User login
FDA grants orphan designation to gilteritinib in AML
The US Food and Drug Administration (FDA) has granted orphan drug designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib, an inhibitor of FLT3 and AXL, has demonstrated activity against FLT3 internal tandem duplication (ITD) as well as tyrosine kinase domain, 2 mutations that are seen in up to a third of patients with AML.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were presented at the 2017 ASCO Annual Meeting.
The goal of the study was to determine the tolerability and antileukemic activity of once-daily gilteritinib in a FLT3-ITD-enriched, relapsed/refractory AML population.
The drug exhibited “potent” FLT3 inhibition at doses greater than 80 mg/day. In patients who received such doses, the greatest overall response rate was 52%, and the longest median overall survival was 31 weeks.
The maximum tolerated dose of gilteritinib was 300 mg/day. Dose-limiting toxicities included diarrhea and liver function abnormalities.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib, an inhibitor of FLT3 and AXL, has demonstrated activity against FLT3 internal tandem duplication (ITD) as well as tyrosine kinase domain, 2 mutations that are seen in up to a third of patients with AML.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were presented at the 2017 ASCO Annual Meeting.
The goal of the study was to determine the tolerability and antileukemic activity of once-daily gilteritinib in a FLT3-ITD-enriched, relapsed/refractory AML population.
The drug exhibited “potent” FLT3 inhibition at doses greater than 80 mg/day. In patients who received such doses, the greatest overall response rate was 52%, and the longest median overall survival was 31 weeks.
The maximum tolerated dose of gilteritinib was 300 mg/day. Dose-limiting toxicities included diarrhea and liver function abnormalities.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib, an inhibitor of FLT3 and AXL, has demonstrated activity against FLT3 internal tandem duplication (ITD) as well as tyrosine kinase domain, 2 mutations that are seen in up to a third of patients with AML.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were presented at the 2017 ASCO Annual Meeting.
The goal of the study was to determine the tolerability and antileukemic activity of once-daily gilteritinib in a FLT3-ITD-enriched, relapsed/refractory AML population.
The drug exhibited “potent” FLT3 inhibition at doses greater than 80 mg/day. In patients who received such doses, the greatest overall response rate was 52%, and the longest median overall survival was 31 weeks.
The maximum tolerated dose of gilteritinib was 300 mg/day. Dose-limiting toxicities included diarrhea and liver function abnormalities.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
FDA approves generic tranexamic acid
Zydus Cadila has received approval from the US Food and Drug Administration (FDA) to market a tranexamic acid product for use in patients with hemophilia.
The company’s product—Tranexamic Acid Injection, 1000 mg/10 mL (100 mg/mL) Single Dose Vial—can be used to prevent or reduce bleeding in hemophilia patients undergoing tooth extraction.
Zydus Cadila’s tranexamic acid will be produced at a manufacturing facility in Moraiya, Gujarat, India. ![]()
Zydus Cadila has received approval from the US Food and Drug Administration (FDA) to market a tranexamic acid product for use in patients with hemophilia.
The company’s product—Tranexamic Acid Injection, 1000 mg/10 mL (100 mg/mL) Single Dose Vial—can be used to prevent or reduce bleeding in hemophilia patients undergoing tooth extraction.
Zydus Cadila’s tranexamic acid will be produced at a manufacturing facility in Moraiya, Gujarat, India. ![]()
Zydus Cadila has received approval from the US Food and Drug Administration (FDA) to market a tranexamic acid product for use in patients with hemophilia.
The company’s product—Tranexamic Acid Injection, 1000 mg/10 mL (100 mg/mL) Single Dose Vial—can be used to prevent or reduce bleeding in hemophilia patients undergoing tooth extraction.
Zydus Cadila’s tranexamic acid will be produced at a manufacturing facility in Moraiya, Gujarat, India. ![]()
Statewide QI learning collaboratives improve asthma care
Care of children with asthma can be improved using statewide quality improvement (QI) learning collaboratives, said Judith C. Dolins, of the American Academy of Pediatrics (AAP), Elk Grove Village, Ill., and her associates.
AAP chapters demonstrated this through their implementation of the Chapter Quality Network (CQN) project, which was supported by the national organization. This project sought to encourage practice changes in asthma care in a number of states using statewide QI learning collaboratives and lead practices to implement the National Heart, Lung, and Blood Institute’s (NHLBI) 2007 asthma guidelines over the course of four time periods, which the researchers referred to as waves. In nine states, 19 AAP chapters engaged 180 practices to participate, and involved 749 pediatricians treating 45,431 patients (Pediatrics. 2017. doi: 10.1542/peds.2016-1612).
Across all waves, practices had reasonably high baseline use of the stepwise approach (81%-89%) and a controller medication for patients with persistent asthma (74%-88%). The patients with a current written asthma action plan increased from 49%-57% to 75%-91%. Physicians’ and parents’ ratings of asthma in children as “well controlled” rose modestly from 58%-63% to 71%-74% and from 67%-73% to 78%-87%, respectively. Patients receiving self-management materials increased from 57%-62% to 62%-88%.
Here’s how the project worked. The CQN had three linked frameworks.: One provided a methodology for spreading practice changes, another outlined the elements of care, and a third provided a framework so the practices could test, implement, and adapt changes.
A national AAP leadership team of experts in asthma care, QI, and primary care practice systems developed a set of key drivers and interventions, and an implementation guide that included resources, tools and methods, and a set of measures for the chapters. They also designed reporting tools and a curriculum fostering QI learning by chapter leaders. Then, in a state chapter leadership learning network and a practice collaborative model in each state, there were “multiple in-person learning sessions and defined action periods, best practices, and tests of change that were spread and incorporated” for the chapters to use, according to the study report.
Chapters in each state had monthly webinars and two in-person learning sessions for participating practices. They also reviewed data reports at the state and practice level and provided coaching for practices.
Practices were asked to “incorporate optimal NHLBI asthma care practices, including assessment of control, a stepwise approach to treatment, appropriate use of controller medication, and an updated asthma action plan for self-management.” Other interventions included use of an asthma encounter form (which collected 16 measures, including outcome and process measures that were entered into a national database at least monthly); introduction of population registries; workflow assessment; motivational interviews; plan-do-study-act cycles for QI; and review of data for QI.
All the physicians were eligible to earn MOC part 4 credit and continuing medical education credit, and 80% of the physicians did get MOC credit across the 4 waves.
“Our findings are notable for achieving improvement in asthma care through training multiple state coordinating entities instead of directly leading the learning collaborative itself. Few other projects have achieved this level of results in pediatric practice improvement in asthma care on such a widespread scale across multiple states. This project may serve as a model for other statewide and national organizations attempting to achieve improvements in population health through support and training for statewide organizations that, in turn, support individual health care providers and practices,” Ms. Dolins and her associates said. “Although none of the waves achieved the preset goal of 90%, all showed substantial improvement and remarkable consistency in the rate of improvement. We, therefore, regarded the project as an overall success.”
The study was funded by the Merck Childhood Asthma Network, American Board of Pediatrics Foundation, American Academy of Pediatrics Friends of Children Fund, the JPB Foundation, and GlaxoSmithKline. Ms. Dolins and Mr. Wise received salary support. Ms. Powell and Dr. Stemmler received consulting fees.
We can do a better job of taking care of our patients. And in no other area is there more room for quality improvement (QI) than in ambulatory care. In the article by Dolins et al., substantial improvements were reported in outpatient management meeting the standard of care for asthma. In my experience, doing so not only gives children a better functional outcome but also saves costs by avoiding unnecessary ED visits and hospitalization and generates new dollars for pediatric offices through the additional services they provide. We have seen similar improvements in our own work in South Carolina and Tennessee. The practices that have wanted to become involved in our asthma QI are those that are already doing a better than average job. Yet, they still generate substantial additional improvements.
The AAP study relied heavily on national experts and standards. Although their input is valued, the true advantage of QI is the opportunity for pediatricians and their staff at the service delivery level to generate their own changes within the context of a learning collaborative. True improvement and innovation is facilitated by allowing flexibility at the local level and sharing the ideas that result. Those that design the QI efforts of the future need to make sure they allow for local expertise rather than leaning too heavily on centrally predetermined change concepts.
Part IV Maintenance of Certification requirements from the American Board of Pediatrics help provide momentum for successful pediatric QI. The National Improvement Partnership Network has formed pediatric outpatient learning collaboratives to share ideas. As we identify more successes with ambulatory care QI, as more and more organizations like AAP state chapters become involved, as all practices – rather than just the best – recognize the obligation to promote quality, we have a tremendous opportunity to improve the developmental and health outcomes of the children. QI can promote work and cost efficiencies that facilitate our work as pediatricians, making our lives more productive and rewarding.
Francis E. Rushton Jr, MD, is a pediatrician and medical director of South Carolina’s QTIP (Quality Through Innovation in Pediatrics) network and the Quality Director for PHIIT (Pediatric Health Improvement In Tennessee). He reported not having any relevant financial disclosures.
We can do a better job of taking care of our patients. And in no other area is there more room for quality improvement (QI) than in ambulatory care. In the article by Dolins et al., substantial improvements were reported in outpatient management meeting the standard of care for asthma. In my experience, doing so not only gives children a better functional outcome but also saves costs by avoiding unnecessary ED visits and hospitalization and generates new dollars for pediatric offices through the additional services they provide. We have seen similar improvements in our own work in South Carolina and Tennessee. The practices that have wanted to become involved in our asthma QI are those that are already doing a better than average job. Yet, they still generate substantial additional improvements.
The AAP study relied heavily on national experts and standards. Although their input is valued, the true advantage of QI is the opportunity for pediatricians and their staff at the service delivery level to generate their own changes within the context of a learning collaborative. True improvement and innovation is facilitated by allowing flexibility at the local level and sharing the ideas that result. Those that design the QI efforts of the future need to make sure they allow for local expertise rather than leaning too heavily on centrally predetermined change concepts.
Part IV Maintenance of Certification requirements from the American Board of Pediatrics help provide momentum for successful pediatric QI. The National Improvement Partnership Network has formed pediatric outpatient learning collaboratives to share ideas. As we identify more successes with ambulatory care QI, as more and more organizations like AAP state chapters become involved, as all practices – rather than just the best – recognize the obligation to promote quality, we have a tremendous opportunity to improve the developmental and health outcomes of the children. QI can promote work and cost efficiencies that facilitate our work as pediatricians, making our lives more productive and rewarding.
Francis E. Rushton Jr, MD, is a pediatrician and medical director of South Carolina’s QTIP (Quality Through Innovation in Pediatrics) network and the Quality Director for PHIIT (Pediatric Health Improvement In Tennessee). He reported not having any relevant financial disclosures.
We can do a better job of taking care of our patients. And in no other area is there more room for quality improvement (QI) than in ambulatory care. In the article by Dolins et al., substantial improvements were reported in outpatient management meeting the standard of care for asthma. In my experience, doing so not only gives children a better functional outcome but also saves costs by avoiding unnecessary ED visits and hospitalization and generates new dollars for pediatric offices through the additional services they provide. We have seen similar improvements in our own work in South Carolina and Tennessee. The practices that have wanted to become involved in our asthma QI are those that are already doing a better than average job. Yet, they still generate substantial additional improvements.
