User login
Hysteroscopic myomectomy using a mechanical approach
Uterine fibroids are a common complaint in gynecology, with an incidence of approximately 30% in women aged 25 to 45 years and a cumulative incidence of 70% to 80% by age 50.1,2 They are more prevalent in women of African descent and are a leading indication for hysterectomy.
Although they can be asymptomatic, submucosal fibroids are frequently associated with:
- abnormal uterine bleeding (AUB)
- dysmenorrhea
- expulsion of an intrauterine device (IUD)
- leukorrhea
- pelvic pain
- urinary frequency
- infertility
- premature labor
- reproductive wastage
- bleeding during hormone replacement therapy.
In postmenopausal women, the risk of malignancy in a leiomyoma ranges from 0.2% to 0.5%.1 The risk is lower in premenopausal women.
In this article, I describe the technique for hysteroscopic myomectomy using a mechanical approach (Truclear Tissue Removal System, Smith & Nephew, Andover, MA), which offers hysteroscopic morcellation as well as quick resection and efficient fluid management. (Note: Unlike open intraperitoneal morcellation, hysteroscopic morcellation carries a low risk of tissue spread.)
Classification of fibroids
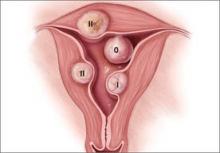
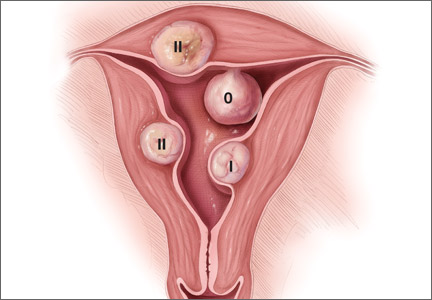
Preoperative classification of leiomyomas makes it possible to determine the best route for surgery. The most commonly used classification system was developed by the European Society of Gynaecological Endoscopy (ESGE) (FIGURE 1), which considers the extent of intramural extension. Each fibroid under that system is classified as:
- Type 0 – no intramural extension
- Type I – less than 50% extension
- Type II – more than 50% extension.
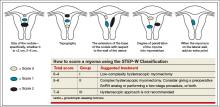
A second classification system recently was devised to take into account additional features of the fibroid. The STEP-W classification considers size, topography, extension, penetration, and the lateral wall (FIGURE 2). In general, the lower the score, the less complex the procedure will be, with a lower risk of fluid intravasation, shorter operative time, and a greater likelihood of complete removal of the fibroid.
A multicenter, prospective study of 449 women who underwent hysteroscopic resection of their fibroids correlated the ESGE and STEP-W systems. All 320 fibroids (100%) with a score of 4 or below on the STEP-W classification system were completely removed, compared with 112 of 145 fibroids (77.2%) with a score greater than 4. All 33 cases of incomplete hysteroscopic resection (100%) had a STEP-W score above 4.3
In the same study, 85 of 86 cases (98.9%) with Type 0 fibroids under the ESGE system had complete resection, along with 278 of 298 Type I fibroids (93.3%), and 69 of 81 Type II fibroids (85.2%).3 Complete removal is a goal because it relieves symptoms and averts the need for additional procedures.
Patient selection
Proper patient selection for hysteroscopic myomectomy is extremely important. The most common indications are AUB, pelvic pain or discomfort, recurrent pregnancy loss, and infertility. In addition, the patient should have a strong wish for uterine preservation and desire a minimally invasive transcervical approach.
AAGL guidelines on the diagnosis and management of submucous fibroids note that, in general, submucous leiomyomas as large as 4 or 5 cm in diameter can be removed hysteroscopically by experienced surgeons.4
A hysteroscopic approach is not advised for women in whom hysteroscopic surgery is contraindicated, such as women with intrauterine pregnancy, active pelvic infection, active herpes infection, or cervical or uterine cancer. Women who have medical comorbidities such as coronary heart disease, significant renal disease, or bleeding diathesis may need perioperative clearance from anesthesia or hematology prior to hysteroscopic surgery and close fluid monitoring during the procedure.
Consider the leiomyoma
Penetration into the myometrium. Women who have a fibroid that penetrates more than 50% into the myometrium may benefit from hysteroscopic myomectomy, provided the surgeon is highly experienced. A skilled hysteroscopist can ensure complete enucleation of a penetrating fibroid in these cases.
If you are still in the learning process for hysteroscopy, however, start with easier cases—ie, polyps and Type 0 and Type I fibroids. Type II fibroids require longer operative time, are associated with increased fluid absorption and intravasation, carry an increased risk of perioperative complications, and may not always be completely resected.
Size of the fibroid also is relevant. As size increases, so does the volume of tissue needing to be removed, adding to overall operative time.
Presence of other fibroids. When a woman has an intracavitary fibroid as well as myomas in other locations, the surgeon should consider whether hysteroscopic removal of the intracavitary lesion alone can provide significant relief of all fibroid-related symptoms. In such cases, laparoscopic, robotic, or abdominal myomectomy may be preferable, especially if the volume of the additional myomas is considerable.
To determine the optimal surgical route, the physician must consider the symptoms present—is AUB the only symptom, or are other fibroid-related conditions present as well, such as bulk, pelvic pain, and other quality-of-life issues? If multiple symptoms exist, then other approaches may be better.
How fibroids affect fertility
Fibroids are present in 5% to 10% of women with infertility. In this population, fibroids are the only abnormal finding in 1.0% to 2.4% of cases.4
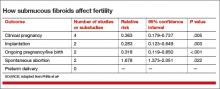
In a meta-analysis of 23 studies evaluating women with fibroids and infertility, Pritts and colleagues found nine studies involving submucosal fibroids.5 These studies included one randomized controlled trial, two prospective studies, and six retrospective analyses. They found that women who had fibroids with a submucosal component had lower pregnancy and implantation rates, compared with their infertile, myoma-free counterparts. Pritts and colleagues concluded that myomectomy is likely to improve fertility in these cases (TABLE).5
Instrumentation
Among the options are monopolar and bipolar resectoscopy and the mechanical approach using the Truclear System, which includes a morcellator. With conventional resectoscopy all chips must be removed, necessitating multiple insertions of the hysteroscope. Monopolar instrumentation, in particular, carries a risk of energy discharge to healthy tissue. The monopolar resectoscope also has a longer learning curve, compared with the mechanical approach.6
In contrast, the Truclear System requires fewer insertions, has a short learning curve, and omits the need for capture of individual chips, as the mechanical morcellator suctions and captures them throughout the procedure.7 In addition, because resection is performed mechanically, there is no risk of energy discharge to healthy tissue.
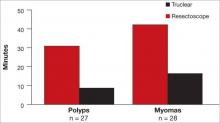
The Truclear system also is associated with a significantly shorter operative time, compared with resectoscopy, which may be advantageous for residents, fellows, and other physicians learning the procedure (FIGURE 3).7 Shorter operative time also may result in lower fluid deficits. In addition, saline distension may reduce the risk of fluid absorption and hyponatremia. The tissue-capture feature allows evaluation of the entire pathologic specimen.
Besides hysteroscopic myomectomy, the Truclear System is appropriate for visual dilatation and curettage (D&C), adhesiolysis, polypectomy, and evacuation of retained products of conception.
Preoperative evaluation
A complete history is vital to document which fibroid-related symptoms are present and how they affect quality of life.
Preoperative imaging also is imperative—using either 2D or 3D saline infusion sonography or a combination of diagnostic hysteroscopy and transvaginal ultrasound—to select patients for hysteroscopy, anticipate blood loss, and ensure that the proper instrumentation is available at the time of surgery. Magnetic resonance imaging, computed tomography, and hysterosalpingography are either prohibitively expensive or of limited value in the initial preoperative assessment of uterine fibroids.
Any woman who has AUB and a risk for endometrial hyperplasia or cancer should undergo endometrial assessment as well.
Use of preoperative medications
In most cases, prophylactic administration of antibiotics is not warranted to prevent infection or endocarditis.
Although some clinicians give gonadotropin-releasing hormone (GnRH) agonists to reduce the size of large fibroids, the drug complicates dissection of the fibroid from the surrounding capsule. For this reason, and because we lack data demonstrating that GnRH agonists decrease blood loss and limit absorption of distension media, I do not administer them to patients.8–12 Moreover, this drug can cause vasomotor symptoms, cervical stenosis, and vaginal hemorrhage (related to estrogen flare).
GnRH agonists may be of value to stimulate transient amenorrhea for several months preoperatively in order to correct iron-deficiency anemia. Intravenous iron also can be administered during this interval.
The risk of bleeding in hysteroscopic myomectomy is 2% to 3%.1 When the mechanical approach is used, rather than resectoscopy, continuous flow coupled with suctioning of the chips during the procedure keeps the image clear. Post-procedure contraction of the uterus stops most bleeding. Intrauterine pressure of the pump can be increased to help tamponade any oozing.
Misoprostol. Cervical stenosis is not uncommon in menopausal women. It can also pose a challenge in nulliparous women. Attempting hysteroscopy in the setting of cervical stenosis increases the risk of cervical laceration, creation of a false passage, and uterine perforation. For this reason, I prescribe oral or vaginal misoprostol 200 to 400 µg nightly for 1 to 2 days before the procedure.
Vasopressin can reduce blood loss during hysteroscopic myomectomy when it is injected into the cervical stroma preoperatively. It also reduces absorption of distension fluid and facilitates cervical dilation.
However, vasopressin must be injected with extreme care, with aspiration to confirm the absence of blood prior to each injection, as intravascular injection can lead to bradycardia, profound hypertension, and even death.13 Always notify the anesthesiologist prior to injection when vasopressin will be administered.
I routinely use vasopressin before hysteroscopic myomectomy (0.5 mg in 20 cc of saline or 20 U in 100 cc), injecting 5 cc of the solution at 3, 6, 9, and 12 o’clock positions.
Anesthesia during hysteroscopic myomectomy typically is “monitored anesthesia care,” or MAC, which consists of local anesthesia with sedation and analgesia. The need for regional or general anesthesia is rare. Consider adding a pericervical block or intravenous ketorolac (Toradol) to provide postoperative analgesia.
Surgical technique
Strict attention to fluid management is required throughout the procedure, preferably in accordance with AAGL guidelines on the management of hysteroscopic distending media.14 With the mechanical approach, because the distension fluid is isotonic (normal saline), it does not increase the risk of hyponatremia but can cause pulmonary edema or congestive heart failure. Intravasation usually is the result of excessive operative time, treatment of deeper myometrial fibroids (Type I or II), or high intrauterine pressure. I operate using intrauterine pressure in the range of 75 to 125 mm Hg.
The steps involved in the mechanical hysteroscopy approach are:
- Insert the hysteroscope into the uterus under direct visualization. In general, the greater the number of insertions, the greater the risk of uterine perforation. Preoperative cervical ripening helps facilitate insertion (see “Misoprostol” above).
- Distend the uterus with saline and inspect the uterine cavity, noting again the size and location of the fibroids and whether they are sessile or pedunculated.
- Locate the fibroid or other pathology to be removed, and place the morcellator window against it to begin cutting. Use the tip of the morcellator to elevate the fibroid for easier cutting. Enucleation is accomplished largely by varying the intrauterine pressure, which permits uterine decompression and myometrial contraction and renders the fibroid capsule more visible. If necessary, the hysteroscope can be withdrawn to stimulate myometrial contraction, which also helps to delineate the fibroid capsule.
- Reinspect the uterus to rule out perforation and remove any additional intrauterine pathology with a targeted view.
- Once all designated fibroids have been removed, withdraw the morcellator and hysteroscope from the uterus.
- Inspect the endocervical landscape to rule out injury and other pathology.
- Careful preoperative evaluation is important, preferably using diagnostic hysteroscopy or saline infusion sonography, to choose the optimal route of myomectomy and plan the surgical approach.
- During the myomectomy, pay close attention to fluid management and adhere strictly to predetermined limits.
- Complete removal of the fibroid is essential to relieve symptoms and avert the need for additional procedures.
Postoperative care
A nonsteroidal anti-inflammatory drug or limited use of narcotics usually is sufficient to relieve any postoperative cramping or vaginal discomfort.
Advise the patient to notify you in the event of increasing pain, foul-smelling vaginal discharge, or fever.
Also counsel her that she can return to most normal activities within 24 to 48 hours. Sexual activity is permissible 1 week after surgery. Early and frequent ambulation is important.
Schedule a follow-up visit 4 to 6 weeks after the procedure.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Perez-Medina T, Font EC, eds. Diagnostic and Operative Hysteroscopy. Tunbridge Wells, Kent, UK: Anshan Publishing; 2007:13.
2. Management of uterine fibroids: an update of the evidence. Agency for Healthcare Research and Quality. http://archive.ahrq.gov/clinic/tp/uteruptp.htm. Published July 2007. Accessed January 14, 2015.
