User login
Low caregiver self-care linked with depression, anxiety
There is increased anxiety and depression among family caregivers who do not take care of themselves, according to a study to be presented at the 2016 ASCO Palliative Care in Oncology Symposium.
Nearly a quarter of 294 caregivers of Medicare patients with advanced cancer reported high depression scores (23%) and 34% reported borderline or high anxiety scores. Worse caregiver anxiety, depression, and mental health–related quality of life scores were significantly associated with lower scores in every self-care measure (P less than .05 for all). Lower self-care behavior scores were associated with longer durations, higher hours, and more days/week of caregiving and with fair or poor patient health.
The cross-sectional survey was conducted in community settings of eight cancer centers in Alabama, Florida, and Tennessee. The family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head & neck, hematologic, or stage IV cancer completed measures of self-care behaviors, including health responsibility, physical activity, nutrition, spiritual growth, interpersonal relations, stress management, and sleep. Caregivers averaged 66 years and were mostly female (72.8%), white (91.2%), Protestant (76.2%), retired (54.4%), and patients’ spouse/partner (60.2%). Approximately half were rural dwellers (46.9%) and had incomes less than $50,000 (53.8%). The majority provided support 6-7 days per week (71%) for greater than 1 year (68%).
“This research serves as an important call to action for the oncology community to implement support networks and services that care for the caregiver,” ASCO representative Andrew Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York, said in a written statement ahead of the symposium.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” lead author James Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham, said in the statement.
On Twitter @jessnicolecraig
There is increased anxiety and depression among family caregivers who do not take care of themselves, according to a study to be presented at the 2016 ASCO Palliative Care in Oncology Symposium.
Nearly a quarter of 294 caregivers of Medicare patients with advanced cancer reported high depression scores (23%) and 34% reported borderline or high anxiety scores. Worse caregiver anxiety, depression, and mental health–related quality of life scores were significantly associated with lower scores in every self-care measure (P less than .05 for all). Lower self-care behavior scores were associated with longer durations, higher hours, and more days/week of caregiving and with fair or poor patient health.
The cross-sectional survey was conducted in community settings of eight cancer centers in Alabama, Florida, and Tennessee. The family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head & neck, hematologic, or stage IV cancer completed measures of self-care behaviors, including health responsibility, physical activity, nutrition, spiritual growth, interpersonal relations, stress management, and sleep. Caregivers averaged 66 years and were mostly female (72.8%), white (91.2%), Protestant (76.2%), retired (54.4%), and patients’ spouse/partner (60.2%). Approximately half were rural dwellers (46.9%) and had incomes less than $50,000 (53.8%). The majority provided support 6-7 days per week (71%) for greater than 1 year (68%).
“This research serves as an important call to action for the oncology community to implement support networks and services that care for the caregiver,” ASCO representative Andrew Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York, said in a written statement ahead of the symposium.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” lead author James Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham, said in the statement.
On Twitter @jessnicolecraig
There is increased anxiety and depression among family caregivers who do not take care of themselves, according to a study to be presented at the 2016 ASCO Palliative Care in Oncology Symposium.
Nearly a quarter of 294 caregivers of Medicare patients with advanced cancer reported high depression scores (23%) and 34% reported borderline or high anxiety scores. Worse caregiver anxiety, depression, and mental health–related quality of life scores were significantly associated with lower scores in every self-care measure (P less than .05 for all). Lower self-care behavior scores were associated with longer durations, higher hours, and more days/week of caregiving and with fair or poor patient health.
The cross-sectional survey was conducted in community settings of eight cancer centers in Alabama, Florida, and Tennessee. The family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head & neck, hematologic, or stage IV cancer completed measures of self-care behaviors, including health responsibility, physical activity, nutrition, spiritual growth, interpersonal relations, stress management, and sleep. Caregivers averaged 66 years and were mostly female (72.8%), white (91.2%), Protestant (76.2%), retired (54.4%), and patients’ spouse/partner (60.2%). Approximately half were rural dwellers (46.9%) and had incomes less than $50,000 (53.8%). The majority provided support 6-7 days per week (71%) for greater than 1 year (68%).
“This research serves as an important call to action for the oncology community to implement support networks and services that care for the caregiver,” ASCO representative Andrew Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York, said in a written statement ahead of the symposium.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” lead author James Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham, said in the statement.
On Twitter @jessnicolecraig
FROM THE 2016 ASCO PALLIATIVE CARE IN ONCOLOGY SYMPOSIUM
Key clinical point: There is increased anxiety and depression among family caregivers who do not take care of themselves.
Major finding: Worse caregiver anxiety, depression, and mental health–related quality of life scores were significantly associated with lower scores in every self-care measure (P less than .05 for all).
Data source: A multistate and cross-sectional survey of 294 family caregivers.
Disclosures: The University of Alabama at Birmingham funded the study. One investigator reported receiving financial compensation and honoraria from Medscape, Carevive Systems, and PackHealth.
Doctors urge Congress to pass Zika funding
Federal health officials, pediatricians, and ob.gyns. are imploring Congress to pass an appropriations bill with sufficient money to fight the growing threat of the Zika virus.
“Funding for Zika research, for prevention, and for control efforts – including mosquito surveillance and control – is essentially all spent,” Beth P. Bell, MD, director of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, said during a press conference. The Obama administration “has already transferred millions of dollars from other important programs to help with the Zika response, [but] without additional resources from Congress, critical public health work may not be accomplished.”
President Obama asked Congress in February to appropriate $1.9 billion to address all aspects of the Zika virus situation in the United States; partisan politics surrounding funding for Planned Parenthood have derailed passage of the legislation to date.
Without additional, specific funding, development of a Zika vaccine would be severely limited, and virtually no funds would be available to conduct multitiered studies that are critical for protecting both women and children from the virus’ devastating effects, Dr. Bell said. Additionally, money allocated to state health departments for the management of patients with Zika virus would no longer be available. Development of tests for early diagnosis would be slowed or halted altogether.
“Allowing this to happen needlessly puts the American people at risk, and will result in more Zika infections and potentially more babies being born with microcephaly and other birth defects,” Dr. Bell added. “Congress has come back from their recess, and we hope that they will do the right thing.”
The American Congress of Obstetricians and Gynecologists “continues to develop, update, and issue guidance on the risks, prevention, assessment, and treatment of the Zika virus,” primarily through its practice advisories and resources available jointly through the CDC, ACOG president Thomas Gellhaus, MD, said.
“The biggest impact Zika has is on babies, and they are our future,” said Karen Remley, MD, executive director and CEO of the American Academy of Pediatricians, adding that funding is crucial to continue monitoring children who have been born with birth defects, as the long-term development of these and other issues is new territory for doctors across the United States and its territories.
As Congress prepared to adjourn in advance of the primary elections, Senate Majority Leader Mitch McConnell noted that some progress is being made on Zika funding.
“We’ve made a lot of important progress already,” Sen. McConnell said Sept. 12 on the Senate floor. “I expect to move forward this week on a continuing resolution through Dec. 9 at last year’s enacted levels and include funds for Zika control and our veterans. Talks are continuing, and leaders from both parties will meet later this afternoon at the White House to discuss the progress and path forward.”
Federal health officials, pediatricians, and ob.gyns. are imploring Congress to pass an appropriations bill with sufficient money to fight the growing threat of the Zika virus.
“Funding for Zika research, for prevention, and for control efforts – including mosquito surveillance and control – is essentially all spent,” Beth P. Bell, MD, director of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, said during a press conference. The Obama administration “has already transferred millions of dollars from other important programs to help with the Zika response, [but] without additional resources from Congress, critical public health work may not be accomplished.”
President Obama asked Congress in February to appropriate $1.9 billion to address all aspects of the Zika virus situation in the United States; partisan politics surrounding funding for Planned Parenthood have derailed passage of the legislation to date.
Without additional, specific funding, development of a Zika vaccine would be severely limited, and virtually no funds would be available to conduct multitiered studies that are critical for protecting both women and children from the virus’ devastating effects, Dr. Bell said. Additionally, money allocated to state health departments for the management of patients with Zika virus would no longer be available. Development of tests for early diagnosis would be slowed or halted altogether.
“Allowing this to happen needlessly puts the American people at risk, and will result in more Zika infections and potentially more babies being born with microcephaly and other birth defects,” Dr. Bell added. “Congress has come back from their recess, and we hope that they will do the right thing.”
The American Congress of Obstetricians and Gynecologists “continues to develop, update, and issue guidance on the risks, prevention, assessment, and treatment of the Zika virus,” primarily through its practice advisories and resources available jointly through the CDC, ACOG president Thomas Gellhaus, MD, said.
“The biggest impact Zika has is on babies, and they are our future,” said Karen Remley, MD, executive director and CEO of the American Academy of Pediatricians, adding that funding is crucial to continue monitoring children who have been born with birth defects, as the long-term development of these and other issues is new territory for doctors across the United States and its territories.
As Congress prepared to adjourn in advance of the primary elections, Senate Majority Leader Mitch McConnell noted that some progress is being made on Zika funding.
“We’ve made a lot of important progress already,” Sen. McConnell said Sept. 12 on the Senate floor. “I expect to move forward this week on a continuing resolution through Dec. 9 at last year’s enacted levels and include funds for Zika control and our veterans. Talks are continuing, and leaders from both parties will meet later this afternoon at the White House to discuss the progress and path forward.”
Federal health officials, pediatricians, and ob.gyns. are imploring Congress to pass an appropriations bill with sufficient money to fight the growing threat of the Zika virus.
“Funding for Zika research, for prevention, and for control efforts – including mosquito surveillance and control – is essentially all spent,” Beth P. Bell, MD, director of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, said during a press conference. The Obama administration “has already transferred millions of dollars from other important programs to help with the Zika response, [but] without additional resources from Congress, critical public health work may not be accomplished.”
President Obama asked Congress in February to appropriate $1.9 billion to address all aspects of the Zika virus situation in the United States; partisan politics surrounding funding for Planned Parenthood have derailed passage of the legislation to date.
Without additional, specific funding, development of a Zika vaccine would be severely limited, and virtually no funds would be available to conduct multitiered studies that are critical for protecting both women and children from the virus’ devastating effects, Dr. Bell said. Additionally, money allocated to state health departments for the management of patients with Zika virus would no longer be available. Development of tests for early diagnosis would be slowed or halted altogether.
“Allowing this to happen needlessly puts the American people at risk, and will result in more Zika infections and potentially more babies being born with microcephaly and other birth defects,” Dr. Bell added. “Congress has come back from their recess, and we hope that they will do the right thing.”
The American Congress of Obstetricians and Gynecologists “continues to develop, update, and issue guidance on the risks, prevention, assessment, and treatment of the Zika virus,” primarily through its practice advisories and resources available jointly through the CDC, ACOG president Thomas Gellhaus, MD, said.
“The biggest impact Zika has is on babies, and they are our future,” said Karen Remley, MD, executive director and CEO of the American Academy of Pediatricians, adding that funding is crucial to continue monitoring children who have been born with birth defects, as the long-term development of these and other issues is new territory for doctors across the United States and its territories.
As Congress prepared to adjourn in advance of the primary elections, Senate Majority Leader Mitch McConnell noted that some progress is being made on Zika funding.
“We’ve made a lot of important progress already,” Sen. McConnell said Sept. 12 on the Senate floor. “I expect to move forward this week on a continuing resolution through Dec. 9 at last year’s enacted levels and include funds for Zika control and our veterans. Talks are continuing, and leaders from both parties will meet later this afternoon at the White House to discuss the progress and path forward.”
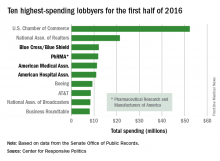
Health sector claims 4 spots among top 10 lobbyers in 2016
Four of the 10 highest-spending lobbyers for the first half of 2016 were in the health sector, with Blue Cross/Blue Shield occupying the sector’s top spot by a relatively small margin, according to the Center for Responsive Politics.
The four health-sectors concerns filled spots 3-6 in the overall top 10. Blue Cross/Blue Shield spent almost $12.1 million on lobbying in the first half of the year, putting it just ahead of the Pharmaceutical Research and Manufacturers of America (PhRMA), which spent $11.8 million. The American Medical Association was next at $11.3 million, followed by the American Hospital Association at $10.9 million, the center reported on OpenSecrets.org.
After those four, the next-highest health-sector spender was Pfizer, which put up almost $6.2 million in lobbying – good for 18th place for the first half of 2016. The health sector itself was the highest spending of the 121 ranked, taking a $266 million bite out of the total $1.6 billion lobbying pie for the year so far, according to the center’s analysis of data downloaded from the Senate Office of Public Records on Aug. 9.
The perennial leading spender on lobbying, the U.S. Chamber of Commerce, was well ahead of second place, with its $52.3 million more than doubling the $21.4 million spent by the National Association of Realtors. The two groups have finished 1-2 in lobbying spending every year since 2012, and the Chamber of Commerce has been the leading spender since 2001, data on OpenSecrets show.
Four of the 10 highest-spending lobbyers for the first half of 2016 were in the health sector, with Blue Cross/Blue Shield occupying the sector’s top spot by a relatively small margin, according to the Center for Responsive Politics.
The four health-sectors concerns filled spots 3-6 in the overall top 10. Blue Cross/Blue Shield spent almost $12.1 million on lobbying in the first half of the year, putting it just ahead of the Pharmaceutical Research and Manufacturers of America (PhRMA), which spent $11.8 million. The American Medical Association was next at $11.3 million, followed by the American Hospital Association at $10.9 million, the center reported on OpenSecrets.org.
After those four, the next-highest health-sector spender was Pfizer, which put up almost $6.2 million in lobbying – good for 18th place for the first half of 2016. The health sector itself was the highest spending of the 121 ranked, taking a $266 million bite out of the total $1.6 billion lobbying pie for the year so far, according to the center’s analysis of data downloaded from the Senate Office of Public Records on Aug. 9.
The perennial leading spender on lobbying, the U.S. Chamber of Commerce, was well ahead of second place, with its $52.3 million more than doubling the $21.4 million spent by the National Association of Realtors. The two groups have finished 1-2 in lobbying spending every year since 2012, and the Chamber of Commerce has been the leading spender since 2001, data on OpenSecrets show.
Four of the 10 highest-spending lobbyers for the first half of 2016 were in the health sector, with Blue Cross/Blue Shield occupying the sector’s top spot by a relatively small margin, according to the Center for Responsive Politics.
The four health-sectors concerns filled spots 3-6 in the overall top 10. Blue Cross/Blue Shield spent almost $12.1 million on lobbying in the first half of the year, putting it just ahead of the Pharmaceutical Research and Manufacturers of America (PhRMA), which spent $11.8 million. The American Medical Association was next at $11.3 million, followed by the American Hospital Association at $10.9 million, the center reported on OpenSecrets.org.
After those four, the next-highest health-sector spender was Pfizer, which put up almost $6.2 million in lobbying – good for 18th place for the first half of 2016. The health sector itself was the highest spending of the 121 ranked, taking a $266 million bite out of the total $1.6 billion lobbying pie for the year so far, according to the center’s analysis of data downloaded from the Senate Office of Public Records on Aug. 9.
The perennial leading spender on lobbying, the U.S. Chamber of Commerce, was well ahead of second place, with its $52.3 million more than doubling the $21.4 million spent by the National Association of Realtors. The two groups have finished 1-2 in lobbying spending every year since 2012, and the Chamber of Commerce has been the leading spender since 2001, data on OpenSecrets show.
Fact or Fiction: Is Orthopedic Follow-Up Worse for Patients Who Sustain Penetrating Trauma?
There is a paucity of literature on how mechanism of injury may be associated with patient retention. Failure to attend outpatient clinics is a form of noncompliance and a major obstacle to safe, effective, and efficient healthcare delivery. Noncompliance may lead to increased patient morbidity and carries substantial financial implications for the healthcare system.1,2 In addition to these direct patient and healthcare issues, loss of patient follow-up or the belief of potential loss of follow-up of penetrating trauma patients may also significantly affect research studies. These patients often may be excluded from studies, even if they might otherwise meet inclusion criteria, because of concerns that they are unlikely to follow-up after leaving hospital. Is this myth or fact? To validate or to disprove this selection bias, we conducted a study in which we retrospectively evaluated long bone fractures caused by either penetrating or blunt trauma.
