User login
Patterns of care with regard to whole-brain radiotherapy technique and delivery among academic centers in the United States
Despite the recent advances in systemic therapy, metastatic spread to the brain continues to be the most common neurologic complication of many cancers. The clinical incidence of brain metastases varies with primary cancer diagnosis, with estimates ranging from 1.2%-19.8%.1,2 Metastatic spread to the brain is even more prevalent at autopsy, with evidence of intracranial tumor being found in 26% of patients in some series.3 It is possible that the clinical incidence of metastatic disease to the brain will continue to increase as newer therapeutic agents improve survival and imaging techniques continue to improve.
The management of brain metastases has changed rapidly as technological improvements have made treatment increasingly safe and efficacious. Traditionally, treatment consisted of radiotherapy to the whole brain, with or without surgical resection.4,5 More recently, stereotactic radiosurgery (SRS) has been adopted on the basis of evidence that it is safe and efficacious alone or in combination with radiotherapy to the whole brain.6 Further evidence is emerging that neurocognitive outcomes are improved when whole-brain radiotherapy (WBRT) is omitted, which possibly contributes to improved patient quality of life.7 Taking into account this and other data, the American Society for Radiation Oncology’s Choosing Wisely campaign now recommends not routinely adding WBRT to radiosurgery in patients with limited brain metastases.8
Despite this recommendation, many patients continue to benefit from WBRT, and it remains a common treatment in radiation oncology clinics across the US for several reasons. Many patients present with multiple brain metastases and are ineligible for radiosurgery. Even for technically eligible patients, WBRT has been shown to improve local control and decrease the rate of distant brain failure over radiosurgery alone.6 With higher rates of subsequent failures, patients receiving radiosurgery alone must adhere to more rigorous follow-up and imaging schedules, which can be difficult for many rural patients who have to travel long distances to centers. Furthermore, there is some suggestion that this decreased failure rate may result in improved survival in highly selected patients with excellent disease and performance status.9 Controversies exist, however, and strong institutional biases persist, contributing to significant differences in practice. We surveyed academic radiation oncologists and in an effort to identify and describe practice patterns in the delivery of WBRT at academic centers.
Methods
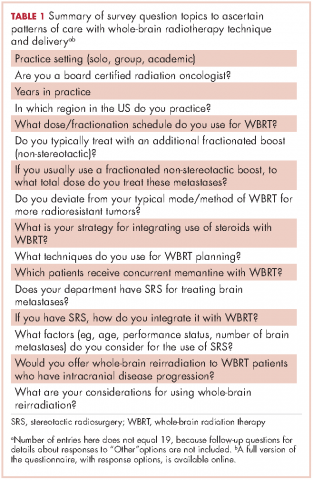
We conducted a thorough review of available literature on radiation for brain metastases and based on our findings, devised a survey 19 questions to ascertain practice patterns and treatment delivery among US academic physicians (Table 1). After obtaining institutional review board approval to do the study, we sent the survey to program coordinators at radiation oncology programs that are accredited by the Accreditation Council for Graduate Medical Education. We instructed coordinators to e-mail the survey to their practicing resident and attending physicians. The surveys were created using SurveyMonkey software. We obtained informed consent from the providers. A total of 3 follow-up e-mails were sent to each recipient of the survey to solicit responses, similar to the Dillman Total Design Survey Method.10
SPSS version 22.0 was used to analyze the data in an exploratory fashion. Statistical methods were used to assess the association of demographic data with SRS and WBRT delivery and treatment technique items when the analyses involved percentages that included the Pearson chi-square statistic and the chi-square test for linear trend. When the analysis focused on ranking data, the Kruskal-Wallis test, Mann-Whitney U test, the Jonckheere-Terpstra and the Kendall tau-b rank correlation were used as appropriate. If there were small sample sizes within some groups, then exact significant levels were assessed. Statistical significance was set by convention at P < .05.
Results
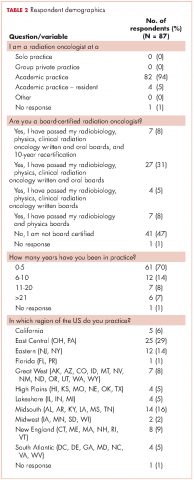
We received 95 responses of which 87 were considered complete for analysis. Forty-seven percent of the 87 respondents were not board-certified, and the remainder had passed their radiobiology and physics boards exams. A majority of respondents (70%, 61 of 87) were physicians who had been in practice for ≤5 years. Fifty-four percent of respondents were located in the Northeast US, 22% in the South, 14% in the West, and 10% in the Midwest and Hawaii (Table 2).
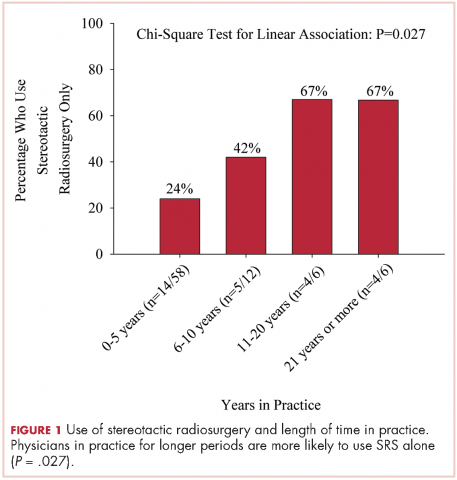
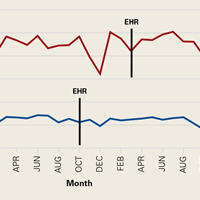
We used the chi-square test for linear trends to assess for a relationship between years of practice and whether respondents deviated from their typical method of WBRT therapy when treating more radioresistant tumors (melanoma, renal cell carcinoma). Respondents were classified by years in practice: 0-5, 6-10, 11-20, and >21 years. The results showed a linear association, with those in practice for longer periods more likely to use SRS alone, P = .027 (Figure 1).
Discussion
The incidence of brain metastases is increasing because of improvements in diagnostic imaging techniques and advancements in systemic therapy control of extracranial disease but not of intracranial disease or metastasis, because therapies do not cross the blood-brain barrier.11,12 Brain metastases are the most common type of brain tumor. Given that most chemotherapeutic agents cannot cross the blood-brain barrier, radiotherapy is considered a means of treatment and of controlling brain metastases. Early data from the 1950s13 and 1960s14 have suggested clinical improvement with brain radiation, making radiotherapy the cornerstone for treatment of brain metastases.
The Radiation Therapy Oncology Group (RTOG) has evaluated several fractionation schedules, with 5 schemas evaluated by the RTOG 6901 and 7361 studies: 30 Gy in 10 fractions, 30 Gy in 15 fractions, 40 Gy in 15 fractions, 40 Gy in 20 fractions, and 20 Gy in 5 fractions. The combined results from these two trials showed that outcomes were similar for patients treated with a shorter regimen than for those treated with a more protracted schedule. In our study, respondents reported that they most frequently treated brain metastases to a total dose of 30 Gy in 10 fractions. Given the results of the aforementioned RTOG trials and practice patterns among academic physicians, we recommend all practitioners consider a shorter hypofractioned course when treating brain metastases with WBRT. This will also reduce delays for patients who are likely to benefit greatly from earlier enrollment into hospice care, because protracted radiation schedules typically are not covered while a patient is in hospice.
Pharmacologic management for patients with brain metastases is important for symptomatic improvement. Glucocorticoids are important for palliation of symptoms from edema and increased intracranial pressure.15 However, steroids have a multitude of side effects and their use in asymptomatic patients is unnecessary. Improvements in imaging and detection11 have allowed us to find smaller and asymptomatic brain tumors. In our survey, it was promising to see a change in former practice patterns, with only 8% of academic practitioners regularly prescribing steroids to all of their patients receiving whole-brain radiation.
Diminished cognitive function and short-term memory loss are troublesome side effects of WBRT. As cancer patients live longer, such cognitive dysfunction will become more than just a nuisance. The RTOG has investigated the use of prophylactic memantine for patients receiving whole-brain radiation to determine if it would aid in the preservation of cognition. It found that patients who received memantine did better and had delayed time to cognitive decline and a reduced rate of memory decline, executive function, and processing speed.16 In our study, about a third of practitioners prescribed memantine and it was reserved for patients who had an otherwise favorable prognosis.
The RTOG has also investigated adjusting treatment technique for patients who receive WBRT. RTOG 0933 was a phase 2 trial that evaluated hippocampal avoidance during deliverance of WBRT with intensity-modulated radiation therapy (IMRT). Results showed that avoiding the hippocampus during WBRT was associated with improved memory preservation and patient quality of life.17 In a survey of practicing radiation oncologists in the US, most reported that they did not use memantine or IMRT for hippocampal sparing when delivering whole-brain radiation.18 Given the positive results of RTOG 0933 and 0614, the NRG Oncology research organization is conducting a phase 3 randomized trial that compares memantine use for patients receiving whole-brain radiation with or without hippocampal sparing to determine if patients will have reduced cognitive decline. All patients receiving WBRT should be considered for enrolment on this trial if they are eligible.
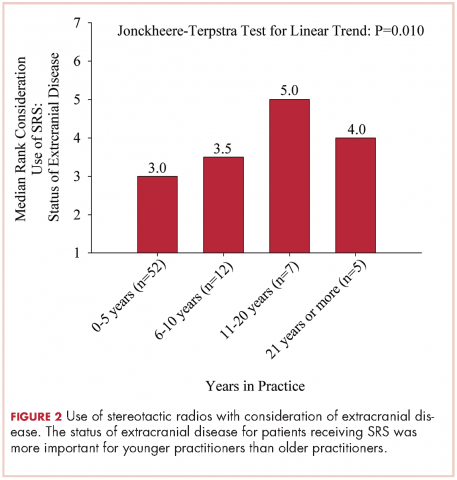
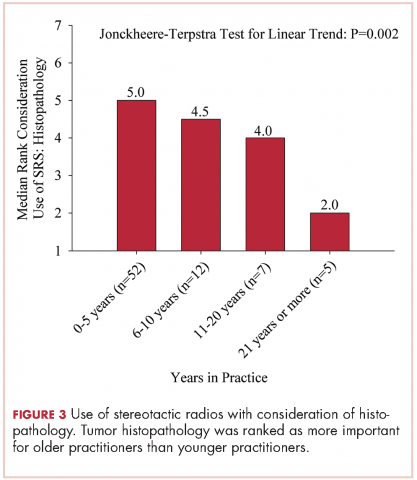
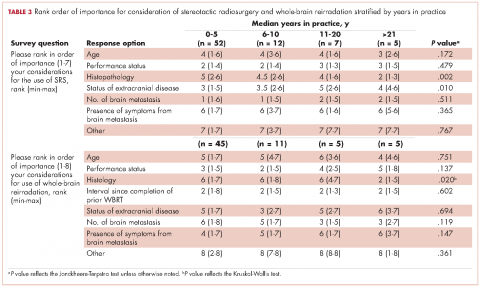
The delivery of brain radiation has continued to change, especially with the introduction of SRS. Recent publication of a meta-analysis of three phase 3 trials evaluating SRS with or without WBRT for 1-4 brain metastases showed that patients aged 50 years or younger experienced a survival benefit with SRS, and the omission of whole-brain radiation did not affect distant brain relapse rates. 19 The authors recommended that for this population, SRS alone is the preferred treatment. In our study, physicians who had been in practice for a longer time were more likely to treat using SRS alone. The results showed a linear association, with those in practice for a longer time being more likely to use SRS alone compared with those practicing for a shorter time (P = .027). Accordingly, 67% of respondents (8 of 12) who had been in practice for 11 or more years used SRS alone, whereas 24% (14 of 58) who had practiced for 0-5 years and 42% (5 of 12) who had practice from 6-10 years used SRS alone (Figure 1). When treating with SRS, younger practitioners placed more importance on the status of extracranial disease, whereas older practitioners placed more importance on tumor histopathology.
The use of repeat whole-brain reirradiation is more controversial among practitioners.20-22 Son and colleagues evaluated patients who needed whole-brain reirradiation after intracranial disease progression.22 The authors noted that patients with stable extracranial disease benefited from reirradiation. In our study, we found that when considering whole-brain reirradiation, older practitioners placed more importance on tumor histology than other factors.
As far as we know, this is the first study evaluating the practices and patterns of care with regard to the delivery of brain radiation in academic centers in the US. We found that time in practice was the most significant predictor of treatment technique and delivery. We also found that older practitioners place more importance on tumor histopathology compared with younger practitioners. A limitation of this study is that we had contact information only for program coordinators at ACGME-accredited programs. As such, we were not able to assess practice patterns among community practitioners. In addition, it seemed that residents and junior faculty were more likely to respond to this survey, likely because of the dissemination pattern. Given the evolution and diversity of treatment regimens for brain metastases, we believe that patients with brain metastases should be managed individually using a multidisciplinary approach.
1. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004;22(14):2865-2872.
2. Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94(10):2698-2705.
3. Takakura K. Metastatic tumors of the central nervous system. Tokyo: Igaku-Shoin; 1982.
4. Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998;280(17):1485-1489.
5. Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. New Engl J Med. 1990;322(8):494-500.
6. Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol Biol Phys. 2015;91(4):710-717.
7. Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10(11):1037-1044.
8. Choosing Wisely [ASTRO]. Don’t routinely add adjuvant whole-brain radiation therapy to stereotactic radiosurgery for limited brain metastases. http://www.choosingwisely.org/clinician-lists/american-society-radiation-oncology-adjunct-whole-brain-radiation-therapy/. Updated June 21, 2016. Accessed November 10, 2016.
9. Aoyama H, Tago M, Shirato H, Japanese Radiation Oncology Study Group I. Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 Randomized Clinical Trial. JAMA Oncol. 2015;1(4):457-464.
10. Hoddinott SN, Bass MJ. The Dillman total design survey method. Can Fam Physician. 1986;32:2366-2368.
11. Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012;14(1):48-54.
12. Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. 2005;75(1):5-14.
13. Chao JH, Phillips R, Nickson JJ. Roentgen-ray therapy of cerebral metastases. Cancer. 1954;7(4):682-689.
14. Nieder C, Niewald M, Schnabel K. Treatment of brain metastases from hypernephroma. Urol Int. 1996;57(1):17-20.
15. Ryken TC, McDermott M, Robinson PD, et al. The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96(1):103-114.
16. Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15(10):1429-1437.
17. Gondi V, Pugh SL, Tome WA, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol. 2014;32(34):3810-3816.
18. Slade AN, Stanic S. The impact of RTOG 0614 and RTOG 0933 trials in routine clinical practice: The US Survey of Utilization of Memantine and IMRT planning for hippocampus sparing in patients receiving whole-brain radiotherapy for brain metastases. Contemp Clin Trials. 2016;47:74-77.
19. Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. International journal of radiation oncology, biology, physics. 2015;91(4):710-717.
20. Hazuka MB, Kinzie JJ. Brain metastases: results and effects of re-irradiation. Int J Radiat Oncol Biol Phys. 1988;15(2):433-437.
21. Sadikov E, Bezjak A, Yi QL, et al. Value of whole-brain re-irradiation for brain metastases — single centre experience. Clin Oncol (R Coll Radiol). 2007;19(7):532-538.
22. Son CH, Jimenez R, Niemierko A, Loeffler JS, Oh KS, Shih HA. outcomes after whole-brain reirradiation in patients with brain metastases. Int J Radiat Oncol Biol Phys. 2012;82(2):e167-e172.
Despite the recent advances in systemic therapy, metastatic spread to the brain continues to be the most common neurologic complication of many cancers. The clinical incidence of brain metastases varies with primary cancer diagnosis, with estimates ranging from 1.2%-19.8%.1,2 Metastatic spread to the brain is even more prevalent at autopsy, with evidence of intracranial tumor being found in 26% of patients in some series.3 It is possible that the clinical incidence of metastatic disease to the brain will continue to increase as newer therapeutic agents improve survival and imaging techniques continue to improve.
The management of brain metastases has changed rapidly as technological improvements have made treatment increasingly safe and efficacious. Traditionally, treatment consisted of radiotherapy to the whole brain, with or without surgical resection.4,5 More recently, stereotactic radiosurgery (SRS) has been adopted on the basis of evidence that it is safe and efficacious alone or in combination with radiotherapy to the whole brain.6 Further evidence is emerging that neurocognitive outcomes are improved when whole-brain radiotherapy (WBRT) is omitted, which possibly contributes to improved patient quality of life.7 Taking into account this and other data, the American Society for Radiation Oncology’s Choosing Wisely campaign now recommends not routinely adding WBRT to radiosurgery in patients with limited brain metastases.8
Despite this recommendation, many patients continue to benefit from WBRT, and it remains a common treatment in radiation oncology clinics across the US for several reasons. Many patients present with multiple brain metastases and are ineligible for radiosurgery. Even for technically eligible patients, WBRT has been shown to improve local control and decrease the rate of distant brain failure over radiosurgery alone.6 With higher rates of subsequent failures, patients receiving radiosurgery alone must adhere to more rigorous follow-up and imaging schedules, which can be difficult for many rural patients who have to travel long distances to centers. Furthermore, there is some suggestion that this decreased failure rate may result in improved survival in highly selected patients with excellent disease and performance status.9 Controversies exist, however, and strong institutional biases persist, contributing to significant differences in practice. We surveyed academic radiation oncologists and in an effort to identify and describe practice patterns in the delivery of WBRT at academic centers.
Methods
We conducted a thorough review of available literature on radiation for brain metastases and based on our findings, devised a survey 19 questions to ascertain practice patterns and treatment delivery among US academic physicians (Table 1). After obtaining institutional review board approval to do the study, we sent the survey to program coordinators at radiation oncology programs that are accredited by the Accreditation Council for Graduate Medical Education. We instructed coordinators to e-mail the survey to their practicing resident and attending physicians. The surveys were created using SurveyMonkey software. We obtained informed consent from the providers. A total of 3 follow-up e-mails were sent to each recipient of the survey to solicit responses, similar to the Dillman Total Design Survey Method.10
SPSS version 22.0 was used to analyze the data in an exploratory fashion. Statistical methods were used to assess the association of demographic data with SRS and WBRT delivery and treatment technique items when the analyses involved percentages that included the Pearson chi-square statistic and the chi-square test for linear trend. When the analysis focused on ranking data, the Kruskal-Wallis test, Mann-Whitney U test, the Jonckheere-Terpstra and the Kendall tau-b rank correlation were used as appropriate. If there were small sample sizes within some groups, then exact significant levels were assessed. Statistical significance was set by convention at P < .05.
Results
We received 95 responses of which 87 were considered complete for analysis. Forty-seven percent of the 87 respondents were not board-certified, and the remainder had passed their radiobiology and physics boards exams. A majority of respondents (70%, 61 of 87) were physicians who had been in practice for ≤5 years. Fifty-four percent of respondents were located in the Northeast US, 22% in the South, 14% in the West, and 10% in the Midwest and Hawaii (Table 2).
We used the chi-square test for linear trends to assess for a relationship between years of practice and whether respondents deviated from their typical method of WBRT therapy when treating more radioresistant tumors (melanoma, renal cell carcinoma). Respondents were classified by years in practice: 0-5, 6-10, 11-20, and >21 years. The results showed a linear association, with those in practice for longer periods more likely to use SRS alone, P = .027 (Figure 1).
Discussion
The incidence of brain metastases is increasing because of improvements in diagnostic imaging techniques and advancements in systemic therapy control of extracranial disease but not of intracranial disease or metastasis, because therapies do not cross the blood-brain barrier.11,12 Brain metastases are the most common type of brain tumor. Given that most chemotherapeutic agents cannot cross the blood-brain barrier, radiotherapy is considered a means of treatment and of controlling brain metastases. Early data from the 1950s13 and 1960s14 have suggested clinical improvement with brain radiation, making radiotherapy the cornerstone for treatment of brain metastases.
The Radiation Therapy Oncology Group (RTOG) has evaluated several fractionation schedules, with 5 schemas evaluated by the RTOG 6901 and 7361 studies: 30 Gy in 10 fractions, 30 Gy in 15 fractions, 40 Gy in 15 fractions, 40 Gy in 20 fractions, and 20 Gy in 5 fractions. The combined results from these two trials showed that outcomes were similar for patients treated with a shorter regimen than for those treated with a more protracted schedule. In our study, respondents reported that they most frequently treated brain metastases to a total dose of 30 Gy in 10 fractions. Given the results of the aforementioned RTOG trials and practice patterns among academic physicians, we recommend all practitioners consider a shorter hypofractioned course when treating brain metastases with WBRT. This will also reduce delays for patients who are likely to benefit greatly from earlier enrollment into hospice care, because protracted radiation schedules typically are not covered while a patient is in hospice.
Pharmacologic management for patients with brain metastases is important for symptomatic improvement. Glucocorticoids are important for palliation of symptoms from edema and increased intracranial pressure.15 However, steroids have a multitude of side effects and their use in asymptomatic patients is unnecessary. Improvements in imaging and detection11 have allowed us to find smaller and asymptomatic brain tumors. In our survey, it was promising to see a change in former practice patterns, with only 8% of academic practitioners regularly prescribing steroids to all of their patients receiving whole-brain radiation.
Diminished cognitive function and short-term memory loss are troublesome side effects of WBRT. As cancer patients live longer, such cognitive dysfunction will become more than just a nuisance. The RTOG has investigated the use of prophylactic memantine for patients receiving whole-brain radiation to determine if it would aid in the preservation of cognition. It found that patients who received memantine did better and had delayed time to cognitive decline and a reduced rate of memory decline, executive function, and processing speed.16 In our study, about a third of practitioners prescribed memantine and it was reserved for patients who had an otherwise favorable prognosis.
The RTOG has also investigated adjusting treatment technique for patients who receive WBRT. RTOG 0933 was a phase 2 trial that evaluated hippocampal avoidance during deliverance of WBRT with intensity-modulated radiation therapy (IMRT). Results showed that avoiding the hippocampus during WBRT was associated with improved memory preservation and patient quality of life.17 In a survey of practicing radiation oncologists in the US, most reported that they did not use memantine or IMRT for hippocampal sparing when delivering whole-brain radiation.18 Given the positive results of RTOG 0933 and 0614, the NRG Oncology research organization is conducting a phase 3 randomized trial that compares memantine use for patients receiving whole-brain radiation with or without hippocampal sparing to determine if patients will have reduced cognitive decline. All patients receiving WBRT should be considered for enrolment on this trial if they are eligible.
The delivery of brain radiation has continued to change, especially with the introduction of SRS. Recent publication of a meta-analysis of three phase 3 trials evaluating SRS with or without WBRT for 1-4 brain metastases showed that patients aged 50 years or younger experienced a survival benefit with SRS, and the omission of whole-brain radiation did not affect distant brain relapse rates. 19 The authors recommended that for this population, SRS alone is the preferred treatment. In our study, physicians who had been in practice for a longer time were more likely to treat using SRS alone. The results showed a linear association, with those in practice for a longer time being more likely to use SRS alone compared with those practicing for a shorter time (P = .027). Accordingly, 67% of respondents (8 of 12) who had been in practice for 11 or more years used SRS alone, whereas 24% (14 of 58) who had practiced for 0-5 years and 42% (5 of 12) who had practice from 6-10 years used SRS alone (Figure 1). When treating with SRS, younger practitioners placed more importance on the status of extracranial disease, whereas older practitioners placed more importance on tumor histopathology.
The use of repeat whole-brain reirradiation is more controversial among practitioners.20-22 Son and colleagues evaluated patients who needed whole-brain reirradiation after intracranial disease progression.22 The authors noted that patients with stable extracranial disease benefited from reirradiation. In our study, we found that when considering whole-brain reirradiation, older practitioners placed more importance on tumor histology than other factors.
As far as we know, this is the first study evaluating the practices and patterns of care with regard to the delivery of brain radiation in academic centers in the US. We found that time in practice was the most significant predictor of treatment technique and delivery. We also found that older practitioners place more importance on tumor histopathology compared with younger practitioners. A limitation of this study is that we had contact information only for program coordinators at ACGME-accredited programs. As such, we were not able to assess practice patterns among community practitioners. In addition, it seemed that residents and junior faculty were more likely to respond to this survey, likely because of the dissemination pattern. Given the evolution and diversity of treatment regimens for brain metastases, we believe that patients with brain metastases should be managed individually using a multidisciplinary approach.
Despite the recent advances in systemic therapy, metastatic spread to the brain continues to be the most common neurologic complication of many cancers. The clinical incidence of brain metastases varies with primary cancer diagnosis, with estimates ranging from 1.2%-19.8%.1,2 Metastatic spread to the brain is even more prevalent at autopsy, with evidence of intracranial tumor being found in 26% of patients in some series.3 It is possible that the clinical incidence of metastatic disease to the brain will continue to increase as newer therapeutic agents improve survival and imaging techniques continue to improve.
The management of brain metastases has changed rapidly as technological improvements have made treatment increasingly safe and efficacious. Traditionally, treatment consisted of radiotherapy to the whole brain, with or without surgical resection.4,5 More recently, stereotactic radiosurgery (SRS) has been adopted on the basis of evidence that it is safe and efficacious alone or in combination with radiotherapy to the whole brain.6 Further evidence is emerging that neurocognitive outcomes are improved when whole-brain radiotherapy (WBRT) is omitted, which possibly contributes to improved patient quality of life.7 Taking into account this and other data, the American Society for Radiation Oncology’s Choosing Wisely campaign now recommends not routinely adding WBRT to radiosurgery in patients with limited brain metastases.8
Despite this recommendation, many patients continue to benefit from WBRT, and it remains a common treatment in radiation oncology clinics across the US for several reasons. Many patients present with multiple brain metastases and are ineligible for radiosurgery. Even for technically eligible patients, WBRT has been shown to improve local control and decrease the rate of distant brain failure over radiosurgery alone.6 With higher rates of subsequent failures, patients receiving radiosurgery alone must adhere to more rigorous follow-up and imaging schedules, which can be difficult for many rural patients who have to travel long distances to centers. Furthermore, there is some suggestion that this decreased failure rate may result in improved survival in highly selected patients with excellent disease and performance status.9 Controversies exist, however, and strong institutional biases persist, contributing to significant differences in practice. We surveyed academic radiation oncologists and in an effort to identify and describe practice patterns in the delivery of WBRT at academic centers.