3. Lasmar RB, Zinmei Z, Indman PD, Celeste RK, Di Spiezo Sardo A. Feasibility of a new system of classification of submucous myomas: a multicenter study. Fertil Steril. 2011;95(6):2073–2077.
4. AAGL Practice Report: practice guidelines for the diagnosis and management of submucous leiomyomas. J Minim Invasive Gynecol. 2012;19(2):152–171.
5. Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009;91(4):1215–1223.
6. Van Dongen H, Emanuel MH, Wolterbeek R, Trimbos JB, Jansen FW. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15(4):466–471.
7. Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12(1):62–66.
8. Emanuel MH, Hart A, Wamsteker K, Lammes F. An analysis of fluid loss during transcervical resection of submucous myomas. Fertil Steril. 1997;68(5):881–886.
9. Taskin O, Sadik S, Onoglu A, et al. Role of endometrial suppression on the frequency of intrauterine adhesions after resectoscopic surgery. J Am Assoc Gynecol Laparosc. 2000;7(3):351.
10. Propst AM, Liberman RF, Harlow BL, Ginsburg ES. Complications of hysteroscopic surgery: predicting patients at risk. Obstet Gynecol. 2000;96(4):517–520.
11. Perino A, Chianchiano N, Petronio M, Cittadini E. Role of leuprolide acetate depot in hysteroscopic surgery: a controlled study. Fertil Steril. 1993;59(3):507–510.
12. Mencaglia L, Tantini C. GnRH agonist analogs and hysteroscopic resection of myomas. Int J Gynaecol Obstet. 1993;43(3):285–288.
13. Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 Pt 2):484–486.
14. Munro MD, Storz K, Abbott JA, et al; AAGL. AAGL Practice Report: practice guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013;20(2):137–148.
Uterine fibroids are a common complaint in gynecology, with an incidence of approximately 30% in women aged 25 to 45 years and a cumulative incidence of 70% to 80% by age 50.1,2 They are more prevalent in women of African descent and are a leading indication for hysterectomy.
Although they can be asymptomatic, submucosal fibroids are frequently associated with:
- abnormal uterine bleeding (AUB)
- dysmenorrhea
- expulsion of an intrauterine device (IUD)
- leukorrhea
- pelvic pain
- urinary frequency
- infertility
- premature labor
- reproductive wastage
- bleeding during hormone replacement therapy.
In postmenopausal women, the risk of malignancy in a leiomyoma ranges from 0.2% to 0.5%.1 The risk is lower in premenopausal women.
In this article, I describe the technique for hysteroscopic myomectomy using a mechanical approach (Truclear Tissue Removal System, Smith & Nephew, Andover, MA), which offers hysteroscopic morcellation as well as quick resection and efficient fluid management. (Note: Unlike open intraperitoneal morcellation, hysteroscopic morcellation carries a low risk of tissue spread.)
Classification of fibroids
Preoperative classification of leiomyomas makes it possible to determine the best route for surgery. The most commonly used classification system was developed by the European Society of Gynaecological Endoscopy (ESGE) (FIGURE 1), which considers the extent of intramural extension. Each fibroid under that system is classified as:
- Type 0 – no intramural extension
- Type I – less than 50% extension
- Type II – more than 50% extension.
A second classification system recently was devised to take into account additional features of the fibroid. The STEP-W classification considers size, topography, extension, penetration, and the lateral wall (FIGURE 2). In general, the lower the score, the less complex the procedure will be, with a lower risk of fluid intravasation, shorter operative time, and a greater likelihood of complete removal of the fibroid.
A multicenter, prospective study of 449 women who underwent hysteroscopic resection of their fibroids correlated the ESGE and STEP-W systems. All 320 fibroids (100%) with a score of 4 or below on the STEP-W classification system were completely removed, compared with 112 of 145 fibroids (77.2%) with a score greater than 4. All 33 cases of incomplete hysteroscopic resection (100%) had a STEP-W score above 4.3
In the same study, 85 of 86 cases (98.9%) with Type 0 fibroids under the ESGE system had complete resection, along with 278 of 298 Type I fibroids (93.3%), and 69 of 81 Type II fibroids (85.2%).3 Complete removal is a goal because it relieves symptoms and averts the need for additional procedures.
Patient selection
Proper patient selection for hysteroscopic myomectomy is extremely important. The most common indications are AUB, pelvic pain or discomfort, recurrent pregnancy loss, and infertility. In addition, the patient should have a strong wish for uterine preservation and desire a minimally invasive transcervical approach.
AAGL guidelines on the diagnosis and management of submucous fibroids note that, in general, submucous leiomyomas as large as 4 or 5 cm in diameter can be removed hysteroscopically by experienced surgeons.4
A hysteroscopic approach is not advised for women in whom hysteroscopic surgery is contraindicated, such as women with intrauterine pregnancy, active pelvic infection, active herpes infection, or cervical or uterine cancer. Women who have medical comorbidities such as coronary heart disease, significant renal disease, or bleeding diathesis may need perioperative clearance from anesthesia or hematology prior to hysteroscopic surgery and close fluid monitoring during the procedure.
Consider the leiomyoma
Penetration into the myometrium. Women who have a fibroid that penetrates more than 50% into the myometrium may benefit from hysteroscopic myomectomy, provided the surgeon is highly experienced. A skilled hysteroscopist can ensure complete enucleation of a penetrating fibroid in these cases.
If you are still in the learning process for hysteroscopy, however, start with easier cases—ie, polyps and Type 0 and Type I fibroids. Type II fibroids require longer operative time, are associated with increased fluid absorption and intravasation, carry an increased risk of perioperative complications, and may not always be completely resected.
Size of the fibroid also is relevant. As size increases, so does the volume of tissue needing to be removed, adding to overall operative time.
Presence of other fibroids. When a woman has an intracavitary fibroid as well as myomas in other locations, the surgeon should consider whether hysteroscopic removal of the intracavitary lesion alone can provide significant relief of all fibroid-related symptoms. In such cases, laparoscopic, robotic, or abdominal myomectomy may be preferable, especially if the volume of the additional myomas is considerable.
To determine the optimal surgical route, the physician must consider the symptoms present—is AUB the only symptom, or are other fibroid-related conditions present as well, such as bulk, pelvic pain, and other quality-of-life issues? If multiple symptoms exist, then other approaches may be better.
How fibroids affect fertility
Fibroids are present in 5% to 10% of women with infertility. In this population, fibroids are the only abnormal finding in 1.0% to 2.4% of cases.4
In a meta-analysis of 23 studies evaluating women with fibroids and infertility, Pritts and colleagues found nine studies involving submucosal fibroids.5 These studies included one randomized controlled trial, two prospective studies, and six retrospective analyses. They found that women who had fibroids with a submucosal component had lower pregnancy and implantation rates, compared with their infertile, myoma-free counterparts. Pritts and colleagues concluded that myomectomy is likely to improve fertility in these cases (TABLE).5
Instrumentation
Among the options are monopolar and bipolar resectoscopy and the mechanical approach using the Truclear System, which includes a morcellator. With conventional resectoscopy all chips must be removed, necessitating multiple insertions of the hysteroscope. Monopolar instrumentation, in particular, carries a risk of energy discharge to healthy tissue. The monopolar resectoscope also has a longer learning curve, compared with the mechanical approach.6
In contrast, the Truclear System requires fewer insertions, has a short learning curve, and omits the need for capture of individual chips, as the mechanical morcellator suctions and captures them throughout the procedure.7 In addition, because resection is performed mechanically, there is no risk of energy discharge to healthy tissue.
The Truclear system also is associated with a significantly shorter operative time, compared with resectoscopy, which may be advantageous for residents, fellows, and other physicians learning the procedure (FIGURE 3).7 Shorter operative time also may result in lower fluid deficits. In addition, saline distension may reduce the risk of fluid absorption and hyponatremia. The tissue-capture feature allows evaluation of the entire pathologic specimen.
Besides hysteroscopic myomectomy, the Truclear System is appropriate for visual dilatation and curettage (D&C), adhesiolysis, polypectomy, and evacuation of retained products of conception.
Preoperative evaluation
A complete history is vital to document which fibroid-related symptoms are present and how they affect quality of life.
Preoperative imaging also is imperative—using either 2D or 3D saline infusion sonography or a combination of diagnostic hysteroscopy and transvaginal ultrasound—to select patients for hysteroscopy, anticipate blood loss, and ensure that the proper instrumentation is available at the time of surgery. Magnetic resonance imaging, computed tomography, and hysterosalpingography are either prohibitively expensive or of limited value in the initial preoperative assessment of uterine fibroids.
Any woman who has AUB and a risk for endometrial hyperplasia or cancer should undergo endometrial assessment as well.
Use of preoperative medications
In most cases, prophylactic administration of antibiotics is not warranted to prevent infection or endocarditis.
Although some clinicians give gonadotropin-releasing hormone (GnRH) agonists to reduce the size of large fibroids, the drug complicates dissection of the fibroid from the surrounding capsule. For this reason, and because we lack data demonstrating that GnRH agonists decrease blood loss and limit absorption of distension media, I do not administer them to patients.8–12 Moreover, this drug can cause vasomotor symptoms, cervical stenosis, and vaginal hemorrhage (related to estrogen flare).
GnRH agonists may be of value to stimulate transient amenorrhea for several months preoperatively in order to correct iron-deficiency anemia. Intravenous iron also can be administered during this interval.
The risk of bleeding in hysteroscopic myomectomy is 2% to 3%.1 When the mechanical approach is used, rather than resectoscopy, continuous flow coupled with suctioning of the chips during the procedure keeps the image clear. Post-procedure contraction of the uterus stops most bleeding. Intrauterine pressure of the pump can be increased to help tamponade any oozing.
Misoprostol. Cervical stenosis is not uncommon in menopausal women. It can also pose a challenge in nulliparous women. Attempting hysteroscopy in the setting of cervical stenosis increases the risk of cervical laceration, creation of a false passage, and uterine perforation. For this reason, I prescribe oral or vaginal misoprostol 200 to 400 µg nightly for 1 to 2 days before the procedure.
Vasopressin can reduce blood loss during hysteroscopic myomectomy when it is injected into the cervical stroma preoperatively. It also reduces absorption of distension fluid and facilitates cervical dilation.
However, vasopressin must be injected with extreme care, with aspiration to confirm the absence of blood prior to each injection, as intravascular injection can lead to bradycardia, profound hypertension, and even death.13 Always notify the anesthesiologist prior to injection when vasopressin will be administered.
I routinely use vasopressin before hysteroscopic myomectomy (0.5 mg in 20 cc of saline or 20 U in 100 cc), injecting 5 cc of the solution at 3, 6, 9, and 12 o’clock positions.
Anesthesia during hysteroscopic myomectomy typically is “monitored anesthesia care,” or MAC, which consists of local anesthesia with sedation and analgesia. The need for regional or general anesthesia is rare. Consider adding a pericervical block or intravenous ketorolac (Toradol) to provide postoperative analgesia.
Surgical technique
Strict attention to fluid management is required throughout the procedure, preferably in accordance with AAGL guidelines on the management of hysteroscopic distending media.14 With the mechanical approach, because the distension fluid is isotonic (normal saline), it does not increase the risk of hyponatremia but can cause pulmonary edema or congestive heart failure. Intravasation usually is the result of excessive operative time, treatment of deeper myometrial fibroids (Type I or II), or high intrauterine pressure. I operate using intrauterine pressure in the range of 75 to 125 mm Hg.
The steps involved in the mechanical hysteroscopy approach are:
- Insert the hysteroscope into the uterus under direct visualization. In general, the greater the number of insertions, the greater the risk of uterine perforation. Preoperative cervical ripening helps facilitate insertion (see “Misoprostol” above).
- Distend the uterus with saline and inspect the uterine cavity, noting again the size and location of the fibroids and whether they are sessile or pedunculated.
- Locate the fibroid or other pathology to be removed, and place the morcellator window against it to begin cutting. Use the tip of the morcellator to elevate the fibroid for easier cutting. Enucleation is accomplished largely by varying the intrauterine pressure, which permits uterine decompression and myometrial contraction and renders the fibroid capsule more visible. If necessary, the hysteroscope can be withdrawn to stimulate myometrial contraction, which also helps to delineate the fibroid capsule.
- Reinspect the uterus to rule out perforation and remove any additional intrauterine pathology with a targeted view.
- Once all designated fibroids have been removed, withdraw the morcellator and hysteroscope from the uterus.
- Inspect the endocervical landscape to rule out injury and other pathology.
- Careful preoperative evaluation is important, preferably using diagnostic hysteroscopy or saline infusion sonography, to choose the optimal route of myomectomy and plan the surgical approach.
- During the myomectomy, pay close attention to fluid management and adhere strictly to predetermined limits.
- Complete removal of the fibroid is essential to relieve symptoms and avert the need for additional procedures.
