User login
Whole brain radiotherapy not beneficial for NSCLC metastasis
Whole brain radiotherapy, a standard treatment for patients with metastatic non–small-cell lung cancer, provided no clinical benefit in a noninferiority trial specifically designed to assess both patient survival and quality of life.
The findings were published online Sept. 4 in the Lancet.
Whole brain radiotherapy, with or without concomitant steroid treatment, has been widely used for decades in that patient population, even though no sufficiently powered, definitive studies support the approach. It is likely that patients and clinicians alike continue to embrace it because of the absence of alternative treatment options.
The Quality of Life After Treatment for Brain Metastases (QUARTZ) trial was intended to assess whether any improvement in survival offered by whole brain radiotherapy is balanced by deterioration in quality of life, said Paula Mulvenna, MBBS, of the Northern Center for Cancer Care, Newcastle (England) Hospitals, and her associates (Lancet 2016 Sep 4. doi: 10.1016/S0140-6736(16)30825-X).
QUARTZ involved 538 adults seen during a 7-year period who had NSCLC with brain metastases and who were not suited for either brain surgery or stereotactic radiotherapy. The median age was 66 years (range, 35-85 years), and 38% had a Karnofsky Performance Status score of less than 70.
The participants were randomly assigned to receive either optimal supportive care plus whole brain radiotherapy (269 patients) or optimal supportive care alone (269 patients) at 69 U.K. and 3 Australian medical centers. They reported on 20 symptoms and adverse effects, as well as health-related quality of life, approximately once per week.
The primary outcome measure – quality-adjusted life-years (QALY), which combines overall survival and quality of life – was 46.4 days with radiotherapy and 41.7 days without it.
Symptoms, adverse effects, and quality of life (QOL) were similar between the two study groups at 4 weeks, except that the radiotherapy group reported more moderate or severe episodes of drowsiness, hair loss, nausea, and dry or itchy scalp. The number and severity of serious adverse events were similar through 12 weeks of follow-up.
The percentage of patients whose QOL was either maintained or improved over time was similar between the two groups at 4 weeks (54% vs. 57%), 8 weeks (44% vs. 51%), and 12 weeks (44% vs. 49%). Changes in Karnofsky scores also were similar.
The study refuted the widely held belief that whole brain radiotherapy allows patients to reduce or discontinue steroid treatment, averting the associated adverse effects. Steroid doses were not significantly different between the two study groups through the first 8 weeks of treatment, which “challenges the dogma that whole brain radiotherapy can be seen as a steroid-sparing modality,” the investigators said.
Taken together, the findings “suggest that whole brain radiotherapy can be omitted and patients treated with optimal supportive care alone, without an important reduction in either overall survival or quality of life,” Dr. Mulvenna and her associates said.
The approximately 5-day difference between the two study groups in median overall survival highlights both the limited benefit offered by radiotherapy and the poor prognosis of this patient population, the researchers added.
Whole brain radiotherapy did offer a small survival benefit to the youngest patients who had good performance status and a “controlled” primary NSCLC. “For all other groups, [it] does not significantly affect QALY or overall survival,” they said.
Cancer Research U.K., the Medical Research Council in the U.K., the Trans Tasman Radiation Oncology Group, and the National Health and Medical Research Council Australia supported the study. Dr. Mulvenna and her associates reported having no relevant financial disclosures.
Managing brain metastases from NSCLC is a challenge, because the lesions may well produce life-threatening symptoms and serious impairment, which could be ameliorated with whole brain radiotherapy.
This is a large and well designed trial, but it was limited in that the maximal benefit of radiotherapy is believed to occur 6 weeks after the end of treatment. Given that median overall survival was only 8 weeks and considering the time it took to deliver the treatment, approximately half of the patients in this study died before an optimal assessment of symptoms could be done.
This might also explain why radiotherapy didn’t have an effect on steroid use in this study. Many patients didn’t live long enough for radiotherapy’s steroid-sparing effect to be observed.
Cécile Le Pechoux, MD, is in the department of radiation oncology at Gustave Roussy Cancer Campus in Villejuif, France. She and her associates reported having no relevant financial disclosures. They made these remarks in a comment accompanying the report on the QUARTZ trial (Lancet 2016 Sep 4. doi: 10.1016/S0140-6736[16]31391-5).
Managing brain metastases from NSCLC is a challenge, because the lesions may well produce life-threatening symptoms and serious impairment, which could be ameliorated with whole brain radiotherapy.
This is a large and well designed trial, but it was limited in that the maximal benefit of radiotherapy is believed to occur 6 weeks after the end of treatment. Given that median overall survival was only 8 weeks and considering the time it took to deliver the treatment, approximately half of the patients in this study died before an optimal assessment of symptoms could be done.
This might also explain why radiotherapy didn’t have an effect on steroid use in this study. Many patients didn’t live long enough for radiotherapy’s steroid-sparing effect to be observed.
Cécile Le Pechoux, MD, is in the department of radiation oncology at Gustave Roussy Cancer Campus in Villejuif, France. She and her associates reported having no relevant financial disclosures. They made these remarks in a comment accompanying the report on the QUARTZ trial (Lancet 2016 Sep 4. doi: 10.1016/S0140-6736[16]31391-5).
Managing brain metastases from NSCLC is a challenge, because the lesions may well produce life-threatening symptoms and serious impairment, which could be ameliorated with whole brain radiotherapy.
This is a large and well designed trial, but it was limited in that the maximal benefit of radiotherapy is believed to occur 6 weeks after the end of treatment. Given that median overall survival was only 8 weeks and considering the time it took to deliver the treatment, approximately half of the patients in this study died before an optimal assessment of symptoms could be done.
This might also explain why radiotherapy didn’t have an effect on steroid use in this study. Many patients didn’t live long enough for radiotherapy’s steroid-sparing effect to be observed.
Cécile Le Pechoux, MD, is in the department of radiation oncology at Gustave Roussy Cancer Campus in Villejuif, France. She and her associates reported having no relevant financial disclosures. They made these remarks in a comment accompanying the report on the QUARTZ trial (Lancet 2016 Sep 4. doi: 10.1016/S0140-6736[16]31391-5).
Whole brain radiotherapy, a standard treatment for patients with metastatic non–small-cell lung cancer, provided no clinical benefit in a noninferiority trial specifically designed to assess both patient survival and quality of life.
The findings were published online Sept. 4 in the Lancet.
Whole brain radiotherapy, with or without concomitant steroid treatment, has been widely used for decades in that patient population, even though no sufficiently powered, definitive studies support the approach. It is likely that patients and clinicians alike continue to embrace it because of the absence of alternative treatment options.
The Quality of Life After Treatment for Brain Metastases (QUARTZ) trial was intended to assess whether any improvement in survival offered by whole brain radiotherapy is balanced by deterioration in quality of life, said Paula Mulvenna, MBBS, of the Northern Center for Cancer Care, Newcastle (England) Hospitals, and her associates (Lancet 2016 Sep 4. doi: 10.1016/S0140-6736(16)30825-X).
QUARTZ involved 538 adults seen during a 7-year period who had NSCLC with brain metastases and who were not suited for either brain surgery or stereotactic radiotherapy. The median age was 66 years (range, 35-85 years), and 38% had a Karnofsky Performance Status score of less than 70.
The participants were randomly assigned to receive either optimal supportive care plus whole brain radiotherapy (269 patients) or optimal supportive care alone (269 patients) at 69 U.K. and 3 Australian medical centers. They reported on 20 symptoms and adverse effects, as well as health-related quality of life, approximately once per week.
The primary outcome measure – quality-adjusted life-years (QALY), which combines overall survival and quality of life – was 46.4 days with radiotherapy and 41.7 days without it.
Symptoms, adverse effects, and quality of life (QOL) were similar between the two study groups at 4 weeks, except that the radiotherapy group reported more moderate or severe episodes of drowsiness, hair loss, nausea, and dry or itchy scalp. The number and severity of serious adverse events were similar through 12 weeks of follow-up.
The percentage of patients whose QOL was either maintained or improved over time was similar between the two groups at 4 weeks (54% vs. 57%), 8 weeks (44% vs. 51%), and 12 weeks (44% vs. 49%). Changes in Karnofsky scores also were similar.
The study refuted the widely held belief that whole brain radiotherapy allows patients to reduce or discontinue steroid treatment, averting the associated adverse effects. Steroid doses were not significantly different between the two study groups through the first 8 weeks of treatment, which “challenges the dogma that whole brain radiotherapy can be seen as a steroid-sparing modality,” the investigators said.
Taken together, the findings “suggest that whole brain radiotherapy can be omitted and patients treated with optimal supportive care alone, without an important reduction in either overall survival or quality of life,” Dr. Mulvenna and her associates said.
The approximately 5-day difference between the two study groups in median overall survival highlights both the limited benefit offered by radiotherapy and the poor prognosis of this patient population, the researchers added.
Whole brain radiotherapy did offer a small survival benefit to the youngest patients who had good performance status and a “controlled” primary NSCLC. “For all other groups, [it] does not significantly affect QALY or overall survival,” they said.
Cancer Research U.K., the Medical Research Council in the U.K., the Trans Tasman Radiation Oncology Group, and the National Health and Medical Research Council Australia supported the study. Dr. Mulvenna and her associates reported having no relevant financial disclosures.
Whole brain radiotherapy, a standard treatment for patients with metastatic non–small-cell lung cancer, provided no clinical benefit in a noninferiority trial specifically designed to assess both patient survival and quality of life.
The findings were published online Sept. 4 in the Lancet.
Whole brain radiotherapy, with or without concomitant steroid treatment, has been widely used for decades in that patient population, even though no sufficiently powered, definitive studies support the approach. It is likely that patients and clinicians alike continue to embrace it because of the absence of alternative treatment options.
The Quality of Life After Treatment for Brain Metastases (QUARTZ) trial was intended to assess whether any improvement in survival offered by whole brain radiotherapy is balanced by deterioration in quality of life, said Paula Mulvenna, MBBS, of the Northern Center for Cancer Care, Newcastle (England) Hospitals, and her associates (Lancet 2016 Sep 4. doi: 10.1016/S0140-6736(16)30825-X).
QUARTZ involved 538 adults seen during a 7-year period who had NSCLC with brain metastases and who were not suited for either brain surgery or stereotactic radiotherapy. The median age was 66 years (range, 35-85 years), and 38% had a Karnofsky Performance Status score of less than 70.
The participants were randomly assigned to receive either optimal supportive care plus whole brain radiotherapy (269 patients) or optimal supportive care alone (269 patients) at 69 U.K. and 3 Australian medical centers. They reported on 20 symptoms and adverse effects, as well as health-related quality of life, approximately once per week.
The primary outcome measure – quality-adjusted life-years (QALY), which combines overall survival and quality of life – was 46.4 days with radiotherapy and 41.7 days without it.
Symptoms, adverse effects, and quality of life (QOL) were similar between the two study groups at 4 weeks, except that the radiotherapy group reported more moderate or severe episodes of drowsiness, hair loss, nausea, and dry or itchy scalp. The number and severity of serious adverse events were similar through 12 weeks of follow-up.
The percentage of patients whose QOL was either maintained or improved over time was similar between the two groups at 4 weeks (54% vs. 57%), 8 weeks (44% vs. 51%), and 12 weeks (44% vs. 49%). Changes in Karnofsky scores also were similar.
The study refuted the widely held belief that whole brain radiotherapy allows patients to reduce or discontinue steroid treatment, averting the associated adverse effects. Steroid doses were not significantly different between the two study groups through the first 8 weeks of treatment, which “challenges the dogma that whole brain radiotherapy can be seen as a steroid-sparing modality,” the investigators said.
Taken together, the findings “suggest that whole brain radiotherapy can be omitted and patients treated with optimal supportive care alone, without an important reduction in either overall survival or quality of life,” Dr. Mulvenna and her associates said.
The approximately 5-day difference between the two study groups in median overall survival highlights both the limited benefit offered by radiotherapy and the poor prognosis of this patient population, the researchers added.
