 30 November 2013 with the onset of stroke-like neurological deficits underwent evaluation and treatment by a neurologist and/or specially trained stroke team. This team consists of the attending neurologist, ED physician, resident physicians, advanced practice nurses, and ED staff nurses and emergency medicine technicians. Team members involved in the evaluation and treatment of these patients undergo routine clinical education and testing to ensure standardization. Patients undergo emergent evaluation including the National Institutes of Health Stroke Scale (NIHSS) and obtain brain imaging with computed tomography (CT).
Patients ≥ 80 years were identified among all those who presented to the ED with ischemic stroke. Patients were included if they were subsequently diagnosed with ischemic stroke or transient ischemic attacks (TIA). They were excluded from analysis if neurological changes were due to primary hemorrhagic stroke, intracranial hemorrhage, subarachnoid hemorrhage, seizure, conversion disorder, or metabolic derangements. They were also excluded from analysis if the acute ischemic stroke treatment included intra-arterial administration of tPA or endovascular revascularization.
Patient data collected included age, NIHSS at presentation to ED, time to presentation at ED, treatment with tPA, contraindications to tPA, discharge disposition, length of stay and in-hospital mortality. Raw NIHSS values were collected at the time of presentation. NIHSS were categorized into mild symptoms (NIHSS < 6), moderate symptoms (NIHSS 6–19), or severe symptoms (NIHSS ≥ 20). Clinical indications for receiving tPA include NIHSS > 4, focal neurological deficit onset < 3 hours (for those ≥ 80 years old), and no evidence of acute hemorrhage or acute infarct on CT. Contraindications include rapidly improving symptoms (repeat NIHSS < 4), active or history of intracranial hemorrhage, history of stroke or head trauma in past 3 months, gastrointestinal or genitourinary hemorrhage within 21 days, major surgery within 14 days, arterial puncture at a noncompressible site in past 7 days, treatment with anticoagulation with therapeutic indices, systolic blood pressure > 185 mm Hg or diastolic blood pressure > 110 mm Hg and not responding to treatment, or platelet count < 100,000/mm3. Patients who were not eligible for tPA based on contraindications with the exception of being outside the treatment window (3 hours) were excluded from comparative analysis. Patient length of stay was rounded to nearest full day. Discharge disposition was categorized as home, acute rehabilitation hospital, skilled nursing facility, home or facility with hospice services, other hospital setting, or death.
Statistics were calculated using SPSS statistical software. Variables were reported as means and percentages. Group means were compared using t tests and differences in proportions were compared using the chi square test. Correlations were performed using Pearson’s correlation. A 2-tailed P < 0.05 was considered statistically significant.
Results
Discussion
Ischemic stroke remains a major cause of morbidity and mortality for very old patients. Though less than 5% of the United States population is over the age of 80 [1], at this community-based hospital 18% of those presenting to the ED with ischemic stroke were in this age-group. With a population of increasing age, more people in this age-group will present with ischemic stroke and need effective treatment to limit the associated morbidity and mortality. Being able to quickly and safely treat acute ischemic stroke may help very old adults maintain independence or prevent institutionalization. While the original studies demonstrating the effectiveness of tPA for acute ischemic stroke excluded or underrepresented those ≥ 80 years, retrospective analysis has not been conclusive regarding its use in very old patients [4–6,10,12,13].However, post-hoc analysis of NINDS and IST-3 data demonstrate efficacy and safety of treatment [12,13].
This study explored the use of tPA at a community-based certified stroke center. Similar to previous studies, it demonstrates the large proportion of patients presenting with acute neurological findings consistent with ischemic stroke are ≥ 80 years old [3,6]. Our incidence of acute ischemic stroke in the oldest patients may be slightly lower than reported elsewhere, which may reflect community differences, with higher rates of younger patients with multiple comorbidities presenting with stroke-like symptoms. Amongst this very old cohort, age was positively correlated with stroke severity. Mortality in patients ≥ 80 years old who present with acute ischemic stroke approaches 25%.
The majority of patients who did not receive tPA had documented contraindications to receiving the medication. The most common reason was rapidly improving symptoms with repeat NIHSS often ≤ 4. The second most common reason was presentation outside the treatment window of 3 hours. We compared those who either arrived too late to receive treatment with tPA or already had ischemic changes on CT to those who received tPA as this suggests the natural history of stroke progression and outcome without effective, early treatment. The outcomes at this institution support this trend. Very old patients who received tPA did not experience harm as evidenced by similar lengths of stay and rates of discharge to home. Also, rates of symptomatic ICH were lower than those reported in the literature. In fact, patients who received tPA were less likely to experience in-hospital death and more likely to be discharged to acute rehabilitation hospitals, suggesting more functional ability to tolerate aggressive recovery efforts.
Very few people who presented with acute ischemic stroke and were eligible for treatment with tPA failed to receive it. This suggests that despite the perceived increased risk to treating these patients with tPA, the specialized stroke team aggressively treats patients age ≥ 80 years who present with acute ischemic stroke. However, those who did not receive tPA were more likely to have presented with mild or severe strokes. This may suggest that treatment time frames are more strongly held, or that treatment teams are more likely to use time frames as a reason to not treat with tPA for patients with mild or severe strokes. Also, very few patients and families who were eligible to receive tPA declined treatment despite the associated risks. This suggests that patients and families are eager for aggressive treatment in attempt to prevent death or disability associated with ischemic stroke.
There are several limitations associated with this evaluation. First, this is a retrospective analysis of a single institution’s acute stroke procedures. Data was collected in an effort to evaluate the processes and outcomes of the specialized stroke team in evaluating and treating this very old cohort who present to a community-based hospital. It involved individualized clinical evaluation and decision making by multiple care providers who may offer different perspectives on the risk of treating patients ≥ 80 years old with tPA, which may result in selection bias. While comparing those who arrived outside treatment windows offers a comparison group who represents the natural course of untreated strokes, patient characteristics that prevented timely evaluation may also impact their outcomes including baseline mobility, care giving availability and underlying medical comorbidities. The similarity in mean presenting NIHSS scores of the two groups, however, argues against this possibility. Lastly, exclusion criteria to receiving tPA may represent intrinsic characteristics that impart higher risk of negative outcomes.
Conculsion
Although there have been no randomized controlled trials that evaluate the safety and efficacy of tPA in the treatment of acute ischemic stroke in very old patients, use at the community-based stroke center was not associated with worse outcomes including symptomatic ICH, hospital length of stay, and in-hospital mortality. In fact, there were trends towards better outcomes in older patients who received tPA, including a significant reduction in in-hospital mortality. This evaluation supports the benefits of using tPA to treat acute ischemic stroke as seen in prior randomized controlled trials that included the treatment of very old patients. Though ongoing research is needed, a growing body of evidence supports the use of tPA to treat acute ischemic stroke in patients ≥ 80 years.
Corresponding author: Jennifer C. Drost, DO, MPH, Summa Health System, 75 Arch St., Ste. G1, Akron, OH 44304, [email protected].
Financial disclosures: None.
Author contributions: Conception and design, JCD, SMB; analysis and interpretation of data, JCD, SMB; drafting of article, JCD; critical revision of the article, JCD, SMB; provision of study materials or patients, SMB; collection and assembly of data, JCD.
1. US Census Bureau. Annual estimates of the resident population for selected age groups by sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2013. Accessed at www.census.gov/popest/index.html.
2. Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med 2010;5:406–9.
3. Marini C, Baldassarre M, Russo T, et al. Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology 2004;62:77–81.
4. Sylaja PN, Cote R, Buchan AM, Hill MD. Thrombolysis in patients older than 80 years with acute ischaemic stroke: Canadian Alteplase for Stroke Effectiveness Study. J Neurol Neurosurg Psychiatry 2006;77:826–9.
5. Heitsch LE, Panagos PD. Treating the elderly stroke patient: complications, controversies, and best care metrics. Clin Geriatr Med 2013;29:231–55.
6. Engelter ST, Bonati LH, Lyrer PA. Intravenous thrombolysis in stroke patients of > or = 80 versus < 80 years of age--a systematic review across cohort studies. Age Ageing 2006;35:572–580.
7. Forti P, Maioli F, Procaccianti G, et al. Independent predictors of ischemic stroke in the elderly: prospective data from a stroke unit. Neurology 2013;80:29–38.
8. Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTischemic stroke, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768–74.
9. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–7.
10. Sung PS, Chen CH, Hsieh HC, et al. Outcome of acute ischemic stroke in very elderly patients: is intravenous thrombolysis beneficial? Eur Neurol 2011;66:110–6.
11. Saposnik G, Guzik AK, Reeves M, et al. Stroke prognostication using age and NIH Stroke Scale: SPAN-100. Neurology 2013;80:21–8.
12. Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA Stroke Trial. Stroke 1997;28:2119–25.
13. Sandercock P, Wardlaw JM, Lindley RI, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 2012;379:2352–63.
14. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke 1997;28:2109–18.
15. Bray BD, Campbell J, Hoffman A, et al. Stroke thrombolysis in England: an age stratified analysis of practice and outcome. Age Ageing 2013;42:240–5.
16. Kono S, Deguchi K, Morimoto N, et al. Intravenous thrombolysis with neuroprotective therapy by edaravone for ischemic stroke patients older than 80 years of age. J Stroke Cerebrovasc Dis 2013;22:1175–83.
17. Berrouschot J, Rother J, Glahn J, et al. Outcome and severe hemorrhagic complications of intravenous thrombolysis with tissue plasminogen activator in very old (> or =80 years) stroke patients. Stroke 2005;36:2421–5.
18. Emberson J, Lees KR, Lyden P, et al; Stroke Thrombolysis Trialists' Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35.
From Summa Health System, Akron, OH.
Abstract
- Background: Ischemic stroke is a major cause of morbidity and mortality for patients ≥ 80 years old. The use of intravenous recombinant tissue plasminogen activator (tPA) in patients ≥ 80 years for treatment of ischemic stroke remains controversial.
- Objective: To examine outcomes in patients ≥ 80 years old who received tPA in our institution.
- Methods: This was a retrospective cohort study at a community-based certified acute stroke center. Individuals age ≥ 80 years evaluated emergently for acute neurologic changes consistent with ischemic stroke were included (n = 184). The comparison groups within this sample were patients who received tPA versus with those who did not because they came to the ED outside of the treatment window. Outcome measures included length of stay, symptomatic intracerebral hemorrhage (ICH), discharge disposition, and in-hospital death
- Results: 38 patients (20.7%) received tPA. 50 patients (27.2%) presented outside of treatment windows and were included in comparative analysis. There was no difference between groups in age (P = 0.26) or initial National Institute of Health Stroke Scale (P = 0.598). One patient (2.6%) who received tPA developed symptomatic ICH. Those receiving tPA were more likely to be discharged to acute rehabilitation hospitals (P = 0.012) and less likely to experience in hospital death (P = 0.048).
- Conclusion: At this institution, the use of tPA in patients ≥ 80 years old is not associated with increased mortality or risk of symptomatic ICH. Those who received tPA were more likely to be discharged to acute rehabilitation hospitals, suggesting greater potential for functional recovery.
Acute ischemic stroke is a major cause of morbidity and mortality in patients 80 years or older. Though less than 5% of the United States population is over the age of 80 [1], studies have shown that up to one-third of patients presenting with ischemic stroke are ≥ 80 years old [2] and among first-time strokes, a third occur in those ≥ 80 [3]. Older adults present with worse symptoms associated with ischemic stroke as measured by the National Institutes of Health Stroke Scale (NIHSS) compared with younger (< 80 years) counterparts [4]. Older patients are more likely to be discharged to a location other than home [5]. Older age is associated with higher hospital, 30-day, and 1-year mortality [3,5,6]. Patients ≥ 80 are significantly more likely to die in the hospital compared to younger patients, 11.7% to 23.6% vs 5.1%, respectively [3,7].
