User login
Access issues looming as more docs eye exit from clinical practice
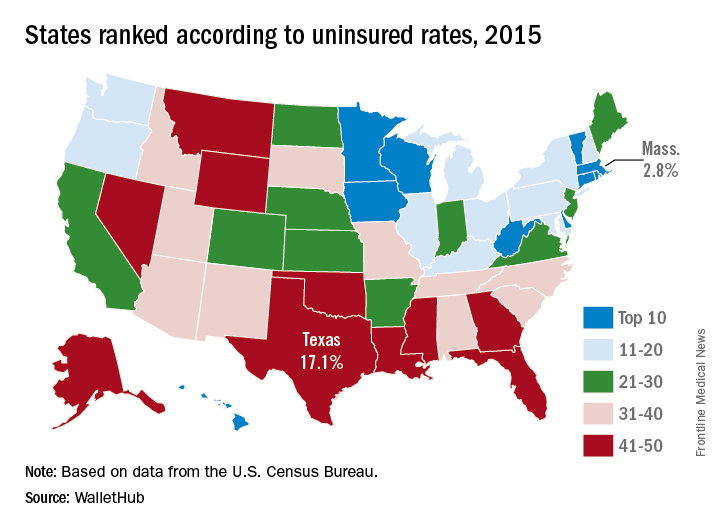
Almost half (47.8%) of physicians surveyed are considering a change in how they practice medicine within the next 1-3 years, including cutting back on hours, retiring, switching to cash/concierge practice, working locum tenens, seeking a nonclinical health care job, seeking employment, or working part time.
That’s according to responses to the 2016 Survey of America’s Physicians Practice Patterns & Perspectives, a biennial survey commissioned by The Physicians Foundation and conducted by Merritt Hawkins. A total of 17,236 physicians responded to the survey.
The percentage looking to change is up from 43.6% in the 2014 survey, but down from the 50.2% of physicians who responded the same way in 2012.
Dr. Ray pointed to a number of findings in the survey that could be driving the growth in those looking to make a change.
“If you think about the last year, the clinical, administrative, and financial changes that have occurred have occurred at a whirlwind pace,” Dr. Ray said. “For instance, continued expansion of the Affordable Care Act has included as many as 20 million new people to the rolls at the same time we have a documented physician shortage where 80% of physicians say that they have all the patients that they can take care of. They are either at capacity or they are overextended.”
Other factors influencing physicians’ employment decisions include the transition to value-based payments under the Medicare Access and CHIP Reauthorization Act (MACRA), the transition to ICD-10, the growth of physician employment, the continued sale of private practices to hospitals and health systems, and the “businessification” of heath care.
“If any of these [changes] occurred in a period of time, it would be impactful,” he said. “But to have all occur simultaneously, we say now that to be a physician is to feel the ground shaking under your feet. This is the landscape in which the survey was taken.”
Given the volume of change, it is no surprise that physician morale is low, Dr. Ray said. “One of the first things that jumps out is morale. The question was ‘what best describes your professional morale about your current feelings and the current state of the medical profession?’ and 54% were somewhat or very negative; 46% were positive/somewhat positive/very positive. The very negatives were twice what the very positives were,” he noted.
Inadequate time to deliver quality care also was cited.
“Only 14% [of respondents] said that they have all the time that they need to provide the highest standards of care; 86% said that their time was either always limited, often limited, or sometimes limited,” Dr. Ray said.
Dr. Ray highlighted another question that provides insight into physicians’ dissatisfaction with their practice environment.
The survey asked, “To what degree is patient care in your practice adversely impacted by external factors such as third party authorizations, treatment protocols, EHR design, etc.”
“The critical term here is ‘adversely impacted,’ not just influenced, but adversely impacted,” Dr. Ray said. “Only 2.3% said not at all; 10% total said either not at all or a little bit. The rest said either somewhat, a good deal, or a great deal. In fact, 72% said a good deal or a great deal.”
All of this is leading to physician burnout, he said.
“I think it all bounces back to interference with the doctor/patient relationship and the fact that [physicians] feel like there are distractions within the practice of medicine due to the regulatory environment,” he said “They are not allowed to make decisions like they want to make in the best interest of their patients based on their training and their studying and their special experience with that patient. It creates this barrier with this professional satisfaction that they want to receive from taking care of patients.”
Almost half (47.8%) of physicians surveyed are considering a change in how they practice medicine within the next 1-3 years, including cutting back on hours, retiring, switching to cash/concierge practice, working locum tenens, seeking a nonclinical health care job, seeking employment, or working part time.
That’s according to responses to the 2016 Survey of America’s Physicians Practice Patterns & Perspectives, a biennial survey commissioned by The Physicians Foundation and conducted by Merritt Hawkins. A total of 17,236 physicians responded to the survey.
The percentage looking to change is up from 43.6% in the 2014 survey, but down from the 50.2% of physicians who responded the same way in 2012.
Dr. Ray pointed to a number of findings in the survey that could be driving the growth in those looking to make a change.
“If you think about the last year, the clinical, administrative, and financial changes that have occurred have occurred at a whirlwind pace,” Dr. Ray said. “For instance, continued expansion of the Affordable Care Act has included as many as 20 million new people to the rolls at the same time we have a documented physician shortage where 80% of physicians say that they have all the patients that they can take care of. They are either at capacity or they are overextended.”
Other factors influencing physicians’ employment decisions include the transition to value-based payments under the Medicare Access and CHIP Reauthorization Act (MACRA), the transition to ICD-10, the growth of physician employment, the continued sale of private practices to hospitals and health systems, and the “businessification” of heath care.
“If any of these [changes] occurred in a period of time, it would be impactful,” he said. “But to have all occur simultaneously, we say now that to be a physician is to feel the ground shaking under your feet. This is the landscape in which the survey was taken.”
Given the volume of change, it is no surprise that physician morale is low, Dr. Ray said. “One of the first things that jumps out is morale. The question was ‘what best describes your professional morale about your current feelings and the current state of the medical profession?’ and 54% were somewhat or very negative; 46% were positive/somewhat positive/very positive. The very negatives were twice what the very positives were,” he noted.
Inadequate time to deliver quality care also was cited.
“Only 14% [of respondents] said that they have all the time that they need to provide the highest standards of care; 86% said that their time was either always limited, often limited, or sometimes limited,” Dr. Ray said.
Dr. Ray highlighted another question that provides insight into physicians’ dissatisfaction with their practice environment.
The survey asked, “To what degree is patient care in your practice adversely impacted by external factors such as third party authorizations, treatment protocols, EHR design, etc.”
“The critical term here is ‘adversely impacted,’ not just influenced, but adversely impacted,” Dr. Ray said. “Only 2.3% said not at all; 10% total said either not at all or a little bit. The rest said either somewhat, a good deal, or a great deal. In fact, 72% said a good deal or a great deal.”
All of this is leading to physician burnout, he said.
“I think it all bounces back to interference with the doctor/patient relationship and the fact that [physicians] feel like there are distractions within the practice of medicine due to the regulatory environment,” he said “They are not allowed to make decisions like they want to make in the best interest of their patients based on their training and their studying and their special experience with that patient. It creates this barrier with this professional satisfaction that they want to receive from taking care of patients.”
Almost half (47.8%) of physicians surveyed are considering a change in how they practice medicine within the next 1-3 years, including cutting back on hours, retiring, switching to cash/concierge practice, working locum tenens, seeking a nonclinical health care job, seeking employment, or working part time.
That’s according to responses to the 2016 Survey of America’s Physicians Practice Patterns & Perspectives, a biennial survey commissioned by The Physicians Foundation and conducted by Merritt Hawkins. A total of 17,236 physicians responded to the survey.
The percentage looking to change is up from 43.6% in the 2014 survey, but down from the 50.2% of physicians who responded the same way in 2012.
Dr. Ray pointed to a number of findings in the survey that could be driving the growth in those looking to make a change.
“If you think about the last year, the clinical, administrative, and financial changes that have occurred have occurred at a whirlwind pace,” Dr. Ray said. “For instance, continued expansion of the Affordable Care Act has included as many as 20 million new people to the rolls at the same time we have a documented physician shortage where 80% of physicians say that they have all the patients that they can take care of. They are either at capacity or they are overextended.”
Other factors influencing physicians’ employment decisions include the transition to value-based payments under the Medicare Access and CHIP Reauthorization Act (MACRA), the transition to ICD-10, the growth of physician employment, the continued sale of private practices to hospitals and health systems, and the “businessification” of heath care.
“If any of these [changes] occurred in a period of time, it would be impactful,” he said. “But to have all occur simultaneously, we say now that to be a physician is to feel the ground shaking under your feet. This is the landscape in which the survey was taken.”
Given the volume of change, it is no surprise that physician morale is low, Dr. Ray said. “One of the first things that jumps out is morale. The question was ‘what best describes your professional morale about your current feelings and the current state of the medical profession?’ and 54% were somewhat or very negative; 46% were positive/somewhat positive/very positive. The very negatives were twice what the very positives were,” he noted.
Inadequate time to deliver quality care also was cited.
“Only 14% [of respondents] said that they have all the time that they need to provide the highest standards of care; 86% said that their time was either always limited, often limited, or sometimes limited,” Dr. Ray said.
Dr. Ray highlighted another question that provides insight into physicians’ dissatisfaction with their practice environment.
The survey asked, “To what degree is patient care in your practice adversely impacted by external factors such as third party authorizations, treatment protocols, EHR design, etc.”
“The critical term here is ‘adversely impacted,’ not just influenced, but adversely impacted,” Dr. Ray said. “Only 2.3% said not at all; 10% total said either not at all or a little bit. The rest said either somewhat, a good deal, or a great deal. In fact, 72% said a good deal or a great deal.”
All of this is leading to physician burnout, he said.
“I think it all bounces back to interference with the doctor/patient relationship and the fact that [physicians] feel like there are distractions within the practice of medicine due to the regulatory environment,” he said “They are not allowed to make decisions like they want to make in the best interest of their patients based on their training and their studying and their special experience with that patient. It creates this barrier with this professional satisfaction that they want to receive from taking care of patients.”
A tool to assess comportment and communication for hospitalists
With the rise of hospital medicine in the United States, the lion’s share of inpatient care is delivered by hospitalists. Both hospitals and hospitalist providers are committed to delivering excellent patient care, but to accomplish this goal, specific feedback is essential.
