User login
Bacterial vaginosis: Meet patients' needs with effective diagnosis and treatment
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Editorial Note
The first Skin of Color column, "Diversity in Dermatology: A Society Devoted to Skin of Color," produced in collaboration with the Skin of Color Society appears on page 322. This column will be published quarterly and will serve to increase the knowledge available to dermatologists to help improve delivery of care to this underserved population.
Look for Skin of Color columns in upcoming issues of Cutis.
The first Skin of Color column, "Diversity in Dermatology: A Society Devoted to Skin of Color," produced in collaboration with the Skin of Color Society appears on page 322. This column will be published quarterly and will serve to increase the knowledge available to dermatologists to help improve delivery of care to this underserved population.
Look for Skin of Color columns in upcoming issues of Cutis.
The first Skin of Color column, "Diversity in Dermatology: A Society Devoted to Skin of Color," produced in collaboration with the Skin of Color Society appears on page 322. This column will be published quarterly and will serve to increase the knowledge available to dermatologists to help improve delivery of care to this underserved population.
Look for Skin of Color columns in upcoming issues of Cutis.
Skin Cancer Mortality in Patients With Skin of Color
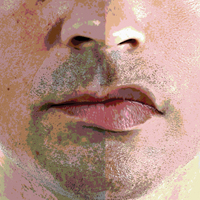
Skin cancers in patients with skin of color are less prevalent but have a higher morbidity and mortality compared to white patients. Challenges to early detection, including clinical differences in presentation, low public awareness, lower index of suspicion among health care providers, and access to specialty care, likely contribute to observed differences in prognosis between skin of color and white populations.
Skin cancer is the most common malignancy in the United States, accounting for approximately 40% of all neoplasms in white patients but only 1% to 4% in Asian American and black patients.1,2 Largely due to the photoprotective effects of increased constitutive epidermal melanin, melanoma is approximately 10 to 20 times less frequent in black patients and 3 to 7 times less common in Hispanics than age-matched whites.1 Nonmelanoma skin cancers including squamous cell carcinoma (SCC) and basal cell carcinoma also are less prevalent in darker skin types.3,4
In the United States, Hispanic, American Indian
Similar to melanoma, the mortality from SCC is disproportionately increased in skin of color populations, ranging from 18% to 29% in black patients.3,10,11 There is a paucity of population-based studies in the United States looking at mortality rates of nonmelanoma skin cancers and their trends over time, but a 1993 study suggests that mortality rates are declining less consistently in black patients than white patients.11
Factors that may contribute to higher mortality rates in patients with skin of color include a greater propensity for inherently aggressive skin cancers (eg, higher risk of SCC) and delays in diagnosis (eg, late-stage diagnosis of melanoma).1,4 For melanoma, increased mortality has been attributed to a predominance of acral lentiginous melanomas, which are more frequently diagnosed at more advanced stages than other melanoma subtypes.6,12,13 Black patients, Hispanics, Asians, and Pacific Islanders are all more likely to present with thicker tumors and metastases on initial presentation than their white counterparts (P<.001).2,8,9,12-14 The higher risk of death from SCC results from the predominance of lesions on non–sun-exposed areas, particularly the legs and anogenital areas, and within sites of chronic scarring or inflammation.4 Unlike sun-induced SCC, the most commonly observed type of SCC in lighter skin types, SCCs that develop in association with chronic inflammatory or ulcerative processes are aggressive and invasive, and they metastasize to distant sites in 20% to 40% of cases (versus 1%–4% in sun-induced SCC).1,3,4 For all skin cancers, poor access to medical care, patients’ unawareness of their skin cancer risk, lack of adequate skin examinations, and prevalence of lesions on uncommon sites that may be inconspicuous or overlooked have all been suggested to delay diagnosis.1,15,16 Given that more advanced disease is associated with worse outcomes, the implications of this delay are enormous and remain a cause for concern.
The alarming skin cancer mortality rates in patients with skin of color are a call to action for the medical community. The consistent use of full-body skin examinations including close inspection of mucosal, acral, and genital areas for all patients independent of skin type and racial/ethnic background is paramount. Advancing skin cancer education in skin of color populations, such as through distribution of patient-directed educational materials produced by organizations such as the American Academy of Dermatology, Skin Cancer Foundation, and Skin of Color Society, is an important step toward increased public awareness.16 Use of social and traditional media outlets as well as community-directed health outreach campaigns also are important strategies to change the common misconception that darker-skinned individuals do not get skin cancer. We hope that with a multipronged approach, disparities in skin cancer mortality will steadily be eliminated.
- Gloster HM Jr, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760; quiz 761-764.
- Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166:1907-1914.
- Mora RG, Perniciaro C. Cancer of the skin in blacks: I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543.
- Halder RM, Bridgeman-Shah S. Skin cancer in African Americans. Cancer. 1995;75:667-673.
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2013. Bethesda, MD: National Cancer Institute; April 2016. http://seer.cancer.gov/csr/1975_2013/. Updated September 12, 2016. Accessed April 7, 2017.
- Bellows CF, Belafsky P, Fortgang IS, et al. Melanoma in African-Americans: trends in biological behavior and clinical characteristics over two decades. J Surg Oncol. 2001;78:10-16.
- Chen L, Jin S. Trends in mortality rates of cutaneous melanoma in East Asian populations. Peer J. 2014;4:e2809.
- Cress RD, Holly EA. Incidence of cutaneous melanoma among non-Hispanic whites, Hispanics, Asians, and blacks: an analysis of California Cancer Registry data. Cancer Causes Control. 1997;8:246-252.
- Johnson DS, Yamane S, Morita S, et al. Malignant melanoma in non-Caucasians: experience from Hawaii. Surg Clin N Am. 2003;83:275-282.
- Fleming ID, Barnawell JR, Burlison PE, et al. Skin cancer in black patients. Cancer. 1975;35:600-605.
- Weinstock MA. Nonmelanoma skin cancer mortality in the United States, 1969 through 1988. Arch Dermatol. 1993;129:1286-1290.
- Byrd KM, Wilson DC, Hoyler SS. Advanced presentation of melanoma in African Americans. J Am Acad Dermatol. 2004;50:142-143.
- Hu S, Parmet Y, Allen G, et al. Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol. 2009;145:1369-1374.
- Black WC, Goldhahn RT, Wiggins C. Melanoma within a southwestern Hispanic population. Arch Dermatol. 1987;123:1331-1334.
- Harvey VM, Oldfield CW, Chen JT, et al. Melanoma disparities among US Hispanics: use of the social ecological model to contextualize reasons for inequitable outcomes and frame a research agenda [published online August 29, 2016]. J Skin Cancer. 2016;2016:4635740.
- Robinson JK, Joshi KM, Ortiz S, et al. Melanoma knowledge, perception, and awareness in ethnic minorities in Chicago: recommendations regarding education. Psychooncology. 2011;20:313-320.
Skin cancers in patients with skin of color are less prevalent but have a higher morbidity and mortality compared to white patients. Challenges to early detection, including clinical differences in presentation, low public awareness, lower index of suspicion among health care providers, and access to specialty care, likely contribute to observed differences in prognosis between skin of color and white populations.
Skin cancer is the most common malignancy in the United States, accounting for approximately 40% of all neoplasms in white patients but only 1% to 4% in Asian American and black patients.1,2 Largely due to the photoprotective effects of increased constitutive epidermal melanin, melanoma is approximately 10 to 20 times less frequent in black patients and 3 to 7 times less common in Hispanics than age-matched whites.1 Nonmelanoma skin cancers including squamous cell carcinoma (SCC) and basal cell carcinoma also are less prevalent in darker skin types.3,4
In the United States, Hispanic, American Indian
Similar to melanoma, the mortality from SCC is disproportionately increased in skin of color populations, ranging from 18% to 29% in black patients.3,10,11 There is a paucity of population-based studies in the United States looking at mortality rates of nonmelanoma skin cancers and their trends over time, but a 1993 study suggests that mortality rates are declining less consistently in black patients than white patients.11
Factors that may contribute to higher mortality rates in patients with skin of color include a greater propensity for inherently aggressive skin cancers (eg, higher risk of SCC) and delays in diagnosis (eg, late-stage diagnosis of melanoma).1,4 For melanoma, increased mortality has been attributed to a predominance of acral lentiginous melanomas, which are more frequently diagnosed at more advanced stages than other melanoma subtypes.6,12,13 Black patients, Hispanics, Asians, and Pacific Islanders are all more likely to present with thicker tumors and metastases on initial presentation than their white counterparts (P<.001).2,8,9,12-14 The higher risk of death from SCC results from the predominance of lesions on non–sun-exposed areas, particularly the legs and anogenital areas, and within sites of chronic scarring or inflammation.4 Unlike sun-induced SCC, the most commonly observed type of SCC in lighter skin types, SCCs that develop in association with chronic inflammatory or ulcerative processes are aggressive and invasive, and they metastasize to distant sites in 20% to 40% of cases (versus 1%–4% in sun-induced SCC).1,3,4 For all skin cancers, poor access to medical care, patients’ unawareness of their skin cancer risk, lack of adequate skin examinations, and prevalence of lesions on uncommon sites that may be inconspicuous or overlooked have all been suggested to delay diagnosis.1,15,16 Given that more advanced disease is associated with worse outcomes, the implications of this delay are enormous and remain a cause for concern.
The alarming skin cancer mortality rates in patients with skin of color are a call to action for the medical community. The consistent use of full-body skin examinations including close inspection of mucosal, acral, and genital areas for all patients independent of skin type and racial/ethnic background is paramount. Advancing skin cancer education in skin of color populations, such as through distribution of patient-directed educational materials produced by organizations such as the American Academy of Dermatology, Skin Cancer Foundation, and Skin of Color Society, is an important step toward increased public awareness.16 Use of social and traditional media outlets as well as community-directed health outreach campaigns also are important strategies to change the common misconception that darker-skinned individuals do not get skin cancer. We hope that with a multipronged approach, disparities in skin cancer mortality will steadily be eliminated.
Skin cancers in patients with skin of color are less prevalent but have a higher morbidity and mortality compared to white patients. Challenges to early detection, including clinical differences in presentation, low public awareness, lower index of suspicion among health care providers, and access to specialty care, likely contribute to observed differences in prognosis between skin of color and white populations.
Skin cancer is the most common malignancy in the United States, accounting for approximately 40% of all neoplasms in white patients but only 1% to 4% in Asian American and black patients.1,2 Largely due to the photoprotective effects of increased constitutive epidermal melanin, melanoma is approximately 10 to 20 times less frequent in black patients and 3 to 7 times less common in Hispanics than age-matched whites.1 Nonmelanoma skin cancers including squamous cell carcinoma (SCC) and basal cell carcinoma also are less prevalent in darker skin types.3,4
In the United States, Hispanic, American Indian
Similar to melanoma, the mortality from SCC is disproportionately increased in skin of color populations, ranging from 18% to 29% in black patients.3,10,11 There is a paucity of population-based studies in the United States looking at mortality rates of nonmelanoma skin cancers and their trends over time, but a 1993 study suggests that mortality rates are declining less consistently in black patients than white patients.11
Factors that may contribute to higher mortality rates in patients with skin of color include a greater propensity for inherently aggressive skin cancers (eg, higher risk of SCC) and delays in diagnosis (eg, late-stage diagnosis of melanoma).1,4 For melanoma, increased mortality has been attributed to a predominance of acral lentiginous melanomas, which are more frequently diagnosed at more advanced stages than other melanoma subtypes.6,12,13 Black patients, Hispanics, Asians, and Pacific Islanders are all more likely to present with thicker tumors and metastases on initial presentation than their white counterparts (P<.001).2,8,9,12-14 The higher risk of death from SCC results from the predominance of lesions on non–sun-exposed areas, particularly the legs and anogenital areas, and within sites of chronic scarring or inflammation.4 Unlike sun-induced SCC, the most commonly observed type of SCC in lighter skin types, SCCs that develop in association with chronic inflammatory or ulcerative processes are aggressive and invasive, and they metastasize to distant sites in 20% to 40% of cases (versus 1%–4% in sun-induced SCC).1,3,4 For all skin cancers, poor access to medical care, patients’ unawareness of their skin cancer risk, lack of adequate skin examinations, and prevalence of lesions on uncommon sites that may be inconspicuous or overlooked have all been suggested to delay diagnosis.1,15,16 Given that more advanced disease is associated with worse outcomes, the implications of this delay are enormous and remain a cause for concern.
The alarming skin cancer mortality rates in patients with skin of color are a call to action for the medical community. The consistent use of full-body skin examinations including close inspection of mucosal, acral, and genital areas for all patients independent of skin type and racial/ethnic background is paramount. Advancing skin cancer education in skin of color populations, such as through distribution of patient-directed educational materials produced by organizations such as the American Academy of Dermatology, Skin Cancer Foundation, and Skin of Color Society, is an important step toward increased public awareness.16 Use of social and traditional media outlets as well as community-directed health outreach campaigns also are important strategies to change the common misconception that darker-skinned individuals do not get skin cancer. We hope that with a multipronged approach, disparities in skin cancer mortality will steadily be eliminated.
- Gloster HM Jr, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760; quiz 761-764.
- Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166:1907-1914.
- Mora RG, Perniciaro C. Cancer of the skin in blacks: I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543.
- Halder RM, Bridgeman-Shah S. Skin cancer in African Americans. Cancer. 1995;75:667-673.
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2013. Bethesda, MD: National Cancer Institute; April 2016. http://seer.cancer.gov/csr/1975_2013/. Updated September 12, 2016. Accessed April 7, 2017.
- Bellows CF, Belafsky P, Fortgang IS, et al. Melanoma in African-Americans: trends in biological behavior and clinical characteristics over two decades. J Surg Oncol. 2001;78:10-16.
- Chen L, Jin S. Trends in mortality rates of cutaneous melanoma in East Asian populations. Peer J. 2014;4:e2809.
- Cress RD, Holly EA. Incidence of cutaneous melanoma among non-Hispanic whites, Hispanics, Asians, and blacks: an analysis of California Cancer Registry data. Cancer Causes Control. 1997;8:246-252.
- Johnson DS, Yamane S, Morita S, et al. Malignant melanoma in non-Caucasians: experience from Hawaii. Surg Clin N Am. 2003;83:275-282.
- Fleming ID, Barnawell JR, Burlison PE, et al. Skin cancer in black patients. Cancer. 1975;35:600-605.
- Weinstock MA. Nonmelanoma skin cancer mortality in the United States, 1969 through 1988. Arch Dermatol. 1993;129:1286-1290.
- Byrd KM, Wilson DC, Hoyler SS. Advanced presentation of melanoma in African Americans. J Am Acad Dermatol. 2004;50:142-143.
- Hu S, Parmet Y, Allen G, et al. Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol. 2009;145:1369-1374.
- Black WC, Goldhahn RT, Wiggins C. Melanoma within a southwestern Hispanic population. Arch Dermatol. 1987;123:1331-1334.
- Harvey VM, Oldfield CW, Chen JT, et al. Melanoma disparities among US Hispanics: use of the social ecological model to contextualize reasons for inequitable outcomes and frame a research agenda [published online August 29, 2016]. J Skin Cancer. 2016;2016:4635740.
- Robinson JK, Joshi KM, Ortiz S, et al. Melanoma knowledge, perception, and awareness in ethnic minorities in Chicago: recommendations regarding education. Psychooncology. 2011;20:313-320.
- Gloster HM Jr, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760; quiz 761-764.
- Cormier JN, Xing Y, Ding M, et al. Ethnic differences among patients with cutaneous melanoma. Arch Intern Med. 2006;166:1907-1914.
- Mora RG, Perniciaro C. Cancer of the skin in blacks: I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543.
- Halder RM, Bridgeman-Shah S. Skin cancer in African Americans. Cancer. 1995;75:667-673.
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2013. Bethesda, MD: National Cancer Institute; April 2016. http://seer.cancer.gov/csr/1975_2013/. Updated September 12, 2016. Accessed April 7, 2017.
- Bellows CF, Belafsky P, Fortgang IS, et al. Melanoma in African-Americans: trends in biological behavior and clinical characteristics over two decades. J Surg Oncol. 2001;78:10-16.
- Chen L, Jin S. Trends in mortality rates of cutaneous melanoma in East Asian populations. Peer J. 2014;4:e2809.
- Cress RD, Holly EA. Incidence of cutaneous melanoma among non-Hispanic whites, Hispanics, Asians, and blacks: an analysis of California Cancer Registry data. Cancer Causes Control. 1997;8:246-252.
- Johnson DS, Yamane S, Morita S, et al. Malignant melanoma in non-Caucasians: experience from Hawaii. Surg Clin N Am. 2003;83:275-282.
- Fleming ID, Barnawell JR, Burlison PE, et al. Skin cancer in black patients. Cancer. 1975;35:600-605.
- Weinstock MA. Nonmelanoma skin cancer mortality in the United States, 1969 through 1988. Arch Dermatol. 1993;129:1286-1290.
- Byrd KM, Wilson DC, Hoyler SS. Advanced presentation of melanoma in African Americans. J Am Acad Dermatol. 2004;50:142-143.
- Hu S, Parmet Y, Allen G, et al. Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol. 2009;145:1369-1374.
- Black WC, Goldhahn RT, Wiggins C. Melanoma within a southwestern Hispanic population. Arch Dermatol. 1987;123:1331-1334.
- Harvey VM, Oldfield CW, Chen JT, et al. Melanoma disparities among US Hispanics: use of the social ecological model to contextualize reasons for inequitable outcomes and frame a research agenda [published online August 29, 2016]. J Skin Cancer. 2016;2016:4635740.
- Robinson JK, Joshi KM, Ortiz S, et al. Melanoma knowledge, perception, and awareness in ethnic minorities in Chicago: recommendations regarding education. Psychooncology. 2011;20:313-320.
Recognizing and Managing Elder Abuse in the Emergency Department
Case
An 85-year-old right-handed woman who recently had been diagnosed with mild cognitive impairment arrived at the ED via emergency medical services (EMS) for evaluation of a reported fall. She was accompanied by her daughter, who resided with the patient and was her primary caregiver. The patient stated that she had tripped on a wet rug in the bathroom of her home, striking her head and face on the edge of the sink without losing consciousness. Her daughter reported that she was not assisting her mother when the fall occurred, but had witnessed the fall from the hallway and called EMS. At the patient’s home, EMS found the patient to be alert, oriented, and ambulatory with normal vital signs that remained stable throughout prehospital transport.
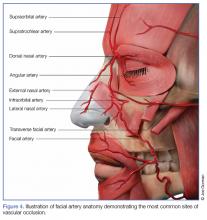
The remainder of the patient’s history was provided almost entirely by her daughter, who constantly interrupted her mother whenever she attempted to directly answer a question or provide information. On physical examination, the patient had bilateral tenderness, edema, and periorbital ecchymoses, and a left eye that was nearly swollen shut. Extraocular movements were normal, visual acuity was intact, and sclerae were noninjected. The patient had tenderness over both maxillary sinuses, and edema and ecchymosis of her left cheek. There was also tenderness, ecchymoses, and edema on the lateral aspects of both forearms, and decreased range of motion of her right lower arm and wrist. With the exception of the patient not knowing the date during the orientation part of the thorough neurological examination, the remainder of the physical examination was unremarkable.
Radiological evaluation found no evidence of traumatic brain injury, but did reveal an acute fracture of the left zygomatic arch, an acute displaced nasal bone fracture, an age-indeterminate fracture of the right zygomatic arch, and an acute right ulnar fracture. Considering all of these findings, particularly the pattern of acute injuries, the emergency physician (EP) considered elder abuse as the possible etiology of the patient’s acute and chronic injuries.
Although the patient had initially agreed with her daughter’s description of the events—including her claim that she had fallen—when the EP questioned the patient alone, she related a history of frequent verbal and less frequent physical abuse by her daughter. The patient further noted that immediately before sustaining the injuries that brought her to the ED, her daughter had been insisting that she sign documents to give her control of her banking and finances. After refusing to sign the papers, the patient said that she and her daughter got into an argument, which she noted “they tended to do frequently.” The patient admitted that during this argument, her daughter struck her in the face repeatedly with the cane that the daughter had grabbed with her right hand.
The EP admitted the patient to the hospital for management of her orthopedic injuries and related pain, and to formulate a safe discharge plan. During admission, additional diagnostic testing revealed multiple old rib fractures, anemia, and a low-serum albumin, which suggested poor nutritional status.
Epidemiology
The term elder abuse refers to harm or the risk of harm to an older adult from either action or negligence committed by someone in a relationship of trust, or when a victim has been targeted because of age or disability. Elder abuse encompasses physical, sexual, or psychological abuse, neglect, and financial exploitation.1-5 Identified victims of elder abuse typically suffer from multiple forms of abuse.1-5
At present, elder abuse annually affects 5% to 10% of community-dwelling older adults,1-6 and nursing-home residents are at increased risk of abuse.7-10 Poor medical outcomes, including depression and dementia,11 and much higher mortality6,12,13 have been linked to victims of elder abuse.
Etiology
When treating older adults, it is critically important for EPs and the ED staff to consider and identify elder abuse in the differential diagnosis.14,15 Presently, only an estimated 1 in 24 cases of abuse is recognized and reported to the authorities,2 and much of the subsequent morbidity and mortality of elder abuse results from poor detection. A visit to the ED for an acute injury or illness may be the only time socially isolated older adults leave their homes.15-17 Additionally, the ED setting is uniquely suited to identify mistreatment, as a patient typically may be evaluated for several hours by providers from multiple disciplines who are able to observe, interact with, and examine the patient.15 The ED already exercises a similar essential role in the identification and initial intervention for both child abuse18,19 and intimate partner violence among younger adults.20,21
Recognition
Unfortunately, at present, ED providers rarely recognize and report elder abuse.22-24 Though the reasons for this are not entirely understood, inadequate training, lack of time and space to conduct complete evaluations, reluctance to become involved with the legal system, and challenges to distinguishing intentional from unintentional injuries may be contributing factors.24,25 A focus on improving EP and ED staff approaches to elder abuse is relevant and timely given the growing elderly population.
Risk Factors
When evaluating elderly patients, providers should consider research suggesting that some older adults may be at particularly high risk for abuse.4,26-29 Notably, individuals who have cognitive impairment are more likely to be victims of abuse.30-32 Health-related demographic characteristics such as poor physical and mental health, substance abuse, low income/socioeconomic status, and social isolation all may increase the potential for mistreatment.
Family History
Similar to situations resulting in intimate partner violence, a family history of abuse and exposure to traumatic events may increase risk, and those responsible for elder abuse often turn out to be spouses, romantic partners, or an adult child living with the elderly parent—though paid caregivers also can be abusive.
Suspicion of abuse should be increased when individuals in caregiving roles have a history or show signs of mental illness, substance abuse, financial dependence on the victim, or caregiver stress. Considering that a caregiver may be overwhelmed is particularly relevant when an elderly patient exhibits behavioral issues.
Medical History
Obtaining a clear and thorough medical history from the patient and caregiver, both together and alone, is paramount to assessing the potential for abuse. Many indicators from the history may suggest the possibility of mistreatment (Table 1)33-37 and although challenging in a busy ED, a comprehensive head-to-toe examination is crucial to adequately assess abuse. Suspicious physical findings and injury patterns of physical abuse, sexual abuse, and neglect are listed in Table 2.33-37 Ongoing research is aimed at improving ED providers’ ability to differentiate accidental injuries, such as fall injuries, from injuries caused by physical elder abuse.
Injury Patterns
Preliminary studies have indicated that physical abuse injuries most commonly occur on the head, neck, and upper extremities.38,39 A study comparing abuse victims to accidental injury sufferers found that abuse victims often had large bruises (>5 cm) on the face, lateral right arm, or posterior torso.40 Preliminary results from a study in progress suggest that injuries to the left periorbital area, neck, and ulnar forearm may be much more common in abuse than in accident.
Imaging Studies
Emergency radiologists are contributing additional concerning findings indicative of elder abuse,38,41,42 such as the concomitant presence of old and new fractures, high-energy fractures inconsistent with the purported mechanism, and distal ulnar diaphyseal fractures.41,42 The ultimate goal is to identify pathognomonic injury patterns similar to those found in child abuse cases, to assist ED providers.
Laboratory Studies
Although there are no laboratory tests to definitively identify abuse or neglect, specific findings that may indicate abuse include anemia, dehydration, malnutrition, hypothermia/hyperthermia, and rhabdomyolysis.43 In addition, inappropriately high- or low-medication levels and the presence of illicit drugs, which are not often checked in elderly patients in the ED, may be a sign of abuse.43
Laboratory studies that reveal undetectable levels of a patient’s prescription medications may indicate a caregiver’s intentional or neglectful withholding of such medications—especially diversion of opioid medications prescribed for painful conditions.43 Likewise, elevated levels of prescribed drugs may point to intentional or unintentional overdose, whereas the presence of nonprescribed drugs or toxins may suggest poisoning.43
Screening Tools
To improve identification of elder abuse in the ED, universal or targeted screening tools are under consideration. Though several screening tools for elder abuse are already available, none have been validated in the ED.15,44,45 Research sponsored by the National Institute of Justice to identify an ED-specific screening tool is ongoing.15
Elder Abuse Suspicion Index
The Elder Abuse Suspicion Index (EASI) is a short screening tool that has been validated for cognitively intact patients being treated in family practice and ambulatory care settings, and may be used in EDs.44 The tool comprises six questions: five for patient response, and a sixth question for clinician response. This tool is available at http://www.nicenet.ca/tools-easi-elder-abuse-suspicion-index.46
Interventional Measures
When elder mistreatment is suspected or confirmed, health care providers must first address any acute medical, traumatic, or psychological issues. Bleeding, orthopedic injuries, metabolic abnormalities, infections, and agitation must be treated and/or stabilized, while neglected or inappropriately managed chronic medical conditions may require treatment.
Hospitalization should be considered for an older adult who needs extended treatment or observation and, in cases of immediate or continued danger of abuse, separation from contact with the suspected abuser. These measures present several challenges, particularly if the suspected abuser is the patient’s health care proxy, in which case early involvement of the hospital’s legal department, social services, and administration may be necessary—especially in navigating the guardianship process.
Engaging security also may be necessary if the patient requires one-to-one patient watch or when the perpetrator must be removed from the ED. Social workers, patient services representatives, and law enforcement officials should be informed when such intervention is necessary.
In instances when a patient is not at risk of immediate harm, interventions can be more individualized. Coordination with primary care physicians (PCPs) must also be facilitated prior to discharge, to ensure consistent longitudinal follow-up care, and social workers should provide any needed out-of-hospital resources to the patient—and caregiver—such as Meals-on-Wheels, medical transportation services, adult day care/senior center participation, and substance abuse treatment.
Patient Decision-Making Capacity
When a patient experiencing abuse declines interventions or services, the EP must evaluate the patient’s decision-making capacity. In unclear cases, a psychiatric evaluation can help to assess decision-making capacity. If the victim is deemed to have capacity with regard to care and/or discharge, the patient’s choice of returning to an unsafe environment must be respected, as is true in instances of intimate partner violence among younger adults—but not in child abuse cases. In such situations, the EP should nevertheless discuss safety planning, offer psychoeducation about violence and abuse, suggest appropriate community referrals, and encourage abused patients to return or call a contact person whenever they desire or feel the need to talk further. For a victim who is deemed not to possess capacity, providers should proceed with treatment considered to be in the best interest of the patient.
Reporting Abuse
Emergency department providers should notify the appropriate authorities when elder abuse is suspected or identified. A report may be made to the local Adult Protective Services (APS), but this agency operates much differently than Child Protective Services. Case workers with APS will not open a case while a patient is in the ED or hospital, as it is deemed a safe environment and any investigation they undertake will only commence upon discharge. Because of this, contacting the local police department prior to discharge should be considered.
Mandatory elder abuse-reporting laws vary from state to state. Health care providers should therefore contact their respective state or city department of health to obtain local legislation.
Multidisciplinary Approach
Ideally, a multidisciplinary, ED-based intervention team modeled on child abuse teams18,19 would help to optimize treatment and ensure the safety and treatment of vulnerable older adults. These teams could conduct thorough medical, forensic, and social work assessments, allowing ED providers to attend to other patients. The team could also assist in arranging for appropriate and safe dispositions. An innovative Vulnerable Elder Protection Team was recently launched at New York-Presbyterian Weill Cornell Medical Center to provide these services, and its impact is currently being evaluated.
Case Conclusion
The EP who treated the patient realized that blows from a blunt object held by a right-handed person would tend to land on the left side of the victim’s face and upper torso, and that a right-handed victim who successfully blocked the blows intended for her face would instead sustain an isolated right ulna or radius midshaft fracture. These findings, together with the concomitant presence of both old and new fractures, led the EP to question the patient alone and, after obtaining a different history of the events that led to the injuries, admit her for further evaluation, treatment, and interventions to prevent continuing abuse.
Summary
Elder abuse has the potential to affect an increasing number of older adults in this growing population, and an ED visit may offer the only opportunity to identify victims and provide intervention, in turn reducing morbidity and mortality. The results of ongoing research will improve the ability of EPs and ED staff to accurately assess the presence or risk of elder abuse and respond more effectively. It is essential that EPs always consider elder abuse and neglect as a possible etiology when evaluating injuries in this population. Moreover, when identified, addressing elder mistreatment may dramatically improve quality of life or save the lives of these vulnerable patients.
1. Elder Mistreatment: Abuse, Neglect, and Exploitation in an Aging America. Bonnie RJ, Wallace RB, eds. Washington, DC: National Academies Press; 2003:1-552. https://www.nap.edu/read/10406/chapter/1. Accessed April 4, 2017.
2. Lifespan of Greater Rochester, Inc; Weill Cornell Medical Center of Cornell University; New York City Department for the Aging. Under the radar: New York state elder abuse prevalence study: self-reported prevalence and documented case surveys 2011.http://ocfs.ny.gov/main/reports/Under%20the%20Radar%2005%2012%2011%20final%20report.pdf. Published May 2011. Accessed April 4, 2017.
3. Connolly MT, Brandl B, Breckman R. The Elder Justice Roadmap: A Stakeholder Initiative to Respond to an Emerging Health, Justice, Financial, and Social Crisis. https://www.justice.gov/elderjustice/file/829266/download. National Center for Elder Abuse. Published January 2014. Accessed April 4, 2017.
4. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297. doi:10.2105/AJPH.2009.163089.
5. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272. doi:10.1016/S0140-6736(04)17144-4.
6. Lachs MS, Pillemer KA. Elder abuse. N Engl J Med. 2015;373(20):1947-1956. doi:10.1056/NEJMra1404688.
7. Ortmann C, Fechner G, Bajanowski T, Brinkmann B. Fatal neglect of the elderly. Int J Legal Med. 2001;114(3):191-193.
8. Schiamberg LB, Oehmke J, Zhang Z, et al. Physical abuse of older adults in nursing homes: a random sample survey of adults with an elderly family member in a nursing home. J Elder Abuse Negl. 2012;24(1):65-83. doi:10.1080/08946566.2011.608056.
9. Rosen T, Pillemer K, Lachs M. Resident-to-resident aggression in long-term care facilities: an understudied problem. Aggress Violent Behav. 2008;13(2):77-87. doi:10.1016/j.avb.2007.12.001.
10. Shinoda-Tagawa T, Leonard R, Pontikas J, McDonough JE, Allen D, Dreyer PI. Resident-to-resident violent incidents in nursing homes. JAMA. 2004;291(5):591-598. doi:10.1001/jama.291.5.591.
11. Dyer CB, Pavlik VN, Murphy KP, Hyman DJ. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205-208.
12. Lachs MS, Williams CS, O’Brien S, Pillemer KA, Charlson ME. The mortality of elder mistreatment. JAMA. 1998;280(5):428-432.
13. Dong XQ, Simon MA, Beck TT, et al. Elder abuse and mortality: the role of psychological and social wellbeing. Gerontology. 2011;57(6):549-658. doi:10.1159/000321881.
14. Stevens TB, Richmond NL, Pereira GF, Shenvi CL, Platts-Mills TF. Prevalence of nonmedical problems among older adults presenting to the emergency department. Acad Emerg Med. 2014;21(6):651-658. doi:10.1111/acem.12395.
15. Rosen T, Hargarten S, Flomenbaum NE, Platts-Mills TF. Identifying elder abuse in the emergency department: toward a multidisciplinary team-based approach. Ann Emerg Med. 2016;68(3):378-382. doi:10.1016/j.annemergmed.2016.01.037.
16. Bond MC, Butler KH. Elder abuse and neglect: definitions, epidemiology, and approaches to emergency department screening. Clin Geriatr Med. 2013;29(1):257-273. doi:10.1016/j.cger.2012.09.004.
17. Heyborne RD. Elder abuse: keeping the unthinkable in the differential. Acad Emerg Med. 2007;14(6):566-567. doi:10.1197/j.aem.2007.01.015.
18. Kistin CJ, Tien I, Bauchner H, Parker V, Leventhal JM. Factors that influence the effectiveness of child protection teams. Pediatrics. 2010;126(1):94-100. doi:10.1542/peds.2009-3446.
19. Hochstadt NJ, Harwicke NJ. How effective is the multidisciplinary approach? A follow-up study. Child Abuse Negl. 1985;9(3):365-372.
20. Choo EK, Gottlieb AS, DeLuca M, Tape C, Colwell L, Zlotnick C. Systematic review of ED-based intimate partner violence intervention research. West J Emerg Med. 2015;16(7):1037-1042. doi:10.5811/westjem.2015.10.27586.
21. Rhodes KV, Rodgers M, Sommers M, et al. Brief motivational intervention for intimate partner violence and heavy drinking in the emergency department: a randomized clinical trial. JAMA. 2015;314(5):466-477. doi:10.1001/jama.2015.8369.
