User login
Atrial fib management pathway lowers hospital admissions
ORLANDO – An atrial fibrillation treatment pathway designed specifically to reduce the proportion of patients with this complaint who are admitted to the hospital from the emergency department was found remarkably effective in a pilot study presented at the annual International AF Symposium.
“In this single-center observational study, a multidisciplinary AF pathway was associated with fivefold reduction in admission rate and 2.5-fold reduction in length of stay for those who were admitted,” reported Jeremy N. Ruskin, MD.
Relative to many other countries, admission rates for AF in the United States are “extremely high,” according to Dr. Ruskin, director of the cardiac arrhythmia service at Massachusetts General Hospital, Boston. Citing 2013 figures from the Nationwide Emergency Department Sample (NEDS) database, rates ranged between 60% and 80% by geographic region with an average of about 66%. In contrast and as an example of lower rates elsewhere, fewer than 40% of AF patients with similar characteristics presenting at emergency departments in Ontario, Can., were admitted. Similarly low admission rates have been reported in Europe.
The AF pathway tested in the study at Mass General was developed through collaboration between electrophysiologists and emergency department physicians. It is suitable for patients presenting with a primary complaint of AF without concomitant diseases, such as sepsis or myocardial infarction. Patients were entered into this study after it was shown that AF was the chief complaint. The first step was to determine whether participants were best suited to a rhythm control or rate control strategy.
“The rhythm control group was anticoagulated and then underwent expedited cardioversion with TEE (transesophageal echocardiogram) if necessary. The rate control group was anticoagulated and then given appropriate pharmacologic therapy,” Dr. Ruskin explained. Once patients were on treatment, an electrophysiologist and an emergency room physician evaluated response. Stable patients were discharged; unstable patients were admitted.
In this nonrandomized observational study conducted over a 1-year period, 94 patients were managed with the AF pathway. Admissions and outcomes in this group were compared with 265 patients who received usual care.
Only 16% of those managed through the AF pathway were admitted versus 80% (P less than .001) in the usual care group. Among those admitted, length of stay was shorter in patients managed along the AF pathway relative to usual care (32 vs. 85 hours; P = .002). Dr. Ruskin also reported that both the cardioversion rate and the proportion of patients discharged on novel oral anticoagulation drugs were higher in the AF pathway group.
The reductions in hospital admissions would be expected to translate into large reductions in costs, particularly as follow-up showed no difference in return visits to the hospital between those entered into the AF pathway relative to those who received routine care, according to Dr. Ruskin. Emphasizing the cost burden of AF admissions, he noted that the estimated charges for the more than 300,000 AF admissions in U.S. hospitals in 2013 exceeded $7 billion.
Currently, there are no guidelines for managing AF in the emergency department, and there is wide variation in practice among centers, according to Dr. Ruskin. He provided data from the NEDS database demonstrating highly significant variations in rates of admission by geographic region (for example, rates were more than 10% higher in the northeast vs. the west) and hospital type (for example, rates were twice as high in metropolitan than nonmetropolitan hospitals).
In the NEDS database, various patient characteristics were associated with increased odds ratios for admission. These included hypertension (OR, 2.3), valvular disease (OR, 3.6), and congestive heart failure (OR, 3.7). However, Dr. Ruskin indicated that patients with these or other characteristics associated with increased likelihood of admission, such as older age, have better outcomes with hospitalization.
The data from this initial observational study were recently published (Am J Cardiol. 2016 Jul 1;118[1]:64-71), and a larger prospective study with this AF pathway is already underway at both Mass General and at Brigham and Women’s Hospital, Boston. If the data confirm that AF admissions can be safely reduced through this pathway, Dr. Ruskin anticipates that implementation will be adopted at other hospitals in the Harvard system.
Dr. Ruskin reported financial relationships with Cardiome, Daiichi Sankyo, Gilead, InCarda Therapeutics, InfoBionic, Laguna Medical, Medtronic, Pfizer, and Portola.
ORLANDO – An atrial fibrillation treatment pathway designed specifically to reduce the proportion of patients with this complaint who are admitted to the hospital from the emergency department was found remarkably effective in a pilot study presented at the annual International AF Symposium.
“In this single-center observational study, a multidisciplinary AF pathway was associated with fivefold reduction in admission rate and 2.5-fold reduction in length of stay for those who were admitted,” reported Jeremy N. Ruskin, MD.
Relative to many other countries, admission rates for AF in the United States are “extremely high,” according to Dr. Ruskin, director of the cardiac arrhythmia service at Massachusetts General Hospital, Boston. Citing 2013 figures from the Nationwide Emergency Department Sample (NEDS) database, rates ranged between 60% and 80% by geographic region with an average of about 66%. In contrast and as an example of lower rates elsewhere, fewer than 40% of AF patients with similar characteristics presenting at emergency departments in Ontario, Can., were admitted. Similarly low admission rates have been reported in Europe.
The AF pathway tested in the study at Mass General was developed through collaboration between electrophysiologists and emergency department physicians. It is suitable for patients presenting with a primary complaint of AF without concomitant diseases, such as sepsis or myocardial infarction. Patients were entered into this study after it was shown that AF was the chief complaint. The first step was to determine whether participants were best suited to a rhythm control or rate control strategy.
“The rhythm control group was anticoagulated and then underwent expedited cardioversion with TEE (transesophageal echocardiogram) if necessary. The rate control group was anticoagulated and then given appropriate pharmacologic therapy,” Dr. Ruskin explained. Once patients were on treatment, an electrophysiologist and an emergency room physician evaluated response. Stable patients were discharged; unstable patients were admitted.
In this nonrandomized observational study conducted over a 1-year period, 94 patients were managed with the AF pathway. Admissions and outcomes in this group were compared with 265 patients who received usual care.
Only 16% of those managed through the AF pathway were admitted versus 80% (P less than .001) in the usual care group. Among those admitted, length of stay was shorter in patients managed along the AF pathway relative to usual care (32 vs. 85 hours; P = .002). Dr. Ruskin also reported that both the cardioversion rate and the proportion of patients discharged on novel oral anticoagulation drugs were higher in the AF pathway group.
The reductions in hospital admissions would be expected to translate into large reductions in costs, particularly as follow-up showed no difference in return visits to the hospital between those entered into the AF pathway relative to those who received routine care, according to Dr. Ruskin. Emphasizing the cost burden of AF admissions, he noted that the estimated charges for the more than 300,000 AF admissions in U.S. hospitals in 2013 exceeded $7 billion.
Currently, there are no guidelines for managing AF in the emergency department, and there is wide variation in practice among centers, according to Dr. Ruskin. He provided data from the NEDS database demonstrating highly significant variations in rates of admission by geographic region (for example, rates were more than 10% higher in the northeast vs. the west) and hospital type (for example, rates were twice as high in metropolitan than nonmetropolitan hospitals).
In the NEDS database, various patient characteristics were associated with increased odds ratios for admission. These included hypertension (OR, 2.3), valvular disease (OR, 3.6), and congestive heart failure (OR, 3.7). However, Dr. Ruskin indicated that patients with these or other characteristics associated with increased likelihood of admission, such as older age, have better outcomes with hospitalization.
The data from this initial observational study were recently published (Am J Cardiol. 2016 Jul 1;118[1]:64-71), and a larger prospective study with this AF pathway is already underway at both Mass General and at Brigham and Women’s Hospital, Boston. If the data confirm that AF admissions can be safely reduced through this pathway, Dr. Ruskin anticipates that implementation will be adopted at other hospitals in the Harvard system.
Dr. Ruskin reported financial relationships with Cardiome, Daiichi Sankyo, Gilead, InCarda Therapeutics, InfoBionic, Laguna Medical, Medtronic, Pfizer, and Portola.
ORLANDO – An atrial fibrillation treatment pathway designed specifically to reduce the proportion of patients with this complaint who are admitted to the hospital from the emergency department was found remarkably effective in a pilot study presented at the annual International AF Symposium.
“In this single-center observational study, a multidisciplinary AF pathway was associated with fivefold reduction in admission rate and 2.5-fold reduction in length of stay for those who were admitted,” reported Jeremy N. Ruskin, MD.
Relative to many other countries, admission rates for AF in the United States are “extremely high,” according to Dr. Ruskin, director of the cardiac arrhythmia service at Massachusetts General Hospital, Boston. Citing 2013 figures from the Nationwide Emergency Department Sample (NEDS) database, rates ranged between 60% and 80% by geographic region with an average of about 66%. In contrast and as an example of lower rates elsewhere, fewer than 40% of AF patients with similar characteristics presenting at emergency departments in Ontario, Can., were admitted. Similarly low admission rates have been reported in Europe.
The AF pathway tested in the study at Mass General was developed through collaboration between electrophysiologists and emergency department physicians. It is suitable for patients presenting with a primary complaint of AF without concomitant diseases, such as sepsis or myocardial infarction. Patients were entered into this study after it was shown that AF was the chief complaint. The first step was to determine whether participants were best suited to a rhythm control or rate control strategy.
