User login
Intensive chemo upfront means DHL patients can skip HSCT
A new study suggests that patients with double-hit lymphoma (DHL) in first remission only benefit from an autologous hematopoietic stem cell transplant (auto-HSCT) if they received standard frontline chemotherapy.
Researchers looked at long-term outcomes for DHL patients who achieved remission and, overall, found that auto-HSCT did not significantly prolong remission or survival.
However, patients who received standard chemotherapy as frontline treatment did appear to benefit from auto-HSCT, as these patients had worse outcomes than patients who received intensive frontline chemotherapy.
This finding led the researchers to recommend that DHL patients receive intensive chemotherapy upfront and forgo subsequent auto-HSCT.
Daniel J. Landsburg, MD, of the University of Pennsylvania in Philadelphia, and his colleagues made these recommendations in the Journal of Clinical Oncology.
“A major dilemma for oncologists who treat [DHL] was whether or not to recommend the potentially harmful therapy of auto-[H]SCT to patients with this disease as a strategy to help keep them in remission,” Dr Landsburg said.
To gain some insight into the issue, Dr Landsburg and his colleagues looked at data on 159 patients from 19 academic medical centers across the US.
Patients were diagnosed with DHL between 2006 and 2015, and all achieved remission following frontline chemotherapy.
Thirty-five patients received standard frontline therapy—R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone).
The remaining patients received intensive frontline chemotherapy:
- 81 received DA-EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab)
- 32 received R-hyperCVAD (rituximab, cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate, and cytarabine)
- 11 received R-CODOX-M/IVAC (rituximab, cyclophosphamide, doxorubicin, vincristine, methotrexate/ifosfamide, etoposide, high-dose cytarabine).
Sixty-two patients underwent auto-HSCT, and 97 patients did not. There were no significant differences between these 2 patient groups at baseline.
“Our result is not explained by differences in patients’ overall health or disease features,” Dr Landsburg said. “The transplant and non-transplant arms of this study were very well-matched.”
Relapse and survival
For the entire patient cohort, the 3-year relapse-free survival (RFS) rate was 80%, and the 3-year overall survival (OS) rate was 87%.
There was no significant difference in RFS or OS between patients who underwent auto-HSCT and those who did not.
The RFS rate was 89% in patients who underwent auto-HSCT and 75% in patients who did not (P=0.12). The OS rate was 91% and 85%, respectively (P=0.74).
“Once these patients achieve remission, the data show they are likely to stay in remission,” Dr Landsburg said.
“In the absence of a large, randomized, controlled trial, which would be very challenging to carry out in this case, this is the best evidence we have, and it shows there’s no clear benefit to these patients undergoing auto-[H]SCT.”
Impact of frontline therapy
Patients who received R-CHOP upfront had worse RFS and OS than those who received intensive chemotherapy, although the OS difference was not significant.
RFS rates were 56% in patients who received R-CHOP, 88% in those who received DA-EPOCH-R, 87% in those who received R-hyperCVAD, and 91% in those who received R-CODOX-M/IVAC (P=0.003).
OS rates were 77% in patients who received R-CHOP, 87% in those who received DA-EPOCH-R, 90% in those who received R-hyperCVAD, and 100% in those who received R-CODOX-M/IVAC, respectively (P=0.36).
When the 3 intensive regimens were combined, the RFS rate was 88% (vs 56% for R-CHOP, P=0.002), and the OS rate was 90% (vs 77% for R-CHOP, P=0.13).
Frontline therapy and HSCT
Patients who received R-CHOP upfront benefited from auto-HSCT, but patients who received intensive chemotherapy did not.
The RFS was 51% for patients who received R-CHOP and did not undergo auto-HSCT, and it was 75% for patients who received R-CHOP followed by auto-HSCT.
The OS was 75% for patients who received R-CHOP and did not undergo auto-HSCT, and it was 83% for patients who received R-CHOP followed by auto-HSCT.
The RFS was 86% for patients who received intensive chemotherapy and did not undergo auto-HSCT, and it was 91% for patients who received intensive chemotherapy followed by auto-HSCT.
The OS was 89% for patients who received intensive chemotherapy and did not undergo auto-HSCT, and it was 92% for patients who received intensive chemotherapy followed by auto-HSCT.
An intergroup comparison showed a significant difference in RFS (P=0.003), which was driven by a significantly lower rate of RFS for patients who received R-CHOP without auto-HSCT, compared with patients who received intensive chemotherapy without auto-HSCT (P=0.003) or intensive chemotherapy with auto-HSCT (P=0.001).
“[I]f patients do go into remission with R-CHOP, it appears to be less durable, so, in these cases, going forward with auto-[H]SCT may still make sense,” Dr Landsburg said.
On the other hand, there was no significant difference between the groups with regard to OS (P=0.50).
Dr Landsburg said the next step for this research will be to study features of patients who don’t go into remission in order to understand why their disease is resistant to therapy and if that can be overcome with different treatment strategies. He also said it’s important to try to find more effective therapies for DHL patients who relapse. ![]()
A new study suggests that patients with double-hit lymphoma (DHL) in first remission only benefit from an autologous hematopoietic stem cell transplant (auto-HSCT) if they received standard frontline chemotherapy.
Researchers looked at long-term outcomes for DHL patients who achieved remission and, overall, found that auto-HSCT did not significantly prolong remission or survival.
However, patients who received standard chemotherapy as frontline treatment did appear to benefit from auto-HSCT, as these patients had worse outcomes than patients who received intensive frontline chemotherapy.
This finding led the researchers to recommend that DHL patients receive intensive chemotherapy upfront and forgo subsequent auto-HSCT.
Daniel J. Landsburg, MD, of the University of Pennsylvania in Philadelphia, and his colleagues made these recommendations in the Journal of Clinical Oncology.
“A major dilemma for oncologists who treat [DHL] was whether or not to recommend the potentially harmful therapy of auto-[H]SCT to patients with this disease as a strategy to help keep them in remission,” Dr Landsburg said.
To gain some insight into the issue, Dr Landsburg and his colleagues looked at data on 159 patients from 19 academic medical centers across the US.
Patients were diagnosed with DHL between 2006 and 2015, and all achieved remission following frontline chemotherapy.
Thirty-five patients received standard frontline therapy—R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone).
The remaining patients received intensive frontline chemotherapy:
- 81 received DA-EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab)
- 32 received R-hyperCVAD (rituximab, cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate, and cytarabine)
- 11 received R-CODOX-M/IVAC (rituximab, cyclophosphamide, doxorubicin, vincristine, methotrexate/ifosfamide, etoposide, high-dose cytarabine).
Sixty-two patients underwent auto-HSCT, and 97 patients did not. There were no significant differences between these 2 patient groups at baseline.
“Our result is not explained by differences in patients’ overall health or disease features,” Dr Landsburg said. “The transplant and non-transplant arms of this study were very well-matched.”
Relapse and survival
For the entire patient cohort, the 3-year relapse-free survival (RFS) rate was 80%, and the 3-year overall survival (OS) rate was 87%.
There was no significant difference in RFS or OS between patients who underwent auto-HSCT and those who did not.
The RFS rate was 89% in patients who underwent auto-HSCT and 75% in patients who did not (P=0.12). The OS rate was 91% and 85%, respectively (P=0.74).
“Once these patients achieve remission, the data show they are likely to stay in remission,” Dr Landsburg said.
“In the absence of a large, randomized, controlled trial, which would be very challenging to carry out in this case, this is the best evidence we have, and it shows there’s no clear benefit to these patients undergoing auto-[H]SCT.”
Impact of frontline therapy
Patients who received R-CHOP upfront had worse RFS and OS than those who received intensive chemotherapy, although the OS difference was not significant.
RFS rates were 56% in patients who received R-CHOP, 88% in those who received DA-EPOCH-R, 87% in those who received R-hyperCVAD, and 91% in those who received R-CODOX-M/IVAC (P=0.003).
OS rates were 77% in patients who received R-CHOP, 87% in those who received DA-EPOCH-R, 90% in those who received R-hyperCVAD, and 100% in those who received R-CODOX-M/IVAC, respectively (P=0.36).
When the 3 intensive regimens were combined, the RFS rate was 88% (vs 56% for R-CHOP, P=0.002), and the OS rate was 90% (vs 77% for R-CHOP, P=0.13).
Frontline therapy and HSCT
Patients who received R-CHOP upfront benefited from auto-HSCT, but patients who received intensive chemotherapy did not.
The RFS was 51% for patients who received R-CHOP and did not undergo auto-HSCT, and it was 75% for patients who received R-CHOP followed by auto-HSCT.
The OS was 75% for patients who received R-CHOP and did not undergo auto-HSCT, and it was 83% for patients who received R-CHOP followed by auto-HSCT.
The RFS was 86% for patients who received intensive chemotherapy and did not undergo auto-HSCT, and it was 91% for patients who received intensive chemotherapy followed by auto-HSCT.
The OS was 89% for patients who received intensive chemotherapy and did not undergo auto-HSCT, and it was 92% for patients who received intensive chemotherapy followed by auto-HSCT.
An intergroup comparison showed a significant difference in RFS (P=0.003), which was driven by a significantly lower rate of RFS for patients who received R-CHOP without auto-HSCT, compared with patients who received intensive chemotherapy without auto-HSCT (P=0.003) or intensive chemotherapy with auto-HSCT (P=0.001).
“[I]f patients do go into remission with R-CHOP, it appears to be less durable, so, in these cases, going forward with auto-[H]SCT may still make sense,” Dr Landsburg said.
On the other hand, there was no significant difference between the groups with regard to OS (P=0.50).
Dr Landsburg said the next step for this research will be to study features of patients who don’t go into remission in order to understand why their disease is resistant to therapy and if that can be overcome with different treatment strategies. He also said it’s important to try to find more effective therapies for DHL patients who relapse. ![]()
A new study suggests that patients with double-hit lymphoma (DHL) in first remission only benefit from an autologous hematopoietic stem cell transplant (auto-HSCT) if they received standard frontline chemotherapy.
Researchers looked at long-term outcomes for DHL patients who achieved remission and, overall, found that auto-HSCT did not significantly prolong remission or survival.
However, patients who received standard chemotherapy as frontline treatment did appear to benefit from auto-HSCT, as these patients had worse outcomes than patients who received intensive frontline chemotherapy.
This finding led the researchers to recommend that DHL patients receive intensive chemotherapy upfront and forgo subsequent auto-HSCT.
Daniel J. Landsburg, MD, of the University of Pennsylvania in Philadelphia, and his colleagues made these recommendations in the Journal of Clinical Oncology.
“A major dilemma for oncologists who treat [DHL] was whether or not to recommend the potentially harmful therapy of auto-[H]SCT to patients with this disease as a strategy to help keep them in remission,” Dr Landsburg said.
To gain some insight into the issue, Dr Landsburg and his colleagues looked at data on 159 patients from 19 academic medical centers across the US.
Patients were diagnosed with DHL between 2006 and 2015, and all achieved remission following frontline chemotherapy.
Thirty-five patients received standard frontline therapy—R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone).
The remaining patients received intensive frontline chemotherapy:
- 81 received DA-EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab)
- 32 received R-hyperCVAD (rituximab, cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate, and cytarabine)
- 11 received R-CODOX-M/IVAC (rituximab, cyclophosphamide, doxorubicin, vincristine, methotrexate/ifosfamide, etoposide, high-dose cytarabine).
Sixty-two patients underwent auto-HSCT, and 97 patients did not. There were no significant differences between these 2 patient groups at baseline.
“Our result is not explained by differences in patients’ overall health or disease features,” Dr Landsburg said. “The transplant and non-transplant arms of this study were very well-matched.”
Relapse and survival
For the entire patient cohort, the 3-year relapse-free survival (RFS) rate was 80%, and the 3-year overall survival (OS) rate was 87%.
There was no significant difference in RFS or OS between patients who underwent auto-HSCT and those who did not.
The RFS rate was 89% in patients who underwent auto-HSCT and 75% in patients who did not (P=0.12). The OS rate was 91% and 85%, respectively (P=0.74).
“Once these patients achieve remission, the data show they are likely to stay in remission,” Dr Landsburg said.
“In the absence of a large, randomized, controlled trial, which would be very challenging to carry out in this case, this is the best evidence we have, and it shows there’s no clear benefit to these patients undergoing auto-[H]SCT.”
Impact of frontline therapy
Patients who received R-CHOP upfront had worse RFS and OS than those who received intensive chemotherapy, although the OS difference was not significant.
RFS rates were 56% in patients who received R-CHOP, 88% in those who received DA-EPOCH-R, 87% in those who received R-hyperCVAD, and 91% in those who received R-CODOX-M/IVAC (P=0.003).
OS rates were 77% in patients who received R-CHOP, 87% in those who received DA-EPOCH-R, 90% in those who received R-hyperCVAD, and 100% in those who received R-CODOX-M/IVAC, respectively (P=0.36).
When the 3 intensive regimens were combined, the RFS rate was 88% (vs 56% for R-CHOP, P=0.002), and the OS rate was 90% (vs 77% for R-CHOP, P=0.13).
