User login
Experts endorse routine screening for pediatric psoriasis comorbidities
Pediatric psoriasis patients should be screened regularly to identify risk factors for comorbidities including depression, gastrointestinal problems, diabetes, and dyslipidemia, according to the debut guidelines issued by an expert panel.
The National Psoriasis Foundation and the Pediatric Dermatology Research Alliance joined forces to assess the literature and develop recommendations for screening comorbidities for children with psoriasis. The National Psoriasis Foundation has guidelines for comorbidity screening in adults with psoriasis, but no guidelines previously existed for children, wrote Emily Osier, MD, of Eastern Virginia Medical School, Norfolk, and her colleagues (JAMA Dermatol 2017 May 17. doi: 10.1001/jamadermatol.2017.0499).
The panelists reviewed the literature on psoriasis and comorbidities published between 1999 and 2015 and identified 153 studies, 26 of which involved children.
“The screening recommendations derived are largely consistent with those endorsed by the AAP for the general pediatric patient,” the researchers noted.
Although many young children are screened for a range of comorbid conditions at annual checkups, preteens and teenagers may be less likely to receive preventive services in primary care, they said. “Thus, all health care providers caring for patients with pediatric psoriasis should help assess and ensure that appropriate screening has been performed,” they emphasized.
Some notable recommendations include the following:
• Screen children with psoriasis for overweight and obesity annually using body mass index percentiles.
• Screen for diabetes every 3 years starting at age 10 years.
• Perform universal lipid screening at ages 9-11 years and 17-21 years.
• Screen for nonalcoholic fatty liver disease every 2-3 years starting at age 9-11 years.
• Screen for hypertension annually starting at age 3 years.
• Screen for arthritis at the time of psoriasis diagnosis and periodically.
• Screen yearly for depression and anxiety at all ages, with yearly screening for substance abuse starting at age 11 years.
Uveitis screening is recommended only for children with psoriatic arthritis, the researchers said.
In addition, clinicians “should recognize the profound psychosocial ramifications of psoriasis and the potential significant impact on quality of life of patients and caregivers,” the researchers wrote. Clinicians may consider a formal quality of life measurement, such as the Children’s Dermatology Life Quality Index, or at least asking questions about the impact of psoriasis on the child’s life at home, at school, and during other activities.
Awareness of comorbidities also impacts potential psoriasis treatment, the researchers said. “Direct baseline screening and monitoring tests should be performed as indicated by each individual’s therapeutic plan,” they said.
The consensus statement is a starting point for screening that will be refined over time, and may include stratifying patients by age, disease subtype, or disease severity, the researchers noted.
“Communication and collaboration between dermatologists, primary care providers, and other pediatric specialists will be critical to accomplish the recommended screenings and to limit the sequelae of this disorder,” they wrote.
The National Psoriasis Foundation and the University of California, San Diego, Eczema and Inflammatory Skin Disease Center supported the study. Dr. Osier was supported in part by a Medical Dermatology Research Fellowship grant from the National Psoriasis Foundation in 2014-2016, but she had no financial conflicts to disclose.
Pediatric psoriasis patients should be screened regularly to identify risk factors for comorbidities including depression, gastrointestinal problems, diabetes, and dyslipidemia, according to the debut guidelines issued by an expert panel.
The National Psoriasis Foundation and the Pediatric Dermatology Research Alliance joined forces to assess the literature and develop recommendations for screening comorbidities for children with psoriasis. The National Psoriasis Foundation has guidelines for comorbidity screening in adults with psoriasis, but no guidelines previously existed for children, wrote Emily Osier, MD, of Eastern Virginia Medical School, Norfolk, and her colleagues (JAMA Dermatol 2017 May 17. doi: 10.1001/jamadermatol.2017.0499).
The panelists reviewed the literature on psoriasis and comorbidities published between 1999 and 2015 and identified 153 studies, 26 of which involved children.
“The screening recommendations derived are largely consistent with those endorsed by the AAP for the general pediatric patient,” the researchers noted.
Although many young children are screened for a range of comorbid conditions at annual checkups, preteens and teenagers may be less likely to receive preventive services in primary care, they said. “Thus, all health care providers caring for patients with pediatric psoriasis should help assess and ensure that appropriate screening has been performed,” they emphasized.
Some notable recommendations include the following:
• Screen children with psoriasis for overweight and obesity annually using body mass index percentiles.
• Screen for diabetes every 3 years starting at age 10 years.
• Perform universal lipid screening at ages 9-11 years and 17-21 years.
• Screen for nonalcoholic fatty liver disease every 2-3 years starting at age 9-11 years.
• Screen for hypertension annually starting at age 3 years.
• Screen for arthritis at the time of psoriasis diagnosis and periodically.
• Screen yearly for depression and anxiety at all ages, with yearly screening for substance abuse starting at age 11 years.
Uveitis screening is recommended only for children with psoriatic arthritis, the researchers said.
In addition, clinicians “should recognize the profound psychosocial ramifications of psoriasis and the potential significant impact on quality of life of patients and caregivers,” the researchers wrote. Clinicians may consider a formal quality of life measurement, such as the Children’s Dermatology Life Quality Index, or at least asking questions about the impact of psoriasis on the child’s life at home, at school, and during other activities.
Awareness of comorbidities also impacts potential psoriasis treatment, the researchers said. “Direct baseline screening and monitoring tests should be performed as indicated by each individual’s therapeutic plan,” they said.
The consensus statement is a starting point for screening that will be refined over time, and may include stratifying patients by age, disease subtype, or disease severity, the researchers noted.
“Communication and collaboration between dermatologists, primary care providers, and other pediatric specialists will be critical to accomplish the recommended screenings and to limit the sequelae of this disorder,” they wrote.
The National Psoriasis Foundation and the University of California, San Diego, Eczema and Inflammatory Skin Disease Center supported the study. Dr. Osier was supported in part by a Medical Dermatology Research Fellowship grant from the National Psoriasis Foundation in 2014-2016, but she had no financial conflicts to disclose.
Pediatric psoriasis patients should be screened regularly to identify risk factors for comorbidities including depression, gastrointestinal problems, diabetes, and dyslipidemia, according to the debut guidelines issued by an expert panel.
The National Psoriasis Foundation and the Pediatric Dermatology Research Alliance joined forces to assess the literature and develop recommendations for screening comorbidities for children with psoriasis. The National Psoriasis Foundation has guidelines for comorbidity screening in adults with psoriasis, but no guidelines previously existed for children, wrote Emily Osier, MD, of Eastern Virginia Medical School, Norfolk, and her colleagues (JAMA Dermatol 2017 May 17. doi: 10.1001/jamadermatol.2017.0499).
The panelists reviewed the literature on psoriasis and comorbidities published between 1999 and 2015 and identified 153 studies, 26 of which involved children.
“The screening recommendations derived are largely consistent with those endorsed by the AAP for the general pediatric patient,” the researchers noted.
Although many young children are screened for a range of comorbid conditions at annual checkups, preteens and teenagers may be less likely to receive preventive services in primary care, they said. “Thus, all health care providers caring for patients with pediatric psoriasis should help assess and ensure that appropriate screening has been performed,” they emphasized.
Some notable recommendations include the following:
• Screen children with psoriasis for overweight and obesity annually using body mass index percentiles.
• Screen for diabetes every 3 years starting at age 10 years.
• Perform universal lipid screening at ages 9-11 years and 17-21 years.
• Screen for nonalcoholic fatty liver disease every 2-3 years starting at age 9-11 years.
• Screen for hypertension annually starting at age 3 years.
• Screen for arthritis at the time of psoriasis diagnosis and periodically.
• Screen yearly for depression and anxiety at all ages, with yearly screening for substance abuse starting at age 11 years.
Uveitis screening is recommended only for children with psoriatic arthritis, the researchers said.
In addition, clinicians “should recognize the profound psychosocial ramifications of psoriasis and the potential significant impact on quality of life of patients and caregivers,” the researchers wrote. Clinicians may consider a formal quality of life measurement, such as the Children’s Dermatology Life Quality Index, or at least asking questions about the impact of psoriasis on the child’s life at home, at school, and during other activities.
