User login
Drug could fight bortezomib resistance in MM
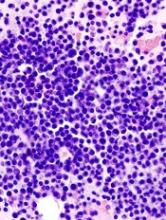
The E-selectin antagonist GMI-1271 can restore sensitivity to bortezomib in resistant multiple myeloma (MM), according to preclinical research published in Leukemia.
Researchers found evidence to suggest that E-selectin ligands induce an aggressive form of MM that is resistant to treatment with bortezomib.
However, treatment with GMI-1271 was able to overcome this resistance in a mouse model of the disease.
“The results in this preclinical study demonstrate that targeting E-selectin may provide a novel approach to treatment of patients with multiple myeloma and could potentially restore sensitivity to chemotherapy and, in particular, proteasome inhibitor therapy,” said John L. Magnani, PhD, vice-president and chief scientific officer of GlycoMimetics Inc., the company developing GMI-1271.
This research was supported by GlycoMimetics, and some of the researchers involved are employees of the company.
The researchers noted that E-selectin ligands are recognized by an antibody known as HECA452. So the team screened 9 MM cell lines for E-selectin ligands using HECA452.
Most of the cell lines were negative for HECA452. However, a minority of cells in 2 of the cell lines—11.2% of RPMI8226 cells and 2.4% of MM1S cells—were positive for HECA452.
So the researchers established HECA452-enriched cell lines from the RPMI8226 and MM1S cells to investigate the biology of E-selectin ligands in MM.
The team said they found that “HECA452-enriched cells express functional E-selectin ligands and exhibit enhanced rolling and adhesion capabilities on E-selectin, which are amenable to therapeutic intervention.”
Experiments in mice
To build on their in vitro findings, the researchers compared the effects of parental MM1S cells and HECA452-enriched MM1S cells in mice.
The team found that animals transplanted with HECA452-enriched cells had significantly shorter survival than those transplanted with parental MM1S cells.
The researchers said this difference is unlikely to be due to a different proliferation rate between the 2 cell types because they demonstrated comparable proliferation and clonogenic capacity in vitro.
The team then tested treatments in a second cohort of mice transplanted with parental or HECA452-enriched MM1S cells. The mice received saline, GMI-1271 alone, bortezomib alone, or GMI-1271 plus bortezomib.
In mice with parental MM1S cells, the median survival was 33 days in the saline group, 31 days in the GMI-1271 group, 42 days in the bortezomib group (P=0.0622 vs saline), and 60 days in the GMI-1271 plus bortezomib group (P=0.0101 vs saline, P=0.0363 vs bortezomib alone).
In mice with HECA452-enriched MM1S cells, the median survival was 25.5 days in the saline group, 30 days in the GMI-1271 group, 24 days in the bortezomib group (P=0.6743 vs saline), and 56.5 days in the GMI-1271 plus bortezomib group (P=0.0028 vs saline, P=0.0123 vs bortezomib alone).
The researchers said additional experiments in mice revealed that GMI-1271 mobilizes HECA452-positive human MM cells from the bone marrow into the peripheral blood.
Investigation in patients
Finally, the researchers evaluated the role of E-selectin and its ligands in patients with MM.
The team looked for HECA452-positive plasma cells in bone marrow samples from MM patients and found these cells were more common in patients with relapsed or refractory MM (14/50) than in those with newly diagnosed MM (1/33, P=0.009).
Next, the researchers analyzed RNA sequencing data from the CoMMpass study and found that increased expression of genes involved in E-selectin ligand synthesis (ST3Gal-6 or ST3Gal-4 and FUT7) is associated with poor progression-free survival (hazard ratio=1.37, P=0.02).
The team concluded that their results “provide compelling evidence that E-selectin and its ligands play an important role in disease progression and drug resistance in MM.” And there is “a strong rationale” for targeting E-selectin and its ligands in patients with MM. ![]()
The E-selectin antagonist GMI-1271 can restore sensitivity to bortezomib in resistant multiple myeloma (MM), according to preclinical research published in Leukemia.
Researchers found evidence to suggest that E-selectin ligands induce an aggressive form of MM that is resistant to treatment with bortezomib.
However, treatment with GMI-1271 was able to overcome this resistance in a mouse model of the disease.
“The results in this preclinical study demonstrate that targeting E-selectin may provide a novel approach to treatment of patients with multiple myeloma and could potentially restore sensitivity to chemotherapy and, in particular, proteasome inhibitor therapy,” said John L. Magnani, PhD, vice-president and chief scientific officer of GlycoMimetics Inc., the company developing GMI-1271.
This research was supported by GlycoMimetics, and some of the researchers involved are employees of the company.
The researchers noted that E-selectin ligands are recognized by an antibody known as HECA452. So the team screened 9 MM cell lines for E-selectin ligands using HECA452.
Most of the cell lines were negative for HECA452. However, a minority of cells in 2 of the cell lines—11.2% of RPMI8226 cells and 2.4% of MM1S cells—were positive for HECA452.
So the researchers established HECA452-enriched cell lines from the RPMI8226 and MM1S cells to investigate the biology of E-selectin ligands in MM.
The team said they found that “HECA452-enriched cells express functional E-selectin ligands and exhibit enhanced rolling and adhesion capabilities on E-selectin, which are amenable to therapeutic intervention.”
Experiments in mice
To build on their in vitro findings, the researchers compared the effects of parental MM1S cells and HECA452-enriched MM1S cells in mice.
The team found that animals transplanted with HECA452-enriched cells had significantly shorter survival than those transplanted with parental MM1S cells.
The researchers said this difference is unlikely to be due to a different proliferation rate between the 2 cell types because they demonstrated comparable proliferation and clonogenic capacity in vitro.
The team then tested treatments in a second cohort of mice transplanted with parental or HECA452-enriched MM1S cells. The mice received saline, GMI-1271 alone, bortezomib alone, or GMI-1271 plus bortezomib.
In mice with parental MM1S cells, the median survival was 33 days in the saline group, 31 days in the GMI-1271 group, 42 days in the bortezomib group (P=0.0622 vs saline), and 60 days in the GMI-1271 plus bortezomib group (P=0.0101 vs saline, P=0.0363 vs bortezomib alone).
In mice with HECA452-enriched MM1S cells, the median survival was 25.5 days in the saline group, 30 days in the GMI-1271 group, 24 days in the bortezomib group (P=0.6743 vs saline), and 56.5 days in the GMI-1271 plus bortezomib group (P=0.0028 vs saline, P=0.0123 vs bortezomib alone).
The researchers said additional experiments in mice revealed that GMI-1271 mobilizes HECA452-positive human MM cells from the bone marrow into the peripheral blood.
Investigation in patients
Finally, the researchers evaluated the role of E-selectin and its ligands in patients with MM.
The team looked for HECA452-positive plasma cells in bone marrow samples from MM patients and found these cells were more common in patients with relapsed or refractory MM (14/50) than in those with newly diagnosed MM (1/33, P=0.009).
Next, the researchers analyzed RNA sequencing data from the CoMMpass study and found that increased expression of genes involved in E-selectin ligand synthesis (ST3Gal-6 or ST3Gal-4 and FUT7) is associated with poor progression-free survival (hazard ratio=1.37, P=0.02).
The team concluded that their results “provide compelling evidence that E-selectin and its ligands play an important role in disease progression and drug resistance in MM.” And there is “a strong rationale” for targeting E-selectin and its ligands in patients with MM. ![]()
The E-selectin antagonist GMI-1271 can restore sensitivity to bortezomib in resistant multiple myeloma (MM), according to preclinical research published in Leukemia.
Researchers found evidence to suggest that E-selectin ligands induce an aggressive form of MM that is resistant to treatment with bortezomib.
However, treatment with GMI-1271 was able to overcome this resistance in a mouse model of the disease.
“The results in this preclinical study demonstrate that targeting E-selectin may provide a novel approach to treatment of patients with multiple myeloma and could potentially restore sensitivity to chemotherapy and, in particular, proteasome inhibitor therapy,” said John L. Magnani, PhD, vice-president and chief scientific officer of GlycoMimetics Inc., the company developing GMI-1271.
This research was supported by GlycoMimetics, and some of the researchers involved are employees of the company.
The researchers noted that E-selectin ligands are recognized by an antibody known as HECA452. So the team screened 9 MM cell lines for E-selectin ligands using HECA452.
Most of the cell lines were negative for HECA452. However, a minority of cells in 2 of the cell lines—11.2% of RPMI8226 cells and 2.4% of MM1S cells—were positive for HECA452.
So the researchers established HECA452-enriched cell lines from the RPMI8226 and MM1S cells to investigate the biology of E-selectin ligands in MM.
The team said they found that “HECA452-enriched cells express functional E-selectin ligands and exhibit enhanced rolling and adhesion capabilities on E-selectin, which are amenable to therapeutic intervention.”
Experiments in mice
To build on their in vitro findings, the researchers compared the effects of parental MM1S cells and HECA452-enriched MM1S cells in mice.
The team found that animals transplanted with HECA452-enriched cells had significantly shorter survival than those transplanted with parental MM1S cells.
The researchers said this difference is unlikely to be due to a different proliferation rate between the 2 cell types because they demonstrated comparable proliferation and clonogenic capacity in vitro.
The team then tested treatments in a second cohort of mice transplanted with parental or HECA452-enriched MM1S cells. The mice received saline, GMI-1271 alone, bortezomib alone, or GMI-1271 plus bortezomib.
In mice with parental MM1S cells, the median survival was 33 days in the saline group, 31 days in the GMI-1271 group, 42 days in the bortezomib group (P=0.0622 vs saline), and 60 days in the GMI-1271 plus bortezomib group (P=0.0101 vs saline, P=0.0363 vs bortezomib alone).
In mice with HECA452-enriched MM1S cells, the median survival was 25.5 days in the saline group, 30 days in the GMI-1271 group, 24 days in the bortezomib group (P=0.6743 vs saline), and 56.5 days in the GMI-1271 plus bortezomib group (P=0.0028 vs saline, P=0.0123 vs bortezomib alone).
The researchers said additional experiments in mice revealed that GMI-1271 mobilizes HECA452-positive human MM cells from the bone marrow into the peripheral blood.
Investigation in patients
Finally, the researchers evaluated the role of E-selectin and its ligands in patients with MM.
The team looked for HECA452-positive plasma cells in bone marrow samples from MM patients and found these cells were more common in patients with relapsed or refractory MM (14/50) than in those with newly diagnosed MM (1/33, P=0.009).
Next, the researchers analyzed RNA sequencing data from the CoMMpass study and found that increased expression of genes involved in E-selectin ligand synthesis (ST3Gal-6 or ST3Gal-4 and FUT7) is associated with poor progression-free survival (hazard ratio=1.37, P=0.02).
The team concluded that their results “provide compelling evidence that E-selectin and its ligands play an important role in disease progression and drug resistance in MM.” And there is “a strong rationale” for targeting E-selectin and its ligands in patients with MM. ![]()
Restrictions on pharma reps change docs’ prescribing behavior
New research indicates that limiting how pharmaceutical sales representatives can market their products to physicians changes the physicians’ prescribing behaviors.
Researchers examined the effects of restrictions on pharmaceutical representatives’ visits to doctors’ offices at 19 academic medical centers in 5 US states.
The team found these restrictions were associated with “modest but significant” reductions in prescribing promoted drugs.
“Social science has long demonstrated that professionals, even well-meaning ones, are powerfully influenced by conflicts of interest,” said George Loewenstein, PhD, of Carnegie Mellon University in Pittsburgh, Pennsylvania.
