User login
Merkel cell carcinoma most likely to recur within 2 years of diagnosis
PORTLAND, ORE. – The first 2 years after diagnosis are crucial when conducting surveillance for recurrence of Merkel cell carcinoma (MCC), Aubriana McEvoy said at the annual meeting of the Society for Investigative Dermatology.
Regardless of stage at diagnosis, the risk of recurrence peaked at about 1 year and leveled off by about year 2 in a retrospective cohort study, according to Ms. McEvoy, a medical student at the University of Washington, Seattle, who conducted the study with colleagues under the mentorship of Paul Nghiem, MD, PhD, professor and head of the division of dermatology. The study also inversely linked primary MCC stage with subsequent recurrence-free survival, highlighted the role of imaging for surveillance of patients who have advanced primary disease, and linked distant metastatic recurrence with significantly worse survival, compared with local or nodal recurrence.
“Patients with Merkel cell carcinoma always ask about recurrence,” Ms. McEvoy said. “Now, for the first time, we have the data to answer their questions.”
Surveillance of MCC is increasingly important, she said: The “treatment landscape is evolving quickly, and immunotherapies such as pembrolizumab can have a good response rate, especially in the setting of lower burden of disease.” But follow-up is costly on several fronts, making it crucial to aim for “enough” and not “too much” surveillance, she added.
“Imaging often costs thousands of dollars, and that’s only one piece of the pie. There’s also the cost of office visits, time spent by the patient and their family, and the emotional investment and uncertainty a patient goes through every time they have to come for a follow-up visit and scan,” Ms. McEvoy said.
Comprehensive, stage-specific guidelines can help clinicians and patients balance the benefits and costs of surveillance, but are lacking in MCC because no published study has characterized recurrence by stage, she said. To fill this gap, she and her associates analyzed 10 years of longitudinal MCC surveillance data on 468 patients who underwent pathologic staging and were followed at the Nghiem laboratory.
The risk of recurrence was highest within the first 2 years after diagnosis, regardless of whether patients had local (pathologic stage I–II) or nodal (stage III) MCC. However, the probability of recurrence-free survival correlated inversely with pathologic stage of primary MCC (P = .003). Median recurrence-free survival time was not reached by the 186 patients with local disease and small (2-cm maximum dimension) primary lesions, or by 135 patients with clinically occult nodal disease.
In contrast, median recurrence-free survival was about 6 years among 84 patients with local disease and lesions measuring more than 2 cm; was less than 2 years among 35 patients with clinically apparent, pathologically confirmed nodal disease or in-transit metastases; and was less than 1 year among patients with distant metastatic disease.
The researchers also investigated the risk of distant metastatic recurrence to confirm which patients need most intensive follow-up. Among 138 individuals with available data, 40% of stage I primary MCC patients developed a distant metastatic recurrence, as did 60% of patients with stage IIA or stage IIB primary MCC. And 80% of recurrences among patients with stage IIIA or stage IIIB primary disease were distant metastases. “I think it’s safe to say that stage III patients should receive appropriate, if not vigilant, surveillance,” Ms. McEvoy said. The site of recurrence also was significantly (P less than .001) tied to the risk of subsequent death from recurrent MCC; median survival time was not reached when recurrence was local or nodal, but was less than 2 years when it was distant or metastatic.
Early in 2018, the American Joint Committee on Cancer will update its MCC staging system to distinguish clinical versus pathologic staging. “This is important, because pathologic staging remains the gold standard, providing a much more in-depth view of the patient’s disease,” Ms. McEvoy commented. Ideally, clinicians would use more information to help predict the prognosis of MCC, including sex and immune and viral status, she noted. “But we hope these data provide information for more consistency across the country, so we can catch recurrences earlier, and avoid unnecessary visits and imaging scans for lower-risk patients.”
The study was supported by the National Institutes of Health, the Seattle Cancer Care Alliance, the University of Washington, and the Institute of Translational Health Sciences. Ms. McEvoy had no conflicts of interest.
PORTLAND, ORE. – The first 2 years after diagnosis are crucial when conducting surveillance for recurrence of Merkel cell carcinoma (MCC), Aubriana McEvoy said at the annual meeting of the Society for Investigative Dermatology.
Regardless of stage at diagnosis, the risk of recurrence peaked at about 1 year and leveled off by about year 2 in a retrospective cohort study, according to Ms. McEvoy, a medical student at the University of Washington, Seattle, who conducted the study with colleagues under the mentorship of Paul Nghiem, MD, PhD, professor and head of the division of dermatology. The study also inversely linked primary MCC stage with subsequent recurrence-free survival, highlighted the role of imaging for surveillance of patients who have advanced primary disease, and linked distant metastatic recurrence with significantly worse survival, compared with local or nodal recurrence.
“Patients with Merkel cell carcinoma always ask about recurrence,” Ms. McEvoy said. “Now, for the first time, we have the data to answer their questions.”
Surveillance of MCC is increasingly important, she said: The “treatment landscape is evolving quickly, and immunotherapies such as pembrolizumab can have a good response rate, especially in the setting of lower burden of disease.” But follow-up is costly on several fronts, making it crucial to aim for “enough” and not “too much” surveillance, she added.
“Imaging often costs thousands of dollars, and that’s only one piece of the pie. There’s also the cost of office visits, time spent by the patient and their family, and the emotional investment and uncertainty a patient goes through every time they have to come for a follow-up visit and scan,” Ms. McEvoy said.
Comprehensive, stage-specific guidelines can help clinicians and patients balance the benefits and costs of surveillance, but are lacking in MCC because no published study has characterized recurrence by stage, she said. To fill this gap, she and her associates analyzed 10 years of longitudinal MCC surveillance data on 468 patients who underwent pathologic staging and were followed at the Nghiem laboratory.
The risk of recurrence was highest within the first 2 years after diagnosis, regardless of whether patients had local (pathologic stage I–II) or nodal (stage III) MCC. However, the probability of recurrence-free survival correlated inversely with pathologic stage of primary MCC (P = .003). Median recurrence-free survival time was not reached by the 186 patients with local disease and small (2-cm maximum dimension) primary lesions, or by 135 patients with clinically occult nodal disease.
In contrast, median recurrence-free survival was about 6 years among 84 patients with local disease and lesions measuring more than 2 cm; was less than 2 years among 35 patients with clinically apparent, pathologically confirmed nodal disease or in-transit metastases; and was less than 1 year among patients with distant metastatic disease.
The researchers also investigated the risk of distant metastatic recurrence to confirm which patients need most intensive follow-up. Among 138 individuals with available data, 40% of stage I primary MCC patients developed a distant metastatic recurrence, as did 60% of patients with stage IIA or stage IIB primary MCC. And 80% of recurrences among patients with stage IIIA or stage IIIB primary disease were distant metastases. “I think it’s safe to say that stage III patients should receive appropriate, if not vigilant, surveillance,” Ms. McEvoy said. The site of recurrence also was significantly (P less than .001) tied to the risk of subsequent death from recurrent MCC; median survival time was not reached when recurrence was local or nodal, but was less than 2 years when it was distant or metastatic.
Early in 2018, the American Joint Committee on Cancer will update its MCC staging system to distinguish clinical versus pathologic staging. “This is important, because pathologic staging remains the gold standard, providing a much more in-depth view of the patient’s disease,” Ms. McEvoy commented. Ideally, clinicians would use more information to help predict the prognosis of MCC, including sex and immune and viral status, she noted. “But we hope these data provide information for more consistency across the country, so we can catch recurrences earlier, and avoid unnecessary visits and imaging scans for lower-risk patients.”
The study was supported by the National Institutes of Health, the Seattle Cancer Care Alliance, the University of Washington, and the Institute of Translational Health Sciences. Ms. McEvoy had no conflicts of interest.
PORTLAND, ORE. – The first 2 years after diagnosis are crucial when conducting surveillance for recurrence of Merkel cell carcinoma (MCC), Aubriana McEvoy said at the annual meeting of the Society for Investigative Dermatology.
Regardless of stage at diagnosis, the risk of recurrence peaked at about 1 year and leveled off by about year 2 in a retrospective cohort study, according to Ms. McEvoy, a medical student at the University of Washington, Seattle, who conducted the study with colleagues under the mentorship of Paul Nghiem, MD, PhD, professor and head of the division of dermatology. The study also inversely linked primary MCC stage with subsequent recurrence-free survival, highlighted the role of imaging for surveillance of patients who have advanced primary disease, and linked distant metastatic recurrence with significantly worse survival, compared with local or nodal recurrence.
“Patients with Merkel cell carcinoma always ask about recurrence,” Ms. McEvoy said. “Now, for the first time, we have the data to answer their questions.”
Surveillance of MCC is increasingly important, she said: The “treatment landscape is evolving quickly, and immunotherapies such as pembrolizumab can have a good response rate, especially in the setting of lower burden of disease.” But follow-up is costly on several fronts, making it crucial to aim for “enough” and not “too much” surveillance, she added.
“Imaging often costs thousands of dollars, and that’s only one piece of the pie. There’s also the cost of office visits, time spent by the patient and their family, and the emotional investment and uncertainty a patient goes through every time they have to come for a follow-up visit and scan,” Ms. McEvoy said.
Comprehensive, stage-specific guidelines can help clinicians and patients balance the benefits and costs of surveillance, but are lacking in MCC because no published study has characterized recurrence by stage, she said. To fill this gap, she and her associates analyzed 10 years of longitudinal MCC surveillance data on 468 patients who underwent pathologic staging and were followed at the Nghiem laboratory.
The risk of recurrence was highest within the first 2 years after diagnosis, regardless of whether patients had local (pathologic stage I–II) or nodal (stage III) MCC. However, the probability of recurrence-free survival correlated inversely with pathologic stage of primary MCC (P = .003). Median recurrence-free survival time was not reached by the 186 patients with local disease and small (2-cm maximum dimension) primary lesions, or by 135 patients with clinically occult nodal disease.
In contrast, median recurrence-free survival was about 6 years among 84 patients with local disease and lesions measuring more than 2 cm; was less than 2 years among 35 patients with clinically apparent, pathologically confirmed nodal disease or in-transit metastases; and was less than 1 year among patients with distant metastatic disease.
The researchers also investigated the risk of distant metastatic recurrence to confirm which patients need most intensive follow-up. Among 138 individuals with available data, 40% of stage I primary MCC patients developed a distant metastatic recurrence, as did 60% of patients with stage IIA or stage IIB primary MCC. And 80% of recurrences among patients with stage IIIA or stage IIIB primary disease were distant metastases. “I think it’s safe to say that stage III patients should receive appropriate, if not vigilant, surveillance,” Ms. McEvoy said. The site of recurrence also was significantly (P less than .001) tied to the risk of subsequent death from recurrent MCC; median survival time was not reached when recurrence was local or nodal, but was less than 2 years when it was distant or metastatic.
Early in 2018, the American Joint Committee on Cancer will update its MCC staging system to distinguish clinical versus pathologic staging. “This is important, because pathologic staging remains the gold standard, providing a much more in-depth view of the patient’s disease,” Ms. McEvoy commented. Ideally, clinicians would use more information to help predict the prognosis of MCC, including sex and immune and viral status, she noted. “But we hope these data provide information for more consistency across the country, so we can catch recurrences earlier, and avoid unnecessary visits and imaging scans for lower-risk patients.”
The study was supported by the National Institutes of Health, the Seattle Cancer Care Alliance, the University of Washington, and the Institute of Translational Health Sciences. Ms. McEvoy had no conflicts of interest.
AT SID 2017
Key clinical point:
Major finding: The risk of recurrence peaked about 1 year after diagnosis and leveled off at about year 2, regardless of whether patients had local (pathologic stage I–II) or nodal (stage III) disease.
