User login
A Heart Failure Management Program Using Shared Medical Appointments
Rising health care costs have led to threats of nonreimbursement for rehospitalization within 30 days postdischarge.1,2 Heart failure (HF) in particular is characterized by the highest 30-day rehospitalization rate (23.5% in 2013), which accounts for more than two-thirds of HF expenditures.3,4
Much of HF-related health care costs can be addressed with effective self-management by patients with HF. Therefore, developing and implementing effective disease management programs for this high-risk patient population is essential. Heart failure management programs may include optimizing HF medications, improving patient understanding of the importance of appropriate diet and physical activity, and cultivating psychological health and well-being. In a 2013 systematic review and meta-analysis, Wakefield and colleagues found that disease management programs improved nearly all HF outcomes, including lower mortality rates, lower hospital readmission rates, fewer clinic visits, higher satisfaction with care, and higher quality of life, compared with a no-treatment control or standard care.5 Moreover, these programs demonstrated cost-effectiveness by reducing HF-related hospitalizations and health care expenditures.5
One method to deliver specialized disease management programs to a greater number of patients may be to use shared medical appointments (SMAs). In a randomized controlled trial, Smith and colleagues demonstrated improved HF outcomes through 7 months among veterans who attended SMAs for HF management.6 However, the trial enrolled only 25% of patients screened, and 63% of the patients who did not enroll were classified as not interested. These findings suggest that patients with HF, and veterans in particular, may face additional barriers to enrolling in HF management programs, and these results may not be fully representative of veterans with HF.
In this study, the authors used a naturalistic study design via retrospective review of the electronic health record (EHR) to evaluate whether patients with acute HF who chose to attend SMAs promoting self-management skills for HF would have better hospitalization outcomes compared with those who received individual disease management instructions in a HF specialty clinic (ie, usual care). The authors hypothesized that veterans who participated in the HF SMA clinic would have fewer 12-month HF-related and all-cause hospitalizations, fewer days in the hospital, and more days to first hospitalization compared with patients in usual care.
Methods
The clinic for veterans with acute HF was initiated in October, 2010 at the Jesse Brown VAMC (JBVAMC) in Chicago, Illinois, to reduce readmissions by targeting patients who had been previously hospitalized for HF. In September 2011, the multidisciplinary SMA clinic was developed within the HF clinic to provide enhanced care focused on self-management strategies for patients with HF. The HF SMA program comprised 4 weekly face-to-face sessions co-led by a nurse practitioner (NP), a dietitian, and a clinical psychologist, similar to what has been shown to be successful and cost-effective in nonveteran populations.6-8 Patients attended at least 4 sessions before graduating to the advanced HF SMA program where they could attend monthly booster sessions. The program promoted self-management by providing education about and support for the HF process, HF medications, diet adherence, physical activity, psychological well-being, and stress management via interactive presentations. During the visit, patients’ medication and food logs were reviewed. Patients were encouraged to discuss successes and obstacles in achieving their goals. All study procedures were approved by the institutional review board at JBVAMC.
Study Design
Data were collected by retrospective review of the JBVAMC EHR. The EHR was reviewed for all veterans scheduled for ≥ 1 SMA clinic visit within the HF specialty clinic using predetermined, convenient selection between January 1, 2012, and December 31, 2013. Outcome data were collected through 12-month follow-up (through December 31, 2014).
Patients in both treatment arms received HF care through the HF clinic, including one-on-one education regarding HF self-management provided by a NP. Patients were assigned to the HF SMA group if they also attended the HF SMA clinic within 3 months of their initial HF clinic consult. The number of SMAs attended was included as a covariate in the models. Patients who were scheduled for, but did not attend, the HF SMA clinic were assigned to the HF clinic group. Patients who attended the initial HF consult before September 1, 2011, were excluded, thereby ensuring that all patients included in the present analyses had the opportunity to attend the HF SMA appointment within the predetermined period of chart review.
Data for all VA hospitalizations that occurred between January 1, 2012 and December 31, 2014, were extracted from the EHR. Extracted data included admission date, discharge date, and discharge diagnoses. From these data, the authors assessed 4 hospitalization outcomes for each HF hospitalization and all-cause hospitalization within 12 months of the initial HF clinic consult date: hospitalization (yes/no), number of hospitalizations, number of days in the hospital, and days to first hospitalization.
Data Analysis
Demographic, HF characteristics, and HF outcome variables for the HF SMA and HF clinic groups were compared using t tests and chi-square analyses. Logistic regressions were used to predict 12-month hospitalization, linear regressions were used to predict number of hospitalizations and number of days hospitalized, and Cox proportional hazards regressions were used to predict time from initial HF consult to first hospitalization for each HF-related hospitalization variable and all-cause hospitalization variable. A separate logistic regression was conducted to predict 12-month all-cause mortality. The primary predictor variable of interest for all models was group membership (HF SMA vs HF clinic). Covariates in all models included race (black vs nonblack), ethnicity (Hispanic/Latino vs non-Hispanic/Latino), age, and number of HF SMAs attended.
Results
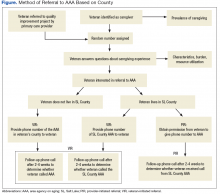
Of 709 HF SMA clinic appointments made for 141 patients between January 1, 2012, and December 31, 2013, 54 patients were assigned to the HF SMA group and 37 patients were assigned to the HF clinic group (Figure). The majority of the sample was black (87%), non-Hispanic/Latino (96%), and the average age was 68 years. Patients were more likely to have nonischemic (rather than ischemic) cardiomyopathy (66%) and more likely to have HF with reduced (rather than preserved) ejection fraction (76%; ie, systolic HF). Furthermore, 40% of the sample was diagnosed with atrial fibrillation (AF) or atrial flutter (A-flutter), and 24% had an implantable cardioverter-defibrillator or pacemaker. There were no significant differences in demographics or HF characteristics between the HF SMA group and the HF clinic group (Table).
HF Hospitalization Outcomes
During the 12-month follow-up, 32 patients were hospitalized for HF, 18 (33.3%) in the SMA group and 14 (37.8%) in the HF clinic group, P = .658. Patients were hospitalized up to 4 times for between 1 and 38 days, and from 1 to 352 days postconsult. No differences between the HF SMA group and HF clinic group were observed on any of the HF hospitalization outcomes (Table). Group membership did not predict HF hospitalization (odds ratio [OR]: 0.39, 95% confidence interval [CI]: 0.11-1.42), number of HF hospitalizations (β: 0.15, SE: 0.29), number of days hospitalized for HF (β: 0.1.66, SE: 2.01), or time to first HF hospitalization (hazard ratio [HR]: 1.35, 95% CI: 0.66-2.77), all Ps > .10. In the Cox proportional hazards regression predicting time to HF hospitalization, the coefficients did not converge when the model included demographic covariates; therefore, the model was run only with HF group as a predictor variable. For all other models, no covariates significantly predicted HF hospitalization outcomes.
All-Cause Hospitalization Outcomes
During the 12-month follow-up, 57 patients were hospitalized for any cause (including HF hospitalizations), 32 (59.3%) in the SMA group and 25 (67.6%) in the HF clinic group, P = .421. Patients were hospitalized up to 6 times for between 1 and 106 days and from 1 to 352 days postconsult. No differences were observed between the groups on any of the all-cause hospitalization outcomes (Table). Group membership did not predict all-cause hospitalization (OR: 0.34, 95% CI: 0.10-1.19), number of all-cause hospitalizations (β: 0.49, SE: 0.41), number of days hospitalized for any cause (β: 5.15, SE: 5.15), or time to first all-cause hospitalization (HR: 0.98, 95% CI: 0.56-1.72), all P > .05. None of the covariates predicted any of the all-cause hospitalization outcomes.
All-Cause Mortality Outcomes
During the 12-month follow-up, 14 patients (15%) died of any cause, 8 (15%) in the SMA group and 6 (16%) in the HF clinic group, P = .856. Group membership did not predict all-cause mortality (OR: 2.32, 95% CI: 0.44-12.18), and likewise none of the covariates were associated with 12-month all-cause mortality.
Discussion
This study was a naturalistic, retrospective examination of a HF management program promoting self-management delivered via multidisciplinary SMAs among veterans who enrolled in an acute HF specialty clinic. The authors’ hypothesis was not supported: patients who attended the HF SMA clinic did not have lower 12-month hospitalization or mortality rates, shorter hospital stays, or longer time to hospitalization compared with patients in the HF clinic only.
In contrast to the patient-centered approach of this study, a randomized trial delivering a similar disease management program found that patients with acute HF in the SMA group had better short-term (< 7 months) hospitalization outcomes, specifically greater time to first HF-related hospitalization (HR 0.45, 95% CI: 0.21-0.98), but this effect did not last through 12 months when compared with patients in standard care.6 These disparate findings may be explained by the gap in bench-to-bedside research, where despite scientific evidence indicating better outcomes among patients randomized to an intervention, when patients are given a choice, they may not choose to engage in the best option for their HF treatment.
In the present study, veterans who chose not to attend the HF SMA clinic may have done so for numerous reasons that may have influenced the outcomes. For example, those veterans who did not attend the HF SMA clinic may have had higher health literacy and less need for an educational program. Health literacy has been inversely associated with HF outcomes, such that patients with HF with lower health literacy have greater risk of HF rehospitalization or mortality.9,10 In addition, many of the veterans who were followed in the HF clinic were taught the same disease management strategies by the NP during one-on-one visits, and they may have gained the same self-management skills in a different setting.
Another possibility is that the veterans enrolled in the HF clinic were less likely to be followed exclusively at the VA and therefore may have had external hospitalizations not recorded in their VA health records. In 2000, more than half the veterans who received health care services at the VA reported that they did not receive their care exclusively at the VA.11 This may be especially true since the Veteran’s Choice Program permits veterans who reside > 40 miles from a VA hospital to receive care closer to home.
Disease Management Programs
Disease management programs for HF in general promote better outcomes and lower health care expenditures.5,12 Self-management instruction delivered via SMAs may have greater potential for reducing HF-associated health care costs if it were to be integrated earlier in the continuum of care. The sample in this study was composed of veterans who were referred to a specialty clinic only after being hospitalized for HF. These patients likely were experiencing more advanced disease and/or low adherence, as indicated by the relatively high prevalence of AF diagnoses and pacemakers; these null findings are consistent with those from a randomized controlled trial of a disease management program among veterans with heavy HF symptom burden and impaired functional status.13 However, integrating self-management programs earlier in HF clinical care (eg, primary care or cardiology clinics) may be more effective in promoting proactive disease management and delaying or preventing initial HF hospitalizations.
For example, a disease management plan implemented by general practitioners for veterans with HF in Australia was associated with a 23% reduction in potentially preventable hospitalization rates.14 Veterans with HF enrolled in a NP-led disease management intervention, relative to those followed only in primary care, had significantly fewer hospitalizations and nearly half the risk mortality (15% vs 28% after 2 years; HR 0.55).15 Furthermore, some have suggested that SMAs may be more effective for patients for whom risk of disease is high but current disease burden (ie, symptoms) is low, such as diabetes mellitus management programs.16 Early intervention also may allow providers to reach more patients more quickly and before they experience advanced symptoms, thereby reducing specialty clinic wait times and overall health expenditures. Developing more effective disease management programs for patients with acute HF and veterans in particular remains a critical matter for future study.
Additional and novel components of HF management programs show promise for future interventions. First, various facets of social support, including emotional support, instrumental/tangible support, informational support, and appraisal support, are associated with improved self-care.17 For example, the levels of family functioning and family support predict HF outcomes, perhaps because between-appointment monitoring allows patients to report problems that might otherwise go unidentified and receive more external feedback about their disease and symptoms.18,19 Patients report that family members or especially supportive members of their health care team are invaluable contributors to their successful management of HF.20 A recently published feasibility trial of a couple-based disease management program observed positive trends in HF management for veterans, as well as improvements in caregiver’s depressive symptoms and burden, indicating that even support from informal caregivers may improve HF outcomes.21
Advances in technology-delivered disease management programs show promise in improving adherence to chronic disease management programs.22,23 Specifically for HF, veterans who enrolled in a daily telehealth intervention employing daily vital signs and symptom reporting, automated reminders and tips for self-management, and proactive monitoring and intervention telephone calls from a nurse successfully lowered their blood pressure, lost weight, reduced their HF medication dosages, and spent 80% fewer days in the hospital.24 Among patients with coronary artery disease, a text messaging service was shown to improve a number of cardiovascular risk factors.25 Moreover, mobile applications can be used to support informal caregivers of patients with HF.26 To the authors knowledge, no research studies have been conducted using text messaging or mobile applications among veterans with HF.
Limitations
Some limitations of the present study warrant discussion. First, as discussed earlier, patients were not randomized to the treatment arms. Second, veterans are referred to the HF clinic only after being hospitalized for HF. As a result, all the referred veterans likely were experiencing more advanced disease and/or low adherence, and these results may not be representative of patients with less advanced disease. Finally, the sample used in the present analysis was a small, homogeneous group of 91 male veterans who were 85% black and 95% non-Hispanic. These demographics are largely representative of the JBVAMC. Therefore, the present results may not be generalizable to more racially or ethnically diverse populations, women, or nonveterans.
Conclusion
Minimizing rehospitalization rates for patients with HF continues to be a priority. Health care costs of HF are more than double those of patients in the general population, primarily due to hospitalizations—in 2013, HF hospitalization costs in the U.S. exceeded $10 billion.27,28 Given the current emphasis on economical, patient-centered care, SMAs may be a cost-effective alternative to individualized disease management plans while continuing to allow providers to tailor treatment to individual patient needs.
Although this study did not find better outcomes among veterans whose specialty HF care was augmented by clinic-based SMAs, the authors believe that this type of program has great potential. Heart failure SMAs may improve HF outcomes, enhance efficiency of health care delivery, and reduce overall HF-associated health care costs if it is integrated earlier along the continuum of care or if other novel components, such as caregiver support or technology-based delivery, is included. Further studies are needed to systematically evaluate HF management programs delivered via SMAs to improve outcomes and reduce the economic burden that HF places on the health care system.
1. Boccuti C, Casillas G. Aiming for fewer hospital U-turns: the Medicare hospital readmissions reduction program. http://kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/. Published September 30, 2016. Accessed March 6, 2017.
2. Barrett ML, Wier LM, Jiang HJ, Steiner CA. All-cause readmissions by payer and age, 2009-2013. Statistical Brief #199. https://www.hcup-us.ahrq .gov/reports/statbriefs/sb199-Readmissions-Payer -Age.jsp. Published December 2015. Accessed March 6, 2017.
3. Fingar K, Washington R. Trends in hospital readmissions for four high-volume conditions, 2009-2013. Statistical Brief #196. https://www.hcup-us .ahrq.gov/reports/statbriefs/sb196-Readmissions -Trends-High-Volume-Conditions.jsp. Published November 2015. Accessed March 6, 2017.
4. McMurray JJ, Adamopoulos S, Anker SD, et al; ESC Committee for Practice Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33(14):1787-1847.
5. Wakefield BJ, Boren SA, Groves PS, Conn VS. Heart failure care management programs: a review of study interventions and meta-analysis of outcomes. J Cardiovasc Nurs. 2013;28(1):8-19.
6. Smith CE, Piamjariyakul U, Wick JA, et al. Multidisciplinary group clinic appointments: the Self-Management and Care of Heart Failure (SMAC-HF) trial. Circ Heart Fail. 2014;7(6):888-894.
7. Sochalski J, Jaarsma T, Krumholz HM, et al. What works in chronic care management: the case of heart failure. Health Aff (Millwood). 2009;28(1): 179-189.
8. Ågren S, Evangelista LS, Davidson T, Strömberg A. Cost-effectiveness of a nurse-led education and psychosocial programme for patients with chronic heart failure and their partners. J Clin Nurs. 2013;22(15-16):2347-2353.
9. Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21(8):612-618.
10. McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. 2015;4(6). pii:e001799.
11. Nelson KM, Starkebaum GA, Reiber GE. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Rep. 2007;122(1):93-100.
12. Whellan DJ, Hasselblad V, Peterson E, O’Connor CM, Schulman KA. Metaanalysis and review of heart failure disease management randomized controlled clinical trials. Am Heart J. 2005;149(4):722-729.
13. Bekelman DB, Plomondon ME, Carey EP, et al. Primary results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study: a randomized clinical trial. JAMA Intern Med. 2015;175(5):725-732.
14. Vitry AI, Nguyen TA, Ramsay EN, et al. General practitioner management plans delaying time to next potentially preventable hospitalisation for patients with heart failure. Intern Med J. 2014;44(11):1117-1123.
15. Lowery J, Hopp F, Subramanian U, et al. Evaluation of a nurse practitioner disease management model for chronic heart failure: a multi-site implementation study. Congest Heart Fail. 2012;18(1):64-71.
16. Edelman D, McDuffie JR, Oddone E, Gierisch JM, Nagi A, Williams JW Jr. Shared medical appointments for chronic medical conditions: a systematic review. VAESP Project #09-010. http://www.hsrd.research.va.gov/publications/esp/shared -med- appt-REPORT.pdf. Published July 2012. Accessed March 6, 2017.
17. Graven LJ, Grant JS. Social support and self-care behaviors in individuals with heart failure: an integrative review. Int J Nurs Stud. 2014;51(2):320-333.
18. Dunbar SB, Clark PC, Quinn C, Gary RA, Kaslow NJ. Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs. 2008;23(3):258-265.
19. Piette JD, Gregor MA, Share D, et al. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congest Heart Fail. 2008;14(1):12-18.
20. Skaperdas E, Tuepker A, Nicolaidis C, Robb JK, Kansagara D, Hickam DH. Congestive heart failure self-management among US veterans: the role of personal and professional advocates. Patient Educ Couns. 2014;95(3):371-377.
21. Trivedi R, Slightam C, Fan VS, et al. A couples’ based self-management program for heart failure: results of a feasibility study. Front Public Health. 2016;4:171.
22. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg SA. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52.
23. Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362.
24. Schofield RS, Kline SE, Schmalfuss CM, et al. Early outcomes of a care coordination-enhanced telehome care program for elderly veterans with chronic heart failure. Telemed J E Health. 2005;11(1):20-27.
25. Chow CK, Redfern J, Hillis GS, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255-1263.
26. Piette JD, Striplin D, Marinec N, et al. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative efficacy trial. J Med Internet Res. 2015;17(6):e142.
27. Mejhert M, Lindgren P, Schill O, Edner M, Persson H, Kahan T. Long term health care consumption and cost expenditure in systolic heart failure. Eur J Intern Med. 2013;24(3):260-265.
28. Torio CM, Moore BJ. National inpatient hospital costs: the most expensive conditions by payer, 2013. Statistical Brief #204. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp. Published May 2016. Accessed March 6, 2017.
Rising health care costs have led to threats of nonreimbursement for rehospitalization within 30 days postdischarge.1,2 Heart failure (HF) in particular is characterized by the highest 30-day rehospitalization rate (23.5% in 2013), which accounts for more than two-thirds of HF expenditures.3,4
Much of HF-related health care costs can be addressed with effective self-management by patients with HF. Therefore, developing and implementing effective disease management programs for this high-risk patient population is essential. Heart failure management programs may include optimizing HF medications, improving patient understanding of the importance of appropriate diet and physical activity, and cultivating psychological health and well-being. In a 2013 systematic review and meta-analysis, Wakefield and colleagues found that disease management programs improved nearly all HF outcomes, including lower mortality rates, lower hospital readmission rates, fewer clinic visits, higher satisfaction with care, and higher quality of life, compared with a no-treatment control or standard care.5 Moreover, these programs demonstrated cost-effectiveness by reducing HF-related hospitalizations and health care expenditures.5
One method to deliver specialized disease management programs to a greater number of patients may be to use shared medical appointments (SMAs). In a randomized controlled trial, Smith and colleagues demonstrated improved HF outcomes through 7 months among veterans who attended SMAs for HF management.6 However, the trial enrolled only 25% of patients screened, and 63% of the patients who did not enroll were classified as not interested. These findings suggest that patients with HF, and veterans in particular, may face additional barriers to enrolling in HF management programs, and these results may not be fully representative of veterans with HF.
In this study, the authors used a naturalistic study design via retrospective review of the electronic health record (EHR) to evaluate whether patients with acute HF who chose to attend SMAs promoting self-management skills for HF would have better hospitalization outcomes compared with those who received individual disease management instructions in a HF specialty clinic (ie, usual care). The authors hypothesized that veterans who participated in the HF SMA clinic would have fewer 12-month HF-related and all-cause hospitalizations, fewer days in the hospital, and more days to first hospitalization compared with patients in usual care.
Methods
The clinic for veterans with acute HF was initiated in October, 2010 at the Jesse Brown VAMC (JBVAMC) in Chicago, Illinois, to reduce readmissions by targeting patients who had been previously hospitalized for HF. In September 2011, the multidisciplinary SMA clinic was developed within the HF clinic to provide enhanced care focused on self-management strategies for patients with HF. The HF SMA program comprised 4 weekly face-to-face sessions co-led by a nurse practitioner (NP), a dietitian, and a clinical psychologist, similar to what has been shown to be successful and cost-effective in nonveteran populations.6-8 Patients attended at least 4 sessions before graduating to the advanced HF SMA program where they could attend monthly booster sessions. The program promoted self-management by providing education about and support for the HF process, HF medications, diet adherence, physical activity, psychological well-being, and stress management via interactive presentations. During the visit, patients’ medication and food logs were reviewed. Patients were encouraged to discuss successes and obstacles in achieving their goals. All study procedures were approved by the institutional review board at JBVAMC.
