User login
AAP, NASPAG issue joint guidance on menstruation management in teens with disabilities
For the first time, the American Academy of Pediatrics is offering guidance on managing menstruation and sexuality education in adolescents with disabilities.
Written jointly with the North American Society for Pediatric and Adolescent Gynecology, the clinical report offers guidance on options for menstrual management, sexual education and expression, and protection from sexual abuse. The report gives guidance regarding the care of adolescents with physical and/or intellectual abilities, but not for those with psychiatric illnesses (Pediatrics. 2016 April. doi: 10.1542/peds.2016-0295).
“Taking care of teens with disabilities and figuring out what to do with menstrual management has been all over the map,” Dr. Cora Collette Breuner, chair of the AAP’s committee on adolescence, said in an interview. “So, we tried to clarify it and help clinicians know what to do and when.”
A particular concern for the two groups was the threat of adverse events. “We wanted to cover what’s safe and what’s not in menstruation management, especially around bone health and thromboembolic events,” said Dr. Breuner, a professor of pediatrics and adolescent medicine at the University of Washington, Seattle.
Some of the information will not surprise clinicians, but there are some data that will perhaps come as news, said Dr. Breuner, including the recommendation that long-acting reversible contraception (LARC), such as the levonorgestrel intrauterine device or the progesterone implant rod should be considered first-line management therapies. “We point out that a number of studies show that these are safe.”
The report emphasizes offering anticipatory guidance before menses begins, noting that most teens with disabilities mature at the same rate as teens without disabilities. The report does not recommend premenarchal suppression in these patients, because doing so can interfere with normal bone growth. Such suppression also prevents patients and their families and caregivers from discovering that coping with the onset of menses is perhaps not as difficult as they might fear, the report states.
Although combined oral contraceptives are not contraindicated in teens with mobility issues, to guard against the threat of thromboembolic events in teens who use wheelchairs, the report recommends taking a thorough family history to rule out inherited thrombophilia. Otherwise, the recommendation is to prescribe the lowest-dose estrogen with a first- or second-generation progestin, as these are associated with lower rates of venous thrombotic events.
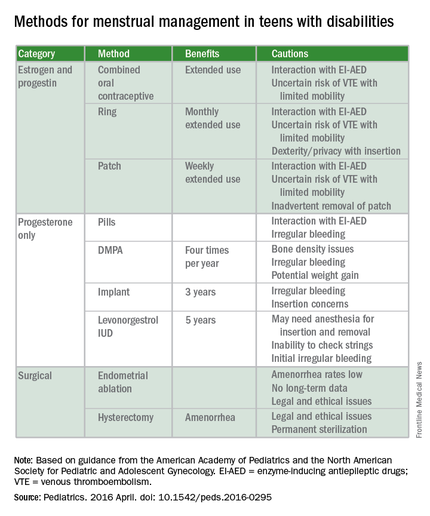
The guidance states that if cycles are creating difficulties in the patient’s life, “as determined by health care providers, patients, and families,” then menstrual management is appropriate. Even though it may take up to 3 years before a menstrual cycle becomes regular, the report cites irregularities caused by certain medications can be reason enough for menstrual management. Specific drugs noted include those affecting the dopaminergic system, valproic acid, and medications that elevate prolactin. Teens with obesity, seizure disorders, and polycystic ovary syndrome also can experience higher rates of irregularity.
The report also warns against the assumption that teens with disabilities are asexual or uninterested in sex. When appropriate, they should be offered the same confidential conversations about sexuality as are recommended for all teenagers by the AAP and the American College of Obstetricians and Gynecologists. “Teenagers with physical disabilities are just as likely to be sexually active as their peers and have a higher incidence of sexual abuse,” the report states. It is typically when a patient is cognitively impaired that consent to confidential services may require “discussion about legal guardianship or medical power of attorney status for families,” according to the report.
The report’s comprehensive review of four main menstrual management techniques – estrogen-containing, progestin-only, nonhormonal methods, and surgical requests and options – begins with the caveat that regardless of the method used, the threat of abuse or sexually transmitted infections remain. When a patient’s family or caregivers request suppression of menarche in a patient, stating fears of abuse or pregnancy, further investigation into the patient’s circumstances is warranted, the report states.
“It’s always worth reminding physicians that in this cohort, endometrial ablation can have legal implications, and it’s not recommended in this age group,” Dr. Breuner said.
On average, 1.5 hormonal methods are tried before achieving management goals, according to the report. Data cited in the study showed that at 42%, oral contraception is the preferred method of menstrual suppression, followed by the patch at 20%. Expectant management was third at 15%, followed by DMPA (depot medroxyprogesterone acetate) at 12%. The least utilized method was the levonorgestrel intrauterine device at 3%. No data were provided for the implantable contraceptive rod.
The clinical report is a companion document to another AAP clinical report, “Sexuality of Children and Adolescents with Developmental Disabilities” (Pediatrics. 2006. doi: 10.1542/peds.2006-1115).
AAP guidance on these matters in teens with psychiatric illnesses is expected to be issued within a few years, Dr. Breuner said.
There was no external funding and the authors have no relevant financial disclosures.
On Twitter @whitneymcknight
Although this guideline focuses on menstrual management and the guidance for you to help teens with disabilities through the pubertal transition, it’s very important to put this topic also into the context of sexuality. I think you have a great opportunity to do this because, often, you already have developed long-term relationships with these teenagers and their families, so the trust is already there. You should be the one to ensure all patients have appropriate sex education and help families with this.

|
Dr. Elisabeth Quint |
For some of these teens who are cognitively impaired, the initial conversations about sex may focus more on safety and abuse prevention. For example, which parts of their body should not be touched by other people. You can help the families really be the educators. Parents can be the ones to teach their kids how to protect themselves by rehearsing the answers to questions like, “What do you do if someone touches you? Who do you tell? Where do you go? What if it happens at school?” As part of the safety aspects, you also can help families assess whether the patient will be able to have a consensual sexual relationship. It’s the teens who have mild cognitive impairment that I worry about most, because often they are friendly and open to people, and can be taken advantage of. You just want to make sure they have the right information at their appropriate level.
Adolescents with physical disabilities are going to be just as interested in sex as any other teens and should be helped with any potential issues that they may have around that issue. They will likely get sex education in schools, but are still often viewed as not interested in sex or sexually active, and they may not get the usual confidential teen questions or appropriate screenings. Menstrual management and sexuality education both are important aspects of reproductive health care for teens with disabilities.
Dr. Elisabeth Quint, lead author of the AAP clinical report “Menstrual Management for Adolescents,” is a clinical professor of obstetrics and gynecology at the University of Michigan, Ann Arbor. She is also a past president of the North American Society for Pediatric and Adolescent Gynecology.
Although this guideline focuses on menstrual management and the guidance for you to help teens with disabilities through the pubertal transition, it’s very important to put this topic also into the context of sexuality. I think you have a great opportunity to do this because, often, you already have developed long-term relationships with these teenagers and their families, so the trust is already there. You should be the one to ensure all patients have appropriate sex education and help families with this.

|
Dr. Elisabeth Quint |
For some of these teens who are cognitively impaired, the initial conversations about sex may focus more on safety and abuse prevention. For example, which parts of their body should not be touched by other people. You can help the families really be the educators. Parents can be the ones to teach their kids how to protect themselves by rehearsing the answers to questions like, “What do you do if someone touches you? Who do you tell? Where do you go? What if it happens at school?” As part of the safety aspects, you also can help families assess whether the patient will be able to have a consensual sexual relationship. It’s the teens who have mild cognitive impairment that I worry about most, because often they are friendly and open to people, and can be taken advantage of. You just want to make sure they have the right information at their appropriate level.
Adolescents with physical disabilities are going to be just as interested in sex as any other teens and should be helped with any potential issues that they may have around that issue. They will likely get sex education in schools, but are still often viewed as not interested in sex or sexually active, and they may not get the usual confidential teen questions or appropriate screenings. Menstrual management and sexuality education both are important aspects of reproductive health care for teens with disabilities.
Dr. Elisabeth Quint, lead author of the AAP clinical report “Menstrual Management for Adolescents,” is a clinical professor of obstetrics and gynecology at the University of Michigan, Ann Arbor. She is also a past president of the North American Society for Pediatric and Adolescent Gynecology.
Although this guideline focuses on menstrual management and the guidance for you to help teens with disabilities through the pubertal transition, it’s very important to put this topic also into the context of sexuality. I think you have a great opportunity to do this because, often, you already have developed long-term relationships with these teenagers and their families, so the trust is already there. You should be the one to ensure all patients have appropriate sex education and help families with this.

|
Dr. Elisabeth Quint |
For some of these teens who are cognitively impaired, the initial conversations about sex may focus more on safety and abuse prevention. For example, which parts of their body should not be touched by other people. You can help the families really be the educators. Parents can be the ones to teach their kids how to protect themselves by rehearsing the answers to questions like, “What do you do if someone touches you? Who do you tell? Where do you go? What if it happens at school?” As part of the safety aspects, you also can help families assess whether the patient will be able to have a consensual sexual relationship. It’s the teens who have mild cognitive impairment that I worry about most, because often they are friendly and open to people, and can be taken advantage of. You just want to make sure they have the right information at their appropriate level.
Adolescents with physical disabilities are going to be just as interested in sex as any other teens and should be helped with any potential issues that they may have around that issue. They will likely get sex education in schools, but are still often viewed as not interested in sex or sexually active, and they may not get the usual confidential teen questions or appropriate screenings. Menstrual management and sexuality education both are important aspects of reproductive health care for teens with disabilities.
Dr. Elisabeth Quint, lead author of the AAP clinical report “Menstrual Management for Adolescents,” is a clinical professor of obstetrics and gynecology at the University of Michigan, Ann Arbor. She is also a past president of the North American Society for Pediatric and Adolescent Gynecology.
For the first time, the American Academy of Pediatrics is offering guidance on managing menstruation and sexuality education in adolescents with disabilities.
Written jointly with the North American Society for Pediatric and Adolescent Gynecology, the clinical report offers guidance on options for menstrual management, sexual education and expression, and protection from sexual abuse. The report gives guidance regarding the care of adolescents with physical and/or intellectual abilities, but not for those with psychiatric illnesses (Pediatrics. 2016 April. doi: 10.1542/peds.2016-0295).
“Taking care of teens with disabilities and figuring out what to do with menstrual management has been all over the map,” Dr. Cora Collette Breuner, chair of the AAP’s committee on adolescence, said in an interview. “So, we tried to clarify it and help clinicians know what to do and when.”
A particular concern for the two groups was the threat of adverse events. “We wanted to cover what’s safe and what’s not in menstruation management, especially around bone health and thromboembolic events,” said Dr. Breuner, a professor of pediatrics and adolescent medicine at the University of Washington, Seattle.