Data source: A retrospective cohort study of 544 patients with Merkel cell carcinoma (468 with pathologic stage disease).
Disclosures: The study was supported by the National Institutes of Health, the Seattle Cancer Care Alliance, the University of Washington, and the Institute of Translational Health Sciences. Ms. McEvoy had no conflicts of interest.
CRC in Lynch syndrome is lower than previously reported
CHICAGO – Lynch syndrome can predispose individuals to a number of different cancer types, including colorectal tumors, but the results of a preliminary study found that the incidence may be lower than what has been previously reported.
New findings presented at Digestive Disease Week® showed that the incidence of colorectal cancer after screening with colonoscopy ranged from 6.3% to 25.9%, depending on the specific mutated gene. This is in contrast to other reports which have found a 50% increase in the incidence of colorectal cancer in individuals with Lynch syndrome.
“We looked at the incidence of colorectal cancer and other associated cancers in individuals with Lynch syndrome and how screening can have an impact on that,” said study author Ariadna Sanchez, MD, from the Hospital Clínic de Barcelona, Spain.
She emphasized that the results being presented at the meeting are preliminary and, thus, will need further confirmation, but it is a multicenter study and is being conducted in more than 1,100 patients.
“The diagnosis of colorectal cancer with screening colonoscopy is lower than results that have been previously published,” she said. “This finding reinforces the importance of screening colonoscopies in patients with Lynch syndrome.”
As to why their rates are lower, Dr. Sanchez speculated that it may be because precancerous polyps are being removed with screening.
“Our thinking is that, as we perform screening and remove the polyps, then in theory, cancer will be prevented,” she explained, “since they didn’t have the opportunity to continue to progress into cancer.”
In other words, screening this high-risk population may not only identify those who have cancer but may prevent it from developing in others.
Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is an inherited disorder that increases the risk of many types of cancer, including colorectal and cancers of the stomach, small intestine, liver, gallbladder ducts, upper urinary tract, brain, skin, ovaries, and endometrium.
Caused by germline mutations in the mismatch DNA repair system (MLH1, MSH2, MSH6, PMS2), it has been difficult to make precise estimates of cancer risk in individuals with the syndrome because of retrospective studies and small cohorts.
Dr. Sanchez and her colleagues conducted a multicenter nation-wide study in Spain with the goal of establishing the cumulative incidence of colorectal cancer and other tumor types in Lynch syndrome and to evaluate the effect of screening surveillance on cancer incidence. Cancer-specific survival will also be assessed.
The cohort included 1,108 patients with Lynch syndrome from 25 centers, who were followed-up for a mean of 67.5 (± 57.8 months).
The first colonoscopy screening detected cancer in 49 patients (MLH1, n = 23/268; MSH2, n = 18/249; MSH6, n = 4/154; PMS2, n = 2/47; EPCAM, n = 2/13), extrapolating to a cumulative incidence of 25.6% for MLH1, 22.1% for MSH2, 6.3% for MSH6, and 25.9% for PMS2 mutation carriers.
Most patients were diagnosed with stage 1 disease (45.7%) and, to a lesser degree, with stage II (28.6%), stage III (22.9%), and stage IV (2.9%).
The 10-year cumulative incidences for subsequent colorectal cancers for patients who had a previous diagnosis of the disease were 9.4% (95% CI, 5-17) for MLH1, 12.6% (95% CI, 5.6-27.6) for MSH2, and 17.2% (95% CI, 6.6-40) for MSH6.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
CHICAGO – Lynch syndrome can predispose individuals to a number of different cancer types, including colorectal tumors, but the results of a preliminary study found that the incidence may be lower than what has been previously reported.
New findings presented at Digestive Disease Week® showed that the incidence of colorectal cancer after screening with colonoscopy ranged from 6.3% to 25.9%, depending on the specific mutated gene. This is in contrast to other reports which have found a 50% increase in the incidence of colorectal cancer in individuals with Lynch syndrome.
“We looked at the incidence of colorectal cancer and other associated cancers in individuals with Lynch syndrome and how screening can have an impact on that,” said study author Ariadna Sanchez, MD, from the Hospital Clínic de Barcelona, Spain.
She emphasized that the results being presented at the meeting are preliminary and, thus, will need further confirmation, but it is a multicenter study and is being conducted in more than 1,100 patients.
“The diagnosis of colorectal cancer with screening colonoscopy is lower than results that have been previously published,” she said. “This finding reinforces the importance of screening colonoscopies in patients with Lynch syndrome.”
As to why their rates are lower, Dr. Sanchez speculated that it may be because precancerous polyps are being removed with screening.
“Our thinking is that, as we perform screening and remove the polyps, then in theory, cancer will be prevented,” she explained, “since they didn’t have the opportunity to continue to progress into cancer.”
In other words, screening this high-risk population may not only identify those who have cancer but may prevent it from developing in others.
Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is an inherited disorder that increases the risk of many types of cancer, including colorectal and cancers of the stomach, small intestine, liver, gallbladder ducts, upper urinary tract, brain, skin, ovaries, and endometrium.
Caused by germline mutations in the mismatch DNA repair system (MLH1, MSH2, MSH6, PMS2), it has been difficult to make precise estimates of cancer risk in individuals with the syndrome because of retrospective studies and small cohorts.
Dr. Sanchez and her colleagues conducted a multicenter nation-wide study in Spain with the goal of establishing the cumulative incidence of colorectal cancer and other tumor types in Lynch syndrome and to evaluate the effect of screening surveillance on cancer incidence. Cancer-specific survival will also be assessed.
The cohort included 1,108 patients with Lynch syndrome from 25 centers, who were followed-up for a mean of 67.5 (± 57.8 months).
The first colonoscopy screening detected cancer in 49 patients (MLH1, n = 23/268; MSH2, n = 18/249; MSH6, n = 4/154; PMS2, n = 2/47; EPCAM, n = 2/13), extrapolating to a cumulative incidence of 25.6% for MLH1, 22.1% for MSH2, 6.3% for MSH6, and 25.9% for PMS2 mutation carriers.
Most patients were diagnosed with stage 1 disease (45.7%) and, to a lesser degree, with stage II (28.6%), stage III (22.9%), and stage IV (2.9%).
The 10-year cumulative incidences for subsequent colorectal cancers for patients who had a previous diagnosis of the disease were 9.4% (95% CI, 5-17) for MLH1, 12.6% (95% CI, 5.6-27.6) for MSH2, and 17.2% (95% CI, 6.6-40) for MSH6.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
CHICAGO – Lynch syndrome can predispose individuals to a number of different cancer types, including colorectal tumors, but the results of a preliminary study found that the incidence may be lower than what has been previously reported.
New findings presented at Digestive Disease Week® showed that the incidence of colorectal cancer after screening with colonoscopy ranged from 6.3% to 25.9%, depending on the specific mutated gene. This is in contrast to other reports which have found a 50% increase in the incidence of colorectal cancer in individuals with Lynch syndrome.
“We looked at the incidence of colorectal cancer and other associated cancers in individuals with Lynch syndrome and how screening can have an impact on that,” said study author Ariadna Sanchez, MD, from the Hospital Clínic de Barcelona, Spain.
She emphasized that the results being presented at the meeting are preliminary and, thus, will need further confirmation, but it is a multicenter study and is being conducted in more than 1,100 patients.
“The diagnosis of colorectal cancer with screening colonoscopy is lower than results that have been previously published,” she said. “This finding reinforces the importance of screening colonoscopies in patients with Lynch syndrome.”
As to why their rates are lower, Dr. Sanchez speculated that it may be because precancerous polyps are being removed with screening.
“Our thinking is that, as we perform screening and remove the polyps, then in theory, cancer will be prevented,” she explained, “since they didn’t have the opportunity to continue to progress into cancer.”
In other words, screening this high-risk population may not only identify those who have cancer but may prevent it from developing in others.
Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is an inherited disorder that increases the risk of many types of cancer, including colorectal and cancers of the stomach, small intestine, liver, gallbladder ducts, upper urinary tract, brain, skin, ovaries, and endometrium.
Caused by germline mutations in the mismatch DNA repair system (MLH1, MSH2, MSH6, PMS2), it has been difficult to make precise estimates of cancer risk in individuals with the syndrome because of retrospective studies and small cohorts.
Dr. Sanchez and her colleagues conducted a multicenter nation-wide study in Spain with the goal of establishing the cumulative incidence of colorectal cancer and other tumor types in Lynch syndrome and to evaluate the effect of screening surveillance on cancer incidence. Cancer-specific survival will also be assessed.
The cohort included 1,108 patients with Lynch syndrome from 25 centers, who were followed-up for a mean of 67.5 (± 57.8 months).
The first colonoscopy screening detected cancer in 49 patients (MLH1, n = 23/268; MSH2, n = 18/249; MSH6, n = 4/154; PMS2, n = 2/47; EPCAM, n = 2/13), extrapolating to a cumulative incidence of 25.6% for MLH1, 22.1% for MSH2, 6.3% for MSH6, and 25.9% for PMS2 mutation carriers.
Most patients were diagnosed with stage 1 disease (45.7%) and, to a lesser degree, with stage II (28.6%), stage III (22.9%), and stage IV (2.9%).
The 10-year cumulative incidences for subsequent colorectal cancers for patients who had a previous diagnosis of the disease were 9.4% (95% CI, 5-17) for MLH1, 12.6% (95% CI, 5.6-27.6) for MSH2, and 17.2% (95% CI, 6.6-40) for MSH6.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
Key clinical point: Colorectal cancer screening may lower the incidence of disease in a high-risk population of individuals with Lynch syndrome.
Major finding: The incidence of colorectal cancer was lower than has been previously reported in Lynch syndrome, possibly because of the removal of polyps during screening.
Data source: Prospective multicenter study that included 1,108 patients with Lynch syndrome who underwent colonoscopy screening.
Disclosures: Dr. Sanchez has no disclosures.
Buprenorphine is an alternative to morphine in treating NAS
SAN FRANCISCO – The phase III, single-center Blinded Buprenorphine or Neonatal Morphine Solution (BBORN) clinical trial has established the efficacy of buprenorphine as an alternative to morphine for treatment of newborns with neonatal abstinence syndrome (NAS).
The strategy cuts the treatment time needed to relieve the withdrawal symptoms of the infants by nearly half, the researchers reported. The study results, presented at the Pediatric Academic Societies meeting, were simultaneously published in the New England Journal of Medicine (2017. doi: 10.1056/NEJMoa1614835).
“For those infants who ultimately require pharmacologic treatment, the BBORN trial demonstrated that buprenorphine has similar safety and improved efficacy in length of treatment and length of stay compared to morphine, which is used in 80% of neonatal intensive care units,” said Walter K. Kraft, MD, of Thomas Jefferson University, Philadelphia,.
In the trial, 63 term infants (greater than and equal to 37 weeks of gestation) exposed to opioids prior to birth and who displayed signs of NAS were randomized to receive sublingual buprenorphine or oral morphine. Prior exposure to benzodiazepine in the 30 days before birth, medical or neurologic illness, and elevated bilirubin were grounds for exclusion.
The primary endpoint was the length of treatment needed to deal with the withdrawal symptoms. Secondary endpoints included length of hospitalization, need for supplementary treatment with phenobarbital, and safety.
The groups were comparable at baseline, with the exception of median gestational age in the buprenorphine group (38.5 vs. 39.0 weeks, P = .03). Most of the infants were white. Almost all mothers were on maintenance methadone therapy and almost all were current smokers. Thirty-three infants were randomized to receive buprenorphine. Three withdrew and were treated with open-label morphine. Thirty infants received morphine, with two withdrawing to the open-label treatment.
