User login
Lower-dose aluminum hydroxide–adjuvanted polio vaccine noninferior to standard IPV
Aluminum hydroxide–adjuvanted vaccines with reduced doses of inactivated polio vaccine (IPV-Al) were noninferior to standard inactivated poliovirus vaccine (IPV) in a large trial in the Dominican Republic, said Luis Rivera, MD, of the Hospital Maternidad Nuestra Señora de la Altagracia, Santo Domingo, Dominican Republic, and his associates.
If these findings are replicated in phase III trials and regulatory approval follows, such vaccines could be low-cost replacements for standard IPV and oral poliovirus vaccines in low-resource countries, the study authors suggested.
In this phase II, blinded, randomized trial with three investigational IPV-Al groups and one IPV group, the vaccines were given at 6 weeks, 10 weeks, 14 weeks, and 18 weeks to 823 infants who had not previously received any polio vaccination. The three new IPV-Al vaccines all proved to be noninferior to IPV for poliovirus types 1, 2, and 3.
For 1/10 IPV-Al, the seroconversion rates for the different poliovirus types were 98.5% (type 1), 94.6% (type 2), and 99.5% (type 3), compared with 100% (type 1), 98.5% (type 2), and 100% (type 3) for IPV.
This and the results from other studies “have paved the way for further clinical investigations of IPV-Al in phase III trials,” Dr. Rivera and his associates wrote.
“The low frequency of adverse events in this phase II trial suggests that a safety evaluation is not necessarily justified,” they concluded.
The Bill & Melinda Gates Foundation funded the study. The authors had no disclosures.
Read more in the Lancet Infectious Diseases (2017 Apr 25. doi: 10.1016/S1473-3099(17)30177-9).
Aluminum hydroxide–adjuvanted vaccines with reduced doses of inactivated polio vaccine (IPV-Al) were noninferior to standard inactivated poliovirus vaccine (IPV) in a large trial in the Dominican Republic, said Luis Rivera, MD, of the Hospital Maternidad Nuestra Señora de la Altagracia, Santo Domingo, Dominican Republic, and his associates.
If these findings are replicated in phase III trials and regulatory approval follows, such vaccines could be low-cost replacements for standard IPV and oral poliovirus vaccines in low-resource countries, the study authors suggested.
In this phase II, blinded, randomized trial with three investigational IPV-Al groups and one IPV group, the vaccines were given at 6 weeks, 10 weeks, 14 weeks, and 18 weeks to 823 infants who had not previously received any polio vaccination. The three new IPV-Al vaccines all proved to be noninferior to IPV for poliovirus types 1, 2, and 3.
For 1/10 IPV-Al, the seroconversion rates for the different poliovirus types were 98.5% (type 1), 94.6% (type 2), and 99.5% (type 3), compared with 100% (type 1), 98.5% (type 2), and 100% (type 3) for IPV.
This and the results from other studies “have paved the way for further clinical investigations of IPV-Al in phase III trials,” Dr. Rivera and his associates wrote.
“The low frequency of adverse events in this phase II trial suggests that a safety evaluation is not necessarily justified,” they concluded.
The Bill & Melinda Gates Foundation funded the study. The authors had no disclosures.
Read more in the Lancet Infectious Diseases (2017 Apr 25. doi: 10.1016/S1473-3099(17)30177-9).
Aluminum hydroxide–adjuvanted vaccines with reduced doses of inactivated polio vaccine (IPV-Al) were noninferior to standard inactivated poliovirus vaccine (IPV) in a large trial in the Dominican Republic, said Luis Rivera, MD, of the Hospital Maternidad Nuestra Señora de la Altagracia, Santo Domingo, Dominican Republic, and his associates.
If these findings are replicated in phase III trials and regulatory approval follows, such vaccines could be low-cost replacements for standard IPV and oral poliovirus vaccines in low-resource countries, the study authors suggested.
In this phase II, blinded, randomized trial with three investigational IPV-Al groups and one IPV group, the vaccines were given at 6 weeks, 10 weeks, 14 weeks, and 18 weeks to 823 infants who had not previously received any polio vaccination. The three new IPV-Al vaccines all proved to be noninferior to IPV for poliovirus types 1, 2, and 3.
For 1/10 IPV-Al, the seroconversion rates for the different poliovirus types were 98.5% (type 1), 94.6% (type 2), and 99.5% (type 3), compared with 100% (type 1), 98.5% (type 2), and 100% (type 3) for IPV.
This and the results from other studies “have paved the way for further clinical investigations of IPV-Al in phase III trials,” Dr. Rivera and his associates wrote.
“The low frequency of adverse events in this phase II trial suggests that a safety evaluation is not necessarily justified,” they concluded.
The Bill & Melinda Gates Foundation funded the study. The authors had no disclosures.
Read more in the Lancet Infectious Diseases (2017 Apr 25. doi: 10.1016/S1473-3099(17)30177-9).
FROM THE LANCET INFECTIOUS DISEASES
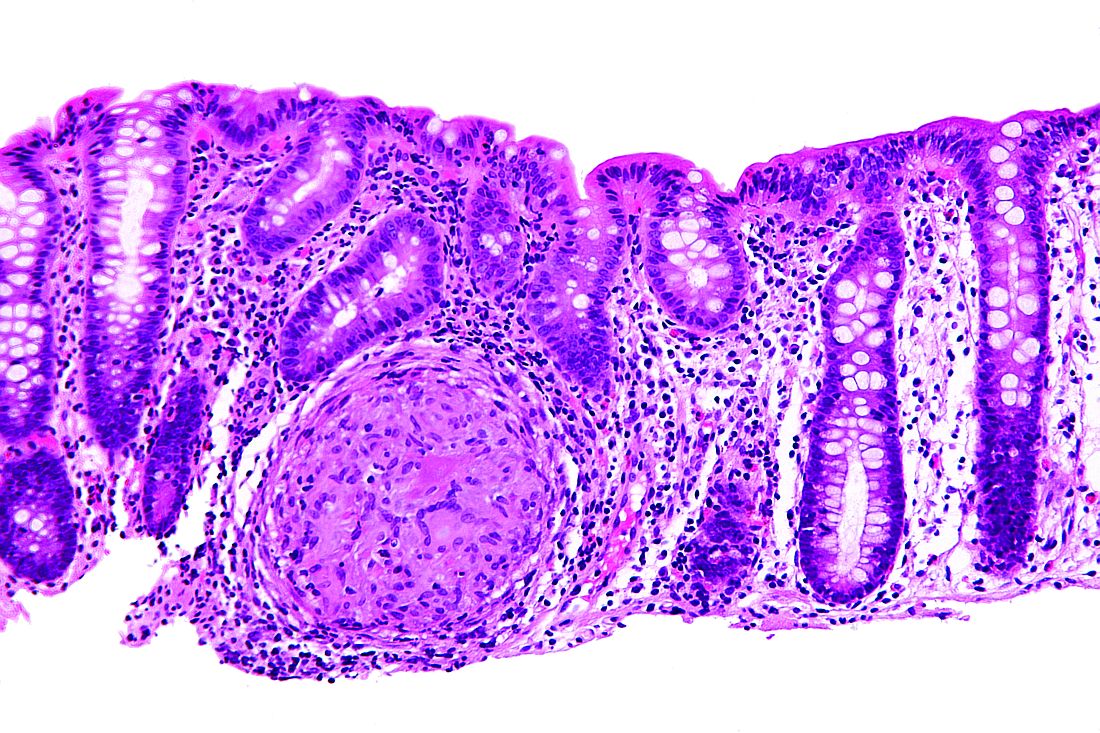
Consider strongyloidiasis before giving oral steroids
SYDNEY – Think twice before prescribing oral steroids for patients who have urticarial dermatitis, diarrhea, and cough, especially if they have lived in or recently traveled to tropical areas, Ian McCrossin, MD, said at the annual meeting of the Australasian College of Dermatologists.
Strongyloides stercoralis, or threadworm, infection can flare dramatically when patients take oral steroids. “You get thousands of worms, and they punch their way through the bowel wall and take the bowel organisms with them; that’s when you get septicaemia,” Dr. McCrossin, a dermatologist from Liverpool Hospital, Sydney, said in an interview.
Dr. McCrossin cited an Australian study that found a strongyloides infection was present in 11.6% of 309 Vietnam veterans living in South Australia.
Risk factors for Strongyloides hyperinfection include compromised immunity, human T-cell lymphotropic virus type 1, alcohol use disorder, malnutrition, and oral steroid use. Mortality rates from the resulting sepsis are as high as 87%, Dr. McCrossin said.
IgG ELISA is a reliable test for established strongyloidiasis, but is less effective for recent infection, hyperinfection, and in patients who are immunosuppressed. Eosinophilia has a poor predictive value. Light microscopy of stool samples may require evaluation of multiple stool samples unless the patient had hyperinfection.