The AAP study relied heavily on national experts and standards. Although their input is valued, the true advantage of QI is the opportunity for pediatricians and their staff at the service delivery level to generate their own changes within the context of a learning collaborative. True improvement and innovation is facilitated by allowing flexibility at the local level and sharing the ideas that result. Those that design the QI efforts of the future need to make sure they allow for local expertise rather than leaning too heavily on centrally predetermined change concepts.
Part IV Maintenance of Certification requirements from the American Board of Pediatrics help provide momentum for successful pediatric QI. The National Improvement Partnership Network has formed pediatric outpatient learning collaboratives to share ideas. As we identify more successes with ambulatory care QI, as more and more organizations like AAP state chapters become involved, as all practices – rather than just the best – recognize the obligation to promote quality, we have a tremendous opportunity to improve the developmental and health outcomes of the children. QI can promote work and cost efficiencies that facilitate our work as pediatricians, making our lives more productive and rewarding.
Francis E. Rushton Jr, MD, is a pediatrician and medical director of South Carolina’s QTIP (Quality Through Innovation in Pediatrics) network and the Quality Director for PHIIT (Pediatric Health Improvement In Tennessee). He reported not having any relevant financial disclosures.
Care of children with asthma can be improved using statewide quality improvement (QI) learning collaboratives, said Judith C. Dolins, of the American Academy of Pediatrics (AAP), Elk Grove Village, Ill., and her associates.
AAP chapters demonstrated this through their implementation of the Chapter Quality Network (CQN) project, which was supported by the national organization. This project sought to encourage practice changes in asthma care in a number of states using statewide QI learning collaboratives and lead practices to implement the National Heart, Lung, and Blood Institute’s (NHLBI) 2007 asthma guidelines over the course of four time periods, which the researchers referred to as waves. In nine states, 19 AAP chapters engaged 180 practices to participate, and involved 749 pediatricians treating 45,431 patients (Pediatrics. 2017. doi: 10.1542/peds.2016-1612).
Across all waves, practices had reasonably high baseline use of the stepwise approach (81%-89%) and a controller medication for patients with persistent asthma (74%-88%). The patients with a current written asthma action plan increased from 49%-57% to 75%-91%. Physicians’ and parents’ ratings of asthma in children as “well controlled” rose modestly from 58%-63% to 71%-74% and from 67%-73% to 78%-87%, respectively. Patients receiving self-management materials increased from 57%-62% to 62%-88%.
Here’s how the project worked. The CQN had three linked frameworks.: One provided a methodology for spreading practice changes, another outlined the elements of care, and a third provided a framework so the practices could test, implement, and adapt changes.
A national AAP leadership team of experts in asthma care, QI, and primary care practice systems developed a set of key drivers and interventions, and an implementation guide that included resources, tools and methods, and a set of measures for the chapters. They also designed reporting tools and a curriculum fostering QI learning by chapter leaders. Then, in a state chapter leadership learning network and a practice collaborative model in each state, there were “multiple in-person learning sessions and defined action periods, best practices, and tests of change that were spread and incorporated” for the chapters to use, according to the study report.
Chapters in each state had monthly webinars and two in-person learning sessions for participating practices. They also reviewed data reports at the state and practice level and provided coaching for practices.
Practices were asked to “incorporate optimal NHLBI asthma care practices, including assessment of control, a stepwise approach to treatment, appropriate use of controller medication, and an updated asthma action plan for self-management.” Other interventions included use of an asthma encounter form (which collected 16 measures, including outcome and process measures that were entered into a national database at least monthly); introduction of population registries; workflow assessment; motivational interviews; plan-do-study-act cycles for QI; and review of data for QI.
All the physicians were eligible to earn MOC part 4 credit and continuing medical education credit, and 80% of the physicians did get MOC credit across the 4 waves.
“Our findings are notable for achieving improvement in asthma care through training multiple state coordinating entities instead of directly leading the learning collaborative itself. Few other projects have achieved this level of results in pediatric practice improvement in asthma care on such a widespread scale across multiple states. This project may serve as a model for other statewide and national organizations attempting to achieve improvements in population health through support and training for statewide organizations that, in turn, support individual health care providers and practices,” Ms. Dolins and her associates said. “Although none of the waves achieved the preset goal of 90%, all showed substantial improvement and remarkable consistency in the rate of improvement. We, therefore, regarded the project as an overall success.”
The study was funded by the Merck Childhood Asthma Network, American Board of Pediatrics Foundation, American Academy of Pediatrics Friends of Children Fund, the JPB Foundation, and GlaxoSmithKline. Ms. Dolins and Mr. Wise received salary support. Ms. Powell and Dr. Stemmler received consulting fees.
Care of children with asthma can be improved using statewide quality improvement (QI) learning collaboratives, said Judith C. Dolins, of the American Academy of Pediatrics (AAP), Elk Grove Village, Ill., and her associates.
AAP chapters demonstrated this through their implementation of the Chapter Quality Network (CQN) project, which was supported by the national organization. This project sought to encourage practice changes in asthma care in a number of states using statewide QI learning collaboratives and lead practices to implement the National Heart, Lung, and Blood Institute’s (NHLBI) 2007 asthma guidelines over the course of four time periods, which the researchers referred to as waves. In nine states, 19 AAP chapters engaged 180 practices to participate, and involved 749 pediatricians treating 45,431 patients (Pediatrics. 2017. doi: 10.1542/peds.2016-1612).
Across all waves, practices had reasonably high baseline use of the stepwise approach (81%-89%) and a controller medication for patients with persistent asthma (74%-88%). The patients with a current written asthma action plan increased from 49%-57% to 75%-91%. Physicians’ and parents’ ratings of asthma in children as “well controlled” rose modestly from 58%-63% to 71%-74% and from 67%-73% to 78%-87%, respectively. Patients receiving self-management materials increased from 57%-62% to 62%-88%.
Here’s how the project worked. The CQN had three linked frameworks.: One provided a methodology for spreading practice changes, another outlined the elements of care, and a third provided a framework so the practices could test, implement, and adapt changes.
A national AAP leadership team of experts in asthma care, QI, and primary care practice systems developed a set of key drivers and interventions, and an implementation guide that included resources, tools and methods, and a set of measures for the chapters. They also designed reporting tools and a curriculum fostering QI learning by chapter leaders. Then, in a state chapter leadership learning network and a practice collaborative model in each state, there were “multiple in-person learning sessions and defined action periods, best practices, and tests of change that were spread and incorporated” for the chapters to use, according to the study report.
Chapters in each state had monthly webinars and two in-person learning sessions for participating practices. They also reviewed data reports at the state and practice level and provided coaching for practices.
Practices were asked to “incorporate optimal NHLBI asthma care practices, including assessment of control, a stepwise approach to treatment, appropriate use of controller medication, and an updated asthma action plan for self-management.” Other interventions included use of an asthma encounter form (which collected 16 measures, including outcome and process measures that were entered into a national database at least monthly); introduction of population registries; workflow assessment; motivational interviews; plan-do-study-act cycles for QI; and review of data for QI.
All the physicians were eligible to earn MOC part 4 credit and continuing medical education credit, and 80% of the physicians did get MOC credit across the 4 waves.
“Our findings are notable for achieving improvement in asthma care through training multiple state coordinating entities instead of directly leading the learning collaborative itself. Few other projects have achieved this level of results in pediatric practice improvement in asthma care on such a widespread scale across multiple states. This project may serve as a model for other statewide and national organizations attempting to achieve improvements in population health through support and training for statewide organizations that, in turn, support individual health care providers and practices,” Ms. Dolins and her associates said. “Although none of the waves achieved the preset goal of 90%, all showed substantial improvement and remarkable consistency in the rate of improvement. We, therefore, regarded the project as an overall success.”
The study was funded by the Merck Childhood Asthma Network, American Board of Pediatrics Foundation, American Academy of Pediatrics Friends of Children Fund, the JPB Foundation, and GlaxoSmithKline. Ms. Dolins and Mr. Wise received salary support. Ms. Powell and Dr. Stemmler received consulting fees.
FROM PEDIATRICS
Key clinical point:
Major finding: In wave 4, during which data were collected for 9 months, the rate of optimal asthma care at each encounter improved from 38% to 72%.
Data source: In nine states, 19 AAP chapters engaged 180 practices to participate in quality improvement learning collaboratives, which involved 749 pediatricians treating 45,431 patients.
Disclosures: The study was funded by the Merck Childhood Asthma Network, American Board of Pediatrics Foundation, American Academy of Pediatrics Friends of Children Fund, the JPB Foundation, and GlaxoSmithKline. Ms. Dolins and Mr. Wise received salary support. Ms. Powell and Dr. Stemmler received consulting fees.
Rivaroxaban or aspirin for extended treatment of VTE
TITLE: Low-dose or full-dose rivaroxaban is superior to aspirin for long-term anticoagulation
CLINICAL QUESTION: Is full or lower intensity rivaroxaban better for extended treatment of venous thromboembolism (VTE) as compared to aspirin?
STUDY DESIGN: Multicenter randomized double-blinded phase III trial.
SETTING: 230 Medical centers worldwide in 20 countries.
SYNOPSIS: 3,365 patients with a history of VTE who had undergone 6-12 months of initial anticoagulation therapy and in whom continuation of therapy was thought to be beneficial were enrolled. Patients were randomly assigned to daily high-dose rivaroxaban (20 mg) or daily low-dose rivaroxaban (10 mg) or aspirin (100 mg). After a median of 351 days, symptomatic recurrent VTE or unexplained death occurred in 17 of the 1,107 patients (1.5%) who were assigned to the high-dose group, in 13 of 1,127 patients (1.2%) who were assigned to the low-dose group, and in 50 of 1,131 patients (4.4%) who were assigned to aspirin. Bleeding rates were not significantly different between the three groups (2%-3%). The major limitation of this study is the short duration of follow-up and the lack of power to demonstrate noninferiority of the low-dose as compared to the high-dose regimen for rivaroxaban.
BOTTOM LINE: In patients with a history of VTE, in whom prolonged anticoagulation could be beneficial, low or high-dose rivaroxaban is superior to aspirin in preventing recurrent VTE without increasing bleeding risk.
CITATION: Weitz JI, Lensing MH, Prins R, et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017; 376:1211-22.
Dr. Mayasy is assistant professor in the department of hospital medicine at the University of New Mexico.
TITLE: Low-dose or full-dose rivaroxaban is superior to aspirin for long-term anticoagulation
CLINICAL QUESTION: Is full or lower intensity rivaroxaban better for extended treatment of venous thromboembolism (VTE) as compared to aspirin?
STUDY DESIGN: Multicenter randomized double-blinded phase III trial.
SETTING: 230 Medical centers worldwide in 20 countries.
SYNOPSIS: 3,365 patients with a history of VTE who had undergone 6-12 months of initial anticoagulation therapy and in whom continuation of therapy was thought to be beneficial were enrolled. Patients were randomly assigned to daily high-dose rivaroxaban (20 mg) or daily low-dose rivaroxaban (10 mg) or aspirin (100 mg). After a median of 351 days, symptomatic recurrent VTE or unexplained death occurred in 17 of the 1,107 patients (1.5%) who were assigned to the high-dose group, in 13 of 1,127 patients (1.2%) who were assigned to the low-dose group, and in 50 of 1,131 patients (4.4%) who were assigned to aspirin. Bleeding rates were not significantly different between the three groups (2%-3%). The major limitation of this study is the short duration of follow-up and the lack of power to demonstrate noninferiority of the low-dose as compared to the high-dose regimen for rivaroxaban.