Those receiving buprenorphine displayed significantly shorter median duration of treatment (15 vs. 28 days) and median length of hospital stay (21 vs. 33 days) (both P less than .001). The use of supplemental phenobarbital was similar in both groups.
Occurrence of adverse events was similar, with 13 events in 7 infants in the buprenorphine group and 10 events in 8 infants in the morphine group. One serious event occurred in each group; neither was treatment related.
“The trial only proves that buprenorphine works but does not answer how. We suspect a long half-life is a part of the answer, though methadone also has a long half-life. We have not compared buprenorphine to methadone for treatment of infants with neonatal abstinence syndrome. We conjecture that as a partial agonist, weaning may be smoother. In our trial, it was a shorter wean time, rather than quicker control of symptoms, in which buprenorphine was more effective than morphine. Buprenorphine has effects on other receptors, but it is very unclear if this added to efficacy relative to morphine,” explained Dr. Kraft.
“Regarding mechanism, it is believed that the somatic (as opposed to the drug craving) symptoms of opiate withdrawal in the adult arise from areas of the brainstem called the locus coeruleus and periaqueductal gray, which express opiate receptors. These areas are undergoing major developmental changes in utero and at the time of birth. Therefore, although we hypothesize that the withdrawal symptoms in the infants are likely arising from the same regions, it has not been proven, and is actually something we are investigating in rodent models,” explained the study’s main author, Michelle Ehrlich, MD, of Icahn School of Medicine at Mount Sinai, New York.
While the trial’s findings presented at PAS 17 are an advance in the armamentarium of care for NAS, the researchers are adamant that the approach should not be seen as a stand-alone treatment.
“I would stress than an approach to treatment of neonatal abstinence syndrome most importantly be multidisciplinary and use a uniform institutional protocol. For example, there should be standardization of Finnegan scoring with continuous quality improvement. All babies should have nonpharmacologic treatment of breastfeeding, rooming in, and minimization of excessive stimuli,” explained Dr. Kraft.
Next steps include clarifying the pharmacokinetics to optimize the dose, and to assess the influence of buprenorphine on neurobehavior. “We suspect the mechanism of action to be similar to that of adults. However, how the biology of neonatal abstinence syndrome differs from opioid withdrawal of adults is not known and [is] an area in need of more investigation. We did collect pharmacokinetic samples, and these data are currently being analyzed,” said Dr. Kraft.
Thomas Jefferson University sponsored the study, which was funded by the National Institute on Drug Abuse. Dr. Kraft reported serving as an unpaid consultant to Chiesi Farmaceutici S.p.A. Dr. Ehrlich disclosed receipt of buprenorphine from Indivior for the study and grants from NIDA.
SAN FRANCISCO – The phase III, single-center Blinded Buprenorphine or Neonatal Morphine Solution (BBORN) clinical trial has established the efficacy of buprenorphine as an alternative to morphine for treatment of newborns with neonatal abstinence syndrome (NAS).
The strategy cuts the treatment time needed to relieve the withdrawal symptoms of the infants by nearly half, the researchers reported. The study results, presented at the Pediatric Academic Societies meeting, were simultaneously published in the New England Journal of Medicine (2017. doi: 10.1056/NEJMoa1614835).
“For those infants who ultimately require pharmacologic treatment, the BBORN trial demonstrated that buprenorphine has similar safety and improved efficacy in length of treatment and length of stay compared to morphine, which is used in 80% of neonatal intensive care units,” said Walter K. Kraft, MD, of Thomas Jefferson University, Philadelphia,.
In the trial, 63 term infants (greater than and equal to 37 weeks of gestation) exposed to opioids prior to birth and who displayed signs of NAS were randomized to receive sublingual buprenorphine or oral morphine. Prior exposure to benzodiazepine in the 30 days before birth, medical or neurologic illness, and elevated bilirubin were grounds for exclusion.
The primary endpoint was the length of treatment needed to deal with the withdrawal symptoms. Secondary endpoints included length of hospitalization, need for supplementary treatment with phenobarbital, and safety.
The groups were comparable at baseline, with the exception of median gestational age in the buprenorphine group (38.5 vs. 39.0 weeks, P = .03). Most of the infants were white. Almost all mothers were on maintenance methadone therapy and almost all were current smokers. Thirty-three infants were randomized to receive buprenorphine. Three withdrew and were treated with open-label morphine. Thirty infants received morphine, with two withdrawing to the open-label treatment.
Those receiving buprenorphine displayed significantly shorter median duration of treatment (15 vs. 28 days) and median length of hospital stay (21 vs. 33 days) (both P less than .001). The use of supplemental phenobarbital was similar in both groups.
Occurrence of adverse events was similar, with 13 events in 7 infants in the buprenorphine group and 10 events in 8 infants in the morphine group. One serious event occurred in each group; neither was treatment related.
“The trial only proves that buprenorphine works but does not answer how. We suspect a long half-life is a part of the answer, though methadone also has a long half-life. We have not compared buprenorphine to methadone for treatment of infants with neonatal abstinence syndrome. We conjecture that as a partial agonist, weaning may be smoother. In our trial, it was a shorter wean time, rather than quicker control of symptoms, in which buprenorphine was more effective than morphine. Buprenorphine has effects on other receptors, but it is very unclear if this added to efficacy relative to morphine,” explained Dr. Kraft.
“Regarding mechanism, it is believed that the somatic (as opposed to the drug craving) symptoms of opiate withdrawal in the adult arise from areas of the brainstem called the locus coeruleus and periaqueductal gray, which express opiate receptors. These areas are undergoing major developmental changes in utero and at the time of birth. Therefore, although we hypothesize that the withdrawal symptoms in the infants are likely arising from the same regions, it has not been proven, and is actually something we are investigating in rodent models,” explained the study’s main author, Michelle Ehrlich, MD, of Icahn School of Medicine at Mount Sinai, New York.
While the trial’s findings presented at PAS 17 are an advance in the armamentarium of care for NAS, the researchers are adamant that the approach should not be seen as a stand-alone treatment.
“I would stress than an approach to treatment of neonatal abstinence syndrome most importantly be multidisciplinary and use a uniform institutional protocol. For example, there should be standardization of Finnegan scoring with continuous quality improvement. All babies should have nonpharmacologic treatment of breastfeeding, rooming in, and minimization of excessive stimuli,” explained Dr. Kraft.
Next steps include clarifying the pharmacokinetics to optimize the dose, and to assess the influence of buprenorphine on neurobehavior. “We suspect the mechanism of action to be similar to that of adults. However, how the biology of neonatal abstinence syndrome differs from opioid withdrawal of adults is not known and [is] an area in need of more investigation. We did collect pharmacokinetic samples, and these data are currently being analyzed,” said Dr. Kraft.
Thomas Jefferson University sponsored the study, which was funded by the National Institute on Drug Abuse. Dr. Kraft reported serving as an unpaid consultant to Chiesi Farmaceutici S.p.A. Dr. Ehrlich disclosed receipt of buprenorphine from Indivior for the study and grants from NIDA.
SAN FRANCISCO – The phase III, single-center Blinded Buprenorphine or Neonatal Morphine Solution (BBORN) clinical trial has established the efficacy of buprenorphine as an alternative to morphine for treatment of newborns with neonatal abstinence syndrome (NAS).
The strategy cuts the treatment time needed to relieve the withdrawal symptoms of the infants by nearly half, the researchers reported. The study results, presented at the Pediatric Academic Societies meeting, were simultaneously published in the New England Journal of Medicine (2017. doi: 10.1056/NEJMoa1614835).
“For those infants who ultimately require pharmacologic treatment, the BBORN trial demonstrated that buprenorphine has similar safety and improved efficacy in length of treatment and length of stay compared to morphine, which is used in 80% of neonatal intensive care units,” said Walter K. Kraft, MD, of Thomas Jefferson University, Philadelphia,.
In the trial, 63 term infants (greater than and equal to 37 weeks of gestation) exposed to opioids prior to birth and who displayed signs of NAS were randomized to receive sublingual buprenorphine or oral morphine. Prior exposure to benzodiazepine in the 30 days before birth, medical or neurologic illness, and elevated bilirubin were grounds for exclusion.
The primary endpoint was the length of treatment needed to deal with the withdrawal symptoms. Secondary endpoints included length of hospitalization, need for supplementary treatment with phenobarbital, and safety.
The groups were comparable at baseline, with the exception of median gestational age in the buprenorphine group (38.5 vs. 39.0 weeks, P = .03). Most of the infants were white. Almost all mothers were on maintenance methadone therapy and almost all were current smokers. Thirty-three infants were randomized to receive buprenorphine. Three withdrew and were treated with open-label morphine. Thirty infants received morphine, with two withdrawing to the open-label treatment.
Those receiving buprenorphine displayed significantly shorter median duration of treatment (15 vs. 28 days) and median length of hospital stay (21 vs. 33 days) (both P less than .001). The use of supplemental phenobarbital was similar in both groups.
Occurrence of adverse events was similar, with 13 events in 7 infants in the buprenorphine group and 10 events in 8 infants in the morphine group. One serious event occurred in each group; neither was treatment related.
“The trial only proves that buprenorphine works but does not answer how. We suspect a long half-life is a part of the answer, though methadone also has a long half-life. We have not compared buprenorphine to methadone for treatment of infants with neonatal abstinence syndrome. We conjecture that as a partial agonist, weaning may be smoother. In our trial, it was a shorter wean time, rather than quicker control of symptoms, in which buprenorphine was more effective than morphine. Buprenorphine has effects on other receptors, but it is very unclear if this added to efficacy relative to morphine,” explained Dr. Kraft.
“Regarding mechanism, it is believed that the somatic (as opposed to the drug craving) symptoms of opiate withdrawal in the adult arise from areas of the brainstem called the locus coeruleus and periaqueductal gray, which express opiate receptors. These areas are undergoing major developmental changes in utero and at the time of birth. Therefore, although we hypothesize that the withdrawal symptoms in the infants are likely arising from the same regions, it has not been proven, and is actually something we are investigating in rodent models,” explained the study’s main author, Michelle Ehrlich, MD, of Icahn School of Medicine at Mount Sinai, New York.
While the trial’s findings presented at PAS 17 are an advance in the armamentarium of care for NAS, the researchers are adamant that the approach should not be seen as a stand-alone treatment.
“I would stress than an approach to treatment of neonatal abstinence syndrome most importantly be multidisciplinary and use a uniform institutional protocol. For example, there should be standardization of Finnegan scoring with continuous quality improvement. All babies should have nonpharmacologic treatment of breastfeeding, rooming in, and minimization of excessive stimuli,” explained Dr. Kraft.
Next steps include clarifying the pharmacokinetics to optimize the dose, and to assess the influence of buprenorphine on neurobehavior. “We suspect the mechanism of action to be similar to that of adults. However, how the biology of neonatal abstinence syndrome differs from opioid withdrawal of adults is not known and [is] an area in need of more investigation. We did collect pharmacokinetic samples, and these data are currently being analyzed,” said Dr. Kraft.
Thomas Jefferson University sponsored the study, which was funded by the National Institute on Drug Abuse. Dr. Kraft reported serving as an unpaid consultant to Chiesi Farmaceutici S.p.A. Dr. Ehrlich disclosed receipt of buprenorphine from Indivior for the study and grants from NIDA.
AT PAS 17
Key clinical point:
Major finding: Buprenorphine reduced median length of treatment (15 vs. 28 days, P less than .001) and median length of stay (21 vs. 34.5 days, P less than .001), compared with morphine.
Data source: Double-blind, double-dummy, single-site, randomized clinical trial (NCT01452789).
