User login
Executive order aims to reform specialized visa program
A recent executive order by President Trump that aims to overhaul a specialized visa program for foreign workers appears to have more bark than bite, immigration experts say.
The order, published April 21 in the Federal Register, calls upon federal agencies to propose new rules, guidance, and reforms to ensure that H-1B visas are granted only to fill the most highly skilled positions. The H-1B visa program allows U.S. employers to temporarily employ highly skilled foreign workers in specialty occupations; foreign physicians and medical students regularly use the program to practice and train in the United States.
In a statement, the White House said the order is intended to prevent companies from abusing the H-1B visa program by replacing American workers with lower-paid foreign workers. While the program is designed to bring in skilled workers, the majority of approved applications are for the two lowest wage levels allowed, according to a White House statement.
“This executive order targets the abusive use of waivers and exceptions that undermine ‘Buy American’ laws meant to promote taxpayer money going to American companies,” according to the statement. “President Trump is making sure the immigration system isn’t abused to displace hard-working American workers for cheaper foreign labor.”
But the executive order will have no immediate effect on the H-1B program or foreign physicians applying for such visas, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“[There is] no immediate impact on the H-1B at all, just a promise to look at the program and ‘crack down’ on the alleged abuse and fraud,” Ms. Minear said in an interview. “I view this as a way of scaring people and looking to sound tough while actually doing nothing to change the system.”
Many of the changes proposed by the Trump administration would require legislation or a lengthy rule-making process, according to Adam Cohen, a Memphis immigration attorney. Some of the proposed changes have included changing the H-1B lottery system, altering the way prevailing wages are calculated, and charging higher processing fees.
“[The executive order] reflects a desire to move toward H-1B reforms but does not signal any immediate or concrete change,” Mr. Cohen said in an interview.
It remains to be seen what the new toughness on potential fraud and abuse may look like, Ms. Minear said. Added enforcement could include additional hurdles during visa processing due to heightened suspicion and review of all H-1B applicants. Depending on the extent of enforcement, it’s possible the changes could end up before a court, she said.
“If the administration oversteps in terms of enforcements and inappropriate scrutinizing of the program, there will be litigation in a heartbeat,” she predicted.
Meanwhile, there is still no word whether U.S. Citizenship and Immigration Services (USCIS) may exempt physicians from the
On April 3, USCIS temporarily suspended its expedited processing of H-1B visas, a program by which applicants could pay for expedited processing and a response within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
The International Medical Graduate Taskforce and a group of U.S. senators have urged USCIS to exempt physicians from the premium processing ban.
USCIS officials have not said whether the agency will exempt physicians. In an interview, a spokeswoman said the agency will be monitoring the situation during the coming months and will evaluate any time-sensitive impacts prior to the resumption of premium processing services.
[email protected]
On Twitter @legal_med
A recent executive order by President Trump that aims to overhaul a specialized visa program for foreign workers appears to have more bark than bite, immigration experts say.
The order, published April 21 in the Federal Register, calls upon federal agencies to propose new rules, guidance, and reforms to ensure that H-1B visas are granted only to fill the most highly skilled positions. The H-1B visa program allows U.S. employers to temporarily employ highly skilled foreign workers in specialty occupations; foreign physicians and medical students regularly use the program to practice and train in the United States.
In a statement, the White House said the order is intended to prevent companies from abusing the H-1B visa program by replacing American workers with lower-paid foreign workers. While the program is designed to bring in skilled workers, the majority of approved applications are for the two lowest wage levels allowed, according to a White House statement.
“This executive order targets the abusive use of waivers and exceptions that undermine ‘Buy American’ laws meant to promote taxpayer money going to American companies,” according to the statement. “President Trump is making sure the immigration system isn’t abused to displace hard-working American workers for cheaper foreign labor.”
But the executive order will have no immediate effect on the H-1B program or foreign physicians applying for such visas, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“[There is] no immediate impact on the H-1B at all, just a promise to look at the program and ‘crack down’ on the alleged abuse and fraud,” Ms. Minear said in an interview. “I view this as a way of scaring people and looking to sound tough while actually doing nothing to change the system.”
Many of the changes proposed by the Trump administration would require legislation or a lengthy rule-making process, according to Adam Cohen, a Memphis immigration attorney. Some of the proposed changes have included changing the H-1B lottery system, altering the way prevailing wages are calculated, and charging higher processing fees.
“[The executive order] reflects a desire to move toward H-1B reforms but does not signal any immediate or concrete change,” Mr. Cohen said in an interview.
It remains to be seen what the new toughness on potential fraud and abuse may look like, Ms. Minear said. Added enforcement could include additional hurdles during visa processing due to heightened suspicion and review of all H-1B applicants. Depending on the extent of enforcement, it’s possible the changes could end up before a court, she said.
“If the administration oversteps in terms of enforcements and inappropriate scrutinizing of the program, there will be litigation in a heartbeat,” she predicted.
Meanwhile, there is still no word whether U.S. Citizenship and Immigration Services (USCIS) may exempt physicians from the
On April 3, USCIS temporarily suspended its expedited processing of H-1B visas, a program by which applicants could pay for expedited processing and a response within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
The International Medical Graduate Taskforce and a group of U.S. senators have urged USCIS to exempt physicians from the premium processing ban.
USCIS officials have not said whether the agency will exempt physicians. In an interview, a spokeswoman said the agency will be monitoring the situation during the coming months and will evaluate any time-sensitive impacts prior to the resumption of premium processing services.
[email protected]
On Twitter @legal_med
A recent executive order by President Trump that aims to overhaul a specialized visa program for foreign workers appears to have more bark than bite, immigration experts say.
The order, published April 21 in the Federal Register, calls upon federal agencies to propose new rules, guidance, and reforms to ensure that H-1B visas are granted only to fill the most highly skilled positions. The H-1B visa program allows U.S. employers to temporarily employ highly skilled foreign workers in specialty occupations; foreign physicians and medical students regularly use the program to practice and train in the United States.
In a statement, the White House said the order is intended to prevent companies from abusing the H-1B visa program by replacing American workers with lower-paid foreign workers. While the program is designed to bring in skilled workers, the majority of approved applications are for the two lowest wage levels allowed, according to a White House statement.
“This executive order targets the abusive use of waivers and exceptions that undermine ‘Buy American’ laws meant to promote taxpayer money going to American companies,” according to the statement. “President Trump is making sure the immigration system isn’t abused to displace hard-working American workers for cheaper foreign labor.”
But the executive order will have no immediate effect on the H-1B program or foreign physicians applying for such visas, said Jennifer A. Minear, a Richmond, Va.–based attorney and national treasurer for the American Immigration Lawyers Association.
“[There is] no immediate impact on the H-1B at all, just a promise to look at the program and ‘crack down’ on the alleged abuse and fraud,” Ms. Minear said in an interview. “I view this as a way of scaring people and looking to sound tough while actually doing nothing to change the system.”
Many of the changes proposed by the Trump administration would require legislation or a lengthy rule-making process, according to Adam Cohen, a Memphis immigration attorney. Some of the proposed changes have included changing the H-1B lottery system, altering the way prevailing wages are calculated, and charging higher processing fees.
“[The executive order] reflects a desire to move toward H-1B reforms but does not signal any immediate or concrete change,” Mr. Cohen said in an interview.
It remains to be seen what the new toughness on potential fraud and abuse may look like, Ms. Minear said. Added enforcement could include additional hurdles during visa processing due to heightened suspicion and review of all H-1B applicants. Depending on the extent of enforcement, it’s possible the changes could end up before a court, she said.
“If the administration oversteps in terms of enforcements and inappropriate scrutinizing of the program, there will be litigation in a heartbeat,” she predicted.
Meanwhile, there is still no word whether U.S. Citizenship and Immigration Services (USCIS) may exempt physicians from the
On April 3, USCIS temporarily suspended its expedited processing of H-1B visas, a program by which applicants could pay for expedited processing and a response within 15 days. Standard processing of H-1B applications takes 6-10 months. USCIS is terminating the expedited reviews for up to 6 months to address long-standing H-1B petitions and to reduce backlogs, according to a March announcement by the agency.
The International Medical Graduate Taskforce and a group of U.S. senators have urged USCIS to exempt physicians from the premium processing ban.
USCIS officials have not said whether the agency will exempt physicians. In an interview, a spokeswoman said the agency will be monitoring the situation during the coming months and will evaluate any time-sensitive impacts prior to the resumption of premium processing services.
[email protected]
On Twitter @legal_med
Sun Protection for Infants: Parent Behaviors and Beliefs in Miami, Florida
Sun exposure and sunburns sustained during childhood are linked to an increased risk for development of skin cancers in adulthood. In infants, the skin is particularly vulnerable and is considered to be at increased risk for UV radiation damage,1 even as early as the first 6 months of life.2 Sun-safe behaviors instituted from a young age may help reduce the risk for future skin cancers.3 To effectively teach parents proper sun-safe practices, it is essential to understand their existing perceptions and behaviors. This study sought to examine differences in infant sun-safety practices during the first 6 months of life among black, Hispanic, and non-Hispanic white (NHW) parents in Miami, Florida.
Methods
Parents presenting to the University of Miami general pediatrics clinic from February 2015 through April 2015 with a child younger than 5 years were administered a 15-item questionnaire that included items on demographics, sun-safety strategies, sunburns and tanning, beliefs and limitations regarding sunscreen, and primary information source regarding sun safety (eg, physician, Internet, media, instincts). Parents were approached by the investigators consecutively for participation in scheduled blocks, with the exception of those who were otherwise engaged in appointment-related tasks (eg, paperwork). The study was approved by the University of Miami Miller School of Medicine institutional review board. The primary objective of this study was to determine the sun protection behaviors that black and Hispanic parents in Miami, Florida, employ in infants younger than 6 months. Secondary objectives included determining if this patient population is at risk for infant sunburns and tanning, beliefs among parents regarding sunscreen's efficacy in the prevention of skin cancers, and limitations of sunscreen use.
All data were analyzed using SAS software version 9.3. Wilcoxon signed rank test, Kruskal-Wallis test, Fisher exact test, and proportional-odds cumulative logit model were used to compare nonparametric data. Parents reporting on the full first 6 months of life (ie, the child was older than 6 months at the time of study completion) were included for analysis of sun-safety strategies. All survey respondents were included for analysis of secondary objectives. Responses from parents of infants of mixed racial and ethnic backgrounds were excluded from applicable subgroup analyses.
Results
Ninety-eight parents were approached for participation in the study; 97 consented to participate and 95 completed the survey. Seventy parents had children who were at least 6 months of age and were included for analysis of the primary objectives (ie, sun-protection strategies in the first 6 months of life). The cohort included 49 Hispanic parents, 26 black parents, and 9 NHW parents; 5 parents indicated their child was of mixed racial and ethnic background. Six respondents indicated another minority group (eg, Native American, Pacific Islander). Eighty-three respondents were mothers, 72 were educated beyond high school, and 14 were Spanish-speaking only. Four reported a known family history of skin cancer.