“A large body of research also shows that simply disclosing conflicts of interests is insufficient to reduce their influence and may even exacerbate it. The results from this study underline the effectiveness of, and need for, centralized rules and regulations.”
Dr Loewenstein and his colleagues reported the results of this study in JAMA.
The researchers noted that pharmaceutical sales representatives’ visits to doctors, which are known as “detailing,” are the most common form of interaction between physicians and industry. However, little was known about how practice-level detailing restrictions affect physician prescribing.
To gain some insight, Dr Loewenstein and his colleagues looked at the prescribing behavior of doctors whose practices did and did not have restrictions on detailing.
The team assessed the prescribing behavior of 2126 doctors at 19 academic medical centers in 5 states (California, Illinois, Massachusetts, Pennsylvania, and New York) before and after the centers introduced policies restricting detailing.
The researchers compared the prescribing behavior of these doctors with the prescribing behavior of a control group of 24,593 physicians practicing in the same geographic regions who were not subject to detailing restrictions.
The data covered 262 drugs in 8 major drug classes—ranging from statins to antidepressants—representing more than $60 billion in aggregate sales in the US.
In all, there were 16,121,483 prescriptions written between January 2006 and June 2012 by both intervention and control physicians.
Overall results
The researchers found the enactment of detailing restrictions was associated with a significant decrease in the prescribing of detailed drugs (1.67 percentage points of market share) and a significant increase in the prescribing of nondetailed drugs (0.84 percentage points, P<0.001 for both).
The mean market share of detailed drugs was 19.3% prior to the enactment of restrictions, so the 1.67 percentage-point reduction represented an 8.7% relative decrease in market share.
The mean market share of nondetailed drugs was 14.2% prior to the enactment of restrictions, so the 0.84 percentage-point increase represented a 5.6% relative increase in market share.
“The study cannot definitively prove a causal link between policies that regulated detailing and changes in physician prescribing, but, absent a randomized control, this evidence is as definitive as possible,” said study author Ian Larkin, PhD, of the University of California, Los Angeles.
“We investigated 19 different policy implementations that happened over a 6-year period, included a control group of highly similar physicians not subject to detailing restrictions, and looked at effects in 8 large drug classes. The results were remarkably robust. After the introduction of policies, about 5% to 10% of physician prescribing behavior changed.”
Results by drug class, medical center
The researchers said detailing restrictions were associated with significant changes in market share for 6 of the 8 drug classes studied (lipid-lowering drugs, gastroesophageal reflux disease drugs, antihypertensive drugs, sleep aids, attention-deficit/hyperactivity disorder drugs, and antidepressants).
Looking at the medical centers individually, the researchers found that detailing restrictions were associated with significant changes in market share for detailed drugs at 9 centers and for nondetailed drugs at 8 centers.
The team noted that detailing restrictions differed among the centers.
Eleven of the centers regulated gifts to physicians, restricted sales representatives’ access to facilities, and had explicit enforcement policies. For 8 of these 11 centers, there was a significant change in prescribing practices.
The remaining 8 centers had less stringent restrictions in that they did not cover all 3 areas of restriction (regulating gifts, restricting access, and having enforcement policies). There was a significant change in prescribing practices for only 1 of these centers.
“No medical center completely barred salesperson visits,” Dr Larkin noted. “Salespeople could and did continue to visit physicians at all medical centers in the study. The most common restriction put in place was a ban on meals and other small gifts.”
“The fact that regulating gifts while still allowing sales calls still led to a switch to cheaper, generic drugs may suggest that gifts such as meals play an important role in influencing physicians. The correlation between meals and prescribing has been well established in the literature, but our study suggests this relationship may be causal in nature.” ![]()
New research indicates that limiting how pharmaceutical sales representatives can market their products to physicians changes the physicians’ prescribing behaviors.
Researchers examined the effects of restrictions on pharmaceutical representatives’ visits to doctors’ offices at 19 academic medical centers in 5 US states.
The team found these restrictions were associated with “modest but significant” reductions in prescribing promoted drugs.
“Social science has long demonstrated that professionals, even well-meaning ones, are powerfully influenced by conflicts of interest,” said George Loewenstein, PhD, of Carnegie Mellon University in Pittsburgh, Pennsylvania.
“A large body of research also shows that simply disclosing conflicts of interests is insufficient to reduce their influence and may even exacerbate it. The results from this study underline the effectiveness of, and need for, centralized rules and regulations.”
Dr Loewenstein and his colleagues reported the results of this study in JAMA.
The researchers noted that pharmaceutical sales representatives’ visits to doctors, which are known as “detailing,” are the most common form of interaction between physicians and industry. However, little was known about how practice-level detailing restrictions affect physician prescribing.
To gain some insight, Dr Loewenstein and his colleagues looked at the prescribing behavior of doctors whose practices did and did not have restrictions on detailing.
The team assessed the prescribing behavior of 2126 doctors at 19 academic medical centers in 5 states (California, Illinois, Massachusetts, Pennsylvania, and New York) before and after the centers introduced policies restricting detailing.
The researchers compared the prescribing behavior of these doctors with the prescribing behavior of a control group of 24,593 physicians practicing in the same geographic regions who were not subject to detailing restrictions.
The data covered 262 drugs in 8 major drug classes—ranging from statins to antidepressants—representing more than $60 billion in aggregate sales in the US.
In all, there were 16,121,483 prescriptions written between January 2006 and June 2012 by both intervention and control physicians.
Overall results
The researchers found the enactment of detailing restrictions was associated with a significant decrease in the prescribing of detailed drugs (1.67 percentage points of market share) and a significant increase in the prescribing of nondetailed drugs (0.84 percentage points, P<0.001 for both).
The mean market share of detailed drugs was 19.3% prior to the enactment of restrictions, so the 1.67 percentage-point reduction represented an 8.7% relative decrease in market share.
The mean market share of nondetailed drugs was 14.2% prior to the enactment of restrictions, so the 0.84 percentage-point increase represented a 5.6% relative increase in market share.
“The study cannot definitively prove a causal link between policies that regulated detailing and changes in physician prescribing, but, absent a randomized control, this evidence is as definitive as possible,” said study author Ian Larkin, PhD, of the University of California, Los Angeles.
“We investigated 19 different policy implementations that happened over a 6-year period, included a control group of highly similar physicians not subject to detailing restrictions, and looked at effects in 8 large drug classes. The results were remarkably robust. After the introduction of policies, about 5% to 10% of physician prescribing behavior changed.”
Results by drug class, medical center
The researchers said detailing restrictions were associated with significant changes in market share for 6 of the 8 drug classes studied (lipid-lowering drugs, gastroesophageal reflux disease drugs, antihypertensive drugs, sleep aids, attention-deficit/hyperactivity disorder drugs, and antidepressants).
Looking at the medical centers individually, the researchers found that detailing restrictions were associated with significant changes in market share for detailed drugs at 9 centers and for nondetailed drugs at 8 centers.
The team noted that detailing restrictions differed among the centers.
Eleven of the centers regulated gifts to physicians, restricted sales representatives’ access to facilities, and had explicit enforcement policies. For 8 of these 11 centers, there was a significant change in prescribing practices.
The remaining 8 centers had less stringent restrictions in that they did not cover all 3 areas of restriction (regulating gifts, restricting access, and having enforcement policies). There was a significant change in prescribing practices for only 1 of these centers.
“No medical center completely barred salesperson visits,” Dr Larkin noted. “Salespeople could and did continue to visit physicians at all medical centers in the study. The most common restriction put in place was a ban on meals and other small gifts.”
“The fact that regulating gifts while still allowing sales calls still led to a switch to cheaper, generic drugs may suggest that gifts such as meals play an important role in influencing physicians. The correlation between meals and prescribing has been well established in the literature, but our study suggests this relationship may be causal in nature.” ![]()
New research indicates that limiting how pharmaceutical sales representatives can market their products to physicians changes the physicians’ prescribing behaviors.
Researchers examined the effects of restrictions on pharmaceutical representatives’ visits to doctors’ offices at 19 academic medical centers in 5 US states.
The team found these restrictions were associated with “modest but significant” reductions in prescribing promoted drugs.
“Social science has long demonstrated that professionals, even well-meaning ones, are powerfully influenced by conflicts of interest,” said George Loewenstein, PhD, of Carnegie Mellon University in Pittsburgh, Pennsylvania.
“A large body of research also shows that simply disclosing conflicts of interests is insufficient to reduce their influence and may even exacerbate it. The results from this study underline the effectiveness of, and need for, centralized rules and regulations.”
Dr Loewenstein and his colleagues reported the results of this study in JAMA.
The researchers noted that pharmaceutical sales representatives’ visits to doctors, which are known as “detailing,” are the most common form of interaction between physicians and industry. However, little was known about how practice-level detailing restrictions affect physician prescribing.
To gain some insight, Dr Loewenstein and his colleagues looked at the prescribing behavior of doctors whose practices did and did not have restrictions on detailing.
The team assessed the prescribing behavior of 2126 doctors at 19 academic medical centers in 5 states (California, Illinois, Massachusetts, Pennsylvania, and New York) before and after the centers introduced policies restricting detailing.
The researchers compared the prescribing behavior of these doctors with the prescribing behavior of a control group of 24,593 physicians practicing in the same geographic regions who were not subject to detailing restrictions.
The data covered 262 drugs in 8 major drug classes—ranging from statins to antidepressants—representing more than $60 billion in aggregate sales in the US.
In all, there were 16,121,483 prescriptions written between January 2006 and June 2012 by both intervention and control physicians.
Overall results
The researchers found the enactment of detailing restrictions was associated with a significant decrease in the prescribing of detailed drugs (1.67 percentage points of market share) and a significant increase in the prescribing of nondetailed drugs (0.84 percentage points, P<0.001 for both).
The mean market share of detailed drugs was 19.3% prior to the enactment of restrictions, so the 1.67 percentage-point reduction represented an 8.7% relative decrease in market share.
The mean market share of nondetailed drugs was 14.2% prior to the enactment of restrictions, so the 0.84 percentage-point increase represented a 5.6% relative increase in market share.
“The study cannot definitively prove a causal link between policies that regulated detailing and changes in physician prescribing, but, absent a randomized control, this evidence is as definitive as possible,” said study author Ian Larkin, PhD, of the University of California, Los Angeles.
“We investigated 19 different policy implementations that happened over a 6-year period, included a control group of highly similar physicians not subject to detailing restrictions, and looked at effects in 8 large drug classes. The results were remarkably robust. After the introduction of policies, about 5% to 10% of physician prescribing behavior changed.”
Results by drug class, medical center
The researchers said detailing restrictions were associated with significant changes in market share for 6 of the 8 drug classes studied (lipid-lowering drugs, gastroesophageal reflux disease drugs, antihypertensive drugs, sleep aids, attention-deficit/hyperactivity disorder drugs, and antidepressants).
Looking at the medical centers individually, the researchers found that detailing restrictions were associated with significant changes in market share for detailed drugs at 9 centers and for nondetailed drugs at 8 centers.
The team noted that detailing restrictions differed among the centers.
Eleven of the centers regulated gifts to physicians, restricted sales representatives’ access to facilities, and had explicit enforcement policies. For 8 of these 11 centers, there was a significant change in prescribing practices.
The remaining 8 centers had less stringent restrictions in that they did not cover all 3 areas of restriction (regulating gifts, restricting access, and having enforcement policies). There was a significant change in prescribing practices for only 1 of these centers.
“No medical center completely barred salesperson visits,” Dr Larkin noted. “Salespeople could and did continue to visit physicians at all medical centers in the study. The most common restriction put in place was a ban on meals and other small gifts.”
