User login
NETWORKS Health-care weaponization, PTSD, depression in caregivers Disaster Response Practice Operations Transplant Women’s Health
The tragic weaponization of health care
The Syrian conflict has highlighted the dangers to health-care workers (HCWs) in humanitarian crises. The Lancet-American University of Beirut Commission on Syria reports on the weaponization of health care in Syria – a strategy of depriving people of their health-care needs. Targeting of HCWs was recognized early in the Syrian war with targeting of health-care facilities being frequently reported throughout the conflict. HCWs facing extreme supply shortages have been reported to resort to desperate measures: using urine bags with added anticoagulants for blood collection and crafting homemade external fixators for fractures. Sadly, the Syrian conflict is not unique. The International Committee of the Red Cross (ICRC) documented 2,398 episodes of violence directed at health facilities in 11 countries affected by armed conflict between 2012 and 2014 alone. In Syria and elsewhere, the exodus of trained medical personnel, due to lack of medical training in trauma, emergency medicine, and intensive care, puts populations at further risk in these regions. The Inte
Dr. Maves is a military service member. The opinions expressed herein are his own and do not necessarily reflect the official opinions of the Department of the Navy, Department of Defense, or the US Government.
Rashmi Mishra, MD
Fellow-in-Training Member
Ryan Maves, MD, FCCP
Steering Committee Member
The House AHCA /Senate BCRA compared with ACA (Affordable Care Act)
Health-care costs are a fundamental driver of insurance costs, which leads to challenges to coverage affordability for millions of families. There is ongoing debate whether the current law (Affordable Care Act [ACA/Obamacare]) and the republican alternatives (American Healthcare Act [AHCA] and Better Care Reconciliation Act [BCRA]) do enough to address the cost challenges. Here is a brief summary of the key similarities and differences.
Similarities: (1) Children will be covered up to age 26. (2) Coverage of pre-existing conditions continues (high risk pools will be subsidized by a state government but premiums are up to twice as much as individual coverage). (3) Tax credit (based on age and family size rather than income level). (4) Insurance can charge older customers more than younger (up to 3X under ACA, 5X under AHCA/BCRA). (5) No annual or lifetime payout limit (but states may apply waivers allowing insurers to apply limits).
Differences: (1) Insurance will no longer be mandatory (no individual or employer mandates, but there is a 30% increase in premiums for 1 year for not maintaining individual continuous coverage). (2) Medicaid expansion (expanded under ACA to 133% of po
Health-care reform undoubtedly is complicated, and there are a lot of questions in the air about the future of health care under the Trump Administration. Few certainties: change is coming, MACRA is here to stay.
Adel Bassily-Marcus, MD, FCCP
NetWork Chair
Posttraumatic Stress Disorder Post-Lung Transplant
The majority of transplant physicians are mainly concerned with issues posttransplant that are focused on the graft function. But recently, neurocognition and posttransplant posttraumatic stress disorder have been found to have significant impact on quality of life and mortality after transplantation. Posttraumatic stress disorder (PTSD) is described as re-experiencing a traumatic event in addition to having avoidant and hyperarousal symptoms, which last for a period of at least 1 month. Studies of PTSD in solid organ transplant recipients have revealed a significantly higher prevalence of PTSD symptoms (10% to 17%) compared with the general population (prevalence of 3.5% to 6%). In one study of heart transplant recipients, patients who met the criteria for PTSD in the first year posttransplant had a higher risk for 3-year mortality (OR=13.74) [Dew et al. J Heart Lung Transplant. 1999;18[6]:549-562].
Lung transplant recipients are at a high risk for developing PTSD due to exposure to several traumatic events, such as a life-threatening exacerbation of the underlying lung disease, undergoing transplant surgery, intensive care unit stay, delirium and episodes of infection, and acute and chronic rejection. However, data regarding the prevalence and risk factors for PTSD post-lung transplant are limited.
The prevalence of PTSD post lung transplantation has been reported to be 12.6% to 15.8%. In lung transplant recipients with clinically significant PTSD symptomatology; the presence of symptoms of re-experiencing (29.5%) and arousal (33.8%) were more common than avoidant symptoms (18.4%) [Gries et al. J Heart Lung Transplant. 2013; 32[5]: 525-532]. In another study by Dew et al, in 178 lung transplant recipients, all PTSD occurred in the early months posttransplant with a median duration of symptoms of 12 months (IQR 7.2 to 18.5 months) [Dew et al. Gen. Hosp Psychiatry. 2012;34:127-138]. A higher burden of PTSD is noted in patients who are younger, have a lo
The challenges that remain include determining the true prevalence of PTSD in the lung transplant recipient in the LAS era using standard diagnostic criteria, documenting the adverse effects of PTSD on medical compliance, morbidity, and mortality; and developing interventions to mitigate the adverse effects of PTSD through well-designed multicenter prospective studies.
Vivek Ahya, MD
Steering Committee Member
Caregiver Burden in the ICU and Beyond
Family members of patients in the ICU who transition to the role of caregivers following discharge are at high risk for psychosocial distress. Post-intensive care syndrome-family (PICS-F) describes the symptoms of depression, posttraumatic stress, and anxiety commonly found in this population (Davidson et al. Crit Care Med. 2012;4(2):618-624). Women are more commonly called upon to adopt the role of caregiver for family members with chronic medical conditions or mental illnesses. Worldwide estimates indicate that 57% to 81% of all caregivers are women (Sharma et al. World J Psych. 2016;6[2]:7-17).
Family burden begins during the acute phase of critical illness. As surrogate decision-makers, they frequently face decisional conflict and decisional regret, especially in scenarios that limit life-sustaining therapies (Long et al. Curr Opin Crit Care. 2016;22:613-620). The prevalence of PICS-F is high as family members attempt to balance their role in the ICU with personal obligations (Choi et al. J Korean Acad Nurs. 2016;[46]2:159-167). Those who perceive that they are not receiving complete information from the medical team, and who do not find their physician comforting, have been shown to suffer a greater symptom burden (Davidson et al).
With the growing older adult population, and increased ICU survival, family members are often called upon to serve as caretakers to the chronically critically ill (Choi et al.). These caregivers have more depressive symptoms, worse health outcomes, and significant professional and personal lifestyle disruptions (Cameron, et al. N Engl J Med. 2016;[374]19:1831-1841). In many caregivers, depressive symptoms persist at 1 year after ICU admission, with rates comparable to caretakers of patients with dementia (Haines et al. Crit Care Med. 2015;(43)5:1112-1120). Caregivers who are younger, female, minorities, and those with pre-existing depression are at especially high risk for worse mental health outcomes (Davidson et al; Cameron et al).
Caregivers of ICU survivors are vulnerable and undersupported. Interventions such as ICU diaries, telephone-based mindfulness exercises, and stress management strategies have shown promise in alleviating PICS-F symptoms (Choi et al.). During the acute ICU stay, how medical providers communicate, and how we help family members make sense of what has happened and their new roles as caregivers have an impact (Davidson et al.). From an individual in a study of psychosocial morbidity in caregivers of ICU survivors: “Leaving the hospital is not the end for some people. The next place is just as hard, sometimes worse” (Haines et al. Further studies are needed to identify interventions that will truly address this population’s unique needs.
Margaret Pisani, MD, FCCP
Steering Committee Member
Nicole Bournival, MD
Fellow-in-Training Member
The tragic weaponization of health care
The Syrian conflict has highlighted the dangers to health-care workers (HCWs) in humanitarian crises. The Lancet-American University of Beirut Commission on Syria reports on the weaponization of health care in Syria – a strategy of depriving people of their health-care needs. Targeting of HCWs was recognized early in the Syrian war with targeting of health-care facilities being frequently reported throughout the conflict. HCWs facing extreme supply shortages have been reported to resort to desperate measures: using urine bags with added anticoagulants for blood collection and crafting homemade external fixators for fractures. Sadly, the Syrian conflict is not unique. The International Committee of the Red Cross (ICRC) documented 2,398 episodes of violence directed at health facilities in 11 countries affected by armed conflict between 2012 and 2014 alone. In Syria and elsewhere, the exodus of trained medical personnel, due to lack of medical training in trauma, emergency medicine, and intensive care, puts populations at further risk in these regions. The Inte
Dr. Maves is a military service member. The opinions expressed herein are his own and do not necessarily reflect the official opinions of the Department of the Navy, Department of Defense, or the US Government.
Rashmi Mishra, MD
Fellow-in-Training Member
Ryan Maves, MD, FCCP
Steering Committee Member
The House AHCA /Senate BCRA compared with ACA (Affordable Care Act)
Health-care costs are a fundamental driver of insurance costs, which leads to challenges to coverage affordability for millions of families. There is ongoing debate whether the current law (Affordable Care Act [ACA/Obamacare]) and the republican alternatives (American Healthcare Act [AHCA] and Better Care Reconciliation Act [BCRA]) do enough to address the cost challenges. Here is a brief summary of the key similarities and differences.
Similarities: (1) Children will be covered up to age 26. (2) Coverage of pre-existing conditions continues (high risk pools will be subsidized by a state government but premiums are up to twice as much as individual coverage). (3) Tax credit (based on age and family size rather than income level). (4) Insurance can charge older customers more than younger (up to 3X under ACA, 5X under AHCA/BCRA). (5) No annual or lifetime payout limit (but states may apply waivers allowing insurers to apply limits).
Differences: (1) Insurance will no longer be mandatory (no individual or employer mandates, but there is a 30% increase in premiums for 1 year for not maintaining individual continuous coverage). (2) Medicaid expansion (expanded under ACA to 133% of po
Health-care reform undoubtedly is complicated, and there are a lot of questions in the air about the future of health care under the Trump Administration. Few certainties: change is coming, MACRA is here to stay.
Adel Bassily-Marcus, MD, FCCP
NetWork Chair
Posttraumatic Stress Disorder Post-Lung Transplant
The majority of transplant physicians are mainly concerned with issues posttransplant that are focused on the graft function. But recently, neurocognition and posttransplant posttraumatic stress disorder have been found to have significant impact on quality of life and mortality after transplantation. Posttraumatic stress disorder (PTSD) is described as re-experiencing a traumatic event in addition to having avoidant and hyperarousal symptoms, which last for a period of at least 1 month. Studies of PTSD in solid organ transplant recipients have revealed a significantly higher prevalence of PTSD symptoms (10% to 17%) compared with the general population (prevalence of 3.5% to 6%). In one study of heart transplant recipients, patients who met the criteria for PTSD in the first year posttransplant had a higher risk for 3-year mortality (OR=13.74) [Dew et al. J Heart Lung Transplant. 1999;18[6]:549-562].
Lung transplant recipients are at a high risk for developing PTSD due to exposure to several traumatic events, such as a life-threatening exacerbation of the underlying lung disease, undergoing transplant surgery, intensive care unit stay, delirium and episodes of infection, and acute and chronic rejection. However, data regarding the prevalence and risk factors for PTSD post-lung transplant are limited.
The prevalence of PTSD post lung transplantation has been reported to be 12.6% to 15.8%. In lung transplant recipients with clinically significant PTSD symptomatology; the presence of symptoms of re-experiencing (29.5%) and arousal (33.8%) were more common than avoidant symptoms (18.4%) [Gries et al. J Heart Lung Transplant. 2013; 32[5]: 525-532]. In another study by Dew et al, in 178 lung transplant recipients, all PTSD occurred in the early months posttransplant with a median duration of symptoms of 12 months (IQR 7.2 to 18.5 months) [Dew et al. Gen. Hosp Psychiatry. 2012;34:127-138]. A higher burden of PTSD is noted in patients who are younger, have a lo
The challenges that remain include determining the true prevalence of PTSD in the lung transplant recipient in the LAS era using standard diagnostic criteria, documenting the adverse effects of PTSD on medical compliance, morbidity, and mortality; and developing interventions to mitigate the adverse effects of PTSD through well-designed multicenter prospective studies.
Vivek Ahya, MD
Steering Committee Member
Caregiver Burden in the ICU and Beyond
Family members of patients in the ICU who transition to the role of caregivers following discharge are at high risk for psychosocial distress. Post-intensive care syndrome-family (PICS-F) describes the symptoms of depression, posttraumatic stress, and anxiety commonly found in this population (Davidson et al. Crit Care Med. 2012;4(2):618-624). Women are more commonly called upon to adopt the role of caregiver for family members with chronic medical conditions or mental illnesses. Worldwide estimates indicate that 57% to 81% of all caregivers are women (Sharma et al. World J Psych. 2016;6[2]:7-17).