“The rhythm control group was anticoagulated and then underwent expedited cardioversion with TEE (transesophageal echocardiogram) if necessary. The rate control group was anticoagulated and then given appropriate pharmacologic therapy,” Dr. Ruskin explained. Once patients were on treatment, an electrophysiologist and an emergency room physician evaluated response. Stable patients were discharged; unstable patients were admitted.
In this nonrandomized observational study conducted over a 1-year period, 94 patients were managed with the AF pathway. Admissions and outcomes in this group were compared with 265 patients who received usual care.
Only 16% of those managed through the AF pathway were admitted versus 80% (P less than .001) in the usual care group. Among those admitted, length of stay was shorter in patients managed along the AF pathway relative to usual care (32 vs. 85 hours; P = .002). Dr. Ruskin also reported that both the cardioversion rate and the proportion of patients discharged on novel oral anticoagulation drugs were higher in the AF pathway group.
The reductions in hospital admissions would be expected to translate into large reductions in costs, particularly as follow-up showed no difference in return visits to the hospital between those entered into the AF pathway relative to those who received routine care, according to Dr. Ruskin. Emphasizing the cost burden of AF admissions, he noted that the estimated charges for the more than 300,000 AF admissions in U.S. hospitals in 2013 exceeded $7 billion.
Currently, there are no guidelines for managing AF in the emergency department, and there is wide variation in practice among centers, according to Dr. Ruskin. He provided data from the NEDS database demonstrating highly significant variations in rates of admission by geographic region (for example, rates were more than 10% higher in the northeast vs. the west) and hospital type (for example, rates were twice as high in metropolitan than nonmetropolitan hospitals).
In the NEDS database, various patient characteristics were associated with increased odds ratios for admission. These included hypertension (OR, 2.3), valvular disease (OR, 3.6), and congestive heart failure (OR, 3.7). However, Dr. Ruskin indicated that patients with these or other characteristics associated with increased likelihood of admission, such as older age, have better outcomes with hospitalization.
The data from this initial observational study were recently published (Am J Cardiol. 2016 Jul 1;118[1]:64-71), and a larger prospective study with this AF pathway is already underway at both Mass General and at Brigham and Women’s Hospital, Boston. If the data confirm that AF admissions can be safely reduced through this pathway, Dr. Ruskin anticipates that implementation will be adopted at other hospitals in the Harvard system.
Dr. Ruskin reported financial relationships with Cardiome, Daiichi Sankyo, Gilead, InCarda Therapeutics, InfoBionic, Laguna Medical, Medtronic, Pfizer, and Portola.
Key clinical point: An atrial fibrillation (AF) treatment pathway in the emergency department reduces hospital admission rates.
Major finding: Once implemented, the AF hospital admission rate at one institution fell significantly, from 80% to 16%.
Data source: Prospective observational study.
Disclosures: Dr. Ruskin reports financial relationships with Cardiome, Daiichi Sankyo, Gilead, InCarda Therapeutics, InfoBionic, Laguna Medical, Medtronic, Pfizer, and Portola.
21 Medicare health plans warned to fix provider directory errors
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.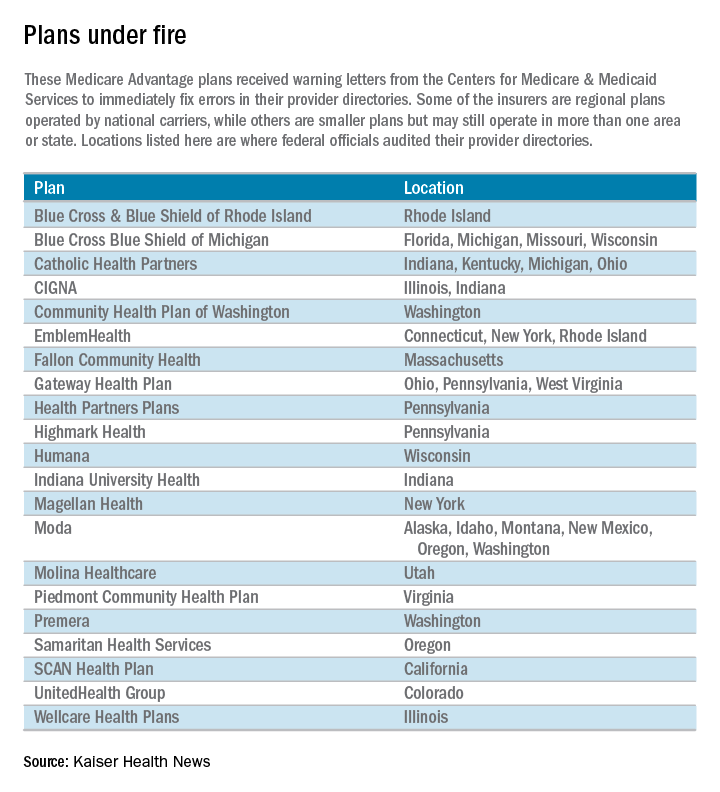
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.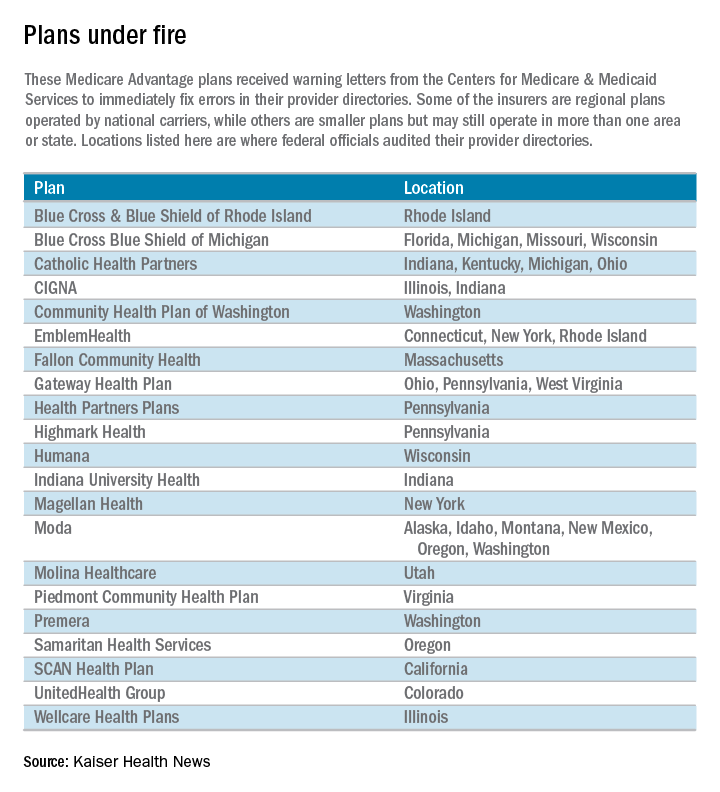
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.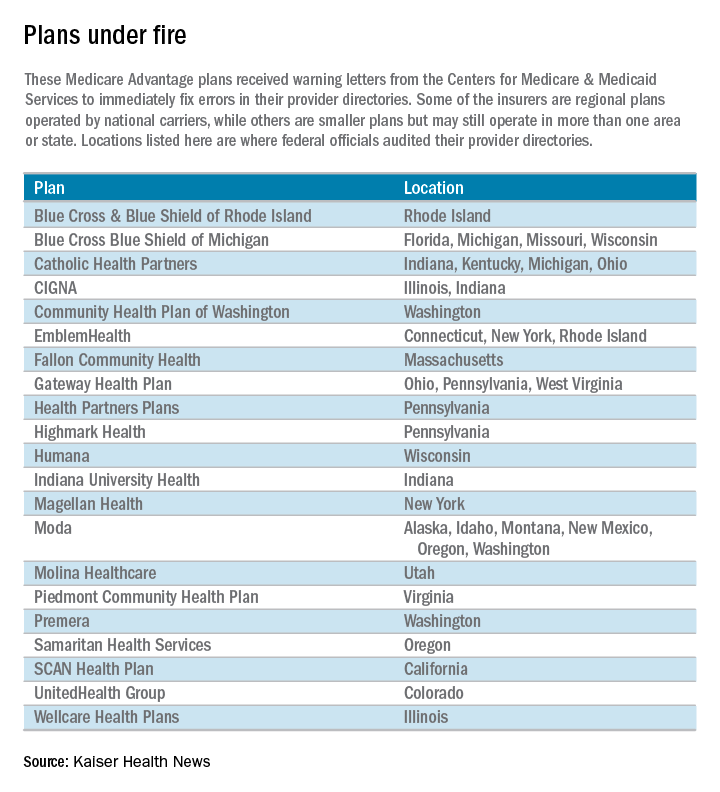
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Ultrashort course antibiotics may be enough in stable VAP
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Key clinical point: Ultrashort antibiotic courses yielded outcomes that were similar to those with longer courses in patients with suspected ventilator-associated pneumonia but minimal and stable ventilator settings.
Major finding: The groups did not significantly differ based on time to extubation alive (hazard ratio, 1.2), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).