Frontline therapy and HSCT
Patients who received R-CHOP upfront benefited from auto-HSCT, but patients who received intensive chemotherapy did not.
The RFS was 51% for patients who received R-CHOP and did not undergo auto-HSCT, and it was 75% for patients who received R-CHOP followed by auto-HSCT.
The OS was 75% for patients who received R-CHOP and did not undergo auto-HSCT, and it was 83% for patients who received R-CHOP followed by auto-HSCT.
The RFS was 86% for patients who received intensive chemotherapy and did not undergo auto-HSCT, and it was 91% for patients who received intensive chemotherapy followed by auto-HSCT.
The OS was 89% for patients who received intensive chemotherapy and did not undergo auto-HSCT, and it was 92% for patients who received intensive chemotherapy followed by auto-HSCT.
An intergroup comparison showed a significant difference in RFS (P=0.003), which was driven by a significantly lower rate of RFS for patients who received R-CHOP without auto-HSCT, compared with patients who received intensive chemotherapy without auto-HSCT (P=0.003) or intensive chemotherapy with auto-HSCT (P=0.001).
“[I]f patients do go into remission with R-CHOP, it appears to be less durable, so, in these cases, going forward with auto-[H]SCT may still make sense,” Dr Landsburg said.
On the other hand, there was no significant difference between the groups with regard to OS (P=0.50).
Dr Landsburg said the next step for this research will be to study features of patients who don’t go into remission in order to understand why their disease is resistant to therapy and if that can be overcome with different treatment strategies. He also said it’s important to try to find more effective therapies for DHL patients who relapse. ![]()
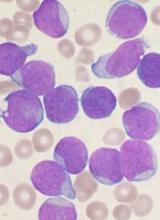
Antibody shows potential for treating AML, B-ALL
Endoglin may be a promising therapeutic target in acute myeloid leukemia (AML) and B-cell acute lymphoblastic leukemia (B-ALL), according to researchers.
The group identified endoglin expression on the majority of blasts from patients with AML and B-ALL.
The team also found that an endoglin antibody, TRC105 (carotuximab), exhibited activity against AML and B-ALL in vivo, and combining the drug with chemotherapeutic agents enhanced this activity.
Rita Perlingeiro, PhD, of the University of Minnesota in Minneapolis, and her colleagues reported these findings in Blood.
The researchers first discovered that endoglin, which is also known as CD105, was “highly expressed” in leukemic blasts.
In samples from AML patients, 47.6% to 98.5% of blasts were CD105+. In samples from B-ALL patients, 92.6% to 99% of blasts were CD105+.
“We have been studying the function of endoglin in hematopoiesis for more than a decade, and the consistent expression of this receptor in the majority of acute leukemias was intriguing,” Dr Perlingeiro said.
She and her colleagues also found that CD105+ blasts had superior leukemogenic activity and reduced survival in mice when compared to CD105- blasts.
Mice injected with AML CD105+ blasts had all died at day 110 after injection, but mice injected with CD105- AML blasts survived until day 140.
Mice injected with CD105+ ALL blasts died 3 months after injection, but mice injected with CD105- ALL blasts were still alive and showed no signs of disease at the time of sacrifice, which was 5 months after injection.
TRC105 monotherapy
Several experiments showed that TRC105 could reduce leukemic activity in vivo.
TRC105 reduced blast counts in the peripheral blood of mice that had been injected with AML blasts. The drug also reduced blasts in the bone marrow initially, though blast counts were comparable in treated mice and controls by week 12.
On the other hand, mice treated with TRC105 did not experience the weight loss and splenomegaly observed in control mice. And TRC105 suppressed the ability of AML blasts to give rise to leukemia in secondary recipient mice.
In mice injected with ALL blasts, TRC105 initially decreased blast counts. However, by week 8, blast counts in the peripheral blood, bone marrow, and spleen of treated mice were similar to those observed in controls. The researchers said this suggests that TRC105 only slows the development of ALL.
The team then evaluated the effects of TRC105 after disease had been established. Mice with established AML received TRC105 for 8 weeks, and mice with established ALL received TRC105 for 4 weeks.
In mice with AML, TRC105 reduced blasts in the peripheral blood and spleen but not the bone marrow. The treatment also prevented splenomegaly and weight loss and prolonged survival.
“Our hypothesis that endoglin expression was linked to leukemia-forming activity was proven to be true, and it was even more rewarding to witness the robust anti-leukemogenic effect of blocking endoglin signaling with TRC105, even when leukemia had already been established in the mouse,” Dr Perlingeiro said.
However, in mice with established ALL, TRC105 had no effect on leukemia progression.
The researchers said this could be due to expression of soluble endoglin (sENG), which would titrate the TRC105 antibody, limiting its ability to bind to membrane-bound endoglin on leukemic cells. Results of additional experiments supported this idea.
TRC105 in combination
The researchers also tested TRC105 in combination with chemotherapy in the mouse models. The team combined the antibody with cytarabine to treat AML and cyclophosphamide to treat ALL.
In mice with AML, cytarabine and TRC105 significantly reduced levels of leukemic cells in the peripheral blood.
In mice with ALL, cyclophosphamide and TRC105 suppressed leukemia development more effectively and more quickly than cyclophosphamide alone.
The researchers detected high levels of sENG in untreated mice with ALL, but levels were lower in the TRC105-treated mice. And there was “no significant detection” of sENG in mice that received cyclophosphamide and TRC105 or cyclophosphamide alone.
Dr Perlingeiro and her colleagues said this suggests the inhibitory effects of sENG can be circumvented by suppressing tumor burden, which results in the combination therapy demonstrating potent antileukemic activity. ![]()
Endoglin may be a promising therapeutic target in acute myeloid leukemia (AML) and B-cell acute lymphoblastic leukemia (B-ALL), according to researchers.
The group identified endoglin expression on the majority of blasts from patients with AML and B-ALL.
The team also found that an endoglin antibody, TRC105 (carotuximab), exhibited activity against AML and B-ALL in vivo, and combining the drug with chemotherapeutic agents enhanced this activity.
Rita Perlingeiro, PhD, of the University of Minnesota in Minneapolis, and her colleagues reported these findings in Blood.
The researchers first discovered that endoglin, which is also known as CD105, was “highly expressed” in leukemic blasts.
In samples from AML patients, 47.6% to 98.5% of blasts were CD105+. In samples from B-ALL patients, 92.6% to 99% of blasts were CD105+.
“We have been studying the function of endoglin in hematopoiesis for more than a decade, and the consistent expression of this receptor in the majority of acute leukemias was intriguing,” Dr Perlingeiro said.
She and her colleagues also found that CD105+ blasts had superior leukemogenic activity and reduced survival in mice when compared to CD105- blasts.
Mice injected with AML CD105+ blasts had all died at day 110 after injection, but mice injected with CD105- AML blasts survived until day 140.
Mice injected with CD105+ ALL blasts died 3 months after injection, but mice injected with CD105- ALL blasts were still alive and showed no signs of disease at the time of sacrifice, which was 5 months after injection.
TRC105 monotherapy
Several experiments showed that TRC105 could reduce leukemic activity in vivo.
TRC105 reduced blast counts in the peripheral blood of mice that had been injected with AML blasts. The drug also reduced blasts in the bone marrow initially, though blast counts were comparable in treated mice and controls by week 12.
On the other hand, mice treated with TRC105 did not experience the weight loss and splenomegaly observed in control mice. And TRC105 suppressed the ability of AML blasts to give rise to leukemia in secondary recipient mice.
In mice injected with ALL blasts, TRC105 initially decreased blast counts. However, by week 8, blast counts in the peripheral blood, bone marrow, and spleen of treated mice were similar to those observed in controls. The researchers said this suggests that TRC105 only slows the development of ALL.
The team then evaluated the effects of TRC105 after disease had been established. Mice with established AML received TRC105 for 8 weeks, and mice with established ALL received TRC105 for 4 weeks.
In mice with AML, TRC105 reduced blasts in the peripheral blood and spleen but not the bone marrow. The treatment also prevented splenomegaly and weight loss and prolonged survival.
“Our hypothesis that endoglin expression was linked to leukemia-forming activity was proven to be true, and it was even more rewarding to witness the robust anti-leukemogenic effect of blocking endoglin signaling with TRC105, even when leukemia had already been established in the mouse,” Dr Perlingeiro said.
However, in mice with established ALL, TRC105 had no effect on leukemia progression.
The researchers said this could be due to expression of soluble endoglin (sENG), which would titrate the TRC105 antibody, limiting its ability to bind to membrane-bound endoglin on leukemic cells. Results of additional experiments supported this idea.
TRC105 in combination
The researchers also tested TRC105 in combination with chemotherapy in the mouse models. The team combined the antibody with cytarabine to treat AML and cyclophosphamide to treat ALL.
In mice with AML, cytarabine and TRC105 significantly reduced levels of leukemic cells in the peripheral blood.
In mice with ALL, cyclophosphamide and TRC105 suppressed leukemia development more effectively and more quickly than cyclophosphamide alone.
The researchers detected high levels of sENG in untreated mice with ALL, but levels were lower in the TRC105-treated mice. And there was “no significant detection” of sENG in mice that received cyclophosphamide and TRC105 or cyclophosphamide alone.
Dr Perlingeiro and her colleagues said this suggests the inhibitory effects of sENG can be circumvented by suppressing tumor burden, which results in the combination therapy demonstrating potent antileukemic activity. ![]()
Endoglin may be a promising therapeutic target in acute myeloid leukemia (AML) and B-cell acute lymphoblastic leukemia (B-ALL), according to researchers.
The group identified endoglin expression on the majority of blasts from patients with AML and B-ALL.
The team also found that an endoglin antibody, TRC105 (carotuximab), exhibited activity against AML and B-ALL in vivo, and combining the drug with chemotherapeutic agents enhanced this activity.
Rita Perlingeiro, PhD, of the University of Minnesota in Minneapolis, and her colleagues reported these findings in Blood.
The researchers first discovered that endoglin, which is also known as CD105, was “highly expressed” in leukemic blasts.
In samples from AML patients, 47.6% to 98.5% of blasts were CD105+. In samples from B-ALL patients, 92.6% to 99% of blasts were CD105+.
“We have been studying the function of endoglin in hematopoiesis for more than a decade, and the consistent expression of this receptor in the majority of acute leukemias was intriguing,” Dr Perlingeiro said.
She and her colleagues also found that CD105+ blasts had superior leukemogenic activity and reduced survival in mice when compared to CD105- blasts.
Mice injected with AML CD105+ blasts had all died at day 110 after injection, but mice injected with CD105- AML blasts survived until day 140.
Mice injected with CD105+ ALL blasts died 3 months after injection, but mice injected with CD105- ALL blasts were still alive and showed no signs of disease at the time of sacrifice, which was 5 months after injection.
TRC105 monotherapy
Several experiments showed that TRC105 could reduce leukemic activity in vivo.
TRC105 reduced blast counts in the peripheral blood of mice that had been injected with AML blasts. The drug also reduced blasts in the bone marrow initially, though blast counts were comparable in treated mice and controls by week 12.
On the other hand, mice treated with TRC105 did not experience the weight loss and splenomegaly observed in control mice. And TRC105 suppressed the ability of AML blasts to give rise to leukemia in secondary recipient mice.
In mice injected with ALL blasts, TRC105 initially decreased blast counts. However, by week 8, blast counts in the peripheral blood, bone marrow, and spleen of treated mice were similar to those observed in controls. The researchers said this suggests that TRC105 only slows the development of ALL.
The team then evaluated the effects of TRC105 after disease had been established. Mice with established AML received TRC105 for 8 weeks, and mice with established ALL received TRC105 for 4 weeks.
In mice with AML, TRC105 reduced blasts in the peripheral blood and spleen but not the bone marrow. The treatment also prevented splenomegaly and weight loss and prolonged survival.
“Our hypothesis that endoglin expression was linked to leukemia-forming activity was proven to be true, and it was even more rewarding to witness the robust anti-leukemogenic effect of blocking endoglin signaling with TRC105, even when leukemia had already been established in the mouse,” Dr Perlingeiro said.
However, in mice with established ALL, TRC105 had no effect on leukemia progression.
The researchers said this could be due to expression of soluble endoglin (sENG), which would titrate the TRC105 antibody, limiting its ability to bind to membrane-bound endoglin on leukemic cells. Results of additional experiments supported this idea.
TRC105 in combination
The researchers also tested TRC105 in combination with chemotherapy in the mouse models. The team combined the antibody with cytarabine to treat AML and cyclophosphamide to treat ALL.
In mice with AML, cytarabine and TRC105 significantly reduced levels of leukemic cells in the peripheral blood.
In mice with ALL, cyclophosphamide and TRC105 suppressed leukemia development more effectively and more quickly than cyclophosphamide alone.
The researchers detected high levels of sENG in untreated mice with ALL, but levels were lower in the TRC105-treated mice. And there was “no significant detection” of sENG in mice that received cyclophosphamide and TRC105 or cyclophosphamide alone.