Family burden begins during the acute phase of critical illness. As surrogate decision-makers, they frequently face decisional conflict and decisional regret, especially in scenarios that limit life-sustaining therapies (Long et al. Curr Opin Crit Care. 2016;22:613-620). The prevalence of PICS-F is high as family members attempt to balance their role in the ICU with personal obligations (Choi et al. J Korean Acad Nurs. 2016;[46]2:159-167). Those who perceive that they are not receiving complete information from the medical team, and who do not find their physician comforting, have been shown to suffer a greater symptom burden (Davidson et al).
With the growing older adult population, and increased ICU survival, family members are often called upon to serve as caretakers to the chronically critically ill (Choi et al.). These caregivers have more depressive symptoms, worse health outcomes, and significant professional and personal lifestyle disruptions (Cameron, et al. N Engl J Med. 2016;[374]19:1831-1841). In many caregivers, depressive symptoms persist at 1 year after ICU admission, with rates comparable to caretakers of patients with dementia (Haines et al. Crit Care Med. 2015;(43)5:1112-1120). Caregivers who are younger, female, minorities, and those with pre-existing depression are at especially high risk for worse mental health outcomes (Davidson et al; Cameron et al).
Caregivers of ICU survivors are vulnerable and undersupported. Interventions such as ICU diaries, telephone-based mindfulness exercises, and stress management strategies have shown promise in alleviating PICS-F symptoms (Choi et al.). During the acute ICU stay, how medical providers communicate, and how we help family members make sense of what has happened and their new roles as caregivers have an impact (Davidson et al.). From an individual in a study of psychosocial morbidity in caregivers of ICU survivors: “Leaving the hospital is not the end for some people. The next place is just as hard, sometimes worse” (Haines et al. Further studies are needed to identify interventions that will truly address this population’s unique needs.
Margaret Pisani, MD, FCCP
Steering Committee Member
Nicole Bournival, MD
Fellow-in-Training Member
The tragic weaponization of health care
The Syrian conflict has highlighted the dangers to health-care workers (HCWs) in humanitarian crises. The Lancet-American University of Beirut Commission on Syria reports on the weaponization of health care in Syria – a strategy of depriving people of their health-care needs. Targeting of HCWs was recognized early in the Syrian war with targeting of health-care facilities being frequently reported throughout the conflict. HCWs facing extreme supply shortages have been reported to resort to desperate measures: using urine bags with added anticoagulants for blood collection and crafting homemade external fixators for fractures. Sadly, the Syrian conflict is not unique. The International Committee of the Red Cross (ICRC) documented 2,398 episodes of violence directed at health facilities in 11 countries affected by armed conflict between 2012 and 2014 alone. In Syria and elsewhere, the exodus of trained medical personnel, due to lack of medical training in trauma, emergency medicine, and intensive care, puts populations at further risk in these regions. The Inte
Dr. Maves is a military service member. The opinions expressed herein are his own and do not necessarily reflect the official opinions of the Department of the Navy, Department of Defense, or the US Government.
Rashmi Mishra, MD
Fellow-in-Training Member
Ryan Maves, MD, FCCP
Steering Committee Member
The House AHCA /Senate BCRA compared with ACA (Affordable Care Act)
Health-care costs are a fundamental driver of insurance costs, which leads to challenges to coverage affordability for millions of families. There is ongoing debate whether the current law (Affordable Care Act [ACA/Obamacare]) and the republican alternatives (American Healthcare Act [AHCA] and Better Care Reconciliation Act [BCRA]) do enough to address the cost challenges. Here is a brief summary of the key similarities and differences.
Similarities: (1) Children will be covered up to age 26. (2) Coverage of pre-existing conditions continues (high risk pools will be subsidized by a state government but premiums are up to twice as much as individual coverage). (3) Tax credit (based on age and family size rather than income level). (4) Insurance can charge older customers more than younger (up to 3X under ACA, 5X under AHCA/BCRA). (5) No annual or lifetime payout limit (but states may apply waivers allowing insurers to apply limits).
Differences: (1) Insurance will no longer be mandatory (no individual or employer mandates, but there is a 30% increase in premiums for 1 year for not maintaining individual continuous coverage). (2) Medicaid expansion (expanded under ACA to 133% of po
Health-care reform undoubtedly is complicated, and there are a lot of questions in the air about the future of health care under the Trump Administration. Few certainties: change is coming, MACRA is here to stay.
Adel Bassily-Marcus, MD, FCCP
NetWork Chair
Posttraumatic Stress Disorder Post-Lung Transplant
The majority of transplant physicians are mainly concerned with issues posttransplant that are focused on the graft function. But recently, neurocognition and posttransplant posttraumatic stress disorder have been found to have significant impact on quality of life and mortality after transplantation. Posttraumatic stress disorder (PTSD) is described as re-experiencing a traumatic event in addition to having avoidant and hyperarousal symptoms, which last for a period of at least 1 month. Studies of PTSD in solid organ transplant recipients have revealed a significantly higher prevalence of PTSD symptoms (10% to 17%) compared with the general population (prevalence of 3.5% to 6%). In one study of heart transplant recipients, patients who met the criteria for PTSD in the first year posttransplant had a higher risk for 3-year mortality (OR=13.74) [Dew et al. J Heart Lung Transplant. 1999;18[6]:549-562].
Lung transplant recipients are at a high risk for developing PTSD due to exposure to several traumatic events, such as a life-threatening exacerbation of the underlying lung disease, undergoing transplant surgery, intensive care unit stay, delirium and episodes of infection, and acute and chronic rejection. However, data regarding the prevalence and risk factors for PTSD post-lung transplant are limited.
The prevalence of PTSD post lung transplantation has been reported to be 12.6% to 15.8%. In lung transplant recipients with clinically significant PTSD symptomatology; the presence of symptoms of re-experiencing (29.5%) and arousal (33.8%) were more common than avoidant symptoms (18.4%) [Gries et al. J Heart Lung Transplant. 2013; 32[5]: 525-532]. In another study by Dew et al, in 178 lung transplant recipients, all PTSD occurred in the early months posttransplant with a median duration of symptoms of 12 months (IQR 7.2 to 18.5 months) [Dew et al. Gen. Hosp Psychiatry. 2012;34:127-138]. A higher burden of PTSD is noted in patients who are younger, have a lo
The challenges that remain include determining the true prevalence of PTSD in the lung transplant recipient in the LAS era using standard diagnostic criteria, documenting the adverse effects of PTSD on medical compliance, morbidity, and mortality; and developing interventions to mitigate the adverse effects of PTSD through well-designed multicenter prospective studies.
Vivek Ahya, MD
Steering Committee Member
Caregiver Burden in the ICU and Beyond
Family members of patients in the ICU who transition to the role of caregivers following discharge are at high risk for psychosocial distress. Post-intensive care syndrome-family (PICS-F) describes the symptoms of depression, posttraumatic stress, and anxiety commonly found in this population (Davidson et al. Crit Care Med. 2012;4(2):618-624). Women are more commonly called upon to adopt the role of caregiver for family members with chronic medical conditions or mental illnesses. Worldwide estimates indicate that 57% to 81% of all caregivers are women (Sharma et al. World J Psych. 2016;6[2]:7-17).
Family burden begins during the acute phase of critical illness. As surrogate decision-makers, they frequently face decisional conflict and decisional regret, especially in scenarios that limit life-sustaining therapies (Long et al. Curr Opin Crit Care. 2016;22:613-620). The prevalence of PICS-F is high as family members attempt to balance their role in the ICU with personal obligations (Choi et al. J Korean Acad Nurs. 2016;[46]2:159-167). Those who perceive that they are not receiving complete information from the medical team, and who do not find their physician comforting, have been shown to suffer a greater symptom burden (Davidson et al).
With the growing older adult population, and increased ICU survival, family members are often called upon to serve as caretakers to the chronically critically ill (Choi et al.). These caregivers have more depressive symptoms, worse health outcomes, and significant professional and personal lifestyle disruptions (Cameron, et al. N Engl J Med. 2016;[374]19:1831-1841). In many caregivers, depressive symptoms persist at 1 year after ICU admission, with rates comparable to caretakers of patients with dementia (Haines et al. Crit Care Med. 2015;(43)5:1112-1120). Caregivers who are younger, female, minorities, and those with pre-existing depression are at especially high risk for worse mental health outcomes (Davidson et al; Cameron et al).
Caregivers of ICU survivors are vulnerable and undersupported. Interventions such as ICU diaries, telephone-based mindfulness exercises, and stress management strategies have shown promise in alleviating PICS-F symptoms (Choi et al.). During the acute ICU stay, how medical providers communicate, and how we help family members make sense of what has happened and their new roles as caregivers have an impact (Davidson et al.). From an individual in a study of psychosocial morbidity in caregivers of ICU survivors: “Leaving the hospital is not the end for some people. The next place is just as hard, sometimes worse” (Haines et al. Further studies are needed to identify interventions that will truly address this population’s unique needs.
Margaret Pisani, MD, FCCP
Steering Committee Member
Nicole Bournival, MD
Fellow-in-Training Member
High-flow nasal cannula safe outside of pediatric ICU, but may up length of stay
NASHVILLE, TENN. – Young children with acute bronchiolitis do not need to be admitted to the pediatric ICU for high-flow nasal cannula treatment of up to 6 L/min and 50% oxygen; it is safe to administer it on the floor, according to a review of 6,804 acute bronchiolitis cases in children younger than 2 years treated at the University of Texas Southwestern Medical Center, Dallas.
Use of high-flow nasal cannulas (HFNC) has increased dramatically in recent years at UT Southwestern and elsewhere. It soothes children and can rapidly improve breathing without the nasal edema and nose bleeds common with cooler, drier, 100% oxygen. At Southwestern, HFNC use on the pediatric wards increased from 5% of acute bronchiolitis cases in the September 2010 to April 2011 season to 60% in the 2015-2016 season. Use for bronchiolitis in the PICU increased from 82% to 98% over the same period.
The increase correlated with a drop in intubation for acute bronchiolitis from 14% of children in 2010-2011 to just 2% in 2015-2016. The only HFNC adverse events were minor air leaks in two children.
As HFNC became more common, however, the Dallas team found that length of stay for acute bronchiolitis increased from 1.8 days in 2011-2012 to 2.4 days in 2015-2016, perhaps because the use of HFNC gives providers the impression that children are sicker than they actually are.
To counter the problem, lead investigator Vineeta Mittal, MD, associate professor of pediatrics, and her colleagues created an HFNC weaning protocol that gradually steps down treatment based on blood oxygen saturation levels and breathing effort, leading ultimately to a room-air challenge. It helped; the mean length of stay as of November 2016 was 1.7 days.
There’s been pushback in some places about giving HFNC on the floor: Intensivists sometimes consider it a form of ventilation that should be administered in the PICU. At levels up to 6 L/min and 50% oxygen, though, HFNC is “safe to give on the floor, because there’s no pneumothorax risk,” Dr. Mittal explained. HFNC “is not a ventilator; it’s an effective form of noninvasive respiratory support in children with moderate to severe respiratory distress from bronchiolitis.”
At Southwestern, “we are managing 80% of cases on the floor” with the help of HFNC, Dr. Mittal said at Pediatric Hospital Medicine.
At least for now, children at Southwestern go to the PICU if they need higher flow rates, but Dr. Mittal said it’s not clear if that’s necessary. “We said [6 L/min] is safe,” but maybe “we could even use 8 L/min or even 12 L/min” – the maximum delivered in the PICU over the study period – “because we know it’s safe,” she said. In addition, keeping kids on the floor also saves money, she noted at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Dr. Mittal is concerned HFNC might be overused. “We have gotten so used to this machine that the moment we see distress, we put the kid on high flow,” rather than observing them for a bit to see if they recover on their own. More data are needed to determine when HFNC should be initiated, and when to pull the plug on HFNC and intubate, she said.
Dr. Mittal had no disclosures.
NASHVILLE, TENN. – Young children with acute bronchiolitis do not need to be admitted to the pediatric ICU for high-flow nasal cannula treatment of up to 6 L/min and 50% oxygen; it is safe to administer it on the floor, according to a review of 6,804 acute bronchiolitis cases in children younger than 2 years treated at the University of Texas Southwestern Medical Center, Dallas.
