User login
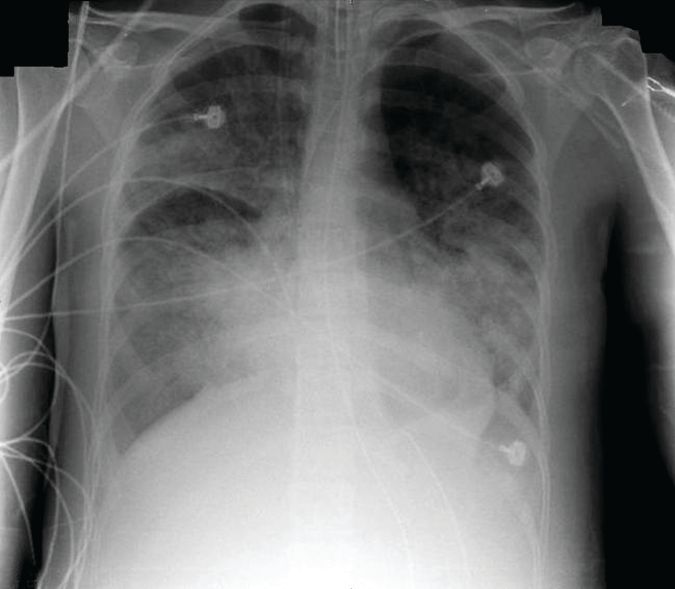
Bedside imaging finds best PEEP settings
A noninvasive bedside imaging technique can individually calibrate positive end-expiratory pressure settings in patients on extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS), a study showed.
The step-down PEEP (positive end-expiratory pressure) trial could not identify a single PEEP setting that optimally balanced lung overdistension and lung collapse for all 15 patients. But, electrical impedance tomography (EIT) allowed investigators to individually titrate PEEP settings for each patient, Guillaume Franchineau, MD, wrote (Am J Respir Crit Care Med. 2017;196[4]:447-57. doi: 10.1164/rccm.201605-1055OC).
The 4-month study involved 15 patients (aged, 18-79 years) who were in acute respiratory distress syndrome for a variety of reasons, including influenza (7 patients), pneumonia (3), leukemia (2), and 1 case each of Pneumocystis, antisynthetase syndrome, and trauma. All patients were receiving ECMO with a constant driving pressure of 14 cm H2O. After verifying that the inspiratory flow was 0 at the end of inspiration, PEEP was increased to 20 cm H2O (PEEP 20) with a peak inspiratory pressure of 34 cm H2O. PEEP 20 was held for 20 minutes and then lowered by 5-cm H2O decrements with the potential of reaching PEEP 0.
The EIT device, consisting of a silicone belt with 16 surface electrodes, was placed around the thorax aligning with the sixth intercostal parasternal space and connected to a monitor. By measuring conductivity and impeditivity in the underlying tissues, the device generates a low-resolution, two-dimensional image. The image was sufficient to show lung distension and collapse as the PEEP settings changed. Investigators looked for the best compromise between overdistension and collapsed zones, which they defined as the lowest pressure able to limit EIT-assessed collapse to no more than 15% with the least overdistension.
There was no one-size-fits-all PEEP setting, the authors found. The setting that minimized both overdistension and collapse was PEEP 15 in seven patients, PEEP 10 in six patients, and PEEP 5 in two patients.
At each patient’s optimal PEEP setting, the median tidal volume was similar: 3.8 mL/kg ideal body weight for PEEP 15, 3.9 mL/kg ideal body weight for PEEP 10, and 4.3 mL/kg ideal body weight for PEEP 5.
Respiratory system compliance was also similar among the groups, at 20 mL/cm H2O, 18 mL/cm H2O, and 21 mL/cm H2O, respectively. However, arterial partial pressure of oxygen decreased as the PEEP setting decreased, dropping from 148 mm Hg to 128 mm Hg to 100 mm Hg, respectively. Conversely, arterial partial pressure of CO2 increased (32-41 mm Hg).
EIT also allowed clinicians to pinpoint areas of distension or collapse. As PEEP decreased, there was steady ventilation loss in the medial-dorsal and dorsal regions, which shifted to the medial-ventral and ventral regions.
“Most end-expiratory lung impedances were located in medial-dorsal and medial-ventral regions, whereas the dorsal region constantly contributed less than 10% of total end-expiratory lung impedance,” the authors noted.
“The broad variability of EIT-based best compromise PEEPs in these patients with severe ARDS reinforces the need to provide ventilation settings individually tailored to the regional ARDS-lesion distribution,” they concluded. “To achieve that goal, EIT seems to be an interesting bedside noninvasive tool to provide real-time monitoring of the PEEP effect and ventilation distribution on ECMO.”
Positive PEEP trial, but questions remain
This first study to examine EIT in patients under extracorporeal membrane oxygenation shows important clinical potential, but also raises important questions, Claude Guerin, MD, wrote in an accompanying editorial. (Am J Respir Crit Care Med. doi: 10.1164/rccm.201701-0167ed).
The ability to titrate PEEP settings to a patient’s individual needs could substantially reduce the risk of lung derecruitment or damage by overdistension.
The current study, however, has limitations that must be addressed in the next phase of research, before this technique can be adopted into clinical practice, noted Dr. Guerin, a pulmonologist at the Hospital de la Croix Rousse, Lyon, France. The 5-cm H20 PEEP steps may be too large to detect relevant changes, he said.
In several other studies, PEEP was reduced more gradually in 2- to 3-cm H2O increments. “Surprisingly, PEEP was reduced to 0 cm H2O in this study, with this step maintained for 20 minutes, raising the risk of derecruitment and further stretching once higher PEEP levels were resumed.”
The investigators did not perform any recruitment maneuvers before proceeding with PEEP adjustment. This is contrary to what has been done in prior animal and human studies.
The computation of driving pressure was done without taking total PEEP into account. “As total PEEP is frequently greater than PEEP in patients with [acute respiratory distress syndrome], driving pressure can be overestimated with the common computation.”
The optimal PEEP that the investigators aimed for was determined retrospectively from an offline analysis of the data; this technique would not be suitable for bedside management. “When ‘optimal’ PEEP was defined from [EIT criteria], from a higher PaO2 [arterial partial pressure of oxygen] or from a higher compliance of the respiratory system during the decremental PEEP trial, these three criteria were observed together in only four patients with [acute respiratory distress syndrome].”
The study was done only once and cannot comply with the need for regular PEEP-level assessments over time, as could be done with some other strategies.
“Further studies should also consider taking into account the role of chest wall mechanics,” Dr. Guerin said.
Nevertheless, he concluded, EIT-based PEEP titration for each individual patient represents a prospective tool for assisting with the treatment of acute respiratory distress syndrome, and should be fully investigated in a large, prospective trial.
Dr. Franchineau reported receiving speakers fees from Mapquet. Dr. Guerin had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
A noninvasive bedside imaging technique can individually calibrate positive end-expiratory pressure settings in patients on extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS), a study showed.
The step-down PEEP (positive end-expiratory pressure) trial could not identify a single PEEP setting that optimally balanced lung overdistension and lung collapse for all 15 patients. But, electrical impedance tomography (EIT) allowed investigators to individually titrate PEEP settings for each patient, Guillaume Franchineau, MD, wrote (Am J Respir Crit Care Med. 2017;196[4]:447-57. doi: 10.1164/rccm.201605-1055OC).
The 4-month study involved 15 patients (aged, 18-79 years) who were in acute respiratory distress syndrome for a variety of reasons, including influenza (7 patients), pneumonia (3), leukemia (2), and 1 case each of Pneumocystis, antisynthetase syndrome, and trauma. All patients were receiving ECMO with a constant driving pressure of 14 cm H2O. After verifying that the inspiratory flow was 0 at the end of inspiration, PEEP was increased to 20 cm H2O (PEEP 20) with a peak inspiratory pressure of 34 cm H2O. PEEP 20 was held for 20 minutes and then lowered by 5-cm H2O decrements with the potential of reaching PEEP 0.
The EIT device, consisting of a silicone belt with 16 surface electrodes, was placed around the thorax aligning with the sixth intercostal parasternal space and connected to a monitor. By measuring conductivity and impeditivity in the underlying tissues, the device generates a low-resolution, two-dimensional image. The image was sufficient to show lung distension and collapse as the PEEP settings changed. Investigators looked for the best compromise between overdistension and collapsed zones, which they defined as the lowest pressure able to limit EIT-assessed collapse to no more than 15% with the least overdistension.
There was no one-size-fits-all PEEP setting, the authors found. The setting that minimized both overdistension and collapse was PEEP 15 in seven patients, PEEP 10 in six patients, and PEEP 5 in two patients.
At each patient’s optimal PEEP setting, the median tidal volume was similar: 3.8 mL/kg ideal body weight for PEEP 15, 3.9 mL/kg ideal body weight for PEEP 10, and 4.3 mL/kg ideal body weight for PEEP 5.
Respiratory system compliance was also similar among the groups, at 20 mL/cm H2O, 18 mL/cm H2O, and 21 mL/cm H2O, respectively. However, arterial partial pressure of oxygen decreased as the PEEP setting decreased, dropping from 148 mm Hg to 128 mm Hg to 100 mm Hg, respectively. Conversely, arterial partial pressure of CO2 increased (32-41 mm Hg).
EIT also allowed clinicians to pinpoint areas of distension or collapse. As PEEP decreased, there was steady ventilation loss in the medial-dorsal and dorsal regions, which shifted to the medial-ventral and ventral regions.
“Most end-expiratory lung impedances were located in medial-dorsal and medial-ventral regions, whereas the dorsal region constantly contributed less than 10% of total end-expiratory lung impedance,” the authors noted.
“The broad variability of EIT-based best compromise PEEPs in these patients with severe ARDS reinforces the need to provide ventilation settings individually tailored to the regional ARDS-lesion distribution,” they concluded. “To achieve that goal, EIT seems to be an interesting bedside noninvasive tool to provide real-time monitoring of the PEEP effect and ventilation distribution on ECMO.”
Positive PEEP trial, but questions remain
This first study to examine EIT in patients under extracorporeal membrane oxygenation shows important clinical potential, but also raises important questions, Claude Guerin, MD, wrote in an accompanying editorial. (Am J Respir Crit Care Med. doi: 10.1164/rccm.201701-0167ed).
The ability to titrate PEEP settings to a patient’s individual needs could substantially reduce the risk of lung derecruitment or damage by overdistension.
The current study, however, has limitations that must be addressed in the next phase of research, before this technique can be adopted into clinical practice, noted Dr. Guerin, a pulmonologist at the Hospital de la Croix Rousse, Lyon, France. The 5-cm H20 PEEP steps may be too large to detect relevant changes, he said.
In several other studies, PEEP was reduced more gradually in 2- to 3-cm H2O increments. “Surprisingly, PEEP was reduced to 0 cm H2O in this study, with this step maintained for 20 minutes, raising the risk of derecruitment and further stretching once higher PEEP levels were resumed.”