Methods
After obtaining Institutional Review Board approval for this study, we used the trauma database of an American College of Surgeons–verified level I trauma center in a major Midwest metropolitan area to compile a list of all cases of long bone fractures caused by penetrating trauma between 2006 and 2009 (N = 132). Gunshot wounds were the mechanism of injury for the penetrating trauma. We also compiled a list of control cases—long bone fractures caused by blunt trauma in patients demographically matched to the penetrating group patients on sex, race, and age (N = 104) (Table).
We retrospectively performed chart reviews to obtain patient follow-up data 3, 6, 9, and 12 months after injury from penetrating or blunt trauma. Patients scheduled to return on an as-needed basis were considered to have completed follow-up. The 2 groups were also statistically compared with respect to sex, race, age, surgical fixation, and history of tobacco, alcohol, or drug use.
SAS/STAT Version 8 (SAS Institute) was used to test the equality of survival functions (patient retention) for the penetrating and blunt trauma patient groups. A similar comparison was made for the categories of sex, race, and age. Pearson χ2 test was used to compare the 12-month survival rates of the 2 treatment groups across sex and race. Binary logistic regression was used to compare the 12-month survival rates of the 2 treatment groups removing the effect of age. A comparison of the frequency distributions of the 2 treatment groups with respect to alcohol use, tobacco use, drug use, and surgical intervention was also performed. Power analysis showed power of more than 90% in detecting at least a 20% difference in the follow-up rates between the penetrating and blunt trauma groups based on our sample size.
Results
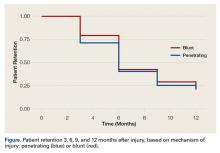
There was no statistically significant difference (P = .736) between the penetrating and blunt trauma patients in terms of follow-up within 1 year after injury. At 1 year, 103 (78%) of the 132 penetrating trauma patients and 83 (80%) of the 104 blunt trauma patients were lost to follow-up (Figure).
Discussion
Trauma outcomes historically have been difficult to determine because of lack of patient follow-up. In a simulation series, Zelle and colleagues3 found that the turning point from significant to nonsignificant varied from 15% to 75% loss of follow-up, thus compromising the validity of a study. They and others have emphasized the importance of establishing research protocols to minimize follow-up loss and eliminate reporting bias, ensure randomization, and report accurate outcomes.3-7
Very few have tried to investigate factors associated with failure to follow up after trauma.1,2,4 Leukhardt and colleagues4 evaluated the medical services that trauma patients follow up with most often. Orthopedic surgery had the largest portion of follow-up visits (37%), followed by the trauma surgery clinic and the emergency department (19% each). The authors also found that penetrating trauma patients were more likely to follow up, though more than 90% of the authors’ patients had blunt trauma. Although our study did not support their finding, it does call into question the commonly held belief that penetrating trauma patients are less likely to follow up, as our study found no difference in follow-up between penetrating and blunt trauma patients.
One of the most interesting findings in this retrospective study is that almost 80% of patients were lost to follow-up regardless of mechanism of injury. Most prospective studies try to reduce loss to follow-up to below 10%. This difference may be attributable to having a dedicated research team and the resources required to ensure follow-up of research patients to improve follow-up beyond baseline values. At our institution, 13 prospective studies (most multicenter) are currently enrolling patients, and the worst loss to follow-up has been 30%. The majority of the studies have loss to follow-up of 15% or less. This low rate represents a significant difference from the 80% “baseline” clinical loss to follow-up for the blunt and penetrating trauma patients treated at our institution, based on the findings of this study. We have been improving follow-up by having dedicated research coordinators call patients to remind them of their appointments (all clinic patients who are not research patients receive a recorded reminder); by having the hospital agree that research patients can be seen without charge (by the facility or the physician), which helps defray costs to the patient; and by excluding patients the principal investigator thinks are unlikely to follow up. Patients unlikely to follow up are routinely excluded by all centers that enroll in prospective studies. Although it is difficult to quantitate, this factor may play a large role in reducing loss to follow-up. Penetrating trauma patients historically routinely biased investigators to exclude them from studies, regardless of whether being considered unlikely to follow-up was an exclusion criterion. Our study results suggest this bias may not be valid.
Our study evaluated the role of mechanism of injury, penetrating or blunt trauma, and the respective orthopedic follow-up. There was no statistically significant difference in the 1-year follow-up rate based on the mechanism of injury. Our study was conducted with a well-matched control group that eliminated potential confounding variables, such as sex, race, age, tobacco use, and alcohol use. Although the prevalence of drug use was higher in the penetrating trauma group, patient retention seemed not to be affected by it. Surprisingly, patient loss to follow-up was extremely high (almost 80%) for both the penetrating and blunt trauma patient groups at the 1-year mark. Our findings call into question the commonly accepted theory that patients with penetrating injuries are less likely to follow up, at least in an academic level I trauma center population. We suggest that the commonly held belief that penetrating trauma patients are less likely to follow up may not be valid and that, when prospective studies are designed, it may not be appropriate to exclude penetrating trauma patients on this basis alone.
The primary limitation of this study is that it was performed at a single institution. Eighty-five percent of blunt trauma patients and 93% of penetrating trauma patients live in the county that is predominantly served by our institution, and electronic medical records from all major hospitals in the metropolitan area are linked, suggesting that the large majority of patients lost to follow-up do not seek further medical care, at least not from local facilities in our metropolitan area. A prospective multicenter study is being designed to help us gain a better understanding of the variables that affect musculoskeletal trauma patient follow-up and learn interventional strategies that can be used to improve patient retention.
Dr. Turner is an Orthopedic Surgeon, Rockwood Clinic, Spokane, Washington. Dr. Turner was a resident at the time the article was written. Dr. Hiatt is an Anesthesia Resident, University of Louisville Department of Anesthesiology and Perioperative Medicine, Louisville, Kentucky. Dr. Mullis is Chief of the Orthopaedic Trauma Service, Eskenazi Health, and Professor & Program Director, Indiana University School of Medicine Department of Orthopaedics, Indianapolis, Indiana.
Acknowledgments: This study was first reported in a poster presentation at the annual meeting of the Orthopaedic Trauma Association, October 2013, Phoenix, Arizona.
The authors gratefully acknowledge and thank Jyoti Sarkar, PhD, for his assistance with statistical analysis and manuscript preparation.
Am J Orthop. 2016;45(6):E331-E334. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Sciberras N, Gregori A, Holt G. The ethical and practical challenges of patient noncompliance in orthopaedic surgery. J Bone Joint Surg Am. 2013;95(9):e61.
2. Sharma H, Crane E, Syme B, Foxworthy M. Non-compliance in orthopaedic surgery and its ethical challenges. Orthop Trauma. 2007;21(4):310-313.
3. Zelle BA, Bhandari M, Sanchez AI, Probst C, Pape HC. Loss of follow-up in orthopaedic trauma: is 80% follow-up still acceptable? J Orthop Trauma. 2013;27(3):177-181.
4. Leukhardt WH, Golob JF, McCoy AM, Fadlalla AM, Malangoni MA, Claridge JA. Follow-up disparities after trauma: a real problem for outcomes research. Am J Surg. 2010;199(3):348-352.
5. Shumaker SA, Dugan E, Bowen DJ. Enhancing adherence in randomized controlled clinical trials. Control Clin Trials. 2000;21(5 suppl):226S-232S.
6. Smith JS, Watts HG. Methods for locating missing patients for the purpose of long-term clinical studies. J Bone Joint Surg Am. 1998;80(3):431-438.
7. Sprague S, Leece P, Bhandari M, Tornetta P 3rd, Schemitsch E, Swiontkowski MF; S.P.R.I.N.T. Investigators. Limiting loss to follow-up in a multicenter randomized trial in orthopedic surgery. Control Clin Trials. 2003;24(6):719-725.
There is a paucity of literature on how mechanism of injury may be associated with patient retention. Failure to attend outpatient clinics is a form of noncompliance and a major obstacle to safe, effective, and efficient healthcare delivery. Noncompliance may lead to increased patient morbidity and carries substantial financial implications for the healthcare system.1,2 In addition to these direct patient and healthcare issues, loss of patient follow-up or the belief of potential loss of follow-up of penetrating trauma patients may also significantly affect research studies. These patients often may be excluded from studies, even if they might otherwise meet inclusion criteria, because of concerns that they are unlikely to follow-up after leaving hospital. Is this myth or fact? To validate or to disprove this selection bias, we conducted a study in which we retrospectively evaluated long bone fractures caused by either penetrating or blunt trauma.
Methods
After obtaining Institutional Review Board approval for this study, we used the trauma database of an American College of Surgeons–verified level I trauma center in a major Midwest metropolitan area to compile a list of all cases of long bone fractures caused by penetrating trauma between 2006 and 2009 (N = 132). Gunshot wounds were the mechanism of injury for the penetrating trauma. We also compiled a list of control cases—long bone fractures caused by blunt trauma in patients demographically matched to the penetrating group patients on sex, race, and age (N = 104) (Table).
We retrospectively performed chart reviews to obtain patient follow-up data 3, 6, 9, and 12 months after injury from penetrating or blunt trauma. Patients scheduled to return on an as-needed basis were considered to have completed follow-up. The 2 groups were also statistically compared with respect to sex, race, age, surgical fixation, and history of tobacco, alcohol, or drug use.
SAS/STAT Version 8 (SAS Institute) was used to test the equality of survival functions (patient retention) for the penetrating and blunt trauma patient groups. A similar comparison was made for the categories of sex, race, and age. Pearson χ2 test was used to compare the 12-month survival rates of the 2 treatment groups across sex and race. Binary logistic regression was used to compare the 12-month survival rates of the 2 treatment groups removing the effect of age. A comparison of the frequency distributions of the 2 treatment groups with respect to alcohol use, tobacco use, drug use, and surgical intervention was also performed. Power analysis showed power of more than 90% in detecting at least a 20% difference in the follow-up rates between the penetrating and blunt trauma groups based on our sample size.
Results
There was no statistically significant difference (P = .736) between the penetrating and blunt trauma patients in terms of follow-up within 1 year after injury. At 1 year, 103 (78%) of the 132 penetrating trauma patients and 83 (80%) of the 104 blunt trauma patients were lost to follow-up (Figure).
Discussion
Trauma outcomes historically have been difficult to determine because of lack of patient follow-up. In a simulation series, Zelle and colleagues3 found that the turning point from significant to nonsignificant varied from 15% to 75% loss of follow-up, thus compromising the validity of a study. They and others have emphasized the importance of establishing research protocols to minimize follow-up loss and eliminate reporting bias, ensure randomization, and report accurate outcomes.3-7
Very few have tried to investigate factors associated with failure to follow up after trauma.1,2,4 Leukhardt and colleagues4 evaluated the medical services that trauma patients follow up with most often. Orthopedic surgery had the largest portion of follow-up visits (37%), followed by the trauma surgery clinic and the emergency department (19% each). The authors also found that penetrating trauma patients were more likely to follow up, though more than 90% of the authors’ patients had blunt trauma. Although our study did not support their finding, it does call into question the commonly held belief that penetrating trauma patients are less likely to follow up, as our study found no difference in follow-up between penetrating and blunt trauma patients.
One of the most interesting findings in this retrospective study is that almost 80% of patients were lost to follow-up regardless of mechanism of injury. Most prospective studies try to reduce loss to follow-up to below 10%. This difference may be attributable to having a dedicated research team and the resources required to ensure follow-up of research patients to improve follow-up beyond baseline values. At our institution, 13 prospective studies (most multicenter) are currently enrolling patients, and the worst loss to follow-up has been 30%. The majority of the studies have loss to follow-up of 15% or less. This low rate represents a significant difference from the 80% “baseline” clinical loss to follow-up for the blunt and penetrating trauma patients treated at our institution, based on the findings of this study. We have been improving follow-up by having dedicated research coordinators call patients to remind them of their appointments (all clinic patients who are not research patients receive a recorded reminder); by having the hospital agree that research patients can be seen without charge (by the facility or the physician), which helps defray costs to the patient; and by excluding patients the principal investigator thinks are unlikely to follow up. Patients unlikely to follow up are routinely excluded by all centers that enroll in prospective studies. Although it is difficult to quantitate, this factor may play a large role in reducing loss to follow-up. Penetrating trauma patients historically routinely biased investigators to exclude them from studies, regardless of whether being considered unlikely to follow-up was an exclusion criterion. Our study results suggest this bias may not be valid.
Our study evaluated the role of mechanism of injury, penetrating or blunt trauma, and the respective orthopedic follow-up. There was no statistically significant difference in the 1-year follow-up rate based on the mechanism of injury. Our study was conducted with a well-matched control group that eliminated potential confounding variables, such as sex, race, age, tobacco use, and alcohol use. Although the prevalence of drug use was higher in the penetrating trauma group, patient retention seemed not to be affected by it. Surprisingly, patient loss to follow-up was extremely high (almost 80%) for both the penetrating and blunt trauma patient groups at the 1-year mark. Our findings call into question the commonly accepted theory that patients with penetrating injuries are less likely to follow up, at least in an academic level I trauma center population. We suggest that the commonly held belief that penetrating trauma patients are less likely to follow up may not be valid and that, when prospective studies are designed, it may not be appropriate to exclude penetrating trauma patients on this basis alone.
The primary limitation of this study is that it was performed at a single institution. Eighty-five percent of blunt trauma patients and 93% of penetrating trauma patients live in the county that is predominantly served by our institution, and electronic medical records from all major hospitals in the metropolitan area are linked, suggesting that the large majority of patients lost to follow-up do not seek further medical care, at least not from local facilities in our metropolitan area. A prospective multicenter study is being designed to help us gain a better understanding of the variables that affect musculoskeletal trauma patient follow-up and learn interventional strategies that can be used to improve patient retention.
Dr. Turner is an Orthopedic Surgeon, Rockwood Clinic, Spokane, Washington. Dr. Turner was a resident at the time the article was written. Dr. Hiatt is an Anesthesia Resident, University of Louisville Department of Anesthesiology and Perioperative Medicine, Louisville, Kentucky. Dr. Mullis is Chief of the Orthopaedic Trauma Service, Eskenazi Health, and Professor & Program Director, Indiana University School of Medicine Department of Orthopaedics, Indianapolis, Indiana.
Acknowledgments: This study was first reported in a poster presentation at the annual meeting of the Orthopaedic Trauma Association, October 2013, Phoenix, Arizona.
The authors gratefully acknowledge and thank Jyoti Sarkar, PhD, for his assistance with statistical analysis and manuscript preparation.
Am J Orthop. 2016;45(6):E331-E334. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
There is a paucity of literature on how mechanism of injury may be associated with patient retention. Failure to attend outpatient clinics is a form of noncompliance and a major obstacle to safe, effective, and efficient healthcare delivery. Noncompliance may lead to increased patient morbidity and carries substantial financial implications for the healthcare system.1,2 In addition to these direct patient and healthcare issues, loss of patient follow-up or the belief of potential loss of follow-up of penetrating trauma patients may also significantly affect research studies. These patients often may be excluded from studies, even if they might otherwise meet inclusion criteria, because of concerns that they are unlikely to follow-up after leaving hospital. Is this myth or fact? To validate or to disprove this selection bias, we conducted a study in which we retrospectively evaluated long bone fractures caused by either penetrating or blunt trauma.
Methods
After obtaining Institutional Review Board approval for this study, we used the trauma database of an American College of Surgeons–verified level I trauma center in a major Midwest metropolitan area to compile a list of all cases of long bone fractures caused by penetrating trauma between 2006 and 2009 (N = 132). Gunshot wounds were the mechanism of injury for the penetrating trauma. We also compiled a list of control cases—long bone fractures caused by blunt trauma in patients demographically matched to the penetrating group patients on sex, race, and age (N = 104) (Table).