Methods
We conducted a thorough review of available literature on radiation for brain metastases and based on our findings, devised a survey 19 questions to ascertain practice patterns and treatment delivery among US academic physicians (Table 1). After obtaining institutional review board approval to do the study, we sent the survey to program coordinators at radiation oncology programs that are accredited by the Accreditation Council for Graduate Medical Education. We instructed coordinators to e-mail the survey to their practicing resident and attending physicians. The surveys were created using SurveyMonkey software. We obtained informed consent from the providers. A total of 3 follow-up e-mails were sent to each recipient of the survey to solicit responses, similar to the Dillman Total Design Survey Method.10
SPSS version 22.0 was used to analyze the data in an exploratory fashion. Statistical methods were used to assess the association of demographic data with SRS and WBRT delivery and treatment technique items when the analyses involved percentages that included the Pearson chi-square statistic and the chi-square test for linear trend. When the analysis focused on ranking data, the Kruskal-Wallis test, Mann-Whitney U test, the Jonckheere-Terpstra and the Kendall tau-b rank correlation were used as appropriate. If there were small sample sizes within some groups, then exact significant levels were assessed. Statistical significance was set by convention at P < .05.
Results
We received 95 responses of which 87 were considered complete for analysis. Forty-seven percent of the 87 respondents were not board-certified, and the remainder had passed their radiobiology and physics boards exams. A majority of respondents (70%, 61 of 87) were physicians who had been in practice for ≤5 years. Fifty-four percent of respondents were located in the Northeast US, 22% in the South, 14% in the West, and 10% in the Midwest and Hawaii (Table 2).
We used the chi-square test for linear trends to assess for a relationship between years of practice and whether respondents deviated from their typical method of WBRT therapy when treating more radioresistant tumors (melanoma, renal cell carcinoma). Respondents were classified by years in practice: 0-5, 6-10, 11-20, and >21 years. The results showed a linear association, with those in practice for longer periods more likely to use SRS alone, P = .027 (Figure 1).
Discussion
The incidence of brain metastases is increasing because of improvements in diagnostic imaging techniques and advancements in systemic therapy control of extracranial disease but not of intracranial disease or metastasis, because therapies do not cross the blood-brain barrier.11,12 Brain metastases are the most common type of brain tumor. Given that most chemotherapeutic agents cannot cross the blood-brain barrier, radiotherapy is considered a means of treatment and of controlling brain metastases. Early data from the 1950s13 and 1960s14 have suggested clinical improvement with brain radiation, making radiotherapy the cornerstone for treatment of brain metastases.
The Radiation Therapy Oncology Group (RTOG) has evaluated several fractionation schedules, with 5 schemas evaluated by the RTOG 6901 and 7361 studies: 30 Gy in 10 fractions, 30 Gy in 15 fractions, 40 Gy in 15 fractions, 40 Gy in 20 fractions, and 20 Gy in 5 fractions. The combined results from these two trials showed that outcomes were similar for patients treated with a shorter regimen than for those treated with a more protracted schedule. In our study, respondents reported that they most frequently treated brain metastases to a total dose of 30 Gy in 10 fractions. Given the results of the aforementioned RTOG trials and practice patterns among academic physicians, we recommend all practitioners consider a shorter hypofractioned course when treating brain metastases with WBRT. This will also reduce delays for patients who are likely to benefit greatly from earlier enrollment into hospice care, because protracted radiation schedules typically are not covered while a patient is in hospice.
Pharmacologic management for patients with brain metastases is important for symptomatic improvement. Glucocorticoids are important for palliation of symptoms from edema and increased intracranial pressure.15 However, steroids have a multitude of side effects and their use in asymptomatic patients is unnecessary. Improvements in imaging and detection11 have allowed us to find smaller and asymptomatic brain tumors. In our survey, it was promising to see a change in former practice patterns, with only 8% of academic practitioners regularly prescribing steroids to all of their patients receiving whole-brain radiation.
Diminished cognitive function and short-term memory loss are troublesome side effects of WBRT. As cancer patients live longer, such cognitive dysfunction will become more than just a nuisance. The RTOG has investigated the use of prophylactic memantine for patients receiving whole-brain radiation to determine if it would aid in the preservation of cognition. It found that patients who received memantine did better and had delayed time to cognitive decline and a reduced rate of memory decline, executive function, and processing speed.16 In our study, about a third of practitioners prescribed memantine and it was reserved for patients who had an otherwise favorable prognosis.
The RTOG has also investigated adjusting treatment technique for patients who receive WBRT. RTOG 0933 was a phase 2 trial that evaluated hippocampal avoidance during deliverance of WBRT with intensity-modulated radiation therapy (IMRT). Results showed that avoiding the hippocampus during WBRT was associated with improved memory preservation and patient quality of life.17 In a survey of practicing radiation oncologists in the US, most reported that they did not use memantine or IMRT for hippocampal sparing when delivering whole-brain radiation.18 Given the positive results of RTOG 0933 and 0614, the NRG Oncology research organization is conducting a phase 3 randomized trial that compares memantine use for patients receiving whole-brain radiation with or without hippocampal sparing to determine if patients will have reduced cognitive decline. All patients receiving WBRT should be considered for enrolment on this trial if they are eligible.
The delivery of brain radiation has continued to change, especially with the introduction of SRS. Recent publication of a meta-analysis of three phase 3 trials evaluating SRS with or without WBRT for 1-4 brain metastases showed that patients aged 50 years or younger experienced a survival benefit with SRS, and the omission of whole-brain radiation did not affect distant brain relapse rates. 19 The authors recommended that for this population, SRS alone is the preferred treatment. In our study, physicians who had been in practice for a longer time were more likely to treat using SRS alone. The results showed a linear association, with those in practice for a longer time being more likely to use SRS alone compared with those practicing for a shorter time (P = .027). Accordingly, 67% of respondents (8 of 12) who had been in practice for 11 or more years used SRS alone, whereas 24% (14 of 58) who had practiced for 0-5 years and 42% (5 of 12) who had practice from 6-10 years used SRS alone (Figure 1). When treating with SRS, younger practitioners placed more importance on the status of extracranial disease, whereas older practitioners placed more importance on tumor histopathology.
The use of repeat whole-brain reirradiation is more controversial among practitioners.20-22 Son and colleagues evaluated patients who needed whole-brain reirradiation after intracranial disease progression.22 The authors noted that patients with stable extracranial disease benefited from reirradiation. In our study, we found that when considering whole-brain reirradiation, older practitioners placed more importance on tumor histology than other factors.
As far as we know, this is the first study evaluating the practices and patterns of care with regard to the delivery of brain radiation in academic centers in the US. We found that time in practice was the most significant predictor of treatment technique and delivery. We also found that older practitioners place more importance on tumor histopathology compared with younger practitioners. A limitation of this study is that we had contact information only for program coordinators at ACGME-accredited programs. As such, we were not able to assess practice patterns among community practitioners. In addition, it seemed that residents and junior faculty were more likely to respond to this survey, likely because of the dissemination pattern. Given the evolution and diversity of treatment regimens for brain metastases, we believe that patients with brain metastases should be managed individually using a multidisciplinary approach.
1. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004;22(14):2865-2872.
2. Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94(10):2698-2705.
3. Takakura K. Metastatic tumors of the central nervous system. Tokyo: Igaku-Shoin; 1982.
4. Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998;280(17):1485-1489.
5. Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. New Engl J Med. 1990;322(8):494-500.
6. Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol Biol Phys. 2015;91(4):710-717.
7. Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10(11):1037-1044.
8. Choosing Wisely [ASTRO]. Don’t routinely add adjuvant whole-brain radiation therapy to stereotactic radiosurgery for limited brain metastases. http://www.choosingwisely.org/clinician-lists/american-society-radiation-oncology-adjunct-whole-brain-radiation-therapy/. Updated June 21, 2016. Accessed November 10, 2016.
9. Aoyama H, Tago M, Shirato H, Japanese Radiation Oncology Study Group I. Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 Randomized Clinical Trial. JAMA Oncol. 2015;1(4):457-464.
10. Hoddinott SN, Bass MJ. The Dillman total design survey method. Can Fam Physician. 1986;32:2366-2368.
11. Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012;14(1):48-54.
12. Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. 2005;75(1):5-14.
13. Chao JH, Phillips R, Nickson JJ. Roentgen-ray therapy of cerebral metastases. Cancer. 1954;7(4):682-689.
14. Nieder C, Niewald M, Schnabel K. Treatment of brain metastases from hypernephroma. Urol Int. 1996;57(1):17-20.
15. Ryken TC, McDermott M, Robinson PD, et al. The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96(1):103-114.
16. Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15(10):1429-1437.
17. Gondi V, Pugh SL, Tome WA, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol. 2014;32(34):3810-3816.
18. Slade AN, Stanic S. The impact of RTOG 0614 and RTOG 0933 trials in routine clinical practice: The US Survey of Utilization of Memantine and IMRT planning for hippocampus sparing in patients receiving whole-brain radiotherapy for brain metastases. Contemp Clin Trials. 2016;47:74-77.
19. Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. International journal of radiation oncology, biology, physics. 2015;91(4):710-717.
20. Hazuka MB, Kinzie JJ. Brain metastases: results and effects of re-irradiation. Int J Radiat Oncol Biol Phys. 1988;15(2):433-437.
21. Sadikov E, Bezjak A, Yi QL, et al. Value of whole-brain re-irradiation for brain metastases — single centre experience. Clin Oncol (R Coll Radiol). 2007;19(7):532-538.
22. Son CH, Jimenez R, Niemierko A, Loeffler JS, Oh KS, Shih HA. outcomes after whole-brain reirradiation in patients with brain metastases. Int J Radiat Oncol Biol Phys. 2012;82(2):e167-e172.
1. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004;22(14):2865-2872.
2. Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94(10):2698-2705.
3. Takakura K. Metastatic tumors of the central nervous system. Tokyo: Igaku-Shoin; 1982.
4. Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998;280(17):1485-1489.
5. Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. New Engl J Med. 1990;322(8):494-500.
6. Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol Biol Phys. 2015;91(4):710-717.
7. Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10(11):1037-1044.
8. Choosing Wisely [ASTRO]. Don’t routinely add adjuvant whole-brain radiation therapy to stereotactic radiosurgery for limited brain metastases. http://www.choosingwisely.org/clinician-lists/american-society-radiation-oncology-adjunct-whole-brain-radiation-therapy/. Updated June 21, 2016. Accessed November 10, 2016.
9. Aoyama H, Tago M, Shirato H, Japanese Radiation Oncology Study Group I. Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 Randomized Clinical Trial. JAMA Oncol. 2015;1(4):457-464.
10. Hoddinott SN, Bass MJ. The Dillman total design survey method. Can Fam Physician. 1986;32:2366-2368.
11. Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012;14(1):48-54.
12. Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. 2005;75(1):5-14.
13. Chao JH, Phillips R, Nickson JJ. Roentgen-ray therapy of cerebral metastases. Cancer. 1954;7(4):682-689.
14. Nieder C, Niewald M, Schnabel K. Treatment of brain metastases from hypernephroma. Urol Int. 1996;57(1):17-20.
15. Ryken TC, McDermott M, Robinson PD, et al. The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96(1):103-114.
16. Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15(10):1429-1437.
17. Gondi V, Pugh SL, Tome WA, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol. 2014;32(34):3810-3816.
18. Slade AN, Stanic S. The impact of RTOG 0614 and RTOG 0933 trials in routine clinical practice: The US Survey of Utilization of Memantine and IMRT planning for hippocampus sparing in patients receiving whole-brain radiotherapy for brain metastases. Contemp Clin Trials. 2016;47:74-77.
19. Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. International journal of radiation oncology, biology, physics. 2015;91(4):710-717.
20. Hazuka MB, Kinzie JJ. Brain metastases: results and effects of re-irradiation. Int J Radiat Oncol Biol Phys. 1988;15(2):433-437.
21. Sadikov E, Bezjak A, Yi QL, et al. Value of whole-brain re-irradiation for brain metastases — single centre experience. Clin Oncol (R Coll Radiol). 2007;19(7):532-538.
22. Son CH, Jimenez R, Niemierko A, Loeffler JS, Oh KS, Shih HA. outcomes after whole-brain reirradiation in patients with brain metastases. Int J Radiat Oncol Biol Phys. 2012;82(2):e167-e172.
Distress management in cancer patients in Puerto Rico
A comprehensive, patient-centered approach is required to accomplish cancer best standards of care.1 This approach reflects the holistic conceptualization of health in which the physical, emotional, and social dimensions of the human being are considered when providing medical care. As a result, to look after all patient needs, interdisciplinary and well-coordinated interventions are recommended. Cancer patients should be provided not only with diagnostic, treatment, and follow-up clinical service, but also with the supportive assistance that may positively influence all aspects of their health.
To appraise physical, social, emotional and spiritual issues and to develop supportive interventional action plans, the National Comprehensive Cancer Network (NCCN) recommends screening all cancer patients for distress.2 In particular, screening the emotional component of distress occupies a prominent place in this process because it is now recognized as the sixth vital sign in oncology.3 Even though the influence of emotional distress over cancer mortality rates and disease progression is still under scrutiny,4 its plausible implications over treatment compliance have been pointed out. Patients with higher levels of emotional distress show lower adherence to treatment and poorer health outcomes.5 Furthermore, prevalence rates of emotional distress in cancer patients from ambulatory settings6 and oncology surgical units have been studied and have provided justification for distress management.7 Studies have shown low ability among oncologists to identify patients in distress and oncologists’ tendency to judge distress higher than the patients themselves.8 As a consequence, to achieve systematic distress evaluations and appropriate referrals for care, guidelines for distress management should be implemented in clinical settings. It is recommended that tests are conducted to find brief screening instruments and procedures to assure accurate interventions according to patient specific needs.
This article presents the process of implementing a distress management program at HIMA-San Pablo Oncologic Hospital in Caguas, Puerto Rico, with particular emphasis on the management of emotional distress, which has been defined as the feeling of suffering that cancer patients may experience after diagnosis. In addition, we have included data from a pilot study that was completed for content validation of the Patient Health Questionnaire (PHQ-9) to estimate depression levels in Puerto Rican cancer patients.
Methods
HIMA-San Pablo operates a group of privately owned hospitals in Puerto Rico. It established a cancer center in Caguas in 2007, recruiting a multispecialty medical faculty to provide cancer care and bone marrow transplants for adult and pediatric patients. The cancer center, currently named HIMA-San Pablo Oncologic Hospital (HSPOH), is a hospital within a hospital licensed by the Puerto Rico Department of Health. In 2007, a cancer committee was established as the steering committee to ensure the delivery of cancer care according to best standards of care. The committee took responsibility for developing all activities needed to achieve the American College of Surgeons’ Commission on Cancer (CoC) accreditation under the category of Comprehensive Community Cancer Center. The committee established a psychosocial team to develop a protocol for the delivery of distress management for adult patients. (The psychosocial needs of pediatric patients are assessed through other procedures.)
To develop the protocol, principles of input-output model of research and quality analysis in health care were applied.9 The input-output model, with its origin in engineering, helped map systematic activities to transform empirical data on cancer psychosocial care into operational procedures. Focus was given to data gathering (input), information organization and analysis (throughput), and the schematization of emotional distress management care (output).
The input phase
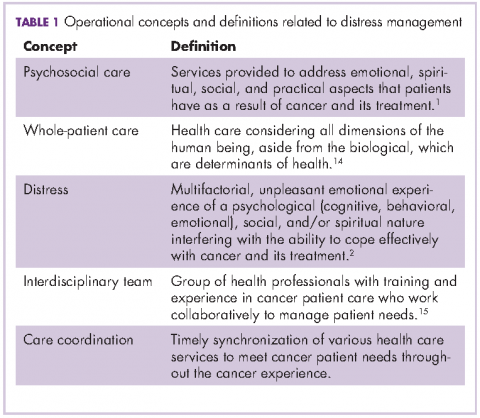
In the input phase, elements of psychosocial care and operational definitions related to distress management in general were identified through literature review (Table 1). Basic parameters for distress management were clarified, resulting in a conceptual framework based in four remarks: First, according to NCCN, distress is a multifactorial unpleasant emotional experience of a psychological, social, and spiritual nature. It may interfere with the ability to cope effectively with cancer, its symptoms and its treatment. Its intensity may fluctuate from feelings of suffering and fear to incapacitating manifestations of anxiety and depression2 and its severity may hamper patient quality of life and treatment compliance.
Second, distress management requires the intervention of an interdisciplinary team with both medical and allied health professionals. This may include mental health specialists and other professionals with training and experience in cancer-related issues, who work with reciprocal channels of communication for the exchange of patient information.
Third, NCCN recommends using the Distress Thermometer for patient initial distress screening.10-12 It consists of a numeric scale ranging from 0 (no distress) to 10 (severe distress) in which patients classify their level of distress. The numeric scale is followed by a section in which patients identify areas of practical, familiar, emotional, spiritual/ religious, and physical concerns. Based on responses, interviews may follow to set distress management interventions.
Fourth, screening and assessment are different but sequential and complementary stages of distress management. Screening is viewed as a rapid strategy to identify cancer patients in distress. Assessment looks out for a broader appraisal and documentation of factors with repercussions over patient distress level and resiliency capability.13 In many instances, the patient’s emotional distress is better understood in the assessment phase.
The throughput phase
Within the throughput phase of information organization and analysis, an inventory of health professionals and other in-house consultants needed for distress management was completed. Roles and procedures for information sharing were determined, and we established collaborative agreements with professionals in the community who could contribute to distress management. Members of the psychosocial team held workshops to discuss elements of NCCN guidelines for distress management and to create an action plan for the implementation of the protocol. Data analyses were performed to create a demographic profile of the oncology population at the hospital and assess patient willingness to receive emotional support services,16 which led to the implementation of support group meetings at which additional substantive information was collected about issues affecting cancer patients’ emotions.
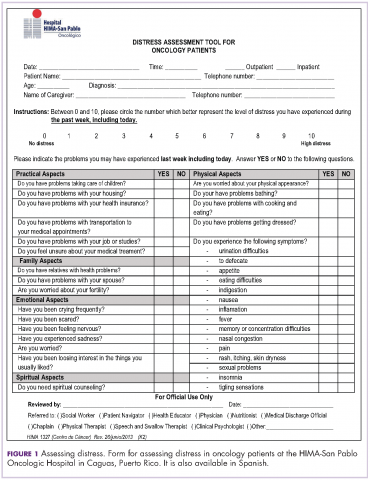
The NCCN Distress Thermometer for measuring distress was translated to Spanish. Its format was adapted, and it was identified as a distress screening tool (DST), which we named Distress Assessment Tool for Oncology Patients (Figure 1). The instrument helps for rapid screening of patient needs and proper determination of initial interventions. In addition, psychometric properties of several instruments were reviewed for instances when patient emotional distress could not be clearly determined. We decided to proceed with the validation of the 9-item Patient Health Questionnaire (PHQ-9) to estimate patient depression level. A proposal for content validation of the PHQ-9 was approved by the University of Puerto Rico institutional review board, and patients were recruited to participate in the pilot study.
The PHQ-9. The PHQ-9 is a self-report version of the PRIME-MD instrument developed to assess mental disorders in clinical settings. It is based on DSM-IV diagnostic criteria.17 The PHQ-9 is the depression module with nine depression symptoms to check off if they become the cause of emotional impairment. Respondents categorized depression symptoms in four frequency degrees representing numeric values: 0 (not at all), 1 (several days), 2 (more than half the days), 3 (nearly every day). Measures of depression severity are subsequently determined in a Likert-type scale according to numeric calculations of responses: 0-4 (none severe depression), 5-9 (mild), 10-14 (moderate), 15-19 (moderately severe), and 20-27 (severe-major depression).
The instrument is widely used because of its validity in small and large populations. It showed adequate reliability and validity in a small sample of head and neck cancer patients, with a Cronbach’s alpha of 0.80 and a correlation coefficient of 0.71.18 Similarly, it showed good performance in identifying major depression in 4264 cancer outpatients, with sensitivity of 93%, specificity of 81%, and a positive predictive value (PPV) of 25% and negative predictive value (NPV) of 99%.19 Even when administered on a touch screen computer, the instrument showed valid data of depression from patients in treatment.20
The Beck Depression Inventory. We used the Beck Depression Inventory (BDI-II) Spanish version as the gold standard measure for the validation study. It is a 22-items inventory that measures attitudes and symptoms of depression.21 It can be administered in 10 minutes and has shown good psychometric measures when administered in Spain and Puerto Rico.22, 23
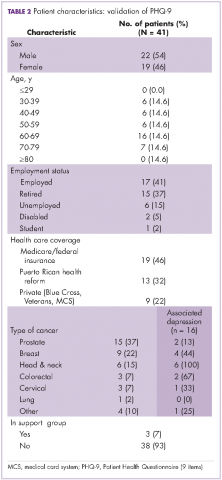
The pilot study. In all, 44 cancer patients who were receiving outpatient treatment at the radiotherapy unit agreed to participate in the study. The participants signed a consent form after the confidentiality protection measures and the main objectives of the study had been explained to them. Patients were interviewed individually during November and December 2012, with the Spanish versions of the PHQ-9 and BDI-II administered by one of two interviewers. At the beginning of each interview, the patient was asked 10 questions so that we could gather demographic data and confirm participant eligibility: aged 21 years or older, born and raised in Puerto Rico, being a Spanish speaker, and having a primary cancer diagnosis with no previous disease. Three patients were excluded from the sample because they either had cancer previously or had a recurrence or metastasis. The final sample consisted of 41 outpatients (N = 41).
Data analysis for demographics was completed with STATA v.12 software. Measures of central tendency and dispersion as well as PHQ-9 internal consistency analysis were made through Cronbach alpha with SPSS.
From a total of 41 patients surveyed, 22 (54%) were men and 19 (46%) were women, with an overall median age of 61 years. Among the men, 15 (68%) had a prostate cancer diagnosis and among women, 9 (47.4%) had a breast cancer diagnosis. In regard to health insurance, 19 (46%) had Medicare or Veterans/federal insurance coverage, and 13 (32%) had Reforma, the Puerto Rican government health insurance program partially funded by Medicaid funds. In addition, 8 participants (20%) were unemployed or disabled. As previously stated, all of the patients were in ambulatory care. Only 3 (7%) were participating in support groups.
Of all the respondents, 16 (39%) reported some level of depression. In particular, 2 (5%) showed severe-major depression, 4 (10%) moderately severe depression, and 10 (24%) moderate depression. Of those with depression, 8 (50%) were women, 8 (50%) were men. All 6 of the patients with head and neck cancer showed moderate or moderately severe depression (Table 2).
When respondent PHQ-9 scoring reflected moderate to severe depression (>10), a letter was sent to the patient’s radio-oncologist for referral to counseling and clinical psychological evaluation. All participants had access to the support group program, to a radiotherapy education program meeting weekly, and written information about their cancer diagnosis and treatment. They also were interviewed by the psychosocial coordinator or patient navigator for further assessment.
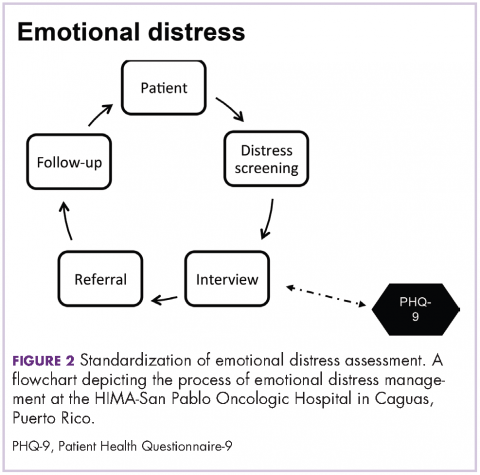
The output phase
In the output phase, a graphic representing the process of emotional assessment at the institution was created and then modified. PHQ-9 was added to the process when it was found suitable to assess level of depression contributing to the identification of patients requiring psychological and psychiatric assistance which by other means would be missed. PHQ-9 was useful in the busy clinical setting as it was completed, scored and interpreted in minutes. It showed the potential for routine evaluations when looking to identify improvement or deterioration in depression levels thus helping to monitor responses to treatment and providing insights for follow up interventions. As stated by NCCN guidelines, distress should be monitored, documented and managed at all stages of the cancer continuum.
Results and discussion
The protocol for distress management at HSPOH is based on the 2013 NCCN guidelines. Cancer patients are screened for levels of distress in all settings (inpatients and outpatients). Screening is held with the DST Spanish translation at the moment of diagnosis or as soon as possible after a diagnosis is made. Screening for distress is also done before or after surgery, in recurrence or progression, and when clinically indicated. Patients are informed that distress management is an essential part of their care and are encouraged to provide information so that we can make a proper need assessment.
Patients are screened by the psychosocial coordinator or patient navigator who administers the DST followed by in-depth interviews for additional appraisal. An action plan is designed based on patient needs, which include their intervention and the intervention of other members of the psychosocial team from the institution and/or from the community. Additional in-house health professionals contributing in distress management include, but are not limited to: physicians; clinical psychologists; health educators; social workers; dietitians; chaplains; and physical, respiratory, speech, and/or swallow therapists. Follow-up and rescreening sessions are scheduled to assure coordination of services between those health professionals as well as to secure continuity of distress management during all stages of the cancer continuum.
The results of the DST are filed in patient medical records. Members of the psychosocial team also document their interventions in the patient medical record, which helps in the exchange of information among the cancer care team. The psychosocial team meets once a month – or as required for extraordinary cases – to review and discuss the cases, determine the best options for distress management, and identify areas for psychosocial care improvement. Those findings and the results of distress management in patient level of satisfaction are then reported and discussed quarterly by the psychosocial coordinator and the cancer committee.