Awareness of comorbidities also impacts potential psoriasis treatment, the researchers said. “Direct baseline screening and monitoring tests should be performed as indicated by each individual’s therapeutic plan,” they said.
The consensus statement is a starting point for screening that will be refined over time, and may include stratifying patients by age, disease subtype, or disease severity, the researchers noted.
“Communication and collaboration between dermatologists, primary care providers, and other pediatric specialists will be critical to accomplish the recommended screenings and to limit the sequelae of this disorder,” they wrote.
The National Psoriasis Foundation and the University of California, San Diego, Eczema and Inflammatory Skin Disease Center supported the study. Dr. Osier was supported in part by a Medical Dermatology Research Fellowship grant from the National Psoriasis Foundation in 2014-2016, but she had no financial conflicts to disclose.
FROM JAMA DERMATOLOGY
Osteoarthritis contributes more to difficulty walking than do diabetes, CVD
Hip and knee osteoarthritis on their own predict difficulty walking in adults aged 55 years and older to a greater extent than do diabetes or cardiovascular disease individually, according to findings from a Canadian population-based study.
The ability of hip and knee osteoarthritis (OA) to predict difficulty walking also increased with the number of joints affected and acted additively with either diabetes or cardiovascular disease (CVD) or both to raise the odds for walking problems, reported Lauren K. King, MBBS, of the University of Toronto, and colleagues.
To determine the impact of hip and knee OA on difficulty walking, the researchers reviewed data from 18,490 adults recruited between 1996 and 1998. The average age of the participants was 68 years, 60% were women, and 25% reported difficulty with walking during the past 3 months (Arthritis Care Res. 2017 May 17 doi: 10.1002/acr.23250). They completed questionnaires about their health conditions, and the researchers developed a clinical nomogram using their final multivariate logistic model.
The researchers calculated that the predicted probability of difficulty walking for a 60-year-old, middle-income, normal-weight woman with no health conditions was 5%-10%. However, the probability of walking problems was 10%-20% for the same woman with diabetes and CVD; 40% with osteoarthritis in two hips/knees; 60%-70% with diabetes, CVD, and osteoarthritis in two hips/knees; and 80% with diabetes, CVD, and osteoarthritis in all hips/knees.
Overall, 10% of the participants met criteria for hip OA and 15% met criteria for knee OA. The most common chronic conditions were hypertension (43%), diabetes (11%), and CVD (11%).
In a multivariate analysis, individuals with knee or hip OA had the highest odds of reporting walking difficulty, and the odds increased with the number of joints affected.
The results were limited by the cross-sectional nature of the study and the use of self-reports, the researchers noted.
However, “Given the high prevalence of OA and the substantial physical, social, and psychological consequences of walking difficulty, we believe our findings have high clinical relevance to primary care physicians and internal medicine specialists beyond rheumatology,” they said.
“Further research is warranted to understand the mechanisms by which chronic conditions affect mobility, physical activity, and sedentary behavior, and to elucidate safe and effective management approaches to reduce OA-related walking difficulty,” they added.
None of the investigators had relevant financial disclosures to report.
Hip and knee osteoarthritis on their own predict difficulty walking in adults aged 55 years and older to a greater extent than do diabetes or cardiovascular disease individually, according to findings from a Canadian population-based study.
The ability of hip and knee osteoarthritis (OA) to predict difficulty walking also increased with the number of joints affected and acted additively with either diabetes or cardiovascular disease (CVD) or both to raise the odds for walking problems, reported Lauren K. King, MBBS, of the University of Toronto, and colleagues.
To determine the impact of hip and knee OA on difficulty walking, the researchers reviewed data from 18,490 adults recruited between 1996 and 1998. The average age of the participants was 68 years, 60% were women, and 25% reported difficulty with walking during the past 3 months (Arthritis Care Res. 2017 May 17 doi: 10.1002/acr.23250). They completed questionnaires about their health conditions, and the researchers developed a clinical nomogram using their final multivariate logistic model.
The researchers calculated that the predicted probability of difficulty walking for a 60-year-old, middle-income, normal-weight woman with no health conditions was 5%-10%. However, the probability of walking problems was 10%-20% for the same woman with diabetes and CVD; 40% with osteoarthritis in two hips/knees; 60%-70% with diabetes, CVD, and osteoarthritis in two hips/knees; and 80% with diabetes, CVD, and osteoarthritis in all hips/knees.
Overall, 10% of the participants met criteria for hip OA and 15% met criteria for knee OA. The most common chronic conditions were hypertension (43%), diabetes (11%), and CVD (11%).
In a multivariate analysis, individuals with knee or hip OA had the highest odds of reporting walking difficulty, and the odds increased with the number of joints affected.
The results were limited by the cross-sectional nature of the study and the use of self-reports, the researchers noted.
However, “Given the high prevalence of OA and the substantial physical, social, and psychological consequences of walking difficulty, we believe our findings have high clinical relevance to primary care physicians and internal medicine specialists beyond rheumatology,” they said.
“Further research is warranted to understand the mechanisms by which chronic conditions affect mobility, physical activity, and sedentary behavior, and to elucidate safe and effective management approaches to reduce OA-related walking difficulty,” they added.
None of the investigators had relevant financial disclosures to report.
Hip and knee osteoarthritis on their own predict difficulty walking in adults aged 55 years and older to a greater extent than do diabetes or cardiovascular disease individually, according to findings from a Canadian population-based study.
The ability of hip and knee osteoarthritis (OA) to predict difficulty walking also increased with the number of joints affected and acted additively with either diabetes or cardiovascular disease (CVD) or both to raise the odds for walking problems, reported Lauren K. King, MBBS, of the University of Toronto, and colleagues.
To determine the impact of hip and knee OA on difficulty walking, the researchers reviewed data from 18,490 adults recruited between 1996 and 1998. The average age of the participants was 68 years, 60% were women, and 25% reported difficulty with walking during the past 3 months (Arthritis Care Res. 2017 May 17 doi: 10.1002/acr.23250). They completed questionnaires about their health conditions, and the researchers developed a clinical nomogram using their final multivariate logistic model.
The researchers calculated that the predicted probability of difficulty walking for a 60-year-old, middle-income, normal-weight woman with no health conditions was 5%-10%. However, the probability of walking problems was 10%-20% for the same woman with diabetes and CVD; 40% with osteoarthritis in two hips/knees; 60%-70% with diabetes, CVD, and osteoarthritis in two hips/knees; and 80% with diabetes, CVD, and osteoarthritis in all hips/knees.
Overall, 10% of the participants met criteria for hip OA and 15% met criteria for knee OA. The most common chronic conditions were hypertension (43%), diabetes (11%), and CVD (11%).
In a multivariate analysis, individuals with knee or hip OA had the highest odds of reporting walking difficulty, and the odds increased with the number of joints affected.
The results were limited by the cross-sectional nature of the study and the use of self-reports, the researchers noted.
However, “Given the high prevalence of OA and the substantial physical, social, and psychological consequences of walking difficulty, we believe our findings have high clinical relevance to primary care physicians and internal medicine specialists beyond rheumatology,” they said.
“Further research is warranted to understand the mechanisms by which chronic conditions affect mobility, physical activity, and sedentary behavior, and to elucidate safe and effective management approaches to reduce OA-related walking difficulty,” they added.
None of the investigators had relevant financial disclosures to report.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: The probability of difficulty walking was 40% for a 60-year-old, middle-income, normal-weight woman with OA in two hips or knees vs. 5% in the same woman with no health conditions.
Data source: A population-based cohort study of 18,490 adults aged 55 years and older.
Disclosures: None of the investigators had relevant financial disclosures to report.
HM17 session summary: CT to PET scans – What every hospitalist needs to know
Presenter
Timothy Kasprzak, MD, MBA
Session summary
“What imaging study should I order for this patient?” is a question that comes up frequently in the hospital. Dr. Kasprzak, the director of abdominopelvic and oncologic imaging at Case Western MetroHealth, Cleveland, offered some practical advice for inpatient clinicians during a rapid-fire session at HM17.
The session also touched on the risks and benefits of contrast media for CT scans and MRIs. As with other tests and treatments in medicine, the use of contrast is always a “risk-benefit.” The main benefit of both forms of contrast is to improve the “conspicuity” of findings on imaging studies – many diagnoses that are visible with contrast (such as vascular lesions, solid organ lesions, or extravasations) are invisible without it.
