User login
How Does TMS Benefit Patients With Parkinson’s Disease?
In conjunction with exercise, TMS improves motor function, but sham stimulation provides similar results.
MIAMI—For patients with Parkinson’s disease, a regime of transcranial magnetic stimulation (TMS) and aerobic exercise results in motor improvements that are sustained for one month, according to a study presented at the Second Pan American Parkinson’s Disease and Movement Disorders Congress. Another study by the same researchers indicates that stimulation of two regions in the premotor associative cortex, compared with stimulation of one region, improves axial symptoms in Parkinson’s disease. Both studies suggest that TMS prolongs the cortical silent period.
TMS Prolonged Cortical Silent Period
Aerobic exercise improves the motor symptoms of Parkinson’s disease. A proposed mechanism for this improvement is the enhancement of brain-derived neurotrophic factor (BDNF) signaling or activity. TMS also improves motor symptoms of Parkinson’s disease, and rat studies indicate that it enhances BDNF-tropomyosin receptor kinase B (TrkB) signaling, which is a biomarker of plasticity.
Milton C. Biagioni, MD, Assistant Professor of Neurology at the Marlene and Paolo Fresco Institute for Parkinson’s and Movement Disorders at NYU Langone Health in New York, and colleagues studied differences in BDNF-TrkB signaling between 16 patients with Parkinson’s disease and five healthy controls. Levels of all TrkB signaling biomarkers were significantly higher in healthy controls than in patients with Parkinson’s disease.
Dr. Biagioni and colleagues also investigated the biologic effects, motor outcomes, and physiologic outcomes of repetitive TMS and aerobic exercise in patients with Parkinson’s disease in a randomized, double-blind trial. In this trial, 16 patients with Parkinson’s disease participated in daily 40-minute sessions of aerobic exercise. Participants were randomized 1:1 to receive high-frequency repetitive TMS or sham stimulation over the motor cortex. Patients exercised on a recumbent linear cross trainer.
Motor outcomes included the Unified Parkinson’s Disease Rating Scale (UPDRS) and Timed Up and Go (TUG) test. Neurophysiologic outcomes included the cortical silent period, motor threshold, and paired-associative stimulation (PAS-25). The researchers obtained peripheral blood lymphocytes from participants in the morning to measure BDNF activity. Outcomes were measured at baseline, two weeks after the intervention, and one month after the intervention.
Among patients with Parkinson’s disease, mean age was about 65. Mean disease duration was eight years, and mean UPDRS III score was 46.4. The researchers found no significant differences at baseline between patients randomized to TMS and those randomized to sham.
BDNF-TrkB signaling increased by 29.3% in the sham group and by 36.6% in the TMS group. Both increases were statistically significant, but the difference between groups was not significant. At one month, the cortical silent period was significantly prolonged after TMS, compared with sham. All patients had significant improvement in UPDRS III. Improvements in UPDRS III and TUG were sustained for one month in the TMS group.
Multifocal Stimulation Improved Axial Score
A previous study indicated that low-frequency repetitive TMS over the supplementary motor area (SMA) effectively improves motor symptoms in Parkinson’s disease. Like the SMA, the dorsal premotor cortex (PMd) is involved in motor planning and motor control. Researchers had not previously studied multifocal TMS over both targets, and Dr. Biagioni and colleagues decided to examine this technique.
They conducted a parallel, active-controlled, double-blind, randomized study of four weekly sessions of low-frequency repetitive TMS in 22 patients with Parkinson’s disease. The control group received TMS over the SMA and sham stimulation over the PMd. The experimental group received TMS over both areas. The study outcomes included all components of the UPDRS, as well as UPDRS III axial, tremor, rigidity, and bradykinesia scores. Dr. Biagioni and colleagues assessed patients in the on state at baseline and at four weeks after treatment.
Participants’ mean age was 65, and eight patients were female. Mean disease duration was approximately nine years, mean UPDRS total score was 53.1, and mean UPDRS III score was 35.9. The only significant difference between the control and experimental groups at baseline was Montreal Cognitive Assessment score, which was 24.2 in the control group and 26.4 in the experimental group.
Both interventions were well tolerated. After one month, UPDRS III decreased by 5.5 points in the control group and by 6.5 points in the experimental group. Both changes were statistically significant, but the difference between groups was not significant. The researchers found no difference between groups in total UPDRS and UPDRS III after one month. Axial score significantly decreased in the experimental group, compared with the control group, but the researchers found no significant differences between groups in rigidity, tremor, or bradykinesia scores. In addition, the cortical silent period was significantly prolonged in the experimental group, compared with the control group.
—Erik Greb
Suggested Reading
Chou YH, Hickey PT, Sundman M, et al. Effects of repetitive transcranial magnetic stimulation on motor symptoms in Parkinson disease: a systematic review and meta-analysis. JAMA Neurol. 2015;72(4):432-440.
Shirota Y, Ohtsu H, Hamada M, et al. Supplementary motor area stimulation for Parkinson disease: a randomized controlled study. Neurology. 2013;80(15):1400-1405.
In conjunction with exercise, TMS improves motor function, but sham stimulation provides similar results.
In conjunction with exercise, TMS improves motor function, but sham stimulation provides similar results.
MIAMI—For patients with Parkinson’s disease, a regime of transcranial magnetic stimulation (TMS) and aerobic exercise results in motor improvements that are sustained for one month, according to a study presented at the Second Pan American Parkinson’s Disease and Movement Disorders Congress. Another study by the same researchers indicates that stimulation of two regions in the premotor associative cortex, compared with stimulation of one region, improves axial symptoms in Parkinson’s disease. Both studies suggest that TMS prolongs the cortical silent period.
TMS Prolonged Cortical Silent Period
Aerobic exercise improves the motor symptoms of Parkinson’s disease. A proposed mechanism for this improvement is the enhancement of brain-derived neurotrophic factor (BDNF) signaling or activity. TMS also improves motor symptoms of Parkinson’s disease, and rat studies indicate that it enhances BDNF-tropomyosin receptor kinase B (TrkB) signaling, which is a biomarker of plasticity.
Milton C. Biagioni, MD, Assistant Professor of Neurology at the Marlene and Paolo Fresco Institute for Parkinson’s and Movement Disorders at NYU Langone Health in New York, and colleagues studied differences in BDNF-TrkB signaling between 16 patients with Parkinson’s disease and five healthy controls. Levels of all TrkB signaling biomarkers were significantly higher in healthy controls than in patients with Parkinson’s disease.
Dr. Biagioni and colleagues also investigated the biologic effects, motor outcomes, and physiologic outcomes of repetitive TMS and aerobic exercise in patients with Parkinson’s disease in a randomized, double-blind trial. In this trial, 16 patients with Parkinson’s disease participated in daily 40-minute sessions of aerobic exercise. Participants were randomized 1:1 to receive high-frequency repetitive TMS or sham stimulation over the motor cortex. Patients exercised on a recumbent linear cross trainer.
Motor outcomes included the Unified Parkinson’s Disease Rating Scale (UPDRS) and Timed Up and Go (TUG) test. Neurophysiologic outcomes included the cortical silent period, motor threshold, and paired-associative stimulation (PAS-25). The researchers obtained peripheral blood lymphocytes from participants in the morning to measure BDNF activity. Outcomes were measured at baseline, two weeks after the intervention, and one month after the intervention.
Among patients with Parkinson’s disease, mean age was about 65. Mean disease duration was eight years, and mean UPDRS III score was 46.4. The researchers found no significant differences at baseline between patients randomized to TMS and those randomized to sham.
BDNF-TrkB signaling increased by 29.3% in the sham group and by 36.6% in the TMS group. Both increases were statistically significant, but the difference between groups was not significant. At one month, the cortical silent period was significantly prolonged after TMS, compared with sham. All patients had significant improvement in UPDRS III. Improvements in UPDRS III and TUG were sustained for one month in the TMS group.
Multifocal Stimulation Improved Axial Score
A previous study indicated that low-frequency repetitive TMS over the supplementary motor area (SMA) effectively improves motor symptoms in Parkinson’s disease. Like the SMA, the dorsal premotor cortex (PMd) is involved in motor planning and motor control. Researchers had not previously studied multifocal TMS over both targets, and Dr. Biagioni and colleagues decided to examine this technique.
They conducted a parallel, active-controlled, double-blind, randomized study of four weekly sessions of low-frequency repetitive TMS in 22 patients with Parkinson’s disease. The control group received TMS over the SMA and sham stimulation over the PMd. The experimental group received TMS over both areas. The study outcomes included all components of the UPDRS, as well as UPDRS III axial, tremor, rigidity, and bradykinesia scores. Dr. Biagioni and colleagues assessed patients in the on state at baseline and at four weeks after treatment.
Participants’ mean age was 65, and eight patients were female. Mean disease duration was approximately nine years, mean UPDRS total score was 53.1, and mean UPDRS III score was 35.9. The only significant difference between the control and experimental groups at baseline was Montreal Cognitive Assessment score, which was 24.2 in the control group and 26.4 in the experimental group.
Both interventions were well tolerated. After one month, UPDRS III decreased by 5.5 points in the control group and by 6.5 points in the experimental group. Both changes were statistically significant, but the difference between groups was not significant. The researchers found no difference between groups in total UPDRS and UPDRS III after one month. Axial score significantly decreased in the experimental group, compared with the control group, but the researchers found no significant differences between groups in rigidity, tremor, or bradykinesia scores. In addition, the cortical silent period was significantly prolonged in the experimental group, compared with the control group.
—Erik Greb
Suggested Reading
Chou YH, Hickey PT, Sundman M, et al. Effects of repetitive transcranial magnetic stimulation on motor symptoms in Parkinson disease: a systematic review and meta-analysis. JAMA Neurol. 2015;72(4):432-440.
Shirota Y, Ohtsu H, Hamada M, et al. Supplementary motor area stimulation for Parkinson disease: a randomized controlled study. Neurology. 2013;80(15):1400-1405.
MIAMI—For patients with Parkinson’s disease, a regime of transcranial magnetic stimulation (TMS) and aerobic exercise results in motor improvements that are sustained for one month, according to a study presented at the Second Pan American Parkinson’s Disease and Movement Disorders Congress. Another study by the same researchers indicates that stimulation of two regions in the premotor associative cortex, compared with stimulation of one region, improves axial symptoms in Parkinson’s disease. Both studies suggest that TMS prolongs the cortical silent period.
TMS Prolonged Cortical Silent Period
Aerobic exercise improves the motor symptoms of Parkinson’s disease. A proposed mechanism for this improvement is the enhancement of brain-derived neurotrophic factor (BDNF) signaling or activity. TMS also improves motor symptoms of Parkinson’s disease, and rat studies indicate that it enhances BDNF-tropomyosin receptor kinase B (TrkB) signaling, which is a biomarker of plasticity.
Milton C. Biagioni, MD, Assistant Professor of Neurology at the Marlene and Paolo Fresco Institute for Parkinson’s and Movement Disorders at NYU Langone Health in New York, and colleagues studied differences in BDNF-TrkB signaling between 16 patients with Parkinson’s disease and five healthy controls. Levels of all TrkB signaling biomarkers were significantly higher in healthy controls than in patients with Parkinson’s disease.
Dr. Biagioni and colleagues also investigated the biologic effects, motor outcomes, and physiologic outcomes of repetitive TMS and aerobic exercise in patients with Parkinson’s disease in a randomized, double-blind trial. In this trial, 16 patients with Parkinson’s disease participated in daily 40-minute sessions of aerobic exercise. Participants were randomized 1:1 to receive high-frequency repetitive TMS or sham stimulation over the motor cortex. Patients exercised on a recumbent linear cross trainer.
Motor outcomes included the Unified Parkinson’s Disease Rating Scale (UPDRS) and Timed Up and Go (TUG) test. Neurophysiologic outcomes included the cortical silent period, motor threshold, and paired-associative stimulation (PAS-25). The researchers obtained peripheral blood lymphocytes from participants in the morning to measure BDNF activity. Outcomes were measured at baseline, two weeks after the intervention, and one month after the intervention.
Among patients with Parkinson’s disease, mean age was about 65. Mean disease duration was eight years, and mean UPDRS III score was 46.4. The researchers found no significant differences at baseline between patients randomized to TMS and those randomized to sham.
BDNF-TrkB signaling increased by 29.3% in the sham group and by 36.6% in the TMS group. Both increases were statistically significant, but the difference between groups was not significant. At one month, the cortical silent period was significantly prolonged after TMS, compared with sham. All patients had significant improvement in UPDRS III. Improvements in UPDRS III and TUG were sustained for one month in the TMS group.
Multifocal Stimulation Improved Axial Score
A previous study indicated that low-frequency repetitive TMS over the supplementary motor area (SMA) effectively improves motor symptoms in Parkinson’s disease. Like the SMA, the dorsal premotor cortex (PMd) is involved in motor planning and motor control. Researchers had not previously studied multifocal TMS over both targets, and Dr. Biagioni and colleagues decided to examine this technique.
They conducted a parallel, active-controlled, double-blind, randomized study of four weekly sessions of low-frequency repetitive TMS in 22 patients with Parkinson’s disease. The control group received TMS over the SMA and sham stimulation over the PMd. The experimental group received TMS over both areas. The study outcomes included all components of the UPDRS, as well as UPDRS III axial, tremor, rigidity, and bradykinesia scores. Dr. Biagioni and colleagues assessed patients in the on state at baseline and at four weeks after treatment.
Participants’ mean age was 65, and eight patients were female. Mean disease duration was approximately nine years, mean UPDRS total score was 53.1, and mean UPDRS III score was 35.9. The only significant difference between the control and experimental groups at baseline was Montreal Cognitive Assessment score, which was 24.2 in the control group and 26.4 in the experimental group.
Both interventions were well tolerated. After one month, UPDRS III decreased by 5.5 points in the control group and by 6.5 points in the experimental group. Both changes were statistically significant, but the difference between groups was not significant. The researchers found no difference between groups in total UPDRS and UPDRS III after one month. Axial score significantly decreased in the experimental group, compared with the control group, but the researchers found no significant differences between groups in rigidity, tremor, or bradykinesia scores. In addition, the cortical silent period was significantly prolonged in the experimental group, compared with the control group.
—Erik Greb
Suggested Reading
Chou YH, Hickey PT, Sundman M, et al. Effects of repetitive transcranial magnetic stimulation on motor symptoms in Parkinson disease: a systematic review and meta-analysis. JAMA Neurol. 2015;72(4):432-440.
Shirota Y, Ohtsu H, Hamada M, et al. Supplementary motor area stimulation for Parkinson disease: a randomized controlled study. Neurology. 2013;80(15):1400-1405.
'Follow your passion' not always good career advice
“Follow your passion” has long been a self-help mantra when it comes to a career. The idea has been that doing what you love will provide the fuel for success. The thinking goes back decades to Richard Bolles’s self-published 1972 classic “What Color is Your Parachute”. The thinking has inspired countless career aspirants, including business titans.
“You’ve got to find what you love. … The only way to do great work is to love what you do. If you haven’t found it yet, keep looking, and don’t settle,” related the late Apple founder Steve Jobs in a commencement address delivered in 2005 at Stanford (Calif.) University. For Mr. Jobs and others over the past 4 decades, the bedrock foundation of a career is passion for the work and dreaming the big dream.
Cal Newport, the author of “So Good They Can’t Ignore You” (New York: Business Plus, 2012), takes the polar opposite view. The job-passion trail has little to do with why most people love the work they do, and can spawn anxiety and a pattern of moving from one job to another, according to Mr. Newport. Rather, passion for the job comes after the hours of hard work that are needed to become really good at something. How the work is done is more important than what the work is.
In “Designing Your Life” (New York: Alfred A. Knopf, 2016), Bill Burnett and Dave Evans go even further, arguing that a career based on passion is usually useless and sometimes dangerous, since many people don’t know what they are passionate about or are passionate about something that is a clunker from a career perspective. Following your passion can lead to chasing pipe dreams.
A better tact might be to insert “interest” instead of “passion” when pondering career choices, according to Crystal Holly, PhD, a clinical psychologist in Ottawa. she said in an interview for the article published on the website of the Canadian Broadcasting Corporation (CBC).
Looking at interests more abstractly, rather than setting up a score sheet of definitive career goals, can be helpful, according to career coach Jen Polk, PhD, since that approach can lead to work areas not previously considered, which prove to be satisfying and fulfilling.
The path of job passion worked for Steve Jobs. But it might not be the way for many people.
Click here to read the CBC article.
“Follow your passion” has long been a self-help mantra when it comes to a career. The idea has been that doing what you love will provide the fuel for success. The thinking goes back decades to Richard Bolles’s self-published 1972 classic “What Color is Your Parachute”. The thinking has inspired countless career aspirants, including business titans.
“You’ve got to find what you love. … The only way to do great work is to love what you do. If you haven’t found it yet, keep looking, and don’t settle,” related the late Apple founder Steve Jobs in a commencement address delivered in 2005 at Stanford (Calif.) University. For Mr. Jobs and others over the past 4 decades, the bedrock foundation of a career is passion for the work and dreaming the big dream.
Cal Newport, the author of “So Good They Can’t Ignore You” (New York: Business Plus, 2012), takes the polar opposite view. The job-passion trail has little to do with why most people love the work they do, and can spawn anxiety and a pattern of moving from one job to another, according to Mr. Newport. Rather, passion for the job comes after the hours of hard work that are needed to become really good at something. How the work is done is more important than what the work is.
In “Designing Your Life” (New York: Alfred A. Knopf, 2016), Bill Burnett and Dave Evans go even further, arguing that a career based on passion is usually useless and sometimes dangerous, since many people don’t know what they are passionate about or are passionate about something that is a clunker from a career perspective. Following your passion can lead to chasing pipe dreams.
A better tact might be to insert “interest” instead of “passion” when pondering career choices, according to Crystal Holly, PhD, a clinical psychologist in Ottawa. she said in an interview for the article published on the website of the Canadian Broadcasting Corporation (CBC).
Looking at interests more abstractly, rather than setting up a score sheet of definitive career goals, can be helpful, according to career coach Jen Polk, PhD, since that approach can lead to work areas not previously considered, which prove to be satisfying and fulfilling.
The path of job passion worked for Steve Jobs. But it might not be the way for many people.
Click here to read the CBC article.
“Follow your passion” has long been a self-help mantra when it comes to a career. The idea has been that doing what you love will provide the fuel for success. The thinking goes back decades to Richard Bolles’s self-published 1972 classic “What Color is Your Parachute”. The thinking has inspired countless career aspirants, including business titans.
“You’ve got to find what you love. … The only way to do great work is to love what you do. If you haven’t found it yet, keep looking, and don’t settle,” related the late Apple founder Steve Jobs in a commencement address delivered in 2005 at Stanford (Calif.) University. For Mr. Jobs and others over the past 4 decades, the bedrock foundation of a career is passion for the work and dreaming the big dream.
Cal Newport, the author of “So Good They Can’t Ignore You” (New York: Business Plus, 2012), takes the polar opposite view. The job-passion trail has little to do with why most people love the work they do, and can spawn anxiety and a pattern of moving from one job to another, according to Mr. Newport. Rather, passion for the job comes after the hours of hard work that are needed to become really good at something. How the work is done is more important than what the work is.
In “Designing Your Life” (New York: Alfred A. Knopf, 2016), Bill Burnett and Dave Evans go even further, arguing that a career based on passion is usually useless and sometimes dangerous, since many people don’t know what they are passionate about or are passionate about something that is a clunker from a career perspective. Following your passion can lead to chasing pipe dreams.
A better tact might be to insert “interest” instead of “passion” when pondering career choices, according to Crystal Holly, PhD, a clinical psychologist in Ottawa. she said in an interview for the article published on the website of the Canadian Broadcasting Corporation (CBC).
Looking at interests more abstractly, rather than setting up a score sheet of definitive career goals, can be helpful, according to career coach Jen Polk, PhD, since that approach can lead to work areas not previously considered, which prove to be satisfying and fulfilling.
The path of job passion worked for Steve Jobs. But it might not be the way for many people.
Click here to read the CBC article.
Putting the brakes on ‘virality’
The Internet can be the antithesis of pondering before doing. “Take a breath,” “count to 10,” and “sleep on it” are all pearls of wisdom meant to keep people from doing or saying something that they will regret later. But the world of Facebook, Twitter, and WhatsApp is rife with rude responses and is a conduit for “virality” – the global dissemination of information.
The information can be silly and harmless. But it also can be false and damaging. A compelling example of the latter is the meddling in the 2016 U.S. presidential election by Russian operatives via Facebook.
The information also can prove lethal. An article in The Economist cites the example of at least two dozen people who were killed in India after stories linking them (falsely) to child abductions went viral on WhatsApp, a messaging service owned by Facebook.
Part of the problem with WhatsApp has been the capability of mass dissemination of a post. Since WhatsApp is not fueled by advertiser revenue, a drop in traffic does not affect the financial bottom line. A similar limit on Facebook and Twitter seems harder to envision.
And yet, the move could prove wise, according to the article. “The short-term pain caused by a decline in virality may be in the long-term interest of the social networks. Fake news and concerns about digital addiction, among other things, have already damaged the reputations of tech platforms. Moves to slow sharing could help see off draconian action by regulators and lawmakers,” according to the authors.
More than half the population of the planet uses the Internet. Fostering a climate of honest exchange of information and limiting the spread of malicious information could have a transformative effect.
Click here to read The Economist article.
The Internet can be the antithesis of pondering before doing. “Take a breath,” “count to 10,” and “sleep on it” are all pearls of wisdom meant to keep people from doing or saying something that they will regret later. But the world of Facebook, Twitter, and WhatsApp is rife with rude responses and is a conduit for “virality” – the global dissemination of information.
The information can be silly and harmless. But it also can be false and damaging. A compelling example of the latter is the meddling in the 2016 U.S. presidential election by Russian operatives via Facebook.
The information also can prove lethal. An article in The Economist cites the example of at least two dozen people who were killed in India after stories linking them (falsely) to child abductions went viral on WhatsApp, a messaging service owned by Facebook.
Part of the problem with WhatsApp has been the capability of mass dissemination of a post. Since WhatsApp is not fueled by advertiser revenue, a drop in traffic does not affect the financial bottom line. A similar limit on Facebook and Twitter seems harder to envision.
And yet, the move could prove wise, according to the article. “The short-term pain caused by a decline in virality may be in the long-term interest of the social networks. Fake news and concerns about digital addiction, among other things, have already damaged the reputations of tech platforms. Moves to slow sharing could help see off draconian action by regulators and lawmakers,” according to the authors.
More than half the population of the planet uses the Internet. Fostering a climate of honest exchange of information and limiting the spread of malicious information could have a transformative effect.
Click here to read The Economist article.
The Internet can be the antithesis of pondering before doing. “Take a breath,” “count to 10,” and “sleep on it” are all pearls of wisdom meant to keep people from doing or saying something that they will regret later. But the world of Facebook, Twitter, and WhatsApp is rife with rude responses and is a conduit for “virality” – the global dissemination of information.
The information can be silly and harmless. But it also can be false and damaging. A compelling example of the latter is the meddling in the 2016 U.S. presidential election by Russian operatives via Facebook.
The information also can prove lethal. An article in The Economist cites the example of at least two dozen people who were killed in India after stories linking them (falsely) to child abductions went viral on WhatsApp, a messaging service owned by Facebook.
Part of the problem with WhatsApp has been the capability of mass dissemination of a post. Since WhatsApp is not fueled by advertiser revenue, a drop in traffic does not affect the financial bottom line. A similar limit on Facebook and Twitter seems harder to envision.
And yet, the move could prove wise, according to the article. “The short-term pain caused by a decline in virality may be in the long-term interest of the social networks. Fake news and concerns about digital addiction, among other things, have already damaged the reputations of tech platforms. Moves to slow sharing could help see off draconian action by regulators and lawmakers,” according to the authors.
More than half the population of the planet uses the Internet. Fostering a climate of honest exchange of information and limiting the spread of malicious information could have a transformative effect.
Click here to read The Economist article.
Labor induction at 39 weeks reduced cesarean rate for low-risk, first-time mothers
Nulliparous women who were induced at 39 weeks had the same relative risk of adverse perinatal outcomes but a lower risk of a cesarean delivery, compared with women who received expectant management, results that researchers say contrast traditional recommendations for perinatal care, according to study from the New England Journal of Medicine.
“These findings contradict the conclusions of multiple observational studies that have suggested that labor induction is associated with an increased risk of adverse maternal and perinatal outcomes,” William A. Grobman, MD, the Arthur Hale Curtis, MD, Professor of Obstetrics and Gynecology at Northwestern University in Chicago, and his colleagues wrote. “These studies, however, compared women who underwent labor induction with those who had spontaneous labor, which is not a comparison that is useful to guide clinical decision making.”
Dr. Grobman and his colleagues evaluated the deliveries of 3,062 women who underwent labor induction between 39 weeks of gestation and 39 weeks and 4 days of gestation, and compared them with outcomes of 3,044 women who received expectant management until 40 weeks and 5 days of gestation. Women in both groups had a singleton fetus, no indication of early delivery, and did not plan on delivering by C-section. The participants were assessed again at about 38 weeks of gestation and randomly assigned to receive labor induction or expectant management as part of a multicenter randomized, controlled, parallel-group, unmasked trial in 41 maternal-fetal medicine departments in hospitals participating in the Eunice Kennedy Shriver National Institute of Child Health and Human Development network screened between March 2014, and August 2017.
Primary perinatal outcomes and components were defined as perinatal death, respiratory support, an Apgar score of 3 or less at 5 minutes, hypoxic-ischemic encephalopathy, seizure, infection, meconium aspiration syndrome, birth trauma, intracranial or subgaleal hemorrhage, or hypotension that requires vasopressor support. The principal secondary outcome was cesarean delivery, but other secondary outcomes included neonatal or intensive care, infection, postpartum hospital stay, and hypertension, among others.
Dr. Grobman and his colleagues found 132 (4.3%) of neonates in the induction group and 164 (5.4%) in the expectant-management group experienced a primary composite outcome (relative risk, 0.80; 95% confidence interval, 0.64-1.00; P = .049).
Regarding secondary outcomes, there was a significantly lower risk of cesarean delivery in the induction group, with 18.6% of women undergoing a cesarean delivery, compared with 22.2% of women in the expectant-management group (RR, 0.84; 95% CI, 0.76-0.93; P less than .001). Women in the labor induction group had a significantly lower relative risk of hypertensive disorders of pregnancy (9.1%), compared with the expectant-management (14.1%) group (RR, 0.64; 95% CI, 0.56-0.74; P less than .001). The investigators said women who underwent induced labor had lower 10-point Likert scale scores, were more likely to have “extensions of the uterine incision during cesarean delivery,” perceived they had “more control” during delivery, and had a shorter postpartum stay in the hospital, compared with women who received expectant management. However, women in the induced labor group also had a longer stay in the labor and delivery units, they said.
The researchers noted the limitations in this study, which included its unmasked design, lack of power to detect infrequent outcome differences, and the lack of information surrounding labor induction at 39 weeks in low-risk nulliparous women.
“These results suggest that policies aimed at the avoidance of elective labor induction among low-risk nulliparous women at 39 weeks of gestation are unlikely to reduce the rate of cesarean delivery on a population level; the trial provides information that can be incorporated into discussions that rely on principles of shared decision making,” Dr. Grobman and his colleagues wrote.
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Silver reports receiving personal fees from Gestavision. The other authors report no relevant financial disclosures.
SOURCE: Grobman WA et al. N Engl J Med. 2018 Aug 9. doi: 10.1056/NEJMoa1800566.
Of the more than 50,000 women screened for the study by Grobman et al., there were more than 44,000 women excluded and more than 16,000 did not participate in the trial. Further, the study participants tended to be younger and comprised more black or Hispanic women than the general population of mothers in the United States, Michael F. Greene, MD, said in a related editorial.
“Readers can only speculate as to why so many women declined to participate in the trial and what implications the demographics of the participants may have for the generalizability of the trial results and the acceptability of elective induction of labor at 39 weeks among women in the United States more generally,” Dr. Greene said. “If induction at 39 weeks becomes a widely popular option, busy obstetrical centers will need to find new ways to accommodate larger numbers of women with longer lengths of stay in the labor and delivery unit.”
Nevertheless, the study reflects a “public preference for a less interventionist approach” to delivery, Dr. Greene said, and the interest is backed by available data. He cited a meta-analysis of 20 randomized trials that found inducing labor at 39 weeks may reduce perinatal morality while not increasing the risk of operative deliveries. Specifically, he noted a randomized trial from the United Kingdom found induction of labor among 619 women at 39 weeks who were at least 35 years old did not affect the participants’ perception of delivery or increase the number of operative deliveries.
“These results across multiple obstetrical centers in the United States, however, should reassure women that elective induction of labor at 39 weeks is a reasonable choice that is very unlikely to result in poorer obstetrical outcomes,” he said.
Dr. Greene is chief of obstetrics and gynecology at Massachusetts General Hospital in Boston. He reported no relevant conflicts of interest. These comments summarize his editorial accompanying the article by Dr. Grobman and his associates ( N Engl J Med. 2018 Aug 9;379[6]:580-1 ).
Of the more than 50,000 women screened for the study by Grobman et al., there were more than 44,000 women excluded and more than 16,000 did not participate in the trial. Further, the study participants tended to be younger and comprised more black or Hispanic women than the general population of mothers in the United States, Michael F. Greene, MD, said in a related editorial.
“Readers can only speculate as to why so many women declined to participate in the trial and what implications the demographics of the participants may have for the generalizability of the trial results and the acceptability of elective induction of labor at 39 weeks among women in the United States more generally,” Dr. Greene said. “If induction at 39 weeks becomes a widely popular option, busy obstetrical centers will need to find new ways to accommodate larger numbers of women with longer lengths of stay in the labor and delivery unit.”
Nevertheless, the study reflects a “public preference for a less interventionist approach” to delivery, Dr. Greene said, and the interest is backed by available data. He cited a meta-analysis of 20 randomized trials that found inducing labor at 39 weeks may reduce perinatal morality while not increasing the risk of operative deliveries. Specifically, he noted a randomized trial from the United Kingdom found induction of labor among 619 women at 39 weeks who were at least 35 years old did not affect the participants’ perception of delivery or increase the number of operative deliveries.
“These results across multiple obstetrical centers in the United States, however, should reassure women that elective induction of labor at 39 weeks is a reasonable choice that is very unlikely to result in poorer obstetrical outcomes,” he said.
Dr. Greene is chief of obstetrics and gynecology at Massachusetts General Hospital in Boston. He reported no relevant conflicts of interest. These comments summarize his editorial accompanying the article by Dr. Grobman and his associates ( N Engl J Med. 2018 Aug 9;379[6]:580-1 ).
Of the more than 50,000 women screened for the study by Grobman et al., there were more than 44,000 women excluded and more than 16,000 did not participate in the trial. Further, the study participants tended to be younger and comprised more black or Hispanic women than the general population of mothers in the United States, Michael F. Greene, MD, said in a related editorial.
“Readers can only speculate as to why so many women declined to participate in the trial and what implications the demographics of the participants may have for the generalizability of the trial results and the acceptability of elective induction of labor at 39 weeks among women in the United States more generally,” Dr. Greene said. “If induction at 39 weeks becomes a widely popular option, busy obstetrical centers will need to find new ways to accommodate larger numbers of women with longer lengths of stay in the labor and delivery unit.”
Nevertheless, the study reflects a “public preference for a less interventionist approach” to delivery, Dr. Greene said, and the interest is backed by available data. He cited a meta-analysis of 20 randomized trials that found inducing labor at 39 weeks may reduce perinatal morality while not increasing the risk of operative deliveries. Specifically, he noted a randomized trial from the United Kingdom found induction of labor among 619 women at 39 weeks who were at least 35 years old did not affect the participants’ perception of delivery or increase the number of operative deliveries.
“These results across multiple obstetrical centers in the United States, however, should reassure women that elective induction of labor at 39 weeks is a reasonable choice that is very unlikely to result in poorer obstetrical outcomes,” he said.
Dr. Greene is chief of obstetrics and gynecology at Massachusetts General Hospital in Boston. He reported no relevant conflicts of interest. These comments summarize his editorial accompanying the article by Dr. Grobman and his associates ( N Engl J Med. 2018 Aug 9;379[6]:580-1 ).
Nulliparous women who were induced at 39 weeks had the same relative risk of adverse perinatal outcomes but a lower risk of a cesarean delivery, compared with women who received expectant management, results that researchers say contrast traditional recommendations for perinatal care, according to study from the New England Journal of Medicine.
“These findings contradict the conclusions of multiple observational studies that have suggested that labor induction is associated with an increased risk of adverse maternal and perinatal outcomes,” William A. Grobman, MD, the Arthur Hale Curtis, MD, Professor of Obstetrics and Gynecology at Northwestern University in Chicago, and his colleagues wrote. “These studies, however, compared women who underwent labor induction with those who had spontaneous labor, which is not a comparison that is useful to guide clinical decision making.”
Dr. Grobman and his colleagues evaluated the deliveries of 3,062 women who underwent labor induction between 39 weeks of gestation and 39 weeks and 4 days of gestation, and compared them with outcomes of 3,044 women who received expectant management until 40 weeks and 5 days of gestation. Women in both groups had a singleton fetus, no indication of early delivery, and did not plan on delivering by C-section. The participants were assessed again at about 38 weeks of gestation and randomly assigned to receive labor induction or expectant management as part of a multicenter randomized, controlled, parallel-group, unmasked trial in 41 maternal-fetal medicine departments in hospitals participating in the Eunice Kennedy Shriver National Institute of Child Health and Human Development network screened between March 2014, and August 2017.
Primary perinatal outcomes and components were defined as perinatal death, respiratory support, an Apgar score of 3 or less at 5 minutes, hypoxic-ischemic encephalopathy, seizure, infection, meconium aspiration syndrome, birth trauma, intracranial or subgaleal hemorrhage, or hypotension that requires vasopressor support. The principal secondary outcome was cesarean delivery, but other secondary outcomes included neonatal or intensive care, infection, postpartum hospital stay, and hypertension, among others.
Dr. Grobman and his colleagues found 132 (4.3%) of neonates in the induction group and 164 (5.4%) in the expectant-management group experienced a primary composite outcome (relative risk, 0.80; 95% confidence interval, 0.64-1.00; P = .049).
Regarding secondary outcomes, there was a significantly lower risk of cesarean delivery in the induction group, with 18.6% of women undergoing a cesarean delivery, compared with 22.2% of women in the expectant-management group (RR, 0.84; 95% CI, 0.76-0.93; P less than .001). Women in the labor induction group had a significantly lower relative risk of hypertensive disorders of pregnancy (9.1%), compared with the expectant-management (14.1%) group (RR, 0.64; 95% CI, 0.56-0.74; P less than .001). The investigators said women who underwent induced labor had lower 10-point Likert scale scores, were more likely to have “extensions of the uterine incision during cesarean delivery,” perceived they had “more control” during delivery, and had a shorter postpartum stay in the hospital, compared with women who received expectant management. However, women in the induced labor group also had a longer stay in the labor and delivery units, they said.
The researchers noted the limitations in this study, which included its unmasked design, lack of power to detect infrequent outcome differences, and the lack of information surrounding labor induction at 39 weeks in low-risk nulliparous women.
“These results suggest that policies aimed at the avoidance of elective labor induction among low-risk nulliparous women at 39 weeks of gestation are unlikely to reduce the rate of cesarean delivery on a population level; the trial provides information that can be incorporated into discussions that rely on principles of shared decision making,” Dr. Grobman and his colleagues wrote.
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Silver reports receiving personal fees from Gestavision. The other authors report no relevant financial disclosures.
SOURCE: Grobman WA et al. N Engl J Med. 2018 Aug 9. doi: 10.1056/NEJMoa1800566.
Nulliparous women who were induced at 39 weeks had the same relative risk of adverse perinatal outcomes but a lower risk of a cesarean delivery, compared with women who received expectant management, results that researchers say contrast traditional recommendations for perinatal care, according to study from the New England Journal of Medicine.
“These findings contradict the conclusions of multiple observational studies that have suggested that labor induction is associated with an increased risk of adverse maternal and perinatal outcomes,” William A. Grobman, MD, the Arthur Hale Curtis, MD, Professor of Obstetrics and Gynecology at Northwestern University in Chicago, and his colleagues wrote. “These studies, however, compared women who underwent labor induction with those who had spontaneous labor, which is not a comparison that is useful to guide clinical decision making.”
Dr. Grobman and his colleagues evaluated the deliveries of 3,062 women who underwent labor induction between 39 weeks of gestation and 39 weeks and 4 days of gestation, and compared them with outcomes of 3,044 women who received expectant management until 40 weeks and 5 days of gestation. Women in both groups had a singleton fetus, no indication of early delivery, and did not plan on delivering by C-section. The participants were assessed again at about 38 weeks of gestation and randomly assigned to receive labor induction or expectant management as part of a multicenter randomized, controlled, parallel-group, unmasked trial in 41 maternal-fetal medicine departments in hospitals participating in the Eunice Kennedy Shriver National Institute of Child Health and Human Development network screened between March 2014, and August 2017.
Primary perinatal outcomes and components were defined as perinatal death, respiratory support, an Apgar score of 3 or less at 5 minutes, hypoxic-ischemic encephalopathy, seizure, infection, meconium aspiration syndrome, birth trauma, intracranial or subgaleal hemorrhage, or hypotension that requires vasopressor support. The principal secondary outcome was cesarean delivery, but other secondary outcomes included neonatal or intensive care, infection, postpartum hospital stay, and hypertension, among others.
Dr. Grobman and his colleagues found 132 (4.3%) of neonates in the induction group and 164 (5.4%) in the expectant-management group experienced a primary composite outcome (relative risk, 0.80; 95% confidence interval, 0.64-1.00; P = .049).
Regarding secondary outcomes, there was a significantly lower risk of cesarean delivery in the induction group, with 18.6% of women undergoing a cesarean delivery, compared with 22.2% of women in the expectant-management group (RR, 0.84; 95% CI, 0.76-0.93; P less than .001). Women in the labor induction group had a significantly lower relative risk of hypertensive disorders of pregnancy (9.1%), compared with the expectant-management (14.1%) group (RR, 0.64; 95% CI, 0.56-0.74; P less than .001). The investigators said women who underwent induced labor had lower 10-point Likert scale scores, were more likely to have “extensions of the uterine incision during cesarean delivery,” perceived they had “more control” during delivery, and had a shorter postpartum stay in the hospital, compared with women who received expectant management. However, women in the induced labor group also had a longer stay in the labor and delivery units, they said.
The researchers noted the limitations in this study, which included its unmasked design, lack of power to detect infrequent outcome differences, and the lack of information surrounding labor induction at 39 weeks in low-risk nulliparous women.
“These results suggest that policies aimed at the avoidance of elective labor induction among low-risk nulliparous women at 39 weeks of gestation are unlikely to reduce the rate of cesarean delivery on a population level; the trial provides information that can be incorporated into discussions that rely on principles of shared decision making,” Dr. Grobman and his colleagues wrote.
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Silver reports receiving personal fees from Gestavision. The other authors report no relevant financial disclosures.
SOURCE: Grobman WA et al. N Engl J Med. 2018 Aug 9. doi: 10.1056/NEJMoa1800566.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: 18.6% of women in the induced labor group underwent cesarean delivery, compared with 22.2% in the expectant management group.
Study details: A multicenter randomized, controlled, parallel-group, unmasked trial of 6,106 women from 41 maternal-fetal medicine departments in hospitals participating in the Eunice Kennedy Shriver National Institute of Child Health and Human Development network screened between March 2014 and August 2017.
Disclosures: This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Silver reports receiving personal fees from Gestavision. The other authors report no relevant financial disclosures..
Source: Grobman WA et al. N Engl J Med. 2018 Aug 9. doi: 10.1056/NEJMoa1800566.
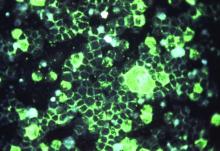
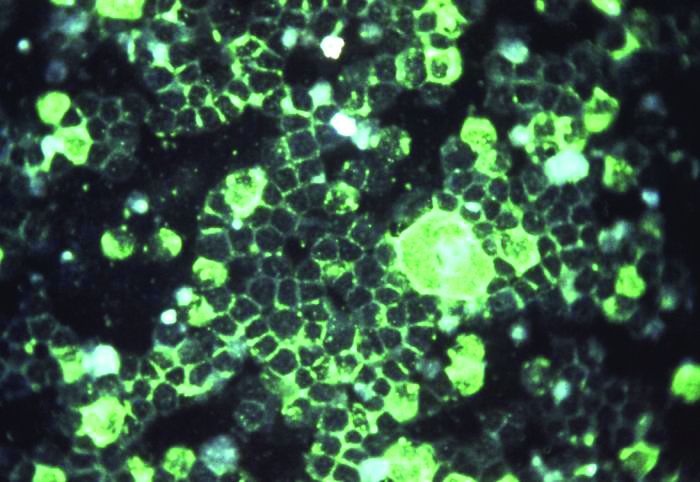
Frequent BCCs linked to blood cancers
New research suggests people who develop frequent cases of basal cell carcinoma (BCC) have an increased risk of leukemias, lymphomas, and other cancers.
“We discovered that people who develop 6 or more basal cell carcinomas during a 10-year period are about 3 times more likely than the general population to develop other, unrelated cancers,” said Kavita Sarin, MD, PhD, of Stanford University School of Medicine in California.
“We’re hopeful that this finding could be a way to identify people at an increased risk for a life-threatening malignancy before those cancers develop.”
Dr Sarin and her colleagues reported their findings in JCI Insight.
Stanford cohort
The researchers first studied 61 patients treated at Stanford Health Care for unusually frequent BCCs—an average of 11 per patient over a 10-year period. The team investigated whether these patients may have mutations in 29 genes that code for DNA damage repair proteins.
“We found that about 20% of the people with frequent basal cell carcinomas have a mutation in one of the genes responsible for repairing DNA damage, versus about 3% of the general population,” Dr Sarin said. “That’s shockingly high.”
Specifically, there were 12 BCC patients (19.7%) who had 13 pathogenic mutations in 12 genes—APC, BARD1, BRCA1, BRCA2, CDH1, CHEK2, MLH1, MSH2, MSH6, MUTYH, NBN, and PALB2. And 3.0% of non-Finnish European subjects in the Exome Aggregation Consortium had pathogenic mutations in these 12 genes.
Furthermore, 21 of the 61 BCC patients (64.4%) had a history of additional cancers. This included 5 hematologic malignancies (leukemia/lymphoma), 5 invasive melanomas, and 2 breast, 2 colon, and 5 prostate cancers.
When the researchers compared the cancer prevalence in these patients to the Surveillance, Epidemiology, and End Results-estimated prevalence of cancer in the 60- to 69-year-old population of European descent, the BCC cohort had an increased risk of any cancer—a relative risk (RR) of 3.5 (P<0.001).
The RR was 3.5 for leukemia and lymphoma (P=0.004), 11.9 for invasive melanoma (P<0.001), 4.5 for colon cancer (P=0.030), 5.6 for breast cancer (P=0.009), and 4.7 for prostate cancer (P<0.001).
Insurance cohort
To confirm the findings in the Stanford cohort, the researchers applied a similar analysis to a large medical insurance claims database, Truven MarketScan.
The database contained 111,562 patients with 1 case of BCC, 13,264 patients with 6 or more BCCs, and 2920 patients with 12 or more BCCs. Truven patients with no history of BCC served as controls.
The researchers adjusted for age and sex and found that patients with 1 BCC, 6 or more BCCs, and 12 or more BCCs had an increased risk of any cancer compared to controls.
The odds ratio (OR) for any cancer was 1.61 for patients with 1 BCC, 3.12 for those with 6 or more BCCs, and 4.15 for patients with 12 or more BCCs.
The OR for Hodgkin lymphoma was 2.27 for patients with 1 BCC, 8.94 for patients with 6 or more BCCs, and 15.41 for patients with 12 or more BCCs.
The OR for non-Hodgkin lymphoma was 1.40 for patients with 1 BCC, 2.59 for patients with 6 or more BCCs, and 3.10 for patients with 12 or more BCCs.
The OR for leukemia was 1.76 for patients with 1 BCC, 3.23 for patients with 6 or more BCCs, and 5.78 for patients with 12 or more BCCs.
The researchers pointed out that, the more BCCs an individual had, the more likely that person was to have had other cancers as well.
“I was surprised to see such a strong correlation, but it’s also very gratifying,” Dr Sarin said. “Now, we can ask patients with repeated basal cell carcinomas whether they have family members with other types of cancers and perhaps suggest that they consider genetic testing and increased screening.”
The researchers are continuing to enroll Stanford patients in their study to learn whether particular mutations in genes responsible for repairing DNA damage are linked to the development of specific malignancies. The team would also like to conduct a similar study in patients with frequent melanomas.
The current study was supported by the Dermatology Foundation, the Stanford Society of Physician Scholars, the American Skin Association, and Pellepharm Inc.
New research suggests people who develop frequent cases of basal cell carcinoma (BCC) have an increased risk of leukemias, lymphomas, and other cancers.
“We discovered that people who develop 6 or more basal cell carcinomas during a 10-year period are about 3 times more likely than the general population to develop other, unrelated cancers,” said Kavita Sarin, MD, PhD, of Stanford University School of Medicine in California.
“We’re hopeful that this finding could be a way to identify people at an increased risk for a life-threatening malignancy before those cancers develop.”
Dr Sarin and her colleagues reported their findings in JCI Insight.
Stanford cohort
The researchers first studied 61 patients treated at Stanford Health Care for unusually frequent BCCs—an average of 11 per patient over a 10-year period. The team investigated whether these patients may have mutations in 29 genes that code for DNA damage repair proteins.
“We found that about 20% of the people with frequent basal cell carcinomas have a mutation in one of the genes responsible for repairing DNA damage, versus about 3% of the general population,” Dr Sarin said. “That’s shockingly high.”
Specifically, there were 12 BCC patients (19.7%) who had 13 pathogenic mutations in 12 genes—APC, BARD1, BRCA1, BRCA2, CDH1, CHEK2, MLH1, MSH2, MSH6, MUTYH, NBN, and PALB2. And 3.0% of non-Finnish European subjects in the Exome Aggregation Consortium had pathogenic mutations in these 12 genes.
Furthermore, 21 of the 61 BCC patients (64.4%) had a history of additional cancers. This included 5 hematologic malignancies (leukemia/lymphoma), 5 invasive melanomas, and 2 breast, 2 colon, and 5 prostate cancers.
When the researchers compared the cancer prevalence in these patients to the Surveillance, Epidemiology, and End Results-estimated prevalence of cancer in the 60- to 69-year-old population of European descent, the BCC cohort had an increased risk of any cancer—a relative risk (RR) of 3.5 (P<0.001).
The RR was 3.5 for leukemia and lymphoma (P=0.004), 11.9 for invasive melanoma (P<0.001), 4.5 for colon cancer (P=0.030), 5.6 for breast cancer (P=0.009), and 4.7 for prostate cancer (P<0.001).
Insurance cohort
To confirm the findings in the Stanford cohort, the researchers applied a similar analysis to a large medical insurance claims database, Truven MarketScan.
The database contained 111,562 patients with 1 case of BCC, 13,264 patients with 6 or more BCCs, and 2920 patients with 12 or more BCCs. Truven patients with no history of BCC served as controls.
The researchers adjusted for age and sex and found that patients with 1 BCC, 6 or more BCCs, and 12 or more BCCs had an increased risk of any cancer compared to controls.
The odds ratio (OR) for any cancer was 1.61 for patients with 1 BCC, 3.12 for those with 6 or more BCCs, and 4.15 for patients with 12 or more BCCs.
The OR for Hodgkin lymphoma was 2.27 for patients with 1 BCC, 8.94 for patients with 6 or more BCCs, and 15.41 for patients with 12 or more BCCs.
The OR for non-Hodgkin lymphoma was 1.40 for patients with 1 BCC, 2.59 for patients with 6 or more BCCs, and 3.10 for patients with 12 or more BCCs.
The OR for leukemia was 1.76 for patients with 1 BCC, 3.23 for patients with 6 or more BCCs, and 5.78 for patients with 12 or more BCCs.
The researchers pointed out that, the more BCCs an individual had, the more likely that person was to have had other cancers as well.
“I was surprised to see such a strong correlation, but it’s also very gratifying,” Dr Sarin said. “Now, we can ask patients with repeated basal cell carcinomas whether they have family members with other types of cancers and perhaps suggest that they consider genetic testing and increased screening.”
The researchers are continuing to enroll Stanford patients in their study to learn whether particular mutations in genes responsible for repairing DNA damage are linked to the development of specific malignancies. The team would also like to conduct a similar study in patients with frequent melanomas.
The current study was supported by the Dermatology Foundation, the Stanford Society of Physician Scholars, the American Skin Association, and Pellepharm Inc.
New research suggests people who develop frequent cases of basal cell carcinoma (BCC) have an increased risk of leukemias, lymphomas, and other cancers.
“We discovered that people who develop 6 or more basal cell carcinomas during a 10-year period are about 3 times more likely than the general population to develop other, unrelated cancers,” said Kavita Sarin, MD, PhD, of Stanford University School of Medicine in California.
“We’re hopeful that this finding could be a way to identify people at an increased risk for a life-threatening malignancy before those cancers develop.”
Dr Sarin and her colleagues reported their findings in JCI Insight.
Stanford cohort
The researchers first studied 61 patients treated at Stanford Health Care for unusually frequent BCCs—an average of 11 per patient over a 10-year period. The team investigated whether these patients may have mutations in 29 genes that code for DNA damage repair proteins.
“We found that about 20% of the people with frequent basal cell carcinomas have a mutation in one of the genes responsible for repairing DNA damage, versus about 3% of the general population,” Dr Sarin said. “That’s shockingly high.”
Specifically, there were 12 BCC patients (19.7%) who had 13 pathogenic mutations in 12 genes—APC, BARD1, BRCA1, BRCA2, CDH1, CHEK2, MLH1, MSH2, MSH6, MUTYH, NBN, and PALB2. And 3.0% of non-Finnish European subjects in the Exome Aggregation Consortium had pathogenic mutations in these 12 genes.
Furthermore, 21 of the 61 BCC patients (64.4%) had a history of additional cancers. This included 5 hematologic malignancies (leukemia/lymphoma), 5 invasive melanomas, and 2 breast, 2 colon, and 5 prostate cancers.
When the researchers compared the cancer prevalence in these patients to the Surveillance, Epidemiology, and End Results-estimated prevalence of cancer in the 60- to 69-year-old population of European descent, the BCC cohort had an increased risk of any cancer—a relative risk (RR) of 3.5 (P<0.001).
The RR was 3.5 for leukemia and lymphoma (P=0.004), 11.9 for invasive melanoma (P<0.001), 4.5 for colon cancer (P=0.030), 5.6 for breast cancer (P=0.009), and 4.7 for prostate cancer (P<0.001).
Insurance cohort
To confirm the findings in the Stanford cohort, the researchers applied a similar analysis to a large medical insurance claims database, Truven MarketScan.
The database contained 111,562 patients with 1 case of BCC, 13,264 patients with 6 or more BCCs, and 2920 patients with 12 or more BCCs. Truven patients with no history of BCC served as controls.
The researchers adjusted for age and sex and found that patients with 1 BCC, 6 or more BCCs, and 12 or more BCCs had an increased risk of any cancer compared to controls.
The odds ratio (OR) for any cancer was 1.61 for patients with 1 BCC, 3.12 for those with 6 or more BCCs, and 4.15 for patients with 12 or more BCCs.
The OR for Hodgkin lymphoma was 2.27 for patients with 1 BCC, 8.94 for patients with 6 or more BCCs, and 15.41 for patients with 12 or more BCCs.
The OR for non-Hodgkin lymphoma was 1.40 for patients with 1 BCC, 2.59 for patients with 6 or more BCCs, and 3.10 for patients with 12 or more BCCs.
The OR for leukemia was 1.76 for patients with 1 BCC, 3.23 for patients with 6 or more BCCs, and 5.78 for patients with 12 or more BCCs.
The researchers pointed out that, the more BCCs an individual had, the more likely that person was to have had other cancers as well.
“I was surprised to see such a strong correlation, but it’s also very gratifying,” Dr Sarin said. “Now, we can ask patients with repeated basal cell carcinomas whether they have family members with other types of cancers and perhaps suggest that they consider genetic testing and increased screening.”
The researchers are continuing to enroll Stanford patients in their study to learn whether particular mutations in genes responsible for repairing DNA damage are linked to the development of specific malignancies. The team would also like to conduct a similar study in patients with frequent melanomas.
The current study was supported by the Dermatology Foundation, the Stanford Society of Physician Scholars, the American Skin Association, and Pellepharm Inc.
NIAAA Ends Funding for Alcohol and CV Health Study
After just 4 months, the National Institute of Alcohol Abuse and Alcoholism (NIAAA) is ending funding for the Moderate Alcohol and Cardiovascular Health (MACH) trial, citing concerns about the study design.
The MACH study was designed as a multicenter randomized trial to determine the effects of 1 serving of alcohol (approximately 15 g) a day compared with no alcohol intake on the rate of new cases of cardiovascular disease and new cases of diabetes among participants free of diabetes at baseline. The study was launched because some epidemiologic research had shown that moderate alcohol consumption had health benefits by reducing risk for coronary artery disease, type 2 diabetes, and rheumatoid arthritis.
The study began enrollment in February 2018 and was suspended on May 10. The NIAAA expected to commit $20 million to the project over 10 years, of which $4 million has been spent; remaining funding came from private donations of $67.7 million, of which $11.8 million has been spent.
The “orderly closeout” is based on recommendations from the advisory committee to the director working group, which found “significant process irregularities in the development of funding opportunities for the MACH funding awards undermined the integrity of the research process.” Additionally, a preliminary report from the National Institutes of Health (NIH) Office of Management Assessment determined that a small number of NIAAA employees violated NIH policies in soliciting gift funding and circumvented standard operating procedures.
After just 4 months, the National Institute of Alcohol Abuse and Alcoholism (NIAAA) is ending funding for the Moderate Alcohol and Cardiovascular Health (MACH) trial, citing concerns about the study design.
The MACH study was designed as a multicenter randomized trial to determine the effects of 1 serving of alcohol (approximately 15 g) a day compared with no alcohol intake on the rate of new cases of cardiovascular disease and new cases of diabetes among participants free of diabetes at baseline. The study was launched because some epidemiologic research had shown that moderate alcohol consumption had health benefits by reducing risk for coronary artery disease, type 2 diabetes, and rheumatoid arthritis.
The study began enrollment in February 2018 and was suspended on May 10. The NIAAA expected to commit $20 million to the project over 10 years, of which $4 million has been spent; remaining funding came from private donations of $67.7 million, of which $11.8 million has been spent.
The “orderly closeout” is based on recommendations from the advisory committee to the director working group, which found “significant process irregularities in the development of funding opportunities for the MACH funding awards undermined the integrity of the research process.” Additionally, a preliminary report from the National Institutes of Health (NIH) Office of Management Assessment determined that a small number of NIAAA employees violated NIH policies in soliciting gift funding and circumvented standard operating procedures.
After just 4 months, the National Institute of Alcohol Abuse and Alcoholism (NIAAA) is ending funding for the Moderate Alcohol and Cardiovascular Health (MACH) trial, citing concerns about the study design.
The MACH study was designed as a multicenter randomized trial to determine the effects of 1 serving of alcohol (approximately 15 g) a day compared with no alcohol intake on the rate of new cases of cardiovascular disease and new cases of diabetes among participants free of diabetes at baseline. The study was launched because some epidemiologic research had shown that moderate alcohol consumption had health benefits by reducing risk for coronary artery disease, type 2 diabetes, and rheumatoid arthritis.
The study began enrollment in February 2018 and was suspended on May 10. The NIAAA expected to commit $20 million to the project over 10 years, of which $4 million has been spent; remaining funding came from private donations of $67.7 million, of which $11.8 million has been spent.
The “orderly closeout” is based on recommendations from the advisory committee to the director working group, which found “significant process irregularities in the development of funding opportunities for the MACH funding awards undermined the integrity of the research process.” Additionally, a preliminary report from the National Institutes of Health (NIH) Office of Management Assessment determined that a small number of NIAAA employees violated NIH policies in soliciting gift funding and circumvented standard operating procedures.
Comprehensive sequencing informs treatment for MM
A comprehensive RNA and DNA sequencing platform can guide treatment decisions for late-stage and drug-resistant multiple myeloma (MM), according to a study published in JCO Precision Oncology.
Researchers used the platform to generate treatment suggestions for 64 MM patients who had exhausted all approved treatment options.
Of the 21 evaluable patients who received the sequencing-recommended therapies, 67% achieved a response. Five patients had ongoing responses at the end of the trial.
“Our study shows how a precision medicine approach incorporating RNA sequencing may identify viable and effective therapeutic options beyond the current FDA-approved armamentarium for multiple myeloma patients,” said study author Samir Parekh, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York.
“The trial has allowed us to test the accuracy of our platform, laying the foundation for our next-generation precision medicine framework.”
Dr Parekh and his colleagues used DNA and RNA sequencing data to generate personalized treatment recommendations for 64 heavily pretreated MM patients.
The patients had received a median of 7 lines of therapy. Most patients (61%) were male, their median age was 59 (range, 40-85), and 67% had high-risk cytogenetics.
The sequencing data yielded treatment recommendations for 63 patients. Twenty-six patients (42%) actually received at least 1 of the recommended treatments.
The treatments (given alone or in combination) were:
- Trametinib (n=16)—recommended because of mutations in NRAS or KRAS
- Venetoclax (n=8)—recommended because of high BCL2 expression
- Panobinostat (n=6)—recommended due to activation of the HDAC pathway and/or by RNA-based drug repurposing selecting the pan-HDAC inhibitor vorinostat
- Dabrafenib (n=1)—recommended because of concurrent BRAF and RAS mutations
- Etoposide (n=2)—selected by RNA-based drug repurposing.
Twenty-one patients were evaluable for response. The researchers noted that 11 of these patients received treatment based on RNA findings, 8 based on DNA, and 2 based on both.
One patient achieved a complete response, 3 had a very good partial response, 10 had a partial response, 2 had a minimal response (25% reduction of disease marker), 3 had stable disease, and 2 progressed.
That means the overall response rate was 66.6% (14/21), and the clinical benefit rate (minimal response or better) was 76.2% (16/21).
The median duration of response was 131 days (range, 37-372), and 5 patients were still in response at the end of the study (September, 1, 2017).
Mount Sinai researchers have received funding to develop a clinical trial that will incorporate machine learning algorithms into this precision medicine platform, which will implement interactive learning techniques to refine the predictions based on a patient’s success with the therapies and a physician’s opinion of the treatment plan.
“This research is part of an accelerating paradigm shift in cancer therapy where treatment may be given based on the specific genomic alterations observed in a patient’s tumor rather than on the tumor histology or tissue type,” said study author Joel Dudley, PhD, of the Icahn School of Medicine at Mount Sinai.
“RNA sequencing will likely complement current precision medicine strategies in the near future due to its ability to capture more dynamic aspects of unique tumor biology and provide information beyond what is capable with DNA alone.”
A comprehensive RNA and DNA sequencing platform can guide treatment decisions for late-stage and drug-resistant multiple myeloma (MM), according to a study published in JCO Precision Oncology.
Researchers used the platform to generate treatment suggestions for 64 MM patients who had exhausted all approved treatment options.
Of the 21 evaluable patients who received the sequencing-recommended therapies, 67% achieved a response. Five patients had ongoing responses at the end of the trial.
“Our study shows how a precision medicine approach incorporating RNA sequencing may identify viable and effective therapeutic options beyond the current FDA-approved armamentarium for multiple myeloma patients,” said study author Samir Parekh, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York.
“The trial has allowed us to test the accuracy of our platform, laying the foundation for our next-generation precision medicine framework.”
Dr Parekh and his colleagues used DNA and RNA sequencing data to generate personalized treatment recommendations for 64 heavily pretreated MM patients.
The patients had received a median of 7 lines of therapy. Most patients (61%) were male, their median age was 59 (range, 40-85), and 67% had high-risk cytogenetics.
The sequencing data yielded treatment recommendations for 63 patients. Twenty-six patients (42%) actually received at least 1 of the recommended treatments.
The treatments (given alone or in combination) were:
- Trametinib (n=16)—recommended because of mutations in NRAS or KRAS
- Venetoclax (n=8)—recommended because of high BCL2 expression
- Panobinostat (n=6)—recommended due to activation of the HDAC pathway and/or by RNA-based drug repurposing selecting the pan-HDAC inhibitor vorinostat
- Dabrafenib (n=1)—recommended because of concurrent BRAF and RAS mutations
- Etoposide (n=2)—selected by RNA-based drug repurposing.
Twenty-one patients were evaluable for response. The researchers noted that 11 of these patients received treatment based on RNA findings, 8 based on DNA, and 2 based on both.
One patient achieved a complete response, 3 had a very good partial response, 10 had a partial response, 2 had a minimal response (25% reduction of disease marker), 3 had stable disease, and 2 progressed.
That means the overall response rate was 66.6% (14/21), and the clinical benefit rate (minimal response or better) was 76.2% (16/21).
The median duration of response was 131 days (range, 37-372), and 5 patients were still in response at the end of the study (September, 1, 2017).
Mount Sinai researchers have received funding to develop a clinical trial that will incorporate machine learning algorithms into this precision medicine platform, which will implement interactive learning techniques to refine the predictions based on a patient’s success with the therapies and a physician’s opinion of the treatment plan.
“This research is part of an accelerating paradigm shift in cancer therapy where treatment may be given based on the specific genomic alterations observed in a patient’s tumor rather than on the tumor histology or tissue type,” said study author Joel Dudley, PhD, of the Icahn School of Medicine at Mount Sinai.
“RNA sequencing will likely complement current precision medicine strategies in the near future due to its ability to capture more dynamic aspects of unique tumor biology and provide information beyond what is capable with DNA alone.”
A comprehensive RNA and DNA sequencing platform can guide treatment decisions for late-stage and drug-resistant multiple myeloma (MM), according to a study published in JCO Precision Oncology.
Researchers used the platform to generate treatment suggestions for 64 MM patients who had exhausted all approved treatment options.
Of the 21 evaluable patients who received the sequencing-recommended therapies, 67% achieved a response. Five patients had ongoing responses at the end of the trial.
“Our study shows how a precision medicine approach incorporating RNA sequencing may identify viable and effective therapeutic options beyond the current FDA-approved armamentarium for multiple myeloma patients,” said study author Samir Parekh, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York.
“The trial has allowed us to test the accuracy of our platform, laying the foundation for our next-generation precision medicine framework.”
Dr Parekh and his colleagues used DNA and RNA sequencing data to generate personalized treatment recommendations for 64 heavily pretreated MM patients.
The patients had received a median of 7 lines of therapy. Most patients (61%) were male, their median age was 59 (range, 40-85), and 67% had high-risk cytogenetics.
The sequencing data yielded treatment recommendations for 63 patients. Twenty-six patients (42%) actually received at least 1 of the recommended treatments.
The treatments (given alone or in combination) were:
- Trametinib (n=16)—recommended because of mutations in NRAS or KRAS
- Venetoclax (n=8)—recommended because of high BCL2 expression
- Panobinostat (n=6)—recommended due to activation of the HDAC pathway and/or by RNA-based drug repurposing selecting the pan-HDAC inhibitor vorinostat
- Dabrafenib (n=1)—recommended because of concurrent BRAF and RAS mutations
- Etoposide (n=2)—selected by RNA-based drug repurposing.
Twenty-one patients were evaluable for response. The researchers noted that 11 of these patients received treatment based on RNA findings, 8 based on DNA, and 2 based on both.
One patient achieved a complete response, 3 had a very good partial response, 10 had a partial response, 2 had a minimal response (25% reduction of disease marker), 3 had stable disease, and 2 progressed.
That means the overall response rate was 66.6% (14/21), and the clinical benefit rate (minimal response or better) was 76.2% (16/21).
The median duration of response was 131 days (range, 37-372), and 5 patients were still in response at the end of the study (September, 1, 2017).
Mount Sinai researchers have received funding to develop a clinical trial that will incorporate machine learning algorithms into this precision medicine platform, which will implement interactive learning techniques to refine the predictions based on a patient’s success with the therapies and a physician’s opinion of the treatment plan.
“This research is part of an accelerating paradigm shift in cancer therapy where treatment may be given based on the specific genomic alterations observed in a patient’s tumor rather than on the tumor histology or tissue type,” said study author Joel Dudley, PhD, of the Icahn School of Medicine at Mount Sinai.
“RNA sequencing will likely complement current precision medicine strategies in the near future due to its ability to capture more dynamic aspects of unique tumor biology and provide information beyond what is capable with DNA alone.”
Tool identifies potential treatment for resistant MM
Researchers say they have developed a computational platform that can be used to identify optimal treatments for multiple myeloma (MM).
Using this tool, the quadratic phenotypic optimization platform (QPOP), the researchers identified a 2-drug combination that proved effective against bortezomib-resistant MM in vitro.
The combination—decitabine and mitomycin C—also decreased tumor volume and prolonged survival in a mouse model of bortezomib-resistant MM.
Masturah Bte Mohd Abdul Rashid, of the Cancer Science Institute of Singapore, and her colleagues reported these results in Science Translational Medicine.
The researchers explained that QPOP approximates biological responses to therapies using advanced mathematical equations. Unlike conventional models, QPOP doesn’t require predetermined information about the mechanisms or composition of a drug.
To test QPOP’s utility in MM, the researchers began by identifying candidate drugs that might be effective against bortezomib-resistant MM. They screened 114 approved oncology drugs on 2 MM cell lines—RPMI 8226 and bortezomib-resistant RPMI 8226 (P100v).
The drugs that proved most effective against P100v were dactinomycin, decitabine, mechlorethamine hydrochloride, and mitomycin C.
The researchers wanted to identify optimal drug combinations, so they conducted a QPOP analysis including the 4 most effective drugs and an additional 10 drugs used to treat MM. The 10 drugs were bortezomib, carfilzomib, cyclophosphamide monohydrate, dexamethasone, doxorubucin, lenalidomide, panobinostat, plerixafor, thalidomide, and zoledronic acid.
The team tested 2 dosages of the 14 drugs in 128 combinations, then narrowed the list to 9 drugs and tested them at 3 dosages in 155 combinations.
This revealed the top 3 combinations:
- Decitabine and mitomycin C
- Mechlorethamine hydrochloride, decitabine, and mitomycin C
- Bortezomib, mechlorethamine hydrochloride, and mitomycin C.
The researchers said these combinations act by reversing the DNA methylation and tumor suppressor silencing that often occurs after acquired bortezomib resistance.
The team noted that the top 3 combinations had synergistic interactions, but the QPOP analysis revealed antagonistic interactions as well. For example, bortezomib and dexamethasone proved antagonistic, as did bortezomib and panobinostat.
The researchers conducted further testing to determine the optimal dosage of decitabine and mitomycin C. Results suggested both drugs should be given at 1.5 mg/kg.
The team then treated P100v tumor-bearing mice with decitabine and mitomycin C, both at 1.5 mg/kg, either alone or in combination.
Mice that received the combination had a decrease in tumor size and prolonged survival compared to mice that received DMSO (P=0.0130), decitabine alone (P=0.0121), or mitomycin C alone (P=0.00174).
The researchers also compared decitabine and mitomycin C in combination to 2 bortezomib-based combinations used to treat MM—bortezomib/dexamethasone/melphalan and bortezomib/dexamethasone/lenalidomide—in P100v tumor-bearing mice.
There was a significant decrease in tumor volume with decitabine/mitomycin C compared to bortezomib/dexamethasone/melphalan (P=0.000376) and bortezomib/dexamethasone/lenalidomide (P=0.000691).
Mice that received decitabine/mitomycin C had significantly longer survival than mice that received bortezomib/dexamethasone/melphalan (P=0.0389) or bortezomib/dexamethasone/lenalidomide (P=0.0246).
Neither survival times nor tumor volumes were significantly different between the mice that received DMSO and those that received either of the bortezomib-based combinations.
Researchers say they have developed a computational platform that can be used to identify optimal treatments for multiple myeloma (MM).
Using this tool, the quadratic phenotypic optimization platform (QPOP), the researchers identified a 2-drug combination that proved effective against bortezomib-resistant MM in vitro.
The combination—decitabine and mitomycin C—also decreased tumor volume and prolonged survival in a mouse model of bortezomib-resistant MM.
Masturah Bte Mohd Abdul Rashid, of the Cancer Science Institute of Singapore, and her colleagues reported these results in Science Translational Medicine.
The researchers explained that QPOP approximates biological responses to therapies using advanced mathematical equations. Unlike conventional models, QPOP doesn’t require predetermined information about the mechanisms or composition of a drug.
To test QPOP’s utility in MM, the researchers began by identifying candidate drugs that might be effective against bortezomib-resistant MM. They screened 114 approved oncology drugs on 2 MM cell lines—RPMI 8226 and bortezomib-resistant RPMI 8226 (P100v).
The drugs that proved most effective against P100v were dactinomycin, decitabine, mechlorethamine hydrochloride, and mitomycin C.
The researchers wanted to identify optimal drug combinations, so they conducted a QPOP analysis including the 4 most effective drugs and an additional 10 drugs used to treat MM. The 10 drugs were bortezomib, carfilzomib, cyclophosphamide monohydrate, dexamethasone, doxorubucin, lenalidomide, panobinostat, plerixafor, thalidomide, and zoledronic acid.
The team tested 2 dosages of the 14 drugs in 128 combinations, then narrowed the list to 9 drugs and tested them at 3 dosages in 155 combinations.
This revealed the top 3 combinations:
- Decitabine and mitomycin C
- Mechlorethamine hydrochloride, decitabine, and mitomycin C
- Bortezomib, mechlorethamine hydrochloride, and mitomycin C.
The researchers said these combinations act by reversing the DNA methylation and tumor suppressor silencing that often occurs after acquired bortezomib resistance.
The team noted that the top 3 combinations had synergistic interactions, but the QPOP analysis revealed antagonistic interactions as well. For example, bortezomib and dexamethasone proved antagonistic, as did bortezomib and panobinostat.
The researchers conducted further testing to determine the optimal dosage of decitabine and mitomycin C. Results suggested both drugs should be given at 1.5 mg/kg.
The team then treated P100v tumor-bearing mice with decitabine and mitomycin C, both at 1.5 mg/kg, either alone or in combination.
Mice that received the combination had a decrease in tumor size and prolonged survival compared to mice that received DMSO (P=0.0130), decitabine alone (P=0.0121), or mitomycin C alone (P=0.00174).
The researchers also compared decitabine and mitomycin C in combination to 2 bortezomib-based combinations used to treat MM—bortezomib/dexamethasone/melphalan and bortezomib/dexamethasone/lenalidomide—in P100v tumor-bearing mice.
There was a significant decrease in tumor volume with decitabine/mitomycin C compared to bortezomib/dexamethasone/melphalan (P=0.000376) and bortezomib/dexamethasone/lenalidomide (P=0.000691).
Mice that received decitabine/mitomycin C had significantly longer survival than mice that received bortezomib/dexamethasone/melphalan (P=0.0389) or bortezomib/dexamethasone/lenalidomide (P=0.0246).
Neither survival times nor tumor volumes were significantly different between the mice that received DMSO and those that received either of the bortezomib-based combinations.
Researchers say they have developed a computational platform that can be used to identify optimal treatments for multiple myeloma (MM).
Using this tool, the quadratic phenotypic optimization platform (QPOP), the researchers identified a 2-drug combination that proved effective against bortezomib-resistant MM in vitro.
The combination—decitabine and mitomycin C—also decreased tumor volume and prolonged survival in a mouse model of bortezomib-resistant MM.
Masturah Bte Mohd Abdul Rashid, of the Cancer Science Institute of Singapore, and her colleagues reported these results in Science Translational Medicine.
The researchers explained that QPOP approximates biological responses to therapies using advanced mathematical equations. Unlike conventional models, QPOP doesn’t require predetermined information about the mechanisms or composition of a drug.
To test QPOP’s utility in MM, the researchers began by identifying candidate drugs that might be effective against bortezomib-resistant MM. They screened 114 approved oncology drugs on 2 MM cell lines—RPMI 8226 and bortezomib-resistant RPMI 8226 (P100v).
The drugs that proved most effective against P100v were dactinomycin, decitabine, mechlorethamine hydrochloride, and mitomycin C.
The researchers wanted to identify optimal drug combinations, so they conducted a QPOP analysis including the 4 most effective drugs and an additional 10 drugs used to treat MM. The 10 drugs were bortezomib, carfilzomib, cyclophosphamide monohydrate, dexamethasone, doxorubucin, lenalidomide, panobinostat, plerixafor, thalidomide, and zoledronic acid.
The team tested 2 dosages of the 14 drugs in 128 combinations, then narrowed the list to 9 drugs and tested them at 3 dosages in 155 combinations.
This revealed the top 3 combinations:
- Decitabine and mitomycin C
- Mechlorethamine hydrochloride, decitabine, and mitomycin C
- Bortezomib, mechlorethamine hydrochloride, and mitomycin C.
The researchers said these combinations act by reversing the DNA methylation and tumor suppressor silencing that often occurs after acquired bortezomib resistance.
The team noted that the top 3 combinations had synergistic interactions, but the QPOP analysis revealed antagonistic interactions as well. For example, bortezomib and dexamethasone proved antagonistic, as did bortezomib and panobinostat.
The researchers conducted further testing to determine the optimal dosage of decitabine and mitomycin C. Results suggested both drugs should be given at 1.5 mg/kg.
The team then treated P100v tumor-bearing mice with decitabine and mitomycin C, both at 1.5 mg/kg, either alone or in combination.
Mice that received the combination had a decrease in tumor size and prolonged survival compared to mice that received DMSO (P=0.0130), decitabine alone (P=0.0121), or mitomycin C alone (P=0.00174).
The researchers also compared decitabine and mitomycin C in combination to 2 bortezomib-based combinations used to treat MM—bortezomib/dexamethasone/melphalan and bortezomib/dexamethasone/lenalidomide—in P100v tumor-bearing mice.
There was a significant decrease in tumor volume with decitabine/mitomycin C compared to bortezomib/dexamethasone/melphalan (P=0.000376) and bortezomib/dexamethasone/lenalidomide (P=0.000691).
Mice that received decitabine/mitomycin C had significantly longer survival than mice that received bortezomib/dexamethasone/melphalan (P=0.0389) or bortezomib/dexamethasone/lenalidomide (P=0.0246).
Neither survival times nor tumor volumes were significantly different between the mice that received DMSO and those that received either of the bortezomib-based combinations.
RSV-related risk of hospitalization higher in Down syndrome patients
reported Andrea Beckhaus, MD, and Jose Castro-Rodriguez, MD, PhD, at the Pontificia Universidad Católica de Chile in Santiago.
Because DS is the most common chromosomal disorder, affecting 1 in every 800 children born worldwide, and respiratory infections are the leading cause of hospitalization in children with DS, especially during the first year of life, the results of this study are important and have considerable consequences for public health, the authors observed.
The economic burden on families of children with DS and the health care systems that treat them is, not surprisingly, significantly higher given their sevenfold higher need for supplemental oxygen therapy, threefold likely increased risk of ICU admission, fivefold higher likely need for ventilator support, and average increased length of hospital stay by nearly 5 days.
In the 15 years from 1997 to 2012, RSV-related hospital charges for infants with DS increased by nearly 80% from $10,141 (US dollars) to $18,217, compared with charges for infants not at high risk, which increased by more than 60% from $6,983 to $11,273 during the same period, according to a study (PLoS One. 2016;11[4]:e0152208).
Dr. Beckhaus and Dr. Castro-Rodriguez conducted their systematic review and meta-analysis to evaluate RSV-associated morbidity in children with DS. Following a search of four electronic data bases, a total of 12 studies published between 2004 and 2017 across 10 different countries were identified, including six in Europe, three in Asia, two in the United States, and one in Latin America. Altogether, 3,662 children with DS and 1,145,509 without DS were included in the review.
“Any potential strategy to reduce RSV infection (e.g., prophylaxis with monoclonal antibodies or new vaccines) in children with DS could decrease their morbidity and mortality,” the authors noted. Specifically, they cited the humanized monoclonal antibody palivizumab, which is used for prophylaxis against RSV. Palivizumab is known to reduce hospitalizations in children at high risk from comorbid conditions, including chronic lung disease, hemodynamically significant congenital heart disease (CHD), neuromuscular disease, immunodeficiency, and prematurity. At present, palivizumab is not recommended by the American Academy of Pediatrics for routine use to prevent RSV infection in patients with DS who are not already qualified for other reasons because there are insufficient data to recommend routine prophylactic use of the drug in children with Down syndrome.
The authors cited recent studies in Canada and Japan that may warrant further reconsideration of the AAP’s recommendations, however. A fourfold lowering of RSV-related hospitalizations was observed during the first 2 years of life among 532 children with DS receiving palivizumab who were included in a recent prospective Canadian study. The drug also was found to be safe and effective for preventing lower respiratory tract infections caused by RSV in a recent Japanese multicenter postmarketing surveillance study that evaluated palivizumab prophylaxis for RSV infection in 138 children with DS who did not have hemodynamically significant CHD; only 2 of the children treated required hospitalization.
“More cost-utility studies used to determine the efficacy of RSV immunoprophylaxis in this specific high-risk patient population need to be done,” Dr. Beckhaus and Dr. Castro-Rodriguez recommended.
The review was not without limitations. Not all of the studies included subgroups of participants with DS with CHD and without CHD or other additional risk factors. However, when only those studies were considered that had data for participants with DS without other risk factors, almost all results were similar.
One key strength of the study concerned the study methodology. Using the Newcastle–Ottawa scale, the risk of bias among the 12 studies was generally low, the total number of participants was considerably high, and the outcomes selected had importance for the patients and also public health implications. “It is important to remark that the vast majority of the outcomes that were analyzed had no or unimportant bias,” they said.
Dr. Beckhaus and Dr. Castro-Rodriguez had no relevant disclosures to disclose.
SOURCE: Beckhaus A et al. J Pediatrics. 2018;142(3):e20180225.
reported Andrea Beckhaus, MD, and Jose Castro-Rodriguez, MD, PhD, at the Pontificia Universidad Católica de Chile in Santiago.
Because DS is the most common chromosomal disorder, affecting 1 in every 800 children born worldwide, and respiratory infections are the leading cause of hospitalization in children with DS, especially during the first year of life, the results of this study are important and have considerable consequences for public health, the authors observed.
The economic burden on families of children with DS and the health care systems that treat them is, not surprisingly, significantly higher given their sevenfold higher need for supplemental oxygen therapy, threefold likely increased risk of ICU admission, fivefold higher likely need for ventilator support, and average increased length of hospital stay by nearly 5 days.
In the 15 years from 1997 to 2012, RSV-related hospital charges for infants with DS increased by nearly 80% from $10,141 (US dollars) to $18,217, compared with charges for infants not at high risk, which increased by more than 60% from $6,983 to $11,273 during the same period, according to a study (PLoS One. 2016;11[4]:e0152208).
Dr. Beckhaus and Dr. Castro-Rodriguez conducted their systematic review and meta-analysis to evaluate RSV-associated morbidity in children with DS. Following a search of four electronic data bases, a total of 12 studies published between 2004 and 2017 across 10 different countries were identified, including six in Europe, three in Asia, two in the United States, and one in Latin America. Altogether, 3,662 children with DS and 1,145,509 without DS were included in the review.
“Any potential strategy to reduce RSV infection (e.g., prophylaxis with monoclonal antibodies or new vaccines) in children with DS could decrease their morbidity and mortality,” the authors noted. Specifically, they cited the humanized monoclonal antibody palivizumab, which is used for prophylaxis against RSV. Palivizumab is known to reduce hospitalizations in children at high risk from comorbid conditions, including chronic lung disease, hemodynamically significant congenital heart disease (CHD), neuromuscular disease, immunodeficiency, and prematurity. At present, palivizumab is not recommended by the American Academy of Pediatrics for routine use to prevent RSV infection in patients with DS who are not already qualified for other reasons because there are insufficient data to recommend routine prophylactic use of the drug in children with Down syndrome.
The authors cited recent studies in Canada and Japan that may warrant further reconsideration of the AAP’s recommendations, however. A fourfold lowering of RSV-related hospitalizations was observed during the first 2 years of life among 532 children with DS receiving palivizumab who were included in a recent prospective Canadian study. The drug also was found to be safe and effective for preventing lower respiratory tract infections caused by RSV in a recent Japanese multicenter postmarketing surveillance study that evaluated palivizumab prophylaxis for RSV infection in 138 children with DS who did not have hemodynamically significant CHD; only 2 of the children treated required hospitalization.
“More cost-utility studies used to determine the efficacy of RSV immunoprophylaxis in this specific high-risk patient population need to be done,” Dr. Beckhaus and Dr. Castro-Rodriguez recommended.
The review was not without limitations. Not all of the studies included subgroups of participants with DS with CHD and without CHD or other additional risk factors. However, when only those studies were considered that had data for participants with DS without other risk factors, almost all results were similar.
One key strength of the study concerned the study methodology. Using the Newcastle–Ottawa scale, the risk of bias among the 12 studies was generally low, the total number of participants was considerably high, and the outcomes selected had importance for the patients and also public health implications. “It is important to remark that the vast majority of the outcomes that were analyzed had no or unimportant bias,” they said.
Dr. Beckhaus and Dr. Castro-Rodriguez had no relevant disclosures to disclose.
SOURCE: Beckhaus A et al. J Pediatrics. 2018;142(3):e20180225.
reported Andrea Beckhaus, MD, and Jose Castro-Rodriguez, MD, PhD, at the Pontificia Universidad Católica de Chile in Santiago.
Because DS is the most common chromosomal disorder, affecting 1 in every 800 children born worldwide, and respiratory infections are the leading cause of hospitalization in children with DS, especially during the first year of life, the results of this study are important and have considerable consequences for public health, the authors observed.
The economic burden on families of children with DS and the health care systems that treat them is, not surprisingly, significantly higher given their sevenfold higher need for supplemental oxygen therapy, threefold likely increased risk of ICU admission, fivefold higher likely need for ventilator support, and average increased length of hospital stay by nearly 5 days.
In the 15 years from 1997 to 2012, RSV-related hospital charges for infants with DS increased by nearly 80% from $10,141 (US dollars) to $18,217, compared with charges for infants not at high risk, which increased by more than 60% from $6,983 to $11,273 during the same period, according to a study (PLoS One. 2016;11[4]:e0152208).
Dr. Beckhaus and Dr. Castro-Rodriguez conducted their systematic review and meta-analysis to evaluate RSV-associated morbidity in children with DS. Following a search of four electronic data bases, a total of 12 studies published between 2004 and 2017 across 10 different countries were identified, including six in Europe, three in Asia, two in the United States, and one in Latin America. Altogether, 3,662 children with DS and 1,145,509 without DS were included in the review.
“Any potential strategy to reduce RSV infection (e.g., prophylaxis with monoclonal antibodies or new vaccines) in children with DS could decrease their morbidity and mortality,” the authors noted. Specifically, they cited the humanized monoclonal antibody palivizumab, which is used for prophylaxis against RSV. Palivizumab is known to reduce hospitalizations in children at high risk from comorbid conditions, including chronic lung disease, hemodynamically significant congenital heart disease (CHD), neuromuscular disease, immunodeficiency, and prematurity. At present, palivizumab is not recommended by the American Academy of Pediatrics for routine use to prevent RSV infection in patients with DS who are not already qualified for other reasons because there are insufficient data to recommend routine prophylactic use of the drug in children with Down syndrome.
The authors cited recent studies in Canada and Japan that may warrant further reconsideration of the AAP’s recommendations, however. A fourfold lowering of RSV-related hospitalizations was observed during the first 2 years of life among 532 children with DS receiving palivizumab who were included in a recent prospective Canadian study. The drug also was found to be safe and effective for preventing lower respiratory tract infections caused by RSV in a recent Japanese multicenter postmarketing surveillance study that evaluated palivizumab prophylaxis for RSV infection in 138 children with DS who did not have hemodynamically significant CHD; only 2 of the children treated required hospitalization.
“More cost-utility studies used to determine the efficacy of RSV immunoprophylaxis in this specific high-risk patient population need to be done,” Dr. Beckhaus and Dr. Castro-Rodriguez recommended.
The review was not without limitations. Not all of the studies included subgroups of participants with DS with CHD and without CHD or other additional risk factors. However, when only those studies were considered that had data for participants with DS without other risk factors, almost all results were similar.
One key strength of the study concerned the study methodology. Using the Newcastle–Ottawa scale, the risk of bias among the 12 studies was generally low, the total number of participants was considerably high, and the outcomes selected had importance for the patients and also public health implications. “It is important to remark that the vast majority of the outcomes that were analyzed had no or unimportant bias,” they said.
Dr. Beckhaus and Dr. Castro-Rodriguez had no relevant disclosures to disclose.
SOURCE: Beckhaus A et al. J Pediatrics. 2018;142(3):e20180225.
FROM PEDIATRICS
Key clinical point: Strategies to reduce RSV are needed to decrease morbidity and mortality in children with Down syndrome.
Major finding: Down syndrome children with RSV-related hospitalization had sevenfold higher need for supplemental oxygen therapy, threefold likely increased risk of ICU admission, fivefold higher likely need for ventilator support, and average increased length of hospital stay by nearly 5 days.
Study details: Systematic review and 12-study meta-analysis of 3,662 children with DS and 1,145,509 without DS.
Disclosures: The authors had no relevant financial disclosures.
Source: Beckhaus A et al. J Pediatrics. 2018;142(3):e20180225.
Maternal obesity plus diabetes lead to psychiatric disorders in offspring
Women who were obese and had diabetes before becoming pregnant were sixfold more likely to have children with psychiatric and neurodevelopmental disorders by age 11 years, as compared to women with normal body mass indexes (BMIs), based on results of a large, prospective, population-based, cohort study published in Pediatrics.
The risks to offspring whose mothers were obese and had pregestational diabetes mellitus (PGDM) were far greater than the risks seen when mothers had either condition alone or had gestational diabetes mellitus (GDM) in the study, reported Linghua Kong of the Karolinska Institute, Stockholm, and colleagues. The study is based on data from various national registries in Finland regarding 649,043 live births during 2004-2014 and data regarding psychiatric diagnoses from the Finnish Care Registers for Health Care.
Of the children in the cohort, 7.67% had mothers who were obese and 3.66% had mothers who were severely obese based on standard World Health Organization criteria; mothers had PGDM in 0.62% of the births and GDM in 15.7% of the births.
Overall, 5.4% of the children were diagnosed with a psychiatric disorder by age 11 years.
Compared with children born to mothers of normal weight (BMI less than 25 kg/m2), those born to mothers with severe maternal obesity alone (BMI greater than 35) had higher rates of developmental disorders or speech, language, motor, and scholastic skills (hazard ratio, 1.69; 95% confidence interval 1.54-1.86); ADHD and/or conduct disorder (HR, 1.88; 95% CI, 1.58-2.23); and psychosis and mood and anxiety disorders (HR, 1.67; 95% CI, 1.31-2.13). Increased risk of psychiatric disorders were only slightly statistically significant in the offspring of women with severe obesity and GDM.
The risks were significantly elevated, however, for children born to obese women who also had PGDM. The hazard ratio for autism spectrum disorder was 6.49 (95% CI, 3.08-13.69), and the HR for ADHD and/or conduct disorder was 6.03 (95% CI, 3.23-11.24). The risks were fourfold higher for mixed disorders of emotions and conduct, disorders of social function, and tics (HR, 4.29; 95% CI, 2.14-8.60).
Limitations of the study included basing results on shorter follow-up times for those born later in the study period, grouping of offspring’s disorder diagnoses, basing the definition of PGDM on insulin prescription, and using BMI measurements taken at only one time point during pregnancy.
The researchers were supported by the National Institute for Health and Welfare: Drugs and Pregnancy project, the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. Pediatrics. 2018 Sep;142(3):1-11.
Women who were obese and had diabetes before becoming pregnant were sixfold more likely to have children with psychiatric and neurodevelopmental disorders by age 11 years, as compared to women with normal body mass indexes (BMIs), based on results of a large, prospective, population-based, cohort study published in Pediatrics.
The risks to offspring whose mothers were obese and had pregestational diabetes mellitus (PGDM) were far greater than the risks seen when mothers had either condition alone or had gestational diabetes mellitus (GDM) in the study, reported Linghua Kong of the Karolinska Institute, Stockholm, and colleagues. The study is based on data from various national registries in Finland regarding 649,043 live births during 2004-2014 and data regarding psychiatric diagnoses from the Finnish Care Registers for Health Care.
Of the children in the cohort, 7.67% had mothers who were obese and 3.66% had mothers who were severely obese based on standard World Health Organization criteria; mothers had PGDM in 0.62% of the births and GDM in 15.7% of the births.
Overall, 5.4% of the children were diagnosed with a psychiatric disorder by age 11 years.
Compared with children born to mothers of normal weight (BMI less than 25 kg/m2), those born to mothers with severe maternal obesity alone (BMI greater than 35) had higher rates of developmental disorders or speech, language, motor, and scholastic skills (hazard ratio, 1.69; 95% confidence interval 1.54-1.86); ADHD and/or conduct disorder (HR, 1.88; 95% CI, 1.58-2.23); and psychosis and mood and anxiety disorders (HR, 1.67; 95% CI, 1.31-2.13). Increased risk of psychiatric disorders were only slightly statistically significant in the offspring of women with severe obesity and GDM.
The risks were significantly elevated, however, for children born to obese women who also had PGDM. The hazard ratio for autism spectrum disorder was 6.49 (95% CI, 3.08-13.69), and the HR for ADHD and/or conduct disorder was 6.03 (95% CI, 3.23-11.24). The risks were fourfold higher for mixed disorders of emotions and conduct, disorders of social function, and tics (HR, 4.29; 95% CI, 2.14-8.60).
Limitations of the study included basing results on shorter follow-up times for those born later in the study period, grouping of offspring’s disorder diagnoses, basing the definition of PGDM on insulin prescription, and using BMI measurements taken at only one time point during pregnancy.
The researchers were supported by the National Institute for Health and Welfare: Drugs and Pregnancy project, the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. Pediatrics. 2018 Sep;142(3):1-11.
Women who were obese and had diabetes before becoming pregnant were sixfold more likely to have children with psychiatric and neurodevelopmental disorders by age 11 years, as compared to women with normal body mass indexes (BMIs), based on results of a large, prospective, population-based, cohort study published in Pediatrics.
The risks to offspring whose mothers were obese and had pregestational diabetes mellitus (PGDM) were far greater than the risks seen when mothers had either condition alone or had gestational diabetes mellitus (GDM) in the study, reported Linghua Kong of the Karolinska Institute, Stockholm, and colleagues. The study is based on data from various national registries in Finland regarding 649,043 live births during 2004-2014 and data regarding psychiatric diagnoses from the Finnish Care Registers for Health Care.
Of the children in the cohort, 7.67% had mothers who were obese and 3.66% had mothers who were severely obese based on standard World Health Organization criteria; mothers had PGDM in 0.62% of the births and GDM in 15.7% of the births.
Overall, 5.4% of the children were diagnosed with a psychiatric disorder by age 11 years.
Compared with children born to mothers of normal weight (BMI less than 25 kg/m2), those born to mothers with severe maternal obesity alone (BMI greater than 35) had higher rates of developmental disorders or speech, language, motor, and scholastic skills (hazard ratio, 1.69; 95% confidence interval 1.54-1.86); ADHD and/or conduct disorder (HR, 1.88; 95% CI, 1.58-2.23); and psychosis and mood and anxiety disorders (HR, 1.67; 95% CI, 1.31-2.13). Increased risk of psychiatric disorders were only slightly statistically significant in the offspring of women with severe obesity and GDM.
The risks were significantly elevated, however, for children born to obese women who also had PGDM. The hazard ratio for autism spectrum disorder was 6.49 (95% CI, 3.08-13.69), and the HR for ADHD and/or conduct disorder was 6.03 (95% CI, 3.23-11.24). The risks were fourfold higher for mixed disorders of emotions and conduct, disorders of social function, and tics (HR, 4.29; 95% CI, 2.14-8.60).
Limitations of the study included basing results on shorter follow-up times for those born later in the study period, grouping of offspring’s disorder diagnoses, basing the definition of PGDM on insulin prescription, and using BMI measurements taken at only one time point during pregnancy.
The researchers were supported by the National Institute for Health and Welfare: Drugs and Pregnancy project, the Swedish Research Council, the regional agreement on medical training and clinical research between Stockholm County Council and Karolinska Institutet Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. Pediatrics. 2018 Sep;142(3):1-11.
FROM PEDIATRICS