Dr Perlingeiro and her colleagues said this suggests the inhibitory effects of sENG can be circumvented by suppressing tumor burden, which results in the combination therapy demonstrating potent antileukemic activity. ![]()
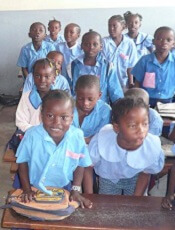
Maternal education can reduce risk of childhood malaria
One way to reduce the risk of malaria infection in children is to educate their mothers, according to a study published in Pathogens and Global Health.
The study suggested that educating mothers can be more effective in preventing childhood malaria than the malaria vaccine candidate RTS,S (Mosquirix).
Researchers said this finding can be explained by the fact that educated mothers know of ways to prevent malaria infection, such as using bed nets and taking their children for treatment if they develop a fever.
For this study, the researchers performed malaria testing in 647 children in the Democratic Republic of Congo (DRC) who were between the ages of 2 months and 5 years.
The team also had the children’s parent or guardian fill out a survey related to demographics, socioeconomic status, maternal education, bed net use, and recent illness involving fever.
Results showed that mothers with a higher education level had children with a lower risk of malaria infection.
“This was not a small effect,” said study author Michael Hawkes, MD, PhD, of the University of Alberta in Edmonton, Alberta, Canada.
“Maternal education had an enormous effect—equivalent to or greater than the leading biomedical vaccine against malaria.”
Overall, 19% of the children studied (123/647) tested positive for malaria.
The prevalence of malaria was 30% in children of mothers with no education, 17% in children of mothers with primary education, and 15% in children of mothers with education beyond primary school (P=0.001).
In a multivariate analysis adjusted for the effect of a child’s age and the study site, maternal education was still a significant predictor of malaria antigenemia.
“It doesn’t take a lot of education to teach a mom how to take simple precautions to prevent malaria in her child,” said study author Cary Ma, a medical student at the University of Alberta.
“All it takes is knowing the importance of using a bed net and knowing the importance of seeking care when your child has a fever. These are fairly straightforward, simple messages in the context of health and hygiene that can easily be conveyed, usually at an elementary or primary school level.”
“The World Health Organization is rolling out a new vaccine [RTS,S] in countries across Africa that has an efficacy of about 30%,” Dr Hawkes added.
“But children whose mothers are educated beyond the primary level have a 53% reduction in their malaria rates. So educating the mom has as profound an effect on childhood malaria as hundreds of millions of dollars spent on a vaccine.”
The researchers said this work builds upon previous studies that have shown the importance of maternal education in reducing child mortality and disease in other countries around the world.
The team noted that maternal education isn’t a magic bullet by itself, but they do believe it is part of the solution. They hope the lessons learned via this study can help lead policymakers to strengthen efforts to educate girls and women in the DRC and other malaria hotspots around the world. ![]()
One way to reduce the risk of malaria infection in children is to educate their mothers, according to a study published in Pathogens and Global Health.
The study suggested that educating mothers can be more effective in preventing childhood malaria than the malaria vaccine candidate RTS,S (Mosquirix).
Researchers said this finding can be explained by the fact that educated mothers know of ways to prevent malaria infection, such as using bed nets and taking their children for treatment if they develop a fever.
For this study, the researchers performed malaria testing in 647 children in the Democratic Republic of Congo (DRC) who were between the ages of 2 months and 5 years.
The team also had the children’s parent or guardian fill out a survey related to demographics, socioeconomic status, maternal education, bed net use, and recent illness involving fever.
Results showed that mothers with a higher education level had children with a lower risk of malaria infection.
“This was not a small effect,” said study author Michael Hawkes, MD, PhD, of the University of Alberta in Edmonton, Alberta, Canada.
“Maternal education had an enormous effect—equivalent to or greater than the leading biomedical vaccine against malaria.”
Overall, 19% of the children studied (123/647) tested positive for malaria.
The prevalence of malaria was 30% in children of mothers with no education, 17% in children of mothers with primary education, and 15% in children of mothers with education beyond primary school (P=0.001).
In a multivariate analysis adjusted for the effect of a child’s age and the study site, maternal education was still a significant predictor of malaria antigenemia.
“It doesn’t take a lot of education to teach a mom how to take simple precautions to prevent malaria in her child,” said study author Cary Ma, a medical student at the University of Alberta.
“All it takes is knowing the importance of using a bed net and knowing the importance of seeking care when your child has a fever. These are fairly straightforward, simple messages in the context of health and hygiene that can easily be conveyed, usually at an elementary or primary school level.”
“The World Health Organization is rolling out a new vaccine [RTS,S] in countries across Africa that has an efficacy of about 30%,” Dr Hawkes added.
“But children whose mothers are educated beyond the primary level have a 53% reduction in their malaria rates. So educating the mom has as profound an effect on childhood malaria as hundreds of millions of dollars spent on a vaccine.”
The researchers said this work builds upon previous studies that have shown the importance of maternal education in reducing child mortality and disease in other countries around the world.
The team noted that maternal education isn’t a magic bullet by itself, but they do believe it is part of the solution. They hope the lessons learned via this study can help lead policymakers to strengthen efforts to educate girls and women in the DRC and other malaria hotspots around the world. ![]()
One way to reduce the risk of malaria infection in children is to educate their mothers, according to a study published in Pathogens and Global Health.
The study suggested that educating mothers can be more effective in preventing childhood malaria than the malaria vaccine candidate RTS,S (Mosquirix).
Researchers said this finding can be explained by the fact that educated mothers know of ways to prevent malaria infection, such as using bed nets and taking their children for treatment if they develop a fever.
For this study, the researchers performed malaria testing in 647 children in the Democratic Republic of Congo (DRC) who were between the ages of 2 months and 5 years.
The team also had the children’s parent or guardian fill out a survey related to demographics, socioeconomic status, maternal education, bed net use, and recent illness involving fever.
Results showed that mothers with a higher education level had children with a lower risk of malaria infection.
“This was not a small effect,” said study author Michael Hawkes, MD, PhD, of the University of Alberta in Edmonton, Alberta, Canada.
“Maternal education had an enormous effect—equivalent to or greater than the leading biomedical vaccine against malaria.”
Overall, 19% of the children studied (123/647) tested positive for malaria.
The prevalence of malaria was 30% in children of mothers with no education, 17% in children of mothers with primary education, and 15% in children of mothers with education beyond primary school (P=0.001).
In a multivariate analysis adjusted for the effect of a child’s age and the study site, maternal education was still a significant predictor of malaria antigenemia.
“It doesn’t take a lot of education to teach a mom how to take simple precautions to prevent malaria in her child,” said study author Cary Ma, a medical student at the University of Alberta.
“All it takes is knowing the importance of using a bed net and knowing the importance of seeking care when your child has a fever. These are fairly straightforward, simple messages in the context of health and hygiene that can easily be conveyed, usually at an elementary or primary school level.”
“The World Health Organization is rolling out a new vaccine [RTS,S] in countries across Africa that has an efficacy of about 30%,” Dr Hawkes added.
“But children whose mothers are educated beyond the primary level have a 53% reduction in their malaria rates. So educating the mom has as profound an effect on childhood malaria as hundreds of millions of dollars spent on a vaccine.”
The researchers said this work builds upon previous studies that have shown the importance of maternal education in reducing child mortality and disease in other countries around the world.
The team noted that maternal education isn’t a magic bullet by itself, but they do believe it is part of the solution. They hope the lessons learned via this study can help lead policymakers to strengthen efforts to educate girls and women in the DRC and other malaria hotspots around the world. ![]()
Racial, ethnic differences exist ADHD treatment of Medicaid-enrolled youth
, reported Janet R. Cummings, PhD, and her associates at the Rollins School of Public Health at Emory University, Atlanta.
Overall, quality of care for Medicaid-enrolled children receiving ADHD treatment is poor. Of those who initiated medications, 59% visited a provider within 30 days, 64% received at least two other doctor visits, and 38% received combined treatment with any psychotherapy visit. Sixty percent did not fill the ADHD prescription for enough days, 70% had no psychotherapy visit, and 42% stopped treatment.
The percentage that had any follow-up visit in the initiation phase was lower among African American children than among white children (56% vs. 61%, P less than .001), while Hispanic children were more likely than were white children to receive adequate follow-up in the initiation phase (63% vs. 61%; P less than .001) as well as in the C&M phase (71% vs. 63%; P less than .001). In children who continued medication, African American and Hispanic children were more likely than were white children to receive any psychotherapy (42% and 49% vs. 35%; P less than .001).
“The adjusted rate of discontinuing medication was 22.4% points higher (P less than .001) among African American versus white youth and 16.7% points higher (P less than .001) among Hispanic versus white youth,” Dr. Cummings and her associates said. “These findings are in line with research indicating that racial/ethnic minority parents may prefer psychosocial treatments over medication for ADHD.”
In terms of stopping treatment, the percentages were significantly higher among African American (51%) and Hispanic (45%) children than among white children at 36% (P less than .001).
“Higher rates of medication discontinuation among minority youth could be due to differences in cultural health beliefs and/or concerns about ADHD medication treatment. African American parents are less likely than white parents to conceptualize ADHD as a medical condition requiring treatment and may be less willing to administer psychotropic medication to a child due to beliefs about medication efficacy and side effects. ADHD medication is associated with an increased risk of adverse effects ... and a substantial proportion of treatment discontinuation is due to these adverse effects,” the researchers said.
Read more in Pediatrics (2017 May 16. doi: 10.1542/ peds. 2016-2444).
, reported Janet R. Cummings, PhD, and her associates at the Rollins School of Public Health at Emory University, Atlanta.
Overall, quality of care for Medicaid-enrolled children receiving ADHD treatment is poor. Of those who initiated medications, 59% visited a provider within 30 days, 64% received at least two other doctor visits, and 38% received combined treatment with any psychotherapy visit. Sixty percent did not fill the ADHD prescription for enough days, 70% had no psychotherapy visit, and 42% stopped treatment.
The percentage that had any follow-up visit in the initiation phase was lower among African American children than among white children (56% vs. 61%, P less than .001), while Hispanic children were more likely than were white children to receive adequate follow-up in the initiation phase (63% vs. 61%; P less than .001) as well as in the C&M phase (71% vs. 63%; P less than .001). In children who continued medication, African American and Hispanic children were more likely than were white children to receive any psychotherapy (42% and 49% vs. 35%; P less than .001).
“The adjusted rate of discontinuing medication was 22.4% points higher (P less than .001) among African American versus white youth and 16.7% points higher (P less than .001) among Hispanic versus white youth,” Dr. Cummings and her associates said. “These findings are in line with research indicating that racial/ethnic minority parents may prefer psychosocial treatments over medication for ADHD.”
In terms of stopping treatment, the percentages were significantly higher among African American (51%) and Hispanic (45%) children than among white children at 36% (P less than .001).
“Higher rates of medication discontinuation among minority youth could be due to differences in cultural health beliefs and/or concerns about ADHD medication treatment. African American parents are less likely than white parents to conceptualize ADHD as a medical condition requiring treatment and may be less willing to administer psychotropic medication to a child due to beliefs about medication efficacy and side effects. ADHD medication is associated with an increased risk of adverse effects ... and a substantial proportion of treatment discontinuation is due to these adverse effects,” the researchers said.
Read more in Pediatrics (2017 May 16. doi: 10.1542/ peds. 2016-2444).
, reported Janet R. Cummings, PhD, and her associates at the Rollins School of Public Health at Emory University, Atlanta.
Overall, quality of care for Medicaid-enrolled children receiving ADHD treatment is poor. Of those who initiated medications, 59% visited a provider within 30 days, 64% received at least two other doctor visits, and 38% received combined treatment with any psychotherapy visit. Sixty percent did not fill the ADHD prescription for enough days, 70% had no psychotherapy visit, and 42% stopped treatment.
The percentage that had any follow-up visit in the initiation phase was lower among African American children than among white children (56% vs. 61%, P less than .001), while Hispanic children were more likely than were white children to receive adequate follow-up in the initiation phase (63% vs. 61%; P less than .001) as well as in the C&M phase (71% vs. 63%; P less than .001). In children who continued medication, African American and Hispanic children were more likely than were white children to receive any psychotherapy (42% and 49% vs. 35%; P less than .001).
“The adjusted rate of discontinuing medication was 22.4% points higher (P less than .001) among African American versus white youth and 16.7% points higher (P less than .001) among Hispanic versus white youth,” Dr. Cummings and her associates said. “These findings are in line with research indicating that racial/ethnic minority parents may prefer psychosocial treatments over medication for ADHD.”
In terms of stopping treatment, the percentages were significantly higher among African American (51%) and Hispanic (45%) children than among white children at 36% (P less than .001).
“Higher rates of medication discontinuation among minority youth could be due to differences in cultural health beliefs and/or concerns about ADHD medication treatment. African American parents are less likely than white parents to conceptualize ADHD as a medical condition requiring treatment and may be less willing to administer psychotropic medication to a child due to beliefs about medication efficacy and side effects. ADHD medication is associated with an increased risk of adverse effects ... and a substantial proportion of treatment discontinuation is due to these adverse effects,” the researchers said.
Read more in Pediatrics (2017 May 16. doi: 10.1542/ peds. 2016-2444).