Use of high-flow nasal cannulas (HFNC) has increased dramatically in recent years at UT Southwestern and elsewhere. It soothes children and can rapidly improve breathing without the nasal edema and nose bleeds common with cooler, drier, 100% oxygen. At Southwestern, HFNC use on the pediatric wards increased from 5% of acute bronchiolitis cases in the September 2010 to April 2011 season to 60% in the 2015-2016 season. Use for bronchiolitis in the PICU increased from 82% to 98% over the same period.
The increase correlated with a drop in intubation for acute bronchiolitis from 14% of children in 2010-2011 to just 2% in 2015-2016. The only HFNC adverse events were minor air leaks in two children.
As HFNC became more common, however, the Dallas team found that length of stay for acute bronchiolitis increased from 1.8 days in 2011-2012 to 2.4 days in 2015-2016, perhaps because the use of HFNC gives providers the impression that children are sicker than they actually are.
To counter the problem, lead investigator Vineeta Mittal, MD, associate professor of pediatrics, and her colleagues created an HFNC weaning protocol that gradually steps down treatment based on blood oxygen saturation levels and breathing effort, leading ultimately to a room-air challenge. It helped; the mean length of stay as of November 2016 was 1.7 days.
There’s been pushback in some places about giving HFNC on the floor: Intensivists sometimes consider it a form of ventilation that should be administered in the PICU. At levels up to 6 L/min and 50% oxygen, though, HFNC is “safe to give on the floor, because there’s no pneumothorax risk,” Dr. Mittal explained. HFNC “is not a ventilator; it’s an effective form of noninvasive respiratory support in children with moderate to severe respiratory distress from bronchiolitis.”
At Southwestern, “we are managing 80% of cases on the floor” with the help of HFNC, Dr. Mittal said at Pediatric Hospital Medicine.
At least for now, children at Southwestern go to the PICU if they need higher flow rates, but Dr. Mittal said it’s not clear if that’s necessary. “We said [6 L/min] is safe,” but maybe “we could even use 8 L/min or even 12 L/min” – the maximum delivered in the PICU over the study period – “because we know it’s safe,” she said. In addition, keeping kids on the floor also saves money, she noted at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Dr. Mittal is concerned HFNC might be overused. “We have gotten so used to this machine that the moment we see distress, we put the kid on high flow,” rather than observing them for a bit to see if they recover on their own. More data are needed to determine when HFNC should be initiated, and when to pull the plug on HFNC and intubate, she said.
Dr. Mittal had no disclosures.
NASHVILLE, TENN. – Young children with acute bronchiolitis do not need to be admitted to the pediatric ICU for high-flow nasal cannula treatment of up to 6 L/min and 50% oxygen; it is safe to administer it on the floor, according to a review of 6,804 acute bronchiolitis cases in children younger than 2 years treated at the University of Texas Southwestern Medical Center, Dallas.
Use of high-flow nasal cannulas (HFNC) has increased dramatically in recent years at UT Southwestern and elsewhere. It soothes children and can rapidly improve breathing without the nasal edema and nose bleeds common with cooler, drier, 100% oxygen. At Southwestern, HFNC use on the pediatric wards increased from 5% of acute bronchiolitis cases in the September 2010 to April 2011 season to 60% in the 2015-2016 season. Use for bronchiolitis in the PICU increased from 82% to 98% over the same period.
The increase correlated with a drop in intubation for acute bronchiolitis from 14% of children in 2010-2011 to just 2% in 2015-2016. The only HFNC adverse events were minor air leaks in two children.
As HFNC became more common, however, the Dallas team found that length of stay for acute bronchiolitis increased from 1.8 days in 2011-2012 to 2.4 days in 2015-2016, perhaps because the use of HFNC gives providers the impression that children are sicker than they actually are.
To counter the problem, lead investigator Vineeta Mittal, MD, associate professor of pediatrics, and her colleagues created an HFNC weaning protocol that gradually steps down treatment based on blood oxygen saturation levels and breathing effort, leading ultimately to a room-air challenge. It helped; the mean length of stay as of November 2016 was 1.7 days.
There’s been pushback in some places about giving HFNC on the floor: Intensivists sometimes consider it a form of ventilation that should be administered in the PICU. At levels up to 6 L/min and 50% oxygen, though, HFNC is “safe to give on the floor, because there’s no pneumothorax risk,” Dr. Mittal explained. HFNC “is not a ventilator; it’s an effective form of noninvasive respiratory support in children with moderate to severe respiratory distress from bronchiolitis.”
At Southwestern, “we are managing 80% of cases on the floor” with the help of HFNC, Dr. Mittal said at Pediatric Hospital Medicine.
At least for now, children at Southwestern go to the PICU if they need higher flow rates, but Dr. Mittal said it’s not clear if that’s necessary. “We said [6 L/min] is safe,” but maybe “we could even use 8 L/min or even 12 L/min” – the maximum delivered in the PICU over the study period – “because we know it’s safe,” she said. In addition, keeping kids on the floor also saves money, she noted at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Dr. Mittal is concerned HFNC might be overused. “We have gotten so used to this machine that the moment we see distress, we put the kid on high flow,” rather than observing them for a bit to see if they recover on their own. More data are needed to determine when HFNC should be initiated, and when to pull the plug on HFNC and intubate, she said.
Dr. Mittal had no disclosures.
AT PHM 2017
Key clinical point:
Major finding: The increased use of HFNC corresponded with an increase in length of stay for acute bronchiolitis, from 1.8 days in the 2011-2012 season to 2.4 days in the 2015-2016 season.
Data source: A single-center review of almost 7,000 acute bronchiolitis cases.
Disclosures: The lead investigator had no disclosures.
Learn What's New in Billing, Coding
Learn the latest in billing, coding and reimbursement at the 2017 Coding and Reimbursement Workshop for vascular surgeons, Oct. 13-14 in Chicago.
Cost is $880 for SVS members or staff; $955 for non-members and $250 for residents and trainees.
The program will address and review 2018 updates and include information about the global surgical package and how it impacts billing and reimbursement, along with the application of modifiers for streamlined reimbursement.
An optional workshop on Evaluation and Management (E&M) coding will be held from 9 a.m. to noon Oct. 13.
Learn the latest in billing, coding and reimbursement at the 2017 Coding and Reimbursement Workshop for vascular surgeons, Oct. 13-14 in Chicago.
Cost is $880 for SVS members or staff; $955 for non-members and $250 for residents and trainees.
The program will address and review 2018 updates and include information about the global surgical package and how it impacts billing and reimbursement, along with the application of modifiers for streamlined reimbursement.
An optional workshop on Evaluation and Management (E&M) coding will be held from 9 a.m. to noon Oct. 13.
Learn the latest in billing, coding and reimbursement at the 2017 Coding and Reimbursement Workshop for vascular surgeons, Oct. 13-14 in Chicago.
Cost is $880 for SVS members or staff; $955 for non-members and $250 for residents and trainees.
The program will address and review 2018 updates and include information about the global surgical package and how it impacts billing and reimbursement, along with the application of modifiers for streamlined reimbursement.
An optional workshop on Evaluation and Management (E&M) coding will be held from 9 a.m. to noon Oct. 13.
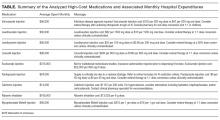
Impact of Displaying Inpatient Pharmaceutical Costs at the Time of Order Entry: Lessons From a Tertiary Care Center
Secondary to rising healthcare costs in the United States, broad efforts are underway to identify and reduce waste in the health system.1,2 A recent systematic review exhibited that many physicians inaccurately estimate the cost of medications.3 Raising awareness of medication costs among prescribers is one potential way to promote high-value care.
Some evidence suggests that cost transparency may help prescribers understand how medication orders drive costs. In a previous study carried out at the Johns Hopkins Hospital, fee data were displayed to providers for diagnostic laboratory tests.4 An 8.6% decrease (95% confidence interval [CI], –8.99% to –8.19%) in test ordering was observed when costs were displayed vs a 5.6% increase (95% CI, 4.90% to 6.39%) in ordering when costs were not displayed during a 6-month intervention period (P < 0.001). Conversely, a similar study that investigated the impact of cost transparency on inpatient imaging utilization did not demonstrate a significant influence of cost display.5 This suggests that cost transparency may work in some areas of care but not in others. A systematic review that investigated price-display interventions for imaging, laboratory studies, and medications reported 10 studies that demonstrated a statistically significant decrease in expenditures without an effect on patient safety.6
Informing prescribers of institution-specific medication costs within and between drug classes may enable the selection of less expensive, therapeutically equivalent drugs. Prior studies investigating the effect of medication cost display were conducted in a variety of patient care settings, including ambulatory clinics,7 urgent care centers,8 and operating rooms,9,10 with some yielding positive results in terms of ordering and cost11,12 and others having no impact.13,14 Currently, there is little evidence specifically addressing the effect of cost display for medications in the inpatient setting.
As part of an institutional initiative to control pharmaceutical expenditures, informational messaging for several high-cost drugs was initiated at our tertiary care hospital in April 2015. The goal of our study was to assess the effect of these medication cost messages on ordering practices. We hypothesized that the display of inpatient pharmaceutical costs at the time of order entry would result in a reduction in ordering.
METHODS
Setting, Intervention, and Participants
As part of an effort to educate prescribers about the high cost of medications, 9 intravenous (IV) medications were selected by the Johns Hopkins Hospital Pharmacy and Therapeutics Committee as targets for drug cost messaging. The intention of the committee was to implement a rapid, low-cost, proof-of-concept, quality-improvement project that was not designed as prospective research. Representatives from the pharmacy and clinicians from relevant clinical areas participated in preimplementation discussions to help identify medications that were subjectively felt to be overused at our institution and potentially modifiable through provider education. The criteria for selecting drug targets included a variety of factors, such as medications infrequently ordered but representing a significant cost per dose (eg, eculizumab and ribavirin), frequently ordered medications with less expensive substitutes (eg, linezolid and voriconazole), and high-cost medications without direct therapeutic alternatives (eg, calcitonin). From April 10, 2015, to October 5, 2015, the computerized Provider Order Entry System (cPOE), Sunrise Clinical Manager (Allscripts Corporation, Chicago, IL), displayed the cost for targeted medications. Seven of the medication alerts also included a reasonable therapeutic alternative and its cost. There were no restrictions placed on ordering; prescribers were able to choose the high-cost medications at their discretion.
Despite the fact that this initiative was not designed as a research project, we felt it was important to formally evaluate the impact of the drug cost messaging effort to inform future quality-improvement interventions. Each medication was compared to its preintervention baseline utilization dating back to January 1, 2013. For the 7 medications with alternatives offered, we also analyzed use of the suggested alternative during these time periods.
Data Sources and Measurement
Our study utilized data obtained from the pharmacy order verification system and the cPOE database. Data were collected over a period of 143 weeks from January 1, 2013, to October 5, 2015, to allow for a baseline period (January 1, 2013, to April 9, 2015) and an intervention period (April 10, 2015, to October 5, 2015). Data elements extracted included drug characteristics (dosage form, route, cost, strength, name, and quantity), patient characteristics (race, gender, and age), clinical setting (facility location, inpatient or outpatient), and billing information (provider name, doses dispensed from pharmacy, order number, revenue or procedure code, record number, date of service, and unique billing number) for each admission. Using these elements, we generated the following 8 variables to use in our analyses: week, month, period identifier, drug name, dosage form, weekly orders, weekly patient days, and number of weekly orders per 10,000 patient days. Average wholesale price (AWP), referred to as medication cost in this manuscript, was used to report all drug costs in all associated cost calculations. While the actual cost of acquisition and price charged to the patient may vary based on several factors, including manufacturer and payer, we chose to use AWP as a generalizable estimate of the cost of acquisition of the drug for the hospital.
Variables
“Week” and “month” were defined as the week and month of our study, respectively. The “period identifier” was a binary variable that identified the time period before and after the intervention. “Weekly orders” was defined as the total number of new orders placed per week for each specified drug included in our study. For example, if a patient received 2 discrete, new orders for a medication in a given week, 2 orders would be counted toward the “weekly orders” variable. “Patient days,” defined as the total number of patients treated at our facility, was summated for each week of our study to yield “weekly patient days.” To derive the “number of weekly orders per 10,000 patient days,” we divided weekly orders by weekly patient days and multiplied the resultant figure by 10,000.