Patient satisfaction surveys that assess provider performance, such as Press Ganey (PG)1 and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS),2 do not truly provide feedback at the encounter level with valid attribution, and these data are not sent to providers in a timely manner.
In the analyses, the HMCCOT scores were moderately correlated with the hospitalists’ PG scores. Higher scores on the HMCCOT took an average of 13 minutes per patient encounter, giving further credence to the fact that excellent communication and comportment can be rapidly established at the bedside.
Patients’ complaints about doctors often relate to comportment and communication; the grievances are most commonly about feeling rushed, not being heard, and that information was not conveyed in a clear manner.4 Patient-centeredness has been shown to improve patient satisfaction as well as clinical outcomes, in part because they feel like partners in the mutually agreed upon treatment plans.5 Many of the components of the HMCCOT are at the heart of patient-centered care. While comportment may not be a frequently used term in patient care, respectful behaviors performed at the opening of any encounter [etiquette-based medicine which includes introducing oneself to patients and smiling] set the tone for the doctor-patient interaction.
Demonstrating genuine interest in the patient as a person is a core component of excellent patient care. Sir William Osler famously observed “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.”6 A common method of “demonstrating interest in the patient as a person” recorded by the HMCCOT was physicians asking about patient’s personal history and of their interests. It is not difficult to fathom how knowing about patients’ personal interests and perspectives can help to most effectively engage them in establishing their goals of care and with therapeutic decisions.
Because hospitalists spend only a small proportion of their clinical time in direct patient care at the bedside, they need to make every moment count. HMCCOT allows for the identification of providers who are excellent in communication and comportment. Once identified, these exemplars can watch their peers and become the trainers to establish a culture of excellence.
Larger studies will be needed in the future to assess whether interventions that translate into improved comportment and communication among hospitalists will definitively augment patient satisfaction and ameliorate clinical outcomes.
1. Press Ganey. Accessed Dec. 15, 2015.
2. HCAHPS. Accessed Feb. 2, 2016.
3. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Aug 13. doi: 10.1002/jhm.2647.
4. Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994 Nov 23-30;272(20):1583-7.
5. Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.
6. Taylor RB. White Coat Tales: Medicine’s Heroes, Heritage, and Misadventure. New York: Springer; 2007:126.
Susrutha Kotwal, MD, and Scott Wright, MD, are based in the department of medicine, division of hospital medicine, Johns Hopkins Bayview Medical Center and Johns Hopkins University, Baltimore.
With the rise of hospital medicine in the United States, the lion’s share of inpatient care is delivered by hospitalists. Both hospitals and hospitalist providers are committed to delivering excellent patient care, but to accomplish this goal, specific feedback is essential.
Patient satisfaction surveys that assess provider performance, such as Press Ganey (PG)1 and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS),2 do not truly provide feedback at the encounter level with valid attribution, and these data are not sent to providers in a timely manner.
In the analyses, the HMCCOT scores were moderately correlated with the hospitalists’ PG scores. Higher scores on the HMCCOT took an average of 13 minutes per patient encounter, giving further credence to the fact that excellent communication and comportment can be rapidly established at the bedside.
Patients’ complaints about doctors often relate to comportment and communication; the grievances are most commonly about feeling rushed, not being heard, and that information was not conveyed in a clear manner.4 Patient-centeredness has been shown to improve patient satisfaction as well as clinical outcomes, in part because they feel like partners in the mutually agreed upon treatment plans.5 Many of the components of the HMCCOT are at the heart of patient-centered care. While comportment may not be a frequently used term in patient care, respectful behaviors performed at the opening of any encounter [etiquette-based medicine which includes introducing oneself to patients and smiling] set the tone for the doctor-patient interaction.
Demonstrating genuine interest in the patient as a person is a core component of excellent patient care. Sir William Osler famously observed “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.”6 A common method of “demonstrating interest in the patient as a person” recorded by the HMCCOT was physicians asking about patient’s personal history and of their interests. It is not difficult to fathom how knowing about patients’ personal interests and perspectives can help to most effectively engage them in establishing their goals of care and with therapeutic decisions.
Because hospitalists spend only a small proportion of their clinical time in direct patient care at the bedside, they need to make every moment count. HMCCOT allows for the identification of providers who are excellent in communication and comportment. Once identified, these exemplars can watch their peers and become the trainers to establish a culture of excellence.
Larger studies will be needed in the future to assess whether interventions that translate into improved comportment and communication among hospitalists will definitively augment patient satisfaction and ameliorate clinical outcomes.
1. Press Ganey. Accessed Dec. 15, 2015.
2. HCAHPS. Accessed Feb. 2, 2016.
3. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Aug 13. doi: 10.1002/jhm.2647.
4. Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994 Nov 23-30;272(20):1583-7.
5. Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.
6. Taylor RB. White Coat Tales: Medicine’s Heroes, Heritage, and Misadventure. New York: Springer; 2007:126.
Susrutha Kotwal, MD, and Scott Wright, MD, are based in the department of medicine, division of hospital medicine, Johns Hopkins Bayview Medical Center and Johns Hopkins University, Baltimore.
With the rise of hospital medicine in the United States, the lion’s share of inpatient care is delivered by hospitalists. Both hospitals and hospitalist providers are committed to delivering excellent patient care, but to accomplish this goal, specific feedback is essential.
Patient satisfaction surveys that assess provider performance, such as Press Ganey (PG)1 and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS),2 do not truly provide feedback at the encounter level with valid attribution, and these data are not sent to providers in a timely manner.
In the analyses, the HMCCOT scores were moderately correlated with the hospitalists’ PG scores. Higher scores on the HMCCOT took an average of 13 minutes per patient encounter, giving further credence to the fact that excellent communication and comportment can be rapidly established at the bedside.
Patients’ complaints about doctors often relate to comportment and communication; the grievances are most commonly about feeling rushed, not being heard, and that information was not conveyed in a clear manner.4 Patient-centeredness has been shown to improve patient satisfaction as well as clinical outcomes, in part because they feel like partners in the mutually agreed upon treatment plans.5 Many of the components of the HMCCOT are at the heart of patient-centered care. While comportment may not be a frequently used term in patient care, respectful behaviors performed at the opening of any encounter [etiquette-based medicine which includes introducing oneself to patients and smiling] set the tone for the doctor-patient interaction.
Demonstrating genuine interest in the patient as a person is a core component of excellent patient care. Sir William Osler famously observed “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.”6 A common method of “demonstrating interest in the patient as a person” recorded by the HMCCOT was physicians asking about patient’s personal history and of their interests. It is not difficult to fathom how knowing about patients’ personal interests and perspectives can help to most effectively engage them in establishing their goals of care and with therapeutic decisions.
Because hospitalists spend only a small proportion of their clinical time in direct patient care at the bedside, they need to make every moment count. HMCCOT allows for the identification of providers who are excellent in communication and comportment. Once identified, these exemplars can watch their peers and become the trainers to establish a culture of excellence.
Larger studies will be needed in the future to assess whether interventions that translate into improved comportment and communication among hospitalists will definitively augment patient satisfaction and ameliorate clinical outcomes.
1. Press Ganey. Accessed Dec. 15, 2015.
2. HCAHPS. Accessed Feb. 2, 2016.
3. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Aug 13. doi: 10.1002/jhm.2647.
4. Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994 Nov 23-30;272(20):1583-7.
5. Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.
6. Taylor RB. White Coat Tales: Medicine’s Heroes, Heritage, and Misadventure. New York: Springer; 2007:126.
Susrutha Kotwal, MD, and Scott Wright, MD, are based in the department of medicine, division of hospital medicine, Johns Hopkins Bayview Medical Center and Johns Hopkins University, Baltimore.
Benefits of dental sealant programs for low-income children exceed costs
Cavities and fillings were approximately three times more likely among low-income children aged 7-11 years whose teeth were not treated with dental sealants, compared to those treated with sealants, based on data from the National Health and Nutrition Examination Survey (NHANES) from 2011-2014.
Overall, 43% of children and 39% of low-income children in the United States were treated at least once with dental sealant.
Although sealant use in children increased overall from 31% to 44% in a comparison of 1999-2004 and 2011-2014 NHANES data, sealant use was less common among low-income children compared with high-income children (39% vs. 48%) in the 2011-2014 period after increases of 16% and 9%, respectively, during 2011-2014.
School-based programs to provide sealants could increase their use among low-income children, wrote Susan O. Griffin, PhD, of the Centers for Disease Control and Prevention in Atlanta, and her associates. The researchers reviewed data from 1,371 low-income children aged 6-11 years, and found that 60% (approximately 6.5 million children), had not been treated with dental sealants. “The systematic review of economic evaluations of school-based sealant programs (SBSP) conducted for the Task Force found that SBSP became cost-saving within 2 years of placing sealants,” the researchers noted.
The data were published in the CDC’s Morbidity and Mortality Weekly Report (MMWR 2016 Oct 21;65[41];1141-5).
Cavities and fillings were approximately three times more likely among low-income children aged 7-11 years whose teeth were not treated with dental sealants, compared to those treated with sealants, based on data from the National Health and Nutrition Examination Survey (NHANES) from 2011-2014.
Overall, 43% of children and 39% of low-income children in the United States were treated at least once with dental sealant.
Although sealant use in children increased overall from 31% to 44% in a comparison of 1999-2004 and 2011-2014 NHANES data, sealant use was less common among low-income children compared with high-income children (39% vs. 48%) in the 2011-2014 period after increases of 16% and 9%, respectively, during 2011-2014.
School-based programs to provide sealants could increase their use among low-income children, wrote Susan O. Griffin, PhD, of the Centers for Disease Control and Prevention in Atlanta, and her associates. The researchers reviewed data from 1,371 low-income children aged 6-11 years, and found that 60% (approximately 6.5 million children), had not been treated with dental sealants. “The systematic review of economic evaluations of school-based sealant programs (SBSP) conducted for the Task Force found that SBSP became cost-saving within 2 years of placing sealants,” the researchers noted.
The data were published in the CDC’s Morbidity and Mortality Weekly Report (MMWR 2016 Oct 21;65[41];1141-5).