BOTTOM LINE: In patients with a history of VTE, in whom prolonged anticoagulation could be beneficial, low or high-dose rivaroxaban is superior to aspirin in preventing recurrent VTE without increasing bleeding risk.
CITATION: Weitz JI, Lensing MH, Prins R, et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017; 376:1211-22.
Dr. Mayasy is assistant professor in the department of hospital medicine at the University of New Mexico.
TITLE: Low-dose or full-dose rivaroxaban is superior to aspirin for long-term anticoagulation
CLINICAL QUESTION: Is full or lower intensity rivaroxaban better for extended treatment of venous thromboembolism (VTE) as compared to aspirin?
STUDY DESIGN: Multicenter randomized double-blinded phase III trial.
SETTING: 230 Medical centers worldwide in 20 countries.
SYNOPSIS: 3,365 patients with a history of VTE who had undergone 6-12 months of initial anticoagulation therapy and in whom continuation of therapy was thought to be beneficial were enrolled. Patients were randomly assigned to daily high-dose rivaroxaban (20 mg) or daily low-dose rivaroxaban (10 mg) or aspirin (100 mg). After a median of 351 days, symptomatic recurrent VTE or unexplained death occurred in 17 of the 1,107 patients (1.5%) who were assigned to the high-dose group, in 13 of 1,127 patients (1.2%) who were assigned to the low-dose group, and in 50 of 1,131 patients (4.4%) who were assigned to aspirin. Bleeding rates were not significantly different between the three groups (2%-3%). The major limitation of this study is the short duration of follow-up and the lack of power to demonstrate noninferiority of the low-dose as compared to the high-dose regimen for rivaroxaban.
BOTTOM LINE: In patients with a history of VTE, in whom prolonged anticoagulation could be beneficial, low or high-dose rivaroxaban is superior to aspirin in preventing recurrent VTE without increasing bleeding risk.
CITATION: Weitz JI, Lensing MH, Prins R, et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017; 376:1211-22.
Dr. Mayasy is assistant professor in the department of hospital medicine at the University of New Mexico.
Life-long risk reduction could cut late-life dementia by up to 35%
LONDON – As many as a third of dementia cases could be prevented worldwide if society could adopt a life course–focused approach of supporting brain health with mostly common-sense measures.
Improving childhood education, controlling blood pressure and cholesterol, keeping socially and intellectually active, exercising, and ceasing tobacco use are among the recommendations to reduce the incidence of dementia made by a worldwide panel of expert clinicians and researchers.
The findings are part of an exhaustive report commission by The Lancet and released at the Alzheimer’s Association International Conference. The report has concluded that nine lifestyle factors, most of which are modifiable from childhood though middle age, account for 35% of dementia that strikes elderly persons, Gillian Livingston, MD, said at the conference. The report was simultaneously published.
Being homozygous for the ApoE4 allele confers about an immutable 7% increased chance of developing Alzheimer’s disease. But two of the other factors identified in the Lancet report, low education in childhood and hearing loss at middle age, confer even higher individual risks of 8% and 9%. And when combined with other mid-life risks of hypertension and obesity, and late-life risks imposed by smoking, depression, inactivity, social isolation, and diabetes, these factors not only dwarf the potential impact of ApoE4, but offer a lifelong chance to forestall or even prevent dementia.
The findings, all gathered from an exhaustive literature review, bolster the notion that public health interventions could block the tsunami of dementia cases that threaten to overwhelm the world’s health care resources by 2050, Dr. Livingston said.
“While public health interventions won’t prevent or cure all potentially modifiable dementia, intervention for cardiovascular risk factors, mental health, and hearing may push back the onset in many people for years. Even if only some of this promise is realized, it could make a huge difference. We have, in fact, already seen that in some populations dementia is being delayed for years. If we could achieve an overall delay of onset by 5 years, we could cut the global prevalence by half.”
The Lancet commissioned the panel of global dementia experts to review the extant literature and construct a lifespan-focused risk model. In addition to examining risk and making recommendations to ameliorate it, the panel issued recommendations about treating cognition and psychiatric and behavioral problems; protecting dementia patients in both home and long-term care settings; supporting the family members who provide most of the care for dementia patients; and helping patients and families navigate end-of-life situations.
The literature review identified nine modifiable risk factors that account for 35% of dementia risk worldwide:
• Education in youth. Less education in childhood, which the commission identified as a lack of secondary schooling, increased the risk of dementia by 8%. Improving education at this age would remove this portion of the population attributable risk factor (PAF), Dr. Livingston said.
This finding represents an enormous opportunity for improvement: The decline in dementia incidence seen in some populations occurs mostly among the better-educated. “The mechanism of prevention here appears to be increasing brain resilience,” said Lon Schneider, MD, a member of the Lancet panel.
Tackling poor childhood education is a daunting task and requires commitment from both public and private sectors, the report noted, but its importance cannot be overstated.
• Hearing loss at mid-life. This emerged as the most powerful risk factor in the analysis, conferring an independent 9% increased risk of dementia, “a relatively new idea that has not been included in previous calculations of population attributable factors,” the commission wrote. The mechanism of increased risk isn’t clear, but may be a combination of neurodegeneration and social isolation imposed by being shut out of easy communication. It’s unclear whether hearing aids can mitigate the effects of hearing loss on dementia risk, the report noted.
• Hypertension, obesity, and diabetes. Respectively, these accounted for 2%, 1%, and 1% of the PAF. Obesity is linked to prediabetes and diabetes, which are in turn linked to insulin resistance, decreased brain amyloid clearance, high blood glucose, and inflammation – all risks for Alzheimer’s disease.
The report recommends that anyone aged 45-65 years who has hypertension should be actively treated for the disorder.
• Smoking. At 5%, smoking posted the third-highest PAF. The risk is probably mediated through smoking’s detrimental effects on cardiovascular health. But the report noted that tobacco smoke contains known neurotoxins as well.
Preventing the smoking/dementia connection is simple, Dr. Livingston said. “Simply stop smoking. If you’re smoking, just stop. Please.”
• Depression. Depression in late life imposed a 4% PAF. The evidence reviewed suggested that depression is not, in fact, linked to dementia when experienced at mid-life. But late-life depression may be a prodromal symptom of dementia and biologically linked to increased stress hormones, decreased neuronal growth factors, and decreased hippocampal volume. The commission noted animal models that suggest some antidepressants, including citalopram, decrease amyloid progression.
• Social isolation. Associated with a 2% PAF, social isolation may, like depression, be a prodromal symptom. But, the report said, there is growing evidence that it actually is an independent risk factor as well. It has been shown to also increase the risk of hypertension, cardiovascular disease, and depression, all dementia risk factors in their own right.
Longitudinal studies suggest that social activities and personal connections may prevent or delay dementia, although top-grade evidence is lacking. Still, maintaining a rich social network not only reduces the chance of isolation, but helps prevent depression as well.
• Physical inactivity. Sedentary lifestyle carried a 3% PAF for dementia. Older adults who maintain physical activity are more likely to remain cognitively intact. Physical exercise improves mood, reduces the risk of falls, and maintains normal physical function. The report cited a meta-analysis of 16 studies and almost 164,000 participants without dementia; it concluded that those in the highest level of activity had a 25% decreased risk of all-cause dementia and a 45% decreased risk of Alzheimer’s disease.
The strongest evidence for exercise’s benefit on cognition may be from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Patients with a high risk of dementia who completed the lifestyle modification program of healthy diet cognitive training, vascular risk factor management, and aerobic exercise showed a slowing of cognitive decline and improvements in executive function and processing speed.
Becoming aware of the risk factors is one thing, the report said. Doing something about them is another. In general, the first step is to “be ambitious” about prevention.
“Prevention is always better than treatment,” Dr. Livingston said in an interview. “We need to start thinking about dementia not as something that simply happens outside our control, but as something that we can have an effect on.”
The Lancet commissioned the report. Dr. Livingston did not have any financial declarations but many of the other authors reported multiple relationships with pharmaceutical companies.
[email protected]
On Twitter @alz_gal
LONDON – As many as a third of dementia cases could be prevented worldwide if society could adopt a life course–focused approach of supporting brain health with mostly common-sense measures.
Improving childhood education, controlling blood pressure and cholesterol, keeping socially and intellectually active, exercising, and ceasing tobacco use are among the recommendations to reduce the incidence of dementia made by a worldwide panel of expert clinicians and researchers.
The findings are part of an exhaustive report commission by The Lancet and released at the Alzheimer’s Association International Conference. The report has concluded that nine lifestyle factors, most of which are modifiable from childhood though middle age, account for 35% of dementia that strikes elderly persons, Gillian Livingston, MD, said at the conference. The report was simultaneously published.
Being homozygous for the ApoE4 allele confers about an immutable 7% increased chance of developing Alzheimer’s disease. But two of the other factors identified in the Lancet report, low education in childhood and hearing loss at middle age, confer even higher individual risks of 8% and 9%. And when combined with other mid-life risks of hypertension and obesity, and late-life risks imposed by smoking, depression, inactivity, social isolation, and diabetes, these factors not only dwarf the potential impact of ApoE4, but offer a lifelong chance to forestall or even prevent dementia.
The findings, all gathered from an exhaustive literature review, bolster the notion that public health interventions could block the tsunami of dementia cases that threaten to overwhelm the world’s health care resources by 2050, Dr. Livingston said.
“While public health interventions won’t prevent or cure all potentially modifiable dementia, intervention for cardiovascular risk factors, mental health, and hearing may push back the onset in many people for years. Even if only some of this promise is realized, it could make a huge difference. We have, in fact, already seen that in some populations dementia is being delayed for years. If we could achieve an overall delay of onset by 5 years, we could cut the global prevalence by half.”
The Lancet commissioned the panel of global dementia experts to review the extant literature and construct a lifespan-focused risk model. In addition to examining risk and making recommendations to ameliorate it, the panel issued recommendations about treating cognition and psychiatric and behavioral problems; protecting dementia patients in both home and long-term care settings; supporting the family members who provide most of the care for dementia patients; and helping patients and families navigate end-of-life situations.
The literature review identified nine modifiable risk factors that account for 35% of dementia risk worldwide:
• Education in youth. Less education in childhood, which the commission identified as a lack of secondary schooling, increased the risk of dementia by 8%. Improving education at this age would remove this portion of the population attributable risk factor (PAF), Dr. Livingston said.
This finding represents an enormous opportunity for improvement: The decline in dementia incidence seen in some populations occurs mostly among the better-educated. “The mechanism of prevention here appears to be increasing brain resilience,” said Lon Schneider, MD, a member of the Lancet panel.
Tackling poor childhood education is a daunting task and requires commitment from both public and private sectors, the report noted, but its importance cannot be overstated.
• Hearing loss at mid-life. This emerged as the most powerful risk factor in the analysis, conferring an independent 9% increased risk of dementia, “a relatively new idea that has not been included in previous calculations of population attributable factors,” the commission wrote. The mechanism of increased risk isn’t clear, but may be a combination of neurodegeneration and social isolation imposed by being shut out of easy communication. It’s unclear whether hearing aids can mitigate the effects of hearing loss on dementia risk, the report noted.