The investigators did not perform any recruitment maneuvers before proceeding with PEEP adjustment. This is contrary to what has been done in prior animal and human studies.
The computation of driving pressure was done without taking total PEEP into account. “As total PEEP is frequently greater than PEEP in patients with [acute respiratory distress syndrome], driving pressure can be overestimated with the common computation.”
The optimal PEEP that the investigators aimed for was determined retrospectively from an offline analysis of the data; this technique would not be suitable for bedside management. “When ‘optimal’ PEEP was defined from [EIT criteria], from a higher PaO2 [arterial partial pressure of oxygen] or from a higher compliance of the respiratory system during the decremental PEEP trial, these three criteria were observed together in only four patients with [acute respiratory distress syndrome].”
The study was done only once and cannot comply with the need for regular PEEP-level assessments over time, as could be done with some other strategies.
“Further studies should also consider taking into account the role of chest wall mechanics,” Dr. Guerin said.
Nevertheless, he concluded, EIT-based PEEP titration for each individual patient represents a prospective tool for assisting with the treatment of acute respiratory distress syndrome, and should be fully investigated in a large, prospective trial.
Dr. Franchineau reported receiving speakers fees from Mapquet. Dr. Guerin had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
A noninvasive bedside imaging technique can individually calibrate positive end-expiratory pressure settings in patients on extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS), a study showed.
The step-down PEEP (positive end-expiratory pressure) trial could not identify a single PEEP setting that optimally balanced lung overdistension and lung collapse for all 15 patients. But, electrical impedance tomography (EIT) allowed investigators to individually titrate PEEP settings for each patient, Guillaume Franchineau, MD, wrote (Am J Respir Crit Care Med. 2017;196[4]:447-57. doi: 10.1164/rccm.201605-1055OC).
The 4-month study involved 15 patients (aged, 18-79 years) who were in acute respiratory distress syndrome for a variety of reasons, including influenza (7 patients), pneumonia (3), leukemia (2), and 1 case each of Pneumocystis, antisynthetase syndrome, and trauma. All patients were receiving ECMO with a constant driving pressure of 14 cm H2O. After verifying that the inspiratory flow was 0 at the end of inspiration, PEEP was increased to 20 cm H2O (PEEP 20) with a peak inspiratory pressure of 34 cm H2O. PEEP 20 was held for 20 minutes and then lowered by 5-cm H2O decrements with the potential of reaching PEEP 0.
The EIT device, consisting of a silicone belt with 16 surface electrodes, was placed around the thorax aligning with the sixth intercostal parasternal space and connected to a monitor. By measuring conductivity and impeditivity in the underlying tissues, the device generates a low-resolution, two-dimensional image. The image was sufficient to show lung distension and collapse as the PEEP settings changed. Investigators looked for the best compromise between overdistension and collapsed zones, which they defined as the lowest pressure able to limit EIT-assessed collapse to no more than 15% with the least overdistension.
There was no one-size-fits-all PEEP setting, the authors found. The setting that minimized both overdistension and collapse was PEEP 15 in seven patients, PEEP 10 in six patients, and PEEP 5 in two patients.
At each patient’s optimal PEEP setting, the median tidal volume was similar: 3.8 mL/kg ideal body weight for PEEP 15, 3.9 mL/kg ideal body weight for PEEP 10, and 4.3 mL/kg ideal body weight for PEEP 5.
Respiratory system compliance was also similar among the groups, at 20 mL/cm H2O, 18 mL/cm H2O, and 21 mL/cm H2O, respectively. However, arterial partial pressure of oxygen decreased as the PEEP setting decreased, dropping from 148 mm Hg to 128 mm Hg to 100 mm Hg, respectively. Conversely, arterial partial pressure of CO2 increased (32-41 mm Hg).
EIT also allowed clinicians to pinpoint areas of distension or collapse. As PEEP decreased, there was steady ventilation loss in the medial-dorsal and dorsal regions, which shifted to the medial-ventral and ventral regions.
“Most end-expiratory lung impedances were located in medial-dorsal and medial-ventral regions, whereas the dorsal region constantly contributed less than 10% of total end-expiratory lung impedance,” the authors noted.
“The broad variability of EIT-based best compromise PEEPs in these patients with severe ARDS reinforces the need to provide ventilation settings individually tailored to the regional ARDS-lesion distribution,” they concluded. “To achieve that goal, EIT seems to be an interesting bedside noninvasive tool to provide real-time monitoring of the PEEP effect and ventilation distribution on ECMO.”
Positive PEEP trial, but questions remain
This first study to examine EIT in patients under extracorporeal membrane oxygenation shows important clinical potential, but also raises important questions, Claude Guerin, MD, wrote in an accompanying editorial. (Am J Respir Crit Care Med. doi: 10.1164/rccm.201701-0167ed).
The ability to titrate PEEP settings to a patient’s individual needs could substantially reduce the risk of lung derecruitment or damage by overdistension.
The current study, however, has limitations that must be addressed in the next phase of research, before this technique can be adopted into clinical practice, noted Dr. Guerin, a pulmonologist at the Hospital de la Croix Rousse, Lyon, France. The 5-cm H20 PEEP steps may be too large to detect relevant changes, he said.
In several other studies, PEEP was reduced more gradually in 2- to 3-cm H2O increments. “Surprisingly, PEEP was reduced to 0 cm H2O in this study, with this step maintained for 20 minutes, raising the risk of derecruitment and further stretching once higher PEEP levels were resumed.”
The investigators did not perform any recruitment maneuvers before proceeding with PEEP adjustment. This is contrary to what has been done in prior animal and human studies.
The computation of driving pressure was done without taking total PEEP into account. “As total PEEP is frequently greater than PEEP in patients with [acute respiratory distress syndrome], driving pressure can be overestimated with the common computation.”
The optimal PEEP that the investigators aimed for was determined retrospectively from an offline analysis of the data; this technique would not be suitable for bedside management. “When ‘optimal’ PEEP was defined from [EIT criteria], from a higher PaO2 [arterial partial pressure of oxygen] or from a higher compliance of the respiratory system during the decremental PEEP trial, these three criteria were observed together in only four patients with [acute respiratory distress syndrome].”
The study was done only once and cannot comply with the need for regular PEEP-level assessments over time, as could be done with some other strategies.
“Further studies should also consider taking into account the role of chest wall mechanics,” Dr. Guerin said.
Nevertheless, he concluded, EIT-based PEEP titration for each individual patient represents a prospective tool for assisting with the treatment of acute respiratory distress syndrome, and should be fully investigated in a large, prospective trial.
Dr. Franchineau reported receiving speakers fees from Mapquet. Dr. Guerin had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
Tezepelumab reduces exacerbations in asthma
Patients whose asthma remains uncontrolled despite treatment may benefit from a new monoclonal antibody that targets an inflammatory cytokine known to be promoted in asthmatic airways, according to data presented at the annual congress of the European Respiratory Society.
Writing in the Sept. 7 issue of the New England Journal of Medicine, researchers reported on a phase 2, randomized placebo-controlled trial of three dosing regimens of subcutaneous tezepelumab, which targets the epithelial cell–derived cytokine thymic stromal lymphopoietin (TSLP). The trial involved 584 patients with uncontrolled asthma, despite treatment with long-acting beta-agonists and medium to high doses of inhaled glucocorticoids.
At 70 mg every 4 weeks, exacerbation rates were 61% lower than in the placebo group; at 210 mg every 4 weeks, they were 71% lower; and at 280 mg every 2 weeks, they were 66% lower (P was less than .001 in comparisons between each group and the placebo).The overall annualized exacerbation rates by week 52 were 0.26 for the 70-mg group, 0.19 for the 210-mg group, and 0.22 for the 280-mg group, compared with 0.67 in the placebo group, regardless of a patient’s baseline eosinophil count. Patients treated with tezepelumab had a longer time to first asthma exacerbation. They also experienced a significantly higher change from baseline in their prebronchodilator forced expiratory volume in 1 second at week 52, when compared with patients on the placebo. “The observed improvements in disease control in patients who received tezepelumab highlight the potential pathogenic role of TSLP across different asthma phenotypes,” reported Jonathan Corren, MD, of the University of California, Los Angeles, and his coauthors. “... Although TSLP is central to the regulation of type 2 immunity, many cell types that are activated by or respond to TSLP, such as mast cells, basophils, natural killer T cells, innate lymphoid cells, and neutrophils, may play a role in inflammation in asthma beyond type 2 inflammation.”The incidences of adverse events and serious adverse events were similar across all groups in the study. Three serious adverse events – pneumonia and stroke in the same patient and one case of Guillain-Barré syndrome – in patients taking tezepelumab, were deemed to be related to the treatment.
Tezepelumab ‘most promising’ asthma biologic to date
Tezepelumab is the first biologic that has a substantial positive effect on two important markers of the inflammation of asthma – namely, blood eosinophil counts and the fraction of exhaled nitric oxide, noted Elisabeth H. Bel, MD, PhD, in an editorial accompanying the New England Journal of Medicine’s publication of this study (2017;377:989-91). It appears to be the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date, said Dr. Bel, of the department of respiratory medicine, Academic Medical Center, the University of Amsterdam.
The observation that tezepelumab reduces the level of both inflammatory markers shows that it hits a more upstream target and that it blocks at least two relevant inflammatory pathways in asthma, she noted. This is likely to be clinically relevant, since simultaneously increased exhaled nitric oxide levels and blood eosinophil counts are related to increased morbidity due to asthma.
The study was supported by tezepelumab manufacturers MedImmune (a member of the AstraZeneca group) and Amgen. Six of the seven authors are employees of MedImmune or Amgen. One author declared support and honoraria from several pharmaceutical companies, one declared a related patent, and five also had stock options in either MedImmune or Amgen.
Dr. Bel declared consultancies and grants from pharmaceutical companies including AstraZeneca.
Patients whose asthma remains uncontrolled despite treatment may benefit from a new monoclonal antibody that targets an inflammatory cytokine known to be promoted in asthmatic airways, according to data presented at the annual congress of the European Respiratory Society.
Writing in the Sept. 7 issue of the New England Journal of Medicine, researchers reported on a phase 2, randomized placebo-controlled trial of three dosing regimens of subcutaneous tezepelumab, which targets the epithelial cell–derived cytokine thymic stromal lymphopoietin (TSLP). The trial involved 584 patients with uncontrolled asthma, despite treatment with long-acting beta-agonists and medium to high doses of inhaled glucocorticoids.