Treatment generally consists of ivermectin, 200 mcg/kg orally for 1-2 days. Follow-up stool exams should be performed 2-4 weeks after treatment to confirm clearance of infection. In those patients with hyperinfections, ivermectin 200 mcg/kg orally is given daily until stool and/or sputum exams are negative for 2 weeks.
Dr. McCrossin declared no conflicts of interest.
SYDNEY – Think twice before prescribing oral steroids for patients who have urticarial dermatitis, diarrhea, and cough, especially if they have lived in or recently traveled to tropical areas, Ian McCrossin, MD, said at the annual meeting of the Australasian College of Dermatologists.
Strongyloides stercoralis, or threadworm, infection can flare dramatically when patients take oral steroids. “You get thousands of worms, and they punch their way through the bowel wall and take the bowel organisms with them; that’s when you get septicaemia,” Dr. McCrossin, a dermatologist from Liverpool Hospital, Sydney, said in an interview.
Dr. McCrossin cited an Australian study that found a strongyloides infection was present in 11.6% of 309 Vietnam veterans living in South Australia.
Risk factors for Strongyloides hyperinfection include compromised immunity, human T-cell lymphotropic virus type 1, alcohol use disorder, malnutrition, and oral steroid use. Mortality rates from the resulting sepsis are as high as 87%, Dr. McCrossin said.
IgG ELISA is a reliable test for established strongyloidiasis, but is less effective for recent infection, hyperinfection, and in patients who are immunosuppressed. Eosinophilia has a poor predictive value. Light microscopy of stool samples may require evaluation of multiple stool samples unless the patient had hyperinfection.
Treatment generally consists of ivermectin, 200 mcg/kg orally for 1-2 days. Follow-up stool exams should be performed 2-4 weeks after treatment to confirm clearance of infection. In those patients with hyperinfections, ivermectin 200 mcg/kg orally is given daily until stool and/or sputum exams are negative for 2 weeks.
Dr. McCrossin declared no conflicts of interest.
SYDNEY – Think twice before prescribing oral steroids for patients who have urticarial dermatitis, diarrhea, and cough, especially if they have lived in or recently traveled to tropical areas, Ian McCrossin, MD, said at the annual meeting of the Australasian College of Dermatologists.
Strongyloides stercoralis, or threadworm, infection can flare dramatically when patients take oral steroids. “You get thousands of worms, and they punch their way through the bowel wall and take the bowel organisms with them; that’s when you get septicaemia,” Dr. McCrossin, a dermatologist from Liverpool Hospital, Sydney, said in an interview.
Dr. McCrossin cited an Australian study that found a strongyloides infection was present in 11.6% of 309 Vietnam veterans living in South Australia.
Risk factors for Strongyloides hyperinfection include compromised immunity, human T-cell lymphotropic virus type 1, alcohol use disorder, malnutrition, and oral steroid use. Mortality rates from the resulting sepsis are as high as 87%, Dr. McCrossin said.
IgG ELISA is a reliable test for established strongyloidiasis, but is less effective for recent infection, hyperinfection, and in patients who are immunosuppressed. Eosinophilia has a poor predictive value. Light microscopy of stool samples may require evaluation of multiple stool samples unless the patient had hyperinfection.
Treatment generally consists of ivermectin, 200 mcg/kg orally for 1-2 days. Follow-up stool exams should be performed 2-4 weeks after treatment to confirm clearance of infection. In those patients with hyperinfections, ivermectin 200 mcg/kg orally is given daily until stool and/or sputum exams are negative for 2 weeks.
Dr. McCrossin declared no conflicts of interest.
EXPERT ANALYSIS AT ACDASM 2017
Cutaneous manifestations can signify severe systemic disease in ANCA-associated vasculitis
PORTLAND, ORE. – Clinicians who treat or diagnose ANCA-associated vasculitis should watch for a variety of skin lesions, which can signify severe systemic manifestations of disease, according to the results of a cross-sectional study of 1,184 patients from 130 centers worldwide.
Among patients with granulomatosis with polyangiitis (GPA) or eosinophilic granulomatosis with polyangiitis (EGPA), the presence of skin lesions approximately doubled the likelihood of renal, pulmonary, neurologic, or other severe systemic manifestations of ANCA-associated vasculitis (hazard ratios, 2.0; P less than .03).
This cohort is part of the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS), which aims to develop classification and diagnostic criteria for primary systemic vasculitis. Fully 35% of patients had cutaneous manifestations of ANCA-associated vasculitis, including 47% of those with EGPA, 34% of those with GPA, and 28% of those with microscopic polyangiitis (MPA).
Petechiae/purpura were the most common cutaneous manifestations of all three subtypes, affecting 15% of the overall cohort, 21% of patients with EGPA, 16% of those with GPA, and 9% of those with MPA (P less than .01 for differences among groups). Petechiae/purpura did not more accurately predict systemic disease than other cutaneous findings, and skin lesions were not significantly associated with severe systemic disease in patients with MPA (HR, 0.63; 95% confidence interval, 0.35-1.14; P = .13), the investigators reported.
Besides petechiae/purpura, patients with EGPA most often presented with allergic and nonspecific cutaneous manifestations, such as pruritus (13% of patients), urticaria (8%), and maculopapular rash (8%), they said. In contrast, patients with GPA most often had painful skin lesions (10%) or maculopapular rash (7%), while those with MPA were more likely to have livedo reticularis or racemosa (7%).
Study participants tended to be in their mid-50s to mid-60s at diagnosis, about 48% were male, and most were Northern European, Southern European, or American whites, while 28% of those with MPA were Han Chinese, of another Chinese ethnicity, or Japanese.
“This study demonstrates that skin lesions are quite common and varied in granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis,” the investigators concluded.
Funders included the American College of Rheumatology, the European League Against Rheumatism, the Vasculitis Foundation, and the Dermatology Foundation. Dr. Micheletti had no conflicts of interest.
PORTLAND, ORE. – Clinicians who treat or diagnose ANCA-associated vasculitis should watch for a variety of skin lesions, which can signify severe systemic manifestations of disease, according to the results of a cross-sectional study of 1,184 patients from 130 centers worldwide.
Among patients with granulomatosis with polyangiitis (GPA) or eosinophilic granulomatosis with polyangiitis (EGPA), the presence of skin lesions approximately doubled the likelihood of renal, pulmonary, neurologic, or other severe systemic manifestations of ANCA-associated vasculitis (hazard ratios, 2.0; P less than .03).
This cohort is part of the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS), which aims to develop classification and diagnostic criteria for primary systemic vasculitis. Fully 35% of patients had cutaneous manifestations of ANCA-associated vasculitis, including 47% of those with EGPA, 34% of those with GPA, and 28% of those with microscopic polyangiitis (MPA).
Petechiae/purpura were the most common cutaneous manifestations of all three subtypes, affecting 15% of the overall cohort, 21% of patients with EGPA, 16% of those with GPA, and 9% of those with MPA (P less than .01 for differences among groups). Petechiae/purpura did not more accurately predict systemic disease than other cutaneous findings, and skin lesions were not significantly associated with severe systemic disease in patients with MPA (HR, 0.63; 95% confidence interval, 0.35-1.14; P = .13), the investigators reported.
Besides petechiae/purpura, patients with EGPA most often presented with allergic and nonspecific cutaneous manifestations, such as pruritus (13% of patients), urticaria (8%), and maculopapular rash (8%), they said. In contrast, patients with GPA most often had painful skin lesions (10%) or maculopapular rash (7%), while those with MPA were more likely to have livedo reticularis or racemosa (7%).
Study participants tended to be in their mid-50s to mid-60s at diagnosis, about 48% were male, and most were Northern European, Southern European, or American whites, while 28% of those with MPA were Han Chinese, of another Chinese ethnicity, or Japanese.
“This study demonstrates that skin lesions are quite common and varied in granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis,” the investigators concluded.
Funders included the American College of Rheumatology, the European League Against Rheumatism, the Vasculitis Foundation, and the Dermatology Foundation. Dr. Micheletti had no conflicts of interest.
PORTLAND, ORE. – Clinicians who treat or diagnose ANCA-associated vasculitis should watch for a variety of skin lesions, which can signify severe systemic manifestations of disease, according to the results of a cross-sectional study of 1,184 patients from 130 centers worldwide.
Among patients with granulomatosis with polyangiitis (GPA) or eosinophilic granulomatosis with polyangiitis (EGPA), the presence of skin lesions approximately doubled the likelihood of renal, pulmonary, neurologic, or other severe systemic manifestations of ANCA-associated vasculitis (hazard ratios, 2.0; P less than .03).
This cohort is part of the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS), which aims to develop classification and diagnostic criteria for primary systemic vasculitis. Fully 35% of patients had cutaneous manifestations of ANCA-associated vasculitis, including 47% of those with EGPA, 34% of those with GPA, and 28% of those with microscopic polyangiitis (MPA).