Whole brain radiotherapy did offer a small survival benefit to the youngest patients who had good performance status and a “controlled” primary NSCLC. “For all other groups, [it] does not significantly affect QALY or overall survival,” they said.
Cancer Research U.K., the Medical Research Council in the U.K., the Trans Tasman Radiation Oncology Group, and the National Health and Medical Research Council Australia supported the study. Dr. Mulvenna and her associates reported having no relevant financial disclosures.
FROM THE LANCET
Key clinical point: Whole brain radiotherapy provided no clinically significant benefit for most patients with metastatic NSCLC.
Major finding: The primary outcome measure, quality-adjusted life-years, was 46.4 days with radiotherapy and 41.7 days without it.
Data source: An international, randomized, phase III noninferiority trial involving 538 patients treated during a 7-year period.
Disclosures: Cancer Research U.K., the Medical Research Council in the U.K., the Trans Tasman Radiation Oncology Group, and the Medical Research Council Australia supported the study. Dr. Mulvenna and her associates reported having no relevant financial disclosures.
Clot retrieval devices approved for initial ischemic stroke treatment
Two Trevo clot retrieval devices can now be marketed as an initial therapy to reduce paralysis from strokes that are caused by blood clots, according to a press release from the Food and Drug Administration.
Previously, the only first-line treatment approved for acute ischemic stroke was tissue plasminogen activator (TPA) delivered intravenously. The FDA approved Trevo devices based on a clinical trial in which 29% of patients treated with the Trevo device combined with TPA and medical management of blood pressure and disability symptoms were shown to be functionally independent 3 months after their stroke, compared with only 19% of patients treated with TPA plus medical management alone.
The Trevo devices are approved for usage within 6 hours of symptom onset and only following treatment with TPA, which should be administered within 3 hours of stroke onset. Associated risks with Trevo device usage include failure to retrieve the blood clot, device malfunctions including breakage and navigation difficulties, potential damage of blood vessels, and the chance of perforation or hemorrhage.
The Trevo device was first approved by the FDA in 2012 to remove blood clots in order to restore blood flow in stroke patients who could not receive TPA or for those patients who did not respond to TPA therapy. The current approval expands the devices’ indication to a broader group of patients, according to the release.
“This is the first time FDA has allowed the use of these devices alongside TPA, which has the potential to help further reduce the devastating disabilities associated with strokes compared to the use of TPA alone. Now health care providers and their patients have another tool for treating stroke and potentially preventing long-term disability,” Carlos Peña, PhD, director of the division of neurological and physical medicine devices at the FDA’s Center for Devices and Radiological Health, said in the press release.
Find the full press release on the FDA website.
Two Trevo clot retrieval devices can now be marketed as an initial therapy to reduce paralysis from strokes that are caused by blood clots, according to a press release from the Food and Drug Administration.
Previously, the only first-line treatment approved for acute ischemic stroke was tissue plasminogen activator (TPA) delivered intravenously. The FDA approved Trevo devices based on a clinical trial in which 29% of patients treated with the Trevo device combined with TPA and medical management of blood pressure and disability symptoms were shown to be functionally independent 3 months after their stroke, compared with only 19% of patients treated with TPA plus medical management alone.
The Trevo devices are approved for usage within 6 hours of symptom onset and only following treatment with TPA, which should be administered within 3 hours of stroke onset. Associated risks with Trevo device usage include failure to retrieve the blood clot, device malfunctions including breakage and navigation difficulties, potential damage of blood vessels, and the chance of perforation or hemorrhage.
The Trevo device was first approved by the FDA in 2012 to remove blood clots in order to restore blood flow in stroke patients who could not receive TPA or for those patients who did not respond to TPA therapy. The current approval expands the devices’ indication to a broader group of patients, according to the release.
“This is the first time FDA has allowed the use of these devices alongside TPA, which has the potential to help further reduce the devastating disabilities associated with strokes compared to the use of TPA alone. Now health care providers and their patients have another tool for treating stroke and potentially preventing long-term disability,” Carlos Peña, PhD, director of the division of neurological and physical medicine devices at the FDA’s Center for Devices and Radiological Health, said in the press release.
Find the full press release on the FDA website.
Two Trevo clot retrieval devices can now be marketed as an initial therapy to reduce paralysis from strokes that are caused by blood clots, according to a press release from the Food and Drug Administration.
Previously, the only first-line treatment approved for acute ischemic stroke was tissue plasminogen activator (TPA) delivered intravenously. The FDA approved Trevo devices based on a clinical trial in which 29% of patients treated with the Trevo device combined with TPA and medical management of blood pressure and disability symptoms were shown to be functionally independent 3 months after their stroke, compared with only 19% of patients treated with TPA plus medical management alone.
The Trevo devices are approved for usage within 6 hours of symptom onset and only following treatment with TPA, which should be administered within 3 hours of stroke onset. Associated risks with Trevo device usage include failure to retrieve the blood clot, device malfunctions including breakage and navigation difficulties, potential damage of blood vessels, and the chance of perforation or hemorrhage.
The Trevo device was first approved by the FDA in 2012 to remove blood clots in order to restore blood flow in stroke patients who could not receive TPA or for those patients who did not respond to TPA therapy. The current approval expands the devices’ indication to a broader group of patients, according to the release.
“This is the first time FDA has allowed the use of these devices alongside TPA, which has the potential to help further reduce the devastating disabilities associated with strokes compared to the use of TPA alone. Now health care providers and their patients have another tool for treating stroke and potentially preventing long-term disability,” Carlos Peña, PhD, director of the division of neurological and physical medicine devices at the FDA’s Center for Devices and Radiological Health, said in the press release.
Find the full press release on the FDA website.
Commentary: INR instability in the NOAC era
Progress in the development of new oral anticoagulants (NOACs), as well as agents for their reversal, has lowered the threshold to use these therapeutics as first line agents for the management of nonvalvular atrial fibrillation and venous thromboembolism.1,2 Despite this increase in adoption, however, debate persists as to whether patients chronically maintained on vitamin K antagonists (VKAs), such as warfarin, should be switched to NOACs. The recently published research letter by Pokorney et al. assessed the stability of international normalized ratios (INRs) in patients on long-term warfarin therapy in order to address this question.3
Specifically, prospective registry data from 3,749 patients with at least three INR values in the first 6 months of therapy as well as six or more in the following year were included. Patients were deemed stable if 80% or more of their INRs were in a therapeutic range defined as an INR between 2 and 3.3 During the initiation period, only one in four patients taking warfarin had a stable INR.3 Furthermore, stability in the first 6 months was found to have limited ability to predict stability in the subsequent year (concordance index of 0.61). With regard to time in therapeutic range (TTR), only 32% of patients had a TTR of greater than 80% during the first 6 months with less than half (42%) of these patients able to maintain this in the following year.
Findings from Pokorney et al. add to the growing body of literature demonstrating the difficulty of achieving and maintaining a therapeutic INR while on warfarin therapy.4-7 Clinically, these findings are important, as deviations from TTR have been shown to be associated with increased risk of bleeding and thrombosis as well as increased health care costs.8-10 Mechanistically, patient factors such as differences in vitamin K consumption, comorbid conditions, drug-drug interactions, and medication compliance, as well as genetic differences that impact drug metabolism undoubtedly contribute to the variation of INR noted in patients on warfarin therapy.
Attempts to improve stability have included the administration of low-dose oral vitamin K. However, recent data from a multicenter randomized control trial suggests that while such therapy may help to decrease extreme variations in INR, it does not lead to an increased TTR.11 Furthermore, while significant work has been conducted in identifying specific gene variants, such as CYP2C9 and VKORC, which encode cytochrome P450 and vitamin K epoxide reductase enzymes, respectively, economic analyses suggest that testing for these gene variants would not be cost-effective.12 Additionally, clinical prediction tools, which incorporate important patient factors to help guide anticoagulation explain less than 10% of TTR variability.4
Nonetheless, some caution is warranted in the interpretation of the results reported by Pokorney and his colleagues. The proportion of registry patients treated with warfarin who had a low TTR was much lower than that previously reported by the pivotal U.S. trials of NOACs (55%-68%) and significantly lower than the results of a recent nationwide Swedish registry involving 40,449 patients.13
In the Swedish registry, the mean individual TTR was 70% with more than half the patients having a TTR of 70% or more, emphasizing the importance of health care system effects. Moreover, regardless of whether a patient is on warfarin or a NOAC, patients with a lower TTR have higher rates of diabetes, chronic obstructive pulmonary disease, heart failure, and renal failure, which may contribute to the need for additional therapies that may influence TTR.
For example, INR may be increased by ciprofloxacin or omeprazole when taken with warfarin, and CYP3A4 and P-glycoprotein (P-gp) inducers and inhibitors can result in an increased or decreased anticoagulation effect when used with NOACs. Recent reports have also highlighted variability in the safety of NOACs, particularly among patients with renal or liver insufficiency, African Americans, or patients with a prior history of GI bleeding.14-16 For these subgroups, determining NOAC activity to improve clinical safety of these agents is difficult.
PT or INR testing is largely insensitive or otherwise highly variable and the blood draw time relative to the most recent dose significantly influences the measured level of anti-Xa activity. Importantly, socioeconomic factors and family support systems also influence TTR, as important determinants of access to needed drugs or the ability to sustain related costs over time.
Taken together, prior INR stability on warfarin therapy does not ensure continued stability and, as a consequence, long-term warfarin therapy requires close monitoring in order to remain effective. To this end, further development of point-of-care coagulometers for self-testing and self-management, which have been found to be acceptable and preferred by patients, should be pursued.17 Similarly, attempts to decrease INR variability through research on optimizing computer assisted dosing programs remains warranted.18 NOACs offer an advantage over warfarin therapy in that they have a more predictable pharmacokinetic profile, which precludes the need for routine monitoring of anticoagulation parameters. However, many of the same factors, which influence TTR for warfarin do so for NOACs; NOACs have increased bleeding risk in comparison to warfarin for a number of demographic groups; and the high cost of NOACs may influence patient compliance.
Accordingly, until further data is available, consideration of the conversion of a patient on warfarin with a low TTR to a NOAC should be individualized.
Madhukar S. Patel, MD, is a general surgeon at the Department of Surgery, Massachusetts General Hospital, Boston, and Elliot L. Chaikof, MD, is Surgeon-in-Chief, Beth Israel Deaconess Medical Center, and Chairman, Roberta and Stephen R. Weiner Department of Surgery, Johnson and Johnson Professor of Surgery, Harvard Medical School. Dr. Chaikof is also an associate editor for Vascular Specialist. They have no relevant conflicts.
References
2. Nat Rev Cardiol. 2014;11:693-703.
5. J Thromb Haemost. 2010;8:2182-91.
6. Thromb Haemost. 2009;101:552-6.
7. Am J Cardiovasc Drugs. 2015;15:205-11.
8. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
10. J Med Econ. 2015;18:333-40.
11. Thromb Haemost. 2016;116:480-5.
12. Ann Intern Med. 2009;150:73-83.
13. JAMA Cardiol. 2016;1:172-80.
14. N Engl J Med. 2013;369:2093-104.
15. JAMA Intern Med. 2015;175:18-24.
16. J Am Coll Cardiol. 2014;63:891-900.
Progress in the development of new oral anticoagulants (NOACs), as well as agents for their reversal, has lowered the threshold to use these therapeutics as first line agents for the management of nonvalvular atrial fibrillation and venous thromboembolism.1,2 Despite this increase in adoption, however, debate persists as to whether patients chronically maintained on vitamin K antagonists (VKAs), such as warfarin, should be switched to NOACs. The recently published research letter by Pokorney et al. assessed the stability of international normalized ratios (INRs) in patients on long-term warfarin therapy in order to address this question.3
Specifically, prospective registry data from 3,749 patients with at least three INR values in the first 6 months of therapy as well as six or more in the following year were included. Patients were deemed stable if 80% or more of their INRs were in a therapeutic range defined as an INR between 2 and 3.3 During the initiation period, only one in four patients taking warfarin had a stable INR.3 Furthermore, stability in the first 6 months was found to have limited ability to predict stability in the subsequent year (concordance index of 0.61). With regard to time in therapeutic range (TTR), only 32% of patients had a TTR of greater than 80% during the first 6 months with less than half (42%) of these patients able to maintain this in the following year.