• Hypertension, obesity, and diabetes. Respectively, these accounted for 2%, 1%, and 1% of the PAF. Obesity is linked to prediabetes and diabetes, which are in turn linked to insulin resistance, decreased brain amyloid clearance, high blood glucose, and inflammation – all risks for Alzheimer’s disease.
The report recommends that anyone aged 45-65 years who has hypertension should be actively treated for the disorder.
• Smoking. At 5%, smoking posted the third-highest PAF. The risk is probably mediated through smoking’s detrimental effects on cardiovascular health. But the report noted that tobacco smoke contains known neurotoxins as well.
Preventing the smoking/dementia connection is simple, Dr. Livingston said. “Simply stop smoking. If you’re smoking, just stop. Please.”
• Depression. Depression in late life imposed a 4% PAF. The evidence reviewed suggested that depression is not, in fact, linked to dementia when experienced at mid-life. But late-life depression may be a prodromal symptom of dementia and biologically linked to increased stress hormones, decreased neuronal growth factors, and decreased hippocampal volume. The commission noted animal models that suggest some antidepressants, including citalopram, decrease amyloid progression.
• Social isolation. Associated with a 2% PAF, social isolation may, like depression, be a prodromal symptom. But, the report said, there is growing evidence that it actually is an independent risk factor as well. It has been shown to also increase the risk of hypertension, cardiovascular disease, and depression, all dementia risk factors in their own right.
Longitudinal studies suggest that social activities and personal connections may prevent or delay dementia, although top-grade evidence is lacking. Still, maintaining a rich social network not only reduces the chance of isolation, but helps prevent depression as well.
• Physical inactivity. Sedentary lifestyle carried a 3% PAF for dementia. Older adults who maintain physical activity are more likely to remain cognitively intact. Physical exercise improves mood, reduces the risk of falls, and maintains normal physical function. The report cited a meta-analysis of 16 studies and almost 164,000 participants without dementia; it concluded that those in the highest level of activity had a 25% decreased risk of all-cause dementia and a 45% decreased risk of Alzheimer’s disease.
The strongest evidence for exercise’s benefit on cognition may be from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Patients with a high risk of dementia who completed the lifestyle modification program of healthy diet cognitive training, vascular risk factor management, and aerobic exercise showed a slowing of cognitive decline and improvements in executive function and processing speed.
Becoming aware of the risk factors is one thing, the report said. Doing something about them is another. In general, the first step is to “be ambitious” about prevention.
“Prevention is always better than treatment,” Dr. Livingston said in an interview. “We need to start thinking about dementia not as something that simply happens outside our control, but as something that we can have an effect on.”
The Lancet commissioned the report. Dr. Livingston did not have any financial declarations but many of the other authors reported multiple relationships with pharmaceutical companies.
[email protected]
On Twitter @alz_gal
LONDON – As many as a third of dementia cases could be prevented worldwide if society could adopt a life course–focused approach of supporting brain health with mostly common-sense measures.
Improving childhood education, controlling blood pressure and cholesterol, keeping socially and intellectually active, exercising, and ceasing tobacco use are among the recommendations to reduce the incidence of dementia made by a worldwide panel of expert clinicians and researchers.
The findings are part of an exhaustive report commission by The Lancet and released at the Alzheimer’s Association International Conference. The report has concluded that nine lifestyle factors, most of which are modifiable from childhood though middle age, account for 35% of dementia that strikes elderly persons, Gillian Livingston, MD, said at the conference. The report was simultaneously published.
Being homozygous for the ApoE4 allele confers about an immutable 7% increased chance of developing Alzheimer’s disease. But two of the other factors identified in the Lancet report, low education in childhood and hearing loss at middle age, confer even higher individual risks of 8% and 9%. And when combined with other mid-life risks of hypertension and obesity, and late-life risks imposed by smoking, depression, inactivity, social isolation, and diabetes, these factors not only dwarf the potential impact of ApoE4, but offer a lifelong chance to forestall or even prevent dementia.
The findings, all gathered from an exhaustive literature review, bolster the notion that public health interventions could block the tsunami of dementia cases that threaten to overwhelm the world’s health care resources by 2050, Dr. Livingston said.
“While public health interventions won’t prevent or cure all potentially modifiable dementia, intervention for cardiovascular risk factors, mental health, and hearing may push back the onset in many people for years. Even if only some of this promise is realized, it could make a huge difference. We have, in fact, already seen that in some populations dementia is being delayed for years. If we could achieve an overall delay of onset by 5 years, we could cut the global prevalence by half.”
The Lancet commissioned the panel of global dementia experts to review the extant literature and construct a lifespan-focused risk model. In addition to examining risk and making recommendations to ameliorate it, the panel issued recommendations about treating cognition and psychiatric and behavioral problems; protecting dementia patients in both home and long-term care settings; supporting the family members who provide most of the care for dementia patients; and helping patients and families navigate end-of-life situations.
The literature review identified nine modifiable risk factors that account for 35% of dementia risk worldwide:
• Education in youth. Less education in childhood, which the commission identified as a lack of secondary schooling, increased the risk of dementia by 8%. Improving education at this age would remove this portion of the population attributable risk factor (PAF), Dr. Livingston said.
This finding represents an enormous opportunity for improvement: The decline in dementia incidence seen in some populations occurs mostly among the better-educated. “The mechanism of prevention here appears to be increasing brain resilience,” said Lon Schneider, MD, a member of the Lancet panel.
Tackling poor childhood education is a daunting task and requires commitment from both public and private sectors, the report noted, but its importance cannot be overstated.
• Hearing loss at mid-life. This emerged as the most powerful risk factor in the analysis, conferring an independent 9% increased risk of dementia, “a relatively new idea that has not been included in previous calculations of population attributable factors,” the commission wrote. The mechanism of increased risk isn’t clear, but may be a combination of neurodegeneration and social isolation imposed by being shut out of easy communication. It’s unclear whether hearing aids can mitigate the effects of hearing loss on dementia risk, the report noted.
• Hypertension, obesity, and diabetes. Respectively, these accounted for 2%, 1%, and 1% of the PAF. Obesity is linked to prediabetes and diabetes, which are in turn linked to insulin resistance, decreased brain amyloid clearance, high blood glucose, and inflammation – all risks for Alzheimer’s disease.
The report recommends that anyone aged 45-65 years who has hypertension should be actively treated for the disorder.
• Smoking. At 5%, smoking posted the third-highest PAF. The risk is probably mediated through smoking’s detrimental effects on cardiovascular health. But the report noted that tobacco smoke contains known neurotoxins as well.
Preventing the smoking/dementia connection is simple, Dr. Livingston said. “Simply stop smoking. If you’re smoking, just stop. Please.”
• Depression. Depression in late life imposed a 4% PAF. The evidence reviewed suggested that depression is not, in fact, linked to dementia when experienced at mid-life. But late-life depression may be a prodromal symptom of dementia and biologically linked to increased stress hormones, decreased neuronal growth factors, and decreased hippocampal volume. The commission noted animal models that suggest some antidepressants, including citalopram, decrease amyloid progression.
• Social isolation. Associated with a 2% PAF, social isolation may, like depression, be a prodromal symptom. But, the report said, there is growing evidence that it actually is an independent risk factor as well. It has been shown to also increase the risk of hypertension, cardiovascular disease, and depression, all dementia risk factors in their own right.
Longitudinal studies suggest that social activities and personal connections may prevent or delay dementia, although top-grade evidence is lacking. Still, maintaining a rich social network not only reduces the chance of isolation, but helps prevent depression as well.
• Physical inactivity. Sedentary lifestyle carried a 3% PAF for dementia. Older adults who maintain physical activity are more likely to remain cognitively intact. Physical exercise improves mood, reduces the risk of falls, and maintains normal physical function. The report cited a meta-analysis of 16 studies and almost 164,000 participants without dementia; it concluded that those in the highest level of activity had a 25% decreased risk of all-cause dementia and a 45% decreased risk of Alzheimer’s disease.
The strongest evidence for exercise’s benefit on cognition may be from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Patients with a high risk of dementia who completed the lifestyle modification program of healthy diet cognitive training, vascular risk factor management, and aerobic exercise showed a slowing of cognitive decline and improvements in executive function and processing speed.
Becoming aware of the risk factors is one thing, the report said. Doing something about them is another. In general, the first step is to “be ambitious” about prevention.
“Prevention is always better than treatment,” Dr. Livingston said in an interview. “We need to start thinking about dementia not as something that simply happens outside our control, but as something that we can have an effect on.”
The Lancet commissioned the report. Dr. Livingston did not have any financial declarations but many of the other authors reported multiple relationships with pharmaceutical companies.
[email protected]
On Twitter @alz_gal
AT AAIC 2017
Amyloid PET imaging impacts diagnoses, management for those with MCI and dementia
LONDON – A study to prove the practical clinical utility of amyloid PET scanning appears to be doing just that: The knowledge of patients’ brain amyloid status changed clinical management for 68% of those who had the imaging done.
Interim results of the Imaging Dementia–Evidence for Amyloid Scanning (IDEAS) study far exceeded the 30% change rate that investigators hoped to see, Gil Rabinovici, MD, said at the Alzheimer’s Association International Conference. Not only did many patients receive a more suitable care plan, the scans actually changed diagnoses in three-quarters of those who tested positive, said Dr. Rabinovici of the University of California, San Francisco.
The U.S.-wide, open-label study is being conducted in Medicare beneficiaries who have been diagnosed with mild cognitive impairment (MCI) or dementia of uncertain cause. Its two goals are to show that amyloid PET imaging affects a patient’s care plan within 3 months of the scan and to show an impact on major medical outcomes 12 months later. In diagnostically uncertain cases, investigators theorized, amyloid PET imaging would lead to significant changes in patient management, which would then translate into improved medical outcomes.
At the meeting, Dr. Rabinovici discussed the preplanned interim analysis of 3-month care plan changes. After the scan was completed, physicians related the results to patients and recommended any appropriate management changes. At the 90-day post-scan visit, physicians documented how any changes had been implemented. Data on the 12-month outcomes have not been announced on any portion of the cohort.
The patients were a mean of 76 years old; 64% had a diagnosis of MCI and 36% a diagnosis of dementia. Alzheimer’s disease was the suspected etiology in 74% of the MCI group and in 80% of the dementia group. About one-third of MCI patients and two-thirds of dementia patients were taking Alzheimer’s medications at enrollment.
The scans were positive in 54% of the MCI patients and in 70% of dementia patients. In amyloid-positive patients, the rate of Alzheimer’s diagnosis increased from 78% to 85%. In amyloid-negative patients, the rate of Alzheimer’s diagnosis decreased from 73% to 14%.
More than two-thirds of patients in both groups experienced a change in management after the scans were read. Changes in Alzheimer’s drugs occurred in 48% of both groups, while changes in non-Alzheimer’s drugs occurred in 36% of the MCI group and 32% of the dementia group. In amyloid-positive patients, use of Alzheimer’s drugs increased from 51% to 84%. In amyloid-negative patients, the use of Alzheimer’s drugs decreased from 39% to 31%.
Patient counseling also changed in 24% of the MCI group and 16% of the dementia group.