22. Teaster PB, Dugar TA, Mendiondo MS, et al; The National Committee for the Prevention of Elder Abuse; The National Adult Protective Services Association. The 2004 survey of state adult protective services: abuse of adults 60 years of age and older. http://www.napsa-now.org/wp-content/uploads/2012/09/2-14-06-FINAL-60+REPORT.pdf. Published February 2006. Accessed March 10, 2017.
23. Blakely BE, Dolon R. Another look at the helpfulness of occupational groups in the discovery of elder abuse and neglect. J Elder Abuse Negl. 2003;13:1-23.
24. Evans CS, Hunold KM, Rosen T, Platts-Mills TF. Diagnosis of elder abuse in U.S. emergency departments. J Am Geriatr Soc. 2017;65(1):91-97. doi:10.1111/jgs.14480.
25. Jones JS, Veenstra TR, Seamon JP, Krohmer J. Elder mistreatment: national survey of emergency physicians. Ann Emerg Med. 1997;30(4):473-479.
26. Amstadter AB, Zajac K, Strachan M, Hernandez MA, Kilpatrick DG, Acierno R. Prevalence and correlates of elder mistreatment in South Carolina: the South Carolina elder mistreatment study. J Interpers Violence. 2011;26(15):2947-2972. doi:10.1177/0886260510390959.
27. Friedman LS, Avila S, Tanouye K, Joseph K. A case-control study of severe physical abuse of older adults. J Am Geriatr Soc. 2011;59(3):417-422. doi:10.1111/j.1532-5415.2010.03313.x.
28. Pillemer K, Burnes D, Riffin C, Lachs MS. Elder Abuse: global situation, risk factors, and prevention strategies. Gerontologist. 2016;56 Suppl 2:S194-S205. doi:10.1093/geront/gnw004.
29. Laumann EO, Leitsch SA, Waite LJ. Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J Gerontol B Psychol Sci Soc Sci. 2008;63(4):S248-S254.
30. Cooney C, Howard R, Lawlor B. Abuse of vulnerable people with dementia by their carers: can we identify those most at risk? Int J Geriatr Psychiatry. 2006;21(6):564-571. doi:10.1002/gps.1525.
31. Lachs MS, Williams C, O’Brien S, Hurst L, Horwitz R. Risk factors for reported elder abuse and neglect: a nine-year observational cohort study. Gerontologist. 1997;37(4):469-474.
32. Wiglesworth A, Mosqueda L, Mulnard R, Liao S, Gibbs L, Fitzgerald W. Screening for abuse and neglect of people with dementia. J Am Geriatr Soc. 2010;58(3):493-500. doi:10.1111/j.1532-5415.2010.02737.x.
33. Collins KA. Elder maltreatment: a review. Arch Pathol Lab Med. 2006;130(9):1290-1296. doi:10.1043/1543-2165(2006)130[1290:EMAR]2.0.CO;2.
34. Gibbs LM. Understanding the medical markers of elder abuse and neglect: physical examination findings. Clin Geriatr Med. 2014 Nov;30(4):687-712. doi:10.1016/j.cger.2014.08.002.
35. Palmer M, Brodell RT, Mostow EN. Elder abuse: dermatologic clues and critical solutions. J Am Acad Dermatol. 2013;68(2):e37-e42. doi:10.1016/j.jaad.2011.03.016.
36. Speck PM, Hartig MT, Likes W, et al. Case series of sexual assault in older persons. Clin Geriatr Med. 2014;30(4):779-806. doi:10.1016/j.cger.2014.08.007.
37. Chang AL, Wong JW, Endo JO, Norman RA. Geriatric dermatology: part II. Risk factors and cutaneous signs of elder mistreatment for the dermatologist. J Am Acad Dermatol. 2013;68(4):533.e1-.e10. doi:10.1016/j.jaad.2013.01.001.
38. Murphy K, Waa S, Jaffer H, Sauter A, Chan A. A literature review of findings in physical elder abuse. Can Assoc Radiol J. 2013;64(1):10-14. doi:10.1016/j.carj.2012.12.001.
39. Rosen T, Bloemen EM, LoFaso VM, Clark S, Flomenbaum NE, Lachs MS. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. J Emerg Med. 2016;50(3):518-526. doi:10.1016/j.jemermed.2015.10.037.
40. Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc. 2009;57(7):1191-1196. doi:10.1111/j.1532-5415.2009.02330.x.
41. Rosen T, Bloemen EM, Harpe J, et al. Radiologists’ training, experience, and attitudes about elder abuse detection. AJR Am J Roentgenol. 2016;207:1210-1214.
42. Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J. 2017;68(1):16-20. doi:10.1016/j.carj.2016.06.001.
43. LoFaso VM, Rosen T. Medical and laboratory indicators of elder abuse and neglect. Clin Geriatr Med. 2014;30(4):713-28. doi:10.1016/j.cger.2014.08.003.
44. Fulmer T, Guadagno L, Bitondo Dyer C, Connolly MT. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
45. Yaffe MJ, Wolfson C, Lithwick M, Weiss D. Development and validation of a tool to improve physician identification of elder abuse: the Elder Abuse Suspicion Index (EASI). J Elder Abuse Negl. 2008;20(3):276-300. doi:10.1080/08946560801973168.
46. National Initiative for the Care of the Elderly. EASI: Elder Abuse Suspicion Index. http://www.nicenet.ca/tools-easi-elder-abuse-suspicion-index. Accessed April 5, 2017.
Case
An 85-year-old right-handed woman who recently had been diagnosed with mild cognitive impairment arrived at the ED via emergency medical services (EMS) for evaluation of a reported fall. She was accompanied by her daughter, who resided with the patient and was her primary caregiver. The patient stated that she had tripped on a wet rug in the bathroom of her home, striking her head and face on the edge of the sink without losing consciousness. Her daughter reported that she was not assisting her mother when the fall occurred, but had witnessed the fall from the hallway and called EMS. At the patient’s home, EMS found the patient to be alert, oriented, and ambulatory with normal vital signs that remained stable throughout prehospital transport.
The remainder of the patient’s history was provided almost entirely by her daughter, who constantly interrupted her mother whenever she attempted to directly answer a question or provide information. On physical examination, the patient had bilateral tenderness, edema, and periorbital ecchymoses, and a left eye that was nearly swollen shut. Extraocular movements were normal, visual acuity was intact, and sclerae were noninjected. The patient had tenderness over both maxillary sinuses, and edema and ecchymosis of her left cheek. There was also tenderness, ecchymoses, and edema on the lateral aspects of both forearms, and decreased range of motion of her right lower arm and wrist. With the exception of the patient not knowing the date during the orientation part of the thorough neurological examination, the remainder of the physical examination was unremarkable.
Radiological evaluation found no evidence of traumatic brain injury, but did reveal an acute fracture of the left zygomatic arch, an acute displaced nasal bone fracture, an age-indeterminate fracture of the right zygomatic arch, and an acute right ulnar fracture. Considering all of these findings, particularly the pattern of acute injuries, the emergency physician (EP) considered elder abuse as the possible etiology of the patient’s acute and chronic injuries.
Although the patient had initially agreed with her daughter’s description of the events—including her claim that she had fallen—when the EP questioned the patient alone, she related a history of frequent verbal and less frequent physical abuse by her daughter. The patient further noted that immediately before sustaining the injuries that brought her to the ED, her daughter had been insisting that she sign documents to give her control of her banking and finances. After refusing to sign the papers, the patient said that she and her daughter got into an argument, which she noted “they tended to do frequently.” The patient admitted that during this argument, her daughter struck her in the face repeatedly with the cane that the daughter had grabbed with her right hand.
The EP admitted the patient to the hospital for management of her orthopedic injuries and related pain, and to formulate a safe discharge plan. During admission, additional diagnostic testing revealed multiple old rib fractures, anemia, and a low-serum albumin, which suggested poor nutritional status.
Epidemiology
The term elder abuse refers to harm or the risk of harm to an older adult from either action or negligence committed by someone in a relationship of trust, or when a victim has been targeted because of age or disability. Elder abuse encompasses physical, sexual, or psychological abuse, neglect, and financial exploitation.1-5 Identified victims of elder abuse typically suffer from multiple forms of abuse.1-5
At present, elder abuse annually affects 5% to 10% of community-dwelling older adults,1-6 and nursing-home residents are at increased risk of abuse.7-10 Poor medical outcomes, including depression and dementia,11 and much higher mortality6,12,13 have been linked to victims of elder abuse.
Etiology
When treating older adults, it is critically important for EPs and the ED staff to consider and identify elder abuse in the differential diagnosis.14,15 Presently, only an estimated 1 in 24 cases of abuse is recognized and reported to the authorities,2 and much of the subsequent morbidity and mortality of elder abuse results from poor detection. A visit to the ED for an acute injury or illness may be the only time socially isolated older adults leave their homes.15-17 Additionally, the ED setting is uniquely suited to identify mistreatment, as a patient typically may be evaluated for several hours by providers from multiple disciplines who are able to observe, interact with, and examine the patient.15 The ED already exercises a similar essential role in the identification and initial intervention for both child abuse18,19 and intimate partner violence among younger adults.20,21
Recognition
Unfortunately, at present, ED providers rarely recognize and report elder abuse.22-24 Though the reasons for this are not entirely understood, inadequate training, lack of time and space to conduct complete evaluations, reluctance to become involved with the legal system, and challenges to distinguishing intentional from unintentional injuries may be contributing factors.24,25 A focus on improving EP and ED staff approaches to elder abuse is relevant and timely given the growing elderly population.
Risk Factors
When evaluating elderly patients, providers should consider research suggesting that some older adults may be at particularly high risk for abuse.4,26-29 Notably, individuals who have cognitive impairment are more likely to be victims of abuse.30-32 Health-related demographic characteristics such as poor physical and mental health, substance abuse, low income/socioeconomic status, and social isolation all may increase the potential for mistreatment.
Family History
Similar to situations resulting in intimate partner violence, a family history of abuse and exposure to traumatic events may increase risk, and those responsible for elder abuse often turn out to be spouses, romantic partners, or an adult child living with the elderly parent—though paid caregivers also can be abusive.
Suspicion of abuse should be increased when individuals in caregiving roles have a history or show signs of mental illness, substance abuse, financial dependence on the victim, or caregiver stress. Considering that a caregiver may be overwhelmed is particularly relevant when an elderly patient exhibits behavioral issues.
Medical History
Obtaining a clear and thorough medical history from the patient and caregiver, both together and alone, is paramount to assessing the potential for abuse. Many indicators from the history may suggest the possibility of mistreatment (Table 1)33-37 and although challenging in a busy ED, a comprehensive head-to-toe examination is crucial to adequately assess abuse. Suspicious physical findings and injury patterns of physical abuse, sexual abuse, and neglect are listed in Table 2.33-37 Ongoing research is aimed at improving ED providers’ ability to differentiate accidental injuries, such as fall injuries, from injuries caused by physical elder abuse.
Injury Patterns
Preliminary studies have indicated that physical abuse injuries most commonly occur on the head, neck, and upper extremities.38,39 A study comparing abuse victims to accidental injury sufferers found that abuse victims often had large bruises (>5 cm) on the face, lateral right arm, or posterior torso.40 Preliminary results from a study in progress suggest that injuries to the left periorbital area, neck, and ulnar forearm may be much more common in abuse than in accident.
Imaging Studies
Emergency radiologists are contributing additional concerning findings indicative of elder abuse,38,41,42 such as the concomitant presence of old and new fractures, high-energy fractures inconsistent with the purported mechanism, and distal ulnar diaphyseal fractures.41,42 The ultimate goal is to identify pathognomonic injury patterns similar to those found in child abuse cases, to assist ED providers.
Laboratory Studies
Although there are no laboratory tests to definitively identify abuse or neglect, specific findings that may indicate abuse include anemia, dehydration, malnutrition, hypothermia/hyperthermia, and rhabdomyolysis.43 In addition, inappropriately high- or low-medication levels and the presence of illicit drugs, which are not often checked in elderly patients in the ED, may be a sign of abuse.43
Laboratory studies that reveal undetectable levels of a patient’s prescription medications may indicate a caregiver’s intentional or neglectful withholding of such medications—especially diversion of opioid medications prescribed for painful conditions.43 Likewise, elevated levels of prescribed drugs may point to intentional or unintentional overdose, whereas the presence of nonprescribed drugs or toxins may suggest poisoning.43
Screening Tools
To improve identification of elder abuse in the ED, universal or targeted screening tools are under consideration. Though several screening tools for elder abuse are already available, none have been validated in the ED.15,44,45 Research sponsored by the National Institute of Justice to identify an ED-specific screening tool is ongoing.15
Elder Abuse Suspicion Index
The Elder Abuse Suspicion Index (EASI) is a short screening tool that has been validated for cognitively intact patients being treated in family practice and ambulatory care settings, and may be used in EDs.44 The tool comprises six questions: five for patient response, and a sixth question for clinician response. This tool is available at http://www.nicenet.ca/tools-easi-elder-abuse-suspicion-index.46
Interventional Measures
When elder mistreatment is suspected or confirmed, health care providers must first address any acute medical, traumatic, or psychological issues. Bleeding, orthopedic injuries, metabolic abnormalities, infections, and agitation must be treated and/or stabilized, while neglected or inappropriately managed chronic medical conditions may require treatment.
Hospitalization should be considered for an older adult who needs extended treatment or observation and, in cases of immediate or continued danger of abuse, separation from contact with the suspected abuser. These measures present several challenges, particularly if the suspected abuser is the patient’s health care proxy, in which case early involvement of the hospital’s legal department, social services, and administration may be necessary—especially in navigating the guardianship process.
Engaging security also may be necessary if the patient requires one-to-one patient watch or when the perpetrator must be removed from the ED. Social workers, patient services representatives, and law enforcement officials should be informed when such intervention is necessary.
In instances when a patient is not at risk of immediate harm, interventions can be more individualized. Coordination with primary care physicians (PCPs) must also be facilitated prior to discharge, to ensure consistent longitudinal follow-up care, and social workers should provide any needed out-of-hospital resources to the patient—and caregiver—such as Meals-on-Wheels, medical transportation services, adult day care/senior center participation, and substance abuse treatment.
Patient Decision-Making Capacity
When a patient experiencing abuse declines interventions or services, the EP must evaluate the patient’s decision-making capacity. In unclear cases, a psychiatric evaluation can help to assess decision-making capacity. If the victim is deemed to have capacity with regard to care and/or discharge, the patient’s choice of returning to an unsafe environment must be respected, as is true in instances of intimate partner violence among younger adults—but not in child abuse cases. In such situations, the EP should nevertheless discuss safety planning, offer psychoeducation about violence and abuse, suggest appropriate community referrals, and encourage abused patients to return or call a contact person whenever they desire or feel the need to talk further. For a victim who is deemed not to possess capacity, providers should proceed with treatment considered to be in the best interest of the patient.
Reporting Abuse
Emergency department providers should notify the appropriate authorities when elder abuse is suspected or identified. A report may be made to the local Adult Protective Services (APS), but this agency operates much differently than Child Protective Services. Case workers with APS will not open a case while a patient is in the ED or hospital, as it is deemed a safe environment and any investigation they undertake will only commence upon discharge. Because of this, contacting the local police department prior to discharge should be considered.
Mandatory elder abuse-reporting laws vary from state to state. Health care providers should therefore contact their respective state or city department of health to obtain local legislation.
Multidisciplinary Approach
Ideally, a multidisciplinary, ED-based intervention team modeled on child abuse teams18,19 would help to optimize treatment and ensure the safety and treatment of vulnerable older adults. These teams could conduct thorough medical, forensic, and social work assessments, allowing ED providers to attend to other patients. The team could also assist in arranging for appropriate and safe dispositions. An innovative Vulnerable Elder Protection Team was recently launched at New York-Presbyterian Weill Cornell Medical Center to provide these services, and its impact is currently being evaluated.
Case Conclusion
The EP who treated the patient realized that blows from a blunt object held by a right-handed person would tend to land on the left side of the victim’s face and upper torso, and that a right-handed victim who successfully blocked the blows intended for her face would instead sustain an isolated right ulna or radius midshaft fracture. These findings, together with the concomitant presence of both old and new fractures, led the EP to question the patient alone and, after obtaining a different history of the events that led to the injuries, admit her for further evaluation, treatment, and interventions to prevent continuing abuse.
Summary
Elder abuse has the potential to affect an increasing number of older adults in this growing population, and an ED visit may offer the only opportunity to identify victims and provide intervention, in turn reducing morbidity and mortality. The results of ongoing research will improve the ability of EPs and ED staff to accurately assess the presence or risk of elder abuse and respond more effectively. It is essential that EPs always consider elder abuse and neglect as a possible etiology when evaluating injuries in this population. Moreover, when identified, addressing elder mistreatment may dramatically improve quality of life or save the lives of these vulnerable patients.
Case
An 85-year-old right-handed woman who recently had been diagnosed with mild cognitive impairment arrived at the ED via emergency medical services (EMS) for evaluation of a reported fall. She was accompanied by her daughter, who resided with the patient and was her primary caregiver. The patient stated that she had tripped on a wet rug in the bathroom of her home, striking her head and face on the edge of the sink without losing consciousness. Her daughter reported that she was not assisting her mother when the fall occurred, but had witnessed the fall from the hallway and called EMS. At the patient’s home, EMS found the patient to be alert, oriented, and ambulatory with normal vital signs that remained stable throughout prehospital transport.
The remainder of the patient’s history was provided almost entirely by her daughter, who constantly interrupted her mother whenever she attempted to directly answer a question or provide information. On physical examination, the patient had bilateral tenderness, edema, and periorbital ecchymoses, and a left eye that was nearly swollen shut. Extraocular movements were normal, visual acuity was intact, and sclerae were noninjected. The patient had tenderness over both maxillary sinuses, and edema and ecchymosis of her left cheek. There was also tenderness, ecchymoses, and edema on the lateral aspects of both forearms, and decreased range of motion of her right lower arm and wrist. With the exception of the patient not knowing the date during the orientation part of the thorough neurological examination, the remainder of the physical examination was unremarkable.
Radiological evaluation found no evidence of traumatic brain injury, but did reveal an acute fracture of the left zygomatic arch, an acute displaced nasal bone fracture, an age-indeterminate fracture of the right zygomatic arch, and an acute right ulnar fracture. Considering all of these findings, particularly the pattern of acute injuries, the emergency physician (EP) considered elder abuse as the possible etiology of the patient’s acute and chronic injuries.
Although the patient had initially agreed with her daughter’s description of the events—including her claim that she had fallen—when the EP questioned the patient alone, she related a history of frequent verbal and less frequent physical abuse by her daughter. The patient further noted that immediately before sustaining the injuries that brought her to the ED, her daughter had been insisting that she sign documents to give her control of her banking and finances. After refusing to sign the papers, the patient said that she and her daughter got into an argument, which she noted “they tended to do frequently.” The patient admitted that during this argument, her daughter struck her in the face repeatedly with the cane that the daughter had grabbed with her right hand.
The EP admitted the patient to the hospital for management of her orthopedic injuries and related pain, and to formulate a safe discharge plan. During admission, additional diagnostic testing revealed multiple old rib fractures, anemia, and a low-serum albumin, which suggested poor nutritional status.
Epidemiology
The term elder abuse refers to harm or the risk of harm to an older adult from either action or negligence committed by someone in a relationship of trust, or when a victim has been targeted because of age or disability. Elder abuse encompasses physical, sexual, or psychological abuse, neglect, and financial exploitation.1-5 Identified victims of elder abuse typically suffer from multiple forms of abuse.1-5
At present, elder abuse annually affects 5% to 10% of community-dwelling older adults,1-6 and nursing-home residents are at increased risk of abuse.7-10 Poor medical outcomes, including depression and dementia,11 and much higher mortality6,12,13 have been linked to victims of elder abuse.
Etiology
When treating older adults, it is critically important for EPs and the ED staff to consider and identify elder abuse in the differential diagnosis.14,15 Presently, only an estimated 1 in 24 cases of abuse is recognized and reported to the authorities,2 and much of the subsequent morbidity and mortality of elder abuse results from poor detection. A visit to the ED for an acute injury or illness may be the only time socially isolated older adults leave their homes.15-17 Additionally, the ED setting is uniquely suited to identify mistreatment, as a patient typically may be evaluated for several hours by providers from multiple disciplines who are able to observe, interact with, and examine the patient.15 The ED already exercises a similar essential role in the identification and initial intervention for both child abuse18,19 and intimate partner violence among younger adults.20,21
Recognition
Unfortunately, at present, ED providers rarely recognize and report elder abuse.22-24 Though the reasons for this are not entirely understood, inadequate training, lack of time and space to conduct complete evaluations, reluctance to become involved with the legal system, and challenges to distinguishing intentional from unintentional injuries may be contributing factors.24,25 A focus on improving EP and ED staff approaches to elder abuse is relevant and timely given the growing elderly population.
Risk Factors
When evaluating elderly patients, providers should consider research suggesting that some older adults may be at particularly high risk for abuse.4,26-29 Notably, individuals who have cognitive impairment are more likely to be victims of abuse.30-32 Health-related demographic characteristics such as poor physical and mental health, substance abuse, low income/socioeconomic status, and social isolation all may increase the potential for mistreatment.
Family History
Similar to situations resulting in intimate partner violence, a family history of abuse and exposure to traumatic events may increase risk, and those responsible for elder abuse often turn out to be spouses, romantic partners, or an adult child living with the elderly parent—though paid caregivers also can be abusive.
Suspicion of abuse should be increased when individuals in caregiving roles have a history or show signs of mental illness, substance abuse, financial dependence on the victim, or caregiver stress. Considering that a caregiver may be overwhelmed is particularly relevant when an elderly patient exhibits behavioral issues.
Medical History
Obtaining a clear and thorough medical history from the patient and caregiver, both together and alone, is paramount to assessing the potential for abuse. Many indicators from the history may suggest the possibility of mistreatment (Table 1)33-37 and although challenging in a busy ED, a comprehensive head-to-toe examination is crucial to adequately assess abuse. Suspicious physical findings and injury patterns of physical abuse, sexual abuse, and neglect are listed in Table 2.33-37 Ongoing research is aimed at improving ED providers’ ability to differentiate accidental injuries, such as fall injuries, from injuries caused by physical elder abuse.
Injury Patterns
Preliminary studies have indicated that physical abuse injuries most commonly occur on the head, neck, and upper extremities.38,39 A study comparing abuse victims to accidental injury sufferers found that abuse victims often had large bruises (>5 cm) on the face, lateral right arm, or posterior torso.40 Preliminary results from a study in progress suggest that injuries to the left periorbital area, neck, and ulnar forearm may be much more common in abuse than in accident.
Imaging Studies
Emergency radiologists are contributing additional concerning findings indicative of elder abuse,38,41,42 such as the concomitant presence of old and new fractures, high-energy fractures inconsistent with the purported mechanism, and distal ulnar diaphyseal fractures.41,42 The ultimate goal is to identify pathognomonic injury patterns similar to those found in child abuse cases, to assist ED providers.
Laboratory Studies
Although there are no laboratory tests to definitively identify abuse or neglect, specific findings that may indicate abuse include anemia, dehydration, malnutrition, hypothermia/hyperthermia, and rhabdomyolysis.43 In addition, inappropriately high- or low-medication levels and the presence of illicit drugs, which are not often checked in elderly patients in the ED, may be a sign of abuse.43
Laboratory studies that reveal undetectable levels of a patient’s prescription medications may indicate a caregiver’s intentional or neglectful withholding of such medications—especially diversion of opioid medications prescribed for painful conditions.43 Likewise, elevated levels of prescribed drugs may point to intentional or unintentional overdose, whereas the presence of nonprescribed drugs or toxins may suggest poisoning.43
Screening Tools
To improve identification of elder abuse in the ED, universal or targeted screening tools are under consideration. Though several screening tools for elder abuse are already available, none have been validated in the ED.15,44,45 Research sponsored by the National Institute of Justice to identify an ED-specific screening tool is ongoing.15
Elder Abuse Suspicion Index
The Elder Abuse Suspicion Index (EASI) is a short screening tool that has been validated for cognitively intact patients being treated in family practice and ambulatory care settings, and may be used in EDs.44 The tool comprises six questions: five for patient response, and a sixth question for clinician response. This tool is available at http://www.nicenet.ca/tools-easi-elder-abuse-suspicion-index.46
Interventional Measures
When elder mistreatment is suspected or confirmed, health care providers must first address any acute medical, traumatic, or psychological issues. Bleeding, orthopedic injuries, metabolic abnormalities, infections, and agitation must be treated and/or stabilized, while neglected or inappropriately managed chronic medical conditions may require treatment.
Hospitalization should be considered for an older adult who needs extended treatment or observation and, in cases of immediate or continued danger of abuse, separation from contact with the suspected abuser. These measures present several challenges, particularly if the suspected abuser is the patient’s health care proxy, in which case early involvement of the hospital’s legal department, social services, and administration may be necessary—especially in navigating the guardianship process.
Engaging security also may be necessary if the patient requires one-to-one patient watch or when the perpetrator must be removed from the ED. Social workers, patient services representatives, and law enforcement officials should be informed when such intervention is necessary.
In instances when a patient is not at risk of immediate harm, interventions can be more individualized. Coordination with primary care physicians (PCPs) must also be facilitated prior to discharge, to ensure consistent longitudinal follow-up care, and social workers should provide any needed out-of-hospital resources to the patient—and caregiver—such as Meals-on-Wheels, medical transportation services, adult day care/senior center participation, and substance abuse treatment.
Patient Decision-Making Capacity
When a patient experiencing abuse declines interventions or services, the EP must evaluate the patient’s decision-making capacity. In unclear cases, a psychiatric evaluation can help to assess decision-making capacity. If the victim is deemed to have capacity with regard to care and/or discharge, the patient’s choice of returning to an unsafe environment must be respected, as is true in instances of intimate partner violence among younger adults—but not in child abuse cases. In such situations, the EP should nevertheless discuss safety planning, offer psychoeducation about violence and abuse, suggest appropriate community referrals, and encourage abused patients to return or call a contact person whenever they desire or feel the need to talk further. For a victim who is deemed not to possess capacity, providers should proceed with treatment considered to be in the best interest of the patient.
Reporting Abuse
Emergency department providers should notify the appropriate authorities when elder abuse is suspected or identified. A report may be made to the local Adult Protective Services (APS), but this agency operates much differently than Child Protective Services. Case workers with APS will not open a case while a patient is in the ED or hospital, as it is deemed a safe environment and any investigation they undertake will only commence upon discharge. Because of this, contacting the local police department prior to discharge should be considered.
Mandatory elder abuse-reporting laws vary from state to state. Health care providers should therefore contact their respective state or city department of health to obtain local legislation.
Multidisciplinary Approach
Ideally, a multidisciplinary, ED-based intervention team modeled on child abuse teams18,19 would help to optimize treatment and ensure the safety and treatment of vulnerable older adults. These teams could conduct thorough medical, forensic, and social work assessments, allowing ED providers to attend to other patients. The team could also assist in arranging for appropriate and safe dispositions. An innovative Vulnerable Elder Protection Team was recently launched at New York-Presbyterian Weill Cornell Medical Center to provide these services, and its impact is currently being evaluated.
Case Conclusion
The EP who treated the patient realized that blows from a blunt object held by a right-handed person would tend to land on the left side of the victim’s face and upper torso, and that a right-handed victim who successfully blocked the blows intended for her face would instead sustain an isolated right ulna or radius midshaft fracture. These findings, together with the concomitant presence of both old and new fractures, led the EP to question the patient alone and, after obtaining a different history of the events that led to the injuries, admit her for further evaluation, treatment, and interventions to prevent continuing abuse.
Summary
Elder abuse has the potential to affect an increasing number of older adults in this growing population, and an ED visit may offer the only opportunity to identify victims and provide intervention, in turn reducing morbidity and mortality. The results of ongoing research will improve the ability of EPs and ED staff to accurately assess the presence or risk of elder abuse and respond more effectively. It is essential that EPs always consider elder abuse and neglect as a possible etiology when evaluating injuries in this population. Moreover, when identified, addressing elder mistreatment may dramatically improve quality of life or save the lives of these vulnerable patients.
1. Elder Mistreatment: Abuse, Neglect, and Exploitation in an Aging America. Bonnie RJ, Wallace RB, eds. Washington, DC: National Academies Press; 2003:1-552. https://www.nap.edu/read/10406/chapter/1. Accessed April 4, 2017.
2. Lifespan of Greater Rochester, Inc; Weill Cornell Medical Center of Cornell University; New York City Department for the Aging. Under the radar: New York state elder abuse prevalence study: self-reported prevalence and documented case surveys 2011.http://ocfs.ny.gov/main/reports/Under%20the%20Radar%2005%2012%2011%20final%20report.pdf. Published May 2011. Accessed April 4, 2017.
3. Connolly MT, Brandl B, Breckman R. The Elder Justice Roadmap: A Stakeholder Initiative to Respond to an Emerging Health, Justice, Financial, and Social Crisis. https://www.justice.gov/elderjustice/file/829266/download. National Center for Elder Abuse. Published January 2014. Accessed April 4, 2017.
4. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297. doi:10.2105/AJPH.2009.163089.
5. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272. doi:10.1016/S0140-6736(04)17144-4.
6. Lachs MS, Pillemer KA. Elder abuse. N Engl J Med. 2015;373(20):1947-1956. doi:10.1056/NEJMra1404688.
7. Ortmann C, Fechner G, Bajanowski T, Brinkmann B. Fatal neglect of the elderly. Int J Legal Med. 2001;114(3):191-193.
8. Schiamberg LB, Oehmke J, Zhang Z, et al. Physical abuse of older adults in nursing homes: a random sample survey of adults with an elderly family member in a nursing home. J Elder Abuse Negl. 2012;24(1):65-83. doi:10.1080/08946566.2011.608056.
9. Rosen T, Pillemer K, Lachs M. Resident-to-resident aggression in long-term care facilities: an understudied problem. Aggress Violent Behav. 2008;13(2):77-87. doi:10.1016/j.avb.2007.12.001.
10. Shinoda-Tagawa T, Leonard R, Pontikas J, McDonough JE, Allen D, Dreyer PI. Resident-to-resident violent incidents in nursing homes. JAMA. 2004;291(5):591-598. doi:10.1001/jama.291.5.591.
11. Dyer CB, Pavlik VN, Murphy KP, Hyman DJ. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205-208.
12. Lachs MS, Williams CS, O’Brien S, Pillemer KA, Charlson ME. The mortality of elder mistreatment. JAMA. 1998;280(5):428-432.
13. Dong XQ, Simon MA, Beck TT, et al. Elder abuse and mortality: the role of psychological and social wellbeing. Gerontology. 2011;57(6):549-658. doi:10.1159/000321881.
14. Stevens TB, Richmond NL, Pereira GF, Shenvi CL, Platts-Mills TF. Prevalence of nonmedical problems among older adults presenting to the emergency department. Acad Emerg Med. 2014;21(6):651-658. doi:10.1111/acem.12395.
15. Rosen T, Hargarten S, Flomenbaum NE, Platts-Mills TF. Identifying elder abuse in the emergency department: toward a multidisciplinary team-based approach. Ann Emerg Med. 2016;68(3):378-382. doi:10.1016/j.annemergmed.2016.01.037.
16. Bond MC, Butler KH. Elder abuse and neglect: definitions, epidemiology, and approaches to emergency department screening. Clin Geriatr Med. 2013;29(1):257-273. doi:10.1016/j.cger.2012.09.004.
17. Heyborne RD. Elder abuse: keeping the unthinkable in the differential. Acad Emerg Med. 2007;14(6):566-567. doi:10.1197/j.aem.2007.01.015.
18. Kistin CJ, Tien I, Bauchner H, Parker V, Leventhal JM. Factors that influence the effectiveness of child protection teams. Pediatrics. 2010;126(1):94-100. doi:10.1542/peds.2009-3446.
19. Hochstadt NJ, Harwicke NJ. How effective is the multidisciplinary approach? A follow-up study. Child Abuse Negl. 1985;9(3):365-372.
20. Choo EK, Gottlieb AS, DeLuca M, Tape C, Colwell L, Zlotnick C. Systematic review of ED-based intimate partner violence intervention research. West J Emerg Med. 2015;16(7):1037-1042. doi:10.5811/westjem.2015.10.27586.
21. Rhodes KV, Rodgers M, Sommers M, et al. Brief motivational intervention for intimate partner violence and heavy drinking in the emergency department: a randomized clinical trial. JAMA. 2015;314(5):466-477. doi:10.1001/jama.2015.8369.
22. Teaster PB, Dugar TA, Mendiondo MS, et al; The National Committee for the Prevention of Elder Abuse; The National Adult Protective Services Association. The 2004 survey of state adult protective services: abuse of adults 60 years of age and older. http://www.napsa-now.org/wp-content/uploads/2012/09/2-14-06-FINAL-60+REPORT.pdf. Published February 2006. Accessed March 10, 2017.
23. Blakely BE, Dolon R. Another look at the helpfulness of occupational groups in the discovery of elder abuse and neglect. J Elder Abuse Negl. 2003;13:1-23.
24. Evans CS, Hunold KM, Rosen T, Platts-Mills TF. Diagnosis of elder abuse in U.S. emergency departments. J Am Geriatr Soc. 2017;65(1):91-97. doi:10.1111/jgs.14480.
25. Jones JS, Veenstra TR, Seamon JP, Krohmer J. Elder mistreatment: national survey of emergency physicians. Ann Emerg Med. 1997;30(4):473-479.
26. Amstadter AB, Zajac K, Strachan M, Hernandez MA, Kilpatrick DG, Acierno R. Prevalence and correlates of elder mistreatment in South Carolina: the South Carolina elder mistreatment study. J Interpers Violence. 2011;26(15):2947-2972. doi:10.1177/0886260510390959.