Figure 2 shows in what phase of emotional distress assessment the PHQ-9 was included. Patients reporting four or more of the six areas of concern related to emotional distress in the DST (Figure 1) are automatically referred to a mental health specialist. But when patients report three areas of concern with no clear data on their specific level of depression, PHQ-9 is administered to differentiate those who need a mental health specialist from those who could be adequately supported by health education and support group interventions. In this way detrimental outcomes such as duplicity and over or underuse of services and resources are reduced. In addition, it is recognized that using an interview after the administration of the DST to determine distress management actions does not always provide enough information about a patient’s emotional circumstances and previous comorbidities. Patient responses during interviews may be influenced by the patient’s level of literacy, verbal comprehension, and communication style,24 so emotional distress can go unrecognized during interviews, resulting in delays for treatment and supportive care.
National guidelines in oncology consider such socio-ecological models emphasizing the delivery of patient-centered, interdisciplinary, and evidence-based care. That does not mean that institutions should apply protocols of psychosocial care as previously developed, but that they should test, review, adapt, and improve them during the implementation of the care. In fact, NCCN encourages conducting trials to examine protocols, screening instruments, and models of intervention to determine applicability to particular settings.2
Findings from a study by NCCN member institutions to evaluate progress of implementing distress management guidelines found that 53% (n = 8) of respondent institutions conducted routine distress screening. Of those, 37.5% (3) relied only on interviews. That finding is of concern because if interviews are not standardized and have not been systematically evaluated, then their sensitivity and specificity in identifying distressed patients is unknown.26 Accordingly, the process described in this article and the PHQ-9 validation was an effort to standardize emotional distress management, and was underlined as an achievement during the CoC accreditation visit to the cancer center in December 2013. The hospital was accredited as a comprehensive community cancer center with gold commendations, becoming the first privately owned hospital in Puerto Rico to achieve the accreditation.
1. Commission on Cancer, American College of Surgeons. Cancer Programs Standards 2012: Ensuring Patient-Centered Care. Version 1.2.1. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/programstandards2012.ashx. Published 2012. Accessed March 5, 2013.
2. National Comprehensive Cancer Network clinical practice guidelines in oncology (NCCN guidelines): Distress management. Version I. 2012. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp#supportive. Accessed March 5, 2013.
3. Bultz BD, Groff SL. Screening for distress, the 6th vital sign in oncology: from theory to practice: http://www.oncologyex.com/issue/2009/vol8_no1/8_comment2_1.html. Published February 2009. Accessed February 16, 2017.
4. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009;115:5349-5361.
5. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Int Med. 2000;160:2101-2107.
6. Jadoon NA, Munir W, Shahzad MA, Choudhry ZS. Assessment of depression and anxiety in adult cancer outpatients: a cross sectional study. BMC Cancer. 2010;10:594.
7. Fisher D, Wedel B. Anxiety and depression disorders in cancer patients: incidence, diagnosis and therapy. Mag Eur Med Oncol. 2012;5:52-54.
8. Sollner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived social support, and in need for psychosocial counselling? Br J Cancer. 2001;84:179-185.
9. Scott RD, Solomon SL, McGowan JE. Applying economic principles to health care: special issue. Emerg Infect Dis. 2001;7:282-285.
10. Adler NE, Page AEK. A model for delivering psychosocial health services. In: Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press (US); 2008.
11. Holland JC, Alici Y. Management of distress in cancer patients. J Support Oncol. 2010;8:4-12.
12. Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494-1502.
13. Maihoff SE. Assessment. In Washington CM, Leaver D, eds. Principles and practice of radiation therapy. St Louis, MO: Mosby Elsevier; 2004:243-264.
14. National Academy of Sciences. Adler NE, Page AEK, eds. Cancer care for the whole patient: meeting psychosocial health needs. https://www.ncbi.nlm.nih.gov/books/NBK4015/. Published 2008. Accessed February 22, 2012.
15. Nancarrow SA, Booth A, Ariss
16. Baker-Glenn EA, Park B, Granger L, Symonds P, Mitchell AJ. Desire for psychological support in cancer patients with depression or distress: validation of a simple help question. Psychooncology. 2011;20:525-531.
17. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
18. Omoro SA, Fann JR, Weymuller EA, Macharia IM, Yueh B. Swahili translation and validation of the Patient Health Questionnaire-9 depression scale in the Kenyan head and neck cancer patient population. Int J Psychiatry Med. 2006;36:367-381.
19. Thekkumpurath P, Walker J, Butcher I, et al. Screening for major depression on cancer outpatients: the diagnostic accuracy of the 9-item Patient Health Questionnaire. Cancer. 2011;117:218-227.
20. Fann JR, Berry DL, Wolpin S, et al. Depression screening using the Patient Health Questionnaire-9 administered on a touch screen computer. Psychooncology. 2009;18:14-22.
21. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:651-571.
22. Sanz J, Perdigón AL, Vázquez C. The Spanish adaptation of Beck’s Depression Inventory–II (BDI-II): psychometric properties in the general population. Clínica y Salud. 2003;14:249-280.
23. Bonilla J, Bernal G, Santos A, Santos D. A revised Spanish version of the Beck Depression Inventory: psychometric properties with a Puerto Rican sample of college students. J Clin Psychol. 2004;60:119-130.
24. Alcántara C, Gone JP. Multicultural issues in the clinical interview and diagnostic process. In Leong FTL, ed. APA handbook of multicultural psychology. Vol 2. Applications and training. Washington, DC: American Psychological Association; 2014:153-163.
25. Sharma M, Romas JA. Theoretical foundations of health education and health promotion. 2nd ed. Burlington, MA: Jones & Barlett Learning; 2012.
26. Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5:99-103.
A comprehensive, patient-centered approach is required to accomplish cancer best standards of care.1 This approach reflects the holistic conceptualization of health in which the physical, emotional, and social dimensions of the human being are considered when providing medical care. As a result, to look after all patient needs, interdisciplinary and well-coordinated interventions are recommended. Cancer patients should be provided not only with diagnostic, treatment, and follow-up clinical service, but also with the supportive assistance that may positively influence all aspects of their health.
To appraise physical, social, emotional and spiritual issues and to develop supportive interventional action plans, the National Comprehensive Cancer Network (NCCN) recommends screening all cancer patients for distress.2 In particular, screening the emotional component of distress occupies a prominent place in this process because it is now recognized as the sixth vital sign in oncology.3 Even though the influence of emotional distress over cancer mortality rates and disease progression is still under scrutiny,4 its plausible implications over treatment compliance have been pointed out. Patients with higher levels of emotional distress show lower adherence to treatment and poorer health outcomes.5 Furthermore, prevalence rates of emotional distress in cancer patients from ambulatory settings6 and oncology surgical units have been studied and have provided justification for distress management.7 Studies have shown low ability among oncologists to identify patients in distress and oncologists’ tendency to judge distress higher than the patients themselves.8 As a consequence, to achieve systematic distress evaluations and appropriate referrals for care, guidelines for distress management should be implemented in clinical settings. It is recommended that tests are conducted to find brief screening instruments and procedures to assure accurate interventions according to patient specific needs.
This article presents the process of implementing a distress management program at HIMA-San Pablo Oncologic Hospital in Caguas, Puerto Rico, with particular emphasis on the management of emotional distress, which has been defined as the feeling of suffering that cancer patients may experience after diagnosis. In addition, we have included data from a pilot study that was completed for content validation of the Patient Health Questionnaire (PHQ-9) to estimate depression levels in Puerto Rican cancer patients.
Methods
HIMA-San Pablo operates a group of privately owned hospitals in Puerto Rico. It established a cancer center in Caguas in 2007, recruiting a multispecialty medical faculty to provide cancer care and bone marrow transplants for adult and pediatric patients. The cancer center, currently named HIMA-San Pablo Oncologic Hospital (HSPOH), is a hospital within a hospital licensed by the Puerto Rico Department of Health. In 2007, a cancer committee was established as the steering committee to ensure the delivery of cancer care according to best standards of care. The committee took responsibility for developing all activities needed to achieve the American College of Surgeons’ Commission on Cancer (CoC) accreditation under the category of Comprehensive Community Cancer Center. The committee established a psychosocial team to develop a protocol for the delivery of distress management for adult patients. (The psychosocial needs of pediatric patients are assessed through other procedures.)
To develop the protocol, principles of input-output model of research and quality analysis in health care were applied.9 The input-output model, with its origin in engineering, helped map systematic activities to transform empirical data on cancer psychosocial care into operational procedures. Focus was given to data gathering (input), information organization and analysis (throughput), and the schematization of emotional distress management care (output).
The input phase
In the input phase, elements of psychosocial care and operational definitions related to distress management in general were identified through literature review (Table 1). Basic parameters for distress management were clarified, resulting in a conceptual framework based in four remarks: First, according to NCCN, distress is a multifactorial unpleasant emotional experience of a psychological, social, and spiritual nature. It may interfere with the ability to cope effectively with cancer, its symptoms and its treatment. Its intensity may fluctuate from feelings of suffering and fear to incapacitating manifestations of anxiety and depression2 and its severity may hamper patient quality of life and treatment compliance.
Second, distress management requires the intervention of an interdisciplinary team with both medical and allied health professionals. This may include mental health specialists and other professionals with training and experience in cancer-related issues, who work with reciprocal channels of communication for the exchange of patient information.
Third, NCCN recommends using the Distress Thermometer for patient initial distress screening.10-12 It consists of a numeric scale ranging from 0 (no distress) to 10 (severe distress) in which patients classify their level of distress. The numeric scale is followed by a section in which patients identify areas of practical, familiar, emotional, spiritual/ religious, and physical concerns. Based on responses, interviews may follow to set distress management interventions.
Fourth, screening and assessment are different but sequential and complementary stages of distress management. Screening is viewed as a rapid strategy to identify cancer patients in distress. Assessment looks out for a broader appraisal and documentation of factors with repercussions over patient distress level and resiliency capability.13 In many instances, the patient’s emotional distress is better understood in the assessment phase.
The throughput phase
Within the throughput phase of information organization and analysis, an inventory of health professionals and other in-house consultants needed for distress management was completed. Roles and procedures for information sharing were determined, and we established collaborative agreements with professionals in the community who could contribute to distress management. Members of the psychosocial team held workshops to discuss elements of NCCN guidelines for distress management and to create an action plan for the implementation of the protocol. Data analyses were performed to create a demographic profile of the oncology population at the hospital and assess patient willingness to receive emotional support services,16 which led to the implementation of support group meetings at which additional substantive information was collected about issues affecting cancer patients’ emotions.
The NCCN Distress Thermometer for measuring distress was translated to Spanish. Its format was adapted, and it was identified as a distress screening tool (DST), which we named Distress Assessment Tool for Oncology Patients (Figure 1). The instrument helps for rapid screening of patient needs and proper determination of initial interventions. In addition, psychometric properties of several instruments were reviewed for instances when patient emotional distress could not be clearly determined. We decided to proceed with the validation of the 9-item Patient Health Questionnaire (PHQ-9) to estimate patient depression level. A proposal for content validation of the PHQ-9 was approved by the University of Puerto Rico institutional review board, and patients were recruited to participate in the pilot study.
The PHQ-9. The PHQ-9 is a self-report version of the PRIME-MD instrument developed to assess mental disorders in clinical settings. It is based on DSM-IV diagnostic criteria.17 The PHQ-9 is the depression module with nine depression symptoms to check off if they become the cause of emotional impairment. Respondents categorized depression symptoms in four frequency degrees representing numeric values: 0 (not at all), 1 (several days), 2 (more than half the days), 3 (nearly every day). Measures of depression severity are subsequently determined in a Likert-type scale according to numeric calculations of responses: 0-4 (none severe depression), 5-9 (mild), 10-14 (moderate), 15-19 (moderately severe), and 20-27 (severe-major depression).
The instrument is widely used because of its validity in small and large populations. It showed adequate reliability and validity in a small sample of head and neck cancer patients, with a Cronbach’s alpha of 0.80 and a correlation coefficient of 0.71.18 Similarly, it showed good performance in identifying major depression in 4264 cancer outpatients, with sensitivity of 93%, specificity of 81%, and a positive predictive value (PPV) of 25% and negative predictive value (NPV) of 99%.19 Even when administered on a touch screen computer, the instrument showed valid data of depression from patients in treatment.20
The Beck Depression Inventory. We used the Beck Depression Inventory (BDI-II) Spanish version as the gold standard measure for the validation study. It is a 22-items inventory that measures attitudes and symptoms of depression.21 It can be administered in 10 minutes and has shown good psychometric measures when administered in Spain and Puerto Rico.22, 23
The pilot study. In all, 44 cancer patients who were receiving outpatient treatment at the radiotherapy unit agreed to participate in the study. The participants signed a consent form after the confidentiality protection measures and the main objectives of the study had been explained to them. Patients were interviewed individually during November and December 2012, with the Spanish versions of the PHQ-9 and BDI-II administered by one of two interviewers. At the beginning of each interview, the patient was asked 10 questions so that we could gather demographic data and confirm participant eligibility: aged 21 years or older, born and raised in Puerto Rico, being a Spanish speaker, and having a primary cancer diagnosis with no previous disease. Three patients were excluded from the sample because they either had cancer previously or had a recurrence or metastasis. The final sample consisted of 41 outpatients (N = 41).
Data analysis for demographics was completed with STATA v.12 software. Measures of central tendency and dispersion as well as PHQ-9 internal consistency analysis were made through Cronbach alpha with SPSS.
From a total of 41 patients surveyed, 22 (54%) were men and 19 (46%) were women, with an overall median age of 61 years. Among the men, 15 (68%) had a prostate cancer diagnosis and among women, 9 (47.4%) had a breast cancer diagnosis. In regard to health insurance, 19 (46%) had Medicare or Veterans/federal insurance coverage, and 13 (32%) had Reforma, the Puerto Rican government health insurance program partially funded by Medicaid funds. In addition, 8 participants (20%) were unemployed or disabled. As previously stated, all of the patients were in ambulatory care. Only 3 (7%) were participating in support groups.
Of all the respondents, 16 (39%) reported some level of depression. In particular, 2 (5%) showed severe-major depression, 4 (10%) moderately severe depression, and 10 (24%) moderate depression. Of those with depression, 8 (50%) were women, 8 (50%) were men. All 6 of the patients with head and neck cancer showed moderate or moderately severe depression (Table 2).
When respondent PHQ-9 scoring reflected moderate to severe depression (>10), a letter was sent to the patient’s radio-oncologist for referral to counseling and clinical psychological evaluation. All participants had access to the support group program, to a radiotherapy education program meeting weekly, and written information about their cancer diagnosis and treatment. They also were interviewed by the psychosocial coordinator or patient navigator for further assessment.
The output phase
In the output phase, a graphic representing the process of emotional assessment at the institution was created and then modified. PHQ-9 was added to the process when it was found suitable to assess level of depression contributing to the identification of patients requiring psychological and psychiatric assistance which by other means would be missed. PHQ-9 was useful in the busy clinical setting as it was completed, scored and interpreted in minutes. It showed the potential for routine evaluations when looking to identify improvement or deterioration in depression levels thus helping to monitor responses to treatment and providing insights for follow up interventions. As stated by NCCN guidelines, distress should be monitored, documented and managed at all stages of the cancer continuum.
Results and discussion
The protocol for distress management at HSPOH is based on the 2013 NCCN guidelines. Cancer patients are screened for levels of distress in all settings (inpatients and outpatients). Screening is held with the DST Spanish translation at the moment of diagnosis or as soon as possible after a diagnosis is made. Screening for distress is also done before or after surgery, in recurrence or progression, and when clinically indicated. Patients are informed that distress management is an essential part of their care and are encouraged to provide information so that we can make a proper need assessment.
Patients are screened by the psychosocial coordinator or patient navigator who administers the DST followed by in-depth interviews for additional appraisal. An action plan is designed based on patient needs, which include their intervention and the intervention of other members of the psychosocial team from the institution and/or from the community. Additional in-house health professionals contributing in distress management include, but are not limited to: physicians; clinical psychologists; health educators; social workers; dietitians; chaplains; and physical, respiratory, speech, and/or swallow therapists. Follow-up and rescreening sessions are scheduled to assure coordination of services between those health professionals as well as to secure continuity of distress management during all stages of the cancer continuum.
The results of the DST are filed in patient medical records. Members of the psychosocial team also document their interventions in the patient medical record, which helps in the exchange of information among the cancer care team. The psychosocial team meets once a month – or as required for extraordinary cases – to review and discuss the cases, determine the best options for distress management, and identify areas for psychosocial care improvement. Those findings and the results of distress management in patient level of satisfaction are then reported and discussed quarterly by the psychosocial coordinator and the cancer committee.
Figure 2 shows in what phase of emotional distress assessment the PHQ-9 was included. Patients reporting four or more of the six areas of concern related to emotional distress in the DST (Figure 1) are automatically referred to a mental health specialist. But when patients report three areas of concern with no clear data on their specific level of depression, PHQ-9 is administered to differentiate those who need a mental health specialist from those who could be adequately supported by health education and support group interventions. In this way detrimental outcomes such as duplicity and over or underuse of services and resources are reduced. In addition, it is recognized that using an interview after the administration of the DST to determine distress management actions does not always provide enough information about a patient’s emotional circumstances and previous comorbidities. Patient responses during interviews may be influenced by the patient’s level of literacy, verbal comprehension, and communication style,24 so emotional distress can go unrecognized during interviews, resulting in delays for treatment and supportive care.
National guidelines in oncology consider such socio-ecological models emphasizing the delivery of patient-centered, interdisciplinary, and evidence-based care. That does not mean that institutions should apply protocols of psychosocial care as previously developed, but that they should test, review, adapt, and improve them during the implementation of the care. In fact, NCCN encourages conducting trials to examine protocols, screening instruments, and models of intervention to determine applicability to particular settings.2
Findings from a study by NCCN member institutions to evaluate progress of implementing distress management guidelines found that 53% (n = 8) of respondent institutions conducted routine distress screening. Of those, 37.5% (3) relied only on interviews. That finding is of concern because if interviews are not standardized and have not been systematically evaluated, then their sensitivity and specificity in identifying distressed patients is unknown.26 Accordingly, the process described in this article and the PHQ-9 validation was an effort to standardize emotional distress management, and was underlined as an achievement during the CoC accreditation visit to the cancer center in December 2013. The hospital was accredited as a comprehensive community cancer center with gold commendations, becoming the first privately owned hospital in Puerto Rico to achieve the accreditation.
A comprehensive, patient-centered approach is required to accomplish cancer best standards of care.1 This approach reflects the holistic conceptualization of health in which the physical, emotional, and social dimensions of the human being are considered when providing medical care. As a result, to look after all patient needs, interdisciplinary and well-coordinated interventions are recommended. Cancer patients should be provided not only with diagnostic, treatment, and follow-up clinical service, but also with the supportive assistance that may positively influence all aspects of their health.
To appraise physical, social, emotional and spiritual issues and to develop supportive interventional action plans, the National Comprehensive Cancer Network (NCCN) recommends screening all cancer patients for distress.2 In particular, screening the emotional component of distress occupies a prominent place in this process because it is now recognized as the sixth vital sign in oncology.3 Even though the influence of emotional distress over cancer mortality rates and disease progression is still under scrutiny,4 its plausible implications over treatment compliance have been pointed out. Patients with higher levels of emotional distress show lower adherence to treatment and poorer health outcomes.5 Furthermore, prevalence rates of emotional distress in cancer patients from ambulatory settings6 and oncology surgical units have been studied and have provided justification for distress management.7 Studies have shown low ability among oncologists to identify patients in distress and oncologists’ tendency to judge distress higher than the patients themselves.8 As a consequence, to achieve systematic distress evaluations and appropriate referrals for care, guidelines for distress management should be implemented in clinical settings. It is recommended that tests are conducted to find brief screening instruments and procedures to assure accurate interventions according to patient specific needs.
This article presents the process of implementing a distress management program at HIMA-San Pablo Oncologic Hospital in Caguas, Puerto Rico, with particular emphasis on the management of emotional distress, which has been defined as the feeling of suffering that cancer patients may experience after diagnosis. In addition, we have included data from a pilot study that was completed for content validation of the Patient Health Questionnaire (PHQ-9) to estimate depression levels in Puerto Rican cancer patients.
Methods
HIMA-San Pablo operates a group of privately owned hospitals in Puerto Rico. It established a cancer center in Caguas in 2007, recruiting a multispecialty medical faculty to provide cancer care and bone marrow transplants for adult and pediatric patients. The cancer center, currently named HIMA-San Pablo Oncologic Hospital (HSPOH), is a hospital within a hospital licensed by the Puerto Rico Department of Health. In 2007, a cancer committee was established as the steering committee to ensure the delivery of cancer care according to best standards of care. The committee took responsibility for developing all activities needed to achieve the American College of Surgeons’ Commission on Cancer (CoC) accreditation under the category of Comprehensive Community Cancer Center. The committee established a psychosocial team to develop a protocol for the delivery of distress management for adult patients. (The psychosocial needs of pediatric patients are assessed through other procedures.)
To develop the protocol, principles of input-output model of research and quality analysis in health care were applied.9 The input-output model, with its origin in engineering, helped map systematic activities to transform empirical data on cancer psychosocial care into operational procedures. Focus was given to data gathering (input), information organization and analysis (throughput), and the schematization of emotional distress management care (output).
The input phase
In the input phase, elements of psychosocial care and operational definitions related to distress management in general were identified through literature review (Table 1). Basic parameters for distress management were clarified, resulting in a conceptual framework based in four remarks: First, according to NCCN, distress is a multifactorial unpleasant emotional experience of a psychological, social, and spiritual nature. It may interfere with the ability to cope effectively with cancer, its symptoms and its treatment. Its intensity may fluctuate from feelings of suffering and fear to incapacitating manifestations of anxiety and depression2 and its severity may hamper patient quality of life and treatment compliance.
Second, distress management requires the intervention of an interdisciplinary team with both medical and allied health professionals. This may include mental health specialists and other professionals with training and experience in cancer-related issues, who work with reciprocal channels of communication for the exchange of patient information.
Third, NCCN recommends using the Distress Thermometer for patient initial distress screening.10-12 It consists of a numeric scale ranging from 0 (no distress) to 10 (severe distress) in which patients classify their level of distress. The numeric scale is followed by a section in which patients identify areas of practical, familiar, emotional, spiritual/ religious, and physical concerns. Based on responses, interviews may follow to set distress management interventions.
Fourth, screening and assessment are different but sequential and complementary stages of distress management. Screening is viewed as a rapid strategy to identify cancer patients in distress. Assessment looks out for a broader appraisal and documentation of factors with repercussions over patient distress level and resiliency capability.13 In many instances, the patient’s emotional distress is better understood in the assessment phase.
The throughput phase
Within the throughput phase of information organization and analysis, an inventory of health professionals and other in-house consultants needed for distress management was completed. Roles and procedures for information sharing were determined, and we established collaborative agreements with professionals in the community who could contribute to distress management. Members of the psychosocial team held workshops to discuss elements of NCCN guidelines for distress management and to create an action plan for the implementation of the protocol. Data analyses were performed to create a demographic profile of the oncology population at the hospital and assess patient willingness to receive emotional support services,16 which led to the implementation of support group meetings at which additional substantive information was collected about issues affecting cancer patients’ emotions.
The NCCN Distress Thermometer for measuring distress was translated to Spanish. Its format was adapted, and it was identified as a distress screening tool (DST), which we named Distress Assessment Tool for Oncology Patients (Figure 1). The instrument helps for rapid screening of patient needs and proper determination of initial interventions. In addition, psychometric properties of several instruments were reviewed for instances when patient emotional distress could not be clearly determined. We decided to proceed with the validation of the 9-item Patient Health Questionnaire (PHQ-9) to estimate patient depression level. A proposal for content validation of the PHQ-9 was approved by the University of Puerto Rico institutional review board, and patients were recruited to participate in the pilot study.
The PHQ-9. The PHQ-9 is a self-report version of the PRIME-MD instrument developed to assess mental disorders in clinical settings. It is based on DSM-IV diagnostic criteria.17 The PHQ-9 is the depression module with nine depression symptoms to check off if they become the cause of emotional impairment. Respondents categorized depression symptoms in four frequency degrees representing numeric values: 0 (not at all), 1 (several days), 2 (more than half the days), 3 (nearly every day). Measures of depression severity are subsequently determined in a Likert-type scale according to numeric calculations of responses: 0-4 (none severe depression), 5-9 (mild), 10-14 (moderate), 15-19 (moderately severe), and 20-27 (severe-major depression).
The instrument is widely used because of its validity in small and large populations. It showed adequate reliability and validity in a small sample of head and neck cancer patients, with a Cronbach’s alpha of 0.80 and a correlation coefficient of 0.71.18 Similarly, it showed good performance in identifying major depression in 4264 cancer outpatients, with sensitivity of 93%, specificity of 81%, and a positive predictive value (PPV) of 25% and negative predictive value (NPV) of 99%.19 Even when administered on a touch screen computer, the instrument showed valid data of depression from patients in treatment.20
The Beck Depression Inventory. We used the Beck Depression Inventory (BDI-II) Spanish version as the gold standard measure for the validation study. It is a 22-items inventory that measures attitudes and symptoms of depression.21 It can be administered in 10 minutes and has shown good psychometric measures when administered in Spain and Puerto Rico.22, 23
The pilot study. In all, 44 cancer patients who were receiving outpatient treatment at the radiotherapy unit agreed to participate in the study. The participants signed a consent form after the confidentiality protection measures and the main objectives of the study had been explained to them. Patients were interviewed individually during November and December 2012, with the Spanish versions of the PHQ-9 and BDI-II administered by one of two interviewers. At the beginning of each interview, the patient was asked 10 questions so that we could gather demographic data and confirm participant eligibility: aged 21 years or older, born and raised in Puerto Rico, being a Spanish speaker, and having a primary cancer diagnosis with no previous disease. Three patients were excluded from the sample because they either had cancer previously or had a recurrence or metastasis. The final sample consisted of 41 outpatients (N = 41).