“The fact that regulating gifts while still allowing sales calls still led to a switch to cheaper, generic drugs may suggest that gifts such as meals play an important role in influencing physicians. The correlation between meals and prescribing has been well established in the literature, but our study suggests this relationship may be causal in nature.” ![]()
Lab mice may be ineffective models for immunology research
Laboratory mice may not be effective models for studying immune responses to disease, according to research published in Nature Communications.
Investigators found substantial differences between the immune systems of lab mice and mice taken from the wild.
In fact, the team identified a population of “highly activated” myeloid cells in wild mice that was not present in lab mice.
The results suggest the immune responses observed in lab mice are not necessarily the same as the responses that will occur in the real world, the investigators said.
They therefore advised exercising “considerable caution” in extrapolating results from lab mice to “free-living” animals and human populations.
Mark Viney, PhD, of the University of Bristol in the UK, and his colleagues conducted this research. They studied the immune systems of 460 wild mice taken from 12 sites in the UK and compared them with mice bred in captivity.
The team assessed 62 immunological measures in the mice and found significant differences between the lab mice and the wild mice for 57 of these measures.
The investigators also found that wild mice had “a substantial burden of infection.” They had all been infected with at least 1 pathogen (whereas all lab mice were infection-free).
The wild mice had high concentrations of serum proteins as well. For example, serum concentrations of IgG were 20-fold higher in the wild mice than in lab mice, and serum concentrations of IgE were 200-fold higher in wild mice.
The investigators also found differences in splenocytes between lab mice and wild mice. For instance, wild mice had fewer natural killer (NK) cells and dendritic cells, both in absolute numbers and in proportion to spleen size. (The wild mice had smaller spleens than lab mice, both in direct comparisons and in comparisons with body mass.)
In addition, the wild mice had “highly activated” NK cells. The investigators said this may be a necessary response to the high pathogen load of the wild environment.
The team also identified a novel cell population in the wild mice that was not present in the lab mice. The investigators dubbed the population “hypergranulocytic myeloid cells.” They said more research is needed to understand the role these cells play in immune defense and regulation.
Finally, the investigators found that, compared to lab mice, wild mice had reduced cytokine responses to pathogen-associated molecular patterns, including CpG, peptidoglycan, lipopolysaccharide, and mitogenic stimulation with anti-CD3 and anti-CD28 antibodies.
“It’s remarkable that, despite the enormous number of studies of laboratory mice, ours is the first in-depth study of wild mice immune systems*,” Dr Viney said. “What this shows is that wild mouse immune systems are working at ‘warp-speed’ compared with their lab cousins.”
“These results point to us having to be much more cautious in extrapolating from the lab to the wild, but laboratory mouse models will continue to be hugely important in biological and biomedical research.” ![]()
*In a study published in Nature in 2016, researchers compared the immune systems of lab mice and mice from pet stores.
Laboratory mice may not be effective models for studying immune responses to disease, according to research published in Nature Communications.
Investigators found substantial differences between the immune systems of lab mice and mice taken from the wild.
In fact, the team identified a population of “highly activated” myeloid cells in wild mice that was not present in lab mice.
The results suggest the immune responses observed in lab mice are not necessarily the same as the responses that will occur in the real world, the investigators said.
They therefore advised exercising “considerable caution” in extrapolating results from lab mice to “free-living” animals and human populations.
Mark Viney, PhD, of the University of Bristol in the UK, and his colleagues conducted this research. They studied the immune systems of 460 wild mice taken from 12 sites in the UK and compared them with mice bred in captivity.
The team assessed 62 immunological measures in the mice and found significant differences between the lab mice and the wild mice for 57 of these measures.
The investigators also found that wild mice had “a substantial burden of infection.” They had all been infected with at least 1 pathogen (whereas all lab mice were infection-free).
The wild mice had high concentrations of serum proteins as well. For example, serum concentrations of IgG were 20-fold higher in the wild mice than in lab mice, and serum concentrations of IgE were 200-fold higher in wild mice.
The investigators also found differences in splenocytes between lab mice and wild mice. For instance, wild mice had fewer natural killer (NK) cells and dendritic cells, both in absolute numbers and in proportion to spleen size. (The wild mice had smaller spleens than lab mice, both in direct comparisons and in comparisons with body mass.)
In addition, the wild mice had “highly activated” NK cells. The investigators said this may be a necessary response to the high pathogen load of the wild environment.
The team also identified a novel cell population in the wild mice that was not present in the lab mice. The investigators dubbed the population “hypergranulocytic myeloid cells.” They said more research is needed to understand the role these cells play in immune defense and regulation.
Finally, the investigators found that, compared to lab mice, wild mice had reduced cytokine responses to pathogen-associated molecular patterns, including CpG, peptidoglycan, lipopolysaccharide, and mitogenic stimulation with anti-CD3 and anti-CD28 antibodies.
“It’s remarkable that, despite the enormous number of studies of laboratory mice, ours is the first in-depth study of wild mice immune systems*,” Dr Viney said. “What this shows is that wild mouse immune systems are working at ‘warp-speed’ compared with their lab cousins.”
“These results point to us having to be much more cautious in extrapolating from the lab to the wild, but laboratory mouse models will continue to be hugely important in biological and biomedical research.” ![]()
*In a study published in Nature in 2016, researchers compared the immune systems of lab mice and mice from pet stores.
Laboratory mice may not be effective models for studying immune responses to disease, according to research published in Nature Communications.
Investigators found substantial differences between the immune systems of lab mice and mice taken from the wild.
In fact, the team identified a population of “highly activated” myeloid cells in wild mice that was not present in lab mice.
The results suggest the immune responses observed in lab mice are not necessarily the same as the responses that will occur in the real world, the investigators said.
They therefore advised exercising “considerable caution” in extrapolating results from lab mice to “free-living” animals and human populations.
Mark Viney, PhD, of the University of Bristol in the UK, and his colleagues conducted this research. They studied the immune systems of 460 wild mice taken from 12 sites in the UK and compared them with mice bred in captivity.
The team assessed 62 immunological measures in the mice and found significant differences between the lab mice and the wild mice for 57 of these measures.
The investigators also found that wild mice had “a substantial burden of infection.” They had all been infected with at least 1 pathogen (whereas all lab mice were infection-free).
The wild mice had high concentrations of serum proteins as well. For example, serum concentrations of IgG were 20-fold higher in the wild mice than in lab mice, and serum concentrations of IgE were 200-fold higher in wild mice.
The investigators also found differences in splenocytes between lab mice and wild mice. For instance, wild mice had fewer natural killer (NK) cells and dendritic cells, both in absolute numbers and in proportion to spleen size. (The wild mice had smaller spleens than lab mice, both in direct comparisons and in comparisons with body mass.)
In addition, the wild mice had “highly activated” NK cells. The investigators said this may be a necessary response to the high pathogen load of the wild environment.
The team also identified a novel cell population in the wild mice that was not present in the lab mice. The investigators dubbed the population “hypergranulocytic myeloid cells.” They said more research is needed to understand the role these cells play in immune defense and regulation.
Finally, the investigators found that, compared to lab mice, wild mice had reduced cytokine responses to pathogen-associated molecular patterns, including CpG, peptidoglycan, lipopolysaccharide, and mitogenic stimulation with anti-CD3 and anti-CD28 antibodies.
“It’s remarkable that, despite the enormous number of studies of laboratory mice, ours is the first in-depth study of wild mice immune systems*,” Dr Viney said. “What this shows is that wild mouse immune systems are working at ‘warp-speed’ compared with their lab cousins.”
“These results point to us having to be much more cautious in extrapolating from the lab to the wild, but laboratory mouse models will continue to be hugely important in biological and biomedical research.” ![]()
*In a study published in Nature in 2016, researchers compared the immune systems of lab mice and mice from pet stores.
Group publishes guidance for V/Q imaging in PE
A group of experts from various fields has published appropriate use criteria (AUC) for ventilation/perfusion (V/Q) imaging in patients with pulmonary embolism (PE).
The AUC document lists 21 clinical scenarios and provides scores that indicate whether V/Q imaging is appropriate.
For example, the document says V/Q imaging is appropriate in patients who are considered likely to have PE but are D-dimer-negative and in patients who are considered unlikely to have PE but are D-dimer-positive.
V/Q imaging may be appropriate in patients who are ventilator-dependent and likely have a PE as well as in male or non-pregnant female patients with suspected PE who have a significant abnormal chest radiograph.
However, V/Q imaging is rarely appropriate in patients with recent or prior documentation of a PE with computerized tomography pulmonary angiography (CTPA) and a suspected new PE. And V/Q imaging is rarely appropriate in pregnant patients with likely PE who have a severe abnormal chest radiograph.
The complete AUC document is available for download from the Society of Nuclear Medicine and Molecular Imaging (SNMMI) website. An abbreviated version was published in the May issue of The Journal of Nuclear Medicine.
The AUC are intended to assist referring physicians and ordering professionals in the US so they can fulfill the requirements of the 2014 Protecting Access to Medicare Act.
Beginning January 1, 2018, the act will require referring physicians to consult AUC developed by a provider-led entity to ensure cost-effective and appropriate utilization of advanced diagnostic imaging services.
The AUC were developed by a group consisting of representatives from SNMMI, the European Association of Nuclear Medicine (EANM), the American Society of Hematology (ASH), the Society of Thoracic Surgeons (STS), the American College of Chest Physicians (ACCP), and the American College of Emergency Physicians (ACEP).
Their expertise was supplemented by a systematic review of existing evidence conducted by the Oregon Health Science University’s Evidence-based Practice Center. ![]()
A group of experts from various fields has published appropriate use criteria (AUC) for ventilation/perfusion (V/Q) imaging in patients with pulmonary embolism (PE).
The AUC document lists 21 clinical scenarios and provides scores that indicate whether V/Q imaging is appropriate.
For example, the document says V/Q imaging is appropriate in patients who are considered likely to have PE but are D-dimer-negative and in patients who are considered unlikely to have PE but are D-dimer-positive.
V/Q imaging may be appropriate in patients who are ventilator-dependent and likely have a PE as well as in male or non-pregnant female patients with suspected PE who have a significant abnormal chest radiograph.
However, V/Q imaging is rarely appropriate in patients with recent or prior documentation of a PE with computerized tomography pulmonary angiography (CTPA) and a suspected new PE. And V/Q imaging is rarely appropriate in pregnant patients with likely PE who have a severe abnormal chest radiograph.
The complete AUC document is available for download from the Society of Nuclear Medicine and Molecular Imaging (SNMMI) website. An abbreviated version was published in the May issue of The Journal of Nuclear Medicine.
The AUC are intended to assist referring physicians and ordering professionals in the US so they can fulfill the requirements of the 2014 Protecting Access to Medicare Act.
Beginning January 1, 2018, the act will require referring physicians to consult AUC developed by a provider-led entity to ensure cost-effective and appropriate utilization of advanced diagnostic imaging services.
The AUC were developed by a group consisting of representatives from SNMMI, the European Association of Nuclear Medicine (EANM), the American Society of Hematology (ASH), the Society of Thoracic Surgeons (STS), the American College of Chest Physicians (ACCP), and the American College of Emergency Physicians (ACEP).
Their expertise was supplemented by a systematic review of existing evidence conducted by the Oregon Health Science University’s Evidence-based Practice Center. ![]()
A group of experts from various fields has published appropriate use criteria (AUC) for ventilation/perfusion (V/Q) imaging in patients with pulmonary embolism (PE).