At 70 mg every 4 weeks, exacerbation rates were 61% lower than in the placebo group; at 210 mg every 4 weeks, they were 71% lower; and at 280 mg every 2 weeks, they were 66% lower (P was less than .001 in comparisons between each group and the placebo).The overall annualized exacerbation rates by week 52 were 0.26 for the 70-mg group, 0.19 for the 210-mg group, and 0.22 for the 280-mg group, compared with 0.67 in the placebo group, regardless of a patient’s baseline eosinophil count. Patients treated with tezepelumab had a longer time to first asthma exacerbation. They also experienced a significantly higher change from baseline in their prebronchodilator forced expiratory volume in 1 second at week 52, when compared with patients on the placebo. “The observed improvements in disease control in patients who received tezepelumab highlight the potential pathogenic role of TSLP across different asthma phenotypes,” reported Jonathan Corren, MD, of the University of California, Los Angeles, and his coauthors. “... Although TSLP is central to the regulation of type 2 immunity, many cell types that are activated by or respond to TSLP, such as mast cells, basophils, natural killer T cells, innate lymphoid cells, and neutrophils, may play a role in inflammation in asthma beyond type 2 inflammation.”The incidences of adverse events and serious adverse events were similar across all groups in the study. Three serious adverse events – pneumonia and stroke in the same patient and one case of Guillain-Barré syndrome – in patients taking tezepelumab, were deemed to be related to the treatment.
Tezepelumab ‘most promising’ asthma biologic to date
Tezepelumab is the first biologic that has a substantial positive effect on two important markers of the inflammation of asthma – namely, blood eosinophil counts and the fraction of exhaled nitric oxide, noted Elisabeth H. Bel, MD, PhD, in an editorial accompanying the New England Journal of Medicine’s publication of this study (2017;377:989-91). It appears to be the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date, said Dr. Bel, of the department of respiratory medicine, Academic Medical Center, the University of Amsterdam.
The observation that tezepelumab reduces the level of both inflammatory markers shows that it hits a more upstream target and that it blocks at least two relevant inflammatory pathways in asthma, she noted. This is likely to be clinically relevant, since simultaneously increased exhaled nitric oxide levels and blood eosinophil counts are related to increased morbidity due to asthma.
The study was supported by tezepelumab manufacturers MedImmune (a member of the AstraZeneca group) and Amgen. Six of the seven authors are employees of MedImmune or Amgen. One author declared support and honoraria from several pharmaceutical companies, one declared a related patent, and five also had stock options in either MedImmune or Amgen.
Dr. Bel declared consultancies and grants from pharmaceutical companies including AstraZeneca.
Patients whose asthma remains uncontrolled despite treatment may benefit from a new monoclonal antibody that targets an inflammatory cytokine known to be promoted in asthmatic airways, according to data presented at the annual congress of the European Respiratory Society.
Writing in the Sept. 7 issue of the New England Journal of Medicine, researchers reported on a phase 2, randomized placebo-controlled trial of three dosing regimens of subcutaneous tezepelumab, which targets the epithelial cell–derived cytokine thymic stromal lymphopoietin (TSLP). The trial involved 584 patients with uncontrolled asthma, despite treatment with long-acting beta-agonists and medium to high doses of inhaled glucocorticoids.
At 70 mg every 4 weeks, exacerbation rates were 61% lower than in the placebo group; at 210 mg every 4 weeks, they were 71% lower; and at 280 mg every 2 weeks, they were 66% lower (P was less than .001 in comparisons between each group and the placebo).The overall annualized exacerbation rates by week 52 were 0.26 for the 70-mg group, 0.19 for the 210-mg group, and 0.22 for the 280-mg group, compared with 0.67 in the placebo group, regardless of a patient’s baseline eosinophil count. Patients treated with tezepelumab had a longer time to first asthma exacerbation. They also experienced a significantly higher change from baseline in their prebronchodilator forced expiratory volume in 1 second at week 52, when compared with patients on the placebo. “The observed improvements in disease control in patients who received tezepelumab highlight the potential pathogenic role of TSLP across different asthma phenotypes,” reported Jonathan Corren, MD, of the University of California, Los Angeles, and his coauthors. “... Although TSLP is central to the regulation of type 2 immunity, many cell types that are activated by or respond to TSLP, such as mast cells, basophils, natural killer T cells, innate lymphoid cells, and neutrophils, may play a role in inflammation in asthma beyond type 2 inflammation.”The incidences of adverse events and serious adverse events were similar across all groups in the study. Three serious adverse events – pneumonia and stroke in the same patient and one case of Guillain-Barré syndrome – in patients taking tezepelumab, were deemed to be related to the treatment.
Tezepelumab ‘most promising’ asthma biologic to date
Tezepelumab is the first biologic that has a substantial positive effect on two important markers of the inflammation of asthma – namely, blood eosinophil counts and the fraction of exhaled nitric oxide, noted Elisabeth H. Bel, MD, PhD, in an editorial accompanying the New England Journal of Medicine’s publication of this study (2017;377:989-91). It appears to be the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date, said Dr. Bel, of the department of respiratory medicine, Academic Medical Center, the University of Amsterdam.
The observation that tezepelumab reduces the level of both inflammatory markers shows that it hits a more upstream target and that it blocks at least two relevant inflammatory pathways in asthma, she noted. This is likely to be clinically relevant, since simultaneously increased exhaled nitric oxide levels and blood eosinophil counts are related to increased morbidity due to asthma.
The study was supported by tezepelumab manufacturers MedImmune (a member of the AstraZeneca group) and Amgen. Six of the seven authors are employees of MedImmune or Amgen. One author declared support and honoraria from several pharmaceutical companies, one declared a related patent, and five also had stock options in either MedImmune or Amgen.
Dr. Bel declared consultancies and grants from pharmaceutical companies including AstraZeneca.
Statins linked to lower death rates in COPD
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Larry D. Lynd, PhD, a professor at the at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggest that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of CHEST (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68-0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71- 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts, noted Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, in an editorial published in CHEST (2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the in the STATCOPE study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint, said the editorialists, who are both at the pulmonary and critical care medicine division, University of Maryland, Baltimore.This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE, they said.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis; the others had no conflicts of interest. Neither editorialist had conflicts of interest.
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Larry D. Lynd, PhD, a professor at the at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggest that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of CHEST (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68-0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71- 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts, noted Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, in an editorial published in CHEST (2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the in the STATCOPE study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint, said the editorialists, who are both at the pulmonary and critical care medicine division, University of Maryland, Baltimore.This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE, they said.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis; the others had no conflicts of interest. Neither editorialist had conflicts of interest.
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Larry D. Lynd, PhD, a professor at the at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggest that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of CHEST (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68-0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71- 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts, noted Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, in an editorial published in CHEST (2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the in the STATCOPE study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint, said the editorialists, who are both at the pulmonary and critical care medicine division, University of Maryland, Baltimore.This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE, they said.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis; the others had no conflicts of interest. Neither editorialist had conflicts of interest.
FROM CHEST
Payment gaps seen for child visits
, according to the Agency for Healthcare Research and Quality.
Child visits covered by private insurance brought in a mean $214 for office-based physicians of all specialties in 2015, which was $88 more than the $126 they received for Medicaid-covered visits, the AHRQ said.
That gap has been consistent since 2010, even as payments rose from 2010 to 2013 and fell in 2014 and 2015. The payment gap was even larger in 2015 when looking at the most expensive 10% of child visits: $406 for those that were privately insured and $215 for those covered by Medicaid, the AHRQ reported in a recent Statistical Brief.
Variations in payments also were seen between geographic regions and among the different physician specialties. Mean payments to physicians in the Midwest were highest for both private insurance ($249) and Medicaid ($152), while the lowest payments – $192 from private insurance and $120 from Medicaid – went to physicians in the South. The South also had the smallest gap between private and Medicaid coverage at $72, and the West had the largest gap at an even $100, but none of the variation across regions was significant, the AHRQ said.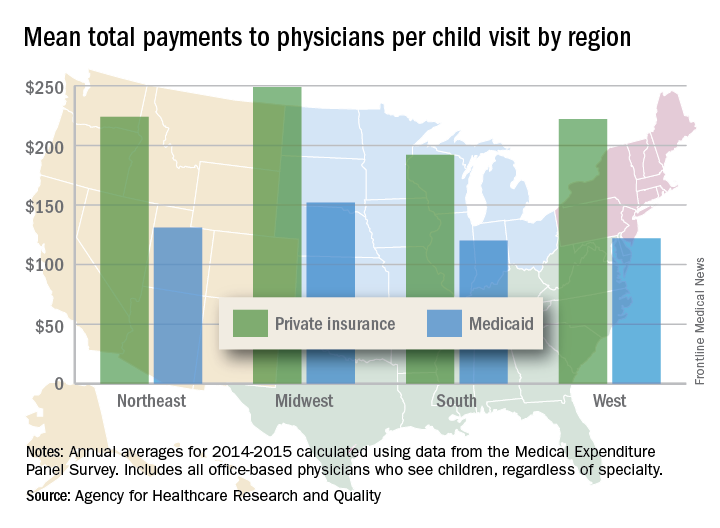
There were statistically significant gaps between private and Medicaid payments by specialty, although only for visits to orthopedists ($423 private – $162 Medicaid = $261) and primary care physicians such as family physicians and internists ($174 private – $122 Medicaid = $52). Payments to pediatricians were $190 private/$115 Medicaid, and the psychiatrists’ $111 mean payment from Medicaid represented the lowest for any specialty, data from Medical Expenditure Panel Survey’s household component show.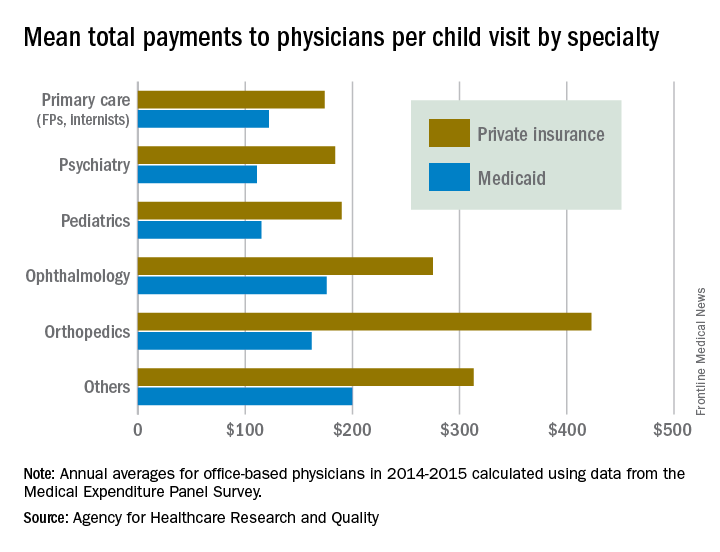
, according to the Agency for Healthcare Research and Quality.
Child visits covered by private insurance brought in a mean $214 for office-based physicians of all specialties in 2015, which was $88 more than the $126 they received for Medicaid-covered visits, the AHRQ said.
That gap has been consistent since 2010, even as payments rose from 2010 to 2013 and fell in 2014 and 2015. The payment gap was even larger in 2015 when looking at the most expensive 10% of child visits: $406 for those that were privately insured and $215 for those covered by Medicaid, the AHRQ reported in a recent Statistical Brief.
