User login
Imatinib is safe, effective long-term, team says
Long-term follow-up of patients treated with imatinib suggests the drug can remain effective beyond 10 years and does not confer “unacceptable” cumulative toxicity, according to researchers.
The group evaluated data on patients who had newly diagnosed, chronic-phase chronic myeloid leukemia (CML) when they began treatment with imatinib.
The median treatment duration was 8.9 years, and the estimated 10-year survival rate ranged from 64.4% to 84.4%.
The researchers said serious adverse events (AEs) thought to be related to imatinib were uncommon and typically occurred early, within the first year of treatment.
These results were reported in NEJM. The research was funded by Novartis Pharmaceuticals, which markets imatinib as Gleevec.
“The long-term success of this treatment confirms the remarkable success we’ve seen since the very first Gleevec trials,” said study author Brian Druker, MD, a physician-scientist at Oregon Health & Science University in Portland, Oregon, who led the original clinical development of Gleevec.
“This study reinforces the notion that we can create effective and non-toxic therapies.”
The study enrolled 1106 newly diagnosed, chronic-phase CML patients at 177 cancer centers in more than 16 countries. Half were assigned to treatment with imatinib (n=533) and the other half to interferon alfa plus cytarabine.
This study allowed for cross-over between the treatment arms, and 65.6% of patients in the cytarabine/interferon alfa arm ultimately crossed over to the imatinib arm.
However, when assessing the effects of imatinib, the researchers focused only on the patients who were first randomized to receive imatinib.
The median follow-up was 10.9 years (range, 0 to 11.7, which included follow-up after patients discontinued study treatment).
Of the patients randomized to imatinib, 48.3% (n=267) completed treatment with the drug. The median duration of first-line imatinib was 8.9 years (range, <0.1 to 11.7).
For patients who did not complete imatinib treatment, reasons for discontinuation included a lack of efficacy (15.9%), withdrawn consent (10.3%), AEs (6.9%), because they proceeded to transplant (3.8%), death (3.4%), protocol violation (3.1%), loss to follow-up (2.7%), cross over to the interferon arm (2.5%), administrative problems (2.2%), abnormal laboratory values (0.5%), or abnormal procedure (0.4%).
Safety
The incidence of serious AEs considered related to imatinib was 9.3% (51/551).
Drug-related serious AEs occurring in at least 2 patients included abdominal pain (n=4), anemia (n=3), congestive cardiac failure (n=3), gastrointestinal hemorrhage (n=3), vomiting (n=3), alanine aminotransferase increase (n=2), cardiac arrest (n=2), conjunctival hemorrhage (n=2), and melana (n=2).
Six patients had a second neoplasm (benign, malignant, or unspecified).
Response
The cumulative rate of complete cytogenetic response (CCR) at the end of the trial was 82.8%.
In the intent-to-treat population, the rate of CCR went from 52.8% in the first year to 22.2% at year 10.
Among evaluable patients, the rate of CCR went from 70.9% (292/412) in the first year to 91.8% (123/134) in year 10.
In the intent-to-treat population, the rate of major molecular response went from 27.7% in the first year to 34.4% at year 10.
Among evaluable patients, the rate of major molecular response went from 50.2% (153/305) in the first year to 93.1% (190/204) in year 10.
Progression and survival
The rate of progression was 6.9% (38/553) in the intent-to-treat population. Most of these patients (n=34) progressed during the first 4 years.
There were 260 patients who were still alive and receiving imatinib at 10 years and 96 patients who were alive but not receiving imatinib.
The researchers did not know the survival status of 111 patients, and there were 86 known deaths at 10 years (89 by the end of the study).
The estimated 10-year survival rate ranged from 64.4% (assuming all 111 patients with unknown status had died) to 84.4% (assuming all 111 were alive).
The cause of death was CML in 50 patients, a secondary malignant condition in 11, a cardiac disorder/cardiovascular disease in 7, infectious disease in 5, and “other” causes in 16 patients. ![]()
Long-term follow-up of patients treated with imatinib suggests the drug can remain effective beyond 10 years and does not confer “unacceptable” cumulative toxicity, according to researchers.
The group evaluated data on patients who had newly diagnosed, chronic-phase chronic myeloid leukemia (CML) when they began treatment with imatinib.
The median treatment duration was 8.9 years, and the estimated 10-year survival rate ranged from 64.4% to 84.4%.
The researchers said serious adverse events (AEs) thought to be related to imatinib were uncommon and typically occurred early, within the first year of treatment.
These results were reported in NEJM. The research was funded by Novartis Pharmaceuticals, which markets imatinib as Gleevec.
“The long-term success of this treatment confirms the remarkable success we’ve seen since the very first Gleevec trials,” said study author Brian Druker, MD, a physician-scientist at Oregon Health & Science University in Portland, Oregon, who led the original clinical development of Gleevec.
“This study reinforces the notion that we can create effective and non-toxic therapies.”
The study enrolled 1106 newly diagnosed, chronic-phase CML patients at 177 cancer centers in more than 16 countries. Half were assigned to treatment with imatinib (n=533) and the other half to interferon alfa plus cytarabine.
This study allowed for cross-over between the treatment arms, and 65.6% of patients in the cytarabine/interferon alfa arm ultimately crossed over to the imatinib arm.
However, when assessing the effects of imatinib, the researchers focused only on the patients who were first randomized to receive imatinib.
The median follow-up was 10.9 years (range, 0 to 11.7, which included follow-up after patients discontinued study treatment).
Of the patients randomized to imatinib, 48.3% (n=267) completed treatment with the drug. The median duration of first-line imatinib was 8.9 years (range, <0.1 to 11.7).
For patients who did not complete imatinib treatment, reasons for discontinuation included a lack of efficacy (15.9%), withdrawn consent (10.3%), AEs (6.9%), because they proceeded to transplant (3.8%), death (3.4%), protocol violation (3.1%), loss to follow-up (2.7%), cross over to the interferon arm (2.5%), administrative problems (2.2%), abnormal laboratory values (0.5%), or abnormal procedure (0.4%).
Safety
The incidence of serious AEs considered related to imatinib was 9.3% (51/551).
Drug-related serious AEs occurring in at least 2 patients included abdominal pain (n=4), anemia (n=3), congestive cardiac failure (n=3), gastrointestinal hemorrhage (n=3), vomiting (n=3), alanine aminotransferase increase (n=2), cardiac arrest (n=2), conjunctival hemorrhage (n=2), and melana (n=2).
Six patients had a second neoplasm (benign, malignant, or unspecified).
Response
The cumulative rate of complete cytogenetic response (CCR) at the end of the trial was 82.8%.
In the intent-to-treat population, the rate of CCR went from 52.8% in the first year to 22.2% at year 10.
Among evaluable patients, the rate of CCR went from 70.9% (292/412) in the first year to 91.8% (123/134) in year 10.
In the intent-to-treat population, the rate of major molecular response went from 27.7% in the first year to 34.4% at year 10.
Among evaluable patients, the rate of major molecular response went from 50.2% (153/305) in the first year to 93.1% (190/204) in year 10.
Progression and survival
The rate of progression was 6.9% (38/553) in the intent-to-treat population. Most of these patients (n=34) progressed during the first 4 years.
There were 260 patients who were still alive and receiving imatinib at 10 years and 96 patients who were alive but not receiving imatinib.
The researchers did not know the survival status of 111 patients, and there were 86 known deaths at 10 years (89 by the end of the study).
The estimated 10-year survival rate ranged from 64.4% (assuming all 111 patients with unknown status had died) to 84.4% (assuming all 111 were alive).
The cause of death was CML in 50 patients, a secondary malignant condition in 11, a cardiac disorder/cardiovascular disease in 7, infectious disease in 5, and “other” causes in 16 patients. ![]()
Long-term follow-up of patients treated with imatinib suggests the drug can remain effective beyond 10 years and does not confer “unacceptable” cumulative toxicity, according to researchers.
The group evaluated data on patients who had newly diagnosed, chronic-phase chronic myeloid leukemia (CML) when they began treatment with imatinib.
The median treatment duration was 8.9 years, and the estimated 10-year survival rate ranged from 64.4% to 84.4%.
The researchers said serious adverse events (AEs) thought to be related to imatinib were uncommon and typically occurred early, within the first year of treatment.
These results were reported in NEJM. The research was funded by Novartis Pharmaceuticals, which markets imatinib as Gleevec.
“The long-term success of this treatment confirms the remarkable success we’ve seen since the very first Gleevec trials,” said study author Brian Druker, MD, a physician-scientist at Oregon Health & Science University in Portland, Oregon, who led the original clinical development of Gleevec.
“This study reinforces the notion that we can create effective and non-toxic therapies.”
The study enrolled 1106 newly diagnosed, chronic-phase CML patients at 177 cancer centers in more than 16 countries. Half were assigned to treatment with imatinib (n=533) and the other half to interferon alfa plus cytarabine.
This study allowed for cross-over between the treatment arms, and 65.6% of patients in the cytarabine/interferon alfa arm ultimately crossed over to the imatinib arm.
However, when assessing the effects of imatinib, the researchers focused only on the patients who were first randomized to receive imatinib.
The median follow-up was 10.9 years (range, 0 to 11.7, which included follow-up after patients discontinued study treatment).
Of the patients randomized to imatinib, 48.3% (n=267) completed treatment with the drug. The median duration of first-line imatinib was 8.9 years (range, <0.1 to 11.7).
For patients who did not complete imatinib treatment, reasons for discontinuation included a lack of efficacy (15.9%), withdrawn consent (10.3%), AEs (6.9%), because they proceeded to transplant (3.8%), death (3.4%), protocol violation (3.1%), loss to follow-up (2.7%), cross over to the interferon arm (2.5%), administrative problems (2.2%), abnormal laboratory values (0.5%), or abnormal procedure (0.4%).
Safety
The incidence of serious AEs considered related to imatinib was 9.3% (51/551).
Drug-related serious AEs occurring in at least 2 patients included abdominal pain (n=4), anemia (n=3), congestive cardiac failure (n=3), gastrointestinal hemorrhage (n=3), vomiting (n=3), alanine aminotransferase increase (n=2), cardiac arrest (n=2), conjunctival hemorrhage (n=2), and melana (n=2).
Six patients had a second neoplasm (benign, malignant, or unspecified).
Response
The cumulative rate of complete cytogenetic response (CCR) at the end of the trial was 82.8%.
In the intent-to-treat population, the rate of CCR went from 52.8% in the first year to 22.2% at year 10.
Among evaluable patients, the rate of CCR went from 70.9% (292/412) in the first year to 91.8% (123/134) in year 10.
In the intent-to-treat population, the rate of major molecular response went from 27.7% in the first year to 34.4% at year 10.
Among evaluable patients, the rate of major molecular response went from 50.2% (153/305) in the first year to 93.1% (190/204) in year 10.
Progression and survival
The rate of progression was 6.9% (38/553) in the intent-to-treat population. Most of these patients (n=34) progressed during the first 4 years.
There were 260 patients who were still alive and receiving imatinib at 10 years and 96 patients who were alive but not receiving imatinib.
The researchers did not know the survival status of 111 patients, and there were 86 known deaths at 10 years (89 by the end of the study).
The estimated 10-year survival rate ranged from 64.4% (assuming all 111 patients with unknown status had died) to 84.4% (assuming all 111 were alive).
The cause of death was CML in 50 patients, a secondary malignant condition in 11, a cardiac disorder/cardiovascular disease in 7, infectious disease in 5, and “other” causes in 16 patients. ![]()
Drug exhibits anti-myeloma activity in mice, humans
An experimental drug called LCL161 stimulates the immune system to fight multiple myeloma (MM), according to research published in Nature Medicine.
Investigators said LCL161 exhibited “robust” activity in a transgenic myeloma mouse model and in patients with relapsed/refractory MM.
Single-agent LCL161 did not produce responses in MM patients, but patients did respond to treatment with LCL161 and cyclophosphamide.
The investigators also found that single-agent LCL161 provided “long-term anti-tumor protection” in mice, and combining LCL161 with an antibody against PD-1 could cure mice of MM.
“The drug, LCL161, was initially developed to promote tumor death,” said study author Marta Chesi, PhD, of Mayo Clinic Arizona in Scottsdale.