The risks of both CT and MRI contrast have been re-evaluated over the past several years. More recent evidence is suggesting the prevalence of contrast-induced nephropathy is lower than previously thought, especially with newer non-ionic contrast. Conversely, there is some recent evidence that CT contrast might accentuate radiation-related DNA damage. Regarding MRIs, gadolinium has been associated with nephrogenic systemic fibrosis, particularly in patients with end-stage renal disease. This appears to be less prevalent with newer gadolinium agents. There are, however, recent reports of gadolinium deposition in the basal ganglia of patients. The clinical significance of this imaging finding is still unknown.
Lastly, Dr. Kasprzak offered advice on the use of PET scans on inpatients. While there are a few indications that would warrant inpatient use (such as evaluation in fever of unknown origin), most PET scans are done for oncologic reasons that do not warrant urgent inpatient use. In addition, some insurance companies don’t reimburse for inpatient PET studies.
Key takeaways for HM
• Utilize appropriate use criteria (such as offered by the ACR) for choosing the most worthwhile imaging study.
• Give relevant clinical history in your order to help the radiologist narrow the differential (and to help prevent the “clinically correlate” phrase as much as possible).
• Consider the risk/benefit of contrast use for all patients getting CT or MRI studies.
• Avoid the use of inpatient PET scans, except for very specific indications (such as obscure infections).
Dr. Sehgal is a hospitalist at the South Texas Veterans Health Care System in San Antonio, an associate professor of medicine at University of Texas Health-San Antonio, and a an editorial board member of The Hospitalist.
Presenter
Timothy Kasprzak, MD, MBA
Session summary
“What imaging study should I order for this patient?” is a question that comes up frequently in the hospital. Dr. Kasprzak, the director of abdominopelvic and oncologic imaging at Case Western MetroHealth, Cleveland, offered some practical advice for inpatient clinicians during a rapid-fire session at HM17.
The session also touched on the risks and benefits of contrast media for CT scans and MRIs. As with other tests and treatments in medicine, the use of contrast is always a “risk-benefit.” The main benefit of both forms of contrast is to improve the “conspicuity” of findings on imaging studies – many diagnoses that are visible with contrast (such as vascular lesions, solid organ lesions, or extravasations) are invisible without it.
The risks of both CT and MRI contrast have been re-evaluated over the past several years. More recent evidence is suggesting the prevalence of contrast-induced nephropathy is lower than previously thought, especially with newer non-ionic contrast. Conversely, there is some recent evidence that CT contrast might accentuate radiation-related DNA damage. Regarding MRIs, gadolinium has been associated with nephrogenic systemic fibrosis, particularly in patients with end-stage renal disease. This appears to be less prevalent with newer gadolinium agents. There are, however, recent reports of gadolinium deposition in the basal ganglia of patients. The clinical significance of this imaging finding is still unknown.
Lastly, Dr. Kasprzak offered advice on the use of PET scans on inpatients. While there are a few indications that would warrant inpatient use (such as evaluation in fever of unknown origin), most PET scans are done for oncologic reasons that do not warrant urgent inpatient use. In addition, some insurance companies don’t reimburse for inpatient PET studies.
Key takeaways for HM
• Utilize appropriate use criteria (such as offered by the ACR) for choosing the most worthwhile imaging study.
• Give relevant clinical history in your order to help the radiologist narrow the differential (and to help prevent the “clinically correlate” phrase as much as possible).
• Consider the risk/benefit of contrast use for all patients getting CT or MRI studies.
• Avoid the use of inpatient PET scans, except for very specific indications (such as obscure infections).
Dr. Sehgal is a hospitalist at the South Texas Veterans Health Care System in San Antonio, an associate professor of medicine at University of Texas Health-San Antonio, and a an editorial board member of The Hospitalist.
Presenter
Timothy Kasprzak, MD, MBA
Session summary
“What imaging study should I order for this patient?” is a question that comes up frequently in the hospital. Dr. Kasprzak, the director of abdominopelvic and oncologic imaging at Case Western MetroHealth, Cleveland, offered some practical advice for inpatient clinicians during a rapid-fire session at HM17.
The session also touched on the risks and benefits of contrast media for CT scans and MRIs. As with other tests and treatments in medicine, the use of contrast is always a “risk-benefit.” The main benefit of both forms of contrast is to improve the “conspicuity” of findings on imaging studies – many diagnoses that are visible with contrast (such as vascular lesions, solid organ lesions, or extravasations) are invisible without it.
The risks of both CT and MRI contrast have been re-evaluated over the past several years. More recent evidence is suggesting the prevalence of contrast-induced nephropathy is lower than previously thought, especially with newer non-ionic contrast. Conversely, there is some recent evidence that CT contrast might accentuate radiation-related DNA damage. Regarding MRIs, gadolinium has been associated with nephrogenic systemic fibrosis, particularly in patients with end-stage renal disease. This appears to be less prevalent with newer gadolinium agents. There are, however, recent reports of gadolinium deposition in the basal ganglia of patients. The clinical significance of this imaging finding is still unknown.
Lastly, Dr. Kasprzak offered advice on the use of PET scans on inpatients. While there are a few indications that would warrant inpatient use (such as evaluation in fever of unknown origin), most PET scans are done for oncologic reasons that do not warrant urgent inpatient use. In addition, some insurance companies don’t reimburse for inpatient PET studies.
Key takeaways for HM
• Utilize appropriate use criteria (such as offered by the ACR) for choosing the most worthwhile imaging study.
• Give relevant clinical history in your order to help the radiologist narrow the differential (and to help prevent the “clinically correlate” phrase as much as possible).
• Consider the risk/benefit of contrast use for all patients getting CT or MRI studies.
• Avoid the use of inpatient PET scans, except for very specific indications (such as obscure infections).
Dr. Sehgal is a hospitalist at the South Texas Veterans Health Care System in San Antonio, an associate professor of medicine at University of Texas Health-San Antonio, and a an editorial board member of The Hospitalist.
SHM group membership strengthens teams, builds leaders at iNDIGO
When it comes to developing, maintaining, and growing an effective hospital medicine team, James W. Levy, PA-C, SFHM, certified physician assistant and managing partner of iNDIGO Health Partners, credits much of the company’s success to a decision to purchase a group SHM membership for its hospital medicine team. Recognizing the value that membership brings, it was an easy decision to extend a group membership to iNDIGO’s hospital medicine team.
“As a company, we are strong supporters of SHM and its mission,” Mr. Levy said. “This seemed like the best way we could support SHM and allow all our providers access to all the personal and professional benefits of SHM membership.”
“We’re strong believers in aggressively fostering the deployment of PAs and NPs in hospital medicine, and, as a PA, I value SHM’s efforts to be a ‘big tent’ organization,” Levy said. “SHM, among professional societies, has been a model of inclusiveness, of encouraging all providers, and [for] providing a forum for like-minded people to collaborate.”
Even prior to the group membership, Dr. Burgess was an active SHM member, citing SHM as a key driver in his development of iNDIGO’s pediatric hospitalist team. He describes how The Pediatric Hospital Medicine Core Competencies, a publication outlining the key clinical skills and objectives for a pediatric hospital medicine team, continues to be critical in onboarding new colleagues and strengthening teams in community hospitals.
“In a community hospital, we’re somewhat removed from the cutting-edge research and programs being implemented at larger academic institutions,” Dr. Burgess said. “SHM provides that information to us and allows us to see trends and connect with colleagues in larger programs.”
Through SHM’s implementation toolkits and online forums, such as the Hospital Medicine Exchange (HMX), iNDIGO hospitalists have access to resources from leaders in the field that are not typically available in a community hospital. Over the last 2 years, Dr. Burgess’ team has implemented the Pediatric Early Warning System (PEWS), a scoring system presented at Hospital Medicine 2013 to aid in the identification of hospitalized patients at risk for clinical deterioration.
