User login
HM17 session summary: The hospitalist’s role in the opioid epidemic
Presenters
Shoshana J. Herzig, MD, MPH, and Hillary J. Mosher, MFA, MD, FHM
Summary
The growth in opiate prescribing and associated increases in adverse events has created unique challenges for hospitalists, including how best to assess pain and opiate use disorders and how to safely prescribe opiates during hospitalization and at discharge.
These challenges are compounded by patient and system factors and a paucity of evidence-based guidelines to help guide safe administration of opiates in hospitalized patients. This can mean frustration for hospitalists and harm for patients.
Key takeaways for HM
- When assessing patients’ pain, it is crucial to differentiate between acute and chronic pain (or both) and whether it is nociceptive or neuropathic. Misclassification of pain contributes to inappropriate exposure and escalation of opiate therapy during hospitalization.
- Always consider nonopioid analgesics such as NSAIDs first and pair them with opiates. Studies in a variety of conditions have demonstrated that these are equally, if not more, effective, even for severe pain, such as with renal colic. Reserve opiates for moderate to severe pain.
- Always assess whether the benefits of initiating or continuing opioid therapy outweigh the risks for individual patients. There is no validated tool to predict risk for adverse events and/or opioid abuse disorder but a careful review of patient history can identify established risk factors (such as a history of mental illness or substance abuse disorders, renal impairment, or other comorbidities). In addition, nearly all states now have Prescription Drug Monitoring Programs, and hospitalists should consult these routinely when prescribing opiates.
- Always clearly discuss expectations and risks of opioid therapy, including the potential for development of opioid use disorders with hospitalized patients prior to initiation. Emphasize pain reduction rather than elimination and focus on functional goals such as improved mobility. Also, set expectations for stepping down treatment up front.
- Use the lowest effective dose of immediate-release opioids (preferably oral route) for shortest duration possible. Long acting opiates are associated with increased risk of adverse events, and their initiation should generally be avoided in hospitalized patients with noncancer pain.
- Minimize risk by avoiding concurrent administration of other medications with sedative properties, especially benzodiazepines, which have been found to significantly increase the risk of adverse events, including overdose.
- Recognize that chronic opioid use often begins with treatment of acute pain during hospitalization. Adopt best practice for discharge, including prescribing shorter courses whenever possible, discussing initiation, and changes or modifications in opiate therapy with patients’ primary care provider, and ensure timely postdischarge follow-up. Also consider coprescription of naloxone at discharge for higher risk patients.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
Presenters
Shoshana J. Herzig, MD, MPH, and Hillary J. Mosher, MFA, MD, FHM
Summary
The growth in opiate prescribing and associated increases in adverse events has created unique challenges for hospitalists, including how best to assess pain and opiate use disorders and how to safely prescribe opiates during hospitalization and at discharge.
These challenges are compounded by patient and system factors and a paucity of evidence-based guidelines to help guide safe administration of opiates in hospitalized patients. This can mean frustration for hospitalists and harm for patients.
Key takeaways for HM
- When assessing patients’ pain, it is crucial to differentiate between acute and chronic pain (or both) and whether it is nociceptive or neuropathic. Misclassification of pain contributes to inappropriate exposure and escalation of opiate therapy during hospitalization.
- Always consider nonopioid analgesics such as NSAIDs first and pair them with opiates. Studies in a variety of conditions have demonstrated that these are equally, if not more, effective, even for severe pain, such as with renal colic. Reserve opiates for moderate to severe pain.
- Always assess whether the benefits of initiating or continuing opioid therapy outweigh the risks for individual patients. There is no validated tool to predict risk for adverse events and/or opioid abuse disorder but a careful review of patient history can identify established risk factors (such as a history of mental illness or substance abuse disorders, renal impairment, or other comorbidities). In addition, nearly all states now have Prescription Drug Monitoring Programs, and hospitalists should consult these routinely when prescribing opiates.
- Always clearly discuss expectations and risks of opioid therapy, including the potential for development of opioid use disorders with hospitalized patients prior to initiation. Emphasize pain reduction rather than elimination and focus on functional goals such as improved mobility. Also, set expectations for stepping down treatment up front.
- Use the lowest effective dose of immediate-release opioids (preferably oral route) for shortest duration possible. Long acting opiates are associated with increased risk of adverse events, and their initiation should generally be avoided in hospitalized patients with noncancer pain.
- Minimize risk by avoiding concurrent administration of other medications with sedative properties, especially benzodiazepines, which have been found to significantly increase the risk of adverse events, including overdose.
- Recognize that chronic opioid use often begins with treatment of acute pain during hospitalization. Adopt best practice for discharge, including prescribing shorter courses whenever possible, discussing initiation, and changes or modifications in opiate therapy with patients’ primary care provider, and ensure timely postdischarge follow-up. Also consider coprescription of naloxone at discharge for higher risk patients.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
Presenters
Shoshana J. Herzig, MD, MPH, and Hillary J. Mosher, MFA, MD, FHM
Summary
The growth in opiate prescribing and associated increases in adverse events has created unique challenges for hospitalists, including how best to assess pain and opiate use disorders and how to safely prescribe opiates during hospitalization and at discharge.
These challenges are compounded by patient and system factors and a paucity of evidence-based guidelines to help guide safe administration of opiates in hospitalized patients. This can mean frustration for hospitalists and harm for patients.
Key takeaways for HM
- When assessing patients’ pain, it is crucial to differentiate between acute and chronic pain (or both) and whether it is nociceptive or neuropathic. Misclassification of pain contributes to inappropriate exposure and escalation of opiate therapy during hospitalization.
- Always consider nonopioid analgesics such as NSAIDs first and pair them with opiates. Studies in a variety of conditions have demonstrated that these are equally, if not more, effective, even for severe pain, such as with renal colic. Reserve opiates for moderate to severe pain.
- Always assess whether the benefits of initiating or continuing opioid therapy outweigh the risks for individual patients. There is no validated tool to predict risk for adverse events and/or opioid abuse disorder but a careful review of patient history can identify established risk factors (such as a history of mental illness or substance abuse disorders, renal impairment, or other comorbidities). In addition, nearly all states now have Prescription Drug Monitoring Programs, and hospitalists should consult these routinely when prescribing opiates.
- Always clearly discuss expectations and risks of opioid therapy, including the potential for development of opioid use disorders with hospitalized patients prior to initiation. Emphasize pain reduction rather than elimination and focus on functional goals such as improved mobility. Also, set expectations for stepping down treatment up front.
- Use the lowest effective dose of immediate-release opioids (preferably oral route) for shortest duration possible. Long acting opiates are associated with increased risk of adverse events, and their initiation should generally be avoided in hospitalized patients with noncancer pain.
- Minimize risk by avoiding concurrent administration of other medications with sedative properties, especially benzodiazepines, which have been found to significantly increase the risk of adverse events, including overdose.
- Recognize that chronic opioid use often begins with treatment of acute pain during hospitalization. Adopt best practice for discharge, including prescribing shorter courses whenever possible, discussing initiation, and changes or modifications in opiate therapy with patients’ primary care provider, and ensure timely postdischarge follow-up. Also consider coprescription of naloxone at discharge for higher risk patients.
Dr. Stella is a hospitalist in Denver and an editorial board member of The Hospitalist.
FRAX Prediction With and Without Bone Mineral Density Testing
In the U.S. about 2 million men have osteoporosis.1 About 1 in 5 men will experience an osteoporotic-related fracture in his lifetime.2 In addition, men with hip fracture have a higher mortality rate compared with that of women with hip fracture.3 The National Osteoporosis Foundation guidelines and the Endocrine Society guidelines recommend that all men aged ≥ 70 years have bone mineral density (BMD) testing. Depending on risk factors, osteoporosis screening may be appropriate for men aged ≥ 50 years. A BMD with a T-score of -2.5 or lower is classified as osteoporosis.2
In addition to osteoporosis, osteopenia also negatively impacts men. Osteopenia is defined as a BMD with a T-score of -1 to -2.5.2 According to the National Health and Nutrition Examination Survey (NHANES), about 30% of men aged ≥ 50 years have osteopenia.4 FRAX is a fracture risk assessment tool that is used to predict the 10-year risk of fracture in untreated patients with osteopenia. The FRAX tool has been validated with the use of BMD testing only at the femoral neck; it has not been validated in other parts of the body. Treatment is indicated if the 10-year fracture risk is > 20% for major osteoporotic fractures and > 3% for hip fractures, based on the FRAX calculation.2
The following risk factors are used in the FRAX calculation: age; sex; weight (kilograms); height (centimeters); previous fracture (yes or no); parental history of hip fracture (yes or no); current smoker (yes or no); oral glucocorticoid exposure currently or for > 3 months in the past (yes or no); rheumatoid arthritis (yes or no); secondary osteoporosis or a disorder strongly associated with osteoporosis, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism, premature menopause, chronic malnutrition, malabsorption, or chronic liver disease (yes or no); 3 or more units of alcohol daily (yes or no); and BMD.5
A dual-energy X-ray absorptiometry (DXA) examination is needed to determine BMD. However, a DXA examination is not always feasible for patients who have limited access, transportation challenges, require the use of assistive devices, and may be unaware of the importance of BMD testing.
The FRAX calculation can be obtained with or without BMD. Gadam and colleagues compared FRAX calculations with and without BMD to predict the 10-year risk of fracture.6 Their study found that 84% of patients had an identical fracture risk prediction whether or not BMD was included. The only risk factor evaluated that was significantly different between those with different treatment predictions and those with identical treatment predictions was age. However, the majority of patients included were female (96%).
No studies existed that compared fracture prediction risk with and without BMD in a male-only population. The purpose of this study was to determine whether FRAX without BMD was as effective as FRAX with BMD to predict the risk of osteoporotic fractures and provide an identical treatment recommendation in male veteran patients at the Lexington VAMC in Kentucky.
Methods
A retrospective chart review was conducted at the Lexington VAMC. Approval was obtained from the Lexington VAMC Institutional Review Board and Research and Development Committee. Patients were identified using the computerized patient record system (CPRS). Included patients were male, ≥ 50 years, had a documented DXA in CPRS from January 2006 to September 2015, and had a previous fracture determined by ICD-9 codes. Patients were excluded if they were diagnosed with osteoporosis or were ever treated for osteoporosis before a DXA scan.
Data collection included patient’s age, gender, race, glucocorticoid use for at least 3 months within 1 year prior to DXA, body weight within 3 months prior to DXA, height within 1 year prior to DXA, family history of fracture, previous fall or fracture, diagnosis of rheumatoid arthritis, smoking status at the time of DXA, alcohol intake of at least 3 drinks per day at the time of DXA, and vitamin D level within 1 year prior to DXA. In order to find a clinically significant difference (P < .05) with a power of 80%, a sample size of 64 patients was needed.
Each patient’s FRAX predictions were calculated with and without BMD. Patients were then separated into 2 groups: those who had an identical treatment recommendation when calculating FRAX with and without BMD, and those who had a different treatment recommendation when calculating FRAX with and without BMD. Binary variables for each group were compared using the Fisher exact test, and numeric variables were compared using a simple Student’s t test.
Results
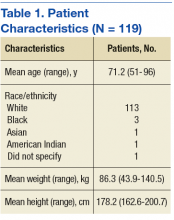
After screening 1,510 patients, only 119 patients met the criteria and were included in the study (Figure). All patients included were male. Mean age was 71.2 years and 113 (95.0%) were white (Table 1).
Of the 119 patients included in the study, 98 patients (82.4%) had the same treatment recommendation when the FRAX score was calculated with and without BMD. The remaining 21 patients (17.6%) had different treatment recommendations when FRAX scores were calculated with BMD compared with FRAX scores calculated without BMD. Treatment was recommended based on risk prediction for 43 of the 98 patients who had identical treatment recommendations. Of the 21 patients who had different treatment recommendations, treatment was recommended based on risk prediction for 14 patients when FRAX scores were calculated with BMD. Treatment was recommended for the other 7 patients when FRAX scores were calculated without BMD.