Statistical Analysis
Segmented regression, a form of interrupted time series analysis, is a quasi-experimental design that was used to determine the immediate and sustained effects of the drug cost messages on the rate of medication ordering.15-17 The model enabled the use of comparison groups (alternative medications, as described above) to enhance internal validity.
In time series data, outcomes may not be independent over time. Autocorrelation of the error terms can arise when outcomes are more similar at time points closer together than outcomes at time points further apart. Failure to account for autocorrelation of the error terms may lead to underestimated standard errors. The presence of autocorrelation, assessed by calculating the Durbin-Watson statistic, was significant among our data. To adjust for this, we employed a Prais-Winsten estimation to adjust the error term (εt) calculated in our models.
Two segmented linear regression models were used to estimate trends in ordering before and after the intervention. The presence or absence of a comparator drug determined which model was to be used. When only single medications were under study, as in the case of eculizumab and calcitonin, our regression model was as follows:
Yt = (β0) + (β1)(Timet) + (β2)(Interventiont) + (β3)(Post-Intervention Timet) + (εt)
In our single-drug model, Yt denoted the number of orders per 10,000 patient days at week “t”; Timet was a continuous variable that indicated the number of weeks prior to or after the study intervention (April 10, 2015) and ranged from –116 to 27 weeks. Post-Intervention Timet was a continuous variable that denoted the number of weeks since the start of the intervention and is coded as zero for all time periods prior to the intervention. β0 was the estimated baseline number of orders per 10,000 patient days at the beginning of the study. β1 is the trend of orders per 10,000 patient days per week during the preintervention period; β2 represents an estimate of the change in the number of orders per 10,000 patient days immediately after the intervention; β3 denotes the difference between preintervention and postintervention slopes; and εt is the “error term,” which represents autocorrelation and random variability of the data.
As mentioned previously, alternative dosage forms of 7 medications included in our study were utilized as comparison groups. In these instances (when multiple drugs were included in our analyses), the following regression model was applied:
Y t = ( β 0 ) + ( β 1 )(Time t ) + ( β 2 )(Intervention t ) + ( β 3 )(Post-Intervention Time t ) + ( β 4 )(Cohort) + ( β 5 )(Cohort)(Time t ) + ( β 6 )(Cohort)(Intervention t ) + ( β 7 )(Cohort)(Post-Intervention Time t ) + ( ε t )
Here, 3 coefficients were added (β4-β7) to describe an additional cohort of orders. Cohort, a binary indicator variable, held a value of either 0 or 1 when the model was used to describe the treatment or comparison group, respectively. The coefficients β4-β7 described the treatment group, and β0-β3 described the comparison group. β4 was the difference in the number of baseline orders per 10,000 patient days between treatment and comparison groups; Β5 represented the difference between the estimated ordering trends of treatment and comparison groups; and Β6 indicated the difference in immediate changes in the number of orders per 10,000 patient days in the 2 groups following the intervention.
The number of orders per week was recorded for each medicine, which enabled a large number of data points to be included in our analyses. This allowed for more accurate and stable estimates to be made in our regression model. A total of 143 data points were collected for each study group, 116 before and 27 following each intervention.
All analyses were conducted by using STATA version 13.1 (StataCorp LP, College Station, TX).
RESULTS
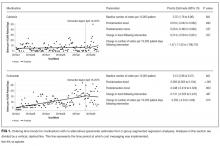
Initial results pertaining to 9 IV medications were examined (Table). Following the implementation of cost messaging, no significant changes were observed in order frequency or trend for IV formulations of eculizumab, calcitonin, levetiracetam, linezolid, mycophenolate, ribavirin, voriconazole, and levothyroxine (Figures 1 and 2). However, a significant decrease in the number of oral ribavirin orders (Figure 2), the control group for the IV form, was observed (–16.3 orders per 10,000 patient days; P = .004; 95% CI, –27.2 to –5.31).
DISCUSSION
Our results suggest that the passive strategy of displaying cost alone was not effective in altering prescriber ordering patterns for the selected medications. This may be due to a lack of awareness regarding direct financial impact on the patient, importance of costs in medical decision-making, or a perceived lack of alternatives or suitability of recommended alternatives. These results may prove valuable to hospital and pharmacy leadership as they develop strategies to curb medication expense.
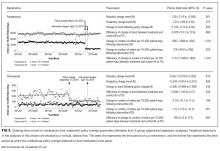
Changes observed in IV pantoprazole ordering are instructive. Due to a national shortage, the IV form of this medication underwent a restriction, which required approval by the pharmacy prior to dispensing. This restriction was instituted independently of our study and led to a 73% decrease from usage rates prior to policy implementation (Figure 3). Ordering was restricted according to defined criteria for IV use. The restriction did not apply to oral pantoprazole, and no significant change in ordering of the oral formulation was noted during the evaluated period (Figure 3).
The dramatic effect of policy changes, as observed with pantoprazole and voriconazole, suggests that a more active strategy may have a greater impact on prescriber behavior when it comes to medication ordering in the inpatient setting. It also highlights several potential sources of confounding that may introduce bias to cost-transparency studies.
This study has multiple limitations. First, as with all observational study designs, causation cannot be drawn with certainty from our results. While we were able to compare medications to their preintervention baselines, the data could have been impacted by longitudinal or seasonal trends in medication ordering, which may have been impacted by seasonal variability in disease prevalence, changes in resistance patterns, and annual cycling of house staff in an academic medical center. While there appear to be potential seasonal patterns regarding prescribing patterns for some of the medications included in this analysis, we also believe the linear regressions capture the overall trends in prescribing adequately. Nonstationarity, or trends in the mean and variance of the outcome that are not related to the intervention, may introduce bias in the interpretation of our findings. However, we believe the parameters included in our models, namely the immediate change in the intercept following the intervention and the change in the trend of the rate of prescribing over time from pre- to postintervention, provide substantial protections from faulty interpretation. Our models are limited to the extent that these parameters do not account for nonstationarity. Additionally, we did not collect data on dosing frequency or duration of treatment, which would have been dependent on factors that are not readily quantified, such as indication, clinical rationale, or patient response. Thus, we were not able to evaluate the impact of the intervention on these factors.
Although intended to enhance internal validity, comparison groups were also subject to external influence. For example, we observed a significant, short-lived rise in oral ribavirin (a control medication) ordering during the preintervention baseline period that appeared to be independent of our intervention and may speak to the unaccounted-for longitudinal variability detailed above.
Finally, the clinical indication and setting may be important. Previous studies performed at the same hospital with price displays showed a reduction in laboratory ordering but no change in imaging.18,19 One might speculate that ordering fewer laboratory tests is viewed by providers as eliminating waste rather than choosing a less expensive option to accomplish the same diagnostic task at hand. Therapeutics may be more similar to radiology tests, because patients presumably need the treatment and often do not have the option of simply not ordering without a concerted effort to reevaluate the treatment plan. Additionally, in a tertiary care teaching center such as ours, a junior clinician, oftentimes at the behest of a more senior colleague, enters most orders. In an environment in which the ordering prescriber has more autonomy or when the order is driven by a junior practitioner rather than an attending (such as daily laboratories), results may be different. Additionally, institutions that incentivize prescribers directly to practice cost-conscious care may experience different results from similar interventions.
We conclude that, in the case of medication cost messaging, a strategy of displaying cost information alone was insufficient to affect prescriber ordering behavior. Coupling cost transparency with educational interventions and active stewardship to impact clinical practice is worthy of further study.
Disclosures: The authors state that there were no external sponsors for this work. The Johns Hopkins Hospital and University “funded” this work by paying the salaries of the authors. The author team maintained independence and made all decisions regarding the study design, data collection, data analysis, interpretation of results, writing of the research report, and decision to submit it for publication. Dr. Shermock had full access to all the study data and takes responsibility for the integrity of the data and accuracy of the data analysis.
1. Berwick DM, Hackbarth AD. Eliminating Waste in US Health Care. JAMA. 2012;307(14):1513-1516. PubMed
2. PricewaterhouseCoopers’ Health Research Institute. The Price of Excess: Identifying Waste in Healthcare Spending. http://www.pwc.com/us/en/healthcare/publications/the-price-of-excess.html. Accessed June 17, 2015.
3. Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283. PubMed
4. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903-908. PubMed
5. Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-113. PubMed
6. Silvestri MT, Bongiovanni TR, Glover JG, Gross CP. Impact of price display on provider ordering: A systematic review. J Hosp Med. 2016;11(1):65-76. PubMed
7. Ornstein SM, MacFarlane LL, Jenkins RG, Pan Q, Wager KA. Medication cost information in a computer-based patient record system. Impact on prescribing in a family medicine clinical practice. Arch Fam Med. 1999;8(2):118-121. PubMed
8. Guterman JJ, Chernof BA, Mares B, Gross-Schulman SG, Gan PG, Thomas D. Modifying provider behavior: A low-tech approach to pharmaceutical ordering. J Gen Intern Med. 2002;17(10):792-796. PubMed
9. McNitt JD, Bode ET, Nelson RE. Long-term pharmaceutical cost reduction using a data management system. Anesth Analg. 1998;87(4):837-842. PubMed
10. Horrow JC, Rosenberg H. Price stickers do not alter drug usage. Can J Anaesth. 1994;41(11):1047-1052. PubMed
11. Guterman JJ, Chernof BA, Mares B, Gross-Schulman SG, Gan PG, Thomas D. Modifying provider behavior: A low-tech approach to pharmaceutical ordering. J Gen Intern Med. 2002;17(10):792-796. PubMed
12. McNitt JD, Bode ET, Nelson RE. Long-term pharmaceutical cost reduction using a data management system. Anesth Analg. 1998;87(4):837-842. PubMed
13. Ornstein SM, MacFarlane LL, Jenkins RG, Pan Q, Wager KA. Medication cost information in a computer-based patient record system. Impact on prescribing in a family medicine clinical practice. Arch Fam Med. 1999;8(2):118-121. PubMed
14. Horrow JC, Rosenberg H. Price stickers do not alter drug usage. Can J Anaesth. 1994;41(11):1047-1052. PubMed
15. Jandoc R, Burden AM, Mamdani M, Levesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J Clin Epidemiol. 2015;68(8):950-56. PubMed
16. Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15(2):480-500.
17. Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231-1238. PubMed
18. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903-908. PubMed
19. Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-113. PubMed
Secondary to rising healthcare costs in the United States, broad efforts are underway to identify and reduce waste in the health system.1,2 A recent systematic review exhibited that many physicians inaccurately estimate the cost of medications.3 Raising awareness of medication costs among prescribers is one potential way to promote high-value care.
Some evidence suggests that cost transparency may help prescribers understand how medication orders drive costs. In a previous study carried out at the Johns Hopkins Hospital, fee data were displayed to providers for diagnostic laboratory tests.4 An 8.6% decrease (95% confidence interval [CI], –8.99% to –8.19%) in test ordering was observed when costs were displayed vs a 5.6% increase (95% CI, 4.90% to 6.39%) in ordering when costs were not displayed during a 6-month intervention period (P < 0.001). Conversely, a similar study that investigated the impact of cost transparency on inpatient imaging utilization did not demonstrate a significant influence of cost display.5 This suggests that cost transparency may work in some areas of care but not in others. A systematic review that investigated price-display interventions for imaging, laboratory studies, and medications reported 10 studies that demonstrated a statistically significant decrease in expenditures without an effect on patient safety.6
Informing prescribers of institution-specific medication costs within and between drug classes may enable the selection of less expensive, therapeutically equivalent drugs. Prior studies investigating the effect of medication cost display were conducted in a variety of patient care settings, including ambulatory clinics,7 urgent care centers,8 and operating rooms,9,10 with some yielding positive results in terms of ordering and cost11,12 and others having no impact.13,14 Currently, there is little evidence specifically addressing the effect of cost display for medications in the inpatient setting.
As part of an institutional initiative to control pharmaceutical expenditures, informational messaging for several high-cost drugs was initiated at our tertiary care hospital in April 2015. The goal of our study was to assess the effect of these medication cost messages on ordering practices. We hypothesized that the display of inpatient pharmaceutical costs at the time of order entry would result in a reduction in ordering.
