User login
MS May Have a Measurable Prodrome
A Large Case–Control Analysis
Previous studies have provided evidence for an MS prodrome that occurs years before a demyelinating event or the onset of clinical symptoms. Many of these studies, however, have been limited by a retrospective design or by the absence of a control group.
To analyze the question further, Dr. Tremlett and colleagues examined data from linked health administrative and clinical databases in the Canadian provinces of British Columbia, Saskatchewan, Manitoba, and Nova Scotia, which were chosen for their geographic diversity and comprehensive data. The researchers created a health administrative cohort, which was based on administrative data, and an MS clinic-derived cohort, which used administrative and clinical data. The study’s primary outcome was all-cause use of health care during each of the five years before the health administrative index date (ie, the first demyelinating disease-related claim) or clinical index date (ie, the date of MS symptom onset).
Health Care Use Increased in Prodromal MS
The health administrative cohort included 14,428 people with MS and 72,059 matched controls. In all, 10,525 (73%) of the patients with MS were women, and their mean age at the health administrative index date was 43. Compared with controls, annual health care use increased steadily between five years and one year before the first demyelinating disease claim in these patients.
The mean number of hospital admissions was 26% higher in people with MS than in controls in the fifth year before the index date, and 78% higher in the year before the index date. The mean number of physician claims was 24% higher in people with MS than in controls in the fifth year before the index date, and 88% higher in people with MS than in controls in the year before the index date. Also, the mean number of prescribed drug classes was 23% higher in people with MS than in matched controls in the fifth year before the index date, and 49% higher in people with MS than in controls in the year before the index date.
The MS clinic cohort included 3,202 people with MS and 16,006 matched controls. In all, 2,368 (74%) of people with MS were women, and the mean age at the clinical index date was approximately 37. Compared with the health administrative cohort, this cohort had similar patterns for physician claims and prescriptions, although the differences in use in each of the five years mostly did not reach statistical significance.
“To gain a better insight into the MS prodrome, the complex reasons for increased health care use will need to be established, for example, through access of additional administrative data such as the specific diagnostic codes related to a hospital admission or physician visit, or the therapeutic drug class for a prescription,” Dr. Tremlett concluded.
—Erik Greb
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017 Apr 20 [Epub ahead of print].
A Large Case–Control Analysis
Previous studies have provided evidence for an MS prodrome that occurs years before a demyelinating event or the onset of clinical symptoms. Many of these studies, however, have been limited by a retrospective design or by the absence of a control group.
To analyze the question further, Dr. Tremlett and colleagues examined data from linked health administrative and clinical databases in the Canadian provinces of British Columbia, Saskatchewan, Manitoba, and Nova Scotia, which were chosen for their geographic diversity and comprehensive data. The researchers created a health administrative cohort, which was based on administrative data, and an MS clinic-derived cohort, which used administrative and clinical data. The study’s primary outcome was all-cause use of health care during each of the five years before the health administrative index date (ie, the first demyelinating disease-related claim) or clinical index date (ie, the date of MS symptom onset).
Health Care Use Increased in Prodromal MS
The health administrative cohort included 14,428 people with MS and 72,059 matched controls. In all, 10,525 (73%) of the patients with MS were women, and their mean age at the health administrative index date was 43. Compared with controls, annual health care use increased steadily between five years and one year before the first demyelinating disease claim in these patients.
The mean number of hospital admissions was 26% higher in people with MS than in controls in the fifth year before the index date, and 78% higher in the year before the index date. The mean number of physician claims was 24% higher in people with MS than in controls in the fifth year before the index date, and 88% higher in people with MS than in controls in the year before the index date. Also, the mean number of prescribed drug classes was 23% higher in people with MS than in matched controls in the fifth year before the index date, and 49% higher in people with MS than in controls in the year before the index date.
The MS clinic cohort included 3,202 people with MS and 16,006 matched controls. In all, 2,368 (74%) of people with MS were women, and the mean age at the clinical index date was approximately 37. Compared with the health administrative cohort, this cohort had similar patterns for physician claims and prescriptions, although the differences in use in each of the five years mostly did not reach statistical significance.
“To gain a better insight into the MS prodrome, the complex reasons for increased health care use will need to be established, for example, through access of additional administrative data such as the specific diagnostic codes related to a hospital admission or physician visit, or the therapeutic drug class for a prescription,” Dr. Tremlett concluded.
—Erik Greb
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017 Apr 20 [Epub ahead of print].
A Large Case–Control Analysis
Previous studies have provided evidence for an MS prodrome that occurs years before a demyelinating event or the onset of clinical symptoms. Many of these studies, however, have been limited by a retrospective design or by the absence of a control group.
To analyze the question further, Dr. Tremlett and colleagues examined data from linked health administrative and clinical databases in the Canadian provinces of British Columbia, Saskatchewan, Manitoba, and Nova Scotia, which were chosen for their geographic diversity and comprehensive data. The researchers created a health administrative cohort, which was based on administrative data, and an MS clinic-derived cohort, which used administrative and clinical data. The study’s primary outcome was all-cause use of health care during each of the five years before the health administrative index date (ie, the first demyelinating disease-related claim) or clinical index date (ie, the date of MS symptom onset).
Health Care Use Increased in Prodromal MS
The health administrative cohort included 14,428 people with MS and 72,059 matched controls. In all, 10,525 (73%) of the patients with MS were women, and their mean age at the health administrative index date was 43. Compared with controls, annual health care use increased steadily between five years and one year before the first demyelinating disease claim in these patients.
The mean number of hospital admissions was 26% higher in people with MS than in controls in the fifth year before the index date, and 78% higher in the year before the index date. The mean number of physician claims was 24% higher in people with MS than in controls in the fifth year before the index date, and 88% higher in people with MS than in controls in the year before the index date. Also, the mean number of prescribed drug classes was 23% higher in people with MS than in matched controls in the fifth year before the index date, and 49% higher in people with MS than in controls in the year before the index date.
The MS clinic cohort included 3,202 people with MS and 16,006 matched controls. In all, 2,368 (74%) of people with MS were women, and the mean age at the clinical index date was approximately 37. Compared with the health administrative cohort, this cohort had similar patterns for physician claims and prescriptions, although the differences in use in each of the five years mostly did not reach statistical significance.
“To gain a better insight into the MS prodrome, the complex reasons for increased health care use will need to be established, for example, through access of additional administrative data such as the specific diagnostic codes related to a hospital admission or physician visit, or the therapeutic drug class for a prescription,” Dr. Tremlett concluded.
—Erik Greb
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017 Apr 20 [Epub ahead of print].
How Can Neurologists Diagnose Traumatic Encephalopathy Syndrome?
BOSTON—Proposed diagnostic criteria for probable or possible chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease associated with repetitive brain trauma, include a history of head impacts and various core clinical and supportive features.
The preliminary criteria, which were presented by Andrew Budson, MD, Professor of Neurology at Boston University School of Medicine, at the 69th Annual Meeting of the American Academy of Neurology, primarily were designed for research purposes, but can serve as a guide for neurologists for the diagnosis of traumatic encephalopathy syndrome. CTE is a neuropathologic diagnosis, whereas traumatic encephalopathy syndrome is a clinical diagnosis. In addition to presenting the general criteria, Dr. Budson shared diagnostic subtypes, potential biomarkers, and treatment options.
General Criteria
There are five general criteria that patients must meet to receive a diagnosis of traumatic encephalopathy syndrome, said Dr. Budson. First, there must be a history of impacts to the head based on types of injuries (eg, mild or severe traumatic brain injury, concussions, or subconcussive trauma) and sources of exposure, such as military service or involvement in contact sports for a minimum of six years, including at least two years at the college level or higher.
Second, patients must not have another neurologic disorder that likely accounts for the clinical features. Third, clinical features must be present for at least 12 months. The fourth requirement is that at least one core clinical feature (ie, cognitive, behavioral, or mood features) must be present and considered a change from baseline. Finally, at least two of nine supportive features must be present.
Core Clinical and Supportive Features
Of the core clinical features, difficulties in cognition must be reported by the patient, an informant, or a clinician and substantiated by standardized tests. Core behavioral clinical features include emotionally explosive behavior or physical and verbal abuse. Core mood clinical features include feeling overly sad, depressed, or hopeless.
In addition to core clinical features, two of the following supportive features must be present: impulsivity, anxiety, apathy, paranoia, suicidality, headache, motor signs (eg, dysarthria, dysgraphia, or other features of parkinsonism), documented decline for at least a year, or delayed onset of clinical features after a significant head impact exposure (usually at least two years).
Syndrome Subtypes
Patients may have one of four possible traumatic encephalopathy syndrome diagnostic subtypes. A behavioral/mood variant is more common among younger patients, whereas a cognitive variant is more common in older populations, said Dr. Budson. Patients also may have a mixed variant or dementia. Patients with the dementia subtype must have a progressive course of cognitive core clinical features, with or without behavior or mood features. In addition, patients with dementia must have cognitive impairment that interferes with their ability to function independently during normal daily activities.
Biomarkers and Treatment
Cavum septum pellucidum, cavum vergae, or fenestrations on neuroimaging are potential CTE biomarkers, said Dr. Budson. Normal beta amyloid CSF levels, elevated CSF p-tau/tau ratio, negative amyloid imaging, as well as cortical atrophy beyond that expected for age could also be signs of CTE. Potential experimental biomarkers include positive tau imaging and cortical thinning based on MRI.
Once physicians have made a diagnosis of probable or possible CTE, there are several treatments that may benefit patients, although no medications are approved for the treatment of CTE. Cholinesterase inhibitors may help to treat memory impairment, said Dr. Budson. For patients with depression and anxiety, selective serotonin reuptake inhibitors may be helpful. For patients with violent or explosive behavior, atypical neuroleptics may be efficacious. Memantine may benefit patients with moderate or severe dementia. Finally, to manage agitation, a combination of dextromethorphan and quinidine may be a treatment option.
—Erica Tricarico
Suggested Reading
Montenigro PH, Baugh CM, Daneshvar DH, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68.
BOSTON—Proposed diagnostic criteria for probable or possible chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease associated with repetitive brain trauma, include a history of head impacts and various core clinical and supportive features.
The preliminary criteria, which were presented by Andrew Budson, MD, Professor of Neurology at Boston University School of Medicine, at the 69th Annual Meeting of the American Academy of Neurology, primarily were designed for research purposes, but can serve as a guide for neurologists for the diagnosis of traumatic encephalopathy syndrome. CTE is a neuropathologic diagnosis, whereas traumatic encephalopathy syndrome is a clinical diagnosis. In addition to presenting the general criteria, Dr. Budson shared diagnostic subtypes, potential biomarkers, and treatment options.
General Criteria
There are five general criteria that patients must meet to receive a diagnosis of traumatic encephalopathy syndrome, said Dr. Budson. First, there must be a history of impacts to the head based on types of injuries (eg, mild or severe traumatic brain injury, concussions, or subconcussive trauma) and sources of exposure, such as military service or involvement in contact sports for a minimum of six years, including at least two years at the college level or higher.