Some of the information will not surprise clinicians, but there are some data that will perhaps come as news, said Dr. Breuner, including the recommendation that long-acting reversible contraception (LARC), such as the levonorgestrel intrauterine device or the progesterone implant rod should be considered first-line management therapies. “We point out that a number of studies show that these are safe.”
The report emphasizes offering anticipatory guidance before menses begins, noting that most teens with disabilities mature at the same rate as teens without disabilities. The report does not recommend premenarchal suppression in these patients, because doing so can interfere with normal bone growth. Such suppression also prevents patients and their families and caregivers from discovering that coping with the onset of menses is perhaps not as difficult as they might fear, the report states.
Although combined oral contraceptives are not contraindicated in teens with mobility issues, to guard against the threat of thromboembolic events in teens who use wheelchairs, the report recommends taking a thorough family history to rule out inherited thrombophilia. Otherwise, the recommendation is to prescribe the lowest-dose estrogen with a first- or second-generation progestin, as these are associated with lower rates of venous thrombotic events.
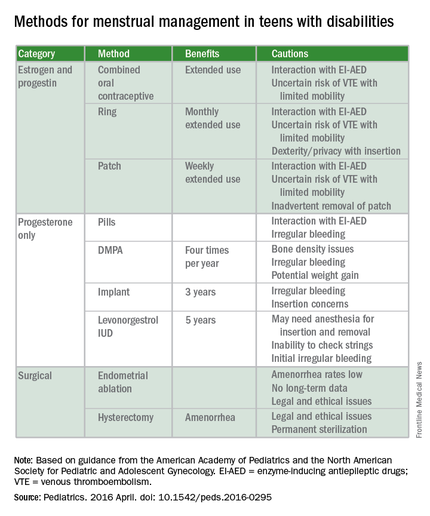
The guidance states that if cycles are creating difficulties in the patient’s life, “as determined by health care providers, patients, and families,” then menstrual management is appropriate. Even though it may take up to 3 years before a menstrual cycle becomes regular, the report cites irregularities caused by certain medications can be reason enough for menstrual management. Specific drugs noted include those affecting the dopaminergic system, valproic acid, and medications that elevate prolactin. Teens with obesity, seizure disorders, and polycystic ovary syndrome also can experience higher rates of irregularity.
The report also warns against the assumption that teens with disabilities are asexual or uninterested in sex. When appropriate, they should be offered the same confidential conversations about sexuality as are recommended for all teenagers by the AAP and the American College of Obstetricians and Gynecologists. “Teenagers with physical disabilities are just as likely to be sexually active as their peers and have a higher incidence of sexual abuse,” the report states. It is typically when a patient is cognitively impaired that consent to confidential services may require “discussion about legal guardianship or medical power of attorney status for families,” according to the report.
The report’s comprehensive review of four main menstrual management techniques – estrogen-containing, progestin-only, nonhormonal methods, and surgical requests and options – begins with the caveat that regardless of the method used, the threat of abuse or sexually transmitted infections remain. When a patient’s family or caregivers request suppression of menarche in a patient, stating fears of abuse or pregnancy, further investigation into the patient’s circumstances is warranted, the report states.
“It’s always worth reminding physicians that in this cohort, endometrial ablation can have legal implications, and it’s not recommended in this age group,” Dr. Breuner said.
On average, 1.5 hormonal methods are tried before achieving management goals, according to the report. Data cited in the study showed that at 42%, oral contraception is the preferred method of menstrual suppression, followed by the patch at 20%. Expectant management was third at 15%, followed by DMPA (depot medroxyprogesterone acetate) at 12%. The least utilized method was the levonorgestrel intrauterine device at 3%. No data were provided for the implantable contraceptive rod.
The clinical report is a companion document to another AAP clinical report, “Sexuality of Children and Adolescents with Developmental Disabilities” (Pediatrics. 2006. doi: 10.1542/peds.2006-1115).
AAP guidance on these matters in teens with psychiatric illnesses is expected to be issued within a few years, Dr. Breuner said.
There was no external funding and the authors have no relevant financial disclosures.
On Twitter @whitneymcknight
For the first time, the American Academy of Pediatrics is offering guidance on managing menstruation and sexuality education in adolescents with disabilities.
Written jointly with the North American Society for Pediatric and Adolescent Gynecology, the clinical report offers guidance on options for menstrual management, sexual education and expression, and protection from sexual abuse. The report gives guidance regarding the care of adolescents with physical and/or intellectual abilities, but not for those with psychiatric illnesses (Pediatrics. 2016 April. doi: 10.1542/peds.2016-0295).
“Taking care of teens with disabilities and figuring out what to do with menstrual management has been all over the map,” Dr. Cora Collette Breuner, chair of the AAP’s committee on adolescence, said in an interview. “So, we tried to clarify it and help clinicians know what to do and when.”
A particular concern for the two groups was the threat of adverse events. “We wanted to cover what’s safe and what’s not in menstruation management, especially around bone health and thromboembolic events,” said Dr. Breuner, a professor of pediatrics and adolescent medicine at the University of Washington, Seattle.
Some of the information will not surprise clinicians, but there are some data that will perhaps come as news, said Dr. Breuner, including the recommendation that long-acting reversible contraception (LARC), such as the levonorgestrel intrauterine device or the progesterone implant rod should be considered first-line management therapies. “We point out that a number of studies show that these are safe.”
The report emphasizes offering anticipatory guidance before menses begins, noting that most teens with disabilities mature at the same rate as teens without disabilities. The report does not recommend premenarchal suppression in these patients, because doing so can interfere with normal bone growth. Such suppression also prevents patients and their families and caregivers from discovering that coping with the onset of menses is perhaps not as difficult as they might fear, the report states.
Although combined oral contraceptives are not contraindicated in teens with mobility issues, to guard against the threat of thromboembolic events in teens who use wheelchairs, the report recommends taking a thorough family history to rule out inherited thrombophilia. Otherwise, the recommendation is to prescribe the lowest-dose estrogen with a first- or second-generation progestin, as these are associated with lower rates of venous thrombotic events.
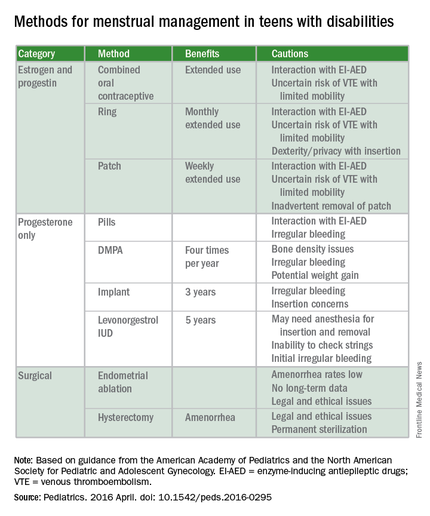
The guidance states that if cycles are creating difficulties in the patient’s life, “as determined by health care providers, patients, and families,” then menstrual management is appropriate. Even though it may take up to 3 years before a menstrual cycle becomes regular, the report cites irregularities caused by certain medications can be reason enough for menstrual management. Specific drugs noted include those affecting the dopaminergic system, valproic acid, and medications that elevate prolactin. Teens with obesity, seizure disorders, and polycystic ovary syndrome also can experience higher rates of irregularity.
The report also warns against the assumption that teens with disabilities are asexual or uninterested in sex. When appropriate, they should be offered the same confidential conversations about sexuality as are recommended for all teenagers by the AAP and the American College of Obstetricians and Gynecologists. “Teenagers with physical disabilities are just as likely to be sexually active as their peers and have a higher incidence of sexual abuse,” the report states. It is typically when a patient is cognitively impaired that consent to confidential services may require “discussion about legal guardianship or medical power of attorney status for families,” according to the report.
The report’s comprehensive review of four main menstrual management techniques – estrogen-containing, progestin-only, nonhormonal methods, and surgical requests and options – begins with the caveat that regardless of the method used, the threat of abuse or sexually transmitted infections remain. When a patient’s family or caregivers request suppression of menarche in a patient, stating fears of abuse or pregnancy, further investigation into the patient’s circumstances is warranted, the report states.
“It’s always worth reminding physicians that in this cohort, endometrial ablation can have legal implications, and it’s not recommended in this age group,” Dr. Breuner said.
On average, 1.5 hormonal methods are tried before achieving management goals, according to the report. Data cited in the study showed that at 42%, oral contraception is the preferred method of menstrual suppression, followed by the patch at 20%. Expectant management was third at 15%, followed by DMPA (depot medroxyprogesterone acetate) at 12%. The least utilized method was the levonorgestrel intrauterine device at 3%. No data were provided for the implantable contraceptive rod.
The clinical report is a companion document to another AAP clinical report, “Sexuality of Children and Adolescents with Developmental Disabilities” (Pediatrics. 2006. doi: 10.1542/peds.2006-1115).
AAP guidance on these matters in teens with psychiatric illnesses is expected to be issued within a few years, Dr. Breuner said.
There was no external funding and the authors have no relevant financial disclosures.
On Twitter @whitneymcknight
FROM PEDIATRICS
Consider Fusobacterium in culture-negative pharyngitis
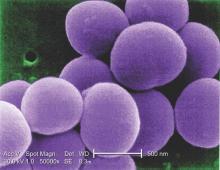
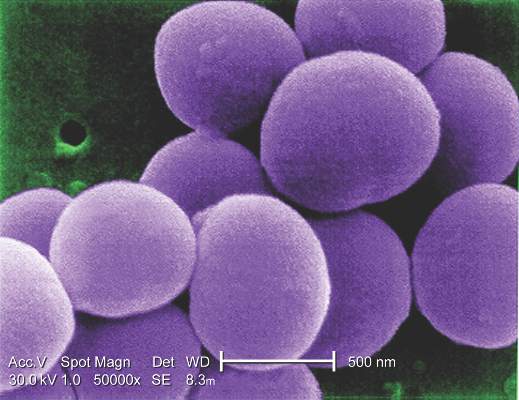
BOSTON – An underappreciated cause of bacterial pharyngitis had a similar clinical presentation to group A Streptococcus (GAS), although prevalence was low in the population of 300 pediatric patients in a single-site study.
The 10 patients (3.3%) who had positive cultures for Fusobacterium necrophorum were about as likely as those with GAS to have fever, sore throat, exudate, and absence of cough. GAS cultures were positive in 57 (19%) of the patients.
F. necrophorum is a common cause of serious bacterial pharyngitis, especially in adolescents and young adults. The gram-negative species, an obligate anaerobe, is a cause of Lemierre’s syndrome, and “has recently been identified to be an important pathogen of bacterial pharyngitis with higher prevalence than group A Streptococcus (GAS) in adolescents and young adults,” wrote Tam Van, Ph.D., and her colleagues in a poster presented at the annual meeting of the American Society for Microbiology.
To examine the prevalence and disease characteristics of F. necrophorum in the emergency department patient population at Children’s Hospital of Los Angeles, Dr Van, a medical microbiology fellow at the hospital, and her colleagues enrolled 300 patients with pharyngitis aged 1-20 years (mean, 7.8 years).