Postoperative care
A nonsteroidal anti-inflammatory drug or limited use of narcotics usually is sufficient to relieve any postoperative cramping or vaginal discomfort.
Advise the patient to notify you in the event of increasing pain, foul-smelling vaginal discharge, or fever.
Also counsel her that she can return to most normal activities within 24 to 48 hours. Sexual activity is permissible 1 week after surgery. Early and frequent ambulation is important.
Schedule a follow-up visit 4 to 6 weeks after the procedure.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Uterine fibroids are a common complaint in gynecology, with an incidence of approximately 30% in women aged 25 to 45 years and a cumulative incidence of 70% to 80% by age 50.1,2 They are more prevalent in women of African descent and are a leading indication for hysterectomy.
Although they can be asymptomatic, submucosal fibroids are frequently associated with:
- abnormal uterine bleeding (AUB)
- dysmenorrhea
- expulsion of an intrauterine device (IUD)
- leukorrhea
- pelvic pain
- urinary frequency
- infertility
- premature labor
- reproductive wastage
- bleeding during hormone replacement therapy.
In postmenopausal women, the risk of malignancy in a leiomyoma ranges from 0.2% to 0.5%.1 The risk is lower in premenopausal women.
In this article, I describe the technique for hysteroscopic myomectomy using a mechanical approach (Truclear Tissue Removal System, Smith & Nephew, Andover, MA), which offers hysteroscopic morcellation as well as quick resection and efficient fluid management. (Note: Unlike open intraperitoneal morcellation, hysteroscopic morcellation carries a low risk of tissue spread.)
Classification of fibroids
Preoperative classification of leiomyomas makes it possible to determine the best route for surgery. The most commonly used classification system was developed by the European Society of Gynaecological Endoscopy (ESGE) (FIGURE 1), which considers the extent of intramural extension. Each fibroid under that system is classified as:
- Type 0 – no intramural extension
- Type I – less than 50% extension
- Type II – more than 50% extension.
A second classification system recently was devised to take into account additional features of the fibroid. The STEP-W classification considers size, topography, extension, penetration, and the lateral wall (FIGURE 2). In general, the lower the score, the less complex the procedure will be, with a lower risk of fluid intravasation, shorter operative time, and a greater likelihood of complete removal of the fibroid.
A multicenter, prospective study of 449 women who underwent hysteroscopic resection of their fibroids correlated the ESGE and STEP-W systems. All 320 fibroids (100%) with a score of 4 or below on the STEP-W classification system were completely removed, compared with 112 of 145 fibroids (77.2%) with a score greater than 4. All 33 cases of incomplete hysteroscopic resection (100%) had a STEP-W score above 4.3
In the same study, 85 of 86 cases (98.9%) with Type 0 fibroids under the ESGE system had complete resection, along with 278 of 298 Type I fibroids (93.3%), and 69 of 81 Type II fibroids (85.2%).3 Complete removal is a goal because it relieves symptoms and averts the need for additional procedures.
Patient selection
Proper patient selection for hysteroscopic myomectomy is extremely important. The most common indications are AUB, pelvic pain or discomfort, recurrent pregnancy loss, and infertility. In addition, the patient should have a strong wish for uterine preservation and desire a minimally invasive transcervical approach.
AAGL guidelines on the diagnosis and management of submucous fibroids note that, in general, submucous leiomyomas as large as 4 or 5 cm in diameter can be removed hysteroscopically by experienced surgeons.4
A hysteroscopic approach is not advised for women in whom hysteroscopic surgery is contraindicated, such as women with intrauterine pregnancy, active pelvic infection, active herpes infection, or cervical or uterine cancer. Women who have medical comorbidities such as coronary heart disease, significant renal disease, or bleeding diathesis may need perioperative clearance from anesthesia or hematology prior to hysteroscopic surgery and close fluid monitoring during the procedure.
Consider the leiomyoma
Penetration into the myometrium. Women who have a fibroid that penetrates more than 50% into the myometrium may benefit from hysteroscopic myomectomy, provided the surgeon is highly experienced. A skilled hysteroscopist can ensure complete enucleation of a penetrating fibroid in these cases.
If you are still in the learning process for hysteroscopy, however, start with easier cases—ie, polyps and Type 0 and Type I fibroids. Type II fibroids require longer operative time, are associated with increased fluid absorption and intravasation, carry an increased risk of perioperative complications, and may not always be completely resected.
Size of the fibroid also is relevant. As size increases, so does the volume of tissue needing to be removed, adding to overall operative time.
Presence of other fibroids. When a woman has an intracavitary fibroid as well as myomas in other locations, the surgeon should consider whether hysteroscopic removal of the intracavitary lesion alone can provide significant relief of all fibroid-related symptoms. In such cases, laparoscopic, robotic, or abdominal myomectomy may be preferable, especially if the volume of the additional myomas is considerable.
To determine the optimal surgical route, the physician must consider the symptoms present—is AUB the only symptom, or are other fibroid-related conditions present as well, such as bulk, pelvic pain, and other quality-of-life issues? If multiple symptoms exist, then other approaches may be better.
How fibroids affect fertility
Fibroids are present in 5% to 10% of women with infertility. In this population, fibroids are the only abnormal finding in 1.0% to 2.4% of cases.4
In a meta-analysis of 23 studies evaluating women with fibroids and infertility, Pritts and colleagues found nine studies involving submucosal fibroids.5 These studies included one randomized controlled trial, two prospective studies, and six retrospective analyses. They found that women who had fibroids with a submucosal component had lower pregnancy and implantation rates, compared with their infertile, myoma-free counterparts. Pritts and colleagues concluded that myomectomy is likely to improve fertility in these cases (TABLE).5
Instrumentation
Among the options are monopolar and bipolar resectoscopy and the mechanical approach using the Truclear System, which includes a morcellator. With conventional resectoscopy all chips must be removed, necessitating multiple insertions of the hysteroscope. Monopolar instrumentation, in particular, carries a risk of energy discharge to healthy tissue. The monopolar resectoscope also has a longer learning curve, compared with the mechanical approach.6
In contrast, the Truclear System requires fewer insertions, has a short learning curve, and omits the need for capture of individual chips, as the mechanical morcellator suctions and captures them throughout the procedure.7 In addition, because resection is performed mechanically, there is no risk of energy discharge to healthy tissue.
The Truclear system also is associated with a significantly shorter operative time, compared with resectoscopy, which may be advantageous for residents, fellows, and other physicians learning the procedure (FIGURE 3).7 Shorter operative time also may result in lower fluid deficits. In addition, saline distension may reduce the risk of fluid absorption and hyponatremia. The tissue-capture feature allows evaluation of the entire pathologic specimen.
Besides hysteroscopic myomectomy, the Truclear System is appropriate for visual dilatation and curettage (D&C), adhesiolysis, polypectomy, and evacuation of retained products of conception.
Preoperative evaluation
A complete history is vital to document which fibroid-related symptoms are present and how they affect quality of life.
Preoperative imaging also is imperative—using either 2D or 3D saline infusion sonography or a combination of diagnostic hysteroscopy and transvaginal ultrasound—to select patients for hysteroscopy, anticipate blood loss, and ensure that the proper instrumentation is available at the time of surgery. Magnetic resonance imaging, computed tomography, and hysterosalpingography are either prohibitively expensive or of limited value in the initial preoperative assessment of uterine fibroids.
Any woman who has AUB and a risk for endometrial hyperplasia or cancer should undergo endometrial assessment as well.
Use of preoperative medications
In most cases, prophylactic administration of antibiotics is not warranted to prevent infection or endocarditis.
Although some clinicians give gonadotropin-releasing hormone (GnRH) agonists to reduce the size of large fibroids, the drug complicates dissection of the fibroid from the surrounding capsule. For this reason, and because we lack data demonstrating that GnRH agonists decrease blood loss and limit absorption of distension media, I do not administer them to patients.8–12 Moreover, this drug can cause vasomotor symptoms, cervical stenosis, and vaginal hemorrhage (related to estrogen flare).
GnRH agonists may be of value to stimulate transient amenorrhea for several months preoperatively in order to correct iron-deficiency anemia. Intravenous iron also can be administered during this interval.
The risk of bleeding in hysteroscopic myomectomy is 2% to 3%.1 When the mechanical approach is used, rather than resectoscopy, continuous flow coupled with suctioning of the chips during the procedure keeps the image clear. Post-procedure contraction of the uterus stops most bleeding. Intrauterine pressure of the pump can be increased to help tamponade any oozing.
Misoprostol. Cervical stenosis is not uncommon in menopausal women. It can also pose a challenge in nulliparous women. Attempting hysteroscopy in the setting of cervical stenosis increases the risk of cervical laceration, creation of a false passage, and uterine perforation. For this reason, I prescribe oral or vaginal misoprostol 200 to 400 µg nightly for 1 to 2 days before the procedure.
Vasopressin can reduce blood loss during hysteroscopic myomectomy when it is injected into the cervical stroma preoperatively. It also reduces absorption of distension fluid and facilitates cervical dilation.
However, vasopressin must be injected with extreme care, with aspiration to confirm the absence of blood prior to each injection, as intravascular injection can lead to bradycardia, profound hypertension, and even death.13 Always notify the anesthesiologist prior to injection when vasopressin will be administered.
I routinely use vasopressin before hysteroscopic myomectomy (0.5 mg in 20 cc of saline or 20 U in 100 cc), injecting 5 cc of the solution at 3, 6, 9, and 12 o’clock positions.
Anesthesia during hysteroscopic myomectomy typically is “monitored anesthesia care,” or MAC, which consists of local anesthesia with sedation and analgesia. The need for regional or general anesthesia is rare. Consider adding a pericervical block or intravenous ketorolac (Toradol) to provide postoperative analgesia.
Surgical technique
Strict attention to fluid management is required throughout the procedure, preferably in accordance with AAGL guidelines on the management of hysteroscopic distending media.14 With the mechanical approach, because the distension fluid is isotonic (normal saline), it does not increase the risk of hyponatremia but can cause pulmonary edema or congestive heart failure. Intravasation usually is the result of excessive operative time, treatment of deeper myometrial fibroids (Type I or II), or high intrauterine pressure. I operate using intrauterine pressure in the range of 75 to 125 mm Hg.
The steps involved in the mechanical hysteroscopy approach are:
- Insert the hysteroscope into the uterus under direct visualization. In general, the greater the number of insertions, the greater the risk of uterine perforation. Preoperative cervical ripening helps facilitate insertion (see “Misoprostol” above).
- Distend the uterus with saline and inspect the uterine cavity, noting again the size and location of the fibroids and whether they are sessile or pedunculated.
- Locate the fibroid or other pathology to be removed, and place the morcellator window against it to begin cutting. Use the tip of the morcellator to elevate the fibroid for easier cutting. Enucleation is accomplished largely by varying the intrauterine pressure, which permits uterine decompression and myometrial contraction and renders the fibroid capsule more visible. If necessary, the hysteroscope can be withdrawn to stimulate myometrial contraction, which also helps to delineate the fibroid capsule.
- Reinspect the uterus to rule out perforation and remove any additional intrauterine pathology with a targeted view.
- Once all designated fibroids have been removed, withdraw the morcellator and hysteroscope from the uterus.
- Inspect the endocervical landscape to rule out injury and other pathology.
- Careful preoperative evaluation is important, preferably using diagnostic hysteroscopy or saline infusion sonography, to choose the optimal route of myomectomy and plan the surgical approach.
- During the myomectomy, pay close attention to fluid management and adhere strictly to predetermined limits.
- Complete removal of the fibroid is essential to relieve symptoms and avert the need for additional procedures.
Postoperative care
A nonsteroidal anti-inflammatory drug or limited use of narcotics usually is sufficient to relieve any postoperative cramping or vaginal discomfort.
Advise the patient to notify you in the event of increasing pain, foul-smelling vaginal discharge, or fever.
Also counsel her that she can return to most normal activities within 24 to 48 hours. Sexual activity is permissible 1 week after surgery. Early and frequent ambulation is important.
Schedule a follow-up visit 4 to 6 weeks after the procedure.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Perez-Medina T, Font EC, eds. Diagnostic and Operative Hysteroscopy. Tunbridge Wells, Kent, UK: Anshan Publishing; 2007:13.
2. Management of uterine fibroids: an update of the evidence. Agency for Healthcare Research and Quality. http://archive.ahrq.gov/clinic/tp/uteruptp.htm. Published July 2007. Accessed January 14, 2015.
3. Lasmar RB, Zinmei Z, Indman PD, Celeste RK, Di Spiezo Sardo A. Feasibility of a new system of classification of submucous myomas: a multicenter study. Fertil Steril. 2011;95(6):2073–2077.
4. AAGL Practice Report: practice guidelines for the diagnosis and management of submucous leiomyomas. J Minim Invasive Gynecol. 2012;19(2):152–171.
5. Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009;91(4):1215–1223.