FROM PEDIATRICS
VIDEO: Care withdrawal becoming more common in ischemic stroke patients
BOSTON – U.S. physicians chose to withdraw life-sustaining care from critically ill ischemic stroke patients at much higher rates in 2011 than in 2006, according to results of a new study, although overall percentages remain low.
The trend was bolstered by big jumps in “withdrawal of care” among patients who underwent thrombolysis or both thrombolysis and endovascular treatment: Over the 5-year period, their likelihood of having care withdrawn increased fivefold.
The study authors don’t know whether the trends have continued over the past 6 years, and it’s not clear why the rates rose so much from 2006 to 2011. The researchers speculate that the increase could be linked to disease severity and the preferences of patients and their families.
Whatever the case, study lead author Malik Muhammad Adil, MD, a neurology resident at the Ochsner Clinic Foundation in New Orleans, cautioned that prematurely withdrawing care can throw off stroke prognostication estimates that are already fuzzy. In an interview, he said this can then lead to “significant consequences, including suboptimal outcomes and higher risk of short-term mortality.”
Dr. Adil defines withdrawal of care as “discontinuation of life-sustaining interventions from a patient who is expected to die without this support.” These interventions include such treatments as intubation, mechanical ventilation, feeding tubes, antibiotics, and brain surgery, he said.
For the new study, researchers examined the Nationwide Inpatient Survey database for the years 2006-2011. They reported their findings at the annual meeting of the American Academy of Neurology.
The study reports the following regarding withdrawal of care among ischemic stroke patients:
- The rate grew in those who received neither thrombolysis nor endovascular treatment from 0.8% in 2006 to 3.0% in 2011 (P less than or equal to .0001).
- In those who received thrombolysis alone, the rate rose from 0.9% to 5.5% (P less than or equal to .0001).
- In those who received endovascular treatment alone, the rate increased from 2.8% to 9.0% (P = .0006).
- In patients who received both thrombolysis and endovascular treatment, the rate grew from 2.0% to 10.3% (P = .0009).
Dr. Adil said several factors can affect rates of withdrawal of care in ischemic stroke patients, such as the level of illness (patients receiving aggressive treatment are sicker), advance directives, and the decisions of family members. Some institutions may be more likely to push for withdrawal of care, too, he said. “At my institution, we are not aggressive with withdrawal of care, and I have seen a few better outcomes than expected,” he said.
Also, the lack of useful data regarding prognosis for these patients may lead to premature decisions regarding withdrawal of care, he said.
“We have few prognostic models/scores that predict mortality, and these models are not very sensitive and specific,” Dr. Adil said. “Often, physicians make these decisions based on their previous experiences. All of this leads to premature withdrawal of care. On the other hand, because of premature withdrawal of care, we do not have the data on long-term outcomes on these patients, leading to errors in prognostication.”
In an interview, Adam G. Kelly, MD, a neurologist at the University of Rochester (N.Y.) and chief of neurology at Highland Hospital in Rochester, said the study is important but lacks crucial information such as the circumstances surrounding the care decisions. He hasn’t noticed trends in withdrawal of care among his patients.
“It’s possible that providers have become better at documenting discussions with patients and families which allowed this information to be better captured,” he said. “As the authors mention, it’s also possible that providers are consciously or unconsciously delivering prognoses that are biased towards negative outcomes, leading patients and families to be more apt to choose a palliative approach.”
Dr. Kelly added that neurologists need to objectively offer prognoses in stroke cases. “When the outcome is in doubt, I recommend time-limited trials of interventions of mechanical ventilation, artificial feeding, and other high-intensity interventions to allow patients and families to make the decision they feel is best,” he said.
What about trends in the years since 2011? Dr. Adil said information regarding the years since 2011 wasn’t available to him, but he hopes to analyze the period from 2012 to 2016.
Dr. Adil discussed his study and its implications in a video interview.
No funding is reported. Dr. Adil reports no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – U.S. physicians chose to withdraw life-sustaining care from critically ill ischemic stroke patients at much higher rates in 2011 than in 2006, according to results of a new study, although overall percentages remain low.
The trend was bolstered by big jumps in “withdrawal of care” among patients who underwent thrombolysis or both thrombolysis and endovascular treatment: Over the 5-year period, their likelihood of having care withdrawn increased fivefold.
The study authors don’t know whether the trends have continued over the past 6 years, and it’s not clear why the rates rose so much from 2006 to 2011. The researchers speculate that the increase could be linked to disease severity and the preferences of patients and their families.
Whatever the case, study lead author Malik Muhammad Adil, MD, a neurology resident at the Ochsner Clinic Foundation in New Orleans, cautioned that prematurely withdrawing care can throw off stroke prognostication estimates that are already fuzzy. In an interview, he said this can then lead to “significant consequences, including suboptimal outcomes and higher risk of short-term mortality.”
Dr. Adil defines withdrawal of care as “discontinuation of life-sustaining interventions from a patient who is expected to die without this support.” These interventions include such treatments as intubation, mechanical ventilation, feeding tubes, antibiotics, and brain surgery, he said.
For the new study, researchers examined the Nationwide Inpatient Survey database for the years 2006-2011. They reported their findings at the annual meeting of the American Academy of Neurology.
The study reports the following regarding withdrawal of care among ischemic stroke patients:
- The rate grew in those who received neither thrombolysis nor endovascular treatment from 0.8% in 2006 to 3.0% in 2011 (P less than or equal to .0001).
- In those who received thrombolysis alone, the rate rose from 0.9% to 5.5% (P less than or equal to .0001).
- In those who received endovascular treatment alone, the rate increased from 2.8% to 9.0% (P = .0006).
- In patients who received both thrombolysis and endovascular treatment, the rate grew from 2.0% to 10.3% (P = .0009).
Dr. Adil said several factors can affect rates of withdrawal of care in ischemic stroke patients, such as the level of illness (patients receiving aggressive treatment are sicker), advance directives, and the decisions of family members. Some institutions may be more likely to push for withdrawal of care, too, he said. “At my institution, we are not aggressive with withdrawal of care, and I have seen a few better outcomes than expected,” he said.
Also, the lack of useful data regarding prognosis for these patients may lead to premature decisions regarding withdrawal of care, he said.
“We have few prognostic models/scores that predict mortality, and these models are not very sensitive and specific,” Dr. Adil said. “Often, physicians make these decisions based on their previous experiences. All of this leads to premature withdrawal of care. On the other hand, because of premature withdrawal of care, we do not have the data on long-term outcomes on these patients, leading to errors in prognostication.”
In an interview, Adam G. Kelly, MD, a neurologist at the University of Rochester (N.Y.) and chief of neurology at Highland Hospital in Rochester, said the study is important but lacks crucial information such as the circumstances surrounding the care decisions. He hasn’t noticed trends in withdrawal of care among his patients.
“It’s possible that providers have become better at documenting discussions with patients and families which allowed this information to be better captured,” he said. “As the authors mention, it’s also possible that providers are consciously or unconsciously delivering prognoses that are biased towards negative outcomes, leading patients and families to be more apt to choose a palliative approach.”
Dr. Kelly added that neurologists need to objectively offer prognoses in stroke cases. “When the outcome is in doubt, I recommend time-limited trials of interventions of mechanical ventilation, artificial feeding, and other high-intensity interventions to allow patients and families to make the decision they feel is best,” he said.
What about trends in the years since 2011? Dr. Adil said information regarding the years since 2011 wasn’t available to him, but he hopes to analyze the period from 2012 to 2016.
Dr. Adil discussed his study and its implications in a video interview.
No funding is reported. Dr. Adil reports no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – U.S. physicians chose to withdraw life-sustaining care from critically ill ischemic stroke patients at much higher rates in 2011 than in 2006, according to results of a new study, although overall percentages remain low.
The trend was bolstered by big jumps in “withdrawal of care” among patients who underwent thrombolysis or both thrombolysis and endovascular treatment: Over the 5-year period, their likelihood of having care withdrawn increased fivefold.
The study authors don’t know whether the trends have continued over the past 6 years, and it’s not clear why the rates rose so much from 2006 to 2011. The researchers speculate that the increase could be linked to disease severity and the preferences of patients and their families.
Whatever the case, study lead author Malik Muhammad Adil, MD, a neurology resident at the Ochsner Clinic Foundation in New Orleans, cautioned that prematurely withdrawing care can throw off stroke prognostication estimates that are already fuzzy. In an interview, he said this can then lead to “significant consequences, including suboptimal outcomes and higher risk of short-term mortality.”
Dr. Adil defines withdrawal of care as “discontinuation of life-sustaining interventions from a patient who is expected to die without this support.” These interventions include such treatments as intubation, mechanical ventilation, feeding tubes, antibiotics, and brain surgery, he said.
For the new study, researchers examined the Nationwide Inpatient Survey database for the years 2006-2011. They reported their findings at the annual meeting of the American Academy of Neurology.
The study reports the following regarding withdrawal of care among ischemic stroke patients:
- The rate grew in those who received neither thrombolysis nor endovascular treatment from 0.8% in 2006 to 3.0% in 2011 (P less than or equal to .0001).
- In those who received thrombolysis alone, the rate rose from 0.9% to 5.5% (P less than or equal to .0001).
- In those who received endovascular treatment alone, the rate increased from 2.8% to 9.0% (P = .0006).
- In patients who received both thrombolysis and endovascular treatment, the rate grew from 2.0% to 10.3% (P = .0009).
Dr. Adil said several factors can affect rates of withdrawal of care in ischemic stroke patients, such as the level of illness (patients receiving aggressive treatment are sicker), advance directives, and the decisions of family members. Some institutions may be more likely to push for withdrawal of care, too, he said. “At my institution, we are not aggressive with withdrawal of care, and I have seen a few better outcomes than expected,” he said.
Also, the lack of useful data regarding prognosis for these patients may lead to premature decisions regarding withdrawal of care, he said.
“We have few prognostic models/scores that predict mortality, and these models are not very sensitive and specific,” Dr. Adil said. “Often, physicians make these decisions based on their previous experiences. All of this leads to premature withdrawal of care. On the other hand, because of premature withdrawal of care, we do not have the data on long-term outcomes on these patients, leading to errors in prognostication.”
In an interview, Adam G. Kelly, MD, a neurologist at the University of Rochester (N.Y.) and chief of neurology at Highland Hospital in Rochester, said the study is important but lacks crucial information such as the circumstances surrounding the care decisions. He hasn’t noticed trends in withdrawal of care among his patients.
“It’s possible that providers have become better at documenting discussions with patients and families which allowed this information to be better captured,” he said. “As the authors mention, it’s also possible that providers are consciously or unconsciously delivering prognoses that are biased towards negative outcomes, leading patients and families to be more apt to choose a palliative approach.”
Dr. Kelly added that neurologists need to objectively offer prognoses in stroke cases. “When the outcome is in doubt, I recommend time-limited trials of interventions of mechanical ventilation, artificial feeding, and other high-intensity interventions to allow patients and families to make the decision they feel is best,” he said.
What about trends in the years since 2011? Dr. Adil said information regarding the years since 2011 wasn’t available to him, but he hopes to analyze the period from 2012 to 2016.
Dr. Adil discussed his study and its implications in a video interview.
No funding is reported. Dr. Adil reports no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Key clinical point:
Major finding: The percentages of ischemic stroke patients whose care was withdrawn grew from 0.8%-2.8% in 2006 to 3.0%-10.3% in 2011, depending on the kind of treatment they received (thrombolysis, endovascular treatment, both, or neither).
Data source: Nationwide Inpatient Survey database.
Disclosures: No funding is reported. Dr. Adil reports no relevant disclosures.
Long-term TNFi tapering possible for some with ankylosing spondylitis
BIRMINGHAM, ENGLAND – A proportion of patients with ankylosing spondylitis (AS) were able to remain on a reduced-dose regimen of a tumor necrosis factor inhibitor (TNFi) for almost 4 years, according to data from a small study presented at the British Society for Rheumatology annual conference.
In an extension of the ANSWERS (Ankylosing Spondylitis with Etanercept Regimens) trial, 4 of 12 patients receiving a once-weekly 25-mg dose of etanercept (Enbrel) had a sustained response as did 14 of 21 patients who remained on the usual once-weekly dose of 50 mg.
“Although a minority of patients maintained response to the lower dose of etanercept over the longer term, the costs savings are substantial,” said Lauren Steel and coauthors from the Norfolk and Norwich Hospitals NHS Foundation Trust in a poster presentation. Almost 18,000 pounds sterling ($23,000) could be saved per each patient who is able to stay on the lower dose for 50 months.
Further, patients who did not maintain a response on the lower dose were usually able to regain their responses when the higher dose therapy was reinstituted. On average, disease control was reestablished in three out of four patients within 14 months of reverting to standard therapy.
ANSWERS was an open-label, multicenter, randomized, pilot study that sought to determine if tapering the dose of etanercept from the recommended 50 mg to 25 mg was feasible in 47 patients with AS (J Rheumatol. 2015;42:1177–85). The premise was that dose tapering in patients who achieved a response would perhaps reduce the risk for side effects in the long term, as well as provide considerable cost savings.