All patients’ throats were swabbed, and investigators conducted a rapid antigen detection test (RADT) for group A beta-hemolytic Streptococcus and cultured samples for Streptococcus on a blood agar plate, according to usual care; samples also were cultured anaerobically and tested via polymerase chain reaction (PCR) for F. necrophorum.
A total of 67 patients had positive culture or PCR results for both species. Fifteen of the RADT tests were positive, while 57 cultures returned positive for GAS growth. Nine of the 10 positive F. necrophorum PCR tests correlated with positive culture results for that species.
Luckily, said Dr. Van, penicillin is an effective treatment for F. necrophorum, although it’s a gram-negative bacterium, so if a patient is coinfected with F. necrophorum and GAS, or treated for GAS empirically, then standard of care treatment should be effective, she said. However, since the species is associated with serious complications such as Lemierre’s disease, close follow-up and a low threshold for aggressive treatment are warranted if F. necrophorum is suspected or identified.
The relatively low positive culture rate of 3.3% for F. necrophorum in the study population was a bit surprising, Dr. Van said in an interview but was perhaps accounted for by the relatively young age of the Children’s Hospital Los Angeles patients. “Previous reports looked at adolescents and young adults,” wrote Dr. Van and her colleagues, while two-thirds of the patients in their study were under the age of 10 years. “This may contribute to the difference in prevalence.”
“Although rare, recovery of F. necrophorum correlated with true signs and symptoms of bacterial pharyngitis,” wrote Dr. Van and her colleagues. Serious pharyngitis with a negative rapid test and culture for group A Streptococcus should prompt clinical suspicion for F. necrophorum, especially in older adolescents and young adults, said Dr. Tam.
Dr. Tam and her coauthors reported no outside sources of funding and reported no relevant financial disclosures.
On Twitter @karioakes
BOSTON – An underappreciated cause of bacterial pharyngitis had a similar clinical presentation to group A Streptococcus (GAS), although prevalence was low in the population of 300 pediatric patients in a single-site study.
The 10 patients (3.3%) who had positive cultures for Fusobacterium necrophorum were about as likely as those with GAS to have fever, sore throat, exudate, and absence of cough. GAS cultures were positive in 57 (19%) of the patients.
F. necrophorum is a common cause of serious bacterial pharyngitis, especially in adolescents and young adults. The gram-negative species, an obligate anaerobe, is a cause of Lemierre’s syndrome, and “has recently been identified to be an important pathogen of bacterial pharyngitis with higher prevalence than group A Streptococcus (GAS) in adolescents and young adults,” wrote Tam Van, Ph.D., and her colleagues in a poster presented at the annual meeting of the American Society for Microbiology.
To examine the prevalence and disease characteristics of F. necrophorum in the emergency department patient population at Children’s Hospital of Los Angeles, Dr Van, a medical microbiology fellow at the hospital, and her colleagues enrolled 300 patients with pharyngitis aged 1-20 years (mean, 7.8 years).
All patients’ throats were swabbed, and investigators conducted a rapid antigen detection test (RADT) for group A beta-hemolytic Streptococcus and cultured samples for Streptococcus on a blood agar plate, according to usual care; samples also were cultured anaerobically and tested via polymerase chain reaction (PCR) for F. necrophorum.
A total of 67 patients had positive culture or PCR results for both species. Fifteen of the RADT tests were positive, while 57 cultures returned positive for GAS growth. Nine of the 10 positive F. necrophorum PCR tests correlated with positive culture results for that species.
Luckily, said Dr. Van, penicillin is an effective treatment for F. necrophorum, although it’s a gram-negative bacterium, so if a patient is coinfected with F. necrophorum and GAS, or treated for GAS empirically, then standard of care treatment should be effective, she said. However, since the species is associated with serious complications such as Lemierre’s disease, close follow-up and a low threshold for aggressive treatment are warranted if F. necrophorum is suspected or identified.
The relatively low positive culture rate of 3.3% for F. necrophorum in the study population was a bit surprising, Dr. Van said in an interview but was perhaps accounted for by the relatively young age of the Children’s Hospital Los Angeles patients. “Previous reports looked at adolescents and young adults,” wrote Dr. Van and her colleagues, while two-thirds of the patients in their study were under the age of 10 years. “This may contribute to the difference in prevalence.”
“Although rare, recovery of F. necrophorum correlated with true signs and symptoms of bacterial pharyngitis,” wrote Dr. Van and her colleagues. Serious pharyngitis with a negative rapid test and culture for group A Streptococcus should prompt clinical suspicion for F. necrophorum, especially in older adolescents and young adults, said Dr. Tam.
Dr. Tam and her coauthors reported no outside sources of funding and reported no relevant financial disclosures.
On Twitter @karioakes
BOSTON – An underappreciated cause of bacterial pharyngitis had a similar clinical presentation to group A Streptococcus (GAS), although prevalence was low in the population of 300 pediatric patients in a single-site study.
The 10 patients (3.3%) who had positive cultures for Fusobacterium necrophorum were about as likely as those with GAS to have fever, sore throat, exudate, and absence of cough. GAS cultures were positive in 57 (19%) of the patients.
F. necrophorum is a common cause of serious bacterial pharyngitis, especially in adolescents and young adults. The gram-negative species, an obligate anaerobe, is a cause of Lemierre’s syndrome, and “has recently been identified to be an important pathogen of bacterial pharyngitis with higher prevalence than group A Streptococcus (GAS) in adolescents and young adults,” wrote Tam Van, Ph.D., and her colleagues in a poster presented at the annual meeting of the American Society for Microbiology.
To examine the prevalence and disease characteristics of F. necrophorum in the emergency department patient population at Children’s Hospital of Los Angeles, Dr Van, a medical microbiology fellow at the hospital, and her colleagues enrolled 300 patients with pharyngitis aged 1-20 years (mean, 7.8 years).
All patients’ throats were swabbed, and investigators conducted a rapid antigen detection test (RADT) for group A beta-hemolytic Streptococcus and cultured samples for Streptococcus on a blood agar plate, according to usual care; samples also were cultured anaerobically and tested via polymerase chain reaction (PCR) for F. necrophorum.
A total of 67 patients had positive culture or PCR results for both species. Fifteen of the RADT tests were positive, while 57 cultures returned positive for GAS growth. Nine of the 10 positive F. necrophorum PCR tests correlated with positive culture results for that species.
Luckily, said Dr. Van, penicillin is an effective treatment for F. necrophorum, although it’s a gram-negative bacterium, so if a patient is coinfected with F. necrophorum and GAS, or treated for GAS empirically, then standard of care treatment should be effective, she said. However, since the species is associated with serious complications such as Lemierre’s disease, close follow-up and a low threshold for aggressive treatment are warranted if F. necrophorum is suspected or identified.
The relatively low positive culture rate of 3.3% for F. necrophorum in the study population was a bit surprising, Dr. Van said in an interview but was perhaps accounted for by the relatively young age of the Children’s Hospital Los Angeles patients. “Previous reports looked at adolescents and young adults,” wrote Dr. Van and her colleagues, while two-thirds of the patients in their study were under the age of 10 years. “This may contribute to the difference in prevalence.”
“Although rare, recovery of F. necrophorum correlated with true signs and symptoms of bacterial pharyngitis,” wrote Dr. Van and her colleagues. Serious pharyngitis with a negative rapid test and culture for group A Streptococcus should prompt clinical suspicion for F. necrophorum, especially in older adolescents and young adults, said Dr. Tam.
Dr. Tam and her coauthors reported no outside sources of funding and reported no relevant financial disclosures.
On Twitter @karioakes
AT ASM MICROBE 2016
Key clinical point: Fusobacterium necrophorum has a similar presentation to group A Streptococcus (GAS) pharyngitis.
Major finding: Pediatric patients with F. necrophorum pharyngitis were about as likely as those with GAS to have fever, exudates, adenopathy, and no cough.
Data source: 300 pediatric emergency department patients with pharyngitis who received antigen testing, cultures, and PCR to identify both causative agents.
Disclosures: The study investigators reported no disclosures.
Debunking Psoriasis Myths: Can Diet Clear Psoriasis?
Myth: Psoriasis Can Be Treated By Eating or Avoiding Certain Foods
Patients who Google “diet and psoriasis” are flooded with search results of diets claiming to cure psoriasis. This misinformation is dangerous for patients, as there is no scientific evidence that any specific psoriasis diet can treat the condition. Patients may wish to improve their diet to prevent comorbidities such as cardiovascular disease and metabolic syndrome. Even though it may not be a cure, encouraging patients to eat healthy is never a bad thing.
In a 2014 analysis of psoriasis, obesity, body mass index (BMI), and diet literature, an increased risk for psoriasis development in the setting of obesity was discussed. There is evidence suggesting that a BMI greater than 30 kg/m2 may potentially play a role in the ability to achieve a full therapeutic effect of psoriasis therapy. “This could be for two possible reasons,” Debbaneh et al reported. “It may be a consequence of decreased drug distribution into the body due to increased body mass, or it may be a consequence of increased pro-inflammatory cytokine release as a result of increased adipocyte count.” However, this finding may be treatment specific. For example, higher body weight was an independent predictor of response to ustekinumab, providing the rationale for offering 2 weight-based dosing regimens of the drug. Overweight and obese patients also were less likely to experience clearance with adalimumab. However, studies have found no association between BMI and biologic treatment.
Weight loss through a low-calorie diet has been reported to achieve a greater reduction in psoriasis severity and a slower rebound of disease. “Interestingly, studies have shown that caloric restriction in obese subjects lowers the level of circulating inflammatory cytokines,” reported Debbaneh et al. “This may contribute to the observed beneficial effect in psoriatic disease.”
In patients whose disease has had a significant impact on quality of life, it is important that they are consulting resources online that will help them maintain a healthy lifestyle. The National Psoriasis Foundation provides useful information on diet and psoriasis, emphasizing that diet is not going to cure psoriatic disease but eating healthier can only help.
Expert Commentary
Many of my psoriasis patients ask me what should they avoid eating to prevent the psoriasis from worsening, or what did they eat to cause psoriasis to occur in the first place. I stress to patients that what they eat is not likely the cause of their psoriasis nor will avoiding certain foods prevent a flare. However, alcohol use may induce a psoriasis flare.
—Jashin J. Wu, MD (Los Angeles, California)
Debbaneh M, Millsop JW, Bhatia BK, et al. Diet and psoriasis: part I. impact of weight loss interventions. J Am Acad Dermatol. 2014;71:133-140.
National Psoriasis Foundation. Diet and psoriasis. https://www.psoriasis.org/about-psoriasis/treatments/alternative/diet-supplements. Accessed June 20, 2016.
Myth: Psoriasis Can Be Treated By Eating or Avoiding Certain Foods
Patients who Google “diet and psoriasis” are flooded with search results of diets claiming to cure psoriasis. This misinformation is dangerous for patients, as there is no scientific evidence that any specific psoriasis diet can treat the condition. Patients may wish to improve their diet to prevent comorbidities such as cardiovascular disease and metabolic syndrome. Even though it may not be a cure, encouraging patients to eat healthy is never a bad thing.