Study Design
Data were collected by retrospective review of the JBVAMC EHR. The EHR was reviewed for all veterans scheduled for ≥ 1 SMA clinic visit within the HF specialty clinic using predetermined, convenient selection between January 1, 2012, and December 31, 2013. Outcome data were collected through 12-month follow-up (through December 31, 2014).
Patients in both treatment arms received HF care through the HF clinic, including one-on-one education regarding HF self-management provided by a NP. Patients were assigned to the HF SMA group if they also attended the HF SMA clinic within 3 months of their initial HF clinic consult. The number of SMAs attended was included as a covariate in the models. Patients who were scheduled for, but did not attend, the HF SMA clinic were assigned to the HF clinic group. Patients who attended the initial HF consult before September 1, 2011, were excluded, thereby ensuring that all patients included in the present analyses had the opportunity to attend the HF SMA appointment within the predetermined period of chart review.
Data for all VA hospitalizations that occurred between January 1, 2012 and December 31, 2014, were extracted from the EHR. Extracted data included admission date, discharge date, and discharge diagnoses. From these data, the authors assessed 4 hospitalization outcomes for each HF hospitalization and all-cause hospitalization within 12 months of the initial HF clinic consult date: hospitalization (yes/no), number of hospitalizations, number of days in the hospital, and days to first hospitalization.
Data Analysis
Demographic, HF characteristics, and HF outcome variables for the HF SMA and HF clinic groups were compared using t tests and chi-square analyses. Logistic regressions were used to predict 12-month hospitalization, linear regressions were used to predict number of hospitalizations and number of days hospitalized, and Cox proportional hazards regressions were used to predict time from initial HF consult to first hospitalization for each HF-related hospitalization variable and all-cause hospitalization variable. A separate logistic regression was conducted to predict 12-month all-cause mortality. The primary predictor variable of interest for all models was group membership (HF SMA vs HF clinic). Covariates in all models included race (black vs nonblack), ethnicity (Hispanic/Latino vs non-Hispanic/Latino), age, and number of HF SMAs attended.
Results
Of 709 HF SMA clinic appointments made for 141 patients between January 1, 2012, and December 31, 2013, 54 patients were assigned to the HF SMA group and 37 patients were assigned to the HF clinic group (Figure). The majority of the sample was black (87%), non-Hispanic/Latino (96%), and the average age was 68 years. Patients were more likely to have nonischemic (rather than ischemic) cardiomyopathy (66%) and more likely to have HF with reduced (rather than preserved) ejection fraction (76%; ie, systolic HF). Furthermore, 40% of the sample was diagnosed with atrial fibrillation (AF) or atrial flutter (A-flutter), and 24% had an implantable cardioverter-defibrillator or pacemaker. There were no significant differences in demographics or HF characteristics between the HF SMA group and the HF clinic group (Table).
HF Hospitalization Outcomes
During the 12-month follow-up, 32 patients were hospitalized for HF, 18 (33.3%) in the SMA group and 14 (37.8%) in the HF clinic group, P = .658. Patients were hospitalized up to 4 times for between 1 and 38 days, and from 1 to 352 days postconsult. No differences between the HF SMA group and HF clinic group were observed on any of the HF hospitalization outcomes (Table). Group membership did not predict HF hospitalization (odds ratio [OR]: 0.39, 95% confidence interval [CI]: 0.11-1.42), number of HF hospitalizations (β: 0.15, SE: 0.29), number of days hospitalized for HF (β: 0.1.66, SE: 2.01), or time to first HF hospitalization (hazard ratio [HR]: 1.35, 95% CI: 0.66-2.77), all Ps > .10. In the Cox proportional hazards regression predicting time to HF hospitalization, the coefficients did not converge when the model included demographic covariates; therefore, the model was run only with HF group as a predictor variable. For all other models, no covariates significantly predicted HF hospitalization outcomes.
All-Cause Hospitalization Outcomes
During the 12-month follow-up, 57 patients were hospitalized for any cause (including HF hospitalizations), 32 (59.3%) in the SMA group and 25 (67.6%) in the HF clinic group, P = .421. Patients were hospitalized up to 6 times for between 1 and 106 days and from 1 to 352 days postconsult. No differences were observed between the groups on any of the all-cause hospitalization outcomes (Table). Group membership did not predict all-cause hospitalization (OR: 0.34, 95% CI: 0.10-1.19), number of all-cause hospitalizations (β: 0.49, SE: 0.41), number of days hospitalized for any cause (β: 5.15, SE: 5.15), or time to first all-cause hospitalization (HR: 0.98, 95% CI: 0.56-1.72), all P > .05. None of the covariates predicted any of the all-cause hospitalization outcomes.
All-Cause Mortality Outcomes
During the 12-month follow-up, 14 patients (15%) died of any cause, 8 (15%) in the SMA group and 6 (16%) in the HF clinic group, P = .856. Group membership did not predict all-cause mortality (OR: 2.32, 95% CI: 0.44-12.18), and likewise none of the covariates were associated with 12-month all-cause mortality.
Discussion
This study was a naturalistic, retrospective examination of a HF management program promoting self-management delivered via multidisciplinary SMAs among veterans who enrolled in an acute HF specialty clinic. The authors’ hypothesis was not supported: patients who attended the HF SMA clinic did not have lower 12-month hospitalization or mortality rates, shorter hospital stays, or longer time to hospitalization compared with patients in the HF clinic only.
In contrast to the patient-centered approach of this study, a randomized trial delivering a similar disease management program found that patients with acute HF in the SMA group had better short-term (< 7 months) hospitalization outcomes, specifically greater time to first HF-related hospitalization (HR 0.45, 95% CI: 0.21-0.98), but this effect did not last through 12 months when compared with patients in standard care.6 These disparate findings may be explained by the gap in bench-to-bedside research, where despite scientific evidence indicating better outcomes among patients randomized to an intervention, when patients are given a choice, they may not choose to engage in the best option for their HF treatment.
In the present study, veterans who chose not to attend the HF SMA clinic may have done so for numerous reasons that may have influenced the outcomes. For example, those veterans who did not attend the HF SMA clinic may have had higher health literacy and less need for an educational program. Health literacy has been inversely associated with HF outcomes, such that patients with HF with lower health literacy have greater risk of HF rehospitalization or mortality.9,10 In addition, many of the veterans who were followed in the HF clinic were taught the same disease management strategies by the NP during one-on-one visits, and they may have gained the same self-management skills in a different setting.
Another possibility is that the veterans enrolled in the HF clinic were less likely to be followed exclusively at the VA and therefore may have had external hospitalizations not recorded in their VA health records. In 2000, more than half the veterans who received health care services at the VA reported that they did not receive their care exclusively at the VA.11 This may be especially true since the Veteran’s Choice Program permits veterans who reside > 40 miles from a VA hospital to receive care closer to home.
Disease Management Programs
Disease management programs for HF in general promote better outcomes and lower health care expenditures.5,12 Self-management instruction delivered via SMAs may have greater potential for reducing HF-associated health care costs if it were to be integrated earlier in the continuum of care. The sample in this study was composed of veterans who were referred to a specialty clinic only after being hospitalized for HF. These patients likely were experiencing more advanced disease and/or low adherence, as indicated by the relatively high prevalence of AF diagnoses and pacemakers; these null findings are consistent with those from a randomized controlled trial of a disease management program among veterans with heavy HF symptom burden and impaired functional status.13 However, integrating self-management programs earlier in HF clinical care (eg, primary care or cardiology clinics) may be more effective in promoting proactive disease management and delaying or preventing initial HF hospitalizations.
For example, a disease management plan implemented by general practitioners for veterans with HF in Australia was associated with a 23% reduction in potentially preventable hospitalization rates.14 Veterans with HF enrolled in a NP-led disease management intervention, relative to those followed only in primary care, had significantly fewer hospitalizations and nearly half the risk mortality (15% vs 28% after 2 years; HR 0.55).15 Furthermore, some have suggested that SMAs may be more effective for patients for whom risk of disease is high but current disease burden (ie, symptoms) is low, such as diabetes mellitus management programs.16 Early intervention also may allow providers to reach more patients more quickly and before they experience advanced symptoms, thereby reducing specialty clinic wait times and overall health expenditures. Developing more effective disease management programs for patients with acute HF and veterans in particular remains a critical matter for future study.
Additional and novel components of HF management programs show promise for future interventions. First, various facets of social support, including emotional support, instrumental/tangible support, informational support, and appraisal support, are associated with improved self-care.17 For example, the levels of family functioning and family support predict HF outcomes, perhaps because between-appointment monitoring allows patients to report problems that might otherwise go unidentified and receive more external feedback about their disease and symptoms.18,19 Patients report that family members or especially supportive members of their health care team are invaluable contributors to their successful management of HF.20 A recently published feasibility trial of a couple-based disease management program observed positive trends in HF management for veterans, as well as improvements in caregiver’s depressive symptoms and burden, indicating that even support from informal caregivers may improve HF outcomes.21
Advances in technology-delivered disease management programs show promise in improving adherence to chronic disease management programs.22,23 Specifically for HF, veterans who enrolled in a daily telehealth intervention employing daily vital signs and symptom reporting, automated reminders and tips for self-management, and proactive monitoring and intervention telephone calls from a nurse successfully lowered their blood pressure, lost weight, reduced their HF medication dosages, and spent 80% fewer days in the hospital.24 Among patients with coronary artery disease, a text messaging service was shown to improve a number of cardiovascular risk factors.25 Moreover, mobile applications can be used to support informal caregivers of patients with HF.26 To the authors knowledge, no research studies have been conducted using text messaging or mobile applications among veterans with HF.
Limitations
Some limitations of the present study warrant discussion. First, as discussed earlier, patients were not randomized to the treatment arms. Second, veterans are referred to the HF clinic only after being hospitalized for HF. As a result, all the referred veterans likely were experiencing more advanced disease and/or low adherence, and these results may not be representative of patients with less advanced disease. Finally, the sample used in the present analysis was a small, homogeneous group of 91 male veterans who were 85% black and 95% non-Hispanic. These demographics are largely representative of the JBVAMC. Therefore, the present results may not be generalizable to more racially or ethnically diverse populations, women, or nonveterans.
Conclusion
Minimizing rehospitalization rates for patients with HF continues to be a priority. Health care costs of HF are more than double those of patients in the general population, primarily due to hospitalizations—in 2013, HF hospitalization costs in the U.S. exceeded $10 billion.27,28 Given the current emphasis on economical, patient-centered care, SMAs may be a cost-effective alternative to individualized disease management plans while continuing to allow providers to tailor treatment to individual patient needs.
Although this study did not find better outcomes among veterans whose specialty HF care was augmented by clinic-based SMAs, the authors believe that this type of program has great potential. Heart failure SMAs may improve HF outcomes, enhance efficiency of health care delivery, and reduce overall HF-associated health care costs if it is integrated earlier along the continuum of care or if other novel components, such as caregiver support or technology-based delivery, is included. Further studies are needed to systematically evaluate HF management programs delivered via SMAs to improve outcomes and reduce the economic burden that HF places on the health care system.
Rising health care costs have led to threats of nonreimbursement for rehospitalization within 30 days postdischarge.1,2 Heart failure (HF) in particular is characterized by the highest 30-day rehospitalization rate (23.5% in 2013), which accounts for more than two-thirds of HF expenditures.3,4
Much of HF-related health care costs can be addressed with effective self-management by patients with HF. Therefore, developing and implementing effective disease management programs for this high-risk patient population is essential. Heart failure management programs may include optimizing HF medications, improving patient understanding of the importance of appropriate diet and physical activity, and cultivating psychological health and well-being. In a 2013 systematic review and meta-analysis, Wakefield and colleagues found that disease management programs improved nearly all HF outcomes, including lower mortality rates, lower hospital readmission rates, fewer clinic visits, higher satisfaction with care, and higher quality of life, compared with a no-treatment control or standard care.5 Moreover, these programs demonstrated cost-effectiveness by reducing HF-related hospitalizations and health care expenditures.5
One method to deliver specialized disease management programs to a greater number of patients may be to use shared medical appointments (SMAs). In a randomized controlled trial, Smith and colleagues demonstrated improved HF outcomes through 7 months among veterans who attended SMAs for HF management.6 However, the trial enrolled only 25% of patients screened, and 63% of the patients who did not enroll were classified as not interested. These findings suggest that patients with HF, and veterans in particular, may face additional barriers to enrolling in HF management programs, and these results may not be fully representative of veterans with HF.
In this study, the authors used a naturalistic study design via retrospective review of the electronic health record (EHR) to evaluate whether patients with acute HF who chose to attend SMAs promoting self-management skills for HF would have better hospitalization outcomes compared with those who received individual disease management instructions in a HF specialty clinic (ie, usual care). The authors hypothesized that veterans who participated in the HF SMA clinic would have fewer 12-month HF-related and all-cause hospitalizations, fewer days in the hospital, and more days to first hospitalization compared with patients in usual care.
Methods
The clinic for veterans with acute HF was initiated in October, 2010 at the Jesse Brown VAMC (JBVAMC) in Chicago, Illinois, to reduce readmissions by targeting patients who had been previously hospitalized for HF. In September 2011, the multidisciplinary SMA clinic was developed within the HF clinic to provide enhanced care focused on self-management strategies for patients with HF. The HF SMA program comprised 4 weekly face-to-face sessions co-led by a nurse practitioner (NP), a dietitian, and a clinical psychologist, similar to what has been shown to be successful and cost-effective in nonveteran populations.6-8 Patients attended at least 4 sessions before graduating to the advanced HF SMA program where they could attend monthly booster sessions. The program promoted self-management by providing education about and support for the HF process, HF medications, diet adherence, physical activity, psychological well-being, and stress management via interactive presentations. During the visit, patients’ medication and food logs were reviewed. Patients were encouraged to discuss successes and obstacles in achieving their goals. All study procedures were approved by the institutional review board at JBVAMC.
Study Design
Data were collected by retrospective review of the JBVAMC EHR. The EHR was reviewed for all veterans scheduled for ≥ 1 SMA clinic visit within the HF specialty clinic using predetermined, convenient selection between January 1, 2012, and December 31, 2013. Outcome data were collected through 12-month follow-up (through December 31, 2014).
Patients in both treatment arms received HF care through the HF clinic, including one-on-one education regarding HF self-management provided by a NP. Patients were assigned to the HF SMA group if they also attended the HF SMA clinic within 3 months of their initial HF clinic consult. The number of SMAs attended was included as a covariate in the models. Patients who were scheduled for, but did not attend, the HF SMA clinic were assigned to the HF clinic group. Patients who attended the initial HF consult before September 1, 2011, were excluded, thereby ensuring that all patients included in the present analyses had the opportunity to attend the HF SMA appointment within the predetermined period of chart review.
Data for all VA hospitalizations that occurred between January 1, 2012 and December 31, 2014, were extracted from the EHR. Extracted data included admission date, discharge date, and discharge diagnoses. From these data, the authors assessed 4 hospitalization outcomes for each HF hospitalization and all-cause hospitalization within 12 months of the initial HF clinic consult date: hospitalization (yes/no), number of hospitalizations, number of days in the hospital, and days to first hospitalization.
Data Analysis
Demographic, HF characteristics, and HF outcome variables for the HF SMA and HF clinic groups were compared using t tests and chi-square analyses. Logistic regressions were used to predict 12-month hospitalization, linear regressions were used to predict number of hospitalizations and number of days hospitalized, and Cox proportional hazards regressions were used to predict time from initial HF consult to first hospitalization for each HF-related hospitalization variable and all-cause hospitalization variable. A separate logistic regression was conducted to predict 12-month all-cause mortality. The primary predictor variable of interest for all models was group membership (HF SMA vs HF clinic). Covariates in all models included race (black vs nonblack), ethnicity (Hispanic/Latino vs non-Hispanic/Latino), age, and number of HF SMAs attended.
Results
Of 709 HF SMA clinic appointments made for 141 patients between January 1, 2012, and December 31, 2013, 54 patients were assigned to the HF SMA group and 37 patients were assigned to the HF clinic group (Figure). The majority of the sample was black (87%), non-Hispanic/Latino (96%), and the average age was 68 years. Patients were more likely to have nonischemic (rather than ischemic) cardiomyopathy (66%) and more likely to have HF with reduced (rather than preserved) ejection fraction (76%; ie, systolic HF). Furthermore, 40% of the sample was diagnosed with atrial fibrillation (AF) or atrial flutter (A-flutter), and 24% had an implantable cardioverter-defibrillator or pacemaker. There were no significant differences in demographics or HF characteristics between the HF SMA group and the HF clinic group (Table).
HF Hospitalization Outcomes
During the 12-month follow-up, 32 patients were hospitalized for HF, 18 (33.3%) in the SMA group and 14 (37.8%) in the HF clinic group, P = .658. Patients were hospitalized up to 4 times for between 1 and 38 days, and from 1 to 352 days postconsult. No differences between the HF SMA group and HF clinic group were observed on any of the HF hospitalization outcomes (Table). Group membership did not predict HF hospitalization (odds ratio [OR]: 0.39, 95% confidence interval [CI]: 0.11-1.42), number of HF hospitalizations (β: 0.15, SE: 0.29), number of days hospitalized for HF (β: 0.1.66, SE: 2.01), or time to first HF hospitalization (hazard ratio [HR]: 1.35, 95% CI: 0.66-2.77), all Ps > .10. In the Cox proportional hazards regression predicting time to HF hospitalization, the coefficients did not converge when the model included demographic covariates; therefore, the model was run only with HF group as a predictor variable. For all other models, no covariates significantly predicted HF hospitalization outcomes.
All-Cause Hospitalization Outcomes
During the 12-month follow-up, 57 patients were hospitalized for any cause (including HF hospitalizations), 32 (59.3%) in the SMA group and 25 (67.6%) in the HF clinic group, P = .421. Patients were hospitalized up to 6 times for between 1 and 106 days and from 1 to 352 days postconsult. No differences were observed between the groups on any of the all-cause hospitalization outcomes (Table). Group membership did not predict all-cause hospitalization (OR: 0.34, 95% CI: 0.10-1.19), number of all-cause hospitalizations (β: 0.49, SE: 0.41), number of days hospitalized for any cause (β: 5.15, SE: 5.15), or time to first all-cause hospitalization (HR: 0.98, 95% CI: 0.56-1.72), all P > .05. None of the covariates predicted any of the all-cause hospitalization outcomes.
All-Cause Mortality Outcomes
During the 12-month follow-up, 14 patients (15%) died of any cause, 8 (15%) in the SMA group and 6 (16%) in the HF clinic group, P = .856. Group membership did not predict all-cause mortality (OR: 2.32, 95% CI: 0.44-12.18), and likewise none of the covariates were associated with 12-month all-cause mortality.
Discussion
This study was a naturalistic, retrospective examination of a HF management program promoting self-management delivered via multidisciplinary SMAs among veterans who enrolled in an acute HF specialty clinic. The authors’ hypothesis was not supported: patients who attended the HF SMA clinic did not have lower 12-month hospitalization or mortality rates, shorter hospital stays, or longer time to hospitalization compared with patients in the HF clinic only.
In contrast to the patient-centered approach of this study, a randomized trial delivering a similar disease management program found that patients with acute HF in the SMA group had better short-term (< 7 months) hospitalization outcomes, specifically greater time to first HF-related hospitalization (HR 0.45, 95% CI: 0.21-0.98), but this effect did not last through 12 months when compared with patients in standard care.6 These disparate findings may be explained by the gap in bench-to-bedside research, where despite scientific evidence indicating better outcomes among patients randomized to an intervention, when patients are given a choice, they may not choose to engage in the best option for their HF treatment.
In the present study, veterans who chose not to attend the HF SMA clinic may have done so for numerous reasons that may have influenced the outcomes. For example, those veterans who did not attend the HF SMA clinic may have had higher health literacy and less need for an educational program. Health literacy has been inversely associated with HF outcomes, such that patients with HF with lower health literacy have greater risk of HF rehospitalization or mortality.9,10 In addition, many of the veterans who were followed in the HF clinic were taught the same disease management strategies by the NP during one-on-one visits, and they may have gained the same self-management skills in a different setting.
Another possibility is that the veterans enrolled in the HF clinic were less likely to be followed exclusively at the VA and therefore may have had external hospitalizations not recorded in their VA health records. In 2000, more than half the veterans who received health care services at the VA reported that they did not receive their care exclusively at the VA.11 This may be especially true since the Veteran’s Choice Program permits veterans who reside > 40 miles from a VA hospital to receive care closer to home.
Disease Management Programs
Disease management programs for HF in general promote better outcomes and lower health care expenditures.5,12 Self-management instruction delivered via SMAs may have greater potential for reducing HF-associated health care costs if it were to be integrated earlier in the continuum of care. The sample in this study was composed of veterans who were referred to a specialty clinic only after being hospitalized for HF. These patients likely were experiencing more advanced disease and/or low adherence, as indicated by the relatively high prevalence of AF diagnoses and pacemakers; these null findings are consistent with those from a randomized controlled trial of a disease management program among veterans with heavy HF symptom burden and impaired functional status.13 However, integrating self-management programs earlier in HF clinical care (eg, primary care or cardiology clinics) may be more effective in promoting proactive disease management and delaying or preventing initial HF hospitalizations.
For example, a disease management plan implemented by general practitioners for veterans with HF in Australia was associated with a 23% reduction in potentially preventable hospitalization rates.14 Veterans with HF enrolled in a NP-led disease management intervention, relative to those followed only in primary care, had significantly fewer hospitalizations and nearly half the risk mortality (15% vs 28% after 2 years; HR 0.55).15 Furthermore, some have suggested that SMAs may be more effective for patients for whom risk of disease is high but current disease burden (ie, symptoms) is low, such as diabetes mellitus management programs.16 Early intervention also may allow providers to reach more patients more quickly and before they experience advanced symptoms, thereby reducing specialty clinic wait times and overall health expenditures. Developing more effective disease management programs for patients with acute HF and veterans in particular remains a critical matter for future study.