We retrospectively performed chart reviews to obtain patient follow-up data 3, 6, 9, and 12 months after injury from penetrating or blunt trauma. Patients scheduled to return on an as-needed basis were considered to have completed follow-up. The 2 groups were also statistically compared with respect to sex, race, age, surgical fixation, and history of tobacco, alcohol, or drug use.
SAS/STAT Version 8 (SAS Institute) was used to test the equality of survival functions (patient retention) for the penetrating and blunt trauma patient groups. A similar comparison was made for the categories of sex, race, and age. Pearson χ2 test was used to compare the 12-month survival rates of the 2 treatment groups across sex and race. Binary logistic regression was used to compare the 12-month survival rates of the 2 treatment groups removing the effect of age. A comparison of the frequency distributions of the 2 treatment groups with respect to alcohol use, tobacco use, drug use, and surgical intervention was also performed. Power analysis showed power of more than 90% in detecting at least a 20% difference in the follow-up rates between the penetrating and blunt trauma groups based on our sample size.
Results
There was no statistically significant difference (P = .736) between the penetrating and blunt trauma patients in terms of follow-up within 1 year after injury. At 1 year, 103 (78%) of the 132 penetrating trauma patients and 83 (80%) of the 104 blunt trauma patients were lost to follow-up (Figure).
Discussion
Trauma outcomes historically have been difficult to determine because of lack of patient follow-up. In a simulation series, Zelle and colleagues3 found that the turning point from significant to nonsignificant varied from 15% to 75% loss of follow-up, thus compromising the validity of a study. They and others have emphasized the importance of establishing research protocols to minimize follow-up loss and eliminate reporting bias, ensure randomization, and report accurate outcomes.3-7
Very few have tried to investigate factors associated with failure to follow up after trauma.1,2,4 Leukhardt and colleagues4 evaluated the medical services that trauma patients follow up with most often. Orthopedic surgery had the largest portion of follow-up visits (37%), followed by the trauma surgery clinic and the emergency department (19% each). The authors also found that penetrating trauma patients were more likely to follow up, though more than 90% of the authors’ patients had blunt trauma. Although our study did not support their finding, it does call into question the commonly held belief that penetrating trauma patients are less likely to follow up, as our study found no difference in follow-up between penetrating and blunt trauma patients.
One of the most interesting findings in this retrospective study is that almost 80% of patients were lost to follow-up regardless of mechanism of injury. Most prospective studies try to reduce loss to follow-up to below 10%. This difference may be attributable to having a dedicated research team and the resources required to ensure follow-up of research patients to improve follow-up beyond baseline values. At our institution, 13 prospective studies (most multicenter) are currently enrolling patients, and the worst loss to follow-up has been 30%. The majority of the studies have loss to follow-up of 15% or less. This low rate represents a significant difference from the 80% “baseline” clinical loss to follow-up for the blunt and penetrating trauma patients treated at our institution, based on the findings of this study. We have been improving follow-up by having dedicated research coordinators call patients to remind them of their appointments (all clinic patients who are not research patients receive a recorded reminder); by having the hospital agree that research patients can be seen without charge (by the facility or the physician), which helps defray costs to the patient; and by excluding patients the principal investigator thinks are unlikely to follow up. Patients unlikely to follow up are routinely excluded by all centers that enroll in prospective studies. Although it is difficult to quantitate, this factor may play a large role in reducing loss to follow-up. Penetrating trauma patients historically routinely biased investigators to exclude them from studies, regardless of whether being considered unlikely to follow-up was an exclusion criterion. Our study results suggest this bias may not be valid.
Our study evaluated the role of mechanism of injury, penetrating or blunt trauma, and the respective orthopedic follow-up. There was no statistically significant difference in the 1-year follow-up rate based on the mechanism of injury. Our study was conducted with a well-matched control group that eliminated potential confounding variables, such as sex, race, age, tobacco use, and alcohol use. Although the prevalence of drug use was higher in the penetrating trauma group, patient retention seemed not to be affected by it. Surprisingly, patient loss to follow-up was extremely high (almost 80%) for both the penetrating and blunt trauma patient groups at the 1-year mark. Our findings call into question the commonly accepted theory that patients with penetrating injuries are less likely to follow up, at least in an academic level I trauma center population. We suggest that the commonly held belief that penetrating trauma patients are less likely to follow up may not be valid and that, when prospective studies are designed, it may not be appropriate to exclude penetrating trauma patients on this basis alone.
The primary limitation of this study is that it was performed at a single institution. Eighty-five percent of blunt trauma patients and 93% of penetrating trauma patients live in the county that is predominantly served by our institution, and electronic medical records from all major hospitals in the metropolitan area are linked, suggesting that the large majority of patients lost to follow-up do not seek further medical care, at least not from local facilities in our metropolitan area. A prospective multicenter study is being designed to help us gain a better understanding of the variables that affect musculoskeletal trauma patient follow-up and learn interventional strategies that can be used to improve patient retention.
Dr. Turner is an Orthopedic Surgeon, Rockwood Clinic, Spokane, Washington. Dr. Turner was a resident at the time the article was written. Dr. Hiatt is an Anesthesia Resident, University of Louisville Department of Anesthesiology and Perioperative Medicine, Louisville, Kentucky. Dr. Mullis is Chief of the Orthopaedic Trauma Service, Eskenazi Health, and Professor & Program Director, Indiana University School of Medicine Department of Orthopaedics, Indianapolis, Indiana.
Acknowledgments: This study was first reported in a poster presentation at the annual meeting of the Orthopaedic Trauma Association, October 2013, Phoenix, Arizona.
The authors gratefully acknowledge and thank Jyoti Sarkar, PhD, for his assistance with statistical analysis and manuscript preparation.
Am J Orthop. 2016;45(6):E331-E334. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Sciberras N, Gregori A, Holt G. The ethical and practical challenges of patient noncompliance in orthopaedic surgery. J Bone Joint Surg Am. 2013;95(9):e61.
2. Sharma H, Crane E, Syme B, Foxworthy M. Non-compliance in orthopaedic surgery and its ethical challenges. Orthop Trauma. 2007;21(4):310-313.
3. Zelle BA, Bhandari M, Sanchez AI, Probst C, Pape HC. Loss of follow-up in orthopaedic trauma: is 80% follow-up still acceptable? J Orthop Trauma. 2013;27(3):177-181.
4. Leukhardt WH, Golob JF, McCoy AM, Fadlalla AM, Malangoni MA, Claridge JA. Follow-up disparities after trauma: a real problem for outcomes research. Am J Surg. 2010;199(3):348-352.
5. Shumaker SA, Dugan E, Bowen DJ. Enhancing adherence in randomized controlled clinical trials. Control Clin Trials. 2000;21(5 suppl):226S-232S.
6. Smith JS, Watts HG. Methods for locating missing patients for the purpose of long-term clinical studies. J Bone Joint Surg Am. 1998;80(3):431-438.
7. Sprague S, Leece P, Bhandari M, Tornetta P 3rd, Schemitsch E, Swiontkowski MF; S.P.R.I.N.T. Investigators. Limiting loss to follow-up in a multicenter randomized trial in orthopedic surgery. Control Clin Trials. 2003;24(6):719-725.
1. Sciberras N, Gregori A, Holt G. The ethical and practical challenges of patient noncompliance in orthopaedic surgery. J Bone Joint Surg Am. 2013;95(9):e61.
2. Sharma H, Crane E, Syme B, Foxworthy M. Non-compliance in orthopaedic surgery and its ethical challenges. Orthop Trauma. 2007;21(4):310-313.
3. Zelle BA, Bhandari M, Sanchez AI, Probst C, Pape HC. Loss of follow-up in orthopaedic trauma: is 80% follow-up still acceptable? J Orthop Trauma. 2013;27(3):177-181.
4. Leukhardt WH, Golob JF, McCoy AM, Fadlalla AM, Malangoni MA, Claridge JA. Follow-up disparities after trauma: a real problem for outcomes research. Am J Surg. 2010;199(3):348-352.
5. Shumaker SA, Dugan E, Bowen DJ. Enhancing adherence in randomized controlled clinical trials. Control Clin Trials. 2000;21(5 suppl):226S-232S.
6. Smith JS, Watts HG. Methods for locating missing patients for the purpose of long-term clinical studies. J Bone Joint Surg Am. 1998;80(3):431-438.
7. Sprague S, Leece P, Bhandari M, Tornetta P 3rd, Schemitsch E, Swiontkowski MF; S.P.R.I.N.T. Investigators. Limiting loss to follow-up in a multicenter randomized trial in orthopedic surgery. Control Clin Trials. 2003;24(6):719-725.
New drugs poised to stem tide of antibacterial resistance in gonorrhea
ANNAPOLIS, MD. – Three novel treatments for gonorrhea, currently in late stages of development, could give clinicians an edge in the fight against antibacterial resistance, according to a federal health official.
The pathogen Neisseria gonorrhoeae is already showing signs of besting first-line therapy ceftriaxone in Japan and parts of Europe, said Carolyn Deal, PhD, chief of the sexually transmitted diseases branch at the National Institute of Allergy and Infectious Diseases (NIAID). And the Centers for Disease Control and Prevention lists N. gonorrhoeae among its “urgent” antibiotic resistance threats.
“I think we have a new superbug,” Dr. Deal said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. “In my opinion, it’s just a matter of time in this country.”
But three agents in late-stage clinical trials for uncomplicated urogenital gonorrhea offer promise in fighting the gram-negative bacteria, according to Dr. Deal. The first is solithromycin, manufactured by Cempra. The company has a phase III study underway to compare a single dose of oral solithromycin with intramuscular ceftriaxone plus oral azithromycin for urogenital gonorrhea.
The other two drugs are first-in-class antibacterial agents. In partnership with the NIAID, the company Entasis recently completed a phase II study of zoliflodacin, an oral agent in a novel class of topoisomerase inhibitors. A phase III trial is expected to begin in 2017, also in partnership with the NIAID, according to an Entasis document. The third agent is gepotidacin, a novel triazaacenaphthylene antibacterial agent currently being investigated by GlaxoSmithKline in a phase II study.
Because N. gonorrhoeae poses such an urgent threat, waiting to develop a vaccine is less feasible than working with companies to develop additional antibacterial agents, Dr. Deal said. But taking a compound out of the basic research lab and having enough data to get into the investigational new drug phase is a significant investment, she said, so pharmaceutical manufacturers look for as many indications for a drug as possible.
For instance, solithromycin was initially investigated for community-acquired pneumonia. Gepotidacin initially was developed in partnership with the NIAID and the Biomedical Advanced Research and Development Authority in case of an anthrax attack, Dr. Deal said. “The Entasis product is the only one specifically developed for Neisseria gonorrhoeae,” she said.
One reason that two of the drugs in the pipeline include N. gonorrhoeae as an indication is that the Food and Drug Administration has issued guidance on developing drugs in the area of uncomplicated gonorrhea. That guidance is lacking for nasopharyngeal and rectal gonorrhea, leaving a “vacuum” in the pipeline, Dr. Deal said. “Many of us have come to the conclusion that developing vaccines is the only real long-term solution.”
On Twitter @whitneymcknight
ANNAPOLIS, MD. – Three novel treatments for gonorrhea, currently in late stages of development, could give clinicians an edge in the fight against antibacterial resistance, according to a federal health official.
The pathogen Neisseria gonorrhoeae is already showing signs of besting first-line therapy ceftriaxone in Japan and parts of Europe, said Carolyn Deal, PhD, chief of the sexually transmitted diseases branch at the National Institute of Allergy and Infectious Diseases (NIAID). And the Centers for Disease Control and Prevention lists N. gonorrhoeae among its “urgent” antibiotic resistance threats.
“I think we have a new superbug,” Dr. Deal said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. “In my opinion, it’s just a matter of time in this country.”
But three agents in late-stage clinical trials for uncomplicated urogenital gonorrhea offer promise in fighting the gram-negative bacteria, according to Dr. Deal. The first is solithromycin, manufactured by Cempra. The company has a phase III study underway to compare a single dose of oral solithromycin with intramuscular ceftriaxone plus oral azithromycin for urogenital gonorrhea.
The other two drugs are first-in-class antibacterial agents. In partnership with the NIAID, the company Entasis recently completed a phase II study of zoliflodacin, an oral agent in a novel class of topoisomerase inhibitors. A phase III trial is expected to begin in 2017, also in partnership with the NIAID, according to an Entasis document. The third agent is gepotidacin, a novel triazaacenaphthylene antibacterial agent currently being investigated by GlaxoSmithKline in a phase II study.
Because N. gonorrhoeae poses such an urgent threat, waiting to develop a vaccine is less feasible than working with companies to develop additional antibacterial agents, Dr. Deal said. But taking a compound out of the basic research lab and having enough data to get into the investigational new drug phase is a significant investment, she said, so pharmaceutical manufacturers look for as many indications for a drug as possible.
For instance, solithromycin was initially investigated for community-acquired pneumonia. Gepotidacin initially was developed in partnership with the NIAID and the Biomedical Advanced Research and Development Authority in case of an anthrax attack, Dr. Deal said. “The Entasis product is the only one specifically developed for Neisseria gonorrhoeae,” she said.
One reason that two of the drugs in the pipeline include N. gonorrhoeae as an indication is that the Food and Drug Administration has issued guidance on developing drugs in the area of uncomplicated gonorrhea. That guidance is lacking for nasopharyngeal and rectal gonorrhea, leaving a “vacuum” in the pipeline, Dr. Deal said. “Many of us have come to the conclusion that developing vaccines is the only real long-term solution.”
On Twitter @whitneymcknight
ANNAPOLIS, MD. – Three novel treatments for gonorrhea, currently in late stages of development, could give clinicians an edge in the fight against antibacterial resistance, according to a federal health official.
The pathogen Neisseria gonorrhoeae is already showing signs of besting first-line therapy ceftriaxone in Japan and parts of Europe, said Carolyn Deal, PhD, chief of the sexually transmitted diseases branch at the National Institute of Allergy and Infectious Diseases (NIAID). And the Centers for Disease Control and Prevention lists N. gonorrhoeae among its “urgent” antibiotic resistance threats.
“I think we have a new superbug,” Dr. Deal said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. “In my opinion, it’s just a matter of time in this country.”
But three agents in late-stage clinical trials for uncomplicated urogenital gonorrhea offer promise in fighting the gram-negative bacteria, according to Dr. Deal. The first is solithromycin, manufactured by Cempra. The company has a phase III study underway to compare a single dose of oral solithromycin with intramuscular ceftriaxone plus oral azithromycin for urogenital gonorrhea.
The other two drugs are first-in-class antibacterial agents. In partnership with the NIAID, the company Entasis recently completed a phase II study of zoliflodacin, an oral agent in a novel class of topoisomerase inhibitors. A phase III trial is expected to begin in 2017, also in partnership with the NIAID, according to an Entasis document. The third agent is gepotidacin, a novel triazaacenaphthylene antibacterial agent currently being investigated by GlaxoSmithKline in a phase II study.
Because N. gonorrhoeae poses such an urgent threat, waiting to develop a vaccine is less feasible than working with companies to develop additional antibacterial agents, Dr. Deal said. But taking a compound out of the basic research lab and having enough data to get into the investigational new drug phase is a significant investment, she said, so pharmaceutical manufacturers look for as many indications for a drug as possible.
For instance, solithromycin was initially investigated for community-acquired pneumonia. Gepotidacin initially was developed in partnership with the NIAID and the Biomedical Advanced Research and Development Authority in case of an anthrax attack, Dr. Deal said. “The Entasis product is the only one specifically developed for Neisseria gonorrhoeae,” she said.
One reason that two of the drugs in the pipeline include N. gonorrhoeae as an indication is that the Food and Drug Administration has issued guidance on developing drugs in the area of uncomplicated gonorrhea. That guidance is lacking for nasopharyngeal and rectal gonorrhea, leaving a “vacuum” in the pipeline, Dr. Deal said. “Many of us have come to the conclusion that developing vaccines is the only real long-term solution.”