Disclosures: Thomas Jefferson University sponsored the study, which was funded by the National Institute on Drug Abuse. Dr. Kraft reported serving as an unpaid consultant to Chiesi Farmaceutici S.p.A. Dr. Ehrlich disclosed receipt of buprenorphine from Indivior for the study and grants from NIDA.
Nomogram may direct diabetes patients to best operation
PHILADELPHIA – A nomogram that assigns a disease severity score to individuals with type 2 diabetes may provide a tool that helps surgeons, endocrinologists, and primary care physicians determine which weight-loss surgical procedure would be most effective, according to an analysis of 900 patients from Cleveland Clinic and University Hospital Clinic, Barcelona, reported at the annual meeting of the American Surgical Association.
“This is the largest reported cohort with long-term glycemic follow-up data that categorizes diabetes into three validated stages of severity to guide procedure selection,” said Ali Aminian, MD, of Cleveland Clinic. The study also highlighted the importance of surgery in early diabetes. The study involved a modeling cohort of 659 patients who had bariatric procedures at Cleveland Clinic from 2005 to 2011 and a separate data set of 241 patients from Barcelona to validate the findings. Roux-en-Y gastric bypass (RYGB) was performed in 78% of the Cleveland Clinic group and 49% of the Barcelona group, with the remainder having sleeve gastrectomy (SG).
RYGB and SG account for more than 95% of all bariatric procedures in people with type 2 diabetes, Dr. Aminian said, but outcomes of clinical trials have been variable, some reporting up to half of patients having long-term relapses. The Cleveland Clinic study involved all patients with type 2 diabetes who had RYGB or SG from 2005 to 2011 with 5 years or more of glycemic data, with a median follow-up of 7 years. The study used American Diabetes Association targets to define remission and glycemic control.
“Long-term response after bariatric surgery in patients with diabetes significantly differs according to diabetes severity,” Dr. Aminian said. “For example, the outcome of surgery in a patient who has diabetes for 2 years is significantly different than a patient who has diabetes for 15 years taking three medications, including insulin.”
The researchers generated the nomogram based on these four independent preoperative factors:
- Number of preoperative diabetes medications (P less than .0001).
- Insulin use (P = .002).
- Duration of diabetes (P less than .0001).
- Glycemic control (P = .002).
“These factors are readily available in clinical practice and are considered a proxy of functional pancreatic beta-cell reserve,” Dr. Aminian said. The nomogram scores the severity of each factor on a scale of 0 to 100. For example, one preoperative medication scores 12, but five scores 63; duration of diabetes of 1 year scores five points, but 16 years scores 60. The patient’s total points represent the Individualized Metabolic Surgery score.
The researchers assigned three categories: A score of 25 or less represents mild disease, a score of 25-95 represents moderate, and 95 to the maximum 180 is severe disease.
Based on the Cleveland Clinic and Barcelona cohorts, the researchers next developed recommendations for average risk patients in each category.
RYGB is “suggested” in mild disease based on remission rates of 92% in the Cleveland subgroup and 91% in the Barcelona subgroup vs. SG remission rates of 74% and 91%, respectively. On the other end of the spectrum, in patients with severe diabetes, both procedures were less effective in achieving long-term diabetes remission. The disparities were more pronounced for the moderate group: 60% and 70% for RYGB and 25% and 56% for SG in the Cleveland Clinic and Barcelona subgroups, respectively. Hence the nomogram highly “recommends” RYGB. An online calculator to determine Individualized Metabolic Surgery score is available at http://riskcalc.org/Metabolic_Surgery_Score/.
“Obviously, this is the first attempt toward individualized procedure selection and more work needs to be done,” Dr. Aminian said. “Our findings also highlight the importance of surgical intervention in early stages of diabetes in order to achieve sustainable remission.”
In his discussion, Matthew M. Hutter, MD, FACS, of Harvard Medical School, Boston, offered to “quibble” with Dr. Aminian’s conclusions. “I challenge you on your conclusion for the mild and severe categories,” Dr. Hutter said. “My rate-of-cure data makes me want to recommend bypass for any patient with diabetes – mild, moderate or severe.”
Dr. Aminian acknowledged that the number of SG cases in the severe subgroup – 51 – was not great, and long-term diabetes remission was comparable between the two procedures. The key distinguishing measure in the severe category was a net 8% difference between two procedures in glycemic control at last follow-up. “This is the difference that we must decide whether it’s clinically important or not – whether we’re willing to recommend a riskier procedure for an extra 8% achieving glycemic control,” Dr. Aminian said. “If someone thinks it’s worth the risk, then they may suggest gastric bypass. If someone thinks it’s not worth the risk, then they may suggest a sleeve gastrectomy. But, we should remember that patients in the severe group are very high-risk patients.”
Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
PHILADELPHIA – A nomogram that assigns a disease severity score to individuals with type 2 diabetes may provide a tool that helps surgeons, endocrinologists, and primary care physicians determine which weight-loss surgical procedure would be most effective, according to an analysis of 900 patients from Cleveland Clinic and University Hospital Clinic, Barcelona, reported at the annual meeting of the American Surgical Association.
“This is the largest reported cohort with long-term glycemic follow-up data that categorizes diabetes into three validated stages of severity to guide procedure selection,” said Ali Aminian, MD, of Cleveland Clinic. The study also highlighted the importance of surgery in early diabetes. The study involved a modeling cohort of 659 patients who had bariatric procedures at Cleveland Clinic from 2005 to 2011 and a separate data set of 241 patients from Barcelona to validate the findings. Roux-en-Y gastric bypass (RYGB) was performed in 78% of the Cleveland Clinic group and 49% of the Barcelona group, with the remainder having sleeve gastrectomy (SG).
RYGB and SG account for more than 95% of all bariatric procedures in people with type 2 diabetes, Dr. Aminian said, but outcomes of clinical trials have been variable, some reporting up to half of patients having long-term relapses. The Cleveland Clinic study involved all patients with type 2 diabetes who had RYGB or SG from 2005 to 2011 with 5 years or more of glycemic data, with a median follow-up of 7 years. The study used American Diabetes Association targets to define remission and glycemic control.
“Long-term response after bariatric surgery in patients with diabetes significantly differs according to diabetes severity,” Dr. Aminian said. “For example, the outcome of surgery in a patient who has diabetes for 2 years is significantly different than a patient who has diabetes for 15 years taking three medications, including insulin.”
The researchers generated the nomogram based on these four independent preoperative factors:
- Number of preoperative diabetes medications (P less than .0001).
- Insulin use (P = .002).
- Duration of diabetes (P less than .0001).
- Glycemic control (P = .002).
“These factors are readily available in clinical practice and are considered a proxy of functional pancreatic beta-cell reserve,” Dr. Aminian said. The nomogram scores the severity of each factor on a scale of 0 to 100. For example, one preoperative medication scores 12, but five scores 63; duration of diabetes of 1 year scores five points, but 16 years scores 60. The patient’s total points represent the Individualized Metabolic Surgery score.
The researchers assigned three categories: A score of 25 or less represents mild disease, a score of 25-95 represents moderate, and 95 to the maximum 180 is severe disease.
Based on the Cleveland Clinic and Barcelona cohorts, the researchers next developed recommendations for average risk patients in each category.
RYGB is “suggested” in mild disease based on remission rates of 92% in the Cleveland subgroup and 91% in the Barcelona subgroup vs. SG remission rates of 74% and 91%, respectively. On the other end of the spectrum, in patients with severe diabetes, both procedures were less effective in achieving long-term diabetes remission. The disparities were more pronounced for the moderate group: 60% and 70% for RYGB and 25% and 56% for SG in the Cleveland Clinic and Barcelona subgroups, respectively. Hence the nomogram highly “recommends” RYGB. An online calculator to determine Individualized Metabolic Surgery score is available at http://riskcalc.org/Metabolic_Surgery_Score/.
“Obviously, this is the first attempt toward individualized procedure selection and more work needs to be done,” Dr. Aminian said. “Our findings also highlight the importance of surgical intervention in early stages of diabetes in order to achieve sustainable remission.”
In his discussion, Matthew M. Hutter, MD, FACS, of Harvard Medical School, Boston, offered to “quibble” with Dr. Aminian’s conclusions. “I challenge you on your conclusion for the mild and severe categories,” Dr. Hutter said. “My rate-of-cure data makes me want to recommend bypass for any patient with diabetes – mild, moderate or severe.”
Dr. Aminian acknowledged that the number of SG cases in the severe subgroup – 51 – was not great, and long-term diabetes remission was comparable between the two procedures. The key distinguishing measure in the severe category was a net 8% difference between two procedures in glycemic control at last follow-up. “This is the difference that we must decide whether it’s clinically important or not – whether we’re willing to recommend a riskier procedure for an extra 8% achieving glycemic control,” Dr. Aminian said. “If someone thinks it’s worth the risk, then they may suggest gastric bypass. If someone thinks it’s not worth the risk, then they may suggest a sleeve gastrectomy. But, we should remember that patients in the severe group are very high-risk patients.”
Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
PHILADELPHIA – A nomogram that assigns a disease severity score to individuals with type 2 diabetes may provide a tool that helps surgeons, endocrinologists, and primary care physicians determine which weight-loss surgical procedure would be most effective, according to an analysis of 900 patients from Cleveland Clinic and University Hospital Clinic, Barcelona, reported at the annual meeting of the American Surgical Association.
“This is the largest reported cohort with long-term glycemic follow-up data that categorizes diabetes into three validated stages of severity to guide procedure selection,” said Ali Aminian, MD, of Cleveland Clinic. The study also highlighted the importance of surgery in early diabetes. The study involved a modeling cohort of 659 patients who had bariatric procedures at Cleveland Clinic from 2005 to 2011 and a separate data set of 241 patients from Barcelona to validate the findings. Roux-en-Y gastric bypass (RYGB) was performed in 78% of the Cleveland Clinic group and 49% of the Barcelona group, with the remainder having sleeve gastrectomy (SG).
RYGB and SG account for more than 95% of all bariatric procedures in people with type 2 diabetes, Dr. Aminian said, but outcomes of clinical trials have been variable, some reporting up to half of patients having long-term relapses. The Cleveland Clinic study involved all patients with type 2 diabetes who had RYGB or SG from 2005 to 2011 with 5 years or more of glycemic data, with a median follow-up of 7 years. The study used American Diabetes Association targets to define remission and glycemic control.
“Long-term response after bariatric surgery in patients with diabetes significantly differs according to diabetes severity,” Dr. Aminian said. “For example, the outcome of surgery in a patient who has diabetes for 2 years is significantly different than a patient who has diabetes for 15 years taking three medications, including insulin.”
The researchers generated the nomogram based on these four independent preoperative factors:
- Number of preoperative diabetes medications (P less than .0001).
- Insulin use (P = .002).
- Duration of diabetes (P less than .0001).
- Glycemic control (P = .002).
“These factors are readily available in clinical practice and are considered a proxy of functional pancreatic beta-cell reserve,” Dr. Aminian said. The nomogram scores the severity of each factor on a scale of 0 to 100. For example, one preoperative medication scores 12, but five scores 63; duration of diabetes of 1 year scores five points, but 16 years scores 60. The patient’s total points represent the Individualized Metabolic Surgery score.
The researchers assigned three categories: A score of 25 or less represents mild disease, a score of 25-95 represents moderate, and 95 to the maximum 180 is severe disease.
Based on the Cleveland Clinic and Barcelona cohorts, the researchers next developed recommendations for average risk patients in each category.