Cavities and fillings were approximately three times more likely among low-income children aged 7-11 years whose teeth were not treated with dental sealants, compared to those treated with sealants, based on data from the National Health and Nutrition Examination Survey (NHANES) from 2011-2014.
Overall, 43% of children and 39% of low-income children in the United States were treated at least once with dental sealant.
Although sealant use in children increased overall from 31% to 44% in a comparison of 1999-2004 and 2011-2014 NHANES data, sealant use was less common among low-income children compared with high-income children (39% vs. 48%) in the 2011-2014 period after increases of 16% and 9%, respectively, during 2011-2014.
School-based programs to provide sealants could increase their use among low-income children, wrote Susan O. Griffin, PhD, of the Centers for Disease Control and Prevention in Atlanta, and her associates. The researchers reviewed data from 1,371 low-income children aged 6-11 years, and found that 60% (approximately 6.5 million children), had not been treated with dental sealants. “The systematic review of economic evaluations of school-based sealant programs (SBSP) conducted for the Task Force found that SBSP became cost-saving within 2 years of placing sealants,” the researchers noted.
The data were published in the CDC’s Morbidity and Mortality Weekly Report (MMWR 2016 Oct 21;65[41];1141-5).
FROM MMWR
CMS offering educational webinars on MACRA
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
Enhanced recovery pathways in gynecology
Enhanced recovery surgical principles were first described in the 1990s.1 These principles postulate that the body’s stress response to surgical injury and deviation from normal physiology is the source of postoperative morbidity. Thus, enhanced recovery programs are designed around perioperative interventions that mitigate and help the body cope with the surgical stress response.
Many of these interventions run counter to traditional perioperative care paradigms. Enhanced recovery protocols are diverse but have common themes of avoiding preoperative fasting and bowel preparation, early oral intake, limiting use of drains and catheters, multimodal analgesia, early ambulation, and prioritizing euvolemia and normothermia. Individual interventions in these areas are combined to create a master protocol, which is implemented as a bundle to improve surgical outcomes.
Current components
Minimizing preoperative fasting, early postoperative refeeding, and preoperative carbohydrate-loading drinks are all key aspects of enhanced recovery protocols. “NPO after midnight” has been a longstanding rule due to the risk of aspiration with intubation. However, a Cochrane review found no evidence that a shortened period of fasting was associated with an increased risk of aspiration or related morbidity. Currently, the American Society of Anesthesiologists recommends only a 6-hour fast for solid foods and 2 hours for clear liquids.2,3
Preoperative fasting causes depletion of glycogen stores leading to insulin resistance and hyperglycemia, which are both associated with postoperative complications and morbidity.4 Preoperative carbohydrate-loading drinks can reverse some of the effects of limited preoperative fasting including preventing insulin resistance and hyperglycemia.5
Postoperative fasting should also be avoided. Early enteral intake is very important to decrease time spent in a catabolic state and decrease insulin resistance. In gynecology patients, early refeeding is associated with a faster return of bowel function and a decreased length of stay without an increase in postoperative complications.6 Notably, patients undergoing early feeding consistently experience more nausea and vomiting, but this is not associated with complications.7
The fluid management goal in enhanced recovery is to maintain perioperative euvolemia, as both hypovolemia and hypervolemia have negative physiologic consequences. When studied, fluid protocols designed to minimize the use of postoperative fluids have resulted in decreased cardiopulmonary complications, decreased postoperative morbidity, faster return of bowel function, and shorter hospital stays.8 Given the morbidity associated with fluid overload, enhanced recovery protocols recommend that minimal fluids be given in the operating room and intravenous fluids be removed as quickly as possible, often with first oral intake or postoperative day 1 at the latest.
Engagement of the patient in their perioperative recovery with patient education materials and expectations for postoperative tasks, such as early refeeding, spirometry, and ambulation are all important components of enhanced recovery. Patients become partners in achieving postoperative milestones, and this results in improved outcomes such as decreased pain scores and shorter recoveries.
Evidence in gynecology
Enhanced recovery has been studied in many surgical disciplines including urology, colorectal surgery, hepatobiliary surgery, and gynecology. High-quality studies of abdominal and vaginal hysterectomy patients have consistently found a decrease in length of stay with no difference in readmission or postoperative complication rates.9 An interesting study also found that an enhanced recovery program was associated with decreased nursing time required for patient care.10
For ovarian cancer patients, enhanced recovery is associated with decreased length of stay, decreased time to return of bowel function, and improved quality of life. Enhanced recovery is also cost saving, saving $257-$697 per vaginal hysterectomy patient and $5,410-$7,600 per ovarian cancer patient.11
Enhanced recovery protocols are safe, evidenced based, cost saving, and are increasingly being adopted as clinicians and health systems become aware of their benefits.
References
1. Br J Anaesth. 1997 May;78(5):606-17.
2. Cochrane Database Syst Rev. 2003 Oct 20;(4):CD004423.
3. Anesthesiology. 1999 Mar;90(3):896-905.
4. J Am Coll Surg. 2012 Jan;214(1):68-80.
5. Clin Nutr. 1998 Apr;17(2):65-71.
6. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD004508.
7. Obstet Gynecol. 1998 Jul;92(1):94-7.
8. Br J Surg. 2009 Apr;96(4):331-41.
9. Obstet Gynecol. 2013 Aug;122(2 Pt 1):319-28.
10. Qual Saf Health Care. 2009 Jun;18(3):236-40.
11. Gynecol Oncol. 2008 Feb;108(2):282-6.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Barber is a third-year fellow in gynecologic oncology at the university. They reported having no financial disclosures relevant to this column. Email them at [email protected].
Enhanced recovery surgical principles were first described in the 1990s.1 These principles postulate that the body’s stress response to surgical injury and deviation from normal physiology is the source of postoperative morbidity. Thus, enhanced recovery programs are designed around perioperative interventions that mitigate and help the body cope with the surgical stress response.
Many of these interventions run counter to traditional perioperative care paradigms. Enhanced recovery protocols are diverse but have common themes of avoiding preoperative fasting and bowel preparation, early oral intake, limiting use of drains and catheters, multimodal analgesia, early ambulation, and prioritizing euvolemia and normothermia. Individual interventions in these areas are combined to create a master protocol, which is implemented as a bundle to improve surgical outcomes.
Current components
Minimizing preoperative fasting, early postoperative refeeding, and preoperative carbohydrate-loading drinks are all key aspects of enhanced recovery protocols. “NPO after midnight” has been a longstanding rule due to the risk of aspiration with intubation. However, a Cochrane review found no evidence that a shortened period of fasting was associated with an increased risk of aspiration or related morbidity. Currently, the American Society of Anesthesiologists recommends only a 6-hour fast for solid foods and 2 hours for clear liquids.2,3
Preoperative fasting causes depletion of glycogen stores leading to insulin resistance and hyperglycemia, which are both associated with postoperative complications and morbidity.4 Preoperative carbohydrate-loading drinks can reverse some of the effects of limited preoperative fasting including preventing insulin resistance and hyperglycemia.5
Postoperative fasting should also be avoided. Early enteral intake is very important to decrease time spent in a catabolic state and decrease insulin resistance. In gynecology patients, early refeeding is associated with a faster return of bowel function and a decreased length of stay without an increase in postoperative complications.6 Notably, patients undergoing early feeding consistently experience more nausea and vomiting, but this is not associated with complications.7
The fluid management goal in enhanced recovery is to maintain perioperative euvolemia, as both hypovolemia and hypervolemia have negative physiologic consequences. When studied, fluid protocols designed to minimize the use of postoperative fluids have resulted in decreased cardiopulmonary complications, decreased postoperative morbidity, faster return of bowel function, and shorter hospital stays.8 Given the morbidity associated with fluid overload, enhanced recovery protocols recommend that minimal fluids be given in the operating room and intravenous fluids be removed as quickly as possible, often with first oral intake or postoperative day 1 at the latest.
Engagement of the patient in their perioperative recovery with patient education materials and expectations for postoperative tasks, such as early refeeding, spirometry, and ambulation are all important components of enhanced recovery. Patients become partners in achieving postoperative milestones, and this results in improved outcomes such as decreased pain scores and shorter recoveries.
Evidence in gynecology
Enhanced recovery has been studied in many surgical disciplines including urology, colorectal surgery, hepatobiliary surgery, and gynecology. High-quality studies of abdominal and vaginal hysterectomy patients have consistently found a decrease in length of stay with no difference in readmission or postoperative complication rates.9 An interesting study also found that an enhanced recovery program was associated with decreased nursing time required for patient care.10
For ovarian cancer patients, enhanced recovery is associated with decreased length of stay, decreased time to return of bowel function, and improved quality of life. Enhanced recovery is also cost saving, saving $257-$697 per vaginal hysterectomy patient and $5,410-$7,600 per ovarian cancer patient.11
Enhanced recovery protocols are safe, evidenced based, cost saving, and are increasingly being adopted as clinicians and health systems become aware of their benefits.
References
1. Br J Anaesth. 1997 May;78(5):606-17.
2. Cochrane Database Syst Rev. 2003 Oct 20;(4):CD004423.
3. Anesthesiology. 1999 Mar;90(3):896-905.
4. J Am Coll Surg. 2012 Jan;214(1):68-80.
5. Clin Nutr. 1998 Apr;17(2):65-71.
6. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD004508.
7. Obstet Gynecol. 1998 Jul;92(1):94-7.
8. Br J Surg. 2009 Apr;96(4):331-41.
9. Obstet Gynecol. 2013 Aug;122(2 Pt 1):319-28.
10. Qual Saf Health Care. 2009 Jun;18(3):236-40.
11. Gynecol Oncol. 2008 Feb;108(2):282-6.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Barber is a third-year fellow in gynecologic oncology at the university. They reported having no financial disclosures relevant to this column. Email them at [email protected].
Enhanced recovery surgical principles were first described in the 1990s.1 These principles postulate that the body’s stress response to surgical injury and deviation from normal physiology is the source of postoperative morbidity. Thus, enhanced recovery programs are designed around perioperative interventions that mitigate and help the body cope with the surgical stress response.
Many of these interventions run counter to traditional perioperative care paradigms. Enhanced recovery protocols are diverse but have common themes of avoiding preoperative fasting and bowel preparation, early oral intake, limiting use of drains and catheters, multimodal analgesia, early ambulation, and prioritizing euvolemia and normothermia. Individual interventions in these areas are combined to create a master protocol, which is implemented as a bundle to improve surgical outcomes.