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM IDSOG
Impact of a Musculoskeletal Clerkship on Orthopedic Surgery Applicant Diversity
As the United States becomes increasingly diverse, with predictions that by 2045 minorities will comprise 50% or more of the population,1 the demographics of the orthopedic surgery population will also likely diversify. It is important that orthopedic surgeons shift in their diversity as well. Lack of diversity in orthopedics (women and racial minorities are underrepresented) relative to the national population and other surgical specialties and their training programs is well documented.2-8
More concerning, the diversity of orthopedic residents does not compare favorably with that of medical school attendees.4,9 The difference suggests the greatest loss of potential diversity occurs during the transition from medical school to residency. A national study demonstrated that instruction in musculoskeletal medicine led to an increase in application rates nationally.10 However, the authors of that study stated they were unexpectedly limited by its large size—they could not validate the accuracy of curriculum data and could not differentiate between a 1-day required experience and a 4-week rotation.
In the present study, which accounted for curricular factors, we compared our medical students’ application rates to orthopedics residencies based on sex and race before and after introduction of a required third-year musculoskeletal clerkship. We hypothesized that making the curriculum a requirement would increase the number of applicants and increase the diversity of applicants in terms of both women and underrepresented minorities. This hypothesis was based on the rationale that these groups might not consider an orthopedics residency without first being directly exposed to orthopedics. We also wanted to determine what factors influenced applicants to choose orthopedic surgery.
Methods
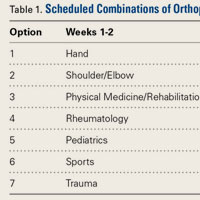
Curriculum
Before 2006, third-year students spent 3 months completing a surgery clerkship. Some students interested in orthopedic surgery would have to wait until their fourth year to complete an elective in orthopedic surgery, and uninterested students would not be exposed at all. Starting in 2006, 1 month of the third-year surgery clerkship was required to be completed in musculoskeletal surgery: orthopedic surgery, plastic surgery, or neurosurgical spine. Plastic surgery was an option, as it exposed students to hand surgery and flap reconstruction.
During the 12-year study period, overall teaching hours in the preclinical curriculum did not change, and there were no other structural changes to the preclinical or clinical curriculum. The orthopedics department increased its faculty from 23 in 2000 to 34 in 2012. Number of female faculty increased from 1 to 3, representing a 4% to 9% increase in department faculty. Throughout the 12 years, there were no underrepresented minority faculty. Total number of residents increased from 26 in 2000 to 30 in 2012. Number of female residents varied year to year, from a low of 3 in the period 2003–2004 to a high of 11 in the period 2009–2010. Number of underrepresented minority residents varied yearly as well, from 1 to 2.
Data Collection
After this study was granted exempt status by our Institutional Review Board, we obtained student data from our registrar. Data included graduation year, self-identified sex and race, exposure to orthopedic surgery during clerkships, and matching residency specialty. National data were obtained from the Electronic Residency Application Service for the periods 2002–2007 and 2009–2012. These data included all US allopathic medical students’ self-identified sex and race, and applied-to primary residency specialty. National data from 2008 and national data on sex differences in orthopedic applications from 2009 were not available.
Graduates who matched into orthopedic surgery were asked to complete an anonymous survey on what influenced their decision to apply to orthopedic surgery and when this decision was made. Our goal with the survey was to substantiate or refute the conclusion that application rates depended on third-year exposure to musculoskeletal medicine.
Statistical Methods
Students were divided into 2 groups: precurriculum (graduated within 7-year period, 2000–2006) and postcurriculum (graduated within 6-year period, 2007–2012). A 2-sample test for proportions was used to compare percentage of total students who applied to orthopedics in each group. In the group of students who applied to orthopedics, we compared precurriculum and postcurriculum proportions of women and underrepresented minorities (non-white, non-Asian). We also compared these proportions with national data (using 2-sample tests for proportions) to determine if any change in diversity of our institution’s applicants was mirroring a national trend. Our definition of underrepresented minority was based on work that showed that the proportion of Asian matriculants in medical school and the proportion of applicants to orthopedics are higher than their respective national proportions.5 Survey data are reported descriptively. Statistical significance was defined with a 2-tailed α of 0.05 for all tests.
Results
Over the 2000–2012 period, 1507 students from our institution successfully applied to residency programs: 792 in the precurriculum group and 715 in the postcurriculum group. Of these students, 91 successfully applied to orthopedic surgery: 48 in the precurriculum group (applied before introduction of the required clerkship) and 43 in the postcurriculum group (applied afterward).
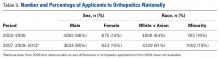
Over the 2002–2012 period, 10,100 US allopathic medical students applied to orthopedic residency programs: 4769 students between 2002 and 2006 and 5331 students between 2007 and 2012.
Before the musculoskeletal clerkship was required, 317 (40%) of the 792 precurriculum students were exposed to orthopedics during their third year. During this period, 42 of the 48 orthopedic surgery applicants completed an orthopedic surgery rotation during their third year of medical school. After the clerkship was required, 465 (65%) of the 715 postcurriculum students were exposed to orthopedics during their third year, including all 43 orthopedic surgery applicants (100% of students were exposed to musculoskeletal surgery, including plastic surgery and neurologic spine). The 25% increase in exposure to orthopedic surgery during the third year was statistically significant (P < .0001), but there was no resultant increase in overall percentage of students applying to orthopedic residencies (6% in each case; P = .98).
Over the 12-year study period, the proportion of female medical students at our institution declined from 50% (395/792) to 46% (328/715) (P = .13). However, there was an 81% relative increase, from 17% (8/48) before introduction of the clerkship to 30% (13/43) afterward, in the proportion of female applicants to orthopedic surgery. This contrasted with national data showing the percentage of female applicants to orthopedic surgery remained stable from 2002–2006 (14%, 675/4758) to 2007–2012 (15%, 643/4277). Before the clerkship was required, the proportion of female applicants from our institution was similar to national rates (P = .50). Afterward, our institution produced a significantly higher proportion of female applicants compared with the national proportion (P = .026).
Over the 12-year period, our self-identified underrepresented minority medical student population increased significantly (P = .02), from 13% (103/792) to 17% (124/715). The relative proportion of underrepresented minority orthopedic surgery applicants increased by 101%, from 10% (5/48) before the clerkship was required to 21% (9/43) afterward. Nationally, over the same period, underrepresented minorities’ orthopedic surgery application rates increased significantly (P < .001), from 16% (763/4769) to 19% (1002/5331). The proportion of underrepresented racial minorities that applied did not differ significantly between our institution and nationally for the years either before (P = .97) or after (P = .68) introduction of the curriculum.
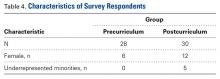
Surveys were completed by 58 (64%) of 91 graduates (21 women, 70 men). Respondents’ characteristics are listed in Table 4.
Discussion
Orthopedic surgery needs a more diverse workforce11-17 in order to better mirror the population served, bring care to underserved areas,18-26 and provide better training environments.27 Several hypotheses about the lack of diversity have been posited: stereotypes about the specialty,28-31 lack of interest among minority medical students, and lack of exposure to the specialty.5,6,32,33
Lack of exposure deserves scrutiny, as a large proportion of medical students who choose to apply to orthopedic surgery make their decision before entering medical school, which is not typical.33 Such a finding suggests that exposure to orthopedic surgery is lacking, especially given that an orthopedic surgery rotation is usually not required during the clinical years. The idea that increased exposure to orthopedics affects application patterns is logical, as clinical exposure has been shown to play a role in medical students’ choice of specialty.34
Exposure helps in several key areas. Firsthand experience can help dispel stereotypes, such as the idea that success in orthopedic surgery depends on physical strength and that only former athletes pursue orthopedics.28-31 Authors have also reported on a perceived negative bias against women: Orthopedics is an “old boys’ network”; women will not fit in and need not apply; the orthopedic lifestyle is difficult and not conducive to a satisfying personal life.9 Requiring exposure ensures that all students, but especially women, can gain firsthand experience that can show these stereotypes to be false. Beyond dispelling these stereotypes, exposure to orthopedic surgery is essential for women, as studies have shown that clinical rotations play a larger role in determining specialty choice for women compared to men,33 and this would be particularly critical for specialties they may not be initially considering.
A national study found that requiring an orthopedic/musculoskeletal clerkship led to a 12% relative increase in the application rate, from 5.1% to 5.7%, and to an increase in applicant diversity (race, sex).10 However, the investigators could not determine individual reasons for specialty choice or the exact nature of each institution’s musculoskeletal curriculum. Confirming these factors, we found an 81% increase in number of female applicants and a 101% increase in number of underrepresented minority applicants after introduction of the required third-year musculoskeletal surgery clerkship at our institution.
We were unable to replicate the 12% relative increase in the overall application rate; our orthopedic surgery match rate remained 6%. Our findings cannot directly explain this, but we have several hypotheses. First, whereas other studies measured the application rate, we measured the successful match rate, given our data structure. This difference in data definition could account for some of the discrepancy. Second, we did not account for individuals’ academic success, and career counseling is paramount in decisions regarding residency specialties. It is possible we are substituting qualified female and underrepresented minority candidates for less-than-qualified male applicants. Third, the 25% increase in medical student exposure to orthopedic surgery led to a corresponding increase in number of orthopedic faculty providing undergraduate medical education. Some of these faculty could have been inexperienced in undergraduate medical education, and thus the teaching environment may not have been optimal.
Our study had several limitations. First, our institution has limited racial diversity. Over the past 12 years, only 15% of our students have been underrepresented minorities. (Nationally, the proportion is closer to 18%.) This may have limited the ability of our orthopedic rotation to affect the proportion of underrepresented minority applicants. Second, this study involved medical students at only one institution, which limits generalizability of findings. Third, we were unable to obtain records specifying which faculty and residents interacted with which medical students, and the increased number of female faculty and residents coinciding with the curriculum change may also be a factor. However, we expect that, without the curriculum change, these students would have had smaller odds of interacting with these potential female role models in orthopedics, negating any affect they may have had. Last, although we contacted former students to ask about their reasons for choosing the orthopedics residency, those findings are limited by a potential respondent selection bias.
The qualities and characteristics of successful orthopedic surgeons, as presented in both medical and lay cultures, are subject to numerous stereotypes. By increasing medical student exposure to orthopedics during the third year of medical school, we are giving a larger proportion of our students direct clinical experience in a field they may not have been considering. This exposure allows students to interact with mentors who can be positive role models—orthopedic surgeons who are dispelling stereotypes. By increasing medical student exposure and reaching students who may not have been considering orthopedics, we have increased diversity among our applicants. Third-year medical students’ exposure to orthopedic surgery is essential in promoting a more diverse workforce.
Am J Orthop. 2016;45(6):E347-E351. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. US Census Bureau. 2012 National Population Projections: Summary Tables. http://www.census.gov/population/projections/data/national/2012/summarytables.html. Accessed April 15, 2013.
2. Blakemore LC, Hall JM, Biermann JS. Women in surgical residency training programs. J Bone Joint Surg Am. 2003;85(12):2477-2480.
3. Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92(13):2328-2335.
4. Lewis VO, Scherl SA, O’Connor MI. Women in orthopaedics—way behind the number curve. J Bone Joint Surg Am. 2012;94(5):e30.
5. Okike K, Utuk ME, White AA. Racial and ethnic diversity in orthopaedic surgery residency programs. J Bone Joint Surg Am. 2011;93(18):e107.
6. Salsberg ES, Grover A, Simon MA, Frick SL, Kuremsky MA, Goodman DC. An AOA critical issue. Future physician workforce requirements: implications for orthopaedic surgery education. J Bone Joint Surg Am. 2008;90(5):1143-1159.
7. American Academy of Orthopaedic Surgeons. Orthopaedic Practice in the US 2008. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2009.
8. White AA 3rd. Alfred R. Shands, Jr., lecture: our humanitarian orthopaedic opportunity. J Bone Joint Surg Am. 2002;84(3):478-484.
9. Templeton K, Wood VJ, Haynes R. Women and minorities in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S37-S41.
10. Bernstein J, Dicaprio MR, Mehta S. The relationship between required medical school instruction in musculoskeletal medicine and application rates to orthopaedic surgery residency programs. J Bone Joint Surg Am. 2004;86(10):2335-2338.
11. Dykes DC, White AA. Getting to equal: strategies to understand and eliminate general and orthopaedic healthcare disparities. Clin Orthop Relat Res. 2009;467(10):2598-2605.
12. Gebhardt MC. Improving diversity in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S49-S50.
13. Hammond RA. The moral imperatives for diversity. Clin Orthop Relat Res. 1999;(362):102-106.
14. Lindsey RW. The role of the department chair in promoting diversity. J Am Acad Orthop Surg. 2007;15(suppl 1):S65-S69.
15. Satcher RL. African Americans and orthopaedic surgery. A resident’s perspective. Clin Orthop Relat Res. 1999;(362):114-116.
16. White AA. Justifications and needs for diversity in orthopaedics. Clin Orthop Relat Res. 1999;(362):22-33.
17. White AA. Resident selection: are we putting the cart before the horse? Clin Orthop Relat Res. 2002;(399):255-259.
18. Dominick KL, Baker TA. Racial and ethnic differences in osteoarthritis: prevalence, outcomes, and medical care. Ethn Dis. 2004;14(4):558-566.
19. Furstenberg AL, Mezey MD. Differences in outcome between black and white elderly hip fracture patients. J Chronic Dis. 1987;40(10):931-938.
20. Ibrahim SA. Racial and ethnic disparities in hip and knee joint replacement: a review of research in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S87-S94.
21. Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334(20):1305-1310.
22. Moy E, Bartman BA. Physician race and care of minority and medically indigent patients. JAMA. 1995;273(19):1515-1520.
23. Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15(suppl 1):S13-S17.
24. Rowley DL, Jenkins BC, Frazier E. Utilization of joint arthroplasty: racial and ethnic disparities in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S43-S48.
25. Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350-1359.
26. Steel N, Clark A, Lang LA, Wallace RB, Melzer D. Racial disparities in receipt of hip and knee joint replacements are not explained by need: the Health and Retirement Study 1998-2004. J Gerontol A Biol Sci Med Sci. 2008;63(6):629-634.
27. Whitla DK, Orfield G, Silen W, Teperow C, Howard C, Reede J. Educational benefits of diversity in medical school: a survey of students. Acad Med. 2003;78(5):460-466.
28. Barrett DS. Are orthopaedic surgeons gorillas? Br Med J. 1988;297(6664):1638-1639.
29. Brenkel IJ, Pearse M, Gregg PJ. A “cracking” complication of hemiarthroplasty of the hip. Br Med J. 1986;293(6562):1648.
30. Fox JS, Bell GR, Sweeney PJ. Are orthopaedic surgeons really gorillas? Br Med J. 1990;301(6766):1425-1426.
31. Subramanian P, Kantharuban S, Subramanian V, Willis-Owen SA, Willis-Owen CA. Orthopaedic surgeons: as strong as an ox and almost twice as clever? Multicentre prospective comparative study. Br Med J. 2011;343:d7506.
32. Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011;34(12):e919-e932.
33. Johnson AL, Sharma J, Chinchilli VM, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94(11):e78.
34. Wilson FC. Teaching by residents. Clin Orthop Relat Res. 2007;(454):247-250.
As the United States becomes increasingly diverse, with predictions that by 2045 minorities will comprise 50% or more of the population,1 the demographics of the orthopedic surgery population will also likely diversify. It is important that orthopedic surgeons shift in their diversity as well. Lack of diversity in orthopedics (women and racial minorities are underrepresented) relative to the national population and other surgical specialties and their training programs is well documented.2-8
More concerning, the diversity of orthopedic residents does not compare favorably with that of medical school attendees.4,9 The difference suggests the greatest loss of potential diversity occurs during the transition from medical school to residency. A national study demonstrated that instruction in musculoskeletal medicine led to an increase in application rates nationally.10 However, the authors of that study stated they were unexpectedly limited by its large size—they could not validate the accuracy of curriculum data and could not differentiate between a 1-day required experience and a 4-week rotation.
