User login
Commentary: JAK Inhibitors and Comorbidities in AD, December 2023
Schlösser and colleagues provide a real-world report of 48 patients treated with upadacitinib for atopic dermatitis, many of whom had previously been treated with cyclosporine and dupilumab. The upbeat authors concluded, "Overall, adverse events were mostly well tolerated." Being a cynical, glass-is-half-empty kind of person, I wondered what that meant. Most patients (56%) reported adverse events, the most common being acne (25% of patients treated), nausea (13%), respiratory tract infections (10%), and herpes virus (8%). The herpes virus signal is not just a bit of a concern for me, but it also makes it hard for me to convince patients to take a Janus kinase (JAK) inhibitor, as when I even mention herpes, patients reply, often rather emphatically, "I don't want herpes!" I'll be encouraging patients to get vaccinated for shingles when starting them on JAK inhibitors.
Dupilumab seems to work great in real-life use. In Martinez-Cabriales and colleagues' study of 62 children age < 12 with atopic dermatitis, only four discontinued the treatment. One of these was a nonresponder who took only one injection and had flushing, and one of the other three discontinued because their skin had completely cleared.
When I saw the title of Rand and colleagues' article, "Matching-Adjusted Indirect Comparison of the Long-Term Efficacy Maintenance and Adverse Event Rates of Lebrikizumab Versus Dupilumab in Moderate-to-Severe Atopic Dermatitis," I thought, Oh, this is great — a head-to-head, long-term trial comparing lebrikizumab and dupilumab. I was disappointed to find that this was simply a retrospective analysis of data reported from different studies. The study found little difference in efficacy or safety of the two drugs. Both seem to be excellent medications for atopic dermatitis.
Here's another study (Zhou et al) that reports possible increased risk for a comorbidity (cognitive dysfunction) associated with atopic dermatitis. This study reports that there is an elevated hazard ratio that is statistically significant; the article fails to report what the increased absolute risk is for cognitive dysfunction associated with atopic dermatitis. My guess is that it is small and probably clinically unimportant. The hazard ratio for developing dementia was 1.16. It's hard to know how that translates into absolute risk, but my brilliant friend and former partner, Dr Alan Fleischer, once told me that the odds ratio for smoking and lung cancer is something like 100; the hazard ratio is in the range of 20. On the basis of a hazard ratio of 1.16, I don't think patients with atopic dermatitis need to be any more worried about dementia than those without. (Though, to be honest, I think we can all be worried about developing dementia.)
In this tour de force analysis of 83 trials with over 20,000 participants, Drucker and colleagues determined that high doses of abrocitinib and upadacitinib are more effective than even dupilumab for atopic dermatitis. The standard doses of these JAK inhibitors were similar in efficacy to dupilumab. I think it's safe to say that JAK inhibitors are, at least at their high doses, more effective than dupilumab, but safety remains a critical factor in treatment decision-making. I think JAK inhibitors are a great option for patients who need the most effective treatment or who fail to respond to dupilumab.
The title of the article by Oh and colleagues, "Increased Risk of Renal Malignancy in Patients With Moderate to Severe Atopic Dermatitis," seems like it could terrify patients. The study involved an analysis of an enormous number of people, including tens of thousands with atopic dermatitis and millions of controls. The investigators did find statistically significant differences in the rate of malignancy. The rate of renal cancer was about 1.6 per 10,000 person-years for people without atopic dermatitis or people with mild atopic dermatitis; the rate was about 2.5 per 10,000 people for patients with moderate to severe atopic dermatitis. While the rate of renal cancer was statistically significantly higher in patients with moderate to severe atopic dermatitis (ie, the higher rate was unlikely to be occurring due to chance alone), these patients have very little risk for renal malignancy. The authors' conclusion that regular checkups for renal malignancy are recommended for patients with severe atopic dermatitis seems unnecessary to me.
Schlösser and colleagues provide a real-world report of 48 patients treated with upadacitinib for atopic dermatitis, many of whom had previously been treated with cyclosporine and dupilumab. The upbeat authors concluded, "Overall, adverse events were mostly well tolerated." Being a cynical, glass-is-half-empty kind of person, I wondered what that meant. Most patients (56%) reported adverse events, the most common being acne (25% of patients treated), nausea (13%), respiratory tract infections (10%), and herpes virus (8%). The herpes virus signal is not just a bit of a concern for me, but it also makes it hard for me to convince patients to take a Janus kinase (JAK) inhibitor, as when I even mention herpes, patients reply, often rather emphatically, "I don't want herpes!" I'll be encouraging patients to get vaccinated for shingles when starting them on JAK inhibitors.
Dupilumab seems to work great in real-life use. In Martinez-Cabriales and colleagues' study of 62 children age < 12 with atopic dermatitis, only four discontinued the treatment. One of these was a nonresponder who took only one injection and had flushing, and one of the other three discontinued because their skin had completely cleared.
When I saw the title of Rand and colleagues' article, "Matching-Adjusted Indirect Comparison of the Long-Term Efficacy Maintenance and Adverse Event Rates of Lebrikizumab Versus Dupilumab in Moderate-to-Severe Atopic Dermatitis," I thought, Oh, this is great — a head-to-head, long-term trial comparing lebrikizumab and dupilumab. I was disappointed to find that this was simply a retrospective analysis of data reported from different studies. The study found little difference in efficacy or safety of the two drugs. Both seem to be excellent medications for atopic dermatitis.
Here's another study (Zhou et al) that reports possible increased risk for a comorbidity (cognitive dysfunction) associated with atopic dermatitis. This study reports that there is an elevated hazard ratio that is statistically significant; the article fails to report what the increased absolute risk is for cognitive dysfunction associated with atopic dermatitis. My guess is that it is small and probably clinically unimportant. The hazard ratio for developing dementia was 1.16. It's hard to know how that translates into absolute risk, but my brilliant friend and former partner, Dr Alan Fleischer, once told me that the odds ratio for smoking and lung cancer is something like 100; the hazard ratio is in the range of 20. On the basis of a hazard ratio of 1.16, I don't think patients with atopic dermatitis need to be any more worried about dementia than those without. (Though, to be honest, I think we can all be worried about developing dementia.)
In this tour de force analysis of 83 trials with over 20,000 participants, Drucker and colleagues determined that high doses of abrocitinib and upadacitinib are more effective than even dupilumab for atopic dermatitis. The standard doses of these JAK inhibitors were similar in efficacy to dupilumab. I think it's safe to say that JAK inhibitors are, at least at their high doses, more effective than dupilumab, but safety remains a critical factor in treatment decision-making. I think JAK inhibitors are a great option for patients who need the most effective treatment or who fail to respond to dupilumab.
The title of the article by Oh and colleagues, "Increased Risk of Renal Malignancy in Patients With Moderate to Severe Atopic Dermatitis," seems like it could terrify patients. The study involved an analysis of an enormous number of people, including tens of thousands with atopic dermatitis and millions of controls. The investigators did find statistically significant differences in the rate of malignancy. The rate of renal cancer was about 1.6 per 10,000 person-years for people without atopic dermatitis or people with mild atopic dermatitis; the rate was about 2.5 per 10,000 people for patients with moderate to severe atopic dermatitis. While the rate of renal cancer was statistically significantly higher in patients with moderate to severe atopic dermatitis (ie, the higher rate was unlikely to be occurring due to chance alone), these patients have very little risk for renal malignancy. The authors' conclusion that regular checkups for renal malignancy are recommended for patients with severe atopic dermatitis seems unnecessary to me.
Schlösser and colleagues provide a real-world report of 48 patients treated with upadacitinib for atopic dermatitis, many of whom had previously been treated with cyclosporine and dupilumab. The upbeat authors concluded, "Overall, adverse events were mostly well tolerated." Being a cynical, glass-is-half-empty kind of person, I wondered what that meant. Most patients (56%) reported adverse events, the most common being acne (25% of patients treated), nausea (13%), respiratory tract infections (10%), and herpes virus (8%). The herpes virus signal is not just a bit of a concern for me, but it also makes it hard for me to convince patients to take a Janus kinase (JAK) inhibitor, as when I even mention herpes, patients reply, often rather emphatically, "I don't want herpes!" I'll be encouraging patients to get vaccinated for shingles when starting them on JAK inhibitors.
Dupilumab seems to work great in real-life use. In Martinez-Cabriales and colleagues' study of 62 children age < 12 with atopic dermatitis, only four discontinued the treatment. One of these was a nonresponder who took only one injection and had flushing, and one of the other three discontinued because their skin had completely cleared.
When I saw the title of Rand and colleagues' article, "Matching-Adjusted Indirect Comparison of the Long-Term Efficacy Maintenance and Adverse Event Rates of Lebrikizumab Versus Dupilumab in Moderate-to-Severe Atopic Dermatitis," I thought, Oh, this is great — a head-to-head, long-term trial comparing lebrikizumab and dupilumab. I was disappointed to find that this was simply a retrospective analysis of data reported from different studies. The study found little difference in efficacy or safety of the two drugs. Both seem to be excellent medications for atopic dermatitis.
Here's another study (Zhou et al) that reports possible increased risk for a comorbidity (cognitive dysfunction) associated with atopic dermatitis. This study reports that there is an elevated hazard ratio that is statistically significant; the article fails to report what the increased absolute risk is for cognitive dysfunction associated with atopic dermatitis. My guess is that it is small and probably clinically unimportant. The hazard ratio for developing dementia was 1.16. It's hard to know how that translates into absolute risk, but my brilliant friend and former partner, Dr Alan Fleischer, once told me that the odds ratio for smoking and lung cancer is something like 100; the hazard ratio is in the range of 20. On the basis of a hazard ratio of 1.16, I don't think patients with atopic dermatitis need to be any more worried about dementia than those without. (Though, to be honest, I think we can all be worried about developing dementia.)
In this tour de force analysis of 83 trials with over 20,000 participants, Drucker and colleagues determined that high doses of abrocitinib and upadacitinib are more effective than even dupilumab for atopic dermatitis. The standard doses of these JAK inhibitors were similar in efficacy to dupilumab. I think it's safe to say that JAK inhibitors are, at least at their high doses, more effective than dupilumab, but safety remains a critical factor in treatment decision-making. I think JAK inhibitors are a great option for patients who need the most effective treatment or who fail to respond to dupilumab.
The title of the article by Oh and colleagues, "Increased Risk of Renal Malignancy in Patients With Moderate to Severe Atopic Dermatitis," seems like it could terrify patients. The study involved an analysis of an enormous number of people, including tens of thousands with atopic dermatitis and millions of controls. The investigators did find statistically significant differences in the rate of malignancy. The rate of renal cancer was about 1.6 per 10,000 person-years for people without atopic dermatitis or people with mild atopic dermatitis; the rate was about 2.5 per 10,000 people for patients with moderate to severe atopic dermatitis. While the rate of renal cancer was statistically significantly higher in patients with moderate to severe atopic dermatitis (ie, the higher rate was unlikely to be occurring due to chance alone), these patients have very little risk for renal malignancy. The authors' conclusion that regular checkups for renal malignancy are recommended for patients with severe atopic dermatitis seems unnecessary to me.
Do patients follow up on referrals after telehealth visits?
Telehealth has been a boon for modern-day patients, allowing people who might have difficulty accessing in-person appointments to continue seeing their physicians. But how many patients actually follow through on their physician’s recommendations afterward?
A new study suggests that
Investigators retrospectively examined test and referral orders for more than 4,000 patients to see how many complied with recommendations to have a colonoscopy, consult a dermatologist for a suspicious skin lesion, or undergo a cardiac stress test.
Completion of a recommended test or specialty referral was termed “diagnostic loop closure.” In particular, the researchers wanted to compare loop closure after telehealth versus in-person visits.
Rates of loop closure were low across all visit modalities but were lower for tests and referrals ordered during telehealth visits, compared with in-person visits – especially for colonoscopies.
“The take-home message for practicing clinicians is that they should be especially aware of follow-up for tests or referrals ordered during telehealth visits,” said corresponding author Maëlys Amat, MD, MBA, a primary care physician at Healthcare Associates, Beth Israel Deaconess Medical Center, Boston.
The study was published online on in JAMA Network Open.
‘Unintended side effects’
“Diagnostic errors present a huge safety concern, impacting many patient lives and costing the health care system billions of dollars, said Dr. Amat, who is also an instructor at Harvard Medical School.
“Telehealth utilization increased rapidly during the COVID pandemic, and although there are clear benefits to utilizing telehealth, our team sought to investigate unintended side effects of this technology and highlight opportunities for improvement,” she said.
To investigate the question, the researchers reviewed medical records of 4,113 patients, with a mean age of 59 years, at two Boston-based primary care sites: an urban hospital–based primary care practice and an affiliated community health center.
Orders for tests or referrals in both centers were placed electronically through the medical record. During an in-person visit, the patient was handed a form with a phone number to call to schedule the test or referral. Patients with limited English proficiency or complex needs may have received help with the scheduling the referral during check-out.
For telehealth visits, the clinician gave the patient the phone number to call to schedule the test or referral during the visit itself. In all scenarios, patients did not receive communication after the visit reminding them about the referral or test.
A loop was considered “closed” if the orders were completed within 365 days, 90 days, or 45 days for colonoscopy, dermatology visits, or cardiac stress testing, respectively.
Of the tests, 52.4% were ordered during an in-person visit, 27.8% were ordered during a telehealth visit, and 19.7% were ordered without a visit.
Tracking systems, virtual checkout
Fewer than half of the orders (42.6%) placed during a telehealth visit were completed within the designated time frame, compared with 58.4% of the orders placed during an in-person visit and 57.4% placed without a visit.
Patients who had telehealth visits were roughly half as likely as those who had in-person visits to close the loop on high-risk tests and referrals, even in an analysis that adjusted for test type, patient demographic characteristics, comorbidities, clinical site, clinician type, and patient engagement (odds ratio, 0.55; 95% confidence interval, 0.47-0.64).
Only 39.8% of colonoscopy referrals ordered during a telehealth visit were completed during the 365-day time period, compared with 56.9% ordered during an in-person visit and 56.7% ordered without a visit.
Follow-through with dermatology referrals within 90 days was roughly the same across all types of visits (63.1% for telehealth, 61.5% for in-person, and 62.9% for no visit). No significant differences were found between telehealth and in-person visits or orders placed without a visit.
Although patients seen via telehealth were less likely than those seen in person to follow through on cardiac stress tests within the 45-day window (59.1% vs. 63.2%), this difference didn’t reach statistical significance.
“Ideally, clinicians would implement automatic tracking systems to help ensure that an ordered test or referral is completed,” Dr. Amat commented. “However, if these systems aren’t yet in place, we strongly encourage clinicians to create their own work flows for tracking tests to completion.”
Additionally, “clinicians should consider implementing a virtual checkout system, similar to what is done during in-person visits, to help patients better understand recommended next steps,” she continued.
Other potentially helpful ways to improve loop closure include automatic tracking for outstanding tests, interventions such as telephone outreach to patients, automated text and email reminders, and the use of referral managers – especially in remote, rural areas or for “disadvantaged patients with limited health care access and literacy.”
Education is key
Kisha Davis, MD, MPH, member of the board of directors of the American Academy of Family Physicians, said in an interview that being able to see a provider virtually can make the difference between a person receiving or not receiving medical care. She regards telehealth as another tool in the toolkit her practice offers to provide comprehensive health care.
Dr. Davis, a family physician in Gaithersburg, Md., who wasn’t involved with the study, described a patient with hypertension who was an Uber driver. “During the pandemic, Uber rides were down, and he couldn›t afford to pass up any opportunities, so he pulled over to the side of the road after one of his rides, did his telehealth visit, reviewed his medications, and went on to his next ride.”
The key is to make sure that patients receive adequate follow-up from the office, which Dr. Davis arranged for this patient.
She noted that telehealth “is best done if there’s an established physician-patient relationship but harder to accomplish successfully if you’ve only met the patient on telehealth and never in person.”
The study didn’t specify whether the physicians had an established relationship with their patients.
During the checkout process after an in-person appointment, patients often receive a sheet of paper with the follow-up referrals. “I can see where patients are less likely to follow through if they don’t have someone handing them that paper,” she said.
In her practice, patients’ charts are color-coded “to keep track and make sure it’s not just the ‘squeaky wheels’ that get all the attention,” she said. “The onus is on the physician and the practice, in today’s world of value-based care, to make sure that patients who don’t come into the office are getting the care they need.”
This is facilitated by a “system of care coordination” in which the office team – such as a nurse or medical assistant – follows up with patients to see if they’ve “gotten everything done without barriers,” Dr. Davis said. “Did they have trouble filling that prescription? Did they have difficulty with the referral? Or do they not think it’s necessary – for example, a patient might not go to physical therapy because the injury has improved.”
Dr. Davis wasn’t surprised that patients were less likely to close the loop for colonoscopies compared with seeking out a stress test or treatment for skin lesions.
“People who have a skin lesion may be concerned about their appearance or about skin cancer, and people who need a stress test may have had cardiac symptoms or be worried about their heart.” But a routine screening such as a colonoscopy may not mobilize the patient’s concern to the same degree.
“Additionally, a colonoscopy has an ‘ick factor,’ so there aren’t a whole lot of people who are jumping to have the procedure done.” She suggested considering newer FDA-approved stool tests to screen for colon cancer.
Dr. Amat and Dr. Davis both emphasized that educating patients – both during and after the visit – and making sure they understand the importance of their referral for tests or specialists referrals are key to ensuring that they follow through on the recommendations.
The study was funded by the Agency for Healthcare Research and Quality. Dr. Amat was supported by the Arnold Tofias and Leo Condakes Quality Scholarship Program. Dr. Amat declared no relevant financial relationships. Dr. Davis is the chief health officer for Montgomery County in Maryland.
A version of this article first appeared on Medscape.com.
Telehealth has been a boon for modern-day patients, allowing people who might have difficulty accessing in-person appointments to continue seeing their physicians. But how many patients actually follow through on their physician’s recommendations afterward?
A new study suggests that
Investigators retrospectively examined test and referral orders for more than 4,000 patients to see how many complied with recommendations to have a colonoscopy, consult a dermatologist for a suspicious skin lesion, or undergo a cardiac stress test.
Completion of a recommended test or specialty referral was termed “diagnostic loop closure.” In particular, the researchers wanted to compare loop closure after telehealth versus in-person visits.
Rates of loop closure were low across all visit modalities but were lower for tests and referrals ordered during telehealth visits, compared with in-person visits – especially for colonoscopies.
“The take-home message for practicing clinicians is that they should be especially aware of follow-up for tests or referrals ordered during telehealth visits,” said corresponding author Maëlys Amat, MD, MBA, a primary care physician at Healthcare Associates, Beth Israel Deaconess Medical Center, Boston.
The study was published online on in JAMA Network Open.
‘Unintended side effects’
“Diagnostic errors present a huge safety concern, impacting many patient lives and costing the health care system billions of dollars, said Dr. Amat, who is also an instructor at Harvard Medical School.
“Telehealth utilization increased rapidly during the COVID pandemic, and although there are clear benefits to utilizing telehealth, our team sought to investigate unintended side effects of this technology and highlight opportunities for improvement,” she said.
To investigate the question, the researchers reviewed medical records of 4,113 patients, with a mean age of 59 years, at two Boston-based primary care sites: an urban hospital–based primary care practice and an affiliated community health center.
Orders for tests or referrals in both centers were placed electronically through the medical record. During an in-person visit, the patient was handed a form with a phone number to call to schedule the test or referral. Patients with limited English proficiency or complex needs may have received help with the scheduling the referral during check-out.
For telehealth visits, the clinician gave the patient the phone number to call to schedule the test or referral during the visit itself. In all scenarios, patients did not receive communication after the visit reminding them about the referral or test.
A loop was considered “closed” if the orders were completed within 365 days, 90 days, or 45 days for colonoscopy, dermatology visits, or cardiac stress testing, respectively.
Of the tests, 52.4% were ordered during an in-person visit, 27.8% were ordered during a telehealth visit, and 19.7% were ordered without a visit.
Tracking systems, virtual checkout
Fewer than half of the orders (42.6%) placed during a telehealth visit were completed within the designated time frame, compared with 58.4% of the orders placed during an in-person visit and 57.4% placed without a visit.
Patients who had telehealth visits were roughly half as likely as those who had in-person visits to close the loop on high-risk tests and referrals, even in an analysis that adjusted for test type, patient demographic characteristics, comorbidities, clinical site, clinician type, and patient engagement (odds ratio, 0.55; 95% confidence interval, 0.47-0.64).
Only 39.8% of colonoscopy referrals ordered during a telehealth visit were completed during the 365-day time period, compared with 56.9% ordered during an in-person visit and 56.7% ordered without a visit.
Follow-through with dermatology referrals within 90 days was roughly the same across all types of visits (63.1% for telehealth, 61.5% for in-person, and 62.9% for no visit). No significant differences were found between telehealth and in-person visits or orders placed without a visit.
