User login
Soccer injuries up 111% in children
The rate of soccer injuries treated at U.S. emergency departments among patients aged 7-17 years rose by 111%, and that of soccer-related concussions and closed-head injuries increased by 1,595%, during the last 25 years, according to a report published online Sept. 12 in Pediatrics.
These increases underscore the need to improve injury prevention in this patient population. In particular, concussion prevention should focus on reducing player-to-player contact, especially during illegal moves. “Education of players, coaches, referees or officials, and parents about the importance of following the rules of the game, and enforcement of those rules, are critical first steps,” said Nicholas A. Smith of the Center for Injury Research and Policy, the Research Institute at Nationwide Children’s Hospital, Columbus, and his associates.
In what they described as the first study to comprehensively examine the epidemiology of U.S. youth soccer-related injuries treated at EDs, the investigators analyzed data from a nationally representative injury surveillance system between 1990 and 2014. Almost 3 million children were treated during that period for concussions/closed-head injuries, fractures, dislocations, sprains or strains, soft-tissue injuries such as abrasions or hematomas, lacerations, nondental avulsions, or punctures sustained during soccer practice or games.
The annual rate of soccer-related injury per 10,000 participants rose by 111%, and the annual number of such injuries rose by 78%. Much of this increase was attributed to a 1,595% rise in the annual rate of concussions/closed-head injuries and a 1,332% rise in the number of concussions/closed-head injuries. Patients with head injuries were twice as likely to be admitted to the hospital as were those with other types of injury, highlighting the severity of head injuries, the investigators noted.
The majority of injuries (73%) occurred in older children aged 12-17 years; their injury rate was more than three times higher than that in younger children, “probably because of the more aggressive play and the higher-energy impacts associated with the older age group,” Mr. Smith and his associates wrote (Pediatrics. 2016 Sep 12. doi: 10.1542/peds.2016-0346).
The increase in soccer-related injuries was much greater among girls than among boys, paralleling the much larger increase in soccer participation among girls than among boys during the study period.
This study underestimates the actual number of soccer-related injuries because it didn’t include patients who were treated in health care settings other than the ED and patients who were not treated at all, the investigators added.
The rate of soccer injuries treated at U.S. emergency departments among patients aged 7-17 years rose by 111%, and that of soccer-related concussions and closed-head injuries increased by 1,595%, during the last 25 years, according to a report published online Sept. 12 in Pediatrics.
These increases underscore the need to improve injury prevention in this patient population. In particular, concussion prevention should focus on reducing player-to-player contact, especially during illegal moves. “Education of players, coaches, referees or officials, and parents about the importance of following the rules of the game, and enforcement of those rules, are critical first steps,” said Nicholas A. Smith of the Center for Injury Research and Policy, the Research Institute at Nationwide Children’s Hospital, Columbus, and his associates.
In what they described as the first study to comprehensively examine the epidemiology of U.S. youth soccer-related injuries treated at EDs, the investigators analyzed data from a nationally representative injury surveillance system between 1990 and 2014. Almost 3 million children were treated during that period for concussions/closed-head injuries, fractures, dislocations, sprains or strains, soft-tissue injuries such as abrasions or hematomas, lacerations, nondental avulsions, or punctures sustained during soccer practice or games.
The annual rate of soccer-related injury per 10,000 participants rose by 111%, and the annual number of such injuries rose by 78%. Much of this increase was attributed to a 1,595% rise in the annual rate of concussions/closed-head injuries and a 1,332% rise in the number of concussions/closed-head injuries. Patients with head injuries were twice as likely to be admitted to the hospital as were those with other types of injury, highlighting the severity of head injuries, the investigators noted.
The majority of injuries (73%) occurred in older children aged 12-17 years; their injury rate was more than three times higher than that in younger children, “probably because of the more aggressive play and the higher-energy impacts associated with the older age group,” Mr. Smith and his associates wrote (Pediatrics. 2016 Sep 12. doi: 10.1542/peds.2016-0346).
The increase in soccer-related injuries was much greater among girls than among boys, paralleling the much larger increase in soccer participation among girls than among boys during the study period.
This study underestimates the actual number of soccer-related injuries because it didn’t include patients who were treated in health care settings other than the ED and patients who were not treated at all, the investigators added.
The rate of soccer injuries treated at U.S. emergency departments among patients aged 7-17 years rose by 111%, and that of soccer-related concussions and closed-head injuries increased by 1,595%, during the last 25 years, according to a report published online Sept. 12 in Pediatrics.
These increases underscore the need to improve injury prevention in this patient population. In particular, concussion prevention should focus on reducing player-to-player contact, especially during illegal moves. “Education of players, coaches, referees or officials, and parents about the importance of following the rules of the game, and enforcement of those rules, are critical first steps,” said Nicholas A. Smith of the Center for Injury Research and Policy, the Research Institute at Nationwide Children’s Hospital, Columbus, and his associates.
In what they described as the first study to comprehensively examine the epidemiology of U.S. youth soccer-related injuries treated at EDs, the investigators analyzed data from a nationally representative injury surveillance system between 1990 and 2014. Almost 3 million children were treated during that period for concussions/closed-head injuries, fractures, dislocations, sprains or strains, soft-tissue injuries such as abrasions or hematomas, lacerations, nondental avulsions, or punctures sustained during soccer practice or games.
The annual rate of soccer-related injury per 10,000 participants rose by 111%, and the annual number of such injuries rose by 78%. Much of this increase was attributed to a 1,595% rise in the annual rate of concussions/closed-head injuries and a 1,332% rise in the number of concussions/closed-head injuries. Patients with head injuries were twice as likely to be admitted to the hospital as were those with other types of injury, highlighting the severity of head injuries, the investigators noted.
The majority of injuries (73%) occurred in older children aged 12-17 years; their injury rate was more than three times higher than that in younger children, “probably because of the more aggressive play and the higher-energy impacts associated with the older age group,” Mr. Smith and his associates wrote (Pediatrics. 2016 Sep 12. doi: 10.1542/peds.2016-0346).
The increase in soccer-related injuries was much greater among girls than among boys, paralleling the much larger increase in soccer participation among girls than among boys during the study period.
This study underestimates the actual number of soccer-related injuries because it didn’t include patients who were treated in health care settings other than the ED and patients who were not treated at all, the investigators added.
FROM PEDIATRICS
Key clinical point: Soccer injuries treated at U.S. emergency departments rose by 111% during the last 25 years among children aged 7-17 years.
Major finding: Much of the increase in soccer-related injuries was attributed to a 1,595% rise in the annual rate of concussions/closed-head injuries.
Data source: A retrospective analysis of a nationally representative database involving almost 3 million pediatric soccer injuries over a 25-year period.
Disclosures: This study was supported by the Research Institute at Nationwide Children’s Hospital and Ohio State University. Mr. Smith and his associates reported having no relevant financial disclosures.
Antibiotic stewardship lacking at many hospital nurseries
Nearly one-third of hospital newborn nurseries and neonatal ICUs do not have an antibiotic stewardship program, according to a survey of 146 hospital nursery centers across all 50 states.
Researchers randomly selected a level III NICU in each state using the 2014 American Hospital Association annual survey, then selected a level I and level II nursery in the same city. They collected data on the hospital, nursery, and antibiotic stewardship program characteristics and interviewed staff pharmacists and infectious diseases physicians (J Pediatric Infect Dis Soc. 2016 Jul 15. doi: 10.1093/jpids/piw040).
A total of 104 (71%) of responding hospitals had an antibiotic stewardship program in place for their nurseries. Hospitals with a nursery-based antibiotic stewardship programs tended to be larger, have more full-time equivalent staff dedicated to the antibiotic stewardship program, have higher level nurses, and be affiliated with a university, according to Joseph B. Cantey, MD, and his colleagues from the Texas A&M Health Science Center in Temple.
Geographic region and core stewardship strategies did not influence the likelihood of a nursery-based antibiotic stewardship program in place.
From the interviews, the researchers identified several barriers to implementation of antibiotic stewardship programs, and themes such as unwanted coverage, unnecessary coverage, and need for communication.
“Many [antibiotic stewardship program] and nursery representatives stated that nursery [antibiotic stewardship program] coverage was not important, either because antibiotic consumption was perceived as low (theme 1), narrow-spectrum (theme 2), or both,” the authors wrote.
Some nursery providers also argued that participating in stewardship programs was time consuming and not valuable, which the authors said was often related to a lack of pediatric expertise in the program providers. Some of those interviewed also spoke of issues relating to jurisdiction and responsibility for the programs, and there was also a common perception that antibiotic stewardship programs were more concerned with cost savings than patient care.
“Barriers to effective nursery stewardship are exacerbated by lack of communication between stewardship providers and their nursery counterparts,” the authors reported.
No conflicts of interest were declared.
Nearly one-third of hospital newborn nurseries and neonatal ICUs do not have an antibiotic stewardship program, according to a survey of 146 hospital nursery centers across all 50 states.
Researchers randomly selected a level III NICU in each state using the 2014 American Hospital Association annual survey, then selected a level I and level II nursery in the same city. They collected data on the hospital, nursery, and antibiotic stewardship program characteristics and interviewed staff pharmacists and infectious diseases physicians (J Pediatric Infect Dis Soc. 2016 Jul 15. doi: 10.1093/jpids/piw040).
A total of 104 (71%) of responding hospitals had an antibiotic stewardship program in place for their nurseries. Hospitals with a nursery-based antibiotic stewardship programs tended to be larger, have more full-time equivalent staff dedicated to the antibiotic stewardship program, have higher level nurses, and be affiliated with a university, according to Joseph B. Cantey, MD, and his colleagues from the Texas A&M Health Science Center in Temple.
Geographic region and core stewardship strategies did not influence the likelihood of a nursery-based antibiotic stewardship program in place.
From the interviews, the researchers identified several barriers to implementation of antibiotic stewardship programs, and themes such as unwanted coverage, unnecessary coverage, and need for communication.
“Many [antibiotic stewardship program] and nursery representatives stated that nursery [antibiotic stewardship program] coverage was not important, either because antibiotic consumption was perceived as low (theme 1), narrow-spectrum (theme 2), or both,” the authors wrote.
Some nursery providers also argued that participating in stewardship programs was time consuming and not valuable, which the authors said was often related to a lack of pediatric expertise in the program providers. Some of those interviewed also spoke of issues relating to jurisdiction and responsibility for the programs, and there was also a common perception that antibiotic stewardship programs were more concerned with cost savings than patient care.
“Barriers to effective nursery stewardship are exacerbated by lack of communication between stewardship providers and their nursery counterparts,” the authors reported.
No conflicts of interest were declared.
Nearly one-third of hospital newborn nurseries and neonatal ICUs do not have an antibiotic stewardship program, according to a survey of 146 hospital nursery centers across all 50 states.
Researchers randomly selected a level III NICU in each state using the 2014 American Hospital Association annual survey, then selected a level I and level II nursery in the same city. They collected data on the hospital, nursery, and antibiotic stewardship program characteristics and interviewed staff pharmacists and infectious diseases physicians (J Pediatric Infect Dis Soc. 2016 Jul 15. doi: 10.1093/jpids/piw040).