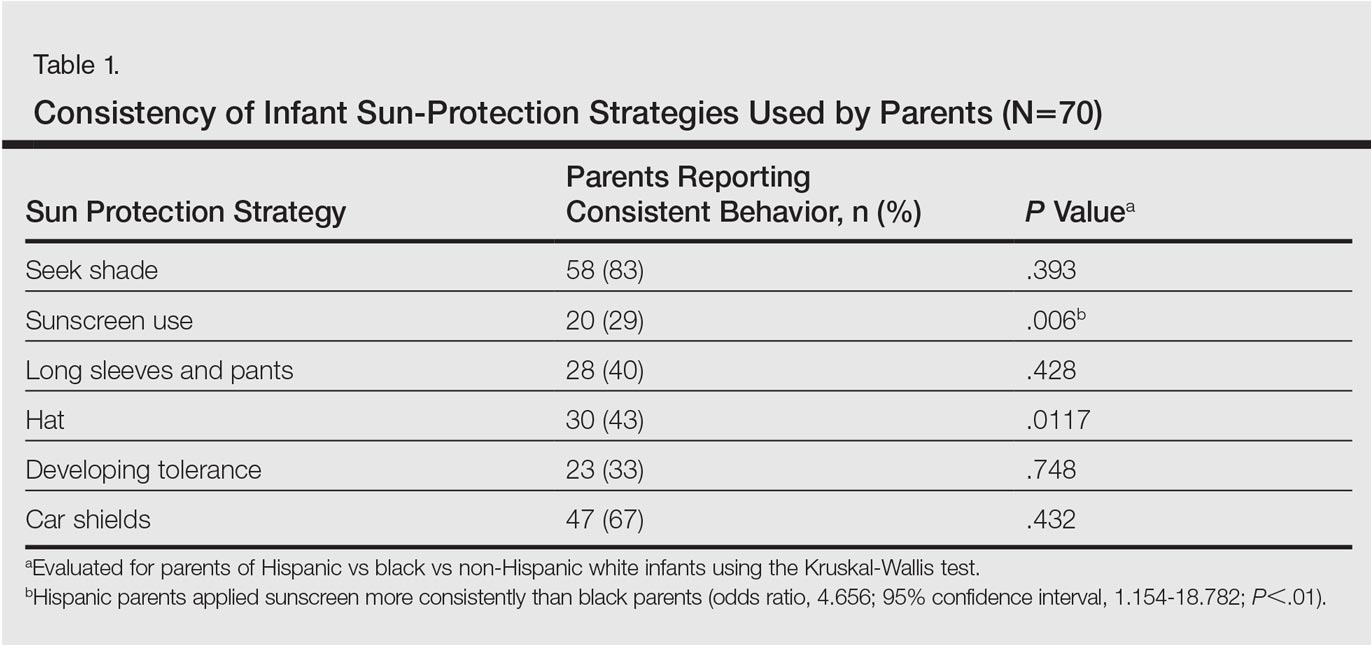
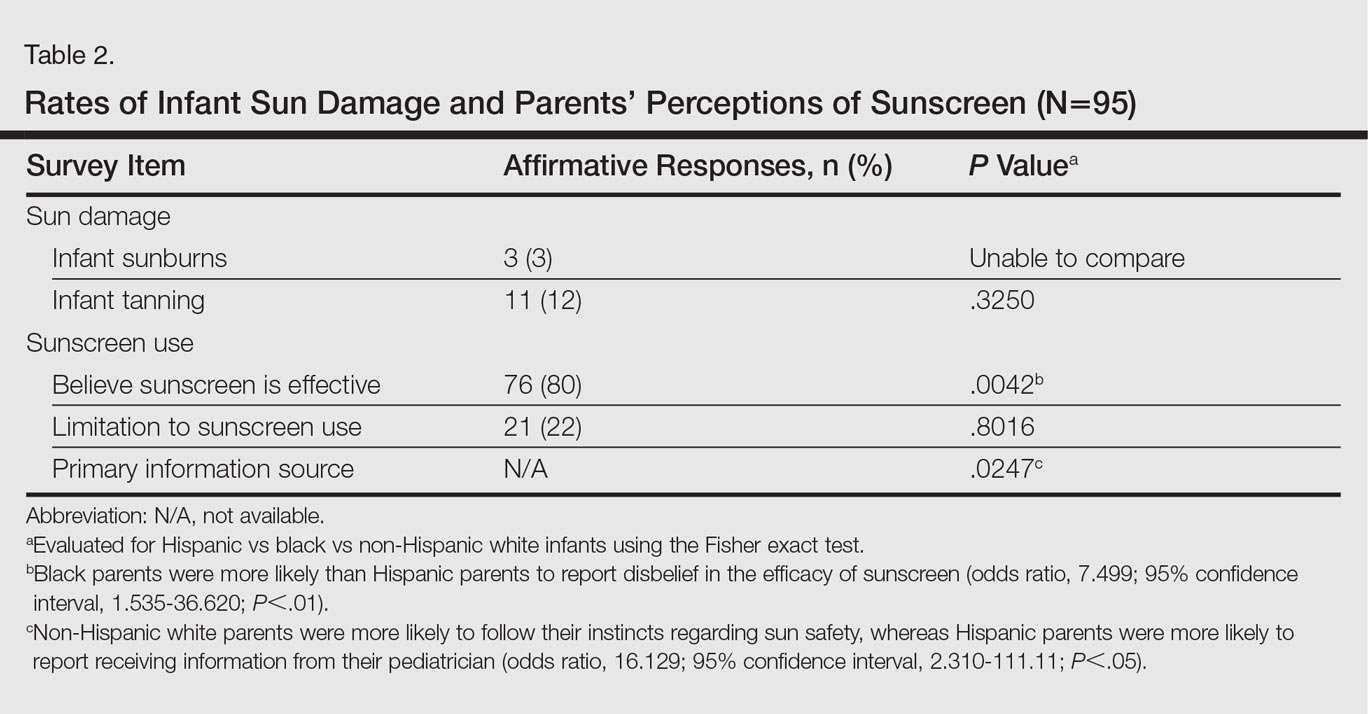
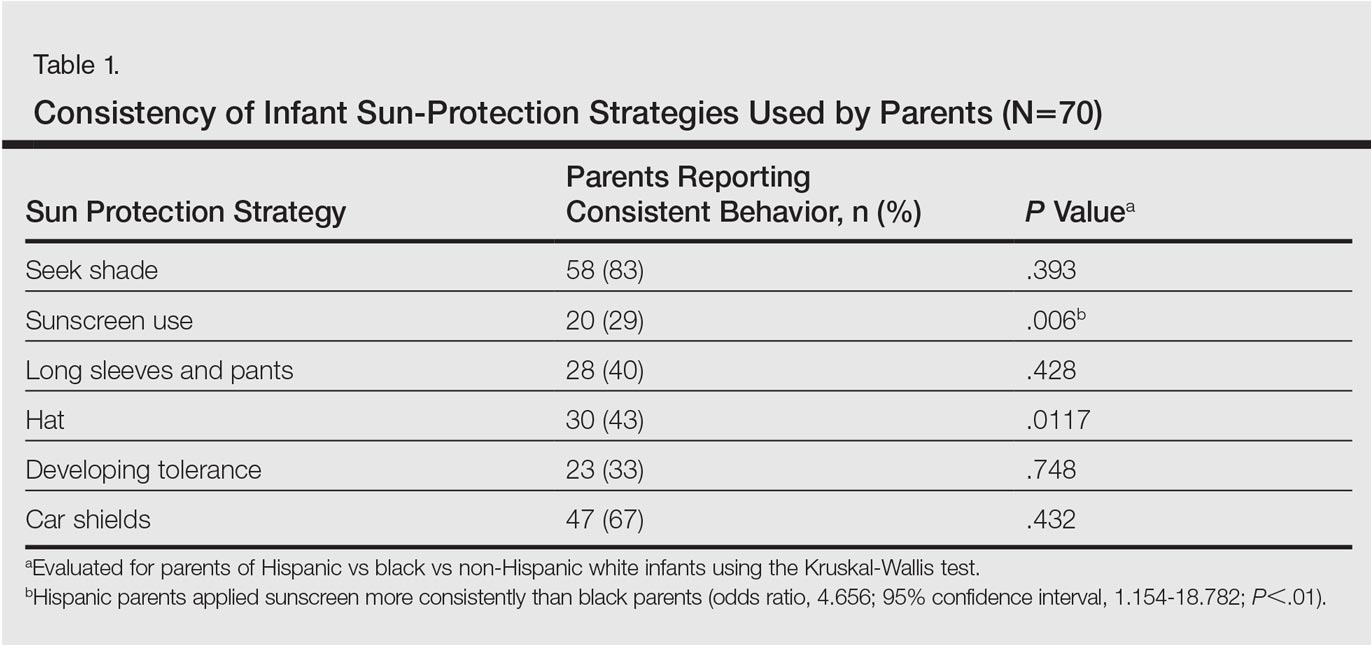
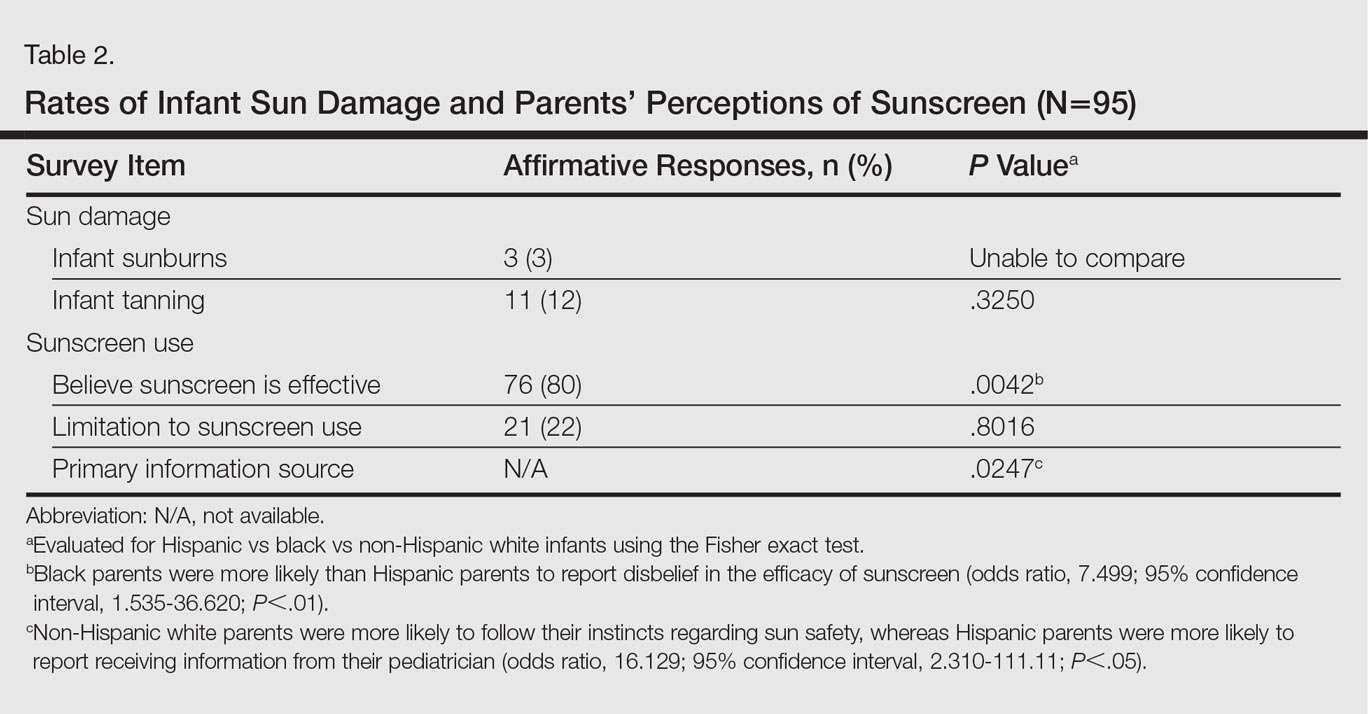
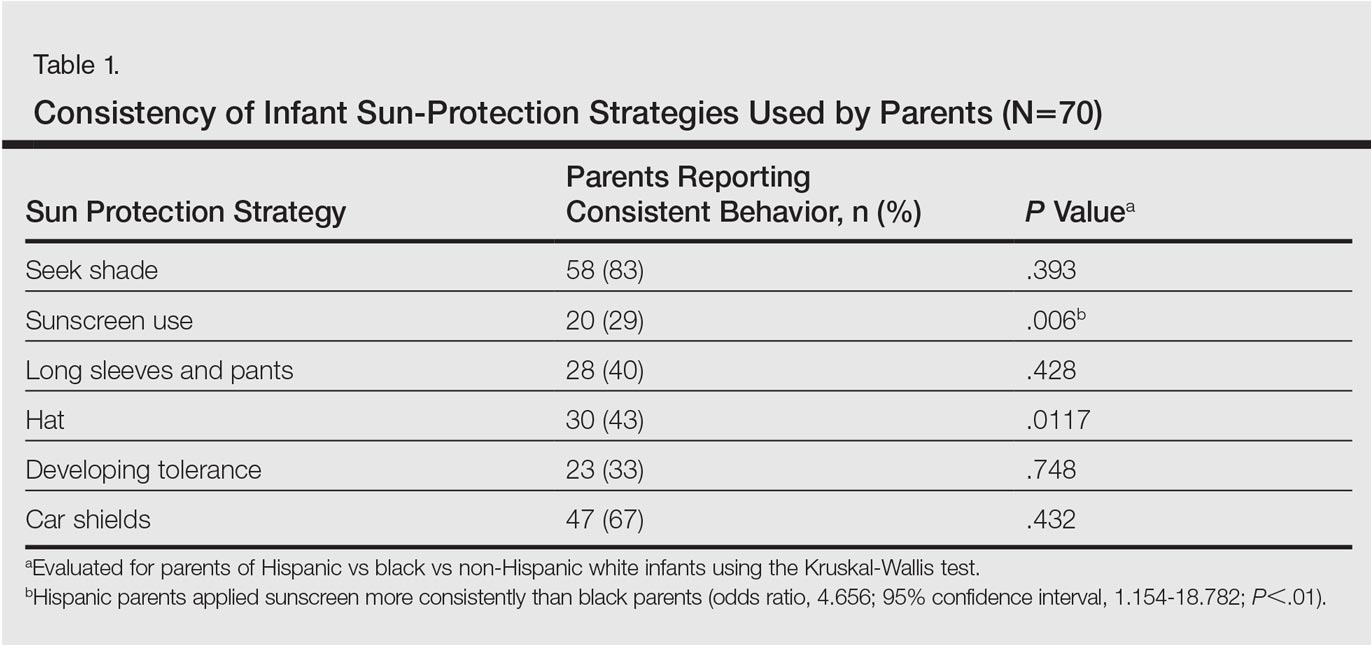
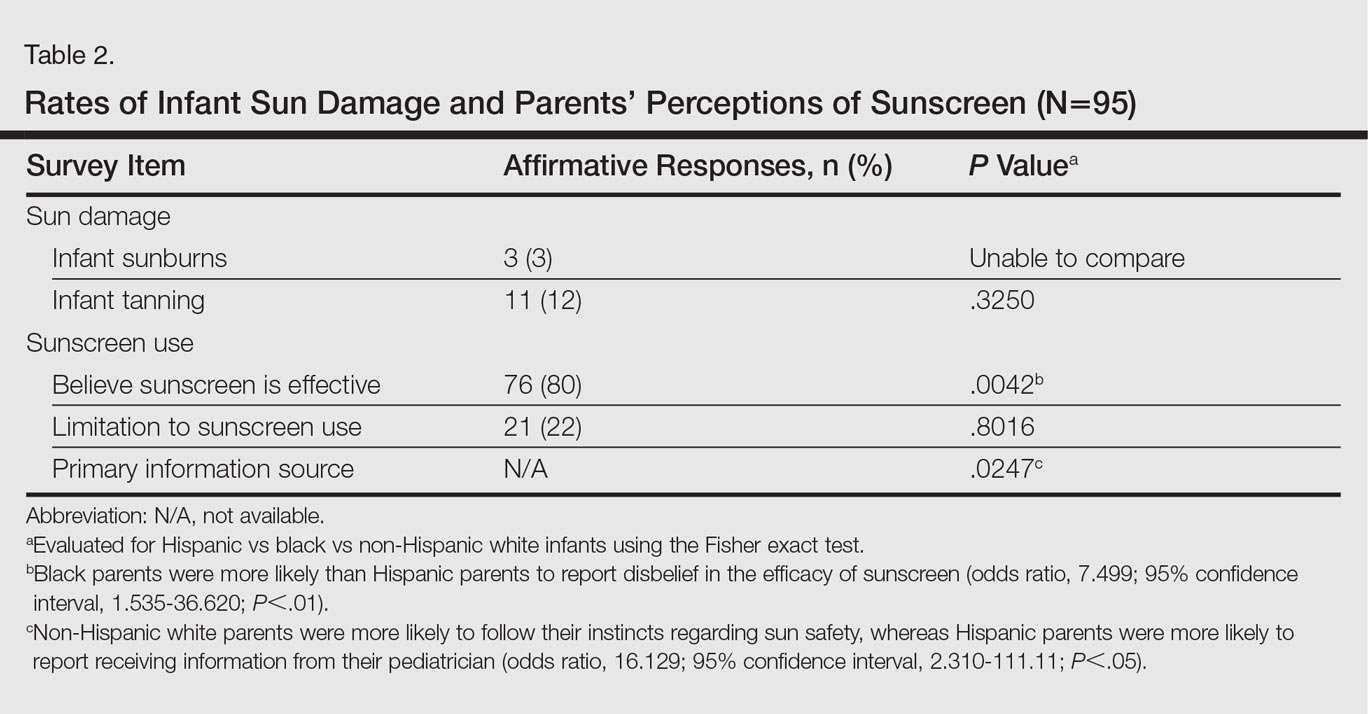
There were notable differences in application of sunscreen, belief in the efficacy of sunscreen, and primary source of information between parents (Tables 1 and 2). Hispanic parents reported applying sunscreen more consistently than black parents (odds ratio, 4.656; 95% confidence interval, 1.154-18.782; P<.01). Hispanic parents also were more likely than black parents to believe sunscreen is effective in the prevention of skin cancers (odds ratio, 7.499; 95% confidence interval, 1.535-36.620; P<.01). Hispanic parents were more likely to report receiving information regarding sun-safety practices for infants from their pediatrician, whereas NHW parents were more likely to follow their instincts regarding how and if infants should be exposed to the sun (P<.05). No significant differences were found in the reported primary source of information in black versus Hispanic parents or in black versus NHW parents. Three percent (3/95) of respondents reported a sunburn in the infant's first 6 months of life, and 12% (11/95) reported tanning of infants' skin from sun exposure. Tanning was associated with inconsistent shade (P<.01), inconsistent clothing coverage (P<.01), and consistently allowing infants to "develop tolerance to the sun's rays by slowly increasing sun exposure each day" (P<.05).
Comment
The survey results indicated suboptimal sun-protection practices among parents of black and Hispanic infants in Miami. Although the majority of respondents (83% [58/70]) reported keeping their infants in the shade, less than half of parents consistently covered their infants adequately with clothing and hats (40% [28/70] and 43% [30/70], respectively). More alarmingly, one-third of parents reported intentionally increasing their infant's level of sun exposure to develop his/her tolerance to the sun. A minority of parents reported sunburns (3%) and tanning (12%) within the first 6 months of life. Twenty-nine percent of parents (20/70) reported consistently applying sunscreen to their infants who were younger than 6 months despite limited safety data available for this age group.
Although our study included a limited sample size and represents a narrow geographic distribution, these results suggest that shortcomings in current practices in sun protection for black and Hispanic infants younger than 6 months may be a widespread problem. Black and Hispanic patients have a lower incidence of skin cancer, but the diagnosis often is delayed and the mortality is higher when skin cancer does occur.4 The common perception among laypeople as well as many health care providers that black and Hispanic individuals are not at risk for skin cancer may limit sun-safety counseling as well as the overall knowledge base of this patient demographic. As demonstrated by the results of this study, there is a need for counseling on sun-safe behaviors from a young age among this population.
Conclusion
This study highlights potential shortcomings in current sun-protection practices for black and Hispanic infants younger than 6 months. Sun-safe behaviors instituted from a young age may help reduce the risk for future skin cancers.3 Additional studies are needed to further define sun-safety behaviors in black and Hispanic children across the United States. Further, additional studies should focus on developing interventions that positively influence sun-safety behaviors in this patient population.
- Paller AS, Hawk JL, Honig P, et al. New insights about infant and toddler skin: implications for sun protection. Pediatrics. 2011;128:92-102.
- Benjes LS, Brooks DR, Zhang Z, et al. Changing patterns of sun protection between the first and second summers for very young children. Arch Dermatol. 2004;140:925-930.
- Oliveria SA, Saraiya M, Geller AC, et al. Sun exposure and risk of melanoma. Arch Dis Child. 2006;91:131-138.
- Wu XC, Eide MJ, King J, et al. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999-2006. J Am Acad Dermatol. 2011;65(5 suppl 1):S26-S37.
Sun exposure and sunburns sustained during childhood are linked to an increased risk for development of skin cancers in adulthood. In infants, the skin is particularly vulnerable and is considered to be at increased risk for UV radiation damage,1 even as early as the first 6 months of life.2 Sun-safe behaviors instituted from a young age may help reduce the risk for future skin cancers.3 To effectively teach parents proper sun-safe practices, it is essential to understand their existing perceptions and behaviors. This study sought to examine differences in infant sun-safety practices during the first 6 months of life among black, Hispanic, and non-Hispanic white (NHW) parents in Miami, Florida.
Methods
Parents presenting to the University of Miami general pediatrics clinic from February 2015 through April 2015 with a child younger than 5 years were administered a 15-item questionnaire that included items on demographics, sun-safety strategies, sunburns and tanning, beliefs and limitations regarding sunscreen, and primary information source regarding sun safety (eg, physician, Internet, media, instincts). Parents were approached by the investigators consecutively for participation in scheduled blocks, with the exception of those who were otherwise engaged in appointment-related tasks (eg, paperwork). The study was approved by the University of Miami Miller School of Medicine institutional review board. The primary objective of this study was to determine the sun protection behaviors that black and Hispanic parents in Miami, Florida, employ in infants younger than 6 months. Secondary objectives included determining if this patient population is at risk for infant sunburns and tanning, beliefs among parents regarding sunscreen's efficacy in the prevention of skin cancers, and limitations of sunscreen use.