Although patients seen via telehealth were less likely than those seen in person to follow through on cardiac stress tests within the 45-day window (59.1% vs. 63.2%), this difference didn’t reach statistical significance.
“Ideally, clinicians would implement automatic tracking systems to help ensure that an ordered test or referral is completed,” Dr. Amat commented. “However, if these systems aren’t yet in place, we strongly encourage clinicians to create their own work flows for tracking tests to completion.”
Additionally, “clinicians should consider implementing a virtual checkout system, similar to what is done during in-person visits, to help patients better understand recommended next steps,” she continued.
Other potentially helpful ways to improve loop closure include automatic tracking for outstanding tests, interventions such as telephone outreach to patients, automated text and email reminders, and the use of referral managers – especially in remote, rural areas or for “disadvantaged patients with limited health care access and literacy.”
Education is key
Kisha Davis, MD, MPH, member of the board of directors of the American Academy of Family Physicians, said in an interview that being able to see a provider virtually can make the difference between a person receiving or not receiving medical care. She regards telehealth as another tool in the toolkit her practice offers to provide comprehensive health care.
Dr. Davis, a family physician in Gaithersburg, Md., who wasn’t involved with the study, described a patient with hypertension who was an Uber driver. “During the pandemic, Uber rides were down, and he couldn›t afford to pass up any opportunities, so he pulled over to the side of the road after one of his rides, did his telehealth visit, reviewed his medications, and went on to his next ride.”
The key is to make sure that patients receive adequate follow-up from the office, which Dr. Davis arranged for this patient.
She noted that telehealth “is best done if there’s an established physician-patient relationship but harder to accomplish successfully if you’ve only met the patient on telehealth and never in person.”
The study didn’t specify whether the physicians had an established relationship with their patients.
During the checkout process after an in-person appointment, patients often receive a sheet of paper with the follow-up referrals. “I can see where patients are less likely to follow through if they don’t have someone handing them that paper,” she said.
In her practice, patients’ charts are color-coded “to keep track and make sure it’s not just the ‘squeaky wheels’ that get all the attention,” she said. “The onus is on the physician and the practice, in today’s world of value-based care, to make sure that patients who don’t come into the office are getting the care they need.”
This is facilitated by a “system of care coordination” in which the office team – such as a nurse or medical assistant – follows up with patients to see if they’ve “gotten everything done without barriers,” Dr. Davis said. “Did they have trouble filling that prescription? Did they have difficulty with the referral? Or do they not think it’s necessary – for example, a patient might not go to physical therapy because the injury has improved.”
Dr. Davis wasn’t surprised that patients were less likely to close the loop for colonoscopies compared with seeking out a stress test or treatment for skin lesions.
“People who have a skin lesion may be concerned about their appearance or about skin cancer, and people who need a stress test may have had cardiac symptoms or be worried about their heart.” But a routine screening such as a colonoscopy may not mobilize the patient’s concern to the same degree.
“Additionally, a colonoscopy has an ‘ick factor,’ so there aren’t a whole lot of people who are jumping to have the procedure done.” She suggested considering newer FDA-approved stool tests to screen for colon cancer.
Dr. Amat and Dr. Davis both emphasized that educating patients – both during and after the visit – and making sure they understand the importance of their referral for tests or specialists referrals are key to ensuring that they follow through on the recommendations.
The study was funded by the Agency for Healthcare Research and Quality. Dr. Amat was supported by the Arnold Tofias and Leo Condakes Quality Scholarship Program. Dr. Amat declared no relevant financial relationships. Dr. Davis is the chief health officer for Montgomery County in Maryland.
A version of this article first appeared on Medscape.com.
Telehealth has been a boon for modern-day patients, allowing people who might have difficulty accessing in-person appointments to continue seeing their physicians. But how many patients actually follow through on their physician’s recommendations afterward?
A new study suggests that
Investigators retrospectively examined test and referral orders for more than 4,000 patients to see how many complied with recommendations to have a colonoscopy, consult a dermatologist for a suspicious skin lesion, or undergo a cardiac stress test.
Completion of a recommended test or specialty referral was termed “diagnostic loop closure.” In particular, the researchers wanted to compare loop closure after telehealth versus in-person visits.
Rates of loop closure were low across all visit modalities but were lower for tests and referrals ordered during telehealth visits, compared with in-person visits – especially for colonoscopies.
“The take-home message for practicing clinicians is that they should be especially aware of follow-up for tests or referrals ordered during telehealth visits,” said corresponding author Maëlys Amat, MD, MBA, a primary care physician at Healthcare Associates, Beth Israel Deaconess Medical Center, Boston.
The study was published online on in JAMA Network Open.
‘Unintended side effects’
“Diagnostic errors present a huge safety concern, impacting many patient lives and costing the health care system billions of dollars, said Dr. Amat, who is also an instructor at Harvard Medical School.
“Telehealth utilization increased rapidly during the COVID pandemic, and although there are clear benefits to utilizing telehealth, our team sought to investigate unintended side effects of this technology and highlight opportunities for improvement,” she said.
To investigate the question, the researchers reviewed medical records of 4,113 patients, with a mean age of 59 years, at two Boston-based primary care sites: an urban hospital–based primary care practice and an affiliated community health center.
Orders for tests or referrals in both centers were placed electronically through the medical record. During an in-person visit, the patient was handed a form with a phone number to call to schedule the test or referral. Patients with limited English proficiency or complex needs may have received help with the scheduling the referral during check-out.
For telehealth visits, the clinician gave the patient the phone number to call to schedule the test or referral during the visit itself. In all scenarios, patients did not receive communication after the visit reminding them about the referral or test.
A loop was considered “closed” if the orders were completed within 365 days, 90 days, or 45 days for colonoscopy, dermatology visits, or cardiac stress testing, respectively.
Of the tests, 52.4% were ordered during an in-person visit, 27.8% were ordered during a telehealth visit, and 19.7% were ordered without a visit.
Tracking systems, virtual checkout
Fewer than half of the orders (42.6%) placed during a telehealth visit were completed within the designated time frame, compared with 58.4% of the orders placed during an in-person visit and 57.4% placed without a visit.
Patients who had telehealth visits were roughly half as likely as those who had in-person visits to close the loop on high-risk tests and referrals, even in an analysis that adjusted for test type, patient demographic characteristics, comorbidities, clinical site, clinician type, and patient engagement (odds ratio, 0.55; 95% confidence interval, 0.47-0.64).
Only 39.8% of colonoscopy referrals ordered during a telehealth visit were completed during the 365-day time period, compared with 56.9% ordered during an in-person visit and 56.7% ordered without a visit.
Follow-through with dermatology referrals within 90 days was roughly the same across all types of visits (63.1% for telehealth, 61.5% for in-person, and 62.9% for no visit). No significant differences were found between telehealth and in-person visits or orders placed without a visit.
Although patients seen via telehealth were less likely than those seen in person to follow through on cardiac stress tests within the 45-day window (59.1% vs. 63.2%), this difference didn’t reach statistical significance.
“Ideally, clinicians would implement automatic tracking systems to help ensure that an ordered test or referral is completed,” Dr. Amat commented. “However, if these systems aren’t yet in place, we strongly encourage clinicians to create their own work flows for tracking tests to completion.”
Additionally, “clinicians should consider implementing a virtual checkout system, similar to what is done during in-person visits, to help patients better understand recommended next steps,” she continued.
Other potentially helpful ways to improve loop closure include automatic tracking for outstanding tests, interventions such as telephone outreach to patients, automated text and email reminders, and the use of referral managers – especially in remote, rural areas or for “disadvantaged patients with limited health care access and literacy.”
Education is key
Kisha Davis, MD, MPH, member of the board of directors of the American Academy of Family Physicians, said in an interview that being able to see a provider virtually can make the difference between a person receiving or not receiving medical care. She regards telehealth as another tool in the toolkit her practice offers to provide comprehensive health care.
Dr. Davis, a family physician in Gaithersburg, Md., who wasn’t involved with the study, described a patient with hypertension who was an Uber driver. “During the pandemic, Uber rides were down, and he couldn›t afford to pass up any opportunities, so he pulled over to the side of the road after one of his rides, did his telehealth visit, reviewed his medications, and went on to his next ride.”
The key is to make sure that patients receive adequate follow-up from the office, which Dr. Davis arranged for this patient.
She noted that telehealth “is best done if there’s an established physician-patient relationship but harder to accomplish successfully if you’ve only met the patient on telehealth and never in person.”
The study didn’t specify whether the physicians had an established relationship with their patients.
During the checkout process after an in-person appointment, patients often receive a sheet of paper with the follow-up referrals. “I can see where patients are less likely to follow through if they don’t have someone handing them that paper,” she said.
In her practice, patients’ charts are color-coded “to keep track and make sure it’s not just the ‘squeaky wheels’ that get all the attention,” she said. “The onus is on the physician and the practice, in today’s world of value-based care, to make sure that patients who don’t come into the office are getting the care they need.”
This is facilitated by a “system of care coordination” in which the office team – such as a nurse or medical assistant – follows up with patients to see if they’ve “gotten everything done without barriers,” Dr. Davis said. “Did they have trouble filling that prescription? Did they have difficulty with the referral? Or do they not think it’s necessary – for example, a patient might not go to physical therapy because the injury has improved.”
Dr. Davis wasn’t surprised that patients were less likely to close the loop for colonoscopies compared with seeking out a stress test or treatment for skin lesions.
“People who have a skin lesion may be concerned about their appearance or about skin cancer, and people who need a stress test may have had cardiac symptoms or be worried about their heart.” But a routine screening such as a colonoscopy may not mobilize the patient’s concern to the same degree.
“Additionally, a colonoscopy has an ‘ick factor,’ so there aren’t a whole lot of people who are jumping to have the procedure done.” She suggested considering newer FDA-approved stool tests to screen for colon cancer.
Dr. Amat and Dr. Davis both emphasized that educating patients – both during and after the visit – and making sure they understand the importance of their referral for tests or specialists referrals are key to ensuring that they follow through on the recommendations.
The study was funded by the Agency for Healthcare Research and Quality. Dr. Amat was supported by the Arnold Tofias and Leo Condakes Quality Scholarship Program. Dr. Amat declared no relevant financial relationships. Dr. Davis is the chief health officer for Montgomery County in Maryland.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Is most Parkinson’s disease man-made and therefore preventable?
This transcript has been edited for clarity.
Indu Subramanian, MD: It’s my pleasure to have Ray Dorsey on our program today. Ray is a professor of neurology at the University of Rochester and has been doing some amazing advocacy work in largely the space of trying to end Parkinson’s disease.
E. Ray Dorsey, MD: Thanks very much for having me, Indu. I’m delighted to be with you.
Trichloroethylene and PD
Dr. Subramanian: I wanted to first that we talk about as something that is in pretty much everywhere. This paper came out, and you wrote a commentary in JAMA Neurology as well. Perhaps we can summarize the paper and its findings.
Dr. Dorsey: Like most people, I didn’t know what TCE was until about 5 or 6 years ago. TCE is a very simple molecule. It’s got six atoms – two carbon atoms, one hydrogen atom, and three chlorine atoms — hence, its name “trichloroethylene.” There’s a very similar chemical called perchloroethylene, which is widely used in dry cleaning. It’s got one additional chlorine atom, and the prefix “per-” means “four.” I’ll talk about TCE predominantly, but both of these chemicals probably have similar toxicity with respect to Parkinson’s disease.
Research done by Dr. Carlie Tanner and Dr. Sam Goldman about a decade ago showed that in twins who were exposed to this through their work (it’s widely used as a degreasing agent) or hobbies (it’s used in printing and painting, by varnish workers, or by anyone that needs it as a solvent) had a 500% increased risk of developing Parkinson’s disease. Importantly, in that study, they showed that there was a lag time of 10-40 years between exposure to that chemical and the diagnosis of the disease. Because TCE was so widely used, they said that public health implications could be substantial.
What’s Camp Lejeune? Camp Lejeune is a Marine base in North Carolina where many Marines are trained. Between 1953 and 1987 at that Marine base, the drinking water was contaminated with TCE, perchloroethylene, and other toxic chemicals. The reason Camp Lejeune is so infamous is because the Marines knew about the contamination for many years and covered it up.
Indeed, this story only came to the forefront because Jennie Ensminger, the daughter of a Marine drill instructor, developed leukemia at age 6 and died at age 9. Her father, Jerry Ensminger, a retired master sergeant, found out after the fact that these cancer-causing chemicals, including TCE, a known carcinogen, were found at the Marine base and could be an explanation for why his daughter developed and died of leukemia.
Dr. Sam Goldman and Dr. Carlie Tanner and colleagues from UCSF looked at the rates of Parkinson’s among Marines who served at Camp Lejeune during the 1970s and compared that with rates in Marines who served Camp Pendleton on the West Coast. It turned out that the Marines who served at Camp Lejeune had a 70% higher risk of developing Parkinson’s disease than the Marines who served at Camp Pendleton.
Importantly, these Marines, by definition, were healthy. They were young. They were only 20 years old, on average, when they were at Camp Lejeune. They stayed at a Marine base for a short period of time, so on average, they were only there for 2 years. Yet 30 years later, they had a 70% increased risk of developing Parkinson’s disease.
Ending Parkinson’s disease
Dr. Subramanian: Wow, that’s pretty profound. You’ve done a large amount of work, and in fact you, along with some of our colleagues wrote a book about ending Parkinson’s disease. I read that book when it came out a couple of years ago, and I was really struck by a few things. Parkinson’s has doubled in the past 40 years and is going to double again in the next 20 years. Can you tell me a little bit about that statistic and why that is? It’s not just because people are aging. What is the sense of that? How do we interpret that?
Dr. Dorsey: According to the Global Burden of Disease study, which I was fortunate to be part of, the number of people with Parkinson’s disease has more than doubled in the past 25 years. A conservative projection based on aging alone suggests that it’s going to double again unless we change something about it. It’s now the world’s fastest-growing brain disease, and it is growing faster than can be explained by aging alone.
If you look at the map of Parkinson’s disease, if you thought it was purely genetic, you would have a relatively uniform map of rates of Parkinson’s disease. In fact, we don’t see that. Rates of Parkinson’s are five times higher in industrialized parts of the world, like the United States and Canada, than they are in sub-Saharan Africa. Rates of Parkinson’s disease are increasing most rapidly in areas of world that are undergoing the most rapid industrialization, such as India and China, where adjusted for age, the rates of Parkinson’s have more than doubled in the past 25 years.
The thesis of our book is that much of Parkinson’s disease is man-made. Work done by your colleagues at UCLA, including Jeff Bronstein and Beate Ritz, have demonstrated that air pollution and certain pesticides are likely fueling the rise of Parkinson’s disease.
Given that in the United States, rates of Parkinson’s disease are actually higher in urban and suburban areas than they are in rural areas, I think that this dry-cleaning chemical – which was widely used in the 1970s in everything from typewriter correction fluid to decaffeinated coffee and [over] 2 pounds per American [was produced] – could be one of the most important causes or contributing factors to Parkinson’s disease.
What to tell patients
Dr. Subramanian: For the general neurologists or practitioners out there watching this, what can they do? If you have a patient whom you suspect may have been exposed to toxins, what should we tell people who aren’t patients yet who are at risk? What are some things that you think would be helpful?
Dr. Dorsey: I think one of the shortcomings of American medicine is that we often just go from diagnosis to treatment. You’re depressed, you get an antidepressant; you have Parkinson’s disease, you get levodopa; you have seizures, you get put on an antiepileptic medication.
I think we need to spend a couple of minutes at least, maybe at the beginning, to go to the diagnosis of the condition and why you have this disease. If you just do a brief occupational history, after you start the exam – things like finding out what people do for a living or did for a living or how they spend their time – I think you’ll find many of these risk factors are actually present.
It’s pretty easy to identify whether people grew up in a rural area and drank well water, which is prone to be contaminated with pesticides. We know that people who drink [contaminated] well water have about a 75% increased risk of developing Parkinson’s disease. I think you can find for people, especially when they grew up, when they were young, that the most relevant exposure might be that when people were young children.
It’s a little bit harder to identify all exposure to TCE. The Marines at Camp Lejeune didn’t know they were drinking the water that was contaminated with this and only found out about it after the fact because Jerry Ensminger launched a 26-year campaign to bring justice for the Marines and their dependents.
Some people who know that they work with chemicals or with solvents might know about this. In New York City, these chemicals are widely used in dry cleaning. They’re readily volatile. These chemicals can evaporate from dry-cleaning buildings and go into the indoor air of apartments above dry cleaners, for example, in New York City. That can be in toxic levels. These readily dissolve in fat, hence their use in degreasing.
There have been studies, for example, in Germany, that found that supermarkets that are simply near a dry cleaner will have TCE or perchloroethylene in the butter and the cheese that they’re selling.
It gets even worse. For example, you bring your daughter into the dry-cleaning building and she’s eating an ice cream cone. When she leaves, she’s eating perchloroethylene and TCE.
It’s a little bit harder to find it, but I think it’s relevant because some people might be still being exposed and some people might still be drinking well water and they rarely have their well tested. For those people, I recommend they get their well tested and I recommend all my patients to get a carbon filter to decrease exposure to pesticides and chemicals. A carbon filter is just like what Brita and Pure and other brands are.
Because they’re chemicals known to cause cancer, I get a little bit concerned about cancer screening. This is most strongly tied to non-Hodgkin lymphoma, liver cancer, and renal cancer. It’s also linked to multiple myeloma, prostate cancer, probably brain cancer, and probably breast cancer, especially in men.
I tell people to be concerned about those, and then I tell people to avoid pesticides if they have Parkinson’s disease in all its forms, not only in the drinking water but in the produce you buy, the food you eat, what you put on your lawn, what’s on the golf course where you play, and the like.
Dr. Subramanian: I would say, just from the wellness perspective, if people are at risk for degenerative disease in terms of their brain health, things like sleep, mind-body practices, exercise, diet (Mediterranean or organic, if you can), and avoiding pesticides are all important. Social connection is important as well – the things that we think are helpful in general as people age and to prevent Alzheimer’s and other things like that.
Dr. Dorsey: These are fantastic ways to modify disease course. The evidence for them is only increasing. There’s an analogy I like to use. If someone is diagnosed with lung cancer, the first thing we tell them to do is to stop smoking. If someone’s diagnosed with Parkinson’s, we don’t tell them to stop getting exposure to pesticides. We don’t tell them to stop dry cleaning their clothes. We don’t tell them to avoid air pollution. These are all risk factors that are increasingly well established for Parkinson’s disease.
I think Parkinson’s disease, fundamentally for the vast majority of people, is an entirely preventable disease. We’re not taking actions to prevent people from getting this very disabling and very deadly disease.
Advocacy work
Dr. Subramanian: You and I are quite interested in the sense of being advocates as neurologists, and I think it fuels our passion and helps us to wake up every morning feeling like we have something that is meaningful and purposeful in our lives. Could you describe this as your passion and how it may prevent burnout and what it’s given you as a neurologist?
Dr. Dorsey: The credit for much of this is Dr. Carlie Tanner at UC San Francisco. I had the gift of sabbatical and I started reading the literature, I started reading her literature, and I came away with that, over the past 25 years, she detailed these environmental risk factors that are linked to Parkinson’s disease. Pesticides, these dry-cleaning chemicals, and air pollution. When I read it, I just realized that this was the case.
The same time I was reading her work, I read this book called “How to Survive a Plague,” by David France, who was a member of a group called Act Up, which was a group of men in New York City who reacted to the emergence of HIV in the 1980s. If you remember the 1980s, there was no federal response to HIV. People were blamed for the diseases that they were developing. It was only because brave men and women in New York City and in San Francisco banded together and organized that they changed the course of HIV.
They didn’t just do it for themselves. They did it for all of us. You and I and many people may not have HIV because of their courage. They made HIV a treatable condition. It’s actually more treatable than Parkinson’s disease. It’s associated with a near-normal life expectancy. They also made it a preventable disease. Thousands, if not millions, of us don’t have HIV because of their work. It’s an increasingly less common disease. Rates of HIV are actually decreasing, which is something that you or I would never have expected when we were in medical training.
I can’t think of a better outcome for a neurologist or any physician than to make the diseases that they’re caring for nonexistent ... than if we lived in a world that didn’t have HIV, we lived in a world where lung cancer largely didn’t exist. We’ve had worlds in the past where Parkinson’s probably didn’t exist or existed in extremely small numbers. That might be true for diffuse Lewy body disease and others, and if these diseases are preventable, we can take actions as individuals and as a society to lower our risk.
What a wonderful gift for future generations and many generations to come, hopefully, to live in a world that’s largely devoid of Parkinson’s disease. Just like we live in a world free of typhus. We live in a world free of smallpox. We live in a world where polio is extraordinarily uncommon. We don’t even have treatments for polio because we just don’t have polio. I think we can do the same thing for Parkinson’s disease for the vast majority.