Second, patients must not have another neurologic disorder that likely accounts for the clinical features. Third, clinical features must be present for at least 12 months. The fourth requirement is that at least one core clinical feature (ie, cognitive, behavioral, or mood features) must be present and considered a change from baseline. Finally, at least two of nine supportive features must be present.
Core Clinical and Supportive Features
Of the core clinical features, difficulties in cognition must be reported by the patient, an informant, or a clinician and substantiated by standardized tests. Core behavioral clinical features include emotionally explosive behavior or physical and verbal abuse. Core mood clinical features include feeling overly sad, depressed, or hopeless.
In addition to core clinical features, two of the following supportive features must be present: impulsivity, anxiety, apathy, paranoia, suicidality, headache, motor signs (eg, dysarthria, dysgraphia, or other features of parkinsonism), documented decline for at least a year, or delayed onset of clinical features after a significant head impact exposure (usually at least two years).
Syndrome Subtypes
Patients may have one of four possible traumatic encephalopathy syndrome diagnostic subtypes. A behavioral/mood variant is more common among younger patients, whereas a cognitive variant is more common in older populations, said Dr. Budson. Patients also may have a mixed variant or dementia. Patients with the dementia subtype must have a progressive course of cognitive core clinical features, with or without behavior or mood features. In addition, patients with dementia must have cognitive impairment that interferes with their ability to function independently during normal daily activities.
Biomarkers and Treatment
Cavum septum pellucidum, cavum vergae, or fenestrations on neuroimaging are potential CTE biomarkers, said Dr. Budson. Normal beta amyloid CSF levels, elevated CSF p-tau/tau ratio, negative amyloid imaging, as well as cortical atrophy beyond that expected for age could also be signs of CTE. Potential experimental biomarkers include positive tau imaging and cortical thinning based on MRI.
Once physicians have made a diagnosis of probable or possible CTE, there are several treatments that may benefit patients, although no medications are approved for the treatment of CTE. Cholinesterase inhibitors may help to treat memory impairment, said Dr. Budson. For patients with depression and anxiety, selective serotonin reuptake inhibitors may be helpful. For patients with violent or explosive behavior, atypical neuroleptics may be efficacious. Memantine may benefit patients with moderate or severe dementia. Finally, to manage agitation, a combination of dextromethorphan and quinidine may be a treatment option.
—Erica Tricarico
Suggested Reading
Montenigro PH, Baugh CM, Daneshvar DH, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68.
BOSTON—Proposed diagnostic criteria for probable or possible chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease associated with repetitive brain trauma, include a history of head impacts and various core clinical and supportive features.
The preliminary criteria, which were presented by Andrew Budson, MD, Professor of Neurology at Boston University School of Medicine, at the 69th Annual Meeting of the American Academy of Neurology, primarily were designed for research purposes, but can serve as a guide for neurologists for the diagnosis of traumatic encephalopathy syndrome. CTE is a neuropathologic diagnosis, whereas traumatic encephalopathy syndrome is a clinical diagnosis. In addition to presenting the general criteria, Dr. Budson shared diagnostic subtypes, potential biomarkers, and treatment options.
General Criteria
There are five general criteria that patients must meet to receive a diagnosis of traumatic encephalopathy syndrome, said Dr. Budson. First, there must be a history of impacts to the head based on types of injuries (eg, mild or severe traumatic brain injury, concussions, or subconcussive trauma) and sources of exposure, such as military service or involvement in contact sports for a minimum of six years, including at least two years at the college level or higher.
Second, patients must not have another neurologic disorder that likely accounts for the clinical features. Third, clinical features must be present for at least 12 months. The fourth requirement is that at least one core clinical feature (ie, cognitive, behavioral, or mood features) must be present and considered a change from baseline. Finally, at least two of nine supportive features must be present.
Core Clinical and Supportive Features
Of the core clinical features, difficulties in cognition must be reported by the patient, an informant, or a clinician and substantiated by standardized tests. Core behavioral clinical features include emotionally explosive behavior or physical and verbal abuse. Core mood clinical features include feeling overly sad, depressed, or hopeless.
In addition to core clinical features, two of the following supportive features must be present: impulsivity, anxiety, apathy, paranoia, suicidality, headache, motor signs (eg, dysarthria, dysgraphia, or other features of parkinsonism), documented decline for at least a year, or delayed onset of clinical features after a significant head impact exposure (usually at least two years).
Syndrome Subtypes
Patients may have one of four possible traumatic encephalopathy syndrome diagnostic subtypes. A behavioral/mood variant is more common among younger patients, whereas a cognitive variant is more common in older populations, said Dr. Budson. Patients also may have a mixed variant or dementia. Patients with the dementia subtype must have a progressive course of cognitive core clinical features, with or without behavior or mood features. In addition, patients with dementia must have cognitive impairment that interferes with their ability to function independently during normal daily activities.
Biomarkers and Treatment
Cavum septum pellucidum, cavum vergae, or fenestrations on neuroimaging are potential CTE biomarkers, said Dr. Budson. Normal beta amyloid CSF levels, elevated CSF p-tau/tau ratio, negative amyloid imaging, as well as cortical atrophy beyond that expected for age could also be signs of CTE. Potential experimental biomarkers include positive tau imaging and cortical thinning based on MRI.
Once physicians have made a diagnosis of probable or possible CTE, there are several treatments that may benefit patients, although no medications are approved for the treatment of CTE. Cholinesterase inhibitors may help to treat memory impairment, said Dr. Budson. For patients with depression and anxiety, selective serotonin reuptake inhibitors may be helpful. For patients with violent or explosive behavior, atypical neuroleptics may be efficacious. Memantine may benefit patients with moderate or severe dementia. Finally, to manage agitation, a combination of dextromethorphan and quinidine may be a treatment option.
—Erica Tricarico
Suggested Reading
Montenigro PH, Baugh CM, Daneshvar DH, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68.
Breast cancer liquid biopsies don’t change outcomes....yet
LAS VEGAS – Although circulating tumor cells are prognostic in breast cancer, they aren’t likely to become a part of routine practice until they’ve been shown to improve outcomes, and that hasn’t happened yet, according to Anthony Lucci, MD, professor of breast surgical oncology at MD Anderson Cancer Center, Houston.
MD Anderson and other institutions have established that in breast cancer, from baseline through treatment follow-up, the presence of circulating tumor cells (CTCs) in the blood predicts worse outcomes in both metastatic and local disease, even among women who have a pathologic complete response to treatment.
That knowledge has not yet translated into better outcomes. In a pivotal trial, survival was no better in metastatic breast cancer when women were switched to an alternative chemotherapy regimen after their CTC levels did not fall in response to first-line treatment, compared with women who remained on their initial agent despite persistently high CTCs (J Clin Oncol. 2014 Nov 1;32[31]:3483-9).
“When we tried to switch chemotherapy” based on CTCs, “it really didn’t make a difference, so no one is really quite sure yet what to do with this information. We can’t tell a patient that they are likely to have a much worse outcome, but there’s nothing we can do about it,” and “I don’t think payers will pay” for CTC testing in breast cancer until “we establish a predictive benefit, and show what agents will reduce CTCs and improve outcomes,” Dr. Lucci said at the American Society of Breast Surgeons annual meeting.
Even so, the promise of CTCs as a clinical tool is too great to abandon research, and work continues at MD Anderson and elsewhere. It’s thought that tumor cells in the blood aren’t simply a marker of disease, but rather microscopic disease in themselves that contributes to recurrence and progression. It’s possible that cells shed by tumors lie dormant in the bone marrow, then reactivate and reseed the original tumor site or give rise to distant metastases.
CTCs are similar to tumor cells that have been found in the bone marrow of women with apparently quiescent breast cancer, but finding them in the blood means “you don’t have to poke a needle in someone’s bone. You can just take a sample of their blood, and it tells you the same information,” Dr. Lucci said.
CTCs have been shown in breast cancer to rise and fall depending on tumor response. “In the future, I do think we will [use them] as a serial monitoring tool and a guide to therapy.” There might even be a role for breast cancer screening, he said.
Analyzing the blood for evidence of solid tumors – popularly called “liquid biopsy” – has shown benefits in a variety of cancers, particularly for identifying disease, and in some cases mutations, sooner than with conventional methods. Science is catching up to the old-school notion that cancer spreads through the blood.
Another approach is to look for circulating tumor DNA, which has been shown to be useful for early detection in gynecologic cancers. The idea is that a few tumor cells shatter and spill their genetic material into the blood early on. “In the majority of breast cancer patients,” however, “you don’t find actionable mutations” with circulating tumor DNA, especially in earlier-stage, nonmetastatic disease. “There’s not enough DNA released into the blood,” Dr. Lucci said.
But “we need to be monitoring the blood on a routine basis” for breast cancer clues. “That, I think, is the wave of the future. Just looking at x-rays and waiting for something to happen is too late,” he said.
Dr. Lucci had no disclosures related to his talk.
LAS VEGAS – Although circulating tumor cells are prognostic in breast cancer, they aren’t likely to become a part of routine practice until they’ve been shown to improve outcomes, and that hasn’t happened yet, according to Anthony Lucci, MD, professor of breast surgical oncology at MD Anderson Cancer Center, Houston.
MD Anderson and other institutions have established that in breast cancer, from baseline through treatment follow-up, the presence of circulating tumor cells (CTCs) in the blood predicts worse outcomes in both metastatic and local disease, even among women who have a pathologic complete response to treatment.
That knowledge has not yet translated into better outcomes. In a pivotal trial, survival was no better in metastatic breast cancer when women were switched to an alternative chemotherapy regimen after their CTC levels did not fall in response to first-line treatment, compared with women who remained on their initial agent despite persistently high CTCs (J Clin Oncol. 2014 Nov 1;32[31]:3483-9).
“When we tried to switch chemotherapy” based on CTCs, “it really didn’t make a difference, so no one is really quite sure yet what to do with this information. We can’t tell a patient that they are likely to have a much worse outcome, but there’s nothing we can do about it,” and “I don’t think payers will pay” for CTC testing in breast cancer until “we establish a predictive benefit, and show what agents will reduce CTCs and improve outcomes,” Dr. Lucci said at the American Society of Breast Surgeons annual meeting.
Even so, the promise of CTCs as a clinical tool is too great to abandon research, and work continues at MD Anderson and elsewhere. It’s thought that tumor cells in the blood aren’t simply a marker of disease, but rather microscopic disease in themselves that contributes to recurrence and progression. It’s possible that cells shed by tumors lie dormant in the bone marrow, then reactivate and reseed the original tumor site or give rise to distant metastases.
CTCs are similar to tumor cells that have been found in the bone marrow of women with apparently quiescent breast cancer, but finding them in the blood means “you don’t have to poke a needle in someone’s bone. You can just take a sample of their blood, and it tells you the same information,” Dr. Lucci said.