27. Friedman LS, Avila S, Tanouye K, Joseph K. A case-control study of severe physical abuse of older adults. J Am Geriatr Soc. 2011;59(3):417-422. doi:10.1111/j.1532-5415.2010.03313.x.
28. Pillemer K, Burnes D, Riffin C, Lachs MS. Elder Abuse: global situation, risk factors, and prevention strategies. Gerontologist. 2016;56 Suppl 2:S194-S205. doi:10.1093/geront/gnw004.
29. Laumann EO, Leitsch SA, Waite LJ. Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J Gerontol B Psychol Sci Soc Sci. 2008;63(4):S248-S254.
30. Cooney C, Howard R, Lawlor B. Abuse of vulnerable people with dementia by their carers: can we identify those most at risk? Int J Geriatr Psychiatry. 2006;21(6):564-571. doi:10.1002/gps.1525.
31. Lachs MS, Williams C, O’Brien S, Hurst L, Horwitz R. Risk factors for reported elder abuse and neglect: a nine-year observational cohort study. Gerontologist. 1997;37(4):469-474.
32. Wiglesworth A, Mosqueda L, Mulnard R, Liao S, Gibbs L, Fitzgerald W. Screening for abuse and neglect of people with dementia. J Am Geriatr Soc. 2010;58(3):493-500. doi:10.1111/j.1532-5415.2010.02737.x.
33. Collins KA. Elder maltreatment: a review. Arch Pathol Lab Med. 2006;130(9):1290-1296. doi:10.1043/1543-2165(2006)130[1290:EMAR]2.0.CO;2.
34. Gibbs LM. Understanding the medical markers of elder abuse and neglect: physical examination findings. Clin Geriatr Med. 2014 Nov;30(4):687-712. doi:10.1016/j.cger.2014.08.002.
35. Palmer M, Brodell RT, Mostow EN. Elder abuse: dermatologic clues and critical solutions. J Am Acad Dermatol. 2013;68(2):e37-e42. doi:10.1016/j.jaad.2011.03.016.
36. Speck PM, Hartig MT, Likes W, et al. Case series of sexual assault in older persons. Clin Geriatr Med. 2014;30(4):779-806. doi:10.1016/j.cger.2014.08.007.
37. Chang AL, Wong JW, Endo JO, Norman RA. Geriatric dermatology: part II. Risk factors and cutaneous signs of elder mistreatment for the dermatologist. J Am Acad Dermatol. 2013;68(4):533.e1-.e10. doi:10.1016/j.jaad.2013.01.001.
38. Murphy K, Waa S, Jaffer H, Sauter A, Chan A. A literature review of findings in physical elder abuse. Can Assoc Radiol J. 2013;64(1):10-14. doi:10.1016/j.carj.2012.12.001.
39. Rosen T, Bloemen EM, LoFaso VM, Clark S, Flomenbaum NE, Lachs MS. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. J Emerg Med. 2016;50(3):518-526. doi:10.1016/j.jemermed.2015.10.037.
40. Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc. 2009;57(7):1191-1196. doi:10.1111/j.1532-5415.2009.02330.x.
41. Rosen T, Bloemen EM, Harpe J, et al. Radiologists’ training, experience, and attitudes about elder abuse detection. AJR Am J Roentgenol. 2016;207:1210-1214.
42. Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J. 2017;68(1):16-20. doi:10.1016/j.carj.2016.06.001.
43. LoFaso VM, Rosen T. Medical and laboratory indicators of elder abuse and neglect. Clin Geriatr Med. 2014;30(4):713-28. doi:10.1016/j.cger.2014.08.003.
44. Fulmer T, Guadagno L, Bitondo Dyer C, Connolly MT. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
45. Yaffe MJ, Wolfson C, Lithwick M, Weiss D. Development and validation of a tool to improve physician identification of elder abuse: the Elder Abuse Suspicion Index (EASI). J Elder Abuse Negl. 2008;20(3):276-300. doi:10.1080/08946560801973168.
46. National Initiative for the Care of the Elderly. EASI: Elder Abuse Suspicion Index. http://www.nicenet.ca/tools-easi-elder-abuse-suspicion-index. Accessed April 5, 2017.
1. Elder Mistreatment: Abuse, Neglect, and Exploitation in an Aging America. Bonnie RJ, Wallace RB, eds. Washington, DC: National Academies Press; 2003:1-552. https://www.nap.edu/read/10406/chapter/1. Accessed April 4, 2017.
2. Lifespan of Greater Rochester, Inc; Weill Cornell Medical Center of Cornell University; New York City Department for the Aging. Under the radar: New York state elder abuse prevalence study: self-reported prevalence and documented case surveys 2011.http://ocfs.ny.gov/main/reports/Under%20the%20Radar%2005%2012%2011%20final%20report.pdf. Published May 2011. Accessed April 4, 2017.
3. Connolly MT, Brandl B, Breckman R. The Elder Justice Roadmap: A Stakeholder Initiative to Respond to an Emerging Health, Justice, Financial, and Social Crisis. https://www.justice.gov/elderjustice/file/829266/download. National Center for Elder Abuse. Published January 2014. Accessed April 4, 2017.
4. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297. doi:10.2105/AJPH.2009.163089.
5. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272. doi:10.1016/S0140-6736(04)17144-4.
6. Lachs MS, Pillemer KA. Elder abuse. N Engl J Med. 2015;373(20):1947-1956. doi:10.1056/NEJMra1404688.
7. Ortmann C, Fechner G, Bajanowski T, Brinkmann B. Fatal neglect of the elderly. Int J Legal Med. 2001;114(3):191-193.
8. Schiamberg LB, Oehmke J, Zhang Z, et al. Physical abuse of older adults in nursing homes: a random sample survey of adults with an elderly family member in a nursing home. J Elder Abuse Negl. 2012;24(1):65-83. doi:10.1080/08946566.2011.608056.
9. Rosen T, Pillemer K, Lachs M. Resident-to-resident aggression in long-term care facilities: an understudied problem. Aggress Violent Behav. 2008;13(2):77-87. doi:10.1016/j.avb.2007.12.001.
10. Shinoda-Tagawa T, Leonard R, Pontikas J, McDonough JE, Allen D, Dreyer PI. Resident-to-resident violent incidents in nursing homes. JAMA. 2004;291(5):591-598. doi:10.1001/jama.291.5.591.
11. Dyer CB, Pavlik VN, Murphy KP, Hyman DJ. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205-208.
12. Lachs MS, Williams CS, O’Brien S, Pillemer KA, Charlson ME. The mortality of elder mistreatment. JAMA. 1998;280(5):428-432.
13. Dong XQ, Simon MA, Beck TT, et al. Elder abuse and mortality: the role of psychological and social wellbeing. Gerontology. 2011;57(6):549-658. doi:10.1159/000321881.
14. Stevens TB, Richmond NL, Pereira GF, Shenvi CL, Platts-Mills TF. Prevalence of nonmedical problems among older adults presenting to the emergency department. Acad Emerg Med. 2014;21(6):651-658. doi:10.1111/acem.12395.
15. Rosen T, Hargarten S, Flomenbaum NE, Platts-Mills TF. Identifying elder abuse in the emergency department: toward a multidisciplinary team-based approach. Ann Emerg Med. 2016;68(3):378-382. doi:10.1016/j.annemergmed.2016.01.037.
16. Bond MC, Butler KH. Elder abuse and neglect: definitions, epidemiology, and approaches to emergency department screening. Clin Geriatr Med. 2013;29(1):257-273. doi:10.1016/j.cger.2012.09.004.
17. Heyborne RD. Elder abuse: keeping the unthinkable in the differential. Acad Emerg Med. 2007;14(6):566-567. doi:10.1197/j.aem.2007.01.015.
18. Kistin CJ, Tien I, Bauchner H, Parker V, Leventhal JM. Factors that influence the effectiveness of child protection teams. Pediatrics. 2010;126(1):94-100. doi:10.1542/peds.2009-3446.
19. Hochstadt NJ, Harwicke NJ. How effective is the multidisciplinary approach? A follow-up study. Child Abuse Negl. 1985;9(3):365-372.
20. Choo EK, Gottlieb AS, DeLuca M, Tape C, Colwell L, Zlotnick C. Systematic review of ED-based intimate partner violence intervention research. West J Emerg Med. 2015;16(7):1037-1042. doi:10.5811/westjem.2015.10.27586.
21. Rhodes KV, Rodgers M, Sommers M, et al. Brief motivational intervention for intimate partner violence and heavy drinking in the emergency department: a randomized clinical trial. JAMA. 2015;314(5):466-477. doi:10.1001/jama.2015.8369.
22. Teaster PB, Dugar TA, Mendiondo MS, et al; The National Committee for the Prevention of Elder Abuse; The National Adult Protective Services Association. The 2004 survey of state adult protective services: abuse of adults 60 years of age and older. http://www.napsa-now.org/wp-content/uploads/2012/09/2-14-06-FINAL-60+REPORT.pdf. Published February 2006. Accessed March 10, 2017.
23. Blakely BE, Dolon R. Another look at the helpfulness of occupational groups in the discovery of elder abuse and neglect. J Elder Abuse Negl. 2003;13:1-23.
24. Evans CS, Hunold KM, Rosen T, Platts-Mills TF. Diagnosis of elder abuse in U.S. emergency departments. J Am Geriatr Soc. 2017;65(1):91-97. doi:10.1111/jgs.14480.
25. Jones JS, Veenstra TR, Seamon JP, Krohmer J. Elder mistreatment: national survey of emergency physicians. Ann Emerg Med. 1997;30(4):473-479.
26. Amstadter AB, Zajac K, Strachan M, Hernandez MA, Kilpatrick DG, Acierno R. Prevalence and correlates of elder mistreatment in South Carolina: the South Carolina elder mistreatment study. J Interpers Violence. 2011;26(15):2947-2972. doi:10.1177/0886260510390959.
27. Friedman LS, Avila S, Tanouye K, Joseph K. A case-control study of severe physical abuse of older adults. J Am Geriatr Soc. 2011;59(3):417-422. doi:10.1111/j.1532-5415.2010.03313.x.
28. Pillemer K, Burnes D, Riffin C, Lachs MS. Elder Abuse: global situation, risk factors, and prevention strategies. Gerontologist. 2016;56 Suppl 2:S194-S205. doi:10.1093/geront/gnw004.
29. Laumann EO, Leitsch SA, Waite LJ. Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J Gerontol B Psychol Sci Soc Sci. 2008;63(4):S248-S254.
30. Cooney C, Howard R, Lawlor B. Abuse of vulnerable people with dementia by their carers: can we identify those most at risk? Int J Geriatr Psychiatry. 2006;21(6):564-571. doi:10.1002/gps.1525.
31. Lachs MS, Williams C, O’Brien S, Hurst L, Horwitz R. Risk factors for reported elder abuse and neglect: a nine-year observational cohort study. Gerontologist. 1997;37(4):469-474.
32. Wiglesworth A, Mosqueda L, Mulnard R, Liao S, Gibbs L, Fitzgerald W. Screening for abuse and neglect of people with dementia. J Am Geriatr Soc. 2010;58(3):493-500. doi:10.1111/j.1532-5415.2010.02737.x.
33. Collins KA. Elder maltreatment: a review. Arch Pathol Lab Med. 2006;130(9):1290-1296. doi:10.1043/1543-2165(2006)130[1290:EMAR]2.0.CO;2.
34. Gibbs LM. Understanding the medical markers of elder abuse and neglect: physical examination findings. Clin Geriatr Med. 2014 Nov;30(4):687-712. doi:10.1016/j.cger.2014.08.002.
35. Palmer M, Brodell RT, Mostow EN. Elder abuse: dermatologic clues and critical solutions. J Am Acad Dermatol. 2013;68(2):e37-e42. doi:10.1016/j.jaad.2011.03.016.
36. Speck PM, Hartig MT, Likes W, et al. Case series of sexual assault in older persons. Clin Geriatr Med. 2014;30(4):779-806. doi:10.1016/j.cger.2014.08.007.
37. Chang AL, Wong JW, Endo JO, Norman RA. Geriatric dermatology: part II. Risk factors and cutaneous signs of elder mistreatment for the dermatologist. J Am Acad Dermatol. 2013;68(4):533.e1-.e10. doi:10.1016/j.jaad.2013.01.001.
38. Murphy K, Waa S, Jaffer H, Sauter A, Chan A. A literature review of findings in physical elder abuse. Can Assoc Radiol J. 2013;64(1):10-14. doi:10.1016/j.carj.2012.12.001.
39. Rosen T, Bloemen EM, LoFaso VM, Clark S, Flomenbaum NE, Lachs MS. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. J Emerg Med. 2016;50(3):518-526. doi:10.1016/j.jemermed.2015.10.037.
40. Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc. 2009;57(7):1191-1196. doi:10.1111/j.1532-5415.2009.02330.x.
41. Rosen T, Bloemen EM, Harpe J, et al. Radiologists’ training, experience, and attitudes about elder abuse detection. AJR Am J Roentgenol. 2016;207:1210-1214.
42. Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J. 2017;68(1):16-20. doi:10.1016/j.carj.2016.06.001.
43. LoFaso VM, Rosen T. Medical and laboratory indicators of elder abuse and neglect. Clin Geriatr Med. 2014;30(4):713-28. doi:10.1016/j.cger.2014.08.003.
44. Fulmer T, Guadagno L, Bitondo Dyer C, Connolly MT. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
45. Yaffe MJ, Wolfson C, Lithwick M, Weiss D. Development and validation of a tool to improve physician identification of elder abuse: the Elder Abuse Suspicion Index (EASI). J Elder Abuse Negl. 2008;20(3):276-300. doi:10.1080/08946560801973168.
46. National Initiative for the Care of the Elderly. EASI: Elder Abuse Suspicion Index. http://www.nicenet.ca/tools-easi-elder-abuse-suspicion-index. Accessed April 5, 2017.
Case Studies in Toxicology: Angioedema Post-tPA: Hemorrhage Is Not the Only Risk Factor
Case
A 49-year-old man with a history of hypertension, for which he was taking aspirin, carvedilol, hydralazine, and nifedipine, presented to the ED with complaints of left-sided weakness that started 3 hours before he came to the ED. Initial vital signs were: blood pressure, 158/90 mm Hg; heart rate, 74 beats/min; respiratory rate, 18 breaths/min; and temperature, 98°F. Oxygen saturation was 100% on room air, and a finger-stick glucose test was 106 mg/dL.
Physical examination revealed slowed speech with mild dysarthria, mild left facial droop, 2/5 strength in all muscle groups in the left upper and lower extremities, and decreased sensation to light touch on the left side. The patient also had left-sided sensory neglect and an abnormal gait, and dragged his left foot on the floor when walking. The rest of his examination was normal.
The stroke team was activated, and the patient was immediately transferred to the ED radiology department for imaging studies. A noncontrast head computed tomography (CT) was negative for any acute intracranial hemorrhage or cerebral edema. A CT angiogram (CTA) also was performed, which revealed atherosclerosis but no arterial occlusion. Based on these findings and the existing protocol, the patient received an intravenous (IV) bolus of tissue plasminogen activator (tPA). Approximately 17 minutes after tPA administration, the patient developed left-sided upper and lower lip swelling. There was no voice change, tongue swelling, or uvular deviation.
What is the differential diagnosis of swelling of the lip?
The differential diagnoses for lip swelling includes trauma, allergic reaction, and angioedema (hereditary, or angiotensin converting enzyme inhibitor [ACEI]-induced). The patient in this case denied any trauma to the lip, and no bleeding was noted from the lip; however, his entire left lip (upper and lower) was swollen. He was not taking any ACEIs or angiotensin-receptor blockers (ARBs). He also denied a family history of angioedema or any prior similar episodes. The patient further denied exposure to any new medications, foods, or other substances and had no respiratory distress, urticaria, or other findings consistent with an allergy.
What are the common adverse effects of tPA?
The only US Food and Drug-approved pharmacological treatment for ischemic stroke is tPA (also known as IV rtPA). Tissue plasminogen activator hydrolyzes plasminogen to plasmin, which exerts a fibrinolytic effect. Based on the ability of tPA to lyse thrombus, it is also a standard therapy for hemodynamically unstable patients with confirmed pulmonary embolism, as well as for patients with myocardial infarction in whom percutaneous intervention is contraindicated or unavailable. Despite the beneficial effects of tPA, significant adverse effects are associated with the drug. For example, thrombolysis may result in conversion of an ischemic stroke into a hemorrhagic event, resulting in generalized bleeding from mucosal surfaces.
The increase in plasmin may play a role in the development of angioedema by activating the kinin pathway, leading to the formation of the vasodilator bradykinin (Figure). Plasmin also activates the complement system and leads to the production of anaphylatoxins C3a, C4a, and C5a, which also cause mast cell degranulation and histamine release.1
When does post-tPA angioedema occur?
In the few published case reports available, tPA-induced angioedema was shown to typically occur in the stroke distribution (which was attributed to the left-sided swelling in this patient).2 Following tPA administration, the onset of angioedema reportedly varies from as early as 10 to 15 minutes from initiation until about 1 hour postinfusion. The short half-life of tPA (approximately 7 minutes)2 limits the outer- time window for the initial development of angioedema, but progression can continue well beyond this timeframe.
What is the treatment for tPA-induced angioedema?
The first priority of acute management of angioedema is discontinuation of the inciting substance, if possible—in this case, the tPA infusion.3 Assessment and maintenance of a patent airway are of utmost concern. Patients with posterior oropharyngeal effects or who are progressing should be admitted to an intensive care unit (ICU) for observation.4-6
Endotracheal Intubation. Providers should have a low threshold for endotracheal intubation, which should ideally be performed in any patient at risk for airway compromise.4 Due to the extensive airway swelling that can occur in the setting of angioedema, airway intervention should optimally be performed by an available clinician with the most skill and experience in this area. It is wise to be prepared to utilize advanced airway techniques, if available, including fiberoptic laryngoscopy or potentially cricothyrotomy.
Histamine Agonists. Standard therapy for patients who develop angioedema should include histamine antagonists, such as diphenhydramine (H1 antagonist) and famotidine (H2 antagonist) along with corticosteroids. Although these therapies are unlikely to be helpful in the treatment of tPA-induced angioedema, the difficulty in excluding allergic angioedema and the low risk of adverse effects associated with these medications support their use.
Fresh Frozen Plasma. Fresh frozen plasma (FFP) should be considered for patients who have a history of hereditary angioedema. Fresh frozen plasma contains enzymes that degrade bradykinin. Although FFP has been used successfully in the treatment of ACEI-induced angioedema, its use (or benefit) in tPA-related cases is not clear.
Icatibant. A selective bradykinin B2-receptor antagonist, icatibant has been used to treat patients with ACEI-induced angioedema because of its effects on bradykinin receptors. Comparison of the efficacy of icatibant to the prevailing treatment strategy of diphenhydramine, famotidine, and methylprednisolone found a shorter time to symptom relief with icatibant.7 However, icatibant is extremely expensive ($23,000/30 mg). As previously mentioned, based on its similar mechanism of action, lower cost, and safety profile, FFP can be given (off label) in this situation.
Case Conclusion
The patient was given diphenhydramine, famotidine, and methylprednisolone, but did not show any improvement. His upper/lower lip swelling continued to worsen, and 30 minutes after the onset of angioedema, he was unable to open his mouth more than 1 cm.
Multiple attempts to perform awake fiberoptic intubation failed due to inadequate sedation; however, intubation was successfully performed following light sedation. The patient self-extubated in the ICU on hospital day 3, and the angioedema had progressively decreased. Angioedema and weakness completely resolved by hospital day 4, and he was discharged home on hospital day 7.
1. Molinaro G, Gervais N, Adam A. Biochemical basis of angioedema associated with recombinant tissue plasminogen activator treatment: an in vitro experimental approach. Stroke. 2002;33(6):1712-1716.
2. Madden B, Chebl RB. Hemi orolingual angioedema after tPA administration for acute ischemic stroke. West J Emerg Med. 2015;16(1):175-177. doi:10.5811/westjem.2014.12.24210.
3. Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-1527.
4. Temiño VM, Peebles RS Jr. The spectrum and treatment of angioedema. Am J Med. 2008;121(4):282-286. doi:10.1016/j.amjmed.2007.09.024.
5. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281-1284.
6. Maertins M, Wold R, Swider M. Angioedema after administration of tPA for ischemic stroke: case report. Air Med J. 2011;30(5):276-278. doi:10.1016/j.amj.2010.12.011.
7. Baş M, Greve J, Stelter K, et al. A randomized trial of icatibant in ACE-inhibitor-induced angioedema. N Engl J Med. 2015;372(5):418-425. doi:10.1056/NEJMoa1312524.
Case
A 49-year-old man with a history of hypertension, for which he was taking aspirin, carvedilol, hydralazine, and nifedipine, presented to the ED with complaints of left-sided weakness that started 3 hours before he came to the ED. Initial vital signs were: blood pressure, 158/90 mm Hg; heart rate, 74 beats/min; respiratory rate, 18 breaths/min; and temperature, 98°F. Oxygen saturation was 100% on room air, and a finger-stick glucose test was 106 mg/dL.
Physical examination revealed slowed speech with mild dysarthria, mild left facial droop, 2/5 strength in all muscle groups in the left upper and lower extremities, and decreased sensation to light touch on the left side. The patient also had left-sided sensory neglect and an abnormal gait, and dragged his left foot on the floor when walking. The rest of his examination was normal.
The stroke team was activated, and the patient was immediately transferred to the ED radiology department for imaging studies. A noncontrast head computed tomography (CT) was negative for any acute intracranial hemorrhage or cerebral edema. A CT angiogram (CTA) also was performed, which revealed atherosclerosis but no arterial occlusion. Based on these findings and the existing protocol, the patient received an intravenous (IV) bolus of tissue plasminogen activator (tPA). Approximately 17 minutes after tPA administration, the patient developed left-sided upper and lower lip swelling. There was no voice change, tongue swelling, or uvular deviation.
What is the differential diagnosis of swelling of the lip?
The differential diagnoses for lip swelling includes trauma, allergic reaction, and angioedema (hereditary, or angiotensin converting enzyme inhibitor [ACEI]-induced). The patient in this case denied any trauma to the lip, and no bleeding was noted from the lip; however, his entire left lip (upper and lower) was swollen. He was not taking any ACEIs or angiotensin-receptor blockers (ARBs). He also denied a family history of angioedema or any prior similar episodes. The patient further denied exposure to any new medications, foods, or other substances and had no respiratory distress, urticaria, or other findings consistent with an allergy.
What are the common adverse effects of tPA?
The only US Food and Drug-approved pharmacological treatment for ischemic stroke is tPA (also known as IV rtPA). Tissue plasminogen activator hydrolyzes plasminogen to plasmin, which exerts a fibrinolytic effect. Based on the ability of tPA to lyse thrombus, it is also a standard therapy for hemodynamically unstable patients with confirmed pulmonary embolism, as well as for patients with myocardial infarction in whom percutaneous intervention is contraindicated or unavailable. Despite the beneficial effects of tPA, significant adverse effects are associated with the drug. For example, thrombolysis may result in conversion of an ischemic stroke into a hemorrhagic event, resulting in generalized bleeding from mucosal surfaces.
The increase in plasmin may play a role in the development of angioedema by activating the kinin pathway, leading to the formation of the vasodilator bradykinin (Figure). Plasmin also activates the complement system and leads to the production of anaphylatoxins C3a, C4a, and C5a, which also cause mast cell degranulation and histamine release.1
When does post-tPA angioedema occur?
In the few published case reports available, tPA-induced angioedema was shown to typically occur in the stroke distribution (which was attributed to the left-sided swelling in this patient).2 Following tPA administration, the onset of angioedema reportedly varies from as early as 10 to 15 minutes from initiation until about 1 hour postinfusion. The short half-life of tPA (approximately 7 minutes)2 limits the outer- time window for the initial development of angioedema, but progression can continue well beyond this timeframe.
What is the treatment for tPA-induced angioedema?
The first priority of acute management of angioedema is discontinuation of the inciting substance, if possible—in this case, the tPA infusion.3 Assessment and maintenance of a patent airway are of utmost concern. Patients with posterior oropharyngeal effects or who are progressing should be admitted to an intensive care unit (ICU) for observation.4-6
Endotracheal Intubation. Providers should have a low threshold for endotracheal intubation, which should ideally be performed in any patient at risk for airway compromise.4 Due to the extensive airway swelling that can occur in the setting of angioedema, airway intervention should optimally be performed by an available clinician with the most skill and experience in this area. It is wise to be prepared to utilize advanced airway techniques, if available, including fiberoptic laryngoscopy or potentially cricothyrotomy.
Histamine Agonists. Standard therapy for patients who develop angioedema should include histamine antagonists, such as diphenhydramine (H1 antagonist) and famotidine (H2 antagonist) along with corticosteroids. Although these therapies are unlikely to be helpful in the treatment of tPA-induced angioedema, the difficulty in excluding allergic angioedema and the low risk of adverse effects associated with these medications support their use.
Fresh Frozen Plasma. Fresh frozen plasma (FFP) should be considered for patients who have a history of hereditary angioedema. Fresh frozen plasma contains enzymes that degrade bradykinin. Although FFP has been used successfully in the treatment of ACEI-induced angioedema, its use (or benefit) in tPA-related cases is not clear.
Icatibant. A selective bradykinin B2-receptor antagonist, icatibant has been used to treat patients with ACEI-induced angioedema because of its effects on bradykinin receptors. Comparison of the efficacy of icatibant to the prevailing treatment strategy of diphenhydramine, famotidine, and methylprednisolone found a shorter time to symptom relief with icatibant.7 However, icatibant is extremely expensive ($23,000/30 mg). As previously mentioned, based on its similar mechanism of action, lower cost, and safety profile, FFP can be given (off label) in this situation.
Case Conclusion
The patient was given diphenhydramine, famotidine, and methylprednisolone, but did not show any improvement. His upper/lower lip swelling continued to worsen, and 30 minutes after the onset of angioedema, he was unable to open his mouth more than 1 cm.
Multiple attempts to perform awake fiberoptic intubation failed due to inadequate sedation; however, intubation was successfully performed following light sedation. The patient self-extubated in the ICU on hospital day 3, and the angioedema had progressively decreased. Angioedema and weakness completely resolved by hospital day 4, and he was discharged home on hospital day 7.
Case
A 49-year-old man with a history of hypertension, for which he was taking aspirin, carvedilol, hydralazine, and nifedipine, presented to the ED with complaints of left-sided weakness that started 3 hours before he came to the ED. Initial vital signs were: blood pressure, 158/90 mm Hg; heart rate, 74 beats/min; respiratory rate, 18 breaths/min; and temperature, 98°F. Oxygen saturation was 100% on room air, and a finger-stick glucose test was 106 mg/dL.
Physical examination revealed slowed speech with mild dysarthria, mild left facial droop, 2/5 strength in all muscle groups in the left upper and lower extremities, and decreased sensation to light touch on the left side. The patient also had left-sided sensory neglect and an abnormal gait, and dragged his left foot on the floor when walking. The rest of his examination was normal.
The stroke team was activated, and the patient was immediately transferred to the ED radiology department for imaging studies. A noncontrast head computed tomography (CT) was negative for any acute intracranial hemorrhage or cerebral edema. A CT angiogram (CTA) also was performed, which revealed atherosclerosis but no arterial occlusion. Based on these findings and the existing protocol, the patient received an intravenous (IV) bolus of tissue plasminogen activator (tPA). Approximately 17 minutes after tPA administration, the patient developed left-sided upper and lower lip swelling. There was no voice change, tongue swelling, or uvular deviation.
What is the differential diagnosis of swelling of the lip?
The differential diagnoses for lip swelling includes trauma, allergic reaction, and angioedema (hereditary, or angiotensin converting enzyme inhibitor [ACEI]-induced). The patient in this case denied any trauma to the lip, and no bleeding was noted from the lip; however, his entire left lip (upper and lower) was swollen. He was not taking any ACEIs or angiotensin-receptor blockers (ARBs). He also denied a family history of angioedema or any prior similar episodes. The patient further denied exposure to any new medications, foods, or other substances and had no respiratory distress, urticaria, or other findings consistent with an allergy.
What are the common adverse effects of tPA?
The only US Food and Drug-approved pharmacological treatment for ischemic stroke is tPA (also known as IV rtPA). Tissue plasminogen activator hydrolyzes plasminogen to plasmin, which exerts a fibrinolytic effect. Based on the ability of tPA to lyse thrombus, it is also a standard therapy for hemodynamically unstable patients with confirmed pulmonary embolism, as well as for patients with myocardial infarction in whom percutaneous intervention is contraindicated or unavailable. Despite the beneficial effects of tPA, significant adverse effects are associated with the drug. For example, thrombolysis may result in conversion of an ischemic stroke into a hemorrhagic event, resulting in generalized bleeding from mucosal surfaces.
The increase in plasmin may play a role in the development of angioedema by activating the kinin pathway, leading to the formation of the vasodilator bradykinin (Figure). Plasmin also activates the complement system and leads to the production of anaphylatoxins C3a, C4a, and C5a, which also cause mast cell degranulation and histamine release.1
When does post-tPA angioedema occur?
In the few published case reports available, tPA-induced angioedema was shown to typically occur in the stroke distribution (which was attributed to the left-sided swelling in this patient).2 Following tPA administration, the onset of angioedema reportedly varies from as early as 10 to 15 minutes from initiation until about 1 hour postinfusion. The short half-life of tPA (approximately 7 minutes)2 limits the outer- time window for the initial development of angioedema, but progression can continue well beyond this timeframe.
What is the treatment for tPA-induced angioedema?
The first priority of acute management of angioedema is discontinuation of the inciting substance, if possible—in this case, the tPA infusion.3 Assessment and maintenance of a patent airway are of utmost concern. Patients with posterior oropharyngeal effects or who are progressing should be admitted to an intensive care unit (ICU) for observation.4-6
Endotracheal Intubation. Providers should have a low threshold for endotracheal intubation, which should ideally be performed in any patient at risk for airway compromise.4 Due to the extensive airway swelling that can occur in the setting of angioedema, airway intervention should optimally be performed by an available clinician with the most skill and experience in this area. It is wise to be prepared to utilize advanced airway techniques, if available, including fiberoptic laryngoscopy or potentially cricothyrotomy.
Histamine Agonists. Standard therapy for patients who develop angioedema should include histamine antagonists, such as diphenhydramine (H1 antagonist) and famotidine (H2 antagonist) along with corticosteroids. Although these therapies are unlikely to be helpful in the treatment of tPA-induced angioedema, the difficulty in excluding allergic angioedema and the low risk of adverse effects associated with these medications support their use.
Fresh Frozen Plasma. Fresh frozen plasma (FFP) should be considered for patients who have a history of hereditary angioedema. Fresh frozen plasma contains enzymes that degrade bradykinin. Although FFP has been used successfully in the treatment of ACEI-induced angioedema, its use (or benefit) in tPA-related cases is not clear.
Icatibant. A selective bradykinin B2-receptor antagonist, icatibant has been used to treat patients with ACEI-induced angioedema because of its effects on bradykinin receptors. Comparison of the efficacy of icatibant to the prevailing treatment strategy of diphenhydramine, famotidine, and methylprednisolone found a shorter time to symptom relief with icatibant.7 However, icatibant is extremely expensive ($23,000/30 mg). As previously mentioned, based on its similar mechanism of action, lower cost, and safety profile, FFP can be given (off label) in this situation.
Case Conclusion
The patient was given diphenhydramine, famotidine, and methylprednisolone, but did not show any improvement. His upper/lower lip swelling continued to worsen, and 30 minutes after the onset of angioedema, he was unable to open his mouth more than 1 cm.
Multiple attempts to perform awake fiberoptic intubation failed due to inadequate sedation; however, intubation was successfully performed following light sedation. The patient self-extubated in the ICU on hospital day 3, and the angioedema had progressively decreased. Angioedema and weakness completely resolved by hospital day 4, and he was discharged home on hospital day 7.
1. Molinaro G, Gervais N, Adam A. Biochemical basis of angioedema associated with recombinant tissue plasminogen activator treatment: an in vitro experimental approach. Stroke. 2002;33(6):1712-1716.
2. Madden B, Chebl RB. Hemi orolingual angioedema after tPA administration for acute ischemic stroke. West J Emerg Med. 2015;16(1):175-177. doi:10.5811/westjem.2014.12.24210.
3. Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-1527.
4. Temiño VM, Peebles RS Jr. The spectrum and treatment of angioedema. Am J Med. 2008;121(4):282-286. doi:10.1016/j.amjmed.2007.09.024.
5. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281-1284.
6. Maertins M, Wold R, Swider M. Angioedema after administration of tPA for ischemic stroke: case report. Air Med J. 2011;30(5):276-278. doi:10.1016/j.amj.2010.12.011.
7. Baş M, Greve J, Stelter K, et al. A randomized trial of icatibant in ACE-inhibitor-induced angioedema. N Engl J Med. 2015;372(5):418-425. doi:10.1056/NEJMoa1312524.
1. Molinaro G, Gervais N, Adam A. Biochemical basis of angioedema associated with recombinant tissue plasminogen activator treatment: an in vitro experimental approach. Stroke. 2002;33(6):1712-1716.
2. Madden B, Chebl RB. Hemi orolingual angioedema after tPA administration for acute ischemic stroke. West J Emerg Med. 2015;16(1):175-177. doi:10.5811/westjem.2014.12.24210.
3. Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-1527.
4. Temiño VM, Peebles RS Jr. The spectrum and treatment of angioedema. Am J Med. 2008;121(4):282-286. doi:10.1016/j.amjmed.2007.09.024.
5. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281-1284.
6. Maertins M, Wold R, Swider M. Angioedema after administration of tPA for ischemic stroke: case report. Air Med J. 2011;30(5):276-278. doi:10.1016/j.amj.2010.12.011.
7. Baş M, Greve J, Stelter K, et al. A randomized trial of icatibant in ACE-inhibitor-induced angioedema. N Engl J Med. 2015;372(5):418-425. doi:10.1056/NEJMoa1312524.
Treatment Protocol for Acute Arterial Occlusion Secondary to Facial Revolumization Procedures
Artificial dermal fillers and autologous fat grafting have become increasingly popular in recent years, primarily because they augment existing soft tissue volumes, thus producing aesthetic improvements at a lower cost than traditional plastic surgery (ie, facelift), and with nearly no recovery time. According to the American Society for Aesthetic Plastic Surgery, more than 2 million hyaluronic acid (HA) dermal filler procedures were performed in 2016, an increase of 3% from 2015.1 In addition, 80,000 autologous fat grafting procedures were performed in 2016, an increase of 13% from 2015. In total, there were 2.6 million soft tissue filler procedures in 2016, an increase of 2% from 2015.1
With the increased demand and access to both artificial dermal fillers and autologous fat grafting, there has been a plethora of reported adverse events, ranging from expected erythema to acute blindness and stroke. Emergency physicians should have a thorough understanding of facial vascular anatomy, as well as the effects of available facial volumization products, including potential complications and treatment options. Through our review of two patient cases, we propose a simplified protocol for the treatment of patients with acute arterial occlusion secondary to facial volumization procedures.
Case 1
A 38-year-old white woman presented to the ED for evaluation of transient blurred vision and blanching of the left cheek and upper lip, which began approximately 40 minutes prior to presentation, immediately after her primary care physician (PCP) injected her left nasolabial fold with calcium hydroxyapatite (CaHA). The patient stated that her vision became blurry and her eyes began to tear within 1 minute of receiving the injection. She further noted that these visual changes were painless and lasted for approximately 30 seconds.
The patient’s PCP believed these symptoms were due to pain at the injection site. While the patient was at her PCP’s office, the reception clerk noticed the blanching of the patient’s left cheek and informed the PCP, who referred the patient to our ED for evaluation.
Workup
The patient’s vital signs at presentation were normal. Her medical history was unremarkable and negative for smoking, alcohol, or drug use. She was not taking any medications and had no known drug allergies. The patient’s history was negative for any prior cosmetic procedures, and she confirmed this was the first and only time had a facial revolumization.
Facial examination revealed a Fitzpatrick scale (FS; a numerical scoring system used to assess a patient’s reaction to ultraviolet radiation) score of type 3. She also had left-sided blanching that extended from the midpoint of the nose diagonally to the lateral midbuccal cheek to the level of the oral commissure, including the cutaneous upper lip, alar, and nasal side wall. There was minimal capillary refill with compression at the affected site, and sensation was diminished to fine touch and pinprick. The facial muscles were intact, and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal.
The ophthalmic examination revealed a reactive pupil at 2 mm, white sclera, pink conjunctiva, red reflex, and normal fundoscopic vessels. The patient’s bedside Snellen visual acuity and visual field assessments were normal. The neurological examination was likewise normal, and no other physical findings were noted.
Laboratory evaluation included complete blood count (CBC), Chem 7 panel (creatinine, blood urea nitrogen [BUN], carbon dioxide, chloride, glucose, sodium, and potassium), and international normalized ratio (INR), which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion and transient retinal artery embolism secondary to facial volumization with CaHA. She was treated with oral acetylsalicylic acid aspirin (ASA) 325 mg, prednisone 40 mg, and sildenafil 50 mg; and subcutaneous (SC) enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Ophthalmology and plastic surgery services were contacted for consultation. Based on no acute findings on examination, the ophthalmologist provided no additional treatment recommendations. The patient was observed in the ED for 4 hours, during which time the facial blanching resolved and her capillary refill time returned to normal at 2 seconds.
After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral ASA and sildenafil, as well as a methylprednisolone dose pack for 6 days. He also recommended the patient begin hyperbaric oxygen (HBO) therapy the day after discharge, since there was no HBO chamber available during her hospital stay.
The patient complied with all discharge instructions, including HBO therapy. At plastic surgery follow-up, the patient had no long-term adverse effects from the CaHA injection.
Case 2
A 54-year-old Asian woman presented to the ED for evaluation of a 24-hour history of progressive and persistent pain, swelling, and discoloration of the nasolabial and upper lip region. She stated her symptoms began within 1 hour of receiving a fat graft injection into the affected area by her cosmetic surgeon. After examining the patient, the cosmetic surgeon referred her to the ED for further evaluation. The patient stated that she had undergone six prior facial revolumization procedures, but noted the recent procedure was her first autologous fat graft.
Workup
The patient’s medical history was unremarkable. Her social history was positive for one glass of wine per day and negative for smoking. The patient was not taking any medications and had no known drug allergies.
The patient’s vital signs at presentation were normal. She was evaluated approximately 30 hours after the fat graft procedure. Facial examination revealed an FS of type 4 with right-sided ischemia along the cutaneous upper lip, alar, and cheek (Figure 1).
Capillary refill time with compression was 0 in the affected area. Sensation to fine touch and pinprick was 0. The facial muscles were intact and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal. The neurological examination was likewise normal, and no other physical findings were noted. Laboratory evaluation included CBC, Chem 7 panel, and INR, which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion with soft tissue ischemia secondary to facial revolumization with autologous fat grafting. She was given oral acyclovir 800 mg, ASA 325 mg, cephalexin 500 mg, prednisone 40 mg, and sildenafil 50 mg; and SC enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Plastic surgery services were contacted for consultation. After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral acyclovir, ASA, cephalexin, prednisone, and sildenafil for 6 days. He also recommended the patient start HBO therapy the day after discharge home.
The patient refused HBO therapy, but did visit a plastic surgeon for a follow-up examination 3 days after discharge from the ED. A photograph of the patient’s nasolabial and upper lip region taken during this visit is presented in Figure 2.
Five days after discharge from the ED, the patient presented to a plastic surgery clinic for evaluation; a photograph was also obtained at this visit (Figure 3). The plastic surgeon at this clinic referred the patient to a tertiary center for a second opinion regarding the need for HBO therapy. The plastic surgeon at the tertiary center affirmed the initial plastic surgeon’s diagnosis and recommendation for HBO therapy. Although the patient did not return for further evaluation, she underwent 10 HBO treatments at the tertiary center with an acceptable aesthetic result.
Noninvasive Injectable Cosmetic Facial Augmentation
Facial augmentation procedures include the use of autologous adipose bovine collagen, HA gels, CaHA, and plastic compounds to fill wrinkles, folds, or soft tissue defects due to normal aging or trauma. Plastic surgeons traditionally use adipose and manufactured products for scar revision, midfacial restoration of volume loss from aging or trauma, cheek and chin augmentation, tear-trough correction (the diagonal crease running from the inner eye canthus to the maxilla resulting in a groove that creates a tired appearance), nose reshaping, lip enhancement, and correction of facial asymmetry.
Today the use of manufactured soft tissue revolumization products (ie, fillers) is no longer solely in the purview of plastic surgeons, but rather has become ubiquitous with nonsurgeons and allied health care professionals. As the overall number of revolumization procedures increases, so too does the risk for local and distant vascular complications.
Dermal Fillers
Dermal fillers vary widely in their respective properties, solubility, injection-technique flow requirements, and inherent complication risks. Regardless of type, all dermal fillers have the potential to cause serious complications. Most adverse events are related to substance type, volume, and injection technique. Bruising and trauma-related edema following dermal filler procedures are considered normal.
Though complications from dermal filler injections are rarely lethal, serious adverse events can result in permanent functional and aesthetic deficits. With proper physician training, planning, and injection technique, most adverse events can be avoided.
Hyaluronic Acid. Hyaluronic acid (HA)-containing injectable gel fillers (eg, Belotero, Juvederm, Perlane, and Restylane) are one of the most commonly used volumization products—especially by nonplastic surgeons. These gel fillers, which vary in viscosity and elasticity, may be injected from the superficial dermis to the periosteum. Dilution, dispersion, and degradation may be achieved in vivo either by high arterial flow or hyaluronidase.
Calcium Hydroxylapatite. Calcium hydroxylapatite (Radiesse) microsphere fillers consist of a very viscous paste that is mixed with lidocaine prior to injection to increase its flowability. The CaHA solution is injected at the deep dermis to periosteum level. Since CaHA is not easily diluted, dispersed, or degraded by high arterial flow, it tends to retain its consistency. When this procedure is performed by a novice, it can result in complete occlusion at the injection site or through embolization via antegrade or retrograde flow.
Poly-L-lactic Acid. Poly-L-lactic acid (PLLA; Sculptra) is a low-viscosity fluid comprised of synthetic polymer beads. The PLLA microparticles are not dissolvable or degradable by high arterial flow, and are designed to induce an inflammatory response with neocollagenesis.
Polymethyl Methacrylate. Polymethyl methacrylate (PMMA; Bellafil) consists of a combination of microscopic synthetic polymer beads suspended in a variety of substances. For facial enhancement, PMMA is usually suspended in HA or bovine collagen. Off-label use of silicon oils and gels such as PMMA are gaining in popularity—often with disastrous consequences such as acute arterial occlusion, bone erosion, and skin ulcerations.2,3
Autologous Adipose Tissue. Plastic surgeons primarily use autologous adipose tissue to volumize the face, breasts, buttocks, and scars. Autologous fat grafts are typically placed in fat, superficial and deep muscles, and deep fat pads through a 2- to 2.5-mm facial fat grafting cannula using a multichannel technique that leaves minute amounts of fat in each channel. Fat embolization may occur when a nonfacial fat graft cannula or needle used to transplant the fat graft enters an artery either through direct sharp puncture or traumatic tear cannulation.4-9
Adverse Events
The first recorded manufactured adverse event from an injectable dermal filler was in 1991. At that time, the US Food and Drug Administration warned of adverse events secondary to collagen injections, including open sores, abscess formation associated with delayed healing of the skin, and partial blindness.10
Arterial Embolization and Cannulation. The most serious complications from dermal fillers are accidental injection and/or embolization of the filler into the arterial system. Since 1991, an increased number of cases of soft tissue necrosis, blindness, and stroke have been reported as a result of injection of fillers in the glabella, forehead creases, temple, crow’s feet, nose, cheeks, nasolabial folds, and lower lip.11-15
Accidental cannulation and inadvertent injection of fillers into the arterial vessels can have catastrophic complications. The potential of such inadvertent complications occurs despite skill level of the practitioner or surgeon. Therefore, recognition and treatment of a vascular occlusion must be immediate and aggressive to avoid devastating and potentially irreversible complications including blindness, stroke, and death.11-15
Acute Blindness and Stroke. The issues and concerns associated with local intra-arterial dermal filler injection and distal embolism are well described in the literature. However, the mechanism of retinal artery occlusion is much more complex given the need for deep placement of products and the force necessary to cause distention and elevation of the dermis. Hence, higher g-forces are applied via the plunger, forcing the intra-arterial filler proximally past the origin of the retinal artery. When the clinician stops the injection, the arterial systolic pressure immediately embolizes the filler into the distal branches of the ophthalmic artery. This causes acute pain and blindness (Figure 5). Depending on the g-force applied, filler can enter into the internal carotid artery and embolize resulting in cerebral ischemia. Signs of cerebral ischemia may be mild or overt.4-9
Intra-arterial placement results in pain out of proportion to the procedure and results in almost immediate skin blanching. Depending upon the duration of ischemia, there is progressive necrosis of the end target tissue (nasolabial dermis, mucosal and dermis lip, alar and nasal tip cartilage with dermis).14,16-19 Areas of tissue necrosis are also subject to secondary bacterial or viral infections, which is why the patient in Case 2 was given a course of acyclovir and cephalosporin.
Management
Patients with intra-arterial dermal filler injection constitute a medical emergency requiring immediate intervention. We recommend clinicians initiate the treatment protocols outlined in the Box and Table 1.
Hyaluronidase. Injection of hyaluronidase may assist in degrading the HA around the arterial puncture site, relieving compression, which may increase blood flow. There is a risk of distal embolization from a dislodged HA emboli.
Fat Graft Injections. There are no known degradation products for fat, CaHA, PLLA, or PMMA products. The use of normal saline or hyaluronidase has no proven efficacy and may increase the compression pressure in the artery and surrounding tissue, causing further ischemia.
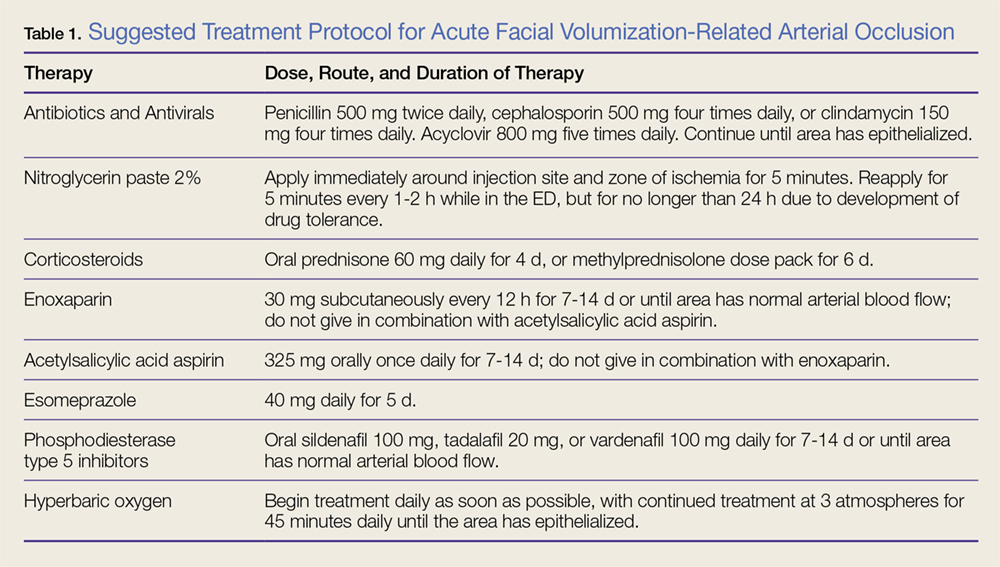
Nitroglycerin. The use of topical nitroglycerin 2% will dilate the superficial vasculature with possible draw of blood from surrounding cross-feeding vessels. The nitroglycerin should be applied for 5-minute intervals every 1 to 2 hours. Adjusting the duration and frequency is necessary if the patient experiences headache or lightheadedness.
Corticosteroids. As corticosteroids help to decrease the inflammatory response in tissue ischemia, including edema, treatment should be initiated immediately. High doses (eg, 60 mg) of an oral corticosteroid for 4 days or a methylprednisolone dose pack for 6 days are both acceptable treatment options. There is no increased efficacy to giving corticosteroids via the intramuscular or intravenous (IV) route. Corticosteroid use in diabetic patients may increase blood glucose levels.
Subcutaneous enoxaparin. A low molecular weight heparin, enoxaparin should be given at a dose of 30 mg SC twice daily in patients in whom there is no known contraindication to heparins. Enoxaparin should not be given in combination with ASA therapy.
Acetylsalicylic Acid Aspirin. Patients should be given 325 mg ASA orally, which may assist fibrinolysis. Prophylactic treatment with an antacid is recommended to prevent gastritis/esophagitis associated with ASA therapy. Acetylsalicylic acid aspirin should not be given to patients in whom contraindications exist, or used in combination with enoxaparin.
Phosphodiesterase Type 5 Inhibitors. Phosphodiesterase type 5 inhibitors (eg, tadalafil, sildenafil, vardenafil) inhibit the degradation of cyclic guanosine monophosphate, allowing arterial muscle wall relaxation and increased vasodilation.
Antibiotic and Antiviral Therapy. Tissue ischemia requires treatment with prophylactic antibiotics and antivirals. Oral broad-spectrum coverage for gram-positive bacteria should be initiated (cephalosporin or penicillin). If the oral mucosa is compromised, the clinician should consider clindamycin.
Consultations. Ophthalmology consultation should be obtained if the patient has symptoms of retinal or ophthalmic artery compromise. Plastic surgery consultation should be obtained for possible HBO therapy and for possible surgical intervention. A neurology consultation should be obtained if the patient has symptoms of cerebral ischemia (Table 2).
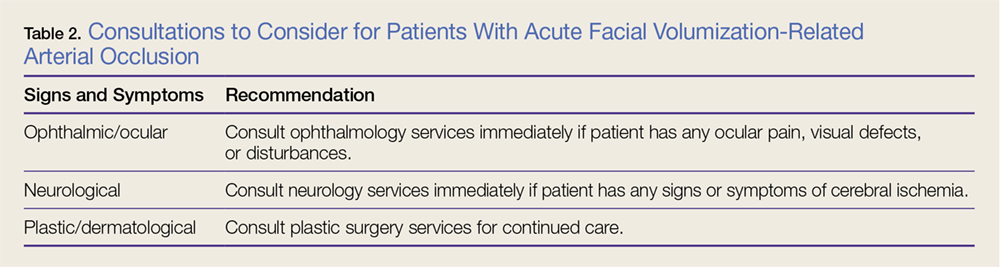
Hyperbaric Oxygen Therapy. Patients in whom HBO therapy is recommended should receive treatment at 3 atmospheres of pressure for 45 minutes to drive oxygen into deep structures, raising the tissue oxygen tension 100-fold. Hyperbaric oxygen limits ischemic damage, cell death, and inflammation by decreasing lactate production and tissue acidosis. It also promotes collagen synthesis and angiogenesis.
Long-term Sequelae
Despite aggressive intervention, permanent complications of cerebral ischemia, blindness, and severe soft tissue necrosis may occur. In six cases in the literature, patients treated with ocular massage therapy,7,14 carbon dioxide rebreathing,14 HBO therapy,7,14 oral and IV corticosteroids,6-9 antiplatelet drugs,6 and fibrinolytic agents,7,16 or mechanical thrombolysis16 showed no clinical effects. Neither the treated nor the untreated patients in any of these case studies had any return of vision.4-7,9,20-27
Conclusion
Although artificial dermal fillers such as HA, CaHA, PLLA, and PMMA, and autologous adipose tissue grafts offer a minimally invasive alternative to plastic surgical procedures, they are not without complication or adverse effects, such as the acute arterial occlusion experienced by both of our patients. Patients presenting to the ED with adverse effects from such procedures must be managed promptly, employing the suggested management and treatment protocol, including consultation with ophthalmology, plastic surgery, and neurological services as indicated, to avoid permanent sequela and damage.
1. American Society of Plastic Surgeons. 2016 National Plastic Surgery Statistics. https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2016/2016-plastic-surgery-statistics-report.pdf. Accessed April 13, 2017.
2. Hilinski JM, Cohen SR. Soft tissue augmentation with ArteFill. Facial Plast Surg. 2009;25(2):114-119. doi:10.1055/s-0029-1220651.
3. Liu HL, Cheung WY. Complications of polyacrylamide hydrogel (PAAG) injection in facial augmentation. J Plast Reconstr Aesthet Surg. 2010;63(1):e9-e12. doi:10.1016/j.bjps.2009.05.013.
4. Danesh-Meyer HV, Savino PJ, Sergott RC. Case reports and small case series: ocular and cerebral ischemia following facial injection of autologous fat. Arch Ophthalmol. 2001;119(5):777-778.
5. Feinendegen DL, Baumgartner RW, Vuadens P, et al. Autologous fat injection for soft tissue augmentation in the face: a safe procedure? Aesthetic Plast Surg. 1998;22(3):163-167.
6. Egido JA, Arroyo R, Marcos A, Jiménez-Alfaro I. Middle cerebral artery embolism and unilateral visual loss after autologous fat injection into the glabellar area. Stroke. 1993;24(4):615-616.
7. Lee DH, Yang HN, Kim JC, Shyn KH. Sudden unilateral visual loss and brain infarction after autologous fat injection into nasolabial groove. Br J Ophthalmol. 1996;80(11):1026-1027.
8. Thaunat O, Thaler F, Loirat P, Decroix JP, Boulin A. Cerebral fat embolism induced by facial fat injection. Plast Reconstr Surg. 2004;113(7):2235-2236.
9. Yoon SS, Chang DI, Chung KC. Acute fatal stroke immediately following autologous fat injection into the face. Neurology. 2003;61(8):1151-1152.
10. US Food and Drug Administration. Current and Useful Information on Collagen and Liquid Silicone Injections. FDA Backgrounder, August 1991. BG91-2.0.
11. Kwon SG, Hong JW, Roh TS, Kim YS, Rah DK, Kim SS. Ischemic oculomotor nerve palsy and skin necrosis caused by vascular embolization after hyaluronic Acid filler injection: a case report. Ann Plast Surg. 2013;71(4):333-334. doi:10.1097/SAP.0b013e31824f21da.
12. Peter S, Mennel S. Retinal branch artery occlusion following injection of hyaluronic acid (Restylane). Clin Exp Ophthalmol. 2006;34(4):363-364. doi:10.1111/j.1442-9071.2006.01224.x.
13. Kim YJ, Kim SS, Song WK, Lee SY, Yoon JS. Ocular ischemia with hypotony after injection of hyaluronic acid gel. Ophthal Plast Reconstr Surg. 2011;27(6):e152-e155. doi:10.1097/IOP.0b013e3182082f37.
14. Grunebaum LD, Bogdan Allemann I, Dayan S, Mandy S, Baumann L. Dermatol Surg. 2009;35 Suppl 2:1635-1640. doi:10.1111/j.1524-4725.2009.01342.x.
15. Schanz S, Schippert W, Ulmer A, Rassner G, Fierlbeck G. Arterial embolization caused by injection of hyaluronic acid (Restylane). Br J Dermatol. 2002;146(5):928-929.
16. Georgescu D, Jones Y, McCann JD, Anderson RL. Skin necrosis after calcium hydroxylapatite injection into the glabellar and nasolabial folds. Ophthal Plast Reconstr Surg. 2009;25(6):498-499. doi:10.1097/IOP.0b013e3181b81082.
17. Kassir R, Kolluru A, Kassir M. Extensive necrosis after injection of hyaluronic acid filler: case report and review of the literature. J Cosmet Dermatol. 2011;10(3):224-231. doi:10.1111/j.1473-2165.2011.00562.x.
18. Glaich AS, Cohen JL, Goldberg LH. Injection necrosis of the glabella: protocol for prevention and treatment after use of dermal fillers. Dermatol Surg. 2006;32(2):276-281.
19. Burt B, Nakra T, Isaacs DK, Goldberg RA. Alar necrosis after facial injection of hyaluronic acid. Plast Reconstr Surg. 2010;125(5):199e-200e. doi:10.1097/PRS.0b013e3181d5152e.
20. Teimourian B. Blindness following fat injections. Plast Reconstr Surg. 1988;82(2):361.
21. Dreizen NG, Framm L. Sudden unilateral visual loss after autologous fat injection into the glabellar area. Am J Ophthalmol. 1989;107(1):85-87.
22. Coleman SR. Avoidance of arterial occlusion from injection of soft tissue fillers. Aesthet Surg J. 2002;22(6):555-557. doi:10.1067/maj.2002.129625.
23. Allali J, Bernard A, Assaraf E, Bourges JL, Renard G. Multiple embolizations of the branches of the ophthalmic artery: an unknown serious complication of facial surgeries. [Article in French] J Fr Ophtalmol. 2006;29(1):51-57.
24. Mori K, Ohta K, Nagano S, Toshinori M, Yago T, Ichinose Y. A case of ophthalmic artery obstruction following autologous fat injection in the glabellar area. [Article in Japanese] Nippon Ganka Gakkai Zasshi. 2007;111(1):22-25.
25. Park SH, Sun HJ, Choi KS. Sudden unilateral visual loss after autologous fat injection into the nasolabial fold. Clin Ophthalmol. 2008;2(3):679-683.
26. Lee YJ, Kim HJ, Choi KD, Choi HY. MRI restricted diffusion in optic nerve infarction after autologous fat transplantation. J Neuroophthalmol. 2010;30(3):216-218. doi:10.1097/WNO.0b013e3181c5d147.
27. Park SJ, Woo SJ, Park KH, et al. Partial recovery after intraarterial pharmacomechanical thrombolysis in ophthalmic artery occlusion following nasal autologous fat injection. J Vasc Interv Radiol. 2011;22(2):251-254. doi:10.1016/j.jvir.2010.10.023.
Artificial dermal fillers and autologous fat grafting have become increasingly popular in recent years, primarily because they augment existing soft tissue volumes, thus producing aesthetic improvements at a lower cost than traditional plastic surgery (ie, facelift), and with nearly no recovery time. According to the American Society for Aesthetic Plastic Surgery, more than 2 million hyaluronic acid (HA) dermal filler procedures were performed in 2016, an increase of 3% from 2015.1 In addition, 80,000 autologous fat grafting procedures were performed in 2016, an increase of 13% from 2015. In total, there were 2.6 million soft tissue filler procedures in 2016, an increase of 2% from 2015.1
With the increased demand and access to both artificial dermal fillers and autologous fat grafting, there has been a plethora of reported adverse events, ranging from expected erythema to acute blindness and stroke. Emergency physicians should have a thorough understanding of facial vascular anatomy, as well as the effects of available facial volumization products, including potential complications and treatment options. Through our review of two patient cases, we propose a simplified protocol for the treatment of patients with acute arterial occlusion secondary to facial volumization procedures.
Case 1
A 38-year-old white woman presented to the ED for evaluation of transient blurred vision and blanching of the left cheek and upper lip, which began approximately 40 minutes prior to presentation, immediately after her primary care physician (PCP) injected her left nasolabial fold with calcium hydroxyapatite (CaHA). The patient stated that her vision became blurry and her eyes began to tear within 1 minute of receiving the injection. She further noted that these visual changes were painless and lasted for approximately 30 seconds.
The patient’s PCP believed these symptoms were due to pain at the injection site. While the patient was at her PCP’s office, the reception clerk noticed the blanching of the patient’s left cheek and informed the PCP, who referred the patient to our ED for evaluation.
Workup
The patient’s vital signs at presentation were normal. Her medical history was unremarkable and negative for smoking, alcohol, or drug use. She was not taking any medications and had no known drug allergies. The patient’s history was negative for any prior cosmetic procedures, and she confirmed this was the first and only time had a facial revolumization.
Facial examination revealed a Fitzpatrick scale (FS; a numerical scoring system used to assess a patient’s reaction to ultraviolet radiation) score of type 3. She also had left-sided blanching that extended from the midpoint of the nose diagonally to the lateral midbuccal cheek to the level of the oral commissure, including the cutaneous upper lip, alar, and nasal side wall. There was minimal capillary refill with compression at the affected site, and sensation was diminished to fine touch and pinprick. The facial muscles were intact, and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal.
The ophthalmic examination revealed a reactive pupil at 2 mm, white sclera, pink conjunctiva, red reflex, and normal fundoscopic vessels. The patient’s bedside Snellen visual acuity and visual field assessments were normal. The neurological examination was likewise normal, and no other physical findings were noted.
Laboratory evaluation included complete blood count (CBC), Chem 7 panel (creatinine, blood urea nitrogen [BUN], carbon dioxide, chloride, glucose, sodium, and potassium), and international normalized ratio (INR), which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion and transient retinal artery embolism secondary to facial volumization with CaHA. She was treated with oral acetylsalicylic acid aspirin (ASA) 325 mg, prednisone 40 mg, and sildenafil 50 mg; and subcutaneous (SC) enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Ophthalmology and plastic surgery services were contacted for consultation. Based on no acute findings on examination, the ophthalmologist provided no additional treatment recommendations. The patient was observed in the ED for 4 hours, during which time the facial blanching resolved and her capillary refill time returned to normal at 2 seconds.
After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral ASA and sildenafil, as well as a methylprednisolone dose pack for 6 days. He also recommended the patient begin hyperbaric oxygen (HBO) therapy the day after discharge, since there was no HBO chamber available during her hospital stay.
The patient complied with all discharge instructions, including HBO therapy. At plastic surgery follow-up, the patient had no long-term adverse effects from the CaHA injection.
Case 2
A 54-year-old Asian woman presented to the ED for evaluation of a 24-hour history of progressive and persistent pain, swelling, and discoloration of the nasolabial and upper lip region. She stated her symptoms began within 1 hour of receiving a fat graft injection into the affected area by her cosmetic surgeon. After examining the patient, the cosmetic surgeon referred her to the ED for further evaluation. The patient stated that she had undergone six prior facial revolumization procedures, but noted the recent procedure was her first autologous fat graft.
Workup
The patient’s medical history was unremarkable. Her social history was positive for one glass of wine per day and negative for smoking. The patient was not taking any medications and had no known drug allergies.
The patient’s vital signs at presentation were normal. She was evaluated approximately 30 hours after the fat graft procedure. Facial examination revealed an FS of type 4 with right-sided ischemia along the cutaneous upper lip, alar, and cheek (Figure 1).
Capillary refill time with compression was 0 in the affected area. Sensation to fine touch and pinprick was 0. The facial muscles were intact and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal. The neurological examination was likewise normal, and no other physical findings were noted. Laboratory evaluation included CBC, Chem 7 panel, and INR, which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion with soft tissue ischemia secondary to facial revolumization with autologous fat grafting. She was given oral acyclovir 800 mg, ASA 325 mg, cephalexin 500 mg, prednisone 40 mg, and sildenafil 50 mg; and SC enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Plastic surgery services were contacted for consultation. After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral acyclovir, ASA, cephalexin, prednisone, and sildenafil for 6 days. He also recommended the patient start HBO therapy the day after discharge home.
The patient refused HBO therapy, but did visit a plastic surgeon for a follow-up examination 3 days after discharge from the ED. A photograph of the patient’s nasolabial and upper lip region taken during this visit is presented in Figure 2.
Five days after discharge from the ED, the patient presented to a plastic surgery clinic for evaluation; a photograph was also obtained at this visit (Figure 3). The plastic surgeon at this clinic referred the patient to a tertiary center for a second opinion regarding the need for HBO therapy. The plastic surgeon at the tertiary center affirmed the initial plastic surgeon’s diagnosis and recommendation for HBO therapy. Although the patient did not return for further evaluation, she underwent 10 HBO treatments at the tertiary center with an acceptable aesthetic result.
Noninvasive Injectable Cosmetic Facial Augmentation
Facial augmentation procedures include the use of autologous adipose bovine collagen, HA gels, CaHA, and plastic compounds to fill wrinkles, folds, or soft tissue defects due to normal aging or trauma. Plastic surgeons traditionally use adipose and manufactured products for scar revision, midfacial restoration of volume loss from aging or trauma, cheek and chin augmentation, tear-trough correction (the diagonal crease running from the inner eye canthus to the maxilla resulting in a groove that creates a tired appearance), nose reshaping, lip enhancement, and correction of facial asymmetry.
Today the use of manufactured soft tissue revolumization products (ie, fillers) is no longer solely in the purview of plastic surgeons, but rather has become ubiquitous with nonsurgeons and allied health care professionals. As the overall number of revolumization procedures increases, so too does the risk for local and distant vascular complications.
Dermal Fillers
Dermal fillers vary widely in their respective properties, solubility, injection-technique flow requirements, and inherent complication risks. Regardless of type, all dermal fillers have the potential to cause serious complications. Most adverse events are related to substance type, volume, and injection technique. Bruising and trauma-related edema following dermal filler procedures are considered normal.
Though complications from dermal filler injections are rarely lethal, serious adverse events can result in permanent functional and aesthetic deficits. With proper physician training, planning, and injection technique, most adverse events can be avoided.
Hyaluronic Acid. Hyaluronic acid (HA)-containing injectable gel fillers (eg, Belotero, Juvederm, Perlane, and Restylane) are one of the most commonly used volumization products—especially by nonplastic surgeons. These gel fillers, which vary in viscosity and elasticity, may be injected from the superficial dermis to the periosteum. Dilution, dispersion, and degradation may be achieved in vivo either by high arterial flow or hyaluronidase.
Calcium Hydroxylapatite. Calcium hydroxylapatite (Radiesse) microsphere fillers consist of a very viscous paste that is mixed with lidocaine prior to injection to increase its flowability. The CaHA solution is injected at the deep dermis to periosteum level. Since CaHA is not easily diluted, dispersed, or degraded by high arterial flow, it tends to retain its consistency. When this procedure is performed by a novice, it can result in complete occlusion at the injection site or through embolization via antegrade or retrograde flow.
Poly-L-lactic Acid. Poly-L-lactic acid (PLLA; Sculptra) is a low-viscosity fluid comprised of synthetic polymer beads. The PLLA microparticles are not dissolvable or degradable by high arterial flow, and are designed to induce an inflammatory response with neocollagenesis.