In a 2014 analysis of psoriasis, obesity, body mass index (BMI), and diet literature, an increased risk for psoriasis development in the setting of obesity was discussed. There is evidence suggesting that a BMI greater than 30 kg/m2 may potentially play a role in the ability to achieve a full therapeutic effect of psoriasis therapy. “This could be for two possible reasons,” Debbaneh et al reported. “It may be a consequence of decreased drug distribution into the body due to increased body mass, or it may be a consequence of increased pro-inflammatory cytokine release as a result of increased adipocyte count.” However, this finding may be treatment specific. For example, higher body weight was an independent predictor of response to ustekinumab, providing the rationale for offering 2 weight-based dosing regimens of the drug. Overweight and obese patients also were less likely to experience clearance with adalimumab. However, studies have found no association between BMI and biologic treatment.
Weight loss through a low-calorie diet has been reported to achieve a greater reduction in psoriasis severity and a slower rebound of disease. “Interestingly, studies have shown that caloric restriction in obese subjects lowers the level of circulating inflammatory cytokines,” reported Debbaneh et al. “This may contribute to the observed beneficial effect in psoriatic disease.”
In patients whose disease has had a significant impact on quality of life, it is important that they are consulting resources online that will help them maintain a healthy lifestyle. The National Psoriasis Foundation provides useful information on diet and psoriasis, emphasizing that diet is not going to cure psoriatic disease but eating healthier can only help.
Expert Commentary
Many of my psoriasis patients ask me what should they avoid eating to prevent the psoriasis from worsening, or what did they eat to cause psoriasis to occur in the first place. I stress to patients that what they eat is not likely the cause of their psoriasis nor will avoiding certain foods prevent a flare. However, alcohol use may induce a psoriasis flare.
—Jashin J. Wu, MD (Los Angeles, California)
Myth: Psoriasis Can Be Treated By Eating or Avoiding Certain Foods
Patients who Google “diet and psoriasis” are flooded with search results of diets claiming to cure psoriasis. This misinformation is dangerous for patients, as there is no scientific evidence that any specific psoriasis diet can treat the condition. Patients may wish to improve their diet to prevent comorbidities such as cardiovascular disease and metabolic syndrome. Even though it may not be a cure, encouraging patients to eat healthy is never a bad thing.
In a 2014 analysis of psoriasis, obesity, body mass index (BMI), and diet literature, an increased risk for psoriasis development in the setting of obesity was discussed. There is evidence suggesting that a BMI greater than 30 kg/m2 may potentially play a role in the ability to achieve a full therapeutic effect of psoriasis therapy. “This could be for two possible reasons,” Debbaneh et al reported. “It may be a consequence of decreased drug distribution into the body due to increased body mass, or it may be a consequence of increased pro-inflammatory cytokine release as a result of increased adipocyte count.” However, this finding may be treatment specific. For example, higher body weight was an independent predictor of response to ustekinumab, providing the rationale for offering 2 weight-based dosing regimens of the drug. Overweight and obese patients also were less likely to experience clearance with adalimumab. However, studies have found no association between BMI and biologic treatment.
Weight loss through a low-calorie diet has been reported to achieve a greater reduction in psoriasis severity and a slower rebound of disease. “Interestingly, studies have shown that caloric restriction in obese subjects lowers the level of circulating inflammatory cytokines,” reported Debbaneh et al. “This may contribute to the observed beneficial effect in psoriatic disease.”
In patients whose disease has had a significant impact on quality of life, it is important that they are consulting resources online that will help them maintain a healthy lifestyle. The National Psoriasis Foundation provides useful information on diet and psoriasis, emphasizing that diet is not going to cure psoriatic disease but eating healthier can only help.
Expert Commentary
Many of my psoriasis patients ask me what should they avoid eating to prevent the psoriasis from worsening, or what did they eat to cause psoriasis to occur in the first place. I stress to patients that what they eat is not likely the cause of their psoriasis nor will avoiding certain foods prevent a flare. However, alcohol use may induce a psoriasis flare.
—Jashin J. Wu, MD (Los Angeles, California)
Debbaneh M, Millsop JW, Bhatia BK, et al. Diet and psoriasis: part I. impact of weight loss interventions. J Am Acad Dermatol. 2014;71:133-140.
National Psoriasis Foundation. Diet and psoriasis. https://www.psoriasis.org/about-psoriasis/treatments/alternative/diet-supplements. Accessed June 20, 2016.
Debbaneh M, Millsop JW, Bhatia BK, et al. Diet and psoriasis: part I. impact of weight loss interventions. J Am Acad Dermatol. 2014;71:133-140.
National Psoriasis Foundation. Diet and psoriasis. https://www.psoriasis.org/about-psoriasis/treatments/alternative/diet-supplements. Accessed June 20, 2016.
Challenging ‘dogma’ of allografts in infectious endocarditis
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Use of homografts showed no significant benefit, compared with conventional prosthetic valves when the patient has infective endocarditis involving the aortic valve.
Major finding: The homograft group had more than twice the rate of early death than the conventional group, 19.8% vs. 9.2%, but in longer-term follow-up, the survival rates did not differ between groups.
Data source: 304 consecutive adult patients from the perspective database of two tertiary academic centers who had surgery for active infective endocarditis involving the aortic valve from 2002 to 2014.
Disclosures: Coauthor Dr. Sundt, disclosed he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
Debunking Psoriasis Myths: Do Biologics Cause Cancer?
Myth: Biologics Cause Cancer
Biologics generally are safe and well-tolerated therapies; however, due to their immunosuppressive properties, the risk for lymphoma has been of potential concern, leading patients to believe that biologics cause cancer. The risk of some cancers, including some solid cancers, hematologic cancers, and skin cancers, appears to be increased in patients with psoriasis, possibly associated with chronic inflammation. Some psoriasis therapies may increase the risk for malignancy, including phototherapy with psoralen plus UVA, cyclosporine, and methotrexate.
Many studies have supported a favorable safety profile for biologics in terms of the risk for developing malignancy. In a 2015 analysis of 12,093 patients enrolled in PSOLAR (Psoriasis Longitudinal Assessment and Registry), none of the biologics were found to be associated with increased risk for malignancy.
In psoriasis patients with existing or prior malignancies, the benefits of biologic therapy to improve quality of life often outweigh the negligible risks for malignancy. However, coordinated care with oncology is recommended for psoriasis patients with a history of prior malignancy.
General recommendations from the American Academy of Dermatology indicate one should carefully consider the decision to use a tumor necrosis factor (TNF) antagonist in patients with a history of malignancy, particularly lymphoma. Short-term treatment with biologics (up to 4 years) appears to be safe with respect to lymphoma risk, especially with TNF-α inhibitors. The potential risk for melanoma, cutaneous T-cell lymphoma, and nonmelanoma skin cancer in patients treated with TNF inhibitors also has been raised.
Expert Commentary
OBSERVE-5 was a 5-year phase 4, prospective, multicenter surveillance registry of 2510 psoriasis patients with at least a baseline dose of etanercept (Kimball et al, 2015). There was no increased risk for cancer when compared to the Truven Health MarketScan database, which is a proxy for the general population.
ESPRIT is an ongoing, 10-year, international, prospective, observational registry of 6059 psoriasis patients with at least a baseline dose of adalimumab (Menter et al). There are no signals of increased risk for cancer.
We do not have enough numbers of psoriasis patients on secukinumab or ixekizumab yet, but their phase 3 trials also do not seem to indicate an increased risk for cancer.
—Jashin J. Wu, MD (Los Angeles, California)
American Academy of Dermatology. Psoriasis: TNF inhibitors general recommendations. https://www.aad.org/practice-tools/quality-care/clinical-guidelines/psoriasis/biologics/tnf-inhibitors-recommendations. Accessed June 14, 2016.
Dommasch E, Gelfand JM. Is there truly a risk of lymphoma from biologic therapies? Dermatol Ther. 2009;22:418-430.
Kimball AB, Rothman KJ, Kricorian G, et al. OBSERVE-5: Observational postmarketing safety surveillance registry of etanercept for the treatment of psoriasis final 5-year results. J Am Acad Dermatol. 2015;72:115-122.
Kimball AB, Schenfeld J, Accortt NA, et al. 5-year incidence rates of malignancies in psoriasis patients compared with the general US population. Poster presented at: Summer Meeting of the American Academy of Dermatology; August 6-10, 2014; Chicago, IL.
Menter A, Thaçi D, Papp KA, et al. Five-year analysis from the ESPRIT 10-year postmarketing surveillance registry of adalimumab treatment for moderate to severe psoriasis. J Am Acad Dermatol. 2015;73:410-419.e6.
Papp K, Gottlieb AB, Naldi L, et al. Safety surveillance for ustekinumab and other psoriasis treatments from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Drugs Dermatol. 2015;14:706-714.
Patel S, Patel T, Kerdel FA. The risk of malignancy or progression of existing malignancy in patients with psoriasis treated with biologics: case report and review of the literature. Int J Dermatol. 2016;55:487-493.
Myth: Biologics Cause Cancer
Biologics generally are safe and well-tolerated therapies; however, due to their immunosuppressive properties, the risk for lymphoma has been of potential concern, leading patients to believe that biologics cause cancer. The risk of some cancers, including some solid cancers, hematologic cancers, and skin cancers, appears to be increased in patients with psoriasis, possibly associated with chronic inflammation. Some psoriasis therapies may increase the risk for malignancy, including phototherapy with psoralen plus UVA, cyclosporine, and methotrexate.
Many studies have supported a favorable safety profile for biologics in terms of the risk for developing malignancy. In a 2015 analysis of 12,093 patients enrolled in PSOLAR (Psoriasis Longitudinal Assessment and Registry), none of the biologics were found to be associated with increased risk for malignancy.
In psoriasis patients with existing or prior malignancies, the benefits of biologic therapy to improve quality of life often outweigh the negligible risks for malignancy. However, coordinated care with oncology is recommended for psoriasis patients with a history of prior malignancy.
General recommendations from the American Academy of Dermatology indicate one should carefully consider the decision to use a tumor necrosis factor (TNF) antagonist in patients with a history of malignancy, particularly lymphoma. Short-term treatment with biologics (up to 4 years) appears to be safe with respect to lymphoma risk, especially with TNF-α inhibitors. The potential risk for melanoma, cutaneous T-cell lymphoma, and nonmelanoma skin cancer in patients treated with TNF inhibitors also has been raised.
Expert Commentary
OBSERVE-5 was a 5-year phase 4, prospective, multicenter surveillance registry of 2510 psoriasis patients with at least a baseline dose of etanercept (Kimball et al, 2015). There was no increased risk for cancer when compared to the Truven Health MarketScan database, which is a proxy for the general population.