About half of the patients studied achieved a response to full-dose etanercept and were able to reduce their dose. At 6 months, a clinical response was maintained by 52% of the patients taking 25 mg and 92% of the patients taking 50 mg (P = .003).
The current prospective extension of the study looked at the longer-term outcomes of the patients who successfully maintained a response to the lower dose of etanercept.
Maintenance of response was defined as no change in the primary outcome of a reduction of 50% or more or a fall of at least 2 units in the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), and at least a 2-unit reduction in spinal pain measured using a 10-point scale.
In all, 12 patients, 9 of them male, with a mean age of 52 years entered the extension study. The comparator group consisted of 21 patients who had continued taking the 50-mg dose, 20 of them male, with a mean age of 60 years.
Of the 12 patients in the 25-mg group, 1 discontinued treatment because of side effects and did not restart any further biologic treatment; 7 patients experienced a disease flare after a median of 16 months and were retreated with the 50-mg dose. Five of the seven patients who reverted to the higher dose of etanercept regained a good response; the other two patients were switched to adalimumab (Humira) because of a loss of efficacy.
Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
BIRMINGHAM, ENGLAND – A proportion of patients with ankylosing spondylitis (AS) were able to remain on a reduced-dose regimen of a tumor necrosis factor inhibitor (TNFi) for almost 4 years, according to data from a small study presented at the British Society for Rheumatology annual conference.
In an extension of the ANSWERS (Ankylosing Spondylitis with Etanercept Regimens) trial, 4 of 12 patients receiving a once-weekly 25-mg dose of etanercept (Enbrel) had a sustained response as did 14 of 21 patients who remained on the usual once-weekly dose of 50 mg.
“Although a minority of patients maintained response to the lower dose of etanercept over the longer term, the costs savings are substantial,” said Lauren Steel and coauthors from the Norfolk and Norwich Hospitals NHS Foundation Trust in a poster presentation. Almost 18,000 pounds sterling ($23,000) could be saved per each patient who is able to stay on the lower dose for 50 months.
Further, patients who did not maintain a response on the lower dose were usually able to regain their responses when the higher dose therapy was reinstituted. On average, disease control was reestablished in three out of four patients within 14 months of reverting to standard therapy.
ANSWERS was an open-label, multicenter, randomized, pilot study that sought to determine if tapering the dose of etanercept from the recommended 50 mg to 25 mg was feasible in 47 patients with AS (J Rheumatol. 2015;42:1177–85). The premise was that dose tapering in patients who achieved a response would perhaps reduce the risk for side effects in the long term, as well as provide considerable cost savings.
About half of the patients studied achieved a response to full-dose etanercept and were able to reduce their dose. At 6 months, a clinical response was maintained by 52% of the patients taking 25 mg and 92% of the patients taking 50 mg (P = .003).
The current prospective extension of the study looked at the longer-term outcomes of the patients who successfully maintained a response to the lower dose of etanercept.
Maintenance of response was defined as no change in the primary outcome of a reduction of 50% or more or a fall of at least 2 units in the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), and at least a 2-unit reduction in spinal pain measured using a 10-point scale.
In all, 12 patients, 9 of them male, with a mean age of 52 years entered the extension study. The comparator group consisted of 21 patients who had continued taking the 50-mg dose, 20 of them male, with a mean age of 60 years.
Of the 12 patients in the 25-mg group, 1 discontinued treatment because of side effects and did not restart any further biologic treatment; 7 patients experienced a disease flare after a median of 16 months and were retreated with the 50-mg dose. Five of the seven patients who reverted to the higher dose of etanercept regained a good response; the other two patients were switched to adalimumab (Humira) because of a loss of efficacy.
Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
BIRMINGHAM, ENGLAND – A proportion of patients with ankylosing spondylitis (AS) were able to remain on a reduced-dose regimen of a tumor necrosis factor inhibitor (TNFi) for almost 4 years, according to data from a small study presented at the British Society for Rheumatology annual conference.
In an extension of the ANSWERS (Ankylosing Spondylitis with Etanercept Regimens) trial, 4 of 12 patients receiving a once-weekly 25-mg dose of etanercept (Enbrel) had a sustained response as did 14 of 21 patients who remained on the usual once-weekly dose of 50 mg.
“Although a minority of patients maintained response to the lower dose of etanercept over the longer term, the costs savings are substantial,” said Lauren Steel and coauthors from the Norfolk and Norwich Hospitals NHS Foundation Trust in a poster presentation. Almost 18,000 pounds sterling ($23,000) could be saved per each patient who is able to stay on the lower dose for 50 months.
Further, patients who did not maintain a response on the lower dose were usually able to regain their responses when the higher dose therapy was reinstituted. On average, disease control was reestablished in three out of four patients within 14 months of reverting to standard therapy.
ANSWERS was an open-label, multicenter, randomized, pilot study that sought to determine if tapering the dose of etanercept from the recommended 50 mg to 25 mg was feasible in 47 patients with AS (J Rheumatol. 2015;42:1177–85). The premise was that dose tapering in patients who achieved a response would perhaps reduce the risk for side effects in the long term, as well as provide considerable cost savings.
About half of the patients studied achieved a response to full-dose etanercept and were able to reduce their dose. At 6 months, a clinical response was maintained by 52% of the patients taking 25 mg and 92% of the patients taking 50 mg (P = .003).
The current prospective extension of the study looked at the longer-term outcomes of the patients who successfully maintained a response to the lower dose of etanercept.
Maintenance of response was defined as no change in the primary outcome of a reduction of 50% or more or a fall of at least 2 units in the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), and at least a 2-unit reduction in spinal pain measured using a 10-point scale.
In all, 12 patients, 9 of them male, with a mean age of 52 years entered the extension study. The comparator group consisted of 21 patients who had continued taking the 50-mg dose, 20 of them male, with a mean age of 60 years.
Of the 12 patients in the 25-mg group, 1 discontinued treatment because of side effects and did not restart any further biologic treatment; 7 patients experienced a disease flare after a median of 16 months and were retreated with the 50-mg dose. Five of the seven patients who reverted to the higher dose of etanercept regained a good response; the other two patients were switched to adalimumab (Humira) because of a loss of efficacy.
Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
AT RHEUMATOLOGY 2017
Key clinical point:
Major finding: Four of 12 patients treated with etanercept 25 mg once weekly maintained a response at 50 months.
Data source: An extension study of 33 patients in the open-label, multicenter, randomized Ankylosing Spondylitis with Etanercept Regimens (ANSWERS) trial.
Disclosures: Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
Consider invasive mediastinal staging in higher risk NSCLC patients, despite guidelines
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) appears to be cost effective for use in non–small cell lung cancer (NSCLC) staging if the prevalence of mediastinal lymph node metastasis (MLNM) is greater than or equal to 2.5%, according to the results of single institution modeling study. In addition, the study found that confirmatory mediastinoscopy should be performed in high-risk patients in cases of negative EBUS-TBNA.
Katarzyna Czarnecka-Kujawa, MD, of the University of Toronto and Toronto General Hospital, and her colleagues performed a decision analysis to compare health outcomes and costs of four mediastinal staging strategies. They assessed the following: no invasive staging, endobronchial ultrasound-guided transbronchial need aspiration (EBUS-TBNA), mediastinoscopy, and EBUS-TBNA followed by mediastinoscopy if EBUS-TBNA results were negative. They determined incremental cost-effectiveness ratios (ICER) for all strategies and performed comprehensive sensitivity analyses using a willingness to pay threshold of $80,000 [Canadian]/quality adjusted life-year (QALY).
They used data obtained for staging, outcomes, and costs from the patients in the lung cancer program at the Toronto General Hospital from Jan. 1, 2005 to Dec. 31, 2014, as detailed in a report published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2017. doi: 10.1016/j.jtcvs.2016.12.048).
After exclusions, they utilized a final case count of 499 cases for developing their surgical and procedure cost analysis, and a total of 750 cases in their endoscopy database for endoscopy analysis. For the base-case analysis, they assumed a prevalence of mediastinal metastasis of 9%, and obtained the prevalence of a pathologic lymph nodal stage disease following EBUS-TBNA from their institutional data.
Their results showed that EBUS-TBNA followed by mediastinoscopy was the strategy that resulted in the highest QALYs, but that it had a prohibitive ICER of greater than $1.4 million/QALY. Accordingly, it may not be justifiable to use mediastinoscopy after negative EBUS-TBNA in all patients, the researchers noted. However, the researchers’ data suggest that invasive screening may be justified in a very-low-risk population (MLNM above 2.5%).
In addition, the researchers stated that “[the] benefit conveyed by detecting mediastinal metastatic disease becomes more apparent as the prevalence of MLNM increases, with confirmatory mediastinoscopy becoming cost effective in cases of negative EBUS-TBNA in patients with moderate to high probability of MLNM” (greater than 57%).
Our model points out that there is a well-defined role for the use of different modalities, including mediastinoscopy. This stresses the need for ongoing focus on maintenance of competency and skill acquisition in mediastinoscopy and EBUS-TBNA by currently practicing and future thoracic surgeons respectively,” the researchers concluded.
Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
The authors make a compelling argument for invasive mediastinal staging in patients with clinical stage I non–small cell lung cancer and acknowledge that this conflicts with current guidelines, according to Biniam Kidane, MD, of the University of Manitoba, Winnipeg, in his invited comments on the study in the Journal of Thoracic and Cardiovascular Surgery (2017 Mar 10. doi: 10.1016/j.jtcvs.2017.02.051).
Their single-payer system is likely to have a different willingness-to-pay threshold, compared with those in other countries, especially the United States, where the EBUS-TBNA strategy without invasive staging is likely to remain the cost-effective choice.
“Cost-economic analyses such as these provide a window into the factors necessary to bridge guidelines from the realm of the abstract to the realm of local reality. When interpreting these findings, clinicians should consider: 1) What EBUS resources are available? (2) What is your local EBUS sensitivity? 3) What is the prevalence of MLNM?” Dr. Kidane concluded, with the caveat that such studies are not infallible and models are based on assumptions and must be treated with care.
Dr. Kidane reported no disclosures with regard to commercial support.
The authors make a compelling argument for invasive mediastinal staging in patients with clinical stage I non–small cell lung cancer and acknowledge that this conflicts with current guidelines, according to Biniam Kidane, MD, of the University of Manitoba, Winnipeg, in his invited comments on the study in the Journal of Thoracic and Cardiovascular Surgery (2017 Mar 10. doi: 10.1016/j.jtcvs.2017.02.051).
Their single-payer system is likely to have a different willingness-to-pay threshold, compared with those in other countries, especially the United States, where the EBUS-TBNA strategy without invasive staging is likely to remain the cost-effective choice.
“Cost-economic analyses such as these provide a window into the factors necessary to bridge guidelines from the realm of the abstract to the realm of local reality. When interpreting these findings, clinicians should consider: 1) What EBUS resources are available? (2) What is your local EBUS sensitivity? 3) What is the prevalence of MLNM?” Dr. Kidane concluded, with the caveat that such studies are not infallible and models are based on assumptions and must be treated with care.
Dr. Kidane reported no disclosures with regard to commercial support.
The authors make a compelling argument for invasive mediastinal staging in patients with clinical stage I non–small cell lung cancer and acknowledge that this conflicts with current guidelines, according to Biniam Kidane, MD, of the University of Manitoba, Winnipeg, in his invited comments on the study in the Journal of Thoracic and Cardiovascular Surgery (2017 Mar 10. doi: 10.1016/j.jtcvs.2017.02.051).
Their single-payer system is likely to have a different willingness-to-pay threshold, compared with those in other countries, especially the United States, where the EBUS-TBNA strategy without invasive staging is likely to remain the cost-effective choice.
“Cost-economic analyses such as these provide a window into the factors necessary to bridge guidelines from the realm of the abstract to the realm of local reality. When interpreting these findings, clinicians should consider: 1) What EBUS resources are available? (2) What is your local EBUS sensitivity? 3) What is the prevalence of MLNM?” Dr. Kidane concluded, with the caveat that such studies are not infallible and models are based on assumptions and must be treated with care.
Dr. Kidane reported no disclosures with regard to commercial support.
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) appears to be cost effective for use in non–small cell lung cancer (NSCLC) staging if the prevalence of mediastinal lymph node metastasis (MLNM) is greater than or equal to 2.5%, according to the results of single institution modeling study. In addition, the study found that confirmatory mediastinoscopy should be performed in high-risk patients in cases of negative EBUS-TBNA.
Katarzyna Czarnecka-Kujawa, MD, of the University of Toronto and Toronto General Hospital, and her colleagues performed a decision analysis to compare health outcomes and costs of four mediastinal staging strategies. They assessed the following: no invasive staging, endobronchial ultrasound-guided transbronchial need aspiration (EBUS-TBNA), mediastinoscopy, and EBUS-TBNA followed by mediastinoscopy if EBUS-TBNA results were negative. They determined incremental cost-effectiveness ratios (ICER) for all strategies and performed comprehensive sensitivity analyses using a willingness to pay threshold of $80,000 [Canadian]/quality adjusted life-year (QALY).