Data analysis for demographics was completed with STATA v.12 software. Measures of central tendency and dispersion as well as PHQ-9 internal consistency analysis were made through Cronbach alpha with SPSS.
From a total of 41 patients surveyed, 22 (54%) were men and 19 (46%) were women, with an overall median age of 61 years. Among the men, 15 (68%) had a prostate cancer diagnosis and among women, 9 (47.4%) had a breast cancer diagnosis. In regard to health insurance, 19 (46%) had Medicare or Veterans/federal insurance coverage, and 13 (32%) had Reforma, the Puerto Rican government health insurance program partially funded by Medicaid funds. In addition, 8 participants (20%) were unemployed or disabled. As previously stated, all of the patients were in ambulatory care. Only 3 (7%) were participating in support groups.
Of all the respondents, 16 (39%) reported some level of depression. In particular, 2 (5%) showed severe-major depression, 4 (10%) moderately severe depression, and 10 (24%) moderate depression. Of those with depression, 8 (50%) were women, 8 (50%) were men. All 6 of the patients with head and neck cancer showed moderate or moderately severe depression (Table 2).
When respondent PHQ-9 scoring reflected moderate to severe depression (>10), a letter was sent to the patient’s radio-oncologist for referral to counseling and clinical psychological evaluation. All participants had access to the support group program, to a radiotherapy education program meeting weekly, and written information about their cancer diagnosis and treatment. They also were interviewed by the psychosocial coordinator or patient navigator for further assessment.
The output phase
In the output phase, a graphic representing the process of emotional assessment at the institution was created and then modified. PHQ-9 was added to the process when it was found suitable to assess level of depression contributing to the identification of patients requiring psychological and psychiatric assistance which by other means would be missed. PHQ-9 was useful in the busy clinical setting as it was completed, scored and interpreted in minutes. It showed the potential for routine evaluations when looking to identify improvement or deterioration in depression levels thus helping to monitor responses to treatment and providing insights for follow up interventions. As stated by NCCN guidelines, distress should be monitored, documented and managed at all stages of the cancer continuum.
Results and discussion
The protocol for distress management at HSPOH is based on the 2013 NCCN guidelines. Cancer patients are screened for levels of distress in all settings (inpatients and outpatients). Screening is held with the DST Spanish translation at the moment of diagnosis or as soon as possible after a diagnosis is made. Screening for distress is also done before or after surgery, in recurrence or progression, and when clinically indicated. Patients are informed that distress management is an essential part of their care and are encouraged to provide information so that we can make a proper need assessment.
Patients are screened by the psychosocial coordinator or patient navigator who administers the DST followed by in-depth interviews for additional appraisal. An action plan is designed based on patient needs, which include their intervention and the intervention of other members of the psychosocial team from the institution and/or from the community. Additional in-house health professionals contributing in distress management include, but are not limited to: physicians; clinical psychologists; health educators; social workers; dietitians; chaplains; and physical, respiratory, speech, and/or swallow therapists. Follow-up and rescreening sessions are scheduled to assure coordination of services between those health professionals as well as to secure continuity of distress management during all stages of the cancer continuum.
The results of the DST are filed in patient medical records. Members of the psychosocial team also document their interventions in the patient medical record, which helps in the exchange of information among the cancer care team. The psychosocial team meets once a month – or as required for extraordinary cases – to review and discuss the cases, determine the best options for distress management, and identify areas for psychosocial care improvement. Those findings and the results of distress management in patient level of satisfaction are then reported and discussed quarterly by the psychosocial coordinator and the cancer committee.
Figure 2 shows in what phase of emotional distress assessment the PHQ-9 was included. Patients reporting four or more of the six areas of concern related to emotional distress in the DST (Figure 1) are automatically referred to a mental health specialist. But when patients report three areas of concern with no clear data on their specific level of depression, PHQ-9 is administered to differentiate those who need a mental health specialist from those who could be adequately supported by health education and support group interventions. In this way detrimental outcomes such as duplicity and over or underuse of services and resources are reduced. In addition, it is recognized that using an interview after the administration of the DST to determine distress management actions does not always provide enough information about a patient’s emotional circumstances and previous comorbidities. Patient responses during interviews may be influenced by the patient’s level of literacy, verbal comprehension, and communication style,24 so emotional distress can go unrecognized during interviews, resulting in delays for treatment and supportive care.
National guidelines in oncology consider such socio-ecological models emphasizing the delivery of patient-centered, interdisciplinary, and evidence-based care. That does not mean that institutions should apply protocols of psychosocial care as previously developed, but that they should test, review, adapt, and improve them during the implementation of the care. In fact, NCCN encourages conducting trials to examine protocols, screening instruments, and models of intervention to determine applicability to particular settings.2
Findings from a study by NCCN member institutions to evaluate progress of implementing distress management guidelines found that 53% (n = 8) of respondent institutions conducted routine distress screening. Of those, 37.5% (3) relied only on interviews. That finding is of concern because if interviews are not standardized and have not been systematically evaluated, then their sensitivity and specificity in identifying distressed patients is unknown.26 Accordingly, the process described in this article and the PHQ-9 validation was an effort to standardize emotional distress management, and was underlined as an achievement during the CoC accreditation visit to the cancer center in December 2013. The hospital was accredited as a comprehensive community cancer center with gold commendations, becoming the first privately owned hospital in Puerto Rico to achieve the accreditation.
1. Commission on Cancer, American College of Surgeons. Cancer Programs Standards 2012: Ensuring Patient-Centered Care. Version 1.2.1. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/programstandards2012.ashx. Published 2012. Accessed March 5, 2013.
2. National Comprehensive Cancer Network clinical practice guidelines in oncology (NCCN guidelines): Distress management. Version I. 2012. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp#supportive. Accessed March 5, 2013.
3. Bultz BD, Groff SL. Screening for distress, the 6th vital sign in oncology: from theory to practice: http://www.oncologyex.com/issue/2009/vol8_no1/8_comment2_1.html. Published February 2009. Accessed February 16, 2017.
4. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009;115:5349-5361.
5. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Int Med. 2000;160:2101-2107.
6. Jadoon NA, Munir W, Shahzad MA, Choudhry ZS. Assessment of depression and anxiety in adult cancer outpatients: a cross sectional study. BMC Cancer. 2010;10:594.
7. Fisher D, Wedel B. Anxiety and depression disorders in cancer patients: incidence, diagnosis and therapy. Mag Eur Med Oncol. 2012;5:52-54.
8. Sollner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived social support, and in need for psychosocial counselling? Br J Cancer. 2001;84:179-185.
9. Scott RD, Solomon SL, McGowan JE. Applying economic principles to health care: special issue. Emerg Infect Dis. 2001;7:282-285.
10. Adler NE, Page AEK. A model for delivering psychosocial health services. In: Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press (US); 2008.
11. Holland JC, Alici Y. Management of distress in cancer patients. J Support Oncol. 2010;8:4-12.
12. Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494-1502.
13. Maihoff SE. Assessment. In Washington CM, Leaver D, eds. Principles and practice of radiation therapy. St Louis, MO: Mosby Elsevier; 2004:243-264.
14. National Academy of Sciences. Adler NE, Page AEK, eds. Cancer care for the whole patient: meeting psychosocial health needs. https://www.ncbi.nlm.nih.gov/books/NBK4015/. Published 2008. Accessed February 22, 2012.
15. Nancarrow SA, Booth A, Ariss
16. Baker-Glenn EA, Park B, Granger L, Symonds P, Mitchell AJ. Desire for psychological support in cancer patients with depression or distress: validation of a simple help question. Psychooncology. 2011;20:525-531.
17. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
18. Omoro SA, Fann JR, Weymuller EA, Macharia IM, Yueh B. Swahili translation and validation of the Patient Health Questionnaire-9 depression scale in the Kenyan head and neck cancer patient population. Int J Psychiatry Med. 2006;36:367-381.
19. Thekkumpurath P, Walker J, Butcher I, et al. Screening for major depression on cancer outpatients: the diagnostic accuracy of the 9-item Patient Health Questionnaire. Cancer. 2011;117:218-227.
20. Fann JR, Berry DL, Wolpin S, et al. Depression screening using the Patient Health Questionnaire-9 administered on a touch screen computer. Psychooncology. 2009;18:14-22.
21. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:651-571.
22. Sanz J, Perdigón AL, Vázquez C. The Spanish adaptation of Beck’s Depression Inventory–II (BDI-II): psychometric properties in the general population. Clínica y Salud. 2003;14:249-280.
23. Bonilla J, Bernal G, Santos A, Santos D. A revised Spanish version of the Beck Depression Inventory: psychometric properties with a Puerto Rican sample of college students. J Clin Psychol. 2004;60:119-130.
24. Alcántara C, Gone JP. Multicultural issues in the clinical interview and diagnostic process. In Leong FTL, ed. APA handbook of multicultural psychology. Vol 2. Applications and training. Washington, DC: American Psychological Association; 2014:153-163.
25. Sharma M, Romas JA. Theoretical foundations of health education and health promotion. 2nd ed. Burlington, MA: Jones & Barlett Learning; 2012.
26. Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5:99-103.
1. Commission on Cancer, American College of Surgeons. Cancer Programs Standards 2012: Ensuring Patient-Centered Care. Version 1.2.1. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/programstandards2012.ashx. Published 2012. Accessed March 5, 2013.
2. National Comprehensive Cancer Network clinical practice guidelines in oncology (NCCN guidelines): Distress management. Version I. 2012. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp#supportive. Accessed March 5, 2013.
3. Bultz BD, Groff SL. Screening for distress, the 6th vital sign in oncology: from theory to practice: http://www.oncologyex.com/issue/2009/vol8_no1/8_comment2_1.html. Published February 2009. Accessed February 16, 2017.
4. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009;115:5349-5361.
5. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Int Med. 2000;160:2101-2107.
6. Jadoon NA, Munir W, Shahzad MA, Choudhry ZS. Assessment of depression and anxiety in adult cancer outpatients: a cross sectional study. BMC Cancer. 2010;10:594.
7. Fisher D, Wedel B. Anxiety and depression disorders in cancer patients: incidence, diagnosis and therapy. Mag Eur Med Oncol. 2012;5:52-54.
8. Sollner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived social support, and in need for psychosocial counselling? Br J Cancer. 2001;84:179-185.
9. Scott RD, Solomon SL, McGowan JE. Applying economic principles to health care: special issue. Emerg Infect Dis. 2001;7:282-285.
10. Adler NE, Page AEK. A model for delivering psychosocial health services. In: Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press (US); 2008.
11. Holland JC, Alici Y. Management of distress in cancer patients. J Support Oncol. 2010;8:4-12.
12. Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494-1502.
13. Maihoff SE. Assessment. In Washington CM, Leaver D, eds. Principles and practice of radiation therapy. St Louis, MO: Mosby Elsevier; 2004:243-264.
14. National Academy of Sciences. Adler NE, Page AEK, eds. Cancer care for the whole patient: meeting psychosocial health needs. https://www.ncbi.nlm.nih.gov/books/NBK4015/. Published 2008. Accessed February 22, 2012.
15. Nancarrow SA, Booth A, Ariss
16. Baker-Glenn EA, Park B, Granger L, Symonds P, Mitchell AJ. Desire for psychological support in cancer patients with depression or distress: validation of a simple help question. Psychooncology. 2011;20:525-531.
17. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
18. Omoro SA, Fann JR, Weymuller EA, Macharia IM, Yueh B. Swahili translation and validation of the Patient Health Questionnaire-9 depression scale in the Kenyan head and neck cancer patient population. Int J Psychiatry Med. 2006;36:367-381.
19. Thekkumpurath P, Walker J, Butcher I, et al. Screening for major depression on cancer outpatients: the diagnostic accuracy of the 9-item Patient Health Questionnaire. Cancer. 2011;117:218-227.
20. Fann JR, Berry DL, Wolpin S, et al. Depression screening using the Patient Health Questionnaire-9 administered on a touch screen computer. Psychooncology. 2009;18:14-22.
21. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:651-571.
22. Sanz J, Perdigón AL, Vázquez C. The Spanish adaptation of Beck’s Depression Inventory–II (BDI-II): psychometric properties in the general population. Clínica y Salud. 2003;14:249-280.
23. Bonilla J, Bernal G, Santos A, Santos D. A revised Spanish version of the Beck Depression Inventory: psychometric properties with a Puerto Rican sample of college students. J Clin Psychol. 2004;60:119-130.
24. Alcántara C, Gone JP. Multicultural issues in the clinical interview and diagnostic process. In Leong FTL, ed. APA handbook of multicultural psychology. Vol 2. Applications and training. Washington, DC: American Psychological Association; 2014:153-163.
25. Sharma M, Romas JA. Theoretical foundations of health education and health promotion. 2nd ed. Burlington, MA: Jones & Barlett Learning; 2012.
26. Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5:99-103.
Electronic Health Record Implementation Is Associated With a Negligible Change in Outpatient Volume and Billing
Take-Home Points
- With EHR implementation there are small changes in the level of billing coding.
- Although these changes may be statistically significant they are relatively minor.
- In the general internal medicine department, level 4 coding increased by 1.2% while level 3 coding decreased by 0.5%.
- In the orthopedics department, level 4 coding increased by 3.3% while level 3 coding decreased by 3.1%.
- Reports in the lay media regarding dramatic up-coding after EHR implementation may be misleading.
The Health Information Technology for Economic and Clinical Health (HITECH) Act, which was signed into law in 2009, mandated that hospitals that care for Medicare patients either begin using electronic health records (EHRs) or pay a nontrivial penalty.1 By now, the majority of orthopedic surgeons have implemented EHRs in their practices.2 Despite ongoing debate in the orthopedic literature,3 EHRs are expected to improve coordination of care, reduce duplicate testing, and reduce costs over the long term as healthcare insurance coverage is extended to millions more Americans.
In early coverage, however, media reported that EHR implementation at some hospitals was correlated with substantial increases in Medicare payments.4 Journalists suggested the billion dollars more paid by Medicare to hospitals in 2010 than in 2005 were partly attributable to up-coding facilitated by EHRs.5 The secretary of the Department of Health and Human Services (DHHS) and the attorney general of the Department of Justice also weighed in on this controversy by expressing their concerns in a letter to the presidents of 5 hospital associations.6 The inspector general of DHHS also published a report critical of Medicare officials’ oversight of EHRs.7Responding to the critical reception of EHR implementations, investigators studied the validity of the early reports and anecdotes. Some initial reports cited the emergency department (ED) as an area at high risk for using the convenience of EHRs to up-code visits.5 The DHHS Office of the Inspector General noted that, between 2001 and 2010, the proportion of claims for lower reimbursement categories of American Medical Association Current Procedural Terminology (CPT) codes decreased while the proportion for higher-paid billing codes increased for all visit types.8 Addressing these concerns, the American Hospital Association9 issued a brief that noted that any observed coding increases were more likely attributable to more ED use by Medicare patients and increased average illness severity. In a thoughtful perspective, Pitts10 conceded that, though utilization and illness severity may explain part of the trend, the trend may also be related to technological innovations and changes in culture and practice style in the ED.
Because these studies and reports variously suggested that EHR implementation affects patient volume and up-coding, and because none of the reports specifically addressed orthopedics, we conducted a study to determine whether any significant up-coding or change in patient volumes occurred around the time of EHR implementation in ambulatory practices at our academic medical center. In a recent national study, Adler-Milstein and Jha11 compared billing data of hospitals that adopted EHRs and hospitals that did not. Although both groups showed increased billing trends, the increases were not significantly different between the EHR adopters and nonadopters. To more effectively control for the confounding differences between groups of EHR adopters and nonadopters, we studied individual departments during EHR implementation at our institution.
Methods
In 2011, our academic medical center began the transition to EHRs (Epic). We examined our center’s trends in patient volumes and billing coding around the time of the transition in the outpatient practice of the general internal medicine (GIM) department (EHR transition, October 2011) and the outpatient practice of the orthopedics department (EHR transition, March 2012). These departments were chosen because they are representative of a GIM practice and a subspecialty practice, and because a recent study found that GIM practitioners and orthopedic surgeons were among those specialists who used EHRs the most.12
After this study was approved by our Human Investigations Committee, we began using CPT codes to identify all outpatient visits (new, consultation, and return) on a monthly basis. We compared the volume of patient visits and the billing coding level in the GIM and orthopedics departments before and after EHR implementation. Pearson χ2 test was used when appropriate, and statistical analyses were performed with SPSS for Windows Version 16.0.
Results
In the GIM department, mean monthly volume of patient visits in the 12 months before EHR implementation was similar to that in the 12 months afterward (613 vs 587; P = .439). Even when normalized for changes in provider availability (maternity leave), the decrease in volume of patient visits after EHR implementation in the GIM department was not significant (6.9%; P = .107). Likewise, in the orthopedics department, mean monthly volume of patient visits in the 17 months before EHR implementation was similar to that in the 7 months afterward (2157 vs 2317; P = .156). In fact, patient volumes remained constant during the EHR transition (Figure 1).
EHR implementation brought small changes in billing coding levels. In the GIM department, the largest change was a 1.2% increase in level 4 billing coding—an increase accompanied by a 0.5% decrease in level 3 coding.
Discussion
It is remarkable that the volumes of patient visits in the GIM and orthopedics departments at our academic center were not affected by EHR implementation.
Rather than reduce scheduling during the EHR transition, surgeons in our practice either added or lengthened clinic sessions, and the level of ancillary staffing was adjusted accordingly. As staffing costs at any given time are multifactorial and vary widely, estimating the cost of these staffing changes during the EHR transition is difficult. We should note that extending ancillary staff hours during the transition very likely increased costs, and it is unclear whether they were higher or lower than the costs that would have been incurred had we reduced scheduling or tried some combination of these strategies.
Although billing coding levels changed with EHR implementation, the changes were small. In the GIM department, level 4 CPT coded visits as percentages of all visits increased to 59.5% from 58.3%, and level 5 visits increased to 6.2% from 6.0%; in the orthopedics department, level 4 visits increased to 40.2% from 37.1%, and level 5 visits increased to 5.5% from 3.8% (Table). The 1.2% and 0.2% absolute increases in level 4 and level 5 visits in the GIM department represent 2.1% and 3.3% relative increases in level 4 and level 5 visits, and the 3.3% and 1.7% absolute increases in the orthopedics department represent 8.4% and 44.7% relative increases in level 4 and level 5 visits after EHR implementation.
Although the absolute increases in level 4 and level 5 visits were relatively minor, popular media have raised the alarm about 43% and 82% relative increases in level 5 visits after EHR implementation in some hospitals’ EDs.4 Although our orthopedics department showed a 44.7% relative increase in level 5 visits after EHR implementation, this represented an increase of only 1.7% of patient visits overall. Our findings therefore indicate that lay media reports could be misleading. Nevertheless, the small changes we found were statistically significant.
One explanation for these small changes is that EHRs facilitate better documentation of services provided. Therefore, what seem to be billing coding changes could be more accurate reports of high-level care that is the same as before. In addition, because of meaningful use mandates that coincided with the requirement to implement EHRs, additional data elements are now being consistently collected and reviewed (these may not necessarily have been collected and reviewed before). In some patient encounters, these additional data elements may have contributed to higher levels of service, and this effect could be especially apparent in EDs.
Some have suggested a potential for large-scale up-coding during EHR transitions. Others have contended that coding level increases are a consequence of a time-intensive data entry process, collection and review of additional data, and more accurate reporting of services already being provided. We are not convinced that large coding changes are attributable solely to EHR implementation, as the changes at our center have been relatively small.
Nevertheless, minor coding level changes could translate to large changes in healthcare costs when scaled nationally. Although causes may be innocuous, any increases in national healthcare costs are concerning in our time of limited budgets and scrutinized healthcare utilization.
This study had its limitations. First, including billing data from only 2 departments at a single center may limit the generalizability of findings. However, we specifically selected a GIM department and a specialty (orthopedics) department in an attempt to capture a representative sample of practices. Another limitation is that we investigated billing codes over only 2 years, around the implementation of EHRs in these departments, and therefore may have captured only short-term changes. However, as patient volumes and billing are subject to many factors, including staffing changes (eg, new partners, new hires, retirements, other departures), we attempted to limit the effect of confounding variables by limiting the period of analysis.
Overall, changes in patient volume and coded level of service during EHR implementation at our institution were relatively small. Although the trend toward higher billing coding levels was statistically significant, these 0.2% and 1.7% increases in level 5 coding hardly deserve the negative attention from lay media. These small increases are unlikely caused by intentional up-coding, and more likely reflect better documentation of an already high level of care. We hope these findings allay the concern that up-coding increased dramatically with EHR implementation.
Am J Orthop. 2017;46(3):E172-E176. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Centers for Medicare & Medicaid Services. Electronic health records (EHR) incentive programs. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms. Accessed February 5, 2015.
2. American Academy of Orthopaedic Surgeons Practice Management Committee. EMR: A Primer for Orthopaedic Surgeons. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010.
3. Ries MD. Electronic medical records: friends or foes? Clin Orthop Relat Res. 2014;472(1):16-21.
4. Abelson R. Medicare is faulted on shift to electronic records. New York Times. November 29, 2012;B1. http://www.nytimes.com/2012/11/29/business/medicare-is-faulted-in-electronic-medical-records-conversion.html. Accessed February 5, 2015.
5. Abelson R, Creswell J, Palmer G. Medicare bills rise as records turn electronic. New York Times. September 22, 2012;A1. http://www.nytimes.com/2012/09/22/business/medicare-billing-rises-at-hospitals-with-electronic-records.html. Accessed February 5, 2015.
6. Carlson J. Warning bell. Potential for fraud through use of EHRs draws federal scrutiny. Mod Healthc. 2012;42(40):8-9.
7. Levinson DR. Early assessment finds that CMS faces obstacles in overseeing the Medicare EHR Incentive Program. Dept of Health and Human Services, Office of Inspector General website. https://oig.hss.gov/oei/reports/oei-05-11-00250.pdf. Publication OEI-05-11-00250. Published November 2012. Accessed February 5, 2015.
8. Levinson DR. Coding trends of Medicare evaluation and management services. Dept of Health and Human Services, Office of Inspector General website. https://oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Publication OEI-04-10-00180. Published May 2012. Accessed February 5, 2015.
9. American Hospital Association. Sicker, more complex patients are driving up intensity of ED care [issue brief]. http://www.aha.org/content/13/13issuebrief-ed.pdf. Published May 2, 2013. Accessed February 5, 2015.
10. Pitts SR. Higher-complexity ED billing codes—sicker patients, more intensive practice, or improper payments? N Engl J Med. 2012;367(26):2465-2467.
11. Adler-Milstein J, Jha AK. No evidence found that hospitals are using new electronic health records to increase Medicare reimbursements. Health Aff (Millwood). 2014;33(7):1271-1277.
12. Kokkonen EW, Davis SA, Lin HC, Dabade TS, Feldman SR, Fleischer AB Jr. Use of electronic medical records differs by specialty and office settings. J Am Med Inform Assoc. 2013;20(e1):e33-e38.
13. Samaan ZM, Klein MD, Mansour ME, DeWitt TG. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage. 2009;32(3):180-187.
Take-Home Points
- With EHR implementation there are small changes in the level of billing coding.
- Although these changes may be statistically significant they are relatively minor.
- In the general internal medicine department, level 4 coding increased by 1.2% while level 3 coding decreased by 0.5%.
- In the orthopedics department, level 4 coding increased by 3.3% while level 3 coding decreased by 3.1%.
- Reports in the lay media regarding dramatic up-coding after EHR implementation may be misleading.
The Health Information Technology for Economic and Clinical Health (HITECH) Act, which was signed into law in 2009, mandated that hospitals that care for Medicare patients either begin using electronic health records (EHRs) or pay a nontrivial penalty.1 By now, the majority of orthopedic surgeons have implemented EHRs in their practices.2 Despite ongoing debate in the orthopedic literature,3 EHRs are expected to improve coordination of care, reduce duplicate testing, and reduce costs over the long term as healthcare insurance coverage is extended to millions more Americans.
In early coverage, however, media reported that EHR implementation at some hospitals was correlated with substantial increases in Medicare payments.4 Journalists suggested the billion dollars more paid by Medicare to hospitals in 2010 than in 2005 were partly attributable to up-coding facilitated by EHRs.5 The secretary of the Department of Health and Human Services (DHHS) and the attorney general of the Department of Justice also weighed in on this controversy by expressing their concerns in a letter to the presidents of 5 hospital associations.6 The inspector general of DHHS also published a report critical of Medicare officials’ oversight of EHRs.7Responding to the critical reception of EHR implementations, investigators studied the validity of the early reports and anecdotes. Some initial reports cited the emergency department (ED) as an area at high risk for using the convenience of EHRs to up-code visits.5 The DHHS Office of the Inspector General noted that, between 2001 and 2010, the proportion of claims for lower reimbursement categories of American Medical Association Current Procedural Terminology (CPT) codes decreased while the proportion for higher-paid billing codes increased for all visit types.8 Addressing these concerns, the American Hospital Association9 issued a brief that noted that any observed coding increases were more likely attributable to more ED use by Medicare patients and increased average illness severity. In a thoughtful perspective, Pitts10 conceded that, though utilization and illness severity may explain part of the trend, the trend may also be related to technological innovations and changes in culture and practice style in the ED.
Because these studies and reports variously suggested that EHR implementation affects patient volume and up-coding, and because none of the reports specifically addressed orthopedics, we conducted a study to determine whether any significant up-coding or change in patient volumes occurred around the time of EHR implementation in ambulatory practices at our academic medical center. In a recent national study, Adler-Milstein and Jha11 compared billing data of hospitals that adopted EHRs and hospitals that did not. Although both groups showed increased billing trends, the increases were not significantly different between the EHR adopters and nonadopters. To more effectively control for the confounding differences between groups of EHR adopters and nonadopters, we studied individual departments during EHR implementation at our institution.