Polymethyl Methacrylate. Polymethyl methacrylate (PMMA; Bellafil) consists of a combination of microscopic synthetic polymer beads suspended in a variety of substances. For facial enhancement, PMMA is usually suspended in HA or bovine collagen. Off-label use of silicon oils and gels such as PMMA are gaining in popularity—often with disastrous consequences such as acute arterial occlusion, bone erosion, and skin ulcerations.2,3
Autologous Adipose Tissue. Plastic surgeons primarily use autologous adipose tissue to volumize the face, breasts, buttocks, and scars. Autologous fat grafts are typically placed in fat, superficial and deep muscles, and deep fat pads through a 2- to 2.5-mm facial fat grafting cannula using a multichannel technique that leaves minute amounts of fat in each channel. Fat embolization may occur when a nonfacial fat graft cannula or needle used to transplant the fat graft enters an artery either through direct sharp puncture or traumatic tear cannulation.4-9
Adverse Events
The first recorded manufactured adverse event from an injectable dermal filler was in 1991. At that time, the US Food and Drug Administration warned of adverse events secondary to collagen injections, including open sores, abscess formation associated with delayed healing of the skin, and partial blindness.10
Arterial Embolization and Cannulation. The most serious complications from dermal fillers are accidental injection and/or embolization of the filler into the arterial system. Since 1991, an increased number of cases of soft tissue necrosis, blindness, and stroke have been reported as a result of injection of fillers in the glabella, forehead creases, temple, crow’s feet, nose, cheeks, nasolabial folds, and lower lip.11-15
Accidental cannulation and inadvertent injection of fillers into the arterial vessels can have catastrophic complications. The potential of such inadvertent complications occurs despite skill level of the practitioner or surgeon. Therefore, recognition and treatment of a vascular occlusion must be immediate and aggressive to avoid devastating and potentially irreversible complications including blindness, stroke, and death.11-15
Acute Blindness and Stroke. The issues and concerns associated with local intra-arterial dermal filler injection and distal embolism are well described in the literature. However, the mechanism of retinal artery occlusion is much more complex given the need for deep placement of products and the force necessary to cause distention and elevation of the dermis. Hence, higher g-forces are applied via the plunger, forcing the intra-arterial filler proximally past the origin of the retinal artery. When the clinician stops the injection, the arterial systolic pressure immediately embolizes the filler into the distal branches of the ophthalmic artery. This causes acute pain and blindness (Figure 5). Depending on the g-force applied, filler can enter into the internal carotid artery and embolize resulting in cerebral ischemia. Signs of cerebral ischemia may be mild or overt.4-9
Intra-arterial placement results in pain out of proportion to the procedure and results in almost immediate skin blanching. Depending upon the duration of ischemia, there is progressive necrosis of the end target tissue (nasolabial dermis, mucosal and dermis lip, alar and nasal tip cartilage with dermis).14,16-19 Areas of tissue necrosis are also subject to secondary bacterial or viral infections, which is why the patient in Case 2 was given a course of acyclovir and cephalosporin.
Management
Patients with intra-arterial dermal filler injection constitute a medical emergency requiring immediate intervention. We recommend clinicians initiate the treatment protocols outlined in the Box and Table 1.
Hyaluronidase. Injection of hyaluronidase may assist in degrading the HA around the arterial puncture site, relieving compression, which may increase blood flow. There is a risk of distal embolization from a dislodged HA emboli.
Fat Graft Injections. There are no known degradation products for fat, CaHA, PLLA, or PMMA products. The use of normal saline or hyaluronidase has no proven efficacy and may increase the compression pressure in the artery and surrounding tissue, causing further ischemia.
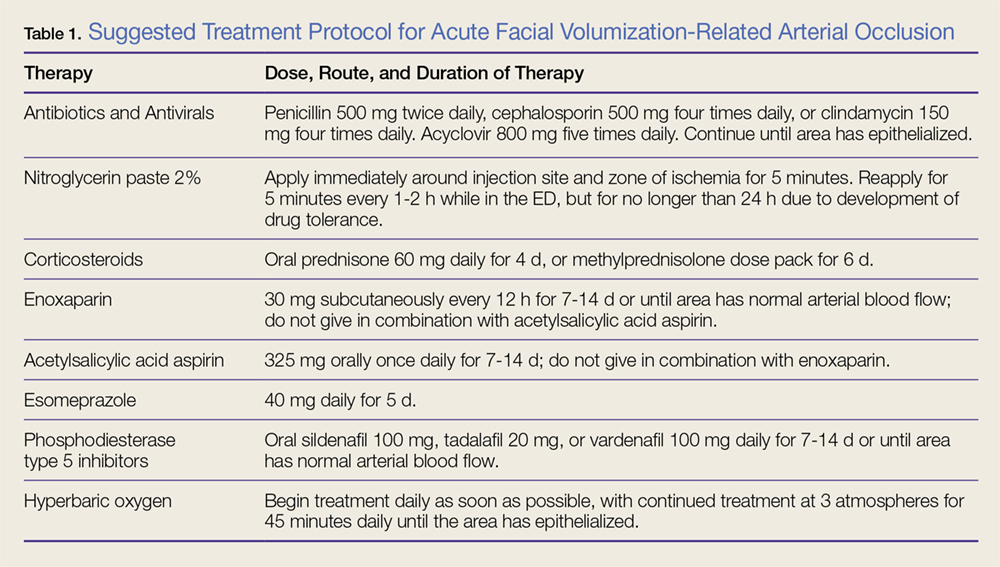
Nitroglycerin. The use of topical nitroglycerin 2% will dilate the superficial vasculature with possible draw of blood from surrounding cross-feeding vessels. The nitroglycerin should be applied for 5-minute intervals every 1 to 2 hours. Adjusting the duration and frequency is necessary if the patient experiences headache or lightheadedness.
Corticosteroids. As corticosteroids help to decrease the inflammatory response in tissue ischemia, including edema, treatment should be initiated immediately. High doses (eg, 60 mg) of an oral corticosteroid for 4 days or a methylprednisolone dose pack for 6 days are both acceptable treatment options. There is no increased efficacy to giving corticosteroids via the intramuscular or intravenous (IV) route. Corticosteroid use in diabetic patients may increase blood glucose levels.
Subcutaneous enoxaparin. A low molecular weight heparin, enoxaparin should be given at a dose of 30 mg SC twice daily in patients in whom there is no known contraindication to heparins. Enoxaparin should not be given in combination with ASA therapy.
Acetylsalicylic Acid Aspirin. Patients should be given 325 mg ASA orally, which may assist fibrinolysis. Prophylactic treatment with an antacid is recommended to prevent gastritis/esophagitis associated with ASA therapy. Acetylsalicylic acid aspirin should not be given to patients in whom contraindications exist, or used in combination with enoxaparin.
Phosphodiesterase Type 5 Inhibitors. Phosphodiesterase type 5 inhibitors (eg, tadalafil, sildenafil, vardenafil) inhibit the degradation of cyclic guanosine monophosphate, allowing arterial muscle wall relaxation and increased vasodilation.
Antibiotic and Antiviral Therapy. Tissue ischemia requires treatment with prophylactic antibiotics and antivirals. Oral broad-spectrum coverage for gram-positive bacteria should be initiated (cephalosporin or penicillin). If the oral mucosa is compromised, the clinician should consider clindamycin.
Consultations. Ophthalmology consultation should be obtained if the patient has symptoms of retinal or ophthalmic artery compromise. Plastic surgery consultation should be obtained for possible HBO therapy and for possible surgical intervention. A neurology consultation should be obtained if the patient has symptoms of cerebral ischemia (Table 2).
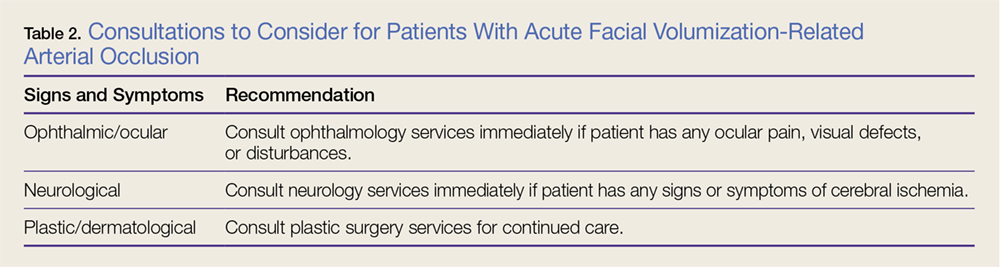
Hyperbaric Oxygen Therapy. Patients in whom HBO therapy is recommended should receive treatment at 3 atmospheres of pressure for 45 minutes to drive oxygen into deep structures, raising the tissue oxygen tension 100-fold. Hyperbaric oxygen limits ischemic damage, cell death, and inflammation by decreasing lactate production and tissue acidosis. It also promotes collagen synthesis and angiogenesis.
Long-term Sequelae
Despite aggressive intervention, permanent complications of cerebral ischemia, blindness, and severe soft tissue necrosis may occur. In six cases in the literature, patients treated with ocular massage therapy,7,14 carbon dioxide rebreathing,14 HBO therapy,7,14 oral and IV corticosteroids,6-9 antiplatelet drugs,6 and fibrinolytic agents,7,16 or mechanical thrombolysis16 showed no clinical effects. Neither the treated nor the untreated patients in any of these case studies had any return of vision.4-7,9,20-27
Conclusion
Although artificial dermal fillers such as HA, CaHA, PLLA, and PMMA, and autologous adipose tissue grafts offer a minimally invasive alternative to plastic surgical procedures, they are not without complication or adverse effects, such as the acute arterial occlusion experienced by both of our patients. Patients presenting to the ED with adverse effects from such procedures must be managed promptly, employing the suggested management and treatment protocol, including consultation with ophthalmology, plastic surgery, and neurological services as indicated, to avoid permanent sequela and damage.
Artificial dermal fillers and autologous fat grafting have become increasingly popular in recent years, primarily because they augment existing soft tissue volumes, thus producing aesthetic improvements at a lower cost than traditional plastic surgery (ie, facelift), and with nearly no recovery time. According to the American Society for Aesthetic Plastic Surgery, more than 2 million hyaluronic acid (HA) dermal filler procedures were performed in 2016, an increase of 3% from 2015.1 In addition, 80,000 autologous fat grafting procedures were performed in 2016, an increase of 13% from 2015. In total, there were 2.6 million soft tissue filler procedures in 2016, an increase of 2% from 2015.1
With the increased demand and access to both artificial dermal fillers and autologous fat grafting, there has been a plethora of reported adverse events, ranging from expected erythema to acute blindness and stroke. Emergency physicians should have a thorough understanding of facial vascular anatomy, as well as the effects of available facial volumization products, including potential complications and treatment options. Through our review of two patient cases, we propose a simplified protocol for the treatment of patients with acute arterial occlusion secondary to facial volumization procedures.
Case 1
A 38-year-old white woman presented to the ED for evaluation of transient blurred vision and blanching of the left cheek and upper lip, which began approximately 40 minutes prior to presentation, immediately after her primary care physician (PCP) injected her left nasolabial fold with calcium hydroxyapatite (CaHA). The patient stated that her vision became blurry and her eyes began to tear within 1 minute of receiving the injection. She further noted that these visual changes were painless and lasted for approximately 30 seconds.
The patient’s PCP believed these symptoms were due to pain at the injection site. While the patient was at her PCP’s office, the reception clerk noticed the blanching of the patient’s left cheek and informed the PCP, who referred the patient to our ED for evaluation.
Workup
The patient’s vital signs at presentation were normal. Her medical history was unremarkable and negative for smoking, alcohol, or drug use. She was not taking any medications and had no known drug allergies. The patient’s history was negative for any prior cosmetic procedures, and she confirmed this was the first and only time had a facial revolumization.
Facial examination revealed a Fitzpatrick scale (FS; a numerical scoring system used to assess a patient’s reaction to ultraviolet radiation) score of type 3. She also had left-sided blanching that extended from the midpoint of the nose diagonally to the lateral midbuccal cheek to the level of the oral commissure, including the cutaneous upper lip, alar, and nasal side wall. There was minimal capillary refill with compression at the affected site, and sensation was diminished to fine touch and pinprick. The facial muscles were intact, and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal.
The ophthalmic examination revealed a reactive pupil at 2 mm, white sclera, pink conjunctiva, red reflex, and normal fundoscopic vessels. The patient’s bedside Snellen visual acuity and visual field assessments were normal. The neurological examination was likewise normal, and no other physical findings were noted.
Laboratory evaluation included complete blood count (CBC), Chem 7 panel (creatinine, blood urea nitrogen [BUN], carbon dioxide, chloride, glucose, sodium, and potassium), and international normalized ratio (INR), which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion and transient retinal artery embolism secondary to facial volumization with CaHA. She was treated with oral acetylsalicylic acid aspirin (ASA) 325 mg, prednisone 40 mg, and sildenafil 50 mg; and subcutaneous (SC) enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Ophthalmology and plastic surgery services were contacted for consultation. Based on no acute findings on examination, the ophthalmologist provided no additional treatment recommendations. The patient was observed in the ED for 4 hours, during which time the facial blanching resolved and her capillary refill time returned to normal at 2 seconds.
After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral ASA and sildenafil, as well as a methylprednisolone dose pack for 6 days. He also recommended the patient begin hyperbaric oxygen (HBO) therapy the day after discharge, since there was no HBO chamber available during her hospital stay.
The patient complied with all discharge instructions, including HBO therapy. At plastic surgery follow-up, the patient had no long-term adverse effects from the CaHA injection.
Case 2
A 54-year-old Asian woman presented to the ED for evaluation of a 24-hour history of progressive and persistent pain, swelling, and discoloration of the nasolabial and upper lip region. She stated her symptoms began within 1 hour of receiving a fat graft injection into the affected area by her cosmetic surgeon. After examining the patient, the cosmetic surgeon referred her to the ED for further evaluation. The patient stated that she had undergone six prior facial revolumization procedures, but noted the recent procedure was her first autologous fat graft.
Workup
The patient’s medical history was unremarkable. Her social history was positive for one glass of wine per day and negative for smoking. The patient was not taking any medications and had no known drug allergies.
The patient’s vital signs at presentation were normal. She was evaluated approximately 30 hours after the fat graft procedure. Facial examination revealed an FS of type 4 with right-sided ischemia along the cutaneous upper lip, alar, and cheek (Figure 1).
Capillary refill time with compression was 0 in the affected area. Sensation to fine touch and pinprick was 0. The facial muscles were intact and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal. The neurological examination was likewise normal, and no other physical findings were noted. Laboratory evaluation included CBC, Chem 7 panel, and INR, which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion with soft tissue ischemia secondary to facial revolumization with autologous fat grafting. She was given oral acyclovir 800 mg, ASA 325 mg, cephalexin 500 mg, prednisone 40 mg, and sildenafil 50 mg; and SC enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Plastic surgery services were contacted for consultation. After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral acyclovir, ASA, cephalexin, prednisone, and sildenafil for 6 days. He also recommended the patient start HBO therapy the day after discharge home.
The patient refused HBO therapy, but did visit a plastic surgeon for a follow-up examination 3 days after discharge from the ED. A photograph of the patient’s nasolabial and upper lip region taken during this visit is presented in Figure 2.
Five days after discharge from the ED, the patient presented to a plastic surgery clinic for evaluation; a photograph was also obtained at this visit (Figure 3). The plastic surgeon at this clinic referred the patient to a tertiary center for a second opinion regarding the need for HBO therapy. The plastic surgeon at the tertiary center affirmed the initial plastic surgeon’s diagnosis and recommendation for HBO therapy. Although the patient did not return for further evaluation, she underwent 10 HBO treatments at the tertiary center with an acceptable aesthetic result.
Noninvasive Injectable Cosmetic Facial Augmentation
Facial augmentation procedures include the use of autologous adipose bovine collagen, HA gels, CaHA, and plastic compounds to fill wrinkles, folds, or soft tissue defects due to normal aging or trauma. Plastic surgeons traditionally use adipose and manufactured products for scar revision, midfacial restoration of volume loss from aging or trauma, cheek and chin augmentation, tear-trough correction (the diagonal crease running from the inner eye canthus to the maxilla resulting in a groove that creates a tired appearance), nose reshaping, lip enhancement, and correction of facial asymmetry.
Today the use of manufactured soft tissue revolumization products (ie, fillers) is no longer solely in the purview of plastic surgeons, but rather has become ubiquitous with nonsurgeons and allied health care professionals. As the overall number of revolumization procedures increases, so too does the risk for local and distant vascular complications.
Dermal Fillers
Dermal fillers vary widely in their respective properties, solubility, injection-technique flow requirements, and inherent complication risks. Regardless of type, all dermal fillers have the potential to cause serious complications. Most adverse events are related to substance type, volume, and injection technique. Bruising and trauma-related edema following dermal filler procedures are considered normal.
Though complications from dermal filler injections are rarely lethal, serious adverse events can result in permanent functional and aesthetic deficits. With proper physician training, planning, and injection technique, most adverse events can be avoided.
Hyaluronic Acid. Hyaluronic acid (HA)-containing injectable gel fillers (eg, Belotero, Juvederm, Perlane, and Restylane) are one of the most commonly used volumization products—especially by nonplastic surgeons. These gel fillers, which vary in viscosity and elasticity, may be injected from the superficial dermis to the periosteum. Dilution, dispersion, and degradation may be achieved in vivo either by high arterial flow or hyaluronidase.
Calcium Hydroxylapatite. Calcium hydroxylapatite (Radiesse) microsphere fillers consist of a very viscous paste that is mixed with lidocaine prior to injection to increase its flowability. The CaHA solution is injected at the deep dermis to periosteum level. Since CaHA is not easily diluted, dispersed, or degraded by high arterial flow, it tends to retain its consistency. When this procedure is performed by a novice, it can result in complete occlusion at the injection site or through embolization via antegrade or retrograde flow.
Poly-L-lactic Acid. Poly-L-lactic acid (PLLA; Sculptra) is a low-viscosity fluid comprised of synthetic polymer beads. The PLLA microparticles are not dissolvable or degradable by high arterial flow, and are designed to induce an inflammatory response with neocollagenesis.
Polymethyl Methacrylate. Polymethyl methacrylate (PMMA; Bellafil) consists of a combination of microscopic synthetic polymer beads suspended in a variety of substances. For facial enhancement, PMMA is usually suspended in HA or bovine collagen. Off-label use of silicon oils and gels such as PMMA are gaining in popularity—often with disastrous consequences such as acute arterial occlusion, bone erosion, and skin ulcerations.2,3
Autologous Adipose Tissue. Plastic surgeons primarily use autologous adipose tissue to volumize the face, breasts, buttocks, and scars. Autologous fat grafts are typically placed in fat, superficial and deep muscles, and deep fat pads through a 2- to 2.5-mm facial fat grafting cannula using a multichannel technique that leaves minute amounts of fat in each channel. Fat embolization may occur when a nonfacial fat graft cannula or needle used to transplant the fat graft enters an artery either through direct sharp puncture or traumatic tear cannulation.4-9
Adverse Events
The first recorded manufactured adverse event from an injectable dermal filler was in 1991. At that time, the US Food and Drug Administration warned of adverse events secondary to collagen injections, including open sores, abscess formation associated with delayed healing of the skin, and partial blindness.10
Arterial Embolization and Cannulation. The most serious complications from dermal fillers are accidental injection and/or embolization of the filler into the arterial system. Since 1991, an increased number of cases of soft tissue necrosis, blindness, and stroke have been reported as a result of injection of fillers in the glabella, forehead creases, temple, crow’s feet, nose, cheeks, nasolabial folds, and lower lip.11-15
Accidental cannulation and inadvertent injection of fillers into the arterial vessels can have catastrophic complications. The potential of such inadvertent complications occurs despite skill level of the practitioner or surgeon. Therefore, recognition and treatment of a vascular occlusion must be immediate and aggressive to avoid devastating and potentially irreversible complications including blindness, stroke, and death.11-15
Acute Blindness and Stroke. The issues and concerns associated with local intra-arterial dermal filler injection and distal embolism are well described in the literature. However, the mechanism of retinal artery occlusion is much more complex given the need for deep placement of products and the force necessary to cause distention and elevation of the dermis. Hence, higher g-forces are applied via the plunger, forcing the intra-arterial filler proximally past the origin of the retinal artery. When the clinician stops the injection, the arterial systolic pressure immediately embolizes the filler into the distal branches of the ophthalmic artery. This causes acute pain and blindness (Figure 5). Depending on the g-force applied, filler can enter into the internal carotid artery and embolize resulting in cerebral ischemia. Signs of cerebral ischemia may be mild or overt.4-9
Intra-arterial placement results in pain out of proportion to the procedure and results in almost immediate skin blanching. Depending upon the duration of ischemia, there is progressive necrosis of the end target tissue (nasolabial dermis, mucosal and dermis lip, alar and nasal tip cartilage with dermis).14,16-19 Areas of tissue necrosis are also subject to secondary bacterial or viral infections, which is why the patient in Case 2 was given a course of acyclovir and cephalosporin.
Management
Patients with intra-arterial dermal filler injection constitute a medical emergency requiring immediate intervention. We recommend clinicians initiate the treatment protocols outlined in the Box and Table 1.
Hyaluronidase. Injection of hyaluronidase may assist in degrading the HA around the arterial puncture site, relieving compression, which may increase blood flow. There is a risk of distal embolization from a dislodged HA emboli.
Fat Graft Injections. There are no known degradation products for fat, CaHA, PLLA, or PMMA products. The use of normal saline or hyaluronidase has no proven efficacy and may increase the compression pressure in the artery and surrounding tissue, causing further ischemia.
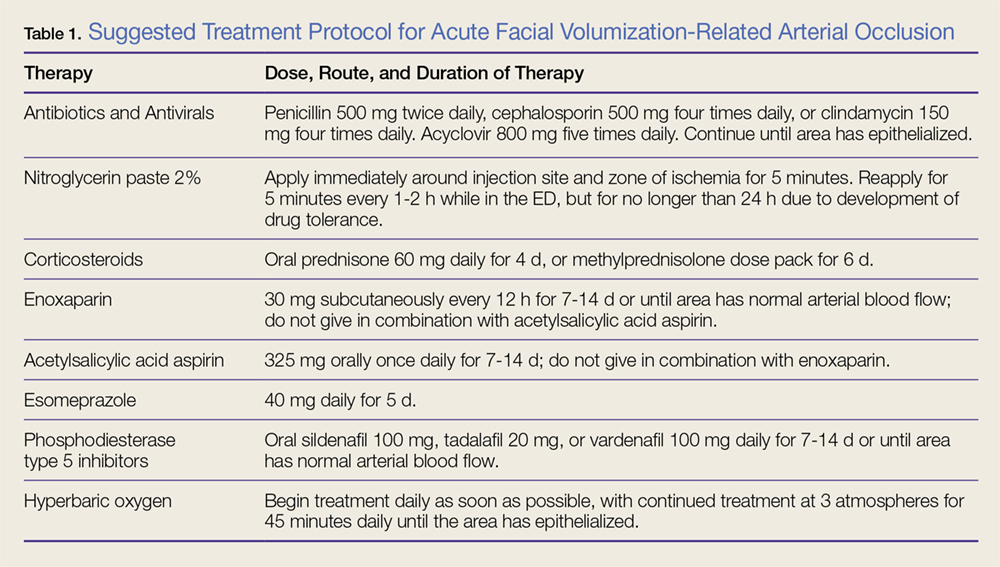
Nitroglycerin. The use of topical nitroglycerin 2% will dilate the superficial vasculature with possible draw of blood from surrounding cross-feeding vessels. The nitroglycerin should be applied for 5-minute intervals every 1 to 2 hours. Adjusting the duration and frequency is necessary if the patient experiences headache or lightheadedness.
Corticosteroids. As corticosteroids help to decrease the inflammatory response in tissue ischemia, including edema, treatment should be initiated immediately. High doses (eg, 60 mg) of an oral corticosteroid for 4 days or a methylprednisolone dose pack for 6 days are both acceptable treatment options. There is no increased efficacy to giving corticosteroids via the intramuscular or intravenous (IV) route. Corticosteroid use in diabetic patients may increase blood glucose levels.
Subcutaneous enoxaparin. A low molecular weight heparin, enoxaparin should be given at a dose of 30 mg SC twice daily in patients in whom there is no known contraindication to heparins. Enoxaparin should not be given in combination with ASA therapy.
Acetylsalicylic Acid Aspirin. Patients should be given 325 mg ASA orally, which may assist fibrinolysis. Prophylactic treatment with an antacid is recommended to prevent gastritis/esophagitis associated with ASA therapy. Acetylsalicylic acid aspirin should not be given to patients in whom contraindications exist, or used in combination with enoxaparin.
Phosphodiesterase Type 5 Inhibitors. Phosphodiesterase type 5 inhibitors (eg, tadalafil, sildenafil, vardenafil) inhibit the degradation of cyclic guanosine monophosphate, allowing arterial muscle wall relaxation and increased vasodilation.
Antibiotic and Antiviral Therapy. Tissue ischemia requires treatment with prophylactic antibiotics and antivirals. Oral broad-spectrum coverage for gram-positive bacteria should be initiated (cephalosporin or penicillin). If the oral mucosa is compromised, the clinician should consider clindamycin.
Consultations. Ophthalmology consultation should be obtained if the patient has symptoms of retinal or ophthalmic artery compromise. Plastic surgery consultation should be obtained for possible HBO therapy and for possible surgical intervention. A neurology consultation should be obtained if the patient has symptoms of cerebral ischemia (Table 2).
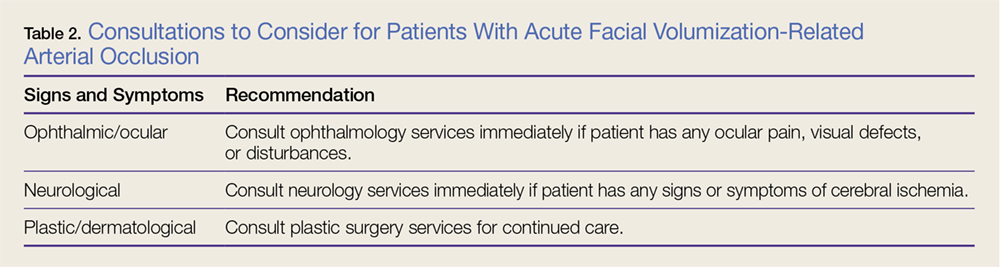
Hyperbaric Oxygen Therapy. Patients in whom HBO therapy is recommended should receive treatment at 3 atmospheres of pressure for 45 minutes to drive oxygen into deep structures, raising the tissue oxygen tension 100-fold. Hyperbaric oxygen limits ischemic damage, cell death, and inflammation by decreasing lactate production and tissue acidosis. It also promotes collagen synthesis and angiogenesis.
Long-term Sequelae
Despite aggressive intervention, permanent complications of cerebral ischemia, blindness, and severe soft tissue necrosis may occur. In six cases in the literature, patients treated with ocular massage therapy,7,14 carbon dioxide rebreathing,14 HBO therapy,7,14 oral and IV corticosteroids,6-9 antiplatelet drugs,6 and fibrinolytic agents,7,16 or mechanical thrombolysis16 showed no clinical effects. Neither the treated nor the untreated patients in any of these case studies had any return of vision.4-7,9,20-27
Conclusion
Although artificial dermal fillers such as HA, CaHA, PLLA, and PMMA, and autologous adipose tissue grafts offer a minimally invasive alternative to plastic surgical procedures, they are not without complication or adverse effects, such as the acute arterial occlusion experienced by both of our patients. Patients presenting to the ED with adverse effects from such procedures must be managed promptly, employing the suggested management and treatment protocol, including consultation with ophthalmology, plastic surgery, and neurological services as indicated, to avoid permanent sequela and damage.
1. American Society of Plastic Surgeons. 2016 National Plastic Surgery Statistics. https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2016/2016-plastic-surgery-statistics-report.pdf. Accessed April 13, 2017.
2. Hilinski JM, Cohen SR. Soft tissue augmentation with ArteFill. Facial Plast Surg. 2009;25(2):114-119. doi:10.1055/s-0029-1220651.
3. Liu HL, Cheung WY. Complications of polyacrylamide hydrogel (PAAG) injection in facial augmentation. J Plast Reconstr Aesthet Surg. 2010;63(1):e9-e12. doi:10.1016/j.bjps.2009.05.013.
4. Danesh-Meyer HV, Savino PJ, Sergott RC. Case reports and small case series: ocular and cerebral ischemia following facial injection of autologous fat. Arch Ophthalmol. 2001;119(5):777-778.
5. Feinendegen DL, Baumgartner RW, Vuadens P, et al. Autologous fat injection for soft tissue augmentation in the face: a safe procedure? Aesthetic Plast Surg. 1998;22(3):163-167.
6. Egido JA, Arroyo R, Marcos A, Jiménez-Alfaro I. Middle cerebral artery embolism and unilateral visual loss after autologous fat injection into the glabellar area. Stroke. 1993;24(4):615-616.
7. Lee DH, Yang HN, Kim JC, Shyn KH. Sudden unilateral visual loss and brain infarction after autologous fat injection into nasolabial groove. Br J Ophthalmol. 1996;80(11):1026-1027.
8. Thaunat O, Thaler F, Loirat P, Decroix JP, Boulin A. Cerebral fat embolism induced by facial fat injection. Plast Reconstr Surg. 2004;113(7):2235-2236.
9. Yoon SS, Chang DI, Chung KC. Acute fatal stroke immediately following autologous fat injection into the face. Neurology. 2003;61(8):1151-1152.
10. US Food and Drug Administration. Current and Useful Information on Collagen and Liquid Silicone Injections. FDA Backgrounder, August 1991. BG91-2.0.
11. Kwon SG, Hong JW, Roh TS, Kim YS, Rah DK, Kim SS. Ischemic oculomotor nerve palsy and skin necrosis caused by vascular embolization after hyaluronic Acid filler injection: a case report. Ann Plast Surg. 2013;71(4):333-334. doi:10.1097/SAP.0b013e31824f21da.
12. Peter S, Mennel S. Retinal branch artery occlusion following injection of hyaluronic acid (Restylane). Clin Exp Ophthalmol. 2006;34(4):363-364. doi:10.1111/j.1442-9071.2006.01224.x.
13. Kim YJ, Kim SS, Song WK, Lee SY, Yoon JS. Ocular ischemia with hypotony after injection of hyaluronic acid gel. Ophthal Plast Reconstr Surg. 2011;27(6):e152-e155. doi:10.1097/IOP.0b013e3182082f37.
14. Grunebaum LD, Bogdan Allemann I, Dayan S, Mandy S, Baumann L. Dermatol Surg. 2009;35 Suppl 2:1635-1640. doi:10.1111/j.1524-4725.2009.01342.x.
15. Schanz S, Schippert W, Ulmer A, Rassner G, Fierlbeck G. Arterial embolization caused by injection of hyaluronic acid (Restylane). Br J Dermatol. 2002;146(5):928-929.
16. Georgescu D, Jones Y, McCann JD, Anderson RL. Skin necrosis after calcium hydroxylapatite injection into the glabellar and nasolabial folds. Ophthal Plast Reconstr Surg. 2009;25(6):498-499. doi:10.1097/IOP.0b013e3181b81082.
17. Kassir R, Kolluru A, Kassir M. Extensive necrosis after injection of hyaluronic acid filler: case report and review of the literature. J Cosmet Dermatol. 2011;10(3):224-231. doi:10.1111/j.1473-2165.2011.00562.x.
18. Glaich AS, Cohen JL, Goldberg LH. Injection necrosis of the glabella: protocol for prevention and treatment after use of dermal fillers. Dermatol Surg. 2006;32(2):276-281.
19. Burt B, Nakra T, Isaacs DK, Goldberg RA. Alar necrosis after facial injection of hyaluronic acid. Plast Reconstr Surg. 2010;125(5):199e-200e. doi:10.1097/PRS.0b013e3181d5152e.
20. Teimourian B. Blindness following fat injections. Plast Reconstr Surg. 1988;82(2):361.
21. Dreizen NG, Framm L. Sudden unilateral visual loss after autologous fat injection into the glabellar area. Am J Ophthalmol. 1989;107(1):85-87.
22. Coleman SR. Avoidance of arterial occlusion from injection of soft tissue fillers. Aesthet Surg J. 2002;22(6):555-557. doi:10.1067/maj.2002.129625.
23. Allali J, Bernard A, Assaraf E, Bourges JL, Renard G. Multiple embolizations of the branches of the ophthalmic artery: an unknown serious complication of facial surgeries. [Article in French] J Fr Ophtalmol. 2006;29(1):51-57.
24. Mori K, Ohta K, Nagano S, Toshinori M, Yago T, Ichinose Y. A case of ophthalmic artery obstruction following autologous fat injection in the glabellar area. [Article in Japanese] Nippon Ganka Gakkai Zasshi. 2007;111(1):22-25.
25. Park SH, Sun HJ, Choi KS. Sudden unilateral visual loss after autologous fat injection into the nasolabial fold. Clin Ophthalmol. 2008;2(3):679-683.
26. Lee YJ, Kim HJ, Choi KD, Choi HY. MRI restricted diffusion in optic nerve infarction after autologous fat transplantation. J Neuroophthalmol. 2010;30(3):216-218. doi:10.1097/WNO.0b013e3181c5d147.
27. Park SJ, Woo SJ, Park KH, et al. Partial recovery after intraarterial pharmacomechanical thrombolysis in ophthalmic artery occlusion following nasal autologous fat injection. J Vasc Interv Radiol. 2011;22(2):251-254. doi:10.1016/j.jvir.2010.10.023.
1. American Society of Plastic Surgeons. 2016 National Plastic Surgery Statistics. https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2016/2016-plastic-surgery-statistics-report.pdf. Accessed April 13, 2017.
2. Hilinski JM, Cohen SR. Soft tissue augmentation with ArteFill. Facial Plast Surg. 2009;25(2):114-119. doi:10.1055/s-0029-1220651.
3. Liu HL, Cheung WY. Complications of polyacrylamide hydrogel (PAAG) injection in facial augmentation. J Plast Reconstr Aesthet Surg. 2010;63(1):e9-e12. doi:10.1016/j.bjps.2009.05.013.
4. Danesh-Meyer HV, Savino PJ, Sergott RC. Case reports and small case series: ocular and cerebral ischemia following facial injection of autologous fat. Arch Ophthalmol. 2001;119(5):777-778.
5. Feinendegen DL, Baumgartner RW, Vuadens P, et al. Autologous fat injection for soft tissue augmentation in the face: a safe procedure? Aesthetic Plast Surg. 1998;22(3):163-167.