Data source: A single-center retrospective observational study of 1,290 patients with suspected ventilator-associated pneumonia.
Disclosures: The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Risk tool bests CDC criteria for initiating PrEP
A risk-assessment tool that incorporates more data on patient and partner behavior is more specific than are the CDC criteria for initiating HIV preexposure prophylaxis and would allow more targeted treatment, according to a report published in the January issue of Sexually Transmitted Diseases.
To construct a risk-assessment tool that incorporated the most relevant information for predicting HIV acquisition, researchers collected data for all the men who have sex with men who underwent serial HIV testing at a single Los Angeles facility during a 4-year period. These 9,481 men were HIV negative at their baseline visit and were followed for a mean of 2 years (range, from less than 1 year to more than 4 years) for seroconversion, said Matthew R. Beymer, PhD, of the Los Angeles LGBT Center and the University of California, Los Angeles, and his associates.
A total of 370 of these men acquired HIV infection during 16,894 person-years of follow-up.
The investigators constructed a risk-assessment tool to guide the initiation of PrEP, which included seven factors that were the most predictive of HIV seroconversion: Hispanic or African-American ethnicity; a self-reported history of chlamydia, gonorrhea, and/or syphilis; not using a condom during their last occasion of receptive anal sex; having more than three sexual partners during the preceding month or more than five during the preceding 3 months; being of the same ethnicity as the last sexual partner; experiencing intimate partner violence; and using methamphetamines or inhaled nitrates during the preceding year.
“If all individuals in our population who had a risk score of greater than or equal to 5 (51%) had been given PrEP [at baseline], 75% of HIV infections would [have been] averted during follow-up, assuming adequate regimen adherence and near complete effectiveness,” Dr. Beymer and his associates said (Sex Transm Dis. 2017;44[1]:49-57).
In contrast, CDC criteria would have selected 69% of this cohort to begin PrEP. The additional behavioral data incorporated into the risk-assessment tool “allowed for more targeted PrEP. Physicians, their patients, and other interested individuals can obtain their own personalized risk score by visiting www.IsPrEPforMe.org,” the investigators said.
They recommend that men with a risk score of 5 or higher on this instrument begin PrEP, and strongly recommend that men with a risk score of 8 or higher do so. “For individuals whose risk score is less than 5 but who request PrEP, we believe the provider should consider it in light of their patient’s overall concerns.”
Using this tool instead of CDC criteria permits a more personalized recommendation, the authors wrote. Also, those at risk will be better informed about what actions and circumstances specifically lead to their increased HIV risk, which can aid in deciding “to initiate PrEP, reduce sexual risk, or make a plan that incorporates both PrEP initiation and sexual risk reduction,” Dr. Beymer and his associates said.
The Center for HIV Identification, Prevention, and Treatment; the National Institute of Mental Health; and the UCLA Center for AIDS Research supported the study. Dr. Beymer and his associates reported having no relevant disclosures.
A risk-assessment tool that incorporates more data on patient and partner behavior is more specific than are the CDC criteria for initiating HIV preexposure prophylaxis and would allow more targeted treatment, according to a report published in the January issue of Sexually Transmitted Diseases.
To construct a risk-assessment tool that incorporated the most relevant information for predicting HIV acquisition, researchers collected data for all the men who have sex with men who underwent serial HIV testing at a single Los Angeles facility during a 4-year period. These 9,481 men were HIV negative at their baseline visit and were followed for a mean of 2 years (range, from less than 1 year to more than 4 years) for seroconversion, said Matthew R. Beymer, PhD, of the Los Angeles LGBT Center and the University of California, Los Angeles, and his associates.
A total of 370 of these men acquired HIV infection during 16,894 person-years of follow-up.
The investigators constructed a risk-assessment tool to guide the initiation of PrEP, which included seven factors that were the most predictive of HIV seroconversion: Hispanic or African-American ethnicity; a self-reported history of chlamydia, gonorrhea, and/or syphilis; not using a condom during their last occasion of receptive anal sex; having more than three sexual partners during the preceding month or more than five during the preceding 3 months; being of the same ethnicity as the last sexual partner; experiencing intimate partner violence; and using methamphetamines or inhaled nitrates during the preceding year.
“If all individuals in our population who had a risk score of greater than or equal to 5 (51%) had been given PrEP [at baseline], 75% of HIV infections would [have been] averted during follow-up, assuming adequate regimen adherence and near complete effectiveness,” Dr. Beymer and his associates said (Sex Transm Dis. 2017;44[1]:49-57).
In contrast, CDC criteria would have selected 69% of this cohort to begin PrEP. The additional behavioral data incorporated into the risk-assessment tool “allowed for more targeted PrEP. Physicians, their patients, and other interested individuals can obtain their own personalized risk score by visiting www.IsPrEPforMe.org,” the investigators said.
They recommend that men with a risk score of 5 or higher on this instrument begin PrEP, and strongly recommend that men with a risk score of 8 or higher do so. “For individuals whose risk score is less than 5 but who request PrEP, we believe the provider should consider it in light of their patient’s overall concerns.”
Using this tool instead of CDC criteria permits a more personalized recommendation, the authors wrote. Also, those at risk will be better informed about what actions and circumstances specifically lead to their increased HIV risk, which can aid in deciding “to initiate PrEP, reduce sexual risk, or make a plan that incorporates both PrEP initiation and sexual risk reduction,” Dr. Beymer and his associates said.
The Center for HIV Identification, Prevention, and Treatment; the National Institute of Mental Health; and the UCLA Center for AIDS Research supported the study. Dr. Beymer and his associates reported having no relevant disclosures.
A risk-assessment tool that incorporates more data on patient and partner behavior is more specific than are the CDC criteria for initiating HIV preexposure prophylaxis and would allow more targeted treatment, according to a report published in the January issue of Sexually Transmitted Diseases.
To construct a risk-assessment tool that incorporated the most relevant information for predicting HIV acquisition, researchers collected data for all the men who have sex with men who underwent serial HIV testing at a single Los Angeles facility during a 4-year period. These 9,481 men were HIV negative at their baseline visit and were followed for a mean of 2 years (range, from less than 1 year to more than 4 years) for seroconversion, said Matthew R. Beymer, PhD, of the Los Angeles LGBT Center and the University of California, Los Angeles, and his associates.
A total of 370 of these men acquired HIV infection during 16,894 person-years of follow-up.
The investigators constructed a risk-assessment tool to guide the initiation of PrEP, which included seven factors that were the most predictive of HIV seroconversion: Hispanic or African-American ethnicity; a self-reported history of chlamydia, gonorrhea, and/or syphilis; not using a condom during their last occasion of receptive anal sex; having more than three sexual partners during the preceding month or more than five during the preceding 3 months; being of the same ethnicity as the last sexual partner; experiencing intimate partner violence; and using methamphetamines or inhaled nitrates during the preceding year.
“If all individuals in our population who had a risk score of greater than or equal to 5 (51%) had been given PrEP [at baseline], 75% of HIV infections would [have been] averted during follow-up, assuming adequate regimen adherence and near complete effectiveness,” Dr. Beymer and his associates said (Sex Transm Dis. 2017;44[1]:49-57).
In contrast, CDC criteria would have selected 69% of this cohort to begin PrEP. The additional behavioral data incorporated into the risk-assessment tool “allowed for more targeted PrEP. Physicians, their patients, and other interested individuals can obtain their own personalized risk score by visiting www.IsPrEPforMe.org,” the investigators said.
They recommend that men with a risk score of 5 or higher on this instrument begin PrEP, and strongly recommend that men with a risk score of 8 or higher do so. “For individuals whose risk score is less than 5 but who request PrEP, we believe the provider should consider it in light of their patient’s overall concerns.”
Using this tool instead of CDC criteria permits a more personalized recommendation, the authors wrote. Also, those at risk will be better informed about what actions and circumstances specifically lead to their increased HIV risk, which can aid in deciding “to initiate PrEP, reduce sexual risk, or make a plan that incorporates both PrEP initiation and sexual risk reduction,” Dr. Beymer and his associates said.
The Center for HIV Identification, Prevention, and Treatment; the National Institute of Mental Health; and the UCLA Center for AIDS Research supported the study. Dr. Beymer and his associates reported having no relevant disclosures.
FROM SEXUALLY TRANSMITTED DISEASES
Key clinical point: A risk-assessment tool that incorporates behavioral data is more specific than are CDC criteria for initiating PrEP and would allow more targeted treatment.
Major finding: If all the men in this cohort who had a risk score of 5 or higher (51%) had been given PrEP at baseline, 75% of HIV infections acquired during follow-up would have been averted.
Data source: A retrospective single-center cohort study involving 9,481 men who have sex with men who underwent HIV testing during a 4-year period and were followed for 2 years for the acquisition of HIV.
Disclosures: The Center for HIV Identification, Prevention, and Treatment; the National Institute of Mental Health; and the UCLA Center for AIDS Research supported the study. Dr. Beymer and his associates reported having no relevant disclosures.