Petechiae/purpura were the most common cutaneous manifestations of all three subtypes, affecting 15% of the overall cohort, 21% of patients with EGPA, 16% of those with GPA, and 9% of those with MPA (P less than .01 for differences among groups). Petechiae/purpura did not more accurately predict systemic disease than other cutaneous findings, and skin lesions were not significantly associated with severe systemic disease in patients with MPA (HR, 0.63; 95% confidence interval, 0.35-1.14; P = .13), the investigators reported.
Besides petechiae/purpura, patients with EGPA most often presented with allergic and nonspecific cutaneous manifestations, such as pruritus (13% of patients), urticaria (8%), and maculopapular rash (8%), they said. In contrast, patients with GPA most often had painful skin lesions (10%) or maculopapular rash (7%), while those with MPA were more likely to have livedo reticularis or racemosa (7%).
Study participants tended to be in their mid-50s to mid-60s at diagnosis, about 48% were male, and most were Northern European, Southern European, or American whites, while 28% of those with MPA were Han Chinese, of another Chinese ethnicity, or Japanese.
“This study demonstrates that skin lesions are quite common and varied in granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis,” the investigators concluded.
Funders included the American College of Rheumatology, the European League Against Rheumatism, the Vasculitis Foundation, and the Dermatology Foundation. Dr. Micheletti had no conflicts of interest.
AT SID 2017
Key clinical point: Skin lesions can be a red flag for severe systemic disease in patients with ANCA-associated vasculitis.
Major finding: Among patients with granulomatosis with polyangiitis or eosinophilic granulomatosis with polyangiitis, the presence of skin lesions approximately doubled the likelihood of renal, pulmonary, neurologic, or other severe systemic manifestations of ANCA-associated vasculitis (HR, 2.0, P less than .03). The hazard ratio was not elevated in patients with microscopic polyangiitis.
Data source: A cross-sectional study of 1,184 patients with ANCA-associated vasculitis from 130 centers worldwide.
Disclosures: Funders included the American College of Rheumatology, the European League Against Rheumatism, the Vasculitis Foundation, and the Dermatology Foundation. Dr. Micheletti had no conflicts of interest.
Why Is Skin Cancer Mortality Higher in Patients With Skin of Color?
FDA approves avelumab for advanced urothelial carcinoma
The Food and Drug Administration has granted accelerated approval to avelumab for the treatment of patients with locally advanced or metastatic urothelial carcinoma whose disease progressed during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy.
Approval was based on a confirmed overall response rate (ORR) of 16.1% in 26 patients who had been followed for at least 6 months in a single-arm, multicenter study that enrolled 242 patients with locally advanced or metastatic urothelial carcinoma whose disease progressed following platinum-containing neoadjuvant or adjuvant chemotherapy. The ORR was 13.3% among 30 patients who had been followed for at least 13 weeks. Median time to response was 2.0 months (range 1.3-11.0). The median response duration had not been reached in patients followed for at least 13 weeks or at least 6 months, but ranged from 1.4+ to 17.4+ months in both groups, the FDA said in a statement.
Serious adverse reactions, including urinary tract infection/urosepsis, abdominal pain, musculoskeletal pain, creatinine increased/renal failure, dehydration, hematuria/urinary tract hemorrhage, intestinal obstruction/small intestinal obstruction, and pyrexia, were reported in 41% of patients, causing death in 6% of patients. The most common adverse reactions were infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection.
The FDA recommended an intravenous infusion of 10 mg/kg over 60 minutes every 2 weeks, and premedication with an antihistamine and acetaminophen prior to the first four infusions of avelumab.
Full prescribing information is available here.
The drug is being marketed as Bavencio by EMD Serono.
The Food and Drug Administration has granted accelerated approval to avelumab for the treatment of patients with locally advanced or metastatic urothelial carcinoma whose disease progressed during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy.
Approval was based on a confirmed overall response rate (ORR) of 16.1% in 26 patients who had been followed for at least 6 months in a single-arm, multicenter study that enrolled 242 patients with locally advanced or metastatic urothelial carcinoma whose disease progressed following platinum-containing neoadjuvant or adjuvant chemotherapy. The ORR was 13.3% among 30 patients who had been followed for at least 13 weeks. Median time to response was 2.0 months (range 1.3-11.0). The median response duration had not been reached in patients followed for at least 13 weeks or at least 6 months, but ranged from 1.4+ to 17.4+ months in both groups, the FDA said in a statement.
Serious adverse reactions, including urinary tract infection/urosepsis, abdominal pain, musculoskeletal pain, creatinine increased/renal failure, dehydration, hematuria/urinary tract hemorrhage, intestinal obstruction/small intestinal obstruction, and pyrexia, were reported in 41% of patients, causing death in 6% of patients. The most common adverse reactions were infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection.
The FDA recommended an intravenous infusion of 10 mg/kg over 60 minutes every 2 weeks, and premedication with an antihistamine and acetaminophen prior to the first four infusions of avelumab.
Full prescribing information is available here.
The drug is being marketed as Bavencio by EMD Serono.
The Food and Drug Administration has granted accelerated approval to avelumab for the treatment of patients with locally advanced or metastatic urothelial carcinoma whose disease progressed during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy.
Approval was based on a confirmed overall response rate (ORR) of 16.1% in 26 patients who had been followed for at least 6 months in a single-arm, multicenter study that enrolled 242 patients with locally advanced or metastatic urothelial carcinoma whose disease progressed following platinum-containing neoadjuvant or adjuvant chemotherapy. The ORR was 13.3% among 30 patients who had been followed for at least 13 weeks. Median time to response was 2.0 months (range 1.3-11.0). The median response duration had not been reached in patients followed for at least 13 weeks or at least 6 months, but ranged from 1.4+ to 17.4+ months in both groups, the FDA said in a statement.
Serious adverse reactions, including urinary tract infection/urosepsis, abdominal pain, musculoskeletal pain, creatinine increased/renal failure, dehydration, hematuria/urinary tract hemorrhage, intestinal obstruction/small intestinal obstruction, and pyrexia, were reported in 41% of patients, causing death in 6% of patients. The most common adverse reactions were infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection.
The FDA recommended an intravenous infusion of 10 mg/kg over 60 minutes every 2 weeks, and premedication with an antihistamine and acetaminophen prior to the first four infusions of avelumab.
Full prescribing information is available here.
The drug is being marketed as Bavencio by EMD Serono.
Dalbavancin proves highly effective in osteomyelitis
VIENNA – Two infusions of the long-acting lipoglycopeptide antibiotic dalbavancin showed a favorable clinical benefit for treatment of adult osteomyelitis in a phase II study.
Dalbavancin (Dalvance) showed positive results while avoiding the complexities of standard therapies that require longer, more frequent dosing, Urania Rappo, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Dalbavancin already is approved for acute bacterial skin and skin structure infections, and its long terminal half-life of 14 days and high bone penetration made it a natural candidate for evaluation in the treatment of osteomyelitis, said Dr. Rappo, director of clinical development (anti-infectives) at Allergan, which markets the drug and sponsored the study.
Dalbavancin is a glycopeptide antibiotic with a lipid tail that prolongs its half-life, compared with other drugs in this category, such as vancomycin and teicoplanin, to which it is structurally related. It is highly potent against gram-positive bacterial infections, including methicillin-resistant Staphylococcus aureus.
The drug’s MIC90 for S. aureus is 0.06 mcg/mL; vancomycin’s, in comparison, is 1 mcg/mL. A 2015 bone penetration study found that the bone level 12 hours after a 1,000-mg infusion was 6.3 mcg/g. This remained elevated for 14 days; the concentration at 2 weeks was 4 mcg/g (Antimicrob Agents Chemother. 2015 Apr;59[4]:1849-55).
“The mean bone-to-plasma penetration ratio was 13%, and drug levels in bone were very similar to free drug levels in serum, so we expect that much of this is free drug in the bone, available for antimicrobial activity,” Dr. Rappo noted. “It’s not only long lasting, but highly potent, meaning we need less drug to kill the infecting organism.”
Dalbavancin was administered as two 1,500-mg IV infusions, 1 week apart in Dr. Rappo’s randomized, open-label, phase II study – the first clinical trial to examine the drug’s effect in osteomyelitis in adults. The study is ongoing; she presented interim results on 68 patients, 59 of whom took dalbavancin. The nine patients in the standard-of-care arm were treated according to the investigator’s clinical judgment. Vancomycin was the most commonly employed therapy. Three patients received vancomycin infusions for 4 weeks. Four received a regimen of 4-16 days of intravenous vancomycin followed by intravenous linezolid or levofloxacin to complete a 4- to 6-week course of therapy. Adjunctive aztreonam was permitted for presumed coinfection with a gram-negative pathogen and a switch to oral antibiotic for gram-negative coverage was allowed after clinical improvement.
The primary endpoint was clinical cure at 42 days in the clinically evaluable population, defined as recovery without need for further antibiotic therapy. Failure was defined as the need for additional antibiotics; more than 6 weeks of treatment in the comparator arm; new purulence; amputation due to infection progression; or death. Indeterminate response was defined as loss to follow-up or amputation due to vascular insufficiency.