6. Egido JA, Arroyo R, Marcos A, Jiménez-Alfaro I. Middle cerebral artery embolism and unilateral visual loss after autologous fat injection into the glabellar area. Stroke. 1993;24(4):615-616.
7. Lee DH, Yang HN, Kim JC, Shyn KH. Sudden unilateral visual loss and brain infarction after autologous fat injection into nasolabial groove. Br J Ophthalmol. 1996;80(11):1026-1027.
8. Thaunat O, Thaler F, Loirat P, Decroix JP, Boulin A. Cerebral fat embolism induced by facial fat injection. Plast Reconstr Surg. 2004;113(7):2235-2236.
9. Yoon SS, Chang DI, Chung KC. Acute fatal stroke immediately following autologous fat injection into the face. Neurology. 2003;61(8):1151-1152.
10. US Food and Drug Administration. Current and Useful Information on Collagen and Liquid Silicone Injections. FDA Backgrounder, August 1991. BG91-2.0.
11. Kwon SG, Hong JW, Roh TS, Kim YS, Rah DK, Kim SS. Ischemic oculomotor nerve palsy and skin necrosis caused by vascular embolization after hyaluronic Acid filler injection: a case report. Ann Plast Surg. 2013;71(4):333-334. doi:10.1097/SAP.0b013e31824f21da.
12. Peter S, Mennel S. Retinal branch artery occlusion following injection of hyaluronic acid (Restylane). Clin Exp Ophthalmol. 2006;34(4):363-364. doi:10.1111/j.1442-9071.2006.01224.x.
13. Kim YJ, Kim SS, Song WK, Lee SY, Yoon JS. Ocular ischemia with hypotony after injection of hyaluronic acid gel. Ophthal Plast Reconstr Surg. 2011;27(6):e152-e155. doi:10.1097/IOP.0b013e3182082f37.
14. Grunebaum LD, Bogdan Allemann I, Dayan S, Mandy S, Baumann L. Dermatol Surg. 2009;35 Suppl 2:1635-1640. doi:10.1111/j.1524-4725.2009.01342.x.
15. Schanz S, Schippert W, Ulmer A, Rassner G, Fierlbeck G. Arterial embolization caused by injection of hyaluronic acid (Restylane). Br J Dermatol. 2002;146(5):928-929.
16. Georgescu D, Jones Y, McCann JD, Anderson RL. Skin necrosis after calcium hydroxylapatite injection into the glabellar and nasolabial folds. Ophthal Plast Reconstr Surg. 2009;25(6):498-499. doi:10.1097/IOP.0b013e3181b81082.
17. Kassir R, Kolluru A, Kassir M. Extensive necrosis after injection of hyaluronic acid filler: case report and review of the literature. J Cosmet Dermatol. 2011;10(3):224-231. doi:10.1111/j.1473-2165.2011.00562.x.
18. Glaich AS, Cohen JL, Goldberg LH. Injection necrosis of the glabella: protocol for prevention and treatment after use of dermal fillers. Dermatol Surg. 2006;32(2):276-281.
19. Burt B, Nakra T, Isaacs DK, Goldberg RA. Alar necrosis after facial injection of hyaluronic acid. Plast Reconstr Surg. 2010;125(5):199e-200e. doi:10.1097/PRS.0b013e3181d5152e.
20. Teimourian B. Blindness following fat injections. Plast Reconstr Surg. 1988;82(2):361.
21. Dreizen NG, Framm L. Sudden unilateral visual loss after autologous fat injection into the glabellar area. Am J Ophthalmol. 1989;107(1):85-87.
22. Coleman SR. Avoidance of arterial occlusion from injection of soft tissue fillers. Aesthet Surg J. 2002;22(6):555-557. doi:10.1067/maj.2002.129625.
23. Allali J, Bernard A, Assaraf E, Bourges JL, Renard G. Multiple embolizations of the branches of the ophthalmic artery: an unknown serious complication of facial surgeries. [Article in French] J Fr Ophtalmol. 2006;29(1):51-57.
24. Mori K, Ohta K, Nagano S, Toshinori M, Yago T, Ichinose Y. A case of ophthalmic artery obstruction following autologous fat injection in the glabellar area. [Article in Japanese] Nippon Ganka Gakkai Zasshi. 2007;111(1):22-25.
25. Park SH, Sun HJ, Choi KS. Sudden unilateral visual loss after autologous fat injection into the nasolabial fold. Clin Ophthalmol. 2008;2(3):679-683.
26. Lee YJ, Kim HJ, Choi KD, Choi HY. MRI restricted diffusion in optic nerve infarction after autologous fat transplantation. J Neuroophthalmol. 2010;30(3):216-218. doi:10.1097/WNO.0b013e3181c5d147.
27. Park SJ, Woo SJ, Park KH, et al. Partial recovery after intraarterial pharmacomechanical thrombolysis in ophthalmic artery occlusion following nasal autologous fat injection. J Vasc Interv Radiol. 2011;22(2):251-254. doi:10.1016/j.jvir.2010.10.023.
Elder Abuse: A New Old Problem
Emergency physicians (EPs) are trained to recognize and treat conditions that most severely affect patients at the extremes of age. For decades, the recognition and management of child neglect and abuse has been part of emergency medicine (EM) residency training and most states now require physicians to complete a child abuse course for licensing. In this issue, “Recognizing and Managing Elder Abuse in the Emergency Department” by Rosen et al describes abuse at the other age extreme. The thorough discussion following an illustrative case presentation raises serious concerns that the occurrence of elder neglect and abuse may be increasing in frequency in a rapidly aging population.
Child abuse and elder abuse share several common features along with some notable differences. When a member of either age group presents to the ED with fractures and/or soft tissue injuries, EPs must maintain a high index of suspicion for abuse, obtain a carefully directed history, and be able to recognize the characteristic patterns of injury. Hallmarks of both child abuse and elder abuse include a history provided by the caregiver that is not consistent with the actual injuries; an often-unobtainable independent history from an infant or baby not yet able to speak or an older adult with dementia; and a physical exam revealing bruises in areas that are not over bony prominences. A radiographic skeletal survey may show multiple fractures in various stages of healing, and laboratory testing may reveal nutritional evidence of neglect, medication over- or underdosing, or the presence of medications that have not been prescribed for the patient.
Patterns of abuse injuries in the two age groups differ. As noted by Colbourne and Clarke in Tintinalli’s Emergency Medicine (8th ed, p. 1001), nonaccidental bruises in children are more common on the torso, neck, ears, cheeks, buttocks, and back; appear in clusters; are frequently symmetrical; and tend to be larger and more numerous than accidental injuries. Hand or implement patterns on the skin may be observed. Rib and metaphyseal fractures are unusual in children, as are all fractures at a very young age.
In the midst of an epidemic of elderly fall injuries, abuse injuries, as described in the pages ahead, most commonly occur on the head, neck, and upper extremities, and include large bruises on the face, lateral arm, or posterior torso. Based on preliminary results from an ongoing study, left periorbital, neck, and ulnar forearm injuries appear to be particularly indicative of abuse rather than accidental. An elderly person may be abused by an adult-child or relative living in the same household attempting to gain control over the victim’s wealth or residence.
Interventional resources required for both types of abuse, as well as for intimate partner abuse, are also similar and include safe facilities for extended treatment and separation from a suspected abuser; hospital security, legal, and administrative support; social services; law enforcement; psychiatric evaluation of adult capacity; and child or adult protective services, which, as Rosen et al note, operate very differently from one another. All states, except one, now require reporting of both child abuse and elder abuse.*
None of these comparisons of child abuse and elder abuse are meant to suggest equivalency—moral or otherwise. Children are not “little adults,” and the frail elderly are not truly “child-like.” Each incident of a child “slipping through the cracks” of the protective measures currently in place underscores the need for sufficient resources to deal with child abuse alone, and an increasing number of elder abuse cases should not compete with these needs. But implementing greater awareness, preventive measures, and physical and human resources to address these problems at both extremes of age cannot be put off for the future.
When I started the first geriatric emergency medicine fellowship in the country in 2005, elder abuse was not even on my radar screen. Now it must be considered a serious and growing problem by all.
*New York State alone does not require reporting of elder abuse.
Emergency physicians (EPs) are trained to recognize and treat conditions that most severely affect patients at the extremes of age. For decades, the recognition and management of child neglect and abuse has been part of emergency medicine (EM) residency training and most states now require physicians to complete a child abuse course for licensing. In this issue, “Recognizing and Managing Elder Abuse in the Emergency Department” by Rosen et al describes abuse at the other age extreme. The thorough discussion following an illustrative case presentation raises serious concerns that the occurrence of elder neglect and abuse may be increasing in frequency in a rapidly aging population.
Child abuse and elder abuse share several common features along with some notable differences. When a member of either age group presents to the ED with fractures and/or soft tissue injuries, EPs must maintain a high index of suspicion for abuse, obtain a carefully directed history, and be able to recognize the characteristic patterns of injury. Hallmarks of both child abuse and elder abuse include a history provided by the caregiver that is not consistent with the actual injuries; an often-unobtainable independent history from an infant or baby not yet able to speak or an older adult with dementia; and a physical exam revealing bruises in areas that are not over bony prominences. A radiographic skeletal survey may show multiple fractures in various stages of healing, and laboratory testing may reveal nutritional evidence of neglect, medication over- or underdosing, or the presence of medications that have not been prescribed for the patient.
Patterns of abuse injuries in the two age groups differ. As noted by Colbourne and Clarke in Tintinalli’s Emergency Medicine (8th ed, p. 1001), nonaccidental bruises in children are more common on the torso, neck, ears, cheeks, buttocks, and back; appear in clusters; are frequently symmetrical; and tend to be larger and more numerous than accidental injuries. Hand or implement patterns on the skin may be observed. Rib and metaphyseal fractures are unusual in children, as are all fractures at a very young age.
In the midst of an epidemic of elderly fall injuries, abuse injuries, as described in the pages ahead, most commonly occur on the head, neck, and upper extremities, and include large bruises on the face, lateral arm, or posterior torso. Based on preliminary results from an ongoing study, left periorbital, neck, and ulnar forearm injuries appear to be particularly indicative of abuse rather than accidental. An elderly person may be abused by an adult-child or relative living in the same household attempting to gain control over the victim’s wealth or residence.
Interventional resources required for both types of abuse, as well as for intimate partner abuse, are also similar and include safe facilities for extended treatment and separation from a suspected abuser; hospital security, legal, and administrative support; social services; law enforcement; psychiatric evaluation of adult capacity; and child or adult protective services, which, as Rosen et al note, operate very differently from one another. All states, except one, now require reporting of both child abuse and elder abuse.*
None of these comparisons of child abuse and elder abuse are meant to suggest equivalency—moral or otherwise. Children are not “little adults,” and the frail elderly are not truly “child-like.” Each incident of a child “slipping through the cracks” of the protective measures currently in place underscores the need for sufficient resources to deal with child abuse alone, and an increasing number of elder abuse cases should not compete with these needs. But implementing greater awareness, preventive measures, and physical and human resources to address these problems at both extremes of age cannot be put off for the future.
When I started the first geriatric emergency medicine fellowship in the country in 2005, elder abuse was not even on my radar screen. Now it must be considered a serious and growing problem by all.
*New York State alone does not require reporting of elder abuse.
Emergency physicians (EPs) are trained to recognize and treat conditions that most severely affect patients at the extremes of age. For decades, the recognition and management of child neglect and abuse has been part of emergency medicine (EM) residency training and most states now require physicians to complete a child abuse course for licensing. In this issue, “Recognizing and Managing Elder Abuse in the Emergency Department” by Rosen et al describes abuse at the other age extreme. The thorough discussion following an illustrative case presentation raises serious concerns that the occurrence of elder neglect and abuse may be increasing in frequency in a rapidly aging population.
Child abuse and elder abuse share several common features along with some notable differences. When a member of either age group presents to the ED with fractures and/or soft tissue injuries, EPs must maintain a high index of suspicion for abuse, obtain a carefully directed history, and be able to recognize the characteristic patterns of injury. Hallmarks of both child abuse and elder abuse include a history provided by the caregiver that is not consistent with the actual injuries; an often-unobtainable independent history from an infant or baby not yet able to speak or an older adult with dementia; and a physical exam revealing bruises in areas that are not over bony prominences. A radiographic skeletal survey may show multiple fractures in various stages of healing, and laboratory testing may reveal nutritional evidence of neglect, medication over- or underdosing, or the presence of medications that have not been prescribed for the patient.
Patterns of abuse injuries in the two age groups differ. As noted by Colbourne and Clarke in Tintinalli’s Emergency Medicine (8th ed, p. 1001), nonaccidental bruises in children are more common on the torso, neck, ears, cheeks, buttocks, and back; appear in clusters; are frequently symmetrical; and tend to be larger and more numerous than accidental injuries. Hand or implement patterns on the skin may be observed. Rib and metaphyseal fractures are unusual in children, as are all fractures at a very young age.
In the midst of an epidemic of elderly fall injuries, abuse injuries, as described in the pages ahead, most commonly occur on the head, neck, and upper extremities, and include large bruises on the face, lateral arm, or posterior torso. Based on preliminary results from an ongoing study, left periorbital, neck, and ulnar forearm injuries appear to be particularly indicative of abuse rather than accidental. An elderly person may be abused by an adult-child or relative living in the same household attempting to gain control over the victim’s wealth or residence.
Interventional resources required for both types of abuse, as well as for intimate partner abuse, are also similar and include safe facilities for extended treatment and separation from a suspected abuser; hospital security, legal, and administrative support; social services; law enforcement; psychiatric evaluation of adult capacity; and child or adult protective services, which, as Rosen et al note, operate very differently from one another. All states, except one, now require reporting of both child abuse and elder abuse.*
None of these comparisons of child abuse and elder abuse are meant to suggest equivalency—moral or otherwise. Children are not “little adults,” and the frail elderly are not truly “child-like.” Each incident of a child “slipping through the cracks” of the protective measures currently in place underscores the need for sufficient resources to deal with child abuse alone, and an increasing number of elder abuse cases should not compete with these needs. But implementing greater awareness, preventive measures, and physical and human resources to address these problems at both extremes of age cannot be put off for the future.
When I started the first geriatric emergency medicine fellowship in the country in 2005, elder abuse was not even on my radar screen. Now it must be considered a serious and growing problem by all.
*New York State alone does not require reporting of elder abuse.
Kratom: An Emerging Drug of Abuse
Editor’s Note: This article has been adapted from an article originally published in Federal Practitioner (Tavakoli HR, et al. Kratom: a new product in an expanding substance abuse market. Fed Prac. 2016;33[11]:132-136. http://www.fedprac.com).
According to the United Nations Office on Drugs and Crime, the last decade saw an alarming rise in the use of recreational substances.1 There was an escalation not only in the use of the more well-known street drugs (cannabis, stimulants, opioids, and hallucinogens), but also an exponential increase in the abuse of novel psychoactive substances. Although most emergency physicians (EPs) are at least relatively familiar with some of these designer drugs—often synthesized analogues of common street drugs—region-specific herbal products with psychoactive properties are now entering the market worldwide. Certainly, the cause of this increased use is multifactorial: Ease of access to these drugs and ambiguous legality are believed to be among the largest contributors. Infrastructure established through globalization promotes easy drug transportation and distribution across borders, and widespread Internet use makes knowledge of and accessibility to such substances exceedingly simple.2,3
In particular, widespread online access has permanently altered the acquisition of knowledge in all realms—including drug use. Although Erowid Center remains one of the oldest and best-known of this type of Web site and bills itself as providing “harm reduction,” others have cropped up online and disseminate information about many forms of potentially psychoactive substances. Despite the purported raison d’être of these Web sites, recent studies have demonstrated these sites’ efficacy in promoting drug use under the guise of safety, particularly among adolescents and young adults. Among these is a qualitative study by Boyer et al4 of 12 drug users admitted to a pediatric psychiatry unit. Through extensive questioning about the patients’ digital habits, the researchers demonstrated that the majority of subjects used these Web sites and, as a result, either increased their drug use or learned about (and tried) new substances.
One drug that has benefited from globalization and the Internet is kratom (Mitragyna speciosa korth). This formerly regionally confined herbal psychoactive substance is native to Southeast Asia, where it has been used (and abused) for centuries as a mild stimulant, to prevent opioid withdrawal, and for recreational purposes. In recent years, kratom has been marketed as a psychotropic drug and has become increasingly popular in the United States and in the United Kingdom.2,5,6 In the United States, this poses a problem for EPs who often are unaware of this plant’s existence, much less its abuse potential or health effects.2 Also known as ketum, kakuam, thang, thom, or biak, kratom is marketed in stores and online as a cheap, safe alternative to opioids.
Although considered a “substance of concern” without any approved medical use by the US Drug Enforcement Agency (DEA
To that end, users consider kratom a legal high, and it is easily purchased online. A 2010 study in the United Kingdom examined Web sites where kratom and many other quasilegal substances (including Salvia divinorum and legal precursors to LSD) could be purchased for an average of £10 (about $13 US currency).5 This study’s authors also noted a significant lack of product information on these marketplaces. As these products are not overseen by any regulatory body, the risk of overdose or adulteration is extremely high.2,3,6-8 In fact, Krypton, a kratom product sold online, was found to be adulterated with O-desmethyltramadol—the active metabolite of the synthetic opiate tramadol—and implicated in at least nine deaths.7
This article presents a case of kratom abuse. It describes a brief history of the substance, its pharmacological characteristics, the clinical presentation of kratom abuse, and the treatment of kratom-related illness and evaluation of potential toxic sequelae. In light of the rapid proliferation of kratom in the United States, a basic working knowledge of the drug is quickly becoming a must for EPs.
Case Presentation
At his employer’s request, a 33-year-old man presented to his family physician for a worsening of his uncontrolled back pain from a herniated lumbar disk resulting from a motor vehicle collision 3 months before. At his physician’s office he stated, “I don’t care if I live or die, I’m tired of the pain,” and “I’m going to go off on somebody if I can’t get this pain under control.” He also endorsed having auditory hallucinations for several years and a history of violence and homicide. The problem arose precipitously after he became concerned that he was abusing his opioid medication, and it was discontinued. The patient was transferred to the local ED and admitted to the psychiatric service for his suicidal ideations and risk of harming self and others.
On admission to the psychiatric service, the patient complained of body aches, chills, rhinorrhea, and significantly worsened irritability from his baseline, consistent with opioid withdrawal. Initial point-of-care (POC) admission drug testing had been negative as had expanded urine tests looking for synthetic opioids, cannabinoids, and cathinones. The patient reported no opioid use but was unable to explain his current symptom patterns, which were worsening his chronic pain and hampering any attempt to build rapport. On hospital day 3, the patient’s opioid withdrawal resolved, and psychiatric treatment was able to progress fully. On hospital day 4, the inpatient treatment team received a message from the patient’s primary care manager stating that a friend of the patient had found a bottle of herbal pills in the patient’s car. This was later revealed to be a kratom formulation that he had purchased online.
Background
Kratom is the colloquial name of a tree that is native to Thailand, Malaysia, and other countries in Southeast Asia. These trees, which can grow to 50 feet high and 15 feet wide, have long been the source of herbal remedies in Southeast Asia.2,3 The leaves of these trees contain psychoactive substances that have a variety of effects when consumed. At low doses, kratom causes a stimulant effect (akin to the leaves of the coca plant in South America); laborers and farmers often use it to help boost their energy. At higher doses, kratom causes an opioid-like effect, which at mega doses produces an intense euphoric state and has led to a steady growth in abuse worldwide. Although the government of Thailand banned the planting of Mitragyna speciosa as early as 1943, its continued proliferation in Southeast Asia and throughout the world has not ceased.2,3,6
In the United Kingdom, kratom is currently the second most common drug that is considered a legal high, only behind salvia (Salvia divinorum), a hallucinogenic herb that is better known as a result of its use by young celebrities over the past decade.5,8
Kratom can be taken in a variety of ways: Crushed leaves often are placed in gel caps and swallowed; it can be drunk as a tea, juice, or boiled syrup; and it can be smoked or insufflated.2,3,5,6
Pharmacology and Clinical Presentation
More than 20 psychoactive compounds have been isolated from kratom. Although a discussion of all these compounds is beyond the scope of this review, the two major compounds are mitragynine and 7-hydroxymitragynine.
Mitragynine
Mitragynine, the most abundant psychoactive compound found in kratom, is an indole alkaloid (Figure 1). Extraction and analysis of this compound has demonstrated numerous effects on multiple receptors, including mu-, delta-, and kappa-opioid receptors, leading to its opioid-like effects, including analgesia and euphoria. Also similar to common opioids, withdrawal symptomatology can present after only 5 days of daily use. There is limited evidence that mitragynine can activate postsynaptic alpha-2 adrenergic receptors, which may act synergistically with the mu-agonist with regard to its analgesic effect.2,5
7-Hydroxymitragynine
7-hydroxymitragynine, despite being far less concentrated in kratom preparations, is about 13 times more potent than morphine and 46 times more potent than mitragynine. It is thought that its hydroxyl side chain added to C7 (Figure 2) adds to its lipophilicity and ability to cross the blood-brain barrier at a far more rapid rate than that of mitragynine.2
Mitragynine and 7-hydroxymitragynine remain the best-studied psychoactive components of kratom at this time. Other compounds that have been isolated, such as speciociliatine, paynantheine, and speciogynine, may play a role in kratom’s analgesic and psychoactive effects. Animal studies have demonstrated antimuscarinic properties in these compounds, but the properties do not seem to have any demonstrable effect at the opioid receptors.2
Intoxication and Withdrawal
Due to its increasing worldwide popularity, it is now imperative for EPs to be aware of the presentation of patients with kratom abuse as well as the management of withdrawal in light of its dependence potential. However, large-scale studies have not been performed, and much of the evidence comes not from the medical literature but from Web sites such as Erowid or SageWisdom.2,5-9 To that end, such information will be discussed along with the limited research and expert consensuses available in peer-reviewed medical literature.
Kratom seems to have dose-dependent effects. At low doses (1-5 g of raw crushed leaves), kratom abusers often report a mild energizing effect, thought to be secondary to the stimulant properties of kratom’s multiple alkaloids. Users have reported mild euphoria and highs similar to those of the abuse of methylphenidate or modafinil.2,9,10 Also similar to abuse of those substances, users have reported anxiety, irritability, and aggressiveness as a result of the stimulant-like effects.
At moderate-to-high doses (5-15 g of raw crushed leaves), it is believed that the mu-opiate receptor agonism overtakes the stimulant effects, leading to the euphoria, relaxation, and analgesia seen with conventional opioid use and abuse.2,10 In light of the drug’s substantial binding and agonism of all opioid receptors, constipation and itching also are seen.2 As such, if an individual is intoxicated, he or she should be managed with supportive and symptomatic care and continuous monitoring of heart rate, blood pressure, respiratory rate, and oxygen saturation.2,10 Kratom intoxication can precipitate psychotic episodes similar to those caused by opiate intoxication, so monitoring for agitation or psychotic behaviors is also indicated.9,10
The medical management of a patient with an acute kratom overdose (typically requiring ingestion of >15 g of crushed leaves) begins with addressing airway support, breathing, and circulation along with continuous vital sign monitoring and laboratory testing, including POC glucose testing, complete blood count, electrolytes, lactate, venous blood gas, and measurable drug levels (ethanol, acetaminophen, tricyclic antidepressants, as indicated).11 If it is determined that kratom was the intoxicant, the greatest concern of death is similar to that of opioid overdose: respiratory depression. Although there are no large-scale human studies demonstrating efficacy, multiple authors suggest the use of naloxone in kratom-related hypoventilation.9,10
The development of dependence on kratom and its subsequent withdrawal phenomena are thought to be similar to that of opioids, in light of its strong mu agonism.2,5,9,10 Indeed, kratom has a long history of being used by opioid-dependent patients as an attempt to quit drug abuse or stave off debilitating withdrawal symptoms when they are unable to acquire their substance of choice.2,5-10 As such, withdrawal and the treatment thereof will also mimic that of opioid withdrawal.
The kratom-dependent individual will often present with rhinorrhea, lacrimation, dry mouth, hostility, aggression, and emotional lability similar to the case study described earlier.2,9,10 Kratom withdrawal, much like intoxication, also may precipitate or worsen psychotic symptoms, and monitoring is necessary throughout the detoxification process.2,5,10 Withdrawal management should proceed along ambulatory clinic or hospital opioid withdrawal protocols that include step-down administration of opioids or with nonopioid medications for symptomatic relief, including muscle relaxants, alpha-2 agonists, and antidiarrheal agents.5,9,10
Kratom Toxicity
A review of the available medical literature has demonstrated a number of toxic effects with kratom abuse, either as the sole agent or in concert with prescribed medications, recreational coingestants, or as a result of manufacturer’s adulteration with other chemicals or drugs. Of particular interest to EPs are manic or psychotic episode precipitation, seizure, hypothyroidism, intrahepatic cholestatic injury, and even sudden cardiac death.2,3,5-10 In addition to the basic history, physical, and laboratory examination, the workup of patients identified as kratom users should include the following:
- Fastidious medication reconciliation with drug-interaction check;
- Exhaustive substance abuse history;
- Identification of the brand name and source of kratom purchased, to determine whether there are advertised coingestants or reports of adulteration;
- Electrocardiogram;
- Thyroid function testing;
- Hepatic function testing; and
- Comprehensive neurological and mental status examinations.
In chronic users of kratom, a number of effects have been seen whose etiologies have not yet been determined. These effects include depression, anxiety, tremulousness, weight loss, and psychosis.3-7 Additionally, a study by Kittirattanapaiboon et al12 correlated drug use by those with concurrent mental health disorders (in particular, kratom, which was used in 59% of the ≥14,000 individuals included in the study sample) with statistically significant higher suicide risk.
Detection
Because kratom is a relatively new compound in the United States, medical and forensic laboratories are only now implementing kratom detection protocols. Many laboratories now use high-performance liquid chromatography to analyze for mitragynine, 7-hydroxymitragynine, and two metabolites of mitragynine in urine.7 Le et al13 were able to detect mitragynine in the urine in levels as low as 1 ng/mL, which is clinically useful as mitragynine has a half-life determined in animal studies to be 3.85 hours. Similar detection limits for mitragynine and 7-hydroxymitragynine are used only at the Naval Medical Center Portsmouth in Virginia; however, kratom was not detected in the case study patient’s urine because a urine test was not done until hospital day 5.
Case Conclusion
When gently confronted about the kratom found in his car, the case study patient admitted that he had purchased kratom online after he was “cut off” from prescription opioids for his pain. He admitted that although it was beneficial for his pain, he did notice worsening in his aggression toward his spouse and coworkers. This progressed to an exacerbation of his psychotic symptoms of hallucinations and persecutory delusions. These symptoms remained well hidden—but were present for years prior to his presentation at the hospital. The patient was discharged from the inpatient psychiatric unit on hospital day 16 with a diagnosis of schizoaffective disorder, depressive type in addition to opioid-use disorder. The patient agreed to seek a pain management specialist and discontinue kratom use.
Conclusion
Kratom is an emerging drug of abuse in the Western world. Although significant research is being conducted on its possible medical uses, little is known about kratom beyond the “trip reports” of kratom users posted online. Because of its technically legal status in the United States and multiple other Western countries, kratom is easily accessible. Emergency physicians need to be aware of kratom, and during their evaluations, question appropriate patients about kratom and other legal highs.
1. United Nations Office of Drug and Crime. World Drug Report 2014. https://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf. Published June 2014. Accessed September 26, 2016.
2. Prozialeck WC, Jivan JK, Andurkar SV. Pharmacology of kratom: an emerging botanical agent with stimulant, analgesic and opioid-like effects. J Am Osteopath Assoc. 2012;112(12):792-799.
3. U.S. Drug Enforcement Administration, Office of Diversion Control. Kratom (Mitragyna speciosa korth). http://www.deadiversion.usdoj.gov/drug _chem_info/kratom.pdf. Published January 2013. Accessed September 26, 2016.
4. Boyer EW, Shannon M, Hibberd PL. The Internet and psychoactive substance use among innovative drug users. Pediatrics. 2005;115(2):302-305.
5. Yusoff NH, Suhaimi FW, Vadivelu RK, et al. Abuse potential and adverse cognitive effects of mitragynine (kratom). Addict Biol. 2016;21(1):98-110.
6. Schmidt MM, Sharma A, Schifano F, Feinmann C. “Legal highs” on the net-evaluation of UK-based websites, products and product information. Forensic Sci Int. 2011;206(1-3):92-97.
7. Kronstrand R, Roman M, Thelander G, Eriksson A. Unintentional fatal intoxications with mitragynine and O-desmethyltramadol from the herbal blend Krypton. J Anal Toxicol. 2011;35(4):242-247.
8. Holler JM, Vorce SP, McDonough-Bender PC, Magluilo J Jr, Solomon CJ, Levine B. A drug toxicity death involving propylhexedrine and mitragynine. J Anal Toxicol. 2011;35(1):54-59.
9. Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow…and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. J Med Toxicol. 2012;8(1):15-32.
10. Rech MA, Donahey E, Cappiello Dziedzic JM, Oh L, Greenhalgh E. New drugs of abuse. Pharmacotherapy. 2015;35(2):189-197.
11. Silvilotti MLA. Initial management of the critically ill adult with an unknown overdose. http://www.uptodate.com/contents/initial-management-of-the -critically-ill-adult-with-an-unknown-overdose. Updated August 27, 2015. Accessed September 26, 2016.
12. Kittirattanapaiboon P, Suttajit S, Junsirimongkol B, Likhitsathian S, Srisurapanont M. Suicide risk among Thai illicit drug users with and without mental/alcohol use disorders. Neuropsychiatr Dis Treat. 2014;10:453-458.
13. Le D, Goggin MM, Janis GC. Analysis of mitragynine and metabolites in human urine for detecting the use of the psychoactive plant kratom. J Anal Toxicol. 2012;36(9):616-625.
Editor’s Note: This article has been adapted from an article originally published in Federal Practitioner (Tavakoli HR, et al. Kratom: a new product in an expanding substance abuse market. Fed Prac. 2016;33[11]:132-136. http://www.fedprac.com).
According to the United Nations Office on Drugs and Crime, the last decade saw an alarming rise in the use of recreational substances.1 There was an escalation not only in the use of the more well-known street drugs (cannabis, stimulants, opioids, and hallucinogens), but also an exponential increase in the abuse of novel psychoactive substances. Although most emergency physicians (EPs) are at least relatively familiar with some of these designer drugs—often synthesized analogues of common street drugs—region-specific herbal products with psychoactive properties are now entering the market worldwide. Certainly, the cause of this increased use is multifactorial: Ease of access to these drugs and ambiguous legality are believed to be among the largest contributors. Infrastructure established through globalization promotes easy drug transportation and distribution across borders, and widespread Internet use makes knowledge of and accessibility to such substances exceedingly simple.2,3
In particular, widespread online access has permanently altered the acquisition of knowledge in all realms—including drug use. Although Erowid Center remains one of the oldest and best-known of this type of Web site and bills itself as providing “harm reduction,” others have cropped up online and disseminate information about many forms of potentially psychoactive substances. Despite the purported raison d’être of these Web sites, recent studies have demonstrated these sites’ efficacy in promoting drug use under the guise of safety, particularly among adolescents and young adults. Among these is a qualitative study by Boyer et al4 of 12 drug users admitted to a pediatric psychiatry unit. Through extensive questioning about the patients’ digital habits, the researchers demonstrated that the majority of subjects used these Web sites and, as a result, either increased their drug use or learned about (and tried) new substances.
One drug that has benefited from globalization and the Internet is kratom (Mitragyna speciosa korth). This formerly regionally confined herbal psychoactive substance is native to Southeast Asia, where it has been used (and abused) for centuries as a mild stimulant, to prevent opioid withdrawal, and for recreational purposes. In recent years, kratom has been marketed as a psychotropic drug and has become increasingly popular in the United States and in the United Kingdom.2,5,6 In the United States, this poses a problem for EPs who often are unaware of this plant’s existence, much less its abuse potential or health effects.2 Also known as ketum, kakuam, thang, thom, or biak, kratom is marketed in stores and online as a cheap, safe alternative to opioids.
Although considered a “substance of concern” without any approved medical use by the US Drug Enforcement Agency (DEA
To that end, users consider kratom a legal high, and it is easily purchased online. A 2010 study in the United Kingdom examined Web sites where kratom and many other quasilegal substances (including Salvia divinorum and legal precursors to LSD) could be purchased for an average of £10 (about $13 US currency).5 This study’s authors also noted a significant lack of product information on these marketplaces. As these products are not overseen by any regulatory body, the risk of overdose or adulteration is extremely high.2,3,6-8 In fact, Krypton, a kratom product sold online, was found to be adulterated with O-desmethyltramadol—the active metabolite of the synthetic opiate tramadol—and implicated in at least nine deaths.7
This article presents a case of kratom abuse. It describes a brief history of the substance, its pharmacological characteristics, the clinical presentation of kratom abuse, and the treatment of kratom-related illness and evaluation of potential toxic sequelae. In light of the rapid proliferation of kratom in the United States, a basic working knowledge of the drug is quickly becoming a must for EPs.
Case Presentation
At his employer’s request, a 33-year-old man presented to his family physician for a worsening of his uncontrolled back pain from a herniated lumbar disk resulting from a motor vehicle collision 3 months before. At his physician’s office he stated, “I don’t care if I live or die, I’m tired of the pain,” and “I’m going to go off on somebody if I can’t get this pain under control.” He also endorsed having auditory hallucinations for several years and a history of violence and homicide. The problem arose precipitously after he became concerned that he was abusing his opioid medication, and it was discontinued. The patient was transferred to the local ED and admitted to the psychiatric service for his suicidal ideations and risk of harming self and others.