The AUC document lists 21 clinical scenarios and provides scores that indicate whether V/Q imaging is appropriate.
For example, the document says V/Q imaging is appropriate in patients who are considered likely to have PE but are D-dimer-negative and in patients who are considered unlikely to have PE but are D-dimer-positive.
V/Q imaging may be appropriate in patients who are ventilator-dependent and likely have a PE as well as in male or non-pregnant female patients with suspected PE who have a significant abnormal chest radiograph.
However, V/Q imaging is rarely appropriate in patients with recent or prior documentation of a PE with computerized tomography pulmonary angiography (CTPA) and a suspected new PE. And V/Q imaging is rarely appropriate in pregnant patients with likely PE who have a severe abnormal chest radiograph.
The complete AUC document is available for download from the Society of Nuclear Medicine and Molecular Imaging (SNMMI) website. An abbreviated version was published in the May issue of The Journal of Nuclear Medicine.
The AUC are intended to assist referring physicians and ordering professionals in the US so they can fulfill the requirements of the 2014 Protecting Access to Medicare Act.
Beginning January 1, 2018, the act will require referring physicians to consult AUC developed by a provider-led entity to ensure cost-effective and appropriate utilization of advanced diagnostic imaging services.
The AUC were developed by a group consisting of representatives from SNMMI, the European Association of Nuclear Medicine (EANM), the American Society of Hematology (ASH), the Society of Thoracic Surgeons (STS), the American College of Chest Physicians (ACCP), and the American College of Emergency Physicians (ACEP).
Their expertise was supplemented by a systematic review of existing evidence conducted by the Oregon Health Science University’s Evidence-based Practice Center. ![]()
Coin-shaped lesions on arm

The FP noted the coin-like shape of the lesions and made a presumptive diagnosis of nummular eczema (nummular dermatitis). He was also concerned about a possible bacterial superinfection because yellow crusting was visible. However, upon further inquiry, the FP learned that the patient had just completed a 10-day course of doxycycline that was given to him by doctors in the emergency room, who suspected that this was a case of impetigo; the lesions had not improved. The patient also indicated that when the rash first erupted, he had tried an over-the-counter antifungal cream, but it had not helped. The FP still went ahead, though, and scraped the skin for a potassium hydroxide (KOH) preparation. (See a video on how to perform a KOH preparation here: http://www.mdedge.com/jfponline/article/100603/dermatology/koh-preparation.)
Since the patient hadn’t seen any improvement with either the antibiotic or the antifungal cream, the FP felt confident that this was a case of nummular eczema and not impetigo or tinea corporis. He believed that the vesicles, oozing, and crusting were all secondary to the inflammatory process. (And the KOH prep subsequently came back negative.)
Nummular eczema is a type of eczema characterized by circular or oval-shaped scaling plaques with well-defined borders. (“Nummus” is Latin for “coin.”) Nummular eczema produces multiple lesions that are most commonly found on the dorsa of the hands, arms, and legs.
Secondary morphology includes excoriations from scratching, weeping and crusting after the vesicles leak, and scaling and lichenification in more chronic lesions. Excessive weeping and crusting may indicate secondary bacterial infection, but this weeping is often part of the primary inflammatory dermatosis.
In this case, the FP prescribed a high-potency corticosteroid ointment to be applied twice daily. One month later, the patient’s skin was more than 95% improved. Some post-inflammatory hyperpigmentation remained, but the FP reassured the patient that this would likely fade over time. He also explained that the nummular eczema could return and that the steroid could be used again if that were to happen.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Wah Y, Usatine R. Eczema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The FP noted the coin-like shape of the lesions and made a presumptive diagnosis of nummular eczema (nummular dermatitis). He was also concerned about a possible bacterial superinfection because yellow crusting was visible. However, upon further inquiry, the FP learned that the patient had just completed a 10-day course of doxycycline that was given to him by doctors in the emergency room, who suspected that this was a case of impetigo; the lesions had not improved. The patient also indicated that when the rash first erupted, he had tried an over-the-counter antifungal cream, but it had not helped. The FP still went ahead, though, and scraped the skin for a potassium hydroxide (KOH) preparation. (See a video on how to perform a KOH preparation here: http://www.mdedge.com/jfponline/article/100603/dermatology/koh-preparation.)
Since the patient hadn’t seen any improvement with either the antibiotic or the antifungal cream, the FP felt confident that this was a case of nummular eczema and not impetigo or tinea corporis. He believed that the vesicles, oozing, and crusting were all secondary to the inflammatory process. (And the KOH prep subsequently came back negative.)
Nummular eczema is a type of eczema characterized by circular or oval-shaped scaling plaques with well-defined borders. (“Nummus” is Latin for “coin.”) Nummular eczema produces multiple lesions that are most commonly found on the dorsa of the hands, arms, and legs.
Secondary morphology includes excoriations from scratching, weeping and crusting after the vesicles leak, and scaling and lichenification in more chronic lesions. Excessive weeping and crusting may indicate secondary bacterial infection, but this weeping is often part of the primary inflammatory dermatosis.
In this case, the FP prescribed a high-potency corticosteroid ointment to be applied twice daily. One month later, the patient’s skin was more than 95% improved. Some post-inflammatory hyperpigmentation remained, but the FP reassured the patient that this would likely fade over time. He also explained that the nummular eczema could return and that the steroid could be used again if that were to happen.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Wah Y, Usatine R. Eczema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The FP noted the coin-like shape of the lesions and made a presumptive diagnosis of nummular eczema (nummular dermatitis). He was also concerned about a possible bacterial superinfection because yellow crusting was visible. However, upon further inquiry, the FP learned that the patient had just completed a 10-day course of doxycycline that was given to him by doctors in the emergency room, who suspected that this was a case of impetigo; the lesions had not improved. The patient also indicated that when the rash first erupted, he had tried an over-the-counter antifungal cream, but it had not helped. The FP still went ahead, though, and scraped the skin for a potassium hydroxide (KOH) preparation. (See a video on how to perform a KOH preparation here: http://www.mdedge.com/jfponline/article/100603/dermatology/koh-preparation.)
Since the patient hadn’t seen any improvement with either the antibiotic or the antifungal cream, the FP felt confident that this was a case of nummular eczema and not impetigo or tinea corporis. He believed that the vesicles, oozing, and crusting were all secondary to the inflammatory process. (And the KOH prep subsequently came back negative.)
Nummular eczema is a type of eczema characterized by circular or oval-shaped scaling plaques with well-defined borders. (“Nummus” is Latin for “coin.”) Nummular eczema produces multiple lesions that are most commonly found on the dorsa of the hands, arms, and legs.
Secondary morphology includes excoriations from scratching, weeping and crusting after the vesicles leak, and scaling and lichenification in more chronic lesions. Excessive weeping and crusting may indicate secondary bacterial infection, but this weeping is often part of the primary inflammatory dermatosis.
In this case, the FP prescribed a high-potency corticosteroid ointment to be applied twice daily. One month later, the patient’s skin was more than 95% improved. Some post-inflammatory hyperpigmentation remained, but the FP reassured the patient that this would likely fade over time. He also explained that the nummular eczema could return and that the steroid could be used again if that were to happen.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Wah Y, Usatine R. Eczema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Clearing the Air
The month of May marks peak season for asthma and allergies. Coincidentally, May is also Asthma and Allergy Awareness and Clean Air month. Seems a perfect match, don’t you agree? Air quality plays a menacing role in the manifestation of asthma and allergies. Let’s take a closer look at that synergy of poor air quality and respiratory sequelae and discuss approaches to mitigate these problems.
Clean air has a natural balance of gases (ie, oxygen, nitrogen, carbon dioxide) and does not contain pollutants or allergens.1 The Environmental Protection Agency (EPA), whose mission is to protect human health and the environment, identifies six common air pollutants: particulate matter (eg, dust, dirt, soot, smoke), photochemical oxidants (including ozone), carbon monoxide, sulfur dioxide, nitrogen dioxide, and lead.2 The EPA has five goals in their strategic plan, the first of which is “Addressing Climate Change and Improving Air Quality.”3 The agency is working with a multitude of stakeholders to achieve its mission of reducing air pollution. One major way we can contribute to this goal is to use public transportation, walk, or ride a bike instead of driving a car.
As we know, pollutants have detrimental consequences not only on air quality, but the environment as a whole. Pollutants infiltrate our lakes and rivers and can also damage plants and trees. Recall from your early science classes the role that plants and trees have as natural air cleaners—scrubbers, if you will. They rid the air of carbon dioxide and can also remove formaldehyde, benzene, and a host of other toxins. Trees can eradicate gaseous pollutants and airborne particles.4 But these natural air scrubbers are slowly being destroyed by the overwhelming amount of pollutants—and our short- and long-term health will ultimately pay the price. These pollutants contribute to the risk for cardiovascular and respiratory diseases, primarily asthma.5
Surveillance data show the deadly, disruptive, and costly impact asthma has on the nation.6 Asthma is a serious, potentially life-threatening chronic respiratory disease that affects quality of life in more than 24 million Americans, including an estimated six million children.7 Moreover, it is one of the most common diseases associated with poor air quality. Environmental asthma triggers include pollen, chemicals, extreme weather changes, and smoke. Educating patients with asthma on how to avoid these triggers will help them manage their disease and lessen the disruption it can cause. Additionally, a concerted effort to minimize our contribution to air pollution will assist in reducing the incidence of asthma caused by external factors.
Creating an “asthma-friendly environment” is recommended by the American Lung Association. Some might view this as a major undertaking, but simple steps such as avoiding use of aerosol products, changing the air filter in HVAC units, and dusting and vacuuming the house frequently are low-cost, effective approaches to clean the air. Avoiding perfumes and perfumed products is another way to reduce indoor triggers.
In addition to trigger avoidance, proper management of asthma is essential. Vigilance in screening for early indicators of asthma and prompt initiation of treatment can decrease or eliminate the development of long-term consequences, such as COPD and asthma-COPD overlap syndrome.8
Allergies, which affect more than 50 million people in the US, can also result from poor air quality.9 In some cases, allergies are food-based and therefore fairly easy to evade. But others are induced by pollen, pet dander, and other air-based allergens. How do we manage these pesky allergens so we can breathe easy? While the field of allergy research continues to grow, we rely heavily on allergen-specific immunotherapy as a potentially curative treat
In order for a house to be allergen-free, it should also be plant-free, right? Contrary to popular belief, this is not the case! Not all plants are problematic. A houseplant can remove formaldehyde, benzene, and a multitude of other toxins that typically reside in indoor air. Plants such as areca palm, pothos (known as Mother-in-Law’s Tongue), and the Money Plant have been shown to improve air quality.10 Additionally, decreasing or eliminating the use of room deodorizers and other allergen-containing products can reduce flare-ups. More and more frequently, we see notices in offices and at conferences to avoid the use of perfumes; this is an effective measure for the safety and comfort of those with allergies.
Alas, outdoor allergens are a bit more difficult to manage. Airborne allergens exist in such high quantities that they are nearly impossible to elude when in season.11 Keeping windows closed, wiping down surfaces where pollen and dust collects, and avoiding flowering plants can help reduce contact with allergens.
Lowering the incidence of air pollution and the symptoms of allergies and asthma can improve quality of life. By implementing these approaches to contribute to cleaner air and reduce triggers, we can help our patients and ourselves.
1. Clean air month 2017. www.whathealth.com/awareness/event/cleanairmonth.html. Accessed April 4, 2017.
2. United States Environmental Protection Agency (EPA). Particulate matter (PM) pollution. www.epa.gov/pm-pollution. Accessed April 19, 2017.