Dr. Subramanian: Thank you so much, Ray, for your advocacy. We’re getting to the point in neurology, which is exciting to me, of possibly primary prevention of some of these disorders. I think we have a role in that, which is exciting for the future.
Dr. Dorsey: Absolutely.
Dr. Subramanian is clinical professor, department of neurology, University of California Los Angeles, and director of PADRECC (Parkinson’s Disease Research, Education, and Clinical Centers), West Los Angeles Veterans Association, Los Angeles. She disclosed ties with Acorda Pharma. Dr. Dorsey is the David M. Levy Professor of Neurology, University of Rochester (N.Y.). He disclosed ties to Abbott, AbbVie, Acadia, Acorda Therapeutics, Averitas Pharma, Biogen, BioSensics, Boehringer Ingelheim, Burroughs Wellcome Fund, Caraway Therapeutics, CuraSen, DConsult2, Denali Therapeutics, Eli Lilly, Genentech, Health & Wellness Partners, HMP Education, Included Health, Karger, KOL Groups, Life Sciences, Mediflix, Medrhythms, Merck; MJH Holdings, North American Center for Continuing Medical Education, Novartis, Otsuka, Pfizer, Photopharmics, Praxis Medicine, Roche, Safra Foundation, Sanofi, Seelos Therapeutics, SemCap, Spark Therapeutics, Springer Healthcare, Synapticure, Theravance Biopharmaceuticals, and WebMD.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Indu Subramanian, MD: It’s my pleasure to have Ray Dorsey on our program today. Ray is a professor of neurology at the University of Rochester and has been doing some amazing advocacy work in largely the space of trying to end Parkinson’s disease.
E. Ray Dorsey, MD: Thanks very much for having me, Indu. I’m delighted to be with you.
Trichloroethylene and PD
Dr. Subramanian: I wanted to first that we talk about as something that is in pretty much everywhere. This paper came out, and you wrote a commentary in JAMA Neurology as well. Perhaps we can summarize the paper and its findings.
Dr. Dorsey: Like most people, I didn’t know what TCE was until about 5 or 6 years ago. TCE is a very simple molecule. It’s got six atoms – two carbon atoms, one hydrogen atom, and three chlorine atoms — hence, its name “trichloroethylene.” There’s a very similar chemical called perchloroethylene, which is widely used in dry cleaning. It’s got one additional chlorine atom, and the prefix “per-” means “four.” I’ll talk about TCE predominantly, but both of these chemicals probably have similar toxicity with respect to Parkinson’s disease.
Research done by Dr. Carlie Tanner and Dr. Sam Goldman about a decade ago showed that in twins who were exposed to this through their work (it’s widely used as a degreasing agent) or hobbies (it’s used in printing and painting, by varnish workers, or by anyone that needs it as a solvent) had a 500% increased risk of developing Parkinson’s disease. Importantly, in that study, they showed that there was a lag time of 10-40 years between exposure to that chemical and the diagnosis of the disease. Because TCE was so widely used, they said that public health implications could be substantial.
What’s Camp Lejeune? Camp Lejeune is a Marine base in North Carolina where many Marines are trained. Between 1953 and 1987 at that Marine base, the drinking water was contaminated with TCE, perchloroethylene, and other toxic chemicals. The reason Camp Lejeune is so infamous is because the Marines knew about the contamination for many years and covered it up.
Indeed, this story only came to the forefront because Jennie Ensminger, the daughter of a Marine drill instructor, developed leukemia at age 6 and died at age 9. Her father, Jerry Ensminger, a retired master sergeant, found out after the fact that these cancer-causing chemicals, including TCE, a known carcinogen, were found at the Marine base and could be an explanation for why his daughter developed and died of leukemia.
Dr. Sam Goldman and Dr. Carlie Tanner and colleagues from UCSF looked at the rates of Parkinson’s among Marines who served at Camp Lejeune during the 1970s and compared that with rates in Marines who served Camp Pendleton on the West Coast. It turned out that the Marines who served at Camp Lejeune had a 70% higher risk of developing Parkinson’s disease than the Marines who served at Camp Pendleton.
Importantly, these Marines, by definition, were healthy. They were young. They were only 20 years old, on average, when they were at Camp Lejeune. They stayed at a Marine base for a short period of time, so on average, they were only there for 2 years. Yet 30 years later, they had a 70% increased risk of developing Parkinson’s disease.
Ending Parkinson’s disease
Dr. Subramanian: Wow, that’s pretty profound. You’ve done a large amount of work, and in fact you, along with some of our colleagues wrote a book about ending Parkinson’s disease. I read that book when it came out a couple of years ago, and I was really struck by a few things. Parkinson’s has doubled in the past 40 years and is going to double again in the next 20 years. Can you tell me a little bit about that statistic and why that is? It’s not just because people are aging. What is the sense of that? How do we interpret that?
Dr. Dorsey: According to the Global Burden of Disease study, which I was fortunate to be part of, the number of people with Parkinson’s disease has more than doubled in the past 25 years. A conservative projection based on aging alone suggests that it’s going to double again unless we change something about it. It’s now the world’s fastest-growing brain disease, and it is growing faster than can be explained by aging alone.
If you look at the map of Parkinson’s disease, if you thought it was purely genetic, you would have a relatively uniform map of rates of Parkinson’s disease. In fact, we don’t see that. Rates of Parkinson’s are five times higher in industrialized parts of the world, like the United States and Canada, than they are in sub-Saharan Africa. Rates of Parkinson’s disease are increasing most rapidly in areas of world that are undergoing the most rapid industrialization, such as India and China, where adjusted for age, the rates of Parkinson’s have more than doubled in the past 25 years.
The thesis of our book is that much of Parkinson’s disease is man-made. Work done by your colleagues at UCLA, including Jeff Bronstein and Beate Ritz, have demonstrated that air pollution and certain pesticides are likely fueling the rise of Parkinson’s disease.
Given that in the United States, rates of Parkinson’s disease are actually higher in urban and suburban areas than they are in rural areas, I think that this dry-cleaning chemical – which was widely used in the 1970s in everything from typewriter correction fluid to decaffeinated coffee and [over] 2 pounds per American [was produced] – could be one of the most important causes or contributing factors to Parkinson’s disease.
What to tell patients
Dr. Subramanian: For the general neurologists or practitioners out there watching this, what can they do? If you have a patient whom you suspect may have been exposed to toxins, what should we tell people who aren’t patients yet who are at risk? What are some things that you think would be helpful?
Dr. Dorsey: I think one of the shortcomings of American medicine is that we often just go from diagnosis to treatment. You’re depressed, you get an antidepressant; you have Parkinson’s disease, you get levodopa; you have seizures, you get put on an antiepileptic medication.
I think we need to spend a couple of minutes at least, maybe at the beginning, to go to the diagnosis of the condition and why you have this disease. If you just do a brief occupational history, after you start the exam – things like finding out what people do for a living or did for a living or how they spend their time – I think you’ll find many of these risk factors are actually present.
It’s pretty easy to identify whether people grew up in a rural area and drank well water, which is prone to be contaminated with pesticides. We know that people who drink [contaminated] well water have about a 75% increased risk of developing Parkinson’s disease. I think you can find for people, especially when they grew up, when they were young, that the most relevant exposure might be that when people were young children.
It’s a little bit harder to identify all exposure to TCE. The Marines at Camp Lejeune didn’t know they were drinking the water that was contaminated with this and only found out about it after the fact because Jerry Ensminger launched a 26-year campaign to bring justice for the Marines and their dependents.
Some people who know that they work with chemicals or with solvents might know about this. In New York City, these chemicals are widely used in dry cleaning. They’re readily volatile. These chemicals can evaporate from dry-cleaning buildings and go into the indoor air of apartments above dry cleaners, for example, in New York City. That can be in toxic levels. These readily dissolve in fat, hence their use in degreasing.
There have been studies, for example, in Germany, that found that supermarkets that are simply near a dry cleaner will have TCE or perchloroethylene in the butter and the cheese that they’re selling.
It gets even worse. For example, you bring your daughter into the dry-cleaning building and she’s eating an ice cream cone. When she leaves, she’s eating perchloroethylene and TCE.
It’s a little bit harder to find it, but I think it’s relevant because some people might be still being exposed and some people might still be drinking well water and they rarely have their well tested. For those people, I recommend they get their well tested and I recommend all my patients to get a carbon filter to decrease exposure to pesticides and chemicals. A carbon filter is just like what Brita and Pure and other brands are.
Because they’re chemicals known to cause cancer, I get a little bit concerned about cancer screening. This is most strongly tied to non-Hodgkin lymphoma, liver cancer, and renal cancer. It’s also linked to multiple myeloma, prostate cancer, probably brain cancer, and probably breast cancer, especially in men.
I tell people to be concerned about those, and then I tell people to avoid pesticides if they have Parkinson’s disease in all its forms, not only in the drinking water but in the produce you buy, the food you eat, what you put on your lawn, what’s on the golf course where you play, and the like.
Dr. Subramanian: I would say, just from the wellness perspective, if people are at risk for degenerative disease in terms of their brain health, things like sleep, mind-body practices, exercise, diet (Mediterranean or organic, if you can), and avoiding pesticides are all important. Social connection is important as well – the things that we think are helpful in general as people age and to prevent Alzheimer’s and other things like that.
Dr. Dorsey: These are fantastic ways to modify disease course. The evidence for them is only increasing. There’s an analogy I like to use. If someone is diagnosed with lung cancer, the first thing we tell them to do is to stop smoking. If someone’s diagnosed with Parkinson’s, we don’t tell them to stop getting exposure to pesticides. We don’t tell them to stop dry cleaning their clothes. We don’t tell them to avoid air pollution. These are all risk factors that are increasingly well established for Parkinson’s disease.
I think Parkinson’s disease, fundamentally for the vast majority of people, is an entirely preventable disease. We’re not taking actions to prevent people from getting this very disabling and very deadly disease.
Advocacy work
Dr. Subramanian: You and I are quite interested in the sense of being advocates as neurologists, and I think it fuels our passion and helps us to wake up every morning feeling like we have something that is meaningful and purposeful in our lives. Could you describe this as your passion and how it may prevent burnout and what it’s given you as a neurologist?
Dr. Dorsey: The credit for much of this is Dr. Carlie Tanner at UC San Francisco. I had the gift of sabbatical and I started reading the literature, I started reading her literature, and I came away with that, over the past 25 years, she detailed these environmental risk factors that are linked to Parkinson’s disease. Pesticides, these dry-cleaning chemicals, and air pollution. When I read it, I just realized that this was the case.
The same time I was reading her work, I read this book called “How to Survive a Plague,” by David France, who was a member of a group called Act Up, which was a group of men in New York City who reacted to the emergence of HIV in the 1980s. If you remember the 1980s, there was no federal response to HIV. People were blamed for the diseases that they were developing. It was only because brave men and women in New York City and in San Francisco banded together and organized that they changed the course of HIV.
They didn’t just do it for themselves. They did it for all of us. You and I and many people may not have HIV because of their courage. They made HIV a treatable condition. It’s actually more treatable than Parkinson’s disease. It’s associated with a near-normal life expectancy. They also made it a preventable disease. Thousands, if not millions, of us don’t have HIV because of their work. It’s an increasingly less common disease. Rates of HIV are actually decreasing, which is something that you or I would never have expected when we were in medical training.
I can’t think of a better outcome for a neurologist or any physician than to make the diseases that they’re caring for nonexistent ... than if we lived in a world that didn’t have HIV, we lived in a world where lung cancer largely didn’t exist. We’ve had worlds in the past where Parkinson’s probably didn’t exist or existed in extremely small numbers. That might be true for diffuse Lewy body disease and others, and if these diseases are preventable, we can take actions as individuals and as a society to lower our risk.
What a wonderful gift for future generations and many generations to come, hopefully, to live in a world that’s largely devoid of Parkinson’s disease. Just like we live in a world free of typhus. We live in a world free of smallpox. We live in a world where polio is extraordinarily uncommon. We don’t even have treatments for polio because we just don’t have polio. I think we can do the same thing for Parkinson’s disease for the vast majority.
Dr. Subramanian: Thank you so much, Ray, for your advocacy. We’re getting to the point in neurology, which is exciting to me, of possibly primary prevention of some of these disorders. I think we have a role in that, which is exciting for the future.
Dr. Dorsey: Absolutely.
Dr. Subramanian is clinical professor, department of neurology, University of California Los Angeles, and director of PADRECC (Parkinson’s Disease Research, Education, and Clinical Centers), West Los Angeles Veterans Association, Los Angeles. She disclosed ties with Acorda Pharma. Dr. Dorsey is the David M. Levy Professor of Neurology, University of Rochester (N.Y.). He disclosed ties to Abbott, AbbVie, Acadia, Acorda Therapeutics, Averitas Pharma, Biogen, BioSensics, Boehringer Ingelheim, Burroughs Wellcome Fund, Caraway Therapeutics, CuraSen, DConsult2, Denali Therapeutics, Eli Lilly, Genentech, Health & Wellness Partners, HMP Education, Included Health, Karger, KOL Groups, Life Sciences, Mediflix, Medrhythms, Merck; MJH Holdings, North American Center for Continuing Medical Education, Novartis, Otsuka, Pfizer, Photopharmics, Praxis Medicine, Roche, Safra Foundation, Sanofi, Seelos Therapeutics, SemCap, Spark Therapeutics, Springer Healthcare, Synapticure, Theravance Biopharmaceuticals, and WebMD.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Indu Subramanian, MD: It’s my pleasure to have Ray Dorsey on our program today. Ray is a professor of neurology at the University of Rochester and has been doing some amazing advocacy work in largely the space of trying to end Parkinson’s disease.
E. Ray Dorsey, MD: Thanks very much for having me, Indu. I’m delighted to be with you.
Trichloroethylene and PD
Dr. Subramanian: I wanted to first that we talk about as something that is in pretty much everywhere. This paper came out, and you wrote a commentary in JAMA Neurology as well. Perhaps we can summarize the paper and its findings.
Dr. Dorsey: Like most people, I didn’t know what TCE was until about 5 or 6 years ago. TCE is a very simple molecule. It’s got six atoms – two carbon atoms, one hydrogen atom, and three chlorine atoms — hence, its name “trichloroethylene.” There’s a very similar chemical called perchloroethylene, which is widely used in dry cleaning. It’s got one additional chlorine atom, and the prefix “per-” means “four.” I’ll talk about TCE predominantly, but both of these chemicals probably have similar toxicity with respect to Parkinson’s disease.
Research done by Dr. Carlie Tanner and Dr. Sam Goldman about a decade ago showed that in twins who were exposed to this through their work (it’s widely used as a degreasing agent) or hobbies (it’s used in printing and painting, by varnish workers, or by anyone that needs it as a solvent) had a 500% increased risk of developing Parkinson’s disease. Importantly, in that study, they showed that there was a lag time of 10-40 years between exposure to that chemical and the diagnosis of the disease. Because TCE was so widely used, they said that public health implications could be substantial.
What’s Camp Lejeune? Camp Lejeune is a Marine base in North Carolina where many Marines are trained. Between 1953 and 1987 at that Marine base, the drinking water was contaminated with TCE, perchloroethylene, and other toxic chemicals. The reason Camp Lejeune is so infamous is because the Marines knew about the contamination for many years and covered it up.
Indeed, this story only came to the forefront because Jennie Ensminger, the daughter of a Marine drill instructor, developed leukemia at age 6 and died at age 9. Her father, Jerry Ensminger, a retired master sergeant, found out after the fact that these cancer-causing chemicals, including TCE, a known carcinogen, were found at the Marine base and could be an explanation for why his daughter developed and died of leukemia.
Dr. Sam Goldman and Dr. Carlie Tanner and colleagues from UCSF looked at the rates of Parkinson’s among Marines who served at Camp Lejeune during the 1970s and compared that with rates in Marines who served Camp Pendleton on the West Coast. It turned out that the Marines who served at Camp Lejeune had a 70% higher risk of developing Parkinson’s disease than the Marines who served at Camp Pendleton.
Importantly, these Marines, by definition, were healthy. They were young. They were only 20 years old, on average, when they were at Camp Lejeune. They stayed at a Marine base for a short period of time, so on average, they were only there for 2 years. Yet 30 years later, they had a 70% increased risk of developing Parkinson’s disease.
Ending Parkinson’s disease
Dr. Subramanian: Wow, that’s pretty profound. You’ve done a large amount of work, and in fact you, along with some of our colleagues wrote a book about ending Parkinson’s disease. I read that book when it came out a couple of years ago, and I was really struck by a few things. Parkinson’s has doubled in the past 40 years and is going to double again in the next 20 years. Can you tell me a little bit about that statistic and why that is? It’s not just because people are aging. What is the sense of that? How do we interpret that?
Dr. Dorsey: According to the Global Burden of Disease study, which I was fortunate to be part of, the number of people with Parkinson’s disease has more than doubled in the past 25 years. A conservative projection based on aging alone suggests that it’s going to double again unless we change something about it. It’s now the world’s fastest-growing brain disease, and it is growing faster than can be explained by aging alone.
If you look at the map of Parkinson’s disease, if you thought it was purely genetic, you would have a relatively uniform map of rates of Parkinson’s disease. In fact, we don’t see that. Rates of Parkinson’s are five times higher in industrialized parts of the world, like the United States and Canada, than they are in sub-Saharan Africa. Rates of Parkinson’s disease are increasing most rapidly in areas of world that are undergoing the most rapid industrialization, such as India and China, where adjusted for age, the rates of Parkinson’s have more than doubled in the past 25 years.
The thesis of our book is that much of Parkinson’s disease is man-made. Work done by your colleagues at UCLA, including Jeff Bronstein and Beate Ritz, have demonstrated that air pollution and certain pesticides are likely fueling the rise of Parkinson’s disease.
Given that in the United States, rates of Parkinson’s disease are actually higher in urban and suburban areas than they are in rural areas, I think that this dry-cleaning chemical – which was widely used in the 1970s in everything from typewriter correction fluid to decaffeinated coffee and [over] 2 pounds per American [was produced] – could be one of the most important causes or contributing factors to Parkinson’s disease.
What to tell patients
Dr. Subramanian: For the general neurologists or practitioners out there watching this, what can they do? If you have a patient whom you suspect may have been exposed to toxins, what should we tell people who aren’t patients yet who are at risk? What are some things that you think would be helpful?
Dr. Dorsey: I think one of the shortcomings of American medicine is that we often just go from diagnosis to treatment. You’re depressed, you get an antidepressant; you have Parkinson’s disease, you get levodopa; you have seizures, you get put on an antiepileptic medication.
I think we need to spend a couple of minutes at least, maybe at the beginning, to go to the diagnosis of the condition and why you have this disease. If you just do a brief occupational history, after you start the exam – things like finding out what people do for a living or did for a living or how they spend their time – I think you’ll find many of these risk factors are actually present.
It’s pretty easy to identify whether people grew up in a rural area and drank well water, which is prone to be contaminated with pesticides. We know that people who drink [contaminated] well water have about a 75% increased risk of developing Parkinson’s disease. I think you can find for people, especially when they grew up, when they were young, that the most relevant exposure might be that when people were young children.
It’s a little bit harder to identify all exposure to TCE. The Marines at Camp Lejeune didn’t know they were drinking the water that was contaminated with this and only found out about it after the fact because Jerry Ensminger launched a 26-year campaign to bring justice for the Marines and their dependents.
Some people who know that they work with chemicals or with solvents might know about this. In New York City, these chemicals are widely used in dry cleaning. They’re readily volatile. These chemicals can evaporate from dry-cleaning buildings and go into the indoor air of apartments above dry cleaners, for example, in New York City. That can be in toxic levels. These readily dissolve in fat, hence their use in degreasing.
There have been studies, for example, in Germany, that found that supermarkets that are simply near a dry cleaner will have TCE or perchloroethylene in the butter and the cheese that they’re selling.
It gets even worse. For example, you bring your daughter into the dry-cleaning building and she’s eating an ice cream cone. When she leaves, she’s eating perchloroethylene and TCE.
It’s a little bit harder to find it, but I think it’s relevant because some people might be still being exposed and some people might still be drinking well water and they rarely have their well tested. For those people, I recommend they get their well tested and I recommend all my patients to get a carbon filter to decrease exposure to pesticides and chemicals. A carbon filter is just like what Brita and Pure and other brands are.
Because they’re chemicals known to cause cancer, I get a little bit concerned about cancer screening. This is most strongly tied to non-Hodgkin lymphoma, liver cancer, and renal cancer. It’s also linked to multiple myeloma, prostate cancer, probably brain cancer, and probably breast cancer, especially in men.
I tell people to be concerned about those, and then I tell people to avoid pesticides if they have Parkinson’s disease in all its forms, not only in the drinking water but in the produce you buy, the food you eat, what you put on your lawn, what’s on the golf course where you play, and the like.