“However, we found that the drug does not kill tumor cells directly. Rather, it makes them more visible to the immune system that recognizes them as foreign invaders and eliminates them.”
Dr Chesi and her colleagues explained that the cellular inhibitors of apoptosis (cIAP) 1 and 2 have been identified as potential therapeutic targets in some cancers.
And LCL161 is a small-molecule IAP antagonist that induces tumor necrosis factor-mediated apoptosis in cancer cells. However, the investigators found that LCL161 was not directly cytotoxic to MM cells.
Instead, the drug upregulated tumor-cell-autonomous type I interferon signaling and induced an acute inflammatory response. This led to the activation of macrophages and dendritic cells, which prompted phagocytosis in MM cells.
Results in mice
The investigators first tested LCL161 alone (at a dose previously shown to be well-tolerated) in Vk*MYC transgenic mice with established MM.
The team said they observed a reduction in tumor burden that was comparable to that observed in response to drugs currently used to treat MM—carfilzomib, bortezomib, melphalan, cyclophosphamide, panobinostat, dexamethasone, and pomalidomide.
The investigators then tested the combination of LCL161 and a PD1 antibody in Vk12598-tumor-bearing mice.
The team said the combination was curative in all mice that completed 2 weeks of treatment. In fact, it was more effective than combination treatment with LCL161 and cyclophosphamide.
Results in patients
Dr Chesi and her colleagues conducted a phase 2 trial of LCL161 in 25 patients with relapsed/refractory MM. Patients could receive cyclophosphamide if they failed to respond or progressed after 8 weeks of treatment with LCL161 alone.
The patients’ median age was 68 (range, 47-90), and they had a median of 3 prior therapies (range, 1-6). Forty-four percent of patients had high-risk features, 28% had relapsed disease, and 72% had relapsed and refractory disease.
Four patients experienced grade 2 cytokine release syndrome when they received LCL161 at a dose of 1800 mg weekly, so the dose was lowered to 1200 mg.
None of the patients responded to single-agent LCL161. So 23 of the patients received 500 mg of weekly cyclophosphamide as well.
There was 1 complete response to the combination therapy, 1 very good partial response, 2 partial responses, and 1 minimal response. The median progression-free survival in these patients was 10 months.
Grade 3 adverse events included decrease in neutrophil count (28%), decrease in lymphocyte count (28%), anemia (24%), fatigue (16%), hyperglycemia (12%), syncope (12%), decrease in white blood cell count (12%), decrease in platelet count (8%), increase in lymphocyte count (8%), nausea (4%), vomiting (4%), diarrhea (4%), maculo-papular rash (4%), hypotension (4%), lung infection (4%), pain in extremity (4%), and urticaria (4%).
Grade 4 events included decrease in lymphocyte count (24%), decrease in neutrophil count (8%), decrease in white blood cell count (8%), hyperuricemia (4%), decrease in platelet count (4%), and sepsis (4%).
Based on these results, the investigators said the combination of LCL161 and cyclophosphamide is “an attractive platform for future trials,” and the same is true for LCL161 in combination with anti-PD1 therapy.
The phase 2 trial was sponsored by Mayo Clinic and the National Cancer Institute. Novartis provided LCL161 for this research and supported the trial. ![]()
An experimental drug called LCL161 stimulates the immune system to fight multiple myeloma (MM), according to research published in Nature Medicine.
Investigators said LCL161 exhibited “robust” activity in a transgenic myeloma mouse model and in patients with relapsed/refractory MM.
Single-agent LCL161 did not produce responses in MM patients, but patients did respond to treatment with LCL161 and cyclophosphamide.
The investigators also found that single-agent LCL161 provided “long-term anti-tumor protection” in mice, and combining LCL161 with an antibody against PD-1 could cure mice of MM.
“The drug, LCL161, was initially developed to promote tumor death,” said study author Marta Chesi, PhD, of Mayo Clinic Arizona in Scottsdale.
“However, we found that the drug does not kill tumor cells directly. Rather, it makes them more visible to the immune system that recognizes them as foreign invaders and eliminates them.”
Dr Chesi and her colleagues explained that the cellular inhibitors of apoptosis (cIAP) 1 and 2 have been identified as potential therapeutic targets in some cancers.
And LCL161 is a small-molecule IAP antagonist that induces tumor necrosis factor-mediated apoptosis in cancer cells. However, the investigators found that LCL161 was not directly cytotoxic to MM cells.
Instead, the drug upregulated tumor-cell-autonomous type I interferon signaling and induced an acute inflammatory response. This led to the activation of macrophages and dendritic cells, which prompted phagocytosis in MM cells.
Results in mice
The investigators first tested LCL161 alone (at a dose previously shown to be well-tolerated) in Vk*MYC transgenic mice with established MM.
The team said they observed a reduction in tumor burden that was comparable to that observed in response to drugs currently used to treat MM—carfilzomib, bortezomib, melphalan, cyclophosphamide, panobinostat, dexamethasone, and pomalidomide.
The investigators then tested the combination of LCL161 and a PD1 antibody in Vk12598-tumor-bearing mice.
The team said the combination was curative in all mice that completed 2 weeks of treatment. In fact, it was more effective than combination treatment with LCL161 and cyclophosphamide.
Results in patients
Dr Chesi and her colleagues conducted a phase 2 trial of LCL161 in 25 patients with relapsed/refractory MM. Patients could receive cyclophosphamide if they failed to respond or progressed after 8 weeks of treatment with LCL161 alone.
The patients’ median age was 68 (range, 47-90), and they had a median of 3 prior therapies (range, 1-6). Forty-four percent of patients had high-risk features, 28% had relapsed disease, and 72% had relapsed and refractory disease.
Four patients experienced grade 2 cytokine release syndrome when they received LCL161 at a dose of 1800 mg weekly, so the dose was lowered to 1200 mg.
None of the patients responded to single-agent LCL161. So 23 of the patients received 500 mg of weekly cyclophosphamide as well.
There was 1 complete response to the combination therapy, 1 very good partial response, 2 partial responses, and 1 minimal response. The median progression-free survival in these patients was 10 months.
Grade 3 adverse events included decrease in neutrophil count (28%), decrease in lymphocyte count (28%), anemia (24%), fatigue (16%), hyperglycemia (12%), syncope (12%), decrease in white blood cell count (12%), decrease in platelet count (8%), increase in lymphocyte count (8%), nausea (4%), vomiting (4%), diarrhea (4%), maculo-papular rash (4%), hypotension (4%), lung infection (4%), pain in extremity (4%), and urticaria (4%).
Grade 4 events included decrease in lymphocyte count (24%), decrease in neutrophil count (8%), decrease in white blood cell count (8%), hyperuricemia (4%), decrease in platelet count (4%), and sepsis (4%).
Based on these results, the investigators said the combination of LCL161 and cyclophosphamide is “an attractive platform for future trials,” and the same is true for LCL161 in combination with anti-PD1 therapy.
The phase 2 trial was sponsored by Mayo Clinic and the National Cancer Institute. Novartis provided LCL161 for this research and supported the trial. ![]()
An experimental drug called LCL161 stimulates the immune system to fight multiple myeloma (MM), according to research published in Nature Medicine.
Investigators said LCL161 exhibited “robust” activity in a transgenic myeloma mouse model and in patients with relapsed/refractory MM.
Single-agent LCL161 did not produce responses in MM patients, but patients did respond to treatment with LCL161 and cyclophosphamide.
The investigators also found that single-agent LCL161 provided “long-term anti-tumor protection” in mice, and combining LCL161 with an antibody against PD-1 could cure mice of MM.
“The drug, LCL161, was initially developed to promote tumor death,” said study author Marta Chesi, PhD, of Mayo Clinic Arizona in Scottsdale.
“However, we found that the drug does not kill tumor cells directly. Rather, it makes them more visible to the immune system that recognizes them as foreign invaders and eliminates them.”
Dr Chesi and her colleagues explained that the cellular inhibitors of apoptosis (cIAP) 1 and 2 have been identified as potential therapeutic targets in some cancers.
And LCL161 is a small-molecule IAP antagonist that induces tumor necrosis factor-mediated apoptosis in cancer cells. However, the investigators found that LCL161 was not directly cytotoxic to MM cells.
Instead, the drug upregulated tumor-cell-autonomous type I interferon signaling and induced an acute inflammatory response. This led to the activation of macrophages and dendritic cells, which prompted phagocytosis in MM cells.
Results in mice
The investigators first tested LCL161 alone (at a dose previously shown to be well-tolerated) in Vk*MYC transgenic mice with established MM.
The team said they observed a reduction in tumor burden that was comparable to that observed in response to drugs currently used to treat MM—carfilzomib, bortezomib, melphalan, cyclophosphamide, panobinostat, dexamethasone, and pomalidomide.
The investigators then tested the combination of LCL161 and a PD1 antibody in Vk12598-tumor-bearing mice.
The team said the combination was curative in all mice that completed 2 weeks of treatment. In fact, it was more effective than combination treatment with LCL161 and cyclophosphamide.
Results in patients
Dr Chesi and her colleagues conducted a phase 2 trial of LCL161 in 25 patients with relapsed/refractory MM. Patients could receive cyclophosphamide if they failed to respond or progressed after 8 weeks of treatment with LCL161 alone.
The patients’ median age was 68 (range, 47-90), and they had a median of 3 prior therapies (range, 1-6). Forty-four percent of patients had high-risk features, 28% had relapsed disease, and 72% had relapsed and refractory disease.
Four patients experienced grade 2 cytokine release syndrome when they received LCL161 at a dose of 1800 mg weekly, so the dose was lowered to 1200 mg.
None of the patients responded to single-agent LCL161. So 23 of the patients received 500 mg of weekly cyclophosphamide as well.
There was 1 complete response to the combination therapy, 1 very good partial response, 2 partial responses, and 1 minimal response. The median progression-free survival in these patients was 10 months.
Grade 3 adverse events included decrease in neutrophil count (28%), decrease in lymphocyte count (28%), anemia (24%), fatigue (16%), hyperglycemia (12%), syncope (12%), decrease in white blood cell count (12%), decrease in platelet count (8%), increase in lymphocyte count (8%), nausea (4%), vomiting (4%), diarrhea (4%), maculo-papular rash (4%), hypotension (4%), lung infection (4%), pain in extremity (4%), and urticaria (4%).
Grade 4 events included decrease in lymphocyte count (24%), decrease in neutrophil count (8%), decrease in white blood cell count (8%), hyperuricemia (4%), decrease in platelet count (4%), and sepsis (4%).
Based on these results, the investigators said the combination of LCL161 and cyclophosphamide is “an attractive platform for future trials,” and the same is true for LCL161 in combination with anti-PD1 therapy.
The phase 2 trial was sponsored by Mayo Clinic and the National Cancer Institute. Novartis provided LCL161 for this research and supported the trial. ![]()
Transfusion practice may harm certain patients
A retrospective study indicates that a high transfusion ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) may not be beneficial for surgical patients who do not have traumatic injuries.
In fact, the data suggest a high FFP:RBC ratio may be harmful for some of these patients.
“The strategy of giving patients requiring massive transfusion greater amounts of fresh frozen plasma, relative to the amount of red blood cells, has spilled over from trauma patients into unstudied patient populations,” said Daniel Dante Yeh, MD, of Massachusetts General Hospital in Boston.
“This may have important consequences, since our results suggest that certain populations may be harmed by this practice.”
Dr Yeh and his colleagues reported these results in JAMA Surgery.
The researchers reviewed all massive transfusions performed at Massachusetts General Hospital from January 1, 2009, through December 31, 2012.
A transfusion qualified as “massive” if at least 10 units of RBCs were given in the first 24 hours after a patient’s admission to the operating room, emergency department, or intensive care unit.
The researchers included all patients who received massive transfusions during the study period and survived more than 30 minutes after hospital arrival.
According to these criteria, there were 865 massive transfusion events. The total number of units transfused was 16,569 for RBCs, 13,933 for FFP, 5228 for cryoprecipitate, and 22,635 for platelets.
A majority of the massive transfusion recipients were not trauma patients (88.7%). Most of the transfusions were performed for intraoperative bleeding (62.9%).