CTCs have been shown in breast cancer to rise and fall depending on tumor response. “In the future, I do think we will [use them] as a serial monitoring tool and a guide to therapy.” There might even be a role for breast cancer screening, he said.
Analyzing the blood for evidence of solid tumors – popularly called “liquid biopsy” – has shown benefits in a variety of cancers, particularly for identifying disease, and in some cases mutations, sooner than with conventional methods. Science is catching up to the old-school notion that cancer spreads through the blood.
Another approach is to look for circulating tumor DNA, which has been shown to be useful for early detection in gynecologic cancers. The idea is that a few tumor cells shatter and spill their genetic material into the blood early on. “In the majority of breast cancer patients,” however, “you don’t find actionable mutations” with circulating tumor DNA, especially in earlier-stage, nonmetastatic disease. “There’s not enough DNA released into the blood,” Dr. Lucci said.
But “we need to be monitoring the blood on a routine basis” for breast cancer clues. “That, I think, is the wave of the future. Just looking at x-rays and waiting for something to happen is too late,” he said.
Dr. Lucci had no disclosures related to his talk.
LAS VEGAS – Although circulating tumor cells are prognostic in breast cancer, they aren’t likely to become a part of routine practice until they’ve been shown to improve outcomes, and that hasn’t happened yet, according to Anthony Lucci, MD, professor of breast surgical oncology at MD Anderson Cancer Center, Houston.
MD Anderson and other institutions have established that in breast cancer, from baseline through treatment follow-up, the presence of circulating tumor cells (CTCs) in the blood predicts worse outcomes in both metastatic and local disease, even among women who have a pathologic complete response to treatment.
That knowledge has not yet translated into better outcomes. In a pivotal trial, survival was no better in metastatic breast cancer when women were switched to an alternative chemotherapy regimen after their CTC levels did not fall in response to first-line treatment, compared with women who remained on their initial agent despite persistently high CTCs (J Clin Oncol. 2014 Nov 1;32[31]:3483-9).
“When we tried to switch chemotherapy” based on CTCs, “it really didn’t make a difference, so no one is really quite sure yet what to do with this information. We can’t tell a patient that they are likely to have a much worse outcome, but there’s nothing we can do about it,” and “I don’t think payers will pay” for CTC testing in breast cancer until “we establish a predictive benefit, and show what agents will reduce CTCs and improve outcomes,” Dr. Lucci said at the American Society of Breast Surgeons annual meeting.
Even so, the promise of CTCs as a clinical tool is too great to abandon research, and work continues at MD Anderson and elsewhere. It’s thought that tumor cells in the blood aren’t simply a marker of disease, but rather microscopic disease in themselves that contributes to recurrence and progression. It’s possible that cells shed by tumors lie dormant in the bone marrow, then reactivate and reseed the original tumor site or give rise to distant metastases.
CTCs are similar to tumor cells that have been found in the bone marrow of women with apparently quiescent breast cancer, but finding them in the blood means “you don’t have to poke a needle in someone’s bone. You can just take a sample of their blood, and it tells you the same information,” Dr. Lucci said.
CTCs have been shown in breast cancer to rise and fall depending on tumor response. “In the future, I do think we will [use them] as a serial monitoring tool and a guide to therapy.” There might even be a role for breast cancer screening, he said.
Analyzing the blood for evidence of solid tumors – popularly called “liquid biopsy” – has shown benefits in a variety of cancers, particularly for identifying disease, and in some cases mutations, sooner than with conventional methods. Science is catching up to the old-school notion that cancer spreads through the blood.
Another approach is to look for circulating tumor DNA, which has been shown to be useful for early detection in gynecologic cancers. The idea is that a few tumor cells shatter and spill their genetic material into the blood early on. “In the majority of breast cancer patients,” however, “you don’t find actionable mutations” with circulating tumor DNA, especially in earlier-stage, nonmetastatic disease. “There’s not enough DNA released into the blood,” Dr. Lucci said.
But “we need to be monitoring the blood on a routine basis” for breast cancer clues. “That, I think, is the wave of the future. Just looking at x-rays and waiting for something to happen is too late,” he said.
Dr. Lucci had no disclosures related to his talk.
AT ASBS 2017
Desmoplastic trichoepithelioma may co-occur with BCC
SYDNEY, AUSTRALIA – Watchful waiting may not be the safest approach for managing patients with desmoplastic trichoepithelioma, according to a speaker at the annual meeting of the Australasian College of Dermatologists, who described five cases of the benign tumor combined with basal cell carcinoma.
Desmoplastic trichoepithelioma (DTE), a rare benign tumor that typically presents as a small, slow-growing, asymptomatic, skin-colored lesion on the face, with a depressed nonulcerated center and often raised edges, is managed with watchful waiting or local excision. While its key histopathologic features are narrow cords or strands of basaloid cells, numerous small keratin-filled cysts, and a surrounding desmoplastic core, DTE can be confused with morpheaform basal cell carcinoma (BCC), Tristan Blake, MD, dermatology registrar at Royal Brisbane and Womens’ Hospital, Brisbane, Australia, said at the meeting.
“At this stage, there’s no way to confidently say, looking at the slides, if those cases were desmoplastic trichoepithelioma arising in basal cell carcinoma or vice versa, or if they were a single tumor with divergent differentiation, or an occlusion of two separate tumors,” he said.
Dr. Blake added that this was the first time, to his knowledge, that such a combination had been reported, and that the finding had the potential to change the way DTE is managed.
“How can you now confidently elect to leave or watch the desmoplastic trichoepithelioma patients you have, knowing that not an insignificant portion might also harbor BCC or develop BCC in the future?” he said. This dilemma is made more acute by the fact that DTEs are typically found in younger patients and on the face, he added.
Two dermatopathologists involved in the retrospective review of cases reported that histochemistry was not particularly useful in differentiating DTE from other tumors, he noted.
Patients in the study were also interviewed about their tumors and reported no symptoms; when asked how long the lesions had been there prior to diagnosis, those who could recall said the lesions had likely been present for decades.
In an interview, Dr. Blake said that the discovery of coexisting DTE and BCC was a surprise, and cast doubt on the practice of watchful waiting.
No conflicts of interest were declared.
SYDNEY, AUSTRALIA – Watchful waiting may not be the safest approach for managing patients with desmoplastic trichoepithelioma, according to a speaker at the annual meeting of the Australasian College of Dermatologists, who described five cases of the benign tumor combined with basal cell carcinoma.
Desmoplastic trichoepithelioma (DTE), a rare benign tumor that typically presents as a small, slow-growing, asymptomatic, skin-colored lesion on the face, with a depressed nonulcerated center and often raised edges, is managed with watchful waiting or local excision. While its key histopathologic features are narrow cords or strands of basaloid cells, numerous small keratin-filled cysts, and a surrounding desmoplastic core, DTE can be confused with morpheaform basal cell carcinoma (BCC), Tristan Blake, MD, dermatology registrar at Royal Brisbane and Womens’ Hospital, Brisbane, Australia, said at the meeting.
“At this stage, there’s no way to confidently say, looking at the slides, if those cases were desmoplastic trichoepithelioma arising in basal cell carcinoma or vice versa, or if they were a single tumor with divergent differentiation, or an occlusion of two separate tumors,” he said.
Dr. Blake added that this was the first time, to his knowledge, that such a combination had been reported, and that the finding had the potential to change the way DTE is managed.
“How can you now confidently elect to leave or watch the desmoplastic trichoepithelioma patients you have, knowing that not an insignificant portion might also harbor BCC or develop BCC in the future?” he said. This dilemma is made more acute by the fact that DTEs are typically found in younger patients and on the face, he added.
Two dermatopathologists involved in the retrospective review of cases reported that histochemistry was not particularly useful in differentiating DTE from other tumors, he noted.
Patients in the study were also interviewed about their tumors and reported no symptoms; when asked how long the lesions had been there prior to diagnosis, those who could recall said the lesions had likely been present for decades.
In an interview, Dr. Blake said that the discovery of coexisting DTE and BCC was a surprise, and cast doubt on the practice of watchful waiting.
No conflicts of interest were declared.
SYDNEY, AUSTRALIA – Watchful waiting may not be the safest approach for managing patients with desmoplastic trichoepithelioma, according to a speaker at the annual meeting of the Australasian College of Dermatologists, who described five cases of the benign tumor combined with basal cell carcinoma.
Desmoplastic trichoepithelioma (DTE), a rare benign tumor that typically presents as a small, slow-growing, asymptomatic, skin-colored lesion on the face, with a depressed nonulcerated center and often raised edges, is managed with watchful waiting or local excision. While its key histopathologic features are narrow cords or strands of basaloid cells, numerous small keratin-filled cysts, and a surrounding desmoplastic core, DTE can be confused with morpheaform basal cell carcinoma (BCC), Tristan Blake, MD, dermatology registrar at Royal Brisbane and Womens’ Hospital, Brisbane, Australia, said at the meeting.
“At this stage, there’s no way to confidently say, looking at the slides, if those cases were desmoplastic trichoepithelioma arising in basal cell carcinoma or vice versa, or if they were a single tumor with divergent differentiation, or an occlusion of two separate tumors,” he said.
Dr. Blake added that this was the first time, to his knowledge, that such a combination had been reported, and that the finding had the potential to change the way DTE is managed.
“How can you now confidently elect to leave or watch the desmoplastic trichoepithelioma patients you have, knowing that not an insignificant portion might also harbor BCC or develop BCC in the future?” he said. This dilemma is made more acute by the fact that DTEs are typically found in younger patients and on the face, he added.
Two dermatopathologists involved in the retrospective review of cases reported that histochemistry was not particularly useful in differentiating DTE from other tumors, he noted.
Patients in the study were also interviewed about their tumors and reported no symptoms; when asked how long the lesions had been there prior to diagnosis, those who could recall said the lesions had likely been present for decades.
In an interview, Dr. Blake said that the discovery of coexisting DTE and BCC was a surprise, and cast doubt on the practice of watchful waiting.
No conflicts of interest were declared.
AT ACDASM 2017
Key clinical point: Watchful waiting may no longer be the obvious choice for desmoplastic trichoepithelioma, with evidence that the benign tumor may co-occur with basal cell carcinoma.
Major finding: Researchers reported five cases in which both DTE and BCC were identified in the same pathology specimen.
Data source: A retrospective review of 27 patients with DTE, which included reexamination of specimens.
Disclosures: No conflicts of interest were declared.
Alzheimer’s mortality in U.S. grew from 1999 to 2014
The rate of death attributable to Alzheimer’s disease increased by more than 50% from 1999 to 2014 in the United States, according to a report from the Centers for Disease Control and Prevention.