ESPRIT is an ongoing, 10-year, international, prospective, observational registry of 6059 psoriasis patients with at least a baseline dose of adalimumab (Menter et al). There are no signals of increased risk for cancer.
We do not have enough numbers of psoriasis patients on secukinumab or ixekizumab yet, but their phase 3 trials also do not seem to indicate an increased risk for cancer.
—Jashin J. Wu, MD (Los Angeles, California)
Myth: Biologics Cause Cancer
Biologics generally are safe and well-tolerated therapies; however, due to their immunosuppressive properties, the risk for lymphoma has been of potential concern, leading patients to believe that biologics cause cancer. The risk of some cancers, including some solid cancers, hematologic cancers, and skin cancers, appears to be increased in patients with psoriasis, possibly associated with chronic inflammation. Some psoriasis therapies may increase the risk for malignancy, including phototherapy with psoralen plus UVA, cyclosporine, and methotrexate.
Many studies have supported a favorable safety profile for biologics in terms of the risk for developing malignancy. In a 2015 analysis of 12,093 patients enrolled in PSOLAR (Psoriasis Longitudinal Assessment and Registry), none of the biologics were found to be associated with increased risk for malignancy.
In psoriasis patients with existing or prior malignancies, the benefits of biologic therapy to improve quality of life often outweigh the negligible risks for malignancy. However, coordinated care with oncology is recommended for psoriasis patients with a history of prior malignancy.
General recommendations from the American Academy of Dermatology indicate one should carefully consider the decision to use a tumor necrosis factor (TNF) antagonist in patients with a history of malignancy, particularly lymphoma. Short-term treatment with biologics (up to 4 years) appears to be safe with respect to lymphoma risk, especially with TNF-α inhibitors. The potential risk for melanoma, cutaneous T-cell lymphoma, and nonmelanoma skin cancer in patients treated with TNF inhibitors also has been raised.
Expert Commentary
OBSERVE-5 was a 5-year phase 4, prospective, multicenter surveillance registry of 2510 psoriasis patients with at least a baseline dose of etanercept (Kimball et al, 2015). There was no increased risk for cancer when compared to the Truven Health MarketScan database, which is a proxy for the general population.
ESPRIT is an ongoing, 10-year, international, prospective, observational registry of 6059 psoriasis patients with at least a baseline dose of adalimumab (Menter et al). There are no signals of increased risk for cancer.
We do not have enough numbers of psoriasis patients on secukinumab or ixekizumab yet, but their phase 3 trials also do not seem to indicate an increased risk for cancer.
—Jashin J. Wu, MD (Los Angeles, California)
American Academy of Dermatology. Psoriasis: TNF inhibitors general recommendations. https://www.aad.org/practice-tools/quality-care/clinical-guidelines/psoriasis/biologics/tnf-inhibitors-recommendations. Accessed June 14, 2016.
Dommasch E, Gelfand JM. Is there truly a risk of lymphoma from biologic therapies? Dermatol Ther. 2009;22:418-430.
Kimball AB, Rothman KJ, Kricorian G, et al. OBSERVE-5: Observational postmarketing safety surveillance registry of etanercept for the treatment of psoriasis final 5-year results. J Am Acad Dermatol. 2015;72:115-122.
Kimball AB, Schenfeld J, Accortt NA, et al. 5-year incidence rates of malignancies in psoriasis patients compared with the general US population. Poster presented at: Summer Meeting of the American Academy of Dermatology; August 6-10, 2014; Chicago, IL.
Menter A, Thaçi D, Papp KA, et al. Five-year analysis from the ESPRIT 10-year postmarketing surveillance registry of adalimumab treatment for moderate to severe psoriasis. J Am Acad Dermatol. 2015;73:410-419.e6.
Papp K, Gottlieb AB, Naldi L, et al. Safety surveillance for ustekinumab and other psoriasis treatments from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Drugs Dermatol. 2015;14:706-714.
Patel S, Patel T, Kerdel FA. The risk of malignancy or progression of existing malignancy in patients with psoriasis treated with biologics: case report and review of the literature. Int J Dermatol. 2016;55:487-493.
American Academy of Dermatology. Psoriasis: TNF inhibitors general recommendations. https://www.aad.org/practice-tools/quality-care/clinical-guidelines/psoriasis/biologics/tnf-inhibitors-recommendations. Accessed June 14, 2016.
Dommasch E, Gelfand JM. Is there truly a risk of lymphoma from biologic therapies? Dermatol Ther. 2009;22:418-430.
Kimball AB, Rothman KJ, Kricorian G, et al. OBSERVE-5: Observational postmarketing safety surveillance registry of etanercept for the treatment of psoriasis final 5-year results. J Am Acad Dermatol. 2015;72:115-122.
Kimball AB, Schenfeld J, Accortt NA, et al. 5-year incidence rates of malignancies in psoriasis patients compared with the general US population. Poster presented at: Summer Meeting of the American Academy of Dermatology; August 6-10, 2014; Chicago, IL.
Menter A, Thaçi D, Papp KA, et al. Five-year analysis from the ESPRIT 10-year postmarketing surveillance registry of adalimumab treatment for moderate to severe psoriasis. J Am Acad Dermatol. 2015;73:410-419.e6.
Papp K, Gottlieb AB, Naldi L, et al. Safety surveillance for ustekinumab and other psoriasis treatments from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Drugs Dermatol. 2015;14:706-714.
Patel S, Patel T, Kerdel FA. The risk of malignancy or progression of existing malignancy in patients with psoriasis treated with biologics: case report and review of the literature. Int J Dermatol. 2016;55:487-493.
FDA reports shortage of doxorubicin for injection, initiates importation
A critical shortage of doxorubicin hydrochloride 50 mg powder for injection has been reported to the Food and Drug Administration.
Doxorubicin is approved to treat acute lymphoblastic leukemia, acute myeloid leukemia, breast cancer, gastric cancer, ovarian cancer, neuroblastoma, and other cancer types.
To increase availability, the pharmaceutical company Hospira (a Pfizer company) is coordinating with the FDA to import the drug from Ahmedabad, India, where it is manufactured by Zydus Hospira Oncology Private Ltd. at an FDA-inspected facility that is in compliance with current good manufacturing practice requirements.
“It is important to note that there are substantive differences in the format and content of the labeling between the U.S.-approved doxorubicin hydrochloride for injection, USP and the Hospira Limited’s doxorubicin hydrochloride 50 mg powder for injection,” Hospira reported in a letter to health care providers.
To place an order or to get questions answered, contact Hospira directly by calling customer care at 1-877-946-7747 (Mondays-Fridays, 7 a.m.-6 p.m. Central time).
For clinical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or email [email protected].
According to the letter, adverse events or quality problems associated with use of this product should be reported by calling Hospira Global Complaint Management by phone, 1-800-441-4100; by sending an email to [email protected]; or by submitting a report online to Medwatch.
On Twitter @jessnicolecraig
A critical shortage of doxorubicin hydrochloride 50 mg powder for injection has been reported to the Food and Drug Administration.
Doxorubicin is approved to treat acute lymphoblastic leukemia, acute myeloid leukemia, breast cancer, gastric cancer, ovarian cancer, neuroblastoma, and other cancer types.
To increase availability, the pharmaceutical company Hospira (a Pfizer company) is coordinating with the FDA to import the drug from Ahmedabad, India, where it is manufactured by Zydus Hospira Oncology Private Ltd. at an FDA-inspected facility that is in compliance with current good manufacturing practice requirements.
“It is important to note that there are substantive differences in the format and content of the labeling between the U.S.-approved doxorubicin hydrochloride for injection, USP and the Hospira Limited’s doxorubicin hydrochloride 50 mg powder for injection,” Hospira reported in a letter to health care providers.
To place an order or to get questions answered, contact Hospira directly by calling customer care at 1-877-946-7747 (Mondays-Fridays, 7 a.m.-6 p.m. Central time).
For clinical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or email [email protected].
According to the letter, adverse events or quality problems associated with use of this product should be reported by calling Hospira Global Complaint Management by phone, 1-800-441-4100; by sending an email to [email protected]; or by submitting a report online to Medwatch.
On Twitter @jessnicolecraig
A critical shortage of doxorubicin hydrochloride 50 mg powder for injection has been reported to the Food and Drug Administration.
Doxorubicin is approved to treat acute lymphoblastic leukemia, acute myeloid leukemia, breast cancer, gastric cancer, ovarian cancer, neuroblastoma, and other cancer types.
To increase availability, the pharmaceutical company Hospira (a Pfizer company) is coordinating with the FDA to import the drug from Ahmedabad, India, where it is manufactured by Zydus Hospira Oncology Private Ltd. at an FDA-inspected facility that is in compliance with current good manufacturing practice requirements.
“It is important to note that there are substantive differences in the format and content of the labeling between the U.S.-approved doxorubicin hydrochloride for injection, USP and the Hospira Limited’s doxorubicin hydrochloride 50 mg powder for injection,” Hospira reported in a letter to health care providers.
To place an order or to get questions answered, contact Hospira directly by calling customer care at 1-877-946-7747 (Mondays-Fridays, 7 a.m.-6 p.m. Central time).
For clinical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or email [email protected].
According to the letter, adverse events or quality problems associated with use of this product should be reported by calling Hospira Global Complaint Management by phone, 1-800-441-4100; by sending an email to [email protected]; or by submitting a report online to Medwatch.
On Twitter @jessnicolecraig
New HCV test approach could cut costs, streamline diagnosis
Substituting a less-expensive hepatitis C core antigen test into the standard two-step process for diagnosing active hepatitis C virus (HCV) infection could streamline and cut the cost of HCV detection.
The standard two-step approach – detection of HCV antibodies followed by nucleic acid testing (NAT) as a marker for HCV viremia – may be improved by replacing NAT with the HCV core antigen (HCVcAg) test, according to the results of a study published in Annals of Internal Medicine.
Dr. J. Morgan Freiman, of the Boston Medical Center, and her colleagues conducted a systematic literature review to identify 44 case-control, cross-sectional, cohort, or randomized trials that compared any of five HCVcAg screening tests with a NAT reference standard.
The investigators performed a meta-analysis to assess the sensitivity (proportion of samples with a positive NAT and HCVcAg) and specificity (proportion of samples with a negative NAT and HCVcAg) associated with the five HCVcAg tests, as well as how they correlated with NAT-derived HCV RNA levels greater than 3,000 IU/mL.
The two best-performing HCVcAg tests of the five assessed were the Abbott ARCHITECT HCV Ag and the Ortho HCV Ag ELISA, based on their sensitivity (93.4%and 93.2%, respectively), specificity (98.8% and 99.2%, respectively), and positive (80.6 and 116.5, respectively) and negative (0.06 and 0.06, respectively) likelihood ratios.
Although limited data were available, the results of three quantitative studies showed that Abbott ARCHITECT HCVcAg was well correlated with HCV RNA levels greater than 3,000 IU/mL.