All data were analyzed using SAS software version 9.3. Wilcoxon signed rank test, Kruskal-Wallis test, Fisher exact test, and proportional-odds cumulative logit model were used to compare nonparametric data. Parents reporting on the full first 6 months of life (ie, the child was older than 6 months at the time of study completion) were included for analysis of sun-safety strategies. All survey respondents were included for analysis of secondary objectives. Responses from parents of infants of mixed racial and ethnic backgrounds were excluded from applicable subgroup analyses.
Results
Ninety-eight parents were approached for participation in the study; 97 consented to participate and 95 completed the survey. Seventy parents had children who were at least 6 months of age and were included for analysis of the primary objectives (ie, sun-protection strategies in the first 6 months of life). The cohort included 49 Hispanic parents, 26 black parents, and 9 NHW parents; 5 parents indicated their child was of mixed racial and ethnic background. Six respondents indicated another minority group (eg, Native American, Pacific Islander). Eighty-three respondents were mothers, 72 were educated beyond high school, and 14 were Spanish-speaking only. Four reported a known family history of skin cancer.
There were notable differences in application of sunscreen, belief in the efficacy of sunscreen, and primary source of information between parents (Tables 1 and 2). Hispanic parents reported applying sunscreen more consistently than black parents (odds ratio, 4.656; 95% confidence interval, 1.154-18.782; P<.01). Hispanic parents also were more likely than black parents to believe sunscreen is effective in the prevention of skin cancers (odds ratio, 7.499; 95% confidence interval, 1.535-36.620; P<.01). Hispanic parents were more likely to report receiving information regarding sun-safety practices for infants from their pediatrician, whereas NHW parents were more likely to follow their instincts regarding how and if infants should be exposed to the sun (P<.05). No significant differences were found in the reported primary source of information in black versus Hispanic parents or in black versus NHW parents. Three percent (3/95) of respondents reported a sunburn in the infant's first 6 months of life, and 12% (11/95) reported tanning of infants' skin from sun exposure. Tanning was associated with inconsistent shade (P<.01), inconsistent clothing coverage (P<.01), and consistently allowing infants to "develop tolerance to the sun's rays by slowly increasing sun exposure each day" (P<.05).
Comment
The survey results indicated suboptimal sun-protection practices among parents of black and Hispanic infants in Miami. Although the majority of respondents (83% [58/70]) reported keeping their infants in the shade, less than half of parents consistently covered their infants adequately with clothing and hats (40% [28/70] and 43% [30/70], respectively). More alarmingly, one-third of parents reported intentionally increasing their infant's level of sun exposure to develop his/her tolerance to the sun. A minority of parents reported sunburns (3%) and tanning (12%) within the first 6 months of life. Twenty-nine percent of parents (20/70) reported consistently applying sunscreen to their infants who were younger than 6 months despite limited safety data available for this age group.
Although our study included a limited sample size and represents a narrow geographic distribution, these results suggest that shortcomings in current practices in sun protection for black and Hispanic infants younger than 6 months may be a widespread problem. Black and Hispanic patients have a lower incidence of skin cancer, but the diagnosis often is delayed and the mortality is higher when skin cancer does occur.4 The common perception among laypeople as well as many health care providers that black and Hispanic individuals are not at risk for skin cancer may limit sun-safety counseling as well as the overall knowledge base of this patient demographic. As demonstrated by the results of this study, there is a need for counseling on sun-safe behaviors from a young age among this population.
Conclusion
This study highlights potential shortcomings in current sun-protection practices for black and Hispanic infants younger than 6 months. Sun-safe behaviors instituted from a young age may help reduce the risk for future skin cancers.3 Additional studies are needed to further define sun-safety behaviors in black and Hispanic children across the United States. Further, additional studies should focus on developing interventions that positively influence sun-safety behaviors in this patient population.
Sun exposure and sunburns sustained during childhood are linked to an increased risk for development of skin cancers in adulthood. In infants, the skin is particularly vulnerable and is considered to be at increased risk for UV radiation damage,1 even as early as the first 6 months of life.2 Sun-safe behaviors instituted from a young age may help reduce the risk for future skin cancers.3 To effectively teach parents proper sun-safe practices, it is essential to understand their existing perceptions and behaviors. This study sought to examine differences in infant sun-safety practices during the first 6 months of life among black, Hispanic, and non-Hispanic white (NHW) parents in Miami, Florida.