Of the numeric variables evaluated, mean age, femoral neck BMD, and T-score were all significantly different between the 2 groups (Table 2). Patients with an identical treatment recommendation were a mean age of 67.9 years (SD: 10.2 y), and patients with different treatment recommendations were a mean age of 62.2 years (SD: 8.9 y) (P = .011). Patients with an identical treatment recommendation had a mean BMD of 0.9 (SD: 0.2), and patients with different treatment recommendations had a mean BMD of 0.8 (SD: 0.1) (P = .021). Patients with an identical treatment recommendation had a mean T-score of -1.7 (SD: 1.2), and patients with different treatment recommendations had a mean T-score of -2.3 (SD: 1.1) (P = .031). Mean weight, height, and vitamin D level were not statistically significantly different between the 2 groups.
Of the binary variables evaluated, only glucocorticoid use was significantly different between the 2 groups. Of the patients with an identical treatment recommendation, 4 (4.1%) received a glucocorticoid.
Discussion
The purpose of this retrospective study was to determine whether using FRAX without BMD was as effective as using FRAX with BMD in predicting the risk of osteoporotic fractures and in providing identical treatment recommendations in male veteran patients. The results of this study revealed that FRAX calculations without BMD provided identical treatment recommendations as FRAX calculations with BMD for 82.4% of male veteran patients. These findings were similar to the findings of another study by Gadam and colleagues, in which 84% of patients had identical treatment recommendations when calculating FRAX scores with and without BMD.6 In contrast, a prospective cohort study by Ettinger and colleagues found that the addition of BMD to the FRAX calculation enhanced the performance of the FRAX tool by correctly identifying more patients who experienced a fracture within the following 10 years.8
Several of the risk factors evaluated in the present study were indicative of an identical treatment recommendation. Age was one of the risk factors that differed significantly between the 2 groups. The mean age of patients with an identical treatment recommendation was 67.9 years, and the mean age of patients with different treatment recommendations was 62.2 years (P = .011). These findings opposed the findings in the Gadam and colleagues’ study.6 The results of that study revealed that younger age rather than older age was more indicative of an identical treatment recommendation. The study by Gadam and colleagues included both male and female patients; however, the majority of patients included in the Gadam study were female (96%).6 Because the present study included only male patients, a comparison of the results was difficult because of the different patient populations.
A higher T-score (P = .031) and a higher BMD (P = .021) were the other 2 risk factors associated with an identical treatment recommendation with and without BMD. The Gadam and colleagues study did not find these to be significant risk factors for identifying an identical treatment recommendation.6
The FRAX calculation without BMD identified all the patients meeting treatment criteria based on the FRAX calculation with BMD except for 14 of the 119 patients (11.8%). Therefore, > 88% of patients who met treatment criteria based on FRAX calculated with BMD also met treatment criteria based on FRAX without BMD.
The FRAX calculation has several advantages, including risk stratification in men and identifying those with other conditions that may predispose them to a fracture.7 Therefore, before obtaining a DXA scan, it would be reasonable to calculate a FRAX score without BMD to identify patients who are at high risk for fracture but who may not receive treatment because they are not considered to need a DXA scan or a DXA scan is not feasible.
Limitations
Currently, FRAX is validated only using femoral neck BMD. This study was a retrospective chart review only; no information was obtained from communicating with the patient, including the patient’s past medical history and family history. Also, this study had a small sample size: Of the 1,510 patients screened, only 119 met inclusion criteria. None of the 119 patients evaluated had a family history of fracture documented in their CPRS. Therefore, several of the patient’s 10-year fracture risk scores may be underestimated if one or both of their parents experienced a fracture. Last, the majority of patients included in this study were white, so the results of this study cannot necessarily be generalized to other races.
Conclusion
The majority of male patients had an identical treatment recommendation when a FRAX score was calculated with and without BMD. Older age, higher BMD, and higher T-score were all indicative of an identical treatment recommendation. Larger studies are necessary in order to validate the FRAX tool without the use of femoral neck BMD. However, the FRAX tool alone can be beneficial to identify male patients who should have a DXA scan performed to obtain a BMD. If a male patient’s FRAX score suggests risk for osteoporotic fracture, then a DXA scan should be completed to obtain a BMD if feasible.
Additionally, when obtaining a BMD is not feasible to predict fracture risk, the FRAX tool alone may be useful a majority of the time to accurately determine treatment recommendations in male patients aged > 65 years. The results of this study lead the authors to believe that FRAX without BMD in male patients aged > 65 years will appropriately identify more patients for treatment. ˜
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Lexington VA Medical Center.
1. Sweet MG, Sweet JM, Jeremiah MP, Galazka SS. Diagnosis and treatment of osteoporosis. Am Fam Physician. 2009;79(3):193-200.
2. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
3. Khan AA, Hodsman AB, Papaioannou A, Kendler D, Brown JP, Olszynski WP. Management of osteoporosis in men: an update and case example. CMAJ. 2007;176(3):345-348.
4. Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64-71.
5. Kanas JA; World Health Organization Scientific Group. Assessment of osteoporosis at the primary health care level. https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Published 2007. Accessed March 29, 2017.
6. Gadam RK, Schlauch K, Izuora KE. FRAX prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013;19(5):780-784.
7. Siris E, Delmas PD. Assessment of 10-year absolute fracture risk: a new paradigm with worldwide application. Osteoporosis Int. 2008;19(4):383-384.
8. Ettinger B, Liu H, Blackwell T, et al. Validation of FRC, a fracture risk assessment tool, in a cohort of older men: the osteoporotic fractures in men (MrOS) study. J Clin Densitom. 2012;15(3):334-342.
In the U.S. about 2 million men have osteoporosis.1 About 1 in 5 men will experience an osteoporotic-related fracture in his lifetime.2 In addition, men with hip fracture have a higher mortality rate compared with that of women with hip fracture.3 The National Osteoporosis Foundation guidelines and the Endocrine Society guidelines recommend that all men aged ≥ 70 years have bone mineral density (BMD) testing. Depending on risk factors, osteoporosis screening may be appropriate for men aged ≥ 50 years. A BMD with a T-score of -2.5 or lower is classified as osteoporosis.2
In addition to osteoporosis, osteopenia also negatively impacts men. Osteopenia is defined as a BMD with a T-score of -1 to -2.5.2 According to the National Health and Nutrition Examination Survey (NHANES), about 30% of men aged ≥ 50 years have osteopenia.4 FRAX is a fracture risk assessment tool that is used to predict the 10-year risk of fracture in untreated patients with osteopenia. The FRAX tool has been validated with the use of BMD testing only at the femoral neck; it has not been validated in other parts of the body. Treatment is indicated if the 10-year fracture risk is > 20% for major osteoporotic fractures and > 3% for hip fractures, based on the FRAX calculation.2
The following risk factors are used in the FRAX calculation: age; sex; weight (kilograms); height (centimeters); previous fracture (yes or no); parental history of hip fracture (yes or no); current smoker (yes or no); oral glucocorticoid exposure currently or for > 3 months in the past (yes or no); rheumatoid arthritis (yes or no); secondary osteoporosis or a disorder strongly associated with osteoporosis, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism, premature menopause, chronic malnutrition, malabsorption, or chronic liver disease (yes or no); 3 or more units of alcohol daily (yes or no); and BMD.5
A dual-energy X-ray absorptiometry (DXA) examination is needed to determine BMD. However, a DXA examination is not always feasible for patients who have limited access, transportation challenges, require the use of assistive devices, and may be unaware of the importance of BMD testing.
The FRAX calculation can be obtained with or without BMD. Gadam and colleagues compared FRAX calculations with and without BMD to predict the 10-year risk of fracture.6 Their study found that 84% of patients had an identical fracture risk prediction whether or not BMD was included. The only risk factor evaluated that was significantly different between those with different treatment predictions and those with identical treatment predictions was age. However, the majority of patients included were female (96%).
No studies existed that compared fracture prediction risk with and without BMD in a male-only population. The purpose of this study was to determine whether FRAX without BMD was as effective as FRAX with BMD to predict the risk of osteoporotic fractures and provide an identical treatment recommendation in male veteran patients at the Lexington VAMC in Kentucky.
Methods
A retrospective chart review was conducted at the Lexington VAMC. Approval was obtained from the Lexington VAMC Institutional Review Board and Research and Development Committee. Patients were identified using the computerized patient record system (CPRS). Included patients were male, ≥ 50 years, had a documented DXA in CPRS from January 2006 to September 2015, and had a previous fracture determined by ICD-9 codes. Patients were excluded if they were diagnosed with osteoporosis or were ever treated for osteoporosis before a DXA scan.
Data collection included patient’s age, gender, race, glucocorticoid use for at least 3 months within 1 year prior to DXA, body weight within 3 months prior to DXA, height within 1 year prior to DXA, family history of fracture, previous fall or fracture, diagnosis of rheumatoid arthritis, smoking status at the time of DXA, alcohol intake of at least 3 drinks per day at the time of DXA, and vitamin D level within 1 year prior to DXA. In order to find a clinically significant difference (P < .05) with a power of 80%, a sample size of 64 patients was needed.
Each patient’s FRAX predictions were calculated with and without BMD. Patients were then separated into 2 groups: those who had an identical treatment recommendation when calculating FRAX with and without BMD, and those who had a different treatment recommendation when calculating FRAX with and without BMD. Binary variables for each group were compared using the Fisher exact test, and numeric variables were compared using a simple Student’s t test.
Results
After screening 1,510 patients, only 119 patients met the criteria and were included in the study (Figure). All patients included were male. Mean age was 71.2 years and 113 (95.0%) were white (Table 1).
Of the 119 patients included in the study, 98 patients (82.4%) had the same treatment recommendation when the FRAX score was calculated with and without BMD. The remaining 21 patients (17.6%) had different treatment recommendations when FRAX scores were calculated with BMD compared with FRAX scores calculated without BMD. Treatment was recommended based on risk prediction for 43 of the 98 patients who had identical treatment recommendations. Of the 21 patients who had different treatment recommendations, treatment was recommended based on risk prediction for 14 patients when FRAX scores were calculated with BMD. Treatment was recommended for the other 7 patients when FRAX scores were calculated without BMD.
Of the numeric variables evaluated, mean age, femoral neck BMD, and T-score were all significantly different between the 2 groups (Table 2). Patients with an identical treatment recommendation were a mean age of 67.9 years (SD: 10.2 y), and patients with different treatment recommendations were a mean age of 62.2 years (SD: 8.9 y) (P = .011). Patients with an identical treatment recommendation had a mean BMD of 0.9 (SD: 0.2), and patients with different treatment recommendations had a mean BMD of 0.8 (SD: 0.1) (P = .021). Patients with an identical treatment recommendation had a mean T-score of -1.7 (SD: 1.2), and patients with different treatment recommendations had a mean T-score of -2.3 (SD: 1.1) (P = .031). Mean weight, height, and vitamin D level were not statistically significantly different between the 2 groups.
Of the binary variables evaluated, only glucocorticoid use was significantly different between the 2 groups. Of the patients with an identical treatment recommendation, 4 (4.1%) received a glucocorticoid.