There were several secondary endpoints: clinical improvement at day 21, including changes in C-reactive protein level and clinical response in patients who had follow-up at days 42, 180, and 365.
In the dalbavancin arm, patients had a mean age of 51 years. All had undergone surgical debridement and bone culture. The most common site of infection was the foot or leg (about 83%). The baseline mean CRP level was 41.8 mg/L. About half of the patients had methicillin-susceptible S. aureus on bone culture. Coagulase-negative staphylococci were present in 20%. About 22% had gram-negative pathogens, mostly present in a mixed infection along with gram-positive pathogens. Five patients (three on dalbavancin, two on standard of care) discontinued the study drug early because they were solely infected with gram-negative pathogens.
At day 42, clinical cure was seen in all the dalbavancin patients and six of the standard treatment patients. In the group with treatment data out to 180 days (54 on dalbavancin and 5 on standard therapy), clinical cure rates were similar.
At 180 days, clinical cure continued in 93% of the dalbavancin patients (50 of 54). Two patients were defined as failures, and two patients were indeterminate because of loss to follow-up. In the standard therapy group at 180 days, four of five standard therapy patients maintained clinical cure; none of these patients has reached the 365-day outcome.
There were no treatment-emergent adverse events (TEAEs) in the standard therapy group. In the dalbavancin group, 10 patients experienced TEAEs, only one of whom had TEAEs related to the study drug, which were not serious, Dr. Rappo said.
This study was performed at a single center in the Ukraine, and an additional phase II study in the United States has begun, she added.
[email protected]
On Twitter @alz_gal
VIENNA – Two infusions of the long-acting lipoglycopeptide antibiotic dalbavancin showed a favorable clinical benefit for treatment of adult osteomyelitis in a phase II study.
Dalbavancin (Dalvance) showed positive results while avoiding the complexities of standard therapies that require longer, more frequent dosing, Urania Rappo, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Dalbavancin already is approved for acute bacterial skin and skin structure infections, and its long terminal half-life of 14 days and high bone penetration made it a natural candidate for evaluation in the treatment of osteomyelitis, said Dr. Rappo, director of clinical development (anti-infectives) at Allergan, which markets the drug and sponsored the study.
Dalbavancin is a glycopeptide antibiotic with a lipid tail that prolongs its half-life, compared with other drugs in this category, such as vancomycin and teicoplanin, to which it is structurally related. It is highly potent against gram-positive bacterial infections, including methicillin-resistant Staphylococcus aureus.
The drug’s MIC90 for S. aureus is 0.06 mcg/mL; vancomycin’s, in comparison, is 1 mcg/mL. A 2015 bone penetration study found that the bone level 12 hours after a 1,000-mg infusion was 6.3 mcg/g. This remained elevated for 14 days; the concentration at 2 weeks was 4 mcg/g (Antimicrob Agents Chemother. 2015 Apr;59[4]:1849-55).
“The mean bone-to-plasma penetration ratio was 13%, and drug levels in bone were very similar to free drug levels in serum, so we expect that much of this is free drug in the bone, available for antimicrobial activity,” Dr. Rappo noted. “It’s not only long lasting, but highly potent, meaning we need less drug to kill the infecting organism.”
Dalbavancin was administered as two 1,500-mg IV infusions, 1 week apart in Dr. Rappo’s randomized, open-label, phase II study – the first clinical trial to examine the drug’s effect in osteomyelitis in adults. The study is ongoing; she presented interim results on 68 patients, 59 of whom took dalbavancin. The nine patients in the standard-of-care arm were treated according to the investigator’s clinical judgment. Vancomycin was the most commonly employed therapy. Three patients received vancomycin infusions for 4 weeks. Four received a regimen of 4-16 days of intravenous vancomycin followed by intravenous linezolid or levofloxacin to complete a 4- to 6-week course of therapy. Adjunctive aztreonam was permitted for presumed coinfection with a gram-negative pathogen and a switch to oral antibiotic for gram-negative coverage was allowed after clinical improvement.
The primary endpoint was clinical cure at 42 days in the clinically evaluable population, defined as recovery without need for further antibiotic therapy. Failure was defined as the need for additional antibiotics; more than 6 weeks of treatment in the comparator arm; new purulence; amputation due to infection progression; or death. Indeterminate response was defined as loss to follow-up or amputation due to vascular insufficiency.
There were several secondary endpoints: clinical improvement at day 21, including changes in C-reactive protein level and clinical response in patients who had follow-up at days 42, 180, and 365.
In the dalbavancin arm, patients had a mean age of 51 years. All had undergone surgical debridement and bone culture. The most common site of infection was the foot or leg (about 83%). The baseline mean CRP level was 41.8 mg/L. About half of the patients had methicillin-susceptible S. aureus on bone culture. Coagulase-negative staphylococci were present in 20%. About 22% had gram-negative pathogens, mostly present in a mixed infection along with gram-positive pathogens. Five patients (three on dalbavancin, two on standard of care) discontinued the study drug early because they were solely infected with gram-negative pathogens.
At day 42, clinical cure was seen in all the dalbavancin patients and six of the standard treatment patients. In the group with treatment data out to 180 days (54 on dalbavancin and 5 on standard therapy), clinical cure rates were similar.
At 180 days, clinical cure continued in 93% of the dalbavancin patients (50 of 54). Two patients were defined as failures, and two patients were indeterminate because of loss to follow-up. In the standard therapy group at 180 days, four of five standard therapy patients maintained clinical cure; none of these patients has reached the 365-day outcome.
There were no treatment-emergent adverse events (TEAEs) in the standard therapy group. In the dalbavancin group, 10 patients experienced TEAEs, only one of whom had TEAEs related to the study drug, which were not serious, Dr. Rappo said.
This study was performed at a single center in the Ukraine, and an additional phase II study in the United States has begun, she added.
[email protected]
On Twitter @alz_gal
VIENNA – Two infusions of the long-acting lipoglycopeptide antibiotic dalbavancin showed a favorable clinical benefit for treatment of adult osteomyelitis in a phase II study.
Dalbavancin (Dalvance) showed positive results while avoiding the complexities of standard therapies that require longer, more frequent dosing, Urania Rappo, MD, said at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
Dalbavancin already is approved for acute bacterial skin and skin structure infections, and its long terminal half-life of 14 days and high bone penetration made it a natural candidate for evaluation in the treatment of osteomyelitis, said Dr. Rappo, director of clinical development (anti-infectives) at Allergan, which markets the drug and sponsored the study.
Dalbavancin is a glycopeptide antibiotic with a lipid tail that prolongs its half-life, compared with other drugs in this category, such as vancomycin and teicoplanin, to which it is structurally related. It is highly potent against gram-positive bacterial infections, including methicillin-resistant Staphylococcus aureus.
The drug’s MIC90 for S. aureus is 0.06 mcg/mL; vancomycin’s, in comparison, is 1 mcg/mL. A 2015 bone penetration study found that the bone level 12 hours after a 1,000-mg infusion was 6.3 mcg/g. This remained elevated for 14 days; the concentration at 2 weeks was 4 mcg/g (Antimicrob Agents Chemother. 2015 Apr;59[4]:1849-55).
“The mean bone-to-plasma penetration ratio was 13%, and drug levels in bone were very similar to free drug levels in serum, so we expect that much of this is free drug in the bone, available for antimicrobial activity,” Dr. Rappo noted. “It’s not only long lasting, but highly potent, meaning we need less drug to kill the infecting organism.”
Dalbavancin was administered as two 1,500-mg IV infusions, 1 week apart in Dr. Rappo’s randomized, open-label, phase II study – the first clinical trial to examine the drug’s effect in osteomyelitis in adults. The study is ongoing; she presented interim results on 68 patients, 59 of whom took dalbavancin. The nine patients in the standard-of-care arm were treated according to the investigator’s clinical judgment. Vancomycin was the most commonly employed therapy. Three patients received vancomycin infusions for 4 weeks. Four received a regimen of 4-16 days of intravenous vancomycin followed by intravenous linezolid or levofloxacin to complete a 4- to 6-week course of therapy. Adjunctive aztreonam was permitted for presumed coinfection with a gram-negative pathogen and a switch to oral antibiotic for gram-negative coverage was allowed after clinical improvement.
The primary endpoint was clinical cure at 42 days in the clinically evaluable population, defined as recovery without need for further antibiotic therapy. Failure was defined as the need for additional antibiotics; more than 6 weeks of treatment in the comparator arm; new purulence; amputation due to infection progression; or death. Indeterminate response was defined as loss to follow-up or amputation due to vascular insufficiency.
There were several secondary endpoints: clinical improvement at day 21, including changes in C-reactive protein level and clinical response in patients who had follow-up at days 42, 180, and 365.