6. Van Dongen H, Emanuel MH, Wolterbeek R, Trimbos JB, Jansen FW. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15(4):466–471.
7. Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12(1):62–66.
8. Emanuel MH, Hart A, Wamsteker K, Lammes F. An analysis of fluid loss during transcervical resection of submucous myomas. Fertil Steril. 1997;68(5):881–886.
9. Taskin O, Sadik S, Onoglu A, et al. Role of endometrial suppression on the frequency of intrauterine adhesions after resectoscopic surgery. J Am Assoc Gynecol Laparosc. 2000;7(3):351.
10. Propst AM, Liberman RF, Harlow BL, Ginsburg ES. Complications of hysteroscopic surgery: predicting patients at risk. Obstet Gynecol. 2000;96(4):517–520.
11. Perino A, Chianchiano N, Petronio M, Cittadini E. Role of leuprolide acetate depot in hysteroscopic surgery: a controlled study. Fertil Steril. 1993;59(3):507–510.
12. Mencaglia L, Tantini C. GnRH agonist analogs and hysteroscopic resection of myomas. Int J Gynaecol Obstet. 1993;43(3):285–288.
13. Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 Pt 2):484–486.
14. Munro MD, Storz K, Abbott JA, et al; AAGL. AAGL Practice Report: practice guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013;20(2):137–148.
1. Perez-Medina T, Font EC, eds. Diagnostic and Operative Hysteroscopy. Tunbridge Wells, Kent, UK: Anshan Publishing; 2007:13.
2. Management of uterine fibroids: an update of the evidence. Agency for Healthcare Research and Quality. http://archive.ahrq.gov/clinic/tp/uteruptp.htm. Published July 2007. Accessed January 14, 2015.
3. Lasmar RB, Zinmei Z, Indman PD, Celeste RK, Di Spiezo Sardo A. Feasibility of a new system of classification of submucous myomas: a multicenter study. Fertil Steril. 2011;95(6):2073–2077.
4. AAGL Practice Report: practice guidelines for the diagnosis and management of submucous leiomyomas. J Minim Invasive Gynecol. 2012;19(2):152–171.
5. Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009;91(4):1215–1223.
6. Van Dongen H, Emanuel MH, Wolterbeek R, Trimbos JB, Jansen FW. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15(4):466–471.
7. Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12(1):62–66.
8. Emanuel MH, Hart A, Wamsteker K, Lammes F. An analysis of fluid loss during transcervical resection of submucous myomas. Fertil Steril. 1997;68(5):881–886.
9. Taskin O, Sadik S, Onoglu A, et al. Role of endometrial suppression on the frequency of intrauterine adhesions after resectoscopic surgery. J Am Assoc Gynecol Laparosc. 2000;7(3):351.
10. Propst AM, Liberman RF, Harlow BL, Ginsburg ES. Complications of hysteroscopic surgery: predicting patients at risk. Obstet Gynecol. 2000;96(4):517–520.
11. Perino A, Chianchiano N, Petronio M, Cittadini E. Role of leuprolide acetate depot in hysteroscopic surgery: a controlled study. Fertil Steril. 1993;59(3):507–510.
12. Mencaglia L, Tantini C. GnRH agonist analogs and hysteroscopic resection of myomas. Int J Gynaecol Obstet. 1993;43(3):285–288.
13. Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 Pt 2):484–486.
14. Munro MD, Storz K, Abbott JA, et al; AAGL. AAGL Practice Report: practice guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013;20(2):137–148.
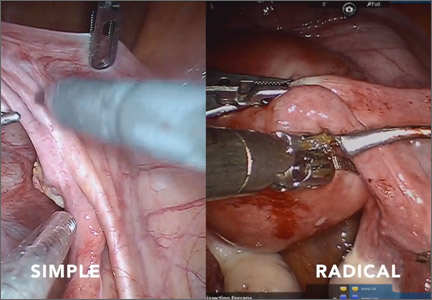
Simple versus radical hysterectomy
Hysterectomy is one of the fundamental surgical procedures in gynecology. Understanding the nuances of both the anatomy and the surgical dissection techniques of this procedure is especially important when approaching complex cases in either benign or oncologic settings.
This month’s surgical video contribution is by my gynecologic oncology colleagues, who highlight the key differences between the simple and radical hysterectomy. They emphasize key surgical principles for the benefit of both benign and oncologic surgeons.
The objectives of this video are to:
- compare the surgical techniques of a simple versus radical hysterectomy
- review the relevant anatomy as it relates to the varying types of hysterectomy
- provide an educational review of the different types of hysterectomy.
This video does an excellent job of achieving its objectives. I hope you share it with your colleagues and residents.

Share your thoughts on this video! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Hysterectomy is one of the fundamental surgical procedures in gynecology. Understanding the nuances of both the anatomy and the surgical dissection techniques of this procedure is especially important when approaching complex cases in either benign or oncologic settings.
This month’s surgical video contribution is by my gynecologic oncology colleagues, who highlight the key differences between the simple and radical hysterectomy. They emphasize key surgical principles for the benefit of both benign and oncologic surgeons.
The objectives of this video are to:
- compare the surgical techniques of a simple versus radical hysterectomy
- review the relevant anatomy as it relates to the varying types of hysterectomy
- provide an educational review of the different types of hysterectomy.
This video does an excellent job of achieving its objectives. I hope you share it with your colleagues and residents.

Share your thoughts on this video! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Hysterectomy is one of the fundamental surgical procedures in gynecology. Understanding the nuances of both the anatomy and the surgical dissection techniques of this procedure is especially important when approaching complex cases in either benign or oncologic settings.
This month’s surgical video contribution is by my gynecologic oncology colleagues, who highlight the key differences between the simple and radical hysterectomy. They emphasize key surgical principles for the benefit of both benign and oncologic surgeons.
The objectives of this video are to:
- compare the surgical techniques of a simple versus radical hysterectomy
- review the relevant anatomy as it relates to the varying types of hysterectomy
- provide an educational review of the different types of hysterectomy.
This video does an excellent job of achieving its objectives. I hope you share it with your colleagues and residents.

Share your thoughts on this video! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Product Update
LITHOTOMY STIRRUPS FOR PATIENT COMFORT
Frontier Medical Innovations says its new GStirrup® is designed to provide patients stable and comfortable foot positioning for extended periods of time during office-based surgical procedures. The GStirrup is a pair of cushioned lithotomy boots that attach to examination-table foot rests. Straps secure the patient’s feet and legs; weights in the base make it difficult for the patient to lift the boot off the footrest. GStirrups fit most footrests and are helpful for patients who have hip or knee replacement, low back pain, arthritis, or neurologic conditions such as multiple sclerosis or Parkinson’s disease.
FOR MORE INFORMATION, VISIT www.gstirrup.com
PREGNANCY, BIRTH, AND BREASTFEEDING APP
Totally Pregnant, an app for pregnant women and health-care providers, is now partnering with Lamaze International to provide access to online parenting classes for pregnancy, childbirth, and early parenting. By using the Totally Pregnant app, women can personalize their pregnancy experience and clinicians can connect with their patients. Available for iPhone, iPad, Android, and desktop.
FOR MORE INFORMATION, VISIT www.iamtotally.com
PREDICTING IVF SUCCESS
Univfy®offers fertility predictive analytics to help prospective parents understand the probability for the success of in vitro fertilization (IVF) and estimated costs. The PreIVF™ calculator helps to decide whether or when to start IVF; the PredictIVF™ helps determine if another IVF cycle is the right option. The IVF Cost Calculator offers a cost comparison tailored to the patient’s IVF success rate. Your Fertility™ is an interactive multimedia blog offering educational material.
FOR MORE INFORMATION, VISIT www.univfy.com
SECURE WAY TO CARRY MEDS
FusionWrap is a waist/hip wrap with two 7-inch pockets to carry small personal belongings. Besides providing secure space for identification and money, it also allows those with asthma, diabetes, allergies, or other chronic diseases to carry medications at all times. Made of stretch fabric that is moisture wicking and antimicrobial, FusionWrap comes in various colors and sizes for women, men, and children.
FOR MORE INFORMATION, VISIT www.fusion-wrap.com
BREAST IMAGING TOOLS
Volpara Solutions offers multiple volumetric breast-imaging software tools designed to improve clinical decision making and the early detection of breast cancer. Volpara®Density™ is a breast-density assessment tool available for clinical use with 2D mammography and digital breast tomosynthesis (3D mammography) platforms from multiple manufacturers.
FOR MORE INFORMATION, VISIT www.volparadensity.com
SMOKE EVACUATION PENCIL
The PlumePen® Elite is an electrosurgical smoke pencil with a compact, ergonomic design that is smaller but offers more flow than competitive smoke pencils, claims Buffalo Filter. The adjustable capture port allows for optimum visibility regardless of blade length. The one-piece molded design prevents buttons from sticking and improves grip. The PlumePen Elite connects to most surgical plume evacuators and generators.
FOR MORE INFORMATION, VISIT www.buffalofilter.com
SURGICAL CO2 LASER
Lumenis designed the AcuPulse Smart CO2 Laser with SurgiTouch™ Automation System for tissue ablation during gynecologic surgery to increase speed, precision, and convenience over other electrosurgical devices. Robotic, computer-controlled laser-beam movement provides more precision than hand-held lasers and offers reproducible outcomes. Brief laser-tissue interaction reduces thermal damage.
FOR MORE INFORMATION, VISIT www.lumenis.com
REUSABLE FORNIX FOR LAP HYSTERECTOMY
The Banyan Colpo-Port Vaginal Fornix Delineator is a reusable uterine elevator/vaginal fornix delineator for laparoscopic hysterectomy. Inserted vaginally, the distal tip has a canted, beveled cup that fits securely in the vaginal fornix. The Calibrated Uterine Elevator (CUE) passes through the inner diameter of the delineator body, through the cervix, and into the uterine cavity. The CUE can be locked at preset depths to prevent uterine perforation. The device is easy to clean using standard sterilization procedures.
FOR MORE INFORMATION, VISIT www.banyanmedllc.com
OVARIAN MALIGNANCY ALGORITHM
The Risk of Ovarian Malignancy Algorithm (ROMA™) from Fujirebio is a quantitative serum test intended to assess the risk of finding malignancy at surgery in a premenopausal or postmenopausal woman with an ovarian mass. ROMA, a risk stratification tool, combines the results of human epididymis protein 4 (HE4), cancer antigen 125 (CA125), and menopausal status into a numerical score.
FOR MORE INFORMATION, VISIT www.he4test.com
PORT-SITE CLOSURE DEVICE
neoClose® AnchorGuide facilitates rapid trocar exchange and precise AutoAnchor placement to help prevent port-site hernia. The AnchorGuide design facilitates the delivery of absorbable AutoAnchors through soft tissue during surgery; allows for the VectorX method of port approximation for reduced tension at wound sites; and helps desufflate to remove CO2 at the end of surgery. AnchorGuide comes in 8–15 mm and 5–12 mm sizes compatible with 8 mm robotic ports.
FOR MORE INFORMATION, VISIT www.neosurgical.com
LITHOTOMY STIRRUPS FOR PATIENT COMFORT
Frontier Medical Innovations says its new GStirrup® is designed to provide patients stable and comfortable foot positioning for extended periods of time during office-based surgical procedures. The GStirrup is a pair of cushioned lithotomy boots that attach to examination-table foot rests. Straps secure the patient’s feet and legs; weights in the base make it difficult for the patient to lift the boot off the footrest. GStirrups fit most footrests and are helpful for patients who have hip or knee replacement, low back pain, arthritis, or neurologic conditions such as multiple sclerosis or Parkinson’s disease.
FOR MORE INFORMATION, VISIT www.gstirrup.com
PREGNANCY, BIRTH, AND BREASTFEEDING APP
Totally Pregnant, an app for pregnant women and health-care providers, is now partnering with Lamaze International to provide access to online parenting classes for pregnancy, childbirth, and early parenting. By using the Totally Pregnant app, women can personalize their pregnancy experience and clinicians can connect with their patients. Available for iPhone, iPad, Android, and desktop.
FOR MORE INFORMATION, VISIT www.iamtotally.com
PREDICTING IVF SUCCESS
Univfy®offers fertility predictive analytics to help prospective parents understand the probability for the success of in vitro fertilization (IVF) and estimated costs. The PreIVF™ calculator helps to decide whether or when to start IVF; the PredictIVF™ helps determine if another IVF cycle is the right option. The IVF Cost Calculator offers a cost comparison tailored to the patient’s IVF success rate. Your Fertility™ is an interactive multimedia blog offering educational material.
FOR MORE INFORMATION, VISIT www.univfy.com
SECURE WAY TO CARRY MEDS
FusionWrap is a waist/hip wrap with two 7-inch pockets to carry small personal belongings. Besides providing secure space for identification and money, it also allows those with asthma, diabetes, allergies, or other chronic diseases to carry medications at all times. Made of stretch fabric that is moisture wicking and antimicrobial, FusionWrap comes in various colors and sizes for women, men, and children.