Additional and novel components of HF management programs show promise for future interventions. First, various facets of social support, including emotional support, instrumental/tangible support, informational support, and appraisal support, are associated with improved self-care.17 For example, the levels of family functioning and family support predict HF outcomes, perhaps because between-appointment monitoring allows patients to report problems that might otherwise go unidentified and receive more external feedback about their disease and symptoms.18,19 Patients report that family members or especially supportive members of their health care team are invaluable contributors to their successful management of HF.20 A recently published feasibility trial of a couple-based disease management program observed positive trends in HF management for veterans, as well as improvements in caregiver’s depressive symptoms and burden, indicating that even support from informal caregivers may improve HF outcomes.21
Advances in technology-delivered disease management programs show promise in improving adherence to chronic disease management programs.22,23 Specifically for HF, veterans who enrolled in a daily telehealth intervention employing daily vital signs and symptom reporting, automated reminders and tips for self-management, and proactive monitoring and intervention telephone calls from a nurse successfully lowered their blood pressure, lost weight, reduced their HF medication dosages, and spent 80% fewer days in the hospital.24 Among patients with coronary artery disease, a text messaging service was shown to improve a number of cardiovascular risk factors.25 Moreover, mobile applications can be used to support informal caregivers of patients with HF.26 To the authors knowledge, no research studies have been conducted using text messaging or mobile applications among veterans with HF.
Limitations
Some limitations of the present study warrant discussion. First, as discussed earlier, patients were not randomized to the treatment arms. Second, veterans are referred to the HF clinic only after being hospitalized for HF. As a result, all the referred veterans likely were experiencing more advanced disease and/or low adherence, and these results may not be representative of patients with less advanced disease. Finally, the sample used in the present analysis was a small, homogeneous group of 91 male veterans who were 85% black and 95% non-Hispanic. These demographics are largely representative of the JBVAMC. Therefore, the present results may not be generalizable to more racially or ethnically diverse populations, women, or nonveterans.
Conclusion
Minimizing rehospitalization rates for patients with HF continues to be a priority. Health care costs of HF are more than double those of patients in the general population, primarily due to hospitalizations—in 2013, HF hospitalization costs in the U.S. exceeded $10 billion.27,28 Given the current emphasis on economical, patient-centered care, SMAs may be a cost-effective alternative to individualized disease management plans while continuing to allow providers to tailor treatment to individual patient needs.
Although this study did not find better outcomes among veterans whose specialty HF care was augmented by clinic-based SMAs, the authors believe that this type of program has great potential. Heart failure SMAs may improve HF outcomes, enhance efficiency of health care delivery, and reduce overall HF-associated health care costs if it is integrated earlier along the continuum of care or if other novel components, such as caregiver support or technology-based delivery, is included. Further studies are needed to systematically evaluate HF management programs delivered via SMAs to improve outcomes and reduce the economic burden that HF places on the health care system.
1. Boccuti C, Casillas G. Aiming for fewer hospital U-turns: the Medicare hospital readmissions reduction program. http://kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/. Published September 30, 2016. Accessed March 6, 2017.
2. Barrett ML, Wier LM, Jiang HJ, Steiner CA. All-cause readmissions by payer and age, 2009-2013. Statistical Brief #199. https://www.hcup-us.ahrq .gov/reports/statbriefs/sb199-Readmissions-Payer -Age.jsp. Published December 2015. Accessed March 6, 2017.
3. Fingar K, Washington R. Trends in hospital readmissions for four high-volume conditions, 2009-2013. Statistical Brief #196. https://www.hcup-us .ahrq.gov/reports/statbriefs/sb196-Readmissions -Trends-High-Volume-Conditions.jsp. Published November 2015. Accessed March 6, 2017.
4. McMurray JJ, Adamopoulos S, Anker SD, et al; ESC Committee for Practice Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33(14):1787-1847.
5. Wakefield BJ, Boren SA, Groves PS, Conn VS. Heart failure care management programs: a review of study interventions and meta-analysis of outcomes. J Cardiovasc Nurs. 2013;28(1):8-19.
6. Smith CE, Piamjariyakul U, Wick JA, et al. Multidisciplinary group clinic appointments: the Self-Management and Care of Heart Failure (SMAC-HF) trial. Circ Heart Fail. 2014;7(6):888-894.
7. Sochalski J, Jaarsma T, Krumholz HM, et al. What works in chronic care management: the case of heart failure. Health Aff (Millwood). 2009;28(1): 179-189.
8. Ågren S, Evangelista LS, Davidson T, Strömberg A. Cost-effectiveness of a nurse-led education and psychosocial programme for patients with chronic heart failure and their partners. J Clin Nurs. 2013;22(15-16):2347-2353.
9. Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21(8):612-618.
10. McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. 2015;4(6). pii:e001799.
11. Nelson KM, Starkebaum GA, Reiber GE. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Rep. 2007;122(1):93-100.
12. Whellan DJ, Hasselblad V, Peterson E, O’Connor CM, Schulman KA. Metaanalysis and review of heart failure disease management randomized controlled clinical trials. Am Heart J. 2005;149(4):722-729.
13. Bekelman DB, Plomondon ME, Carey EP, et al. Primary results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study: a randomized clinical trial. JAMA Intern Med. 2015;175(5):725-732.
14. Vitry AI, Nguyen TA, Ramsay EN, et al. General practitioner management plans delaying time to next potentially preventable hospitalisation for patients with heart failure. Intern Med J. 2014;44(11):1117-1123.
15. Lowery J, Hopp F, Subramanian U, et al. Evaluation of a nurse practitioner disease management model for chronic heart failure: a multi-site implementation study. Congest Heart Fail. 2012;18(1):64-71.
16. Edelman D, McDuffie JR, Oddone E, Gierisch JM, Nagi A, Williams JW Jr. Shared medical appointments for chronic medical conditions: a systematic review. VAESP Project #09-010. http://www.hsrd.research.va.gov/publications/esp/shared -med- appt-REPORT.pdf. Published July 2012. Accessed March 6, 2017.
17. Graven LJ, Grant JS. Social support and self-care behaviors in individuals with heart failure: an integrative review. Int J Nurs Stud. 2014;51(2):320-333.
18. Dunbar SB, Clark PC, Quinn C, Gary RA, Kaslow NJ. Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs. 2008;23(3):258-265.
19. Piette JD, Gregor MA, Share D, et al. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congest Heart Fail. 2008;14(1):12-18.
20. Skaperdas E, Tuepker A, Nicolaidis C, Robb JK, Kansagara D, Hickam DH. Congestive heart failure self-management among US veterans: the role of personal and professional advocates. Patient Educ Couns. 2014;95(3):371-377.
21. Trivedi R, Slightam C, Fan VS, et al. A couples’ based self-management program for heart failure: results of a feasibility study. Front Public Health. 2016;4:171.
22. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg SA. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52.
23. Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362.
24. Schofield RS, Kline SE, Schmalfuss CM, et al. Early outcomes of a care coordination-enhanced telehome care program for elderly veterans with chronic heart failure. Telemed J E Health. 2005;11(1):20-27.
25. Chow CK, Redfern J, Hillis GS, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255-1263.
26. Piette JD, Striplin D, Marinec N, et al. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative efficacy trial. J Med Internet Res. 2015;17(6):e142.
27. Mejhert M, Lindgren P, Schill O, Edner M, Persson H, Kahan T. Long term health care consumption and cost expenditure in systolic heart failure. Eur J Intern Med. 2013;24(3):260-265.
28. Torio CM, Moore BJ. National inpatient hospital costs: the most expensive conditions by payer, 2013. Statistical Brief #204. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp. Published May 2016. Accessed March 6, 2017.
1. Boccuti C, Casillas G. Aiming for fewer hospital U-turns: the Medicare hospital readmissions reduction program. http://kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/. Published September 30, 2016. Accessed March 6, 2017.
2. Barrett ML, Wier LM, Jiang HJ, Steiner CA. All-cause readmissions by payer and age, 2009-2013. Statistical Brief #199. https://www.hcup-us.ahrq .gov/reports/statbriefs/sb199-Readmissions-Payer -Age.jsp. Published December 2015. Accessed March 6, 2017.
3. Fingar K, Washington R. Trends in hospital readmissions for four high-volume conditions, 2009-2013. Statistical Brief #196. https://www.hcup-us .ahrq.gov/reports/statbriefs/sb196-Readmissions -Trends-High-Volume-Conditions.jsp. Published November 2015. Accessed March 6, 2017.
4. McMurray JJ, Adamopoulos S, Anker SD, et al; ESC Committee for Practice Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33(14):1787-1847.
5. Wakefield BJ, Boren SA, Groves PS, Conn VS. Heart failure care management programs: a review of study interventions and meta-analysis of outcomes. J Cardiovasc Nurs. 2013;28(1):8-19.
6. Smith CE, Piamjariyakul U, Wick JA, et al. Multidisciplinary group clinic appointments: the Self-Management and Care of Heart Failure (SMAC-HF) trial. Circ Heart Fail. 2014;7(6):888-894.
7. Sochalski J, Jaarsma T, Krumholz HM, et al. What works in chronic care management: the case of heart failure. Health Aff (Millwood). 2009;28(1): 179-189.
8. Ågren S, Evangelista LS, Davidson T, Strömberg A. Cost-effectiveness of a nurse-led education and psychosocial programme for patients with chronic heart failure and their partners. J Clin Nurs. 2013;22(15-16):2347-2353.
9. Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21(8):612-618.
10. McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. 2015;4(6). pii:e001799.
11. Nelson KM, Starkebaum GA, Reiber GE. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Rep. 2007;122(1):93-100.
12. Whellan DJ, Hasselblad V, Peterson E, O’Connor CM, Schulman KA. Metaanalysis and review of heart failure disease management randomized controlled clinical trials. Am Heart J. 2005;149(4):722-729.
13. Bekelman DB, Plomondon ME, Carey EP, et al. Primary results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study: a randomized clinical trial. JAMA Intern Med. 2015;175(5):725-732.
14. Vitry AI, Nguyen TA, Ramsay EN, et al. General practitioner management plans delaying time to next potentially preventable hospitalisation for patients with heart failure. Intern Med J. 2014;44(11):1117-1123.
15. Lowery J, Hopp F, Subramanian U, et al. Evaluation of a nurse practitioner disease management model for chronic heart failure: a multi-site implementation study. Congest Heart Fail. 2012;18(1):64-71.
16. Edelman D, McDuffie JR, Oddone E, Gierisch JM, Nagi A, Williams JW Jr. Shared medical appointments for chronic medical conditions: a systematic review. VAESP Project #09-010. http://www.hsrd.research.va.gov/publications/esp/shared -med- appt-REPORT.pdf. Published July 2012. Accessed March 6, 2017.
17. Graven LJ, Grant JS. Social support and self-care behaviors in individuals with heart failure: an integrative review. Int J Nurs Stud. 2014;51(2):320-333.
18. Dunbar SB, Clark PC, Quinn C, Gary RA, Kaslow NJ. Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs. 2008;23(3):258-265.
19. Piette JD, Gregor MA, Share D, et al. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congest Heart Fail. 2008;14(1):12-18.
20. Skaperdas E, Tuepker A, Nicolaidis C, Robb JK, Kansagara D, Hickam DH. Congestive heart failure self-management among US veterans: the role of personal and professional advocates. Patient Educ Couns. 2014;95(3):371-377.
21. Trivedi R, Slightam C, Fan VS, et al. A couples’ based self-management program for heart failure: results of a feasibility study. Front Public Health. 2016;4:171.
22. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg SA. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52.
23. Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362.
24. Schofield RS, Kline SE, Schmalfuss CM, et al. Early outcomes of a care coordination-enhanced telehome care program for elderly veterans with chronic heart failure. Telemed J E Health. 2005;11(1):20-27.
25. Chow CK, Redfern J, Hillis GS, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255-1263.
26. Piette JD, Striplin D, Marinec N, et al. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative efficacy trial. J Med Internet Res. 2015;17(6):e142.
27. Mejhert M, Lindgren P, Schill O, Edner M, Persson H, Kahan T. Long term health care consumption and cost expenditure in systolic heart failure. Eur J Intern Med. 2013;24(3):260-265.
28. Torio CM, Moore BJ. National inpatient hospital costs: the most expensive conditions by payer, 2013. Statistical Brief #204. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp. Published May 2016. Accessed March 6, 2017.
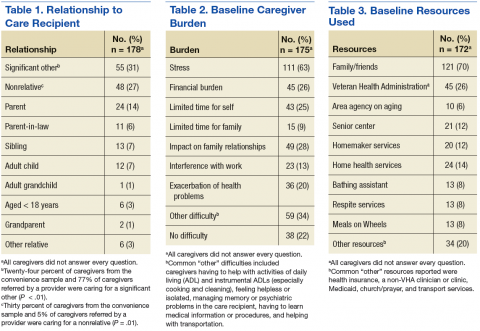
Veterans as Caregivers:Those Who Continue to Serve
More than 20% of the U.S. population will be aged ≥ 65 years by 2030, an increase from 13% in 2012.1 The likelihood of needing assistance with activities of daily living (ADLs) increases with age.2 People who need such assistance often depend on informal and unpaid assistance from friends and family. In 2009, about 65.7 million Americans (28.5%) provided informal care for people with an illness or disability, and that number only is expected to rise.3 These informal caregivers provide up to 80% of the total care hours needed by community-dwelling older adults—an estimated economic value of $450 billion in unpaid contributions in 2009.4,5
Caregiving can lead to significant physical, psychological, social, and financial burdens.6 The caregiving burden is associated with a host of adverse health behaviors and outcomes such as poor diet, lack of exercise and sleep, smoking, decreased participation in preventive health care, anxiety, depression, relationship difficulties, employment disruption, financial hardship, suicide, and higher mortality compared with that of noncaregivers.6-10 Additionally, care recipients are at increased risk for abuse or neglect when the caregiver is experiencing a significant burden.11 Therefore, efforts to improve caregiver support are important for both partners in the caregiver/care recipient dyad.
Caregiver support is beneficial to the health of caregivers and care recipients.10,12 For example, the Resources for Enhancing Alzheimer’s Caregiver Health (REACH) program has been shown to reduce the stress of informal caregiving and the risk of depression in caregivers.13,14 This program showed similar effects when implemented within the VHA.14 In the Partners in Dementia Care project, the VHA and Alzheimer’s Association coordinated care and support for veterans with dementia and their family and friends. This intervention resulted in lower caregiver strain and depression scores among participants.15
With a growing medical literature that shows the benefits of caregiver support interventions, the VHA developed a robust support program for informal caregivers of veterans. The VA caregiver support website (www.caregiver.va.gov) provides information and resources targeted to caregivers for veterans, including psychosocial and functional support for caregivers. The psychosocial support provided by the VA includes caregiver education, counseling, access to caregiver support coordinators, a caregiver support line, support groups, and referral to community support organizations.16 Functional support on the site includes financial assistance toward skilled home care, home hospice care, adult day care, home-based primary care, homemaker and home health aide services, telehealth, and respite care.16 Veterans who are caregiving for nonveterans have access to VHA psychosocial support but not to functional support services. For these veterans, functional caregiver support must come from family or referral to community organizations.
Background
In the U.S., about 11% of caregivers are veterans, but the availability of data about these caregivers is limited to veteran subgroups.3 For example, a 2011 study reported that 20% of veterans aged ≥ 60 years are caregivers.17 However, this estimate included child care for unimpaired children, which is not commonly included in other caregiving estimates. In another study, 30% of middle-aged active-duty officers reported helping their parents with instrumental ADLs (IADLs).18 These data suggest a significant proportion of veterans may be caregivers; however, the estimates do not identify prevalence of caregiving among a population of VHA enrolled veterans.
Likewise, few studies discuss the burden veterans experience from caregiving. A study of the 2009/2010 CDC Behavioral Risk Factor Surveillance System data found that female caregivers were more likely to report problems with sleep and mental health if they were veterans vs nonveterans.19 In a second study, caregiving veterans frequently reported physical (39%) and emotional (53%) strain, with emotional strain relating to depressive symptoms. The study of active-duty officers noted that worry was prevalent among military officers caregiving for parents from a distance.18 In contrast to the negative outcomes of caregiving, Monin and colleagues found that many veterans perceived caregiving as rewarding. Since caregiving may be a positive experience, veterans may benefit and be a potential resource for care to elderly and disabled citizens.17
Project Rationale and Goals
Social workers are the cornerstone of caregiver support at the George E. Wahlen VA Salt Lake City Health Care System (VASLCHCS) in Utah. They educate veterans and caregivers about VA resources to support caregivers of veterans. For those veterans who are caregiving for a nonveteran, the VASLCHCS social workers provide psychosocial support and help veterans connect to a local area agency on aging (AAA) for access to functional support. In practice, primary care clinic (PCC) providers have observed that directing a veteran to call the AAA does not usually result in a phone call. Therefore, an aim of this quality improvement (QI) project was to determine the most effective means of completing a successful AAA referral.
The VASLCHCS Geriatric Research Education and Clinical Center collaborates with the Utah Aging and Disability Resource Connection (ADRC) to improve awareness of available resources for veterans. Building on this collaborative project, the authors created a formal referral process for veterans needing local AAA services. This QI project had 3 aims: (1) estimate the prevalence of caregiving among veterans in the VASLCHCS primary care clinic; (2) identify perceived caregiving difficulties and resource use difficulty in caregiving tasks; and (3) test different strategies to connect veterans with a referral to community resources through the AAA.
The authors hypothesized that a veteran would be more likely to connect with the AAA if contact was initiated by the AAA rather than the standard practice of asking the veteran to make the call. However, the authors also hypothesized that a veteran who took the time to make the call would be more likely to use AAA resources compared with veterans who were called by the AAA.
Methods
The VASLCHCS Research and Development Office reviewed this project and determined that it met the definition of QI. Therefore, it did not require IRB approval.
The study drew from a convenience sample of veterans who were waiting for appointments in the PCC and who were referred by their health care provider (HCP). To identify caregivers, veterans were asked: “People may provide regular care or assistance to a friend or family member who has a health problem, long-term illness, or disability. During the past month, did you provide any such care or assistance to a friend or family member?” Referrals from HCPs were included in all calculations except the prevalence estimate.
The authors interviewed veterans over a 3-month period in 2015. As of November 2014, the clinic was serving about 11,000 veterans, of which 6,589 lived in Salt Lake County. The clinic also serves veterans who live in other counties in Utah, Nevada, Wyoming, Idaho, and Colorado.
Intervention and Partnering With Community Resources
All willing caregivers were provided a referral to a local AAA (Figure). Salt Lake County veterans interested in referral to the AAA were randomized to 1 of 2 referral methods: veteran-initiated referral (VIR), in which the veteran was given a handout with the phone number of the Salt Lake County caregiver support program (CSP), or provider-initiated referral (PIR), in which the veteran’s phone number was given to the CSP. Caregiving veterans living outside Salt Lake County were provided the AAA phone number in their area and instructed to call for information.
The interview form was randomized using an even or odd number before the interview. Some veterans who were randomized to a PIR needed to be moved into the VIR intervention arm because of the following reasons: the veteran’s care recipient was aged < 18 years (3); the veteran lived outside of Salt Lake County (20); the veteran did not want his/her name given to an outside agency (5); or the interviewer mistakenly gave the veteran the AAA contact information (4).
The primary author called caregivers in the PIR and VIR groups 2 to 4 weeks after the referral to determine whether they had contacted or were contacted by the AAA. Ten call attempts were made before participants were considered lost to follow-up. Caregivers that had been in contact with the AAA reported in open-ended fashion the resources to which they had been referred and whether those resources had been helpful.
Analysis
In this evaluation, the primary outcome of interest was whether contact between the veteran and AAA occurred. For the VIR group, contact was defined as the veteran having called the AAA, regardless of whether he or she actually spoke to someone. For the PIR group, contact occurred if the veteran reported receiving a phone call from AAA regardless of whether he or she had actually spoken with someone (eg, if the veteran reported that the AAA had left a voice mail, this was considered contact). Veterans also were asked whether connecting with the AAA led to resource referrals and whether these referrals were useful.
To achieve a power of 80% with a 95% confidence interval, 20 people were needed in each intervention group to detect a 40% difference in the rate of contact between the 2 groups. STATA12 (College Station, TX) was used to calculate Fisher exact and chi-square values to evaluate differences between groups.
Results
For the study, 433 PCC veterans were interviewed, and 157 (36%) self-identified as a caregiver. An additional 22 referrals were included for a total of 179 caregivers. Caregiver and care recipient characteristics, caregiver burden, and resource utilization were calculated for all 179 caregivers; however, all caregivers did not answer every question. Ninety-eight percent (176) of caregivers were men; 64% (109/170) were from Salt Lake County, and 5% were from outside Utah (8). Twelve percent (21) of the 179 caregivers were providing care for > 1 person. Of 177 caregivers, 3% (5) were caring for both a veteran and a nonveteran, 69% (122) were caring for a nonveteran only, and 28% (49) were caring for another veteran only (Table 1).
The most common burden reported by caregivers was stress (63%); 70% endorsed family/friends as a resource (Table 2). Just 6% (10) of caregivers used the AAA, whereas 26% (45) received VHA support. Of the 54 veterans who were caring for a veteran, 40 reported using the VHA as a resource. Five people caring for nonveterans reported using the VHA as a resource; however, data about which resources those caregivers were accessing were not collected (Table 3).