The Food and Drug Administration (FDA) approved the use of intravenous recombinant tissue plasminogen activator (tPA) in 1996 for the treatment of ischemic stroke [8]. Studies evaluating the safety and efficacy of tPA in ischemic stroke excluded or underrepresented patients ≥ 80 [8,9]. The use of tPA in those ≥ 80 has not been shown consistently to improve outcomes [6,10,11]. Post-hoc analysis of the National Institute of Neurologic Disorders and Stroke (NINDS) study did not show worse outcomes or harms to older adults treated with tPA [12]. Likewise, data from the International Stroke Treatment (IST-3) collaborative group show that treatment with tPA up to 6 hours from the onset of symptoms improves outcomes in the elderly [13]. Use of tPA in the oldest adults remains controversial due to perceived higher risk of symptomatic intracerebral hemorrhage (ICH). Published data suggest overall ICH risk of 4.3% to 6.4% across all age-groups [9,14,15].Studies have failed to demonstrate an increased risk in the oldest adults [4,10,16,17], though they may have higher mortality rates associated with ICH [15]. Despite this, trends suggest increasing use of tPA in those ≥ 80 over the past decade [2]. Along with primary data from NINDS [12] and IST-3 [13], a meta-analysis conducted in 2014 suggests that regardless of age, patients have improved outcomes with tPA [18].With the increasing age of the population, effective treatment of strokes in patients ≥ 80 will continue to be an important clinical and research endeavor.
This study evaluates the outcomes of clinical use of tPA for treatment of patients ≥ 80 years old who present to a community-based certified stroke center with ischemic stroke.
Methods
The study setting was a 540-bed acute care hospital that is a community-based certified stroke center. This study was deemed nonhuman subjects research by the institutional review board as the goal was to evaluate processes and outcomes of this institution’s stroke team in treating a subgroup of patients according to clinically accepted practice (quality improvement initiative). All patients presenting to the emergency department (ED) between 1 January 2011 and 30 November 2013 with the onset of stroke-like neurological deficits underwent evaluation and treatment by a neurologist and/or specially trained stroke team. This team consists of the attending neurologist, ED physician, resident physicians, advanced practice nurses, and ED staff nurses and emergency medicine technicians. Team members involved in the evaluation and treatment of these patients undergo routine clinical education and testing to ensure standardization. Patients undergo emergent evaluation including the National Institutes of Health Stroke Scale (NIHSS) and obtain brain imaging with computed tomography (CT).
Patients ≥ 80 years were identified among all those who presented to the ED with ischemic stroke. Patients were included if they were subsequently diagnosed with ischemic stroke or transient ischemic attacks (TIA). They were excluded from analysis if neurological changes were due to primary hemorrhagic stroke, intracranial hemorrhage, subarachnoid hemorrhage, seizure, conversion disorder, or metabolic derangements. They were also excluded from analysis if the acute ischemic stroke treatment included intra-arterial administration of tPA or endovascular revascularization.
Patient data collected included age, NIHSS at presentation to ED, time to presentation at ED, treatment with tPA, contraindications to tPA, discharge disposition, length of stay and in-hospital mortality. Raw NIHSS values were collected at the time of presentation. NIHSS were categorized into mild symptoms (NIHSS < 6), moderate symptoms (NIHSS 6–19), or severe symptoms (NIHSS ≥ 20). Clinical indications for receiving tPA include NIHSS > 4, focal neurological deficit onset < 3 hours (for those ≥ 80 years old), and no evidence of acute hemorrhage or acute infarct on CT. Contraindications include rapidly improving symptoms (repeat NIHSS < 4), active or history of intracranial hemorrhage, history of stroke or head trauma in past 3 months, gastrointestinal or genitourinary hemorrhage within 21 days, major surgery within 14 days, arterial puncture at a noncompressible site in past 7 days, treatment with anticoagulation with therapeutic indices, systolic blood pressure > 185 mm Hg or diastolic blood pressure > 110 mm Hg and not responding to treatment, or platelet count < 100,000/mm3. Patients who were not eligible for tPA based on contraindications with the exception of being outside the treatment window (3 hours) were excluded from comparative analysis. Patient length of stay was rounded to nearest full day. Discharge disposition was categorized as home, acute rehabilitation hospital, skilled nursing facility, home or facility with hospice services, other hospital setting, or death.
Statistics were calculated using SPSS statistical software. Variables were reported as means and percentages. Group means were compared using t tests and differences in proportions were compared using the chi square test. Correlations were performed using Pearson’s correlation. A 2-tailed P < 0.05 was considered statistically significant.
Results
Discussion
Ischemic stroke remains a major cause of morbidity and mortality for very old patients. Though less than 5% of the United States population is over the age of 80 [1], at this community-based hospital 18% of those presenting to the ED with ischemic stroke were in this age-group. With a population of increasing age, more people in this age-group will present with ischemic stroke and need effective treatment to limit the associated morbidity and mortality. Being able to quickly and safely treat acute ischemic stroke may help very old adults maintain independence or prevent institutionalization. While the original studies demonstrating the effectiveness of tPA for acute ischemic stroke excluded or underrepresented those ≥ 80 years, retrospective analysis has not been conclusive regarding its use in very old patients [4–6,10,12,13].However, post-hoc analysis of NINDS and IST-3 data demonstrate efficacy and safety of treatment [12,13].
This study explored the use of tPA at a community-based certified stroke center. Similar to previous studies, it demonstrates the large proportion of patients presenting with acute neurological findings consistent with ischemic stroke are ≥ 80 years old [3,6]. Our incidence of acute ischemic stroke in the oldest patients may be slightly lower than reported elsewhere, which may reflect community differences, with higher rates of younger patients with multiple comorbidities presenting with stroke-like symptoms. Amongst this very old cohort, age was positively correlated with stroke severity. Mortality in patients ≥ 80 years old who present with acute ischemic stroke approaches 25%.
The majority of patients who did not receive tPA had documented contraindications to receiving the medication. The most common reason was rapidly improving symptoms with repeat NIHSS often ≤ 4. The second most common reason was presentation outside the treatment window of 3 hours. We compared those who either arrived too late to receive treatment with tPA or already had ischemic changes on CT to those who received tPA as this suggests the natural history of stroke progression and outcome without effective, early treatment. The outcomes at this institution support this trend. Very old patients who received tPA did not experience harm as evidenced by similar lengths of stay and rates of discharge to home. Also, rates of symptomatic ICH were lower than those reported in the literature. In fact, patients who received tPA were less likely to experience in-hospital death and more likely to be discharged to acute rehabilitation hospitals, suggesting more functional ability to tolerate aggressive recovery efforts.
Very few people who presented with acute ischemic stroke and were eligible for treatment with tPA failed to receive it. This suggests that despite the perceived increased risk to treating these patients with tPA, the specialized stroke team aggressively treats patients age ≥ 80 years who present with acute ischemic stroke. However, those who did not receive tPA were more likely to have presented with mild or severe strokes. This may suggest that treatment time frames are more strongly held, or that treatment teams are more likely to use time frames as a reason to not treat with tPA for patients with mild or severe strokes. Also, very few patients and families who were eligible to receive tPA declined treatment despite the associated risks. This suggests that patients and families are eager for aggressive treatment in attempt to prevent death or disability associated with ischemic stroke.
There are several limitations associated with this evaluation. First, this is a retrospective analysis of a single institution’s acute stroke procedures. Data was collected in an effort to evaluate the processes and outcomes of the specialized stroke team in evaluating and treating this very old cohort who present to a community-based hospital. It involved individualized clinical evaluation and decision making by multiple care providers who may offer different perspectives on the risk of treating patients ≥ 80 years old with tPA, which may result in selection bias. While comparing those who arrived outside treatment windows offers a comparison group who represents the natural course of untreated strokes, patient characteristics that prevented timely evaluation may also impact their outcomes including baseline mobility, care giving availability and underlying medical comorbidities. The similarity in mean presenting NIHSS scores of the two groups, however, argues against this possibility. Lastly, exclusion criteria to receiving tPA may represent intrinsic characteristics that impart higher risk of negative outcomes.
Conculsion
Although there have been no randomized controlled trials that evaluate the safety and efficacy of tPA in the treatment of acute ischemic stroke in very old patients, use at the community-based stroke center was not associated with worse outcomes including symptomatic ICH, hospital length of stay, and in-hospital mortality. In fact, there were trends towards better outcomes in older patients who received tPA, including a significant reduction in in-hospital mortality. This evaluation supports the benefits of using tPA to treat acute ischemic stroke as seen in prior randomized controlled trials that included the treatment of very old patients. Though ongoing research is needed, a growing body of evidence supports the use of tPA to treat acute ischemic stroke in patients ≥ 80 years.
Corresponding author: Jennifer C. Drost, DO, MPH, Summa Health System, 75 Arch St., Ste. G1, Akron, OH 44304, [email protected].
Financial disclosures: None.
Author contributions: Conception and design, JCD, SMB; analysis and interpretation of data, JCD, SMB; drafting of article, JCD; critical revision of the article, JCD, SMB; provision of study materials or patients, SMB; collection and assembly of data, JCD.
From Summa Health System, Akron, OH.
Abstract
- Background: Ischemic stroke is a major cause of morbidity and mortality for patients ≥ 80 years old. The use of intravenous recombinant tissue plasminogen activator (tPA) in patients ≥ 80 years for treatment of ischemic stroke remains controversial.
- Objective: To examine outcomes in patients ≥ 80 years old who received tPA in our institution.
- Methods: This was a retrospective cohort study at a community-based certified acute stroke center. Individuals age ≥ 80 years evaluated emergently for acute neurologic changes consistent with ischemic stroke were included (n = 184). The comparison groups within this sample were patients who received tPA versus with those who did not because they came to the ED outside of the treatment window. Outcome measures included length of stay, symptomatic intracerebral hemorrhage (ICH), discharge disposition, and in-hospital death
- Results: 38 patients (20.7%) received tPA. 50 patients (27.2%) presented outside of treatment windows and were included in comparative analysis. There was no difference between groups in age (P = 0.26) or initial National Institute of Health Stroke Scale (P = 0.598). One patient (2.6%) who received tPA developed symptomatic ICH. Those receiving tPA were more likely to be discharged to acute rehabilitation hospitals (P = 0.012) and less likely to experience in hospital death (P = 0.048).
- Conclusion: At this institution, the use of tPA in patients ≥ 80 years old is not associated with increased mortality or risk of symptomatic ICH. Those who received tPA were more likely to be discharged to acute rehabilitation hospitals, suggesting greater potential for functional recovery.
Acute ischemic stroke is a major cause of morbidity and mortality in patients 80 years or older. Though less than 5% of the United States population is over the age of 80 [1], studies have shown that up to one-third of patients presenting with ischemic stroke are ≥ 80 years old [2] and among first-time strokes, a third occur in those ≥ 80 [3]. Older adults present with worse symptoms associated with ischemic stroke as measured by the National Institutes of Health Stroke Scale (NIHSS) compared with younger (< 80 years) counterparts [4]. Older patients are more likely to be discharged to a location other than home [5]. Older age is associated with higher hospital, 30-day, and 1-year mortality [3,5,6]. Patients ≥ 80 are significantly more likely to die in the hospital compared to younger patients, 11.7% to 23.6% vs 5.1%, respectively [3,7].
The Food and Drug Administration (FDA) approved the use of intravenous recombinant tissue plasminogen activator (tPA) in 1996 for the treatment of ischemic stroke [8]. Studies evaluating the safety and efficacy of tPA in ischemic stroke excluded or underrepresented patients ≥ 80 [8,9]. The use of tPA in those ≥ 80 has not been shown consistently to improve outcomes [6,10,11]. Post-hoc analysis of the National Institute of Neurologic Disorders and Stroke (NINDS) study did not show worse outcomes or harms to older adults treated with tPA [12]. Likewise, data from the International Stroke Treatment (IST-3) collaborative group show that treatment with tPA up to 6 hours from the onset of symptoms improves outcomes in the elderly [13]. Use of tPA in the oldest adults remains controversial due to perceived higher risk of symptomatic intracerebral hemorrhage (ICH). Published data suggest overall ICH risk of 4.3% to 6.4% across all age-groups [9,14,15].Studies have failed to demonstrate an increased risk in the oldest adults [4,10,16,17], though they may have higher mortality rates associated with ICH [15]. Despite this, trends suggest increasing use of tPA in those ≥ 80 over the past decade [2]. Along with primary data from NINDS [12] and IST-3 [13], a meta-analysis conducted in 2014 suggests that regardless of age, patients have improved outcomes with tPA [18].With the increasing age of the population, effective treatment of strokes in patients ≥ 80 will continue to be an important clinical and research endeavor.