A total of 104 (71%) of responding hospitals had an antibiotic stewardship program in place for their nurseries. Hospitals with a nursery-based antibiotic stewardship programs tended to be larger, have more full-time equivalent staff dedicated to the antibiotic stewardship program, have higher level nurses, and be affiliated with a university, according to Joseph B. Cantey, MD, and his colleagues from the Texas A&M Health Science Center in Temple.
Geographic region and core stewardship strategies did not influence the likelihood of a nursery-based antibiotic stewardship program in place.
From the interviews, the researchers identified several barriers to implementation of antibiotic stewardship programs, and themes such as unwanted coverage, unnecessary coverage, and need for communication.
“Many [antibiotic stewardship program] and nursery representatives stated that nursery [antibiotic stewardship program] coverage was not important, either because antibiotic consumption was perceived as low (theme 1), narrow-spectrum (theme 2), or both,” the authors wrote.
Some nursery providers also argued that participating in stewardship programs was time consuming and not valuable, which the authors said was often related to a lack of pediatric expertise in the program providers. Some of those interviewed also spoke of issues relating to jurisdiction and responsibility for the programs, and there was also a common perception that antibiotic stewardship programs were more concerned with cost savings than patient care.
“Barriers to effective nursery stewardship are exacerbated by lack of communication between stewardship providers and their nursery counterparts,” the authors reported.
No conflicts of interest were declared.
FROM JOURNAL OF THE PEDIATRIC INFECTIOUS DISEASES SOCIETY
Key clinical point: Many hospital newborn nurseries or neonatal ICUs do not have an antibiotic stewardship program in place.
Major finding: 29% of hospital nurseries surveyed did not have an antibiotic stewardship program.
Data source: Survey of 146 hospital nursery centers in 50 states.
Disclosures: No conflicts of interest were declared.
Zika’s not the only mosquito-borne virus to worry about
NEWPORT BEACH, CALIF. – As the spread of Zika virus continues to garner attention in the national spotlight, two other mosquito-borne viral infections pose a potential threat to the United States: dengue fever and chikungunya.
At the annual meeting of the Pacific Dermatologic Association, Iris Z. Ahronowitz, MD, shared tips on how to spot and diagnose patients with these viral infections.
“You really need to use all the data at your disposal, including a thorough symptom history, a thorough exposure history, and of course, our most important tool in all of this: our eyes,” said Dr. Ahronowitz, a dermatologist at the University of Southern California, Los Angeles. Reaching a diagnosis involves asking about epidemiologic exposure, symptoms, morphology, and performing confirmatory testing by PCR and/or ELISA. “Unfortunately we are not getting these results very quickly,” she said. “Sometimes the turn-around time can be 3 weeks or longer.”
She discussed the case of a 32-year-old woman who had returned from travel to Central Mexico (J Am Acad Dermatol. 2008;58[2]:308-16). Two days later, she developed fever, fatigue, and retro-orbital headache, as well as flushing macular erythema over the chest. Three days later, she developed a generalized morbilliform eruption. Her white blood cell count was 1.5, platelets were 37, aspartate aminotransferase was 124 and alanine aminotransferase was 87.
The differential diagnosis for morbilliform eruption plus fever in a returning traveler is extensive, Dr. Ahronowitz said, including measles, chikungunya, West Nile virus, O’nyong-nyong fever, Mayaro virus, Sindbis virus, Ross river disease, Ebola/Marburg, dengue, and Zika. Bacterial/rickettsial possibilities include typhoid fever, typhus, and leptospirosis.
The patient was ultimately diagnosed with dengue virus, a mosquito-borne flavivirus. Five serotypes have been identified, the most recent in 2013. According to Dr. Ahronowitz, dengue ranks as the most common febrile illness in travelers returning from the Caribbean, South American, and Southeast Asia. “There are up to 100 million cases every year, 40% of the world population is at risk, and an estimated 80% of people are asymptomatic carriers, which is facilitating the spread of this disease,” she said. The most common vector is Aedes aegypti, a daytime biting mosquito that is endemic to the tropics and subtropics. But a new vector is emerging, A. albopictus, which is common in temperate areas. “Both types of mosquitoes are in the United States, and they’re spreading rapidly,” she said. “This is probably due to a combination of climate change and international travel.”
Dengue classically presents with sudden onset of fevers, headaches, and particularly retro-orbital pain, severe myalgia; 50%-82% of cases develop a distinctive rash. “While most viruses have nonspecific lab abnormalities, one that can be very helpful to you with suspected dengue is thrombocytopenia,” she said. “The incubation period ranges from 3 to 14 days.”
Rashes associated with dengue are classically biphasic and sequential. The initial rash occurs within 24-48 hours of symptom onset and is often mistaken for sunburn, with a flushing erythema of the face, neck, and chest. Three to five days later, a subsequent rash develops that starts out as a generalized morbilliform eruption but becomes confluent with petechiae and islands of sparing. “It’s been described as white islands in a sea of red,” Dr. Ahronowitz said.
A more severe form of the disease, dengue hemorrhagic fever, is characterized by extensive purpura and bleeding from mucosa, GI tract, and injection sites. “The patients who get this have prior immunity to a different serotype,” she said. “This is thought to be due to a phenomenon called antibody-dependent enhancement whereby the presence of preexisting antibodies facilitates entry of the virus and produces a more robust inflammatory response. Most of these patients, even the ones with severe dengue, recover fully. The most common long-term sequela we’re seeing is chronic fatigue.”
The diagnosis is made with viral PCR from serum less than 7 days from onset of symptoms, or IgM ELISA more than 4 days from onset of symptoms. The treatment is supportive care with fluid resuscitation and analgesia; there’s no specific treatment. “Do not give NSAIDs, which can potentiate hemorrhage; give acetaminophen for pain and fevers,” she advised. “A tetravalent vaccine is now available for dengue. Prevention is so important because there is no treatment.”
Next, Dr. Ahronowitz discussed the case of a 38-year-old man who returned from travel to Bangladesh (Int J Dermatol. 2008;47[1]:1148-52). Two days after returning he developed fever to 104 degrees, headaches, and cervical lymphadenopathy. Three days after returning, he developed severe pain in the wrist, knees, and ankles, and a rash. “This rash was not specific, it was a morbilliform eruption primarily on the chest,” she said.
The patient was ultimately diagnosed with chikungunya, a single-strand RNA mosquito-borne virus with the same vectors as dengue. “This has been wreaking havoc across the Caribbean in the past few years,” Dr. Ahronowitz said. “Chikungunya was first identified in the Americas in 2013, and there have been hundreds of thousands of cases in the Caribbean.” The first case acquired in the United States occurred in Florida in the summer of 2014. As of January 2016 there were 679 imported cases of the infection in the United States. “Fortunately, this most recent epidemic is slowing down a bit, but it’s important to be aware of,” she said.
Clinical presentation of chikungunya includes an incubation period of 3-7 days, acute onset of high fevers, chills, and myalgia. Nonspecific exanthem around 3 days occurs in 40%-75% of cases, and symmetric polyarthralgias are common in the fingers, wrists, and ankles. Labs may reveal lymphopenia, AKI, and elevated AST/ALT. Acute symptoms resolve within 7-10 days.
Besides the rash, other cutaneous signs of the disease include aphthous-like ulcers and anogenital ulcers, particularly around the scrotum. Other patients may present with controfacial hyperpigmentation, also known as “brownie nose,” that appears with the rash. In babies, bullous lesions can occur. More than 20% of patients who acquire chikungunya still have severe joint pain 1 year after initial presentation. “This can be really debilitating,” she said. “A subset of patients will develop an inflammatory seronegative rheumatoid-like arthritis. It’s generally not a fatal condition except in the extremes of age and in people with a lot of comorbidities. Most people recover fully.”
As in dengue, clinicians can diagnose chikungunya by viral culture in the first 3 days of illness, and by RT-PCR in the first 8 days of illness. On serology, IgM is positive by 5 days of symptom onset.
“If testing is not available locally, contact the [Centers for Disease Control and Prevention],” Dr. Ahronowitz said. “Treatment is supportive. Evaluate for and treat potential coinfections, including dengue, malaria, and bacterial infections. If dengue is in the differential diagnosis, avoid NSAIDs.” A new vaccine for chikungunya is currently in phase II trials.
Dr. Ahronowitz reported having no relevant disclosures.
NEWPORT BEACH, CALIF. – As the spread of Zika virus continues to garner attention in the national spotlight, two other mosquito-borne viral infections pose a potential threat to the United States: dengue fever and chikungunya.
At the annual meeting of the Pacific Dermatologic Association, Iris Z. Ahronowitz, MD, shared tips on how to spot and diagnose patients with these viral infections.
“You really need to use all the data at your disposal, including a thorough symptom history, a thorough exposure history, and of course, our most important tool in all of this: our eyes,” said Dr. Ahronowitz, a dermatologist at the University of Southern California, Los Angeles. Reaching a diagnosis involves asking about epidemiologic exposure, symptoms, morphology, and performing confirmatory testing by PCR and/or ELISA. “Unfortunately we are not getting these results very quickly,” she said. “Sometimes the turn-around time can be 3 weeks or longer.”
She discussed the case of a 32-year-old woman who had returned from travel to Central Mexico (J Am Acad Dermatol. 2008;58[2]:308-16). Two days later, she developed fever, fatigue, and retro-orbital headache, as well as flushing macular erythema over the chest. Three days later, she developed a generalized morbilliform eruption. Her white blood cell count was 1.5, platelets were 37, aspartate aminotransferase was 124 and alanine aminotransferase was 87.
The differential diagnosis for morbilliform eruption plus fever in a returning traveler is extensive, Dr. Ahronowitz said, including measles, chikungunya, West Nile virus, O’nyong-nyong fever, Mayaro virus, Sindbis virus, Ross river disease, Ebola/Marburg, dengue, and Zika. Bacterial/rickettsial possibilities include typhoid fever, typhus, and leptospirosis.
The patient was ultimately diagnosed with dengue virus, a mosquito-borne flavivirus. Five serotypes have been identified, the most recent in 2013. According to Dr. Ahronowitz, dengue ranks as the most common febrile illness in travelers returning from the Caribbean, South American, and Southeast Asia. “There are up to 100 million cases every year, 40% of the world population is at risk, and an estimated 80% of people are asymptomatic carriers, which is facilitating the spread of this disease,” she said. The most common vector is Aedes aegypti, a daytime biting mosquito that is endemic to the tropics and subtropics. But a new vector is emerging, A. albopictus, which is common in temperate areas. “Both types of mosquitoes are in the United States, and they’re spreading rapidly,” she said. “This is probably due to a combination of climate change and international travel.”
Dengue classically presents with sudden onset of fevers, headaches, and particularly retro-orbital pain, severe myalgia; 50%-82% of cases develop a distinctive rash. “While most viruses have nonspecific lab abnormalities, one that can be very helpful to you with suspected dengue is thrombocytopenia,” she said. “The incubation period ranges from 3 to 14 days.”