Dr. Subramanian: I would say, just from the wellness perspective, if people are at risk for degenerative disease in terms of their brain health, things like sleep, mind-body practices, exercise, diet (Mediterranean or organic, if you can), and avoiding pesticides are all important. Social connection is important as well – the things that we think are helpful in general as people age and to prevent Alzheimer’s and other things like that.
Dr. Dorsey: These are fantastic ways to modify disease course. The evidence for them is only increasing. There’s an analogy I like to use. If someone is diagnosed with lung cancer, the first thing we tell them to do is to stop smoking. If someone’s diagnosed with Parkinson’s, we don’t tell them to stop getting exposure to pesticides. We don’t tell them to stop dry cleaning their clothes. We don’t tell them to avoid air pollution. These are all risk factors that are increasingly well established for Parkinson’s disease.
I think Parkinson’s disease, fundamentally for the vast majority of people, is an entirely preventable disease. We’re not taking actions to prevent people from getting this very disabling and very deadly disease.
Advocacy work
Dr. Subramanian: You and I are quite interested in the sense of being advocates as neurologists, and I think it fuels our passion and helps us to wake up every morning feeling like we have something that is meaningful and purposeful in our lives. Could you describe this as your passion and how it may prevent burnout and what it’s given you as a neurologist?
Dr. Dorsey: The credit for much of this is Dr. Carlie Tanner at UC San Francisco. I had the gift of sabbatical and I started reading the literature, I started reading her literature, and I came away with that, over the past 25 years, she detailed these environmental risk factors that are linked to Parkinson’s disease. Pesticides, these dry-cleaning chemicals, and air pollution. When I read it, I just realized that this was the case.
The same time I was reading her work, I read this book called “How to Survive a Plague,” by David France, who was a member of a group called Act Up, which was a group of men in New York City who reacted to the emergence of HIV in the 1980s. If you remember the 1980s, there was no federal response to HIV. People were blamed for the diseases that they were developing. It was only because brave men and women in New York City and in San Francisco banded together and organized that they changed the course of HIV.
They didn’t just do it for themselves. They did it for all of us. You and I and many people may not have HIV because of their courage. They made HIV a treatable condition. It’s actually more treatable than Parkinson’s disease. It’s associated with a near-normal life expectancy. They also made it a preventable disease. Thousands, if not millions, of us don’t have HIV because of their work. It’s an increasingly less common disease. Rates of HIV are actually decreasing, which is something that you or I would never have expected when we were in medical training.
I can’t think of a better outcome for a neurologist or any physician than to make the diseases that they’re caring for nonexistent ... than if we lived in a world that didn’t have HIV, we lived in a world where lung cancer largely didn’t exist. We’ve had worlds in the past where Parkinson’s probably didn’t exist or existed in extremely small numbers. That might be true for diffuse Lewy body disease and others, and if these diseases are preventable, we can take actions as individuals and as a society to lower our risk.
What a wonderful gift for future generations and many generations to come, hopefully, to live in a world that’s largely devoid of Parkinson’s disease. Just like we live in a world free of typhus. We live in a world free of smallpox. We live in a world where polio is extraordinarily uncommon. We don’t even have treatments for polio because we just don’t have polio. I think we can do the same thing for Parkinson’s disease for the vast majority.
Dr. Subramanian: Thank you so much, Ray, for your advocacy. We’re getting to the point in neurology, which is exciting to me, of possibly primary prevention of some of these disorders. I think we have a role in that, which is exciting for the future.
Dr. Dorsey: Absolutely.
Dr. Subramanian is clinical professor, department of neurology, University of California Los Angeles, and director of PADRECC (Parkinson’s Disease Research, Education, and Clinical Centers), West Los Angeles Veterans Association, Los Angeles. She disclosed ties with Acorda Pharma. Dr. Dorsey is the David M. Levy Professor of Neurology, University of Rochester (N.Y.). He disclosed ties to Abbott, AbbVie, Acadia, Acorda Therapeutics, Averitas Pharma, Biogen, BioSensics, Boehringer Ingelheim, Burroughs Wellcome Fund, Caraway Therapeutics, CuraSen, DConsult2, Denali Therapeutics, Eli Lilly, Genentech, Health & Wellness Partners, HMP Education, Included Health, Karger, KOL Groups, Life Sciences, Mediflix, Medrhythms, Merck; MJH Holdings, North American Center for Continuing Medical Education, Novartis, Otsuka, Pfizer, Photopharmics, Praxis Medicine, Roche, Safra Foundation, Sanofi, Seelos Therapeutics, SemCap, Spark Therapeutics, Springer Healthcare, Synapticure, Theravance Biopharmaceuticals, and WebMD.
A version of this article appeared on Medscape.com.
What to tell your patients about anti-amyloids for Alzheimer’s disease
Recorded October 13, 2023. This transcript has been edited for clarity.
Kathrin LaFaver, MD: I’ll be talking today with Dr. Meredith Wicklund, senior associate consultant and behavioral neurologist specialist at Mayo Clinic in Arizona. Welcome, Meredith.
Meredith Wicklund, MD: Thank you.
Lecanemab data
Dr. LaFaver: I’m very excited about our topic. Could you give us a brief overview of why there has been so much research interest in this topic of anti-amyloid antibodies?
Dr. Wicklund: The pathologic component of what defines something as Alzheimer’s disease is, by definition, presence of amyloid plaques and tau tangles. When it was first discovered in the 1980s that the component of the plaques was actually the amyloid protein – beta amyloid specifically – interest went right from there to developing therapies to directly target the pathology that is Alzheimer’s disease.
Dr. LaFaver: Lecanemab is the first FDA-approved disease-modifying antibody in that realm. Could you review the study data, especially as it applies to both of us in daily neurology clinic?
Dr. Wicklund: The study data from a phase 3 trial did show, for the primary outcome, that there was a 27% slowing of decline compared with individuals on placebo. It’s important to point out that this was slowing of decline. It was not stabilizing decline. It was not improving decline.
I think it’s important that we inform our patients that really, even with this therapy, there’s no prospect of stabilizing or restoring cognition or function. We do progress at a slower rate compared with individuals not on this treatment, which, given that this medication is for individuals in mild disease who have relatively preserved functional status, that can be potentially very meaningful to families.
The overall benefit was small. It essentially amounts to half a point on an 18-point scale, which is statistically significant. How much clinical meaningfulness that actually leads to is unclear. Finding clinical meaningfulness cannot be defined by a particular test. It really can only be defined on the individual level, what is meaningful to them.
Recommended tests
Dr. LaFaver: It is my understanding that, to qualify for lecanemab use, one needs to have a biomarker-supported diagnosis of Alzheimer’s disease, either via an amyloid PET scan or CSF biomarkers. What would your recommendation be for a neurologist in practice to go about these requirements?
Dr. Wicklund: Since this medication is directly targeting the amyloid pathology, and it does convey a potential risk, we want to make sure that the actual pathology is present in the individuals before we treat them and potentially expose them to risk. The best way of doing that is through either an amyloid PET scan or spinal fluid testing of beta amyloid and tau.
There are several plasma-based biomarkers in development. However, I would avoid using those currently. There are still many unknowns in terms of what exactly is the right species of tau that we should be looking at, the right mechanism of the lab test, how minority status may influence it, and how different comorbidities may influence it.
I would recommend, at this time, sticking with amyloid PET or CSF testing. Given that amyloid PET is not widely available in many community practices, generally only available at academic centers, and is quite costly, many insurances do not cover it – although Medicare has a proposal to potentially start covering it – I generally go with spinal fluid testing, which is more widely available. There are several labs across the country that can process that testing in a reliable way.
Amyloid-related imaging abnormalities
Dr. LaFaver: That’s very helpful to know. There’s been a large amount of buzz just these past couple of weeks about the blood biomarker coming up. I think, as you point out, this wasn’t the marker used in the clinical studies and there are still unknowns. Maybe it’s not quite time for clinical use, unfortunately.
We also have learned that there are significant potential risks involved. One issue that’s really been a focus is ARIA – amyloid-related imaging abnormalities. Could you speak a bit about that and requirements for monitoring?
Dr. Wicklund: ARIA essentially amounts to either vasogenic edema, microhemorrhages, or superficial siderosis that develops as a result of treatment. It relates to activation of the immune system with these passive monoclonal antibodies that’s going to occur with targeting against the plaques. In the parenchyma, it will cause edema. If you have amyloid in the walls of the blood vessels, it can cause microhemorrhages.
While the term “ARIA” implies an imaging-related abnormality, and it largely is purely an imaging finding, it’s not solely an imaging-related finding. It can cause symptoms, including very serious symptoms.
Overall, with lecanemab, the incidence of ARIA within the treatment group in the phase 3 study, combined between both ARIA-E (edema/effusion) and ARIA-H (hemorrhage), was 21.5%, with about 17% being ARIA-H and about 12.5% being ARIA-E. Of course, they can occur at the same time.
Overall, in terms of people in the clinical trials, for most it was purely an imaging-related finding. About 3% developed symptomatic ARIA. Some of those were very serious symptoms, including things like seizures and need to be hospitalized. A couple of deaths have been attributed to ARIA as well.
Patients on anticoagulation
Dr. LaFaver: Along those lines, any additional words to say for people who might be on anticoagulation or might require medications for a stroke, for example?
Dr. Wicklund: While individuals on anticoagulation were allowed in the clinical trials, the current, published appropriate-use guideline is recommending against its use, as several of the serious adverse effects, including the deaths, were for the most part attributed to anticoagulation use.
When it comes to acute stroke treatment, one must carefully consider use of tPA, as two of the three deaths were tPA associated in the clinical trials. It shouldn’t necessarily be an absolute contraindication, but it can make the clinical picture very muddy. If an individual is on lecanemab and comes to the ER with acute stroke-like symptoms, it’s more likely that they’re going to be having an ARIA side effect rather than an acute stroke.
A general recommendation would be to obtain an acute head CT with a CTA, and if there is a large vessel occlusion, proceed to thrombectomy. However, if there isn’t a large vessel occlusion, if you have the ability to get a rapid MRI with diffusion-weighted imaging to screen for acute stroke changes or tissue flair with acute edema changes suggestive of ARIA, that would be preferred before proceeding with thrombolysis. These are all relative contraindications and are going to depend on what’s available near you.
Donanemab approval pending
Dr. LaFaver: This will be an issue because the population we’re talking about is definitely at risk for stroke as well as Alzheimer’s disease. Where do you see this field going as far as amyloid antibody therapy is concerned, with another agent, donanemab, possibly getting FDA approval later this year as well?
Dr. Wicklund: We’re anticipating that donanemab will get FDA approval in the next coming months. Donanemab also targets the amyloid in the brain, although lecanemab and donanemab target different aspects of the production of the amyloid plaque. They were both shown to have roughly equal efficacy in their phase 3 clinical trials. Donanemab has the benefit of being a once-monthly infusion as opposed to twice-monthly infusions with lecanemab. It does have a slightly higher risk for ARIA compared with lecanemab.
Those are just some things to take into consideration when talking with your patients. In terms of where we’re going from here, we’re moving even earlier in terms of disease state. The lecanemab and donanemab phase 3 trials were done in individuals with mild cognitive impairment or mild dementia due to Alzheimer’s disease. They should not be used in individuals with moderate or more advanced Alzheimer’s disease.
There are ongoing, large, national, multicenter clinical trials of both lecanemab and donanemab in a preclinical state of Alzheimer’s disease. These individuals have evidence of amyloidosis, either through PET imaging or through CSF, but are clinically asymptomatic and do not yet have any signs of cognitive impairment or functional decline. We look forward to those results in the next few years. Hopefully, they’ll be able to show even greater benefit when moving into these early disease states in terms of delaying or even preventing cognitive decline.
Dr. LaFaver: That’s definitely very interesting to hear about. Where can people go for more information?
Dr. Wicklund: There’s a guideline on the use of lecanemab through the American Academy of Neurology. I encourage you to look at that. Also, look at the appropriate-use recommendations that were published this year in The Journal of Prevention of Alzheimer’s Disease.
Dr. LaFaver: Wonderful. With that being said, thank you so much for talking to me. I learned a lot. Thanks, everyone, for listening.
Dr. LaFaver is a neurologist at Saratoga Hospital Medical Group, Saratoga Springs, N.Y. She disclosed having no relevant financial relationships. Dr. Wicklund is senior associate consultant in the department of Neurology at Mayo Clinic, Phoenix, Ariz. She disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Recorded October 13, 2023. This transcript has been edited for clarity.
Kathrin LaFaver, MD: I’ll be talking today with Dr. Meredith Wicklund, senior associate consultant and behavioral neurologist specialist at Mayo Clinic in Arizona. Welcome, Meredith.
Meredith Wicklund, MD: Thank you.
Lecanemab data
Dr. LaFaver: I’m very excited about our topic. Could you give us a brief overview of why there has been so much research interest in this topic of anti-amyloid antibodies?
Dr. Wicklund: The pathologic component of what defines something as Alzheimer’s disease is, by definition, presence of amyloid plaques and tau tangles. When it was first discovered in the 1980s that the component of the plaques was actually the amyloid protein – beta amyloid specifically – interest went right from there to developing therapies to directly target the pathology that is Alzheimer’s disease.
Dr. LaFaver: Lecanemab is the first FDA-approved disease-modifying antibody in that realm. Could you review the study data, especially as it applies to both of us in daily neurology clinic?
Dr. Wicklund: The study data from a phase 3 trial did show, for the primary outcome, that there was a 27% slowing of decline compared with individuals on placebo. It’s important to point out that this was slowing of decline. It was not stabilizing decline. It was not improving decline.
I think it’s important that we inform our patients that really, even with this therapy, there’s no prospect of stabilizing or restoring cognition or function. We do progress at a slower rate compared with individuals not on this treatment, which, given that this medication is for individuals in mild disease who have relatively preserved functional status, that can be potentially very meaningful to families.
The overall benefit was small. It essentially amounts to half a point on an 18-point scale, which is statistically significant. How much clinical meaningfulness that actually leads to is unclear. Finding clinical meaningfulness cannot be defined by a particular test. It really can only be defined on the individual level, what is meaningful to them.
Recommended tests
Dr. LaFaver: It is my understanding that, to qualify for lecanemab use, one needs to have a biomarker-supported diagnosis of Alzheimer’s disease, either via an amyloid PET scan or CSF biomarkers. What would your recommendation be for a neurologist in practice to go about these requirements?
Dr. Wicklund: Since this medication is directly targeting the amyloid pathology, and it does convey a potential risk, we want to make sure that the actual pathology is present in the individuals before we treat them and potentially expose them to risk. The best way of doing that is through either an amyloid PET scan or spinal fluid testing of beta amyloid and tau.
There are several plasma-based biomarkers in development. However, I would avoid using those currently. There are still many unknowns in terms of what exactly is the right species of tau that we should be looking at, the right mechanism of the lab test, how minority status may influence it, and how different comorbidities may influence it.
I would recommend, at this time, sticking with amyloid PET or CSF testing. Given that amyloid PET is not widely available in many community practices, generally only available at academic centers, and is quite costly, many insurances do not cover it – although Medicare has a proposal to potentially start covering it – I generally go with spinal fluid testing, which is more widely available. There are several labs across the country that can process that testing in a reliable way.
Amyloid-related imaging abnormalities
Dr. LaFaver: That’s very helpful to know. There’s been a large amount of buzz just these past couple of weeks about the blood biomarker coming up. I think, as you point out, this wasn’t the marker used in the clinical studies and there are still unknowns. Maybe it’s not quite time for clinical use, unfortunately.
We also have learned that there are significant potential risks involved. One issue that’s really been a focus is ARIA – amyloid-related imaging abnormalities. Could you speak a bit about that and requirements for monitoring?
Dr. Wicklund: ARIA essentially amounts to either vasogenic edema, microhemorrhages, or superficial siderosis that develops as a result of treatment. It relates to activation of the immune system with these passive monoclonal antibodies that’s going to occur with targeting against the plaques. In the parenchyma, it will cause edema. If you have amyloid in the walls of the blood vessels, it can cause microhemorrhages.
While the term “ARIA” implies an imaging-related abnormality, and it largely is purely an imaging finding, it’s not solely an imaging-related finding. It can cause symptoms, including very serious symptoms.
Overall, with lecanemab, the incidence of ARIA within the treatment group in the phase 3 study, combined between both ARIA-E (edema/effusion) and ARIA-H (hemorrhage), was 21.5%, with about 17% being ARIA-H and about 12.5% being ARIA-E. Of course, they can occur at the same time.
Overall, in terms of people in the clinical trials, for most it was purely an imaging-related finding. About 3% developed symptomatic ARIA. Some of those were very serious symptoms, including things like seizures and need to be hospitalized. A couple of deaths have been attributed to ARIA as well.
Patients on anticoagulation
Dr. LaFaver: Along those lines, any additional words to say for people who might be on anticoagulation or might require medications for a stroke, for example?
Dr. Wicklund: While individuals on anticoagulation were allowed in the clinical trials, the current, published appropriate-use guideline is recommending against its use, as several of the serious adverse effects, including the deaths, were for the most part attributed to anticoagulation use.
When it comes to acute stroke treatment, one must carefully consider use of tPA, as two of the three deaths were tPA associated in the clinical trials. It shouldn’t necessarily be an absolute contraindication, but it can make the clinical picture very muddy. If an individual is on lecanemab and comes to the ER with acute stroke-like symptoms, it’s more likely that they’re going to be having an ARIA side effect rather than an acute stroke.
A general recommendation would be to obtain an acute head CT with a CTA, and if there is a large vessel occlusion, proceed to thrombectomy. However, if there isn’t a large vessel occlusion, if you have the ability to get a rapid MRI with diffusion-weighted imaging to screen for acute stroke changes or tissue flair with acute edema changes suggestive of ARIA, that would be preferred before proceeding with thrombolysis. These are all relative contraindications and are going to depend on what’s available near you.
Donanemab approval pending
Dr. LaFaver: This will be an issue because the population we’re talking about is definitely at risk for stroke as well as Alzheimer’s disease. Where do you see this field going as far as amyloid antibody therapy is concerned, with another agent, donanemab, possibly getting FDA approval later this year as well?
Dr. Wicklund: We’re anticipating that donanemab will get FDA approval in the next coming months. Donanemab also targets the amyloid in the brain, although lecanemab and donanemab target different aspects of the production of the amyloid plaque. They were both shown to have roughly equal efficacy in their phase 3 clinical trials. Donanemab has the benefit of being a once-monthly infusion as opposed to twice-monthly infusions with lecanemab. It does have a slightly higher risk for ARIA compared with lecanemab.
Those are just some things to take into consideration when talking with your patients. In terms of where we’re going from here, we’re moving even earlier in terms of disease state. The lecanemab and donanemab phase 3 trials were done in individuals with mild cognitive impairment or mild dementia due to Alzheimer’s disease. They should not be used in individuals with moderate or more advanced Alzheimer’s disease.
There are ongoing, large, national, multicenter clinical trials of both lecanemab and donanemab in a preclinical state of Alzheimer’s disease. These individuals have evidence of amyloidosis, either through PET imaging or through CSF, but are clinically asymptomatic and do not yet have any signs of cognitive impairment or functional decline. We look forward to those results in the next few years. Hopefully, they’ll be able to show even greater benefit when moving into these early disease states in terms of delaying or even preventing cognitive decline.
Dr. LaFaver: That’s definitely very interesting to hear about. Where can people go for more information?
Dr. Wicklund: There’s a guideline on the use of lecanemab through the American Academy of Neurology. I encourage you to look at that. Also, look at the appropriate-use recommendations that were published this year in The Journal of Prevention of Alzheimer’s Disease.
Dr. LaFaver: Wonderful. With that being said, thank you so much for talking to me. I learned a lot. Thanks, everyone, for listening.
Dr. LaFaver is a neurologist at Saratoga Hospital Medical Group, Saratoga Springs, N.Y. She disclosed having no relevant financial relationships. Dr. Wicklund is senior associate consultant in the department of Neurology at Mayo Clinic, Phoenix, Ariz. She disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Recorded October 13, 2023. This transcript has been edited for clarity.
Kathrin LaFaver, MD: I’ll be talking today with Dr. Meredith Wicklund, senior associate consultant and behavioral neurologist specialist at Mayo Clinic in Arizona. Welcome, Meredith.
Meredith Wicklund, MD: Thank you.
Lecanemab data
Dr. LaFaver: I’m very excited about our topic. Could you give us a brief overview of why there has been so much research interest in this topic of anti-amyloid antibodies?
Dr. Wicklund: The pathologic component of what defines something as Alzheimer’s disease is, by definition, presence of amyloid plaques and tau tangles. When it was first discovered in the 1980s that the component of the plaques was actually the amyloid protein – beta amyloid specifically – interest went right from there to developing therapies to directly target the pathology that is Alzheimer’s disease.