It is not only SHM’s resources that enhance iNDIGO’s hospital medicine practice. “As a former member of SHM’s Public Policy Committee, I especially respect the advocacy that SHM does so effectively in Washington to ensure that federal policy being developed positively affects hospitalists and the patients they serve,” Levy said. SHM’s recent advocacy efforts include work on observation status as well as physician payment and the Medicare Access and CHIP Reauthorization Act (MACRA).
iNDIGO continues to seek out partnerships with SHM at a local and national level, bringing best practices and innovative ideas – like a flexible scheduling system not reflective of the typical 7-on/7-off hospitalist schedule – to SHM and its members throughout the country.
From quality improvement and leadership training to advocacy and education, SHM helps hospital medicine professionals to build successful teams. “One of our goals is to develop great teams rather than just staffing programs,” Levy said. “Great teams need great leaders, and SHM’s resources promote and strengthen our on-the-ground leaders.”
To learn more about the membership opportunities available to you and your hospital medicine team, visit joinshm.org.
Brett Radler is SHM’s communications specialist.
When it comes to developing, maintaining, and growing an effective hospital medicine team, James W. Levy, PA-C, SFHM, certified physician assistant and managing partner of iNDIGO Health Partners, credits much of the company’s success to a decision to purchase a group SHM membership for its hospital medicine team. Recognizing the value that membership brings, it was an easy decision to extend a group membership to iNDIGO’s hospital medicine team.
“As a company, we are strong supporters of SHM and its mission,” Mr. Levy said. “This seemed like the best way we could support SHM and allow all our providers access to all the personal and professional benefits of SHM membership.”
“We’re strong believers in aggressively fostering the deployment of PAs and NPs in hospital medicine, and, as a PA, I value SHM’s efforts to be a ‘big tent’ organization,” Levy said. “SHM, among professional societies, has been a model of inclusiveness, of encouraging all providers, and [for] providing a forum for like-minded people to collaborate.”
Even prior to the group membership, Dr. Burgess was an active SHM member, citing SHM as a key driver in his development of iNDIGO’s pediatric hospitalist team. He describes how The Pediatric Hospital Medicine Core Competencies, a publication outlining the key clinical skills and objectives for a pediatric hospital medicine team, continues to be critical in onboarding new colleagues and strengthening teams in community hospitals.
“In a community hospital, we’re somewhat removed from the cutting-edge research and programs being implemented at larger academic institutions,” Dr. Burgess said. “SHM provides that information to us and allows us to see trends and connect with colleagues in larger programs.”
Through SHM’s implementation toolkits and online forums, such as the Hospital Medicine Exchange (HMX), iNDIGO hospitalists have access to resources from leaders in the field that are not typically available in a community hospital. Over the last 2 years, Dr. Burgess’ team has implemented the Pediatric Early Warning System (PEWS), a scoring system presented at Hospital Medicine 2013 to aid in the identification of hospitalized patients at risk for clinical deterioration.
It is not only SHM’s resources that enhance iNDIGO’s hospital medicine practice. “As a former member of SHM’s Public Policy Committee, I especially respect the advocacy that SHM does so effectively in Washington to ensure that federal policy being developed positively affects hospitalists and the patients they serve,” Levy said. SHM’s recent advocacy efforts include work on observation status as well as physician payment and the Medicare Access and CHIP Reauthorization Act (MACRA).
iNDIGO continues to seek out partnerships with SHM at a local and national level, bringing best practices and innovative ideas – like a flexible scheduling system not reflective of the typical 7-on/7-off hospitalist schedule – to SHM and its members throughout the country.
From quality improvement and leadership training to advocacy and education, SHM helps hospital medicine professionals to build successful teams. “One of our goals is to develop great teams rather than just staffing programs,” Levy said. “Great teams need great leaders, and SHM’s resources promote and strengthen our on-the-ground leaders.”
To learn more about the membership opportunities available to you and your hospital medicine team, visit joinshm.org.
Brett Radler is SHM’s communications specialist.
When it comes to developing, maintaining, and growing an effective hospital medicine team, James W. Levy, PA-C, SFHM, certified physician assistant and managing partner of iNDIGO Health Partners, credits much of the company’s success to a decision to purchase a group SHM membership for its hospital medicine team. Recognizing the value that membership brings, it was an easy decision to extend a group membership to iNDIGO’s hospital medicine team.
“As a company, we are strong supporters of SHM and its mission,” Mr. Levy said. “This seemed like the best way we could support SHM and allow all our providers access to all the personal and professional benefits of SHM membership.”
“We’re strong believers in aggressively fostering the deployment of PAs and NPs in hospital medicine, and, as a PA, I value SHM’s efforts to be a ‘big tent’ organization,” Levy said. “SHM, among professional societies, has been a model of inclusiveness, of encouraging all providers, and [for] providing a forum for like-minded people to collaborate.”
Even prior to the group membership, Dr. Burgess was an active SHM member, citing SHM as a key driver in his development of iNDIGO’s pediatric hospitalist team. He describes how The Pediatric Hospital Medicine Core Competencies, a publication outlining the key clinical skills and objectives for a pediatric hospital medicine team, continues to be critical in onboarding new colleagues and strengthening teams in community hospitals.
“In a community hospital, we’re somewhat removed from the cutting-edge research and programs being implemented at larger academic institutions,” Dr. Burgess said. “SHM provides that information to us and allows us to see trends and connect with colleagues in larger programs.”
Through SHM’s implementation toolkits and online forums, such as the Hospital Medicine Exchange (HMX), iNDIGO hospitalists have access to resources from leaders in the field that are not typically available in a community hospital. Over the last 2 years, Dr. Burgess’ team has implemented the Pediatric Early Warning System (PEWS), a scoring system presented at Hospital Medicine 2013 to aid in the identification of hospitalized patients at risk for clinical deterioration.
It is not only SHM’s resources that enhance iNDIGO’s hospital medicine practice. “As a former member of SHM’s Public Policy Committee, I especially respect the advocacy that SHM does so effectively in Washington to ensure that federal policy being developed positively affects hospitalists and the patients they serve,” Levy said. SHM’s recent advocacy efforts include work on observation status as well as physician payment and the Medicare Access and CHIP Reauthorization Act (MACRA).
iNDIGO continues to seek out partnerships with SHM at a local and national level, bringing best practices and innovative ideas – like a flexible scheduling system not reflective of the typical 7-on/7-off hospitalist schedule – to SHM and its members throughout the country.
From quality improvement and leadership training to advocacy and education, SHM helps hospital medicine professionals to build successful teams. “One of our goals is to develop great teams rather than just staffing programs,” Levy said. “Great teams need great leaders, and SHM’s resources promote and strengthen our on-the-ground leaders.”
To learn more about the membership opportunities available to you and your hospital medicine team, visit joinshm.org.
Brett Radler is SHM’s communications specialist.
Diabetes Programs: Referral Isn’t Enough
Many patients who could benefit from intensive lifestyle interventions to reduce and prevent diabetes may not be getting the opportunity, according to researchers at Montefiore Health System (MHS).
Beginning in 2010, MHS partnered with the YMCA of Greater New York to provide the YMCA’s 1-year Diabetes Prevention Program (DPP) to patients in Bronx-based primary care clinics. During an office visit, eligible patients were told of their risk for developing diabetes and asked whether they were interested in participating. Physicians referred patients who said yes. Schedule and location for 16 core sessions were based on availability of coaches, space for the sessions, and patient demand.
Over the study period, 1,249 patients were referred to the DPP. For up to 1 year after referral, MHS placed patients in 66 core groups. “Placed” meant they were scheduled to attend a session. Patients who attended ≥ 3 sessions were considered “enrolled.” Of MHS patients referred to the YMCA’s DPP, only 34% were placed. Of those, 47% attended ≥ 3 sessions.
More than half (53%) of placed patients were never enrolled. But when they do enroll the study shows patients have good results. One-third of patients lost ≥ 5% of their body weight during their enrollment. The average weight loss was 3.4%.
The study points to some areas for improvement, the researchers say. Reducing the lag time between referral and the start of the sessions, for instance, would maximize the likelihood of enrollment. Patients who started their sessions within 2 months of their referral date were more often enrolled compared with those who had to wait ≥ 4 months (54% vs 22%). The researchers also note that the timing of referrals and sessions are important considerations, and efforts should be made to coordinate them.