Current components
Minimizing preoperative fasting, early postoperative refeeding, and preoperative carbohydrate-loading drinks are all key aspects of enhanced recovery protocols. “NPO after midnight” has been a longstanding rule due to the risk of aspiration with intubation. However, a Cochrane review found no evidence that a shortened period of fasting was associated with an increased risk of aspiration or related morbidity. Currently, the American Society of Anesthesiologists recommends only a 6-hour fast for solid foods and 2 hours for clear liquids.2,3
Preoperative fasting causes depletion of glycogen stores leading to insulin resistance and hyperglycemia, which are both associated with postoperative complications and morbidity.4 Preoperative carbohydrate-loading drinks can reverse some of the effects of limited preoperative fasting including preventing insulin resistance and hyperglycemia.5
Postoperative fasting should also be avoided. Early enteral intake is very important to decrease time spent in a catabolic state and decrease insulin resistance. In gynecology patients, early refeeding is associated with a faster return of bowel function and a decreased length of stay without an increase in postoperative complications.6 Notably, patients undergoing early feeding consistently experience more nausea and vomiting, but this is not associated with complications.7
The fluid management goal in enhanced recovery is to maintain perioperative euvolemia, as both hypovolemia and hypervolemia have negative physiologic consequences. When studied, fluid protocols designed to minimize the use of postoperative fluids have resulted in decreased cardiopulmonary complications, decreased postoperative morbidity, faster return of bowel function, and shorter hospital stays.8 Given the morbidity associated with fluid overload, enhanced recovery protocols recommend that minimal fluids be given in the operating room and intravenous fluids be removed as quickly as possible, often with first oral intake or postoperative day 1 at the latest.
Engagement of the patient in their perioperative recovery with patient education materials and expectations for postoperative tasks, such as early refeeding, spirometry, and ambulation are all important components of enhanced recovery. Patients become partners in achieving postoperative milestones, and this results in improved outcomes such as decreased pain scores and shorter recoveries.
Evidence in gynecology
Enhanced recovery has been studied in many surgical disciplines including urology, colorectal surgery, hepatobiliary surgery, and gynecology. High-quality studies of abdominal and vaginal hysterectomy patients have consistently found a decrease in length of stay with no difference in readmission or postoperative complication rates.9 An interesting study also found that an enhanced recovery program was associated with decreased nursing time required for patient care.10
For ovarian cancer patients, enhanced recovery is associated with decreased length of stay, decreased time to return of bowel function, and improved quality of life. Enhanced recovery is also cost saving, saving $257-$697 per vaginal hysterectomy patient and $5,410-$7,600 per ovarian cancer patient.11
Enhanced recovery protocols are safe, evidenced based, cost saving, and are increasingly being adopted as clinicians and health systems become aware of their benefits.
References
1. Br J Anaesth. 1997 May;78(5):606-17.
2. Cochrane Database Syst Rev. 2003 Oct 20;(4):CD004423.
3. Anesthesiology. 1999 Mar;90(3):896-905.
4. J Am Coll Surg. 2012 Jan;214(1):68-80.
5. Clin Nutr. 1998 Apr;17(2):65-71.
6. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD004508.
7. Obstet Gynecol. 1998 Jul;92(1):94-7.
8. Br J Surg. 2009 Apr;96(4):331-41.
9. Obstet Gynecol. 2013 Aug;122(2 Pt 1):319-28.
10. Qual Saf Health Care. 2009 Jun;18(3):236-40.
11. Gynecol Oncol. 2008 Feb;108(2):282-6.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Barber is a third-year fellow in gynecologic oncology at the university. They reported having no financial disclosures relevant to this column. Email them at [email protected].
FDA approves atezolizumab for advanced NSCLC
The Food and Drug Administration has approved the programmed death-ligand 1 (PD-L1) blocking antibody atezolizumab for the treatment of patients with metastatic non–small cell lung cancer (NSCLC) whose disease has progressed during or following platinum-containing chemotherapy.
The FDA previously approved atezolizumab (Tecentriq) for the treatment of locally advanced or metastatic urothelial carcinoma that has progressed after platinum-containing chemotherapy.
Approval for treatment of NSCLC was based on results from the phase III OAK and phase II POPLAR trials that enrolled a total of 1,137 patients with NSCLC whose disease had progressed on platinum-containing chemotherapy. In OAK, median overall survival for patients assigned to atezolizumab was 13.8 months, compared with 9.6 months for patients assigned to docetaxel, as recently reported at the European Society for Medical Oncology Congress.
In POPLAR, overall survival was 12.6 months for patients receiving atezolizumab versus 9.7 months for those assigned to docetaxel, as reported at the European Cancer Congress in 2015.
The most common (greater than or equal to 20%) adverse reactions in patients treated with atezolizumab were fatigue, decreased appetite, dyspnea, cough, nausea, musculoskeletal pain, and constipation, according to the FDA website. The most common (greater than or equal to 2%) grade 3-4 adverse events in patients treated with atezolizumab were dyspnea, pneumonia, hypoxia, hyponatremia, fatigue, anemia, musculoskeletal pain, AST increase, ALT increase, dysphagia, and arthralgia. Clinically significant immune-related adverse events for patients receiving atezolizumab have included pneumonitis, hepatitis, colitis, and thyroid disease.
The recommended dose is 1,200 mg administered as an intravenous infusion over 60 minutes every 3 weeks until disease progression or unacceptable toxicity.
Patients with EGFR or ALK genomic tumor aberrations should not receive atezolizumab before having disease progression on FDA-approved therapy for these aberrations, the FDA said.
Full prescribing information is available on the FDA website.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has approved the programmed death-ligand 1 (PD-L1) blocking antibody atezolizumab for the treatment of patients with metastatic non–small cell lung cancer (NSCLC) whose disease has progressed during or following platinum-containing chemotherapy.
The FDA previously approved atezolizumab (Tecentriq) for the treatment of locally advanced or metastatic urothelial carcinoma that has progressed after platinum-containing chemotherapy.
Approval for treatment of NSCLC was based on results from the phase III OAK and phase II POPLAR trials that enrolled a total of 1,137 patients with NSCLC whose disease had progressed on platinum-containing chemotherapy. In OAK, median overall survival for patients assigned to atezolizumab was 13.8 months, compared with 9.6 months for patients assigned to docetaxel, as recently reported at the European Society for Medical Oncology Congress.
In POPLAR, overall survival was 12.6 months for patients receiving atezolizumab versus 9.7 months for those assigned to docetaxel, as reported at the European Cancer Congress in 2015.
The most common (greater than or equal to 20%) adverse reactions in patients treated with atezolizumab were fatigue, decreased appetite, dyspnea, cough, nausea, musculoskeletal pain, and constipation, according to the FDA website. The most common (greater than or equal to 2%) grade 3-4 adverse events in patients treated with atezolizumab were dyspnea, pneumonia, hypoxia, hyponatremia, fatigue, anemia, musculoskeletal pain, AST increase, ALT increase, dysphagia, and arthralgia. Clinically significant immune-related adverse events for patients receiving atezolizumab have included pneumonitis, hepatitis, colitis, and thyroid disease.
The recommended dose is 1,200 mg administered as an intravenous infusion over 60 minutes every 3 weeks until disease progression or unacceptable toxicity.
Patients with EGFR or ALK genomic tumor aberrations should not receive atezolizumab before having disease progression on FDA-approved therapy for these aberrations, the FDA said.
Full prescribing information is available on the FDA website.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has approved the programmed death-ligand 1 (PD-L1) blocking antibody atezolizumab for the treatment of patients with metastatic non–small cell lung cancer (NSCLC) whose disease has progressed during or following platinum-containing chemotherapy.
The FDA previously approved atezolizumab (Tecentriq) for the treatment of locally advanced or metastatic urothelial carcinoma that has progressed after platinum-containing chemotherapy.
Approval for treatment of NSCLC was based on results from the phase III OAK and phase II POPLAR trials that enrolled a total of 1,137 patients with NSCLC whose disease had progressed on platinum-containing chemotherapy. In OAK, median overall survival for patients assigned to atezolizumab was 13.8 months, compared with 9.6 months for patients assigned to docetaxel, as recently reported at the European Society for Medical Oncology Congress.
In POPLAR, overall survival was 12.6 months for patients receiving atezolizumab versus 9.7 months for those assigned to docetaxel, as reported at the European Cancer Congress in 2015.
The most common (greater than or equal to 20%) adverse reactions in patients treated with atezolizumab were fatigue, decreased appetite, dyspnea, cough, nausea, musculoskeletal pain, and constipation, according to the FDA website. The most common (greater than or equal to 2%) grade 3-4 adverse events in patients treated with atezolizumab were dyspnea, pneumonia, hypoxia, hyponatremia, fatigue, anemia, musculoskeletal pain, AST increase, ALT increase, dysphagia, and arthralgia. Clinically significant immune-related adverse events for patients receiving atezolizumab have included pneumonitis, hepatitis, colitis, and thyroid disease.
The recommended dose is 1,200 mg administered as an intravenous infusion over 60 minutes every 3 weeks until disease progression or unacceptable toxicity.
Patients with EGFR or ALK genomic tumor aberrations should not receive atezolizumab before having disease progression on FDA-approved therapy for these aberrations, the FDA said.
Full prescribing information is available on the FDA website.
[email protected]
On Twitter @nikolaideslaura
Psychological stress did not harm IVF outcomes
SALT LAKE CITY – Self-reported psychological distress and biological markers of stress did not affect the chances of pregnancy after in vitro fertilization, according to a single-center prospective cohort study of 186 women.
Rates of ultrasound-confirmed pregnancy were 36% among first-time IVF recipients and 30% among women undergoing their third round of IVF, and did not differ based on self-reported depressive symptoms, stress, anxiety, or serum levels of adrenocorticotropic hormone (ACTH), cortisol, or interleukin-6, Maria Costantini-Ferrando, MD, PhD, said at the annual meeting of the American Society for Reproductive Medicine.
Nonetheless, IVF recipients reported more depressive symptoms than oocyte donors did, especially after a negative pregnancy test, reported Dr. Costantini-Ferrando, a reproductive endocrinologist in Englewood, N.J.