RYGB is “suggested” in mild disease based on remission rates of 92% in the Cleveland subgroup and 91% in the Barcelona subgroup vs. SG remission rates of 74% and 91%, respectively. On the other end of the spectrum, in patients with severe diabetes, both procedures were less effective in achieving long-term diabetes remission. The disparities were more pronounced for the moderate group: 60% and 70% for RYGB and 25% and 56% for SG in the Cleveland Clinic and Barcelona subgroups, respectively. Hence the nomogram highly “recommends” RYGB. An online calculator to determine Individualized Metabolic Surgery score is available at http://riskcalc.org/Metabolic_Surgery_Score/.
“Obviously, this is the first attempt toward individualized procedure selection and more work needs to be done,” Dr. Aminian said. “Our findings also highlight the importance of surgical intervention in early stages of diabetes in order to achieve sustainable remission.”
In his discussion, Matthew M. Hutter, MD, FACS, of Harvard Medical School, Boston, offered to “quibble” with Dr. Aminian’s conclusions. “I challenge you on your conclusion for the mild and severe categories,” Dr. Hutter said. “My rate-of-cure data makes me want to recommend bypass for any patient with diabetes – mild, moderate or severe.”
Dr. Aminian acknowledged that the number of SG cases in the severe subgroup – 51 – was not great, and long-term diabetes remission was comparable between the two procedures. The key distinguishing measure in the severe category was a net 8% difference between two procedures in glycemic control at last follow-up. “This is the difference that we must decide whether it’s clinically important or not – whether we’re willing to recommend a riskier procedure for an extra 8% achieving glycemic control,” Dr. Aminian said. “If someone thinks it’s worth the risk, then they may suggest gastric bypass. If someone thinks it’s not worth the risk, then they may suggest a sleeve gastrectomy. But, we should remember that patients in the severe group are very high-risk patients.”
Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: A nomogram has been developed that assigns an Individualized Metabolic Surgery score to individuals with type 2 diabetes to help determine which type of bariatric procedure would provide best outcomes.
Major finding: In mild diabetes (Individualized Metabolic Surgery score less than or equal to 25), Roux-en-Y gastric bypass and sleeve gastrectomy significantly improve diabetes. For patients with severe diabetes (IMS Score greater than 95), both procedures have similarly low efficacy for diabetes remission.
Data source: Analysis of 900 patients with type 2 diabetes who had either Roux-en-Y gastric bypass or sleeve gastrectomy with a minimum 5-year follow-up.
Disclosure: Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
12 things pharmacists want hospitalists to know
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
Monitoring Programs Cut Down on Doctor Shopping
Prescription-drug monitoring programs (PDMPs), which require physicians to check drug registries before writing prescriptions, dramatically cut the odds of doctor shopping for opioid pain relievers, according to researchers from the Substance Abuse and Mental Health Services Administration (SAMHSA).
The PDMPs are electronic databases that track prescribing of controlled substances and identify people at high risk of misusing the drugs. The researchers analyzed annual nationwide surveys of drug use and health from 2004 to 2014, when 36 states implemented PDMPs. Their paper is the first to examine the role of PDMPs on individual-level opioid-related outcomes.
Every state except Missouri now has a PDMP. In some states it is mandatory to have a PDMP, but in some states it is voluntarily implemented. In states with mandatory checking, the odds that ≥ 2 doctors would be giving pain relievers for nonmedical purposes to a single patient were reduced by 80%. In states with voluntary monitoring, the odds dropped by 56%.
PDMPs also were associated with 10 to 20 fewer days of use of painkillers for nonmedical purposes in the previous year.
Prescription-drug monitoring programs (PDMPs), which require physicians to check drug registries before writing prescriptions, dramatically cut the odds of doctor shopping for opioid pain relievers, according to researchers from the Substance Abuse and Mental Health Services Administration (SAMHSA).
The PDMPs are electronic databases that track prescribing of controlled substances and identify people at high risk of misusing the drugs. The researchers analyzed annual nationwide surveys of drug use and health from 2004 to 2014, when 36 states implemented PDMPs. Their paper is the first to examine the role of PDMPs on individual-level opioid-related outcomes.
Every state except Missouri now has a PDMP. In some states it is mandatory to have a PDMP, but in some states it is voluntarily implemented. In states with mandatory checking, the odds that ≥ 2 doctors would be giving pain relievers for nonmedical purposes to a single patient were reduced by 80%. In states with voluntary monitoring, the odds dropped by 56%.
PDMPs also were associated with 10 to 20 fewer days of use of painkillers for nonmedical purposes in the previous year.
Prescription-drug monitoring programs (PDMPs), which require physicians to check drug registries before writing prescriptions, dramatically cut the odds of doctor shopping for opioid pain relievers, according to researchers from the Substance Abuse and Mental Health Services Administration (SAMHSA).
The PDMPs are electronic databases that track prescribing of controlled substances and identify people at high risk of misusing the drugs. The researchers analyzed annual nationwide surveys of drug use and health from 2004 to 2014, when 36 states implemented PDMPs. Their paper is the first to examine the role of PDMPs on individual-level opioid-related outcomes.
Every state except Missouri now has a PDMP. In some states it is mandatory to have a PDMP, but in some states it is voluntarily implemented. In states with mandatory checking, the odds that ≥ 2 doctors would be giving pain relievers for nonmedical purposes to a single patient were reduced by 80%. In states with voluntary monitoring, the odds dropped by 56%.
PDMPs also were associated with 10 to 20 fewer days of use of painkillers for nonmedical purposes in the previous year.
Novel inhibitor proves ‘potent’ in hematologic malignancies
BOSTON—A pair of preclinical studies suggest the FLT3/BTK inhibitor CG’806 is active in a range of hematologic malignancies.
In one of the studies, CG’806 proved particularly effective against acute myeloid leukemia (AML) cells harboring mutant forms of FLT3, and the compound was able to eradicate AML in mice.
In another study, researchers found CG’806 exhibited “broad potency” against leukemias, lymphomas, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs).
Both studies were presented as posters at Hematologic Malignancies: Translating Discoveries to Novel Therapies (poster 25 and poster 44).
Both studies involved researchers from Aptose Biosciences, the company developing CG’806.
Poster 25
Weiguo Zhang, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues presented poster 25, “CG’806, a first-in-class FLT3/BTK inhibitor, exerts superior potency against AML cells harboring ITD, TKD and gatekeeper mutated FLT3 or wild-type FLT3.”
The researchers tested CG’806 and other FLT3 inhibitors in human or murine leukemia cell lines with wild-type (WT) FLT3, FLT3-ITD mutations, FLT3 TKD domain mutations, or ITD plus TKD mutations.
Compared to second-generation FLT3 inhibitors (quizartinib, gilteritinib, or crenolanib), CG’806 showed more pronounced anti-proliferative effects in leukemia cells with ITD mutations, D835 mutations, ITD plus F691I/Y842D/D835 mutations, or in FLT3 WT cells.
With CG’086, the IC50s in human AML cell lines were 0.17 nM for MV4-11 (FLT3-ITD) and 0.82 nM for MOLM13 (FLT3-ITD).
The IC50s in the murine leukemia cell lines were 9.49 nM for Ba/F3 (FLT3-WT), 0.30 nM for Ba/F3 (FLT3-ITD), 8.26 nM for Ba/F3 (FLT3-D835Y), 9.72 nM for Ba/F3 (FLT3-ITD+D835Y), and 0.43 nM for Ba/F3 (FLT3-ITD+F691L).
The researchers also found that CG’806 “triggers marked apoptosis” in FLT3-ITD-mutated primary AML samples but minimal apoptosis in normal bone marrow cells.
Another finding was that once-daily oral dosing of CG’806 in a murine model of AML (MV4-11) resulted in sustained micromolar plasma concentration over a 24-hour period.
This was accompanied by complete elimination of AML FLT3-ITD tumors without toxicity, the researchers said.
Poster 44
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented poster 44, “CG’806, a First-in-Class FLT3/BTK Inhibitor, Exhibits Potent Activity against AML Patient Samples with Mutant or Wild-Type FLT3, as well as Other Hematologic Malignancy Subtypes.”
The researchers tested CG’806 in samples from patients with AML (n=82), MDS/MPNs (n=15), acute lymphoblastic leukemia (ALL, n=17), chronic lymphocytic leukemia (CLL, n=58), and chronic myeloid leukemia (CML, n=4).
The team observed “broad sensitivity” to CG’806, with 59% (48/82) of AML, 53% (8/15) of MDS/MPN, 40% (23/58) of CLL, 29% (5/17) of ALL, and 25% (1/4) of CML cases exhibiting an IC50 of less than 100 nM.
Among the 38 tested AML samples with known FLT3 mutational status, the FLT3-ITD+ AML samples tended to have enhanced sensitivity to CG’806 (median IC50 = 20 nM, n=8) relative to the FLT3-WT samples (median IC50 = 120 nM, n=30).
The researchers also found that CG’806 exerted potent anti-proliferative activity against human AML, B-ALL, mantle cell lymphoma, Burkitt lymphoma, and diffuse large B-cell lymphoma cell lines.
“The analyses of CG’806 against primary hematologic malignancy patient samples and cultured cell lines show evidence of potent and broad drug activity in AML and other disease subtypes and support further development of this agent for hematologic malignancies,” Dr Kurtz said. ![]()
BOSTON—A pair of preclinical studies suggest the FLT3/BTK inhibitor CG’806 is active in a range of hematologic malignancies.
In one of the studies, CG’806 proved particularly effective against acute myeloid leukemia (AML) cells harboring mutant forms of FLT3, and the compound was able to eradicate AML in mice.
In another study, researchers found CG’806 exhibited “broad potency” against leukemias, lymphomas, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs).
Both studies were presented as posters at Hematologic Malignancies: Translating Discoveries to Novel Therapies (poster 25 and poster 44).
Both studies involved researchers from Aptose Biosciences, the company developing CG’806.
Poster 25
Weiguo Zhang, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues presented poster 25, “CG’806, a first-in-class FLT3/BTK inhibitor, exerts superior potency against AML cells harboring ITD, TKD and gatekeeper mutated FLT3 or wild-type FLT3.”
The researchers tested CG’806 and other FLT3 inhibitors in human or murine leukemia cell lines with wild-type (WT) FLT3, FLT3-ITD mutations, FLT3 TKD domain mutations, or ITD plus TKD mutations.
Compared to second-generation FLT3 inhibitors (quizartinib, gilteritinib, or crenolanib), CG’806 showed more pronounced anti-proliferative effects in leukemia cells with ITD mutations, D835 mutations, ITD plus F691I/Y842D/D835 mutations, or in FLT3 WT cells.
With CG’086, the IC50s in human AML cell lines were 0.17 nM for MV4-11 (FLT3-ITD) and 0.82 nM for MOLM13 (FLT3-ITD).
The IC50s in the murine leukemia cell lines were 9.49 nM for Ba/F3 (FLT3-WT), 0.30 nM for Ba/F3 (FLT3-ITD), 8.26 nM for Ba/F3 (FLT3-D835Y), 9.72 nM for Ba/F3 (FLT3-ITD+D835Y), and 0.43 nM for Ba/F3 (FLT3-ITD+F691L).
The researchers also found that CG’806 “triggers marked apoptosis” in FLT3-ITD-mutated primary AML samples but minimal apoptosis in normal bone marrow cells.
Another finding was that once-daily oral dosing of CG’806 in a murine model of AML (MV4-11) resulted in sustained micromolar plasma concentration over a 24-hour period.
This was accompanied by complete elimination of AML FLT3-ITD tumors without toxicity, the researchers said.
Poster 44
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented poster 44, “CG’806, a First-in-Class FLT3/BTK Inhibitor, Exhibits Potent Activity against AML Patient Samples with Mutant or Wild-Type FLT3, as well as Other Hematologic Malignancy Subtypes.”