A sweet new solution for rosacea
VIENNA – A medical-grade topical honey product proved safe and effective for the treatment of rosacea in a randomized, placebo-controlled clinical trial, Brigitte Dreno, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
The product, known as Honevo, is a cream consisting of 90% New Zealand kanuka honey and 10% glycerine. It is applied twice daily as a face mask. Honevo is designed to wash off easily and is less sticky than honey.
The primary outcome in the trial was at least a 2-point improvement from baseline on the 7-point Investigator Global Assessment of Rosacea Severity Score (IGA-RSS) as assessed by blinded investigators. This outcome, which reflects a clinical improvement from severe to moderate or from moderate to mild, was achieved in 34% of the Honevo group, compared with 17% of controls. Significant improvement in the honey group was seen after 2 weeks.
Rosacea resolved in 13% of the Honevo group and in 3% of controls, based on a week 8 IGA-RSS of zero, noted Dr. Dreno, professor and chair of the department of dermatology at the University of Nantes (France).
The investigators, from the Medical Research Institute of New Zealand and the University of Otago in Wellington, observed that the study outcomes look at least as good as the results of placebo-controlled studies of topical metronidazole or azelaic cream. They plan to conduct randomized, head-to-head comparative trials of those prescription drugs versus Honevo, which is an OTC product.
The mechanism of action of kanuka honey in treating rosacea is believed to involve its previously reported antibacterial and anti-inflammatory effects, according to the investigators (BMJ Open. 2015 Jun 24;5[6]:e007651. doi: 10.1136/bmjopen-2015-007651).
The researchers noted that many rosacea patients aren’t interested in long-term antibiotic therapy. They want a natural product that doesn’t contribute to the global antibiotic resistance problem and is available OTC. And Honevo is one of the few natural or complementary medicine therapies backed by data from a rigorous clinical trial, in this case one registered in the Australian New Zealand Clinical Trials Registry (ACTRN12614000004662).
Dr. Dreno wasn’t involved in the study but included it in a talk in which she examined the strengths and weaknesses of current rosacea therapies. She is waiting for a confirmatory study before she incorporates Honevo in her own treatment algorithm. She said that she also would like to see studies examining whether combining the topical honey product with prescription drugs for rosacea provides synergistic efficacy.
HoneyLab, which funded the clinical trial and markets Honevo, ships the product to customers worldwide from its New Zealand headquarters.
VIENNA – A medical-grade topical honey product proved safe and effective for the treatment of rosacea in a randomized, placebo-controlled clinical trial, Brigitte Dreno, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
The product, known as Honevo, is a cream consisting of 90% New Zealand kanuka honey and 10% glycerine. It is applied twice daily as a face mask. Honevo is designed to wash off easily and is less sticky than honey.
The primary outcome in the trial was at least a 2-point improvement from baseline on the 7-point Investigator Global Assessment of Rosacea Severity Score (IGA-RSS) as assessed by blinded investigators. This outcome, which reflects a clinical improvement from severe to moderate or from moderate to mild, was achieved in 34% of the Honevo group, compared with 17% of controls. Significant improvement in the honey group was seen after 2 weeks.
Rosacea resolved in 13% of the Honevo group and in 3% of controls, based on a week 8 IGA-RSS of zero, noted Dr. Dreno, professor and chair of the department of dermatology at the University of Nantes (France).
The investigators, from the Medical Research Institute of New Zealand and the University of Otago in Wellington, observed that the study outcomes look at least as good as the results of placebo-controlled studies of topical metronidazole or azelaic cream. They plan to conduct randomized, head-to-head comparative trials of those prescription drugs versus Honevo, which is an OTC product.
The mechanism of action of kanuka honey in treating rosacea is believed to involve its previously reported antibacterial and anti-inflammatory effects, according to the investigators (BMJ Open. 2015 Jun 24;5[6]:e007651. doi: 10.1136/bmjopen-2015-007651).
The researchers noted that many rosacea patients aren’t interested in long-term antibiotic therapy. They want a natural product that doesn’t contribute to the global antibiotic resistance problem and is available OTC. And Honevo is one of the few natural or complementary medicine therapies backed by data from a rigorous clinical trial, in this case one registered in the Australian New Zealand Clinical Trials Registry (ACTRN12614000004662).
Dr. Dreno wasn’t involved in the study but included it in a talk in which she examined the strengths and weaknesses of current rosacea therapies. She is waiting for a confirmatory study before she incorporates Honevo in her own treatment algorithm. She said that she also would like to see studies examining whether combining the topical honey product with prescription drugs for rosacea provides synergistic efficacy.
HoneyLab, which funded the clinical trial and markets Honevo, ships the product to customers worldwide from its New Zealand headquarters.
VIENNA – A medical-grade topical honey product proved safe and effective for the treatment of rosacea in a randomized, placebo-controlled clinical trial, Brigitte Dreno, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
The product, known as Honevo, is a cream consisting of 90% New Zealand kanuka honey and 10% glycerine. It is applied twice daily as a face mask. Honevo is designed to wash off easily and is less sticky than honey.
The primary outcome in the trial was at least a 2-point improvement from baseline on the 7-point Investigator Global Assessment of Rosacea Severity Score (IGA-RSS) as assessed by blinded investigators. This outcome, which reflects a clinical improvement from severe to moderate or from moderate to mild, was achieved in 34% of the Honevo group, compared with 17% of controls. Significant improvement in the honey group was seen after 2 weeks.
Rosacea resolved in 13% of the Honevo group and in 3% of controls, based on a week 8 IGA-RSS of zero, noted Dr. Dreno, professor and chair of the department of dermatology at the University of Nantes (France).
The investigators, from the Medical Research Institute of New Zealand and the University of Otago in Wellington, observed that the study outcomes look at least as good as the results of placebo-controlled studies of topical metronidazole or azelaic cream. They plan to conduct randomized, head-to-head comparative trials of those prescription drugs versus Honevo, which is an OTC product.
The mechanism of action of kanuka honey in treating rosacea is believed to involve its previously reported antibacterial and anti-inflammatory effects, according to the investigators (BMJ Open. 2015 Jun 24;5[6]:e007651. doi: 10.1136/bmjopen-2015-007651).
The researchers noted that many rosacea patients aren’t interested in long-term antibiotic therapy. They want a natural product that doesn’t contribute to the global antibiotic resistance problem and is available OTC. And Honevo is one of the few natural or complementary medicine therapies backed by data from a rigorous clinical trial, in this case one registered in the Australian New Zealand Clinical Trials Registry (ACTRN12614000004662).
Dr. Dreno wasn’t involved in the study but included it in a talk in which she examined the strengths and weaknesses of current rosacea therapies. She is waiting for a confirmatory study before she incorporates Honevo in her own treatment algorithm. She said that she also would like to see studies examining whether combining the topical honey product with prescription drugs for rosacea provides synergistic efficacy.
HoneyLab, which funded the clinical trial and markets Honevo, ships the product to customers worldwide from its New Zealand headquarters.
AT THE EADV CONGRESS
Key clinical point:
Major finding: 34% of rosacea patients experienced clinically meaningful improvement in response to twice-daily kanuka honey face masks, a rate twice that in controls.
Data source: This was a randomized, placebo-controlled, single-blind, 8-week clinical trial involving 138 adults with rosacea.
Disclosures: The presenter reported having no financial conflicts of interest regarding the study.
Palliative care improves quality of life after HCT
Inpatient palliative care can help maintain quality of life (QoL) in patients undergoing hematopoietic stem cell transplantation (HCT), based on the results of a randomized clinical trial to assess the effect of inpatient palliative care on patient and caregiver-reported outcomes while hospitalized for HCT and for 3 months after transplantation.
During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone. The difference was statistically significant (JAMA. 2016;316[20]:2094-2103. doi:10.1001/jama.2016.16786).
In addition to the QoL results, Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston, and coauthors, noted that “exploratory secondary outcomes also showed that patients in the palliative care group benefited, with less increase in their depression symptoms, lower anxiety symptoms, and less increase in symptom burden compared with those receiving standard transplant care.
“Thus, palliative care may help to lessen the decline in QoL experienced by patients during hospitalization for HCT, which has long been perceived as a natural aspect of the transplantation process.”
The study cohort comprised 160 adults with hematologic malignancies undergoing autologous/allogeneic HCT, and 94 caregivers.
A total of 81 patients were assigned to the intervention, and were seen by palliative care clinicians at least twice a week while they were hospitalized. The palliative care intervention focused on managing both physical and psychological symptoms, and those who were assigned to the standard care arm (n = 79) could also request to be seen by the palliative care team.
Quality of life was measured based on mean FACT-BMT score. In the palliative care group, the FACT-BMT score was 110.26 at hospitalization and 95.46 at 2 weeks after transplant (mean change, −14.72). For the standard care group, FACT-BMT score was 106.83 at hospitalization and 85.42 at 2 weeks after transplant (mean change, −21.54) The −6.82 difference between the group groups was statistically significant (95% CI, −13.48 to −0.16; P = .045).