According to data collected from the National Vital Statistics System, the total number of Alzheimer’s deaths was 44,536 in 1999 and 93,541 in 2014. The mortality in 1999 was 16.5 per 100,000 people, and in 2014 it was 25.4 per 100,000 people, a rate increase of 54.5%. Alzheimer’s was the sixth most common cause of death in 2014, accounting for 3.6% of all U.S. deaths.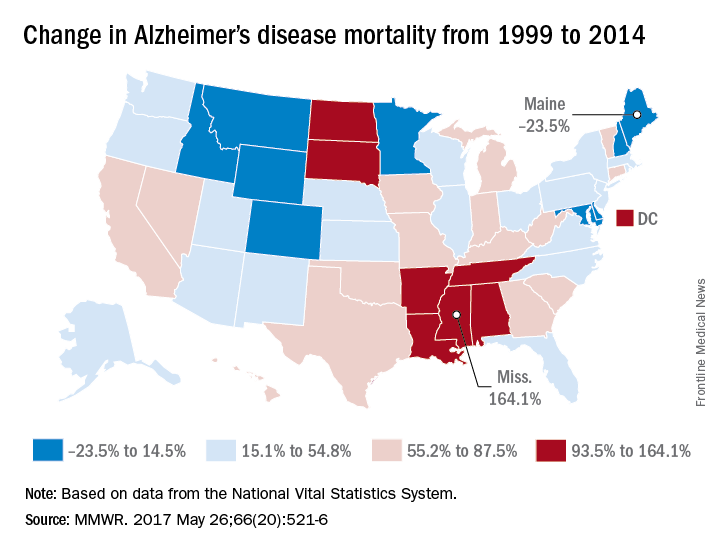
Mississippi, Louisiana, Arkansas, South Dakota, and Tennessee had mortality increases of more than 100%; Mississippi’s 164.1% increase from 13.3 to 35.2 per 100,000 people was the greatest during the study period. Maine, Montana, and Maryland saw decreases in mortality, with the percentages falling 23.5%, 9.9%, and 6.1%, respectively.
“An increasing number of Alzheimer’s deaths coupled with an increasing number of patients dying at home suggests that there is an increasing number of caregivers of persons with Alzheimer’s. It is likely that these caregivers might benefit from interventions such as education, respite care, and case management that can lessen the potential burden of caregiving,” the CDC investigators concluded.
Find the full study in MMWR (2017;66[20]:521-6).
The rate of death attributable to Alzheimer’s disease increased by more than 50% from 1999 to 2014 in the United States, according to a report from the Centers for Disease Control and Prevention.
According to data collected from the National Vital Statistics System, the total number of Alzheimer’s deaths was 44,536 in 1999 and 93,541 in 2014. The mortality in 1999 was 16.5 per 100,000 people, and in 2014 it was 25.4 per 100,000 people, a rate increase of 54.5%. Alzheimer’s was the sixth most common cause of death in 2014, accounting for 3.6% of all U.S. deaths.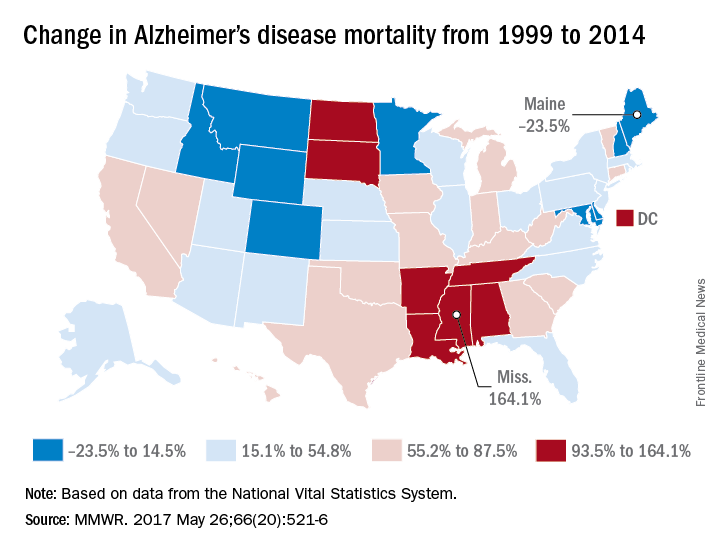
Mississippi, Louisiana, Arkansas, South Dakota, and Tennessee had mortality increases of more than 100%; Mississippi’s 164.1% increase from 13.3 to 35.2 per 100,000 people was the greatest during the study period. Maine, Montana, and Maryland saw decreases in mortality, with the percentages falling 23.5%, 9.9%, and 6.1%, respectively.
“An increasing number of Alzheimer’s deaths coupled with an increasing number of patients dying at home suggests that there is an increasing number of caregivers of persons with Alzheimer’s. It is likely that these caregivers might benefit from interventions such as education, respite care, and case management that can lessen the potential burden of caregiving,” the CDC investigators concluded.
Find the full study in MMWR (2017;66[20]:521-6).
The rate of death attributable to Alzheimer’s disease increased by more than 50% from 1999 to 2014 in the United States, according to a report from the Centers for Disease Control and Prevention.
According to data collected from the National Vital Statistics System, the total number of Alzheimer’s deaths was 44,536 in 1999 and 93,541 in 2014. The mortality in 1999 was 16.5 per 100,000 people, and in 2014 it was 25.4 per 100,000 people, a rate increase of 54.5%. Alzheimer’s was the sixth most common cause of death in 2014, accounting for 3.6% of all U.S. deaths.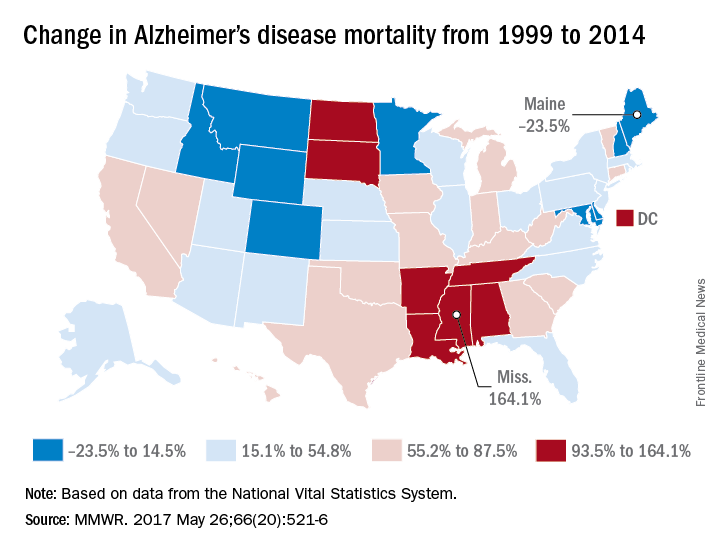
Mississippi, Louisiana, Arkansas, South Dakota, and Tennessee had mortality increases of more than 100%; Mississippi’s 164.1% increase from 13.3 to 35.2 per 100,000 people was the greatest during the study period. Maine, Montana, and Maryland saw decreases in mortality, with the percentages falling 23.5%, 9.9%, and 6.1%, respectively.
“An increasing number of Alzheimer’s deaths coupled with an increasing number of patients dying at home suggests that there is an increasing number of caregivers of persons with Alzheimer’s. It is likely that these caregivers might benefit from interventions such as education, respite care, and case management that can lessen the potential burden of caregiving,” the CDC investigators concluded.
Find the full study in MMWR (2017;66[20]:521-6).
FROM MMWR
My face is all red!
My grandson is almost 3. He is, of course, very advanced in many areas, including self-awareness.
At the moment he is suffering from Fifth Disease. (See how advanced he is – he skipped right over Diseases One through Four!) Every now and then his face clouds over as he announces, to anyone and no one, “My face is all red!”
I am not worried about long-term psychic harm. A moment later his face lights up as he looks up at the sky. “It’s a helicopter!” he declares.
By the way, does his behavior remind you of anyone else you’ve met? How about all your patients with rosacea or facial keratosis pilaris who stop by the office to say, “My face is all red!” If they didn’t notice this themselves, others have been happy to help. “You’re all red!” say their family, friends, and coworkers. “Are you all right?”
What about patients like those? Would you call them vain, or cosmetically oriented?
It seems to me that the behavior of little kids – too young to elaborate their psychological musings – sheds light on the way their elders behave, or the way they will themselves when they grow up. Years ago, I was about to laser the face of a woman with an old pulsed-dye unit that left deep-purple bruises. Her job was to train monkeys for the blind. “I need makeup,” she said. “When my monkeys see red spots on my face, they get very upset and start to point at me.”
“Not just monkeys,” I replied.
To take another example, many years ago I saw a little tyke about 18 months old. His parents were concerned about a mole on his palm.
He was not happy to let me examine him, and he let me know. “It’s OK,” I said, in my most condescending, clueless adult voice. “Your Mom and Dad just asked me to check your boo-boo.”
That set him off. “No boo-boo!” he shouted. “No boo-boo!”
Well, silly me, I later realized. The tyke was right: Of course it was not a boo-boo. A boo-boo is an assault on the integrity of the body: a cut, a scrape, a burn, something new, painful, hard to look at. That is why 9.8 out of 10 people whom we freeze, burn, or puncture look the other way while we do it. It’s also why kids dial their screams down to whimpers when we hide what we froze, burned, or punctured by covering it with a Band-Aid. Now the boo-boo is out of sight.
The tyke’s mole, on the other hand, is not an insult to the body but a part of it. It’s him.
Fast forward 15 years and ask a teen with a large (but not giant) hairy congenital nevus if she wants it off. She does not. “That’s me,” she explains.
Or ask an adult with what you would think is a disfiguring facial port-wine stain what growing up with that was like. “It was fine,” they reply. “Strangers sometimes commented, but my friends knew that was just how I looked.”
Or listen to folks who want their liver spots lasered off. They point to a dozen or so, then add, “But don’t take off that one! That’s always been there. That’s just me.”
If you listen for it, you can pick up how early a lot of adult behavior starts. Little ones destined to be lifetime pickers start scraping off anything that’s raised above the skin. Teens finicky about facial moles or minute perturbations in their complexion grow into fussy adults.
We grownups learn to embroider our primal responses with words, thoughts, feeling, explanations. Kids just come out and say what they think – “My face is all red!”
Soon my grandson will have overcome his Fifth Disease without, I hope, graduating to any higher numbers. His other grandfather is a retired engineer who used to design helicopters. By next year I expect that our mutual grandson will be able to identify anything flying overhead by make and model number.
As I said, he’s very advanced.
Also cute as all get-out, (temporary) red face and all.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected]
My grandson is almost 3. He is, of course, very advanced in many areas, including self-awareness.
At the moment he is suffering from Fifth Disease. (See how advanced he is – he skipped right over Diseases One through Four!) Every now and then his face clouds over as he announces, to anyone and no one, “My face is all red!”
I am not worried about long-term psychic harm. A moment later his face lights up as he looks up at the sky. “It’s a helicopter!” he declares.
By the way, does his behavior remind you of anyone else you’ve met? How about all your patients with rosacea or facial keratosis pilaris who stop by the office to say, “My face is all red!” If they didn’t notice this themselves, others have been happy to help. “You’re all red!” say their family, friends, and coworkers. “Are you all right?”