3. United States Environmental Protection Agency (EPA). EPA strategic plan. www.epa.gov/planandbudget/strategicplan. Accessed April 4, 2017.
4. Downing A. Air: what’s a tree got to do with it? www.ecology.com/2011/09/02/air-and-trees. Accessed April 4, 2017.
5. World Health Organization. Ambient (outdoor) air quality and health. www.who.int/mediacentre/factsheets/fs313/en. Ac-cessed April 4, 2017.
6. CDC. Asthma’s impact on the nation. www.cdc.gov/asthma/impacts_nation/default.htm. Accessed April 4, 2017.
7. CDC. Asthma. www.cdc.gov/asthma/default.htm. Accessed April 4, 2017.
8. Bui DS, Burgess JA, Lowe AJ, et al. Childhood lung function predicts adult COPD and asthma-COPD overlap syndrome (ACOS). Am J Respir Crit Care Med. 2017 Feb 1. [Epub ahead of print]
9. Doheny K. Living with severe allergies. www.webmd.com/allergies/features/severe-allergies#1. Accessed April 4, 2017.
10. Gromicko N, Tarasenko K. Plants and indoor air quality. www.nachi.org/plants-indoor-air-quality.htm. Accessed April 4, 2017.
11. Asthma and Allergy Foundation of America. Fight the cause of allergy. http://fightthecauseofallergy.org/page/fight. Accessed April 4, 2017.
The month of May marks peak season for asthma and allergies. Coincidentally, May is also Asthma and Allergy Awareness and Clean Air month. Seems a perfect match, don’t you agree? Air quality plays a menacing role in the manifestation of asthma and allergies. Let’s take a closer look at that synergy of poor air quality and respiratory sequelae and discuss approaches to mitigate these problems.
Clean air has a natural balance of gases (ie, oxygen, nitrogen, carbon dioxide) and does not contain pollutants or allergens.1 The Environmental Protection Agency (EPA), whose mission is to protect human health and the environment, identifies six common air pollutants: particulate matter (eg, dust, dirt, soot, smoke), photochemical oxidants (including ozone), carbon monoxide, sulfur dioxide, nitrogen dioxide, and lead.2 The EPA has five goals in their strategic plan, the first of which is “Addressing Climate Change and Improving Air Quality.”3 The agency is working with a multitude of stakeholders to achieve its mission of reducing air pollution. One major way we can contribute to this goal is to use public transportation, walk, or ride a bike instead of driving a car.
As we know, pollutants have detrimental consequences not only on air quality, but the environment as a whole. Pollutants infiltrate our lakes and rivers and can also damage plants and trees. Recall from your early science classes the role that plants and trees have as natural air cleaners—scrubbers, if you will. They rid the air of carbon dioxide and can also remove formaldehyde, benzene, and a host of other toxins. Trees can eradicate gaseous pollutants and airborne particles.4 But these natural air scrubbers are slowly being destroyed by the overwhelming amount of pollutants—and our short- and long-term health will ultimately pay the price. These pollutants contribute to the risk for cardiovascular and respiratory diseases, primarily asthma.5
Surveillance data show the deadly, disruptive, and costly impact asthma has on the nation.6 Asthma is a serious, potentially life-threatening chronic respiratory disease that affects quality of life in more than 24 million Americans, including an estimated six million children.7 Moreover, it is one of the most common diseases associated with poor air quality. Environmental asthma triggers include pollen, chemicals, extreme weather changes, and smoke. Educating patients with asthma on how to avoid these triggers will help them manage their disease and lessen the disruption it can cause. Additionally, a concerted effort to minimize our contribution to air pollution will assist in reducing the incidence of asthma caused by external factors.
Creating an “asthma-friendly environment” is recommended by the American Lung Association. Some might view this as a major undertaking, but simple steps such as avoiding use of aerosol products, changing the air filter in HVAC units, and dusting and vacuuming the house frequently are low-cost, effective approaches to clean the air. Avoiding perfumes and perfumed products is another way to reduce indoor triggers.
In addition to trigger avoidance, proper management of asthma is essential. Vigilance in screening for early indicators of asthma and prompt initiation of treatment can decrease or eliminate the development of long-term consequences, such as COPD and asthma-COPD overlap syndrome.8
Allergies, which affect more than 50 million people in the US, can also result from poor air quality.9 In some cases, allergies are food-based and therefore fairly easy to evade. But others are induced by pollen, pet dander, and other air-based allergens. How do we manage these pesky allergens so we can breathe easy? While the field of allergy research continues to grow, we rely heavily on allergen-specific immunotherapy as a potentially curative treat
In order for a house to be allergen-free, it should also be plant-free, right? Contrary to popular belief, this is not the case! Not all plants are problematic. A houseplant can remove formaldehyde, benzene, and a multitude of other toxins that typically reside in indoor air. Plants such as areca palm, pothos (known as Mother-in-Law’s Tongue), and the Money Plant have been shown to improve air quality.10 Additionally, decreasing or eliminating the use of room deodorizers and other allergen-containing products can reduce flare-ups. More and more frequently, we see notices in offices and at conferences to avoid the use of perfumes; this is an effective measure for the safety and comfort of those with allergies.
Alas, outdoor allergens are a bit more difficult to manage. Airborne allergens exist in such high quantities that they are nearly impossible to elude when in season.11 Keeping windows closed, wiping down surfaces where pollen and dust collects, and avoiding flowering plants can help reduce contact with allergens.
Lowering the incidence of air pollution and the symptoms of allergies and asthma can improve quality of life. By implementing these approaches to contribute to cleaner air and reduce triggers, we can help our patients and ourselves.
The month of May marks peak season for asthma and allergies. Coincidentally, May is also Asthma and Allergy Awareness and Clean Air month. Seems a perfect match, don’t you agree? Air quality plays a menacing role in the manifestation of asthma and allergies. Let’s take a closer look at that synergy of poor air quality and respiratory sequelae and discuss approaches to mitigate these problems.
Clean air has a natural balance of gases (ie, oxygen, nitrogen, carbon dioxide) and does not contain pollutants or allergens.1 The Environmental Protection Agency (EPA), whose mission is to protect human health and the environment, identifies six common air pollutants: particulate matter (eg, dust, dirt, soot, smoke), photochemical oxidants (including ozone), carbon monoxide, sulfur dioxide, nitrogen dioxide, and lead.2 The EPA has five goals in their strategic plan, the first of which is “Addressing Climate Change and Improving Air Quality.”3 The agency is working with a multitude of stakeholders to achieve its mission of reducing air pollution. One major way we can contribute to this goal is to use public transportation, walk, or ride a bike instead of driving a car.
As we know, pollutants have detrimental consequences not only on air quality, but the environment as a whole. Pollutants infiltrate our lakes and rivers and can also damage plants and trees. Recall from your early science classes the role that plants and trees have as natural air cleaners—scrubbers, if you will. They rid the air of carbon dioxide and can also remove formaldehyde, benzene, and a host of other toxins. Trees can eradicate gaseous pollutants and airborne particles.4 But these natural air scrubbers are slowly being destroyed by the overwhelming amount of pollutants—and our short- and long-term health will ultimately pay the price. These pollutants contribute to the risk for cardiovascular and respiratory diseases, primarily asthma.5
Surveillance data show the deadly, disruptive, and costly impact asthma has on the nation.6 Asthma is a serious, potentially life-threatening chronic respiratory disease that affects quality of life in more than 24 million Americans, including an estimated six million children.7 Moreover, it is one of the most common diseases associated with poor air quality. Environmental asthma triggers include pollen, chemicals, extreme weather changes, and smoke. Educating patients with asthma on how to avoid these triggers will help them manage their disease and lessen the disruption it can cause. Additionally, a concerted effort to minimize our contribution to air pollution will assist in reducing the incidence of asthma caused by external factors.
Creating an “asthma-friendly environment” is recommended by the American Lung Association. Some might view this as a major undertaking, but simple steps such as avoiding use of aerosol products, changing the air filter in HVAC units, and dusting and vacuuming the house frequently are low-cost, effective approaches to clean the air. Avoiding perfumes and perfumed products is another way to reduce indoor triggers.
In addition to trigger avoidance, proper management of asthma is essential. Vigilance in screening for early indicators of asthma and prompt initiation of treatment can decrease or eliminate the development of long-term consequences, such as COPD and asthma-COPD overlap syndrome.8
Allergies, which affect more than 50 million people in the US, can also result from poor air quality.9 In some cases, allergies are food-based and therefore fairly easy to evade. But others are induced by pollen, pet dander, and other air-based allergens. How do we manage these pesky allergens so we can breathe easy? While the field of allergy research continues to grow, we rely heavily on allergen-specific immunotherapy as a potentially curative treat
In order for a house to be allergen-free, it should also be plant-free, right? Contrary to popular belief, this is not the case! Not all plants are problematic. A houseplant can remove formaldehyde, benzene, and a multitude of other toxins that typically reside in indoor air. Plants such as areca palm, pothos (known as Mother-in-Law’s Tongue), and the Money Plant have been shown to improve air quality.10 Additionally, decreasing or eliminating the use of room deodorizers and other allergen-containing products can reduce flare-ups. More and more frequently, we see notices in offices and at conferences to avoid the use of perfumes; this is an effective measure for the safety and comfort of those with allergies.
Alas, outdoor allergens are a bit more difficult to manage. Airborne allergens exist in such high quantities that they are nearly impossible to elude when in season.11 Keeping windows closed, wiping down surfaces where pollen and dust collects, and avoiding flowering plants can help reduce contact with allergens.
Lowering the incidence of air pollution and the symptoms of allergies and asthma can improve quality of life. By implementing these approaches to contribute to cleaner air and reduce triggers, we can help our patients and ourselves.
1. Clean air month 2017. www.whathealth.com/awareness/event/cleanairmonth.html. Accessed April 4, 2017.
2. United States Environmental Protection Agency (EPA). Particulate matter (PM) pollution. www.epa.gov/pm-pollution. Accessed April 19, 2017.
3. United States Environmental Protection Agency (EPA). EPA strategic plan. www.epa.gov/planandbudget/strategicplan. Accessed April 4, 2017.
4. Downing A. Air: what’s a tree got to do with it? www.ecology.com/2011/09/02/air-and-trees. Accessed April 4, 2017.
5. World Health Organization. Ambient (outdoor) air quality and health. www.who.int/mediacentre/factsheets/fs313/en. Ac-cessed April 4, 2017.
6. CDC. Asthma’s impact on the nation. www.cdc.gov/asthma/impacts_nation/default.htm. Accessed April 4, 2017.
7. CDC. Asthma. www.cdc.gov/asthma/default.htm. Accessed April 4, 2017.
8. Bui DS, Burgess JA, Lowe AJ, et al. Childhood lung function predicts adult COPD and asthma-COPD overlap syndrome (ACOS). Am J Respir Crit Care Med. 2017 Feb 1. [Epub ahead of print]
9. Doheny K. Living with severe allergies. www.webmd.com/allergies/features/severe-allergies#1. Accessed April 4, 2017.
10. Gromicko N, Tarasenko K. Plants and indoor air quality. www.nachi.org/plants-indoor-air-quality.htm. Accessed April 4, 2017.
11. Asthma and Allergy Foundation of America. Fight the cause of allergy. http://fightthecauseofallergy.org/page/fight. Accessed April 4, 2017.
1. Clean air month 2017. www.whathealth.com/awareness/event/cleanairmonth.html. Accessed April 4, 2017.
2. United States Environmental Protection Agency (EPA). Particulate matter (PM) pollution. www.epa.gov/pm-pollution. Accessed April 19, 2017.