Rashes associated with dengue are classically biphasic and sequential. The initial rash occurs within 24-48 hours of symptom onset and is often mistaken for sunburn, with a flushing erythema of the face, neck, and chest. Three to five days later, a subsequent rash develops that starts out as a generalized morbilliform eruption but becomes confluent with petechiae and islands of sparing. “It’s been described as white islands in a sea of red,” Dr. Ahronowitz said.
A more severe form of the disease, dengue hemorrhagic fever, is characterized by extensive purpura and bleeding from mucosa, GI tract, and injection sites. “The patients who get this have prior immunity to a different serotype,” she said. “This is thought to be due to a phenomenon called antibody-dependent enhancement whereby the presence of preexisting antibodies facilitates entry of the virus and produces a more robust inflammatory response. Most of these patients, even the ones with severe dengue, recover fully. The most common long-term sequela we’re seeing is chronic fatigue.”
The diagnosis is made with viral PCR from serum less than 7 days from onset of symptoms, or IgM ELISA more than 4 days from onset of symptoms. The treatment is supportive care with fluid resuscitation and analgesia; there’s no specific treatment. “Do not give NSAIDs, which can potentiate hemorrhage; give acetaminophen for pain and fevers,” she advised. “A tetravalent vaccine is now available for dengue. Prevention is so important because there is no treatment.”
Next, Dr. Ahronowitz discussed the case of a 38-year-old man who returned from travel to Bangladesh (Int J Dermatol. 2008;47[1]:1148-52). Two days after returning he developed fever to 104 degrees, headaches, and cervical lymphadenopathy. Three days after returning, he developed severe pain in the wrist, knees, and ankles, and a rash. “This rash was not specific, it was a morbilliform eruption primarily on the chest,” she said.
The patient was ultimately diagnosed with chikungunya, a single-strand RNA mosquito-borne virus with the same vectors as dengue. “This has been wreaking havoc across the Caribbean in the past few years,” Dr. Ahronowitz said. “Chikungunya was first identified in the Americas in 2013, and there have been hundreds of thousands of cases in the Caribbean.” The first case acquired in the United States occurred in Florida in the summer of 2014. As of January 2016 there were 679 imported cases of the infection in the United States. “Fortunately, this most recent epidemic is slowing down a bit, but it’s important to be aware of,” she said.
Clinical presentation of chikungunya includes an incubation period of 3-7 days, acute onset of high fevers, chills, and myalgia. Nonspecific exanthem around 3 days occurs in 40%-75% of cases, and symmetric polyarthralgias are common in the fingers, wrists, and ankles. Labs may reveal lymphopenia, AKI, and elevated AST/ALT. Acute symptoms resolve within 7-10 days.
Besides the rash, other cutaneous signs of the disease include aphthous-like ulcers and anogenital ulcers, particularly around the scrotum. Other patients may present with controfacial hyperpigmentation, also known as “brownie nose,” that appears with the rash. In babies, bullous lesions can occur. More than 20% of patients who acquire chikungunya still have severe joint pain 1 year after initial presentation. “This can be really debilitating,” she said. “A subset of patients will develop an inflammatory seronegative rheumatoid-like arthritis. It’s generally not a fatal condition except in the extremes of age and in people with a lot of comorbidities. Most people recover fully.”
As in dengue, clinicians can diagnose chikungunya by viral culture in the first 3 days of illness, and by RT-PCR in the first 8 days of illness. On serology, IgM is positive by 5 days of symptom onset.
“If testing is not available locally, contact the [Centers for Disease Control and Prevention],” Dr. Ahronowitz said. “Treatment is supportive. Evaluate for and treat potential coinfections, including dengue, malaria, and bacterial infections. If dengue is in the differential diagnosis, avoid NSAIDs.” A new vaccine for chikungunya is currently in phase II trials.
Dr. Ahronowitz reported having no relevant disclosures.
NEWPORT BEACH, CALIF. – As the spread of Zika virus continues to garner attention in the national spotlight, two other mosquito-borne viral infections pose a potential threat to the United States: dengue fever and chikungunya.
At the annual meeting of the Pacific Dermatologic Association, Iris Z. Ahronowitz, MD, shared tips on how to spot and diagnose patients with these viral infections.
“You really need to use all the data at your disposal, including a thorough symptom history, a thorough exposure history, and of course, our most important tool in all of this: our eyes,” said Dr. Ahronowitz, a dermatologist at the University of Southern California, Los Angeles. Reaching a diagnosis involves asking about epidemiologic exposure, symptoms, morphology, and performing confirmatory testing by PCR and/or ELISA. “Unfortunately we are not getting these results very quickly,” she said. “Sometimes the turn-around time can be 3 weeks or longer.”
She discussed the case of a 32-year-old woman who had returned from travel to Central Mexico (J Am Acad Dermatol. 2008;58[2]:308-16). Two days later, she developed fever, fatigue, and retro-orbital headache, as well as flushing macular erythema over the chest. Three days later, she developed a generalized morbilliform eruption. Her white blood cell count was 1.5, platelets were 37, aspartate aminotransferase was 124 and alanine aminotransferase was 87.
The differential diagnosis for morbilliform eruption plus fever in a returning traveler is extensive, Dr. Ahronowitz said, including measles, chikungunya, West Nile virus, O’nyong-nyong fever, Mayaro virus, Sindbis virus, Ross river disease, Ebola/Marburg, dengue, and Zika. Bacterial/rickettsial possibilities include typhoid fever, typhus, and leptospirosis.
The patient was ultimately diagnosed with dengue virus, a mosquito-borne flavivirus. Five serotypes have been identified, the most recent in 2013. According to Dr. Ahronowitz, dengue ranks as the most common febrile illness in travelers returning from the Caribbean, South American, and Southeast Asia. “There are up to 100 million cases every year, 40% of the world population is at risk, and an estimated 80% of people are asymptomatic carriers, which is facilitating the spread of this disease,” she said. The most common vector is Aedes aegypti, a daytime biting mosquito that is endemic to the tropics and subtropics. But a new vector is emerging, A. albopictus, which is common in temperate areas. “Both types of mosquitoes are in the United States, and they’re spreading rapidly,” she said. “This is probably due to a combination of climate change and international travel.”
Dengue classically presents with sudden onset of fevers, headaches, and particularly retro-orbital pain, severe myalgia; 50%-82% of cases develop a distinctive rash. “While most viruses have nonspecific lab abnormalities, one that can be very helpful to you with suspected dengue is thrombocytopenia,” she said. “The incubation period ranges from 3 to 14 days.”
Rashes associated with dengue are classically biphasic and sequential. The initial rash occurs within 24-48 hours of symptom onset and is often mistaken for sunburn, with a flushing erythema of the face, neck, and chest. Three to five days later, a subsequent rash develops that starts out as a generalized morbilliform eruption but becomes confluent with petechiae and islands of sparing. “It’s been described as white islands in a sea of red,” Dr. Ahronowitz said.
A more severe form of the disease, dengue hemorrhagic fever, is characterized by extensive purpura and bleeding from mucosa, GI tract, and injection sites. “The patients who get this have prior immunity to a different serotype,” she said. “This is thought to be due to a phenomenon called antibody-dependent enhancement whereby the presence of preexisting antibodies facilitates entry of the virus and produces a more robust inflammatory response. Most of these patients, even the ones with severe dengue, recover fully. The most common long-term sequela we’re seeing is chronic fatigue.”
The diagnosis is made with viral PCR from serum less than 7 days from onset of symptoms, or IgM ELISA more than 4 days from onset of symptoms. The treatment is supportive care with fluid resuscitation and analgesia; there’s no specific treatment. “Do not give NSAIDs, which can potentiate hemorrhage; give acetaminophen for pain and fevers,” she advised. “A tetravalent vaccine is now available for dengue. Prevention is so important because there is no treatment.”
Next, Dr. Ahronowitz discussed the case of a 38-year-old man who returned from travel to Bangladesh (Int J Dermatol. 2008;47[1]:1148-52). Two days after returning he developed fever to 104 degrees, headaches, and cervical lymphadenopathy. Three days after returning, he developed severe pain in the wrist, knees, and ankles, and a rash. “This rash was not specific, it was a morbilliform eruption primarily on the chest,” she said.
The patient was ultimately diagnosed with chikungunya, a single-strand RNA mosquito-borne virus with the same vectors as dengue. “This has been wreaking havoc across the Caribbean in the past few years,” Dr. Ahronowitz said. “Chikungunya was first identified in the Americas in 2013, and there have been hundreds of thousands of cases in the Caribbean.” The first case acquired in the United States occurred in Florida in the summer of 2014. As of January 2016 there were 679 imported cases of the infection in the United States. “Fortunately, this most recent epidemic is slowing down a bit, but it’s important to be aware of,” she said.
Clinical presentation of chikungunya includes an incubation period of 3-7 days, acute onset of high fevers, chills, and myalgia. Nonspecific exanthem around 3 days occurs in 40%-75% of cases, and symmetric polyarthralgias are common in the fingers, wrists, and ankles. Labs may reveal lymphopenia, AKI, and elevated AST/ALT. Acute symptoms resolve within 7-10 days.
Besides the rash, other cutaneous signs of the disease include aphthous-like ulcers and anogenital ulcers, particularly around the scrotum. Other patients may present with controfacial hyperpigmentation, also known as “brownie nose,” that appears with the rash. In babies, bullous lesions can occur. More than 20% of patients who acquire chikungunya still have severe joint pain 1 year after initial presentation. “This can be really debilitating,” she said. “A subset of patients will develop an inflammatory seronegative rheumatoid-like arthritis. It’s generally not a fatal condition except in the extremes of age and in people with a lot of comorbidities. Most people recover fully.”
As in dengue, clinicians can diagnose chikungunya by viral culture in the first 3 days of illness, and by RT-PCR in the first 8 days of illness. On serology, IgM is positive by 5 days of symptom onset.
“If testing is not available locally, contact the [Centers for Disease Control and Prevention],” Dr. Ahronowitz said. “Treatment is supportive. Evaluate for and treat potential coinfections, including dengue, malaria, and bacterial infections. If dengue is in the differential diagnosis, avoid NSAIDs.” A new vaccine for chikungunya is currently in phase II trials.
Dr. Ahronowitz reported having no relevant disclosures.
EXPERT ANALYSIS AT PDA 2016
FDA, ACOG recommend against using ovarian cancer screening tests
No marketed screening test has been clinically proven to accurately diagnose ovarian cancer, according to a MedWatch announcement from the Food and Drug Administration.
Despite extensive research and published studies, there are currently no screening tests for ovarian cancer that are sensitive enough to reliably screen for ovarian cancer without a high number of inaccurate results,” FDA officials said in a statement.
Officials with the American Congress of Obstetricians and Gynecologists echoed the FDA’s concern, pointing out that several ovarian cancer screening tests, including the CA-125 test and the Risk of Ovarian Cancer Algorithm test, are currently available and claim to detect ovarian cancer before symptoms occur. These claims are “not based on data,” ACOG president Thomas Gellhaus, MD, said in a statement.
The FDA and ACOG both expressed concern that the use of these tests could delay treatment for asymptomatic women with early-stage ovarian cancer and also may result in unnecessary medical procedures for women who receive positive test results even though no cancer is present.