Findings from Pokorney et al. add to the growing body of literature demonstrating the difficulty of achieving and maintaining a therapeutic INR while on warfarin therapy.4-7 Clinically, these findings are important, as deviations from TTR have been shown to be associated with increased risk of bleeding and thrombosis as well as increased health care costs.8-10 Mechanistically, patient factors such as differences in vitamin K consumption, comorbid conditions, drug-drug interactions, and medication compliance, as well as genetic differences that impact drug metabolism undoubtedly contribute to the variation of INR noted in patients on warfarin therapy.
Attempts to improve stability have included the administration of low-dose oral vitamin K. However, recent data from a multicenter randomized control trial suggests that while such therapy may help to decrease extreme variations in INR, it does not lead to an increased TTR.11 Furthermore, while significant work has been conducted in identifying specific gene variants, such as CYP2C9 and VKORC, which encode cytochrome P450 and vitamin K epoxide reductase enzymes, respectively, economic analyses suggest that testing for these gene variants would not be cost-effective.12 Additionally, clinical prediction tools, which incorporate important patient factors to help guide anticoagulation explain less than 10% of TTR variability.4
Nonetheless, some caution is warranted in the interpretation of the results reported by Pokorney and his colleagues. The proportion of registry patients treated with warfarin who had a low TTR was much lower than that previously reported by the pivotal U.S. trials of NOACs (55%-68%) and significantly lower than the results of a recent nationwide Swedish registry involving 40,449 patients.13
In the Swedish registry, the mean individual TTR was 70% with more than half the patients having a TTR of 70% or more, emphasizing the importance of health care system effects. Moreover, regardless of whether a patient is on warfarin or a NOAC, patients with a lower TTR have higher rates of diabetes, chronic obstructive pulmonary disease, heart failure, and renal failure, which may contribute to the need for additional therapies that may influence TTR.
For example, INR may be increased by ciprofloxacin or omeprazole when taken with warfarin, and CYP3A4 and P-glycoprotein (P-gp) inducers and inhibitors can result in an increased or decreased anticoagulation effect when used with NOACs. Recent reports have also highlighted variability in the safety of NOACs, particularly among patients with renal or liver insufficiency, African Americans, or patients with a prior history of GI bleeding.14-16 For these subgroups, determining NOAC activity to improve clinical safety of these agents is difficult.
PT or INR testing is largely insensitive or otherwise highly variable and the blood draw time relative to the most recent dose significantly influences the measured level of anti-Xa activity. Importantly, socioeconomic factors and family support systems also influence TTR, as important determinants of access to needed drugs or the ability to sustain related costs over time.
Taken together, prior INR stability on warfarin therapy does not ensure continued stability and, as a consequence, long-term warfarin therapy requires close monitoring in order to remain effective. To this end, further development of point-of-care coagulometers for self-testing and self-management, which have been found to be acceptable and preferred by patients, should be pursued.17 Similarly, attempts to decrease INR variability through research on optimizing computer assisted dosing programs remains warranted.18 NOACs offer an advantage over warfarin therapy in that they have a more predictable pharmacokinetic profile, which precludes the need for routine monitoring of anticoagulation parameters. However, many of the same factors, which influence TTR for warfarin do so for NOACs; NOACs have increased bleeding risk in comparison to warfarin for a number of demographic groups; and the high cost of NOACs may influence patient compliance.
Accordingly, until further data is available, consideration of the conversion of a patient on warfarin with a low TTR to a NOAC should be individualized.
Madhukar S. Patel, MD, is a general surgeon at the Department of Surgery, Massachusetts General Hospital, Boston, and Elliot L. Chaikof, MD, is Surgeon-in-Chief, Beth Israel Deaconess Medical Center, and Chairman, Roberta and Stephen R. Weiner Department of Surgery, Johnson and Johnson Professor of Surgery, Harvard Medical School. Dr. Chaikof is also an associate editor for Vascular Specialist. They have no relevant conflicts.
References
2. Nat Rev Cardiol. 2014;11:693-703.
5. J Thromb Haemost. 2010;8:2182-91.
6. Thromb Haemost. 2009;101:552-6.
7. Am J Cardiovasc Drugs. 2015;15:205-11.
8. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
10. J Med Econ. 2015;18:333-40.
11. Thromb Haemost. 2016;116:480-5.
12. Ann Intern Med. 2009;150:73-83.
13. JAMA Cardiol. 2016;1:172-80.
14. N Engl J Med. 2013;369:2093-104.
15. JAMA Intern Med. 2015;175:18-24.
16. J Am Coll Cardiol. 2014;63:891-900.
Progress in the development of new oral anticoagulants (NOACs), as well as agents for their reversal, has lowered the threshold to use these therapeutics as first line agents for the management of nonvalvular atrial fibrillation and venous thromboembolism.1,2 Despite this increase in adoption, however, debate persists as to whether patients chronically maintained on vitamin K antagonists (VKAs), such as warfarin, should be switched to NOACs. The recently published research letter by Pokorney et al. assessed the stability of international normalized ratios (INRs) in patients on long-term warfarin therapy in order to address this question.3
Specifically, prospective registry data from 3,749 patients with at least three INR values in the first 6 months of therapy as well as six or more in the following year were included. Patients were deemed stable if 80% or more of their INRs were in a therapeutic range defined as an INR between 2 and 3.3 During the initiation period, only one in four patients taking warfarin had a stable INR.3 Furthermore, stability in the first 6 months was found to have limited ability to predict stability in the subsequent year (concordance index of 0.61). With regard to time in therapeutic range (TTR), only 32% of patients had a TTR of greater than 80% during the first 6 months with less than half (42%) of these patients able to maintain this in the following year.
Findings from Pokorney et al. add to the growing body of literature demonstrating the difficulty of achieving and maintaining a therapeutic INR while on warfarin therapy.4-7 Clinically, these findings are important, as deviations from TTR have been shown to be associated with increased risk of bleeding and thrombosis as well as increased health care costs.8-10 Mechanistically, patient factors such as differences in vitamin K consumption, comorbid conditions, drug-drug interactions, and medication compliance, as well as genetic differences that impact drug metabolism undoubtedly contribute to the variation of INR noted in patients on warfarin therapy.
Attempts to improve stability have included the administration of low-dose oral vitamin K. However, recent data from a multicenter randomized control trial suggests that while such therapy may help to decrease extreme variations in INR, it does not lead to an increased TTR.11 Furthermore, while significant work has been conducted in identifying specific gene variants, such as CYP2C9 and VKORC, which encode cytochrome P450 and vitamin K epoxide reductase enzymes, respectively, economic analyses suggest that testing for these gene variants would not be cost-effective.12 Additionally, clinical prediction tools, which incorporate important patient factors to help guide anticoagulation explain less than 10% of TTR variability.4
Nonetheless, some caution is warranted in the interpretation of the results reported by Pokorney and his colleagues. The proportion of registry patients treated with warfarin who had a low TTR was much lower than that previously reported by the pivotal U.S. trials of NOACs (55%-68%) and significantly lower than the results of a recent nationwide Swedish registry involving 40,449 patients.13
In the Swedish registry, the mean individual TTR was 70% with more than half the patients having a TTR of 70% or more, emphasizing the importance of health care system effects. Moreover, regardless of whether a patient is on warfarin or a NOAC, patients with a lower TTR have higher rates of diabetes, chronic obstructive pulmonary disease, heart failure, and renal failure, which may contribute to the need for additional therapies that may influence TTR.
For example, INR may be increased by ciprofloxacin or omeprazole when taken with warfarin, and CYP3A4 and P-glycoprotein (P-gp) inducers and inhibitors can result in an increased or decreased anticoagulation effect when used with NOACs. Recent reports have also highlighted variability in the safety of NOACs, particularly among patients with renal or liver insufficiency, African Americans, or patients with a prior history of GI bleeding.14-16 For these subgroups, determining NOAC activity to improve clinical safety of these agents is difficult.
PT or INR testing is largely insensitive or otherwise highly variable and the blood draw time relative to the most recent dose significantly influences the measured level of anti-Xa activity. Importantly, socioeconomic factors and family support systems also influence TTR, as important determinants of access to needed drugs or the ability to sustain related costs over time.
Taken together, prior INR stability on warfarin therapy does not ensure continued stability and, as a consequence, long-term warfarin therapy requires close monitoring in order to remain effective. To this end, further development of point-of-care coagulometers for self-testing and self-management, which have been found to be acceptable and preferred by patients, should be pursued.17 Similarly, attempts to decrease INR variability through research on optimizing computer assisted dosing programs remains warranted.18 NOACs offer an advantage over warfarin therapy in that they have a more predictable pharmacokinetic profile, which precludes the need for routine monitoring of anticoagulation parameters. However, many of the same factors, which influence TTR for warfarin do so for NOACs; NOACs have increased bleeding risk in comparison to warfarin for a number of demographic groups; and the high cost of NOACs may influence patient compliance.
Accordingly, until further data is available, consideration of the conversion of a patient on warfarin with a low TTR to a NOAC should be individualized.
Madhukar S. Patel, MD, is a general surgeon at the Department of Surgery, Massachusetts General Hospital, Boston, and Elliot L. Chaikof, MD, is Surgeon-in-Chief, Beth Israel Deaconess Medical Center, and Chairman, Roberta and Stephen R. Weiner Department of Surgery, Johnson and Johnson Professor of Surgery, Harvard Medical School. Dr. Chaikof is also an associate editor for Vascular Specialist. They have no relevant conflicts.
References
2. Nat Rev Cardiol. 2014;11:693-703.
5. J Thromb Haemost. 2010;8:2182-91.
6. Thromb Haemost. 2009;101:552-6.
7. Am J Cardiovasc Drugs. 2015;15:205-11.
8. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
10. J Med Econ. 2015;18:333-40.
11. Thromb Haemost. 2016;116:480-5.
12. Ann Intern Med. 2009;150:73-83.
13. JAMA Cardiol. 2016;1:172-80.
14. N Engl J Med. 2013;369:2093-104.
15. JAMA Intern Med. 2015;175:18-24.
16. J Am Coll Cardiol. 2014;63:891-900.
Antibiotic susceptibility differs in transplant recipients
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
FROM DIAGNOSTIC MICROBIOLOGY AND INFECTIOUS DISEASE
Key clinical point: Antibiotic susceptibility in bacteria cultured from transplant recipients differs markedly from that in hospital-wide antibiograms.
Major finding: In the transplant recipients, E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin.
Data source: A single-center study comparing the antibiotic susceptibility of 1,889 bacterial isolates from transplant recipients with 10,439 isolates from other patients.
Disclosures: This study was not supported by funding from any public, commercial, or not-for-profit entities. Dr. Rosa and her associates reported having no relevant financial disclosures.
Size does matter
I grew up in a small town. I went to a small college. And I live and practiced in a small town in a sparsely populated state. Clearly, I’m partial to smallness. I have practiced in a two-man partnership, a solo practice, a small group, and finally in a large multicenter organization. The 10 years I practiced by myself were the most productive. It was also the most rewarding period of my life both professionally and financially.
The small group environment was a close second as a far as job satisfaction. What little I lost in autonomy was almost balanced by professional stimulation and camaraderie or working shoulder to shoulder with peers. However, all that was lost as our small group was engulfed by a larger entity. Our overhead inflated to a point that it was almost unsustainable. Meetings gobbled up productive office time. Even making little changes that might have allowed us to adapt to the changing clinical landscape seemed to take forever. That is, if they ever happened at all.
From my personal experience, health care delivery doesn’t benefit from the economics of scale that is claimed by other industries. Bigger is not better for health care delivery.
When the promoters of the Affordable Care Act promised that it would encourage cost saving and quality enhancing mergers of health delivery organizations, many other physicians and I had serious doubts about this claim. It turns that our concerns were well founded. The consolidations that were predicted and so eagerly anticipated by the architects of the ACA have occurred, but have not resulted in the promised cost savings or quality improvement.