The researchers tested CG’806 in samples from patients with AML (n=82), MDS/MPNs (n=15), acute lymphoblastic leukemia (ALL, n=17), chronic lymphocytic leukemia (CLL, n=58), and chronic myeloid leukemia (CML, n=4).
The team observed “broad sensitivity” to CG’806, with 59% (48/82) of AML, 53% (8/15) of MDS/MPN, 40% (23/58) of CLL, 29% (5/17) of ALL, and 25% (1/4) of CML cases exhibiting an IC50 of less than 100 nM.
Among the 38 tested AML samples with known FLT3 mutational status, the FLT3-ITD+ AML samples tended to have enhanced sensitivity to CG’806 (median IC50 = 20 nM, n=8) relative to the FLT3-WT samples (median IC50 = 120 nM, n=30).
The researchers also found that CG’806 exerted potent anti-proliferative activity against human AML, B-ALL, mantle cell lymphoma, Burkitt lymphoma, and diffuse large B-cell lymphoma cell lines.
“The analyses of CG’806 against primary hematologic malignancy patient samples and cultured cell lines show evidence of potent and broad drug activity in AML and other disease subtypes and support further development of this agent for hematologic malignancies,” Dr Kurtz said. ![]()
BOSTON—A pair of preclinical studies suggest the FLT3/BTK inhibitor CG’806 is active in a range of hematologic malignancies.
In one of the studies, CG’806 proved particularly effective against acute myeloid leukemia (AML) cells harboring mutant forms of FLT3, and the compound was able to eradicate AML in mice.
In another study, researchers found CG’806 exhibited “broad potency” against leukemias, lymphomas, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs).
Both studies were presented as posters at Hematologic Malignancies: Translating Discoveries to Novel Therapies (poster 25 and poster 44).
Both studies involved researchers from Aptose Biosciences, the company developing CG’806.
Poster 25
Weiguo Zhang, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues presented poster 25, “CG’806, a first-in-class FLT3/BTK inhibitor, exerts superior potency against AML cells harboring ITD, TKD and gatekeeper mutated FLT3 or wild-type FLT3.”
The researchers tested CG’806 and other FLT3 inhibitors in human or murine leukemia cell lines with wild-type (WT) FLT3, FLT3-ITD mutations, FLT3 TKD domain mutations, or ITD plus TKD mutations.
Compared to second-generation FLT3 inhibitors (quizartinib, gilteritinib, or crenolanib), CG’806 showed more pronounced anti-proliferative effects in leukemia cells with ITD mutations, D835 mutations, ITD plus F691I/Y842D/D835 mutations, or in FLT3 WT cells.
With CG’086, the IC50s in human AML cell lines were 0.17 nM for MV4-11 (FLT3-ITD) and 0.82 nM for MOLM13 (FLT3-ITD).
The IC50s in the murine leukemia cell lines were 9.49 nM for Ba/F3 (FLT3-WT), 0.30 nM for Ba/F3 (FLT3-ITD), 8.26 nM for Ba/F3 (FLT3-D835Y), 9.72 nM for Ba/F3 (FLT3-ITD+D835Y), and 0.43 nM for Ba/F3 (FLT3-ITD+F691L).
The researchers also found that CG’806 “triggers marked apoptosis” in FLT3-ITD-mutated primary AML samples but minimal apoptosis in normal bone marrow cells.
Another finding was that once-daily oral dosing of CG’806 in a murine model of AML (MV4-11) resulted in sustained micromolar plasma concentration over a 24-hour period.
This was accompanied by complete elimination of AML FLT3-ITD tumors without toxicity, the researchers said.
Poster 44
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented poster 44, “CG’806, a First-in-Class FLT3/BTK Inhibitor, Exhibits Potent Activity against AML Patient Samples with Mutant or Wild-Type FLT3, as well as Other Hematologic Malignancy Subtypes.”
The researchers tested CG’806 in samples from patients with AML (n=82), MDS/MPNs (n=15), acute lymphoblastic leukemia (ALL, n=17), chronic lymphocytic leukemia (CLL, n=58), and chronic myeloid leukemia (CML, n=4).
The team observed “broad sensitivity” to CG’806, with 59% (48/82) of AML, 53% (8/15) of MDS/MPN, 40% (23/58) of CLL, 29% (5/17) of ALL, and 25% (1/4) of CML cases exhibiting an IC50 of less than 100 nM.
Among the 38 tested AML samples with known FLT3 mutational status, the FLT3-ITD+ AML samples tended to have enhanced sensitivity to CG’806 (median IC50 = 20 nM, n=8) relative to the FLT3-WT samples (median IC50 = 120 nM, n=30).
The researchers also found that CG’806 exerted potent anti-proliferative activity against human AML, B-ALL, mantle cell lymphoma, Burkitt lymphoma, and diffuse large B-cell lymphoma cell lines.
“The analyses of CG’806 against primary hematologic malignancy patient samples and cultured cell lines show evidence of potent and broad drug activity in AML and other disease subtypes and support further development of this agent for hematologic malignancies,” Dr Kurtz said. ![]()
IV and SC rituximab produce similar results in FL
In a phase 3 trial, subcutaneous (SC) and intravenous (IV) rituximab produced comparable results as part of a first-line treatment regimen for follicular lymphoma (FL).
Overall response rates (ORR) were similar in patients who received SC rituximab and those who received IV rituximab, first in combination with chemotherapy and then alone as maintenance therapy.
Although patients who received SC rituximab had administration-related reactions that weren’t observed in the IV rituximab group, these events were largely mild-to-moderate local injection-site reactions.
Andrew Davies, PhD, of the University of Southampton in the UK, and his colleagues reported these results in The Lancet Haematology.
Data from stage 1 of this study, known as SABRINA, were previously published in The Lancet Oncology. The current publication includes stage 2 data.
The study was funded by Roche, which markets rituximab as Rituxan and MabThera.
The trial enrolled 410 patients with previously untreated, grade 1-3a, CD20-positive FL.
Patients were randomized to receive IV rituximab at 375 mg/m2 (n=205) or SC rituximab at 1400 mg (n=205) plus chemotherapy.
Chemotherapy consisted of 6 to 8 cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) or 8 cycles of cyclophosphamide, vincristine, and prednisone (CVP) every 3 weeks during induction.
Patients then received rituximab maintenance every 8 weeks.
The researchers said baseline characteristics were balanced between the treatment arms, although there were more females in the SC arm than the IV arm—120 (59%) and 99 (48%), respectively.
Efficacy
In stage 1 of this study, the primary endpoint was the ratio of observed rituximab serum trough concentrations (Ctrough) between the treatment arms at cycle 7.
The results suggested SC rituximab was non-inferior to the IV formulation. The geometric mean Ctrough was 83.13 μg/mL in the IV arm and 134.58 μg/mL in the SC arm (ratio=1.62).
In stage 2, the primary endpoint was efficacy, or ORR, at the end of induction based on the researchers’ assessments and confirmed by an independent review panel of radiologists.
At the end of induction, the ORR was 84.9% (174/205) in the IV arm and 84.4% (173/205) in the SC arm. The complete response rate was 32.2% (n=66) in both arms.
At the end of maintenance therapy, the ORR was 78.1% (139/178) in the IV arm and 77.9% (134/172) in the SC arm. The complete response rates were 56.2% (n=100) and 50.6% (n=87), respectively.
At a median follow-up of 37 months, there was no significant difference between the arms with regard to progression-free survival (hazard ratio[HR]=0.84), event-free survival (HR=0.91), or overall survival (HR=0.81).
Safety
The incidence of adverse events (AEs) was similar between the treatment arms—95% in the IV arm and 96% in the SC arm. The incidence of grade 3 or higher AEs was 55% and 56%, respectively, and the incidence of serious AEs was 34% and 37%, respectively.
Overall, the most common AEs were gastrointestinal disorders (60% in the IV arm and 66% in the SC arm), infections and infestations (64% and 67%, respectively), and general or administration site conditions (50% and 60%, respectively).
Administration-related reactions were more common in the SC arm than the IV arm—48% and 35%, respectively. The most common of these reactions were chills (7%) and pruritus (6%) in the IV arm and injection-site erythema (11%), pruritus (6%), rash (5%), and injection-site pain (5%) in the SC arm.
Neutropenia was the most common grade 3 or higher AE, occurring in 34% of patients in the IV arm and 37% in the SC arm. Febrile neutropenia was the most frequent serious AE, occurring in 5% and 6%, respectively.
The researchers said these results suggest the SC formulation of rituximab has similar efficacy and a similar safety profile as IV rituximab in the first-line treatment of FL. ![]()
In a phase 3 trial, subcutaneous (SC) and intravenous (IV) rituximab produced comparable results as part of a first-line treatment regimen for follicular lymphoma (FL).
Overall response rates (ORR) were similar in patients who received SC rituximab and those who received IV rituximab, first in combination with chemotherapy and then alone as maintenance therapy.
Although patients who received SC rituximab had administration-related reactions that weren’t observed in the IV rituximab group, these events were largely mild-to-moderate local injection-site reactions.
Andrew Davies, PhD, of the University of Southampton in the UK, and his colleagues reported these results in The Lancet Haematology.
Data from stage 1 of this study, known as SABRINA, were previously published in The Lancet Oncology. The current publication includes stage 2 data.
The study was funded by Roche, which markets rituximab as Rituxan and MabThera.
The trial enrolled 410 patients with previously untreated, grade 1-3a, CD20-positive FL.
Patients were randomized to receive IV rituximab at 375 mg/m2 (n=205) or SC rituximab at 1400 mg (n=205) plus chemotherapy.
Chemotherapy consisted of 6 to 8 cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) or 8 cycles of cyclophosphamide, vincristine, and prednisone (CVP) every 3 weeks during induction.
Patients then received rituximab maintenance every 8 weeks.
The researchers said baseline characteristics were balanced between the treatment arms, although there were more females in the SC arm than the IV arm—120 (59%) and 99 (48%), respectively.
Efficacy
In stage 1 of this study, the primary endpoint was the ratio of observed rituximab serum trough concentrations (Ctrough) between the treatment arms at cycle 7.
The results suggested SC rituximab was non-inferior to the IV formulation. The geometric mean Ctrough was 83.13 μg/mL in the IV arm and 134.58 μg/mL in the SC arm (ratio=1.62).
In stage 2, the primary endpoint was efficacy, or ORR, at the end of induction based on the researchers’ assessments and confirmed by an independent review panel of radiologists.
At the end of induction, the ORR was 84.9% (174/205) in the IV arm and 84.4% (173/205) in the SC arm. The complete response rate was 32.2% (n=66) in both arms.
At the end of maintenance therapy, the ORR was 78.1% (139/178) in the IV arm and 77.9% (134/172) in the SC arm. The complete response rates were 56.2% (n=100) and 50.6% (n=87), respectively.
At a median follow-up of 37 months, there was no significant difference between the arms with regard to progression-free survival (hazard ratio[HR]=0.84), event-free survival (HR=0.91), or overall survival (HR=0.81).
Safety
The incidence of adverse events (AEs) was similar between the treatment arms—95% in the IV arm and 96% in the SC arm. The incidence of grade 3 or higher AEs was 55% and 56%, respectively, and the incidence of serious AEs was 34% and 37%, respectively.
Overall, the most common AEs were gastrointestinal disorders (60% in the IV arm and 66% in the SC arm), infections and infestations (64% and 67%, respectively), and general or administration site conditions (50% and 60%, respectively).
Administration-related reactions were more common in the SC arm than the IV arm—48% and 35%, respectively. The most common of these reactions were chills (7%) and pruritus (6%) in the IV arm and injection-site erythema (11%), pruritus (6%), rash (5%), and injection-site pain (5%) in the SC arm.