“Using unproven ovarian cancer screening tests also may be harmful for women with increased risk for developing ovarian cancer,” the FDA wrote and added that “women at high risk for developing ovarian cancer should not use any currently offered test that claims to screen for ovarian cancer.”
Instead, women at high risk of developing ovarian cancer, including those with BRCA mutations, should be referred to a genetic counselor, gynecologic oncologist, or other appropriate health care provider for more specialized care, the FDA recommended. “Currently, it appears that the best way to detect ovarian cancer is for both the patient and her clinician to have a high index of suspicion of the diagnosis in symptomatic women. Persistent and progressive symptoms, such as an increase in bloating, pelvic or abdominal pain, or difficulty eating or feeling full quickly, should be evaluated,” Dr. Gellhaus added.
On Twitter @jessnicolecraig
No marketed screening test has been clinically proven to accurately diagnose ovarian cancer, according to a MedWatch announcement from the Food and Drug Administration.
Despite extensive research and published studies, there are currently no screening tests for ovarian cancer that are sensitive enough to reliably screen for ovarian cancer without a high number of inaccurate results,” FDA officials said in a statement.
Officials with the American Congress of Obstetricians and Gynecologists echoed the FDA’s concern, pointing out that several ovarian cancer screening tests, including the CA-125 test and the Risk of Ovarian Cancer Algorithm test, are currently available and claim to detect ovarian cancer before symptoms occur. These claims are “not based on data,” ACOG president Thomas Gellhaus, MD, said in a statement.
The FDA and ACOG both expressed concern that the use of these tests could delay treatment for asymptomatic women with early-stage ovarian cancer and also may result in unnecessary medical procedures for women who receive positive test results even though no cancer is present.
“Using unproven ovarian cancer screening tests also may be harmful for women with increased risk for developing ovarian cancer,” the FDA wrote and added that “women at high risk for developing ovarian cancer should not use any currently offered test that claims to screen for ovarian cancer.”
Instead, women at high risk of developing ovarian cancer, including those with BRCA mutations, should be referred to a genetic counselor, gynecologic oncologist, or other appropriate health care provider for more specialized care, the FDA recommended. “Currently, it appears that the best way to detect ovarian cancer is for both the patient and her clinician to have a high index of suspicion of the diagnosis in symptomatic women. Persistent and progressive symptoms, such as an increase in bloating, pelvic or abdominal pain, or difficulty eating or feeling full quickly, should be evaluated,” Dr. Gellhaus added.
On Twitter @jessnicolecraig
No marketed screening test has been clinically proven to accurately diagnose ovarian cancer, according to a MedWatch announcement from the Food and Drug Administration.
Despite extensive research and published studies, there are currently no screening tests for ovarian cancer that are sensitive enough to reliably screen for ovarian cancer without a high number of inaccurate results,” FDA officials said in a statement.
Officials with the American Congress of Obstetricians and Gynecologists echoed the FDA’s concern, pointing out that several ovarian cancer screening tests, including the CA-125 test and the Risk of Ovarian Cancer Algorithm test, are currently available and claim to detect ovarian cancer before symptoms occur. These claims are “not based on data,” ACOG president Thomas Gellhaus, MD, said in a statement.
The FDA and ACOG both expressed concern that the use of these tests could delay treatment for asymptomatic women with early-stage ovarian cancer and also may result in unnecessary medical procedures for women who receive positive test results even though no cancer is present.
“Using unproven ovarian cancer screening tests also may be harmful for women with increased risk for developing ovarian cancer,” the FDA wrote and added that “women at high risk for developing ovarian cancer should not use any currently offered test that claims to screen for ovarian cancer.”
Instead, women at high risk of developing ovarian cancer, including those with BRCA mutations, should be referred to a genetic counselor, gynecologic oncologist, or other appropriate health care provider for more specialized care, the FDA recommended. “Currently, it appears that the best way to detect ovarian cancer is for both the patient and her clinician to have a high index of suspicion of the diagnosis in symptomatic women. Persistent and progressive symptoms, such as an increase in bloating, pelvic or abdominal pain, or difficulty eating or feeling full quickly, should be evaluated,” Dr. Gellhaus added.
On Twitter @jessnicolecraig
Study: One hour with patients means two hours on EHR
Physicians are spending twice as much time on electronic health records as they are face to face with patients, according to a new study by the American Medical Association.
Researchers observed 57 physicians in four specialties (family medicine, internal medicine, cardiology, and orthopedics) and found that for every hour of direct clinical face time with patients, nearly 2 additional hours is spent on EHR and desk work within the clinic day. Additionally, based on diaries kept by 21 of the participating physicians, another 1-2 hours of personal time were spent each night doing additional computer and clerical work, according to the study published Sept. 5 in Annals of Internal Medicine (2016. doi: 10.7326/M16-0961).
“Over the years, doctors have recognized that more and more of their time was spent on nonpatient care, activities but probably haven’t recognized the magnitude of that change,” Christine Sinsky, MD, vice president of professional satisfaction at the AMA and lead author on the study, said in an interview. “Our study was able to help to quantify that and paint that picture.”
Overall, physicians spent 27% of their day dealing directly with patients, while 49% of the time was spent on EHR and desk work. In the examination room with patients, physicians spent 53% of time on direct clinical face time and 37% on EHR and desk work.
The situation “is the cumulative effect of many, many well-intended efforts that individually might have made sense, but taken collectively have paradoxically made it harder for physicians to deliver quality of care and harder for patients to get the quality of care they deserve,” she said.
EHR development should be focused on reducing the time-cost of providing care on their platforms, Dr. Sinsky recommended.
She noted that for her practice, it takes 32 clicks to order and record a flu shot. “I think vendors have a responsibility to minimize time, to minimize clicks involved in a task.”
She added that “regulators have a responsibility to not just add more and more regulations without first identifying the time-cost of complying with that regulation and without adding up the total cost of complying with regulation.”
Future regulations on EHRs must add flexibility when it comes to who is entering information into the system, she said. “Many regulations are either written with the explicit statement – or it is implied or an institution might overinterpret the regulation – that the physician is the one who must do the keyboarding into the record,” she said, noting that although not primarily studied in the research, preliminary data suggests that doctors who had documentation support were able to spend more time with their patients.
Finally, physicians themselves need to be stronger advocates for the changes they need to enable them to better serve their patients.
In addition to Dr. Sinsky, three other study authors are employed by AMA, which funded the study. No other financial conflicts were reported.
Physicians are spending twice as much time on electronic health records as they are face to face with patients, according to a new study by the American Medical Association.
Researchers observed 57 physicians in four specialties (family medicine, internal medicine, cardiology, and orthopedics) and found that for every hour of direct clinical face time with patients, nearly 2 additional hours is spent on EHR and desk work within the clinic day. Additionally, based on diaries kept by 21 of the participating physicians, another 1-2 hours of personal time were spent each night doing additional computer and clerical work, according to the study published Sept. 5 in Annals of Internal Medicine (2016. doi: 10.7326/M16-0961).
“Over the years, doctors have recognized that more and more of their time was spent on nonpatient care, activities but probably haven’t recognized the magnitude of that change,” Christine Sinsky, MD, vice president of professional satisfaction at the AMA and lead author on the study, said in an interview. “Our study was able to help to quantify that and paint that picture.”
Overall, physicians spent 27% of their day dealing directly with patients, while 49% of the time was spent on EHR and desk work. In the examination room with patients, physicians spent 53% of time on direct clinical face time and 37% on EHR and desk work.
The situation “is the cumulative effect of many, many well-intended efforts that individually might have made sense, but taken collectively have paradoxically made it harder for physicians to deliver quality of care and harder for patients to get the quality of care they deserve,” she said.
EHR development should be focused on reducing the time-cost of providing care on their platforms, Dr. Sinsky recommended.
She noted that for her practice, it takes 32 clicks to order and record a flu shot. “I think vendors have a responsibility to minimize time, to minimize clicks involved in a task.”
She added that “regulators have a responsibility to not just add more and more regulations without first identifying the time-cost of complying with that regulation and without adding up the total cost of complying with regulation.”
Future regulations on EHRs must add flexibility when it comes to who is entering information into the system, she said. “Many regulations are either written with the explicit statement – or it is implied or an institution might overinterpret the regulation – that the physician is the one who must do the keyboarding into the record,” she said, noting that although not primarily studied in the research, preliminary data suggests that doctors who had documentation support were able to spend more time with their patients.
Finally, physicians themselves need to be stronger advocates for the changes they need to enable them to better serve their patients.
In addition to Dr. Sinsky, three other study authors are employed by AMA, which funded the study. No other financial conflicts were reported.
Physicians are spending twice as much time on electronic health records as they are face to face with patients, according to a new study by the American Medical Association.
Researchers observed 57 physicians in four specialties (family medicine, internal medicine, cardiology, and orthopedics) and found that for every hour of direct clinical face time with patients, nearly 2 additional hours is spent on EHR and desk work within the clinic day. Additionally, based on diaries kept by 21 of the participating physicians, another 1-2 hours of personal time were spent each night doing additional computer and clerical work, according to the study published Sept. 5 in Annals of Internal Medicine (2016. doi: 10.7326/M16-0961).
“Over the years, doctors have recognized that more and more of their time was spent on nonpatient care, activities but probably haven’t recognized the magnitude of that change,” Christine Sinsky, MD, vice president of professional satisfaction at the AMA and lead author on the study, said in an interview. “Our study was able to help to quantify that and paint that picture.”
Overall, physicians spent 27% of their day dealing directly with patients, while 49% of the time was spent on EHR and desk work. In the examination room with patients, physicians spent 53% of time on direct clinical face time and 37% on EHR and desk work.
The situation “is the cumulative effect of many, many well-intended efforts that individually might have made sense, but taken collectively have paradoxically made it harder for physicians to deliver quality of care and harder for patients to get the quality of care they deserve,” she said.
EHR development should be focused on reducing the time-cost of providing care on their platforms, Dr. Sinsky recommended.
She noted that for her practice, it takes 32 clicks to order and record a flu shot. “I think vendors have a responsibility to minimize time, to minimize clicks involved in a task.”
She added that “regulators have a responsibility to not just add more and more regulations without first identifying the time-cost of complying with that regulation and without adding up the total cost of complying with regulation.”
Future regulations on EHRs must add flexibility when it comes to who is entering information into the system, she said. “Many regulations are either written with the explicit statement – or it is implied or an institution might overinterpret the regulation – that the physician is the one who must do the keyboarding into the record,” she said, noting that although not primarily studied in the research, preliminary data suggests that doctors who had documentation support were able to spend more time with their patients.
Finally, physicians themselves need to be stronger advocates for the changes they need to enable them to better serve their patients.
In addition to Dr. Sinsky, three other study authors are employed by AMA, which funded the study. No other financial conflicts were reported.
FROM ANNALS OF INTERNAL MEDICINE
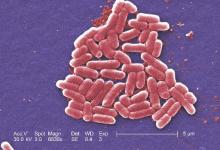
Fourth U.S. case of mcr-1–resistance gene reported
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Wartime Lessons Inform Civilian Medicine
Recent wars have led to innovations in military trauma care that can be applied to civilians, say the authors of a JAMA Viewpoint published in June.1
During the Afghanistan and Iraq wars, the percentage of wounded soldiers who died as a result of their injuries reached its lowest point in recorded history, writes lead author Donald M. Berwick, MD, MPP, of the Institute for Healthcare Improvement in Cambridge, Mass., along with colleagues from the National Academies of Sciences, Engineering, and Medicine in Washington, D.C.