The results have been so disappointing that Dr. Bob Kocher, special assistant to President Obama for health care and economic policy from 2009 to 2010, has felt the need to issue a mea culpa in the form of an op-ed piece in the Wall Street Journal (“How I Was Wrong About ObamaCare,” July 31, 2016). Although Dr. Kocher still believes organizing medicine into networks “that can share information, coordinate care for patients, and manage risk is critical for delivering higher-quality care, generating cost savings and improving the experience for patients,” he acknowledges, “having every provider in health care ‘owned’ by a single organization is more likely to be a barrier to better care.”
He cites recent evidence that “savings and quality improvement are generated much more often by independent primary care doctors than large hospital-centric health systems.” Small independent practices know their patients better. Unencumbered by the weight of multiple organizational layers, they can more nimbly adjust to change. And there will always be change.
Dr. Kocher also admits that he and his co-crafters of the ACA were mistaken in their belief that “it would take three to five years for physicians to use electronic health records effectively.” Unfortunately, he places the failure on what he views as delay tactics by organized medicine. Sadly, he shares this blind spot with too many other former and current government health care officials, most of whom who have never suffered under the burden of a user-unfriendly, free time–wasting, electronic medical record system.
While it is nice of Dr. Kocher to acknowledge his revelation about size, it comes too late. The bridges have already been burned. Most of the smaller independent practices he now realizes could have provided a solution to the accelerating cost of medical care are gone. In some cases, one of forces driving small practices to merge was the cost and complexity of converting to electronic medical records.
The mea culpa that we really need to hear now is the one admitting that the roll out of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009 and meaningful use requirements were poorly conceived and implemented. Electronic health record systems that are capable of seamlessly communicating with one another, and are inexpensive, intuitive, and user friendly might have allowed more small independent practices to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a small town. I went to a small college. And I live and practiced in a small town in a sparsely populated state. Clearly, I’m partial to smallness. I have practiced in a two-man partnership, a solo practice, a small group, and finally in a large multicenter organization. The 10 years I practiced by myself were the most productive. It was also the most rewarding period of my life both professionally and financially.
The small group environment was a close second as a far as job satisfaction. What little I lost in autonomy was almost balanced by professional stimulation and camaraderie or working shoulder to shoulder with peers. However, all that was lost as our small group was engulfed by a larger entity. Our overhead inflated to a point that it was almost unsustainable. Meetings gobbled up productive office time. Even making little changes that might have allowed us to adapt to the changing clinical landscape seemed to take forever. That is, if they ever happened at all.
From my personal experience, health care delivery doesn’t benefit from the economics of scale that is claimed by other industries. Bigger is not better for health care delivery.
When the promoters of the Affordable Care Act promised that it would encourage cost saving and quality enhancing mergers of health delivery organizations, many other physicians and I had serious doubts about this claim. It turns that our concerns were well founded. The consolidations that were predicted and so eagerly anticipated by the architects of the ACA have occurred, but have not resulted in the promised cost savings or quality improvement.
The results have been so disappointing that Dr. Bob Kocher, special assistant to President Obama for health care and economic policy from 2009 to 2010, has felt the need to issue a mea culpa in the form of an op-ed piece in the Wall Street Journal (“How I Was Wrong About ObamaCare,” July 31, 2016). Although Dr. Kocher still believes organizing medicine into networks “that can share information, coordinate care for patients, and manage risk is critical for delivering higher-quality care, generating cost savings and improving the experience for patients,” he acknowledges, “having every provider in health care ‘owned’ by a single organization is more likely to be a barrier to better care.”
He cites recent evidence that “savings and quality improvement are generated much more often by independent primary care doctors than large hospital-centric health systems.” Small independent practices know their patients better. Unencumbered by the weight of multiple organizational layers, they can more nimbly adjust to change. And there will always be change.
Dr. Kocher also admits that he and his co-crafters of the ACA were mistaken in their belief that “it would take three to five years for physicians to use electronic health records effectively.” Unfortunately, he places the failure on what he views as delay tactics by organized medicine. Sadly, he shares this blind spot with too many other former and current government health care officials, most of whom who have never suffered under the burden of a user-unfriendly, free time–wasting, electronic medical record system.
While it is nice of Dr. Kocher to acknowledge his revelation about size, it comes too late. The bridges have already been burned. Most of the smaller independent practices he now realizes could have provided a solution to the accelerating cost of medical care are gone. In some cases, one of forces driving small practices to merge was the cost and complexity of converting to electronic medical records.
The mea culpa that we really need to hear now is the one admitting that the roll out of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009 and meaningful use requirements were poorly conceived and implemented. Electronic health record systems that are capable of seamlessly communicating with one another, and are inexpensive, intuitive, and user friendly might have allowed more small independent practices to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a small town. I went to a small college. And I live and practiced in a small town in a sparsely populated state. Clearly, I’m partial to smallness. I have practiced in a two-man partnership, a solo practice, a small group, and finally in a large multicenter organization. The 10 years I practiced by myself were the most productive. It was also the most rewarding period of my life both professionally and financially.
The small group environment was a close second as a far as job satisfaction. What little I lost in autonomy was almost balanced by professional stimulation and camaraderie or working shoulder to shoulder with peers. However, all that was lost as our small group was engulfed by a larger entity. Our overhead inflated to a point that it was almost unsustainable. Meetings gobbled up productive office time. Even making little changes that might have allowed us to adapt to the changing clinical landscape seemed to take forever. That is, if they ever happened at all.
From my personal experience, health care delivery doesn’t benefit from the economics of scale that is claimed by other industries. Bigger is not better for health care delivery.
When the promoters of the Affordable Care Act promised that it would encourage cost saving and quality enhancing mergers of health delivery organizations, many other physicians and I had serious doubts about this claim. It turns that our concerns were well founded. The consolidations that were predicted and so eagerly anticipated by the architects of the ACA have occurred, but have not resulted in the promised cost savings or quality improvement.
The results have been so disappointing that Dr. Bob Kocher, special assistant to President Obama for health care and economic policy from 2009 to 2010, has felt the need to issue a mea culpa in the form of an op-ed piece in the Wall Street Journal (“How I Was Wrong About ObamaCare,” July 31, 2016). Although Dr. Kocher still believes organizing medicine into networks “that can share information, coordinate care for patients, and manage risk is critical for delivering higher-quality care, generating cost savings and improving the experience for patients,” he acknowledges, “having every provider in health care ‘owned’ by a single organization is more likely to be a barrier to better care.”
He cites recent evidence that “savings and quality improvement are generated much more often by independent primary care doctors than large hospital-centric health systems.” Small independent practices know their patients better. Unencumbered by the weight of multiple organizational layers, they can more nimbly adjust to change. And there will always be change.
Dr. Kocher also admits that he and his co-crafters of the ACA were mistaken in their belief that “it would take three to five years for physicians to use electronic health records effectively.” Unfortunately, he places the failure on what he views as delay tactics by organized medicine. Sadly, he shares this blind spot with too many other former and current government health care officials, most of whom who have never suffered under the burden of a user-unfriendly, free time–wasting, electronic medical record system.
While it is nice of Dr. Kocher to acknowledge his revelation about size, it comes too late. The bridges have already been burned. Most of the smaller independent practices he now realizes could have provided a solution to the accelerating cost of medical care are gone. In some cases, one of forces driving small practices to merge was the cost and complexity of converting to electronic medical records.
The mea culpa that we really need to hear now is the one admitting that the roll out of the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009 and meaningful use requirements were poorly conceived and implemented. Electronic health record systems that are capable of seamlessly communicating with one another, and are inexpensive, intuitive, and user friendly might have allowed more small independent practices to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
USPSTF: Screen for tuberculosis in those at greatest risk
Screening for latent tuberculosis infection (LTBI) can help prevent progression to active disease, and the availability of effective tests supports screening asymptomatic adults aged 18 years and older at increased risk for infection, according to new recommendations from the U.S. Preventive Services Task Force.
The recommendations were published online Sept. 6 in JAMA.
“The USPSTF concludes with moderate certainty that the net benefit of screening for LTBI in persons at increased risk for tuberculosis is moderate,” wrote lead author Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco, and her colleagues (JAMA 2016 Sep 6;316[9]:962-9).
TB infection spreads through the coughing or sneezing of someone with active disease. Individuals at high risk for TB include those who are immunocompromised, residents of long-term care facilities or correctional facilities, or homeless individuals, as well as those born in countries known to have a high incidence of TB, including China, India, Mexico, and Vietnam.
Other populations at increased risk for TB are contacts of patients with active TB, health care workers, and workers in high-risk settings, the researchers noted.
TB remains a preventable disease in the United States, with a prevalence of approximately 5%, the researchers said. The two most effective screening tests, tuberculin skin test (TST) and interferon-gamma release assays (IGRA), demonstrated sensitivity and specificity of 79% and 97%, and at least 80% and 95%, respectively.
The recommendations are supported by an evidence review, also published in JAMA (2016 Sep 6;316[9]:970-83). The review included 72 studies and 51,711 adults.
The studies in the evidence review did not assess the benefits vs. harms of TB screening, compared with no screening, noted Leila C. Kahwati, MD, of RTI International in Research Triangle Park, N.C., and her colleagues.
“The applicability of the evidence on accuracy and reliability of screening tests to primary care practice settings and populations is uncertain for several reasons,” the investigators said. However, the findings suggest that “treatment reduced the risk of active TB among the populations included in this review.”
The researchers had no financial conflicts to disclose.
Screening for latent tuberculosis infection (LTBI) can help prevent progression to active disease, and the availability of effective tests supports screening asymptomatic adults aged 18 years and older at increased risk for infection, according to new recommendations from the U.S. Preventive Services Task Force.
The recommendations were published online Sept. 6 in JAMA.
“The USPSTF concludes with moderate certainty that the net benefit of screening for LTBI in persons at increased risk for tuberculosis is moderate,” wrote lead author Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco, and her colleagues (JAMA 2016 Sep 6;316[9]:962-9).
TB infection spreads through the coughing or sneezing of someone with active disease. Individuals at high risk for TB include those who are immunocompromised, residents of long-term care facilities or correctional facilities, or homeless individuals, as well as those born in countries known to have a high incidence of TB, including China, India, Mexico, and Vietnam.
Other populations at increased risk for TB are contacts of patients with active TB, health care workers, and workers in high-risk settings, the researchers noted.
TB remains a preventable disease in the United States, with a prevalence of approximately 5%, the researchers said. The two most effective screening tests, tuberculin skin test (TST) and interferon-gamma release assays (IGRA), demonstrated sensitivity and specificity of 79% and 97%, and at least 80% and 95%, respectively.
The recommendations are supported by an evidence review, also published in JAMA (2016 Sep 6;316[9]:970-83). The review included 72 studies and 51,711 adults.
The studies in the evidence review did not assess the benefits vs. harms of TB screening, compared with no screening, noted Leila C. Kahwati, MD, of RTI International in Research Triangle Park, N.C., and her colleagues.
“The applicability of the evidence on accuracy and reliability of screening tests to primary care practice settings and populations is uncertain for several reasons,” the investigators said. However, the findings suggest that “treatment reduced the risk of active TB among the populations included in this review.”
The researchers had no financial conflicts to disclose.
Screening for latent tuberculosis infection (LTBI) can help prevent progression to active disease, and the availability of effective tests supports screening asymptomatic adults aged 18 years and older at increased risk for infection, according to new recommendations from the U.S. Preventive Services Task Force.
The recommendations were published online Sept. 6 in JAMA.
“The USPSTF concludes with moderate certainty that the net benefit of screening for LTBI in persons at increased risk for tuberculosis is moderate,” wrote lead author Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco, and her colleagues (JAMA 2016 Sep 6;316[9]:962-9).
TB infection spreads through the coughing or sneezing of someone with active disease. Individuals at high risk for TB include those who are immunocompromised, residents of long-term care facilities or correctional facilities, or homeless individuals, as well as those born in countries known to have a high incidence of TB, including China, India, Mexico, and Vietnam.