FOR MORE INFORMATION, VISIT www.fusion-wrap.com
BREAST IMAGING TOOLS
Volpara Solutions offers multiple volumetric breast-imaging software tools designed to improve clinical decision making and the early detection of breast cancer. Volpara®Density™ is a breast-density assessment tool available for clinical use with 2D mammography and digital breast tomosynthesis (3D mammography) platforms from multiple manufacturers.
FOR MORE INFORMATION, VISIT www.volparadensity.com
SMOKE EVACUATION PENCIL
The PlumePen® Elite is an electrosurgical smoke pencil with a compact, ergonomic design that is smaller but offers more flow than competitive smoke pencils, claims Buffalo Filter. The adjustable capture port allows for optimum visibility regardless of blade length. The one-piece molded design prevents buttons from sticking and improves grip. The PlumePen Elite connects to most surgical plume evacuators and generators.
FOR MORE INFORMATION, VISIT www.buffalofilter.com
SURGICAL CO2 LASER
Lumenis designed the AcuPulse Smart CO2 Laser with SurgiTouch™ Automation System for tissue ablation during gynecologic surgery to increase speed, precision, and convenience over other electrosurgical devices. Robotic, computer-controlled laser-beam movement provides more precision than hand-held lasers and offers reproducible outcomes. Brief laser-tissue interaction reduces thermal damage.
FOR MORE INFORMATION, VISIT www.lumenis.com
REUSABLE FORNIX FOR LAP HYSTERECTOMY
The Banyan Colpo-Port Vaginal Fornix Delineator is a reusable uterine elevator/vaginal fornix delineator for laparoscopic hysterectomy. Inserted vaginally, the distal tip has a canted, beveled cup that fits securely in the vaginal fornix. The Calibrated Uterine Elevator (CUE) passes through the inner diameter of the delineator body, through the cervix, and into the uterine cavity. The CUE can be locked at preset depths to prevent uterine perforation. The device is easy to clean using standard sterilization procedures.
FOR MORE INFORMATION, VISIT www.banyanmedllc.com
OVARIAN MALIGNANCY ALGORITHM
The Risk of Ovarian Malignancy Algorithm (ROMA™) from Fujirebio is a quantitative serum test intended to assess the risk of finding malignancy at surgery in a premenopausal or postmenopausal woman with an ovarian mass. ROMA, a risk stratification tool, combines the results of human epididymis protein 4 (HE4), cancer antigen 125 (CA125), and menopausal status into a numerical score.
FOR MORE INFORMATION, VISIT www.he4test.com
PORT-SITE CLOSURE DEVICE
neoClose® AnchorGuide facilitates rapid trocar exchange and precise AutoAnchor placement to help prevent port-site hernia. The AnchorGuide design facilitates the delivery of absorbable AutoAnchors through soft tissue during surgery; allows for the VectorX method of port approximation for reduced tension at wound sites; and helps desufflate to remove CO2 at the end of surgery. AnchorGuide comes in 8–15 mm and 5–12 mm sizes compatible with 8 mm robotic ports.
FOR MORE INFORMATION, VISIT www.neosurgical.com
LITHOTOMY STIRRUPS FOR PATIENT COMFORT
Frontier Medical Innovations says its new GStirrup® is designed to provide patients stable and comfortable foot positioning for extended periods of time during office-based surgical procedures. The GStirrup is a pair of cushioned lithotomy boots that attach to examination-table foot rests. Straps secure the patient’s feet and legs; weights in the base make it difficult for the patient to lift the boot off the footrest. GStirrups fit most footrests and are helpful for patients who have hip or knee replacement, low back pain, arthritis, or neurologic conditions such as multiple sclerosis or Parkinson’s disease.
FOR MORE INFORMATION, VISIT www.gstirrup.com
PREGNANCY, BIRTH, AND BREASTFEEDING APP
Totally Pregnant, an app for pregnant women and health-care providers, is now partnering with Lamaze International to provide access to online parenting classes for pregnancy, childbirth, and early parenting. By using the Totally Pregnant app, women can personalize their pregnancy experience and clinicians can connect with their patients. Available for iPhone, iPad, Android, and desktop.
FOR MORE INFORMATION, VISIT www.iamtotally.com
PREDICTING IVF SUCCESS
Univfy®offers fertility predictive analytics to help prospective parents understand the probability for the success of in vitro fertilization (IVF) and estimated costs. The PreIVF™ calculator helps to decide whether or when to start IVF; the PredictIVF™ helps determine if another IVF cycle is the right option. The IVF Cost Calculator offers a cost comparison tailored to the patient’s IVF success rate. Your Fertility™ is an interactive multimedia blog offering educational material.
FOR MORE INFORMATION, VISIT www.univfy.com
SECURE WAY TO CARRY MEDS
FusionWrap is a waist/hip wrap with two 7-inch pockets to carry small personal belongings. Besides providing secure space for identification and money, it also allows those with asthma, diabetes, allergies, or other chronic diseases to carry medications at all times. Made of stretch fabric that is moisture wicking and antimicrobial, FusionWrap comes in various colors and sizes for women, men, and children.
FOR MORE INFORMATION, VISIT www.fusion-wrap.com
BREAST IMAGING TOOLS
Volpara Solutions offers multiple volumetric breast-imaging software tools designed to improve clinical decision making and the early detection of breast cancer. Volpara®Density™ is a breast-density assessment tool available for clinical use with 2D mammography and digital breast tomosynthesis (3D mammography) platforms from multiple manufacturers.
FOR MORE INFORMATION, VISIT www.volparadensity.com
SMOKE EVACUATION PENCIL
The PlumePen® Elite is an electrosurgical smoke pencil with a compact, ergonomic design that is smaller but offers more flow than competitive smoke pencils, claims Buffalo Filter. The adjustable capture port allows for optimum visibility regardless of blade length. The one-piece molded design prevents buttons from sticking and improves grip. The PlumePen Elite connects to most surgical plume evacuators and generators.
FOR MORE INFORMATION, VISIT www.buffalofilter.com
SURGICAL CO2 LASER
Lumenis designed the AcuPulse Smart CO2 Laser with SurgiTouch™ Automation System for tissue ablation during gynecologic surgery to increase speed, precision, and convenience over other electrosurgical devices. Robotic, computer-controlled laser-beam movement provides more precision than hand-held lasers and offers reproducible outcomes. Brief laser-tissue interaction reduces thermal damage.
FOR MORE INFORMATION, VISIT www.lumenis.com
REUSABLE FORNIX FOR LAP HYSTERECTOMY
The Banyan Colpo-Port Vaginal Fornix Delineator is a reusable uterine elevator/vaginal fornix delineator for laparoscopic hysterectomy. Inserted vaginally, the distal tip has a canted, beveled cup that fits securely in the vaginal fornix. The Calibrated Uterine Elevator (CUE) passes through the inner diameter of the delineator body, through the cervix, and into the uterine cavity. The CUE can be locked at preset depths to prevent uterine perforation. The device is easy to clean using standard sterilization procedures.
FOR MORE INFORMATION, VISIT www.banyanmedllc.com
OVARIAN MALIGNANCY ALGORITHM
The Risk of Ovarian Malignancy Algorithm (ROMA™) from Fujirebio is a quantitative serum test intended to assess the risk of finding malignancy at surgery in a premenopausal or postmenopausal woman with an ovarian mass. ROMA, a risk stratification tool, combines the results of human epididymis protein 4 (HE4), cancer antigen 125 (CA125), and menopausal status into a numerical score.
FOR MORE INFORMATION, VISIT www.he4test.com
PORT-SITE CLOSURE DEVICE
neoClose® AnchorGuide facilitates rapid trocar exchange and precise AutoAnchor placement to help prevent port-site hernia. The AnchorGuide design facilitates the delivery of absorbable AutoAnchors through soft tissue during surgery; allows for the VectorX method of port approximation for reduced tension at wound sites; and helps desufflate to remove CO2 at the end of surgery. AnchorGuide comes in 8–15 mm and 5–12 mm sizes compatible with 8 mm robotic ports.
FOR MORE INFORMATION, VISIT www.neosurgical.com
RBC transfusions during CABG increase risk of pneumonia

Credit: Elise Amendola
SAN DIEGO—Patients who receive red blood cell (RBC) transfusions during coronary artery bypass grafting (CABG) surgery are at an increased risk of
developing pneumonia, according to research presented at the 51st Annual Meeting of The Society of Thoracic Surgeons.
And the risk appears to increase with the volume of RBCs transfused. Patients who received 6 or more units had a 14 times higher risk of developing pneumonia than their untransfused peers.
“Pneumonia is a known risk following CABG surgery, and developing it has been shown to significantly increase a patient’s risk of morbidity and mortality,” said study investigator Donald S. Likosky, PhD, of the University of Michigan Health System in Ann Arbor.
“Previous research has shown that 1 in every 20 CABG patients develop a major infection, with pneumonia being the most common type of infection.”
For this study, Dr Liksoky and his colleagues examined data on 16,182 patients who underwent CABG between 2011 and 2013 at any of the 33 hospitals participating in the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
They used propensity scoring to match the 4585 patients (32.3%) who received RBCs to the 9612 who did not (total=14,197). The team matched patients based on age, sex, body mass index, history of smoking, congestive heart failure, chronic obstructive pulmonary disease, diabetes, prior cardiac surgery, vascular disease, ejection fraction, preoperative hematocrit, and preoperative pneumonia.
The researchers then calculated adjusted odds ratios (ORs) reflecting the association between the number of RBC units transfused (0 to 6+) and postoperative pneumonia.
In all, 450 patients (3.2%) developed pneumonia. And the analysis revealed a significant association between any RBC transfusion and pneumonia (OR=4.0, P<0.001), as well as associations between the number of units transfused and the odds of developing pneumonia.
The OR was 1.6 (P=0.02) for patients who received 1 RBC unit, 2.1 for those who received 2 units (P<0.001), 4.9 for those who received 3 units (P<0.001), 5.5 for those who received 4 units (P<0.001), 8.9 for those who received 5 units (P<0.001), and 14.4 for patients who received 6 or more units (P<0.001).
“The ability to store and transfuse blood is one of medicine’s greatest accomplishments, but we are continuing to see that receiving a blood transfusion may alter a patient’s ability to fight infection,” said James R. Edgerton, MD, from The Heart Hospital Baylor Plano in Texas, who was not affiliated with this study.
“In their study, Dr Likosky and colleagues have identified an increased risk of pneumonia after transfusion, which is an important breakthrough because it allows physicians to remain vigilant for the onset of pneumonia and initiate therapy early in hopes of shortening its course and severity. It also enables physicians to initiate preventive therapies in patients who have been transfused, which will contribute to better care of our patients.”
“Patients should receive red blood cell transfusions based on clinical need,” Dr Likosky added. “Surgical teams may have opportunities to reduce the need for transfusions among patients, thereby reducing the risk of secondary complications.” ![]()

Credit: Elise Amendola
SAN DIEGO—Patients who receive red blood cell (RBC) transfusions during coronary artery bypass grafting (CABG) surgery are at an increased risk of
developing pneumonia, according to research presented at the 51st Annual Meeting of The Society of Thoracic Surgeons.
And the risk appears to increase with the volume of RBCs transfused. Patients who received 6 or more units had a 14 times higher risk of developing pneumonia than their untransfused peers.
“Pneumonia is a known risk following CABG surgery, and developing it has been shown to significantly increase a patient’s risk of morbidity and mortality,” said study investigator Donald S. Likosky, PhD, of the University of Michigan Health System in Ann Arbor.
“Previous research has shown that 1 in every 20 CABG patients develop a major infection, with pneumonia being the most common type of infection.”
For this study, Dr Liksoky and his colleagues examined data on 16,182 patients who underwent CABG between 2011 and 2013 at any of the 33 hospitals participating in the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
They used propensity scoring to match the 4585 patients (32.3%) who received RBCs to the 9612 who did not (total=14,197). The team matched patients based on age, sex, body mass index, history of smoking, congestive heart failure, chronic obstructive pulmonary disease, diabetes, prior cardiac surgery, vascular disease, ejection fraction, preoperative hematocrit, and preoperative pneumonia.
The researchers then calculated adjusted odds ratios (ORs) reflecting the association between the number of RBC units transfused (0 to 6+) and postoperative pneumonia.
In all, 450 patients (3.2%) developed pneumonia. And the analysis revealed a significant association between any RBC transfusion and pneumonia (OR=4.0, P<0.001), as well as associations between the number of units transfused and the odds of developing pneumonia.
The OR was 1.6 (P=0.02) for patients who received 1 RBC unit, 2.1 for those who received 2 units (P<0.001), 4.9 for those who received 3 units (P<0.001), 5.5 for those who received 4 units (P<0.001), 8.9 for those who received 5 units (P<0.001), and 14.4 for patients who received 6 or more units (P<0.001).