On admission to the psychiatric service, the patient complained of body aches, chills, rhinorrhea, and significantly worsened irritability from his baseline, consistent with opioid withdrawal. Initial point-of-care (POC) admission drug testing had been negative as had expanded urine tests looking for synthetic opioids, cannabinoids, and cathinones. The patient reported no opioid use but was unable to explain his current symptom patterns, which were worsening his chronic pain and hampering any attempt to build rapport. On hospital day 3, the patient’s opioid withdrawal resolved, and psychiatric treatment was able to progress fully. On hospital day 4, the inpatient treatment team received a message from the patient’s primary care manager stating that a friend of the patient had found a bottle of herbal pills in the patient’s car. This was later revealed to be a kratom formulation that he had purchased online.
Background
Kratom is the colloquial name of a tree that is native to Thailand, Malaysia, and other countries in Southeast Asia. These trees, which can grow to 50 feet high and 15 feet wide, have long been the source of herbal remedies in Southeast Asia.2,3 The leaves of these trees contain psychoactive substances that have a variety of effects when consumed. At low doses, kratom causes a stimulant effect (akin to the leaves of the coca plant in South America); laborers and farmers often use it to help boost their energy. At higher doses, kratom causes an opioid-like effect, which at mega doses produces an intense euphoric state and has led to a steady growth in abuse worldwide. Although the government of Thailand banned the planting of Mitragyna speciosa as early as 1943, its continued proliferation in Southeast Asia and throughout the world has not ceased.2,3,6
In the United Kingdom, kratom is currently the second most common drug that is considered a legal high, only behind salvia (Salvia divinorum), a hallucinogenic herb that is better known as a result of its use by young celebrities over the past decade.5,8
Kratom can be taken in a variety of ways: Crushed leaves often are placed in gel caps and swallowed; it can be drunk as a tea, juice, or boiled syrup; and it can be smoked or insufflated.2,3,5,6
Pharmacology and Clinical Presentation
More than 20 psychoactive compounds have been isolated from kratom. Although a discussion of all these compounds is beyond the scope of this review, the two major compounds are mitragynine and 7-hydroxymitragynine.
Mitragynine
Mitragynine, the most abundant psychoactive compound found in kratom, is an indole alkaloid (Figure 1). Extraction and analysis of this compound has demonstrated numerous effects on multiple receptors, including mu-, delta-, and kappa-opioid receptors, leading to its opioid-like effects, including analgesia and euphoria. Also similar to common opioids, withdrawal symptomatology can present after only 5 days of daily use. There is limited evidence that mitragynine can activate postsynaptic alpha-2 adrenergic receptors, which may act synergistically with the mu-agonist with regard to its analgesic effect.2,5
7-Hydroxymitragynine
7-hydroxymitragynine, despite being far less concentrated in kratom preparations, is about 13 times more potent than morphine and 46 times more potent than mitragynine. It is thought that its hydroxyl side chain added to C7 (Figure 2) adds to its lipophilicity and ability to cross the blood-brain barrier at a far more rapid rate than that of mitragynine.2
Mitragynine and 7-hydroxymitragynine remain the best-studied psychoactive components of kratom at this time. Other compounds that have been isolated, such as speciociliatine, paynantheine, and speciogynine, may play a role in kratom’s analgesic and psychoactive effects. Animal studies have demonstrated antimuscarinic properties in these compounds, but the properties do not seem to have any demonstrable effect at the opioid receptors.2
Intoxication and Withdrawal
Due to its increasing worldwide popularity, it is now imperative for EPs to be aware of the presentation of patients with kratom abuse as well as the management of withdrawal in light of its dependence potential. However, large-scale studies have not been performed, and much of the evidence comes not from the medical literature but from Web sites such as Erowid or SageWisdom.2,5-9 To that end, such information will be discussed along with the limited research and expert consensuses available in peer-reviewed medical literature.
Kratom seems to have dose-dependent effects. At low doses (1-5 g of raw crushed leaves), kratom abusers often report a mild energizing effect, thought to be secondary to the stimulant properties of kratom’s multiple alkaloids. Users have reported mild euphoria and highs similar to those of the abuse of methylphenidate or modafinil.2,9,10 Also similar to abuse of those substances, users have reported anxiety, irritability, and aggressiveness as a result of the stimulant-like effects.
At moderate-to-high doses (5-15 g of raw crushed leaves), it is believed that the mu-opiate receptor agonism overtakes the stimulant effects, leading to the euphoria, relaxation, and analgesia seen with conventional opioid use and abuse.2,10 In light of the drug’s substantial binding and agonism of all opioid receptors, constipation and itching also are seen.2 As such, if an individual is intoxicated, he or she should be managed with supportive and symptomatic care and continuous monitoring of heart rate, blood pressure, respiratory rate, and oxygen saturation.2,10 Kratom intoxication can precipitate psychotic episodes similar to those caused by opiate intoxication, so monitoring for agitation or psychotic behaviors is also indicated.9,10
The medical management of a patient with an acute kratom overdose (typically requiring ingestion of >15 g of crushed leaves) begins with addressing airway support, breathing, and circulation along with continuous vital sign monitoring and laboratory testing, including POC glucose testing, complete blood count, electrolytes, lactate, venous blood gas, and measurable drug levels (ethanol, acetaminophen, tricyclic antidepressants, as indicated).11 If it is determined that kratom was the intoxicant, the greatest concern of death is similar to that of opioid overdose: respiratory depression. Although there are no large-scale human studies demonstrating efficacy, multiple authors suggest the use of naloxone in kratom-related hypoventilation.9,10
The development of dependence on kratom and its subsequent withdrawal phenomena are thought to be similar to that of opioids, in light of its strong mu agonism.2,5,9,10 Indeed, kratom has a long history of being used by opioid-dependent patients as an attempt to quit drug abuse or stave off debilitating withdrawal symptoms when they are unable to acquire their substance of choice.2,5-10 As such, withdrawal and the treatment thereof will also mimic that of opioid withdrawal.
The kratom-dependent individual will often present with rhinorrhea, lacrimation, dry mouth, hostility, aggression, and emotional lability similar to the case study described earlier.2,9,10 Kratom withdrawal, much like intoxication, also may precipitate or worsen psychotic symptoms, and monitoring is necessary throughout the detoxification process.2,5,10 Withdrawal management should proceed along ambulatory clinic or hospital opioid withdrawal protocols that include step-down administration of opioids or with nonopioid medications for symptomatic relief, including muscle relaxants, alpha-2 agonists, and antidiarrheal agents.5,9,10
Kratom Toxicity
A review of the available medical literature has demonstrated a number of toxic effects with kratom abuse, either as the sole agent or in concert with prescribed medications, recreational coingestants, or as a result of manufacturer’s adulteration with other chemicals or drugs. Of particular interest to EPs are manic or psychotic episode precipitation, seizure, hypothyroidism, intrahepatic cholestatic injury, and even sudden cardiac death.2,3,5-10 In addition to the basic history, physical, and laboratory examination, the workup of patients identified as kratom users should include the following:
- Fastidious medication reconciliation with drug-interaction check;
- Exhaustive substance abuse history;
- Identification of the brand name and source of kratom purchased, to determine whether there are advertised coingestants or reports of adulteration;
- Electrocardiogram;
- Thyroid function testing;
- Hepatic function testing; and
- Comprehensive neurological and mental status examinations.
In chronic users of kratom, a number of effects have been seen whose etiologies have not yet been determined. These effects include depression, anxiety, tremulousness, weight loss, and psychosis.3-7 Additionally, a study by Kittirattanapaiboon et al12 correlated drug use by those with concurrent mental health disorders (in particular, kratom, which was used in 59% of the ≥14,000 individuals included in the study sample) with statistically significant higher suicide risk.
Detection
Because kratom is a relatively new compound in the United States, medical and forensic laboratories are only now implementing kratom detection protocols. Many laboratories now use high-performance liquid chromatography to analyze for mitragynine, 7-hydroxymitragynine, and two metabolites of mitragynine in urine.7 Le et al13 were able to detect mitragynine in the urine in levels as low as 1 ng/mL, which is clinically useful as mitragynine has a half-life determined in animal studies to be 3.85 hours. Similar detection limits for mitragynine and 7-hydroxymitragynine are used only at the Naval Medical Center Portsmouth in Virginia; however, kratom was not detected in the case study patient’s urine because a urine test was not done until hospital day 5.
Case Conclusion
When gently confronted about the kratom found in his car, the case study patient admitted that he had purchased kratom online after he was “cut off” from prescription opioids for his pain. He admitted that although it was beneficial for his pain, he did notice worsening in his aggression toward his spouse and coworkers. This progressed to an exacerbation of his psychotic symptoms of hallucinations and persecutory delusions. These symptoms remained well hidden—but were present for years prior to his presentation at the hospital. The patient was discharged from the inpatient psychiatric unit on hospital day 16 with a diagnosis of schizoaffective disorder, depressive type in addition to opioid-use disorder. The patient agreed to seek a pain management specialist and discontinue kratom use.
Conclusion
Kratom is an emerging drug of abuse in the Western world. Although significant research is being conducted on its possible medical uses, little is known about kratom beyond the “trip reports” of kratom users posted online. Because of its technically legal status in the United States and multiple other Western countries, kratom is easily accessible. Emergency physicians need to be aware of kratom, and during their evaluations, question appropriate patients about kratom and other legal highs.
Editor’s Note: This article has been adapted from an article originally published in Federal Practitioner (Tavakoli HR, et al. Kratom: a new product in an expanding substance abuse market. Fed Prac. 2016;33[11]:132-136. http://www.fedprac.com).
According to the United Nations Office on Drugs and Crime, the last decade saw an alarming rise in the use of recreational substances.1 There was an escalation not only in the use of the more well-known street drugs (cannabis, stimulants, opioids, and hallucinogens), but also an exponential increase in the abuse of novel psychoactive substances. Although most emergency physicians (EPs) are at least relatively familiar with some of these designer drugs—often synthesized analogues of common street drugs—region-specific herbal products with psychoactive properties are now entering the market worldwide. Certainly, the cause of this increased use is multifactorial: Ease of access to these drugs and ambiguous legality are believed to be among the largest contributors. Infrastructure established through globalization promotes easy drug transportation and distribution across borders, and widespread Internet use makes knowledge of and accessibility to such substances exceedingly simple.2,3
In particular, widespread online access has permanently altered the acquisition of knowledge in all realms—including drug use. Although Erowid Center remains one of the oldest and best-known of this type of Web site and bills itself as providing “harm reduction,” others have cropped up online and disseminate information about many forms of potentially psychoactive substances. Despite the purported raison d’être of these Web sites, recent studies have demonstrated these sites’ efficacy in promoting drug use under the guise of safety, particularly among adolescents and young adults. Among these is a qualitative study by Boyer et al4 of 12 drug users admitted to a pediatric psychiatry unit. Through extensive questioning about the patients’ digital habits, the researchers demonstrated that the majority of subjects used these Web sites and, as a result, either increased their drug use or learned about (and tried) new substances.
One drug that has benefited from globalization and the Internet is kratom (Mitragyna speciosa korth). This formerly regionally confined herbal psychoactive substance is native to Southeast Asia, where it has been used (and abused) for centuries as a mild stimulant, to prevent opioid withdrawal, and for recreational purposes. In recent years, kratom has been marketed as a psychotropic drug and has become increasingly popular in the United States and in the United Kingdom.2,5,6 In the United States, this poses a problem for EPs who often are unaware of this plant’s existence, much less its abuse potential or health effects.2 Also known as ketum, kakuam, thang, thom, or biak, kratom is marketed in stores and online as a cheap, safe alternative to opioids.
Although considered a “substance of concern” without any approved medical use by the US Drug Enforcement Agency (DEA
To that end, users consider kratom a legal high, and it is easily purchased online. A 2010 study in the United Kingdom examined Web sites where kratom and many other quasilegal substances (including Salvia divinorum and legal precursors to LSD) could be purchased for an average of £10 (about $13 US currency).5 This study’s authors also noted a significant lack of product information on these marketplaces. As these products are not overseen by any regulatory body, the risk of overdose or adulteration is extremely high.2,3,6-8 In fact, Krypton, a kratom product sold online, was found to be adulterated with O-desmethyltramadol—the active metabolite of the synthetic opiate tramadol—and implicated in at least nine deaths.7
This article presents a case of kratom abuse. It describes a brief history of the substance, its pharmacological characteristics, the clinical presentation of kratom abuse, and the treatment of kratom-related illness and evaluation of potential toxic sequelae. In light of the rapid proliferation of kratom in the United States, a basic working knowledge of the drug is quickly becoming a must for EPs.
Case Presentation
At his employer’s request, a 33-year-old man presented to his family physician for a worsening of his uncontrolled back pain from a herniated lumbar disk resulting from a motor vehicle collision 3 months before. At his physician’s office he stated, “I don’t care if I live or die, I’m tired of the pain,” and “I’m going to go off on somebody if I can’t get this pain under control.” He also endorsed having auditory hallucinations for several years and a history of violence and homicide. The problem arose precipitously after he became concerned that he was abusing his opioid medication, and it was discontinued. The patient was transferred to the local ED and admitted to the psychiatric service for his suicidal ideations and risk of harming self and others.
On admission to the psychiatric service, the patient complained of body aches, chills, rhinorrhea, and significantly worsened irritability from his baseline, consistent with opioid withdrawal. Initial point-of-care (POC) admission drug testing had been negative as had expanded urine tests looking for synthetic opioids, cannabinoids, and cathinones. The patient reported no opioid use but was unable to explain his current symptom patterns, which were worsening his chronic pain and hampering any attempt to build rapport. On hospital day 3, the patient’s opioid withdrawal resolved, and psychiatric treatment was able to progress fully. On hospital day 4, the inpatient treatment team received a message from the patient’s primary care manager stating that a friend of the patient had found a bottle of herbal pills in the patient’s car. This was later revealed to be a kratom formulation that he had purchased online.
Background
Kratom is the colloquial name of a tree that is native to Thailand, Malaysia, and other countries in Southeast Asia. These trees, which can grow to 50 feet high and 15 feet wide, have long been the source of herbal remedies in Southeast Asia.2,3 The leaves of these trees contain psychoactive substances that have a variety of effects when consumed. At low doses, kratom causes a stimulant effect (akin to the leaves of the coca plant in South America); laborers and farmers often use it to help boost their energy. At higher doses, kratom causes an opioid-like effect, which at mega doses produces an intense euphoric state and has led to a steady growth in abuse worldwide. Although the government of Thailand banned the planting of Mitragyna speciosa as early as 1943, its continued proliferation in Southeast Asia and throughout the world has not ceased.2,3,6
In the United Kingdom, kratom is currently the second most common drug that is considered a legal high, only behind salvia (Salvia divinorum), a hallucinogenic herb that is better known as a result of its use by young celebrities over the past decade.5,8
Kratom can be taken in a variety of ways: Crushed leaves often are placed in gel caps and swallowed; it can be drunk as a tea, juice, or boiled syrup; and it can be smoked or insufflated.2,3,5,6
Pharmacology and Clinical Presentation
More than 20 psychoactive compounds have been isolated from kratom. Although a discussion of all these compounds is beyond the scope of this review, the two major compounds are mitragynine and 7-hydroxymitragynine.
Mitragynine
Mitragynine, the most abundant psychoactive compound found in kratom, is an indole alkaloid (Figure 1). Extraction and analysis of this compound has demonstrated numerous effects on multiple receptors, including mu-, delta-, and kappa-opioid receptors, leading to its opioid-like effects, including analgesia and euphoria. Also similar to common opioids, withdrawal symptomatology can present after only 5 days of daily use. There is limited evidence that mitragynine can activate postsynaptic alpha-2 adrenergic receptors, which may act synergistically with the mu-agonist with regard to its analgesic effect.2,5
7-Hydroxymitragynine
7-hydroxymitragynine, despite being far less concentrated in kratom preparations, is about 13 times more potent than morphine and 46 times more potent than mitragynine. It is thought that its hydroxyl side chain added to C7 (Figure 2) adds to its lipophilicity and ability to cross the blood-brain barrier at a far more rapid rate than that of mitragynine.2
Mitragynine and 7-hydroxymitragynine remain the best-studied psychoactive components of kratom at this time. Other compounds that have been isolated, such as speciociliatine, paynantheine, and speciogynine, may play a role in kratom’s analgesic and psychoactive effects. Animal studies have demonstrated antimuscarinic properties in these compounds, but the properties do not seem to have any demonstrable effect at the opioid receptors.2
Intoxication and Withdrawal
Due to its increasing worldwide popularity, it is now imperative for EPs to be aware of the presentation of patients with kratom abuse as well as the management of withdrawal in light of its dependence potential. However, large-scale studies have not been performed, and much of the evidence comes not from the medical literature but from Web sites such as Erowid or SageWisdom.2,5-9 To that end, such information will be discussed along with the limited research and expert consensuses available in peer-reviewed medical literature.
Kratom seems to have dose-dependent effects. At low doses (1-5 g of raw crushed leaves), kratom abusers often report a mild energizing effect, thought to be secondary to the stimulant properties of kratom’s multiple alkaloids. Users have reported mild euphoria and highs similar to those of the abuse of methylphenidate or modafinil.2,9,10 Also similar to abuse of those substances, users have reported anxiety, irritability, and aggressiveness as a result of the stimulant-like effects.
At moderate-to-high doses (5-15 g of raw crushed leaves), it is believed that the mu-opiate receptor agonism overtakes the stimulant effects, leading to the euphoria, relaxation, and analgesia seen with conventional opioid use and abuse.2,10 In light of the drug’s substantial binding and agonism of all opioid receptors, constipation and itching also are seen.2 As such, if an individual is intoxicated, he or she should be managed with supportive and symptomatic care and continuous monitoring of heart rate, blood pressure, respiratory rate, and oxygen saturation.2,10 Kratom intoxication can precipitate psychotic episodes similar to those caused by opiate intoxication, so monitoring for agitation or psychotic behaviors is also indicated.9,10
The medical management of a patient with an acute kratom overdose (typically requiring ingestion of >15 g of crushed leaves) begins with addressing airway support, breathing, and circulation along with continuous vital sign monitoring and laboratory testing, including POC glucose testing, complete blood count, electrolytes, lactate, venous blood gas, and measurable drug levels (ethanol, acetaminophen, tricyclic antidepressants, as indicated).11 If it is determined that kratom was the intoxicant, the greatest concern of death is similar to that of opioid overdose: respiratory depression. Although there are no large-scale human studies demonstrating efficacy, multiple authors suggest the use of naloxone in kratom-related hypoventilation.9,10
The development of dependence on kratom and its subsequent withdrawal phenomena are thought to be similar to that of opioids, in light of its strong mu agonism.2,5,9,10 Indeed, kratom has a long history of being used by opioid-dependent patients as an attempt to quit drug abuse or stave off debilitating withdrawal symptoms when they are unable to acquire their substance of choice.2,5-10 As such, withdrawal and the treatment thereof will also mimic that of opioid withdrawal.
The kratom-dependent individual will often present with rhinorrhea, lacrimation, dry mouth, hostility, aggression, and emotional lability similar to the case study described earlier.2,9,10 Kratom withdrawal, much like intoxication, also may precipitate or worsen psychotic symptoms, and monitoring is necessary throughout the detoxification process.2,5,10 Withdrawal management should proceed along ambulatory clinic or hospital opioid withdrawal protocols that include step-down administration of opioids or with nonopioid medications for symptomatic relief, including muscle relaxants, alpha-2 agonists, and antidiarrheal agents.5,9,10
Kratom Toxicity
A review of the available medical literature has demonstrated a number of toxic effects with kratom abuse, either as the sole agent or in concert with prescribed medications, recreational coingestants, or as a result of manufacturer’s adulteration with other chemicals or drugs. Of particular interest to EPs are manic or psychotic episode precipitation, seizure, hypothyroidism, intrahepatic cholestatic injury, and even sudden cardiac death.2,3,5-10 In addition to the basic history, physical, and laboratory examination, the workup of patients identified as kratom users should include the following:
- Fastidious medication reconciliation with drug-interaction check;
- Exhaustive substance abuse history;
- Identification of the brand name and source of kratom purchased, to determine whether there are advertised coingestants or reports of adulteration;
- Electrocardiogram;
- Thyroid function testing;
- Hepatic function testing; and
- Comprehensive neurological and mental status examinations.
In chronic users of kratom, a number of effects have been seen whose etiologies have not yet been determined. These effects include depression, anxiety, tremulousness, weight loss, and psychosis.3-7 Additionally, a study by Kittirattanapaiboon et al12 correlated drug use by those with concurrent mental health disorders (in particular, kratom, which was used in 59% of the ≥14,000 individuals included in the study sample) with statistically significant higher suicide risk.
Detection
Because kratom is a relatively new compound in the United States, medical and forensic laboratories are only now implementing kratom detection protocols. Many laboratories now use high-performance liquid chromatography to analyze for mitragynine, 7-hydroxymitragynine, and two metabolites of mitragynine in urine.7 Le et al13 were able to detect mitragynine in the urine in levels as low as 1 ng/mL, which is clinically useful as mitragynine has a half-life determined in animal studies to be 3.85 hours. Similar detection limits for mitragynine and 7-hydroxymitragynine are used only at the Naval Medical Center Portsmouth in Virginia; however, kratom was not detected in the case study patient’s urine because a urine test was not done until hospital day 5.
Case Conclusion
When gently confronted about the kratom found in his car, the case study patient admitted that he had purchased kratom online after he was “cut off” from prescription opioids for his pain. He admitted that although it was beneficial for his pain, he did notice worsening in his aggression toward his spouse and coworkers. This progressed to an exacerbation of his psychotic symptoms of hallucinations and persecutory delusions. These symptoms remained well hidden—but were present for years prior to his presentation at the hospital. The patient was discharged from the inpatient psychiatric unit on hospital day 16 with a diagnosis of schizoaffective disorder, depressive type in addition to opioid-use disorder. The patient agreed to seek a pain management specialist and discontinue kratom use.
Conclusion
Kratom is an emerging drug of abuse in the Western world. Although significant research is being conducted on its possible medical uses, little is known about kratom beyond the “trip reports” of kratom users posted online. Because of its technically legal status in the United States and multiple other Western countries, kratom is easily accessible. Emergency physicians need to be aware of kratom, and during their evaluations, question appropriate patients about kratom and other legal highs.
1. United Nations Office of Drug and Crime. World Drug Report 2014. https://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf. Published June 2014. Accessed September 26, 2016.
2. Prozialeck WC, Jivan JK, Andurkar SV. Pharmacology of kratom: an emerging botanical agent with stimulant, analgesic and opioid-like effects. J Am Osteopath Assoc. 2012;112(12):792-799.
3. U.S. Drug Enforcement Administration, Office of Diversion Control. Kratom (Mitragyna speciosa korth). http://www.deadiversion.usdoj.gov/drug _chem_info/kratom.pdf. Published January 2013. Accessed September 26, 2016.
4. Boyer EW, Shannon M, Hibberd PL. The Internet and psychoactive substance use among innovative drug users. Pediatrics. 2005;115(2):302-305.
5. Yusoff NH, Suhaimi FW, Vadivelu RK, et al. Abuse potential and adverse cognitive effects of mitragynine (kratom). Addict Biol. 2016;21(1):98-110.
6. Schmidt MM, Sharma A, Schifano F, Feinmann C. “Legal highs” on the net-evaluation of UK-based websites, products and product information. Forensic Sci Int. 2011;206(1-3):92-97.
7. Kronstrand R, Roman M, Thelander G, Eriksson A. Unintentional fatal intoxications with mitragynine and O-desmethyltramadol from the herbal blend Krypton. J Anal Toxicol. 2011;35(4):242-247.
8. Holler JM, Vorce SP, McDonough-Bender PC, Magluilo J Jr, Solomon CJ, Levine B. A drug toxicity death involving propylhexedrine and mitragynine. J Anal Toxicol. 2011;35(1):54-59.
9. Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow…and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. J Med Toxicol. 2012;8(1):15-32.
10. Rech MA, Donahey E, Cappiello Dziedzic JM, Oh L, Greenhalgh E. New drugs of abuse. Pharmacotherapy. 2015;35(2):189-197.
11. Silvilotti MLA. Initial management of the critically ill adult with an unknown overdose. http://www.uptodate.com/contents/initial-management-of-the -critically-ill-adult-with-an-unknown-overdose. Updated August 27, 2015. Accessed September 26, 2016.
12. Kittirattanapaiboon P, Suttajit S, Junsirimongkol B, Likhitsathian S, Srisurapanont M. Suicide risk among Thai illicit drug users with and without mental/alcohol use disorders. Neuropsychiatr Dis Treat. 2014;10:453-458.
13. Le D, Goggin MM, Janis GC. Analysis of mitragynine and metabolites in human urine for detecting the use of the psychoactive plant kratom. J Anal Toxicol. 2012;36(9):616-625.
1. United Nations Office of Drug and Crime. World Drug Report 2014. https://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf. Published June 2014. Accessed September 26, 2016.
2. Prozialeck WC, Jivan JK, Andurkar SV. Pharmacology of kratom: an emerging botanical agent with stimulant, analgesic and opioid-like effects. J Am Osteopath Assoc. 2012;112(12):792-799.
3. U.S. Drug Enforcement Administration, Office of Diversion Control. Kratom (Mitragyna speciosa korth). http://www.deadiversion.usdoj.gov/drug _chem_info/kratom.pdf. Published January 2013. Accessed September 26, 2016.
4. Boyer EW, Shannon M, Hibberd PL. The Internet and psychoactive substance use among innovative drug users. Pediatrics. 2005;115(2):302-305.
5. Yusoff NH, Suhaimi FW, Vadivelu RK, et al. Abuse potential and adverse cognitive effects of mitragynine (kratom). Addict Biol. 2016;21(1):98-110.
6. Schmidt MM, Sharma A, Schifano F, Feinmann C. “Legal highs” on the net-evaluation of UK-based websites, products and product information. Forensic Sci Int. 2011;206(1-3):92-97.
7. Kronstrand R, Roman M, Thelander G, Eriksson A. Unintentional fatal intoxications with mitragynine and O-desmethyltramadol from the herbal blend Krypton. J Anal Toxicol. 2011;35(4):242-247.
8. Holler JM, Vorce SP, McDonough-Bender PC, Magluilo J Jr, Solomon CJ, Levine B. A drug toxicity death involving propylhexedrine and mitragynine. J Anal Toxicol. 2011;35(1):54-59.
9. Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow…and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. J Med Toxicol. 2012;8(1):15-32.
10. Rech MA, Donahey E, Cappiello Dziedzic JM, Oh L, Greenhalgh E. New drugs of abuse. Pharmacotherapy. 2015;35(2):189-197.
11. Silvilotti MLA. Initial management of the critically ill adult with an unknown overdose. http://www.uptodate.com/contents/initial-management-of-the -critically-ill-adult-with-an-unknown-overdose. Updated August 27, 2015. Accessed September 26, 2016.
12. Kittirattanapaiboon P, Suttajit S, Junsirimongkol B, Likhitsathian S, Srisurapanont M. Suicide risk among Thai illicit drug users with and without mental/alcohol use disorders. Neuropsychiatr Dis Treat. 2014;10:453-458.
13. Le D, Goggin MM, Janis GC. Analysis of mitragynine and metabolites in human urine for detecting the use of the psychoactive plant kratom. J Anal Toxicol. 2012;36(9):616-625.
Emergency Ultrasound: Tendon Evaluation With Ultrasonography
The vast majority of musculotendinous injuries occur secondary to violent contraction or excessive stretching.1 Ligamentous injuries, on the other hand, are due to an abnormal motion of joints. The magnitude of inciting forces results in a spectrum of pathology, ranging from a minor tear to a complete disruption of structures.
Ultrasonography provides a detailed assessment of soft tissue anatomy and dynamic functionality, and in some instances can be comparable or even superior to magnetic resonance imaging2 because the structural characteristics of certain tendons make them ideal for imaging via ultrasonography. We describe some of these characteristics and highlight their utility in diagnostic imaging.
Anatomical Structure
Tendons consist of tightly packed type I collagen fibers forming subfascicles that are arranged in a parallel distribution as fascicles. These bundles are held together by loose soft tissue, and the entire structure is covered by a thick fibroelastic epitendineum sheath. This linear distribution of structures yields a uniquely linear “fibrillary” pattern when viewed along the longitudinal axis of the structure (Figure 1a). In the short-axis view, the tendon appears as a well-circumscribed structure with speckled pattern of hyperechoic foci (Figure 1b). 3
Imaging Technique
The optimal scanning technique involves the use of a high-frequency linear transducer. Higher frequencies yield more detailed images, but may be limited in patients with deeper structures due to body habitus. A key concept in tendon evaluation is an artifact known as “anisotropy.” This refers to change in appearance of the tendon based on the incident angle of the ultrasound beam. For example, when the probe is held perpendicular to the structure of interest, parallel fibers will reflect the emitted beam toward the probe and thus appear as hyperechoic and speckled, a characteristic of these fibers (Figures 1a and 1b). Contrarily, if the probe is held at a nonperpendicular angle, the reflected beam will not return to the probe, resulting in a hypoechoic appearance (Figure 2).
Pathology
Tendon strains result in varying degrees of fibrous tearing. These tears can range from first-degree tears (a few fibers) to third-degree tears (complete disruption). Partial tears result in focal hematoma formation (Figure 3a) at the region of disruption, appearing on ultrasound as a hypoechoic fluid collection within a hyperechoic fibrillary or speckled tendon structure. If the disruption occurs along the surface of the tendon, a focus of anechoic fluid may be seen surrounding the tendon. Complete tendon ruptures, on the other hand, appear as a hypoechoic void with retracted tendon fragments visualized on either side4 (Figures 3b and 3c). Although complete tears can be more apparent clinically in areas in which a group of tendons performs a cohesive movement (ie, rotator cuff), ultrasound can significantly reduce the rate of delayed diagnosis when physical examination is equivocal.
In the appropriate clinical setting, ultrasonography can provide rapid and dynamic assessment of musculotendinous injuries. Lower extremity injuries, including those affecting the Achilles (Figure 1), quadriceps, (Figures 4a and 4b) and patellar tendons (Figure 5), are easier clinical applications.
Assessment of rotator cuff tendons, although more difficult, can provide a specific assessment of shoulder pain.5 In such scenarios, ultrasound can serve a very useful role as an adjunct to the physical examination.
An important point to recognize is that tendons will appear hypoechoic at the insertion point on bone (anthesis) due to increased curvature resulting in lack of anisotropy. This can appear as a pathological finding, but can be accounted for by simply performing a heel-toe or tilt maneuver to arrange the beam perpendicular to the tendon fibers (Figures 6a and 6b).
Summary
Musculotendinous injuries many times present as nonspecific symptoms of pain and/or swelling. In the case of an equivocal physical examination, musculotendinous injuries can be diagnosed with increased accuracy through the use of ultrasound. Understanding the artifactual component of tendon ultrasound can aid the clinician in diagnosing these injuries, enhancing patient care and satisfaction.
1. Geiderman J, Katz D. Geneneral principles in orthopedic injuries. In: Marx JA, Hockberger RS, Walls RM, Biros MH, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Philadelphia, PA: Elsevier Saunders; 2014:49:511-533.
2. Jacobson, Jon A. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am. 1999;37(4):713-735.
3. O’Neill J, ed. Musculoskeletal Ultrasound: Anatomy and Technique. New York, NY: Springer Science+Business Media. 2008:3-17.
4. Dawson M, Mallin M. Introduction to bedside ultrasound. Vol 1. Emergency ultrasound solutions. Lexington, KY: Emergency Ultrasound Solutions; 2012;25:245-248. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/327852/Introduction_to_Bedside_Ultrasound_Volume_1_-_Matt_and_Mike.pdf. Accessed April 12, 2017.
5. Tran G, Hensor EM, Ray A, Kingsbury SR, O’Connor P, Conaghan PG. Ultrasound-detected pathologies cluster into groups with different clinical outcomes: data from 3000 community referrals for shoulder pain. Arthritis Res Ther. 2017;19(1):30. doi:10.1186/s13075-017-1235-y.
The vast majority of musculotendinous injuries occur secondary to violent contraction or excessive stretching.1 Ligamentous injuries, on the other hand, are due to an abnormal motion of joints. The magnitude of inciting forces results in a spectrum of pathology, ranging from a minor tear to a complete disruption of structures.
Ultrasonography provides a detailed assessment of soft tissue anatomy and dynamic functionality, and in some instances can be comparable or even superior to magnetic resonance imaging2 because the structural characteristics of certain tendons make them ideal for imaging via ultrasonography. We describe some of these characteristics and highlight their utility in diagnostic imaging.
Anatomical Structure
Tendons consist of tightly packed type I collagen fibers forming subfascicles that are arranged in a parallel distribution as fascicles. These bundles are held together by loose soft tissue, and the entire structure is covered by a thick fibroelastic epitendineum sheath. This linear distribution of structures yields a uniquely linear “fibrillary” pattern when viewed along the longitudinal axis of the structure (Figure 1a). In the short-axis view, the tendon appears as a well-circumscribed structure with speckled pattern of hyperechoic foci (Figure 1b). 3
Imaging Technique
The optimal scanning technique involves the use of a high-frequency linear transducer. Higher frequencies yield more detailed images, but may be limited in patients with deeper structures due to body habitus. A key concept in tendon evaluation is an artifact known as “anisotropy.” This refers to change in appearance of the tendon based on the incident angle of the ultrasound beam. For example, when the probe is held perpendicular to the structure of interest, parallel fibers will reflect the emitted beam toward the probe and thus appear as hyperechoic and speckled, a characteristic of these fibers (Figures 1a and 1b). Contrarily, if the probe is held at a nonperpendicular angle, the reflected beam will not return to the probe, resulting in a hypoechoic appearance (Figure 2).