“Patients undergoing IVF do experience real psychological distress. The efficiency of IVF in controlling the hypothalamic-pituitary-adrenal and the hypothalamic-pituitary-gonadal axes may overshadow any deleterious effect of heightened stress, but it will not eliminate patients’ experience of it,” she said.
Patients need support and follow-up to help lessen the psychological burden of treatment and decrease drop-out, she said.
Women in the study were aged 22-44 years, and the IVF recipients had a mean age of 37 years. In all, 75 women (40%) were first-time IVF patients, 29% were undergoing their third cycle of IVF, and 31% were oocyte donors. Among the IVF recipients, 22% were in psychotherapy, and 4% were on psychotropic medications. None of the women had other medical comorbidities. Patients were assessed at baseline, time of oocyte retrieval, time of embryo transfer, and on the day of the pregnancy test.
Patients with infertility reported significantly worse depressive symptoms at baseline compared with oocyte donors, with average Beck Depression Inventory scores of 11, compared with 2.3 (P less than .01). This difference persisted at the time of vaginal oocyte retrieval. First-time and third-time IVF recipients tended to have similar Beck Depression Inventory scores until pregnancy testing, when the average scores of third-time recipients increased by about five additional points.
Scores on the daily stress questionnaire echoed these findings. Patients who were receiving IVF reported significantly more stress than did oocyte donors, with the highest increase at the time of the pregnancy test among patients with previous IVF failures. However, both recipients and donors reported mild to moderate anxiety based on the State-Trait Anxiety Inventory, Dr. Costantini-Ferrando said.
All groups had low interleukin-6 levels when starting IVF, but donors had the highest levels of both ACTH and cortisol. Levels of these hormones dropped over time, and then rose at the time of pregnancy testing. That trend suggests that IVF was an acute “procedural” stressor for both recipients and donors, but that the magnitude of the stress response lessened somewhat over time with repeated exposure to the stressor, Dr. Costantini-Ferrando noted.
“The complexity of this interaction may explain why it is difficult to elucidate the true impact of stress on IVF outcome,” she said.
Ultimately, these findings support a shift in focus, she added. Instead of asking if stress decreases reproductive potential, clinicians and researchers can instead explore how to address psychological distress to maximize reproductive potential. “This is important to keep patients engaged in infertility treatment and facilitate the difficult process of decision making during treatment,” she added.
The paper won a prize from the ASRM Mental Health Professional Group.
The National Institutes of Health provided funding for the study. Dr. Costantini-Ferrando reported having no relevant financial disclosures.
SALT LAKE CITY – Self-reported psychological distress and biological markers of stress did not affect the chances of pregnancy after in vitro fertilization, according to a single-center prospective cohort study of 186 women.
Rates of ultrasound-confirmed pregnancy were 36% among first-time IVF recipients and 30% among women undergoing their third round of IVF, and did not differ based on self-reported depressive symptoms, stress, anxiety, or serum levels of adrenocorticotropic hormone (ACTH), cortisol, or interleukin-6, Maria Costantini-Ferrando, MD, PhD, said at the annual meeting of the American Society for Reproductive Medicine.
Nonetheless, IVF recipients reported more depressive symptoms than oocyte donors did, especially after a negative pregnancy test, reported Dr. Costantini-Ferrando, a reproductive endocrinologist in Englewood, N.J.
“Patients undergoing IVF do experience real psychological distress. The efficiency of IVF in controlling the hypothalamic-pituitary-adrenal and the hypothalamic-pituitary-gonadal axes may overshadow any deleterious effect of heightened stress, but it will not eliminate patients’ experience of it,” she said.
Patients need support and follow-up to help lessen the psychological burden of treatment and decrease drop-out, she said.
Women in the study were aged 22-44 years, and the IVF recipients had a mean age of 37 years. In all, 75 women (40%) were first-time IVF patients, 29% were undergoing their third cycle of IVF, and 31% were oocyte donors. Among the IVF recipients, 22% were in psychotherapy, and 4% were on psychotropic medications. None of the women had other medical comorbidities. Patients were assessed at baseline, time of oocyte retrieval, time of embryo transfer, and on the day of the pregnancy test.
Patients with infertility reported significantly worse depressive symptoms at baseline compared with oocyte donors, with average Beck Depression Inventory scores of 11, compared with 2.3 (P less than .01). This difference persisted at the time of vaginal oocyte retrieval. First-time and third-time IVF recipients tended to have similar Beck Depression Inventory scores until pregnancy testing, when the average scores of third-time recipients increased by about five additional points.
Scores on the daily stress questionnaire echoed these findings. Patients who were receiving IVF reported significantly more stress than did oocyte donors, with the highest increase at the time of the pregnancy test among patients with previous IVF failures. However, both recipients and donors reported mild to moderate anxiety based on the State-Trait Anxiety Inventory, Dr. Costantini-Ferrando said.
All groups had low interleukin-6 levels when starting IVF, but donors had the highest levels of both ACTH and cortisol. Levels of these hormones dropped over time, and then rose at the time of pregnancy testing. That trend suggests that IVF was an acute “procedural” stressor for both recipients and donors, but that the magnitude of the stress response lessened somewhat over time with repeated exposure to the stressor, Dr. Costantini-Ferrando noted.
“The complexity of this interaction may explain why it is difficult to elucidate the true impact of stress on IVF outcome,” she said.
Ultimately, these findings support a shift in focus, she added. Instead of asking if stress decreases reproductive potential, clinicians and researchers can instead explore how to address psychological distress to maximize reproductive potential. “This is important to keep patients engaged in infertility treatment and facilitate the difficult process of decision making during treatment,” she added.
The paper won a prize from the ASRM Mental Health Professional Group.
The National Institutes of Health provided funding for the study. Dr. Costantini-Ferrando reported having no relevant financial disclosures.
SALT LAKE CITY – Self-reported psychological distress and biological markers of stress did not affect the chances of pregnancy after in vitro fertilization, according to a single-center prospective cohort study of 186 women.
Rates of ultrasound-confirmed pregnancy were 36% among first-time IVF recipients and 30% among women undergoing their third round of IVF, and did not differ based on self-reported depressive symptoms, stress, anxiety, or serum levels of adrenocorticotropic hormone (ACTH), cortisol, or interleukin-6, Maria Costantini-Ferrando, MD, PhD, said at the annual meeting of the American Society for Reproductive Medicine.
Nonetheless, IVF recipients reported more depressive symptoms than oocyte donors did, especially after a negative pregnancy test, reported Dr. Costantini-Ferrando, a reproductive endocrinologist in Englewood, N.J.
“Patients undergoing IVF do experience real psychological distress. The efficiency of IVF in controlling the hypothalamic-pituitary-adrenal and the hypothalamic-pituitary-gonadal axes may overshadow any deleterious effect of heightened stress, but it will not eliminate patients’ experience of it,” she said.
Patients need support and follow-up to help lessen the psychological burden of treatment and decrease drop-out, she said.
Women in the study were aged 22-44 years, and the IVF recipients had a mean age of 37 years. In all, 75 women (40%) were first-time IVF patients, 29% were undergoing their third cycle of IVF, and 31% were oocyte donors. Among the IVF recipients, 22% were in psychotherapy, and 4% were on psychotropic medications. None of the women had other medical comorbidities. Patients were assessed at baseline, time of oocyte retrieval, time of embryo transfer, and on the day of the pregnancy test.
Patients with infertility reported significantly worse depressive symptoms at baseline compared with oocyte donors, with average Beck Depression Inventory scores of 11, compared with 2.3 (P less than .01). This difference persisted at the time of vaginal oocyte retrieval. First-time and third-time IVF recipients tended to have similar Beck Depression Inventory scores until pregnancy testing, when the average scores of third-time recipients increased by about five additional points.
Scores on the daily stress questionnaire echoed these findings. Patients who were receiving IVF reported significantly more stress than did oocyte donors, with the highest increase at the time of the pregnancy test among patients with previous IVF failures. However, both recipients and donors reported mild to moderate anxiety based on the State-Trait Anxiety Inventory, Dr. Costantini-Ferrando said.
All groups had low interleukin-6 levels when starting IVF, but donors had the highest levels of both ACTH and cortisol. Levels of these hormones dropped over time, and then rose at the time of pregnancy testing. That trend suggests that IVF was an acute “procedural” stressor for both recipients and donors, but that the magnitude of the stress response lessened somewhat over time with repeated exposure to the stressor, Dr. Costantini-Ferrando noted.
“The complexity of this interaction may explain why it is difficult to elucidate the true impact of stress on IVF outcome,” she said.
Ultimately, these findings support a shift in focus, she added. Instead of asking if stress decreases reproductive potential, clinicians and researchers can instead explore how to address psychological distress to maximize reproductive potential. “This is important to keep patients engaged in infertility treatment and facilitate the difficult process of decision making during treatment,” she added.
The paper won a prize from the ASRM Mental Health Professional Group.
The National Institutes of Health provided funding for the study. Dr. Costantini-Ferrando reported having no relevant financial disclosures.
Key clinical point:
Major finding: Rates of pregnancy were 36% among first-time IVF recipients and 30% among third-time IVF recipients, and did not correlate with self-reported depressive symptoms, stress, anxiety, or serum levels of adrenocorticotropic hormone, cortisol, or interleukin-6.
Data source: A single-center prospective study of 186 IVF patients.
Disclosures: The National Institutes of Health provided funding for the study. Dr. Costantini-Ferrando reported having no financial disclosures.
Use of 2D bar coding with vaccines may be the future in pediatric practice
ATLANTA – Since the first bar coded consumer product, a pack of gum, was scanned in June of 1974, the soon widespread use of bar codes changed little until 2D bar codes arrived toward the end of last century. Today, the increasing use of 2D bar code technology with vaccines offers practices the potential for greater accuracy and efficiency with vaccine administration and data entry – if they have the resources to take the plunge.
An overview of 2D bar code use with vaccines, presented at a conference sponsored by the Centers for Disease Control and Prevention, provided a glimpse into both the types of changes practices might see with adoption of the technology and the way some clinics have made the transition.
Ken Gerlach, MPH, of the Immunization Services Division at the CDC in Atlanta, outlined the history of bar code use in immunizations, starting with a November 1999 Institute of Medicine report that identified the contribution of human error to disease and led the Food and Drug Administration to begin requiring linear bar codes on pharmaceutical unit-of-use products to reduce errors.