When looking at secondary outcomes, those in the intervention group had lower mean depression scores at 2 weeks based on the HADS-D measure. For the intervention group, the mean baseline score was 3.95 and the mean week 2 score was 6.39. For the control group, the baseline score was 4.94 and the week 2 score was 8.86. The difference between the groups was 1.49 (95% CI, 0.20-2.78; P = .02). Depression scores remained lower in the intervention group at 3 months.
The intervention group also reported a decrease in anxiety symptoms, but the control group reported an increase in anxiety symptoms from baseline to week 2 on the HADS-A measure. The mean difference in score between the two groups was 1.92; (95% CI, 0.83-3.01; P less than .001). However, there was no significant difference between the two groups at 3 months after transplant.
The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
Inpatient palliative care can help maintain quality of life (QoL) in patients undergoing hematopoietic stem cell transplantation (HCT), based on the results of a randomized clinical trial to assess the effect of inpatient palliative care on patient and caregiver-reported outcomes while hospitalized for HCT and for 3 months after transplantation.
During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone. The difference was statistically significant (JAMA. 2016;316[20]:2094-2103. doi:10.1001/jama.2016.16786).
In addition to the QoL results, Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston, and coauthors, noted that “exploratory secondary outcomes also showed that patients in the palliative care group benefited, with less increase in their depression symptoms, lower anxiety symptoms, and less increase in symptom burden compared with those receiving standard transplant care.
“Thus, palliative care may help to lessen the decline in QoL experienced by patients during hospitalization for HCT, which has long been perceived as a natural aspect of the transplantation process.”
The study cohort comprised 160 adults with hematologic malignancies undergoing autologous/allogeneic HCT, and 94 caregivers.
A total of 81 patients were assigned to the intervention, and were seen by palliative care clinicians at least twice a week while they were hospitalized. The palliative care intervention focused on managing both physical and psychological symptoms, and those who were assigned to the standard care arm (n = 79) could also request to be seen by the palliative care team.
Quality of life was measured based on mean FACT-BMT score. In the palliative care group, the FACT-BMT score was 110.26 at hospitalization and 95.46 at 2 weeks after transplant (mean change, −14.72). For the standard care group, FACT-BMT score was 106.83 at hospitalization and 85.42 at 2 weeks after transplant (mean change, −21.54) The −6.82 difference between the group groups was statistically significant (95% CI, −13.48 to −0.16; P = .045).
When looking at secondary outcomes, those in the intervention group had lower mean depression scores at 2 weeks based on the HADS-D measure. For the intervention group, the mean baseline score was 3.95 and the mean week 2 score was 6.39. For the control group, the baseline score was 4.94 and the week 2 score was 8.86. The difference between the groups was 1.49 (95% CI, 0.20-2.78; P = .02). Depression scores remained lower in the intervention group at 3 months.
The intervention group also reported a decrease in anxiety symptoms, but the control group reported an increase in anxiety symptoms from baseline to week 2 on the HADS-A measure. The mean difference in score between the two groups was 1.92; (95% CI, 0.83-3.01; P less than .001). However, there was no significant difference between the two groups at 3 months after transplant.
The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
Inpatient palliative care can help maintain quality of life (QoL) in patients undergoing hematopoietic stem cell transplantation (HCT), based on the results of a randomized clinical trial to assess the effect of inpatient palliative care on patient and caregiver-reported outcomes while hospitalized for HCT and for 3 months after transplantation.
During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone. The difference was statistically significant (JAMA. 2016;316[20]:2094-2103. doi:10.1001/jama.2016.16786).
In addition to the QoL results, Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston, and coauthors, noted that “exploratory secondary outcomes also showed that patients in the palliative care group benefited, with less increase in their depression symptoms, lower anxiety symptoms, and less increase in symptom burden compared with those receiving standard transplant care.
“Thus, palliative care may help to lessen the decline in QoL experienced by patients during hospitalization for HCT, which has long been perceived as a natural aspect of the transplantation process.”
The study cohort comprised 160 adults with hematologic malignancies undergoing autologous/allogeneic HCT, and 94 caregivers.
A total of 81 patients were assigned to the intervention, and were seen by palliative care clinicians at least twice a week while they were hospitalized. The palliative care intervention focused on managing both physical and psychological symptoms, and those who were assigned to the standard care arm (n = 79) could also request to be seen by the palliative care team.
Quality of life was measured based on mean FACT-BMT score. In the palliative care group, the FACT-BMT score was 110.26 at hospitalization and 95.46 at 2 weeks after transplant (mean change, −14.72). For the standard care group, FACT-BMT score was 106.83 at hospitalization and 85.42 at 2 weeks after transplant (mean change, −21.54) The −6.82 difference between the group groups was statistically significant (95% CI, −13.48 to −0.16; P = .045).
When looking at secondary outcomes, those in the intervention group had lower mean depression scores at 2 weeks based on the HADS-D measure. For the intervention group, the mean baseline score was 3.95 and the mean week 2 score was 6.39. For the control group, the baseline score was 4.94 and the week 2 score was 8.86. The difference between the groups was 1.49 (95% CI, 0.20-2.78; P = .02). Depression scores remained lower in the intervention group at 3 months.
The intervention group also reported a decrease in anxiety symptoms, but the control group reported an increase in anxiety symptoms from baseline to week 2 on the HADS-A measure. The mean difference in score between the two groups was 1.92; (95% CI, 0.83-3.01; P less than .001). However, there was no significant difference between the two groups at 3 months after transplant.
The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
FROM JAMA
Key clinical point: Inpatient palliative care can help maintain quality of life in patients undergoing hematopoietic stem cell transplantation.
Major finding: During the 2-week period following their transplants, patients who received inpatient palliative care experienced a 14.72-point decrease in QoL, compared with a 21.54-point decrease in QoL for those assigned to standard transplant care alone.
Data source: Randomized clinical trial among 160 adults with hematologic malignancies who underwent HCT, and their caregivers (n = 94).
Disclosures: The study was supported by the National Palliative Care Research Foundation and grant K24 CA 181253 from the National Cancer Institute. Dr. El-Jawahri reported no disclosures.
Discussing the ADHD ‘controversy’ with patients and parents
There are many topics within the child psychiatry community that are controversial. How many kids really deserve a diagnosis of bipolar disorder? Which type of therapy works best? Is cannabis a gateway drug? The existence of attention-deficit/hyperactivity disorder as a legitimate psychiatric entity, however, is not one of them.
Despite this fact, there remains considerable controversy in the public about how “real” ADHD actually is. Social media, blogs, and even entire books have been written that disparage the diagnosis and even suggest that ADHD was fabricated by the pharmaceutical industry to sell medications. Although these publications and posts generally ignore the scientific literature or at least twist it beyond recognition, there are several aspects of ADHD that legitimately cause more confusion and less confidence about the diagnosis, relative to other common pediatric problems. This column attempts to describe and contextualize these elements so that pediatricians can be more fully informed when they are called to respond to some of the allegations against ADHD that often are brought up by families.
Case summary
Hunter is a 6-year-old boy who presents with his mother and father for “behavioral concerns.” He always has been an energetic child, but the school has been having increasing difficulties with his behavior. Hunter struggles to stay in his seat and take part in quiet activities. His teacher needs to give multiple reminders per day about not interrupting others or speaking out in class. Without redirection, Hunter typically loses focus in class and does not complete his work. Because of these difficulties, the question of ADHD arose during a recent parent-teacher conference. While Hunter’s mother acknowledges these behaviors and notes similar ones at home, the father is resisting any further evaluation, claiming that Hunter “is just being a boy.” The father notes that he acted similarly as a child and “turned out okay.” When the mother tried to research ADHD online, she encountered several sites that claimed that the diagnosis of ADHD was “made up” by drug companies wanting “to turn kids into zombies.” At the appointment, the parents state that they want their son to succeed and be happy, but are concerned about some of the things they have read on the Internet.
Discussion
This example represents a common dilemma for parents who encounter so many mixed messages when doing background research on ADHD. Although the legitimacy of ADHD has been supported in literally hundreds of research studies that have examined areas such as genetics, neuropsychological testing, and brain imaging1,2, some of the lingering doubts about ADHD validity are rooted in characteristics of the diagnosis that do differ from some nonpsychiatric diagnoses. At the same time, however, further inspection reveals that these qualities exist for many other entities that have received far less public criticism. Three of these main qualities include the following:
1. ADHD is a dimensional rather than binary entity. Despite the fact that the current nomenclature continues to frame ADHD as an all-or-nothing diagnosis, there is now overwhelming scientific evidence that it is much more accurately conceptualized as a dimension3. As such, there is no clear-cut boundary between what should be judged as “typical” levels of attention and activity and ADHD. As written in a previous column4, in some ways the label of ADHD is a lot like the label of someone being tall, with some individuals clearly falling into the category of “tall” or “not tall,” while many others could be considered in-between. However, many of the most common nonpsychiatric conditions such as hypertension and hypercholesterolemia also exist this way without high levels of public controversy.