“Effective bleeding-control measures, improved resuscitation techniques, and aggressive neurocritical care interventions are among many advances that saved lives on the battlefield that otherwise would have been lost,” they write.
The reduction in injury-related deaths is in part due to the Military Health System and its Joint Trauma System embracing a culture of continuous performance improvement and an agile approach, a model called “focused empiricism,” the authors say. A new report from the National Academies of Sciences, Engineering, and Medicine clarifies the components of such a learning health system, which can also be applied to civilian care:
- Leadership and a culture of learning: “A learning health system must be stewarded by leadership committed to nurturing a culture of continuous learning and improvement. ... Such a system should unite military and civilian trauma care leaders around a common, core aim established at the highest level in the nation; namely, to achieve zero preventable deaths after injury and minimize trauma-related disability.”
- Transparency and incentives for quality trauma care: “Trauma care practitioners at all levels, including trauma surgeons and other physicians, nurses, technicians, and prehospital care personnel, should have access to data on their performance relative to that of their peers.”
- Systems for ensuring an expert trauma care workforce: “A joint, integrated network of military and civilian trauma centers should be created as a training platform to prepare and sustain an expert workforce and to promote the translation of best practices between sectors.”
The progress made by the military’s trauma system could be lost, the writers conclude, without concerted efforts to disseminate and maintain the advances. The authors note that in the United States, there are nearly 150,000 deaths from trauma each year, and injury is the third-leading cause of death.
The “hundreds of thousands of civilians who have sustained trauma deserve the benefits of care improvements achieved in military medicine,” they conclude.
Reference
- Berwick DM, Downey AS, Cornett EA. A national trauma care system to achieve zero preventable deaths after injury: recommendations from a National Academies of Sciences, Engineering, and Medicine report [published online ahead of print June 17, 2006]. JAMA. doi:10.1001/jama.2016.8524.
Quick Byte
Rating RTLS Options
The healthcare industry typically uses real-time location systems (RTLS) to help improve care quality, workflow efficiency, and bottom lines, according to a recent article in HealthcareITNews. The research firm KLAS rated 11 RTLS vendors and gave Centrak the highest overall performance score, beating competitors including AwarePoint, Cerner, GE Healthcare, and Intelligent Insights.
Reference
- Siwicki B. KLAS ranks real-time location systems from AwarePoint, Cerner, CenTrak, Versus and others. HealthcareITNews website. Accessed July 13, 2016.
Recent wars have led to innovations in military trauma care that can be applied to civilians, say the authors of a JAMA Viewpoint published in June.1
During the Afghanistan and Iraq wars, the percentage of wounded soldiers who died as a result of their injuries reached its lowest point in recorded history, writes lead author Donald M. Berwick, MD, MPP, of the Institute for Healthcare Improvement in Cambridge, Mass., along with colleagues from the National Academies of Sciences, Engineering, and Medicine in Washington, D.C.
“Effective bleeding-control measures, improved resuscitation techniques, and aggressive neurocritical care interventions are among many advances that saved lives on the battlefield that otherwise would have been lost,” they write.
The reduction in injury-related deaths is in part due to the Military Health System and its Joint Trauma System embracing a culture of continuous performance improvement and an agile approach, a model called “focused empiricism,” the authors say. A new report from the National Academies of Sciences, Engineering, and Medicine clarifies the components of such a learning health system, which can also be applied to civilian care:
- Leadership and a culture of learning: “A learning health system must be stewarded by leadership committed to nurturing a culture of continuous learning and improvement. ... Such a system should unite military and civilian trauma care leaders around a common, core aim established at the highest level in the nation; namely, to achieve zero preventable deaths after injury and minimize trauma-related disability.”
- Transparency and incentives for quality trauma care: “Trauma care practitioners at all levels, including trauma surgeons and other physicians, nurses, technicians, and prehospital care personnel, should have access to data on their performance relative to that of their peers.”
- Systems for ensuring an expert trauma care workforce: “A joint, integrated network of military and civilian trauma centers should be created as a training platform to prepare and sustain an expert workforce and to promote the translation of best practices between sectors.”
The progress made by the military’s trauma system could be lost, the writers conclude, without concerted efforts to disseminate and maintain the advances. The authors note that in the United States, there are nearly 150,000 deaths from trauma each year, and injury is the third-leading cause of death.
The “hundreds of thousands of civilians who have sustained trauma deserve the benefits of care improvements achieved in military medicine,” they conclude.
Reference
- Berwick DM, Downey AS, Cornett EA. A national trauma care system to achieve zero preventable deaths after injury: recommendations from a National Academies of Sciences, Engineering, and Medicine report [published online ahead of print June 17, 2006]. JAMA. doi:10.1001/jama.2016.8524.
Quick Byte
Rating RTLS Options
The healthcare industry typically uses real-time location systems (RTLS) to help improve care quality, workflow efficiency, and bottom lines, according to a recent article in HealthcareITNews. The research firm KLAS rated 11 RTLS vendors and gave Centrak the highest overall performance score, beating competitors including AwarePoint, Cerner, GE Healthcare, and Intelligent Insights.
Reference
- Siwicki B. KLAS ranks real-time location systems from AwarePoint, Cerner, CenTrak, Versus and others. HealthcareITNews website. Accessed July 13, 2016.
Recent wars have led to innovations in military trauma care that can be applied to civilians, say the authors of a JAMA Viewpoint published in June.1
During the Afghanistan and Iraq wars, the percentage of wounded soldiers who died as a result of their injuries reached its lowest point in recorded history, writes lead author Donald M. Berwick, MD, MPP, of the Institute for Healthcare Improvement in Cambridge, Mass., along with colleagues from the National Academies of Sciences, Engineering, and Medicine in Washington, D.C.
“Effective bleeding-control measures, improved resuscitation techniques, and aggressive neurocritical care interventions are among many advances that saved lives on the battlefield that otherwise would have been lost,” they write.
The reduction in injury-related deaths is in part due to the Military Health System and its Joint Trauma System embracing a culture of continuous performance improvement and an agile approach, a model called “focused empiricism,” the authors say. A new report from the National Academies of Sciences, Engineering, and Medicine clarifies the components of such a learning health system, which can also be applied to civilian care:
- Leadership and a culture of learning: “A learning health system must be stewarded by leadership committed to nurturing a culture of continuous learning and improvement. ... Such a system should unite military and civilian trauma care leaders around a common, core aim established at the highest level in the nation; namely, to achieve zero preventable deaths after injury and minimize trauma-related disability.”
- Transparency and incentives for quality trauma care: “Trauma care practitioners at all levels, including trauma surgeons and other physicians, nurses, technicians, and prehospital care personnel, should have access to data on their performance relative to that of their peers.”
- Systems for ensuring an expert trauma care workforce: “A joint, integrated network of military and civilian trauma centers should be created as a training platform to prepare and sustain an expert workforce and to promote the translation of best practices between sectors.”
The progress made by the military’s trauma system could be lost, the writers conclude, without concerted efforts to disseminate and maintain the advances. The authors note that in the United States, there are nearly 150,000 deaths from trauma each year, and injury is the third-leading cause of death.
The “hundreds of thousands of civilians who have sustained trauma deserve the benefits of care improvements achieved in military medicine,” they conclude.
Reference
- Berwick DM, Downey AS, Cornett EA. A national trauma care system to achieve zero preventable deaths after injury: recommendations from a National Academies of Sciences, Engineering, and Medicine report [published online ahead of print June 17, 2006]. JAMA. doi:10.1001/jama.2016.8524.
Quick Byte
Rating RTLS Options
The healthcare industry typically uses real-time location systems (RTLS) to help improve care quality, workflow efficiency, and bottom lines, according to a recent article in HealthcareITNews. The research firm KLAS rated 11 RTLS vendors and gave Centrak the highest overall performance score, beating competitors including AwarePoint, Cerner, GE Healthcare, and Intelligent Insights.
Reference
- Siwicki B. KLAS ranks real-time location systems from AwarePoint, Cerner, CenTrak, Versus and others. HealthcareITNews website. Accessed July 13, 2016.
Cancer patients’ caregivers may carry greater burden

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—New research suggests caring for a loved one with cancer may be more burdensome than caring for a loved one with a different condition.
Researchers analyzed data from “Caregiving in the U.S. 2015,” an online panel study of unpaid adult caregivers.
The team compared cancer and non-cancer caregivers to determine similarities and differences in characteristics and experiences.
The findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 4).
The study included 1248 caregivers, age 18 and older at the time they were surveyed, who provided care to an adult patient. Seven percent of these caregivers were looking after patients with cancer.
Cancer caregivers reported spending more hours per week providing care than non-cancer caregivers—32.9 and 23.9 hours, respectively.
In addition, cancer caregivers were more likely than other caregivers to communicate with healthcare professionals (82% and 62%, respectively), monitor and adjust patients’ care (76% and 66%, respectively), and advocate on behalf of patients (62% and 49%, respectively).
Despite high levels of engagement with providers, cancer caregivers were nearly twice as likely as non-cancer caregivers to report needing more help and information with making end-of-life decisions—40% and 21%, respectively.
“Our research demonstrates the ripple effect that cancer has on families and patient support systems,” said study investigator Erin Kent, PhD, of the National Cancer Institute in Rockville, Maryland.
“Caregiving can be extremely stressful and demanding—physically, emotionally, and financially. The data show we need to do a better job of supporting these individuals, as their wellbeing is essential to the patient’s quality of life and outcomes.”
Dr Kent emphasized the cyclical nature of cancer care, often requiring short, highly intense periods of time where patients undergo active treatment as a possible reason for the increased intensity in caregiving. She noted that such intensity is also associated with increased caregiver stress and depression.
“Based on our findings, it’s clear we need additional research on caregiving to better understand at what point providers and clinicians should intervene to assess the wellbeing of caregivers,” Dr Kent said.
“Technology, combined with use of a clinical distress rating system, could be promising in the future as a means to ensure caregivers are being supported in a meaningful way.” ![]()

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—New research suggests caring for a loved one with cancer may be more burdensome than caring for a loved one with a different condition.
Researchers analyzed data from “Caregiving in the U.S. 2015,” an online panel study of unpaid adult caregivers.
The team compared cancer and non-cancer caregivers to determine similarities and differences in characteristics and experiences.
The findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 4).
The study included 1248 caregivers, age 18 and older at the time they were surveyed, who provided care to an adult patient. Seven percent of these caregivers were looking after patients with cancer.
Cancer caregivers reported spending more hours per week providing care than non-cancer caregivers—32.9 and 23.9 hours, respectively.
In addition, cancer caregivers were more likely than other caregivers to communicate with healthcare professionals (82% and 62%, respectively), monitor and adjust patients’ care (76% and 66%, respectively), and advocate on behalf of patients (62% and 49%, respectively).