In the present study, which accounted for curricular factors, we compared our medical students’ application rates to orthopedics residencies based on sex and race before and after introduction of a required third-year musculoskeletal clerkship. We hypothesized that making the curriculum a requirement would increase the number of applicants and increase the diversity of applicants in terms of both women and underrepresented minorities. This hypothesis was based on the rationale that these groups might not consider an orthopedics residency without first being directly exposed to orthopedics. We also wanted to determine what factors influenced applicants to choose orthopedic surgery.
Methods
Curriculum
Before 2006, third-year students spent 3 months completing a surgery clerkship. Some students interested in orthopedic surgery would have to wait until their fourth year to complete an elective in orthopedic surgery, and uninterested students would not be exposed at all. Starting in 2006, 1 month of the third-year surgery clerkship was required to be completed in musculoskeletal surgery: orthopedic surgery, plastic surgery, or neurosurgical spine. Plastic surgery was an option, as it exposed students to hand surgery and flap reconstruction.
During the 12-year study period, overall teaching hours in the preclinical curriculum did not change, and there were no other structural changes to the preclinical or clinical curriculum. The orthopedics department increased its faculty from 23 in 2000 to 34 in 2012. Number of female faculty increased from 1 to 3, representing a 4% to 9% increase in department faculty. Throughout the 12 years, there were no underrepresented minority faculty. Total number of residents increased from 26 in 2000 to 30 in 2012. Number of female residents varied year to year, from a low of 3 in the period 2003–2004 to a high of 11 in the period 2009–2010. Number of underrepresented minority residents varied yearly as well, from 1 to 2.
Data Collection
After this study was granted exempt status by our Institutional Review Board, we obtained student data from our registrar. Data included graduation year, self-identified sex and race, exposure to orthopedic surgery during clerkships, and matching residency specialty. National data were obtained from the Electronic Residency Application Service for the periods 2002–2007 and 2009–2012. These data included all US allopathic medical students’ self-identified sex and race, and applied-to primary residency specialty. National data from 2008 and national data on sex differences in orthopedic applications from 2009 were not available.
Graduates who matched into orthopedic surgery were asked to complete an anonymous survey on what influenced their decision to apply to orthopedic surgery and when this decision was made. Our goal with the survey was to substantiate or refute the conclusion that application rates depended on third-year exposure to musculoskeletal medicine.
Statistical Methods
Students were divided into 2 groups: precurriculum (graduated within 7-year period, 2000–2006) and postcurriculum (graduated within 6-year period, 2007–2012). A 2-sample test for proportions was used to compare percentage of total students who applied to orthopedics in each group. In the group of students who applied to orthopedics, we compared precurriculum and postcurriculum proportions of women and underrepresented minorities (non-white, non-Asian). We also compared these proportions with national data (using 2-sample tests for proportions) to determine if any change in diversity of our institution’s applicants was mirroring a national trend. Our definition of underrepresented minority was based on work that showed that the proportion of Asian matriculants in medical school and the proportion of applicants to orthopedics are higher than their respective national proportions.5 Survey data are reported descriptively. Statistical significance was defined with a 2-tailed α of 0.05 for all tests.
Results
Over the 2000–2012 period, 1507 students from our institution successfully applied to residency programs: 792 in the precurriculum group and 715 in the postcurriculum group. Of these students, 91 successfully applied to orthopedic surgery: 48 in the precurriculum group (applied before introduction of the required clerkship) and 43 in the postcurriculum group (applied afterward).
Over the 2002–2012 period, 10,100 US allopathic medical students applied to orthopedic residency programs: 4769 students between 2002 and 2006 and 5331 students between 2007 and 2012.
Before the musculoskeletal clerkship was required, 317 (40%) of the 792 precurriculum students were exposed to orthopedics during their third year. During this period, 42 of the 48 orthopedic surgery applicants completed an orthopedic surgery rotation during their third year of medical school. After the clerkship was required, 465 (65%) of the 715 postcurriculum students were exposed to orthopedics during their third year, including all 43 orthopedic surgery applicants (100% of students were exposed to musculoskeletal surgery, including plastic surgery and neurologic spine). The 25% increase in exposure to orthopedic surgery during the third year was statistically significant (P < .0001), but there was no resultant increase in overall percentage of students applying to orthopedic residencies (6% in each case; P = .98).
Over the 12-year study period, the proportion of female medical students at our institution declined from 50% (395/792) to 46% (328/715) (P = .13). However, there was an 81% relative increase, from 17% (8/48) before introduction of the clerkship to 30% (13/43) afterward, in the proportion of female applicants to orthopedic surgery. This contrasted with national data showing the percentage of female applicants to orthopedic surgery remained stable from 2002–2006 (14%, 675/4758) to 2007–2012 (15%, 643/4277). Before the clerkship was required, the proportion of female applicants from our institution was similar to national rates (P = .50). Afterward, our institution produced a significantly higher proportion of female applicants compared with the national proportion (P = .026).
Over the 12-year period, our self-identified underrepresented minority medical student population increased significantly (P = .02), from 13% (103/792) to 17% (124/715). The relative proportion of underrepresented minority orthopedic surgery applicants increased by 101%, from 10% (5/48) before the clerkship was required to 21% (9/43) afterward. Nationally, over the same period, underrepresented minorities’ orthopedic surgery application rates increased significantly (P < .001), from 16% (763/4769) to 19% (1002/5331). The proportion of underrepresented racial minorities that applied did not differ significantly between our institution and nationally for the years either before (P = .97) or after (P = .68) introduction of the curriculum.
Surveys were completed by 58 (64%) of 91 graduates (21 women, 70 men). Respondents’ characteristics are listed in Table 4.
Discussion
Orthopedic surgery needs a more diverse workforce11-17 in order to better mirror the population served, bring care to underserved areas,18-26 and provide better training environments.27 Several hypotheses about the lack of diversity have been posited: stereotypes about the specialty,28-31 lack of interest among minority medical students, and lack of exposure to the specialty.5,6,32,33
Lack of exposure deserves scrutiny, as a large proportion of medical students who choose to apply to orthopedic surgery make their decision before entering medical school, which is not typical.33 Such a finding suggests that exposure to orthopedic surgery is lacking, especially given that an orthopedic surgery rotation is usually not required during the clinical years. The idea that increased exposure to orthopedics affects application patterns is logical, as clinical exposure has been shown to play a role in medical students’ choice of specialty.34
Exposure helps in several key areas. Firsthand experience can help dispel stereotypes, such as the idea that success in orthopedic surgery depends on physical strength and that only former athletes pursue orthopedics.28-31 Authors have also reported on a perceived negative bias against women: Orthopedics is an “old boys’ network”; women will not fit in and need not apply; the orthopedic lifestyle is difficult and not conducive to a satisfying personal life.9 Requiring exposure ensures that all students, but especially women, can gain firsthand experience that can show these stereotypes to be false. Beyond dispelling these stereotypes, exposure to orthopedic surgery is essential for women, as studies have shown that clinical rotations play a larger role in determining specialty choice for women compared to men,33 and this would be particularly critical for specialties they may not be initially considering.
A national study found that requiring an orthopedic/musculoskeletal clerkship led to a 12% relative increase in the application rate, from 5.1% to 5.7%, and to an increase in applicant diversity (race, sex).10 However, the investigators could not determine individual reasons for specialty choice or the exact nature of each institution’s musculoskeletal curriculum. Confirming these factors, we found an 81% increase in number of female applicants and a 101% increase in number of underrepresented minority applicants after introduction of the required third-year musculoskeletal surgery clerkship at our institution.
We were unable to replicate the 12% relative increase in the overall application rate; our orthopedic surgery match rate remained 6%. Our findings cannot directly explain this, but we have several hypotheses. First, whereas other studies measured the application rate, we measured the successful match rate, given our data structure. This difference in data definition could account for some of the discrepancy. Second, we did not account for individuals’ academic success, and career counseling is paramount in decisions regarding residency specialties. It is possible we are substituting qualified female and underrepresented minority candidates for less-than-qualified male applicants. Third, the 25% increase in medical student exposure to orthopedic surgery led to a corresponding increase in number of orthopedic faculty providing undergraduate medical education. Some of these faculty could have been inexperienced in undergraduate medical education, and thus the teaching environment may not have been optimal.
Our study had several limitations. First, our institution has limited racial diversity. Over the past 12 years, only 15% of our students have been underrepresented minorities. (Nationally, the proportion is closer to 18%.) This may have limited the ability of our orthopedic rotation to affect the proportion of underrepresented minority applicants. Second, this study involved medical students at only one institution, which limits generalizability of findings. Third, we were unable to obtain records specifying which faculty and residents interacted with which medical students, and the increased number of female faculty and residents coinciding with the curriculum change may also be a factor. However, we expect that, without the curriculum change, these students would have had smaller odds of interacting with these potential female role models in orthopedics, negating any affect they may have had. Last, although we contacted former students to ask about their reasons for choosing the orthopedics residency, those findings are limited by a potential respondent selection bias.
The qualities and characteristics of successful orthopedic surgeons, as presented in both medical and lay cultures, are subject to numerous stereotypes. By increasing medical student exposure to orthopedics during the third year of medical school, we are giving a larger proportion of our students direct clinical experience in a field they may not have been considering. This exposure allows students to interact with mentors who can be positive role models—orthopedic surgeons who are dispelling stereotypes. By increasing medical student exposure and reaching students who may not have been considering orthopedics, we have increased diversity among our applicants. Third-year medical students’ exposure to orthopedic surgery is essential in promoting a more diverse workforce.
Am J Orthop. 2016;45(6):E347-E351. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
As the United States becomes increasingly diverse, with predictions that by 2045 minorities will comprise 50% or more of the population,1 the demographics of the orthopedic surgery population will also likely diversify. It is important that orthopedic surgeons shift in their diversity as well. Lack of diversity in orthopedics (women and racial minorities are underrepresented) relative to the national population and other surgical specialties and their training programs is well documented.2-8
More concerning, the diversity of orthopedic residents does not compare favorably with that of medical school attendees.4,9 The difference suggests the greatest loss of potential diversity occurs during the transition from medical school to residency. A national study demonstrated that instruction in musculoskeletal medicine led to an increase in application rates nationally.10 However, the authors of that study stated they were unexpectedly limited by its large size—they could not validate the accuracy of curriculum data and could not differentiate between a 1-day required experience and a 4-week rotation.
In the present study, which accounted for curricular factors, we compared our medical students’ application rates to orthopedics residencies based on sex and race before and after introduction of a required third-year musculoskeletal clerkship. We hypothesized that making the curriculum a requirement would increase the number of applicants and increase the diversity of applicants in terms of both women and underrepresented minorities. This hypothesis was based on the rationale that these groups might not consider an orthopedics residency without first being directly exposed to orthopedics. We also wanted to determine what factors influenced applicants to choose orthopedic surgery.
Methods
Curriculum
Before 2006, third-year students spent 3 months completing a surgery clerkship. Some students interested in orthopedic surgery would have to wait until their fourth year to complete an elective in orthopedic surgery, and uninterested students would not be exposed at all. Starting in 2006, 1 month of the third-year surgery clerkship was required to be completed in musculoskeletal surgery: orthopedic surgery, plastic surgery, or neurosurgical spine. Plastic surgery was an option, as it exposed students to hand surgery and flap reconstruction.
During the 12-year study period, overall teaching hours in the preclinical curriculum did not change, and there were no other structural changes to the preclinical or clinical curriculum. The orthopedics department increased its faculty from 23 in 2000 to 34 in 2012. Number of female faculty increased from 1 to 3, representing a 4% to 9% increase in department faculty. Throughout the 12 years, there were no underrepresented minority faculty. Total number of residents increased from 26 in 2000 to 30 in 2012. Number of female residents varied year to year, from a low of 3 in the period 2003–2004 to a high of 11 in the period 2009–2010. Number of underrepresented minority residents varied yearly as well, from 1 to 2.
Data Collection
After this study was granted exempt status by our Institutional Review Board, we obtained student data from our registrar. Data included graduation year, self-identified sex and race, exposure to orthopedic surgery during clerkships, and matching residency specialty. National data were obtained from the Electronic Residency Application Service for the periods 2002–2007 and 2009–2012. These data included all US allopathic medical students’ self-identified sex and race, and applied-to primary residency specialty. National data from 2008 and national data on sex differences in orthopedic applications from 2009 were not available.
Graduates who matched into orthopedic surgery were asked to complete an anonymous survey on what influenced their decision to apply to orthopedic surgery and when this decision was made. Our goal with the survey was to substantiate or refute the conclusion that application rates depended on third-year exposure to musculoskeletal medicine.
Statistical Methods
Students were divided into 2 groups: precurriculum (graduated within 7-year period, 2000–2006) and postcurriculum (graduated within 6-year period, 2007–2012). A 2-sample test for proportions was used to compare percentage of total students who applied to orthopedics in each group. In the group of students who applied to orthopedics, we compared precurriculum and postcurriculum proportions of women and underrepresented minorities (non-white, non-Asian). We also compared these proportions with national data (using 2-sample tests for proportions) to determine if any change in diversity of our institution’s applicants was mirroring a national trend. Our definition of underrepresented minority was based on work that showed that the proportion of Asian matriculants in medical school and the proportion of applicants to orthopedics are higher than their respective national proportions.5 Survey data are reported descriptively. Statistical significance was defined with a 2-tailed α of 0.05 for all tests.
Results
Over the 2000–2012 period, 1507 students from our institution successfully applied to residency programs: 792 in the precurriculum group and 715 in the postcurriculum group. Of these students, 91 successfully applied to orthopedic surgery: 48 in the precurriculum group (applied before introduction of the required clerkship) and 43 in the postcurriculum group (applied afterward).
Over the 2002–2012 period, 10,100 US allopathic medical students applied to orthopedic residency programs: 4769 students between 2002 and 2006 and 5331 students between 2007 and 2012.
Before the musculoskeletal clerkship was required, 317 (40%) of the 792 precurriculum students were exposed to orthopedics during their third year. During this period, 42 of the 48 orthopedic surgery applicants completed an orthopedic surgery rotation during their third year of medical school. After the clerkship was required, 465 (65%) of the 715 postcurriculum students were exposed to orthopedics during their third year, including all 43 orthopedic surgery applicants (100% of students were exposed to musculoskeletal surgery, including plastic surgery and neurologic spine). The 25% increase in exposure to orthopedic surgery during the third year was statistically significant (P < .0001), but there was no resultant increase in overall percentage of students applying to orthopedic residencies (6% in each case; P = .98).
Over the 12-year study period, the proportion of female medical students at our institution declined from 50% (395/792) to 46% (328/715) (P = .13). However, there was an 81% relative increase, from 17% (8/48) before introduction of the clerkship to 30% (13/43) afterward, in the proportion of female applicants to orthopedic surgery. This contrasted with national data showing the percentage of female applicants to orthopedic surgery remained stable from 2002–2006 (14%, 675/4758) to 2007–2012 (15%, 643/4277). Before the clerkship was required, the proportion of female applicants from our institution was similar to national rates (P = .50). Afterward, our institution produced a significantly higher proportion of female applicants compared with the national proportion (P = .026).
Over the 12-year period, our self-identified underrepresented minority medical student population increased significantly (P = .02), from 13% (103/792) to 17% (124/715). The relative proportion of underrepresented minority orthopedic surgery applicants increased by 101%, from 10% (5/48) before the clerkship was required to 21% (9/43) afterward. Nationally, over the same period, underrepresented minorities’ orthopedic surgery application rates increased significantly (P < .001), from 16% (763/4769) to 19% (1002/5331). The proportion of underrepresented racial minorities that applied did not differ significantly between our institution and nationally for the years either before (P = .97) or after (P = .68) introduction of the curriculum.
Surveys were completed by 58 (64%) of 91 graduates (21 women, 70 men). Respondents’ characteristics are listed in Table 4.