METHODS
Setting, Intervention, and Participants
As part of an effort to educate prescribers about the high cost of medications, 9 intravenous (IV) medications were selected by the Johns Hopkins Hospital Pharmacy and Therapeutics Committee as targets for drug cost messaging. The intention of the committee was to implement a rapid, low-cost, proof-of-concept, quality-improvement project that was not designed as prospective research. Representatives from the pharmacy and clinicians from relevant clinical areas participated in preimplementation discussions to help identify medications that were subjectively felt to be overused at our institution and potentially modifiable through provider education. The criteria for selecting drug targets included a variety of factors, such as medications infrequently ordered but representing a significant cost per dose (eg, eculizumab and ribavirin), frequently ordered medications with less expensive substitutes (eg, linezolid and voriconazole), and high-cost medications without direct therapeutic alternatives (eg, calcitonin). From April 10, 2015, to October 5, 2015, the computerized Provider Order Entry System (cPOE), Sunrise Clinical Manager (Allscripts Corporation, Chicago, IL), displayed the cost for targeted medications. Seven of the medication alerts also included a reasonable therapeutic alternative and its cost. There were no restrictions placed on ordering; prescribers were able to choose the high-cost medications at their discretion.
Despite the fact that this initiative was not designed as a research project, we felt it was important to formally evaluate the impact of the drug cost messaging effort to inform future quality-improvement interventions. Each medication was compared to its preintervention baseline utilization dating back to January 1, 2013. For the 7 medications with alternatives offered, we also analyzed use of the suggested alternative during these time periods.
Data Sources and Measurement
Our study utilized data obtained from the pharmacy order verification system and the cPOE database. Data were collected over a period of 143 weeks from January 1, 2013, to October 5, 2015, to allow for a baseline period (January 1, 2013, to April 9, 2015) and an intervention period (April 10, 2015, to October 5, 2015). Data elements extracted included drug characteristics (dosage form, route, cost, strength, name, and quantity), patient characteristics (race, gender, and age), clinical setting (facility location, inpatient or outpatient), and billing information (provider name, doses dispensed from pharmacy, order number, revenue or procedure code, record number, date of service, and unique billing number) for each admission. Using these elements, we generated the following 8 variables to use in our analyses: week, month, period identifier, drug name, dosage form, weekly orders, weekly patient days, and number of weekly orders per 10,000 patient days. Average wholesale price (AWP), referred to as medication cost in this manuscript, was used to report all drug costs in all associated cost calculations. While the actual cost of acquisition and price charged to the patient may vary based on several factors, including manufacturer and payer, we chose to use AWP as a generalizable estimate of the cost of acquisition of the drug for the hospital.
Variables
“Week” and “month” were defined as the week and month of our study, respectively. The “period identifier” was a binary variable that identified the time period before and after the intervention. “Weekly orders” was defined as the total number of new orders placed per week for each specified drug included in our study. For example, if a patient received 2 discrete, new orders for a medication in a given week, 2 orders would be counted toward the “weekly orders” variable. “Patient days,” defined as the total number of patients treated at our facility, was summated for each week of our study to yield “weekly patient days.” To derive the “number of weekly orders per 10,000 patient days,” we divided weekly orders by weekly patient days and multiplied the resultant figure by 10,000.
Statistical Analysis
Segmented regression, a form of interrupted time series analysis, is a quasi-experimental design that was used to determine the immediate and sustained effects of the drug cost messages on the rate of medication ordering.15-17 The model enabled the use of comparison groups (alternative medications, as described above) to enhance internal validity.
In time series data, outcomes may not be independent over time. Autocorrelation of the error terms can arise when outcomes are more similar at time points closer together than outcomes at time points further apart. Failure to account for autocorrelation of the error terms may lead to underestimated standard errors. The presence of autocorrelation, assessed by calculating the Durbin-Watson statistic, was significant among our data. To adjust for this, we employed a Prais-Winsten estimation to adjust the error term (εt) calculated in our models.
Two segmented linear regression models were used to estimate trends in ordering before and after the intervention. The presence or absence of a comparator drug determined which model was to be used. When only single medications were under study, as in the case of eculizumab and calcitonin, our regression model was as follows:
Yt = (β0) + (β1)(Timet) + (β2)(Interventiont) + (β3)(Post-Intervention Timet) + (εt)
In our single-drug model, Yt denoted the number of orders per 10,000 patient days at week “t”; Timet was a continuous variable that indicated the number of weeks prior to or after the study intervention (April 10, 2015) and ranged from –116 to 27 weeks. Post-Intervention Timet was a continuous variable that denoted the number of weeks since the start of the intervention and is coded as zero for all time periods prior to the intervention. β0 was the estimated baseline number of orders per 10,000 patient days at the beginning of the study. β1 is the trend of orders per 10,000 patient days per week during the preintervention period; β2 represents an estimate of the change in the number of orders per 10,000 patient days immediately after the intervention; β3 denotes the difference between preintervention and postintervention slopes; and εt is the “error term,” which represents autocorrelation and random variability of the data.
As mentioned previously, alternative dosage forms of 7 medications included in our study were utilized as comparison groups. In these instances (when multiple drugs were included in our analyses), the following regression model was applied:
Y t = ( β 0 ) + ( β 1 )(Time t ) + ( β 2 )(Intervention t ) + ( β 3 )(Post-Intervention Time t ) + ( β 4 )(Cohort) + ( β 5 )(Cohort)(Time t ) + ( β 6 )(Cohort)(Intervention t ) + ( β 7 )(Cohort)(Post-Intervention Time t ) + ( ε t )
Here, 3 coefficients were added (β4-β7) to describe an additional cohort of orders. Cohort, a binary indicator variable, held a value of either 0 or 1 when the model was used to describe the treatment or comparison group, respectively. The coefficients β4-β7 described the treatment group, and β0-β3 described the comparison group. β4 was the difference in the number of baseline orders per 10,000 patient days between treatment and comparison groups; Β5 represented the difference between the estimated ordering trends of treatment and comparison groups; and Β6 indicated the difference in immediate changes in the number of orders per 10,000 patient days in the 2 groups following the intervention.
The number of orders per week was recorded for each medicine, which enabled a large number of data points to be included in our analyses. This allowed for more accurate and stable estimates to be made in our regression model. A total of 143 data points were collected for each study group, 116 before and 27 following each intervention.
All analyses were conducted by using STATA version 13.1 (StataCorp LP, College Station, TX).
RESULTS
Initial results pertaining to 9 IV medications were examined (Table). Following the implementation of cost messaging, no significant changes were observed in order frequency or trend for IV formulations of eculizumab, calcitonin, levetiracetam, linezolid, mycophenolate, ribavirin, voriconazole, and levothyroxine (Figures 1 and 2). However, a significant decrease in the number of oral ribavirin orders (Figure 2), the control group for the IV form, was observed (–16.3 orders per 10,000 patient days; P = .004; 95% CI, –27.2 to –5.31).
DISCUSSION
Our results suggest that the passive strategy of displaying cost alone was not effective in altering prescriber ordering patterns for the selected medications. This may be due to a lack of awareness regarding direct financial impact on the patient, importance of costs in medical decision-making, or a perceived lack of alternatives or suitability of recommended alternatives. These results may prove valuable to hospital and pharmacy leadership as they develop strategies to curb medication expense.
Changes observed in IV pantoprazole ordering are instructive. Due to a national shortage, the IV form of this medication underwent a restriction, which required approval by the pharmacy prior to dispensing. This restriction was instituted independently of our study and led to a 73% decrease from usage rates prior to policy implementation (Figure 3). Ordering was restricted according to defined criteria for IV use. The restriction did not apply to oral pantoprazole, and no significant change in ordering of the oral formulation was noted during the evaluated period (Figure 3).
The dramatic effect of policy changes, as observed with pantoprazole and voriconazole, suggests that a more active strategy may have a greater impact on prescriber behavior when it comes to medication ordering in the inpatient setting. It also highlights several potential sources of confounding that may introduce bias to cost-transparency studies.
This study has multiple limitations. First, as with all observational study designs, causation cannot be drawn with certainty from our results. While we were able to compare medications to their preintervention baselines, the data could have been impacted by longitudinal or seasonal trends in medication ordering, which may have been impacted by seasonal variability in disease prevalence, changes in resistance patterns, and annual cycling of house staff in an academic medical center. While there appear to be potential seasonal patterns regarding prescribing patterns for some of the medications included in this analysis, we also believe the linear regressions capture the overall trends in prescribing adequately. Nonstationarity, or trends in the mean and variance of the outcome that are not related to the intervention, may introduce bias in the interpretation of our findings. However, we believe the parameters included in our models, namely the immediate change in the intercept following the intervention and the change in the trend of the rate of prescribing over time from pre- to postintervention, provide substantial protections from faulty interpretation. Our models are limited to the extent that these parameters do not account for nonstationarity. Additionally, we did not collect data on dosing frequency or duration of treatment, which would have been dependent on factors that are not readily quantified, such as indication, clinical rationale, or patient response. Thus, we were not able to evaluate the impact of the intervention on these factors.
Although intended to enhance internal validity, comparison groups were also subject to external influence. For example, we observed a significant, short-lived rise in oral ribavirin (a control medication) ordering during the preintervention baseline period that appeared to be independent of our intervention and may speak to the unaccounted-for longitudinal variability detailed above.
Finally, the clinical indication and setting may be important. Previous studies performed at the same hospital with price displays showed a reduction in laboratory ordering but no change in imaging.18,19 One might speculate that ordering fewer laboratory tests is viewed by providers as eliminating waste rather than choosing a less expensive option to accomplish the same diagnostic task at hand. Therapeutics may be more similar to radiology tests, because patients presumably need the treatment and often do not have the option of simply not ordering without a concerted effort to reevaluate the treatment plan. Additionally, in a tertiary care teaching center such as ours, a junior clinician, oftentimes at the behest of a more senior colleague, enters most orders. In an environment in which the ordering prescriber has more autonomy or when the order is driven by a junior practitioner rather than an attending (such as daily laboratories), results may be different. Additionally, institutions that incentivize prescribers directly to practice cost-conscious care may experience different results from similar interventions.
We conclude that, in the case of medication cost messaging, a strategy of displaying cost information alone was insufficient to affect prescriber ordering behavior. Coupling cost transparency with educational interventions and active stewardship to impact clinical practice is worthy of further study.
Disclosures: The authors state that there were no external sponsors for this work. The Johns Hopkins Hospital and University “funded” this work by paying the salaries of the authors. The author team maintained independence and made all decisions regarding the study design, data collection, data analysis, interpretation of results, writing of the research report, and decision to submit it for publication. Dr. Shermock had full access to all the study data and takes responsibility for the integrity of the data and accuracy of the data analysis.
Secondary to rising healthcare costs in the United States, broad efforts are underway to identify and reduce waste in the health system.1,2 A recent systematic review exhibited that many physicians inaccurately estimate the cost of medications.3 Raising awareness of medication costs among prescribers is one potential way to promote high-value care.
Some evidence suggests that cost transparency may help prescribers understand how medication orders drive costs. In a previous study carried out at the Johns Hopkins Hospital, fee data were displayed to providers for diagnostic laboratory tests.4 An 8.6% decrease (95% confidence interval [CI], –8.99% to –8.19%) in test ordering was observed when costs were displayed vs a 5.6% increase (95% CI, 4.90% to 6.39%) in ordering when costs were not displayed during a 6-month intervention period (P < 0.001). Conversely, a similar study that investigated the impact of cost transparency on inpatient imaging utilization did not demonstrate a significant influence of cost display.5 This suggests that cost transparency may work in some areas of care but not in others. A systematic review that investigated price-display interventions for imaging, laboratory studies, and medications reported 10 studies that demonstrated a statistically significant decrease in expenditures without an effect on patient safety.6
Informing prescribers of institution-specific medication costs within and between drug classes may enable the selection of less expensive, therapeutically equivalent drugs. Prior studies investigating the effect of medication cost display were conducted in a variety of patient care settings, including ambulatory clinics,7 urgent care centers,8 and operating rooms,9,10 with some yielding positive results in terms of ordering and cost11,12 and others having no impact.13,14 Currently, there is little evidence specifically addressing the effect of cost display for medications in the inpatient setting.
As part of an institutional initiative to control pharmaceutical expenditures, informational messaging for several high-cost drugs was initiated at our tertiary care hospital in April 2015. The goal of our study was to assess the effect of these medication cost messages on ordering practices. We hypothesized that the display of inpatient pharmaceutical costs at the time of order entry would result in a reduction in ordering.