3. United States Environmental Protection Agency (EPA). EPA strategic plan. www.epa.gov/planandbudget/strategicplan. Accessed April 4, 2017.
4. Downing A. Air: what’s a tree got to do with it? www.ecology.com/2011/09/02/air-and-trees. Accessed April 4, 2017.
5. World Health Organization. Ambient (outdoor) air quality and health. www.who.int/mediacentre/factsheets/fs313/en. Ac-cessed April 4, 2017.
6. CDC. Asthma’s impact on the nation. www.cdc.gov/asthma/impacts_nation/default.htm. Accessed April 4, 2017.
7. CDC. Asthma. www.cdc.gov/asthma/default.htm. Accessed April 4, 2017.
8. Bui DS, Burgess JA, Lowe AJ, et al. Childhood lung function predicts adult COPD and asthma-COPD overlap syndrome (ACOS). Am J Respir Crit Care Med. 2017 Feb 1. [Epub ahead of print]
9. Doheny K. Living with severe allergies. www.webmd.com/allergies/features/severe-allergies#1. Accessed April 4, 2017.
10. Gromicko N, Tarasenko K. Plants and indoor air quality. www.nachi.org/plants-indoor-air-quality.htm. Accessed April 4, 2017.
11. Asthma and Allergy Foundation of America. Fight the cause of allergy. http://fightthecauseofallergy.org/page/fight. Accessed April 4, 2017.
Antipsychotics ineffective for symptoms of delirium in palliative care
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Do antipsychotics provide symptomatic benefit for delirium in palliative care?
BACKGROUND: Antipsychotics are frequently used for the treatment of delirium and guideline recommended for delirium-associated distress. However, a 2016 meta-analysis found antipsychotics are not associated with change in delirium duration or severity. Antipsychotics for palliative management of delirium at end of life is not well studied.
STUDY DESIGN: Double-blind randomized controlled trial with placebo, haloperidol, and risperidone arms.
SETTING: Eleven Australian inpatient hospice or palliative care services.
SYNOPSIS: 247 patients (mean age, 74.9 years; 88.3% with cancer) with advanced incurable disease and active delirium were studied. Most had mild-moderate severity delirium. All received nonpharmacological measures and plan to address reversible precipitants. Patients were randomized to placebo (84), haloperidol (81), or risperidone (82) for 72 hours. Dose titration was allowed based on delirium symptoms. In intention to treat analysis the delirium severity scores were statistically higher in haloperidol and risperidone arms, compared with placebo. This reached statistical significance although less than the minimum clinically significant difference. Mortality, use of rescue medicines, and extrapyramidal symptoms were higher in antipsychotic groups.
BOTTOM LINE: Antipsychotics cause side effects without efficacy in palliation of symptoms of delirium.
CITATIONS: Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017 Jan;177:34-42.
Dr. Cumbler is the associate chief of hospital medicine, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Stump the Professor event entertains, educates
Gurpreet Dhaliwal, MD, professor of medicine at the University of California, San Francisco, joked that participating in a “Stump the Professor” event is “like taking an oral exam in front of 300 or 400 people.”
Dr. Dhaliwal passed his “exam” with flying colors on Wednesday at HM17, correctly making a diagnosis of a case of leptospirosis described by his co-presenter Daniel Brotman, MD, SFHM, professor of medicine and director of the hospitalist program at Johns Hopkins University, Baltimore.
While the format is intended to be fun and entertaining, he said that there is no doubt that learning is taking place – both by him and by the audience.
“The most important goal by far and away is to put our most important procedure on display, which is thinking,” he said. “We don’t always make our thinking explicit, and we don’t often open it to scrutiny. So the goal of this session is to do both.”
Talking through his uncertainty can be one of the most interesting aspects of the session, Dr. Dhaliwal told attendees.
“If I can’t say something insightful, let me try to capture my uncertainty and crystallize that for you so you recognize that as a real part of medicine,” he said.
The HM17 audience seemed to enjoy trying to solve the case and thinking through the clinical reasoning as Dr. Dhaliwal did the same. The diagnosis of leptospirosis in Wednesday’s case surprised the audience, many of whom shook their heads in amazement.
“I pick cases based on being dramatic and/or unusual enough to provide some clinical excitement and diagnostic challenge,” he said.
An “important bonus,” Dr. Dhaliwal said, is that the audience would learn something about the disease that’s being discussed.
“I suspect I learn the most, especially if I get the case wrong,” he told attendees. “After living it on stage, there’s a lot that I upload in my memory for the next time I see something like this in real life.”
He said he’s probably batting about 0.500 on getting the cases right.
“I’ve had plenty of experiences where I’ve pulled the rabbit out of the hat at the last minute, and it’s been glorious, and I’ve had plenty of experiences where I’ve fallen flat on my face, and I didn’t have a prayer of knowing it, either, because my thinking was off, my knowledge was deficient, or it was something I had never heard of before,” he said. “The one thing that’s always rewarding is that people are always very appreciative that I shared my thinking, whether it’s a flash of insight or a total stumble or an uncertainty that I have.”
It might seem that the event has more of a potential downside than upside: If he gets a case right, he’s doing what he should do; if he gets one wrong, it might be embarrassing. He doesn’t see it that way, he told the crowd.
“It’s a total joy to be up here,” Dr. Dhaliwal said. “There’s no doubt that standing in front of a crowd induces a little bit of anxiety, but it is a lot of fun to do. And I had mentors who did this, and then I started to learn it myself, and at some point, you get past the anxiety of being right or wrong, and you just enjoy being up there.”
Gurpreet Dhaliwal, MD, professor of medicine at the University of California, San Francisco, joked that participating in a “Stump the Professor” event is “like taking an oral exam in front of 300 or 400 people.”
Dr. Dhaliwal passed his “exam” with flying colors on Wednesday at HM17, correctly making a diagnosis of a case of leptospirosis described by his co-presenter Daniel Brotman, MD, SFHM, professor of medicine and director of the hospitalist program at Johns Hopkins University, Baltimore.
While the format is intended to be fun and entertaining, he said that there is no doubt that learning is taking place – both by him and by the audience.
“The most important goal by far and away is to put our most important procedure on display, which is thinking,” he said. “We don’t always make our thinking explicit, and we don’t often open it to scrutiny. So the goal of this session is to do both.”
Talking through his uncertainty can be one of the most interesting aspects of the session, Dr. Dhaliwal told attendees.
“If I can’t say something insightful, let me try to capture my uncertainty and crystallize that for you so you recognize that as a real part of medicine,” he said.
The HM17 audience seemed to enjoy trying to solve the case and thinking through the clinical reasoning as Dr. Dhaliwal did the same. The diagnosis of leptospirosis in Wednesday’s case surprised the audience, many of whom shook their heads in amazement.
“I pick cases based on being dramatic and/or unusual enough to provide some clinical excitement and diagnostic challenge,” he said.
An “important bonus,” Dr. Dhaliwal said, is that the audience would learn something about the disease that’s being discussed.
“I suspect I learn the most, especially if I get the case wrong,” he told attendees. “After living it on stage, there’s a lot that I upload in my memory for the next time I see something like this in real life.”
He said he’s probably batting about 0.500 on getting the cases right.
“I’ve had plenty of experiences where I’ve pulled the rabbit out of the hat at the last minute, and it’s been glorious, and I’ve had plenty of experiences where I’ve fallen flat on my face, and I didn’t have a prayer of knowing it, either, because my thinking was off, my knowledge was deficient, or it was something I had never heard of before,” he said. “The one thing that’s always rewarding is that people are always very appreciative that I shared my thinking, whether it’s a flash of insight or a total stumble or an uncertainty that I have.”
It might seem that the event has more of a potential downside than upside: If he gets a case right, he’s doing what he should do; if he gets one wrong, it might be embarrassing. He doesn’t see it that way, he told the crowd.
“It’s a total joy to be up here,” Dr. Dhaliwal said. “There’s no doubt that standing in front of a crowd induces a little bit of anxiety, but it is a lot of fun to do. And I had mentors who did this, and then I started to learn it myself, and at some point, you get past the anxiety of being right or wrong, and you just enjoy being up there.”
Gurpreet Dhaliwal, MD, professor of medicine at the University of California, San Francisco, joked that participating in a “Stump the Professor” event is “like taking an oral exam in front of 300 or 400 people.”
Dr. Dhaliwal passed his “exam” with flying colors on Wednesday at HM17, correctly making a diagnosis of a case of leptospirosis described by his co-presenter Daniel Brotman, MD, SFHM, professor of medicine and director of the hospitalist program at Johns Hopkins University, Baltimore.
While the format is intended to be fun and entertaining, he said that there is no doubt that learning is taking place – both by him and by the audience.
“The most important goal by far and away is to put our most important procedure on display, which is thinking,” he said. “We don’t always make our thinking explicit, and we don’t often open it to scrutiny. So the goal of this session is to do both.”
Talking through his uncertainty can be one of the most interesting aspects of the session, Dr. Dhaliwal told attendees.
“If I can’t say something insightful, let me try to capture my uncertainty and crystallize that for you so you recognize that as a real part of medicine,” he said.
The HM17 audience seemed to enjoy trying to solve the case and thinking through the clinical reasoning as Dr. Dhaliwal did the same. The diagnosis of leptospirosis in Wednesday’s case surprised the audience, many of whom shook their heads in amazement.
“I pick cases based on being dramatic and/or unusual enough to provide some clinical excitement and diagnostic challenge,” he said.
An “important bonus,” Dr. Dhaliwal said, is that the audience would learn something about the disease that’s being discussed.
“I suspect I learn the most, especially if I get the case wrong,” he told attendees. “After living it on stage, there’s a lot that I upload in my memory for the next time I see something like this in real life.”
He said he’s probably batting about 0.500 on getting the cases right.
“I’ve had plenty of experiences where I’ve pulled the rabbit out of the hat at the last minute, and it’s been glorious, and I’ve had plenty of experiences where I’ve fallen flat on my face, and I didn’t have a prayer of knowing it, either, because my thinking was off, my knowledge was deficient, or it was something I had never heard of before,” he said. “The one thing that’s always rewarding is that people are always very appreciative that I shared my thinking, whether it’s a flash of insight or a total stumble or an uncertainty that I have.”
It might seem that the event has more of a potential downside than upside: If he gets a case right, he’s doing what he should do; if he gets one wrong, it might be embarrassing. He doesn’t see it that way, he told the crowd.
“It’s a total joy to be up here,” Dr. Dhaliwal said. “There’s no doubt that standing in front of a crowd induces a little bit of anxiety, but it is a lot of fun to do. And I had mentors who did this, and then I started to learn it myself, and at some point, you get past the anxiety of being right or wrong, and you just enjoy being up there.”
For bone and joint infections, oral antibiotics match IV, cost less
VIENNA – Oral antibiotic therapy is just as effective as intravenous treatment in curing bone and joint infections, but costs about $3,500 less.
Treating these infections with oral agents also “improves patient autonomy, as it’s not necessary to have IV lines at home,” and represents a generally wiser use of powerful antibiotics, Matthew Scarborough, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
OVIVA (Oral vs. Intravenous Antibiotics for Bone and Joint Infection) was conducted at 26 sites in the United Kingdom. It randomized 1,054 adults with bone or joint infections to 6 weeks of either oral or intravenous treatment.
An important aspect of the trial was that both oral and IV treatment choices were made before randomization, Dr. Scarborough said. However, the decisions on what drug to use were left up to the treating physician and depended on the infection site and pathogen.