What about patients like those? Would you call them vain, or cosmetically oriented?
It seems to me that the behavior of little kids – too young to elaborate their psychological musings – sheds light on the way their elders behave, or the way they will themselves when they grow up. Years ago, I was about to laser the face of a woman with an old pulsed-dye unit that left deep-purple bruises. Her job was to train monkeys for the blind. “I need makeup,” she said. “When my monkeys see red spots on my face, they get very upset and start to point at me.”
“Not just monkeys,” I replied.
To take another example, many years ago I saw a little tyke about 18 months old. His parents were concerned about a mole on his palm.
He was not happy to let me examine him, and he let me know. “It’s OK,” I said, in my most condescending, clueless adult voice. “Your Mom and Dad just asked me to check your boo-boo.”
That set him off. “No boo-boo!” he shouted. “No boo-boo!”
Well, silly me, I later realized. The tyke was right: Of course it was not a boo-boo. A boo-boo is an assault on the integrity of the body: a cut, a scrape, a burn, something new, painful, hard to look at. That is why 9.8 out of 10 people whom we freeze, burn, or puncture look the other way while we do it. It’s also why kids dial their screams down to whimpers when we hide what we froze, burned, or punctured by covering it with a Band-Aid. Now the boo-boo is out of sight.
The tyke’s mole, on the other hand, is not an insult to the body but a part of it. It’s him.
Fast forward 15 years and ask a teen with a large (but not giant) hairy congenital nevus if she wants it off. She does not. “That’s me,” she explains.
Or ask an adult with what you would think is a disfiguring facial port-wine stain what growing up with that was like. “It was fine,” they reply. “Strangers sometimes commented, but my friends knew that was just how I looked.”
Or listen to folks who want their liver spots lasered off. They point to a dozen or so, then add, “But don’t take off that one! That’s always been there. That’s just me.”
If you listen for it, you can pick up how early a lot of adult behavior starts. Little ones destined to be lifetime pickers start scraping off anything that’s raised above the skin. Teens finicky about facial moles or minute perturbations in their complexion grow into fussy adults.
We grownups learn to embroider our primal responses with words, thoughts, feeling, explanations. Kids just come out and say what they think – “My face is all red!”
Soon my grandson will have overcome his Fifth Disease without, I hope, graduating to any higher numbers. His other grandfather is a retired engineer who used to design helicopters. By next year I expect that our mutual grandson will be able to identify anything flying overhead by make and model number.
As I said, he’s very advanced.
Also cute as all get-out, (temporary) red face and all.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected]
My grandson is almost 3. He is, of course, very advanced in many areas, including self-awareness.
At the moment he is suffering from Fifth Disease. (See how advanced he is – he skipped right over Diseases One through Four!) Every now and then his face clouds over as he announces, to anyone and no one, “My face is all red!”
I am not worried about long-term psychic harm. A moment later his face lights up as he looks up at the sky. “It’s a helicopter!” he declares.
By the way, does his behavior remind you of anyone else you’ve met? How about all your patients with rosacea or facial keratosis pilaris who stop by the office to say, “My face is all red!” If they didn’t notice this themselves, others have been happy to help. “You’re all red!” say their family, friends, and coworkers. “Are you all right?”
What about patients like those? Would you call them vain, or cosmetically oriented?
It seems to me that the behavior of little kids – too young to elaborate their psychological musings – sheds light on the way their elders behave, or the way they will themselves when they grow up. Years ago, I was about to laser the face of a woman with an old pulsed-dye unit that left deep-purple bruises. Her job was to train monkeys for the blind. “I need makeup,” she said. “When my monkeys see red spots on my face, they get very upset and start to point at me.”
“Not just monkeys,” I replied.
To take another example, many years ago I saw a little tyke about 18 months old. His parents were concerned about a mole on his palm.
He was not happy to let me examine him, and he let me know. “It’s OK,” I said, in my most condescending, clueless adult voice. “Your Mom and Dad just asked me to check your boo-boo.”
That set him off. “No boo-boo!” he shouted. “No boo-boo!”
Well, silly me, I later realized. The tyke was right: Of course it was not a boo-boo. A boo-boo is an assault on the integrity of the body: a cut, a scrape, a burn, something new, painful, hard to look at. That is why 9.8 out of 10 people whom we freeze, burn, or puncture look the other way while we do it. It’s also why kids dial their screams down to whimpers when we hide what we froze, burned, or punctured by covering it with a Band-Aid. Now the boo-boo is out of sight.
The tyke’s mole, on the other hand, is not an insult to the body but a part of it. It’s him.
Fast forward 15 years and ask a teen with a large (but not giant) hairy congenital nevus if she wants it off. She does not. “That’s me,” she explains.
Or ask an adult with what you would think is a disfiguring facial port-wine stain what growing up with that was like. “It was fine,” they reply. “Strangers sometimes commented, but my friends knew that was just how I looked.”
Or listen to folks who want their liver spots lasered off. They point to a dozen or so, then add, “But don’t take off that one! That’s always been there. That’s just me.”
If you listen for it, you can pick up how early a lot of adult behavior starts. Little ones destined to be lifetime pickers start scraping off anything that’s raised above the skin. Teens finicky about facial moles or minute perturbations in their complexion grow into fussy adults.
We grownups learn to embroider our primal responses with words, thoughts, feeling, explanations. Kids just come out and say what they think – “My face is all red!”
Soon my grandson will have overcome his Fifth Disease without, I hope, graduating to any higher numbers. His other grandfather is a retired engineer who used to design helicopters. By next year I expect that our mutual grandson will be able to identify anything flying overhead by make and model number.
As I said, he’s very advanced.
Also cute as all get-out, (temporary) red face and all.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected]
Recognizing and treating pediatric bug infestations
Pruritic bug infestations are a common problem among school-age children, Albert C. Yan, MD, said at a pediatric dermatology meeting sponsored by Rady Children’s Hospital-San Diego and UC San Diego School of Medicine.
– and it is essential for you to be able to recognize and treat these appropriately. You also need to know resistance patterns, and how to counsel patient on full treatment protocol.
Carpet beetle dermatitis presents in children with a history of spending lots of time on a carpet, presenting with nondescript itchy patches on skin areas that were in contact with the carpet. Carpet beetle dermatitis is becoming more common on the east coast. Patients can actually find these beetles, which have tiger-striped coloring and have little prickly hairs that stick out of them, in their carpets. The beetles do not bite; rather, the rash is a reaction from exposure to insect blood or the larval hairs. The adult beetles tend to feed on carpet fabrics, wool, grains of food products, animal material, or nectar and pollen in flowers. The treatment is to get rid of the beetles. To rid the house of the beetles, it is recommended to vacuum, remove contaminated food sources, freeze stuffed animals for 10-14 days, and have an exterminator visit the home. Bringing in fresh cut flowers from the garden without rinsing them may bring the beetles into the house.
Scabies tends to be an itchy, widespread dermatosis. It is associated with extensive small skin papules scattered across the body with linear or curvilinear burrows, and tends to present from the elbows or knees distally, and especially in webbed areas, such as between the fingers. Keeping these geographic locations in mind makes it easier to differentiate scabies from hand dermatitis and eczema, said Dr. Yan, chief of pediatric dermatology at Children’s Hospital of Philadelphia and professor of pediatrics and dermatology at the University of Pennsylvania, Philadelphia.
To help diagnose this infestation, scrape the lesion and visualize the mite, the scybala or mite feces, or the oval eggs under the microscope.
The treatment is a “permethrin party.” Luckily, the scabies mite has very little documented resistance to permethrin 5% cream. However, with recurrent treatment, resistance starts to develop, he said. Proper administration is critical in controlling the infestation. For an adult, use 3 ounces or one tube, and for a child, use about 1.5 ounces for a child or one-half a tube. Apply it to the skin from neck down, leave it on for 8 hours overnight. Treat the patient and family members or close contacts. Repeat this application in 1 week. Oral ivermectin is effective and is useful in older kids who may not adhere to the permethrin.
A commonly encountered problem is apparent treatment failure. The scabies may be identified, treated, and then they appear to recur. Some patients have persistent postscabetic itch – the patients are still itchy afterward, but the lesions look excoriated and different than the original scabies lesions. The patient does not need retreatment, Dr. Yan emphasized. Rather, use topical corticosteroids or antihistamines to treat the itch.
Another explanation is improper use of medication – for instance, only certain parts of the skin were treated or all family members had not been treated. In this case, everyone needs to be retreated, he said. Reinfection is possible, but resistance is unlikely. Patients with scabies sometimes develop scabetic nodules or hypersensitivity nodules. Often, these are leftover areas of inflammation that can remain for up to 1 year. Dr. Yan recommends treating these areas with low-dose topical steroids.
The last phenomena presents with recurrent crops of pustules in the acral area, which is acropustulosis of infancy or postscabetic pustulosis. This is a variant of acropustulosis of infancy, in that it is more likely to involve the torso than is traditional acropustulosis and tends to be cyclical in that it reappears every few weeks.
Recently, the Journal of Medical Entomology published study findings in which head lice genetics were assessed, raising the concern about the development of “super lice.” However, this information has not yet brought treatment changes.
The conventional treatments include Nix, Rid, Triple X, but there can be a fair amount of resistance with these OTC treatment. Other options include mayonnaise and olive oil, however, not much data support the efficacy of this treatment. There are three prescription medications available: benzyl alcohol lotion, spinosad topical suspension, and ivermectin lotion. Start with these treatments quickly when dealing with lice that are resistant. Oral ivermectin also is effective. Dr. Yan concluded his lecture with discussion of other techniques that have been Food and Drug Administration–cleared, such as blowing drying them off the head, if one is okay with them landing in the office!
Dr. Yan reported no relevant financial disclosures.
Pruritic bug infestations are a common problem among school-age children, Albert C. Yan, MD, said at a pediatric dermatology meeting sponsored by Rady Children’s Hospital-San Diego and UC San Diego School of Medicine.
– and it is essential for you to be able to recognize and treat these appropriately. You also need to know resistance patterns, and how to counsel patient on full treatment protocol.
Carpet beetle dermatitis presents in children with a history of spending lots of time on a carpet, presenting with nondescript itchy patches on skin areas that were in contact with the carpet. Carpet beetle dermatitis is becoming more common on the east coast. Patients can actually find these beetles, which have tiger-striped coloring and have little prickly hairs that stick out of them, in their carpets. The beetles do not bite; rather, the rash is a reaction from exposure to insect blood or the larval hairs. The adult beetles tend to feed on carpet fabrics, wool, grains of food products, animal material, or nectar and pollen in flowers. The treatment is to get rid of the beetles. To rid the house of the beetles, it is recommended to vacuum, remove contaminated food sources, freeze stuffed animals for 10-14 days, and have an exterminator visit the home. Bringing in fresh cut flowers from the garden without rinsing them may bring the beetles into the house.