They used data obtained for staging, outcomes, and costs from the patients in the lung cancer program at the Toronto General Hospital from Jan. 1, 2005 to Dec. 31, 2014, as detailed in a report published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2017. doi: 10.1016/j.jtcvs.2016.12.048).
After exclusions, they utilized a final case count of 499 cases for developing their surgical and procedure cost analysis, and a total of 750 cases in their endoscopy database for endoscopy analysis. For the base-case analysis, they assumed a prevalence of mediastinal metastasis of 9%, and obtained the prevalence of a pathologic lymph nodal stage disease following EBUS-TBNA from their institutional data.
Their results showed that EBUS-TBNA followed by mediastinoscopy was the strategy that resulted in the highest QALYs, but that it had a prohibitive ICER of greater than $1.4 million/QALY. Accordingly, it may not be justifiable to use mediastinoscopy after negative EBUS-TBNA in all patients, the researchers noted. However, the researchers’ data suggest that invasive screening may be justified in a very-low-risk population (MLNM above 2.5%).
In addition, the researchers stated that “[the] benefit conveyed by detecting mediastinal metastatic disease becomes more apparent as the prevalence of MLNM increases, with confirmatory mediastinoscopy becoming cost effective in cases of negative EBUS-TBNA in patients with moderate to high probability of MLNM” (greater than 57%).
Our model points out that there is a well-defined role for the use of different modalities, including mediastinoscopy. This stresses the need for ongoing focus on maintenance of competency and skill acquisition in mediastinoscopy and EBUS-TBNA by currently practicing and future thoracic surgeons respectively,” the researchers concluded.
Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) appears to be cost effective for use in non–small cell lung cancer (NSCLC) staging if the prevalence of mediastinal lymph node metastasis (MLNM) is greater than or equal to 2.5%, according to the results of single institution modeling study. In addition, the study found that confirmatory mediastinoscopy should be performed in high-risk patients in cases of negative EBUS-TBNA.
Katarzyna Czarnecka-Kujawa, MD, of the University of Toronto and Toronto General Hospital, and her colleagues performed a decision analysis to compare health outcomes and costs of four mediastinal staging strategies. They assessed the following: no invasive staging, endobronchial ultrasound-guided transbronchial need aspiration (EBUS-TBNA), mediastinoscopy, and EBUS-TBNA followed by mediastinoscopy if EBUS-TBNA results were negative. They determined incremental cost-effectiveness ratios (ICER) for all strategies and performed comprehensive sensitivity analyses using a willingness to pay threshold of $80,000 [Canadian]/quality adjusted life-year (QALY).
They used data obtained for staging, outcomes, and costs from the patients in the lung cancer program at the Toronto General Hospital from Jan. 1, 2005 to Dec. 31, 2014, as detailed in a report published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2017. doi: 10.1016/j.jtcvs.2016.12.048).
After exclusions, they utilized a final case count of 499 cases for developing their surgical and procedure cost analysis, and a total of 750 cases in their endoscopy database for endoscopy analysis. For the base-case analysis, they assumed a prevalence of mediastinal metastasis of 9%, and obtained the prevalence of a pathologic lymph nodal stage disease following EBUS-TBNA from their institutional data.
Their results showed that EBUS-TBNA followed by mediastinoscopy was the strategy that resulted in the highest QALYs, but that it had a prohibitive ICER of greater than $1.4 million/QALY. Accordingly, it may not be justifiable to use mediastinoscopy after negative EBUS-TBNA in all patients, the researchers noted. However, the researchers’ data suggest that invasive screening may be justified in a very-low-risk population (MLNM above 2.5%).
In addition, the researchers stated that “[the] benefit conveyed by detecting mediastinal metastatic disease becomes more apparent as the prevalence of MLNM increases, with confirmatory mediastinoscopy becoming cost effective in cases of negative EBUS-TBNA in patients with moderate to high probability of MLNM” (greater than 57%).
Our model points out that there is a well-defined role for the use of different modalities, including mediastinoscopy. This stresses the need for ongoing focus on maintenance of competency and skill acquisition in mediastinoscopy and EBUS-TBNA by currently practicing and future thoracic surgeons respectively,” the researchers concluded.
Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:
Major finding: Once the pathologic lymph nodal stage reaches 57%, EBUS-TBNA followed by mediastinoscopy is cost effective.
Data source: A model of health care outcomes and costs was developed from data obtained from patients treated over a 10-year period at a single institution.
Disclosures: Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
Educate patients about dense breasts and cancer risk
Monica Saini, MD, a radiologist in Santa Fe, New Mexico, and JoAnn Pushkin, executive director of the nonprofit educational website DenseBreast-info.org, engaged ObGyn attendees on “Breast density: Why it matters and what to do” at the American College of Obstetricians and Gynecologists (ACOG) 2017 Annual Clinical and Scientific Meeting (May 6–9, 2017) in San Diego, California. The program was sponsored by GE Healthcare.
DENSE BREASTS ARE A RISK FACTOR FOR CANCER
Breast density is the second largest risk factor for breast cancer after radiation treatment to the chest, so it is important to identify patients with dense breasts, according to Dr. Saini. The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) classifies breast density into 4 groups: 1) almost entirely fatty, 2) scattered fibroglandular densities, 3) heterogeneously dense, and 4) extremely dense. A woman whose mammograms show heterogeneously dense or extremely dense breasts is considered to have “dense breasts.”
Cancer is often difficult to identify with mammography in dense breasts because masses or lumps appear as white on a white (dense tissue) background; by contrast, a tumor in a nondense (fatty) breast would appear as white on a dark, fatty tissue background. Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, said Dr. Saini.
Having dense breasts is not an abnormal condition, however, and is actually common—about 40% of women aged 40 or older have dense breasts.
Supplement mammography with other screening modalities
While screening mammograms can save lives, mammography should not be viewed as a one-size-fits-all modality. Screening for breast cancer should be personalized, based on, among other factors, a woman’s personal and family history, age, genetic risk, lifestyle factors, and breast density.
Key point. Women with dense breasts should continue to have screening mammograms. In addition, mammography for these patients should be supplemented with other technologies, such as 3D mammography (digital tomosynthesis), handheld ultrasound, or automated breast ultrasound (ABUS). In women at higher risk (presence of BRCA1 or BRCA2 gene mutation, strong family history of breast cancer, or radiation treatment to the chest) magnetic resonance imaging (MRI) may be considered.
Data on adjunct screening modalities. Dr. Saini discussed the results of the ASTOUND trial, a prospective multicenter study that compared ultrasound and tomosynthesis for the detection of breast cancer in mammography-negative dense breasts.1 Among the 3,231 asymptomatic women included in the trial, 13 breast cancers were detected with tomosynthesis (incremental cancer detection rate [CDR], 4 per 1,000 screens; 95% confidence interval [CI], 1.8–6.2) and 23 were detected with ultrasound (incremental CDR, 7.1 per 1,000 screens; 95% CI, 4.4–10.0), P = .006. There were 107 false-positive results: 53 with tomosynthesis and 65 with ultrasound, a difference that was not statistically significant. The study authors noted that while ultrasound had better incremental breast cancer detection than tomosynthesis, and at a similar false-positive recall rate, tomosynthesis did detect more than half of the additional breast cancers in these women.1
Make screening easier for the patient
Dr. Saini noted that for women with dense breasts, performing mammography and adjunctive screening at the same visit is convenient for the patient. Physicians can also write prescriptions for follow-up based on density findings, for example, “3D mammography if available, if dense, order ultrasound.”
Read how to answer patient questions about breast density
ARE YOU READY TO ANSWER PATIENT QUESTIONS ABOUT BREAST DENSITY?
That is the question JoAnn Pushkin, executive director of DenseBreast-info.org, asked in her presentation. You should discuss with patients exactly what it means to have dense breasts, breast density as an independent risk factor for cancer, the breast imaging technologies available for screening (mammography, tomosynthesis, ultrasound, contrast-enhanced MRI), the risks and benefits of each screening modality, and surveillance intervals for women with dense breasts. Good communication with the patient’s radiology team assists in formulating an individualized screening strategy.
Patients may have concerns about the information provided—or not provided—in their state’s breast density notification letter after a mammogram. Currently, 31 states mandate some type of breast density notification, while 4 states have efforts for density reporting or education that do not require notification. The information given to patients and how they will be informed varies by state. Some states, for example, require that patients who have heterogeneously or extremely dense breasts be informed of this by letter, while other states require that all patients receive the same notification with information about dense breasts but does not tell them whether or not they have dense breasts.
A go-to resource for ObGyns and patients
The website of the nonprofit DenseBreast-Info.org (http://densebreast-info.org/), co-founded by Wendie Berg, MD, PhD, who serves as Chief Scientific Advisor to the organization and is Professor of Radiology at the University of Pittsburgh School of Medicine/Magee-Women’s Hospital of UPMC, provides an interactive US map that features state-by-state breast density reporting guidelines so you can stay up-to-date on notification legislation in your area.
Sections for patients offer comprehensive and clearly written information on categories of breast density, a patient risk checklist, screening test descriptions, frequently asked questions, educational videos, and a patient brochure in English and Spanish.
For health care providers, resources include:
- a screening decision support tool flowchart to help assess which patients need more screening
- a table summarizing the cancer detection rates for mammography alone and mammography plus another screening modality (tomosynthesis, ultrasound, MRI)
- a comparison of breast cancer screening guidelines from various medical societies, including the American College of Radiology/Society of Breast Imaging, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the US Preventive Services Task Force.
A special section covers screening technology, and each page includes descriptions, benefits, and considerations for use. Photos of the equipment and images of breast scans with explanatory captions enhance understanding.
Screening for high-risk women
Ms. Pushkin noted that for high-risk patients with dense breasts, mammography plus MRI annually would be an appropriate option.
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2015]. J Clin Oncol. doi:10.1200/JCO.2015.63.4147.
Monica Saini, MD, a radiologist in Santa Fe, New Mexico, and JoAnn Pushkin, executive director of the nonprofit educational website DenseBreast-info.org, engaged ObGyn attendees on “Breast density: Why it matters and what to do” at the American College of Obstetricians and Gynecologists (ACOG) 2017 Annual Clinical and Scientific Meeting (May 6–9, 2017) in San Diego, California. The program was sponsored by GE Healthcare.
DENSE BREASTS ARE A RISK FACTOR FOR CANCER
Breast density is the second largest risk factor for breast cancer after radiation treatment to the chest, so it is important to identify patients with dense breasts, according to Dr. Saini. The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) classifies breast density into 4 groups: 1) almost entirely fatty, 2) scattered fibroglandular densities, 3) heterogeneously dense, and 4) extremely dense. A woman whose mammograms show heterogeneously dense or extremely dense breasts is considered to have “dense breasts.”
Cancer is often difficult to identify with mammography in dense breasts because masses or lumps appear as white on a white (dense tissue) background; by contrast, a tumor in a nondense (fatty) breast would appear as white on a dark, fatty tissue background. Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, said Dr. Saini.
Having dense breasts is not an abnormal condition, however, and is actually common—about 40% of women aged 40 or older have dense breasts.
Supplement mammography with other screening modalities
While screening mammograms can save lives, mammography should not be viewed as a one-size-fits-all modality. Screening for breast cancer should be personalized, based on, among other factors, a woman’s personal and family history, age, genetic risk, lifestyle factors, and breast density.
Key point. Women with dense breasts should continue to have screening mammograms. In addition, mammography for these patients should be supplemented with other technologies, such as 3D mammography (digital tomosynthesis), handheld ultrasound, or automated breast ultrasound (ABUS). In women at higher risk (presence of BRCA1 or BRCA2 gene mutation, strong family history of breast cancer, or radiation treatment to the chest) magnetic resonance imaging (MRI) may be considered.
Data on adjunct screening modalities. Dr. Saini discussed the results of the ASTOUND trial, a prospective multicenter study that compared ultrasound and tomosynthesis for the detection of breast cancer in mammography-negative dense breasts.1 Among the 3,231 asymptomatic women included in the trial, 13 breast cancers were detected with tomosynthesis (incremental cancer detection rate [CDR], 4 per 1,000 screens; 95% confidence interval [CI], 1.8–6.2) and 23 were detected with ultrasound (incremental CDR, 7.1 per 1,000 screens; 95% CI, 4.4–10.0), P = .006. There were 107 false-positive results: 53 with tomosynthesis and 65 with ultrasound, a difference that was not statistically significant. The study authors noted that while ultrasound had better incremental breast cancer detection than tomosynthesis, and at a similar false-positive recall rate, tomosynthesis did detect more than half of the additional breast cancers in these women.1
Make screening easier for the patient
Dr. Saini noted that for women with dense breasts, performing mammography and adjunctive screening at the same visit is convenient for the patient. Physicians can also write prescriptions for follow-up based on density findings, for example, “3D mammography if available, if dense, order ultrasound.”
Read how to answer patient questions about breast density
ARE YOU READY TO ANSWER PATIENT QUESTIONS ABOUT BREAST DENSITY?