Discussion
The purpose of this retrospective study was to determine whether using FRAX without BMD was as effective as using FRAX with BMD in predicting the risk of osteoporotic fractures and in providing identical treatment recommendations in male veteran patients. The results of this study revealed that FRAX calculations without BMD provided identical treatment recommendations as FRAX calculations with BMD for 82.4% of male veteran patients. These findings were similar to the findings of another study by Gadam and colleagues, in which 84% of patients had identical treatment recommendations when calculating FRAX scores with and without BMD.6 In contrast, a prospective cohort study by Ettinger and colleagues found that the addition of BMD to the FRAX calculation enhanced the performance of the FRAX tool by correctly identifying more patients who experienced a fracture within the following 10 years.8
Several of the risk factors evaluated in the present study were indicative of an identical treatment recommendation. Age was one of the risk factors that differed significantly between the 2 groups. The mean age of patients with an identical treatment recommendation was 67.9 years, and the mean age of patients with different treatment recommendations was 62.2 years (P = .011). These findings opposed the findings in the Gadam and colleagues’ study.6 The results of that study revealed that younger age rather than older age was more indicative of an identical treatment recommendation. The study by Gadam and colleagues included both male and female patients; however, the majority of patients included in the Gadam study were female (96%).6 Because the present study included only male patients, a comparison of the results was difficult because of the different patient populations.
A higher T-score (P = .031) and a higher BMD (P = .021) were the other 2 risk factors associated with an identical treatment recommendation with and without BMD. The Gadam and colleagues study did not find these to be significant risk factors for identifying an identical treatment recommendation.6
The FRAX calculation without BMD identified all the patients meeting treatment criteria based on the FRAX calculation with BMD except for 14 of the 119 patients (11.8%). Therefore, > 88% of patients who met treatment criteria based on FRAX calculated with BMD also met treatment criteria based on FRAX without BMD.
The FRAX calculation has several advantages, including risk stratification in men and identifying those with other conditions that may predispose them to a fracture.7 Therefore, before obtaining a DXA scan, it would be reasonable to calculate a FRAX score without BMD to identify patients who are at high risk for fracture but who may not receive treatment because they are not considered to need a DXA scan or a DXA scan is not feasible.
Limitations
Currently, FRAX is validated only using femoral neck BMD. This study was a retrospective chart review only; no information was obtained from communicating with the patient, including the patient’s past medical history and family history. Also, this study had a small sample size: Of the 1,510 patients screened, only 119 met inclusion criteria. None of the 119 patients evaluated had a family history of fracture documented in their CPRS. Therefore, several of the patient’s 10-year fracture risk scores may be underestimated if one or both of their parents experienced a fracture. Last, the majority of patients included in this study were white, so the results of this study cannot necessarily be generalized to other races.
Conclusion
The majority of male patients had an identical treatment recommendation when a FRAX score was calculated with and without BMD. Older age, higher BMD, and higher T-score were all indicative of an identical treatment recommendation. Larger studies are necessary in order to validate the FRAX tool without the use of femoral neck BMD. However, the FRAX tool alone can be beneficial to identify male patients who should have a DXA scan performed to obtain a BMD. If a male patient’s FRAX score suggests risk for osteoporotic fracture, then a DXA scan should be completed to obtain a BMD if feasible.
Additionally, when obtaining a BMD is not feasible to predict fracture risk, the FRAX tool alone may be useful a majority of the time to accurately determine treatment recommendations in male patients aged > 65 years. The results of this study lead the authors to believe that FRAX without BMD in male patients aged > 65 years will appropriately identify more patients for treatment. ˜
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Lexington VA Medical Center.
In the U.S. about 2 million men have osteoporosis.1 About 1 in 5 men will experience an osteoporotic-related fracture in his lifetime.2 In addition, men with hip fracture have a higher mortality rate compared with that of women with hip fracture.3 The National Osteoporosis Foundation guidelines and the Endocrine Society guidelines recommend that all men aged ≥ 70 years have bone mineral density (BMD) testing. Depending on risk factors, osteoporosis screening may be appropriate for men aged ≥ 50 years. A BMD with a T-score of -2.5 or lower is classified as osteoporosis.2
In addition to osteoporosis, osteopenia also negatively impacts men. Osteopenia is defined as a BMD with a T-score of -1 to -2.5.2 According to the National Health and Nutrition Examination Survey (NHANES), about 30% of men aged ≥ 50 years have osteopenia.4 FRAX is a fracture risk assessment tool that is used to predict the 10-year risk of fracture in untreated patients with osteopenia. The FRAX tool has been validated with the use of BMD testing only at the femoral neck; it has not been validated in other parts of the body. Treatment is indicated if the 10-year fracture risk is > 20% for major osteoporotic fractures and > 3% for hip fractures, based on the FRAX calculation.2
The following risk factors are used in the FRAX calculation: age; sex; weight (kilograms); height (centimeters); previous fracture (yes or no); parental history of hip fracture (yes or no); current smoker (yes or no); oral glucocorticoid exposure currently or for > 3 months in the past (yes or no); rheumatoid arthritis (yes or no); secondary osteoporosis or a disorder strongly associated with osteoporosis, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism, premature menopause, chronic malnutrition, malabsorption, or chronic liver disease (yes or no); 3 or more units of alcohol daily (yes or no); and BMD.5
A dual-energy X-ray absorptiometry (DXA) examination is needed to determine BMD. However, a DXA examination is not always feasible for patients who have limited access, transportation challenges, require the use of assistive devices, and may be unaware of the importance of BMD testing.
The FRAX calculation can be obtained with or without BMD. Gadam and colleagues compared FRAX calculations with and without BMD to predict the 10-year risk of fracture.6 Their study found that 84% of patients had an identical fracture risk prediction whether or not BMD was included. The only risk factor evaluated that was significantly different between those with different treatment predictions and those with identical treatment predictions was age. However, the majority of patients included were female (96%).
No studies existed that compared fracture prediction risk with and without BMD in a male-only population. The purpose of this study was to determine whether FRAX without BMD was as effective as FRAX with BMD to predict the risk of osteoporotic fractures and provide an identical treatment recommendation in male veteran patients at the Lexington VAMC in Kentucky.
Methods
A retrospective chart review was conducted at the Lexington VAMC. Approval was obtained from the Lexington VAMC Institutional Review Board and Research and Development Committee. Patients were identified using the computerized patient record system (CPRS). Included patients were male, ≥ 50 years, had a documented DXA in CPRS from January 2006 to September 2015, and had a previous fracture determined by ICD-9 codes. Patients were excluded if they were diagnosed with osteoporosis or were ever treated for osteoporosis before a DXA scan.
Data collection included patient’s age, gender, race, glucocorticoid use for at least 3 months within 1 year prior to DXA, body weight within 3 months prior to DXA, height within 1 year prior to DXA, family history of fracture, previous fall or fracture, diagnosis of rheumatoid arthritis, smoking status at the time of DXA, alcohol intake of at least 3 drinks per day at the time of DXA, and vitamin D level within 1 year prior to DXA. In order to find a clinically significant difference (P < .05) with a power of 80%, a sample size of 64 patients was needed.
Each patient’s FRAX predictions were calculated with and without BMD. Patients were then separated into 2 groups: those who had an identical treatment recommendation when calculating FRAX with and without BMD, and those who had a different treatment recommendation when calculating FRAX with and without BMD. Binary variables for each group were compared using the Fisher exact test, and numeric variables were compared using a simple Student’s t test.
Results
After screening 1,510 patients, only 119 patients met the criteria and were included in the study (Figure). All patients included were male. Mean age was 71.2 years and 113 (95.0%) were white (Table 1).
Of the 119 patients included in the study, 98 patients (82.4%) had the same treatment recommendation when the FRAX score was calculated with and without BMD. The remaining 21 patients (17.6%) had different treatment recommendations when FRAX scores were calculated with BMD compared with FRAX scores calculated without BMD. Treatment was recommended based on risk prediction for 43 of the 98 patients who had identical treatment recommendations. Of the 21 patients who had different treatment recommendations, treatment was recommended based on risk prediction for 14 patients when FRAX scores were calculated with BMD. Treatment was recommended for the other 7 patients when FRAX scores were calculated without BMD.
Of the numeric variables evaluated, mean age, femoral neck BMD, and T-score were all significantly different between the 2 groups (Table 2). Patients with an identical treatment recommendation were a mean age of 67.9 years (SD: 10.2 y), and patients with different treatment recommendations were a mean age of 62.2 years (SD: 8.9 y) (P = .011). Patients with an identical treatment recommendation had a mean BMD of 0.9 (SD: 0.2), and patients with different treatment recommendations had a mean BMD of 0.8 (SD: 0.1) (P = .021). Patients with an identical treatment recommendation had a mean T-score of -1.7 (SD: 1.2), and patients with different treatment recommendations had a mean T-score of -2.3 (SD: 1.1) (P = .031). Mean weight, height, and vitamin D level were not statistically significantly different between the 2 groups.
Of the binary variables evaluated, only glucocorticoid use was significantly different between the 2 groups. Of the patients with an identical treatment recommendation, 4 (4.1%) received a glucocorticoid.
Discussion
The purpose of this retrospective study was to determine whether using FRAX without BMD was as effective as using FRAX with BMD in predicting the risk of osteoporotic fractures and in providing identical treatment recommendations in male veteran patients. The results of this study revealed that FRAX calculations without BMD provided identical treatment recommendations as FRAX calculations with BMD for 82.4% of male veteran patients. These findings were similar to the findings of another study by Gadam and colleagues, in which 84% of patients had identical treatment recommendations when calculating FRAX scores with and without BMD.6 In contrast, a prospective cohort study by Ettinger and colleagues found that the addition of BMD to the FRAX calculation enhanced the performance of the FRAX tool by correctly identifying more patients who experienced a fracture within the following 10 years.8
Several of the risk factors evaluated in the present study were indicative of an identical treatment recommendation. Age was one of the risk factors that differed significantly between the 2 groups. The mean age of patients with an identical treatment recommendation was 67.9 years, and the mean age of patients with different treatment recommendations was 62.2 years (P = .011). These findings opposed the findings in the Gadam and colleagues’ study.6 The results of that study revealed that younger age rather than older age was more indicative of an identical treatment recommendation. The study by Gadam and colleagues included both male and female patients; however, the majority of patients included in the Gadam study were female (96%).6 Because the present study included only male patients, a comparison of the results was difficult because of the different patient populations.
A higher T-score (P = .031) and a higher BMD (P = .021) were the other 2 risk factors associated with an identical treatment recommendation with and without BMD. The Gadam and colleagues study did not find these to be significant risk factors for identifying an identical treatment recommendation.6
The FRAX calculation without BMD identified all the patients meeting treatment criteria based on the FRAX calculation with BMD except for 14 of the 119 patients (11.8%). Therefore, > 88% of patients who met treatment criteria based on FRAX calculated with BMD also met treatment criteria based on FRAX without BMD.
The FRAX calculation has several advantages, including risk stratification in men and identifying those with other conditions that may predispose them to a fracture.7 Therefore, before obtaining a DXA scan, it would be reasonable to calculate a FRAX score without BMD to identify patients who are at high risk for fracture but who may not receive treatment because they are not considered to need a DXA scan or a DXA scan is not feasible.
Limitations
Currently, FRAX is validated only using femoral neck BMD. This study was a retrospective chart review only; no information was obtained from communicating with the patient, including the patient’s past medical history and family history. Also, this study had a small sample size: Of the 1,510 patients screened, only 119 met inclusion criteria. None of the 119 patients evaluated had a family history of fracture documented in their CPRS. Therefore, several of the patient’s 10-year fracture risk scores may be underestimated if one or both of their parents experienced a fracture. Last, the majority of patients included in this study were white, so the results of this study cannot necessarily be generalized to other races.
Conclusion
The majority of male patients had an identical treatment recommendation when a FRAX score was calculated with and without BMD. Older age, higher BMD, and higher T-score were all indicative of an identical treatment recommendation. Larger studies are necessary in order to validate the FRAX tool without the use of femoral neck BMD. However, the FRAX tool alone can be beneficial to identify male patients who should have a DXA scan performed to obtain a BMD. If a male patient’s FRAX score suggests risk for osteoporotic fracture, then a DXA scan should be completed to obtain a BMD if feasible.