Variations in payments also were seen between geographic regions and among the different physician specialties. Mean payments to physicians in the Midwest were highest for both private insurance ($249) and Medicaid ($152), while the lowest payments – $192 from private insurance and $120 from Medicaid – went to physicians in the South. The South also had the smallest gap between private and Medicaid coverage at $72, and the West had the largest gap at an even $100, but none of the variation across regions was significant, the AHRQ said.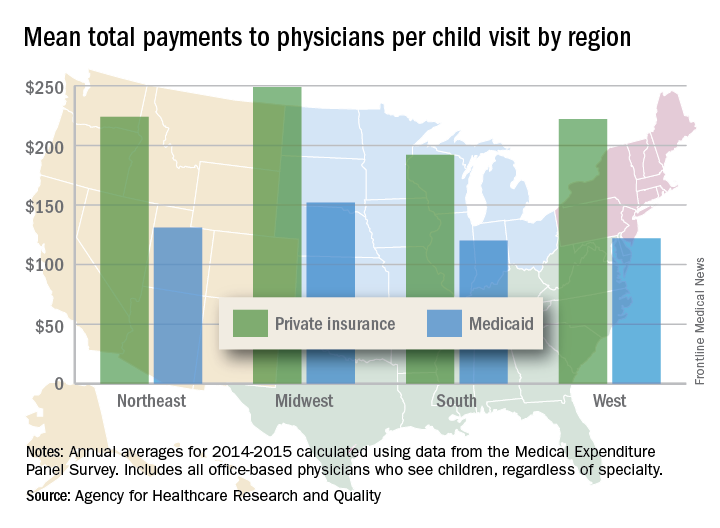
There were statistically significant gaps between private and Medicaid payments by specialty, although only for visits to orthopedists ($423 private – $162 Medicaid = $261) and primary care physicians such as family physicians and internists ($174 private – $122 Medicaid = $52). Payments to pediatricians were $190 private/$115 Medicaid, and the psychiatrists’ $111 mean payment from Medicaid represented the lowest for any specialty, data from Medical Expenditure Panel Survey’s household component show.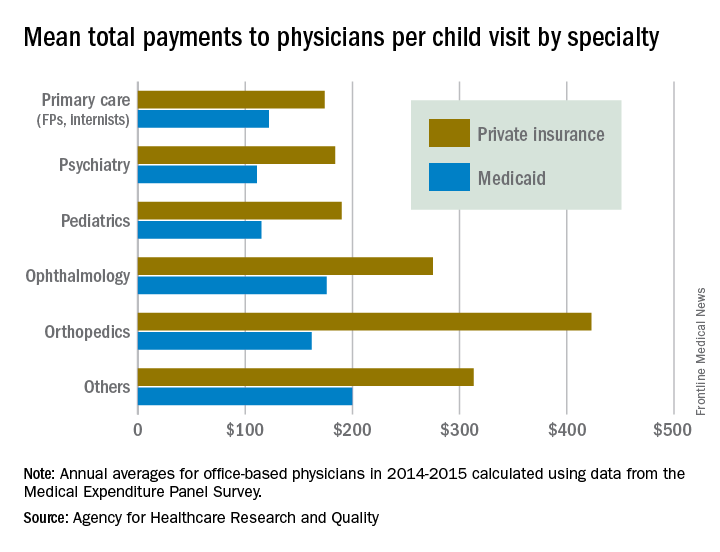
, according to the Agency for Healthcare Research and Quality.
Child visits covered by private insurance brought in a mean $214 for office-based physicians of all specialties in 2015, which was $88 more than the $126 they received for Medicaid-covered visits, the AHRQ said.
That gap has been consistent since 2010, even as payments rose from 2010 to 2013 and fell in 2014 and 2015. The payment gap was even larger in 2015 when looking at the most expensive 10% of child visits: $406 for those that were privately insured and $215 for those covered by Medicaid, the AHRQ reported in a recent Statistical Brief.
Variations in payments also were seen between geographic regions and among the different physician specialties. Mean payments to physicians in the Midwest were highest for both private insurance ($249) and Medicaid ($152), while the lowest payments – $192 from private insurance and $120 from Medicaid – went to physicians in the South. The South also had the smallest gap between private and Medicaid coverage at $72, and the West had the largest gap at an even $100, but none of the variation across regions was significant, the AHRQ said.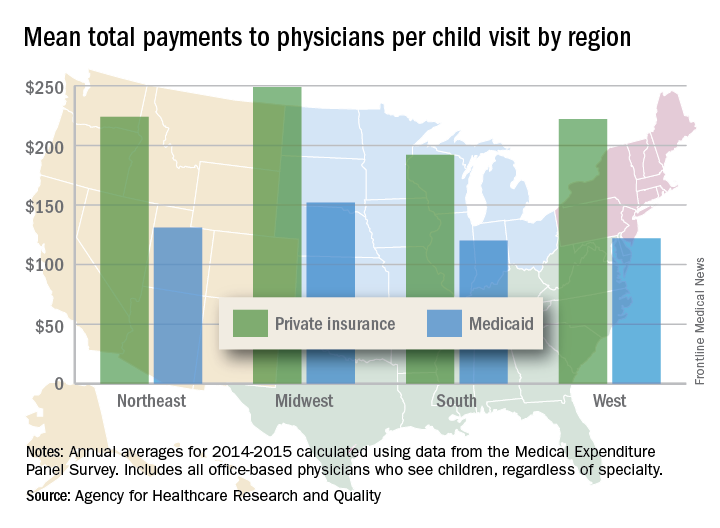
There were statistically significant gaps between private and Medicaid payments by specialty, although only for visits to orthopedists ($423 private – $162 Medicaid = $261) and primary care physicians such as family physicians and internists ($174 private – $122 Medicaid = $52). Payments to pediatricians were $190 private/$115 Medicaid, and the psychiatrists’ $111 mean payment from Medicaid represented the lowest for any specialty, data from Medical Expenditure Panel Survey’s household component show.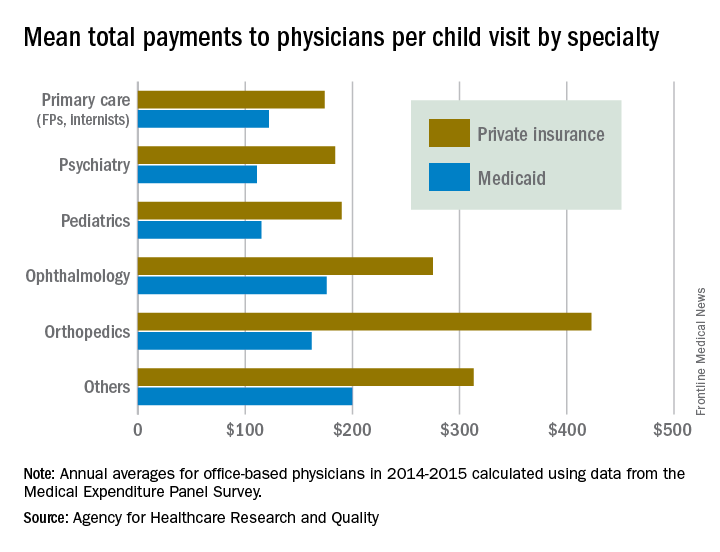
Tdap during pregnancy, or before, offers infants pertussis protection
during the early months of life, according to Tami H. Skoff of the Centers for Disease Control and Prevention, Atlanta, and her associates.
In an analysis of 240 infants younger than 2 months with pertussis cough onset between 2011 and 2015 and 535 control infants, 57% of case mothers and 67% of control mothers had at least one valid Tdap dose; 13% of vaccinated case mothers and 14% of vaccinated control mothers had more than one valid dose of Tdap reported.
Of Tdap doses received during pregnancy in 22 cases and 117 controls, 77% were received during the third trimester, most during the Advisory Committee on Immunization Practices’ recommended 27-36 weeks of gestation. Of the Tdap doses received before pregnancy in mothers of 24 cases and 67 controls, 25% of the case mothers and 67% of the control mothers received Tdap 2 or fewer years before pregnancy.
The effectiveness of Tdap vaccination during the third trimester of pregnancy was 78%, and effectiveness during the first or second trimester was 64%. Effectiveness of Tdap given 2 or fewer years before pregnancy was 83%. This study was not powered to determine a difference if the vaccine was administered in the ACIP-recommended time period during the third trimester.
A reported 49% of U.S. pregnant women received Tdap during the 2015-2016 flu season, an increase of 22% from the 2013-2014 season, according to a CDC Internet panel survey.
“While maternal immunization during pregnancy will help bridge the gap until next-generation pertussis vaccines are licensed and available for use, this highly effective strategy will likely remain an integral component of pertussis prevention and control, even in the setting of new vaccines,” the investigators said.
Read more in Clinical Infectious Diseases (2017 Sep 28. doi: 10.1093/cid/cix724).
during the early months of life, according to Tami H. Skoff of the Centers for Disease Control and Prevention, Atlanta, and her associates.
In an analysis of 240 infants younger than 2 months with pertussis cough onset between 2011 and 2015 and 535 control infants, 57% of case mothers and 67% of control mothers had at least one valid Tdap dose; 13% of vaccinated case mothers and 14% of vaccinated control mothers had more than one valid dose of Tdap reported.
Of Tdap doses received during pregnancy in 22 cases and 117 controls, 77% were received during the third trimester, most during the Advisory Committee on Immunization Practices’ recommended 27-36 weeks of gestation. Of the Tdap doses received before pregnancy in mothers of 24 cases and 67 controls, 25% of the case mothers and 67% of the control mothers received Tdap 2 or fewer years before pregnancy.
The effectiveness of Tdap vaccination during the third trimester of pregnancy was 78%, and effectiveness during the first or second trimester was 64%. Effectiveness of Tdap given 2 or fewer years before pregnancy was 83%. This study was not powered to determine a difference if the vaccine was administered in the ACIP-recommended time period during the third trimester.
A reported 49% of U.S. pregnant women received Tdap during the 2015-2016 flu season, an increase of 22% from the 2013-2014 season, according to a CDC Internet panel survey.
“While maternal immunization during pregnancy will help bridge the gap until next-generation pertussis vaccines are licensed and available for use, this highly effective strategy will likely remain an integral component of pertussis prevention and control, even in the setting of new vaccines,” the investigators said.
Read more in Clinical Infectious Diseases (2017 Sep 28. doi: 10.1093/cid/cix724).
during the early months of life, according to Tami H. Skoff of the Centers for Disease Control and Prevention, Atlanta, and her associates.
In an analysis of 240 infants younger than 2 months with pertussis cough onset between 2011 and 2015 and 535 control infants, 57% of case mothers and 67% of control mothers had at least one valid Tdap dose; 13% of vaccinated case mothers and 14% of vaccinated control mothers had more than one valid dose of Tdap reported.
Of Tdap doses received during pregnancy in 22 cases and 117 controls, 77% were received during the third trimester, most during the Advisory Committee on Immunization Practices’ recommended 27-36 weeks of gestation. Of the Tdap doses received before pregnancy in mothers of 24 cases and 67 controls, 25% of the case mothers and 67% of the control mothers received Tdap 2 or fewer years before pregnancy.