Discussion
Orthopedic surgery needs a more diverse workforce11-17 in order to better mirror the population served, bring care to underserved areas,18-26 and provide better training environments.27 Several hypotheses about the lack of diversity have been posited: stereotypes about the specialty,28-31 lack of interest among minority medical students, and lack of exposure to the specialty.5,6,32,33
Lack of exposure deserves scrutiny, as a large proportion of medical students who choose to apply to orthopedic surgery make their decision before entering medical school, which is not typical.33 Such a finding suggests that exposure to orthopedic surgery is lacking, especially given that an orthopedic surgery rotation is usually not required during the clinical years. The idea that increased exposure to orthopedics affects application patterns is logical, as clinical exposure has been shown to play a role in medical students’ choice of specialty.34
Exposure helps in several key areas. Firsthand experience can help dispel stereotypes, such as the idea that success in orthopedic surgery depends on physical strength and that only former athletes pursue orthopedics.28-31 Authors have also reported on a perceived negative bias against women: Orthopedics is an “old boys’ network”; women will not fit in and need not apply; the orthopedic lifestyle is difficult and not conducive to a satisfying personal life.9 Requiring exposure ensures that all students, but especially women, can gain firsthand experience that can show these stereotypes to be false. Beyond dispelling these stereotypes, exposure to orthopedic surgery is essential for women, as studies have shown that clinical rotations play a larger role in determining specialty choice for women compared to men,33 and this would be particularly critical for specialties they may not be initially considering.
A national study found that requiring an orthopedic/musculoskeletal clerkship led to a 12% relative increase in the application rate, from 5.1% to 5.7%, and to an increase in applicant diversity (race, sex).10 However, the investigators could not determine individual reasons for specialty choice or the exact nature of each institution’s musculoskeletal curriculum. Confirming these factors, we found an 81% increase in number of female applicants and a 101% increase in number of underrepresented minority applicants after introduction of the required third-year musculoskeletal surgery clerkship at our institution.
We were unable to replicate the 12% relative increase in the overall application rate; our orthopedic surgery match rate remained 6%. Our findings cannot directly explain this, but we have several hypotheses. First, whereas other studies measured the application rate, we measured the successful match rate, given our data structure. This difference in data definition could account for some of the discrepancy. Second, we did not account for individuals’ academic success, and career counseling is paramount in decisions regarding residency specialties. It is possible we are substituting qualified female and underrepresented minority candidates for less-than-qualified male applicants. Third, the 25% increase in medical student exposure to orthopedic surgery led to a corresponding increase in number of orthopedic faculty providing undergraduate medical education. Some of these faculty could have been inexperienced in undergraduate medical education, and thus the teaching environment may not have been optimal.
Our study had several limitations. First, our institution has limited racial diversity. Over the past 12 years, only 15% of our students have been underrepresented minorities. (Nationally, the proportion is closer to 18%.) This may have limited the ability of our orthopedic rotation to affect the proportion of underrepresented minority applicants. Second, this study involved medical students at only one institution, which limits generalizability of findings. Third, we were unable to obtain records specifying which faculty and residents interacted with which medical students, and the increased number of female faculty and residents coinciding with the curriculum change may also be a factor. However, we expect that, without the curriculum change, these students would have had smaller odds of interacting with these potential female role models in orthopedics, negating any affect they may have had. Last, although we contacted former students to ask about their reasons for choosing the orthopedics residency, those findings are limited by a potential respondent selection bias.
The qualities and characteristics of successful orthopedic surgeons, as presented in both medical and lay cultures, are subject to numerous stereotypes. By increasing medical student exposure to orthopedics during the third year of medical school, we are giving a larger proportion of our students direct clinical experience in a field they may not have been considering. This exposure allows students to interact with mentors who can be positive role models—orthopedic surgeons who are dispelling stereotypes. By increasing medical student exposure and reaching students who may not have been considering orthopedics, we have increased diversity among our applicants. Third-year medical students’ exposure to orthopedic surgery is essential in promoting a more diverse workforce.
Am J Orthop. 2016;45(6):E347-E351. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. US Census Bureau. 2012 National Population Projections: Summary Tables. http://www.census.gov/population/projections/data/national/2012/summarytables.html. Accessed April 15, 2013.
2. Blakemore LC, Hall JM, Biermann JS. Women in surgical residency training programs. J Bone Joint Surg Am. 2003;85(12):2477-2480.
3. Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92(13):2328-2335.
4. Lewis VO, Scherl SA, O’Connor MI. Women in orthopaedics—way behind the number curve. J Bone Joint Surg Am. 2012;94(5):e30.
5. Okike K, Utuk ME, White AA. Racial and ethnic diversity in orthopaedic surgery residency programs. J Bone Joint Surg Am. 2011;93(18):e107.
6. Salsberg ES, Grover A, Simon MA, Frick SL, Kuremsky MA, Goodman DC. An AOA critical issue. Future physician workforce requirements: implications for orthopaedic surgery education. J Bone Joint Surg Am. 2008;90(5):1143-1159.
7. American Academy of Orthopaedic Surgeons. Orthopaedic Practice in the US 2008. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2009.
8. White AA 3rd. Alfred R. Shands, Jr., lecture: our humanitarian orthopaedic opportunity. J Bone Joint Surg Am. 2002;84(3):478-484.
9. Templeton K, Wood VJ, Haynes R. Women and minorities in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S37-S41.
10. Bernstein J, Dicaprio MR, Mehta S. The relationship between required medical school instruction in musculoskeletal medicine and application rates to orthopaedic surgery residency programs. J Bone Joint Surg Am. 2004;86(10):2335-2338.
11. Dykes DC, White AA. Getting to equal: strategies to understand and eliminate general and orthopaedic healthcare disparities. Clin Orthop Relat Res. 2009;467(10):2598-2605.
12. Gebhardt MC. Improving diversity in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S49-S50.
13. Hammond RA. The moral imperatives for diversity. Clin Orthop Relat Res. 1999;(362):102-106.
14. Lindsey RW. The role of the department chair in promoting diversity. J Am Acad Orthop Surg. 2007;15(suppl 1):S65-S69.
15. Satcher RL. African Americans and orthopaedic surgery. A resident’s perspective. Clin Orthop Relat Res. 1999;(362):114-116.
16. White AA. Justifications and needs for diversity in orthopaedics. Clin Orthop Relat Res. 1999;(362):22-33.
17. White AA. Resident selection: are we putting the cart before the horse? Clin Orthop Relat Res. 2002;(399):255-259.
18. Dominick KL, Baker TA. Racial and ethnic differences in osteoarthritis: prevalence, outcomes, and medical care. Ethn Dis. 2004;14(4):558-566.
19. Furstenberg AL, Mezey MD. Differences in outcome between black and white elderly hip fracture patients. J Chronic Dis. 1987;40(10):931-938.
20. Ibrahim SA. Racial and ethnic disparities in hip and knee joint replacement: a review of research in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S87-S94.
21. Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334(20):1305-1310.
22. Moy E, Bartman BA. Physician race and care of minority and medically indigent patients. JAMA. 1995;273(19):1515-1520.
23. Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15(suppl 1):S13-S17.
24. Rowley DL, Jenkins BC, Frazier E. Utilization of joint arthroplasty: racial and ethnic disparities in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S43-S48.
25. Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350-1359.
26. Steel N, Clark A, Lang LA, Wallace RB, Melzer D. Racial disparities in receipt of hip and knee joint replacements are not explained by need: the Health and Retirement Study 1998-2004. J Gerontol A Biol Sci Med Sci. 2008;63(6):629-634.
27. Whitla DK, Orfield G, Silen W, Teperow C, Howard C, Reede J. Educational benefits of diversity in medical school: a survey of students. Acad Med. 2003;78(5):460-466.
28. Barrett DS. Are orthopaedic surgeons gorillas? Br Med J. 1988;297(6664):1638-1639.
29. Brenkel IJ, Pearse M, Gregg PJ. A “cracking” complication of hemiarthroplasty of the hip. Br Med J. 1986;293(6562):1648.
30. Fox JS, Bell GR, Sweeney PJ. Are orthopaedic surgeons really gorillas? Br Med J. 1990;301(6766):1425-1426.
31. Subramanian P, Kantharuban S, Subramanian V, Willis-Owen SA, Willis-Owen CA. Orthopaedic surgeons: as strong as an ox and almost twice as clever? Multicentre prospective comparative study. Br Med J. 2011;343:d7506.
32. Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011;34(12):e919-e932.
33. Johnson AL, Sharma J, Chinchilli VM, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94(11):e78.
34. Wilson FC. Teaching by residents. Clin Orthop Relat Res. 2007;(454):247-250.
1. US Census Bureau. 2012 National Population Projections: Summary Tables. http://www.census.gov/population/projections/data/national/2012/summarytables.html. Accessed April 15, 2013.
2. Blakemore LC, Hall JM, Biermann JS. Women in surgical residency training programs. J Bone Joint Surg Am. 2003;85(12):2477-2480.
3. Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92(13):2328-2335.
4. Lewis VO, Scherl SA, O’Connor MI. Women in orthopaedics—way behind the number curve. J Bone Joint Surg Am. 2012;94(5):e30.
5. Okike K, Utuk ME, White AA. Racial and ethnic diversity in orthopaedic surgery residency programs. J Bone Joint Surg Am. 2011;93(18):e107.
6. Salsberg ES, Grover A, Simon MA, Frick SL, Kuremsky MA, Goodman DC. An AOA critical issue. Future physician workforce requirements: implications for orthopaedic surgery education. J Bone Joint Surg Am. 2008;90(5):1143-1159.
7. American Academy of Orthopaedic Surgeons. Orthopaedic Practice in the US 2008. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2009.
8. White AA 3rd. Alfred R. Shands, Jr., lecture: our humanitarian orthopaedic opportunity. J Bone Joint Surg Am. 2002;84(3):478-484.
9. Templeton K, Wood VJ, Haynes R. Women and minorities in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S37-S41.
10. Bernstein J, Dicaprio MR, Mehta S. The relationship between required medical school instruction in musculoskeletal medicine and application rates to orthopaedic surgery residency programs. J Bone Joint Surg Am. 2004;86(10):2335-2338.
11. Dykes DC, White AA. Getting to equal: strategies to understand and eliminate general and orthopaedic healthcare disparities. Clin Orthop Relat Res. 2009;467(10):2598-2605.
12. Gebhardt MC. Improving diversity in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(suppl 1):S49-S50.
13. Hammond RA. The moral imperatives for diversity. Clin Orthop Relat Res. 1999;(362):102-106.
14. Lindsey RW. The role of the department chair in promoting diversity. J Am Acad Orthop Surg. 2007;15(suppl 1):S65-S69.
15. Satcher RL. African Americans and orthopaedic surgery. A resident’s perspective. Clin Orthop Relat Res. 1999;(362):114-116.
16. White AA. Justifications and needs for diversity in orthopaedics. Clin Orthop Relat Res. 1999;(362):22-33.
17. White AA. Resident selection: are we putting the cart before the horse? Clin Orthop Relat Res. 2002;(399):255-259.
18. Dominick KL, Baker TA. Racial and ethnic differences in osteoarthritis: prevalence, outcomes, and medical care. Ethn Dis. 2004;14(4):558-566.
19. Furstenberg AL, Mezey MD. Differences in outcome between black and white elderly hip fracture patients. J Chronic Dis. 1987;40(10):931-938.
20. Ibrahim SA. Racial and ethnic disparities in hip and knee joint replacement: a review of research in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S87-S94.
21. Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334(20):1305-1310.
22. Moy E, Bartman BA. Physician race and care of minority and medically indigent patients. JAMA. 1995;273(19):1515-1520.
23. Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15(suppl 1):S13-S17.
24. Rowley DL, Jenkins BC, Frazier E. Utilization of joint arthroplasty: racial and ethnic disparities in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S43-S48.
25. Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350-1359.
26. Steel N, Clark A, Lang LA, Wallace RB, Melzer D. Racial disparities in receipt of hip and knee joint replacements are not explained by need: the Health and Retirement Study 1998-2004. J Gerontol A Biol Sci Med Sci. 2008;63(6):629-634.
27. Whitla DK, Orfield G, Silen W, Teperow C, Howard C, Reede J. Educational benefits of diversity in medical school: a survey of students. Acad Med. 2003;78(5):460-466.
28. Barrett DS. Are orthopaedic surgeons gorillas? Br Med J. 1988;297(6664):1638-1639.
29. Brenkel IJ, Pearse M, Gregg PJ. A “cracking” complication of hemiarthroplasty of the hip. Br Med J. 1986;293(6562):1648.
30. Fox JS, Bell GR, Sweeney PJ. Are orthopaedic surgeons really gorillas? Br Med J. 1990;301(6766):1425-1426.
31. Subramanian P, Kantharuban S, Subramanian V, Willis-Owen SA, Willis-Owen CA. Orthopaedic surgeons: as strong as an ox and almost twice as clever? Multicentre prospective comparative study. Br Med J. 2011;343:d7506.
32. Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011;34(12):e919-e932.
33. Johnson AL, Sharma J, Chinchilli VM, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94(11):e78.
34. Wilson FC. Teaching by residents. Clin Orthop Relat Res. 2007;(454):247-250.
In Orbit

When using biologic therapies for psoriasis, it is important to evaluate long-term efficacy (>4 years of follow-up). Biologic drug survival in psoriasis reflects long-term performance in real-life settings. Prior studies have yielded inconsistent results.
Vilarrasa et al (J Am Acad Dermatol. 2016;74:1066-1072) conducted an observational retrospective study called ORBIT (Outcome and Retention Rate of Biologic Treatments for Psoriasis) to determine drug survival (the mean length of time patients remain on a drug) in a cohort of 427 patients (63.5% male; mean age, 50.2 years) with moderate to severe psoriasis vulgaris (mean baseline psoriasis area and severity index [PASI], 16.4). In addition to determining mean drug survival times for etanercept, infliximab, adalimumab, and ustekinumab, investigators searched for variables that positively or negatively affected drug survival times. Data were extracted from clinical records of patients treated with biologic agents over a 4-year period. Drug survival was analyzed using the Kaplan-Meier method and the influence of several covariates was assessed using Cox regression.
The investigators evaluated 703 treatment courses. The overall median drug survival was 31.0 months. Cumulative probability of drug survival was lower in obese patients (23.0 months; 95% CI, 17.4-28.6) than in patients with body mass index less than 30 (37.3 months; 95% CI, 29.4-45.1; P=.001). Drug survival was significantly higher for ustekinumab than for any other biologic agent (log-rank test, P<.001). Multivariate analysis showed that obesity, etanercept treatment, and strict adherence to approved doses were associated with an increased probability of drug withdrawal, whereas ustekinumab treatment and PASI 75 and PASI 90 responses at week 16 prolonged drug survival. Data were collected retrospectively.
What’s the issue?
These results should help to educate patients and to manage expectations about drug efficacy.

When using biologic therapies for psoriasis, it is important to evaluate long-term efficacy (>4 years of follow-up). Biologic drug survival in psoriasis reflects long-term performance in real-life settings. Prior studies have yielded inconsistent results.
Vilarrasa et al (J Am Acad Dermatol. 2016;74:1066-1072) conducted an observational retrospective study called ORBIT (Outcome and Retention Rate of Biologic Treatments for Psoriasis) to determine drug survival (the mean length of time patients remain on a drug) in a cohort of 427 patients (63.5% male; mean age, 50.2 years) with moderate to severe psoriasis vulgaris (mean baseline psoriasis area and severity index [PASI], 16.4). In addition to determining mean drug survival times for etanercept, infliximab, adalimumab, and ustekinumab, investigators searched for variables that positively or negatively affected drug survival times. Data were extracted from clinical records of patients treated with biologic agents over a 4-year period. Drug survival was analyzed using the Kaplan-Meier method and the influence of several covariates was assessed using Cox regression.