2. ADHD lacks a specific known neurobiologic marker that can be measured by a lab or neuroimaging test. As mentioned, there is a vast literature supporting the idea that the brains of people with ADHD are different from those without ADHD, but these differences tend to describe quantitative differences in regional brain volume, cortical thickness, activity levels, or connectivity rather than a discrete “thing” that a radiologist can point to on a scan. Given the dimensional nature of ADHD and the broad brain processes required for complex functions such as attention and motor activity, the lack of a specific and universal “lesion” underlying ADHD is to be expected, yet it still remains easy ammunition for those who criticize the diagnosis. Again, very similar cases can be made for other entities such as autism or low intelligence, which few argue are not real but also have no reliable biomarker to support them.
3. Medications often are used to treat ADHD. The diagnosis of ADHD would probably be far less controversial if one of its primary treatments did not involve psychiatric medications. While it is probably fair to say that the many nonpharmacologic approaches to ADHD are quite underutilized, it seems a stretch to use potential overreliance on medication as a legitimate reason to question the validity of a diagnosis. Opiate abuse also is a problem in this country, but that doesn’t mean a person’s pain doesn’t exist. As a practical tip, it can be reassuring for families to hear explicitly from their physician that “zombification” is not considered an acceptable medical outcome and that the prescribing clinician will promptly deal with any side effects that might occur with treatment5.
Understanding these aspects about ADHD and how they are misinterpreted in the media can help families make more informed and comfortable decisions about their child’s care in collaboration with their pediatrician. It also is important for pediatricians to be proactive in distributing reliable and science-backed material to the public in this new age of information overload.
Case follow-up
The pediatrician hears the family’s concerns and discusses the evidence supporting the scientific legitimacy of ADHD, as well as some of the qualities of the diagnosis that have led to its controversy. The parents are reassured but would like to proceed carefully and cautiously with further work-up and treatment. The pediatrician sends the family home with some quantitative rating scales to be completed by Hunter’s parents and teacher. She also makes a plan to begin monitoring several health promotion areas that could be impacting Hunter’s behavior including sleep quality, physical activity, screen time, and nutrition.
References
1. Psychiatr Clin North Am. 2010 Mar;33(1):159-80.
2. Dev Neuropsychol. 2013;38(4):211-25.3. Can Fam Physician. 2016 Dec;62(12):979-82.
4. ADHD boundaries with normal behavior. Pediatric News; published online Aug. 27, 2014.
5. Zombification is not an acceptable medical outcome. Psychology Today, ABCs of Child Psychiatry blog; published online Oct. 18, 2013.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych.
There are many topics within the child psychiatry community that are controversial. How many kids really deserve a diagnosis of bipolar disorder? Which type of therapy works best? Is cannabis a gateway drug? The existence of attention-deficit/hyperactivity disorder as a legitimate psychiatric entity, however, is not one of them.
Despite this fact, there remains considerable controversy in the public about how “real” ADHD actually is. Social media, blogs, and even entire books have been written that disparage the diagnosis and even suggest that ADHD was fabricated by the pharmaceutical industry to sell medications. Although these publications and posts generally ignore the scientific literature or at least twist it beyond recognition, there are several aspects of ADHD that legitimately cause more confusion and less confidence about the diagnosis, relative to other common pediatric problems. This column attempts to describe and contextualize these elements so that pediatricians can be more fully informed when they are called to respond to some of the allegations against ADHD that often are brought up by families.
Case summary
Hunter is a 6-year-old boy who presents with his mother and father for “behavioral concerns.” He always has been an energetic child, but the school has been having increasing difficulties with his behavior. Hunter struggles to stay in his seat and take part in quiet activities. His teacher needs to give multiple reminders per day about not interrupting others or speaking out in class. Without redirection, Hunter typically loses focus in class and does not complete his work. Because of these difficulties, the question of ADHD arose during a recent parent-teacher conference. While Hunter’s mother acknowledges these behaviors and notes similar ones at home, the father is resisting any further evaluation, claiming that Hunter “is just being a boy.” The father notes that he acted similarly as a child and “turned out okay.” When the mother tried to research ADHD online, she encountered several sites that claimed that the diagnosis of ADHD was “made up” by drug companies wanting “to turn kids into zombies.” At the appointment, the parents state that they want their son to succeed and be happy, but are concerned about some of the things they have read on the Internet.
Discussion
This example represents a common dilemma for parents who encounter so many mixed messages when doing background research on ADHD. Although the legitimacy of ADHD has been supported in literally hundreds of research studies that have examined areas such as genetics, neuropsychological testing, and brain imaging1,2, some of the lingering doubts about ADHD validity are rooted in characteristics of the diagnosis that do differ from some nonpsychiatric diagnoses. At the same time, however, further inspection reveals that these qualities exist for many other entities that have received far less public criticism. Three of these main qualities include the following:
1. ADHD is a dimensional rather than binary entity. Despite the fact that the current nomenclature continues to frame ADHD as an all-or-nothing diagnosis, there is now overwhelming scientific evidence that it is much more accurately conceptualized as a dimension3. As such, there is no clear-cut boundary between what should be judged as “typical” levels of attention and activity and ADHD. As written in a previous column4, in some ways the label of ADHD is a lot like the label of someone being tall, with some individuals clearly falling into the category of “tall” or “not tall,” while many others could be considered in-between. However, many of the most common nonpsychiatric conditions such as hypertension and hypercholesterolemia also exist this way without high levels of public controversy.
2. ADHD lacks a specific known neurobiologic marker that can be measured by a lab or neuroimaging test. As mentioned, there is a vast literature supporting the idea that the brains of people with ADHD are different from those without ADHD, but these differences tend to describe quantitative differences in regional brain volume, cortical thickness, activity levels, or connectivity rather than a discrete “thing” that a radiologist can point to on a scan. Given the dimensional nature of ADHD and the broad brain processes required for complex functions such as attention and motor activity, the lack of a specific and universal “lesion” underlying ADHD is to be expected, yet it still remains easy ammunition for those who criticize the diagnosis. Again, very similar cases can be made for other entities such as autism or low intelligence, which few argue are not real but also have no reliable biomarker to support them.
3. Medications often are used to treat ADHD. The diagnosis of ADHD would probably be far less controversial if one of its primary treatments did not involve psychiatric medications. While it is probably fair to say that the many nonpharmacologic approaches to ADHD are quite underutilized, it seems a stretch to use potential overreliance on medication as a legitimate reason to question the validity of a diagnosis. Opiate abuse also is a problem in this country, but that doesn’t mean a person’s pain doesn’t exist. As a practical tip, it can be reassuring for families to hear explicitly from their physician that “zombification” is not considered an acceptable medical outcome and that the prescribing clinician will promptly deal with any side effects that might occur with treatment5.
Understanding these aspects about ADHD and how they are misinterpreted in the media can help families make more informed and comfortable decisions about their child’s care in collaboration with their pediatrician. It also is important for pediatricians to be proactive in distributing reliable and science-backed material to the public in this new age of information overload.
Case follow-up
The pediatrician hears the family’s concerns and discusses the evidence supporting the scientific legitimacy of ADHD, as well as some of the qualities of the diagnosis that have led to its controversy. The parents are reassured but would like to proceed carefully and cautiously with further work-up and treatment. The pediatrician sends the family home with some quantitative rating scales to be completed by Hunter’s parents and teacher. She also makes a plan to begin monitoring several health promotion areas that could be impacting Hunter’s behavior including sleep quality, physical activity, screen time, and nutrition.
References
1. Psychiatr Clin North Am. 2010 Mar;33(1):159-80.
2. Dev Neuropsychol. 2013;38(4):211-25.3. Can Fam Physician. 2016 Dec;62(12):979-82.
4. ADHD boundaries with normal behavior. Pediatric News; published online Aug. 27, 2014.
5. Zombification is not an acceptable medical outcome. Psychology Today, ABCs of Child Psychiatry blog; published online Oct. 18, 2013.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych.
There are many topics within the child psychiatry community that are controversial. How many kids really deserve a diagnosis of bipolar disorder? Which type of therapy works best? Is cannabis a gateway drug? The existence of attention-deficit/hyperactivity disorder as a legitimate psychiatric entity, however, is not one of them.
Despite this fact, there remains considerable controversy in the public about how “real” ADHD actually is. Social media, blogs, and even entire books have been written that disparage the diagnosis and even suggest that ADHD was fabricated by the pharmaceutical industry to sell medications. Although these publications and posts generally ignore the scientific literature or at least twist it beyond recognition, there are several aspects of ADHD that legitimately cause more confusion and less confidence about the diagnosis, relative to other common pediatric problems. This column attempts to describe and contextualize these elements so that pediatricians can be more fully informed when they are called to respond to some of the allegations against ADHD that often are brought up by families.