Dr. LaFaver: Lecanemab is the first FDA-approved disease-modifying antibody in that realm. Could you review the study data, especially as it applies to both of us in daily neurology clinic?
Dr. Wicklund: The study data from a phase 3 trial did show, for the primary outcome, that there was a 27% slowing of decline compared with individuals on placebo. It’s important to point out that this was slowing of decline. It was not stabilizing decline. It was not improving decline.
I think it’s important that we inform our patients that really, even with this therapy, there’s no prospect of stabilizing or restoring cognition or function. We do progress at a slower rate compared with individuals not on this treatment, which, given that this medication is for individuals in mild disease who have relatively preserved functional status, that can be potentially very meaningful to families.
The overall benefit was small. It essentially amounts to half a point on an 18-point scale, which is statistically significant. How much clinical meaningfulness that actually leads to is unclear. Finding clinical meaningfulness cannot be defined by a particular test. It really can only be defined on the individual level, what is meaningful to them.
Recommended tests
Dr. LaFaver: It is my understanding that, to qualify for lecanemab use, one needs to have a biomarker-supported diagnosis of Alzheimer’s disease, either via an amyloid PET scan or CSF biomarkers. What would your recommendation be for a neurologist in practice to go about these requirements?
Dr. Wicklund: Since this medication is directly targeting the amyloid pathology, and it does convey a potential risk, we want to make sure that the actual pathology is present in the individuals before we treat them and potentially expose them to risk. The best way of doing that is through either an amyloid PET scan or spinal fluid testing of beta amyloid and tau.
There are several plasma-based biomarkers in development. However, I would avoid using those currently. There are still many unknowns in terms of what exactly is the right species of tau that we should be looking at, the right mechanism of the lab test, how minority status may influence it, and how different comorbidities may influence it.
I would recommend, at this time, sticking with amyloid PET or CSF testing. Given that amyloid PET is not widely available in many community practices, generally only available at academic centers, and is quite costly, many insurances do not cover it – although Medicare has a proposal to potentially start covering it – I generally go with spinal fluid testing, which is more widely available. There are several labs across the country that can process that testing in a reliable way.
Amyloid-related imaging abnormalities
Dr. LaFaver: That’s very helpful to know. There’s been a large amount of buzz just these past couple of weeks about the blood biomarker coming up. I think, as you point out, this wasn’t the marker used in the clinical studies and there are still unknowns. Maybe it’s not quite time for clinical use, unfortunately.
We also have learned that there are significant potential risks involved. One issue that’s really been a focus is ARIA – amyloid-related imaging abnormalities. Could you speak a bit about that and requirements for monitoring?
Dr. Wicklund: ARIA essentially amounts to either vasogenic edema, microhemorrhages, or superficial siderosis that develops as a result of treatment. It relates to activation of the immune system with these passive monoclonal antibodies that’s going to occur with targeting against the plaques. In the parenchyma, it will cause edema. If you have amyloid in the walls of the blood vessels, it can cause microhemorrhages.
While the term “ARIA” implies an imaging-related abnormality, and it largely is purely an imaging finding, it’s not solely an imaging-related finding. It can cause symptoms, including very serious symptoms.
Overall, with lecanemab, the incidence of ARIA within the treatment group in the phase 3 study, combined between both ARIA-E (edema/effusion) and ARIA-H (hemorrhage), was 21.5%, with about 17% being ARIA-H and about 12.5% being ARIA-E. Of course, they can occur at the same time.
Overall, in terms of people in the clinical trials, for most it was purely an imaging-related finding. About 3% developed symptomatic ARIA. Some of those were very serious symptoms, including things like seizures and need to be hospitalized. A couple of deaths have been attributed to ARIA as well.
Patients on anticoagulation
Dr. LaFaver: Along those lines, any additional words to say for people who might be on anticoagulation or might require medications for a stroke, for example?
Dr. Wicklund: While individuals on anticoagulation were allowed in the clinical trials, the current, published appropriate-use guideline is recommending against its use, as several of the serious adverse effects, including the deaths, were for the most part attributed to anticoagulation use.
When it comes to acute stroke treatment, one must carefully consider use of tPA, as two of the three deaths were tPA associated in the clinical trials. It shouldn’t necessarily be an absolute contraindication, but it can make the clinical picture very muddy. If an individual is on lecanemab and comes to the ER with acute stroke-like symptoms, it’s more likely that they’re going to be having an ARIA side effect rather than an acute stroke.
A general recommendation would be to obtain an acute head CT with a CTA, and if there is a large vessel occlusion, proceed to thrombectomy. However, if there isn’t a large vessel occlusion, if you have the ability to get a rapid MRI with diffusion-weighted imaging to screen for acute stroke changes or tissue flair with acute edema changes suggestive of ARIA, that would be preferred before proceeding with thrombolysis. These are all relative contraindications and are going to depend on what’s available near you.
Donanemab approval pending
Dr. LaFaver: This will be an issue because the population we’re talking about is definitely at risk for stroke as well as Alzheimer’s disease. Where do you see this field going as far as amyloid antibody therapy is concerned, with another agent, donanemab, possibly getting FDA approval later this year as well?
Dr. Wicklund: We’re anticipating that donanemab will get FDA approval in the next coming months. Donanemab also targets the amyloid in the brain, although lecanemab and donanemab target different aspects of the production of the amyloid plaque. They were both shown to have roughly equal efficacy in their phase 3 clinical trials. Donanemab has the benefit of being a once-monthly infusion as opposed to twice-monthly infusions with lecanemab. It does have a slightly higher risk for ARIA compared with lecanemab.
Those are just some things to take into consideration when talking with your patients. In terms of where we’re going from here, we’re moving even earlier in terms of disease state. The lecanemab and donanemab phase 3 trials were done in individuals with mild cognitive impairment or mild dementia due to Alzheimer’s disease. They should not be used in individuals with moderate or more advanced Alzheimer’s disease.
There are ongoing, large, national, multicenter clinical trials of both lecanemab and donanemab in a preclinical state of Alzheimer’s disease. These individuals have evidence of amyloidosis, either through PET imaging or through CSF, but are clinically asymptomatic and do not yet have any signs of cognitive impairment or functional decline. We look forward to those results in the next few years. Hopefully, they’ll be able to show even greater benefit when moving into these early disease states in terms of delaying or even preventing cognitive decline.
Dr. LaFaver: That’s definitely very interesting to hear about. Where can people go for more information?
Dr. Wicklund: There’s a guideline on the use of lecanemab through the American Academy of Neurology. I encourage you to look at that. Also, look at the appropriate-use recommendations that were published this year in The Journal of Prevention of Alzheimer’s Disease.
Dr. LaFaver: Wonderful. With that being said, thank you so much for talking to me. I learned a lot. Thanks, everyone, for listening.
Dr. LaFaver is a neurologist at Saratoga Hospital Medical Group, Saratoga Springs, N.Y. She disclosed having no relevant financial relationships. Dr. Wicklund is senior associate consultant in the department of Neurology at Mayo Clinic, Phoenix, Ariz. She disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Headache after drinking red wine? This could be why
This transcript has been edited for clarity.
Robert Louis Stevenson famously said, “Wine is bottled poetry.” And I think it works quite well. I’ve had wines that are simple, elegant, and unpretentious like Emily Dickinson, and passionate and mysterious like Pablo Neruda. And I’ve had wines that are more analogous to the limerick you might read scrawled on a rest-stop bathroom wall. Those ones give me headaches.
– and apparently it’s not just the alcohol.
Headaches are common, and headaches after drinking alcohol are particularly common. An interesting epidemiologic phenomenon, not yet adequately explained, is why red wine is associated with more headache than other forms of alcohol. There have been many studies fingering many suspects, from sulfites to tannins to various phenolic compounds, but none have really provided a concrete explanation for what might be going on.
A new hypothesis came to the fore on Nov. 20 in the journal Scientific Reports:
To understand the idea, first a reminder of what happens when you drink alcohol, physiologically.
Alcohol is metabolized by the enzyme alcohol dehydrogenase in the gut and then in the liver. That turns it into acetaldehyde, a toxic metabolite. In most of us, aldehyde dehydrogenase (ALDH) quickly metabolizes acetaldehyde to the inert acetate, which can be safely excreted.
I say “most of us” because some populations, particularly those with East Asian ancestry, have a mutation in the ALDH gene which can lead to accumulation of toxic acetaldehyde with alcohol consumption – leading to facial flushing, nausea, and headache.
We can also inhibit the enzyme medically. That’s what the drug disulfiram, also known as Antabuse, does. It doesn’t prevent you from wanting to drink; it makes the consequences of drinking incredibly aversive.
The researchers focused in on the aldehyde dehydrogenase enzyme and conducted a screening study. Are there any compounds in red wine that naturally inhibit ALDH?
The results pointed squarely at quercetin, and particularly its metabolite quercetin glucuronide, which, at 20 micromolar concentrations, inhibited about 80% of ALDH activity.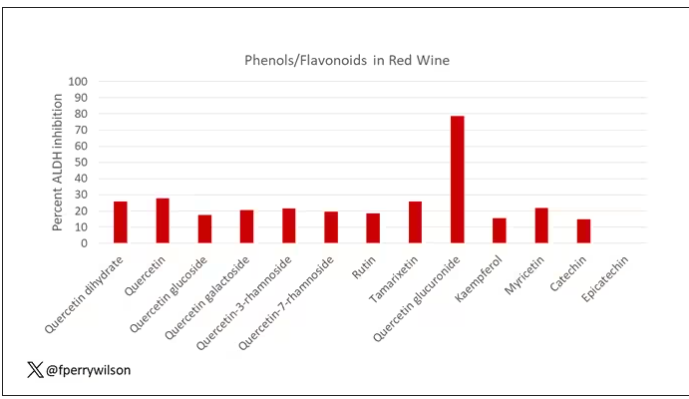
Quercetin is a flavonoid – a compound that gives color to a variety of vegetables and fruits, including grapes. In a test tube, it is an antioxidant, which is enough evidence to spawn a small quercetin-as-supplement industry, but there is no convincing evidence that it is medically useful. The authors then examined the concentration of quercetin glucuronide to achieve various inhibitions of ALDH, as you can see in this graph here.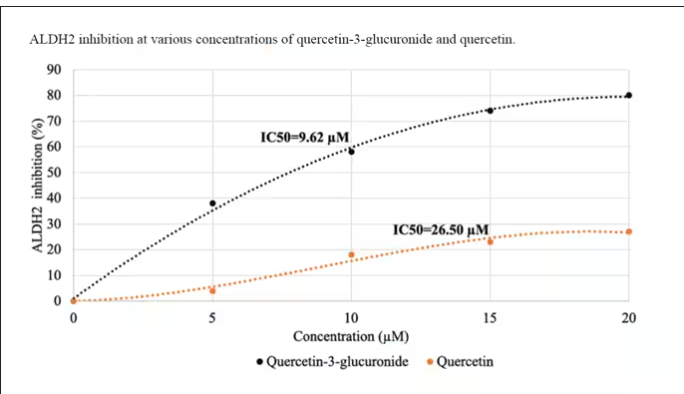
By about 10 micromolar, we see a decent amount of inhibition. Disulfiram is about 10 times more potent than that, but then again, you don’t drink three glasses of disulfiram with Thanksgiving dinner.
This is where this study stops. But it obviously tells us very little about what might be happening in the human body. For that, we need to ask the question: Can we get our quercetin levels to 10 micromolar? Is that remotely achievable?
Let’s start with how much quercetin there is in red wine. Like all things wine, it varies, but this study examining Australian wines found mean concentrations of 11 mg/L. The highest value I saw was close to 50 mg/L.
So let’s do some math. To make the numbers easy, let’s say you drank a liter of Australian wine, taking in 50 mg of quercetin glucuronide.
How much of that gets into your bloodstream? Some studies suggest a bioavailability of less than 1%, which basically means none and should probably put the quercetin hypothesis to bed. But there is some variation here too; it seems to depend on the form of quercetin you ingest.
Let’s say all 50 mg gets into your bloodstream. What blood concentration would that lead to? Well, I’ll keep the stoichiometry in the graphics and just say that if we assume that the volume of distribution of the compound is restricted to plasma alone, then you could achieve similar concentrations to what was done in petri dishes during this study.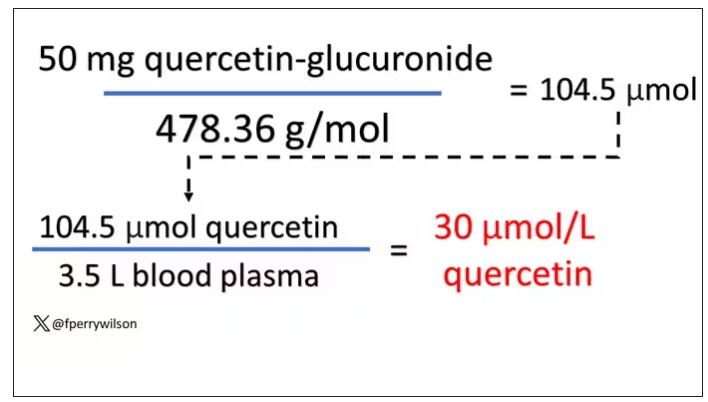
Of course, if quercetin is really the culprit behind red wine headache, I have some questions: Why aren’t the Amazon reviews of quercetin supplements chock full of warnings not to take them with alcohol? And other foods have way higher quercetin concentration than wine, but you don’t hear people warning not to take your red onions with alcohol, or your capers, or lingonberries.
There’s some more work to be done here – most importantly, some human studies. Let’s give people wine with different amounts of quercetin and see what happens. Sign me up. Seriously.
As for Thanksgiving, it’s worth noting that cranberries have a lot of quercetin in them. So between the cranberry sauce, the Beaujolais, and your uncle ranting about the contrails again, the probability of headache is pretty darn high. Stay safe out there, and Happy Thanksgiving.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Robert Louis Stevenson famously said, “Wine is bottled poetry.” And I think it works quite well. I’ve had wines that are simple, elegant, and unpretentious like Emily Dickinson, and passionate and mysterious like Pablo Neruda. And I’ve had wines that are more analogous to the limerick you might read scrawled on a rest-stop bathroom wall. Those ones give me headaches.
– and apparently it’s not just the alcohol.
Headaches are common, and headaches after drinking alcohol are particularly common. An interesting epidemiologic phenomenon, not yet adequately explained, is why red wine is associated with more headache than other forms of alcohol. There have been many studies fingering many suspects, from sulfites to tannins to various phenolic compounds, but none have really provided a concrete explanation for what might be going on.
A new hypothesis came to the fore on Nov. 20 in the journal Scientific Reports:
To understand the idea, first a reminder of what happens when you drink alcohol, physiologically.
Alcohol is metabolized by the enzyme alcohol dehydrogenase in the gut and then in the liver. That turns it into acetaldehyde, a toxic metabolite. In most of us, aldehyde dehydrogenase (ALDH) quickly metabolizes acetaldehyde to the inert acetate, which can be safely excreted.
I say “most of us” because some populations, particularly those with East Asian ancestry, have a mutation in the ALDH gene which can lead to accumulation of toxic acetaldehyde with alcohol consumption – leading to facial flushing, nausea, and headache.
We can also inhibit the enzyme medically. That’s what the drug disulfiram, also known as Antabuse, does. It doesn’t prevent you from wanting to drink; it makes the consequences of drinking incredibly aversive.
The researchers focused in on the aldehyde dehydrogenase enzyme and conducted a screening study. Are there any compounds in red wine that naturally inhibit ALDH?
The results pointed squarely at quercetin, and particularly its metabolite quercetin glucuronide, which, at 20 micromolar concentrations, inhibited about 80% of ALDH activity.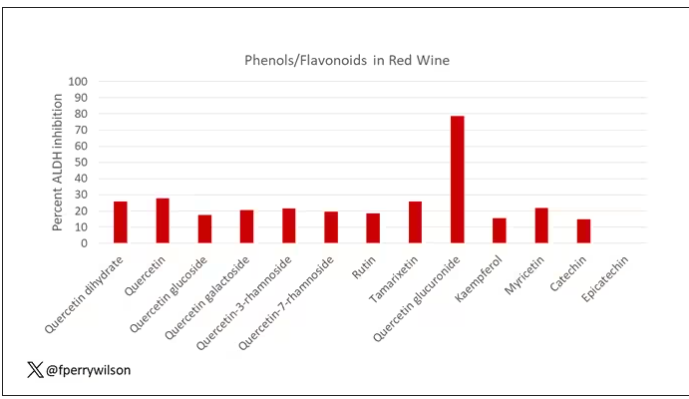
Quercetin is a flavonoid – a compound that gives color to a variety of vegetables and fruits, including grapes. In a test tube, it is an antioxidant, which is enough evidence to spawn a small quercetin-as-supplement industry, but there is no convincing evidence that it is medically useful. The authors then examined the concentration of quercetin glucuronide to achieve various inhibitions of ALDH, as you can see in this graph here.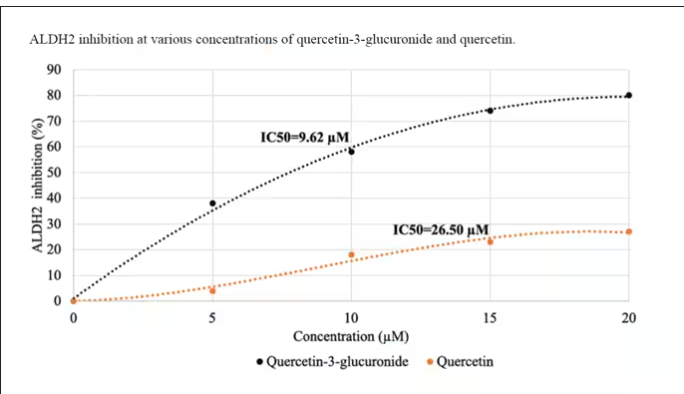
By about 10 micromolar, we see a decent amount of inhibition. Disulfiram is about 10 times more potent than that, but then again, you don’t drink three glasses of disulfiram with Thanksgiving dinner.
This is where this study stops. But it obviously tells us very little about what might be happening in the human body. For that, we need to ask the question: Can we get our quercetin levels to 10 micromolar? Is that remotely achievable?
Let’s start with how much quercetin there is in red wine. Like all things wine, it varies, but this study examining Australian wines found mean concentrations of 11 mg/L. The highest value I saw was close to 50 mg/L.
So let’s do some math. To make the numbers easy, let’s say you drank a liter of Australian wine, taking in 50 mg of quercetin glucuronide.
How much of that gets into your bloodstream? Some studies suggest a bioavailability of less than 1%, which basically means none and should probably put the quercetin hypothesis to bed. But there is some variation here too; it seems to depend on the form of quercetin you ingest.
Let’s say all 50 mg gets into your bloodstream. What blood concentration would that lead to? Well, I’ll keep the stoichiometry in the graphics and just say that if we assume that the volume of distribution of the compound is restricted to plasma alone, then you could achieve similar concentrations to what was done in petri dishes during this study.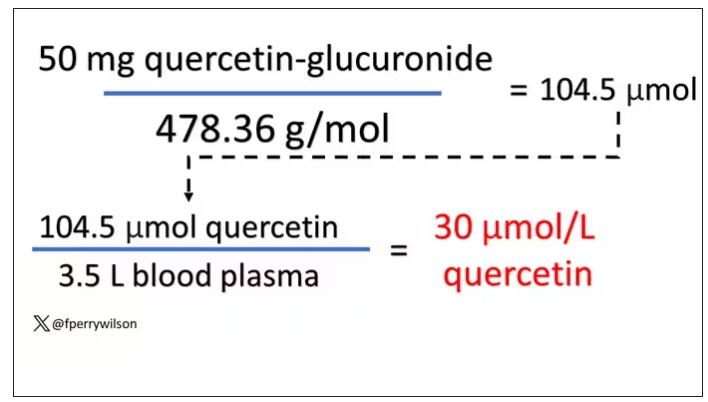
Of course, if quercetin is really the culprit behind red wine headache, I have some questions: Why aren’t the Amazon reviews of quercetin supplements chock full of warnings not to take them with alcohol? And other foods have way higher quercetin concentration than wine, but you don’t hear people warning not to take your red onions with alcohol, or your capers, or lingonberries.
There’s some more work to be done here – most importantly, some human studies. Let’s give people wine with different amounts of quercetin and see what happens. Sign me up. Seriously.
As for Thanksgiving, it’s worth noting that cranberries have a lot of quercetin in them. So between the cranberry sauce, the Beaujolais, and your uncle ranting about the contrails again, the probability of headache is pretty darn high. Stay safe out there, and Happy Thanksgiving.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Robert Louis Stevenson famously said, “Wine is bottled poetry.” And I think it works quite well. I’ve had wines that are simple, elegant, and unpretentious like Emily Dickinson, and passionate and mysterious like Pablo Neruda. And I’ve had wines that are more analogous to the limerick you might read scrawled on a rest-stop bathroom wall. Those ones give me headaches.