In the dalbavancin arm, patients had a mean age of 51 years. All had undergone surgical debridement and bone culture. The most common site of infection was the foot or leg (about 83%). The baseline mean CRP level was 41.8 mg/L. About half of the patients had methicillin-susceptible S. aureus on bone culture. Coagulase-negative staphylococci were present in 20%. About 22% had gram-negative pathogens, mostly present in a mixed infection along with gram-positive pathogens. Five patients (three on dalbavancin, two on standard of care) discontinued the study drug early because they were solely infected with gram-negative pathogens.
At day 42, clinical cure was seen in all the dalbavancin patients and six of the standard treatment patients. In the group with treatment data out to 180 days (54 on dalbavancin and 5 on standard therapy), clinical cure rates were similar.
At 180 days, clinical cure continued in 93% of the dalbavancin patients (50 of 54). Two patients were defined as failures, and two patients were indeterminate because of loss to follow-up. In the standard therapy group at 180 days, four of five standard therapy patients maintained clinical cure; none of these patients has reached the 365-day outcome.
There were no treatment-emergent adverse events (TEAEs) in the standard therapy group. In the dalbavancin group, 10 patients experienced TEAEs, only one of whom had TEAEs related to the study drug, which were not serious, Dr. Rappo said.
This study was performed at a single center in the Ukraine, and an additional phase II study in the United States has begun, she added.
[email protected]
On Twitter @alz_gal
Key clinical point:
Major finding: At 42 days, 100% of patients taking the drug were clear of infection.
Data source: A phase II trial involving 68 patients, 59 of whom were randomized to the study drug; the remainder were on standard treatment.
Disclosures: Allergan sponsored the study; Dr. Rappo is a company employee.
Changing gloves before closure cut wound-related cesarean complications
SAN DIEGO – Changing gloves before closure during cesarean deliveries can reduce overall wound morbidity, a study showed.
Glove changing during the study had a number needed to treat (NNT) of 14 to see benefit, no demonstrated risk, and a total cost per procedure of about $5.
Researchers led by Buvana Reddy, MD, an ob.gyn. in group practice in Woodbury, Minn., used a randomized trial design to determine whether donning a fresh pair of gloves makes a difference in the rate of surgical complications during cesarean delivery. .
Just one previous study had shown a reduced wound infection rate when gloves were changed after placental delivery (J Reprod Med. 2004 Jan;49[1]:13-6). The study showed a statistically significant drop in wound infections, but Dr. Scrafford said that the sample size was small, and the point at which glove changing was performed is not very practical in terms of the flow of surgery.
Building on this study, Dr. Scrafford and his colleagues designed a trial that was meant to be larger, incorporated a composite wound outcome score rather than just focusing strictly on infection, and switched the timing of glove change to just before abdominal closure.
The randomized controlled trial included all women who underwent nonemergent cesarean delivery at the investigators’ home facility during a 15-month period. The patient allocation was not known until the presurgical “time-out.” Patients allocated to the control condition did not have any change in operative procedures; the surgical team of patients allocated to the intervention arm changed their outer gloves immediately before peritoneal or fascial closure.
The composite primary outcome measure assessed wound seroma, hematoma, or dehiscence (defined as a separation of at least 1 cm), as well as wound infection and any other wound abnormality. Secondary outcome measures included whether patients had a fever or peri-incisional cellulitis.
A total of 553 patients were randomized. Follow-up was high, so Dr. Scrafford and his colleagues were able to analyze data from a total of 250 patients in the control arm and 236 patients who received the glove-changing intervention.
Patient demographics and comorbidities were similar between groups, as was the surgical time and estimated blood loss. Dr. Scrafford noted that significantly more patients in the glove-changing group than in the control group received presurgical vaginal preparation with antiseptic solution (20.3% vs. 10.5%; P = .001). However, he reported, statistical analysis showed that this difference had no effect on the results.
Overall, 15 (6.4%) of the patients in the glove-changing group met the criteria for wound complication, compared with 34 (13.6%) in the control group (P = .008). Of the individual components of the primary outcome measure, the difference in incidence of skin separation was also significant; separation was experienced by five patients (2.1%) in the glove-changing group, compared with 14 (5.6%) in the control group (P = .01).
The rate of wound infections was numerically lower in the intervention group, compared with the control group (8 vs. 14), but the difference was not statistically significant.
There were no significant differences between the groups when secondary outcomes were analyzed, Dr. Scrafford said.
The lack of block randomization in the study left open the potential for historical bias, Dr. Scrafford said. Since surgeons couldn’t be blinded as to study arm, the potential for observer bias also existed. Still, he said, the study’s strengths included its large size, and the real-world applicability of the broad inclusion criteria and diverse patient population.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
SAN DIEGO – Changing gloves before closure during cesarean deliveries can reduce overall wound morbidity, a study showed.
Glove changing during the study had a number needed to treat (NNT) of 14 to see benefit, no demonstrated risk, and a total cost per procedure of about $5.
Researchers led by Buvana Reddy, MD, an ob.gyn. in group practice in Woodbury, Minn., used a randomized trial design to determine whether donning a fresh pair of gloves makes a difference in the rate of surgical complications during cesarean delivery. .
Just one previous study had shown a reduced wound infection rate when gloves were changed after placental delivery (J Reprod Med. 2004 Jan;49[1]:13-6). The study showed a statistically significant drop in wound infections, but Dr. Scrafford said that the sample size was small, and the point at which glove changing was performed is not very practical in terms of the flow of surgery.
Building on this study, Dr. Scrafford and his colleagues designed a trial that was meant to be larger, incorporated a composite wound outcome score rather than just focusing strictly on infection, and switched the timing of glove change to just before abdominal closure.
The randomized controlled trial included all women who underwent nonemergent cesarean delivery at the investigators’ home facility during a 15-month period. The patient allocation was not known until the presurgical “time-out.” Patients allocated to the control condition did not have any change in operative procedures; the surgical team of patients allocated to the intervention arm changed their outer gloves immediately before peritoneal or fascial closure.
The composite primary outcome measure assessed wound seroma, hematoma, or dehiscence (defined as a separation of at least 1 cm), as well as wound infection and any other wound abnormality. Secondary outcome measures included whether patients had a fever or peri-incisional cellulitis.
A total of 553 patients were randomized. Follow-up was high, so Dr. Scrafford and his colleagues were able to analyze data from a total of 250 patients in the control arm and 236 patients who received the glove-changing intervention.
Patient demographics and comorbidities were similar between groups, as was the surgical time and estimated blood loss. Dr. Scrafford noted that significantly more patients in the glove-changing group than in the control group received presurgical vaginal preparation with antiseptic solution (20.3% vs. 10.5%; P = .001). However, he reported, statistical analysis showed that this difference had no effect on the results.
Overall, 15 (6.4%) of the patients in the glove-changing group met the criteria for wound complication, compared with 34 (13.6%) in the control group (P = .008). Of the individual components of the primary outcome measure, the difference in incidence of skin separation was also significant; separation was experienced by five patients (2.1%) in the glove-changing group, compared with 14 (5.6%) in the control group (P = .01).
The rate of wound infections was numerically lower in the intervention group, compared with the control group (8 vs. 14), but the difference was not statistically significant.
There were no significant differences between the groups when secondary outcomes were analyzed, Dr. Scrafford said.
The lack of block randomization in the study left open the potential for historical bias, Dr. Scrafford said. Since surgeons couldn’t be blinded as to study arm, the potential for observer bias also existed. Still, he said, the study’s strengths included its large size, and the real-world applicability of the broad inclusion criteria and diverse patient population.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
SAN DIEGO – Changing gloves before closure during cesarean deliveries can reduce overall wound morbidity, a study showed.
Glove changing during the study had a number needed to treat (NNT) of 14 to see benefit, no demonstrated risk, and a total cost per procedure of about $5.
Researchers led by Buvana Reddy, MD, an ob.gyn. in group practice in Woodbury, Minn., used a randomized trial design to determine whether donning a fresh pair of gloves makes a difference in the rate of surgical complications during cesarean delivery. .
Just one previous study had shown a reduced wound infection rate when gloves were changed after placental delivery (J Reprod Med. 2004 Jan;49[1]:13-6). The study showed a statistically significant drop in wound infections, but Dr. Scrafford said that the sample size was small, and the point at which glove changing was performed is not very practical in terms of the flow of surgery.
Building on this study, Dr. Scrafford and his colleagues designed a trial that was meant to be larger, incorporated a composite wound outcome score rather than just focusing strictly on infection, and switched the timing of glove change to just before abdominal closure.
The randomized controlled trial included all women who underwent nonemergent cesarean delivery at the investigators’ home facility during a 15-month period. The patient allocation was not known until the presurgical “time-out.” Patients allocated to the control condition did not have any change in operative procedures; the surgical team of patients allocated to the intervention arm changed their outer gloves immediately before peritoneal or fascial closure.
The composite primary outcome measure assessed wound seroma, hematoma, or dehiscence (defined as a separation of at least 1 cm), as well as wound infection and any other wound abnormality. Secondary outcome measures included whether patients had a fever or peri-incisional cellulitis.