Other populations at increased risk for TB are contacts of patients with active TB, health care workers, and workers in high-risk settings, the researchers noted.
TB remains a preventable disease in the United States, with a prevalence of approximately 5%, the researchers said. The two most effective screening tests, tuberculin skin test (TST) and interferon-gamma release assays (IGRA), demonstrated sensitivity and specificity of 79% and 97%, and at least 80% and 95%, respectively.
The recommendations are supported by an evidence review, also published in JAMA (2016 Sep 6;316[9]:970-83). The review included 72 studies and 51,711 adults.
The studies in the evidence review did not assess the benefits vs. harms of TB screening, compared with no screening, noted Leila C. Kahwati, MD, of RTI International in Research Triangle Park, N.C., and her colleagues.
“The applicability of the evidence on accuracy and reliability of screening tests to primary care practice settings and populations is uncertain for several reasons,” the investigators said. However, the findings suggest that “treatment reduced the risk of active TB among the populations included in this review.”
The researchers had no financial conflicts to disclose.
FROM JAMA
Key clinical point: Latent tuberculosis infection is a significant problem, and both the tuberculin skin test (TST) and interferon-gamma release assays (IGRA) were moderately sensitive and highly specific in areas with a low tuberculosis burden.
Major finding: Approximately 5%-10% of individuals with latent TB progress to active disease, according to the USPSTF, and treatment reduces the risk of progression.
Data source: An evidence review including 72 studies and 51,711 individuals.
Disclosures: The researchers had no financial conflicts to disclose.
Help at a cost
Have you read the study with the weighty title of “Fully Capitated Payment Breakeven Rate for a Mid-Size Pediatric Practice?” (Pediatrics. 2016, July 29. doi: 10.1542/peds.2015-4367). You should! Of course, it’s easy for me to admonish you because my active practice days are behind me, and I have the time to read things with intimidating titles. But if you have had the time it takes to read the handwriting on the wall, you know that fee for service (FFS) is on the endangered list and is being replaced by a variety of other payment models, many of which are based on some form of capitation. Even just a cursory reading of this study from the Center of Healthcare Innovation and Policy Research at George Washington University should help you appreciate the complexities implicit in the transition from FFS to capitation and give you a sense of how it might affect the way you practice.
To amass the data they needed to run their computer models, the investigators had to make some assumptions. Here are just a few: The average pediatrician salary was pegged at $180,000, and she/he would be seeing 25 patients per day for 220 clinical days in the year. The practice she/he is working in has a staff to physician ratio of 3.2. Do you even know what your practice’s staff to physician ratio is? Is it ever discussed? How do their assumptions square with your reality?
The researchers also assumed that when practices transition to a capitated system many of them also adopt a primary care medical home (PCMH) model that often includes changes in staffing ratios almost always resulting in a higher staff to physician ratio. When the researchers fed their model even modest increases in staff to physician ratio from 3.2 to 4.0 or 4.4, the result was an increase in the break-even payment rate of between 12% and 23%. However, this study doesn’t answer whether related changes in panel size and patient outcome would make these increases sustainable.
It also doesn’t include the complexities that are inherent in the trend toward part-time employment. How good is your practice at optimizing physician to staff ratios when several physicians have chosen to work part-time? Are the physicians’ schedules arranged to minimize resource-wasting overlap in staffing? How efficient are you at utilizing support staff? For example, do you do your own measurements as part of your exam and give immunizations? How does this compare with your peers? Is your efficiency paying for some of their overhead?
If you are already using a PCMH model, how efficient have you been in using the additional support staff that it requires? Measuring the improvement in quality the change has created is difficult, but it should be fairly easy to determine the cost of the added staffing.
The investigators acknowledge that they have not included the cost of immunization in their models, and I don’t think that they expect to us take their numbers too seriously. But the first line in the authors’ conclusion is the reason that you should take the time to read this study. “Practices are more likely to succeed in capitated models if pediatricians understand how these models alter practice finances.”
You may have gone into pediatrics because of the noble causes that the specialty espouses. But it’s time to swallow hard and acknowledge that this is one of those situations in which it is all about the money. You need to keep informed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Have you read the study with the weighty title of “Fully Capitated Payment Breakeven Rate for a Mid-Size Pediatric Practice?” (Pediatrics. 2016, July 29. doi: 10.1542/peds.2015-4367). You should! Of course, it’s easy for me to admonish you because my active practice days are behind me, and I have the time to read things with intimidating titles. But if you have had the time it takes to read the handwriting on the wall, you know that fee for service (FFS) is on the endangered list and is being replaced by a variety of other payment models, many of which are based on some form of capitation. Even just a cursory reading of this study from the Center of Healthcare Innovation and Policy Research at George Washington University should help you appreciate the complexities implicit in the transition from FFS to capitation and give you a sense of how it might affect the way you practice.
To amass the data they needed to run their computer models, the investigators had to make some assumptions. Here are just a few: The average pediatrician salary was pegged at $180,000, and she/he would be seeing 25 patients per day for 220 clinical days in the year. The practice she/he is working in has a staff to physician ratio of 3.2. Do you even know what your practice’s staff to physician ratio is? Is it ever discussed? How do their assumptions square with your reality?
The researchers also assumed that when practices transition to a capitated system many of them also adopt a primary care medical home (PCMH) model that often includes changes in staffing ratios almost always resulting in a higher staff to physician ratio. When the researchers fed their model even modest increases in staff to physician ratio from 3.2 to 4.0 or 4.4, the result was an increase in the break-even payment rate of between 12% and 23%. However, this study doesn’t answer whether related changes in panel size and patient outcome would make these increases sustainable.
It also doesn’t include the complexities that are inherent in the trend toward part-time employment. How good is your practice at optimizing physician to staff ratios when several physicians have chosen to work part-time? Are the physicians’ schedules arranged to minimize resource-wasting overlap in staffing? How efficient are you at utilizing support staff? For example, do you do your own measurements as part of your exam and give immunizations? How does this compare with your peers? Is your efficiency paying for some of their overhead?
If you are already using a PCMH model, how efficient have you been in using the additional support staff that it requires? Measuring the improvement in quality the change has created is difficult, but it should be fairly easy to determine the cost of the added staffing.
The investigators acknowledge that they have not included the cost of immunization in their models, and I don’t think that they expect to us take their numbers too seriously. But the first line in the authors’ conclusion is the reason that you should take the time to read this study. “Practices are more likely to succeed in capitated models if pediatricians understand how these models alter practice finances.”
You may have gone into pediatrics because of the noble causes that the specialty espouses. But it’s time to swallow hard and acknowledge that this is one of those situations in which it is all about the money. You need to keep informed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Have you read the study with the weighty title of “Fully Capitated Payment Breakeven Rate for a Mid-Size Pediatric Practice?” (Pediatrics. 2016, July 29. doi: 10.1542/peds.2015-4367). You should! Of course, it’s easy for me to admonish you because my active practice days are behind me, and I have the time to read things with intimidating titles. But if you have had the time it takes to read the handwriting on the wall, you know that fee for service (FFS) is on the endangered list and is being replaced by a variety of other payment models, many of which are based on some form of capitation. Even just a cursory reading of this study from the Center of Healthcare Innovation and Policy Research at George Washington University should help you appreciate the complexities implicit in the transition from FFS to capitation and give you a sense of how it might affect the way you practice.
To amass the data they needed to run their computer models, the investigators had to make some assumptions. Here are just a few: The average pediatrician salary was pegged at $180,000, and she/he would be seeing 25 patients per day for 220 clinical days in the year. The practice she/he is working in has a staff to physician ratio of 3.2. Do you even know what your practice’s staff to physician ratio is? Is it ever discussed? How do their assumptions square with your reality?
The researchers also assumed that when practices transition to a capitated system many of them also adopt a primary care medical home (PCMH) model that often includes changes in staffing ratios almost always resulting in a higher staff to physician ratio. When the researchers fed their model even modest increases in staff to physician ratio from 3.2 to 4.0 or 4.4, the result was an increase in the break-even payment rate of between 12% and 23%. However, this study doesn’t answer whether related changes in panel size and patient outcome would make these increases sustainable.
It also doesn’t include the complexities that are inherent in the trend toward part-time employment. How good is your practice at optimizing physician to staff ratios when several physicians have chosen to work part-time? Are the physicians’ schedules arranged to minimize resource-wasting overlap in staffing? How efficient are you at utilizing support staff? For example, do you do your own measurements as part of your exam and give immunizations? How does this compare with your peers? Is your efficiency paying for some of their overhead?
If you are already using a PCMH model, how efficient have you been in using the additional support staff that it requires? Measuring the improvement in quality the change has created is difficult, but it should be fairly easy to determine the cost of the added staffing.
The investigators acknowledge that they have not included the cost of immunization in their models, and I don’t think that they expect to us take their numbers too seriously. But the first line in the authors’ conclusion is the reason that you should take the time to read this study. “Practices are more likely to succeed in capitated models if pediatricians understand how these models alter practice finances.”
You may have gone into pediatrics because of the noble causes that the specialty espouses. But it’s time to swallow hard and acknowledge that this is one of those situations in which it is all about the money. You need to keep informed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Pneumonitis with nivolumab treatment shows common radiographic patterns
A study of cancer patients enrolled in trials of the programmed cell death-1 inhibiting medicine nivolumab found that among a minority who developed pneumonitis during treatment, distinct radiographic patterns were significantly associated with the level of pneumonitis severity.
Investigators found that cryptic organizing pneumonia pattern (COP) was the most common, though not the most severe. Led by Mizuki Nishino, MD, of Brigham and Women’s Hospital, Boston, the researchers looked at the 20 patients out of a cohort of 170 (11.8%) who had developed pneumonitis, and found that radiologic patterns indicating acute interstitial pneumonia/acute respiratory distress syndrome (n = 2) had the highest severity grade on a scale of 1-5 (median 3), followed by those with COP pattern (n = 13, median grade 2), hypersensitivity pneumonitis (n = 2, median grade 1), and nonspecific interstitial pneumonia (n = 3, median grade 1). The pattern was significantly associated with severity (P = .0006).
The study cohort included patients being treated with nivolumab for lung cancer, melanoma, and lymphoma; the COP patten was the most common across tumor types and observed in patients receiving monotherapy and combination therapy alike. Therapy with nivolumab was suspended for all 20 pneumonitis patients, and most (n = 17) received treatment for pneumonitis with corticosteroids with or without infliximab, for a median treatment time of 6 weeks. Seven patients were able to restart nivolumab, though pneumonitis recurred in two, the investigators reported (Clin Cancer Res. 2016 Aug 17. doi: 10.1158/1078-0432.CCR-16-1320).
“Time from initiation of therapy to the development of pneumonitis had a wide range (0.5-11.5 months), indicating an importance of careful observation and follow-up for signs and symptoms of pneumonitis throughout treatment,” Dr. Nishino and colleagues wrote in their analysis, adding that shorter times were observed for lung cancer patients, possibly because of their higher pulmonary burden, a lower threshold for performing chest scans in these patients, or both. “In most patients, clinical and radiographic improvements were noted after treatment, indicating that [PD-1 inhibitor-related pneumonitis], although potentially serious, is treatable if diagnosed and managed appropriately. The observation emphasizes the importance of timely recognition, accurate diagnosis, and early intervention.”
The lead author and several coauthors disclosed funding from Bristol-Myers Squibb, which sponsored the trial, as well as from other manufacturers.
A study of cancer patients enrolled in trials of the programmed cell death-1 inhibiting medicine nivolumab found that among a minority who developed pneumonitis during treatment, distinct radiographic patterns were significantly associated with the level of pneumonitis severity.
Investigators found that cryptic organizing pneumonia pattern (COP) was the most common, though not the most severe. Led by Mizuki Nishino, MD, of Brigham and Women’s Hospital, Boston, the researchers looked at the 20 patients out of a cohort of 170 (11.8%) who had developed pneumonitis, and found that radiologic patterns indicating acute interstitial pneumonia/acute respiratory distress syndrome (n = 2) had the highest severity grade on a scale of 1-5 (median 3), followed by those with COP pattern (n = 13, median grade 2), hypersensitivity pneumonitis (n = 2, median grade 1), and nonspecific interstitial pneumonia (n = 3, median grade 1). The pattern was significantly associated with severity (P = .0006).