Then, a meeting organized by the American Academy of Pediatrics in January 2009 with the FDA, CDC, vaccine manufacturers, and other stakeholders led to a bar code rule change by the FDA in August 2011 that allowed alternatives to the traditional linear bar codes on vaccine vials and syringes.
“They essentially indicated to the pharmaceutical companies that it’s okay to add 2D bar codes, and this is essentially the point where things began to take off,” Mr. Gerlach explained. Until then, there had been no 2D bar codes on vaccines, but today the majority of vaccine products have them, as do all Vaccine Information Statements. In addition to the standard information included on traditional bar codes – Global Trade Item Number (GTIN), lot and serial numbers, and the expiration date – 2D bar codes also can include most relevant patient information that would go into the EMR except the injection site and immunization route. But a practice cannot simply jump over to scanning the 2D bar codes without ensuring that its EMR system is configured to accept the scanning.
Mr. Gerlach described a three-part project by the CDC, from 2011 through 2017, that assesses the impact of 2D coding on vaccination data quality and work flow, facilitates the adoption of 2D bar code scanning in health care practices, and then assesses the potential for expanding 2D bar code use in a large health care system. The first part of the project, which ran from 2011 to 2014, involved two vaccine manufacturers and 217 health care practices with more than 1.4 million de-identified vaccination records, 18.1% of which had been 2D bar coded.
Analysis of data quality from that pilot revealed an 8% increase in the correctness of lot numbers and 11% increase for expiration dates, with a time savings of 3.4 seconds per vaccine administration. Among the 116 staff users who completed surveys, 86% agreed that 2D bar coding improves accuracy and completeness, and 60% agreed it was easy to integrate the bar coding into their usual data recording process.
The pilot revealed challenges as well, however: not all individuals units of vaccines were 2D bar coded, users did not always consistently scan the bar codes, and some bar codes were difficult to read, such as one that was brown and wouldn’t scan. Another obstacle was having different lot numbers on the unit of use versus the unit of sale with 10% of the vaccines. Further, because inventory management typically involves unit of sale, it does not always match well with scanning unit of use.
Clinicians’ beliefs and attitudes toward 2D bar coding
As more practices consider adopting the technology, buy-in will important. At the conference, Sharon Humiston, MD, and Jill Hernandez, MPH, of Children’s Mercy Hospital in Kansas City, Mo., shared the findings of an online questionnaire about 2D bar coding and practices’ current systems for vaccine inventory and recording patient immunization information. The researchers distributed the questionnaire link to various AAP sections and committees in listservs and emails. Those eligible to complete the 15-minute survey were primary care personnel who used EMRs but not 2D bar code scanning for vaccines. They also needed to be key decision makers in the process of purchasing technology for the practice, and their practice needed to be enrolled in the Vaccines for Children program.
Among the 77 respondents who met all the inclusion criteria (61% of all who started the survey), 1 in 5 were private practices with one or two physicians, just over a third (36%) were private practices with more than two physicians, and a quarter were multispecialty group practices. Overall, respondents administered an average 116 doses of DTaP and 50 doses of Tdap each month.
Protocols for immunization management varied considerably across the respondents. For recording vaccine information, 49% reported that an administrator pre-entered it into an EMR, but 43% reported that staff manually enter it into an EMR. About 55% of practices entered the information before vaccine administration, and 42% entered it afterward. Although 57% of respondents’ practices upload the vaccination information directly from the EMR to their state’s Immunization Information System (IIS), 30% must enter it both into the EMR and into the state IIS separately, and 11% don’t enter it into a state IIS.
More than half (56%) of the respondents were extremely interested in having a bar code scanner system, and 31% were moderately to strongly interested, rating a 6 to 9 on a scale of 1 to 10. If provided evidence that 2D bar codes reduced errors in vaccine documentation, 56% of respondents said it would greatly increase their interest, and 32% said it would somewhat increase it. Only 23% said their interest would greatly increase if the bar code technology allowed the vaccine information statement to be scanned into EMRs.
Nearly all the respondents agreed that 2D bar code scanning technology would improve efficiency and accuracy of entering vaccine information into medical records and tracking vaccine inventory. Further, 81% believed it would reduce medical malpractice liability, and 85% believed it would reduce risk of harm to patients. However, 23% thought bar code technology would disrupt office work flow, and a quarter believed the technology’s costs would exceeds its benefits.
Despite the strong interest overall, respondents reported a number of barriers to adopting 2D bar code technology. The greatest barrier, reported by more than 70%, was the upfront cost of purchasing software for the EMR interface, followed by the cost of the bar code scanners. Other barriers, reported by 25%-45% of respondents, were the need for staff training, the need to service and maintain electronics for the technology, and the purchase of additional computers for scanner sites. If a bar code system cost less than $5,000, then 80% of the respondents would definitely or probably adopt such a system. Few would adopt it if the system cost $10,000 or more, but 42% probably would if it cost between $5,000 and $9,999. Even this small survey of self-selected volunteers, however, suggested strong interest in using 2D bar code technology for vaccines – although initial costs for a system presented a significant barrier to most practices.
One influenza vaccine clinic’s experience
Interest based on hypothetical questions is one thing. The process of actually implementing a 2D bar code scanning system into a health care center is another. In a separate presentation, Jane Glaser, MSN, RN, executive director of Campbell County Public Health in Gillette, Wyo., reviewed how such a system was implemented for mass influenza vaccination.
Campbell County, in the northeast corner of Wyoming, covers more than 4,800 square miles, has a population base of nearly 50,000 people, and also serves individuals from Montana, South Dakota, and North Dakota. Although the community as a whole works 24/7 in the county because of the oil, mining, and farming industries, the mass flu clinic is open 7 a.m. to 7 p.m., during which it provides an estimated 700 to 1,500 flu vaccines daily. Personnel comprises 13 public health nurses, 5 administrative assistants, and 3-4 community volunteers.
After 20 years of using an IIS, the clinic’s leadership decided to begin using 2D bar code scanners in October 2011 after observing it at a state immunization conference. Their goals in changing systems were to increase clinic flow, decrease registration time, and decrease overtime due to data entry. The new work flow went as follows: Those with Wyoming driver licenses or state ID cards have the linear bar code on their ID scanned in the immunization registry, which automatically populates the patient’s record. Then the staff member enters the vaccine information directly into the IIS registry in real time after the client receives the vaccine.
Ms. Glaser describes a number of improvements that resulted from use of the bar code scanning system, starting with reduced time for clinic registration and improved clinic flow. They also found that using bar code scanning reduced manual entry errors and improved the efficiency of assessing vaccination status and needed vaccines. Entering data in real time at point of care reduced time spent on data entry later on, thereby leading to a decrease in overtime and subsequent cost savings.
For providers and practices interested in learning more about 2D bar coding, the CDC offers a current list of 2D bar coded vaccines, data from the pilot program, training materials, and AAP guidance about 2D bar code use.
None of three presentations noted external funding, and all the researchers reported no financial relationships with companies that profit from bar code scanning technology. Deloitte Consulting, was involved in the three-part project conducted by the CDC.
ATLANTA – Since the first bar coded consumer product, a pack of gum, was scanned in June of 1974, the soon widespread use of bar codes changed little until 2D bar codes arrived toward the end of last century. Today, the increasing use of 2D bar code technology with vaccines offers practices the potential for greater accuracy and efficiency with vaccine administration and data entry – if they have the resources to take the plunge.
An overview of 2D bar code use with vaccines, presented at a conference sponsored by the Centers for Disease Control and Prevention, provided a glimpse into both the types of changes practices might see with adoption of the technology and the way some clinics have made the transition.
Ken Gerlach, MPH, of the Immunization Services Division at the CDC in Atlanta, outlined the history of bar code use in immunizations, starting with a November 1999 Institute of Medicine report that identified the contribution of human error to disease and led the Food and Drug Administration to begin requiring linear bar codes on pharmaceutical unit-of-use products to reduce errors.
Then, a meeting organized by the American Academy of Pediatrics in January 2009 with the FDA, CDC, vaccine manufacturers, and other stakeholders led to a bar code rule change by the FDA in August 2011 that allowed alternatives to the traditional linear bar codes on vaccine vials and syringes.
“They essentially indicated to the pharmaceutical companies that it’s okay to add 2D bar codes, and this is essentially the point where things began to take off,” Mr. Gerlach explained. Until then, there had been no 2D bar codes on vaccines, but today the majority of vaccine products have them, as do all Vaccine Information Statements. In addition to the standard information included on traditional bar codes – Global Trade Item Number (GTIN), lot and serial numbers, and the expiration date – 2D bar codes also can include most relevant patient information that would go into the EMR except the injection site and immunization route. But a practice cannot simply jump over to scanning the 2D bar codes without ensuring that its EMR system is configured to accept the scanning.
Mr. Gerlach described a three-part project by the CDC, from 2011 through 2017, that assesses the impact of 2D coding on vaccination data quality and work flow, facilitates the adoption of 2D bar code scanning in health care practices, and then assesses the potential for expanding 2D bar code use in a large health care system. The first part of the project, which ran from 2011 to 2014, involved two vaccine manufacturers and 217 health care practices with more than 1.4 million de-identified vaccination records, 18.1% of which had been 2D bar coded.
Analysis of data quality from that pilot revealed an 8% increase in the correctness of lot numbers and 11% increase for expiration dates, with a time savings of 3.4 seconds per vaccine administration. Among the 116 staff users who completed surveys, 86% agreed that 2D bar coding improves accuracy and completeness, and 60% agreed it was easy to integrate the bar coding into their usual data recording process.
The pilot revealed challenges as well, however: not all individuals units of vaccines were 2D bar coded, users did not always consistently scan the bar codes, and some bar codes were difficult to read, such as one that was brown and wouldn’t scan. Another obstacle was having different lot numbers on the unit of use versus the unit of sale with 10% of the vaccines. Further, because inventory management typically involves unit of sale, it does not always match well with scanning unit of use.