AAA Referral and Randomization
Sixty-five percent of caregivers accepted AAA referrals. Of 109 Salt Lake County caregivers, 70% accepted referral to the AAA. There was no statistically significant difference in referral acceptance rates when comparing Salt Lake County residents with nonresidents (P = .09).The authors were unable to obtain the phone number for 1 caregiver who had accepted a referral, and 1 caregiver who accepted referral did not want a follow-up. This left 111 caregivers available for follow-up, 75 in Salt Lake County. Fifty Salt Lake County veterans were randomly assigned to the VIR group and 25 to the PIR group. The 36 caregivers who accepted referrals outside Salt Lake County also were placed in the VIR group, for a total of 86 caregivers.
Follow-up
Ninety-eight percent of caregivers were reached for follow-up. Both people lost to follow-up were in Salt Lake County (1 in each group).
In Salt Lake County, 12% (6) of the VIR group and 64% (16) of the PIR group had connected with the AAA (P < .01). Although 64% of those in the PIR group reported having been called by the AAA, the AAA representative reported all 25 had been called. The AAA records showed 9 of those called were reached by voice mail, 6 were provided information about caregiving resources, 2 formally joined the support program, 5 declined help, 1 was no longer caregiving, 1 was too busy to talk, and 1 was the wrong phone number (and was lost to follow-up as well).
Outside of Salt Lake County 19% (7) reported calling the local AAA. There was no difference in referral completion between the Salt Lake County/non-Salt Lake County VIR groups (P = .4).
Fifteen percent of all VIR caregivers reported calling the AAA. There were no statistical differences between Salt Lake County VIR and non-Salt Lake County VIR for reasons why the veteran had not called the AAA (Table 4).
Of 28 people who connected with the AAA, 16 (57%) said they had received access to a needed resource as a result of the phone call. Seven caregivers (25%) said they had not been referred to other resources as a result of the call. The VIR group was more likely to be referred to other resources after contacting the AAA than was the PIR group, although this difference did not reach significance (69% vs 47%, P = .28).
Discussion
More than one-third (36%) of veterans seen in the VASLCHCS PCC are caregivers. This prevalence is higher than that reported for the general U.S. population and higher than that reported in other veteran groups.5,17,18 Most caregivers in this project were caring for nonveterans and only had access to VHA psychosocial caregiver support programs because VHA functional caregiver support (eg, respite, homemaker services) is not available to veterans who care for nonveterans. A majority (78%) of caregiving veterans reported some caregiver burden. Despite the burden, most are not using community resources. However when offered, more than half the caregivers were interested in an AAA referral.
Although the VHA does not provide functional caregiver support resources to veterans caring for nonveterans, there are other agencies that can assist veterans: AAAs for care recipients aged ≥ 60 years and the ADRCs for younger veterans. Through AAAs, caregivers can access a variety of support services, including transportation, adult day care, caregiver support, and health promotion programs. Partnership between agencies such as the VHA and the AAAs could benefit caregiving veterans. This QI project suggests ways to strengthen interagency cooperation.
This study also suggests that a provider or clinic-initiated referral is more likely to connect veterans with information and resources than the current practice of recommending that the veteran initiate the referral. Once in contact with the AAA, most caregivers were referred to needed resources. The next step will be to establish an efficient way for clinic staff to identify caregiving veterans and make referrals to community programs. Referrals could be made by any member of the patient aligned care team (PACT) to further standardize and streamline the process.
Thirty-one percent of veterans in this project were eligible for the VHA caregiver support program because they cared for a veteran. However, 25% of these caregiving veterans were not accessing this resource. Increasing awareness of the VHA caregiver support program among veterans caring for other veterans would improve caregiver support to both caregiving and care recipient veterans.
Limitations
One limitation of this project was the intentional exclusion of the women’s clinic from the sampling process. For consistency, the authors wanted to limit the intervention to 1 PCC and so they chose the clinic that serves the majority of the veterans who receive primary care at VASLCHCS. Additionally, the literature showed that male caregivers compared with women caregivers20,21 have different characteristics in regards to caregiver burden, and a well-designed study of women caregivers already has been published.19
Also, this study did not obtain data on age, health problems, or socioeconomic status of the caregivers to avoid identifying information. Last, the authors did not ask about time spent caregiving or type of care provided. These questions may be important for future studies. Future investigations should evaluate health care use and health of caregivers vs noncaregivers in the veteran population. It also could be important to determine methods for building bridges between the VHA, AAAs, and other community services.
Conclusion
To minimize the disruption that a research study might have caused to normal clinical workflow, the primary author played the role that a medical social worker or other PACT member might play in the future. This project sheds light on how to improve outcomes for community referrals and an important future step in this research would be to develop and test a process that would integrate the PACT into the referral process.
More than one-third of veterans seen in the VASLCHCS PCC are caregivers. To the authors’ knowledge, this is the first estimate of prevalence of caregiving in veterans who receive primary care from the VHA. About 63% of caregiving veterans perceived some burden due to caregiving, and 66% accepted referral to community resources. However, only 12% who were asked to self-refer made contact with the AAA compared with 64% when a provider made the referral for them. Provider referral is more effective in connecting caregiving veterans with resources. Development of interagency partnerships should be fostered to help veterans decrease caregiving burden.
This project is one of the few studies looking at this special group of caregivers: veterans who serve as caregivers. It highlights the need for the VHA to establish policies and partnerships to improve caregiver support to this valuable group of veterans.
1. Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States: population estimates and projections. http://www.census .gov/prod/2014pubs/p25-1140.pdf. Published May 2014. Accessed March 9, 2017.
2. Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA Intern Med. 2013;173(16):1506-1513.
3. National Alliance for Caregiving, American Association of Retired Persons. Caregiving in the U.S. 2009 executive summary. http://assets.aarp.org/rgcenter/il/caregiving_09_es.pdf. Published November 2009. Accessed March 9, 2017.
4. Spillman BC, Wolff J, Freedman VA, Kasper JD; Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Informal caregiving for older Americans: an analysis of the 2011 national study of caregiving. https://aspe.hhs.gov/report/informal-caregiving-older-americans-analysis-2011-national-study-caregiving. Published April 1, 2014. Accessed March 9, 2017.
5. Feinberg L, Reinhard SC, Houser A, Choula R; AARP Public Policy Institute. Valuing the invaluable: 2011 update. The growing contributions and costs of family caregiving. https://assets.aarp .org/rgcenter/ppi/ltc/i51-caregiving.pdf. Published June 2011. Accessed March 9, 2017.
6. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052-1059.
7. Burton LC, Newsom JT, Schulz R, Hirsch CH, German PS. Preventive health behaviors among spousal caregivers. Prev Med. 1997;26(2):162-169.
8. Talley RC, Crews JE. Framing the public health of caregiving. Am J Public Health. 2007;97(2):224-228.
9. Hoffman GJ, Lee J, Mendez-Luck CA. Health behaviors among baby boomer informal caregivers. Gerontologist. 2012;52(2):219-230.
10. National Alliance for Caregiving. Caregivers of veterans—serving on the homefront: report of study findings. http://www.caregiving.org/data/2010 _Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed March 9, 2017.
11. Johannesen M, LoGuidice D. Elder abuse: a systematic review of risk factors in community dwelling elders. Age Ageing. 2013;42(3):292-298.
12. Goy E, Kansagara D, Freeman M;Department of Veterans Affairs, Health Services Research & Development Service. A systematic evidence review of interventions for non-professional caregivers of individuals with dementia. http://www.hsrd.research .va.gov/publications/esp/DementiaCaregivers-EXEC .pdf. Published October 2010. Accessed March 9, 2017.
13. Belle SH, Burgio L, Burns R, et al; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized controlled trial. Ann Intern Med. 2006;145(10):727-738.
14. Nichols LO, Martindale-Adams J, Burns R, Graney MJ, Zuber J. Translation of a dementia caregiver support program in a health care system—REACH VA. Arch Intern Med. 2011;171(4):353-359.
15. Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377-1386.
16. U.S. Department of Veteran Affairs. VA caregiver support: caregiver services. http://www.caregiver .va.gov/support/support_services.asp. Updated June 3, 2015. Accessed March 9, 2017.
17. Monin JK, Levy BR, Pietrzak RH. From serving in the military to serving loved ones: unique experiences of older veteran caregivers. Am J Geriatr Psychiatry. 2014;22(6):570-579.
18. Parker MW, Call VR, Dunkle R, Vaitkus M. “Out of sight” but not “out of mind”: parent contact and worry among senior ranking male officers in the military who live long distances from parents. Milit Psychol. 2002;14(4):257-277.
19. Lavela SL, Etingen B, Louise-Bender Pape T. Caregiving experiences and health conditions of women veteran and non-veteran caregivers. Womens Health Issues. 2013;23(4):e225-e232.
20. Yee JL, Schultz RS. Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist. 2000;40(2):147-164.
21. Collins CR. Men as caregivers of the elderly: support for the contributions of sons. J Multidiscip Healthc. 2014;7:525-531.
More than 20% of the U.S. population will be aged ≥ 65 years by 2030, an increase from 13% in 2012.1 The likelihood of needing assistance with activities of daily living (ADLs) increases with age.2 People who need such assistance often depend on informal and unpaid assistance from friends and family. In 2009, about 65.7 million Americans (28.5%) provided informal care for people with an illness or disability, and that number only is expected to rise.3 These informal caregivers provide up to 80% of the total care hours needed by community-dwelling older adults—an estimated economic value of $450 billion in unpaid contributions in 2009.4,5
Caregiving can lead to significant physical, psychological, social, and financial burdens.6 The caregiving burden is associated with a host of adverse health behaviors and outcomes such as poor diet, lack of exercise and sleep, smoking, decreased participation in preventive health care, anxiety, depression, relationship difficulties, employment disruption, financial hardship, suicide, and higher mortality compared with that of noncaregivers.6-10 Additionally, care recipients are at increased risk for abuse or neglect when the caregiver is experiencing a significant burden.11 Therefore, efforts to improve caregiver support are important for both partners in the caregiver/care recipient dyad.
Caregiver support is beneficial to the health of caregivers and care recipients.10,12 For example, the Resources for Enhancing Alzheimer’s Caregiver Health (REACH) program has been shown to reduce the stress of informal caregiving and the risk of depression in caregivers.13,14 This program showed similar effects when implemented within the VHA.14 In the Partners in Dementia Care project, the VHA and Alzheimer’s Association coordinated care and support for veterans with dementia and their family and friends. This intervention resulted in lower caregiver strain and depression scores among participants.15
With a growing medical literature that shows the benefits of caregiver support interventions, the VHA developed a robust support program for informal caregivers of veterans. The VA caregiver support website (www.caregiver.va.gov) provides information and resources targeted to caregivers for veterans, including psychosocial and functional support for caregivers. The psychosocial support provided by the VA includes caregiver education, counseling, access to caregiver support coordinators, a caregiver support line, support groups, and referral to community support organizations.16 Functional support on the site includes financial assistance toward skilled home care, home hospice care, adult day care, home-based primary care, homemaker and home health aide services, telehealth, and respite care.16 Veterans who are caregiving for nonveterans have access to VHA psychosocial support but not to functional support services. For these veterans, functional caregiver support must come from family or referral to community organizations.
Background
In the U.S., about 11% of caregivers are veterans, but the availability of data about these caregivers is limited to veteran subgroups.3 For example, a 2011 study reported that 20% of veterans aged ≥ 60 years are caregivers.17 However, this estimate included child care for unimpaired children, which is not commonly included in other caregiving estimates. In another study, 30% of middle-aged active-duty officers reported helping their parents with instrumental ADLs (IADLs).18 These data suggest a significant proportion of veterans may be caregivers; however, the estimates do not identify prevalence of caregiving among a population of VHA enrolled veterans.
Likewise, few studies discuss the burden veterans experience from caregiving. A study of the 2009/2010 CDC Behavioral Risk Factor Surveillance System data found that female caregivers were more likely to report problems with sleep and mental health if they were veterans vs nonveterans.19 In a second study, caregiving veterans frequently reported physical (39%) and emotional (53%) strain, with emotional strain relating to depressive symptoms. The study of active-duty officers noted that worry was prevalent among military officers caregiving for parents from a distance.18 In contrast to the negative outcomes of caregiving, Monin and colleagues found that many veterans perceived caregiving as rewarding. Since caregiving may be a positive experience, veterans may benefit and be a potential resource for care to elderly and disabled citizens.17
Project Rationale and Goals
Social workers are the cornerstone of caregiver support at the George E. Wahlen VA Salt Lake City Health Care System (VASLCHCS) in Utah. They educate veterans and caregivers about VA resources to support caregivers of veterans. For those veterans who are caregiving for a nonveteran, the VASLCHCS social workers provide psychosocial support and help veterans connect to a local area agency on aging (AAA) for access to functional support. In practice, primary care clinic (PCC) providers have observed that directing a veteran to call the AAA does not usually result in a phone call. Therefore, an aim of this quality improvement (QI) project was to determine the most effective means of completing a successful AAA referral.
The VASLCHCS Geriatric Research Education and Clinical Center collaborates with the Utah Aging and Disability Resource Connection (ADRC) to improve awareness of available resources for veterans. Building on this collaborative project, the authors created a formal referral process for veterans needing local AAA services. This QI project had 3 aims: (1) estimate the prevalence of caregiving among veterans in the VASLCHCS primary care clinic; (2) identify perceived caregiving difficulties and resource use difficulty in caregiving tasks; and (3) test different strategies to connect veterans with a referral to community resources through the AAA.
The authors hypothesized that a veteran would be more likely to connect with the AAA if contact was initiated by the AAA rather than the standard practice of asking the veteran to make the call. However, the authors also hypothesized that a veteran who took the time to make the call would be more likely to use AAA resources compared with veterans who were called by the AAA.
Methods
The VASLCHCS Research and Development Office reviewed this project and determined that it met the definition of QI. Therefore, it did not require IRB approval.
The study drew from a convenience sample of veterans who were waiting for appointments in the PCC and who were referred by their health care provider (HCP). To identify caregivers, veterans were asked: “People may provide regular care or assistance to a friend or family member who has a health problem, long-term illness, or disability. During the past month, did you provide any such care or assistance to a friend or family member?” Referrals from HCPs were included in all calculations except the prevalence estimate.
The authors interviewed veterans over a 3-month period in 2015. As of November 2014, the clinic was serving about 11,000 veterans, of which 6,589 lived in Salt Lake County. The clinic also serves veterans who live in other counties in Utah, Nevada, Wyoming, Idaho, and Colorado.
Intervention and Partnering With Community Resources
All willing caregivers were provided a referral to a local AAA (Figure). Salt Lake County veterans interested in referral to the AAA were randomized to 1 of 2 referral methods: veteran-initiated referral (VIR), in which the veteran was given a handout with the phone number of the Salt Lake County caregiver support program (CSP), or provider-initiated referral (PIR), in which the veteran’s phone number was given to the CSP. Caregiving veterans living outside Salt Lake County were provided the AAA phone number in their area and instructed to call for information.
The interview form was randomized using an even or odd number before the interview. Some veterans who were randomized to a PIR needed to be moved into the VIR intervention arm because of the following reasons: the veteran’s care recipient was aged < 18 years (3); the veteran lived outside of Salt Lake County (20); the veteran did not want his/her name given to an outside agency (5); or the interviewer mistakenly gave the veteran the AAA contact information (4).
The primary author called caregivers in the PIR and VIR groups 2 to 4 weeks after the referral to determine whether they had contacted or were contacted by the AAA. Ten call attempts were made before participants were considered lost to follow-up. Caregivers that had been in contact with the AAA reported in open-ended fashion the resources to which they had been referred and whether those resources had been helpful.
Analysis
In this evaluation, the primary outcome of interest was whether contact between the veteran and AAA occurred. For the VIR group, contact was defined as the veteran having called the AAA, regardless of whether he or she actually spoke to someone. For the PIR group, contact occurred if the veteran reported receiving a phone call from AAA regardless of whether he or she had actually spoken with someone (eg, if the veteran reported that the AAA had left a voice mail, this was considered contact). Veterans also were asked whether connecting with the AAA led to resource referrals and whether these referrals were useful.
To achieve a power of 80% with a 95% confidence interval, 20 people were needed in each intervention group to detect a 40% difference in the rate of contact between the 2 groups. STATA12 (College Station, TX) was used to calculate Fisher exact and chi-square values to evaluate differences between groups.
Results
For the study, 433 PCC veterans were interviewed, and 157 (36%) self-identified as a caregiver. An additional 22 referrals were included for a total of 179 caregivers. Caregiver and care recipient characteristics, caregiver burden, and resource utilization were calculated for all 179 caregivers; however, all caregivers did not answer every question. Ninety-eight percent (176) of caregivers were men; 64% (109/170) were from Salt Lake County, and 5% were from outside Utah (8). Twelve percent (21) of the 179 caregivers were providing care for > 1 person. Of 177 caregivers, 3% (5) were caring for both a veteran and a nonveteran, 69% (122) were caring for a nonveteran only, and 28% (49) were caring for another veteran only (Table 1).
The most common burden reported by caregivers was stress (63%); 70% endorsed family/friends as a resource (Table 2). Just 6% (10) of caregivers used the AAA, whereas 26% (45) received VHA support. Of the 54 veterans who were caring for a veteran, 40 reported using the VHA as a resource. Five people caring for nonveterans reported using the VHA as a resource; however, data about which resources those caregivers were accessing were not collected (Table 3).
AAA Referral and Randomization
Sixty-five percent of caregivers accepted AAA referrals. Of 109 Salt Lake County caregivers, 70% accepted referral to the AAA. There was no statistically significant difference in referral acceptance rates when comparing Salt Lake County residents with nonresidents (P = .09).The authors were unable to obtain the phone number for 1 caregiver who had accepted a referral, and 1 caregiver who accepted referral did not want a follow-up. This left 111 caregivers available for follow-up, 75 in Salt Lake County. Fifty Salt Lake County veterans were randomly assigned to the VIR group and 25 to the PIR group. The 36 caregivers who accepted referrals outside Salt Lake County also were placed in the VIR group, for a total of 86 caregivers.
Follow-up
Ninety-eight percent of caregivers were reached for follow-up. Both people lost to follow-up were in Salt Lake County (1 in each group).
In Salt Lake County, 12% (6) of the VIR group and 64% (16) of the PIR group had connected with the AAA (P < .01). Although 64% of those in the PIR group reported having been called by the AAA, the AAA representative reported all 25 had been called. The AAA records showed 9 of those called were reached by voice mail, 6 were provided information about caregiving resources, 2 formally joined the support program, 5 declined help, 1 was no longer caregiving, 1 was too busy to talk, and 1 was the wrong phone number (and was lost to follow-up as well).
Outside of Salt Lake County 19% (7) reported calling the local AAA. There was no difference in referral completion between the Salt Lake County/non-Salt Lake County VIR groups (P = .4).
Fifteen percent of all VIR caregivers reported calling the AAA. There were no statistical differences between Salt Lake County VIR and non-Salt Lake County VIR for reasons why the veteran had not called the AAA (Table 4).
Of 28 people who connected with the AAA, 16 (57%) said they had received access to a needed resource as a result of the phone call. Seven caregivers (25%) said they had not been referred to other resources as a result of the call. The VIR group was more likely to be referred to other resources after contacting the AAA than was the PIR group, although this difference did not reach significance (69% vs 47%, P = .28).
Discussion
More than one-third (36%) of veterans seen in the VASLCHCS PCC are caregivers. This prevalence is higher than that reported for the general U.S. population and higher than that reported in other veteran groups.5,17,18 Most caregivers in this project were caring for nonveterans and only had access to VHA psychosocial caregiver support programs because VHA functional caregiver support (eg, respite, homemaker services) is not available to veterans who care for nonveterans. A majority (78%) of caregiving veterans reported some caregiver burden. Despite the burden, most are not using community resources. However when offered, more than half the caregivers were interested in an AAA referral.
Although the VHA does not provide functional caregiver support resources to veterans caring for nonveterans, there are other agencies that can assist veterans: AAAs for care recipients aged ≥ 60 years and the ADRCs for younger veterans. Through AAAs, caregivers can access a variety of support services, including transportation, adult day care, caregiver support, and health promotion programs. Partnership between agencies such as the VHA and the AAAs could benefit caregiving veterans. This QI project suggests ways to strengthen interagency cooperation.
This study also suggests that a provider or clinic-initiated referral is more likely to connect veterans with information and resources than the current practice of recommending that the veteran initiate the referral. Once in contact with the AAA, most caregivers were referred to needed resources. The next step will be to establish an efficient way for clinic staff to identify caregiving veterans and make referrals to community programs. Referrals could be made by any member of the patient aligned care team (PACT) to further standardize and streamline the process.
Thirty-one percent of veterans in this project were eligible for the VHA caregiver support program because they cared for a veteran. However, 25% of these caregiving veterans were not accessing this resource. Increasing awareness of the VHA caregiver support program among veterans caring for other veterans would improve caregiver support to both caregiving and care recipient veterans.
Limitations
One limitation of this project was the intentional exclusion of the women’s clinic from the sampling process. For consistency, the authors wanted to limit the intervention to 1 PCC and so they chose the clinic that serves the majority of the veterans who receive primary care at VASLCHCS. Additionally, the literature showed that male caregivers compared with women caregivers20,21 have different characteristics in regards to caregiver burden, and a well-designed study of women caregivers already has been published.19
Also, this study did not obtain data on age, health problems, or socioeconomic status of the caregivers to avoid identifying information. Last, the authors did not ask about time spent caregiving or type of care provided. These questions may be important for future studies. Future investigations should evaluate health care use and health of caregivers vs noncaregivers in the veteran population. It also could be important to determine methods for building bridges between the VHA, AAAs, and other community services.