The investigators evaluated 703 treatment courses. The overall median drug survival was 31.0 months. Cumulative probability of drug survival was lower in obese patients (23.0 months; 95% CI, 17.4-28.6) than in patients with body mass index less than 30 (37.3 months; 95% CI, 29.4-45.1; P=.001). Drug survival was significantly higher for ustekinumab than for any other biologic agent (log-rank test, P<.001). Multivariate analysis showed that obesity, etanercept treatment, and strict adherence to approved doses were associated with an increased probability of drug withdrawal, whereas ustekinumab treatment and PASI 75 and PASI 90 responses at week 16 prolonged drug survival. Data were collected retrospectively.
What’s the issue?
These results should help to educate patients and to manage expectations about drug efficacy.

When using biologic therapies for psoriasis, it is important to evaluate long-term efficacy (>4 years of follow-up). Biologic drug survival in psoriasis reflects long-term performance in real-life settings. Prior studies have yielded inconsistent results.
Vilarrasa et al (J Am Acad Dermatol. 2016;74:1066-1072) conducted an observational retrospective study called ORBIT (Outcome and Retention Rate of Biologic Treatments for Psoriasis) to determine drug survival (the mean length of time patients remain on a drug) in a cohort of 427 patients (63.5% male; mean age, 50.2 years) with moderate to severe psoriasis vulgaris (mean baseline psoriasis area and severity index [PASI], 16.4). In addition to determining mean drug survival times for etanercept, infliximab, adalimumab, and ustekinumab, investigators searched for variables that positively or negatively affected drug survival times. Data were extracted from clinical records of patients treated with biologic agents over a 4-year period. Drug survival was analyzed using the Kaplan-Meier method and the influence of several covariates was assessed using Cox regression.
The investigators evaluated 703 treatment courses. The overall median drug survival was 31.0 months. Cumulative probability of drug survival was lower in obese patients (23.0 months; 95% CI, 17.4-28.6) than in patients with body mass index less than 30 (37.3 months; 95% CI, 29.4-45.1; P=.001). Drug survival was significantly higher for ustekinumab than for any other biologic agent (log-rank test, P<.001). Multivariate analysis showed that obesity, etanercept treatment, and strict adherence to approved doses were associated with an increased probability of drug withdrawal, whereas ustekinumab treatment and PASI 75 and PASI 90 responses at week 16 prolonged drug survival. Data were collected retrospectively.
What’s the issue?
These results should help to educate patients and to manage expectations about drug efficacy.
Leveraging what is available
Illicit drug use in the United States continues to rise. In 2014, 27 million people reported using an illicit drug in the previous 30 days. This corresponds to nearly 1 in every 10 Americans.
Use of marijuana has the highest prevalence, followed distantly by pain relievers, tranquilizers, stimulants, and cocaine. Resources for drug users who want to quit are difficult to access – and even if those resources are available, they may be constrained.
For patients struggling with alcohol dependence who want to quit, Alcoholics Anonymous (AA) is the most well-known and ubiquitous 12-step mutual help organization (MHO). Other MHOs, such as Narcotics Anonymous (NA), exist for illicit substances such as opiates (e.g., heroin), stimulants, or cannabis. Shared experiences are hypothesized to maximize therapeutic benefit.
But what, then, should we do if somebody struggling with illicit substance dependence wants to remain abstinent from drugs and there are only AA groups around?
Harvard investigators suggest that support from AA for patients with illicit substance addiction is not associated with early discontinuation or compromised recovery. To evaluate this, researchers examined treatment outcomes among young adults participating in residential treatment in Minnesota (Alcohol Alcohol. 2014 Nov;49[6]:645-3).
Four groups of patients with drug use disorder were evaluated: alcohol, cannabis, opiates, or stimulants. The goal was to compare the relative success of individuals with fellowship “mismatch” (e.g., attending AA but was a primary user of cannabis), compared with those who had a fellowship match. Success during aftercare was defined as percentage of days abstinent and attendance at the MHO.
Investigators observed that in the first 3 months after discharge from the residential treatment program, a significant proportion (79%) of the meetings attended by the cannabis, opiates, or stimulant users were AA meetings. This mismatch was unrelated to 12-step attendance at 6 and 12 months, or to percentage of days abstinent.
Available literature suggests that 12-step MHO participation is a predictor of better treatment outcomes. The findings from this study suggest that AA attendance among patients recovering from cannabis, opiates, or stimulant use disorder is beneficial. Patients with illicit drug use disorder should be encouraged to attend AA if other MHOs are not accessible.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
Illicit drug use in the United States continues to rise. In 2014, 27 million people reported using an illicit drug in the previous 30 days. This corresponds to nearly 1 in every 10 Americans.
Use of marijuana has the highest prevalence, followed distantly by pain relievers, tranquilizers, stimulants, and cocaine. Resources for drug users who want to quit are difficult to access – and even if those resources are available, they may be constrained.
For patients struggling with alcohol dependence who want to quit, Alcoholics Anonymous (AA) is the most well-known and ubiquitous 12-step mutual help organization (MHO). Other MHOs, such as Narcotics Anonymous (NA), exist for illicit substances such as opiates (e.g., heroin), stimulants, or cannabis. Shared experiences are hypothesized to maximize therapeutic benefit.
But what, then, should we do if somebody struggling with illicit substance dependence wants to remain abstinent from drugs and there are only AA groups around?
Harvard investigators suggest that support from AA for patients with illicit substance addiction is not associated with early discontinuation or compromised recovery. To evaluate this, researchers examined treatment outcomes among young adults participating in residential treatment in Minnesota (Alcohol Alcohol. 2014 Nov;49[6]:645-3).
Four groups of patients with drug use disorder were evaluated: alcohol, cannabis, opiates, or stimulants. The goal was to compare the relative success of individuals with fellowship “mismatch” (e.g., attending AA but was a primary user of cannabis), compared with those who had a fellowship match. Success during aftercare was defined as percentage of days abstinent and attendance at the MHO.
Investigators observed that in the first 3 months after discharge from the residential treatment program, a significant proportion (79%) of the meetings attended by the cannabis, opiates, or stimulant users were AA meetings. This mismatch was unrelated to 12-step attendance at 6 and 12 months, or to percentage of days abstinent.
Available literature suggests that 12-step MHO participation is a predictor of better treatment outcomes. The findings from this study suggest that AA attendance among patients recovering from cannabis, opiates, or stimulant use disorder is beneficial. Patients with illicit drug use disorder should be encouraged to attend AA if other MHOs are not accessible.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
Illicit drug use in the United States continues to rise. In 2014, 27 million people reported using an illicit drug in the previous 30 days. This corresponds to nearly 1 in every 10 Americans.
Use of marijuana has the highest prevalence, followed distantly by pain relievers, tranquilizers, stimulants, and cocaine. Resources for drug users who want to quit are difficult to access – and even if those resources are available, they may be constrained.
For patients struggling with alcohol dependence who want to quit, Alcoholics Anonymous (AA) is the most well-known and ubiquitous 12-step mutual help organization (MHO). Other MHOs, such as Narcotics Anonymous (NA), exist for illicit substances such as opiates (e.g., heroin), stimulants, or cannabis. Shared experiences are hypothesized to maximize therapeutic benefit.
But what, then, should we do if somebody struggling with illicit substance dependence wants to remain abstinent from drugs and there are only AA groups around?
Harvard investigators suggest that support from AA for patients with illicit substance addiction is not associated with early discontinuation or compromised recovery. To evaluate this, researchers examined treatment outcomes among young adults participating in residential treatment in Minnesota (Alcohol Alcohol. 2014 Nov;49[6]:645-3).
Four groups of patients with drug use disorder were evaluated: alcohol, cannabis, opiates, or stimulants. The goal was to compare the relative success of individuals with fellowship “mismatch” (e.g., attending AA but was a primary user of cannabis), compared with those who had a fellowship match. Success during aftercare was defined as percentage of days abstinent and attendance at the MHO.
Investigators observed that in the first 3 months after discharge from the residential treatment program, a significant proportion (79%) of the meetings attended by the cannabis, opiates, or stimulant users were AA meetings. This mismatch was unrelated to 12-step attendance at 6 and 12 months, or to percentage of days abstinent.
Available literature suggests that 12-step MHO participation is a predictor of better treatment outcomes. The findings from this study suggest that AA attendance among patients recovering from cannabis, opiates, or stimulant use disorder is beneficial. Patients with illicit drug use disorder should be encouraged to attend AA if other MHOs are not accessible.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
Debunking Psoriasis Myths: Is Psoriasis Infectious?
Myth: Psoriasis Is Infectious The precise cause of psoriasis is unknown, but researchers believe the immune system and genetics play major roles in its development, according to the National Psoriasis Foundation. The skin cells in patients with psoriasis grow at an abnormally fast rate, which causes the buildup of psoriasis lesions. Usually, something triggers psoriasis to flare.
A common misconception among patients is that psoriasis is caused by an infection. Psoriasis is not contagious and psoriasis lesions are not infectious.
However, psoriasis patients are more prone to infections than those without psoriasis. Risk factors for serious infections in psoriasis patients include immune dysregulation, systemic immunosuppressive medications, and comorbid health conditions such as diabetes mellitus or obesity. A 2016 study revealed an increased incidence of serious infections (eg, cellulitis, herpes simplex virus infection, any fungal infection, infectious arthritis, methicillin-resistant Staphylococcus aureus) in hospitalized patients with psoriasis. Higher rates were seen among nonwhite and non-privately insured patients.
In a 2011 study, the likelihood of infectious diseases in patients with psoriasis was twice as high as the reference population. The risk was highest in patients with more severe psoriasis but was not associated with recent systemic antipsoriatic drug dispensing. Respiratory tract, abdominal, and skin infections occurred most frequently in patients with psoriasis.
Poor access to adequate dermatologic care may contribute to higher rates of infections. Dermatologists must closely monitor patients with psoriasis for infection. More research is needed to develop interventions for prevention.
Expert Commentary Psoriasis patients have long faced discrimination because of an irrational fear that their disease was somehow contagious. In fact this is completely false. This highlights the need for education of the public, so that they understand the true causes and nature of the disease.
—Jeffrey M. Weinberg, MD (New York, New York)
About psoriasis. National Psoriasis Foundation website. http://www.psoriasis.org/about-psoriasis. Accessed September 9, 2016.
Hsu DY, Gordon K, Silverberg JI. Serious infections in hospitalized patients with psoriasis in the United States [published online June 17, 2016]. J Am Acad Dermatol. 2016;75:287-296.
Wakkee M, de Vries E, van den Haak P, et al. Increased risk of infectious disease requiring hospitalization among patients with psoriasis: a population-based cohort. J Am Acad Dermatol. 2011;65:1135-1144.
Myth: Psoriasis Is Infectious The precise cause of psoriasis is unknown, but researchers believe the immune system and genetics play major roles in its development, according to the National Psoriasis Foundation. The skin cells in patients with psoriasis grow at an abnormally fast rate, which causes the buildup of psoriasis lesions. Usually, something triggers psoriasis to flare.
A common misconception among patients is that psoriasis is caused by an infection. Psoriasis is not contagious and psoriasis lesions are not infectious.
However, psoriasis patients are more prone to infections than those without psoriasis. Risk factors for serious infections in psoriasis patients include immune dysregulation, systemic immunosuppressive medications, and comorbid health conditions such as diabetes mellitus or obesity. A 2016 study revealed an increased incidence of serious infections (eg, cellulitis, herpes simplex virus infection, any fungal infection, infectious arthritis, methicillin-resistant Staphylococcus aureus) in hospitalized patients with psoriasis. Higher rates were seen among nonwhite and non-privately insured patients.
In a 2011 study, the likelihood of infectious diseases in patients with psoriasis was twice as high as the reference population. The risk was highest in patients with more severe psoriasis but was not associated with recent systemic antipsoriatic drug dispensing. Respiratory tract, abdominal, and skin infections occurred most frequently in patients with psoriasis.
Poor access to adequate dermatologic care may contribute to higher rates of infections. Dermatologists must closely monitor patients with psoriasis for infection. More research is needed to develop interventions for prevention.
Expert Commentary Psoriasis patients have long faced discrimination because of an irrational fear that their disease was somehow contagious. In fact this is completely false. This highlights the need for education of the public, so that they understand the true causes and nature of the disease.
—Jeffrey M. Weinberg, MD (New York, New York)
Myth: Psoriasis Is Infectious The precise cause of psoriasis is unknown, but researchers believe the immune system and genetics play major roles in its development, according to the National Psoriasis Foundation. The skin cells in patients with psoriasis grow at an abnormally fast rate, which causes the buildup of psoriasis lesions. Usually, something triggers psoriasis to flare.
A common misconception among patients is that psoriasis is caused by an infection. Psoriasis is not contagious and psoriasis lesions are not infectious.
However, psoriasis patients are more prone to infections than those without psoriasis. Risk factors for serious infections in psoriasis patients include immune dysregulation, systemic immunosuppressive medications, and comorbid health conditions such as diabetes mellitus or obesity. A 2016 study revealed an increased incidence of serious infections (eg, cellulitis, herpes simplex virus infection, any fungal infection, infectious arthritis, methicillin-resistant Staphylococcus aureus) in hospitalized patients with psoriasis. Higher rates were seen among nonwhite and non-privately insured patients.
In a 2011 study, the likelihood of infectious diseases in patients with psoriasis was twice as high as the reference population. The risk was highest in patients with more severe psoriasis but was not associated with recent systemic antipsoriatic drug dispensing. Respiratory tract, abdominal, and skin infections occurred most frequently in patients with psoriasis.
Poor access to adequate dermatologic care may contribute to higher rates of infections. Dermatologists must closely monitor patients with psoriasis for infection. More research is needed to develop interventions for prevention.
Expert Commentary Psoriasis patients have long faced discrimination because of an irrational fear that their disease was somehow contagious. In fact this is completely false. This highlights the need for education of the public, so that they understand the true causes and nature of the disease.
—Jeffrey M. Weinberg, MD (New York, New York)
About psoriasis. National Psoriasis Foundation website. http://www.psoriasis.org/about-psoriasis. Accessed September 9, 2016.
Hsu DY, Gordon K, Silverberg JI. Serious infections in hospitalized patients with psoriasis in the United States [published online June 17, 2016]. J Am Acad Dermatol. 2016;75:287-296.
Wakkee M, de Vries E, van den Haak P, et al. Increased risk of infectious disease requiring hospitalization among patients with psoriasis: a population-based cohort. J Am Acad Dermatol. 2011;65:1135-1144.
About psoriasis. National Psoriasis Foundation website. http://www.psoriasis.org/about-psoriasis. Accessed September 9, 2016.
Hsu DY, Gordon K, Silverberg JI. Serious infections in hospitalized patients with psoriasis in the United States [published online June 17, 2016]. J Am Acad Dermatol. 2016;75:287-296.
Wakkee M, de Vries E, van den Haak P, et al. Increased risk of infectious disease requiring hospitalization among patients with psoriasis: a population-based cohort. J Am Acad Dermatol. 2011;65:1135-1144.
Direct-to-Consumer Marketing: Implications for Patient Care and Orthopedic Education
Direct-to-consumer marketing (DTCM) is the promotion of health-related products or services directly to patients. Although this topic is not new to orthopedics, several emerging trends hold troubling implications for patients as well as orthopedic surgeons, particularly surgeons in training.