METHODS
Setting, Intervention, and Participants
As part of an effort to educate prescribers about the high cost of medications, 9 intravenous (IV) medications were selected by the Johns Hopkins Hospital Pharmacy and Therapeutics Committee as targets for drug cost messaging. The intention of the committee was to implement a rapid, low-cost, proof-of-concept, quality-improvement project that was not designed as prospective research. Representatives from the pharmacy and clinicians from relevant clinical areas participated in preimplementation discussions to help identify medications that were subjectively felt to be overused at our institution and potentially modifiable through provider education. The criteria for selecting drug targets included a variety of factors, such as medications infrequently ordered but representing a significant cost per dose (eg, eculizumab and ribavirin), frequently ordered medications with less expensive substitutes (eg, linezolid and voriconazole), and high-cost medications without direct therapeutic alternatives (eg, calcitonin). From April 10, 2015, to October 5, 2015, the computerized Provider Order Entry System (cPOE), Sunrise Clinical Manager (Allscripts Corporation, Chicago, IL), displayed the cost for targeted medications. Seven of the medication alerts also included a reasonable therapeutic alternative and its cost. There were no restrictions placed on ordering; prescribers were able to choose the high-cost medications at their discretion.
Despite the fact that this initiative was not designed as a research project, we felt it was important to formally evaluate the impact of the drug cost messaging effort to inform future quality-improvement interventions. Each medication was compared to its preintervention baseline utilization dating back to January 1, 2013. For the 7 medications with alternatives offered, we also analyzed use of the suggested alternative during these time periods.
Data Sources and Measurement
Our study utilized data obtained from the pharmacy order verification system and the cPOE database. Data were collected over a period of 143 weeks from January 1, 2013, to October 5, 2015, to allow for a baseline period (January 1, 2013, to April 9, 2015) and an intervention period (April 10, 2015, to October 5, 2015). Data elements extracted included drug characteristics (dosage form, route, cost, strength, name, and quantity), patient characteristics (race, gender, and age), clinical setting (facility location, inpatient or outpatient), and billing information (provider name, doses dispensed from pharmacy, order number, revenue or procedure code, record number, date of service, and unique billing number) for each admission. Using these elements, we generated the following 8 variables to use in our analyses: week, month, period identifier, drug name, dosage form, weekly orders, weekly patient days, and number of weekly orders per 10,000 patient days. Average wholesale price (AWP), referred to as medication cost in this manuscript, was used to report all drug costs in all associated cost calculations. While the actual cost of acquisition and price charged to the patient may vary based on several factors, including manufacturer and payer, we chose to use AWP as a generalizable estimate of the cost of acquisition of the drug for the hospital.
Variables
“Week” and “month” were defined as the week and month of our study, respectively. The “period identifier” was a binary variable that identified the time period before and after the intervention. “Weekly orders” was defined as the total number of new orders placed per week for each specified drug included in our study. For example, if a patient received 2 discrete, new orders for a medication in a given week, 2 orders would be counted toward the “weekly orders” variable. “Patient days,” defined as the total number of patients treated at our facility, was summated for each week of our study to yield “weekly patient days.” To derive the “number of weekly orders per 10,000 patient days,” we divided weekly orders by weekly patient days and multiplied the resultant figure by 10,000.
Statistical Analysis
Segmented regression, a form of interrupted time series analysis, is a quasi-experimental design that was used to determine the immediate and sustained effects of the drug cost messages on the rate of medication ordering.15-17 The model enabled the use of comparison groups (alternative medications, as described above) to enhance internal validity.
In time series data, outcomes may not be independent over time. Autocorrelation of the error terms can arise when outcomes are more similar at time points closer together than outcomes at time points further apart. Failure to account for autocorrelation of the error terms may lead to underestimated standard errors. The presence of autocorrelation, assessed by calculating the Durbin-Watson statistic, was significant among our data. To adjust for this, we employed a Prais-Winsten estimation to adjust the error term (εt) calculated in our models.
Two segmented linear regression models were used to estimate trends in ordering before and after the intervention. The presence or absence of a comparator drug determined which model was to be used. When only single medications were under study, as in the case of eculizumab and calcitonin, our regression model was as follows:
Yt = (β0) + (β1)(Timet) + (β2)(Interventiont) + (β3)(Post-Intervention Timet) + (εt)
In our single-drug model, Yt denoted the number of orders per 10,000 patient days at week “t”; Timet was a continuous variable that indicated the number of weeks prior to or after the study intervention (April 10, 2015) and ranged from –116 to 27 weeks. Post-Intervention Timet was a continuous variable that denoted the number of weeks since the start of the intervention and is coded as zero for all time periods prior to the intervention. β0 was the estimated baseline number of orders per 10,000 patient days at the beginning of the study. β1 is the trend of orders per 10,000 patient days per week during the preintervention period; β2 represents an estimate of the change in the number of orders per 10,000 patient days immediately after the intervention; β3 denotes the difference between preintervention and postintervention slopes; and εt is the “error term,” which represents autocorrelation and random variability of the data.
As mentioned previously, alternative dosage forms of 7 medications included in our study were utilized as comparison groups. In these instances (when multiple drugs were included in our analyses), the following regression model was applied:
Y t = ( β 0 ) + ( β 1 )(Time t ) + ( β 2 )(Intervention t ) + ( β 3 )(Post-Intervention Time t ) + ( β 4 )(Cohort) + ( β 5 )(Cohort)(Time t ) + ( β 6 )(Cohort)(Intervention t ) + ( β 7 )(Cohort)(Post-Intervention Time t ) + ( ε t )
Here, 3 coefficients were added (β4-β7) to describe an additional cohort of orders. Cohort, a binary indicator variable, held a value of either 0 or 1 when the model was used to describe the treatment or comparison group, respectively. The coefficients β4-β7 described the treatment group, and β0-β3 described the comparison group. β4 was the difference in the number of baseline orders per 10,000 patient days between treatment and comparison groups; Β5 represented the difference between the estimated ordering trends of treatment and comparison groups; and Β6 indicated the difference in immediate changes in the number of orders per 10,000 patient days in the 2 groups following the intervention.
The number of orders per week was recorded for each medicine, which enabled a large number of data points to be included in our analyses. This allowed for more accurate and stable estimates to be made in our regression model. A total of 143 data points were collected for each study group, 116 before and 27 following each intervention.
All analyses were conducted by using STATA version 13.1 (StataCorp LP, College Station, TX).
RESULTS
Initial results pertaining to 9 IV medications were examined (Table). Following the implementation of cost messaging, no significant changes were observed in order frequency or trend for IV formulations of eculizumab, calcitonin, levetiracetam, linezolid, mycophenolate, ribavirin, voriconazole, and levothyroxine (Figures 1 and 2). However, a significant decrease in the number of oral ribavirin orders (Figure 2), the control group for the IV form, was observed (–16.3 orders per 10,000 patient days; P = .004; 95% CI, –27.2 to –5.31).
DISCUSSION
Our results suggest that the passive strategy of displaying cost alone was not effective in altering prescriber ordering patterns for the selected medications. This may be due to a lack of awareness regarding direct financial impact on the patient, importance of costs in medical decision-making, or a perceived lack of alternatives or suitability of recommended alternatives. These results may prove valuable to hospital and pharmacy leadership as they develop strategies to curb medication expense.
Changes observed in IV pantoprazole ordering are instructive. Due to a national shortage, the IV form of this medication underwent a restriction, which required approval by the pharmacy prior to dispensing. This restriction was instituted independently of our study and led to a 73% decrease from usage rates prior to policy implementation (Figure 3). Ordering was restricted according to defined criteria for IV use. The restriction did not apply to oral pantoprazole, and no significant change in ordering of the oral formulation was noted during the evaluated period (Figure 3).
The dramatic effect of policy changes, as observed with pantoprazole and voriconazole, suggests that a more active strategy may have a greater impact on prescriber behavior when it comes to medication ordering in the inpatient setting. It also highlights several potential sources of confounding that may introduce bias to cost-transparency studies.
This study has multiple limitations. First, as with all observational study designs, causation cannot be drawn with certainty from our results. While we were able to compare medications to their preintervention baselines, the data could have been impacted by longitudinal or seasonal trends in medication ordering, which may have been impacted by seasonal variability in disease prevalence, changes in resistance patterns, and annual cycling of house staff in an academic medical center. While there appear to be potential seasonal patterns regarding prescribing patterns for some of the medications included in this analysis, we also believe the linear regressions capture the overall trends in prescribing adequately. Nonstationarity, or trends in the mean and variance of the outcome that are not related to the intervention, may introduce bias in the interpretation of our findings. However, we believe the parameters included in our models, namely the immediate change in the intercept following the intervention and the change in the trend of the rate of prescribing over time from pre- to postintervention, provide substantial protections from faulty interpretation. Our models are limited to the extent that these parameters do not account for nonstationarity. Additionally, we did not collect data on dosing frequency or duration of treatment, which would have been dependent on factors that are not readily quantified, such as indication, clinical rationale, or patient response. Thus, we were not able to evaluate the impact of the intervention on these factors.
Although intended to enhance internal validity, comparison groups were also subject to external influence. For example, we observed a significant, short-lived rise in oral ribavirin (a control medication) ordering during the preintervention baseline period that appeared to be independent of our intervention and may speak to the unaccounted-for longitudinal variability detailed above.
Finally, the clinical indication and setting may be important. Previous studies performed at the same hospital with price displays showed a reduction in laboratory ordering but no change in imaging.18,19 One might speculate that ordering fewer laboratory tests is viewed by providers as eliminating waste rather than choosing a less expensive option to accomplish the same diagnostic task at hand. Therapeutics may be more similar to radiology tests, because patients presumably need the treatment and often do not have the option of simply not ordering without a concerted effort to reevaluate the treatment plan. Additionally, in a tertiary care teaching center such as ours, a junior clinician, oftentimes at the behest of a more senior colleague, enters most orders. In an environment in which the ordering prescriber has more autonomy or when the order is driven by a junior practitioner rather than an attending (such as daily laboratories), results may be different. Additionally, institutions that incentivize prescribers directly to practice cost-conscious care may experience different results from similar interventions.
We conclude that, in the case of medication cost messaging, a strategy of displaying cost information alone was insufficient to affect prescriber ordering behavior. Coupling cost transparency with educational interventions and active stewardship to impact clinical practice is worthy of further study.
Disclosures: The authors state that there were no external sponsors for this work. The Johns Hopkins Hospital and University “funded” this work by paying the salaries of the authors. The author team maintained independence and made all decisions regarding the study design, data collection, data analysis, interpretation of results, writing of the research report, and decision to submit it for publication. Dr. Shermock had full access to all the study data and takes responsibility for the integrity of the data and accuracy of the data analysis.
1. Berwick DM, Hackbarth AD. Eliminating Waste in US Health Care. JAMA. 2012;307(14):1513-1516. PubMed
2. PricewaterhouseCoopers’ Health Research Institute. The Price of Excess: Identifying Waste in Healthcare Spending. http://www.pwc.com/us/en/healthcare/publications/the-price-of-excess.html. Accessed June 17, 2015.
3. Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283. PubMed
4. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903-908. PubMed
5. Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-113. PubMed
6. Silvestri MT, Bongiovanni TR, Glover JG, Gross CP. Impact of price display on provider ordering: A systematic review. J Hosp Med. 2016;11(1):65-76. PubMed
7. Ornstein SM, MacFarlane LL, Jenkins RG, Pan Q, Wager KA. Medication cost information in a computer-based patient record system. Impact on prescribing in a family medicine clinical practice. Arch Fam Med. 1999;8(2):118-121. PubMed
8. Guterman JJ, Chernof BA, Mares B, Gross-Schulman SG, Gan PG, Thomas D. Modifying provider behavior: A low-tech approach to pharmaceutical ordering. J Gen Intern Med. 2002;17(10):792-796. PubMed
9. McNitt JD, Bode ET, Nelson RE. Long-term pharmaceutical cost reduction using a data management system. Anesth Analg. 1998;87(4):837-842. PubMed
10. Horrow JC, Rosenberg H. Price stickers do not alter drug usage. Can J Anaesth. 1994;41(11):1047-1052. PubMed
11. Guterman JJ, Chernof BA, Mares B, Gross-Schulman SG, Gan PG, Thomas D. Modifying provider behavior: A low-tech approach to pharmaceutical ordering. J Gen Intern Med. 2002;17(10):792-796. PubMed
12. McNitt JD, Bode ET, Nelson RE. Long-term pharmaceutical cost reduction using a data management system. Anesth Analg. 1998;87(4):837-842. PubMed
13. Ornstein SM, MacFarlane LL, Jenkins RG, Pan Q, Wager KA. Medication cost information in a computer-based patient record system. Impact on prescribing in a family medicine clinical practice. Arch Fam Med. 1999;8(2):118-121. PubMed
14. Horrow JC, Rosenberg H. Price stickers do not alter drug usage. Can J Anaesth. 1994;41(11):1047-1052. PubMed
15. Jandoc R, Burden AM, Mamdani M, Levesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J Clin Epidemiol. 2015;68(8):950-56. PubMed
16. Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15(2):480-500.
17. Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231-1238. PubMed
18. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903-908. PubMed
19. Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-113. PubMed
1. Berwick DM, Hackbarth AD. Eliminating Waste in US Health Care. JAMA. 2012;307(14):1513-1516. PubMed
2. PricewaterhouseCoopers’ Health Research Institute. The Price of Excess: Identifying Waste in Healthcare Spending. http://www.pwc.com/us/en/healthcare/publications/the-price-of-excess.html. Accessed June 17, 2015.
3. Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283. PubMed
4. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903-908. PubMed
5. Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-113. PubMed
6. Silvestri MT, Bongiovanni TR, Glover JG, Gross CP. Impact of price display on provider ordering: A systematic review. J Hosp Med. 2016;11(1):65-76. PubMed
7. Ornstein SM, MacFarlane LL, Jenkins RG, Pan Q, Wager KA. Medication cost information in a computer-based patient record system. Impact on prescribing in a family medicine clinical practice. Arch Fam Med. 1999;8(2):118-121. PubMed
8. Guterman JJ, Chernof BA, Mares B, Gross-Schulman SG, Gan PG, Thomas D. Modifying provider behavior: A low-tech approach to pharmaceutical ordering. J Gen Intern Med. 2002;17(10):792-796. PubMed
9. McNitt JD, Bode ET, Nelson RE. Long-term pharmaceutical cost reduction using a data management system. Anesth Analg. 1998;87(4):837-842. PubMed
10. Horrow JC, Rosenberg H. Price stickers do not alter drug usage. Can J Anaesth. 1994;41(11):1047-1052. PubMed
11. Guterman JJ, Chernof BA, Mares B, Gross-Schulman SG, Gan PG, Thomas D. Modifying provider behavior: A low-tech approach to pharmaceutical ordering. J Gen Intern Med. 2002;17(10):792-796. PubMed
12. McNitt JD, Bode ET, Nelson RE. Long-term pharmaceutical cost reduction using a data management system. Anesth Analg. 1998;87(4):837-842. PubMed
13. Ornstein SM, MacFarlane LL, Jenkins RG, Pan Q, Wager KA. Medication cost information in a computer-based patient record system. Impact on prescribing in a family medicine clinical practice. Arch Fam Med. 1999;8(2):118-121. PubMed
14. Horrow JC, Rosenberg H. Price stickers do not alter drug usage. Can J Anaesth. 1994;41(11):1047-1052. PubMed
15. Jandoc R, Burden AM, Mamdani M, Levesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J Clin Epidemiol. 2015;68(8):950-56. PubMed
16. Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15(2):480-500.
17. Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231-1238. PubMed
18. Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173(10):903-908. PubMed
19. Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-113. PubMed
© 2017 Society of Hospital Medicine
This Month in CHEST: Editor’s picks
Giants in Chest Medicine:
Steven E. Weinberger, MD, FCCP
By Dr. J. Mandel
Editorial
Precision Medicine Urgency: The Case of Inhaled Corticosteroids in COPD By Drs. S. Suissa and P. Ernst
Original Research
Physician Assessment of Pretest Probability of Malignancy and Adherence With Guidelines for Pulmonary Nodule Evaluation By Dr. N. T. Tanner, et al.
The Long-Term Effect of Bacille Calmette-Guérin Vaccination on Tuberculin Skin Testing: A 55-Year Follow-Up Study By Dr. J. D. Mancuso, et al.
Clinical Characteristics of Pertussis-Associated Cough in Adults and Children: A Diagnostic Systematic Review and Meta-Analysis By Dr. A. Moore, et al.
Giants in Chest Medicine:
Steven E. Weinberger, MD, FCCP
By Dr. J. Mandel
Editorial
Precision Medicine Urgency: The Case of Inhaled Corticosteroids in COPD By Drs. S. Suissa and P. Ernst
Original Research
Physician Assessment of Pretest Probability of Malignancy and Adherence With Guidelines for Pulmonary Nodule Evaluation By Dr. N. T. Tanner, et al.
The Long-Term Effect of Bacille Calmette-Guérin Vaccination on Tuberculin Skin Testing: A 55-Year Follow-Up Study By Dr. J. D. Mancuso, et al.
Clinical Characteristics of Pertussis-Associated Cough in Adults and Children: A Diagnostic Systematic Review and Meta-Analysis By Dr. A. Moore, et al.
Giants in Chest Medicine:
Steven E. Weinberger, MD, FCCP
By Dr. J. Mandel
Editorial
Precision Medicine Urgency: The Case of Inhaled Corticosteroids in COPD By Drs. S. Suissa and P. Ernst
Original Research
Physician Assessment of Pretest Probability of Malignancy and Adherence With Guidelines for Pulmonary Nodule Evaluation By Dr. N. T. Tanner, et al.
The Long-Term Effect of Bacille Calmette-Guérin Vaccination on Tuberculin Skin Testing: A 55-Year Follow-Up Study By Dr. J. D. Mancuso, et al.
Clinical Characteristics of Pertussis-Associated Cough in Adults and Children: A Diagnostic Systematic Review and Meta-Analysis By Dr. A. Moore, et al.
CHEST Membership News
Introducing CHEST Participation Points
Everyday, you commit your time to helping patients. We recognize your dedication not only to your profession but to the CHEST community.
We’re happy to introduce CHEST Participation Points, designed to increase member recognition and reward you for participating and contributing to our diverse community. Wherever you are in your career, you can earn points for the things you do within the CHEST community.
Once you receive 50, 100, or 150 points, you can redeem your points for CHEST-branded apparel or discounts on courses and products.
Point accrual started on July 5, so you’ve already been earning points. If you are an FCCP, you began with 30 points awarded for becoming FCCP—that’s only 20 points away from the first tier of prizes. To accrue or redeem points, you must be an active member and current with your dues.
Log in to your CHEST account, and access Participation Points in the left column to see your points.
Start earning more points today! Learn more at chestnet.org/participationpoints.
Introducing CHEST Participation Points
Everyday, you commit your time to helping patients. We recognize your dedication not only to your profession but to the CHEST community.
We’re happy to introduce CHEST Participation Points, designed to increase member recognition and reward you for participating and contributing to our diverse community. Wherever you are in your career, you can earn points for the things you do within the CHEST community.
Once you receive 50, 100, or 150 points, you can redeem your points for CHEST-branded apparel or discounts on courses and products.
Point accrual started on July 5, so you’ve already been earning points. If you are an FCCP, you began with 30 points awarded for becoming FCCP—that’s only 20 points away from the first tier of prizes. To accrue or redeem points, you must be an active member and current with your dues.
Log in to your CHEST account, and access Participation Points in the left column to see your points.
Start earning more points today! Learn more at chestnet.org/participationpoints.
Introducing CHEST Participation Points
Everyday, you commit your time to helping patients. We recognize your dedication not only to your profession but to the CHEST community.
We’re happy to introduce CHEST Participation Points, designed to increase member recognition and reward you for participating and contributing to our diverse community. Wherever you are in your career, you can earn points for the things you do within the CHEST community.
Once you receive 50, 100, or 150 points, you can redeem your points for CHEST-branded apparel or discounts on courses and products.
Point accrual started on July 5, so you’ve already been earning points. If you are an FCCP, you began with 30 points awarded for becoming FCCP—that’s only 20 points away from the first tier of prizes. To accrue or redeem points, you must be an active member and current with your dues.
Log in to your CHEST account, and access Participation Points in the left column to see your points.
Start earning more points today! Learn more at chestnet.org/participationpoints.
CHEST ® journal — new online home
We are excited to share that the journal CHEST® has a new website with improved navigation, better search capabilities, alert sign-ups, and more multimedia elements. We are asking members to take a few minutes to activate their new account.
In order to maintain continuous access to the online journal, members will have to register for a free account and claim their subscription. If you go to chestjournal.org, CHEST members can then complete a 1- to 2-minute registration process.
CHEST members should have received an email with step-by-step instructions. Still have questions or need help? Contact Online Journal Support at 800/654-2452 (US and Canada) or +44 (0) 1865-843177 (Europe).
We are excited to share that the journal CHEST® has a new website with improved navigation, better search capabilities, alert sign-ups, and more multimedia elements. We are asking members to take a few minutes to activate their new account.
In order to maintain continuous access to the online journal, members will have to register for a free account and claim their subscription. If you go to chestjournal.org, CHEST members can then complete a 1- to 2-minute registration process.
CHEST members should have received an email with step-by-step instructions. Still have questions or need help? Contact Online Journal Support at 800/654-2452 (US and Canada) or +44 (0) 1865-843177 (Europe).
We are excited to share that the journal CHEST® has a new website with improved navigation, better search capabilities, alert sign-ups, and more multimedia elements. We are asking members to take a few minutes to activate their new account.
In order to maintain continuous access to the online journal, members will have to register for a free account and claim their subscription. If you go to chestjournal.org, CHEST members can then complete a 1- to 2-minute registration process.
CHEST members should have received an email with step-by-step instructions. Still have questions or need help? Contact Online Journal Support at 800/654-2452 (US and Canada) or +44 (0) 1865-843177 (Europe).
New Tools in Campaign to Fight Asthma
The Allergy & Asthma NetWork, the nation’s leading patient education and advocacy organization for people with allergy and asthma, has once again joined forces with the CHEST Foundation in an effort to empower patients suffering from severe asthma.
The campaign’s focus is to educate health-care providers, patients, parents of asthmatics, and the public about the most current treatment options for asthma, highlight the importance of referring to specialists to improve patient outcomes, and bring to light the role of the entire health-care team in the care of a patient with severe or difficult-to-control asthma.
Severity Assessment Tool
Available online and in print, the severity assessment tool was designed to help a patient, and the clinician, understand the severity of their asthma. Not only does the tool evaluate the severity of their condition, but it also helps the patient become more aware of their symptoms. The seven-question assessment includes questions on usage of quick-relief or rescue inhalers, visits to the ED/hospital, physical activity, controller medication, and quality of sleep.
Patient and Caregiver Testimonials
The campaign features several patient and caregiver testimonials that tell the stories of patients and parents of children with severe asthma.
“What we want people to understand, is that at the time of Ben’s passing, he was on a preventive med. He was going to the doctor routinely. We had actually just been to the asthma doctor. We were seeing somebody, had an action plan, and everybody knew what they had to do. Even with all of that, it still came to this. Benjamin still lost his life, and we never knew this was something that could happen,” stated Cristin Buckley, mother of Benjamin Buckley who was 7 years old at the time of his death. These testimonial videos will be used to raise awareness of the condition, and the importance of managing and monitoring symptoms.
Shared Decision Making Tool
Thank You to Our Supporters
The CHEST Foundation and Allergy and Asthma Network would like to thank our generous supporters, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, and Novartis for making this campaign possible. It is through supporters, who are active participants in helping grow this campaign, that these important materials are able to have an impact on patient outcomes and create long-lasting social change.
To view the campaign materials, visit us at asthma.chestnet.org.
The Allergy & Asthma NetWork, the nation’s leading patient education and advocacy organization for people with allergy and asthma, has once again joined forces with the CHEST Foundation in an effort to empower patients suffering from severe asthma.
The campaign’s focus is to educate health-care providers, patients, parents of asthmatics, and the public about the most current treatment options for asthma, highlight the importance of referring to specialists to improve patient outcomes, and bring to light the role of the entire health-care team in the care of a patient with severe or difficult-to-control asthma.
Severity Assessment Tool
Available online and in print, the severity assessment tool was designed to help a patient, and the clinician, understand the severity of their asthma. Not only does the tool evaluate the severity of their condition, but it also helps the patient become more aware of their symptoms. The seven-question assessment includes questions on usage of quick-relief or rescue inhalers, visits to the ED/hospital, physical activity, controller medication, and quality of sleep.
Patient and Caregiver Testimonials
The campaign features several patient and caregiver testimonials that tell the stories of patients and parents of children with severe asthma.