Conclusion
To minimize the disruption that a research study might have caused to normal clinical workflow, the primary author played the role that a medical social worker or other PACT member might play in the future. This project sheds light on how to improve outcomes for community referrals and an important future step in this research would be to develop and test a process that would integrate the PACT into the referral process.
More than one-third of veterans seen in the VASLCHCS PCC are caregivers. To the authors’ knowledge, this is the first estimate of prevalence of caregiving in veterans who receive primary care from the VHA. About 63% of caregiving veterans perceived some burden due to caregiving, and 66% accepted referral to community resources. However, only 12% who were asked to self-refer made contact with the AAA compared with 64% when a provider made the referral for them. Provider referral is more effective in connecting caregiving veterans with resources. Development of interagency partnerships should be fostered to help veterans decrease caregiving burden.
This project is one of the few studies looking at this special group of caregivers: veterans who serve as caregivers. It highlights the need for the VHA to establish policies and partnerships to improve caregiver support to this valuable group of veterans.
More than 20% of the U.S. population will be aged ≥ 65 years by 2030, an increase from 13% in 2012.1 The likelihood of needing assistance with activities of daily living (ADLs) increases with age.2 People who need such assistance often depend on informal and unpaid assistance from friends and family. In 2009, about 65.7 million Americans (28.5%) provided informal care for people with an illness or disability, and that number only is expected to rise.3 These informal caregivers provide up to 80% of the total care hours needed by community-dwelling older adults—an estimated economic value of $450 billion in unpaid contributions in 2009.4,5
Caregiving can lead to significant physical, psychological, social, and financial burdens.6 The caregiving burden is associated with a host of adverse health behaviors and outcomes such as poor diet, lack of exercise and sleep, smoking, decreased participation in preventive health care, anxiety, depression, relationship difficulties, employment disruption, financial hardship, suicide, and higher mortality compared with that of noncaregivers.6-10 Additionally, care recipients are at increased risk for abuse or neglect when the caregiver is experiencing a significant burden.11 Therefore, efforts to improve caregiver support are important for both partners in the caregiver/care recipient dyad.
Caregiver support is beneficial to the health of caregivers and care recipients.10,12 For example, the Resources for Enhancing Alzheimer’s Caregiver Health (REACH) program has been shown to reduce the stress of informal caregiving and the risk of depression in caregivers.13,14 This program showed similar effects when implemented within the VHA.14 In the Partners in Dementia Care project, the VHA and Alzheimer’s Association coordinated care and support for veterans with dementia and their family and friends. This intervention resulted in lower caregiver strain and depression scores among participants.15
With a growing medical literature that shows the benefits of caregiver support interventions, the VHA developed a robust support program for informal caregivers of veterans. The VA caregiver support website (www.caregiver.va.gov) provides information and resources targeted to caregivers for veterans, including psychosocial and functional support for caregivers. The psychosocial support provided by the VA includes caregiver education, counseling, access to caregiver support coordinators, a caregiver support line, support groups, and referral to community support organizations.16 Functional support on the site includes financial assistance toward skilled home care, home hospice care, adult day care, home-based primary care, homemaker and home health aide services, telehealth, and respite care.16 Veterans who are caregiving for nonveterans have access to VHA psychosocial support but not to functional support services. For these veterans, functional caregiver support must come from family or referral to community organizations.
Background
In the U.S., about 11% of caregivers are veterans, but the availability of data about these caregivers is limited to veteran subgroups.3 For example, a 2011 study reported that 20% of veterans aged ≥ 60 years are caregivers.17 However, this estimate included child care for unimpaired children, which is not commonly included in other caregiving estimates. In another study, 30% of middle-aged active-duty officers reported helping their parents with instrumental ADLs (IADLs).18 These data suggest a significant proportion of veterans may be caregivers; however, the estimates do not identify prevalence of caregiving among a population of VHA enrolled veterans.
Likewise, few studies discuss the burden veterans experience from caregiving. A study of the 2009/2010 CDC Behavioral Risk Factor Surveillance System data found that female caregivers were more likely to report problems with sleep and mental health if they were veterans vs nonveterans.19 In a second study, caregiving veterans frequently reported physical (39%) and emotional (53%) strain, with emotional strain relating to depressive symptoms. The study of active-duty officers noted that worry was prevalent among military officers caregiving for parents from a distance.18 In contrast to the negative outcomes of caregiving, Monin and colleagues found that many veterans perceived caregiving as rewarding. Since caregiving may be a positive experience, veterans may benefit and be a potential resource for care to elderly and disabled citizens.17
Project Rationale and Goals
Social workers are the cornerstone of caregiver support at the George E. Wahlen VA Salt Lake City Health Care System (VASLCHCS) in Utah. They educate veterans and caregivers about VA resources to support caregivers of veterans. For those veterans who are caregiving for a nonveteran, the VASLCHCS social workers provide psychosocial support and help veterans connect to a local area agency on aging (AAA) for access to functional support. In practice, primary care clinic (PCC) providers have observed that directing a veteran to call the AAA does not usually result in a phone call. Therefore, an aim of this quality improvement (QI) project was to determine the most effective means of completing a successful AAA referral.
The VASLCHCS Geriatric Research Education and Clinical Center collaborates with the Utah Aging and Disability Resource Connection (ADRC) to improve awareness of available resources for veterans. Building on this collaborative project, the authors created a formal referral process for veterans needing local AAA services. This QI project had 3 aims: (1) estimate the prevalence of caregiving among veterans in the VASLCHCS primary care clinic; (2) identify perceived caregiving difficulties and resource use difficulty in caregiving tasks; and (3) test different strategies to connect veterans with a referral to community resources through the AAA.
The authors hypothesized that a veteran would be more likely to connect with the AAA if contact was initiated by the AAA rather than the standard practice of asking the veteran to make the call. However, the authors also hypothesized that a veteran who took the time to make the call would be more likely to use AAA resources compared with veterans who were called by the AAA.
Methods
The VASLCHCS Research and Development Office reviewed this project and determined that it met the definition of QI. Therefore, it did not require IRB approval.
The study drew from a convenience sample of veterans who were waiting for appointments in the PCC and who were referred by their health care provider (HCP). To identify caregivers, veterans were asked: “People may provide regular care or assistance to a friend or family member who has a health problem, long-term illness, or disability. During the past month, did you provide any such care or assistance to a friend or family member?” Referrals from HCPs were included in all calculations except the prevalence estimate.
The authors interviewed veterans over a 3-month period in 2015. As of November 2014, the clinic was serving about 11,000 veterans, of which 6,589 lived in Salt Lake County. The clinic also serves veterans who live in other counties in Utah, Nevada, Wyoming, Idaho, and Colorado.
Intervention and Partnering With Community Resources
All willing caregivers were provided a referral to a local AAA (Figure). Salt Lake County veterans interested in referral to the AAA were randomized to 1 of 2 referral methods: veteran-initiated referral (VIR), in which the veteran was given a handout with the phone number of the Salt Lake County caregiver support program (CSP), or provider-initiated referral (PIR), in which the veteran’s phone number was given to the CSP. Caregiving veterans living outside Salt Lake County were provided the AAA phone number in their area and instructed to call for information.
The interview form was randomized using an even or odd number before the interview. Some veterans who were randomized to a PIR needed to be moved into the VIR intervention arm because of the following reasons: the veteran’s care recipient was aged < 18 years (3); the veteran lived outside of Salt Lake County (20); the veteran did not want his/her name given to an outside agency (5); or the interviewer mistakenly gave the veteran the AAA contact information (4).
The primary author called caregivers in the PIR and VIR groups 2 to 4 weeks after the referral to determine whether they had contacted or were contacted by the AAA. Ten call attempts were made before participants were considered lost to follow-up. Caregivers that had been in contact with the AAA reported in open-ended fashion the resources to which they had been referred and whether those resources had been helpful.
Analysis
In this evaluation, the primary outcome of interest was whether contact between the veteran and AAA occurred. For the VIR group, contact was defined as the veteran having called the AAA, regardless of whether he or she actually spoke to someone. For the PIR group, contact occurred if the veteran reported receiving a phone call from AAA regardless of whether he or she had actually spoken with someone (eg, if the veteran reported that the AAA had left a voice mail, this was considered contact). Veterans also were asked whether connecting with the AAA led to resource referrals and whether these referrals were useful.
To achieve a power of 80% with a 95% confidence interval, 20 people were needed in each intervention group to detect a 40% difference in the rate of contact between the 2 groups. STATA12 (College Station, TX) was used to calculate Fisher exact and chi-square values to evaluate differences between groups.
Results
For the study, 433 PCC veterans were interviewed, and 157 (36%) self-identified as a caregiver. An additional 22 referrals were included for a total of 179 caregivers. Caregiver and care recipient characteristics, caregiver burden, and resource utilization were calculated for all 179 caregivers; however, all caregivers did not answer every question. Ninety-eight percent (176) of caregivers were men; 64% (109/170) were from Salt Lake County, and 5% were from outside Utah (8). Twelve percent (21) of the 179 caregivers were providing care for > 1 person. Of 177 caregivers, 3% (5) were caring for both a veteran and a nonveteran, 69% (122) were caring for a nonveteran only, and 28% (49) were caring for another veteran only (Table 1).
The most common burden reported by caregivers was stress (63%); 70% endorsed family/friends as a resource (Table 2). Just 6% (10) of caregivers used the AAA, whereas 26% (45) received VHA support. Of the 54 veterans who were caring for a veteran, 40 reported using the VHA as a resource. Five people caring for nonveterans reported using the VHA as a resource; however, data about which resources those caregivers were accessing were not collected (Table 3).
AAA Referral and Randomization
Sixty-five percent of caregivers accepted AAA referrals. Of 109 Salt Lake County caregivers, 70% accepted referral to the AAA. There was no statistically significant difference in referral acceptance rates when comparing Salt Lake County residents with nonresidents (P = .09).The authors were unable to obtain the phone number for 1 caregiver who had accepted a referral, and 1 caregiver who accepted referral did not want a follow-up. This left 111 caregivers available for follow-up, 75 in Salt Lake County. Fifty Salt Lake County veterans were randomly assigned to the VIR group and 25 to the PIR group. The 36 caregivers who accepted referrals outside Salt Lake County also were placed in the VIR group, for a total of 86 caregivers.
Follow-up
Ninety-eight percent of caregivers were reached for follow-up. Both people lost to follow-up were in Salt Lake County (1 in each group).
In Salt Lake County, 12% (6) of the VIR group and 64% (16) of the PIR group had connected with the AAA (P < .01). Although 64% of those in the PIR group reported having been called by the AAA, the AAA representative reported all 25 had been called. The AAA records showed 9 of those called were reached by voice mail, 6 were provided information about caregiving resources, 2 formally joined the support program, 5 declined help, 1 was no longer caregiving, 1 was too busy to talk, and 1 was the wrong phone number (and was lost to follow-up as well).
Outside of Salt Lake County 19% (7) reported calling the local AAA. There was no difference in referral completion between the Salt Lake County/non-Salt Lake County VIR groups (P = .4).
Fifteen percent of all VIR caregivers reported calling the AAA. There were no statistical differences between Salt Lake County VIR and non-Salt Lake County VIR for reasons why the veteran had not called the AAA (Table 4).
Of 28 people who connected with the AAA, 16 (57%) said they had received access to a needed resource as a result of the phone call. Seven caregivers (25%) said they had not been referred to other resources as a result of the call. The VIR group was more likely to be referred to other resources after contacting the AAA than was the PIR group, although this difference did not reach significance (69% vs 47%, P = .28).
Discussion
More than one-third (36%) of veterans seen in the VASLCHCS PCC are caregivers. This prevalence is higher than that reported for the general U.S. population and higher than that reported in other veteran groups.5,17,18 Most caregivers in this project were caring for nonveterans and only had access to VHA psychosocial caregiver support programs because VHA functional caregiver support (eg, respite, homemaker services) is not available to veterans who care for nonveterans. A majority (78%) of caregiving veterans reported some caregiver burden. Despite the burden, most are not using community resources. However when offered, more than half the caregivers were interested in an AAA referral.
Although the VHA does not provide functional caregiver support resources to veterans caring for nonveterans, there are other agencies that can assist veterans: AAAs for care recipients aged ≥ 60 years and the ADRCs for younger veterans. Through AAAs, caregivers can access a variety of support services, including transportation, adult day care, caregiver support, and health promotion programs. Partnership between agencies such as the VHA and the AAAs could benefit caregiving veterans. This QI project suggests ways to strengthen interagency cooperation.
This study also suggests that a provider or clinic-initiated referral is more likely to connect veterans with information and resources than the current practice of recommending that the veteran initiate the referral. Once in contact with the AAA, most caregivers were referred to needed resources. The next step will be to establish an efficient way for clinic staff to identify caregiving veterans and make referrals to community programs. Referrals could be made by any member of the patient aligned care team (PACT) to further standardize and streamline the process.
Thirty-one percent of veterans in this project were eligible for the VHA caregiver support program because they cared for a veteran. However, 25% of these caregiving veterans were not accessing this resource. Increasing awareness of the VHA caregiver support program among veterans caring for other veterans would improve caregiver support to both caregiving and care recipient veterans.
Limitations
One limitation of this project was the intentional exclusion of the women’s clinic from the sampling process. For consistency, the authors wanted to limit the intervention to 1 PCC and so they chose the clinic that serves the majority of the veterans who receive primary care at VASLCHCS. Additionally, the literature showed that male caregivers compared with women caregivers20,21 have different characteristics in regards to caregiver burden, and a well-designed study of women caregivers already has been published.19
Also, this study did not obtain data on age, health problems, or socioeconomic status of the caregivers to avoid identifying information. Last, the authors did not ask about time spent caregiving or type of care provided. These questions may be important for future studies. Future investigations should evaluate health care use and health of caregivers vs noncaregivers in the veteran population. It also could be important to determine methods for building bridges between the VHA, AAAs, and other community services.
Conclusion
To minimize the disruption that a research study might have caused to normal clinical workflow, the primary author played the role that a medical social worker or other PACT member might play in the future. This project sheds light on how to improve outcomes for community referrals and an important future step in this research would be to develop and test a process that would integrate the PACT into the referral process.
More than one-third of veterans seen in the VASLCHCS PCC are caregivers. To the authors’ knowledge, this is the first estimate of prevalence of caregiving in veterans who receive primary care from the VHA. About 63% of caregiving veterans perceived some burden due to caregiving, and 66% accepted referral to community resources. However, only 12% who were asked to self-refer made contact with the AAA compared with 64% when a provider made the referral for them. Provider referral is more effective in connecting caregiving veterans with resources. Development of interagency partnerships should be fostered to help veterans decrease caregiving burden.
This project is one of the few studies looking at this special group of caregivers: veterans who serve as caregivers. It highlights the need for the VHA to establish policies and partnerships to improve caregiver support to this valuable group of veterans.
1. Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States: population estimates and projections. http://www.census .gov/prod/2014pubs/p25-1140.pdf. Published May 2014. Accessed March 9, 2017.
2. Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA Intern Med. 2013;173(16):1506-1513.
3. National Alliance for Caregiving, American Association of Retired Persons. Caregiving in the U.S. 2009 executive summary. http://assets.aarp.org/rgcenter/il/caregiving_09_es.pdf. Published November 2009. Accessed March 9, 2017.
4. Spillman BC, Wolff J, Freedman VA, Kasper JD; Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Informal caregiving for older Americans: an analysis of the 2011 national study of caregiving. https://aspe.hhs.gov/report/informal-caregiving-older-americans-analysis-2011-national-study-caregiving. Published April 1, 2014. Accessed March 9, 2017.
5. Feinberg L, Reinhard SC, Houser A, Choula R; AARP Public Policy Institute. Valuing the invaluable: 2011 update. The growing contributions and costs of family caregiving. https://assets.aarp .org/rgcenter/ppi/ltc/i51-caregiving.pdf. Published June 2011. Accessed March 9, 2017.
6. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052-1059.
7. Burton LC, Newsom JT, Schulz R, Hirsch CH, German PS. Preventive health behaviors among spousal caregivers. Prev Med. 1997;26(2):162-169.
8. Talley RC, Crews JE. Framing the public health of caregiving. Am J Public Health. 2007;97(2):224-228.
9. Hoffman GJ, Lee J, Mendez-Luck CA. Health behaviors among baby boomer informal caregivers. Gerontologist. 2012;52(2):219-230.
10. National Alliance for Caregiving. Caregivers of veterans—serving on the homefront: report of study findings. http://www.caregiving.org/data/2010 _Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed March 9, 2017.
11. Johannesen M, LoGuidice D. Elder abuse: a systematic review of risk factors in community dwelling elders. Age Ageing. 2013;42(3):292-298.
12. Goy E, Kansagara D, Freeman M;Department of Veterans Affairs, Health Services Research & Development Service. A systematic evidence review of interventions for non-professional caregivers of individuals with dementia. http://www.hsrd.research .va.gov/publications/esp/DementiaCaregivers-EXEC .pdf. Published October 2010. Accessed March 9, 2017.
13. Belle SH, Burgio L, Burns R, et al; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized controlled trial. Ann Intern Med. 2006;145(10):727-738.
14. Nichols LO, Martindale-Adams J, Burns R, Graney MJ, Zuber J. Translation of a dementia caregiver support program in a health care system—REACH VA. Arch Intern Med. 2011;171(4):353-359.
15. Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377-1386.
16. U.S. Department of Veteran Affairs. VA caregiver support: caregiver services. http://www.caregiver .va.gov/support/support_services.asp. Updated June 3, 2015. Accessed March 9, 2017.
17. Monin JK, Levy BR, Pietrzak RH. From serving in the military to serving loved ones: unique experiences of older veteran caregivers. Am J Geriatr Psychiatry. 2014;22(6):570-579.
18. Parker MW, Call VR, Dunkle R, Vaitkus M. “Out of sight” but not “out of mind”: parent contact and worry among senior ranking male officers in the military who live long distances from parents. Milit Psychol. 2002;14(4):257-277.
19. Lavela SL, Etingen B, Louise-Bender Pape T. Caregiving experiences and health conditions of women veteran and non-veteran caregivers. Womens Health Issues. 2013;23(4):e225-e232.
20. Yee JL, Schultz RS. Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist. 2000;40(2):147-164.
21. Collins CR. Men as caregivers of the elderly: support for the contributions of sons. J Multidiscip Healthc. 2014;7:525-531.
1. Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States: population estimates and projections. http://www.census .gov/prod/2014pubs/p25-1140.pdf. Published May 2014. Accessed March 9, 2017.
2. Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA Intern Med. 2013;173(16):1506-1513.
3. National Alliance for Caregiving, American Association of Retired Persons. Caregiving in the U.S. 2009 executive summary. http://assets.aarp.org/rgcenter/il/caregiving_09_es.pdf. Published November 2009. Accessed March 9, 2017.
4. Spillman BC, Wolff J, Freedman VA, Kasper JD; Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Informal caregiving for older Americans: an analysis of the 2011 national study of caregiving. https://aspe.hhs.gov/report/informal-caregiving-older-americans-analysis-2011-national-study-caregiving. Published April 1, 2014. Accessed March 9, 2017.
5. Feinberg L, Reinhard SC, Houser A, Choula R; AARP Public Policy Institute. Valuing the invaluable: 2011 update. The growing contributions and costs of family caregiving. https://assets.aarp .org/rgcenter/ppi/ltc/i51-caregiving.pdf. Published June 2011. Accessed March 9, 2017.
6. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052-1059.
7. Burton LC, Newsom JT, Schulz R, Hirsch CH, German PS. Preventive health behaviors among spousal caregivers. Prev Med. 1997;26(2):162-169.
8. Talley RC, Crews JE. Framing the public health of caregiving. Am J Public Health. 2007;97(2):224-228.
9. Hoffman GJ, Lee J, Mendez-Luck CA. Health behaviors among baby boomer informal caregivers. Gerontologist. 2012;52(2):219-230.
10. National Alliance for Caregiving. Caregivers of veterans—serving on the homefront: report of study findings. http://www.caregiving.org/data/2010 _Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed March 9, 2017.
11. Johannesen M, LoGuidice D. Elder abuse: a systematic review of risk factors in community dwelling elders. Age Ageing. 2013;42(3):292-298.
12. Goy E, Kansagara D, Freeman M;Department of Veterans Affairs, Health Services Research & Development Service. A systematic evidence review of interventions for non-professional caregivers of individuals with dementia. http://www.hsrd.research .va.gov/publications/esp/DementiaCaregivers-EXEC .pdf. Published October 2010. Accessed March 9, 2017.
13. Belle SH, Burgio L, Burns R, et al; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized controlled trial. Ann Intern Med. 2006;145(10):727-738.
14. Nichols LO, Martindale-Adams J, Burns R, Graney MJ, Zuber J. Translation of a dementia caregiver support program in a health care system—REACH VA. Arch Intern Med. 2011;171(4):353-359.
15. Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377-1386.
16. U.S. Department of Veteran Affairs. VA caregiver support: caregiver services. http://www.caregiver .va.gov/support/support_services.asp. Updated June 3, 2015. Accessed March 9, 2017.
17. Monin JK, Levy BR, Pietrzak RH. From serving in the military to serving loved ones: unique experiences of older veteran caregivers. Am J Geriatr Psychiatry. 2014;22(6):570-579.
18. Parker MW, Call VR, Dunkle R, Vaitkus M. “Out of sight” but not “out of mind”: parent contact and worry among senior ranking male officers in the military who live long distances from parents. Milit Psychol. 2002;14(4):257-277.
19. Lavela SL, Etingen B, Louise-Bender Pape T. Caregiving experiences and health conditions of women veteran and non-veteran caregivers. Womens Health Issues. 2013;23(4):e225-e232.