Methods
Parents presenting to the University of Miami general pediatrics clinic from February 2015 through April 2015 with a child younger than 5 years were administered a 15-item questionnaire that included items on demographics, sun-safety strategies, sunburns and tanning, beliefs and limitations regarding sunscreen, and primary information source regarding sun safety (eg, physician, Internet, media, instincts). Parents were approached by the investigators consecutively for participation in scheduled blocks, with the exception of those who were otherwise engaged in appointment-related tasks (eg, paperwork). The study was approved by the University of Miami Miller School of Medicine institutional review board. The primary objective of this study was to determine the sun protection behaviors that black and Hispanic parents in Miami, Florida, employ in infants younger than 6 months. Secondary objectives included determining if this patient population is at risk for infant sunburns and tanning, beliefs among parents regarding sunscreen's efficacy in the prevention of skin cancers, and limitations of sunscreen use.
All data were analyzed using SAS software version 9.3. Wilcoxon signed rank test, Kruskal-Wallis test, Fisher exact test, and proportional-odds cumulative logit model were used to compare nonparametric data. Parents reporting on the full first 6 months of life (ie, the child was older than 6 months at the time of study completion) were included for analysis of sun-safety strategies. All survey respondents were included for analysis of secondary objectives. Responses from parents of infants of mixed racial and ethnic backgrounds were excluded from applicable subgroup analyses.
Results
Ninety-eight parents were approached for participation in the study; 97 consented to participate and 95 completed the survey. Seventy parents had children who were at least 6 months of age and were included for analysis of the primary objectives (ie, sun-protection strategies in the first 6 months of life). The cohort included 49 Hispanic parents, 26 black parents, and 9 NHW parents; 5 parents indicated their child was of mixed racial and ethnic background. Six respondents indicated another minority group (eg, Native American, Pacific Islander). Eighty-three respondents were mothers, 72 were educated beyond high school, and 14 were Spanish-speaking only. Four reported a known family history of skin cancer.
There were notable differences in application of sunscreen, belief in the efficacy of sunscreen, and primary source of information between parents (Tables 1 and 2). Hispanic parents reported applying sunscreen more consistently than black parents (odds ratio, 4.656; 95% confidence interval, 1.154-18.782; P<.01). Hispanic parents also were more likely than black parents to believe sunscreen is effective in the prevention of skin cancers (odds ratio, 7.499; 95% confidence interval, 1.535-36.620; P<.01). Hispanic parents were more likely to report receiving information regarding sun-safety practices for infants from their pediatrician, whereas NHW parents were more likely to follow their instincts regarding how and if infants should be exposed to the sun (P<.05). No significant differences were found in the reported primary source of information in black versus Hispanic parents or in black versus NHW parents. Three percent (3/95) of respondents reported a sunburn in the infant's first 6 months of life, and 12% (11/95) reported tanning of infants' skin from sun exposure. Tanning was associated with inconsistent shade (P<.01), inconsistent clothing coverage (P<.01), and consistently allowing infants to "develop tolerance to the sun's rays by slowly increasing sun exposure each day" (P<.05).
Comment
The survey results indicated suboptimal sun-protection practices among parents of black and Hispanic infants in Miami. Although the majority of respondents (83% [58/70]) reported keeping their infants in the shade, less than half of parents consistently covered their infants adequately with clothing and hats (40% [28/70] and 43% [30/70], respectively). More alarmingly, one-third of parents reported intentionally increasing their infant's level of sun exposure to develop his/her tolerance to the sun. A minority of parents reported sunburns (3%) and tanning (12%) within the first 6 months of life. Twenty-nine percent of parents (20/70) reported consistently applying sunscreen to their infants who were younger than 6 months despite limited safety data available for this age group.
Although our study included a limited sample size and represents a narrow geographic distribution, these results suggest that shortcomings in current practices in sun protection for black and Hispanic infants younger than 6 months may be a widespread problem. Black and Hispanic patients have a lower incidence of skin cancer, but the diagnosis often is delayed and the mortality is higher when skin cancer does occur.4 The common perception among laypeople as well as many health care providers that black and Hispanic individuals are not at risk for skin cancer may limit sun-safety counseling as well as the overall knowledge base of this patient demographic. As demonstrated by the results of this study, there is a need for counseling on sun-safe behaviors from a young age among this population.
Conclusion
This study highlights potential shortcomings in current sun-protection practices for black and Hispanic infants younger than 6 months. Sun-safe behaviors instituted from a young age may help reduce the risk for future skin cancers.3 Additional studies are needed to further define sun-safety behaviors in black and Hispanic children across the United States. Further, additional studies should focus on developing interventions that positively influence sun-safety behaviors in this patient population.
- Paller AS, Hawk JL, Honig P, et al. New insights about infant and toddler skin: implications for sun protection. Pediatrics. 2011;128:92-102.
- Benjes LS, Brooks DR, Zhang Z, et al. Changing patterns of sun protection between the first and second summers for very young children. Arch Dermatol. 2004;140:925-930.
- Oliveria SA, Saraiya M, Geller AC, et al. Sun exposure and risk of melanoma. Arch Dis Child. 2006;91:131-138.
- Wu XC, Eide MJ, King J, et al. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999-2006. J Am Acad Dermatol. 2011;65(5 suppl 1):S26-S37.
- Paller AS, Hawk JL, Honig P, et al. New insights about infant and toddler skin: implications for sun protection. Pediatrics. 2011;128:92-102.
- Benjes LS, Brooks DR, Zhang Z, et al. Changing patterns of sun protection between the first and second summers for very young children. Arch Dermatol. 2004;140:925-930.
- Oliveria SA, Saraiya M, Geller AC, et al. Sun exposure and risk of melanoma. Arch Dis Child. 2006;91:131-138.
- Wu XC, Eide MJ, King J, et al. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999-2006. J Am Acad Dermatol. 2011;65(5 suppl 1):S26-S37.
Practice Points
- Infants of all racial and ethnic backgrounds need protection from the sun's rays. Remember to counsel parents on the importance of sun protection.
- Instruct parents to keep infants in the shade when outdoors and to dress infants in a long-sleeved shirt, pants, and a hat. Intentional sun exposure for infants is not recommended.
- The American Academy of Dermatology currently recommends that parents begin sunscreen application when their child reaches 6 months of age. Broad-spectrum barrier sunscreens containing zinc oxide or titanium dioxide are preferred and should provide a sun protection factor of 30 or greater.
Keys to de-escalating endocrine emergencies
It’s a fine line between compensated and decompensated endocrine conditions, and often, there is an underlying non–endocrine component complicating the diagnosis.
That’s according to Marilyn Tan, MD, a clinical assistant professor of medicine at Stanford (Calif.) University, where she is chief of the endocrinology clinic. She spoke about endocrinology emergencies during a case-based, rapid-fire session at HM17.
“Endocrine emergencies are usually due to an excess or a deficiency of a hormone,” Dr. Tan said, noting that these can take time to bring into balance. This is one reason Dr. Tan counseled not waiting for laboratory results before administering treatment.
To diagnose and treat diabetic ketoacidosis, combined with a hyperosmolar hyperglycemic state, Dr. Tan recommended checking hypoglycemia levels, which she said are often mild, and to check anion gap, pH, and ketones. It’s also important to be generous with IV fluids, to administer insulin only if the ketoacidosis level is greater than 3.3 mEq/L, and to not take the patient off an insulin drip too early or inappropriately. To prevent readmissions, the patient on discharge should have adequate diabetes supplies, education on their condition, and timely follow-up, Dr. Tan recommended.
For patients experiencing a thyroid storm, Dr. Tan advised that thyroid function tests are a poor surrogate for predicting who will decompensate. The clinical distinction is made by documentation of acute organ dysfunction. Reducing T3 to T4 conversion means propylthiouracil is preferred over methimazole.
Ongoing management of a myxedema coma means monitoring the clinical parameters of the patient’s mental status, cardiac and pulmonary functions, while keeping the levothyroxine dose steady and checking lab values every 1-2 days to ensure the patient is progressing.
Suspect pituitary apoplexy in cases of hypertension, major surgery, trauma, anticoagulation, pregnancy, or if there is a large sellar mass. If choosing to image a patient, Dr. Tan recommended using an MRI rather than a CT scan, which she said is less sensitive. Immediate hydrocortisone treatment must be administered, she said. About 90% of cases of acute hypercalcemia are caused by hyperparathyroidism in the outpatient setting, and malignancy in the inpatient setting, Dr. Tan said. Also, these patients tend to be volume depleted, so assessment of their ability to tolerate hydration is essential.
Regarding all endocrine emergencies, Dr. Tan said, “When in doubt, be more aggressive with treatment.”
Dr. Tan had no relevant financial disclosures.
It’s a fine line between compensated and decompensated endocrine conditions, and often, there is an underlying non–endocrine component complicating the diagnosis.
That’s according to Marilyn Tan, MD, a clinical assistant professor of medicine at Stanford (Calif.) University, where she is chief of the endocrinology clinic. She spoke about endocrinology emergencies during a case-based, rapid-fire session at HM17.
“Endocrine emergencies are usually due to an excess or a deficiency of a hormone,” Dr. Tan said, noting that these can take time to bring into balance. This is one reason Dr. Tan counseled not waiting for laboratory results before administering treatment.
To diagnose and treat diabetic ketoacidosis, combined with a hyperosmolar hyperglycemic state, Dr. Tan recommended checking hypoglycemia levels, which she said are often mild, and to check anion gap, pH, and ketones. It’s also important to be generous with IV fluids, to administer insulin only if the ketoacidosis level is greater than 3.3 mEq/L, and to not take the patient off an insulin drip too early or inappropriately. To prevent readmissions, the patient on discharge should have adequate diabetes supplies, education on their condition, and timely follow-up, Dr. Tan recommended.
For patients experiencing a thyroid storm, Dr. Tan advised that thyroid function tests are a poor surrogate for predicting who will decompensate. The clinical distinction is made by documentation of acute organ dysfunction. Reducing T3 to T4 conversion means propylthiouracil is preferred over methimazole.
Ongoing management of a myxedema coma means monitoring the clinical parameters of the patient’s mental status, cardiac and pulmonary functions, while keeping the levothyroxine dose steady and checking lab values every 1-2 days to ensure the patient is progressing.
Suspect pituitary apoplexy in cases of hypertension, major surgery, trauma, anticoagulation, pregnancy, or if there is a large sellar mass. If choosing to image a patient, Dr. Tan recommended using an MRI rather than a CT scan, which she said is less sensitive. Immediate hydrocortisone treatment must be administered, she said. About 90% of cases of acute hypercalcemia are caused by hyperparathyroidism in the outpatient setting, and malignancy in the inpatient setting, Dr. Tan said. Also, these patients tend to be volume depleted, so assessment of their ability to tolerate hydration is essential.
Regarding all endocrine emergencies, Dr. Tan said, “When in doubt, be more aggressive with treatment.”
Dr. Tan had no relevant financial disclosures.
It’s a fine line between compensated and decompensated endocrine conditions, and often, there is an underlying non–endocrine component complicating the diagnosis.
That’s according to Marilyn Tan, MD, a clinical assistant professor of medicine at Stanford (Calif.) University, where she is chief of the endocrinology clinic. She spoke about endocrinology emergencies during a case-based, rapid-fire session at HM17.
“Endocrine emergencies are usually due to an excess or a deficiency of a hormone,” Dr. Tan said, noting that these can take time to bring into balance. This is one reason Dr. Tan counseled not waiting for laboratory results before administering treatment.
To diagnose and treat diabetic ketoacidosis, combined with a hyperosmolar hyperglycemic state, Dr. Tan recommended checking hypoglycemia levels, which she said are often mild, and to check anion gap, pH, and ketones. It’s also important to be generous with IV fluids, to administer insulin only if the ketoacidosis level is greater than 3.3 mEq/L, and to not take the patient off an insulin drip too early or inappropriately. To prevent readmissions, the patient on discharge should have adequate diabetes supplies, education on their condition, and timely follow-up, Dr. Tan recommended.
For patients experiencing a thyroid storm, Dr. Tan advised that thyroid function tests are a poor surrogate for predicting who will decompensate. The clinical distinction is made by documentation of acute organ dysfunction. Reducing T3 to T4 conversion means propylthiouracil is preferred over methimazole.
Ongoing management of a myxedema coma means monitoring the clinical parameters of the patient’s mental status, cardiac and pulmonary functions, while keeping the levothyroxine dose steady and checking lab values every 1-2 days to ensure the patient is progressing.