The study cohort included patients being treated with nivolumab for lung cancer, melanoma, and lymphoma; the COP patten was the most common across tumor types and observed in patients receiving monotherapy and combination therapy alike. Therapy with nivolumab was suspended for all 20 pneumonitis patients, and most (n = 17) received treatment for pneumonitis with corticosteroids with or without infliximab, for a median treatment time of 6 weeks. Seven patients were able to restart nivolumab, though pneumonitis recurred in two, the investigators reported (Clin Cancer Res. 2016 Aug 17. doi: 10.1158/1078-0432.CCR-16-1320).
“Time from initiation of therapy to the development of pneumonitis had a wide range (0.5-11.5 months), indicating an importance of careful observation and follow-up for signs and symptoms of pneumonitis throughout treatment,” Dr. Nishino and colleagues wrote in their analysis, adding that shorter times were observed for lung cancer patients, possibly because of their higher pulmonary burden, a lower threshold for performing chest scans in these patients, or both. “In most patients, clinical and radiographic improvements were noted after treatment, indicating that [PD-1 inhibitor-related pneumonitis], although potentially serious, is treatable if diagnosed and managed appropriately. The observation emphasizes the importance of timely recognition, accurate diagnosis, and early intervention.”
The lead author and several coauthors disclosed funding from Bristol-Myers Squibb, which sponsored the trial, as well as from other manufacturers.
A study of cancer patients enrolled in trials of the programmed cell death-1 inhibiting medicine nivolumab found that among a minority who developed pneumonitis during treatment, distinct radiographic patterns were significantly associated with the level of pneumonitis severity.
Investigators found that cryptic organizing pneumonia pattern (COP) was the most common, though not the most severe. Led by Mizuki Nishino, MD, of Brigham and Women’s Hospital, Boston, the researchers looked at the 20 patients out of a cohort of 170 (11.8%) who had developed pneumonitis, and found that radiologic patterns indicating acute interstitial pneumonia/acute respiratory distress syndrome (n = 2) had the highest severity grade on a scale of 1-5 (median 3), followed by those with COP pattern (n = 13, median grade 2), hypersensitivity pneumonitis (n = 2, median grade 1), and nonspecific interstitial pneumonia (n = 3, median grade 1). The pattern was significantly associated with severity (P = .0006).
The study cohort included patients being treated with nivolumab for lung cancer, melanoma, and lymphoma; the COP patten was the most common across tumor types and observed in patients receiving monotherapy and combination therapy alike. Therapy with nivolumab was suspended for all 20 pneumonitis patients, and most (n = 17) received treatment for pneumonitis with corticosteroids with or without infliximab, for a median treatment time of 6 weeks. Seven patients were able to restart nivolumab, though pneumonitis recurred in two, the investigators reported (Clin Cancer Res. 2016 Aug 17. doi: 10.1158/1078-0432.CCR-16-1320).
“Time from initiation of therapy to the development of pneumonitis had a wide range (0.5-11.5 months), indicating an importance of careful observation and follow-up for signs and symptoms of pneumonitis throughout treatment,” Dr. Nishino and colleagues wrote in their analysis, adding that shorter times were observed for lung cancer patients, possibly because of their higher pulmonary burden, a lower threshold for performing chest scans in these patients, or both. “In most patients, clinical and radiographic improvements were noted after treatment, indicating that [PD-1 inhibitor-related pneumonitis], although potentially serious, is treatable if diagnosed and managed appropriately. The observation emphasizes the importance of timely recognition, accurate diagnosis, and early intervention.”
The lead author and several coauthors disclosed funding from Bristol-Myers Squibb, which sponsored the trial, as well as from other manufacturers.
FROM CLINICAL CANCER RESEARCH
Key clinical point: Pneumonitis related to treatment with PD-1 inhibitors showed distinct radiographic patterns associated with severity; most cases resolved with corticosteroid treatment.
Major finding: Of 20 patients in nivolumab trials who developed pneumonitis, a COP pattern was seen in 13, and other patterns in 7; different patterns were significantly associated with pneumonitis severity (P = .006).
Data source: 170 patients with melanoma, lung cancer or lymphoma enrolled in single-site open-label clinical trial of nivolumab.
Disclosures: The lead author and several coauthors disclosed funding from Bristol-Myers Squibb, which sponsored the trial, as well as from other manufacturers.
Commentary: Should board exams include a technical skill assessment? A European perspective
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
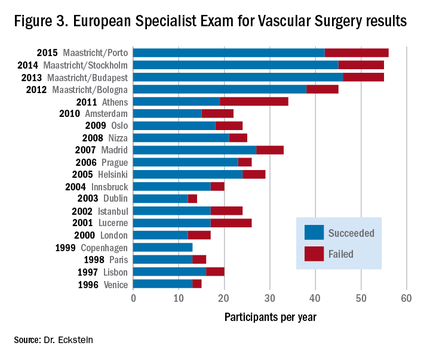
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8
 |
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.
 |
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.
 |
Dr. Malachi Sheahan III |
Dr. Eckstein’s excellent review highlights the challenges the European Union faces in trying to standardize its certification in vascular surgery. Among European nations, the training pathways in vascular surgery are extremely varied, yet the European Economic Union calls for a medical specialist who is certified in one country to be able to practice that specialty in any EEU nation. While participation in the Fellowship of the European Board in Vascular Surgery is still mostly optional, it does provide a path toward a standard of quality that includes competence in open and endovascular procedures. In the United States, we face a similar dilemma with the advent of the integrated vascular residencies. Curricula, case volumes, and rotations still vary wildly between programs and in comparison with traditional fellowships. One solution is the Fundamentals of Vascular and Endovascular Surgery (FVEVS) project. Currently in its pilot stage, the FVEVS is designed to ensure the attainment of basic technical competencies by the mid-trainee level so the later years are focused on advanced open and endovascular training.
Dr. Malachi Sheahan III is the Associate Medical Editor for Vascular Specialist.
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
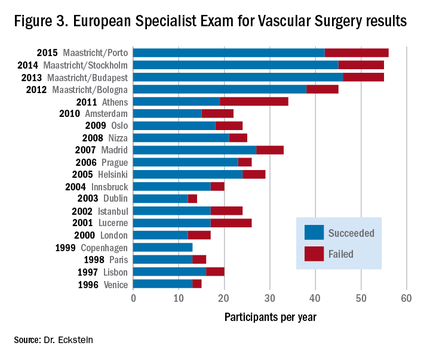
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8
The incidence of vascular diseases is steadily increasing because of an aging population. Vascular surgery is the only specialty that can offer all modalities of vascular therapy (endovascular, open, and conservative). It is therefore necessary to ensure implementation of all these modalities in a modern vascular surgical curricula. The creation of a vascular specialist curriculum is undoubtedly the best way to overcome further fragmentation of vascular provision and to prevent the increasingly financially-driven incentives that can mislead treatment. For obvious reasons this would be a major benefit for our patients and for our specialty.
Another reason for updating the vascular surgical curricula is the significant reduction of open aortic and peripheral vascular surgical training cases, such as abdominal aortic aneurysms and superficial femoral artery occlusions.1 Since the vast majority of these patients are now treated by endovascular means, the remaining vascular disease morphologies can technically be very demanding when requiring open vascular surgery procedures.
Nevertheless, the public and our patients quite understandably expect to be treated by well trained and competent vascular surgeons/specialists. As in all other professions, a proper assessment of all vascular competencies is therefore considered to be mandatory at the end of the training period for a vascular specialist. To this end, several proposals have been made to improve both the structure and different assessment tools including the Vascular Surgical Milestones Project,2 the Vascular Surgery In-Training Examinations (VSITE),3 the use of procedure-based assessments (PBA),4 or objective structured assessments of technical skills (OSATS).5 In addition, simulation workshops (using computer- or life-like synthetic models) play an increasing role in teaching vascular residents the ever-increasing number of different open and endovascular surgical techniques.6,7
Traditionally, the final board examination at the end of the vascular surgical training period consists of an oral assessment or a computer-based test. The obvious crucial question is whether a practical examination should be a added as a mandatory part of a vascular exit exam. This article gives an overview of the board examination of the European Board of Vascular Surgery (EBVS) at the UEMS (Union of European Medical Specialists), which adopted a technical skills assessment in 2006.
The European Vascular Surgical Examination
The UEMS was founded in 1958 as an official body of the European Union (EU). The UEMS has the remits to accredit medical meetings,8 to promote free professional movement of all doctors within Europe, and to ensure high quality of training and associated specialist standards via UEMS examinations.9,10 Currently, the UEMS represents the national medical societies of 37 member states. To date there are 42 UEMS Specialist Sections (separate and independent disciplines), UEMS Divisions (key areas within the independent disciplines, such as Interventional Radiology) and some so-called “Multidisciplinary Joint Committees” (such as Phlebology).
Since 2005, vascular surgery has been represented as an independent medical discipline within the UEMS.Politically, this was a tremendously important step that has helped many European countries to establish vascular surgery on a national level as a separate specialty. The most recent examples are Switzerland (since 2014) and Austria (since 2015).
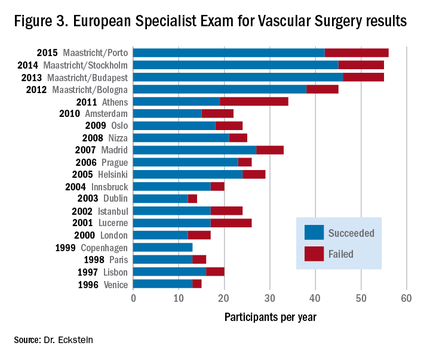
European vascular surgical examinations have been offered since 1996. The Fellowship of the European Board in Vascular Surgery (FEBVS) is voluntary in most European countries, but in some countries, such as Switzerland and the Netherlands, the European exam has now replaced the national specialist exam.12 Other countries also are in the process of accepting this European standard as a national standard, including Romania, Austria, and Sweden.
The European exam consists of a written section and a combined oral and practical exam. Candidates must be in possession of a national specialist title for surgery or vascular surgery (in countries with a monospecialty). Applications from non-EU countries also are accepted.
Applications must be made in writing, giving details of open-operative and endovascular experience. A distinction is made between assisted operations, independently performed surgery with assistance, and actual independently performed surgical procedures without specialist tutorial assistance. All candidates admitted to the examination have to pass a one-day oral and practical examination, which includes questioning on theoretical background knowledge and its practical application. This takes place mostly in the context of specific clinical case studies as well as via practical examinations on pulsatile perfused lifelike models.
The following procedures are assessed: an infrarenal aortic anastomosis, a carotid endarterectomy, and a distal bypass anastomosis.6,13,14 In the endovascular part of the examination, the applicant’s ability to introduce a guide-wire into the renal artery is assessed.15 Unlike the case in many national tests, FEBVS candidates are also presented with a specialist English-language publication (usually from the European Journal of Vascular and Endovascular Surgery). This article is then discussed with two examiners, with respect to its quality as well as its methodological content and significance. Many examination candidates fear this hurdle the most, but in fact very few participants fail this part of the test.
The European exam is designed to be unbiased and fair, with two examiners at each test station who carry out their assessments independent of each other. During the course of the examination, each candidate is interviewed by approximately 10 assessors. The assessment is validated by way of an evaluation form. The assessing auditors’ communications skills are themselves judged by observers. In the event of communication difficulties, observers are subsequently consulted.
Despite the challenging test procedures, the number of participants in the European Specialist Exam for Vascular Surgery has steadily increased in recent years. For this reason, since 2012, two examination sessions per year have been offered, one during the Annual Meeting of the European Society for Vascular Surgery (ESVS) and one at the European Vascular Course (EVC) in Maastricht. The failure rate each year fluctuates around 20%.