That is the question JoAnn Pushkin, executive director of DenseBreast-info.org, asked in her presentation. You should discuss with patients exactly what it means to have dense breasts, breast density as an independent risk factor for cancer, the breast imaging technologies available for screening (mammography, tomosynthesis, ultrasound, contrast-enhanced MRI), the risks and benefits of each screening modality, and surveillance intervals for women with dense breasts. Good communication with the patient’s radiology team assists in formulating an individualized screening strategy.
Patients may have concerns about the information provided—or not provided—in their state’s breast density notification letter after a mammogram. Currently, 31 states mandate some type of breast density notification, while 4 states have efforts for density reporting or education that do not require notification. The information given to patients and how they will be informed varies by state. Some states, for example, require that patients who have heterogeneously or extremely dense breasts be informed of this by letter, while other states require that all patients receive the same notification with information about dense breasts but does not tell them whether or not they have dense breasts.
A go-to resource for ObGyns and patients
The website of the nonprofit DenseBreast-Info.org (http://densebreast-info.org/), co-founded by Wendie Berg, MD, PhD, who serves as Chief Scientific Advisor to the organization and is Professor of Radiology at the University of Pittsburgh School of Medicine/Magee-Women’s Hospital of UPMC, provides an interactive US map that features state-by-state breast density reporting guidelines so you can stay up-to-date on notification legislation in your area.
Sections for patients offer comprehensive and clearly written information on categories of breast density, a patient risk checklist, screening test descriptions, frequently asked questions, educational videos, and a patient brochure in English and Spanish.
For health care providers, resources include:
- a screening decision support tool flowchart to help assess which patients need more screening
- a table summarizing the cancer detection rates for mammography alone and mammography plus another screening modality (tomosynthesis, ultrasound, MRI)
- a comparison of breast cancer screening guidelines from various medical societies, including the American College of Radiology/Society of Breast Imaging, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the US Preventive Services Task Force.
A special section covers screening technology, and each page includes descriptions, benefits, and considerations for use. Photos of the equipment and images of breast scans with explanatory captions enhance understanding.
Screening for high-risk women
Ms. Pushkin noted that for high-risk patients with dense breasts, mammography plus MRI annually would be an appropriate option.
Monica Saini, MD, a radiologist in Santa Fe, New Mexico, and JoAnn Pushkin, executive director of the nonprofit educational website DenseBreast-info.org, engaged ObGyn attendees on “Breast density: Why it matters and what to do” at the American College of Obstetricians and Gynecologists (ACOG) 2017 Annual Clinical and Scientific Meeting (May 6–9, 2017) in San Diego, California. The program was sponsored by GE Healthcare.
DENSE BREASTS ARE A RISK FACTOR FOR CANCER
Breast density is the second largest risk factor for breast cancer after radiation treatment to the chest, so it is important to identify patients with dense breasts, according to Dr. Saini. The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) classifies breast density into 4 groups: 1) almost entirely fatty, 2) scattered fibroglandular densities, 3) heterogeneously dense, and 4) extremely dense. A woman whose mammograms show heterogeneously dense or extremely dense breasts is considered to have “dense breasts.”
Cancer is often difficult to identify with mammography in dense breasts because masses or lumps appear as white on a white (dense tissue) background; by contrast, a tumor in a nondense (fatty) breast would appear as white on a dark, fatty tissue background. Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, said Dr. Saini.
Having dense breasts is not an abnormal condition, however, and is actually common—about 40% of women aged 40 or older have dense breasts.
Supplement mammography with other screening modalities
While screening mammograms can save lives, mammography should not be viewed as a one-size-fits-all modality. Screening for breast cancer should be personalized, based on, among other factors, a woman’s personal and family history, age, genetic risk, lifestyle factors, and breast density.
Key point. Women with dense breasts should continue to have screening mammograms. In addition, mammography for these patients should be supplemented with other technologies, such as 3D mammography (digital tomosynthesis), handheld ultrasound, or automated breast ultrasound (ABUS). In women at higher risk (presence of BRCA1 or BRCA2 gene mutation, strong family history of breast cancer, or radiation treatment to the chest) magnetic resonance imaging (MRI) may be considered.
Data on adjunct screening modalities. Dr. Saini discussed the results of the ASTOUND trial, a prospective multicenter study that compared ultrasound and tomosynthesis for the detection of breast cancer in mammography-negative dense breasts.1 Among the 3,231 asymptomatic women included in the trial, 13 breast cancers were detected with tomosynthesis (incremental cancer detection rate [CDR], 4 per 1,000 screens; 95% confidence interval [CI], 1.8–6.2) and 23 were detected with ultrasound (incremental CDR, 7.1 per 1,000 screens; 95% CI, 4.4–10.0), P = .006. There were 107 false-positive results: 53 with tomosynthesis and 65 with ultrasound, a difference that was not statistically significant. The study authors noted that while ultrasound had better incremental breast cancer detection than tomosynthesis, and at a similar false-positive recall rate, tomosynthesis did detect more than half of the additional breast cancers in these women.1
Make screening easier for the patient
Dr. Saini noted that for women with dense breasts, performing mammography and adjunctive screening at the same visit is convenient for the patient. Physicians can also write prescriptions for follow-up based on density findings, for example, “3D mammography if available, if dense, order ultrasound.”
Read how to answer patient questions about breast density
ARE YOU READY TO ANSWER PATIENT QUESTIONS ABOUT BREAST DENSITY?
That is the question JoAnn Pushkin, executive director of DenseBreast-info.org, asked in her presentation. You should discuss with patients exactly what it means to have dense breasts, breast density as an independent risk factor for cancer, the breast imaging technologies available for screening (mammography, tomosynthesis, ultrasound, contrast-enhanced MRI), the risks and benefits of each screening modality, and surveillance intervals for women with dense breasts. Good communication with the patient’s radiology team assists in formulating an individualized screening strategy.
Patients may have concerns about the information provided—or not provided—in their state’s breast density notification letter after a mammogram. Currently, 31 states mandate some type of breast density notification, while 4 states have efforts for density reporting or education that do not require notification. The information given to patients and how they will be informed varies by state. Some states, for example, require that patients who have heterogeneously or extremely dense breasts be informed of this by letter, while other states require that all patients receive the same notification with information about dense breasts but does not tell them whether or not they have dense breasts.
A go-to resource for ObGyns and patients
The website of the nonprofit DenseBreast-Info.org (http://densebreast-info.org/), co-founded by Wendie Berg, MD, PhD, who serves as Chief Scientific Advisor to the organization and is Professor of Radiology at the University of Pittsburgh School of Medicine/Magee-Women’s Hospital of UPMC, provides an interactive US map that features state-by-state breast density reporting guidelines so you can stay up-to-date on notification legislation in your area.
Sections for patients offer comprehensive and clearly written information on categories of breast density, a patient risk checklist, screening test descriptions, frequently asked questions, educational videos, and a patient brochure in English and Spanish.
For health care providers, resources include:
- a screening decision support tool flowchart to help assess which patients need more screening
- a table summarizing the cancer detection rates for mammography alone and mammography plus another screening modality (tomosynthesis, ultrasound, MRI)
- a comparison of breast cancer screening guidelines from various medical societies, including the American College of Radiology/Society of Breast Imaging, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the US Preventive Services Task Force.
A special section covers screening technology, and each page includes descriptions, benefits, and considerations for use. Photos of the equipment and images of breast scans with explanatory captions enhance understanding.
Screening for high-risk women
Ms. Pushkin noted that for high-risk patients with dense breasts, mammography plus MRI annually would be an appropriate option.
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2015]. J Clin Oncol. doi:10.1200/JCO.2015.63.4147.
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2015]. J Clin Oncol. doi:10.1200/JCO.2015.63.4147.
Los Angeles County encourages LARC use to decrease Zika cases
Los Angeles County, California, has been identified as one of 7 areas in the nation with the highest risk of local Zika transmission by the Centers for Disease Control and Prevention (CDC), advise Adriana Ramos and colleagues from Los Angeles County Department of Public Health (DPH), Maternal, Child & Adolescent Health Programs.1 One factor for this classification is the county’s high birth rate. According to Ramos at el the CDC recommends that, before a Zika outbreak occurs, health departments in areas with Aedes species mosquitos increase access to and use of effective contraception.1 Long-acting reversible contraceptives (LARCs), including the intrauterine device (IUD) and the implant, are proven most effective methods.1
In a poster presented at the American College of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting in San Diego, California, Ramos and colleagues summarized contraceptive use within LA County using data from the Los Angeles Mommy and Baby (LAMB) project, conducted by the Maternal, Child, and Adolescent Health (MCAH) Programs of the LA County DPH, which surveyed mothers who recently delivered a live baby about their preconception and perinatal experiences. In 2012, 6,893 mothers participated. In 2014, MCAH re-interviewed the 2012 LAMB respondents, excluding those with a subsequent pregnancy after the 2012 survey or who had not originally answered questions about family planning, leaving 3,175 respondents. Findings, weighted to the 2012 live-birth cohort, estimated the weighted population at 115,284 live births.1
The study defined contraception use by efficacy, identifying no contraception use, condoms, withdrawal, and the rhythm method as less effective; oral contraceptive pills and vaginal ring as moderately effective; and LARCs and sterilization as highly effective. Unintended births account for 47% of births in LAC and more than 59% of women report using less effective contraceptive methods.1
Results of the study
As a result of their study, MCAH researchers Adriana Ramos, Shin Chao, MD, MPH, and Diana E. Ramos, MD, MPH, conclude that educating providers to place LARC contraceptives and educating the public on the most effective contraceptive methods can decrease the neonatal Zika complication rates by preventing unplanned pregnancy. LAC is undertaking these activities to decrease the number of neonatal Zika cases.1
- Ramos A, Chao S, Ramos DE. Zika: Preconception & perinatal opportunities in Los Angeles County. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 6, 2017; San Diego, California.
Los Angeles County, California, has been identified as one of 7 areas in the nation with the highest risk of local Zika transmission by the Centers for Disease Control and Prevention (CDC), advise Adriana Ramos and colleagues from Los Angeles County Department of Public Health (DPH), Maternal, Child & Adolescent Health Programs.1 One factor for this classification is the county’s high birth rate. According to Ramos at el the CDC recommends that, before a Zika outbreak occurs, health departments in areas with Aedes species mosquitos increase access to and use of effective contraception.1 Long-acting reversible contraceptives (LARCs), including the intrauterine device (IUD) and the implant, are proven most effective methods.1
In a poster presented at the American College of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting in San Diego, California, Ramos and colleagues summarized contraceptive use within LA County using data from the Los Angeles Mommy and Baby (LAMB) project, conducted by the Maternal, Child, and Adolescent Health (MCAH) Programs of the LA County DPH, which surveyed mothers who recently delivered a live baby about their preconception and perinatal experiences. In 2012, 6,893 mothers participated. In 2014, MCAH re-interviewed the 2012 LAMB respondents, excluding those with a subsequent pregnancy after the 2012 survey or who had not originally answered questions about family planning, leaving 3,175 respondents. Findings, weighted to the 2012 live-birth cohort, estimated the weighted population at 115,284 live births.1
The study defined contraception use by efficacy, identifying no contraception use, condoms, withdrawal, and the rhythm method as less effective; oral contraceptive pills and vaginal ring as moderately effective; and LARCs and sterilization as highly effective. Unintended births account for 47% of births in LAC and more than 59% of women report using less effective contraceptive methods.1
Results of the study
As a result of their study, MCAH researchers Adriana Ramos, Shin Chao, MD, MPH, and Diana E. Ramos, MD, MPH, conclude that educating providers to place LARC contraceptives and educating the public on the most effective contraceptive methods can decrease the neonatal Zika complication rates by preventing unplanned pregnancy. LAC is undertaking these activities to decrease the number of neonatal Zika cases.1
Los Angeles County, California, has been identified as one of 7 areas in the nation with the highest risk of local Zika transmission by the Centers for Disease Control and Prevention (CDC), advise Adriana Ramos and colleagues from Los Angeles County Department of Public Health (DPH), Maternal, Child & Adolescent Health Programs.1 One factor for this classification is the county’s high birth rate. According to Ramos at el the CDC recommends that, before a Zika outbreak occurs, health departments in areas with Aedes species mosquitos increase access to and use of effective contraception.1 Long-acting reversible contraceptives (LARCs), including the intrauterine device (IUD) and the implant, are proven most effective methods.1
In a poster presented at the American College of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting in San Diego, California, Ramos and colleagues summarized contraceptive use within LA County using data from the Los Angeles Mommy and Baby (LAMB) project, conducted by the Maternal, Child, and Adolescent Health (MCAH) Programs of the LA County DPH, which surveyed mothers who recently delivered a live baby about their preconception and perinatal experiences. In 2012, 6,893 mothers participated. In 2014, MCAH re-interviewed the 2012 LAMB respondents, excluding those with a subsequent pregnancy after the 2012 survey or who had not originally answered questions about family planning, leaving 3,175 respondents. Findings, weighted to the 2012 live-birth cohort, estimated the weighted population at 115,284 live births.1
The study defined contraception use by efficacy, identifying no contraception use, condoms, withdrawal, and the rhythm method as less effective; oral contraceptive pills and vaginal ring as moderately effective; and LARCs and sterilization as highly effective. Unintended births account for 47% of births in LAC and more than 59% of women report using less effective contraceptive methods.1
Results of the study
As a result of their study, MCAH researchers Adriana Ramos, Shin Chao, MD, MPH, and Diana E. Ramos, MD, MPH, conclude that educating providers to place LARC contraceptives and educating the public on the most effective contraceptive methods can decrease the neonatal Zika complication rates by preventing unplanned pregnancy. LAC is undertaking these activities to decrease the number of neonatal Zika cases.1
- Ramos A, Chao S, Ramos DE. Zika: Preconception & perinatal opportunities in Los Angeles County. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 6, 2017; San Diego, California.