Neutropenia was the most common grade 3 or higher AE, occurring in 34% of patients in the IV arm and 37% in the SC arm. Febrile neutropenia was the most frequent serious AE, occurring in 5% and 6%, respectively.
The researchers said these results suggest the SC formulation of rituximab has similar efficacy and a similar safety profile as IV rituximab in the first-line treatment of FL. ![]()
In a phase 3 trial, subcutaneous (SC) and intravenous (IV) rituximab produced comparable results as part of a first-line treatment regimen for follicular lymphoma (FL).
Overall response rates (ORR) were similar in patients who received SC rituximab and those who received IV rituximab, first in combination with chemotherapy and then alone as maintenance therapy.
Although patients who received SC rituximab had administration-related reactions that weren’t observed in the IV rituximab group, these events were largely mild-to-moderate local injection-site reactions.
Andrew Davies, PhD, of the University of Southampton in the UK, and his colleagues reported these results in The Lancet Haematology.
Data from stage 1 of this study, known as SABRINA, were previously published in The Lancet Oncology. The current publication includes stage 2 data.
The study was funded by Roche, which markets rituximab as Rituxan and MabThera.
The trial enrolled 410 patients with previously untreated, grade 1-3a, CD20-positive FL.
Patients were randomized to receive IV rituximab at 375 mg/m2 (n=205) or SC rituximab at 1400 mg (n=205) plus chemotherapy.
Chemotherapy consisted of 6 to 8 cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) or 8 cycles of cyclophosphamide, vincristine, and prednisone (CVP) every 3 weeks during induction.
Patients then received rituximab maintenance every 8 weeks.
The researchers said baseline characteristics were balanced between the treatment arms, although there were more females in the SC arm than the IV arm—120 (59%) and 99 (48%), respectively.
Efficacy
In stage 1 of this study, the primary endpoint was the ratio of observed rituximab serum trough concentrations (Ctrough) between the treatment arms at cycle 7.
The results suggested SC rituximab was non-inferior to the IV formulation. The geometric mean Ctrough was 83.13 μg/mL in the IV arm and 134.58 μg/mL in the SC arm (ratio=1.62).
In stage 2, the primary endpoint was efficacy, or ORR, at the end of induction based on the researchers’ assessments and confirmed by an independent review panel of radiologists.
At the end of induction, the ORR was 84.9% (174/205) in the IV arm and 84.4% (173/205) in the SC arm. The complete response rate was 32.2% (n=66) in both arms.
At the end of maintenance therapy, the ORR was 78.1% (139/178) in the IV arm and 77.9% (134/172) in the SC arm. The complete response rates were 56.2% (n=100) and 50.6% (n=87), respectively.
At a median follow-up of 37 months, there was no significant difference between the arms with regard to progression-free survival (hazard ratio[HR]=0.84), event-free survival (HR=0.91), or overall survival (HR=0.81).
Safety
The incidence of adverse events (AEs) was similar between the treatment arms—95% in the IV arm and 96% in the SC arm. The incidence of grade 3 or higher AEs was 55% and 56%, respectively, and the incidence of serious AEs was 34% and 37%, respectively.
Overall, the most common AEs were gastrointestinal disorders (60% in the IV arm and 66% in the SC arm), infections and infestations (64% and 67%, respectively), and general or administration site conditions (50% and 60%, respectively).
Administration-related reactions were more common in the SC arm than the IV arm—48% and 35%, respectively. The most common of these reactions were chills (7%) and pruritus (6%) in the IV arm and injection-site erythema (11%), pruritus (6%), rash (5%), and injection-site pain (5%) in the SC arm.
Neutropenia was the most common grade 3 or higher AE, occurring in 34% of patients in the IV arm and 37% in the SC arm. Febrile neutropenia was the most frequent serious AE, occurring in 5% and 6%, respectively.
The researchers said these results suggest the SC formulation of rituximab has similar efficacy and a similar safety profile as IV rituximab in the first-line treatment of FL. ![]()
Study provides new insight into HSC dormancy
Preclinical research has revealed new insights regarding hematopoietic stem cells’ (HSCs) transition from a dormant state to an active one.
Investigators said they found the transition to be “a continuous developmental path” that is different for each individual cell, rather than a stepwise progression, as researchers previously believed.
The team also found the transition was characterized by low levels of Myc and high expression of retinoic acid.
In fact, the group’s experiments suggested that a diet lacking vitamin A can have a detrimental effect on HSCs.
Nina Cabezas-Wallscheid, PhD, of the German Cancer Research Center (DKFZ) in Heidelberg, Germany, and her colleagues conducted this research and reported their findings in Cell.
The investigators used single-cell RNA sequencing to show that HSCs’ transition from dormant to active cells is “a continuous stream-like progression of steadily increasing metabolic activity and preparation for cell-cycle entry without the apparent presence of accumulating cellular intermediates.”
The team said they observed robust downregulation of biosynthetic processes in dormant HSCs (compared to active HSCs) that was associated with the downregulation of Myc target genes.
The investigators also found that retinoic acid-induced signaling was “highly enriched” in dormant HSCs, and all-trans retinoic acid (ATRA) treatment maintained dormant HSCs in vitro.
In mice, ATRA protected dormant HSCs from activation.
The investigators exposed mice to a few different HSC activation conditions, including bacterial liposaccharide, the double-stranded RNA analog polyI:polyC, and the chemotherapeutic agent 5-fluorouracil. But pre-treatment with ATRA allowed HSCs to maintain a quiescent state in all 3 cases.
Finally, the investigators evaluated the effects of a vitamin A-free diet on HSCs. Adult mice fed a vitamin A-free diet for 14 to 17 weeks lost HSCs, particularly dormant HSCs. And without vitamin A, active HSCs were unable to return to a dormant state.
“Thus, we can prove, for the first time, that vitamin A has a direct impact on blood stem cells,” Dr Cabezas-Wallscheid said. “This shows how vitally important it is to have a sufficient intake of vitamin A from a balanced diet.”
The investigators also believe these findings could be applied in cancer research, as there is evidence to suggest that cancer cells rest in a state of dormancy, which makes them resistant to chemotherapy.
“Once we understand in detail how vitamin A or retinoic acid, respectively, sends normal and malignant stem cells into dormancy, we can try to turn the tables,” said study author Andreas Trumpp, PhD, also of DKFZ.
“If we could make cancer cells temporarily enter an active state, we could thus make them vulnerable to modern therapies.” ![]()
Preclinical research has revealed new insights regarding hematopoietic stem cells’ (HSCs) transition from a dormant state to an active one.
Investigators said they found the transition to be “a continuous developmental path” that is different for each individual cell, rather than a stepwise progression, as researchers previously believed.
The team also found the transition was characterized by low levels of Myc and high expression of retinoic acid.
In fact, the group’s experiments suggested that a diet lacking vitamin A can have a detrimental effect on HSCs.
Nina Cabezas-Wallscheid, PhD, of the German Cancer Research Center (DKFZ) in Heidelberg, Germany, and her colleagues conducted this research and reported their findings in Cell.
The investigators used single-cell RNA sequencing to show that HSCs’ transition from dormant to active cells is “a continuous stream-like progression of steadily increasing metabolic activity and preparation for cell-cycle entry without the apparent presence of accumulating cellular intermediates.”
The team said they observed robust downregulation of biosynthetic processes in dormant HSCs (compared to active HSCs) that was associated with the downregulation of Myc target genes.
The investigators also found that retinoic acid-induced signaling was “highly enriched” in dormant HSCs, and all-trans retinoic acid (ATRA) treatment maintained dormant HSCs in vitro.
In mice, ATRA protected dormant HSCs from activation.
The investigators exposed mice to a few different HSC activation conditions, including bacterial liposaccharide, the double-stranded RNA analog polyI:polyC, and the chemotherapeutic agent 5-fluorouracil. But pre-treatment with ATRA allowed HSCs to maintain a quiescent state in all 3 cases.
Finally, the investigators evaluated the effects of a vitamin A-free diet on HSCs. Adult mice fed a vitamin A-free diet for 14 to 17 weeks lost HSCs, particularly dormant HSCs. And without vitamin A, active HSCs were unable to return to a dormant state.
“Thus, we can prove, for the first time, that vitamin A has a direct impact on blood stem cells,” Dr Cabezas-Wallscheid said. “This shows how vitally important it is to have a sufficient intake of vitamin A from a balanced diet.”
The investigators also believe these findings could be applied in cancer research, as there is evidence to suggest that cancer cells rest in a state of dormancy, which makes them resistant to chemotherapy.
“Once we understand in detail how vitamin A or retinoic acid, respectively, sends normal and malignant stem cells into dormancy, we can try to turn the tables,” said study author Andreas Trumpp, PhD, also of DKFZ.
“If we could make cancer cells temporarily enter an active state, we could thus make them vulnerable to modern therapies.” ![]()
Preclinical research has revealed new insights regarding hematopoietic stem cells’ (HSCs) transition from a dormant state to an active one.
Investigators said they found the transition to be “a continuous developmental path” that is different for each individual cell, rather than a stepwise progression, as researchers previously believed.
The team also found the transition was characterized by low levels of Myc and high expression of retinoic acid.
In fact, the group’s experiments suggested that a diet lacking vitamin A can have a detrimental effect on HSCs.
Nina Cabezas-Wallscheid, PhD, of the German Cancer Research Center (DKFZ) in Heidelberg, Germany, and her colleagues conducted this research and reported their findings in Cell.
The investigators used single-cell RNA sequencing to show that HSCs’ transition from dormant to active cells is “a continuous stream-like progression of steadily increasing metabolic activity and preparation for cell-cycle entry without the apparent presence of accumulating cellular intermediates.”
The team said they observed robust downregulation of biosynthetic processes in dormant HSCs (compared to active HSCs) that was associated with the downregulation of Myc target genes.
The investigators also found that retinoic acid-induced signaling was “highly enriched” in dormant HSCs, and all-trans retinoic acid (ATRA) treatment maintained dormant HSCs in vitro.
In mice, ATRA protected dormant HSCs from activation.
The investigators exposed mice to a few different HSC activation conditions, including bacterial liposaccharide, the double-stranded RNA analog polyI:polyC, and the chemotherapeutic agent 5-fluorouracil. But pre-treatment with ATRA allowed HSCs to maintain a quiescent state in all 3 cases.
Finally, the investigators evaluated the effects of a vitamin A-free diet on HSCs. Adult mice fed a vitamin A-free diet for 14 to 17 weeks lost HSCs, particularly dormant HSCs. And without vitamin A, active HSCs were unable to return to a dormant state.
“Thus, we can prove, for the first time, that vitamin A has a direct impact on blood stem cells,” Dr Cabezas-Wallscheid said. “This shows how vitally important it is to have a sufficient intake of vitamin A from a balanced diet.”
The investigators also believe these findings could be applied in cancer research, as there is evidence to suggest that cancer cells rest in a state of dormancy, which makes them resistant to chemotherapy.
“Once we understand in detail how vitamin A or retinoic acid, respectively, sends normal and malignant stem cells into dormancy, we can try to turn the tables,” said study author Andreas Trumpp, PhD, also of DKFZ.