Orthopedics DTCM most commonly involves television and print advertisements. Supporters contend DTCM is an empowering educational tool that increases awareness of medical ailments and encourages patients to seek treatment. Opponents point to inaccuracies and misleading claims. Bhattacharyya and colleagues1 found that about half the claims in orthopedic print advertisements were not supported by clinical evidence. Woloshin and colleagues2 found that information in DTCM was vague and often was designed to act on the emotions. Patients misled by these claims and innately seeking improvement could present with unreasonable expectations and difficult discussions that can be detrimental to the patient–physician relationship.3Given changing patient demographics and the information revolution, the effects of DTCM likely will continue to grow. Total joint arthroplasty (TJA), which represents Medicare’s largest expenditure,4 is a classic example. Today’s TJA patients are younger, more active, and better educated, and they live longer, have higher expectations, and are more reliant on the media.5 Television is no longer our main medium—the internet is the source of healthcare education for 70% of adults in the United States.6Healthcare reform has also brought significant changes in the delivery of DTCM. In an era of competition for market share brought by increased demand and decreased reimbursement, DTCM has evolved into sales pitches by hospitals and physicians. Robotic joint replacement, minimally invasive surgery (MIS), use of the anterior hip approach, use of sex-specific or high-flexion knee implants, and other practices have become popular marketing tools for surgery centers competing for new patients. As a result, patients often present not only with a complaint but with a request for a particular procedure.4,5 Labovitch and colleagues7 found that 70% of MIS information on the internet was produced by hospitals and private medical groups, and only 6% was produced by industry. Although the vast majority of the sources reported on the advantages of MIS, only 15% explained patient eligibility, and a mere 9% supplied references for examination of peer-reviewed data. Another unfortunate consequence of DCTM is “physician shopping.” Bozic and colleagues4 found that patients exposed to DCTM were more likely to demand a specific surgery, approach, or implant and were less open to alternatives; in addition, they saw more than one surgeon before deciding on joint arthroplasty.
The effects of DTCM on resident and fellowship training require serious consideration. An emphasis on technology has come at the expense of learning the science and art of orthopedics.8 Physicians in training are pressured both to produce more and to use whichever specific technique or product a patient requests.4 Similarly, orthopedic surgeons are seeing job advertisements that read, “Training in robotic surgery or anterior approach is preferred.” Employer pressure can have profound implications for residents and fellows, who may feel compelled to learn these techniques. To a large degree, residents and fellows learn by accompanying their mentors and closely observing their decision-making processes and interactions with patients. Decisions regarding fellowships should not be influenced by surgical techniques or implant choices but by the quality and breadth of clinical experience.
DTCM likely will continue to shape all aspects of care. Claims made by physicians and hospitals are especially troubling because patients trust these sources. We face the challenge of reaffirming our commitment to patients and orthopedic surgeons. As the leader in musculoskeletal education, the American Academy of Orthopaedic Surgeons (AAOS) not only must provide educational material that is compatible with current technological media but must address current controversies and misleading claims. Toward that end, AAOS can expand its patient website, OrthoInfo, to include information on new technologies and surgical techniques pertaining to each musculoskeletal condition. Educating the public about risk factors for poor surgical outcomes is equally important in order to moderate unrealistic expectations and stimulate discussions on risks involved in unnecessary or potentially harmful technologies. The American Association of Hip and Knee Surgeons (AAHKS) has already embarked on this approach. Orthopedic surgeons should continue to abide by the standards of professionalism—maintaining the tenet of “First do no harm,” resisting the temptations of consumerism, and giving patients accurate information. Taking these measures may help reduce physician shopping and strengthen the patient–physician relationship. We physicians are the guardians of patients’ well-being. We also owe it to orthopedic surgeons in training to provide well-balanced, unbiased education. The focus of training should not be on techniques for gaining market edge but on learning evidence-based medicine and surgical principles. In our burdened healthcare system, curbing DTCM has the potential to decrease unnecessary use of resources and improve the quality of education and patient care.
Am J Orthop. 2016;45(6):E335-E336. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Bhattacharyya T, Tornetta P 3rd, Healy WL, Einhorn TA. The validity of claims made in orthopaedic print advertisements. J Bone Joint Surgery Am. 2003;85(7):1224-1228.
2. Woloshin S, Schwartz LM, Tremmel J, Welch HG. Direct-to-consumer advertisements for prescription drugs: what are Americans being sold? Lancet. 2001;358(9288):1141-1146.
3. Robinson AR, Hohmann KB, Rifkin JI, et al. Direct-to-consumer pharmaceutical advertising: physician and public opinion and potential effects on the physician-patient relationship. Arch Intern Med. 2004;164(4):427-432.
4. Bozic KJ, Smith AR, Hariri S, et al. The 2007 ABJS Marshall Urist award: the impact of direct-to-consumer advertising in orthopaedics. Clin Orthop Relat Res. 2007;(458):202-219.
5. Mason JB. The new demands by patients in the modern era of total joint arthroplasty: a point of view. Clin Orthop Relat Res. 2008;466(1):146-152.
6. Weinstein SL. Words from a “wise old hand”—guideposts for the future. Professor Stuart L. Weinstein. Iowa Orthop J. 2008;28:94-97.
7. Labovitch RS, Bozic KJ, Hansen E. An evaluation of information available on the internet regarding minimally invasive hip arthroplasty. J Arthroplasty. 2006;21(1):1-5.
8. Buckwalter JA. Advancing the science and art of orthopaedics. Lessons from history. J Bone Joint Surg Am. 2000;82(12):1782-1803.
Direct-to-consumer marketing (DTCM) is the promotion of health-related products or services directly to patients. Although this topic is not new to orthopedics, several emerging trends hold troubling implications for patients as well as orthopedic surgeons, particularly surgeons in training.
Orthopedics DTCM most commonly involves television and print advertisements. Supporters contend DTCM is an empowering educational tool that increases awareness of medical ailments and encourages patients to seek treatment. Opponents point to inaccuracies and misleading claims. Bhattacharyya and colleagues1 found that about half the claims in orthopedic print advertisements were not supported by clinical evidence. Woloshin and colleagues2 found that information in DTCM was vague and often was designed to act on the emotions. Patients misled by these claims and innately seeking improvement could present with unreasonable expectations and difficult discussions that can be detrimental to the patient–physician relationship.3Given changing patient demographics and the information revolution, the effects of DTCM likely will continue to grow. Total joint arthroplasty (TJA), which represents Medicare’s largest expenditure,4 is a classic example. Today’s TJA patients are younger, more active, and better educated, and they live longer, have higher expectations, and are more reliant on the media.5 Television is no longer our main medium—the internet is the source of healthcare education for 70% of adults in the United States.6Healthcare reform has also brought significant changes in the delivery of DTCM. In an era of competition for market share brought by increased demand and decreased reimbursement, DTCM has evolved into sales pitches by hospitals and physicians. Robotic joint replacement, minimally invasive surgery (MIS), use of the anterior hip approach, use of sex-specific or high-flexion knee implants, and other practices have become popular marketing tools for surgery centers competing for new patients. As a result, patients often present not only with a complaint but with a request for a particular procedure.4,5 Labovitch and colleagues7 found that 70% of MIS information on the internet was produced by hospitals and private medical groups, and only 6% was produced by industry. Although the vast majority of the sources reported on the advantages of MIS, only 15% explained patient eligibility, and a mere 9% supplied references for examination of peer-reviewed data. Another unfortunate consequence of DCTM is “physician shopping.” Bozic and colleagues4 found that patients exposed to DCTM were more likely to demand a specific surgery, approach, or implant and were less open to alternatives; in addition, they saw more than one surgeon before deciding on joint arthroplasty.
The effects of DTCM on resident and fellowship training require serious consideration. An emphasis on technology has come at the expense of learning the science and art of orthopedics.8 Physicians in training are pressured both to produce more and to use whichever specific technique or product a patient requests.4 Similarly, orthopedic surgeons are seeing job advertisements that read, “Training in robotic surgery or anterior approach is preferred.” Employer pressure can have profound implications for residents and fellows, who may feel compelled to learn these techniques. To a large degree, residents and fellows learn by accompanying their mentors and closely observing their decision-making processes and interactions with patients. Decisions regarding fellowships should not be influenced by surgical techniques or implant choices but by the quality and breadth of clinical experience.
DTCM likely will continue to shape all aspects of care. Claims made by physicians and hospitals are especially troubling because patients trust these sources. We face the challenge of reaffirming our commitment to patients and orthopedic surgeons. As the leader in musculoskeletal education, the American Academy of Orthopaedic Surgeons (AAOS) not only must provide educational material that is compatible with current technological media but must address current controversies and misleading claims. Toward that end, AAOS can expand its patient website, OrthoInfo, to include information on new technologies and surgical techniques pertaining to each musculoskeletal condition. Educating the public about risk factors for poor surgical outcomes is equally important in order to moderate unrealistic expectations and stimulate discussions on risks involved in unnecessary or potentially harmful technologies. The American Association of Hip and Knee Surgeons (AAHKS) has already embarked on this approach. Orthopedic surgeons should continue to abide by the standards of professionalism—maintaining the tenet of “First do no harm,” resisting the temptations of consumerism, and giving patients accurate information. Taking these measures may help reduce physician shopping and strengthen the patient–physician relationship. We physicians are the guardians of patients’ well-being. We also owe it to orthopedic surgeons in training to provide well-balanced, unbiased education. The focus of training should not be on techniques for gaining market edge but on learning evidence-based medicine and surgical principles. In our burdened healthcare system, curbing DTCM has the potential to decrease unnecessary use of resources and improve the quality of education and patient care.
Am J Orthop. 2016;45(6):E335-E336. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
Direct-to-consumer marketing (DTCM) is the promotion of health-related products or services directly to patients. Although this topic is not new to orthopedics, several emerging trends hold troubling implications for patients as well as orthopedic surgeons, particularly surgeons in training.
Orthopedics DTCM most commonly involves television and print advertisements. Supporters contend DTCM is an empowering educational tool that increases awareness of medical ailments and encourages patients to seek treatment. Opponents point to inaccuracies and misleading claims. Bhattacharyya and colleagues1 found that about half the claims in orthopedic print advertisements were not supported by clinical evidence. Woloshin and colleagues2 found that information in DTCM was vague and often was designed to act on the emotions. Patients misled by these claims and innately seeking improvement could present with unreasonable expectations and difficult discussions that can be detrimental to the patient–physician relationship.3Given changing patient demographics and the information revolution, the effects of DTCM likely will continue to grow. Total joint arthroplasty (TJA), which represents Medicare’s largest expenditure,4 is a classic example. Today’s TJA patients are younger, more active, and better educated, and they live longer, have higher expectations, and are more reliant on the media.5 Television is no longer our main medium—the internet is the source of healthcare education for 70% of adults in the United States.6Healthcare reform has also brought significant changes in the delivery of DTCM. In an era of competition for market share brought by increased demand and decreased reimbursement, DTCM has evolved into sales pitches by hospitals and physicians. Robotic joint replacement, minimally invasive surgery (MIS), use of the anterior hip approach, use of sex-specific or high-flexion knee implants, and other practices have become popular marketing tools for surgery centers competing for new patients. As a result, patients often present not only with a complaint but with a request for a particular procedure.4,5 Labovitch and colleagues7 found that 70% of MIS information on the internet was produced by hospitals and private medical groups, and only 6% was produced by industry. Although the vast majority of the sources reported on the advantages of MIS, only 15% explained patient eligibility, and a mere 9% supplied references for examination of peer-reviewed data. Another unfortunate consequence of DCTM is “physician shopping.” Bozic and colleagues4 found that patients exposed to DCTM were more likely to demand a specific surgery, approach, or implant and were less open to alternatives; in addition, they saw more than one surgeon before deciding on joint arthroplasty.
The effects of DTCM on resident and fellowship training require serious consideration. An emphasis on technology has come at the expense of learning the science and art of orthopedics.8 Physicians in training are pressured both to produce more and to use whichever specific technique or product a patient requests.4 Similarly, orthopedic surgeons are seeing job advertisements that read, “Training in robotic surgery or anterior approach is preferred.” Employer pressure can have profound implications for residents and fellows, who may feel compelled to learn these techniques. To a large degree, residents and fellows learn by accompanying their mentors and closely observing their decision-making processes and interactions with patients. Decisions regarding fellowships should not be influenced by surgical techniques or implant choices but by the quality and breadth of clinical experience.
DTCM likely will continue to shape all aspects of care. Claims made by physicians and hospitals are especially troubling because patients trust these sources. We face the challenge of reaffirming our commitment to patients and orthopedic surgeons. As the leader in musculoskeletal education, the American Academy of Orthopaedic Surgeons (AAOS) not only must provide educational material that is compatible with current technological media but must address current controversies and misleading claims. Toward that end, AAOS can expand its patient website, OrthoInfo, to include information on new technologies and surgical techniques pertaining to each musculoskeletal condition. Educating the public about risk factors for poor surgical outcomes is equally important in order to moderate unrealistic expectations and stimulate discussions on risks involved in unnecessary or potentially harmful technologies. The American Association of Hip and Knee Surgeons (AAHKS) has already embarked on this approach. Orthopedic surgeons should continue to abide by the standards of professionalism—maintaining the tenet of “First do no harm,” resisting the temptations of consumerism, and giving patients accurate information. Taking these measures may help reduce physician shopping and strengthen the patient–physician relationship. We physicians are the guardians of patients’ well-being. We also owe it to orthopedic surgeons in training to provide well-balanced, unbiased education. The focus of training should not be on techniques for gaining market edge but on learning evidence-based medicine and surgical principles. In our burdened healthcare system, curbing DTCM has the potential to decrease unnecessary use of resources and improve the quality of education and patient care.
Am J Orthop. 2016;45(6):E335-E336. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Bhattacharyya T, Tornetta P 3rd, Healy WL, Einhorn TA. The validity of claims made in orthopaedic print advertisements. J Bone Joint Surgery Am. 2003;85(7):1224-1228.
2. Woloshin S, Schwartz LM, Tremmel J, Welch HG. Direct-to-consumer advertisements for prescription drugs: what are Americans being sold? Lancet. 2001;358(9288):1141-1146.
3. Robinson AR, Hohmann KB, Rifkin JI, et al. Direct-to-consumer pharmaceutical advertising: physician and public opinion and potential effects on the physician-patient relationship. Arch Intern Med. 2004;164(4):427-432.
4. Bozic KJ, Smith AR, Hariri S, et al. The 2007 ABJS Marshall Urist award: the impact of direct-to-consumer advertising in orthopaedics. Clin Orthop Relat Res. 2007;(458):202-219.
5. Mason JB. The new demands by patients in the modern era of total joint arthroplasty: a point of view. Clin Orthop Relat Res. 2008;466(1):146-152.
6. Weinstein SL. Words from a “wise old hand”—guideposts for the future. Professor Stuart L. Weinstein. Iowa Orthop J. 2008;28:94-97.
7. Labovitch RS, Bozic KJ, Hansen E. An evaluation of information available on the internet regarding minimally invasive hip arthroplasty. J Arthroplasty. 2006;21(1):1-5.
8. Buckwalter JA. Advancing the science and art of orthopaedics. Lessons from history. J Bone Joint Surg Am. 2000;82(12):1782-1803.
1. Bhattacharyya T, Tornetta P 3rd, Healy WL, Einhorn TA. The validity of claims made in orthopaedic print advertisements. J Bone Joint Surgery Am. 2003;85(7):1224-1228.
2. Woloshin S, Schwartz LM, Tremmel J, Welch HG. Direct-to-consumer advertisements for prescription drugs: what are Americans being sold? Lancet. 2001;358(9288):1141-1146.
3. Robinson AR, Hohmann KB, Rifkin JI, et al. Direct-to-consumer pharmaceutical advertising: physician and public opinion and potential effects on the physician-patient relationship. Arch Intern Med. 2004;164(4):427-432.
4. Bozic KJ, Smith AR, Hariri S, et al. The 2007 ABJS Marshall Urist award: the impact of direct-to-consumer advertising in orthopaedics. Clin Orthop Relat Res. 2007;(458):202-219.
5. Mason JB. The new demands by patients in the modern era of total joint arthroplasty: a point of view. Clin Orthop Relat Res. 2008;466(1):146-152.
6. Weinstein SL. Words from a “wise old hand”—guideposts for the future. Professor Stuart L. Weinstein. Iowa Orthop J. 2008;28:94-97.
7. Labovitch RS, Bozic KJ, Hansen E. An evaluation of information available on the internet regarding minimally invasive hip arthroplasty. J Arthroplasty. 2006;21(1):1-5.
8. Buckwalter JA. Advancing the science and art of orthopaedics. Lessons from history. J Bone Joint Surg Am. 2000;82(12):1782-1803.