Clinicians’ beliefs and attitudes toward 2D bar coding
As more practices consider adopting the technology, buy-in will important. At the conference, Sharon Humiston, MD, and Jill Hernandez, MPH, of Children’s Mercy Hospital in Kansas City, Mo., shared the findings of an online questionnaire about 2D bar coding and practices’ current systems for vaccine inventory and recording patient immunization information. The researchers distributed the questionnaire link to various AAP sections and committees in listservs and emails. Those eligible to complete the 15-minute survey were primary care personnel who used EMRs but not 2D bar code scanning for vaccines. They also needed to be key decision makers in the process of purchasing technology for the practice, and their practice needed to be enrolled in the Vaccines for Children program.
Among the 77 respondents who met all the inclusion criteria (61% of all who started the survey), 1 in 5 were private practices with one or two physicians, just over a third (36%) were private practices with more than two physicians, and a quarter were multispecialty group practices. Overall, respondents administered an average 116 doses of DTaP and 50 doses of Tdap each month.
Protocols for immunization management varied considerably across the respondents. For recording vaccine information, 49% reported that an administrator pre-entered it into an EMR, but 43% reported that staff manually enter it into an EMR. About 55% of practices entered the information before vaccine administration, and 42% entered it afterward. Although 57% of respondents’ practices upload the vaccination information directly from the EMR to their state’s Immunization Information System (IIS), 30% must enter it both into the EMR and into the state IIS separately, and 11% don’t enter it into a state IIS.
More than half (56%) of the respondents were extremely interested in having a bar code scanner system, and 31% were moderately to strongly interested, rating a 6 to 9 on a scale of 1 to 10. If provided evidence that 2D bar codes reduced errors in vaccine documentation, 56% of respondents said it would greatly increase their interest, and 32% said it would somewhat increase it. Only 23% said their interest would greatly increase if the bar code technology allowed the vaccine information statement to be scanned into EMRs.
Nearly all the respondents agreed that 2D bar code scanning technology would improve efficiency and accuracy of entering vaccine information into medical records and tracking vaccine inventory. Further, 81% believed it would reduce medical malpractice liability, and 85% believed it would reduce risk of harm to patients. However, 23% thought bar code technology would disrupt office work flow, and a quarter believed the technology’s costs would exceeds its benefits.
Despite the strong interest overall, respondents reported a number of barriers to adopting 2D bar code technology. The greatest barrier, reported by more than 70%, was the upfront cost of purchasing software for the EMR interface, followed by the cost of the bar code scanners. Other barriers, reported by 25%-45% of respondents, were the need for staff training, the need to service and maintain electronics for the technology, and the purchase of additional computers for scanner sites. If a bar code system cost less than $5,000, then 80% of the respondents would definitely or probably adopt such a system. Few would adopt it if the system cost $10,000 or more, but 42% probably would if it cost between $5,000 and $9,999. Even this small survey of self-selected volunteers, however, suggested strong interest in using 2D bar code technology for vaccines – although initial costs for a system presented a significant barrier to most practices.
One influenza vaccine clinic’s experience
Interest based on hypothetical questions is one thing. The process of actually implementing a 2D bar code scanning system into a health care center is another. In a separate presentation, Jane Glaser, MSN, RN, executive director of Campbell County Public Health in Gillette, Wyo., reviewed how such a system was implemented for mass influenza vaccination.
Campbell County, in the northeast corner of Wyoming, covers more than 4,800 square miles, has a population base of nearly 50,000 people, and also serves individuals from Montana, South Dakota, and North Dakota. Although the community as a whole works 24/7 in the county because of the oil, mining, and farming industries, the mass flu clinic is open 7 a.m. to 7 p.m., during which it provides an estimated 700 to 1,500 flu vaccines daily. Personnel comprises 13 public health nurses, 5 administrative assistants, and 3-4 community volunteers.
After 20 years of using an IIS, the clinic’s leadership decided to begin using 2D bar code scanners in October 2011 after observing it at a state immunization conference. Their goals in changing systems were to increase clinic flow, decrease registration time, and decrease overtime due to data entry. The new work flow went as follows: Those with Wyoming driver licenses or state ID cards have the linear bar code on their ID scanned in the immunization registry, which automatically populates the patient’s record. Then the staff member enters the vaccine information directly into the IIS registry in real time after the client receives the vaccine.
Ms. Glaser describes a number of improvements that resulted from use of the bar code scanning system, starting with reduced time for clinic registration and improved clinic flow. They also found that using bar code scanning reduced manual entry errors and improved the efficiency of assessing vaccination status and needed vaccines. Entering data in real time at point of care reduced time spent on data entry later on, thereby leading to a decrease in overtime and subsequent cost savings.
For providers and practices interested in learning more about 2D bar coding, the CDC offers a current list of 2D bar coded vaccines, data from the pilot program, training materials, and AAP guidance about 2D bar code use.
None of three presentations noted external funding, and all the researchers reported no financial relationships with companies that profit from bar code scanning technology. Deloitte Consulting, was involved in the three-part project conducted by the CDC.
ATLANTA – Since the first bar coded consumer product, a pack of gum, was scanned in June of 1974, the soon widespread use of bar codes changed little until 2D bar codes arrived toward the end of last century. Today, the increasing use of 2D bar code technology with vaccines offers practices the potential for greater accuracy and efficiency with vaccine administration and data entry – if they have the resources to take the plunge.
An overview of 2D bar code use with vaccines, presented at a conference sponsored by the Centers for Disease Control and Prevention, provided a glimpse into both the types of changes practices might see with adoption of the technology and the way some clinics have made the transition.
Ken Gerlach, MPH, of the Immunization Services Division at the CDC in Atlanta, outlined the history of bar code use in immunizations, starting with a November 1999 Institute of Medicine report that identified the contribution of human error to disease and led the Food and Drug Administration to begin requiring linear bar codes on pharmaceutical unit-of-use products to reduce errors.
Then, a meeting organized by the American Academy of Pediatrics in January 2009 with the FDA, CDC, vaccine manufacturers, and other stakeholders led to a bar code rule change by the FDA in August 2011 that allowed alternatives to the traditional linear bar codes on vaccine vials and syringes.
“They essentially indicated to the pharmaceutical companies that it’s okay to add 2D bar codes, and this is essentially the point where things began to take off,” Mr. Gerlach explained. Until then, there had been no 2D bar codes on vaccines, but today the majority of vaccine products have them, as do all Vaccine Information Statements. In addition to the standard information included on traditional bar codes – Global Trade Item Number (GTIN), lot and serial numbers, and the expiration date – 2D bar codes also can include most relevant patient information that would go into the EMR except the injection site and immunization route. But a practice cannot simply jump over to scanning the 2D bar codes without ensuring that its EMR system is configured to accept the scanning.
Mr. Gerlach described a three-part project by the CDC, from 2011 through 2017, that assesses the impact of 2D coding on vaccination data quality and work flow, facilitates the adoption of 2D bar code scanning in health care practices, and then assesses the potential for expanding 2D bar code use in a large health care system. The first part of the project, which ran from 2011 to 2014, involved two vaccine manufacturers and 217 health care practices with more than 1.4 million de-identified vaccination records, 18.1% of which had been 2D bar coded.
Analysis of data quality from that pilot revealed an 8% increase in the correctness of lot numbers and 11% increase for expiration dates, with a time savings of 3.4 seconds per vaccine administration. Among the 116 staff users who completed surveys, 86% agreed that 2D bar coding improves accuracy and completeness, and 60% agreed it was easy to integrate the bar coding into their usual data recording process.
The pilot revealed challenges as well, however: not all individuals units of vaccines were 2D bar coded, users did not always consistently scan the bar codes, and some bar codes were difficult to read, such as one that was brown and wouldn’t scan. Another obstacle was having different lot numbers on the unit of use versus the unit of sale with 10% of the vaccines. Further, because inventory management typically involves unit of sale, it does not always match well with scanning unit of use.
Clinicians’ beliefs and attitudes toward 2D bar coding
As more practices consider adopting the technology, buy-in will important. At the conference, Sharon Humiston, MD, and Jill Hernandez, MPH, of Children’s Mercy Hospital in Kansas City, Mo., shared the findings of an online questionnaire about 2D bar coding and practices’ current systems for vaccine inventory and recording patient immunization information. The researchers distributed the questionnaire link to various AAP sections and committees in listservs and emails. Those eligible to complete the 15-minute survey were primary care personnel who used EMRs but not 2D bar code scanning for vaccines. They also needed to be key decision makers in the process of purchasing technology for the practice, and their practice needed to be enrolled in the Vaccines for Children program.
Among the 77 respondents who met all the inclusion criteria (61% of all who started the survey), 1 in 5 were private practices with one or two physicians, just over a third (36%) were private practices with more than two physicians, and a quarter were multispecialty group practices. Overall, respondents administered an average 116 doses of DTaP and 50 doses of Tdap each month.
Protocols for immunization management varied considerably across the respondents. For recording vaccine information, 49% reported that an administrator pre-entered it into an EMR, but 43% reported that staff manually enter it into an EMR. About 55% of practices entered the information before vaccine administration, and 42% entered it afterward. Although 57% of respondents’ practices upload the vaccination information directly from the EMR to their state’s Immunization Information System (IIS), 30% must enter it both into the EMR and into the state IIS separately, and 11% don’t enter it into a state IIS.
More than half (56%) of the respondents were extremely interested in having a bar code scanner system, and 31% were moderately to strongly interested, rating a 6 to 9 on a scale of 1 to 10. If provided evidence that 2D bar codes reduced errors in vaccine documentation, 56% of respondents said it would greatly increase their interest, and 32% said it would somewhat increase it. Only 23% said their interest would greatly increase if the bar code technology allowed the vaccine information statement to be scanned into EMRs.
Nearly all the respondents agreed that 2D bar code scanning technology would improve efficiency and accuracy of entering vaccine information into medical records and tracking vaccine inventory. Further, 81% believed it would reduce medical malpractice liability, and 85% believed it would reduce risk of harm to patients. However, 23% thought bar code technology would disrupt office work flow, and a quarter believed the technology’s costs would exceeds its benefits.
Despite the strong interest overall, respondents reported a number of barriers to adopting 2D bar code technology. The greatest barrier, reported by more than 70%, was the upfront cost of purchasing software for the EMR interface, followed by the cost of the bar code scanners. Other barriers, reported by 25%-45% of respondents, were the need for staff training, the need to service and maintain electronics for the technology, and the purchase of additional computers for scanner sites. If a bar code system cost less than $5,000, then 80% of the respondents would definitely or probably adopt such a system. Few would adopt it if the system cost $10,000 or more, but 42% probably would if it cost between $5,000 and $9,999. Even this small survey of self-selected volunteers, however, suggested strong interest in using 2D bar code technology for vaccines – although initial costs for a system presented a significant barrier to most practices.