“If we could make cancer cells temporarily enter an active state, we could thus make them vulnerable to modern therapies.” ![]()
Woman’s Weakness is Worsening
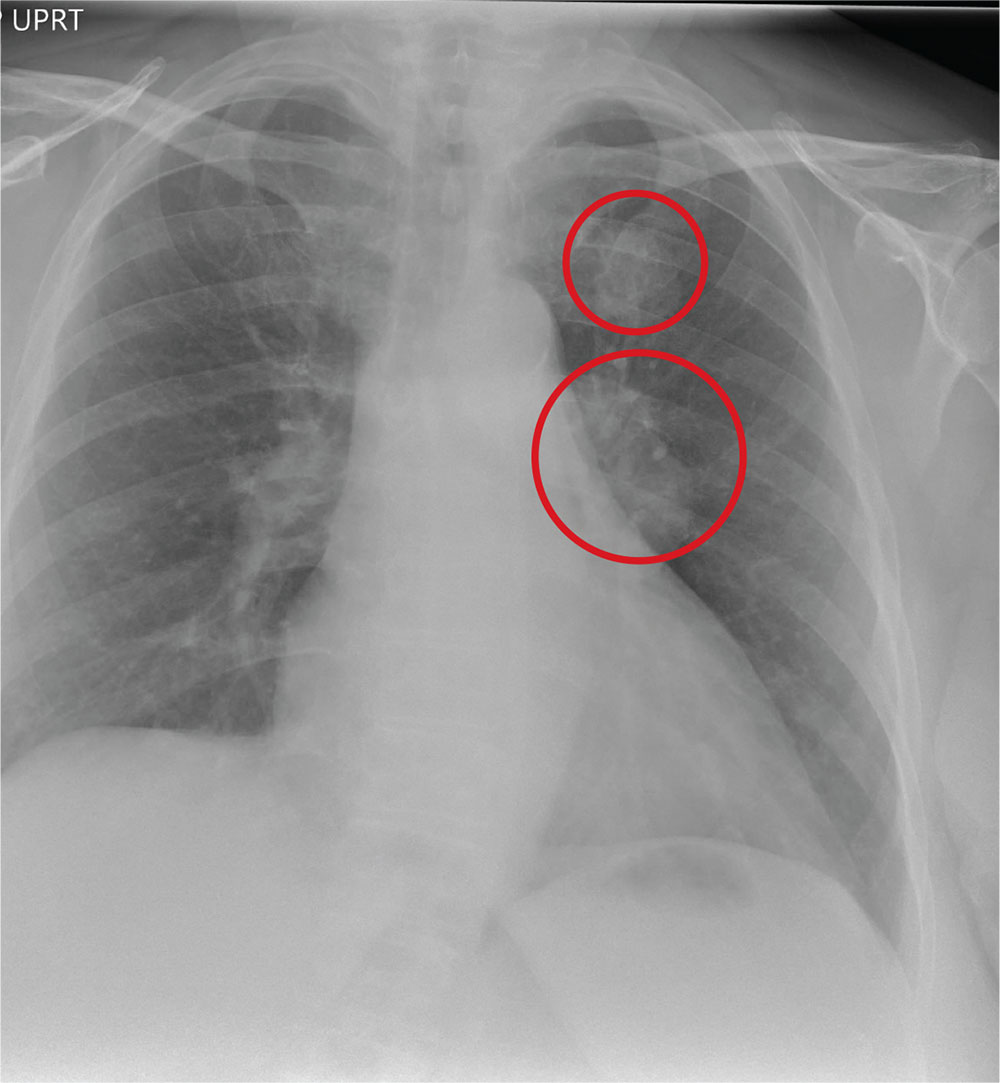
ANSWER
The radiograph shows a large, hyperdense mass within the left hilum. A second hyperdense mass is seen within the left upper lobe. Both are concerning for neoplastic processes and warrant further evaluation with contrast-enhanced CT.
Although thorough work-up and biopsy is needed, the presumptive diagnosis is a primary lung mass with likely metastasis to the brain.
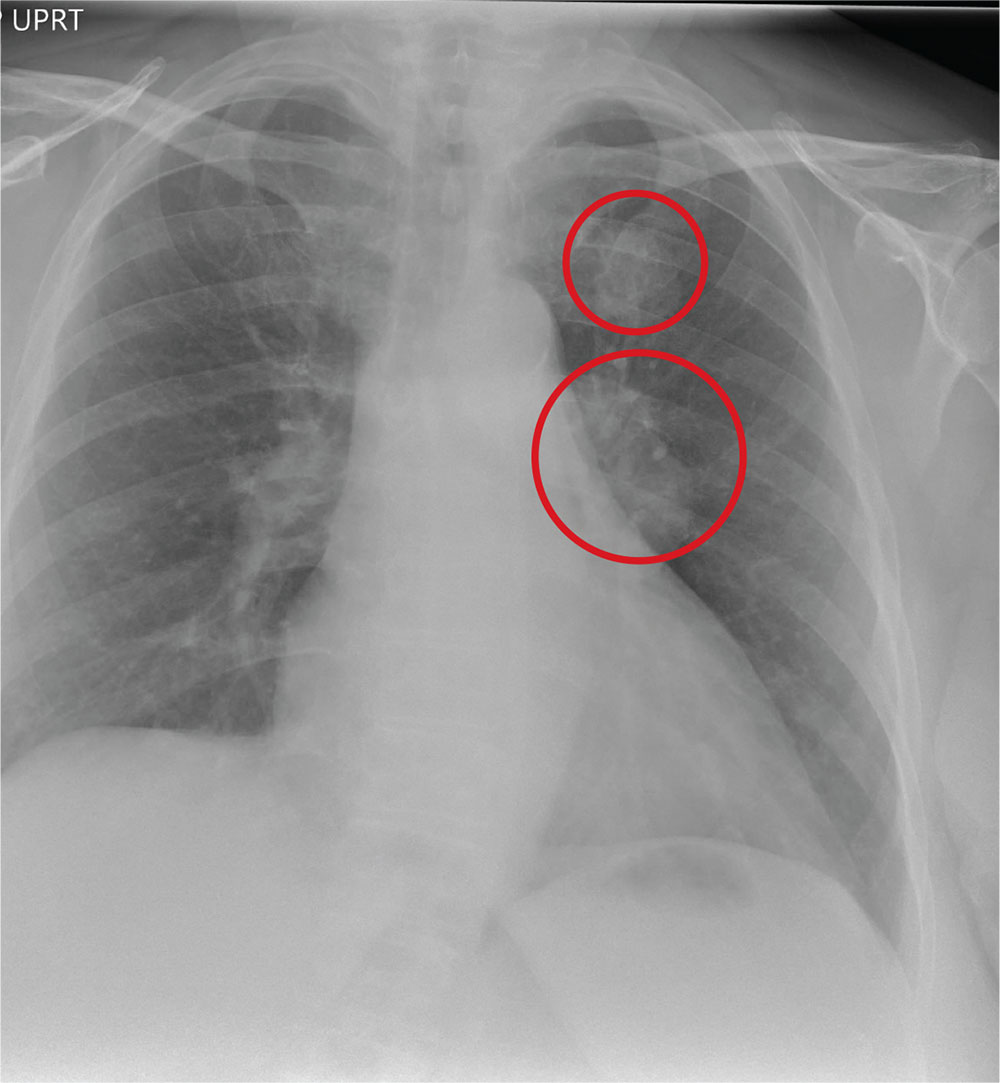
ANSWER
The radiograph shows a large, hyperdense mass within the left hilum. A second hyperdense mass is seen within the left upper lobe. Both are concerning for neoplastic processes and warrant further evaluation with contrast-enhanced CT.
Although thorough work-up and biopsy is needed, the presumptive diagnosis is a primary lung mass with likely metastasis to the brain.
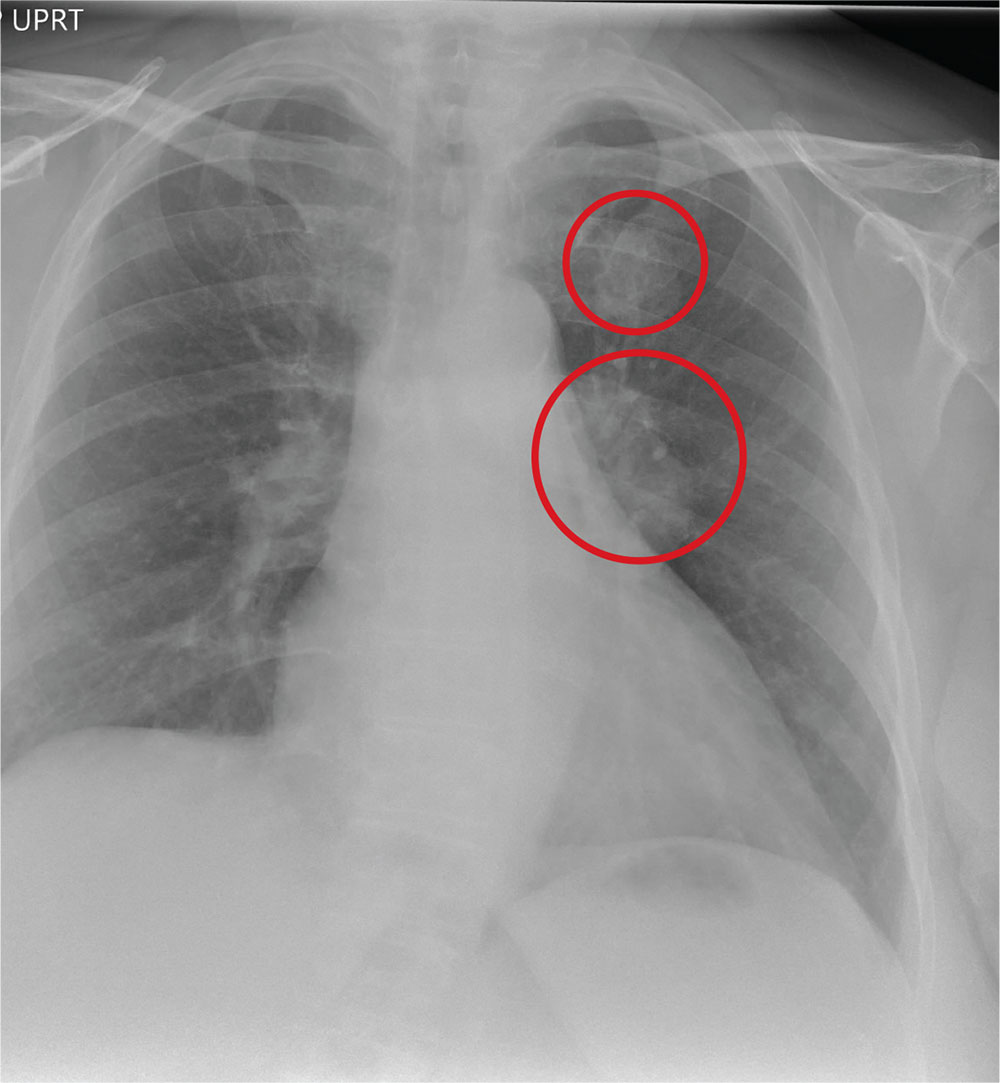
ANSWER
The radiograph shows a large, hyperdense mass within the left hilum. A second hyperdense mass is seen within the left upper lobe. Both are concerning for neoplastic processes and warrant further evaluation with contrast-enhanced CT.
Although thorough work-up and biopsy is needed, the presumptive diagnosis is a primary lung mass with likely metastasis to the brain.

A 65-year-old woman is transferred to your facility for evaluation of left-side weakness she has been experiencing for more than two months. She states that it is worsening with time but denies any other symptoms. Outpatient MRI of the brain, obtained by the referring provider, is reported to show a right parietal mass with surrounding edema.
Medical history is significant for hypertension, diabetes, and hypercholesterolemia, which are controlled with medication. The patient reports smoking nearly two packs of cigarettes daily for at least 30 years.
Physical examination reveals normal vital signs and no apparent distress. The patient does have left hemiparesis; her left upper extremity is approximately 4/5 throughout, and her left lower extremity is approximately 2/5 throughout. The exam is otherwise normal.
As you review her admission lab results, you note that a chest radiograph was obtained (shown). What is your impression?