A total of 553 patients were randomized. Follow-up was high, so Dr. Scrafford and his colleagues were able to analyze data from a total of 250 patients in the control arm and 236 patients who received the glove-changing intervention.
Patient demographics and comorbidities were similar between groups, as was the surgical time and estimated blood loss. Dr. Scrafford noted that significantly more patients in the glove-changing group than in the control group received presurgical vaginal preparation with antiseptic solution (20.3% vs. 10.5%; P = .001). However, he reported, statistical analysis showed that this difference had no effect on the results.
Overall, 15 (6.4%) of the patients in the glove-changing group met the criteria for wound complication, compared with 34 (13.6%) in the control group (P = .008). Of the individual components of the primary outcome measure, the difference in incidence of skin separation was also significant; separation was experienced by five patients (2.1%) in the glove-changing group, compared with 14 (5.6%) in the control group (P = .01).
The rate of wound infections was numerically lower in the intervention group, compared with the control group (8 vs. 14), but the difference was not statistically significant.
There were no significant differences between the groups when secondary outcomes were analyzed, Dr. Scrafford said.
The lack of block randomization in the study left open the potential for historical bias, Dr. Scrafford said. Since surgeons couldn’t be blinded as to study arm, the potential for observer bias also existed. Still, he said, the study’s strengths included its large size, and the real-world applicability of the broad inclusion criteria and diverse patient population.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: The number needed to treat to see benefit from glove changing was 14; the cost per procedure was about $5.
Data source: A randomized controlled trial of 553 patients undergoing nonemergent cesarean delivery.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Antacid use in infants linked to increased fracture risk
SAN FRANCISCO – Children were more likely to experience a fracture if they were prescribed antacids before age 1 year, according to a study of military families.
The large study revealed that use of proton pump inhibitors (PPIs) before age 1 year was linked to a 22% increased risk of fracture, compared with those not prescribed antacids. Similarly, children prescribed both PPIs and H2 blockers before age 1 year were 31% more likely to have a fracture compared to those not taking the drugs.
“A lot of data are coming out that proton pump inhibitors are not quite as benign as we used to think, and we are seeing that fracture risk is increased with use,” U.S. Air Force Capt. Laura Malchodi, MD, a pediatrics resident at Walter Reed National Military Medical Center in Bethesda, Md., told colleagues at the Pediatric Academic Societies meeting.
Antacid use has been increasing among both adults and children, but the biggest rise has been in children under age 1 year, she said. Previous research into adult use of antacids has revealed an increased incidence of fractures, so Dr. Malchodi investigated the incidence of fractures in children under age 1 year among those who had taken PPIs, H2 blockers, neither, or both.
“What this means for doctors is that when you do start to think of using proton pump inhibitors or any antacid therapy in children, we should really think of limiting it to one type if possible – H2 blockers are now preferable – and for the shortest amount of time as possible,” Dr. Malchodi said of her findings.
The retrospective study’s cohort comprised 874,447 children born between 2001 and 2013 who had been in the U.S. Military Health System for at least 2 years. Children who took antacids after age 1, spent more than a week in a neonatal intensive care unit, or had nonaccidental trauma (abuse) or osteogenesis imperfecta were excluded.
Ninety percent of the cohort had not received prescriptions for any antacids (789,631 children) in their first year of life, and 1.2% had received prescriptions for both PPIs and H2 blockers before age 1 year. Of the remaining children, 7.7% had received prescriptions for H2 blockers, and 0.8% for PPIs.
The children who had and had not been prescribed antacids were similar in median years enrolled in the system, but nearly twice as many who received antacid prescription had been preterm (6.4% vs. 3.5%, P less than .05). Similarly, 3.7% of those prescribed antacids had a low birth weight, compared with 2.2% of those not prescribed antacids (P less than .05). The median age of fracture also differed for the two groups: 3.9 years for those prescribed antacids and 4.5 years for those not (P less than .05).
In using medical records during their analysis, the researchers excluded follow-up visits for the same fracture within the previous 6 months. Before adjustment for covariates, boys had a slightly increased risk of fracture (hazard ratio [HR], 1.08), and those with a previous fracture had an 85% increased risk (HR, 1.85). Compared with children not prescribed antacids, those prescribed PPIs had a 23% increased risk of fracture (HR, 1.23), and those prescribed H2 blockers had a 13% increased risk (HR, 1.13). Those prescribed combination antacid therapy had a 32% increased risk of fractures (HR, 1.32).
Adjustment for preterm birth, low birth weight, sex, and a previous fracture barely reduced those risks: 22% increased risk for PPI use, 4% increased risk for H2 blocker use, and 31% increased risk for using both. The vast majority of children who took antacids had been prescribed them in their first 6 months, so the researchers calculated adjusted risk by age of exposure. For H2 blockers, no statistically significant increased risk of fracture existed in those taking them before or after 6 months old.
Those taking PPIs, however, had a 25% increased risk of fracture if they took them before 6 months old, compared with a 20% increased risk if prescribed PPIs between 6 and 12 months. Likewise, children taking both PPIs and H2 blockers before 6 months old had a 32% increased risk of fracture, compared with a 23% increased risk between 6 and 12 months old.
Analysis of the duration of children’s use of antacids revealed a dose-response relationship, with an increasing risk alongside increasing days taking the medication. For example, those on PPIs for a month or less had a 19% increased risk of fracture, compared with children not prescribed antacids, but that rose to a 23% increased risk for those taking PPIs from 60 to 150 days and to a 42% increased risk for taking them longer than 150 days.
Similarly, the risk of fracture after having taken H2 blockers for up to a month was 14%, which increased to 22% for medication durations over 120 days. Children on combination therapy took the medication for much longer than did children prescribed either antacid. The risk of fracture was 17% greater for those taking them for up to 4 months, but that increased to a 50% greater risk for children taking both antacids for longer than 338 days.
“A couple of decades ago, we thought these medications were super safe, that there could be no problem with them,” Dr. Malchodi said, suggesting that their availability over the counter for adults may contribute to that perception. “With this growing evidence, there’s at least a lot more caution about using them,” she said.
Because the study relied on prescriptions for antacids, the researchers could not take into account which children actually took the antacids. Another limitation was their inability to consider other potential confounders, such as socioeconomic status or comorbidities that may later increase the risk of fracture. Further, exclusion of 6 months of follow-up after one fracture may have missed new fractures in that time period. Using a military cohort, on the other hand, meant having a geographically and socioeconomically diverse population with less risk of care bias because all the children had universal health care coverage.
No external funding was used. Dr. Malchodi reported having no disclosures.
*The View on the News was added on 6/13/17.
Acid suppression is frequently prescribed in infants for the treatment of symptoms such as fussiness, arching, and poor feeding, despite randomized controlled trials showing no benefit for these symptoms over placebo. These medications are often prescribed because physicians think they are useful; families are frustrated, exhausted, and worried about the infant’s symptoms; and these medications are considered safe and well tolerated. Recent adult studies have raised the possibility that these medications may not be as safe as once thought, with case-controlled studies linking them to increased risk of infectious, renal, cardiac, neurologic, and orthopedic complications. While there are pediatric studies supporting an increased infectious risk from both PPI and H2 antagonist use, there are no pediatric studies that address other complications. In this study by Dr. Malchodi et al., acid suppression use in infants under the age of 1 year was associated with an increased risk of fractures over the duration of enrollment in the U.S. Military Health System. They also found a dose-dependent effect, which further strengthens the conclusions that acid suppression may predispose patients to fractures. This research is a critical first step in elucidating the relationship of acid suppression and fracture risk in infants.
As with all database studies, there are some limitations to this study. First, patients taking acid suppression often have more comorbidities than do patients who are not taking the medications; because these patients are sicker, they may have more risk factors including compromised nutritional status and malabsorption predisposing them to fractures. The authors controlled for some of these comorbidities, but future studies should address additional ones. Second, as with all case-control studies, proving causality, not just association, is difficult so any future prospective acid suppression trials should include an assessment of bone health. Third, because the dosing per kilogram is not included, it is difficult to determine if there is a safe level of acid suppression for those children who need it. Fourth, because this is a database review, it is not clear if patients actually took the prescribed medication.
Because of the safety concerns regarding acid suppression as well as the lack of benefit in reducing symptoms in infants, nonpharmacologic therapies should be considered as first-line therapy for the treatment of bothersome symptoms. In the fussy, arching, or irritable child, changing the frequency or volume of feeds, thickening feeds, or changing to partially hydrolyzed formulas or eliminating dairy from the maternal diet (for breastfed infants) should be considered before starting acid suppression therapy. Other diagnoses besides gastroesophageal reflux disease, such as colic and cow’s milk protein allergy, need to be considered as well to ensure that the therapy matches the diagnosis. For those patients in whom acid suppression is required, using the lowest dose possible for the shortest amount of time is critical. Finally, for patients on multiple medications that may impact fracture risk (such as acid suppression, steroids), extra vigilance is needed to stop unnecessary medications as soon as possible.