This study evaluates the outcomes of clinical use of tPA for treatment of patients ≥ 80 years old who present to a community-based certified stroke center with ischemic stroke.
Methods
The study setting was a 540-bed acute care hospital that is a community-based certified stroke center. This study was deemed nonhuman subjects research by the institutional review board as the goal was to evaluate processes and outcomes of this institution’s stroke team in treating a subgroup of patients according to clinically accepted practice (quality improvement initiative). All patients presenting to the emergency department (ED) between 1 January 2011 and 30 November 2013 with the onset of stroke-like neurological deficits underwent evaluation and treatment by a neurologist and/or specially trained stroke team. This team consists of the attending neurologist, ED physician, resident physicians, advanced practice nurses, and ED staff nurses and emergency medicine technicians. Team members involved in the evaluation and treatment of these patients undergo routine clinical education and testing to ensure standardization. Patients undergo emergent evaluation including the National Institutes of Health Stroke Scale (NIHSS) and obtain brain imaging with computed tomography (CT).
Patients ≥ 80 years were identified among all those who presented to the ED with ischemic stroke. Patients were included if they were subsequently diagnosed with ischemic stroke or transient ischemic attacks (TIA). They were excluded from analysis if neurological changes were due to primary hemorrhagic stroke, intracranial hemorrhage, subarachnoid hemorrhage, seizure, conversion disorder, or metabolic derangements. They were also excluded from analysis if the acute ischemic stroke treatment included intra-arterial administration of tPA or endovascular revascularization.
Patient data collected included age, NIHSS at presentation to ED, time to presentation at ED, treatment with tPA, contraindications to tPA, discharge disposition, length of stay and in-hospital mortality. Raw NIHSS values were collected at the time of presentation. NIHSS were categorized into mild symptoms (NIHSS < 6), moderate symptoms (NIHSS 6–19), or severe symptoms (NIHSS ≥ 20). Clinical indications for receiving tPA include NIHSS > 4, focal neurological deficit onset < 3 hours (for those ≥ 80 years old), and no evidence of acute hemorrhage or acute infarct on CT. Contraindications include rapidly improving symptoms (repeat NIHSS < 4), active or history of intracranial hemorrhage, history of stroke or head trauma in past 3 months, gastrointestinal or genitourinary hemorrhage within 21 days, major surgery within 14 days, arterial puncture at a noncompressible site in past 7 days, treatment with anticoagulation with therapeutic indices, systolic blood pressure > 185 mm Hg or diastolic blood pressure > 110 mm Hg and not responding to treatment, or platelet count < 100,000/mm3. Patients who were not eligible for tPA based on contraindications with the exception of being outside the treatment window (3 hours) were excluded from comparative analysis. Patient length of stay was rounded to nearest full day. Discharge disposition was categorized as home, acute rehabilitation hospital, skilled nursing facility, home or facility with hospice services, other hospital setting, or death.
Statistics were calculated using SPSS statistical software. Variables were reported as means and percentages. Group means were compared using t tests and differences in proportions were compared using the chi square test. Correlations were performed using Pearson’s correlation. A 2-tailed P < 0.05 was considered statistically significant.
Results
Discussion
Ischemic stroke remains a major cause of morbidity and mortality for very old patients. Though less than 5% of the United States population is over the age of 80 [1], at this community-based hospital 18% of those presenting to the ED with ischemic stroke were in this age-group. With a population of increasing age, more people in this age-group will present with ischemic stroke and need effective treatment to limit the associated morbidity and mortality. Being able to quickly and safely treat acute ischemic stroke may help very old adults maintain independence or prevent institutionalization. While the original studies demonstrating the effectiveness of tPA for acute ischemic stroke excluded or underrepresented those ≥ 80 years, retrospective analysis has not been conclusive regarding its use in very old patients [4–6,10,12,13].However, post-hoc analysis of NINDS and IST-3 data demonstrate efficacy and safety of treatment [12,13].
This study explored the use of tPA at a community-based certified stroke center. Similar to previous studies, it demonstrates the large proportion of patients presenting with acute neurological findings consistent with ischemic stroke are ≥ 80 years old [3,6]. Our incidence of acute ischemic stroke in the oldest patients may be slightly lower than reported elsewhere, which may reflect community differences, with higher rates of younger patients with multiple comorbidities presenting with stroke-like symptoms. Amongst this very old cohort, age was positively correlated with stroke severity. Mortality in patients ≥ 80 years old who present with acute ischemic stroke approaches 25%.
The majority of patients who did not receive tPA had documented contraindications to receiving the medication. The most common reason was rapidly improving symptoms with repeat NIHSS often ≤ 4. The second most common reason was presentation outside the treatment window of 3 hours. We compared those who either arrived too late to receive treatment with tPA or already had ischemic changes on CT to those who received tPA as this suggests the natural history of stroke progression and outcome without effective, early treatment. The outcomes at this institution support this trend. Very old patients who received tPA did not experience harm as evidenced by similar lengths of stay and rates of discharge to home. Also, rates of symptomatic ICH were lower than those reported in the literature. In fact, patients who received tPA were less likely to experience in-hospital death and more likely to be discharged to acute rehabilitation hospitals, suggesting more functional ability to tolerate aggressive recovery efforts.
Very few people who presented with acute ischemic stroke and were eligible for treatment with tPA failed to receive it. This suggests that despite the perceived increased risk to treating these patients with tPA, the specialized stroke team aggressively treats patients age ≥ 80 years who present with acute ischemic stroke. However, those who did not receive tPA were more likely to have presented with mild or severe strokes. This may suggest that treatment time frames are more strongly held, or that treatment teams are more likely to use time frames as a reason to not treat with tPA for patients with mild or severe strokes. Also, very few patients and families who were eligible to receive tPA declined treatment despite the associated risks. This suggests that patients and families are eager for aggressive treatment in attempt to prevent death or disability associated with ischemic stroke.
There are several limitations associated with this evaluation. First, this is a retrospective analysis of a single institution’s acute stroke procedures. Data was collected in an effort to evaluate the processes and outcomes of the specialized stroke team in evaluating and treating this very old cohort who present to a community-based hospital. It involved individualized clinical evaluation and decision making by multiple care providers who may offer different perspectives on the risk of treating patients ≥ 80 years old with tPA, which may result in selection bias. While comparing those who arrived outside treatment windows offers a comparison group who represents the natural course of untreated strokes, patient characteristics that prevented timely evaluation may also impact their outcomes including baseline mobility, care giving availability and underlying medical comorbidities. The similarity in mean presenting NIHSS scores of the two groups, however, argues against this possibility. Lastly, exclusion criteria to receiving tPA may represent intrinsic characteristics that impart higher risk of negative outcomes.
Conculsion
Although there have been no randomized controlled trials that evaluate the safety and efficacy of tPA in the treatment of acute ischemic stroke in very old patients, use at the community-based stroke center was not associated with worse outcomes including symptomatic ICH, hospital length of stay, and in-hospital mortality. In fact, there were trends towards better outcomes in older patients who received tPA, including a significant reduction in in-hospital mortality. This evaluation supports the benefits of using tPA to treat acute ischemic stroke as seen in prior randomized controlled trials that included the treatment of very old patients. Though ongoing research is needed, a growing body of evidence supports the use of tPA to treat acute ischemic stroke in patients ≥ 80 years.
Corresponding author: Jennifer C. Drost, DO, MPH, Summa Health System, 75 Arch St., Ste. G1, Akron, OH 44304, [email protected].
Financial disclosures: None.
Author contributions: Conception and design, JCD, SMB; analysis and interpretation of data, JCD, SMB; drafting of article, JCD; critical revision of the article, JCD, SMB; provision of study materials or patients, SMB; collection and assembly of data, JCD.
1. US Census Bureau. Annual estimates of the resident population for selected age groups by sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2013. Accessed at www.census.gov/popest/index.html.
2. Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med 2010;5:406–9.
3. Marini C, Baldassarre M, Russo T, et al. Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology 2004;62:77–81.
4. Sylaja PN, Cote R, Buchan AM, Hill MD. Thrombolysis in patients older than 80 years with acute ischaemic stroke: Canadian Alteplase for Stroke Effectiveness Study. J Neurol Neurosurg Psychiatry 2006;77:826–9.
5. Heitsch LE, Panagos PD. Treating the elderly stroke patient: complications, controversies, and best care metrics. Clin Geriatr Med 2013;29:231–55.
6. Engelter ST, Bonati LH, Lyrer PA. Intravenous thrombolysis in stroke patients of > or = 80 versus < 80 years of age--a systematic review across cohort studies. Age Ageing 2006;35:572–580.
7. Forti P, Maioli F, Procaccianti G, et al. Independent predictors of ischemic stroke in the elderly: prospective data from a stroke unit. Neurology 2013;80:29–38.
8. Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTischemic stroke, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768–74.
9. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–7.
10. Sung PS, Chen CH, Hsieh HC, et al. Outcome of acute ischemic stroke in very elderly patients: is intravenous thrombolysis beneficial? Eur Neurol 2011;66:110–6.
11. Saposnik G, Guzik AK, Reeves M, et al. Stroke prognostication using age and NIH Stroke Scale: SPAN-100. Neurology 2013;80:21–8.
12. Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA Stroke Trial. Stroke 1997;28:2119–25.
13. Sandercock P, Wardlaw JM, Lindley RI, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 2012;379:2352–63.
14. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke 1997;28:2109–18.
15. Bray BD, Campbell J, Hoffman A, et al. Stroke thrombolysis in England: an age stratified analysis of practice and outcome. Age Ageing 2013;42:240–5.
16. Kono S, Deguchi K, Morimoto N, et al. Intravenous thrombolysis with neuroprotective therapy by edaravone for ischemic stroke patients older than 80 years of age. J Stroke Cerebrovasc Dis 2013;22:1175–83.
17. Berrouschot J, Rother J, Glahn J, et al. Outcome and severe hemorrhagic complications of intravenous thrombolysis with tissue plasminogen activator in very old (> or =80 years) stroke patients. Stroke 2005;36:2421–5.
18. Emberson J, Lees KR, Lyden P, et al; Stroke Thrombolysis Trialists' Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35.
1. US Census Bureau. Annual estimates of the resident population for selected age groups by sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2013. Accessed at www.census.gov/popest/index.html.
2. Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med 2010;5:406–9.
3. Marini C, Baldassarre M, Russo T, et al. Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology 2004;62:77–81.
4. Sylaja PN, Cote R, Buchan AM, Hill MD. Thrombolysis in patients older than 80 years with acute ischaemic stroke: Canadian Alteplase for Stroke Effectiveness Study. J Neurol Neurosurg Psychiatry 2006;77:826–9.
5. Heitsch LE, Panagos PD. Treating the elderly stroke patient: complications, controversies, and best care metrics. Clin Geriatr Med 2013;29:231–55.
6. Engelter ST, Bonati LH, Lyrer PA. Intravenous thrombolysis in stroke patients of > or = 80 versus < 80 years of age--a systematic review across cohort studies. Age Ageing 2006;35:572–580.
7. Forti P, Maioli F, Procaccianti G, et al. Independent predictors of ischemic stroke in the elderly: prospective data from a stroke unit. Neurology 2013;80:29–38.
8. Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTischemic stroke, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768–74.
9. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–7.
10. Sung PS, Chen CH, Hsieh HC, et al. Outcome of acute ischemic stroke in very elderly patients: is intravenous thrombolysis beneficial? Eur Neurol 2011;66:110–6.
11. Saposnik G, Guzik AK, Reeves M, et al. Stroke prognostication using age and NIH Stroke Scale: SPAN-100. Neurology 2013;80:21–8.
12. Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA Stroke Trial. Stroke 1997;28:2119–25.