Methods
In 2011, our academic medical center began the transition to EHRs (Epic). We examined our center’s trends in patient volumes and billing coding around the time of the transition in the outpatient practice of the general internal medicine (GIM) department (EHR transition, October 2011) and the outpatient practice of the orthopedics department (EHR transition, March 2012). These departments were chosen because they are representative of a GIM practice and a subspecialty practice, and because a recent study found that GIM practitioners and orthopedic surgeons were among those specialists who used EHRs the most.12
After this study was approved by our Human Investigations Committee, we began using CPT codes to identify all outpatient visits (new, consultation, and return) on a monthly basis. We compared the volume of patient visits and the billing coding level in the GIM and orthopedics departments before and after EHR implementation. Pearson χ2 test was used when appropriate, and statistical analyses were performed with SPSS for Windows Version 16.0.
Results
In the GIM department, mean monthly volume of patient visits in the 12 months before EHR implementation was similar to that in the 12 months afterward (613 vs 587; P = .439). Even when normalized for changes in provider availability (maternity leave), the decrease in volume of patient visits after EHR implementation in the GIM department was not significant (6.9%; P = .107). Likewise, in the orthopedics department, mean monthly volume of patient visits in the 17 months before EHR implementation was similar to that in the 7 months afterward (2157 vs 2317; P = .156). In fact, patient volumes remained constant during the EHR transition (Figure 1).
EHR implementation brought small changes in billing coding levels. In the GIM department, the largest change was a 1.2% increase in level 4 billing coding—an increase accompanied by a 0.5% decrease in level 3 coding.
Discussion
It is remarkable that the volumes of patient visits in the GIM and orthopedics departments at our academic center were not affected by EHR implementation.
Rather than reduce scheduling during the EHR transition, surgeons in our practice either added or lengthened clinic sessions, and the level of ancillary staffing was adjusted accordingly. As staffing costs at any given time are multifactorial and vary widely, estimating the cost of these staffing changes during the EHR transition is difficult. We should note that extending ancillary staff hours during the transition very likely increased costs, and it is unclear whether they were higher or lower than the costs that would have been incurred had we reduced scheduling or tried some combination of these strategies.
Although billing coding levels changed with EHR implementation, the changes were small. In the GIM department, level 4 CPT coded visits as percentages of all visits increased to 59.5% from 58.3%, and level 5 visits increased to 6.2% from 6.0%; in the orthopedics department, level 4 visits increased to 40.2% from 37.1%, and level 5 visits increased to 5.5% from 3.8% (Table). The 1.2% and 0.2% absolute increases in level 4 and level 5 visits in the GIM department represent 2.1% and 3.3% relative increases in level 4 and level 5 visits, and the 3.3% and 1.7% absolute increases in the orthopedics department represent 8.4% and 44.7% relative increases in level 4 and level 5 visits after EHR implementation.
Although the absolute increases in level 4 and level 5 visits were relatively minor, popular media have raised the alarm about 43% and 82% relative increases in level 5 visits after EHR implementation in some hospitals’ EDs.4 Although our orthopedics department showed a 44.7% relative increase in level 5 visits after EHR implementation, this represented an increase of only 1.7% of patient visits overall. Our findings therefore indicate that lay media reports could be misleading. Nevertheless, the small changes we found were statistically significant.
One explanation for these small changes is that EHRs facilitate better documentation of services provided. Therefore, what seem to be billing coding changes could be more accurate reports of high-level care that is the same as before. In addition, because of meaningful use mandates that coincided with the requirement to implement EHRs, additional data elements are now being consistently collected and reviewed (these may not necessarily have been collected and reviewed before). In some patient encounters, these additional data elements may have contributed to higher levels of service, and this effect could be especially apparent in EDs.
Some have suggested a potential for large-scale up-coding during EHR transitions. Others have contended that coding level increases are a consequence of a time-intensive data entry process, collection and review of additional data, and more accurate reporting of services already being provided. We are not convinced that large coding changes are attributable solely to EHR implementation, as the changes at our center have been relatively small.
Nevertheless, minor coding level changes could translate to large changes in healthcare costs when scaled nationally. Although causes may be innocuous, any increases in national healthcare costs are concerning in our time of limited budgets and scrutinized healthcare utilization.
This study had its limitations. First, including billing data from only 2 departments at a single center may limit the generalizability of findings. However, we specifically selected a GIM department and a specialty (orthopedics) department in an attempt to capture a representative sample of practices. Another limitation is that we investigated billing codes over only 2 years, around the implementation of EHRs in these departments, and therefore may have captured only short-term changes. However, as patient volumes and billing are subject to many factors, including staffing changes (eg, new partners, new hires, retirements, other departures), we attempted to limit the effect of confounding variables by limiting the period of analysis.
Overall, changes in patient volume and coded level of service during EHR implementation at our institution were relatively small. Although the trend toward higher billing coding levels was statistically significant, these 0.2% and 1.7% increases in level 5 coding hardly deserve the negative attention from lay media. These small increases are unlikely caused by intentional up-coding, and more likely reflect better documentation of an already high level of care. We hope these findings allay the concern that up-coding increased dramatically with EHR implementation.
Am J Orthop. 2017;46(3):E172-E176. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- With EHR implementation there are small changes in the level of billing coding.
- Although these changes may be statistically significant they are relatively minor.
- In the general internal medicine department, level 4 coding increased by 1.2% while level 3 coding decreased by 0.5%.
- In the orthopedics department, level 4 coding increased by 3.3% while level 3 coding decreased by 3.1%.
- Reports in the lay media regarding dramatic up-coding after EHR implementation may be misleading.
The Health Information Technology for Economic and Clinical Health (HITECH) Act, which was signed into law in 2009, mandated that hospitals that care for Medicare patients either begin using electronic health records (EHRs) or pay a nontrivial penalty.1 By now, the majority of orthopedic surgeons have implemented EHRs in their practices.2 Despite ongoing debate in the orthopedic literature,3 EHRs are expected to improve coordination of care, reduce duplicate testing, and reduce costs over the long term as healthcare insurance coverage is extended to millions more Americans.
In early coverage, however, media reported that EHR implementation at some hospitals was correlated with substantial increases in Medicare payments.4 Journalists suggested the billion dollars more paid by Medicare to hospitals in 2010 than in 2005 were partly attributable to up-coding facilitated by EHRs.5 The secretary of the Department of Health and Human Services (DHHS) and the attorney general of the Department of Justice also weighed in on this controversy by expressing their concerns in a letter to the presidents of 5 hospital associations.6 The inspector general of DHHS also published a report critical of Medicare officials’ oversight of EHRs.7Responding to the critical reception of EHR implementations, investigators studied the validity of the early reports and anecdotes. Some initial reports cited the emergency department (ED) as an area at high risk for using the convenience of EHRs to up-code visits.5 The DHHS Office of the Inspector General noted that, between 2001 and 2010, the proportion of claims for lower reimbursement categories of American Medical Association Current Procedural Terminology (CPT) codes decreased while the proportion for higher-paid billing codes increased for all visit types.8 Addressing these concerns, the American Hospital Association9 issued a brief that noted that any observed coding increases were more likely attributable to more ED use by Medicare patients and increased average illness severity. In a thoughtful perspective, Pitts10 conceded that, though utilization and illness severity may explain part of the trend, the trend may also be related to technological innovations and changes in culture and practice style in the ED.
Because these studies and reports variously suggested that EHR implementation affects patient volume and up-coding, and because none of the reports specifically addressed orthopedics, we conducted a study to determine whether any significant up-coding or change in patient volumes occurred around the time of EHR implementation in ambulatory practices at our academic medical center. In a recent national study, Adler-Milstein and Jha11 compared billing data of hospitals that adopted EHRs and hospitals that did not. Although both groups showed increased billing trends, the increases were not significantly different between the EHR adopters and nonadopters. To more effectively control for the confounding differences between groups of EHR adopters and nonadopters, we studied individual departments during EHR implementation at our institution.
Methods
In 2011, our academic medical center began the transition to EHRs (Epic). We examined our center’s trends in patient volumes and billing coding around the time of the transition in the outpatient practice of the general internal medicine (GIM) department (EHR transition, October 2011) and the outpatient practice of the orthopedics department (EHR transition, March 2012). These departments were chosen because they are representative of a GIM practice and a subspecialty practice, and because a recent study found that GIM practitioners and orthopedic surgeons were among those specialists who used EHRs the most.12
After this study was approved by our Human Investigations Committee, we began using CPT codes to identify all outpatient visits (new, consultation, and return) on a monthly basis. We compared the volume of patient visits and the billing coding level in the GIM and orthopedics departments before and after EHR implementation. Pearson χ2 test was used when appropriate, and statistical analyses were performed with SPSS for Windows Version 16.0.
Results
In the GIM department, mean monthly volume of patient visits in the 12 months before EHR implementation was similar to that in the 12 months afterward (613 vs 587; P = .439). Even when normalized for changes in provider availability (maternity leave), the decrease in volume of patient visits after EHR implementation in the GIM department was not significant (6.9%; P = .107). Likewise, in the orthopedics department, mean monthly volume of patient visits in the 17 months before EHR implementation was similar to that in the 7 months afterward (2157 vs 2317; P = .156). In fact, patient volumes remained constant during the EHR transition (Figure 1).
EHR implementation brought small changes in billing coding levels. In the GIM department, the largest change was a 1.2% increase in level 4 billing coding—an increase accompanied by a 0.5% decrease in level 3 coding.
Discussion
It is remarkable that the volumes of patient visits in the GIM and orthopedics departments at our academic center were not affected by EHR implementation.
Rather than reduce scheduling during the EHR transition, surgeons in our practice either added or lengthened clinic sessions, and the level of ancillary staffing was adjusted accordingly. As staffing costs at any given time are multifactorial and vary widely, estimating the cost of these staffing changes during the EHR transition is difficult. We should note that extending ancillary staff hours during the transition very likely increased costs, and it is unclear whether they were higher or lower than the costs that would have been incurred had we reduced scheduling or tried some combination of these strategies.
Although billing coding levels changed with EHR implementation, the changes were small. In the GIM department, level 4 CPT coded visits as percentages of all visits increased to 59.5% from 58.3%, and level 5 visits increased to 6.2% from 6.0%; in the orthopedics department, level 4 visits increased to 40.2% from 37.1%, and level 5 visits increased to 5.5% from 3.8% (Table). The 1.2% and 0.2% absolute increases in level 4 and level 5 visits in the GIM department represent 2.1% and 3.3% relative increases in level 4 and level 5 visits, and the 3.3% and 1.7% absolute increases in the orthopedics department represent 8.4% and 44.7% relative increases in level 4 and level 5 visits after EHR implementation.
Although the absolute increases in level 4 and level 5 visits were relatively minor, popular media have raised the alarm about 43% and 82% relative increases in level 5 visits after EHR implementation in some hospitals’ EDs.4 Although our orthopedics department showed a 44.7% relative increase in level 5 visits after EHR implementation, this represented an increase of only 1.7% of patient visits overall. Our findings therefore indicate that lay media reports could be misleading. Nevertheless, the small changes we found were statistically significant.
One explanation for these small changes is that EHRs facilitate better documentation of services provided. Therefore, what seem to be billing coding changes could be more accurate reports of high-level care that is the same as before. In addition, because of meaningful use mandates that coincided with the requirement to implement EHRs, additional data elements are now being consistently collected and reviewed (these may not necessarily have been collected and reviewed before). In some patient encounters, these additional data elements may have contributed to higher levels of service, and this effect could be especially apparent in EDs.
Some have suggested a potential for large-scale up-coding during EHR transitions. Others have contended that coding level increases are a consequence of a time-intensive data entry process, collection and review of additional data, and more accurate reporting of services already being provided. We are not convinced that large coding changes are attributable solely to EHR implementation, as the changes at our center have been relatively small.
Nevertheless, minor coding level changes could translate to large changes in healthcare costs when scaled nationally. Although causes may be innocuous, any increases in national healthcare costs are concerning in our time of limited budgets and scrutinized healthcare utilization.
This study had its limitations. First, including billing data from only 2 departments at a single center may limit the generalizability of findings. However, we specifically selected a GIM department and a specialty (orthopedics) department in an attempt to capture a representative sample of practices. Another limitation is that we investigated billing codes over only 2 years, around the implementation of EHRs in these departments, and therefore may have captured only short-term changes. However, as patient volumes and billing are subject to many factors, including staffing changes (eg, new partners, new hires, retirements, other departures), we attempted to limit the effect of confounding variables by limiting the period of analysis.
Overall, changes in patient volume and coded level of service during EHR implementation at our institution were relatively small. Although the trend toward higher billing coding levels was statistically significant, these 0.2% and 1.7% increases in level 5 coding hardly deserve the negative attention from lay media. These small increases are unlikely caused by intentional up-coding, and more likely reflect better documentation of an already high level of care. We hope these findings allay the concern that up-coding increased dramatically with EHR implementation.
Am J Orthop. 2017;46(3):E172-E176. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Centers for Medicare & Medicaid Services. Electronic health records (EHR) incentive programs. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms. Accessed February 5, 2015.
2. American Academy of Orthopaedic Surgeons Practice Management Committee. EMR: A Primer for Orthopaedic Surgeons. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010.
3. Ries MD. Electronic medical records: friends or foes? Clin Orthop Relat Res. 2014;472(1):16-21.
4. Abelson R. Medicare is faulted on shift to electronic records. New York Times. November 29, 2012;B1. http://www.nytimes.com/2012/11/29/business/medicare-is-faulted-in-electronic-medical-records-conversion.html. Accessed February 5, 2015.
5. Abelson R, Creswell J, Palmer G. Medicare bills rise as records turn electronic. New York Times. September 22, 2012;A1. http://www.nytimes.com/2012/09/22/business/medicare-billing-rises-at-hospitals-with-electronic-records.html. Accessed February 5, 2015.
6. Carlson J. Warning bell. Potential for fraud through use of EHRs draws federal scrutiny. Mod Healthc. 2012;42(40):8-9.
7. Levinson DR. Early assessment finds that CMS faces obstacles in overseeing the Medicare EHR Incentive Program. Dept of Health and Human Services, Office of Inspector General website. https://oig.hss.gov/oei/reports/oei-05-11-00250.pdf. Publication OEI-05-11-00250. Published November 2012. Accessed February 5, 2015.
8. Levinson DR. Coding trends of Medicare evaluation and management services. Dept of Health and Human Services, Office of Inspector General website. https://oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Publication OEI-04-10-00180. Published May 2012. Accessed February 5, 2015.
9. American Hospital Association. Sicker, more complex patients are driving up intensity of ED care [issue brief]. http://www.aha.org/content/13/13issuebrief-ed.pdf. Published May 2, 2013. Accessed February 5, 2015.
10. Pitts SR. Higher-complexity ED billing codes—sicker patients, more intensive practice, or improper payments? N Engl J Med. 2012;367(26):2465-2467.
11. Adler-Milstein J, Jha AK. No evidence found that hospitals are using new electronic health records to increase Medicare reimbursements. Health Aff (Millwood). 2014;33(7):1271-1277.
12. Kokkonen EW, Davis SA, Lin HC, Dabade TS, Feldman SR, Fleischer AB Jr. Use of electronic medical records differs by specialty and office settings. J Am Med Inform Assoc. 2013;20(e1):e33-e38.
13. Samaan ZM, Klein MD, Mansour ME, DeWitt TG. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage. 2009;32(3):180-187.
1. Centers for Medicare & Medicaid Services. Electronic health records (EHR) incentive programs. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms. Accessed February 5, 2015.
2. American Academy of Orthopaedic Surgeons Practice Management Committee. EMR: A Primer for Orthopaedic Surgeons. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010.
3. Ries MD. Electronic medical records: friends or foes? Clin Orthop Relat Res. 2014;472(1):16-21.
4. Abelson R. Medicare is faulted on shift to electronic records. New York Times. November 29, 2012;B1. http://www.nytimes.com/2012/11/29/business/medicare-is-faulted-in-electronic-medical-records-conversion.html. Accessed February 5, 2015.
5. Abelson R, Creswell J, Palmer G. Medicare bills rise as records turn electronic. New York Times. September 22, 2012;A1. http://www.nytimes.com/2012/09/22/business/medicare-billing-rises-at-hospitals-with-electronic-records.html. Accessed February 5, 2015.
6. Carlson J. Warning bell. Potential for fraud through use of EHRs draws federal scrutiny. Mod Healthc. 2012;42(40):8-9.
7. Levinson DR. Early assessment finds that CMS faces obstacles in overseeing the Medicare EHR Incentive Program. Dept of Health and Human Services, Office of Inspector General website. https://oig.hss.gov/oei/reports/oei-05-11-00250.pdf. Publication OEI-05-11-00250. Published November 2012. Accessed February 5, 2015.
8. Levinson DR. Coding trends of Medicare evaluation and management services. Dept of Health and Human Services, Office of Inspector General website. https://oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Publication OEI-04-10-00180. Published May 2012. Accessed February 5, 2015.
9. American Hospital Association. Sicker, more complex patients are driving up intensity of ED care [issue brief]. http://www.aha.org/content/13/13issuebrief-ed.pdf. Published May 2, 2013. Accessed February 5, 2015.
10. Pitts SR. Higher-complexity ED billing codes—sicker patients, more intensive practice, or improper payments? N Engl J Med. 2012;367(26):2465-2467.
11. Adler-Milstein J, Jha AK. No evidence found that hospitals are using new electronic health records to increase Medicare reimbursements. Health Aff (Millwood). 2014;33(7):1271-1277.
12. Kokkonen EW, Davis SA, Lin HC, Dabade TS, Feldman SR, Fleischer AB Jr. Use of electronic medical records differs by specialty and office settings. J Am Med Inform Assoc. 2013;20(e1):e33-e38.
13. Samaan ZM, Klein MD, Mansour ME, DeWitt TG. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage. 2009;32(3):180-187.
Repeal and replace? How about retain, review, and refine?
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
A suggestion for Congress: keep what’s working in the Patient Protection and Affordable Care Act (PPACA), adjust what isn’t working – just make the whole thing better and call it what you will.
A good thing, but needing work
The PPACA, which is also referred to as Obama care, had a lot in it that any reasonable person would consider good. Let’s take a look. As Dr Valerie Arkoosh wrote in our journal in 2012,2 the law attempted to expand access to health care to the embarrassingly large 30 million or more Americans who were not insured. How would it do this? By expanding Medicaid, enhancing consumer protections in the private health insurance market, requiring large employers to offer insurance or pay a fine, giving tax credits to increase affordability of insurance for small businesses, creating state-based competitive market places, and requiring individuals to purchase health insurance plans (the so-called insurance mandate), thereby creating a pool of large numbers of healthy people who would help defray the costs of those not so fortunate.The law also guaranteed insurability despite any preexisting condition, surely a step in the right direction. Likewise, the need for employers to provide health insurance, the state-based health insurance exchanges, and especially the individual mandate to buy insurance or pay a fine, were all steps in the right direction.
And the law went further – it also addressed preventive care. Medicare and all new insurance plans would have to cover, without copay, co-insurance, or deductible, high-certainty preventive services such as screening for breast, cervical, colorectal, lung, and skin cancers, the annual well-woman visit, breast cancer preventative medications, and many others.3 Medicare recipients would be eligible for one non-copay annual wellness visit to their caregiver. Beyond providing increased access to health care, the PPACA added incentives to caregivers who were coming out of training programs to serve in underserved areas and benefit from a decrease in their med school loans or in their loan repayments.
Finally, and especially important, under the PPACA, our age-old insurance system of fee for service, which tends to incentivize more care, would change to incentivizing high-quality, outcomes-based care , thus replacing “quantity of care” with quality of care. So what’s wrong with the features of the law outlined in the preceding paragraphs? Well, of course, for every 100 ideas, only a few will be implemented and actually pay off. Certainly some of the PPACA could have been better implemented, and perhaps the task now facing Congress, if it could ever abandon its current pitched-camp approach, should be to take the ideas that health care policy scientists have established as being valid and find a way to make them work. Surely that would be best for all players, rather than carping about the repeal-replace approach versus staying with the PPACA.
So my response to the repeal-replace assertion? Retain, review, and refine.
Practitioner-friendly content
Health care calamities notwithstanding, we have a line-up of articles in this issue that uniformly address some of the pressing needs many of us face in our daily practice. Barry and colleagues examined the patterns of care with regard to whole brain radiotherapy technique and delivery at US-based academic centers. Their results show some interesting differences in the way younger and older practitioners deliver that care, with older practitioners placing more importance on tumor histopathology when considering brain irradiation. Speaking of access to care in the context of health reform, how often do our cancer patients use the emergency department? Lash and colleagues looked at the ED-use numbers from two databases in California and found that patients go to the ED at higher rates than previously reported and with notable variability by cancer type. Now we need to examine the reasons for those visits and establish ways to identify predictors of ED use to improve patient quality of care and rein in the higher costs of ED use.
In regard to symptom management, we can never have enough about nausea and vomiting prevention. Schwartzberg and colleagues report on a trial in which they evaluated the clinical benefits of APF530, a subcutaneous formulation of granisetron, compared with ondansetron in patients who had received cisplatin therapy. This longer-acting formulation of granisetron performed very well against a standard of care and might give our patients another option in the clinic for highly emetogenic chemotherapy.
Still on the topic of symptom management, preventing and treating mTOR-inhibitor–associated stomatitis (mIAS) is the subject of a review by Ramchandran and colleagues. The inhibitors have been approved for treatment in renal cell, neuroendocrine, and breast cancers, but of course, many of our newer molecules have some associated toxicity. Based on their literature scan, the authors report that management of mIAS should focus on three major approaches: prevention, early aggressive treatment, and, when needed, more aggressive pain management. Early recognition and diagnosis of mIAS facilitate early intervention to limit potential sequelae of mIAS and minimize the need for mTOR inhibitor dose reduction and interruption.
In a way, stress management could also fall under the symptom management category. I often remember being told during my training that we should always discuss with your patients their level of anxiety and depression. But I think sometimes we are so busy addressing the cancer, its treatment, and treatment side effects, we overlook the fact that the patient is suffering psychologically and might need additional intervention in the form of talk therapy and/or medication. Ramírez-Solá and colleagues describe in our How We Do It section the process of developing and implementing a psychosocial distress management program at their institution in Puerto Rico. The authors also summarize the results of a pilot study to validate the Patient Health Questionnaire (PHQ-9) as a measure to improve the process of emotional distress management in particular.
In recent years, the number of approvals and new indications for therapies for different cancer types has increased significantly. We highlight two such approvals in this issue. One is the PARP inhibitor, rucaparib, which was approved in both the platinum-sensitive and -resistant settings for BRCA1- and BRCA2-mutant patients with ovarian cancer. The other is the new CD38 antibody daratumumab, which was originally approved as a single-agent therapy for relapsed myeloma and which has now received a second approval with demonstrated improvement of progression-free survival when given with the lenalidomide-dexamethasone or bortezomib-dexamethasone combinations.
When it comes to new therapies, immunotherapies are at the cutting edge. Who hasn’t heard of the new checkpoint inhibitor drugs for a range of cancers that have either been approved or are in trial? Until now, we have used these immunotherapies as single agents, but Jane de Lartigue writes of the potential of combining more than one immunotherapy drug and/or combining an immune checkpoint inhibitor with a chemotherapy drug. The key behind this concept is that the more antigenic differentiation and tumor infiltrating lymphocytes in the system, the better the immunotherapy might work.
In the previous issue of the journal, one of our Editors, Thomas Strouse, discussed the issue of physician aid in dying (PAD)4 and asserted he had come to view “active non-participation” in legal PAD as a “toxic form of patient abandonment.” This is, of course, a very challenging and complex topic, and one that we likely have to address on a weekly basis with some of our cancer patients: if palliative care and end-of-life is the goal, how can we most humanely achieve that ethically and legally in concert with our patients’ wishes? Is it right or wrong to aid in some way in the dying process? Dr Alva Weir responds to Dr Strouse’s editorial, taking the view point that physician-assisted suicide is toxic abandonment. Dr Strauss responds, and I encourage you to read this very interesting exchange that highlights the point-counterpoint views of physician involvement in the dying process.
We round off the issue with a bumper crop of Case Reports. They include two that document diagnostic challenges: one in a patient with pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion and another in which atraumatic splenic rupture is the initial presentation of CML. Also included is a report on a case of primary cardiac prosthetic valve-associated lymphoma and another on how a collaborative effort between oncologists and dermatologists contributed to the resolution of palmoplantar exacerbation of psoriasis in a patient who had been treated with nivolumab.
Going digital
I will close by remarking that the Journal of Community and Supportive Oncology, or JCSO, will be going digital only after this print issue. We will continue publishing the same content as a bimonthly digital issue, posting articles directly to our website, and mailing out our regular electronic newsletters. So visit the website, www.jcso-online.com, where you can read the articles as soon as they are posted and also find instructions for downloading the app for the digital edition – it’s quick, easy, and free, in case you were wondering. For a shortcut to the download the app, you can also use http://bit.ly/2nCEPIa.
Finally, if you would like to submit a paper to us for consideration for publication, you can do so by going to www.editorialmanager.com/jso/. We will consider submissions in original research, reviews, How We Do It, case reports, and tumor board summaries – you’ll find all the information you need to submit a paper at the EditorialManager platform. And let’s not forget social media – we’re on Twitter where our handle is @jcs_onc, my personal Twitter handle is @davidhenrymd, so connect with us – follow us, like us, and retweet us.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
1. Pear R, Kelly K. Trump concedes health law overhaul is ‘unbelievably complex.’ https://www.nytimes.com/2017/02/27/us/politics/trump-concedes-health-law-overhaul-is-unbelievably-complex.html?_r=0. New York Times. February 27, 2017. Accessed April 4, 2017.