Acid suppression is frequently prescribed in infants for the treatment of symptoms such as fussiness, arching, and poor feeding, despite randomized controlled trials showing no benefit for these symptoms over placebo. These medications are often prescribed because physicians think they are useful; families are frustrated, exhausted, and worried about the infant’s symptoms; and these medications are considered safe and well tolerated. Recent adult studies have raised the possibility that these medications may not be as safe as once thought, with case-controlled studies linking them to increased risk of infectious, renal, cardiac, neurologic, and orthopedic complications. While there are pediatric studies supporting an increased infectious risk from both PPI and H2 antagonist use, there are no pediatric studies that address other complications. In this study by Dr. Malchodi et al., acid suppression use in infants under the age of 1 year was associated with an increased risk of fractures over the duration of enrollment in the U.S. Military Health System. They also found a dose-dependent effect, which further strengthens the conclusions that acid suppression may predispose patients to fractures. This research is a critical first step in elucidating the relationship of acid suppression and fracture risk in infants.
As with all database studies, there are some limitations to this study. First, patients taking acid suppression often have more comorbidities than do patients who are not taking the medications; because these patients are sicker, they may have more risk factors including compromised nutritional status and malabsorption predisposing them to fractures. The authors controlled for some of these comorbidities, but future studies should address additional ones. Second, as with all case-control studies, proving causality, not just association, is difficult so any future prospective acid suppression trials should include an assessment of bone health. Third, because the dosing per kilogram is not included, it is difficult to determine if there is a safe level of acid suppression for those children who need it. Fourth, because this is a database review, it is not clear if patients actually took the prescribed medication.
Because of the safety concerns regarding acid suppression as well as the lack of benefit in reducing symptoms in infants, nonpharmacologic therapies should be considered as first-line therapy for the treatment of bothersome symptoms. In the fussy, arching, or irritable child, changing the frequency or volume of feeds, thickening feeds, or changing to partially hydrolyzed formulas or eliminating dairy from the maternal diet (for breastfed infants) should be considered before starting acid suppression therapy. Other diagnoses besides gastroesophageal reflux disease, such as colic and cow’s milk protein allergy, need to be considered as well to ensure that the therapy matches the diagnosis. For those patients in whom acid suppression is required, using the lowest dose possible for the shortest amount of time is critical. Finally, for patients on multiple medications that may impact fracture risk (such as acid suppression, steroids), extra vigilance is needed to stop unnecessary medications as soon as possible.
Acid suppression is frequently prescribed in infants for the treatment of symptoms such as fussiness, arching, and poor feeding, despite randomized controlled trials showing no benefit for these symptoms over placebo. These medications are often prescribed because physicians think they are useful; families are frustrated, exhausted, and worried about the infant’s symptoms; and these medications are considered safe and well tolerated. Recent adult studies have raised the possibility that these medications may not be as safe as once thought, with case-controlled studies linking them to increased risk of infectious, renal, cardiac, neurologic, and orthopedic complications. While there are pediatric studies supporting an increased infectious risk from both PPI and H2 antagonist use, there are no pediatric studies that address other complications. In this study by Dr. Malchodi et al., acid suppression use in infants under the age of 1 year was associated with an increased risk of fractures over the duration of enrollment in the U.S. Military Health System. They also found a dose-dependent effect, which further strengthens the conclusions that acid suppression may predispose patients to fractures. This research is a critical first step in elucidating the relationship of acid suppression and fracture risk in infants.
As with all database studies, there are some limitations to this study. First, patients taking acid suppression often have more comorbidities than do patients who are not taking the medications; because these patients are sicker, they may have more risk factors including compromised nutritional status and malabsorption predisposing them to fractures. The authors controlled for some of these comorbidities, but future studies should address additional ones. Second, as with all case-control studies, proving causality, not just association, is difficult so any future prospective acid suppression trials should include an assessment of bone health. Third, because the dosing per kilogram is not included, it is difficult to determine if there is a safe level of acid suppression for those children who need it. Fourth, because this is a database review, it is not clear if patients actually took the prescribed medication.
Because of the safety concerns regarding acid suppression as well as the lack of benefit in reducing symptoms in infants, nonpharmacologic therapies should be considered as first-line therapy for the treatment of bothersome symptoms. In the fussy, arching, or irritable child, changing the frequency or volume of feeds, thickening feeds, or changing to partially hydrolyzed formulas or eliminating dairy from the maternal diet (for breastfed infants) should be considered before starting acid suppression therapy. Other diagnoses besides gastroesophageal reflux disease, such as colic and cow’s milk protein allergy, need to be considered as well to ensure that the therapy matches the diagnosis. For those patients in whom acid suppression is required, using the lowest dose possible for the shortest amount of time is critical. Finally, for patients on multiple medications that may impact fracture risk (such as acid suppression, steroids), extra vigilance is needed to stop unnecessary medications as soon as possible.
SAN FRANCISCO – Children were more likely to experience a fracture if they were prescribed antacids before age 1 year, according to a study of military families.
The large study revealed that use of proton pump inhibitors (PPIs) before age 1 year was linked to a 22% increased risk of fracture, compared with those not prescribed antacids. Similarly, children prescribed both PPIs and H2 blockers before age 1 year were 31% more likely to have a fracture compared to those not taking the drugs.
“A lot of data are coming out that proton pump inhibitors are not quite as benign as we used to think, and we are seeing that fracture risk is increased with use,” U.S. Air Force Capt. Laura Malchodi, MD, a pediatrics resident at Walter Reed National Military Medical Center in Bethesda, Md., told colleagues at the Pediatric Academic Societies meeting.
Antacid use has been increasing among both adults and children, but the biggest rise has been in children under age 1 year, she said. Previous research into adult use of antacids has revealed an increased incidence of fractures, so Dr. Malchodi investigated the incidence of fractures in children under age 1 year among those who had taken PPIs, H2 blockers, neither, or both.
“What this means for doctors is that when you do start to think of using proton pump inhibitors or any antacid therapy in children, we should really think of limiting it to one type if possible – H2 blockers are now preferable – and for the shortest amount of time as possible,” Dr. Malchodi said of her findings.
The retrospective study’s cohort comprised 874,447 children born between 2001 and 2013 who had been in the U.S. Military Health System for at least 2 years. Children who took antacids after age 1, spent more than a week in a neonatal intensive care unit, or had nonaccidental trauma (abuse) or osteogenesis imperfecta were excluded.
Ninety percent of the cohort had not received prescriptions for any antacids (789,631 children) in their first year of life, and 1.2% had received prescriptions for both PPIs and H2 blockers before age 1 year. Of the remaining children, 7.7% had received prescriptions for H2 blockers, and 0.8% for PPIs.
The children who had and had not been prescribed antacids were similar in median years enrolled in the system, but nearly twice as many who received antacid prescription had been preterm (6.4% vs. 3.5%, P less than .05). Similarly, 3.7% of those prescribed antacids had a low birth weight, compared with 2.2% of those not prescribed antacids (P less than .05). The median age of fracture also differed for the two groups: 3.9 years for those prescribed antacids and 4.5 years for those not (P less than .05).
In using medical records during their analysis, the researchers excluded follow-up visits for the same fracture within the previous 6 months. Before adjustment for covariates, boys had a slightly increased risk of fracture (hazard ratio [HR], 1.08), and those with a previous fracture had an 85% increased risk (HR, 1.85). Compared with children not prescribed antacids, those prescribed PPIs had a 23% increased risk of fracture (HR, 1.23), and those prescribed H2 blockers had a 13% increased risk (HR, 1.13). Those prescribed combination antacid therapy had a 32% increased risk of fractures (HR, 1.32).
Adjustment for preterm birth, low birth weight, sex, and a previous fracture barely reduced those risks: 22% increased risk for PPI use, 4% increased risk for H2 blocker use, and 31% increased risk for using both. The vast majority of children who took antacids had been prescribed them in their first 6 months, so the researchers calculated adjusted risk by age of exposure. For H2 blockers, no statistically significant increased risk of fracture existed in those taking them before or after 6 months old.
Those taking PPIs, however, had a 25% increased risk of fracture if they took them before 6 months old, compared with a 20% increased risk if prescribed PPIs between 6 and 12 months. Likewise, children taking both PPIs and H2 blockers before 6 months old had a 32% increased risk of fracture, compared with a 23% increased risk between 6 and 12 months old.
Analysis of the duration of children’s use of antacids revealed a dose-response relationship, with an increasing risk alongside increasing days taking the medication. For example, those on PPIs for a month or less had a 19% increased risk of fracture, compared with children not prescribed antacids, but that rose to a 23% increased risk for those taking PPIs from 60 to 150 days and to a 42% increased risk for taking them longer than 150 days.
Similarly, the risk of fracture after having taken H2 blockers for up to a month was 14%, which increased to 22% for medication durations over 120 days. Children on combination therapy took the medication for much longer than did children prescribed either antacid. The risk of fracture was 17% greater for those taking them for up to 4 months, but that increased to a 50% greater risk for children taking both antacids for longer than 338 days.