Suspect pituitary apoplexy in cases of hypertension, major surgery, trauma, anticoagulation, pregnancy, or if there is a large sellar mass. If choosing to image a patient, Dr. Tan recommended using an MRI rather than a CT scan, which she said is less sensitive. Immediate hydrocortisone treatment must be administered, she said. About 90% of cases of acute hypercalcemia are caused by hyperparathyroidism in the outpatient setting, and malignancy in the inpatient setting, Dr. Tan said. Also, these patients tend to be volume depleted, so assessment of their ability to tolerate hydration is essential.
Regarding all endocrine emergencies, Dr. Tan said, “When in doubt, be more aggressive with treatment.”
Dr. Tan had no relevant financial disclosures.
Mobile App for Medical-Assisted Treatment
In 2015, nearly 2.4 million Americans had an opioid use disorder. Close to 80% did not receive treatment. To help change those numbers, the Substance Abuse and Mental Health Services Administration (SAMHSA) has developed a free mobile application called MATx that supports medication-assisted treatment. The app “empowers health care practitioners to provide effective, evidence-based care for people with opioid use disorder.” Features include the following:
- Information on treatment approaches and medications approved by the FDA for use in treating opioid use disorders;
- A buprenorphine prescribing guide, including information on the Drug Addiction Treatment Act of 2000 waiver process and patient limits;
- Clinical support tools, such as treatment guidelines, ICD-10 coding, and recommendations for working with special populations;
- Access to critical helplines and SAMHSA’s treatment locators.
For more information on the app, visit http://store.samhsa.gov/apps/mat/tools/index.html?WT.ac=PEPAdSpreadWord20161018Prof.
In 2015, nearly 2.4 million Americans had an opioid use disorder. Close to 80% did not receive treatment. To help change those numbers, the Substance Abuse and Mental Health Services Administration (SAMHSA) has developed a free mobile application called MATx that supports medication-assisted treatment. The app “empowers health care practitioners to provide effective, evidence-based care for people with opioid use disorder.” Features include the following:
- Information on treatment approaches and medications approved by the FDA for use in treating opioid use disorders;
- A buprenorphine prescribing guide, including information on the Drug Addiction Treatment Act of 2000 waiver process and patient limits;
- Clinical support tools, such as treatment guidelines, ICD-10 coding, and recommendations for working with special populations;
- Access to critical helplines and SAMHSA’s treatment locators.
For more information on the app, visit http://store.samhsa.gov/apps/mat/tools/index.html?WT.ac=PEPAdSpreadWord20161018Prof.
In 2015, nearly 2.4 million Americans had an opioid use disorder. Close to 80% did not receive treatment. To help change those numbers, the Substance Abuse and Mental Health Services Administration (SAMHSA) has developed a free mobile application called MATx that supports medication-assisted treatment. The app “empowers health care practitioners to provide effective, evidence-based care for people with opioid use disorder.” Features include the following:
- Information on treatment approaches and medications approved by the FDA for use in treating opioid use disorders;
- A buprenorphine prescribing guide, including information on the Drug Addiction Treatment Act of 2000 waiver process and patient limits;
- Clinical support tools, such as treatment guidelines, ICD-10 coding, and recommendations for working with special populations;
- Access to critical helplines and SAMHSA’s treatment locators.
For more information on the app, visit http://store.samhsa.gov/apps/mat/tools/index.html?WT.ac=PEPAdSpreadWord20161018Prof.
Highlights of Day 4
Sometimes the final day of a convention is nothing more than the “getaway day.”
But not at HM17. Not this year.
The finale of the 2017 annual meeting is capped off, as has become tradition, by a speech from the dean of hospital medicine: Robert Wachter, MD, MHM. The last time Dr. Wachter gave his address from a Vegas stage, it ended with him in head-to-toe Elton John regalia. While there’s no guarantee of a wardrobe reprisal, the annual address from the man who helped name the specialty promises to entertain and inform, said HM17 course director Lenny Feldman, MD, SFHM.
However, Dr. Wachter’s words – this year titled “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” – aren’t the final day’s only lure.
Two of this year’s newest educational tracks – Health Policy and Medical Education – debut today and offer five courses focusing on niche areas interesting to many hospitalists. Also today is the annual Potpurri track, which highlights off-beat topics such as “Case-Based Approach to Difficult Conversations” and “The History of Medicine: Discoveries that Shaped Our Profession.”
“These sessions are unique but have a wide range of appeal,” Dr. Feldman said. “Attendees are going to have a great time delving into these topics.”
Sometimes the final day of a convention is nothing more than the “getaway day.”
But not at HM17. Not this year.
The finale of the 2017 annual meeting is capped off, as has become tradition, by a speech from the dean of hospital medicine: Robert Wachter, MD, MHM. The last time Dr. Wachter gave his address from a Vegas stage, it ended with him in head-to-toe Elton John regalia. While there’s no guarantee of a wardrobe reprisal, the annual address from the man who helped name the specialty promises to entertain and inform, said HM17 course director Lenny Feldman, MD, SFHM.
However, Dr. Wachter’s words – this year titled “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” – aren’t the final day’s only lure.
Two of this year’s newest educational tracks – Health Policy and Medical Education – debut today and offer five courses focusing on niche areas interesting to many hospitalists. Also today is the annual Potpurri track, which highlights off-beat topics such as “Case-Based Approach to Difficult Conversations” and “The History of Medicine: Discoveries that Shaped Our Profession.”
“These sessions are unique but have a wide range of appeal,” Dr. Feldman said. “Attendees are going to have a great time delving into these topics.”
Sometimes the final day of a convention is nothing more than the “getaway day.”
But not at HM17. Not this year.
The finale of the 2017 annual meeting is capped off, as has become tradition, by a speech from the dean of hospital medicine: Robert Wachter, MD, MHM. The last time Dr. Wachter gave his address from a Vegas stage, it ended with him in head-to-toe Elton John regalia. While there’s no guarantee of a wardrobe reprisal, the annual address from the man who helped name the specialty promises to entertain and inform, said HM17 course director Lenny Feldman, MD, SFHM.
However, Dr. Wachter’s words – this year titled “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” – aren’t the final day’s only lure.
Two of this year’s newest educational tracks – Health Policy and Medical Education – debut today and offer five courses focusing on niche areas interesting to many hospitalists. Also today is the annual Potpurri track, which highlights off-beat topics such as “Case-Based Approach to Difficult Conversations” and “The History of Medicine: Discoveries that Shaped Our Profession.”
“These sessions are unique but have a wide range of appeal,” Dr. Feldman said. “Attendees are going to have a great time delving into these topics.”
Hope and change
Robert M. Wachter, MD, MHM, has given the last plenary address at every SHM annual meeting since 2007. The talks are peppered with his one-of-a-kind take on the confluence of medicine, politics, and policy. Then there was the time when he broke into an Elton John parody.
Where does that point of view come from? Well, as the dean of hospital medicine says in his ever-popular Twitter bio, he is “what happens when a poli-sci major becomes an academic physician.”
That’s a needed perspective this year, as the level of political upheaval in the United States has added to the tumult in the health care field. Questions surrounding the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the continued struggles that doctors face when using electronic health records (EHRs) are among the topics that he will address in his this final discussion.
“While [President Donald] Trump brings massive uncertainly, the shift to value and the increasing importance of building a strong culture, a method to continuously improve, and a way to use the EHR to make things better is unlikely to go away,” said Dr. Wachter, whose address is titled, “Mergers, MACRA, and Mission-Creep: Can Hospitalists Thrive in the New World of Healthcare?”
Dr. Wachter, chair of the department of medicine at the University of California, San Francisco, said that the Trump administration is a once-in-a-lifetime anomaly that understandably has made both physicians and patients nervous – particularly at a time when health care reform appeared to be stabilizing.
The new president “adds an amazing wild card, at every level,” he said. “If it weren’t for his administration, I think we’d be on a fairly stable, predictable path. Not that that path doesn’t include a ton of change, but at least it had a predictable path.”
The defeat of Republicans’ plan to replace the Affordable Care Act (ACA) with the American Health Care Act (AHCA) showed that the divide over health care extends even to intraparty discussions.
“The implosion of the AHCA shows how difficult health reform is and how quickly the ACA became the de facto standard,” Dr. Wachter said. “It is now that status quo that is so difficult to change.”
Dr. Wachter, who famously helped coined the term “hospitalist” in the 1996 New England Journal of Medicine paper that propelled the nascent specialty, said that one big challenge to HM is determining the future of how hospitals get paid – and how they pay their workers (335[7]:514-7).
“The business model for hospitals will be massively challenged, and it could get worse if a lot of your patients lose insurance or [if] their payments go way down,” he predicted.
What that means for the daily schedules of hospitalists remains to be seen, but Dr. Wachter doesn’t expect much in the short term.
“The job will be the same,” he said. “Take care of patients well, make them happy, satisfy your bosses and colleagues, and do it for less money. The biggest shift is likely to be that more and more people/systems – doing the same thing – will find that they don’t need as many hospital days, which means that we’ll have fewer patients and fewer hospitals. But we knew that.”
Dr. Wachter is more interested to see what will happen in postacute and other nonhospital facilities, how quickly technology continues to disrupt, and who hospitalists will work for (be it staffing companies, medical groups, or “something new”).
The veteran physician in him says not to get too distracted “by all of the zigs and zags,” he noted, while the political idealist in him says not to ever forget that the “core values and imperatives remain.”
If the past decade of wise words ending SHM’s annual meeting are any indication, Dr. Wachter’s message of trepidation and concern will end on a high note for attendees.
Robert M. Wachter, MD, MHM, has given the last plenary address at every SHM annual meeting since 2007. The talks are peppered with his one-of-a-kind take on the confluence of medicine, politics, and policy. Then there was the time when he broke into an Elton John parody.
Where does that point of view come from? Well, as the dean of hospital medicine says in his ever-popular Twitter bio, he is “what happens when a poli-sci major becomes an academic physician.”
That’s a needed perspective this year, as the level of political upheaval in the United States has added to the tumult in the health care field. Questions surrounding the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the continued struggles that doctors face when using electronic health records (EHRs) are among the topics that he will address in his this final discussion.
“While [President Donald] Trump brings massive uncertainly, the shift to value and the increasing importance of building a strong culture, a method to continuously improve, and a way to use the EHR to make things better is unlikely to go away,” said Dr. Wachter, whose address is titled, “Mergers, MACRA, and Mission-Creep: Can Hospitalists Thrive in the New World of Healthcare?”
Dr. Wachter, chair of the department of medicine at the University of California, San Francisco, said that the Trump administration is a once-in-a-lifetime anomaly that understandably has made both physicians and patients nervous – particularly at a time when health care reform appeared to be stabilizing.
The new president “adds an amazing wild card, at every level,” he said. “If it weren’t for his administration, I think we’d be on a fairly stable, predictable path. Not that that path doesn’t include a ton of change, but at least it had a predictable path.”
The defeat of Republicans’ plan to replace the Affordable Care Act (ACA) with the American Health Care Act (AHCA) showed that the divide over health care extends even to intraparty discussions.
“The implosion of the AHCA shows how difficult health reform is and how quickly the ACA became the de facto standard,” Dr. Wachter said. “It is now that status quo that is so difficult to change.”
Dr. Wachter, who famously helped coined the term “hospitalist” in the 1996 New England Journal of Medicine paper that propelled the nascent specialty, said that one big challenge to HM is determining the future of how hospitals get paid – and how they pay their workers (335[7]:514-7).
“The business model for hospitals will be massively challenged, and it could get worse if a lot of your patients lose insurance or [if] their payments go way down,” he predicted.
What that means for the daily schedules of hospitalists remains to be seen, but Dr. Wachter doesn’t expect much in the short term.
“The job will be the same,” he said. “Take care of patients well, make them happy, satisfy your bosses and colleagues, and do it for less money. The biggest shift is likely to be that more and more people/systems – doing the same thing – will find that they don’t need as many hospital days, which means that we’ll have fewer patients and fewer hospitals. But we knew that.”
Dr. Wachter is more interested to see what will happen in postacute and other nonhospital facilities, how quickly technology continues to disrupt, and who hospitalists will work for (be it staffing companies, medical groups, or “something new”).
The veteran physician in him says not to get too distracted “by all of the zigs and zags,” he noted, while the political idealist in him says not to ever forget that the “core values and imperatives remain.”
If the past decade of wise words ending SHM’s annual meeting are any indication, Dr. Wachter’s message of trepidation and concern will end on a high note for attendees.
Robert M. Wachter, MD, MHM, has given the last plenary address at every SHM annual meeting since 2007. The talks are peppered with his one-of-a-kind take on the confluence of medicine, politics, and policy. Then there was the time when he broke into an Elton John parody.
Where does that point of view come from? Well, as the dean of hospital medicine says in his ever-popular Twitter bio, he is “what happens when a poli-sci major becomes an academic physician.”