13. Sandercock P, Wardlaw JM, Lindley RI, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 2012;379:2352–63.
14. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke 1997;28:2109–18.
15. Bray BD, Campbell J, Hoffman A, et al. Stroke thrombolysis in England: an age stratified analysis of practice and outcome. Age Ageing 2013;42:240–5.
16. Kono S, Deguchi K, Morimoto N, et al. Intravenous thrombolysis with neuroprotective therapy by edaravone for ischemic stroke patients older than 80 years of age. J Stroke Cerebrovasc Dis 2013;22:1175–83.
17. Berrouschot J, Rother J, Glahn J, et al. Outcome and severe hemorrhagic complications of intravenous thrombolysis with tissue plasminogen activator in very old (> or =80 years) stroke patients. Stroke 2005;36:2421–5.
18. Emberson J, Lees KR, Lyden P, et al; Stroke Thrombolysis Trialists' Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35.
Comparison of Parent and Child versus Child-Only Weight Management Interventions in the Patient-Centered Medical Home
Study Overview
Objective. To determine the efficacy, both short and long term, of a behavioral intervention targeting overweight parents and their children simultaneously versus an intervention focused on weight management only for the child within the patient-centered medical home (PCMH).
Design. 4-center, 2-arm, randomized controlled trial.
Setting and participants. Study participants were recruited from 4 urban/suburban pediatric practices. Primary care providers (PCPs) recruited patients at the time of well or sick visits based on body mass index (BMI) flagged prior to the visit by Patient Enhancement Assistants (PEAs). 171 parent/child dyads were assessed for eligibility and 105 were randomized in blocks of 12 dyads using a random number generator and stratified by child’s gender. Pediatricians were blind to their patient’s group assignments. Inclusion criteria were as follows: children aged 2–5 with a BMI higher than the 85th percentile for both age and gender, and 1 parent with a BMI greater than 25. Exclusion criteria were limited to children who were small for gestational age and/or short stature, and child or parent inability to perform physical activity. Specific precautions were taken to prevent contamination between intervention and information control (IC) groups [1].
Intervention. Three PEAs who held a masters or bachelors degree in psychology, nutrition, exercise science, or equivalent, or were registered dietitians, were embedded within each PCMH practice. For both the intervention and IC groups, parents attended 13 one-hour group sessions led by a PEA over a 12-month period, followed by a 12-month follow-up period with 3 additional meetings. The PEA telephoned parents between scheduled meetings. Pediatricians reviewed child’s weight changes every 6 months during scheduled appointments and the PEA sent progress notes in between these visits [2]. Dietary, physical, and sedentary activity guidelines were given based on the recommendations of a national multi-organizational expert committee [3]. Parents were given specific goals for their child, including a 0.5- to 1-pound per week loss, 60 minutes per day of physical activity, and limiting TV and screen time to less than 2 hours per day.
In addition, the intervention group received parenting and behavior change strategies to promote both parent and child weight loss. Parents were instructed to weigh themselves and their child once per week and monitor physical activity and diet. They received individual meetings with the PEA before or after group meetings to review goal setting and food/physical activity diaries. Parents were also given a weight loss goal of 1 to 2 pounds per week and were advised to model physical activity by engaging in active play with their child for at least 10 minutes per day.
Main outcome measures. The main outcome measures were %0BMI and z-BMI. Percent 0BMI is defined as [(child’s BMI – 50th percentile BMI)/50th percentile BMI] x 100 [2]. The authors chose %0BMI as the primary outcome measure because z-BMI can diminish the effect of weight change in heavier children [4]. Both measures were expressed as mean ± standard error (SEM). Parent weight change was measured using BMI alone.
The child’s weight was measured at each session and height was measured at baseline, 3, 6, 12, 18, and 24 months. Parent weight was measured every session in the intervention group, but only at baseline, 6, 12, 18, and 24 months in the IC group. A standardized protocol was followed for all height and weight measurements. An intention to treat analysis (ITT) was conducted on all parent/child dyads, regardless of whether or not they completed the study (n = 96).
Results. Research assistants assessed 171 parent/child dyads for eligibility. 66 were excluded for either not meeting inclusion criteria (n = 24) or declining to participate (n = 42). 105 dyads were randomized, but 9 did not receive the allocated intervention because they did not start the study, resulting in a total of 96 dyads included in analysis: 46 in the intervention group and 50 in the IC. Twelve- and 24-month completion rates were 83% and 73% respectively; there was no difference in attrition between intervention and IC groups.
The mean child ages of the intervention and IC groups were 4.6 ± 0.2 and 4.4 ± 0.2 years, respectively. 33 of the 46 children in the intervention group and 37 of the 50 children in the IC group were identified as non-Hispanic white. The mean yearly income of all families was $65,729 ± $3068, with only 8.3% of families below $20,000.
The intervention group had greater decreases in child %0BMI from baseline to 6, 12, 18, and 24 months than the IC group. Similar trends were seen with child z-BMI. A slower increase in height was observed in the intervention group when compared with the IC at both 18 months (P < 0.001) and at 24 months (P < 0.02). Parents showed greater overall BMI reduction in the intervention group as opposed to the IC group at all time points (P < 0.001). BMI changes achieved at 6 months were maintained at 24 months. %0BMI and parent BMI changes were correlated from baseline to 12, 18, and 24 months. No significant baseline moderators were found among the children in either group.
Conclusion. This study demonstrated that within the PCMH model of pediatric primary care, an intervention focused on joint behavior change and weight modification treatment of parents and children led to better initial and sustained improvements in %0BMI and z-BMI (in children) and BMI (in parents) than a child-focused IC.
Commentary
Over one-third of children and adolescents are considered to be overweight or have obesity, a number that has doubled in the past 30 years [5]. Pediatrician and primary care physician visits are optimal places to identify overweight children who are at risk for obesity and begin prevention measures, although identifying overweight and obese younger children can be difficult [6]. This study used PEAs to aid physicians in identification, implementation, and delivery. With increasing evidence to support pediatrician involvement in intensive weight management in a primary versus specialty care setting, embedding PEAs within the PCMH model may be an important way to help deliver care for overweight/obese children [7].
Although many approaches have been considered to target childhood obesity, this study represents an important contribution to the literature because it demonstrates that a primary care–based intervention targeting parents as well as their young children is more efficacious for weight management than a more traditional, child-only focused intervention. In addition, the intervention included many different evidence-based components such as teaching behavior modification techniques to parents, consideration of parenting styles and techniques, and encouraging simultaneous parental weight modification. While the U.S. Preventive Services Task Force (USPSTF) recommends intensive interventions with 30 sessions over 2 years [8], this study was able to accomplish significant weight change in 13 sessions.
This intervention is unique in its integration of parenting techniques with other evidence-based strategies for child weight management. Although it has been shown in the literature that certain parenting styles can positively impact children’s health behaviors [9], namely the use of positive reinforcement and monitoring children’s health practices [10], only a few studies have looked at the impact of parenting interventions on childhood obesity. Mazzeo et al demonstrated a significant reduction in child BMI with a parenting-only intervention in the NOURISH trial [11], Slusser et al found a significant child BMI reduction using parent training for low-income, 2- to 4-year-old children [12], and Brotman et al conducted a longitudinal study demonstrating that a family intervention could decrease BMI and improve overall child health behaviors [13]. Despite these aforementioned studies, there is a lack of longitudinal data on the association between general parenting style and weight [14], and this study addresses this gap in literature by providing 2-year follow-up and demonstrating sustained impact on the intervention group.
This study had many additional strengths, including randomized design, primary care physician blinding, use of intention to treat analysis, standardization of measurement tools, clear justification of sample size, long-term follow-up, and the use of child-appropriate BMI measures (eg, %0BMI vs. z-BMI as primary outcome measure). In addition, the intervention setting in a PCMH follows the trend of increasing interest in exploring this model of health care delivery [15,16]. It is also important to note that the intervention and IC groups received the same number of group visits and phone calls, the only difference being the content and the extra 1:1 PEA sessions received by the intervention group.
The few weaknesses include that the PEAs could not be blinded to treatment allocation, and generalizability is limited by the mostly non-Hispanic white population and that only 8.3% of the study population had an annual household income of less than $20,000. All parents included in this study were on the high end of the obese range (BMI 30–39.9), with baseline BMI values of 37.2 and 36.2 in the intervention and IC groups respectively. In addition, the age of the children included in the study were on the high end of the designated 2- to 5-year-old range: 4.6 years (IC) and 4.4 years (intervention). Although findings were promising within this specific population, further research in younger and more diverse populations is necessary [11].
Finally, it is unclear whether this intervention is scalable, and a cost-effectiveness analysis of this intervention is needed. This study was designed to limit the PCP’s role and simplify the process of identifying and intervening on overweight children and their parents, yet this required 3 part-time PEAs and a project coordinator responsible for delivering all of the group sessions and providing follow-up counseling to both intervention and IC groups.
Applications for Clinical Practice
This study demonstrates that in a mostly white, urban/suburban population, a parenting and behavior modification intervention focused on both parent and child leads to greater improvements in %0BMI and z-BMI in the child and BMI reduction in parents compared with an intervention focused on the child alone within pediatric PCMH practices. This intervention should be tested in more diverse populations. This study also suggests further exploration of the use of PEAs to help clinicians address obesity within the PCMH model of primary care.
—Natalie Berner, BA, and Melanie Jay, MD, MS
1. Quattrin T, Roemmich JN, Paluch R, et al. Efficacy of family-based weight control program for preschool children in primary care. Pediatrics 2012;130:660–6.
2. Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol 2007;19:487–94.
3. Barlow SE, for the Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120(suppl 4):S164–S192.
4. Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005;59: 419–25.
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.
6. Miller JL, Silverstein JH. Management approaches for pediatric obesity. Nature Clinical Practice Endocrin Metab 2007;3:810–8.
7. Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr 2007; 19:354–61.
8. Barton M; US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics 2010;125:361–7.
9. Institute of Medicine. Early childhood obesity prevention policies. Washington, DC: National Academies Press; 2011.
10. Arredondo EM, Elder JP, Ayala GX,et al. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Educ Res 2006;21:862–71.
11. Mazzeo SE, Kelly NR, Stern M, et al. Parent skills training to enhance weight loss in overweight children: Evaluation of NOURISH. Eat Behav 2014;15:225–9.
12. Slusser W, Frankel F, Robison K, et al. Pediatric overweight prevention through a parent training program for 2-4 year old Latino children. Child Obesity 2012;8:52–9.
13. Brotman LM, Dawson-McClure S, Huang K, et al. Early childhood obesity family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics 2012;129:e621–e628.
14. Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 2008;5:15.
15. Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med 200;21:427–40.
16. Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med 2013;158:169–78.
Study Overview
Objective. To determine the efficacy, both short and long term, of a behavioral intervention targeting overweight parents and their children simultaneously versus an intervention focused on weight management only for the child within the patient-centered medical home (PCMH).
Design. 4-center, 2-arm, randomized controlled trial.
Setting and participants. Study participants were recruited from 4 urban/suburban pediatric practices. Primary care providers (PCPs) recruited patients at the time of well or sick visits based on body mass index (BMI) flagged prior to the visit by Patient Enhancement Assistants (PEAs). 171 parent/child dyads were assessed for eligibility and 105 were randomized in blocks of 12 dyads using a random number generator and stratified by child’s gender. Pediatricians were blind to their patient’s group assignments. Inclusion criteria were as follows: children aged 2–5 with a BMI higher than the 85th percentile for both age and gender, and 1 parent with a BMI greater than 25. Exclusion criteria were limited to children who were small for gestational age and/or short stature, and child or parent inability to perform physical activity. Specific precautions were taken to prevent contamination between intervention and information control (IC) groups [1].