“What we want people to understand, is that at the time of Ben’s passing, he was on a preventive med. He was going to the doctor routinely. We had actually just been to the asthma doctor. We were seeing somebody, had an action plan, and everybody knew what they had to do. Even with all of that, it still came to this. Benjamin still lost his life, and we never knew this was something that could happen,” stated Cristin Buckley, mother of Benjamin Buckley who was 7 years old at the time of his death. These testimonial videos will be used to raise awareness of the condition, and the importance of managing and monitoring symptoms.
Shared Decision Making Tool
Thank You to Our Supporters
The CHEST Foundation and Allergy and Asthma Network would like to thank our generous supporters, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, and Novartis for making this campaign possible. It is through supporters, who are active participants in helping grow this campaign, that these important materials are able to have an impact on patient outcomes and create long-lasting social change.
To view the campaign materials, visit us at asthma.chestnet.org.
The Allergy & Asthma NetWork, the nation’s leading patient education and advocacy organization for people with allergy and asthma, has once again joined forces with the CHEST Foundation in an effort to empower patients suffering from severe asthma.
The campaign’s focus is to educate health-care providers, patients, parents of asthmatics, and the public about the most current treatment options for asthma, highlight the importance of referring to specialists to improve patient outcomes, and bring to light the role of the entire health-care team in the care of a patient with severe or difficult-to-control asthma.
Severity Assessment Tool
Available online and in print, the severity assessment tool was designed to help a patient, and the clinician, understand the severity of their asthma. Not only does the tool evaluate the severity of their condition, but it also helps the patient become more aware of their symptoms. The seven-question assessment includes questions on usage of quick-relief or rescue inhalers, visits to the ED/hospital, physical activity, controller medication, and quality of sleep.
Patient and Caregiver Testimonials
The campaign features several patient and caregiver testimonials that tell the stories of patients and parents of children with severe asthma.
“What we want people to understand, is that at the time of Ben’s passing, he was on a preventive med. He was going to the doctor routinely. We had actually just been to the asthma doctor. We were seeing somebody, had an action plan, and everybody knew what they had to do. Even with all of that, it still came to this. Benjamin still lost his life, and we never knew this was something that could happen,” stated Cristin Buckley, mother of Benjamin Buckley who was 7 years old at the time of his death. These testimonial videos will be used to raise awareness of the condition, and the importance of managing and monitoring symptoms.
Shared Decision Making Tool
Thank You to Our Supporters
The CHEST Foundation and Allergy and Asthma Network would like to thank our generous supporters, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, and Novartis for making this campaign possible. It is through supporters, who are active participants in helping grow this campaign, that these important materials are able to have an impact on patient outcomes and create long-lasting social change.
To view the campaign materials, visit us at asthma.chestnet.org.
CHEST Joint Congress in Basel, Switzerland
Members of CHEST leadership, faculty, and staff traveled to Basel, Switzerland, in June, to participate in the CHEST Joint Congress, which was co-hosted with the Swiss Respiratory Society, Schweizersche Gesellschaft Fur Pneumologie (SPG). Overall, there were approximately 1,100 total attendees, representing over 40 countries, who enjoyed the scientific program and gained valuable chest medicine knowledge.
The CHEST Joint Congress in Basel represented the second collaborative scientific conference endeavor with a third party, the first being the CHEST Conference held in Amsterdam May 6-9, COPD: Current Excellence and Future Development.
Members of CHEST leadership, faculty, and staff traveled to Basel, Switzerland, in June, to participate in the CHEST Joint Congress, which was co-hosted with the Swiss Respiratory Society, Schweizersche Gesellschaft Fur Pneumologie (SPG). Overall, there were approximately 1,100 total attendees, representing over 40 countries, who enjoyed the scientific program and gained valuable chest medicine knowledge.
The CHEST Joint Congress in Basel represented the second collaborative scientific conference endeavor with a third party, the first being the CHEST Conference held in Amsterdam May 6-9, COPD: Current Excellence and Future Development.
Members of CHEST leadership, faculty, and staff traveled to Basel, Switzerland, in June, to participate in the CHEST Joint Congress, which was co-hosted with the Swiss Respiratory Society, Schweizersche Gesellschaft Fur Pneumologie (SPG). Overall, there were approximately 1,100 total attendees, representing over 40 countries, who enjoyed the scientific program and gained valuable chest medicine knowledge.
The CHEST Joint Congress in Basel represented the second collaborative scientific conference endeavor with a third party, the first being the CHEST Conference held in Amsterdam May 6-9, COPD: Current Excellence and Future Development.
PHM17 session summary: Demonstrating teaching excellence with an educator’s portfolio
NASHVILLE, TENN. – Development of a medical educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process, according to an expert panel at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Promote yourself: Demonstrating teaching excellence with an educator’s portfolio
Presenters
Michael Ryan, MD, MEHP; Ashlie Tseng, MD; Jocelyn Schiller, MD; Rebecca Tenney-Soeiro, MD, MEd; Michele Long, MD; Corki Lehmann, MD, MEd; Amy Fleming, MD; and H. Barrett Fromme, MD, MHPE
Session summary
Development of an educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process. Each institution has its own specific requirements for the educator’s portfolio, but there are several general themes that should be considered for inclusion:
1. Develop an educational philosophy. This is a personal statement that frames the rest of the portfolio and describes how this philosophy is used by the educator in his/her approach to education.
2. Teaching. Include teaching activities that are both formal (i.e. lectures) and sessions that encourage more active participation (i.e. small group discussions). This can be accomplished by generating a teaching activities report, which helps to categorize these activities. This will not only demonstrate the volume of teaching experience, but also help to demonstrate the diversity of an educator’s teaching activities. In this section, an educator also should include teaching awards received.
3. Learner evaluations. A qualitative summary of comments will provide a narrative of the educator’s teaching skills. This section also may include summaries of annual reviews of teaching.
4. Curriculum development. Demonstrate the educator’s active engagement in the development of a novel curriculum or the improvement of a pre-existing curriculum and the successful outcomes of those improvements.
5. Mentoring and advising. Generating a list of advisees and highlighting their accomplishments reflects on the ability of the educator to guide and promote success in his/her learners.
6. Educational leadership and administration. This is a description of the past and present leadership roles that the educator has held, including courses or clerkships directed. This should allow the educator the opportunity to provide a narrative description of his/her involvement beyond what is typically stated on the curriculum vitae.
7. Professional development. The educator should develop a list of activities, including formal degree programs, certificate programs, and educational workshops, in which he/she has participated as a learner and have enhanced his/her skills as an educator.
8. Products of educational scholarship. Generate a list of education-related peer-reviewed publications authored, other educational products (such as a syllabus or curriculum) developed, and educational workshops that the educator was invited to give.
For clinician educators interested in developing an educator’s portfolio, there are several resources available, including the Academic Pediatric Association’s website and several MedEdPORTAL publications.
Key takeaways for Pediatric HM
• While each institution has its own specific requirements, there are general themes to consider including in an educator’s portfolio.
• Resources such as the Academic Pediatric Association’s website can help guide an educator in the development of his/her portfolio.
Dr. Player is a pediatric hospitalist at Children’s Hospital of Wisconsin and assistant professor at the Medical College of Wisconsin, Milwaukee.
NASHVILLE, TENN. – Development of a medical educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process, according to an expert panel at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Promote yourself: Demonstrating teaching excellence with an educator’s portfolio
Presenters
Michael Ryan, MD, MEHP; Ashlie Tseng, MD; Jocelyn Schiller, MD; Rebecca Tenney-Soeiro, MD, MEd; Michele Long, MD; Corki Lehmann, MD, MEd; Amy Fleming, MD; and H. Barrett Fromme, MD, MHPE
Session summary
Development of an educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process. Each institution has its own specific requirements for the educator’s portfolio, but there are several general themes that should be considered for inclusion:
1. Develop an educational philosophy. This is a personal statement that frames the rest of the portfolio and describes how this philosophy is used by the educator in his/her approach to education.
2. Teaching. Include teaching activities that are both formal (i.e. lectures) and sessions that encourage more active participation (i.e. small group discussions). This can be accomplished by generating a teaching activities report, which helps to categorize these activities. This will not only demonstrate the volume of teaching experience, but also help to demonstrate the diversity of an educator’s teaching activities. In this section, an educator also should include teaching awards received.
3. Learner evaluations. A qualitative summary of comments will provide a narrative of the educator’s teaching skills. This section also may include summaries of annual reviews of teaching.
4. Curriculum development. Demonstrate the educator’s active engagement in the development of a novel curriculum or the improvement of a pre-existing curriculum and the successful outcomes of those improvements.
5. Mentoring and advising. Generating a list of advisees and highlighting their accomplishments reflects on the ability of the educator to guide and promote success in his/her learners.
6. Educational leadership and administration. This is a description of the past and present leadership roles that the educator has held, including courses or clerkships directed. This should allow the educator the opportunity to provide a narrative description of his/her involvement beyond what is typically stated on the curriculum vitae.
7. Professional development. The educator should develop a list of activities, including formal degree programs, certificate programs, and educational workshops, in which he/she has participated as a learner and have enhanced his/her skills as an educator.
8. Products of educational scholarship. Generate a list of education-related peer-reviewed publications authored, other educational products (such as a syllabus or curriculum) developed, and educational workshops that the educator was invited to give.
For clinician educators interested in developing an educator’s portfolio, there are several resources available, including the Academic Pediatric Association’s website and several MedEdPORTAL publications.
Key takeaways for Pediatric HM
• While each institution has its own specific requirements, there are general themes to consider including in an educator’s portfolio.
• Resources such as the Academic Pediatric Association’s website can help guide an educator in the development of his/her portfolio.
Dr. Player is a pediatric hospitalist at Children’s Hospital of Wisconsin and assistant professor at the Medical College of Wisconsin, Milwaukee.
NASHVILLE, TENN. – Development of a medical educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process, according to an expert panel at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Promote yourself: Demonstrating teaching excellence with an educator’s portfolio
Presenters
Michael Ryan, MD, MEHP; Ashlie Tseng, MD; Jocelyn Schiller, MD; Rebecca Tenney-Soeiro, MD, MEd; Michele Long, MD; Corki Lehmann, MD, MEd; Amy Fleming, MD; and H. Barrett Fromme, MD, MHPE
Session summary
Development of an educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process. Each institution has its own specific requirements for the educator’s portfolio, but there are several general themes that should be considered for inclusion:
1. Develop an educational philosophy. This is a personal statement that frames the rest of the portfolio and describes how this philosophy is used by the educator in his/her approach to education.
2. Teaching. Include teaching activities that are both formal (i.e. lectures) and sessions that encourage more active participation (i.e. small group discussions). This can be accomplished by generating a teaching activities report, which helps to categorize these activities. This will not only demonstrate the volume of teaching experience, but also help to demonstrate the diversity of an educator’s teaching activities. In this section, an educator also should include teaching awards received.
3. Learner evaluations. A qualitative summary of comments will provide a narrative of the educator’s teaching skills. This section also may include summaries of annual reviews of teaching.
4. Curriculum development. Demonstrate the educator’s active engagement in the development of a novel curriculum or the improvement of a pre-existing curriculum and the successful outcomes of those improvements.
5. Mentoring and advising. Generating a list of advisees and highlighting their accomplishments reflects on the ability of the educator to guide and promote success in his/her learners.
6. Educational leadership and administration. This is a description of the past and present leadership roles that the educator has held, including courses or clerkships directed. This should allow the educator the opportunity to provide a narrative description of his/her involvement beyond what is typically stated on the curriculum vitae.
7. Professional development. The educator should develop a list of activities, including formal degree programs, certificate programs, and educational workshops, in which he/she has participated as a learner and have enhanced his/her skills as an educator.
8. Products of educational scholarship. Generate a list of education-related peer-reviewed publications authored, other educational products (such as a syllabus or curriculum) developed, and educational workshops that the educator was invited to give.
For clinician educators interested in developing an educator’s portfolio, there are several resources available, including the Academic Pediatric Association’s website and several MedEdPORTAL publications.
Key takeaways for Pediatric HM
• While each institution has its own specific requirements, there are general themes to consider including in an educator’s portfolio.
• Resources such as the Academic Pediatric Association’s website can help guide an educator in the development of his/her portfolio.
Dr. Player is a pediatric hospitalist at Children’s Hospital of Wisconsin and assistant professor at the Medical College of Wisconsin, Milwaukee.
At PHM 2017