Scabies tends to be an itchy, widespread dermatosis. It is associated with extensive small skin papules scattered across the body with linear or curvilinear burrows, and tends to present from the elbows or knees distally, and especially in webbed areas, such as between the fingers. Keeping these geographic locations in mind makes it easier to differentiate scabies from hand dermatitis and eczema, said Dr. Yan, chief of pediatric dermatology at Children’s Hospital of Philadelphia and professor of pediatrics and dermatology at the University of Pennsylvania, Philadelphia.
To help diagnose this infestation, scrape the lesion and visualize the mite, the scybala or mite feces, or the oval eggs under the microscope.
The treatment is a “permethrin party.” Luckily, the scabies mite has very little documented resistance to permethrin 5% cream. However, with recurrent treatment, resistance starts to develop, he said. Proper administration is critical in controlling the infestation. For an adult, use 3 ounces or one tube, and for a child, use about 1.5 ounces for a child or one-half a tube. Apply it to the skin from neck down, leave it on for 8 hours overnight. Treat the patient and family members or close contacts. Repeat this application in 1 week. Oral ivermectin is effective and is useful in older kids who may not adhere to the permethrin.
A commonly encountered problem is apparent treatment failure. The scabies may be identified, treated, and then they appear to recur. Some patients have persistent postscabetic itch – the patients are still itchy afterward, but the lesions look excoriated and different than the original scabies lesions. The patient does not need retreatment, Dr. Yan emphasized. Rather, use topical corticosteroids or antihistamines to treat the itch.
Another explanation is improper use of medication – for instance, only certain parts of the skin were treated or all family members had not been treated. In this case, everyone needs to be retreated, he said. Reinfection is possible, but resistance is unlikely. Patients with scabies sometimes develop scabetic nodules or hypersensitivity nodules. Often, these are leftover areas of inflammation that can remain for up to 1 year. Dr. Yan recommends treating these areas with low-dose topical steroids.
The last phenomena presents with recurrent crops of pustules in the acral area, which is acropustulosis of infancy or postscabetic pustulosis. This is a variant of acropustulosis of infancy, in that it is more likely to involve the torso than is traditional acropustulosis and tends to be cyclical in that it reappears every few weeks.
Recently, the Journal of Medical Entomology published study findings in which head lice genetics were assessed, raising the concern about the development of “super lice.” However, this information has not yet brought treatment changes.
The conventional treatments include Nix, Rid, Triple X, but there can be a fair amount of resistance with these OTC treatment. Other options include mayonnaise and olive oil, however, not much data support the efficacy of this treatment. There are three prescription medications available: benzyl alcohol lotion, spinosad topical suspension, and ivermectin lotion. Start with these treatments quickly when dealing with lice that are resistant. Oral ivermectin also is effective. Dr. Yan concluded his lecture with discussion of other techniques that have been Food and Drug Administration–cleared, such as blowing drying them off the head, if one is okay with them landing in the office!
Dr. Yan reported no relevant financial disclosures.
Pruritic bug infestations are a common problem among school-age children, Albert C. Yan, MD, said at a pediatric dermatology meeting sponsored by Rady Children’s Hospital-San Diego and UC San Diego School of Medicine.
– and it is essential for you to be able to recognize and treat these appropriately. You also need to know resistance patterns, and how to counsel patient on full treatment protocol.
Carpet beetle dermatitis presents in children with a history of spending lots of time on a carpet, presenting with nondescript itchy patches on skin areas that were in contact with the carpet. Carpet beetle dermatitis is becoming more common on the east coast. Patients can actually find these beetles, which have tiger-striped coloring and have little prickly hairs that stick out of them, in their carpets. The beetles do not bite; rather, the rash is a reaction from exposure to insect blood or the larval hairs. The adult beetles tend to feed on carpet fabrics, wool, grains of food products, animal material, or nectar and pollen in flowers. The treatment is to get rid of the beetles. To rid the house of the beetles, it is recommended to vacuum, remove contaminated food sources, freeze stuffed animals for 10-14 days, and have an exterminator visit the home. Bringing in fresh cut flowers from the garden without rinsing them may bring the beetles into the house.
Scabies tends to be an itchy, widespread dermatosis. It is associated with extensive small skin papules scattered across the body with linear or curvilinear burrows, and tends to present from the elbows or knees distally, and especially in webbed areas, such as between the fingers. Keeping these geographic locations in mind makes it easier to differentiate scabies from hand dermatitis and eczema, said Dr. Yan, chief of pediatric dermatology at Children’s Hospital of Philadelphia and professor of pediatrics and dermatology at the University of Pennsylvania, Philadelphia.
To help diagnose this infestation, scrape the lesion and visualize the mite, the scybala or mite feces, or the oval eggs under the microscope.
The treatment is a “permethrin party.” Luckily, the scabies mite has very little documented resistance to permethrin 5% cream. However, with recurrent treatment, resistance starts to develop, he said. Proper administration is critical in controlling the infestation. For an adult, use 3 ounces or one tube, and for a child, use about 1.5 ounces for a child or one-half a tube. Apply it to the skin from neck down, leave it on for 8 hours overnight. Treat the patient and family members or close contacts. Repeat this application in 1 week. Oral ivermectin is effective and is useful in older kids who may not adhere to the permethrin.
A commonly encountered problem is apparent treatment failure. The scabies may be identified, treated, and then they appear to recur. Some patients have persistent postscabetic itch – the patients are still itchy afterward, but the lesions look excoriated and different than the original scabies lesions. The patient does not need retreatment, Dr. Yan emphasized. Rather, use topical corticosteroids or antihistamines to treat the itch.
Another explanation is improper use of medication – for instance, only certain parts of the skin were treated or all family members had not been treated. In this case, everyone needs to be retreated, he said. Reinfection is possible, but resistance is unlikely. Patients with scabies sometimes develop scabetic nodules or hypersensitivity nodules. Often, these are leftover areas of inflammation that can remain for up to 1 year. Dr. Yan recommends treating these areas with low-dose topical steroids.
The last phenomena presents with recurrent crops of pustules in the acral area, which is acropustulosis of infancy or postscabetic pustulosis. This is a variant of acropustulosis of infancy, in that it is more likely to involve the torso than is traditional acropustulosis and tends to be cyclical in that it reappears every few weeks.
Recently, the Journal of Medical Entomology published study findings in which head lice genetics were assessed, raising the concern about the development of “super lice.” However, this information has not yet brought treatment changes.
The conventional treatments include Nix, Rid, Triple X, but there can be a fair amount of resistance with these OTC treatment. Other options include mayonnaise and olive oil, however, not much data support the efficacy of this treatment. There are three prescription medications available: benzyl alcohol lotion, spinosad topical suspension, and ivermectin lotion. Start with these treatments quickly when dealing with lice that are resistant. Oral ivermectin also is effective. Dr. Yan concluded his lecture with discussion of other techniques that have been Food and Drug Administration–cleared, such as blowing drying them off the head, if one is okay with them landing in the office!
Dr. Yan reported no relevant financial disclosures.
Pooled Data Show Benefits of Cladribine Tablets on Relapse Rates and Disability Progression in Patients With MS
NEW ORLEANS—Analysis of pooled data from the CLARITY and ONWARD studies showed that cladribine tablets 3.5 mg/kg decreased annualized relapse rate by 57% and reduced the risk for six-month confirmed disability progression by 39% versus placebo in a population of patients with active relapsing multiple sclerosis (MS). These findings were presented at the 31st Annual Meeting of the Consortium of MS Centers.
Treatment with cladribine tablets in the CLARITY and ONWARD studies demonstrated efficacy versus placebo across a range of patients with active MS. “Combining efficacy data from the double-blind periods of these studies allows assessment of the efficacy of two years’ treatment with cladribine tablets 3.5 mg/kg,” said Gavin Giovannoni, MBBCh, PhD, on behalf of his research colleagues. Dr. Giovannoni is a Professor at the Blizard Institute at Barts and the London School of Medicine and Dentistry in London.
Dr. Giovannoni and colleagues used pooled data from the two-year, double-blind periods of CLARITY and ONWARD to analyze the efficacy of cladribine tablets 3.5 mg/kg in patients with relapsing MS (n = 1,067) and in subgroups defined by baseline characteristics. Patients from ONWARD on cladribine tablets or placebo were also taking interferon beta. Annualized relapse rates and three-month and six-month confirmed disability progression were compared using relative risk ratios from a Poisson regression model, hazard ratios from a Cox proportional hazard model, and 95% confidence intervals for patients treated with cladribine tablets 3.5 mg/kg or placebo. The subgroups analyzed included, among others, patients with no T1 gadolinium-enhancing lesions (n = 759) or one or more T1 gadolinium-enhancing lesions (n = 308) and patients with an Expanded Disability Status Scale (EDSS) score of 3.0 or lower (n = 653) or 3.5 or greater (n = 414).
For annualized relapse rate, consistent benefits were seen with cladribine tablets 3.5 mg/kg versus placebo in the overall population (relative risk ratio: 0.43) and in the subgroups: no T1 gadolinium-enhancing lesions, 0.46; one or more T1 gadolinium-enhancing lesions, 0.38; EDSS of 3.0 or lower, 0.40; EDSS of 3.5 or greater, 0.47. Benefits favored cladribine tablets 3.5 mg/kg versus placebo in the overall population for time to three-month confirmed disability progression (hazard ratio: 0.64) and six-month confirmed disability progression (hazard ratio: 0.61) and in each of these outcomes in a majority of subgroups. For three-month confirmed disability progression: no T1 gadolinium-enhancing lesions, hazard ratio: 0.59; one or more T1 gadolinium-enhancing lesions, hazard ratio: 0.75; EDSS of 3.0 or lower, hazard ratio: 0.76; EDSS of 3.5 or greater, hazard ratio: 0.55. For six-month confirmed disability progression: no T1 gadolinium-enhancing lesions, hazard ratio: 0.59; one or more T1 gadolinium-enhancing lesions, hazard ratio: 0.66; EDSS of 3.0 or lower, hazard ratio: 0.75; EDSS of 3.5 or greater, hazard ratio: 0.51.
This study was supported by EMD Serono.
NEW ORLEANS—Analysis of pooled data from the CLARITY and ONWARD studies showed that cladribine tablets 3.5 mg/kg decreased annualized relapse rate by 57% and reduced the risk for six-month confirmed disability progression by 39% versus placebo in a population of patients with active relapsing multiple sclerosis (MS). These findings were presented at the 31st Annual Meeting of the Consortium of MS Centers.
Treatment with cladribine tablets in the CLARITY and ONWARD studies demonstrated efficacy versus placebo across a range of patients with active MS. “Combining efficacy data from the double-blind periods of these studies allows assessment of the efficacy of two years’ treatment with cladribine tablets 3.5 mg/kg,” said Gavin Giovannoni, MBBCh, PhD, on behalf of his research colleagues. Dr. Giovannoni is a Professor at the Blizard Institute at Barts and the London School of Medicine and Dentistry in London.