Additionally, when obtaining a BMD is not feasible to predict fracture risk, the FRAX tool alone may be useful a majority of the time to accurately determine treatment recommendations in male patients aged > 65 years. The results of this study lead the authors to believe that FRAX without BMD in male patients aged > 65 years will appropriately identify more patients for treatment. ˜
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Lexington VA Medical Center.
1. Sweet MG, Sweet JM, Jeremiah MP, Galazka SS. Diagnosis and treatment of osteoporosis. Am Fam Physician. 2009;79(3):193-200.
2. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
3. Khan AA, Hodsman AB, Papaioannou A, Kendler D, Brown JP, Olszynski WP. Management of osteoporosis in men: an update and case example. CMAJ. 2007;176(3):345-348.
4. Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64-71.
5. Kanas JA; World Health Organization Scientific Group. Assessment of osteoporosis at the primary health care level. https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Published 2007. Accessed March 29, 2017.
6. Gadam RK, Schlauch K, Izuora KE. FRAX prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013;19(5):780-784.
7. Siris E, Delmas PD. Assessment of 10-year absolute fracture risk: a new paradigm with worldwide application. Osteoporosis Int. 2008;19(4):383-384.
8. Ettinger B, Liu H, Blackwell T, et al. Validation of FRC, a fracture risk assessment tool, in a cohort of older men: the osteoporotic fractures in men (MrOS) study. J Clin Densitom. 2012;15(3):334-342.
1. Sweet MG, Sweet JM, Jeremiah MP, Galazka SS. Diagnosis and treatment of osteoporosis. Am Fam Physician. 2009;79(3):193-200.
2. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
3. Khan AA, Hodsman AB, Papaioannou A, Kendler D, Brown JP, Olszynski WP. Management of osteoporosis in men: an update and case example. CMAJ. 2007;176(3):345-348.
4. Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64-71.
5. Kanas JA; World Health Organization Scientific Group. Assessment of osteoporosis at the primary health care level. https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Published 2007. Accessed March 29, 2017.
6. Gadam RK, Schlauch K, Izuora KE. FRAX prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013;19(5):780-784.
7. Siris E, Delmas PD. Assessment of 10-year absolute fracture risk: a new paradigm with worldwide application. Osteoporosis Int. 2008;19(4):383-384.
8. Ettinger B, Liu H, Blackwell T, et al. Validation of FRC, a fracture risk assessment tool, in a cohort of older men: the osteoporotic fractures in men (MrOS) study. J Clin Densitom. 2012;15(3):334-342.
Finding could lead to ‘Holy Grail’ of antithrombotic therapy
The protein CIB1 may be a superior target for antithrombotic therapy, according to researchers.
The team found that CIB1 plays a role in thrombus development but not in initial clot formation.
“The Holy Grail of our field is to reduce unwanted thrombus formation without completely blocking other important platelet functions,” said study author Ulhas Naik, PhD, of Thomas Jefferson University in Philadelphia, Pennsylvania.
He and his colleagues believe targeting CIB1 may do just that.
In earlier work, the researchers showed that CIB1 was involved in thrombus formation. They found mice that lacked the CIB1 gene were less likely to form a thrombus.
That work also indicated that mice lacking the CIB1 were still able to form a platelet plug, suggesting this gene was involved only in the process of thrombus formation.
To investigate this possibility further and to demonstrate that the process was relevant to human physiology, Dr Naik and his colleagues conducted the current study.
The team described this work in PLOS ONE.
The researchers studied human platelets and probed the molecules that interacted with CIB1 at different time points after platelet activation.
The team found that CIB1 does not begin to bind and interact with platelet molecular machinery until after filopodia formation, which allows platelets to cross-link to one another and begin to form a plug.
The study also elucidated a number of molecules that CIB1 interacts with during outside-in signaling and thrombus formation.
“This work demonstrates that CIB1 could be a good antithrombotic drug target,” Dr Naik said. “If we block CIB1, it hampers thrombus formation without interfering with platelet plug formation. If developed further, blocking CIB1 could reduce the risk of heart attack and stroke without increasing the risk for excessive bleeding that is the trade-off of current medication.”
The next step for Dr Naik and his colleagues is screening for small-molecule compounds that would inhibit CIB1 and could be developed into new therapies. ![]()
The protein CIB1 may be a superior target for antithrombotic therapy, according to researchers.
The team found that CIB1 plays a role in thrombus development but not in initial clot formation.
“The Holy Grail of our field is to reduce unwanted thrombus formation without completely blocking other important platelet functions,” said study author Ulhas Naik, PhD, of Thomas Jefferson University in Philadelphia, Pennsylvania.
He and his colleagues believe targeting CIB1 may do just that.
In earlier work, the researchers showed that CIB1 was involved in thrombus formation. They found mice that lacked the CIB1 gene were less likely to form a thrombus.
That work also indicated that mice lacking the CIB1 were still able to form a platelet plug, suggesting this gene was involved only in the process of thrombus formation.
To investigate this possibility further and to demonstrate that the process was relevant to human physiology, Dr Naik and his colleagues conducted the current study.
The team described this work in PLOS ONE.
The researchers studied human platelets and probed the molecules that interacted with CIB1 at different time points after platelet activation.
The team found that CIB1 does not begin to bind and interact with platelet molecular machinery until after filopodia formation, which allows platelets to cross-link to one another and begin to form a plug.
The study also elucidated a number of molecules that CIB1 interacts with during outside-in signaling and thrombus formation.
“This work demonstrates that CIB1 could be a good antithrombotic drug target,” Dr Naik said. “If we block CIB1, it hampers thrombus formation without interfering with platelet plug formation. If developed further, blocking CIB1 could reduce the risk of heart attack and stroke without increasing the risk for excessive bleeding that is the trade-off of current medication.”
The next step for Dr Naik and his colleagues is screening for small-molecule compounds that would inhibit CIB1 and could be developed into new therapies. ![]()
The protein CIB1 may be a superior target for antithrombotic therapy, according to researchers.
The team found that CIB1 plays a role in thrombus development but not in initial clot formation.
“The Holy Grail of our field is to reduce unwanted thrombus formation without completely blocking other important platelet functions,” said study author Ulhas Naik, PhD, of Thomas Jefferson University in Philadelphia, Pennsylvania.
He and his colleagues believe targeting CIB1 may do just that.
In earlier work, the researchers showed that CIB1 was involved in thrombus formation. They found mice that lacked the CIB1 gene were less likely to form a thrombus.
That work also indicated that mice lacking the CIB1 were still able to form a platelet plug, suggesting this gene was involved only in the process of thrombus formation.
To investigate this possibility further and to demonstrate that the process was relevant to human physiology, Dr Naik and his colleagues conducted the current study.
The team described this work in PLOS ONE.
The researchers studied human platelets and probed the molecules that interacted with CIB1 at different time points after platelet activation.
The team found that CIB1 does not begin to bind and interact with platelet molecular machinery until after filopodia formation, which allows platelets to cross-link to one another and begin to form a plug.
The study also elucidated a number of molecules that CIB1 interacts with during outside-in signaling and thrombus formation.
“This work demonstrates that CIB1 could be a good antithrombotic drug target,” Dr Naik said. “If we block CIB1, it hampers thrombus formation without interfering with platelet plug formation. If developed further, blocking CIB1 could reduce the risk of heart attack and stroke without increasing the risk for excessive bleeding that is the trade-off of current medication.”
The next step for Dr Naik and his colleagues is screening for small-molecule compounds that would inhibit CIB1 and could be developed into new therapies. ![]()
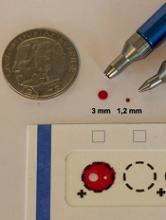
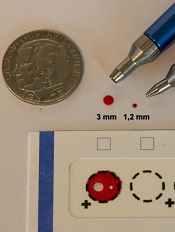
Study supports wider use of dried blood samples
Researchers have found evidence to suggest that dried blood samples may sometimes be a suitable alternative to conventional blood sampling.
The team measured levels of 92 proteins in millimeter-sized circles punched out of dried blood samples.
They found that, in many cases, little happens to these proteins when they are allowed to dry.
Most of the proteins remain unaltered after 30 years, or they change only minimally.
However, the proteins can be affected by storage temperatures.
Still, the researchers believe these results suggest dried blood samples could be used more widely—for routine health checks and to set up large-scale biobanks, with patients collecting the blood samples themselves.
“[Y]ou can prick your own finger and send in a dried blood spot by post,” study author Ulf Landegren, MD, PhD, of Uppsala University in Sweden.
“[A]t a minimal cost, it will be possible to build gigantic biobanks of samples obtained on a routine clinical basis. This means that samples can be taken before the clinical debut of a disease to identify markers of value for early diagnosis, improving the scope for curative treatment.”
Dr Landegren and his colleagues discussed these possibilities in a paper published in Molecular and Cellular Proteomics.
The researchers analyzed dried blood samples, measuring levels of 92 proteins that are relevant in oncology. To determine the effects of long-term storage, the team examined what happens to protein detection as an effect of the drying process.
Some of the dried blood samples analyzed had been collected recently, while others had been preserved for up to 30 years in biobanks in Sweden and Denmark. These 2 biobanks keep their dried blood samples at different temperatures: the Swedish one at +4°C and the Danish one at -24°C.
The researchers also looked at wet plasma samples kept at -70°C for corresponding periods of time.
“Our conclusion is that we can measure levels of 92 proteins with very high precision and sensitivity using PEA [proximity extension assay] technology in the tiny, punched-out discs from a dried blood spot,” said study author Johan Björkesten, a doctoral student at Uppsala University.
“The actual drying process has a negligible effect on the various proteins, and the effect is reproducible, which means that it can be included in the calculation.”
The researchers did find that long-term storage affects the detectability of certain proteins more than others.
Most proteins remain completely intact after 30 years or exhibit minimal changes. However, levels of some proteins decrease so that half the quantity remains after a period of between 10 and 50 years.
The researchers also found that a relatively low storage temperature is preferable for proteins that are affected by storage.
Protein detection was less affected when dried blood samples were stored at -24°C than when they were stored at +4°C. Over the 30-year period, detectability was not affected for 34% of proteins stored at +4°C and 76% of proteins stored at -24°C.
However, storing wet plasma at -70°C preserved proteins better than dried blood sample storage at -24°C. Detectability decreased for 5% of the proteins stored wet at -70°C for 45 years, compared to 24% for proteins in dried samples stored at -24°C for 30 years.
The researchers did note, though, that this part of their analysis was complicated by some confounding factors, so this was not a clear, direct comparison between wet and dry samples. ![]()
Researchers have found evidence to suggest that dried blood samples may sometimes be a suitable alternative to conventional blood sampling.
The team measured levels of 92 proteins in millimeter-sized circles punched out of dried blood samples.
They found that, in many cases, little happens to these proteins when they are allowed to dry.
Most of the proteins remain unaltered after 30 years, or they change only minimally.
However, the proteins can be affected by storage temperatures.
Still, the researchers believe these results suggest dried blood samples could be used more widely—for routine health checks and to set up large-scale biobanks, with patients collecting the blood samples themselves.
“[Y]ou can prick your own finger and send in a dried blood spot by post,” study author Ulf Landegren, MD, PhD, of Uppsala University in Sweden.
“[A]t a minimal cost, it will be possible to build gigantic biobanks of samples obtained on a routine clinical basis. This means that samples can be taken before the clinical debut of a disease to identify markers of value for early diagnosis, improving the scope for curative treatment.”
Dr Landegren and his colleagues discussed these possibilities in a paper published in Molecular and Cellular Proteomics.