The primary outcome was definite treatment failure (bacteriologic, histologic, and clinical). Patients were followed for 1 year.
Patients were a median of 60 years old. All had surgical treatment before antibiotic therapy, including debridement and, in those with implants, removal of infected devices. The lower limb was involved in 81%, including hip, knee, and foot. The infection was in an upper limb in 10% and in the spine in 7%.
Staphylococcus aureus was present in 38% of cases, coagulase-negative staphylococci in 27%, and streptococci in 15%. Gram-negative bacteria were found in 22%.
For those patients randomized to IV therapy, glycopeptides and cephalosporins were most commonly employed (41% and 33%, respectively). For oral therapy, quinolones and penicillins were most common (37% and 16%). Most patients (74%) continued antibiotic treatment for more than 6 weeks. Forty patients were lost to follow-up.
In the primary intent-to-treat analysis, the failure rate was 13% for oral therapy and 14% for IV therapy, not a significant difference. Results were similar in the other analyses, including a modified intent to treat with only patients who had complete 1-year data, and a per-protocol analysis. All of the point prevalence numbers favored oral therapy, but crossed the null. Curves in the time-to-treatment-failure analysis were virtually superimposable, as were curves in time to discontinuation of therapy.
Another subgroup analysis examined treatment failure by infective organism; again, there were no significant treatment differences in any of the pathogen subgroups examined (S. aureus, coagulase-negative staph, streptococci species, and other gram-negative bacteria).
Nor did the type of antibiotic significantly affect failure rate, Dr. Scarborough noted. The median length of stay was 14 days for patients on IV treatment and 11 days for those taking oral medications. The incidence of serious adverse events was very similar – about 86% in each group.
On a visual analog scale that assessed health-related quality of life, patients taking oral treatment reported better mobility, self-care, and activity level, and less pain, discomfort, anxiety, and depression than those taking IV medications.
Cost represented the other significant difference between the groups. Over 1 year, the mean IV treatment cost was the equivalent of $17,152, and the mean oral treatment cost was $13,611 – a significant difference of $3,541.
“This represents a potential savings to the National Health Service of 16-25 million pounds sterling ($20.6 million-$32.3 million) per year,” Dr. Scarborough said. “All coming at no expense of good clinical outcomes.”
OVIVA was sponsored by the U.K. National Institute of Health Research. Dr. Scarborough had no financial disclosures.
[email protected]
On Twitter @alz_gal
VIENNA – Oral antibiotic therapy is just as effective as intravenous treatment in curing bone and joint infections, but costs about $3,500 less.
Treating these infections with oral agents also “improves patient autonomy, as it’s not necessary to have IV lines at home,” and represents a generally wiser use of powerful antibiotics, Matthew Scarborough, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
OVIVA (Oral vs. Intravenous Antibiotics for Bone and Joint Infection) was conducted at 26 sites in the United Kingdom. It randomized 1,054 adults with bone or joint infections to 6 weeks of either oral or intravenous treatment.
An important aspect of the trial was that both oral and IV treatment choices were made before randomization, Dr. Scarborough said. However, the decisions on what drug to use were left up to the treating physician and depended on the infection site and pathogen.
The primary outcome was definite treatment failure (bacteriologic, histologic, and clinical). Patients were followed for 1 year.
Patients were a median of 60 years old. All had surgical treatment before antibiotic therapy, including debridement and, in those with implants, removal of infected devices. The lower limb was involved in 81%, including hip, knee, and foot. The infection was in an upper limb in 10% and in the spine in 7%.
Staphylococcus aureus was present in 38% of cases, coagulase-negative staphylococci in 27%, and streptococci in 15%. Gram-negative bacteria were found in 22%.
For those patients randomized to IV therapy, glycopeptides and cephalosporins were most commonly employed (41% and 33%, respectively). For oral therapy, quinolones and penicillins were most common (37% and 16%). Most patients (74%) continued antibiotic treatment for more than 6 weeks. Forty patients were lost to follow-up.
In the primary intent-to-treat analysis, the failure rate was 13% for oral therapy and 14% for IV therapy, not a significant difference. Results were similar in the other analyses, including a modified intent to treat with only patients who had complete 1-year data, and a per-protocol analysis. All of the point prevalence numbers favored oral therapy, but crossed the null. Curves in the time-to-treatment-failure analysis were virtually superimposable, as were curves in time to discontinuation of therapy.
Another subgroup analysis examined treatment failure by infective organism; again, there were no significant treatment differences in any of the pathogen subgroups examined (S. aureus, coagulase-negative staph, streptococci species, and other gram-negative bacteria).
Nor did the type of antibiotic significantly affect failure rate, Dr. Scarborough noted. The median length of stay was 14 days for patients on IV treatment and 11 days for those taking oral medications. The incidence of serious adverse events was very similar – about 86% in each group.
On a visual analog scale that assessed health-related quality of life, patients taking oral treatment reported better mobility, self-care, and activity level, and less pain, discomfort, anxiety, and depression than those taking IV medications.
Cost represented the other significant difference between the groups. Over 1 year, the mean IV treatment cost was the equivalent of $17,152, and the mean oral treatment cost was $13,611 – a significant difference of $3,541.
“This represents a potential savings to the National Health Service of 16-25 million pounds sterling ($20.6 million-$32.3 million) per year,” Dr. Scarborough said. “All coming at no expense of good clinical outcomes.”
OVIVA was sponsored by the U.K. National Institute of Health Research. Dr. Scarborough had no financial disclosures.
[email protected]
On Twitter @alz_gal
VIENNA – Oral antibiotic therapy is just as effective as intravenous treatment in curing bone and joint infections, but costs about $3,500 less.
Treating these infections with oral agents also “improves patient autonomy, as it’s not necessary to have IV lines at home,” and represents a generally wiser use of powerful antibiotics, Matthew Scarborough, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
OVIVA (Oral vs. Intravenous Antibiotics for Bone and Joint Infection) was conducted at 26 sites in the United Kingdom. It randomized 1,054 adults with bone or joint infections to 6 weeks of either oral or intravenous treatment.
An important aspect of the trial was that both oral and IV treatment choices were made before randomization, Dr. Scarborough said. However, the decisions on what drug to use were left up to the treating physician and depended on the infection site and pathogen.
The primary outcome was definite treatment failure (bacteriologic, histologic, and clinical). Patients were followed for 1 year.
Patients were a median of 60 years old. All had surgical treatment before antibiotic therapy, including debridement and, in those with implants, removal of infected devices. The lower limb was involved in 81%, including hip, knee, and foot. The infection was in an upper limb in 10% and in the spine in 7%.
Staphylococcus aureus was present in 38% of cases, coagulase-negative staphylococci in 27%, and streptococci in 15%. Gram-negative bacteria were found in 22%.
For those patients randomized to IV therapy, glycopeptides and cephalosporins were most commonly employed (41% and 33%, respectively). For oral therapy, quinolones and penicillins were most common (37% and 16%). Most patients (74%) continued antibiotic treatment for more than 6 weeks. Forty patients were lost to follow-up.
In the primary intent-to-treat analysis, the failure rate was 13% for oral therapy and 14% for IV therapy, not a significant difference. Results were similar in the other analyses, including a modified intent to treat with only patients who had complete 1-year data, and a per-protocol analysis. All of the point prevalence numbers favored oral therapy, but crossed the null. Curves in the time-to-treatment-failure analysis were virtually superimposable, as were curves in time to discontinuation of therapy.
Another subgroup analysis examined treatment failure by infective organism; again, there were no significant treatment differences in any of the pathogen subgroups examined (S. aureus, coagulase-negative staph, streptococci species, and other gram-negative bacteria).
Nor did the type of antibiotic significantly affect failure rate, Dr. Scarborough noted. The median length of stay was 14 days for patients on IV treatment and 11 days for those taking oral medications. The incidence of serious adverse events was very similar – about 86% in each group.
On a visual analog scale that assessed health-related quality of life, patients taking oral treatment reported better mobility, self-care, and activity level, and less pain, discomfort, anxiety, and depression than those taking IV medications.
Cost represented the other significant difference between the groups. Over 1 year, the mean IV treatment cost was the equivalent of $17,152, and the mean oral treatment cost was $13,611 – a significant difference of $3,541.
“This represents a potential savings to the National Health Service of 16-25 million pounds sterling ($20.6 million-$32.3 million) per year,” Dr. Scarborough said. “All coming at no expense of good clinical outcomes.”
OVIVA was sponsored by the U.K. National Institute of Health Research. Dr. Scarborough had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT ECCMID 2017
Key clinical point:
Major finding: At 1 year, cure rates were identical, but oral treatment cost about $3,500 less than IV treatment.
Data source: The study randomized 1,054 patients.
Disclosures: OVIVA was sponsored by the U.K. National Institute of Health Research. Dr. Scarborough had no financial disclosures.
Declining bullying rates in Maryland study contradict common misconception
Rates of bullying among students in grades 4-12 decreased over the past 10 years in a state study, contradicting a common perception of a rising trend in schools, according to a study.
The rate of self-reported, frequent bullying victimization fell from 28% in 2005 to 13% in 2014, reported Tracy Evian Waasdorp, PhD, at the Children’s Hospital of Philadelphia and the Center for the Prevention of Youth Violence at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and her associates. “These findings do contradict the public’s [mis]perception that bullying is increasing.”
Data collected through a survey of 246,306 students in grades 4-12 from 109 schools in Maryland in 2005-2014 found significant decreases in 10 of 13 bullying indicators (Pediatrics. 2017. doi: 10.1542/peds.2016-2615).
In the survey, students anonymously reported if they had been a frequent victim of bullying – two or more times within the past month – as defined by the World Health Organization and Center for Disease Control and Prevention’s definition: “A person is bullied when he or she is exposed, repeatedly and over time, to negative actions on the part of one or more other persons. Bullying often occurs in situations where there is a power or status difference. Bullying includes actions like threatening, teasing, name-calling, ignoring, rumor spreading, sending hurtful emails and text messages, and leaving someone out on purpose.”
The investigators found victimization decreased across indicators including pushing (beta = –0.03), hitting (beta = –0.03), threats (beta = –0.02), cyberbullying (beta = –0.01), and rumors (beta = –0.02), according to the researchers. All values were determined with a P value less than .001.
“It was hypothesized that cyberbullying might increase, but consistent with the other forms of bullying, cyberbullying also decreased,” the researchers wrote. “However, given the rapid change of technology and new social media platforms used by youth and increasingly at younger ages, the nature and quality of cyberbullying may change.”
Dr. Waasdorp and her colleagues also had children report if and how often they had participated in bullying or had witnessed bullying, both of which also declined, from 21% to 7% of students and 66% to 43% of students, respectively.
Along with bullying, students were asked how safe they felt in school and if adults in their school were doing enough to prevent bullying, both of which sentiments increased over the course of the study. While 80% of students reported feeling safe in the school, the number of those who felt as though they belonged remained relatively unchanged.
While decreases in each category were relatively small from year to year, “some of these changes were fairly substantial across 10 years, as indicated by the effect size estimates comparing the first and last years (average difference = 0.325),” according to the researchers.
In fact, Dr. Waasdorp and her peers found the final year of the study to have the greatest improvement, which they estimate may come from more comprehensive bullying laws and school practices.
Looking across grade levels, Dr. Waasdorp and her colleagues found greater declines in witnessing bullying and school safety in high schoolers than middle schoolers, which they say may indicate more support in middle school systems, where bullying peaks.
Because of the large number of outcomes, significant associations between school levels and bullying indicators were limited. The anonymous nature of the survey limited the ability of the researchers to link student data across years. The investigators also did not collect data on why changes to the bullying indicators occurred.