Intervention. Three PEAs who held a masters or bachelors degree in psychology, nutrition, exercise science, or equivalent, or were registered dietitians, were embedded within each PCMH practice. For both the intervention and IC groups, parents attended 13 one-hour group sessions led by a PEA over a 12-month period, followed by a 12-month follow-up period with 3 additional meetings. The PEA telephoned parents between scheduled meetings. Pediatricians reviewed child’s weight changes every 6 months during scheduled appointments and the PEA sent progress notes in between these visits [2]. Dietary, physical, and sedentary activity guidelines were given based on the recommendations of a national multi-organizational expert committee [3]. Parents were given specific goals for their child, including a 0.5- to 1-pound per week loss, 60 minutes per day of physical activity, and limiting TV and screen time to less than 2 hours per day.
In addition, the intervention group received parenting and behavior change strategies to promote both parent and child weight loss. Parents were instructed to weigh themselves and their child once per week and monitor physical activity and diet. They received individual meetings with the PEA before or after group meetings to review goal setting and food/physical activity diaries. Parents were also given a weight loss goal of 1 to 2 pounds per week and were advised to model physical activity by engaging in active play with their child for at least 10 minutes per day.
Main outcome measures. The main outcome measures were %0BMI and z-BMI. Percent 0BMI is defined as [(child’s BMI – 50th percentile BMI)/50th percentile BMI] x 100 [2]. The authors chose %0BMI as the primary outcome measure because z-BMI can diminish the effect of weight change in heavier children [4]. Both measures were expressed as mean ± standard error (SEM). Parent weight change was measured using BMI alone.
The child’s weight was measured at each session and height was measured at baseline, 3, 6, 12, 18, and 24 months. Parent weight was measured every session in the intervention group, but only at baseline, 6, 12, 18, and 24 months in the IC group. A standardized protocol was followed for all height and weight measurements. An intention to treat analysis (ITT) was conducted on all parent/child dyads, regardless of whether or not they completed the study (n = 96).
Results. Research assistants assessed 171 parent/child dyads for eligibility. 66 were excluded for either not meeting inclusion criteria (n = 24) or declining to participate (n = 42). 105 dyads were randomized, but 9 did not receive the allocated intervention because they did not start the study, resulting in a total of 96 dyads included in analysis: 46 in the intervention group and 50 in the IC. Twelve- and 24-month completion rates were 83% and 73% respectively; there was no difference in attrition between intervention and IC groups.
The mean child ages of the intervention and IC groups were 4.6 ± 0.2 and 4.4 ± 0.2 years, respectively. 33 of the 46 children in the intervention group and 37 of the 50 children in the IC group were identified as non-Hispanic white. The mean yearly income of all families was $65,729 ± $3068, with only 8.3% of families below $20,000.
The intervention group had greater decreases in child %0BMI from baseline to 6, 12, 18, and 24 months than the IC group. Similar trends were seen with child z-BMI. A slower increase in height was observed in the intervention group when compared with the IC at both 18 months (P < 0.001) and at 24 months (P < 0.02). Parents showed greater overall BMI reduction in the intervention group as opposed to the IC group at all time points (P < 0.001). BMI changes achieved at 6 months were maintained at 24 months. %0BMI and parent BMI changes were correlated from baseline to 12, 18, and 24 months. No significant baseline moderators were found among the children in either group.
Conclusion. This study demonstrated that within the PCMH model of pediatric primary care, an intervention focused on joint behavior change and weight modification treatment of parents and children led to better initial and sustained improvements in %0BMI and z-BMI (in children) and BMI (in parents) than a child-focused IC.
Commentary
Over one-third of children and adolescents are considered to be overweight or have obesity, a number that has doubled in the past 30 years [5]. Pediatrician and primary care physician visits are optimal places to identify overweight children who are at risk for obesity and begin prevention measures, although identifying overweight and obese younger children can be difficult [6]. This study used PEAs to aid physicians in identification, implementation, and delivery. With increasing evidence to support pediatrician involvement in intensive weight management in a primary versus specialty care setting, embedding PEAs within the PCMH model may be an important way to help deliver care for overweight/obese children [7].
Although many approaches have been considered to target childhood obesity, this study represents an important contribution to the literature because it demonstrates that a primary care–based intervention targeting parents as well as their young children is more efficacious for weight management than a more traditional, child-only focused intervention. In addition, the intervention included many different evidence-based components such as teaching behavior modification techniques to parents, consideration of parenting styles and techniques, and encouraging simultaneous parental weight modification. While the U.S. Preventive Services Task Force (USPSTF) recommends intensive interventions with 30 sessions over 2 years [8], this study was able to accomplish significant weight change in 13 sessions.
This intervention is unique in its integration of parenting techniques with other evidence-based strategies for child weight management. Although it has been shown in the literature that certain parenting styles can positively impact children’s health behaviors [9], namely the use of positive reinforcement and monitoring children’s health practices [10], only a few studies have looked at the impact of parenting interventions on childhood obesity. Mazzeo et al demonstrated a significant reduction in child BMI with a parenting-only intervention in the NOURISH trial [11], Slusser et al found a significant child BMI reduction using parent training for low-income, 2- to 4-year-old children [12], and Brotman et al conducted a longitudinal study demonstrating that a family intervention could decrease BMI and improve overall child health behaviors [13]. Despite these aforementioned studies, there is a lack of longitudinal data on the association between general parenting style and weight [14], and this study addresses this gap in literature by providing 2-year follow-up and demonstrating sustained impact on the intervention group.
This study had many additional strengths, including randomized design, primary care physician blinding, use of intention to treat analysis, standardization of measurement tools, clear justification of sample size, long-term follow-up, and the use of child-appropriate BMI measures (eg, %0BMI vs. z-BMI as primary outcome measure). In addition, the intervention setting in a PCMH follows the trend of increasing interest in exploring this model of health care delivery [15,16]. It is also important to note that the intervention and IC groups received the same number of group visits and phone calls, the only difference being the content and the extra 1:1 PEA sessions received by the intervention group.
The few weaknesses include that the PEAs could not be blinded to treatment allocation, and generalizability is limited by the mostly non-Hispanic white population and that only 8.3% of the study population had an annual household income of less than $20,000. All parents included in this study were on the high end of the obese range (BMI 30–39.9), with baseline BMI values of 37.2 and 36.2 in the intervention and IC groups respectively. In addition, the age of the children included in the study were on the high end of the designated 2- to 5-year-old range: 4.6 years (IC) and 4.4 years (intervention). Although findings were promising within this specific population, further research in younger and more diverse populations is necessary [11].
Finally, it is unclear whether this intervention is scalable, and a cost-effectiveness analysis of this intervention is needed. This study was designed to limit the PCP’s role and simplify the process of identifying and intervening on overweight children and their parents, yet this required 3 part-time PEAs and a project coordinator responsible for delivering all of the group sessions and providing follow-up counseling to both intervention and IC groups.
Applications for Clinical Practice
This study demonstrates that in a mostly white, urban/suburban population, a parenting and behavior modification intervention focused on both parent and child leads to greater improvements in %0BMI and z-BMI in the child and BMI reduction in parents compared with an intervention focused on the child alone within pediatric PCMH practices. This intervention should be tested in more diverse populations. This study also suggests further exploration of the use of PEAs to help clinicians address obesity within the PCMH model of primary care.
—Natalie Berner, BA, and Melanie Jay, MD, MS
Study Overview
Objective. To determine the efficacy, both short and long term, of a behavioral intervention targeting overweight parents and their children simultaneously versus an intervention focused on weight management only for the child within the patient-centered medical home (PCMH).
Design. 4-center, 2-arm, randomized controlled trial.
Setting and participants. Study participants were recruited from 4 urban/suburban pediatric practices. Primary care providers (PCPs) recruited patients at the time of well or sick visits based on body mass index (BMI) flagged prior to the visit by Patient Enhancement Assistants (PEAs). 171 parent/child dyads were assessed for eligibility and 105 were randomized in blocks of 12 dyads using a random number generator and stratified by child’s gender. Pediatricians were blind to their patient’s group assignments. Inclusion criteria were as follows: children aged 2–5 with a BMI higher than the 85th percentile for both age and gender, and 1 parent with a BMI greater than 25. Exclusion criteria were limited to children who were small for gestational age and/or short stature, and child or parent inability to perform physical activity. Specific precautions were taken to prevent contamination between intervention and information control (IC) groups [1].
Intervention. Three PEAs who held a masters or bachelors degree in psychology, nutrition, exercise science, or equivalent, or were registered dietitians, were embedded within each PCMH practice. For both the intervention and IC groups, parents attended 13 one-hour group sessions led by a PEA over a 12-month period, followed by a 12-month follow-up period with 3 additional meetings. The PEA telephoned parents between scheduled meetings. Pediatricians reviewed child’s weight changes every 6 months during scheduled appointments and the PEA sent progress notes in between these visits [2]. Dietary, physical, and sedentary activity guidelines were given based on the recommendations of a national multi-organizational expert committee [3]. Parents were given specific goals for their child, including a 0.5- to 1-pound per week loss, 60 minutes per day of physical activity, and limiting TV and screen time to less than 2 hours per day.
In addition, the intervention group received parenting and behavior change strategies to promote both parent and child weight loss. Parents were instructed to weigh themselves and their child once per week and monitor physical activity and diet. They received individual meetings with the PEA before or after group meetings to review goal setting and food/physical activity diaries. Parents were also given a weight loss goal of 1 to 2 pounds per week and were advised to model physical activity by engaging in active play with their child for at least 10 minutes per day.
Main outcome measures. The main outcome measures were %0BMI and z-BMI. Percent 0BMI is defined as [(child’s BMI – 50th percentile BMI)/50th percentile BMI] x 100 [2]. The authors chose %0BMI as the primary outcome measure because z-BMI can diminish the effect of weight change in heavier children [4]. Both measures were expressed as mean ± standard error (SEM). Parent weight change was measured using BMI alone.
The child’s weight was measured at each session and height was measured at baseline, 3, 6, 12, 18, and 24 months. Parent weight was measured every session in the intervention group, but only at baseline, 6, 12, 18, and 24 months in the IC group. A standardized protocol was followed for all height and weight measurements. An intention to treat analysis (ITT) was conducted on all parent/child dyads, regardless of whether or not they completed the study (n = 96).
Results. Research assistants assessed 171 parent/child dyads for eligibility. 66 were excluded for either not meeting inclusion criteria (n = 24) or declining to participate (n = 42). 105 dyads were randomized, but 9 did not receive the allocated intervention because they did not start the study, resulting in a total of 96 dyads included in analysis: 46 in the intervention group and 50 in the IC. Twelve- and 24-month completion rates were 83% and 73% respectively; there was no difference in attrition between intervention and IC groups.
The mean child ages of the intervention and IC groups were 4.6 ± 0.2 and 4.4 ± 0.2 years, respectively. 33 of the 46 children in the intervention group and 37 of the 50 children in the IC group were identified as non-Hispanic white. The mean yearly income of all families was $65,729 ± $3068, with only 8.3% of families below $20,000.
The intervention group had greater decreases in child %0BMI from baseline to 6, 12, 18, and 24 months than the IC group. Similar trends were seen with child z-BMI. A slower increase in height was observed in the intervention group when compared with the IC at both 18 months (P < 0.001) and at 24 months (P < 0.02). Parents showed greater overall BMI reduction in the intervention group as opposed to the IC group at all time points (P < 0.001). BMI changes achieved at 6 months were maintained at 24 months. %0BMI and parent BMI changes were correlated from baseline to 12, 18, and 24 months. No significant baseline moderators were found among the children in either group.
Conclusion. This study demonstrated that within the PCMH model of pediatric primary care, an intervention focused on joint behavior change and weight modification treatment of parents and children led to better initial and sustained improvements in %0BMI and z-BMI (in children) and BMI (in parents) than a child-focused IC.
Commentary
Over one-third of children and adolescents are considered to be overweight or have obesity, a number that has doubled in the past 30 years [5]. Pediatrician and primary care physician visits are optimal places to identify overweight children who are at risk for obesity and begin prevention measures, although identifying overweight and obese younger children can be difficult [6]. This study used PEAs to aid physicians in identification, implementation, and delivery. With increasing evidence to support pediatrician involvement in intensive weight management in a primary versus specialty care setting, embedding PEAs within the PCMH model may be an important way to help deliver care for overweight/obese children [7].