Despite high levels of engagement with providers, cancer caregivers were nearly twice as likely as non-cancer caregivers to report needing more help and information with making end-of-life decisions—40% and 21%, respectively.
“Our research demonstrates the ripple effect that cancer has on families and patient support systems,” said study investigator Erin Kent, PhD, of the National Cancer Institute in Rockville, Maryland.
“Caregiving can be extremely stressful and demanding—physically, emotionally, and financially. The data show we need to do a better job of supporting these individuals, as their wellbeing is essential to the patient’s quality of life and outcomes.”
Dr Kent emphasized the cyclical nature of cancer care, often requiring short, highly intense periods of time where patients undergo active treatment as a possible reason for the increased intensity in caregiving. She noted that such intensity is also associated with increased caregiver stress and depression.
“Based on our findings, it’s clear we need additional research on caregiving to better understand at what point providers and clinicians should intervene to assess the wellbeing of caregivers,” Dr Kent said.
“Technology, combined with use of a clinical distress rating system, could be promising in the future as a means to ensure caregivers are being supported in a meaningful way.” ![]()

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—New research suggests caring for a loved one with cancer may be more burdensome than caring for a loved one with a different condition.
Researchers analyzed data from “Caregiving in the U.S. 2015,” an online panel study of unpaid adult caregivers.
The team compared cancer and non-cancer caregivers to determine similarities and differences in characteristics and experiences.
The findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 4).
The study included 1248 caregivers, age 18 and older at the time they were surveyed, who provided care to an adult patient. Seven percent of these caregivers were looking after patients with cancer.
Cancer caregivers reported spending more hours per week providing care than non-cancer caregivers—32.9 and 23.9 hours, respectively.
In addition, cancer caregivers were more likely than other caregivers to communicate with healthcare professionals (82% and 62%, respectively), monitor and adjust patients’ care (76% and 66%, respectively), and advocate on behalf of patients (62% and 49%, respectively).
Despite high levels of engagement with providers, cancer caregivers were nearly twice as likely as non-cancer caregivers to report needing more help and information with making end-of-life decisions—40% and 21%, respectively.
“Our research demonstrates the ripple effect that cancer has on families and patient support systems,” said study investigator Erin Kent, PhD, of the National Cancer Institute in Rockville, Maryland.
“Caregiving can be extremely stressful and demanding—physically, emotionally, and financially. The data show we need to do a better job of supporting these individuals, as their wellbeing is essential to the patient’s quality of life and outcomes.”
Dr Kent emphasized the cyclical nature of cancer care, often requiring short, highly intense periods of time where patients undergo active treatment as a possible reason for the increased intensity in caregiving. She noted that such intensity is also associated with increased caregiver stress and depression.
“Based on our findings, it’s clear we need additional research on caregiving to better understand at what point providers and clinicians should intervene to assess the wellbeing of caregivers,” Dr Kent said.
“Technology, combined with use of a clinical distress rating system, could be promising in the future as a means to ensure caregivers are being supported in a meaningful way.” ![]()
10 tips to mitigate legal risks of opioid prescribing
Opioid-related lawsuits against physicians are on the rise. Common allegations include unnecessary prescribing, failing to heed contraindications, and missing warning signs of a likely overdose, said Ericka L. Adler, a Chicago-based health law attorney. To mitigate your risk of getting sued, legal and clinical experts offer the following advice.
1. Identify at-risk patients
Consider the full range of patient risk factors before prescribing or continuing opioids, said Ilene R. Robeck, MD, director of virtual pain education at Richmond VA Medical Center in St. Petersburg, Fla., and cochair of the National VA PACT Pain Champions Initiative.
“When we look at the overdose data, there used to be a perception that people who overdosed were not taking their medication as prescribed, and that’s not true all the time,” she said. “In fact, in some [studies], half the people who overdose take their medication exactly as prescribed. The problems are related to dose, mixing the opioids with other medications, [patient] age, and underlying medical problems.”
Ensure that therapy considerations related to opioids address the full patient picture, Dr. Robeck advised. For example, patients with liver disease, sleep apnea, chronic obstructive pulmonary disease (COPD), asthma, and kidney disease are more prone to overdose. In addition, while nonmedical use of prescription drugs is highest in patients aged 18-25 years, opioid overdose rates are highest among patients aged 25-54 years, according to the Centers for Disease Control and Prevention.
2. Monitor midlevel providers
Closely monitor and limit opioid prescribing by the midlevel providers you supervise, said pharmacologist and consultant James T. O’Donnell, PharmD. A fair share of medical malpractice lawsuits result from failing to supervise a physician assistant (PA) or nurse practitioner (NP) prescribing or treating pain patients.
“Excessive or inappropriate opiate prescribing will result in legal actions against the supervising physician,” Dr. O’Donnell said. “Close monitoring of midlevel providers requires establishing guidelines for opiate prescribing.”
Develop practice protocols that track and regulate midlevel prescribing and regularly discuss prescribing dangers with staff. Know your state law; the extent to which an NP or PA can prescribe varies widely.
3. Document
Keep detailed records of patient encounters that include specifics of what the patient tells you, said Ms. Adler.
Clear documentation about prior conditions, interactions with other health care providers, and past and current treatments help protect the doctor should liability later arise. In the case of a dishonest patient, clear record keeping could help show that a patient lied or omitted facts if the notes later become evidence in a lawsuit, she said.
“I also think [doctors] should document their policies, so there is clarity and understanding in the relationship,” Ms. Adler said. “Showing a policy where national standards/recommendations are followed will help protect the practice.”
4. Restrict refills
Require prescriber review before patients can obtain refills or new prescriptions for patients who run out of medicine before their next appointment, Dr. O’Donnell said.
“Excessive or early refills for opiate prescriptions are signs of abuse,” he said. “This creates risk to the patient and malpractice risk to the physician.”
It’s also helpful to limit the number of pharmacies used for opioid prescriptions, Ms. Adler said. This makes it easier track medications and narrows the pathway between prescription and drug obtainment.
5. Partner with pharmacists
Work closely with other health providers, such as psychiatrists, therapists, and pharmacists to ensure safe prescribing decisions. Pharmacists have a corresponding responsibility in dispensing opiates, Dr. O’Donnell said.
“Take the pharmacists’ calls regarding your opiates prescriptions,” he advised. “The pharmacist will know what other medicines the patient is taking and may advise of dangerous dosage or interactions.”
6. Require patient agreements
Opioid treatment agreements aid in patient accountability and promote education of drug risks, Dr. Robeck noted. In such contracts, patients agree to fully comply with all aspects of the treatment program and acknowledge that they will not use medication with harmful substances. Other terms can include that patients:
• Only obtain opioid prescriptions from one provider.
• Agree to keep all scheduled medical appointments.
• Promise to undergo urine drug screens as indicated.
• Agree not to share or sell medication.
• Agree not to drive or operate heavy machinery until medication-related drowsiness clears.
Contracts can help patients remain informed about the dangers and benefits of medications, while protecting the physician’s right to terminate treatment if the patient violates the agreement, Ms. Adler said. One sample agreement can be found here.
7. Involve family members
Family members and caregivers are critical to a patient’s opioid therapy plan, Dr. Robeck said. Discuss with patients ahead of time the potential for family member involvement. Family or the patient’s support system should be educated about the patient’s medications, the risks, and how to respond in an emergency.
“It may be life saving,” Dr. Robeck said. “It’s very important for the physician to communicate with the family. There may be times you want the family to come [to appointments].”
Such communication can ensure that family members’ concerns about a patient are conveyed to physicians. Family and caregivers can also have a role in improving home conditions to assist with pain management for the patient, she said. Family education in using a naloxone rescue kit in the event of a possible overdose is essential.
“Giving the patient naloxone to prevent an overdose is more than just handing them the nasal spray or the self-injector, it’s also about educating them and the family about the true risks of these medications,” Dr. Robeck said.
8. Watch for red flags
Be cognizant of warning signs that patients may be addicted, Ms. Adler advised. Patients who demand medications, act impatiently about waiting for refills, or refuse to answer questions about their history should raise alarm bells, she said. Patients who travel long distances for pain medication also should raise question marks, Dr. O’Donnell adds.
“If the patient is in too much of a hurry to wait for records or to get a urine test, that’s a red flag,” Ms. Adler said. “When doctors are not sure, the safest bet is to refer to a pain specialist.”
Consider the criteria for opioid use disorder, Dr. Robeck noted. The condition is defined as a problematic pattern of opioid use leading to clinically significant impairment or distress. Signs of opioid use disorder include recurrent use by patients resulting in a failure to fulfill major role obligations at work or home, continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by opioids, and spending a great deal of time in activities necessary to obtain the opioid, use the opioid, or recover from use, according to the American Psychiatric Association.
9. Develop an exit plan
Before starting a patient on opioid therapy, have a plan in place in case something goes awry, Dr. Robeck said. Create an exit strategy that includes both pharmacological and nonpharmacological resources from which to draw from should problems arise. Make sure you have a plan for tapering patients off opioids when necessary. This may include getting help from other clinicians in the community, she said.
“Those patients need very careful follow-up,” Dr. Robeck. “The rate of the taper needs to occur based on level of risk. Whenever possible, we try to taper patients slowly.”
10. Do your research
Always check your state’s prescription drug–monitoring program (PDMP) when prescribing an opiate to a new patient, Mr. O’Donnell advised.
Currently, 49 states and Guam have operational PDMP databases. The PDMP Training and Technical Assistance Center offers information about each PDMP, state pharmacy and practitioner data, drug schedules monitored, patient information data, and legislation dates and citations.
Perhaps most importantly, know best prescribing practices, Dr. Robeck said. Earlier this year, the CDC released guidelines for prescribing opioids for chronic pain.
“Thoroughly understand the CDC guidelines,” she said. “These are the keys to understanding where opioids fit into your plan of medications and nonpharmacological therapies for pain.”
On Twitter @legal_med
Opioid-related lawsuits against physicians are on the rise. Common allegations include unnecessary prescribing, failing to heed contraindications, and missing warning signs of a likely overdose, said Ericka L. Adler, a Chicago-based health law attorney. To mitigate your risk of getting sued, legal and clinical experts offer the following advice.
1. Identify at-risk patients
Consider the full range of patient risk factors before prescribing or continuing opioids, said Ilene R. Robeck, MD, director of virtual pain education at Richmond VA Medical Center in St. Petersburg, Fla., and cochair of the National VA PACT Pain Champions Initiative.
“When we look at the overdose data, there used to be a perception that people who overdosed were not taking their medication as prescribed, and that’s not true all the time,” she said. “In fact, in some [studies], half the people who overdose take their medication exactly as prescribed. The problems are related to dose, mixing the opioids with other medications, [patient] age, and underlying medical problems.”
Ensure that therapy considerations related to opioids address the full patient picture, Dr. Robeck advised. For example, patients with liver disease, sleep apnea, chronic obstructive pulmonary disease (COPD), asthma, and kidney disease are more prone to overdose. In addition, while nonmedical use of prescription drugs is highest in patients aged 18-25 years, opioid overdose rates are highest among patients aged 25-54 years, according to the Centers for Disease Control and Prevention.