“This systematic review concludes that a well-performing HCVcAg test can achieve similar diagnostic accuracy to NAT for identification of active HCV infection when the viral load exceeds 3,000 IU/mL,” Dr. Freiman and her colleagues noted.
HCVcAg testing should be researched further as a potentially viable and less-expensive alternative to NAT, the investigators said, with the goal of simplifying detection at the point of care and increasing the rate of patient diagnosis (Ann Intern Med. 2016 Jun 21; doi: 10.7326/M16-0065).
The National Institutes of Health funded the study. Dr. White disclosed grant support from the funding source. Dr. Ongarello and Dr. Denkinger reported relationships with the Foundation for Innovative New Diagnostics. No additional authors reported conflicts of interest.
Substituting a less-expensive hepatitis C core antigen test into the standard two-step process for diagnosing active hepatitis C virus (HCV) infection could streamline and cut the cost of HCV detection.
The standard two-step approach – detection of HCV antibodies followed by nucleic acid testing (NAT) as a marker for HCV viremia – may be improved by replacing NAT with the HCV core antigen (HCVcAg) test, according to the results of a study published in Annals of Internal Medicine.
Dr. J. Morgan Freiman, of the Boston Medical Center, and her colleagues conducted a systematic literature review to identify 44 case-control, cross-sectional, cohort, or randomized trials that compared any of five HCVcAg screening tests with a NAT reference standard.
The investigators performed a meta-analysis to assess the sensitivity (proportion of samples with a positive NAT and HCVcAg) and specificity (proportion of samples with a negative NAT and HCVcAg) associated with the five HCVcAg tests, as well as how they correlated with NAT-derived HCV RNA levels greater than 3,000 IU/mL.
The two best-performing HCVcAg tests of the five assessed were the Abbott ARCHITECT HCV Ag and the Ortho HCV Ag ELISA, based on their sensitivity (93.4%and 93.2%, respectively), specificity (98.8% and 99.2%, respectively), and positive (80.6 and 116.5, respectively) and negative (0.06 and 0.06, respectively) likelihood ratios.
Although limited data were available, the results of three quantitative studies showed that Abbott ARCHITECT HCVcAg was well correlated with HCV RNA levels greater than 3,000 IU/mL.
“This systematic review concludes that a well-performing HCVcAg test can achieve similar diagnostic accuracy to NAT for identification of active HCV infection when the viral load exceeds 3,000 IU/mL,” Dr. Freiman and her colleagues noted.
HCVcAg testing should be researched further as a potentially viable and less-expensive alternative to NAT, the investigators said, with the goal of simplifying detection at the point of care and increasing the rate of patient diagnosis (Ann Intern Med. 2016 Jun 21; doi: 10.7326/M16-0065).
The National Institutes of Health funded the study. Dr. White disclosed grant support from the funding source. Dr. Ongarello and Dr. Denkinger reported relationships with the Foundation for Innovative New Diagnostics. No additional authors reported conflicts of interest.
Substituting a less-expensive hepatitis C core antigen test into the standard two-step process for diagnosing active hepatitis C virus (HCV) infection could streamline and cut the cost of HCV detection.
The standard two-step approach – detection of HCV antibodies followed by nucleic acid testing (NAT) as a marker for HCV viremia – may be improved by replacing NAT with the HCV core antigen (HCVcAg) test, according to the results of a study published in Annals of Internal Medicine.
Dr. J. Morgan Freiman, of the Boston Medical Center, and her colleagues conducted a systematic literature review to identify 44 case-control, cross-sectional, cohort, or randomized trials that compared any of five HCVcAg screening tests with a NAT reference standard.
The investigators performed a meta-analysis to assess the sensitivity (proportion of samples with a positive NAT and HCVcAg) and specificity (proportion of samples with a negative NAT and HCVcAg) associated with the five HCVcAg tests, as well as how they correlated with NAT-derived HCV RNA levels greater than 3,000 IU/mL.
The two best-performing HCVcAg tests of the five assessed were the Abbott ARCHITECT HCV Ag and the Ortho HCV Ag ELISA, based on their sensitivity (93.4%and 93.2%, respectively), specificity (98.8% and 99.2%, respectively), and positive (80.6 and 116.5, respectively) and negative (0.06 and 0.06, respectively) likelihood ratios.
Although limited data were available, the results of three quantitative studies showed that Abbott ARCHITECT HCVcAg was well correlated with HCV RNA levels greater than 3,000 IU/mL.
“This systematic review concludes that a well-performing HCVcAg test can achieve similar diagnostic accuracy to NAT for identification of active HCV infection when the viral load exceeds 3,000 IU/mL,” Dr. Freiman and her colleagues noted.
HCVcAg testing should be researched further as a potentially viable and less-expensive alternative to NAT, the investigators said, with the goal of simplifying detection at the point of care and increasing the rate of patient diagnosis (Ann Intern Med. 2016 Jun 21; doi: 10.7326/M16-0065).
The National Institutes of Health funded the study. Dr. White disclosed grant support from the funding source. Dr. Ongarello and Dr. Denkinger reported relationships with the Foundation for Innovative New Diagnostics. No additional authors reported conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: The diagnostic rate of chronic hepatitis C virus may be increased by point of care hepatitis C virus core antigen assessment.
Major finding: For patients with chronic HCV infection and viral loads exceeding 3,000 IU/mL, an HCVcAg screen performed as well as nucleic acid testing.
Data sources: Case-control, cross-sectional, cohort, or randomized trials that compared any of five HCVcAg tests with a NAT reference standard.
Disclosures: The National Institutes of Health funded the study. Dr. White disclosed grant support from the funding source. Dr. Ongarello and Dr. Denkinger reported relationships with the Foundation for Innovative New Diagnostics. No additional authors reported conflicts of interest.
Psychiatry’s role rising in hospital care
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
Additional antibiotics needed when implanting cryopreserved human aortic grafts
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The infection resistance of cryopreserved human allografts (CHAs) depends on antibiotic pretreatment during processing.
Major finding: Cardiac surgeons can recommend CHAs to patients either with active destructive infections or at high risk of reinfection, but they may want to apply additional antibiotic agents during implantation to enhance bacterial resistance.
Data source: Pieces of 10 CHAs were microbiologically tested in vitro and exposed to bacterial contamination and the number of attached bacteria quantified.
Disclosures: Dr. Steffen and her coauthors had no financial relationships to disclose.
Zika virus: The path to fetal infection
The question of how viruses can enter the intrauterine compartment and infect the fetus has long been a focus of research. It is of particular urgency today as the Zika virus spreads and causes perinatal infection that threatens the developing fetus with serious adverse outcomes such microcephaly and other brain anomalies, placental insufficiency, and fetal growth restriction.
We know that viruses can take a variety of routes to the fetal compartment, but we have also learned that the placenta has a robust level of inherent resistance to viruses. This resistance likely explains why we don’t see more viral infections in pregnancy.
Recent studies performed at our institution suggest that placental trophoblasts – the placenta’s primary line of defense – have inherent resistance to viruses such as Zika. It appears, therefore, that the Zika virus invades the intrauterine cavity by crossing the trophoblasts, perhaps earlier in pregnancy and prior to the development of full trophoblast resistance, by entering through breaks in this outer layer, or by utilizing alternative pathways to access the fetal compartment.
Further study of the placenta and its various cell types and mechanisms of viral defense will be critical for designing therapeutic strategies for preventing perinatal infections.
Various routes and affinities
Viruses have long been known to affect mothers and their unborn children. The rubella virus, for instance, posed a significant threat to the fetus until a vaccine program was introduced almost 50 years ago. Cytomegalovirus (CMV), on the other hand, continues be passed from mothers to their unborn children. While not as threatening as rubella once was, it can in some cases cause severe defects.
One might expect viruses to infect the placenta and then secondarily infect the fetus. While this may indeed occur, direct placental infection is not the only route by which viruses may enter the intrauterine compartment. Some viruses may be carried by macrophages or other immune cells through the placenta and into the fetal compartment, while others colonize the uterine cavity prior to conception, ready to proliferate during pregnancy.
In still other cases, viruses may be inadvertently introduced during medical procedures such as amniocentesis or transmitted through transvaginal ascending infection, most likely after rupture of the membranes. Viruses may also be transported through infected sperm (this appears to be one of the Zika virus’s modes of transportation), and as is the case with HIV and herpes simplex viruses, transmission sometimes occurs during delivery.
When we investigate whether or not the fetus is protected against particular viruses, we must therefore think about the multifaceted mechanisms by which viruses may be transmitted. With respect to the placenta specifically, we seek to understand how viruses enter the placenta, and how the placenta resists the propagation of some viruses while allowing other viruses to gain entry to the intrauterine compartment.
An additional consideration – one that is of utmost importance in the case of Zika – is whether viruses have any special affinity for particular fetal tissues. Some viruses, like CMV, infect multiple types of fetal tissue. The Zika virus, on the other hand, appears to target neuronal tissue in the fetus. In May, investigators of two studies reported that a strain of the Zika virus efficiently infected human cortical neural progenitor cells (Cell Stem Cell. 2016 May 5;18[5]:587-90), and that Zika infection of mice early in pregnancy resulted in infection of the placenta and of the fetal brain (Cell. 2016 May 19;165[5]:1081-91).
Interestingly, other flaviviruses such as the dengue and chikungunya viruses have not been associated with microcephaly or other congenital disorders. This suggests that the Zika virus employs unique mechanisms to infect or bypass the placental barrier and, in turn, to cause neuronal-focused damage.
Placental passage
The villous trophoblasts, cells that are bathed in maternal blood, form the placenta’s first line of defense. Viruses, including the Zika virus, must cross or somehow bypass this initial barrier before crossing the placental basement membrane and endothelial cells, if they are to potentially invade the intrauterine cavity and infect the fetal brain and other tissues.
Research has demonstrated that cells of various types of tissue may express certain proteins, such as AXL, MER and TYRO3. While not yet proven, these proteins may mediate the entry of viruses such as Zika, enabling them to cross the placental trophoblast layer. These proteins are indeed expressed in trophoblasts, especially in early pregnancy, but we do not yet know if the proteins actually aid Zika’s passage through the placenta.
Another mechanism that has been postulated in the case of Zika infection is antibody-dependent enhancement, a process by which a current infection is enhanced by prior infection with another virus from the same family. Some experts believe that pre-existing immunity to the dengue virus – another member of the flavivirus family that has been endemic in Brazil – may be enhancing the spread of Zika infection as antibodies against dengue cross-react with the Zika virus.
While antibody-dependent enhancement has been shown to occur and to advance infection in various body systems, it has not been proven to affect the placenta. Until we learn more, we must simply appreciate that the presence of antibodies from another member of a family of viruses does not necessarily confer resistance. Instead, it may enable new infections to advance.
One might view pregnancy as a time of immune compromise, but we have shown in our laboratories that trophoblasts in fact have inherent resistance to a number of viruses. In a recent study, we found that trophoblasts are refractory to direct infection with the Zika virus. We isolated trophoblast cells from healthy full-term human placentas, cultured these cells for several days, and infected them with the Zika virus. We then measured viral replication and compared the infectivity of these cells with the infectivity of human brain microvascular endothelial cells – nontrophoblast cells that served as a control.