Benefits of being a Fellow of the European Board of Vascular Surgery (FEBVS)
There are a number of very good reasons to sit a European examination and acquire the title of Fellow of the European Board of Vascular Surgery (FEBVS). Some of them are:
Evidence of competency in job applications. Many managers know that the European exam is theoretically and practically challenging, and comprehensive. Confidence in candidates (specialists and senior physicians) who have passed the European test is therefore higher. That in turn increases the chances of getting the desired position especially when applying abroad!
Verification of open surgical and endovascular skills. Filling in the logbook16 helps to maintain a transparent open/endovascular portfolio. It is an extremely sophisticated tool to capture expertise and experience.
Commitment to the need for a European standard. The UEMS has set itself the goal of setting a European standard for medical specialists at the highest level. The European specialist exam projects this. All FEBVS support this goal via their application.
Commitment to academic knowledge-based vascular surgery. The European Vascular Surgery specialist exam covers theoretical background, knowledge of the main studies, basic academic skills, and the ability to comprehensively apply this knowledge to case studies from the entire vascular field. By obtaining this exam, all FEBVS confirm their commitment to an evidence-based approach to vascular surgery.
Commitment to competency-based vascular surgery. The European Vascular Surgery specialist exam covers a practical assessment on open vascular surgical and endovascular key competencies. By passing this part of the exam, all FEBVS give evidence that they are technically competent vascular surgeons.
Desire to belong to the best of the profession. The European specialist exam is certainly more demanding than many national board certifications. However, it offers an opportunity to belong to the European vascular surgical elite.
In conclusion, the European experience on board examinations including skills assessment shows pretty clearly that this sort of comprehensive examination is feasible. Moreover, the increasing number of applications indicates the growing attractiveness of the European certification and qualification as FEBVS. The long-term goal will be to make this examination mandatory for all EU countries – still a long way to go. By the way, since the status of FEBVS is also achievable by non-EU countries, Brexit will not prevent vascular surgeons from the United Kingdom to qualify as FEBVS in the future!
Dr. Eckstein is the Past President of the Board and Section of Vascular Surgery at the Union of European Medical Specialists (UEMS) and Past President of the German Vascular Society (DGG), and an associate editor for Vascular Specialist.
References
1. J Vasc Surg. 2014;60:945-49
2. J Vasc Surg. 2009;49:1140-6
3. Vascular surgery qualifying examination and Vsite
4. Health Technol Assess. 2011;15:i-xxi, 1-162
6. J Vasc Surg. 2013;57:1422-8
8. International Angiology. 2007;26:361-6
9. Eur J Vasc Endovasc Surg. 2009;37:109-15
10. J Vasc Surg. 2008;48:69S-75S; discussion 75S
12. Eur J Vasc Endovasc Surg. 2013;46:719-25
13. J Vasc Surg. 2013;57:1148-54
14. Brit J Surg. 2006;93:1132-8
Current Tx for blistering disorders lacks evidence-based science
NEWPORT BEACH, CALIF. – Current treatment of autoimmune blistering diseases is not backed by evidence-based medicine and solid randomized, controlled trials, according to David T. Woodley, MD.
“These are rare diseases; there’s no consensus on the treatment of choice,” Dr. Woodley said at the annual meeting of the Pacific Dermatologic Association.
Dr. Woodley, professor of dermatology at the University of Southern California, Los Angeles, limited his discussion to pemphigus vulgaris (PV), pemphigus foliaceus (PF), and bullous pemphigoid (BP). The histologic hallmark of PV and PF is acantholysis. “Because these are intraepidermal blistering diseases, you don’t see the blister very often; maybe you’ll have a few intact loose sacklike blisters, but you mostly see erosions and crusting,” he said. “PV often only begins with mouth lesions.”
Work-up for a suspected autoimmune blistering disease includes a physical exam, histology, direct and indirect immunofluorescence, and serologic tests. The diagnosis should be based on the target autoantigen in the skin. PV and PF can appear identical on direct immunofluorescence, even though the blister cleavage plane is very high in PF and usually just above the basal keratinocytes in PV. “PF can have an intercellular keratinocyte cell surface staining pattern throughout the full epidermis or sometimes only the upper epidermal layers,” Dr. Woodley said.
At an international meeting on pemphigus in 2015, Dr. Woodley and his associates presented results from an ongoing study that is following 44 pemphigus patients at Keck Hospital of USC (a private university health care system) and 40 patients at Los Angeles County and USC Medical Center (a public safety net health care system). “The question we asked was, When the same doctors treat patients with a serious complicated disease requiring lots of details and follow-up at two very different health care systems, were there any differences in the outcomes of these patients?”
They found that the rates of clinical and immunologic remission were identical at both hospitals. However, at the county hospital, there was a higher incidence of relapses (59% vs. 30%). In addition, complications between the county and private hospitals differed in terms of hyperglycemia (38% vs. 11%, respectively), infections (79% vs. 37%), deaths (1 vs. none), medication dosage nonadherence (68% vs. 22%), and inappropriate discontinuation of one or more medications (68% vs. 15%). “Current research goals are to determine what factors cause medication compliance and noncompliance,” he said.
Dr. Woodley noted that one autoimmune blistering disease can evolve into another because of the phenomenon of epitope spreading. “The concept is that inflammation from one autoimmune blistering disease creates skin injury and reveals new neoautoantigens that get recognized by the patient’s immune system,” he said.
For example, a patient who had PF and high-titer autoantibodies to desmoglein 1 after a couple of years began to have blisters and erosions in her mouth, which is not supposed to happen in PF. Immunologic testing of this patient showed that in addition to antibodies against desmoglein 1, she began making high-titer autoantibodies against desmoglein 3 and had transformed into PV.
Bullous pemphigoid is another well-characterized autoimmune bullous disease that usually occurs in elderly patients. The blister is beneath the epidermis at the dermal-epidermal junction. These patients may have oral involvement. BP is characterized by tense subepidermal bullae on inflammatory bases. Histology reveals epidermal-dermal separation, many eosinophils and mast cells, and sometimes many polymorphonuclear leukocytes. “Many of these patients have very high IgE antibodies as well as IgG,” he said.
Features of BP include IgG and C3 deposits at the dermal-epidermal junction by direct immunofluorescence and by indirect immunofluorescence. “On salt-split human skin substrate, these antibodies bind to the epidermal roof of the separation and not to the dermal floor,” Dr. Woodley said. “You can send off the patient’s serum for ELISA [enzyme-linked immunosorbent assay] testing to detect autoantibodies against the BP230 antigen and the BP180 antigen to confirm the diagnosis. Autoantibodies to the BP180 antigen often correlate with the patient’s disease activity. The sensitivity of indirect immunofluorescence and ELISA are both above 95%.”
BP can present with urticarial plaques and pruritus and without blisters. Also, recent research has demonstrated that BP can present with just pruritus and no skin lesions. “So that’s something to keep in mind in refractory pruritus patients,” he said.
The incidence of BP seems to be increasing, from an estimated 7 cases per million in 1995 to 43 cases per million in 2008, Dr. Woodley said. “It may be that it is associated with some drugs like loop diuretics and spironolactone, but the precise reason is not known,” he said. “If your patient has dementia or Parkinson’s disease, he or she has a fourfold increased chance that they will have BP, because the BP180 and BP230 antigens are also in neuronal cells. Parkinson’s patients are known to make antibodies to the BP180 antigen, but not to the NC16A domain of the BP180 antigen. The development of BP in a Parkinson’s patient occurs when he or she begins to also make autoantibodies against the NC16A domain.”
The standard of treatment for autoimmune blistering diseases is prednisone 0.7-2 mg/kg. Nonsteroidal immunosuppressive agents are also helpful, including methotrexate, azathioprine, cyclophosphamide, and mycophenolate mofetil. Emerging evidence suggests that rituximab is the drug of choice for PV and PF, and should be the first-line therapy. Rituximab is a chimeric monoclonal antibody that targets CD20–positive B lymphocytes. “It removes cells that are ready to transform into autoantibody-producing short-lived plasma cells,” Dr. Woodley said. “The depletion lasts 6-12 months.”
Another new development in BP is the use of omalizumab, a monoclonal antibody to IgE. “Omalizumab inhibits the IgE antibody binding to the BP180,” Dr. Woodley said.
“It’s thought that the BP180 antigen is released from basal keratinocytes into the high papillary dermis. In BP patients, there are numerous mast cells at that location. IgE binds to the mast cells, which have IgE receptors on their surface, and in the presence of the BP180 antigen, forms dimers on the mast cells, and causes them to release inflammatory cytokines, some of which recruit eosinophils. This is likely why BP is such an inflammatory disorder. You cannot follow the IgE levels; you have to follow the eosinophils. The IgE is still high, but it’s nullified and inactive.”
Other biologics that have been successfully used in PV, PF, and BP include tumor necrosis factor–alpha inhibitors and rituximab (Rituxan). Common dosing for rituximab is 325 mg/m2 per week for 4 weeks. Infusion reactions are the most common side effect, he said, but other reported adverse reactions include infections, transient hypogammaglobulinemia, neutropenia, deep vein thrombosis, and pulmonary embolism. “The incidence of side effects seems to be going down, because we are now premedicating patients with antihistamines and IV hydrocortisone before giving them rituximab,” Dr. Woodley noted.
The development of progressive multifocal leukoencephalopathy has also been reported with the use of rituximab. “This is exceedingly rare with rituximab but has been described, and this is what keeps doctors who use this drug awake at night,” he said.
Elderly patients with mild BP sometimes can get by without using immunosuppressive agents to manage their disease. One option is potent topical steroids plus niacinamide 0.5-2 g after each meal as an anti-inflammatory B vitamin. “Doxycycline 100 mg b.i.d. also works to inhibit neutrophils,” he said. “Antihistamines can also be helpful, and some French dermatologists have found total body clobetasol to be useful.”
Dr. Woodley disclosed that he holds patents on human recombinant type VII collagen. He is also a consultant for Shire Pharmaceuticals and a speaker for Biofusion.
NEWPORT BEACH, CALIF. – Current treatment of autoimmune blistering diseases is not backed by evidence-based medicine and solid randomized, controlled trials, according to David T. Woodley, MD.
“These are rare diseases; there’s no consensus on the treatment of choice,” Dr. Woodley said at the annual meeting of the Pacific Dermatologic Association.
Dr. Woodley, professor of dermatology at the University of Southern California, Los Angeles, limited his discussion to pemphigus vulgaris (PV), pemphigus foliaceus (PF), and bullous pemphigoid (BP). The histologic hallmark of PV and PF is acantholysis. “Because these are intraepidermal blistering diseases, you don’t see the blister very often; maybe you’ll have a few intact loose sacklike blisters, but you mostly see erosions and crusting,” he said. “PV often only begins with mouth lesions.”
Work-up for a suspected autoimmune blistering disease includes a physical exam, histology, direct and indirect immunofluorescence, and serologic tests. The diagnosis should be based on the target autoantigen in the skin. PV and PF can appear identical on direct immunofluorescence, even though the blister cleavage plane is very high in PF and usually just above the basal keratinocytes in PV. “PF can have an intercellular keratinocyte cell surface staining pattern throughout the full epidermis or sometimes only the upper epidermal layers,” Dr. Woodley said.
At an international meeting on pemphigus in 2015, Dr. Woodley and his associates presented results from an ongoing study that is following 44 pemphigus patients at Keck Hospital of USC (a private university health care system) and 40 patients at Los Angeles County and USC Medical Center (a public safety net health care system). “The question we asked was, When the same doctors treat patients with a serious complicated disease requiring lots of details and follow-up at two very different health care systems, were there any differences in the outcomes of these patients?”
They found that the rates of clinical and immunologic remission were identical at both hospitals. However, at the county hospital, there was a higher incidence of relapses (59% vs. 30%). In addition, complications between the county and private hospitals differed in terms of hyperglycemia (38% vs. 11%, respectively), infections (79% vs. 37%), deaths (1 vs. none), medication dosage nonadherence (68% vs. 22%), and inappropriate discontinuation of one or more medications (68% vs. 15%). “Current research goals are to determine what factors cause medication compliance and noncompliance,” he said.