The effectiveness of Tdap vaccination during the third trimester of pregnancy was 78%, and effectiveness during the first or second trimester was 64%. Effectiveness of Tdap given 2 or fewer years before pregnancy was 83%. This study was not powered to determine a difference if the vaccine was administered in the ACIP-recommended time period during the third trimester.
A reported 49% of U.S. pregnant women received Tdap during the 2015-2016 flu season, an increase of 22% from the 2013-2014 season, according to a CDC Internet panel survey.
“While maternal immunization during pregnancy will help bridge the gap until next-generation pertussis vaccines are licensed and available for use, this highly effective strategy will likely remain an integral component of pertussis prevention and control, even in the setting of new vaccines,” the investigators said.
Read more in Clinical Infectious Diseases (2017 Sep 28. doi: 10.1093/cid/cix724).
FROM CLINICAL INFECTIOUS DISEASES
Avoid sildenafil for pulmonary hypertension after corrected valvular disease
BARCELONA – Off-label use of the phosphodiesterase-5 inhibitor sildenafil to treat residual pulmonary hypertension after successful correction of valvular heart disease is not merely ineffective, it’s counterproductive, according to the results of the randomized, placebo-controlled SIOVAC study.
“We believe based upon our results that off-label use of sildenafil in patients with left heart disease-pulmonary hypertension due to valvular disease should be discouraged,” Javier Bermejo, MD, declared at the annual congress of the European Society of Cardiology.

Sildenafil is approved with a solid, evidence-based indication for treating some other types of pulmonary hypertension. Many cardiologists also prescribe the drug off label for residual pulmonary hypertension in patients with corrected valve disease, hoping that it will be of benefit, since there is currently no approved treatment for this common and serious condition associated with increased mortality. But because the anecdotal literature on sildenafil for this specific type of pulmonary hypertension is mixed, Dr. Bermejo and his coinvestigators in the Spanish Network Center for Cardiovascular Research decided to conduct a multicenter randomized trial.
SIOVAC (Sildenafil for Improving Clinical Outcomes After Valvular Correction) comprised 200 patients with residual pulmonary hypertension after corrected valvular heart disease at 17 Spanish general hospitals. The patients were randomized to receive sildenafil at 40 mg t.i.d. or placebo for 6 months in this double-blind trial.
The primary endpoint was a standardized composite clinical score widely used in heart failure trials. It consists of all-cause mortality, hospital admission for heart failure, worsening exercise tolerance, and deterioration in a global self-assessment rating.
The shocker for the investigators – who had expected a positive study – was that 33% of patients in the sildenafil group worsened significantly on the composite clinical score at 6 months, compared with 14% of placebo-treated controls, said Dr. Bermejo, a cardiologist at Gregorio Marañón University Hospital in Madrid.
Moreover, only 27% of the sildenafil group improved, compared with 44% of controls. About one-third of patients in both groups remained unchanged over the course of the 6-month trial.
Dr. Bermejo noted that valvular disease is considered the next cardiac epidemic because of its strong association with advancing age and the rapid aging of the population worldwide. Pulmonary hypertension occurs is virtually all patients with severe mitral disease and in up to two-thirds of those with asymptomatic aortic stenosis. Regression of the pulmonary hypertension is often incomplete after successful surgical or transcatheter correction of the valvular lesion.
Discussant Irene M. Lang, MD, called SIOVAC “a very clear study.” It convincingly establishes that sildenafil – a vasodilator – is ineffective for the treatment of what the current ESC/European Respiratory Society guidelines on pulmonary hypertension call isolated post-capillary pulmonary hypertension, a condition defined hemodynamically by a diastolic pulmonary vascular pressure gradient of less than 7 mm Hg and/or a pulmonary vascular resistance below 3 Wood units (Eur Heart J. 2016 Jan 1;37[1]:67-119.)
The SIOVAC findings underscore the strong IIIC recommendation in the European guidelines that the use of approved therapies for pulmonary arterial hypertension is not recommended in patients with left heart disease-pulmonary hypertension, added Dr. Lang, a coauthor of the guidelines and professor of vascular biology at the Medical University of Vienna.
The Spanish government funded SIOVAC. Dr. Bermejo reported having no financial conflicts of interest.
BARCELONA – Off-label use of the phosphodiesterase-5 inhibitor sildenafil to treat residual pulmonary hypertension after successful correction of valvular heart disease is not merely ineffective, it’s counterproductive, according to the results of the randomized, placebo-controlled SIOVAC study.
“We believe based upon our results that off-label use of sildenafil in patients with left heart disease-pulmonary hypertension due to valvular disease should be discouraged,” Javier Bermejo, MD, declared at the annual congress of the European Society of Cardiology.

Sildenafil is approved with a solid, evidence-based indication for treating some other types of pulmonary hypertension. Many cardiologists also prescribe the drug off label for residual pulmonary hypertension in patients with corrected valve disease, hoping that it will be of benefit, since there is currently no approved treatment for this common and serious condition associated with increased mortality. But because the anecdotal literature on sildenafil for this specific type of pulmonary hypertension is mixed, Dr. Bermejo and his coinvestigators in the Spanish Network Center for Cardiovascular Research decided to conduct a multicenter randomized trial.
SIOVAC (Sildenafil for Improving Clinical Outcomes After Valvular Correction) comprised 200 patients with residual pulmonary hypertension after corrected valvular heart disease at 17 Spanish general hospitals. The patients were randomized to receive sildenafil at 40 mg t.i.d. or placebo for 6 months in this double-blind trial.
The primary endpoint was a standardized composite clinical score widely used in heart failure trials. It consists of all-cause mortality, hospital admission for heart failure, worsening exercise tolerance, and deterioration in a global self-assessment rating.
The shocker for the investigators – who had expected a positive study – was that 33% of patients in the sildenafil group worsened significantly on the composite clinical score at 6 months, compared with 14% of placebo-treated controls, said Dr. Bermejo, a cardiologist at Gregorio Marañón University Hospital in Madrid.
Moreover, only 27% of the sildenafil group improved, compared with 44% of controls. About one-third of patients in both groups remained unchanged over the course of the 6-month trial.
Dr. Bermejo noted that valvular disease is considered the next cardiac epidemic because of its strong association with advancing age and the rapid aging of the population worldwide. Pulmonary hypertension occurs is virtually all patients with severe mitral disease and in up to two-thirds of those with asymptomatic aortic stenosis. Regression of the pulmonary hypertension is often incomplete after successful surgical or transcatheter correction of the valvular lesion.
Discussant Irene M. Lang, MD, called SIOVAC “a very clear study.” It convincingly establishes that sildenafil – a vasodilator – is ineffective for the treatment of what the current ESC/European Respiratory Society guidelines on pulmonary hypertension call isolated post-capillary pulmonary hypertension, a condition defined hemodynamically by a diastolic pulmonary vascular pressure gradient of less than 7 mm Hg and/or a pulmonary vascular resistance below 3 Wood units (Eur Heart J. 2016 Jan 1;37[1]:67-119.)
The SIOVAC findings underscore the strong IIIC recommendation in the European guidelines that the use of approved therapies for pulmonary arterial hypertension is not recommended in patients with left heart disease-pulmonary hypertension, added Dr. Lang, a coauthor of the guidelines and professor of vascular biology at the Medical University of Vienna.
The Spanish government funded SIOVAC. Dr. Bermejo reported having no financial conflicts of interest.
BARCELONA – Off-label use of the phosphodiesterase-5 inhibitor sildenafil to treat residual pulmonary hypertension after successful correction of valvular heart disease is not merely ineffective, it’s counterproductive, according to the results of the randomized, placebo-controlled SIOVAC study.
“We believe based upon our results that off-label use of sildenafil in patients with left heart disease-pulmonary hypertension due to valvular disease should be discouraged,” Javier Bermejo, MD, declared at the annual congress of the European Society of Cardiology.

Sildenafil is approved with a solid, evidence-based indication for treating some other types of pulmonary hypertension. Many cardiologists also prescribe the drug off label for residual pulmonary hypertension in patients with corrected valve disease, hoping that it will be of benefit, since there is currently no approved treatment for this common and serious condition associated with increased mortality. But because the anecdotal literature on sildenafil for this specific type of pulmonary hypertension is mixed, Dr. Bermejo and his coinvestigators in the Spanish Network Center for Cardiovascular Research decided to conduct a multicenter randomized trial.
SIOVAC (Sildenafil for Improving Clinical Outcomes After Valvular Correction) comprised 200 patients with residual pulmonary hypertension after corrected valvular heart disease at 17 Spanish general hospitals. The patients were randomized to receive sildenafil at 40 mg t.i.d. or placebo for 6 months in this double-blind trial.
The primary endpoint was a standardized composite clinical score widely used in heart failure trials. It consists of all-cause mortality, hospital admission for heart failure, worsening exercise tolerance, and deterioration in a global self-assessment rating.
The shocker for the investigators – who had expected a positive study – was that 33% of patients in the sildenafil group worsened significantly on the composite clinical score at 6 months, compared with 14% of placebo-treated controls, said Dr. Bermejo, a cardiologist at Gregorio Marañón University Hospital in Madrid.
Moreover, only 27% of the sildenafil group improved, compared with 44% of controls. About one-third of patients in both groups remained unchanged over the course of the 6-month trial.
Dr. Bermejo noted that valvular disease is considered the next cardiac epidemic because of its strong association with advancing age and the rapid aging of the population worldwide. Pulmonary hypertension occurs is virtually all patients with severe mitral disease and in up to two-thirds of those with asymptomatic aortic stenosis. Regression of the pulmonary hypertension is often incomplete after successful surgical or transcatheter correction of the valvular lesion.
Discussant Irene M. Lang, MD, called SIOVAC “a very clear study.” It convincingly establishes that sildenafil – a vasodilator – is ineffective for the treatment of what the current ESC/European Respiratory Society guidelines on pulmonary hypertension call isolated post-capillary pulmonary hypertension, a condition defined hemodynamically by a diastolic pulmonary vascular pressure gradient of less than 7 mm Hg and/or a pulmonary vascular resistance below 3 Wood units (Eur Heart J. 2016 Jan 1;37[1]:67-119.)
The SIOVAC findings underscore the strong IIIC recommendation in the European guidelines that the use of approved therapies for pulmonary arterial hypertension is not recommended in patients with left heart disease-pulmonary hypertension, added Dr. Lang, a coauthor of the guidelines and professor of vascular biology at the Medical University of Vienna.
The Spanish government funded SIOVAC. Dr. Bermejo reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: One-third of patients with residual pulmonary hypertension after successful correction of valvular heart disease experienced significant clinical worsening during 6 months of sildenafil therapy, compared with 14% on placebo.
Data source: SIOVAC, a 6-month, double-blind, placebo-controlled study of 200 patients with residual pulmonary hypertension after correction for valvular heart disease.