“The ability to store and transfuse blood is one of medicine’s greatest accomplishments, but we are continuing to see that receiving a blood transfusion may alter a patient’s ability to fight infection,” said James R. Edgerton, MD, from The Heart Hospital Baylor Plano in Texas, who was not affiliated with this study.
“In their study, Dr Likosky and colleagues have identified an increased risk of pneumonia after transfusion, which is an important breakthrough because it allows physicians to remain vigilant for the onset of pneumonia and initiate therapy early in hopes of shortening its course and severity. It also enables physicians to initiate preventive therapies in patients who have been transfused, which will contribute to better care of our patients.”
“Patients should receive red blood cell transfusions based on clinical need,” Dr Likosky added. “Surgical teams may have opportunities to reduce the need for transfusions among patients, thereby reducing the risk of secondary complications.” ![]()

Credit: Elise Amendola
SAN DIEGO—Patients who receive red blood cell (RBC) transfusions during coronary artery bypass grafting (CABG) surgery are at an increased risk of
developing pneumonia, according to research presented at the 51st Annual Meeting of The Society of Thoracic Surgeons.
And the risk appears to increase with the volume of RBCs transfused. Patients who received 6 or more units had a 14 times higher risk of developing pneumonia than their untransfused peers.
“Pneumonia is a known risk following CABG surgery, and developing it has been shown to significantly increase a patient’s risk of morbidity and mortality,” said study investigator Donald S. Likosky, PhD, of the University of Michigan Health System in Ann Arbor.
“Previous research has shown that 1 in every 20 CABG patients develop a major infection, with pneumonia being the most common type of infection.”
For this study, Dr Liksoky and his colleagues examined data on 16,182 patients who underwent CABG between 2011 and 2013 at any of the 33 hospitals participating in the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative.
They used propensity scoring to match the 4585 patients (32.3%) who received RBCs to the 9612 who did not (total=14,197). The team matched patients based on age, sex, body mass index, history of smoking, congestive heart failure, chronic obstructive pulmonary disease, diabetes, prior cardiac surgery, vascular disease, ejection fraction, preoperative hematocrit, and preoperative pneumonia.
The researchers then calculated adjusted odds ratios (ORs) reflecting the association between the number of RBC units transfused (0 to 6+) and postoperative pneumonia.
In all, 450 patients (3.2%) developed pneumonia. And the analysis revealed a significant association between any RBC transfusion and pneumonia (OR=4.0, P<0.001), as well as associations between the number of units transfused and the odds of developing pneumonia.
The OR was 1.6 (P=0.02) for patients who received 1 RBC unit, 2.1 for those who received 2 units (P<0.001), 4.9 for those who received 3 units (P<0.001), 5.5 for those who received 4 units (P<0.001), 8.9 for those who received 5 units (P<0.001), and 14.4 for patients who received 6 or more units (P<0.001).
“The ability to store and transfuse blood is one of medicine’s greatest accomplishments, but we are continuing to see that receiving a blood transfusion may alter a patient’s ability to fight infection,” said James R. Edgerton, MD, from The Heart Hospital Baylor Plano in Texas, who was not affiliated with this study.
“In their study, Dr Likosky and colleagues have identified an increased risk of pneumonia after transfusion, which is an important breakthrough because it allows physicians to remain vigilant for the onset of pneumonia and initiate therapy early in hopes of shortening its course and severity. It also enables physicians to initiate preventive therapies in patients who have been transfused, which will contribute to better care of our patients.”
“Patients should receive red blood cell transfusions based on clinical need,” Dr Likosky added. “Surgical teams may have opportunities to reduce the need for transfusions among patients, thereby reducing the risk of secondary complications.” ![]()
Most cardiologists misstep on aspirin in ACS
SNOWMASS, COLO. – U.S. cardiologists are glaringly out of touch with the guidelines on maintenance aspirin dosing in patients with acute coronary syndrome, American College of Cardiology President Dr. Patrick T. O’Gara said at the Annual Cardiovascular Conference at Snowmass.
The latest AHA/ACC guidelines state that maintenance aspirin therapy at 81 mg/day to be continued indefinitely is preferred over 325 mg/day in patients with ACS, regardless of whether they have received a coronary stent or noninvasive medical management (Circulation 2014 Dec 23;130(25):e344-426).
“This statement has been out there in the guidelines for several years now. Yet the last time we interrogated the NCDR [National Cardiovascular Data Registry], 70% of patients with ACS were discharged on 325 mg/day of aspirin in the U.S.,” said Dr. O’Gara, professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, Boston.
The recommendation in the guidelines is based on several solid studies, including OASIS 7, which in more than 25,000 randomized patients showed no difference in outcomes when aspirin at 75-100 mg/day was compared with 300-325 mg/day, but an increased incidence of bleeding at the higher dose (N. Engl. J. Med. 2010;363:930-42).
“Aspirin at 81 mg/day is not inferior with respect to clinical efficacy and it’s superior with respect to its safety outcome. But here in the United States we are still very much wedded to using 325 mg of aspirin. I’m not exactly sure of the reasons for that. Maybe it’s a catch up phenomenon,” Dr. O’Gara commented.
In the setting of percutaneous coronary intervention with a bare metal or drug-eluting stent for patients with either non–ST-elevation ACS or ST-elevation MI, the AHA/ACC guidelines give a class I recommendation for at least 12 months of dual-antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor. Either ticagrelor (Brilinta) at 90 mg twice daily or prasugrel (Effient) once daily at 10 mg is recommended over clopidogrel at 75 mg/day in patients who can take those medications safely; this guidance is based on ticagrelor’s superior efficacy compared with clopidogrel as shown in TRITON TIMI-38 (N. Engl. J. Med. 2007;357:2001-15) and prasugrel’s superiority in the PLATO trial (N. Engl. J. Med. 2009;361:1045-57).
The AHA/ACC guidelines give a relatively tepid level IIb recommendation that continuation of DAPT beyond 12 months may be considered in stent recipients. Many observers expect a stronger endorsement in the next iteration of the guidelines on the strength of the recent DAPT study, which showed that 30 months of DAPT was better than 12 in terms of major adverse cardiac and cerebrovascular events (N. Engl. J. Med. 2014;371:2155-66).
“Interestingly enough, the mechanism of benefit had less to do with prevention of stent thrombosis than it did with prevention of recurrent MI and stroke. This renders into much sharper focus the question of whether we’re treating the patient or we’re treating the stent. This result would imply that we’re treating the patient,” Dr. O’Gara observed.
The guidelines also include a bail-out option which states that if the risk of bleeding outweighs the anticipated benefit, it’s reasonable to discontinue DAPT before 12 months.
“I don’t know a single practitioner who’s not had to withdraw one or both elements of DAPT because of bleeding or because of the need for unanticipated noncardiac surgery. It’s a fact of life, and sometimes you have to just hope for the best,” the cardiologist said.
He reported having no financial conflicts of interest.
SNOWMASS, COLO. – U.S. cardiologists are glaringly out of touch with the guidelines on maintenance aspirin dosing in patients with acute coronary syndrome, American College of Cardiology President Dr. Patrick T. O’Gara said at the Annual Cardiovascular Conference at Snowmass.
The latest AHA/ACC guidelines state that maintenance aspirin therapy at 81 mg/day to be continued indefinitely is preferred over 325 mg/day in patients with ACS, regardless of whether they have received a coronary stent or noninvasive medical management (Circulation 2014 Dec 23;130(25):e344-426).
“This statement has been out there in the guidelines for several years now. Yet the last time we interrogated the NCDR [National Cardiovascular Data Registry], 70% of patients with ACS were discharged on 325 mg/day of aspirin in the U.S.,” said Dr. O’Gara, professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, Boston.
The recommendation in the guidelines is based on several solid studies, including OASIS 7, which in more than 25,000 randomized patients showed no difference in outcomes when aspirin at 75-100 mg/day was compared with 300-325 mg/day, but an increased incidence of bleeding at the higher dose (N. Engl. J. Med. 2010;363:930-42).
“Aspirin at 81 mg/day is not inferior with respect to clinical efficacy and it’s superior with respect to its safety outcome. But here in the United States we are still very much wedded to using 325 mg of aspirin. I’m not exactly sure of the reasons for that. Maybe it’s a catch up phenomenon,” Dr. O’Gara commented.
In the setting of percutaneous coronary intervention with a bare metal or drug-eluting stent for patients with either non–ST-elevation ACS or ST-elevation MI, the AHA/ACC guidelines give a class I recommendation for at least 12 months of dual-antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor. Either ticagrelor (Brilinta) at 90 mg twice daily or prasugrel (Effient) once daily at 10 mg is recommended over clopidogrel at 75 mg/day in patients who can take those medications safely; this guidance is based on ticagrelor’s superior efficacy compared with clopidogrel as shown in TRITON TIMI-38 (N. Engl. J. Med. 2007;357:2001-15) and prasugrel’s superiority in the PLATO trial (N. Engl. J. Med. 2009;361:1045-57).
The AHA/ACC guidelines give a relatively tepid level IIb recommendation that continuation of DAPT beyond 12 months may be considered in stent recipients. Many observers expect a stronger endorsement in the next iteration of the guidelines on the strength of the recent DAPT study, which showed that 30 months of DAPT was better than 12 in terms of major adverse cardiac and cerebrovascular events (N. Engl. J. Med. 2014;371:2155-66).
“Interestingly enough, the mechanism of benefit had less to do with prevention of stent thrombosis than it did with prevention of recurrent MI and stroke. This renders into much sharper focus the question of whether we’re treating the patient or we’re treating the stent. This result would imply that we’re treating the patient,” Dr. O’Gara observed.
The guidelines also include a bail-out option which states that if the risk of bleeding outweighs the anticipated benefit, it’s reasonable to discontinue DAPT before 12 months.
“I don’t know a single practitioner who’s not had to withdraw one or both elements of DAPT because of bleeding or because of the need for unanticipated noncardiac surgery. It’s a fact of life, and sometimes you have to just hope for the best,” the cardiologist said.
He reported having no financial conflicts of interest.
SNOWMASS, COLO. – U.S. cardiologists are glaringly out of touch with the guidelines on maintenance aspirin dosing in patients with acute coronary syndrome, American College of Cardiology President Dr. Patrick T. O’Gara said at the Annual Cardiovascular Conference at Snowmass.
The latest AHA/ACC guidelines state that maintenance aspirin therapy at 81 mg/day to be continued indefinitely is preferred over 325 mg/day in patients with ACS, regardless of whether they have received a coronary stent or noninvasive medical management (Circulation 2014 Dec 23;130(25):e344-426).
“This statement has been out there in the guidelines for several years now. Yet the last time we interrogated the NCDR [National Cardiovascular Data Registry], 70% of patients with ACS were discharged on 325 mg/day of aspirin in the U.S.,” said Dr. O’Gara, professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, Boston.
The recommendation in the guidelines is based on several solid studies, including OASIS 7, which in more than 25,000 randomized patients showed no difference in outcomes when aspirin at 75-100 mg/day was compared with 300-325 mg/day, but an increased incidence of bleeding at the higher dose (N. Engl. J. Med. 2010;363:930-42).
“Aspirin at 81 mg/day is not inferior with respect to clinical efficacy and it’s superior with respect to its safety outcome. But here in the United States we are still very much wedded to using 325 mg of aspirin. I’m not exactly sure of the reasons for that. Maybe it’s a catch up phenomenon,” Dr. O’Gara commented.
In the setting of percutaneous coronary intervention with a bare metal or drug-eluting stent for patients with either non–ST-elevation ACS or ST-elevation MI, the AHA/ACC guidelines give a class I recommendation for at least 12 months of dual-antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor. Either ticagrelor (Brilinta) at 90 mg twice daily or prasugrel (Effient) once daily at 10 mg is recommended over clopidogrel at 75 mg/day in patients who can take those medications safely; this guidance is based on ticagrelor’s superior efficacy compared with clopidogrel as shown in TRITON TIMI-38 (N. Engl. J. Med. 2007;357:2001-15) and prasugrel’s superiority in the PLATO trial (N. Engl. J. Med. 2009;361:1045-57).
The AHA/ACC guidelines give a relatively tepid level IIb recommendation that continuation of DAPT beyond 12 months may be considered in stent recipients. Many observers expect a stronger endorsement in the next iteration of the guidelines on the strength of the recent DAPT study, which showed that 30 months of DAPT was better than 12 in terms of major adverse cardiac and cerebrovascular events (N. Engl. J. Med. 2014;371:2155-66).
“Interestingly enough, the mechanism of benefit had less to do with prevention of stent thrombosis than it did with prevention of recurrent MI and stroke. This renders into much sharper focus the question of whether we’re treating the patient or we’re treating the stent. This result would imply that we’re treating the patient,” Dr. O’Gara observed.