Dr. Rabinovici was cautiously optimistic about the interim results. “The study has two aims, and Medicare has made it clear that we need to complete both before they will consider covering the scans. I hope they understand that these changes in management are incredibly important, but they also want to see that they result in improved outcomes. That will take a year from when we enroll our last patient.”
Although the study is designed to show change in clinical outcomes, it’s also changing something less tangible, but no less important: patients’ understanding of their situation.
“We may be looking at objective changes in management, but we are also seeing that patients really want to know what’s going on in their brain, what the cause of their cognitive impairment is. They don’t want to be told that it’s normal aging, because they know it isn’t. There is a real value to getting that diagnosis, even if it’s the bad news that there are amyloid plaques in the brain. It leads to a clear plan in terms of what drugs to use, the possibility of enrolling in clinical trials, and getting some clarity about what’s going on. A lot of times, the certainty is better than the uncertainty.”
As of June, IDEAS had recruited 12,484 patients and completed 11,712 amyloid PET scans. Dr. Rabinovici hopes the recruitment will be completed by late this year, or early 2018.
IDEAS is being funded by the Centers for Medicare & Medicaid Services, Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, Piramal Imaging, the Alzheimer’s Association, and the American College of Radiology. Dr. Rabinovici has received honoraria or consulting fees from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche.
[email protected]
On Twitter @alz_gal
LONDON – A study to prove the practical clinical utility of amyloid PET scanning appears to be doing just that: The knowledge of patients’ brain amyloid status changed clinical management for 68% of those who had the imaging done.
Interim results of the Imaging Dementia–Evidence for Amyloid Scanning (IDEAS) study far exceeded the 30% change rate that investigators hoped to see, Gil Rabinovici, MD, said at the Alzheimer’s Association International Conference. Not only did many patients receive a more suitable care plan, the scans actually changed diagnoses in three-quarters of those who tested positive, said Dr. Rabinovici of the University of California, San Francisco.
The U.S.-wide, open-label study is being conducted in Medicare beneficiaries who have been diagnosed with mild cognitive impairment (MCI) or dementia of uncertain cause. Its two goals are to show that amyloid PET imaging affects a patient’s care plan within 3 months of the scan and to show an impact on major medical outcomes 12 months later. In diagnostically uncertain cases, investigators theorized, amyloid PET imaging would lead to significant changes in patient management, which would then translate into improved medical outcomes.
At the meeting, Dr. Rabinovici discussed the preplanned interim analysis of 3-month care plan changes. After the scan was completed, physicians related the results to patients and recommended any appropriate management changes. At the 90-day post-scan visit, physicians documented how any changes had been implemented. Data on the 12-month outcomes have not been announced on any portion of the cohort.
The patients were a mean of 76 years old; 64% had a diagnosis of MCI and 36% a diagnosis of dementia. Alzheimer’s disease was the suspected etiology in 74% of the MCI group and in 80% of the dementia group. About one-third of MCI patients and two-thirds of dementia patients were taking Alzheimer’s medications at enrollment.
The scans were positive in 54% of the MCI patients and in 70% of dementia patients. In amyloid-positive patients, the rate of Alzheimer’s diagnosis increased from 78% to 85%. In amyloid-negative patients, the rate of Alzheimer’s diagnosis decreased from 73% to 14%.
More than two-thirds of patients in both groups experienced a change in management after the scans were read. Changes in Alzheimer’s drugs occurred in 48% of both groups, while changes in non-Alzheimer’s drugs occurred in 36% of the MCI group and 32% of the dementia group. In amyloid-positive patients, use of Alzheimer’s drugs increased from 51% to 84%. In amyloid-negative patients, the use of Alzheimer’s drugs decreased from 39% to 31%.
Patient counseling also changed in 24% of the MCI group and 16% of the dementia group.
Dr. Rabinovici was cautiously optimistic about the interim results. “The study has two aims, and Medicare has made it clear that we need to complete both before they will consider covering the scans. I hope they understand that these changes in management are incredibly important, but they also want to see that they result in improved outcomes. That will take a year from when we enroll our last patient.”
Although the study is designed to show change in clinical outcomes, it’s also changing something less tangible, but no less important: patients’ understanding of their situation.
“We may be looking at objective changes in management, but we are also seeing that patients really want to know what’s going on in their brain, what the cause of their cognitive impairment is. They don’t want to be told that it’s normal aging, because they know it isn’t. There is a real value to getting that diagnosis, even if it’s the bad news that there are amyloid plaques in the brain. It leads to a clear plan in terms of what drugs to use, the possibility of enrolling in clinical trials, and getting some clarity about what’s going on. A lot of times, the certainty is better than the uncertainty.”
As of June, IDEAS had recruited 12,484 patients and completed 11,712 amyloid PET scans. Dr. Rabinovici hopes the recruitment will be completed by late this year, or early 2018.
IDEAS is being funded by the Centers for Medicare & Medicaid Services, Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, Piramal Imaging, the Alzheimer’s Association, and the American College of Radiology. Dr. Rabinovici has received honoraria or consulting fees from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche.
[email protected]
On Twitter @alz_gal
LONDON – A study to prove the practical clinical utility of amyloid PET scanning appears to be doing just that: The knowledge of patients’ brain amyloid status changed clinical management for 68% of those who had the imaging done.
Interim results of the Imaging Dementia–Evidence for Amyloid Scanning (IDEAS) study far exceeded the 30% change rate that investigators hoped to see, Gil Rabinovici, MD, said at the Alzheimer’s Association International Conference. Not only did many patients receive a more suitable care plan, the scans actually changed diagnoses in three-quarters of those who tested positive, said Dr. Rabinovici of the University of California, San Francisco.
The U.S.-wide, open-label study is being conducted in Medicare beneficiaries who have been diagnosed with mild cognitive impairment (MCI) or dementia of uncertain cause. Its two goals are to show that amyloid PET imaging affects a patient’s care plan within 3 months of the scan and to show an impact on major medical outcomes 12 months later. In diagnostically uncertain cases, investigators theorized, amyloid PET imaging would lead to significant changes in patient management, which would then translate into improved medical outcomes.
At the meeting, Dr. Rabinovici discussed the preplanned interim analysis of 3-month care plan changes. After the scan was completed, physicians related the results to patients and recommended any appropriate management changes. At the 90-day post-scan visit, physicians documented how any changes had been implemented. Data on the 12-month outcomes have not been announced on any portion of the cohort.
The patients were a mean of 76 years old; 64% had a diagnosis of MCI and 36% a diagnosis of dementia. Alzheimer’s disease was the suspected etiology in 74% of the MCI group and in 80% of the dementia group. About one-third of MCI patients and two-thirds of dementia patients were taking Alzheimer’s medications at enrollment.
The scans were positive in 54% of the MCI patients and in 70% of dementia patients. In amyloid-positive patients, the rate of Alzheimer’s diagnosis increased from 78% to 85%. In amyloid-negative patients, the rate of Alzheimer’s diagnosis decreased from 73% to 14%.
More than two-thirds of patients in both groups experienced a change in management after the scans were read. Changes in Alzheimer’s drugs occurred in 48% of both groups, while changes in non-Alzheimer’s drugs occurred in 36% of the MCI group and 32% of the dementia group. In amyloid-positive patients, use of Alzheimer’s drugs increased from 51% to 84%. In amyloid-negative patients, the use of Alzheimer’s drugs decreased from 39% to 31%.
Patient counseling also changed in 24% of the MCI group and 16% of the dementia group.
Dr. Rabinovici was cautiously optimistic about the interim results. “The study has two aims, and Medicare has made it clear that we need to complete both before they will consider covering the scans. I hope they understand that these changes in management are incredibly important, but they also want to see that they result in improved outcomes. That will take a year from when we enroll our last patient.”
Although the study is designed to show change in clinical outcomes, it’s also changing something less tangible, but no less important: patients’ understanding of their situation.
“We may be looking at objective changes in management, but we are also seeing that patients really want to know what’s going on in their brain, what the cause of their cognitive impairment is. They don’t want to be told that it’s normal aging, because they know it isn’t. There is a real value to getting that diagnosis, even if it’s the bad news that there are amyloid plaques in the brain. It leads to a clear plan in terms of what drugs to use, the possibility of enrolling in clinical trials, and getting some clarity about what’s going on. A lot of times, the certainty is better than the uncertainty.”
As of June, IDEAS had recruited 12,484 patients and completed 11,712 amyloid PET scans. Dr. Rabinovici hopes the recruitment will be completed by late this year, or early 2018.
IDEAS is being funded by the Centers for Medicare & Medicaid Services, Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, Piramal Imaging, the Alzheimer’s Association, and the American College of Radiology. Dr. Rabinovici has received honoraria or consulting fees from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche.
[email protected]
On Twitter @alz_gal
AT AAIC 2017
Key clinical point:
Major finding: Amyloid status changed clinical management in 68% of patients diagnosed with mild cognitive impairment or dementia.
Data source: An interim analysis of 4,000 out of 18,500 planned for enrollment in the IDEAS study.
Disclosures: IDEAS is being funded by the Centers for Medicare & Medicaid Services, Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, Piramal Imaging, the Alzheimer’s Association, and the American College of Radiology. Dr. Rabinovici has received honoraria or consulting fees from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche.
Crohn’s & Colitis Congress registration open
Join the Crohn’s & Colitis Foundation and AGA for the inaugural Crohn’s & Colitis Congress™. Expand your knowledge, network with inflammatory bowel diseases (IBD) leaders across multiple disciplines and get inspired to improve patient care.
The Crohn’s & Colitis Congress, taking place Jan. 18-20, 2018 in Las Vegas, combines the strengths of the nation’s leading IBD patient organization, Crohn’s & Colitis Foundation, and the premier GI professional association, AGA. Together we are committed to convening the greatest minds in IBD to transform patient care and accelerate the pace of research.
The Crohn’s & Colitis Congress offers a bold multidisciplinary, clinically focused and forward-thinking program. The organizing committee and faculty represent key disciplines involved in the comprehensive care of IBD patients, as well as the foremost minds in research.
Sessions will emphasize case studies with multidisciplinary panel discussions covering:
- • Management of complicated IBD
- • Defining optimal treatment algorithms
- • Clinical and research challenges
Take a critical step toward finding cures and improving the lives of adults and children living with IBD. Learn more about the congress and register today by visiting www.crohnscolitiscongress.org.
Join the Crohn’s & Colitis Foundation and AGA for the inaugural Crohn’s & Colitis Congress™. Expand your knowledge, network with inflammatory bowel diseases (IBD) leaders across multiple disciplines and get inspired to improve patient care.
The Crohn’s & Colitis Congress, taking place Jan. 18-20, 2018 in Las Vegas, combines the strengths of the nation’s leading IBD patient organization, Crohn’s & Colitis Foundation, and the premier GI professional association, AGA. Together we are committed to convening the greatest minds in IBD to transform patient care and accelerate the pace of research.
The Crohn’s & Colitis Congress offers a bold multidisciplinary, clinically focused and forward-thinking program. The organizing committee and faculty represent key disciplines involved in the comprehensive care of IBD patients, as well as the foremost minds in research.