That’s a needed perspective this year, as the level of political upheaval in the United States has added to the tumult in the health care field. Questions surrounding the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the continued struggles that doctors face when using electronic health records (EHRs) are among the topics that he will address in his this final discussion.
“While [President Donald] Trump brings massive uncertainly, the shift to value and the increasing importance of building a strong culture, a method to continuously improve, and a way to use the EHR to make things better is unlikely to go away,” said Dr. Wachter, whose address is titled, “Mergers, MACRA, and Mission-Creep: Can Hospitalists Thrive in the New World of Healthcare?”
Dr. Wachter, chair of the department of medicine at the University of California, San Francisco, said that the Trump administration is a once-in-a-lifetime anomaly that understandably has made both physicians and patients nervous – particularly at a time when health care reform appeared to be stabilizing.
The new president “adds an amazing wild card, at every level,” he said. “If it weren’t for his administration, I think we’d be on a fairly stable, predictable path. Not that that path doesn’t include a ton of change, but at least it had a predictable path.”
The defeat of Republicans’ plan to replace the Affordable Care Act (ACA) with the American Health Care Act (AHCA) showed that the divide over health care extends even to intraparty discussions.
“The implosion of the AHCA shows how difficult health reform is and how quickly the ACA became the de facto standard,” Dr. Wachter said. “It is now that status quo that is so difficult to change.”
Dr. Wachter, who famously helped coined the term “hospitalist” in the 1996 New England Journal of Medicine paper that propelled the nascent specialty, said that one big challenge to HM is determining the future of how hospitals get paid – and how they pay their workers (335[7]:514-7).
“The business model for hospitals will be massively challenged, and it could get worse if a lot of your patients lose insurance or [if] their payments go way down,” he predicted.
What that means for the daily schedules of hospitalists remains to be seen, but Dr. Wachter doesn’t expect much in the short term.
“The job will be the same,” he said. “Take care of patients well, make them happy, satisfy your bosses and colleagues, and do it for less money. The biggest shift is likely to be that more and more people/systems – doing the same thing – will find that they don’t need as many hospital days, which means that we’ll have fewer patients and fewer hospitals. But we knew that.”
Dr. Wachter is more interested to see what will happen in postacute and other nonhospital facilities, how quickly technology continues to disrupt, and who hospitalists will work for (be it staffing companies, medical groups, or “something new”).
The veteran physician in him says not to get too distracted “by all of the zigs and zags,” he noted, while the political idealist in him says not to ever forget that the “core values and imperatives remain.”
If the past decade of wise words ending SHM’s annual meeting are any indication, Dr. Wachter’s message of trepidation and concern will end on a high note for attendees.
Welcome to the third and final day of HM17!
Welcome to the third and final day of HM17!
Although it is the shortest day of the conference, day 3 is full of quality content, starting at 7:40 a.m. with a mini-track.
If you are interested in hearing about the impact of November’s election on health care reform, join me at the Health Policy Mini-Track starting first thing in the morning. The mini-track will begin with a session called “Hot Topics in Health Policy for Hospitalists” and will be followed by a panel of visitors from our nation’s capital who will weigh in on events in D.C. that will have an impact on our careers.
There are also three workshops in the morning including one on negotiation that I hope to attend. The second set of workshops includes one with the provocative title of “Cutting Out Things We Do for No Reason.”
And while there are too many great sessions to be able to call out each one, the prize for most creative title clearly goes to “Take Your PICC: Choosing the Right Vascular Access.”
The day, and the meeting, ends as it traditionally does with a talk by the venerable Bob Wachter, MD, MHM, who will treat us to a discussion on “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” We may even see some of his famed humor and wit as we have in past years. Everyone who has ever heard Bob speak knows that this is a session that should not be missed!
Your afternoon is free to travel home or to hit the casinos one last time.
As I begin my year as SHM President, I continue to be energized by the opportunity to meet so many of you at our Annual Meeting and to be part of an organization that continues to have such a positive impact on our nation’s health care system.
The coming year will see a continued reshaping of our delivery system, driven by emerging federal policy including the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and anticipated changes in the Affordable Care Act. It will continue to be a priority for SHM to make sure that the voice of Hospital Medicine is heard loud and clear as decisions are made that will affect our patients and our careers. I will be asking our members to help ensure that we have a prominent place in these decision making processes. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build and maintain a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen our system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them along with their colleagues.
And, of course, SHM will continue to be the only organization created to represent our nation’s hospitalists and to be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy.
I hope you enjoyed what turned out to be the largest and best Annual Meeting in our history. And I hope to see you at Hospital Medicine 2018 in Orlando.
Welcome to the third and final day of HM17!
Although it is the shortest day of the conference, day 3 is full of quality content, starting at 7:40 a.m. with a mini-track.
If you are interested in hearing about the impact of November’s election on health care reform, join me at the Health Policy Mini-Track starting first thing in the morning. The mini-track will begin with a session called “Hot Topics in Health Policy for Hospitalists” and will be followed by a panel of visitors from our nation’s capital who will weigh in on events in D.C. that will have an impact on our careers.
There are also three workshops in the morning including one on negotiation that I hope to attend. The second set of workshops includes one with the provocative title of “Cutting Out Things We Do for No Reason.”
And while there are too many great sessions to be able to call out each one, the prize for most creative title clearly goes to “Take Your PICC: Choosing the Right Vascular Access.”
The day, and the meeting, ends as it traditionally does with a talk by the venerable Bob Wachter, MD, MHM, who will treat us to a discussion on “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” We may even see some of his famed humor and wit as we have in past years. Everyone who has ever heard Bob speak knows that this is a session that should not be missed!
Your afternoon is free to travel home or to hit the casinos one last time.
As I begin my year as SHM President, I continue to be energized by the opportunity to meet so many of you at our Annual Meeting and to be part of an organization that continues to have such a positive impact on our nation’s health care system.
The coming year will see a continued reshaping of our delivery system, driven by emerging federal policy including the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and anticipated changes in the Affordable Care Act. It will continue to be a priority for SHM to make sure that the voice of Hospital Medicine is heard loud and clear as decisions are made that will affect our patients and our careers. I will be asking our members to help ensure that we have a prominent place in these decision making processes. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build and maintain a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen our system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them along with their colleagues.
And, of course, SHM will continue to be the only organization created to represent our nation’s hospitalists and to be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy.
I hope you enjoyed what turned out to be the largest and best Annual Meeting in our history. And I hope to see you at Hospital Medicine 2018 in Orlando.
Welcome to the third and final day of HM17!
Although it is the shortest day of the conference, day 3 is full of quality content, starting at 7:40 a.m. with a mini-track.
If you are interested in hearing about the impact of November’s election on health care reform, join me at the Health Policy Mini-Track starting first thing in the morning. The mini-track will begin with a session called “Hot Topics in Health Policy for Hospitalists” and will be followed by a panel of visitors from our nation’s capital who will weigh in on events in D.C. that will have an impact on our careers.
There are also three workshops in the morning including one on negotiation that I hope to attend. The second set of workshops includes one with the provocative title of “Cutting Out Things We Do for No Reason.”
And while there are too many great sessions to be able to call out each one, the prize for most creative title clearly goes to “Take Your PICC: Choosing the Right Vascular Access.”
The day, and the meeting, ends as it traditionally does with a talk by the venerable Bob Wachter, MD, MHM, who will treat us to a discussion on “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” We may even see some of his famed humor and wit as we have in past years. Everyone who has ever heard Bob speak knows that this is a session that should not be missed!
Your afternoon is free to travel home or to hit the casinos one last time.
As I begin my year as SHM President, I continue to be energized by the opportunity to meet so many of you at our Annual Meeting and to be part of an organization that continues to have such a positive impact on our nation’s health care system.
The coming year will see a continued reshaping of our delivery system, driven by emerging federal policy including the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and anticipated changes in the Affordable Care Act. It will continue to be a priority for SHM to make sure that the voice of Hospital Medicine is heard loud and clear as decisions are made that will affect our patients and our careers. I will be asking our members to help ensure that we have a prominent place in these decision making processes. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build and maintain a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen our system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them along with their colleagues.
And, of course, SHM will continue to be the only organization created to represent our nation’s hospitalists and to be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy.
I hope you enjoyed what turned out to be the largest and best Annual Meeting in our history. And I hope to see you at Hospital Medicine 2018 in Orlando.
Does Ultrasonography Help Predict Thyroid Tumors?
Is ultrasonography really useful in distinguishing between benign and malignant thyroid nodules? The reality facing many physicians, say researchers from the University of Alberta, is that ultrasonography reports originate from multiple sites and are dictated by physicians of varying experience, practice volumes, and styles of documentation. The researchers say although thyroid ultrasonography provides accurate results, few ultrasound reports contain the necessary information to predict malignancy and guide management.
The Thyroid Imaging and Reporting System (TI-RADS) was developed to standardize risk stratification according to nodule characteristics: size, marked hypoechogenicity, taller-than-wide shape, microcalcifications, irregular margins, and solid component. The researchers reviewed ultrasound reports using TI-RADS criteria for 329 patients who had undergone thyroidectomy and then assessed whether individual or multiple criteria were associated with malignancy.
Related: New Treatment Options for Metastatic Thyroid Cancer
About 42% of the nodules were malignant. The most common carcinoma was papillary thyroid cancer. Benign disease was predominantly cases of multinodular goiter. The difference in size between benign and malignant neoplasms was not significant. About 11% of the specimens exhibited incidental microcarcionomas.
Nearly all the reports documented nodule size. But > 90% noted ≤ 3 of the remaining TI-RADS criteria. In fact, nearly 40% included 1 or no criterion beyond the description of size. The number of features reported did not reflect an increased risk of malignancy. The researchers found no associations among reporting criteria—for example, the presence of microcalcifications did not trigger targeted comments about any other factor—and this was true for all of the criteria, they note.
Half of the reports with a comment noted solid or cystic nodules and echogenicity. The description of a hypoechoic nodule or a solid nodule was significantly more likely to be identified in malignant neoplasms. The presence of microcalcifications was the most sensitive marker of malignancy (90%), and documentation of irregular margins was the most specific indicator.
Overall, the researchers say, it was clear that microcalcifications, hypoechogenicity, irregular margins, and solid nodules were significantly more likely to be found in malignant neoplasms. The absence of these nodules predicted benign disease. But because so few reports consistently documented all criteria, the overall ability of thyroid ultrasonography to discriminate between lower- and higher-risk nodules is limited.
Source:
Gamme G, Parrington T, Wiebe E, et al. Can J Surg. 2017;60(2):134-139
doi:10.1503/cjs.010316
Is ultrasonography really useful in distinguishing between benign and malignant thyroid nodules? The reality facing many physicians, say researchers from the University of Alberta, is that ultrasonography reports originate from multiple sites and are dictated by physicians of varying experience, practice volumes, and styles of documentation. The researchers say although thyroid ultrasonography provides accurate results, few ultrasound reports contain the necessary information to predict malignancy and guide management.
The Thyroid Imaging and Reporting System (TI-RADS) was developed to standardize risk stratification according to nodule characteristics: size, marked hypoechogenicity, taller-than-wide shape, microcalcifications, irregular margins, and solid component. The researchers reviewed ultrasound reports using TI-RADS criteria for 329 patients who had undergone thyroidectomy and then assessed whether individual or multiple criteria were associated with malignancy.
Related: New Treatment Options for Metastatic Thyroid Cancer
About 42% of the nodules were malignant. The most common carcinoma was papillary thyroid cancer. Benign disease was predominantly cases of multinodular goiter. The difference in size between benign and malignant neoplasms was not significant. About 11% of the specimens exhibited incidental microcarcionomas.
Nearly all the reports documented nodule size. But > 90% noted ≤ 3 of the remaining TI-RADS criteria. In fact, nearly 40% included 1 or no criterion beyond the description of size. The number of features reported did not reflect an increased risk of malignancy. The researchers found no associations among reporting criteria—for example, the presence of microcalcifications did not trigger targeted comments about any other factor—and this was true for all of the criteria, they note.
Half of the reports with a comment noted solid or cystic nodules and echogenicity. The description of a hypoechoic nodule or a solid nodule was significantly more likely to be identified in malignant neoplasms. The presence of microcalcifications was the most sensitive marker of malignancy (90%), and documentation of irregular margins was the most specific indicator.
Overall, the researchers say, it was clear that microcalcifications, hypoechogenicity, irregular margins, and solid nodules were significantly more likely to be found in malignant neoplasms. The absence of these nodules predicted benign disease. But because so few reports consistently documented all criteria, the overall ability of thyroid ultrasonography to discriminate between lower- and higher-risk nodules is limited.