The researchers analyzed dried blood samples, measuring levels of 92 proteins that are relevant in oncology. To determine the effects of long-term storage, the team examined what happens to protein detection as an effect of the drying process.
Some of the dried blood samples analyzed had been collected recently, while others had been preserved for up to 30 years in biobanks in Sweden and Denmark. These 2 biobanks keep their dried blood samples at different temperatures: the Swedish one at +4°C and the Danish one at -24°C.
The researchers also looked at wet plasma samples kept at -70°C for corresponding periods of time.
“Our conclusion is that we can measure levels of 92 proteins with very high precision and sensitivity using PEA [proximity extension assay] technology in the tiny, punched-out discs from a dried blood spot,” said study author Johan Björkesten, a doctoral student at Uppsala University.
“The actual drying process has a negligible effect on the various proteins, and the effect is reproducible, which means that it can be included in the calculation.”
The researchers did find that long-term storage affects the detectability of certain proteins more than others.
Most proteins remain completely intact after 30 years or exhibit minimal changes. However, levels of some proteins decrease so that half the quantity remains after a period of between 10 and 50 years.
The researchers also found that a relatively low storage temperature is preferable for proteins that are affected by storage.
Protein detection was less affected when dried blood samples were stored at -24°C than when they were stored at +4°C. Over the 30-year period, detectability was not affected for 34% of proteins stored at +4°C and 76% of proteins stored at -24°C.
However, storing wet plasma at -70°C preserved proteins better than dried blood sample storage at -24°C. Detectability decreased for 5% of the proteins stored wet at -70°C for 45 years, compared to 24% for proteins in dried samples stored at -24°C for 30 years.
The researchers did note, though, that this part of their analysis was complicated by some confounding factors, so this was not a clear, direct comparison between wet and dry samples. ![]()
Researchers have found evidence to suggest that dried blood samples may sometimes be a suitable alternative to conventional blood sampling.
The team measured levels of 92 proteins in millimeter-sized circles punched out of dried blood samples.
They found that, in many cases, little happens to these proteins when they are allowed to dry.
Most of the proteins remain unaltered after 30 years, or they change only minimally.
However, the proteins can be affected by storage temperatures.
Still, the researchers believe these results suggest dried blood samples could be used more widely—for routine health checks and to set up large-scale biobanks, with patients collecting the blood samples themselves.
“[Y]ou can prick your own finger and send in a dried blood spot by post,” study author Ulf Landegren, MD, PhD, of Uppsala University in Sweden.
“[A]t a minimal cost, it will be possible to build gigantic biobanks of samples obtained on a routine clinical basis. This means that samples can be taken before the clinical debut of a disease to identify markers of value for early diagnosis, improving the scope for curative treatment.”
Dr Landegren and his colleagues discussed these possibilities in a paper published in Molecular and Cellular Proteomics.
The researchers analyzed dried blood samples, measuring levels of 92 proteins that are relevant in oncology. To determine the effects of long-term storage, the team examined what happens to protein detection as an effect of the drying process.
Some of the dried blood samples analyzed had been collected recently, while others had been preserved for up to 30 years in biobanks in Sweden and Denmark. These 2 biobanks keep their dried blood samples at different temperatures: the Swedish one at +4°C and the Danish one at -24°C.
The researchers also looked at wet plasma samples kept at -70°C for corresponding periods of time.
“Our conclusion is that we can measure levels of 92 proteins with very high precision and sensitivity using PEA [proximity extension assay] technology in the tiny, punched-out discs from a dried blood spot,” said study author Johan Björkesten, a doctoral student at Uppsala University.
“The actual drying process has a negligible effect on the various proteins, and the effect is reproducible, which means that it can be included in the calculation.”
The researchers did find that long-term storage affects the detectability of certain proteins more than others.
Most proteins remain completely intact after 30 years or exhibit minimal changes. However, levels of some proteins decrease so that half the quantity remains after a period of between 10 and 50 years.
The researchers also found that a relatively low storage temperature is preferable for proteins that are affected by storage.
Protein detection was less affected when dried blood samples were stored at -24°C than when they were stored at +4°C. Over the 30-year period, detectability was not affected for 34% of proteins stored at +4°C and 76% of proteins stored at -24°C.
However, storing wet plasma at -70°C preserved proteins better than dried blood sample storage at -24°C. Detectability decreased for 5% of the proteins stored wet at -70°C for 45 years, compared to 24% for proteins in dried samples stored at -24°C for 30 years.
The researchers did note, though, that this part of their analysis was complicated by some confounding factors, so this was not a clear, direct comparison between wet and dry samples. ![]()
EC grants drug orphan designation for AML
The European Commission (EC) has granted orphan designation to GMI-1271 for the treatment of acute myeloid leukemia (AML).
GMI-1271 is an E-selectin antagonist being developed by GlycoMimetics, Inc.
The product also has orphan designation, fast track designation, and breakthrough therapy designation in the US.
GMI-1271 is currently being evaluated in a phase 1/2 trial of patients with relapsed or refractory AML and patients age 60 and older with newly diagnosed AML.
The patients are receiving GM-1271 in combination with chemotherapy. The relapsed/refractory group is receiving mitoxantrone, etoposide, and cytarabine. The newly diagnosed patients are receiving cytarabine and idarubicin (7+3).
GlycoMimetics plans to present data from this trial at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting as abstracts 2520 and 2560.
The company also plans to present the research at the 22nd Congress of the European Hematology Association (EHA) as abstracts P547 and P203.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the EC for a final decision. The EC typically makes a decision within 30 days of that submission. ![]()
The European Commission (EC) has granted orphan designation to GMI-1271 for the treatment of acute myeloid leukemia (AML).
GMI-1271 is an E-selectin antagonist being developed by GlycoMimetics, Inc.
The product also has orphan designation, fast track designation, and breakthrough therapy designation in the US.
GMI-1271 is currently being evaluated in a phase 1/2 trial of patients with relapsed or refractory AML and patients age 60 and older with newly diagnosed AML.
The patients are receiving GM-1271 in combination with chemotherapy. The relapsed/refractory group is receiving mitoxantrone, etoposide, and cytarabine. The newly diagnosed patients are receiving cytarabine and idarubicin (7+3).
GlycoMimetics plans to present data from this trial at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting as abstracts 2520 and 2560.
The company also plans to present the research at the 22nd Congress of the European Hematology Association (EHA) as abstracts P547 and P203.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the EC for a final decision. The EC typically makes a decision within 30 days of that submission. ![]()
The European Commission (EC) has granted orphan designation to GMI-1271 for the treatment of acute myeloid leukemia (AML).
GMI-1271 is an E-selectin antagonist being developed by GlycoMimetics, Inc.
The product also has orphan designation, fast track designation, and breakthrough therapy designation in the US.
GMI-1271 is currently being evaluated in a phase 1/2 trial of patients with relapsed or refractory AML and patients age 60 and older with newly diagnosed AML.
The patients are receiving GM-1271 in combination with chemotherapy. The relapsed/refractory group is receiving mitoxantrone, etoposide, and cytarabine. The newly diagnosed patients are receiving cytarabine and idarubicin (7+3).
GlycoMimetics plans to present data from this trial at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting as abstracts 2520 and 2560.
The company also plans to present the research at the 22nd Congress of the European Hematology Association (EHA) as abstracts P547 and P203.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the EC for a final decision. The EC typically makes a decision within 30 days of that submission. ![]()
President’s budget: Malpractice reform but deep health care cuts
President Trump’s proposed budget for fiscal 2018 could mean crushing blows for some of the nation’s largest health care programs, if it makes it through Congress.
The proposed budget “clearly reflects the priorities of the Trump administration, which is to cut taxes, to increase defense spending and spending on boarder security, and also to cut domestic spending,” Timothy S. Jost, a health law professor at Washington and Lee University in Lexington, Va., said in an interview*.
The proposed CHIP reduction would eliminate the increased federal match provided by the Affordable Care Act and cap eligibility for federal CHIP funding at 250% of the federal poverty level, according to a summary of the proposal by the Kaiser Family Foundation. States would be able to transfer children in families with incomes below 133% of the poverty line who were moved from CHIP to Medicaid under the ACA back to CHIP.
If the cuts are approved, physicians face the challenge of caring for more uninsured and underinsured patients, said John D. Abramson, MD, a family physician and health policy lecturer at Harvard Medical School in Boston. He notes that the budget’s proposed Medicaid cuts come on top of Medicaid reductions included in the AHCA.
Meanwhile, the Food and Drug Administration stands to lose $850 million for 2018 through the budget, although medical product user fees would increase, resulting in a program increase of about $450 million. The President proposes to cut CDC funds by $1.3 billion and withdraw $252 million in funding from the Substance Abuse and Mental Health Services Administration. The cuts and savings are further outlined in a U.S. Department of Health & Human Services budget summary.
The cuts to mental health care funding would no doubt affect mental health care providers and the patients they seek to treat, Mr. Jost said. “Given the seriousness of the opioid crisis, it doesn’t seem like a great time to be cutting funding for substance abuse treatment.”
Medical research may also suffer under the proposed budget. The President intends to cut funding for the National Institutes of Health by $5.8 billion, while eliminating the Agency for Health Care Research and Quality as a stand alone agency and folding it into the NIH with less funding.
The American Association for the Advancement of Science expressed concern that the research cuts could devastate the country’s science and technology enterprise and weaken the nation’s economic growth.
“Slashing funding of critically important federal agencies threatens our nation’s ability to advance cures for disease, develop new energy technologies, improve public health, train the next generation of scientists and engineers and grow the American economy,” Rush Holt, association CEO said in a statement.
Other proposals in the budget could be positive for health care, experts say.
IPAB “really hasn’t had any impact on health care over the past 7 years,” Dr. Ayanian said. ““That’s potentially one area of compromise as senators and representatives discuss ways in which the Affordable Care Act can be reformed.”
Medical malpractice reforms are also included in the proposed budget. The proposal includes a $250,000 cap on noneconomic damages, a 3-year statute of limitations, and an established safe harbor for clinicians following evidence-based clinical practice guidelines. The changes are estimated to save the federal government $55 billion over 10 years.
“That’s an area of frequent concern for practicing physicians,” Dr. Ayanian said. “To the extent that reforms can be developed that are acceptable to patients and physicians that create the right incentives for improving health care quality and avoiding medical errors, that could be a positive. It’ll depend very much on the reform proposals that are developed. I think there is potential for bipartisan agreement in this area.”
Ms. Carpenter stressed that the President’s budget is only the first step in a lengthy budget process that will include congressional hearings and debate before legislators draft budget resolutions. “I expect Congress to debate some of the cuts to domestic spending, including things like NIH. There seems to be a good bit of alignment in terms of repeal and replace of the [ACA] and potentially some of the Medicaid reforms.”
“Trump’s budget breaks his promise not to touch Social Security, which at its core is lifeline insurance for Americans who can no longer work, not just in retirement, but also due to a disability,” Sen. Wyden said in a statement. “It also slashes Medicaid by over $600 billion beyond the damage done by Trumpcare, further threatening pediatric care, the nursing home benefit, special education programs in schools, and other health care like substance misuse treatment.”
House Energy and Commerce Committee Chairman Greg Walden (R-Ore.) commended the budget proposal as one that demonstrates President Trump’s commitment to balancing the budget and responsibly prioritizing taxpayer dollars.
“The initiatives modernizing our energy infrastructure and promoting our nation’s energy abundance would undoubtedly make positive impacts on our constituents’ lives,” he said in a statement. “The president’s proposals show the difficult choices facing the country as we work to reduce the deficit, protect our security, and grow jobs.”
Additional proposals in the President’s budget include:
• Nearly $70 billion in cuts for Social Security disability benefits over the next 10 years.