- Ramos A, Chao S, Ramos DE. Zika: Preconception & perinatal opportunities in Los Angeles County. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 6, 2017; San Diego, California.
Embolism major cause of stroke after open arch surgery in patients with carotid/intracranial stenosis
Embolization was the major cause of permanent stroke in patients with moderate or severe carotid or intracranial atherosclerosis who underwent elective open aortic arch surgery at a single institution, according to the results of a retrospective study.
Preoperative craniocervical and aortic screening may aid in modifying the operative strategy to reduce the incidence of stroke in these patients, according to a report published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Preventing stroke in this patient population is an important consideration, because perioperative stroke is approximately 4 times more common in open aortic arch surgery (OAAS) than in coronary artery bypass grafting or valve surgery, according to Ken-ichi Imasaka, MD, and his colleagues at the National Hospital Organization Kyushu Medical Center, Fukuoka, Japan.
The study population comprised 200 consecutive patients undergoing elective OAAS at the institution between October 2008 and October 2015, including 34% women and with a mean patient age of 71 years (J Thorac Cardiovasc Surg. 2017;153:1045-53).
After preoperative screening, 21% of patients were diagnosed with carotid or intracranial artery disease (CIAD). None of these patients were diagnosed with impaired cerebral perfusion reserve on brain SPECT (single-photon emission computed tomography). A total of 92% of patients underwent ascending aorta or aortic arch replacement through a median sternotomy, while the remaining 8% underwent extended aortic arch replacement via L-incision (15 patients) or combined median sternotomy and left posterior lateral thoracotomy (1 patient). Among the patients, 16% underwent ascending aorta replacement; 8% had partial arch replacement; and the remaining 76% had total arch replacement.
Shaggy aorta was present in 19% of the patients, with 51% of these showing CIAD (P less than .0001). A total of 30% of the patients with shaggy aorta had the total arch replacement through an L-incision or combined median sternotomy and left posterior lateral thoracotomy, a significant difference (P less than .0001).
The overall in-hospital mortality rate was 3.5%. The overall incidence of permanent stroke and paraplegia or paraparesis was 4% (8 patients) and 2% (4 patients), respectively. Three (37.5%) of the 8 permanent stroke patients died during the postoperative hospital stay, compared with 2.1% of the 192 patients without stroke.
Univariate analysis indicated that previous cerebrovascular accident (P = .0002), shaggy aorta (P less than .0001), cardiopulmonary bypass time (P = .003), selective antegrade cerebral perfusion time (P = .004), operation time (P = .02), and extended aortic repair through L-incision or combined median sternotomy and left posterior lateral thoracotomy (P = .0002) were significant risk factors for neurologic morbidity.
“Preoperative intensive screening of carotid and intracranial artery disease is a useful step to identify patients at higher risk of hemodynamic ischemic stroke. Advanced systemic atherosclerosis may be a crucial determinant of perioperative stroke due to atherothrombotic embolization. Antiembolic measures during surgery are essential to prevent perioperative stroke,” the researchers concluded.
The authors reported that they had no disclosures.
During aortic arch surgery, the lack of blood supply as a result of emboli, rather than atherosclerosis itself, kills the cerebral neurons, according to Ourania Preventza, MD, and Joseph S. Coselli, MD, of the Baylor College of Medicine, Houston, in their invited commentary (J Thorac Cardiovasc Surg. 2017;153:1054-5).
Patients with carotid and intracranial disease should indeed have more intensive screening before undergoing major aortic surgery, they agreed, but pointed out that in the absence of carotid disease, large or complex aortic atheromas can be seen in the arch, indicating that, even though atherosclerosis is a systemic disease, using different sites of prediction can be uncertain.
This requires a broader approach to prevent stroke, including careful selection of the cannulation site in patients with diffuse and heavy arch atherosclerosis or currently ulcerated plaque, they added.
“To minimize postoperative neurologic morbidities after aortic arch surgery, an individually tailored perioperative approach should be in the armamentarium of cardiac surgeons,” Dr. Preventza and Dr. Coselli concluded.
Dr. Preventza consults for Medtronic and W. L. Gore & Associates. Dr. Coselli participates in clinical research trials conducted by GlaxoSmithKline, Edwards Lifesciences, and Bolton Medical, and consults for various companies.
During aortic arch surgery, the lack of blood supply as a result of emboli, rather than atherosclerosis itself, kills the cerebral neurons, according to Ourania Preventza, MD, and Joseph S. Coselli, MD, of the Baylor College of Medicine, Houston, in their invited commentary (J Thorac Cardiovasc Surg. 2017;153:1054-5).
Patients with carotid and intracranial disease should indeed have more intensive screening before undergoing major aortic surgery, they agreed, but pointed out that in the absence of carotid disease, large or complex aortic atheromas can be seen in the arch, indicating that, even though atherosclerosis is a systemic disease, using different sites of prediction can be uncertain.
This requires a broader approach to prevent stroke, including careful selection of the cannulation site in patients with diffuse and heavy arch atherosclerosis or currently ulcerated plaque, they added.
“To minimize postoperative neurologic morbidities after aortic arch surgery, an individually tailored perioperative approach should be in the armamentarium of cardiac surgeons,” Dr. Preventza and Dr. Coselli concluded.
Dr. Preventza consults for Medtronic and W. L. Gore & Associates. Dr. Coselli participates in clinical research trials conducted by GlaxoSmithKline, Edwards Lifesciences, and Bolton Medical, and consults for various companies.
During aortic arch surgery, the lack of blood supply as a result of emboli, rather than atherosclerosis itself, kills the cerebral neurons, according to Ourania Preventza, MD, and Joseph S. Coselli, MD, of the Baylor College of Medicine, Houston, in their invited commentary (J Thorac Cardiovasc Surg. 2017;153:1054-5).
Patients with carotid and intracranial disease should indeed have more intensive screening before undergoing major aortic surgery, they agreed, but pointed out that in the absence of carotid disease, large or complex aortic atheromas can be seen in the arch, indicating that, even though atherosclerosis is a systemic disease, using different sites of prediction can be uncertain.
This requires a broader approach to prevent stroke, including careful selection of the cannulation site in patients with diffuse and heavy arch atherosclerosis or currently ulcerated plaque, they added.
“To minimize postoperative neurologic morbidities after aortic arch surgery, an individually tailored perioperative approach should be in the armamentarium of cardiac surgeons,” Dr. Preventza and Dr. Coselli concluded.
Dr. Preventza consults for Medtronic and W. L. Gore & Associates. Dr. Coselli participates in clinical research trials conducted by GlaxoSmithKline, Edwards Lifesciences, and Bolton Medical, and consults for various companies.
Embolization was the major cause of permanent stroke in patients with moderate or severe carotid or intracranial atherosclerosis who underwent elective open aortic arch surgery at a single institution, according to the results of a retrospective study.
Preoperative craniocervical and aortic screening may aid in modifying the operative strategy to reduce the incidence of stroke in these patients, according to a report published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Preventing stroke in this patient population is an important consideration, because perioperative stroke is approximately 4 times more common in open aortic arch surgery (OAAS) than in coronary artery bypass grafting or valve surgery, according to Ken-ichi Imasaka, MD, and his colleagues at the National Hospital Organization Kyushu Medical Center, Fukuoka, Japan.
The study population comprised 200 consecutive patients undergoing elective OAAS at the institution between October 2008 and October 2015, including 34% women and with a mean patient age of 71 years (J Thorac Cardiovasc Surg. 2017;153:1045-53).
After preoperative screening, 21% of patients were diagnosed with carotid or intracranial artery disease (CIAD). None of these patients were diagnosed with impaired cerebral perfusion reserve on brain SPECT (single-photon emission computed tomography). A total of 92% of patients underwent ascending aorta or aortic arch replacement through a median sternotomy, while the remaining 8% underwent extended aortic arch replacement via L-incision (15 patients) or combined median sternotomy and left posterior lateral thoracotomy (1 patient). Among the patients, 16% underwent ascending aorta replacement; 8% had partial arch replacement; and the remaining 76% had total arch replacement.
Shaggy aorta was present in 19% of the patients, with 51% of these showing CIAD (P less than .0001). A total of 30% of the patients with shaggy aorta had the total arch replacement through an L-incision or combined median sternotomy and left posterior lateral thoracotomy, a significant difference (P less than .0001).
The overall in-hospital mortality rate was 3.5%. The overall incidence of permanent stroke and paraplegia or paraparesis was 4% (8 patients) and 2% (4 patients), respectively. Three (37.5%) of the 8 permanent stroke patients died during the postoperative hospital stay, compared with 2.1% of the 192 patients without stroke.
Univariate analysis indicated that previous cerebrovascular accident (P = .0002), shaggy aorta (P less than .0001), cardiopulmonary bypass time (P = .003), selective antegrade cerebral perfusion time (P = .004), operation time (P = .02), and extended aortic repair through L-incision or combined median sternotomy and left posterior lateral thoracotomy (P = .0002) were significant risk factors for neurologic morbidity.
“Preoperative intensive screening of carotid and intracranial artery disease is a useful step to identify patients at higher risk of hemodynamic ischemic stroke. Advanced systemic atherosclerosis may be a crucial determinant of perioperative stroke due to atherothrombotic embolization. Antiembolic measures during surgery are essential to prevent perioperative stroke,” the researchers concluded.
The authors reported that they had no disclosures.
Embolization was the major cause of permanent stroke in patients with moderate or severe carotid or intracranial atherosclerosis who underwent elective open aortic arch surgery at a single institution, according to the results of a retrospective study.
Preoperative craniocervical and aortic screening may aid in modifying the operative strategy to reduce the incidence of stroke in these patients, according to a report published in the May issue of the Journal of Thoracic and Cardiovascular Surgery.
Preventing stroke in this patient population is an important consideration, because perioperative stroke is approximately 4 times more common in open aortic arch surgery (OAAS) than in coronary artery bypass grafting or valve surgery, according to Ken-ichi Imasaka, MD, and his colleagues at the National Hospital Organization Kyushu Medical Center, Fukuoka, Japan.
The study population comprised 200 consecutive patients undergoing elective OAAS at the institution between October 2008 and October 2015, including 34% women and with a mean patient age of 71 years (J Thorac Cardiovasc Surg. 2017;153:1045-53).
After preoperative screening, 21% of patients were diagnosed with carotid or intracranial artery disease (CIAD). None of these patients were diagnosed with impaired cerebral perfusion reserve on brain SPECT (single-photon emission computed tomography). A total of 92% of patients underwent ascending aorta or aortic arch replacement through a median sternotomy, while the remaining 8% underwent extended aortic arch replacement via L-incision (15 patients) or combined median sternotomy and left posterior lateral thoracotomy (1 patient). Among the patients, 16% underwent ascending aorta replacement; 8% had partial arch replacement; and the remaining 76% had total arch replacement.
Shaggy aorta was present in 19% of the patients, with 51% of these showing CIAD (P less than .0001). A total of 30% of the patients with shaggy aorta had the total arch replacement through an L-incision or combined median sternotomy and left posterior lateral thoracotomy, a significant difference (P less than .0001).
The overall in-hospital mortality rate was 3.5%. The overall incidence of permanent stroke and paraplegia or paraparesis was 4% (8 patients) and 2% (4 patients), respectively. Three (37.5%) of the 8 permanent stroke patients died during the postoperative hospital stay, compared with 2.1% of the 192 patients without stroke.
Univariate analysis indicated that previous cerebrovascular accident (P = .0002), shaggy aorta (P less than .0001), cardiopulmonary bypass time (P = .003), selective antegrade cerebral perfusion time (P = .004), operation time (P = .02), and extended aortic repair through L-incision or combined median sternotomy and left posterior lateral thoracotomy (P = .0002) were significant risk factors for neurologic morbidity.
“Preoperative intensive screening of carotid and intracranial artery disease is a useful step to identify patients at higher risk of hemodynamic ischemic stroke. Advanced systemic atherosclerosis may be a crucial determinant of perioperative stroke due to atherothrombotic embolization. Antiembolic measures during surgery are essential to prevent perioperative stroke,” the researchers concluded.
The authors reported that they had no disclosures.
Key clinical point:
Major finding: Previous cerebrovascular accident and shaggy aorta were significant determinants of neurologic morbidity.
Data source: Retrospective study of 200 consecutive patients undergoing elective aortic arch surgery at a single institution.
Disclosures: The authors reported having no conflicts of interest.