Although many approaches have been considered to target childhood obesity, this study represents an important contribution to the literature because it demonstrates that a primary care–based intervention targeting parents as well as their young children is more efficacious for weight management than a more traditional, child-only focused intervention. In addition, the intervention included many different evidence-based components such as teaching behavior modification techniques to parents, consideration of parenting styles and techniques, and encouraging simultaneous parental weight modification. While the U.S. Preventive Services Task Force (USPSTF) recommends intensive interventions with 30 sessions over 2 years [8], this study was able to accomplish significant weight change in 13 sessions.
This intervention is unique in its integration of parenting techniques with other evidence-based strategies for child weight management. Although it has been shown in the literature that certain parenting styles can positively impact children’s health behaviors [9], namely the use of positive reinforcement and monitoring children’s health practices [10], only a few studies have looked at the impact of parenting interventions on childhood obesity. Mazzeo et al demonstrated a significant reduction in child BMI with a parenting-only intervention in the NOURISH trial [11], Slusser et al found a significant child BMI reduction using parent training for low-income, 2- to 4-year-old children [12], and Brotman et al conducted a longitudinal study demonstrating that a family intervention could decrease BMI and improve overall child health behaviors [13]. Despite these aforementioned studies, there is a lack of longitudinal data on the association between general parenting style and weight [14], and this study addresses this gap in literature by providing 2-year follow-up and demonstrating sustained impact on the intervention group.
This study had many additional strengths, including randomized design, primary care physician blinding, use of intention to treat analysis, standardization of measurement tools, clear justification of sample size, long-term follow-up, and the use of child-appropriate BMI measures (eg, %0BMI vs. z-BMI as primary outcome measure). In addition, the intervention setting in a PCMH follows the trend of increasing interest in exploring this model of health care delivery [15,16]. It is also important to note that the intervention and IC groups received the same number of group visits and phone calls, the only difference being the content and the extra 1:1 PEA sessions received by the intervention group.
The few weaknesses include that the PEAs could not be blinded to treatment allocation, and generalizability is limited by the mostly non-Hispanic white population and that only 8.3% of the study population had an annual household income of less than $20,000. All parents included in this study were on the high end of the obese range (BMI 30–39.9), with baseline BMI values of 37.2 and 36.2 in the intervention and IC groups respectively. In addition, the age of the children included in the study were on the high end of the designated 2- to 5-year-old range: 4.6 years (IC) and 4.4 years (intervention). Although findings were promising within this specific population, further research in younger and more diverse populations is necessary [11].
Finally, it is unclear whether this intervention is scalable, and a cost-effectiveness analysis of this intervention is needed. This study was designed to limit the PCP’s role and simplify the process of identifying and intervening on overweight children and their parents, yet this required 3 part-time PEAs and a project coordinator responsible for delivering all of the group sessions and providing follow-up counseling to both intervention and IC groups.
Applications for Clinical Practice
This study demonstrates that in a mostly white, urban/suburban population, a parenting and behavior modification intervention focused on both parent and child leads to greater improvements in %0BMI and z-BMI in the child and BMI reduction in parents compared with an intervention focused on the child alone within pediatric PCMH practices. This intervention should be tested in more diverse populations. This study also suggests further exploration of the use of PEAs to help clinicians address obesity within the PCMH model of primary care.
—Natalie Berner, BA, and Melanie Jay, MD, MS
1. Quattrin T, Roemmich JN, Paluch R, et al. Efficacy of family-based weight control program for preschool children in primary care. Pediatrics 2012;130:660–6.
2. Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol 2007;19:487–94.
3. Barlow SE, for the Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120(suppl 4):S164–S192.
4. Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005;59: 419–25.
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.
6. Miller JL, Silverstein JH. Management approaches for pediatric obesity. Nature Clinical Practice Endocrin Metab 2007;3:810–8.
7. Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr 2007; 19:354–61.
8. Barton M; US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics 2010;125:361–7.
9. Institute of Medicine. Early childhood obesity prevention policies. Washington, DC: National Academies Press; 2011.
10. Arredondo EM, Elder JP, Ayala GX,et al. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Educ Res 2006;21:862–71.
11. Mazzeo SE, Kelly NR, Stern M, et al. Parent skills training to enhance weight loss in overweight children: Evaluation of NOURISH. Eat Behav 2014;15:225–9.
12. Slusser W, Frankel F, Robison K, et al. Pediatric overweight prevention through a parent training program for 2-4 year old Latino children. Child Obesity 2012;8:52–9.
13. Brotman LM, Dawson-McClure S, Huang K, et al. Early childhood obesity family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics 2012;129:e621–e628.
14. Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 2008;5:15.
15. Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med 200;21:427–40.
16. Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med 2013;158:169–78.
1. Quattrin T, Roemmich JN, Paluch R, et al. Efficacy of family-based weight control program for preschool children in primary care. Pediatrics 2012;130:660–6.
2. Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol 2007;19:487–94.
3. Barlow SE, for the Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120(suppl 4):S164–S192.
4. Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005;59: 419–25.
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.
6. Miller JL, Silverstein JH. Management approaches for pediatric obesity. Nature Clinical Practice Endocrin Metab 2007;3:810–8.
7. Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr 2007; 19:354–61.
8. Barton M; US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics 2010;125:361–7.
9. Institute of Medicine. Early childhood obesity prevention policies. Washington, DC: National Academies Press; 2011.
10. Arredondo EM, Elder JP, Ayala GX,et al. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Educ Res 2006;21:862–71.
11. Mazzeo SE, Kelly NR, Stern M, et al. Parent skills training to enhance weight loss in overweight children: Evaluation of NOURISH. Eat Behav 2014;15:225–9.
12. Slusser W, Frankel F, Robison K, et al. Pediatric overweight prevention through a parent training program for 2-4 year old Latino children. Child Obesity 2012;8:52–9.
13. Brotman LM, Dawson-McClure S, Huang K, et al. Early childhood obesity family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics 2012;129:e621–e628.
14. Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 2008;5:15.
15. Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med 200;21:427–40.
16. Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med 2013;158:169–78.
Mogamulizumab in PTCL: Europe vs Japan
SAN FRANCISCO—Two phase 2 studies testing mogamulizumab in peripheral T-cell lymphomas (PTCLs) suggest that higher response rates don’t necessarily translate to an improvement in progression-free survival (PFS).
The anti-CCR4 antibody produced a higher overall response rate (ORR) in a Japanese study than in a European study—34% and 11%, respectively.
However, median PFS times were similar—about 2 months in both studies.
This similarity is all the more interesting because the studies enrolled different types of patients and followed different dosing schedules, according to Pier Luigi Zinzani, MD, PhD, of the University of Bologna in Italy.
Dr Zinzani discussed details of the European experience testing mogamulizumab in PTCL, comparing it to the Japanese experience, in a presentation at the 7th Annual T-cell Lymphoma Forum.
Kensei Tobinai, MD, PhD, of the National Cancer Center Hospital in Tokyo, Japan, also reviewed the Japanese experience (TCLF 2013, JCO 2014) during the meeting’s keynote address and presented data from an ancillary analysis of this study (which is unpublished).
All of the research was sponsored by Kyowa Hakko Kirin Co., Ltd., the company developing mogamulizumab.
The Japanese experience
The Japanese study included 29 patients with PTCL and 8 with cutaneous T-cell lymphoma (CTCL). All patients had relapsed after their last chemotherapy regimen, and none had received an allogeneic stem cell transplant (allo-SCT). The PTCL patients had a median age of 67, and 69% were male.
All patients received mogamulizumab at 1.0 mg/kg/day weekly for 8 weeks. The ORR was 35%—34% for PTCL patients and 38% for CTCL patients.
Among PTCL patients, there were 5 complete responses (CRs) and 5 partial responses (PRs). Nine patients had stable disease (SD), and 10 progressed.
Of the 16 patients with PTCL-not otherwise specified (PTCL-NOS), 1 had a CR, 2 had a PR, 6 had SD, and 7 progressed. Of the 12 patients with angioimmunoblastic T-cell lymphoma (AITL), 3 had a CR, 3 had a PR, 3 had SD, and 3 progressed. The only patient with ALK- anaplastic large-cell lymphoma (ALCL) had an unconfirmed CR.
The ancillary analysis showed that tumor shrinkage of the target lesions occurred in 72% (21/29) of patients with PTCL. The patients’ median duration of response was 6.4 months, and the median time to response was 1.9 months.
Overall, the median PFS was 3.0 months—2.0 months in patients with PTCL and 3.4 months in patients with CTCL.
Common adverse events (for both PTCL and CTCL patients) included lymphopenia (81%), skin disorders (51%), leukopenia (43%), neutropenia (38%), thrombocytopenia (38%), pyrexia (30%), acute infusion reactions (24%), and anemia (14%).
Dr Tobinai noted that these results are not as favorable as those observed when patients with adult T-cell leukemia-lymphoma receive mogamulizumab.
“But compared to the efficacy rate of other approved agents—pralatrexate and romidepsin—this antibody has promising efficacy,” he said.
In fact, the results of this study prompted the December approval of mogamulizumab to treat PTCL and CTCL patients in Japan.
The European experience
The European study differed from the Japanese study in a few ways, Dr Zinzani pointed out. The European study only enrolled patients with PTCL. And it included patients with relapsed (49%) or refractory (51%) disease, whereas the Japanese study only included relapsed patients.
Furthermore, the Japanese study did not include any patients with an ECOG performance status of 2, while the European study did (39%). And the dosing schedule differed between the 2 studies.
In the European study, patients received mogamulizumab at 1 mg/kg once weekly for 4 weeks and then once every 2 weeks until they progressed or developed unacceptable toxicity.
There were 38 patients in the safety analysis. They had a median age of 58.5 years, and 61% were male.
Thirty-five of these patients were included in the efficacy analysis. They had a median of 2 prior treatments (range, 1-8), and 17 patients (49%) had responded to their last therapy.
The patients had PTCL-NOS (43%, 15/35), AITL (34%, 12), transformed mycosis fungoides (9%, 3), ALK- ALCL (11%, 4), and ALK+ ALCL (3%, 1).
The ORR was 11% (n=4), and 46% of patients (n=16) had SD or better. Two patients with PTCL-NOS responded, as did 2 with AITL.
Six patients with PTCL-NOS had SD, as did 3 with AITL, 1 with transformed mycosis fungoides, and 2 with ALK- ALCL.
The median duration of response (including SD) was 2.9 months. And the median PFS was 2.1 months. Two patients (1 with ALK- ALCL and 1 with PTCL-NOS) went on to allo-SCT.
The most frequent adverse events (occurring in at least 10% of patients) were drug eruption (n=12), pyrexia (n=9), pruritus (n=7), diarrhea (n=7), cough (n=6), vomiting (n=6), thrombocytopenia (n=6), hypotension (n=4), headache (n=4), peripheral edema (n=4), asthenia (n=4), nausea (n=4), anemia (n=4), and neutropenia (n=4).
“For the European experience, there were some differences from the Japanese experience,” Dr Zinzani said in closing. “It was worse in terms of overall response rate—only 11%—but roughly 50% of patients attained at least stable disease. And there was an acceptable safety profile in these really heavily pretreated, relapsed/refractory PTCL patients.” ![]()
SAN FRANCISCO—Two phase 2 studies testing mogamulizumab in peripheral T-cell lymphomas (PTCLs) suggest that higher response rates don’t necessarily translate to an improvement in progression-free survival (PFS).
The anti-CCR4 antibody produced a higher overall response rate (ORR) in a Japanese study than in a European study—34% and 11%, respectively.
However, median PFS times were similar—about 2 months in both studies.
This similarity is all the more interesting because the studies enrolled different types of patients and followed different dosing schedules, according to Pier Luigi Zinzani, MD, PhD, of the University of Bologna in Italy.
Dr Zinzani discussed details of the European experience testing mogamulizumab in PTCL, comparing it to the Japanese experience, in a presentation at the 7th Annual T-cell Lymphoma Forum.
Kensei Tobinai, MD, PhD, of the National Cancer Center Hospital in Tokyo, Japan, also reviewed the Japanese experience (TCLF 2013, JCO 2014) during the meeting’s keynote address and presented data from an ancillary analysis of this study (which is unpublished).