Our findings were extremely interesting to us: The trophoblast cells appeared to be significantly more resistant to the Zika virus than the nontrophoblast cells.
We learned, moreover, that this resistance was mediated by a particular interferon released by the trophoblast cells – type III interferon IFN1 – and that this type III interferon appeared to protect not only the trophoblasts but the nontrophoblast cells as well. It acted in both an autocrine and a paracrine manner to protect cells from the Zika virus. When we blocked the antiviral signaling of this interferon, resistance to the virus was attenuated.
These findings suggest that while Zika appears able to cross through the placenta and infect the fetus, the mechanism does not involve direct infection of the trophoblasts, at least in the later stages of pregnancy. The virus must either evade the type III interferon antiviral signals generated by the trophoblasts or somehow bypass these cells to cross the placenta (Cell Host Microbe. 2016 May 11;19[5]:705-12).
Interestingly, the Cell study mentioned above, in which Zika infection of mice early in pregnancy infected placental cells and the brain, also showed reduced Zika presence in the mouse mononuclear trophoblasts and syncytiotrophoblasts, in areas of the placenta analogous to the human villi.
Some experts have suggested, based the study of other viruses, that the Zika virus is better able to infect the placenta when the infection occurs early in the first trimester or the second trimester. It is indeed possible – and makes intuitive sense – that first-trimester trophoblasts confer less resistance and a lower level of protection than the mature trophoblasts we studied. At this point, however, we cannot say with certainty whether or not the placenta is more or less permissive to Zika infection at different points in pregnancy.
Interestingly, investigators who prospectively followed a small cohort of pregnant women in Brazil with suspected Zika infection identified abnormalities in fetuses of women who were infected at various points of their pregnancies, even in the third trimester. Fetuses infected in the first trimester had findings suggestive of pathologic change during embryogenesis, but central nervous system abnormalities were seen in fetuses infected as late as 27 weeks of gestation, the investigators said (N Engl J Med. 2016 Mar 4. doi: 10.1056/NEJMoa1602412).
The interferon-conferred resistance demonstrated in our recent study is one of two mechanisms we’ve identified by which placental trophoblasts orchestrate resistance to viral infection. In earlier research, we found that resistance can be conferred to nontrophoblast cells by the delivery of micro-RNAs. These micro-RNAs (C19MC miRNAs) are uniquely expressed in the placenta and packaged within trophoblast-derived nanovesicles called exosomes. The nanovesicles can latch onto other cells in the vicinity of the trophoblasts, attenuating viral replication in these recipient cells.
This earlier in-vitro study involved a panel of diverse and unrelated viruses, including coxsackievirus B3, poliovirus, vesicular stomatitis virus, and human cytomegalovirus (Proc Natl Acad Sci U S A. 2013 Jul 16;110[29]:12048-53). It did not include the Zika virus, but our ongoing preliminary research suggests that the same mechanisms might be active against Zika.
Furthering research
Research at our institution and in other laboratories has shed light on various ways in which the fetus is protected from viruses, but we must learn more in order to understand how particular viruses, such as Zika, are able to reach the fetal compartment and cause particular birth defects.
We must further investigate the role and importance of antibody-dependent enhancement, and we must continue to study the placenta and its various cell types. Continuing efforts to better elucidate the placenta’s defense mechanisms and to identify cell types that are more or less resistant to the Zika virus – and understand their differences – may lead us to potential therapeutic strategies.
Dr. Sadovsky is scientific director of the Magee-Womens Research Institute, Elsie Hilliard Hillman Chair of Women’s Health Research, and professor of ob.gyn., reproductive sciences, microbiology, and molecular genetics at the University of Pittsburgh. Dr. Coyne is associate professor of microbiology and molecular genetics, and ob.gyn. and reproductive sciences, at the University of Pittsburgh.* Their research addressed in this Master Class was supported by grants from the National Institutes of Health, State of Pennsylvania Formula Research Funds, and Burroughs Wellcome Fund.
*Correction, 7/05/2016: An earlier version of this article misstated Dr. Coyne's academic title.
The question of how viruses can enter the intrauterine compartment and infect the fetus has long been a focus of research. It is of particular urgency today as the Zika virus spreads and causes perinatal infection that threatens the developing fetus with serious adverse outcomes such microcephaly and other brain anomalies, placental insufficiency, and fetal growth restriction.
We know that viruses can take a variety of routes to the fetal compartment, but we have also learned that the placenta has a robust level of inherent resistance to viruses. This resistance likely explains why we don’t see more viral infections in pregnancy.
Recent studies performed at our institution suggest that placental trophoblasts – the placenta’s primary line of defense – have inherent resistance to viruses such as Zika. It appears, therefore, that the Zika virus invades the intrauterine cavity by crossing the trophoblasts, perhaps earlier in pregnancy and prior to the development of full trophoblast resistance, by entering through breaks in this outer layer, or by utilizing alternative pathways to access the fetal compartment.
Further study of the placenta and its various cell types and mechanisms of viral defense will be critical for designing therapeutic strategies for preventing perinatal infections.
Various routes and affinities
Viruses have long been known to affect mothers and their unborn children. The rubella virus, for instance, posed a significant threat to the fetus until a vaccine program was introduced almost 50 years ago. Cytomegalovirus (CMV), on the other hand, continues be passed from mothers to their unborn children. While not as threatening as rubella once was, it can in some cases cause severe defects.
One might expect viruses to infect the placenta and then secondarily infect the fetus. While this may indeed occur, direct placental infection is not the only route by which viruses may enter the intrauterine compartment. Some viruses may be carried by macrophages or other immune cells through the placenta and into the fetal compartment, while others colonize the uterine cavity prior to conception, ready to proliferate during pregnancy.
In still other cases, viruses may be inadvertently introduced during medical procedures such as amniocentesis or transmitted through transvaginal ascending infection, most likely after rupture of the membranes. Viruses may also be transported through infected sperm (this appears to be one of the Zika virus’s modes of transportation), and as is the case with HIV and herpes simplex viruses, transmission sometimes occurs during delivery.
When we investigate whether or not the fetus is protected against particular viruses, we must therefore think about the multifaceted mechanisms by which viruses may be transmitted. With respect to the placenta specifically, we seek to understand how viruses enter the placenta, and how the placenta resists the propagation of some viruses while allowing other viruses to gain entry to the intrauterine compartment.
An additional consideration – one that is of utmost importance in the case of Zika – is whether viruses have any special affinity for particular fetal tissues. Some viruses, like CMV, infect multiple types of fetal tissue. The Zika virus, on the other hand, appears to target neuronal tissue in the fetus. In May, investigators of two studies reported that a strain of the Zika virus efficiently infected human cortical neural progenitor cells (Cell Stem Cell. 2016 May 5;18[5]:587-90), and that Zika infection of mice early in pregnancy resulted in infection of the placenta and of the fetal brain (Cell. 2016 May 19;165[5]:1081-91).
Interestingly, other flaviviruses such as the dengue and chikungunya viruses have not been associated with microcephaly or other congenital disorders. This suggests that the Zika virus employs unique mechanisms to infect or bypass the placental barrier and, in turn, to cause neuronal-focused damage.
Placental passage
The villous trophoblasts, cells that are bathed in maternal blood, form the placenta’s first line of defense. Viruses, including the Zika virus, must cross or somehow bypass this initial barrier before crossing the placental basement membrane and endothelial cells, if they are to potentially invade the intrauterine cavity and infect the fetal brain and other tissues.
Research has demonstrated that cells of various types of tissue may express certain proteins, such as AXL, MER and TYRO3. While not yet proven, these proteins may mediate the entry of viruses such as Zika, enabling them to cross the placental trophoblast layer. These proteins are indeed expressed in trophoblasts, especially in early pregnancy, but we do not yet know if the proteins actually aid Zika’s passage through the placenta.
Another mechanism that has been postulated in the case of Zika infection is antibody-dependent enhancement, a process by which a current infection is enhanced by prior infection with another virus from the same family. Some experts believe that pre-existing immunity to the dengue virus – another member of the flavivirus family that has been endemic in Brazil – may be enhancing the spread of Zika infection as antibodies against dengue cross-react with the Zika virus.
While antibody-dependent enhancement has been shown to occur and to advance infection in various body systems, it has not been proven to affect the placenta. Until we learn more, we must simply appreciate that the presence of antibodies from another member of a family of viruses does not necessarily confer resistance. Instead, it may enable new infections to advance.
One might view pregnancy as a time of immune compromise, but we have shown in our laboratories that trophoblasts in fact have inherent resistance to a number of viruses. In a recent study, we found that trophoblasts are refractory to direct infection with the Zika virus. We isolated trophoblast cells from healthy full-term human placentas, cultured these cells for several days, and infected them with the Zika virus. We then measured viral replication and compared the infectivity of these cells with the infectivity of human brain microvascular endothelial cells – nontrophoblast cells that served as a control.
Our findings were extremely interesting to us: The trophoblast cells appeared to be significantly more resistant to the Zika virus than the nontrophoblast cells.
We learned, moreover, that this resistance was mediated by a particular interferon released by the trophoblast cells – type III interferon IFN1 – and that this type III interferon appeared to protect not only the trophoblasts but the nontrophoblast cells as well. It acted in both an autocrine and a paracrine manner to protect cells from the Zika virus. When we blocked the antiviral signaling of this interferon, resistance to the virus was attenuated.
These findings suggest that while Zika appears able to cross through the placenta and infect the fetus, the mechanism does not involve direct infection of the trophoblasts, at least in the later stages of pregnancy. The virus must either evade the type III interferon antiviral signals generated by the trophoblasts or somehow bypass these cells to cross the placenta (Cell Host Microbe. 2016 May 11;19[5]:705-12).
Interestingly, the Cell study mentioned above, in which Zika infection of mice early in pregnancy infected placental cells and the brain, also showed reduced Zika presence in the mouse mononuclear trophoblasts and syncytiotrophoblasts, in areas of the placenta analogous to the human villi.
Some experts have suggested, based the study of other viruses, that the Zika virus is better able to infect the placenta when the infection occurs early in the first trimester or the second trimester. It is indeed possible – and makes intuitive sense – that first-trimester trophoblasts confer less resistance and a lower level of protection than the mature trophoblasts we studied. At this point, however, we cannot say with certainty whether or not the placenta is more or less permissive to Zika infection at different points in pregnancy.
Interestingly, investigators who prospectively followed a small cohort of pregnant women in Brazil with suspected Zika infection identified abnormalities in fetuses of women who were infected at various points of their pregnancies, even in the third trimester. Fetuses infected in the first trimester had findings suggestive of pathologic change during embryogenesis, but central nervous system abnormalities were seen in fetuses infected as late as 27 weeks of gestation, the investigators said (N Engl J Med. 2016 Mar 4. doi: 10.1056/NEJMoa1602412).