One influenza vaccine clinic’s experience
Interest based on hypothetical questions is one thing. The process of actually implementing a 2D bar code scanning system into a health care center is another. In a separate presentation, Jane Glaser, MSN, RN, executive director of Campbell County Public Health in Gillette, Wyo., reviewed how such a system was implemented for mass influenza vaccination.
Campbell County, in the northeast corner of Wyoming, covers more than 4,800 square miles, has a population base of nearly 50,000 people, and also serves individuals from Montana, South Dakota, and North Dakota. Although the community as a whole works 24/7 in the county because of the oil, mining, and farming industries, the mass flu clinic is open 7 a.m. to 7 p.m., during which it provides an estimated 700 to 1,500 flu vaccines daily. Personnel comprises 13 public health nurses, 5 administrative assistants, and 3-4 community volunteers.
After 20 years of using an IIS, the clinic’s leadership decided to begin using 2D bar code scanners in October 2011 after observing it at a state immunization conference. Their goals in changing systems were to increase clinic flow, decrease registration time, and decrease overtime due to data entry. The new work flow went as follows: Those with Wyoming driver licenses or state ID cards have the linear bar code on their ID scanned in the immunization registry, which automatically populates the patient’s record. Then the staff member enters the vaccine information directly into the IIS registry in real time after the client receives the vaccine.
Ms. Glaser describes a number of improvements that resulted from use of the bar code scanning system, starting with reduced time for clinic registration and improved clinic flow. They also found that using bar code scanning reduced manual entry errors and improved the efficiency of assessing vaccination status and needed vaccines. Entering data in real time at point of care reduced time spent on data entry later on, thereby leading to a decrease in overtime and subsequent cost savings.
For providers and practices interested in learning more about 2D bar coding, the CDC offers a current list of 2D bar coded vaccines, data from the pilot program, training materials, and AAP guidance about 2D bar code use.
None of three presentations noted external funding, and all the researchers reported no financial relationships with companies that profit from bar code scanning technology. Deloitte Consulting, was involved in the three-part project conducted by the CDC.
EXPERT ANALYSIS FROM AAP 16
Key clinical point: 2D bar coding with vaccines offers benefits and challenges.
Major finding:
Data source: A CDC study, an online questionnaire, and experience in a Wyoming flu clinic.
Disclosures: None of three presentations noted external funding, and all researchers reported no financial relationships with companies that profit from bar code scanning technology. Deloitte Consulting was involved in the three-part project conducted by the CDC.
FDA grants accelerated approval to olaratumab for soft tissue sarcoma
The Food and Drug Administration has granted accelerated approval to olaratumab with doxorubicin for the treatment of adult patients with certain types of soft tissue sarcoma.
“This is the first new therapy approved by the FDA for the initial treatment of soft tissue sarcoma since doxorubicin’s approval more than 40 years ago,” Richard Pazdur, MD, director of the office of hematology and oncology products in the FDA Center for Drug Evaluation and Research and acting director of the FDA Oncology Center of Excellence, said in a statement.
Approval was based on a statistically significant improvement in survival in a randomized trial involving 133 patients with more than 25 different subtypes of metastatic soft tissue sarcoma. Patients received olaratumab (Lartruvo) with doxorubicin or doxorubicin alone. Median survival was 26.5 months for patients who received both drugs, compared with 14.7 months for patients who received doxorubicin alone. Median progression-free survival was 8.2 months for patients who received both drugs and 4.4 months for patients who received doxorubicin alone.
The most common adverse reactions from olaratumab were nausea, fatigue, neutropenia, musculoskeletal pain, mucositis, alopecia, vomiting, diarrhea, decreased appetite, abdominal pain, neuropathy, and headache. There are serious risks of infusion-related reactions and embryo-fetal harm, the FDA warned.
Olaratumab was approved under the FDA’s accelerated approval program after receiving fast track designation, breakthrough therapy designation, and a priority review status. The drug also received an orphan drug designation. Drug maker Eli Lilly is currently conducting a larger study of olaratumab across multiple subtypes of soft tissue sarcoma.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has granted accelerated approval to olaratumab with doxorubicin for the treatment of adult patients with certain types of soft tissue sarcoma.
“This is the first new therapy approved by the FDA for the initial treatment of soft tissue sarcoma since doxorubicin’s approval more than 40 years ago,” Richard Pazdur, MD, director of the office of hematology and oncology products in the FDA Center for Drug Evaluation and Research and acting director of the FDA Oncology Center of Excellence, said in a statement.
Approval was based on a statistically significant improvement in survival in a randomized trial involving 133 patients with more than 25 different subtypes of metastatic soft tissue sarcoma. Patients received olaratumab (Lartruvo) with doxorubicin or doxorubicin alone. Median survival was 26.5 months for patients who received both drugs, compared with 14.7 months for patients who received doxorubicin alone. Median progression-free survival was 8.2 months for patients who received both drugs and 4.4 months for patients who received doxorubicin alone.
The most common adverse reactions from olaratumab were nausea, fatigue, neutropenia, musculoskeletal pain, mucositis, alopecia, vomiting, diarrhea, decreased appetite, abdominal pain, neuropathy, and headache. There are serious risks of infusion-related reactions and embryo-fetal harm, the FDA warned.
Olaratumab was approved under the FDA’s accelerated approval program after receiving fast track designation, breakthrough therapy designation, and a priority review status. The drug also received an orphan drug designation. Drug maker Eli Lilly is currently conducting a larger study of olaratumab across multiple subtypes of soft tissue sarcoma.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has granted accelerated approval to olaratumab with doxorubicin for the treatment of adult patients with certain types of soft tissue sarcoma.
“This is the first new therapy approved by the FDA for the initial treatment of soft tissue sarcoma since doxorubicin’s approval more than 40 years ago,” Richard Pazdur, MD, director of the office of hematology and oncology products in the FDA Center for Drug Evaluation and Research and acting director of the FDA Oncology Center of Excellence, said in a statement.
Approval was based on a statistically significant improvement in survival in a randomized trial involving 133 patients with more than 25 different subtypes of metastatic soft tissue sarcoma. Patients received olaratumab (Lartruvo) with doxorubicin or doxorubicin alone. Median survival was 26.5 months for patients who received both drugs, compared with 14.7 months for patients who received doxorubicin alone. Median progression-free survival was 8.2 months for patients who received both drugs and 4.4 months for patients who received doxorubicin alone.
The most common adverse reactions from olaratumab were nausea, fatigue, neutropenia, musculoskeletal pain, mucositis, alopecia, vomiting, diarrhea, decreased appetite, abdominal pain, neuropathy, and headache. There are serious risks of infusion-related reactions and embryo-fetal harm, the FDA warned.
Olaratumab was approved under the FDA’s accelerated approval program after receiving fast track designation, breakthrough therapy designation, and a priority review status. The drug also received an orphan drug designation. Drug maker Eli Lilly is currently conducting a larger study of olaratumab across multiple subtypes of soft tissue sarcoma.
[email protected]
On Twitter @nikolaideslaura
Uninsured rate lowest in Massachusetts
Massachusetts had the nation’s lowest uninsured rate in 2015, and Texas had the highest, according to the personal finance website WalletHub.
Massachusetts’ uninsured rate of 2.8% was followed by Vermont at 3.8%, Hawaii at 4%, Minnesota at 4.5%, and Iowa at 5%, WalletHub reported.
Nevada, which was 44th overall in 2015, had the largest reduction (–10.3%) in its uninsured rate from 2010 to 2015. Oregon had the next-largest drop (10.1%) and Massachusetts had the smallest decrease at –1.6%, meaning that no state saw an increase over the 5-year period, the WalletHub report showed.
A quick run through some subgroups shows that Vermont had the lowest percentage of uninsured children (1%) and Alaska had the highest (10.6%), Massachusetts was lowest for whites (2.2%) and Hispanics (5.3%) while Mississippi was highest (10.9% white and 37.6% Hispanic). Hawaii had the lowest rate (3.8%) for blacks, and Montana had the highest (17.4%), WalletHub said.
Massachusetts had the nation’s lowest uninsured rate in 2015, and Texas had the highest, according to the personal finance website WalletHub.
Massachusetts’ uninsured rate of 2.8% was followed by Vermont at 3.8%, Hawaii at 4%, Minnesota at 4.5%, and Iowa at 5%, WalletHub reported.
Nevada, which was 44th overall in 2015, had the largest reduction (–10.3%) in its uninsured rate from 2010 to 2015. Oregon had the next-largest drop (10.1%) and Massachusetts had the smallest decrease at –1.6%, meaning that no state saw an increase over the 5-year period, the WalletHub report showed.
A quick run through some subgroups shows that Vermont had the lowest percentage of uninsured children (1%) and Alaska had the highest (10.6%), Massachusetts was lowest for whites (2.2%) and Hispanics (5.3%) while Mississippi was highest (10.9% white and 37.6% Hispanic). Hawaii had the lowest rate (3.8%) for blacks, and Montana had the highest (17.4%), WalletHub said.
Massachusetts had the nation’s lowest uninsured rate in 2015, and Texas had the highest, according to the personal finance website WalletHub.
Massachusetts’ uninsured rate of 2.8% was followed by Vermont at 3.8%, Hawaii at 4%, Minnesota at 4.5%, and Iowa at 5%, WalletHub reported.
Nevada, which was 44th overall in 2015, had the largest reduction (–10.3%) in its uninsured rate from 2010 to 2015. Oregon had the next-largest drop (10.1%) and Massachusetts had the smallest decrease at –1.6%, meaning that no state saw an increase over the 5-year period, the WalletHub report showed.
A quick run through some subgroups shows that Vermont had the lowest percentage of uninsured children (1%) and Alaska had the highest (10.6%), Massachusetts was lowest for whites (2.2%) and Hispanics (5.3%) while Mississippi was highest (10.9% white and 37.6% Hispanic). Hawaii had the lowest rate (3.8%) for blacks, and Montana had the highest (17.4%), WalletHub said.