All of the research was sponsored by Kyowa Hakko Kirin Co., Ltd., the company developing mogamulizumab.
The Japanese experience
The Japanese study included 29 patients with PTCL and 8 with cutaneous T-cell lymphoma (CTCL). All patients had relapsed after their last chemotherapy regimen, and none had received an allogeneic stem cell transplant (allo-SCT). The PTCL patients had a median age of 67, and 69% were male.
All patients received mogamulizumab at 1.0 mg/kg/day weekly for 8 weeks. The ORR was 35%—34% for PTCL patients and 38% for CTCL patients.
Among PTCL patients, there were 5 complete responses (CRs) and 5 partial responses (PRs). Nine patients had stable disease (SD), and 10 progressed.
Of the 16 patients with PTCL-not otherwise specified (PTCL-NOS), 1 had a CR, 2 had a PR, 6 had SD, and 7 progressed. Of the 12 patients with angioimmunoblastic T-cell lymphoma (AITL), 3 had a CR, 3 had a PR, 3 had SD, and 3 progressed. The only patient with ALK- anaplastic large-cell lymphoma (ALCL) had an unconfirmed CR.
The ancillary analysis showed that tumor shrinkage of the target lesions occurred in 72% (21/29) of patients with PTCL. The patients’ median duration of response was 6.4 months, and the median time to response was 1.9 months.
Overall, the median PFS was 3.0 months—2.0 months in patients with PTCL and 3.4 months in patients with CTCL.
Common adverse events (for both PTCL and CTCL patients) included lymphopenia (81%), skin disorders (51%), leukopenia (43%), neutropenia (38%), thrombocytopenia (38%), pyrexia (30%), acute infusion reactions (24%), and anemia (14%).
Dr Tobinai noted that these results are not as favorable as those observed when patients with adult T-cell leukemia-lymphoma receive mogamulizumab.
“But compared to the efficacy rate of other approved agents—pralatrexate and romidepsin—this antibody has promising efficacy,” he said.
In fact, the results of this study prompted the December approval of mogamulizumab to treat PTCL and CTCL patients in Japan.
The European experience
The European study differed from the Japanese study in a few ways, Dr Zinzani pointed out. The European study only enrolled patients with PTCL. And it included patients with relapsed (49%) or refractory (51%) disease, whereas the Japanese study only included relapsed patients.
Furthermore, the Japanese study did not include any patients with an ECOG performance status of 2, while the European study did (39%). And the dosing schedule differed between the 2 studies.
In the European study, patients received mogamulizumab at 1 mg/kg once weekly for 4 weeks and then once every 2 weeks until they progressed or developed unacceptable toxicity.
There were 38 patients in the safety analysis. They had a median age of 58.5 years, and 61% were male.
Thirty-five of these patients were included in the efficacy analysis. They had a median of 2 prior treatments (range, 1-8), and 17 patients (49%) had responded to their last therapy.
The patients had PTCL-NOS (43%, 15/35), AITL (34%, 12), transformed mycosis fungoides (9%, 3), ALK- ALCL (11%, 4), and ALK+ ALCL (3%, 1).
The ORR was 11% (n=4), and 46% of patients (n=16) had SD or better. Two patients with PTCL-NOS responded, as did 2 with AITL.
Six patients with PTCL-NOS had SD, as did 3 with AITL, 1 with transformed mycosis fungoides, and 2 with ALK- ALCL.
The median duration of response (including SD) was 2.9 months. And the median PFS was 2.1 months. Two patients (1 with ALK- ALCL and 1 with PTCL-NOS) went on to allo-SCT.
The most frequent adverse events (occurring in at least 10% of patients) were drug eruption (n=12), pyrexia (n=9), pruritus (n=7), diarrhea (n=7), cough (n=6), vomiting (n=6), thrombocytopenia (n=6), hypotension (n=4), headache (n=4), peripheral edema (n=4), asthenia (n=4), nausea (n=4), anemia (n=4), and neutropenia (n=4).
“For the European experience, there were some differences from the Japanese experience,” Dr Zinzani said in closing. “It was worse in terms of overall response rate—only 11%—but roughly 50% of patients attained at least stable disease. And there was an acceptable safety profile in these really heavily pretreated, relapsed/refractory PTCL patients.” ![]()
SAN FRANCISCO—Two phase 2 studies testing mogamulizumab in peripheral T-cell lymphomas (PTCLs) suggest that higher response rates don’t necessarily translate to an improvement in progression-free survival (PFS).
The anti-CCR4 antibody produced a higher overall response rate (ORR) in a Japanese study than in a European study—34% and 11%, respectively.
However, median PFS times were similar—about 2 months in both studies.
This similarity is all the more interesting because the studies enrolled different types of patients and followed different dosing schedules, according to Pier Luigi Zinzani, MD, PhD, of the University of Bologna in Italy.
Dr Zinzani discussed details of the European experience testing mogamulizumab in PTCL, comparing it to the Japanese experience, in a presentation at the 7th Annual T-cell Lymphoma Forum.
Kensei Tobinai, MD, PhD, of the National Cancer Center Hospital in Tokyo, Japan, also reviewed the Japanese experience (TCLF 2013, JCO 2014) during the meeting’s keynote address and presented data from an ancillary analysis of this study (which is unpublished).
All of the research was sponsored by Kyowa Hakko Kirin Co., Ltd., the company developing mogamulizumab.
The Japanese experience
The Japanese study included 29 patients with PTCL and 8 with cutaneous T-cell lymphoma (CTCL). All patients had relapsed after their last chemotherapy regimen, and none had received an allogeneic stem cell transplant (allo-SCT). The PTCL patients had a median age of 67, and 69% were male.
All patients received mogamulizumab at 1.0 mg/kg/day weekly for 8 weeks. The ORR was 35%—34% for PTCL patients and 38% for CTCL patients.
Among PTCL patients, there were 5 complete responses (CRs) and 5 partial responses (PRs). Nine patients had stable disease (SD), and 10 progressed.
Of the 16 patients with PTCL-not otherwise specified (PTCL-NOS), 1 had a CR, 2 had a PR, 6 had SD, and 7 progressed. Of the 12 patients with angioimmunoblastic T-cell lymphoma (AITL), 3 had a CR, 3 had a PR, 3 had SD, and 3 progressed. The only patient with ALK- anaplastic large-cell lymphoma (ALCL) had an unconfirmed CR.
The ancillary analysis showed that tumor shrinkage of the target lesions occurred in 72% (21/29) of patients with PTCL. The patients’ median duration of response was 6.4 months, and the median time to response was 1.9 months.
Overall, the median PFS was 3.0 months—2.0 months in patients with PTCL and 3.4 months in patients with CTCL.
Common adverse events (for both PTCL and CTCL patients) included lymphopenia (81%), skin disorders (51%), leukopenia (43%), neutropenia (38%), thrombocytopenia (38%), pyrexia (30%), acute infusion reactions (24%), and anemia (14%).
Dr Tobinai noted that these results are not as favorable as those observed when patients with adult T-cell leukemia-lymphoma receive mogamulizumab.
“But compared to the efficacy rate of other approved agents—pralatrexate and romidepsin—this antibody has promising efficacy,” he said.
In fact, the results of this study prompted the December approval of mogamulizumab to treat PTCL and CTCL patients in Japan.
The European experience
The European study differed from the Japanese study in a few ways, Dr Zinzani pointed out. The European study only enrolled patients with PTCL. And it included patients with relapsed (49%) or refractory (51%) disease, whereas the Japanese study only included relapsed patients.
Furthermore, the Japanese study did not include any patients with an ECOG performance status of 2, while the European study did (39%). And the dosing schedule differed between the 2 studies.
In the European study, patients received mogamulizumab at 1 mg/kg once weekly for 4 weeks and then once every 2 weeks until they progressed or developed unacceptable toxicity.
There were 38 patients in the safety analysis. They had a median age of 58.5 years, and 61% were male.
Thirty-five of these patients were included in the efficacy analysis. They had a median of 2 prior treatments (range, 1-8), and 17 patients (49%) had responded to their last therapy.
The patients had PTCL-NOS (43%, 15/35), AITL (34%, 12), transformed mycosis fungoides (9%, 3), ALK- ALCL (11%, 4), and ALK+ ALCL (3%, 1).
The ORR was 11% (n=4), and 46% of patients (n=16) had SD or better. Two patients with PTCL-NOS responded, as did 2 with AITL.
Six patients with PTCL-NOS had SD, as did 3 with AITL, 1 with transformed mycosis fungoides, and 2 with ALK- ALCL.
The median duration of response (including SD) was 2.9 months. And the median PFS was 2.1 months. Two patients (1 with ALK- ALCL and 1 with PTCL-NOS) went on to allo-SCT.
The most frequent adverse events (occurring in at least 10% of patients) were drug eruption (n=12), pyrexia (n=9), pruritus (n=7), diarrhea (n=7), cough (n=6), vomiting (n=6), thrombocytopenia (n=6), hypotension (n=4), headache (n=4), peripheral edema (n=4), asthenia (n=4), nausea (n=4), anemia (n=4), and neutropenia (n=4).
“For the European experience, there were some differences from the Japanese experience,” Dr Zinzani said in closing. “It was worse in terms of overall response rate—only 11%—but roughly 50% of patients attained at least stable disease. And there was an acceptable safety profile in these really heavily pretreated, relapsed/refractory PTCL patients.” ![]()
Though costly, blood cancer drugs appear cost-effective

Photo by Bill Branson
A new analysis indicates that certain high-cost therapies for hematologic malignancies provide reasonable value for money spent.
Most cost-effectiveness ratios were lower than thresholds commonly used to establish cost-effectiveness in the US—$50,000 or $100,000 per quality-adjusted life year (QALY) gained.
The median cost-effectiveness ratio was highest for chronic myeloid leukemia (CML), at $55,000/QALY, and lowest for non-Hodgkin lymphoma (NHL), at $21,500/QALY.
Researchers presented these data in Blood.
“Given the increased discussion about the high cost of these treatments, we were somewhat surprised to discover that their cost-effectiveness ratios were lower than expected,” said study author Peter J. Neumann, ScD, of Tufts Medical Center in Boston.
“Our analysis had a small sample size and included both industry- and non-industry-funded studies. In addition, cost-effectiveness ratios may have changed over time as associated costs or benefits have changed. However, the study underscores that debates in healthcare should consider the value of breakthrough drugs and not just costs.”
With that issue in mind, Dr Neumann and his colleagues had conducted a systematic review of studies published between 1996 and 2012 that examined the cost utility of agents for hematologic malignancies. The cost utility of a drug was depicted as a ratio of a drug’s total cost per patient QALY gained.
The researchers identified 29 studies, 22 of which were industry-funded. Nine studies were conducted from a US perspective, 6 from the UK, 3 from Norway, 3 from Sweden, 2 from France, 1 from Canada, 1 from Finland, and 4 from “other” countries.
The team grouped studies according to malignancy—CML, chronic lymphocytic leukemia (CLL), NHL, and multiple myeloma (MM)—as well as by treatment—α interferon, alemtuzumab, bendamustine, bortezomib, dasatinib, imatinib, lenalidomide, rituximab alone or in combination, and thalidomide.
The studies reported 44 cost-effectiveness ratios, most concerning interventions for NHL (41%) or CML (30%). Most ratios pertained to rituximab (43%), α interferon (18%), or imatinib (16%), and the most common intervention-disease combination was rituximab (alone or in combination) for NHL (36%).
The median cost-effectiveness ratios fluctuated over time, rising from $35,000/QALY (1996-2002) to $52,000/QALY (2003-2006), then falling to $22,000/QALY (2007-2012).
The median cost-effectiveness ratio reported by industry-funded studies was lower ($26,000/QALY) than for non-industry-funded studies ($33,000/QALY).
Four cost-effectiveness ratios, 1 from an industry-funded study, exceeded $100,000/QALY. This included 2 studies of bortezomib in MM, 1 of α interferon in CML, and 1 of imatinib in CML.