Source:
Gamme G, Parrington T, Wiebe E, et al. Can J Surg. 2017;60(2):134-139
doi:10.1503/cjs.010316
Is ultrasonography really useful in distinguishing between benign and malignant thyroid nodules? The reality facing many physicians, say researchers from the University of Alberta, is that ultrasonography reports originate from multiple sites and are dictated by physicians of varying experience, practice volumes, and styles of documentation. The researchers say although thyroid ultrasonography provides accurate results, few ultrasound reports contain the necessary information to predict malignancy and guide management.
The Thyroid Imaging and Reporting System (TI-RADS) was developed to standardize risk stratification according to nodule characteristics: size, marked hypoechogenicity, taller-than-wide shape, microcalcifications, irregular margins, and solid component. The researchers reviewed ultrasound reports using TI-RADS criteria for 329 patients who had undergone thyroidectomy and then assessed whether individual or multiple criteria were associated with malignancy.
Related: New Treatment Options for Metastatic Thyroid Cancer
About 42% of the nodules were malignant. The most common carcinoma was papillary thyroid cancer. Benign disease was predominantly cases of multinodular goiter. The difference in size between benign and malignant neoplasms was not significant. About 11% of the specimens exhibited incidental microcarcionomas.
Nearly all the reports documented nodule size. But > 90% noted ≤ 3 of the remaining TI-RADS criteria. In fact, nearly 40% included 1 or no criterion beyond the description of size. The number of features reported did not reflect an increased risk of malignancy. The researchers found no associations among reporting criteria—for example, the presence of microcalcifications did not trigger targeted comments about any other factor—and this was true for all of the criteria, they note.
Half of the reports with a comment noted solid or cystic nodules and echogenicity. The description of a hypoechoic nodule or a solid nodule was significantly more likely to be identified in malignant neoplasms. The presence of microcalcifications was the most sensitive marker of malignancy (90%), and documentation of irregular margins was the most specific indicator.
Overall, the researchers say, it was clear that microcalcifications, hypoechogenicity, irregular margins, and solid nodules were significantly more likely to be found in malignant neoplasms. The absence of these nodules predicted benign disease. But because so few reports consistently documented all criteria, the overall ability of thyroid ultrasonography to discriminate between lower- and higher-risk nodules is limited.
Source:
Gamme G, Parrington T, Wiebe E, et al. Can J Surg. 2017;60(2):134-139
doi:10.1503/cjs.010316
Providing Mental Health Care to All Veterans Regardless of Discharge Status
During his testimony before the House Committee on Veterans Affairs on March 7, 2017, Secretary of Veterans Affairs David J. Shulkin, MD, expressed his intent to remove the administrative barrier prohibiting other-than-honorably (OTH) discharged service members from receiving VHA mental health care. This is the first time in VA history to integrate those veterans whose OTH discharge status had previously disenfranchised them.
In his comments to Congress, Dr. Shulkin voiced his gratitude to Rep. Mike Coffman (R-CO) for helping him to “better understand the urgency of getting this right.” In March 2016, Rep. Coffman introduced the
Veterans Fairness Act, which would permit OTH discharged combat veterans to obtain emergency mental health services. Rep. Coffman cited that 22,000 U.S. Army veterans were discharged for misconduct since 2009, most with a traumatic brain injury (TBI) or mental illness.1 Veterans often refer to OTH discharges as having “bad paper.” In 2013, National Public Radio produced a series on OTH discharged service members that underscored their struggles.2 Those reports estimated that more than 100,000 veterans left the service with OTH discharges in the decade before the story.2
These individuals, many of whom have already lost a great deal as a result of their military service, lose much more when they are OTH discharged. They are unable to apply for the GI Bill, which enables them to further their education and livelihood; they cannot get a VA home loan to help them house their families; and they are ineligible for disability even for combat-related conditions like posttraumatic stress disorder (PTSD) and TBI. Most damaging of all, until Dr. Shulkin’s historic announcement, they also could not get VA health care. In effect, OTH discharge status creates a second class of service men and women, even though the discharge may have been the result of injury and illness related to their time in uniform. That consequence makes Dr. Shulkin’s proposal not only an administrative change, but also an ethical decision regarding the civil and human rights of service members, which is the reason most major veterans service and advocacy organizations have long endorsed it.
Although research on OTH discharged veterans has been limited, studies have found a high rate of mental health problems. The OTH discharged service members are significantly represented in the cohorts who face some of the most serious public health problems that the VA has tried to address through new programs that were initiated during the prior administration and continued by the current one, such as ending homelessness and preventing suicide.
A 2017 study compared rates of mental illness and substance use among veterans with routine discharges with those who had nonroutine separations from the military.3 The results showed that there was a higher rate of almost every psychiatric diagnosis in the nonroutine discharges; the rates were particularly high for those discharged for misconduct.3 Because of the established correlation of multiple deployments to Afghanistan and Iraq and incidence of TBI, PTSD, and substance use and the association of these disorders with behaviors that contribute to OTH discharge status, a clear duty to care for these men and women emerges.
Similarly, the ethical principle of nonmalfeasance provides persuasive justification for Dr. Shulkin’s proposed change in VA eligibility for mental health care. The study also found that even if not previously entitled to VA services, these veterans share the increased risk of suicide found in all those who have worn a uniform for their country and similarly need compassionate, competent veteran-centered care.3
Recent research showed that patients who receive mental health care within the VA have lower rates of suicide than that of those who receive care in the community.4 The results of this study contribute to the ethical imperative to grant these former service members access to potentially life-saving mental health treatment more urgent.
The elevated suicide risk of those veterans who do not have VA mental health services makes this extension of care clinically and ethically imperative and urgent. In his testimony at the hearing, Dr. Shulkin underscored this rationale, “The President and I have made it clear that suicide prevention is one of our top priorities,” Shulkin added. “We know the rate of death by suicide among veterans who do not use VA care is increasing at a greater rate than veterans who use VA care. This is a national emergency that requires bold action. We must and we will do all that we can to help former service members who may be at risk. When we say even one veteran suicide is one too many, we mean it.
The downstream consequences of OTH discharge status are the most detrimental to the veteran and have negative effects on the veteran’s family and community. Nonroutinely discharged veterans are more likely to be homeless. The new initiative would open a variety of VA mental health services to OTH discharged service members, including those available in VA emergency departments, Vet Centers, and the Veterans Crisis Line. In developing the plan to expand coverage to OTH discharged veterans, Dr. Shulkin indicated that he would consult with Veterans Service Organizations and the DoD.
We can hope that additional services will be opened to OTH discharged service members, such as case management and housing assistance, which have proven so successful in reintegrating those service members with routine discharges.
1. Roeder T. Rep. Coffman renews push for mental health care for all veterans who need it. http://gazette.com/rep.-coffman-renews-push-for-mental-health-care-for-all-veterans-who-need-it/article/1596355. Updated February 9, 2017. Access April 10, 2017.
2. Peñaloza M, Lawrence Q. Veterans and otherthan-honorable discharges. http://www.npr.orgseries/250013036/veterans-and-other-than-honorable-discharges. Published December 12, 2013. Accessed April 10, 2017.
3. Brignone E, Fargo JD, Blais RK, Carter ME, Samore MH, Gundlapalli AV. Non-routine discharge from military service: mental illness, substance use disorders, and suicidality. Am J Prev Med. 2017;52(5):557-565.
4. Hoffmire CA, Kemp Je, Bossarte RM. Changes in suicide mortality for veterans and non-veterans by gender and history of VHA service use, 2000-2010. Psychiatr Serv. 2015;66(9):959-965.
During his testimony before the House Committee on Veterans Affairs on March 7, 2017, Secretary of Veterans Affairs David J. Shulkin, MD, expressed his intent to remove the administrative barrier prohibiting other-than-honorably (OTH) discharged service members from receiving VHA mental health care. This is the first time in VA history to integrate those veterans whose OTH discharge status had previously disenfranchised them.
In his comments to Congress, Dr. Shulkin voiced his gratitude to Rep. Mike Coffman (R-CO) for helping him to “better understand the urgency of getting this right.” In March 2016, Rep. Coffman introduced the
Veterans Fairness Act, which would permit OTH discharged combat veterans to obtain emergency mental health services. Rep. Coffman cited that 22,000 U.S. Army veterans were discharged for misconduct since 2009, most with a traumatic brain injury (TBI) or mental illness.1 Veterans often refer to OTH discharges as having “bad paper.” In 2013, National Public Radio produced a series on OTH discharged service members that underscored their struggles.2 Those reports estimated that more than 100,000 veterans left the service with OTH discharges in the decade before the story.2
These individuals, many of whom have already lost a great deal as a result of their military service, lose much more when they are OTH discharged. They are unable to apply for the GI Bill, which enables them to further their education and livelihood; they cannot get a VA home loan to help them house their families; and they are ineligible for disability even for combat-related conditions like posttraumatic stress disorder (PTSD) and TBI. Most damaging of all, until Dr. Shulkin’s historic announcement, they also could not get VA health care. In effect, OTH discharge status creates a second class of service men and women, even though the discharge may have been the result of injury and illness related to their time in uniform. That consequence makes Dr. Shulkin’s proposal not only an administrative change, but also an ethical decision regarding the civil and human rights of service members, which is the reason most major veterans service and advocacy organizations have long endorsed it.
Although research on OTH discharged veterans has been limited, studies have found a high rate of mental health problems. The OTH discharged service members are significantly represented in the cohorts who face some of the most serious public health problems that the VA has tried to address through new programs that were initiated during the prior administration and continued by the current one, such as ending homelessness and preventing suicide.
A 2017 study compared rates of mental illness and substance use among veterans with routine discharges with those who had nonroutine separations from the military.3 The results showed that there was a higher rate of almost every psychiatric diagnosis in the nonroutine discharges; the rates were particularly high for those discharged for misconduct.3 Because of the established correlation of multiple deployments to Afghanistan and Iraq and incidence of TBI, PTSD, and substance use and the association of these disorders with behaviors that contribute to OTH discharge status, a clear duty to care for these men and women emerges.
Similarly, the ethical principle of nonmalfeasance provides persuasive justification for Dr. Shulkin’s proposed change in VA eligibility for mental health care. The study also found that even if not previously entitled to VA services, these veterans share the increased risk of suicide found in all those who have worn a uniform for their country and similarly need compassionate, competent veteran-centered care.3
Recent research showed that patients who receive mental health care within the VA have lower rates of suicide than that of those who receive care in the community.4 The results of this study contribute to the ethical imperative to grant these former service members access to potentially life-saving mental health treatment more urgent.
The elevated suicide risk of those veterans who do not have VA mental health services makes this extension of care clinically and ethically imperative and urgent. In his testimony at the hearing, Dr. Shulkin underscored this rationale, “The President and I have made it clear that suicide prevention is one of our top priorities,” Shulkin added. “We know the rate of death by suicide among veterans who do not use VA care is increasing at a greater rate than veterans who use VA care. This is a national emergency that requires bold action. We must and we will do all that we can to help former service members who may be at risk. When we say even one veteran suicide is one too many, we mean it.
The downstream consequences of OTH discharge status are the most detrimental to the veteran and have negative effects on the veteran’s family and community. Nonroutinely discharged veterans are more likely to be homeless. The new initiative would open a variety of VA mental health services to OTH discharged service members, including those available in VA emergency departments, Vet Centers, and the Veterans Crisis Line. In developing the plan to expand coverage to OTH discharged veterans, Dr. Shulkin indicated that he would consult with Veterans Service Organizations and the DoD.
We can hope that additional services will be opened to OTH discharged service members, such as case management and housing assistance, which have proven so successful in reintegrating those service members with routine discharges.
During his testimony before the House Committee on Veterans Affairs on March 7, 2017, Secretary of Veterans Affairs David J. Shulkin, MD, expressed his intent to remove the administrative barrier prohibiting other-than-honorably (OTH) discharged service members from receiving VHA mental health care. This is the first time in VA history to integrate those veterans whose OTH discharge status had previously disenfranchised them.