Dr. Giovannoni and colleagues used pooled data from the two-year, double-blind periods of CLARITY and ONWARD to analyze the efficacy of cladribine tablets 3.5 mg/kg in patients with relapsing MS (n = 1,067) and in subgroups defined by baseline characteristics. Patients from ONWARD on cladribine tablets or placebo were also taking interferon beta. Annualized relapse rates and three-month and six-month confirmed disability progression were compared using relative risk ratios from a Poisson regression model, hazard ratios from a Cox proportional hazard model, and 95% confidence intervals for patients treated with cladribine tablets 3.5 mg/kg or placebo. The subgroups analyzed included, among others, patients with no T1 gadolinium-enhancing lesions (n = 759) or one or more T1 gadolinium-enhancing lesions (n = 308) and patients with an Expanded Disability Status Scale (EDSS) score of 3.0 or lower (n = 653) or 3.5 or greater (n = 414).
For annualized relapse rate, consistent benefits were seen with cladribine tablets 3.5 mg/kg versus placebo in the overall population (relative risk ratio: 0.43) and in the subgroups: no T1 gadolinium-enhancing lesions, 0.46; one or more T1 gadolinium-enhancing lesions, 0.38; EDSS of 3.0 or lower, 0.40; EDSS of 3.5 or greater, 0.47. Benefits favored cladribine tablets 3.5 mg/kg versus placebo in the overall population for time to three-month confirmed disability progression (hazard ratio: 0.64) and six-month confirmed disability progression (hazard ratio: 0.61) and in each of these outcomes in a majority of subgroups. For three-month confirmed disability progression: no T1 gadolinium-enhancing lesions, hazard ratio: 0.59; one or more T1 gadolinium-enhancing lesions, hazard ratio: 0.75; EDSS of 3.0 or lower, hazard ratio: 0.76; EDSS of 3.5 or greater, hazard ratio: 0.55. For six-month confirmed disability progression: no T1 gadolinium-enhancing lesions, hazard ratio: 0.59; one or more T1 gadolinium-enhancing lesions, hazard ratio: 0.66; EDSS of 3.0 or lower, hazard ratio: 0.75; EDSS of 3.5 or greater, hazard ratio: 0.51.
This study was supported by EMD Serono.
NEW ORLEANS—Analysis of pooled data from the CLARITY and ONWARD studies showed that cladribine tablets 3.5 mg/kg decreased annualized relapse rate by 57% and reduced the risk for six-month confirmed disability progression by 39% versus placebo in a population of patients with active relapsing multiple sclerosis (MS). These findings were presented at the 31st Annual Meeting of the Consortium of MS Centers.
Treatment with cladribine tablets in the CLARITY and ONWARD studies demonstrated efficacy versus placebo across a range of patients with active MS. “Combining efficacy data from the double-blind periods of these studies allows assessment of the efficacy of two years’ treatment with cladribine tablets 3.5 mg/kg,” said Gavin Giovannoni, MBBCh, PhD, on behalf of his research colleagues. Dr. Giovannoni is a Professor at the Blizard Institute at Barts and the London School of Medicine and Dentistry in London.
Dr. Giovannoni and colleagues used pooled data from the two-year, double-blind periods of CLARITY and ONWARD to analyze the efficacy of cladribine tablets 3.5 mg/kg in patients with relapsing MS (n = 1,067) and in subgroups defined by baseline characteristics. Patients from ONWARD on cladribine tablets or placebo were also taking interferon beta. Annualized relapse rates and three-month and six-month confirmed disability progression were compared using relative risk ratios from a Poisson regression model, hazard ratios from a Cox proportional hazard model, and 95% confidence intervals for patients treated with cladribine tablets 3.5 mg/kg or placebo. The subgroups analyzed included, among others, patients with no T1 gadolinium-enhancing lesions (n = 759) or one or more T1 gadolinium-enhancing lesions (n = 308) and patients with an Expanded Disability Status Scale (EDSS) score of 3.0 or lower (n = 653) or 3.5 or greater (n = 414).
For annualized relapse rate, consistent benefits were seen with cladribine tablets 3.5 mg/kg versus placebo in the overall population (relative risk ratio: 0.43) and in the subgroups: no T1 gadolinium-enhancing lesions, 0.46; one or more T1 gadolinium-enhancing lesions, 0.38; EDSS of 3.0 or lower, 0.40; EDSS of 3.5 or greater, 0.47. Benefits favored cladribine tablets 3.5 mg/kg versus placebo in the overall population for time to three-month confirmed disability progression (hazard ratio: 0.64) and six-month confirmed disability progression (hazard ratio: 0.61) and in each of these outcomes in a majority of subgroups. For three-month confirmed disability progression: no T1 gadolinium-enhancing lesions, hazard ratio: 0.59; one or more T1 gadolinium-enhancing lesions, hazard ratio: 0.75; EDSS of 3.0 or lower, hazard ratio: 0.76; EDSS of 3.5 or greater, hazard ratio: 0.55. For six-month confirmed disability progression: no T1 gadolinium-enhancing lesions, hazard ratio: 0.59; one or more T1 gadolinium-enhancing lesions, hazard ratio: 0.66; EDSS of 3.0 or lower, hazard ratio: 0.75; EDSS of 3.5 or greater, hazard ratio: 0.51.
This study was supported by EMD Serono.
Preliminary Results Suggest Ublituximab Is Safe in Relapsing Multiple Sclerosis
NEW ORLEANS—Ublituximab, a novel glycoengineered anti-CD20 antibody, is well tolerated and demonstrates rapid and robust B-cell depletion, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “Unlike other anti-CD20s, ublituximab can be delivered in shorter infusions, providing a convenience benefit for patients,” reported Amy Lovett-Racke, PhD, and her research colleagues. Dr. Lovett-Racke is a Professor in the Department of Microbial Infection and Immunity at Ohio State University Medical Center in Columbus.
Patients with relapsing or primary progressive forms of multiple sclerosis (MS) have shown significant clinical improvement after B-cell depletion with an anti-CD20 antibody. Ublituximab is a chimeric monoclonal antibody that targets a unique epitope on the CD20 antigen. It has been glycoengineered to enhance affinity for all variants of FcgRIIIa receptors, demonstrating greater antibody-dependent cellular cytotoxicity (ADCC) activity than rituximab. Ublituximab is currently in phase III trials for the treatment of hematologic malignancies.
To determine the level of B-cell depletion by ublituximab in subjects with relapsing MS, Dr. Lovett-Racke and colleagues conducted a 52-week, phase II, placebo-controlled, multicenter study that was designed to assess the infusion time and optimal dose as well as the safety and tolerability of ublituximab in patients with relapsing MS. The investigators also performed radiologic and clinical analyses. Optimal dosing was determined by B-cell depletion, defined as percentage of CD19+ B cells present following ublituximab administration. This percentage was calculated by gating the entire lymphocyte/myeloid population. Within this population, CD19+ CD3− cells were gated, and the percentage of CD19+ B cells was determined.
To date, B-cell data from 11 subjects have been analyzed up to week four of the 52-week study, encompassing two infusions of ublituximab. No severe adverse events have been reported, including in subjects receiving rapid infusions. Only patients whose B-cell levels were within a normal range (≥ 5% of total lymphocytes) at screening were included in the study. At week four (one week post second infusion), median B-cell depletion was 99% from baseline in ublituximab-treated subjects, while controls maintained similar B-cell levels, as compared with baseline.
This study was supported by TG Therapeutics.
NEW ORLEANS—Ublituximab, a novel glycoengineered anti-CD20 antibody, is well tolerated and demonstrates rapid and robust B-cell depletion, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “Unlike other anti-CD20s, ublituximab can be delivered in shorter infusions, providing a convenience benefit for patients,” reported Amy Lovett-Racke, PhD, and her research colleagues. Dr. Lovett-Racke is a Professor in the Department of Microbial Infection and Immunity at Ohio State University Medical Center in Columbus.
Patients with relapsing or primary progressive forms of multiple sclerosis (MS) have shown significant clinical improvement after B-cell depletion with an anti-CD20 antibody. Ublituximab is a chimeric monoclonal antibody that targets a unique epitope on the CD20 antigen. It has been glycoengineered to enhance affinity for all variants of FcgRIIIa receptors, demonstrating greater antibody-dependent cellular cytotoxicity (ADCC) activity than rituximab. Ublituximab is currently in phase III trials for the treatment of hematologic malignancies.
To determine the level of B-cell depletion by ublituximab in subjects with relapsing MS, Dr. Lovett-Racke and colleagues conducted a 52-week, phase II, placebo-controlled, multicenter study that was designed to assess the infusion time and optimal dose as well as the safety and tolerability of ublituximab in patients with relapsing MS. The investigators also performed radiologic and clinical analyses. Optimal dosing was determined by B-cell depletion, defined as percentage of CD19+ B cells present following ublituximab administration. This percentage was calculated by gating the entire lymphocyte/myeloid population. Within this population, CD19+ CD3− cells were gated, and the percentage of CD19+ B cells was determined.
To date, B-cell data from 11 subjects have been analyzed up to week four of the 52-week study, encompassing two infusions of ublituximab. No severe adverse events have been reported, including in subjects receiving rapid infusions. Only patients whose B-cell levels were within a normal range (≥ 5% of total lymphocytes) at screening were included in the study. At week four (one week post second infusion), median B-cell depletion was 99% from baseline in ublituximab-treated subjects, while controls maintained similar B-cell levels, as compared with baseline.
This study was supported by TG Therapeutics.
NEW ORLEANS—Ublituximab, a novel glycoengineered anti-CD20 antibody, is well tolerated and demonstrates rapid and robust B-cell depletion, according to a report presented at the 31st Annual Meeting of the Consortium of Multiple Sclerosis Centers. “Unlike other anti-CD20s, ublituximab can be delivered in shorter infusions, providing a convenience benefit for patients,” reported Amy Lovett-Racke, PhD, and her research colleagues. Dr. Lovett-Racke is a Professor in the Department of Microbial Infection and Immunity at Ohio State University Medical Center in Columbus.
Patients with relapsing or primary progressive forms of multiple sclerosis (MS) have shown significant clinical improvement after B-cell depletion with an anti-CD20 antibody. Ublituximab is a chimeric monoclonal antibody that targets a unique epitope on the CD20 antigen. It has been glycoengineered to enhance affinity for all variants of FcgRIIIa receptors, demonstrating greater antibody-dependent cellular cytotoxicity (ADCC) activity than rituximab. Ublituximab is currently in phase III trials for the treatment of hematologic malignancies.
To determine the level of B-cell depletion by ublituximab in subjects with relapsing MS, Dr. Lovett-Racke and colleagues conducted a 52-week, phase II, placebo-controlled, multicenter study that was designed to assess the infusion time and optimal dose as well as the safety and tolerability of ublituximab in patients with relapsing MS. The investigators also performed radiologic and clinical analyses. Optimal dosing was determined by B-cell depletion, defined as percentage of CD19+ B cells present following ublituximab administration. This percentage was calculated by gating the entire lymphocyte/myeloid population. Within this population, CD19+ CD3− cells were gated, and the percentage of CD19+ B cells was determined.