The researchers said these results suggest that many new treatments for hematologic malignancies may confer reasonable value for money spent. The distribution of cost-effectiveness ratios is comparable to those for cancers overall and for other healthcare fields, they said.
This study was funded by internal resources at the Center for the Evaluation of Value and Risk in Health. The center receives funding from federal, private foundation, and pharmaceutical industry sources. ![]()

Photo by Bill Branson
A new analysis indicates that certain high-cost therapies for hematologic malignancies provide reasonable value for money spent.
Most cost-effectiveness ratios were lower than thresholds commonly used to establish cost-effectiveness in the US—$50,000 or $100,000 per quality-adjusted life year (QALY) gained.
The median cost-effectiveness ratio was highest for chronic myeloid leukemia (CML), at $55,000/QALY, and lowest for non-Hodgkin lymphoma (NHL), at $21,500/QALY.
Researchers presented these data in Blood.
“Given the increased discussion about the high cost of these treatments, we were somewhat surprised to discover that their cost-effectiveness ratios were lower than expected,” said study author Peter J. Neumann, ScD, of Tufts Medical Center in Boston.
“Our analysis had a small sample size and included both industry- and non-industry-funded studies. In addition, cost-effectiveness ratios may have changed over time as associated costs or benefits have changed. However, the study underscores that debates in healthcare should consider the value of breakthrough drugs and not just costs.”
With that issue in mind, Dr Neumann and his colleagues had conducted a systematic review of studies published between 1996 and 2012 that examined the cost utility of agents for hematologic malignancies. The cost utility of a drug was depicted as a ratio of a drug’s total cost per patient QALY gained.
The researchers identified 29 studies, 22 of which were industry-funded. Nine studies were conducted from a US perspective, 6 from the UK, 3 from Norway, 3 from Sweden, 2 from France, 1 from Canada, 1 from Finland, and 4 from “other” countries.
The team grouped studies according to malignancy—CML, chronic lymphocytic leukemia (CLL), NHL, and multiple myeloma (MM)—as well as by treatment—α interferon, alemtuzumab, bendamustine, bortezomib, dasatinib, imatinib, lenalidomide, rituximab alone or in combination, and thalidomide.
The studies reported 44 cost-effectiveness ratios, most concerning interventions for NHL (41%) or CML (30%). Most ratios pertained to rituximab (43%), α interferon (18%), or imatinib (16%), and the most common intervention-disease combination was rituximab (alone or in combination) for NHL (36%).
The median cost-effectiveness ratios fluctuated over time, rising from $35,000/QALY (1996-2002) to $52,000/QALY (2003-2006), then falling to $22,000/QALY (2007-2012).
The median cost-effectiveness ratio reported by industry-funded studies was lower ($26,000/QALY) than for non-industry-funded studies ($33,000/QALY).
Four cost-effectiveness ratios, 1 from an industry-funded study, exceeded $100,000/QALY. This included 2 studies of bortezomib in MM, 1 of α interferon in CML, and 1 of imatinib in CML.
The researchers said these results suggest that many new treatments for hematologic malignancies may confer reasonable value for money spent. The distribution of cost-effectiveness ratios is comparable to those for cancers overall and for other healthcare fields, they said.
This study was funded by internal resources at the Center for the Evaluation of Value and Risk in Health. The center receives funding from federal, private foundation, and pharmaceutical industry sources. ![]()

Photo by Bill Branson
A new analysis indicates that certain high-cost therapies for hematologic malignancies provide reasonable value for money spent.
Most cost-effectiveness ratios were lower than thresholds commonly used to establish cost-effectiveness in the US—$50,000 or $100,000 per quality-adjusted life year (QALY) gained.
The median cost-effectiveness ratio was highest for chronic myeloid leukemia (CML), at $55,000/QALY, and lowest for non-Hodgkin lymphoma (NHL), at $21,500/QALY.
Researchers presented these data in Blood.
“Given the increased discussion about the high cost of these treatments, we were somewhat surprised to discover that their cost-effectiveness ratios were lower than expected,” said study author Peter J. Neumann, ScD, of Tufts Medical Center in Boston.
“Our analysis had a small sample size and included both industry- and non-industry-funded studies. In addition, cost-effectiveness ratios may have changed over time as associated costs or benefits have changed. However, the study underscores that debates in healthcare should consider the value of breakthrough drugs and not just costs.”
With that issue in mind, Dr Neumann and his colleagues had conducted a systematic review of studies published between 1996 and 2012 that examined the cost utility of agents for hematologic malignancies. The cost utility of a drug was depicted as a ratio of a drug’s total cost per patient QALY gained.
The researchers identified 29 studies, 22 of which were industry-funded. Nine studies were conducted from a US perspective, 6 from the UK, 3 from Norway, 3 from Sweden, 2 from France, 1 from Canada, 1 from Finland, and 4 from “other” countries.
The team grouped studies according to malignancy—CML, chronic lymphocytic leukemia (CLL), NHL, and multiple myeloma (MM)—as well as by treatment—α interferon, alemtuzumab, bendamustine, bortezomib, dasatinib, imatinib, lenalidomide, rituximab alone or in combination, and thalidomide.
The studies reported 44 cost-effectiveness ratios, most concerning interventions for NHL (41%) or CML (30%). Most ratios pertained to rituximab (43%), α interferon (18%), or imatinib (16%), and the most common intervention-disease combination was rituximab (alone or in combination) for NHL (36%).
The median cost-effectiveness ratios fluctuated over time, rising from $35,000/QALY (1996-2002) to $52,000/QALY (2003-2006), then falling to $22,000/QALY (2007-2012).
The median cost-effectiveness ratio reported by industry-funded studies was lower ($26,000/QALY) than for non-industry-funded studies ($33,000/QALY).
Four cost-effectiveness ratios, 1 from an industry-funded study, exceeded $100,000/QALY. This included 2 studies of bortezomib in MM, 1 of α interferon in CML, and 1 of imatinib in CML.
The researchers said these results suggest that many new treatments for hematologic malignancies may confer reasonable value for money spent. The distribution of cost-effectiveness ratios is comparable to those for cancers overall and for other healthcare fields, they said.
This study was funded by internal resources at the Center for the Evaluation of Value and Risk in Health. The center receives funding from federal, private foundation, and pharmaceutical industry sources. ![]()
Hand rejuvenation
The three most exposed areas of the body that give away a person’s age are the face, neck, and hands. Rejuvenation of the hands is an often simple and nice addition to facial and neck aesthetic rejuvenation.
When examining aging hands, the three most prominent features are decreased volume in the interosseous spaces (leading to increased crepiness of the skin and increased show of extensor tendons), lentigines, and prominent veins. Therefore, the treatment for hands is quite simple: Restore volume, treat the pigmented lesions, and if needed, treat the prominent veins.
The anatomy of the dorsal hand can be divided into three major compartments. First, the skin, which on the dorsal hand is quite pliable. Second, the subcutaneous tissue, which consists of a loose areolar tissue where the lymphatics and veins lie. Third, beneath the subcutaneous tissue is the dorsal fascia of the hand, which is contiguous with extensor tendons and underlying compartments. It is in the subcutaneous layer (or loose areolar tissue) where fillers or fat are placed to treat volume loss.
While several fillers are currently used off label for hand rejuvenation, the Food and Drug Administration is meeting in February to consider officially approving Radiesse for this indication. Currently, hyaluronic acid (HA) fillers, calcium- hydroxylapatite (Radiesse), poly-L-lactic acid, and autologous fat are all utilized. I tend to use HAs in this location because of the reversibility, if needed, and decreased risk of nodule formation. Several techniques exist, including injecting between each tendon space vs. a bolus technique. I tend to use a bolus technique, where one or two boluses are injected while tenting the skin up to ensure injection into the correct plane and to avoid the vessels. Subsequently, the boluses are massaged into place while the patient makes a fist.
Once the interosseous spaces have been treated, the veins often appear less prominent and often don’t require direct treatment. I typically do not treat the dorsal hand veins, but sclerotherapy can be performed. Lentigines may be treated with a variety of devices including intense pulse light, Q-switched lasers, and fractionated nonablative lasers. Chemical peels and topical antipigment agents also may help to a lesser degree or also may be used for maintenance to keep the lentigines away.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Dermatology News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
The three most exposed areas of the body that give away a person’s age are the face, neck, and hands. Rejuvenation of the hands is an often simple and nice addition to facial and neck aesthetic rejuvenation.
When examining aging hands, the three most prominent features are decreased volume in the interosseous spaces (leading to increased crepiness of the skin and increased show of extensor tendons), lentigines, and prominent veins. Therefore, the treatment for hands is quite simple: Restore volume, treat the pigmented lesions, and if needed, treat the prominent veins.
The anatomy of the dorsal hand can be divided into three major compartments. First, the skin, which on the dorsal hand is quite pliable. Second, the subcutaneous tissue, which consists of a loose areolar tissue where the lymphatics and veins lie. Third, beneath the subcutaneous tissue is the dorsal fascia of the hand, which is contiguous with extensor tendons and underlying compartments. It is in the subcutaneous layer (or loose areolar tissue) where fillers or fat are placed to treat volume loss.
While several fillers are currently used off label for hand rejuvenation, the Food and Drug Administration is meeting in February to consider officially approving Radiesse for this indication. Currently, hyaluronic acid (HA) fillers, calcium- hydroxylapatite (Radiesse), poly-L-lactic acid, and autologous fat are all utilized. I tend to use HAs in this location because of the reversibility, if needed, and decreased risk of nodule formation. Several techniques exist, including injecting between each tendon space vs. a bolus technique. I tend to use a bolus technique, where one or two boluses are injected while tenting the skin up to ensure injection into the correct plane and to avoid the vessels. Subsequently, the boluses are massaged into place while the patient makes a fist.
Once the interosseous spaces have been treated, the veins often appear less prominent and often don’t require direct treatment. I typically do not treat the dorsal hand veins, but sclerotherapy can be performed. Lentigines may be treated with a variety of devices including intense pulse light, Q-switched lasers, and fractionated nonablative lasers. Chemical peels and topical antipigment agents also may help to a lesser degree or also may be used for maintenance to keep the lentigines away.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Dermatology News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
The three most exposed areas of the body that give away a person’s age are the face, neck, and hands. Rejuvenation of the hands is an often simple and nice addition to facial and neck aesthetic rejuvenation.
When examining aging hands, the three most prominent features are decreased volume in the interosseous spaces (leading to increased crepiness of the skin and increased show of extensor tendons), lentigines, and prominent veins. Therefore, the treatment for hands is quite simple: Restore volume, treat the pigmented lesions, and if needed, treat the prominent veins.
The anatomy of the dorsal hand can be divided into three major compartments. First, the skin, which on the dorsal hand is quite pliable. Second, the subcutaneous tissue, which consists of a loose areolar tissue where the lymphatics and veins lie. Third, beneath the subcutaneous tissue is the dorsal fascia of the hand, which is contiguous with extensor tendons and underlying compartments. It is in the subcutaneous layer (or loose areolar tissue) where fillers or fat are placed to treat volume loss.
While several fillers are currently used off label for hand rejuvenation, the Food and Drug Administration is meeting in February to consider officially approving Radiesse for this indication. Currently, hyaluronic acid (HA) fillers, calcium- hydroxylapatite (Radiesse), poly-L-lactic acid, and autologous fat are all utilized. I tend to use HAs in this location because of the reversibility, if needed, and decreased risk of nodule formation. Several techniques exist, including injecting between each tendon space vs. a bolus technique. I tend to use a bolus technique, where one or two boluses are injected while tenting the skin up to ensure injection into the correct plane and to avoid the vessels. Subsequently, the boluses are massaged into place while the patient makes a fist.
Once the interosseous spaces have been treated, the veins often appear less prominent and often don’t require direct treatment. I typically do not treat the dorsal hand veins, but sclerotherapy can be performed. Lentigines may be treated with a variety of devices including intense pulse light, Q-switched lasers, and fractionated nonablative lasers. Chemical peels and topical antipigment agents also may help to a lesser degree or also may be used for maintenance to keep the lentigines away.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Dermatology News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.