– and apparently it’s not just the alcohol.
Headaches are common, and headaches after drinking alcohol are particularly common. An interesting epidemiologic phenomenon, not yet adequately explained, is why red wine is associated with more headache than other forms of alcohol. There have been many studies fingering many suspects, from sulfites to tannins to various phenolic compounds, but none have really provided a concrete explanation for what might be going on.
A new hypothesis came to the fore on Nov. 20 in the journal Scientific Reports:
To understand the idea, first a reminder of what happens when you drink alcohol, physiologically.
Alcohol is metabolized by the enzyme alcohol dehydrogenase in the gut and then in the liver. That turns it into acetaldehyde, a toxic metabolite. In most of us, aldehyde dehydrogenase (ALDH) quickly metabolizes acetaldehyde to the inert acetate, which can be safely excreted.
I say “most of us” because some populations, particularly those with East Asian ancestry, have a mutation in the ALDH gene which can lead to accumulation of toxic acetaldehyde with alcohol consumption – leading to facial flushing, nausea, and headache.
We can also inhibit the enzyme medically. That’s what the drug disulfiram, also known as Antabuse, does. It doesn’t prevent you from wanting to drink; it makes the consequences of drinking incredibly aversive.
The researchers focused in on the aldehyde dehydrogenase enzyme and conducted a screening study. Are there any compounds in red wine that naturally inhibit ALDH?
The results pointed squarely at quercetin, and particularly its metabolite quercetin glucuronide, which, at 20 micromolar concentrations, inhibited about 80% of ALDH activity.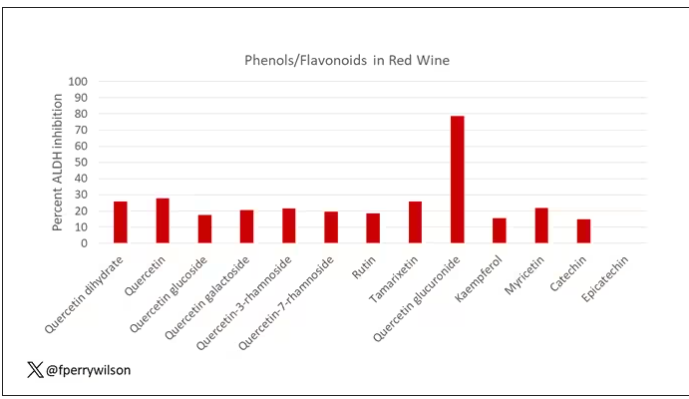
Quercetin is a flavonoid – a compound that gives color to a variety of vegetables and fruits, including grapes. In a test tube, it is an antioxidant, which is enough evidence to spawn a small quercetin-as-supplement industry, but there is no convincing evidence that it is medically useful. The authors then examined the concentration of quercetin glucuronide to achieve various inhibitions of ALDH, as you can see in this graph here.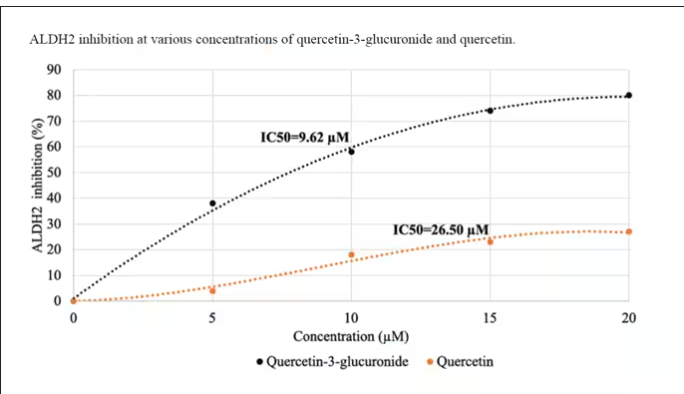
By about 10 micromolar, we see a decent amount of inhibition. Disulfiram is about 10 times more potent than that, but then again, you don’t drink three glasses of disulfiram with Thanksgiving dinner.
This is where this study stops. But it obviously tells us very little about what might be happening in the human body. For that, we need to ask the question: Can we get our quercetin levels to 10 micromolar? Is that remotely achievable?
Let’s start with how much quercetin there is in red wine. Like all things wine, it varies, but this study examining Australian wines found mean concentrations of 11 mg/L. The highest value I saw was close to 50 mg/L.
So let’s do some math. To make the numbers easy, let’s say you drank a liter of Australian wine, taking in 50 mg of quercetin glucuronide.
How much of that gets into your bloodstream? Some studies suggest a bioavailability of less than 1%, which basically means none and should probably put the quercetin hypothesis to bed. But there is some variation here too; it seems to depend on the form of quercetin you ingest.
Let’s say all 50 mg gets into your bloodstream. What blood concentration would that lead to? Well, I’ll keep the stoichiometry in the graphics and just say that if we assume that the volume of distribution of the compound is restricted to plasma alone, then you could achieve similar concentrations to what was done in petri dishes during this study.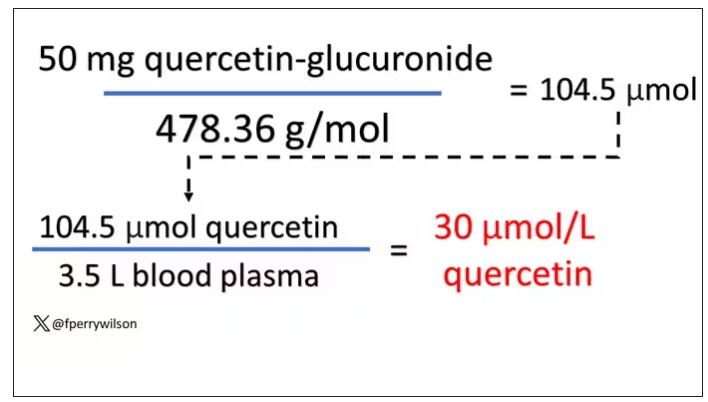
Of course, if quercetin is really the culprit behind red wine headache, I have some questions: Why aren’t the Amazon reviews of quercetin supplements chock full of warnings not to take them with alcohol? And other foods have way higher quercetin concentration than wine, but you don’t hear people warning not to take your red onions with alcohol, or your capers, or lingonberries.
There’s some more work to be done here – most importantly, some human studies. Let’s give people wine with different amounts of quercetin and see what happens. Sign me up. Seriously.
As for Thanksgiving, it’s worth noting that cranberries have a lot of quercetin in them. So between the cranberry sauce, the Beaujolais, and your uncle ranting about the contrails again, the probability of headache is pretty darn high. Stay safe out there, and Happy Thanksgiving.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
New insights into how omega-3 fatty acids improve NASH
TOPLINE:
that contributes to liver fibrosis and progression to cirrhosis and liver cancer, new data suggest.
METHODOLOGY:
- Because omega-3 polyunsaturated fatty acids have been shown to reduce hepatic dysfunction in NASH, but the molecular underpinnings of this action were elusive, researchers conducted a multiomic network analysis applied to a mouse model of Western diet–induced NASH to identify the key mechanisms involved.
- They also performed a meta-analysis of human liver cancer transcriptome data to evaluate which aspects of NASH pathogenesis leading to cancer are reversed by omega-3 polyunsaturated fatty acids.
TAKEAWAY:
- BTC, an epidermal growth factor–binding protein, was consistently upregulated in liver cancer and downregulated by omega-3 polyunsaturated fatty acids in mice and humans with NASH.
- BTC promotes NASH fibrosis by activating dormant hepatic stellate cells to produce transforming growth factor beta-2 and increase collagen production. It also exacerbates toll-like receptor-dependent inflammatory processes in NASH.
- By downregulating BTC, omega-3 polyunsaturated fatty acids have therapeutic potential in NASH and could serve as a novel drug target.
IN PRACTICE:
“BTC represents a candidate master regulator inducing two most important factors (collagens and integrins) contributing to liver fibrosis and consequently promoting liver cancer,” the researchers write. “Future studies should investigate if BTC-triggered gene expression signatures can serve as biomarkers guiding personalized [omega-3 polyunsaturated fatty acid] therapy, as targets of new NAFLD/NASH drugs, and finally as a predictors of hepatic cancer risk in humans.”
SOURCE:
The study, with lead first author Jyothi Padiadpu, PhD, Oregon State University College of Pharmacy, Corvallis, was published online in EMBO Molecular Medicine (2023. doi: 10.15252/emmm.202318367).
LIMITATIONS:
The study authors report no limitations. However, the findings are based on mouse model and human transcriptome data.
DISCLOSURES:
This research was supported by the National Institute of Diabetes and Digestive Kidney Diseases and the U.S. Department of Agriculture. The authors report no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
that contributes to liver fibrosis and progression to cirrhosis and liver cancer, new data suggest.
METHODOLOGY:
- Because omega-3 polyunsaturated fatty acids have been shown to reduce hepatic dysfunction in NASH, but the molecular underpinnings of this action were elusive, researchers conducted a multiomic network analysis applied to a mouse model of Western diet–induced NASH to identify the key mechanisms involved.
- They also performed a meta-analysis of human liver cancer transcriptome data to evaluate which aspects of NASH pathogenesis leading to cancer are reversed by omega-3 polyunsaturated fatty acids.
TAKEAWAY:
- BTC, an epidermal growth factor–binding protein, was consistently upregulated in liver cancer and downregulated by omega-3 polyunsaturated fatty acids in mice and humans with NASH.
- BTC promotes NASH fibrosis by activating dormant hepatic stellate cells to produce transforming growth factor beta-2 and increase collagen production. It also exacerbates toll-like receptor-dependent inflammatory processes in NASH.
- By downregulating BTC, omega-3 polyunsaturated fatty acids have therapeutic potential in NASH and could serve as a novel drug target.
IN PRACTICE:
“BTC represents a candidate master regulator inducing two most important factors (collagens and integrins) contributing to liver fibrosis and consequently promoting liver cancer,” the researchers write. “Future studies should investigate if BTC-triggered gene expression signatures can serve as biomarkers guiding personalized [omega-3 polyunsaturated fatty acid] therapy, as targets of new NAFLD/NASH drugs, and finally as a predictors of hepatic cancer risk in humans.”
SOURCE:
The study, with lead first author Jyothi Padiadpu, PhD, Oregon State University College of Pharmacy, Corvallis, was published online in EMBO Molecular Medicine (2023. doi: 10.15252/emmm.202318367).
LIMITATIONS:
The study authors report no limitations. However, the findings are based on mouse model and human transcriptome data.
DISCLOSURES:
This research was supported by the National Institute of Diabetes and Digestive Kidney Diseases and the U.S. Department of Agriculture. The authors report no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
that contributes to liver fibrosis and progression to cirrhosis and liver cancer, new data suggest.
METHODOLOGY:
- Because omega-3 polyunsaturated fatty acids have been shown to reduce hepatic dysfunction in NASH, but the molecular underpinnings of this action were elusive, researchers conducted a multiomic network analysis applied to a mouse model of Western diet–induced NASH to identify the key mechanisms involved.
- They also performed a meta-analysis of human liver cancer transcriptome data to evaluate which aspects of NASH pathogenesis leading to cancer are reversed by omega-3 polyunsaturated fatty acids.
TAKEAWAY:
- BTC, an epidermal growth factor–binding protein, was consistently upregulated in liver cancer and downregulated by omega-3 polyunsaturated fatty acids in mice and humans with NASH.
- BTC promotes NASH fibrosis by activating dormant hepatic stellate cells to produce transforming growth factor beta-2 and increase collagen production. It also exacerbates toll-like receptor-dependent inflammatory processes in NASH.
- By downregulating BTC, omega-3 polyunsaturated fatty acids have therapeutic potential in NASH and could serve as a novel drug target.
IN PRACTICE:
“BTC represents a candidate master regulator inducing two most important factors (collagens and integrins) contributing to liver fibrosis and consequently promoting liver cancer,” the researchers write. “Future studies should investigate if BTC-triggered gene expression signatures can serve as biomarkers guiding personalized [omega-3 polyunsaturated fatty acid] therapy, as targets of new NAFLD/NASH drugs, and finally as a predictors of hepatic cancer risk in humans.”
SOURCE:
The study, with lead first author Jyothi Padiadpu, PhD, Oregon State University College of Pharmacy, Corvallis, was published online in EMBO Molecular Medicine (2023. doi: 10.15252/emmm.202318367).
LIMITATIONS:
The study authors report no limitations. However, the findings are based on mouse model and human transcriptome data.
DISCLOSURES:
This research was supported by the National Institute of Diabetes and Digestive Kidney Diseases and the U.S. Department of Agriculture. The authors report no conflicts of interest.
A version of this article appeared on Medscape.com.
UHC accused of using AI to skirt doctors’ orders, deny claims
.
In a class action suit filed in Minnesota district court, the attorneys for the families of two deceased UHC Medicare Advantage plan policyholders say that the company uses the technology to systematically deny skilled nursing facility (SNF) claims and shirk its responsibility to adhere to Medicare’s coverage determination standards.
The case raises ethical and legal questions about whether AI can replace or supplement human tasks and interactions, particularly in a field as complex as health care. California-based public advocacy firm Clarkson Law filed a similar complaint against Cigna earlier this year and has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ data to train their AI systems.
Clarkson Law represents the plaintiffs and says that the policyholders had to pay thousands in out-of-pocket costs or forgo the recommended postacute care owing to UHC’s faulty AI model, nH Predict. The tool has a 90% error rate, says the lawsuit, as evidenced by the number of claims that are reversed following review by a medical professional. Still, just 0.2% of policyholders appeal the denials.
nH Predict was created by naviHealth and was acquired by UnitedHealth Group, UHC’s parent company, in 2020. In a statement to Bloomberg Law, a spokesperson for naviHealth said that the lawsuit has no merit and the model was not used for making coverage determinations.
According to the complaint, nH Predict determines the appropriate amount of SNF, home health, or rehabilitation services a patient requires on the basis of the diagnosis, age, and living situation. The model compares the patient with its database of 6 million patients and estimates the ideal length of stay and target discharge date, “pinpointing the precise moment when [UHC] will cut off payment for a patient’s treatment.”
The lawsuit says that employees are instructed to strictly adhere to the AI model’s predictions, and those who do not are disciplined and terminated, even when additional care for the patient is warranted. Employees are told that the generated reports contain proprietary information and that they cannot share them with physicians and patients who inquire about extending care.
“Every patient is entitled to a nuanced evaluation of their health care needs,” Zarrina Ozari, senior associate at Clarkson Law, said in a prepared statement. “By replacing licensed practitioners with unchecked AI, UHC is telling its patients that they are completely interchangeable with one another and undervaluing the expertise of the physicians devoted to key elements of care.”
According to the complaint, Gene Lokken fell in May 2022 and fractured his leg and ankle. After a 1-month SNF stay, the 91-year-old man’s doctor ordered physical therapy. However, the insurer said Mr. Lokken was safe to be discharged home two and a half weeks later, conflicting with a physical therapist’s notes that indicated he still had paralyzed and weak muscles. The insurer denied Mr. Lokken’s appeal. He remained in the facility for another year until his death, paying about $150,000 in out-of-pocket expenses, according to the lawsuit.
Another patient, Dale H. Tetzloff, initially spent just 20 days in a SNF for stroke rehabilitation before UHC denied coverage. An appeal later extended the stay to 40 days, short of the 100 days recommended by his physician. Requests for further extensions were unsuccessful, and Mr. Tetzloff ultimately paid about $70,000 in out-of-pocket expenses over the next 10 months, according to the complaint.
New federal rules prohibit Medicare Advantage plans from relying on an algorithm or software to make medically necessary determinations instead of an individual’s specific circumstances. Any medical necessity denial must be “reviewed by a physician or other appropriate health care professional with expertise in the field of medicine or health care that is appropriate for the service at issue.”
Clarkson is demanding a jury trial and has asked the court to certify the case as a federal class action, which could open the suit to any U.S. resident who purchased a UHC Medicare Advantage plan in the past 4 years.
A version of this article appeared on Medscape.com.
.
In a class action suit filed in Minnesota district court, the attorneys for the families of two deceased UHC Medicare Advantage plan policyholders say that the company uses the technology to systematically deny skilled nursing facility (SNF) claims and shirk its responsibility to adhere to Medicare’s coverage determination standards.
The case raises ethical and legal questions about whether AI can replace or supplement human tasks and interactions, particularly in a field as complex as health care. California-based public advocacy firm Clarkson Law filed a similar complaint against Cigna earlier this year and has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ data to train their AI systems.
Clarkson Law represents the plaintiffs and says that the policyholders had to pay thousands in out-of-pocket costs or forgo the recommended postacute care owing to UHC’s faulty AI model, nH Predict. The tool has a 90% error rate, says the lawsuit, as evidenced by the number of claims that are reversed following review by a medical professional. Still, just 0.2% of policyholders appeal the denials.
nH Predict was created by naviHealth and was acquired by UnitedHealth Group, UHC’s parent company, in 2020. In a statement to Bloomberg Law, a spokesperson for naviHealth said that the lawsuit has no merit and the model was not used for making coverage determinations.
According to the complaint, nH Predict determines the appropriate amount of SNF, home health, or rehabilitation services a patient requires on the basis of the diagnosis, age, and living situation. The model compares the patient with its database of 6 million patients and estimates the ideal length of stay and target discharge date, “pinpointing the precise moment when [UHC] will cut off payment for a patient’s treatment.”
The lawsuit says that employees are instructed to strictly adhere to the AI model’s predictions, and those who do not are disciplined and terminated, even when additional care for the patient is warranted. Employees are told that the generated reports contain proprietary information and that they cannot share them with physicians and patients who inquire about extending care.
“Every patient is entitled to a nuanced evaluation of their health care needs,” Zarrina Ozari, senior associate at Clarkson Law, said in a prepared statement. “By replacing licensed practitioners with unchecked AI, UHC is telling its patients that they are completely interchangeable with one another and undervaluing the expertise of the physicians devoted to key elements of care.”
According to the complaint, Gene Lokken fell in May 2022 and fractured his leg and ankle. After a 1-month SNF stay, the 91-year-old man’s doctor ordered physical therapy. However, the insurer said Mr. Lokken was safe to be discharged home two and a half weeks later, conflicting with a physical therapist’s notes that indicated he still had paralyzed and weak muscles. The insurer denied Mr. Lokken’s appeal. He remained in the facility for another year until his death, paying about $150,000 in out-of-pocket expenses, according to the lawsuit.
Another patient, Dale H. Tetzloff, initially spent just 20 days in a SNF for stroke rehabilitation before UHC denied coverage. An appeal later extended the stay to 40 days, short of the 100 days recommended by his physician. Requests for further extensions were unsuccessful, and Mr. Tetzloff ultimately paid about $70,000 in out-of-pocket expenses over the next 10 months, according to the complaint.
New federal rules prohibit Medicare Advantage plans from relying on an algorithm or software to make medically necessary determinations instead of an individual’s specific circumstances. Any medical necessity denial must be “reviewed by a physician or other appropriate health care professional with expertise in the field of medicine or health care that is appropriate for the service at issue.”
Clarkson is demanding a jury trial and has asked the court to certify the case as a federal class action, which could open the suit to any U.S. resident who purchased a UHC Medicare Advantage plan in the past 4 years.
A version of this article appeared on Medscape.com.
.
In a class action suit filed in Minnesota district court, the attorneys for the families of two deceased UHC Medicare Advantage plan policyholders say that the company uses the technology to systematically deny skilled nursing facility (SNF) claims and shirk its responsibility to adhere to Medicare’s coverage determination standards.
The case raises ethical and legal questions about whether AI can replace or supplement human tasks and interactions, particularly in a field as complex as health care. California-based public advocacy firm Clarkson Law filed a similar complaint against Cigna earlier this year and has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ data to train their AI systems.
Clarkson Law represents the plaintiffs and says that the policyholders had to pay thousands in out-of-pocket costs or forgo the recommended postacute care owing to UHC’s faulty AI model, nH Predict. The tool has a 90% error rate, says the lawsuit, as evidenced by the number of claims that are reversed following review by a medical professional. Still, just 0.2% of policyholders appeal the denials.
nH Predict was created by naviHealth and was acquired by UnitedHealth Group, UHC’s parent company, in 2020. In a statement to Bloomberg Law, a spokesperson for naviHealth said that the lawsuit has no merit and the model was not used for making coverage determinations.
According to the complaint, nH Predict determines the appropriate amount of SNF, home health, or rehabilitation services a patient requires on the basis of the diagnosis, age, and living situation. The model compares the patient with its database of 6 million patients and estimates the ideal length of stay and target discharge date, “pinpointing the precise moment when [UHC] will cut off payment for a patient’s treatment.”
The lawsuit says that employees are instructed to strictly adhere to the AI model’s predictions, and those who do not are disciplined and terminated, even when additional care for the patient is warranted. Employees are told that the generated reports contain proprietary information and that they cannot share them with physicians and patients who inquire about extending care.
“Every patient is entitled to a nuanced evaluation of their health care needs,” Zarrina Ozari, senior associate at Clarkson Law, said in a prepared statement. “By replacing licensed practitioners with unchecked AI, UHC is telling its patients that they are completely interchangeable with one another and undervaluing the expertise of the physicians devoted to key elements of care.”
According to the complaint, Gene Lokken fell in May 2022 and fractured his leg and ankle. After a 1-month SNF stay, the 91-year-old man’s doctor ordered physical therapy. However, the insurer said Mr. Lokken was safe to be discharged home two and a half weeks later, conflicting with a physical therapist’s notes that indicated he still had paralyzed and weak muscles. The insurer denied Mr. Lokken’s appeal. He remained in the facility for another year until his death, paying about $150,000 in out-of-pocket expenses, according to the lawsuit.
Another patient, Dale H. Tetzloff, initially spent just 20 days in a SNF for stroke rehabilitation before UHC denied coverage. An appeal later extended the stay to 40 days, short of the 100 days recommended by his physician. Requests for further extensions were unsuccessful, and Mr. Tetzloff ultimately paid about $70,000 in out-of-pocket expenses over the next 10 months, according to the complaint.
New federal rules prohibit Medicare Advantage plans from relying on an algorithm or software to make medically necessary determinations instead of an individual’s specific circumstances. Any medical necessity denial must be “reviewed by a physician or other appropriate health care professional with expertise in the field of medicine or health care that is appropriate for the service at issue.”
Clarkson is demanding a jury trial and has asked the court to certify the case as a federal class action, which could open the suit to any U.S. resident who purchased a UHC Medicare Advantage plan in the past 4 years.
A version of this article appeared on Medscape.com.
Before signing an offer letter: Read this
You’ve just received an offer letter from that job you interviewed for. Sometimes you want to let the employer know right away how interested you are. The verbiage says the letter isn’t “binding.” So you eagerly sign on the dotted line. Everything looks great ... until it isn’t.
Attorney Ericka Adler, JD, LLM, a partner at Roetzel & Andress, a Chicago-based law firm that represents physicians and health care professionals nationwide, described her client who was in this predicament. The physician, a dermatologist, left a practice where she had been employed because she had received an “amazing” offer letter that included promises about her new work location, staffing, equipment, and hours. She signed and immediately gave notice to her previous employer.
“When she received the actual employment contract, none of those details from the offer letter – which is also called a letter of intent [LOI] – were included,” Ms. Adler told this news organization. The physician wanted to have the details from the LOI formally spelled out in the contract, but the employer refused.
“Basically, they said, ‘This is our standard contract and you’ll just have to trust us that we’ll keep our word. We meant what we said in the LOI, but we cannot include those details in the actual agreement because everyone has the same form of agreement.’ “ The physician decided to sign the contract and accept the position.
She contacted Ms. Adler after she had been at her new position for a month. “She had received none of the things they had promised her in the LOI,” Ms. Adler reported. “She lacked the NP and PA support, she lacked the equipment, she didn’t have enough exam rooms. As soon as she started, someone with whom she was sharing call coverage left, and she was expected to take over. The LOI had a cap on the amount of call she would be required to take, but that verbiage didn’t make it into the contract.”
Ms. Adler tried to address this issue with the employer. “We couldn’t say they had literally breached the agreement, but we did list the things that were mentioned in the LOI but on which they hadn’t delivered. We asked them to fix the issue within 10 days.”
The employer argued “that they didn’t have to fulfill anything that wasn’t spelled out in the contract, even if it was in the LOI. In fact, the contract specified clearly that the signed employment agreement was the only agreement and replaced any previous written or oral agreements between the parties.”
The dermatologist ultimately left the new position. “She might have been able to have a legal claim against the employer for breach or perhaps ‘detrimental reliance’ – meaning, she might have argued that she had been financially harmed due to the false promises made to her. But it would have been difficult and expensive for her to litigate the issue,” said Ms. Adler.
“It also didn’t seem like the physician could remain in the job and develop a positive work relationship with the employer, given that she felt betrayed and misled, and didn’t like the terms of employment, which didn’t match her needs or expectations,” said Ms. Adler.
She added that “most employers are not as unscrupulous and dishonest as this one was. But some employers do play on the fact that younger doctors – especially residents and fellows – tend to be trusting or feel they don’t have negotiation power. They’re often excited to get an offer and sign it without a second thought.”
That’s why she advises physicians to “review the terms of the LOI carefully and make sure you’re comfortable with them before signing it; but know that the real contract to negotiate will be the actual Employment Agreement.”
She also advises physicians not to give notice at their current place of employment until they’ve signed the final contract with the new employer.
On the same page?
Anu Murthy, JD, an attorney and associate contract review specialist at Contract Diagnostics, explained that the LOI is a document that the candidate receives after an interview but before a full contract. Sometimes, the LOI is preceded by a verbal or e-mailed offer, which is less formal.
“An LOI is sometimes called a Term Sheet or Memorandum of Understanding,“ Ms. Murthy told this news organization. “Typically, it lays out key provisions, such as compensation, initial term of the contract, location, and recruitment incentives.” Sometimes it includes mention of staffing, call schedule, malpractice, noncompete covenants, and other components of the position.
Justin Nabity, founder and CEO of Physicians Thrive, a physician financial advisory group, said that LOIs are “a way for employers to gauge a prospective employee’s level of interest.”
The employer “doesn’t want to send a contract with a lot of details before determining whether the candidate is really serious about the position, so the offer letter doesn’t show the whole picture,” Mr. Nabity told this news organization.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, agreed.
“Another way of putting it is that the employer wants to see whether the prospective employee is on the same page. The LOI will typically include some key components that will later appear in a more complete and formal contract, together with other topics and details. Agreeing to those key components signals that indeed you and the employer are in accord,” said Mr. Hursh.
But are you really on the same page with your prospective employer? And if you seem to be on the same page, and you sign the LOI, is that a guarantee that the employer will honor its terms?
Not necessarily, according to the experts. In fact, many LOIs contain some verbiage stating that the letter isn’t binding, which can be confusing. Others suggest that it is binding, but the candidate doesn’t realize that the letter isn’t a formal contract and that the contract may contain details not included in the LOI or may omit details mentioned in the LOI, as happened to Ms. Adler’s unfortunate client.
“One of the pitfalls I see is that doctors sign the LOI without recognizing whether it’s binding or nonbinding,” Ms. Murthy said. “If it’s binding, it creates a legal obligation on your part and could preclude you from further negotiation once you see the contract and feel you’d like to negotiate some of its terms.”
Binding letters are typically offered to candidates after some back-and-forth between the parties, and important terms have been agreed to, which can happen either verbally or via e-mail. Once these agreements have been reached, they’re summarized in a “binding” letter before being extended into a full contract.
“But even if you’ve agreed on the terms verbally, it’s still important to have someone more experienced review the offer letter before signing it,” Ms. Murthy said. “It’s important to understand the ‘legalese’ and what your rights and obligations are before agreeing to anything.”
And certainly, if you receive a binding LOI, you shouldn’t sign anything until you’re sure you’re comfortable with its contents and have more details.
Are “nonbinding” LOIs really not binding?
Even if the LOI is nonbinding, that doesn’t necessarily mean you can sign it and expect to negotiate later. “I see people tripped up when they sign the LOI, thinking they’ll negotiate later,” said Mr. Hursh. “They may not like the terms – for example, they think the compensation is too low – and they figure they’ll work it out at the contract stage, because the LOI is ‘not legally binding.’ “
But because the candidate signed the LOI, “the employer is under the impression that the compensation was acceptable, so now you’ve tied your hands – and the hands of any attorney you may consult down the road – to negotiate those terms.”
Mr. Hursh said he is often consulted by physicians who signed the contract “to get the ball rolling,” thinking that the LOI was “just a meaningless bureaucratic paper.” They need to understand “that the employer wants to make sure they’re in agreement on the basic points before getting into the details,” he said. “Large hospitals with in-house counsel may not want to use their legal department’s valuable time in redrafting terms they thought were acceptable to the candidate, and most practices don’t want to pay a lawyer to draft an LOI and then come back and say, ‘Actually, the physician wants more compensation.’ “
Mr. Nabity summarized: “The LOI is essentially a negotiation tactic to take some of the cards out of the hands of the doctor and commit him or her to something they’re not ready to commit to.” Employers may be playing on the sense of pressure and candidate’s fear that the job will slip through their fingers if they wait too long to sign. “But it’s better to wait longer at this stage before signing even a nonbinding LOI,” he said.
What to do before signing
So how should physicians relate to the LOI? Mr. Nabity advises “working through the details of the offer letter first, going through it carefully and identifying areas of concern, bearing in mind that employers never begin with their best offer.”
He pointed out that physicians “rarely know their value and usually don’t know how to work through the dynamics of compensation, call schedules, additional incentives, bonuses, and productivity,” so they need to be informed about these areas before signing anything.
Ms. Murthy recommended “going back and saying [to the prospective employer], ‘Thank you, but I need time to consider and evaluate this offer.’ Then, do some due diligence.”
At that point, you can hire an attorney to go over the offer, educate yourself about compensation benchmarks and what your worth actually is, or consult another trained professional or more experienced individual who can review the LOI before you sign it.
That’s what Dominique Cleveland, MD, a Texas-based ob.gyn., did when she received an LOI 5 years ago.
“The offer letter from the group practice contained a statement that the group wanted me to come on board, what the salary would be, and the time frame that would be covered in the contract,” she told this news organization. “It mentioned benefits and incentives and relocation, but it was only a short document – maybe one or two pages long.”
At the time that she received her LOI, Dr. Cleveland was completing her residency. She consulted experienced faculty members from her institution to find out whether the terms laid out in the LOI “were the norm and were reasonable.” She was “fairly certain” that the salary was low and this was confirmed by the faculty members she talked to. “So I felt comfortable asking for more [compensation],” she said.
The employer was receptive to her proposed changes, which were included in the more detailed contract that followed. “I can’t say there were any surprises per se in the contract because I had negotiated my salary after receiving the offer letter,” she said. She accepted the position and has been working there ever since.
Dr. Cleveland advises physicians “not to make a decision without speaking to someone who’s experienced and can help you compare what’s out there.”
She also encourages physicians to ask for what they want, whether it’s compensation or something else, such as call schedule or vacation time, without being afraid. “I’m a firm believer that you won’t know what you can get if you don’t ask for it,” she said.
Negotiation tips
Mr. Nabity recommended not agreeing to any terms until you are ready to enter into negotiation, recognizing that negotiation is an “art” that requires skill and training. “Either get trained in negotiation, perhaps taking courses to advocate for yourself – which is rare, and most doctors aren’t likely to do this – or go to a trained advocate, such as a lawyer, who can do so on your behalf.”
You might share your concerns with the person who interviewed you, with the person whose name is on the LOI, or with the recruiter who can advocate on your behalf, Ms. Murthy said. “You can reach out to the recruiter and say, ‘I really appreciate the opportunity, but there are some things in the offer letter I’d like to continue discussing.’ “
When you’re ready to negotiate, be sure to assemble all of your “asks” in a single document rather than going back to the prospective employer with “multiple individual questions multiple times,” Ms. Murthy advised. It’s more efficient and the employer or recruiter will appreciate that.
She also advised couching your request in language that expresses your appreciation for the offer and stating that you would like the agreement to serve the best interests of both parties. “Use open-ended language like that, and ask if it’s all right for you to send back some questions, ask for clarification, or share concerns.”
Most employers “will be fine with that,” Ms. Murthy said. “Most won’t say, ‘This is it, take it or leave it.’ If they do, that’s a red flag for you to reconsider whether you really want to work for this particular employer.”
Mr. Hursh suggested that if you choose to sign the LOI immediately, so as to rapidly let the prospective employer know of your interest, “you should add some type of qualification such as, ‘I’m signing this to express my interest, but accepting the position will be dependent upon a more thorough review of compensation benchmarks,’ for example.”
Mr. Nabity agreed: “You can add a handwritten note to the signed LOI expressing that you’re eager to move forward and proceed with the position, but it shouldn’t be construed as accepting the terms of the LOI until you’ve seen the full contract.
“Remember, health care can’t exist without doctors,” Mr. Nabity said. “Doctors are the star players and should go into the negotiation process recognizing their true worth.”
A version of this article appeared on Medscape.com.
You’ve just received an offer letter from that job you interviewed for. Sometimes you want to let the employer know right away how interested you are. The verbiage says the letter isn’t “binding.” So you eagerly sign on the dotted line. Everything looks great ... until it isn’t.
Attorney Ericka Adler, JD, LLM, a partner at Roetzel & Andress, a Chicago-based law firm that represents physicians and health care professionals nationwide, described her client who was in this predicament. The physician, a dermatologist, left a practice where she had been employed because she had received an “amazing” offer letter that included promises about her new work location, staffing, equipment, and hours. She signed and immediately gave notice to her previous employer.
“When she received the actual employment contract, none of those details from the offer letter – which is also called a letter of intent [LOI] – were included,” Ms. Adler told this news organization. The physician wanted to have the details from the LOI formally spelled out in the contract, but the employer refused.
“Basically, they said, ‘This is our standard contract and you’ll just have to trust us that we’ll keep our word. We meant what we said in the LOI, but we cannot include those details in the actual agreement because everyone has the same form of agreement.’ “ The physician decided to sign the contract and accept the position.
She contacted Ms. Adler after she had been at her new position for a month. “She had received none of the things they had promised her in the LOI,” Ms. Adler reported. “She lacked the NP and PA support, she lacked the equipment, she didn’t have enough exam rooms. As soon as she started, someone with whom she was sharing call coverage left, and she was expected to take over. The LOI had a cap on the amount of call she would be required to take, but that verbiage didn’t make it into the contract.”
Ms. Adler tried to address this issue with the employer. “We couldn’t say they had literally breached the agreement, but we did list the things that were mentioned in the LOI but on which they hadn’t delivered. We asked them to fix the issue within 10 days.”
The employer argued “that they didn’t have to fulfill anything that wasn’t spelled out in the contract, even if it was in the LOI. In fact, the contract specified clearly that the signed employment agreement was the only agreement and replaced any previous written or oral agreements between the parties.”
The dermatologist ultimately left the new position. “She might have been able to have a legal claim against the employer for breach or perhaps ‘detrimental reliance’ – meaning, she might have argued that she had been financially harmed due to the false promises made to her. But it would have been difficult and expensive for her to litigate the issue,” said Ms. Adler.
“It also didn’t seem like the physician could remain in the job and develop a positive work relationship with the employer, given that she felt betrayed and misled, and didn’t like the terms of employment, which didn’t match her needs or expectations,” said Ms. Adler.
She added that “most employers are not as unscrupulous and dishonest as this one was. But some employers do play on the fact that younger doctors – especially residents and fellows – tend to be trusting or feel they don’t have negotiation power. They’re often excited to get an offer and sign it without a second thought.”
That’s why she advises physicians to “review the terms of the LOI carefully and make sure you’re comfortable with them before signing it; but know that the real contract to negotiate will be the actual Employment Agreement.”
She also advises physicians not to give notice at their current place of employment until they’ve signed the final contract with the new employer.
On the same page?
Anu Murthy, JD, an attorney and associate contract review specialist at Contract Diagnostics, explained that the LOI is a document that the candidate receives after an interview but before a full contract. Sometimes, the LOI is preceded by a verbal or e-mailed offer, which is less formal.
“An LOI is sometimes called a Term Sheet or Memorandum of Understanding,“ Ms. Murthy told this news organization. “Typically, it lays out key provisions, such as compensation, initial term of the contract, location, and recruitment incentives.” Sometimes it includes mention of staffing, call schedule, malpractice, noncompete covenants, and other components of the position.
Justin Nabity, founder and CEO of Physicians Thrive, a physician financial advisory group, said that LOIs are “a way for employers to gauge a prospective employee’s level of interest.”
The employer “doesn’t want to send a contract with a lot of details before determining whether the candidate is really serious about the position, so the offer letter doesn’t show the whole picture,” Mr. Nabity told this news organization.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, agreed.
“Another way of putting it is that the employer wants to see whether the prospective employee is on the same page. The LOI will typically include some key components that will later appear in a more complete and formal contract, together with other topics and details. Agreeing to those key components signals that indeed you and the employer are in accord,” said Mr. Hursh.
But are you really on the same page with your prospective employer? And if you seem to be on the same page, and you sign the LOI, is that a guarantee that the employer will honor its terms?
Not necessarily, according to the experts. In fact, many LOIs contain some verbiage stating that the letter isn’t binding, which can be confusing. Others suggest that it is binding, but the candidate doesn’t realize that the letter isn’t a formal contract and that the contract may contain details not included in the LOI or may omit details mentioned in the LOI, as happened to Ms. Adler’s unfortunate client.
“One of the pitfalls I see is that doctors sign the LOI without recognizing whether it’s binding or nonbinding,” Ms. Murthy said. “If it’s binding, it creates a legal obligation on your part and could preclude you from further negotiation once you see the contract and feel you’d like to negotiate some of its terms.”
Binding letters are typically offered to candidates after some back-and-forth between the parties, and important terms have been agreed to, which can happen either verbally or via e-mail. Once these agreements have been reached, they’re summarized in a “binding” letter before being extended into a full contract.
“But even if you’ve agreed on the terms verbally, it’s still important to have someone more experienced review the offer letter before signing it,” Ms. Murthy said. “It’s important to understand the ‘legalese’ and what your rights and obligations are before agreeing to anything.”
And certainly, if you receive a binding LOI, you shouldn’t sign anything until you’re sure you’re comfortable with its contents and have more details.
Are “nonbinding” LOIs really not binding?
Even if the LOI is nonbinding, that doesn’t necessarily mean you can sign it and expect to negotiate later. “I see people tripped up when they sign the LOI, thinking they’ll negotiate later,” said Mr. Hursh. “They may not like the terms – for example, they think the compensation is too low – and they figure they’ll work it out at the contract stage, because the LOI is ‘not legally binding.’ “
But because the candidate signed the LOI, “the employer is under the impression that the compensation was acceptable, so now you’ve tied your hands – and the hands of any attorney you may consult down the road – to negotiate those terms.”
Mr. Hursh said he is often consulted by physicians who signed the contract “to get the ball rolling,” thinking that the LOI was “just a meaningless bureaucratic paper.” They need to understand “that the employer wants to make sure they’re in agreement on the basic points before getting into the details,” he said. “Large hospitals with in-house counsel may not want to use their legal department’s valuable time in redrafting terms they thought were acceptable to the candidate, and most practices don’t want to pay a lawyer to draft an LOI and then come back and say, ‘Actually, the physician wants more compensation.’ “
Mr. Nabity summarized: “The LOI is essentially a negotiation tactic to take some of the cards out of the hands of the doctor and commit him or her to something they’re not ready to commit to.” Employers may be playing on the sense of pressure and candidate’s fear that the job will slip through their fingers if they wait too long to sign. “But it’s better to wait longer at this stage before signing even a nonbinding LOI,” he said.
What to do before signing
So how should physicians relate to the LOI? Mr. Nabity advises “working through the details of the offer letter first, going through it carefully and identifying areas of concern, bearing in mind that employers never begin with their best offer.”
He pointed out that physicians “rarely know their value and usually don’t know how to work through the dynamics of compensation, call schedules, additional incentives, bonuses, and productivity,” so they need to be informed about these areas before signing anything.
Ms. Murthy recommended “going back and saying [to the prospective employer], ‘Thank you, but I need time to consider and evaluate this offer.’ Then, do some due diligence.”
At that point, you can hire an attorney to go over the offer, educate yourself about compensation benchmarks and what your worth actually is, or consult another trained professional or more experienced individual who can review the LOI before you sign it.
That’s what Dominique Cleveland, MD, a Texas-based ob.gyn., did when she received an LOI 5 years ago.
“The offer letter from the group practice contained a statement that the group wanted me to come on board, what the salary would be, and the time frame that would be covered in the contract,” she told this news organization. “It mentioned benefits and incentives and relocation, but it was only a short document – maybe one or two pages long.”
At the time that she received her LOI, Dr. Cleveland was completing her residency. She consulted experienced faculty members from her institution to find out whether the terms laid out in the LOI “were the norm and were reasonable.” She was “fairly certain” that the salary was low and this was confirmed by the faculty members she talked to. “So I felt comfortable asking for more [compensation],” she said.
The employer was receptive to her proposed changes, which were included in the more detailed contract that followed. “I can’t say there were any surprises per se in the contract because I had negotiated my salary after receiving the offer letter,” she said. She accepted the position and has been working there ever since.
Dr. Cleveland advises physicians “not to make a decision without speaking to someone who’s experienced and can help you compare what’s out there.”
She also encourages physicians to ask for what they want, whether it’s compensation or something else, such as call schedule or vacation time, without being afraid. “I’m a firm believer that you won’t know what you can get if you don’t ask for it,” she said.
Negotiation tips
Mr. Nabity recommended not agreeing to any terms until you are ready to enter into negotiation, recognizing that negotiation is an “art” that requires skill and training. “Either get trained in negotiation, perhaps taking courses to advocate for yourself – which is rare, and most doctors aren’t likely to do this – or go to a trained advocate, such as a lawyer, who can do so on your behalf.”
You might share your concerns with the person who interviewed you, with the person whose name is on the LOI, or with the recruiter who can advocate on your behalf, Ms. Murthy said. “You can reach out to the recruiter and say, ‘I really appreciate the opportunity, but there are some things in the offer letter I’d like to continue discussing.’ “
When you’re ready to negotiate, be sure to assemble all of your “asks” in a single document rather than going back to the prospective employer with “multiple individual questions multiple times,” Ms. Murthy advised. It’s more efficient and the employer or recruiter will appreciate that.
She also advised couching your request in language that expresses your appreciation for the offer and stating that you would like the agreement to serve the best interests of both parties. “Use open-ended language like that, and ask if it’s all right for you to send back some questions, ask for clarification, or share concerns.”
Most employers “will be fine with that,” Ms. Murthy said. “Most won’t say, ‘This is it, take it or leave it.’ If they do, that’s a red flag for you to reconsider whether you really want to work for this particular employer.”
Mr. Hursh suggested that if you choose to sign the LOI immediately, so as to rapidly let the prospective employer know of your interest, “you should add some type of qualification such as, ‘I’m signing this to express my interest, but accepting the position will be dependent upon a more thorough review of compensation benchmarks,’ for example.”
Mr. Nabity agreed: “You can add a handwritten note to the signed LOI expressing that you’re eager to move forward and proceed with the position, but it shouldn’t be construed as accepting the terms of the LOI until you’ve seen the full contract.
“Remember, health care can’t exist without doctors,” Mr. Nabity said. “Doctors are the star players and should go into the negotiation process recognizing their true worth.”
A version of this article appeared on Medscape.com.
You’ve just received an offer letter from that job you interviewed for. Sometimes you want to let the employer know right away how interested you are. The verbiage says the letter isn’t “binding.” So you eagerly sign on the dotted line. Everything looks great ... until it isn’t.
Attorney Ericka Adler, JD, LLM, a partner at Roetzel & Andress, a Chicago-based law firm that represents physicians and health care professionals nationwide, described her client who was in this predicament. The physician, a dermatologist, left a practice where she had been employed because she had received an “amazing” offer letter that included promises about her new work location, staffing, equipment, and hours. She signed and immediately gave notice to her previous employer.
“When she received the actual employment contract, none of those details from the offer letter – which is also called a letter of intent [LOI] – were included,” Ms. Adler told this news organization. The physician wanted to have the details from the LOI formally spelled out in the contract, but the employer refused.
“Basically, they said, ‘This is our standard contract and you’ll just have to trust us that we’ll keep our word. We meant what we said in the LOI, but we cannot include those details in the actual agreement because everyone has the same form of agreement.’ “ The physician decided to sign the contract and accept the position.
She contacted Ms. Adler after she had been at her new position for a month. “She had received none of the things they had promised her in the LOI,” Ms. Adler reported. “She lacked the NP and PA support, she lacked the equipment, she didn’t have enough exam rooms. As soon as she started, someone with whom she was sharing call coverage left, and she was expected to take over. The LOI had a cap on the amount of call she would be required to take, but that verbiage didn’t make it into the contract.”
Ms. Adler tried to address this issue with the employer. “We couldn’t say they had literally breached the agreement, but we did list the things that were mentioned in the LOI but on which they hadn’t delivered. We asked them to fix the issue within 10 days.”
The employer argued “that they didn’t have to fulfill anything that wasn’t spelled out in the contract, even if it was in the LOI. In fact, the contract specified clearly that the signed employment agreement was the only agreement and replaced any previous written or oral agreements between the parties.”
The dermatologist ultimately left the new position. “She might have been able to have a legal claim against the employer for breach or perhaps ‘detrimental reliance’ – meaning, she might have argued that she had been financially harmed due to the false promises made to her. But it would have been difficult and expensive for her to litigate the issue,” said Ms. Adler.
“It also didn’t seem like the physician could remain in the job and develop a positive work relationship with the employer, given that she felt betrayed and misled, and didn’t like the terms of employment, which didn’t match her needs or expectations,” said Ms. Adler.
She added that “most employers are not as unscrupulous and dishonest as this one was. But some employers do play on the fact that younger doctors – especially residents and fellows – tend to be trusting or feel they don’t have negotiation power. They’re often excited to get an offer and sign it without a second thought.”
That’s why she advises physicians to “review the terms of the LOI carefully and make sure you’re comfortable with them before signing it; but know that the real contract to negotiate will be the actual Employment Agreement.”
She also advises physicians not to give notice at their current place of employment until they’ve signed the final contract with the new employer.
On the same page?
Anu Murthy, JD, an attorney and associate contract review specialist at Contract Diagnostics, explained that the LOI is a document that the candidate receives after an interview but before a full contract. Sometimes, the LOI is preceded by a verbal or e-mailed offer, which is less formal.
“An LOI is sometimes called a Term Sheet or Memorandum of Understanding,“ Ms. Murthy told this news organization. “Typically, it lays out key provisions, such as compensation, initial term of the contract, location, and recruitment incentives.” Sometimes it includes mention of staffing, call schedule, malpractice, noncompete covenants, and other components of the position.
Justin Nabity, founder and CEO of Physicians Thrive, a physician financial advisory group, said that LOIs are “a way for employers to gauge a prospective employee’s level of interest.”
The employer “doesn’t want to send a contract with a lot of details before determining whether the candidate is really serious about the position, so the offer letter doesn’t show the whole picture,” Mr. Nabity told this news organization.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, agreed.
“Another way of putting it is that the employer wants to see whether the prospective employee is on the same page. The LOI will typically include some key components that will later appear in a more complete and formal contract, together with other topics and details. Agreeing to those key components signals that indeed you and the employer are in accord,” said Mr. Hursh.
But are you really on the same page with your prospective employer? And if you seem to be on the same page, and you sign the LOI, is that a guarantee that the employer will honor its terms?
Not necessarily, according to the experts. In fact, many LOIs contain some verbiage stating that the letter isn’t binding, which can be confusing. Others suggest that it is binding, but the candidate doesn’t realize that the letter isn’t a formal contract and that the contract may contain details not included in the LOI or may omit details mentioned in the LOI, as happened to Ms. Adler’s unfortunate client.
“One of the pitfalls I see is that doctors sign the LOI without recognizing whether it’s binding or nonbinding,” Ms. Murthy said. “If it’s binding, it creates a legal obligation on your part and could preclude you from further negotiation once you see the contract and feel you’d like to negotiate some of its terms.”
Binding letters are typically offered to candidates after some back-and-forth between the parties, and important terms have been agreed to, which can happen either verbally or via e-mail. Once these agreements have been reached, they’re summarized in a “binding” letter before being extended into a full contract.
“But even if you’ve agreed on the terms verbally, it’s still important to have someone more experienced review the offer letter before signing it,” Ms. Murthy said. “It’s important to understand the ‘legalese’ and what your rights and obligations are before agreeing to anything.”
And certainly, if you receive a binding LOI, you shouldn’t sign anything until you’re sure you’re comfortable with its contents and have more details.
Are “nonbinding” LOIs really not binding?
Even if the LOI is nonbinding, that doesn’t necessarily mean you can sign it and expect to negotiate later. “I see people tripped up when they sign the LOI, thinking they’ll negotiate later,” said Mr. Hursh. “They may not like the terms – for example, they think the compensation is too low – and they figure they’ll work it out at the contract stage, because the LOI is ‘not legally binding.’ “
But because the candidate signed the LOI, “the employer is under the impression that the compensation was acceptable, so now you’ve tied your hands – and the hands of any attorney you may consult down the road – to negotiate those terms.”
Mr. Hursh said he is often consulted by physicians who signed the contract “to get the ball rolling,” thinking that the LOI was “just a meaningless bureaucratic paper.” They need to understand “that the employer wants to make sure they’re in agreement on the basic points before getting into the details,” he said. “Large hospitals with in-house counsel may not want to use their legal department’s valuable time in redrafting terms they thought were acceptable to the candidate, and most practices don’t want to pay a lawyer to draft an LOI and then come back and say, ‘Actually, the physician wants more compensation.’ “
Mr. Nabity summarized: “The LOI is essentially a negotiation tactic to take some of the cards out of the hands of the doctor and commit him or her to something they’re not ready to commit to.” Employers may be playing on the sense of pressure and candidate’s fear that the job will slip through their fingers if they wait too long to sign. “But it’s better to wait longer at this stage before signing even a nonbinding LOI,” he said.
What to do before signing
So how should physicians relate to the LOI? Mr. Nabity advises “working through the details of the offer letter first, going through it carefully and identifying areas of concern, bearing in mind that employers never begin with their best offer.”
He pointed out that physicians “rarely know their value and usually don’t know how to work through the dynamics of compensation, call schedules, additional incentives, bonuses, and productivity,” so they need to be informed about these areas before signing anything.
Ms. Murthy recommended “going back and saying [to the prospective employer], ‘Thank you, but I need time to consider and evaluate this offer.’ Then, do some due diligence.”
At that point, you can hire an attorney to go over the offer, educate yourself about compensation benchmarks and what your worth actually is, or consult another trained professional or more experienced individual who can review the LOI before you sign it.
That’s what Dominique Cleveland, MD, a Texas-based ob.gyn., did when she received an LOI 5 years ago.
“The offer letter from the group practice contained a statement that the group wanted me to come on board, what the salary would be, and the time frame that would be covered in the contract,” she told this news organization. “It mentioned benefits and incentives and relocation, but it was only a short document – maybe one or two pages long.”
At the time that she received her LOI, Dr. Cleveland was completing her residency. She consulted experienced faculty members from her institution to find out whether the terms laid out in the LOI “were the norm and were reasonable.” She was “fairly certain” that the salary was low and this was confirmed by the faculty members she talked to. “So I felt comfortable asking for more [compensation],” she said.
The employer was receptive to her proposed changes, which were included in the more detailed contract that followed. “I can’t say there were any surprises per se in the contract because I had negotiated my salary after receiving the offer letter,” she said. She accepted the position and has been working there ever since.
Dr. Cleveland advises physicians “not to make a decision without speaking to someone who’s experienced and can help you compare what’s out there.”
She also encourages physicians to ask for what they want, whether it’s compensation or something else, such as call schedule or vacation time, without being afraid. “I’m a firm believer that you won’t know what you can get if you don’t ask for it,” she said.
Negotiation tips
Mr. Nabity recommended not agreeing to any terms until you are ready to enter into negotiation, recognizing that negotiation is an “art” that requires skill and training. “Either get trained in negotiation, perhaps taking courses to advocate for yourself – which is rare, and most doctors aren’t likely to do this – or go to a trained advocate, such as a lawyer, who can do so on your behalf.”
You might share your concerns with the person who interviewed you, with the person whose name is on the LOI, or with the recruiter who can advocate on your behalf, Ms. Murthy said. “You can reach out to the recruiter and say, ‘I really appreciate the opportunity, but there are some things in the offer letter I’d like to continue discussing.’ “
When you’re ready to negotiate, be sure to assemble all of your “asks” in a single document rather than going back to the prospective employer with “multiple individual questions multiple times,” Ms. Murthy advised. It’s more efficient and the employer or recruiter will appreciate that.
She also advised couching your request in language that expresses your appreciation for the offer and stating that you would like the agreement to serve the best interests of both parties. “Use open-ended language like that, and ask if it’s all right for you to send back some questions, ask for clarification, or share concerns.”
Most employers “will be fine with that,” Ms. Murthy said. “Most won’t say, ‘This is it, take it or leave it.’ If they do, that’s a red flag for you to reconsider whether you really want to work for this particular employer.”
Mr. Hursh suggested that if you choose to sign the LOI immediately, so as to rapidly let the prospective employer know of your interest, “you should add some type of qualification such as, ‘I’m signing this to express my interest, but accepting the position will be dependent upon a more thorough review of compensation benchmarks,’ for example.”
Mr. Nabity agreed: “You can add a handwritten note to the signed LOI expressing that you’re eager to move forward and proceed with the position, but it shouldn’t be construed as accepting the terms of the LOI until you’ve seen the full contract.
“Remember, health care can’t exist without doctors,” Mr. Nabity said. “Doctors are the star players and should go into the negotiation process recognizing their true worth.”
A version of this article appeared on Medscape.com.
Surgery is falling out of favor in rectal cancer
TOPLINE:
METHODOLOGY:
- The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
- To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
- The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
- Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
- The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
- In that time frame, organ preservation increased from 19.5% to 32.5% – a percent increase of about 67% – for patients with stage 2A-C disease, 16.2% to 29.1% – a percent increase of about 80% – for patients with stage 3A-C disease, and 16.5% to 26.6% – a percent increase of about 60% – for those with unknown stages.
- However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer – from 20.3% to 26.4%.
- Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors concluded. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester (N.Y.), was published online in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
- To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
- The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
- Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
- The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
- In that time frame, organ preservation increased from 19.5% to 32.5% – a percent increase of about 67% – for patients with stage 2A-C disease, 16.2% to 29.1% – a percent increase of about 80% – for patients with stage 3A-C disease, and 16.5% to 26.6% – a percent increase of about 60% – for those with unknown stages.
- However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer – from 20.3% to 26.4%.
- Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors concluded. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester (N.Y.), was published online in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
- To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
- The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
- Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
- The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
- In that time frame, organ preservation increased from 19.5% to 32.5% – a percent increase of about 67% – for patients with stage 2A-C disease, 16.2% to 29.1% – a percent increase of about 80% – for patients with stage 3A-C disease, and 16.5% to 26.6% – a percent increase of about 60% – for those with unknown stages.
- However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer – from 20.3% to 26.4%.
- Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors concluded. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester (N.Y.), was published online in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA OKs symplicity renal denervation system for hypertension
the company has announced.
The Symplicity Spyral system, also known as the Symplicity blood pressure procedure, provides a catheter-based approach to denervate the renal arteries using radiofrequency energy.
Back in August, the FDA’s Circulatory System Devices Panel unanimously agreed that the Symplicity Spyral system is safe, but the panel was split on its efficacy and whether the benefits outweighed the risks associated with its use.
As part of the Medtronic SPYRAL HTN Global Clinical Program, more than 25,000 patients have been treated worldwide, both in the presence and absence of medication, and in patients with high baseline cardiovascular risk.
The SPYRAL HTN-OFF study enrolled patients with hypertension whose medications could be stopped at the start of the trial.
The primary effectiveness endpoint was the mean difference in the baseline adjusted 24-hour ambulatory systolic blood pressure (ASBP) from baseline to 3 months after renal denervation or sham procedure. The study showed a statistically significant reduction of 3.9 mm Hg ASBP in patients who received the device, compared with sham-control patients.
The SPYRAL HTN-ON study evaluated patients with uncontrolled hypertension who continued taking their BP medications during treatment with either the Spyral renal denervation device or a sham device.
The primary endpoint was the mean difference in the baseline adjusted 24-hour ambulatory systolic blood pressure at 6 months. The study showed a nonsignificant 24-hour 0.03 mm Hg reduction in ASBP in active-treatment patients, compared with sham-control patients.
“The Symplicity blood pressure procedure is safe and effective, providing significant ‘always-on’ blood pressure reductions for patients,” David Kandzari, MD, chief, Piedmont Heart Institute, Atlanta, and co–principal investigator of the SPYRAL clinical program, said in the news release.
“This approval paves the way for a transformation in hypertension treatment, offering a solution that complements medication and lifestyle changes,” added co–principal investigator Raymond Townsend, MD, with University of Pennsylvania, Philadelphia.
Medtronic notes that patient preference and shared decision-making are key components when considering the Symplicity blood pressure procedure.
In a patient preference study led by Medtronic, when presented with an interventional treatment with BP reduction and potential risks in line with those of the Symplicity blood pressure procedure, approximately one-third of patients were likely to choose the interventional treatment.
Earlier in November, the FDA also approved the Paradise Ultrasound Renal Denervation system (Recor Medical, Otsuka Medical Devices) for the treatment of hypertension.
A version of this article first appeared on Medscape.com.
the company has announced.
The Symplicity Spyral system, also known as the Symplicity blood pressure procedure, provides a catheter-based approach to denervate the renal arteries using radiofrequency energy.
Back in August, the FDA’s Circulatory System Devices Panel unanimously agreed that the Symplicity Spyral system is safe, but the panel was split on its efficacy and whether the benefits outweighed the risks associated with its use.
As part of the Medtronic SPYRAL HTN Global Clinical Program, more than 25,000 patients have been treated worldwide, both in the presence and absence of medication, and in patients with high baseline cardiovascular risk.
The SPYRAL HTN-OFF study enrolled patients with hypertension whose medications could be stopped at the start of the trial.
The primary effectiveness endpoint was the mean difference in the baseline adjusted 24-hour ambulatory systolic blood pressure (ASBP) from baseline to 3 months after renal denervation or sham procedure. The study showed a statistically significant reduction of 3.9 mm Hg ASBP in patients who received the device, compared with sham-control patients.
The SPYRAL HTN-ON study evaluated patients with uncontrolled hypertension who continued taking their BP medications during treatment with either the Spyral renal denervation device or a sham device.
The primary endpoint was the mean difference in the baseline adjusted 24-hour ambulatory systolic blood pressure at 6 months. The study showed a nonsignificant 24-hour 0.03 mm Hg reduction in ASBP in active-treatment patients, compared with sham-control patients.
“The Symplicity blood pressure procedure is safe and effective, providing significant ‘always-on’ blood pressure reductions for patients,” David Kandzari, MD, chief, Piedmont Heart Institute, Atlanta, and co–principal investigator of the SPYRAL clinical program, said in the news release.
“This approval paves the way for a transformation in hypertension treatment, offering a solution that complements medication and lifestyle changes,” added co–principal investigator Raymond Townsend, MD, with University of Pennsylvania, Philadelphia.
Medtronic notes that patient preference and shared decision-making are key components when considering the Symplicity blood pressure procedure.
In a patient preference study led by Medtronic, when presented with an interventional treatment with BP reduction and potential risks in line with those of the Symplicity blood pressure procedure, approximately one-third of patients were likely to choose the interventional treatment.
Earlier in November, the FDA also approved the Paradise Ultrasound Renal Denervation system (Recor Medical, Otsuka Medical Devices) for the treatment of hypertension.
A version of this article first appeared on Medscape.com.
the company has announced.
The Symplicity Spyral system, also known as the Symplicity blood pressure procedure, provides a catheter-based approach to denervate the renal arteries using radiofrequency energy.
Back in August, the FDA’s Circulatory System Devices Panel unanimously agreed that the Symplicity Spyral system is safe, but the panel was split on its efficacy and whether the benefits outweighed the risks associated with its use.
As part of the Medtronic SPYRAL HTN Global Clinical Program, more than 25,000 patients have been treated worldwide, both in the presence and absence of medication, and in patients with high baseline cardiovascular risk.
The SPYRAL HTN-OFF study enrolled patients with hypertension whose medications could be stopped at the start of the trial.
The primary effectiveness endpoint was the mean difference in the baseline adjusted 24-hour ambulatory systolic blood pressure (ASBP) from baseline to 3 months after renal denervation or sham procedure. The study showed a statistically significant reduction of 3.9 mm Hg ASBP in patients who received the device, compared with sham-control patients.
The SPYRAL HTN-ON study evaluated patients with uncontrolled hypertension who continued taking their BP medications during treatment with either the Spyral renal denervation device or a sham device.
The primary endpoint was the mean difference in the baseline adjusted 24-hour ambulatory systolic blood pressure at 6 months. The study showed a nonsignificant 24-hour 0.03 mm Hg reduction in ASBP in active-treatment patients, compared with sham-control patients.
“The Symplicity blood pressure procedure is safe and effective, providing significant ‘always-on’ blood pressure reductions for patients,” David Kandzari, MD, chief, Piedmont Heart Institute, Atlanta, and co–principal investigator of the SPYRAL clinical program, said in the news release.
“This approval paves the way for a transformation in hypertension treatment, offering a solution that complements medication and lifestyle changes,” added co–principal investigator Raymond Townsend, MD, with University of Pennsylvania, Philadelphia.
Medtronic notes that patient preference and shared decision-making are key components when considering the Symplicity blood pressure procedure.
In a patient preference study led by Medtronic, when presented with an interventional treatment with BP reduction and potential risks in line with those of the Symplicity blood pressure procedure, approximately one-third of patients were likely to choose the interventional treatment.
Earlier in November, the FDA also approved the Paradise Ultrasound Renal Denervation system (Recor Medical, Otsuka Medical Devices) for the treatment of hypertension.
A version of this article first appeared on Medscape.com.