To date, B-cell data from 11 subjects have been analyzed up to week four of the 52-week study, encompassing two infusions of ublituximab. No severe adverse events have been reported, including in subjects receiving rapid infusions. Only patients whose B-cell levels were within a normal range (≥ 5% of total lymphocytes) at screening were included in the study. At week four (one week post second infusion), median B-cell depletion was 99% from baseline in ublituximab-treated subjects, while controls maintained similar B-cell levels, as compared with baseline.
This study was supported by TG Therapeutics.
Five year survival doubles for younger women with de novo MBC
Nearly 155,000 women in the United States are living with metastatic breast cancer (MBC), three-fourths of whom were initially diagnosed with lower-stage disease that progressed to stage IV, based on estimated prevalence data.
The estimates, derived from national breast cancer mortality and survival data, also show positive trends in breast cancer care, especially a doubling of 5-year survival rates among younger women diagnosed with de novo metastatic disease from the 1990s to the 2000s, reported Angela B. Mariotto, PhD, of the National Cancer Institute and her colleagues.
“Despite the progressive and incurable nature of almost all MBC, median survival after diagnosis with metastatic disease has been increasing, resulting in a growing number of women living with MBC in the United States. The increased survival is especially noted for women diagnosed at younger ages,” they wrote in Cancer Epidemiology, Biomarkers, & Prevention (2017 May 18. doi: 10.1158/1055-9965.epi-16-088).
Patients with advanced breast cancer require extensive care and intensive use of medical and other resources, but, until this study, there were no reliable estimates of the number of women actually living with metastatic disease in the United States, the authors said.
To get a clearer picture of the prevalence of advanced breast cancer in the United States, they worked backward from Surveillance, Epidemiology, and End Results data on breast cancer deaths and survival, working on the assumption that each observed breast cancer death is the result of metastatic disease, either in women whose initial diagnosis was stage IV disease (de novo metastatic disease) or disease recurrence with metastases.
They estimated that, in 2013, the most recent year for which there were observed data, the prevalence of metastatic breast cancer was 138,622, and that 38,897 (28%) of survivors were diagnosed with metastatic disease. The remaining 99,725 survivors (72%) were women who were initially diagnosed with stage I-III disease that either recurred or metastasized.
The authors calculated that 50,344 women were diagnosed with de novo metastatic disease in 2013, 12,966 of whom (26%) had de novo metastatic breast cancer and 37,378 of whom had recurrent disease. They projected that, as of Jan. 1, 2017, there are 154,794 women living with metastatic breast cancer in the United States.
They also estimated changes over time in survival and found that, for women diagnosed from the ages of 15 to 49 during the 1992-1994 surveillance period, median survival time was 22.3 months, which improved to 38.7 months during the 2005-2012 surveillance period. The respective survival times for women 50-64 years were 19.1 months and 29.7 months.
For women 15-49 years who were diagnosed with de novo metastatic breast cancer, the 5-year relative survival rates doubled from 18% during 1992-1994 to 36% during 2005-2012.
“Despite a poor prognosis, there is a small but meaningful percentage of these cases who survive 10 years or more. More than 11% of women diagnosed between 2000-2004 under the age of 64 years survived 10 years or more. Younger women diagnosed with de novo MBC have higher survival than women diagnosed at older ages,” Dr. Mariotto and her colleagues wrote.
The investigators pointed to the population size, population-based data, long follow-up, and use of consistent staging definitions over time as study strengths but acknowledged that the study was limited by the absence of population-based estimates of survival following recurrence of metastatic breast cancer.
“To our knowledge, this is the first time that the number of women living with MBC in the United States has been estimated. These estimates provide a new perspective on the population burden of breast cancer and have great potential significance to the research and advocacy community working on behalf of patients with MBC and their families,” the authors wrote.
The study was supported by the National Cancer Institute. The authors reported no relevant financial disclosures.
This article was updated June 5, 2017.
Nearly 155,000 women in the United States are living with metastatic breast cancer (MBC), three-fourths of whom were initially diagnosed with lower-stage disease that progressed to stage IV, based on estimated prevalence data.
The estimates, derived from national breast cancer mortality and survival data, also show positive trends in breast cancer care, especially a doubling of 5-year survival rates among younger women diagnosed with de novo metastatic disease from the 1990s to the 2000s, reported Angela B. Mariotto, PhD, of the National Cancer Institute and her colleagues.
“Despite the progressive and incurable nature of almost all MBC, median survival after diagnosis with metastatic disease has been increasing, resulting in a growing number of women living with MBC in the United States. The increased survival is especially noted for women diagnosed at younger ages,” they wrote in Cancer Epidemiology, Biomarkers, & Prevention (2017 May 18. doi: 10.1158/1055-9965.epi-16-088).
Patients with advanced breast cancer require extensive care and intensive use of medical and other resources, but, until this study, there were no reliable estimates of the number of women actually living with metastatic disease in the United States, the authors said.
To get a clearer picture of the prevalence of advanced breast cancer in the United States, they worked backward from Surveillance, Epidemiology, and End Results data on breast cancer deaths and survival, working on the assumption that each observed breast cancer death is the result of metastatic disease, either in women whose initial diagnosis was stage IV disease (de novo metastatic disease) or disease recurrence with metastases.
They estimated that, in 2013, the most recent year for which there were observed data, the prevalence of metastatic breast cancer was 138,622, and that 38,897 (28%) of survivors were diagnosed with metastatic disease. The remaining 99,725 survivors (72%) were women who were initially diagnosed with stage I-III disease that either recurred or metastasized.
The authors calculated that 50,344 women were diagnosed with de novo metastatic disease in 2013, 12,966 of whom (26%) had de novo metastatic breast cancer and 37,378 of whom had recurrent disease. They projected that, as of Jan. 1, 2017, there are 154,794 women living with metastatic breast cancer in the United States.
They also estimated changes over time in survival and found that, for women diagnosed from the ages of 15 to 49 during the 1992-1994 surveillance period, median survival time was 22.3 months, which improved to 38.7 months during the 2005-2012 surveillance period. The respective survival times for women 50-64 years were 19.1 months and 29.7 months.
For women 15-49 years who were diagnosed with de novo metastatic breast cancer, the 5-year relative survival rates doubled from 18% during 1992-1994 to 36% during 2005-2012.
“Despite a poor prognosis, there is a small but meaningful percentage of these cases who survive 10 years or more. More than 11% of women diagnosed between 2000-2004 under the age of 64 years survived 10 years or more. Younger women diagnosed with de novo MBC have higher survival than women diagnosed at older ages,” Dr. Mariotto and her colleagues wrote.
The investigators pointed to the population size, population-based data, long follow-up, and use of consistent staging definitions over time as study strengths but acknowledged that the study was limited by the absence of population-based estimates of survival following recurrence of metastatic breast cancer.
“To our knowledge, this is the first time that the number of women living with MBC in the United States has been estimated. These estimates provide a new perspective on the population burden of breast cancer and have great potential significance to the research and advocacy community working on behalf of patients with MBC and their families,” the authors wrote.
The study was supported by the National Cancer Institute. The authors reported no relevant financial disclosures.
This article was updated June 5, 2017.
Nearly 155,000 women in the United States are living with metastatic breast cancer (MBC), three-fourths of whom were initially diagnosed with lower-stage disease that progressed to stage IV, based on estimated prevalence data.
The estimates, derived from national breast cancer mortality and survival data, also show positive trends in breast cancer care, especially a doubling of 5-year survival rates among younger women diagnosed with de novo metastatic disease from the 1990s to the 2000s, reported Angela B. Mariotto, PhD, of the National Cancer Institute and her colleagues.
“Despite the progressive and incurable nature of almost all MBC, median survival after diagnosis with metastatic disease has been increasing, resulting in a growing number of women living with MBC in the United States. The increased survival is especially noted for women diagnosed at younger ages,” they wrote in Cancer Epidemiology, Biomarkers, & Prevention (2017 May 18. doi: 10.1158/1055-9965.epi-16-088).
Patients with advanced breast cancer require extensive care and intensive use of medical and other resources, but, until this study, there were no reliable estimates of the number of women actually living with metastatic disease in the United States, the authors said.
To get a clearer picture of the prevalence of advanced breast cancer in the United States, they worked backward from Surveillance, Epidemiology, and End Results data on breast cancer deaths and survival, working on the assumption that each observed breast cancer death is the result of metastatic disease, either in women whose initial diagnosis was stage IV disease (de novo metastatic disease) or disease recurrence with metastases.
They estimated that, in 2013, the most recent year for which there were observed data, the prevalence of metastatic breast cancer was 138,622, and that 38,897 (28%) of survivors were diagnosed with metastatic disease. The remaining 99,725 survivors (72%) were women who were initially diagnosed with stage I-III disease that either recurred or metastasized.
The authors calculated that 50,344 women were diagnosed with de novo metastatic disease in 2013, 12,966 of whom (26%) had de novo metastatic breast cancer and 37,378 of whom had recurrent disease. They projected that, as of Jan. 1, 2017, there are 154,794 women living with metastatic breast cancer in the United States.
They also estimated changes over time in survival and found that, for women diagnosed from the ages of 15 to 49 during the 1992-1994 surveillance period, median survival time was 22.3 months, which improved to 38.7 months during the 2005-2012 surveillance period. The respective survival times for women 50-64 years were 19.1 months and 29.7 months.
For women 15-49 years who were diagnosed with de novo metastatic breast cancer, the 5-year relative survival rates doubled from 18% during 1992-1994 to 36% during 2005-2012.
“Despite a poor prognosis, there is a small but meaningful percentage of these cases who survive 10 years or more. More than 11% of women diagnosed between 2000-2004 under the age of 64 years survived 10 years or more. Younger women diagnosed with de novo MBC have higher survival than women diagnosed at older ages,” Dr. Mariotto and her colleagues wrote.
The investigators pointed to the population size, population-based data, long follow-up, and use of consistent staging definitions over time as study strengths but acknowledged that the study was limited by the absence of population-based estimates of survival following recurrence of metastatic breast cancer.
“To our knowledge, this is the first time that the number of women living with MBC in the United States has been estimated. These estimates provide a new perspective on the population burden of breast cancer and have great potential significance to the research and advocacy community working on behalf of patients with MBC and their families,” the authors wrote.
The study was supported by the National Cancer Institute. The authors reported no relevant financial disclosures.
This article was updated June 5, 2017.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS & PREVENTION
Key clinical point: An estimated 155,000 women are living with metastatic breast cancer in the United States.
Major finding: Among women diagnosed from ages 15 to 49 with de novo metastatic breast cancer, the 5-year relative survival doubled from 18% during 1992-1994 to 36% during 2005-2012.
Data source: An epidemiologic estimate of metastatic breast cancer prevalence in the United States using SEER data.
Disclosures: The study was supported by the National Cancer Institute. The authors reported no relevant financial disclosures.
