2. Monitor midlevel providers
Closely monitor and limit opioid prescribing by the midlevel providers you supervise, said pharmacologist and consultant James T. O’Donnell, PharmD. A fair share of medical malpractice lawsuits result from failing to supervise a physician assistant (PA) or nurse practitioner (NP) prescribing or treating pain patients.
“Excessive or inappropriate opiate prescribing will result in legal actions against the supervising physician,” Dr. O’Donnell said. “Close monitoring of midlevel providers requires establishing guidelines for opiate prescribing.”
Develop practice protocols that track and regulate midlevel prescribing and regularly discuss prescribing dangers with staff. Know your state law; the extent to which an NP or PA can prescribe varies widely.
3. Document
Keep detailed records of patient encounters that include specifics of what the patient tells you, said Ms. Adler.
Clear documentation about prior conditions, interactions with other health care providers, and past and current treatments help protect the doctor should liability later arise. In the case of a dishonest patient, clear record keeping could help show that a patient lied or omitted facts if the notes later become evidence in a lawsuit, she said.
“I also think [doctors] should document their policies, so there is clarity and understanding in the relationship,” Ms. Adler said. “Showing a policy where national standards/recommendations are followed will help protect the practice.”
4. Restrict refills
Require prescriber review before patients can obtain refills or new prescriptions for patients who run out of medicine before their next appointment, Dr. O’Donnell said.
“Excessive or early refills for opiate prescriptions are signs of abuse,” he said. “This creates risk to the patient and malpractice risk to the physician.”
It’s also helpful to limit the number of pharmacies used for opioid prescriptions, Ms. Adler said. This makes it easier track medications and narrows the pathway between prescription and drug obtainment.
5. Partner with pharmacists
Work closely with other health providers, such as psychiatrists, therapists, and pharmacists to ensure safe prescribing decisions. Pharmacists have a corresponding responsibility in dispensing opiates, Dr. O’Donnell said.
“Take the pharmacists’ calls regarding your opiates prescriptions,” he advised. “The pharmacist will know what other medicines the patient is taking and may advise of dangerous dosage or interactions.”
6. Require patient agreements
Opioid treatment agreements aid in patient accountability and promote education of drug risks, Dr. Robeck noted. In such contracts, patients agree to fully comply with all aspects of the treatment program and acknowledge that they will not use medication with harmful substances. Other terms can include that patients:
• Only obtain opioid prescriptions from one provider.
• Agree to keep all scheduled medical appointments.
• Promise to undergo urine drug screens as indicated.
• Agree not to share or sell medication.
• Agree not to drive or operate heavy machinery until medication-related drowsiness clears.
Contracts can help patients remain informed about the dangers and benefits of medications, while protecting the physician’s right to terminate treatment if the patient violates the agreement, Ms. Adler said. One sample agreement can be found here.
7. Involve family members
Family members and caregivers are critical to a patient’s opioid therapy plan, Dr. Robeck said. Discuss with patients ahead of time the potential for family member involvement. Family or the patient’s support system should be educated about the patient’s medications, the risks, and how to respond in an emergency.
“It may be life saving,” Dr. Robeck said. “It’s very important for the physician to communicate with the family. There may be times you want the family to come [to appointments].”
Such communication can ensure that family members’ concerns about a patient are conveyed to physicians. Family and caregivers can also have a role in improving home conditions to assist with pain management for the patient, she said. Family education in using a naloxone rescue kit in the event of a possible overdose is essential.
“Giving the patient naloxone to prevent an overdose is more than just handing them the nasal spray or the self-injector, it’s also about educating them and the family about the true risks of these medications,” Dr. Robeck said.
8. Watch for red flags
Be cognizant of warning signs that patients may be addicted, Ms. Adler advised. Patients who demand medications, act impatiently about waiting for refills, or refuse to answer questions about their history should raise alarm bells, she said. Patients who travel long distances for pain medication also should raise question marks, Dr. O’Donnell adds.
“If the patient is in too much of a hurry to wait for records or to get a urine test, that’s a red flag,” Ms. Adler said. “When doctors are not sure, the safest bet is to refer to a pain specialist.”
Consider the criteria for opioid use disorder, Dr. Robeck noted. The condition is defined as a problematic pattern of opioid use leading to clinically significant impairment or distress. Signs of opioid use disorder include recurrent use by patients resulting in a failure to fulfill major role obligations at work or home, continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by opioids, and spending a great deal of time in activities necessary to obtain the opioid, use the opioid, or recover from use, according to the American Psychiatric Association.
9. Develop an exit plan
Before starting a patient on opioid therapy, have a plan in place in case something goes awry, Dr. Robeck said. Create an exit strategy that includes both pharmacological and nonpharmacological resources from which to draw from should problems arise. Make sure you have a plan for tapering patients off opioids when necessary. This may include getting help from other clinicians in the community, she said.
“Those patients need very careful follow-up,” Dr. Robeck. “The rate of the taper needs to occur based on level of risk. Whenever possible, we try to taper patients slowly.”
10. Do your research
Always check your state’s prescription drug–monitoring program (PDMP) when prescribing an opiate to a new patient, Mr. O’Donnell advised.
Currently, 49 states and Guam have operational PDMP databases. The PDMP Training and Technical Assistance Center offers information about each PDMP, state pharmacy and practitioner data, drug schedules monitored, patient information data, and legislation dates and citations.
Perhaps most importantly, know best prescribing practices, Dr. Robeck said. Earlier this year, the CDC released guidelines for prescribing opioids for chronic pain.
“Thoroughly understand the CDC guidelines,” she said. “These are the keys to understanding where opioids fit into your plan of medications and nonpharmacological therapies for pain.”
On Twitter @legal_med
Opioid-related lawsuits against physicians are on the rise. Common allegations include unnecessary prescribing, failing to heed contraindications, and missing warning signs of a likely overdose, said Ericka L. Adler, a Chicago-based health law attorney. To mitigate your risk of getting sued, legal and clinical experts offer the following advice.
1. Identify at-risk patients
Consider the full range of patient risk factors before prescribing or continuing opioids, said Ilene R. Robeck, MD, director of virtual pain education at Richmond VA Medical Center in St. Petersburg, Fla., and cochair of the National VA PACT Pain Champions Initiative.
“When we look at the overdose data, there used to be a perception that people who overdosed were not taking their medication as prescribed, and that’s not true all the time,” she said. “In fact, in some [studies], half the people who overdose take their medication exactly as prescribed. The problems are related to dose, mixing the opioids with other medications, [patient] age, and underlying medical problems.”
Ensure that therapy considerations related to opioids address the full patient picture, Dr. Robeck advised. For example, patients with liver disease, sleep apnea, chronic obstructive pulmonary disease (COPD), asthma, and kidney disease are more prone to overdose. In addition, while nonmedical use of prescription drugs is highest in patients aged 18-25 years, opioid overdose rates are highest among patients aged 25-54 years, according to the Centers for Disease Control and Prevention.
2. Monitor midlevel providers
Closely monitor and limit opioid prescribing by the midlevel providers you supervise, said pharmacologist and consultant James T. O’Donnell, PharmD. A fair share of medical malpractice lawsuits result from failing to supervise a physician assistant (PA) or nurse practitioner (NP) prescribing or treating pain patients.
“Excessive or inappropriate opiate prescribing will result in legal actions against the supervising physician,” Dr. O’Donnell said. “Close monitoring of midlevel providers requires establishing guidelines for opiate prescribing.”
Develop practice protocols that track and regulate midlevel prescribing and regularly discuss prescribing dangers with staff. Know your state law; the extent to which an NP or PA can prescribe varies widely.
3. Document
Keep detailed records of patient encounters that include specifics of what the patient tells you, said Ms. Adler.
Clear documentation about prior conditions, interactions with other health care providers, and past and current treatments help protect the doctor should liability later arise. In the case of a dishonest patient, clear record keeping could help show that a patient lied or omitted facts if the notes later become evidence in a lawsuit, she said.
“I also think [doctors] should document their policies, so there is clarity and understanding in the relationship,” Ms. Adler said. “Showing a policy where national standards/recommendations are followed will help protect the practice.”
4. Restrict refills
Require prescriber review before patients can obtain refills or new prescriptions for patients who run out of medicine before their next appointment, Dr. O’Donnell said.
“Excessive or early refills for opiate prescriptions are signs of abuse,” he said. “This creates risk to the patient and malpractice risk to the physician.”
It’s also helpful to limit the number of pharmacies used for opioid prescriptions, Ms. Adler said. This makes it easier track medications and narrows the pathway between prescription and drug obtainment.
5. Partner with pharmacists
Work closely with other health providers, such as psychiatrists, therapists, and pharmacists to ensure safe prescribing decisions. Pharmacists have a corresponding responsibility in dispensing opiates, Dr. O’Donnell said.
“Take the pharmacists’ calls regarding your opiates prescriptions,” he advised. “The pharmacist will know what other medicines the patient is taking and may advise of dangerous dosage or interactions.”
6. Require patient agreements
Opioid treatment agreements aid in patient accountability and promote education of drug risks, Dr. Robeck noted. In such contracts, patients agree to fully comply with all aspects of the treatment program and acknowledge that they will not use medication with harmful substances. Other terms can include that patients:
• Only obtain opioid prescriptions from one provider.
• Agree to keep all scheduled medical appointments.
• Promise to undergo urine drug screens as indicated.
• Agree not to share or sell medication.
• Agree not to drive or operate heavy machinery until medication-related drowsiness clears.
Contracts can help patients remain informed about the dangers and benefits of medications, while protecting the physician’s right to terminate treatment if the patient violates the agreement, Ms. Adler said. One sample agreement can be found here.
7. Involve family members
Family members and caregivers are critical to a patient’s opioid therapy plan, Dr. Robeck said. Discuss with patients ahead of time the potential for family member involvement. Family or the patient’s support system should be educated about the patient’s medications, the risks, and how to respond in an emergency.
“It may be life saving,” Dr. Robeck said. “It’s very important for the physician to communicate with the family. There may be times you want the family to come [to appointments].”
Such communication can ensure that family members’ concerns about a patient are conveyed to physicians. Family and caregivers can also have a role in improving home conditions to assist with pain management for the patient, she said. Family education in using a naloxone rescue kit in the event of a possible overdose is essential.
“Giving the patient naloxone to prevent an overdose is more than just handing them the nasal spray or the self-injector, it’s also about educating them and the family about the true risks of these medications,” Dr. Robeck said.
8. Watch for red flags
Be cognizant of warning signs that patients may be addicted, Ms. Adler advised. Patients who demand medications, act impatiently about waiting for refills, or refuse to answer questions about their history should raise alarm bells, she said. Patients who travel long distances for pain medication also should raise question marks, Dr. O’Donnell adds.
“If the patient is in too much of a hurry to wait for records or to get a urine test, that’s a red flag,” Ms. Adler said. “When doctors are not sure, the safest bet is to refer to a pain specialist.”
Consider the criteria for opioid use disorder, Dr. Robeck noted. The condition is defined as a problematic pattern of opioid use leading to clinically significant impairment or distress. Signs of opioid use disorder include recurrent use by patients resulting in a failure to fulfill major role obligations at work or home, continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by opioids, and spending a great deal of time in activities necessary to obtain the opioid, use the opioid, or recover from use, according to the American Psychiatric Association.