In his comments to Congress, Dr. Shulkin voiced his gratitude to Rep. Mike Coffman (R-CO) for helping him to “better understand the urgency of getting this right.” In March 2016, Rep. Coffman introduced the
Veterans Fairness Act, which would permit OTH discharged combat veterans to obtain emergency mental health services. Rep. Coffman cited that 22,000 U.S. Army veterans were discharged for misconduct since 2009, most with a traumatic brain injury (TBI) or mental illness.1 Veterans often refer to OTH discharges as having “bad paper.” In 2013, National Public Radio produced a series on OTH discharged service members that underscored their struggles.2 Those reports estimated that more than 100,000 veterans left the service with OTH discharges in the decade before the story.2
These individuals, many of whom have already lost a great deal as a result of their military service, lose much more when they are OTH discharged. They are unable to apply for the GI Bill, which enables them to further their education and livelihood; they cannot get a VA home loan to help them house their families; and they are ineligible for disability even for combat-related conditions like posttraumatic stress disorder (PTSD) and TBI. Most damaging of all, until Dr. Shulkin’s historic announcement, they also could not get VA health care. In effect, OTH discharge status creates a second class of service men and women, even though the discharge may have been the result of injury and illness related to their time in uniform. That consequence makes Dr. Shulkin’s proposal not only an administrative change, but also an ethical decision regarding the civil and human rights of service members, which is the reason most major veterans service and advocacy organizations have long endorsed it.
Although research on OTH discharged veterans has been limited, studies have found a high rate of mental health problems. The OTH discharged service members are significantly represented in the cohorts who face some of the most serious public health problems that the VA has tried to address through new programs that were initiated during the prior administration and continued by the current one, such as ending homelessness and preventing suicide.
A 2017 study compared rates of mental illness and substance use among veterans with routine discharges with those who had nonroutine separations from the military.3 The results showed that there was a higher rate of almost every psychiatric diagnosis in the nonroutine discharges; the rates were particularly high for those discharged for misconduct.3 Because of the established correlation of multiple deployments to Afghanistan and Iraq and incidence of TBI, PTSD, and substance use and the association of these disorders with behaviors that contribute to OTH discharge status, a clear duty to care for these men and women emerges.
Similarly, the ethical principle of nonmalfeasance provides persuasive justification for Dr. Shulkin’s proposed change in VA eligibility for mental health care. The study also found that even if not previously entitled to VA services, these veterans share the increased risk of suicide found in all those who have worn a uniform for their country and similarly need compassionate, competent veteran-centered care.3
Recent research showed that patients who receive mental health care within the VA have lower rates of suicide than that of those who receive care in the community.4 The results of this study contribute to the ethical imperative to grant these former service members access to potentially life-saving mental health treatment more urgent.
The elevated suicide risk of those veterans who do not have VA mental health services makes this extension of care clinically and ethically imperative and urgent. In his testimony at the hearing, Dr. Shulkin underscored this rationale, “The President and I have made it clear that suicide prevention is one of our top priorities,” Shulkin added. “We know the rate of death by suicide among veterans who do not use VA care is increasing at a greater rate than veterans who use VA care. This is a national emergency that requires bold action. We must and we will do all that we can to help former service members who may be at risk. When we say even one veteran suicide is one too many, we mean it.
The downstream consequences of OTH discharge status are the most detrimental to the veteran and have negative effects on the veteran’s family and community. Nonroutinely discharged veterans are more likely to be homeless. The new initiative would open a variety of VA mental health services to OTH discharged service members, including those available in VA emergency departments, Vet Centers, and the Veterans Crisis Line. In developing the plan to expand coverage to OTH discharged veterans, Dr. Shulkin indicated that he would consult with Veterans Service Organizations and the DoD.
We can hope that additional services will be opened to OTH discharged service members, such as case management and housing assistance, which have proven so successful in reintegrating those service members with routine discharges.
1. Roeder T. Rep. Coffman renews push for mental health care for all veterans who need it. http://gazette.com/rep.-coffman-renews-push-for-mental-health-care-for-all-veterans-who-need-it/article/1596355. Updated February 9, 2017. Access April 10, 2017.
2. Peñaloza M, Lawrence Q. Veterans and otherthan-honorable discharges. http://www.npr.orgseries/250013036/veterans-and-other-than-honorable-discharges. Published December 12, 2013. Accessed April 10, 2017.
3. Brignone E, Fargo JD, Blais RK, Carter ME, Samore MH, Gundlapalli AV. Non-routine discharge from military service: mental illness, substance use disorders, and suicidality. Am J Prev Med. 2017;52(5):557-565.
4. Hoffmire CA, Kemp Je, Bossarte RM. Changes in suicide mortality for veterans and non-veterans by gender and history of VHA service use, 2000-2010. Psychiatr Serv. 2015;66(9):959-965.
1. Roeder T. Rep. Coffman renews push for mental health care for all veterans who need it. http://gazette.com/rep.-coffman-renews-push-for-mental-health-care-for-all-veterans-who-need-it/article/1596355. Updated February 9, 2017. Access April 10, 2017.
2. Peñaloza M, Lawrence Q. Veterans and otherthan-honorable discharges. http://www.npr.orgseries/250013036/veterans-and-other-than-honorable-discharges. Published December 12, 2013. Accessed April 10, 2017.
3. Brignone E, Fargo JD, Blais RK, Carter ME, Samore MH, Gundlapalli AV. Non-routine discharge from military service: mental illness, substance use disorders, and suicidality. Am J Prev Med. 2017;52(5):557-565.
4. Hoffmire CA, Kemp Je, Bossarte RM. Changes in suicide mortality for veterans and non-veterans by gender and history of VHA service use, 2000-2010. Psychiatr Serv. 2015;66(9):959-965.
Talk About Premature Balding...
Several months ago, this 8-year-old boy began losing hair from his scalp. Other than mild itching, there are no associated symptoms. The patient has no pets at home, but he spends his after-school hours with his cousin, who does.
The child is allergy prone but otherwise healthy. No one else in the family (ie, his two younger siblings) has been similarly affected.
EXAMINATION
About three-quarters of the hair is missing from a 6-cm oval patch on the parietal scalp. A few short hairs remain. The skin in this area is slightly edematous, with focal areas of broken, scaly skin.
Palpation of the head and neck reveals adenopathy in the nuchal area of the affected side. A KOH prep is performed with a #10 blade; the sample includes hairs as well as skin.

What is the diagnosis?
DISCUSSION
Examination of the sample revealed endothrix, in which fungal spores and hyphae are found inside the broken-off hairs, especially near the roots. A fungal culture confirmed the presence of Trychophyton tonsurans.
T tonsurans is the most common culprit in tinea captitis cases in the United States. This dermatophytic infection of the scalp is a common diagnosis in children, who typically contract it from other children. (Some causative species—such as Microsporum audouinii—spread via contact with animals, but these organisms are generally rare in the US.) Tinea capitis is seen more frequently in boys than in girls, and African-American patients are especially at risk.
Tinea capitis infects the deep hair shaft but spares the skin. Diagnosis requires a combination of clinical signs and identification of the organism in the hair shaft; the latter will also help to guide treatment. In contrast, tinea corporis is diagnosed by clinical features and KOH examination of external scales where the organism resides. Traditionally, infected hairs have needed to be removed for KOH exam—but practical experience has shown that a vigorous scrape that captures infected hairs can accomplish the same thing.
The results of fungal culture may take a month or more to finalize; in the interim, patients such as this one may be treated with griseofulvin (10 mg/kg/d) and application of topical ciclopirox cream bid to reduce infectivity. Total clearance will take at least two months.
Tinea capitis has several forms including inflammatory (which manifests with a large, swollen, inflamed mass) and black dot (named for the tips of broken hair shafts that remain in the affected areas). The differential includes psoriasis, alopecia areata, and seborrhea.
TAKE-HOME LEARNING POINTS
- Tinea capitis is a dermatophytic infection of the scalp usually caused by the dermatophytes Trychophyton tonsurans or T rubrum.
- These infections involve the hair shaft below the skin line, rather than the surface of the skin.
- The organisms that commonly cause tinea capitis in the US typically spread through contact with another person.
- Diagnosis can be made from clinical findings only, including reactive adenopathy. KOH and culture can be necessary in questionable cases, and because of the length of treatment.
Several months ago, this 8-year-old boy began losing hair from his scalp. Other than mild itching, there are no associated symptoms. The patient has no pets at home, but he spends his after-school hours with his cousin, who does.
The child is allergy prone but otherwise healthy. No one else in the family (ie, his two younger siblings) has been similarly affected.
EXAMINATION
About three-quarters of the hair is missing from a 6-cm oval patch on the parietal scalp. A few short hairs remain. The skin in this area is slightly edematous, with focal areas of broken, scaly skin.
Palpation of the head and neck reveals adenopathy in the nuchal area of the affected side. A KOH prep is performed with a #10 blade; the sample includes hairs as well as skin.

What is the diagnosis?
DISCUSSION
Examination of the sample revealed endothrix, in which fungal spores and hyphae are found inside the broken-off hairs, especially near the roots. A fungal culture confirmed the presence of Trychophyton tonsurans.
T tonsurans is the most common culprit in tinea captitis cases in the United States. This dermatophytic infection of the scalp is a common diagnosis in children, who typically contract it from other children. (Some causative species—such as Microsporum audouinii—spread via contact with animals, but these organisms are generally rare in the US.) Tinea capitis is seen more frequently in boys than in girls, and African-American patients are especially at risk.
Tinea capitis infects the deep hair shaft but spares the skin. Diagnosis requires a combination of clinical signs and identification of the organism in the hair shaft; the latter will also help to guide treatment. In contrast, tinea corporis is diagnosed by clinical features and KOH examination of external scales where the organism resides. Traditionally, infected hairs have needed to be removed for KOH exam—but practical experience has shown that a vigorous scrape that captures infected hairs can accomplish the same thing.
The results of fungal culture may take a month or more to finalize; in the interim, patients such as this one may be treated with griseofulvin (10 mg/kg/d) and application of topical ciclopirox cream bid to reduce infectivity. Total clearance will take at least two months.
Tinea capitis has several forms including inflammatory (which manifests with a large, swollen, inflamed mass) and black dot (named for the tips of broken hair shafts that remain in the affected areas). The differential includes psoriasis, alopecia areata, and seborrhea.
TAKE-HOME LEARNING POINTS
- Tinea capitis is a dermatophytic infection of the scalp usually caused by the dermatophytes Trychophyton tonsurans or T rubrum.
- These infections involve the hair shaft below the skin line, rather than the surface of the skin.
- The organisms that commonly cause tinea capitis in the US typically spread through contact with another person.
- Diagnosis can be made from clinical findings only, including reactive adenopathy. KOH and culture can be necessary in questionable cases, and because of the length of treatment.
Several months ago, this 8-year-old boy began losing hair from his scalp. Other than mild itching, there are no associated symptoms. The patient has no pets at home, but he spends his after-school hours with his cousin, who does.
The child is allergy prone but otherwise healthy. No one else in the family (ie, his two younger siblings) has been similarly affected.
EXAMINATION
About three-quarters of the hair is missing from a 6-cm oval patch on the parietal scalp. A few short hairs remain. The skin in this area is slightly edematous, with focal areas of broken, scaly skin.
Palpation of the head and neck reveals adenopathy in the nuchal area of the affected side. A KOH prep is performed with a #10 blade; the sample includes hairs as well as skin.

What is the diagnosis?
DISCUSSION
Examination of the sample revealed endothrix, in which fungal spores and hyphae are found inside the broken-off hairs, especially near the roots. A fungal culture confirmed the presence of Trychophyton tonsurans.
T tonsurans is the most common culprit in tinea captitis cases in the United States. This dermatophytic infection of the scalp is a common diagnosis in children, who typically contract it from other children. (Some causative species—such as Microsporum audouinii—spread via contact with animals, but these organisms are generally rare in the US.) Tinea capitis is seen more frequently in boys than in girls, and African-American patients are especially at risk.
Tinea capitis infects the deep hair shaft but spares the skin. Diagnosis requires a combination of clinical signs and identification of the organism in the hair shaft; the latter will also help to guide treatment. In contrast, tinea corporis is diagnosed by clinical features and KOH examination of external scales where the organism resides. Traditionally, infected hairs have needed to be removed for KOH exam—but practical experience has shown that a vigorous scrape that captures infected hairs can accomplish the same thing.
The results of fungal culture may take a month or more to finalize; in the interim, patients such as this one may be treated with griseofulvin (10 mg/kg/d) and application of topical ciclopirox cream bid to reduce infectivity. Total clearance will take at least two months.
Tinea capitis has several forms including inflammatory (which manifests with a large, swollen, inflamed mass) and black dot (named for the tips of broken hair shafts that remain in the affected areas). The differential includes psoriasis, alopecia areata, and seborrhea.
TAKE-HOME LEARNING POINTS
- Tinea capitis is a dermatophytic infection of the scalp usually caused by the dermatophytes Trychophyton tonsurans or T rubrum.
- These infections involve the hair shaft below the skin line, rather than the surface of the skin.
- The organisms that commonly cause tinea capitis in the US typically spread through contact with another person.
- Diagnosis can be made from clinical findings only, including reactive adenopathy. KOH and culture can be necessary in questionable cases, and because of the length of treatment.