2. Arkoosh VA. The Patient Protection and Affordable Care Act: no rhetoric, just the facts. Commun Oncol. 2012;9(6):206-209.
3. USPSTF A and B Recommendations. US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/. January 2017. Accessed April 4, 2017.
4. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Community Support Oncol. 2017;15(1):1-3.
Study supports link between pediatric MS and remote viral infections
BOSTON – Prior Epstein-Barr virus (EBV) infection and prior herpes simplex virus (HSV) infection each appear to be associated with development of pediatric-onset multiple sclerosis (MS), according to findings from a large national case-control study.
Samples from 360 children with MS or clinically isolated syndrome and 496 frequency-matched controls recruited from 16 pediatric MS centers across the United States were tested for EBV, cytomegalovirus (CMV), and HSV antibodies and for 25-(OH)-vitamin D levels. After adjusting for age, sex, and race/ethnicity, evidence of a remote infection with EBV was strongly associated with higher risk of pediatric-onset MS (odds ratio, 3.6), Bardia Nourbakhsh, MD, reported at the annual meeting of the American Academy of Neurology.
“We didn’t see an association between CMV and the risk of developing pediatric MS,” he said, noting that prior studies had shown a protective effect of prior CMV.
There was a trend toward an association between lower serum vitamin D levels and the risk of developing pediatric MS, but the findings are questionable because of vitamin D supplementation started after diagnosis in most patients, he noted.
Further, analysis showed that race also played a role in the relationships between prior infections and MS.
The association between HSV-1 and -2 infection was significant only among white patients, the association between prior EBV and MS was much stronger in whites than non-whites, and the association between EBV and MS was stronger in non-Hispanics than in Hispanics, he said.
The MS risk variant HLA DRB1*1501 also played a role in the associations. The association between prior HSV-1 and -2 infection and MS risk was apparent only in DRB1-negative individuals, and, conversely, the association between prior EBV and MS risk was much stronger in those who were DRB1-positive, he said.
Patients included in the study had a mean age of 15.2 years, 64% were girls, and the mean disease duration was 354 days. Controls had a mean age of 14.3 years.
“Remote viral infections have been known as one of the most commonly cited risk factors for adult and pediatric MS,” Dr. Nourbakhsh said, noting that a prior case-control study showed these associations and that other studies suggested associations with vitamin D deficiency.
The current study was conducted in an attempt to replicate those prior findings, he said.
The results of this large study support an association between prior EBV and HSV infections and MS risk and a possible association between vitamin D deficiency and MS risk but are limited by lack of testing before disease development and by vitamin D supplementation in almost all patients after diagnosis, he said.
“In the future, hopefully, we can look further at the interaction of genes and environment and the heterogeneity of the effect of risk factors in different subpopulations,” he concluded.
Dr. Nourbakhsh reported having no disclosures.
BOSTON – Prior Epstein-Barr virus (EBV) infection and prior herpes simplex virus (HSV) infection each appear to be associated with development of pediatric-onset multiple sclerosis (MS), according to findings from a large national case-control study.
Samples from 360 children with MS or clinically isolated syndrome and 496 frequency-matched controls recruited from 16 pediatric MS centers across the United States were tested for EBV, cytomegalovirus (CMV), and HSV antibodies and for 25-(OH)-vitamin D levels. After adjusting for age, sex, and race/ethnicity, evidence of a remote infection with EBV was strongly associated with higher risk of pediatric-onset MS (odds ratio, 3.6), Bardia Nourbakhsh, MD, reported at the annual meeting of the American Academy of Neurology.
“We didn’t see an association between CMV and the risk of developing pediatric MS,” he said, noting that prior studies had shown a protective effect of prior CMV.
There was a trend toward an association between lower serum vitamin D levels and the risk of developing pediatric MS, but the findings are questionable because of vitamin D supplementation started after diagnosis in most patients, he noted.
Further, analysis showed that race also played a role in the relationships between prior infections and MS.
The association between HSV-1 and -2 infection was significant only among white patients, the association between prior EBV and MS was much stronger in whites than non-whites, and the association between EBV and MS was stronger in non-Hispanics than in Hispanics, he said.
The MS risk variant HLA DRB1*1501 also played a role in the associations. The association between prior HSV-1 and -2 infection and MS risk was apparent only in DRB1-negative individuals, and, conversely, the association between prior EBV and MS risk was much stronger in those who were DRB1-positive, he said.
Patients included in the study had a mean age of 15.2 years, 64% were girls, and the mean disease duration was 354 days. Controls had a mean age of 14.3 years.
“Remote viral infections have been known as one of the most commonly cited risk factors for adult and pediatric MS,” Dr. Nourbakhsh said, noting that a prior case-control study showed these associations and that other studies suggested associations with vitamin D deficiency.
The current study was conducted in an attempt to replicate those prior findings, he said.
The results of this large study support an association between prior EBV and HSV infections and MS risk and a possible association between vitamin D deficiency and MS risk but are limited by lack of testing before disease development and by vitamin D supplementation in almost all patients after diagnosis, he said.
“In the future, hopefully, we can look further at the interaction of genes and environment and the heterogeneity of the effect of risk factors in different subpopulations,” he concluded.
Dr. Nourbakhsh reported having no disclosures.
BOSTON – Prior Epstein-Barr virus (EBV) infection and prior herpes simplex virus (HSV) infection each appear to be associated with development of pediatric-onset multiple sclerosis (MS), according to findings from a large national case-control study.
Samples from 360 children with MS or clinically isolated syndrome and 496 frequency-matched controls recruited from 16 pediatric MS centers across the United States were tested for EBV, cytomegalovirus (CMV), and HSV antibodies and for 25-(OH)-vitamin D levels. After adjusting for age, sex, and race/ethnicity, evidence of a remote infection with EBV was strongly associated with higher risk of pediatric-onset MS (odds ratio, 3.6), Bardia Nourbakhsh, MD, reported at the annual meeting of the American Academy of Neurology.
“We didn’t see an association between CMV and the risk of developing pediatric MS,” he said, noting that prior studies had shown a protective effect of prior CMV.
There was a trend toward an association between lower serum vitamin D levels and the risk of developing pediatric MS, but the findings are questionable because of vitamin D supplementation started after diagnosis in most patients, he noted.
Further, analysis showed that race also played a role in the relationships between prior infections and MS.
The association between HSV-1 and -2 infection was significant only among white patients, the association between prior EBV and MS was much stronger in whites than non-whites, and the association between EBV and MS was stronger in non-Hispanics than in Hispanics, he said.
The MS risk variant HLA DRB1*1501 also played a role in the associations. The association between prior HSV-1 and -2 infection and MS risk was apparent only in DRB1-negative individuals, and, conversely, the association between prior EBV and MS risk was much stronger in those who were DRB1-positive, he said.
Patients included in the study had a mean age of 15.2 years, 64% were girls, and the mean disease duration was 354 days. Controls had a mean age of 14.3 years.
“Remote viral infections have been known as one of the most commonly cited risk factors for adult and pediatric MS,” Dr. Nourbakhsh said, noting that a prior case-control study showed these associations and that other studies suggested associations with vitamin D deficiency.
The current study was conducted in an attempt to replicate those prior findings, he said.
The results of this large study support an association between prior EBV and HSV infections and MS risk and a possible association between vitamin D deficiency and MS risk but are limited by lack of testing before disease development and by vitamin D supplementation in almost all patients after diagnosis, he said.
“In the future, hopefully, we can look further at the interaction of genes and environment and the heterogeneity of the effect of risk factors in different subpopulations,” he concluded.
Dr. Nourbakhsh reported having no disclosures.
Key clinical point:
Major finding: Remote infections with EBV and HSV were associated with higher risk of pediatric-onset MS (odds ratios, 3.6 and 1.5, respectively).
Data source: A study of 360 pediatric MS patients and 496 controls.
Disclosures: Dr. Nourbakhsh reported having no disclosures.
Toxic abandonment: a case for non-participation in physician-assisted suicide
I recently read with interest Dr Thomas Strouse’s article written to support physician aid in dying. Within the article he made the following statement: “I have come to view ‘active non-participation’ in legal PAD [physician aid in dying] – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment.”1 Within the article, Dr Strouse lays out for us thoughtful precautions in the aid-in-dying laws, attempting to demonstrate that no vulnerable population is abused. Such precautions are important but provide the same result for all participants: the death of a patient. This is the central problem with aid in dying. Certainly there is nothing wrong with dying, and we all will have that opportunity. Though most of us would choose to put that moment off a while, for some, the suffering in this life makes death seem a welcome relief.
What is a physician’s central responsibility in the care of his or her patients near the end of their lives?
As program director for the hematology and oncology fellowship at my institution, I impress upon my fellows the importance of goal-oriented decision-making. I specifically teach them that there are only four goals worth achieving in any therapeutic or diagnostic decision making: to cure the disease; to help patients live longer despite the disease; to maximize the patient’s quality of life, and to prevent impending disasters. I know of no other worthwhile goal in any decision we are to make for our patients. I can point to none of these goals that physician aid in dying achieves. When it comes to physician-assisted suicide, some would argue that selecting an early death is a way of “maximizing quality of life.” And certainly our task is to make life the best it can be for our patients while they live through the dying process, but I am unaware of any published quality of life formula that calculates the end of life as a positive measure.
The question for us is the role of the doctor. Dr Strouse raises two issues with those whom he accuses of toxic abandonment. The first is whether physicians should provide aid in death, and the second is whether physicians should refer for the same service if they believe it is wrong for their patients.
It certainly has not been well established that physician-assisted suicide is a good thing rather than a tragic thing. A 2012 statement from the Ethics, Professionalism and Human Rights Committee of the American College of Physicians suggests otherwise: “After much consideration, the College concluded that making physician-assisted suicide legal raised serious ethical, clinical and social concerns and that the practice might undermine patient trust; distract from reform in end-of-life care; and be used in vulnerable patients, including those who are poor, are disabled, or are unable to speak for themselves or minority groups who have experienced discrimination.”2 The disability rights group, Not Dead Yet, has agreed with the ACP: “It cannot be seriously maintained that assisted suicide laws can or do limit assisted suicide to people who are imminently dying, and voluntarily request and consume a lethal dose, free of inappropriate pressures from family or society. Rather, assisted suicide laws ensure legal immunity for physicians who already devalue the lives of older and disabled people and have significant economic incentives to at least agree with their suicides, if not encourage them, or worse.”3
Such statements sound prophetic within both our present cost containment health care culture and in the real world of personal family economic pressures that can lead a patient toward the understanding that a right to die is actually a “duty to die.”
As society is driving physicians to be technicians to carry out their bidding, physicians should be clinging tightly to their role as trusted advocates for their patients. Certainly our patients have fears and pain that would at times lead them to prefer death to living, but a patient’s move to nonexistence is not the task of the physician. Our task as physicians was well described recently by Yang and Curlin: “Many patients with terminal illnesses fear unbearable pain or other symptoms. The physician’s role is to care for them in their illness so as to relieve pain or otherwise help them bear up under the symptoms they endure. Many patients loathe the prospect of abject debility. The physician’s role is to maintain solidarity with those whose health is diminished, not to not to imply that debility renders a patient’s life not worth living.”4
Statements such as these by reasoned people suggest we, as a country, have no consensus for the question whether aid in dying is possibly good or seriously bad for our patients. So it is quite reasonable for compassionate physicians to refuse to administer lethal medicines to their patients in order to “do no harm.”
The second question Dr Strouse explores is whether physicians who disapprove of physician-assisted suicide are abandoning their patients because they do not refer them to a provider who will provide such services. Dr Edmund Pelligrino, a well-respected medical ethicist, in his discussion of moral absolutes in medicine establishes the moral absolute, “Do not kill” and then addresses the ethical problem of complicity in killing. “Formal cooperation is absolutely and always, forbidden. This is the case when the physician shares the evil intent, partakes directly and freely, or in any way facilitates an intrinsically evil act like abortion or assisted suicide.”5 Though personally I would not use the word, “evil,” as he does, since evil implies motive; I would substitute the word “harm” and suggest that we should never be complicit in an act that we feel brings the harm of death to our patients. I would suggest that the expectation that physicians referring for aid in dying is analogous with the patient who comes to me demanding a chemotherapy that I know would cause her harm. I would refuse to give it to her and refuse to send her to a doctor who would be willing to give to her. Referral to produce harm is complicity with causing the harm itself. Our society should never go there. Our society should never ask a physician to cross the boundary line of conscience that is the ultimate protection for vulnerable patients.
I know what it is like to watch our patients suffer. I know what it is like to watch our loved ones suffer. I pushed the morphine at my father’s bedside until he quit screaming in pain. But I did not kill him. I cared for him. Such is the physician’s role. If society decides to allow patients the autonomy to end their lives early and wishes to provide skilled technical help in doing so, let it do so at their peril. But let it choose and train technicians to do it. Do not compromise the one person whom our patients should trust totally to never do them harm.
Alva B Weir, III, MD, FACP ([email protected])
West Cancer Center, Memphis, Tennessee
1. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Commun and Support Oncol. 2017;15(1):1-3.
2. Snyder L. American College of Physicians ethics manual: sixth edition. Ann Int Med. 2012;156(1, part 2)73-104.
3. Coleman D. Assisted suicide laws create discriminatory double standard for who gets suicide prevention and who gets suicide assistance: Not Dead Yet Responds to Autonomy Inc. Disabil Health. http://www.disabilityandhealthjnl.com/article/S1936-6574(09)00089-2/fulltext. Published January 2010. Accessed on March 12, 2017.
4. Yang YT, Curlin FA. Why physicians should oppose assisted suicide. JAMA 2016;315(3):247-248.
5. Pelligrino E. Some things ought never be done: moral absolutes in clinical ethics. Theo Med Bioeth. 2005;26:469-486.
I recently read with interest Dr Thomas Strouse’s article written to support physician aid in dying. Within the article he made the following statement: “I have come to view ‘active non-participation’ in legal PAD [physician aid in dying] – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment.”1 Within the article, Dr Strouse lays out for us thoughtful precautions in the aid-in-dying laws, attempting to demonstrate that no vulnerable population is abused. Such precautions are important but provide the same result for all participants: the death of a patient. This is the central problem with aid in dying. Certainly there is nothing wrong with dying, and we all will have that opportunity. Though most of us would choose to put that moment off a while, for some, the suffering in this life makes death seem a welcome relief.
What is a physician’s central responsibility in the care of his or her patients near the end of their lives?
As program director for the hematology and oncology fellowship at my institution, I impress upon my fellows the importance of goal-oriented decision-making. I specifically teach them that there are only four goals worth achieving in any therapeutic or diagnostic decision making: to cure the disease; to help patients live longer despite the disease; to maximize the patient’s quality of life, and to prevent impending disasters. I know of no other worthwhile goal in any decision we are to make for our patients. I can point to none of these goals that physician aid in dying achieves. When it comes to physician-assisted suicide, some would argue that selecting an early death is a way of “maximizing quality of life.” And certainly our task is to make life the best it can be for our patients while they live through the dying process, but I am unaware of any published quality of life formula that calculates the end of life as a positive measure.
The question for us is the role of the doctor. Dr Strouse raises two issues with those whom he accuses of toxic abandonment. The first is whether physicians should provide aid in death, and the second is whether physicians should refer for the same service if they believe it is wrong for their patients.
It certainly has not been well established that physician-assisted suicide is a good thing rather than a tragic thing. A 2012 statement from the Ethics, Professionalism and Human Rights Committee of the American College of Physicians suggests otherwise: “After much consideration, the College concluded that making physician-assisted suicide legal raised serious ethical, clinical and social concerns and that the practice might undermine patient trust; distract from reform in end-of-life care; and be used in vulnerable patients, including those who are poor, are disabled, or are unable to speak for themselves or minority groups who have experienced discrimination.”2 The disability rights group, Not Dead Yet, has agreed with the ACP: “It cannot be seriously maintained that assisted suicide laws can or do limit assisted suicide to people who are imminently dying, and voluntarily request and consume a lethal dose, free of inappropriate pressures from family or society. Rather, assisted suicide laws ensure legal immunity for physicians who already devalue the lives of older and disabled people and have significant economic incentives to at least agree with their suicides, if not encourage them, or worse.”3
Such statements sound prophetic within both our present cost containment health care culture and in the real world of personal family economic pressures that can lead a patient toward the understanding that a right to die is actually a “duty to die.”
As society is driving physicians to be technicians to carry out their bidding, physicians should be clinging tightly to their role as trusted advocates for their patients. Certainly our patients have fears and pain that would at times lead them to prefer death to living, but a patient’s move to nonexistence is not the task of the physician. Our task as physicians was well described recently by Yang and Curlin: “Many patients with terminal illnesses fear unbearable pain or other symptoms. The physician’s role is to care for them in their illness so as to relieve pain or otherwise help them bear up under the symptoms they endure. Many patients loathe the prospect of abject debility. The physician’s role is to maintain solidarity with those whose health is diminished, not to not to imply that debility renders a patient’s life not worth living.”4
Statements such as these by reasoned people suggest we, as a country, have no consensus for the question whether aid in dying is possibly good or seriously bad for our patients. So it is quite reasonable for compassionate physicians to refuse to administer lethal medicines to their patients in order to “do no harm.”
The second question Dr Strouse explores is whether physicians who disapprove of physician-assisted suicide are abandoning their patients because they do not refer them to a provider who will provide such services. Dr Edmund Pelligrino, a well-respected medical ethicist, in his discussion of moral absolutes in medicine establishes the moral absolute, “Do not kill” and then addresses the ethical problem of complicity in killing. “Formal cooperation is absolutely and always, forbidden. This is the case when the physician shares the evil intent, partakes directly and freely, or in any way facilitates an intrinsically evil act like abortion or assisted suicide.”5 Though personally I would not use the word, “evil,” as he does, since evil implies motive; I would substitute the word “harm” and suggest that we should never be complicit in an act that we feel brings the harm of death to our patients. I would suggest that the expectation that physicians referring for aid in dying is analogous with the patient who comes to me demanding a chemotherapy that I know would cause her harm. I would refuse to give it to her and refuse to send her to a doctor who would be willing to give to her. Referral to produce harm is complicity with causing the harm itself. Our society should never go there. Our society should never ask a physician to cross the boundary line of conscience that is the ultimate protection for vulnerable patients.
I know what it is like to watch our patients suffer. I know what it is like to watch our loved ones suffer. I pushed the morphine at my father’s bedside until he quit screaming in pain. But I did not kill him. I cared for him. Such is the physician’s role. If society decides to allow patients the autonomy to end their lives early and wishes to provide skilled technical help in doing so, let it do so at their peril. But let it choose and train technicians to do it. Do not compromise the one person whom our patients should trust totally to never do them harm.
Alva B Weir, III, MD, FACP ([email protected])
West Cancer Center, Memphis, Tennessee
I recently read with interest Dr Thomas Strouse’s article written to support physician aid in dying. Within the article he made the following statement: “I have come to view ‘active non-participation’ in legal PAD [physician aid in dying] – that is, decisions by individual physicians and/or health systems not only to not provide, but also not refer patients to possibly willing providers and systems without regard for specific clinical contexts – as a toxic form of patient abandonment.”1 Within the article, Dr Strouse lays out for us thoughtful precautions in the aid-in-dying laws, attempting to demonstrate that no vulnerable population is abused. Such precautions are important but provide the same result for all participants: the death of a patient. This is the central problem with aid in dying. Certainly there is nothing wrong with dying, and we all will have that opportunity. Though most of us would choose to put that moment off a while, for some, the suffering in this life makes death seem a welcome relief.
What is a physician’s central responsibility in the care of his or her patients near the end of their lives?
As program director for the hematology and oncology fellowship at my institution, I impress upon my fellows the importance of goal-oriented decision-making. I specifically teach them that there are only four goals worth achieving in any therapeutic or diagnostic decision making: to cure the disease; to help patients live longer despite the disease; to maximize the patient’s quality of life, and to prevent impending disasters. I know of no other worthwhile goal in any decision we are to make for our patients. I can point to none of these goals that physician aid in dying achieves. When it comes to physician-assisted suicide, some would argue that selecting an early death is a way of “maximizing quality of life.” And certainly our task is to make life the best it can be for our patients while they live through the dying process, but I am unaware of any published quality of life formula that calculates the end of life as a positive measure.
The question for us is the role of the doctor. Dr Strouse raises two issues with those whom he accuses of toxic abandonment. The first is whether physicians should provide aid in death, and the second is whether physicians should refer for the same service if they believe it is wrong for their patients.
It certainly has not been well established that physician-assisted suicide is a good thing rather than a tragic thing. A 2012 statement from the Ethics, Professionalism and Human Rights Committee of the American College of Physicians suggests otherwise: “After much consideration, the College concluded that making physician-assisted suicide legal raised serious ethical, clinical and social concerns and that the practice might undermine patient trust; distract from reform in end-of-life care; and be used in vulnerable patients, including those who are poor, are disabled, or are unable to speak for themselves or minority groups who have experienced discrimination.”2 The disability rights group, Not Dead Yet, has agreed with the ACP: “It cannot be seriously maintained that assisted suicide laws can or do limit assisted suicide to people who are imminently dying, and voluntarily request and consume a lethal dose, free of inappropriate pressures from family or society. Rather, assisted suicide laws ensure legal immunity for physicians who already devalue the lives of older and disabled people and have significant economic incentives to at least agree with their suicides, if not encourage them, or worse.”3
Such statements sound prophetic within both our present cost containment health care culture and in the real world of personal family economic pressures that can lead a patient toward the understanding that a right to die is actually a “duty to die.”
As society is driving physicians to be technicians to carry out their bidding, physicians should be clinging tightly to their role as trusted advocates for their patients. Certainly our patients have fears and pain that would at times lead them to prefer death to living, but a patient’s move to nonexistence is not the task of the physician. Our task as physicians was well described recently by Yang and Curlin: “Many patients with terminal illnesses fear unbearable pain or other symptoms. The physician’s role is to care for them in their illness so as to relieve pain or otherwise help them bear up under the symptoms they endure. Many patients loathe the prospect of abject debility. The physician’s role is to maintain solidarity with those whose health is diminished, not to not to imply that debility renders a patient’s life not worth living.”4
Statements such as these by reasoned people suggest we, as a country, have no consensus for the question whether aid in dying is possibly good or seriously bad for our patients. So it is quite reasonable for compassionate physicians to refuse to administer lethal medicines to their patients in order to “do no harm.”
The second question Dr Strouse explores is whether physicians who disapprove of physician-assisted suicide are abandoning their patients because they do not refer them to a provider who will provide such services. Dr Edmund Pelligrino, a well-respected medical ethicist, in his discussion of moral absolutes in medicine establishes the moral absolute, “Do not kill” and then addresses the ethical problem of complicity in killing. “Formal cooperation is absolutely and always, forbidden. This is the case when the physician shares the evil intent, partakes directly and freely, or in any way facilitates an intrinsically evil act like abortion or assisted suicide.”5 Though personally I would not use the word, “evil,” as he does, since evil implies motive; I would substitute the word “harm” and suggest that we should never be complicit in an act that we feel brings the harm of death to our patients. I would suggest that the expectation that physicians referring for aid in dying is analogous with the patient who comes to me demanding a chemotherapy that I know would cause her harm. I would refuse to give it to her and refuse to send her to a doctor who would be willing to give to her. Referral to produce harm is complicity with causing the harm itself. Our society should never go there. Our society should never ask a physician to cross the boundary line of conscience that is the ultimate protection for vulnerable patients.
I know what it is like to watch our patients suffer. I know what it is like to watch our loved ones suffer. I pushed the morphine at my father’s bedside until he quit screaming in pain. But I did not kill him. I cared for him. Such is the physician’s role. If society decides to allow patients the autonomy to end their lives early and wishes to provide skilled technical help in doing so, let it do so at their peril. But let it choose and train technicians to do it. Do not compromise the one person whom our patients should trust totally to never do them harm.
Alva B Weir, III, MD, FACP ([email protected])
West Cancer Center, Memphis, Tennessee
1. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Commun and Support Oncol. 2017;15(1):1-3.
2. Snyder L. American College of Physicians ethics manual: sixth edition. Ann Int Med. 2012;156(1, part 2)73-104.
3. Coleman D. Assisted suicide laws create discriminatory double standard for who gets suicide prevention and who gets suicide assistance: Not Dead Yet Responds to Autonomy Inc. Disabil Health. http://www.disabilityandhealthjnl.com/article/S1936-6574(09)00089-2/fulltext. Published January 2010. Accessed on March 12, 2017.
4. Yang YT, Curlin FA. Why physicians should oppose assisted suicide. JAMA 2016;315(3):247-248.
5. Pelligrino E. Some things ought never be done: moral absolutes in clinical ethics. Theo Med Bioeth. 2005;26:469-486.
1. Strouse T. End-of-life options and the legal pathways to physician aid in dying. J Commun and Support Oncol. 2017;15(1):1-3.
2. Snyder L. American College of Physicians ethics manual: sixth edition. Ann Int Med. 2012;156(1, part 2)73-104.
3. Coleman D. Assisted suicide laws create discriminatory double standard for who gets suicide prevention and who gets suicide assistance: Not Dead Yet Responds to Autonomy Inc. Disabil Health. http://www.disabilityandhealthjnl.com/article/S1936-6574(09)00089-2/fulltext. Published January 2010. Accessed on March 12, 2017.