Targeting younger patients and Spanish-speaking adults also would help. Attrition among younger participants is of “particular concern,” the researchers say, given that about 26% of adults aged < 60 years have prediabetes. Patients aged 18 to 44 years, the bulk of the patients referred, were least often placed compared with patients aged ≥ 45 years. Patients who preferred sessions in Spanish were less often placed than those who preferred English.
Finally, the researchers point out that health care providers have an important role in placing patients: The number of referrals that a provider made was associated with whether or not the patient was placed.
Many patients who could benefit from intensive lifestyle interventions to reduce and prevent diabetes may not be getting the opportunity, according to researchers at Montefiore Health System (MHS).
Beginning in 2010, MHS partnered with the YMCA of Greater New York to provide the YMCA’s 1-year Diabetes Prevention Program (DPP) to patients in Bronx-based primary care clinics. During an office visit, eligible patients were told of their risk for developing diabetes and asked whether they were interested in participating. Physicians referred patients who said yes. Schedule and location for 16 core sessions were based on availability of coaches, space for the sessions, and patient demand.
Over the study period, 1,249 patients were referred to the DPP. For up to 1 year after referral, MHS placed patients in 66 core groups. “Placed” meant they were scheduled to attend a session. Patients who attended ≥ 3 sessions were considered “enrolled.” Of MHS patients referred to the YMCA’s DPP, only 34% were placed. Of those, 47% attended ≥ 3 sessions.
More than half (53%) of placed patients were never enrolled. But when they do enroll the study shows patients have good results. One-third of patients lost ≥ 5% of their body weight during their enrollment. The average weight loss was 3.4%.
The study points to some areas for improvement, the researchers say. Reducing the lag time between referral and the start of the sessions, for instance, would maximize the likelihood of enrollment. Patients who started their sessions within 2 months of their referral date were more often enrolled compared with those who had to wait ≥ 4 months (54% vs 22%). The researchers also note that the timing of referrals and sessions are important considerations, and efforts should be made to coordinate them.
Targeting younger patients and Spanish-speaking adults also would help. Attrition among younger participants is of “particular concern,” the researchers say, given that about 26% of adults aged < 60 years have prediabetes. Patients aged 18 to 44 years, the bulk of the patients referred, were least often placed compared with patients aged ≥ 45 years. Patients who preferred sessions in Spanish were less often placed than those who preferred English.
Finally, the researchers point out that health care providers have an important role in placing patients: The number of referrals that a provider made was associated with whether or not the patient was placed.
Many patients who could benefit from intensive lifestyle interventions to reduce and prevent diabetes may not be getting the opportunity, according to researchers at Montefiore Health System (MHS).
Beginning in 2010, MHS partnered with the YMCA of Greater New York to provide the YMCA’s 1-year Diabetes Prevention Program (DPP) to patients in Bronx-based primary care clinics. During an office visit, eligible patients were told of their risk for developing diabetes and asked whether they were interested in participating. Physicians referred patients who said yes. Schedule and location for 16 core sessions were based on availability of coaches, space for the sessions, and patient demand.
Over the study period, 1,249 patients were referred to the DPP. For up to 1 year after referral, MHS placed patients in 66 core groups. “Placed” meant they were scheduled to attend a session. Patients who attended ≥ 3 sessions were considered “enrolled.” Of MHS patients referred to the YMCA’s DPP, only 34% were placed. Of those, 47% attended ≥ 3 sessions.
More than half (53%) of placed patients were never enrolled. But when they do enroll the study shows patients have good results. One-third of patients lost ≥ 5% of their body weight during their enrollment. The average weight loss was 3.4%.
The study points to some areas for improvement, the researchers say. Reducing the lag time between referral and the start of the sessions, for instance, would maximize the likelihood of enrollment. Patients who started their sessions within 2 months of their referral date were more often enrolled compared with those who had to wait ≥ 4 months (54% vs 22%). The researchers also note that the timing of referrals and sessions are important considerations, and efforts should be made to coordinate them.
Targeting younger patients and Spanish-speaking adults also would help. Attrition among younger participants is of “particular concern,” the researchers say, given that about 26% of adults aged < 60 years have prediabetes. Patients aged 18 to 44 years, the bulk of the patients referred, were least often placed compared with patients aged ≥ 45 years. Patients who preferred sessions in Spanish were less often placed than those who preferred English.
Finally, the researchers point out that health care providers have an important role in placing patients: The number of referrals that a provider made was associated with whether or not the patient was placed.
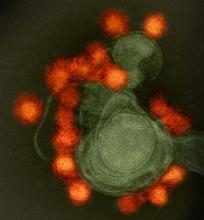
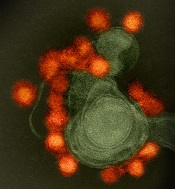
Zika virus spread undetected in the Americas, team says
New research suggests the Zika virus spread quickly in the Americas and then diverged into distinct genetic groups.
Researchers performed genetic analysis on samples collected as the virus spread throughout the Americas after its introduction in 2013 or 2014.
The team found that Zika circulated undetected for up to a year in some regions before it came to the attention of public health authorities.
Genetic sequencing also enabled the researchers to recreate the epidemiological and evolutionary paths the virus took as it spread and split into the distinct subtypes—or clades—that have been detected in the Americas.
Hayden C. Metsky, a PhD student at the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported these findings in Nature.
The researchers reconstructed Zika’s dispersal by sequencing genetic material collected from hundreds of patients in 10 countries and territories.
The team eventually amassed a database of 110 complete or partial Zika virus genomes—the largest collection to date—which they analyzed along with 64 published and publicly shared genomes.
Based on changes to the viral genome that accumulated as the disease moved through new populations, the researchers concluded that Zika virus spread rapidly upon its initial introduction in Brazil, likely sometime in 2013.
Later, at several points in early to mid-2015, the virus separated into at least 3 clades—distinct genetic groups whose members share a common ancestor—in Colombia, Honduras, and Puerto Rico, as well as a fourth type found in parts of the Caribbean and the continental US.
The researchers believe these findings could have a direct impact on public health, informing disease surveillance and the development of diagnostic tests. ![]()
New research suggests the Zika virus spread quickly in the Americas and then diverged into distinct genetic groups.
Researchers performed genetic analysis on samples collected as the virus spread throughout the Americas after its introduction in 2013 or 2014.
The team found that Zika circulated undetected for up to a year in some regions before it came to the attention of public health authorities.
Genetic sequencing also enabled the researchers to recreate the epidemiological and evolutionary paths the virus took as it spread and split into the distinct subtypes—or clades—that have been detected in the Americas.
Hayden C. Metsky, a PhD student at the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported these findings in Nature.
The researchers reconstructed Zika’s dispersal by sequencing genetic material collected from hundreds of patients in 10 countries and territories.
The team eventually amassed a database of 110 complete or partial Zika virus genomes—the largest collection to date—which they analyzed along with 64 published and publicly shared genomes.
Based on changes to the viral genome that accumulated as the disease moved through new populations, the researchers concluded that Zika virus spread rapidly upon its initial introduction in Brazil, likely sometime in 2013.
Later, at several points in early to mid-2015, the virus separated into at least 3 clades—distinct genetic groups whose members share a common ancestor—in Colombia, Honduras, and Puerto Rico, as well as a fourth type found in parts of the Caribbean and the continental US.
The researchers believe these findings could have a direct impact on public health, informing disease surveillance and the development of diagnostic tests. ![]()
New research suggests the Zika virus spread quickly in the Americas and then diverged into distinct genetic groups.
Researchers performed genetic analysis on samples collected as the virus spread throughout the Americas after its introduction in 2013 or 2014.
The team found that Zika circulated undetected for up to a year in some regions before it came to the attention of public health authorities.
Genetic sequencing also enabled the researchers to recreate the epidemiological and evolutionary paths the virus took as it spread and split into the distinct subtypes—or clades—that have been detected in the Americas.
Hayden C. Metsky, a PhD student at the Broad Institute of MIT and Harvard, Cambridge, Massachusetts, and his colleagues reported these findings in Nature.
The researchers reconstructed Zika’s dispersal by sequencing genetic material collected from hundreds of patients in 10 countries and territories.
The team eventually amassed a database of 110 complete or partial Zika virus genomes—the largest collection to date—which they analyzed along with 64 published and publicly shared genomes.