Pathology
Tendon strains result in varying degrees of fibrous tearing. These tears can range from first-degree tears (a few fibers) to third-degree tears (complete disruption). Partial tears result in focal hematoma formation (Figure 3a) at the region of disruption, appearing on ultrasound as a hypoechoic fluid collection within a hyperechoic fibrillary or speckled tendon structure. If the disruption occurs along the surface of the tendon, a focus of anechoic fluid may be seen surrounding the tendon. Complete tendon ruptures, on the other hand, appear as a hypoechoic void with retracted tendon fragments visualized on either side4 (Figures 3b and 3c). Although complete tears can be more apparent clinically in areas in which a group of tendons performs a cohesive movement (ie, rotator cuff), ultrasound can significantly reduce the rate of delayed diagnosis when physical examination is equivocal.
In the appropriate clinical setting, ultrasonography can provide rapid and dynamic assessment of musculotendinous injuries. Lower extremity injuries, including those affecting the Achilles (Figure 1), quadriceps, (Figures 4a and 4b) and patellar tendons (Figure 5), are easier clinical applications.
Assessment of rotator cuff tendons, although more difficult, can provide a specific assessment of shoulder pain.5 In such scenarios, ultrasound can serve a very useful role as an adjunct to the physical examination.
An important point to recognize is that tendons will appear hypoechoic at the insertion point on bone (anthesis) due to increased curvature resulting in lack of anisotropy. This can appear as a pathological finding, but can be accounted for by simply performing a heel-toe or tilt maneuver to arrange the beam perpendicular to the tendon fibers (Figures 6a and 6b).
Summary
Musculotendinous injuries many times present as nonspecific symptoms of pain and/or swelling. In the case of an equivocal physical examination, musculotendinous injuries can be diagnosed with increased accuracy through the use of ultrasound. Understanding the artifactual component of tendon ultrasound can aid the clinician in diagnosing these injuries, enhancing patient care and satisfaction.
The vast majority of musculotendinous injuries occur secondary to violent contraction or excessive stretching.1 Ligamentous injuries, on the other hand, are due to an abnormal motion of joints. The magnitude of inciting forces results in a spectrum of pathology, ranging from a minor tear to a complete disruption of structures.
Ultrasonography provides a detailed assessment of soft tissue anatomy and dynamic functionality, and in some instances can be comparable or even superior to magnetic resonance imaging2 because the structural characteristics of certain tendons make them ideal for imaging via ultrasonography. We describe some of these characteristics and highlight their utility in diagnostic imaging.
Anatomical Structure
Tendons consist of tightly packed type I collagen fibers forming subfascicles that are arranged in a parallel distribution as fascicles. These bundles are held together by loose soft tissue, and the entire structure is covered by a thick fibroelastic epitendineum sheath. This linear distribution of structures yields a uniquely linear “fibrillary” pattern when viewed along the longitudinal axis of the structure (Figure 1a). In the short-axis view, the tendon appears as a well-circumscribed structure with speckled pattern of hyperechoic foci (Figure 1b). 3
Imaging Technique
The optimal scanning technique involves the use of a high-frequency linear transducer. Higher frequencies yield more detailed images, but may be limited in patients with deeper structures due to body habitus. A key concept in tendon evaluation is an artifact known as “anisotropy.” This refers to change in appearance of the tendon based on the incident angle of the ultrasound beam. For example, when the probe is held perpendicular to the structure of interest, parallel fibers will reflect the emitted beam toward the probe and thus appear as hyperechoic and speckled, a characteristic of these fibers (Figures 1a and 1b). Contrarily, if the probe is held at a nonperpendicular angle, the reflected beam will not return to the probe, resulting in a hypoechoic appearance (Figure 2).
Pathology
Tendon strains result in varying degrees of fibrous tearing. These tears can range from first-degree tears (a few fibers) to third-degree tears (complete disruption). Partial tears result in focal hematoma formation (Figure 3a) at the region of disruption, appearing on ultrasound as a hypoechoic fluid collection within a hyperechoic fibrillary or speckled tendon structure. If the disruption occurs along the surface of the tendon, a focus of anechoic fluid may be seen surrounding the tendon. Complete tendon ruptures, on the other hand, appear as a hypoechoic void with retracted tendon fragments visualized on either side4 (Figures 3b and 3c). Although complete tears can be more apparent clinically in areas in which a group of tendons performs a cohesive movement (ie, rotator cuff), ultrasound can significantly reduce the rate of delayed diagnosis when physical examination is equivocal.
In the appropriate clinical setting, ultrasonography can provide rapid and dynamic assessment of musculotendinous injuries. Lower extremity injuries, including those affecting the Achilles (Figure 1), quadriceps, (Figures 4a and 4b) and patellar tendons (Figure 5), are easier clinical applications.
Assessment of rotator cuff tendons, although more difficult, can provide a specific assessment of shoulder pain.5 In such scenarios, ultrasound can serve a very useful role as an adjunct to the physical examination.
An important point to recognize is that tendons will appear hypoechoic at the insertion point on bone (anthesis) due to increased curvature resulting in lack of anisotropy. This can appear as a pathological finding, but can be accounted for by simply performing a heel-toe or tilt maneuver to arrange the beam perpendicular to the tendon fibers (Figures 6a and 6b).
Summary
Musculotendinous injuries many times present as nonspecific symptoms of pain and/or swelling. In the case of an equivocal physical examination, musculotendinous injuries can be diagnosed with increased accuracy through the use of ultrasound. Understanding the artifactual component of tendon ultrasound can aid the clinician in diagnosing these injuries, enhancing patient care and satisfaction.
1. Geiderman J, Katz D. Geneneral principles in orthopedic injuries. In: Marx JA, Hockberger RS, Walls RM, Biros MH, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Philadelphia, PA: Elsevier Saunders; 2014:49:511-533.
2. Jacobson, Jon A. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am. 1999;37(4):713-735.
3. O’Neill J, ed. Musculoskeletal Ultrasound: Anatomy and Technique. New York, NY: Springer Science+Business Media. 2008:3-17.
4. Dawson M, Mallin M. Introduction to bedside ultrasound. Vol 1. Emergency ultrasound solutions. Lexington, KY: Emergency Ultrasound Solutions; 2012;25:245-248. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/327852/Introduction_to_Bedside_Ultrasound_Volume_1_-_Matt_and_Mike.pdf. Accessed April 12, 2017.
5. Tran G, Hensor EM, Ray A, Kingsbury SR, O’Connor P, Conaghan PG. Ultrasound-detected pathologies cluster into groups with different clinical outcomes: data from 3000 community referrals for shoulder pain. Arthritis Res Ther. 2017;19(1):30. doi:10.1186/s13075-017-1235-y.
1. Geiderman J, Katz D. Geneneral principles in orthopedic injuries. In: Marx JA, Hockberger RS, Walls RM, Biros MH, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Philadelphia, PA: Elsevier Saunders; 2014:49:511-533.
2. Jacobson, Jon A. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am. 1999;37(4):713-735.
3. O’Neill J, ed. Musculoskeletal Ultrasound: Anatomy and Technique. New York, NY: Springer Science+Business Media. 2008:3-17.
4. Dawson M, Mallin M. Introduction to bedside ultrasound. Vol 1. Emergency ultrasound solutions. Lexington, KY: Emergency Ultrasound Solutions; 2012;25:245-248. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/327852/Introduction_to_Bedside_Ultrasound_Volume_1_-_Matt_and_Mike.pdf. Accessed April 12, 2017.
5. Tran G, Hensor EM, Ray A, Kingsbury SR, O’Connor P, Conaghan PG. Ultrasound-detected pathologies cluster into groups with different clinical outcomes: data from 3000 community referrals for shoulder pain. Arthritis Res Ther. 2017;19(1):30. doi:10.1186/s13075-017-1235-y.
First EDition: Medical “Merit Badges” for EPs, more
In a historic collaboration, 10 major emergency medicine organizations have joined forces to create The Coalition to Oppose Medical Merit Badges (COMMB). In its news release, the Coalition stated it “…believes that board-certified emergency physicians who actively maintain their board certification should not be required to complete short-course certification or acquire condition-specific continuing medical education credits in advanced
The COMMB consists of the American Academy of Emergency Medicine (AAEM), American Academy of Emergency Medicine/Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Association of Academic Chairs of Emergency Medicine (AACEM), Council of Emergency Medicine Residency Directors (CORD), Emergency Medicine Residents’ Association (EMRA), Society for Academic Emergency Medicine (SAEM), American Osteopathic Board of Emergency Medicine (AOBEM), and American College of Osteopathic Emergency Physicians (ACOEP).
In a written statement signed by the president/chair of each member organization, COMMB further asserted:
Similarly, mandatory targeted continuing medical education (CME) requirements do not offer any meaningful value for the public or for the emergency physician who has achieved and maintained board certification. Such requirements are often promulgated by others who incompletely understand the foundation of knowledge and skills acquired by successfully completing an Accreditation Council for Graduate Medical Education-accredited or American Osteopathic Association-approved Emergency Medicine Residency Program. These “merit badges” add no additional value for board-certified emergency physicians. Instead, they devalue the board certification process, failing to recognize the rigor of the ABEM Maintenance of Certification (MOC) Program. In essence, medical merit badges set a lower bar than a diplomate’s education, training, and ongoing learning, as measured by initial board certification and maintenance of certification.
The Coalition finds no rational justification to require medical merit badges for board-certified emergency physicians who maintain their board certification. Our committed professional organizations provide the best opportunities for continuous professional development and medical merit badges dismiss the quality of those educational efforts.
Opposing the requirements for medical merit badges will be a long and challenging struggle. It will take time to help administrators and regulatory bodies to better understand the rigorous standards to which we adhere as board-certified emergency physicians. In the coming months, we will develop our long-term strategy to create success and a pathway to recognize clinical excellence. We welcome your thoughts and suggestions as to how we can best succeed. In the near future, we will ask for strong support and a loud and unified voice.
We will persist and we are up to the challenge—we are board-certified emergency physicians. Opposing medical merit badges is the right thing to do for our specialty. We will forever demonstrate a lifelong commitment to caring for anyone who is ill or injured, at any time, for any reason.
Study Nixed Magnesium for Infants With Acute Bronchiolitis
AMY KARON
FRONTLINE MEDICAL news
Intravenous (IV) magnesium does not benefit, and may harm, infants with moderate-to-severe acute bronchiolitis, investigators reported. Compared with placebo, adding a single IV dose of magnesium sulfate (100 mg/kg) to usual care did not reduce time to medical readiness for discharge, even when patients had eczema or a family history of asthma, and was tied to a more than 3-fold rise in the rate of short-term readmissions, Khalid Al Ansari, MD, of Hamad Medical Corp in Doha, Qatar, and his associates wrote in Chest. “To our knowledge, this is the first randomized study to investigate the effect of intravenous magnesium in a bronchiolitis population,” they added.
Bronchiolitis lacks new, inexpensive, readily available treatments, despite being a common reason for hospital admission, the researchers noted. For older children with moderate-to-severe exacerbations of asthma, a meta-analysis found that the addition of magnesium to usual care appeared to cut readmissions and shorten lengths of stay, compared with placebo. To explore magnesium therapy in younger children, the investigators enrolled 162 previously healthy infants up to 18 months old who had been admitted to the short-stay unit of a pediatric emergency center with a diagnosis of moderate-to-severe viral bronchiolitis. Patients received usual care with oral dexamethasone and nebulized 5% hypertonic saline in 1 mL of 1:1000 epinephrine, plus a 60-minute IV infusion with a blinded syringe of either 0.9% saline placebo or magnesium sulfate (100 mg/kg).
The primary endpoint, time to medical readiness for discharge, did not statistically differ between groups, averaging 24.1 (95% confidence interval [CI], 20.0-29.1) hours with magnesium and 25.3 (95% CI, 20.3-31.5) hours with placebo (P = .91). Among patients with a history of eczema or a family history of asthma, mean times to readiness for discharge resembled those for the entire cohort and did not statistically differ based on treatment. Average Wang bronchiolitis severity scores also were similar between groups, as were rates of outpatient clinic visits (33.8% with magnesium and 27.2% with placebo). Thus, the trial identified “no benefit in adding intravenous magnesium for infant bronchiolitis, even in patients characterized to be at a higher risk for asthma,” the researchers concluded.
Strikingly, 2-week readmission rates were 19.5% with magnesium (95% CI, 11.3-30.1) and 6.2% with placebo (95% CI, 0.02-13.8; P = .016). Among patients with eczema or a family history of asthma, 2-week readmission rates also were significantly higher with magnesium (26.3%; 95% CI, 13.4-43.1) than with placebo (7.5%; 95% CI, 1.6-20.4; P = .034) These might have been chance findings, or magnesium might have masked worse bronchiolitis, prolonged the disease course, or interacted with 5% hypertonic saline or systemic corticosteroids, the investigators said. Intravenous magnesium might contribute to secondary relapse, especially among patients with eczema or a family history of asthma, they added.
Patients in this study had a median age of 3.7 months (range, 22 days to 17.6 months), about half had eczema or a family history of asthma, and 86% had positive nasopharyngeal virus swabs. Cardiopulmonary monitoring revealed no acute events during treatment. Of 16 readmissions in the magnesium group, 11 entered the infirmary and four entered the hospital. The five placebo readmissions included four to the infirmary and one to the hospital.
“As with other ‘negative studies,’ we may have failed to identify a benefit from intravenous magnesium in a patient subgroup because of our limited sample size,” the investigators wrote. “But we think our findings are generalizable to a similarly heterogeneous group of patients presenting for bronchiolitis care in a busy urban emergency department.”
Alansari K, Sayyed R, Davidson BL, Al Jawala S, Ghadier M. Intravenous magnesium sulfate for bronchiolitis: A randomized trial. Chest. 2017;pii:S0012-3692(17):30361-30366. doi:10.1016/j.chest.2017.03.002. [Epub ahead of print]
CDC: Some Shigella Strains Show Reduced Ciprofloxacin Susceptibility
SHARON WORCESTER
FRONTLINE MEDICAL NEWS
The Centers for Disease Control and Prevention (CDC) has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
- Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
- Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
- Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
- Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible—with special attention given to the MIC for fluoroquinolone antibiotics.
- Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
- Consult local or state health departments for guidance on when patients may return to childcare, school, or work.
- Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition, and all cases should be reported to one’s local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
Prenotification, Unequivocal Stroke Promote Ultrafast Door-to-Needle Time
SHARON WORCESTER
FRONTLINE MEDICAL NEWS
Ultrafast door-to-needle times (DNTs) of 10 minutes or less for IV acute ischemic stroke thrombolysis can be safely achieved in carefully selected cases, according to a review of cases at an Austrian teaching hospital.
Raffi Topakian, MD, and his colleagues at the Academic Teaching Hospital Wels-Grieskirchen in Wels, Austria, followed a multidisciplinary intervention to reinforce key components of the well-known Helsinki model of acute stroke care to improve the IV thrombolysis rate and the median DNT at the teaching hospital, and analyzed data from 361 patients who underwent intravenous thrombolysis (IVT) for stroke there between July 2014 and September 2016. The IVT rate increased from 19% to about 27% after intervention, and the DNT during the study period was 60 minutes or less in 316 patients (87.5%), 30 minutes or less in 181 patients (50.1%), and 10 minutes or less in 63 patients (17.5%).
“Over the study period, we reduced the DNT time from 49 minutes to 25 minutes. This was significant, and the door-to-needle times were astonishingly similar for the in-hours service and the out-of-hour service,” he said at the annual meeting of the American Academy of Neurology.
Further, the rate of prenotifications from emergency medical services (EMS) rose from about 30% to 63% during the study period.
Patients with ultrafast DNT vs those with slower DNT were older, had more chronic heart failure, had more severe stroke (National Institutes of Health Stroke Scale score of 10 vs 5), had more anterior circulation stroke and cardioembolic stroke, and had clear onset of stroke. Independent predictors of ultrafast DNT included prenotification by EMS, anterior circulation syndrome, chronic heart failure, and having a stroke neurologist on duty, Dr Topakian said.
“Ultrashort DNTs can be achieved safely. The key is that we are prenotified by the EMS, that we can get all the relevant history details during transport, that there is a dedicated multidisciplinary stroke team and EMS staff, and that we have a seemingly unequivocal clinical scenario,” he said. “Out-of-hours DNT matched in-hours DNT, but the caveat is we’re talking about highly selected candidates; safety must not be sacrificed for the sake of speed, in all of our patients.”
In a historic collaboration, 10 major emergency medicine organizations have joined forces to create The Coalition to Oppose Medical Merit Badges (COMMB). In its news release, the Coalition stated it “…believes that board-certified emergency physicians who actively maintain their board certification should not be required to complete short-course certification or acquire condition-specific continuing medical education credits in advanced
The COMMB consists of the American Academy of Emergency Medicine (AAEM), American Academy of Emergency Medicine/Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Association of Academic Chairs of Emergency Medicine (AACEM), Council of Emergency Medicine Residency Directors (CORD), Emergency Medicine Residents’ Association (EMRA), Society for Academic Emergency Medicine (SAEM), American Osteopathic Board of Emergency Medicine (AOBEM), and American College of Osteopathic Emergency Physicians (ACOEP).
In a written statement signed by the president/chair of each member organization, COMMB further asserted:
Similarly, mandatory targeted continuing medical education (CME) requirements do not offer any meaningful value for the public or for the emergency physician who has achieved and maintained board certification. Such requirements are often promulgated by others who incompletely understand the foundation of knowledge and skills acquired by successfully completing an Accreditation Council for Graduate Medical Education-accredited or American Osteopathic Association-approved Emergency Medicine Residency Program. These “merit badges” add no additional value for board-certified emergency physicians. Instead, they devalue the board certification process, failing to recognize the rigor of the ABEM Maintenance of Certification (MOC) Program. In essence, medical merit badges set a lower bar than a diplomate’s education, training, and ongoing learning, as measured by initial board certification and maintenance of certification.
The Coalition finds no rational justification to require medical merit badges for board-certified emergency physicians who maintain their board certification. Our committed professional organizations provide the best opportunities for continuous professional development and medical merit badges dismiss the quality of those educational efforts.
Opposing the requirements for medical merit badges will be a long and challenging struggle. It will take time to help administrators and regulatory bodies to better understand the rigorous standards to which we adhere as board-certified emergency physicians. In the coming months, we will develop our long-term strategy to create success and a pathway to recognize clinical excellence. We welcome your thoughts and suggestions as to how we can best succeed. In the near future, we will ask for strong support and a loud and unified voice.
We will persist and we are up to the challenge—we are board-certified emergency physicians. Opposing medical merit badges is the right thing to do for our specialty. We will forever demonstrate a lifelong commitment to caring for anyone who is ill or injured, at any time, for any reason.
Study Nixed Magnesium for Infants With Acute Bronchiolitis
AMY KARON
FRONTLINE MEDICAL news
Intravenous (IV) magnesium does not benefit, and may harm, infants with moderate-to-severe acute bronchiolitis, investigators reported. Compared with placebo, adding a single IV dose of magnesium sulfate (100 mg/kg) to usual care did not reduce time to medical readiness for discharge, even when patients had eczema or a family history of asthma, and was tied to a more than 3-fold rise in the rate of short-term readmissions, Khalid Al Ansari, MD, of Hamad Medical Corp in Doha, Qatar, and his associates wrote in Chest. “To our knowledge, this is the first randomized study to investigate the effect of intravenous magnesium in a bronchiolitis population,” they added.
Bronchiolitis lacks new, inexpensive, readily available treatments, despite being a common reason for hospital admission, the researchers noted. For older children with moderate-to-severe exacerbations of asthma, a meta-analysis found that the addition of magnesium to usual care appeared to cut readmissions and shorten lengths of stay, compared with placebo. To explore magnesium therapy in younger children, the investigators enrolled 162 previously healthy infants up to 18 months old who had been admitted to the short-stay unit of a pediatric emergency center with a diagnosis of moderate-to-severe viral bronchiolitis. Patients received usual care with oral dexamethasone and nebulized 5% hypertonic saline in 1 mL of 1:1000 epinephrine, plus a 60-minute IV infusion with a blinded syringe of either 0.9% saline placebo or magnesium sulfate (100 mg/kg).
The primary endpoint, time to medical readiness for discharge, did not statistically differ between groups, averaging 24.1 (95% confidence interval [CI], 20.0-29.1) hours with magnesium and 25.3 (95% CI, 20.3-31.5) hours with placebo (P = .91). Among patients with a history of eczema or a family history of asthma, mean times to readiness for discharge resembled those for the entire cohort and did not statistically differ based on treatment. Average Wang bronchiolitis severity scores also were similar between groups, as were rates of outpatient clinic visits (33.8% with magnesium and 27.2% with placebo). Thus, the trial identified “no benefit in adding intravenous magnesium for infant bronchiolitis, even in patients characterized to be at a higher risk for asthma,” the researchers concluded.
Strikingly, 2-week readmission rates were 19.5% with magnesium (95% CI, 11.3-30.1) and 6.2% with placebo (95% CI, 0.02-13.8; P = .016). Among patients with eczema or a family history of asthma, 2-week readmission rates also were significantly higher with magnesium (26.3%; 95% CI, 13.4-43.1) than with placebo (7.5%; 95% CI, 1.6-20.4; P = .034) These might have been chance findings, or magnesium might have masked worse bronchiolitis, prolonged the disease course, or interacted with 5% hypertonic saline or systemic corticosteroids, the investigators said. Intravenous magnesium might contribute to secondary relapse, especially among patients with eczema or a family history of asthma, they added.
Patients in this study had a median age of 3.7 months (range, 22 days to 17.6 months), about half had eczema or a family history of asthma, and 86% had positive nasopharyngeal virus swabs. Cardiopulmonary monitoring revealed no acute events during treatment. Of 16 readmissions in the magnesium group, 11 entered the infirmary and four entered the hospital. The five placebo readmissions included four to the infirmary and one to the hospital.
“As with other ‘negative studies,’ we may have failed to identify a benefit from intravenous magnesium in a patient subgroup because of our limited sample size,” the investigators wrote. “But we think our findings are generalizable to a similarly heterogeneous group of patients presenting for bronchiolitis care in a busy urban emergency department.”
Alansari K, Sayyed R, Davidson BL, Al Jawala S, Ghadier M. Intravenous magnesium sulfate for bronchiolitis: A randomized trial. Chest. 2017;pii:S0012-3692(17):30361-30366. doi:10.1016/j.chest.2017.03.002. [Epub ahead of print]
CDC: Some Shigella Strains Show Reduced Ciprofloxacin Susceptibility
SHARON WORCESTER
FRONTLINE MEDICAL NEWS
The Centers for Disease Control and Prevention (CDC) has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
- Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
- Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
- Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
- Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible—with special attention given to the MIC for fluoroquinolone antibiotics.
- Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
- Consult local or state health departments for guidance on when patients may return to childcare, school, or work.
- Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition, and all cases should be reported to one’s local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
Prenotification, Unequivocal Stroke Promote Ultrafast Door-to-Needle Time
SHARON WORCESTER
FRONTLINE MEDICAL NEWS
Ultrafast door-to-needle times (DNTs) of 10 minutes or less for IV acute ischemic stroke thrombolysis can be safely achieved in carefully selected cases, according to a review of cases at an Austrian teaching hospital.
Raffi Topakian, MD, and his colleagues at the Academic Teaching Hospital Wels-Grieskirchen in Wels, Austria, followed a multidisciplinary intervention to reinforce key components of the well-known Helsinki model of acute stroke care to improve the IV thrombolysis rate and the median DNT at the teaching hospital, and analyzed data from 361 patients who underwent intravenous thrombolysis (IVT) for stroke there between July 2014 and September 2016. The IVT rate increased from 19% to about 27% after intervention, and the DNT during the study period was 60 minutes or less in 316 patients (87.5%), 30 minutes or less in 181 patients (50.1%), and 10 minutes or less in 63 patients (17.5%).
“Over the study period, we reduced the DNT time from 49 minutes to 25 minutes. This was significant, and the door-to-needle times were astonishingly similar for the in-hours service and the out-of-hour service,” he said at the annual meeting of the American Academy of Neurology.
Further, the rate of prenotifications from emergency medical services (EMS) rose from about 30% to 63% during the study period.
Patients with ultrafast DNT vs those with slower DNT were older, had more chronic heart failure, had more severe stroke (National Institutes of Health Stroke Scale score of 10 vs 5), had more anterior circulation stroke and cardioembolic stroke, and had clear onset of stroke. Independent predictors of ultrafast DNT included prenotification by EMS, anterior circulation syndrome, chronic heart failure, and having a stroke neurologist on duty, Dr Topakian said.
“Ultrashort DNTs can be achieved safely. The key is that we are prenotified by the EMS, that we can get all the relevant history details during transport, that there is a dedicated multidisciplinary stroke team and EMS staff, and that we have a seemingly unequivocal clinical scenario,” he said. “Out-of-hours DNT matched in-hours DNT, but the caveat is we’re talking about highly selected candidates; safety must not be sacrificed for the sake of speed, in all of our patients.”
In a historic collaboration, 10 major emergency medicine organizations have joined forces to create The Coalition to Oppose Medical Merit Badges (COMMB). In its news release, the Coalition stated it “…believes that board-certified emergency physicians who actively maintain their board certification should not be required to complete short-course certification or acquire condition-specific continuing medical education credits in advanced
The COMMB consists of the American Academy of Emergency Medicine (AAEM), American Academy of Emergency Medicine/Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Association of Academic Chairs of Emergency Medicine (AACEM), Council of Emergency Medicine Residency Directors (CORD), Emergency Medicine Residents’ Association (EMRA), Society for Academic Emergency Medicine (SAEM), American Osteopathic Board of Emergency Medicine (AOBEM), and American College of Osteopathic Emergency Physicians (ACOEP).
In a written statement signed by the president/chair of each member organization, COMMB further asserted:
Similarly, mandatory targeted continuing medical education (CME) requirements do not offer any meaningful value for the public or for the emergency physician who has achieved and maintained board certification. Such requirements are often promulgated by others who incompletely understand the foundation of knowledge and skills acquired by successfully completing an Accreditation Council for Graduate Medical Education-accredited or American Osteopathic Association-approved Emergency Medicine Residency Program. These “merit badges” add no additional value for board-certified emergency physicians. Instead, they devalue the board certification process, failing to recognize the rigor of the ABEM Maintenance of Certification (MOC) Program. In essence, medical merit badges set a lower bar than a diplomate’s education, training, and ongoing learning, as measured by initial board certification and maintenance of certification.
The Coalition finds no rational justification to require medical merit badges for board-certified emergency physicians who maintain their board certification. Our committed professional organizations provide the best opportunities for continuous professional development and medical merit badges dismiss the quality of those educational efforts.
Opposing the requirements for medical merit badges will be a long and challenging struggle. It will take time to help administrators and regulatory bodies to better understand the rigorous standards to which we adhere as board-certified emergency physicians. In the coming months, we will develop our long-term strategy to create success and a pathway to recognize clinical excellence. We welcome your thoughts and suggestions as to how we can best succeed. In the near future, we will ask for strong support and a loud and unified voice.
We will persist and we are up to the challenge—we are board-certified emergency physicians. Opposing medical merit badges is the right thing to do for our specialty. We will forever demonstrate a lifelong commitment to caring for anyone who is ill or injured, at any time, for any reason.
Study Nixed Magnesium for Infants With Acute Bronchiolitis
AMY KARON
FRONTLINE MEDICAL news
Intravenous (IV) magnesium does not benefit, and may harm, infants with moderate-to-severe acute bronchiolitis, investigators reported. Compared with placebo, adding a single IV dose of magnesium sulfate (100 mg/kg) to usual care did not reduce time to medical readiness for discharge, even when patients had eczema or a family history of asthma, and was tied to a more than 3-fold rise in the rate of short-term readmissions, Khalid Al Ansari, MD, of Hamad Medical Corp in Doha, Qatar, and his associates wrote in Chest. “To our knowledge, this is the first randomized study to investigate the effect of intravenous magnesium in a bronchiolitis population,” they added.
Bronchiolitis lacks new, inexpensive, readily available treatments, despite being a common reason for hospital admission, the researchers noted. For older children with moderate-to-severe exacerbations of asthma, a meta-analysis found that the addition of magnesium to usual care appeared to cut readmissions and shorten lengths of stay, compared with placebo. To explore magnesium therapy in younger children, the investigators enrolled 162 previously healthy infants up to 18 months old who had been admitted to the short-stay unit of a pediatric emergency center with a diagnosis of moderate-to-severe viral bronchiolitis. Patients received usual care with oral dexamethasone and nebulized 5% hypertonic saline in 1 mL of 1:1000 epinephrine, plus a 60-minute IV infusion with a blinded syringe of either 0.9% saline placebo or magnesium sulfate (100 mg/kg).
The primary endpoint, time to medical readiness for discharge, did not statistically differ between groups, averaging 24.1 (95% confidence interval [CI], 20.0-29.1) hours with magnesium and 25.3 (95% CI, 20.3-31.5) hours with placebo (P = .91). Among patients with a history of eczema or a family history of asthma, mean times to readiness for discharge resembled those for the entire cohort and did not statistically differ based on treatment. Average Wang bronchiolitis severity scores also were similar between groups, as were rates of outpatient clinic visits (33.8% with magnesium and 27.2% with placebo). Thus, the trial identified “no benefit in adding intravenous magnesium for infant bronchiolitis, even in patients characterized to be at a higher risk for asthma,” the researchers concluded.
Strikingly, 2-week readmission rates were 19.5% with magnesium (95% CI, 11.3-30.1) and 6.2% with placebo (95% CI, 0.02-13.8; P = .016). Among patients with eczema or a family history of asthma, 2-week readmission rates also were significantly higher with magnesium (26.3%; 95% CI, 13.4-43.1) than with placebo (7.5%; 95% CI, 1.6-20.4; P = .034) These might have been chance findings, or magnesium might have masked worse bronchiolitis, prolonged the disease course, or interacted with 5% hypertonic saline or systemic corticosteroids, the investigators said. Intravenous magnesium might contribute to secondary relapse, especially among patients with eczema or a family history of asthma, they added.
Patients in this study had a median age of 3.7 months (range, 22 days to 17.6 months), about half had eczema or a family history of asthma, and 86% had positive nasopharyngeal virus swabs. Cardiopulmonary monitoring revealed no acute events during treatment. Of 16 readmissions in the magnesium group, 11 entered the infirmary and four entered the hospital. The five placebo readmissions included four to the infirmary and one to the hospital.
“As with other ‘negative studies,’ we may have failed to identify a benefit from intravenous magnesium in a patient subgroup because of our limited sample size,” the investigators wrote. “But we think our findings are generalizable to a similarly heterogeneous group of patients presenting for bronchiolitis care in a busy urban emergency department.”
Alansari K, Sayyed R, Davidson BL, Al Jawala S, Ghadier M. Intravenous magnesium sulfate for bronchiolitis: A randomized trial. Chest. 2017;pii:S0012-3692(17):30361-30366. doi:10.1016/j.chest.2017.03.002. [Epub ahead of print]
CDC: Some Shigella Strains Show Reduced Ciprofloxacin Susceptibility
SHARON WORCESTER
FRONTLINE MEDICAL NEWS
The Centers for Disease Control and Prevention (CDC) has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
- Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
- Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
- Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
- Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible—with special attention given to the MIC for fluoroquinolone antibiotics.
- Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
- Consult local or state health departments for guidance on when patients may return to childcare, school, or work.
- Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition, and all cases should be reported to one’s local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
Prenotification, Unequivocal Stroke Promote Ultrafast Door-to-Needle Time
SHARON WORCESTER
FRONTLINE MEDICAL NEWS
Ultrafast door-to-needle times (DNTs) of 10 minutes or less for IV acute ischemic stroke thrombolysis can be safely achieved in carefully selected cases, according to a review of cases at an Austrian teaching hospital.
Raffi Topakian, MD, and his colleagues at the Academic Teaching Hospital Wels-Grieskirchen in Wels, Austria, followed a multidisciplinary intervention to reinforce key components of the well-known Helsinki model of acute stroke care to improve the IV thrombolysis rate and the median DNT at the teaching hospital, and analyzed data from 361 patients who underwent intravenous thrombolysis (IVT) for stroke there between July 2014 and September 2016. The IVT rate increased from 19% to about 27% after intervention, and the DNT during the study period was 60 minutes or less in 316 patients (87.5%), 30 minutes or less in 181 patients (50.1%), and 10 minutes or less in 63 patients (17.5%).
“Over the study period, we reduced the DNT time from 49 minutes to 25 minutes. This was significant, and the door-to-needle times were astonishingly similar for the in-hours service and the out-of-hour service,” he said at the annual meeting of the American Academy of Neurology.
Further, the rate of prenotifications from emergency medical services (EMS) rose from about 30% to 63% during the study period.
Patients with ultrafast DNT vs those with slower DNT were older, had more chronic heart failure, had more severe stroke (National Institutes of Health Stroke Scale score of 10 vs 5), had more anterior circulation stroke and cardioembolic stroke, and had clear onset of stroke. Independent predictors of ultrafast DNT included prenotification by EMS, anterior circulation syndrome, chronic heart failure, and having a stroke neurologist on duty, Dr Topakian said.
“Ultrashort DNTs can be achieved safely. The key is that we are prenotified by the EMS, that we can get all the relevant history details during transport, that there is a dedicated multidisciplinary stroke team and EMS staff, and that we have a seemingly unequivocal clinical scenario,” he said. “Out-of-hours DNT matched in-hours DNT, but the caveat is we’re talking about highly selected candidates; safety must not be sacrificed for the sake of speed, in all of our patients.”