Sessions will emphasize case studies with multidisciplinary panel discussions covering:
- • Management of complicated IBD
- • Defining optimal treatment algorithms
- • Clinical and research challenges
Take a critical step toward finding cures and improving the lives of adults and children living with IBD. Learn more about the congress and register today by visiting www.crohnscolitiscongress.org.
Join the Crohn’s & Colitis Foundation and AGA for the inaugural Crohn’s & Colitis Congress™. Expand your knowledge, network with inflammatory bowel diseases (IBD) leaders across multiple disciplines and get inspired to improve patient care.
The Crohn’s & Colitis Congress, taking place Jan. 18-20, 2018 in Las Vegas, combines the strengths of the nation’s leading IBD patient organization, Crohn’s & Colitis Foundation, and the premier GI professional association, AGA. Together we are committed to convening the greatest minds in IBD to transform patient care and accelerate the pace of research.
The Crohn’s & Colitis Congress offers a bold multidisciplinary, clinically focused and forward-thinking program. The organizing committee and faculty represent key disciplines involved in the comprehensive care of IBD patients, as well as the foremost minds in research.
Sessions will emphasize case studies with multidisciplinary panel discussions covering:
- • Management of complicated IBD
- • Defining optimal treatment algorithms
- • Clinical and research challenges
Take a critical step toward finding cures and improving the lives of adults and children living with IBD. Learn more about the congress and register today by visiting www.crohnscolitiscongress.org.
Nomadic Mongolian skin care practices
In a large country of only 3 million people (where wild horses outnumber people), with an estimated 2 million who live in the capital and 1 million who live a traditional nomadic lifestyle, traditional skin care and beauty practices can still be found.
In the capital city of Ulaanbaatar, women practice many of the same beauty regimens as those of women in other parts of mainstream Asia, with access to department store beauty counters and shopping malls found in major cities throughout the world. With the influx of movies and media into Mongolia from South Korea in the late 1990s, South Korean beauty regimens and standards have weaved their way into the urban culture. However, in rural Mongolia, where a nomadic way of life still predominates, certain beauty and cultural practices remain intact without the influence of mainstream culture.
Homemade yogurt, a staple in rural Mongolia, is used on the face to help brighten the skin. In rural Mongolia, the yogurt is made and eaten fresh, thus lasts for 1-2 days if not refrigerated. The yogurt comes from cows and goats (rarely from other animals) that graze on open land without pesticides and are not fed hormones and grains. My personal diet doesn’t consist of much dairy, but I can say firsthand that in my opinion, it is delicious there. Yogurt is also applied to the skin to treat acne, but for acne the yogurt is fermented more than usual, so there is more acid to reduce the skin inflammation. (Lactic acid is typically what is found in fermented yogurt.)
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Resource:
In a large country of only 3 million people (where wild horses outnumber people), with an estimated 2 million who live in the capital and 1 million who live a traditional nomadic lifestyle, traditional skin care and beauty practices can still be found.
In the capital city of Ulaanbaatar, women practice many of the same beauty regimens as those of women in other parts of mainstream Asia, with access to department store beauty counters and shopping malls found in major cities throughout the world. With the influx of movies and media into Mongolia from South Korea in the late 1990s, South Korean beauty regimens and standards have weaved their way into the urban culture. However, in rural Mongolia, where a nomadic way of life still predominates, certain beauty and cultural practices remain intact without the influence of mainstream culture.
Homemade yogurt, a staple in rural Mongolia, is used on the face to help brighten the skin. In rural Mongolia, the yogurt is made and eaten fresh, thus lasts for 1-2 days if not refrigerated. The yogurt comes from cows and goats (rarely from other animals) that graze on open land without pesticides and are not fed hormones and grains. My personal diet doesn’t consist of much dairy, but I can say firsthand that in my opinion, it is delicious there. Yogurt is also applied to the skin to treat acne, but for acne the yogurt is fermented more than usual, so there is more acid to reduce the skin inflammation. (Lactic acid is typically what is found in fermented yogurt.)
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Resource:
In a large country of only 3 million people (where wild horses outnumber people), with an estimated 2 million who live in the capital and 1 million who live a traditional nomadic lifestyle, traditional skin care and beauty practices can still be found.
In the capital city of Ulaanbaatar, women practice many of the same beauty regimens as those of women in other parts of mainstream Asia, with access to department store beauty counters and shopping malls found in major cities throughout the world. With the influx of movies and media into Mongolia from South Korea in the late 1990s, South Korean beauty regimens and standards have weaved their way into the urban culture. However, in rural Mongolia, where a nomadic way of life still predominates, certain beauty and cultural practices remain intact without the influence of mainstream culture.
Homemade yogurt, a staple in rural Mongolia, is used on the face to help brighten the skin. In rural Mongolia, the yogurt is made and eaten fresh, thus lasts for 1-2 days if not refrigerated. The yogurt comes from cows and goats (rarely from other animals) that graze on open land without pesticides and are not fed hormones and grains. My personal diet doesn’t consist of much dairy, but I can say firsthand that in my opinion, it is delicious there. Yogurt is also applied to the skin to treat acne, but for acne the yogurt is fermented more than usual, so there is more acid to reduce the skin inflammation. (Lactic acid is typically what is found in fermented yogurt.)
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Resource:
New classification system for systemic lupus erythematosus moves forward
MADRID – A proposed classification scheme for systemic lupus erythematosus (SLE) relies on a combination of antinuclear antibody titer and the weighted scoring of signs and symptoms in seven clinical and three immunologic domains.
Anyone with an ANA titer of at least 1:80 on immunofluorescence and 84 points accumulated from the domains can be classified as having the disease, according to the proposed system. An international collaboration between the American College of Rheumatology and the European League Against Rheumatism, the system is the first classification scheme update since 2012, said Sindhu Johnson, MD, PhD, who discussed it during the European Congress of Rheumatology.
[polldaddy:9802068]
The proposed system is not intended to be a diagnostic tool, Dr. Johnson said in an interview. Rather, it’s meant to better stratify patients into research studies. “The prior criteria were missing patients. And, since classification criteria are used to decide whether patients can get into a clinical trial, we all felt that we were doing patients an injustice if the criteria were excluding some and denying them an opportunity to receive a novel therapy.”
There are currently two classification criteria in use: the 1982 American College of Rheumatology criteria and the Systemic Lupus International Collaborating Clinics Criteria (SLICC 2012). New understandings of SLE pathogenesis have rendered the 1982 ACR criteria outdated, according to a recently published paper (Arthritis Care Res. 2017 July 10. doi: 10.1002/acr.23317). While the SLICC 2012 criteria incorporated some of the new concepts and have increased sensitivity, compared with the 1982 ACR criteria, their specificity actually declined, partially because the document assigned equal weight to each of the clinical and immunologic criteria. The ACR/EULAR project takes a different tack. Criteria are weighted to reflect the clinical impact of different signs and symptoms, Dr. Johnson said.
“In clinical practice, if someone has class III/IV lupus nephritis, that’s a very different patient than someone who has leukopenia. As clinicians, we weight things differently, and so do these criteria, putting more weight on serious or internal organ manifestations of SLE.”
The ACR/EULAR criteria begin with a confirmed ANA titer of at least 1:80. “This has never been a requirement before, but the consensus now is that you need to have a positive ANA to be classified.”
Once that baseline is established, patients can be assessed in seven clinical domains and three immunologic domains. Each contains a subgroup of weighted signs and symptoms. These are ordered from those with least impact to those with most impact. Within each domain, only the highest-scoring criterion is counted toward the total score. When assessing, clinicians should not score any symptom if a cause other than SLE is more likely. The symptoms are not time-bound either, Dr. Johnson said. A symptom may have occurred only one time in the past, and that’s sufficient to earn a score. At least one clinical criterion must be present to be classified as SLE-positive.
The clinical domains
Constitutional: Fever (13 points). The only symptom in this domain, it’s never before been assessed in SLE criteria, Dr. Johnson said. “Our inclusion of fever is new, but our work in phase 1 of this project found that fever is a feature that can distinguish early lupus from mimickers. We want to identify patients as early in the disease course as possible so we can intervene, and fever appears to improve the ability to detect those patients.”
Cutaneous: Nonscarring alopecia (13), oral ulcers (14), subacute cutaneous or discoid lupus (29), and acute cutaneous lupus (38).
“Skin has long been recognized as an important part of lupus, but it got a lot of weight that some people felt was inappropriate. These criteria still include skin, but a patient can’t be classified on skin findings alone. There is concern that skin findings by themselves may not be lupus but something else, and some people even consider that cutaneous and systemic lupus are two different things.”
Arthritis: Synovitis in at least two joints (34).
Neurologic: Delirium (12), psychosis (20), and seizure (34).
Serositis: Pleural or pericardial effusion (34) and acute pericarditis (38).
Hematologic: Leukopenia (12), thrombocytopenia (26), and autoimmune hemolysis (28).
Renal: Proteinuria more than 0.5 g/24 hours (27), renal biopsy with class II or V lupus nephritis (55), and renal biopsy with class III or IV lupus nephritis (74).
The immunologic domains
Antiphospholipid antibodies: Anticardiolipin immunoglobulin G more than 40 GPL units, anti-beta2GP1 IgG more than 40 units, or lupus anticoagulant positive (13).
Complement proteins: Low C3 or low C4 (19) and low C3 and low C4 (27).
Highly specific antibodies: Anti-dsDNA antibody (38) and anti-Smith antibody (40).
Moving forward
Screening 10 domains with their attendant components may seem a bit clunky now, Dr. Johnson noted, but the final iteration should be more streamlined. Plus, she said, the system will be presented on a computer application that makes calculation much easier. “We’re aiming for feasibility and simplicity, but, at the same time, when you have a complex disease, you don’t want oversimplification. You may lose sensitivity and specificity.”
After further streamlining, Dr. Johnson said, the next step will be validating in a large retrospective patient cohort. “Right now, we are still collecting data for the validation cohort, which will be drawn from 36 centers. We’ll analyze sensitivity and specificity, comparing this system with the other two. We hope to present all these data at the ACR meeting in the fall.”
While research classification is the system’s raison d’être, it will undoubtedly influence diagnosis and clinical assessment as well, Dr. Johnson said. “ACR and EULAR are very clear that they only support the validation of classification criteria. The diagnosis of SLE is still within the hands of the physician. But, we know that classification criteria do inform our concept of the disease, so it’s likely these will shift the way we think about diagnosing lupus as well. We do hope to identify patients with earlier disease, so they have the opportunity to be involved in research” that may modify their disease course and, ultimately, prevent permanent damage and improve quality of life.
Dr. Johnson had no disclosures related to the development of the classification criteria.
[email protected]
On Twitter @alz_gal
This joint ACR/EULAR effort is very large, involving over 40 international SLE experts and centers, including many Systemic Lupus International Collaborating Clinics Criteria members. The goals are to develop new criteria that will be both sensitive and specific for SLE, which is a very heterogeneous and often elusive disease, using newer rigorous expert opinion–based and data-driven methodologies (as has been accomplished recently for rheumatoid arthritis, scleroderma, and gout).
This is a tall order! While genetic and cytokine-based biomarkers are being developed for the identification of SLE, unfortunately, we were not able incorporate them as they are not available for routine use at this time. The SLE classification criteria are used worldwide for inclusion in clinical trials and studies.