Disclosures: The Spanish government funded SIOVAC. The presenter reported having no financial conflicts of interest.
Walking the halls of power
Hospital medicine may be a young specialty, but it is already playing a significant role in both front-line patient care and, increasingly, in shaping public policy. Case in point: Two hospitalists serving currently in key roles in the federal government, and two former top civil servants, each of whom are examples of the growing influence of the hospitalist perspective.
“The hospitalist viewpoint of the health care system is a unique one, and it lends itself very well to the challenges of our current delivery system reform. We’re reforming the health care system to deliver care more cost effectively,” said Ron Greeno, MD, FCCP, MHM, SHM president and chair of the SHM Public Policy committee. “Hospitalists are trained to do that – they go to work every day to do that.”
Leading the FDA
“He’s the perfect person for that job and is looking to shake things up,” Dr. Greeno said. “There are a lot of things that can improve in terms of how drugs get to market, including lower cost generic drugs.” That’s an issue Dr. Gottlieb has been championing for years, and his understanding of the issue also makes him well prepared to take this position now, Dr. Greeno said.
“Dr. Gottlieb’s nomination comes at a momentous time for the agency, which Mr. Trump has promised to significantly remake,” the New York Times wrote on March 29, prior to his confirmation. “The next commissioner will be charged with putting into practice a far-reaching law, passed in December, aimed at bringing drugs to market more quickly.”
In addition to his work at the AEI, Dr. Gottlieb served on SHM’s Public Policy committee. He was a clinical assistant professor at New York University School of Medicine and advised the U.S. Department of Health and Human Services as a member of the Federal Health IT Policy committee.
Steering national quality programs
Kate Goodrich’s preparation for her government role included experience with several sides of the health care system: Dr. Goodrich, MD, MHS, was the director of the Division of Hospital Medicine at George Washington University Hospital, one of the first hospitalist programs in the Washington area. She worked at an inpatient rehab facility and has practiced in ambulatory care.
Now, as chief medical officer of CMS and director of the Center for Clinical Standards and Quality (CCSQ), she’s helping drive those policy decisions, overseeing multiple quality measurement and value-based purchasing programs and health and safety standards for hospitals.
Dr. Goodrich still makes rounds at George Washington Hospital on weekends. “It allows me to have a sort of in-your-bones understanding of the challenges of frontline providers,” she said. “I’m able to understand the clinician point of view in our policy decisions.” She’s also able to see first-hand the effects of those policy decisions on clinicians, patients, and health care systems.
As physician leaders within their organizations, hospitalists fit naturally into other leadership positions, she said. “Hospitalists often take leadership roles around quality of care and efficiency and flow and those sorts of thing,” Dr. Goodrich said. “I think it is a very natural progression for hospitalists to get interested in health care and medicine from that viewpoint, which then might allow them to make a leap into another type of field.”
An innovator at CMS
Until very recently, pediatric hospitalist Patrick Conway, MD, FAAP, MHM, served as deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation. On Oct. 1, he took on a new challenge, becoming president and CEO of Blue Cross and Blue Shield of North Carolina (Blue Cross NC).
Dr. Conway was selected as a Master of Hospital Medicine by SHM, and received the HHS Secretary’s Award for Distinguished Service, the Secretary’s highest distinction for excellence. The Patient Safety Movement Foundation gave him their Humanitarian Award, and in February 2017, he received the AMA’s Dr. Nathan Davis Award for Outstanding Government Service. He also was elected to the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine in 2014.
Prior to joining CMS, Dr. Conway oversaw clinical operations and research at Cincinnati Children’s Hospital Medical Center as director of hospital medicine, with a focus on improving patient outcomes across the health system.
Improving the country’s health
Obesity, tobacco-related disease, mental illness, and addiction are some of the issues Vivek H. Murthy, MD, MBA, targeted while serving as the 19th U.S. Surgeon General. He was appointed to the position by President Obama in 2014, and was relieved of his duties by President Trump in April 2017.
Dr. Murthy has said that addiction should be seen as a chronic illness, not a character flaw, and last year sent a letter to 2.3 million health care providers nationwide, encouraging them to join a national effort to reform prescribing practices.
According to Dr. Greeno, each of these hospitalists illuminates new paths for others in the field. “I think for young people who are trying to identify what career path they want to pursue, this is something that can’t be anything but good for our specialty – and good for the health system,” he said. “Hospitalists have the perfect clinical background and mindset to help our health care system get to where it needs to go. It’s a huge challenge. It’s going to be a ton of work, and the stakes are very, very high.”
Reference
1. Thomas K. F.D.A. Nominee, Paid Millions by Industry, Says He’ll Recuse Himself if Needed. New York Times. March 29, 2017. https://www.nytimes.com/2017/03/29/health/fda-nominee-scott-gottlieb-recuse-conflicts.html?_r=0. Accessed March 31, 2017.
Hospital medicine may be a young specialty, but it is already playing a significant role in both front-line patient care and, increasingly, in shaping public policy. Case in point: Two hospitalists serving currently in key roles in the federal government, and two former top civil servants, each of whom are examples of the growing influence of the hospitalist perspective.
“The hospitalist viewpoint of the health care system is a unique one, and it lends itself very well to the challenges of our current delivery system reform. We’re reforming the health care system to deliver care more cost effectively,” said Ron Greeno, MD, FCCP, MHM, SHM president and chair of the SHM Public Policy committee. “Hospitalists are trained to do that – they go to work every day to do that.”
Leading the FDA
“He’s the perfect person for that job and is looking to shake things up,” Dr. Greeno said. “There are a lot of things that can improve in terms of how drugs get to market, including lower cost generic drugs.” That’s an issue Dr. Gottlieb has been championing for years, and his understanding of the issue also makes him well prepared to take this position now, Dr. Greeno said.
“Dr. Gottlieb’s nomination comes at a momentous time for the agency, which Mr. Trump has promised to significantly remake,” the New York Times wrote on March 29, prior to his confirmation. “The next commissioner will be charged with putting into practice a far-reaching law, passed in December, aimed at bringing drugs to market more quickly.”
In addition to his work at the AEI, Dr. Gottlieb served on SHM’s Public Policy committee. He was a clinical assistant professor at New York University School of Medicine and advised the U.S. Department of Health and Human Services as a member of the Federal Health IT Policy committee.
Steering national quality programs
Kate Goodrich’s preparation for her government role included experience with several sides of the health care system: Dr. Goodrich, MD, MHS, was the director of the Division of Hospital Medicine at George Washington University Hospital, one of the first hospitalist programs in the Washington area. She worked at an inpatient rehab facility and has practiced in ambulatory care.
Now, as chief medical officer of CMS and director of the Center for Clinical Standards and Quality (CCSQ), she’s helping drive those policy decisions, overseeing multiple quality measurement and value-based purchasing programs and health and safety standards for hospitals.
Dr. Goodrich still makes rounds at George Washington Hospital on weekends. “It allows me to have a sort of in-your-bones understanding of the challenges of frontline providers,” she said. “I’m able to understand the clinician point of view in our policy decisions.” She’s also able to see first-hand the effects of those policy decisions on clinicians, patients, and health care systems.
As physician leaders within their organizations, hospitalists fit naturally into other leadership positions, she said. “Hospitalists often take leadership roles around quality of care and efficiency and flow and those sorts of thing,” Dr. Goodrich said. “I think it is a very natural progression for hospitalists to get interested in health care and medicine from that viewpoint, which then might allow them to make a leap into another type of field.”
An innovator at CMS
Until very recently, pediatric hospitalist Patrick Conway, MD, FAAP, MHM, served as deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation. On Oct. 1, he took on a new challenge, becoming president and CEO of Blue Cross and Blue Shield of North Carolina (Blue Cross NC).
Dr. Conway was selected as a Master of Hospital Medicine by SHM, and received the HHS Secretary’s Award for Distinguished Service, the Secretary’s highest distinction for excellence. The Patient Safety Movement Foundation gave him their Humanitarian Award, and in February 2017, he received the AMA’s Dr. Nathan Davis Award for Outstanding Government Service. He also was elected to the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine in 2014.
Prior to joining CMS, Dr. Conway oversaw clinical operations and research at Cincinnati Children’s Hospital Medical Center as director of hospital medicine, with a focus on improving patient outcomes across the health system.
Improving the country’s health
Obesity, tobacco-related disease, mental illness, and addiction are some of the issues Vivek H. Murthy, MD, MBA, targeted while serving as the 19th U.S. Surgeon General. He was appointed to the position by President Obama in 2014, and was relieved of his duties by President Trump in April 2017.
Dr. Murthy has said that addiction should be seen as a chronic illness, not a character flaw, and last year sent a letter to 2.3 million health care providers nationwide, encouraging them to join a national effort to reform prescribing practices.
According to Dr. Greeno, each of these hospitalists illuminates new paths for others in the field. “I think for young people who are trying to identify what career path they want to pursue, this is something that can’t be anything but good for our specialty – and good for the health system,” he said. “Hospitalists have the perfect clinical background and mindset to help our health care system get to where it needs to go. It’s a huge challenge. It’s going to be a ton of work, and the stakes are very, very high.”
Reference
1. Thomas K. F.D.A. Nominee, Paid Millions by Industry, Says He’ll Recuse Himself if Needed. New York Times. March 29, 2017. https://www.nytimes.com/2017/03/29/health/fda-nominee-scott-gottlieb-recuse-conflicts.html?_r=0. Accessed March 31, 2017.
Hospital medicine may be a young specialty, but it is already playing a significant role in both front-line patient care and, increasingly, in shaping public policy. Case in point: Two hospitalists serving currently in key roles in the federal government, and two former top civil servants, each of whom are examples of the growing influence of the hospitalist perspective.
“The hospitalist viewpoint of the health care system is a unique one, and it lends itself very well to the challenges of our current delivery system reform. We’re reforming the health care system to deliver care more cost effectively,” said Ron Greeno, MD, FCCP, MHM, SHM president and chair of the SHM Public Policy committee. “Hospitalists are trained to do that – they go to work every day to do that.”
Leading the FDA
“He’s the perfect person for that job and is looking to shake things up,” Dr. Greeno said. “There are a lot of things that can improve in terms of how drugs get to market, including lower cost generic drugs.” That’s an issue Dr. Gottlieb has been championing for years, and his understanding of the issue also makes him well prepared to take this position now, Dr. Greeno said.
“Dr. Gottlieb’s nomination comes at a momentous time for the agency, which Mr. Trump has promised to significantly remake,” the New York Times wrote on March 29, prior to his confirmation. “The next commissioner will be charged with putting into practice a far-reaching law, passed in December, aimed at bringing drugs to market more quickly.”
In addition to his work at the AEI, Dr. Gottlieb served on SHM’s Public Policy committee. He was a clinical assistant professor at New York University School of Medicine and advised the U.S. Department of Health and Human Services as a member of the Federal Health IT Policy committee.