9. Develop an exit plan
Before starting a patient on opioid therapy, have a plan in place in case something goes awry, Dr. Robeck said. Create an exit strategy that includes both pharmacological and nonpharmacological resources from which to draw from should problems arise. Make sure you have a plan for tapering patients off opioids when necessary. This may include getting help from other clinicians in the community, she said.
“Those patients need very careful follow-up,” Dr. Robeck. “The rate of the taper needs to occur based on level of risk. Whenever possible, we try to taper patients slowly.”
10. Do your research
Always check your state’s prescription drug–monitoring program (PDMP) when prescribing an opiate to a new patient, Mr. O’Donnell advised.
Currently, 49 states and Guam have operational PDMP databases. The PDMP Training and Technical Assistance Center offers information about each PDMP, state pharmacy and practitioner data, drug schedules monitored, patient information data, and legislation dates and citations.
Perhaps most importantly, know best prescribing practices, Dr. Robeck said. Earlier this year, the CDC released guidelines for prescribing opioids for chronic pain.
“Thoroughly understand the CDC guidelines,” she said. “These are the keys to understanding where opioids fit into your plan of medications and nonpharmacological therapies for pain.”
On Twitter @legal_med
LABA withdrawal does not worsen asthma control
LONDON – Real-life experience shows that stopping treatment with a long-acting beta-agonist (LABA) does not worsen asthma control, nor does it lead to any immediate decline in lung function.
Spirometric parameters were similar before and 3 weeks after stopping LABA therapy in an observational study of 58 patients who had stable asthma and were being treated with an inhaled corticosteroid (ICS) and a LABA.
The forced expiratory volume in 1 second (FEV1) was 88.8% at baseline and 89.5% at the 3-week visit after stepping down their LABA therapy (P = .55). Patients’ average peak expiratory flow rate was 462 L/min both before and after LABA withdrawal.
In addition, no changes were seen in lung function based on impulse oscillometry, a noninvasive method for measuring airway resistance and reactance (Chest. 2014;146[3]:841-7). Similar levels of fractional exhaled nitric oxide (FeNO, 38 and 36 ppb) were recorded.
The findings were presented at the annual congress of the European Respiratory Society (ERS) and have been published in an early online edition of the Annals of Allergy, Asthma & Immunology (doi: 10.1016/j.anai.2016.07.022).
“About 45% of the UK adult asthma population are taking step 3 GINA [Global Initiative for Asthma] therapy, which is ICS/LABA,” explained Sunny Jabbal, MD, of the Scottish Centre for Respiratory Research at Ninewells Hospital in Dundee, Scotland, where the study was conducted. Patients should be on the lowest of the five steps in the 2016 GINA guidelines that achieve asthma control and should be regularly reviewed.
To test whether the LABA could be safely withdrawn, that is stepped down to ICS only [GINA step 2], Dr. Jabbal and colleagues studied 58 patients with a mean age of 39 years. All had well-controlled asthma, and had been receiving ICS/LABA for at least 3 months with no asthma exacerbations requiring treatment. None of the patients were current smokers.
At study entry, patients underwent spirometry, impulse oscillometry, and had FeNO measured. Their LABA was then stopped, and patients were reassessed 3 weeks later. “In accordance with GINA, their ICS dose was also reduced by approximately 25%,” Dr. Jabbal said.
Patients recorded their symptoms and short-term reliever (albuterol) use on simple diary cards. They were also given a 24-hour emergency mobile number, but no calls were received and no adverse events reported. The mean daily symptom score recorded during the step down process was 0.4 (out of a possible score of 3), and the mean albuterol usage was one puff per day.
One of the chairs of the session, Omar Usmani, MD, of Imperial College London noted that some clinicians are “very apprehensive” about stopping LABA and stepping down ICS therapy in their patients.
This was a short-term study, Dr. Jabbal acknowledged. Although a follow-up of 3 weeks may be enough to determine the effects of stopping a LABA, that time may not be sufficient to assess the effects of stepping down the ICS. Further real-life studies are needed to evaluate outcomes such as exacerbations and overall quality of life.
Improved adherence with ICS therapy after LABA withdrawal might explain the lack of deleterious effects, or perhaps some patients may not have initially needed an ICS/LABA combination, he speculated. Maybe even the steroid dose could be reduced further in this particular patient population.
The study received no commercial funding. Dr. Jabbal had no conflicts of interest related to his presentation.
LONDON – Real-life experience shows that stopping treatment with a long-acting beta-agonist (LABA) does not worsen asthma control, nor does it lead to any immediate decline in lung function.
Spirometric parameters were similar before and 3 weeks after stopping LABA therapy in an observational study of 58 patients who had stable asthma and were being treated with an inhaled corticosteroid (ICS) and a LABA.
The forced expiratory volume in 1 second (FEV1) was 88.8% at baseline and 89.5% at the 3-week visit after stepping down their LABA therapy (P = .55). Patients’ average peak expiratory flow rate was 462 L/min both before and after LABA withdrawal.
In addition, no changes were seen in lung function based on impulse oscillometry, a noninvasive method for measuring airway resistance and reactance (Chest. 2014;146[3]:841-7). Similar levels of fractional exhaled nitric oxide (FeNO, 38 and 36 ppb) were recorded.
The findings were presented at the annual congress of the European Respiratory Society (ERS) and have been published in an early online edition of the Annals of Allergy, Asthma & Immunology (doi: 10.1016/j.anai.2016.07.022).
“About 45% of the UK adult asthma population are taking step 3 GINA [Global Initiative for Asthma] therapy, which is ICS/LABA,” explained Sunny Jabbal, MD, of the Scottish Centre for Respiratory Research at Ninewells Hospital in Dundee, Scotland, where the study was conducted. Patients should be on the lowest of the five steps in the 2016 GINA guidelines that achieve asthma control and should be regularly reviewed.
To test whether the LABA could be safely withdrawn, that is stepped down to ICS only [GINA step 2], Dr. Jabbal and colleagues studied 58 patients with a mean age of 39 years. All had well-controlled asthma, and had been receiving ICS/LABA for at least 3 months with no asthma exacerbations requiring treatment. None of the patients were current smokers.
At study entry, patients underwent spirometry, impulse oscillometry, and had FeNO measured. Their LABA was then stopped, and patients were reassessed 3 weeks later. “In accordance with GINA, their ICS dose was also reduced by approximately 25%,” Dr. Jabbal said.
Patients recorded their symptoms and short-term reliever (albuterol) use on simple diary cards. They were also given a 24-hour emergency mobile number, but no calls were received and no adverse events reported. The mean daily symptom score recorded during the step down process was 0.4 (out of a possible score of 3), and the mean albuterol usage was one puff per day.
One of the chairs of the session, Omar Usmani, MD, of Imperial College London noted that some clinicians are “very apprehensive” about stopping LABA and stepping down ICS therapy in their patients.
This was a short-term study, Dr. Jabbal acknowledged. Although a follow-up of 3 weeks may be enough to determine the effects of stopping a LABA, that time may not be sufficient to assess the effects of stepping down the ICS. Further real-life studies are needed to evaluate outcomes such as exacerbations and overall quality of life.
Improved adherence with ICS therapy after LABA withdrawal might explain the lack of deleterious effects, or perhaps some patients may not have initially needed an ICS/LABA combination, he speculated. Maybe even the steroid dose could be reduced further in this particular patient population.
The study received no commercial funding. Dr. Jabbal had no conflicts of interest related to his presentation.
LONDON – Real-life experience shows that stopping treatment with a long-acting beta-agonist (LABA) does not worsen asthma control, nor does it lead to any immediate decline in lung function.
Spirometric parameters were similar before and 3 weeks after stopping LABA therapy in an observational study of 58 patients who had stable asthma and were being treated with an inhaled corticosteroid (ICS) and a LABA.
The forced expiratory volume in 1 second (FEV1) was 88.8% at baseline and 89.5% at the 3-week visit after stepping down their LABA therapy (P = .55). Patients’ average peak expiratory flow rate was 462 L/min both before and after LABA withdrawal.
In addition, no changes were seen in lung function based on impulse oscillometry, a noninvasive method for measuring airway resistance and reactance (Chest. 2014;146[3]:841-7). Similar levels of fractional exhaled nitric oxide (FeNO, 38 and 36 ppb) were recorded.
The findings were presented at the annual congress of the European Respiratory Society (ERS) and have been published in an early online edition of the Annals of Allergy, Asthma & Immunology (doi: 10.1016/j.anai.2016.07.022).
“About 45% of the UK adult asthma population are taking step 3 GINA [Global Initiative for Asthma] therapy, which is ICS/LABA,” explained Sunny Jabbal, MD, of the Scottish Centre for Respiratory Research at Ninewells Hospital in Dundee, Scotland, where the study was conducted. Patients should be on the lowest of the five steps in the 2016 GINA guidelines that achieve asthma control and should be regularly reviewed.
To test whether the LABA could be safely withdrawn, that is stepped down to ICS only [GINA step 2], Dr. Jabbal and colleagues studied 58 patients with a mean age of 39 years. All had well-controlled asthma, and had been receiving ICS/LABA for at least 3 months with no asthma exacerbations requiring treatment. None of the patients were current smokers.
At study entry, patients underwent spirometry, impulse oscillometry, and had FeNO measured. Their LABA was then stopped, and patients were reassessed 3 weeks later. “In accordance with GINA, their ICS dose was also reduced by approximately 25%,” Dr. Jabbal said.
Patients recorded their symptoms and short-term reliever (albuterol) use on simple diary cards. They were also given a 24-hour emergency mobile number, but no calls were received and no adverse events reported. The mean daily symptom score recorded during the step down process was 0.4 (out of a possible score of 3), and the mean albuterol usage was one puff per day.
One of the chairs of the session, Omar Usmani, MD, of Imperial College London noted that some clinicians are “very apprehensive” about stopping LABA and stepping down ICS therapy in their patients.
This was a short-term study, Dr. Jabbal acknowledged. Although a follow-up of 3 weeks may be enough to determine the effects of stopping a LABA, that time may not be sufficient to assess the effects of stepping down the ICS. Further real-life studies are needed to evaluate outcomes such as exacerbations and overall quality of life.
Improved adherence with ICS therapy after LABA withdrawal might explain the lack of deleterious effects, or perhaps some patients may not have initially needed an ICS/LABA combination, he speculated. Maybe even the steroid dose could be reduced further in this particular patient population.
The study received no commercial funding. Dr. Jabbal had no conflicts of interest related to his presentation.
AT THE ERS CONGRESS 2016
Key clinical point: Step-down treatment works well in routine asthma care, with no loss of control or lung function decline.
Major finding: No significant changes in FEV1 (88.8% vs. 89.5%), PEF (462 L/min vs. 462 L/min), or other lung function variables were seen before or 3 weeks after LABA withdrawal.
Data source: Observational study of 58 stable asthmatic patients being treated with ICS/LABA (GINA step 3).
Disclosures: The study received no commercial funding. Dr. Jabbal had no conflicts of interest related to his presentation.