• A funding increase for the Veterans Administration, including $29 billion over the next decade for a program that enables veterans to seek outside health services from private doctors.
• A ban on funds for clinics and medical centers that provide abortions, such as Planned Parenthood.
• A $70 million increase for Medicare and Medicaid fraud prevention efforts in 2018.
• A $114 million funding increase for the Center for Medicare and Medicaid Innovation.
[email protected]
On Twitter @legal_med
*This story was updated May 26, 2017
President Trump’s proposed budget for fiscal 2018 could mean crushing blows for some of the nation’s largest health care programs, if it makes it through Congress.
The proposed budget “clearly reflects the priorities of the Trump administration, which is to cut taxes, to increase defense spending and spending on boarder security, and also to cut domestic spending,” Timothy S. Jost, a health law professor at Washington and Lee University in Lexington, Va., said in an interview*.
The proposed CHIP reduction would eliminate the increased federal match provided by the Affordable Care Act and cap eligibility for federal CHIP funding at 250% of the federal poverty level, according to a summary of the proposal by the Kaiser Family Foundation. States would be able to transfer children in families with incomes below 133% of the poverty line who were moved from CHIP to Medicaid under the ACA back to CHIP.
If the cuts are approved, physicians face the challenge of caring for more uninsured and underinsured patients, said John D. Abramson, MD, a family physician and health policy lecturer at Harvard Medical School in Boston. He notes that the budget’s proposed Medicaid cuts come on top of Medicaid reductions included in the AHCA.
Meanwhile, the Food and Drug Administration stands to lose $850 million for 2018 through the budget, although medical product user fees would increase, resulting in a program increase of about $450 million. The President proposes to cut CDC funds by $1.3 billion and withdraw $252 million in funding from the Substance Abuse and Mental Health Services Administration. The cuts and savings are further outlined in a U.S. Department of Health & Human Services budget summary.
The cuts to mental health care funding would no doubt affect mental health care providers and the patients they seek to treat, Mr. Jost said. “Given the seriousness of the opioid crisis, it doesn’t seem like a great time to be cutting funding for substance abuse treatment.”
Medical research may also suffer under the proposed budget. The President intends to cut funding for the National Institutes of Health by $5.8 billion, while eliminating the Agency for Health Care Research and Quality as a stand alone agency and folding it into the NIH with less funding.
The American Association for the Advancement of Science expressed concern that the research cuts could devastate the country’s science and technology enterprise and weaken the nation’s economic growth.
“Slashing funding of critically important federal agencies threatens our nation’s ability to advance cures for disease, develop new energy technologies, improve public health, train the next generation of scientists and engineers and grow the American economy,” Rush Holt, association CEO said in a statement.
Other proposals in the budget could be positive for health care, experts say.
IPAB “really hasn’t had any impact on health care over the past 7 years,” Dr. Ayanian said. ““That’s potentially one area of compromise as senators and representatives discuss ways in which the Affordable Care Act can be reformed.”
Medical malpractice reforms are also included in the proposed budget. The proposal includes a $250,000 cap on noneconomic damages, a 3-year statute of limitations, and an established safe harbor for clinicians following evidence-based clinical practice guidelines. The changes are estimated to save the federal government $55 billion over 10 years.
“That’s an area of frequent concern for practicing physicians,” Dr. Ayanian said. “To the extent that reforms can be developed that are acceptable to patients and physicians that create the right incentives for improving health care quality and avoiding medical errors, that could be a positive. It’ll depend very much on the reform proposals that are developed. I think there is potential for bipartisan agreement in this area.”
Ms. Carpenter stressed that the President’s budget is only the first step in a lengthy budget process that will include congressional hearings and debate before legislators draft budget resolutions. “I expect Congress to debate some of the cuts to domestic spending, including things like NIH. There seems to be a good bit of alignment in terms of repeal and replace of the [ACA] and potentially some of the Medicaid reforms.”
“Trump’s budget breaks his promise not to touch Social Security, which at its core is lifeline insurance for Americans who can no longer work, not just in retirement, but also due to a disability,” Sen. Wyden said in a statement. “It also slashes Medicaid by over $600 billion beyond the damage done by Trumpcare, further threatening pediatric care, the nursing home benefit, special education programs in schools, and other health care like substance misuse treatment.”
House Energy and Commerce Committee Chairman Greg Walden (R-Ore.) commended the budget proposal as one that demonstrates President Trump’s commitment to balancing the budget and responsibly prioritizing taxpayer dollars.
“The initiatives modernizing our energy infrastructure and promoting our nation’s energy abundance would undoubtedly make positive impacts on our constituents’ lives,” he said in a statement. “The president’s proposals show the difficult choices facing the country as we work to reduce the deficit, protect our security, and grow jobs.”
Additional proposals in the President’s budget include:
• Nearly $70 billion in cuts for Social Security disability benefits over the next 10 years.
• A funding increase for the Veterans Administration, including $29 billion over the next decade for a program that enables veterans to seek outside health services from private doctors.
• A ban on funds for clinics and medical centers that provide abortions, such as Planned Parenthood.
• A $70 million increase for Medicare and Medicaid fraud prevention efforts in 2018.
• A $114 million funding increase for the Center for Medicare and Medicaid Innovation.
[email protected]
On Twitter @legal_med
*This story was updated May 26, 2017
President Trump’s proposed budget for fiscal 2018 could mean crushing blows for some of the nation’s largest health care programs, if it makes it through Congress.
The proposed budget “clearly reflects the priorities of the Trump administration, which is to cut taxes, to increase defense spending and spending on boarder security, and also to cut domestic spending,” Timothy S. Jost, a health law professor at Washington and Lee University in Lexington, Va., said in an interview*.
The proposed CHIP reduction would eliminate the increased federal match provided by the Affordable Care Act and cap eligibility for federal CHIP funding at 250% of the federal poverty level, according to a summary of the proposal by the Kaiser Family Foundation. States would be able to transfer children in families with incomes below 133% of the poverty line who were moved from CHIP to Medicaid under the ACA back to CHIP.
If the cuts are approved, physicians face the challenge of caring for more uninsured and underinsured patients, said John D. Abramson, MD, a family physician and health policy lecturer at Harvard Medical School in Boston. He notes that the budget’s proposed Medicaid cuts come on top of Medicaid reductions included in the AHCA.
Meanwhile, the Food and Drug Administration stands to lose $850 million for 2018 through the budget, although medical product user fees would increase, resulting in a program increase of about $450 million. The President proposes to cut CDC funds by $1.3 billion and withdraw $252 million in funding from the Substance Abuse and Mental Health Services Administration. The cuts and savings are further outlined in a U.S. Department of Health & Human Services budget summary.
The cuts to mental health care funding would no doubt affect mental health care providers and the patients they seek to treat, Mr. Jost said. “Given the seriousness of the opioid crisis, it doesn’t seem like a great time to be cutting funding for substance abuse treatment.”
Medical research may also suffer under the proposed budget. The President intends to cut funding for the National Institutes of Health by $5.8 billion, while eliminating the Agency for Health Care Research and Quality as a stand alone agency and folding it into the NIH with less funding.
The American Association for the Advancement of Science expressed concern that the research cuts could devastate the country’s science and technology enterprise and weaken the nation’s economic growth.
“Slashing funding of critically important federal agencies threatens our nation’s ability to advance cures for disease, develop new energy technologies, improve public health, train the next generation of scientists and engineers and grow the American economy,” Rush Holt, association CEO said in a statement.
Other proposals in the budget could be positive for health care, experts say.
IPAB “really hasn’t had any impact on health care over the past 7 years,” Dr. Ayanian said. ““That’s potentially one area of compromise as senators and representatives discuss ways in which the Affordable Care Act can be reformed.”
Medical malpractice reforms are also included in the proposed budget. The proposal includes a $250,000 cap on noneconomic damages, a 3-year statute of limitations, and an established safe harbor for clinicians following evidence-based clinical practice guidelines. The changes are estimated to save the federal government $55 billion over 10 years.
“That’s an area of frequent concern for practicing physicians,” Dr. Ayanian said. “To the extent that reforms can be developed that are acceptable to patients and physicians that create the right incentives for improving health care quality and avoiding medical errors, that could be a positive. It’ll depend very much on the reform proposals that are developed. I think there is potential for bipartisan agreement in this area.”
Ms. Carpenter stressed that the President’s budget is only the first step in a lengthy budget process that will include congressional hearings and debate before legislators draft budget resolutions. “I expect Congress to debate some of the cuts to domestic spending, including things like NIH. There seems to be a good bit of alignment in terms of repeal and replace of the [ACA] and potentially some of the Medicaid reforms.”
“Trump’s budget breaks his promise not to touch Social Security, which at its core is lifeline insurance for Americans who can no longer work, not just in retirement, but also due to a disability,” Sen. Wyden said in a statement. “It also slashes Medicaid by over $600 billion beyond the damage done by Trumpcare, further threatening pediatric care, the nursing home benefit, special education programs in schools, and other health care like substance misuse treatment.”
House Energy and Commerce Committee Chairman Greg Walden (R-Ore.) commended the budget proposal as one that demonstrates President Trump’s commitment to balancing the budget and responsibly prioritizing taxpayer dollars.
“The initiatives modernizing our energy infrastructure and promoting our nation’s energy abundance would undoubtedly make positive impacts on our constituents’ lives,” he said in a statement. “The president’s proposals show the difficult choices facing the country as we work to reduce the deficit, protect our security, and grow jobs.”
Additional proposals in the President’s budget include:
• Nearly $70 billion in cuts for Social Security disability benefits over the next 10 years.
• A funding increase for the Veterans Administration, including $29 billion over the next decade for a program that enables veterans to seek outside health services from private doctors.
• A ban on funds for clinics and medical centers that provide abortions, such as Planned Parenthood.
• A $70 million increase for Medicare and Medicaid fraud prevention efforts in 2018.
• A $114 million funding increase for the Center for Medicare and Medicaid Innovation.
[email protected]
On Twitter @legal_med
*This story was updated May 26, 2017
App Identifies Stress and Missed Sleep as Seizure Triggers
BOSTON—Research using an Apple Watch app to track seizures in people with epilepsy finds that common triggers include stress and missed sleep, according to a preliminary study presented at the 69th Annual Meeting of the American Academy of Neurology.
Gregory Krauss, MD, Professor of Neurology at Johns Hopkins University in Baltimore, and colleagues conducted the study to identify common seizure triggers and estimate their relative frequency in a US population of people with epilepsy. For the 10-month study, 598 people signed up to track their seizures with an app called EpiWatch that had been created using ResearchKit, a software framework designed by Apple to make it easy for researchers to gather data more frequently and more accurately from participants using an iPhone or Apple Watch.
When a participant felt a seizure aura starting, he or she opened the app. Using the Apple Watch's biosensors, EpiWatch recorded the participant's heart rate and movements for 10 minutes. The app asked him or her to perform tasks to test responsiveness. After the seizure ended, the participant was given a brief survey about seizure type, aura, loss of awareness, and possible seizure triggers.
"The data collected will help researchers better understand epilepsy, while helping people with epilepsy keep a more complete history of their seizures," said Dr. Krauss. "The app also provides helpful tracking of seizures, prescription medication use, and drug side effects--activities that are important in helping people manage their condition."
In all, 40% of the group tracked a total of 1,485 seizures, and 177 participants reported what triggered their seizures. Stress was the most common trigger and was linked to 37% of seizures. Participants also identified lack of sleep as a trigger for 18% of the seizures, menstruation for 12%, and overexertion for 11%. Other reported triggers included diet (9%), missed medications (7%), and fever or infection (6%). Demographics and seizure types were generally similar between participants who reported seizure triggers and those who did not. Seizure triggers did not vary by the type of seizure people had.