Steering national quality programs
Kate Goodrich’s preparation for her government role included experience with several sides of the health care system: Dr. Goodrich, MD, MHS, was the director of the Division of Hospital Medicine at George Washington University Hospital, one of the first hospitalist programs in the Washington area. She worked at an inpatient rehab facility and has practiced in ambulatory care.
Now, as chief medical officer of CMS and director of the Center for Clinical Standards and Quality (CCSQ), she’s helping drive those policy decisions, overseeing multiple quality measurement and value-based purchasing programs and health and safety standards for hospitals.
Dr. Goodrich still makes rounds at George Washington Hospital on weekends. “It allows me to have a sort of in-your-bones understanding of the challenges of frontline providers,” she said. “I’m able to understand the clinician point of view in our policy decisions.” She’s also able to see first-hand the effects of those policy decisions on clinicians, patients, and health care systems.
As physician leaders within their organizations, hospitalists fit naturally into other leadership positions, she said. “Hospitalists often take leadership roles around quality of care and efficiency and flow and those sorts of thing,” Dr. Goodrich said. “I think it is a very natural progression for hospitalists to get interested in health care and medicine from that viewpoint, which then might allow them to make a leap into another type of field.”
An innovator at CMS
Until very recently, pediatric hospitalist Patrick Conway, MD, FAAP, MHM, served as deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation. On Oct. 1, he took on a new challenge, becoming president and CEO of Blue Cross and Blue Shield of North Carolina (Blue Cross NC).
Dr. Conway was selected as a Master of Hospital Medicine by SHM, and received the HHS Secretary’s Award for Distinguished Service, the Secretary’s highest distinction for excellence. The Patient Safety Movement Foundation gave him their Humanitarian Award, and in February 2017, he received the AMA’s Dr. Nathan Davis Award for Outstanding Government Service. He also was elected to the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine in 2014.
Prior to joining CMS, Dr. Conway oversaw clinical operations and research at Cincinnati Children’s Hospital Medical Center as director of hospital medicine, with a focus on improving patient outcomes across the health system.
Improving the country’s health
Obesity, tobacco-related disease, mental illness, and addiction are some of the issues Vivek H. Murthy, MD, MBA, targeted while serving as the 19th U.S. Surgeon General. He was appointed to the position by President Obama in 2014, and was relieved of his duties by President Trump in April 2017.
Dr. Murthy has said that addiction should be seen as a chronic illness, not a character flaw, and last year sent a letter to 2.3 million health care providers nationwide, encouraging them to join a national effort to reform prescribing practices.
According to Dr. Greeno, each of these hospitalists illuminates new paths for others in the field. “I think for young people who are trying to identify what career path they want to pursue, this is something that can’t be anything but good for our specialty – and good for the health system,” he said. “Hospitalists have the perfect clinical background and mindset to help our health care system get to where it needs to go. It’s a huge challenge. It’s going to be a ton of work, and the stakes are very, very high.”
Reference
1. Thomas K. F.D.A. Nominee, Paid Millions by Industry, Says He’ll Recuse Himself if Needed. New York Times. March 29, 2017. https://www.nytimes.com/2017/03/29/health/fda-nominee-scott-gottlieb-recuse-conflicts.html?_r=0. Accessed March 31, 2017.
Febuxostat prevents early gout flares
The urate-lowering therapy febuxostat reduced the number of disease flares that people with early gout experienced relative to placebo in a double-blind, placebo-controlled study.
Febuxostat (Uloric) produced a 12.1% reduction in the overall percentage of patients who experienced at least one gout flare in comparison to placebo (29.3% vs. 41.4%; P less than .05).
Treatment with febuxostat also significantly improved control of serum uric acid, compared with the placebo-treated patients (64.3% vs. 5.7%; P less than .001), as well as synovitis as measured via the rheumatoid arthritis magnetic resonance imaging score (RAMRIS) score (–0.43 vs. –0.07; P less than .001).
“This study indicates that even for people who have only had one or two prior gout flares, urate-lowering therapy to reduce serum urate below 6 mg/dL may have benefit in reduction future flares,” said Dr. Dalbeth of the University of Auckland (New Zealand).
Febuxostat is a xanthine oxidase inhibitor indicated for the chronic management of excess uric acid in the blood in people diagnosed with gout. It is not indicated for use in people who have high serum uric acid levels without a history of gout.
“Although acute self-limiting flares are the most common clinical presentation of gout, joint damage is a frequent complication of the disease,” Dr. Dalbeth and her associates wrote.
“Joint damage is typically a late feature of long-standing gout,” they added, but “longitudinal observational data have indicated that joint damage can occur in some patients with early disease.” Increased urate crystal deposition could be associated with bone erosions, they explained, and the primary aim of the study was to look the rate of bone erosions over the course of 2 years’ treatment.
However, despite this reasoning and some prior clinical evidence, the researchers found no noticeable differences between the study groups in terms of radiologic joint erosion. This was assessed over 2 years in a single-affected joint. The mean change from baseline to month 24 in modified Sharp-van der Heijde erosion scores was 0.01 for both febuxostat and placebo (P = .47).
This was a phase 2 study conducted in 56 centers in the United States that screened 798 subjects and enrolled 314 adults with early gout. For inclusion, patients had to have hyperuricemia, defined as a serum uric acid level of 7.0 mg/dL or higher, and they had to have experienced no more than two gout flares in the past year.
Patients were randomized to once-daily treatment with febuxostat or placebo, with those randomized to the active treatment started at a dose of 40 mg, which could be increased to 80 mg after 2 weeks if serum uric acid levels remained high, at 6.0 mg/dL or above.
“To our knowledge, this is the first randomized, controlled trial examining the effects of [urate-lowering therapy] in patients with early gout,” the authors observed.
Although the primary endpoint was not met, the study “provides important new information about the natural history of joint damage in subjects with gout,” they suggested. In contrast to other inflammatory joint diseases, such as rheumatoid arthritis, joint erosions on plain radiographs were “infrequently observed at baseline” and over the 2-year study period. The fact the there was a change in MRI synovitis suggests that perhaps there may be some underlying joint damage occurring, although the clinical significance of this is uncertain.
Takeda, which makes febuxostat, funded the study. Dr. Dalbeth has received consulting fees, speaker fees, or research grants from Takeda, CymaBay, Ardea Biosciences, AstraZeneca, and Horizon. A couple of her coauthors disclosed acting as consultants to or receiving research funding from Takeda, and three were current or past employees of the company.
The urate-lowering therapy febuxostat reduced the number of disease flares that people with early gout experienced relative to placebo in a double-blind, placebo-controlled study.
Febuxostat (Uloric) produced a 12.1% reduction in the overall percentage of patients who experienced at least one gout flare in comparison to placebo (29.3% vs. 41.4%; P less than .05).
Treatment with febuxostat also significantly improved control of serum uric acid, compared with the placebo-treated patients (64.3% vs. 5.7%; P less than .001), as well as synovitis as measured via the rheumatoid arthritis magnetic resonance imaging score (RAMRIS) score (–0.43 vs. –0.07; P less than .001).
“This study indicates that even for people who have only had one or two prior gout flares, urate-lowering therapy to reduce serum urate below 6 mg/dL may have benefit in reduction future flares,” said Dr. Dalbeth of the University of Auckland (New Zealand).
Febuxostat is a xanthine oxidase inhibitor indicated for the chronic management of excess uric acid in the blood in people diagnosed with gout. It is not indicated for use in people who have high serum uric acid levels without a history of gout.
“Although acute self-limiting flares are the most common clinical presentation of gout, joint damage is a frequent complication of the disease,” Dr. Dalbeth and her associates wrote.
“Joint damage is typically a late feature of long-standing gout,” they added, but “longitudinal observational data have indicated that joint damage can occur in some patients with early disease.” Increased urate crystal deposition could be associated with bone erosions, they explained, and the primary aim of the study was to look the rate of bone erosions over the course of 2 years’ treatment.
However, despite this reasoning and some prior clinical evidence, the researchers found no noticeable differences between the study groups in terms of radiologic joint erosion. This was assessed over 2 years in a single-affected joint. The mean change from baseline to month 24 in modified Sharp-van der Heijde erosion scores was 0.01 for both febuxostat and placebo (P = .47).
This was a phase 2 study conducted in 56 centers in the United States that screened 798 subjects and enrolled 314 adults with early gout. For inclusion, patients had to have hyperuricemia, defined as a serum uric acid level of 7.0 mg/dL or higher, and they had to have experienced no more than two gout flares in the past year.
Patients were randomized to once-daily treatment with febuxostat or placebo, with those randomized to the active treatment started at a dose of 40 mg, which could be increased to 80 mg after 2 weeks if serum uric acid levels remained high, at 6.0 mg/dL or above.
“To our knowledge, this is the first randomized, controlled trial examining the effects of [urate-lowering therapy] in patients with early gout,” the authors observed.
Although the primary endpoint was not met, the study “provides important new information about the natural history of joint damage in subjects with gout,” they suggested. In contrast to other inflammatory joint diseases, such as rheumatoid arthritis, joint erosions on plain radiographs were “infrequently observed at baseline” and over the 2-year study period. The fact the there was a change in MRI synovitis suggests that perhaps there may be some underlying joint damage occurring, although the clinical significance of this is uncertain.
Takeda, which makes febuxostat, funded the study. Dr. Dalbeth has received consulting fees, speaker fees, or research grants from Takeda, CymaBay, Ardea Biosciences, AstraZeneca, and Horizon. A couple of her coauthors disclosed acting as consultants to or receiving research funding from Takeda, and three were current or past employees of the company.
The urate-lowering therapy febuxostat reduced the number of disease flares that people with early gout experienced relative to placebo in a double-blind, placebo-controlled study.
Febuxostat (Uloric) produced a 12.1% reduction in the overall percentage of patients who experienced at least one gout flare in comparison to placebo (29.3% vs. 41.4%; P less than .05).
Treatment with febuxostat also significantly improved control of serum uric acid, compared with the placebo-treated patients (64.3% vs. 5.7%; P less than .001), as well as synovitis as measured via the rheumatoid arthritis magnetic resonance imaging score (RAMRIS) score (–0.43 vs. –0.07; P less than .001).
“This study indicates that even for people who have only had one or two prior gout flares, urate-lowering therapy to reduce serum urate below 6 mg/dL may have benefit in reduction future flares,” said Dr. Dalbeth of the University of Auckland (New Zealand).
Febuxostat is a xanthine oxidase inhibitor indicated for the chronic management of excess uric acid in the blood in people diagnosed with gout. It is not indicated for use in people who have high serum uric acid levels without a history of gout.
“Although acute self-limiting flares are the most common clinical presentation of gout, joint damage is a frequent complication of the disease,” Dr. Dalbeth and her associates wrote.
“Joint damage is typically a late feature of long-standing gout,” they added, but “longitudinal observational data have indicated that joint damage can occur in some patients with early disease.” Increased urate crystal deposition could be associated with bone erosions, they explained, and the primary aim of the study was to look the rate of bone erosions over the course of 2 years’ treatment.