20. Yee JL, Schultz RS. Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist. 2000;40(2):147-164.
21. Collins CR. Men as caregivers of the elderly: support for the contributions of sons. J Multidiscip Healthc. 2014;7:525-531.
Cells are key to specification of HSCs, team says
Experiments in zebrafish embryos have suggested that trunk neural crest cells play a key role in the specification of hematopoietic stem cells (HSCs).
Researchers believe this finding could be used to aid the creation of HSCs in the lab and ultimately help improve access to HSC transplant.
“The research will likely open new avenues of investigation in stem cell biology and blood development and provide insight to aid efforts to make transplantable hematopoietic stem cells in the lab,” said Wilson Clements, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Clements and Erich W. Damm, PhD, also of St. Jude, described this research in Nature Cell Biology.
The researchers noted that scientists have yet to achieve in vitro specification of normal HSCs with a high level of engraftment and normal multilineage potential. And this suggests key specification signals remain unknown.
The pair pointed out that, in all vertebrates, HSCs arise from hemogenic endothelium in the ventral floor of the dorsal aorta. And stromal cells residing in stem cell microenvironments often act as a niche to contribute cues that regulate behavior.
“Researchers have speculated that the endothelial cells that give rise to blood-forming stem cells are surrounded by a support niche of other cells whose identity and origins were unknown,” Dr Damm said. “Our results support the existence of a niche and identify trunk neural crest cells as an occupant.”
Trunk neural crest cells are made in the developing spinal cord and migrate throughout the embryo. The cells eventually give rise to a variety of adult cells, including neurons and glial cells in the sympathetic and parasympathetic nervous system.
Using time-lapse video, Drs Clements and Damm tracked the migration of neural crest cells in the transparent embryos of zebrafish. (Zebrafish and humans share nearly identical blood systems.)
After about 20 hours, the neural crest cells had reached the developing aorta. After hour 24, the migrating cells had cozied up to the endothelial cells in the aorta, which then turned on genes, such as runx1, indicating their conversion to HSCs.
Additional experiments revealed that migration of neural crest cells to the dorsal aorta is dependent on platelet-derived growth factor signaling, and this signaling is required for HSC specification.
Likewise, the physical association of neural crest cells with the pre-hematopoietic dorsal aorta is required for initiation of the hematopoietic program and HSC specification.
Drs Clements and Damm said these results suggest neural crest cells are key cellular components of the HSC specification niche that can be profiled to identify unknown HSC specification signals. ![]()
Experiments in zebrafish embryos have suggested that trunk neural crest cells play a key role in the specification of hematopoietic stem cells (HSCs).
Researchers believe this finding could be used to aid the creation of HSCs in the lab and ultimately help improve access to HSC transplant.
“The research will likely open new avenues of investigation in stem cell biology and blood development and provide insight to aid efforts to make transplantable hematopoietic stem cells in the lab,” said Wilson Clements, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Clements and Erich W. Damm, PhD, also of St. Jude, described this research in Nature Cell Biology.
The researchers noted that scientists have yet to achieve in vitro specification of normal HSCs with a high level of engraftment and normal multilineage potential. And this suggests key specification signals remain unknown.
The pair pointed out that, in all vertebrates, HSCs arise from hemogenic endothelium in the ventral floor of the dorsal aorta. And stromal cells residing in stem cell microenvironments often act as a niche to contribute cues that regulate behavior.
“Researchers have speculated that the endothelial cells that give rise to blood-forming stem cells are surrounded by a support niche of other cells whose identity and origins were unknown,” Dr Damm said. “Our results support the existence of a niche and identify trunk neural crest cells as an occupant.”
Trunk neural crest cells are made in the developing spinal cord and migrate throughout the embryo. The cells eventually give rise to a variety of adult cells, including neurons and glial cells in the sympathetic and parasympathetic nervous system.
Using time-lapse video, Drs Clements and Damm tracked the migration of neural crest cells in the transparent embryos of zebrafish. (Zebrafish and humans share nearly identical blood systems.)
After about 20 hours, the neural crest cells had reached the developing aorta. After hour 24, the migrating cells had cozied up to the endothelial cells in the aorta, which then turned on genes, such as runx1, indicating their conversion to HSCs.
Additional experiments revealed that migration of neural crest cells to the dorsal aorta is dependent on platelet-derived growth factor signaling, and this signaling is required for HSC specification.
Likewise, the physical association of neural crest cells with the pre-hematopoietic dorsal aorta is required for initiation of the hematopoietic program and HSC specification.
Drs Clements and Damm said these results suggest neural crest cells are key cellular components of the HSC specification niche that can be profiled to identify unknown HSC specification signals. ![]()
Experiments in zebrafish embryos have suggested that trunk neural crest cells play a key role in the specification of hematopoietic stem cells (HSCs).
Researchers believe this finding could be used to aid the creation of HSCs in the lab and ultimately help improve access to HSC transplant.
“The research will likely open new avenues of investigation in stem cell biology and blood development and provide insight to aid efforts to make transplantable hematopoietic stem cells in the lab,” said Wilson Clements, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Clements and Erich W. Damm, PhD, also of St. Jude, described this research in Nature Cell Biology.
The researchers noted that scientists have yet to achieve in vitro specification of normal HSCs with a high level of engraftment and normal multilineage potential. And this suggests key specification signals remain unknown.
The pair pointed out that, in all vertebrates, HSCs arise from hemogenic endothelium in the ventral floor of the dorsal aorta. And stromal cells residing in stem cell microenvironments often act as a niche to contribute cues that regulate behavior.
“Researchers have speculated that the endothelial cells that give rise to blood-forming stem cells are surrounded by a support niche of other cells whose identity and origins were unknown,” Dr Damm said. “Our results support the existence of a niche and identify trunk neural crest cells as an occupant.”
Trunk neural crest cells are made in the developing spinal cord and migrate throughout the embryo. The cells eventually give rise to a variety of adult cells, including neurons and glial cells in the sympathetic and parasympathetic nervous system.
Using time-lapse video, Drs Clements and Damm tracked the migration of neural crest cells in the transparent embryos of zebrafish. (Zebrafish and humans share nearly identical blood systems.)
After about 20 hours, the neural crest cells had reached the developing aorta. After hour 24, the migrating cells had cozied up to the endothelial cells in the aorta, which then turned on genes, such as runx1, indicating their conversion to HSCs.
Additional experiments revealed that migration of neural crest cells to the dorsal aorta is dependent on platelet-derived growth factor signaling, and this signaling is required for HSC specification.
Likewise, the physical association of neural crest cells with the pre-hematopoietic dorsal aorta is required for initiation of the hematopoietic program and HSC specification.
Drs Clements and Damm said these results suggest neural crest cells are key cellular components of the HSC specification niche that can be profiled to identify unknown HSC specification signals. ![]()
Cancer risk, burden expected to shift in HIV population
WASHINGTON, DC—New research suggests HIV-positive adults in the US will see a shift in cancer risk and burden in the coming years.
The study indicates that, through 2030, people living with HIV will see a decrease in AIDS-defining cancers, such as non-Hodgkin lymphoma (NHL) and Kaposi sarcoma.
But this group will also see an increase in cancers not linked to AIDS, such as prostate and liver cancers.
Researchers made these projections in a presentation at the AACR Annual Meeting 2017 (abstract 5302).
“Declines in cancer incidence rates, particularly for AIDS-defining cancers, are likely driven by widespread treatment with modern antiretroviral therapies, which reduce immune suppression and decrease risk of some cancers,” said Jessica Y. Islam, a doctoral student at the University of North Carolina Gillings School of Global Public Health in Chapel Hill.
She and her collaborators estimated future cancer risk and burden for HIV-positive people using age-specific cancer incidence data from the National Cancer Institute HIV/AIDS Cancer Match (HACM) Study, and projected HIV prevalence data from the Centers for Disease Control and Prevention.
Cancer incidence
From 2000 to 2012, there were 23,907 cancers reported in 463,300 HIV-infected adults in the HACM Study. Based on trends in this study, the researchers made projections for cancer incidence through 2030.
They projected that HIV-positive adults of all ages will see a significant decrease over time in the incidence of NHL, Kaposi sarcoma, cervical cancer, anal cancer among men who have sex with men (MSM), lung cancer, and Hodgkin lymphoma.
Patients age 65 and older will see a significant decrease in colon cancer incidence over time. However, there will be no significant change for patients younger than 65.
HIV-positive adults of all ages will see no significant change over time in the incidence of liver cancer, oral cavity cancer, anal cancer among non-MSMs, and breast cancer.
The incidence of prostate cancer will increase significantly among patients ages 35 to 44 and among patients ages 45 to 64.
Cancer burden
The researchers said the number of adults living with HIV in the US is projected to increase from 1.06 million in 2006 to 1.17 million in 2018, but it is expected to decline to 1.09 million in 2030.
The team noted that, in 2006, there were an estimated 8241 cancers in patients with HIV—3522 AIDS-defining cancers and 4719 malignancies not associated with AIDS.
In 2030, the total number of cancers in the HIV-positive population is projected to be 6692, with decreases in AIDS-defining cancers (n=716) and increases in other cancers (n=5976) from the 2006 data.
In 2010, the most common cancers among HIV-positive patients were estimated to be NHL (n=1488), Kaposi sarcoma (n=1133), and lung cancer (n=815).
But in 2030, the most common cancers are projected to be prostate (n=1587), lung (n=1027), and liver cancers (n=483).
“It is critical to understand both incidence rates and burden over time, as rates capture changes in cancer risk, and burden quantifies the actual number of cancer cases expected to occur,” said study investigator Meredith S. Shiels, PhD, of the National Cancer Institute in Bethesda, Maryland.
“For example, lung cancer rates are expected to decrease in the future, but the burden is expected to increase due to the growing number of older people living with HIV.” ![]()
WASHINGTON, DC—New research suggests HIV-positive adults in the US will see a shift in cancer risk and burden in the coming years.
The study indicates that, through 2030, people living with HIV will see a decrease in AIDS-defining cancers, such as non-Hodgkin lymphoma (NHL) and Kaposi sarcoma.
But this group will also see an increase in cancers not linked to AIDS, such as prostate and liver cancers.
Researchers made these projections in a presentation at the AACR Annual Meeting 2017 (abstract 5302).
“Declines in cancer incidence rates, particularly for AIDS-defining cancers, are likely driven by widespread treatment with modern antiretroviral therapies, which reduce immune suppression and decrease risk of some cancers,” said Jessica Y. Islam, a doctoral student at the University of North Carolina Gillings School of Global Public Health in Chapel Hill.
She and her collaborators estimated future cancer risk and burden for HIV-positive people using age-specific cancer incidence data from the National Cancer Institute HIV/AIDS Cancer Match (HACM) Study, and projected HIV prevalence data from the Centers for Disease Control and Prevention.
Cancer incidence
From 2000 to 2012, there were 23,907 cancers reported in 463,300 HIV-infected adults in the HACM Study. Based on trends in this study, the researchers made projections for cancer incidence through 2030.
They projected that HIV-positive adults of all ages will see a significant decrease over time in the incidence of NHL, Kaposi sarcoma, cervical cancer, anal cancer among men who have sex with men (MSM), lung cancer, and Hodgkin lymphoma.
Patients age 65 and older will see a significant decrease in colon cancer incidence over time. However, there will be no significant change for patients younger than 65.
HIV-positive adults of all ages will see no significant change over time in the incidence of liver cancer, oral cavity cancer, anal cancer among non-MSMs, and breast cancer.
The incidence of prostate cancer will increase significantly among patients ages 35 to 44 and among patients ages 45 to 64.
Cancer burden
The researchers said the number of adults living with HIV in the US is projected to increase from 1.06 million in 2006 to 1.17 million in 2018, but it is expected to decline to 1.09 million in 2030.
The team noted that, in 2006, there were an estimated 8241 cancers in patients with HIV—3522 AIDS-defining cancers and 4719 malignancies not associated with AIDS.
In 2030, the total number of cancers in the HIV-positive population is projected to be 6692, with decreases in AIDS-defining cancers (n=716) and increases in other cancers (n=5976) from the 2006 data.
In 2010, the most common cancers among HIV-positive patients were estimated to be NHL (n=1488), Kaposi sarcoma (n=1133), and lung cancer (n=815).
But in 2030, the most common cancers are projected to be prostate (n=1587), lung (n=1027), and liver cancers (n=483).
“It is critical to understand both incidence rates and burden over time, as rates capture changes in cancer risk, and burden quantifies the actual number of cancer cases expected to occur,” said study investigator Meredith S. Shiels, PhD, of the National Cancer Institute in Bethesda, Maryland.
“For example, lung cancer rates are expected to decrease in the future, but the burden is expected to increase due to the growing number of older people living with HIV.” ![]()
WASHINGTON, DC—New research suggests HIV-positive adults in the US will see a shift in cancer risk and burden in the coming years.
The study indicates that, through 2030, people living with HIV will see a decrease in AIDS-defining cancers, such as non-Hodgkin lymphoma (NHL) and Kaposi sarcoma.
But this group will also see an increase in cancers not linked to AIDS, such as prostate and liver cancers.
Researchers made these projections in a presentation at the AACR Annual Meeting 2017 (abstract 5302).
“Declines in cancer incidence rates, particularly for AIDS-defining cancers, are likely driven by widespread treatment with modern antiretroviral therapies, which reduce immune suppression and decrease risk of some cancers,” said Jessica Y. Islam, a doctoral student at the University of North Carolina Gillings School of Global Public Health in Chapel Hill.
She and her collaborators estimated future cancer risk and burden for HIV-positive people using age-specific cancer incidence data from the National Cancer Institute HIV/AIDS Cancer Match (HACM) Study, and projected HIV prevalence data from the Centers for Disease Control and Prevention.
Cancer incidence
From 2000 to 2012, there were 23,907 cancers reported in 463,300 HIV-infected adults in the HACM Study. Based on trends in this study, the researchers made projections for cancer incidence through 2030.
They projected that HIV-positive adults of all ages will see a significant decrease over time in the incidence of NHL, Kaposi sarcoma, cervical cancer, anal cancer among men who have sex with men (MSM), lung cancer, and Hodgkin lymphoma.
Patients age 65 and older will see a significant decrease in colon cancer incidence over time. However, there will be no significant change for patients younger than 65.
HIV-positive adults of all ages will see no significant change over time in the incidence of liver cancer, oral cavity cancer, anal cancer among non-MSMs, and breast cancer.
The incidence of prostate cancer will increase significantly among patients ages 35 to 44 and among patients ages 45 to 64.
Cancer burden
The researchers said the number of adults living with HIV in the US is projected to increase from 1.06 million in 2006 to 1.17 million in 2018, but it is expected to decline to 1.09 million in 2030.
The team noted that, in 2006, there were an estimated 8241 cancers in patients with HIV—3522 AIDS-defining cancers and 4719 malignancies not associated with AIDS.
In 2030, the total number of cancers in the HIV-positive population is projected to be 6692, with decreases in AIDS-defining cancers (n=716) and increases in other cancers (n=5976) from the 2006 data.
In 2010, the most common cancers among HIV-positive patients were estimated to be NHL (n=1488), Kaposi sarcoma (n=1133), and lung cancer (n=815).
But in 2030, the most common cancers are projected to be prostate (n=1587), lung (n=1027), and liver cancers (n=483).
“It is critical to understand both incidence rates and burden over time, as rates capture changes in cancer risk, and burden quantifies the actual number of cancer cases expected to occur,” said study investigator Meredith S. Shiels, PhD, of the National Cancer Institute in Bethesda, Maryland.
“For example, lung cancer rates are expected to decrease in the future, but the burden is expected to increase due to the growing number of older people living with HIV.” ![]()
Factor IX therapy seems safe, effective in young kids
SCOTTSDALE, ARIZONA—The recombinant factor IX product trenonacog alfa appears safe and effective for previously treated patients with hemophilia B who are younger than 12 years of age, according to researchers.
The team conducted a pooled analysis of 2 studies, which included a total of 12 patients.
The median annualized bleeding rate (ABR) was low among patients who received trenonacog alfa as prophylaxis.
Among all patients, 72% of bleeding episodes were resolved with a single infusion of trenonacog alfa.
None of the patients developed factor IX inhibitors, and treatment-related adverse events consisted of fever and hyperhidrosis.
These results were presented in a poster at the Hemostasis and Thrombosis Research Society 2017 Scientific Symposium.
The research was conducted by employees of Aptevo Therapeutics, the company marketing trenonacog alfa as IXINITY®. The poster is available on the company’s website.
The researchers conducted a pooled analysis of 2 prospective, non-randomized studies of 12 children with hemophilia B under the age of 12.
The patients’ median age was 9.5 (range, 2-11). All patients were male. Half were Asian, 3 were white, 2 were Pacific Islanders, and 1 belonged to an “other” racial/ethnic group.
Eleven patients received trenonacog alfa as prophylaxis, and 1 patient received the treatment on demand.
Among the patients on prophylaxis, the median number of exposure days was 254 (range, 111-404), and the median dose per infusion was 75.3 IU/kg (range, 25.3-111.0).
For the patients on prophylaxis, the median number of bleeding episodes was 1.0 (range, 0-11), and the median ABR was 0.3 (range, 0-4.0). Two patients had no bleeding episodes.
The patient who received trenonacog alfa on demand had 23 bleeding episodes and an ABR of 11.1.
There were a total of 61 bleeding episodes in this study. Most (72%, n=44) resolved after 1 infusion of trenonacog alfa, and 10% (n=6) resolved without any infusions.
Eight percent of the bleeding episodes (n=5) required 2 infusions of trenonacog alfa, and 10% (n=6) required 3, 4, or 5 infusions.
Adverse events thought to be related to trenonacog alfa were hyperhidrosis and fever in 1 patient, and hyperhidrosis in another patient. ![]()
SCOTTSDALE, ARIZONA—The recombinant factor IX product trenonacog alfa appears safe and effective for previously treated patients with hemophilia B who are younger than 12 years of age, according to researchers.
The team conducted a pooled analysis of 2 studies, which included a total of 12 patients.
The median annualized bleeding rate (ABR) was low among patients who received trenonacog alfa as prophylaxis.
Among all patients, 72% of bleeding episodes were resolved with a single infusion of trenonacog alfa.
None of the patients developed factor IX inhibitors, and treatment-related adverse events consisted of fever and hyperhidrosis.
These results were presented in a poster at the Hemostasis and Thrombosis Research Society 2017 Scientific Symposium.
The research was conducted by employees of Aptevo Therapeutics, the company marketing trenonacog alfa as IXINITY®. The poster is available on the company’s website.
The researchers conducted a pooled analysis of 2 prospective, non-randomized studies of 12 children with hemophilia B under the age of 12.
The patients’ median age was 9.5 (range, 2-11). All patients were male. Half were Asian, 3 were white, 2 were Pacific Islanders, and 1 belonged to an “other” racial/ethnic group.
Eleven patients received trenonacog alfa as prophylaxis, and 1 patient received the treatment on demand.
Among the patients on prophylaxis, the median number of exposure days was 254 (range, 111-404), and the median dose per infusion was 75.3 IU/kg (range, 25.3-111.0).
For the patients on prophylaxis, the median number of bleeding episodes was 1.0 (range, 0-11), and the median ABR was 0.3 (range, 0-4.0). Two patients had no bleeding episodes.
The patient who received trenonacog alfa on demand had 23 bleeding episodes and an ABR of 11.1.
There were a total of 61 bleeding episodes in this study. Most (72%, n=44) resolved after 1 infusion of trenonacog alfa, and 10% (n=6) resolved without any infusions.
Eight percent of the bleeding episodes (n=5) required 2 infusions of trenonacog alfa, and 10% (n=6) required 3, 4, or 5 infusions.
Adverse events thought to be related to trenonacog alfa were hyperhidrosis and fever in 1 patient, and hyperhidrosis in another patient. ![]()
SCOTTSDALE, ARIZONA—The recombinant factor IX product trenonacog alfa appears safe and effective for previously treated patients with hemophilia B who are younger than 12 years of age, according to researchers.
The team conducted a pooled analysis of 2 studies, which included a total of 12 patients.
The median annualized bleeding rate (ABR) was low among patients who received trenonacog alfa as prophylaxis.
Among all patients, 72% of bleeding episodes were resolved with a single infusion of trenonacog alfa.
None of the patients developed factor IX inhibitors, and treatment-related adverse events consisted of fever and hyperhidrosis.
These results were presented in a poster at the Hemostasis and Thrombosis Research Society 2017 Scientific Symposium.
The research was conducted by employees of Aptevo Therapeutics, the company marketing trenonacog alfa as IXINITY®. The poster is available on the company’s website.
The researchers conducted a pooled analysis of 2 prospective, non-randomized studies of 12 children with hemophilia B under the age of 12.
The patients’ median age was 9.5 (range, 2-11). All patients were male. Half were Asian, 3 were white, 2 were Pacific Islanders, and 1 belonged to an “other” racial/ethnic group.
Eleven patients received trenonacog alfa as prophylaxis, and 1 patient received the treatment on demand.
Among the patients on prophylaxis, the median number of exposure days was 254 (range, 111-404), and the median dose per infusion was 75.3 IU/kg (range, 25.3-111.0).
For the patients on prophylaxis, the median number of bleeding episodes was 1.0 (range, 0-11), and the median ABR was 0.3 (range, 0-4.0). Two patients had no bleeding episodes.
The patient who received trenonacog alfa on demand had 23 bleeding episodes and an ABR of 11.1.
There were a total of 61 bleeding episodes in this study. Most (72%, n=44) resolved after 1 infusion of trenonacog alfa, and 10% (n=6) resolved without any infusions.