Based on changes to the viral genome that accumulated as the disease moved through new populations, the researchers concluded that Zika virus spread rapidly upon its initial introduction in Brazil, likely sometime in 2013.
Later, at several points in early to mid-2015, the virus separated into at least 3 clades—distinct genetic groups whose members share a common ancestor—in Colombia, Honduras, and Puerto Rico, as well as a fourth type found in parts of the Caribbean and the continental US.
The researchers believe these findings could have a direct impact on public health, informing disease surveillance and the development of diagnostic tests. ![]()
Before the Parade Passes By, Be Sure to Cross the Street
Are we in Pamplona, Spain, or San Diego, California?
The differences might blur Saturday morning; it won’t be Pamplona’s running of the bulls in front of the San Diego Convention Center, but a cattle drive of long-horned cattle. And this frontier drive may create a few difficulties getting to and from the Vascular Annual Meeting.
The cattle will travel on Harbor Drive, the street directly in front of the San Diego Convention Center, VAM’s home and the VAM headquarters hotel, the Marriot Marquis San Diego Marina.
The route will affect the ability to cross Harbor Drive (from other hotels, for example) and will delay anyone attempting to leave the Marriott via car or taxi while the parade is passing by.
For those staying in San Diego after VAM, the fair opens June 2 and runs through July 4. Fun includes panning for gold, a Wild West saloon with an old-fashioned player piano, and chance encounters with notorious outlaws such as Jesse James and Black Bart.
Are we in Pamplona, Spain, or San Diego, California?
The differences might blur Saturday morning; it won’t be Pamplona’s running of the bulls in front of the San Diego Convention Center, but a cattle drive of long-horned cattle. And this frontier drive may create a few difficulties getting to and from the Vascular Annual Meeting.
The cattle will travel on Harbor Drive, the street directly in front of the San Diego Convention Center, VAM’s home and the VAM headquarters hotel, the Marriot Marquis San Diego Marina.
The route will affect the ability to cross Harbor Drive (from other hotels, for example) and will delay anyone attempting to leave the Marriott via car or taxi while the parade is passing by.
For those staying in San Diego after VAM, the fair opens June 2 and runs through July 4. Fun includes panning for gold, a Wild West saloon with an old-fashioned player piano, and chance encounters with notorious outlaws such as Jesse James and Black Bart.
Are we in Pamplona, Spain, or San Diego, California?
The differences might blur Saturday morning; it won’t be Pamplona’s running of the bulls in front of the San Diego Convention Center, but a cattle drive of long-horned cattle. And this frontier drive may create a few difficulties getting to and from the Vascular Annual Meeting.
The cattle will travel on Harbor Drive, the street directly in front of the San Diego Convention Center, VAM’s home and the VAM headquarters hotel, the Marriot Marquis San Diego Marina.
The route will affect the ability to cross Harbor Drive (from other hotels, for example) and will delay anyone attempting to leave the Marriott via car or taxi while the parade is passing by.
For those staying in San Diego after VAM, the fair opens June 2 and runs through July 4. Fun includes panning for gold, a Wild West saloon with an old-fashioned player piano, and chance encounters with notorious outlaws such as Jesse James and Black Bart.
How to Welcome a Patient Advisor to Your Research Team
When it comes to caring for those with vascular disease, who better to tell surgeons and researchers the effects of various treatments than … patients?
Patients who have completed a comprehensive Patient Advisors Course will provide their perspective Thursday afternoon in “Patient Advisors Program,” 2:30 to 3:30 p.m., with a reception to further the conversation immediately afterward, from 3:30 to 4:30 p.m.
This session has been more than a year in the making, the fruition of a project funded by the Patient-Centered Outcomes Research Institute on “Connecting Patients and Researchers to Engage in Patient-Centered Vascular Disease Research.” Adrienne Faerber, PhD, at the Dartmouth Institute for Health Policy and Clinical Research is leading the project in partnership with SVS member Philip Goodney, MD.
The patients attending VAM have completed an online course aimed at patient collaboration with researchers and clinicians. Researchers, clinicians, and clinical leaders all should find the session valuable, said Dr. Faerber. Major funding agencies are moving toward requiring patients to give their input on research proposals, she said.
“And clinicians who want to improve their care of patients and clinical leaders who want to learn about leading change initiatives will want to listen to what they have to say as well.
“Patients are the experts in living with vascular diseases and we should be listening to them.”
Their experience encompasses far more than just their treatment, Dr. Faerber said of patients, with questions – even if they don’t know to ask them – that involve far more than “stent or surgery.”
“Surgeons tend to think of risks and benefits of procedures. But patients find the post-operative recovery a really important part of the experience,” she said. Surgeons should discuss pain management and any lifestyle restrictions; for example, a patient might not know until after surgery that he cannot drive for six or eight weeks.
“In the patient-centered view, that’s a huge issue,” she said.
“Providing good care goes beyond recommending a treatment,” said Dr. Faerber. “Clinicians need their patients’ input as to what they want, their values and beliefs.” Considering all those factors, plus lifestyle, “may change your thinking on the treatment decision.”
The Thursday session includes an orientation to patient-centered research and patient advisors, conversations with patients about their experiences and how clinics and hospitals can improve the patient experience of those with vascular care plus clinician and researcher reactions.
Dr. Matthew Corriere will discuss parallels between the patients’ stories to his work evaluating what matters to patients undergoing treatment, and Dr. Philip Goodney will describe how patient advisors have helped him improve his research portfolio.
The reception following the session will provide an opportunity to talk with the patient advisors and find out more about adding a Patient Advisor to a research or quality improvement team.
For more information, visit patientadvisorscourse.com.
Thursday, June 1
2:30 – 3:30 p.m.
SDCC, Room 17B
Patient Advisors Program
Moderators: Adrienne Faerber, PhD and Philip Goodney, MD
3:30 – 4:30 p.m.
SDCC, Room 17B
Patient Advisors Program Reception
When it comes to caring for those with vascular disease, who better to tell surgeons and researchers the effects of various treatments than … patients?
Patients who have completed a comprehensive Patient Advisors Course will provide their perspective Thursday afternoon in “Patient Advisors Program,” 2:30 to 3:30 p.m., with a reception to further the conversation immediately afterward, from 3:30 to 4:30 p.m.
This session has been more than a year in the making, the fruition of a project funded by the Patient-Centered Outcomes Research Institute on “Connecting Patients and Researchers to Engage in Patient-Centered Vascular Disease Research.” Adrienne Faerber, PhD, at the Dartmouth Institute for Health Policy and Clinical Research is leading the project in partnership with SVS member Philip Goodney, MD.
The patients attending VAM have completed an online course aimed at patient collaboration with researchers and clinicians. Researchers, clinicians, and clinical leaders all should find the session valuable, said Dr. Faerber. Major funding agencies are moving toward requiring patients to give their input on research proposals, she said.
“And clinicians who want to improve their care of patients and clinical leaders who want to learn about leading change initiatives will want to listen to what they have to say as well.
“Patients are the experts in living with vascular diseases and we should be listening to them.”
Their experience encompasses far more than just their treatment, Dr. Faerber said of patients, with questions – even if they don’t know to ask them – that involve far more than “stent or surgery.”
“Surgeons tend to think of risks and benefits of procedures. But patients find the post-operative recovery a really important part of the experience,” she said. Surgeons should discuss pain management and any lifestyle restrictions; for example, a patient might not know until after surgery that he cannot drive for six or eight weeks.
“In the patient-centered view, that’s a huge issue,” she said.
“Providing good care goes beyond recommending a treatment,” said Dr. Faerber. “Clinicians need their patients’ input as to what they want, their values and beliefs.” Considering all those factors, plus lifestyle, “may change your thinking on the treatment decision.”
The Thursday session includes an orientation to patient-centered research and patient advisors, conversations with patients about their experiences and how clinics and hospitals can improve the patient experience of those with vascular care plus clinician and researcher reactions.
Dr. Matthew Corriere will discuss parallels between the patients’ stories to his work evaluating what matters to patients undergoing treatment, and Dr. Philip Goodney will describe how patient advisors have helped him improve his research portfolio.
The reception following the session will provide an opportunity to talk with the patient advisors and find out more about adding a Patient Advisor to a research or quality improvement team.