During the study, the researchers were supported in part by grants from the U.S. Department of Education, the William T. Grant Foundation, and the National Institute of Justice. The authors reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
The Waasdorp et al. study is a comprehensive one using a sophisticated longitudinal design and a number of covariates to give a better comprehension of current bullying trends.
While it is encouraging to hear of the declining trends across many forms of bullying, it is important to remember 48% of children still reported bullying as an issue in their lives, with nearly as many reporting witnessing bullying against others.
We must be watchful for instances of bullying and active in getting rid of it both in and out of the classroom.
This means calling on educators to implement programs that not only sound like they will work, but have been tested and proven to be the best choice for the entire community. Programs that build empathy and encourage students to figure out productive conflict-management solutions often are good choices.
The responsibility to end bullying is not just with educators, but with pediatricians as well. Bullying can have serious mental and physical ramifications for patients, and clinicians must be vigilant for signs of victimization, such as anxiety, depression, or social withdrawal. If it seems as though a patient has been the victim or is the perpetrator of bullying, clinicians may want to talk with the child and their parents about finding a counselor at school where bullying might occur most often, encourage the child to talk with his or her parents about any problems at school, build a stronger communication between parents and the school, and help to support at least one peer friendship, which has been found to be a strong buffer against peer victimization.
This study is a good example of the progress made so far, but there is still plenty of work to be done.
Stephen S. Leff, PhD, is a psychologist in the department of child and adolescent psychiatry and behavioral sciences and codirector of the Violence Prevention Initiative at the Children’s Hospital of Philadelphia and Chris Feudtner, MD, PhD, is director of the department of medical ethics at the hospital. This a summary of their comments from an editorial accompanying the report by Waasdorp et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-0504 ) Neither Dr. Leff nor Dr. Feudtner reported any relevant disclosures.
The Waasdorp et al. study is a comprehensive one using a sophisticated longitudinal design and a number of covariates to give a better comprehension of current bullying trends.
While it is encouraging to hear of the declining trends across many forms of bullying, it is important to remember 48% of children still reported bullying as an issue in their lives, with nearly as many reporting witnessing bullying against others.
We must be watchful for instances of bullying and active in getting rid of it both in and out of the classroom.
This means calling on educators to implement programs that not only sound like they will work, but have been tested and proven to be the best choice for the entire community. Programs that build empathy and encourage students to figure out productive conflict-management solutions often are good choices.
The responsibility to end bullying is not just with educators, but with pediatricians as well. Bullying can have serious mental and physical ramifications for patients, and clinicians must be vigilant for signs of victimization, such as anxiety, depression, or social withdrawal. If it seems as though a patient has been the victim or is the perpetrator of bullying, clinicians may want to talk with the child and their parents about finding a counselor at school where bullying might occur most often, encourage the child to talk with his or her parents about any problems at school, build a stronger communication between parents and the school, and help to support at least one peer friendship, which has been found to be a strong buffer against peer victimization.
This study is a good example of the progress made so far, but there is still plenty of work to be done.
Stephen S. Leff, PhD, is a psychologist in the department of child and adolescent psychiatry and behavioral sciences and codirector of the Violence Prevention Initiative at the Children’s Hospital of Philadelphia and Chris Feudtner, MD, PhD, is director of the department of medical ethics at the hospital. This a summary of their comments from an editorial accompanying the report by Waasdorp et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-0504 ) Neither Dr. Leff nor Dr. Feudtner reported any relevant disclosures.
The Waasdorp et al. study is a comprehensive one using a sophisticated longitudinal design and a number of covariates to give a better comprehension of current bullying trends.
While it is encouraging to hear of the declining trends across many forms of bullying, it is important to remember 48% of children still reported bullying as an issue in their lives, with nearly as many reporting witnessing bullying against others.
We must be watchful for instances of bullying and active in getting rid of it both in and out of the classroom.
This means calling on educators to implement programs that not only sound like they will work, but have been tested and proven to be the best choice for the entire community. Programs that build empathy and encourage students to figure out productive conflict-management solutions often are good choices.
The responsibility to end bullying is not just with educators, but with pediatricians as well. Bullying can have serious mental and physical ramifications for patients, and clinicians must be vigilant for signs of victimization, such as anxiety, depression, or social withdrawal. If it seems as though a patient has been the victim or is the perpetrator of bullying, clinicians may want to talk with the child and their parents about finding a counselor at school where bullying might occur most often, encourage the child to talk with his or her parents about any problems at school, build a stronger communication between parents and the school, and help to support at least one peer friendship, which has been found to be a strong buffer against peer victimization.
This study is a good example of the progress made so far, but there is still plenty of work to be done.
Stephen S. Leff, PhD, is a psychologist in the department of child and adolescent psychiatry and behavioral sciences and codirector of the Violence Prevention Initiative at the Children’s Hospital of Philadelphia and Chris Feudtner, MD, PhD, is director of the department of medical ethics at the hospital. This a summary of their comments from an editorial accompanying the report by Waasdorp et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-0504 ) Neither Dr. Leff nor Dr. Feudtner reported any relevant disclosures.
Rates of bullying among students in grades 4-12 decreased over the past 10 years in a state study, contradicting a common perception of a rising trend in schools, according to a study.
The rate of self-reported, frequent bullying victimization fell from 28% in 2005 to 13% in 2014, reported Tracy Evian Waasdorp, PhD, at the Children’s Hospital of Philadelphia and the Center for the Prevention of Youth Violence at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and her associates. “These findings do contradict the public’s [mis]perception that bullying is increasing.”
Data collected through a survey of 246,306 students in grades 4-12 from 109 schools in Maryland in 2005-2014 found significant decreases in 10 of 13 bullying indicators (Pediatrics. 2017. doi: 10.1542/peds.2016-2615).
In the survey, students anonymously reported if they had been a frequent victim of bullying – two or more times within the past month – as defined by the World Health Organization and Center for Disease Control and Prevention’s definition: “A person is bullied when he or she is exposed, repeatedly and over time, to negative actions on the part of one or more other persons. Bullying often occurs in situations where there is a power or status difference. Bullying includes actions like threatening, teasing, name-calling, ignoring, rumor spreading, sending hurtful emails and text messages, and leaving someone out on purpose.”
The investigators found victimization decreased across indicators including pushing (beta = –0.03), hitting (beta = –0.03), threats (beta = –0.02), cyberbullying (beta = –0.01), and rumors (beta = –0.02), according to the researchers. All values were determined with a P value less than .001.
“It was hypothesized that cyberbullying might increase, but consistent with the other forms of bullying, cyberbullying also decreased,” the researchers wrote. “However, given the rapid change of technology and new social media platforms used by youth and increasingly at younger ages, the nature and quality of cyberbullying may change.”
Dr. Waasdorp and her colleagues also had children report if and how often they had participated in bullying or had witnessed bullying, both of which also declined, from 21% to 7% of students and 66% to 43% of students, respectively.
Along with bullying, students were asked how safe they felt in school and if adults in their school were doing enough to prevent bullying, both of which sentiments increased over the course of the study. While 80% of students reported feeling safe in the school, the number of those who felt as though they belonged remained relatively unchanged.
While decreases in each category were relatively small from year to year, “some of these changes were fairly substantial across 10 years, as indicated by the effect size estimates comparing the first and last years (average difference = 0.325),” according to the researchers.
In fact, Dr. Waasdorp and her peers found the final year of the study to have the greatest improvement, which they estimate may come from more comprehensive bullying laws and school practices.
Looking across grade levels, Dr. Waasdorp and her colleagues found greater declines in witnessing bullying and school safety in high schoolers than middle schoolers, which they say may indicate more support in middle school systems, where bullying peaks.
Because of the large number of outcomes, significant associations between school levels and bullying indicators were limited. The anonymous nature of the survey limited the ability of the researchers to link student data across years. The investigators also did not collect data on why changes to the bullying indicators occurred.
During the study, the researchers were supported in part by grants from the U.S. Department of Education, the William T. Grant Foundation, and the National Institute of Justice. The authors reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
Rates of bullying among students in grades 4-12 decreased over the past 10 years in a state study, contradicting a common perception of a rising trend in schools, according to a study.
The rate of self-reported, frequent bullying victimization fell from 28% in 2005 to 13% in 2014, reported Tracy Evian Waasdorp, PhD, at the Children’s Hospital of Philadelphia and the Center for the Prevention of Youth Violence at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and her associates. “These findings do contradict the public’s [mis]perception that bullying is increasing.”
Data collected through a survey of 246,306 students in grades 4-12 from 109 schools in Maryland in 2005-2014 found significant decreases in 10 of 13 bullying indicators (Pediatrics. 2017. doi: 10.1542/peds.2016-2615).
In the survey, students anonymously reported if they had been a frequent victim of bullying – two or more times within the past month – as defined by the World Health Organization and Center for Disease Control and Prevention’s definition: “A person is bullied when he or she is exposed, repeatedly and over time, to negative actions on the part of one or more other persons. Bullying often occurs in situations where there is a power or status difference. Bullying includes actions like threatening, teasing, name-calling, ignoring, rumor spreading, sending hurtful emails and text messages, and leaving someone out on purpose.”
The investigators found victimization decreased across indicators including pushing (beta = –0.03), hitting (beta = –0.03), threats (beta = –0.02), cyberbullying (beta = –0.01), and rumors (beta = –0.02), according to the researchers. All values were determined with a P value less than .001.
“It was hypothesized that cyberbullying might increase, but consistent with the other forms of bullying, cyberbullying also decreased,” the researchers wrote. “However, given the rapid change of technology and new social media platforms used by youth and increasingly at younger ages, the nature and quality of cyberbullying may change.”
Dr. Waasdorp and her colleagues also had children report if and how often they had participated in bullying or had witnessed bullying, both of which also declined, from 21% to 7% of students and 66% to 43% of students, respectively.
Along with bullying, students were asked how safe they felt in school and if adults in their school were doing enough to prevent bullying, both of which sentiments increased over the course of the study. While 80% of students reported feeling safe in the school, the number of those who felt as though they belonged remained relatively unchanged.
While decreases in each category were relatively small from year to year, “some of these changes were fairly substantial across 10 years, as indicated by the effect size estimates comparing the first and last years (average difference = 0.325),” according to the researchers.
In fact, Dr. Waasdorp and her peers found the final year of the study to have the greatest improvement, which they estimate may come from more comprehensive bullying laws and school practices.
Looking across grade levels, Dr. Waasdorp and her colleagues found greater declines in witnessing bullying and school safety in high schoolers than middle schoolers, which they say may indicate more support in middle school systems, where bullying peaks.
Because of the large number of outcomes, significant associations between school levels and bullying indicators were limited. The anonymous nature of the survey limited the ability of the researchers to link student data across years. The investigators also did not collect data on why changes to the bullying indicators occurred.
During the study, the researchers were supported in part by grants from the U.S. Department of Education, the William T. Grant Foundation, and the National Institute of Justice. The authors reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
FROM PEDIATRICS
Key clinical point:
Major finding: Reports of victimization overall among Maryland students in grades 4-12 decreased from 28% to 13% over a decade, with decreases in 10 of 13 bullying indicators in the study.
Data source: Self-reported survey of 246,306 students in grades 4-12 from 109 Maryland schools in 2005-2014, analyzed using a longitudinal hierarchical linear model.
Disclosures: During the study, researchers were supported in part by grants from the U.S. Department of Education, the William T. Grant Foundation, and the National Institute of Justice. The authors reported no relevant financial disclosures.