The work has been preceding in phases: phase 1, item generation; phase 2, item reduction and definition of criteria; phase 3, multicriteria decision analysis and threshold identification; and phase 4, validation. Phases 1-3 involved many iterative, group discussions, data collection and review, and novel “forced choice” methodologies for arriving at group consensus. In phase 4 (validation), the goal is to compare classification using these criteria with the existing ACR and SLICC criteria, as well as SLE expert physician diagnosis. We will see how they do after all this effort!
Karen H. Costenbader, MD, is the lupus program director at Brigham and Women’s Hospital, Boston. She is a member of the classification criteria steering committee and is the senior author on a paper describing the process to develop the draft classification criteria (Arthritis Care Res. 2017 July 10. doi: 10.1002/acr.23317).
This joint ACR/EULAR effort is very large, involving over 40 international SLE experts and centers, including many Systemic Lupus International Collaborating Clinics Criteria members. The goals are to develop new criteria that will be both sensitive and specific for SLE, which is a very heterogeneous and often elusive disease, using newer rigorous expert opinion–based and data-driven methodologies (as has been accomplished recently for rheumatoid arthritis, scleroderma, and gout).
This is a tall order! While genetic and cytokine-based biomarkers are being developed for the identification of SLE, unfortunately, we were not able incorporate them as they are not available for routine use at this time. The SLE classification criteria are used worldwide for inclusion in clinical trials and studies.
The work has been preceding in phases: phase 1, item generation; phase 2, item reduction and definition of criteria; phase 3, multicriteria decision analysis and threshold identification; and phase 4, validation. Phases 1-3 involved many iterative, group discussions, data collection and review, and novel “forced choice” methodologies for arriving at group consensus. In phase 4 (validation), the goal is to compare classification using these criteria with the existing ACR and SLICC criteria, as well as SLE expert physician diagnosis. We will see how they do after all this effort!
Karen H. Costenbader, MD, is the lupus program director at Brigham and Women’s Hospital, Boston. She is a member of the classification criteria steering committee and is the senior author on a paper describing the process to develop the draft classification criteria (Arthritis Care Res. 2017 July 10. doi: 10.1002/acr.23317).
This joint ACR/EULAR effort is very large, involving over 40 international SLE experts and centers, including many Systemic Lupus International Collaborating Clinics Criteria members. The goals are to develop new criteria that will be both sensitive and specific for SLE, which is a very heterogeneous and often elusive disease, using newer rigorous expert opinion–based and data-driven methodologies (as has been accomplished recently for rheumatoid arthritis, scleroderma, and gout).
This is a tall order! While genetic and cytokine-based biomarkers are being developed for the identification of SLE, unfortunately, we were not able incorporate them as they are not available for routine use at this time. The SLE classification criteria are used worldwide for inclusion in clinical trials and studies.
The work has been preceding in phases: phase 1, item generation; phase 2, item reduction and definition of criteria; phase 3, multicriteria decision analysis and threshold identification; and phase 4, validation. Phases 1-3 involved many iterative, group discussions, data collection and review, and novel “forced choice” methodologies for arriving at group consensus. In phase 4 (validation), the goal is to compare classification using these criteria with the existing ACR and SLICC criteria, as well as SLE expert physician diagnosis. We will see how they do after all this effort!
Karen H. Costenbader, MD, is the lupus program director at Brigham and Women’s Hospital, Boston. She is a member of the classification criteria steering committee and is the senior author on a paper describing the process to develop the draft classification criteria (Arthritis Care Res. 2017 July 10. doi: 10.1002/acr.23317).
MADRID – A proposed classification scheme for systemic lupus erythematosus (SLE) relies on a combination of antinuclear antibody titer and the weighted scoring of signs and symptoms in seven clinical and three immunologic domains.
Anyone with an ANA titer of at least 1:80 on immunofluorescence and 84 points accumulated from the domains can be classified as having the disease, according to the proposed system. An international collaboration between the American College of Rheumatology and the European League Against Rheumatism, the system is the first classification scheme update since 2012, said Sindhu Johnson, MD, PhD, who discussed it during the European Congress of Rheumatology.
[polldaddy:9802068]
The proposed system is not intended to be a diagnostic tool, Dr. Johnson said in an interview. Rather, it’s meant to better stratify patients into research studies. “The prior criteria were missing patients. And, since classification criteria are used to decide whether patients can get into a clinical trial, we all felt that we were doing patients an injustice if the criteria were excluding some and denying them an opportunity to receive a novel therapy.”
There are currently two classification criteria in use: the 1982 American College of Rheumatology criteria and the Systemic Lupus International Collaborating Clinics Criteria (SLICC 2012). New understandings of SLE pathogenesis have rendered the 1982 ACR criteria outdated, according to a recently published paper (Arthritis Care Res. 2017 July 10. doi: 10.1002/acr.23317). While the SLICC 2012 criteria incorporated some of the new concepts and have increased sensitivity, compared with the 1982 ACR criteria, their specificity actually declined, partially because the document assigned equal weight to each of the clinical and immunologic criteria. The ACR/EULAR project takes a different tack. Criteria are weighted to reflect the clinical impact of different signs and symptoms, Dr. Johnson said.
“In clinical practice, if someone has class III/IV lupus nephritis, that’s a very different patient than someone who has leukopenia. As clinicians, we weight things differently, and so do these criteria, putting more weight on serious or internal organ manifestations of SLE.”
The ACR/EULAR criteria begin with a confirmed ANA titer of at least 1:80. “This has never been a requirement before, but the consensus now is that you need to have a positive ANA to be classified.”
Once that baseline is established, patients can be assessed in seven clinical domains and three immunologic domains. Each contains a subgroup of weighted signs and symptoms. These are ordered from those with least impact to those with most impact. Within each domain, only the highest-scoring criterion is counted toward the total score. When assessing, clinicians should not score any symptom if a cause other than SLE is more likely. The symptoms are not time-bound either, Dr. Johnson said. A symptom may have occurred only one time in the past, and that’s sufficient to earn a score. At least one clinical criterion must be present to be classified as SLE-positive.
The clinical domains
Constitutional: Fever (13 points). The only symptom in this domain, it’s never before been assessed in SLE criteria, Dr. Johnson said. “Our inclusion of fever is new, but our work in phase 1 of this project found that fever is a feature that can distinguish early lupus from mimickers. We want to identify patients as early in the disease course as possible so we can intervene, and fever appears to improve the ability to detect those patients.”
Cutaneous: Nonscarring alopecia (13), oral ulcers (14), subacute cutaneous or discoid lupus (29), and acute cutaneous lupus (38).
“Skin has long been recognized as an important part of lupus, but it got a lot of weight that some people felt was inappropriate. These criteria still include skin, but a patient can’t be classified on skin findings alone. There is concern that skin findings by themselves may not be lupus but something else, and some people even consider that cutaneous and systemic lupus are two different things.”
Arthritis: Synovitis in at least two joints (34).
Neurologic: Delirium (12), psychosis (20), and seizure (34).
Serositis: Pleural or pericardial effusion (34) and acute pericarditis (38).
Hematologic: Leukopenia (12), thrombocytopenia (26), and autoimmune hemolysis (28).
Renal: Proteinuria more than 0.5 g/24 hours (27), renal biopsy with class II or V lupus nephritis (55), and renal biopsy with class III or IV lupus nephritis (74).
The immunologic domains
Antiphospholipid antibodies: Anticardiolipin immunoglobulin G more than 40 GPL units, anti-beta2GP1 IgG more than 40 units, or lupus anticoagulant positive (13).
Complement proteins: Low C3 or low C4 (19) and low C3 and low C4 (27).
Highly specific antibodies: Anti-dsDNA antibody (38) and anti-Smith antibody (40).
Moving forward
Screening 10 domains with their attendant components may seem a bit clunky now, Dr. Johnson noted, but the final iteration should be more streamlined. Plus, she said, the system will be presented on a computer application that makes calculation much easier. “We’re aiming for feasibility and simplicity, but, at the same time, when you have a complex disease, you don’t want oversimplification. You may lose sensitivity and specificity.”
After further streamlining, Dr. Johnson said, the next step will be validating in a large retrospective patient cohort. “Right now, we are still collecting data for the validation cohort, which will be drawn from 36 centers. We’ll analyze sensitivity and specificity, comparing this system with the other two. We hope to present all these data at the ACR meeting in the fall.”
While research classification is the system’s raison d’être, it will undoubtedly influence diagnosis and clinical assessment as well, Dr. Johnson said. “ACR and EULAR are very clear that they only support the validation of classification criteria. The diagnosis of SLE is still within the hands of the physician. But, we know that classification criteria do inform our concept of the disease, so it’s likely these will shift the way we think about diagnosing lupus as well. We do hope to identify patients with earlier disease, so they have the opportunity to be involved in research” that may modify their disease course and, ultimately, prevent permanent damage and improve quality of life.
Dr. Johnson had no disclosures related to the development of the classification criteria.
[email protected]
On Twitter @alz_gal
MADRID – A proposed classification scheme for systemic lupus erythematosus (SLE) relies on a combination of antinuclear antibody titer and the weighted scoring of signs and symptoms in seven clinical and three immunologic domains.
Anyone with an ANA titer of at least 1:80 on immunofluorescence and 84 points accumulated from the domains can be classified as having the disease, according to the proposed system. An international collaboration between the American College of Rheumatology and the European League Against Rheumatism, the system is the first classification scheme update since 2012, said Sindhu Johnson, MD, PhD, who discussed it during the European Congress of Rheumatology.
[polldaddy:9802068]
The proposed system is not intended to be a diagnostic tool, Dr. Johnson said in an interview. Rather, it’s meant to better stratify patients into research studies. “The prior criteria were missing patients. And, since classification criteria are used to decide whether patients can get into a clinical trial, we all felt that we were doing patients an injustice if the criteria were excluding some and denying them an opportunity to receive a novel therapy.”
There are currently two classification criteria in use: the 1982 American College of Rheumatology criteria and the Systemic Lupus International Collaborating Clinics Criteria (SLICC 2012). New understandings of SLE pathogenesis have rendered the 1982 ACR criteria outdated, according to a recently published paper (Arthritis Care Res. 2017 July 10. doi: 10.1002/acr.23317). While the SLICC 2012 criteria incorporated some of the new concepts and have increased sensitivity, compared with the 1982 ACR criteria, their specificity actually declined, partially because the document assigned equal weight to each of the clinical and immunologic criteria. The ACR/EULAR project takes a different tack. Criteria are weighted to reflect the clinical impact of different signs and symptoms, Dr. Johnson said.
“In clinical practice, if someone has class III/IV lupus nephritis, that’s a very different patient than someone who has leukopenia. As clinicians, we weight things differently, and so do these criteria, putting more weight on serious or internal organ manifestations of SLE.”
The ACR/EULAR criteria begin with a confirmed ANA titer of at least 1:80. “This has never been a requirement before, but the consensus now is that you need to have a positive ANA to be classified.”
Once that baseline is established, patients can be assessed in seven clinical domains and three immunologic domains. Each contains a subgroup of weighted signs and symptoms. These are ordered from those with least impact to those with most impact. Within each domain, only the highest-scoring criterion is counted toward the total score. When assessing, clinicians should not score any symptom if a cause other than SLE is more likely. The symptoms are not time-bound either, Dr. Johnson said. A symptom may have occurred only one time in the past, and that’s sufficient to earn a score. At least one clinical criterion must be present to be classified as SLE-positive.