Eight percent of the bleeding episodes (n=5) required 2 infusions of trenonacog alfa, and 10% (n=6) required 3, 4, or 5 infusions.
Adverse events thought to be related to trenonacog alfa were hyperhidrosis and fever in 1 patient, and hyperhidrosis in another patient. ![]()
New Drugs to Treat Hyperkalemia
Q)I have heard talk about the development of new drugs to treat hyperkalemia. What is the status of these?
Hyperkalemia is a commonly seen electrolyte imbalance in clinical practice. Risks associated with moderate-to-severe hyperkalemia include potentially fatal cardiac conduction abnormalities/arrhythmias, making identification and management critical. An in-depth discussion of hyperkalemia diagnosis can be found in our March 2017 CE/CME activity (2017;27[3]:40-49).
Risk factors for hyperkalemia include excess intake or supplementation of potassium, type 2 diabetes, liver cirrhosis, congestive heart failure (CHF), and chronic kidney disease (CKD). The kidneys excrete 90% to 95% of ingested potassium, and the gut excretes the rest. Normal kidneys take six to 12 hours to excrete an acute potassium load. As kidney function decreases, risk for hyperkalemia increases.1 Hyperkalemia rates as high as 26% have been observed in patients with CKD stages 3 to 5 (glomerular filtration rate [GFR], < 60 mL/min).2
Renin-angiotensin-aldosterone system (RAAS) inhibitors—including ACE inhibitors (ACEis), angiotensin-receptor blockers, and aldosterone agonists—are associated with hyperkalemia. While RAAS therapy can play an important role in the management of CKD and cardiovascular disease (CVD), the development of hyperkalemia can necessitate a dose reduction or discontinuation of these medications, limiting their therapeutic benefit. Other medications that elevate risk for hyperkalemia include NSAIDs, heparin, cyclosporine, amiloride, triamterene, and nonselective ß-blockers.1
Therapeutic options for nonurgent treatment of hyperkalemia are limited. In addition to reducing or discontinuing associated medications, strategies include use of diuretics (as appropriate), treatment of metabolic acidosis, and dietary restrictions (ie, limiting high-potassium foods).1 Pharmacologically, there has been one (less than ideal) option—until recently.
Sodium polystyrene sulfonate (SPS), an ion-exchange resin approved in 1958, can be used to treat hyperkalemia.3 It comes in an enema and an oral form; the former has a faster onset, but the latter is more effective, with an onset of action of one to two hours and a duration of four to six hours.1 However, each gram of SPS contains 100 g of sodium, and the typical dose of SPS is 15 g to 60 g.4 The resulting increase in sodium load can be a concern for patients with CHF, severe hypertension, or severe edema.5
Data from randomized controlled trials (RCTs) are limited; however, one double-blind RCT investigated the effect of SPS on 33 patients with CKD and mild-to-moderate hyperkalemia (potassium level, 5 mEq/L to 5.9 mEq/L). The researchers found that patients who took 30 g/d of SPS for seven days experienced a 73% reduction in serum potassium, compared with a 38% reduction in patients who took a placebo. Of note, more gastrointestinal issues were observed in the SPS group.6
Additionally, a retrospective chart review of 14 patients with CKD and heart disease found low-dose SPS to be safe and effective when used as a secondary measure for hyperkalemia prevention in those taking RAAS therapy.7 However, a systematic review found that SPS use with and without concurrent sorbitol may be associated with serious and fatal gastrointestinal injuries.8 In 2011, the FDA issued a black box warning regarding increased risk for intestinal necrosis when SPS is used with sorbitol.9 In 2015, the FDA recommended separating SPS from other oral medications by at least six hours, due to its potential to bind with other medications.10
Patiromer, a new potassium binder, was approved by the FDA in 2015. This sodium-free, nonabsorbed, spherical polymer uses calcium as the exchange cation to bind potassium in the gastrointestinal tract. Its onset of action is seven hours, with a 24-hour duration of action. It is not approved for emergency use. There are no renal dosing adjustment considerations with patiromer.
In RCTs, patiromer has been associated with a significant reduction in serum potassium in patients with CKD (with or without diabetes) taking RAAS therapy. The starting dose is 8.4 g/d mixed with water, taken with food; this can be increased by 8.4 g each week as needed, to a maximum dosage of 25.2 g/d. Patiromer binds between 8.5 mEq to 8.8 mEq of potassium per gram of polymer.
The original approval included a black box warning to take patiromer six hours before and after other medications, due to concern for binding with certain medications. However, after an additional study in 2016, the FDA removed this warning and approved a change in administration to three hours before and after taking other medications.
Use of patiromer is not advised in those with severe constipation, bowel obstruction/impaction, or allergies to any of its components.11 Adverse reactions associated with patiromer include constipation (which generally improves with time), hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. A 52-week RCT of 304 patients with CKD on RAAS found the most common adverse event to be mild-to-moderate constipation (6.3% of patients), with two patients discontinuing therapy as a result.4 In clinical trials, 9% of patients developed hypomagnesemia (serum magnesium value, < 1.4 mg/dL). It is recommended that serum magnesium levels be monitored and supplementation offered, when appropriate.11
Sodium zirconium cyclosilicate (ZS-9) is among the potassium-lowering medications on the horizon. In 2016, the FDA accepted a new drug application for this insoluble, unabsorbed cation exchanger that also works in the GI tract and uses sodium and hydrogen as exchange cations.12
For now, however, dietary education remains a mainstay of treatment for patients with elevated serum potassium levels. It is particularly important to inform your patients that many salt substitutes and low-sodium products contain potassium chloride. They should therefore exercise caution when incorporating sodium-reducing components into their diet. —CS
Cynthia Smith, DNP, CNN-NP, APRN, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virginia
1. Gilbert S, Weiner D, Gipson D, eds; National Kidney Foundation. Primer on Kidney Diseases. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014.
2. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162.
3. Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol: a preliminary report. N Engl J Med. 1961;264:111-115.
4. Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 suppl): s307-s315.
5. Li L, Harrison SD, Cope MJ, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456-465.
6. Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015; 10(12):2136-2142.
7. Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35(1):32-36.
8. Harel Z, Harel S, Shah PS, et al. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126(3):264.e9-e24.
9. FDA. Safety warning: Kayexalate (sodium polystyrene sulfonate) powder. www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed February 15, 2017.
10. FDA. FDA drug safety communication: FDA required drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Accessed March 1, 2017.
11. Veltassa® (patiromer) [package insert]. Redwood City, CA: Relypsa, Inc; 2016. www.veltassa.com/pi.pdf. Accessed March 1, 2017.
12. AstraZeneca. FDA accepts for review New Drug Application for sodium zirconium cyclosilicate (ZS-9) for the treatment of hyperkalaemia. www.astrazeneca.com/investor-relations/Stock-exchange-announcements/fda-accepts-for-review-new-drug-application-for-sodium-zirconium-18102016.html. Accessed March 1, 2017.
Q)I have heard talk about the development of new drugs to treat hyperkalemia. What is the status of these?
Hyperkalemia is a commonly seen electrolyte imbalance in clinical practice. Risks associated with moderate-to-severe hyperkalemia include potentially fatal cardiac conduction abnormalities/arrhythmias, making identification and management critical. An in-depth discussion of hyperkalemia diagnosis can be found in our March 2017 CE/CME activity (2017;27[3]:40-49).
Risk factors for hyperkalemia include excess intake or supplementation of potassium, type 2 diabetes, liver cirrhosis, congestive heart failure (CHF), and chronic kidney disease (CKD). The kidneys excrete 90% to 95% of ingested potassium, and the gut excretes the rest. Normal kidneys take six to 12 hours to excrete an acute potassium load. As kidney function decreases, risk for hyperkalemia increases.1 Hyperkalemia rates as high as 26% have been observed in patients with CKD stages 3 to 5 (glomerular filtration rate [GFR], < 60 mL/min).2
Renin-angiotensin-aldosterone system (RAAS) inhibitors—including ACE inhibitors (ACEis), angiotensin-receptor blockers, and aldosterone agonists—are associated with hyperkalemia. While RAAS therapy can play an important role in the management of CKD and cardiovascular disease (CVD), the development of hyperkalemia can necessitate a dose reduction or discontinuation of these medications, limiting their therapeutic benefit. Other medications that elevate risk for hyperkalemia include NSAIDs, heparin, cyclosporine, amiloride, triamterene, and nonselective ß-blockers.1
Therapeutic options for nonurgent treatment of hyperkalemia are limited. In addition to reducing or discontinuing associated medications, strategies include use of diuretics (as appropriate), treatment of metabolic acidosis, and dietary restrictions (ie, limiting high-potassium foods).1 Pharmacologically, there has been one (less than ideal) option—until recently.
Sodium polystyrene sulfonate (SPS), an ion-exchange resin approved in 1958, can be used to treat hyperkalemia.3 It comes in an enema and an oral form; the former has a faster onset, but the latter is more effective, with an onset of action of one to two hours and a duration of four to six hours.1 However, each gram of SPS contains 100 g of sodium, and the typical dose of SPS is 15 g to 60 g.4 The resulting increase in sodium load can be a concern for patients with CHF, severe hypertension, or severe edema.5
Data from randomized controlled trials (RCTs) are limited; however, one double-blind RCT investigated the effect of SPS on 33 patients with CKD and mild-to-moderate hyperkalemia (potassium level, 5 mEq/L to 5.9 mEq/L). The researchers found that patients who took 30 g/d of SPS for seven days experienced a 73% reduction in serum potassium, compared with a 38% reduction in patients who took a placebo. Of note, more gastrointestinal issues were observed in the SPS group.6
Additionally, a retrospective chart review of 14 patients with CKD and heart disease found low-dose SPS to be safe and effective when used as a secondary measure for hyperkalemia prevention in those taking RAAS therapy.7 However, a systematic review found that SPS use with and without concurrent sorbitol may be associated with serious and fatal gastrointestinal injuries.8 In 2011, the FDA issued a black box warning regarding increased risk for intestinal necrosis when SPS is used with sorbitol.9 In 2015, the FDA recommended separating SPS from other oral medications by at least six hours, due to its potential to bind with other medications.10
Patiromer, a new potassium binder, was approved by the FDA in 2015. This sodium-free, nonabsorbed, spherical polymer uses calcium as the exchange cation to bind potassium in the gastrointestinal tract. Its onset of action is seven hours, with a 24-hour duration of action. It is not approved for emergency use. There are no renal dosing adjustment considerations with patiromer.
In RCTs, patiromer has been associated with a significant reduction in serum potassium in patients with CKD (with or without diabetes) taking RAAS therapy. The starting dose is 8.4 g/d mixed with water, taken with food; this can be increased by 8.4 g each week as needed, to a maximum dosage of 25.2 g/d. Patiromer binds between 8.5 mEq to 8.8 mEq of potassium per gram of polymer.
The original approval included a black box warning to take patiromer six hours before and after other medications, due to concern for binding with certain medications. However, after an additional study in 2016, the FDA removed this warning and approved a change in administration to three hours before and after taking other medications.
Use of patiromer is not advised in those with severe constipation, bowel obstruction/impaction, or allergies to any of its components.11 Adverse reactions associated with patiromer include constipation (which generally improves with time), hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. A 52-week RCT of 304 patients with CKD on RAAS found the most common adverse event to be mild-to-moderate constipation (6.3% of patients), with two patients discontinuing therapy as a result.4 In clinical trials, 9% of patients developed hypomagnesemia (serum magnesium value, < 1.4 mg/dL). It is recommended that serum magnesium levels be monitored and supplementation offered, when appropriate.11
Sodium zirconium cyclosilicate (ZS-9) is among the potassium-lowering medications on the horizon. In 2016, the FDA accepted a new drug application for this insoluble, unabsorbed cation exchanger that also works in the GI tract and uses sodium and hydrogen as exchange cations.12
For now, however, dietary education remains a mainstay of treatment for patients with elevated serum potassium levels. It is particularly important to inform your patients that many salt substitutes and low-sodium products contain potassium chloride. They should therefore exercise caution when incorporating sodium-reducing components into their diet. —CS
Cynthia Smith, DNP, CNN-NP, APRN, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virginia
Q)I have heard talk about the development of new drugs to treat hyperkalemia. What is the status of these?
Hyperkalemia is a commonly seen electrolyte imbalance in clinical practice. Risks associated with moderate-to-severe hyperkalemia include potentially fatal cardiac conduction abnormalities/arrhythmias, making identification and management critical. An in-depth discussion of hyperkalemia diagnosis can be found in our March 2017 CE/CME activity (2017;27[3]:40-49).
Risk factors for hyperkalemia include excess intake or supplementation of potassium, type 2 diabetes, liver cirrhosis, congestive heart failure (CHF), and chronic kidney disease (CKD). The kidneys excrete 90% to 95% of ingested potassium, and the gut excretes the rest. Normal kidneys take six to 12 hours to excrete an acute potassium load. As kidney function decreases, risk for hyperkalemia increases.1 Hyperkalemia rates as high as 26% have been observed in patients with CKD stages 3 to 5 (glomerular filtration rate [GFR], < 60 mL/min).2
Renin-angiotensin-aldosterone system (RAAS) inhibitors—including ACE inhibitors (ACEis), angiotensin-receptor blockers, and aldosterone agonists—are associated with hyperkalemia. While RAAS therapy can play an important role in the management of CKD and cardiovascular disease (CVD), the development of hyperkalemia can necessitate a dose reduction or discontinuation of these medications, limiting their therapeutic benefit. Other medications that elevate risk for hyperkalemia include NSAIDs, heparin, cyclosporine, amiloride, triamterene, and nonselective ß-blockers.1
Therapeutic options for nonurgent treatment of hyperkalemia are limited. In addition to reducing or discontinuing associated medications, strategies include use of diuretics (as appropriate), treatment of metabolic acidosis, and dietary restrictions (ie, limiting high-potassium foods).1 Pharmacologically, there has been one (less than ideal) option—until recently.
Sodium polystyrene sulfonate (SPS), an ion-exchange resin approved in 1958, can be used to treat hyperkalemia.3 It comes in an enema and an oral form; the former has a faster onset, but the latter is more effective, with an onset of action of one to two hours and a duration of four to six hours.1 However, each gram of SPS contains 100 g of sodium, and the typical dose of SPS is 15 g to 60 g.4 The resulting increase in sodium load can be a concern for patients with CHF, severe hypertension, or severe edema.5
Data from randomized controlled trials (RCTs) are limited; however, one double-blind RCT investigated the effect of SPS on 33 patients with CKD and mild-to-moderate hyperkalemia (potassium level, 5 mEq/L to 5.9 mEq/L). The researchers found that patients who took 30 g/d of SPS for seven days experienced a 73% reduction in serum potassium, compared with a 38% reduction in patients who took a placebo. Of note, more gastrointestinal issues were observed in the SPS group.6
Additionally, a retrospective chart review of 14 patients with CKD and heart disease found low-dose SPS to be safe and effective when used as a secondary measure for hyperkalemia prevention in those taking RAAS therapy.7 However, a systematic review found that SPS use with and without concurrent sorbitol may be associated with serious and fatal gastrointestinal injuries.8 In 2011, the FDA issued a black box warning regarding increased risk for intestinal necrosis when SPS is used with sorbitol.9 In 2015, the FDA recommended separating SPS from other oral medications by at least six hours, due to its potential to bind with other medications.10
Patiromer, a new potassium binder, was approved by the FDA in 2015. This sodium-free, nonabsorbed, spherical polymer uses calcium as the exchange cation to bind potassium in the gastrointestinal tract. Its onset of action is seven hours, with a 24-hour duration of action. It is not approved for emergency use. There are no renal dosing adjustment considerations with patiromer.
In RCTs, patiromer has been associated with a significant reduction in serum potassium in patients with CKD (with or without diabetes) taking RAAS therapy. The starting dose is 8.4 g/d mixed with water, taken with food; this can be increased by 8.4 g each week as needed, to a maximum dosage of 25.2 g/d. Patiromer binds between 8.5 mEq to 8.8 mEq of potassium per gram of polymer.
The original approval included a black box warning to take patiromer six hours before and after other medications, due to concern for binding with certain medications. However, after an additional study in 2016, the FDA removed this warning and approved a change in administration to three hours before and after taking other medications.
Use of patiromer is not advised in those with severe constipation, bowel obstruction/impaction, or allergies to any of its components.11 Adverse reactions associated with patiromer include constipation (which generally improves with time), hypomagnesemia, diarrhea, nausea, abdominal discomfort, and flatulence. A 52-week RCT of 304 patients with CKD on RAAS found the most common adverse event to be mild-to-moderate constipation (6.3% of patients), with two patients discontinuing therapy as a result.4 In clinical trials, 9% of patients developed hypomagnesemia (serum magnesium value, < 1.4 mg/dL). It is recommended that serum magnesium levels be monitored and supplementation offered, when appropriate.11
Sodium zirconium cyclosilicate (ZS-9) is among the potassium-lowering medications on the horizon. In 2016, the FDA accepted a new drug application for this insoluble, unabsorbed cation exchanger that also works in the GI tract and uses sodium and hydrogen as exchange cations.12
For now, however, dietary education remains a mainstay of treatment for patients with elevated serum potassium levels. It is particularly important to inform your patients that many salt substitutes and low-sodium products contain potassium chloride. They should therefore exercise caution when incorporating sodium-reducing components into their diet. —CS
Cynthia Smith, DNP, CNN-NP, APRN, FNP-BC
Renal Consultants, PLLC, South Charleston, West Virginia
1. Gilbert S, Weiner D, Gipson D, eds; National Kidney Foundation. Primer on Kidney Diseases. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014.
2. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162.
3. Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol: a preliminary report. N Engl J Med. 1961;264:111-115.
4. Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 suppl): s307-s315.
5. Li L, Harrison SD, Cope MJ, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456-465.
6. Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015; 10(12):2136-2142.
7. Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35(1):32-36.
8. Harel Z, Harel S, Shah PS, et al. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126(3):264.e9-e24.
9. FDA. Safety warning: Kayexalate (sodium polystyrene sulfonate) powder. www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed February 15, 2017.
10. FDA. FDA drug safety communication: FDA required drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Accessed March 1, 2017.
11. Veltassa® (patiromer) [package insert]. Redwood City, CA: Relypsa, Inc; 2016. www.veltassa.com/pi.pdf. Accessed March 1, 2017.
12. AstraZeneca. FDA accepts for review New Drug Application for sodium zirconium cyclosilicate (ZS-9) for the treatment of hyperkalaemia. www.astrazeneca.com/investor-relations/Stock-exchange-announcements/fda-accepts-for-review-new-drug-application-for-sodium-zirconium-18102016.html. Accessed March 1, 2017.
1. Gilbert S, Weiner D, Gipson D, eds; National Kidney Foundation. Primer on Kidney Diseases. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014.
2. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162.
3. Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol: a preliminary report. N Engl J Med. 1961;264:111-115.
4. Dunn JD, Benton WW, Orozco-Torrentera E, Adamson RT. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 suppl): s307-s315.
5. Li L, Harrison SD, Cope MJ, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456-465.
6. Lepage L, Dufour AC, Doiron J, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015; 10(12):2136-2142.
7. Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary prevention of hyperkalemia with sodium polystyrene sulfonate in cardiac and kidney patients on renin-angiotensin-aldosterone system inhibition therapy. Clin Cardiol. 2012;35(1):32-36.
8. Harel Z, Harel S, Shah PS, et al. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126(3):264.e9-e24.
9. FDA. Safety warning: Kayexalate (sodium polystyrene sulfonate) powder. www.fda.gov/Safety/MedWatch/SafetyInformation/ucm186845.htm. Accessed February 15, 2017.
10. FDA. FDA drug safety communication: FDA required drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Accessed March 1, 2017.
11. Veltassa® (patiromer) [package insert]. Redwood City, CA: Relypsa, Inc; 2016. www.veltassa.com/pi.pdf. Accessed March 1, 2017.
12. AstraZeneca. FDA accepts for review New Drug Application for sodium zirconium cyclosilicate (ZS-9) for the treatment of hyperkalaemia. www.astrazeneca.com/investor-relations/Stock-exchange-announcements/fda-accepts-for-review-new-drug-application-for-sodium-zirconium-18102016.html. Accessed March 1, 2017.
Decline in U.S. flu activity puts end of season within sight
Outpatient visits for influenza were down again in the United States during the week ending April 1, and the number of states at the highest level of flu activity dropped from seven to four, according to the Centers for Disease Control and Prevention.
The national proportion of outpatient visits for influenza-like illness (ILI) was 2.9% for the week ending April 1, compared with 3.2% the week before, the CDC’s Outpatient Influenza-like Illness Surveillance Network reported. The national baseline level is 2.2%.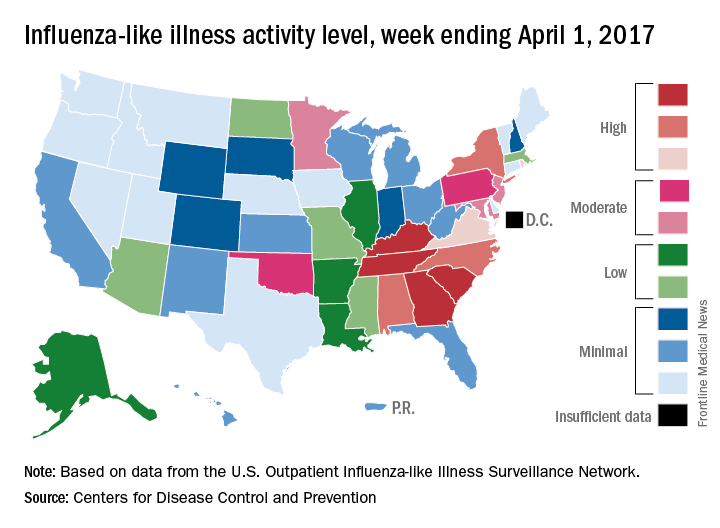
There were 7 flu-related pediatric deaths reported for the week ending April 1 – six of the deaths occurred in previous weeks – which brings the total for the 2016-2017 season to 68, the CDC said. The largest share of those deaths by age group has been among 5- to 11-year-olds (36.8%), followed by those aged 12-17 years (26.5%), 6-23 months (16.2%), 2-4 years (14.7%), and 0-5 months (5.9%).