For more information, visit patientadvisorscourse.com.
Thursday, June 1
2:30 – 3:30 p.m.
SDCC, Room 17B
Patient Advisors Program
Moderators: Adrienne Faerber, PhD and Philip Goodney, MD
3:30 – 4:30 p.m.
SDCC, Room 17B
Patient Advisors Program Reception
When it comes to caring for those with vascular disease, who better to tell surgeons and researchers the effects of various treatments than … patients?
Patients who have completed a comprehensive Patient Advisors Course will provide their perspective Thursday afternoon in “Patient Advisors Program,” 2:30 to 3:30 p.m., with a reception to further the conversation immediately afterward, from 3:30 to 4:30 p.m.
This session has been more than a year in the making, the fruition of a project funded by the Patient-Centered Outcomes Research Institute on “Connecting Patients and Researchers to Engage in Patient-Centered Vascular Disease Research.” Adrienne Faerber, PhD, at the Dartmouth Institute for Health Policy and Clinical Research is leading the project in partnership with SVS member Philip Goodney, MD.
The patients attending VAM have completed an online course aimed at patient collaboration with researchers and clinicians. Researchers, clinicians, and clinical leaders all should find the session valuable, said Dr. Faerber. Major funding agencies are moving toward requiring patients to give their input on research proposals, she said.
“And clinicians who want to improve their care of patients and clinical leaders who want to learn about leading change initiatives will want to listen to what they have to say as well.
“Patients are the experts in living with vascular diseases and we should be listening to them.”
Their experience encompasses far more than just their treatment, Dr. Faerber said of patients, with questions – even if they don’t know to ask them – that involve far more than “stent or surgery.”
“Surgeons tend to think of risks and benefits of procedures. But patients find the post-operative recovery a really important part of the experience,” she said. Surgeons should discuss pain management and any lifestyle restrictions; for example, a patient might not know until after surgery that he cannot drive for six or eight weeks.
“In the patient-centered view, that’s a huge issue,” she said.
“Providing good care goes beyond recommending a treatment,” said Dr. Faerber. “Clinicians need their patients’ input as to what they want, their values and beliefs.” Considering all those factors, plus lifestyle, “may change your thinking on the treatment decision.”
The Thursday session includes an orientation to patient-centered research and patient advisors, conversations with patients about their experiences and how clinics and hospitals can improve the patient experience of those with vascular care plus clinician and researcher reactions.
Dr. Matthew Corriere will discuss parallels between the patients’ stories to his work evaluating what matters to patients undergoing treatment, and Dr. Philip Goodney will describe how patient advisors have helped him improve his research portfolio.
The reception following the session will provide an opportunity to talk with the patient advisors and find out more about adding a Patient Advisor to a research or quality improvement team.
For more information, visit patientadvisorscourse.com.
Thursday, June 1
2:30 – 3:30 p.m.
SDCC, Room 17B
Patient Advisors Program
Moderators: Adrienne Faerber, PhD and Philip Goodney, MD
3:30 – 4:30 p.m.
SDCC, Room 17B
Patient Advisors Program Reception
On Tap – Thursday
Here are some of the events your colleagues will be talking about later. You won’t want to miss:
Thursday, June 1
Stop by the Exhibit Hall, opening at noon, and its popular Vascular Live presentations.
8:00 to 8:30 a.m. – Opening Ceremony. Don’t miss the kickoff of our 2017 Vascular Annual Meeting events. Find out who is here and what you’ll want to attend. SDCC, Room 6 A/B.
8:30-10:15 a.m. – William J. von Liebig Forum. The first big event in our opening day lineup. Top issues moderated by Drs. Ronald Fairman and Ronald Dalman. SDCC, Room A/B.
10:30 a.m. to 12:00 p.m. – The E. Stanley Crawford Critical Issues Forum. “How to Navigate a Value-Based Reimbursement System: What you Need to Know,” the event will bring in experts on the changing reimbursements landscape. SVS President-Elect Dr. R. Clement Darling III, will moderate. SDCC, Room A/B.
2:30 - 3:30 p.m. – Patient Advisors Program. New this year! Patients advisors, trained in an innovative new program, will share stories of their diagnoses and treatments and discuss how patients and researchers can collaborate on patient-centered research projects. SDCC, Room 17B, with a reception to further the conversation following from 3:30 to 4:30 p.m.
3:00 to 3:30 p.m. – The Roy Greenberg Distinguished Lecture. “Aneurysms Don’t Know Borders” will be delivered by Dr. Tara Mastracci, of the Royal Free Foundation Trust in London. SDCC, Room 6 A/B.
6:30-7:30 p.m. – The Networking Reception for Women, Diversity and Young Surgeons, Marriott, Santa Rosa room, followed by the popular Alumni Receptions (see Program Book or the VAM mobile app for times and rooms).
Here are some of the events your colleagues will be talking about later. You won’t want to miss:
Thursday, June 1
Stop by the Exhibit Hall, opening at noon, and its popular Vascular Live presentations.
8:00 to 8:30 a.m. – Opening Ceremony. Don’t miss the kickoff of our 2017 Vascular Annual Meeting events. Find out who is here and what you’ll want to attend. SDCC, Room 6 A/B.
8:30-10:15 a.m. – William J. von Liebig Forum. The first big event in our opening day lineup. Top issues moderated by Drs. Ronald Fairman and Ronald Dalman. SDCC, Room A/B.
10:30 a.m. to 12:00 p.m. – The E. Stanley Crawford Critical Issues Forum. “How to Navigate a Value-Based Reimbursement System: What you Need to Know,” the event will bring in experts on the changing reimbursements landscape. SVS President-Elect Dr. R. Clement Darling III, will moderate. SDCC, Room A/B.
2:30 - 3:30 p.m. – Patient Advisors Program. New this year! Patients advisors, trained in an innovative new program, will share stories of their diagnoses and treatments and discuss how patients and researchers can collaborate on patient-centered research projects. SDCC, Room 17B, with a reception to further the conversation following from 3:30 to 4:30 p.m.
3:00 to 3:30 p.m. – The Roy Greenberg Distinguished Lecture. “Aneurysms Don’t Know Borders” will be delivered by Dr. Tara Mastracci, of the Royal Free Foundation Trust in London. SDCC, Room 6 A/B.
6:30-7:30 p.m. – The Networking Reception for Women, Diversity and Young Surgeons, Marriott, Santa Rosa room, followed by the popular Alumni Receptions (see Program Book or the VAM mobile app for times and rooms).
Here are some of the events your colleagues will be talking about later. You won’t want to miss:
Thursday, June 1
Stop by the Exhibit Hall, opening at noon, and its popular Vascular Live presentations.
8:00 to 8:30 a.m. – Opening Ceremony. Don’t miss the kickoff of our 2017 Vascular Annual Meeting events. Find out who is here and what you’ll want to attend. SDCC, Room 6 A/B.
8:30-10:15 a.m. – William J. von Liebig Forum. The first big event in our opening day lineup. Top issues moderated by Drs. Ronald Fairman and Ronald Dalman. SDCC, Room A/B.
10:30 a.m. to 12:00 p.m. – The E. Stanley Crawford Critical Issues Forum. “How to Navigate a Value-Based Reimbursement System: What you Need to Know,” the event will bring in experts on the changing reimbursements landscape. SVS President-Elect Dr. R. Clement Darling III, will moderate. SDCC, Room A/B.
2:30 - 3:30 p.m. – Patient Advisors Program. New this year! Patients advisors, trained in an innovative new program, will share stories of their diagnoses and treatments and discuss how patients and researchers can collaborate on patient-centered research projects. SDCC, Room 17B, with a reception to further the conversation following from 3:30 to 4:30 p.m.
3:00 to 3:30 p.m. – The Roy Greenberg Distinguished Lecture. “Aneurysms Don’t Know Borders” will be delivered by Dr. Tara Mastracci, of the Royal Free Foundation Trust in London. SDCC, Room 6 A/B.
6:30-7:30 p.m. – The Networking Reception for Women, Diversity and Young Surgeons, Marriott, Santa Rosa room, followed by the popular Alumni Receptions (see Program Book or the VAM mobile app for times and rooms).