However, despite this reasoning and some prior clinical evidence, the researchers found no noticeable differences between the study groups in terms of radiologic joint erosion. This was assessed over 2 years in a single-affected joint. The mean change from baseline to month 24 in modified Sharp-van der Heijde erosion scores was 0.01 for both febuxostat and placebo (P = .47).
This was a phase 2 study conducted in 56 centers in the United States that screened 798 subjects and enrolled 314 adults with early gout. For inclusion, patients had to have hyperuricemia, defined as a serum uric acid level of 7.0 mg/dL or higher, and they had to have experienced no more than two gout flares in the past year.
Patients were randomized to once-daily treatment with febuxostat or placebo, with those randomized to the active treatment started at a dose of 40 mg, which could be increased to 80 mg after 2 weeks if serum uric acid levels remained high, at 6.0 mg/dL or above.
“To our knowledge, this is the first randomized, controlled trial examining the effects of [urate-lowering therapy] in patients with early gout,” the authors observed.
Although the primary endpoint was not met, the study “provides important new information about the natural history of joint damage in subjects with gout,” they suggested. In contrast to other inflammatory joint diseases, such as rheumatoid arthritis, joint erosions on plain radiographs were “infrequently observed at baseline” and over the 2-year study period. The fact the there was a change in MRI synovitis suggests that perhaps there may be some underlying joint damage occurring, although the clinical significance of this is uncertain.
Takeda, which makes febuxostat, funded the study. Dr. Dalbeth has received consulting fees, speaker fees, or research grants from Takeda, CymaBay, Ardea Biosciences, AstraZeneca, and Horizon. A couple of her coauthors disclosed acting as consultants to or receiving research funding from Takeda, and three were current or past employees of the company.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: Gout flares over 2 years occurred in 29.3% of subjects treated with febuxostat versus 41.4% of those given placebo (P less than .05)
Data source Randomized, double-blind, placebo-controlled study assessing febuxostat versus placebo effects on joint damage in 314 hyperuricemic subjects with early gout.
Disclosures: Takeda, which makes febuxostat, funded the study. Dr. Dalbeth has received consulting fees, speaker fees, or research grants from Takeda, CymaBay, Ardea Biosciences, AstraZeneca, and Horizon. A couple of her coauthors disclosed acting as consultants to or receiving research funding from Takeda, and three were current or past employees of the company.
Innovations in Dermatology: Brodalumab for Plaque Psoriasis
Study supports routine rapid HCV testing for at-risk youth
Routine finger-stick testing for hepatitis C virus infection is the best screening strategy for 15- to 30-year-olds, provided that at least 6 in every 1,000 have injected drugs, according to the results of a modeling study.
“Currently, nearly all hepatitis C virus (HCV) transmission in the United States occurs among young persons who inject drugs,” wrote Sabrina A. Assoumou, MD, of Boston Medical Center and Boston University and her associates. “We show that routine testing provides the most clinical benefit and best value for money in an urban community health setting where HCV prevalence is high.”
Rapid routine testing consistently yielded more quality-adjusted life years (QALYs) at a lower cost than did the current practice of reflexive, risk-based venipuncture testing, the researchers said. They recommended that urban health centers either replace venipuncture diagnostics with routine finger-stick testing or that they ensure follow-up RNA testing when needed so they can link HCV-positive patients to treatment (Clin Infect Dis. 2017 Sep 9. doi: 10.1093/cid/cix798).
The Centers for Disease Control and Prevention has recommended risk-based HCV testing, but studies indicate that primary care providers often miss the chance to test and have trouble identifying high-risk patients, Dr. Assoumou and her associates said. The standard HCV test is a blood draw for antibody testing followed by confirmatory RNA testing, but a two-step process complicates follow-up.
To compare one-time HCV screening strategies in high-risk settings, the researchers created a decision analytic model using TreeAge Pro 2014 software and input data on prevalence, mortality, treatment costs, and efficacy from an extensive literature review.
Compared with targeted risk-based HCV testing, routine rapid testing performed by dedicated counselors yielded an incremental cost-effectiveness ratio of less than $100,000 per quality-adjusted life year unless the prevalence of injection drug use was less than 0.59%, the prevalence of HCV infection among injection drug users was less than 16%, the reinfection rate exceeded 26 cases per 100 person-years, or all venipuncture antibody tests were followed by confirmatory testing. Routine rapid testing identified 20% of HCV infections in the model, which is four times the rate under current practice. Rates of sustained virologic response were 18% with routine rapid testing and 2% with standard practice.
Routine rapid testing did not dramatically boost QALYs at a population level, the researchers acknowledged, but diagnosing and treating an injection drug user increased life span by an average of 2 years and saved $214,000 per patient in additional costs.
“Rapid testing always provided greater life expectancy than venipuncture testing at either a lower lifetime medical cost or a lower cost/QALY gained,” the investigators concluded. “Future studies are needed to define the programmatic effectiveness of HCV treatment among youth, and testing and treatment acceptability in this population.”
The National Institute on Drug Abuse and the National Institute of Allergy and Infectious Diseases provided funding. The researchers reported having no conflicts of interest.
Routine finger-stick testing for hepatitis C virus infection is the best screening strategy for 15- to 30-year-olds, provided that at least 6 in every 1,000 have injected drugs, according to the results of a modeling study.
“Currently, nearly all hepatitis C virus (HCV) transmission in the United States occurs among young persons who inject drugs,” wrote Sabrina A. Assoumou, MD, of Boston Medical Center and Boston University and her associates. “We show that routine testing provides the most clinical benefit and best value for money in an urban community health setting where HCV prevalence is high.”
Rapid routine testing consistently yielded more quality-adjusted life years (QALYs) at a lower cost than did the current practice of reflexive, risk-based venipuncture testing, the researchers said. They recommended that urban health centers either replace venipuncture diagnostics with routine finger-stick testing or that they ensure follow-up RNA testing when needed so they can link HCV-positive patients to treatment (Clin Infect Dis. 2017 Sep 9. doi: 10.1093/cid/cix798).
The Centers for Disease Control and Prevention has recommended risk-based HCV testing, but studies indicate that primary care providers often miss the chance to test and have trouble identifying high-risk patients, Dr. Assoumou and her associates said. The standard HCV test is a blood draw for antibody testing followed by confirmatory RNA testing, but a two-step process complicates follow-up.
To compare one-time HCV screening strategies in high-risk settings, the researchers created a decision analytic model using TreeAge Pro 2014 software and input data on prevalence, mortality, treatment costs, and efficacy from an extensive literature review.
Compared with targeted risk-based HCV testing, routine rapid testing performed by dedicated counselors yielded an incremental cost-effectiveness ratio of less than $100,000 per quality-adjusted life year unless the prevalence of injection drug use was less than 0.59%, the prevalence of HCV infection among injection drug users was less than 16%, the reinfection rate exceeded 26 cases per 100 person-years, or all venipuncture antibody tests were followed by confirmatory testing. Routine rapid testing identified 20% of HCV infections in the model, which is four times the rate under current practice. Rates of sustained virologic response were 18% with routine rapid testing and 2% with standard practice.
Routine rapid testing did not dramatically boost QALYs at a population level, the researchers acknowledged, but diagnosing and treating an injection drug user increased life span by an average of 2 years and saved $214,000 per patient in additional costs.
“Rapid testing always provided greater life expectancy than venipuncture testing at either a lower lifetime medical cost or a lower cost/QALY gained,” the investigators concluded. “Future studies are needed to define the programmatic effectiveness of HCV treatment among youth, and testing and treatment acceptability in this population.”
The National Institute on Drug Abuse and the National Institute of Allergy and Infectious Diseases provided funding. The researchers reported having no conflicts of interest.
Routine finger-stick testing for hepatitis C virus infection is the best screening strategy for 15- to 30-year-olds, provided that at least 6 in every 1,000 have injected drugs, according to the results of a modeling study.
“Currently, nearly all hepatitis C virus (HCV) transmission in the United States occurs among young persons who inject drugs,” wrote Sabrina A. Assoumou, MD, of Boston Medical Center and Boston University and her associates. “We show that routine testing provides the most clinical benefit and best value for money in an urban community health setting where HCV prevalence is high.”
Rapid routine testing consistently yielded more quality-adjusted life years (QALYs) at a lower cost than did the current practice of reflexive, risk-based venipuncture testing, the researchers said. They recommended that urban health centers either replace venipuncture diagnostics with routine finger-stick testing or that they ensure follow-up RNA testing when needed so they can link HCV-positive patients to treatment (Clin Infect Dis. 2017 Sep 9. doi: 10.1093/cid/cix798).
The Centers for Disease Control and Prevention has recommended risk-based HCV testing, but studies indicate that primary care providers often miss the chance to test and have trouble identifying high-risk patients, Dr. Assoumou and her associates said. The standard HCV test is a blood draw for antibody testing followed by confirmatory RNA testing, but a two-step process complicates follow-up.
To compare one-time HCV screening strategies in high-risk settings, the researchers created a decision analytic model using TreeAge Pro 2014 software and input data on prevalence, mortality, treatment costs, and efficacy from an extensive literature review.
Compared with targeted risk-based HCV testing, routine rapid testing performed by dedicated counselors yielded an incremental cost-effectiveness ratio of less than $100,000 per quality-adjusted life year unless the prevalence of injection drug use was less than 0.59%, the prevalence of HCV infection among injection drug users was less than 16%, the reinfection rate exceeded 26 cases per 100 person-years, or all venipuncture antibody tests were followed by confirmatory testing. Routine rapid testing identified 20% of HCV infections in the model, which is four times the rate under current practice. Rates of sustained virologic response were 18% with routine rapid testing and 2% with standard practice.
Routine rapid testing did not dramatically boost QALYs at a population level, the researchers acknowledged, but diagnosing and treating an injection drug user increased life span by an average of 2 years and saved $214,000 per patient in additional costs.
“Rapid testing always provided greater life expectancy than venipuncture testing at either a lower lifetime medical cost or a lower cost/QALY gained,” the investigators concluded. “Future studies are needed to define the programmatic effectiveness of HCV treatment among youth, and testing and treatment acceptability in this population.”
The National Institute on Drug Abuse and the National Institute of Allergy and Infectious Diseases provided funding. The researchers reported having no conflicts of interest.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Routine finger-stick testing was the most cost-effective way to screen urban adolescents and young adults for hepatitis C virus infection.
Major finding: The incremental cost-effectiveness ratio was less than $100,000 per quality-adjusted life year unless prevalence of injection drug use was less than 0.59%, less than 16% of injection drug users had HCV infection, the reinfection rate exceeded 26 cases per 100 person-years, or all venipuncture antibody tests were followed by confirmatory testing.
Data source: A decision analytic model created with TreeAge Pro 2014 and data from an extensive literature review.
Disclosures: The National Institute on Drug Abuse and the National Institute of Allergy and Infectious Diseases provided funding. The researchers reported having no conflicts of interest.