The interferon-conferred resistance demonstrated in our recent study is one of two mechanisms we’ve identified by which placental trophoblasts orchestrate resistance to viral infection. In earlier research, we found that resistance can be conferred to nontrophoblast cells by the delivery of micro-RNAs. These micro-RNAs (C19MC miRNAs) are uniquely expressed in the placenta and packaged within trophoblast-derived nanovesicles called exosomes. The nanovesicles can latch onto other cells in the vicinity of the trophoblasts, attenuating viral replication in these recipient cells.
This earlier in-vitro study involved a panel of diverse and unrelated viruses, including coxsackievirus B3, poliovirus, vesicular stomatitis virus, and human cytomegalovirus (Proc Natl Acad Sci U S A. 2013 Jul 16;110[29]:12048-53). It did not include the Zika virus, but our ongoing preliminary research suggests that the same mechanisms might be active against Zika.
Furthering research
Research at our institution and in other laboratories has shed light on various ways in which the fetus is protected from viruses, but we must learn more in order to understand how particular viruses, such as Zika, are able to reach the fetal compartment and cause particular birth defects.
We must further investigate the role and importance of antibody-dependent enhancement, and we must continue to study the placenta and its various cell types. Continuing efforts to better elucidate the placenta’s defense mechanisms and to identify cell types that are more or less resistant to the Zika virus – and understand their differences – may lead us to potential therapeutic strategies.
Dr. Sadovsky is scientific director of the Magee-Womens Research Institute, Elsie Hilliard Hillman Chair of Women’s Health Research, and professor of ob.gyn., reproductive sciences, microbiology, and molecular genetics at the University of Pittsburgh. Dr. Coyne is associate professor of microbiology and molecular genetics, and ob.gyn. and reproductive sciences, at the University of Pittsburgh.* Their research addressed in this Master Class was supported by grants from the National Institutes of Health, State of Pennsylvania Formula Research Funds, and Burroughs Wellcome Fund.
*Correction, 7/05/2016: An earlier version of this article misstated Dr. Coyne's academic title.
The question of how viruses can enter the intrauterine compartment and infect the fetus has long been a focus of research. It is of particular urgency today as the Zika virus spreads and causes perinatal infection that threatens the developing fetus with serious adverse outcomes such microcephaly and other brain anomalies, placental insufficiency, and fetal growth restriction.
We know that viruses can take a variety of routes to the fetal compartment, but we have also learned that the placenta has a robust level of inherent resistance to viruses. This resistance likely explains why we don’t see more viral infections in pregnancy.
Recent studies performed at our institution suggest that placental trophoblasts – the placenta’s primary line of defense – have inherent resistance to viruses such as Zika. It appears, therefore, that the Zika virus invades the intrauterine cavity by crossing the trophoblasts, perhaps earlier in pregnancy and prior to the development of full trophoblast resistance, by entering through breaks in this outer layer, or by utilizing alternative pathways to access the fetal compartment.
Further study of the placenta and its various cell types and mechanisms of viral defense will be critical for designing therapeutic strategies for preventing perinatal infections.
Various routes and affinities
Viruses have long been known to affect mothers and their unborn children. The rubella virus, for instance, posed a significant threat to the fetus until a vaccine program was introduced almost 50 years ago. Cytomegalovirus (CMV), on the other hand, continues be passed from mothers to their unborn children. While not as threatening as rubella once was, it can in some cases cause severe defects.
One might expect viruses to infect the placenta and then secondarily infect the fetus. While this may indeed occur, direct placental infection is not the only route by which viruses may enter the intrauterine compartment. Some viruses may be carried by macrophages or other immune cells through the placenta and into the fetal compartment, while others colonize the uterine cavity prior to conception, ready to proliferate during pregnancy.
In still other cases, viruses may be inadvertently introduced during medical procedures such as amniocentesis or transmitted through transvaginal ascending infection, most likely after rupture of the membranes. Viruses may also be transported through infected sperm (this appears to be one of the Zika virus’s modes of transportation), and as is the case with HIV and herpes simplex viruses, transmission sometimes occurs during delivery.
When we investigate whether or not the fetus is protected against particular viruses, we must therefore think about the multifaceted mechanisms by which viruses may be transmitted. With respect to the placenta specifically, we seek to understand how viruses enter the placenta, and how the placenta resists the propagation of some viruses while allowing other viruses to gain entry to the intrauterine compartment.
An additional consideration – one that is of utmost importance in the case of Zika – is whether viruses have any special affinity for particular fetal tissues. Some viruses, like CMV, infect multiple types of fetal tissue. The Zika virus, on the other hand, appears to target neuronal tissue in the fetus. In May, investigators of two studies reported that a strain of the Zika virus efficiently infected human cortical neural progenitor cells (Cell Stem Cell. 2016 May 5;18[5]:587-90), and that Zika infection of mice early in pregnancy resulted in infection of the placenta and of the fetal brain (Cell. 2016 May 19;165[5]:1081-91).
Interestingly, other flaviviruses such as the dengue and chikungunya viruses have not been associated with microcephaly or other congenital disorders. This suggests that the Zika virus employs unique mechanisms to infect or bypass the placental barrier and, in turn, to cause neuronal-focused damage.
Placental passage
The villous trophoblasts, cells that are bathed in maternal blood, form the placenta’s first line of defense. Viruses, including the Zika virus, must cross or somehow bypass this initial barrier before crossing the placental basement membrane and endothelial cells, if they are to potentially invade the intrauterine cavity and infect the fetal brain and other tissues.
Research has demonstrated that cells of various types of tissue may express certain proteins, such as AXL, MER and TYRO3. While not yet proven, these proteins may mediate the entry of viruses such as Zika, enabling them to cross the placental trophoblast layer. These proteins are indeed expressed in trophoblasts, especially in early pregnancy, but we do not yet know if the proteins actually aid Zika’s passage through the placenta.
Another mechanism that has been postulated in the case of Zika infection is antibody-dependent enhancement, a process by which a current infection is enhanced by prior infection with another virus from the same family. Some experts believe that pre-existing immunity to the dengue virus – another member of the flavivirus family that has been endemic in Brazil – may be enhancing the spread of Zika infection as antibodies against dengue cross-react with the Zika virus.
While antibody-dependent enhancement has been shown to occur and to advance infection in various body systems, it has not been proven to affect the placenta. Until we learn more, we must simply appreciate that the presence of antibodies from another member of a family of viruses does not necessarily confer resistance. Instead, it may enable new infections to advance.
One might view pregnancy as a time of immune compromise, but we have shown in our laboratories that trophoblasts in fact have inherent resistance to a number of viruses. In a recent study, we found that trophoblasts are refractory to direct infection with the Zika virus. We isolated trophoblast cells from healthy full-term human placentas, cultured these cells for several days, and infected them with the Zika virus. We then measured viral replication and compared the infectivity of these cells with the infectivity of human brain microvascular endothelial cells – nontrophoblast cells that served as a control.
Our findings were extremely interesting to us: The trophoblast cells appeared to be significantly more resistant to the Zika virus than the nontrophoblast cells.
We learned, moreover, that this resistance was mediated by a particular interferon released by the trophoblast cells – type III interferon IFN1 – and that this type III interferon appeared to protect not only the trophoblasts but the nontrophoblast cells as well. It acted in both an autocrine and a paracrine manner to protect cells from the Zika virus. When we blocked the antiviral signaling of this interferon, resistance to the virus was attenuated.
These findings suggest that while Zika appears able to cross through the placenta and infect the fetus, the mechanism does not involve direct infection of the trophoblasts, at least in the later stages of pregnancy. The virus must either evade the type III interferon antiviral signals generated by the trophoblasts or somehow bypass these cells to cross the placenta (Cell Host Microbe. 2016 May 11;19[5]:705-12).
Interestingly, the Cell study mentioned above, in which Zika infection of mice early in pregnancy infected placental cells and the brain, also showed reduced Zika presence in the mouse mononuclear trophoblasts and syncytiotrophoblasts, in areas of the placenta analogous to the human villi.
Some experts have suggested, based the study of other viruses, that the Zika virus is better able to infect the placenta when the infection occurs early in the first trimester or the second trimester. It is indeed possible – and makes intuitive sense – that first-trimester trophoblasts confer less resistance and a lower level of protection than the mature trophoblasts we studied. At this point, however, we cannot say with certainty whether or not the placenta is more or less permissive to Zika infection at different points in pregnancy.
Interestingly, investigators who prospectively followed a small cohort of pregnant women in Brazil with suspected Zika infection identified abnormalities in fetuses of women who were infected at various points of their pregnancies, even in the third trimester. Fetuses infected in the first trimester had findings suggestive of pathologic change during embryogenesis, but central nervous system abnormalities were seen in fetuses infected as late as 27 weeks of gestation, the investigators said (N Engl J Med. 2016 Mar 4. doi: 10.1056/NEJMoa1602412).
The interferon-conferred resistance demonstrated in our recent study is one of two mechanisms we’ve identified by which placental trophoblasts orchestrate resistance to viral infection. In earlier research, we found that resistance can be conferred to nontrophoblast cells by the delivery of micro-RNAs. These micro-RNAs (C19MC miRNAs) are uniquely expressed in the placenta and packaged within trophoblast-derived nanovesicles called exosomes. The nanovesicles can latch onto other cells in the vicinity of the trophoblasts, attenuating viral replication in these recipient cells.
This earlier in-vitro study involved a panel of diverse and unrelated viruses, including coxsackievirus B3, poliovirus, vesicular stomatitis virus, and human cytomegalovirus (Proc Natl Acad Sci U S A. 2013 Jul 16;110[29]:12048-53). It did not include the Zika virus, but our ongoing preliminary research suggests that the same mechanisms might be active against Zika.
Furthering research
Research at our institution and in other laboratories has shed light on various ways in which the fetus is protected from viruses, but we must learn more in order to understand how particular viruses, such as Zika, are able to reach the fetal compartment and cause particular birth defects.
We must further investigate the role and importance of antibody-dependent enhancement, and we must continue to study the placenta and its various cell types. Continuing efforts to better elucidate the placenta’s defense mechanisms and to identify cell types that are more or less resistant to the Zika virus – and understand their differences – may lead us to potential therapeutic strategies.
Dr. Sadovsky is scientific director of the Magee-Womens Research Institute, Elsie Hilliard Hillman Chair of Women’s Health Research, and professor of ob.gyn., reproductive sciences, microbiology, and molecular genetics at the University of Pittsburgh. Dr. Coyne is associate professor of microbiology and molecular genetics, and ob.gyn. and reproductive sciences, at the University of Pittsburgh.* Their research addressed in this Master Class was supported by grants from the National Institutes of Health, State of Pennsylvania Formula Research Funds, and Burroughs Wellcome Fund.
*Correction, 7/05/2016: An earlier version of this article misstated Dr. Coyne's academic title.