“A couple of decades ago, we thought these medications were super safe, that there could be no problem with them,” Dr. Malchodi said, suggesting that their availability over the counter for adults may contribute to that perception. “With this growing evidence, there’s at least a lot more caution about using them,” she said.
Because the study relied on prescriptions for antacids, the researchers could not take into account which children actually took the antacids. Another limitation was their inability to consider other potential confounders, such as socioeconomic status or comorbidities that may later increase the risk of fracture. Further, exclusion of 6 months of follow-up after one fracture may have missed new fractures in that time period. Using a military cohort, on the other hand, meant having a geographically and socioeconomically diverse population with less risk of care bias because all the children had universal health care coverage.
No external funding was used. Dr. Malchodi reported having no disclosures.
*The View on the News was added on 6/13/17.
SAN FRANCISCO – Children were more likely to experience a fracture if they were prescribed antacids before age 1 year, according to a study of military families.
The large study revealed that use of proton pump inhibitors (PPIs) before age 1 year was linked to a 22% increased risk of fracture, compared with those not prescribed antacids. Similarly, children prescribed both PPIs and H2 blockers before age 1 year were 31% more likely to have a fracture compared to those not taking the drugs.
“A lot of data are coming out that proton pump inhibitors are not quite as benign as we used to think, and we are seeing that fracture risk is increased with use,” U.S. Air Force Capt. Laura Malchodi, MD, a pediatrics resident at Walter Reed National Military Medical Center in Bethesda, Md., told colleagues at the Pediatric Academic Societies meeting.
Antacid use has been increasing among both adults and children, but the biggest rise has been in children under age 1 year, she said. Previous research into adult use of antacids has revealed an increased incidence of fractures, so Dr. Malchodi investigated the incidence of fractures in children under age 1 year among those who had taken PPIs, H2 blockers, neither, or both.
“What this means for doctors is that when you do start to think of using proton pump inhibitors or any antacid therapy in children, we should really think of limiting it to one type if possible – H2 blockers are now preferable – and for the shortest amount of time as possible,” Dr. Malchodi said of her findings.
The retrospective study’s cohort comprised 874,447 children born between 2001 and 2013 who had been in the U.S. Military Health System for at least 2 years. Children who took antacids after age 1, spent more than a week in a neonatal intensive care unit, or had nonaccidental trauma (abuse) or osteogenesis imperfecta were excluded.
Ninety percent of the cohort had not received prescriptions for any antacids (789,631 children) in their first year of life, and 1.2% had received prescriptions for both PPIs and H2 blockers before age 1 year. Of the remaining children, 7.7% had received prescriptions for H2 blockers, and 0.8% for PPIs.
The children who had and had not been prescribed antacids were similar in median years enrolled in the system, but nearly twice as many who received antacid prescription had been preterm (6.4% vs. 3.5%, P less than .05). Similarly, 3.7% of those prescribed antacids had a low birth weight, compared with 2.2% of those not prescribed antacids (P less than .05). The median age of fracture also differed for the two groups: 3.9 years for those prescribed antacids and 4.5 years for those not (P less than .05).
In using medical records during their analysis, the researchers excluded follow-up visits for the same fracture within the previous 6 months. Before adjustment for covariates, boys had a slightly increased risk of fracture (hazard ratio [HR], 1.08), and those with a previous fracture had an 85% increased risk (HR, 1.85). Compared with children not prescribed antacids, those prescribed PPIs had a 23% increased risk of fracture (HR, 1.23), and those prescribed H2 blockers had a 13% increased risk (HR, 1.13). Those prescribed combination antacid therapy had a 32% increased risk of fractures (HR, 1.32).
Adjustment for preterm birth, low birth weight, sex, and a previous fracture barely reduced those risks: 22% increased risk for PPI use, 4% increased risk for H2 blocker use, and 31% increased risk for using both. The vast majority of children who took antacids had been prescribed them in their first 6 months, so the researchers calculated adjusted risk by age of exposure. For H2 blockers, no statistically significant increased risk of fracture existed in those taking them before or after 6 months old.
Those taking PPIs, however, had a 25% increased risk of fracture if they took them before 6 months old, compared with a 20% increased risk if prescribed PPIs between 6 and 12 months. Likewise, children taking both PPIs and H2 blockers before 6 months old had a 32% increased risk of fracture, compared with a 23% increased risk between 6 and 12 months old.
Analysis of the duration of children’s use of antacids revealed a dose-response relationship, with an increasing risk alongside increasing days taking the medication. For example, those on PPIs for a month or less had a 19% increased risk of fracture, compared with children not prescribed antacids, but that rose to a 23% increased risk for those taking PPIs from 60 to 150 days and to a 42% increased risk for taking them longer than 150 days.
Similarly, the risk of fracture after having taken H2 blockers for up to a month was 14%, which increased to 22% for medication durations over 120 days. Children on combination therapy took the medication for much longer than did children prescribed either antacid. The risk of fracture was 17% greater for those taking them for up to 4 months, but that increased to a 50% greater risk for children taking both antacids for longer than 338 days.
“A couple of decades ago, we thought these medications were super safe, that there could be no problem with them,” Dr. Malchodi said, suggesting that their availability over the counter for adults may contribute to that perception. “With this growing evidence, there’s at least a lot more caution about using them,” she said.
Because the study relied on prescriptions for antacids, the researchers could not take into account which children actually took the antacids. Another limitation was their inability to consider other potential confounders, such as socioeconomic status or comorbidities that may later increase the risk of fracture. Further, exclusion of 6 months of follow-up after one fracture may have missed new fractures in that time period. Using a military cohort, on the other hand, meant having a geographically and socioeconomically diverse population with less risk of care bias because all the children had universal health care coverage.
No external funding was used. Dr. Malchodi reported having no disclosures.
*The View on the News was added on 6/13/17.
AT PAS 17
Key clinical point:
Major finding: Risk of fracture increased 22% among children who took proton pump inhibitors in their first year of life and increased 31% among children taking both PPIs and H2 blockers.
Data source: A retrospective cohort study of 874,447 children born between 2001 and 2013 and who were in the U.S. Military Health System for at least 2 years.
Disclosures: No external funding was used. Dr. Malchodi reported having no relevant financial disclosures.
RIV spotlights HM-focused research in real-time
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
Adalimumab is good first-line anti-TNF therapy for pediatric Crohn’s disease
Adalimumab (ADA) as a first-line anti–tumor necrosis factor therapy induced and maintained clinical remission in children with Crohn’s disease, said Víctor Manuel Navas-López, MD, PhD, of the Hospital Materno Infantil, Málaga, Spain, and his associates.
Infliximab is the usual first-line anti–tumor necrosis factor treatment given to children with Crohn’s disease, with ADA used in patients who don’t respond or who develop tolerance to infliximab.
Dose escalation was necessary for 26% of the 62 patients. Thirty-nine percent of patients had growth retardation.
“ADA treatment significantly improved z-score growth rate in children with Crohn’s disease, especially in those with severe growth failure at baseline,” the researchers said. Only 13% of patients reported adverse events, none of them severe.
Read more in the Anales de Pediatría (2017 Apr 14. doi: 10.1016/j.anpedi.2017.01.013).
Adalimumab (ADA) as a first-line anti–tumor necrosis factor therapy induced and maintained clinical remission in children with Crohn’s disease, said Víctor Manuel Navas-López, MD, PhD, of the Hospital Materno Infantil, Málaga, Spain, and his associates.
Infliximab is the usual first-line anti–tumor necrosis factor treatment given to children with Crohn’s disease, with ADA used in patients who don’t respond or who develop tolerance to infliximab.
Dose escalation was necessary for 26% of the 62 patients. Thirty-nine percent of patients had growth retardation.
“ADA treatment significantly improved z-score growth rate in children with Crohn’s disease, especially in those with severe growth failure at baseline,” the researchers said. Only 13% of patients reported adverse events, none of them severe.
Read more in the Anales de Pediatría (2017 Apr 14. doi: 10.1016/j.anpedi.2017.01.013).
Adalimumab (ADA) as a first-line anti–tumor necrosis factor therapy induced and maintained clinical remission in children with Crohn’s disease, said Víctor Manuel Navas-López, MD, PhD, of the Hospital Materno Infantil, Málaga, Spain, and his associates.
Infliximab is the usual first-line anti–tumor necrosis factor treatment given to children with Crohn’s disease, with ADA used in patients who don’t respond or who develop tolerance to infliximab.
Dose escalation was necessary for 26% of the 62 patients. Thirty-nine percent of patients had growth retardation.
“ADA treatment significantly improved z-score growth rate in children with Crohn’s disease, especially in those with severe growth failure at baseline,” the researchers said. Only 13% of patients reported adverse events, none of them severe.
Read more in the Anales de Pediatría (2017 Apr 14. doi: 10.1016/j.anpedi.2017.01.013).
FROM ANALES DE PEDIATRIA