Case summary
Hunter is a 6-year-old boy who presents with his mother and father for “behavioral concerns.” He always has been an energetic child, but the school has been having increasing difficulties with his behavior. Hunter struggles to stay in his seat and take part in quiet activities. His teacher needs to give multiple reminders per day about not interrupting others or speaking out in class. Without redirection, Hunter typically loses focus in class and does not complete his work. Because of these difficulties, the question of ADHD arose during a recent parent-teacher conference. While Hunter’s mother acknowledges these behaviors and notes similar ones at home, the father is resisting any further evaluation, claiming that Hunter “is just being a boy.” The father notes that he acted similarly as a child and “turned out okay.” When the mother tried to research ADHD online, she encountered several sites that claimed that the diagnosis of ADHD was “made up” by drug companies wanting “to turn kids into zombies.” At the appointment, the parents state that they want their son to succeed and be happy, but are concerned about some of the things they have read on the Internet.
Discussion
This example represents a common dilemma for parents who encounter so many mixed messages when doing background research on ADHD. Although the legitimacy of ADHD has been supported in literally hundreds of research studies that have examined areas such as genetics, neuropsychological testing, and brain imaging1,2, some of the lingering doubts about ADHD validity are rooted in characteristics of the diagnosis that do differ from some nonpsychiatric diagnoses. At the same time, however, further inspection reveals that these qualities exist for many other entities that have received far less public criticism. Three of these main qualities include the following:
1. ADHD is a dimensional rather than binary entity. Despite the fact that the current nomenclature continues to frame ADHD as an all-or-nothing diagnosis, there is now overwhelming scientific evidence that it is much more accurately conceptualized as a dimension3. As such, there is no clear-cut boundary between what should be judged as “typical” levels of attention and activity and ADHD. As written in a previous column4, in some ways the label of ADHD is a lot like the label of someone being tall, with some individuals clearly falling into the category of “tall” or “not tall,” while many others could be considered in-between. However, many of the most common nonpsychiatric conditions such as hypertension and hypercholesterolemia also exist this way without high levels of public controversy.
2. ADHD lacks a specific known neurobiologic marker that can be measured by a lab or neuroimaging test. As mentioned, there is a vast literature supporting the idea that the brains of people with ADHD are different from those without ADHD, but these differences tend to describe quantitative differences in regional brain volume, cortical thickness, activity levels, or connectivity rather than a discrete “thing” that a radiologist can point to on a scan. Given the dimensional nature of ADHD and the broad brain processes required for complex functions such as attention and motor activity, the lack of a specific and universal “lesion” underlying ADHD is to be expected, yet it still remains easy ammunition for those who criticize the diagnosis. Again, very similar cases can be made for other entities such as autism or low intelligence, which few argue are not real but also have no reliable biomarker to support them.
3. Medications often are used to treat ADHD. The diagnosis of ADHD would probably be far less controversial if one of its primary treatments did not involve psychiatric medications. While it is probably fair to say that the many nonpharmacologic approaches to ADHD are quite underutilized, it seems a stretch to use potential overreliance on medication as a legitimate reason to question the validity of a diagnosis. Opiate abuse also is a problem in this country, but that doesn’t mean a person’s pain doesn’t exist. As a practical tip, it can be reassuring for families to hear explicitly from their physician that “zombification” is not considered an acceptable medical outcome and that the prescribing clinician will promptly deal with any side effects that might occur with treatment5.
Understanding these aspects about ADHD and how they are misinterpreted in the media can help families make more informed and comfortable decisions about their child’s care in collaboration with their pediatrician. It also is important for pediatricians to be proactive in distributing reliable and science-backed material to the public in this new age of information overload.
Case follow-up
The pediatrician hears the family’s concerns and discusses the evidence supporting the scientific legitimacy of ADHD, as well as some of the qualities of the diagnosis that have led to its controversy. The parents are reassured but would like to proceed carefully and cautiously with further work-up and treatment. The pediatrician sends the family home with some quantitative rating scales to be completed by Hunter’s parents and teacher. She also makes a plan to begin monitoring several health promotion areas that could be impacting Hunter’s behavior including sleep quality, physical activity, screen time, and nutrition.
References
1. Psychiatr Clin North Am. 2010 Mar;33(1):159-80.
2. Dev Neuropsychol. 2013;38(4):211-25.3. Can Fam Physician. 2016 Dec;62(12):979-82.
4. ADHD boundaries with normal behavior. Pediatric News; published online Aug. 27, 2014.
5. Zombification is not an acceptable medical outcome. Psychology Today, ABCs of Child Psychiatry blog; published online Oct. 18, 2013.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych.
VIDEO: First multicenter trial of CAR T cells shows response in DLBCL
SAN DIEGO – Aggressive, refractory non-Hodgkin lymphomas responded to anti-CD19 chimeric antigen receptor T cells in ZUMA-1, the first multicenter trial of the cellular immunotherapy, based on early data reported at the annual meeting of the American Society of Hematology.
In an interim analysis of 51 patients with diffuse large B-cell lymphomas, 47% had complete remissions and 29% had partial remissions. But the remission rate declined to 33% complete remissions and 6% partial remissions after 3 months.
There have really been no new treatments in the last 20 years for patients with non-Hodgkin lymphoma that does not respond to chemotherapy or recurs after autologous stem cell transplant. With median overall survival of 6 months, and about 8% complete remissions with existing therapies, CAR T cells might be a solution for these patients, said ZUMA-1 investigator Sattva S. Neelapu, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In our video interview at the meeting, Dr. Neelapu discussed initial results in the real-world setting of 22 participating centers, most of which had no previous experience with CAR T-cell therapy. With an efficient production and logistics plan, 91% of 110 patients were able to receive the investigational product, known as KTE-C19.
ZUMA-1 is funded by Kite, which makes KTE-C19, and the Leukemia & Lymphoma Society Therapy Acceleration Program. Dr. Neelapu receives research support from and is an advisor to Kite.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @maryjodales
SAN DIEGO – Aggressive, refractory non-Hodgkin lymphomas responded to anti-CD19 chimeric antigen receptor T cells in ZUMA-1, the first multicenter trial of the cellular immunotherapy, based on early data reported at the annual meeting of the American Society of Hematology.
In an interim analysis of 51 patients with diffuse large B-cell lymphomas, 47% had complete remissions and 29% had partial remissions. But the remission rate declined to 33% complete remissions and 6% partial remissions after 3 months.
There have really been no new treatments in the last 20 years for patients with non-Hodgkin lymphoma that does not respond to chemotherapy or recurs after autologous stem cell transplant. With median overall survival of 6 months, and about 8% complete remissions with existing therapies, CAR T cells might be a solution for these patients, said ZUMA-1 investigator Sattva S. Neelapu, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In our video interview at the meeting, Dr. Neelapu discussed initial results in the real-world setting of 22 participating centers, most of which had no previous experience with CAR T-cell therapy. With an efficient production and logistics plan, 91% of 110 patients were able to receive the investigational product, known as KTE-C19.
ZUMA-1 is funded by Kite, which makes KTE-C19, and the Leukemia & Lymphoma Society Therapy Acceleration Program. Dr. Neelapu receives research support from and is an advisor to Kite.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @maryjodales
SAN DIEGO – Aggressive, refractory non-Hodgkin lymphomas responded to anti-CD19 chimeric antigen receptor T cells in ZUMA-1, the first multicenter trial of the cellular immunotherapy, based on early data reported at the annual meeting of the American Society of Hematology.
In an interim analysis of 51 patients with diffuse large B-cell lymphomas, 47% had complete remissions and 29% had partial remissions. But the remission rate declined to 33% complete remissions and 6% partial remissions after 3 months.
There have really been no new treatments in the last 20 years for patients with non-Hodgkin lymphoma that does not respond to chemotherapy or recurs after autologous stem cell transplant. With median overall survival of 6 months, and about 8% complete remissions with existing therapies, CAR T cells might be a solution for these patients, said ZUMA-1 investigator Sattva S. Neelapu, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In our video interview at the meeting, Dr. Neelapu discussed initial results in the real-world setting of 22 participating centers, most of which had no previous experience with CAR T-cell therapy. With an efficient production and logistics plan, 91% of 110 patients were able to receive the investigational product, known as KTE-C19.
ZUMA-1 is funded by Kite, which makes KTE-C19, and the Leukemia & Lymphoma Society Therapy Acceleration Program. Dr. Neelapu receives research support from and is an advisor to Kite.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @maryjodales
Preventing EMR problems means foreseeing them first
SAN FRANCISCO – Are electronic medical records wreaking havoc for you? Herschel R. Lessin, MD, vice president of the Children’s Medical Group in Poughkeepsie, N.Y., had some EMR recommendations.
In his presentation entitled “Help! My EMR Threw Me Under the Bus!” at the annual meeting of the American Academy of Pediatrics, Dr. Lessin offered the following recommendations for troubleshooting or preventing EMR problems, starting with customizing your EMR right away to reduce alert fatigue.
• Document the specifics of a particular condition, treatment, history, or other note when checking boxes.
• Document your thinking in terms of differential diagnoses.
• Document a follow-up plan beyond just checking the box of a patient’s return date.
• Be wary of cutting and pasting too quickly or relying on the template as a standard of care instead of thoughtful application of the evidence.