The guidelines also include a bail-out option which states that if the risk of bleeding outweighs the anticipated benefit, it’s reasonable to discontinue DAPT before 12 months.
“I don’t know a single practitioner who’s not had to withdraw one or both elements of DAPT because of bleeding or because of the need for unanticipated noncardiac surgery. It’s a fact of life, and sometimes you have to just hope for the best,” the cardiologist said.
He reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Your practice moves but your address on the Internet doesn’t
I moved offices in April 2014, for the first time in my career. Overall, it went quite smoothly.
But one problem persists, thanks to the Internet age.
The majority of search engines and rate-a-doc sites haven’t updated my address. I’ve e-mailed them about it, but get either no response or (even better) a response saying “We’ve reviewed your note and found our information is correct.” Apparently, I don’t know my correct address, in spite of driving there every day.
But what’s even more frustrating is when my patients follow these instructions. My secretary is quite conscientious about giving patients, new and old, the correct location when they make the appointment. My practice website even has a map.
Despite this, we still have a roughly 20% rate of people going to my old office across the street, then calling to see where we went. Worse, this even happens with patients who were never even seen at that office, yet have been to my new one several times.
Then they come in and yell at my staff for giving them the wrong address. They claim my website has the wrong address. It doesn’t, but I can’t control other sites.
The problem is that most don’t trust other people as much as they trust their phones. Rather than writing down my address when talking to my secretary, it’s easier to just tell Siri, “find Dr. Allan Block’s office.” Siri checks the Internet, where the majority of incorrect listings drown out my dinky little practice site. So people follow the phone’s instructions without questioning them. Even those who’ve previously been to this office, or think, “that doesn’t sound right,” will often follow the directions without question. After all, the Internet knows best.
I’m not knocking the rise of the smartphone. They’re awesome. I rely on Siri myself a great deal. But the phone is only as good as the data supplied, and isn’t capable of questioning it. If most sites list an incorrect address, then who am I to argue? I’m just the guy who’s actually renting the place.
The problem is that information itself is often unhelpful and misleading, and the Internet isn’t always right.
When I dictate an EEG report, I often end it with “clinical correlation is advised.” We need to keep that in mind for everyday life, too.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I moved offices in April 2014, for the first time in my career. Overall, it went quite smoothly.
But one problem persists, thanks to the Internet age.
The majority of search engines and rate-a-doc sites haven’t updated my address. I’ve e-mailed them about it, but get either no response or (even better) a response saying “We’ve reviewed your note and found our information is correct.” Apparently, I don’t know my correct address, in spite of driving there every day.
But what’s even more frustrating is when my patients follow these instructions. My secretary is quite conscientious about giving patients, new and old, the correct location when they make the appointment. My practice website even has a map.
Despite this, we still have a roughly 20% rate of people going to my old office across the street, then calling to see where we went. Worse, this even happens with patients who were never even seen at that office, yet have been to my new one several times.
Then they come in and yell at my staff for giving them the wrong address. They claim my website has the wrong address. It doesn’t, but I can’t control other sites.
The problem is that most don’t trust other people as much as they trust their phones. Rather than writing down my address when talking to my secretary, it’s easier to just tell Siri, “find Dr. Allan Block’s office.” Siri checks the Internet, where the majority of incorrect listings drown out my dinky little practice site. So people follow the phone’s instructions without questioning them. Even those who’ve previously been to this office, or think, “that doesn’t sound right,” will often follow the directions without question. After all, the Internet knows best.
I’m not knocking the rise of the smartphone. They’re awesome. I rely on Siri myself a great deal. But the phone is only as good as the data supplied, and isn’t capable of questioning it. If most sites list an incorrect address, then who am I to argue? I’m just the guy who’s actually renting the place.
The problem is that information itself is often unhelpful and misleading, and the Internet isn’t always right.
When I dictate an EEG report, I often end it with “clinical correlation is advised.” We need to keep that in mind for everyday life, too.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I moved offices in April 2014, for the first time in my career. Overall, it went quite smoothly.
But one problem persists, thanks to the Internet age.
The majority of search engines and rate-a-doc sites haven’t updated my address. I’ve e-mailed them about it, but get either no response or (even better) a response saying “We’ve reviewed your note and found our information is correct.” Apparently, I don’t know my correct address, in spite of driving there every day.
But what’s even more frustrating is when my patients follow these instructions. My secretary is quite conscientious about giving patients, new and old, the correct location when they make the appointment. My practice website even has a map.
Despite this, we still have a roughly 20% rate of people going to my old office across the street, then calling to see where we went. Worse, this even happens with patients who were never even seen at that office, yet have been to my new one several times.
Then they come in and yell at my staff for giving them the wrong address. They claim my website has the wrong address. It doesn’t, but I can’t control other sites.
The problem is that most don’t trust other people as much as they trust their phones. Rather than writing down my address when talking to my secretary, it’s easier to just tell Siri, “find Dr. Allan Block’s office.” Siri checks the Internet, where the majority of incorrect listings drown out my dinky little practice site. So people follow the phone’s instructions without questioning them. Even those who’ve previously been to this office, or think, “that doesn’t sound right,” will often follow the directions without question. After all, the Internet knows best.
I’m not knocking the rise of the smartphone. They’re awesome. I rely on Siri myself a great deal. But the phone is only as good as the data supplied, and isn’t capable of questioning it. If most sites list an incorrect address, then who am I to argue? I’m just the guy who’s actually renting the place.
The problem is that information itself is often unhelpful and misleading, and the Internet isn’t always right.
When I dictate an EEG report, I often end it with “clinical correlation is advised.” We need to keep that in mind for everyday life, too.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Early initiation of postpartum contraception decreases rapid repeat pregnancy in teens
In an effort to determine how to curb rapid repeat adolescent pregnancy, researchers at MedStar Washington Hospital Center in Washington, DC, conducted a retrospective cohort study with first-time adolescent mothers, aged 19 years or younger. The repeat pregnancy rate at 2 years was 35% (n = 340). The average (SD) time from delivery to the second pregnancy was 9.9 (6.4) months.
Damle and colleagues found that leaving the hospital after giving birth without initiating any contraception was associated with more than double the risk of repeat pregnancy (odds ratio [OR], 2.447; 95% confidence interval [CI], 1.326–4.515). Follow-up in clinic within an 8-week postpartum period significantly reduced the chance of repeat pregnancy (OR, 0.322; 95% CI, 0.172–0.603). And placement of a long-acting reversible contraception (LARC), including intrauterine device or etonogestrel subdermal implant, by 8 weeks’ postpartum decreased the chance of rapid repeat pregnancy (OR, 0.118; 95% CI, 0.035-0.397).
Researchers Damle and colleagues concluded that adolescent mothers who begin to use a LARC within 8 weeks’ postpartum are less likely to have a repeat pregnancy within 2 years than those who chose another method or no contraception at all.
“First time adolescent mothers should be counseled about this advantage of using LARC,” wrote the authors.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
1. Damle LF, Gohari AC, McEvoy AK, Desale SY, Gomez-Lobo V. Early initiation of postpartum contraception: does it decrease rapid repeat pregnancy in adolescents? J Pediatr Adolesc Gynecol. 2015;28(1):57–62.
In an effort to determine how to curb rapid repeat adolescent pregnancy, researchers at MedStar Washington Hospital Center in Washington, DC, conducted a retrospective cohort study with first-time adolescent mothers, aged 19 years or younger. The repeat pregnancy rate at 2 years was 35% (n = 340). The average (SD) time from delivery to the second pregnancy was 9.9 (6.4) months.
Damle and colleagues found that leaving the hospital after giving birth without initiating any contraception was associated with more than double the risk of repeat pregnancy (odds ratio [OR], 2.447; 95% confidence interval [CI], 1.326–4.515). Follow-up in clinic within an 8-week postpartum period significantly reduced the chance of repeat pregnancy (OR, 0.322; 95% CI, 0.172–0.603). And placement of a long-acting reversible contraception (LARC), including intrauterine device or etonogestrel subdermal implant, by 8 weeks’ postpartum decreased the chance of rapid repeat pregnancy (OR, 0.118; 95% CI, 0.035-0.397).
Researchers Damle and colleagues concluded that adolescent mothers who begin to use a LARC within 8 weeks’ postpartum are less likely to have a repeat pregnancy within 2 years than those who chose another method or no contraception at all.
“First time adolescent mothers should be counseled about this advantage of using LARC,” wrote the authors.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In an effort to determine how to curb rapid repeat adolescent pregnancy, researchers at MedStar Washington Hospital Center in Washington, DC, conducted a retrospective cohort study with first-time adolescent mothers, aged 19 years or younger. The repeat pregnancy rate at 2 years was 35% (n = 340). The average (SD) time from delivery to the second pregnancy was 9.9 (6.4) months.
Damle and colleagues found that leaving the hospital after giving birth without initiating any contraception was associated with more than double the risk of repeat pregnancy (odds ratio [OR], 2.447; 95% confidence interval [CI], 1.326–4.515). Follow-up in clinic within an 8-week postpartum period significantly reduced the chance of repeat pregnancy (OR, 0.322; 95% CI, 0.172–0.603). And placement of a long-acting reversible contraception (LARC), including intrauterine device or etonogestrel subdermal implant, by 8 weeks’ postpartum decreased the chance of rapid repeat pregnancy (OR, 0.118; 95% CI, 0.035-0.397).
Researchers Damle and colleagues concluded that adolescent mothers who begin to use a LARC within 8 weeks’ postpartum are less likely to have a repeat pregnancy within 2 years than those who chose another method or no contraception at all.
“First time adolescent mothers should be counseled about this advantage of using LARC,” wrote the authors.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
1. Damle LF, Gohari AC, McEvoy AK, Desale SY, Gomez-Lobo V. Early initiation of postpartum contraception: does it decrease rapid repeat pregnancy in adolescents? J Pediatr Adolesc Gynecol. 2015;28(1):57–62.
Reference
1. Damle LF, Gohari AC, McEvoy AK, Desale SY, Gomez-Lobo V. Early initiation of postpartum contraception: does it decrease rapid repeat pregnancy in adolescents? J Pediatr Adolesc Gynecol. 2015;28(1):57–62.
FDA approves ibrutinib for WM

Credit: CDC
The US Food and Drug Administration (FDA) has granted approval for ibrutinib (Imbruvica) as the first and only treatment for patients with Waldenstrom’s macroglobulinemia (WM).
The drug is now approved as a single agent for use in all lines of therapy.
This is the fourth indication for ibrutinib, which is also FDA-approved to treat patients with chronic lymphocytic leukemia (CLL) who have received at least one prior therapy, CLL patients with del 17p, and patients with mantle cell lymphoma.
Ibrutinib is being jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc.
The latest FDA approval is based on results from a multicenter, phase 2 study in which researchers evaluated the efficacy and tolerability of ibrutinib in 63 patients with previously treated WM.
The response rate, according to an independent review committee, was 62%. Eleven percent of patients had a very good partial response rate, and 51% had a partial response rate.
The median duration of response has not been reached, with a range of 2.8 to 18.8 months.
The most commonly occurring adverse events (>20%) were neutropenia, thrombocytopenia, diarrhea, rash, nausea, muscle spasms, and fatigue.
Six percent of patients discontinued treatment due to adverse events. Events leading to dose reduction occurred in 11% of patients.
For more details, see the full prescribing information. ![]()

Credit: CDC
The US Food and Drug Administration (FDA) has granted approval for ibrutinib (Imbruvica) as the first and only treatment for patients with Waldenstrom’s macroglobulinemia (WM).
The drug is now approved as a single agent for use in all lines of therapy.
This is the fourth indication for ibrutinib, which is also FDA-approved to treat patients with chronic lymphocytic leukemia (CLL) who have received at least one prior therapy, CLL patients with del 17p, and patients with mantle cell lymphoma.
Ibrutinib is being jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc.
The latest FDA approval is based on results from a multicenter, phase 2 study in which researchers evaluated the efficacy and tolerability of ibrutinib in 63 patients with previously treated WM.
The response rate, according to an independent review committee, was 62%. Eleven percent of patients had a very good partial response rate, and 51% had a partial response rate.
The median duration of response has not been reached, with a range of 2.8 to 18.8 months.
The most commonly occurring adverse events (>20%) were neutropenia, thrombocytopenia, diarrhea, rash, nausea, muscle spasms, and fatigue.
Six percent of patients discontinued treatment due to adverse events. Events leading to dose reduction occurred in 11% of patients.
For more details, see the full prescribing information. ![]()

Credit: CDC
The US Food and Drug Administration (FDA) has granted approval for ibrutinib (Imbruvica) as the first and only treatment for patients with Waldenstrom’s macroglobulinemia (WM).
The drug is now approved as a single agent for use in all lines of therapy.