Outpatient visits for influenza were down again in the United States during the week ending April 1, and the number of states at the highest level of flu activity dropped from seven to four, according to the Centers for Disease Control and Prevention.
The national proportion of outpatient visits for influenza-like illness (ILI) was 2.9% for the week ending April 1, compared with 3.2% the week before, the CDC’s Outpatient Influenza-like Illness Surveillance Network reported. The national baseline level is 2.2%.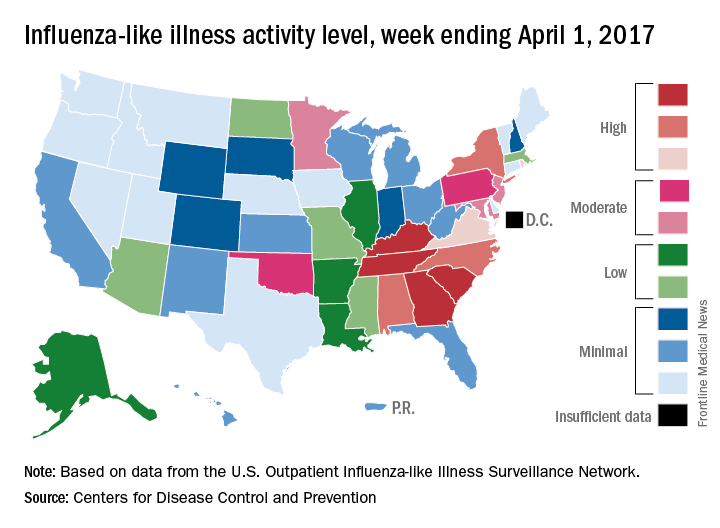
There were 7 flu-related pediatric deaths reported for the week ending April 1 – six of the deaths occurred in previous weeks – which brings the total for the 2016-2017 season to 68, the CDC said. The largest share of those deaths by age group has been among 5- to 11-year-olds (36.8%), followed by those aged 12-17 years (26.5%), 6-23 months (16.2%), 2-4 years (14.7%), and 0-5 months (5.9%).
Outpatient visits for influenza were down again in the United States during the week ending April 1, and the number of states at the highest level of flu activity dropped from seven to four, according to the Centers for Disease Control and Prevention.
The national proportion of outpatient visits for influenza-like illness (ILI) was 2.9% for the week ending April 1, compared with 3.2% the week before, the CDC’s Outpatient Influenza-like Illness Surveillance Network reported. The national baseline level is 2.2%.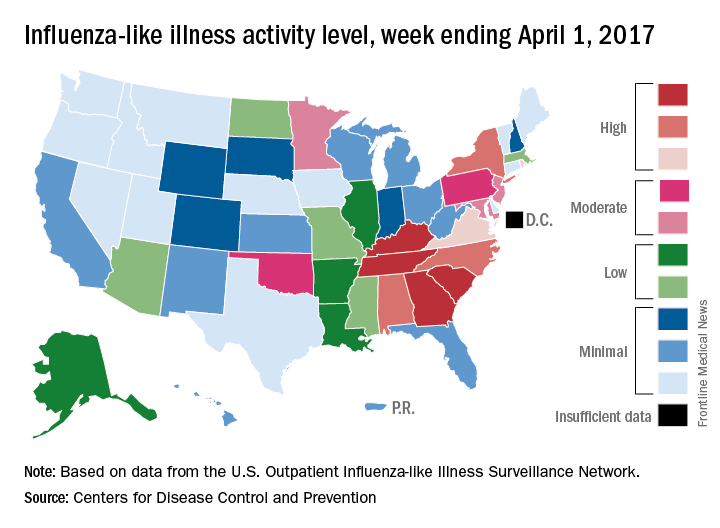
There were 7 flu-related pediatric deaths reported for the week ending April 1 – six of the deaths occurred in previous weeks – which brings the total for the 2016-2017 season to 68, the CDC said. The largest share of those deaths by age group has been among 5- to 11-year-olds (36.8%), followed by those aged 12-17 years (26.5%), 6-23 months (16.2%), 2-4 years (14.7%), and 0-5 months (5.9%).
Death watch intensifies for HDL-based interventions
WASHINGTON – Is it finally time to give up on HDL cholesterol–based interventions to treat atherosclerotic disease?
The approach “is on life support,” admitted Stephen J. Nicholls, MD, a long-time leader in the field who has reported results from a series of studies during the past 10 or so years that tested various approaches to juicing HDL cholesterol activity in patients, only to see each and every candidate intervention result in an inability to budge clinical outcomes.
The latest disappointment he reported was for CER-001, an engineered HDL mimetic agent. In a placebo-controlled international study, CARAT (CER-001 Atherosclerosis Regression ACS Trial), with 301 randomized patients and 272 completers, 10 weekly infusions of CER-001 over the course of 9 weeks failed to produce discernible incremental regression of atherosclerotic plaque volume, compared with standard care measured by serial examination using intravascular ultrasound (IVUS), Dr. Nicholls reported. The absence of any detectable benefit “suggests that this is not a promising strategy,” he said during his report at the meeting.
Enthusiasm for HDL cholesterol–based interventions dates to 2003, when an IVUS study of a first-generation HDL mimetic agent, ETC-216, showed an apparent ability to produce regression of coronary atheroma after five infusions over a 2-week period, compared with placebo-treated patients (JAMA. 2003 Nov 5;290[17]:2292-300). But the successor compound to this agent, MDCO-216, flamed out in an IVUS study with 113 completing patients that Dr. Nicholls reported at the American Heart Association Scientific Sessions in November 2016.
Also lying dead on the trial trail during past years are several cholesterol ester transfer protein inhibitors – torcetrapib, dalcetrapib and evacetrapib – as well as other agents that Dr. Nicholls described in a recent review (Arch Med Sci. 2016 Oct 24;12[6]:1302-7).
“HDL wouldn’t be the first risk factor we’ve seen that is not a modifiable target. Homocysteine is a really good example” of another atherosclerotic disease risk that’s proven immune to intervention, Dr. Nicholls said in an interview at the meeting. “Ultimately we’ll come to a point when the enthusiasm [for potential HDL interventions] will wane, but we’re not quite there yet.”
“There are other players in the HDL field” that remain viable, said Dr. Nicholls, most notably CSL112, plasma-derived apoA1 – the primary functional part of HDL cholesterol – that’s infused into patients to boost HDL activity. Results from a phase II study reported in November 2016 showed it increased cholesterol efflux (Circulation 2016 Nov; doi: 10.1161/CIRCULATIONAHA.116.025687), and is now the subject of additional phase II testing. “But with every negative trial, it will get harder and harder [to fund new HDL research], and we’ll look for other targets,” he said.
One promising alternative target is triglycerides. “HDL has received more attention than triglycerides over the past decade, but I think that will start to change as HDL can’t deliver,” predicted Dr. Nicholls, professor of cardiology at the South Australian Health & Medical Research Institute in Adelaide.
Understandably “financial support is the biggest issue. Do companies and investors still believe in the [HDL] dream?” Dr. Nicholls said that, objectively, looking at the HDL research record should definitely give investors pause before they sink money into new compounds for HDL intervention.
“If I was sitting at the drawing board now, would HDL be the risk factor I’d target? Probably not,” he concluded.
Dr. Nicholls received research support from Cerenis, the company that is developing CER-001, and he has received honoraria and research support from several other companies. Dr. Bhatt has received research support from several drug companies.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – Is it finally time to give up on HDL cholesterol–based interventions to treat atherosclerotic disease?
The approach “is on life support,” admitted Stephen J. Nicholls, MD, a long-time leader in the field who has reported results from a series of studies during the past 10 or so years that tested various approaches to juicing HDL cholesterol activity in patients, only to see each and every candidate intervention result in an inability to budge clinical outcomes.
The latest disappointment he reported was for CER-001, an engineered HDL mimetic agent. In a placebo-controlled international study, CARAT (CER-001 Atherosclerosis Regression ACS Trial), with 301 randomized patients and 272 completers, 10 weekly infusions of CER-001 over the course of 9 weeks failed to produce discernible incremental regression of atherosclerotic plaque volume, compared with standard care measured by serial examination using intravascular ultrasound (IVUS), Dr. Nicholls reported. The absence of any detectable benefit “suggests that this is not a promising strategy,” he said during his report at the meeting.
Enthusiasm for HDL cholesterol–based interventions dates to 2003, when an IVUS study of a first-generation HDL mimetic agent, ETC-216, showed an apparent ability to produce regression of coronary atheroma after five infusions over a 2-week period, compared with placebo-treated patients (JAMA. 2003 Nov 5;290[17]:2292-300). But the successor compound to this agent, MDCO-216, flamed out in an IVUS study with 113 completing patients that Dr. Nicholls reported at the American Heart Association Scientific Sessions in November 2016.
Also lying dead on the trial trail during past years are several cholesterol ester transfer protein inhibitors – torcetrapib, dalcetrapib and evacetrapib – as well as other agents that Dr. Nicholls described in a recent review (Arch Med Sci. 2016 Oct 24;12[6]:1302-7).
“HDL wouldn’t be the first risk factor we’ve seen that is not a modifiable target. Homocysteine is a really good example” of another atherosclerotic disease risk that’s proven immune to intervention, Dr. Nicholls said in an interview at the meeting. “Ultimately we’ll come to a point when the enthusiasm [for potential HDL interventions] will wane, but we’re not quite there yet.”
“There are other players in the HDL field” that remain viable, said Dr. Nicholls, most notably CSL112, plasma-derived apoA1 – the primary functional part of HDL cholesterol – that’s infused into patients to boost HDL activity. Results from a phase II study reported in November 2016 showed it increased cholesterol efflux (Circulation 2016 Nov; doi: 10.1161/CIRCULATIONAHA.116.025687), and is now the subject of additional phase II testing. “But with every negative trial, it will get harder and harder [to fund new HDL research], and we’ll look for other targets,” he said.
One promising alternative target is triglycerides. “HDL has received more attention than triglycerides over the past decade, but I think that will start to change as HDL can’t deliver,” predicted Dr. Nicholls, professor of cardiology at the South Australian Health & Medical Research Institute in Adelaide.
Understandably “financial support is the biggest issue. Do companies and investors still believe in the [HDL] dream?” Dr. Nicholls said that, objectively, looking at the HDL research record should definitely give investors pause before they sink money into new compounds for HDL intervention.
“If I was sitting at the drawing board now, would HDL be the risk factor I’d target? Probably not,” he concluded.
Dr. Nicholls received research support from Cerenis, the company that is developing CER-001, and he has received honoraria and research support from several other companies. Dr. Bhatt has received research support from several drug companies.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – Is it finally time to give up on HDL cholesterol–based interventions to treat atherosclerotic disease?
The approach “is on life support,” admitted Stephen J. Nicholls, MD, a long-time leader in the field who has reported results from a series of studies during the past 10 or so years that tested various approaches to juicing HDL cholesterol activity in patients, only to see each and every candidate intervention result in an inability to budge clinical outcomes.
The latest disappointment he reported was for CER-001, an engineered HDL mimetic agent. In a placebo-controlled international study, CARAT (CER-001 Atherosclerosis Regression ACS Trial), with 301 randomized patients and 272 completers, 10 weekly infusions of CER-001 over the course of 9 weeks failed to produce discernible incremental regression of atherosclerotic plaque volume, compared with standard care measured by serial examination using intravascular ultrasound (IVUS), Dr. Nicholls reported. The absence of any detectable benefit “suggests that this is not a promising strategy,” he said during his report at the meeting.
Enthusiasm for HDL cholesterol–based interventions dates to 2003, when an IVUS study of a first-generation HDL mimetic agent, ETC-216, showed an apparent ability to produce regression of coronary atheroma after five infusions over a 2-week period, compared with placebo-treated patients (JAMA. 2003 Nov 5;290[17]:2292-300). But the successor compound to this agent, MDCO-216, flamed out in an IVUS study with 113 completing patients that Dr. Nicholls reported at the American Heart Association Scientific Sessions in November 2016.
Also lying dead on the trial trail during past years are several cholesterol ester transfer protein inhibitors – torcetrapib, dalcetrapib and evacetrapib – as well as other agents that Dr. Nicholls described in a recent review (Arch Med Sci. 2016 Oct 24;12[6]:1302-7).
“HDL wouldn’t be the first risk factor we’ve seen that is not a modifiable target. Homocysteine is a really good example” of another atherosclerotic disease risk that’s proven immune to intervention, Dr. Nicholls said in an interview at the meeting. “Ultimately we’ll come to a point when the enthusiasm [for potential HDL interventions] will wane, but we’re not quite there yet.”
“There are other players in the HDL field” that remain viable, said Dr. Nicholls, most notably CSL112, plasma-derived apoA1 – the primary functional part of HDL cholesterol – that’s infused into patients to boost HDL activity. Results from a phase II study reported in November 2016 showed it increased cholesterol efflux (Circulation 2016 Nov; doi: 10.1161/CIRCULATIONAHA.116.025687), and is now the subject of additional phase II testing. “But with every negative trial, it will get harder and harder [to fund new HDL research], and we’ll look for other targets,” he said.
One promising alternative target is triglycerides. “HDL has received more attention than triglycerides over the past decade, but I think that will start to change as HDL can’t deliver,” predicted Dr. Nicholls, professor of cardiology at the South Australian Health & Medical Research Institute in Adelaide.
Understandably “financial support is the biggest issue. Do companies and investors still believe in the [HDL] dream?” Dr. Nicholls said that, objectively, looking at the HDL research record should definitely give investors pause before they sink money into new compounds for HDL intervention.
“If I was sitting at the drawing board now, would HDL be the risk factor I’d target? Probably not,” he concluded.
Dr. Nicholls received research support from Cerenis, the company that is developing CER-001, and he has received honoraria and research support from several other companies. Dr. Bhatt has received research support from several drug companies.
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM ACC 17
MicroRNAs linked to treatment response in lupus nephritis
MELBOURNE – Researchers have identified six microRNAs that may indicate a better likelihood of response to cyclophosphamide in patients with lupus nephritis, according to a study presented at an international conference on systemic lupus erythematosus.
“MicroRNA has been shown to be important in systemic lupus in several studies, and they’ve identified several microRNA that have been shown to affect the outcome measures in patients,” said Sarfaraz Hasni, MD, director of the Lupus Clinical Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases in Bethesda, Md., who presented a poster on the study at the meeting.
The aim of this study, involving 71 patients with lupus nephritis, was to look for microRNAs associated with treatment response to cyclophosphamide.
The first stage of the study involved isolating microRNAs from kidney biopsies taken from a first cohort of 17 responders and 15 nonresponders.
Responders were patients who, after 2 years of intravenous cyclophosphamide, showed no active urinary sediments, less than five red blood cells or white blood cells in urine, and proteinuria below 1 g/24 hours.
After analyzing 300-400 microRNAs in these biopsies, the investigators identified 6 that were significantly upregulated in association with treatment outcome in both the first cohort as well as a second validation cohort of 22 responders and 17 nonresponders.
When the researchers looked at the most likely genetic targets of these microRNAs, they identified genes associated with G2/M DNA damage checkpoint regulation, which points to a link with cyclophosphamide efficacy, as well as associations with immunological disease and renal inflammation.
Dr. Hasni said that previous studies of microRNA had looked in the peripheral blood but suggested this may not necessarily reflect what was happening in the kidney.
The next step for researchers is to see if upregulation of these microRNAs is predictive of treatment response.
“If you are giving cyclophosphamide for 2 years, it comes with a high risk of side effects, especially in young women because there is potential for premature ovarian failure,” Dr. Hasni said in an interview. “If we can predict that this patient is not going to respond to cyclophosphamide or will not have a good outcome, we can use alternative therapy, or perhaps use more aggressive or a combination therapy approach rather than keep doing the same thing and 2 years later find out the patient is not going to respond.”
The researchers are also keen to investigate whether these same microRNAs can be isolated from serum or urine, which would reduce the need for kidney biopsy.
“The testing for microRNA is not that hard – it’s the biopsy and extracting the tissue from the biopsy... that’s obviously cumbersome and can only be done in a research setting.”
No conflicts of interest were declared.
MELBOURNE – Researchers have identified six microRNAs that may indicate a better likelihood of response to cyclophosphamide in patients with lupus nephritis, according to a study presented at an international conference on systemic lupus erythematosus.
“MicroRNA has been shown to be important in systemic lupus in several studies, and they’ve identified several microRNA that have been shown to affect the outcome measures in patients,” said Sarfaraz Hasni, MD, director of the Lupus Clinical Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases in Bethesda, Md., who presented a poster on the study at the meeting.
The aim of this study, involving 71 patients with lupus nephritis, was to look for microRNAs associated with treatment response to cyclophosphamide.
The first stage of the study involved isolating microRNAs from kidney biopsies taken from a first cohort of 17 responders and 15 nonresponders.
Responders were patients who, after 2 years of intravenous cyclophosphamide, showed no active urinary sediments, less than five red blood cells or white blood cells in urine, and proteinuria below 1 g/24 hours.
After analyzing 300-400 microRNAs in these biopsies, the investigators identified 6 that were significantly upregulated in association with treatment outcome in both the first cohort as well as a second validation cohort of 22 responders and 17 nonresponders.
When the researchers looked at the most likely genetic targets of these microRNAs, they identified genes associated with G2/M DNA damage checkpoint regulation, which points to a link with cyclophosphamide efficacy, as well as associations with immunological disease and renal inflammation.
Dr. Hasni said that previous studies of microRNA had looked in the peripheral blood but suggested this may not necessarily reflect what was happening in the kidney.
The next step for researchers is to see if upregulation of these microRNAs is predictive of treatment response.
“If you are giving cyclophosphamide for 2 years, it comes with a high risk of side effects, especially in young women because there is potential for premature ovarian failure,” Dr. Hasni said in an interview. “If we can predict that this patient is not going to respond to cyclophosphamide or will not have a good outcome, we can use alternative therapy, or perhaps use more aggressive or a combination therapy approach rather than keep doing the same thing and 2 years later find out the patient is not going to respond.”
The researchers are also keen to investigate whether these same microRNAs can be isolated from serum or urine, which would reduce the need for kidney biopsy.
“The testing for microRNA is not that hard – it’s the biopsy and extracting the tissue from the biopsy... that’s obviously cumbersome and can only be done in a research setting.”
No conflicts of interest were declared.
MELBOURNE – Researchers have identified six microRNAs that may indicate a better likelihood of response to cyclophosphamide in patients with lupus nephritis, according to a study presented at an international conference on systemic lupus erythematosus.
“MicroRNA has been shown to be important in systemic lupus in several studies, and they’ve identified several microRNA that have been shown to affect the outcome measures in patients,” said Sarfaraz Hasni, MD, director of the Lupus Clinical Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases in Bethesda, Md., who presented a poster on the study at the meeting.
The aim of this study, involving 71 patients with lupus nephritis, was to look for microRNAs associated with treatment response to cyclophosphamide.
The first stage of the study involved isolating microRNAs from kidney biopsies taken from a first cohort of 17 responders and 15 nonresponders.
Responders were patients who, after 2 years of intravenous cyclophosphamide, showed no active urinary sediments, less than five red blood cells or white blood cells in urine, and proteinuria below 1 g/24 hours.
After analyzing 300-400 microRNAs in these biopsies, the investigators identified 6 that were significantly upregulated in association with treatment outcome in both the first cohort as well as a second validation cohort of 22 responders and 17 nonresponders.
When the researchers looked at the most likely genetic targets of these microRNAs, they identified genes associated with G2/M DNA damage checkpoint regulation, which points to a link with cyclophosphamide efficacy, as well as associations with immunological disease and renal inflammation.
Dr. Hasni said that previous studies of microRNA had looked in the peripheral blood but suggested this may not necessarily reflect what was happening in the kidney.
The next step for researchers is to see if upregulation of these microRNAs is predictive of treatment response.
“If you are giving cyclophosphamide for 2 years, it comes with a high risk of side effects, especially in young women because there is potential for premature ovarian failure,” Dr. Hasni said in an interview. “If we can predict that this patient is not going to respond to cyclophosphamide or will not have a good outcome, we can use alternative therapy, or perhaps use more aggressive or a combination therapy approach rather than keep doing the same thing and 2 years later find out the patient is not going to respond.”
The researchers are also keen to investigate whether these same microRNAs can be isolated from serum or urine, which would reduce the need for kidney biopsy.
“The testing for microRNA is not that hard – it’s the biopsy and extracting the tissue from the biopsy... that’s obviously cumbersome and can only be done in a research setting.”
No conflicts of interest were declared.
AT LUPUS 2017
Key clinical point:
Major finding: Researchers have identified six microRNAs from kidney biopsies that are significantly upregulated in patients who respond to cyclophosphamide treatment for lupus nephritis.
Data source: Prospective cohort study in 71 patients with lupus nephritis.
Disclosures: No conflicts of interest were declared.
Metformin linked with better survival in RCC patients with diabetes
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Key clinical point:
Major finding: In a pooled analysis of data from eight studies, the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
Data source: A meta-analysis of eight studies including 254,329 patients with renal cell carcinoma.
Disclosures: The authors declared that they had no conflicts of interest.