The clinical domains
Constitutional: Fever (13 points). The only symptom in this domain, it’s never before been assessed in SLE criteria, Dr. Johnson said. “Our inclusion of fever is new, but our work in phase 1 of this project found that fever is a feature that can distinguish early lupus from mimickers. We want to identify patients as early in the disease course as possible so we can intervene, and fever appears to improve the ability to detect those patients.”
Cutaneous: Nonscarring alopecia (13), oral ulcers (14), subacute cutaneous or discoid lupus (29), and acute cutaneous lupus (38).
“Skin has long been recognized as an important part of lupus, but it got a lot of weight that some people felt was inappropriate. These criteria still include skin, but a patient can’t be classified on skin findings alone. There is concern that skin findings by themselves may not be lupus but something else, and some people even consider that cutaneous and systemic lupus are two different things.”
Arthritis: Synovitis in at least two joints (34).
Neurologic: Delirium (12), psychosis (20), and seizure (34).
Serositis: Pleural or pericardial effusion (34) and acute pericarditis (38).
Hematologic: Leukopenia (12), thrombocytopenia (26), and autoimmune hemolysis (28).
Renal: Proteinuria more than 0.5 g/24 hours (27), renal biopsy with class II or V lupus nephritis (55), and renal biopsy with class III or IV lupus nephritis (74).
The immunologic domains
Antiphospholipid antibodies: Anticardiolipin immunoglobulin G more than 40 GPL units, anti-beta2GP1 IgG more than 40 units, or lupus anticoagulant positive (13).
Complement proteins: Low C3 or low C4 (19) and low C3 and low C4 (27).
Highly specific antibodies: Anti-dsDNA antibody (38) and anti-Smith antibody (40).
Moving forward
Screening 10 domains with their attendant components may seem a bit clunky now, Dr. Johnson noted, but the final iteration should be more streamlined. Plus, she said, the system will be presented on a computer application that makes calculation much easier. “We’re aiming for feasibility and simplicity, but, at the same time, when you have a complex disease, you don’t want oversimplification. You may lose sensitivity and specificity.”
After further streamlining, Dr. Johnson said, the next step will be validating in a large retrospective patient cohort. “Right now, we are still collecting data for the validation cohort, which will be drawn from 36 centers. We’ll analyze sensitivity and specificity, comparing this system with the other two. We hope to present all these data at the ACR meeting in the fall.”
While research classification is the system’s raison d’être, it will undoubtedly influence diagnosis and clinical assessment as well, Dr. Johnson said. “ACR and EULAR are very clear that they only support the validation of classification criteria. The diagnosis of SLE is still within the hands of the physician. But, we know that classification criteria do inform our concept of the disease, so it’s likely these will shift the way we think about diagnosing lupus as well. We do hope to identify patients with earlier disease, so they have the opportunity to be involved in research” that may modify their disease course and, ultimately, prevent permanent damage and improve quality of life.
Dr. Johnson had no disclosures related to the development of the classification criteria.
[email protected]
On Twitter @alz_gal
AT THE EULAR 2017 CONGRESS
Over 45% of American adults have type 2 diabetes mellitus or prediabetes
More than 114 million American adults have type 2 diabetes mellitus or prediabetes, according to estimates from the Centers for Disease Control and Prevention.
As of 2015, the combined prevalence of diabetes and prediabetes was 45.4% among adults in the United States: 11.5% (30.3 million) have diabetes and 33.9% have prediabetes, representing 84.1 million people who could develop type 2 diabetes within 5 years, the CDC said in the National Diabetes Statistics Report, 2017.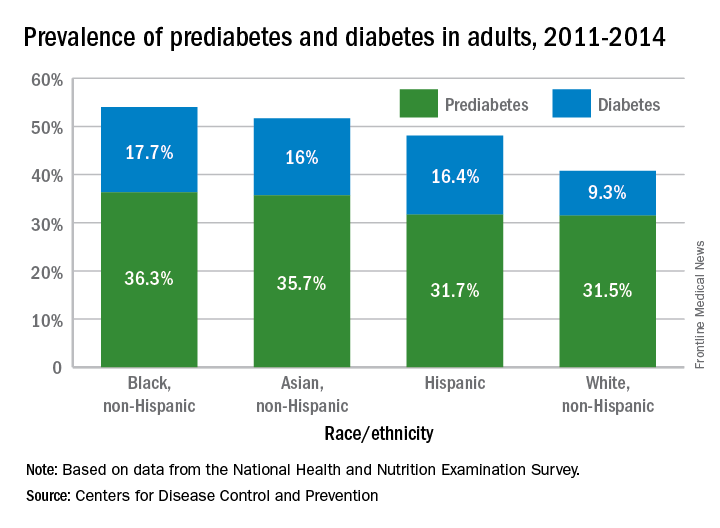
Lack of knowledge about having the disease was common: Almost a quarter (23.8%) of adults with diabetes didn’t know they had it, and the number jumped to 88% for those with prediabetes, based on data from the National Health and Nutrition Examination Survey, which included a blood test for fasting plasma glucose or hemoglobin A1c.
“More than a third of U.S. adults have prediabetes, and the majority don’t know it. Now, more than ever, we must step up our efforts to reduce the burden of this serious disease,” CDC Director Brenda Fitzgerald, MD, said in a statement.
“Diabetes and prediabetes remain serious threats for more than one-third of Americans – the statistics are staggering,” William T. Cefalu, MD, chief scientific, medical, and mission officer of the American Diabetes Association, said in a written statement.
“We must continue to innovate in scientific research and to translate findings to the clinical level to decrease the prevalence of diabetes. These data clearly confirm it is critical for us to continue to provide the education and support needed to improve health outcomes and decrease the daily burden of diabetes. We must reduce the incidence of diabetes and its enormous costs, including both the financial costs and the human toll of lost quality of life,” he said.
“Diabetes and prediabetes remain serious threats for more than one-third of Americans – the statistics are staggering,” William T. Cefalu, MD, chief scientific, medical, and mission officer of the American Diabetes Association, said in a written statement.
“We must continue to innovate in scientific research and to translate findings to the clinical level to decrease the prevalence of diabetes. These data clearly confirm it is critical for us to continue to provide the education and support needed to improve health outcomes and decrease the daily burden of diabetes. We must reduce the incidence of diabetes and its enormous costs, including both the financial costs and the human toll of lost quality of life,” he said.
“Diabetes and prediabetes remain serious threats for more than one-third of Americans – the statistics are staggering,” William T. Cefalu, MD, chief scientific, medical, and mission officer of the American Diabetes Association, said in a written statement.
“We must continue to innovate in scientific research and to translate findings to the clinical level to decrease the prevalence of diabetes. These data clearly confirm it is critical for us to continue to provide the education and support needed to improve health outcomes and decrease the daily burden of diabetes. We must reduce the incidence of diabetes and its enormous costs, including both the financial costs and the human toll of lost quality of life,” he said.
More than 114 million American adults have type 2 diabetes mellitus or prediabetes, according to estimates from the Centers for Disease Control and Prevention.
As of 2015, the combined prevalence of diabetes and prediabetes was 45.4% among adults in the United States: 11.5% (30.3 million) have diabetes and 33.9% have prediabetes, representing 84.1 million people who could develop type 2 diabetes within 5 years, the CDC said in the National Diabetes Statistics Report, 2017.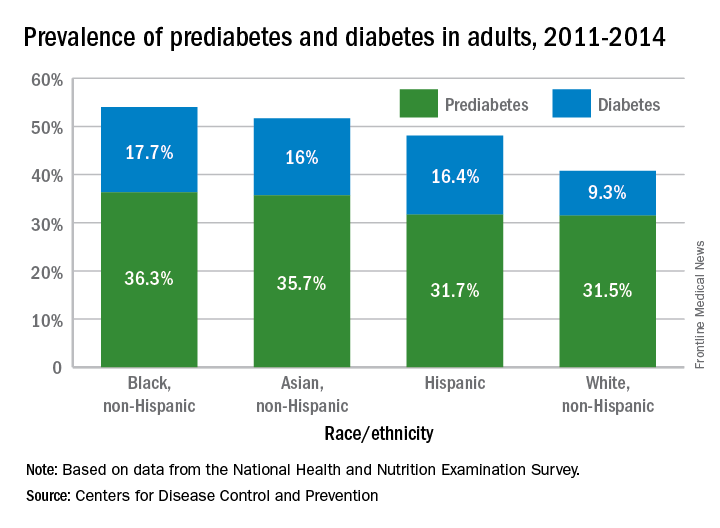
Lack of knowledge about having the disease was common: Almost a quarter (23.8%) of adults with diabetes didn’t know they had it, and the number jumped to 88% for those with prediabetes, based on data from the National Health and Nutrition Examination Survey, which included a blood test for fasting plasma glucose or hemoglobin A1c.
“More than a third of U.S. adults have prediabetes, and the majority don’t know it. Now, more than ever, we must step up our efforts to reduce the burden of this serious disease,” CDC Director Brenda Fitzgerald, MD, said in a statement.
More than 114 million American adults have type 2 diabetes mellitus or prediabetes, according to estimates from the Centers for Disease Control and Prevention.
As of 2015, the combined prevalence of diabetes and prediabetes was 45.4% among adults in the United States: 11.5% (30.3 million) have diabetes and 33.9% have prediabetes, representing 84.1 million people who could develop type 2 diabetes within 5 years, the CDC said in the National Diabetes Statistics Report, 2017.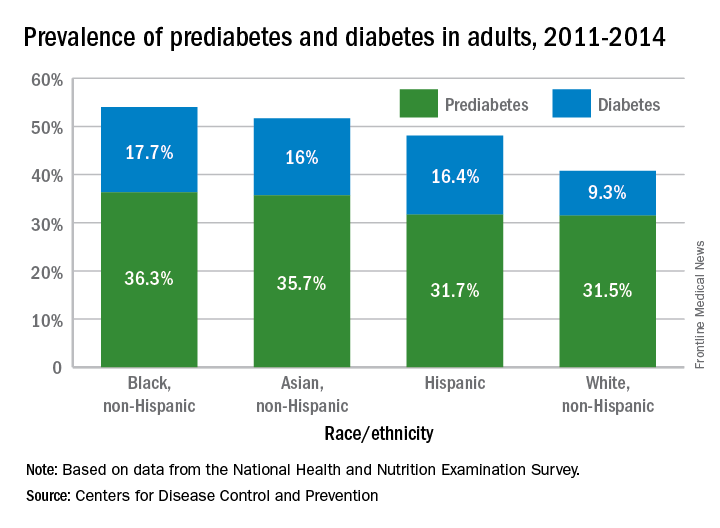
Lack of knowledge about having the disease was common: Almost a quarter (23.8%) of adults with diabetes didn’t know they had it, and the number jumped to 88% for those with prediabetes, based on data from the National Health and Nutrition Examination Survey, which included a blood test for fasting plasma glucose or hemoglobin A1c.
“More than a third of U.S. adults have prediabetes, and the majority don’t know it. Now, more than ever, we must step up our efforts to reduce the burden of this serious disease,” CDC Director Brenda Fitzgerald, MD, said in a statement.



