2017 Resident Research Award: Epigenetic Mechanisms in Type 2 Diabetic Wound Healing
The issue of impaired wound healing in type 2 diabetes is a serious one and the leading cause of lower extremity amputation in the United States. The level of morbidity and mortality associated with diabetic foot ulcers has remained under the radar and, as a result, this important area of research has been understudied.
This year’s Resident Research Award winner, Andrew S. Kimball, MD, of the University of Michigan, will report on the research he and his colleagues performed on the immunologic and epigenetic mechanisms of wound healing in both physiologic and pathophysiologic states.
Dr. Kimball will present the research on Friday, June 2, at 10:00 a.m., discussing the role of specific epigenetic enzymes in the dictation of macrophage phenotype in wound tissue. The talk will cover how diabetes alters those enzymes to influence a deleterious phenotype that promotes inflammation and delays wound healing.
“Our lab specifically looks at the role of monocyte/macrophages in the inflammatory phase of wound healing and how perturbation in the local environment – as occurs in diabetes – affects monocyte/macrophage phenotype, and ultimately, wound healing,” said Dr. Kimball.
He is a PGY5 general surgery resident who will be applying for a vascular surgery fellowship this year.
“This specific project looks at epigenetic changes,” she continued. “It is a newer field, which looks at how variations in the environment can affect changes in the cell. We have found that a particular enzyme, SETDB2, is needed in macrophages for normal wound healing. Diabetics don’t have enough of the enzyme, which results in chronic inflammation.”
The research is important because the at-risk population is vast, and the opportunity for breakthrough research to have an impact has never been greater.
“Despite this,” said Dr. Kimball, “there are no effective treatments for abrogating the impaired wound healing seen in diabetes. And patients continue to suffer significant morbidity and mortality as a result.”
He added, “We hope our fundamental research will identify novel targets for the treatment of impaired wound healing in diabetes.”
Those attending the presentation, Epigenetic Mechanisms of Macrophage Phenotype Regulation in Diabetic Wound Healing, will learn about the immune system’s role in the early stages of wound healing. They will receive a better understanding of the role of epigenetics in influencing the wound cell inflammatory phenotype, and its effect on wound healing. They will also begin to realize how epigenetics influences a cell’s inflammatory phenotype.
Hopefully, the research will be an important first step – leading to new future therapies that target the enzyme and improve macrophage function in diabetic wounds.
“Andrew worked very hard, and I am very proud of his efforts,” said Dr. Gallagher. “He has done a phenomenal job in the lab, and his diligent work has advanced this field tremendously.”
She continued, “I have no doubt that Andrew will continue to make important scientific discoveries in our field in the future. He is certainly deserving of this award.”
Dr. Kimball and his coauthors have no relevant financial disclosures.
Friday, June 2
10:00 a.m.
SDCC, Room 6 A/B
Plenary 5, 2017 Resident Research Award
The issue of impaired wound healing in type 2 diabetes is a serious one and the leading cause of lower extremity amputation in the United States. The level of morbidity and mortality associated with diabetic foot ulcers has remained under the radar and, as a result, this important area of research has been understudied.
This year’s Resident Research Award winner, Andrew S. Kimball, MD, of the University of Michigan, will report on the research he and his colleagues performed on the immunologic and epigenetic mechanisms of wound healing in both physiologic and pathophysiologic states.
Dr. Kimball will present the research on Friday, June 2, at 10:00 a.m., discussing the role of specific epigenetic enzymes in the dictation of macrophage phenotype in wound tissue. The talk will cover how diabetes alters those enzymes to influence a deleterious phenotype that promotes inflammation and delays wound healing.
“Our lab specifically looks at the role of monocyte/macrophages in the inflammatory phase of wound healing and how perturbation in the local environment – as occurs in diabetes – affects monocyte/macrophage phenotype, and ultimately, wound healing,” said Dr. Kimball.
He is a PGY5 general surgery resident who will be applying for a vascular surgery fellowship this year.
“This specific project looks at epigenetic changes,” she continued. “It is a newer field, which looks at how variations in the environment can affect changes in the cell. We have found that a particular enzyme, SETDB2, is needed in macrophages for normal wound healing. Diabetics don’t have enough of the enzyme, which results in chronic inflammation.”
The research is important because the at-risk population is vast, and the opportunity for breakthrough research to have an impact has never been greater.
“Despite this,” said Dr. Kimball, “there are no effective treatments for abrogating the impaired wound healing seen in diabetes. And patients continue to suffer significant morbidity and mortality as a result.”
He added, “We hope our fundamental research will identify novel targets for the treatment of impaired wound healing in diabetes.”
Those attending the presentation, Epigenetic Mechanisms of Macrophage Phenotype Regulation in Diabetic Wound Healing, will learn about the immune system’s role in the early stages of wound healing. They will receive a better understanding of the role of epigenetics in influencing the wound cell inflammatory phenotype, and its effect on wound healing. They will also begin to realize how epigenetics influences a cell’s inflammatory phenotype.
Hopefully, the research will be an important first step – leading to new future therapies that target the enzyme and improve macrophage function in diabetic wounds.
“Andrew worked very hard, and I am very proud of his efforts,” said Dr. Gallagher. “He has done a phenomenal job in the lab, and his diligent work has advanced this field tremendously.”
She continued, “I have no doubt that Andrew will continue to make important scientific discoveries in our field in the future. He is certainly deserving of this award.”
Dr. Kimball and his coauthors have no relevant financial disclosures.
Friday, June 2
10:00 a.m.
SDCC, Room 6 A/B
Plenary 5, 2017 Resident Research Award
The issue of impaired wound healing in type 2 diabetes is a serious one and the leading cause of lower extremity amputation in the United States. The level of morbidity and mortality associated with diabetic foot ulcers has remained under the radar and, as a result, this important area of research has been understudied.
This year’s Resident Research Award winner, Andrew S. Kimball, MD, of the University of Michigan, will report on the research he and his colleagues performed on the immunologic and epigenetic mechanisms of wound healing in both physiologic and pathophysiologic states.
Dr. Kimball will present the research on Friday, June 2, at 10:00 a.m., discussing the role of specific epigenetic enzymes in the dictation of macrophage phenotype in wound tissue. The talk will cover how diabetes alters those enzymes to influence a deleterious phenotype that promotes inflammation and delays wound healing.
“Our lab specifically looks at the role of monocyte/macrophages in the inflammatory phase of wound healing and how perturbation in the local environment – as occurs in diabetes – affects monocyte/macrophage phenotype, and ultimately, wound healing,” said Dr. Kimball.
He is a PGY5 general surgery resident who will be applying for a vascular surgery fellowship this year.
“This specific project looks at epigenetic changes,” she continued. “It is a newer field, which looks at how variations in the environment can affect changes in the cell. We have found that a particular enzyme, SETDB2, is needed in macrophages for normal wound healing. Diabetics don’t have enough of the enzyme, which results in chronic inflammation.”
The research is important because the at-risk population is vast, and the opportunity for breakthrough research to have an impact has never been greater.
“Despite this,” said Dr. Kimball, “there are no effective treatments for abrogating the impaired wound healing seen in diabetes. And patients continue to suffer significant morbidity and mortality as a result.”
He added, “We hope our fundamental research will identify novel targets for the treatment of impaired wound healing in diabetes.”
Those attending the presentation, Epigenetic Mechanisms of Macrophage Phenotype Regulation in Diabetic Wound Healing, will learn about the immune system’s role in the early stages of wound healing. They will receive a better understanding of the role of epigenetics in influencing the wound cell inflammatory phenotype, and its effect on wound healing. They will also begin to realize how epigenetics influences a cell’s inflammatory phenotype.
Hopefully, the research will be an important first step – leading to new future therapies that target the enzyme and improve macrophage function in diabetic wounds.
“Andrew worked very hard, and I am very proud of his efforts,” said Dr. Gallagher. “He has done a phenomenal job in the lab, and his diligent work has advanced this field tremendously.”
She continued, “I have no doubt that Andrew will continue to make important scientific discoveries in our field in the future. He is certainly deserving of this award.”
Dr. Kimball and his coauthors have no relevant financial disclosures.
Friday, June 2
10:00 a.m.
SDCC, Room 6 A/B
Plenary 5, 2017 Resident Research Award