4. Yang YT, Curlin FA. Why physicians should oppose assisted suicide. JAMA 2016;315(3):247-248.
5. Pelligrino E. Some things ought never be done: moral absolutes in clinical ethics. Theo Med Bioeth. 2005;26:469-486.
Pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion: diagnostic dilemma
Pulmonary sarcomatoid carcinoma (PSC) is a rare histological subtype that has an aggressive course with average survival of 11-13 months.1 In clinical practice, the possible presentations of this rare cancer are not widely known, resulting in a misdiagnosis. That is what happened with our patient, who presented with necrotizing cavitary lung lesion and soft tissue necrotizing lymphadenitis. The clinical picture was reminiscent of tuberculosis or granulomatosis with polyangiitis and was further confounded by negative computed-tomography (CT)-guided biopsy and bronchoscopy findings, which added to the delay in diagnosis. With the currently available knowledge, the diagnosis of PSC depends largely on evaluation of the surgically resected specimen, which in most cases is avoided until there is a high suspicion of PSC. Biopsy is not useful due to extensive necrosis, as will be seen in our case. Consequently, most of the data in the literature is based on case series of autopsy specimen, and the clinical characteristics of PSC remain unclear. The rarity of PSC has prevented its characterization in literature. We report here a rare presentation of PSC with necrotizing lung lesion, to add to the paucity of the current data.
Case presentation and summary
A 58-year-old homeless man presented to the Upstate University Hospital, Syracuse, New York, with a 25-pound weight loss during the previous month and associated productive cough and hemoptysis for a week and a painful mass in the nape of his neck. He denied any fever, chest pain, sick contacts, or joint pain. He had a history of about 40 pack-years of smoking, and his brother had recently been diagnosed with lung cancer. A tender fluctuant mass was detected in the nape of his neck on examination (Figure 1).
The patient had presented 9 months earlier with persistent cough and hemoptysis, and at that visit was found to have a cavitary lesion in the right lung measuring 2 cm (0.8 in). He had undergone a computed-tomograpghy (CT)-guided biopsy of the lesion, which had shown acute and chronic inflammation with fibrosis, and he had negative bronchoscopy findings. The patient tested negative for tuberculosis during the first visit but he left the hospital against the medical advice of the physicians and he was lost to follow-up until his re-presentation.
On physical examination at his re-presentation, the patient seemed cachectic, with a blood pressure of 94/62 mm of Hg. The mass in the nape of his neck was about 3 cm (1.2 in) long, with erythema of the surrounding skin (Figure 1). Bronchial breath sounds were heard in the right upper lobe of the lung, likely due to the underlying cavitary lesion (Figure 2).
Given the patient’s advanced disease, he was started on palliative radiotherapy with radiosensitizing chemotherapy with carboplatin (target AUC 6) and paclitaxel (135 mg/m2 over 24 hours). His symptoms of hemoptysis improved transiently after the first cycle, but he became hypotensive and drowsy during the second cycle of therapy, and the family decided to make the patient comfort care and withdraw all further treatment. He was discharged to hospice.
Discussion
PSC is a rare variant of non-small-cell carcinoma lung cancer, accounting for up to 0.4% of lung malignancy.1 It was recently subtyped by the World Health Organization as a non-small cell lung carcinoma with certain amount of differentiation resembling sarcoma or containing elements of sarcoma.2-4 It is not known why both elements co-exist in the tumor, but Franks and colleagues some theories have been postulated in the literature, including possible origin from a single, aberrant stem cell with progenies differentiating in two separate pathways.3
Sarcomatoid carcinoma consists of spectrum of tumors including pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and blastoma.3,4 It usually shows male preponderance, and association with smoking.3 The diagnosis commonly occurs in the sixth decade of life, except for pulmonary blastoma, which is more common in the fourth decade and with equal gender distribution.4
The presenting symptoms can be variable and nonspecific, but predominantly include chest pain, cough, hemoptysis, and/or weight loss.5 Radiologically, pulmonary sarcomatoid cancer presenting as a necrotizing cavitary lesion in the lung is a rare finding, seldom reported in the past.6,7 The presentation in our case, with necrotizing lymphadenitis, was reminiscent of an infectious or autoimmune etiology such as tuberculosis or granulomatosis with polyangiitis. The presence of extensive necrosis in the lesion and the characteristic heterogeneity of the tumor had resulted in inconclusive biopsy findings during the previous presentation. In clinical practice, there is over-reliance on biopsy findings to make the distinction between cancer and other mimicking conditions. This is especially true for rare tumors such as PSC, which often results in misdiagnosis and a delay in administering the proper treatment.
Transbronchial biopsy in cases such as the present case, carries little benefit because the diagnosis depends on the site from which the biopsy is taken and whether the biopsied tissue is representative of the entire mass. The diagnosis can be suspected based on the clinical and radiological findings but confirmation requires a surgical resection to delineate the accurate cytology and architecture.5,6,8 Huang and colleagues showed a misdiagnosis rate of PSC of >70% preoperatively.4 Resective surgery is feasible only in patients with high index of suspicion for a malignancy, which in most cases requires previous confirmation with a biopsy. The rarity of this cancer, its unusual presentations, and the lack of specific testing preclude early diagnosis and timely treatment of this fatal condition.
Initial treatment options for localized or with limited spread disease is resective surgery. The role of chemo- or radiation therapy is not known, but they have not previously shown promising results,6,8 except in some cases when they are used as postoperative adjuvant chemotherapy4 or in bulky, locally invasive tumors.1 The recurrence rate after surgery is very high, resulting in a poor 5-year survival rate.1,8 Experimental therapies, such as antibodies that target epidermal growth factor receptor mutations, have not shown much success either.8 In conclusion, the outlook for patients with PSC with the current available knowledge and treatment protocols, is dismal.
Most of the current knowledge and data in the literature is based on cases from autopsy or early-stage surgical resections rather than on patients with advanced cancer.5 Moreover, the role of surgical resection in PSC is questionable, given the high recurrence rate. Subsequently, the clinical and pathological manifestations have yet to be well characterized.4 There has been advance with the publication of more studies recently. Cytokeratin markers such as CAM 5.2 and AE1/AE3 are commonly useful to support the diagnosis when suspected.3 Other markers, including the carcinoembryonic antigen, CD15, and thyroid transcription factor-1 may be variably positive, based on the differentiation of the cancer. Other exciting prospects in the study of PSC include the suggestion of a modified vimentin histologic score for better characterization of the cancer and the discovery of high platelet-derived growth factor receptor beta immunohistochemistry expression in PSC as a potential target for future therapy.
Conclusion
Pulmonary sarcomatoid lung cancer can present with a predominant necrotizing picture that mimics diseases such as tuberculosis. In such case, transbronchial biopsy carries little benefit because the diagnosis depends on whether the biopsied tissue is representative of the entire mass, often confounded by the extensive necrosis. More data is needed to determine prognostic factors and appropriate therapeutic strategies.
1. Martin LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007;84(3):973-980.
2. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18(6):1059-1068.
3. Franks TJ, Galvin JR. Sarcomatoid carcinoma of the lung: histologic criteria and common lesions in the differential diagnosis. Arch Pathol Lab Med. 2010;134(1):49-54.
4. Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. http://wjso.biomedcentral.com/articles/10.1186/1477-7819-11-252. Published 2013. Accessed March 12, 2017.
5. Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134(11):1645-1658.
6. Pelosi G, Sonzogni A, De Pas T, et al. Review article: pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol. 2010;18(2):103-120.
7. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34(1):91-97.
8. Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3-4):206-213.
Pulmonary sarcomatoid carcinoma (PSC) is a rare histological subtype that has an aggressive course with average survival of 11-13 months.1 In clinical practice, the possible presentations of this rare cancer are not widely known, resulting in a misdiagnosis. That is what happened with our patient, who presented with necrotizing cavitary lung lesion and soft tissue necrotizing lymphadenitis. The clinical picture was reminiscent of tuberculosis or granulomatosis with polyangiitis and was further confounded by negative computed-tomography (CT)-guided biopsy and bronchoscopy findings, which added to the delay in diagnosis. With the currently available knowledge, the diagnosis of PSC depends largely on evaluation of the surgically resected specimen, which in most cases is avoided until there is a high suspicion of PSC. Biopsy is not useful due to extensive necrosis, as will be seen in our case. Consequently, most of the data in the literature is based on case series of autopsy specimen, and the clinical characteristics of PSC remain unclear. The rarity of PSC has prevented its characterization in literature. We report here a rare presentation of PSC with necrotizing lung lesion, to add to the paucity of the current data.
Case presentation and summary
A 58-year-old homeless man presented to the Upstate University Hospital, Syracuse, New York, with a 25-pound weight loss during the previous month and associated productive cough and hemoptysis for a week and a painful mass in the nape of his neck. He denied any fever, chest pain, sick contacts, or joint pain. He had a history of about 40 pack-years of smoking, and his brother had recently been diagnosed with lung cancer. A tender fluctuant mass was detected in the nape of his neck on examination (Figure 1).
The patient had presented 9 months earlier with persistent cough and hemoptysis, and at that visit was found to have a cavitary lesion in the right lung measuring 2 cm (0.8 in). He had undergone a computed-tomograpghy (CT)-guided biopsy of the lesion, which had shown acute and chronic inflammation with fibrosis, and he had negative bronchoscopy findings. The patient tested negative for tuberculosis during the first visit but he left the hospital against the medical advice of the physicians and he was lost to follow-up until his re-presentation.
On physical examination at his re-presentation, the patient seemed cachectic, with a blood pressure of 94/62 mm of Hg. The mass in the nape of his neck was about 3 cm (1.2 in) long, with erythema of the surrounding skin (Figure 1). Bronchial breath sounds were heard in the right upper lobe of the lung, likely due to the underlying cavitary lesion (Figure 2).
Given the patient’s advanced disease, he was started on palliative radiotherapy with radiosensitizing chemotherapy with carboplatin (target AUC 6) and paclitaxel (135 mg/m2 over 24 hours). His symptoms of hemoptysis improved transiently after the first cycle, but he became hypotensive and drowsy during the second cycle of therapy, and the family decided to make the patient comfort care and withdraw all further treatment. He was discharged to hospice.
Discussion
PSC is a rare variant of non-small-cell carcinoma lung cancer, accounting for up to 0.4% of lung malignancy.1 It was recently subtyped by the World Health Organization as a non-small cell lung carcinoma with certain amount of differentiation resembling sarcoma or containing elements of sarcoma.2-4 It is not known why both elements co-exist in the tumor, but Franks and colleagues some theories have been postulated in the literature, including possible origin from a single, aberrant stem cell with progenies differentiating in two separate pathways.3
Sarcomatoid carcinoma consists of spectrum of tumors including pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and blastoma.3,4 It usually shows male preponderance, and association with smoking.3 The diagnosis commonly occurs in the sixth decade of life, except for pulmonary blastoma, which is more common in the fourth decade and with equal gender distribution.4
The presenting symptoms can be variable and nonspecific, but predominantly include chest pain, cough, hemoptysis, and/or weight loss.5 Radiologically, pulmonary sarcomatoid cancer presenting as a necrotizing cavitary lesion in the lung is a rare finding, seldom reported in the past.6,7 The presentation in our case, with necrotizing lymphadenitis, was reminiscent of an infectious or autoimmune etiology such as tuberculosis or granulomatosis with polyangiitis. The presence of extensive necrosis in the lesion and the characteristic heterogeneity of the tumor had resulted in inconclusive biopsy findings during the previous presentation. In clinical practice, there is over-reliance on biopsy findings to make the distinction between cancer and other mimicking conditions. This is especially true for rare tumors such as PSC, which often results in misdiagnosis and a delay in administering the proper treatment.
Transbronchial biopsy in cases such as the present case, carries little benefit because the diagnosis depends on the site from which the biopsy is taken and whether the biopsied tissue is representative of the entire mass. The diagnosis can be suspected based on the clinical and radiological findings but confirmation requires a surgical resection to delineate the accurate cytology and architecture.5,6,8 Huang and colleagues showed a misdiagnosis rate of PSC of >70% preoperatively.4 Resective surgery is feasible only in patients with high index of suspicion for a malignancy, which in most cases requires previous confirmation with a biopsy. The rarity of this cancer, its unusual presentations, and the lack of specific testing preclude early diagnosis and timely treatment of this fatal condition.
Initial treatment options for localized or with limited spread disease is resective surgery. The role of chemo- or radiation therapy is not known, but they have not previously shown promising results,6,8 except in some cases when they are used as postoperative adjuvant chemotherapy4 or in bulky, locally invasive tumors.1 The recurrence rate after surgery is very high, resulting in a poor 5-year survival rate.1,8 Experimental therapies, such as antibodies that target epidermal growth factor receptor mutations, have not shown much success either.8 In conclusion, the outlook for patients with PSC with the current available knowledge and treatment protocols, is dismal.
Most of the current knowledge and data in the literature is based on cases from autopsy or early-stage surgical resections rather than on patients with advanced cancer.5 Moreover, the role of surgical resection in PSC is questionable, given the high recurrence rate. Subsequently, the clinical and pathological manifestations have yet to be well characterized.4 There has been advance with the publication of more studies recently. Cytokeratin markers such as CAM 5.2 and AE1/AE3 are commonly useful to support the diagnosis when suspected.3 Other markers, including the carcinoembryonic antigen, CD15, and thyroid transcription factor-1 may be variably positive, based on the differentiation of the cancer. Other exciting prospects in the study of PSC include the suggestion of a modified vimentin histologic score for better characterization of the cancer and the discovery of high platelet-derived growth factor receptor beta immunohistochemistry expression in PSC as a potential target for future therapy.
Conclusion
Pulmonary sarcomatoid lung cancer can present with a predominant necrotizing picture that mimics diseases such as tuberculosis. In such case, transbronchial biopsy carries little benefit because the diagnosis depends on whether the biopsied tissue is representative of the entire mass, often confounded by the extensive necrosis. More data is needed to determine prognostic factors and appropriate therapeutic strategies.
Pulmonary sarcomatoid carcinoma (PSC) is a rare histological subtype that has an aggressive course with average survival of 11-13 months.1 In clinical practice, the possible presentations of this rare cancer are not widely known, resulting in a misdiagnosis. That is what happened with our patient, who presented with necrotizing cavitary lung lesion and soft tissue necrotizing lymphadenitis. The clinical picture was reminiscent of tuberculosis or granulomatosis with polyangiitis and was further confounded by negative computed-tomography (CT)-guided biopsy and bronchoscopy findings, which added to the delay in diagnosis. With the currently available knowledge, the diagnosis of PSC depends largely on evaluation of the surgically resected specimen, which in most cases is avoided until there is a high suspicion of PSC. Biopsy is not useful due to extensive necrosis, as will be seen in our case. Consequently, most of the data in the literature is based on case series of autopsy specimen, and the clinical characteristics of PSC remain unclear. The rarity of PSC has prevented its characterization in literature. We report here a rare presentation of PSC with necrotizing lung lesion, to add to the paucity of the current data.
Case presentation and summary
A 58-year-old homeless man presented to the Upstate University Hospital, Syracuse, New York, with a 25-pound weight loss during the previous month and associated productive cough and hemoptysis for a week and a painful mass in the nape of his neck. He denied any fever, chest pain, sick contacts, or joint pain. He had a history of about 40 pack-years of smoking, and his brother had recently been diagnosed with lung cancer. A tender fluctuant mass was detected in the nape of his neck on examination (Figure 1).
The patient had presented 9 months earlier with persistent cough and hemoptysis, and at that visit was found to have a cavitary lesion in the right lung measuring 2 cm (0.8 in). He had undergone a computed-tomograpghy (CT)-guided biopsy of the lesion, which had shown acute and chronic inflammation with fibrosis, and he had negative bronchoscopy findings. The patient tested negative for tuberculosis during the first visit but he left the hospital against the medical advice of the physicians and he was lost to follow-up until his re-presentation.
On physical examination at his re-presentation, the patient seemed cachectic, with a blood pressure of 94/62 mm of Hg. The mass in the nape of his neck was about 3 cm (1.2 in) long, with erythema of the surrounding skin (Figure 1). Bronchial breath sounds were heard in the right upper lobe of the lung, likely due to the underlying cavitary lesion (Figure 2).
Given the patient’s advanced disease, he was started on palliative radiotherapy with radiosensitizing chemotherapy with carboplatin (target AUC 6) and paclitaxel (135 mg/m2 over 24 hours). His symptoms of hemoptysis improved transiently after the first cycle, but he became hypotensive and drowsy during the second cycle of therapy, and the family decided to make the patient comfort care and withdraw all further treatment. He was discharged to hospice.
Discussion
PSC is a rare variant of non-small-cell carcinoma lung cancer, accounting for up to 0.4% of lung malignancy.1 It was recently subtyped by the World Health Organization as a non-small cell lung carcinoma with certain amount of differentiation resembling sarcoma or containing elements of sarcoma.2-4 It is not known why both elements co-exist in the tumor, but Franks and colleagues some theories have been postulated in the literature, including possible origin from a single, aberrant stem cell with progenies differentiating in two separate pathways.3
Sarcomatoid carcinoma consists of spectrum of tumors including pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and blastoma.3,4 It usually shows male preponderance, and association with smoking.3 The diagnosis commonly occurs in the sixth decade of life, except for pulmonary blastoma, which is more common in the fourth decade and with equal gender distribution.4
The presenting symptoms can be variable and nonspecific, but predominantly include chest pain, cough, hemoptysis, and/or weight loss.5 Radiologically, pulmonary sarcomatoid cancer presenting as a necrotizing cavitary lesion in the lung is a rare finding, seldom reported in the past.6,7 The presentation in our case, with necrotizing lymphadenitis, was reminiscent of an infectious or autoimmune etiology such as tuberculosis or granulomatosis with polyangiitis. The presence of extensive necrosis in the lesion and the characteristic heterogeneity of the tumor had resulted in inconclusive biopsy findings during the previous presentation. In clinical practice, there is over-reliance on biopsy findings to make the distinction between cancer and other mimicking conditions. This is especially true for rare tumors such as PSC, which often results in misdiagnosis and a delay in administering the proper treatment.
Transbronchial biopsy in cases such as the present case, carries little benefit because the diagnosis depends on the site from which the biopsy is taken and whether the biopsied tissue is representative of the entire mass. The diagnosis can be suspected based on the clinical and radiological findings but confirmation requires a surgical resection to delineate the accurate cytology and architecture.5,6,8 Huang and colleagues showed a misdiagnosis rate of PSC of >70% preoperatively.4 Resective surgery is feasible only in patients with high index of suspicion for a malignancy, which in most cases requires previous confirmation with a biopsy. The rarity of this cancer, its unusual presentations, and the lack of specific testing preclude early diagnosis and timely treatment of this fatal condition.
Initial treatment options for localized or with limited spread disease is resective surgery. The role of chemo- or radiation therapy is not known, but they have not previously shown promising results,6,8 except in some cases when they are used as postoperative adjuvant chemotherapy4 or in bulky, locally invasive tumors.1 The recurrence rate after surgery is very high, resulting in a poor 5-year survival rate.1,8 Experimental therapies, such as antibodies that target epidermal growth factor receptor mutations, have not shown much success either.8 In conclusion, the outlook for patients with PSC with the current available knowledge and treatment protocols, is dismal.
Most of the current knowledge and data in the literature is based on cases from autopsy or early-stage surgical resections rather than on patients with advanced cancer.5 Moreover, the role of surgical resection in PSC is questionable, given the high recurrence rate. Subsequently, the clinical and pathological manifestations have yet to be well characterized.4 There has been advance with the publication of more studies recently. Cytokeratin markers such as CAM 5.2 and AE1/AE3 are commonly useful to support the diagnosis when suspected.3 Other markers, including the carcinoembryonic antigen, CD15, and thyroid transcription factor-1 may be variably positive, based on the differentiation of the cancer. Other exciting prospects in the study of PSC include the suggestion of a modified vimentin histologic score for better characterization of the cancer and the discovery of high platelet-derived growth factor receptor beta immunohistochemistry expression in PSC as a potential target for future therapy.
Conclusion
Pulmonary sarcomatoid lung cancer can present with a predominant necrotizing picture that mimics diseases such as tuberculosis. In such case, transbronchial biopsy carries little benefit because the diagnosis depends on whether the biopsied tissue is representative of the entire mass, often confounded by the extensive necrosis. More data is needed to determine prognostic factors and appropriate therapeutic strategies.
1. Martin LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007;84(3):973-980.
2. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18(6):1059-1068.
3. Franks TJ, Galvin JR. Sarcomatoid carcinoma of the lung: histologic criteria and common lesions in the differential diagnosis. Arch Pathol Lab Med. 2010;134(1):49-54.
4. Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. http://wjso.biomedcentral.com/articles/10.1186/1477-7819-11-252. Published 2013. Accessed March 12, 2017.
5. Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134(11):1645-1658.
6. Pelosi G, Sonzogni A, De Pas T, et al. Review article: pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol. 2010;18(2):103-120.
7. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34(1):91-97.
8. Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3-4):206-213.
1. Martin LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007;84(3):973-980.
2. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18(6):1059-1068.
3. Franks TJ, Galvin JR. Sarcomatoid carcinoma of the lung: histologic criteria and common lesions in the differential diagnosis. Arch Pathol Lab Med. 2010;134(1):49-54.
4. Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. http://wjso.biomedcentral.com/articles/10.1186/1477-7819-11-252. Published 2013. Accessed March 12, 2017.
5. Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134(11):1645-1658.
6. Pelosi G, Sonzogni A, De Pas T, et al. Review article: pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol. 2010;18(2):103-120.
7. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34(1):91-97.
8. Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3-4):206-213.
Palmoplantar exacerbation of psoriasis after nivolumab for lung cancer
Nivolumab is a full human immunoglobulin antibody to the programmed cell death 1 (PD-1) immune checkpoint receptor on T cells. This programmed cell death inhibitor is a targeted immunotherapy used to treat patients with melanoma, among other malignancies.1 More recently, nivolumab has been used for advanced non-small-cell lung cancer (NSCLC) after failure of previous chemotherapeutic agents. It was approved by the US Food and Drug Administration for the NSCLC indication in 2015.2
PD-1 inhibitors are efficacious in treating advanced malignancies, although their immune-mediated functions can lead to undesirable side effects. Patients treated with nivolumab have been reported to develop thyroid disease,1,3,4 diabetes,3 hypophysitis,1,3 hypopituitarism,3 and pneumonitis,4,2 as well as other autoimmune conditions.3 Although nivolumab is often used to treat skin diseases such as melanoma, it can have many cutaneous side effects including pruritus,1,3-6 rash,1,3,4,6,7 vitiligo,1,3,7,6 mouth sores,3 injection site reactions,3,6 and alopecia.5 Herein, we describe a patient who was treated with nivolumab and developed an exacerbation of pre-existing psoriasis.
Case presentation and summary
A 57-year-old man with metastatic NSCLC and a history of plaque psoriasis presented to the dermatology clinic for evaluation of new lesions on his palms and soles. The patient had been previously treated with numerous therapies for NSCLC, including chemotherapy and radiation. Previous chemotherapeutic agents included the cisplatin plus etoposide combination, with doxetaxel and pemetrexed. The patient was not able to tolerate the chemotherapy and instead opted for hospice care. After several months, he chose to restart therapy, and was started on the programmed cell death (PD)-1 inhibitor, nivolumab, at a dose of 3 mg/kg for a total of 6 cycles. He received his first dose 5 weeks before his current presentation to the clinic, and his second dose 2 weeks before.
The patient reported a 20-year history of plaque psoriasis, characterized by psoriatic plaques on the elbows and shins and for which he was treated with topical therapies with good effect. Every few months, he would develop one or two small plaques of psoriasis on his palms and soles. The lesions were inconsequential to the patient, as he never experienced more than one or two small palmoplantar lesions at a time. One week after his second cycle of nivolumab, the patient developed an eruption of lesions on his palms and soles. He observed that the lesions seemed to be similar to his previous palmoplantar psoriatic plaques but with significantly greater skin involvement. The patient denied any new-onset joint pain.
The results of a physical examination revealed a cachectic man in no acute distress, with more than 30 erythematous circular to oval circumscribed plaques with yellow to whitish scales on the bilateral palms (Figure 1) and soles (Figure 2).
The patient also had well-demarcated, thick oval erythematous plaques with micaceous scales on the bilateral elbows (Figure 3), and thin scaly erythematous plaques on the anterior shins (Figure 4). There were no psoriatic plaques on the remainder of the trunk or extremities. Mucosal surfaces, scalp, and nails were uninvolved.
A clinical diagnosis of exacerbation of pre-existing psoriasis owing to nivolumab therapy was made. The patient was started on clobetasol 0.05% ointment twice daily under occlusion with plastic wrap to the affected areas, and he was continued on nivolumab for his NSCLC.
Discussion
Treatment with nivolumab can lead to a range of autoimmune side effects, and as shown in this case, psoriasis is one of the cutaneous findings that could be exacerbated by treatment with nivolumab. To date, two cases of exacerbation of psoriasis in patients treated with nivolumab for melanoma have been reported in the literature.8,9 In the first case, the patient had well-controlled plaque psoriasis at baseline and he subsequently developed psoriatic plaques on the trunk and extremities after the second infusion of nivolumab for metastatic melanoma. A biopsy showed regular acanthosis with hyperkeratosis and parakeratosis in addition to dilated vessels in the papillary dermis.8 In the second case, the patient had a history of psoriasis vulgaris with no active lesions. Three weeks after his first course of nivolumab for metastatic oral mucosal melanoma, he developed new, well-circumscribed erythematous scaly plaques on the trunk and extremities that were clinically diagnosed as psoriasis.9 In a third case, a patient without a prior history of psoriasis experienced a psoriasiform eruption on the trunk and extremities after the fourth dose of nivolumab for oral mucosal melanoma.10 Thus, our case is the third reported case of exacerbation of preexisting psoriasis in a patient treated with nivolumab. Furthermore, our patient is the first reported case of a patient treated with nivolumab for NSCLC to develop this adverse event. Whereas the previously reported cases were characterized by widespread trunk and extremity involvement, our patient developed focal exacerbation of the palmoplantar areas.
Additional studies are needed to more clearly characterize the specific cutaneous toxicities of nivolumab and to determine if particular skin reactions may indicate a better response to the anticancer agent. Side effects such as psoriasis can often be managed with topical therapies and may not require withdrawal of the medication. We encourage the collaboration of dermatologists and oncologists to enhance the diagnosis and management of these cutaneous side effects in cancer patients.
1. Larkin J, Lao CD, Urba WJ, et al. Efficacy and safety of Nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433-440.
2. Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004-2012.
3. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
4. Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257-265.
5. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
6. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311-4318.
7. Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber J. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2015.
8. Matsumura N, Ohtsuka M, Kikuchi N, Yamamoto T. Exacerbation of psoriasis during nivolumab therapy for metastatic melanoma. Acta Derm Venereol. 2016;96(2):259-260.
9. Kato Y, Otsuka A, Miyachi Y, Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30(10):e89-e91.
10. Ohtsuka M, Miura T, Mori T, Ishikawa M, Yamamoto T. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol. 2015;151(7):797-799.
Nivolumab is a full human immunoglobulin antibody to the programmed cell death 1 (PD-1) immune checkpoint receptor on T cells. This programmed cell death inhibitor is a targeted immunotherapy used to treat patients with melanoma, among other malignancies.1 More recently, nivolumab has been used for advanced non-small-cell lung cancer (NSCLC) after failure of previous chemotherapeutic agents. It was approved by the US Food and Drug Administration for the NSCLC indication in 2015.2
PD-1 inhibitors are efficacious in treating advanced malignancies, although their immune-mediated functions can lead to undesirable side effects. Patients treated with nivolumab have been reported to develop thyroid disease,1,3,4 diabetes,3 hypophysitis,1,3 hypopituitarism,3 and pneumonitis,4,2 as well as other autoimmune conditions.3 Although nivolumab is often used to treat skin diseases such as melanoma, it can have many cutaneous side effects including pruritus,1,3-6 rash,1,3,4,6,7 vitiligo,1,3,7,6 mouth sores,3 injection site reactions,3,6 and alopecia.5 Herein, we describe a patient who was treated with nivolumab and developed an exacerbation of pre-existing psoriasis.
Case presentation and summary
A 57-year-old man with metastatic NSCLC and a history of plaque psoriasis presented to the dermatology clinic for evaluation of new lesions on his palms and soles. The patient had been previously treated with numerous therapies for NSCLC, including chemotherapy and radiation. Previous chemotherapeutic agents included the cisplatin plus etoposide combination, with doxetaxel and pemetrexed. The patient was not able to tolerate the chemotherapy and instead opted for hospice care. After several months, he chose to restart therapy, and was started on the programmed cell death (PD)-1 inhibitor, nivolumab, at a dose of 3 mg/kg for a total of 6 cycles. He received his first dose 5 weeks before his current presentation to the clinic, and his second dose 2 weeks before.
The patient reported a 20-year history of plaque psoriasis, characterized by psoriatic plaques on the elbows and shins and for which he was treated with topical therapies with good effect. Every few months, he would develop one or two small plaques of psoriasis on his palms and soles. The lesions were inconsequential to the patient, as he never experienced more than one or two small palmoplantar lesions at a time. One week after his second cycle of nivolumab, the patient developed an eruption of lesions on his palms and soles. He observed that the lesions seemed to be similar to his previous palmoplantar psoriatic plaques but with significantly greater skin involvement. The patient denied any new-onset joint pain.
The results of a physical examination revealed a cachectic man in no acute distress, with more than 30 erythematous circular to oval circumscribed plaques with yellow to whitish scales on the bilateral palms (Figure 1) and soles (Figure 2).
The patient also had well-demarcated, thick oval erythematous plaques with micaceous scales on the bilateral elbows (Figure 3), and thin scaly erythematous plaques on the anterior shins (Figure 4). There were no psoriatic plaques on the remainder of the trunk or extremities. Mucosal surfaces, scalp, and nails were uninvolved.
A clinical diagnosis of exacerbation of pre-existing psoriasis owing to nivolumab therapy was made. The patient was started on clobetasol 0.05% ointment twice daily under occlusion with plastic wrap to the affected areas, and he was continued on nivolumab for his NSCLC.
Discussion
Treatment with nivolumab can lead to a range of autoimmune side effects, and as shown in this case, psoriasis is one of the cutaneous findings that could be exacerbated by treatment with nivolumab. To date, two cases of exacerbation of psoriasis in patients treated with nivolumab for melanoma have been reported in the literature.8,9 In the first case, the patient had well-controlled plaque psoriasis at baseline and he subsequently developed psoriatic plaques on the trunk and extremities after the second infusion of nivolumab for metastatic melanoma. A biopsy showed regular acanthosis with hyperkeratosis and parakeratosis in addition to dilated vessels in the papillary dermis.8 In the second case, the patient had a history of psoriasis vulgaris with no active lesions. Three weeks after his first course of nivolumab for metastatic oral mucosal melanoma, he developed new, well-circumscribed erythematous scaly plaques on the trunk and extremities that were clinically diagnosed as psoriasis.9 In a third case, a patient without a prior history of psoriasis experienced a psoriasiform eruption on the trunk and extremities after the fourth dose of nivolumab for oral mucosal melanoma.10 Thus, our case is the third reported case of exacerbation of preexisting psoriasis in a patient treated with nivolumab. Furthermore, our patient is the first reported case of a patient treated with nivolumab for NSCLC to develop this adverse event. Whereas the previously reported cases were characterized by widespread trunk and extremity involvement, our patient developed focal exacerbation of the palmoplantar areas.
Additional studies are needed to more clearly characterize the specific cutaneous toxicities of nivolumab and to determine if particular skin reactions may indicate a better response to the anticancer agent. Side effects such as psoriasis can often be managed with topical therapies and may not require withdrawal of the medication. We encourage the collaboration of dermatologists and oncologists to enhance the diagnosis and management of these cutaneous side effects in cancer patients.
Nivolumab is a full human immunoglobulin antibody to the programmed cell death 1 (PD-1) immune checkpoint receptor on T cells. This programmed cell death inhibitor is a targeted immunotherapy used to treat patients with melanoma, among other malignancies.1 More recently, nivolumab has been used for advanced non-small-cell lung cancer (NSCLC) after failure of previous chemotherapeutic agents. It was approved by the US Food and Drug Administration for the NSCLC indication in 2015.2
PD-1 inhibitors are efficacious in treating advanced malignancies, although their immune-mediated functions can lead to undesirable side effects. Patients treated with nivolumab have been reported to develop thyroid disease,1,3,4 diabetes,3 hypophysitis,1,3 hypopituitarism,3 and pneumonitis,4,2 as well as other autoimmune conditions.3 Although nivolumab is often used to treat skin diseases such as melanoma, it can have many cutaneous side effects including pruritus,1,3-6 rash,1,3,4,6,7 vitiligo,1,3,7,6 mouth sores,3 injection site reactions,3,6 and alopecia.5 Herein, we describe a patient who was treated with nivolumab and developed an exacerbation of pre-existing psoriasis.
Case presentation and summary
A 57-year-old man with metastatic NSCLC and a history of plaque psoriasis presented to the dermatology clinic for evaluation of new lesions on his palms and soles. The patient had been previously treated with numerous therapies for NSCLC, including chemotherapy and radiation. Previous chemotherapeutic agents included the cisplatin plus etoposide combination, with doxetaxel and pemetrexed. The patient was not able to tolerate the chemotherapy and instead opted for hospice care. After several months, he chose to restart therapy, and was started on the programmed cell death (PD)-1 inhibitor, nivolumab, at a dose of 3 mg/kg for a total of 6 cycles. He received his first dose 5 weeks before his current presentation to the clinic, and his second dose 2 weeks before.
The patient reported a 20-year history of plaque psoriasis, characterized by psoriatic plaques on the elbows and shins and for which he was treated with topical therapies with good effect. Every few months, he would develop one or two small plaques of psoriasis on his palms and soles. The lesions were inconsequential to the patient, as he never experienced more than one or two small palmoplantar lesions at a time. One week after his second cycle of nivolumab, the patient developed an eruption of lesions on his palms and soles. He observed that the lesions seemed to be similar to his previous palmoplantar psoriatic plaques but with significantly greater skin involvement. The patient denied any new-onset joint pain.
The results of a physical examination revealed a cachectic man in no acute distress, with more than 30 erythematous circular to oval circumscribed plaques with yellow to whitish scales on the bilateral palms (Figure 1) and soles (Figure 2).
The patient also had well-demarcated, thick oval erythematous plaques with micaceous scales on the bilateral elbows (Figure 3), and thin scaly erythematous plaques on the anterior shins (Figure 4). There were no psoriatic plaques on the remainder of the trunk or extremities. Mucosal surfaces, scalp, and nails were uninvolved.
A clinical diagnosis of exacerbation of pre-existing psoriasis owing to nivolumab therapy was made. The patient was started on clobetasol 0.05% ointment twice daily under occlusion with plastic wrap to the affected areas, and he was continued on nivolumab for his NSCLC.
Discussion
Treatment with nivolumab can lead to a range of autoimmune side effects, and as shown in this case, psoriasis is one of the cutaneous findings that could be exacerbated by treatment with nivolumab. To date, two cases of exacerbation of psoriasis in patients treated with nivolumab for melanoma have been reported in the literature.8,9 In the first case, the patient had well-controlled plaque psoriasis at baseline and he subsequently developed psoriatic plaques on the trunk and extremities after the second infusion of nivolumab for metastatic melanoma. A biopsy showed regular acanthosis with hyperkeratosis and parakeratosis in addition to dilated vessels in the papillary dermis.8 In the second case, the patient had a history of psoriasis vulgaris with no active lesions. Three weeks after his first course of nivolumab for metastatic oral mucosal melanoma, he developed new, well-circumscribed erythematous scaly plaques on the trunk and extremities that were clinically diagnosed as psoriasis.9 In a third case, a patient without a prior history of psoriasis experienced a psoriasiform eruption on the trunk and extremities after the fourth dose of nivolumab for oral mucosal melanoma.10 Thus, our case is the third reported case of exacerbation of preexisting psoriasis in a patient treated with nivolumab. Furthermore, our patient is the first reported case of a patient treated with nivolumab for NSCLC to develop this adverse event. Whereas the previously reported cases were characterized by widespread trunk and extremity involvement, our patient developed focal exacerbation of the palmoplantar areas.
Additional studies are needed to more clearly characterize the specific cutaneous toxicities of nivolumab and to determine if particular skin reactions may indicate a better response to the anticancer agent. Side effects such as psoriasis can often be managed with topical therapies and may not require withdrawal of the medication. We encourage the collaboration of dermatologists and oncologists to enhance the diagnosis and management of these cutaneous side effects in cancer patients.
1. Larkin J, Lao CD, Urba WJ, et al. Efficacy and safety of Nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433-440.
2. Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004-2012.
3. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
4. Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257-265.
5. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
6. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311-4318.
7. Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber J. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2015.
8. Matsumura N, Ohtsuka M, Kikuchi N, Yamamoto T. Exacerbation of psoriasis during nivolumab therapy for metastatic melanoma. Acta Derm Venereol. 2016;96(2):259-260.
9. Kato Y, Otsuka A, Miyachi Y, Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30(10):e89-e91.
10. Ohtsuka M, Miura T, Mori T, Ishikawa M, Yamamoto T. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol. 2015;151(7):797-799.
1. Larkin J, Lao CD, Urba WJ, et al. Efficacy and safety of Nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433-440.
2. Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004-2012.
3. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
4. Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257-265.
5. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
6. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311-4318.
7. Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber J. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2015.
8. Matsumura N, Ohtsuka M, Kikuchi N, Yamamoto T. Exacerbation of psoriasis during nivolumab therapy for metastatic melanoma. Acta Derm Venereol. 2016;96(2):259-260.
9. Kato Y, Otsuka A, Miyachi Y, Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30(10):e89-e91.
10. Ohtsuka M, Miura T, Mori T, Ishikawa M, Yamamoto T. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol. 2015;151(7):797-799.
Tracking the Relationship Between Unintentional Weight Loss and Cancer
Unintentional weight loss can present diagnostic challenges, according to researchers from University of Barcelona. So many factors are involved, and so many causes are possible, extensive and invasive investigation often is needed. And because cancer may be the underlying cause of weight loss in patients with few or no symptoms, a swift workup is crucial. Most studies of unintentional weight loss (UWL) have been limited by small sample sizes, short or variable follow-up, or focus on older patients, the researchers say. So they conducted the largest and longest prospective study thus far, following 2,677 patients for > 5 years.
The patients were referred to an outpatient diagnosis unit for evaluation of UWL as a dominant or isolated feature of disease and underwent a standard baseline evaluation with laboratory tests and chest X-ray. Those without identifiable causes 6 months after presentation were followed for 60 more months. Older patients also were given an oral cavity examination, a videofluoroscopy or swallowing study, and a depression and cognitive assessment.
At 6 months, 582 patients had unexplained UWL. Of those, 27 had malignancies: 11 patients had pancreatic cancer; nine had lymphoma. Nearly half of the cancers were digestive; of those, pancreatic cancer accounted for 19%, followed by lung (17%); lymphoma (11%); and kidney, ureteral, and bladder cancers (10%). Of 450 nonmalignant organic disorders, 45% were digestive.
Cancer patients had the highest mortality rate (69% vs 5%-6% in other groups). Decreasing weight was substantially more common in survivors with malignancies (66%) than in the rest of the patients studied, as well as in survivors with nonmalignant organic disorders (10%) than in unexplained UWL and psychosocial disorders. Patients with cancers were older, male, and active smokers, with a greater weight loss than patients in other groups. They also were more likely to have accompanying symptoms and abnormalities on physical examination, lab tests, and chest X-ray.
Cancer evading early diagnosis is a major concern, the researchers say. One of the main findings of the study was the long follow-up of patients with unexplained UWL: a mean of 47.5 months. Based on their findings, occult malignancies detected during a follow-up of up to 66 months after presentation “do not seem to be as rare as thought.” Moreover, autopsies of 13 patients showed malignancies in eight.
However, the fact that only 1 in 20 patients received a cancer diagnosis within that period—most notably within the first 28 months after referral for workup—is “fairly reassuring.” However, they recommend continuing to regularly evaluate patients with UWL for longer periods even if they had a normal evaluation and workup.
Unintentional weight loss can present diagnostic challenges, according to researchers from University of Barcelona. So many factors are involved, and so many causes are possible, extensive and invasive investigation often is needed. And because cancer may be the underlying cause of weight loss in patients with few or no symptoms, a swift workup is crucial. Most studies of unintentional weight loss (UWL) have been limited by small sample sizes, short or variable follow-up, or focus on older patients, the researchers say. So they conducted the largest and longest prospective study thus far, following 2,677 patients for > 5 years.
The patients were referred to an outpatient diagnosis unit for evaluation of UWL as a dominant or isolated feature of disease and underwent a standard baseline evaluation with laboratory tests and chest X-ray. Those without identifiable causes 6 months after presentation were followed for 60 more months. Older patients also were given an oral cavity examination, a videofluoroscopy or swallowing study, and a depression and cognitive assessment.
At 6 months, 582 patients had unexplained UWL. Of those, 27 had malignancies: 11 patients had pancreatic cancer; nine had lymphoma. Nearly half of the cancers were digestive; of those, pancreatic cancer accounted for 19%, followed by lung (17%); lymphoma (11%); and kidney, ureteral, and bladder cancers (10%). Of 450 nonmalignant organic disorders, 45% were digestive.
Cancer patients had the highest mortality rate (69% vs 5%-6% in other groups). Decreasing weight was substantially more common in survivors with malignancies (66%) than in the rest of the patients studied, as well as in survivors with nonmalignant organic disorders (10%) than in unexplained UWL and psychosocial disorders. Patients with cancers were older, male, and active smokers, with a greater weight loss than patients in other groups. They also were more likely to have accompanying symptoms and abnormalities on physical examination, lab tests, and chest X-ray.
Cancer evading early diagnosis is a major concern, the researchers say. One of the main findings of the study was the long follow-up of patients with unexplained UWL: a mean of 47.5 months. Based on their findings, occult malignancies detected during a follow-up of up to 66 months after presentation “do not seem to be as rare as thought.” Moreover, autopsies of 13 patients showed malignancies in eight.
However, the fact that only 1 in 20 patients received a cancer diagnosis within that period—most notably within the first 28 months after referral for workup—is “fairly reassuring.” However, they recommend continuing to regularly evaluate patients with UWL for longer periods even if they had a normal evaluation and workup.
Unintentional weight loss can present diagnostic challenges, according to researchers from University of Barcelona. So many factors are involved, and so many causes are possible, extensive and invasive investigation often is needed. And because cancer may be the underlying cause of weight loss in patients with few or no symptoms, a swift workup is crucial. Most studies of unintentional weight loss (UWL) have been limited by small sample sizes, short or variable follow-up, or focus on older patients, the researchers say. So they conducted the largest and longest prospective study thus far, following 2,677 patients for > 5 years.
The patients were referred to an outpatient diagnosis unit for evaluation of UWL as a dominant or isolated feature of disease and underwent a standard baseline evaluation with laboratory tests and chest X-ray. Those without identifiable causes 6 months after presentation were followed for 60 more months. Older patients also were given an oral cavity examination, a videofluoroscopy or swallowing study, and a depression and cognitive assessment.
At 6 months, 582 patients had unexplained UWL. Of those, 27 had malignancies: 11 patients had pancreatic cancer; nine had lymphoma. Nearly half of the cancers were digestive; of those, pancreatic cancer accounted for 19%, followed by lung (17%); lymphoma (11%); and kidney, ureteral, and bladder cancers (10%). Of 450 nonmalignant organic disorders, 45% were digestive.
Cancer patients had the highest mortality rate (69% vs 5%-6% in other groups). Decreasing weight was substantially more common in survivors with malignancies (66%) than in the rest of the patients studied, as well as in survivors with nonmalignant organic disorders (10%) than in unexplained UWL and psychosocial disorders. Patients with cancers were older, male, and active smokers, with a greater weight loss than patients in other groups. They also were more likely to have accompanying symptoms and abnormalities on physical examination, lab tests, and chest X-ray.
Cancer evading early diagnosis is a major concern, the researchers say. One of the main findings of the study was the long follow-up of patients with unexplained UWL: a mean of 47.5 months. Based on their findings, occult malignancies detected during a follow-up of up to 66 months after presentation “do not seem to be as rare as thought.” Moreover, autopsies of 13 patients showed malignancies in eight.
However, the fact that only 1 in 20 patients received a cancer diagnosis within that period—most notably within the first 28 months after referral for workup—is “fairly reassuring.” However, they recommend continuing to regularly evaluate patients with UWL for longer periods even if they had a normal evaluation and workup.
Group prenatal care offers benefits for young mothers
SAN DIEGO – Young women who received group prenatal visits under the CenteringPregnancy model were significantly more likely than were women receiving traditional prenatal care to elect long-acting reversible contraceptives postpartum, results from a small study show.
CenteringPregnancy (CP) – a group prenatal care model for women with due dates around the same time – has been touted as a way to decrease the incidence of preterm deliveries, but little is known about potential additional benefits for other birth-related outcomes, lead study author
CP sessions “follow the regular prenatal visit structure but the care itself is in a group setting,” said Dr. Roussos-Ross, an ob.gyn. at the University of Florida, Gainesville. “Each session lasts an hour and a half to 2 hours. In that group session, patients receive routine prenatal care and increased knowledge of various topics in pregnancy.”
Dr. Roussos-Ross and her associates set out to compare pregnancy-related outcomes in 20 patients aged 18-21 years who received care through the CP model, with a random sample of 20 patients who received care via the traditional care model in women’s health clinics at the University of Florida Health from January to December of 2014. They found that a significantly higher proportion of women in the CP group were African American, compared with those in the control group (85% vs. 55%, respectively; P = .024). In addition, uptake of long-acting reversible contraceptives was significantly higher among the CP group, compared with the control group (32% vs. 0%; P = .0292).
“One of the centering sessions is revolved around the education of different contraceptive uses, so they get information on the different options that they have,” Dr. Roussos-Ross said.
Differences did not reach statistical significance in other birth-related outcomes, but trends favored the CP group in most of the variables studied, including higher rates of flu vaccination (50% vs. 30%; P = .196), Tdap vaccination (60% vs. 35%; P = .11), breastfeeding initiation (95% vs. 90%; P = .579), and breastfeeding at 6 weeks postpartum (42% vs. 20%; P = .2427). Some adverse outcomes were lower in the CP group, such as low birth weight (0% vs. 10%; P = .1468), and the proportion of patients who failed to appear for their postpartum visit (21% vs. 35%; P = .333).
“The CP program was not able to demonstrate an improved preterm delivery outcome in adolescent mothers,” Dr. Roussos-Ross said. “However, this small study was able to demonstrate complementary benefits of CP in adolescent mothers, including improved breastfeeding rates, immunization rates, and [long-acting reversible contraception] usage rates. Offering adolescent mothers group care allows for greater time with their provider, which in turn may lead to increased knowledge and understanding of health and pregnancy-related outcomes.”
The researchers received grant funding from the March of Dimes for start-up costs.
SAN DIEGO – Young women who received group prenatal visits under the CenteringPregnancy model were significantly more likely than were women receiving traditional prenatal care to elect long-acting reversible contraceptives postpartum, results from a small study show.
CenteringPregnancy (CP) – a group prenatal care model for women with due dates around the same time – has been touted as a way to decrease the incidence of preterm deliveries, but little is known about potential additional benefits for other birth-related outcomes, lead study author
CP sessions “follow the regular prenatal visit structure but the care itself is in a group setting,” said Dr. Roussos-Ross, an ob.gyn. at the University of Florida, Gainesville. “Each session lasts an hour and a half to 2 hours. In that group session, patients receive routine prenatal care and increased knowledge of various topics in pregnancy.”
Dr. Roussos-Ross and her associates set out to compare pregnancy-related outcomes in 20 patients aged 18-21 years who received care through the CP model, with a random sample of 20 patients who received care via the traditional care model in women’s health clinics at the University of Florida Health from January to December of 2014. They found that a significantly higher proportion of women in the CP group were African American, compared with those in the control group (85% vs. 55%, respectively; P = .024). In addition, uptake of long-acting reversible contraceptives was significantly higher among the CP group, compared with the control group (32% vs. 0%; P = .0292).
“One of the centering sessions is revolved around the education of different contraceptive uses, so they get information on the different options that they have,” Dr. Roussos-Ross said.
Differences did not reach statistical significance in other birth-related outcomes, but trends favored the CP group in most of the variables studied, including higher rates of flu vaccination (50% vs. 30%; P = .196), Tdap vaccination (60% vs. 35%; P = .11), breastfeeding initiation (95% vs. 90%; P = .579), and breastfeeding at 6 weeks postpartum (42% vs. 20%; P = .2427). Some adverse outcomes were lower in the CP group, such as low birth weight (0% vs. 10%; P = .1468), and the proportion of patients who failed to appear for their postpartum visit (21% vs. 35%; P = .333).
“The CP program was not able to demonstrate an improved preterm delivery outcome in adolescent mothers,” Dr. Roussos-Ross said. “However, this small study was able to demonstrate complementary benefits of CP in adolescent mothers, including improved breastfeeding rates, immunization rates, and [long-acting reversible contraception] usage rates. Offering adolescent mothers group care allows for greater time with their provider, which in turn may lead to increased knowledge and understanding of health and pregnancy-related outcomes.”
The researchers received grant funding from the March of Dimes for start-up costs.
SAN DIEGO – Young women who received group prenatal visits under the CenteringPregnancy model were significantly more likely than were women receiving traditional prenatal care to elect long-acting reversible contraceptives postpartum, results from a small study show.
CenteringPregnancy (CP) – a group prenatal care model for women with due dates around the same time – has been touted as a way to decrease the incidence of preterm deliveries, but little is known about potential additional benefits for other birth-related outcomes, lead study author
CP sessions “follow the regular prenatal visit structure but the care itself is in a group setting,” said Dr. Roussos-Ross, an ob.gyn. at the University of Florida, Gainesville. “Each session lasts an hour and a half to 2 hours. In that group session, patients receive routine prenatal care and increased knowledge of various topics in pregnancy.”
Dr. Roussos-Ross and her associates set out to compare pregnancy-related outcomes in 20 patients aged 18-21 years who received care through the CP model, with a random sample of 20 patients who received care via the traditional care model in women’s health clinics at the University of Florida Health from January to December of 2014. They found that a significantly higher proportion of women in the CP group were African American, compared with those in the control group (85% vs. 55%, respectively; P = .024). In addition, uptake of long-acting reversible contraceptives was significantly higher among the CP group, compared with the control group (32% vs. 0%; P = .0292).
“One of the centering sessions is revolved around the education of different contraceptive uses, so they get information on the different options that they have,” Dr. Roussos-Ross said.
Differences did not reach statistical significance in other birth-related outcomes, but trends favored the CP group in most of the variables studied, including higher rates of flu vaccination (50% vs. 30%; P = .196), Tdap vaccination (60% vs. 35%; P = .11), breastfeeding initiation (95% vs. 90%; P = .579), and breastfeeding at 6 weeks postpartum (42% vs. 20%; P = .2427). Some adverse outcomes were lower in the CP group, such as low birth weight (0% vs. 10%; P = .1468), and the proportion of patients who failed to appear for their postpartum visit (21% vs. 35%; P = .333).
“The CP program was not able to demonstrate an improved preterm delivery outcome in adolescent mothers,” Dr. Roussos-Ross said. “However, this small study was able to demonstrate complementary benefits of CP in adolescent mothers, including improved breastfeeding rates, immunization rates, and [long-acting reversible contraception] usage rates. Offering adolescent mothers group care allows for greater time with their provider, which in turn may lead to increased knowledge and understanding of health and pregnancy-related outcomes.”
The researchers received grant funding from the March of Dimes for start-up costs.
AT ACOG 2017
Key clinical point:
Major finding: Uptake of long-acting reversible contraceptives was significantly higher among the CenteringPregnancy group compared with the control group (32% vs. 0%; P = .0292).
Data source: A chart review of 20 patients aged 18-21 years who received prenatal care via the CenteringPregnancy model, compared with a random sample of 20 patients who received traditional prenatal care.
Disclosures: The researchers received grant funding from the March of Dimes for start-up costs.