The researchers compared patients who survived at least 30 days from hospital arrival to those who did not. Patients who died were older and received more RBCs (P<0.001), FFP (P<0.001), and cryoprecipitate (P=0.008).
However, the FFP:RBC ratios of survivors and non-survivors were similar. The median was 1:1.5 for survivors and 1:1.4 for non-survivors (P=0.43).
Patients without trauma
Among all non-trauma patients (n=767), there was no significant difference in the adjusted odds ratio (aOR) for 30-day mortality between patients who received a transfusion with a high FFP:RBC ratio and those who received one with a low FFP:RBC ratio (aOR=1.10, P=0.65). (The analysis was adjusted for patient age and total units of RBCs transfused.)
Among patients undergoing vascular surgery, those who received transfusions with a high FFP:RBC ratio were less likely to die within 30 days than those who received transfusions with a low FFP:RBC ratio (aOR=0.16, P=0.02).
However, among general surgery and medical service patients, those receiving transfusions with a high FFP:RBC ratio were more likely to die within 30 days than those receiving low-ratio transfusions. The aOR was 4.27 (P=0.02) for general surgery and 8.48 (P=0.02) for medicine.
“Finding evidence of increased mortality in some patients was surprising because that is directly contradictory to what is expected and intended,” Dr Yeh said. “Avoiding unnecessary FFP transfusion is important because there have been reports that associated the use of excess FFP with worse outcomes among patients that required less-than-massive transfusions.”
“Because our study is retrospective, it can only point to the need for further research. Ratio-based transfusion has been studied in trauma patients, most recently in a landmark, multicenter, randomized study called the PROPRR trial. Similar studies now need to be performed in non-trauma patients before the approach can be accepted as standard practice here at MGH [Massachusetts General Hospital] and elsewhere.” ![]()
A retrospective study indicates that a high transfusion ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) may not be beneficial for surgical patients who do not have traumatic injuries.
In fact, the data suggest a high FFP:RBC ratio may be harmful for some of these patients.
“The strategy of giving patients requiring massive transfusion greater amounts of fresh frozen plasma, relative to the amount of red blood cells, has spilled over from trauma patients into unstudied patient populations,” said Daniel Dante Yeh, MD, of Massachusetts General Hospital in Boston.
“This may have important consequences, since our results suggest that certain populations may be harmed by this practice.”
Dr Yeh and his colleagues reported these results in JAMA Surgery.
The researchers reviewed all massive transfusions performed at Massachusetts General Hospital from January 1, 2009, through December 31, 2012.
A transfusion qualified as “massive” if at least 10 units of RBCs were given in the first 24 hours after a patient’s admission to the operating room, emergency department, or intensive care unit.
The researchers included all patients who received massive transfusions during the study period and survived more than 30 minutes after hospital arrival.
According to these criteria, there were 865 massive transfusion events. The total number of units transfused was 16,569 for RBCs, 13,933 for FFP, 5228 for cryoprecipitate, and 22,635 for platelets.
A majority of the massive transfusion recipients were not trauma patients (88.7%). Most of the transfusions were performed for intraoperative bleeding (62.9%).
The researchers compared patients who survived at least 30 days from hospital arrival to those who did not. Patients who died were older and received more RBCs (P<0.001), FFP (P<0.001), and cryoprecipitate (P=0.008).
However, the FFP:RBC ratios of survivors and non-survivors were similar. The median was 1:1.5 for survivors and 1:1.4 for non-survivors (P=0.43).
Patients without trauma
Among all non-trauma patients (n=767), there was no significant difference in the adjusted odds ratio (aOR) for 30-day mortality between patients who received a transfusion with a high FFP:RBC ratio and those who received one with a low FFP:RBC ratio (aOR=1.10, P=0.65). (The analysis was adjusted for patient age and total units of RBCs transfused.)
Among patients undergoing vascular surgery, those who received transfusions with a high FFP:RBC ratio were less likely to die within 30 days than those who received transfusions with a low FFP:RBC ratio (aOR=0.16, P=0.02).
However, among general surgery and medical service patients, those receiving transfusions with a high FFP:RBC ratio were more likely to die within 30 days than those receiving low-ratio transfusions. The aOR was 4.27 (P=0.02) for general surgery and 8.48 (P=0.02) for medicine.
“Finding evidence of increased mortality in some patients was surprising because that is directly contradictory to what is expected and intended,” Dr Yeh said. “Avoiding unnecessary FFP transfusion is important because there have been reports that associated the use of excess FFP with worse outcomes among patients that required less-than-massive transfusions.”
“Because our study is retrospective, it can only point to the need for further research. Ratio-based transfusion has been studied in trauma patients, most recently in a landmark, multicenter, randomized study called the PROPRR trial. Similar studies now need to be performed in non-trauma patients before the approach can be accepted as standard practice here at MGH [Massachusetts General Hospital] and elsewhere.” ![]()
A retrospective study indicates that a high transfusion ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) may not be beneficial for surgical patients who do not have traumatic injuries.
In fact, the data suggest a high FFP:RBC ratio may be harmful for some of these patients.
“The strategy of giving patients requiring massive transfusion greater amounts of fresh frozen plasma, relative to the amount of red blood cells, has spilled over from trauma patients into unstudied patient populations,” said Daniel Dante Yeh, MD, of Massachusetts General Hospital in Boston.
“This may have important consequences, since our results suggest that certain populations may be harmed by this practice.”
Dr Yeh and his colleagues reported these results in JAMA Surgery.
The researchers reviewed all massive transfusions performed at Massachusetts General Hospital from January 1, 2009, through December 31, 2012.
A transfusion qualified as “massive” if at least 10 units of RBCs were given in the first 24 hours after a patient’s admission to the operating room, emergency department, or intensive care unit.
The researchers included all patients who received massive transfusions during the study period and survived more than 30 minutes after hospital arrival.
According to these criteria, there were 865 massive transfusion events. The total number of units transfused was 16,569 for RBCs, 13,933 for FFP, 5228 for cryoprecipitate, and 22,635 for platelets.
A majority of the massive transfusion recipients were not trauma patients (88.7%). Most of the transfusions were performed for intraoperative bleeding (62.9%).
The researchers compared patients who survived at least 30 days from hospital arrival to those who did not. Patients who died were older and received more RBCs (P<0.001), FFP (P<0.001), and cryoprecipitate (P=0.008).
However, the FFP:RBC ratios of survivors and non-survivors were similar. The median was 1:1.5 for survivors and 1:1.4 for non-survivors (P=0.43).
Patients without trauma
Among all non-trauma patients (n=767), there was no significant difference in the adjusted odds ratio (aOR) for 30-day mortality between patients who received a transfusion with a high FFP:RBC ratio and those who received one with a low FFP:RBC ratio (aOR=1.10, P=0.65). (The analysis was adjusted for patient age and total units of RBCs transfused.)
Among patients undergoing vascular surgery, those who received transfusions with a high FFP:RBC ratio were less likely to die within 30 days than those who received transfusions with a low FFP:RBC ratio (aOR=0.16, P=0.02).
However, among general surgery and medical service patients, those receiving transfusions with a high FFP:RBC ratio were more likely to die within 30 days than those receiving low-ratio transfusions. The aOR was 4.27 (P=0.02) for general surgery and 8.48 (P=0.02) for medicine.
“Finding evidence of increased mortality in some patients was surprising because that is directly contradictory to what is expected and intended,” Dr Yeh said. “Avoiding unnecessary FFP transfusion is important because there have been reports that associated the use of excess FFP with worse outcomes among patients that required less-than-massive transfusions.”
“Because our study is retrospective, it can only point to the need for further research. Ratio-based transfusion has been studied in trauma patients, most recently in a landmark, multicenter, randomized study called the PROPRR trial. Similar studies now need to be performed in non-trauma patients before the approach can be accepted as standard practice here at MGH [Massachusetts General Hospital] and elsewhere.” ![]()
FDA lifts clinical hold on AML trials
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
Trump travel policy may affect medical meetings
President Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and could impede assemblies of the world’s top medical experts.
The March 6 executive order bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from those countries from entering the United States for 120 days. The measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban. The new order exempts citizens of the six countries who are legal permanent U.S. residents or who have current visas.
The policy could have detrimental effects on future collaboration between U.S. and international scientists and may ultimately endanger the health and well-being of patients, said International Antiviral Society–U.S.A. executive director and president Donna M. Jacobsen, regarding the original travel ban.
There is “serious reason for concern” that the policy will dissuade scientists and researchers “from traveling to the [United States] in the future overall and sharing their work with colleagues here,” she said.
Thousands of academics from around the world, including physicians, researchers, and professors, have vowed to boycott U.S.-based conferences in light of the Trump administration policy. A Google Docs petition started shortly after the original ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said. A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9. The circuit judges said the plaintiffs were likely to succeed in their arguments and that the president had demonstrated no evidence that his executive order advances national security.
The new executive order excludes Iraq and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
February 7, 2017
The Honorable John F. Kelly
Secretary
U.S. Department of Homeland Security
Washington, DC 20528
Dear Secretary Kelly:
The undersigned organizations are greatly concerned that the executive order signed by President Trump on January 27, 2017 will result in discrimination against foreign-born persons from certain predominantly Muslim countries. We are particularly concerned that by restricting entry of physicians and medical students from seven designated Muslim majority countries, the order will undermine medical education and result in patients losing access to their doctors. We are also greatly concerned that the 120 day ban on accepting refugees, and the indefinite ban on Syrian refugees, will contribute to an ongoing public health crisis for those affected, needlessly subjecting them to violence, injury, illness, deprivation and even death. While we are pleased that the courts have temporarily halted implementation of the executive order, the underlying issues of concern about the harm caused by the executive order remain.
The restrictions in the executive order will hinder the free exchange of information and travel among medical students, residents and physicians around the world and result in Americans having poorer access to care. In 2016, 3,769 non-U.S. citizen international medical graduates (IMGs) obtained first-year residency positions. More than half of internal medicine residency positions were filled by IMGs. Approximately 25% of the nation’s physicians are IMGs and provide a disproportionate share of the care to Americans in underserved communities that have a shortage of U.S. born and trained physicians. They also add necessary diversity and cultural competency to our healthcare workforce. If the executive order prevents IMGs from being able to come to the U.S. this could potentially affect the care for thousands of patients.
Our organizations are also especially concerned about refugees with dire medical conditions who had been approved for visas to enter the U.S. but since the executive order, have been unable to enter the country to receive much needed medical care.
While we urge that the executive order be rescinded and replaced with non-discriminatory policies that support families, public health, and medical education, and are pleased that the courts have temporarily halted implementation, there are steps that DHS can take immediately to selectively ease travel restrictions that impact medical education, access to health care services, and public health for individuals who otherwise meet the criteria for immigration, including those from the seven countries identified in the executive order. Specifically, we urge the Department of Homeland Security to:
1. Reinstate the Visa Interview Waiver Program. Suspension of the program “risks creating substantial backlogs in the processing of new and renewal visas for trainees from any foreign
country — delays that create substantial problems for residency programs with trainees on visas and that could interfere with the residency match process this year.”
2. Remove restrictions on entering the U.S. for physicians from the seven designated countries who have been approved for J-1 or H-1B visas and students from those countries with F-1 visas who have been accepted to U.S. medical schools.
3. Develop and implement a plan to allow physicians from the seven designated countries to obtain travel visas to travel to the U.S. for medical conferences and other medical and research-related engagements.
4. Make it a priority to implement a process to admit refugees, without further delay, who had already been vetted and approved for entry prior to the executive order and who are in need of urgent medical care. We note that even with such revisions, the executive order will still inappropriately bar immigrants and refugees based on discriminatory criteria (religion and country of origin) including family members of physicians and medical students in the U.S.
Our organizations are committed to non-discrimination against physicians, medical students and others in immigration policies and offer our assistance in developing policies that support access to health care services, public health, and medical education while balancing the nation’s security needs. Until or unless the executive order is completely rescinded or permanently blocked, it is essential that DHS move forward to ensure that restrictions on physicians and medical students are not reimposed, and that priority is given to refugees with medical conditions needing treatment.
Sincerely,
Alliance for Academic Internal Medicine
American College of Chest Physicians
American College of Physicians
American Society for Gastrointestinal Endoscopy
American Society of Hematology
American Society of Nephrology
American Thoracic Society
Infectious Diseases Society of America
Renal Physicians Association
Society for Adolescent Health and Medicine
Society of Critical Care Medicine
Society of General Internal Medicine
February 7, 2017
The Honorable John F. Kelly
Secretary
U.S. Department of Homeland Security
Washington, DC 20528
Dear Secretary Kelly:
The undersigned organizations are greatly concerned that the executive order signed by President Trump on January 27, 2017 will result in discrimination against foreign-born persons from certain predominantly Muslim countries. We are particularly concerned that by restricting entry of physicians and medical students from seven designated Muslim majority countries, the order will undermine medical education and result in patients losing access to their doctors. We are also greatly concerned that the 120 day ban on accepting refugees, and the indefinite ban on Syrian refugees, will contribute to an ongoing public health crisis for those affected, needlessly subjecting them to violence, injury, illness, deprivation and even death. While we are pleased that the courts have temporarily halted implementation of the executive order, the underlying issues of concern about the harm caused by the executive order remain.
The restrictions in the executive order will hinder the free exchange of information and travel among medical students, residents and physicians around the world and result in Americans having poorer access to care. In 2016, 3,769 non-U.S. citizen international medical graduates (IMGs) obtained first-year residency positions. More than half of internal medicine residency positions were filled by IMGs. Approximately 25% of the nation’s physicians are IMGs and provide a disproportionate share of the care to Americans in underserved communities that have a shortage of U.S. born and trained physicians. They also add necessary diversity and cultural competency to our healthcare workforce. If the executive order prevents IMGs from being able to come to the U.S. this could potentially affect the care for thousands of patients.
Our organizations are also especially concerned about refugees with dire medical conditions who had been approved for visas to enter the U.S. but since the executive order, have been unable to enter the country to receive much needed medical care.
While we urge that the executive order be rescinded and replaced with non-discriminatory policies that support families, public health, and medical education, and are pleased that the courts have temporarily halted implementation, there are steps that DHS can take immediately to selectively ease travel restrictions that impact medical education, access to health care services, and public health for individuals who otherwise meet the criteria for immigration, including those from the seven countries identified in the executive order. Specifically, we urge the Department of Homeland Security to:
1. Reinstate the Visa Interview Waiver Program. Suspension of the program “risks creating substantial backlogs in the processing of new and renewal visas for trainees from any foreign
country — delays that create substantial problems for residency programs with trainees on visas and that could interfere with the residency match process this year.”
2. Remove restrictions on entering the U.S. for physicians from the seven designated countries who have been approved for J-1 or H-1B visas and students from those countries with F-1 visas who have been accepted to U.S. medical schools.
3. Develop and implement a plan to allow physicians from the seven designated countries to obtain travel visas to travel to the U.S. for medical conferences and other medical and research-related engagements.
4. Make it a priority to implement a process to admit refugees, without further delay, who had already been vetted and approved for entry prior to the executive order and who are in need of urgent medical care. We note that even with such revisions, the executive order will still inappropriately bar immigrants and refugees based on discriminatory criteria (religion and country of origin) including family members of physicians and medical students in the U.S.
Our organizations are committed to non-discrimination against physicians, medical students and others in immigration policies and offer our assistance in developing policies that support access to health care services, public health, and medical education while balancing the nation’s security needs. Until or unless the executive order is completely rescinded or permanently blocked, it is essential that DHS move forward to ensure that restrictions on physicians and medical students are not reimposed, and that priority is given to refugees with medical conditions needing treatment.
Sincerely,
Alliance for Academic Internal Medicine
American College of Chest Physicians
American College of Physicians
American Society for Gastrointestinal Endoscopy
American Society of Hematology
American Society of Nephrology
American Thoracic Society
Infectious Diseases Society of America
Renal Physicians Association
Society for Adolescent Health and Medicine
Society of Critical Care Medicine
Society of General Internal Medicine
February 7, 2017
The Honorable John F. Kelly
Secretary
U.S. Department of Homeland Security
Washington, DC 20528
Dear Secretary Kelly:
The undersigned organizations are greatly concerned that the executive order signed by President Trump on January 27, 2017 will result in discrimination against foreign-born persons from certain predominantly Muslim countries. We are particularly concerned that by restricting entry of physicians and medical students from seven designated Muslim majority countries, the order will undermine medical education and result in patients losing access to their doctors. We are also greatly concerned that the 120 day ban on accepting refugees, and the indefinite ban on Syrian refugees, will contribute to an ongoing public health crisis for those affected, needlessly subjecting them to violence, injury, illness, deprivation and even death. While we are pleased that the courts have temporarily halted implementation of the executive order, the underlying issues of concern about the harm caused by the executive order remain.
The restrictions in the executive order will hinder the free exchange of information and travel among medical students, residents and physicians around the world and result in Americans having poorer access to care. In 2016, 3,769 non-U.S. citizen international medical graduates (IMGs) obtained first-year residency positions. More than half of internal medicine residency positions were filled by IMGs. Approximately 25% of the nation’s physicians are IMGs and provide a disproportionate share of the care to Americans in underserved communities that have a shortage of U.S. born and trained physicians. They also add necessary diversity and cultural competency to our healthcare workforce. If the executive order prevents IMGs from being able to come to the U.S. this could potentially affect the care for thousands of patients.
Our organizations are also especially concerned about refugees with dire medical conditions who had been approved for visas to enter the U.S. but since the executive order, have been unable to enter the country to receive much needed medical care.
While we urge that the executive order be rescinded and replaced with non-discriminatory policies that support families, public health, and medical education, and are pleased that the courts have temporarily halted implementation, there are steps that DHS can take immediately to selectively ease travel restrictions that impact medical education, access to health care services, and public health for individuals who otherwise meet the criteria for immigration, including those from the seven countries identified in the executive order. Specifically, we urge the Department of Homeland Security to:
1. Reinstate the Visa Interview Waiver Program. Suspension of the program “risks creating substantial backlogs in the processing of new and renewal visas for trainees from any foreign
country — delays that create substantial problems for residency programs with trainees on visas and that could interfere with the residency match process this year.”
2. Remove restrictions on entering the U.S. for physicians from the seven designated countries who have been approved for J-1 or H-1B visas and students from those countries with F-1 visas who have been accepted to U.S. medical schools.
3. Develop and implement a plan to allow physicians from the seven designated countries to obtain travel visas to travel to the U.S. for medical conferences and other medical and research-related engagements.
4. Make it a priority to implement a process to admit refugees, without further delay, who had already been vetted and approved for entry prior to the executive order and who are in need of urgent medical care. We note that even with such revisions, the executive order will still inappropriately bar immigrants and refugees based on discriminatory criteria (religion and country of origin) including family members of physicians and medical students in the U.S.
Our organizations are committed to non-discrimination against physicians, medical students and others in immigration policies and offer our assistance in developing policies that support access to health care services, public health, and medical education while balancing the nation’s security needs. Until or unless the executive order is completely rescinded or permanently blocked, it is essential that DHS move forward to ensure that restrictions on physicians and medical students are not reimposed, and that priority is given to refugees with medical conditions needing treatment.
Sincerely,
Alliance for Academic Internal Medicine
American College of Chest Physicians
American College of Physicians
American Society for Gastrointestinal Endoscopy
American Society of Hematology
American Society of Nephrology
American Thoracic Society
Infectious Diseases Society of America
Renal Physicians Association
Society for Adolescent Health and Medicine
Society of Critical Care Medicine
Society of General Internal Medicine
President Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and could impede assemblies of the world’s top medical experts.
The March 6 executive order bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from those countries from entering the United States for 120 days. The measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban. The new order exempts citizens of the six countries who are legal permanent U.S. residents or who have current visas.
The policy could have detrimental effects on future collaboration between U.S. and international scientists and may ultimately endanger the health and well-being of patients, said International Antiviral Society–U.S.A. executive director and president Donna M. Jacobsen, regarding the original travel ban.
There is “serious reason for concern” that the policy will dissuade scientists and researchers “from traveling to the [United States] in the future overall and sharing their work with colleagues here,” she said.
Thousands of academics from around the world, including physicians, researchers, and professors, have vowed to boycott U.S.-based conferences in light of the Trump administration policy. A Google Docs petition started shortly after the original ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said. A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9. The circuit judges said the plaintiffs were likely to succeed in their arguments and that the president had demonstrated no evidence that his executive order advances national security.
The new executive order excludes Iraq and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
President Trump’s revised executive order blocking travelers from six Muslim-majority countries from entering the United States could land a damaging blow to global cooperation in scientific research and could impede assemblies of the world’s top medical experts.
The March 6 executive order bars citizens of Iran, Libya, Somalia, Sudan, Syria, and Yemen from obtaining visas for 90 days and blocks refugees from those countries from entering the United States for 120 days. The measure, which takes effect March 16, supersedes President Trump’s original Jan. 27 travel ban. The new order exempts citizens of the six countries who are legal permanent U.S. residents or who have current visas.
The policy could have detrimental effects on future collaboration between U.S. and international scientists and may ultimately endanger the health and well-being of patients, said International Antiviral Society–U.S.A. executive director and president Donna M. Jacobsen, regarding the original travel ban.
There is “serious reason for concern” that the policy will dissuade scientists and researchers “from traveling to the [United States] in the future overall and sharing their work with colleagues here,” she said.
Thousands of academics from around the world, including physicians, researchers, and professors, have vowed to boycott U.S.-based conferences in light of the Trump administration policy. A Google Docs petition started shortly after the original ban was announced garnered more than 5,000 signatures by professionals acting in solidarity with those affected by the travel restrictions. The academicians who signed the petition said they would not attend international conferences in the United States until those restricted from participating could rejoin their colleagues and freely share their ideas.
The new executive order comes nearly 2 months after President Trump’s original travel ban caused nationwide protests and led to a series of legal challenges. The states of Washington and Minnesota, which sued President Trump over his original ban, argued that such a ban harms the teaching and research missions of their universities and prevents students and faculty from traveling for research and academic collaboration. In addition, the executive order restricts universities from hiring attractive candidates from countries affected by the ban, state officials said. A federal court temporarily blocked the original travel ban on Feb. 3, a decision upheld by the 9th U.S. Circuit Court of Appeals on Feb. 9. The circuit judges said the plaintiffs were likely to succeed in their arguments and that the president had demonstrated no evidence that his executive order advances national security.
The new executive order excludes Iraq and also removes language that had indefinitely banned Syrian refugees. In a March 6 memorandum, the White House said the purpose of the ban is to prevent “foreign nationals who may aid, support, or commit violent, criminal, or terrorist acts,” while the administration enhances the screening and vetting protocols and procedures for granting visas and admission to the United States.
“This nation cannot delay the immediate implementation of additional heightened screening and vetting protocols and procedures for issuing visas to ensure that we strengthen the safety and security of our country,” the memo states.
[email protected]
On Twitter @legal_med
Methotrexate use justified for early RA, disease prevention
Efforts to delay or prevent rheumatoid arthritis (RA) in individuals at high risk for the disease received a boost from the findings of a subgroup analysis of an older Dutch prevention trial involving methotrexate that were published recently in Arthritis & Rheumatology.
However, while the 22-patient subgroup analysis of the 2007 trial, called PROMPT (Probable RA: Methotrexate Versus Placebo Treatment), showed that 1 year of methotrexate prevented the development of rheumatoid arthritis in significantly more individuals at high risk for the disease than did placebo, hindsight has shown that most of these high-risk individuals actually had RA at baseline as defined by the 2010 American College or Rheumatology/European League Against Rheumatism classification criteria.
Even though the “landscape of RA has changed since this study was conceived, enrolled, and performed,” Dr. Sparks noted that the study provides evidence that today’s “standard of care really works” by making use of data that are unobtainable today.
“Nowadays, we wouldn’t be able to do a placebo-controlled trial in early RA because those patients need to be treated, but at the time, it was perfectly fine, based on the treatment landscape, to put these patients in a [placebo-controlled] trial,” he said in an interview.
“It also demonstrates that you really need to find high-risk individuals, because, if you recruit people who are never going to develop RA, you’re just diluting your effect, and you’re not going to find the difference in the groups based on that diluted effect when there could be a true effect in that special subgroup,” he added.
Senior study author Annette van der Helm-van Mil, MD, PhD, and her colleagues at Leiden (the Netherlands) University Medical Center performed the reanalysis after the initial finding that methotrexate had no preventative effect may have been falsely negative because the study included patients with a low risk of progressing to RA (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40062).
In the reanalysis, the investigators defined 22 out of the trial’s 110 participants as high risk based on their score of 8 or higher on the Leiden prediction rule at baseline. Of those 22, 18 also fulfilled the 2010 classification criteria for RA.
This “definition of high risk [in the trial] very much coincided with the new classification criteria and reinforces the standard of care that patients with new diagnosed RA should be treated with DMARDs [disease-modifying antirheumatic drugs] front line,” Dr. Sparks said.
The Leiden prediction rule score is based on ACPA statuses, as well as age, sex, distribution of involved joints, number of swollen and tender joints, severity of morning stiffness, C-reactive protein level, and rheumatoid factor. In previous studies of patients with undifferentiated arthritis, a score of 8 or higher with the prediction rule had a positive predictive value of 84% in patients with undifferentiated arthritis, according to the investigators.
Based on a primary outcome of fulfilling the 1987 classification criteria for RA after 5 years of follow-up, the investigators found that 6 of 11 (55%) in the methotrexate arm developed RA, compared with all 11 patients in the placebo arm (P = .011). “A 1-year course of methotrexate was associated with an absolute risk reduction of 45% on RA development, resulting in a number needed to treat of 2.2 (95% [confidence interval], 1.3-6.2),” the authors wrote.
Furthermore, the time to the development of RA based on the 1987 criteria was longer with methotrexate than with placebo (median of 22.5 months vs. 3 months; P less than .001).
Drug-free remission was also achieved by 4 of 11 (36%) patients taking methotrexate, compared with none of the patients taking placebo (P = .027).
The beneficial effects of methotrexate were seen in ACPA-positive and ACPA-negative high-risk patients but not in patients without a high risk of RA.
For the patients who did not fulfill the 2010 RA criteria at baseline, only one of four of those in the placebo arm did go on to develop RA based on 1987 criteria, whereas only one of three who received methotrexate did.
Overall, the reanalysis of PROMPT trial data illustrates how “noninformative inclusions can blur highly relevant study outcomes, such as prevention of RA,” the study authors concluded.
“As trials are now being conducted to evaluate the efficacy of treatment initiated in the phase of arthralgia, the development of adequate risk prediction models are of importance in order to prevent false-negative study results in the future,” they added.
The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
Small numbers not withstanding, the findings of this reanalysis of the PROMPT trial are exciting, and they address the importance of identifying the right individuals to include in any type of prevention study in RA.
Given the temporal limits of clinical trials, inclusion criteria will need to incorporate both the likelihood of an important outcome and the timing of that outcome – right individuals, right time, right drug/intervention.
It is hoped that investigators will be able to demonstrate conclusively that preventive interventions work for rheumatic disease once these issues are addressed.
Kevin D. Deane, MD, PhD, and his coauthors are with the division of rheumatology at the University of Colorado, Denver, and made these remarks in an editorial accompanying the PROMPT trial reanalysis (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40061).
Small numbers not withstanding, the findings of this reanalysis of the PROMPT trial are exciting, and they address the importance of identifying the right individuals to include in any type of prevention study in RA.
Given the temporal limits of clinical trials, inclusion criteria will need to incorporate both the likelihood of an important outcome and the timing of that outcome – right individuals, right time, right drug/intervention.
It is hoped that investigators will be able to demonstrate conclusively that preventive interventions work for rheumatic disease once these issues are addressed.
Kevin D. Deane, MD, PhD, and his coauthors are with the division of rheumatology at the University of Colorado, Denver, and made these remarks in an editorial accompanying the PROMPT trial reanalysis (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40061).
Small numbers not withstanding, the findings of this reanalysis of the PROMPT trial are exciting, and they address the importance of identifying the right individuals to include in any type of prevention study in RA.
Given the temporal limits of clinical trials, inclusion criteria will need to incorporate both the likelihood of an important outcome and the timing of that outcome – right individuals, right time, right drug/intervention.
It is hoped that investigators will be able to demonstrate conclusively that preventive interventions work for rheumatic disease once these issues are addressed.
Kevin D. Deane, MD, PhD, and his coauthors are with the division of rheumatology at the University of Colorado, Denver, and made these remarks in an editorial accompanying the PROMPT trial reanalysis (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40061).
Efforts to delay or prevent rheumatoid arthritis (RA) in individuals at high risk for the disease received a boost from the findings of a subgroup analysis of an older Dutch prevention trial involving methotrexate that were published recently in Arthritis & Rheumatology.
However, while the 22-patient subgroup analysis of the 2007 trial, called PROMPT (Probable RA: Methotrexate Versus Placebo Treatment), showed that 1 year of methotrexate prevented the development of rheumatoid arthritis in significantly more individuals at high risk for the disease than did placebo, hindsight has shown that most of these high-risk individuals actually had RA at baseline as defined by the 2010 American College or Rheumatology/European League Against Rheumatism classification criteria.
Even though the “landscape of RA has changed since this study was conceived, enrolled, and performed,” Dr. Sparks noted that the study provides evidence that today’s “standard of care really works” by making use of data that are unobtainable today.
“Nowadays, we wouldn’t be able to do a placebo-controlled trial in early RA because those patients need to be treated, but at the time, it was perfectly fine, based on the treatment landscape, to put these patients in a [placebo-controlled] trial,” he said in an interview.
“It also demonstrates that you really need to find high-risk individuals, because, if you recruit people who are never going to develop RA, you’re just diluting your effect, and you’re not going to find the difference in the groups based on that diluted effect when there could be a true effect in that special subgroup,” he added.
Senior study author Annette van der Helm-van Mil, MD, PhD, and her colleagues at Leiden (the Netherlands) University Medical Center performed the reanalysis after the initial finding that methotrexate had no preventative effect may have been falsely negative because the study included patients with a low risk of progressing to RA (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40062).
In the reanalysis, the investigators defined 22 out of the trial’s 110 participants as high risk based on their score of 8 or higher on the Leiden prediction rule at baseline. Of those 22, 18 also fulfilled the 2010 classification criteria for RA.
This “definition of high risk [in the trial] very much coincided with the new classification criteria and reinforces the standard of care that patients with new diagnosed RA should be treated with DMARDs [disease-modifying antirheumatic drugs] front line,” Dr. Sparks said.
The Leiden prediction rule score is based on ACPA statuses, as well as age, sex, distribution of involved joints, number of swollen and tender joints, severity of morning stiffness, C-reactive protein level, and rheumatoid factor. In previous studies of patients with undifferentiated arthritis, a score of 8 or higher with the prediction rule had a positive predictive value of 84% in patients with undifferentiated arthritis, according to the investigators.
Based on a primary outcome of fulfilling the 1987 classification criteria for RA after 5 years of follow-up, the investigators found that 6 of 11 (55%) in the methotrexate arm developed RA, compared with all 11 patients in the placebo arm (P = .011). “A 1-year course of methotrexate was associated with an absolute risk reduction of 45% on RA development, resulting in a number needed to treat of 2.2 (95% [confidence interval], 1.3-6.2),” the authors wrote.
Furthermore, the time to the development of RA based on the 1987 criteria was longer with methotrexate than with placebo (median of 22.5 months vs. 3 months; P less than .001).
Drug-free remission was also achieved by 4 of 11 (36%) patients taking methotrexate, compared with none of the patients taking placebo (P = .027).
The beneficial effects of methotrexate were seen in ACPA-positive and ACPA-negative high-risk patients but not in patients without a high risk of RA.
For the patients who did not fulfill the 2010 RA criteria at baseline, only one of four of those in the placebo arm did go on to develop RA based on 1987 criteria, whereas only one of three who received methotrexate did.
Overall, the reanalysis of PROMPT trial data illustrates how “noninformative inclusions can blur highly relevant study outcomes, such as prevention of RA,” the study authors concluded.
“As trials are now being conducted to evaluate the efficacy of treatment initiated in the phase of arthralgia, the development of adequate risk prediction models are of importance in order to prevent false-negative study results in the future,” they added.
The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
Efforts to delay or prevent rheumatoid arthritis (RA) in individuals at high risk for the disease received a boost from the findings of a subgroup analysis of an older Dutch prevention trial involving methotrexate that were published recently in Arthritis & Rheumatology.
However, while the 22-patient subgroup analysis of the 2007 trial, called PROMPT (Probable RA: Methotrexate Versus Placebo Treatment), showed that 1 year of methotrexate prevented the development of rheumatoid arthritis in significantly more individuals at high risk for the disease than did placebo, hindsight has shown that most of these high-risk individuals actually had RA at baseline as defined by the 2010 American College or Rheumatology/European League Against Rheumatism classification criteria.
Even though the “landscape of RA has changed since this study was conceived, enrolled, and performed,” Dr. Sparks noted that the study provides evidence that today’s “standard of care really works” by making use of data that are unobtainable today.
“Nowadays, we wouldn’t be able to do a placebo-controlled trial in early RA because those patients need to be treated, but at the time, it was perfectly fine, based on the treatment landscape, to put these patients in a [placebo-controlled] trial,” he said in an interview.
“It also demonstrates that you really need to find high-risk individuals, because, if you recruit people who are never going to develop RA, you’re just diluting your effect, and you’re not going to find the difference in the groups based on that diluted effect when there could be a true effect in that special subgroup,” he added.
Senior study author Annette van der Helm-van Mil, MD, PhD, and her colleagues at Leiden (the Netherlands) University Medical Center performed the reanalysis after the initial finding that methotrexate had no preventative effect may have been falsely negative because the study included patients with a low risk of progressing to RA (Arthritis Rheumatol. 2017 Feb 19. doi: 10.1002/art.40062).
In the reanalysis, the investigators defined 22 out of the trial’s 110 participants as high risk based on their score of 8 or higher on the Leiden prediction rule at baseline. Of those 22, 18 also fulfilled the 2010 classification criteria for RA.
This “definition of high risk [in the trial] very much coincided with the new classification criteria and reinforces the standard of care that patients with new diagnosed RA should be treated with DMARDs [disease-modifying antirheumatic drugs] front line,” Dr. Sparks said.
The Leiden prediction rule score is based on ACPA statuses, as well as age, sex, distribution of involved joints, number of swollen and tender joints, severity of morning stiffness, C-reactive protein level, and rheumatoid factor. In previous studies of patients with undifferentiated arthritis, a score of 8 or higher with the prediction rule had a positive predictive value of 84% in patients with undifferentiated arthritis, according to the investigators.
Based on a primary outcome of fulfilling the 1987 classification criteria for RA after 5 years of follow-up, the investigators found that 6 of 11 (55%) in the methotrexate arm developed RA, compared with all 11 patients in the placebo arm (P = .011). “A 1-year course of methotrexate was associated with an absolute risk reduction of 45% on RA development, resulting in a number needed to treat of 2.2 (95% [confidence interval], 1.3-6.2),” the authors wrote.
Furthermore, the time to the development of RA based on the 1987 criteria was longer with methotrexate than with placebo (median of 22.5 months vs. 3 months; P less than .001).
Drug-free remission was also achieved by 4 of 11 (36%) patients taking methotrexate, compared with none of the patients taking placebo (P = .027).
The beneficial effects of methotrexate were seen in ACPA-positive and ACPA-negative high-risk patients but not in patients without a high risk of RA.
For the patients who did not fulfill the 2010 RA criteria at baseline, only one of four of those in the placebo arm did go on to develop RA based on 1987 criteria, whereas only one of three who received methotrexate did.
Overall, the reanalysis of PROMPT trial data illustrates how “noninformative inclusions can blur highly relevant study outcomes, such as prevention of RA,” the study authors concluded.
“As trials are now being conducted to evaluate the efficacy of treatment initiated in the phase of arthralgia, the development of adequate risk prediction models are of importance in order to prevent false-negative study results in the future,” they added.
The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Main finding: In people deemed to be at high risk for RA, a 1-year course of methotrexate was associated with an absolute risk reduction of 45% of RA development, resulting in a number needed to treat of 2.2 (95% CI, 1.3-6.2).
Data source: A reanalysis of the PROMPT trial involving 110 patients with undifferentiated arthritis randomized to a 1-year course of methotrexate or placebo.
Disclosures: The PROMPT trial was supported by the Dutch Arthritis Foundation and the Netherlands Organisation for Scientific Research.
Cutaneous Manifestations of Tick-Borne Diseases
GOP health plan clears first hurdle as opposition lines up
The Republican plan to replace the Affordable Care Act cleared the first legislative hurdle when two house committees passed language that would repeal revenue provisions of the Affordable Care Act and lay the foundation for replacing the health care reform law.
The House Ways and Means Committee–approved legislation would eliminate the individual mandate in favor of allowing insurance companies to penalize individuals by up to 30% of premiums for lapses in coverage and would repeal taxes on high-cost health plans (Cadillac tax), over-the-counter and prescription medications, health savings accounts, tanning, investment, and on health insurers.
The language passed with a party-line vote March 9 with 23 Republicans voting for and 16 Democrats voting against after nearly 18 hours of debate and amendments.
The House Energy and Commerce Committee, after 27 hours of debate that started March 8, also passed its language along party lines with 31 Republicans voting for and 23 Democrats voting against. Their bill would end Medicaid expansion and reset the program’s funding to a per capita allotment based on population indicators, along with block grants, to provide states more flexibility to better manage its population.
A key concern raised in both committee debates was the brief window between the public unveiling of the legislation and the committees’ efforts, especially the lack of financial impact analysis or “score” from the Congressional Budget Office. Democrats efforts in both committees to hold action for a CBO score were voted down on across party lines.
In both committees, Democrats introduced a wide range of amendments, including guarantees there would be no impact from the reduction of Medicaid expansion and on funding to support coverage for mental health, women, children, seniors, and veterans, all of which were voted down. Ways and Means members also offered an amendment to require President Trump to release his income tax filings.
Rep. Frank Pallone (D-N.J.), lead Democrat in the Energy and Commerce Committee, voiced his colleagues’ objections to the bill and the process.
The bill “would rip health care away from millions of Americans, raise costs for working families and seniors, and lead to the rationing of care for 76 million Americans who receive Medicaid. … This has not been a transparent process. We did not go through regular order. The bill was posted less than 2 days before markup. No hearings were held, and we don’t have a CBO score,” Rep. Pallone said during committee debate.
A CBO score of the budget and coverage impacts of the Republican health care proposal could come as early as March 13.
The pace of action in the House even drew criticism from some in the GOP. Sen. Tom Cotton (R-Ark.) took to Twitter with a stern warning to the House.
“House health-care bill can’t pass w/o major changes,” Sen. Cotton tweeted. “To my friends in House: pause, start over. Get it right, don’t get it fast.”
He followed up with two more tweets: “GOP shouldn’t act like Dems did in O’care. No excuse to release bill Mon night, start voting Wed. With no budget estimate!” He added: “What matters in long run is better, more affordable health care for Americans, NOT house leaders’ arbitrary legislative calendar.”
Four Republican senators – Rob Portman (Ohio), Shelley Moore Capito (W.Va.), Cory Gardner (Colo.), and Lisa Murkowski (Alaska) – also expressed concerns regarding how Medicaid will be changed under the repeal/replace effort and vowed not to support any plan “that does not include stability for Medicaid expansion populations or flexibility for states.”
Republicans hold a slim 52-seat majority in the Senate and need only 50 votes to pass any legislation that uses the budget reconciliation process. If those four senators voted with Democrats, who are expected to vote as a party against the repeal effort, the current House Republican legislation would not clear the Senate.
Physicians’ groups also have voiced their opposition. American Medical Association President Andrew Gurman, MD, said in a statement that it is “not legislation we can support. The replacement bill, as written, would reverse the coverage gains of the ACA, causing many Americans to lose the health coverage they have come to depend on.” He added that the proposed changes to Medicaid “would limit states’ ability to respond to changes in service demands and threaten coverage for people with low incomes.”
Likewise, a joint statement issued by the American Academy of Family Physicians, American Academy of Pediatricians, American College of Physicians, American Congress of Obstetricians and Gynecologists and the American Osteopathic Association, expressed concern that the proposal “will likely result in less access to coverage and higher costs for millions of patients.”
The Republican plan to replace the Affordable Care Act cleared the first legislative hurdle when two house committees passed language that would repeal revenue provisions of the Affordable Care Act and lay the foundation for replacing the health care reform law.
The House Ways and Means Committee–approved legislation would eliminate the individual mandate in favor of allowing insurance companies to penalize individuals by up to 30% of premiums for lapses in coverage and would repeal taxes on high-cost health plans (Cadillac tax), over-the-counter and prescription medications, health savings accounts, tanning, investment, and on health insurers.
The language passed with a party-line vote March 9 with 23 Republicans voting for and 16 Democrats voting against after nearly 18 hours of debate and amendments.
The House Energy and Commerce Committee, after 27 hours of debate that started March 8, also passed its language along party lines with 31 Republicans voting for and 23 Democrats voting against. Their bill would end Medicaid expansion and reset the program’s funding to a per capita allotment based on population indicators, along with block grants, to provide states more flexibility to better manage its population.
A key concern raised in both committee debates was the brief window between the public unveiling of the legislation and the committees’ efforts, especially the lack of financial impact analysis or “score” from the Congressional Budget Office. Democrats efforts in both committees to hold action for a CBO score were voted down on across party lines.
In both committees, Democrats introduced a wide range of amendments, including guarantees there would be no impact from the reduction of Medicaid expansion and on funding to support coverage for mental health, women, children, seniors, and veterans, all of which were voted down. Ways and Means members also offered an amendment to require President Trump to release his income tax filings.
Rep. Frank Pallone (D-N.J.), lead Democrat in the Energy and Commerce Committee, voiced his colleagues’ objections to the bill and the process.
The bill “would rip health care away from millions of Americans, raise costs for working families and seniors, and lead to the rationing of care for 76 million Americans who receive Medicaid. … This has not been a transparent process. We did not go through regular order. The bill was posted less than 2 days before markup. No hearings were held, and we don’t have a CBO score,” Rep. Pallone said during committee debate.
A CBO score of the budget and coverage impacts of the Republican health care proposal could come as early as March 13.
The pace of action in the House even drew criticism from some in the GOP. Sen. Tom Cotton (R-Ark.) took to Twitter with a stern warning to the House.
“House health-care bill can’t pass w/o major changes,” Sen. Cotton tweeted. “To my friends in House: pause, start over. Get it right, don’t get it fast.”
He followed up with two more tweets: “GOP shouldn’t act like Dems did in O’care. No excuse to release bill Mon night, start voting Wed. With no budget estimate!” He added: “What matters in long run is better, more affordable health care for Americans, NOT house leaders’ arbitrary legislative calendar.”
Four Republican senators – Rob Portman (Ohio), Shelley Moore Capito (W.Va.), Cory Gardner (Colo.), and Lisa Murkowski (Alaska) – also expressed concerns regarding how Medicaid will be changed under the repeal/replace effort and vowed not to support any plan “that does not include stability for Medicaid expansion populations or flexibility for states.”
Republicans hold a slim 52-seat majority in the Senate and need only 50 votes to pass any legislation that uses the budget reconciliation process. If those four senators voted with Democrats, who are expected to vote as a party against the repeal effort, the current House Republican legislation would not clear the Senate.
Physicians’ groups also have voiced their opposition. American Medical Association President Andrew Gurman, MD, said in a statement that it is “not legislation we can support. The replacement bill, as written, would reverse the coverage gains of the ACA, causing many Americans to lose the health coverage they have come to depend on.” He added that the proposed changes to Medicaid “would limit states’ ability to respond to changes in service demands and threaten coverage for people with low incomes.”
Likewise, a joint statement issued by the American Academy of Family Physicians, American Academy of Pediatricians, American College of Physicians, American Congress of Obstetricians and Gynecologists and the American Osteopathic Association, expressed concern that the proposal “will likely result in less access to coverage and higher costs for millions of patients.”
The Republican plan to replace the Affordable Care Act cleared the first legislative hurdle when two house committees passed language that would repeal revenue provisions of the Affordable Care Act and lay the foundation for replacing the health care reform law.
The House Ways and Means Committee–approved legislation would eliminate the individual mandate in favor of allowing insurance companies to penalize individuals by up to 30% of premiums for lapses in coverage and would repeal taxes on high-cost health plans (Cadillac tax), over-the-counter and prescription medications, health savings accounts, tanning, investment, and on health insurers.
The language passed with a party-line vote March 9 with 23 Republicans voting for and 16 Democrats voting against after nearly 18 hours of debate and amendments.
The House Energy and Commerce Committee, after 27 hours of debate that started March 8, also passed its language along party lines with 31 Republicans voting for and 23 Democrats voting against. Their bill would end Medicaid expansion and reset the program’s funding to a per capita allotment based on population indicators, along with block grants, to provide states more flexibility to better manage its population.
A key concern raised in both committee debates was the brief window between the public unveiling of the legislation and the committees’ efforts, especially the lack of financial impact analysis or “score” from the Congressional Budget Office. Democrats efforts in both committees to hold action for a CBO score were voted down on across party lines.
In both committees, Democrats introduced a wide range of amendments, including guarantees there would be no impact from the reduction of Medicaid expansion and on funding to support coverage for mental health, women, children, seniors, and veterans, all of which were voted down. Ways and Means members also offered an amendment to require President Trump to release his income tax filings.
Rep. Frank Pallone (D-N.J.), lead Democrat in the Energy and Commerce Committee, voiced his colleagues’ objections to the bill and the process.
The bill “would rip health care away from millions of Americans, raise costs for working families and seniors, and lead to the rationing of care for 76 million Americans who receive Medicaid. … This has not been a transparent process. We did not go through regular order. The bill was posted less than 2 days before markup. No hearings were held, and we don’t have a CBO score,” Rep. Pallone said during committee debate.
A CBO score of the budget and coverage impacts of the Republican health care proposal could come as early as March 13.
The pace of action in the House even drew criticism from some in the GOP. Sen. Tom Cotton (R-Ark.) took to Twitter with a stern warning to the House.
“House health-care bill can’t pass w/o major changes,” Sen. Cotton tweeted. “To my friends in House: pause, start over. Get it right, don’t get it fast.”
He followed up with two more tweets: “GOP shouldn’t act like Dems did in O’care. No excuse to release bill Mon night, start voting Wed. With no budget estimate!” He added: “What matters in long run is better, more affordable health care for Americans, NOT house leaders’ arbitrary legislative calendar.”
Four Republican senators – Rob Portman (Ohio), Shelley Moore Capito (W.Va.), Cory Gardner (Colo.), and Lisa Murkowski (Alaska) – also expressed concerns regarding how Medicaid will be changed under the repeal/replace effort and vowed not to support any plan “that does not include stability for Medicaid expansion populations or flexibility for states.”
Republicans hold a slim 52-seat majority in the Senate and need only 50 votes to pass any legislation that uses the budget reconciliation process. If those four senators voted with Democrats, who are expected to vote as a party against the repeal effort, the current House Republican legislation would not clear the Senate.
Physicians’ groups also have voiced their opposition. American Medical Association President Andrew Gurman, MD, said in a statement that it is “not legislation we can support. The replacement bill, as written, would reverse the coverage gains of the ACA, causing many Americans to lose the health coverage they have come to depend on.” He added that the proposed changes to Medicaid “would limit states’ ability to respond to changes in service demands and threaten coverage for people with low incomes.”
Likewise, a joint statement issued by the American Academy of Family Physicians, American Academy of Pediatricians, American College of Physicians, American Congress of Obstetricians and Gynecologists and the American Osteopathic Association, expressed concern that the proposal “will likely result in less access to coverage and higher costs for millions of patients.”
Everything We Say & Do: What PFACs reveal about patient experience
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable tactics that have great potential to positively impact patients’ experience of care.
Patient and Family Advisory Councils (PFACs) provide a tool for understanding the patient perspective and are utilized nationwide. These councils, typically consisting of former and current patients and/or their family members, meet on a regular basis to advise provider communities on a wide range of care-related matters. At my institution, Beth Israel Deaconess Medical Center, our PFAC has weighed in on a wide range of issues, such as how to conduct effective nursing rounds and the best methods for supporting patients with disabilities.
Most recently, we have utilized an innovative approach to both understanding the patient experience and capitalizing on the expertise of our PFAC members. Modeled after a program developed at the Dartmouth-Hitchcock Medical Center, we have trained members of our PFAC to interview inpatients at the bedside about their experience. Time-sensitive information is immediately reported back to the nurse manager, who responds with real-time solutions. Oftentimes, problems can be easily resolved using the right communication, or just providing the “listening ear” of someone to whom the patient relates.
In addition, the information is aggregated to provide us with a broad-based perspective of the patient experience at BIDMC. For example, we found that our patients often discuss issues with volunteers that they have not addressed with providers, suggesting they may at times feel more comfortable disclosing concerns to people outside of their medical team.
The Society of Hospital Medicine (SHM) also recognizes the central role of the patient’s voice in quality medical care. Through the work of its Patient Experience Committee, SHM has convened a nationwide “virtual” PFAC consisting of leaders of PFACs from medical facilities across the country. Members of the SHM PFAC share questions posed by SHM’s committees with their constituents, and the responses are reported back to the Patient Experience Committee.
What lessons have we learned from the SHM PFAC? Make no assumptions. While some of us have been patients ourselves and all of us interact with patients, our ability to understand the patient perspective is blurred by the lenses of medical training, system constraints, and the pressures of the challenging work that we do.
It is often impossible to predict the response when you question a patient about his or her experience. For example, the first question we asked SHM’s nationwide PFAC was: “What is one thing that a hospitalist could do to improve the patient experience?” The most common response we received was: “What is a hospitalist?” These responses suggest that we (hospitalists) need to redirect our efforts in a way that we had not anticipated, with a focus on clarifying who we are and what we do.
Other, more predictable themes emerged as well. Our patients want consistency and continuity throughout their hospitalization. They value a good bedside manner and want us to engage in sensitivity training. They ask us to work on minimizing errors and ensuring accountability both during hospitalization as well as pre- and post hospitalization.
Ultimately we hope that the SHM PFAC will be utilized by all of SHM’s committees, allowing for the patient experience to be a common thread woven through all SHM initiatives.
Amber Moore, MD, MPH, is a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School.
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable tactics that have great potential to positively impact patients’ experience of care.
Patient and Family Advisory Councils (PFACs) provide a tool for understanding the patient perspective and are utilized nationwide. These councils, typically consisting of former and current patients and/or their family members, meet on a regular basis to advise provider communities on a wide range of care-related matters. At my institution, Beth Israel Deaconess Medical Center, our PFAC has weighed in on a wide range of issues, such as how to conduct effective nursing rounds and the best methods for supporting patients with disabilities.
Most recently, we have utilized an innovative approach to both understanding the patient experience and capitalizing on the expertise of our PFAC members. Modeled after a program developed at the Dartmouth-Hitchcock Medical Center, we have trained members of our PFAC to interview inpatients at the bedside about their experience. Time-sensitive information is immediately reported back to the nurse manager, who responds with real-time solutions. Oftentimes, problems can be easily resolved using the right communication, or just providing the “listening ear” of someone to whom the patient relates.
In addition, the information is aggregated to provide us with a broad-based perspective of the patient experience at BIDMC. For example, we found that our patients often discuss issues with volunteers that they have not addressed with providers, suggesting they may at times feel more comfortable disclosing concerns to people outside of their medical team.
The Society of Hospital Medicine (SHM) also recognizes the central role of the patient’s voice in quality medical care. Through the work of its Patient Experience Committee, SHM has convened a nationwide “virtual” PFAC consisting of leaders of PFACs from medical facilities across the country. Members of the SHM PFAC share questions posed by SHM’s committees with their constituents, and the responses are reported back to the Patient Experience Committee.
What lessons have we learned from the SHM PFAC? Make no assumptions. While some of us have been patients ourselves and all of us interact with patients, our ability to understand the patient perspective is blurred by the lenses of medical training, system constraints, and the pressures of the challenging work that we do.
It is often impossible to predict the response when you question a patient about his or her experience. For example, the first question we asked SHM’s nationwide PFAC was: “What is one thing that a hospitalist could do to improve the patient experience?” The most common response we received was: “What is a hospitalist?” These responses suggest that we (hospitalists) need to redirect our efforts in a way that we had not anticipated, with a focus on clarifying who we are and what we do.
Other, more predictable themes emerged as well. Our patients want consistency and continuity throughout their hospitalization. They value a good bedside manner and want us to engage in sensitivity training. They ask us to work on minimizing errors and ensuring accountability both during hospitalization as well as pre- and post hospitalization.
Ultimately we hope that the SHM PFAC will be utilized by all of SHM’s committees, allowing for the patient experience to be a common thread woven through all SHM initiatives.
Amber Moore, MD, MPH, is a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School.
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable tactics that have great potential to positively impact patients’ experience of care.
Patient and Family Advisory Councils (PFACs) provide a tool for understanding the patient perspective and are utilized nationwide. These councils, typically consisting of former and current patients and/or their family members, meet on a regular basis to advise provider communities on a wide range of care-related matters. At my institution, Beth Israel Deaconess Medical Center, our PFAC has weighed in on a wide range of issues, such as how to conduct effective nursing rounds and the best methods for supporting patients with disabilities.
Most recently, we have utilized an innovative approach to both understanding the patient experience and capitalizing on the expertise of our PFAC members. Modeled after a program developed at the Dartmouth-Hitchcock Medical Center, we have trained members of our PFAC to interview inpatients at the bedside about their experience. Time-sensitive information is immediately reported back to the nurse manager, who responds with real-time solutions. Oftentimes, problems can be easily resolved using the right communication, or just providing the “listening ear” of someone to whom the patient relates.
In addition, the information is aggregated to provide us with a broad-based perspective of the patient experience at BIDMC. For example, we found that our patients often discuss issues with volunteers that they have not addressed with providers, suggesting they may at times feel more comfortable disclosing concerns to people outside of their medical team.
The Society of Hospital Medicine (SHM) also recognizes the central role of the patient’s voice in quality medical care. Through the work of its Patient Experience Committee, SHM has convened a nationwide “virtual” PFAC consisting of leaders of PFACs from medical facilities across the country. Members of the SHM PFAC share questions posed by SHM’s committees with their constituents, and the responses are reported back to the Patient Experience Committee.
What lessons have we learned from the SHM PFAC? Make no assumptions. While some of us have been patients ourselves and all of us interact with patients, our ability to understand the patient perspective is blurred by the lenses of medical training, system constraints, and the pressures of the challenging work that we do.
It is often impossible to predict the response when you question a patient about his or her experience. For example, the first question we asked SHM’s nationwide PFAC was: “What is one thing that a hospitalist could do to improve the patient experience?” The most common response we received was: “What is a hospitalist?” These responses suggest that we (hospitalists) need to redirect our efforts in a way that we had not anticipated, with a focus on clarifying who we are and what we do.
Other, more predictable themes emerged as well. Our patients want consistency and continuity throughout their hospitalization. They value a good bedside manner and want us to engage in sensitivity training. They ask us to work on minimizing errors and ensuring accountability both during hospitalization as well as pre- and post hospitalization.
Ultimately we hope that the SHM PFAC will be utilized by all of SHM’s committees, allowing for the patient experience to be a common thread woven through all SHM initiatives.
Amber Moore, MD, MPH, is a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School.
The beginning of the end
No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2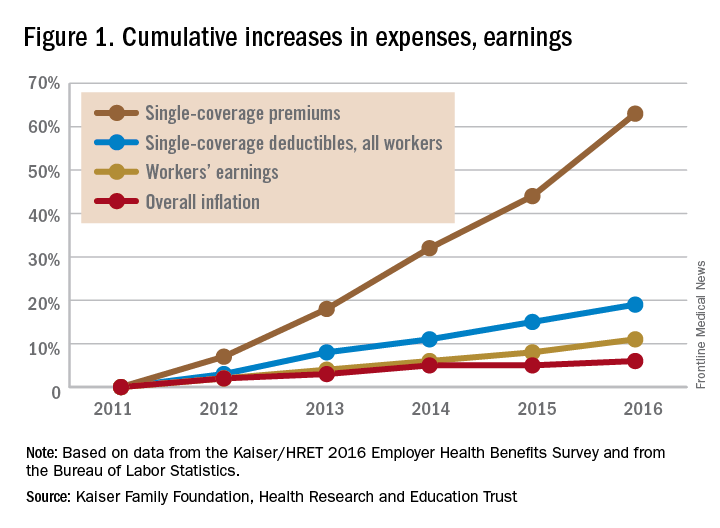
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10
It seems unlikely that a Republican-led government will pursue efforts to decrease out-of-pocket expenses. More likely, new proposals will aim to provide tax benefits to encourage use of health savings accounts (HSAs), continuing the shift of health care to employees.11 HSAs benefit employers, who pay less for the health care costs of employees, but are associated with worsened adherence to recommended treatments for patients.8,12
A 2016 study analyzed health care policies considered by Trump, including the following:
- Full repeal of the ACA.
- Repeal of the ACA plus tax deductions of health insurance premiums.
- Repeal of the ACA plus block grants to states for Medicaid and Children’s Health Insurance Program (CHIP).
- Repeal plus promotion of selling health insurance across state lines.
Not surprisingly, all four scenarios resulted in significant increases in out-of-pocket expenses for those in individual insurance plans.13
Although at the time of writing, the “replace” segment of “repeal-and-replace” is not known, Mr. Trump’s nominee for Secretary of Health and Human Services (HHS), Rep. Tom Price (R-Ga.), has given a hint of what he would champion based on his prior legislative proposals. Along with his support of increasing accessibility of armor-piercing bullets, reduced regulations on cigars, and opposition to expanding the State Children’s Health Insurance Program, he proposed H.R. 2300, “Empower Patients First Act.” This would eliminate the ACA’s Medicaid expansion and replace it with flat tax credits based on age, not income, which turns out to offer greater subsidies relative to income for those with higher incomes. A 30-year-old would, on average, face a premium bill of $2,532, along with a potential out-of-pocket liability of $7,000, with only a $1,200 credit to cover this from Mr. Price’s plan.14
In sum
So what’s a conscientious advocate for the physical and financial health of patients to do? Beyond political action, hospitalists need to keep abreast of the effect of changes in health care policy on their patients, as unpleasant as it may be. Do you know what the copays and out-of-pocket costs are for your patient’s (or your own) health care? Knowing how your recommendations for treatment and follow-up affect your patient’s pocketbook will not only help protect their finances, but will also protect their health, as people are less likely to be compliant with treatment if it involves out-of-pocket costs.
And easy as it would be to simply tune out the partisan rancor, stay engaged as a citizen, if for nothing else, the benefit of your patients.
Dr. Chang is pediatric editor of The Hospitalist. He is associate clinical professor of pediatrics at the University of Massachusetts, Worcester, and chief of pediatric hospital medicine at Baystate Children's Hospital, Springfield, Mass. Send comments and questions to [email protected].
References
1. Horton R. Offline: Looking forward to Donald Trump. The Lancet. 2016;388[10061]:2726.
2. Page L. What Donald Trump would do with the US healthcare system. BMJ. 2016;353:i2996.
3. Uberoi N, Finegold, K. and Gee, E. Health Insurance Coverage and the Affordable Care Act, 2010-2016. Department of Health and Human Services, ASPE Issue Brief, 2016 March 3.
4. Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health Benefits In 2016: Family Premiums Rose Modestly, And Offer Rates Remained Stable. Health Aff (Millwood). 2016 Sep. doi: 10.1377/hlthaff.2016.0951.
5. Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff (Millwood). 2008;27:w318-327.
6. Waters H, Steinhardt L, Oliver TR, Burton A, Milner S. The costs of non-insurance in Maryland. J Health Care Poor Underserved. 2007 Feb;18[1]:139-51.
7. Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14[4]:2259-63.
8. Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57[4]:601-7.
9. Collins SR, Gunja M, Beutel S. How Will the Affordable Care Act’s Cost-Sharing Reductions Affect Consumers’ Out-of-Pocket Costs in 2016? Issue Brief (Commonw Fund) 2016;6:1-17.
10. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6[2]:100-6.
11. Antos J CJ. The House Republicans’ Health Plan. Bethesda, MD: Health Affairs Blog, Project HOPE; 2016 June 22.
12. Fronstin P, Roebuck MC. Health care spending after adopting a full-replacement, high-deductible health plan with a health savings account: a five-year study. EBRI Issue Brief 2013 July:3-15.
13. Saltzman E EC. Donald Trump’s Health Care Reform Proposals: Anticipated Effects on Insurance Coverage, Out-of-Pocket Costs, and the Federal Deficit. The Commonwealth Fund September 2016.
14. Glied SA, Frank RG. Care for the Vulnerable vs. Cash for the Powerful – Trump’s Pick for HHS. N Engl J Med. 2017;376:103-5.
No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2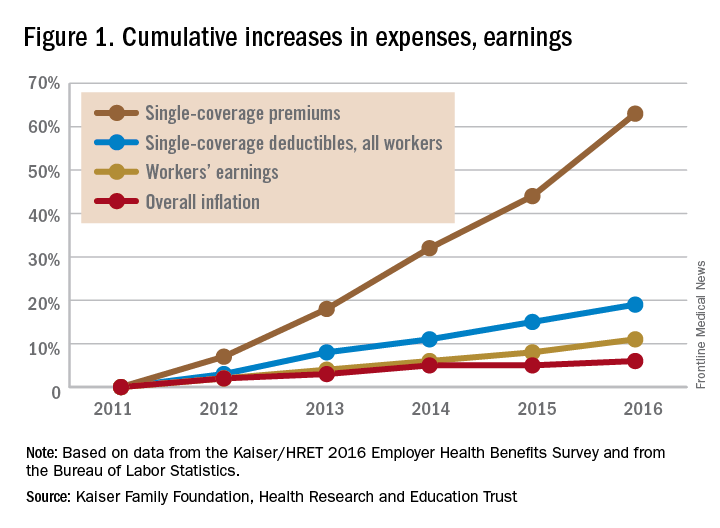
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10
It seems unlikely that a Republican-led government will pursue efforts to decrease out-of-pocket expenses. More likely, new proposals will aim to provide tax benefits to encourage use of health savings accounts (HSAs), continuing the shift of health care to employees.11 HSAs benefit employers, who pay less for the health care costs of employees, but are associated with worsened adherence to recommended treatments for patients.8,12
A 2016 study analyzed health care policies considered by Trump, including the following:
- Full repeal of the ACA.
- Repeal of the ACA plus tax deductions of health insurance premiums.
- Repeal of the ACA plus block grants to states for Medicaid and Children’s Health Insurance Program (CHIP).
- Repeal plus promotion of selling health insurance across state lines.
Not surprisingly, all four scenarios resulted in significant increases in out-of-pocket expenses for those in individual insurance plans.13
Although at the time of writing, the “replace” segment of “repeal-and-replace” is not known, Mr. Trump’s nominee for Secretary of Health and Human Services (HHS), Rep. Tom Price (R-Ga.), has given a hint of what he would champion based on his prior legislative proposals. Along with his support of increasing accessibility of armor-piercing bullets, reduced regulations on cigars, and opposition to expanding the State Children’s Health Insurance Program, he proposed H.R. 2300, “Empower Patients First Act.” This would eliminate the ACA’s Medicaid expansion and replace it with flat tax credits based on age, not income, which turns out to offer greater subsidies relative to income for those with higher incomes. A 30-year-old would, on average, face a premium bill of $2,532, along with a potential out-of-pocket liability of $7,000, with only a $1,200 credit to cover this from Mr. Price’s plan.14
In sum
So what’s a conscientious advocate for the physical and financial health of patients to do? Beyond political action, hospitalists need to keep abreast of the effect of changes in health care policy on their patients, as unpleasant as it may be. Do you know what the copays and out-of-pocket costs are for your patient’s (or your own) health care? Knowing how your recommendations for treatment and follow-up affect your patient’s pocketbook will not only help protect their finances, but will also protect their health, as people are less likely to be compliant with treatment if it involves out-of-pocket costs.
And easy as it would be to simply tune out the partisan rancor, stay engaged as a citizen, if for nothing else, the benefit of your patients.
Dr. Chang is pediatric editor of The Hospitalist. He is associate clinical professor of pediatrics at the University of Massachusetts, Worcester, and chief of pediatric hospital medicine at Baystate Children's Hospital, Springfield, Mass. Send comments and questions to [email protected].
References
1. Horton R. Offline: Looking forward to Donald Trump. The Lancet. 2016;388[10061]:2726.
2. Page L. What Donald Trump would do with the US healthcare system. BMJ. 2016;353:i2996.
3. Uberoi N, Finegold, K. and Gee, E. Health Insurance Coverage and the Affordable Care Act, 2010-2016. Department of Health and Human Services, ASPE Issue Brief, 2016 March 3.
4. Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health Benefits In 2016: Family Premiums Rose Modestly, And Offer Rates Remained Stable. Health Aff (Millwood). 2016 Sep. doi: 10.1377/hlthaff.2016.0951.
5. Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff (Millwood). 2008;27:w318-327.
6. Waters H, Steinhardt L, Oliver TR, Burton A, Milner S. The costs of non-insurance in Maryland. J Health Care Poor Underserved. 2007 Feb;18[1]:139-51.
7. Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14[4]:2259-63.
8. Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57[4]:601-7.
9. Collins SR, Gunja M, Beutel S. How Will the Affordable Care Act’s Cost-Sharing Reductions Affect Consumers’ Out-of-Pocket Costs in 2016? Issue Brief (Commonw Fund) 2016;6:1-17.
10. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6[2]:100-6.
11. Antos J CJ. The House Republicans’ Health Plan. Bethesda, MD: Health Affairs Blog, Project HOPE; 2016 June 22.
12. Fronstin P, Roebuck MC. Health care spending after adopting a full-replacement, high-deductible health plan with a health savings account: a five-year study. EBRI Issue Brief 2013 July:3-15.
13. Saltzman E EC. Donald Trump’s Health Care Reform Proposals: Anticipated Effects on Insurance Coverage, Out-of-Pocket Costs, and the Federal Deficit. The Commonwealth Fund September 2016.
14. Glied SA, Frank RG. Care for the Vulnerable vs. Cash for the Powerful – Trump’s Pick for HHS. N Engl J Med. 2017;376:103-5.
No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2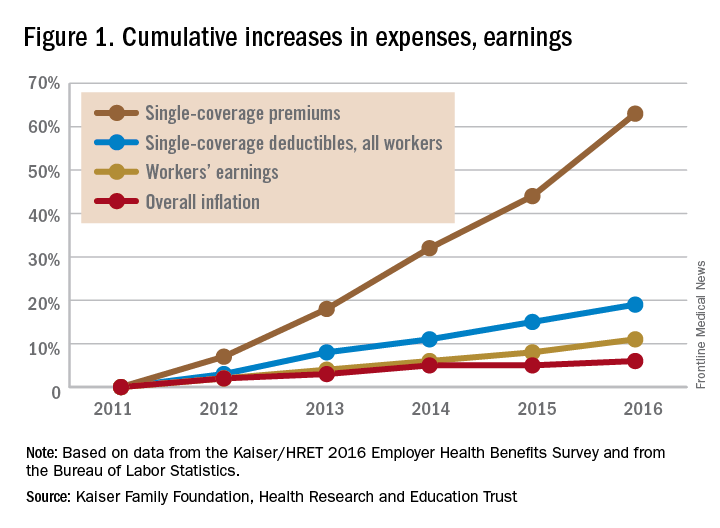
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10
It seems unlikely that a Republican-led government will pursue efforts to decrease out-of-pocket expenses. More likely, new proposals will aim to provide tax benefits to encourage use of health savings accounts (HSAs), continuing the shift of health care to employees.11 HSAs benefit employers, who pay less for the health care costs of employees, but are associated with worsened adherence to recommended treatments for patients.8,12
A 2016 study analyzed health care policies considered by Trump, including the following:
- Full repeal of the ACA.
- Repeal of the ACA plus tax deductions of health insurance premiums.
- Repeal of the ACA plus block grants to states for Medicaid and Children’s Health Insurance Program (CHIP).
- Repeal plus promotion of selling health insurance across state lines.
Not surprisingly, all four scenarios resulted in significant increases in out-of-pocket expenses for those in individual insurance plans.13
Although at the time of writing, the “replace” segment of “repeal-and-replace” is not known, Mr. Trump’s nominee for Secretary of Health and Human Services (HHS), Rep. Tom Price (R-Ga.), has given a hint of what he would champion based on his prior legislative proposals. Along with his support of increasing accessibility of armor-piercing bullets, reduced regulations on cigars, and opposition to expanding the State Children’s Health Insurance Program, he proposed H.R. 2300, “Empower Patients First Act.” This would eliminate the ACA’s Medicaid expansion and replace it with flat tax credits based on age, not income, which turns out to offer greater subsidies relative to income for those with higher incomes. A 30-year-old would, on average, face a premium bill of $2,532, along with a potential out-of-pocket liability of $7,000, with only a $1,200 credit to cover this from Mr. Price’s plan.14
In sum
So what’s a conscientious advocate for the physical and financial health of patients to do? Beyond political action, hospitalists need to keep abreast of the effect of changes in health care policy on their patients, as unpleasant as it may be. Do you know what the copays and out-of-pocket costs are for your patient’s (or your own) health care? Knowing how your recommendations for treatment and follow-up affect your patient’s pocketbook will not only help protect their finances, but will also protect their health, as people are less likely to be compliant with treatment if it involves out-of-pocket costs.
And easy as it would be to simply tune out the partisan rancor, stay engaged as a citizen, if for nothing else, the benefit of your patients.
Dr. Chang is pediatric editor of The Hospitalist. He is associate clinical professor of pediatrics at the University of Massachusetts, Worcester, and chief of pediatric hospital medicine at Baystate Children's Hospital, Springfield, Mass. Send comments and questions to [email protected].
References
1. Horton R. Offline: Looking forward to Donald Trump. The Lancet. 2016;388[10061]:2726.
2. Page L. What Donald Trump would do with the US healthcare system. BMJ. 2016;353:i2996.
3. Uberoi N, Finegold, K. and Gee, E. Health Insurance Coverage and the Affordable Care Act, 2010-2016. Department of Health and Human Services, ASPE Issue Brief, 2016 March 3.
4. Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health Benefits In 2016: Family Premiums Rose Modestly, And Offer Rates Remained Stable. Health Aff (Millwood). 2016 Sep. doi: 10.1377/hlthaff.2016.0951.
5. Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff (Millwood). 2008;27:w318-327.
6. Waters H, Steinhardt L, Oliver TR, Burton A, Milner S. The costs of non-insurance in Maryland. J Health Care Poor Underserved. 2007 Feb;18[1]:139-51.
7. Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14[4]:2259-63.
8. Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57[4]:601-7.
9. Collins SR, Gunja M, Beutel S. How Will the Affordable Care Act’s Cost-Sharing Reductions Affect Consumers’ Out-of-Pocket Costs in 2016? Issue Brief (Commonw Fund) 2016;6:1-17.
10. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6[2]:100-6.
11. Antos J CJ. The House Republicans’ Health Plan. Bethesda, MD: Health Affairs Blog, Project HOPE; 2016 June 22.
12. Fronstin P, Roebuck MC. Health care spending after adopting a full-replacement, high-deductible health plan with a health savings account: a five-year study. EBRI Issue Brief 2013 July:3-15.
13. Saltzman E EC. Donald Trump’s Health Care Reform Proposals: Anticipated Effects on Insurance Coverage, Out-of-Pocket Costs, and the Federal Deficit. The Commonwealth Fund September 2016.
14. Glied SA, Frank RG. Care for the Vulnerable vs. Cash for the Powerful – Trump’s Pick for HHS. N Engl J Med. 2017;376:103-5.


