This is the fourth indication for ibrutinib, which is also FDA-approved to treat patients with chronic lymphocytic leukemia (CLL) who have received at least one prior therapy, CLL patients with del 17p, and patients with mantle cell lymphoma.
Ibrutinib is being jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc.
The latest FDA approval is based on results from a multicenter, phase 2 study in which researchers evaluated the efficacy and tolerability of ibrutinib in 63 patients with previously treated WM.
The response rate, according to an independent review committee, was 62%. Eleven percent of patients had a very good partial response rate, and 51% had a partial response rate.
The median duration of response has not been reached, with a range of 2.8 to 18.8 months.
The most commonly occurring adverse events (>20%) were neutropenia, thrombocytopenia, diarrhea, rash, nausea, muscle spasms, and fatigue.
Six percent of patients discontinued treatment due to adverse events. Events leading to dose reduction occurred in 11% of patients.
For more details, see the full prescribing information. ![]()
Kinase plays key role in leukemia

Credit: Robert Paulson
Inhibiting the cell-cycle kinase CDK6 may prevent leukemic relapse, according to research published in Blood.
Investigators found that CDK6 regulates the activation of hematopoietic stem cells (HSCs) and leukemic stem cells (LSCs), which it does by inhibiting the transcription factor Egr1.
When CDK6 is lost, Egr1 becomes active and prevents stem cells from dividing.
However, the mechanism operates only when HSCs are stressed—such as in leukemia—and not in the normal physiological situation.
“CDK6 is absolutely necessary for leukemic stem cells to induce disease but plays no part in normal hematopoiesis,” said study author Ruth Scheicher, of the University of Veterinary Medicine, Vienna.
“We thus have a novel opportunity to target leukemia at its origin. Inhibiting CDK6 should attack leukemic stem cells while leaving healthy HSCs unaffected.”
Specifically, Scheicher and her colleagues found that Cdk6−/− HSCs did not efficiently repopulate when transplanted into mice. And Cdk6−/− mice could tolerate fewer cycles of treatment with 5-fluorouracil than wild-type mice.
Mice that received BCR-ABLp210+–infected bone marrow harvested from Cdk6−/− mice did not develop leukemia. However, the recipient mice did harbor LSCs.
And knocking down Egr1 in Cdk6−/− BCR-ABLp210+ LSCs enhanced the cells’ ability to form colonies.
The researchers said these results suggest CDK6 is “an important regulator of stem cell activation and an essential component of a transcriptional complex that suppresses Egr1 in HSCs and LSCs.” ![]()

Credit: Robert Paulson
Inhibiting the cell-cycle kinase CDK6 may prevent leukemic relapse, according to research published in Blood.
Investigators found that CDK6 regulates the activation of hematopoietic stem cells (HSCs) and leukemic stem cells (LSCs), which it does by inhibiting the transcription factor Egr1.
When CDK6 is lost, Egr1 becomes active and prevents stem cells from dividing.
However, the mechanism operates only when HSCs are stressed—such as in leukemia—and not in the normal physiological situation.
“CDK6 is absolutely necessary for leukemic stem cells to induce disease but plays no part in normal hematopoiesis,” said study author Ruth Scheicher, of the University of Veterinary Medicine, Vienna.
“We thus have a novel opportunity to target leukemia at its origin. Inhibiting CDK6 should attack leukemic stem cells while leaving healthy HSCs unaffected.”
Specifically, Scheicher and her colleagues found that Cdk6−/− HSCs did not efficiently repopulate when transplanted into mice. And Cdk6−/− mice could tolerate fewer cycles of treatment with 5-fluorouracil than wild-type mice.
Mice that received BCR-ABLp210+–infected bone marrow harvested from Cdk6−/− mice did not develop leukemia. However, the recipient mice did harbor LSCs.
And knocking down Egr1 in Cdk6−/− BCR-ABLp210+ LSCs enhanced the cells’ ability to form colonies.
The researchers said these results suggest CDK6 is “an important regulator of stem cell activation and an essential component of a transcriptional complex that suppresses Egr1 in HSCs and LSCs.” ![]()

Credit: Robert Paulson
Inhibiting the cell-cycle kinase CDK6 may prevent leukemic relapse, according to research published in Blood.
Investigators found that CDK6 regulates the activation of hematopoietic stem cells (HSCs) and leukemic stem cells (LSCs), which it does by inhibiting the transcription factor Egr1.
When CDK6 is lost, Egr1 becomes active and prevents stem cells from dividing.
However, the mechanism operates only when HSCs are stressed—such as in leukemia—and not in the normal physiological situation.
“CDK6 is absolutely necessary for leukemic stem cells to induce disease but plays no part in normal hematopoiesis,” said study author Ruth Scheicher, of the University of Veterinary Medicine, Vienna.
“We thus have a novel opportunity to target leukemia at its origin. Inhibiting CDK6 should attack leukemic stem cells while leaving healthy HSCs unaffected.”
Specifically, Scheicher and her colleagues found that Cdk6−/− HSCs did not efficiently repopulate when transplanted into mice. And Cdk6−/− mice could tolerate fewer cycles of treatment with 5-fluorouracil than wild-type mice.
Mice that received BCR-ABLp210+–infected bone marrow harvested from Cdk6−/− mice did not develop leukemia. However, the recipient mice did harbor LSCs.
And knocking down Egr1 in Cdk6−/− BCR-ABLp210+ LSCs enhanced the cells’ ability to form colonies.
The researchers said these results suggest CDK6 is “an important regulator of stem cell activation and an essential component of a transcriptional complex that suppresses Egr1 in HSCs and LSCs.” ![]()
Group uncovers structure of receptor-chemokine complex
in complex with a chemokine
(purple surface)
Credit: Katya Kadyshevskaya
Researchers have reported the first crystal structure of the cellular receptor CXCR4 bound to the viral chemokine antagonist vMIP-II.
The structure, published in Science, answers longstanding questions about a molecular interaction that plays an important role in human development, immune responses, cancer spread, and HIV infections.
“This new information could ultimately aid the development of better small molecular inhibitors of CXCR4-chemokine interactions—inhibitors that have the potential to block cancer metastasis or viral infections,” said study author Tracy M. Handel, PhD, of the University of California, San Diego.
Dr Handel and her colleagues knew that CXCR4 binds chemokines to transmit messages to the inside of the cell. This signal relay helps cells migrate normally during development and inflammation.
But CXCR4 signaling can also play a role in abnormal cell migration, such as when cancer cells metastasize. And CXCR4 is infamous for another reason: HIV uses it to bind and infect human immune cells.
Despite its far-reaching consequences, researchers have long lacked data to show how exactly the CXCR4-chemokine interaction occurs, or even how many CXCR4 receptors a single chemokine molecule might simultaneously engage.
This is because membrane receptors like CXCR4 are exceptionally challenging structural targets. And the difficulty dramatically increases when studying such receptors in complexes with the proteins they bind.
To overcome these experimental challenges, Dr Handel’s team used a novel approach. They combined computational modeling and a technique known as disulfide trapping to stabilize the complex.
Once it was stabilized, the researchers were able to use X-ray crystallography to determine the CXCR4-chemokine complex’s 3D atomic structure.
This is the first time a receptor like CXCR4 has been crystallized with a protein binding partner, and the results revealed several new insights. First, the new crystal structure shows that one chemokine binds to just one receptor.
Additionally, the structure reveals that the contacts between the receptor and its binding partner are more extensive than previously thought. It is one very large, contiguous surface of interaction rather than two separate binding sites.
“The plasticity of the CXCR4 receptor—its ability to bind many unrelated small molecules, peptides, and proteins—is remarkable,” said Irina Kufareva, PhD, also of UC San Diego.
“Our understanding of this plasticity may impact the design of therapeutics with better inhibition and safety profiles.”
“With more than 800 members, 7-transmembrane receptors like CXCR4 are the largest protein family in the human genome,” added Raymond Stevens, PhD, of the Bridge Institute at the University of Southern California in Los Angeles. “Each new structure opens up so many doors to understanding different aspects of human biology, and this time it is about chemokine signaling.” ![]()
in complex with a chemokine
(purple surface)
Credit: Katya Kadyshevskaya
Researchers have reported the first crystal structure of the cellular receptor CXCR4 bound to the viral chemokine antagonist vMIP-II.
The structure, published in Science, answers longstanding questions about a molecular interaction that plays an important role in human development, immune responses, cancer spread, and HIV infections.
“This new information could ultimately aid the development of better small molecular inhibitors of CXCR4-chemokine interactions—inhibitors that have the potential to block cancer metastasis or viral infections,” said study author Tracy M. Handel, PhD, of the University of California, San Diego.
Dr Handel and her colleagues knew that CXCR4 binds chemokines to transmit messages to the inside of the cell. This signal relay helps cells migrate normally during development and inflammation.
But CXCR4 signaling can also play a role in abnormal cell migration, such as when cancer cells metastasize. And CXCR4 is infamous for another reason: HIV uses it to bind and infect human immune cells.
Despite its far-reaching consequences, researchers have long lacked data to show how exactly the CXCR4-chemokine interaction occurs, or even how many CXCR4 receptors a single chemokine molecule might simultaneously engage.
This is because membrane receptors like CXCR4 are exceptionally challenging structural targets. And the difficulty dramatically increases when studying such receptors in complexes with the proteins they bind.
To overcome these experimental challenges, Dr Handel’s team used a novel approach. They combined computational modeling and a technique known as disulfide trapping to stabilize the complex.
Once it was stabilized, the researchers were able to use X-ray crystallography to determine the CXCR4-chemokine complex’s 3D atomic structure.
This is the first time a receptor like CXCR4 has been crystallized with a protein binding partner, and the results revealed several new insights. First, the new crystal structure shows that one chemokine binds to just one receptor.
Additionally, the structure reveals that the contacts between the receptor and its binding partner are more extensive than previously thought. It is one very large, contiguous surface of interaction rather than two separate binding sites.
“The plasticity of the CXCR4 receptor—its ability to bind many unrelated small molecules, peptides, and proteins—is remarkable,” said Irina Kufareva, PhD, also of UC San Diego.
“Our understanding of this plasticity may impact the design of therapeutics with better inhibition and safety profiles.”
“With more than 800 members, 7-transmembrane receptors like CXCR4 are the largest protein family in the human genome,” added Raymond Stevens, PhD, of the Bridge Institute at the University of Southern California in Los Angeles. “Each new structure opens up so many doors to understanding different aspects of human biology, and this time it is about chemokine signaling.” ![]()
in complex with a chemokine
(purple surface)
Credit: Katya Kadyshevskaya
Researchers have reported the first crystal structure of the cellular receptor CXCR4 bound to the viral chemokine antagonist vMIP-II.
The structure, published in Science, answers longstanding questions about a molecular interaction that plays an important role in human development, immune responses, cancer spread, and HIV infections.
“This new information could ultimately aid the development of better small molecular inhibitors of CXCR4-chemokine interactions—inhibitors that have the potential to block cancer metastasis or viral infections,” said study author Tracy M. Handel, PhD, of the University of California, San Diego.
Dr Handel and her colleagues knew that CXCR4 binds chemokines to transmit messages to the inside of the cell. This signal relay helps cells migrate normally during development and inflammation.
But CXCR4 signaling can also play a role in abnormal cell migration, such as when cancer cells metastasize. And CXCR4 is infamous for another reason: HIV uses it to bind and infect human immune cells.
Despite its far-reaching consequences, researchers have long lacked data to show how exactly the CXCR4-chemokine interaction occurs, or even how many CXCR4 receptors a single chemokine molecule might simultaneously engage.
This is because membrane receptors like CXCR4 are exceptionally challenging structural targets. And the difficulty dramatically increases when studying such receptors in complexes with the proteins they bind.
To overcome these experimental challenges, Dr Handel’s team used a novel approach. They combined computational modeling and a technique known as disulfide trapping to stabilize the complex.
Once it was stabilized, the researchers were able to use X-ray crystallography to determine the CXCR4-chemokine complex’s 3D atomic structure.
This is the first time a receptor like CXCR4 has been crystallized with a protein binding partner, and the results revealed several new insights. First, the new crystal structure shows that one chemokine binds to just one receptor.
Additionally, the structure reveals that the contacts between the receptor and its binding partner are more extensive than previously thought. It is one very large, contiguous surface of interaction rather than two separate binding sites.
“The plasticity of the CXCR4 receptor—its ability to bind many unrelated small molecules, peptides, and proteins—is remarkable,” said Irina Kufareva, PhD, also of UC San Diego.
“Our understanding of this plasticity may impact the design of therapeutics with better inhibition and safety profiles.”
“With more than 800 members, 7-transmembrane receptors like CXCR4 are the largest protein family in the human genome,” added Raymond Stevens, PhD, of the Bridge Institute at the University of Southern California in Los Angeles. “Each new structure opens up so many doors to understanding different aspects of human biology, and this time it is about chemokine signaling.” ![]()