The investigators found that stress was more commonly reported as a trigger for participants who worked full-time (35%), compared with those who worked part-time (21%), were unemployed (27%), or were disabled (29%). Nonadherence to medication was reported slightly more frequently among younger participants (ie, ages 16 to 25), among whom 40% reported a missed medication as a trigger, compared with older participants (ie, ages 26 to 66), among whom 34% reported a missed medication.
"Seizures are very unpredictable," said Dr. Krauss. "Our eventual goal is to be able to use wearable technology to predict an oncoming seizure. This could potentially save lives, as well as give people with epilepsy more freedom. The data collected in this study help us take a step in that direction."
BOSTON—Research using an Apple Watch app to track seizures in people with epilepsy finds that common triggers include stress and missed sleep, according to a preliminary study presented at the 69th Annual Meeting of the American Academy of Neurology.
Gregory Krauss, MD, Professor of Neurology at Johns Hopkins University in Baltimore, and colleagues conducted the study to identify common seizure triggers and estimate their relative frequency in a US population of people with epilepsy. For the 10-month study, 598 people signed up to track their seizures with an app called EpiWatch that had been created using ResearchKit, a software framework designed by Apple to make it easy for researchers to gather data more frequently and more accurately from participants using an iPhone or Apple Watch.
When a participant felt a seizure aura starting, he or she opened the app. Using the Apple Watch's biosensors, EpiWatch recorded the participant's heart rate and movements for 10 minutes. The app asked him or her to perform tasks to test responsiveness. After the seizure ended, the participant was given a brief survey about seizure type, aura, loss of awareness, and possible seizure triggers.
"The data collected will help researchers better understand epilepsy, while helping people with epilepsy keep a more complete history of their seizures," said Dr. Krauss. "The app also provides helpful tracking of seizures, prescription medication use, and drug side effects--activities that are important in helping people manage their condition."
In all, 40% of the group tracked a total of 1,485 seizures, and 177 participants reported what triggered their seizures. Stress was the most common trigger and was linked to 37% of seizures. Participants also identified lack of sleep as a trigger for 18% of the seizures, menstruation for 12%, and overexertion for 11%. Other reported triggers included diet (9%), missed medications (7%), and fever or infection (6%). Demographics and seizure types were generally similar between participants who reported seizure triggers and those who did not. Seizure triggers did not vary by the type of seizure people had.
The investigators found that stress was more commonly reported as a trigger for participants who worked full-time (35%), compared with those who worked part-time (21%), were unemployed (27%), or were disabled (29%). Nonadherence to medication was reported slightly more frequently among younger participants (ie, ages 16 to 25), among whom 40% reported a missed medication as a trigger, compared with older participants (ie, ages 26 to 66), among whom 34% reported a missed medication.
"Seizures are very unpredictable," said Dr. Krauss. "Our eventual goal is to be able to use wearable technology to predict an oncoming seizure. This could potentially save lives, as well as give people with epilepsy more freedom. The data collected in this study help us take a step in that direction."
BOSTON—Research using an Apple Watch app to track seizures in people with epilepsy finds that common triggers include stress and missed sleep, according to a preliminary study presented at the 69th Annual Meeting of the American Academy of Neurology.
Gregory Krauss, MD, Professor of Neurology at Johns Hopkins University in Baltimore, and colleagues conducted the study to identify common seizure triggers and estimate their relative frequency in a US population of people with epilepsy. For the 10-month study, 598 people signed up to track their seizures with an app called EpiWatch that had been created using ResearchKit, a software framework designed by Apple to make it easy for researchers to gather data more frequently and more accurately from participants using an iPhone or Apple Watch.
When a participant felt a seizure aura starting, he or she opened the app. Using the Apple Watch's biosensors, EpiWatch recorded the participant's heart rate and movements for 10 minutes. The app asked him or her to perform tasks to test responsiveness. After the seizure ended, the participant was given a brief survey about seizure type, aura, loss of awareness, and possible seizure triggers.
"The data collected will help researchers better understand epilepsy, while helping people with epilepsy keep a more complete history of their seizures," said Dr. Krauss. "The app also provides helpful tracking of seizures, prescription medication use, and drug side effects--activities that are important in helping people manage their condition."
In all, 40% of the group tracked a total of 1,485 seizures, and 177 participants reported what triggered their seizures. Stress was the most common trigger and was linked to 37% of seizures. Participants also identified lack of sleep as a trigger for 18% of the seizures, menstruation for 12%, and overexertion for 11%. Other reported triggers included diet (9%), missed medications (7%), and fever or infection (6%). Demographics and seizure types were generally similar between participants who reported seizure triggers and those who did not. Seizure triggers did not vary by the type of seizure people had.
The investigators found that stress was more commonly reported as a trigger for participants who worked full-time (35%), compared with those who worked part-time (21%), were unemployed (27%), or were disabled (29%). Nonadherence to medication was reported slightly more frequently among younger participants (ie, ages 16 to 25), among whom 40% reported a missed medication as a trigger, compared with older participants (ie, ages 26 to 66), among whom 34% reported a missed medication.
"Seizures are very unpredictable," said Dr. Krauss. "Our eventual goal is to be able to use wearable technology to predict an oncoming seizure. This could potentially save lives, as well as give people with epilepsy more freedom. The data collected in this study help us take a step in that direction."
Extrapolation of AED Efficacy Data From Adults to Pediatric Patients
BOSTON—Across a likely spectrum of syndromes with generalized seizures, the effect of adjunctive antiepileptic drug (AED) treatment on primary generalized tonic-clonic seizures appears similar between adults and children, according to a report presented at the 69th Annual Meeting of the American Academy of Neurology.
The availability of new AEDs for pediatric patients has been delayed due to the challenges of conducting clinical trials in children. In response to this challenge, the feasibility of extrapolation of adjunctive efficacy results for partial-onset seizures has been previously shown by Pellock et al from adult to pediatric populations when the disease course and pharmacokinetics of drug effects are comparable between populations. In response to a request from the Pediatric Committee of the European Medicines Agency, Douglas Nordli Jr, MD, and colleagues explored the feasibility of extrapolating AED efficacy data from adults to pediatric patients with primary generalized tonic-clonic seizures. Dr. Nordli is the Chief of the Division of Pediatric Neurology and Codirector of the Neurosciences Institute at Children's Hospital Los Angeles.
Dr. Nordli and colleagues conducted literature searches in EMBASE, Medline, and the Cochrane Central Register of Controlled Trials for randomized, placebo-controlled clinical trials of adjunctive AED treatment for primary generalized tonic-clonic seizures in adults and children published from 1970 to 2015. Outcome data, expressed as median percent reduction in seizure frequency and greater than or equal to 50% responder rate, were extracted from eligible trials for adult and pediatric patients receiving adjunctive AEDs or placebo and used to determine the relative strength of baseline-subtracted efficacy measures.
Seven published trials of AED adjunctive therapy for primary generalized tonic-clonic seizures were eligible for quantitative analysis. Dr. Nordli and colleagues found that changes in efficacy measures were similar in adults and children with primary generalized tonic-clonic seizures and were not age-dependent. The 95% confidence intervals for the standardized mean difference in median percent reduction of seizure frequency and estimated risk ratios in greater than or equal to 50% responder rate were consistently in favor of the AED treatment and comparable between adult and pediatric groups.
Dr. Nordli's study was supported by Eisai.
Suggested Reading
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children: a systematic review. Neurology. 2012;79(14):1482-1489.
BOSTON—Across a likely spectrum of syndromes with generalized seizures, the effect of adjunctive antiepileptic drug (AED) treatment on primary generalized tonic-clonic seizures appears similar between adults and children, according to a report presented at the 69th Annual Meeting of the American Academy of Neurology.
The availability of new AEDs for pediatric patients has been delayed due to the challenges of conducting clinical trials in children. In response to this challenge, the feasibility of extrapolation of adjunctive efficacy results for partial-onset seizures has been previously shown by Pellock et al from adult to pediatric populations when the disease course and pharmacokinetics of drug effects are comparable between populations. In response to a request from the Pediatric Committee of the European Medicines Agency, Douglas Nordli Jr, MD, and colleagues explored the feasibility of extrapolating AED efficacy data from adults to pediatric patients with primary generalized tonic-clonic seizures. Dr. Nordli is the Chief of the Division of Pediatric Neurology and Codirector of the Neurosciences Institute at Children's Hospital Los Angeles.
Dr. Nordli and colleagues conducted literature searches in EMBASE, Medline, and the Cochrane Central Register of Controlled Trials for randomized, placebo-controlled clinical trials of adjunctive AED treatment for primary generalized tonic-clonic seizures in adults and children published from 1970 to 2015. Outcome data, expressed as median percent reduction in seizure frequency and greater than or equal to 50% responder rate, were extracted from eligible trials for adult and pediatric patients receiving adjunctive AEDs or placebo and used to determine the relative strength of baseline-subtracted efficacy measures.
Seven published trials of AED adjunctive therapy for primary generalized tonic-clonic seizures were eligible for quantitative analysis. Dr. Nordli and colleagues found that changes in efficacy measures were similar in adults and children with primary generalized tonic-clonic seizures and were not age-dependent. The 95% confidence intervals for the standardized mean difference in median percent reduction of seizure frequency and estimated risk ratios in greater than or equal to 50% responder rate were consistently in favor of the AED treatment and comparable between adult and pediatric groups.
Dr. Nordli's study was supported by Eisai.
Suggested Reading
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children: a systematic review. Neurology. 2012;79(14):1482-1489.
BOSTON—Across a likely spectrum of syndromes with generalized seizures, the effect of adjunctive antiepileptic drug (AED) treatment on primary generalized tonic-clonic seizures appears similar between adults and children, according to a report presented at the 69th Annual Meeting of the American Academy of Neurology.
The availability of new AEDs for pediatric patients has been delayed due to the challenges of conducting clinical trials in children. In response to this challenge, the feasibility of extrapolation of adjunctive efficacy results for partial-onset seizures has been previously shown by Pellock et al from adult to pediatric populations when the disease course and pharmacokinetics of drug effects are comparable between populations. In response to a request from the Pediatric Committee of the European Medicines Agency, Douglas Nordli Jr, MD, and colleagues explored the feasibility of extrapolating AED efficacy data from adults to pediatric patients with primary generalized tonic-clonic seizures. Dr. Nordli is the Chief of the Division of Pediatric Neurology and Codirector of the Neurosciences Institute at Children's Hospital Los Angeles.
Dr. Nordli and colleagues conducted literature searches in EMBASE, Medline, and the Cochrane Central Register of Controlled Trials for randomized, placebo-controlled clinical trials of adjunctive AED treatment for primary generalized tonic-clonic seizures in adults and children published from 1970 to 2015. Outcome data, expressed as median percent reduction in seizure frequency and greater than or equal to 50% responder rate, were extracted from eligible trials for adult and pediatric patients receiving adjunctive AEDs or placebo and used to determine the relative strength of baseline-subtracted efficacy measures.
Seven published trials of AED adjunctive therapy for primary generalized tonic-clonic seizures were eligible for quantitative analysis. Dr. Nordli and colleagues found that changes in efficacy measures were similar in adults and children with primary generalized tonic-clonic seizures and were not age-dependent. The 95% confidence intervals for the standardized mean difference in median percent reduction of seizure frequency and estimated risk ratios in greater than or equal to 50% responder rate were consistently in favor of the AED treatment and comparable between adult and pediatric groups.
Dr. Nordli's study was supported by Eisai.
Suggested Reading
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children: a systematic review. Neurology. 2012;79(14):1482-1489.
Oral GnRH antagonist offers endometriosis pain relief in trials
VANCOUVER – An oral agent reduced dysmenorrhea and nonmenstrual pelvic pain in endometriosis patients, with more fine control over estrogen levels than historically seen with injectable gonadotropin-releasing hormone (GnRH) agonists, according to findings from two randomized controlled trials.
Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist being developed by Neurocrine Biosciences and AbbVie. Its dose can be adjusted in an attempt to achieve estrogen levels in the optimal “therapeutic window” that controls endometriosis pain while reducing menopausal symptoms, according to Hugh S. Taylor, MD, professor of obstetrics, gynecology and reproductive services at Yale University, New Haven, Conn., and chief of obstetrics and gynecology at Yale–New Haven Hospital, who presented the research at the World Congress on Endometriosis.
Results from two phase III clinical trials, simultaneously published in the New England Journal of Medicine, show that two different doses of elagolix – 150 mg once daily or 200 mg twice daily – improved moderate or severe endometriosis-associated pain. However, patients taking the drug experienced heightened frequencies of hot flushes and increased serum lipid levels, and decreases from baseline in bone mineral density (N Engl J Med. 2017 May 19. doi: 10.1056/NEJMoa1700089).
Still, the two doses give physicians options in tailoring the drug for their patients, Dr. Taylor said. The key is to keep the levels within the therapeutic window. “That’s always been the goal, and now we have a drug that does that. You can customize it for your patient, using the stronger dose for those who need it,” he said.
He described the results from two parallel clinical trials, one conducted in the United States and Canada (Elaris Endometriosis I, n = 872) and one conducted at 187 sites on five continents (Elaris Endometriosis II, n = 817).
Patients were allowed to use NSAIDs (500 mg of naproxen) or an opioid, or both, as needed. Dr. Taylor reported the results after 6 months of treatment.
Both doses of the drug outperformed placebo in reducing dysmenorrhea at 3 months. In Elaris EM-I, 75.8% in the high-dose group and 46.4% in the low-dose group had a clinically significant reduction in dysmenorrhea and decreased or stable use of analgesics at 3 months, compared with 19.6% in the placebo group. In Elaris EM-II, 72.4% in the high-dose group and 43.4% in the low-dose group achieved a clinically significant reduction, compared with 22.7% in the placebo group (P less than .001 for all comparisons).
For nonmenstrual pelvic pain, the two doses of elagolix again bested placebo. In Elaris EM-I, 54.5% in the high-dose group and 50.4% in the low-dose group achieved a clinically significant reduction and a decreased or stable use of analgesics, compared with 36.5% on placebo (P less than .001 for all). In Elaris EM-II, 57.8% in the high-dose group and 49.8% in the low-dose group achieved a clinically significant response, compared with 36.5% in the placebo group (P less than .001 and P = .003, respectively).
The responses were sustained at 6 months for both outcomes.
In Elaris EM-I, hot flushes were reported by 7.0% of the placebo group, 23.7% of the low-dose group, and 42.3% of the high-dose group (P less than .001). In Elaris EM-II, they were reported in 10.3% of the placebo group, 22.6% of the low-dose group, and 47.6% of the high-dose group (P less than .001).
Patients in the elagolix groups experienced increases in total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, though the researchers noted that less than 20% of participants in each group had LDL levels higher than 160 mg/dL or triglycerides levels higher than 200 mg/dL at any point during treatment.
There were also decreases in bone mineral density in the elagolix groups, but after 6 months of treatment, a z score of –1.5 or less at the lumbar spine occurred in fewer than 5% of women in the elagolix groups.
The drug should provide a more palatable option to GnRH agonists, according to Dr. Taylor. “This is a big step forward, very effective and much more tolerable. I think having an oral, rapidly acting, reversible drug, with a couple of doses available, will make this much more widely accepted and just as effective.”
The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
VANCOUVER – An oral agent reduced dysmenorrhea and nonmenstrual pelvic pain in endometriosis patients, with more fine control over estrogen levels than historically seen with injectable gonadotropin-releasing hormone (GnRH) agonists, according to findings from two randomized controlled trials.
Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist being developed by Neurocrine Biosciences and AbbVie. Its dose can be adjusted in an attempt to achieve estrogen levels in the optimal “therapeutic window” that controls endometriosis pain while reducing menopausal symptoms, according to Hugh S. Taylor, MD, professor of obstetrics, gynecology and reproductive services at Yale University, New Haven, Conn., and chief of obstetrics and gynecology at Yale–New Haven Hospital, who presented the research at the World Congress on Endometriosis.
Results from two phase III clinical trials, simultaneously published in the New England Journal of Medicine, show that two different doses of elagolix – 150 mg once daily or 200 mg twice daily – improved moderate or severe endometriosis-associated pain. However, patients taking the drug experienced heightened frequencies of hot flushes and increased serum lipid levels, and decreases from baseline in bone mineral density (N Engl J Med. 2017 May 19. doi: 10.1056/NEJMoa1700089).
Still, the two doses give physicians options in tailoring the drug for their patients, Dr. Taylor said. The key is to keep the levels within the therapeutic window. “That’s always been the goal, and now we have a drug that does that. You can customize it for your patient, using the stronger dose for those who need it,” he said.
He described the results from two parallel clinical trials, one conducted in the United States and Canada (Elaris Endometriosis I, n = 872) and one conducted at 187 sites on five continents (Elaris Endometriosis II, n = 817).
Patients were allowed to use NSAIDs (500 mg of naproxen) or an opioid, or both, as needed. Dr. Taylor reported the results after 6 months of treatment.
Both doses of the drug outperformed placebo in reducing dysmenorrhea at 3 months. In Elaris EM-I, 75.8% in the high-dose group and 46.4% in the low-dose group had a clinically significant reduction in dysmenorrhea and decreased or stable use of analgesics at 3 months, compared with 19.6% in the placebo group. In Elaris EM-II, 72.4% in the high-dose group and 43.4% in the low-dose group achieved a clinically significant reduction, compared with 22.7% in the placebo group (P less than .001 for all comparisons).
For nonmenstrual pelvic pain, the two doses of elagolix again bested placebo. In Elaris EM-I, 54.5% in the high-dose group and 50.4% in the low-dose group achieved a clinically significant reduction and a decreased or stable use of analgesics, compared with 36.5% on placebo (P less than .001 for all). In Elaris EM-II, 57.8% in the high-dose group and 49.8% in the low-dose group achieved a clinically significant response, compared with 36.5% in the placebo group (P less than .001 and P = .003, respectively).
The responses were sustained at 6 months for both outcomes.
In Elaris EM-I, hot flushes were reported by 7.0% of the placebo group, 23.7% of the low-dose group, and 42.3% of the high-dose group (P less than .001). In Elaris EM-II, they were reported in 10.3% of the placebo group, 22.6% of the low-dose group, and 47.6% of the high-dose group (P less than .001).
Patients in the elagolix groups experienced increases in total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, though the researchers noted that less than 20% of participants in each group had LDL levels higher than 160 mg/dL or triglycerides levels higher than 200 mg/dL at any point during treatment.
There were also decreases in bone mineral density in the elagolix groups, but after 6 months of treatment, a z score of –1.5 or less at the lumbar spine occurred in fewer than 5% of women in the elagolix groups.
The drug should provide a more palatable option to GnRH agonists, according to Dr. Taylor. “This is a big step forward, very effective and much more tolerable. I think having an oral, rapidly acting, reversible drug, with a couple of doses available, will make this much more widely accepted and just as effective.”
The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
VANCOUVER – An oral agent reduced dysmenorrhea and nonmenstrual pelvic pain in endometriosis patients, with more fine control over estrogen levels than historically seen with injectable gonadotropin-releasing hormone (GnRH) agonists, according to findings from two randomized controlled trials.
Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist being developed by Neurocrine Biosciences and AbbVie. Its dose can be adjusted in an attempt to achieve estrogen levels in the optimal “therapeutic window” that controls endometriosis pain while reducing menopausal symptoms, according to Hugh S. Taylor, MD, professor of obstetrics, gynecology and reproductive services at Yale University, New Haven, Conn., and chief of obstetrics and gynecology at Yale–New Haven Hospital, who presented the research at the World Congress on Endometriosis.
Results from two phase III clinical trials, simultaneously published in the New England Journal of Medicine, show that two different doses of elagolix – 150 mg once daily or 200 mg twice daily – improved moderate or severe endometriosis-associated pain. However, patients taking the drug experienced heightened frequencies of hot flushes and increased serum lipid levels, and decreases from baseline in bone mineral density (N Engl J Med. 2017 May 19. doi: 10.1056/NEJMoa1700089).
Still, the two doses give physicians options in tailoring the drug for their patients, Dr. Taylor said. The key is to keep the levels within the therapeutic window. “That’s always been the goal, and now we have a drug that does that. You can customize it for your patient, using the stronger dose for those who need it,” he said.
He described the results from two parallel clinical trials, one conducted in the United States and Canada (Elaris Endometriosis I, n = 872) and one conducted at 187 sites on five continents (Elaris Endometriosis II, n = 817).
Patients were allowed to use NSAIDs (500 mg of naproxen) or an opioid, or both, as needed. Dr. Taylor reported the results after 6 months of treatment.
Both doses of the drug outperformed placebo in reducing dysmenorrhea at 3 months. In Elaris EM-I, 75.8% in the high-dose group and 46.4% in the low-dose group had a clinically significant reduction in dysmenorrhea and decreased or stable use of analgesics at 3 months, compared with 19.6% in the placebo group. In Elaris EM-II, 72.4% in the high-dose group and 43.4% in the low-dose group achieved a clinically significant reduction, compared with 22.7% in the placebo group (P less than .001 for all comparisons).
For nonmenstrual pelvic pain, the two doses of elagolix again bested placebo. In Elaris EM-I, 54.5% in the high-dose group and 50.4% in the low-dose group achieved a clinically significant reduction and a decreased or stable use of analgesics, compared with 36.5% on placebo (P less than .001 for all). In Elaris EM-II, 57.8% in the high-dose group and 49.8% in the low-dose group achieved a clinically significant response, compared with 36.5% in the placebo group (P less than .001 and P = .003, respectively).
The responses were sustained at 6 months for both outcomes.
In Elaris EM-I, hot flushes were reported by 7.0% of the placebo group, 23.7% of the low-dose group, and 42.3% of the high-dose group (P less than .001). In Elaris EM-II, they were reported in 10.3% of the placebo group, 22.6% of the low-dose group, and 47.6% of the high-dose group (P less than .001).
Patients in the elagolix groups experienced increases in total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, though the researchers noted that less than 20% of participants in each group had LDL levels higher than 160 mg/dL or triglycerides levels higher than 200 mg/dL at any point during treatment.
There were also decreases in bone mineral density in the elagolix groups, but after 6 months of treatment, a z score of –1.5 or less at the lumbar spine occurred in fewer than 5% of women in the elagolix groups.
The drug should provide a more palatable option to GnRH agonists, according to Dr. Taylor. “This is a big step forward, very effective and much more tolerable. I think having an oral, rapidly acting, reversible drug, with a couple of doses available, will make this much more widely accepted and just as effective.”
The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
Key clinical point:
Major finding: At 3 and 6 months, the drug achieved a clinically significant reduction in dysmenorrhea for between 43% and 77% of women, compared with placebo (P less than .001).
Data source: Two phase III controlled trials randomizing nearly 1,700 with surgically confirmed endometriosis.
Disclosures: The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
Infections up the risk for pregnancy-associated stroke in preeclampsia
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
FROM STROKE
Key clinical point:
Major finding: Independent risk factors for pregnancy-associated stroke were severe preeclampsia or eclampsia (OR, 7.2), infections (OR, 3.0), prothrombotic states (OR, 3.5), coagulopathies (OR, 3.1), or chronic hypertension (OR, 3.2).
Data source: A matched, case-control study of 788 women from a New York inpatient database who were hospitalized for preeclampsia.
Disclosures: The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.