Dr. Woodley noted that one autoimmune blistering disease can evolve into another because of the phenomenon of epitope spreading. “The concept is that inflammation from one autoimmune blistering disease creates skin injury and reveals new neoautoantigens that get recognized by the patient’s immune system,” he said.
For example, a patient who had PF and high-titer autoantibodies to desmoglein 1 after a couple of years began to have blisters and erosions in her mouth, which is not supposed to happen in PF. Immunologic testing of this patient showed that in addition to antibodies against desmoglein 1, she began making high-titer autoantibodies against desmoglein 3 and had transformed into PV.
Bullous pemphigoid is another well-characterized autoimmune bullous disease that usually occurs in elderly patients. The blister is beneath the epidermis at the dermal-epidermal junction. These patients may have oral involvement. BP is characterized by tense subepidermal bullae on inflammatory bases. Histology reveals epidermal-dermal separation, many eosinophils and mast cells, and sometimes many polymorphonuclear leukocytes. “Many of these patients have very high IgE antibodies as well as IgG,” he said.
Features of BP include IgG and C3 deposits at the dermal-epidermal junction by direct immunofluorescence and by indirect immunofluorescence. “On salt-split human skin substrate, these antibodies bind to the epidermal roof of the separation and not to the dermal floor,” Dr. Woodley said. “You can send off the patient’s serum for ELISA [enzyme-linked immunosorbent assay] testing to detect autoantibodies against the BP230 antigen and the BP180 antigen to confirm the diagnosis. Autoantibodies to the BP180 antigen often correlate with the patient’s disease activity. The sensitivity of indirect immunofluorescence and ELISA are both above 95%.”
BP can present with urticarial plaques and pruritus and without blisters. Also, recent research has demonstrated that BP can present with just pruritus and no skin lesions. “So that’s something to keep in mind in refractory pruritus patients,” he said.
The incidence of BP seems to be increasing, from an estimated 7 cases per million in 1995 to 43 cases per million in 2008, Dr. Woodley said. “It may be that it is associated with some drugs like loop diuretics and spironolactone, but the precise reason is not known,” he said. “If your patient has dementia or Parkinson’s disease, he or she has a fourfold increased chance that they will have BP, because the BP180 and BP230 antigens are also in neuronal cells. Parkinson’s patients are known to make antibodies to the BP180 antigen, but not to the NC16A domain of the BP180 antigen. The development of BP in a Parkinson’s patient occurs when he or she begins to also make autoantibodies against the NC16A domain.”
The standard of treatment for autoimmune blistering diseases is prednisone 0.7-2 mg/kg. Nonsteroidal immunosuppressive agents are also helpful, including methotrexate, azathioprine, cyclophosphamide, and mycophenolate mofetil. Emerging evidence suggests that rituximab is the drug of choice for PV and PF, and should be the first-line therapy. Rituximab is a chimeric monoclonal antibody that targets CD20–positive B lymphocytes. “It removes cells that are ready to transform into autoantibody-producing short-lived plasma cells,” Dr. Woodley said. “The depletion lasts 6-12 months.”
Another new development in BP is the use of omalizumab, a monoclonal antibody to IgE. “Omalizumab inhibits the IgE antibody binding to the BP180,” Dr. Woodley said.
“It’s thought that the BP180 antigen is released from basal keratinocytes into the high papillary dermis. In BP patients, there are numerous mast cells at that location. IgE binds to the mast cells, which have IgE receptors on their surface, and in the presence of the BP180 antigen, forms dimers on the mast cells, and causes them to release inflammatory cytokines, some of which recruit eosinophils. This is likely why BP is such an inflammatory disorder. You cannot follow the IgE levels; you have to follow the eosinophils. The IgE is still high, but it’s nullified and inactive.”
Other biologics that have been successfully used in PV, PF, and BP include tumor necrosis factor–alpha inhibitors and rituximab (Rituxan). Common dosing for rituximab is 325 mg/m2 per week for 4 weeks. Infusion reactions are the most common side effect, he said, but other reported adverse reactions include infections, transient hypogammaglobulinemia, neutropenia, deep vein thrombosis, and pulmonary embolism. “The incidence of side effects seems to be going down, because we are now premedicating patients with antihistamines and IV hydrocortisone before giving them rituximab,” Dr. Woodley noted.
The development of progressive multifocal leukoencephalopathy has also been reported with the use of rituximab. “This is exceedingly rare with rituximab but has been described, and this is what keeps doctors who use this drug awake at night,” he said.
Elderly patients with mild BP sometimes can get by without using immunosuppressive agents to manage their disease. One option is potent topical steroids plus niacinamide 0.5-2 g after each meal as an anti-inflammatory B vitamin. “Doxycycline 100 mg b.i.d. also works to inhibit neutrophils,” he said. “Antihistamines can also be helpful, and some French dermatologists have found total body clobetasol to be useful.”
Dr. Woodley disclosed that he holds patents on human recombinant type VII collagen. He is also a consultant for Shire Pharmaceuticals and a speaker for Biofusion.
NEWPORT BEACH, CALIF. – Current treatment of autoimmune blistering diseases is not backed by evidence-based medicine and solid randomized, controlled trials, according to David T. Woodley, MD.
“These are rare diseases; there’s no consensus on the treatment of choice,” Dr. Woodley said at the annual meeting of the Pacific Dermatologic Association.
Dr. Woodley, professor of dermatology at the University of Southern California, Los Angeles, limited his discussion to pemphigus vulgaris (PV), pemphigus foliaceus (PF), and bullous pemphigoid (BP). The histologic hallmark of PV and PF is acantholysis. “Because these are intraepidermal blistering diseases, you don’t see the blister very often; maybe you’ll have a few intact loose sacklike blisters, but you mostly see erosions and crusting,” he said. “PV often only begins with mouth lesions.”
Work-up for a suspected autoimmune blistering disease includes a physical exam, histology, direct and indirect immunofluorescence, and serologic tests. The diagnosis should be based on the target autoantigen in the skin. PV and PF can appear identical on direct immunofluorescence, even though the blister cleavage plane is very high in PF and usually just above the basal keratinocytes in PV. “PF can have an intercellular keratinocyte cell surface staining pattern throughout the full epidermis or sometimes only the upper epidermal layers,” Dr. Woodley said.
At an international meeting on pemphigus in 2015, Dr. Woodley and his associates presented results from an ongoing study that is following 44 pemphigus patients at Keck Hospital of USC (a private university health care system) and 40 patients at Los Angeles County and USC Medical Center (a public safety net health care system). “The question we asked was, When the same doctors treat patients with a serious complicated disease requiring lots of details and follow-up at two very different health care systems, were there any differences in the outcomes of these patients?”
They found that the rates of clinical and immunologic remission were identical at both hospitals. However, at the county hospital, there was a higher incidence of relapses (59% vs. 30%). In addition, complications between the county and private hospitals differed in terms of hyperglycemia (38% vs. 11%, respectively), infections (79% vs. 37%), deaths (1 vs. none), medication dosage nonadherence (68% vs. 22%), and inappropriate discontinuation of one or more medications (68% vs. 15%). “Current research goals are to determine what factors cause medication compliance and noncompliance,” he said.
Dr. Woodley noted that one autoimmune blistering disease can evolve into another because of the phenomenon of epitope spreading. “The concept is that inflammation from one autoimmune blistering disease creates skin injury and reveals new neoautoantigens that get recognized by the patient’s immune system,” he said.
For example, a patient who had PF and high-titer autoantibodies to desmoglein 1 after a couple of years began to have blisters and erosions in her mouth, which is not supposed to happen in PF. Immunologic testing of this patient showed that in addition to antibodies against desmoglein 1, she began making high-titer autoantibodies against desmoglein 3 and had transformed into PV.
Bullous pemphigoid is another well-characterized autoimmune bullous disease that usually occurs in elderly patients. The blister is beneath the epidermis at the dermal-epidermal junction. These patients may have oral involvement. BP is characterized by tense subepidermal bullae on inflammatory bases. Histology reveals epidermal-dermal separation, many eosinophils and mast cells, and sometimes many polymorphonuclear leukocytes. “Many of these patients have very high IgE antibodies as well as IgG,” he said.
Features of BP include IgG and C3 deposits at the dermal-epidermal junction by direct immunofluorescence and by indirect immunofluorescence. “On salt-split human skin substrate, these antibodies bind to the epidermal roof of the separation and not to the dermal floor,” Dr. Woodley said. “You can send off the patient’s serum for ELISA [enzyme-linked immunosorbent assay] testing to detect autoantibodies against the BP230 antigen and the BP180 antigen to confirm the diagnosis. Autoantibodies to the BP180 antigen often correlate with the patient’s disease activity. The sensitivity of indirect immunofluorescence and ELISA are both above 95%.”
BP can present with urticarial plaques and pruritus and without blisters. Also, recent research has demonstrated that BP can present with just pruritus and no skin lesions. “So that’s something to keep in mind in refractory pruritus patients,” he said.
The incidence of BP seems to be increasing, from an estimated 7 cases per million in 1995 to 43 cases per million in 2008, Dr. Woodley said. “It may be that it is associated with some drugs like loop diuretics and spironolactone, but the precise reason is not known,” he said. “If your patient has dementia or Parkinson’s disease, he or she has a fourfold increased chance that they will have BP, because the BP180 and BP230 antigens are also in neuronal cells. Parkinson’s patients are known to make antibodies to the BP180 antigen, but not to the NC16A domain of the BP180 antigen. The development of BP in a Parkinson’s patient occurs when he or she begins to also make autoantibodies against the NC16A domain.”
The standard of treatment for autoimmune blistering diseases is prednisone 0.7-2 mg/kg. Nonsteroidal immunosuppressive agents are also helpful, including methotrexate, azathioprine, cyclophosphamide, and mycophenolate mofetil. Emerging evidence suggests that rituximab is the drug of choice for PV and PF, and should be the first-line therapy. Rituximab is a chimeric monoclonal antibody that targets CD20–positive B lymphocytes. “It removes cells that are ready to transform into autoantibody-producing short-lived plasma cells,” Dr. Woodley said. “The depletion lasts 6-12 months.”
Another new development in BP is the use of omalizumab, a monoclonal antibody to IgE. “Omalizumab inhibits the IgE antibody binding to the BP180,” Dr. Woodley said.
“It’s thought that the BP180 antigen is released from basal keratinocytes into the high papillary dermis. In BP patients, there are numerous mast cells at that location. IgE binds to the mast cells, which have IgE receptors on their surface, and in the presence of the BP180 antigen, forms dimers on the mast cells, and causes them to release inflammatory cytokines, some of which recruit eosinophils. This is likely why BP is such an inflammatory disorder. You cannot follow the IgE levels; you have to follow the eosinophils. The IgE is still high, but it’s nullified and inactive.”
Other biologics that have been successfully used in PV, PF, and BP include tumor necrosis factor–alpha inhibitors and rituximab (Rituxan). Common dosing for rituximab is 325 mg/m2 per week for 4 weeks. Infusion reactions are the most common side effect, he said, but other reported adverse reactions include infections, transient hypogammaglobulinemia, neutropenia, deep vein thrombosis, and pulmonary embolism. “The incidence of side effects seems to be going down, because we are now premedicating patients with antihistamines and IV hydrocortisone before giving them rituximab,” Dr. Woodley noted.
The development of progressive multifocal leukoencephalopathy has also been reported with the use of rituximab. “This is exceedingly rare with rituximab but has been described, and this is what keeps doctors who use this drug awake at night,” he said.
Elderly patients with mild BP sometimes can get by without using immunosuppressive agents to manage their disease. One option is potent topical steroids plus niacinamide 0.5-2 g after each meal as an anti-inflammatory B vitamin. “Doxycycline 100 mg b.i.d. also works to inhibit neutrophils,” he said. “Antihistamines can also be helpful, and some French dermatologists have found total body clobetasol to be useful.”
Dr. Woodley disclosed that he holds patents on human recombinant type VII collagen. He is also a consultant for Shire Pharmaceuticals and a speaker for Biofusion.
EXPERT ANALYSIS AT PDA 2016