• Learn the entry fields for diagnosis codes and for medications and their route of administration.
• Double check that you’re clicking the correct patient, medication, and date of service.
• To prevent data breaches, including HIPAA violations, set up different levels of employee access to EMRs and never share your password.
• Narrative notes should be customized and included, even if the records ask many yes/no questions.
• Keep consistent records. Inconsistency in record keeping is one of the fastest ways to end up in litigation, Dr. Lessin warned. Separation of staff duties in filling out different parts of the EMR, failure to review templates, and “hybrid” charts for which the paper and electronic records don’t match are among the biggest risks for inconsistencies.
• Devise a method for tracking and following up with nonresponsive specialists and with patients, checking on their compliance and unique health care needs. “If a patient with diabetes comes in three times between October and February and you don’t give them a flu shot, then when they get the flu, whose fault is that?” he said. “You need some way to track high-risk patients who need immunizations.”
• Enter notes in a timely fashion – knowing that audits will show time and date of entries – and only use addenda to modify notes.
“If you’re going to make any changes in the medical record, you need to do it as an addendum,” Dr. Lessin said. And, of course, never try to erase a record. Even accidental alterations of records that aren’t following the rules can look very bad, he said.
Dr. Lessin is a principal with Physician Integration Consultants in Atlanta.
SAN FRANCISCO – Are electronic medical records wreaking havoc for you? Herschel R. Lessin, MD, vice president of the Children’s Medical Group in Poughkeepsie, N.Y., had some EMR recommendations.
In his presentation entitled “Help! My EMR Threw Me Under the Bus!” at the annual meeting of the American Academy of Pediatrics, Dr. Lessin offered the following recommendations for troubleshooting or preventing EMR problems, starting with customizing your EMR right away to reduce alert fatigue.
• Document the specifics of a particular condition, treatment, history, or other note when checking boxes.
• Document your thinking in terms of differential diagnoses.
• Document a follow-up plan beyond just checking the box of a patient’s return date.
• Be wary of cutting and pasting too quickly or relying on the template as a standard of care instead of thoughtful application of the evidence.
• Learn the entry fields for diagnosis codes and for medications and their route of administration.
• Double check that you’re clicking the correct patient, medication, and date of service.
• To prevent data breaches, including HIPAA violations, set up different levels of employee access to EMRs and never share your password.
• Narrative notes should be customized and included, even if the records ask many yes/no questions.
• Keep consistent records. Inconsistency in record keeping is one of the fastest ways to end up in litigation, Dr. Lessin warned. Separation of staff duties in filling out different parts of the EMR, failure to review templates, and “hybrid” charts for which the paper and electronic records don’t match are among the biggest risks for inconsistencies.
• Devise a method for tracking and following up with nonresponsive specialists and with patients, checking on their compliance and unique health care needs. “If a patient with diabetes comes in three times between October and February and you don’t give them a flu shot, then when they get the flu, whose fault is that?” he said. “You need some way to track high-risk patients who need immunizations.”
• Enter notes in a timely fashion – knowing that audits will show time and date of entries – and only use addenda to modify notes.
“If you’re going to make any changes in the medical record, you need to do it as an addendum,” Dr. Lessin said. And, of course, never try to erase a record. Even accidental alterations of records that aren’t following the rules can look very bad, he said.
Dr. Lessin is a principal with Physician Integration Consultants in Atlanta.
SAN FRANCISCO – Are electronic medical records wreaking havoc for you? Herschel R. Lessin, MD, vice president of the Children’s Medical Group in Poughkeepsie, N.Y., had some EMR recommendations.
In his presentation entitled “Help! My EMR Threw Me Under the Bus!” at the annual meeting of the American Academy of Pediatrics, Dr. Lessin offered the following recommendations for troubleshooting or preventing EMR problems, starting with customizing your EMR right away to reduce alert fatigue.
• Document the specifics of a particular condition, treatment, history, or other note when checking boxes.
• Document your thinking in terms of differential diagnoses.
• Document a follow-up plan beyond just checking the box of a patient’s return date.
• Be wary of cutting and pasting too quickly or relying on the template as a standard of care instead of thoughtful application of the evidence.
• Learn the entry fields for diagnosis codes and for medications and their route of administration.
• Double check that you’re clicking the correct patient, medication, and date of service.
• To prevent data breaches, including HIPAA violations, set up different levels of employee access to EMRs and never share your password.
• Narrative notes should be customized and included, even if the records ask many yes/no questions.
• Keep consistent records. Inconsistency in record keeping is one of the fastest ways to end up in litigation, Dr. Lessin warned. Separation of staff duties in filling out different parts of the EMR, failure to review templates, and “hybrid” charts for which the paper and electronic records don’t match are among the biggest risks for inconsistencies.
• Devise a method for tracking and following up with nonresponsive specialists and with patients, checking on their compliance and unique health care needs. “If a patient with diabetes comes in three times between October and February and you don’t give them a flu shot, then when they get the flu, whose fault is that?” he said. “You need some way to track high-risk patients who need immunizations.”
• Enter notes in a timely fashion – knowing that audits will show time and date of entries – and only use addenda to modify notes.
“If you’re going to make any changes in the medical record, you need to do it as an addendum,” Dr. Lessin said. And, of course, never try to erase a record. Even accidental alterations of records that aren’t following the rules can look very bad, he said.
Dr. Lessin is a principal with Physician Integration Consultants in Atlanta.
AT AAP 16
Childhood psoriasis negatively impacts parental QOL
Parents of children with psoriasis experience significant negative quality-of-life issues, according to Dr. Megha Tollefson and her associates.
In interviews with 31 parents of children with psoriasis, four themes impacting quality of life emerged. Parental health and self-care were negatively affected, with 52% reporting affected sleep patterns and 35% reporting difficulty in maintaining self-care. Mental health issues were common as well, with 65% of parents reporting concern over their child’s condition and nearly half of parents reporting excess stress and sadness, anxiety, or depression.
Family and social functions were adversely affected as well, with parents commonly citing financial difficulty, tension with their spouse or significant other, difficulty in other relationships, a lack of awareness regarding psoriasis, and the burden of care. The final theme highlighted was the sacrifice of personal well-being and life pursuits, with 29% of parents reporting career impacts, 65% reporting a need for special accommodation for their child, and 48% reporting a feeling of having no time.
“The results of this study are a testament to the pervasiveness of childhood psoriasis in a parent’s life. Development of support strategies is recommended for children with psoriasis and their families,” Dr. Tollefson and her coauthors at the Mayo Clinic in Rochester, Minn., concluded.
Find the full study in the Journal of the American Academy of Dermatology (doi:10.1016/j.jaad.2016.09.014).
Parents of children with psoriasis experience significant negative quality-of-life issues, according to Dr. Megha Tollefson and her associates.
In interviews with 31 parents of children with psoriasis, four themes impacting quality of life emerged. Parental health and self-care were negatively affected, with 52% reporting affected sleep patterns and 35% reporting difficulty in maintaining self-care. Mental health issues were common as well, with 65% of parents reporting concern over their child’s condition and nearly half of parents reporting excess stress and sadness, anxiety, or depression.
Family and social functions were adversely affected as well, with parents commonly citing financial difficulty, tension with their spouse or significant other, difficulty in other relationships, a lack of awareness regarding psoriasis, and the burden of care. The final theme highlighted was the sacrifice of personal well-being and life pursuits, with 29% of parents reporting career impacts, 65% reporting a need for special accommodation for their child, and 48% reporting a feeling of having no time.
“The results of this study are a testament to the pervasiveness of childhood psoriasis in a parent’s life. Development of support strategies is recommended for children with psoriasis and their families,” Dr. Tollefson and her coauthors at the Mayo Clinic in Rochester, Minn., concluded.
Find the full study in the Journal of the American Academy of Dermatology (doi:10.1016/j.jaad.2016.09.014).
Parents of children with psoriasis experience significant negative quality-of-life issues, according to Dr. Megha Tollefson and her associates.
In interviews with 31 parents of children with psoriasis, four themes impacting quality of life emerged. Parental health and self-care were negatively affected, with 52% reporting affected sleep patterns and 35% reporting difficulty in maintaining self-care. Mental health issues were common as well, with 65% of parents reporting concern over their child’s condition and nearly half of parents reporting excess stress and sadness, anxiety, or depression.
Family and social functions were adversely affected as well, with parents commonly citing financial difficulty, tension with their spouse or significant other, difficulty in other relationships, a lack of awareness regarding psoriasis, and the burden of care. The final theme highlighted was the sacrifice of personal well-being and life pursuits, with 29% of parents reporting career impacts, 65% reporting a need for special accommodation for their child, and 48% reporting a feeling of having no time.
“The results of this study are a testament to the pervasiveness of childhood psoriasis in a parent’s life. Development of support strategies is recommended for children with psoriasis and their families,” Dr. Tollefson and her coauthors at the Mayo Clinic in Rochester, Minn., concluded.
Find the full study in the Journal of the American Academy of Dermatology (doi:10.1016/j.jaad.2016.09.014).
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY