User login
PPI-responsive eosinophilic esophagitis may be misnomer
PHILADELPHIA – Eosinophilic esophagitis (EoE) responsive to a proton pump inhibitor (PPI) has been characterized as PPI-responsive esophageal eosinophilia (PPI-REE), but there is no compelling evidence that it is a distinct EoE subgroup, according to an expert who updated current thinking about this disease at Digestive Diseases: New Advances.
“Multivariate analyses have not identified any feature that distinguishes PPI-REE from EoE. Why? Because they are probably the same disorder,” reported Stuart J. Spechler, MD, AGAF, codirector of the center for esophageal diseases at Baylor University Medical Center at Dallas.
Although it is true that only a subset of EoE patients respond to PPIs, few therapies are effective for all patients in any disease Dr. Spechler observed. As an example, he noted that ulcerative colitis patients who respond to sulfasalazine are not subclassified as sulfasalazine-responsive ulcerative colitis.
“I do think the term PPI-REE should be retired, although I acknowledge that not everyone in this field is ready to agree,” Dr. Spechler said at the meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The confusion regarding PPI responsiveness in EoE has been driven by the fact that acid control has been widely regarded as the only pertinent mechanism of action from PPIs. Although coexisting gastroesophageal reflux disease could explain symptom relief in some patients with EoE, no evidence of excess acid is found in many responders. Detailed evaluations of the PPI-REE subgroup relative to EOE overall emphasize this point, according to Dr. Spechler.
“Studies have shown that the clinical, endoscopic, histologic, and gene expression features of these two disorders are identical,” he reported.
The lack of distinction is now easier to understand with a growing body of evidence that PPIs have acid-independent effects relevant to benefit in EoE, according to Dr. Spechler. Tracing the advances in understanding the pathogenesis in EoE since it was first described in 1978, Dr. Spechler explained that EoE is now understood to be an antigen-driven expression of food allergy related to up-regulation of the Th2 helper adaptive response. After briefly reviewing several potential anti-inflammatory effects of PPIs, Dr. Spechler focused on evidence that PPIs inhibit the adhesion molecule eotaxin-3.
Specifically, when squamous cells from EoE patients are exposed to the cytokine interleukin-4 (IL-4), “production of eotaxin-3 is increased dramatically but you can block that cytokine Th2 stimulation with [the PPI] omeprazole,” said Dr. Spechler, citing published work by Edaire Cheng, MD, a researcher with whom he has collaborated at the University of Texas Southwestern Medical School, Dallas. This is a potentially important observation, because up-regulation of eotaxin-3 is considered a critical molecular event for the activation of eosinophils and their migration.
The relative importance of this specific mechanism for explaining the benefits of PPIs in EoE requires additional confirmation, but Dr. Spechler indicated that there is strong evidence of acid-independent effects from PPIs. In fact, in outlining an algorithm for treatment of EoE, he listed a trial of PPIs as a reasonable first choice.
“In my opinion, the major reason that we created an arbitrary distinction is this persistent notion that acid inhibition is the only possible therapeutic effect of PPIs,” Dr. Spechler reported. “I hope I have convinced you otherwise.”
In his brief update of EoE treatment in 2017, Dr. Spechler identified a trial of PPIs as first line “simply because they work.” However PPIs have been rendered even more attractive by the evidence of a plausible mechanism of action in EoE. Conversely, he cautioned that steroids are “just a band-aid” because “they cover up the allergy but the allergy remains.” Ultimately, while PPIs are a reasonable first-line therapy to control symptoms, Dr. Spechler suggested that elimination diets are ultimately the best strategy for treating the underlying cause of EoE.
Dr. Spechler reported a financial relationship with Ironwood Pharmaceuticals.
PHILADELPHIA – Eosinophilic esophagitis (EoE) responsive to a proton pump inhibitor (PPI) has been characterized as PPI-responsive esophageal eosinophilia (PPI-REE), but there is no compelling evidence that it is a distinct EoE subgroup, according to an expert who updated current thinking about this disease at Digestive Diseases: New Advances.
“Multivariate analyses have not identified any feature that distinguishes PPI-REE from EoE. Why? Because they are probably the same disorder,” reported Stuart J. Spechler, MD, AGAF, codirector of the center for esophageal diseases at Baylor University Medical Center at Dallas.
Although it is true that only a subset of EoE patients respond to PPIs, few therapies are effective for all patients in any disease Dr. Spechler observed. As an example, he noted that ulcerative colitis patients who respond to sulfasalazine are not subclassified as sulfasalazine-responsive ulcerative colitis.
“I do think the term PPI-REE should be retired, although I acknowledge that not everyone in this field is ready to agree,” Dr. Spechler said at the meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The confusion regarding PPI responsiveness in EoE has been driven by the fact that acid control has been widely regarded as the only pertinent mechanism of action from PPIs. Although coexisting gastroesophageal reflux disease could explain symptom relief in some patients with EoE, no evidence of excess acid is found in many responders. Detailed evaluations of the PPI-REE subgroup relative to EOE overall emphasize this point, according to Dr. Spechler.
“Studies have shown that the clinical, endoscopic, histologic, and gene expression features of these two disorders are identical,” he reported.
The lack of distinction is now easier to understand with a growing body of evidence that PPIs have acid-independent effects relevant to benefit in EoE, according to Dr. Spechler. Tracing the advances in understanding the pathogenesis in EoE since it was first described in 1978, Dr. Spechler explained that EoE is now understood to be an antigen-driven expression of food allergy related to up-regulation of the Th2 helper adaptive response. After briefly reviewing several potential anti-inflammatory effects of PPIs, Dr. Spechler focused on evidence that PPIs inhibit the adhesion molecule eotaxin-3.
Specifically, when squamous cells from EoE patients are exposed to the cytokine interleukin-4 (IL-4), “production of eotaxin-3 is increased dramatically but you can block that cytokine Th2 stimulation with [the PPI] omeprazole,” said Dr. Spechler, citing published work by Edaire Cheng, MD, a researcher with whom he has collaborated at the University of Texas Southwestern Medical School, Dallas. This is a potentially important observation, because up-regulation of eotaxin-3 is considered a critical molecular event for the activation of eosinophils and their migration.
The relative importance of this specific mechanism for explaining the benefits of PPIs in EoE requires additional confirmation, but Dr. Spechler indicated that there is strong evidence of acid-independent effects from PPIs. In fact, in outlining an algorithm for treatment of EoE, he listed a trial of PPIs as a reasonable first choice.
“In my opinion, the major reason that we created an arbitrary distinction is this persistent notion that acid inhibition is the only possible therapeutic effect of PPIs,” Dr. Spechler reported. “I hope I have convinced you otherwise.”
In his brief update of EoE treatment in 2017, Dr. Spechler identified a trial of PPIs as first line “simply because they work.” However PPIs have been rendered even more attractive by the evidence of a plausible mechanism of action in EoE. Conversely, he cautioned that steroids are “just a band-aid” because “they cover up the allergy but the allergy remains.” Ultimately, while PPIs are a reasonable first-line therapy to control symptoms, Dr. Spechler suggested that elimination diets are ultimately the best strategy for treating the underlying cause of EoE.
Dr. Spechler reported a financial relationship with Ironwood Pharmaceuticals.
PHILADELPHIA – Eosinophilic esophagitis (EoE) responsive to a proton pump inhibitor (PPI) has been characterized as PPI-responsive esophageal eosinophilia (PPI-REE), but there is no compelling evidence that it is a distinct EoE subgroup, according to an expert who updated current thinking about this disease at Digestive Diseases: New Advances.
“Multivariate analyses have not identified any feature that distinguishes PPI-REE from EoE. Why? Because they are probably the same disorder,” reported Stuart J. Spechler, MD, AGAF, codirector of the center for esophageal diseases at Baylor University Medical Center at Dallas.
Although it is true that only a subset of EoE patients respond to PPIs, few therapies are effective for all patients in any disease Dr. Spechler observed. As an example, he noted that ulcerative colitis patients who respond to sulfasalazine are not subclassified as sulfasalazine-responsive ulcerative colitis.
“I do think the term PPI-REE should be retired, although I acknowledge that not everyone in this field is ready to agree,” Dr. Spechler said at the meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The confusion regarding PPI responsiveness in EoE has been driven by the fact that acid control has been widely regarded as the only pertinent mechanism of action from PPIs. Although coexisting gastroesophageal reflux disease could explain symptom relief in some patients with EoE, no evidence of excess acid is found in many responders. Detailed evaluations of the PPI-REE subgroup relative to EOE overall emphasize this point, according to Dr. Spechler.
“Studies have shown that the clinical, endoscopic, histologic, and gene expression features of these two disorders are identical,” he reported.
The lack of distinction is now easier to understand with a growing body of evidence that PPIs have acid-independent effects relevant to benefit in EoE, according to Dr. Spechler. Tracing the advances in understanding the pathogenesis in EoE since it was first described in 1978, Dr. Spechler explained that EoE is now understood to be an antigen-driven expression of food allergy related to up-regulation of the Th2 helper adaptive response. After briefly reviewing several potential anti-inflammatory effects of PPIs, Dr. Spechler focused on evidence that PPIs inhibit the adhesion molecule eotaxin-3.
Specifically, when squamous cells from EoE patients are exposed to the cytokine interleukin-4 (IL-4), “production of eotaxin-3 is increased dramatically but you can block that cytokine Th2 stimulation with [the PPI] omeprazole,” said Dr. Spechler, citing published work by Edaire Cheng, MD, a researcher with whom he has collaborated at the University of Texas Southwestern Medical School, Dallas. This is a potentially important observation, because up-regulation of eotaxin-3 is considered a critical molecular event for the activation of eosinophils and their migration.
The relative importance of this specific mechanism for explaining the benefits of PPIs in EoE requires additional confirmation, but Dr. Spechler indicated that there is strong evidence of acid-independent effects from PPIs. In fact, in outlining an algorithm for treatment of EoE, he listed a trial of PPIs as a reasonable first choice.
“In my opinion, the major reason that we created an arbitrary distinction is this persistent notion that acid inhibition is the only possible therapeutic effect of PPIs,” Dr. Spechler reported. “I hope I have convinced you otherwise.”
In his brief update of EoE treatment in 2017, Dr. Spechler identified a trial of PPIs as first line “simply because they work.” However PPIs have been rendered even more attractive by the evidence of a plausible mechanism of action in EoE. Conversely, he cautioned that steroids are “just a band-aid” because “they cover up the allergy but the allergy remains.” Ultimately, while PPIs are a reasonable first-line therapy to control symptoms, Dr. Spechler suggested that elimination diets are ultimately the best strategy for treating the underlying cause of EoE.
Dr. Spechler reported a financial relationship with Ironwood Pharmaceuticals.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Second-Generation Hydrogel Coils May Improve Treatment of Aneurysms
HOUSTON—Compared with standard platinum coils, second-generation hydrogel coils decrease the likelihood of adverse outcomes in the endovascular treatment of medium-sized intracranial aneurysms, according to research presented at the International Stroke Conference 2017. Hydrogel coils provide greater packing density and are associated with decreased risks of aneurysm recurrence and retreatment, compared with standard coils, according to the researchers.
Approximately 85% of subarachnoid hemorrhages result from ruptured intracranial aneurysms, which can be detected with CT angiography. A randomized controlled trial published in 2002 demonstrated that endovascular coiling was superior to neurosurgical clipping in the treatment of ruptured aneurysms. A drawback of coiling, however, is that it entails a relatively high rate of aneurysm recurrence. A novel approach adds a soft hydrogel filament into platinum coils. The hydrogel, once in contact with liquid, increases in volume, resulting in a greater fill of the underlying aneurysm.
Between October 2009 and February 2014, Prof. Taschner and colleagues randomized 513 participants, and 29 patients were excluded from the analysis. The analysis included 243 patients treated with hydrogel coils and 241 patients treated with platinum coils. Of this population, 208 participants (43%) were treated for ruptured aneurysms.
Mean packing density was significantly higher in patients treated with hydrogel coils (39%), compared with patients treated with platinum coils (31%). At 18 months, the major recurrence rate was 12% in patients receiving hydrogel coils and 18% in patients receiving platinum coils. The retreatment rate at 18 months was 3% in patients receiving hydrogel coils and 6% in patients receiving platinum coils. The researchers found no difference in modified Rankin Scale score or mortality rate between groups.
In total, 45 patients in the hydrogel coil group and 66 controls had an adverse composite primary outcome. The hydrogel coils thus reduced the proportion of adverse composite primary outcomes, compared with platinum coils, by 8.4%, said Prof. Taschner.
—Erik Greb
Suggested Reading
Gaba RC, Ansari SA, Roy SS, et al. Embolization of intracranial aneurysms with hydrogel-coated coils versus inert platinum coils: effects on packing density, coil length and quantity, procedure performance, cost, length of hospital stay, and durability of therapy. Stroke. 2006;37(6):1443-1450.
Molyneux AJ, Kerr RS, Yu LM, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366(9488):809-817.
White PM, Lewis SC, Gholkar A, et al. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet. 2011;377(9778):1655-1662.
HOUSTON—Compared with standard platinum coils, second-generation hydrogel coils decrease the likelihood of adverse outcomes in the endovascular treatment of medium-sized intracranial aneurysms, according to research presented at the International Stroke Conference 2017. Hydrogel coils provide greater packing density and are associated with decreased risks of aneurysm recurrence and retreatment, compared with standard coils, according to the researchers.
Approximately 85% of subarachnoid hemorrhages result from ruptured intracranial aneurysms, which can be detected with CT angiography. A randomized controlled trial published in 2002 demonstrated that endovascular coiling was superior to neurosurgical clipping in the treatment of ruptured aneurysms. A drawback of coiling, however, is that it entails a relatively high rate of aneurysm recurrence. A novel approach adds a soft hydrogel filament into platinum coils. The hydrogel, once in contact with liquid, increases in volume, resulting in a greater fill of the underlying aneurysm.
Between October 2009 and February 2014, Prof. Taschner and colleagues randomized 513 participants, and 29 patients were excluded from the analysis. The analysis included 243 patients treated with hydrogel coils and 241 patients treated with platinum coils. Of this population, 208 participants (43%) were treated for ruptured aneurysms.
Mean packing density was significantly higher in patients treated with hydrogel coils (39%), compared with patients treated with platinum coils (31%). At 18 months, the major recurrence rate was 12% in patients receiving hydrogel coils and 18% in patients receiving platinum coils. The retreatment rate at 18 months was 3% in patients receiving hydrogel coils and 6% in patients receiving platinum coils. The researchers found no difference in modified Rankin Scale score or mortality rate between groups.
In total, 45 patients in the hydrogel coil group and 66 controls had an adverse composite primary outcome. The hydrogel coils thus reduced the proportion of adverse composite primary outcomes, compared with platinum coils, by 8.4%, said Prof. Taschner.
—Erik Greb
Suggested Reading
Gaba RC, Ansari SA, Roy SS, et al. Embolization of intracranial aneurysms with hydrogel-coated coils versus inert platinum coils: effects on packing density, coil length and quantity, procedure performance, cost, length of hospital stay, and durability of therapy. Stroke. 2006;37(6):1443-1450.
Molyneux AJ, Kerr RS, Yu LM, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366(9488):809-817.
White PM, Lewis SC, Gholkar A, et al. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet. 2011;377(9778):1655-1662.
HOUSTON—Compared with standard platinum coils, second-generation hydrogel coils decrease the likelihood of adverse outcomes in the endovascular treatment of medium-sized intracranial aneurysms, according to research presented at the International Stroke Conference 2017. Hydrogel coils provide greater packing density and are associated with decreased risks of aneurysm recurrence and retreatment, compared with standard coils, according to the researchers.
Approximately 85% of subarachnoid hemorrhages result from ruptured intracranial aneurysms, which can be detected with CT angiography. A randomized controlled trial published in 2002 demonstrated that endovascular coiling was superior to neurosurgical clipping in the treatment of ruptured aneurysms. A drawback of coiling, however, is that it entails a relatively high rate of aneurysm recurrence. A novel approach adds a soft hydrogel filament into platinum coils. The hydrogel, once in contact with liquid, increases in volume, resulting in a greater fill of the underlying aneurysm.
Between October 2009 and February 2014, Prof. Taschner and colleagues randomized 513 participants, and 29 patients were excluded from the analysis. The analysis included 243 patients treated with hydrogel coils and 241 patients treated with platinum coils. Of this population, 208 participants (43%) were treated for ruptured aneurysms.
Mean packing density was significantly higher in patients treated with hydrogel coils (39%), compared with patients treated with platinum coils (31%). At 18 months, the major recurrence rate was 12% in patients receiving hydrogel coils and 18% in patients receiving platinum coils. The retreatment rate at 18 months was 3% in patients receiving hydrogel coils and 6% in patients receiving platinum coils. The researchers found no difference in modified Rankin Scale score or mortality rate between groups.
In total, 45 patients in the hydrogel coil group and 66 controls had an adverse composite primary outcome. The hydrogel coils thus reduced the proportion of adverse composite primary outcomes, compared with platinum coils, by 8.4%, said Prof. Taschner.
—Erik Greb
Suggested Reading
Gaba RC, Ansari SA, Roy SS, et al. Embolization of intracranial aneurysms with hydrogel-coated coils versus inert platinum coils: effects on packing density, coil length and quantity, procedure performance, cost, length of hospital stay, and durability of therapy. Stroke. 2006;37(6):1443-1450.
Molyneux AJ, Kerr RS, Yu LM, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366(9488):809-817.
White PM, Lewis SC, Gholkar A, et al. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet. 2011;377(9778):1655-1662.
Make the Diagnosis - April 2017
Trichomycosis axillaris
Trichomycosis axillaris (TA) is a bacterial infection of the genus Corynebacterium that affects hairs in the axilla. Predisposing factors include poor local hygiene, hyperhidrosis, obesity, and warm, humid climates. Gram-positive diphtheroids, classically Corynebacterium tenuis, mix with sweat on hair shafts and subsequently produce a cementing material. In the majority of cases, bacterial infection causes keratin damage to the hair shaft with sparing of the cortex. However, recent cases have reported significant invasion of the hair cortex by bacterial structures.
TA is often a clinical diagnosis. Histopathology reveals a discontinuous thick-layer coating of bacterial structures adhered to the hair shafts. Periodic acid–Schiff, gram, and Grocott silver stains are all positive. Examination of hairs with 20% hydrogen peroxide solution can provide a microscopic diagnosis. Wood lamp examination produces a weak, yellow fluorescence, and potassium hydroxide test demonstrates yellowish material of minimal translucency surrounding the hair cortex.
Complete resolution can be achieved by shaving off all the axillary hairs. It is imperative to maintain good hygiene and keep the area dry and clean. To prevent recurrence, topical benzoyl peroxide or topical antibiotics such as erythromycin and clindamycin can be applied. If axillary hyperhidrosis is concurrently present, aluminum chloride hexahydrate solution can decrease sweating and reduce the risk of bacterial regrowth. Injections of botulinum toxin can be used to treat the hyperhidrosis as well.
This patient responded well to topical erythromycin lotion.
This case and photo are courtesy of Jessica Cervantes, University of Miami Miller School of Medicine, and Dr. Bilu Martin.
Donna Bilu Martin, MD, is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/edermatologynews. To submit a case for possible publication, send an email to [email protected].
Trichomycosis axillaris
Trichomycosis axillaris (TA) is a bacterial infection of the genus Corynebacterium that affects hairs in the axilla. Predisposing factors include poor local hygiene, hyperhidrosis, obesity, and warm, humid climates. Gram-positive diphtheroids, classically Corynebacterium tenuis, mix with sweat on hair shafts and subsequently produce a cementing material. In the majority of cases, bacterial infection causes keratin damage to the hair shaft with sparing of the cortex. However, recent cases have reported significant invasion of the hair cortex by bacterial structures.
TA is often a clinical diagnosis. Histopathology reveals a discontinuous thick-layer coating of bacterial structures adhered to the hair shafts. Periodic acid–Schiff, gram, and Grocott silver stains are all positive. Examination of hairs with 20% hydrogen peroxide solution can provide a microscopic diagnosis. Wood lamp examination produces a weak, yellow fluorescence, and potassium hydroxide test demonstrates yellowish material of minimal translucency surrounding the hair cortex.
Complete resolution can be achieved by shaving off all the axillary hairs. It is imperative to maintain good hygiene and keep the area dry and clean. To prevent recurrence, topical benzoyl peroxide or topical antibiotics such as erythromycin and clindamycin can be applied. If axillary hyperhidrosis is concurrently present, aluminum chloride hexahydrate solution can decrease sweating and reduce the risk of bacterial regrowth. Injections of botulinum toxin can be used to treat the hyperhidrosis as well.
This patient responded well to topical erythromycin lotion.
This case and photo are courtesy of Jessica Cervantes, University of Miami Miller School of Medicine, and Dr. Bilu Martin.
Donna Bilu Martin, MD, is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/edermatologynews. To submit a case for possible publication, send an email to [email protected].
Trichomycosis axillaris
Trichomycosis axillaris (TA) is a bacterial infection of the genus Corynebacterium that affects hairs in the axilla. Predisposing factors include poor local hygiene, hyperhidrosis, obesity, and warm, humid climates. Gram-positive diphtheroids, classically Corynebacterium tenuis, mix with sweat on hair shafts and subsequently produce a cementing material. In the majority of cases, bacterial infection causes keratin damage to the hair shaft with sparing of the cortex. However, recent cases have reported significant invasion of the hair cortex by bacterial structures.
TA is often a clinical diagnosis. Histopathology reveals a discontinuous thick-layer coating of bacterial structures adhered to the hair shafts. Periodic acid–Schiff, gram, and Grocott silver stains are all positive. Examination of hairs with 20% hydrogen peroxide solution can provide a microscopic diagnosis. Wood lamp examination produces a weak, yellow fluorescence, and potassium hydroxide test demonstrates yellowish material of minimal translucency surrounding the hair cortex.
Complete resolution can be achieved by shaving off all the axillary hairs. It is imperative to maintain good hygiene and keep the area dry and clean. To prevent recurrence, topical benzoyl peroxide or topical antibiotics such as erythromycin and clindamycin can be applied. If axillary hyperhidrosis is concurrently present, aluminum chloride hexahydrate solution can decrease sweating and reduce the risk of bacterial regrowth. Injections of botulinum toxin can be used to treat the hyperhidrosis as well.
This patient responded well to topical erythromycin lotion.
This case and photo are courtesy of Jessica Cervantes, University of Miami Miller School of Medicine, and Dr. Bilu Martin.
Donna Bilu Martin, MD, is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/edermatologynews. To submit a case for possible publication, send an email to [email protected].
A 35-year-old male with no significant past medical history presented with the chief complaint of occasional malodorous “crust in his underarms.” He used no prior treatments, and he did report axillary hyperhidrosis.
Sublingual Apomorphine Film May Induce On State in Patients With Parkinson’s Disease
MIAMI—Among patients with Parkinson’s disease with well-defined morning off episodes, 83% achieved an on-medication state within 45 minutes of treatment with sublingual apomorphine film, according to research presented at the First Pan American Parkinson’s Disease and Movement Disorders Congress. Investigators presented preliminary results from an open-label dose titration phase of a phase III trial.
The sublingual apomorphine film, known as APL-130277, is being developed by Marlborough, Massachusetts-based Sunovion Pharmaceuticals. Apomorphine injected subcutaneously is approved for the acute, intermittent treatment of off episodes, but it is not widely used, possibly because of its parenteral administration, researchers have said. The dissolvable film consists of an apomorphine drug layer and a second layer that is designed to neutralize acid generation and enhance drug permeability. The film appeared to be effective in a phase II open-label study.
Daily Off Episodes
Participants were older than 18, had idiopathic Parkinson’s disease, and had a modified Hoehn and Yahr stage between 1 and 3 on medication. Participants were responsive to levodopa and had more than two hours of off time per day. Patients were receiving stable doses of levodopa–carbidopa. Investigators excluded patients with psychosis, dementia, or impulse control disorders; mouth cankers or sores; or prior treatment of Parkinson’s disease with a neurosurgical procedure, continuous subcutaneous apomorphine infusion, or levodopa–carbidopa enteral suspension. They also excluded patients who received subcutaneous apomorphine within seven days before screening or were taking 5-HT3 antagonists, dopamine antagonists (other than quetiapine or clozapine), or dopamine-depleting agents.
Three days prior to the dose-titration phase, patients initiated treatment with trimethobenzamide or domperidone, which may reduce nausea and vomiting that can occur during the initiation of apomorphine therapy. Patients arrived at a clinic in an off state, having not taken their regular morning levodopa dose or other adjunctive medication later than midnight, and received 10 mg of APL-130277. Investigators assessed patients using the Unified Parkinson’s Disease Rating Scale Part III prior to dosing and 15, 30, 45, 60, and 90 minutes after dosing. Patients who responded with a fully on response (ie, patients and investigators agreed that medication was benefiting mobility, stiffness, and slowness such that patients had adequate motor function to perform their normal daily activities) were considered to have completed the dose- titration phase and could proceed to randomization for the maintenance treatment phase. Patients who responded to a dose could try the next highest dose at a subsequent titration visit to assess the potential for an improved response at the higher dose. Doses increased by 5-mg increments up to 35 mg.
Of 76 patients who entered the dose-titration phase, 63 (83%) turned fully on with treatment. Among patients who turned fully on, 24 (38%) did so within 15 minutes, and 49 (78%) did so within 30 minutes. The median dose turning patients to fully on was 20 mg. Patients who turned fully on assessed time to onset as between five and 12 minutes.
Safety Data
In a presentation of preliminary safety data from the dose-titration phase, Stuart Isaacson, MD, Director of the Parkinson’s Disease and Movement Disorders Center of Boca Raton in Florida, and colleagues reported that five of the 76 patients who entered the dose-titration phase discontinued the trial due to adverse events—two due to nausea, one due to somnolence, one due to headache, and one due to presyncope. Another two patients withdrew consent, and nine patients who did not turn on at the 35-mg dose were discontinued from the trial. Other reported adverse events included dizziness, yawning, vomiting, and symptomatic hypotension. Most adverse events were considered mild. “In this preliminary analysis, APL-130277 was well tolerated in patients in the dose-titration phase,” Dr. Isaacson and colleagues concluded.
—Jake Remaly
Suggested Reading
Hauser RA, Olanow CW, Dzyngel B, et al. Sublingual apomorphine (APL-130277) for the acute conversion of OFF to ON in Parkinson’s disease. Mov Disord. 2016;31(9):1366-1372.
MIAMI—Among patients with Parkinson’s disease with well-defined morning off episodes, 83% achieved an on-medication state within 45 minutes of treatment with sublingual apomorphine film, according to research presented at the First Pan American Parkinson’s Disease and Movement Disorders Congress. Investigators presented preliminary results from an open-label dose titration phase of a phase III trial.
The sublingual apomorphine film, known as APL-130277, is being developed by Marlborough, Massachusetts-based Sunovion Pharmaceuticals. Apomorphine injected subcutaneously is approved for the acute, intermittent treatment of off episodes, but it is not widely used, possibly because of its parenteral administration, researchers have said. The dissolvable film consists of an apomorphine drug layer and a second layer that is designed to neutralize acid generation and enhance drug permeability. The film appeared to be effective in a phase II open-label study.
Daily Off Episodes
Participants were older than 18, had idiopathic Parkinson’s disease, and had a modified Hoehn and Yahr stage between 1 and 3 on medication. Participants were responsive to levodopa and had more than two hours of off time per day. Patients were receiving stable doses of levodopa–carbidopa. Investigators excluded patients with psychosis, dementia, or impulse control disorders; mouth cankers or sores; or prior treatment of Parkinson’s disease with a neurosurgical procedure, continuous subcutaneous apomorphine infusion, or levodopa–carbidopa enteral suspension. They also excluded patients who received subcutaneous apomorphine within seven days before screening or were taking 5-HT3 antagonists, dopamine antagonists (other than quetiapine or clozapine), or dopamine-depleting agents.
Three days prior to the dose-titration phase, patients initiated treatment with trimethobenzamide or domperidone, which may reduce nausea and vomiting that can occur during the initiation of apomorphine therapy. Patients arrived at a clinic in an off state, having not taken their regular morning levodopa dose or other adjunctive medication later than midnight, and received 10 mg of APL-130277. Investigators assessed patients using the Unified Parkinson’s Disease Rating Scale Part III prior to dosing and 15, 30, 45, 60, and 90 minutes after dosing. Patients who responded with a fully on response (ie, patients and investigators agreed that medication was benefiting mobility, stiffness, and slowness such that patients had adequate motor function to perform their normal daily activities) were considered to have completed the dose- titration phase and could proceed to randomization for the maintenance treatment phase. Patients who responded to a dose could try the next highest dose at a subsequent titration visit to assess the potential for an improved response at the higher dose. Doses increased by 5-mg increments up to 35 mg.
Of 76 patients who entered the dose-titration phase, 63 (83%) turned fully on with treatment. Among patients who turned fully on, 24 (38%) did so within 15 minutes, and 49 (78%) did so within 30 minutes. The median dose turning patients to fully on was 20 mg. Patients who turned fully on assessed time to onset as between five and 12 minutes.
Safety Data
In a presentation of preliminary safety data from the dose-titration phase, Stuart Isaacson, MD, Director of the Parkinson’s Disease and Movement Disorders Center of Boca Raton in Florida, and colleagues reported that five of the 76 patients who entered the dose-titration phase discontinued the trial due to adverse events—two due to nausea, one due to somnolence, one due to headache, and one due to presyncope. Another two patients withdrew consent, and nine patients who did not turn on at the 35-mg dose were discontinued from the trial. Other reported adverse events included dizziness, yawning, vomiting, and symptomatic hypotension. Most adverse events were considered mild. “In this preliminary analysis, APL-130277 was well tolerated in patients in the dose-titration phase,” Dr. Isaacson and colleagues concluded.
—Jake Remaly
Suggested Reading
Hauser RA, Olanow CW, Dzyngel B, et al. Sublingual apomorphine (APL-130277) for the acute conversion of OFF to ON in Parkinson’s disease. Mov Disord. 2016;31(9):1366-1372.
MIAMI—Among patients with Parkinson’s disease with well-defined morning off episodes, 83% achieved an on-medication state within 45 minutes of treatment with sublingual apomorphine film, according to research presented at the First Pan American Parkinson’s Disease and Movement Disorders Congress. Investigators presented preliminary results from an open-label dose titration phase of a phase III trial.
The sublingual apomorphine film, known as APL-130277, is being developed by Marlborough, Massachusetts-based Sunovion Pharmaceuticals. Apomorphine injected subcutaneously is approved for the acute, intermittent treatment of off episodes, but it is not widely used, possibly because of its parenteral administration, researchers have said. The dissolvable film consists of an apomorphine drug layer and a second layer that is designed to neutralize acid generation and enhance drug permeability. The film appeared to be effective in a phase II open-label study.
Daily Off Episodes
Participants were older than 18, had idiopathic Parkinson’s disease, and had a modified Hoehn and Yahr stage between 1 and 3 on medication. Participants were responsive to levodopa and had more than two hours of off time per day. Patients were receiving stable doses of levodopa–carbidopa. Investigators excluded patients with psychosis, dementia, or impulse control disorders; mouth cankers or sores; or prior treatment of Parkinson’s disease with a neurosurgical procedure, continuous subcutaneous apomorphine infusion, or levodopa–carbidopa enteral suspension. They also excluded patients who received subcutaneous apomorphine within seven days before screening or were taking 5-HT3 antagonists, dopamine antagonists (other than quetiapine or clozapine), or dopamine-depleting agents.
Three days prior to the dose-titration phase, patients initiated treatment with trimethobenzamide or domperidone, which may reduce nausea and vomiting that can occur during the initiation of apomorphine therapy. Patients arrived at a clinic in an off state, having not taken their regular morning levodopa dose or other adjunctive medication later than midnight, and received 10 mg of APL-130277. Investigators assessed patients using the Unified Parkinson’s Disease Rating Scale Part III prior to dosing and 15, 30, 45, 60, and 90 minutes after dosing. Patients who responded with a fully on response (ie, patients and investigators agreed that medication was benefiting mobility, stiffness, and slowness such that patients had adequate motor function to perform their normal daily activities) were considered to have completed the dose- titration phase and could proceed to randomization for the maintenance treatment phase. Patients who responded to a dose could try the next highest dose at a subsequent titration visit to assess the potential for an improved response at the higher dose. Doses increased by 5-mg increments up to 35 mg.
Of 76 patients who entered the dose-titration phase, 63 (83%) turned fully on with treatment. Among patients who turned fully on, 24 (38%) did so within 15 minutes, and 49 (78%) did so within 30 minutes. The median dose turning patients to fully on was 20 mg. Patients who turned fully on assessed time to onset as between five and 12 minutes.
Safety Data
In a presentation of preliminary safety data from the dose-titration phase, Stuart Isaacson, MD, Director of the Parkinson’s Disease and Movement Disorders Center of Boca Raton in Florida, and colleagues reported that five of the 76 patients who entered the dose-titration phase discontinued the trial due to adverse events—two due to nausea, one due to somnolence, one due to headache, and one due to presyncope. Another two patients withdrew consent, and nine patients who did not turn on at the 35-mg dose were discontinued from the trial. Other reported adverse events included dizziness, yawning, vomiting, and symptomatic hypotension. Most adverse events were considered mild. “In this preliminary analysis, APL-130277 was well tolerated in patients in the dose-titration phase,” Dr. Isaacson and colleagues concluded.
—Jake Remaly
Suggested Reading
Hauser RA, Olanow CW, Dzyngel B, et al. Sublingual apomorphine (APL-130277) for the acute conversion of OFF to ON in Parkinson’s disease. Mov Disord. 2016;31(9):1366-1372.
Down syndrome in adolescents
Teen years, no doubt, come with expected challenges. For teens with Down syndrome (DS), the challenges are exponentially greater. Although DS is associated with mental retardation, the vast majority of people with DS have only mild to moderate intellectual disability. Still, this can lead to a great deal of internal stress for the adolescent and anxiety and stress for the parents.
Many issues must be considered for the adolescent with DS. Annual surveillance changes as the child ages and the need for intervention do as well. For example, 50% of children with DS are born with congenital heart defect. During infancy, it is important to do echocardiograms to identify and follow specific lesions. Approximately 57% of adolescents with DS will develop mitral valve prolapse and 10% will develop aortic regurgitation.1 Therefore, close evaluation should be done, listening for new onset murmurs, clicks, and unexplained fatigue, and, if these are identified, an echocardiogram should be repeated.
Dysmorphic features such as midfacial hypoplasia, tonsillar hypertrophy, and narrow ear canals also lead to issues that develop in the adolescent years. Chronic otitis, conductive hearing loss because of chronic middle-ear effusion or impacted cerumen, and enlarged tonsils can result in obstructive sleep apnea. As individuals gain weight, these issues are further affected, and a sleep study may be required. Annual hearing screens are recommended.1
Musculoskeletal disorders such as ligamentous laxity and atlantoaxial instability can also present with complications in the adolescent years. Pes planus is a very common finding that can further lead to hip and knee pain. Obesity also further adds to its occurrence (14%-67%).3
Now, the most pressing and, likely, most overlooked issue is the issue of sexuality. We spend a great deal of time educating teens without DS about the risks of unprotected sex and exposures to STIs, but many assume that these issues do not affect teens with DS. Secondary sexual characteristics develop in the same manner and at the same age that they do in children without DS. Therefore, it is a safe assumption that sexual curiosity and arousal do as well. Given that there can be varying levels of mental impairment, the approach to sex education needs to be developmentally appropriate. Normalizing the feelings and having discussions on appropriate and inappropriate expression are important.
As with all teens, acceptance and inclusion are of utmost importance. Physical and learning disabilities set them apart despite shared sexual and emotional development. This can lead to anxiety, depression, and behavior issues. Understanding that these are real issues for the adolescent with DS is important when providing the appropriate resources and support.
Management of the menstrual cycle can add new challenges for both the adolescent and the parent and, thus, should be investigated during health maintenance visits. Amenorrhea can result from introduction of hormonal therapy and should be considered. Sexual abuse also is increased in this age group, so close supervision and awareness of this issue are important.
Assisting parents of children with DS through the teen years is imperative. Making them aware of local support groups and national organizations for children with disabilities will help them navigate these years. The American Academy of Pediatrics has guidelines for health maintenance for DS.2
Dr. Pearce is a pediatrician in Frankfort, Ill. She reported no relevant financial disclosures. Email her at [email protected]
References
1. J Pediatr Health Care. 2006 May-Jun;20(3):198-205.
2. Pediatrics. 2011. doi: 10.1542/peds.2011-1605.
3. Clin Obes. 2015;5(2):52-9.
Correction, 7/26/17: An earlier version of this article misstated a recommendation about radiologic evaluation of the cervical spine in asymptomatic children
Teen years, no doubt, come with expected challenges. For teens with Down syndrome (DS), the challenges are exponentially greater. Although DS is associated with mental retardation, the vast majority of people with DS have only mild to moderate intellectual disability. Still, this can lead to a great deal of internal stress for the adolescent and anxiety and stress for the parents.
Many issues must be considered for the adolescent with DS. Annual surveillance changes as the child ages and the need for intervention do as well. For example, 50% of children with DS are born with congenital heart defect. During infancy, it is important to do echocardiograms to identify and follow specific lesions. Approximately 57% of adolescents with DS will develop mitral valve prolapse and 10% will develop aortic regurgitation.1 Therefore, close evaluation should be done, listening for new onset murmurs, clicks, and unexplained fatigue, and, if these are identified, an echocardiogram should be repeated.
Dysmorphic features such as midfacial hypoplasia, tonsillar hypertrophy, and narrow ear canals also lead to issues that develop in the adolescent years. Chronic otitis, conductive hearing loss because of chronic middle-ear effusion or impacted cerumen, and enlarged tonsils can result in obstructive sleep apnea. As individuals gain weight, these issues are further affected, and a sleep study may be required. Annual hearing screens are recommended.1
Musculoskeletal disorders such as ligamentous laxity and atlantoaxial instability can also present with complications in the adolescent years. Pes planus is a very common finding that can further lead to hip and knee pain. Obesity also further adds to its occurrence (14%-67%).3
Now, the most pressing and, likely, most overlooked issue is the issue of sexuality. We spend a great deal of time educating teens without DS about the risks of unprotected sex and exposures to STIs, but many assume that these issues do not affect teens with DS. Secondary sexual characteristics develop in the same manner and at the same age that they do in children without DS. Therefore, it is a safe assumption that sexual curiosity and arousal do as well. Given that there can be varying levels of mental impairment, the approach to sex education needs to be developmentally appropriate. Normalizing the feelings and having discussions on appropriate and inappropriate expression are important.
As with all teens, acceptance and inclusion are of utmost importance. Physical and learning disabilities set them apart despite shared sexual and emotional development. This can lead to anxiety, depression, and behavior issues. Understanding that these are real issues for the adolescent with DS is important when providing the appropriate resources and support.
Management of the menstrual cycle can add new challenges for both the adolescent and the parent and, thus, should be investigated during health maintenance visits. Amenorrhea can result from introduction of hormonal therapy and should be considered. Sexual abuse also is increased in this age group, so close supervision and awareness of this issue are important.
Assisting parents of children with DS through the teen years is imperative. Making them aware of local support groups and national organizations for children with disabilities will help them navigate these years. The American Academy of Pediatrics has guidelines for health maintenance for DS.2
Dr. Pearce is a pediatrician in Frankfort, Ill. She reported no relevant financial disclosures. Email her at [email protected]
References
1. J Pediatr Health Care. 2006 May-Jun;20(3):198-205.
2. Pediatrics. 2011. doi: 10.1542/peds.2011-1605.
3. Clin Obes. 2015;5(2):52-9.
Correction, 7/26/17: An earlier version of this article misstated a recommendation about radiologic evaluation of the cervical spine in asymptomatic children
Teen years, no doubt, come with expected challenges. For teens with Down syndrome (DS), the challenges are exponentially greater. Although DS is associated with mental retardation, the vast majority of people with DS have only mild to moderate intellectual disability. Still, this can lead to a great deal of internal stress for the adolescent and anxiety and stress for the parents.
Many issues must be considered for the adolescent with DS. Annual surveillance changes as the child ages and the need for intervention do as well. For example, 50% of children with DS are born with congenital heart defect. During infancy, it is important to do echocardiograms to identify and follow specific lesions. Approximately 57% of adolescents with DS will develop mitral valve prolapse and 10% will develop aortic regurgitation.1 Therefore, close evaluation should be done, listening for new onset murmurs, clicks, and unexplained fatigue, and, if these are identified, an echocardiogram should be repeated.
Dysmorphic features such as midfacial hypoplasia, tonsillar hypertrophy, and narrow ear canals also lead to issues that develop in the adolescent years. Chronic otitis, conductive hearing loss because of chronic middle-ear effusion or impacted cerumen, and enlarged tonsils can result in obstructive sleep apnea. As individuals gain weight, these issues are further affected, and a sleep study may be required. Annual hearing screens are recommended.1
Musculoskeletal disorders such as ligamentous laxity and atlantoaxial instability can also present with complications in the adolescent years. Pes planus is a very common finding that can further lead to hip and knee pain. Obesity also further adds to its occurrence (14%-67%).3
Now, the most pressing and, likely, most overlooked issue is the issue of sexuality. We spend a great deal of time educating teens without DS about the risks of unprotected sex and exposures to STIs, but many assume that these issues do not affect teens with DS. Secondary sexual characteristics develop in the same manner and at the same age that they do in children without DS. Therefore, it is a safe assumption that sexual curiosity and arousal do as well. Given that there can be varying levels of mental impairment, the approach to sex education needs to be developmentally appropriate. Normalizing the feelings and having discussions on appropriate and inappropriate expression are important.
As with all teens, acceptance and inclusion are of utmost importance. Physical and learning disabilities set them apart despite shared sexual and emotional development. This can lead to anxiety, depression, and behavior issues. Understanding that these are real issues for the adolescent with DS is important when providing the appropriate resources and support.
Management of the menstrual cycle can add new challenges for both the adolescent and the parent and, thus, should be investigated during health maintenance visits. Amenorrhea can result from introduction of hormonal therapy and should be considered. Sexual abuse also is increased in this age group, so close supervision and awareness of this issue are important.
Assisting parents of children with DS through the teen years is imperative. Making them aware of local support groups and national organizations for children with disabilities will help them navigate these years. The American Academy of Pediatrics has guidelines for health maintenance for DS.2
Dr. Pearce is a pediatrician in Frankfort, Ill. She reported no relevant financial disclosures. Email her at [email protected]
References
1. J Pediatr Health Care. 2006 May-Jun;20(3):198-205.
2. Pediatrics. 2011. doi: 10.1542/peds.2011-1605.
3. Clin Obes. 2015;5(2):52-9.
Correction, 7/26/17: An earlier version of this article misstated a recommendation about radiologic evaluation of the cervical spine in asymptomatic children
The many faces of formaldehyde contact allergy
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
ATLANTA – Formaldehyde has various clinical presentations and variable thresholds to trigger allergic contact dermatitis, so it requires a high index of suspicion, according to Salma de la Feld, MD.
It may present as irritant contact dermatitis, allergic contact dermatitis (especially to the hands and face), airborne allergic contact dermatitis, or systemic allergic contact dermatitis (to aspartame).
From most-releasing to least-releasing, these chemicals include quaternium-15, diazolidinyl urea, DMDM hydantoin, imidazolidinyl urea, and bronopol. Exposure can come from personal care products, prescription topical steroids and acne creams, Brazilian hair keratin, cigarettes, and textiles made of blended fabrics, as well as occupations such as a leather handler, surgical nurse, pathology lab worker, and hairdresser.
“Patients can be allergic to either the formaldehyde that [a product] releases or the non–formaldehyde component or both,” said Dr. de la Feld, who is a dermatologist at Emory University, Atlanta.
Recent studies suggest that the formaldehyde allergen should be tested at 2% instead of at 1%. “You do get a few more irritant reactions [with this approach], but you’re also going to catch more people who have a true positive reaction,” she said. “If you see a borderline papule with a little pink, that might be an irritant. You want to test for the formaldehyde releasers. When you do have a positive reaction, you want to have a high index of suspicion. Patients have to be strict in what personal care products they’re using. Some people might be able to tolerate a low concentration of formaldehyde in some products and that magic number differs between patients.”
From a treatment standpoint, Dr. de la Feld advises patients to avoid all formaldehyde releasers and to wear 100% fabrics in an effort to steer clear of textile exposure. “I like to have people be really strict [in their avoidance] when they’re first starting out,” she said. “They don’t like it, but I’ll say, ‘You’re so itchy. Let’s start really strict to get you clear and better.’ Once they’re better and there’s that one moisturizing cream that they really love, then [you] can do a repeat open application test. If nothing happens, it’s probably safe. If [they] start getting red and itchy there, [they] should probably throw away that moisturizer.”
Fragrance
Fragrance, which was named Allergen of the Year in 2007, is another common contact allergen. An estimated 4%-11% of the worldwide population is allergic to fragrance mix, while 1.6%-10.8% is allergic to balsam of Peru. T.R.U.E. tests for the allergen often yield false-negative results. Clinicians who fail to test for fragrance mix 2 will miss about one-third of fragrance allergic contact dermatitis diagnoses. “If the distribution is scattered, you want to be suspicious for fragrance allergy,” Dr. de la Feld said. “Sometimes patients get exposed inadvertently by their significant other or by a family member who is spraying a fragrant product.” Treatment is avoidance. “You want to tell patients to look for products labeled as fragrance free,” she said. “ ‘Unscented’ does not count. When patients tell you that they’re not using any perfume, you want to ask them if they’ve put any on their clothes.”
Systemic contact dermatitis
Dr. de la Feld finished her presentation by discussing systemic contact dermatitis, which she defined as a rash from systemic exposure to an allergen in someone who was previously sensitized. Alternative names for the condition include endogenous contact eczema, systemically-induced contact dermatitis, and internal-external contact-type hypersensitivity. She acknowledged that not all dermatologists believe systemic contact dermatitis to be a true clinical condition, but she does.
“It’s most classically and commonly reported with nickel and balsam of Peru and more slowly with some other allergens,” she said. “It can have multiple clinical presentations, and it’s not always widespread.” The three most common presentations are dyshidrotic hand eczema, sites of prior contact dermatitis (from contact or patch test), and anogenital and/or flexural areas (Baboon syndrome). There are other reports of systemic contact dermatitis presenting as disseminated patchy dermatitis, generalized erythroderma, cheilitis, and lichen planus of the lip.
Dr. de la Feld reported having no relevant financial disclosures.
Correction, 3/28/17: In an earlier version of this article Dr. de la Feld's name was misstated in the photo caption.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
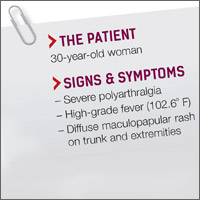
Severe polyarthralgia, high-grade fever, diffuse maculopapular rash on trunk and extremities • Dx?
THE CASE
A 30-year-old woman presented to our emergency department with severe polyarthralgia, a high-grade fever (102.6º F), and a diffuse maculopapular rash on her trunk and extremities. She had returned from her honeymoon in Jamaica 6 days earlier. During her time there, she ate local cuisine, hiked in the jungle, and was bitten by many mosquitoes. The patient was nauseous, and had been experiencing headaches, generalized weakness, and fatigue. Her physical exam revealed a maculopapular rash on her trunk and upper extremities. She had tenderness and pain, as well as decreased range of motion in her ankles, knees, and wrists. The patient had no erythema, swelling, petechiae, or bruising. She had a past medical history of Graves’ disease and had received all of her childhood immunizations.
THE DIAGNOSIS
Our lab work-up included a complete blood count, liver function tests, blood pathogens for malaria, and serologic tests for dengue fever, measles, mumps, rubella, Lyme disease, human immunodeficiency virus (HIV), and parvovirus. We ruled out dengue fever because the patient had no evidence of hemorrhage, thrombocytopenia, rising hematocrit, or neutropenia. HIV antibody screening tests were performed, although, in retrospect, confirmatory HIV quantitative RNA testing should’ve been obtained because of the acute nature of the patient’s symptoms. Regardless, the work-up was negative, with the exception of a positive parvovirus immunoglobulin G (IgG).
Given our patient’s travel history, unremarkable lab results, and physical exam (notably the rash and joint pain), we suspected that she was infected with the chikungunya virus and tested for it. The results of chikungunya serum titers returned 13 days later and were positive for both immunoglobulin M (IgM) and IgG, confirming our suspicion.
DISCUSSION
Chikungunya is a viral infection that is most commonly transmitted to humans via mosquitoes. The infection was first identified in West Africa in the mid-1900s and predominantly occurs in tropical and subtropical regions due to the numbers of mosquitoes in those areas. Since 2000, outbreaks have been most common in Africa and Asia, with the largest outbreaks occurring from 2005 to 2006.1,2 Chikungunya has since become more widespread in the Indian Ocean islands, and in 2013, it was first identified in the Caribbean islands. As of March 2017, over one million cases have been reported in the Americas, according to the Pan American Health Organization.3 In 2014, 12 locally transmitted cases were reported in Florida.4
The most common mosquito vectors for chikungunya are the Aedes albopictus (Asian tiger mosquito) and Aedes aegypti mosquitoes. These mosquitoes also transmit dengue fever, yellow fever, and Zika virus. Both of these mosquitoes are well-adapted to urban areas and can breed in standing water. A aegypti mosquitoes are found only in the southern United States, while A albopictus mosquitoes can be found in more temperate climates—areas like New York, New Jersey, and Pennsylvania.4 Both species are daytime biters, so their activity peaks during the dawn and dusk periods. Because local mosquito vectors exist as far north as New York, local transmission and outbreaks are possible in many parts of the United States.
When to suspect chikungunya, and what to look for
Suspect chikungunya in patients returning from endemic areas. After a 3- to 7-day incubation period, the clinical presentation of chikungunya typically begins with fever and malaise, followed by polyarthralgia that starts 2 to 5 days after the onset of fever. Headache, nausea, and conjunctivitis may also occur. Polyarthralgia and arthritis usually present in symmetrical distal joints and are accompanied by face and trunk flushing that is followed by a maculopapular rash. The rash predominantly appears on the trunk and limbs, but can also occur on the face, palms, and soles. Tendons and ligaments—especially the Achilles tendon—may become inflamed, as well. Symptoms typically resolve within 2 to 3 weeks, although polyarthralgia may last for months or even years.
There is no known risk of transmission through breast milk or in utero, although vertical transmission through vaginal or cesarean birth is common in viremic women. Blood-borne transmission can occur in the laboratory, nosocomially, or through the transfusion of blood products if exposure occurs during the early viremic phase.1,2 Dual infections are possible (typically with yellow fever, malaria, Zika virus, or dengue fever) and should be considered based on the patient’s travel history.5 Abnormal laboratory findings are less common, but may include lymphopenia (most common), thrombocytopenia, elevations in blood urea nitrogen and creatinine (indicating an acute kidney injury), and elevated liver transaminases.
Chikungunya is generally considered a self-limiting disease, but severe atypical manifestations can lead to meningoencephalitis, respiratory failure, and even death. Severe disease is more commonly seen in infants, patients over age 65 years, and in those with chronic medical conditions.
The differential diagnosis for chikungunya virus includes dengue fever, Zika virus, malaria, measles, rubella, parvovirus, primary HIV infection, Lyme disease, and other inflammatory joint conditions. The differential depends on where a patient lives, their travel history, and exposures.
Dengue and chikungunya have similar features, which often make them difficult to distinguish. However, patients with dengue fever present more often with neutropenia, thrombocytopenia, and signs or symptoms of shock or hemorrhage.6 The chikungunya rash is typically a maculopapular rash on the trunk, hands, and feet that appears within the first 2 days of illness, as opposed to dengue, which has a similar rash, but appears later in the disease (Days 2-5). Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) if dengue fever is suspected, as they can worsen hemorrhaging.7
Zika virus typically presents with milder symptoms compared to chikungunya. Patients may have a skin rash and occasionally, conjunctivitis, but limited high fevers or joint pain. Zika rash is maculopapular, but typically starts on the face on the first day of the illness. Zika has been associated with neurological complications such as Guillain-Barré syndrome and microcephaly in fetuses of infected pregnant woman.8
Choice of testing modality depends on when symptoms began
Laboratory diagnosis of chikungunya can be accomplished 3 ways: viral culture, reverse transcriptase-polymerase chain reaction (RT-PCR) viral RNA, and serology.1 The choice of which modality to use depends on the time between the onset of symptoms and the date on which a serum sample is drawn.
- If the patient presents within the first 3 days of illness, viral culture can detect chikungunya. Chikungunya virus testing is available through the Centers for Disease Control and Prevention (CDC), some state laboratories, and one commercial lab.8 Viral cultures are considered the gold standard for diagnosis, but a requirement for an elevated biosafety level, as well as a longer incubation time, make them less useful in the clinical setting.1,9
- If symptoms started less than 5 to 8 days prior, serum should be sent for RT-PCR for viral RNA.
- If symptoms occurred more than 8 days prior, serum should be sent for IgM and IgG serologic testing.
If the acute sample was negative (and chikungunya is still suspected), a second serum sample should be drawn 2 to 3 weeks later during the convalescent phase and sent for IgG serologic testing.
There are no specific treatments or vaccines available for chikungunya, but both live and inactivated vaccines are being tested. To prevent chikungunya virus infection, advise patients traveling to endemic areas to reduce mosquito exposure by avoiding outdoor activities during dusk and dawn, wearing long-sleeved shirts and long pants, and using an insect repellent that contains DEET. Recommend that patients who will be sleeping in a high-risk area use bed netting treated with permethrin. The CDC Web site has excellent additional information, available at http://www.cdc.gov/chikungunya.10
Our patient was briefly hospitalized due to intractable pain. She was discharged after 2 days and given prescriptions for motrin 800 mg and percocet 5/325 mg for breakthrough pain. Her wrist and ankle pain persisted after discharge, but slowly resolved after 2 to 3 months.
THE TAKEAWAY
Chikungunya is becoming more common among travelers returning to the United States from the Caribbean islands, and mosquito vectors found in parts of the United States are enhancing the possibility of local outbreaks. Travel to endemic regions—and the classic symptoms of fever, polyarthralgia, and a maculopapular ras
1. Pan American Health Organization. Preparedness and response for chikungunya virus: Introduction in the Americas. Washington, DC: Pan American Health Organization; 2011:1-149. Available at: http://www1.paho.org/hq/dmdocuments/CHIKV_English.pdf. Accessed March 8, 2017.
2. Enserink M. Infectious diseases. Chikungunya: no longer a third world disease. Science. 2007;318:1860-1861.
3. Pan American Health Organization. Number of reported cases of chikungunya fever in the Americas, by country or territory, 2017. Available at: http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&Itemid=270&gid=38489&lang=en. Accessed March 7, 2017.
4. Centers for Disease Control and Prevention. 2014 final data for the United States. Centers for Disease Control and Prevention Web site. Available at: https://www.cdc.gov/chikungunya/geo/united-states-2014.html. Accessed March 16, 2017.
5. Nayar SK, Noridah O, Paranthaman V, et al. Co-infection of dengue virus and chikungunya virus in two patients with acute febrile illness. Med J Malaysia. 2007;62:335-336.
6. Staples JE, Fischer M. Chikungunya virus in the Americas—what a vectorborne pathogen can do. N Engl J Med. 2014;371:887-889.
7. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition. Geneva: World Health Organization; 2009. Available at: http://www.who.int/tdr/publications/documents/dengue-diagnosis.pdf?ua=1. Accessed March 8, 2017.
8. Centers for Disease Control and Prevention. Chikungunya information for healthcare providers. 2014. Available at: https://www.cdc.gov/chikungunya/pdfs/chikv_clinicians.pdf. Accessed March 8, 2017.
9. Parida MM, Santhosh SR, Dash PK, et al. Rapid and real-time assays for detection and quantification of chikungunya virus. Future Virology. 2008;3:179-192.
10. Centers for Disease Control and Prevention. Chikungunya virus. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/chikungunya. Accessed February 26, 2015.
THE CASE
A 30-year-old woman presented to our emergency department with severe polyarthralgia, a high-grade fever (102.6º F), and a diffuse maculopapular rash on her trunk and extremities. She had returned from her honeymoon in Jamaica 6 days earlier. During her time there, she ate local cuisine, hiked in the jungle, and was bitten by many mosquitoes. The patient was nauseous, and had been experiencing headaches, generalized weakness, and fatigue. Her physical exam revealed a maculopapular rash on her trunk and upper extremities. She had tenderness and pain, as well as decreased range of motion in her ankles, knees, and wrists. The patient had no erythema, swelling, petechiae, or bruising. She had a past medical history of Graves’ disease and had received all of her childhood immunizations.
THE DIAGNOSIS
Our lab work-up included a complete blood count, liver function tests, blood pathogens for malaria, and serologic tests for dengue fever, measles, mumps, rubella, Lyme disease, human immunodeficiency virus (HIV), and parvovirus. We ruled out dengue fever because the patient had no evidence of hemorrhage, thrombocytopenia, rising hematocrit, or neutropenia. HIV antibody screening tests were performed, although, in retrospect, confirmatory HIV quantitative RNA testing should’ve been obtained because of the acute nature of the patient’s symptoms. Regardless, the work-up was negative, with the exception of a positive parvovirus immunoglobulin G (IgG).
Given our patient’s travel history, unremarkable lab results, and physical exam (notably the rash and joint pain), we suspected that she was infected with the chikungunya virus and tested for it. The results of chikungunya serum titers returned 13 days later and were positive for both immunoglobulin M (IgM) and IgG, confirming our suspicion.
DISCUSSION
Chikungunya is a viral infection that is most commonly transmitted to humans via mosquitoes. The infection was first identified in West Africa in the mid-1900s and predominantly occurs in tropical and subtropical regions due to the numbers of mosquitoes in those areas. Since 2000, outbreaks have been most common in Africa and Asia, with the largest outbreaks occurring from 2005 to 2006.1,2 Chikungunya has since become more widespread in the Indian Ocean islands, and in 2013, it was first identified in the Caribbean islands. As of March 2017, over one million cases have been reported in the Americas, according to the Pan American Health Organization.3 In 2014, 12 locally transmitted cases were reported in Florida.4
The most common mosquito vectors for chikungunya are the Aedes albopictus (Asian tiger mosquito) and Aedes aegypti mosquitoes. These mosquitoes also transmit dengue fever, yellow fever, and Zika virus. Both of these mosquitoes are well-adapted to urban areas and can breed in standing water. A aegypti mosquitoes are found only in the southern United States, while A albopictus mosquitoes can be found in more temperate climates—areas like New York, New Jersey, and Pennsylvania.4 Both species are daytime biters, so their activity peaks during the dawn and dusk periods. Because local mosquito vectors exist as far north as New York, local transmission and outbreaks are possible in many parts of the United States.
When to suspect chikungunya, and what to look for
Suspect chikungunya in patients returning from endemic areas. After a 3- to 7-day incubation period, the clinical presentation of chikungunya typically begins with fever and malaise, followed by polyarthralgia that starts 2 to 5 days after the onset of fever. Headache, nausea, and conjunctivitis may also occur. Polyarthralgia and arthritis usually present in symmetrical distal joints and are accompanied by face and trunk flushing that is followed by a maculopapular rash. The rash predominantly appears on the trunk and limbs, but can also occur on the face, palms, and soles. Tendons and ligaments—especially the Achilles tendon—may become inflamed, as well. Symptoms typically resolve within 2 to 3 weeks, although polyarthralgia may last for months or even years.
There is no known risk of transmission through breast milk or in utero, although vertical transmission through vaginal or cesarean birth is common in viremic women. Blood-borne transmission can occur in the laboratory, nosocomially, or through the transfusion of blood products if exposure occurs during the early viremic phase.1,2 Dual infections are possible (typically with yellow fever, malaria, Zika virus, or dengue fever) and should be considered based on the patient’s travel history.5 Abnormal laboratory findings are less common, but may include lymphopenia (most common), thrombocytopenia, elevations in blood urea nitrogen and creatinine (indicating an acute kidney injury), and elevated liver transaminases.
Chikungunya is generally considered a self-limiting disease, but severe atypical manifestations can lead to meningoencephalitis, respiratory failure, and even death. Severe disease is more commonly seen in infants, patients over age 65 years, and in those with chronic medical conditions.
The differential diagnosis for chikungunya virus includes dengue fever, Zika virus, malaria, measles, rubella, parvovirus, primary HIV infection, Lyme disease, and other inflammatory joint conditions. The differential depends on where a patient lives, their travel history, and exposures.
Dengue and chikungunya have similar features, which often make them difficult to distinguish. However, patients with dengue fever present more often with neutropenia, thrombocytopenia, and signs or symptoms of shock or hemorrhage.6 The chikungunya rash is typically a maculopapular rash on the trunk, hands, and feet that appears within the first 2 days of illness, as opposed to dengue, which has a similar rash, but appears later in the disease (Days 2-5). Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) if dengue fever is suspected, as they can worsen hemorrhaging.7
Zika virus typically presents with milder symptoms compared to chikungunya. Patients may have a skin rash and occasionally, conjunctivitis, but limited high fevers or joint pain. Zika rash is maculopapular, but typically starts on the face on the first day of the illness. Zika has been associated with neurological complications such as Guillain-Barré syndrome and microcephaly in fetuses of infected pregnant woman.8
Choice of testing modality depends on when symptoms began
Laboratory diagnosis of chikungunya can be accomplished 3 ways: viral culture, reverse transcriptase-polymerase chain reaction (RT-PCR) viral RNA, and serology.1 The choice of which modality to use depends on the time between the onset of symptoms and the date on which a serum sample is drawn.
- If the patient presents within the first 3 days of illness, viral culture can detect chikungunya. Chikungunya virus testing is available through the Centers for Disease Control and Prevention (CDC), some state laboratories, and one commercial lab.8 Viral cultures are considered the gold standard for diagnosis, but a requirement for an elevated biosafety level, as well as a longer incubation time, make them less useful in the clinical setting.1,9
- If symptoms started less than 5 to 8 days prior, serum should be sent for RT-PCR for viral RNA.
- If symptoms occurred more than 8 days prior, serum should be sent for IgM and IgG serologic testing.
If the acute sample was negative (and chikungunya is still suspected), a second serum sample should be drawn 2 to 3 weeks later during the convalescent phase and sent for IgG serologic testing.
There are no specific treatments or vaccines available for chikungunya, but both live and inactivated vaccines are being tested. To prevent chikungunya virus infection, advise patients traveling to endemic areas to reduce mosquito exposure by avoiding outdoor activities during dusk and dawn, wearing long-sleeved shirts and long pants, and using an insect repellent that contains DEET. Recommend that patients who will be sleeping in a high-risk area use bed netting treated with permethrin. The CDC Web site has excellent additional information, available at http://www.cdc.gov/chikungunya.10
Our patient was briefly hospitalized due to intractable pain. She was discharged after 2 days and given prescriptions for motrin 800 mg and percocet 5/325 mg for breakthrough pain. Her wrist and ankle pain persisted after discharge, but slowly resolved after 2 to 3 months.
THE TAKEAWAY
Chikungunya is becoming more common among travelers returning to the United States from the Caribbean islands, and mosquito vectors found in parts of the United States are enhancing the possibility of local outbreaks. Travel to endemic regions—and the classic symptoms of fever, polyarthralgia, and a maculopapular ras
THE CASE
A 30-year-old woman presented to our emergency department with severe polyarthralgia, a high-grade fever (102.6º F), and a diffuse maculopapular rash on her trunk and extremities. She had returned from her honeymoon in Jamaica 6 days earlier. During her time there, she ate local cuisine, hiked in the jungle, and was bitten by many mosquitoes. The patient was nauseous, and had been experiencing headaches, generalized weakness, and fatigue. Her physical exam revealed a maculopapular rash on her trunk and upper extremities. She had tenderness and pain, as well as decreased range of motion in her ankles, knees, and wrists. The patient had no erythema, swelling, petechiae, or bruising. She had a past medical history of Graves’ disease and had received all of her childhood immunizations.
THE DIAGNOSIS
Our lab work-up included a complete blood count, liver function tests, blood pathogens for malaria, and serologic tests for dengue fever, measles, mumps, rubella, Lyme disease, human immunodeficiency virus (HIV), and parvovirus. We ruled out dengue fever because the patient had no evidence of hemorrhage, thrombocytopenia, rising hematocrit, or neutropenia. HIV antibody screening tests were performed, although, in retrospect, confirmatory HIV quantitative RNA testing should’ve been obtained because of the acute nature of the patient’s symptoms. Regardless, the work-up was negative, with the exception of a positive parvovirus immunoglobulin G (IgG).
Given our patient’s travel history, unremarkable lab results, and physical exam (notably the rash and joint pain), we suspected that she was infected with the chikungunya virus and tested for it. The results of chikungunya serum titers returned 13 days later and were positive for both immunoglobulin M (IgM) and IgG, confirming our suspicion.
DISCUSSION
Chikungunya is a viral infection that is most commonly transmitted to humans via mosquitoes. The infection was first identified in West Africa in the mid-1900s and predominantly occurs in tropical and subtropical regions due to the numbers of mosquitoes in those areas. Since 2000, outbreaks have been most common in Africa and Asia, with the largest outbreaks occurring from 2005 to 2006.1,2 Chikungunya has since become more widespread in the Indian Ocean islands, and in 2013, it was first identified in the Caribbean islands. As of March 2017, over one million cases have been reported in the Americas, according to the Pan American Health Organization.3 In 2014, 12 locally transmitted cases were reported in Florida.4
The most common mosquito vectors for chikungunya are the Aedes albopictus (Asian tiger mosquito) and Aedes aegypti mosquitoes. These mosquitoes also transmit dengue fever, yellow fever, and Zika virus. Both of these mosquitoes are well-adapted to urban areas and can breed in standing water. A aegypti mosquitoes are found only in the southern United States, while A albopictus mosquitoes can be found in more temperate climates—areas like New York, New Jersey, and Pennsylvania.4 Both species are daytime biters, so their activity peaks during the dawn and dusk periods. Because local mosquito vectors exist as far north as New York, local transmission and outbreaks are possible in many parts of the United States.
When to suspect chikungunya, and what to look for
Suspect chikungunya in patients returning from endemic areas. After a 3- to 7-day incubation period, the clinical presentation of chikungunya typically begins with fever and malaise, followed by polyarthralgia that starts 2 to 5 days after the onset of fever. Headache, nausea, and conjunctivitis may also occur. Polyarthralgia and arthritis usually present in symmetrical distal joints and are accompanied by face and trunk flushing that is followed by a maculopapular rash. The rash predominantly appears on the trunk and limbs, but can also occur on the face, palms, and soles. Tendons and ligaments—especially the Achilles tendon—may become inflamed, as well. Symptoms typically resolve within 2 to 3 weeks, although polyarthralgia may last for months or even years.
There is no known risk of transmission through breast milk or in utero, although vertical transmission through vaginal or cesarean birth is common in viremic women. Blood-borne transmission can occur in the laboratory, nosocomially, or through the transfusion of blood products if exposure occurs during the early viremic phase.1,2 Dual infections are possible (typically with yellow fever, malaria, Zika virus, or dengue fever) and should be considered based on the patient’s travel history.5 Abnormal laboratory findings are less common, but may include lymphopenia (most common), thrombocytopenia, elevations in blood urea nitrogen and creatinine (indicating an acute kidney injury), and elevated liver transaminases.
Chikungunya is generally considered a self-limiting disease, but severe atypical manifestations can lead to meningoencephalitis, respiratory failure, and even death. Severe disease is more commonly seen in infants, patients over age 65 years, and in those with chronic medical conditions.
The differential diagnosis for chikungunya virus includes dengue fever, Zika virus, malaria, measles, rubella, parvovirus, primary HIV infection, Lyme disease, and other inflammatory joint conditions. The differential depends on where a patient lives, their travel history, and exposures.
Dengue and chikungunya have similar features, which often make them difficult to distinguish. However, patients with dengue fever present more often with neutropenia, thrombocytopenia, and signs or symptoms of shock or hemorrhage.6 The chikungunya rash is typically a maculopapular rash on the trunk, hands, and feet that appears within the first 2 days of illness, as opposed to dengue, which has a similar rash, but appears later in the disease (Days 2-5). Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) if dengue fever is suspected, as they can worsen hemorrhaging.7
Zika virus typically presents with milder symptoms compared to chikungunya. Patients may have a skin rash and occasionally, conjunctivitis, but limited high fevers or joint pain. Zika rash is maculopapular, but typically starts on the face on the first day of the illness. Zika has been associated with neurological complications such as Guillain-Barré syndrome and microcephaly in fetuses of infected pregnant woman.8
Choice of testing modality depends on when symptoms began
Laboratory diagnosis of chikungunya can be accomplished 3 ways: viral culture, reverse transcriptase-polymerase chain reaction (RT-PCR) viral RNA, and serology.1 The choice of which modality to use depends on the time between the onset of symptoms and the date on which a serum sample is drawn.
- If the patient presents within the first 3 days of illness, viral culture can detect chikungunya. Chikungunya virus testing is available through the Centers for Disease Control and Prevention (CDC), some state laboratories, and one commercial lab.8 Viral cultures are considered the gold standard for diagnosis, but a requirement for an elevated biosafety level, as well as a longer incubation time, make them less useful in the clinical setting.1,9
- If symptoms started less than 5 to 8 days prior, serum should be sent for RT-PCR for viral RNA.
- If symptoms occurred more than 8 days prior, serum should be sent for IgM and IgG serologic testing.
If the acute sample was negative (and chikungunya is still suspected), a second serum sample should be drawn 2 to 3 weeks later during the convalescent phase and sent for IgG serologic testing.
There are no specific treatments or vaccines available for chikungunya, but both live and inactivated vaccines are being tested. To prevent chikungunya virus infection, advise patients traveling to endemic areas to reduce mosquito exposure by avoiding outdoor activities during dusk and dawn, wearing long-sleeved shirts and long pants, and using an insect repellent that contains DEET. Recommend that patients who will be sleeping in a high-risk area use bed netting treated with permethrin. The CDC Web site has excellent additional information, available at http://www.cdc.gov/chikungunya.10
Our patient was briefly hospitalized due to intractable pain. She was discharged after 2 days and given prescriptions for motrin 800 mg and percocet 5/325 mg for breakthrough pain. Her wrist and ankle pain persisted after discharge, but slowly resolved after 2 to 3 months.
THE TAKEAWAY
Chikungunya is becoming more common among travelers returning to the United States from the Caribbean islands, and mosquito vectors found in parts of the United States are enhancing the possibility of local outbreaks. Travel to endemic regions—and the classic symptoms of fever, polyarthralgia, and a maculopapular ras
1. Pan American Health Organization. Preparedness and response for chikungunya virus: Introduction in the Americas. Washington, DC: Pan American Health Organization; 2011:1-149. Available at: http://www1.paho.org/hq/dmdocuments/CHIKV_English.pdf. Accessed March 8, 2017.
2. Enserink M. Infectious diseases. Chikungunya: no longer a third world disease. Science. 2007;318:1860-1861.
3. Pan American Health Organization. Number of reported cases of chikungunya fever in the Americas, by country or territory, 2017. Available at: http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&Itemid=270&gid=38489&lang=en. Accessed March 7, 2017.
4. Centers for Disease Control and Prevention. 2014 final data for the United States. Centers for Disease Control and Prevention Web site. Available at: https://www.cdc.gov/chikungunya/geo/united-states-2014.html. Accessed March 16, 2017.
5. Nayar SK, Noridah O, Paranthaman V, et al. Co-infection of dengue virus and chikungunya virus in two patients with acute febrile illness. Med J Malaysia. 2007;62:335-336.
6. Staples JE, Fischer M. Chikungunya virus in the Americas—what a vectorborne pathogen can do. N Engl J Med. 2014;371:887-889.
7. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition. Geneva: World Health Organization; 2009. Available at: http://www.who.int/tdr/publications/documents/dengue-diagnosis.pdf?ua=1. Accessed March 8, 2017.
8. Centers for Disease Control and Prevention. Chikungunya information for healthcare providers. 2014. Available at: https://www.cdc.gov/chikungunya/pdfs/chikv_clinicians.pdf. Accessed March 8, 2017.
9. Parida MM, Santhosh SR, Dash PK, et al. Rapid and real-time assays for detection and quantification of chikungunya virus. Future Virology. 2008;3:179-192.
10. Centers for Disease Control and Prevention. Chikungunya virus. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/chikungunya. Accessed February 26, 2015.
1. Pan American Health Organization. Preparedness and response for chikungunya virus: Introduction in the Americas. Washington, DC: Pan American Health Organization; 2011:1-149. Available at: http://www1.paho.org/hq/dmdocuments/CHIKV_English.pdf. Accessed March 8, 2017.
2. Enserink M. Infectious diseases. Chikungunya: no longer a third world disease. Science. 2007;318:1860-1861.
3. Pan American Health Organization. Number of reported cases of chikungunya fever in the Americas, by country or territory, 2017. Available at: http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&Itemid=270&gid=38489&lang=en. Accessed March 7, 2017.
4. Centers for Disease Control and Prevention. 2014 final data for the United States. Centers for Disease Control and Prevention Web site. Available at: https://www.cdc.gov/chikungunya/geo/united-states-2014.html. Accessed March 16, 2017.
5. Nayar SK, Noridah O, Paranthaman V, et al. Co-infection of dengue virus and chikungunya virus in two patients with acute febrile illness. Med J Malaysia. 2007;62:335-336.
6. Staples JE, Fischer M. Chikungunya virus in the Americas—what a vectorborne pathogen can do. N Engl J Med. 2014;371:887-889.
7. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition. Geneva: World Health Organization; 2009. Available at: http://www.who.int/tdr/publications/documents/dengue-diagnosis.pdf?ua=1. Accessed March 8, 2017.
8. Centers for Disease Control and Prevention. Chikungunya information for healthcare providers. 2014. Available at: https://www.cdc.gov/chikungunya/pdfs/chikv_clinicians.pdf. Accessed March 8, 2017.
9. Parida MM, Santhosh SR, Dash PK, et al. Rapid and real-time assays for detection and quantification of chikungunya virus. Future Virology. 2008;3:179-192.
10. Centers for Disease Control and Prevention. Chikungunya virus. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/chikungunya. Accessed February 26, 2015.
BEST PRACTICES: Reinforced Reload Stapling in the Thoracic Space
Air leaks have been reported to be frequent and difficult-to-manage sequelae in some lung resection procedures. Click here to learn about a new device being used in the thoracic space
Author:
Mark Ellis Ginsburg,
MD, FACS
Associate Clinical Professor of Surgery
Division of Cardiothoracic Surgery
Columbia University Medical Center
New York, NY
Faculty Disclosure: Dr. Ginsburg has received compensation from Medtronic Inc. for his participation in this article. He has no other conflicts of interest to disclose.
Air leaks have been reported to be frequent and difficult-to-manage sequelae in some lung resection procedures. Click here to learn about a new device being used in the thoracic space
Author:
Mark Ellis Ginsburg,
MD, FACS
Associate Clinical Professor of Surgery
Division of Cardiothoracic Surgery
Columbia University Medical Center
New York, NY
Faculty Disclosure: Dr. Ginsburg has received compensation from Medtronic Inc. for his participation in this article. He has no other conflicts of interest to disclose.
Air leaks have been reported to be frequent and difficult-to-manage sequelae in some lung resection procedures. Click here to learn about a new device being used in the thoracic space
Author:
Mark Ellis Ginsburg,
MD, FACS
Associate Clinical Professor of Surgery
Division of Cardiothoracic Surgery
Columbia University Medical Center
New York, NY
Faculty Disclosure: Dr. Ginsburg has received compensation from Medtronic Inc. for his participation in this article. He has no other conflicts of interest to disclose.
Focus on Reducing the Discomfort, Not the Fever
A child who has a cold, flu, or other acute illness may be what parents often call “fussy”: irritable, teary, and clingy. Such changes in behavior and mood, or “sickness behavior (SB),” are usually thought to be linked to fever. Actually, those symptoms are the immune system’s reactions to invasion by a pathogen, say French researchers—and they may be present whether the child has fever or not. The researchers’ say their multicenter study is the first to show dissociation between SB and the severity of the fever.
The researchers evaluated 6 parameters over the 2 hours preceding consultations with the parents of 200 children with and 200 without fever. Children with particularly painful illnesses and chronic diseases were excluded from the study. Parents used rating scales to report degrees of change in the time the child spent playing, the distance covered (ie. how far from the parent the child roamed), time the child spent seeking comfort, time spent whining or crying, time spent in a state of irritation or anger, most distorted facial expression (on a chart). The researchers also assessed time spent sleeping and appetite in the 24 hours before the consultation. Sickness behavior can’t be reduced to the observation of those 8 behavioral parameters, the researchers note, but they were easy for parents to use and assess.
The mean values of the 8 parameters differed significantly between the 2 groups but were independent of the height of fever in the febrile children. That independence suggests that SB and fever are expressions of 2 autonomous metabolic pathways that are activated simultaneously in febrile conditions, the researchers say, which is in accordance with current pathophysiologic knowledge.
Their findings are in harmony with current treatment recommendations, the researchers say. Because it’s hard to know when behavior changes are due to SB, pain, fatigue, or something else in a febrile child—especially one who is too young to talk about it—it’s more important to focus on relieving the discomfort than in reducing the fever.
Source:
Corrard F, Copin C, Wollner A, et al. PLoS One. 2017;12(3): e0171670.
doi: 10.1371/journal.pone.0171670.
A child who has a cold, flu, or other acute illness may be what parents often call “fussy”: irritable, teary, and clingy. Such changes in behavior and mood, or “sickness behavior (SB),” are usually thought to be linked to fever. Actually, those symptoms are the immune system’s reactions to invasion by a pathogen, say French researchers—and they may be present whether the child has fever or not. The researchers’ say their multicenter study is the first to show dissociation between SB and the severity of the fever.
The researchers evaluated 6 parameters over the 2 hours preceding consultations with the parents of 200 children with and 200 without fever. Children with particularly painful illnesses and chronic diseases were excluded from the study. Parents used rating scales to report degrees of change in the time the child spent playing, the distance covered (ie. how far from the parent the child roamed), time the child spent seeking comfort, time spent whining or crying, time spent in a state of irritation or anger, most distorted facial expression (on a chart). The researchers also assessed time spent sleeping and appetite in the 24 hours before the consultation. Sickness behavior can’t be reduced to the observation of those 8 behavioral parameters, the researchers note, but they were easy for parents to use and assess.
The mean values of the 8 parameters differed significantly between the 2 groups but were independent of the height of fever in the febrile children. That independence suggests that SB and fever are expressions of 2 autonomous metabolic pathways that are activated simultaneously in febrile conditions, the researchers say, which is in accordance with current pathophysiologic knowledge.
Their findings are in harmony with current treatment recommendations, the researchers say. Because it’s hard to know when behavior changes are due to SB, pain, fatigue, or something else in a febrile child—especially one who is too young to talk about it—it’s more important to focus on relieving the discomfort than in reducing the fever.
Source:
Corrard F, Copin C, Wollner A, et al. PLoS One. 2017;12(3): e0171670.
doi: 10.1371/journal.pone.0171670.
A child who has a cold, flu, or other acute illness may be what parents often call “fussy”: irritable, teary, and clingy. Such changes in behavior and mood, or “sickness behavior (SB),” are usually thought to be linked to fever. Actually, those symptoms are the immune system’s reactions to invasion by a pathogen, say French researchers—and they may be present whether the child has fever or not. The researchers’ say their multicenter study is the first to show dissociation between SB and the severity of the fever.
The researchers evaluated 6 parameters over the 2 hours preceding consultations with the parents of 200 children with and 200 without fever. Children with particularly painful illnesses and chronic diseases were excluded from the study. Parents used rating scales to report degrees of change in the time the child spent playing, the distance covered (ie. how far from the parent the child roamed), time the child spent seeking comfort, time spent whining or crying, time spent in a state of irritation or anger, most distorted facial expression (on a chart). The researchers also assessed time spent sleeping and appetite in the 24 hours before the consultation. Sickness behavior can’t be reduced to the observation of those 8 behavioral parameters, the researchers note, but they were easy for parents to use and assess.
The mean values of the 8 parameters differed significantly between the 2 groups but were independent of the height of fever in the febrile children. That independence suggests that SB and fever are expressions of 2 autonomous metabolic pathways that are activated simultaneously in febrile conditions, the researchers say, which is in accordance with current pathophysiologic knowledge.
Their findings are in harmony with current treatment recommendations, the researchers say. Because it’s hard to know when behavior changes are due to SB, pain, fatigue, or something else in a febrile child—especially one who is too young to talk about it—it’s more important to focus on relieving the discomfort than in reducing the fever.
Source:
Corrard F, Copin C, Wollner A, et al. PLoS One. 2017;12(3): e0171670.
doi: 10.1371/journal.pone.0171670.
Walter Reed: A Legacy of Leadership and Service
Walter Reed National Military Medical Center in Bethesda, Maryland, is one of several military and civilian medical facilities named for a U.S. Army doctor.
Walter Reed, MD, was born September 13, 1851 near Gloucester on Virginia’s middle peninsula. His father was the pastor of the Bellamy Methodist Church. The Reed family frequently moved as was required by the church and thus lived in many areas of southeastern Virginia and North Carolina. After the Civil War, Reverend Reed moved his family to Charlottesville, Virginia, where Walter, 15, and 2 of his older brothers were enrolled in the University of Virginia.
After a successful year of study, Reed summoned enough courage to confront the formidably bearded elders of the medical faculty with a bold proposal: If he passed all the courses, would they award him a medical degree regardless of the time it took or his age when he finished? A little more than 2 months shy of this 18th birthday, Reed graduated standing third in a class of 10 remaining from the original 50. He was, then and now, the youngest person ever to graduate from the University of Virginia School of Medicine. Reed went to Bellevue Hospital Medical School in New York for clinical hospital training. In another year, he earned his second medical degree, though it was not awarded until after he had reached the ripe old age of 21.
Reed joined the U.S. Army in 1875, possibly looking for a secure position that allowed him to marry his sweetheart Emily Lawrence in 1876. Over the first 18 years of marriage, they moved about 15 times throughout the west with some eastern assignments.
The selection of George Miller Steinberg as Army Surgeon General in 1893 turned out to be a watershed in Reed’s career. He joined the faculty of the new Army medical school. Reed lived closer to Washington (Minnesota) than did the other candidate (California), which probably helped his candidacy. Reed took full advantage of this opportunity and became a trusted troubleshooter for Sternberg.
After the Spanish-American War, Reed led a U.S. Army board that investigated typhoid fever in stateside camps, which killed more soldiers than died on the battlefield during the war. The findings of this board alone would have made Reed famous, but before these findings were formally published, Reed was sent to Cuba to lead another U.S. Army board to investigate infectious diseases, including yellow fever. Over the course of a few months, with the input and assistance of many others, he designed and carried out a series of human experiments that proved the mosquito as the vector of yellow fever. Application of his findings quickly led to the control of yellow fever in Cuba and later in Panama and throughout the tropics.
Reed died in Washington, DC, in 1902 at age 51, following surgery that discovered a ruptured appendix, which in that pre-antibiotic era was nearly always fatal. William Borden, his surgeon and friend, campaigned for several years for a new U.S. Army hospital in Washington to be named for Reed. Borden was successful with the opening of Walter Reed Army General Hospital in 1909. Renamed Walter Reed Army Medical Center in 1951 on the 100th anniversary of Reed’s birth, the hospital was closed in 2011 and its name transferred to the new Walter Reed National Military Medical Center. Other facilities named for Reed include the Walter Reed Army Institute of Research in Maryland and the civilian Riverside Walter Reed Hospital in Gloucester Courthouse, Virginia.
A particularly interesting resource to learn more about Reed is the Philip Hench Walter Reed Yellow Fever Collection. Most of the collection is available online (http://yellowfever.lib.virginia.edu/reed).
Walter Reed National Military Medical Center in Bethesda, Maryland, is one of several military and civilian medical facilities named for a U.S. Army doctor.
Walter Reed, MD, was born September 13, 1851 near Gloucester on Virginia’s middle peninsula. His father was the pastor of the Bellamy Methodist Church. The Reed family frequently moved as was required by the church and thus lived in many areas of southeastern Virginia and North Carolina. After the Civil War, Reverend Reed moved his family to Charlottesville, Virginia, where Walter, 15, and 2 of his older brothers were enrolled in the University of Virginia.
After a successful year of study, Reed summoned enough courage to confront the formidably bearded elders of the medical faculty with a bold proposal: If he passed all the courses, would they award him a medical degree regardless of the time it took or his age when he finished? A little more than 2 months shy of this 18th birthday, Reed graduated standing third in a class of 10 remaining from the original 50. He was, then and now, the youngest person ever to graduate from the University of Virginia School of Medicine. Reed went to Bellevue Hospital Medical School in New York for clinical hospital training. In another year, he earned his second medical degree, though it was not awarded until after he had reached the ripe old age of 21.
Reed joined the U.S. Army in 1875, possibly looking for a secure position that allowed him to marry his sweetheart Emily Lawrence in 1876. Over the first 18 years of marriage, they moved about 15 times throughout the west with some eastern assignments.
The selection of George Miller Steinberg as Army Surgeon General in 1893 turned out to be a watershed in Reed’s career. He joined the faculty of the new Army medical school. Reed lived closer to Washington (Minnesota) than did the other candidate (California), which probably helped his candidacy. Reed took full advantage of this opportunity and became a trusted troubleshooter for Sternberg.
After the Spanish-American War, Reed led a U.S. Army board that investigated typhoid fever in stateside camps, which killed more soldiers than died on the battlefield during the war. The findings of this board alone would have made Reed famous, but before these findings were formally published, Reed was sent to Cuba to lead another U.S. Army board to investigate infectious diseases, including yellow fever. Over the course of a few months, with the input and assistance of many others, he designed and carried out a series of human experiments that proved the mosquito as the vector of yellow fever. Application of his findings quickly led to the control of yellow fever in Cuba and later in Panama and throughout the tropics.
Reed died in Washington, DC, in 1902 at age 51, following surgery that discovered a ruptured appendix, which in that pre-antibiotic era was nearly always fatal. William Borden, his surgeon and friend, campaigned for several years for a new U.S. Army hospital in Washington to be named for Reed. Borden was successful with the opening of Walter Reed Army General Hospital in 1909. Renamed Walter Reed Army Medical Center in 1951 on the 100th anniversary of Reed’s birth, the hospital was closed in 2011 and its name transferred to the new Walter Reed National Military Medical Center. Other facilities named for Reed include the Walter Reed Army Institute of Research in Maryland and the civilian Riverside Walter Reed Hospital in Gloucester Courthouse, Virginia.
A particularly interesting resource to learn more about Reed is the Philip Hench Walter Reed Yellow Fever Collection. Most of the collection is available online (http://yellowfever.lib.virginia.edu/reed).
Walter Reed National Military Medical Center in Bethesda, Maryland, is one of several military and civilian medical facilities named for a U.S. Army doctor.
Walter Reed, MD, was born September 13, 1851 near Gloucester on Virginia’s middle peninsula. His father was the pastor of the Bellamy Methodist Church. The Reed family frequently moved as was required by the church and thus lived in many areas of southeastern Virginia and North Carolina. After the Civil War, Reverend Reed moved his family to Charlottesville, Virginia, where Walter, 15, and 2 of his older brothers were enrolled in the University of Virginia.
After a successful year of study, Reed summoned enough courage to confront the formidably bearded elders of the medical faculty with a bold proposal: If he passed all the courses, would they award him a medical degree regardless of the time it took or his age when he finished? A little more than 2 months shy of this 18th birthday, Reed graduated standing third in a class of 10 remaining from the original 50. He was, then and now, the youngest person ever to graduate from the University of Virginia School of Medicine. Reed went to Bellevue Hospital Medical School in New York for clinical hospital training. In another year, he earned his second medical degree, though it was not awarded until after he had reached the ripe old age of 21.
Reed joined the U.S. Army in 1875, possibly looking for a secure position that allowed him to marry his sweetheart Emily Lawrence in 1876. Over the first 18 years of marriage, they moved about 15 times throughout the west with some eastern assignments.
The selection of George Miller Steinberg as Army Surgeon General in 1893 turned out to be a watershed in Reed’s career. He joined the faculty of the new Army medical school. Reed lived closer to Washington (Minnesota) than did the other candidate (California), which probably helped his candidacy. Reed took full advantage of this opportunity and became a trusted troubleshooter for Sternberg.
After the Spanish-American War, Reed led a U.S. Army board that investigated typhoid fever in stateside camps, which killed more soldiers than died on the battlefield during the war. The findings of this board alone would have made Reed famous, but before these findings were formally published, Reed was sent to Cuba to lead another U.S. Army board to investigate infectious diseases, including yellow fever. Over the course of a few months, with the input and assistance of many others, he designed and carried out a series of human experiments that proved the mosquito as the vector of yellow fever. Application of his findings quickly led to the control of yellow fever in Cuba and later in Panama and throughout the tropics.
Reed died in Washington, DC, in 1902 at age 51, following surgery that discovered a ruptured appendix, which in that pre-antibiotic era was nearly always fatal. William Borden, his surgeon and friend, campaigned for several years for a new U.S. Army hospital in Washington to be named for Reed. Borden was successful with the opening of Walter Reed Army General Hospital in 1909. Renamed Walter Reed Army Medical Center in 1951 on the 100th anniversary of Reed’s birth, the hospital was closed in 2011 and its name transferred to the new Walter Reed National Military Medical Center. Other facilities named for Reed include the Walter Reed Army Institute of Research in Maryland and the civilian Riverside Walter Reed Hospital in Gloucester Courthouse, Virginia.
A particularly interesting resource to learn more about Reed is the Philip Hench Walter Reed Yellow Fever Collection. Most of the collection is available online (http://yellowfever.lib.virginia.edu/reed).